- Case Report
- Open access
- Published: 25 November 2008

A case of PTSD presenting with psychotic symptomatology: a case report
- Georgios D Floros 1 ,
- Ioanna Charatsidou 1 &
- Grigorios Lavrentiadis 1
Cases Journal volume 1 , Article number: 352 ( 2008 ) Cite this article
30k Accesses
4 Citations
1 Altmetric
Metrics details
A male patient aged 43 presented with psychotic symptomatology after a traumatic event involving accidental mutilation of the fingers. Initial presentation was uncommon although the patient responded well to pharmacotherapy. The theoretical framework, management plan and details of the treatment are presented.
Recent studies have shown that psychotic symptoms can be a hallmark of post-traumatic stress disorder [ 1 , 2 ]. The vast majority of the cases reported concerned war veterans although there were sporadic incidents involving non-combat related trauma (somatic or psychic). There is a biological theoretical framework for the disease [ 3 ] as well as several psychological theories attempting to explain cognitive aspects [ 4 ].
Case presentation
A male patient, aged 43, presented for treatment with complaints tracing back a year ago to a traumatic work-related event involving mutilation of the distal phalanges of his right-hand fingers. Main complaints included mixed hallucinations, irritability, inability to perform everyday tasks and depressive mood. No psychic symptomatology was evident before the event to him or his social milieu.
Mental state examination
The patient was a well-groomed male of short stature, sturdy build and average weight. He was restless but not agitated, with a guarded attitude towards the interviewer. His speech pattern was slow and sparse, his voice low. He described his current mood as 'anxious' without being able to provide with a reason. Patient appeared dysphoric and with blunted affect. He was able to maintain a linear train of thought with no apparent disorganization or irrational connections when expressing himself. Thought content centred on his amputated fingers with a semi-compulsive tendency to gaze to his (gloved) hand. The patient was typically lost in ruminations about his accident with a focus on the precise moment which he experienced as intrusive and affectively charged in a negative and painful way. He could remember wishing for his fingers to re-attach to his hand almost as the accident took place. A trigger in his intrusive thoughts was the painful sensation of neuropathic pain from his half-mutilated fingers, an artefact of surgery.
He denied and thoughts of harming himself and demonstrated no signs of aggression towards others. Hallucinations had a predominantly depressive and ego-dystonic character. He denied any perceptual disturbances at the time of the examination. Their appearance was typically during nighttime especially in the twilight. Initially they were visual only, involving shapes and rocks tumbling down towards the patient, gradually becoming more complex and laden with significance. A mixed visual and tactile hallucination of burning rain came afterwards while in the time of examination a tall stranger clad in black and raiding a tall steed would threaten and ridicule the patient. He scored 21 on a MMSE with trouble in the attention, calculation and recall categories. The patient appeared reliable and candid to the extent of his self-disclosure, gradually opening up to the interviewer but displayed a marked difficulty on describing his emotions and memories of the accident, apparently independent of his conscious will. His judgement was adequate and he had some limited Insight into his difficulties, hesitantly attributing them to his accident.
He was married and a father of three (two boys and a girl aged 7–12) He had no prior medical history for mental or somatic problems and received no medication. He admitted to occasional alcohol consumption although his relatives confirmed that he did not present addiction symptoms. He had some trouble making ends meet for the past five years. Due to rampant unemployment in his hometown, he was periodically employed in various jobs, mostly in the construction sector. One of his children has a congenital deformity, underwent several surgical procedures with mixed results and, before the time of the patient's accident, it was likely that more surgery would be forthcoming. The patient's father was a proud man who worked hard but reportedly was victimized by his brothers, they reaping the benefits of his work in the fields by manipulating his own father. He suffered a nervous breakdown attributed to his low economic status after a failed economic endeavour ending in him being robbed of the profits, seven years before the accident. There was no other relevant family history.
Before the accident the patient was a lively man, heavily involved as a participant and organizer in important local social events from a young age. He was respected by his fellow villagers and felt his involvement as a unique source of pride in an otherwise average existence. Prior to his accident, the patient was repeatedly promised a permanent job as a labourer and fate would have it that his appointment was supposedly approved immediately after the accident only to be subsequently revoked. He viewed himself as an exploited man in his previous jobs, much the same way his father was, while he harboured an extreme bitterness over the unavailability of support for his long-standing problems. His financial status was poor, being in sick-leave from his previous job for the last four months following the accident and hoping to receive some compensation. Although his injuries were considered insufficient for disability pension he could not work to his full capacity since the hand affected was his primary one and he was a manual labourer.
Given that the patient clearly suffered a high level of distress as a result of his hallucinatory experiences he was voluntary admitted to the 2nd Psychiatric Department of the Aristotle University of Thessaloniki for further assessment, observation and treatment. A routine blood workup was ordered with no abnormalities. A Rorschach Inkblot Test was administered in order to gain some insight into patient's dynamics, interpersonal relations and underlying personality characteristics while ruling out any malingering or factitious components in the presentation as suggested in Wilson and Keane [ 5 ]. Results pointed to inadequate reality testing with slight disturbances in perception and a difficulty in separating reality from fantasy, leading to mistaken impressions and a tendency to act without forethought in the face of stress. Uncertainty in particular was unbearable and adjustment to a novel environment hard. Cognitive functions (concentration, attention, information processing, executive functions) were impaired possibly due to cognitive inability or neurological disease. Emotion was controlled with a tendency for impulsive behaviour; however there was difficulty in processing and expressing emotions in an adaptive manner. There were distinct patterns of aggression and anger towards others but expressing those patterns was avoided, switching to passivity and denial rather than succumbing to destructive urges or mature competitiveness. Self-esteem was low with feelings of inferiority and inefficiency.
A neurological examination revealed a left VI cranial nerve paresis, reportedly congenital, resulting in diplopia while gazing to the extreme left, which did not significantly affect the patient. The patient had a chronic complaint of occasional vertigo, to which he partly attributed his accident, although the symptoms were not of a persisting nature.
Initial diagnosis at this stage was 'Psychotic disorder NOS' and pharmacological treatment was initiated. An MRI scan of the brain with gadolinium contrast was ordered to rule out any focal neurological lesions. It was performed fifteen days later and revealed no abnormalities.
Patient was placed on ziprasidone 40 mg bid and lorazepam 1 mg bid. He reported an immediate improvement but when the attending physician enquired as to the nature of the improvement the patient replied that in his hallucinations he told the tall raider that he now had a tall doctor who would help him and the raider promptly left (sic). Apparently, the random assignment of a strikingly tall physician had an unexpected positive effect. Ziprasidone gradually increased to 80 mg bid within three days with no notable effect to the perceptual disturbances but with the development of akathisia for which biperiden was added, 1 mg tid. Duloxetine was added, 60 mg once-daily, in a hope that it could have a positive effect to his mood but also to this neuropathic pain which was frequent and demoralising. The patient had a tough time accommodating to the hospital milieu, although the grounds were extended and there was plenty of opportunity for walks and other activities. He preferred to stay in bed sometimes in obvious agony and with marked insomnia. He presented a strong fear for the welfare of his children, which he could not reason for. Due to the apparent inability of ziprasidone to make a dent in the psychotic symptomatology, medication was switched to amisulpride 400 mg bid and the patient was given a leave for the weekend to visit his home. On his return an improvement in his symptoms was reported by him and close relatives, although he still had excessive anxiety in the hospital setting. It was decided that his leave was to be extended and the patient would return for evaluation every third day. After three appointments he had a marked improvement, denied any psychotic symptoms while his sleep pattern improved. A good working relationship was established with his physician and the patient was with a schedule of follow-up appointments initially every fifteen days and following two months, every thirty days. His exit diagnosis was "Psychotic disorder Not Otherwise Specified – PTSD". He remained asymptomatic for five months and started making in-roads in a cognitively-oriented psychotherapeutic approach but unfortunately further trouble befell him, his wife losing a baby and his claim to an injury compensation rejected. He experienced a mood loss and duloxetine was increased to 120 mg per day to some positive effect. His status remains tenuous but he retains a strong will to make his appointments and work with his physician. A case conceptualization following a cognitive framework [ 6 ] is presented in Figure 1 .
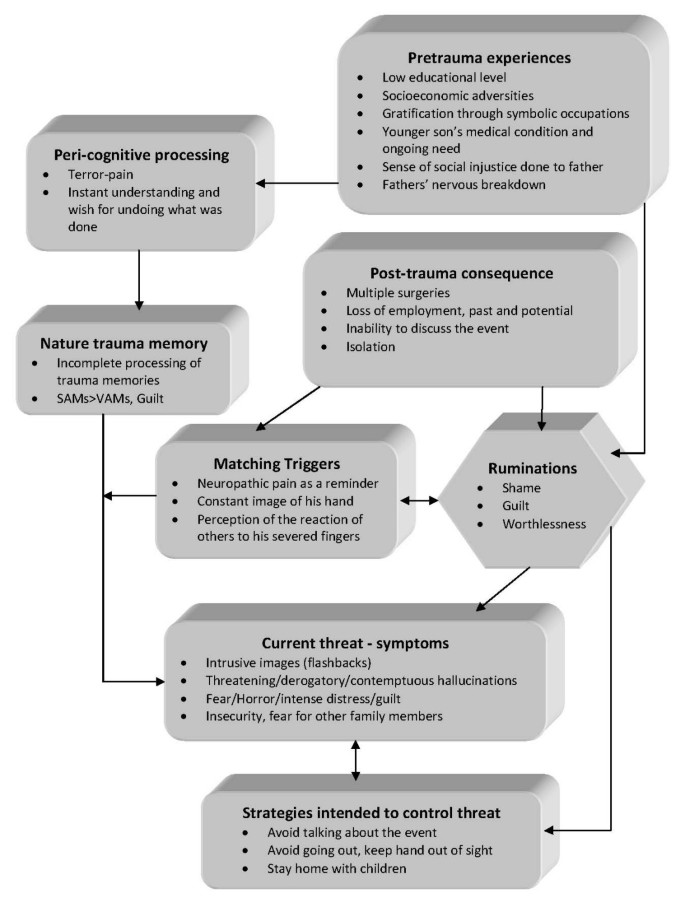
Case formulation – (Persistent PTSD, adapted from Ehlers and Clark [ 6 ] ) . Case formulation following the persistent PTSD model of Ehlers and Clark [ 6 ]. It is suggested that the patient is processing the traumatic information in a way which a sense of immediate threat is perpetuated through negative appraisals of trauma or its consequences and through the nature of the traumatic experience itself. Peri-traumatic influences that operate at encoding, affect the nature of the trauma memory. The memory of the event is poorly elaborated, not given a complete context in time and place, and inadequately integrated into the general database of autobiographical knowledge. Triggers and ruminations serve to re-enact the traumatic information while symptoms and maladaptive coping strategies form a vicious circle. Memories are encoded in the SAM rather than the VAM system, thus preventing cognitive re-appraisal and eventual overcoming of traumatic experience [ 4 ].
The value of a specialized formulation is made clear in complex cases as this one. There is a relationship between the pre-existing cognitive schemas of the individual, thought patterns emerging after the traumatic event and biological triggers. This relationship, best described as a maladaptive cognitive processing style, culminates into feelings of shame, guilt and worthlessness which are unrelated to similar feelings, which emerge during trauma recollection, but nonetheless acts in a positive feedback loop to enhance symptom severity and keep the subject in a constant state of psychotic turmoil. Its central role is addressed in our case formulation under the heading "ruminations" which best describes its ongoing and unrelenting character. The "what if" character of those ruminations may serve as an escape through fantasy from an unbearably stressful cognition. Past experience is relived as current threat and the maladaptive coping strategies serve as negative re-enforcers, perpetuating the emotional suffering.
The psychosocial element in this case report, the patient's involvement with a highly symbolic activity, demonstrates the importance of individualising the case formulation. Apparently the patient had a chronic difficulty in expressing his emotions and integrating into his social surroundings, a difficulty counter-balanced somewhat with his involvement in the local social events which gave him not only a creative way out from any emotional impasse but also status and recognition. His perceived inability to continue with his symbolic activities was not only an indicator of the severity of his troubles but also a stressor in its own right.
Complex cases of PTSD presenting with hallucinatory experiences can be effectively treated with pharmacotherapy and supportive psychotherapy provided a good doctor-patient relationship is established and adverse medication effects rapidly dealt with. A cognitive framework and a Rorschach test can be valuable in deepening the understanding of individuals and obtaining a personalized view of their functioning and character dynamics. A biopsychosocial approach is essential in integrating all aspects of the patients' history in a meaningful way in order to provide adequate help.
Patient's perspective
"My life situation can't seem to get any better. I haven't had any support from anyone in all my life. Leaving home to go anywhere nowadays is hard and I can't seem to be able to stay anyplace else for a long time either. Just getting to the hospital [where the follow-up appointments are held] makes me very nervous, especially the minute I walk in. Can't seem to stay in place at all, just keep pacing while waiting for my appointment. I am only able to open up somewhat to my doctor, whom I thank for his support. Staying in hospital was close to impossible; I was very stressed and particularly concerned for my children, not being able to be close to them. I still need to have them near-by. Getting the MRI scan was also a stressful experience, confined in a small space with all that noise for so long. I succeeded only after getting extra medication.
I hope that things will get better. I don't trust anyone for any help any more; they should have helped me earlier."
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
stands for 'Post Traumatic Stress Disorder'
for 'Verbally Accessible Memory'
for 'Situationally Accessible Memory'
Butler RW, Mueser KT, Sprock J, Braff DL: Positive symptoms of psychosis in posttraumatic stress disorder. Biological Psychiatry. 1996, 39: 839-844. 10.1016/0006-3223(95)00314-2.
Article CAS PubMed Google Scholar
Seedat S, Stein MB, Oosthuizen PP, Emsley RA, Stein DJ: Linking Posttraumatic Stress Disorder and Psychosis: A Look at Epidemiology, Phenomenology, and Treatment. The Journal of Nervous and Mental Disease. 2003, 191: 675-10.1097/01.nmd.0000092177.97317.26.
Article PubMed Google Scholar
Nutt DJ: The psychobiology of posttraumatic stress disorder. J Clin Psychiatry. 2000, 61: 24-29.
CAS PubMed Google Scholar
Brewin CR, Holmes EA: Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003, 23: 339-376. 10.1016/S0272-7358(03)00033-3.
Wilson JP, Keane TM: Assessing Psychological Trauma and PTSD. 2004, The Guilford Press
Google Scholar
Ehlers A, Clark DM: A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000, 38: 319-345. 10.1016/S0005-7967(99)00123-0.
Download references
Acknowledgements
The authors wish to acknowledge the valuable support and direction offered by the department's chair, Professor Ioannis Giouzepas who places the utmost importance in creating a suitable therapeutic environment for our patients and a superb learning environment for the SHO's and registrars in his department.
Author information
Authors and affiliations.
2nd Department of Psychiatry, Psychiatric Hospital of Thessaloniki, 196 Langada str., 564 29, Thessaloniki, Greece
Georgios D Floros, Ioanna Charatsidou & Grigorios Lavrentiadis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Georgios D Floros .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
GF was the attending SHO and the major contributor in writing the manuscript. IC performed the psychological evaluation and Rorschach testing and interpretation. GL provided valuable guidance in diagnosis and handling of the patient. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Floros, G.D., Charatsidou, I. & Lavrentiadis, G. A case of PTSD presenting with psychotic symptomatology: a case report. Cases Journal 1 , 352 (2008). https://doi.org/10.1186/1757-1626-1-352
Download citation
Received : 12 September 2008
Accepted : 25 November 2008
Published : 25 November 2008
DOI : https://doi.org/10.1186/1757-1626-1-352
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ziprasidone
- Psychotic Disorder
- Amisulpride
- Hallucinatory Experience
Cases Journal
ISSN: 1757-1626

CBT Case Studies

Case Study: CBT Treatment – Abby
Case Study: CBT Treatment – Abby Abby witnessed the suicide of a stranger and went on to develop PTSD along with enormous amounts of guilt.

Case Study: CBT Treatment – Holly
Case Study: CBT Treatment – Holly Holly developed PTSD after seeing her Dad who received fatal crush injuries. Following intense flashbacks and intrusive memories, she

Case Study: CBT Treatment – Darren
Case Study: CBT Treatment – Darren Darren lived with PTSD for 8 years before he opened up to his wife about how he was feeling
Hello! Did you find this information useful?
Please consider supporting ptsd uk with a donation to enable us to provide more information & resources to help us to support everyone affected by ptsd, no matter the trauma that caused it, ptsd uk blog.
You’ll find up-to-date news, research and information here along with some great tips to ease your PTSD in our blog.

Rebellious Rebirth – Oran: Guest Blog
Rebellious Rebirth – Oran: Guest Blog In this moving guest blog, PTSD UK Supporter Oran shares her personal story after a traumatic event brought childhood traumas to the surface. Dealing with Complex PTSD, Oran found solace in grounding techniques and

Ralph Fiennes – Trigger Warnings Response
Guest Blog: Response to Ralph Fiennes – Trigger warnings in theatres This thought-provoking article has been written for PTSD UK by one of our supporters, Alex C, and addresses Ralph Fiennes’ recent remarks on trigger warnings in Theatre. Alex sheds

Please don’t tell me I’m brave
Guest Blog: Living With PTSD – Please don’t tell me I’m brave ‘Adapting to living in the wake of trauma can mean maybe you aren’t ready to hear positive affirmations, and that’s ok too.’ and at PTSD UK, we wholeheartedly

Emotional Flashbacks – Rachel
Emotional Flashbacks: Putting Words to a Lifetime of Confusing Feelings PTSD UK was founded with the desire to do what was possible to make sure nobody ever felt as alone, isolated or helpless as our Founder did in the midst

Guest Blog: Calming the ‘riot’ in my head
Guest Blog: ‘Calming the riot’ in my head: Anna In our collective journey to navigate the complexities of PTSD and C-PTSD, finding peace and space within the internal turbulence is vital. In this insightful guest blog, author Anna sheds light

Morning Mile March Challenge
events | walk PTSD UK’s Morning Mile March Challenge Sign up now PTSD UK’s Morning Mile March Challenge The challenge We all know ‘exercise is good for you’, and even a small amount can make a big difference. There are
Treatments for PTSD
It is possible for PTSD to be successfully treated many years after the traumatic event occurred, which means it is never too late to seek help. For some, the first step may be watchful waiting, then exploring therapeutic options such as individual or group therapy – but the main treatment options in the UK are psychological treatments such as Eye Movement Desensitisation Reprogramming (EMDR) and Cognitive Behavioural Therapy (CBT).
Traumatic events can be very difficult to come to terms with, but confronting and understanding your feelings and seeking professional help is often the only way of effectively treating PTSD. You can find out more in the links below, or here .
- International edition
- Australia edition
- Europe edition

Is this actually PTSD? Clinicians divided over redefining borderline personality disorder
Some have argued BPD should be reclassified as a trauma disorder, maintaining those diagnosed are typically women with abuse in their past
- Get our morning and afternoon news emails , free app or daily news podcast
When Prof Andrew Chanen was a trainee psychiatrist in 1993, patients with borderline personality disorder (BPD) who had self-harmed were “vilified” and “treated appallingly”.
“There was this myth that somehow they were indestructible,” he says. Despite what his teachers told him, “most were dead by the end of my training”.
More than three decades later, Chanen is the chief of clinical practice and head of personality disorder research at Orygen, the National Centre of Excellence in Youth Mental Health at the University of Melbourne, and he says BPD remains the most stigmatised and discriminated against mental health disorder in Australia and internationally.
Overwhelmingly diagnosed in women , BPD is characterised by difficulty managing emotions, rapid mood changes, self-harm often accompanied by suicidal thoughts, and an unstable self image.
Some Australian clinicians are calling for BPD to be recognised as a trauma disorder rather than a personality disorder, arguing this would lead to better treatment and outcomes.
The argument for rethinking BPD
American psychoanalyst Adolph Stern introduced the word “borderline” to psychiatric terminology in 1938, using it to describe a group of patients who fitted neither the neurotic nor the psychotic diagnostic categories.
Several studies have shown BPD is associated with child abuse and neglect more than any other personality disorders, but the rates can vary from as high as 90% to as low as 30% . An analysis of 97 studies found 71.1% of people who were diagnosed with the condition reported at least one traumatic childhood experience.
Dr Karen Williams, who runs New South Wales’s Ramsay Clinic Thirroul – Australia’s first women-only trauma hospital – believes BPD “is a gendered diagnosis that is given to women who have got histories of abuse, whereas when we see a man come back from a traumatic event, we [say] he’s got PTSD [post-traumatic stress disorder]”.
“There is no symptom that a borderline personality disordered person has that a PTSD patient doesn’t also have.”
Williams says it often takes several sessions before she can uncover a patient’s abuse. The response of dissociation and forgetting trauma is very common, she says. Also, not all patients recognise their experiences as trauma.
Despite there being no clinical difference between PTSD and BPD, Williams says the clinical response varies markedly. PTSD, particularly among veterans, is treated with sympathy, while women with the diagnosis of BDP are considered “difficult”.

Williams prefers the term “complex post-traumatic stress disorder” to BPD, as does Prof Jayashri Kulkarni, the director of the Monash Alfred Psychiatry Research Centre. Kulkarni says the BPD label implies the behaviour is part of a personality style. There’s an implied “stern moralistic approach” that these people should just be able to control themselves – and that attitude contributes to stigma.
But she says the more she has researched BPD, “the more obvious it seems the women and the men who have been labelled with this condition often have dreadful early life trauma”.
“I really think this is injustice, to say to somebody who’s gone through hell in their early life and onwards, that they’ve got a significant flaw of their inner core.”
The case for the term personality disorder
To Chanen, the term “personality disorder” is useful because it captures the identity and relationship difficulties he says are at the heart of the issue.
He points to a national study of childhood maltreatment published in 2023 which showed nearly two-thirds of the population experience some form of childhood adversity. Despite that, BPD is comparatively rare, occurring in only 1% to 3% of the population.
“There’s something important going on in each individual that interacts with the experience of adversity. While that interaction might give rise to borderline personality disorder, it might also give rise to another disorder, such as depression, or no mental disorder,” he says.
“That’s not to say that the adversity is unimportant, but it’s not inevitable that a person will develop a mental disorder, and certainly not inevitable that they will develop borderline personality disorder.”
Chanen believes any reductionist arguments about causes are “oversimplified, wrong and unfortunately harmful for people living with personality disorder”. He believes the debate around re-naming the disorder as complex PTSD is “not really supported by the science and weakens the moral argument for respect, dignity and equality of access to effective services”.
Chanen is concerned a name change may have the unintended consequence of invalidating the experiences of patients who have not experienced trauma, or prompt clinicians to assume that trauma is present without any evidence. Instead, he believes early intervention is key.
An associate professor at the University of Sydney, Loyola McLean, who identifies as a Yamatji woman, says of the divided opinions within her profession: “It could well be that we’re talking about two halves of the same whole.
“I think we’ve got to keep an open mind that this adverse experience may be contributing, triggering, and for some people will have a causal element,” says McLean, who is a consultation-liaison psychiatrist and psychotherapist.
“Trauma – in particular early trauma, because that’s where the body and brain are really developing – we know that it’s such a huge risk factor for downstream health problems across the spectrum of health problems.”
The physical and the psychological are deeply connected , she says, but “the whole of the western world is still suffering from a kind of a Cartesian divide”.
A shifting approach
The discussion about using BPD or complex post-traumatic stress disorder is about more than words – according to Kulkarni, it changes the whole direction and focus for treatment.
Historically, treatment for BPD has relied upon antidepressants to treat low mood and antipsychotics for paranoid thinking, but it has not addressed underlying cognitive symptoms such as difficulty managing emotions, a disturbed sense of identity, disturbed relationships and impulsivity.
Those symptoms tend to be treated with psychosocial approaches, such as dialectical behaviour therapy, mentalisation-based treatment and high quality care.
Kulkarni and Dr Eveline Mu at Monash Alfred Psychiatry Research Centre are running clinical trials for new drugs to target the neurochemistry they believe drives the symptoms of BPD/complex post-traumatic stress disorder.

The effects of trauma on the body’s stress levels mean the glutamate system – the primary neurotransmitters of the nervous system – is in overdrive, Mu says. Her theory is that this drives cognitive dysfunction.
Since it began in 2022, 200 people have participated in the randomised controlled double blinded clinical trial of memantine, a drug that the regulator has approved for treatment of Alzheimer’s patients, and which blocks the body’s glutamate receptors.
Williams’ women’s-only trauma hospital is also examining new ways of responding to those with acute symptoms. She says the only place where acutely suicidal patients can go are mixed-gender rooms in hospital psychiatric wards , which have no locks and can lack supervision of male patients who are often psychotic, drunk and detoxing. Sexual assault is often rife in such wards.
It’s an environment that exacerbates symptoms, she says.
By contrast, the three-week program her patients undergo involves exercise, self-care, and education about healthy relationships.
“Almost all the time, they don’t just have trauma from their childhood, but they’ve still got it now,” Williams says. “We know that people who have been abused tend to end up in abusive relationships again, because they have such little self value and they don’t know that they deserve to be treated better.”
The hospital’s beds are constantly full with patients who can afford private treatment, with some even coming from interstate. Only one of the hospital’s 40 beds is publicly funded.
Williams says her program has improved the quality of life of her patients, with many able to take on full-time work or go back to study. “Many of them have said: ‘I want to be a nurse, I want to come back and work here.’”
Kulkarni says one of the other new solutions is to get rid of the label. “It’s hurting people … Taking a new look offers us new compassion and new understanding.”
This article was amended on 12 May 2024 to correct the year in which Prof Andrew Chanen was a trainee psychiatrist. It was 1993, not 1983.
In Australia, support is available at Beyond Blue on 1300 22 4636, Lifeline on 13 11 14, and at MensLine on 1300 789 978.
- Mental health
- mental health challenges

Most viewed
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Evid Based Complement Alternat Med
- v.2(4); 2005 Dec

Post-Traumatic Stress Disorder: Evidence-Based Research for the Third Millennium
Javier iribarren.
3 David Geffen School of Medicine at UCLA, Los Angeles, CA, USA
Paolo Prolo
1 UCLA School of Dentistry, Los Angeles, CA, USA
2 Psychoneuroimmunology Group, Inc., Los Angeles, CA, USA
Negoita Neagos
Francesco chiappelli.
The online version of this article has been published under an open access model. Users are entitled to use, reproduce, disseminate, or display the open access version of this article for non-commercial purposes provided that: the original authorship is properly and fully attributed; the Journal and Oxford University Press are attributed as the original place of publication with the correct citation details given; if an article is subsequently reproduced or disseminated not in its entirety but only in part or as a derivative work this must be clearly indicated. For commercial re-use, please contact [email protected]
The stress that results from traumatic events precipitates a spectrum of psycho-emotional and physiopathological outcomes. Post-traumatic stress disorder (PTSD) is a psychiatric disorder that results from the experience or witnessing of traumatic or life-threatening events. PTSD has profound psychobiological correlates, which can impair the person's daily life and be life threatening. In light of current events (e.g. extended combat, terrorism, exposure to certain environmental toxins), a sharp rise in patients with PTSD diagnosis is expected in the next decade. PTSD is a serious public health concern, which compels the search for novel paradigms and theoretical models to deepen the understanding of the condition and to develop new and improved modes of treatment intervention. We review the current knowledge of PTSD and introduce the role of allostasis as a new perspective in fundamental PTSD research. We discuss the domain of evidence-based research in medicine, particularly in the context of complementary medical intervention for patients with PTSD. We present arguments in support of the notion that the future of clinical and translational research in PTSD lies in the systematic evaluation of the research evidence in treatment intervention in order to insure the most effective and efficacious treatment for the benefit of the patient.
Introduction
Post-traumatic stress disorders.
The twenty-first century rose in a ray of hope. The belief was commonly held that an age of worldwide prosperity was beginning with the new millennium. Only a few years ago, people spoke of peace. Today, the general trend in many populations across the globe is fear and anxiety about self and neighbor. Socio-political events have cast a shadow of uneasiness about one's own security and that of significant others at a personal as well as a societal level. (Case in point is Greg, a businessman from Southern California, who happened to be on a business trip in New York city scheduled for September 10–12, 2001. Following the 9/11 attack, which he barely escaped, he immediately attempted to contact his family in the Southland and to leave New York city. He was on the first plane out: but the plane never took off, instead it was boarded by the New York city SWAT team who, at gun point, arrested a passenger seated four seats in front of Greg's. Greg then drove at night to Philadelphia, where he was eventually able to board a plane and return to his anxious family. To this day, Greg does not fly as often as before, is reticent to fly to the east coast and will not return to do business in New York city. His Type II diabetes has considerably worsened.)
Traumatic events are profoundly stressful. The stress that results from traumatic events precipitates a spectrum of psycho-emotional and physiopathological outcomes. In its gravest form, this response is diagnosed as a psychiatric disorder consequential to the experience of traumatic events.
Post-traumatic stress disorder, or PTSD, is the psychiatric disorder that can result from the experience or witnessing of traumatic or life-threatening events such as terrorist attack, violent crime and abuse, military combat, natural disasters, serious accidents or violent personal assaults. Exposure to environmental toxins (e.g. Agent orange, electromagnetic radiation) may result in immune symptoms akin to PTSD in many susceptible patients ( 1 , 2 ).
Subjects with PTSD often relive the experience through nightmares and flashbacks. They report difficulty in sleeping. Their behavior becomes increasingly detached or estranged and is frequently aggravated by related disorders such as depression, substance abuse and problems of memory and cognition. The disorder soon leads to impairment of the ability to function in social or family life, which more often than not results in occupational instability, marital problems and divorces, family discord and difficulties in parenting. The disorder can be severe enough and last long enough to impair the person's daily life and, in the extreme, lead the patient to suicidal tendencies. PTSD is marked by clear biological changes, in addition to the psychological symptoms noted above, and is consequently complicated by a variety of other problems of physical and mental health.
PTSD—A Brief History
Whereas the terminology of PTSD arose relatively soon following the Vietnam conflict, the observation that traumatic events can lead to this plethora of psychobiological manifestations is not new. During the Civil War, a PTSD-like disorder was referred to as the ‘Da Costa's Syndrome’ ( 3 ), from the American internist Jacob Mendez Da Costa (1833–1900; Civil War duty: military hospital in Philadelphia).
The syndrome was first described by ABR Myers (1838–1921) in 1870 as combining effort fatigue, dyspnea, a sighing respiration, palpitation, sweating, tremor, an aching sensation in the left pericardium, utter fatigue, an exaggeration of symptoms upon efforts and occasionally complete syncope. It was noted that the syndrome resembled more closely an abandonment to emotion and fear, rather than the ‘effort’ that normal subjects engage to overcome challenges ( 4 ). This classic observation pertains to what we now know of allostasis, as we discuss below. Da Costa reported in 1871 that the disorder is most commonly seen in soldiers during time of stress, especially when fear was involved ( 3 ). The syndrome became increasingly observed during the Civil War and during World War I.
PTSD in the US Population Today
The National Center for PTSD (US Department of Veterans Affairs) made public estimates that whereas the lifetime prevalence of PTSD in the US population was 5% in men and 10% in women in the mid-to-late 1990s, the prevalence of PTSD among Vietnam veterans at this same time was at 15.2%. About 30% of the men and women who have spent time in more recent war zones experience PTSD.
Whereas the onset and progression of PTSD is characteristic for every individual subject, data suggest that most people who are exposed to a traumatic, stressful event will exhibit early symptoms of PTSD in the days and weeks following exposure. Available data from the National Center for PTSD suggest that ∼8% of men and 20% of women go on to develop PTSD and ∼30% of these individuals develop a chronic form that persists throughout their lifetimes. Complex PTSD, which is also referred to as ‘disorder of extreme stress’, results from exposure to prolonged traumatic circumstances, such as the year-on end threat of insurgent attacks among our military personnel currently in active deployment.
The National Center for PTSD also estimates that under normal and usual socio-political conditions 8% of the US population will experience PTSD at some point in their lives, with women (10.4%) twice as likely as men (5%) to develop PTSD. At the beginning of the millennium, it was estimated that 5–6 million US adults suffered from PTSD. Because of the traumatic developments of recent years, and of ongoing turmoil worldwide, it is possible and even probable that the incidence of PTSD will sharply increase within the next decade and that it may become one among the most significant public health concerns of this new century. This threat is all the more serious considering the fact that PTSD symptoms seldom disappear completely; recovery from PTSD is a lengthy, ongoing, gradual and costly process, which is often hampered by continuing reaction to memories. Treatment usually aims at reducing reactions and to diminishing the acuity of the reactions. Treatments also seek to increase the subject's ability to manage trauma-related emotions and to greater confidence in coping abilities.
Focus of this Review
This work discusses our current understanding about PTSD. It explores current developments in stress research and discusses its applications and implication to the complex psychobiological prognosis of PTSD. The work concludes by presenting a view into the future of PTSD treatment from the perspective of evidence-based medicine, which many regard as the break-open research of the next decades—systematic and critical research on research to establish and determine what is the best available evidence for treatment for the patients. Indeed, this will be particularly true in the case of subjects with PTSD, if the austere predictions of a sharp rise in prevalence consequential to most recent terrorist and war events worldwide that involve US soldiers and civilians prove true.
Current Views on PTSD
There are different psychiatric rating instruments and scales that can be used to assess adult PTSD. Some are part of comprehensive diagnostic manuals or instruments: DSM-IV TR (diagnostic criteria for 309.81 PTSD) ( 5 ); ICD-10 (F43.1 PTSD, from the International Statistical Classification of Diseases and Related Health Problems, 10th revision); the PTSD module, within the Structured Clinical Interview for DSM-IV ( 6 ) or the PTSD Keane scale (PK scale) ( 7 ), within the Minnesota Multiphasic Personality Inventory-2 (MMPI-2).
Some are designed as either self-reports or as clinician-administered instruments specifically assessing adult PTSD: Davidson Trauma Scale ( 8 ); Distressing Event Questionnaire ( 9 ); Impact of Event Scale-Revised ( 10 ); Trauma Symptom Checklist-40 ( 11 ); PTSD Checklist-Civilian Version ( 12 ); Revised Civilian Mississippi Scale for PTSD ( 13 ); the Posttraumatic Stress Diagnostic Scale ( 14 ); Trauma Symptom Inventory ( 11 ); Los Angeles Symptom Checklist ( 15 ) or the Clinician-Administered PTSD Scale (CAPS) ( 16 ).
The underlying phenomena of PTSD are probably centrally mediated. Case in point is a study targeting women with early childhood abuse-related PTSD that found correlates of the emotional Stroop ( 17 ). Subjects with and without PTSD were compared. Both groups underwent PET scanning while performing in the color and emotional Stroop tasks and control condition. The control condition involved naming the color of rows of XXs (red, blue, green and yellow). The active color condition involved naming the color of color words (again with the same four colors), while the semantic context of the word was incongruous with the color. The active emotional condition involved naming the color (again the same four colors) of emotionally charged words (rape, bruise, weapon, and stench). These words have been shown to produce emotional arousal ( 18 ). The study examined the effectiveness of the Stroop task as a probe of anterior cingulate function in PTSD, because of the role of the anterior cingulate and medial prefrontal cortex in stress response and emotional regulation. After comparing it with the color Stroop, the emotional Stroop displayed significantly decreased blood flow among the PTSD subjects in the anterior cingulate. Performance in the color Stroop task produced a non-specific activation of the anterior cingulate in both the PTSD and non-PTSD abused women. However, the emotional Stroop produced a relatively lower level blood flow response of anterior cingulate among PTSD abused women. These observations may indicate that PTSD anterior cingulate dysfunction is specific to the neural circuitry of the processing of emotional stimuli. Shin et al . ( 19 ) confirmed a relative decrease in blood flow in anterior cingulate activation in combat-related PTSD and also displayed a decreased blood flow for the emotional (but not color) Stroop. Taken together, these findings indicate that PTSD may have a neural component, which could significantly alter psychoneuroendocrine-immune regulation, as discussed below.
PTSD Assessment in the Military
Certain scales have been developed that specifically target military personnel.
- PTSD Checklist-Military Version ( 12 ).
- The Mississippi Scale for Combat-Related PTSD (M-PTSD), specifically a screening and diagnostic instrument for combat-related PTSD ( 20 ), which validated as well for treatment seeking ( 21 ) and community samples ( 22 ).
- The Combat Exposure Scale measures the level of war time stress of veterans, an instrument with strong internal consistency (α = 0.85) as well as a high test–retest reliability ( r = 0.97) ( 23 ).
- The PK scale, a subscale of the MMPI-2, whose items were selected based on their ability to differentiate among veterans diagnosed with PTSD and those who were not. This scale has strong reliability (α = 0.95) and good test–retest reliability ( r = 0.94) ( 7 ).
- The SCID PTSD module is frequently used to assess presence of PTSD among veterans as well ( 24 , 25 ).
- Additional scales have been used to target assessment of PTSD among veterans, including the M-PTSD ( 26 – 29 ), the PK scale ( 30 , 31 ) or the CAPS ( 29 , 32 ).
The prevalence of PTSD diagnosis varies depending on the assessment method. One study compared three measures of PTSD among American and Korean War prisoners of war (POWs). It compared an unstructured self-report interview measure, the M-PTSD and the DSM-III-R SCID instrument. The data showed that partially unstructured interviews and the M-PTSD yielded PTSD prevalence rates of 31 and 33%, respectively, which were significantly higher than the rate of 26% yielded by the SCID. Both the unstructured clinical interview and the M-PTSD had equal accuracy, consistently disagreeing with the SCID from 7 to 15% of assessed cases ( 33 ).
Such differences in rates, depending on the assessment instrument may hold significance. According to the study ( 33 ) there may be different explanations; self-report instruments like the M-PTSD do not reflect DSM criteria as comprehensibly as the SCID. Symptoms may differ in both intensity and kind among older and younger prisoners of war. In the paradoxical side, it is possible for an individual to be diagnosed with PTSD while reporting minimal stress levels; in fact, subjective stress can be seen as a confounding factor that can have an influence on diagnosis ( 34 ).
A PTSD-negative clinical interview occurring simultaneously with a PTSD confirmation of PTSD (or also with a moderate-to-low M-PTSD score) may be indicative of chronic, but stable, PTSD. Such chronic and stable PTSD may not be clinically relevant and may not require focused intervention. They recommend to measure symptom intensity with such instruments as the CAPS ( 16 ). Such an approach could decrease PTSD-positive diagnoses among subjects with low levels of distress ( 33 ).
Allostasis and PTSD
Allostasis and the response to stress.
Allostasis refers to the psychobiological regulatory process that brings about stability through change of state consequential to stress. Psycho-emotional stress can be defined as a perceived lack, or loss of fit of one's perceived abilities and the demands of one's inner world or the surrounding environment (i.e. person/environment fit). Traumatic events that trigger PTSD are perfect examples of such onerous demands that lead to the conscious or unconscious perception on the part of the subject of not being able to cope ( 35 ).
The perception of stress is often associated with psychological manifestations of anxiety, irritability and anger, sad and depressed moods, tension and fatigue, and with certain bodily manifestations, including perspiration, blushing or blanching of the face, increased heart beat or decreased blood pressure, and intestinal cramps and discomfort. These signs mirror the spectrum of psychobiological symptoms in PTSD. These manifestations are generally associated with the nature of the stress, its duration, chronicity and severity. A group of symptoms, now referred to as the sickness behavior, is also noted that is associated with clinically relevant changes in the balance between the psychoneuroendocrine and the immune systems ( 35 – 37 ).
It was the renowned nineteenth-century French physiologist, Claude Bernard (1813–1878) who first proposed that defense of the internal milieu ( le milieu intérieur, 1856 ) is a fundamental feature of physiological regulation in mammalian systems, whence the phrase ‘homeostasis’ was coined. By the early 1930s, Walter Cannon (1871–1945) proposed that organisms engage in a dynamic process of adjustment of the physiological balance of the internal milieu in response to changing environmental conditions. Hans Selye (1907–1982) established the cardinal points of the ‘Generalized Stress Response’ in his demonstration of concerted physiological responses to stressful challenges.
Stress alters the regulation of both the sympathetic and the parasympathetic branches of the autonomic nervous system, with consequential alterations in hypothalamic control of the endocrine response controlled by the pituitary gland. Autonomic activation and the elevation of hormones, including those produced by the hypothalamic-pituitary-adrenal axis, play a pivotal role in regulating cell-mediated immune surveillance mechanisms, including the production of cytokines that control inflammatory and healing events ( 35 , 36 ). In brief, the perception of stress leads to a significant load upon physiological regulation, including circadian regulation, sleep and psychoneuroendocrine-immune interaction.
In brief, stress is profound alterations in the cross-regulation and interaction of the hormonal-immune regulatory axis. The experience of stress, as well as that of traumatic events and the anxiety-laden recollections thereof, produce a primary endocrine response, which involves the release of glucocorticoids (GCs). GCs regulate cellular immune activity in vivo systemically and locally. They block the production of pro-inflammatory cytokines (e.g. interleukin[IL]-1β IL-6) and TH1 cytokines (e.g. IL-2) at the molecular level in vitro and in vivo , but may have little effects upon TH2 cytokines (e.g. IL-4). The net effect of challenging immune cells with GC is to impair immune T cell activation and proliferation, while maintaining antibody production. The secretion of GC by the adrenal cortex is under the control of the anterior pituitary adrenocorticotropin hormone (ACTH). Immune challenges release pro-inflammatory cytokines (e.g. IL-1β, IL-6), which induce hypothalamic secretion of the ACTH inducing factor corticotropin releasing factor (CRF) in animal and in human subjects. Stressful stimuli also lead to the significant activation of the sympathetic nervous system and a rise in the levels of pro-inflammatory cytokines (i.e. IL-1β and IL-6). It follows that the consequences of stress are not uniform. The psychopathological and the physiopathological impacts of stress may be significantly greater in certain people, compared with those of others. The impact of stress is dynamic and multifaceted and the same person may exhibit a variety of manifestations of the psychoneuroendocrine-immune stress response with varying degrees of severity at different times. The outcome of stress can be multivalent ( 35 ).
Allostasis and Heterostasis
The term ‘heterostasis’ arose from stress research to describe the situation where the demands upon the organism exceed its inherent physiological limiting capacity. Sterling and Eyer ( 38 ) used the term ‘allostasis’ to describe the events that involve mind–body systemic regulation to recover from stress, rather than local feedback. Allostatic regulation now signifies the recovery and the maintenance of internal balance and viability amidst changing circumstances consequential to stress. It encompasses a range of behavioral and physiological functions that direct the adaptive function of regulating homeostatic systems in response to challenges ( 37 – 39 ).
The cumulative load of the allostatic process is the allostatic load. The pathological side effects of failed adaptation are the allostatic overload. Allostasis pertains to the psychobiological regulatory system with variable set points. These set points are characterized by individual differences. They are associated with anticipatory behavioral and physiological responses and are vulnerable to physiological overload and breakdown of regulatory capacities ( 39 , 40 ).
Type 1 allostatic load utilizes, as it were, stress responses as a means of self-preservation by developing and establishing temporary or permanent adaptation skills. The organism aims at surviving the perturbation in the best condition possible and at normalizing the normal life cycle. In Type 2 allostatic load, the stressful challenge is excessive, sustained or continued and drives allostasis chronically. An escape response cannot be found. Type I versus type II allostatic responses curiously reiterate Myers' observations that his patients seem to abandon themselves to the emotion and the fear that assailed them, rather than engage in the effort to counter and to overcome the challenge, which normal subjects typically undertook. Future research in PTSD from the perspective of allostasis may reveal a learned helplessness component, which could become key in the development and evaluation of treatment interventions ( Fig. 1 ).

Allostasis refers to the psychobiological regulatory process that brings about stability through change of state consequential to stress. Allostatic regulation describes the recovery and the maintenance of internal balance and viability amidst changing circumstances consequential to stress. It encompasses the Type 1 allostatic load that reflects the utilization by the organism of the range of behavioral and physiological functions that direct the adaptive function of regulating homeostatic systems in response to challenges (i.e. stress response) to develop temporary or permanent adaptation skills by means of self-preservation. Type 1 allostatic responses translate the organism aims at surviving the perturbation in the best condition possible and at normalizing the normal life cycle. By contrast, the Type 2 allostatic responses reflect a load to the organism that is excessive, sustained, or continued, and drives allostasis chronically and that precludes effective escape from the stress. The Type 1 and Type 2 allostatic response dichotomy provides a theoretical model for future research and treatment of PTSD and complex PTSD.
It is clear that stress research and PTSD research are intertwined. Psychobiological manifestations in PTSD and in complex PTSD (disorder of extreme stress) evidently pertain to the same domain of mind–body interactions, which are elucidated in psychoneuroimmunology research.
The stress response, more than likely, underlies the psychobiological sequelae of PTSD. The relevance of the field of current research on allostasis to PTSD is all the more evident when one considers that subjects position themselves along a spectrum of allostatic regulation, somewhere between allostasis (i.e. toward regaining physiological balance) and the allostatic overload (i.e. toward physiological collapse and associated potential onset of varied pathologies).
In brief, the recent advances in our understanding of the adaptation of the organism to stressful challenges, the allostatic process, present a new and a rich paradigm for research in the psychobiology of PTSD. Future research must investigate whether or not the dichotomy of Type I and Type II allostatic responses will provide an effective theoretical model for the development of novel and improved modes of intervention to treat PTSD.
PTSD—Paving the Future
The treatment of PTSD is complex, both in terms of available treatments and the myriad of trauma possibilities that cause it. Properly diagnosing PTSD according to DSM-IV criteria should be the first step, including assessing for co-morbidity. This should be followed by treatments with various degrees of demonstrated efficacy ( 41 ).
Historically, it was in the early eighties when research on the treatment efficacy for PTSD began, with multitude of case studies dealing with different kinds of PTSD having been produced since then. Overall, both cognitive behavioral approaches and selective serotonin reuptake inhibitor regimes have been proved to be effective to deal with different kinds of PTSD. At the same time, there is also evidence that other treatment modalities, such as psychodynamic psychotherapy, hypnotherapy, eye movement desensitization and reprocessing can be effective as well; albeit their evidence is derived from less numerous and less well-controlled studies (i.e. open trials or case reports) ( 41 , 42 ). In terms of combined treatments, historically there has not been a systematic effort to address the value of combining medication with psychotherapy and/or combinations of medications. PTSD intervention is complicated further by the fact that co-morbidities (e.g. substance abuse, over-the-counter medication abuse, psychiatric disorders including major depression) are common. Particularly in situations where co-morbidity exists, a combined approached should be considered.
In addition, there are other considerations affecting the treatment appropriateness:
- type of PTSD inducing trauma;
- PTSD chronicity and
- gender, number of times being exposed to trauma and age.
Of interest due to the perilous state of the world (i.e. wars and terrorism) is the issue of the type of PTSD inducing trauma. Combat causes high rates of PTSD and makes it more refractory to treatment than other PTSD-inducing traumas ( 43 ). According to experts, combat veterans with PTSD may be less responsive to treatment that other victims of other traumatic exposures ( 41 , 42 ). It is still unclear why combat-related PTSD is more resistant to treatment than PTSD caused by other traumas. Following is a list of possible reasons:
- a great degree of psychopathology presented by patients seeking help at Veterans Administration hospitals;
- isolation from support and help upon returning home and
- potential for secondary gain, such as disability benefits ( 42 ).
Combat-caused PTSD is often associated with other psychiatric disorders, including depression, anxiety, mood disorders and substance abuse disorders ( 22 ). More specifically, 57–62% of Croatian Balkan war veterans diagnosed with PTSD also met co-morbid diagnoses criteria ( 44 ), with the most common being depression (Muck-Seller et al ., 2003), alcohol, drug abuse, phobias, panic disorders and psychosomatic and psychotic disorders ( 45 ). In terms of PTSD-associated psychotic symptomatology, between 30 and 40% of combat-related PTSD subjects may go on to develop psychotic symptomatology ( 45 , 46 ).
It is usually believed that the most effective treatment results are obtained when both PTSD and the other disorder(s) are treated together rather than one after the other. It is becoming increasingly critical to ascertain this position because the prevalence of PTSD and disorder of complex stress is bound to rise sharply in the next decade consequential to the present multinational state of alert and anxiety following ongoing tragic, wanton and widespread terrorism and particularly with respect to combat-related PTSD in present times.
Psychotherapeutic Interventions
Psychotherapeutic approaches have a long tradition in PTSD treatment, including combat-induced PTSD. Some have more proven efficacy than others. Some of these approaches may be appropriate to address the initial stages of trauma. Psychological debriefing is an intervention given shortly after the occurrence of a traumatic event. The goal is to prevent the subsequent development of negative psychological effects. In fact, psychological debriefing approaches to PTSD can be described as semi-structured interventions aimed at reducing initial psychological stress. Strategies include emotional processing via catharsis, normalization and preparation for future contingencies ( 47 ). Gulf War veterans who underwent psychological debriefing showed no significant differences in their scores of two scales measuring PTSD when compared with the control group ( 48 ). In general, there is little evidence of psychological debriefing approaches effectively acting to prevent psychopathology, although participants seem to be open to it, which may indicate its usefulness as a rapport builder or as a screening tool. In general however, there is a lack of rigorously conducted research in this area. To this day there is paucity in the data to orient the treatment of combat-related PTSD for veterans ( 49 ). The International Consensus Group on Depression and Anxiety supports that exposure psychotherapy is the most appropriate approach for this disorder ( 41 ), although this approach does not show a significant influence on PTSD's negative symptomatology, such as avoidance, impaired relationships or anger control ( 49 ).
In terms of proven efficacy, cognitive behavior therapy and eye movement desensitization and reprocessing are effective approaches to deal with PTSD ( 50 – 54 ), while other psychotherapeutic approaches (e.g. humanistic or psychodynamic interventions) do not have enough evidence to draw strong conclusions on their utility ( 42 ). Cognitive-behavioral psychotherapy encompasses a myriad of approaches (i.e. systematic desensitization, relaxation training, biofeedback, cognitive processing therapy, stress inoculation training, assertiveness training, exposure therapy, combined stress inoculation training and exposure therapy, combined exposure therapy and relaxation training and cognitive therapy). There are empirical studies focusing on PTSD treatment dealing with combat-related PTSD. Vietnam veterans receiving exposure therapy displayed improvement as evidenced in terms of reducing intrusive combat memories ( 55 ), physiological responding, anxiety ( 56 ), depression and feelings of alienation, while also promoting increased vigor and skills confidence ( 57 ). Exposure therapy, combined with a standard treatment also showed effectiveness with other Vietnam veterans in terms of subject self-report symptoms related to the traumatic experiences, sleep and subjective anxiety responding to trauma stimuli ( 58 ).
Pharmacotherapy
Pharmacotherapy is another approach utilized to deal with PTSD, including combat-induced PTSD. In fact, typically, there is a combination of psychotherapy and medication treatments to treat chronic PTSD ( 59 ). In general, the different co-morbidities associated with PTSD play a role in the kinds of pharmacotherapeutic treatments used for its treatment.
Antidepressants and other medications commonly used are tricyclic antidepressants, monoamine oxidase inhibitors, selective serotonin reuptake inhibitors, antianxiety and adrenergic agents and mood stabilizers ( 60 ). Sertraline has been found effective to reduce PTSD symptomatology ( 61 , 62 ). In 1999, the United States Food and Drug Administration (FDA) approved sertraline as an appropriate treatment for PTSD. In fact it is the only drug to receive FDA approval to specifically combat PTSD. Sertraline and fluoxetine have produced clinical improvements among PTSD patients in randomized clinical trials ( 63 ). Paroxetine, another selective serotonin reuptake inhibitor like sertraline, is also habitually used to treat chronic PTSD ( 59 ). Mirtazapine was another successful agent when used in the treatment of PTSD afflicted Korean veterans ( 64 ). In addition, Olanzapine and fluphenazine have been successfully used with combat-induced PTSD subjects from the Balkans. Both medicines were successful in ameliorating both PTSD and psychotic symptomatology ( 43 ).
Rigorous, well-controlled methods are necessary for conducting studies on the efficacy of PTSD treatments. Well-controlled studies are characterized by the following characteristics:
- clearly defined symptoms, as well as inclusion/exclusion criteria;
- measures used are reliable and valid, with solid psychometric properties;
- utilization of blind evaluators in order to minimize expectancy and demand biases;
- properly trained evaluators to ensure reliability and validity;
- the chosen intervention programs are specific, replicable and manualized in order to maximize consistent intervention delivery;
- there is no biased assignment to treatment, which helps maximize that any detected differences and/or similarities are attributable to the treatment technique and not to other causes and
- use of treatment adherence ratings in order to ascertain if intervention parameters were followed ( 41 ).
Research on Research in PTSD: Role of Evidence-Based Research and Complementary Alernative Medicine
Future clinical research in PTSD requires the stringent, rigorous and systematic approach provided by evidence-based medicine. Evidence-based research in medicine goes beyond the routine narrative literature review. It systematically evaluates the strength of the available evidence and generates a consensus statement of the best available evidence in the form of a systematic review of the available research ( Fig. 2 ).

Evidence-based research in medicine follows the 5-step scientific process that includes stating the research question, which in evidence-based research consists of the PIC/PO question (What is the population being examined, e.g. patients with PTSD? What are the interventions being looked at, e.g. conventional treatment versus complementary medicine? Are the interventions being compared or are predictions being drawn, i.e. meta-analysis versus meta-regression approach? What is the outcome of interest, e.g. activities of daily living?). The second step involves methodology, including the sampling of the research literature, and the tools for the critical analysis of the reports. The third step refers to design which usually fall under the acronym CONSORT (i.e. consolidated standards of clinical trials). The fourth step is concerned with the analysis of the data gathered in the evidence-based research process. This commonly entails meta-analytical and meta-regression techniques, as well as individual patient data analysis (e.g. number needed to treat, NNT). Depending upon the tools utilized to evaluate the scientific literature, scores about the completeness and quality of research methodology, design and statistical handling of the findings are generated (SESTA, systematic evaluation of the statistical analysis). These values are analyzed by acceptable sampling statistical protocols to establish whether or not the sample of research reports studied by means of the evidence-based process was statistically acceptable to produce reliable inferences. The last step is a cumulative synthesis, which summarizes the process and the findings. The consensus statement reflects the best available evidence with respect to the stated PIC/PO question. The process is applied to the performance of systematic reviews, which are all-encompassing of the available literature. Best case studies in evidence-based research entail a random performance of the process of evidence-based research with a random sample of the available literature.
The future of clinical and translational research in PTSD lies in the systematic evaluation of the research evidence in treatment intervention for the patients. This type of ‘research on research’ endeavor requires attentive library search of the published materials (e.g. clinical trials) and informal individual communications with the individual researchers and authors. The collected evidence is then evaluated for research quality along certain standards [e.g. the consolidated standards of randomized trials (CONSORT)] and by means of validated instruments (e.g. Timmer scale, Jadad scale and Wong scale) ( 65 ).
The data from separate reports are pooled, when appropriate, for meta-analysis, meta-regression and individual patient data analyses. The data are analyzed from the perspective of Bayesian modeling in order to interpret data from research in the context of external evidence and judgments ( 65 ).
In the context of the treatment of patients with PTSD and co-morbidities, it is important and timely to generate a systematic review of the clinical research evidence for joint and simultaneous treatment of PTSD and the co-morbidities versus a staggered approach. The summative evaluation of the outcome of such a systematic review will generate a consensus statement that will establish whether or not the problem was framed in a clinically relevant manner (e.g. were the patient population, predictor variables and outcome measures clearly identified and relevant to the treatment of PTSD and its co-morbidities within the confines of the research?). The statement must discuss the validity of the process of integration (e.g. were the prospective inclusion and exclusion criteria clearly identified? Was the search comprehensive and explicitly described? Was the validity of the individual studies adequately assessed? Were the process of study selection, searching, assessing validity and data abstraction reliable?). The statement also produces evidence about the rigor of the process by which information was integrated (e.g. were the individual studies sufficiently similar to warrant their combination in an over-arching hypothesis-driven analysis? Are the summary findings representative of the largest and most rigorously performed studies?). The quality, presentation and relevance of the findings must be discussed (e.g. Are the key elements of each study clearly displayed? Is the magnitude of the findings statistically significant? Are the findings homogeneous or heterogeneous? Are sensitivity analyses presented and discussed? Do the findings suggest an overall net benefit for patients with PTSD?). This concerted, systematic and scientific-process driven mode of evaluating current treatment interventions for subjects with PTSD is timely and urgent to insure that the medical establishment will be prepared to handle the fast-approaching wave of PTSD cases in the next decade.
This method-driven approach for the evaluation of clinical data has merit that its product, the consensus statement, must also generate a cost-effectiveness analysis (i.e. a process of decision analysis that incorporates cost) e.g. by a step approach similar as the above method to assess the following:
- whether the problem was framed in a clinically relevant manner,
- the validity of integrated information,
- the rigor of process of integration and
- the presentation and quality of the findings.
The relevant findings in this cost-effectiveness analysis are usually expressed as the incremental cost-effectiveness between joint and simultaneous treatment of PTSD and its co-morbidities versus a staggered approach. The incremental cost-effectiveness ratio, i.e. the difference in costs between the two strategies divided by the difference in effectiveness between the two strategies, is often presented as well.
The consensus statement evaluates each competitive strategy, usually by means of the Markov model-based decision tree. This approach permits to model events that may occur in the future as a direct effect of treatment or as a side effect. The model produces a decision tree that cycles over fixed intervals in time and incorporates probabilities of occurrence. Even if the difference between the two treatment strategies appears quantitatively small, the Markov model outcome reflects the optimal clinical decision, because it is based on the best possible values for probabilities and utilities incorporated in the tree. The outcome produced by the Markov decision analysis is generally obtained by means of the sensitivity analysis to test the stability over a range of probability estimates and thus reflects the most rational treatment choice ( Fig. 3 ).

The purpose of evidence-based research in medicine is to elucidate the best available evidence in response to a stated clinical problem (e.g. is complementary medicine effective with patients with PTSD?). Following the scientific process of evidence-based research and the generation of the consensus statement ( Fig. 2 ), the information is implemented and evaluated by the clinician. Effectiveness and utilities data are estimated (e.g. Markov model) to aid the final clinical decision-making process ( 74 ).
The process of evidence-based research in medicine has begun its integration in the domain of PTSD. Rose et al . ( 66 ) have established by means of a systematic review of the literature that the early optimism about brief early psychological interventions, including debriefing, is actually unfounded and not supported by the research evidence. These findings confirmed earlier Cochrane-based systematic reviews ( 67 , 68 ). In a separate line of study, systematic reviews established clear support of the research evidence for serotonin reuptake inhibitors as the preferred first line treatment for PTSD, whereas mood stabilizers, atypical neuroleptics, adrenergic agents and newer antidepressants were shown to show promise, but to require further controlled trials to establish their efficacy and efficaciousness ( 60 , 69 ).
The future of clinical and translational research in PTSD also lies in its judicious integration of complementary and alternative medicine (CAM). For instance, whereas PTSD symptoms are common in patients with breast cancer, this symptomatology is more effectively reduced by traditional psychosocial interventions compared with CAM-oriented intervention ( 70 ). Research will determine whether this observation is true across all forms of PTSD-inducing stress and trauma and across all subjects.
In conclusion, it is timely to design similar evidence-based research studies to establish the strength of the evidence in support of complementary approaches for the treatment of PTSD. For example, use of complementary therapies (e.g. massage and herbal/food supplements) is widespread among active military veterans and their spouses for stress and co-morbid pain and anxiety. Data indicate that up to 70% of the surveyed subjects want these interventions available at the medical treatment facility (e.g. Veterans Administration Medical Center, VAMC), despite sound supportive research data ( 71 ). This trend appears to be particularly evident among native American veterans, who usually choose not to seek treatment at VAMC facilities, in part because of the preference they hold for alternative and complementary treatments, which are usually not available at those facilities ( 72 ). This population of patients is therefore at serious risk of remaining underserved. Among the civilian population, the need for systematic reviews on the benefit of complementary medicine in the treatment of PTSD is also becoming evident in light of the increasing reports proposing the benefits of massage and acupuncture in individuals exposed to the traumatic events of 9/11 ( 73 ).
Taken together, these developments should produce important novel information about the fundamental nature of PTSD from the perspective of allostasis and about its optimal treatment using the best available evidence obtained from systematic reviews. This concerted approach will be particularly important as the prevalence of PTSD with its complex psychobiological co-morbidity rises and as alternative and complementary medical treatments for PTSD emerge and take hold. Such is, in our view, the future of research in PTSD, in order to establish a registry of regular critical evaluation updates of the available evidence for the immediate service of the clinical research community and the benefit of patients with PTSD, their families and society at large.
Study shows heightened sensitivity to PTSD in autism
For the first time, researchers from the Queensland Brain Institute have proven that a mild stress is enough to trigger post-traumatic stress disorder (PTSD) in mouse models of autism spectrum disorder (ASD).
Dr Shaam Al Abed and Dr Nathalie Dehorter have demonstrated that the two disorders share a reciprocal relationship, identifying a predisposition to PTSD in ASD, and discovering that core autism traits are worsened when traumatic memories are formed.
While recent studies in humans have highlighted the co-occurrence of ASD and PTSD, the link between the disorders is often overlooked and remains poorly understood.
"We set out to determine the occurrence of traumatic stress in ASD, and to understand the neurobiological mechanisms underlying the reported predisposition to PTSD," said Dr Al Abed.
ASD and PTSD share common features, including impaired emotional regulation, altered explicit memory, and difficulties with fear conditioning.
"We demonstrated in four mouse models of ASD that a single mild stress can form a traumatic memory."
"In a control population, on the other hand, PTSD is triggered by extreme stress."
"We wanted to understand this unique perception of stress in ASD that leads to the formation of PTSD."
The prefrontal cortex is a highly specialised area in the front part of the brain that plays a crucial role in social cognition and behaviour.
According to Dr Dehorter, dysfunction in the prefrontal cortex has been linked to both disorders.
"We identified specific cortical circuit alterations that trigger the switch between the formation of a normal memory and a PTSD-like memory during stress," said Dr Dehorter.
The prefrontal cortex contains specialised cells called interneurons, which are crucial for adapted fear memorisation and normal sensory function and play a key role in stress-related disorders.
The formation of PTSD-like memories is triggered by over activation of the prefrontal cortex that is present in ASD and throws out the balance of these cortical circuits.
The capabilities of interneurons to respond to stress is altered in ASD. This alteration worsens autism traits following the formation of a traumatic memory.
"We didn't anticipate that forming a traumatic memory would aggravate the social and behavioural difficulties in ASD."
"What is really promising is once the traumatic memories are successfully recontextualised using behavioural therapy, the ASD traits that were worsened following the stress, are dramatically improved."
This discovery validates the assumption that the two disorders are closely linked and could change the way clinicians treat their patients.
An awareness of the PTSD predisposition and the success of behavioural therapy in treating it could shape the approach to managing stress in ASD.
This paper was published in iScience .
- Mental Health Research
- Psychology Research
- Nervous System
- Accident and Trauma
- Post-traumatic stress disorder
- Psychiatric service dog
- Autistic spectrum
- Mental illness
- Obsessive-compulsive disorder
- Stress (medicine)
Story Source:
Materials provided by University of Queensland . Note: Content may be edited for style and length.
Journal Reference :
- Alice Shaam Al Abed, Tiarne Vickie Allen, Noorya Yasmin Ahmed, Azza Sellami, Yovina Sontani, Elise Caitlin Rawlinson, Aline Marighetto, Aline Desmedt, Nathalie Dehorter. Parvalbumin interneuron activity in autism underlies susceptibility to PTSD-like memory formation . iScience , 2024; 27 (5): 109747 DOI: 10.1016/j.isci.2024.109747
Cite This Page :
Explore More
- Reaching 1,000 Degrees C With Solar Power
- Nature's 3D Printer: Bristle Worms
- Giant ' Cotton Candy' Planet
- A Young Whale's Journey
- No Inner Voice Linked to Poorer Verbal Memory
- Bird Flu A(H5N1) Transmitted from Cow to Human
- Universe's Oldest Stars in Our Galactic Backyard
- Polygenic Embryo Screening for IVF: Opinions
- VR With Cinematoghraphics More Engaging
- 2023 Was the Hottest Summer in 2000 Years
Trending Topics
Strange & offbeat.

As the FDA evaluates ecstasy treatment for PTSD, questions mount about the evidence

In a matter of months, the Food and Drug Administration is expected to decide whether the drug commonly known as ecstasy can be used as a treatment for post-traumatic stress disorder.
An approval by the agency would represent an enormous milestone for the movement to bring psychedelics into the mainstream of mental health care. An FDA rejection of MDMA, the abbreviation of the drug's chemical name, would deal a major setback to the effort.
Clinical trials have inspired optimism in the drug for its potential to help the millions of Americans who experience PTSD. Accounts from some of those who've participated in the trials describe the treatment as transformational.
But new and troubling questions about this research are now threatening to upset the final stretch in the drug's path to market.
The allegations surfaced in a draft report released in March by the Institute for Clinical and Economic Review , a nonprofit that evaluates clinical trials and drug prices, which found "substantial concerns about the validity of the results" of the MDMA clinical trials.
The ICER report was followed in April by a citizen petition to the FDA. In that document, a group of concerned people allege possible misconduct and ethical violations that could compromise the MDMA research. The petition asked the agency to hold a public meeting to address the concerns.
If true, the claims could jeopardize the drug's chances of receiving FDA approval, a decision that is expected to come by early August .
"There's the possibility that the data might not be representative of what's actually happened in clinical trials," says Neşe Devenot , one of the authors of the citizen petition and a senior lecturer in the writing program at Johns Hopkins University who is involved in psychedelic research. "I don't think this has been publicly reckoned with."
That may soon happen. The FDA announced Thursday that it plans to hold a public advisory committee meeting on MDMA-assisted therapy on June 4.
At the heart of the controversy are the organizations that have pioneered research into MDMA: the Multidisciplinary Association for Psychedelic Studies , and the public benefit corporation incubated by MAPS, which was recently rebranded as Lykos Therapeutics .
Lykos sponsored the clinical trials of MDMA. The results are included in the company's application to the FDA seeking approval to market the drug for therapy-assisted PTSD treatment.
Researchers and clinicians involved in the trials have pushed back strongly against the accusations that their clinical data isn't sound.
Jennifer Mitchell , lead author of the published papers from the Phase 3 trials, says she stands behind their findings.
"I didn't feel any pressure from the sponsor to come up with anything different than what the data was providing," says Mitchell, a professor of neurology and psychiatry at the University of California, San Francisco and associate chief of staff for research at the San Francisco VA Medical Center. "I wouldn't have continued to work with them if I had felt that."
Promising MDMA research for PTSD
The Phase 3 trials evaluated MDMA-assisted therapy, a protocol in which the drug is given under the supervision of two therapists.
In the second stage of the trials , 94 people with moderate and severe PTSD received either the drug or a placebo during three sessions, each spaced a month apart. There were also follow up "integration" sessions to help people process their experiences while on MDMA.
By the end of the trial, about 71% of participants in the MDMA arm no longer met the diagnostic criteria for PTSD, compared to about 48% who underwent the same therapy but took a placebo instead. Those findings built on promising results from earlier studies .
The study documented various adverse events in both groups — ranging from nausea and anxiety to heart palpitations — but none of them qualified as serious. The treatment was "generally well tolerated."
"Consistent with PTSD, suicidal ideation was observed in both groups," the authors reported in the journal Nature Medicine , "MDMA did not appear to increase this risk, and no suicidal behavior was observed."
Casey Tylek, a participant in the Phase 3 trials, says he had no experience with the drug prior to the study.
Tylek was in the placebo group, but was later given the opportunity to undergo the therapy with MDMA.
"It was incredibly powerful," says Tylek, a veteran who lives in Massachusetts, "I truly don't know if I would be alive today if I hadn't gone through that trial."
ICER report raises concerns
In its report , ICER acknowledges that the MDMA data suggest it would be an "important addition to treatment options for PTSD," but it questions whether the published findings tell the full story.
Among the concerns, the ICER report details a well-known challenge in psychedelic research around how to make sure study participants don't know if they got the experimental treatment or a placebo. Most of those in the MDMA group were able to identify they had received the drug. It also suggests the method used to assess PTSD — considered the gold-standard — showed improvements in symptoms after the treatment, even though some people were worse overall.
Beyond that, however, the report brings up the possibility that "very strong prior beliefs" among therapists, investigators and patients influenced the results.
"Concerns have been raised by some that therapists encouraged favorable reports by patients and discouraged negative reports by patients including discouraging reports of substantial harms, potentially biasing the recording of benefits and harms," the report states.
ICER does not identify the sources who were interviewed, although it did include two trial participants, a "trial therapist" and those who worked on a podcast called Cover Story , says Dr. David Rind , the chief medical officer for ICER.
"This was a very unusual review," says Rind.
The podcast, produced by New York Magazine and the nonprofit media organization Psymposia , brought to light claims by a participant named Meaghan Buisson, who appeared in a video of two therapists , a married couple, engaged in what Buisson described as inappropriate physical contact while she was under the influence of MDMA at a Phase 2 trial site in Canada.
MAPS determined the therapists "substantially deviated" from the treatment manual. The organization also barred the two therapists from becoming providers of MDMA-assisted therapy in affiliation with MAPS, and health authorities were notified in Canada and the U.S.
The podcast also interviewed two people (their full names were not revealed) who said they received MDMA in the large-scale, or Phase 3, trials and experienced feelings of suicidality and other distress after the studies.
The ICER report is yet to be finalized, but Rind says their analysis showed "there's still a lot of uncertainty" about the treatment.
"You have a group of people who are very upset about how these trials went," he says. "We couldn't tell, even though we talked with people where this happened, whether that represents a tiny fraction of bad events or a number of bad events large enough to have rendered the trial just not believable."
Pushback against the allegations
According to Rind, MAPS and Lykos had "very little" engagement with ICER on the draft report.
But since then, a group of more than 70 clinicians, investigators and others involved in the Phase 3 MDMA trials have published a detailed response , saying that certain aspects of the trials were "misrepresented" and that a number of assertions amount to "hearsay."
Willa Hall , a clinical psychologist in the Phase 3 trials, says she and her colleagues were shocked by how ICER described their work.
"I didn't recognize the study that they were talking about," Hall told NPR. "I think a lot of us felt quite insulted actually by that characterization. I saw nothing like that. I only saw professionalism ."
In their response, Hall and her colleagues write that "[ICER] does not note the many measures taken to train, support, and evaluate therapists on those trials—measures that met, and in some cases exceeded, the accepted standards in the field of psychotherapy research."
They also take issue with ICER relying on "a small number of undisclosed study participants and unnamed 'experts' rather than validated research outcomes." The critiques that participants knew they received the treatment or that the measure of PTSD symptoms might not capture someone's overall condition would also apply to other clinical trials, unrelated to MDMA, they say.
UCSF's Jennifer Mitchell says the clinical trial was designed to safeguard against bias.
Therapists on site were not collecting key data from participants about their PTSD symptoms following the sessions. Instead, that was being done online by "independent assessors" who didn't know who had received the treatment or a placebo.
Hall says therapists "meticulously" captured any adverse events. "We encouraged our participants to be very honest," she says. "We're all invested in knowing how it works and what are the risks for people."
Still, Mitchell acknowledges she doesn't have full insight into what was going on at each trial site on a given day.
"This is my own frustration," she says. "I can't attest to what was happening at one of the sites in Israel on a day to day basis, or on one of the sites in Canada."
But she contends that ICER tried to conduct an investigation without access to the full data.
The FDA granted MDMA "breakthrough therapy" status, she says, which means the agency was involved in the study design and "many aspects" of the trial.
"So there's no keeping things from the FDA," Mitchell says.
The ICER report points out that therapists and participants in the study were "pulled heavily from the existing community of those interested and involved in the use of psychedelics for possible psychological benefits."
For her part though, Mitchell says she's not what some would call a "true believer."
"My personal feeling is that psychedelics are complicated compounds and they do not work for everyone," she says.
Petition adds to controversy ahead of the FDA meeting
On the heels of the ICER report, Neşe Devenot and four others, including Meaghan Buisson, submitted the citizen petition to the FDA calling for a public advisory meeting about the Lykos' application for MDMA.
In it, they ask for extended time for stakeholders who are concerned about the "risks and shortcomings" of the research.
"Evidence from multiple sources indicates that the sponsor has engaged in a pattern of systematic and deliberate omission of adverse events from the public record while minimizing documented harms," the petition states.
It continues: "We cannot rule out the possibility that MAPS/Lykos manipulated clinical trial data to hide adverse events from regulatory agencies."
The petition cites media reports and public statements from figures at Lykos and MAPS — and disclosures from a former employee of the MAPS public benefit corporation "who prefers to maintain anonymity at this juncture."
In addition, the petition alleges that clinical trial investigators would phone MAPS in the event of an incident during the trial to see whether that should be reported as an adverse event and that a suicide attempt during a dosing session was discouraged from being reported.
In an email to NPR, a spokesperson for MAPS rejects the claim.
It's not clear if the FDA's decision to hold a meeting was influenced by Devenot's petition, which has over 80 signatures .
Alaina Jaster , who has a doctorate in pharmacology and toxicology, is another author of the petition.
"We need to listen to people [in the trials] who are having these experiences, instead of telling them that they are liars and that they're going to ruin the psychedelic renaissance," says Jaster who hosts a podcast on psychedelics.
"None of us are against this as a useful tool, or none of us are against treating mental health. We don't have any monetary interests in this not going through," she says.
Neşe Devenot and Brian Pace, another author of the petition, are affiliated with Psymposia , the media organization that produced the podcast, but Devenot says they were not involved in the podcast and are unpaid board members.
In response to the petition's call for a public meeting, a spokesperson for Lykos sent NPR a statement in April saying the company supports holding an advisory meeting. "The voice of the PTSD patient is incredibly important," the email reads.
MAPS "remains fully supportive of comprehensive, high-quality research; careful analysis of safety and efficacy; and stringent regulatory oversight of any psychedelic-assisted therapy research or delivery," according to the statement it also sent to NPR in April. "We stand behind Lykos' execution of the clinical program and support the clinical results."
One of those who signed the petition after seeing it posted online is Dr. Boris Heifets , an anesthesiologist at Stanford University whose lab studies psychedelics, including MDMA.
"I don't know if the allegations are true, it just makes me deeply sad if there was actually malfeasance for such an important trial," says Heifets. "The MDMA Phase 3 trials were very important for mental health, important for a lot of people who may benefit from this therapy."
Learning about MAPS several decades ago was, in part, what inspired Heifets to get involved in this type of research.
He says he donates $100 a year to MAPS and that they have supplied his lab with MDMA. He also consults for one company that's developing a derivative of MDMA.
Heifets says the petition contains some "very strong allegations," particularly the claim that certain adverse events were not disclosed.
"I want to hear MAPS respond," he says. " I would really like to understand the risk profile of this drug before it's approved, not after."
Copyright 2024 NPR

Up to 40pc of mental health conditions are linked to child abuse and neglect, study finds
In 1996, Ange McAuley was just 11 years old when ABC's Four Corners profiled her family living on Brisbane's outskirts.
At the time her mother was pregnant with her sixth child and her father had long ago moved back to Perth.
WARNING: This story contains details that may be distressing to some readers.
It was a story about child protection and the program was profiling the role of community volunteers helping her mother, who had been in and out of mental health wards.
Ange was the eldest and it fell to her to get her younger siblings ready for school.
By the time the new baby arrived, she would stay home and change nappies.
"It was pretty crazy back then — I wasn't going to school a lot," she said.
By that age she was already holding a secret — she'd been sexually abused at age six by her stepfather, who would later be convicted of the crime.
"Back in the nineties, a lot of people kept stuff hidden and it wasn't spoken about outside of the family," she said.
"I've carried all these big burdens that weren't even mine. Sexual abuse happened to me. I didn't ask for it."
She says the trauma triggered a lifetime of mental health problems from substance abuse and self-harm as a teen, right through to post-natal depression.
Hidden source of our mental health crisis
A new study from the University of Sydney's Matilda Centre has established just how much Australia's mental health crisis can be traced back to this kind of childhood abuse and neglect.
The research has found that childhood maltreatment is responsible for up to 41 per cent of common mental health conditions including anxiety, depression, substance abuse, self-harm and suicide attempts.
The research, which draws on a 2023 meta-analysis of 34 research studies covering 54,000 people, found maltreatment accounted for 41 per cent of suicide attempts in Australia, 35 per cent of self-harm cases and 21 per cent of depression episodes.
It defined childhood maltreatment as physical, sexual, emotional abuse, emotional or physical neglect and domestic violence before the age of 18.
Lead researcher Lucy Grummitt said it is the first piece of work to quantify the direct impact of child abuse on long-term mental health.
It found if childhood maltreatment was eradicated it would avert more than 1.8 million cases of depression, anxiety and substance use disorders.
"It shows just how many people in Australia are suffering from mental health conditions that are potentially preventable," she said.
Dr Grummitt said they found in the year 2023 child maltreatment in Australia accounted for 66,143 years of life lost and 118,493 years lived with disability because of the associated mental health conditions.
"We know that when a child is exposed to this level of stress or trauma, it does trigger a lot of changes in the brain and body," Dr Grummitt said.
"Things like altering the body's stress response will make a child hyper-vigilant to threat. It can lead to difficulties with emotion regulation, being able to cope with difficult emotions."
While some areas of maltreatment are trending down, figures from the landmark Australian child maltreatment study last year show rising rates of sexual abuse by adolescents and emotional abuse.
That study found more than one in three females and one in seven males aged 16 to 24 had experienced childhood sexual abuse.
Dr Grummit says childhood trauma can affect how the brain processes emotions once children become teens.
"It could be teenagers struggling to really cope with difficult emotions and certainly trauma can play a huge role in causing those difficult emotions," she said.
Mental health scars emerge early
For Ange, the trauma of her early years first showed itself in adolescence when she started acting out — she remembers punching walls and cars, binge drinking and using drugs.
"I would get angry and just scream," she said.
"I used to talk back to the teachers. I didn't finish school. Mum kicked me out a lot as a teenager. I was back and forth between mum and dad's."
By the time she disclosed her abuse, she was self-harming and at one point tried to take her own life.
"I was just done," she said.
"I was sick of having to get up every day. I didn't want to do it anymore."
Later on, she would have inappropriate relationships with much older men and suffered from depression, including post-natal depression.
"It's definitely affected relationships, it's affected my friendships, it's affected my intimate relationships," she said.
"Flashbacks can come in at the most inappropriate times — you're back in that moment and you feel guilt and shame.
"I feel like it's held me back a lot."
Calls for mental health 'immunisation'
Dr Grummitt said childhood abuse and neglect should be treated as a national public health priority.
In Australia, suicide is the leading cause of death for young people.
"It's critical that we are investing in prevention rather than putting all our investments into treatment of mental health problems," she said.
Her team has suggested child development and mental health check-ins become a regular feature across a person's lifetime and have proposed a mental health "immunisation schedule".
Chief executive of mental health charity Prevention United, Stephen Carbone, said they estimate that less than 1 per cent of mental health funding goes toward prevention.
"There's been a big steady increase in per capita funding for mental health over the last 30 years but that hasn't translated into reductions," Dr Carbone, a GP, said.
"You're not going to be able to prevent mental health conditions unless you start to tackle some of these big causes, in particular child maltreatment."
He said most of Australia's child protection system was about reacting to problems rather than trying to prevent them.
"If you're not tackling the upstream risk factors or putting in place protective factors you just keep getting more and more young people experiencing problems and services being overwhelmed," he said.
Now a mother of two teens herself, Ange says she wants to break the cycle and has been going to therapy regularly to help identify and avoid destructive patterns that she's seen herself fall into.
"I love my girls so much and I want better for them."
- X (formerly Twitter)
Related Stories
Generation overwhelmed: these kids fought back against a national health crisis — and won.
'It's a really massive deal': Unpacking what's going on with Gen Z and ways to improve teen mental health
'The air went out of the room': Shocking new statistics on the abuse and neglect of Australian children
- Child Abuse
- Child Health and Behaviour
- Mental Health
- Post Traumatic Stress Disorder
- University of New South Wales

IMAGES
VIDEO
COMMENTS
CASE STUDY Victor (post-traumatic stress disorder) Case Study Details. Victor is a 27-year-old man who comes to you for help at the urging of his fiancée. He was an infantryman with a local Marine Reserve unit who was honorably discharged in 2014 after serving two tours of duty in Iraq. His fiancé has told him he has "not been the same ...
Philip, a 60-year-old who was in a traffic accident (PDF, 294KB) This case example from the European Journal of Psychotraumatology details an assisted self-study application of cognitive therapy for PTSD. Philip developed PTSD and comorbid major depression following a traffic accident. He was treated in six sessions of cognitive therapy with ...
Monson, C. M. & Shnaider, P. (2014). Treating PTSD with cognitive-behavioral therapies: Interventions that work. Washington, DC: American Psychological Association. Updated July 31, 2017. Date created: 2017. This case example explains how Jill's therapist used a cognitive intervention with a written worksheet as a starting point for engaging in ...
Webinar Notice. It is a continuous challenge living with posttraumatic stress disorder (PTSD), and I've suffered from it for most of my life. I can look back now and gently laugh at all the people who thought I had the perfect life. I was young, beautiful, and talented, but unbeknownst to them, I was terrorized by an undiagnosed debilitating ...
The second case is the victim of a terrible accident at work, causing extensive burns, life-threatening complications, and disfiguring scars. Previous studies indicate that PTSD may be identified in up to 30% of such patients, stressing the need for a dedicated staff psychiatrist in modern burn centers 21, 22).
The first case example about Terry documents the treatment of PTSD using Prolonged Exposure. The second is an example of in-session imaginal exposure with a different client. Prolonged Exposure is strongly recommended by the APA Clinical Practice Guideline for the Treatment of PTSD. Download case study (PDF, 107KB).
The purpose of this report is to illustrate the possibility of treating PTSD in a self-study assisted brief therapy format. The present self-study assisted treatment builds on Cognitive Therapy for PTSD (CT-PTSD), a trauma-focused CBT programme developed by Ehlers, Clark, and colleagues. CT-PTSD is usually delivered in up to 12 weekly sessions ...
A VR-GET case study reported a 20% reduction in the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) - Military Version (PCL-M) score in association with 10 VR-GET sessions for a Navy corpsman . Another VR-GET case study documented that 20 VR-GET sessions conducted with a Seabee, who had ...
This case study follows a 7-year-old boy who presented with symptoms of posttraumatic stress disorder (PTSD) following exposure to domestic violence beginning at a very young age.
This case study follows a 7-year-old boy who presented with symptoms of posttraumatic stress disorder (PTSD) following exposure to domestic violence beginning at a very young age. During evaluation of this young boy's symptoms, it became evident that his mother also was experiencing symptoms of PTSD.
To illustrate IPT for PTSD, we present data from a pilot case that was not included in the current NIMH study, but served as a valuable training case. This patient received open IPT treatment for PTSD because his Clinician-Administered PTSD Scale (CAPS, Blake et al., 1995 ) score of 45, while indicating moderate symptom severity ( Weathers et ...
Case formulation - (Persistent PTSD, adapted from Ehlers and Clark []).Case formulation following the persistent PTSD model of Ehlers and Clark [].It is suggested that the patient is processing the traumatic information in a way which a sense of immediate threat is perpetuated through negative appraisals of trauma or its consequences and through the nature of the traumatic experience itself.
Study participants. This case-control pilot study involved 40 (20 controls; 20 PTSD) age and sex-matched participants recruited in the US between January and June 2019, by Discovery Life Sciences (DLS), California USA, and PrecisionMed, California, USA. Venous blood samples and a detailed clinical history were collected from each study participant.
Two Stories of PTSD. Maria was only 15 when she was attacked by a group of men on the way home from school. They took turns screaming abuse at her and then they each raped her. Finally, they tried ...
Many studies indicate that PTSD is associated with a smaller size of the hippocampus, with meta-analyses reporting that this finding is observed bilaterally 55. A recent consortium study including 1,868 participants (794 with PTSD) found an average smaller size of the hippocampus in those with the disorder 56. The extent to which a smaller ...
Instead of feeling shame and guilt, he said, "I can carry the memory with pride.". Case presentation written by Drs. E.C. Hurley, Louise Maxfield, and Roger M. Solomon. This is a case example for the treatment of PTSD using Eye Movement Desensitization and Reprocessing (EMDR) therapy.
Other responses included reference to the classification of PTSD as an anxiety disorder (10%; n = 5), the idea that PTSD cannot be successfully treated (12%; n = 6) and the idea that individuals who revel in past accomplishments have PTSD. In this last case, one respondent suggested that a "35-year old man consistently at high school football ...
Starting treatment for PTSD can be daunting, but we've gathered case studies about people who've been through treatment to help you understand the process more. At first, CBT (cognitive behavioural therapy) treatment for PTSD can be tricky to understand and so some people are scared to try it, or simply don't believe it can effectively ...
The case study of Rich (see Case Study 1) demonstrates that the body can be an ally and a catalyst in the process of healing from trauma. ... In a large-scale study, 88% of men and 79% of women with PTSD met criteria for another psychiatric disorder. The coexisting disorders most prevalent for men with PTSD were alcohol abuse or dependence (51. ...
for in a traditional PTSD diagnosis. This case study provides an overview of the differences between PTSD and CPTSD, using empirical evidence to illustrate the necessity of distinguishing ... This case study's structure will follow the format of a pragmatic case study as outlined by Fishman (1999; 2013). Thus, it begins with a description of ...
Introduction. The term post-traumatic stress disorder (PTSD) was first coined in Diagnostic and Statistical Manual of Mental Disorders (DSM) 3. The DSM-4 describes three symptom clusters in PTSD: persistent re-experiencing of the trauma (e.g., intrusive memories and flashback experiences, often triggered by exposure to traumatic reminders, and recurring trauma-related nightmares); avoidance of ...
Case Study in the Treatment of Trauma and Suicidality Teri Pentz LPC, NCC, IMH-E® Supervisor Behavioral Health Training Rachel Ludwig LCSW Behavioral Health Therapist III
Acknowledgment. This casebook offers detailed guidance to help practitioners understand and implement the treatments recommended in APA's Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder in Adults. The authors describe the unique factors involved in PTSD treatment, and core competencies necessary for providers.
An analysis of 97 studies found 71.1% of people who were diagnosed with the condition reported at least one ... he's got PTSD [post-traumatic stress disorder]". ... The case for the term ...
One-in-20 develop post-traumatic stress disorder (PTSD). The findings of the first UK inquiry into birth trauma will be presented to ministers on Monday, before Ms Atkins is expected to set out ...
Case in point is a study targeting women with early childhood abuse-related PTSD that found correlates of the emotional Stroop . Subjects with and without PTSD were compared. ... Historically, it was in the early eighties when research on the treatment efficacy for PTSD began, with multitude of case studies dealing with different kinds of PTSD ...
A new study shows that a mild stress is enough to trigger post-traumatic stress disorder (PTSD) in mouse models of autism spectrum disorder (ASD). Researchers demonstrated that the two disorders ...
The study documented various adverse events in both groups — ranging from nausea and anxiety to heart palpitations — but none of them qualified as serious. The treatment was "generally well tolerated." "Consistent with PTSD, suicidal ideation was observed in both groups," the authors reported in the journal Nature Medicine, "MDMA did not ...
Childhood maltreatment is responsible for up to 41 per cent of common mental health conditions including anxiety, depression, substance abuse, self-harm and suicide attempts, according to a new study.