
- Healthcare Executives and Senior Leaders
- Solutions for Physicians and Clinical Staff
- Non-Healthcare Leaders
- Organizational and Cultural Transformation
- Developing Vision and Alignment
- Assessments
- Immersive Experiences
- Coaching and Facilitation
- Speakers and Inspiration
- Academic Journals
- Our Approach
- Solutions for Non-Healthcare Leaders


Lean Management, Patient Experience, Patient Safety, Performance Improvement, Quality and Safety, Quality Improvement
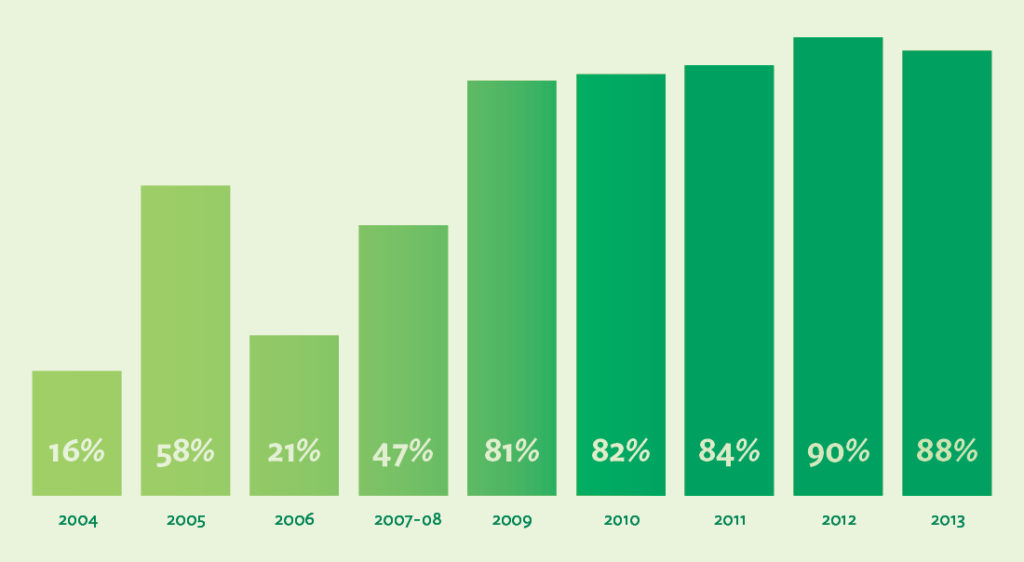
Case study | embedding a system to protect patient safety, patient safety survey participation sharply increases.
Overall staff participation in Virginia Mason’s Culture of Patient Safety survey grew from 16% in 2004 to 88% in the year 2013 alone. Affirmative answers to the survey’s key question — on whether staff speak up freely if they see something that may negatively affect patient safety — were at 80% in 2013.
Protecting Patients, Engaging Staff and Saving Costs
The Patient Safety Alert System™ at Virginia Mason is a project borne of inspiration, innovation, hard work and a dedication to always do what is best for the patient. Virginia Mason employees learn in their first day of employment that it is their duty to report anything that has caused harm or could cause harm to a patient, and the growing number of PSAs support that the organization’s culture of safety is still thriving after more than 10 years. How did Virginia Mason develop the system, and how did they embed it in their culture to continually keep patients safe? How did Virginia Mason meet its goals of dramatically better staff engagement and lower professional liability premiums—and how has the work been sustained?
Inspiration From a Factory Floor in Japan
Before the PSA system was developed, Virginia Mason’s executives viewed their organization as a quality leader that worked every day to best protect its patients. At the turn of the century, however, when they took a hard look at the data, they realized they had a lot of work to do to correct the medical errors that seemed endemic to health care in the U.S. and throughout the world.
In 2002, Virginia Mason executives were tasked with developing new ways to identify and fix the safety problems that threatened the organization’s patients every day. Gary Kaplan, MD, Virginia Mason’s chief executive officer, took them to Japan for two weeks of intensive learning to discover how Toyota had developed the Toyota Production System and worked for decades to create defect-free automobiles that were safe and reliable enough for their customers to drive. Virginia Mason’s team wondered, How did Toyota manage to increase efficiency and eliminate waste, day after day, and sustain this level of excellence?
It was on the factory floor, watching the workers stop the line and work with colleagues to fix the problems with the automobiles as soon as they were discovered, that Cathie Furman, RN, the senior vice president of quality and compliance, saw something she had never witnessed before.
We were so impressed with the [Toyota] culture—the empowerment of high-school-trained assembly-line workers who felt completely comfortable stopping a multi-million-dollar line rather than sending a defective product to their teammate,” Furman says. “That was so different from what we experienced in health care, which has historically been a very blaming, hierarchical culture. 1
As much as she admired what she saw, though, she wondered if they could implement the same kind of system at Virginia Mason so that health care workers could stop a process immediately when a defect was discovered and work collaboratively to fix problems to prevent patient harm. Everyone knew that the complexity of health care meant that mistakes happened every day. Therefore, if every worker at Virginia Mason felt empowered to “stop the line,” wouldn’t that mean that the whole system would never get started again? 2
Implementing a New Patient Safety System in Seattle
The leadership team knew that Toyota’s “stop the line” process could be used to keep patients safer—but they had work to do to develop it for health care. The patient safety system they’d been using for years wasn’t working well. Katherine Galagan, MD, director of clinical laboratories, said that some employees did fill out quality improvement reports, but the reports got funneled to various departments and often ended up “lost in the wash.” It was clear to everyone who had gone to Japan that they needed a new way to galvanize the right people to come together and fix the problems right away, just as they did each day on the line at Toyota. 3
With careful planning, testing and implementation, the team modeled Virginia Mason’s new patient safety system on Toyota’s andon system—which enables any employee to alert managers or colleagues of quality or process defects, small or large. The development of the new system was difficult and time-consuming, and leaders discovered that a culture shift required a new focus on leader responsiveness as well as a degree of transparency that was not familiar to most of Virginia Mason’s employees.
Early on, Virginia Mason leaders agreed to support any staff member who called in a patient safety alert, even when the circumstances were charged. In a 2005 incident that later inspired employees to trust and use the system, a nurse observed that a physician did not follow protocol for a patient procedure. Because she believed that a patient could suffer harm from not following the protocol, she asked the physician to stop the procedure. When the physician refused, the nurse called in a PSA. The leader who responded to the alert thanked the nurse, contacted the physician and ordered him to stop the procedure. Surprised, the physician stopped the procedure but sharply berated the nurse for reporting the incident. The nurse then called in a new PSA, explaining the repercussions she received after acting in the best interest of the patient. The leader who responded to this new alert thanked the nurse and immediately took the physician offline. Virginia Mason thoroughly investigated the incident and provided training for the physician on the organization’s patient safety culture, which necessitated that employees need to feel safe whenever they reported an incident that they believed might cause harm to a patient. From that day forward, many employees knew that Virginia Mason’s top leaders truly respected their actions when they summoned the courage to stop the line. 4
For the program to be successful, it was essential not only that employees would be supported but that the problems would get fixed. As Jamie Leviton, a patient safety manager at Virginia Mason, explains, Virginia Mason’s team set out to develop a system that would consistently encourage safety reporting and transparency, result in a rapid team response and enable leaders to address issues directly with their teams. The system was based on a team vision that patient safety begins and ends on the front line, and that reporting should be “simple, easy and intuitive.” Through years of refinements, the system became capable of enabling all employees at all levels of the organization to submit a patient safety alert by phone or online, as soon as they perceived a patient had experienced harm or could potentially experience harm. 5
In September 2014, Virginia Mason’s 50,000th Patient Safety Alert was reported. By the end of 2014 the average number of PSAs was 879 — a record number for the organization. The goal, promoted at meetings and on the company’s intranet, is to reach an average of 1,000 PSAs per month.
Overall staff participation in Virginia Mason’s Culture of Patient Safety survey grew, from 16% in 2004 to 88% in 2013. Affirmative answers to the survey’s question on whether staff speak up freely if they see something that may negatively affect patient safety reached 80% in 2013.
Additionally, from May 2005 to May 2015, professional liability claims saw a 74% reduction, resulting in considerable savings each year.

Continuous Improvement: Sustaining the Gains
For more than a decade, Virginia Mason has monitored the PSA system and conducted improvement events year after year, with all levels of staff, to make it better. Here are the top key components contributing to the PSA system’s sustained success:
Employees feel safe reporting a patient safety event, near miss or potential problem. For employees to feel safe, they must experience a culture of respect in the workplace. Leaders are responsible for promoting and embodying a culture in which employees feel safe not only speaking up about barriers to patient safety but also voicing and following through on ideas for improvement.
Year after year, the organization’s leaders continually look for ways to keep the program going strong. In 2011, leaders and providers were inspired by Lucian Leape’s powerful presentation at Virginia Mason on the tie between respectful behavior and patient safety—and they knew that they had more work to do to empower employees who still did not feel safe making a PSA. Lynne Chafetz, general counsel at Virginia Mason, said that Leape discussed “not just the obvious—surgeons throwing instruments across the room,” but also “the disrespect that’s more covert.” She knew, and others in the audience also knew, that creating a deeply respectful culture was necessary to empower every employee to speak up for patient safety. That’s when Virginia Mason developed a Respect for People initiative to make the organization’s culture feel even safer for employees. 6
Every PSA is important. In the early years, the PSA program was complex, and it required extensive training throughout the organization to take hold. Later Virginia Mason’s leaders realized that if they wanted staff to report any potential threat to patient safety, no matter how small, they had to make this known. In the Joint Commission Journal on Quality and Public Safety, Furman and Robert Caplan, MD, discussed the program’s dramatic results both in the terms of number of safety reports and the time it took to fix the problems. They also said that to achieve these benefits, the organization needed to keep the door open to all safety concerns. After all, whether a safety concern is “significant” depends on the point of view of the reporter—and no act of speaking up should be dismissed until the matter is investigated and leaders know that patients are safe. 7
For example, Brenda Simon, an organizational development specialist in human resources, relates how even a nonclinical employee at a health care organization can—and should—be a patient safety inspector:
One day I was walking down a stairwell in one of the hospital buildings and noticed that a long strip of yellow tape on one of the steps had come loose. I immediately thought that a patient or team member might trip on this step, so I called in a PSA and explained the situation. When I took the stairs the next day, I saw that the tape had been fixed. All of us are called upon to be on the lookout for threats to patient safety, so I was doing my part—just as the rest of my 5,000 colleagues do every day. 8
Gary Kaplan reinforces the importance of each report when he speaks to staff and to other organizations. He emphasizes the dual benefits of PSAs: “Each patient safety alert not only protects the individual patient, but gives us the opportunity to improve our processes in real time to assure the safety of every patient, every time.” 9
Staff can self-report a PSA without punitive consequences. One of the main differentiators of a lean system—whether it’s in manufacturing or health care—is that a defect signals there’s a problem not with the employee engaged in the procedure but in the organization’s processes that care for its patients. Therefore, it stands to reason that if an employee realizes that his or her own actions have caused harm—or could cause harm—to a patient, then that employee should be able to make a PSA on the incident without punitive action. In one instance, Henry Otero, MD, reported a PSA after his colleague told him a cancer patient’s magnesium level was low. “I didn’t know how I missed it,” Dr. Otero said. “But I realized it’s not about me, it’s about the patient. The process needs to stop me [from] making a mistake.” 10
Staff are supported when they make a PSA after an adverse event. Virginia Mason expects all staff to call in a PSA as soon as any patient suffers an adverse event, and they know that the way leaders respond to PSAs is crucial to keeping employees engaged and helping them see the process as personally meaningful. For every PSA after an adverse event, the leader who responds to it sincerely thanks the employee for reporting and may engage the employee to talk through the incident to help assess the level of urgency and determine next steps. For some PSAs, though, the support goes further. In a survey response, one physician recalled what happened after he called in a PSA:
Last November I undertook an emergent after-hours procedure which tragically ended in a fatal outcome. That morning I filed a PSA as a matter of course and I was surprised when I received a rapid response from the on-call PSA staff member. She facilitated providing support for the family and me that day as well as in the weeks afterwards. The support process was a much appreciated contribution at that challenging time. 11
Leaders support it. When an employee makes a PSA, the senior executive who is responsible for the area responds by ensuring that patients are safe as soon as possible and instigating a team effort to make the targeted process defect-free. Executives learn about patient safety issues in another way, too—by daily rounding. As they meet with staff on the front line, they ask if they know of any instances of patient harm, near misses and ideas for improvement. The leaders take those ideas and determine whether a process needs to be stopped or a worker needs to be taken offline during an investigation. Kaplan emphasizes that executives can’t simply let go of the process. As he says, “Every staff member can and should be a quality and safety inspector, but [he or she] will only do that if that work is supported 24-7 by the executive leadership.” 12
And because the PSA system is central to Virginia Mason’s patients-first culture, no one is surprised when a process is halted for the good of patient safety. As Denise Dubuque, surgical and procedural services administrator, recalls after one PSA, “We escalated an issue and the senior leaders stood behind the team. The staff saw that they were listened to. It was pretty powerful.” 13
Board members support it. When PSAs are reported, notices are sent to Virginia Mason’s board members. Whether it’s a physician’s error that is quickly corrected or a billing mistake that delays care for a patient, the board members get involved to ensure that leaders and staff are addressing the problems in ways that best support the organization’s patients.
When anything goes wrong at Virginia Mason, says board member Julie Morath, I know immediately what happened and what is being done. Those events are not closed until the board says they are. This is not a rubber stamp board. 14
Staff are part of the improvement process. After a PSA is called, leaders use root-cause analysis to determine whether the incident stemmed from a process problem, an individual error or a behavior issue. “Once you realize what the components are in a patient-safety alert, you can deal with correcting them,” says Lucy Glenn, MD, chair of Virginia Mason’s radiology department.
When a PSA reveals that intensive improvement work must be done to correct the problem and keep patients safe, leaders form teams that work in the affected areas. Richard Lee, administrativ director of radiology operations, describes the way leaders begin the process of engaging staff in the improvement work:
We go to the people who are actually doing the work and are in immediate contact with the patients. We have a process where we ask them to generate ideas as to what could be improved, and that’s where it starts—from identifying how our processes could be made better for the patient. 15
Staff are engaged not only from the beginning, but in subsequent meetings, improvement events, testing, implementation and sustainment.
Individuals and teams are recognized. Even in a culture in which employees are told that they’re expected to speak up for patient safety, the act of actually reporting a PSA can seem risky or overwhelming for some. That’s why the organization’s leaders work hard to respond quickly and positively to employees who report—with thank-yous from supervisors and executives; a monthly Good Catch Program, in which a single employee is recognized for a PSA that led to an exceptional solution; and the Mary L. McClinton Patient Safety Award, which is given annually to the team who has done the most to improve patient safety. This last type of recognition is especially meaningful to employees because the event not only commemorates the tragic death of a beloved patient in 2004, but also marks the time when executives chose to be transparent about the error to the staff and the press. Even more, it solidifies the organization’s fervent commitment to make health care safer for all their patients. 16
Feedback continues to make it better. Since the start, the PSA has evolved to make sure the engagement and response time continue to improve. In August 2015 the PSA system introduced easier navigation to enhance reporting. “We made these changes based on feedback from team members, who told us they wanted a simpler reporting system and a way to track how their PSAs are being handled,” says Leviton. “This new version delivers on both requests.” 17 Additionally, as a way to continue the engagement, leaders and staff were invited to sign up for training sessions to learn about the details, ask questions and continue to keep patient safety at the forefront of their work every day at Virginia Mason.
Similar resources
Lean Management, Optimizing Flow, Quality and Safety
Case study | 36-clinic federally qualified health center saves $600k annually improving patient flow.

Case Study | Building a New Outpatient Surgery Center With Patients and Staff in Mind
Lean Management, Patient Safety, Performance Improvement, Quality and Safety
Case study | surgical setup reduction improves patient outcomes, stay connected.
Sign up for our monthly emails to stay up to date with our latest news, resources, case studies, events and more.
Your information will not be shared. Learn more about our privacy policy here .

ASHRM President O’Sullivan’s March Message
We thrive together at ashrm.

Emerging Roles of Risk Managers in Senior Living and Skilled Nursing

Handling Disagreements Between Telehealth Critical Care and Bedside Providers

Strategies for Communication and Apology Are Critical for Front-line Staff

Risk Professionals Ideal to Lead Health Care ESG Journey

- Uncategorized
Case Studies in Patient Safety
- Google Plus
Storytelling has been key to learning since the beginning of humankind. Case studies are a form of storytelling that often includes learning objectives, reflection and analysis. This book by Julie K. Johnson, Helen W. Haskell and Paul R. Barach uses storytelling to explore medical cases from the viewpoints of surviving family members. The amount of effort to collect such stories must have been astounding, but the reader benefits in incalculable ways.
The book’s stories illuminate how the industry might move from a clinician-centered system of care to a patient and family-centered system of care. The authors refer to Paul Batalden’s quote, “Every system is perfectly designed to get the results it gets.” For example, the results of the current medical educations system are knowledgeable diagnosticians who are focused on the individual physician-patient dyad. The authors examined 153 competencies across disciplines internationally that seem to correlate with good outcomes. The book’s stories are organized by these competencies:
- Medical knowledge, patient care
- Professionalism
- Interpersonal/communication skills
- Practice-based learning and improvement
- System-based practice
- Interprofessional collaboration
- Personal and professional development
One sees where professionalism and interpersonal/communication skills are greater important deficits for the families than knowledge or patient care aspects. This sets up the challenge for the reader, as the authors promote, to think differently about how to emotionally and intellectually engage patients and providers in healthcare transformation.
Discussed are 24 cases resulting from in- and out-patient settings in locations throughout the English-speaking world. One poignant case concerned a routine endoscopic procedure, an endoscopic retrograde cholangiopancreatography (ERCP). Post discharge, the patient began regurgitating, perspiring and was in pain. A telephone call to the office nurse resulted in a Tylenol suggestion. Then the physician called and suggested soup. A family member demanded a direct admission. The patient arrived at the emergency room with no forwarding message from the physician so she waited 12 hours for pain meds, but a full workup was achieved. The physician was not returning any emergency room calls as it was after 5 p.m. and the covering colleague said “not my patient.” As the patient deteriorated, a catheter was inserted. Then she was moved to the ICU and then to CCU. Diagnosis: sepsis. No record was ever found for the catheter order nor the ICU or CCU admissions. By now hospital specialists were attending to the patient with no sign of the original surgeon. The first code blue was noted.
With pneumonia and sepsis prevailing, staff placed a ventilator. Physicians mentioned pancreatitis after ERCP. They said it was not uncommon and the patient should recover. Eleven days later the patient had a cardiac arrest and coded. There were conflicting stories whether this occurred during a bath or during some suctioning. The code was unsuccessful. The family was not called by nursing per the protocol.
The CEO called the family back about a month after the death. New management had taken over the hospital. The CEO was trying to set a meeting with the family and physician, but the physician refused. After a year from the death, the physician accepted a meeting. Evidently, he felt comfortable because the family had not requested an autopsy so there was no way to prove whether the surgeon should have done the procedure in the first place or if he had done it wrong. The family regrets the omission of the autopsy because they saw there was no redress possible without it. After a complaint, the state medical board saw no wrong doing on the part of the surgeon. The state’s health services department did cite the emergency room for the lack of care of the patient.
The family felt abandoned by the surgeon, wrote a book about the event and discovered that adverse events were not nearly as common as they were led to believe. The book reviews further insight and notes ERCP is now widely overused.
In conclusion, this book presents poignant case studies that prompt one to think about various sides of stories and how systems, cultures and technical skills intertwine to affect life and death. One sees how the lack of communication can trump all of the aforementioned items to create a disaster. However, the reader is not left depressed, but instead inspired by the people sharing their stories and by the subsequent critical thinking that can occur after reading them.
Johnson, J., Haskell, H., & Barach, P. (2016) Case Studies in Patient Safety. Subury, MA: Jones and Bartlett Learning
You may also like
Building a High-Reliability Organization: A Toolkit for Success

ASHRM Whitepaper – Telemedicine: Risk Management Considerations

Stronger: Develop the Resilience You Need to Succeed
Sign up for ashrm forum updates.
Provide your information below to subscribe to ASHRM email communications
ASHRM Forum
- Submit an Article
Recent Articles
- ASHRM President O’Sullivan’s March Message March 20, 2024
- We thrive together at ASHRM January 10, 2024
- Emerging Roles of Risk Managers in Senior Living and Skilled Nursing October 16, 2023
- Handling Disagreements Between Telehealth Critical Care and Bedside Providers September 12, 2023
- Strategies for Communication and Apology Are Critical for Front-line Staff September 7, 2023
- January 2024
- October 2023
- September 2023
- November 2022
- February 2022
- January 2022
- December 2021
- December 2020
- October 2020
- September 2020
- August 2020
- February 2020
- November 2019
- September 2019
- August 2019
- February 2019
- January 2019
- December 2018
- October 2018
- September 2018
- August 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- February 2017
- November 2016
- October 2016
- September 2016
- ASHRM Academy
- ASHRM President Message
- ASHRM Updates
- Behavioral Health
- Book Review
- Emergency Preparedness
- Enterprise Risk Management (ERM
- Human Capital
- Legal & Regulatory
- Letter from the Chair
- Member Profile
- Operational
- Patient Safety/Clinical Care
- Sustainibility
- Angela Lucas, MSN, BSN, RN, CCRN-K
- Anne Huben-Kearney, RN, BSN, MPA, CPHRM, CPHQ, CPPS, DFASHRM
- Arlene Luu, RN, BSN, JD, CPHRM
- Barbara McCarthy RN, MPH, CIC, CPHQ, CPHRM, FASHRM
- Benedict Hane
- Chad Follmer, ARM, MBA
- Dan Corcoran
- Dan Groszkruger, JD, MPH, CPHRM, DFASHRM
- Deborah Lessard CPHRM, FASHRM, MS and Leigh Ann Yates, AIC, MBA, CPHRM, DFASHRM
- Deborah Lessard, Esq., RN, JD, MA, BSN, CPHRM, FASHRM
- Denise Shope, RN, MHSA, ARM, CPHRM, DFASHRM and Nancy Connelly, RN, BA, CPHRM, DFASHRM
- Denise Winiarski JD, CPHRM Emily Klatt, JD Amir Kazerouninia, MD, PhD
- Ferdinando L. Mirarchi, DO, FAAEM, FACEP
- Forum Task Force Chair Leigh Ann Yates, AIC, MBA, CPHRM, DFASHRM
- Franchesca J. Charney, RN, MS, CPHRM, CPPS, CPSO, DFASHRM and Guy Whittall-Scherfee, MS
- Heidi Harrison, CPHRM
- Jessica J. Ayd, Esq.; Sherri Hobbs, MSM, MSN, RN, CPHQ; Heather Joyce-Byers, MSJ, BS, RN, CCRN-K, CPHRM; Shannon M. Madden, Esq.
- Joan Porcaro, RN, BSN, MM, CPHRM
- John C. West, JD, MHA, DFASHRM, CPHRM,
- John D. Banja, PhD
- Julie Radford, JD, CPHRM
- Karen Garvey, DFASHRM, CPHRM, and CPPS
- Karen Wright RN, BSN, ARM, CPHRM
- Kathleen Shostek, RN ARM FASHRM CPHRM CPPS
- Kenita Hill, MSA, CPHRM, LNHA, LPN
- Larry Veltman, MD, FACOG, CPHRM, DFASHRM
- Leigh Ann Yates and Stephanie Nadasi
- Leigh Ann Yates, MBA, CPHRM, AIC, DFASHRM
- Mackenzie C. Monaco
- Maggie Neustadt, JD CPHRM, FASHRM
- Margaret Curtin, MPA, HCA, CPHRM, DFASHRM
- Mark Dame, MHA, CPHRM, FACHE
- Melanie Osley and Holly Taylor
- Melanie Osley, RN, MBA, CPHRM, CPHQ, CPPS, ARM, DFASHRM
- Melanie Taylor, Esq.
- Melinda Van Niel, BA, MBA and Doug Wojcieszak, MA, MS, BS
- Michael G. Lloyd, MBA, CPCU, ARM, CPHRM
- Monica Cooke BSN, MA, RNC, CPHQ, CPHRM, FASHRM
- Nancy Connelly, RN, BA, CPHRM, DFASHRM
- Nancy Connelly, RN, BA, CPHRM, DFASHRM and Kenita Hill, MSA, CPHRM, LNHA, LPN
- Paula Caballero
- Rhonda DeMeno, RN, MS,MPM, BSHRM, CBIC, CPHRM and Joan Porcaro, RN, BSN, MM, CPHRM
- Rita Barrett-Cosby, CPHRM
- Robin Diamond
- Ryan Solomon, JD
- Sarah B. Roberts, MPH, CHES, CPHQ, CPHRM, ARM, AIS, AINS
- Scripps La Jolla Memorial Quality Team Memorial Quality Team
- Steven D. Weiner and Mario Giannettino
- Sue Boisvert, BSN, MHSA, CPHRM, FASHRM
- Susan Lucot, MSN RN
- Suzanne Natbony
- Tatum O’Sullivan, RN, BSN, MHSA, CPHRM, DFASHRM, CPPS
- Tricia Brooks-Phillips, MSN, RN, CPHRM
- Vallerie H. Propper, JD, MPH
- Vicki J. Missar
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Patient safety review and response case studies by clinical specialty
This page shows case studies, listed by clinical specialty, of where the National Patient Safety Team worked with partners to address issues identified through its review of recorded patient safety events.
Urgent/emergency care
General medicine, intensive care, obstetrics and gynaecology/midwifery, paediatrics and child health, primary care.
You can find out more about our processes for identifying new and under recognised patient safety issues on our using patient safety events data to keep patients safe and reviewing patient safety events and developing advice and guidance web pages.
- COVID-19 swab snapped in tracheostomy
- Risk of dose error when using intraosseous lidocaine in children
- ePrescribing systems and insulin combinations
- Risks of ingestion of alcohol-based hand sanitiser
- Risk of airway obstruction from green anaesthetic swabs
- Dual purpose naso-gastric tubes with ENFit® connectors and the risk of aspiration
- Diagnosis and management of supraglottitis
- Sucrose vial cap identified as potential choking hazard in babies
- The risk of aspiration from orally administered contrast media with spigotted nasogastric tubes
- Metacarpal wrong site surgery – inconsistent terminology used to describe anatomy
- Osmotic Demyelination Syndrome from rapid correction of severe hypo/hypernatraemia
- Ensuring timely updates to clinical risk assessment and management triage tools in emergency departments
- Ingested gel toilet discs
- Delayed oxygenation of neonate during resuscitation when oxygen not ‘flicked’ on
- Equipment falling onto critically ill patients during intrahospital transfers
- Misapplication of spinal collars resulting in harm from unsecured spinal injury
- Ensuring compatibility between defibrillators and associated defibrillator pads
- Ensuring pregnant women with COVID-19 symptoms access appropriate care
- Overdose of oral vitamin D related to frequency and duration of treatment
- Administration of chemotherapy and reactivation of Hepatitis B
- Delay in treatment with prothrombin complex concentrate (PCC)
- Harm from catheterisation in patients with implanted artificial urinary sphincters
- Confusion between different strength preparations of alfentanil
- Distinguishing between haemofilters and plasma filters to reduce mis-selection
- Variation in use of cardiac telemetry
- Ceftazidime as a 24-hour infusion
- Tacrolimus – risk of overdose when converting from oral to intravenous route
- Haloperidol prescribing for confused/agitated/delirious patients
- Ensuring oxygen delivery when using two step humification systems
- Pregnancy tests not performed before anaesthesia
- Ventilator left in standby mode
- Sudden patient deterioration due to secretions blocking heat and moisture exchanger filters
- Anaesthetic machines used as ventilators: issues with circuit set up
- Importance of ‘tug test’ for checking oxygen hose when transferring a patient to a portable ventilator
- Use of trimethoprim in women of child-bearing age
- Assessment of risk of venous thromboembolism (VTE) when prescribing combined hormonal contraceptives
- Harm from prescribing and administering Syntometrine when contraindicated to woman with significantly raised BP
- Unnecessary caesarean section for breech presentation if not scanned on the day
- HIV prophylaxis in women and new-borns
- Ensuring the safe use of plastic cord clamps at caesarean section
- Warning on the use of ethyl chloride during fetal blood sampling
- Risk of babies becoming unwell following move to virtual home midwifery visits
- Testing ammonia levels in children
- Unintentional perforation of oesophagus in neonates from invasive procedures
- Chemical burn to a neonate from use of chlorhexidine
- Risk of harm from spinal administration of anaesthetic agent containing preservative
- Hip cement – different expiry dates for separate components in the same pack
- Bone cement implantation syndrome
- Surgical skin preparation solution entering the eye during surgery
- Retained surgical instrumentation and complex procedures involving multiple teams and equipment
- Unintentional retention of bone cement following hip surgery
- Monitoring patients taking nitrofurantoin for potential lung disease
- Unintended bolus of medication if infused at speed from residual space in giving set
- Infrared temperature screening to detect COVID-19
To read this content please select one of the options below:
Please note you do not have access to teaching notes, case study: more patient safety by design – system-based approaches for hospitals.
Structural Approaches to Address Issues in Patient Safety
ISBN : 978-1-83867-085-6 , eISBN : 978-1-83867-084-9
Publication date: 24 October 2019
Since the publication of the report “To Err Is Human: Building a Safer Health System” by the US Institute of Medicine in 2000, much has changed with regard to patient safety. Many of the more recent initiatives to improve patient safety target the behavior of health care staff (e.g., training, double-checking procedures, and standard operating procedures). System-based interventions have so far received less attention, even though they produce more substantial improvements, being less dependent on individuals’ behavior. One type of system-based intervention that can benefit patient safety involves improvements to hospital design. Given that people’s working environments affect their behavior, good design at a systemic level not only enables staff to work more efficiently; it can also prevent errors and mishaps, which can have serious consequences for patients. While an increasing number of studies have demonstrated the effect of hospital design on patient safety, this knowledge is not easily accessible to clinicians, practitioners, risk managers, and other decision-makers, such as designers and architects of health care facilities. This is why the Swiss Patient Safety Foundation launched its project, “More Patient Safety by Design: Systemic Approaches for Hospitals,” which is presented in this chapter.
- Hospital design
- Information dissemination
- Medical error
- Patient safety
- System-based interventions
- Systemic approach
Acknowledgements
Acknowledgments.
We would like to thank the members of the expert group for their commitment to our project and their valuable input. We are also grateful to the Swiss Federal Office of Public Health, the Swiss Academy of Medical Sciences, and the Swiss National Science Foundation for their financial support, which has helped us not only in completing our project but also in producing our brochure, and in organizing the symposium.
Kobler, I. , Angerer, A. and Schwappach, D. (2019), "Case Study: More Patient Safety by Design – System-based Approaches for Hospitals", Structural Approaches to Address Issues in Patient Safety ( Advances in Health Care Management, Vol. 18 ), Emerald Publishing Limited, Leeds, pp. 1-17. https://doi.org/10.1108/S1474-823120190000018001
Emerald Publishing Limited
Copyright © 2019 Emerald Publishing Limited
We’re listening — tell us what you think
Something didn’t work….
Report bugs here
All feedback is valuable
Please share your general feedback
Join us on our journey
Platform update page.
Visit emeraldpublishing.com/platformupdate to discover the latest news and updates
Questions & More Information
Answers to the most commonly asked questions here
- Open access
- Published: 02 May 2024
Associations between patient safety culture and workplace safety culture in hospital settings
- Brandon Hesgrove 1 ,
- Katarzyna Zebrak 1 ,
- Naomi Yount 1 ,
- Joann Sorra 1 &
- Caren Ginsberg 2
BMC Health Services Research volume 24 , Article number: 568 ( 2024 ) Cite this article
94 Accesses
Metrics details
Strong cultures of workplace safety and patient safety are both critical for advancing safety in healthcare and eliminating harm to both the healthcare workforce and patients. However, there is currently minimal published empirical evidence about the relationship between the perceptions of providers and staff on workplace safety culture and patient safety culture.
This study examined cross-sectional relationships between the core Surveys on Patient Safety Culture™ (SOPS®) Hospital Survey 2.0 patient safety culture measures and supplemental workplace safety culture measures. We used data from a pilot test in 2021 of the Workplace Safety Supplemental Item Set, which consisted of 6,684 respondents from 28 hospitals in 16 states. We performed multiple regressions to examine the relationships between the 11 patient safety culture measures and the 10 workplace safety culture measures.
Sixty-nine (69) of 110 associations were statistically significant (mean standardized β = 0.5; 0.58 < standardized β < 0.95). The largest number of associations for the workplace safety culture measures with the patient safety culture measures were: (1) overall support from hospital leaders to ensure workplace safety; (2) being able to report workplace safety problems without negative consequences; and, (3) overall rating on workplace safety. The two associations with the strongest magnitude were between the overall rating on workplace safety and hospital management support for patient safety (standardized β = 0.95) and hospital management support for workplace safety and hospital management support for patient safety (standardized β = 0.93).
Conclusions
Study results provide evidence that workplace safety culture and patient safety culture are fundamentally linked and both are vital to a strong and healthy culture of safety.
Peer Review reports
About 10% of patients internationally have adverse events Footnote 1 in hospitals, and about half of these adverse events are considered to be preventable [ 1 , 2 ]. About 7% of these adverse events result in death and about half result in temporary or permanent disability. As discussed in the seminal publication To err is human , building a culture of safety is a key component of preventing medical errors and harm to patients [ 3 ]. A growing body of domestic and international research has shown associations between better patient safety culture and reduced adverse events and improved patient experience [ 4 , 5 , 6 , 7 , 8 ].
In 1993, the Health and Safety Commission defined safety culture in the following manner: “The safety culture of an organisation is the product of individual and group values, attitudes, perceptions, competencies, and patterns of behaviour that determine the commitment to, and the style and proficiency of, an organisation’s health and safety management. Organisations with a positive safety culture are characterized by communications founded on mutual trust, by shared perceptions of the importance of safety and by confidence in the efficacy of preventative measures” [ 9 ]. Since then, the concept of safety culture has been applied to the healthcare setting, especially hospitals, and it has been demonstrated that the employer’s safety culture influences the attitude and behaviors of both providers and staff, thus contributing to the overall safety of the organization [ 10 ]. To comprehensively assess safety culture in the hospital setting, the Agency for Healthcare Research and Quality (AHRQ) sponsored the development of the Surveys on Patient Safety Culture® (SOPS®) Hospital Survey that assesses provider and staff perceptions of the extent to which the organizational culture in hospitals supports patient safety [ 11 ].
Although safety culture in healthcare has, until recently, focused on patient safety, several major reports and events, including the World Health Organization’s World Patient Safety Day 2020 [ 12 ], the Institute for Healthcare Improvement (IHI) National Steering Committee for Patient Safety’s National Actional Plan to Advance Patient Safety [ 13 ], and the National Plan for Health Workforce Well-Being [ 14 ], have identified workforce safety as a critical component of advancing patient safety. Workplace safety, including stress and burnout, is a critical issue, as the overexertion injury rate for hospital workers is more than twice the national average of U.S. full time workers [ 15 ]. The most important risk factor for these injuries is the manual lifting, moving, and repositioning of patients [ 16 ]. Further, these injuries are frequently underreported [ 17 , 18 , 19 ]. Additionally, healthcare workers are four times more likely to be victims of verbal and physical workplace violence and aggression than workers in other private industries [ 20 , 21 ]. The COVID-19 pandemic further exacerbated the safety of healthcare workers through shortages of personal protective equipment, high risk and fears over becoming infected and infecting family members with the virus [ 22 , 23 ], and increased patient loads and staffing shortages [ 24 , 25 ].
As a response to this increased concern about the safety of healthcare workers, AHRQ funded the development of the supplemental item set for the SOPS Hospital Survey which focused on the workplace safety of providers and staff in the hospital setting. Recent prominent reports and integrative models of safety culture have shown that not only is workplace safety culture an important factor in patient safety culture, but that they are mutually affected [ 21 , 26 , 27 ]. Both workplace safety culture and patient safety culture are integral to an overall culture of safety and are influenced by overall organizational culture and attitudes toward process improvements, and they are inextricably linked in that improvements in one area influence the other. For example, if providers and staff do not have appropriate equipment or sufficient training to properly use equipment to lift and move patients, patients may fall and providers and staff may also fall or be otherwise injured. Despite this theoretical foundation, there is limited empirical evidence about the crucial relationship between workplace safety culture and patient safety culture. Prior studies have only examined the relationship in single hospitals or hospital units and for a small set of workplace safety culture measures such as workplace violence and burnout [ 28 , 29 , 30 ].
This paper presents evidence regarding this crucial gap by analyzing the associations between workplace safety culture and patient safety culture for a large set of patient safety culture and workplace safety culture measures assessed in a diverse set of hospitals with a wide range of characteristics and geographic locations. To perform this analysis, we used data from a pilot test of the AHRQ Surveys on Patient Safety Culture® (SOPS®) Hospital Survey 2.0 Workplace Safety Supplemental Item Set, which was conducted in 28 hospitals across 16 states, which allows for more generalizable findings than data from a single hospital or unit. We hypothesize that more positive workplace safety culture is associated with more positive patient safety culture.
Data sources and measures
We employed a cross-sectional study design which assessed the associations between patient safety culture measures which are the core items from the AHRQ Surveys on Patient Safety Culture® (SOPS®) Hospital Survey 2.0 [ 31 ] and workplace safety culture measures from the SOPS Workplace Safety Supplemental Item Set for Hospitals [ 32 ]. The SOPS Hospital Survey 2.0, released in 2019, is an update of the original survey released in 2004. Designed to assess hospital provider Footnote 2 and staff Footnote 3 perceptions about patient safety issues and event reporting, the core SOPS Hospital Survey 2.0 includes 32 items aggregated into 10 patient safety culture composite measures and one overall patient safety rating item and one item on the number of events reported (not reported in this study), respectively.
Workplace safety culture is assessed using the Hospital Workplace Safety Supplemental Item Set. This item set was developed by Westat, under contract with AHRQ, in response both to increased concern about healthcare worker safety as a result of the COVID-19 pandemic and a recognition of the importance of workplace safety in ensuring patient safety. The items were developed based on literature on workplace safety in hospitals, interviews with hospital workplace safety experts and researchers, and through feedback from the SOPS Technical Expert Panel (TEP) and workplace safety subject matter experts (SMEs). The development team conducted iterative cognitive testing of the draft survey items with 20 hospital providers and staff and received input from the TEP and SMEs at multiple stages in the development process. The workplace safety supplemental item set includes 16 items aggregated into six composite measures, as well as three single item measures and one overall workplace safety rating.
In 2021, a pilot study was conducted which collected responses to the workplace safety items for 28 hospitals in 16 states across the U.S. The purpose of this pilot study was to obtain data for psychometric analyses to examine the reliability and validity of the Workplace Safety Supplemental Item Set for hospitals. This psychometric analysis of the workplace safety culture measures provided evidence that the measures were reliable and valid [ 33 ]. Psychometric analysis of the SOPS Hospital Survey 2.0 have previously shown that the patient safety culture measures are also reliable and valid [ 34 ].
Recruitment of hospitals occurred through AHRQ SOPS email listserv subscribers, users of the survey, webinar participants, and through outreach to hospital stakeholder organizations. From the list of interested hospitals, a convenience sample of 28 hospitals were selected that varied by several characteristics (e.g., bed size, region, ownership, teaching status), but were not statistically representative of all U.S. hospitals. The pilot study was a web-based survey administered to a census of all providers and staff in the selected hospitals with the workplace safety items near the end of the survey. Each provider and staff member of the selected hospitals received an email with a unique survey link. At the beginning of the survey, the following statement was included: “The survey is voluntary, but your feedback will help your hospital identify areas for patient safety and workplace safety improvement. If you do not wish to answer a question, you may leave it blank. Westat will keep your individual responses to this survey confidential. Only group results will be reported.”
Out of 19,979 surveys distributed, 7,037 providers and staff responded, resulting in a 35% overall response rate. Across all pilot study hospitals, respondents had the following category of staff position: 35% nurses; 2% physician or physician assistant; 18% other clinical position; 11% management; 20% support, and 13% other staff position [ 35 ].
The patient safety measures were as follows, with the number of items in parentheses: Teamwork (3); Staffing and Work Pace (4); Organizational Learning-Continuous Improvement (3); Response to Error (4); Supervisor, Manager, or Clinical Leader Support for Patient Safety (3); Communication About Error (3); Communication Openness (4); Reporting Patient Safety Events (2); Hospital Management Support for Patient Safety (3); Handoffs and Information Exchange (3); and Patient Safety Rating (1) [ 36 ].
The workplace safety measures were as follows, with the number of items in parentheses: Protection from Workplace Hazards (3); Moving, Transferring, or Lifting Patients (3); Addressing Workplace Aggression from Patients or Visitors (2); Workplace Aggression Policies, Procedures, and Training (2); Addressing Verbal Aggression From Providers or Staff (1); Supervisor, Manager, or Clinical Leader Support for Workplace Safety (3); Hospital Management Support for Workplace Safety (3); Workplace Safety and Reporting (1); Work Stress/Burnout (1); and Overall Rating on Workplace Safety for Providers and Staff (1) [ 32 ].
We calculated hospital-level percent positive scores as the percentage of respondents within a hospital who answered positively (% Strongly agree/Agree or Always/Most of the time) for positively worded items, and (% Strongly disagree/Disagree) for negatively worded items for each item. Percent positive scores can range from 0 to 100. These hospital-level percent positive scores for the items within each composite measure were equally weighted and averaged to compute hospital-level composite measure scores. There was one exception to this scoring: Work Stress/Burnout was reported as the percentage of respondents that chose the response ‘3’, Footnote 4 ‘4’, Footnote 5 or ‘5’ Footnote 6 , indicating they had one or more symptoms of work stress or burnout.
Hospital characteristics as Covariates
Three hospital characteristics obtained from the 2020 American Hospital Association (AHA) Annual Survey of Hospitals Database were examined as covariates or control variables. The first control variable was bed size which was categorized into seven categories: 6–24 beds, 25–49 beds, 50–99 beds, 100–199 beds, 200–299 beds, 399 beds, and 400 or more beds. The seven categories were coded as 1 through 7 and this variable was included as a continuous variable modeled linearly in the regression models. The second control variable was ownership status, which was either a government-owned hospital or non-government-owned hospital. The third control variable was teaching status, which was either a teaching or non-teaching hospital. These variables were included because hospital characteristics have been demonstrated to show consistent associations with SOPS Hospital Survey scores [ 37 ] and are also likely to be associated with Hospital Workplace Safety Supplemental Item Set measures.
Analysis sample
All analyses were conducted using the responses of 6,684 providers and staff respondents (353 of the 7,037 respondents did not answer any workplace safety items) from 28 hospitals that participated in the SOPS Hospital Workplace Safety Supplemental Item Set pilot study.
All analyses were conducted using SAS V9 and were at the hospital level.
Descriptive statistics
Means, standard deviations, and ranges for hospital-level percent positive scores (or percent stress/burnout), were calculated for all workplace safety culture and patient safety culture composite measures, as well as the two workplace safety culture single item measures and the overall ratings for both workplace safety culture and patient safety culture. These descriptive statistics show the variation in the patient safety culture and workplace safety culture measures and provide context for interpreting the regression analyses.
Multiple regressions
We conducted a series of multiple regressions to examine the associations between hospital workplace safety culture measures and patient safety culture measures. Specifically, each regression model had one patient safety culture measure as the dependent variable, and one workplace safety culture measure as the independent variable along with the control variables (hospital bed size, teaching status, and ownership). To test a key assumption of linear regression, we confirmed that the percent positive (or negative in the case of burnout) values for each measure were normally distributed.
We included only one workplace safety culture measure in each model because tests of variance inflation factors (VIF) showed substantial evidence of multicollinearity when including all workplace safety culture measures in a single regression. Rules-of-thumb for an indication of substantial multicollinearity are VIFs generally between 4 and 10, with a VIF above 10 indicating substantial multicollinearity [ 38 ]. Tests of VIF when including all workplace safety culture measures in the same regression indicated a VIF of 12.8 for Hospital Management Support for Workplace Safety and a VIF of 12.2 for the Overall Rating on Workplace Safety for Providers and Staff .
Because we are simultaneously conducting multiple hypothesis tests, it is important to adjust the p -values of the hypothesis tests to control the number of false positives due to chance. We adjusted for multiple hypothesis testing by controlling the false discovery rate which is the expected proportion of false rejections (statistically significant estimates) among all rejected tests, using the standard method by Benjamini and Hochberg [ 39 ].
Table 1 shows, for each workplace safety culture and patient safety culture measure, the means and standard deviations for all 28 hospitals of the percentage of individual responses that were positive (except for Work Stress/Burnout ). Percent positive scores for the patient safety culture composite measures ranged from 55.6% ( Staffing and Work Pace ) to 80.6% ( Teamwork) . The Patient Safety Rating percent positive score was 63.9%.
Percent positive scores for the workplace safety composite measures ranged from 58.1% ( Addressing Workplace Aggression From Patients or Visitors ) to 90.3% ( Protection from Workplace Hazards ). Work Stress/Burnout , measured as the overall percentage of respondents in a hospital that reported experiencing symptoms of burnout, was 30.4%. The Overall Rating on Workplace Safety for Providers and Staff percent positive score was 53.1%. These statistics indicate that while the vast majority of providers and staff report they had adequate physical protection, far fewer reported they had adequate protection from workplace aggression from patients or visitors. Further, substantially fewer providers and staff reported positive ratings of overall workplace safety culture than reported positive ratings of overall patient safety culture.
Tables S1 a and S1 b present the results of multiple linear regressions examining associations for workplace safety culture measures with the patient safety culture measures. Table S1 b includes the number of statistically significant associations and the mean and range of the standardized regression coefficients of those statistically significant associations for each workplace safety culture measure. Of the 110 regression estimates, 69 were statistically significant ( p < 0.05). Tables S2 a and S2 b provide model fit statistics of each of the regression models.
Three workplace safety culture measures were significantly associated with all 11 patient safety culture measures and had the largest average magnitude associations ( Overall Rating on Workplace Safety for Providers and Staff , mean β = 0.67; Supervisor, Manager, or Clinical Leader Support for Workplace Safety , mean β = 0.62; and Hospital Management Support for Workplace Safety , mean β = 0.62). These three measures had the largest number of associations with patient safety culture measures on average and represented four of the five largest magnitude associations with patient safety culture measures: Overall Rating on Workplace Safety for Providers and Staff and Hospital Management Support for Patient Safety (β = 0.95); Hospital Management Support for Workplace Safety and Hospital Management Support for Patient Safety ( β = 0.93); Supervisor, Manager, or Clinical Leader for Workplace Safety and Response to Error (β = 0.90); and, Overall Rating on Workplace Safety for Providers and Staff and Overall Patient Safety Rating ( β = 0.85).
Two workplace safety culture measures ( Protection from Workplace Hazards , mean β = 0.57 and Workplace Safety and Reporting , mean β = 0.53) were significantly associated with 10 of the 11 patient safety culture measures. Associations with Protection from Workplace Hazards ranged from 0.39 with Reporting Patient Safety Events to 0.79 with Hospital Management Support for Patient Safety . Associations with Workplace Safety and Reporting ranged from 0.28 with Reporting Patient Safety Events to 0.75 with Response to Error .
Two workplace safety culture measures ( Moving, Transferring, or Lifting Patients and Work Stress/Burnout ) were significantly associated with seven out of 11 patient safety culture measures. Statistically significant associations of Moving, Transferring, or Lifting Patients with patient safety culture measures had an average of β = 0.57, ranging from 0.31 with Reporting Patient Safety Events to 0.87 with Hospital Management Support for Patient Safety . Statistically significant associations of Work Stress/Burnout with patient safety culture measures had an average of β = -0.53, ranging from − 0.47 with Organizational Learning – Continuous Improvement to -0.60 with Staffing and Work Pace . Associations were negative, indicating that higher Work Stress/Burnout was associated with lower patient safety culture.
The three workplace aggression measures ( Addressing Workplace Aggression from Patients or Visitors ; Workplace Aggression Policies, Procedures, and Training ; and Addressing Verbal Aggression from Providers or Staff ) had the lowest number of significant associations and smallest associations on average, with two or fewer significant relationships per measure with the patient safety culture measures. Specifically, Addressing Workplace Aggression from Patients or Visitors was significantly associated with only Communication Openness (β = 0.42); Workplace Aggression Policies, Procedures, and Training was not significantly associated with any patient safety culture measures; and Addressing Verbal Aggression from Providers or Staff was significantly associated with two patient safety culture measures (mean β = 0.56, ranging from 0.50 with Response to Error to 0.61 with Teamwork ).
We examined the relationship between hospital provider and staff perceptions of workplace safety culture and patient safety culture. Our analyses revealed 69 out of 110 statistically significant associations between the workplace safety and patient safety culture measures, while controlling for hospital bed size, ownership, and teaching status, and controlling for multiple comparisons. All workplace safety measures were significantly associated with at least half of the patient safety culture measures, except for the three measures related to addressing workplace aggression from patients or other staff; these measures were only associated with up to two patient safety culture measures.
Theoretical models of organizational culture in health care have posited that the values and strategy of leadership along with characteristics of organizational structure and culture heavily influence the intermediate process domains of staffing; training; employee safety through protection from workplace hazards; resources to safely care for patients and themselves including proper equipment and staffing to move and lift patients safely; and other factors [ 27 ]. These process domains play a key role in how well providers and staff collaborate and are focused on patients and their safety, which in turn influences both satisfaction and intention to leave of providers and staff as well as patient satisfaction and clinical outcomes [ 30 ]. This study provides empirical evidence to support multiple aspects of this model. In particular, hospital management support for and an overall perception of a healthy and robust workplace safety culture have the strongest associations with perceptions of patient safety culture. Additionally, feeling free to report workplace safety incidents without negative consequences, having sufficient resources to protect themselves from hazards, and being able to move and lift patients safely are also strongly associated with staff and providers’ perceptions of patient safety culture.
The strongest association with Work Stress/Burnout was with Staffing and Work Pace , which provides evidence that lower stress and burnout of providers and staff is associated with having sufficient staff, reasonable working hours, and better work pace. The strong relationships between higher burnout and poor patient safety culture are consistent with prior literature [ 29 , 30 , 40 , 41 , 42 , 43 ].
The three measures regarding workplace aggression (policies, procedures, and training; and addressing workplace aggression from patients or visitors and other providers or staff) were not as strongly associated with the patient safety culture measures as the other workplace safety culture measures. We performed a detailed investigation to explore these results and found that two outlier hospitals were the primary reason for the relatively large negative (though nonsignificant) associations between the Workplace Aggression Policies, Procedures, and Training composite measure and the patient safety culture measures. However, these outliers do not explain the low magnitudes and sometimes negative direction of the remaining associations between the workplace aggression and patient safety culture measures. Further research is required to assess why associations between the aggression measures and patient safety culture measures may be smaller or whether these results are limited to this particular sample.
This study has several limitations. First, while the number of hospitals is relatively large among the empirical literature on the relationship between patient safety and workplace safety cultures, the number of hospitals is still relatively small. Second, even though the study hospitals were diverse on a number of characteristics, they were selected as a convenience sample and thus are not representative of all U.S. hospitals. Third, the study is cross-sectional and examines associations, so we were unable to provide evidence on how changes in measures vary with changes in other measures or attribute causal directions to the relationships. That is, although workplace safety culture measures were used as the independent variables in the model, we cannot say definitively that better workplace safety causes better patient safety culture, but only that they are related and likely influence each other.
The analyses presented in this paper revealed relationships between patient safety culture and workplace safety culture measures. We found statistically significant associations between the majority of the workplace safety culture and patient safety culture measures, confirming our hypothesis that these important perceptions would be positively related. Overall, support from hospital management and supervisors, manager, or clinical leaders to ensure workplace safety, being able to report safety problems without negative consequences, and the overall rating of workplace safety culture were the workplace safety culture measures most strongly associated with patient safety culture.
These results provide empirical evidence to support the contention that the concepts of workplace safety culture and patient safety culture are fundamentally linked, and both are integral to a strong and healthy culture of safety. Future research should focus on collecting additional evidence about this relationship using larger sample sizes and additional measures to substantiate these results. This relationship could be assessed outside of hospital settings; nursing homes, for example, could provide fertile ground for additional research, given AHRQ’s recent release of a SOPS Workplace Safety Supplemental Item Set for Nursing Homes. Finally, the relationship between measures of aggression and patient safety culture should be further studied conceptually and empirically to determine whether the weak relationship presented in this study is generalizable to other U.S. hospitals.
Data availability
Some of the de-identified SOPS Hospital Survey 2.0 data are available upon request for research purposes.
An adverse event in healthcare is also known as a “patient safety event” which is defined differently by different government agencies and healthcare organizations. On the Surveys on Patient Safety Culture® (SOPS®), a “patient safety event” is defined as “any type of healthcare-related error, mistake, or incident, regardless of whether or not it results in patient harm.”
Provider refers to physicians, physician assistants, and nurse practitioners who diagnose, treat patients, and prescribe medications.
Staff refers to all other individuals who work in the hospital but are not providers. Examples include medical assistants, administrative staff, housekeeping, and nutrition.
Response option 3 for the Work Stress/Burnout item is: “I am beginning to burn out and have one or more symptoms of burnout, e.g.; emotional exhaustion.”
Response option 4 for the Work Stress/Burnout item is: “The symptoms of burnout I am experiencing won’t go away. I think about work frustrations a lot.”
Response option 5 for the Work Stress/Burnout item is: “I feel completely burned out. I am at the point where I may need to seek help.”
De Vries E, Ramrattan M, Smorenburg S, Gouma D, Boermeester M. The incidence and nature of in-hospital adverse events: a systematic review. BMJ Qual Saf. 2008;17:216–23.
Article Google Scholar
JHA K, Larizgoitia I, Audera-Lopez C, Prasopa-Plaizier N, Waters H, Bates D. The global burden of unsafe medical care: analytic modelling of observational studies. BMJ Qual Saf. 2013;22:809–15.
Article PubMed Google Scholar
Institute of Medicine. To err is human: building a Safer Health System. Washington, DC: National Academy; 1999.
Google Scholar
Bonner A, Castle N, Men A, Handler S. Certified nursing assistants’ perceptions of nursing home patient safety culture: is there a relationship to clinical outcomes. J Am Med Dir Assoc. 2009;10:11–20.
Lawton R, O’Hara J, Sheard L, Reynolds C, Cocks K, Armitage G, Wright J. Can staff and patient perspectives on hospital safety predict harm-free care? An analysis of staff and patient survey data and routinely collected outcomes. BMJ Qual Saf. 2015;24:369–76.
Article PubMed PubMed Central Google Scholar
Mardon R, Khanna K, Sorra J, Dyer N, Famolaro T. Exploring relationships between hospital patient safety culture and adverse events. J Pat Saf. 2010;6:226–32.
Vikan M, Haugen A, Bjørnnes A, Valeberg B, Deilkås E, Danielsen S. The association between patient safety culture and adverse events–a scoping review. BMC Health Serv Res. 2023;23:1–27.
de Bienassis K, Kristensen S, Burtscher M, Brownwood I, Klazinga N. Culture as a cure: Assessments of patient safety culture in OECD countries. 2020.
Health & Safety Commission. ACSNI Human Factors Study Group third report: organising for safety. 1993.
Morello R, Lowthian J, Barker A, McGinnes R, Dunt D, Brand C. Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf. 2013;22:11–8.
Hospital Survey on Patient Safety Culture. https://www.ahrq.gov/sops/surveys/hospital/index.html . Accessed on 3rd March 2023.
Health worker safety: a priority for patient safety. Available online: health-worker-safety-charter-wpsd-17-september-2020-3-1.pdf (who.int). Accessed on. 3rd March 2023.
National Steering Committee for Patient Safety. National Action Plan to Advance Patient Safety ; Institute for Healthcare Improvement: Boston, MA, USA, 2020.
National Academy of Medicine. National Plan for Health Workforce Well-Being. Washington, DC: The National Academies. 2022. https://doi.org/10.17226/26744
U.S. Bureau of Labor Statistics. Injuries, illnesses, and fatalities, table R8 page. Survey of Occupational and Illness Data. Detailed Industry by Selected Events or Exposures (Rate).
Centers for Disease Control and Prevention. The National Institute for Occupational Safety and Health (NIOSH). Safe Patient Handling and Mobility (SPHM) Page.
Centers for Disease Control and Prevention. Workbook for Designing, Implementing, and Evaluating a Sharps Injury Prevention Program.
Bahat H, Hasidov-Gafnim A, Youngster I, Goldman M, Levtzion-Korach O. The prevalence and underreporting of needlestick injuries among hospital workers: a cross-sectional study. Int J Qual Health Care. 2021:33, mzab009.
Boden L, Petrofsky Y, Hopcia K, Wagner G, Hashimoto D. Understanding the hospital sharps injury reporting pathway. Am J Ind Med. 2015;58:282–9.
Philips J. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374:1661–9.
The Joint Commission. Physical and verbal violence against health care workers. Sentin Event Alert. 2018;59:1–7.
Rangachari P, Woods J. Preserving organizational resilience, patient safety, and staff retention during COVID-19 requires a holistic consideration of the psychological safety of healthcare workers. Int J Environ Res Public Health. 2020;17:42–67.
De Kock J, Latham H, Leslie S, Grindle M, Munoz S, Ellis L, Polson R, O’Malley C. A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implicating for supporting psychological well-being. BMC Public Health. 2021;21:104.
Salazar de Pablo G, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, Shin J, Sullivan S, Brondino N, Solmi M, et al. Impact of coronavirus syndromes on physician and mental health of healthcare workers: systematic review and meta-analysis. J Affect Disord. 2020;275:48–57.
Article CAS PubMed PubMed Central Google Scholar
Stericycle. Key insights to Safeguard the Environment and the Environment of Care. Healthcare Workplace Safety Trend Report.
Riehle A, Braun B, Hafiz H. Improving patient and worker safety: exploring opportunities for synergy. J Nurs Care Qual. 2013;28:99–102.
Stone P, Harrison M, Feldman P, Linzer M, Peng T, Roblin D, Williams E. Organizational climate of staff working conditions and safety—an integrative model. Advances in patient safety: from research to implementation (volume 2: concepts and methodology). 2005.
Mossburg S, Himmelfarb C. The association between professional burnout and engagement with patient safety culture and outcomes: a systematic review. J Pat Saf. 2021;17:e1307–19.
Kim S, Kitzmiller R, Baernholdt M, Lynn M, Jones C. Patient safety culture: the impact on workplace violence and health worker burnout. Work Health Saf. 2022;71:78–88.
Zabin L, Zaitoun R, Sweity E, Tantillo L. The relationship between job stress and patient safety culture among nurses: a systematic review. BMC Nurs. 2023;22:39.
SOPS Hospital Survey Version 2.0. https://www.ahrq.gov/sites/default/files/wysiwyg/sops/surveys/hospital/SOPS-Hospital-Survey-2.0-5-26-2021.pdf
SOPS Workplace Safety Supplemental Item Set for the SOPS Hospital Survey. https://www.ahrq.gov/sites/default/files/wysiwyg/sops/surveys/hospital/workplace-safety/Workplace-Safety-Hospitals-2022-1215-ENGLISH_508.pdf . Accessed 31 January 2024.
Famolaro T, Yount N, Sorra J, Zebrak K, Gray L, Carpenter D, Caporaso A, Hare R, Fan L, Liu H. Pilot study results from the AHRQ surveys on Patient Safety Culture (SOPS) Workplace Safety Supplemental items for hospitals. 22 – 0008: AHRQ Publication No; 2021. Accessed 31 January 2024.
Sorra J, Famolaro T, Yount N, Zebrak K, Caporaso A, Behm J, Development. Pilot Test, and Psychometric Analysis of the AHRQ Surveys on Patient Safety Culture (SOPS™) Hospital Survey Version 2.0. AHRQ Publication. 2018.
Zebrak K, Yount N, Sorra J, Famolaro T, Gray L, Carpenter D, Caporaso A. Development, pilot study, and psychometric analysis of the AHRQ surveys on patient safety culture™(SOPS®) workplace safety supplemental items for hospitals. Int Journ Env Res Public Health. 2022;19:6815.
Article CAS Google Scholar
SOPS Hospital Survey Items and Composite Measures. https://www.ahrq.gov/sites/default/files/wysiwyg/sops/surveys/hospital/hospitalsurvey2-items.pdf . Accessed 31 January 2024.
Sorra J, Famolaro T, Dyer N, Nelson D, Khanna K. Hospital Survey on Patient Safety Culture: 2008 comparative database report. Agency for Healthcare Research and Quality. AHRQ Publication No; 2008. pp. 08–0039.
Menard S. Applied logistic regression analysis. Sage; 2002.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J Roy Stat Soc: Ser B (Methodol). 1995;57:289–300.
Sexton B, Sharek P, Thomas E, Gould J, Nisbet C, Amspoker A, Kowalkowski M, Schwendimann R, Profit J. Exposure to Leadership WalkRounds in neonatal intensive care units is associated with a better patient safety culture and less caregiver burnout. BMJ Qual Saf. 2014;23:814–22.
Halbesleben J, Wakefield B, Wakefield D, Cooper L. Nurse burnout and patient safety outcomes: nurse safety perception versus reporting behavior. West J Nurs Res. 2008;30:560–77.
Profit J, Sharek P, Amspoker A, Kowalkowski M, Nisbet C, Thomas E, Chadwick W, Sexton B. Burnout in the NICU setting and its relation to safety culture. BMJ Qual Saf. 2014;23:806–13.
Kim S, Mary R, Baernholdt M, Kitzmiller R, Jones C. How does workplace violence-reporting culture affect workplace violence, nurse burnout, and patient safety? Jour Nurse Care Qual. 2023;38:11–8.
Download references
Acknowledgements
Sylvia Fisher from AHRQ provided helpful comments on the manuscript. We are also grateful to the hospitals and provider and staff respondents of the survey.
This research was funded by the U.S. Agency for Healthcare Research and Quality (AHRQ), Contract No. HHSP233201500026I/HHSP23337004T.
Author information
Authors and affiliations.
Westat, Rockville, MD, USA
Brandon Hesgrove, Katarzyna Zebrak, Naomi Yount & Joann Sorra
Agency for Healthcare Research and Quality, Rockville, MD, USA
Caren Ginsberg
You can also search for this author in PubMed Google Scholar
Contributions
BH, NY, and JS conceptualized the current study and drafted the manuscript. BH conducted all analyses and prepared all tables. KZ, NY, and JS reviewed and provided guidance on all analyses and tables prior to drafting the manuscript. BH, NY, JS, KZ, and CG reviewed and revised the manuscript for BMCHSR. BH, NY, JS, KZ, and CG have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Brandon Hesgrove .
Ethics declarations
Ethics approval and consent to participate.
This study used hospital-level data aggregated from individual-level responses from the SOPS Hospital Survey 2.0. Informed consent language was included at the beginning of the SOPS web survey, along with Westat’s IRB contract information, but we received a waiver of written informed consent for the web survey. The informed consent language was “The survey is voluntary, but your feedback will help your hospital identify areas for patient safety and workplace safety improvement. If you do not wish to answer a question, you may leave it blank. Westat will keep your individual responses to this survey confidential. Only group results will be reported.”
Consent for publication
Not applicable.
Competing interests
CG from AHRQ reviewed and revised the manuscript. CG has a competing interest because she is employed by AHRQ which owns and creates the survey that is the data source for this manuscript. BH, KZ, JS, and NY do not have any competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hesgrove, B., Zebrak, K., Yount, N. et al. Associations between patient safety culture and workplace safety culture in hospital settings. BMC Health Serv Res 24 , 568 (2024). https://doi.org/10.1186/s12913-024-10984-3
Download citation
Received : 30 August 2023
Accepted : 11 April 2024
Published : 02 May 2024
DOI : https://doi.org/10.1186/s12913-024-10984-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care
- Workplace safety
- Patient safety
- Workforce safety
- Safety culture
- Organizational culture
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 6, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Study highlights need for improvement of patient safety in outpatient settings
by Mass General Brigham

Over the last several decades, research has brought nationwide awareness to issues of patient harm in the "inpatient" setting, where patients receive care as part of an overnight stay at a hospital.
A new study reveals that patient safety events are also prevalent and persistent in the outpatient setting— primary care visits, specialty care appointments, day surgeries, visits to the emergency room and other settings where patients receive most of their care. To better understand patient safety in the outpatient setting, a team from Boston area hospitals used data from the SafeCare Study to analyze the care of patients seen in outpatient practices from four health care systems in Massachusetts in 2018.
Led by investigators from Mass General Brigham and sponsored by CRICO, the medical professional liability insurer for the Harvard medical community and its affiliated organizations, the study provides insights into the most common forms of adverse events and populations most at risk, pointing to where interventions are needed most to improve patient safety. Results are published in the Annals of Internal Medicine .
"Our study is an alarm bell. About 1-in-4 people every month are touched by outpatient care, yet we do not know enough about its safety. If we do not measure outpatient safety, we cannot start to improve care for all patients," said corresponding author David Levine, MD, MPH, MA, of the Division of General Internal Medicine and Primary Care at Brigham and Women's Hospital, a founding member of Mass General Brigham. "Our study focuses on data that highlights what is a national and international issue for patients."
Despite how frequently patients receive outpatient care, few studies have focused on this setting, and most of the studies that have done so to date have been limited and their findings have been imprecise.
"While there have been calls to look at safety issues related to inpatient care, we need to examine outpatient care, too," said co-author Luke Sato, MD, of the Division of General Internal Medicine and Primary Care at the Brigham and SVP and CMO at CRICO. "Health care organizations everywhere need to take the first step of measuring patient safety in both inpatient and outpatient settings. This work is groundbreaking, but it's also just the beginning."
For the current study, researchers conducted a retrospective review of adverse events that occurred in the outpatient setting in 2018. They used all available data found in 3,103 electronic health records (EHR) for a random sample of patients aged 18 and over from 11 outpatient care facilities.
Seven nurse reviewers identified possible adverse events by identifying relevant triggers noted in the EHRs. If a nurse found an adverse event in the EHR, they would hand the information to a physician adjudicator who determined whether it was indeed an adverse event. They then ranked the severity of the adverse event, assessed whether it was preventable and rated their confidence using a six-point scale.
They found 7% of patients experienced at least one adverse event in the outpatient setting and 1.9% of patients experienced at least one preventable adverse event. The most common adverse events were adverse drug events (63.8%), health care-associated infections (14.8%), surgical/procedural adverse events (14.2%), patient care adverse events (8.3%) and perinatal/maternal adverse events (0.7%).
The team also found almost half of the adverse events occurred in the physician's office, where patients more frequently receive care—for every 100 ED visits, approximately two adverse events occurred, while adverse events occurred in the physician's office for about one out of every 100 ambulatory encounters.
The researchers also found that adverse events disproportionately affected older adults . Among patients over 85 years old, many had preventable (8.7%) and serious (4.4%) adverse events.
Investigators noted several limitations in the study. Since they analyzed and collected data retrospectively, some patient information may not have been captured in the EHRs. In addition, the team couldn't access relevant data from patients who left the institutions from which the study data was collected. The investigators did not include the safety implications for telemedicine, which is an important aspect of practicing medicine today, but was infrequently practiced in 2018.
"Our results call for urgent measures to curtail outpatient harm," said Levine. "They also have the potential to help inform evidence-based interventions, pointing us to where change could be most effective to help protect patients and prevent adverse events from occurring."
Explore further
Feedback to editors

Research shows altered regulation of genes linked to prostate cancer among firefighters

Biomarker found to help identify cells that can repair damaged blood vessels
2 hours ago

Researchers develop reminder system to enhance memory recall

Years after his death, late scientist's work could yield new cancer treatments
3 hours ago

Cannabis, nicotine use during pregnancy found to increase rate of infant death fourfold
4 hours ago

Study finds genetic link between growth during puberty and long-term health conditions

Using AI and social media to track depression in communities could offer more reliable assessments than surveys
5 hours ago

Mouse study shows intermittent fasting protects against liver inflammation and liver cancer

New genetic mutation identified for congenital thyroid condition
6 hours ago


A potential treatment for inflammatory bowel disease: Engineered yeast can transport medicines and lower inflammation
Related stories.

Study of Massachusetts hospitals underscores importance of patient safety, need for continued improvement
Jan 11, 2023

Drug-drug interactions seen in 21.4% of children with medication exposure
Jan 5, 2024

To what extent are children harmed by medications in pediatric intensive care units?
Dec 8, 2021

US hospital adverse events drop significantly
Jul 12, 2022

Review examines antibiotic prescribing in outpatient telemedicine
Nov 6, 2023

Nearly 1 in 4 hospital patients have harmful event during their stay
Jan 14, 2023
Recommended for you

New analysis links resident physicians' exam scores to patient survival

You're breathing potential carcinogens inside your car, says study
10 hours ago

Improved nutrition, sanitation linked to beneficial changes in child stress and epigenetic programming

Parental deaths due to guns or drugs harmed nearly 100,000 US kids in 2020: Study

Study shows rising child mortality in the US has the most impact on Black and Native American youth
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue Suppl 2
- Interplay between leadership and patient safety in dentistry: a dental hospital-based cross-sectional study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-1709-5793 Muhammad Humza Bin Saeed 1 , 2 ,
- Ulfat Bashir Raja 3 ,
- Yawar Khan 4 ,
- Janice Gidman 5 ,
- Manahil Niazi 1
- 1 Community Dentistry , Riphah International University , Islamabad , Pakistan
- 2 Research, Development & Grants , NHS North Bristol Trust , Bristol , Bristol , UK
- 3 Dentistry , Riphah International University , Islamabad , Pakistan
- 4 Riphah International University Faculty of Health and Medical Sciences , Islamabad , Pakistan
- 5 University of Chester , Chester , Cheshire West and Chester , UK
- Correspondence to Muhammad Humza Bin Saeed; humza.saeed{at}riphah.edu.pk
Objectives The study aimed to study the association of leadership practices and patient safety culture in a dental hospital.
Design Hospital-based, cross-sectional study
Setting Riphah Dental Hospital (RDH), Islamabad, Pakistan.
Participants All dentists working at RDH were invited to participate.
Main outcome measures A questionnaire comprised of the Transformational Leadership Scale (TLS) and the Dental adapted version of the Medical Office Survey of Patient Safety Culture (DMOSOPS) was distributed among the participants. The response rates for each dimension were calculated. The positive responses were added to calculate scores for each of the patient safety and leadership dimensions and the Total Leadership Score (TLS) and total patient safety score (TPSS). Correlational analysis is performed to assess any associations.
Results A total of 104 dentists participated in the study. A high positive response was observed on three of the leadership dimensions: inspirational communication (85.25%), intellectual stimulation (86%), and supportive leadership (75.17%). A low positive response was found on the following items: ‘acknowledges improvement in my quality of work’ (19%) and ‘has a clear sense of where he/she wants our unit to be in 5 years’ (35.64%). The reported positive responses in the patient safety dimensions were high on three of the patient safety dimensions: organisational learning (78.41%), teamwork (82.91%), and patient care tracking/follow-up (77.05%); and low on work pressure and pace (32.02%). A moderately positive correlation was found between TLS and TPSS (r=0.455, p<0.001).
Conclusions Leadership was found to be associated with patient safety culture in a dental hospital. Leadership training programmes should be incorporated during dental training to prepare future leaders who can inspire a positive patient safety culture.
- Patient safety
- Safety culture
Data availability statement
No data are available.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjoq-2023-002376
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Organisational environment and leadership influence staff behaviours and attitudes towards patient safety practices in nursing studies.
WHAT THIS STUDY ADDS
The role of leadership in affecting patient safety practices in a dental hospital is explored in this study.
HOW THIS MIGHT AFFECT RESEARCH, PRACTICE, OR POLICY
The findings may be used to inform policy to train leadership in dental settings.
Introduction
Despite significant progress in the area of ‘patient safety’ over the last 15–20 years, it is still a major public health problem around the world. 1 Medical errors are responsible for 9.5% of all mortalities in the USA, surpassed only by cancer and cardiovascular disease. 2 More than 237 million medication-related errors occur every year in England alone. These errors result in over 1700 deaths every year. 3 4
The modern concept of providing quality healthcare makes patient safety an essential pillar of healthcare practice. 5 Safer primary care is a fundamental part of the United Nation’s Sustainable Development Goals. 6
A WHO report suggests that developing countries lack the facilities and infrastructure required to ensure patient safety protocols are in place. 7 Subsequently, the expected rate of adverse events secondary to medical errors would be even higher than that reported for developed countries. Such an estimate raises major concerns for public health safety.
Dentistry is an important part of primary healthcare. When the topic of patient safety is talked about, dentistry is usually not an area of concern. It has become more of a myth among the healthcare fraternity that dental errors do not cause serious harm. As a result, no specific tool has been designed to measure patient safety incidents in dentistry. 8 In real-world dental practice, severe incidents do occur in dentistry. Using dentistry-related keywords, Thusu et al searched the National Patient Safety Agency database for any patient safety incidents (PSI). A total of over 2000 PSIs were identified, out of which 5.5% (n=111) were medical emergency incidents. 9 Bailey et al 10 reported that patient safety systems in dentistry are still not adequately tested. 10
Medical errors are not performed by healthcare professionals intentionally. It is the complexity of healthcare systems that impacts the performance of professionals and thus, results in errors. 11 Evidence suggests that both human and system factors are responsible for PSIs. The five most commonly reported risk factors for patient safety are active failures, individual factors, communication systems, equipment and supplies, and management of staff and staffing levels. 12 It is interesting to note that all factors are in some manner integrally related to the organisational environment.
Several factors impact the performance of individuals in organisations, thus leading to motivation to perform better. 13 Similarly, in healthcare, a highly motivated workforce is imperative to achieving better outcomes. The characteristics of an organisation, along with the building of social relationships contribute to a workplace environment. 14
The AHRQ’s (Agency for Healthcare Research and Quality) ‘Integrative model of healthcare working conditions on organisational climate and safety’ model suggests that leadership styles impact the characteristics of an organisational climate as well as the management design and workplace culture and environment. Patient care and patient safety outcomes are also affected due to these factors. The satisfaction of healthcare professionals and patient-related outcomes are impacted as well. 15 This model primarily describes the impact of two primary constructs—leadership and organisational climate—on patient and healthcare professionals’ outcomes. Using this model, we have an understanding that healthcare leadership is a significant driving force in contributing towards patient safety in a healthcare working environment. Leadership is a factor that determines the workplace environment. If the leadership does not instil patient safety as a central factor in the hospital environment, employees will not rate safety practice as one of the important factors. Leaders’ behaviours impact the safety culture at the workplace, thereby affecting indicators of patient safety. 16 Furthermore, leadership may affect the employees’ performance in two ways. First, leaders have an indirect effect through their choice of management style. Second, leaders have a direct impact on how employees perform by leading by example and acknowledging their performance. 17 18 Thus, leadership style in healthcare is of paramount importance in the safety realisation of healthcare workers. 19
There is a paucity of literature exploring the impact of leadership on patient safety in a dental work environment. This study aimed to assess the association of leadership style and patient safety practices in a dental work environment.
The study was conducted at Riphah Dental Hospital (RDH), Islamabad. RDH is the largest dental hospital in Islamabad with over 100 dental units and about 120 dentists working in the hospital. Since, it is a teaching hospital, 150 dental students perform their clinical work in the hospital as well.
Ethical considerations
The willingness of the participants to fill out the questionnaires was considered as implied consent. The names of the participants were not recorded on the questionnaire sheets. A unique code number was allotted to each of the participants. The code numbers were written on each of the questionnaires.
Study cohort
A printed copy of the questionnaire was handed out to each participant and then, filled copies were collected at a mutually agreed time. All dentists working at RDH were invited to participate in the study.
Study instrument
Leadership style was assessed from the Transformational Leadership Scale (TLS) derived from the work of House and Podsakoff. 20 The TLS is a valid and reliable 15-item questionnaire with five subdimensions (vision, inspirational communication, intellectual stimulation, supportive leadership, and personal recognition). The items on this scale have been tested for validity and reliability. Each dimension has three items. Each item has five Likert scale responses ranging from 1 (strongly disagree) to 5 (strongly agree). The dental-adapted version of the Medical Office Survey on Patient Safety Culture (MOSOPS) was used to assess the prevalence of PS practices in the dental hospital. 21 The dental-adapted version of the MOSOPS has 44 items under 10 main composite sections and two overall evaluation/supplementary sections. For all of the 44 items, the participants were asked to give their responses on a five-item Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). In the first supplementary section, the participants are presented with nine different scenarios/situations related to ‘Patient Safety and Quality’. They are asked about their estimate of how frequently such an event has occurred in the past 12 months. In the second supplementary section, the participants were asked about information exchange with other settings. They were asked how frequently problems in such exchange had occurred in the past 12 months. In both these supplementary sections, the respondents were asked to report their perception of the frequency of each adverse event on a five-item Likert scale as follows: ‘Daily’, ‘Weekly’, ‘Monthly’, ‘Several Times in the Past 12 Months’, and ‘Never in the Past 12 Months’.
Statistical analysis
All collected data were entered and analysed using the Statistical Package for the Social Sciences (SPSS) V.26.0. For data analysis purposes, the responses for both instruments were dichotomised into ‘positive’ and ‘negative’ responses. Since the instruments included both positive and negative statements, the categorisation was done differently for both types of statements. For positive statements, the ‘Strongly Agree’, ‘Agree’, and ‘Neutral’ responses were categorised as ‘positive responses’, while ‘Disagree’ and ‘Strongly Disagree’ were placed under the ‘negative responses’ category. The negative statements were reverse-coded. For the negative statements, ‘Disagree’ and ‘Strongly Disagree’ were marked as ‘positive responses’, while ‘Strongly Agree’, ‘Agree’, and ‘Neutral’ were marked as ‘negative responses’. Positive response rate was calculated for each item by calculating the frequency and percentage of positive responses. The frequencies and percentages were described for each item and the cumulative categories as well. The responses for ‘Patient Safety and Quality Issues’ and ‘Information Exchange with Other Settings’ were marked in terms of frequency of occurrence. If an event was perceived as occurring ‘Daily’, ‘Weekly’, or ‘Monthly’, it was categorised as a ‘negative response’. However, if the event occurred ‘Several Times in the Past 12 Months’ or ‘Never in the Last 12 Months’, it was categorised as a ‘positive response’.
For further analysis, each positive response was given a score of ‘1’. The total positive responses were added and mean positive responses were calculated for each dimension of Leadership and Patient Safety. The scores of all items were added to calculate the ‘Total Leadership Score’ (TLS) and ‘Total Patient Safety Score’ (TPSS) Mean and SD were described for each of the dimension scores, TLS and TPS. Correlational analysis was then conducted to assess the association between each of the leadership dimensions and TLS with the Patient Safety dimension scores and TPSS. Pearson’s correlation coefficient was described for each correlation.
Out of the 120 dentists working at RDH, 10 were on leave. Six participants refused to participate and a final sample of 104 dentists (response rate=86.7%) participated in the study. Out of these, the maximum of dentists were house officer residents (n=60, 57.7%), followed by 25 (24%) postgraduate residents, seven (6.7%) demonstrators, and 12 (11.6%) consultants.
Among the five leadership dimensions assessed, the lowest positive response was observed for ‘Personal Recognition’ (57.14%), with a significantly low response recorded for the ‘acknowledges improvement in my quality of work’ item (19%). This was followed by the ‘vision’ dimension (61.89%). An interestingly low positive response was observed for the ‘has a clear sense of where he/she wants our unit to be in 5 years’ item (35.64%). A greater than 80% was observed for all the items in the ‘inspirational communication’ and ‘intellectual stimulation’ dimensions. A response of between 70% and 80% was recorded for the ‘supportive leadership’ Dimension ( table 1 ).
- View inline
Positive responses for the leadership dimensions
For patient safety, three of the 10 categories reported a positive response rate of less than 50%. The ‘teamwork’ category had the highest reported positive response rate. The lowest rate was observed for ‘work pressure and pace’ (32%), with the lowest responses recorded for the ‘In this office, we often feel rushed when taking care of patients’ (19.23%) and ‘we have too many patients for the number of providers in this office’ (21.57%) items as shown in online supplemental table 2 .
Supplemental material
The mean scores for leadership and patient safety dimensions are shown in table 2 . Correlational analysis was conducted for the mean scores for PS and leadership ( table 3 ). All of the leadership category scores except ‘vision’ were found to have a significant correlation with the Total Patient Safety Score. ‘Inspirational communication’, ‘intellectual stimulation’, and ‘total leadership’ scores had a weak or moderate correlation with nine of the patient safety categories ( table 3 ). The overall leadership was found to have a positively moderate correlation with overall patient safety (Pearson’s correlation coefficient=0.455; p<0.001). The abbreviations used in table 3 are shown in table 4 .
Mean scores for all leadership and patient safety dimensions
Pearson’s correlation coefficient values between the leadership scores and patient safety scores
Full terms for abbreviations used for terms used in data tables
In the current setting (RDH), ‘intellectual stimulation’ was found to have the highest positive response (86%), which shows that the leadership at RDH inspired critical thinking and ‘out of box’ thinking in the hospital environment. Moreover, ‘inspirational communication’ also had a high response rate (85.25%), suggesting that participants highly valued their association with RDH and accepted the range of professional growth opportunities available to them. Boamah et al 22 reported inspirational motivation to be the strongest factor contributing to nurse and patient outcomes. 22
‘Supportive leadership’ was also observed to have a high response suggesting that the leadership valued and entertained the feelings, interests, and needs of its employees. ‘Personal recognition’ generally had good responses, except for ‘acknowledges improvement in my quality of work’ with a low positive response rate of only 19%. This indicated that despite facilitating the needs of the staff, encouraging, and appreciating the efforts of employees was not a regular practice at RDH. Workplace recognition in dentistry is identified as an important factor for stress management. 23 Lower stress levels lead to better improved workplace performance and thus, leads to better patient outcomes. 24
Finally, while evaluating the ‘vision’ dimension, ‘has a clear sense of where he/she wants our unit to be in 5 years’ had a positive response of only 35.64%. Also, a response rate of 57.28% was reported for ‘has no idea where the organisation is going’. This indicates a deficiency or lack of clarity of vision of leadership. The vision may be defined on paper but the direction of how to achieve the vision and its related goals appears to be unclear. In dentistry, people used to be placed into leadership positions because of the responsibilities that came with their job requirements. A leadership position was not a conscious or intentional choice for dentists until recently. In the last couple of decades, dental leadership has been recognised as an independent identity. Dental leaders have the vision to inspire their team members to work towards collective goals. Busby further describes the concept of this vision in a dental setup in his definition of dental leadership as ‘the ability to continuously define a future practice vision which inspires you and your dental team towards success’. 25 It is this vision that helps the dental team to work towards attainable goals. However, the definition of success can vary, and it is important to understand what success means in a particular setup. Among other outcomes, improved patient outcomes and patient safety must be included in the vision and success criteria of any dental setup.
Busby has described three different dimensions of leadership as being the ‘pillars of leadership’: vision, motivation, and delivering the key outcomes. He further goes on to describe leadership in the dental context as ‘the ability to continuously define a future practice vision which inspires you and your dental team towards success’. 25 Nalliah presented an interesting perspective on the leadership characteristics of dentists. He argued that the professional characteristics that define a good dentist and in contrast to what is required for being a good leader. For instance, he poses the point that a good dental practitioner needs to be autonomous and self-reliant in his practice while paying meticulous attention to finding details. 26 A good leader, on the other hand, exhibits interdependence, is creative, and is focused on the ‘bigger picture’. That need not be the case in practical scenarios. Future leaders are expected to be multifaceted, possessing a range of traits , instead of a set of defined characteristics. 27 A dentist may be focused on the fine details of the contour of restoration while treating a patient, but when he needs to procure equipment for the department, he can exercise delegation and trust in colleagues who have been trained in the process of procuring dental equipment. Also, when a dentist needs to develop a multidisciplinary plan for managing patients, he would trust the opinion of other professionals who are experts in their disciplines. As shown in the present study, participants responded well to the items in the ‘supportive leadership’ subsection, illustrating the point that dentists are comfortable working in an environment where their opinions and needs are valued.
faceted, possessing a range of traits , instead of a set of defined characteristics. 27 A dentist may be focused on the fine details of the contour of restoration while treating a patient, but when he needs to procure equipment for the department, he can exercise delegation and trust in colleagues who have been trained in the process of procuring dental equipment. Also, when a dentist needs to develop a multi-disciplinary plan for managing patients, he would trust the opinion of other professionals who are experts in their disciplines. As shown in the present study, participants responded well to the items in the ‘supportive leadership’ subsection, illustrating the point that dentists are comfortable working in an environment where their opinions and needs are valued.
Recent literature has identified a different type of leadership referred to as ethical leadership (EL ). 19 Based on ethical values, EL is driven by positive psychology, whereby a leader works towards creating a safe working environment for the employees, which in turn leads to improved patient outcomes. 28
Interesting findings were reported for the patient safety section. The ‘overall perception of patient safety and quality’ dimension showed alarming findings. A trend of commonly occurring mistakes and a consequent urgency to complete a greater number of tasks rather than provide quality care was observed. Yansane et al also assessed the patient safety culture in different dental settings using the dental-adapted version of the MOSOPS. They reported that the lowest scores (49%) were reported for the ‘work pressure and pace’ dimension in dental institutions, indicating a higher workload and increased pressure on the dentists. 21
However, a positive trend of adapting office practices to rectify apparent errors was reported with a high positive rate (78.41%). Additionally, a highly positive teamwork spirit was found (82.91%), suggesting that the coherence of the dental team was inspired by good leadership practice. ‘Staff in this office are asked to do tasks they haven’t been trained to do’ had a low positive response of 23.30%. This indicates that although staff training was a regular training feature, the appropriate training was not being conducted.
A high patient load for effective management (23%) and the urgency to complete procedures quickly (19.23%) was perceived as a significant issue impacting patient safety practices. Moreover, a lack of organisation in the departments (41%) was perceived to negatively impact the workflow (32.65%). Although ‘Leadership Support’ was reported to have a high response as a leadership dimension, it was seen as a negatively perceived category from a patient safety perspective. The leadership was reported to not spending an adequate number of resources for improving quality care (positive response=15%); along with overlooking mistakes related to patient care (positive response=31.68%). Management decisions were perceived to be made based on the hospital’s interests rather than those of the patients (positive response=40.35%). This also suggests that the organisation’s interests were not perceived to be aligned with that of the patients in general. The responsibility of ensuring that systems and solutions that focus on patient experience improvement are in place lies on the dental leadership. Punishing the staff for minor mistakes is not considered a practical solution. Instead, efforts to promote a culture that facilitates patient safety practices should be promoted. 21 29
A highly interesting finding was that staff highly felt that their errors were held against them (positive response=17.2%). They were also afraid to ask questions (41.67%) and felt that it was difficult to voice disagreement at the workplace (33.33%). An authoritative or dictatorial leadership style leads to poor performance of healthcare professionals and thereby has a negative impact on patient outcomes. 30 Such a dictatorial style of leadership is highly discouraged in modern medical workplaces. 31
Patients’ follow-up practices were well perceived by the staff at the RDH (positive response=77.05%). Also, the staff generally agreed that the hospital provided evidence-based, cost-effective, and individualised patient care without discriminating against any patient (positive response=85.03%). The participants also perceived that such processes had been put into practice that helped identify patient-related problems (87.63%). Due to the high patient load, getting a timely appointment (46.94%), problems with finding patient records (48.48%), not uploading medication lists (42.57%) and dental equipment failing and needing repair (20.39%) were reported to have low positive responses. This indicates a deficiency in the management practice to handle a high patient volume. Patient flow practices need to be improved with significant barriers identified and removed. Interestingly, few participants believed that the challenging and changing circumstances were opportunities (positive response=17.65%). This suggests that staff need to be trained to appreciate workplace challenges as learning opportunities for professional growth and development. Staff training is propagated as a significant step in preventing patient safety-related incidents. 32
Finally, the staff perceived that information exchange with different medical setups frequently faced some issues (positive response=28.88%). Since all the identified places in this category had a low positive response, this indicates problems in the infrastructure to transport information and/or samples to other places. As the transfer of items/information is of health-related significance, these gaps in the process must be identified and rectified accordingly. Interestingly, Yansane et al reported that dentists reported a higher positive response in the ‘information exchange with other settings’ as compared with their medical counterparts. 21 A simple explanation for this is because of a much lesser exchange of information with other settings in dentistry as compared with medicine. The lower response rate of the current study is hard to explain. Since over 70% of the respondents thought that the frequency of problems in this information exchange is quite frequent, there must be some flaw in the processes of exchange in this particular dental setting. Moreover, the non-response rate for these items was quite high as well. It is quite possible that the participants may not have answered these questions because they did not want to report their opinions on this matter. Not reporting adverse events adversely impacts patient safety. Effective reporting can only be brought into practice by supporting a safety culture where healthcare professionals are encouraged and empowered to report adverse events. 33
Overall, leadership was found to be moderately correlated with patient safety (Pearson’s correlation coefficient=0.455). Ree and Wig studied the association between transformational leadership and patient safety culture among 139 healthcare professionals in-home care services. A multiple regression analysis found transformational leadership to be the strongest predictor for a positive safety culture (β=0.30). 34 Effective leadership can have a positive influence on multiple factors ranging from positive teamwork to situational awareness. These factors contribute to patient safety and quality of care. 16
‘Vision’ had either no or very weak correlations with the different patient safety dimensions. This suggests that although having a future vision is important, it does not significantly impact patient safety culture.
Recommendations
The Collective Leadership for Safety Cultures (Co-Lead) programme was initially designed for multidisciplinary teams. 35 The premise of this programme lies within the concept of collective leadership to promote effective teamwork practices and facilitate a positive patient safety culture. This underlying concept for collective leadership is that leadership is not merely the responsibility of a single individual, rather it is a team responsibility. Since the practice of dentistry involves a collaborative team effort of different specialties, the Co-Lead programme could turn out to be effective in a dental hospital as well.
Effective and evidence-based methods for training leaders in dentistry should be employed by oral healthcare setups to prepare transformational leaders who can inspire their staff to effectively work and create a work environment where patient safety outcomes are incorporated within the very culture of the workplace. Furthermore, future studies should include dental auxiliaries (including dental nurses, technicians, and hygienists), administrative staff, and other supporting staff in future studies.
Limitations
A primary limitation of this study was its cross-sectional study design. Future studies should focus on a longitudinal design that can monitor how leadership styles impact patient safety practices over some time. Moreover, the instruments used for this study relied on a self-reported methodology. Self-reported results are open to bias and results that differ from the ground reality may well be observed in such studies. Furthermore, this was only a single-centre study. 36 Data from multiple hospitals can give a larger overview of the situation providing relatively more generalisable results. 37 Finally, only dentists were included in this study. Including dental nurses, dental technicians, administrative staff, and other supporting staff in the hospital would give a more holistic representation of the workplace environment.
Although all the leadership dimensions did not have a significant association with patient safety culture, the overall association found suggests the presence of a positive relationship between patient safety and leadership in dental settings. Since this association has not been studied in the dental specialty before, this is a novel study and will provide evidence for future research in this area. Moreover, the growing concern regarding patient safety-related adverse events in dentistry warrants that factors contributing to these issues should be addressed. It is suggested that leadership training programmes focusing on effective team building and effective communication should be incorporated for dentists at various levels.
Ethics statements
Patient consent for publication.
Not required.
Ethics approval
Ethical approvals were taken from the Ethical Review Committee of Chester University and the Institutional Review Committee of RDH.
- Makary MA ,
- Elliott RA ,
- Camacho E ,
- Jankovic D , et al
- Fadahunsi KP ,
- Akinlua JT ,
- O’Connor S , et al
- Panesar S ,
- Campbell S , et al
- O’Hara J , et al
- Berberoglu A
- Alotaibi EA ,
- ZienYusoff R ,
- Al-Swidi AK , et al
- Stone PW , et al
- Hyunjie L ,
- V. R. Boedker C ,
- Meagher K ,
- Cogin J , et al
- Atashzadeh-Shoorideh F ,
- Mohtashami J , et al
- Rafferty AE ,
- Yansane A ,
- Hebballi N , et al
- Boamah SA ,
- Spence Laschinger HK ,
- Wong C , et al
- Freeman R ,
- Naicker N , et al
- Yammarino FJ ,
- Dionne SD , et al
- Cummings GG
- Mulenga RM ,
- Kumar RDC ,
- Harrison MI
- De Brún A ,
- Cunningham U , et al
- Benítez‐Silva H ,
- Buchinsky M ,
- Man Chan H , et al
- Sprague S ,
- Bhandari M , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors All authors made significant contributions to the article. HS, guarantor.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Election 2024
- Entertainment
- Newsletters
- Photography
- Personal Finance
- AP Investigations
- AP Buyline Personal Finance
- AP Buyline Shopping
- Press Releases
- Israel-Hamas War
- Russia-Ukraine War
- Global elections
- Asia Pacific
- Latin America
- Middle East
- Election Results
- Delegate Tracker
- AP & Elections
- Auto Racing
- 2024 Paris Olympic Games
- Movie reviews
- Book reviews
- Personal finance
- Financial Markets
- Business Highlights
- Financial wellness
- Artificial Intelligence
- Social Media
Safety lapses contributed to patient assaults at Oregon State Hospital, federal report says
FILE - The general view of the Oregon State Hospital is seen, May 24, 2013, in Salem, Ore. A federal report says safety lapses at the Oregon State Hospital contributed to recent patient-on-patient assaults. (Paul Carter/The Register-Guard via AP, File)
- Copy Link copied
Safety lapses at the Oregon State Hospital contributed to recent patient-on-patient assaults, a federal report on the state’s most secure inpatient psychiatric facility has found.
The investigation by the Centers for Medicare and Medicaid Services found that staff didn’t always adequately supervise their patients and that the hospital didn’t fully investigate acts of aggression, Oregon Public Broadcasting reported.
The federal agency opened the probe after receiving four complaints. Its findings were published following an unannounced, onsite survey conducted at the Salem hospital earlier this year.
A major incident detailed in the report occurred on Feb. 10, when a patient placed another patient in a chokehold until they were unconscious. The victim required “extensive” medical care for their injuries, according to the report.
Investigators also determined that the hospital failed to prevent sexual assault and sexual contact between patients.
In January, a patient was transferred out of a unit due to another patient’s “hypersexual behavior,” the report said. But in the new unit, the patient reported being coerced into sex.
The hospital received the federal report, known as a statement of deficiencies, on May 1. It has 10 calendar days to respond with a plan of correction.
“There will always be things we can improve, and we will continue to do so, but what persists is our dedication to the humans we are privileged to care for,” interim superintendent Sara Walker said in a statement.
Once the Centers for Medicare and Medicaid Services approves the plan, it will conduct another unannounced survey to review its implementation.
The state hospital has long struggled to address staffing shortages, overcrowding and other security lapses.
Just days before receiving the statement of deficiencies, the hospital was placed on “immediate jeopardy status” by CMS after a patient died shortly after arriving at the facility. The federal agency noted that emergency response equipment was not stored in an organized way in the admissions area. They found that while this didn’t contribute to the patient’s death, it presented a potential future safety risk, the Oregon Health Authority said in a statement.
The jeopardy status has since been lifted, state health officials said.
Last summer, a man newly transferred to the hospital managed to escape while fully shackled and drove off in a stolen van. He was found in a pond and then taken into custody, authorities said. An ensuing federal investigation found that the hospital failed to adequately supervise and transport the patient.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Online First
- Assessing quality of direct-to-consumer telemedicine in China: a cross-sectional study using unannounced standardised patients
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Zhen Zeng 1 ,
- Dong (Roman) Xu 2 ,
- Yiyuan Cai 3 ,
- http://orcid.org/0000-0002-7943-4041 Wenjie Gong 1 , 4 , 5
- 1 HER Team and Department of Maternal and Child Health, Xiangya School of Public Health , Central South University , Changsha , China
- 2 SMU Institute for Global Health (SIGHT), School of Health Management and Dermatology Hospital , Southern Medical University (SMU) , Guangzhou , China
- 3 Department of Epidemiology and Health Statistics, School of Public Health , Guizhou Medical University , Guiyang , China
- 4 Institute of Applied Health Research , University of Birmingham , Birmingham B15 2TT , UK
- 5 Department of Psychiatry , University of Rochester , Rochester , New York , USA
- Correspondence to Professor Wenjie Gong, HER Team and Department of Maternal and Child Health, Xiangya School of Public Health, Central South University, Changsha, Hunan, 410078, China; gongwenjie{at}csu.edu.cn
Direct-to-onsumer telemedicine (DTCT) has become popular as an alternative to traditional care. However, uncertainties about the potential risks associated with the lack of comprehensive quality evaluation could influence its long-term development. This study aimed to assess the quality of care provided by DTCT platforms in China using unannounced standardised patients (USP) between July 2021 and January 2022. The study assessed consultation services on both hospital and enterprise-sponsored platforms using the Institute of Medicine quality framework. It employed 10 USP cases, covering conditions such as diabetes, asthma, common cold, gastritis, angina, low back pain, child diarrhoea, child dermatitis, stress urinary incontinence and postpartum depression. Descriptive and regression analyses were employed to examine platform characteristics and compare quality across platform types. The results showed that of 170 USP visits across 107 different telemedicine platforms, enterprise-sponsored platforms achieved a 100% success in access, while hospital-sponsored platforms had a success rate of only 47.5% (56/118). Analysis highlighted a low overall correct diagnosis rate of 45% and inadequate adherence to clinical guidelines across all platforms. Notably, enterprise-sponsored platforms outperformed in accessibility, response time and case management compared with hospital-sponsored platforms. This study highlights the suboptimal quality of DTCT platforms in China, particularly for hospital-sponsored platforms. To further enhance DTCT services, future studies should compare DTCT and in-person care, aiming to identify gaps and potential risks associated with using DTCT as alternatives or supplements to traditional care. The potential of future development in enhancing DTCT services may involve exploring the integration of hospital resources with the technology and market capabilities of enterprise-sponsored platforms.
- Health services research
- Quality measurement
- Performance measures
- Patient-centred care
https://doi.org/10.1136/bmjqs-2024-017072
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Introduction
Direct-to-consumer telemedicine (DTCT) signifies a revolutionary global healthcare delivery model. It involves patients independently initiating medical services remotely, engaging directly with healthcare providers through text messaging or video/phone calls. By bypassing traditional intermediaries like referral clinicians or facilitators, DTCT empowers patients to access medical care swiftly and efficiently. 1 In China, DTCT is burgeoning, boasting over 1700 registered platforms, 2 each serving as an individual website or application for DTCT services. These platforms are categorised into two main types: hospital sponsored and enterprise sponsored. Hospital-sponsored platforms, associated with single physical hospitals, primarily use in-house medical staff and offer streamlined functions due to resource limitations. In contrast, enterprise-sponsored platforms, supported by larger corporations, provide access to a wider network of licensed physicians and offer a diverse range of functions with sophisticated user interfaces. 3 Despite enhanced accessibility and convenience compared with in-person care, DTCT faces quality challenges, such as communication difficulties and antibiotic misuse. 4 5 However, research on DTCT quality remains limited, especially in the context of China. To address this gap, our study employs unannounced standardised patients (USPs)—individuals trained and validated to portray specific medical conditions in a consistent and standardised manner 6 7 —to assess DTCT quality in China across different platform types based on the Institute of Medicine (IOM) quality framework.
This cross-sectional study examined both types of DTCT platforms that offered Chinese language services. The study was conducted between July 2021 and January 2022. Prior informed consent was waived due to minimal risk, and all analyses were performed on fully deidentified aggregated data. 8
To assess consultation service quality, we employed 10 different USP cases, each representing a specific medical condition (details in online supplemental eMethods and online supplemental example of a USP case ). Following thorough training and assessment, we selected 15 qualified USPs from the initial pool of 25 candidates. Each case was assigned at least one USP. As USPs’ initial requests for physician consultations could be denied for various reasons, mirroring real-world scenarios, each case made consultation requests until they completed at least five consultations on each platform type. The USPs captured screenshots and recorded the consultation process, including any failed attempts and reasons for failure. We evaluated the access success rate and assessed consultation quality using the IOM quality framework 9 ( table 1 ).
Supplemental material
- View inline
Quality outcome indicators
We conducted descriptive and regression analyses to evaluate platform characteristics and quality outcomes. Regression analyses compared quality differences using ordinary least squares and logistic regressions, with hospital-sponsored platforms as the benchmark and controlling for patient case fixed effects. Adjusted differences and 95% CIs were reported, adjusted for platform-level clustering. Statistical significance was set at α=0.05. Stata SE (V.16.0) was used for all analyses.
Our study involved 170 visits, with 52 visits on 10 enterprise-sponsored platforms and 118 visits on 97 hospital-sponsored platforms (summarised in online supplemental eTable 1 ). The overall access rate was 63.5% (108/170). Enterprise-sponsored platforms achieved a 100% access rate (52/52), significantly higher than hospital-sponsored ones (56/118, 47.5%) (p<0.001). Common reasons for unsuccessful consultations included incomplete functions, like platforms claiming to offer DTCT services but lacking an accessible feature for initiating online consultations with physicians (25/62, 40.3%), and no response (13/62, 21.0%).
Of 108 successful consultations, 49 consultations (45%) received a correct diagnosis, while adherence to published guidelines was low for consultation (15%) and management decisions (31%). On average, physicians took 3 hours and 47 min to respond, with the total interaction time spanning 12 hours and 19 min. After controlling for disease case fixed effects and adjusting SEs for clustering at platform level, enterprise-sponsored platforms had higher rates of completed management decisions, shorter response times and higher costs ( table 2 ).
Comparison on main quality outcomes between platform types for successful consultations
In this study, we rigorously evaluated the quality of care across two types of DTCT platforms in China using USPs. With 108 successful visits out of 170 attempts, we found a diagnostic accuracy of approximately 45%, along with a decline in completion rates for recommended management decisions to 31%. This may be linked to the limited inquiries during USP encounters, with clinicians asking only about 15% of recommended consultation questions per visit. Besides traditional quality metrics, the timeliness of DTCT services is concerning, with a response time of 3 hours and 47 min and an overall interaction time of 12 hours and 19 min. In China, DTCT predominantly operates asynchronously, leading to these extended durations. Despite offering a more flexible alternative to in-person counselling by eliminating the need for travel, prolonged waiting times may still impact user satisfaction and the perceived effectiveness of DTCT platforms. Future research should prioritise enhancing the timeliness of DTCT services to ensure prompt access and timely interactions. The patient-centredness score averaging 2.4, indicating a medium to low level of patient-centred care, 10 is potentially influenced by less satisfactory outcomes discussed earlier in terms of effectiveness, safety and timeliness. These findings raise concerns about how effective DTCT services are. Further evaluation, including a direct comparison with in-person care, is needed for a clearer understanding of their quality. This can guide improvement measures, especially when DTCT services act as alternatives or supplements to traditional in-person care.
Notably, enterprise-sponsored platforms achieved 100% access success, surpassing hospital-sponsored ones at 47.5%. They exhibited superior performance in response times and completion rates for management decisions. Despite recent growth and policy support, 3 hospital-sponsored platforms seem to be in early developmental stages, potentially limiting medical resource accessibility. These findings challenge a marketing survey suggesting a preference for hospital-sponsored platforms, 11 emphasising higher access denial risks and less timely responses for consumers on these platforms.
This study was limited by the use of a uniform USP for each case. Using standardised scenarios with different USPs potentially allows for a comprehensive assessment of equity. However, due to constraints imposed by scripted scenarios in our study, this aspect was not explored.
Our study highlights the suboptimal quality of DTCT in China, specifically disparities between hospital-sponsored and enterprise-sponsored platforms. These findings likely echo broader challenges and principles inherent in DTCT globally. As DTCT gains momentum after COVID-19, future research becomes critical to effectively address these issues.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study involves human participants and was approved by Xiangya School of Public Health (IRB No XYGW-2021-37). Prior informed consent was waived due to minimal risk and no individually identifiable information on physicians.
Acknowledgments
We sincerely thank Xiaohui Wang, Yaolong Chen, Yun Lu, Xiaojing Fan, Zhongliang Zhou, Jay Pan, and Chengxiang Tang for their unwavering leadership in development and management the SP cases. We also apperciate Lu Liu, Chunping Li, and Huanyu Hu for their their diligent efforts as project assistants, as well as all the standardized patients and study coordinators for their hard work.
- Elliott T ,
- iiMedia Report
- Resneck JS ,
- Steuer M , et al
- Gidengil CA , et al
- Peabody JW ,
- Glassman P , et al
- Colliver JA ,
- Rhodes KV ,
- Institute of Medicine (US) Committee on Quality of Health Care in America
- Tu J , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Contributors WG conceived the study. ZZ coordinated the daily implementation of this study under the supervision of DRX, YC and WG. ZZ carried out data analysis and composed the initial manuscript draft, receiving guidance from WG and DRX. All authors contributed to critical review of the manuscript and approved the final draft.
Funding This study was funded by China Medical Board (20-368), Swiss Agency for Development and Cooperation (81067392) and the National Natural Science Foundation of China (82273643).
Competing interests None declared.
Provenance and peer review Not commissioned; internally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:

An official website of the Department of Health & Human Services
- Search All AHRQ Sites
- Email Updates

1. Use quotes to search for an exact match of a phrase.
2. Put a minus sign just before words you don't want.
3. Enter any important keywords in any order to find entries where all these terms appear.
- The PSNet Collection
- All Content
- Perspectives
- Current Weekly Issue
- Past Weekly Issues
- Curated Libraries
- Clinical Areas
- Patient Safety 101
- The Fundamentals
- Training and Education
- Continuing Education
- WebM&M: Case Studies
- Training Catalog
- Submit a Case
- Improvement Resources
- Innovations
- Submit an Innovation
- About PSNet
- Editorial Team
- Technical Expert Panel
Co-worker unprofessional behaviour and patient safety risks: an analysis of co-worker reports across eight Australian hospitals.
McMullan RD, Churruca K, Hibbert P, et al. Co-worker unprofessional behaviour and patient safety risks: an analysis of co-worker reports across eight Australian hospitals. Int J Qual Health Care. 2024;36(2):mzae030. doi:10.1093/intqhc/mzae030.
Unprofessional behavior negatively impacts teamwork, safety culture, and patient safety . This study analyzed 1,310 reports of unprofessional behavior across eight Australian hospitals between 2017-2020. The researchers found that three in ten reports indicated a risk to patient safety, such as interruptions, poor handover communication, and a lack of adherence to hospital policy or protocol.
Hospital staff reports of coworker positive and unprofessional behaviours across eight hospitals: who reports what about whom? January 31, 2024
Changes in unprofessional behaviour, teamwork, and co-operation among hospital staff during the COVID-19 pandemic. September 28, 2022
Are operating room distractions, interruptions, and disruptions associated with performance and patient safety? A systematic review and meta-analysis. May 19, 2021
Unsafe care in residential settings for older adults. A content analysis of accreditation reports. December 13, 2023
Paediatric medication incident reporting: a multicentre comparison study of medication errors identified at audit, detected by staff and reported to an incident system. May 1, 2024
Middle manager responses to hospital co-workers' unprofessional behaviours within the context of a professional accountability culture change program: a qualitative analysis. November 8, 2023
Speaking up as an extension of socio-cultural dynamics in hospital settings: a study of staff experiences of speaking up across seven hospitals. February 22, 2023
Associations between double-checking and medication administration errors: a direct observational study of paediatric inpatients. August 26, 2020
Short- and long-term effects of an electronic medication management system on paediatric prescribing errors. January 18, 2023
How effective are electronic medication systems in reducing medication error rates and associated harm among hospital inpatients? A systematic review and meta-analysis. December 2, 2020
Effectiveness of a 'Do not interrupt' bundled intervention to reduce interruptions during medication administration: a cluster randomised controlled feasibility study. March 15, 2017
Patient groups, clinicians and healthcare professionals agree—all test results need to be seen, understood and followed up. December 19, 2018
Effectiveness of double checking to reduce medication administration errors: a systematic review. September 18, 2019
Emergency physicians' views of direct notification of laboratory and radiology results to patients using the internet: a multisite survey. March 25, 2015
Managing competing demands through task-switching and multitasking: a multi-setting observational study of 200 clinicians over 1000 hours. February 26, 2014
The safety of electronic prescribing: manifestations, mechanisms, and rates of system-related errors associated with two commercial systems in hospitals. June 12, 2013
Failure to utilize functions of an electronic prescribing system and the subsequent generation of 'technically preventable' computerized alerts. July 25, 2012
Effects of two commercial electronic prescribing systems on prescribing error rates in hospital in-patients: a before and after study. February 15, 2012
Impact of commercial computerized provider order entry (CPOE) and clinical decision support systems (CDSSs) on medication errors, length of stay, and mortality in intensive care units: a systematic review and meta-analysis. April 26, 2017
Allocation of physician time in ambulatory practice: a time and motion study in four specialties. September 7, 2016
Drug-drug interactions and actual harm to hospitalized patients: a multicentre study examining the prevalence pre- and post-electronic medication system implementation. April 10, 2024
Stepped-wedge cluster RCT to assess the effects of an electronic medication system on medication administration errors. March 13, 2024
Clinical decision support alert malfunctions: analysis and empirically derived taxonomy. November 1, 2017
Variation in electronic test results management and its implications for patient safety: a multisite investigation. August 19, 2020
Prevalence and causes of diagnostic errors in hospitalized patients under investigation for COVID-19. April 12, 2023
Seroprevalence of SARS-CoV-2 among frontline health care personnel in a multistate hospital network--13 academic medical centers, April-June 2020. September 23, 2020
The delivery of safe and effective test result communication, management and follow-up. September 27, 2023
The impact of health information technology on the management and follow-up of test results—a systematic review. May 8, 2019
The safety implications of missed test results for hospitalised patients: a systematic review. February 23, 2011
Failure to follow-up test results for ambulatory patients: a systematic review. January 11, 2012
Innovative approaches to analysing aged care falls incident data: International Classification for Patient Safety and correspondence analysis. November 8, 2023
Standardising the classification of harm associated with medication errors: the Harm Associated with Medication Error Classification (HAMEC). May 15, 2019
The prevalence of dose errors among paediatric patients in hospital wards with and without health information technology: a systematic review and meta-analysis. October 24, 2018
Preventable adverse drug events among inpatients: a systematic review. August 29, 2018
The application of the Global Trigger Tool: a systematic review. October 26, 2016
Health service accreditation as a predictor of clinical and organisational performance: a blinded, random, stratified study. March 24, 2010
Association of interruptions with an increased risk and severity of medication administration errors. May 5, 2010
Errors in the administration of intravenous medications in hospital and the role of correct procedures and nurse experience. July 13, 2011
Drivers of unprofessional behaviour between staff in acute care hospitals: a realist review. December 20, 2023
Underlying risk factors for prescribing errors in long-term aged care: a qualitative study. December 9, 2015
Data quality associated with handwritten laboratory test requests: classification and frequency of data-entry errors for outpatient serology tests. November 18, 2015
Disentangling quality and safety indicator data: a longitudinal, comparative study of hand hygiene compliance and accreditation outcomes in 96 Australian hospitals. October 8, 2014
Interruptions and multi-tasking: moving the research agenda in new directions. September 10, 2014
Does computerized provider order entry reduce prescribing errors for hospital inpatients? A systematic review. October 7, 2009
The impact of computerized provider order entry systems on medical-imaging services: a systematic review. January 30, 2011
Non-emergency patient transport: what are the quality and safety issues? A systematic review. February 2, 2011
The impact of interruptions on clinical task completion. July 7, 2010
The effect of computerized provider order entry systems on clinical care and work processes in emergency departments: a systematic review of the quantitative literature. May 22, 2013
Are interventions to reduce interruptions and errors during medication administration effective?: a systematic review. September 11, 2013
Analysis of Australian newspaper coverage of medication errors. January 25, 2012
Health professional networks as a vector for improving healthcare quality and safety: a systematic review. January 11, 2012
Towards an understanding of the information dynamics of the handover process in aged care settings—a prerequisite for the safe and effective use of ICT. April 25, 2012
Improving our understanding of multi-tasking in healthcare: drawing together the cognitive psychology and healthcare literature. March 29, 2017
A work observation study of nuclear medicine technologists: interruptions, resilience and implications for patient safety. November 23, 2016
Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation study. January 31, 2018
Safety and efficiency considerations for the introduction of electronic ordering in a blood bank. July 1, 2009
The effect of physicians' long-term use of CPOE on their test management work practices. September 27, 2006
Toward constructive change after making a medical error: recovery from situations of error theory as a psychosocial model for clinician recovery. August 10, 2022
Evaluation and accurate diagnoses of pediatric diseases using artificial intelligence. February 27, 2019
"Time is of the essence": relationship between hospital staff perceptions of time, safety attitudes and staff wellbeing. December 8, 2021
Dimensions of safety culture: a systematic review of quantitative, qualitative and mixed methods for assessing safety culture in hospitals. September 1, 2021
Predictors of response rates of safety culture questionnaires in healthcare: a systematic review and analysis. October 26, 2022
'Broken hospital windows': debating the theory of spreading disorder and its application to healthcare organizations. May 9, 2018
The MedSafer study-electronic decision support for deprescribing in hospitalized older adults: a cluster randomized clinical trial. February 2, 2022
Guideline for opioid therapy and chronic noncancer pain. May 31, 2017
Team dynamics, clinical work satisfaction, and patient care coordination between primary care providers: a mixed methods study. December 2, 2015
Near miss research in the healthcare system: a scoping review. May 25, 2022
A mixed-methods analysis of patient safety incidents involving opioid substitution treatment with methadone or buprenorphine in community-based care in England and Wales. November 11, 2020
What are the experiences of team members involved in root cause analysis? A qualitative study. December 20, 2023
Improving patient safety governance and systems through learning from successes and failures: qualitative surveys and interviews with international experts. December 6, 2023
Comparing rates of adverse events detected in incident reporting and the Global Trigger Tool: a systematic review. August 16, 2023
The patient died: what about involvement in the investigation process? June 24, 2020
A qualitative content analysis of retained surgical items: learning from root cause analysis investigations. May 27, 2020
Patient safety's missing link: using clinical expertise to recognize, respond to and reduce risks at a population level. November 25, 2015
Diagnostic error in the emergency department: learning from national patient safety incident report analysis. January 15, 2020
Health and social care-associated harm amongst vulnerable children in primary care: mixed methods analysis of national safety reports. April 1, 2020
Repeat prescribing of medications: a system-centred risk management model for primary care organisations. November 8, 2017
Healthcare failure mode and effect analysis (HFMEA) as an effective mechanism in preventing infection caused by accompanying caregivers during COVID-19-experience of a city medical center in Taiwan. January 27, 2021
Findings of a naloxone database and its utilization to improve safety and education in a tertiary care medical center. February 1, 2017
A diagnostic time-out to improve differential diagnosis in pediatric abdominal pain. July 14, 2021
Who do hospital physicians and nurses go to for advice about medications? A social network analysis and examination of prescribing error rates. April 16, 2014
Factors associated with potentially harmful medication prescribing in nursing homes: a scoping review. September 28, 2022
ASPEN parenteral nutrition safety consensus recommendations: translation into practice. May 14, 2014
ASPEN parenteral nutrition safety consensus recommendations. December 11, 2013
Patient safety: Part I. Patient safety and the dermatologist. August 19, 2009
Contextual errors and failures in individualizing patient care: a multicenter study. August 4, 2010
Enabling a learning healthcare system with automated computer protocols that produce replicable and personalized clinician actions. August 4, 2021
Opioid prescribing patterns and complications in the dermatology Medicare population. March 7, 2018
The impact of meaningful use and electronic health records on hospital patient safety. November 2, 2022
When a surgical colleague makes an error. February 24, 2016
Building a Patient Safety Toolkit for use in general practice. July 20, 2016
A patient safety toolkit for family practices. April 25, 2018
The complexities of communication at hospital discharge of older patients: a qualitative study of healthcare professionals' views. November 29, 2023
Early warning systems: the next level of rapid response. January 25, 2012
Preventable adverse drug events causing hospitalisation: identifying root causes and developing a surveillance and learning system at an urban community hospital, a cross-sectional observational study. February 24, 2021
Guidelines for opioid prescribing in children and adolescents after surgery: an expert panel opinion. December 2, 2020
Root cause analysis and actions for the prevention of medical errors: quality improvement and resident education. May 17, 2017
How to perform a root cause analysis for workup and future prevention of medical errors: a review. October 19, 2016
Scoping review of the second victim syndrome among surgeons: understanding the impact, responses, and support systems. March 27, 2024
A systematic review of the effectiveness of interruptive medication prescribing alerts in hospital CPOE systems to change prescriber behavior and improve patient safety. September 27, 2017
Annual Perspective
Nurse leader attitudes and beliefs regarding medical errors. March 6, 2024
Perspective
NPSD Data Spotlight: Patterns of Fall Interventions. November 15, 2023
React, reframe and engage. Establishing a receiver mindset for more effective safety negotiations. November 8, 2023
Impact of leadership walkarounds on operational, cultural and clinical outcomes: a systematic review. October 25, 2023
Exploring the "Black Box" of recommendation generation in local health care incident investigations: a scoping review. October 25, 2023
Bringing the equity lens to patient safety event reporting. October 25, 2023
MHA and MHA Keystone Center Annual Reports. October 20, 2023
When illegitimate tasks threaten patient safety culture: a cross-sectional survey in a tertiary hospital. October 11, 2023
Physician perspectives on responding to clinician-perpetuated interpersonal racism against Black patients with serious illness. September 13, 2023
Incivility in healthcare: the impact of poor communication. August 2, 2023
Implementation of peer messengers to deliver feedback: an observational study to promote professionalism in nursing. January 18, 2023
A failure in the medication delivery system-how disclosure and systems investigation improve patient safety. January 11, 2023
Health system redesign of cardiac monitoring oversight to optimize alarm management, safety, and staff engagement. December 14, 2022
The barriers and enhancers to trust in a just culture in hospital settings: a systematic review. August 17, 2022
Associations between safety outcomes and communication practices among pediatric nurses in the United States. January 19, 2022
The aspects of healthcare quality that are important to health professionals and patients: a qualitative study. December 15, 2021
It's like sending a message in a bottle: a qualitative study of the consequences of one-way communication technologies in hospitals. October 13, 2021
CANDOR Webinar Series. May 27, 2021 - May 27, 2021
I-PASS handover system: a decade of evidence demands action. May 12, 2021
Critical incidents involving the medical emergency team: a 5-year retrospective assessment for healthcare improvement. April 28, 2021
Patient Safety Innovations
The LifePoint National Quality Program Provides Structured Framework for Reducing Inpatient Harm
Nurses' perceptions of open disclosure processes in cancer care: a cross-sectional study. December 16, 2020
Learning from incident reporting? Analysis of incidents resulting in patient injuries in a web-based system in Swedish health care. December 9, 2020
Use of an audit with feedback implementation strategy to promote medication error reporting by nurses. November 25, 2020
A program to provide clinicians with feedback on their diagnostic performance in a learning health system. October 28, 2020
During the pandemic, aspire to identify and prevent medication errors and to avoid blaming attitudes. September 30, 2020

Connect With Us
Sign up for Email Updates
To sign up for updates or to access your subscriber preferences, please enter your email address below.
Agency for Healthcare Research and Quality
5600 Fishers Lane Rockville, MD 20857 Telephone: (301) 427-1364
- Accessibility
- Disclaimers
- Electronic Policies
- HHS Digital Strategy
- HHS Nondiscrimination Notice
- Inspector General
- Plain Writing Act
- Privacy Policy
- Viewers & Players
- U.S. Department of Health & Human Services
- The White House
- Don't have an account? Sign up to PSNet
Submit Your Innovations
Please select your preferred way to submit an innovation.
Continue as a Guest
Track and save your innovation
in My Innovations
Edit your innovation as a draft
Continue Logged In
Please select your preferred way to submit an innovation. Note that even if you have an account, you can still choose to submit an innovation as a guest.
Continue logged in
New users to the psnet site.
Access to quizzes and start earning
CME, CEU, or Trainee Certification.
Get email alerts when new content
matching your topics of interest
in My Innovations.
The ASUS IoT PE200U Enhances Patient Safety in Operating Rooms

Our customer
Smart Sensing Ltd. is an AIoT company incubated by HKSTP for providing smart city and business intelligence solutions with self-developed data analytics platform. The company develops AI-enabled IoT sensing technologies for smart city data acquisition. The sensing technology can be applied to various smart city applications such as property management by improving operational efficiency and customer journey experience. One of company’s recent targeted markets is smart property management in different scenarios including shopping mall, exhibition hall, hotel, museum, hospital, etc. The company has been great success in RF sensing and will extend the sensing technology with video by AI-powered smart cameras.
The Challenge
Maximizing process efficiency while minimizing development costs and human error.
A retained foreign object refers to any type of surgical instrument or material accidentally retained inpatient’s body after surgery or clinical procedure. Because retained surgical objects will cause infection, even internal damage, those situations may lead to constitute medical malpractice. Therefore, most hospitals tend to create checklists, tracking, and routines for surgeons and nurses, decreasing unnecessary harm and medical malpractice.
The solution
Asus pe200u industrial pc with item recognition automatic medical equipment identification solution adopted in hong kong.
Smart-Sensing developed an in-house AI algorithm with ASUS IoT PE200U edge computers for item recognition training models to reduce the risk of guidewire retention in a patient’s body after a clinical procedure or surgery, as known as insertion of a central venous catheter (CVC), and this system is used in hospital operating rooms. The system first will indicate the number of guidewires for the nurse to confirm. Then, the nurse after identifying the guidewires and will take the photo and upload it to the system containing the guidewires and other entangled medical instruments with a smartphone or tablet. Based on the object recognition and data techniques of the AI image-based system, it will detect the guidewires and double-check the manual count in real-time accurately.
The PE200U edge computer comes in a compact size, at 254 mm tall, 147 mm wide and 57 mm long, and it offers stable computing performance and low-power consumption for installation in a 24x7x365 hospital environment. The fan less thermal design not only prevents dust accumulation and establishes quiet operation in operating room, but it also facilitates hygiene control and environment management by avoiding convection that may result in cross-infections. Meanwhile, its diverse I/O interface and expansion options allow integration with multiple medical devices. Moreover, ASUS IoT offers world-class after-sales service and a long-term availability guarantee to accommodate hospital customer needs. Finally, as a global technology powerhouse, ASUS always strives to ensure that customers have the components they need for timely and successful deployment.
The outcome
Precise ai solutions to enhance patient safety in operating rooms.
With the PE200U edge computer, hospitals have successfully reduced the time needed for equipment check-up. Most importantly, have reduce the risk of guidewire retention inpatient's body after having a clinical procedure, also patient safety is much more emphasized.
The new and various techniques, instruments, and technology used for surgical procedures make correct decisions critically important. ASUS IoT which can accurately and promptly recognize all the used guidewires removed from patients’ bodies without missing, is highly reliable in enhancing patient safety. By assisting our customers in implementing smart hospital AI applications, ASUS IoT tries to build a safer operating room and a patient-centric hospital environment. ASUS IoT is a living demonstration proving how smart hospital development can boost efficiency, and make sure patient safety.
Using systems thinking in patient safety: a case study on medicines management
Affiliation.
- 1 School of Healthcare Sciences, Cardiff University, Wales.
- PMID: 28659071
- DOI: 10.7748/nm.2017.e1621
Systems thinking is used as a way of understanding behaviours and actions in complex healthcare organisations. An important premise of the concept is that every action in a system causes a reaction elsewhere in that system. These reactions can lead to unintended consequences, sometimes long after the original action, and so are not always attributed to them. This article applies systems thinking to a medicines management case study, to highlight how quality-improvement practitioners can use the approach to underpin planning and implementation of patient-safety initiatives. The case study is specific to transcribing in children's hospices, but the strategies can be applied to other areas. The article explains that, while root cause analysis tools are useful for identifying the cause of, and possible solutions to, problems, they need to be considered carefully in terms of unintended consequences, and how the system into which the solution is implemented can be affected by the change. Analysis of problems using a systems-thinking approach can help practitioners to develop robust and well informed business cases to present to decision makers.
Keywords: medicines management; nursing management; patient safety; systems thinking; transcribing; unintended consequences; wicked issues.
- Medication Therapy Management*
- Patient Safety*
- Quality Improvement
- Systems Analysis*

IMAGES
VIDEO
COMMENTS
The study sample was designed to include hospitals and patient populations that would provide reliable estimates of safety and safety-related metrics among patients 18 years of age or older at ...
WebM&M: Case Studies. WebM&M (Morbidity & Mortality Rounds on the Web) features expert analysis of medical errors reported anonymously by our readers. Spotlight Cases include interactive learning modules available for CME. Commentaries are written by patient safety experts and published monthly.
Impact Case Studies. AHRQ's evidence-based tools and resources are used by organizations nationwide to improve the quality, safety, effectiveness, and efficiency of health care. The Agency's Impact Case Studies highlight these successes, describing the use and impact of AHRQ-funded tools by State and Federal policy makers, health systems ...
Abstract. Motivated by pressure and a wish to improve, health care organizations are implementing programs to improve patient safety. This article describes six natural experiments in health care safety that show where the safety field is heading and opportunities for and barriers to improvement. All these programs identified organizational ...
Can patient safety incident reports be used to compare hospital safety? Results from a quantitative analysis of the English National Reporting and Learning System data. PLoS One. 2015;10(12):e0144107.
Patient stories can help illustrate the impact of medical harm on patients and their families as well as uncover areas for improvement. This book offers a collection of 24 patient accounts of medical errors with further information from the editors including context, learning objectives, and a case discussion to guide understanding of key health professional competencies and how to integrate ...
By the end of 2014 the average number of PSAs was 879 — a record number for the organization. The goal, promoted at meetings and on the company's intranet, is to reach an average of 1,000 PSAs per month. Overall staff participation in Virginia Mason's Culture of Patient Safety survey grew, from 16% in 2004 to 88% in 2013.
April 2006. ABSTRACT:This report presents 10 case studies of health care organizations, clinical teams, and learning collaborations that have designed innovations in five areas that hold great promise for improving patient safety nationally: promoting an organizational culture of safety, improving teamwork and communication, enhancing rapid ...
This collection of case studies highlights AHRQ-funded patient safety tools, including the Comprehensive Unit-based Safety Program, Re-Engineered Discharge Toolkit, and patient safety culture surveys, to document their successful use in the field. ... Hospital Survey on Patient Safety Culture 2.0. June 1, 2022. Dissemination and Implementation ...
Case Study: More Patient Safety by Design - System-based Approaches for Hospitals Adv Health Care Manag. 2019 Oct 24;18. doi: 10.1108/S1474-823120190000018001. ... One type of system-based intervention that can benefit patient safety involves improvements to hospital design. Given that people's working environments affect their behavior, good ...
Case Study: More Patient Safety by Design - System-based Approaches for Hospitals. Pages 1-17. ... While an increasing number of studies have demonstrated the effect of hospital design on patient safety, this knowledge is not easily accessible to clinicians, practitioners, risk managers, and other decision-makers, such as designers and ...
1.1. Background. Research indicates that there is a potential for patients to improve safety (Davis, Jacklin, Sevdalis, & Vincent, 2007; Vincent & Coulter, 2002) and that patients are willing and able to be involved in safety‐related work (Waterman et al., 2006 Wright et al., 2016).However, several barriers to involving patients in improving patient safety has been identified and organized ...
New management had taken over the hospital. The CEO was trying to set a meeting with the family and physician, but the physician refused. After a year from the death, the physician accepted a meeting. ... Johnson, J., Haskell, H., & Barach, P. (2016) Case Studies in Patient Safety. Subury, MA: Jones and Bartlett Learning . You may also like.
Patient safety review and response case studies by clinical specialty. This page shows case studies, listed by clinical specialty, of where the National Patient Safety Team worked with partners to address issues identified through its review of recorded patient safety events. Urgent/emergency care. General medicine.
Visiting Professor College of Medicine University College Cork Cork, Ireland. Jones & Bartlett Learning books and products are available through most bookstores and online booksellers. To contact Jones & Bartlett Learning directly, call 800-832-0034, fax 978-443-8000, or visit our website, www.jblearning.com.
Thus, this study aimed to examine patient safety attitudes among critical care nurses. Methods: This cross-sectional study was conducted in two hospitals in North Cyprus. Eighty nurses working in critical care units participated in the study. Following ethical approval, data were collected between September and October 2018, using the ...
While an increasing number of studies have demonstrated the effect of hospital design on patient safety, this knowledge is not easily accessible to clinicians, practitioners, risk managers, and other decision-makers, such as designers and architects of health care facilities. ... A. and Schwappach, D. (2019), "Case Study: More Patient Safety by ...
Design/methodology/approach: A descriptive-analytical case study was carried out at Ernesto Dornelles Hospital, a private Brazilian institution. The Brazilian version of the Hospital Survey on Patient Safety Culture was used to assess the perceptions of 618 participants, of whom 315 worked in healthcare assistance and 303 in administrative ...
Patient safety after implementation of a coproduced family centered communication programme: multicenter before and after intervention study. December 19, 2018 Design and implementation of an application and associated services to support interdisciplinary medication reconciliation efforts at an integrated healthcare delivery network.
Data sources and measures. We employed a cross-sectional study design which assessed the associations between patient safety culture measures which are the core items from the AHRQ Surveys on Patient Safety Culture® (SOPS®) Hospital Survey 2.0 [] and workplace safety culture measures from the SOPS Workplace Safety Supplemental Item Set for Hospitals [].
The three had reached a head during the fall 2022 Hospital Safety Grades report and have been trending downward since. Ninety-two percent of hospitals included in the survey have improved their ...
Study of Massachusetts hospitals underscores importance of patient safety, need for continued improvement Jan 11, 2023 Drug-drug interactions seen in 21.4% of children with medication exposure
C. Sample of documentation q shift X 72 hours or until stable using both SOAP and occurrence based documentation. 4/2/04 11pm. Example 1-SOAP. S: Mrs. P has no evidence of injury resulting from her two falls on 4/1/04 at this time.
Objectives The study aimed to study the association of leadership practices and patient safety culture in a dental hospital. Design Hospital-based, cross-sectional study Setting Riphah Dental Hospital (RDH), Islamabad, Pakistan. Participants All dentists working at RDH were invited to participate. Main outcome measures A questionnaire comprised of the Transformational Leadership Scale (TLS ...
The paper reports results from a research project with the objective of studying patient safety, and relates the finding to safety issues within transfusion medicine. ... Patient safety challenges in a case study hospital--of relevance for transfusion processes? Transfus Apher Sci. 2008 Oct;39(2):167-72. doi: 10.1016/j.transci.2008.06.003.
FILE - The general view of the Oregon State Hospital is seen, May 24, 2013, in Salem, Ore. A federal report says safety lapses at the Oregon State Hospital contributed to recent patient-on-patient assaults.
Direct-to-onsumer telemedicine (DTCT) has become popular as an alternative to traditional care. However, uncertainties about the potential risks associated with the lack of comprehensive quality evaluation could influence its long-term development. This study aimed to assess the quality of care provided by DTCT platforms in China using unannounced standardised patients (USP) between July 2021 ...
Unprofessional behavior negatively impacts teamwork, safety culture, and patient safety.This study analyzed 1,310 reports of unprofessional behavior across eight Australian hospitals between 2017-2020. The researchers found that three in ten reports indicated a risk to patient safety, such as interruptions, poor handover communication, and a lack of adherence to hospital policy or protocol.
Precise AI solutions to enhance patient safety in operating rooms. With the PE200U edge computer, hospitals have successfully reduced the time needed for equipment check-up. Most importantly, have reduce the risk of guidewire retention inpatient's body after having a clinical procedure, also patient safety is much more emphasized.
This article applies systems thinking to a medicines management case study, to highlight how quality-improvement practitioners can use the approach to underpin planning and implementation of patient-safety initiatives. The case study is specific to transcribing in children's hospices, but the strategies can be applied to other areas. The ...