Example sentences clinical presentation
Definition of 'clinical' clinical.


Definition of 'present' present
Cobuild collocations clinical presentation.
Browse alphabetically clinical presentation
- clinical pharmacology
- clinical phenotype
- clinical practice
- clinical presentation
- clinical professional
- clinical psychologist
- clinical psychology
- All ENGLISH words that begin with 'C'
Quick word challenge
Quiz Review
Score: 0 / 5
Wordle Helper

Scrabble Tools
Clinical Presentation
Clinical considerations for care of children and adults with confirmed COVID-19
‹ View Table of Contents
- The clinical presentation of COVID-19 ranges from asymptomatic to critical illness.
- An infected person can transmit SARS-CoV-2, the virus that causes COVID-19, before the onset of symptoms. Symptoms can change over the course of illness and can progress in severity.
- Uncommon presentations of COVID-19 can occur, might vary by the age of the patient, and are a challenge to recognize.
- In adults, age is the strongest risk factor for severe COVID-19. The risk of severe COVID-19 increases with increasing age especially for persons over 65 years and with increasing number of certain underlying medical conditions .
Incubation Period
Data suggest that incubation periods may differ by SARS-CoV-2 variant. Meta-analyses of studies published in 2020 identified a pooled mean incubation period of 6.5 days from exposure to symptom onset. (1) A study conducted during high levels of Delta variant transmission reported an incubation period of 4.3 days, (2) and studies performed during high levels of Omicron variant transmission reported a median incubation period of 3–4 days. (3,4)
Presentation
People with COVID-19 may be asymptomatic or may commonly experience one or more of the following symptoms (not a comprehensive list) (5) :
- Fever or chills
- Shortness of breath or difficulty breathing
- Myalgia (Muscle or body aches)
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
The clinical presentation of COVID-19 ranges from asymptomatic to severe illness, and COVID-19 symptoms may change over the course of illness. COVID-19 symptoms can be difficult to differentiate from and can overlap with other viral respiratory illnesses such as influenza(flu) and respiratory syncytial virus (RSV) . Because symptoms may progress quickly, close follow-up is needed, especially for:
- older adults
- people with disabilities
- people with immunocompromising conditions, and
- people with medical conditions that place them at greater risk for severe illness or death.
The NIH COVID-19 Treatment Guidelines group SARS-CoV-2 infection into five categories based on severity of illness:
- Asymptomatic or pre-symptomatic infection : people who test positive for SARS-CoV-2 using a virologic test (i.e., a nucleic acid amplification test [NAAT] or an antigen test) but who have no symptoms that are consistent with COVID-19.
- Mild illness : people who may have any of the various signs and symptoms of COVID-19 but who do not have shortness of breath, dyspnea, or abnormal chest imaging.
- Moderate illness : people who have evidence of lower respiratory disease during clinical assessment or imaging and who have an oxygen saturation (SpO 2 ) ≥94% on room air at sea level.
- Severe illness : people who have oxygen saturation <94% on room air at sea level, a ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO 2 /FiO 2 ) <300 mm Hg, a respiratory rate >30 breaths/min, or lung infiltrates >50%
- Critical illness : people who have respiratory failure, septic shock, or multiple organ dysfunction.
Asymptomatic and presymptomatic presentation
Studies have documented SARS-CoV-2 infection in people who never develop symptoms (asymptomatic presentation) and in people who are asymptomatic when tested but develop symptoms later (presymptomatic presentation). ( 6,7 ) It is unclear what percentage of people who initially appear asymptomatic progress to clinical disease. Multiple publications have reported cases of people with abnormalities on chest imaging that are consistent with COVID-19 very early in the course of illness, even before the onset of symptoms or a positive COVID-19 test. (9)
Radiographic Considerations and Findings
Chest radiographs of patients with severe COVID-19 may demonstrate bilateral air-space consolidation. (23) Chest computed tomography (CT) images from patients with COVID-19 may demonstrate bilateral, peripheral ground glass opacities and consolidation. (24,25) Less common CT findings can include intra- or interlobular septal thickening with ground glass opacities (hazy opacity) or focal and rounded areas of ground glass opacity surrounded by a ring or arc of denser consolidation (reverse halo sign). (24)
Multiple studies suggest that abnormalities on CT or chest radiograph may be present in people who are asymptomatic, pre-symptomatic, or before RT-PCR detection of SARS-CoV-2 RNA in nasopharyngeal specimens. (25)
Common COVID-19 symptoms
Fever, cough, shortness of breath, fatigue, headache, and myalgia are among the most commonly reported symptoms in people with COVID-19. (5) Some people with COVID-19 have gastrointestinal symptoms such as nausea, vomiting, or diarrhea, sometimes prior to having fever or lower respiratory tract signs and symptoms. (10) Loss of smell and taste can occur, although these symptoms are reported to be less common since Omicron began circulating, as compared to earlier during the COVID-19 pandemic. (11,19-21) People can experience SARS-CoV-2 infection (asymptomatic or symptomatic), even if they are up to date with their COVID-19 vaccines or were previously infected. (8)
Several studies have reported ocular symptoms associated with SARS-CoV-2 infection, including redness, tearing, dry eye or foreign body sensation, discharge or increased secretions, and eye itching or pain. (13)
A wide range of dermatologic manifestations have been associated with COVID-19; timing of skin manifestations in relation to other COVID-19 symptoms and signs is variable. (14) Some skin manifestations may be associated with increased disease severity. (15) Images of cutaneous findings in COVID-19 are available from the American Academy of Dermatology .
Uncommon COVID-19 symptoms
Less common presentations of COVID-19 can occur. Older adults may present with different symptoms than children and younger adults. Some older adults can experience SARS-CoV-2 infection accompanied by delirium, falls, reduced mobility or generalized weakness, and glycemic changes. ( 12)
Transmission
People infected with SARS-CoV-2 can transmit the virus even if they are asymptomatic or presymptomatic. ( 16) Peak transmissibility appears to occur early during the infectious period (prior to symptom onset until a few days after), but infected persons can shed infectious virus up to 10 days following infection. (22 ) Both vaccinated and unvaccinated people can transmit SARS-CoV-2. ( 17,18) Clinicians should consider encouraging all people to take the following prevention actions to limit SARS-CoV-2 transmission:
- stay up to date with COVID-19 vaccines,
- test for COVID-19 when symptomatic or exposed to someone with COVID-19, as recommended by CDC,
- wear a high-quality mask when recommended,
- avoiding contact with individuals who have suspected or confirmed COVID-19,
- improving ventilation when possible,
- and follow basic health and hand hygiene guidance .
Clinicians should also recommend that people who are infected with SARS-CoV-2, follow CDC guidelines for isolation.
Table of Contents
- › Clinical Presentation
- Clinical Progression, Management, and Treatment
- Special Clinical Considerations
- Bhaskaran K, Bacon S, Evans SJ, et al. Factors associated with deaths due to COVID-19 versus other causes: population-based cohort analysis of UK primary care data and linked national death registrations within the OpenSAFELY platform. Lancet Reg Health Eur. Jul 2021;6:100109. doi:10.1016/j.lanepe.2021.100109
- Kim L, Garg S, O'Halloran A, et al. Risk Factors for Intensive Care Unit Admission and In-hospital Mortality among Hospitalized Adults Identified through the U.S. Coronavirus Disease 2019 (COVID-19)-Associated Hospitalization Surveillance Network (COVID-NET). Clin Infect Dis. Jul 16 2020;doi:10.1093/cid/ciaa1012
- Kompaniyets L, Pennington AF, Goodman AB, et al. Underlying Medical Conditions and Severe Illness Among 540,667 Adults Hospitalized With COVID-19, March 2020-March 2021. Preventing chronic disease. Jul 1 2021;18:E66. doi:10.5888/pcd18.210123
- Ko JY, Danielson ML, Town M, et al. Risk Factors for COVID-19-associated hospitalization: COVID-19-Associated Hospitalization Surveillance Network and Behavioral Risk Factor Surveillance System. Clin Infect Dis. Sep 18 2020;doi:10.1093/cid/ciaa1419
- Wortham JM, Lee JT, Althomsons S, et al. Characteristics of Persons Who Died with COVID-19 - United States, February 12-May 18, 2020. MMWR Morb Mortal Wkly Rep. Jul 17 2020;69(28):923-929. doi:10.15585/mmwr.mm6928e1
- Yang X, Zhang J, Chen S, et al. Demographic Disparities in Clinical Outcomes of COVID-19: Data From a Statewide Cohort in South Carolina. Open Forum Infect Dis. Sep 2021;8(9):ofab428. doi:10.1093/ofid/ofab428
- Rader B.; Gertz AL, D.; Gilmer, M.; Wronski, L.; Astley, C.; Sewalk, K.; Varrelman, T.; Cohen, J.; Parikh, R.; Reese, H.; Reed, C.; Brownstein J. Use of At-Home COVID-19 Tests — United States, August 23, 2021–March 12, 2022. MMWR Morb Mortal Wkly Rep. April 1, 2022;71(13):489–494. doi:http://dx.doi.org/10.15585/mmwr.mm7113e1
- Pingali C, Meghani M, Razzaghi H, et al. COVID-19 Vaccination Coverage Among Insured Persons Aged >/=16 Years, by Race/Ethnicity and Other Selected Characteristics - Eight Integrated Health Care Organizations, United States, December 14, 2020-May 15, 2021. MMWR Morb Mortal Wkly Rep. Jul 16 2021;70(28):985-990. doi:10.15585/mmwr.mm7028a1
- Wiltz JL, Feehan AK, Molinari NM, et al. Racial and Ethnic Disparities in Receipt of Medications for Treatment of COVID-19 - United States, March 2020-August 2021. MMWR Morb Mortal Wkly Rep. Jan 21 2022;71(3):96-102. doi:10.15585/mmwr.mm7103e1
- Murthy NC, Zell E, Fast HE, et al. Disparities in First Dose COVID-19 Vaccination Coverage among Children 5-11 Years of Age, United States. Emerg Infect Dis. May 2022;28(5):986-989. doi:10.3201/eid2805.220166
- Saelee R, Zell E, Murthy BP, et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties - United States, December 14, 2020-January 31, 2022. MMWR Morb Mortal Wkly Rep. Mar 4 2022;71(9):335-340. doi:10.15585/mmwr.mm7109a2
- Burki TK. The role of antiviral treatment in the COVID-19 pandemic. Lancet Respir Med. Feb 2022;10(2):e18. doi:10.1016/S2213-2600(22)00011-X
- Jayk Bernal A, Gomes da Silva MM, Musungaie DB, et al. Molnupiravir for Oral Treatment of Covid-19 in Nonhospitalized Patients. N Engl J Med. Feb 10 2022;386(6):509-520. doi:10.1056/NEJMoa2116044
- Sjoding MW, Dickson RP, Iwashyna TJ, Gay SE, Valley TS. Racial Bias in Pulse Oximetry Measurement. N Engl J Med. Dec 17 2020;383(25):2477-2478. doi:10.1056/NEJMc2029240
- Jordan TB, Meyers CL, Schrading WA, Donnelly JP. The utility of iPhone oximetry apps: A comparison with standard pulse oximetry measurement in the emergency department. Am J Emerg Med. May 2020;38(5):925-928. doi:10.1016/j.ajem.2019.07.020
- Iuliano AD, Brunkard JM, Boehmer TK, et al. Trends in Disease Severity and Health Care Utilization During the Early Omicron Variant Period Compared with Previous SARS-CoV-2 High Transmission Periods - United States, December 2020-January 2022. MMWR Morb Mortal Wkly Rep. Jan 28 2022;71(4):146-152. doi:10.15585/mmwr.mm7104e4
- Taylor CA, Whitaker M, Anglin O, et al. COVID-19-Associated Hospitalizations Among Adults During SARS-CoV-2 Delta and Omicron Variant Predominance, by Race/Ethnicity and Vaccination Status - COVID-NET, 14 States, July 2021-January 2022. MMWR Morb Mortal Wkly Rep. Mar 25 2022;71(12):466-473. doi:10.15585/mmwr.mm7112e2
- Johnson AG, Amin AB, Ali AR, et al. COVID-19 Incidence and Death Rates Among Unvaccinated and Fully Vaccinated Adults with and Without Booster Doses During Periods of Delta and Omicron Variant Emergence - 25 U.S. Jurisdictions, April 4-December 25, 2021. MMWR Morb Mortal Wkly Rep. Jan 28 2022;71(4):132-138. doi:10.15585/mmwr.mm7104e2
- Danza P, Koo TH, Haddix M, et al. SARS-CoV-2 Infection and Hospitalization Among Adults Aged >/=18 Years, by Vaccination Status, Before and During SARS-CoV-2 B.1.1.529 (Omicron) Variant Predominance - Los Angeles County, California, November 7, 2021-January 8, 2022. MMWR Morb Mortal Wkly Rep. Feb 4 2022;71(5):177-181. doi:10.15585/mmwr.mm7105e1
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Overview and General Information about Oral Presentation
- Daily Presentations During Work Rounds
- The New Patient Presentation
- The Holdover Admission Presentation
- Outpatient Clinic Presentations
- The structure of presentations varies from service to service (e.g. medicine vs. surgery), amongst subspecialties, and between environments (inpatient vs. outpatient). Applying the correct style to the right setting requires that the presenter seek guidance from the listeners at the outset.
- Time available for presenting is rather short, which makes the experience more stressful.
- Individual supervisors (residents, faculty) often have their own (sometimes quirky) preferences regarding presentation styles, adding another layer of variability that the presenter has to manage.
- Students are evaluated/judged on the way in which they present, with faculty using this as one way of gauging a student’s clinical knowledge.
- Done well, presentations promote efficient, excellent care. Done poorly, they promote tedium, low morale, and inefficiency.
General Tips:
- Practice, Practice, Practice! Do this on your own, with colleagues, and/or with anyone who will listen (and offer helpful commentary) before you actually present in front of other clinicians. Speaking "on-the-fly" is difficult, as rapidly organizing and delivering information in a clear and concise fashion is not a naturally occurring skill.
- Immediately following your presentations, seek feedback from your listeners. Ask for specifics about what was done well and what could have been done better – always with an eye towards gaining information that you can apply to improve your performance the next time.
- Listen to presentations that are done well – ask yourself, “Why was it good?” Then try to incorporate those elements into your own presentations.
- Listen to presentations that go poorly – identify the specific things that made it ineffective and avoid those pitfalls when you present.
- Effective presentations require that you have thought through the case beforehand and understand the rationale for your conclusions and plan. This, in turn, requires that you have a good grasp of physiology, pathology, clinical reasoning and decision-making - pushing you to read, pay attention, and in general acquire more knowledge.
- Think about the clinical situation in which you are presenting so that you can provide a summary that is consistent with the expectations of your audience. Work rounds, for example, are clearly different from conferences and therefore mandate a different style of presentation.
- Presentations are the way in which we tell medical stories to one another. When you present, ask yourself if you’ve described the story in an accurate way. Will the listener be able to “see” the patient the same way that you do? Can they come to the correct conclusions? If not, re-calibrate.
- It's O.K. to use notes, though the oral presentation should not simply be reduced to reading the admission note – rather, it requires appropriate editing/shortening.
- In general, try to give your presentations on a particular service using the same order and style for each patient, every day. Following a specific format makes it easier for the listener to follow, as they know what’s coming and when they can expect to hear particular information. Additionally, following a standardized approach makes it easier for you to stay organized, develop a rhythm, and lessens the chance that you’ll omit elements.
Specific types of presentations
There are a number of common presentation-types, each with its own goals and formats. These include:
- Daily presentations during work rounds for patients known to a service.
- Newly admitted patients, where you were the clinician that performed the H&P.
- Newly admitted patients that were “handed off” to the team in the morning, such that the H&P was performed by others.
- Outpatient clinic presentations, covering several common situations.
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics.
Note that there is an acceptable range of how oral presentations can be delivered. Ultimately, your goal is to tell the correct story, in a reasonable amount of time, so that the right care can be delivered. Nuances in the order of presentation, what to include, what to omit, etc. are relatively small points. Don’t let the pursuit of these elements distract you or create undue anxiety.
Daily presentations during work rounds of patients that you’re following:
- Organize the presenter (forces you to think things through)
- Inform the listener(s) of 24 hour events and plan moving forward
- Promote focused discussion amongst your listeners and supervisors
- Opportunity to reassess plan, adjust as indicated
- Demonstrate your knowledge and engagement in the care of the patient
- Rapid (5 min) presentation of the key facts
Key features of presentation:
- Opening one liner: Describe who the patient is, number of days in hospital, and their main clinical issue(s).
- 24-hour events: Highlighting changes in clinical status, procedures, consults, etc.
- Subjective sense from the patient about how they’re feeling, vital signs (ranges), and key physical exam findings (highlighting changes)
- Relevant labs (highlighting changes) and imaging
- Assessment and Plan : Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
Example of a daily presentation for a patient known to a team:
- Opening one liner: This is Mr. Smith, a 65 year old man, Hospital Day #3, being treated for right leg cellulitis
- MRI of the leg, negative for osteomyelitis
- Evaluation by Orthopedics, who I&D’d a superficial abscess in the calf, draining a moderate amount of pus
- Patient appears well, states leg is feeling better, less painful
- T Max 101 yesterday, T Current 98; Pulse range 60-80; BP 140s-160s/70-80s; O2 sat 98% Room Air
- Ins/Outs: 3L in (2 L NS, 1 L po)/Out 4L urine
- Right lower extremity redness now limited to calf, well within inked lines – improved compared with yesterday; bandage removed from the I&D site, and base had small amount of purulence; No evidence of fluctuance or undrained infection.
- Creatinine .8, down from 1.5 yesterday
- WBC 8.7, down from 14
- Blood cultures from admission still negative
- Gram stain of pus from yesterday’s I&D: + PMNS and GPCs; Culture pending
- MRI lower extremity as noted above – negative for osteomyelitis
- Continue Vancomycin for today
- Ortho to reassess I&D site, though looks good
- Follow-up on cultures: if MRSA, will transition to PO Doxycycline; if MSSA, will use PO Dicloxacillin
- Given AKI, will continue to hold ace-inhibitor; will likely wait until outpatient follow-up to restart
- Add back amlodipine 5mg/d today
- Hep lock IV as no need for more IVF
- Continue to hold ace-I as above
- Wound care teaching with RNs today – wife capable and willing to assist. She’ll be in this afternoon.
- Set up follow-up with PMD to reassess wound and cellulitis within 1 week
The Brand New Patient (admitted by you)
- Provide enough information so that the listeners can understand the presentation and generate an appropriate differential diagnosis.
- Present a thoughtful assessment
- Present diagnostic and therapeutic plans
- Provide opportunities for senior listeners to intervene and offer input
- Chief concern: Reason why patient presented to hospital (symptom/event and key past history in one sentence). It often includes a limited listing of their other medical conditions (e.g. diabetes, hypertension, etc.) if these elements might contribute to the reason for admission.
- The history is presented highlighting the relevant events in chronological order.
- 7 days ago, the patient began to notice vague shortness of breath.
- 5 days ago, the breathlessness worsened and they developed a cough productive of green sputum.
- 3 days ago his short of breath worsened to the point where he was winded after walking up a flight of stairs, accompanied by a vague right sided chest pain that was more pronounced with inspiration.
- Enough historical information has to be provided so that the listener can understand the reasons that lead to admission and be able to draw appropriate clinical conclusions.
- Past history that helps to shed light on the current presentation are included towards the end of the HPI and not presented later as “PMH.” This is because knowing this “past” history is actually critical to understanding the current complaint. For example, past cardiac catheterization findings and/or interventions should be presented during the HPI for a patient presenting with chest pain.
- Where relevant, the patient's baseline functional status is described, allowing the listener to understand the degree of impairment caused by the acute medical problem(s).
- It should be explicitly stated if a patient is a poor historian, confused or simply unaware of all the details related to their illness. Historical information obtained from family, friends, etc. should be described as such.
- Review of Systems (ROS): Pertinent positive and negative findings discovered during a review of systems are generally incorporated at the end of the HPI. The listener needs this information to help them put the story in appropriate perspective. Any positive responses to a more inclusive ROS that covers all of the other various organ systems are then noted. If the ROS is completely negative, it is generally acceptable to simply state, "ROS negative.”
- Other Past Medical and Surgical History (PMH/PSH): Past history that relates to the issues that lead to admission are typically mentioned in the HPI and do not have to be repeated here. That said, selective redundancy (i.e. if it’s really important) is OK. Other PMH/PSH are presented here if relevant to the current issues and/or likely to affect the patient’s hospitalization in some way. Unrelated PMH and PSH can be omitted (e.g. if the patient had their gall bladder removed 10y ago and this has no bearing on the admission, then it would be appropriate to leave it out). If the listener really wants to know peripheral details, they can read the admission note, ask the patient themselves, or inquire at the end of the presentation.
- Medications and Allergies: Typically all meds are described, as there’s high potential for adverse reactions or drug-drug interactions.
- Family History: Emphasis is placed on the identification of illnesses within the family (particularly among first degree relatives) that are known to be genetically based and therefore potentially heritable by the patient. This would include: coronary artery disease, diabetes, certain cancers and autoimmune disorders, etc. If the family history is non-contributory, it’s fine to say so.
- Social History, Habits, other → as relates to/informs the presentation or hospitalization. Includes education, work, exposures, hobbies, smoking, alcohol or other substance use/abuse.
- Sexual history if it relates to the active problems.
- Vital signs and relevant findings (or their absence) are provided. As your team develops trust in your ability to identify and report on key problems, it may become acceptable to say “Vital signs stable.”
- Note: Some listeners expect students (and other junior clinicians) to describe what they find in every organ system and will not allow the presenter to say “normal.” The only way to know what to include or omit is to ask beforehand.
- Key labs and imaging: Abnormal findings are highlighted as well as changes from baseline.
- Summary, assessment & plan(s) Presented by problem or organ systems(s), using as many or few as are relevant. Early on, it’s helpful to go through the main categories in your head as a way of making sure that you’re not missing any relevant areas. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- The assessment and plan typically concludes by mentioning appropriate prophylactic considerations (e.g. DVT prevention), code status and disposition.
- Chief Concern: Mr. H is a 50 year old male with AIDS, on HAART, with preserved CD4 count and undetectable viral load, who presents for the evaluation of fever, chills and a cough over the past 7 days.
- Until 1 week ago, he had been quite active, walking up to 2 miles a day without feeling short of breath.
- Approximately 1 week ago, he began to feel dyspneic with moderate activity.
- 3 days ago, he began to develop subjective fevers and chills along with a cough productive of red-green sputum.
- 1 day ago, he was breathless after walking up a single flight of stairs and spent most of the last 24 hours in bed.
- Diagnosed with HIV in 2000, done as a screening test when found to have gonococcal urethritis
- Was not treated with HAART at that time due to concomitant alcohol abuse and non-adherence.
- Diagnosed and treated for PJP pneumonia 2006
- Diagnosed and treated for CMV retinitis 2007
- Became sober in 2008, at which time interested in HAART. Started on Atripla, a combination pill containing: Efavirenz, Tonofovir, and Emtricitabine. He’s taken it ever since, with no adverse effects or issues with adherence. Receives care thru Dr. Smiley at the University HIV clinic.
- CD4 count 3 months ago was 400 and viral load was undetectable.
- He is homosexual though he is currently not sexually active. He has never used intravenous drugs.
- He has no history of asthma, COPD or chronic cardiac or pulmonary condition. No known liver disease. Hepatitis B and C negative. His current problem seems different to him then his past episode of PJP.
- Review of systems: negative for headache, photophobia, stiff neck, focal weakness, chest pain, abdominal pain, diarrhea, nausea, vomiting, urinary symptoms, leg swelling, or other complaints.
- Hypertension x 5 years, no other known vascular disease
- Gonorrhea as above
- Alcohol abuse above and now sober – no known liver disease
- No relevant surgeries
- Atripla, 1 po qd
- Omeprazole 20 mg, 1 PO, qd
- Lisinopril 20mg, qd
- Naprosyn 250 mg, 1-2, PO, BID PRN
- No allergies
- Both of the patient's parents are alive and well (his mother is 78 and father 80). He has 2 brothers, one 45 and the other 55, who are also healthy. There is no family history of heart disease or cancer.
- Patient works as an accountant for a large firm in San Diego. He lives alone in an apartment in the city.
- Smokes 1 pack of cigarettes per day and has done so for 20 years.
- No current alcohol use. Denies any drug use.
- Sexual History as noted above; has sex exclusively with men, last partner 6 months ago.
- Seated on a gurney in the ER, breathing through a face-mask oxygen delivery system. Breathing was labored and accessory muscles were in use. Able to speak in brief sentences, limited by shortness of breath
- Vital signs: Temp 102 F, Pulse 90, BP 150/90, Respiratory Rate 26, O2 Sat (on 40% Face Mask) 95%
- HEENT: No thrush, No adenopathy
- Lungs: Crackles and Bronchial breath sounds noted at right base. E to A changes present. No wheezing or other abnormal sounds noted over any other area of the lung. Dullness to percussion was also appreciated at the right base.
- Cardiac: JVP less than 5 cm; Rhythm was regular. Normal S1 and S2. No murmurs or extra heart sounds noted.
- Abdomen and Genital exams: normal
- Extremities: No clubbing, cyanosis or edema; distal pulses 2+ and equal bilaterally.
- Skin: no eruptions noted.
- Neurological exam: normal
- WBC 18 thousand with 10% bands;
- Normal Chem 7 and LFTs.
- Room air blood gas: pH of 7.47/ PO2 of 55/PCO2 of 30.
- Sputum gram stain remarkable for an abundance of polys along with gram positive diplococci.
- CXR remarkable for dense right lower lobe infiltrate without effusion.
- Monitored care unit, with vigilance for clinical deterioration.
- Hypertension: given significant pneumonia and unclear clinical direction, will hold lisinopril. If BP > 180 and or if clear not developing sepsis, will consider restarting.
- Low molecular weight heparin
- Code Status: Wishes to be full code full care, including intubation and ICU stay if necessary. Has good quality of life and hopes to return to that functional level. Wishes to reconsider if situation ever becomes hopeless. Older brother Tom is surrogate decision maker if the patient can’t speak for himself. Tom lives in San Diego and we have his contact info. He is aware that patient is in the hospital and plans on visiting later today or tomorrow.
- Expected duration of hospitalization unclear – will know more based on response to treatment over next 24 hours.
The holdover admission (presenting data that was generated by other physicians)
- Handoff admissions are very common and present unique challenges
- Understand the reasons why the patient was admitted
- Review key history, exam, imaging and labs to assure that they support the working diagnostic and therapeutic plans
- Does the data support the working diagnosis?
- Do the planned tests and consults make sense?
- What else should be considered (both diagnostically and therapeutically)?
- This process requires that the accepting team thoughtfully review their colleagues efforts with a critical eye – which is not disrespectful but rather constitutes one of the main jobs of the accepting team and is a cornerstone of good care *Note: At some point during the day (likely not during rounds), the team will need to verify all of the data directly with the patient.
- 8-10 minutes
- Chief concern: Reason for admission (symptom and/or event)
- Temporally presented bullets of events leading up to the admission
- Review of systems
- Relevant PMH/PSH – historical information that might affect the patient during their hospitalization.
- Meds and Allergies
- Family and Social History – focusing on information that helps to inform the current presentation.
- Habits and exposures
- Physical exam, imaging and labs that were obtained in the Emergency Department
- Assessment and plan that were generated in the Emergency Department.
- Overnight events (i.e. what happened in the Emergency Dept. and after the patient went to their hospital room)? Responses to treatments, changes in symptoms?
- How does the patient feel this morning? Key exam findings this morning (if seen)? Morning labs (if available)?
- Assessment and Plan , with attention as to whether there needs to be any changes in the working differential or treatment plan. The broad organ system categories include (presented here head-to-toe): Neurological; Psychiatric; Cardiovascular; Pulmonary; Gastrointestinal; Renal/Genitourinary; Hematologic/Oncologic; Endocrine/Metabolic; Infectious; Tubes/lines/drains; Disposition.
- Chief concern: 70 yo male who presented with 10 days of progressive shoulder pain, followed by confusion. He was brought in by his daughter, who felt that her father was no longer able to safely take care for himself.
- 10 days ago, Mr. X developed left shoulder pain, first noted a few days after lifting heavy boxes. He denies falls or direct injury to the shoulder.
- 1 week ago, presented to outside hospital ER for evaluation of left shoulder pain. Records from there were notable for his being afebrile with stable vitals. Exam notable for focal pain anteriorly on palpation, but no obvious deformity. Right shoulder had normal range of motion. Left shoulder reported as diminished range of motion but not otherwise quantified. X-ray negative. Labs remarkable for wbc 8, creat 2.2 (stable). Impression was that the pain was of musculoskeletal origin. Patient was provided with Percocet and told to see PMD in f/u
- Brought to our ER last night by his daughter. Pain in shoulder worse. Also noted to be confused and unable to care for self. Lives alone in the country, home in disarray, no food.
- ROS: negative for falls, prior joint or musculoskeletal problems, fevers, chills, cough, sob, chest pain, head ache, abdominal pain, urinary or bowel symptoms, substance abuse
- Hypertension
- Coronary artery disease, s/p LAD stent for angina 3 y ago, no symptoms since. Normal EF by echo 2 y ago
- Chronic kidney disease stage 3 with creatinine 1.8; felt to be secondary to atherosclerosis and hypertension
- aspirin 81mg qd, atorvastatin 80mg po qd, amlodipine 10 po qd, Prozac 20
- Allergies: none
- Family and Social: lives alone in a rural area of the county, in contact with children every month or so. Retired several years ago from work as truck driver. Otherwise non-contributory.
- Habits: denies alcohol or other drug use.
- Temp 98 Pulse 110 BP 100/70
- Drowsy though arousable; oriented to year but not day or date; knows he’s at a hospital for evaluation of shoulder pain, but doesn’t know the name of the hospital or city
- CV: regular rate and rhythm; normal s1 and s2; no murmurs or extra heart sounds.
- Left shoulder with generalized swelling, warmth and darker coloration compared with Right; generalized pain on palpation, very limited passive or active range of motion in all directions due to pain. Right shoulder appearance and exam normal.
- CXR: normal
- EKG: sr 100; nl intervals, no acute changes
- WBC 13; hemoglobin 14
- Na 134, k 4.6; creat 2.8 (1.8 baseline 4 m ago); bicarb 24
- LFTs and UA normal
- Vancomycin and Zosyn for now
- Orthopedics to see asap to aspirate shoulder for definitive diagnosis
- If aspiration is consistent with infection, will need to go to Operating Room for wash out.
- Urine electrolytes
- Follow-up on creatinine and obtain renal ultrasound if not improved
- Renal dosing of meds
- Strict Ins and Outs.
- follow exam
- obtain additional input from family to assure baseline is, in fact, normal
- Since admission (6 hours) no change in shoulder pain
- This morning, pleasant, easily distracted; knows he’s in the hospital, but not date or year
- T Current 101F Pulse 100 BP 140/80
- Ins and Outs: IVF Normal Saline 3L/Urine output 1.5 liters
- L shoulder with obvious swelling and warmth compared with right; no skin breaks; pain limits any active or passive range of motion to less than 10 degrees in all directions
- Labs this morning remarkable for WBC 10 (from 13), creatinine 2 (down from 2.8)
- Continue with Vancomycin and Zosyn for now
- I already paged Orthopedics this morning, who are en route for aspiration of shoulder, fluid for gram stain, cell count, culture
- If aspirate consistent with infection, then likely to the OR
- Continue IVF at 125/h, follow I/O
- Repeat creatinine later today
- Not on any nephrotoxins, meds renaly dosed
- Continue antibiotics, evaluation for primary source as above
- Discuss with family this morning to establish baseline; possible may have underlying dementia as well
- SC Heparin for DVT prophylaxis
- Code status: full code/full care.
Outpatient-based presentations
There are 4 main types of visits that commonly occur in an outpatient continuity clinic environment, each of which has its own presentation style and purpose. These include the following, each described in detail below.
- The patient who is presenting for their first visit to a primary care clinic and is entirely new to the physician.
- The patient who is returning to primary care for a scheduled follow-up visit.
- The patient who is presenting with an acute problem to a primary care clinic
- The specialty clinic evaluation (new or follow-up)
It’s worth noting that Primary care clinics (Internal Medicine, Family Medicine and Pediatrics) typically take responsibility for covering all of the patient’s issues, though the amount of energy focused on any one topic will depend on the time available, acuity, symptoms, and whether that issue is also followed by a specialty clinic.
The Brand New Primary Care Patient
Purpose of the presentation
- Accurately review all of the patient’s history as well as any new concerns that they might have.
- Identify health related problems that need additional evaluation and/or treatment
- Provide an opportunity for senior listeners to intervene and offer input
Key features of the presentation
- If this is truly their first visit, then one of the main reasons is typically to "establish care" with a new doctor.
- It might well include continuation of therapies and/or evaluations started elsewhere.
- If the patient has other specific goals (medications, referrals, etc.), then this should be stated as well. Note: There may well not be a "chief complaint."
- For a new patient, this is an opportunity to highlight the main issues that might be troubling/bothering them.
- This can include chronic disorders (e.g. diabetes, congestive heart failure, etc.) which cause ongoing symptoms (shortness of breath) and/or generate daily data (finger stick glucoses) that should be discussed.
- Sometimes, there are no specific areas that the patient wishes to discuss up-front.
- Review of systems (ROS): This is typically comprehensive, covering all organ systems. If the patient is known to have certain illnesses (e.g. diabetes), then the ROS should include the search for disorders with high prevalence (e.g. vascular disease). There should also be some consideration for including questions that are epidemiologically appropriate (e.g. based on age and sex).
- Past Medical History (PMH): All known medical conditions (in particular those requiring ongoing treatment) are listed, noting their duration and time of onset. If a condition is followed by a specialist or co-managed with other clinicians, this should be noted as well. If a problem was described in detail during the “acute” history, it doesn’t have to be re-stated here.
- Past Surgical History (PSH): All surgeries, along with the year when they were performed
- Medications and allergies: All meds, including dosage, frequency and over-the-counter preparations. Allergies (and the type of reaction) should be described.
- Social: Work, hobbies, exposures.
- Sexual activity – may include type of activity, number and sex of partner(s), partner’s health.
- Smoking, Alcohol, other drug use: including quantification of consumption, duration of use.
- Family history: Focus on heritable illness amongst first degree relatives. May also include whether patient married, in a relationship, children (and their ages).
- Physical Exam: Vital signs and relevant findings (or their absence).
- Key labs and imaging if they’re available. Also when and where they were obtained.
- Summary, assessment & plan(s) presented by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic. This typically concludes with a “health care maintenance” section, which covers age, sex and risk factor appropriate vaccinations and screening tests.
The Follow-up Visit to a Primary Care Clinic
- Organize the presenter (forces you to think things through).
- Accurately review any relevant interval health care events that might have occurred since the last visit.
- Identification of new symptoms or health related issues that might need additional evaluation and/or treatment
- If the patient has no concerns, then verification that health status is stable
- Review of medications
- Provide an opportunity for listeners to intervene and offer input
- Reason for the visit: Follow-up for whatever the patient’s main issues are, as well as stating when the last visit occurred *Note: There may well not be a “chief complaint,” as patients followed in continuity at any clinic may simply be returning for a visit as directed by their doctor.
- Events since the last visit: This might include emergency room visits, input from other clinicians/specialists, changes in medications, new symptoms, etc.
- Review of Systems (ROS): Depth depends on patient’s risk factors and known illnesses. If the patient has diabetes, then a vascular ROS would be done. On the other hand, if the patient is young and healthy, the ROS could be rather cursory.
- PMH, PSH, Social, Family, Habits are all OMITTED. This is because these facts are already known to the listener and actionable aspects have presumably been added to the problem list (presented at the end). That said, these elements can be restated if the patient has a new symptom or issue related to a historical problem has emerged.
- MEDS : A good idea to review these at every visit.
- Physical exam: Vital signs and pertinent findings (or absence there of) are mentioned.
- Lab and Imaging: The reason why these were done should be mentioned and any key findings mentioned, highlighting changes from baseline.
- Assessment and Plan: This is most clearly done by individually stating all of the conditions/problems that are being addressed (e.g. hypertension, hypothyroidism, depression, etc.) followed by their specific plan(s). If a new or acute issue was identified during the visit, the diagnostic and therapeutic plan for that concern should be described.
The Focused Visit to a Primary Care Clinic
- Accurately review the historical events that lead the patient to make the appointment.
- Identification of risk factors and/or other underlying medical conditions that might affect the diagnostic or therapeutic approach to the new symptom or concern.
- Generate an appropriate assessment and plan
- Allow the listener to comment
Key features of the presentation:
- Reason for the visit
- History of Present illness: Description of the sequence of symptoms and/or events that lead to the patient’s current condition.
- Review of Systems: To an appropriate depth that will allow the listener to grasp the full range of diagnostic possibilities that relate to the presenting problem.
- PMH and PSH: Stating only those elements that might relate to the presenting symptoms/issues.
- PE: Vital signs and key findings (or lack thereof)
- Labs and imaging (if done)
- Assessment and Plan: This is usually very focused and relates directly to the main presenting symptom(s) or issues.
The Specialty Clinic Visit
Specialty clinic visits focus on the health care domains covered by those physicians. For example, Cardiology clinics are interested in cardiovascular disease related symptoms, events, labs, imaging and procedures. Orthopedics clinics will focus on musculoskeletal symptoms, events, imaging and procedures. Information that is unrelated to these disciples will typically be omitted. It’s always a good idea to ask the supervising physician for guidance as to what’s expected to be covered in a particular clinic environment.
- Highlight the reason(s) for the visit
- Review key data
- Provide an opportunity for the listener(s) to comment
- 5-7 minutes
- If it’s a consult, state the main reason(s) that the patient was referred as well as who referred them.
- If it’s a return visit, state the reasons why the patient is being followed in the clinic and when the last visit took place
- If it’s for an acute issue, state up front what the issue is Note: There may well not be a “chief complaint,” as patients followed in continuity in any clinic may simply be returning for a return visit as directed
- For a new patient, this highlights the main things that might be troubling/bothering the patient.
- For a specialty clinic, the history presented typically relates to the symptoms and/or events that are pertinent to that area of care.
- Review of systems , focusing on those elements relevant to that clinic. For a cardiology patient, this will highlight a vascular ROS.
- PMH/PSH that helps to inform the current presentation (e.g. past cardiac catheterization findings/interventions for a patient with chest pain) and/or is otherwise felt to be relevant to that clinic environment.
- Meds and allergies: Typically all meds are described, as there is always the potential for adverse drug interactions.
- Social/Habits/other: as relates to/informs the presentation and/or is relevant to that clinic
- Family history: Focus is on heritable illness amongst first degree relatives
- Physical Exam: VS and relevant findings (or their absence)
- Key labs, imaging: For a cardiology clinic patient, this would include echos, catheterizations, coronary interventions, etc.
- Summary, assessment & plan(s) by organ system and/or problems. As many systems/problems as is necessary to cover all of the active issues that are relevant to that clinic.
- Reason for visit: Patient is a 67 year old male presenting for first office visit after admission for STEMI. He was referred by Dr. Goins, his PMD.
- The patient initially presented to the ER 4 weeks ago with acute CP that started 1 hour prior to his coming in. He was found to be in the midst of a STEMI with ST elevations across the precordial leads.
- Taken urgently to cath, where 95% proximal LAD lesion was stented
- EF preserved by Echo; Peak troponin 10
- In-hospital labs were remarkable for normal cbc, chem; LDL 170, hdl 42, nl lfts
- Uncomplicated hospital course, sent home after 3 days.
- Since home, he states that he feels great.
- Denies chest pain, sob, doe, pnd, edema, or other symptoms.
- No symptoms of stroke or TIA.
- No history of leg or calf pain with ambulation.
- Prior to this admission, he had a history of hypertension which was treated with lisinopril
- 40 pk yr smoking history, quit during hospitalization
- No known prior CAD or vascular disease elsewhere. No known diabetes, no family history of vascular disease; He thinks his cholesterol was always “a little high” but doesn’t know the numbers and was never treated with meds.
- History of depression, well treated with prozac
- Discharge meds included: aspirin, metoprolol 50 bid, lisinopril 10, atorvastatin 80, Plavix; in addition he takes Prozac for depression
- Taking all of them as directed.
- Patient lives with his wife; they have 2 grown children who are no longer at home
- Works as a computer programmer
- Smoking as above
- ETOH: 1 glass of wine w/dinner
- No drug use
- No known history of cardiovascular disease among 2 siblings or parents.
- Well appearing; BP 130/80, Pulse 80 regular, 97% sat on Room Air, weight 175lbs, BMI 32
- Lungs: clear to auscultation
- CV: s1 s2 no s3 s4 murmur
- No carotid bruits
- ABD: no masses
- Ext; no edema; distal pulses 2+
- Cath from 4 weeks ago: R dominant; 95% proximal LAD; 40% Cx.
- EF by TTE 1 day post PCI with mild Anterior Hypokinesis, EF 55%, no valvular disease, moderate LVH
- Labs of note from the hospital following cath: hgb 14, plt 240; creat 1, k 4.2, lfts normal, glucose 100, LDL 170, HDL 42.
- EKG today: SR at 78; nl intervals; nl axis; normal r wave progression, no q waves
- Plan: aspirin 81 indefinitely, Plavix x 1y
- Given nitroglycerine sublingual to have at home.
- Reviewed symptoms that would indicate another MI and what to do if occurred
- Plan: continue with current dosages of meds
- Chem 7 today to check k, creatinine
- Plan: Continue atorvastatin 80mg for life
- Smoking cessation: Doing well since discharge without adjuvant treatments, aware of supports.
- Plan: AAA screening ultrasound
The Clinical Presentation
- First Online: 01 January 2013
Cite this chapter

- Sergio V. Delgado 3 &
- Jeffrey R. Strawn 4
980 Accesses
Presenting case material to colleagues requires preparation, whether the presentation is to be made casually during bedside rounds or in the formal environment of a national meeting. It is rewarding when a presentation is well received, particularly because it may prove helpful to other clinicians, allied health professionals, and researchers. Regardless of the setting, the presenter’s goal is to share their knowledge based on observations they have made and lessons they have learned from the case or cases. The most time-consuming aspect of the patient-oriented presentation is collecting and organizing as much information as possible about the patients, their families, and others who were involved in the patients’ care. Once these tasks are complete, the presenter must summarize the information and place it within the context of treatment data and consensus approaches. Tailoring the talk to the audience is also of paramount importance. Different groups will invariably come from different disciplines, and the presentation will need to be tailored to accommodate each audience’s background, interests and goals.
Make everything as simple as possible, but not simpler —Albert Einstein (1879–1955)
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Altman LK (2006) Socratic dialogue gives way to powerpoint®. New York Times, 12 Dec 2006
Google Scholar
Blechner MJ (2012) Confidentiality: against disguise, for consent. Psychotherapy (Chic) 49(1):16–18
Article Google Scholar
Clifft MA (1986) Writing about psychiatric patients. Guidelines for disguising case material. Bull Menninger Clin 50(6):511–524
PubMed CAS Google Scholar
Copeland HL, Hewson MG, Stoller JK et al (1998) Making the continuing medical education lecture effective. J Contin Educ Health Prof 18:227–234
Gabbard GO (2000) Disguise or consent: problems and recommendations concerning the publication and presentation of clinical material. Int J Psychoanal 81:1071–1086
Article PubMed Google Scholar
Gabbard GO, Williams P (2001) Preserving confidentiality in writing of case reports. Int J Psychoanal 82:1067–1068
Article PubMed CAS Google Scholar
Hull AL, Cullen RJ, Hekelman FP (1989) A retrospective analysis of grand rounds in continuing medical education. J Contin Educ Health Prof 9(4):257–266
Lorin MI, Palazzi DL, Turner TL et al (2008) What is a clinical pearl and what is its role in medical education? Med Teach 30(9–10):870–874
Sackett DL, Rosenberg WM, Gray JA et al (1996) Evidence based medicine: what it is and what it isn’t. Br Med J 312:71–72
Article CAS Google Scholar
Tuckett D (2000) Reporting clinical events in the journal: towards the constructing of a special case. Int J Psychoanal 81:1065–1069
Download references
Author information
Authors and affiliations.
Department of Psychiatry and Child Psychiatry, Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio, USA
Sergio V. Delgado
Department of Psychiatry and Behavioral Neuroscience, University of Cincinnati, Cincinnati, Ohio, USA
Jeffrey R. Strawn
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Delgado, S.V., Strawn, J.R. (2014). The Clinical Presentation. In: Difficult Psychiatric Consultations. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-39552-9_8
Download citation
DOI : https://doi.org/10.1007/978-3-642-39552-9_8
Published : 16 September 2013
Publisher Name : Springer, Berlin, Heidelberg
Print ISBN : 978-3-642-39551-2
Online ISBN : 978-3-642-39552-9
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 November 2020
Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis
- Carlos K. H. Wong 1 , 2 na1 ,
- Janet Y. H. Wong 3 na1 ,
- Eric H. M. Tang 1 ,
- C. H. Au 1 &
- Abraham K. C. Wai 4
Scientific Reports volume 10 , Article number: 19765 ( 2020 ) Cite this article
5978 Accesses
47 Citations
3 Altmetric
Metrics details
- Health care
- Medical research
- Microbiology
- Risk factors
This systematic review and meta-analysis investigated the comorbidities, symptoms, clinical characteristics and treatment of COVID-19 patients. Epidemiological studies published in 2020 (from January–March) on the clinical presentation, laboratory findings and treatments of COVID-19 patients were identified from PubMed/MEDLINE and Embase databases. Studies published in English by 27th March, 2020 with original data were included. Primary outcomes included comorbidities of COVID-19 patients, their symptoms presented on hospital admission, laboratory results, radiological outcomes, and pharmacological and in-patient treatments. 76 studies were included in this meta-analysis, accounting for a total of 11,028 COVID-19 patients in multiple countries. A random-effects model was used to aggregate estimates across eligible studies and produce meta-analytic estimates. The most common comorbidities were hypertension (18.1%, 95% CI 15.4–20.8%). The most frequently identified symptoms were fever (72.4%, 95% CI 67.2–77.7%) and cough (55.5%, 95% CI 50.7–60.3%). For pharmacological treatment, 63.9% (95% CI 52.5–75.3%), 62.4% (95% CI 47.9–76.8%) and 29.7% (95% CI 21.8–37.6%) of patients were given antibiotics, antiviral, and corticosteroid, respectively. Notably, 62.6% (95% CI 39.9–85.4%) and 20.2% (95% CI 14.6–25.9%) of in-patients received oxygen therapy and non-invasive mechanical ventilation, respectively. This meta-analysis informed healthcare providers about the timely status of characteristics and treatments of COVID-19 patients across different countries.
PROSPERO Registration Number: CRD42020176589
Similar content being viewed by others
Global prevalence and effect of comorbidities and smoking status on severity and mortality of COVID-19 in association with age and gender: a systematic review, meta-analysis and meta-regression
Frequency, risk factors, and outcomes of hospital readmissions of COVID-19 patients
Risk factors for severe COVID-19 differ by age for hospitalized adults
Introduction.
Following the possible patient zero of coronavirus infection identified in early December 2019 1 , the Coronavirus Disease 2019 (COVID-19) has been recognized as a pandemic in mid-March 2020 2 , after the increasing global attention to the exponential growth of confirmed cases 3 . As on 29th March, 2020, around 690 thousand persons were confirmed infected, affecting 199 countries and territories around the world, in addition to 2 international conveyances: the Diamond Princess cruise ship harbored in Yokohama, Japan, and the Holland America's MS Zaandam cruise ship. Overall, more than 32 thousand died and about 146 thousand have recovered 4 .
A novel bat-origin virus, 2019 novel coronavirus, was identified by means of deep sequencing analysis. SARS-CoV-2 was closely related (with 88% identity) to two bat-derived severe acute respiratory syndrome (SARS)-like coronaviruses, bat-SL-CoVZC45 and bat-SL-CoVZXC21, but were more distant from SARS-CoV (about 79%) and MERS-CoV (about 50%) 5 , both of which were respectively responsible for two zoonotic human coronavirus epidemics in the early twenty-first century. Following a few initial human infections 6 , the disease could easily be transmitted to a substantial number of individuals with increased social gathering 7 and population mobility during holidays in December and January 8 . An early report has described its high infectivity 9 even before the infected becomes symptomatic 10 . These natural and social factors have potentially influenced the general progression and trajectory of the COVID-19 epidemiology.
By the end of March 2020, there have been approximately 3000 reports about COVID-19 11 . The number of COVID-19-related reports keeps growing everyday, yet it is still far from a clear picture on the spectrum of clinical conditions, transmissibility and mortality, alongside the limitation of medical reports associated with reporting in real time the evolution of an emerging pathogen in its early phase. Previous reports covered mostly the COVID-19 patients in China. With the spread of the virus to other continents, there is an imminent need to review the current knowledge on the clinical features and outcomes of the early patients, so that further research and measures on epidemic control could be developed in this epoch of the pandemic.
Search strategy and selection criteria
The systematic review was conducted according to the protocol registered in the PROSPERO database (CRD42020176589). Following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guideline throughout this review, data were identified by searches of MEDLINE, Embase and references from relevant articles using the search terms "COVID", “SARS-CoV-2”, and “novel coronavirus” (Supplementary material 1 ). Articles published in English up to 27th March, 2020 were included. National containment measures have been implemented at many countries, irrespective of lockdown, curfew, or stay-at-home orders, since the mid of March 2020 12 , except for China where imposed Hubei province lockdown at 23th January 2020, Studies with original data including original articles, short and brief communication, letters, correspondences were included. Editorials, viewpoints, infographics, commentaries, reviews, or studies without original data were excluded. Studies were also excluded if they were animal studies, modelling studies, or did not measure symptoms presentation, laboratory findings, treatment and therapeutics during hospitalization.
After the removal of duplicate records, two reviewers (CW and CHA) independently screened the eligibility criteria of study titles, abstracts and full-texts, and reference lists of the studies retrieved by the literature search. Disagreements regarding the procedures of database search, study selection and eligibility were resolved by discussion. The second and the last authors (JW and AW) verified the eligibility of included studies.
Outcomes definitions
Signs and symptoms were defined as the presentation of fever, cough, sore throat, headache, dyspnea, muscle pain, diarrhea, rhinorrhea, anosmia, and ageusia at the hospital admission 13 .
Laboratory findings included a complete blood count (white blood count, neutrophil, lymphocyte, platelet count), procalcitonin, prothrombin time, urea, and serum biochemical measurements (including electrolytes, renal-function and liver-function values, creatine kinase, lactate dehydrogenase, C-reactive protein, Erythrocyte sedimentation rate), and treatment measures (i.e. antiviral therapy, antibiotics, corticosteroid therapy, mechanical ventilation, intubation, respiratory support, and renal replacement therapy). Radiological outcomes included bilateral involvement identified and pneumonia identified by chest radiograph.
Comorbidities of patients evaluated in this study were hypertension, diabetes, chronic obstructive pulmonary disease (COPD), cardiovascular disease, chronic kidney disease, liver disease and cancer.
In-patient treatment included intensive care unit admission, oxygen therapy, non-invasive ventilation, mechanical ventilation, Extracorporeal membrane oxygenation (ECMO), renal replacement therapy, and pharmacological treatment. Use of antiviral and interferon drugs (Lopinavir/ritonavir, Ribavirin, Umifenovir, Interferon-alpha, or Interferon-beta), antibiotic drugs, corticosteroid, and inotropes (Nor-adrenaline, Adrenaline, Vasopressin, Phenylephrine, Dopamine, or Dobutamine) were considered.
Data analysis
Three authors (CW, EHMT and CHA) extracted data using a standardized spreadsheet to record the article type, country of origin, surname of first author, year of publications, sample size, demographics, comorbidities, symptoms, laboratory and radiology results, pharmacological and non-pharmacological treatments.
We aggregated estimates across 90 eligible studies to produce meta-analytic estimates using a random-effects model. For dichotomous outcomes, we estimated the proportion and its respective 95% confidence interval. For laboratory parameters as continuous outcomes, we estimated the mean and standard deviation from the median and interquartile range if the mean and standard deviation were not available from the study 14 , and calculated the mean and its respective 95% confidence intervals. Random-effect models on DerSimonian and Laird method were adopted due to the significant heterogeneity, checked by the I 2 statistics and the p values. I 2 statistic of < 25%, 25–75% and ≥ 75% is considered as low, moderate, high likelihood of heterogeneity. Pooled estimates were calculated and presented by using forest plots. Publication bias was estimated by Egger’s regression test. Funnel plots of outcomes were also presented to assess publication bias.
All statistical analyses were conducted using the STATA Version 13.0 (Statacorp, College Station, TX). The random effects model was generated by the Stata packages ‘Metaprop’ for proportions 15 and ‘Metan’ for continuous variables 16 .
The selection and screen process are presented in Fig. 1 . A total of 241 studies were found by our searching strategy (71 in PubMed and 170 in Embase). 46 records were excluded due to duplication. After screening the abstracts and titles, 100 English studies were with original data and included in full-text screening. By further excluding 10 studies with not reporting symptoms presentation, laboratory findings, treatment and therapeutics, 90 studies 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 and 76 studies with more than one COVID-19 case 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 34 , 35 , 36 , 37 , 38 , 39 , 42 , 43 , 44 , 45 , 49 , 50 , 51 , 53 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 67 , 69 , 70 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 98 , 100 , 101 , 102 , 103 , 104 , 105 were included in the current systematic review and meta-analysis respectively. 73.3% 66 studies were conducted in China. Newcastle–Ottawa Quality Assessment Scale has been used to assess study quality of each included cohort study 107 . 30% (27/90) of included studies had satisfactory or good quality. The summary of the included study is shown in Table 1 .
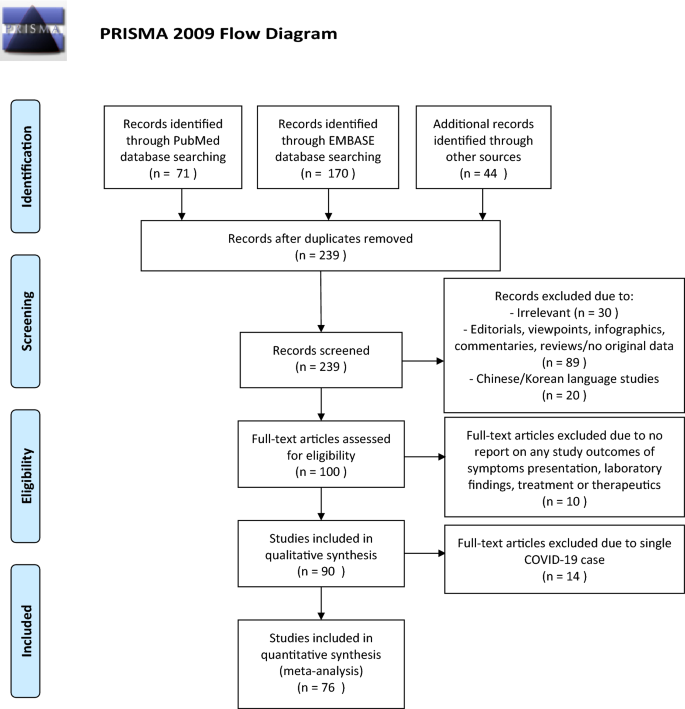
PRISMA flowchart reporting identification, searching and selection processes.
Of those 90 eligible studies, 11,028 COVID-19 patients were identified and included in the systematic review. More than half of patients (6336, 57.5%) were from mainland China. The pooled mean age was 45.8 (95% CI 38.6–52.5) years and 49.3% (pooled 95% CI 45.6–53.0%) of them were male.
For specific comorbidity status, the most prevalent comorbidity was hypertension (18.1%, 95% CI 15.4–20.8%), followed by cardiovascular disease (11.8%, 95% CI 9.4–14.2%) and diabetes (10.4%, 95% CI 8.7–12.1%). The pooled prevalence (95% CI) of COPD, chronic kidney disease, liver disease and cancer were 2.0% (1.3–2.7%), 5.2% (1.7–8.8%), 2.5% (1.7–3.4%) and 2.1% (1.3–2.8%) respectively. Moderate to substantial heterogeneity between reviewed studies were found, with I 2 statistics ranging from 39.4 to 95.9% ( p values between < 0.001–0.041), except for liver disease (I 2 statistics: 1.7%, p = 0.433). Detailed results for comorbidity status are displayed in Fig. 2 .
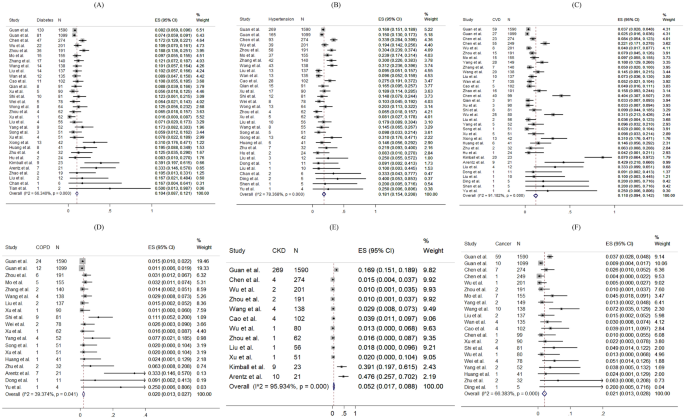
Random-effects meta-analytic estimates for comorbidities. ( A ) Diabetes mellitus, ( B ) Hypertension, ( C ) Cardiovascular disease, ( D ) Chronic obstructive pulmonary disease, ( E ) Chronic kidney disease, ( F ) Cancer.
Regarding the symptoms presented at hospital admission, the most frequent symptoms were fever (pooled prevalence: 72.4%, 95% CI 67.2–77.7%) and cough (pooled prevalence: 55.5%, 95% CI 50.7–60.3%). Sore throat (pooled prevalence: 16.2%, 95% CI 12.7–19.7%), dyspnoea (pooled prevalence: 18.8%, 95% CI 14.7–22.8%) and muscle pain (pooled prevalence: 22.1%, 95% CI 18.6–25.5%) were also common symptoms found in COVID-19 patients, but headache (pooled prevalence: 10.5%, 95% CI 8.7–12.4%), diarrhoea (pooled prevalence: 7.9%, 95% CI 6.3–9.6%), rhinorrhoea (pooled prevalence: 9.2%, 95% CI 5.6–12.8%) were less common. However, none of the included papers reported prevalence of anosmia and ageusia. The I 2 statistics varied from 68.5 to 97.1% (all p values < 0.001), indicating a high heterogeneity exists across studies. Figure 3 shows the pooled proportion of symptoms of patients presented at hospital.
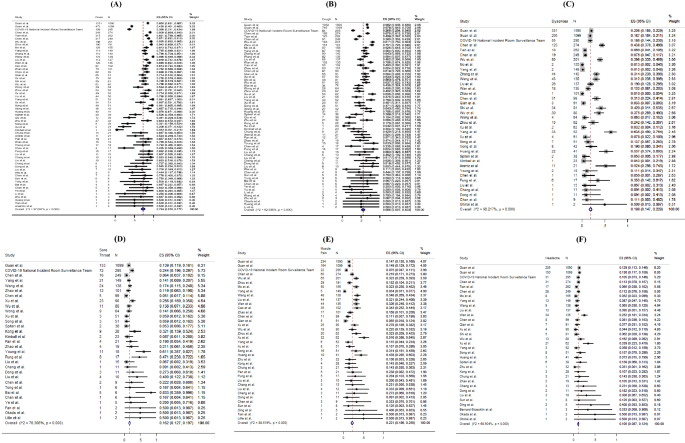
Random-effects meta-analytic estimates for presenting symptoms. ( A ) Fever, ( B ) Cough, ( C ) Dyspnoea, ( D ) Sore throat, ( E ) Muscle pain, ( F ) Headache.
For laboratory parameters, white blood cell (pooled mean: 5.31 × 10 9 /L, 95% CI 5.03–5.58 × 10 9 /L), neutrophil (pooled mean: 3.60 × 10 9 /L, 95% CI 3.31–3.89 × 10 9 /L), lymphocyte (pooled mean: 1.11 × 10 9 /L, 95% CI 1.04–1.17 × 10 9 /L), platelet count (pooled mean: 179.5 U/L, 95% CI 172.6–186.3 U/L), aspartate aminotransferase (pooled mean: 30.3 U/L, 95% CI 27.9–32.7 U/L), alanine aminotransferase (pooled mean: 27.0 U/L, 95% CI 24.4–29.6 U/L) and C-reactive protein (CRP) (pooled mean: 22.0 mg/L, 95% CI 18.3–25.8 mg/L) and D-dimer (0.93 mg/L, 95% CI 0.68–1.18 mg/L) were the common laboratory test taken for COVID-19 patients. Above results and other clinical factors are depicted in Fig. 4 . Same with the comorbidity status and symptoms, high likelihood of heterogeneity was detected by I 2 statistics for a majority of clinical parameters.
Random-effects meta-analytic estimates for laboratory parameters. ( A ) White blood cell, ( B ) Lymphocyte, ( C ) Neutrophil, ( D ) C-creative protein, ( E ) D-dimer, ( F ) Lactate dehydrogenase.
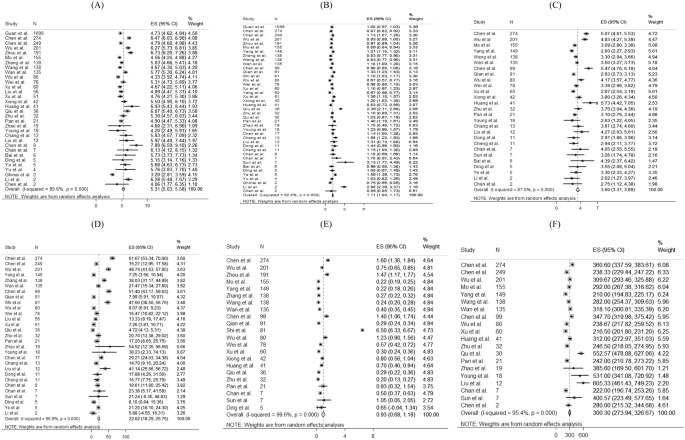
Figure 5 presents the distribution of the pharmacological treatments received for COVID-19 patients. 10.6% of patients admitted to intensive care units (pooled 95% CI 8.1–13.2%). For drug treatment, 63.9% (pooled 95% CI 52.5–75.3%), 62.4% (pooled 95% CI 47.9–76.8%) and 29.7% (pooled 95% CI 21.8–37.6%) patients used antibiotics, antiviral, and corticosteroid, respectively. 41.3% (pooled 95% CI 14.3–68.3%) and 50.7% (pooled 95% CI 9.2–92.3%) reported using Lopinavir/Ritonavir and interferon-alpha as antiviral drug treatment, respectively. Among 14 studies reporting proportion of corticosteroid used, 7 studies (50%) specified the formulation of corticosteroid as systemic corticosteroid. The remaining one specified the use of methylprednisolone. No reviewed studies reported the proportion of patients receiving Ribavirin, Interferon-beta, or inotropes.
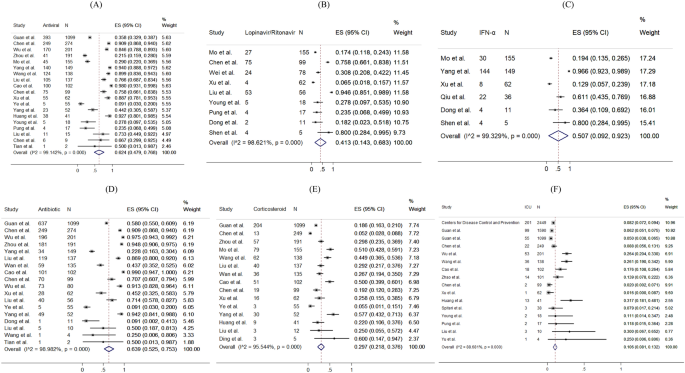
Random-effects meta-analytic estimates for pharmacological treatments and intensive unit care at hospital. ( A ) Antiviral or interferon drugs, ( B ) Lopinavir/Ritonavir, ( C ) Interferon alpha (IFN-α), ( D ) Antibiotic drugs, ( E ) Corticosteroid, ( F ) Admission to Intensive care unit.
The prevalence of radiological outcomes and non-pharmacological treatments were presented in Fig. 6 . Radiology findings detected chest X-ray abnormalities, with 74.4% (95% CI 67.6–81.1%) of patients with bilateral involvement and 74.9% (95% CI 68.0–81.8%) of patients with viral pneumonia. 62.6% (pooled 95% CI 39.9–85.4%), 20.2% (pooled 95% CI 14.6–25.9%), 15.3% (pooled 95% CI 11.0–19.7%), 1.1% (pooled 95% CI 0.4–1.8%) and 4.7% (pooled 95% CI 2.1–7.4%) took oxygen therapy, non-invasive ventilation, mechanical ventilation, ECMO and dialysis respectively.
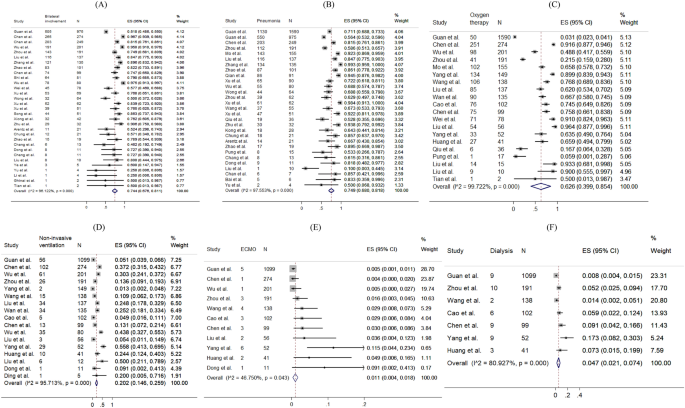
Random-effects meta-analytic estimates for radiological findings and non-pharmacological treatments at hospital. ( A ) Bilateral involvement, ( B ) Pneumonia, ( C ) Oxygen therapy, ( D ) Non-invasive ventilation, ( E ) Extracorporeal membrane oxygenation (ECMO), ( F ) Dialysis.
The funnel plots and results Egger’s test of comorbidity status, symptoms presented, laboratory test and treatment were presented in eFigure 1 – S5 in the Supplement. 63% (19/30) of the funnel plots (eFigure 1 – S5 ) showed significance in the Egger’s test for asymmetry, suggesting the possibility of publication bias or small-study effects caused by clinical heterogeneity.
This meta-analysis reveals the condition of global medical community responding to COVID-19 in the early phase. During the past 4 months, a new major epidemic focus of COVID-19, some without traceable origin, has been identified. Following its first identification in Wuhan, China, the virus has been rapidly spreading to Europe, North America, Asia, and the Middle East, in addition to African and Latin American countries. Three months since Wuhan CDC admitted that there was a cluster of unknown pneumonia cases related to Huanan Seafood Market and a new coronavirus was identified as the cause of the pneumonia 108 , as on 1 April, 2020, there have been 858,371 persons confirmed infected with COVID-19, affecting 202 countries and territories around the world. Although this rapid review is limited by the domination of reports from patients in China, and the patient population is of relative male dominance reflecting the gender imbalance of the Chinese population 109 , it provides essential information.
In this review, the pooled mean age was 45.8 years. Similar to the MERS-CoV pandemic 110 , middle-aged adults were the at-risk group for COVID-19 infections in the initial phase, which was different from the H1N1 influenza pandemic where children and adolescents were more frequently affected 111 . Biological differences may affect the clinical presentations of infections; however, in this review, studies examining the asymptomatic COVID-19 infections or reporting any previous infections were not included. It is suggested that another systematic review should be conducted to compare the age-specific incidence rates between the pre-pandemic and post-pandemic periods, so as to understand the pattern and spread of the disease, and tailor specific strategies in infection control.
Both sexes exhibited clinical presentations similar in symptomatology and frequency to those noted in other severe acute respiratory infections, namely influenza A H1N1 112 and SARS 113 , 114 . These generally included fever, new onset or exacerbation of cough, breathing difficulty, sore throat and muscle pain. Among critically ill patients usually presented with dyspnoea and chest tightness 22 , 29 , 39 , 72 , 141 (4.6%) of them with persistent or progressive hypoxia resulted in the requirement of intubation and mechanical ventilation 115 , while 194 (6.4%) of them required non-invasive ventilation, yielding a total of 11% of patients requiring ventilatory support, which was similar to SARS 116 .
The major comorbidities identified in this review included hypertension, cardiovascular diseases and diabetes mellitus. Meanwhile, the percentages of patients with chronic renal diseases and cancer were relatively low. These chronic conditions influencing the severity of COVID-19 had also been noted to have similar effects in other respiratory illnesses such as SARS, MERS-CoV and influenza 117 , 118 . Higher mortality had been observed among older patients and those with comorbidities.
Early diagnosis of COVID-19 was based on recognition of epidemiological linkages; the presence of typical clinical, laboratory, and radiographic features; and the exclusion of other respiratory pathogens. The case definition had initially been narrow, but was gradually broadened to allow for the detection of more cases, as milder cases and those without epidemiological links to Wuhan or other known cases had been identified 119 , 120 . Laboratory investigations among COVID-19 patients did not reveal specific characteristics—lymphopenia and elevated inflammatory markers such as CRP are some of the most common haematological and biochemical abnormalities, which had also been noticed in SARS 121 . None of these features were specific to COVID-19. Therefore, diagnosis should be confirmed by SARS-CoV–2 specific microbiological and serological studies, although initial management will continue to be based on a clinical and epidemiological assessment of the likelihood of a COVID-19 infection.
Radiology imaging often plays an important role in evaluating patients with acute respiratory distress; however, in this review, radiological findings of SARS-CoV-2 pneumonia were non-specific. Despite chest radiograph usually revealed bilateral involvement and Computed Tomography usually showed bilateral multiple ground-glass opacities or consolidation, there were also patients with normal chest radiograph, implying that chest radiograph might not have high specificity to rule out pneumonia in COVID-19.
Limited clinical data were available for asymptomatic COVID-19 infected persons. Nevertheless, asymptomatic infection could be unknowingly contagious 122 . From some of the official figures, 6.4% of 150 non-travel-related COVID-19 infections in Singapore 123 , 39.9% of cases from the Diamond Princess cruise ship in Japan 124 , and up to 78% of cases in China as extracted on April 1st, 2020, were found to be asymptomatic 122 . 76% (68/90) studies based on hospital setting which provided care and disease management to symptomatic patients had limited number of asymptomatic cases of COVID-19 infection. This review calls for further studies about clinical data of asymptomatic cases. Asymptomatic infection intensifies the challenges of isolation measures. More global reports are crucially needed to give a better picture of the spectrum of presentations among all COVID-19 infected persons. Also, public health policies including social and physical distancing, monitoring and surveillance, as well as contact tracing, are necessary to reduce the spread of COVID-19.
Concerning potential treatment regime, 62.4% of patients received antivirals or interferons (including oseltamivir, lopinavir-ritonavir, interferon alfa), while 63.9% received antibiotics (such as moxifloxacin, and ceftriaxone). In this review, around one-third of patients were given steroid, suggestive as an adjunct to IFN, or sepsis management. Interferon and antiviral agents such as ribavirin, and lopinavir-ritonavir were used during SARS, and the initial uncontrolled reports then noted resolution of fever and improvement in oxygenation and radiographic appearance 113 , 125 , 126 , without further evidence on its effectiveness. At the time of manuscript preparation, there has been no clear evidence guiding the use of antivirals 127 . Further research is needed to inform clinicians of the appropriate use of antivirals for specific groups of infected patients.
Limitations of this meta-analysis should be considered. First, a high statistical heterogeneity was found, which could be related to the highly varied sample sizes (9 to 4226 patients) and study designs. Second, variations of follow-up period may miss the event leading to heterogeneity. In fact, some patients were still hospitalized in the included studies. Third, since only a few studies had compared the comorbidities of severe and non-severe patients, sensitivity analysis and subgroup analysis were not conducted. Fourthly, the frequency and severity of signs and symptoms reported in included studies, primarily based on hospitalized COVID-19 patients were over-estimated. Moreover, different cutoffs for abnormal laboratory findings were applied across countries, and counties within the same countries. Lastly, this meta-analysis reviewed only a limited number of reports written in English, with a predominant patient population from China. This review is expected to inform clinicians of the epidemiology of COVID-19 at this early stage. A recent report estimated the number of confirmed cases in China could reach as high as 232,000 (95% CI 161,000, 359,000) with the case definition adopted in 5th Edition. In this connection, further evidence on the epidemiology is in imminent need.
Oliveira N. Shrimp vendor identified as possible coronavirus ‘patient zero,’ leaked document says. 27 March 2020. New York Daily News. 2020.
World Health Organization. Basic protective measures against the new coronavirus (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 7 Oct 2020.
Google Trend. When will coronavirus end (2020). https://trends.google.com/trends/explore?date=today%203-m&q=when%20will%20coronavirus%20end,%2Fm%2F01cpyy . Accessed 10 Oct 2020.
Worldometer. COVID-19 Coronavirus Pandemic (2020). https://www.worldometers.info/coronavirus/ . Accessed 13 Oct 2020.
Lu, R. et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395 (10224), 565–574 (2020).
Article CAS PubMed PubMed Central Google Scholar
Ralph, R. et al. 2019-nCoV (Wuhan virus), a novel Coronavirus: human-to-human transmission, travel-related cases, and vaccine readiness. J. Infect. Dev. Ctries. 14 (1), 3–17 (2020).
Article CAS PubMed Google Scholar
Sun, Z., Thilakavathy, K., Kumar, S. S., He, G. & Liu, S. V. Potential factors influencing repeated SARS outbreaks in China. Int. J. Environ. Res. Public Health 17 (5), 1633 (2020).
Article CAS PubMed Central Google Scholar
Zhao, S. et al. The association between domestic train transportation and novel coronavirus (2019-nCoV) outbreak in China from 2019 to 2020: a data-driven correlational report. Travel Med. Infect. Dis. 33 , 101568 (2020).
Article PubMed PubMed Central Google Scholar
Li, Q. et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N. Engl. J. Med. 382 (13), 1199–1207 (2020).
Chen, J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 22 (2), 69–71 (2020).
World Health Organization. Database of publications on coronavirus disease (COVID-19) (2020). https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov . Accessed 30 Mar 2020.
Wong, C. K. H. et al. Impact of national containment measures on decelerating the increase in daily new cases of COVID-19 in 54 countries and 4 epicenters of the pandemic: comparative observational study. J. Med. Internet Res. 22 (7), e19904 (2020).
Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19). Symptoms of Coronavirus (2020).
Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 14 (1), 135 (2014).
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch. Public Health 72 (1), 39 (2014).
Harris, R. J. et al. metan: fixed- and random-effects meta-analysis. Stata J. 8 (1), 3–28 (2008).
Article Google Scholar
Xu, X. et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur. J. Nucl. Med. Mol. Imaging 47 (5), 1275–1280 (2020).
Cao, J. et al. Clinical features and short-term outcomes of 18 patients with corona virus disease 2019 in intensive care unit. Intensive Care Med. 46 (5), 851–853 (2020).
Xiong, Y. et al. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest. Radiol. 55 (6), 332–339 (2020).
Arentz, M. et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA 323 (16), 1612–1614 (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 (10223), 497–506 (2020).
Guan, W. J. et al. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382 (18), 1708–1720 (2020).
Zhao, D. et al. A comparative study on the clinical features of coronavirus 2019 (COVID-19) pneumonia with other pneumonias. Clin. Infect. Dis. 71 (15), 756–761 (2020).
Xu, X. W. et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 19 (368), m606 (2020).
Chan, J. F. et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395 (10223), 514–523 (2020).
Chen, N. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395 (10223), 507–513 (2020).
Pung, R. et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet 395 (10229), 1039–1046 (2020).
Wang, D. et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323 (11), 1061–1069 (2020).
Young, B. E. et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 323 (15), 1488–1494 (2020).
Chen, H. et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet 395 (10226), 809–815 (2020).
Huang, W. H. et al. 2019 novel coronavirus disease (COVID-19) in Taiwan: reports of two cases from Wuhan, China. J. Microbiol. Immunol. Infect. 53 (3), 481–484 (2020).
Cheng, S. C. et al. First case of coronavirus disease 2019 (COVID-19) pneumonia in Taiwan. J. Formos. Med. Assoc. 119 (3), 747–751 (2020).
Holshue, M. L. et al. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 382 (10), 929–936 (2020).
Wei, M. et al. Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA 323 (13), 1313–1314 (2020).
Bernard Stoecklin, S. et al. First cases of coronavirus disease 2019 (COVID-19) in France: surveillance, investigations and control measures, January 2020. Euro Surveill. 25 (6), 20–26 (2020).
Shi, H. et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 20 (4), 425–434 (2020).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382 (8), 727–733 (2020).
Ghinai, I. et al. First known person-to-person transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in the USA. Lancet 395 (10230), 1137–1144 (2020).
Zhou, F. et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395 (10229), 1054–1062 (2020).
Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 8 (5), 475–481 (2020).
Kim, J. Y. et al. The first case of 2019 novel coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J. Korean Med. Sci. 35 (5), e61 (2020).
Okada, P. et al . Early transmission patterns of coronavirus disease 2019 (COVID-19) in travellers from Wuhan to Thailand, January 2020. Euro Surveill . 25 (8), 6–10 (2020).
Arashiro, T., Furukawa, K. & Nakamura, A. COVID-19 in 2 persons with mild upper respiratory tract symptoms on a cruise ship, Japan. Emerg. Infect. Dis. 26 (6), 1345–1348 (2020).
Lillie, P. J. et al. Novel coronavirus disease (Covid-19): the first two patients in the UK with person to person transmission. J. Infect. 80 (5), 578–606 (2020).
Tian, S. et al. Pulmonary pathology of early-phase 2019 novel coronavirus (COVID-19) pneumonia in two patients with lung cancer. J. Thorac. Oncol. 15 (5), 700–704 (2020).
Haveri, A. et al . Serological and molecular findings during SARS-CoV-2 infection: the first case study in Finland, January to February 2020. Euro Surveill . 25 (11), 16–21 (2020).
Nicastri, E. et al . Coronavirus disease (COVID-19) in a paucisymptomatic patient: epidemiological and clinical challenge in settings with limited community transmission, Italy, February 2020. Euro Surveill . 25 (11) (2020).
Van Cuong, L. et al. The first Vietnamese case of COVID-19 acquired from China. Lancet Infect Dis. 20 (4), 408–409 (2020).
Spiteri, G. et al . First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveill . 25 (9), 2–7 (2020).
Rothe, C. et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 382 (10), 970–971 (2020).
Tong, Z. D. et al. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerg. Infect. Dis. 26 (5), 1052–1054 (2020).
Bai, Y. et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA 323 (14), 1406–1407 (2020).
Yu, P., Zhu, J., Zhang, Z. & Han, Y. A familial cluster of infection associated with the 2019 novel coronavirus indicating possible person-to-person transmission during the incubation period. J. Infect. Dis. 221 (11), 1757–1761 (2020).
Li, P. et al. Transmission of COVID-19 in the terminal stages of the incubation period: a familial cluster. Int. J. Infect. Dis. 96 , 452–453 (2020).
Tang, A. et al. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg. Infect. Dis. 26 (6), 1337–1339 (2020).
Kam, K. Q. et al. A well infant with coronavirus disease 2019 with high viral load. Clin. Infect. Dis. 71 (15), 847–849 (2020).
Zhou, S., Wang, Y., Zhu, T. & Xia, L. CT Features of Coronavirus Disease 2019 (COVID-19) Pneumonia in 62 Patients in Wuhan. China. AJR Am J Roentgenol. 214 (6), 1287–1294 (2020).
Article PubMed Google Scholar
Zhao, W., Zhong, Z., Xie, X., Yu, Q. & Liu, J. Relation between chest CT findings and clinical conditions of coronavirus disease (COVID-19) pneumonia: a multicenter study. AJR Am. J. Roentgenol. 214 (5), 1072–1077 (2020).
Cheng, Z. et al. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. AJR Am. J. Roentgenol. 215 (1), 121–126 (2020).
Chung, M. et al. CT imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 295 (1), 202–207 (2020).
Liu, K. et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J (Engl). 133 (9), 1025–1031 (2020).
Chang, L. M. et al. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. JAMA 323 (11), 1092–1093 (2020).
Team C-NIRS. COVID-19, Australia: Epidemiology Report 7 (Reporting week ending 19:00 AEDT 14 March 2020). Commun. Dis. Intell. 44 (2018).
Pan, F. et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology 295 (3), 715–721 (2020).
Wang, S. et al. A case report of neonatal 2019 coronavirus disease in China. Clin. Infect. Dis. 71 (15), 853–857 (2020).
Bastola, A. et al. The first 2019 novel coronavirus case in Nepal. Lancet Infect. Dis. 20 (3), 279–280 (2020).
Qiu, H. et al. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect. Dis. 20 (6), 689–696 (2020).
Zhang, J. J. et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 75 (7), 1730–1741 (2020).
Ye, G. et al. Clinical characteristics of severe acute respiratory syndrome coronavirus 2 reactivation. J. Infect. 80 (5), e14–e17 (2020).
Liu, Y. et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 63 (3), 364–374 (2020).
Chen, T. et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 26 (368), m1091 (2020).
Guan, W. J. et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 55 (5), 2000547 (2020).
Wong, H. Y. F. et al. Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology 296 (2), E72–E78 (2020).
Xu, T. et al. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int J Infect Dis. 94 , 68–71 (2020).
Shen, C. et al. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA 323 (16), 1582–1589 (2020).
Kimball, A. et al. Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—King County, Washington, March 2020. Morb. Mortal. Wkly. Rep. 69 (13), 377–381 (2020).
Article CAS Google Scholar
Team CC-R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12-March 16, 2020. Morb. Mortal. Wkly. Rep. 69 (12), 343–346 (2020).
Wu, J. et al. Clinical characteristics of imported cases of coronavirus disease 2019 (COVID-19) in Jiangsu Province: a multicenter descriptive study. Clin. Infect. Dis. 71 (15), 706–712 (2020).
Yang, W. et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J. Infect. 80 (4), 388–393 (2020).
Zhu, L. et al. Successful recovery of COVID-19 pneumonia in a renal transplant recipient with long-term immunosuppression. Am. J. Transplant. 20 (7), 1859–1863 (2020).
Zhu, W. et al. Initial clinical features of suspected coronavirus disease in two emergency departments outside of Hubei, China. J. Med. Virol. 92 , 1525–1532 (2019).
Wu, C. et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 180 (7), 934–943 (2020).
Wang, Z., Chen, X., Lu, Y., Chen, F. & Zhang, W. Clinical characteristics and therapeutic procedure for four cases with 2019 novel coronavirus pneumonia receiving combined Chinese and Western medicine treatment. Biosci. Trends 14 (1), 64–68 (2020).
Wang, Y. et al. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. J. Infect. Dis. 221 (11), 1770–1774 (2020).
Wan, S. et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J. Med.. Virol. 92 (7), 797–806 (2020).
Tian, S. et al. Characteristics of COVID-19 infection in Beijing. J. Infect. 80 (4), 401–406 (2020).
Sun, D. et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center’s observational study. World J. Pediatr. 16 (3), 251–259 (2020).
Song, F. et al. Emerging 2019 novel coronavirus (2019-nCoV) pneumonia. Radiology 295 (1), 210–217 (2020).
Hu, Z. et al. Clinical characteristics of 24 asymptomatic infections with COVID-19 screened among close contacts in Nanjing, China. Sci. China Life Sci. 63 (5), 706–711 (2020).
Qu, R. et al. Platelet-to-lymphocyte ratio is associated with prognosis in patients with coronavirus disease-19. J. Med. Virol. 92 , 1533–1541 (2020).
Qian, G. Q. et al. Epidemiologic and clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM 113 (7), 474–481 (2020).
Mo, P. et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin. Infect. Dis . (2020).
Liu, W. et al. Analysis of factors associated with disease outcomes in hospitalized patients with 2019 novel coronavirus disease. Chin Med. J. (Engl) 133 (9), 1032–1038 (2020).
Liu, K., Chen, Y., Lin, R. & Han, K. Clinical features of COVID-19 in elderly patients: A comparison with young and middle-aged patients. J. Infect. 80 (6), e14–e18 (2020).
Liu, F. et al. Patients of COVID-19 may benefit from sustained Lopinavir-combined regimen and the increase of Eosinophil may predict the outcome of COVID-19 progression. Int. J. Infect. Dis. 95 , 183–191 (2020).
Liu, D. et al. Pregnancy and perinatal outcomes of women with coronavirus disease (COVID-19) pneumonia: a preliminary analysis. AJR Am. J. Roentgenol. 215 (1), 127–132 (2020).
Guillen, E. et al. Case report of COVID-19 in a kidney transplant recipient: does immunosuppression alter the clinical presentation?. Am. J. Transplant. 20 (7), 1875–1878 (2020).
Dong, X. et al. Eleven faces of coronavirus disease 2019. Allergy 75 (7), 1699–1709 (2020).
Fan, C. et al . Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin. Infect. Dis. (2020).
Chen, R. et al. Safety and efficacy of different anesthetic regimens for parturients with COVID-19 undergoing Cesarean delivery: a case series of 17 patients. Can. J. Anaesth. 67 (6), 655–663 (2020).
Chen, L. et al. RNA based mNGS approach identifies a novel human coronavirus from two individual pneumonia cases in 2019 Wuhan outbreak. Emerg. Microbes Infect. 9 (1), 313–319 (2020).
Chen, J. et al. Clinical progression of patients with COVID-19 in Shanghai, China. J. Infect. 80 (5), e1–e6 (2020).
Ding, Q., Lu, P., Fan, Y., Xia, Y. & Liu, M. The clinical characteristics of pneumonia patients coinfected with 2019 novel coronavirus and influenza virus in Wuhan, China. J. Med. Virol. 92 , 1549–1555 (2020).
Covid-19 National Emergency Response Center E & Case Management Team KCfDC, Prevention. Early epidemiological and clinical characteristics of 28 cases of coronavirus disease in South Korea. Osong Public Health Res. Perspect. 11 (1), 8–14 (2020).
Li, Y., Guo, F., Cao, Y., Li, L. & Guo, Y. Insight into COVID-2019 for pediatricians. Pediatr. Pulmonol. 55 (5), E1–E4 (2020).
Ai, J. W., Zhang, Y., Zhang, H. C., Xu, T. & Zhang, W. H. Era of molecular diagnosis for pathogen identification of unexplained pneumonia, lessons to be learned. Emerg Microbes Infect. 9 (1), 597–600 (2020).
Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 25 (9), 603–605 (2010).
Khan N. New virus discovered by Chinese scientists investigating pneumonia outbreak. Wall Street J . (2020).
国家统计局 (National Bureau of Statistics). 2019 年国民经济运行总体平稳 发展主要预期目标较好实现 (In 2019, the overall stable development of the national economic operation is expected to achieve the main goals (2020). http://www.stats.gov.cn/tjsj/zxfb/202001/t20200117_1723383.html . Accessed 30 Mar 2020.
Park, J. E., Jung, S., Kim, A. & Park, J. E. MERS transmission and risk factors: a systematic review. BMC Public Health 18 (1), 574 (2018).
Van Kerkhove, M. D. et al. Risk factors for severe outcomes following 2009 influenza A (H1N1) infection: a global pooled analysis. PLoS Med. 8 (7), e1001053 (2011).
Wang, C. et al. Epidemiological and clinical characteristics of the outbreak of 2009 pandemic influenza A (H1N1) at a middle school in Luoyang, China. Public Health 126 (4), 289–294 (2012).
Lee, N. et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N. Engl. J. Med. 348 (20), 1986–1994 (2003).
Booth, C. M. et al. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA 289 (21), 2801–2809 (2003).
Fowler, R. A. et al. Critically ill patients with severe acute respiratory syndrome. JAMA 290 (3), 367–373 (2003).
Christian, M. D., Poutanen, S. M., Loutfy, M. R., Muller, M. P. & Low, D. E. Severe acute respiratory syndrome. Clin Infect Dis. 38 (10), 1420–1427 (2004).
Mertz, D. et al. Populations at risk for severe or complicated influenza illness: systematic review and meta-analysis. BMJ 23 (347), f5061 (2013).
Badawi, A. & Ryoo, S. G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int. J. Infect. Dis. 49 , 129–133 (2016).
Tsang, T. K. et al. Effect of changing case definitions for COVID-19 on the epidemic curve and transmission parameters in mainland China: a modelling study. Lancet Public Health. 5 (5), e289–e296 (2020).
国家卫生健康委办公厅 (Office of National Health Comission). 新型冠状病毒肺炎诊疗方案 (试行第七版) (Clinical Guideline for Novel Coronavirus Pneumonia—Interim 7th Edition) (2020).
File, T. M. Jr. & Tsang, K. W. Severe acute respiratory syndrome: pertinent clinical characteristics and therapy. Treat. Respir. Med. 4 (2), 95–106 (2005).
Day, M. Covid-19: four fifths of cases are asymptomatic, China figures indicate. BMJ 2 (369), m1375 (2020).
Wei, W. E. et al. Presymptomatic transmission of SARS-CoV-2—Singapore, January 23–March 16, 2020. Morb. Mortal. Wkly. Rep. 69 (14), 411–415 (2020).
Mizumoto, K., Kagaya, K., Zarebski, A. & Chowell, G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro Surveill. 25 (10), 2000180 (2020).
Article PubMed Central Google Scholar
Poutanen, S. M. et al. Identification of severe acute respiratory syndrome in Canada. N. Engl. J .Med. 348 (20), 1995–2005 (2003).
Tsang, K. W. et al. A cluster of cases of severe acute respiratory syndrome in Hong Kong. N. Engl. J. Med. 348 (20), 1977–1985 (2003).
Cao, B. et al. A trial of Lopinavir–Ritonavir in adults hospitalized with severe covid-19. N. Engl. J. Med. 382 (19), 1787–1799 (2020).
Download references
Acknowledgements
There was no funding source for this study.
Author information
These authors contributed equally: Carlos K. H. Wong and Janet Y. H. Wong.
Authors and Affiliations
Department of Family Medicine and Primary Care, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Carlos K. H. Wong, Eric H. M. Tang & C. H. Au
Department of Pharmacology and Pharmacy, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Carlos K. H. Wong
School of Nursing, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Janet Y. H. Wong
Emergency Medicine Unit, Li Ka Shing, Faculty of Medicine, The University of Hong Kong, Hong Kong, China
Abraham K. C. Wai
You can also search for this author in PubMed Google Scholar
Contributions
C.W., J.W. and A.W. contributed equally to all aspects of study design, conduct, data interpretation, and the writing of the manuscript. C.W., E.T. and C.H.A. contributed to eligibility screening, data extraction from eligible studies, and data analysis and interpretation.
Corresponding author
Correspondence to Abraham K. C. Wai .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary figure 1., supplementary figure 2., supplementary figure 3., supplementary figure 4., supplementary figure 5., supplementary material 6., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wong, C.K.H., Wong, J.Y., Tang, E.H.M. et al. Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis. Sci Rep 10 , 19765 (2020). https://doi.org/10.1038/s41598-020-74988-9
Download citation
Received : 04 May 2020
Accepted : 25 September 2020
Published : 13 November 2020
DOI : https://doi.org/10.1038/s41598-020-74988-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Comorbidity genetic risk and pathways impact sars-cov-2 infection outcomes.
- Rachel K. Jaros
- Tayaza Fadason
- Justin M. O’Sullivan
Scientific Reports (2023)
Adrenal function in relation to cytokines and outcome in non-critically ill patients with COVID-19
- N. Athanasiou
- A. Diamantopoulos
- D. A. Vassiliadi
Journal of Endocrinological Investigation (2023)
The Role of Multidimensional Prognostic Index to Identify Hospitalized Older Adults with COVID-19 Who Can Benefit from Remdesivir Treatment: An Observational, Prospective, Multicenter Study
- Carlo Custodero
- Nicola Veronese
- Julia Schlotmann
Drugs & Aging (2023)
Prevalence of hypertension and associated risks in hospitalized patients with COVID-19: a meta-analysis of meta-analyses with 1468 studies and 1,281,510 patients
- Yousof Khairy
- Deniz Naghibi
- Saber Azami-Aghdash
Systematic Reviews (2022)

An alternative approach to determination of Covid-19 personal risk index by using fuzzy logic
- Hakan Şimşek
- Elifnaz Yangın
Health and Technology (2022)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Microbiology newsletter — what matters in microbiology research, free to your inbox weekly.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
CALCULATORS
Related topics.
INTRODUCTION
The epidemiology, definitions, risk factors, clinical presentation, diagnosis, and outcomes of sepsis are reviewed here. The pathophysiology and treatment of sepsis are discussed separately. (See "Pathophysiology of sepsis" and "Evaluation and management of suspected sepsis and septic shock in adults" .)
EPIDEMIOLOGY
Incidence — In the late 1970s, it was estimated that 164,000 cases of sepsis occurred in the United States (US) each year [ 1 ]. Since then, rates of sepsis in the US and elsewhere have on balance increased although many of these are derived from academic institutions or on claims-based analyses [ 2-9 ]:
● One national database analysis of discharge records from hospitals in the US estimated an annual rate of more than 1,665,000 cases of sepsis between 1979 and 2000 [ 2 ].
● Another retrospective population-based analysis reported increased rates of sepsis and septic shock from 13 to 78 cases per 100,000 between 1998 and 2009 [ 3 ].
Tools for the Patient Presentation
The formal patient presentation.
- Posing the Clinical Question
- Searching the Medical Literature for EBM
Sources & Further Reading
First Aid for the Wards
Lingard L, Haber RJ. Teaching and learning communications in medicine: a rhetorical approach . Academic Medicine. 74(5):507-510 1999 May.
Lingard L, Haber RJ. What do we mean by "relevance"? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format . Academic Medicine. 74(10):S124-S127.
The Oral Presentation (A Practical Guide to Clinical Medicine, UCSD School of Medicine) http://meded.ucsd.edu/clinicalmed/oral.htm
"Classically, the formal oral presentation is given in 7 minutes or less. Although it follows the same format as a written report, it is not simply regurgitation. A great presentation requires style as much as substance; your delivery must be succinct and smooth. No time should be wasted on superfluous information; one can read about such matters later in your admit note. Ideally, your presentation should be formulated so that your audience can anticipate your assessment and plan; that is, each piece of information should clue the listener into your thinking process and your most likely diagnosis." [ Le, et al, p. 15 ]
Types of Patient Presentations
New Patient
New patients get the traditional H&P with assessment and plan. Give the chief complaint and a brief and pertinent HPI. Next give important PMH, PSH, etc. The ROS is often left out, as anything important was in the HPI. The PE is reviewed. Only give pertinent positives and negatives. The assessment and plan should include what you think is wrong and, briefly, why. Then, state what you plan to do for the patient, including labs. Be sure to know why things are being done: you will be asked.
The follow-up presentation differs from the presentation of a new patient. It is an abridged presentation, perhaps referencing major patient issues that have been previously presented, but focusing on new information about these issues and/or what has changed. Give the patient’s name, age, date of admission, briefly review the present illness, physical examination and admitting diagnosis. Then report any new finding, laboratory tests, diagnostic procedures and changes in medications.
The attending physician will ask the patient’s permission to have the medical student present their case. After making the proper introductions the attending will let the patient know they may offer input or ask questions at any point. When presenting at bedside the student should try to involve the patient.
Preparing for the Presentation
There are four things you must consider before you do your oral presentation
- Occasion (setting and circumstances)
Ask yourself what do you want the presentation to do
- Present a new patient to your preceptor : the amount of detail will be determined by your preceptor. It is also likely to reflect your development and experience, with less detail being required as you progress.
- Present your patient at working or teaching rounds : the amount of detail will be determined by the customs of the group. The focus of the presentation will be influenced by the learning objectives of working responsibilities of the group.
- Request a consultant’s advice on a clinical problem : the presentation will be focused on the clinical question being posed to the consultant.
- Persuade others about a diagnosis and plan : a shorter presentation which highlights the pertinent positives and negatives that are germane to the diagnosis and/or plan being suggested.
- Enlist cooperation required for patient care : a short presentation focusing on the impact your audience can have in addressing the patient’s issues.
Preparation
- Patient evaluation : history, physical examination, review of tests, studies, procedures, and consultants’ recommendations.
- Selected reading : reference texts; to build a foundational understanding.
- Literature search : for further elucidation of any key references from selected reading, and to bring your understanding up to date, since reference text information is typically three to seven years old.
- Write-up : for oral presentation, just succinct notes to serve as a reminder or reference, since you’re not going to be reading your presentation.
Knowledge (Be prepared to answer questions about the following)
- Pathophysiology
- Complications
- Differential diagnosis
- Course of conditions
- Diagnostic tests
- Medications
- Essential Evidence Plus
Template for Oral Presentations
Chief Complaint (CC)
The opening statement should give an overview of the patient, age, sex, reason for visit and the duration of the complaint. Give marital status, race, or occupation if relevant. If your patient has a history of a major medical problem that bears strongly on the understanding of the present illness, include it. For ongoing care, give a one sentence recap of the history.
History of Present Illness (HPI)
This will be very similar to your written HPI. Present the most important problem first. If there is more than one problem, treat each separately. Present the information chronologically. Cover one system before going onto the next. Characterize the chief complaint – quality, severity, location, duration, progression, and include pertinent negatives. Items from the ROS that are unrelated to the present problem may be mentioned in passing unless you are doing a very formal presentation. When you do your first patient presentation you may be expected to go into detail. For ongoing care, present any new complaints.
Review of Systems (ROS)
Most of the ROS is incorporated at the end of the HPI. Items that are unrelated to the present problem may be briefly mentioned. For ongoing care, present only if new complaints.
Past Medical History (PMH)
Discuss other past medical history that bears directly on the current medical problem. For ongoing care, have the information available to respond to questions.
Past Surgical History
Provide names of procedures, approximate dates, indications, any relevant findings or complications, and pathology reports, if applicable. For ongoing care, have the information available to respond to questions.
Allergies/Medications
Present all current medications along with dosage, route and frequency. For the follow-up presentation just give any changes in medication. For ongoing care, note any changes.
Smoking and Alcohol (and any other substance abuse)
Note frequency and duration. For ongoing care, have the information available to respond to questions.
Social/Work History
Home, environment, work status and sexual history. For ongoing care, have the information available to respond to questions.
Family History Note particular family history of genetically based diseases. For ongoing care, have the information available to respond to questions.
Physical Exam/Labs/Other Tests
Include all significant abnormal findings and any normal findings that contribute to the diagnosis. Give a brief, general description of the patient including physical appearance. Then describe vital signs touching on each major system. Try to find out in advance how thorough you need to be for your presentation. There are times when you will be expected to give more detail on each physical finding, labs and other test results. For ongoing care, mention only further positive findings and relevant negative findings.
Assessment and Plan
Give a summary of the important aspects of the history, physical exam and formulate the differential diagnosis. Make sure to read up on the patient’s case by doing a search of the literature.
- Include only the most essential facts; but be ready to answer ANY questions about all aspects of your patient.
- Keep your presentation lively.
- Do not read the presentation!
- Expect your listeners to ask questions.
- Follow the order of the written case report.
- Keep in mind the limitation of your listeners.
- Beware of jumping back and forth between descriptions of separate problems.
- Use the presentation to build your case.
- Your reasoning process should help the listener consider a differential diagnosis.
- Present the patient as well as the illness .
- << Previous: Home
- Next: Posing the Clinical Question >>
- Last Updated: Jul 19, 2023 10:52 AM
- URL: https://rowanmed.libguides.com/tools
8.1 Clinical Presentation
Section learning objectives.
- Identify and describe the five symptoms of schizophrenia spectrum disorders.
- Describe how schizophrenia presents itself.
- Describe how schizophreniform disorder presents itself.
- Describe how brief psychotic disorder presents itself.
- Describe how schizoaffective disorder presents itself.
- Describe how delusional disorder presents itself.
- Be able to distinguish the five disorders from one another.
8.1.1 Symptoms of Schizophrenia Spectrum and Other Psychotic Disorders
Individuals diagnosed with a schizophrenia spectrum or other psychotic disorder experience psychosis, which is defined as a loss of contact with reality and is manifested by delusions and/or hallucinations. These episodes of psychosis can make it difficult for individuals to perceive and respond to environmental stimuli, which can cause significant disturbances in everyday functioning. While there are a number of symptoms displayed in schizophrenia spectrum and other psychotic disorders, the presentation of symptoms varies greatly among individuals, as there are rarely two cases similar in presentation, triggers, course, or responsiveness to treatment (APA, 2013). We will now turn our attention to the five major symptoms associated with these disorders: delusions, hallucinations, disorganized speech, disorganized behavior, and negative symptoms.
8.1.1.1 Delusions
Delusions are defined as “fixed beliefs that are not amenable to change in light of conflicting evidence” (APA, 2022, pp. 101). This means that despite evidence contradicting one’s thoughts, the individual continues to fixate on a false (i.e., erroneous) belief. There are a variety of delusions that can present in many different ways:
- Grandiose delusions – beliefs they have exceptional abilities, wealth, or fame; the belief they are God or other religious saviors
- Persecutory delusions – beliefs they are going to be harmed, harassed, plotted, or discriminated against by either an individual or an institution
- Referential delusions – beliefs that specific gestures, comments, or even larger environmental cues (e.g., an ad in the newspaper, a terrorist attack) are directed at them
- Delusions of control – beliefs that their thoughts/feelings/actions are controlled by others
- Delusions of thought broadcasting – beliefs that one’s thoughts are transparent and everyone knows what they are thinking
- Delusions of thought withdrawal – belief that one’s thoughts have been removed by another (e.g., alien) source
The most common delusion is persecutory (APA, 2022). It is believed that the presentation of the delusion is largely related to the social, emotional, educational, and cultural background of the individual (Arango & Carpenter, 2010). For example, an individual with schizophrenia who comes from a highly religious family is more likely to experience religious delusions.
8.1.1.2 Hallucinations
Hallucinations are defined as “perception-like experiences that occur without an external stimulus” (APA, 2022; pp. 102). Hallucinations can occur in any of the five senses including hearing (auditory hallucinations), seeing (visual hallucinations), smelling (olfactory hallucinations), touching (tactile hallucinations), or tasting (gustatory hallucinations). Additionally, they can occur in a single modality or present across a combination of modalities (i.e. experiencing both auditory and visual hallucinations). For the most part, individuals recognize that their hallucinations are not real and attempt to engage in normal behavior while simultaneously combating ongoing hallucinations.
According to various research studies, nearly half of all people with schizophrenia report auditory hallucinations, 15% report visual hallucinations, and 5% report tactile hallucinations (DeLeon, Cuesta, & Peralta, 1993). Among the most common types of auditory hallucinations are voices talking to the individual or various voices talking to one another. Generally, these hallucinations are not attributable to any one person that the individual knows. However, they are usually clear, objective, and definite (Arango & Carpenter, 2010) and occur with the same impact as normal perception (APA, 2022). Additionally, the auditory hallucinations can be pleasurable, providing comfort to the individuals; however, in other individuals, the auditory hallucinations can be unsettling as they produce commands or have malicious intent.
8.1.1.3 Disorganized Speech
Among the most common cognitive impairments displayed in individuals with schizophrenia spectrum and other psychotic disorders are disorganized speech and thoughts. More specifically, thoughts and speech patterns may appear to be circumstantial or tangential . For example, individuals with circumstantial speech may give unnecessary details in response to a question before they finally produce the desired response. While the question is eventually answered by individuals with circumstantial speech, those with tangential speech never reach the point or answer the question, but rather jump from topic to topic. Derailment , or the illogical connection in a chain of thoughts, is another common type of disorganized thinking. The most severe form of disorganized speech is incoherence or word salad which is where speech is completely incomprehensible and meaningful sentences are not produced.
These types of distorted thought patterns are often related to concrete thinking. That is, the individual is focused on one aspect of a concept or thing, and neglects all other aspects. This type of thinking makes treatment difficult as individuals lack insight into their illness and symptoms (APA, 2013).
8.1.1.4 Disorganized Behavior
Psychomotor symptoms can also be observed in individuals with schizophrenia spectrum and other psychotic disorders. These behaviors may manifest as awkward movements or even ritualistic/repetitive behaviors. They are often unpredictable and overwhelming, severely impacting the ability to perform daily activities (APA, 2013). Catatonic behavior , or the decrease or even lack of reactivity to the environment, is among the most commonly seen disorganized motor behavior in schizophrenia spectrum disorders. These catatonic behaviors include:
- Negativism – resistance to instruction
- Mutism – complete lack of verbal responses
- Stupor – complete lack of motor responses
- Rigidity – maintaining a rigid or upright posture while resisting efforts to be moved
- Posturing – holding odd, awkward postures for long periods of time
On the opposite side of the spectrum is catatonic excitement, where the individual experiences hyperactivity of motor behavior. This can include echolalia (mimicking the speech of others) and echopraxia (mimicking the movement of others) but may also simply be manifested through excessive and/or purposeless motor behaviors.
8.1.1.5 Negative Symptoms
All symptoms discussed up until this point can be categorized as positive symptoms or symptoms that involve the presence of something that should not be there (e.g., hallucinations and delusions) or disorganized symptoms (disorganized speech and behavior). The final set of symptoms included in the diagnostic criteria of several of the schizophrenia spectrum and other psychotic disorders is negative symptoms , which are defined as the inability, or decreased ability, to initiate actions, speech, express emotion, or feel pleasure (Barch, 2013). Negative symptoms are typically present before positive symptoms and often remain once positive symptoms remit. They account for much of the morbidity in schizophrenia but are not as prominent in the other psychotic disorders (indeed, as you will see, they are not included as a symptom in some of these other disorders). Because of their prevalence through the course of schizophrenia, they are also more indicative of prognosis, with more negative symptoms suggestive of a poorer prognosis. The poorer prognosis may be explained by the lack of effect that traditional antipsychotic medications have in addressing negative symptoms (Kirkpatrick, Fenton, Carpenter, & Marder, 2006) as well as from avolition impacting daily functioning.
There are five main types of negative symptoms seen in individuals with schizophrenia:
- Affective flattening – reduction in emotional expression (i.e., a reduced display of emotional expression)
- Alogia – poverty of speech or speech content
- Anhedonia – decreased ability to experience pleasure
- Asociality – lack of interest in social relationships
- Avolition – lack of motivation for goal-directed behavior
8.1.2 Types of Schizophrenia Spectrum and Other Psychotic Disorders
8.1.2.1 schizophrenia.
As stated above, the hallmark symptoms of schizophrenia include the presence of at least two of the following symptoms for at least one month: (1) delusions, (2) hallucinations, (3) disorganized speech, (4) disorganized/abnormal behavior, (5) negative symptoms. At least one of these must be (1), (2), or (3). These symptoms must create significant impairment in the individual’s ability to engage in normal daily functioning such as work, school, relationships with others, or self-care. It should be noted that the presentation of schizophrenia varies greatly among individuals, as it is a heterogeneous clinical syndrome (APA, 2022).
While the presence of active phase symptoms must persist for a minimum of one month to meet the criteria for a diagnosis of schizophrenia, the total duration of symptoms must persist for at least six months before a diagnosis of schizophrenia can be made. This six-month period can comprise a combination of active, prodromal, and residual phase symptoms. Active phase symptoms represent the “full-blown” symptoms previously described. Prodromal symptoms are “subthreshold” symptoms that precede the active phase of the disorder and residual symptoms are subthreshold symptoms that follow the active phase. These prodromal and residual symptoms are milder forms of symptoms that may not cause significant impairment in functioning, with the exception of negative symptoms (Lieberman et al., 2001). Due to the severity of psychotic symptoms, mood disorder symptoms are also common among individuals with schizophrenia; however, to diagnose schizophrenia there must either be no mood symptoms or if mood symptoms have occurred they must be present for only a minority of the total duration of the illness. The latter helps to distinguish schizophrenia from a mood disorder with psychotic features for which psychotic symptoms are limited to the context of the mood episodes and are never experienced outside a mood episode.
8.1.2.2 Schizophreniform Disorder
Schizophreniform disorder is similar to schizophrenia with the exception of the length of presentation of symptoms and the requirement for impairment in functioning. As described above, a diagnosis of schizophrenia requires impairment in functioning and a six-month minimum duration of symptoms. In contrast, impairment in functioning is not required to diagnose schizophreniform disorder. While many individuals with schizophreniform disorder do display impaired functioning, it is not essential for diagnosis. Moreover, symptoms must last at least one month but less than six-months to diagnose schizophreniform disorder. In this way, the duration of schizophreniform disorder is considered an “intermediate” disorder between schizophrenia and brief psychotic disorder (which we will consider next).
Approximately two-thirds of individuals who are initially diagnosed with schizophreniform disorder will have symptoms that last longer than six months, at which time their diagnosis is changed to schizophrenia (APA, 2013). The other one-third will recover within the six-month time period and schizophreniform disorder will be their final diagnosis.
Finally, as with schizophrenia, psychotic symptoms must be experienced outside of the context of mood episodes (if mood episodes are present). Further, any major mood episodes that are present concurrently with the psychotic features must only be present for a small period of time, otherwise, a diagnosis of schizoaffective disorder may be more appropriate.
8.1.2.3. Brief Psychotic Disorder
A diagnosis of brief psychotic disorder requires one or more of the following symptoms: (1) delusions, (2) hallucinations, (3) disorganized speech, and (4) disorganized behavior. Moreover at least one of these symptoms must be (1), (2), or (3). Notice that negative symptoms are not included in this list. Also notice that while schizophrenia and schizophreniform disorder require a minimum of two symptoms, only one is required for a diagnosis of brief psychotic disorder. To diagnose brief psychotic disorder symptom(s) must be present for at least one day but less than one month (recall: one month is the minimum duration of symptoms required to diagnose schizophreniform disorder). After one-month individuals return to their full premorbid level of functioning. Also, while there is typically very severe impairment in functioning associated with brief psychotic disorder, it is not required for a diagnosis.
8.1.2.4. Schizoaffective Disorder
Schizoaffective disorder is characterized by two or more of the symptoms of schizophrenia (delusions, hallucinations, disorganized speech, disorganized behavior, negative symptoms) and a concurrent uninterrupted period of a major mood episode—either a depressive or manic episode. Those who experience only depressive episodes are diagnosed with the depressive type of schizoaffective disorder while those who experience manic episodes (with or without depressive episodes) are diagnosed with the bipolar type of schizoaffective disorder. It should be noted that because a loss of interest in pleasurable activities is a common symptom of schizophrenia, to meet the criteria for a depressive episode within schizoaffective disorder, the individual must present with a pervasive depressed mood (not just anhedonia). While schizophrenia and schizophreniform disorder do not have a significant mood component, schizoaffective disorder requires the presence of a depressive or manic episode for the majority, if not the total duration of the disorder. While psychotic symptoms are sometimes present in depressive episodes, they remit once the depressive episode is resolved. For individuals with schizoaffective disorder, psychotic symptoms must be present for at least two weeks in the absence of a major mood episode (APA, 2022). This is the key distinguishing feature between schizoaffective disorder and major mood disorders with psychotic features.
8.1.2.5. Delusional Disorder
As suggestive of its title, delusional disorder requires the presence of at least one delusion that lasts for at least one month. It is important to note that any other symptom of schizophrenia (i.e., hallucinations, disorganized behavior, disorganized speech, negative symptoms) rules out a diagnosis of delusional disorder. Therefore the only symptom that can be present is delusions. Unlike most other schizophrenia spectrum and other psychotic disorders, daily functioning is not overtly impacted in individuals with delusional disorder. Additionally, if symptoms of depressive or manic episodes present during delusions, they are typically brief and represent a minority of the total duration of the disorder.
The DSM 5-TR (APA, 2022) has identified several subtypes of delusional disorder in an effort to better categorize the individual’s specific presentation of the disorder. When making a diagnosis of delusional disorder, one of the following specifiers is included.
- Erotomanic type – the individual reports a delusion of another person being in love with them. Generally speaking, the individual whom the convictions are about are of higher status such as a celebrity.
- Grandiose type – involves the conviction of having a great talent or insight. Occasionally, individuals will report they have made an important discovery that benefits the general public. Grandiose delusions may also take on a religious affiliation, as some people believe they are prophets or a God.
- Jealous type – revolves around the conviction that one’s spouse or partner is/has been unfaithful. While many individuals may have this suspicion at some point in their relationship, a jealous delusion is much more extensive and generally based on incorrect inferences that lack evidence.
- Persecutory type – involves beliefs that they are being conspired against, spied on, followed, poisoned or drugged, maliciously maligned, harassed, or obstructed in the pursuit of their long-term goals (APA, 2022). Of all subtypes of delusional disorder, those experiencing persecutory delusions are the most at risk of becoming aggressive or hostile, likely due to the persecutory nature of their beliefs.
- Somatic type – involves delusions regarding bodily functions or sensations. While these delusions can vary significantly, the most common beliefs are that the individual emits a foul odor, that there is an infestation of insects on the skin, or that they have an internal parasite (APA, 2022).
- Mixed type – there are several themes of delusions (e.g., jealousy and persecutory)
- Unspecified type – these are delusions that don’t fit into one of the categories above (e.g., referential delusions without a persecutory or grandiose nature to them).
- Bizarre content – delusions that are clearly not plausible (in one’s culture) and do not stem from ordinary experience (e.g., the delusion that one is an alien or vampire).
Share This Book
- Increase Font Size
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Presentation skills:...
Presentation skills: plan, prepare, phrase, and project
- Related content
- Peer review
- Laura Brammar , careers adviser, C2 Careers
- laura.brammar{at}careers.lon.ac.uk
In the third of her series on getting the dream job, Laura Brammar looks at giving an interview presentation
Many doctors have extensive experience of delivering presentations at conferences, during research projects, or to medical students during their training. Nevertheless, for many medical professionals having to deliver a presentation is still something they dread rather than relish. Equally, candidate presentations are becoming an established feature of selection and assessment for many roles within medicine.
Applicants may be asked to prepare and deliver a presentation as part of the interview process for anything from a salaried general practitioner post to a senior consultant post. For that reason alone, it’s vital to grasp the nettle and strengthen those presentation skills, which you can draw on throughout your medical career.
Break it down to just four P’s
To prepare most effectively for your presentation, you might find considering four main areas particularly useful: planning, preparation, phrasing, and projection.
Planning —A good presentation begins with the early stage of planning. Common complaints about ineffectual and dull presentations revolve around the apparent lack of structure shown by the presenter.
You will generally be given the topic of your presentation in advance. Topics vary, but they usually relate to your specialty—for example, “What do you see as the main current issues/future direction of this specialty?”—or link to contextual factors related to the role—“How, in your opinion, could the current system of X work more effectively?”
Think of the title as your research question or hypothesis and structure your presentation so that you answer that question directly. A simple but effective framework for any presentation is: tell them what you’re going to say, say it, and tell them what you’ve just said. Whether your presentation relates to the latest National Institute for Health and Clinical Excellence (NICE) guidelines for your specialty or a business plan in response to a proposed polyclinic, this structure will help keep your audience engaged and your presentation within the time limit.
Indeed, timing is crucial when giving a presentation. Most candidates are overambitious about what can be squeezed into just five to ten minutes. Be realistic about what you can achieve in the time limit and plan your presentation accordingly. As a rule of thumb, less is almost always more and remember to build in time for questions at the end.
Preparation —Having a clear structure can give you a useful framework that underpins your presentation. In a similar way, using particular resources to support your point can be a good method to employ during a presentation.
While the use of PowerPoint is becoming increasingly popular, in these circumstances you need to check before slaving over your slides. Remember that you are the focus of the presentation, not the screen; avoid distracting animations and excessive detail. Even if PowerPoint is an option you still need to plan for technological meltdowns; bring hard copies and overhead slides as a back-up.
You may consider it worth while to produce a brief summarising handout of the main points. Aim to distribute this before you begin so that you can create a clear and confident start, rather than compete with the rustle of paper as you try to introduce yourself.
Phrasing —Many candidates get anxious about the fact that they may “um” and “er” during a presentation. The vast majority of people feel nervous when they are presenting. Accept that and remember that, to an extent, it is what your audience will expect; from the selectors’ perspective, a completely laidback candidate might appear unmotivated and flippant. So while you want to aim for a fluid and articulate delivery, it’s not the end of the world if you occasionally need to pause between sentences. Indeed pauses can be an excellent way of emphasising your points and retaining your audience’s attention.
Essentially, use your structure to help you—for example, “First, I’d like to talk about . . .; next, let’s look at . . . ; and, finally, in summary . . ..”Also, be aware of your pace and volume.
Projection —Many people associate the term “presentation skills” with aspects of non-verbal communication, such as gestures and facial expression. Even when you feel nervous there are ways successfully to convey confidence to your audience. The following suggestions will help you to show a positive and calm attitude, which in turn will help you to maintain control over your presentation.
Breathe—If you are particularly nervous before you start, take a few moments to slow down your breathing; it may help to think about balancing the length of your inhalation and exhalation and breathe deeply and evenly.
Share your eye contact—If feasible, make eye contact with all your audience throughout your presentation; if you are presenting to a large group, make sure you address both sides of the room during your session.
Take time to pause—Use pauses to illustrate the structure of your session. Brief pauses can also help you to slow down your delivery and maintain the focus of your audience.
Project your voice—Check that those at the back can hear you before you start. Maintain your volume throughout and aim at projecting your voice to the back of the room.
Own the space—If possible, try not to stay stuck to one spot for the duration of the presentation. Clearly, now isn’t the time to try out gestures that feel unnatural or forced. However, convey your confidence through the way you stand and emphasise your message through your body language.
Smile—Despite feeling anxious, displaying a smile can make you feel more relaxed. Even better, it also gives your audience confidence in you and in your message.
Awkward audience moments
While you may have organised thoroughly your planning, preparation, phrasing, and projection, the one area you cannot control or necessarily predict is your audience’s reactions. Many people find the thought of their audience’s responses, especially during the question and answer session, far more terrifying than the presentation itself.
Here are a few suggestions for how to deal with some common difficult situations.
Random interruptions —If someone asks a question in the middle of your presentation, make a decision whether it would be appropriate to deal with it now or later. Don’t be forced to change your structure unless you believe it is really necessary. Acknowledge the question and reassure the person that there will be opportunities to discuss that later. Equally, if it is an unrelated or irrelevant question remember to acknowledge it but make it clear that such a topic isn’t going to be dealt with explicitly on this occasion. You can always offer to research that question for them at a later opportunity.
Audience looks bored —Many people feel they are poor presenters because their audiences can look distracted or even bored. The key thing here is to ask yourself if they are actually bored or whether they are just presenting you with a professional and impartial expression. In your clinical work you need to be able to focus on a task and not be distracted by personal emotional considerations or anxieties; this is no different. Treat the presentation as a professional exercise and move on.
Someone isn’t listening and is talking to someone nearby —Depending on your audience (senior consultants or medical students, for example) you may want to vary your specific response to this. However, a good technique with any audience is to pause in your delivery, look at the culprits while smiling, and wait for their attention before you start again. This is an effective (and non-aggressive) way of acknowledging that they are distracting both you and the rest of the group. That is usually all it takes to get their full attention. However, if they are persistent offenders maintain your professionalism and carry on regardless.
Questions you can’t answer —Sometimes the dread of the questions at the end of a presentation can overshadow the whole experience. Avoid this by framing your question and answer session with a reassurance that you’ll do your best to deal with any questions now and will guarantee to follow up any additional questions after the session. If you are asked a reasonable question which you genuinely can’t answer you may want to try the following:
Acknowledge that it’s a valid question
Invite any suggestions from the audience first
Admit that you can’t give a full answer at this moment; don’t bluff an answer
Offer to follow up a response and email the person later.
Remember that part of good medical practice is to know your limits and work within the parameters of your knowledge; it sounds far more confident and impressive to admit you can’t answer a question fully at this moment, rather than try to cobble together a poor answer and pretend you know.
Want to practise in a supportive environment?
The BMA Careers Service works with many individual medics who wish to improve their presentation skills through a tailormade practice presentation service. A bespoke practice presentation session, based on your actual material, can be excellent preparation for the real thing. During the session you can rehearse your presentation fully, practise answering focused questions, and gain immediate and constructive one to one feedback on your overall performance ( www.bma.org.uk/ap.nsf/Content/Hubcareersadvicefordoctors ).
Competing interests : None declared.
- Cambridge Dictionary +Plus
clinical presentation
Meanings of clinical and presentation.
Your browser doesn't support HTML5 audio
(Definition of clinical and presentation from the Cambridge English Dictionary © Cambridge University Press)
- Examples of clinical presentation

Word of the Day
customer support
help and advice that a company makes available to customers when they have bought something

Varied and diverse (Talking about differences, Part 1)

Learn more with +Plus
- Recent and Recommended {{#preferredDictionaries}} {{name}} {{/preferredDictionaries}}
- Definitions Clear explanations of natural written and spoken English English Learner’s Dictionary Essential British English Essential American English
- Grammar and thesaurus Usage explanations of natural written and spoken English Grammar Thesaurus
- Pronunciation British and American pronunciations with audio English Pronunciation
- English–Chinese (Simplified) Chinese (Simplified)–English
- English–Chinese (Traditional) Chinese (Traditional)–English
- English–Dutch Dutch–English
- English–French French–English
- English–German German–English
- English–Indonesian Indonesian–English
- English–Italian Italian–English
- English–Japanese Japanese–English
- English–Norwegian Norwegian–English
- English–Polish Polish–English
- English–Portuguese Portuguese–English
- English–Spanish Spanish–English
- English–Swedish Swedish–English
- Dictionary +Plus Word Lists
{{message}}
There was a problem sending your report.
- Definition of clinical
- Definition of presentation
- Other collocations with presentation
The National Kidney Foundation’s 2024 Spring Clinical Meetings Late-Breaking Presentation on New Therapy Shows Promising Results for IgAN Patients

(May 14, New York, NY) – During a late-breaking abstract presentation at the annual 2024 NKF Spring Clinical Meetings (SCM) tomorrow Dr. Dana Rizk, from the University of Alabama at Birmingham (UAB) Medical Center, will present data on the impact and safety of Fabhalta (iptacopan) in the treatment of patients with IgA nephropathy (IgAN) also known as Berger disease. Iptacopan was approved by the FDA in 2023 for the treatment of another disease entity, paroxysmal nocturnal hemoglobinuria. IgAN is an incurable glomerular disease that can cause chronic kidney disease (CKD) and is a leading cause of end-stage renal disease (ESRD). The presentation entitled, Efficacy and Safety of Iptacopan in Patients with IgAN: Interim Analysis (IA) of the Phase 3 APPLAUSE-IgAN Study will be held at the Long Beach Convention Center, 300 East Ocean Blvd, on Wednesday, May 15 from 2:30 to 4:30 p.m. (PT).
In the analysis, patients treated with iptacopan in addition to standard supportive care, achieved a 38.3% (p<0.0001) proteinuria reduction (as measured by 24-hour urine protein to creatinine ratio [UPCR]) at 9 months when compared to placebo 1 .) Proteinuria reduction is an increasingly recognized surrogate marker correlating with progression to kidney failure and has been used in IgAN clinical trials to support accelerated approvals 7 . The study also showed that iptacopan was well tolerated by IgAN patients with a favorable safety profile consistent with previously reported data 1,8 .
Quote from Researcher
“In IgAN, part of the immune system called the alternative complement pathway can become overly activated in the kidneys, which causes an inflammatory response, leading to progressive kidney damage and gradual loss of kidney function. The loss of kidney function, together with potential side effects of IgAN treatments available until recently, significantly impact patients’ lives,” said Professor Dana Rizk, Investigator, APPLAUSE-IgAN Steering Committee Member, and Professor in the UAB Division of Nephrology. “Fabhalta is the first potential treatment for IgAN that specifically targets the alternative complement pathway.”
Highlights of the Study
APPLAUSE-IgAN is the first Phase III multicenter, randomized, placebo-controlled study to demonstrate significant proteinuria reduction by targeting the complement system in patients with IgAN. This pre-specified interim analysis included 250 patients for the efficacy analysis and 443 for the safety analysis 1 . The APPLAUSE-IgAN study continues in a double-blind fashion until the final analysis of the primary endpoint related to iptacopan's ability to slow IgAN progression by measuring the annualized total estimated glomerular filtration rate (eGFR) slope over 24 months. Those results are expected at study completion in 2025 9,10 .
The two primary endpoints of the study for the interim and final analysis, respectively, are proteinuria reduction at 9 months as measured by UPCR, and the annualized total eGFR slope over 24 months 9,10 . At the time of final analysis, the following secondary endpoints will also be assessed: the proportion of participants reaching UPCR <1 g/g without receiving corticosteroids/immunosuppressants or other newly approved drugs or initiating new background therapy for treatment of IgAN or initiating kidney replacement therapy (KRT), time from randomization to first occurrence of composite kidney failure endpoint event (reaching either sustained ≥30% decline in eGFR relative to baseline or sustained eGFR <15 mL/min/1.73 m 2 or maintenance dialysis or receipt of kidney transplant or death from kidney failure), change from baseline to 9 months in the fatigue scale measured by the Functional Assessment Of Chronic Illness Therapy-Fatigue questionnaire 9,10 .
The main study population enrolled patients with an eGFR ≥30 mL/min/1.73 m 2 and UPCR ≥1 g/g based on a 24 hr urine collection at baseline 9,10 . In addition, a smaller cohort of patients with severe renal impairment (eGFR 20–30 mL/min/1.73 m 2 at baseline) was also enrolled to provide additional information but will not contribute to the main efficacy analyses 9,10 .
“There is a need for effective, targeted therapies for IgAN patients and the detailed Applause-IgAN study gives valuable, promising insights to healthcare providers and patients living with IgAN,” said NKF President Dr. Sylvia Rosas. “The alternative complement pathway has been implicated in the pathogenesis of IgAN, so it gives patients hope that a novel therapeutic intervention may lead to slowing progression of chronic kidney disease and avoiding kidney failure.”
The annual 2024 NKF Spring Clinical Meetings (SCM) will be held in Long Beach, CA from May 14 – 18.
NKF Spring Clinical Meetings
For the past 32 years, nephrology healthcare professionals from across the country have come to NKF’s Spring Clinical Meetings to learn about the newest developments related to all aspects of nephrology practice; network with colleagues; and present their research findings. The NKF Spring Clinical Meetings is designed for meaningful change in the multidisciplinary healthcare teams’ skills, performance, and patient health outcomes. It is the only conference of its kind that focuses on translating science into practice for the entire healthcare team.
About Kidney Disease
In the United States, more than 37 million adults are estimated to have kidney disease, also known as chronic kidney disease (CKD) - and approximately 90 percent don't know they have it. About 1 in 3 adults in the U.S. are at risk for kidney disease. Risk factors for kidney disease include: diabetes , high blood pressure , heart disease , obesity , and family history . People of Black or African American, Hispanic or Latino, American Indian or Alaska Native, Asian American, or Native Hawaiian or Other Pacific Islander descent are at increased risk for developing the disease. Black or African American people are about four times as likely as White people to have kidney failure. Hispanics experience kidney failure at about double the rate of White people.
NKF Professional Membership
Healthcare professionals can join NKF to receive access to tools and resources for both patients and professionals, discounts on professional education, and access to a network of thousands of individuals who treat patients with kidney disease.
- Perkovic V, Kollins D, Renfurm R, et al. Efficacy and Safety of Iptacopan in Patients with IgA Nephropathy: Interim Results from the Phase 3 APPLAUSE-IgAN Study. Presented at the World Congress of Nephrology (WCN); April 15, 2024; Buenos Aires, Argentina.
- Kidney Disease: Improving Global Outcomes (KDIGO) 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int . 2021;100(4):S1-S276. doi:10.1016/j.kint.2021.05.021
- Rizk DV, Maillard N, Julian BA, et al. The Emerging Role of Complement Proteins as a Target for Therapy of IgA Nephropathy. Front Immunol . 2019;10:504. doi:10.3389/fimmu.2019.00504
- Medjeral-Thomas NR, O'Shaughnessy MM. Complement in IgA Nephropathy: The Role of Complement in the Pathogenesis, Diagnosis, and Future Management of IgA Nephropathy. Adv Chronic Kidney Dis . 2020;27(2):111-119. doi:10.1053/j.ackd.2019.12.004
- Boyd JK, Cheung CK, Molyneux K, Feehally J, Barratt J. An Update on the Pathogenesis and Treatment of IgA Nephropathy. Kidney Int . 2012;81(9):833-843. doi:10.1038/ki.2011.501
- Reich HN, Troyanov SAA, Scholey JW, Cattran DC. Remission of Proteinuria Improves Prognosis in IgA Nephropathy. J Am Soc Nephrol . 2007;18(12):3177-3183. doi:10.1681/ASN.2007050526
- Thompson A, Carroll K, Inker LA, et al. Proteinuria Reduction as a Surrogate End Point in Trials of IgA Nephropathy. Clin J Am Soc Nephrol . 2019;14(3):469-481. doi:10.2215/CJN.08600718
- Zhang H, Rizk DV, Perkovic V, et al. Results of a Randomized Double-Blind Placebo-Controlled Phase 2 Study Propose Iptacopan as an Alternative Complement Pathway Inhibitor for IgA Nephropathy. Kidney Int . 2024;105(1):189-199. doi:10.1016/j.kint.2023.09.027
- Rizk DV, Rovin BH, Zhang H, et al. Targeting the Alternative Complement Pathway with Iptacopan to Treat IgA Nephropathy: Design and Rationale of the APPLAUSE-IgAN Study. Kidney Int Rep . 2023;8(5):968-979. doi:10.1016/j.ekir.2023.01.041
- ClinicalTrials.gov. NCT04578834. A Multi-Center, Randomized, Double-Blind, Placebo-Controlled, Parallel Group, Phase III Study to Evaluate the Efficacy and Safety of LNP023 in Primary IgA Nephropathy Patients. Available from: https://clinicaltrials.gov/ct2/show/NCT04578834 . Accessed April 2024.
- Novartis. Novartis receives FDA approval for Fabhalta® (iptacopan), offering superior hemoglobin improvement in the absence of transfusions as the first oral monotherapy for adults with PNH. Available from: https://www.novartis.com/news/media-releases/novartis-receives-fda-approval-fabhalta-iptacopan-offering-superior-hemoglobin-improvement-absence-transfusions-first-oral-monotherapy-adults-pnh . Accessed April 2024.
- Novartis. Novartis Fabhalta® (iptacopan) receives positive CHMP opinion as first oral monotherapy for adult patients with paroxysmal nocturnal hemoglobinuria (PNH). Available from: https://www.novartis.com/news/media-releases/novartis-fabhalta-iptacopan-receives-positive-chmp-opinion-first-oral-monotherapy-adult-patients-paroxysmal-nocturnal-hemoglobinuria-pnh . Accessed April 2024.
- McGrogan A, Franssen CF, de Vries CS. The Incidence of Primary Glomerulonephritis Worldwide: A Systematic Review of the Literature. Nephrol Dial Transplant . 2011;26(2):414-430. doi:10.1093/ndt/gfq665
- Xie J, Kiryluk K, Wang W, et al. Predicting Progression of IgA Nephropathy: New Clinical Progression Risk Score. PLoS ONE. 2012;7(6):e38904. doi:10.1371/journal.pone.0038904
- Novartis. Novartis completes acquisition of Chinook Therapeutics. Available from: https://www.novartis.com/news/media-releases/novartis-completes-acquisition-chinook-therapeutics . Accessed April 2024.
More From Forbes
Evolve clinical medicine with ai and customization.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
It’s been a few years – so why isn’t AI making medicine better?
Okay, that’s a sort of simplistic question, and yes, AI is advancing medicine in many ways, but there’s still a lot further to go.
“A properly developed and deployed AI, experts say, will be akin to the cavalry riding in to help beleaguered physicians struggling with unrelenting workloads, high administrative burdens, and a tsunami of new clinical data,” wrote Alvin Powell in the Harvard Gazette, and yes, it was 2020, but how much headway have we made in the last three years?
I was listening to a recent presentation by Abhishek Singh, who has been working on these kinds of efforts for a while, at a recent event. He showed how AI might be poised to go a lot further soon.
“Healthcare is full of conflicting evidence,” he said, citing too much reliance on a ‘one-size-fits-all approach’.
In a way, he suggested, what we’re doing now is a lot like exploring the uncharted waters of early geographical exploration, with efforts based on “anecdotes, promised lands, and imprecise data.”
The bottom line? Healthcare needs a Google Maps type of cartography to better personalize medicine!
Netflix: Marvel Dud Among Movies New On Streaming Service This Week
Drake kendrick lamar feud timeline lamar dominates billboard hot 100 with not like us, apple s new chatgpt deal here s what it means for iphone security.
Subway map on smartphone screen. Metro app with metro map. Hand holding mobile phone, finger ... [+] touching screen. Navigation, location concepts. Modern flat design. Vector illustration
“First we track where we are, then we discover where everyone else is, and compare our journey with them, and finally we get a recommended optimal path to go from point A to point B in the fastest way possible,” he said.
Singh also mentioned three bugbears of this process – distrust, disorganization and depersonalization. As he mentions, scattered data makes things harder. So does generic analysis!
Presenting a chart with insights and traffic data, and privacy and health data as values, he explained that a fundamental goal should be to combine both in the problem of discovery – to get a setup where you can get the insights, without violating the privacy.
“In the general healthcare system, there are lots of stakeholders,” he said. “Hospitals, insurance companies, pharma, patients, research institutions – and many of them are not able to exchange information and insights, due to regulation and the overall lack of interoperability.”
However, Singh suggested, with centralization can come a single point of failure, so what about discovery without centralization?
He talked about a clustering of people according to their DNA, which makes their health needs unique.
Mutated DNA and molecules, scientific biotechnology, 3d rendering. Computer digital drawing.
Science Biotechnology Dna Chromosome 3d Rendering High-Res Stock Photo - Getty Images
“Similar to how sailors were building bigger and bigger ships to solve the problem of mapping the world, today's AI is aiming at building bigger and bigger models to improve precision,” he added.
This tracks with things that I've heard from other recent talks by people working in the healthcare field. They suggest that genomics is a way to make healthcare personalized – and that what we have to do largely involves better tracking and better, again, cartography of our personal health systems – in other words, our bodies, and ourselves.
Years ago, we had the move toward electronic medical records and electronic health records. We had all kinds of access challenges, and a lot of those haven’t gone away. In talking about regulation, Singh is probably also referring to HIPAA, which as an overarching rule, has confounded a lot of research activity and efforts.
But if we can make our way from healthcare 2.0 – digital record designs – to healthcare 3.0 – AI analysis and recommendation – we might have the tools we need to build some of what Singh is talking about.

- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Clinical Presentations, Pathogenesis, and Therapy of Sarcoidosis: State of the Art
Francesca polverino.
1 Asthma and Airway Disease Research Center, University of Arizona, Tucson, AZ 85718, USA
Elisabetta Balestro
2 University Hospital of Padua, 35100 Padua, Italy; [email protected] (E.B.); [email protected] (P.S.)
Paolo Spagnolo
Sarcoidosis is a systemic disease of unknown etiology characterized by the presence of noncaseating granulomas that can occur in any organ, most commonly the lungs. Early and accurate diagnosis of sarcoidosis remains challenging because initial presentations may vary, many patients are asymptomatic, and there is no single reliable diagnostic test. Prognosis is variable and depends on epidemiologic factors, mode of onset, initial clinical course, and specific organ involvement. From a pathobiological standpoint, sarcoidosis represents an immune paradox, where an excessive spread of both the innate and the adaptive immune arms of the immune system is accompanied by a state of partial immune anergy. For all these reasons, the optimal treatment for sarcoidosis remains unclear, with corticosteroid therapy being the current gold standard for those patients with significantly symptomatic or progressive pulmonary disease or serious extrapulmonary disease. This review is a state of the art of clinical presentations and immunological features of sarcoidosis, and the current therapeutic approaches used to treat the disease.
1. Definition and Clinical Presentations
Sarcoidosis is a systemic granulomatous disorder that remains an enigma and challenges both researchers and clinicians due to its unknown cause, heterogeneous clinical presentation, and unpredictable outcome, occasionally severe and even lethal, often with no therapy able to change the course of the disease [ 1 ]. This huge variability led scientists to search for clinical patterns of phenotypic variables in order to help the diagnosis and avoid, when possible, invasive procedures. Sarcoidosis can affect individuals of all ages but most commonly affects men aged 30 to 50 years, and women aged 40 to 60 years [ 2 ]. Phenotypic differences in sarcoidosis subsets may relate, at least partially, to the variability of the organs involved.
The frequency of organ involvement at the time of diagnosis is summarized in Table 1 [ 3 , 4 ]. The lung is the most commonly affected organ, although with a frequency that varies according to race, sex, and age. Thoracic involvement occurs in 90% of patients with bilateral symmetrical hilar adenopathy representing the most common thoracic manifestation ( Figure 1 ), whereas unilateral hilar adenopathy occurs in only 3% to 5% of patients.

Acute form of sarcoidosis. Posterior-anterior chest radiograph of a 35-year-old female with Löfgren’s syndrome demonstrating bilateral hilar adenopathy (arrows) without evidence of parenchymal lung involvement.
Overall frequency of organ involvement at the time of diagnosis (patients could have more than one organ involved) adapted from Baughman RP et al., 2001. [ 4 ].
Even though the thorax is the most common site of disease, skin involvement occurs in at least 25% of patients and is often overlooked. Indeed, cutaneous sarcoidosis is often attributed to other causes, mainly due to its wide range of manifestations, which include erythema nodosum, maculopapular lesions, hyper- and hypo pigmentated areas, keloid formation, and subcutaneous nodules [ 5 ]. With the exception of erythema nodosum, which consists of a panniculitis and does not contain granulomas, skin lesions are generally florid areas of granulomatous inflammation, and the diagnosis of sarcoidosis can be readily made by skin biopsy. Erythema nodosum may accompany acute presentations of the disease, is more common in women, and tends to be associated with a favorable prognosis, while manifestations such as lupus pernio [ 6 ], often described in African Americans and Puerto Ricans, are associated with chronic disease and worse prognosis.
Eye involvement may precede the diagnosis of sarcoidosis by years or even decades and occurs in up to 25% of patients depending on race [ 7 ]. For example, only 30% of patients in the United States have sarcoidosis-related eye illness vs. more than 70% in Japan. The most common manifestations are anterior uveitis with acute pain and blurred vision, while photophobia is reported in fewer cases [ 8 ].
Cardiac involvement in sarcoidosis is much more common than clinically appreciated, and it can be present without the involvement of other organs. The three major manifestations of cardiac sarcoidosis are: conduction abnormalities, ventricular arrhythmias, and congestive heart failure. Granulomatous infiltration of the myocardium is responsible for arrhythmias and cardiomyopathy [ 9 ]. In particular, the atrioventricular (AV) block is the most frequent type of arrhythmia, whereas ventricular tachycardia and supraventricular arrhythmia are less common. Chronic heart failure may occur both with reduced ejection fraction from dilated cardiomyopathy and with preserved ejection fraction from restrictive cardiomyopathy [ 10 , 11 ]. Since cardiac sarcoidosis can occur in the absence of apparent disease elsewhere, it should be suspected and investigated in any non-ischemic form of cardiomyopathy, particularly when arrhythmias are prominent [ 12 , 13 ]. Furthermore, cardiac involvement can be observed in patients with advanced pulmonary fibrosis due to Pulmonary Arterial Hypertension (PAH) [ 14 ].
Neurosarcoidosis is reported in 5–10% of sarcoidosis patients and appears to be equally frequent across ethnic groups. Any part of the nervous system can be affected, and among all parts of the central nervous system (CNS), cranial neuropathy and meningeal involvement are the most common manifestations. Furthermore, II, VII, and VIII cranial nerves are the most commonly involved, even if all cranial nerves have been reported to be potentially affected. Meningitis accounts for 10% to 20% of cases of neurosarcoidosis, although the reported frequency of subclinical leptomeningeal damage is much higher [ 15 ]. Finally, brain parenchymal disease is less common, and patients may present with seizure, headache, or cognitive/behavioral problems. Likewise, spinal cord disease and peripheral neuropathy are quite rarely reported [ 16 , 17 , 18 ].
2. Subtypes of Sarcoidosis and Outcomes
The clinical presentation of sarcoidosis is highly heterogeneous, and the onset can be acute or subacute/chronic. It has been hypothesized that different immunologic features underlie these diverse presentations. From both clinical and immunological standpoints, sarcoidosis is mainly classified in Löfgren’s syndrome (LS) and non-Löfgren’s syndrome. In more than half of the cases of LS, the disease resolves spontaneously within 2 years, on average [ 19 , 20 ]. After five years, recovery is much less likely. In terms of clinical development and outcome, sarcoidosis can be classified into acute (≤2 years) and chronic (≥3–5 years).
2.1. Lofgren’s Syndrome (LS)
The typical combination of symptoms with acute onset such as fever, erythema nodosum, and arthritis accompanied by bilateral hilar lymphadenopathy at chest X-ray is defined as LS ( Figure 1 ) [ 21 ]. LS is highly associated with the human leukocyte antigen (HLA) B8 (HLA-B*) serotype [ 22 , 23 ]. Further, a strong association between HLA-B8/DR3 and acute onset of symptoms has been shown in patients with sarcoidosis with bilateral hilar lymphadenopathy, suggesting the key role of immunogenetics in the multifaceted disease presentation [ 24 ]. Rapid onset of acute disease is generally associated with spontaneous resolution and excellent prognosis. LS associated with the HLA-DQB1*0201 allele is associated with good prognosis in European patients, whereas HLA-DRB1*0301 has been associated with an equally favorable prognosis in the Swedish population, even without therapy [ 25 , 26 ]. In the great majority of cases, patients with LS recover from symptoms and/or radiologic abnormalities, either spontaneously or after corticosteroid treatment. The Heerfordt-Waldenström syndrome is another rare form of sarcoidosis with acute presentation and typical signs and symptoms such as parotitis, facial palsy, anterior uveitis, and fever. The radiographic appearance, although nonspecific, shows a typical enlargement of the parotid gland(s) and enlargement of cervical lymph nodes.
2.2. Subacute/Chronic Sarcoidosis
The non-acute form, or non-LS sarcoidosis, is much more heterogeneous than LS and presents with a wide range of nonspecific symptoms and with an insidious/subacute onset [ 27 ]. Subacute to chronic presentation often include cough, shortness of breath, arthralgia, fatigue, chest pain, muscle pain, night sweats, and weight loss. Fatigue is a very common complaint (up to 50–70% of the patients) and leads to impaired quality of life and disability [ 28 ]. Chronic sarcoidosis is associated with an increased risk of developing fibrosis (pulmonary and extrapulmonary), pulmonary arterial hypertension (PAH), and other persistent disabling symptoms, as well as permanent loss of lung function associated with impaired quality of life [ 3 ]. Extrapulmonary manifestations associated with unfavorable prognosis include lupus pernio, chronic uveitis, chronic hypercalcemia, nephrocalcinosis, cystic bone lesions, and myocardial involvement.
Progression to irreversible fibrosis. Pulmonary fibrosis (PF) represents a rare (20% of chronic forms) yet poorly studied phenotype of sarcoidosis ( Figure 2 ). Chronic granulomatous inflammation of the lung may lead to the development of pulmonary fibrosis, which is associated with an increased risk of mortality. Pulmonary fibrosis may manifest as either progressive disease or an exhausted and quiescent process with inactive granulomatous inflammation. Interestingly, a local shift from Th1 to Th2 responses has been associated with progression from granulomatous inflammation to fibrotic disease [ 29 , 30 ]. However, it remains to be clarified whether sarcoidosis-associated PF: (1) is a phenotype that begins early in the course of the disease or whether it develops as a response to an excessive immune response; and (2) once initiated, can progress independently of active granulomatous inflammation. PAH occurs in at least 5% of patients with sarcoidosis, mainly affected by the chronic form. PAH is the most frequent complication of advanced PF and is associated with poor prognosis. A number of mechanisms may underlie the development of PAH, including direct vascular involvement by the granulomatous process, PF, extrinsic arterial compression by lymphadenopathies, or pulmonary veno-occlusive disease [ 31 ]. The majority of patients with end-stage PF show PAH, with a prevalence that is significantly higher than that reported for other fibrotic interstitial lung diseases ( Figure 3 ) [ 32 ]. PF with PAH is generally complicated by the development of respiratory failure and infections such as mycetoma [ 33 ].

Chronic form of sarcoidosis. ( A ) Posterior-anterior chest radiograph of a 55-year-old man with progressive pulmonary fibrosis despite treatment demonstrating permanent, coarse linear opacities, radiating laterally from the hilum upward and outward (arrows). ( B ) high-resolution CT showing intra parenchymal enlargement of pulmonary arteries and enlarged pulmonary trunk at the bifurcation.

Chronic form of sarcoidosis complicated with pulmonary arterial hypertension (PAH). ( A ) Posterior-anterior chest radiograph of a 58-year-old man listed for lung transplant demonstrating extensive parenchymal scarring throughout both lungs, most marked in the upper lungs (arrows) and in the perihilar regions. ( B ) high-resolution CT showing intra-parenchymal enlargement of pulmonary arteries and enlarged pulmonary trunk at the bifurcation.
2.3. Mortality in Sarcoidosis
Patients with sarcoidosis have a lower survival rate than the general population [ 34 ], with a mortality rate reported to be up to 7.6% [ 35 ]. In a study conducted to evaluate mortality rates among French decedents with sarcoidosis from 2002 to 2011, the mean age at death was lower than the general population by about six years [ 36 ]. In addition, in a Swedish cohort, individuals with incident sarcoidosis (2003–2013) had a higher risk of death compared to the general population [ 37 ]. Sarcoidosis was often associated with death because of respiratory failure due to advanced PF, cardiovascular diseases, and neurologic disease with a different rate depending on the country of origin. For example, in western countries, most fatalities were due to end-stage lung disease, whereas in Japan, the main cause of death was heart failure [ 38 ]. Less common causes of mortality include hemoptysis from mycetoma and lymphoma [ 35 ].
3. Pathogenesis of Sarcoidosis
Sarcoidosis is characterized by non-infectious non-caseating granulomas, comprised primarily of macrophages that differentiate to epithelioid cells, which subsequently fuse to form multinucleated giant cells. CD4+ T helper cells, the specificity of which is unknown, are interspersed in the granuloma while CD8+ T cells, regulatory T cells (Tregs), fibroblasts, and B cells surround the periphery [ 39 ]. This heterogeneous cell population suggests that both innate and adaptive immune responses contribute to the onset and the progression of the disease. To date, however, the pathogenesis of sarcoidosis represents an unresolved immunological paradox. In sarcoidosis, affected organs present an intense immune response, yet at the same time, a state of immune anergy is established, as indicated by a reduced delayed-type hypersensitivity to tuberculin and common antigens ( Figure 4 ) [ 40 ].

Pathobiology of sarcoidosis and current therapeutic approaches: An unknown airborne-antigen activates interstitial dendritic cells (DCs) and alveolar macrophages (AMs) simultaneously. The interstitial DCs pick up the antigen and migrate toward the mediastinal lymph nodes, where they serve as antigen-presenting cells (APCs) to T helper (Th)1 and 17 cells by initiating their differentiation and clonal expansion. Simultaneously, AMs: (1) serve as APCs together with DCs; (2) differentiate as M1 and M2 macrophages and further induce the inflammatory process (M1), fibroblasts proliferation, and fibrotic tissue deposition (M2); and (3) produce the pro-inflammatory cytokine tumor necrosis factor-α (TNF-α) via human leukocyte antigen (HLA)-DR, and other chemoattractants such as IL-12 under stimulation of both TNF-α and natural-killer (NK) cell-derived interferon-γ (INF-γ). Persistent stimulation, mediated by APCs leads to continuous recruitment of B cells, plasmacells, Th1/17 cells, monocytes (expressing higher Toll Like Receptor (TLR)2 and TLR4, inducing Th1 and Th2 responses, respectively), and regulatory T cells (Tregs) from the bloodstream to the lung, where they contribute to the granuloma formation. Tregs infiltrating the granuloma fail to diminish the exaggerated immune response, thereby contributing to granuloma persistence and integrity. The therapeutic targets that are currently being used/tested for sarcoidosis are also indicated.
3.1. Putative Antigens
The involvement of both the innate and the adaptive immune cells calls into question the nature of the antigen/s involved in the pathogenesis of sarcoidosis. Thus far, apart from the tuberculin known to trigger the formation of the sarcoid granuloma, many have been the candidate antigens associated with the onset and the progression of the disease. Bacterial DNA has been identified in sarcoidosis lesions [ 41 ] as well as autoantigens belonging to the major histocompatibility complex (MHC) class II molecules on antigen-presenting cells, recognized by the T-cell receptor (TCR) of the responding T-cells of sarcoidosis patients and leading to their clonal expansion [ 42 ]. Strong T cell responses to vimentin, a peptide derived from the cytoskeleton, have been found in a subset of patients with sarcoidosis with a specific HLA type [ 42 ]. Similarly, stimulation of peripheral blood mononuclear cells (PBMCs) from patients with sarcoidosis with vimentin triggers increased secretion of cytokines able to sustain the immune response [ 43 ], suggesting a self-perpetuating mechanism similar to that known to occur in autoimmune diseases.
Overall, the immune cascade triggered by the antigen/s is much better known compared to the nature of the antigen itself. We here describe the role of innate and adaptive immune responses in the onset and the progression of sarcoidosis.
3.2. Innate Immune Cells
Alveolar macrophages (AMs) are involved both in innate and adaptive immune responses in sarcoidosis [ 44 ]. AMs produce a range of pro-inflammatory cytokines, such as tumor necrosis factor-α (TNF-α), which drives granuloma formation in sarcoidosis [ 45 ]. In addition, AMs function as antigen-presenting cells (APCs), interacting with T-cells via human leukocyte antigen (HLA) molecules and T-cell receptors [ 46 ]. Activation of the mammalian target of rapamycin complex 1 (mTORC1) pathway in macrophages promotes excessive granuloma formation in mice and is associated with macrophage proliferation and disease progression in patients with sarcoidosis [ 47 ]. An analysis of peripheral blood monocytes from sarcoidosis patients found enrichment of activated monocytes available to populate sites of granulomatous inflammation and a higher prevalence of cells expressing CD11c, possibly representing a subpopulation of monocyte-derived cells that could differentiate to dendritic cells, thus linking innate and adaptive responses in sarcoidosis [ 48 ]. There is an increased number of phagocytic monocytes in the blood of sarcoidosis patients to control subjects. Similarly, circulating monocytes also display higher Toll Like Receptor TLR2 and TLR4 expression, inducing Th1 and Th2 responses, respectively [ 46 ]. Bronchoalveolar lavage (BAL) cells from patients with sarcoidosis produce more TNF-α and IL-6 in response to TLR2 agonists compared to healthy controls, while PBMCs from sarcoidosis patients have impaired TLR2 responses [ 49 ]. Importantly, macrophage activation status and polarization exert a dominant effect on the outcome of granulomatous inflammation. Granulomatous inflammation in pulmonary sarcoidosis has historically been linked to a compartmentalized elevation of T-helper cell type 1 (Th1) cytokines, including but not limited to IL-2, IFN-γ, and TNF-α. This cytokine milieu is believed to drive classical pro-inflammatory (M1) macrophage activation, whereas the proportion of anti-inflammatory M2 macrophages tends to be higher in other types of interstitial lung disease, including idiopathic pulmonary fibrosis [ 50 ]. However, increases in M2 macrophages have been recently reported in granulomas of patients with sarcoidosis as compared with tuberculous granulomas [ 51 ]. Interestingly, M2 macrophages are capable of differentiating into fibrocyte-like cells that express collagen [ 52 ]. It still needs to be established if the presence of M2 macrophages identifies a profibrotic mechanism inherent to the pathogenesis of sarcoidosis rather than part of a generalized wound-healing response to lung inflammation and injury. AMs are also the main source, together with lung T cells, of interferon gamma (IFN γ ), which is highly expressed in the BALF (Bronchoal Veolar Lavage Fluid) of sarcoidosis patients [ 53 ]. IFN γ inhibits the expression of macrophage peroxisome proliferator-activated receptor γ (PPAR γ ), a negative regulator of inflammation. Under normal physiological conditions, macrophages constitutively express PPAR γ . PPAR γ promotes macrophage IL-10 production, which inhibits the release of TNF α , IL-12, and matrix metalloproteinases (MMPs) from dendritic cells (DCs). In sarcoidosis, PPAR γ activity is deficient in AMs [ 54 ], leading to an increase in the production of TNF α , IL-12, and MMPs, which cause lung damage and fibrosis and induction of T-cell chemotaxis [ 55 ]. Moreover, increased TNF α and decreased IL-10 expression liberate DCs from the inhibition by macrophages, initiating a self-amplifying inflammatory loop (see below)
Peripheral blood DCs from patients with sarcoidosis are less immunostimulatory than normal blood DCs and are less capable of mounting a delayed-type hypersensitivity (DTH) response [ 40 ]. Consistent with this finding, sarcoidosis lung DCs are less able to induce T cell proliferation than normal lung DCs [ 55 ]. A real paradox in sarcoidosis stands in the fact that, despite the partially blunted immunostimulatory capacity of circulating and pulmonary DCs, they are still effective inducers of T cell proliferation, more than macrophages themselves, both through direct TCR and through the secretion of potent inflammatory mediators, such as IL-12. Through IL-12, DCs are able to polarize Th1 T cells, stimulate T cell proliferation, and induce leukocyte chemotactic factors that contribute to granuloma formation [ 56 ]. Overall, the function of DCs in sarcoidosis is paradoxical. On the one hand, they are capable of initiating an antigen-driven, inflammatory oligoclonal T cell responses [ 57 ]. On the other hand, they are anergic and less immunostimulatory than normal DCs [ 40 ].
3.3. Adaptive Immune Cells
3.3.1. t cells.
T-cells, particularly activated CD4+ T-cells, play a key role in the inflammation in sarcoidosis. Different subsets of CD4+ helper T cells participate in the immunopathogenesis of sarcoidosis. The main feature of the acute disease is represented by a Th1/Th17/regulatory T cells (Tregs)-driven inflammatory process involving macrophages both as antigen-presenting cells and key effectors. As discussed above, when triggered by factors as yet unidentified, APCs such as DCs release cytokines (e.g., IL-12) [ 55 ] and other inflammatory factors, leading to a milieu that induces recruitment and activation of Th1 CD4+ T-cells and monocytes to the lungs. In sarcoidosis, the lung homes up to ten times as many CD4+ T-cells as the peripheral blood, thus leading to an elevated CD4/CD8 ratio as measured in BAL fluid [ 58 ]. The CD4+ T cells that trigger the granuloma formation are strongly Th1 polarized. Upon TCR activation, the expression of IFN γ in CD4+ T cells becomes more pronounced. In response to IL-12, CD4+ T-cell production of IL-4 and IL-13 (cytokines that facilitate the fibroproliferative response) is inhibited. IL-12 and IL-18 act synergistically to promote the formation of sarcoid granulomas. As detailed above (see AM section) in sarcoidosis, the deficient PPAR γ activity in AMs [ 54 ] attracts more T cells and myeloid cells into the inflammatory milieu. CD4+ T-cell activation also increases IL-2 production, resulting in increased Th1 polarization. Interestingly, the persistent antigen exposure can induce anergy and/or exhaustion of the pathogenic CD4+ T cells, probably as a defense mechanism to temper down the chronic T cell activation and subsequent inflammation [ 59 ]. Pulmonary CD4+ T cells from patients with sarcoidosis spontaneously secrete IL-2 ex vivo, but upon TCR stimulation, they express less IL-2 and IFN-γ compared to CD4+ T cells from other lung diseases and healthy controls, in line with an anergic/exhausted phenotype [ 60 ]. Other signs of Th1 anergy/exhaustion due to prolonged antigen exposure in sarcoidosis are their reduced proliferative capacity and their higher levels of apoptosis, associated with increased programmed death (PD)-1 expression [ 61 ].
Th17 cells that express IL-17 and a specific master transcription factor, known as RORc [ 62 ], have a key role in the plasticity of granuloma formation and maintenance. They participate in the alveolitic/granuloma phase, the maintenance of granuloma, and the progression towards the fibrotic phase of sarcoidosis [ 63 ]. Th17 cells are increased in the lung and the peripheral blood of patients with active sarcoidosis. Their recruitment to granulomas is due to the release of cytokines and chemoattractants by locally and systemically activated macrophages.
Failure of immune regulatory mechanisms to limit the duration of Th1–Th17 inflammation has been suggested to contribute to persisting granulomatous responses in sarcoidosis. T regulatory cells (Tregs) are vital for the suppression of cell-mediated immune responses. However, Tregs in the sarcoid granulomas (as opposed to peripheral Tregs) that have also been found elevated in BALF from patients with sarcoidosis undergo extensive amplification and are therefore impaired in their ability to repress immune responses [ 64 ]. On the other hand, they secrete pro-inflammatory cytokines (e.g., IL-4), which induces granuloma formation via mast cell activation and fibroblast amplification [ 65 ]. To date, the role of regulatory T cells (Tregs) in the pathogenesis of sarcoidosis remains controversial. Further studies are needed to shed light on the complex interactions between regulatory mechanisms and off-targeted immune responses in the disease.
3.3.2. B Cells
Little is known about B cell immunity in sarcoidosis [ 66 ]. Hypergammaglobulinemia (including autoantibodies) is well-recognized in sarcoidosis, where B cells form prominent infiltrates at the periphery of lung granulomas [ 67 ]. Thus far, whether B cells play a direct role in disease pathogenesis in sarcoidosis is unknown, but altered and/or increased (auto) antibody responses have been reported in these patients. Unlike healthy subjects, patients with sarcoidosis show a direct correlation between the number of BAL T cells and the proportion of BAL cells that secrete IgG [ 68 ]. Additionally, increased numbers of memory IgA-producing B cells are found in patients with sarcoidosis, suggesting that IgA could be involved in granuloma formation [ 69 ]. Interestingly, B cells might also play a role in the autoimmune phenomena associated with the onset and progression of sarcoidosis. In fact, several types of autoantibodies have been found, both circulating and associated with the lung tissue, in patients with sarcoidosis, such as anti-mitochondrial, anti-nuclear antibodies, and autoantibodies to double-stranded DNA [ 70 ]. Case-report evidence of responses to rituximab exists in extrapulmonary sarcoidosis but not for pulmonary disease as yet [ 71 ]. Recently, age-associated B cells (ABCs) [ 72 ], B cell subtypes associated with aging, in which they contribute to inflammation [ 73 ], have been found increased in peripheral blood and BAL (relative to healthy subjects) in patients with sarcoidosis [ 74 ] but their role needs to be clarified.
4. Pharmacological Treatment
In sarcoidosis, the decision to initiate treatment is not straightforward, mainly due to the highly variable and unpredictable course of the disease and the lack of evidence-based management guidelines. Broadly, the treatment is selected based on the presence of life- or organ-threatening disease and very poor quality of life. Figure 4 and Figure 5 summarize the approach to the management of sarcoidosis and the current therapeutic options, as seen by the authors.

Approach to the therapeutic management of sarcoidosis. Abbreviations: AZA: Azathioprine; GCs: glucocorticoids; MMF: mycophenolate mofetil; MTX: methotrexate.
Systemic glucocorticoids (GCs) are the first-line therapy for pulmonary and extrapulmonary sarcoidosis, as they inhibit macrophage and lymphocyte activation and modulate several cytokines that participate in granulomatous inflammation. However, they do not alter the course of the disease, and their long-term use is associated with significant safety and tolerability issues. Therefore, the pros and cons of initiating GC treatment should be carefully weighed, bearing in mind that approximately half of the patients have self-remitting or non-progressive disease, which does not require therapy [ 75 , 76 ]. In patients with pulmonary sarcoidosis, treatment should be considered in the following circumstances: disabling and worsening respiratory symptoms (e.g., dyspnoea, cough, chest discomfort); severe functional impairment or progressive functional deterioration (e.g., TLC (Total Lung Capacity) decline of ≥10% and/or FVC (Forced Ventilatory Capacity) decline of ≥15% and/or DL CO (Diffusion Capacity for Lung Carbon Monoxide) decline of ≥20% over three to six months); or major progression of radiographic abnormalities (e.g., worsening of interstitial opacities, development of cavities or progression of fibrosis with honeycombing) [ 77 ]. Some patients require treatment with GCs because of significant extrapulmonary manifestations such as ocular, cardiac, neurological and renal, and/or hypercalcemia. An additional potential indication for GC therapy includes severely impaired quality of life due to fever, fatigue, arthralgia, or disfiguring skin disease [ 1 , 78 ]. The optimal dose and duration of GC treatment are unknown. We generally initiate therapy with oral prednisone at a daily dose of 0.3–0.5 mg/kg of ideal body weight (usually 20 to 40 mg/day) depending on disease severity. We continue the initial dose for four to six weeks and then re-evaluate the patient. Provided clinical, functional, and radiographic features are stable or improved, we taper the dose by 5 to 10 mg every one to three months for a total treatment period of six to nine months [ 79 , 80 ].
The majority of patients are able to discontinue treatment after one year; however, relapse is common during tapering or after GC discontinuation, with as many as 30% of patients requiring longer-term therapy [ 81 ]. Overall, the GC use is associated with symptomatic and radiographic improvement, at least initially, but their long-term benefit is unclear [ 82 ]. The antimalarial drug hydroxychloroquine may be preferable to GC in patients with skin disease or hypercalcemia [ 83 , 84 ].
Immunosuppressants: for patients experiencing relapse/disease progression despite GC treatment or intolerable side effects of GCs, a step-up approach to second-line agents is recommended. Methotrexate (MTX) is the drug of choice for sarcoidosis selected in several consensus statements [ 85 ]. MTX is an antimetabolite with anti-inflammatory and immunosuppressive properties. Several case series and randomized trials suggest that MTX is safe and effective in sarcoidosis patients with lung, eye, skin, and central nervous system involvement [ 86 ]. A 2-year retrospective study of 200 patients showed that MTX and azathioprine, another immunosuppressant, has similar steroid-sparing capacity, beneficial effects on lung function, and safety and tolerability profiles, although the rate of infection was significantly higher in the azathioprine group [ 87 ]. MTX is generally given at an initial dose of 5–7.5 mg weekly, which is gradually increased weekly, either orally or intramuscularly. MTX has a slow onset of action, and its efficacy should be assessed after at least six months of treatment. Methotrexate is generally well tolerated [ 88 ], but its use may be associated with a variety of adverse effects, including liver and lung toxicity, increased risk of infection, and myelosuppression. In order to reduce the risks of myelosuppression, folic acid supplementation is given at a dose of 5 mg weekly, and tests to monitor blood cell counts and kidney and liver function are performed at regular intervals (i.e., every four to eight weeks). Other immunosuppressants used alternatively to MTX are mycophenolate mofetil (MMF), azathioprine, and leflunomide, although the evidence in support of their efficacy is less robust. In a retrospective study of patients with pulmonary sarcoidosis who either had not responded to a prior immunosuppressive agent or had experienced an adverse event necessitating discontinuation of the drug, addition of MMF allowed a reduction of prednisone dose but was not associated with improved lung function [ 89 ]. In a retrospective case series, patients with sarcoidosis received leflunomide with or without concomitant MTX for the pulmonary or ocular disease [ 86 ]. Complete or partial response to leflunomide was observed in the great majority of patients treated with leflunomide alone and in combination of leflunomide and MTX. Overall, leflunomide was well tolerated and appeared to be as effective as MTX but less toxic.
Biologicals: TNF-α antagonists are generally reserved for patients with active/progressive disease despite being treated with GCs and at least one second-line immunosuppressant agent, particularly in cases of organ- or life-threatening disease. Infliximab is a humanized monoclonal antibody that neutralizes TNF-α. In a phase II, randomized, double-blind, placebo-controlled study, 138 patients with chronic pulmonary sarcoidosis were randomized to receive i.v. infusions of infliximab or placebo at baseline and at weeks 2, 6, 12, 18, and 24 [ 90 ]. Infliximab use was associated with a mean significant increase of 2.5% from baseline to week 24 in the percentage of predicted forced vital capacity (FVC) vs. the placebo group. Post-hoc exploratory analyses suggested that the benefit of infliximab treatment might be greater in patients with more severe disease. Infliximab is safe and well-tolerated, and the proportions of patients who had adverse events are reported to be similar to those in the placebo groups. In a prospective, open-label trial, 56 patients with sarcoidosis refractory to conventional treatment received eight infusions of infliximab [ 91 ]. After 26 weeks of treatment, the infliximab group had a significant increase in FVC predicted vs. the placebo group and a reduction in the active disease in the lung parenchyma, as measured by 18 F-FDG PET (Fluorodeoxyglucose Positron emission tomography) as maximum standardized uptake value (SUV max ). Notably, change in lung function significantly correlated with the level of disease activity. Adalimumab is a fully human anti-TNF-α monoclonal antibody. In an open-label, single-center study, 11 patients with refractory pulmonary sarcoidosis received adalimumab for 45 weeks [ 92 ]. At the 24-week follow-up, FVC improved in four patients and stabilized in seven. In addition, a successful outcome—defined as a reduction in immunosuppressive therapy improvement in FVC of 5% or greater, improvement in 6 MWD (minute walking distance) of 50 m or greater—was observed in 9/11 patients (82%) and 8/10 patients (80%) at weeks 24 and 52, respectively. In addition, among 18 patients who switched from infliximab to adalimumab due to antibody formation or severe adverse events, seven (39%) experienced clinical improvement, six (33%) remained stable, and five (28%) deteriorated [ 93 ]. Severe adverse events occurred in four patients, including one who discontinued adalimumab due to a lupus-like reaction. Current evidence does not support the use of etanercept, which is a soluble TNF-α receptor, in patients with sarcoidosis. Indeed, a prospective, open-label, phase II trial of etanercept 25 mg twice weekly in patients with progressive pulmonary disease was terminated after the enrollment of 17 patients due to excessive clinical deterioration, development of intolerable side effects, and/or need for other immunosuppressive agents [ 94 ]. At present, there is no evidence supporting the routine use of TNF-α antagonists in sarcoidosis. However, they may be useful in selected cases of cardiac and neurological disease refractory to conventional treatment [ 95 , 96 , 97 ].
Besides TNF-α inhibitors, rituximab, a chimeric anti-CD20 monoclonal antibody that induces B cell depletion is the only biologic agent for which there is some evidence of efficacy. Sweiss and colleagues conducted a prospective, open-label, phase I/II trial of rituximab at baseline and two weeks later in patients with refractory pulmonary sarcoidosis ( n = 10) [ 98 ]. At week 24, 5/10 patients had a >5% absolute improvement in FVC % predicted and 4/10 patients had a >10% improvement in FVC % predicted, whereas 2/8 patients had a >10% absolute improvement in FVC % predicted at week 52. Moreover, 6 min walking test (6MWT) improved from the initial value by >30 m in 5/10 patients and by >50 m in 3/10 patients at week 24 and by >50 m in 3/8 patients at week 52. Chest X-rays remained unchanged throughout the study. Whether rituximab may be a viable alternative to anti-TNF-α antibodies for refractory sarcoidosis is unclear and requires further studies.
Other novel therapies: several drugs targeting the immune system are currently being evaluated as future therapeutic strategies for sarcoidosis. The active inflammatory form of sarcoidosis is characterized by an exaggerated production of TNF-α and INF-γ. Fontolizumab, a humanized monoclonal antibody against INF-γ currently tested in Crohn disease [ 99 ], has the potential to depolarize M1 back to an inactive state. Other drugs target the M2 polarization that promotes sarcoidosis-related fibrotic processes in the lung. M2 polarization is regulated by STAT-6, a transcription factor that promotes a signaling cascade that includes the PPAR-γ pathway (see above). Treatment with Leflunomide, a tyrosine kinase inhibitor preventing STAT-6 phosphorylation that regulates inflammation by suppressing Th17 cells and promotes the function of Tregs, may improve lung function in patients with sarcoidosis [ 100 ]. Doxycycline and Dupilumab, two drugs that inhibit the M2 polarization, are also currently being tested in patients with sarcoidosis, but there is still lack of data enough to draw conclusions on their effectiveness. Other treatments, such as nicotine therapy, therapies targeting checkpoint inhibitors, and antibacterial therapy are also in the pipeline for the treatment of patients with sarcoidosis, but the available data are still scant [ 101 ].
Transplant: for highly selected patients with advanced fibrotic lung disease, severe pulmonary hypertension, or both, lung transplantation may be the only therapeutic option for prolonging survival and improving quality of life [ 102 ]. Bilateral lung transplantation is generally favored, as it appears to be associated with slightly better survival compared to single lung transplantation [ 103 ]. Notably, post-transplant survival is similar to that for other indications, such as idiopathic pulmonary fibrosis [ 102 , 104 ]. Heart transplantation has also been successfully performed in patients with cardiac sarcoidosis and end-stage heart failure [ 105 ]. Carefully selected patients with advanced heart failure due to cardiac sarcoidosis have an acceptable outcome after transplantation without evidence of recurrence of the disease in the allograft [ 106 ].
5. Conclusions
Sarcoidosis is a heterogeneous disease with diverse clinical presentations that likely mirror the wide umbrella of underlying immunological endotypes. Thus, a “one size fits all” approach to treating sarcoidosis is not applicable, as some patients may benefit from therapies targeting the excessive spread of the inflammatory responses, while others might benefit from therapies boosting their immune and/or regulatory responses. Further studies aimed at identifying the clinical phenotypes associated with specific blunted and/or exaggerated immune responses are needed in order to shed light on the possible therapeutic approaches for this multifaceted disease.
Author Contributions
F.P., E.B. and P.S. contributed to the writing and editing of the manuscript. All authors have read and agreed to the published version of the manuscript.
Supported by the A2DRC Funds (F.P.), Flight Attendants Medical Research Institute YFAC14004 (F.P.), Parker B. Francis Fellowship (F.P.).
Conflicts of Interest
The authors declare no conflicts of interest.
- Provectus Biopharmaceuticals-stock
- News for Provectus Biopharmaceuticals
Provectus Biopharmaceuticals Announces Eight Presentations of Rose Bengal Photodynamic Antimicrobial Therapy at ARVO 2024 Annual Meeting
- PDAT clinical outcomes for infectious keratitis from Brazil and Mexico
KNOXVILLE, TN, May 14, 2024 (GLOBE NEWSWIRE) -- Provectus Biopharmaceuticals, Inc. (“Provectus” or the “Company”) (OTCQB: PVCT) today announced that clinical and non-clinical data on rose bengal photodynamic antimicrobial therapy (“RB PDAT”) were presented at the annual meeting of the Association for Research in Vision and Ophthalmology (“ARVO”), held May 5-9, 2024 in Seattle, Washington. The ARVO annual meeting brings together approximately 10,000 vision researchers, clinicians, and scientists from around the world for scientific sessions, poster presentations, and invited speaker sessions.
Provectus entered into an exclusive worldwide license agreement with the University of Miami (the “University”) in April 2024 for its intellectual property related to RB PDAT for treating bacterial, fungal, and parasitic (acanthamoeba) eye infections. The Company and University plan to form a start-up biotechnology company (e.g., “Eyecare NewCo”), potentially in the third quarter of 2024, aimed at commercializing the University’s PDAT light source medical device in combination with a drug formulation of Provectus’s proprietary pharmaceutical-grade rose bengal active pharmaceutical ingredient (“RB API”). The Company would contribute the RB PDAT license to and have an exclusive RB API supply arrangement with Eyecare NewCo.
RB PDAT emerged under the leadership of Jean-Marie Parel, IngETS-G, Ph.D., FARVO, Director of Bascom Palmer Eye Institute’s (“BPEI’s”) Ophthalmic Biophysics Center at the University of Miami Miller School of Medicine. Dr. Parel and the OBC team have spent more than ten years advancing RB PDAT technology against different types of infectious keratitis.
ARVO 2024 RB PDAT presentations included:
- Evaluating the Safety of Rose Bengal Photodynamic Therapy , Huang et al., BPEI (Poster no. B0448, Session: Cornea),
- Rose Bengal Photodynamic Antimicrobial Therapy as an Adjuvant Treatment for Infectious Keratitis , Eskenazi-Betech et al., Instituto de Oftalmologia Fundacion Conde de Valenciana IAP (Mexico) (B0338, Cornea),
- Assessment of photosensitizer concentration with a Singlet Oxygen luminescence dosimeter for Photodynamic Antimicrobial Therapy , Carrera et al., BPEI (B0570, Cornea),
- Clinical outcome in patients with infectious keratitis treated with Rose Bengal Photodynamic Antimicrobial Therapy (RB-PDAT) at the Federal University of Sao Paulo (UNIFESP) , Tabuse et al., Universidade Federal de São Paulo (Brazil) (B0575, Cornea),
- Enhanced Fungal Inhibition with High-Dose Rose Bengal Photodynamic Antimiocrobial Therapy , Merikansky et al., BPEI (B0580, Cornea),
- Inhibition of Fungal Isolates via Singlet Oxygen Generation from Erythrosin B and Rose Bengal Photodynamic Antimicrobial Therapy , Ahmed et al., BPEI (Paper no. 4917, Cornea),
- Arginine-Mediated Enhancement of Photodynamic Antimicrobial Therapy to Target the Oxygen-Independent Pathway , Gonzalez et al., BPEI (B0005, Immunology/Microbiology), and
- Preclinical/Poster: Exploring the Combination of Rose Bengal Photodynamic Antimicrobial Therapy and Existing Antifungals , Krishna et al., BPEI (B0010, Immunology/Microbiology).
RB PDAT is the subject of two international Phase 3 randomized controlled trials for acanthamoeba and fungal ( NCT05110001 ) and bacterial ( NCT06271772 ) keratitis, and has been used to treat infectious keratitis patients in four countries to date:
- U.S.: BPEI (first clinical reporting: Naranjo et al. 2019 ),
- India: LV Prasad Eye Institute ( Bagga et al. 2022 ) and Aravind Eye Care System (NCT05110001 data readout planned in Q4 2024),
- Brazil: Universidade Federal de São Paulo (ARVO 2024), and
- Mexico: Instituto de Oftalmología FAP (ARVO 2024).
About Bascom Palmer Eye Institute
Bascom Palmer Eye Institute serves as the Department of Ophthalmology for the University of Miami Miller School of Medicine. The mission of BPEI is to enhance the quality of life by improving sight, preventing blindness, and advancing ophthalmic knowledge through compassionate patient care and innovative research. For 2023-2024, U.S. News & World Report (“U.S. News”) ranked BPEI as the nation’s best in ophthalmology, marking the 22nd time and 20th consecutive year that BPEI has received the No. 1 ranking since U.S. News began surveying American physicians for its annual “Best Hospitals” rankings 34 years ago.
About Provectus
Provectus Biopharmaceuticals, Inc. is a clinical-stage biotechnology company developing immunotherapy medicines for different diseases that are based on a class of synthetic small molecule immuno-catalysts called halogenated xanthenes. Provectus’s lead HX molecule is named rose bengal sodium.
Provectus’s medical science platform includes clinical development programs in oncology, dermatology, and ophthalmology; proof-of-concept in vivo development programs in oncology, hematology, full-thickness cutaneous wound healing, and canine cancers; and in vitro discovery programs in infectious diseases, tissue regeneration and repair, and proprietary targets.
Information about the Company’s clinical trials can be found at the National Institutes of Health (NIH) registry, ClinicalTrials.gov . For additional information about Provectus, please visit the Company’s website at www.provectusbio.com .
FORWARD-LOOKING STATEMENTS: The information provided in this press release may include forward-looking statements, within the meaning of the Private Securities Litigation Reform Act of 1995, relating to the business of Provectus and its affiliates, which are based on currently available information and current assumptions, expectations, and projections about future events and are subject to a variety of risks and uncertainties and other factors that could cause actual events or results to differ materially from those projected in the forward-looking statements. Such statements are made in reliance on the safe harbor provisions of Section 27A of the Securities Act of 1933 and Section 21E of the Securities Exchange Act of 1934. Forward-looking statements are often, but not always, identified by the use of words such as “aim,” “likely,” “outlook,” “seek,” “anticipate,” “budget,” “plan,” “continue,” “estimate,” “expect,” “forecast,” “may,” “will,” “would,” “project,” “projection,” “predict,” “potential,” “targeting,” “intend,” “can,” “could,” “might,” “should,” “believe,” and similar words suggesting future outcomes or statements regarding an outlook.
The safety and efficacy of Provectus’s drug agents and/or their uses under investigation have not been established. There is no guarantee that the agents will receive health authority approval or become commercially available in any country for the uses being investigated or that such agents as products will achieve any revenue levels.
Due to the risks, uncertainties, and assumptions inherent in forward-looking statements, readers should not place undue reliance on these forward-looking statements. The forward-looking statements contained in this press release are made as of the date hereof or as of the date specifically specified herein, and the Company undertakes no obligation to update or revise any forward-looking statements, whether because of new information, future events, or otherwise, except in accordance with applicable securities laws. The forward-looking statements are expressly qualified by this cautionary statement.
Risks, uncertainties, and assumptions include those discussed in the Company’s filings with the Securities and Exchange Commission, including those described in Item 1A of:
- The Company’s Annual Report on Form 10-K for the period ended December 31, 2023 .
Contact: Provectus Biopharmaceuticals, Inc. Heather Raines, CPA Chief Financial Officer Phone: (866) 594-5999

Provectus Biopharmaceuticals News MORE
Related stocks.
- Get 7 Days Free
The National Kidney Foundation's 2024 Spring Clinical Meetings Late-Breaking Presentation on New Therapy Shows Promising Results for IgAN Patients
PR Newswire
NEW YORK, May 14, 2024
NEW YORK, May 14, 2024 /PRNewswire/ -- During a late-breaking abstract presentation at the annual 2024 NKF Spring Clinical Meetings (SCM) tomorrow Dr. Dana Rizk, from the University of Alabama at Birmingham (UAB) Medical Center, will present data on the impact and safety of Fabhalta (iptacopan) in the treatment of patients with IgA nephropathy (IgAN) also known as Berger disease. Iptacopan was approved by the FDA in 2023 for the treatment of another disease entity, paroxysmal nocturnal hemoglobinuria. IgAN is an incurable glomerular disease that can cause chronic kidney disease (CKD) and is a leading cause of end-stage renal disease (ESRD). The presentation entitled, Efficacy and Safety of Iptacopan in Patients with IgAN: Interim Analysis (IA) of the Phase 3 APPLAUSE-IgAN Study will be held at the Long Beach Convention Center, 300 East Ocean Blvd, on Wednesday, May 15 from 2:30 to 4:30 p.m. (PT).

In the analysis, patients treated with iptacopan in addition to standard supportive care, achieved a 38.3% (p<0.0001) proteinuria reduction (as measured by 24-hour urine protein to creatinine ratio [UPCR]) at 9 months when compared to placebo 1 . Proteinuria reduction is an increasingly recognized surrogate marker correlating with progression to kidney failure and has been used in IgAN clinical trials to support accelerated approvals 7 . The study also showed that iptacopan was well tolerated by IgAN patients with a favorable safety profile consistent with previously reported data 1,8 .
Quote from Researcher "In IgAN, part of the immune system called the alternative complement pathway can become overly activated in the kidneys, which causes an inflammatory response, leading to progressive kidney damage and gradual loss of kidney function. The loss of kidney function, together with potential side effects of IgAN treatments available until recently, significantly impact patients' lives," said Professor Dana Rizk, Investigator, APPLAUSE-IgAN Steering Committee Member, and Professor in the UAB Division of Nephrology. "Fabhalta is the first potential treatment for IgAN that specifically targets the alternative complement pathway."
Highlights of the Study APPLAUSE-IgAN is the first Phase III multicenter, randomized, placebo-controlled study to demonstrate significant proteinuria reduction by targeting the complement system in patients with IgAN. This pre-specified interim analysis included 250 patients for the efficacy analysis and 443 for the safety analysis 1 . The APPLAUSE-IgAN study continues in a double-blind fashion until the final analysis of the primary endpoint related to iptacopan's ability to slow IgAN progression by measuring the annualized total estimated glomerular filtration rate (eGFR) slope over 24 months. Those results are expected at study completion in 2025 9,10 .
The two primary endpoints of the study for the interim and final analysis, respectively, are proteinuria reduction at 9 months as measured by UPCR, and the annualized total eGFR slope over 24 months 9,10 . At the time of final analysis, the following secondary endpoints will also be assessed: the proportion of participants reaching UPCR <1 g/g without receiving corticosteroids/immunosuppressants or other newly approved drugs or initiating new background therapy for treatment of IgAN or initiating kidney replacement therapy (KRT), time from randomization to first occurrence of composite kidney failure endpoint event (reaching either sustained ≥30% decline in eGFR relative to baseline or sustained eGFR <15 mL/min/1.73 m 2 or maintenance dialysis or receipt of kidney transplant or death from kidney failure), change from baseline to 9 months in the fatigue scale measured by the Functional Assessment Of Chronic Illness Therapy-Fatigue questionnaire 9,10 .
The main study population enrolled patients with an eGFR ≥30 mL/min/1.73 m 2 and UPCR ≥1 g/g based on a 24 hr urine collection at baseline 9,10 . In addition, a smaller cohort of patients with severe renal impairment (eGFR 20–30 mL/min/1.73 m 2 at baseline) was also enrolled to provide additional information but will not contribute to the main efficacy analyses 9,10 .
"There is a need for effective, targeted therapies for IgAN patients and the detailed Applause-IgAN study gives valuable, promising insights to healthcare providers and patients living with IgAN," said NKF President Dr. Sylvia Rosas. "The alternative complement pathway has been implicated in the pathogenesis of IgAN, so it gives patients hope that a novel therapeutic intervention may lead to slowing progression of chronic kidney disease and avoiding kidney failure."
The annual 2024 NKF Spring Clinical Meetings (SCM) will be held in Long Beach, CA from May 14 – 18.
NKF Spring Clinical Meetings For the past 32 years, nephrology healthcare professionals from across the country have come to NKF's Spring Clinical Meetings to learn about the newest developments related to all aspects of nephrology practice; network with colleagues; and present their research findings. The NKF Spring Clinical Meetings is designed for meaningful change in the multidisciplinary healthcare teams' skills, performance, and patient health outcomes. It is the only conference of its kind that focuses on translating science into practice for the entire healthcare team.
About Kidney Disease In the United States, more than 37 million adults are estimated to have kidney disease, also known as chronic kidney disease (CKD)—and approximately 90 percent don't know they have it. About 1 in 3 adults in the U.S. are at risk for kidney disease. Risk factors for kidney disease include: diabetes , high blood pressure , heart disease , obesity , and family history . People of Black or African American, Hispanic or Latino, American Indian or Alaska Native, Asian American, or Native Hawaiian or Other Pacific Islander descent are at increased risk for developing the disease. Black or African American people are about four times as likely as White people to have kidney failure. Hispanics experience kidney failure at about double the rate of White people.
NKF Professional Membership Healthcare professionals can join NKF to receive access to tools and resources for both patients and professionals, discounts on professional education, and access to a network of thousands of individuals who treat patients with kidney disease.
- Perkovic V, Kollins D, Renfurm R, et al. Efficacy and Safety of Iptacopan in Patients with IgA Nephropathy: Interim Results from the Phase 3 APPLAUSE-IgAN Study. Presented at the World Congress of Nephrology (WCN); April 15, 2024; Buenos Aires, Argentina.
- Kidney Disease: Improving Global Outcomes (KDIGO) 2021 Clinical Practice Guideline for the Management of Glomerular Diseases. Kidney Int . 2021;100(4):S1-S276. doi:10.1016/j.kint.2021.05.021
- Rizk DV, Maillard N, Julian BA, et al. The Emerging Role of Complement Proteins as a Target for Therapy of IgA Nephropathy. Front Immunol . 2019;10:504. doi:10.3389/fimmu.2019.00504
- Medjeral-Thomas NR, O'Shaughnessy MM. Complement in IgA Nephropathy: The Role of Complement in the Pathogenesis, Diagnosis, and Future Management of IgA Nephropathy. Adv Chronic Kidney Dis . 2020;27(2):111-119. doi:10.1053/j.ackd.2019.12.004
- Boyd JK, Cheung CK, Molyneux K, Feehally J, Barratt J. An Update on the Pathogenesis and Treatment of IgA Nephropathy. Kidney Int . 2012;81(9):833-843. doi:10.1038/ki.2011.501
- Reich HN, Troyanov SAA, Scholey JW, Cattran DC. Remission of Proteinuria Improves Prognosis in IgA Nephropathy. J Am Soc Nephrol . 2007;18(12):3177-3183. doi:10.1681/ASN.2007050526
- Thompson A, Carroll K, Inker LA, et al. Proteinuria Reduction as a Surrogate End Point in Trials of IgA Nephropathy. Clin J Am Soc Nephrol . 2019;14(3):469-481. doi:10.2215/CJN.08600718
- Zhang H, Rizk DV, Perkovic V, et al. Results of a Randomized Double-Blind Placebo-Controlled Phase 2 Study Propose Iptacopan as an Alternative Complement Pathway Inhibitor for IgA Nephropathy. Kidney Int . 2024;105(1):189-199. doi:10.1016/j.kint.2023.09.027
- Rizk DV, Rovin BH, Zhang H, et al. Targeting the Alternative Complement Pathway with Iptacopan to Treat IgA Nephropathy: Design and Rationale of the APPLAUSE-IgAN Study. Kidney Int Rep . 2023;8(5):968-979. doi:10.1016/j.ekir.2023.01.041
- ClinicalTrials.gov. NCT04578834. A Multi-Center, Randomized, Double-Blind, Placebo-Controlled, Parallel Group, Phase III Study to Evaluate the Efficacy and Safety of LNP023 in Primary IgA Nephropathy Patients. Available from: https://clinicaltrials.gov/ct2/show/NCT04578834 . Accessed April 2024.
- Novartis. Novartis receives FDA approval for Fabhalta® (iptacopan), offering superior hemoglobin improvement in the absence of transfusions as the first oral monotherapy for adults with PNH. Available from: https://www.novartis.com/news/media-releases/novartis-receives-fda-approval-fabhalta-iptacopan-offering-superior-hemoglobin-improvement-absence-transfusions-first-oral-monotherapy-adults-pnh . Accessed April 2024.
- Novartis. Novartis Fabhalta® (iptacopan) receives positive CHMP opinion as first oral monotherapy for adult patients with paroxysmal nocturnal hemoglobinuria (PNH). Available from: https://www.novartis.com/news/media-releases/novartis-fabhalta-iptacopan-receives-positive-chmp-opinion-first-oral-monotherapy-adult-patients-paroxysmal-nocturnal-hemoglobinuria-pnh . Accessed April 2024.
- McGrogan A, Franssen CF, de Vries CS. The Incidence of Primary Glomerulonephritis Worldwide: A Systematic Review of the Literature. Nephrol Dial Transplant . 2011;26(2):414-430. doi:10.1093/ndt/gfq665
- Xie J, Kiryluk K, Wang W, et al. Predicting Progression of IgA Nephropathy: New Clinical Progression Risk Score. PLoS ONE. 2012;7(6):e38904. doi:10.1371/journal.pone.0038904
- Novartis. Novartis completes acquisition of Chinook Therapeutics. Available from: https://www.novartis.com/news/media-releases/novartis-completes-acquisition-chinook-therapeutics . Accessed April 2024.
SOURCE The National Kidney Foundation
Market Updates
Never mind market efficiency: are the markets sensible, starbucks stock could use a pick-me-up after big selloff; is it a buy, 5 cheap stocks to buy from an attractive part of the market, markets brief: all eyes on inflation, 5 things we learned from the q1 earnings season, after earnings, is palantir stock a buy, a sell, or fairly valued, what’s happening in the markets this week, can the fed declare victory on inflation, stock picks, after earnings and a 56% rally in 2024, is arm stock a buy, a sell, or fairly valued, how morningstar rates stocks, after earnings, is disney stock a buy, a sell, or fairly valued, home depot earnings: macro factors pinch demand, but long-term outlook intact, tariffs on chinese evs offer us automakers a chance to capture demand, the best reits to buy, 3 hot stocks to buy that still look undervalued, after earnings, is eli lilly stock a buy, a sell, or fairly valued, sponsor center.

IMAGES
VIDEO
COMMENTS
CLINICAL PRESENTATION definition | Meaning, pronunciation, translations and examples
The clinical presentation of COVID-19 ranges from asymptomatic to critical illness. An infected person can transmit SARS-CoV-2, the virus that causes COVID-19, before the onset of symptoms. Symptoms can change over the course of illness and can progress in severity. Uncommon presentations of COVID-19 can occur, might vary by the age of the ...
clinical presentation: The constellation of physical signs or symptoms associated with a particular morbid process, the interpretation of which leads to a specific diagnosis
Clinical presenting is the language that doctors use to communicate with each other every day of their working lives. Effective communication between doctors is crucial, considering the collaborative nature of medicine. As a medical student and later as a doctor you will be expected to present cases to peers and senior colleagues.
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence.1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Key elements of each presentation type are described below. Examples of how these would be applied to most situations are provided in italics. The formats are typical of presentations done for internal medicine services and clinics. Note that there is an acceptable range of how oral presentations can be delivered.
Areas covered. Direct person-to-person respiratory transmission has rapidly amplified the spread of coronavirus. In the absence of any clinically proven treatment options, the current clinical management of COVID-19 includes symptom management, infection prevention and control measures, optimized supportive care, and intensive care support in severe or critical illness.
There are a multitude of presentation formats for sharing and discussing clinical cases, diagnostic formulations or dilemmas, treatment approaches, and ethical issues. These presentation formats vary in terms of the number and type of participants, the use of multimedia , the availability of continuing medical education credits, etc. (Hull et ...
Clinical presentation. Similar to other coronaviruses, SARS‐CoV‐2 is predominantly spread by respiratory droplets, although spread by contact with contaminated fomites also occurs, as does transmission by aerosols in certain circumstances.1 Based on the experience in China, the typical incubation period of COVID‐19 infection has been estimated to be a median of 5.1 days (95% CI, 4.5-5. ...
Scientific Reports - Clinical presentations, laboratory and radiological findings, and treatments for 11,028 COVID-19 patients: a systematic review and meta-analysis ... The case definition had ...
Clinical presentation - Patients with CKD may present with symptoms and signs resulting directly from diminished kidney function, such as edema or hypertension. However, many have no clinical symptoms, and kidney disease is often detected in these patients when an elevated serum creatinine, reduced estimated GFR (eGFR), or an abnormal ...
Sepsis is a clinical syndrome that has physiologic, biologic, and biochemical abnormalities caused by a dysregulated host response to infection. Sepsis and the ... The epidemiology, definitions, risk factors, clinical presentation, diagnosis, and outcomes of sepsis are reviewed here. The pathophysiology and treatment of sepsis are discussed ...
2 A well-organized comprehensive knowledge domain has practical implications in clinical problem solving, and appropriate teaching and learning methods play an important role in achieving the educational goals. 3. Clinical presentation (CP) is a relatively new and innovative approach to teaching medicine.
Request a consultant's advice on a clinical problem: the presentation will be focused on the clinical question being posed to the consultant. Persuade others about a diagnosis and plan : a shorter presentation which highlights the pertinent positives and negatives that are germane to the diagnosis and/or plan being suggested.
A clinical presentation is the mode by which a patient presents to a physician and represents the clinical problem a physician is expected to manage. Big picture: The curriculum begins and ends with a focus on the patient, specifically the patient's clinical presentation. Deconstruct and independent learning: Each clinical presentation is ...
It should be noted that the presentation of schizophrenia varies greatly among individuals, as it is a heterogeneous clinical syndrome (APA, 2022). While the presence of active phase symptoms must persist for a minimum of one month to meet the criteria for a diagnosis of schizophrenia, the total duration of symptoms must persist for at least ...
Whether your presentation relates to the latest National Institute for Health and Clinical Excellence (NICE) guidelines for your specialty or a business plan in response to a proposed polyclinic, this structure will help keep your audience engaged and your presentation within the time limit. Indeed, timing is crucial when giving a presentation.
The ancient Egyptians were the first civilization to have trained clinicians to treat physical aliments. Medical papyri, such as the Edwin Smith papyrus (circa 1600 BCE) and the Ebers papyrus (circa 1534 BCE), provided detailed information of management of disease, including wound management with the application of various potions and grease ...
This definition of medical jargon appears to be a dictionary definition. Please rewrite it to present the subject from an encyclopedic point of view. (May 2023) In medicine, a presentation is the appearance in a patient of illness or disease—or signs or symptoms thereof—before a medical professional.
Examples of CLINICAL PRESENTATION in a sentence, how to use it. 16 examples: This review describes the causative organisms, pathogenesis, clinical presentation, epidemiology…
The present manuscript constitutes Part 1 and includes three chapters: (1) definition, epidemiology, and pathogenesis; (2) clinical presentation and natural history and (3) diagnosis (Table 1). The EoETALY Consensus Statements Part 2 includes two final chapters: (4) treatment and (5) monitoring and follow-up.
In England, markers of diagnostic quality have been implemented through Routes to Diagnosis programs that track and categorize patient pathways to cancer diagnosis. 7 Such programs define emergency presentation (EP) of cancer as a diagnosis up to 28 days after unplanned inpatient admission. While this definition does not directly measure diagnostic quality, it has good face validity as it ...
(May 14, New York, NY) - During a late-breaking abstract presentation at the annual 2024 NKF Spring Clinical Meetings (SCM) tomorrow Dr. Dana Rizk, from the University of Alabama at Birmingham (UAB) Medical Center, will present data on the impact and safety of Fabhalta (iptacopan) in the treatment of patients with IgA nephropathy (IgAN) also known as Berger disease. Iptacopan was approved by ...
He showed how AI might be poised to go a lot further soon. "Healthcare is full of conflicting evidence," he said, citing too much reliance on a 'one-size-fits-all approach'. In a way, he ...
1. Definition and Clinical Presentations. Sarcoidosis is a systemic granulomatous disorder that remains an enigma and challenges both researchers and clinicians due to its unknown cause, heterogeneous clinical presentation, and unpredictable outcome, occasionally severe and even lethal, often with no therapy able to change the course of the disease [].
The presentation will summarize updated data from the ongoing Phase 1a/b study of NX-5948 in heavily pretreated patients with relapsed/refractory chronic lymphocytic leukemia (CLL) and non-Hodgkin ...
No other matters were raised by ASCO regarding any data included in the submitted abstract, the planned data intended for presentation at ASCO, or any aspect of the clinical trial. The Company looks forward to sharing the full high-impact data set of our potentially best-in-class IL-2 and emerging results from the ABILITY-1 trial of MDNA11 at a ...
PDAT clinical outcomes for infectious keratitis from Brazil and MexicoKNOXVILLE, TN, May 14, 2024 (GLOBE NEWSWIRE) -- Provectus Biopharmaceutica...
The presentation entitled, Efficacy and Safety of Iptacopan in Patients with IgAN: Interim Analysis (IA) of the Phase 3 APPLAUSE-IgAN Study will be held at the Long Beach Convention Center, 300 ...