We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 5: 10 Real Cases on Acute Heart Failure Syndrome: Diagnosis, Management, and Follow-Up
Swathi Roy; Gayathri Kamalakkannan
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion.
- Full Chapter
- Supplementary Content
Case 1: Diagnosis and Management of New-Onset Heart Failure With Reduced Ejection Fraction
A 54-year-old woman presented to the telemetry floor with shortness of breath (SOB) for 4 months that progressed to an extent that she was unable to perform daily activities. She also used 3 pillows to sleep and often woke up from sleep due to difficulty catching her breath. Her medical history included hypertension, dyslipidemia, diabetes mellitus, and history of triple bypass surgery 4 years ago. Her current home medications included aspirin, atorvastatin, amlodipine, and metformin. No significant social or family history was noted. Her vital signs were stable. Physical examination showed bilateral diffuse crackles in lungs, elevated jugular venous pressure, and 2+ pitting lower extremity edema. ECG showed normal sinus rhythm with left ventricular hypertrophy. Chest x-ray showed vascular congestion. Laboratory results showed a pro-B-type natriuretic peptide (pro-BNP) level of 874 pg/mL and troponin level of 0.22 ng/mL. Thyroid panel was normal. An echocardiogram demonstrated systolic dysfunction, mild mitral regurgitation, a dilated left atrium, and an ejection fraction (EF) of 33%. How would you manage this case?
In this case, a patient with known history of coronary artery disease presented with worsening of shortness of breath with lower extremity edema and jugular venous distension along with crackles in the lung. The sign and symptoms along with labs and imaging findings point to diagnosis of heart failure with reduced EF (HFrEF). She should be treated with diuretics and guideline-directed medical therapy for congestive heart failure (CHF). Telemetry monitoring for arrythmia should be performed, especially with structural heart disease. Electrolyte and urine output monitoring should be continued.
In the initial evaluation of patients who present with signs and symptoms of heart failure, pro-BNP level measurement may be used as both a diagnostic and prognostic tool. Based on left ventricular EF (LVEF), heart failure is classified into heart failure with preserved EF (HFpEF) if LVEF is >50%, HFrEF if LVEF is <40%, and heart failure with mid-range EF (HFmEF) if LVEF is 40% to 50%. All patients with symptomatic heart failure should be started on an angiotensin-converting enzyme (ACE) inhibitor (or angiotensin receptor blocker if ACE inhibitor is not tolerated) and β-blocker, as appropriate. In addition, in patients with New York Heart Association functional classes II through IV, an aldosterone antagonist should be prescribed. In African American patients, hydralazine and nitrates should be added. Recent recommendations also recommend starting an angiotensin receptor-neprilysin inhibitor (ARNI) in patients who are symptomatic on ACE inhibitors.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
Heart Failure Case Studies
- First Online: 30 March 2023
Cite this chapter

- Nicole R. Dellise 3 &
- K. Melissa Smith Hayes 4
558 Accesses
Heart failure patients presenting to primary care clinics often have multiple, complex comorbidities. Several different disease processes and treatment options may need to be considered simultaneously in the setting of acute on chronic exacerbation of symptoms. This chapter will exemplify complex heart failure patient vignettes and provide practical guidance for the primary care provider, highlighting HF guideline-directed medical therapy.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Testani JM, Brisco MA, Turner JM, et al. Loop diuretic efficiency: a metric of diuretic responsiveness with prognostic importance in acute decompensated heart failure. Circ Heart Fail. 2014;7(2):261–70. https://doi.org/10.1161/CIRCHEARTFAILURE.113.000895 .
Article CAS PubMed Google Scholar
Felker GM, Mentz RJ. Diuretics and ultrafiltration in acute decompensated heart failure. J Am Coll Cardiol. 2012;59(24):2145–53. https://doi.org/10.1016/j.jacc.2011.10.910 . PMID: 22676934.
Wagdy K, Nagy S. EMPEROR-preserved: SGLT2 inhibitors breakthrough in the management of heart failure with preserved ejection fraction. Glob Cardiol Sci Pract. 2021;2021(3):e202117. https://doi.org/10.21542/gcsp.2021.17 . PMID: 34805375; PMCID: PMC8587377.
Article PubMed PubMed Central Google Scholar
Heidenreich P, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure. J Am Coll Cardiol. 2022;79(17):e263–421. https://doi.org/10.1016/j.jacc.2021.12.012 .
Article PubMed Google Scholar
Qurie A, Goyal A, Musa R. Allopurinol. [Updated 2021 Jul 7]. In: StatPearls [internet]. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499942/ .
Adamson PB, Abraham WT, Bourge RC, Costanzo MR, Hasan A, Yadav C, et al. Wireless pulmonary artery pressure monitoring guides management to reduce decompensation in heart failure with preserved ejection fraction. Circ Heart Fail. 2014 Nov;7(6):935–44.
Cummings ED, Swoboda HD. Digoxin toxicity. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470568/ .
Otto CM, Nishimura RA, Bonow RO, Carabello BA, Erwin JP 3rd, Gentile F, Jneid H, Krieger EV, Mack M, McLeod C, O’Gara PT, Rigolin VH, Sundt TM III, Thompson A, Toly C. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021;77:e25–197.
Sundt TM, Jneid H. Guideline update on indications for transcatheter aortic valve implantation based on the 2020 American College of Cardiology/American Heart Association guidelines for management of valvular heart disease. JAMA Cardiol. 2021;6(9):1088–9. https://doi.org/10.1001/jamacardio.2021.2534 .
Centers for Medicare and Medicaid Services. Fact Sheet: let Medicaid give you a ride. 2016. Retrieved from https://www.cms.gov/Medicare-Medicaid-Coordination/Fraud-Prevention/Medicaid-Integrity-Education/Downloads/nemt-factsheet.pdf .
Centers for Medicare and Medicaid Services. Medicare and home healthcare. 2020. Retrieved from https://www.medicare.gov/Pubs/pdf/10969-medicare-and-home-health-care.pdf .
Davidson B, Dunham S. The perfect storm: barriers to heart failure treatment options. Crit Care Nurs Clin N Am. 2022;34(2):141–50. https://doi.org/10.1016/j.cnc.2022.02.003 .
Article Google Scholar
Halliday BP, Wassall R, Lota AS, et al. Withdrawal of pharmacological treatment for heart failure in patients with recovered dilated cardiomyopathy (TRED-HF): an open-label, pilot, randomized trial. Lancet. 2019;393:61–73.
Maddox T, Januzzi J, Allen L, et al. 2021 update to the 2017 ACC expert consensus decision pathway for optimization of heart failure treatment: answers to 10 pivotal issues about heart failure with reduced ejection fraction. J Am Coll Cardiol. 2021;77(6):772–810. https://doi.org/10.1016/j.jacc.2020.11.022 .
Download references
Author information
Authors and affiliations.
Centennial Heart, Nashville, TN, USA
Nicole R. Dellise
Vanderbilt University School of Nursing, Nashville, TN, USA
K. Melissa Smith Hayes
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nicole R. Dellise .
Editor information
Editors and affiliations.
Assistant Professor, Vanderbilt University School of Nursing, Nashville, TN, USA
Director, Structural Heart Program, Director, Center for Advanced Heart Failure Therapy, Centennial Heart, Nashville, TN, USA
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Dellise, N.R., Hayes, K.M.S. (2023). Heart Failure Case Studies. In: Hayes, K.M.S., Dellise, N.R. (eds) Managing Heart Failure in Primary Care: A Case Study Approach. Springer, Cham. https://doi.org/10.1007/978-3-031-20193-6_19
Download citation
DOI : https://doi.org/10.1007/978-3-031-20193-6_19
Published : 30 March 2023
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-20192-9
Online ISBN : 978-3-031-20193-6
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Search Menu
- Sign in through your institution
- Author videos
- ESC Content Collections
- Supplements
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About European Heart Journal Supplements
- About the European Society of Cardiology
- ESC Publications
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, case presentation.
- < Previous
Clinical case: heart failure and ischaemic heart disease
- Article contents
- Figures & tables
- Supplementary Data
Giuseppe M C Rosano, Clinical case: heart failure and ischaemic heart disease, European Heart Journal Supplements , Volume 21, Issue Supplement_C, April 2019, Pages C42–C44, https://doi.org/10.1093/eurheartj/suz046
- Permissions Icon Permissions
Patients with ischaemic heart disease that develop heart failure should be treated as per appropriate European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines.
Glucose control in diabetic patients with heart failure should be more lenient that in patients without cardiovascular disease.
Optimization of cardiac metabolism and control of heart rate should be a priority for the treatment of angina in patients with heart failure of ischaemic origin.
This clinical case refers to an 83-year-old man with moderate chronic obstructive pulmonary disease and shows that implementation of appropriate medical therapy according to the European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines improves symptoms and quality of life. 1 The case also illustrates that optimization of glucose metabolism with a more lenient glucose control was most probably important in improving the overall clinical status and functional capacity.
The patient has family history of coronary artery disease as his brother had suffered an acute myocardial infarction (AMI) at the age of 64 and his sister had received coronary artery by-pass. He also has a 14-year diagnosis of arterial hypertension, and he is diabetic on oral glucose-lowering agents since 12 years. He smokes 30 cigarettes per day since childhood.
In February 2009, after 2 weeks of angina for moderate efforts, he suffered an acute anterior myocardial infarction. He presented late (after 14 h since symptom onset) at the hospital where he had been treated conservatively and had been discharged on medical therapy: Atenolol 50 mg o.d., Amlodipine 2.5 mg o.d., Aspirin 100 mg o.d., Atorvastatin 20 mg o.d., Metformin 500 mg tds, Gliclazide 30 mg o.d., Salmeterol 50, and Fluticasone 500 mg oral inhalers.
Four weeks after discharge, he underwent a planned electrocardiogram (ECG) stress test that documented silent effort-induced ST-segment depression (1.5 mm in V4–V6) at 50 W.
He underwent a coronary angiography (June 2009) and left ventriculography that showed a not dilated left ventricle with apical dyskinesia, normal left ventricular ejection fraction (LVEF, 52%); occlusion of proximal LAD, 60% stenosis of circumflex (CX), and 60% stenosis of distal right coronary artery (RCA). An attempt to cross the occluded left anterior descending (LAD) was unsuccessful.
He was therefore discharged on medical therapy with: Atenolol 50 mg o.d., Atorvastatin 20 mg o.d., Amlodipine 2.5 mg o.d., Perindopril 4 mg o.d., oral isosorbide mono-nitrate (ISMN) 60 mg o.d., Aspirin 100 mg o.d., metformin 850 mg tds, Gliclazide 30 mg o.d., Salmeterol 50 mcg, and Fluticasone 500 mcg b.i.d. oral inhalers.
He had been well for a few months but in March 2010 he started to complain of retrosternal constriction associated to dyspnoea for moderate efforts (New York Heart Association (NYHA) II–III, Canadian Class II).
For this reason, he was prescribed a second coronary angiography that showed progression of atherosclerosis with 80% stenosis on the circumflex (after the I obtuse marginal branch) and distal RCA. The LAD was still occluded.
After consultation with the heart team, CABG was avoided because surgical the risk was deemed too high and the patient underwent palliative percutaneous coronary intervention (PCI) of CX and RCA. It was again attempted to cross the occlusion on the LAD. But this attempt was, again, unsuccessful. Collateral circulation from posterior interventricular artery (PDL) to the LAD was found. The pre-PCI echocardiogram documented moderate left ventricular dysfunction (EF 38%), the pre-discharge echocardiogram documented a LVEF of 34%. Because of the reduced LVEF, atenolol was changed for Bisoprolol (5 mg o.d.).
At follow-up visit in December 2012, the clinical status and the haemodynamic conditions had deteriorated. He complained of worsening effort-induced dyspnoea/angina that now occurred for less than a flight of stairs (NYHA III). On clinical examination clear signs of worsening heart failure were detected ( Table 1 ). His medical therapy was modified to: Bisoprolol 5 mg o.d., Atorvastatin 20 mg o.d., Amlodipine 2.5 mg o.d., Perindopil 5 mg o.d., ISMN 60 mg o.d., Aspirin 100 mg o.d., Metformin 500 mg tds, Furosemide 50 mg o.d., Gliclazide 30 mg o.d., Salmeterol 50 mcg oral inhaler, and Fluticasone 500 mcg oral inhaler. A stress perfusion cardiac scintigraphy was requested and revealed dilated ventricles with LVEF 19%, fixed apical perfusion defect and reversible perfusion defect of the antero-septal wall (ischaemic burden <10%, Figure 1 ). He was admitted, and an ICD was implanted.
Clinical parameters during follow-up visits

Myocardial perfusion scintigraphy and left ventriculography showing dilated left ventricle with left ventricular ejection fraction 19%. Reversible perfusion defects on the antero-septal wall and fixed apical perfusion defect.
In March 2013, he felt slightly better but still complained of effort-induced dyspnoea/angina (NYHA III, Table 1 ). Medical therapy was updated with bisoprolol changed with Nebivolol 5 mg o.d. and perindopril changed to Enalapril 10 mg b.i.d. The switch from bisoprolol to nebivolol was undertaken because of the better tolerability and outcome data with nebivolol in elderly patients with heart failure. Perindopril was switched to enalapril because the first one has no indication for the treatment of heart failure.
In September 2013, the clinical conditions were unchanged, he still complained of effort-induced dyspnoea/angina (NYHA III) and did not notice any change in his exercise capacity. His BNP was 1670. He was referred for a 3-month cycle of cardiac rehabilitation during which his medical therapy was changed to: Nebivolol 5 mg o.d., Ivabradine 5 mg b.i.d., uptitrated in October to 7.5 b.i.d., Trimetazidine 20 mg tds, Furosemide 50 mg, Metolazone 5 mg o.d., K-canrenoate 50 mg, Enalapril 10 mg b.i.d., Clopidogrel 75 mg o.d., Atorvastatin 40 mg o.d., Metformin 500 mg b.i.d., Salmeterol 50 mcg oral inhaler, and Fluticasone 500 mcg oral inhaler.
At the follow-up visit in January 2014, he felt much better and had symptomatically, he no longer complained of angina, nor dyspnoea (NYHA Class II, Table 1 ). Trimetazidine was added because of its benefits in heart failure patients of ischaemic origin and because of its effect on functional capacity. Ivabradine was added to reduce heart rate since it was felt that increasing nebivolol, that was already titrated to an effective dose, would have had led to hypotension.
He missed his follow-up visits in June and October 2014 because he was feeling well and he had decided to spend some time at his house in the south of Italy. In January and June 2015, he was well, asymptomatic (NYHA I–II) and able to attend his daily activities. He did not complain of angina nor dyspnoea and reported no limitations in his daily activities. Unfortunately, in November 2015 he was hit by a moped while on the zebra crossing in Rome and he later died in hospital as a consequence of the trauma.
This case highlights the need of optimizing both the heart failure and the anti-anginal medications in patients with heart failure of ischaemic origin. This patient has improved dramatically after the up-titration of diuretics, the control of heart rate with nebivolol and ivabradine and the additional use of trimetazidine. 1–3 All these drugs have contributed to improve the clinical status together with a more lenient control of glucose metabolism. 4 This is another crucial point to take into account in diabetic patients, especially if elderly, with heart failure in whom aggressive glucose control is detrimental for their functional capacity and long-term prognosis. 5
IRCCS San Raffaele - Ricerca corrente Ministero della Salute 2018.
Conflict of interest : none declared. The authors didn’t receive any financial support in terms of honorarium by Servier for the supplement articles.
Ponikowski P , Voors AA , Anker SD , Bueno H , Cleland JG , Coats AJ , Falk V , González-Juanatey JR , Harjola VP , Jankowska EA , Jessup M , Linde C , Nihoyannopoulos P , Parissis JT , Pieske B , Riley JP , Rosano GM , Ruilope LM , Ruschitzka F , Rutten FH , van der Meer P ; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the Special Contribution of the Heart Failure Association (HFA) of the ESC . Eur J Heart Fail 2016 ; 18 : 891 – 975 .
Google Scholar
Rosano GM , Vitale C. Metabolic modulation of cardiac metabolism in heart failure . Card Fail Rev 2018 ; 4 : 99 – 103 .
Vitale C , Ilaria S , Rosano GM. Pharmacological interventions effective in improving exercise capacity in heart failure . Card Fail Rev 2018 ; 4 : 1 – 27 .
Seferović PM , Petrie MC , Filippatos GS , Anker SD , Rosano G , Bauersachs J , Paulus WJ , Komajda M , Cosentino F , de Boer RA , Farmakis D , Doehner W , Lambrinou E , Lopatin Y , Piepoli MF , Theodorakis MJ , Wiggers H , Lekakis J , Mebazaa A , Mamas MA , Tschöpe C , Hoes AW , Seferović JP , Logue J , McDonagh T , Riley JP , Milinković I , Polovina M , van Veldhuisen DJ , Lainscak M , Maggioni AP , Ruschitzka F , McMurray JJV. Type 2 diabetes mellitus and heart failure: a position statement from the Heart Failure Association of the European Society of Cardiology . Eur J Heart Fail 2018 ; 20 : 853 – 872 .
Vitale C , Spoletini I , Rosano GM. Frailty in heart failure: implications for management . Card Fail Rev 2018 ; 4 : 104 – 106 .
- myocardial ischemia
- cardiac rehabilitation
- heart failure
- older adult
Email alerts
More on this topic, related articles in pubmed, citing articles via.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1554-2815
- Print ISSN 1520-765X
- Copyright © 2024 European Society of Cardiology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
This case study involves a 76 year old female named Mary Lou Poppins, who presented to the ED accompanied by her son. She called her son after having symptoms of shortness of breath and confusion. Her past medical history includes hypertension, hyperlipidemia, coronary artery disease, and she was an everyday smoker for 30 years. She reports her home medications are lisinopril, simvastatin, and baby aspirin. Her current lifestyle includes: being a widow of six years, she lives alone, she walks her dog everyday, she drives to her knitting group three days a week, she makes dinner for her grandchildren once a week, she attempts to eat healthy but admits to consuming salty and high fat foods, and she insists on being very independent.
Mary Lou Poppins initial vitals in the emergency department includes a blood pressure of 138/70, heart rate of 108. respiratory rate of 26, temperature 98.9 degrees fahrenheit, and oxygen saturation of 84%. Her initial assessment included alert and oriented to person and place, dyspnea, inspiratory crackles in bilateral lungs, and a cough with pink frothy sputum. Her labs and diagnostics resulted in a BNP of 740 pg/ml, an echocardiogram showing an ejection fraction of 35%, an ECG that read sinus tachycardia, and a chest x-ray that confirmed pulmonary edema.
The Emergency Department physician diagnosed Mary Lou Poppins with left-sided heart failure. The orders included: supplemental oxygen titrated to keep saturation >93%, furosemide IV, enoxaparin subq, and metoprolol PO. Nursing Interventions included: monitoring oxygen saturation, adjusting oxygen route and dosage according to orders, assessing mentation and confusion, obtaining IV access, reassessing vitals, administering medications, and keeping the head of the bed elevated greater than 45 degrees. She was admitted to the telemetry unit for further stabilization, fluid balance monitoring, and oxygen monitoring.
On day one of hospital admission, Mary Lou Poppins required 4L of oxygen via nasal cannula in order to maintain the goal saturation of >93%. Upon assessment, it was determined that she was oriented to person and place. Auscultation of the lungs revealed bilateral crackles throughout, requiring collaboration with respiratory therapy once in the morning, and once in the afternoon. Physical therapy worked with the patient, but she was only able to ambulate for 100 feet. During ambulation, the patient had a decrease of oxygen saturation and dyspnea, requiring her oxygen to be increased to 6L. At the end of the day, strict intake and output monitoring showed an intake of 1200 mL of fluids, with an urinary output of 2L.
On day two of admission, Mary Lou began demonstrating signs of improvement. She only required 2 L of oxygen via nasal cannula with diminished crackles heard upon auscultation. Morning weight showed a weight loss of 1.3 lbs and the patient was oriented to person, place, and sequence of events. During physical therapy, she was able to ambulate 300 feet without required increased oxygen support. Daily fluid intake was 1400 mL with a urinary output of 1900 mL.
On the third and final day of admission, Mary Lou was AOx4 and did not require any type of oxygen support. When physical therapy arrived, the patient was able to ambulate 500 feet, which was close to her pre-hospital status. When the doctor arrived, the patient informed him that she felt so much better and felt confident going home. The doctor placed orders for discharge.
Upon discharge and throughout the patient’s hospital stay, Mary Lou Poppins was educated regarding the disease process of heart failure; symptoms to monitor for and report to her doctor; the importance of daily monitoring of weight, blood pressure, and heart rate; and the importance of adhering to a diet and exercise regime. Education was also provided regarding her medications and the importance of strictly adhering to them in order to prevent exacerbations of heart failure. Smoking cessation was also included in her plan of care. The patient received an informational packet regarding her treatment plan, symptoms to monitor for, and when to call her physician. Upon discharge, the patient was instructed to schedule a follow up appointment with her cardiologist for continued management of her care.
The patient was put in contact with a home health agency to help manage her care. The home health nurse will help to reinforce the information provided to the patient, assess the patient’s home and modify it to meet her physical limitations, and help to create a plan to meet daily dietary and exercise requirements. Regular follow-up appointments were stressed to Mary Lou Poppins in order to assess the progression of her disease. It will be important to monitor her lab values to also assess her disease progression and for any potential side effects associated with her medications. Repeat echocardiograms will be necessary to monitor her ejection fraction; if it does not improve with the treatment plan, an implanted cardiac defibrillator may be necessary to prevent cardiac death.
Open-Ended Questions
- What were the clinical manifestations that Mary Lou Poppins presented with in the ED that suggested the new onset of CHF?
- What factors most likely contributed to the onset of CHF?
- What patient education should Mary Lou Poppins receive on discharge in regards to managing her CHF?
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

- Find a Doctor
- Patients & Visitors
- ER Wait Times
- For Medical Professionals
- Piedmont MyChart

- Toggle navigation --> Back to Piedmont.org
- Piedmont Healthcare
Learning Center
- Education and Resources
- Women's Heart Support Network
- Heart Failure Tools and Resources
Case Study: Acute Heart Failure in a 20-year-old Patient
At Piedmont Heart’s Napa Valley Cardiology Conference, Dr. David Dean presents a challenging case of acute heart failure in a 20-year-old patient. Hear Piedmont’s unusual approach to therapy and tips for success from Dr. Dean, surgical director of Piedmont’s Samsky Advanced Heart Failure Center.
Download the Piedmont Now app
- Indoor Hospital Navigation
- Find & Save Physicians
- Online Scheduling
Download the app today!
Fastest Nurse Insight Engine
- MEDICAL ASSISSTANT
- Abdominal Key
- Anesthesia Key
- Basicmedical Key
- Otolaryngology & Ophthalmology
- Musculoskeletal Key
- Obstetric, Gynecology and Pediatric
- Oncology & Hematology
- Plastic Surgery & Dermatology
- Clinical Dentistry
- Radiology Key
- Thoracic Key
- Veterinary Medicine
- Gold Membership
Case study of a patient with heart failure
13 Case study of a patient with heart failure Chapter aims • To provide you with an example of the nursing care that a patient with heart failure may require • To encourage you to research and deepen your knowledge of heart failure Introduction This chapter provides you with an example of the nursing care that a patient with heart failure may require. The heart failure care plan ( Fig. 13.1 ) has been written by a senior charge nurse for coronary care, Rafael Ripoll, and outlines care for the four stages of heart failure. The case history for Martha will then guide you through the assessment, nursing action and evaluation of a patient with heart failure. Fig 13.1 Heart failure care plan (Reproduced with permission of Rafael Ripoll) Activity A definition of heart failure was given in Chapter 1 and asked you to revise your anatomy and physiology (see Montague et al 2005 ). Before reading the case study, find out the following: 1. What are some of the symptoms of heart failure? 2. What health education could you provide for a patient with heart failure? You can find out the answers to these questions by following the link below. The British Heart Foundation provides free booklets to download: http://www.bhf.org.uk/heart-health/conditions/heart-failure.aspx (accessed July 2011). Patient profile Martha is a 60-year-old lady who is admitted to accident and emergency (A&E) with breathlessness – her respiratory rate is 40 per minute and her oxygen saturation is 89%. On admission, her pulse is 175 beats per minute (bpm) and irregular. Her blood pressure is 90/50 mmHg. Martha is put on high-flow oxygen, a continuous cardiac monitor, hourly observation of vital signs and an intravenous cannula is inserted. Martha is administered intravenous digoxin and furosemide in A&E and is catheterised to enable accurate fluid balance. Martha is married with three grown-up children and smokes 20 cigarettes a day. Martha is then transferred to a medical ward with a cardiac specialty. Assessment on admission Martha is breathless and on oxygen therapy 35% via the mask. She has peripheral oedema and is fluid overloaded. Furosemide is being administered intravenously. She is on stage 2 (see Fig. 13.1 ) of the heart failure care plan but is not receiving glyceryl trinitrate (GTN) due to hypotension. Martha is tachycardic and attached to a cardiac monitor which is showing atrial fibrillation between 110 and 115 bpm. Urinary output is greater than 70 mL/hour. Martha is very distressed but knows where she is and why. She is unable to eat or drink at the moment due to her breathlessness. She is a life-long smoker. She lives with her husband in a third-floor flat with a lift. She still works part time as a cleaner for a local company. Activity See Appendix 4 in Holland et al (2008) for possible questions to consider during the assessment stage of care planning. Many organisations will have a care plan pathway, and Figure 13.1 is an example of one by R. Ripoll (2005 unpublished). This is to ensure that the care of the patient is explicit and standardised. This does not mean that the care becomes less individualised. Martha’s problems Based on your assessment of Martha, the following problems should form the basis of your care plan: • Martha is breathless. • Martha is cardiovascularly unstable due to her condition. • Martha is frightened and distressed. • Martha has a urinary catheter. • Martha is unable to eat or drink adequately due to her condition. • Martha is a life-long smoker and cannot smoke in hospital. Martha’s nursing care plans 1. Problem: Martha is breathless. Goal: To restore normal breathing pattern. Nursing action Rationale Assess Martha’s breathing, respiratory rate and keep oxygen saturation > 95% Observe for signs of cyanosis Administer prescribed oxygen Inform the nurse in charge of any changes to Martha’s condition To observe for any signs of deterioration To ensure that Martha does not become hypoxic Oxygen is a drug and must be prescribed Encourage Martha to sit upright supported by pillows To maximise lung expansion and gaseous exchange To increase comfort Administer any medication as prescribed and ensure that Martha is fully informed about the medication and any side effects For example, explain to Martha why she needs to keep her oxygen mask on Martha is much more likely to comply with her medication if she understands why she needs to have it Refer Martha to the physiotherapist and liaise To maximise gaseous exchange To prevent complications from immobility To ensure consistent treatment from nurses and physiotherapists 2. Problem: Martha is cardiovascularly unstable due to her condition. Goal : To stabilise Martha. Nursing action Rationale Martha needs continuous cardiac monitoring of her condition until it has stabilised Ensure that alarm limits are set within appropriate limits Hourly observations of pulse and blood pressure Inform the nurse in charge and doctor regarding any changes in observations and discuss the frequency of observations required To detect any change in Martha’s condition as soon as possible To be able to respond to these changes and for the team to be informed To check blood urea and electolytes Abnormal potassium levels will increase the risk cardiovascular instability 3. Problem: Martha is frightened and distressed. Goal : To try to relieve Martha’s distress. Nursing action Rationale Spend time with Martha using verbal and non-verbal communication to reassure her Being alone will increase Martha’s distress Always introduce Martha to the nurse who is relieving you or taking over your shift If you need to go to another area, explain to Martha who will be looking after her Explain to Martha how the call bell system works and make sure that it is in easy reach Knowing who is looking after her will help Martha to relax Knowing where her nurse is is important as Martha will know that there is someone identified who is looking after her needs If Martha cannot see her nurse she will understand how to summon help Communicate with Martha’s family and significant others with her permisssion Family and friends may find the environment and equipment daunting Information will help them to understand about Martha’s condition Nurses should never presume that a patient wants her family to know about their condition and it is important to respect Martha’s wishes 4. Problem: Martha has a urinary catheter. Goal: To monitor fluid balance accurately and to prevent infection. Nursing action Rationale Explain to Martha why she requires urinary catheter. Hourly measurements of urine: if below 30 mL/h or above 200 mL/h, report to the nurse in charge and liaise with the doctors when reducing the frequency of the urine output measurements Document urine output on a fluid balance chart To accurately monitor Martha’s fluid balance. Martha is at risk of fluid overload due to her cardiac condition Provide catheter care and hygiene Check the colour of the urine each shift Report any changes to the nurse in charge Provide privacy when providing catheter care To prevent infection To detect any signs of infection or trauma To ensure that Martha’s privacy and dignity needs are met Monitor temperature, pulse and blood pressure and respirations four times a day while Martha has an indwelling urinary catheter Take a catheter specimen of urine for microscopy, culture and sensitivity testing if Martha’s temperature is > 37.5°C and inform the nurse/doctor To detect any infection and treat as soon as possible 5. Problem: Martha is unable to eat or drink adequately due to her condition. Goal: For Martha to have adequate fluid and dietary intake. Nursing action Rationale Ensure a malnutrition risk assessment is undertaken in the first 24 hours (see Ch. 9 ) To determine Martha’s nutritional status Maintain strict food and fluid balance monitoring Martha may be on fluid restriction Inform Martha about this and provide her with rationale Inform the nurse in charge or doctor if Martha’s diet or fluid intake are below the normal limits Due to her cardiac failure, Martha is at risk of fluid overload To ensure that Martha receives adequate fluids and nutrition To prevent complications of dehydration To ensure that there is effective communication within the multidisciplinary team Ensure that nutritional supplements are explained to Martha and encourage her to drink them To keep Martha fully informed Monitor and document observations of her vital signs (see Ch. 7 ) To detect any deterioration/improvement Administer intravenous therapy as prescribed and ensure that a cannula care plan is in place for this (see Ch. 9 ) To reduce the risk of cannula-associated infection/complications Keep Martha informed of her condition To promote and enhance communication 6. Problem: Martha is a life-long smoker and cannot smoke in hospital. Goal: To help Martha deal with any cravings or withdrawal symptoms. Nursing action Rationale To discuss with Martha how she is feeling and discuss prescribing nicotine supplements with the medical team To prevent Martha from suffering from nicotine withdrawal symptoms Once Martha is feeling better, discuss how she feels about smoking after discharge and whether she would accept a referral to the cardiac rehabilitation/heart failure team or smoking cessation team Provide verbal and written information for Martha and her husband To provide health education and promotion to Martha and her family
Share this:
- Click to share on Twitter (Opens in new window)
- Click to share on Facebook (Opens in new window)
Related posts:
- Medical placements
- Revision and future learning
- The end of the journey
- Medicines management
Stay updated, free articles. Join our Telegram channel
Comments are closed for this page.

Full access? Get Clinical Tree

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Congestive heart failure.
Ahmad Malik ; Daniel Brito ; Sarosh Vaqar ; Lovely Chhabra .
Affiliations
Last Update: November 5, 2023 .
- Continuing Education Activity
Congestive heart failure (CHF) is a complex clinical syndrome characterized by inefficient myocardial performance, resulting in compromised blood supply to the body. CHF results from any disorder that impairs ventricular filling or ejection of blood to the systemic circulation. Patients usually present with fatigue and dyspnea, reduced exercise tolerance, and systemic or pulmonary congestion. The etiology of HF is variable and extensive. A comprehensive assessment is required when evaluating a patient with HF. The general management aims at relieving systemic and pulmonary congestion and stabilization of hemodynamic status, regardless of the cause. This activity reviews the evaluation and management of congestive heart failure and highlights the role of the healthcare team in improving care for patients with this condition.
- Apply the staging and classification systems of heart failure.
- Assess and monitor patients with heart failure for signs of decompensation, fluid retention, and response to treatment.
- Select appropriate diagnostic tests, like echocardiography and biomarker assays, to aid in heart failure diagnosis and monitoring.
- Collaborate with multidisciplinary healthcare teams, including cardiologists, nurses, and pharmacists, to ensure coordinated and comprehensive care for heart failure patients.
- Introduction
Congestive heart failure (CHF), as defined by the American College of Cardiology (ACC) and the American Heart Association (AHA), is "a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood.” Ischemic heart disease is the leading cause of death worldwide and also the leading cause of CHF. CHF is a common disorder worldwide with a high morbidity and mortality rate. With an estimated prevalence of 26 million people worldwide, CHF contributes to increased healthcare costs, reduces functional capacity, and significantly affects quality of life. It is imperative to diagnose and effectively treat the disease to prevent recurrent hospitalizations, decrease morbidity and mortality, and enhance patient outcomes. [1]
The etiology of heart failure (HF) is variable and extensive. The general management aims at relieving systemic and pulmonary congestion and stabilization of hemodynamic status, regardless of the cause. The treatment of HF requires a multifaceted approach involving patient education, optimal medication administration, and decreasing acute exacerbations.
Left ventricle ejection fraction (LV EF) is used to classify HF. [1]
- HF with reduced ejection fraction (HFrEF): LV EF ≤ 40%
- HF with mildly reduced ejection fraction: LV EF 41% - 49% and evidence of HF (elevated cardiac biomarkers or elevated filling pressures)
- HF with preserved ejection fraction (HFpEF): LV EF ≥ 50% and evidence of HF (elevated cardiac biomarkers or elevated filling pressures)
- HF with improved ejection fraction: LV EF >40%, with previously documented LV EF ≤ 40%
Patients with HFpEF have traditionally been underdiagnosed but comprise between 44% and 72% of CHF cases. On echocardiogram (echo), LV EF ≥ 50% with evidence of impaired diastolic function. The most significant risk factor is hypertension (HTN), and other risk factors include older age, female sex, and diabetes. [2]
The ACC and the AHA together classify HF by stages, with the first 2 stages being asymptomatic and the second 2 being classified by severity of symptoms.
ACC/AHA Heart Failure Stages
- Stage A: At risk for HF. No symptoms, structural heart disease, or evidence of elevated cardiac biomarkers, but risk factors are present. Risk factors include hypertension, diabetes, metabolic syndrome, cardiotoxic medications, or having a genetic variant for cardiomyopathy.
- Stage B: Pre-HF. Patients have no signs or symptoms of HF but have structural heart disease, evidence of elevated filling pressures (by invasive or noninvasive assessment), or persistently elevated cardiomarkers in the absence of other reasons for elevated markers, like chronic kidney disease or myocarditis.
- Stage C: Patients with structural heart disease and current or past history of HF symptoms.
- Stage D: Patients with refractory symptoms that interfere with daily life or recurrent hospitalization despite targeted guideline-directed medical therapy.
The New York Heart Association Functional Classification is used for patients with symptoms of HF. This system is subjectively determined by clinicians and is widely used in clinical practice to direct therapy.
New York Heart Association Functional Classification
Based on symptoms, the patients can be classified using the New York Heart Association (NYHA) functional classification as follows: [3]
- Class I: Symptom onset with more than ordinary level of activity
- Class II: Symptom onset with an ordinary level of activity
- Class III: Symptom onset with minimal activity
- Class IIIa: No dyspnea at rest
- Class IIIb: Recent onset of dyspnea at rest
- Class IV: Symptoms at rest
There are many etiologies of CHF, and coronary artery disease (CAD) causing ischemic heart disease is the most common cause. Every attempt should be made to identify causative factors to help guide treatment strategies. The etiologies can be broadly classified as intrinsic heart disease and pathologies that are infiltrative, congenital, valvular, myocarditis-related, high-output failure, and secondary to systemic disease. [2] [4] These classifications have significant overlap. The 4 most common etiologies responsible for about two-thirds of CHF cases are ischemic heart disease, chronic obstructive pulmonary disease (COPD), hypertensive heart disease, and rheumatic heart disease. Higher-income countries have higher rates of ischemic heart disease and COPD; lower-income countries have higher rates of hypertensive heart disease, cardiomyopathy, rheumatic heart disease, and myocarditis.
Ischemic heart disease is by far the most common cause of CHF worldwide. Ischemia leads to a lack of blood flow to heart muscles, reducing the EF. Incidence is increasing in developing countries as they adopt a more Western diet and lifestyle, and improved medical care decreases the infectious burden in these countries (myocarditis is often infection-related.)
Valvular heart disease is another common intrinsic heart condition that can cause CHF. Rheumatic heart disease is the most common cause of valvular heart disease in children and young adults worldwide. It is caused by an immune response to group A Streptococcus and primarily causes mitral and aortic stenosis. [5] The most common overall cause of valvular disease is age-related degeneration, and the aortic valve is the most commonly affected valve. Women are more likely to experience mitral valve rheumatic heart disease or mitral valve prolapse, while men are more likely to suffer from aortic valve diseases such as regurgitation or stenosis. Endocarditis is also more common in men.
Hypertension causes CHF even in the absence of CAD or ischemic heart disease. High blood pressure causes mechanical stress by increased afterload and neurohormonal changes that increase ventricular mass. [2] HTN is also strongly associated with other comorbidities for CHF development, and aggressively treating hypertension is shown to lower the incidence of CHF. [2]
Cardiomyopathy is a heterogeneous group of diseases characterized by enlarged ventricles with impaired function not related to secondary causes such as ischemic heart disease, valvular heart disease, hypertension, or congenital heart disease. The most common types of cardiomyopathies are hypertrophic, dilated, restrictive, arrhythmogenic right ventricular, and left ventricular noncompaction. [6] In addition to CHF, cardiomyopathy can present as arrhythmia or sudden cardiac death, further compelling the identification of underlying disorders. Many of these conditions have a genetic basis, and a detailed family history of sudden cardiac death, especially in first-degree relatives older than 35 years, should be taken. There are over 50 identified genes contributing to the development of dilated cardiomyopathy alone. Genetic determinants have variable phenotypic expression, and many nongenetic factors also affect the clinical symptoms. Some of these factors include diabetes, toxic exposure, or pregnancy. Fabry disease is a rare glycogen storage disease that can cause CHF symptoms through a hypertrophic cardiomyopathy pattern. [2] [6]
Inflammatory cardiomyopathy is defined by myocarditis along with ventricular remodeling and cardiac dysfunction. The most common cause is viral infection. Other etiologies are bacterial, fungal, or protozoal infections; toxic substances or drugs; and immune-mediated diseases. Chagas disease is caused by Trypanosoma cruzi, which is endemic in Latin America and commonly causes myocarditis, cardiomyopathy, and CHF. Other viral causes of myocarditis and inflammatory cardiomyopathy include adenoviruses, enteroviruses, herpes virus 6, Epstein-Barr virus, and cytomegalovirus. Viruses can also activate autoimmune myocarditis, including HIV, hepatitis C virus, influenzas A and B, and coronaviruses (including COVID-19). When associated with CHF, these conditions tend to have a poor prognosis. [7]
Infiltrative cardiomyopathies cause a restrictive cardiomyopathy pattern (simar to the genetically determined restrictive cardiomyopathy variant), which is notable for normal ventricular systolic function, but with diastolic dysfunction and restrictive filling dynamics of the LV and RV. This is often associated with a high E/A ratio showing increased early filling and delayed late filling. [6] [8]
Cardiac amyloidosis results from misfolded protein deposits in the heart; this leads to cardiomyocyte separation, cellular toxicity, and tissue stiffness. Patients are preload dependent and are prone to symptomatic hypotension. Currently, tamifidis is the only medication known to prevent cardiac amyloidosis. It prevents, but does not reverse, amyloid deposition. Its high cost is also a limiting factor. [1] [9] [1]
Sarcoidosis is an acquired cardiomyopathy that presents with conduction defects and arrhythmias due to granuloma formation. The most common cardiac manifestation is CHF. Caution must be used when treating with beta-blockers due to the associated conduction abnormalities.
Cardiac hemochromatosis is present in 15% to 20% of patients with hereditary hemochromatosis. This condition initially presents with a restrictive pattern but develops into biventricular systolic dysfunction. [8] Patients with restrictive cardiomyopathy physiology can develop hypotension when treated with traditional CHF medications due to preload dependence, so caution should be used to avoid systemic hypoperfusion. [10]
Takotsubo or stress-induced cardiomyopathy (colloquially broken-heart syndrome) is an underrecognized cause of CHF, which causes transient left-ventricular wall abnormalities that are not localized to a specific vascular territory. It has several proposed pathophysiologic mechanisms, including coronary vasospasm, microcirculatory dysfunction, and increased activation of the sympathetic nervous system. This condition is treated with medications typical for CHF with the addition of antithrombotic medications in certain clinical situations with wall motion abnormalities. Recognized cases increased significantly during the COVID-19 epidemic. [11] [12] [13] [12]
Peripartum cardiomyopathy is a significant cause of maternal mortality. During pregnancy, cardiac output is increased by 20% to 30% due to increased heart rate and stroke volume. It presents with CHF due to LV systolic dysfunction during late pregnancy, postpartum, or up to several months after delivery. There is likely an underlying genetic component, and it is more common in women with advanced maternal age, Black race, and multifetal pregnancies. If wall motion abnormalities are present, anticoagulation is essential due to the hypercoagulable state caused by pregnancy. Recovery is variable by global region and inversely correlates with lowered EF. [14]
Obesity is a leading cause of CHF in patients younger than 40 years, according to the "Candesartan in Heart Failure Assessment of Reduction in Mortality and Morbidity" (the CHARM study). The "obesity paradox" described elsewhere has significant study flaws and is derived from older data. It is thought that up to 10% of CHF cases are attributable to obesity alone. Patients with obesity are more likely to have HFpEF, possibly secondary to adipose-produced cytokines such as IL-1b, IL-8, and TNFα. Adipose tissue also degrades natriuretic peptides. [15] [16] [17]
Tachycardia and arrhythmia can induce a low-output CHF state. There is usually dilation of all cardiac chambers, and there is preservation or thinning of biventricular wall thickness. Electrophysiologic changes, including prologued duration and decreased amplitude of action potentials in the myocytes, accompany this. All of these factors induce the typical neurohormonal response causing CHF. With rate control, these changes are often reversible due to myocardial hibernation. [18]
Thyrotoxicosis is a rare cause of HF despite initiating a hyperdynamic circulatory state. This may be partially due to activation of the renin-angiotensin-aldosterone axis, causing sodium and water retention, as well as upregulation of erythropoietin-stimulating agent, both of which will cause increased blood volume. Sustained tachycardia with or without atrial fibrillation can also cause CHF. [19]
High-output cardiac failure can be associated with thiamine deficiency, which is a rare condition found primarily among patients who are elderly, homeless, or have alcohol abuse disorder. Thiamine deficiency causes decreased ATP production with an accumulation of adenosine, which causes systemic vasodilation. This leads to lowered systemic vascular resistance and increased cardiac output. This evolves to weakened myocardium and decreased EF. Diuretic use can also cause urinary thiamine loss, further compounding the situation. [20] [21] Other common causes of high-output cardiac failure are obesity, liver disease, and arteriovenous shunts. The causative physiologic changes are decreased afterload (ie, systemic vascular resistance) and increased metabolism. These can often present with preserved EF, pulmonary congestion, increased filling pressures, and elevated natriuretic peptides. [22] [23]
- Epidemiology
The global magnitude of the disease cannot be accurately assessed given the significant differences in geographical distribution, assessment methods, lack of imaging modalities, and non-adherence to the uniform staging and diagnosis of the disease. Approximately 1.2 million hospitalizations were due to CHF in 2017, with an increase in the percentage of patients with HFpEF compared to HFrEF. [1]
By some reports, the incidence rate has plateaued; however, the prevalence increases as more patients receive therapy. This has not translated to improved quality of life or a decrease in the number of hospitalizations for patients with CHF. According to the Global Health Data Exchange registry, the current worldwide prevalence of CHF is 64.34 million cases. This translates to 9.91 million years lost due to disability (YLDs) and 346.17 billion US dollars in healthcare expenditure. [24]
Age is a major determinant of HF. Regardless of the cause or the definition used to classify patients with HF, the prevalence of HF increases steeply with age. The Framingham Heart Study showed CHF prevalence to be 8 per 1000 males aged 50 to 59 years, with an increase to 66 per 1000 males aged 80 to 89. [25] The incidence of HF in men doubles with each 10-year age increase after the age of 65, whereas in women, for the same age cohort, the incidence triples. Men have higher rates of heart disease and CHF than women worldwide. [26] [2]
The global registry also notes a predilection for a race with a 25% higher prevalence of HF in Black patients than in White patients. HF is still the primary cause of hospitalization in the elderly population and accounts for 8.5% of cardiovascular-related deaths in the United States. [26]
International statistics regarding the epidemiology of HF are similar. The incidence increases dramatically with age, metabolic risk factors, and a sedentary lifestyle. Ischemic cardiomyopathy and hypertension are significant causes of HF in developing countries. [27] A notable difference based on a review of small cohort studies from these nations is a higher prevalence of isolated right HF. The theoretical cause of this is thought to be due to the higher prevalence of tuberculous, pericardial, and lung diseases. There is a lack of robust data to verify these claims.
- Pathophysiology
HF is a progressive disease. Any acute insult to cardiac structure or acute alteration secondary to genetic mutation, cardiac tissue infiltration, ischemia, valvular heart disease, myocarditis, or acute myocardial injury may initiate the compensatory mechanism, which, once exhausted, results in maladaptation.
In the initial stages of CHF, several compensatory mechanisms attempt to maintain cardiac output and meet the systemic demands. The chronic activation of the sympathetic nervous system results in reduced beta-receptor responsiveness and adrenaline stores. This results in changes in myocyte regeneration, myocardial hypertrophy, and myocardial hypercontractility. [28] The increased sympathetic drive also results in the activation of the renin-angiotensin-aldosterone system (RAAS) system, systemic vasoconstriction, and sodium retention. [28] [29]
A decrease in cardiac output and increased sympathetic drive stimulate the RAAS, leading to increased salt and water retention, along with increased vasoconstriction. This further fuels the maladaptive mechanisms in the heart and causes progressive HF. In addition, the RAAS system releases angiotensin II, which has been shown to increase myocardial cellular hypertrophy and interstitial fibrosis, contributing to myocardial remodeling. [3]
A decrease in cardiac output stimulates the neuroendocrine system with a release of epinephrine, norepinephrine, endothelin-1 (ET-1), and vasopressin. These mediators cause vasoconstriction, leading to increased afterload. There is an increase in cyclic adenosine monophosphate (cAMP), which causes an increase in cytosolic calcium in the myocytes. This increases myocardial contractility and further prevents myocardial relaxation. Increased afterload and myocardial contractility with impaired myocardial relaxation increase myocardial oxygen demand. This paradoxical need for increased cardiac output to meet myocardial demand eventually leads to myocardial cell death and apoptosis. As apoptosis continues, a decrease in cardiac output with increased demand leads to a perpetuating cycle of increased neurohumoral stimulation and maladaptive hemodynamic and myocardial responses. [29] The loss of myocytes decreases EF (cardiac contractility), which leads to incomplete LV emptying. Increased LV volume and pressure cause pulmonary congestion. [30]
Renal hypoperfusion causes the release of antidiuretic hormone (ADH), further potentiating sodium and water retention. Increased central venous and intraabdominal pressure causes reduced renal blood flow, further decreasing GFR. [31]
Decompensated CHF is characterized by peripheral vasoconstriction and increased preload delivery to the overburdened heart. The natriuretic peptides BNP and ANP are secreted but are ineffective in counteracting the excess sodium and water retention. [31]
Neprilysin is an enzyme that breaks down several hormones, including BNP, ANP, and bradykinin; it targets several novel therapeutics. It is always used with an angiotensin receptor blocker because it increases angiotensin II levels, and when administered with an ACE inhibitor, it causes significant angioedema. [32] [33]
Causes of CHF are split about equally between HFrEF and HFpEF but require different treatment plans. In HFpEF, there is a decrease in myocardial relaxation and an increase in the stiffness of the ventricle due to an increase in ventricular afterload. This perpetuates a similar maladaptive hemodynamic compensation and leads to progressive HF. Patients with HFpEF tend to be older, female, and hypertensive. Atrial fibrillation and anemia are also more likely co-occurring conditions. There is some evidence that the prognosis is worse than those with HFrEF. It is possible that appropriate targets have not been identified for optimal therapeutic interventions. [34] [35]
- History and Physical
The diagnosis and classification of HF are primarily based on the presence and severity of symptoms and physical exam findings. It is imperative to obtain a detailed history of symptoms, underlying medical conditions, and functional capacity to treat the patient adequately.
Acute CHF presents primarily with signs of congestion and may also present with organ hypoperfusion or cardiogenic shock. [36] The most commonly reported symptom is shortness of breath. This must be further classified as exertional, positional (orthopnea), and whether acute or chronic. Other commonly reported symptoms of CHF include chest pain, anorexia, and exertional fatigue. Anorexia is due to hepatic congestion, bowel edema, and reduced blood flow to splanchnic circulation. Some patients may present with a recumbent cough due to orthopnea. Patients may also experience abdominal discomfort due to hepatic congestion or ascites. Patients with arrhythmias can present with palpitations, presyncope, or syncope.
Another symptom that increases morbidity is edema, especially of the lower extremities. This can limit mobility and balance; total body water and weight increases of > 20 lbs are not uncommon.
While patients with acute HF present with overt respiratory distress, orthopnea, and paroxysmal nocturnal dyspnea, patients with chronic heart failure tend to curtail their physical activity; hence, symptoms may be obscured. It is essential to identify triggers of acute decompensation such as recent infection, noncompliance with cardiac medications, use of NSAIDs, or increased salt intake.
Physical Examination
The examination findings vary with the stage and acuity of the disease. Patients may have isolated symptoms of left-sided HF, right-sided HF, or combined.
General physical examination: The general appearance of patients with severe CHF or those with acutely decompensated HF includes anxiety, diaphoresis, tachycardia, and tachypnea. Patients with chronic decompensated HF can appear cachexic. On chest examination, the classical finding of pulmonary rales translates to heart failure of moderate-to-severe intensity. Wheezing may be present in acute decompensated heart failure. As the severity of pulmonary congestion increases, frothy and blood-tinged sputum may be seen. It is important to note that the absence of rales does not exclude pulmonary congestion. Jugular venous distention is another classical finding that must be assessed in all patients with HF. In patients with elevated left-sided filling pressures, hepatojugular reflux (sustained increase in JVP of >4 cm after applying pressure over the liver with the patient lying at a 45° angle) is often seen.
Patients with Stage D HF may show signs of poor perfusion, such as hypotension, reduced capillary refill, cold extremities, poor mentation, and reduced urine output. There may be pulsus alternans (an alternating weak and strong pulse), suggestive of severe ventricular dysfunction. The pulse can be irregular in the presence of atrial fibrillation or ectopic beats. Some degree of peripheral edema is present with most HF. [37] Weight gain is another method for assessing volume retention, and precise daily weights can be a useful monitoring tool.
Precordial findings in patients with HF include an S3 gallop, or displaced apex beat (dilated heart). There may be murmurs of associated valvular lesions such as the pansystolic murmur of mitral regurgitation or tricuspid regurgitation, systolic ejection murmur of aortic stenosis, or early diastolic murmur of aortic regurgitation. Patients with pulmonary hypertension may have palpable or loud P2 or parasternal heave. Patients with congenital heart disease may also have associated clubbing, cyanosis, and splitting of the second heart sound.
An S3 gallop is the most significant and early finding associated with HF. [38] Patients with hypertensive heart disease may have an S4 or loud A2. Patients with HF with preserved EF may have an S4 gallop related to ventricular noncompliance.
The commonly used Framingham Diagnostic Criteria for Heart Failure require the presence of 2 major criteria or 1 major and 2 minor criteria to make the diagnosis. This clinical diagnostic tool is highly sensitive for the diagnosis of HF but has a relatively low specificity. The Framingham Diagnostic criteria are as follows: [37]
Major Criteria
- Acute pulmonary edema
- Cardiomegaly
- Hepatojugular reflex
- Neck vein distention
- Paroxysmal nocturnal dyspnea or orthopnea
- Pulmonary rales
- Third heart sound (S3 Gallop)
Minor Criteria
- Ankle edema
- Dyspnea on exertion
- Hepatomegaly
- Nocturnal cough
- Pleural effusion
- Tachycardia (heart rate greater than 120 beats per minute)
A comprehensive assessment is required when evaluating a patient with HF. This includes a complete blood picture, iron profile, renal profile, and liver profile. After the basic metabolic and blood panel, patients require further investigations, depending on the etiology and clinical stage. [1]
A CBC may suggest anemia or leukocytosis suggestive of an infection triggering CHF.
A complete renal profile is necessary for all patients with HF. It indicates the degree of renal injury associated with HF and guides medication choice. It is essential to know baseline renal function before the patient is started on medications, including renin-angiotensin-aldosterone (RAAS) inhibitors, sodium-glucose transporter-2 (SGLT-2) inhibitors, or diuretics. Serum sodium level has prognostic value as a predictor of mortality in patients with chronic HF. "The Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure" (OPTIME-CHF) trial demonstrated a significantly increased risk of in-hospital mortality as well as 30-day mortality in patients with HF who presented with hyponatremia. [39]
A liver profile is usually performed. Hepatic congestion secondary to HF may result in elevated gamma-glutamyl transferase levels, aspartate aminotransferase (AST), and alanine aminotransferase (ALT). [40]
Urine studies can be useful in diagnosis. If amyloidosis is suspected, urine and serum electrophoresis and monoclonal light chain assays should be performed. If clinical suspicion is high despite negative testing for light chains, bone scintigraphy can be performed. [1]
Serum B-type natriuretic peptide (BNP) or N-terminal pro-BNP (NT-ProBNP) levels can aid in differentiating cardiac from noncardiac causes of dyspnea in patients with ambiguous presentations. BNP is an independent predictor of increased left ventricular end-diastolic pressure, and it is used for assessing mortality risk in patients with HF. BNP levels correlate with NYHA classification, and the utility is primarily used as a marker to assess treatment efficacy. NT-ProBNP is the chemically inert N-terminal fragment of BNP and has a longer half-life. The ratio of NT-ProBNP/BNP varies depending on underlying comorbidities and may be a useful tool in the future. [41] In patients with a clear clinical presentation of HF, natriuretic peptides should not be used to drive treatment plans. It is important to remember that BNP and NT-ProBNP levels can be elevated in patients with renal dysfunction, atrial fibrillation, and older patients. Conversely, BNP levels can be falsely low in patients with obesity, hypothyroidism, and advanced HF (due to myocardial fibrosis).
Troponin-I or T suggests ongoing myocardial injury when persistently elevated and predicts adverse outcomes and mortality.
An electrocardiogram may show evidence of prior infarction, chamber enlargement, intraventricular conduction delay, or arrhythmia. It may also give clues to specific etiologies. A low voltage and pseudo infarction pattern of ECG is seen in cardiac amyloidosis. An epsilon wave is seen in ARVC. ECG also suggests the presence of ventricular desynchrony, with a QRS duration of more than 120 msec, predicting the patient's response to device therapy for HF.
Chest radiographs are used to assess the degree of pulmonary congestion and cardiac contour (to determine the presence of cardiomegaly). Findings indicative of CHF on chest radiographs include enlarged cardiac silhouette, edema at the lung bases, and vascular congestion. In florid HF, Kerley B lines may be seen on chest radiographs. The absence of these findings in patients with a suggestive clinical presentation does not rule out CHF. [37]
Echocardiography is the initial choice of modality in patients with suspected HF and is an easily available bedside tool. Echocardiography quantifies right and left ventricular function, denotes structural abnormalities in cardiac chambers and valves, and helps visualize the presence of focal wall motion abnormalities. However, in patients with severe obesity, pregnancy, or mechanical ventilation, it may be challenging to obtain adequate acoustic windows. Transesophageal echocardiography (TEE) is an alternative for these patients. Adequate rate control in patients with tachyarrhythmias is necessary to obtain adequate echocardiographic images. [37]
Cardiac catheterization is often required for diagnosing ischemic cardiomyopathy and can be useful for accurately evaluating intracardiac pressures such as left ventricular end-diastolic pressure or pulmonary artery pressures.
Computed tomography may be used for the assessment of coronary artery disease in a young patient with ventricular dysfunction (older patients are likely to have baseline calcifications). It may also be used in patients with congenital heart diseases causing HF. Cardiac CT may help with the detection of tumors causing HF. CT may also be used for the evaluation of stent patency and graft evaluation.
SPECT-Myocardial Perfusion Imaging helps define the presence of ischemia in patients with newly diagnosed left ventricular dysfunction and not undergoing coronary angiography. It is particularly useful for assessing CAD in patients with no history of ischemia but elevated troponin. ECG-gated myocardial perfusion imaging is used to evaluate LV EF, regional wall motion, and regional wall thickening. EF measurement with this study may be affected in patients with an irregular heart rate, low count density, and extracardiac radiotracer uptake. ECG-gated images are also useful in recognizing artifactual defects seen on SPECT imaging, such as breast tissue and diaphragmatic attenuation. [42]
Cardiac magnetic resonance imaging has evolved as an essential tool when a discrepancy exists between the clinical stage of the disease and echocardiographic findings. It helps with the precise evaluation of volume, chamber sizes, and ventricular function. It also assesses the stage of valvular heart disease in detail. Cardiac MRI also helps with the evaluation of complex congenital heart diseases. The tool can also be used for noninvasive assessment of conditions such as myocarditis, dilated cardiomyopathy, infiltrative cardiomyopathy, or arrhythmogenic right ventricular dysplasia. [43]
Radionuclide multiple-gated acquisition (MUGA) scan is a reliable imaging technique for evaluating EF and is used in patients when there is a disparity of EF measurements from other studies. [42]
Noninvasive stress imaging includes stress echocardiography, stress cardiac MRI, and SPECT imaging. These studies can be used to assess the benefit of coronary revascularization in patients with ischemic cardiomyopathy.
Genetic testing is indicated for identifying genetic variants causing cardiomyopathies, such as Titin, laminin A or C, myosin heavy chain, and cardiac troponin-T mutations. [44]
- Treatment / Management
The goal of therapy for chronic CHF is to improve symptoms and quality of life, decrease hospitalizations, and improve cardiac mortality. The goal of pharmacologic therapy is to control symptoms and to initiate and escalate drugs that reduce mortality and morbidity in HF. [1]
Management for the respective stages of HF is outlined by the American College of Cardiology and the American Heart Association. [1]
For Stage A (At-Risk for HF)
- In patients with hypertension, guideline-directed medical therapy (GDMT) should be used for the management of hypertension.
- In patients with type 2 diabetes, SGLT-2 inhibitors are indicated to reduce HF hospitalizations.
- Lifestyle modifications such as healthy eating, physical activity, maintaining a normal weight, and avoidance of smoking are indicated.
- The use of prognostication scores is recommended in patients with HF to estimate the risk of future HF events. [45] Examples include the Framingham Heart Failure Risk Score (1999), Health ABC Heart Failure Score (2008), ARIC Risk Score (2012), and PCP-HF score (2019).
- There should be optimal management of cardiovascular diseases in patients known to have coronary artery disease.
- Patients at risk for HF due to exposure to cardiotoxic medications (eg, chemotherapy) should be managed with a multidisciplinary approach.
- Natriuretic peptide screening and periodic evaluation are recommended.
For Stage B (Pre-HF)
Management of Stage B is focused on preventing clinical HF and reducing mortality and adverse cardiovascular events.
- For patients with LV EF ≤40%, ACEi should be used to prevent clinical HF and for mortality reduction.
- For patients with LV EF ≤ 40% and evidence of prior or recent acute coronary syndrome or myocardial infarction, the use of a statin and beta-blocker is recommended for reduction of mortality, CHF, and reducing adverse cardiovascular events.
- For patients with LV EF ≤ 30% and receiving optimal medical therapy, with NYHA-class I and an expectation of meaningful survival of more than 1 year, a primary prevention ICD is recommended.
- Beta-blockers are recommended for patients with LV EF ≤ 40%, irrespective of the etiology, to prevent symptomatic HF.
- For patients with LV EF ≤ 50%, the use of thiazolidinediones and non-dihydropyridine calcium channel blockers increases the risk of adverse outcomes and HF hospitalizations, so should be avoided.
- Valve repair, replacement, or interventions have associated guidelines for asymptomatic valvular heart disease.
- Patients with congenital heart disease also have associated guidelines.
For Stage C (HF)
- Multidisciplinary management is indicated for improving self-care and mortality of patients with HF.
- Patient education and social support are required for optimal management.
- Vaccination against respiratory illnesses is effective in reducing mortality.
- It is reasonable to screen patients for frailty, depression, low literacy, low social support, and resource and transport logistics during healthcare encounters.
- A low-sodium diet is recommended.
- Exercise training is effective in improving functional class and quality of life.
- For patients with congestion, diuretics improve symptoms and reduce HF progression.
- A thiazide diuretic (such as metolazone) should be added only to patients who do not respond well to a moderate or high dose of loop diuretics.
- For patients with HFrEF, an ARNi is recommended to reduce mortality and morbidity. ARNi should not be given to patients who are intolerant of ACEi, and an ARB should be substituted. For patients not able to take an ARNi due to economic factors, the use of an ACEi or ARB is indicated. ARNi should not be used within 36 hours of the last dose of ACEi. For patients tolerating ACEi/ARB well, switching to ARNi is recommended, with a high economic value. As with ACEi, ARNi should not be given to patients with a history of angioedema.
- For patients with HFrEF, the use of the beta-blockers carvedilol, bisoprolol, or sustained-release metoprolol is effective in reducing mortality and hospitalization.
- For patients with HFrEF, NYHA class II-IV, an eGFR of more than 30 mL/min/1.73 m2 and a serum potassium of less than 5.0 mEq/L, the use of MRA is recommended. For patients with a serum potassium of more than 5.0 mEq/L, the use of MRA is harmful.
- For patients with HFrEF, the use of SGLT-2 inhibitors is recommended to reduce mortality and HF hospitalization, irrespective of the diabetes status.
- For African American patients with HFrEF and NYHA class III-IV, who are already receiving optimal medical therapy (OMT), the addition of a combination of hydralazine and nitrate is recommended to reduce morbidity and mortality. This is of high economic value.
- For patients with HFrEF and intolerant to RAASi or in whom RAASi is contraindicated due to renal insufficiency, the use of a combination of hydralazine and nitrate might be effective.
- It is recommended to titrate medications aggressively to achieve desired outcomes. This can be done as frequently as 1-2 weeks as tolerated.
- Ivabradine can be useful in patients on OMT with and heart rate of more than 70 bpm, providing mortality benefits, and reducing HF hospitalization.
- Digoxin may be considered in symptomatic patients with sinus rhythm despite adequate goal-directed therapy to reduce the all-cause rate of hospitalizations, but its role is limited.
- In patients with HFrEF and recent HF, an oral soluble guanylate cyclase stimulator (Vericiguat) might be useful in reducing mortality and HF hospitalization. Vericiguat is a soluble guanylate cyclase stimulator that stimulates the intracellular receptor for endogenous NO, which is a potent vasodilator. It also improves cardiac contractility. [46] [47]
- An implantable cardioverter-defibrillator (ICD) is indicated for primary prevention of sudden cardiac death in patients with HF who have an LVEF of less than or equal to 35% and an NYHA functional class of II to III while on goal-directed medical therapy. It is also indicated if a patient has NYHA functional class I and an EF of less than or equal to 30% on adequate medical therapy.
- Cardiac resynchronization therapy (CRT) with biventricular pacing is recommended in patients with HFrEF and an NYHA functional class of II to III or ambulatory class IV with an LVEF less than or equal to 35%, QRS duration ≥ 150 msec, and sinus rhythm with left bundle branch block (LBBB) morphology. It can also be considered in non-LBBB morphology and QRS ≥ 150 msec.
- Revascularization is indicated in selected patients with coronary artery disease and HFrEF while on GDMT.
- Valvular heart disease interventions such as transcatheter edge-to-edge mitral valve repair or mitral valve surgery might be beneficial for patients with HF and on GDMT.
For Stage D (Advanced HF)
- Referral to an HF specialist is indicated.
- It is reasonable to utilize inotropic support and device therapy in patients awaiting mechanical cardiac support or transplant. Inotropic support alone can be used in patients not eligible for a transplant or mechanical cardiac support.
- Mechanical cardiac support such as a durable left ventricle assist device (LVAD) or ECMO can be beneficial as a bridge to transplant.
- For highly selected patients, cardiac transplant is indicated to improve survival and quality of life.
- Goals of care should be decided by shared decision-making. This includes considering comorbid conditions, frailty, and socio-economic support. Palliative care should be offered as indicated after shared decision-making.
- Differential Diagnosis
Diseases that may present with clinical features of volume overload or dyspnea are in the differential for HF. These include acute renal failure, acute respiratory distress syndrome, cirrhosis, pulmonary fibrosis, nephrotic syndrome, and pulmonary embolism.
According to the Centers for Disease Control and Prevention (CDC), in December 2015, the rate of HF-related deaths decreased from 103.1 deaths per 100,000 population in 2000 to 89.5 in 2009 but subsequently increased to 96.9 in 2014. The report noted that the trend correlates with a shift from coronary heart disease as the underlying cause of HF deaths to metabolic diseases and other noncardiac causes of HF, such as obesity, diabetes, malignancies, chronic pulmonary diseases, and renal disease. The mortality rate following hospitalization for HF is estimated at around 10% at 30 days, 22% at 1 year, and 42% at 5 years. This can increase to greater than 50% for patients with stage D HF. [48]
The Ottawa Heart Failure Risk Score is a useful tool for determining prognosis in patients presenting to the emergency department with HF. [49] This score is used to determine the 14-day mortality risk, hospital readmission, and acute coronary syndrome to help arrive at safe disposition planning. Patients with a score of 0 are considered low risk. A score of 1 to 2 is considered moderate risk, a score of 3-4 is considered high risk, and a score of 5 or higher is considered very high risk. The scoring criteria are as follows:
One point for each of the following:
- History of stroke or transient ischemic attack
- Oxygen saturation less than 90%
- Heart rate greater than 110 bpm on the 3-minute walk test
- Acute ischemic ECG changes
- An NT-ProBNP level of greater than 5000 ng/L
Two points for each of the following:
- Prior history of mechanical ventilation for respiratory distress
- Heart rate greater than 110 bpm on presentation
- Blood urea nitrogen (BUN) greater than 33.6 mg/dL (12 mmol/L)
- Serum bicarbonate greater level than 35 mg/d
- Complications
Complications of CHF include:
- Reduced quality of life
- Arrhythmia and sudden cardiac death
- Cardiac cachexia
- Cardiorenal disease
- Liver dysfunction
- Functional valvular insufficiencies (such as functional MR or TR)
- Mural thrombi and risk of thromboembolism (brain, kidney, lung, major limb vessels)
- Recurrent hospitalizations and nosocomial infection
- Consultations
The consultation type depends on the disease stage and the intended management strategy. Commonly consulted specialists include HF specialists, the cardiac transplant team for stage D CHF, cardiam imaging radiologists, cardiac rehabilitation, dieticians, and, if aligned with patient preference, palliative care (also for class D).
- Deterrence and Patient Education
Risk factor reduction and aggressive management of comorbid conditions are crucial to reducing morbidity and mortality associated with HF. In addition to compliance with medications, patients need guidance on self-monitoring of symptoms of HF and avoiding the triggers of HF. These strategies can help prevent the development of HF in patients at high risk for the disease and slow the progression in those who are already diagnosed with it. Patient education is necessary to facilitate self-care and compliance. Close supervision, including surveillance by the patient and family, home-based visits, telephone support, and remote monitoring, is recommended. Socio-economic support is pivotal in the appropriate management of the disease. [1] Patients require close clinical follow-up for assessing volume status, effects of drug therapy, and escalation of care as indicated.
- Enhancing Healthcare Team Outcomes
HF is a complex clinical syndrome with high morbidity and mortality. HF requires a multifaceted treatment approach, including patient education, pharmacologic management, and surgical interventions to optimize clinical outcomes. Specialty-trained HF nurses are an essential component of the multidisciplinary team in educating patients on the importance of lifestyle modifications and medical compliance to help improve morbidity and mortality. Educating patients on symptom assessment and weight management is essential to prevent HF exacerbations and hospital admissions. The HF-trained social worker and case manager can help evaluate the patient in community settings or in-home visits to help the patient adhere to the lifestyle modifications. Clinical pharmacists assist medical providers by reviewing patient medication lists and decreasing potential adverse drug-drug interactions. Primary care medical providers and cardiologists must coordinate care to minimize any adverse outcomes of medical therapy and prevent the progression of this disease. A collaborative interprofessional team can significantly improve the quality of life for patients with HF and decrease mortality.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Congestive Heart Failure Contributed by S Bhimji, MD
Disclosure: Ahmad Malik declares no relevant financial relationships with ineligible companies.
Disclosure: Daniel Brito declares no relevant financial relationships with ineligible companies.
Disclosure: Sarosh Vaqar declares no relevant financial relationships with ineligible companies.
Disclosure: Lovely Chhabra declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Malik A, Brito D, Vaqar S, et al. Congestive Heart Failure. [Updated 2023 Nov 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Heart Failure With Preserved Ejection Fraction (HFpEF). [StatPearls. 2024] Heart Failure With Preserved Ejection Fraction (HFpEF). Golla MSG, Shams P. StatPearls. 2024 Jan
- Biventricular pacing (cardiac resynchronization therapy): an evidence-based analysis. [Ont Health Technol Assess Ser....] Biventricular pacing (cardiac resynchronization therapy): an evidence-based analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2005; 5(13):1-60. Epub 2005 Sep 1.
- Enhanced External Counterpulsation (EECP): An Evidence-Based Analysis. [Ont Health Technol Assess Ser....] Enhanced External Counterpulsation (EECP): An Evidence-Based Analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2006; 6(5):1-70. Epub 2006 Mar 1.
- Review Combination Use of Ivabradine with Sacubitril/Valsartan: A Review of Clinical Effectiveness and Guidelines [ 2020] Review Combination Use of Ivabradine with Sacubitril/Valsartan: A Review of Clinical Effectiveness and Guidelines Pohar R, MacDougall D. 2020 Feb 13
- Review Heart Failure With Preserved Ejection Fraction: A Review. [JAMA. 2023] Review Heart Failure With Preserved Ejection Fraction: A Review. Redfield MM, Borlaug BA. JAMA. 2023 Mar 14; 329(10):827-838.
Recent Activity
- Congestive Heart Failure - StatPearls Congestive Heart Failure - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Survival analysis of heart failure patients: A case study
Roles Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
Affiliation Department of Statistics, Government College University, Faisalabad, Pakistan
Roles Data curation, Formal analysis, Methodology, Writing – original draft
Roles Conceptualization, Methodology, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Roles Formal analysis, Investigation, Methodology, Validation
Roles Methodology, Software, Visualization, Writing – review & editing
- Tanvir Ahmad,
- Assia Munir,
- Sajjad Haider Bhatti,
- Muhammad Aftab,
- Muhammad Ali Raza

- Published: July 20, 2017
- https://doi.org/10.1371/journal.pone.0181001
- Reader Comments
This study was focused on survival analysis of heart failure patients who were admitted to Institute of Cardiology and Allied hospital Faisalabad-Pakistan during April-December (2015). All the patients were aged 40 years or above, having left ventricular systolic dysfunction, belonging to NYHA class III and IV. Cox regression was used to model mortality considering age, ejection fraction, serum creatinine, serum sodium, anemia, platelets, creatinine phosphokinase, blood pressure, gender, diabetes and smoking status as potentially contributing for mortality. Kaplan Meier plot was used to study the general pattern of survival which showed high intensity of mortality in the initial days and then a gradual increase up to the end of study. Martingale residuals were used to assess functional form of variables. Results were validated computing calibration slope and discrimination ability of model via bootstrapping. For graphical prediction of survival probability, a nomogram was constructed. Age, renal dysfunction, blood pressure, ejection fraction and anemia were found as significant risk factors for mortality among heart failure patients.
Citation: Ahmad T, Munir A, Bhatti SH, Aftab M, Raza MA (2017) Survival analysis of heart failure patients: A case study. PLoS ONE 12(7): e0181001. https://doi.org/10.1371/journal.pone.0181001
Editor: Chiara Lazzeri, Azienda Ospedaliero Universitaria Careggi, ITALY
Received: February 26, 2017; Accepted: June 23, 2017; Published: July 20, 2017
Copyright: © 2017 Ahmad et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Heart failure is the state in which muscles in the heart wall get fade and enlarge, limiting heart pumping of blood. The ventricles of heart can get inflexible and do not fill properly between beats. With the passage of time heart fails in fulfilling the proper demand of blood in body and as a consequence person starts feeling difficulty in breathing.
The main reason behind heart failure include coronary heart disease , diabetes , high blood pressure and other diseases like HIV, alcohol abuse or cocaine, thyroid disorders, excess of vitamin E in body, radiation or chemotherapy, etc. As stated by WHO [ 1 ] Cardiovascular Heart Disease (CHD) is now top reason causing 31% of deaths globally. Pakistan is also included in the list of countries where prevalence of CHD is increasing significantly. According to report by Al-Shifa hospital [ 2 ], 33% of Pakistani population above 45 has hypertension, 25% of patients over 45 years suffer diabetes mellitus, and CHD deaths in Pakistan has reached about 200,000 per year i.e. 410/100,000 of the population). All this results in increased prevalence of heart failure. Rate of heart failure patients in Pakistan is estimated to be 110 per million [ 1 ]. Rising stress of economic and social issues in the modern era, greasy food with little exercise results towards increased prevalence of heart failure in Pakistan.
Despite of this alarming situation, Pillai and Ganapathi [ 3 ] have reported that there are no reliable estimates of heart failure incidence and prevalence in this region while they are required due to poor and oily diet, lack of exercise and poor health care policies in this region. There are some projections based on prevalence data only from western countries.
In addition to relative scarcity of studies focusing on heart failure in this region, the present study has specific importance in the Pakistani context, as diet patterns in Pakistan are different with other the countries of South Asia like India, Bangladesh, Nepal and Sri Lanka.
The main objective of this study is to estimate death rates due to heart failure and to investigate its link with some major risk factors by choosing Faisalabad (third most populous city of Pakistan) as study area.
Detail of data
Current study is based on 299 patients of heart failure comprising of 105 women and 194 men. All the patients were more than 40 years old, having left ventricular systolic dysfunction and falling in NYHA class III and IV. Follow up time was 4–285 days with an average of 130 days. Disease was diagnosed by cardiac echo report or notes written by physician. Age, serum sodium, serum creatinine, gender, smoking, Blood Pressure (BP), Ejection Fraction (EF), anemia, platelets, Creatinine Phosphokinase (CPK) and diabetes were considered as potential variables explaining mortality caused by CHD. Age, serum sodium and CPK are continuous variables whereas EF, serum creatinine and platelets were taken as categorical variables. EF was divided into three levels (i.e. EF≤30, 30<EF≤45 and EF>45) and platelets was also divided into three level on the basis of quartiles. Serum creatinine greater than its normal level (1.5) is an indicator of renal dysfunction. Its effect on mortality was studied as creatinine >1.5 vs ≤1.5. Anemia in patients was assessed by their haematocrit level. Following McClellan et al. [ 4 ] the patients with haematocrit less than 36 (minimum normal level of haematocrit) were taken as anemic. The information related to risk factors were taken from blood reports while smoking status and blood pressure were taken from physician’s notes.
The study was approved by Institutional Review Board of Government College University, Faisalabad-Pakistan and the principles of Helsinki Declaration were followed. Informed consent was taken by the patients from whom the information on required characteristics were collected/accessed.
Statistical techniques
Due to the presence of censored data, survival analysis was used to estimate the survival and mortality rates. Kaplan & Meier [ 5 ] product limit estimator was used to make comparisons between survival rates at different levels explanatory variables. Cox regression as presented by Collett [ 6 ] was used to develop a model that can link the hazard of death for an individual with one or more explanatory variables and test the significance of these variables.
For determining the functional form of any particular independent variable following Fitrianto & Jiin [ 7 ] and Gillespie [ 8 ], plot of Martingale residuals versus different values (or levels) of a variable were used. The functional form of CPK was not linear therefore it was log transformed.
Following Pavlou et al. [ 9 ] model validation was assessed by bootstrapping [ 10 – 12 ] with 200 bootstrap replications. Internal validation of model was further checked by calculating calibration slope [ 13 ] for the average linear predictor. The calibration slope helped in estimating the ability of model for survival probability prediction. Discriminating ability of model was assessed by ROC curve [ 14 ]. A nomogram [ 15 ] was also built to predict the survival probabilities graphically.
Up to end of follow-up period, 96 (32%) patients died due to CHD. Table 1 , presents different baseline characteristics of dead and censored patients at the end of follow up period.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0181001.t001
The results of Cox regression model are presented in Table 2 . As Cox regression is semi parametric model, hence estimate of intercept (baseline hazard) was not provided by model fitting. According to Cox model, age was most significant variable.
https://doi.org/10.1371/journal.pone.0181001.t002
Coefficient concerning age indicated that chances of death due to CHD increase with growing age. Hazard of death due to CHD increases by 4% for every additional year of age. EF was another significant factor, hazard rate among patients with EF ≤30 was 67% and 59% higher as compared to the patients with 30<EF≤45 and EF≥45 respectively. In Fig 1(a) , Kaplan Meier survival curve was constructed for each level of EF. It is obvious that survival for EF ≤30 was lower than other two levels. Moreover, relatively small difference between the survival of patients with 30<EF<45 and EF≥45 can be observed. Serum creatinine was significant with p-value = 0.0026. It means death hazard gets more than double for unit increase in Serum creatinine. Serum sodium was significant with p-value = 0.0052 and its one unit (meq/L) increase decreases the hazard by 6%. Anemia was significant variable with p-value = 0.0096 and an anemic patient had 76% more chances of death as compared to non-anemic patient. According to results in Table 2 , gender, smoking, diabetes, CPK and platelets were found to be non-significant.
https://doi.org/10.1371/journal.pone.0181001.g001
Ejection fraction is an important measurement of how well one’s heart is pumping and is used to help classify heart failure and guide treatment. The EF is also found to be significant correlate of deaths among heart failure patients from Cox regression for present sample. Keeping its importance in view, EF is further analyzed through baseline characteristics ( Table 3 ) and Kaplan Meier curves ( Fig 1(a) ) which shows similar pattern as presented in Cox regression results.
https://doi.org/10.1371/journal.pone.0181001.t003
In Fig 1(b) , Kaplan Meier survival curves were constructed for both genders showed almost identical survival pattern.
Model validation
For model validation, calibration slope and ROC curve are developed from 200 bootstrapped samples. Calibration slope was equal to 0.96, which showed that model was not over fitted and predictions made by this model would neither be overestimated nor under estimated.
Discrimination ability was checked by ROC curve in Fig 2(a) . Area under the curve (AUC) was 0.81 at time of 250 days and 0.77 at time of 50 days thus it can be interpreted that the model was able to correctly recognize the event of death for 81% and 77% patients within 250 and 50 days respectively. It shows that discrimination ability of Cox model is higher at longer follow up time. The reason of this difference may be due to the violation of constant effect assumption of EF which is evident in Fig 2(b) which displays that effect of EF increases with the passage of time. As EF is highly significant for mortality (see Table 2 ), hence with passage of time model’s discrimination ability increases.
https://doi.org/10.1371/journal.pone.0181001.g002
Nomogram for prediction
Calibration slope and discrimination ability suggested that Cox model is able to predict probability of survival and hazard sufficiently. On the basis of these results, nomogram is presented in Fig 3 to provide the graphical predictions of probability after assigning different points to each independent variable with respect to their significance. Sum of these points provides an estimate of probability of survival.
https://doi.org/10.1371/journal.pone.0181001.g003
For example, an 80 year old non-smoker female diabetic patient with high blood pressure, EF = 40, haematocrit = 35, sodium = 140, creatinine = 5.2, platelets = 300 thousands and CPK = 3000 have points equal to 50+0+8+3+14+56+50+12+40+10+20 = 263 and probability of her survival is 0.60. The Cox model used for constructing this nomogram was fitted on original values of variables.
The statistical analysis identified age, EF, creatinine, sodium, anemia and BP as the significant variables affecting the likelihood of mortality among heart failure patients. Most of studies [ 16 – 17 ] supported the male gender as predictor of mortality among heart failure patients. However, like Román et al. [ 18 ] in this study odd ratio of men/women is not significant. With respect to significance and importance of variables the findings of the present study are more in lines with Rahimi et al. [ 19 ]. The results are found to be similar with other international studies like [ 20 – 23 ].
The findings that seem surprising are non-significance of smoking and diabetes. However, similar results concerning diabetes and smoking have been reported in other studies [ 24 – 25 ] as well. The reason behind may be smoking and diabetes are basically causes of heart problem at initial stages. We were only concerned with patients of NYHA class III and IV which are advanced stages of heart failure. Up to these stages, these factors (diabetes and smoking) may probably be controlled by medications and hence these factors do not have significant effect on deaths due to heart failure in class III and IV.
Performance of model was checked using calibration slope and ROC curve. Both concluded in adequacy of model for prediction. ROC curves were also used to discuss the goodness of model with respect to time. Nomogram was used to find the probability of survival by graphical method. It was observed that fall of survival probability was almost same for Kaplan Meier plot and nomogram.
It can be concluded that growing age, renal dysfunction (having serum creatinine greater than its normal level 1.5), high BP (higher than normal range), higher level of anaemia and lower values of ejection fraction (EF) are the key factors contributing towards increased risk of mortality among heart failure patients. Increased level of serum sodium can reduce the odds of death. No significant differences were found due to smoking status, diabetes and gender of patients.

Supporting information
S1 data. data_minimal..
https://doi.org/10.1371/journal.pone.0181001.s001
- 1. WHO. Fact sheet on CVDs. Global Hearts. World Health Organization. 2016.
- 2. Al-Shifa IH. Cardiac Diseases in Pakistan [Internet]. 2016 [cited 15 Jun 2017]. http://www.shifa.com.pk/chronic-disease-pakistan/
- View Article
- PubMed/NCBI
- Google Scholar
- 6. Collett D. Modelling Survival Data in Medical Research. 2nd ed. Taylor & Francis; 2003.
- 8. Gillespie B. Checking Assumptions in the Cox Proportional Hazards Regression Model. Midwest SAS Users Group (MWSUG). 2006.
- 11. Efron B, Tibshirani RJ. An Introduction to the Bootstrap. Chapman and Hall, New York; 1993.
- 15. Yang D. Build Prognostic Nomograms for Risk Assessment Using SAS. Proceedings of SAS Global Forum 2013. 2013.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

5: Case Study #4- Heart Failure (HF)
- Last updated
- Save as PDF
- Page ID 9899
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
- 5.1: Learning Objectives
- 5.2: Patient- Meryl Smith
- 5.3: In the Supermarket
- 5.4: Emergency Room
- 5.5: Day 0- Medical Ward
- 5.6: Day 1- Medical Ward
- 5.7: Day 2- Medical Ward
- 5.8: Day 3- Medical Ward
Assessing and managing frailty in advanced heart failure: An International Society for Heart and Lung Transplantation consensus statement
Affiliations.
- 1 School of Nursing, Oregon Health & Science University, Portland, Oregon; Knight Cardiovascular Institute, Oregon Health & Science University, Portland, Oregon. Electronic address: [email protected].
- 2 Faculty of Medicine, University of Notre Dame, Sydney, Australia.
- 3 Division of Cardiology and Gerald Choa Cardiac Research Centre, Department of Medicine & Therapeutics, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong SAR, China; Laboratory for Heart Failure + Circulation Research, Li Ka Shing Institute of Health Sciences, Prince of Wales Hospital, Hong Kong SAR, China; CUHK Medical Centre, Hong Kong and CUHK-Shenzhen School of Medicine, Shenzhen, China.
- 4 Department of Medicine, Health and Caring Sciences, Linköping University, Linköping, Sweden; Department of Nursing Science, Julius Center, University Medical Center Utrecht, Utrecht, the Netherlands.
- 5 Columbia University Irving Medical Center, New York, New York.
- 6 Section on Cardiovascular Medicine, School of Medicine, Wake Forest University, Winston-Salem, North Carolina.
- 7 Division of Cardiology, Jewish General Hospital, McGill University, Montreal, Quebec, Canada; McGill University, Montreal, Quebec, Canada.
- 8 Nursing Science, Department Public Health, University of Basel, Basel, Switzerland.
- 9 Section of Cardiovascular Medicine, Department of Medicine, Yale School of Medicine, New Haven, Connecticut.
- 10 Nursing Science, Department Public Health, University of Basel, Basel, Switzerland; Academic Center of Nursing and Midwifery, Department Public Health and Primary Care, KU Leuven, Belgium.
- 11 Harrington Heart & Vascular Institute, University Hospitals Cleveland Medical Center, Cleveland, Ohio; Case Western Reserve University School of Medicine, Cleveland, Ohio.
- 12 Department of Cardiology, Mater University Hospital, Dublin, Ireland; School of Medicine, University College Dublin, Dublin, Ireland.
- 13 Cedars Sinai Medical Center, Los Angeles, California.
- 14 School of Nursing, Faculty of Science, Medicine and Health, University of Wollongong, New South Wales, Australia; The Centre for Chronic and Complex Care Research, Blacktown Hospital, Western Sydney Local Health District, New South Wales, Australia.
- 15 Department of Clinical Nursing, Faculty of Health Sciences, Wroclaw Medical University, Wroclaw, Poland.
- 16 School of Nursing, University of Connecticut, Storrs, Connecticut.
- 17 Vanderbilt Heart and Vascular Institute, Nashville, Tennessee.
- 18 St Vincent's Hospital, Sydney, Australia; Victor Chang Cardiac Research Institute, Sydney, Australia; University of New South Wales, Sydney, Australia.
- PMID: 38099896
- DOI: 10.1016/j.healun.2023.09.013
Frailty is increasingly recognized as a salient condition in patients with heart failure (HF) as previous studies have determined that frailty is highly prevalent and prognostically significant, particularly in those with advanced HF. Definitions of frailty have included a variety of domains, including physical performance, sarcopenia, disability, comorbidity, and cognitive and psychological impairments, many of which are common in advanced HF. Multiple groups have recently recommended incorporating frailty assessments into clinical practice and research studies, indicating the need to standardize the definition and measurement of frailty in advanced HF. Therefore, the purpose of this consensus statement is to provide an integrated perspective on the definition of frailty in advanced HF and to generate a consensus on how to assess and manage frailty. We convened a group of HF clinicians and researchers who have expertise in frailty and related geriatric conditions in HF, and we focused on the patient with advanced HF. Herein, we provide an overview of frailty and how it has been applied in advanced HF (including potential mechanisms), present a definition of frailty, generate suggested assessments of frailty, provide guidance to differentiate frailty and related terms, and describe the assessment and management in advanced HF, including with surgical and nonsurgical interventions. We conclude by outlining critical evidence gaps, areas for future research, and clinical implementation.
Keywords: frailty; heart failure; heart transplantation; mechanical circulatory support.
Copyright © 2023 International Society for the Heart and Lung Transplantation. Published by Elsevier Inc. All rights reserved.
Publication types
- Practice Guideline

Study finds older adults hospitalized for heart failure had high risk of kidney complications
R esearchers from Brigham and Women's Hospital, a founding member of the Mass General Brigham health care system, have found links between heart failure and kidney disease that support new approaches for integrating the care of these conditions.
In an analysis that included adults ages 65 and older who were hospitalized for heart failure from across 372 sites in the U.S., researchers found that patients had a substantial risk of kidney complications, with approximately 6% progressing to dialysis within a year of being hospitalized for heart failure. The results are published in JAMA Cardiology.
"We know that heart and kidney health are highly interconnected, but management of heart and kidney disease remains relatively siloed, and kidney health often isn't prioritized in patients with heart disease until advanced stages," said first author John Ostrominski, MD, a fellow in Cardiovascular Medicine and Obesity Medicine at the Brigham.
"Declining kidney function is often asymptomatic until late in the disease course, but even less advanced stages of kidney impairment can have important implications for cardiovascular health. Hence, there's a need for analyses that assess kidney outcomes in people with heart failure."
About two thirds of older adults with heart failure have abnormal kidney function. However, few analyses to date have investigated the occurrence of clinically relevant kidney outcomes, such as hospitalization for acute kidney injury or dialysis, in patients with heart failure. Evaluating these more recognizable and patient-centered outcomes, according to Ostrominski, may result in substantial changes to the way that heart and kidney disease are managed together in the clinic.
The study analyzed Medicare claims data from 85,298 patients over the age of 65 who were hospitalized with heart failure between 2021 and 2024.
The data was sourced from the Get with the Guidelines-Heart-Failure Registry, an initiative supported by the American Heart Association that seeks to connect hospitals with current evidence-based guidelines and accurate measurement tools to improve care quality and industry practices. The registry is also proving a valuable source of information for researchers examining trends in health outcomes for patients with heart failure.
In the present study, 63% of patients were discharged with significantly impaired kidney function, as measured by their rate of filtration. The researchers also found that the risk of adverse kidney outcomes increased steeply in patients with lower kidney function. By one year after discharge, 6% of patients were on dialysis, and 7% were either on dialysis or had progressed to end stage kidney disease.
The findings suggest that at the individual provider level, cardiologists should prioritize assessing kidney function—including measuring kidney filtration and looking for evidence of protein in the urine, also known as albuminuria—in all patients with heart failure, and, when indicated, consider heart therapies that are known to improve kidney outcomes.
More broadly, the study emphasizes the need for systemic changes that better support the simultaneous management of heart and kidney disease, including establishing clinics focused on integrating these two care areas, incorporating kidney outcomes into health care performance metrics for cardiovascular diseases, and expanding Medicare reimbursement protocols for interdisciplinary chronic care management.
Researchers at Mass General Brigham are actively engaged as sites for clinical trials evaluating newer treatment strategies for individuals with cardiovascular and kidney disease. The Accelerator for Clinical Transformation team is also developing new ways of delivering care—including medications with established kidney benefits—to eligible patients with and without heart failure.
"The trends we've observed aren't especially surprising given what we know about the links between heart and kidney health, but what's important is that this research emphasizes the scope of the problem and gives us information we can act upon to directly improve clinical outcomes in patients with heart failure," said Ostrominski.
"There are important opportunities for patients and providers, health care institutions, and, at the broader state and national levels, in terms of health care policy that could make a big difference for patients."
More information: Ostrominski, J. et al. Kidney Outcomes Among Medicare Beneficiaries After Hospitalization for Heart Failure, JAMA Cardiology (2024). DOI: 10.1001/jamacardio.2024.1108
Provided by Brigham and Women’s Hospital

- Open access
- Published: 24 May 2024
Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial
- Jian Zhao 1 na1 ,
- Xin Gong 1 na1 ,
- Jian Ding 1 ,
- Kepin Xiong 2 ,
- Kangle Zhuang 3 ,
- Rui Huang 1 ,
- Shu Li 4 &
- Huachun Miao 1
BMC Medical Education volume 24 , Article number: 571 ( 2024 ) Cite this article
275 Accesses
Metrics details
Case-based learning (CBL) methods have gained prominence in medical education, proving especially effective for preclinical training in undergraduate medical education. Tetralogy of Fallot (TOF) is a congenital heart disease characterized by four malformations, presenting a challenge in medical education due to the complexity of its anatomical pathology. Three-dimensional printing (3DP), generating physical replicas from data, offers a valuable tool for illustrating intricate anatomical structures and spatial relationships in the classroom. This study explores the integration of 3DP with CBL teaching for clinical medical undergraduates.
Sixty senior clinical medical undergraduates were randomly assigned to the CBL group and the CBL-3DP group. Computed tomography imaging data from a typical TOF case were exported, processed, and utilized to create four TOF models with a color 3D printer. The CBL group employed CBL teaching methods, while the CBL-3DP group combined CBL with 3D-printed models. Post-class exams and questionnaires assessed the teaching effectiveness of both groups.
The CBL-3DP group exhibited improved performance in post-class examinations, particularly in pathological anatomy and TOF imaging data analysis ( P < 0.05). Questionnaire responses from the CBL-3DP group indicated enhanced satisfaction with teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities ( P < 0.05). These findings underscore the potential of 3D printed models to augment the effectiveness of CBL, aiding students in mastering instructional content and bolstering their interest and self-confidence in learning.
The fusion of CBL with 3D printing models is feasible and effective in TOF instruction to clinical medical undergraduates, and worthy of popularization and application in medical education, especially for courses involving intricate anatomical components.
Peer Review reports
Tetralogy of Fallot (TOF) is the most common cyanotic congenital heart disease(CHD) [ 1 ]. Characterized by four structural anomalies: ventricular septal defect (VSD), pulmonary stenosis (PS), right ventricular hypertrophy (RVH), and overriding aorta (OA), TOF is a focal point and challenge in medical education. Understanding anatomical spatial structures is pivotal for learning and mastering TOF [ 2 ]. Given the constraints of course duration, medical school educators aim to provide students with a comprehensive and intuitive understanding of the disease within a limited timeframe [ 3 ].
The case-based learning (CBL) teaching model incorporates a case-based instructional approach that emphasizes typical clinical cases as a guide in student-centered and teacher-facilitated group discussions [ 4 ]. The CBL instructional methods have garnered widespread attention in medical education as they are particularly appropriate for preclinical training in undergraduate medical education [ 5 , 6 ]. The collection of case data, including medical records and examination results, is essential for case construction [ 7 ]. The anatomical and hemodynamic consequences of TOF can be determined using ultrasonography, computed tomography (CT), and magnetic resonance imaging techniques. However, understanding the anatomical structures from imaging data is a slow and challenging psychological reconstruction process for undergraduate medical students [ 8 ]. Three-dimensional (3D) visualization is valuable for depicting anatomical structures [ 9 ]. 3D printing (3DP), which creates physical replicas based on data, facilitates the demonstration of complex anatomical structures and spatial relationships in the classroom [ 10 ].
During the classroom session, 3D-printed models offer a convenient means for hands-on demonstration and communication, similar to facing a patient, enhancing the efficiency and specificity of intra-team communication and discussion [ 11 ]. In this study, we printed TOF models based on case imaging data, integrated them into CBL teaching, and assessed the effectiveness of classroom instruction.
Research participants
The study employed a prospective, randomized controlled design which received approval from the institutional ethics committee. Senior undergraduate students majoring in clinical medicine at Wannan Medical College were recruited for participation based on predefined inclusion criteria. The researchers implemented recruitment according to the recruitment criteria by contacting the class leaders of the target classes they had previously taught. Notably, these students were in their third year of medical education, with anticipation of progressing to clinical courses in the fourth year, encompassing Internal Medicine, Surgery, Obstetrics, Gynecology, and Pediatrics. Inclusion criteria for participants encompassed the following: (1) proficient communication and comprehension abilities, (2) consistent attendance without absenteeism or truancy, (3) absence of failing grades in prior examinations, and (4) capability to conscientiously fulfill assigned learning tasks. Exclusion criteria were (1) absence from lectures, (2) failure to complete pre-and post-tests, and (3) inadequate completion of questionnaires. For their participation in the study, Students were provided access to the e-book “Localized Anatomy,” authored by the investigators, as an incentive for their participation. Voluntary and anonymous participation was emphasized, with participants retaining the right to withdraw from the study at any time without providing a reason.
The study was conducted between May 1st, 2023, and June 30, 2023, from recruitment to completion of data collection. Drawing upon insights gained from a previous analogous investigation which yielded an effect size of 0.95 [ 10 ]. Sample size was computed, guided by a statistical consultant, with the aim of 0.85 power value, predicated on an effect size of 0.8 and a margin of error set at 0.05. A minimum of 30 participants per group was calculated using G*Power software (latest ver. 3.1.9.7; Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany), resulting in the recruitment of a total of 60 undergraduate students. Each participant was assigned an identification number, with codes placed in boxes. Codes drawn from the boxes determined allocation to either the CBL group or the CBL-3DP group. Subsequently, participants were randomly assigned to either the CBL group, receiving instruction utilizing the CBL methodology, or the CBL-3DP group, which received instruction integrating both CBL and 3D Printed models.
Printing of TOF models
Figure 1 A shows the printing flowchart of the TOF models. A typical TOF case was collected from the Yijishan Hospital of Wannan Medical College. The CT angiography imaging data of the case was exported. Mimics Research 20.0 software (Mimics Innovation Suite version 20, Materialize, Belgium) was used for data processing. The cardiovascular module of the CT-Heart tool was employed to adjust the threshold range, independently obtain the cardiac chambers and vessels, post-process the chambers and vessels to generate a hollow blood pool, and merge it with the myocardial volume to construct a complete heart model. The file was imported into Magics 24.0 software (version 24.0; Materialize, Belgium) for correction using the Shell tool page. After repairs, the model entered the smoothing page, where tools such as triangular surface simplification, local smoothing, refinement and smoothing, subdivision of components, and mesh painting were utilized to achieve varying degrees of smoothness. Finally, optimized data were obtained and exported as stereolithography (STL) files. An experienced cardiothoracic surgeon validated the anatomical accuracy of the digital model.
The STL files were imported into a 3D printer (J401Pro; Sailner 3D Technology, China) for model printing. This printer can produce full-color medical models using different materials. The models were fabricated using two distinct materials: rigid and flexible. Both materials are suitable for the observational discussion of the teaching objectives outlined in our study. From the perspective of observing pathological changes in the TOF, there is no significant difference between the two materials.
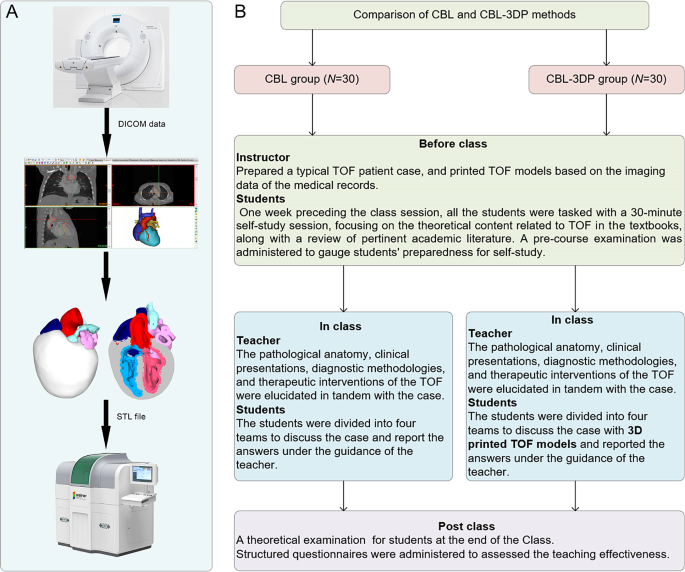
Experimental flow chart of this study. A TOF model printing flow chart. B The instructional framework
Teaching implementation
Figure 1 B illustrates the instructional framework employed in this study. One week preceding the class session, all the students were tasked with a 30-minute self-study session, focusing on the theoretical content related to TOF as outlined in the Pediatrics and Surgery textbooks, along with a review of pertinent academic literature. Both groups received co-supervision from two basic medicine lecturers boasting over a decade of teaching experience, alongside a senior cardiothoracic surgeon. Teaching conditions remained consistent across groups, encompassing uniform assessment criteria and adherence to predefined teaching time frames, all conducted in a Project-Based Learning (PBL) classroom at Wannan Medical College. Additionally, a pre-course examination was administered to gauge students’ preparedness for self-study.
In adherence to the curriculum guidelines, the teaching objectives aimed to empower students to master TOF’s clinical manifestations, diagnostic modalities, and differential diagnoses, while acquainting them with treatment principles and surgical methodologies. Additionally, the objectives sought to cultivate students’ clinical reasoning abilities and problem-solving skills. the duration of instruction for the TOF theory session was standardized to 25 min. The didactic content was integrated with the TOF case study to construct a coherent pedagogical structure.
During the instructional session, both groups underwent teaching utilizing the CBL methodology. Clinical manifestations and case details of TOF cases were presented to stimulate students’ interest and curiosity. Subsequently, the theory of TOF, including its etiology, pathogenesis, pathologic anatomy, clinical manifestations, diagnostic methods, and therapeutic interventions, was briefly elucidated. Emphasis was then placed on the case, wherein selected typical TOF cases were explained, guiding students in analysis and discussion. Students were organized into four teams under the instructors’ supervision, fostering cooperative learning and communication, thereby deepening their understanding of the disease through continuous inquiry and exploration (Fig. 2 L). In the routinely equipped PBL classroom with standard heart models (Fig. 2 J, K), all students had prior exposure to human anatomy and were familiar with these models. Both groups were provided with four standard heart models for reference, while the CBL-3DP group received additional four 3D-printed models depicting TOF anomalies, enriching their learning experience (Fig. 2 D, G). After the lesson, summarization, and feedback sessions were conducted to consolidate group discussions’ outcomes, evaluate teaching effectiveness, and assess learning outcomes.
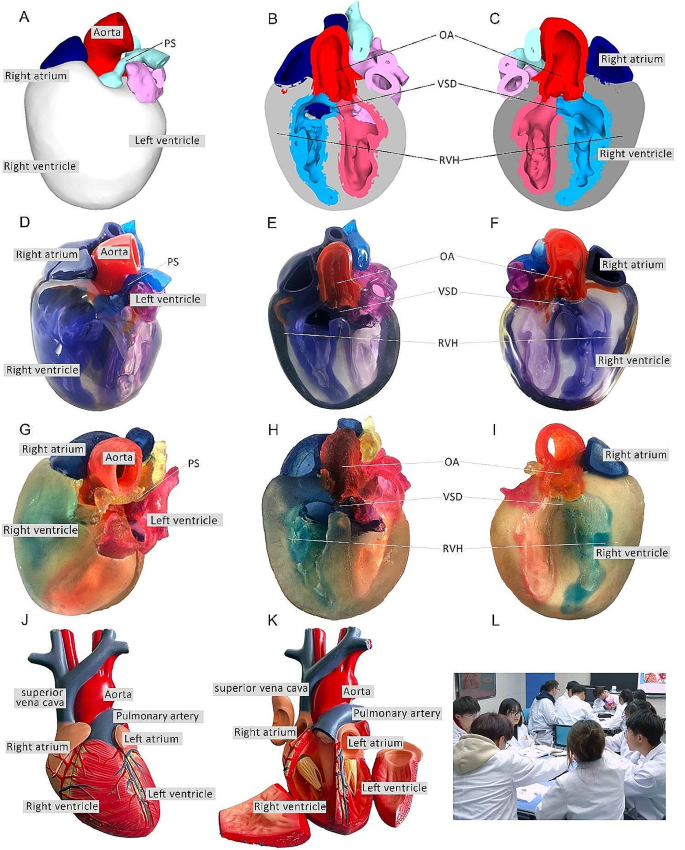
Heart models utilized in instructional sessions. A External perspective of 3D digital models. B, C Cross-sectional views following trans-septal sagittal dissection of the 3D digital model (PS: Pulmonary Stenosis; OA: Overriding Aorta; VSD: Ventricular Septal Defect; RVH: Right Ventricular Hypertrophy). D External depiction of rigid 3D printed model. E, F Sagittal sections of the rigid 3D printed model. G External portrayal of flexible 3D printed model. H, I Sagittal sections of the flexible 3D printed model. J, K The normal heart model employed in the instruction of the CBL group. L Ongoing classroom session
Teaching effectiveness assessment
Following the instructional session, participants from the two groups underwent a theoretical examination to assess their comprehension of the taught material. This assessment covered domains such as pathological anatomy, clinical manifestations, imaging data interpretation, diagnosis, and treatment relevant to TOF. Additionally, structured questionnaires were administered to evaluate the efficacy of the pedagogical approach employed. The questionnaire consisted of six questions designed to gauge participants’ understanding of the teaching content, enhancement of diagnostic skills, cultivation of critical thinking and clinical reasoning abilities, bolstering of confidence in managing TOF cases, satisfaction with the teaching mode, and satisfaction with the CBL methodology.
The questionnaire employed a 5-point Likert scale to gauge responses, with 5 indicating “strongly satisfied/agree,” 4 for “satisfied/agree,” 3 denoting “neutral,” 2 reflecting “dissatisfied/disagree,” and 1 indicating “strongly dissatisfied/disagree.” It comprised six questions, with the initial two probing participants’ knowledge acquisition, questions 3 and 4 exploring satisfaction regarding enhanced competence, and the final two assessing satisfaction with teaching methods and modes. Additionally, participants were encouraged to provide suggestions at the end of the questionnaire. To ensure the questionnaire’s validity, five esteemed lecturers in basic medical sciences with more than 10 years of experience verified its content and assessed its Content Validity Ratio and Content Validity Index to ensure alignment with the study’s objectives.
Statistical analysis
Statistical analyses were conducted utilizing GraphPad Prism 9.0 software. Aggregate score data for both groups were presented as mean ± standard deviation (x ± s). The gender comparisons were analyzed with the chi-square (χ2) test, while the other variables were compared using the Mann-Whitney U test. The threshold for determining statistical significance was set at P < 0.05.
Three-dimensional printing models
After configuring the structural colors of each component (Fig. 2 A, B, C), we printed four color TOF models using both rigid and flexible materials, resulting in four life-sized TOF models. Two color TOF models were created using rigid materials (Fig. 2 D, E, F). These models, exhibiting resistance to deformation, and with a firm texture, smooth and glossy surface, and good transparency, allowing visibility of the internal structures, were deemed conducive to teaching and observation. We also fabricated two color TOF models using flexible materials (Fig. 2 G, H, I), characterized by soft texture, opacity, and deformability, allowing for easy manipulation and cutting. It has potential utility beyond observational purposes. It can serve as a valuable tool for simulating surgical interventions and may be employed to create tomographic anatomical specimens. In this study, both material models were suitable for observation in the classroom. The participants were able to discern the four pathological changes characteristic of TOF from surface examination or cross-sectional analysis.
Baseline characteristics of the students
In total, 60 students were included in this study. The CBL group comprised 30 students (14 males and 16 females), with an average age of (21.20 ± 0.76) years. The CBL-3DP group consisted of 30 students (17 males and 13 females) with an average age of 20.96 years. All the students completed the study procedures. There were no significant differences in age, sex ratio, or pre-class exam scores between the two groups ( P > 0.05), indicating that the baseline scores between the two groups were comparable (Table 1 ).
Theoretical examination results
All students completed the research procedures as planned. The post-class theoretical examination encompassed assessment of pathological anatomy, clinical presentations, imaging data interpretation, diagnosis, and treatment pertinent to TOF. Notably, no statistically significant disparities were observed in the scores on clinical manifestations, diagnosis and treatment components between the cohorts, as delineated in Table 2 . Conversely, discernible distinctions were evident whereby the CBL-3DP group outperformed the CBL group notably in pathological anatomy, imaging data interpretation, and overall aggregate scores ( P < 0.05).
Results of the questionnaires
All the 60 participants submitted the questionnaire. Comparing the CBL and CBL-3DP groups, the scores from the CBL-3DP group showed significant improvements in many areas. This included satisfaction with the teaching mode, promotion of diagnostic skills, bolstering of self-assurance in managing TOF cases, and cultivation of critical thinking and clinical reasoning abilities (Fig. 3 B, C, D, E). All of which improved significantly ( P < 0.05 for the first aspects and P < 0.01 for the rest). However, the two groups were not comparable ( P > 0.05) in terms of understanding of the teaching content and Satisfaction with the CBL methodology (Fig. 3 A, F).
Upon completion of the questionnaires, participants were invited to proffer recommendations. Notably, in the CBL group, seven students expressed challenges in comprehending TOF and indicated a need for additional time for consolidation to enhance understanding. Conversely, within the CBL-3DP group, twelve students advocated for the augmentation of model repertoire and the expansion of disease-related data collection to bolster pedagogical efficacy across other didactic domains.
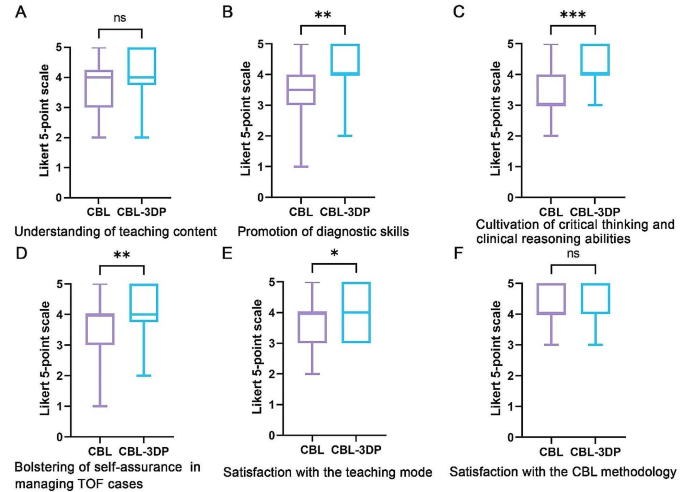
Five-point Likert scores of students’ attitudes in CBL ( n = 30) and CBL-3DP ( n = 30) groups. A Understanding of teaching content. B Promotion of diagnostic skills. C Cultivation of critical thinking and clinical reasoning abilities. D Bolstering of self-assurance in managing TOF cases. E Satisfaction with the teaching mode. F Satisfaction with the CBL methodology. ns No significant difference, * p < 0.05, ** p < 0.01, *** p < 0.001
TOF presents a significant challenge in clinical practice, necessitating a comprehensive understanding for effective diagnosis and treatment [ 12 ]. Traditional teaching methods in medical schools have relied on conventional resources such as textbooks, 2D illustrations, cadaver dissections, and radiographic materials to impart knowledge about complex conditions like TOF [ 13 ]. However, the limitations of these methods in fully engaging students and bridging the gap between theoretical knowledge and practical application have prompted a need for innovative instructional approaches.
CBL has emerged as a valuable tool in medical education, offering students opportunities to engage with authentic clinical cases through group discussions and inquiry-based learning [ 14 ]. By actively involving students in problem-solving and decision-making processes, CBL facilitates the application of theoretical knowledge to real-world scenarios, thus better-preparing students for future clinical practice [ 15 ]. Our investigation revealed that both groups of students exhibited comparable levels of satisfaction with the CBL methodology, devoid of discernible disparities.
CHD presents a formidable challenge due to the intricate nature of anatomical anomalies, the diverse spectrum of conditions, and individual variations [ 16 ]. Utilizing 3D-printed physical models, derived from patient imaging data, can significantly enhance comprehension of complex anatomical structures [ 17 ]. These models have proven invaluable in guiding surgical planning, providing training for junior or inexperienced pediatric residents, and educating healthcare professionals and parents of patients [ 18 ]. Studies indicate that as much as 50% of pediatric surgical decisions can be influenced by the insights gained from 3D printed models [ 19 ]. By providing tangible, anatomically accurate models, 3D printing offers a unique opportunity for people to visualize complex structures and enhance their understanding of anatomical intricacies. Our study utilized full-color, to-scale 3D printed models to illustrate the structural abnormalities associated with TOF, thereby enriching classroom sessions and facilitating a deeper comprehension of the condition.
Comparative analysis between the CBL-3DP group and the CBL group revealed significant improvements in post-test performance, particularly in pathological anatomy and imaging data interpretation. Additionally, questionnaire responses indicated higher levels of satisfaction and confidence among students in the CBL-3DP group, highlighting the positive impact of incorporating 3D printed models into the learning environment, improving the effectiveness of CBL classroom instruction. Despite the merits, our study has limitations. Primarily, participants were exclusively drawn from the same grade level within a single college, possibly engendering bias owing to shared learning backgrounds. Future research could further strengthen these findings by expanding the sample size and including long-term follow-up to assess the retention of knowledge and skills. Additionally, the influence of the 3D models depicting a normal heart on the learning process and its potential to introduce bias into the results warrants consideration, highlighting a need for scrutiny in subsequent studies.
As medical science continues to advance, the need for effective teaching methods becomes increasingly paramount. Our study underscores the potential of combining active learning approaches like CBL with innovative technologies such as 3D printing to enhance teaching effectiveness, improve knowledge acquisition, and foster students’ confidence and enthusiasm in pursuing clinical careers. Moving forward, further research and integration of such methodologies are essential for meeting the evolving demands of medical education, especially in areas involving complex anatomical understanding.
Conclusions
Integrating 3D-printed models with the CBL method is feasible and effective in TOF instruction. The demonstrated success of this method warrants broad implementation in medical education, particularly for complex anatomical topics.
Data availability
All data supporting the conclusions of this research are available upon reasonable request from the corresponding author.
Apitz C, Webb GD, Redington AN. Tetralogy of Fallot. Lancet. 2009;374:1462–71.
Article Google Scholar
Ghosh RM, Jolley MA, Mascio CE, Chen JM, Fuller S, Rome JJ, et al. Clinical 3D modeling to guide pediatric cardiothoracic surgery and intervention using 3D printed anatomic models, computer aided design and virtual reality. 3D Print Med. 2022;8:11.
Chakrabarti R, Wardle K, Wright T, Bennie T, Gishen F. Approaching an undergraduate medical curriculum map: challenges and expectations. BMC Med Educ. 2021;21:341.
Donkin R, Yule H, Fyfe T. Online case-based learning in medical education: a scoping review. BMC Med Educ. 2023;23:564.
Novack JP. Designing cases for case-based immunology teaching in large medical school classes. Front Immunol. 2020;11:995.
Chen HC, Van Den Broek WES, Ten Cate O. The case for use of entrustable professional activities in undergraduate medical education. Acad Med. 2015;90:431–6.
Wang M, Sun Z, Jia M, Wang Y, Wang H, Zhu X, et al. Intelligent virtual case learning system based on real medical records and natural language processing. BMC Med Inf Decis Mak. 2022;22:60.
Yoo S-J, Thabit O, Kim EK, Ide H, Yim D, Dragulescu A, et al. 3D printing in medicine of congenital heart diseases. 3D Print Med. 2015;2:3.
Yammine K, Violato C. A meta-analysis of the educational effectiveness of three-dimensional visualization technologies in teaching anatomy. Anat Sci Educ. 2015;8:525–38.
Miao H, Ding J, Gong X, Zhao J, Li H, Xiong K, et al. Application of 3D-printed pulmonary segment specimens in experimental teaching of sectional anatomy. BMC Surg. 2023;23:109.
Sun Z, Wong YH, Yeong CH. Patient-specific 3D-printed low-cost models in medical education and clinical practice. Micromachines (Basel). 2023;14:464.
Downing TE, Kim YY. Tetralogy of Fallot: general principles of management. Cardiol Clin. 2015;33:531–41. vii–viii.
Jia X, Zeng W, Zhang Q. Combined administration of problem- and lecture-based learning teaching models in medical education in China: a meta-analysis of randomized controlled trials. Med (Baltim). 2018;97:e11366.
McLean SF. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. J Med Educ Curric Dev. 2016;3:JMECD.S20377.
Zeng N, Lu H, Li S, Yang Q, Liu F, Pan H, et al. Application of the combination of CBL teaching method and SEGUE framework to improve the doctor-patient communication skills of resident physicians in otolaryngology department. Bmc Med Educ. 2024;24:201.
Sun Z. Patient-specific 3D-printed models in pediatric congenital heart disease. Children. 2023;10:319.
Meyer-Szary J, Luis MS, Mikulski S, Patel A, Schulz F, Tretiakow D, et al. The role of 3D printing in planning complex medical procedures and training of medical professionals—cross-sectional multispecialty review. IJERPH. 2022;19:3331.
Sun Z, Wee C. 3D printed models in cardiovascular disease: an exciting future to deliver personalized medicine. Micromachines-basel. 2022;13:1575.
Valverde I, Gomez-Ciriza G, Hussain T, Suarez-Mejias C, Velasco-Forte MN, Byrne N, et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: an international multicentre study. Eur J Cardio-thorac. 2017;52:1139–48.
Download references
Acknowledgements
We extend our sincere appreciation to the instructors and students whose invaluable participated in this study.
This paper received support from the Education Department of Anhui Province, China (Grant Numbers 2022jyxm1693, 2022jyxm1694, 2022xskc103, 2018jyxm1280).
Author information
Jian Zhao and Xin Gong are joint first authors.
Authors and Affiliations
Department of Human Anatomy, Wannan Medical College, No.22 West Wenchang Road, Wuhu, 241002, China
Jian Zhao, Xin Gong, Jian Ding, Rui Huang & Huachun Miao
Department of Cardio-Thoracic Surgery, Yijishan Hospital of Wannan Medical College, Wuhu, China
Kepin Xiong
Zhuhai Sailner 3D Technology Co., Ltd., Zhuhai, China
Kangle Zhuang
School of Basic Medical Sciences, Wannan Medical College, Wuhu, China
You can also search for this author in PubMed Google Scholar
Contributions
Jian Zhao and Huachun Miao designed the research. Jian Zhao, Xin Gong, Jian Ding, Kepin Xiong designed the tests and questionnaires. Kangle Zhuang processed the imaging data and printed the models. Xing Gong and Kepin Xiong implemented the teaching. Jian Zhao and Rui Huang collected the data and performed the statistical analysis. Jian Zhao and Huachun Miao prepared the manuscript. Shu Li and Huachun Miao revised the manuscript. Shu Li provided the Funding acquisition. All authors reviewed and approved the final manuscript.
Corresponding authors
Correspondence to Shu Li or Huachun Miao .
Ethics declarations
Ethics approval and consent to participate.
This investigation received ethical approval from the Ethical Committee of School of Basic Medical Sciences, Wannan Medical College (ECBMSWMC2022-1-12). All methodologies adhered strictly to established protocols and guidelines. Written informed consent was obtained from the study participants to take part in the study.
Consent for publication
Written informed consent was obtained from the individuals for the publication of any potentially identifiable images or data included in this article.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Zhao, J., Gong, X., Ding, J. et al. Integration of case-based learning and three-dimensional printing for tetralogy of fallot instruction in clinical medical undergraduates: a randomized controlled trial. BMC Med Educ 24 , 571 (2024). https://doi.org/10.1186/s12909-024-05583-z
Download citation
Received : 03 March 2024
Accepted : 21 May 2024
Published : 24 May 2024
DOI : https://doi.org/10.1186/s12909-024-05583-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Case-based learning
- 3D printing
- Tetralogy of fallot
- Medical undergraduates
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Americans willing to go into debt for travel and entertainment, study finds
Credit card balances have ballooned 32% in the last two years.
(InvestigateTV) — A recent Bankrate survey revealed that 27% of Americans would be willing to go into debt to travel, eat out, or see live entertainment.
Ted Rossman with Bankrate said this was concerning considering the current high interest rates.
“I don’t want to tell anyone they can’t have fun, but I do worry about this in light of credit card rates being at record highs,” Rossman noted. “The average is 20.75%. So, I think a better option for people would be to set a good budget ahead of time.”
Rossman said there’s going to be a lot of temptation to spend this summer and that’s not a bad thing, just make sure to plan for it.
He suggested setting money aside from every paycheck and have it transferred into a savings account.
“We know young adults are very driven by experiences and social things, and again that’s not a bad thing, as long as you’ve accounted for it,” Rossman explained. “I think sometimes also people fall into this trap, ‘Oh, I didn’t know the concert invite was coming’ or ‘the wedding invite was coming.’ You may not know exactly what the invite is, but you do want to put together a good entertainment budget.”
Rossman said a lot of people make the mistake of either not budgeting or if they do, they only account for the necessities. It’s important to put together a fun budget as well.
He said if a trip is budgeted, try to offset the cost with rewards points and miles.
Travelers could also pool resources with friends and share an Airbnb.
Copyright 2024 Gray Media Group, Inc. All rights reserved.

Ponchatoula police officer, 44, died from heart failure while on duty, department says

St. John Sheriff seeks leads after 16-year-old girl murdered in rolling ambush Sunday in Reserve

Louisiana retailers must clear shelves of nitrous oxide by Aug. 1 before enforcement crackdown

Stream news and weather 24/7

6-week-old suffering from life-threatening injuries; teen parents arrested
Latest news.

Heat dome sends temperatures soaring

Congressman’s son steals show on House floor, hamming it up for cameras

Hunter Biden’s federal firearms case is opening after the jury is chosen

Epoch Times CFO is arrested and accused of role in $67M multinational money laundering scheme

Jury selected in Hunter Biden gun trial

IMAGES
VIDEO
COMMENTS
Heart failure is a systemic and complex clinical syndrome, ... Prevalence studies estimate that 23 million individuals worldwide have heart failure and that 2 million new cases are diagnosed annually. ... The patient in this case presented with progressive dyspnea triggered by less than ordinary activities, lower-extremity edema, and ascites ...
On examination, the temperature was 36.4°C, the heart rate 103 beats per minute, the blood pressure 79/51 mm Hg, the respiratory rate 30 breaths per minute, and the oxygen saturation 99% while ...
Presentation of Case. Dr. Amy A. Sarma: A 54-year-old man was evaluated at this hospital because of new heart failure. One month before this evaluation, a nonproductive cough developed after the ...
In this case, a patient with known history of coronary artery disease presented with worsening of shortness of breath with lower extremity edema and jugular venous distension along with crackles in the lung. The sign and symptoms along with labs and imaging findings point to diagnosis of heart failure with reduced EF (HFrEF).
Heart Failure Patient Case Quizzes. Unrecognized HFpEF in a Type 2 DM Patient - Reducing CV and HF Risk ; Untreated HFrEF/Ischemic Cardiomyopathy in Type 2 DM - How to Optimize Medical Therapy to Improve Heart Failure Outcomes ; Restrictive Cardiomyopathies Series: Advanced HF Therapies in ATTR Cardiac Amyloidosis (Certified Patient Case Study)
Less is known about the definition and management of diastolic dysfunction. The following case studies have been chosen to illustrate the basis for therapeutic management of systolic heart failure and outline the remaining gaps in knowledge, of which there are several. The issues apply across the spectrum of patients seen in clinical practice.
Catheter Ablation in End-Stage Heart Failure with Atrial Fibrillation. C. Sohns and OthersN Engl J Med 2023;389:1380-1389. In a randomized trial involving patients with advanced heart failure and ...
About this book. This guide provides a clear and concise overview of heart failure for primary care clinicians. Written by two nurse practitioners for nurses, nurse practitioners, physician assistants, medical students, and pharmacists, it is uniquely designed to bridge the gap between cardiology and primary care.
Clinical background. This case study concerns a 52-year-old woman (Mrs A) with a brief but extremely unfortunate clinical history leading to the development of chronic heart failure. In 1998 Mrs A underwent a mastectomy to remove a breast tumour. In 2001 she developed auxiliary node recurrence with subsequent surgical removal of these nodes ...
Advanced Heart Failure Case Study Patient Case History A 65 y/o man with chronic systolic heart failure comes to the office with progressive heart failure symptoms (dyspnea, fatigue) and a 10# unintentional weight loss. He is having more difficulty carrying on ADLs. He also has nocturnal dyspnea. He complains of chest pain and has
Heart failure patients presenting to primary care clinics often have multiple, complex comorbidities. Several different disease processes and treatment options may need to be considered simultaneously in the setting of acute on chronic exacerbation of symptoms. This...
Introduction. This clinical case refers to an 83-year-old man with moderate chronic obstructive pulmonary disease and shows that implementation of appropriate medical therapy according to the European Society of Cardiology/Heart Failure Association (ESC/HFA) guidelines improves symptoms and quality of life. 1 The case also illustrates that optimization of glucose metabolism with a more lenient ...
Case study: The importance of a robust heart failure system of care. Approximately six million Americans live with heart failure — a number expected to reach epidemic proportions as the population ages.1 Heart failure ranks among the costliest health conditions to treat and takes a tremendous toll on patients' quality of life and longevity.
2364 n engl j med 379;24 nejm.org December 13, 2018 The new england journal of medicine On examination, the temperature was 36.4°C, the heart rate 102 beats per minute, the blood pressure 142/75 ...
This case study involves a 76 year old female named Mary Lou Poppins, who presented to the ED accompanied by her son. ... Mary Lou Poppins was educated regarding the disease process of heart failure; symptoms to monitor for and report to her doctor; the importance of daily monitoring of weight, blood pressure, and heart rate; and the importance ...
Case Study: Acute Heart Failure in a 20-year-old Patient. At Piedmont Heart's Napa Valley Cardiology Conference, Dr. David Dean presents a challenging case of acute heart failure in a 20-year-old patient. Hear Piedmont's unusual approach to therapy and tips for success from Dr. Dean, surgical director of Piedmont's Samsky Advanced Heart ...
Introduction. This chapter provides you with an example of the nursing care that a patient with heart failure may require. The heart failure care plan has been written by a senior charge nurse for coronary care, Rafael Ripoll, and outlines care for the four stages of heart failure.The case history for Martha will then guide you through the assessment, nursing action and evaluation of a patient ...
Efforts to harmonize the definitions, staging, follow-up, and approach to heart failure in children with congenital heart disease are critical to enable the conduct of rigorous scientific studies to advance our understanding of the actual burden of heart failure in this population and to allow the development of evidence-based heart failure ...
Congestive heart failure (CHF), as defined by the American College of Cardiology (ACC) and the American Heart Association (AHA), is "a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood." Ischemic heart disease is the leading cause of death worldwide and also the leading cause of CHF. CHF is a common disorder ...
This study was focused on survival analysis of heart failure patients who were admitted to Institute of Cardiology and Allied hospital Faisalabad-Pakistan during April-December (2015). All the patients were aged 40 years or above, having left ventricular systolic dysfunction, belonging to NYHA class III and IV. Cox regression was used to model mortality considering age, ejection fraction ...
This page titled 5: Case Study #4- Heart Failure (HF) is shared under a CC BY-SA 4.0 license and was authored, remixed, and/or curated by Glynda Rees, Rob Kruger, and Janet Morrison via source content that was edited to the style and standards of the LibreTexts platform; a detailed edit history is available upon request.
The following patients were excluded: patients who did not have a clinical diagnosis of heart failure according to Framingham Heart Study criteria or had a B-type natriuretic peptide level that ...
Frailty is increasingly recognized as a salient condition in patients with heart failure (HF) as previous studies have determined that frailty is highly prevalent and prognostically significant, particularly in those with advanced HF. ... Cleveland, Ohio; Case Western Reserve University School of Medicine, Cleveland, Ohio. 12 Department of ...
The study analyzed Medicare claims data from 85,298 patients over the age of 65 who were hospitalized with heart failure between 2021 and 2024.
Presentation of Case. Dr. Jacqueline B. Henson (Medicine): A 54-year-old man was evaluated at this hospital after cardiac arrest associated with ventricular fibrillation. The patient had been in ...
Background Case-based learning (CBL) methods have gained prominence in medical education, proving especially effective for preclinical training in undergraduate medical education. Tetralogy of Fallot (TOF) is a congenital heart disease characterized by four malformations, presenting a challenge in medical education due to the complexity of its anatomical pathology. Three-dimensional printing ...
Credit card balances have ballooned 32% in the last two years. (InvestigateTV) — A recent Bankrate survey revealed that 27% of Americans would be willing to go into debt to travel, eat out, or ...