Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center


Service Improvement Project
Paper completed for my Nursing degree dissertation. It discusses the implementation of a patients DNACPR status and its identification on a patients wristband. The text follows a hypothetical project to implement the service improvement within an NHS trust; including research, stakeholder engagement and change implementation at a ward level.
Related Papers
Health technology assessment (Winchester, England)
Matthew Breckons
Byung Cheol Lee
Healthcare information systems (e.g., Bar Code Medication Administration (BCMA) system), have been adopted to deliver efficient healthcare services recently. However, though it is seem-ingly simple to use (scanning barcodes before medication), users of the BCMA system (e.g., nurses and pharmacists) often show non-compliance behaviors. Therefore, the goal of this study is to comprehensively understand why such non-compliance behaviors occur with BCMA system. Though comprehensive literature review, we identified 128 instances of causes, which were cate-gorized into the five categories: Poor Visual and Audio Interface, Poor Physical Ergonomic De-sign, Poor Information Integrity, Abnormal Situation for System Use, and User Reluctance and Negligence. The results show that successful use of a BCMA system requires supportive systems and environments, so it is more like an issue of the system, rather than that of an individual user or a device. We believe that the proposed categories could be applicable in investigating non-compliance behaviors in other healthcare information systems as well.
Michelle L Rogers
International Journal of Evidence-based Healthcare
Anesthesia and analgesia
imran bhatti
Difficult airway cases can quickly become emergencies, increasing the risk of life-threatening complications or death. Emergency airway management outside the operating room is particularly challenging. We developed a quality improvement program-the Difficult Airway Response Team (DART)-to improve emergency airway management outside the operating room. DART was implemented by a team of anesthesiologists, otolaryngologists, trauma surgeons, emergency medicine physicians, and risk managers in 2005 at The Johns Hopkins Hospital in Baltimore, Maryland. The DART program had 3 core components: operations, safety, and education. The operations component focused on developing a multidisciplinary difficult airway response team, standardizing the emergency response process, and deploying difficult airway equipment carts throughout the hospital. The safety component focused on real-time monitoring of DART activations and learning from past DART events to continuously improve system-level perfo...
Journal of Evaluation in …
Nick Sevdalis
Graham Cookson
Transfusion
Charles Vincent
Clinical Chemistry and Laboratory Medicine
Pierangelo Bonini
RELATED PAPERS
Joint Commission journal on quality and patient safety / Joint Commission Resources
Etienne Phipps
Cognition, Technology & Work
Emily Patterson
Anesthesiology clinics
Edward R Mariano
BMJ Quality & Safety
Transfusion Medicine
Martha Bruce
Journal of the American Medical Informatics Association
Damian Roland , Alesia Hunt
Andrei Rosin
Claire Goodman , Alison While , Vari M Drennan
Clinics in laboratory medicine
David Novis
Dilek Gümüş
International Journal of Nursing Studies
Laurence Moseley
Tibert Verhagen , Matthijs Noordzij
Implementation Science
Mike English
The practising midwife
Declan Devane
Journal of Advanced Nursing
Robert Crouch
Scandinavian Journal of Caring Sciences
Kjell Grankvist
Kerm Henriksen , Emily Patterson
Quality in primary care
Charles Campion-smith , Peter Wilcock
Alan Tennant
Adam Jowett
Lisa Sharrock , Suzanne K Molesworth
Andrew Booth
Archives of Pathology Laboratory Medicine
peter beresford
BMC Health Services Research
Ivaylo Vassilev , Evridiki Patelarou , christina foss
Amangaly Akanov
Manual Therapy
Janine Leach
Patrick Bolton
Health Service Journal
Omid Shabestari
International Journal of Medical Informatics
Osman Sayan
Panagiotis Siaperas
wendy jessiman
Dr Paul Barach
Irish Journal of Medical Science
Catriona Murphy
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Baillie L, Bromley B, Walker M, Jones R, Mhlanga F Implementing service improvement projects within pre-registration nursing education: A multi-method case study evaluation. Nurse Educ Pract. 2014; 14:(1)62-68 https://doi.org/10.1016/j.nepr.2013.06.006
Bahn D Social Learning Theory: its application in the context of nurse education. Nurse Educ Today. 2001; 21:(2)110-117 https://doi.org/10.1054/nedt.2000.0522
Bandura A Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977; 84:(2)191-215 https://doi.org/10.1037/0033-295X.84.2.191
Bandura A Self-efficacy: the exercise of control.New York: WH Freeman; 1997
Selective moral disengagement in the exercise of moral agency. 2002. https://tinyurl.com/glm79u4 (accessed 27 May 2020)
Batalden PB, Davidoff F What is ‘quality improvement’ and how can it transform healthcare?. Qual Saf Health Care. 2007; 16:(1)2-3 https://doi.org/10.1136/qshc.2006.022046
Baumeister RF, Leary MR The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull. 1995; 117:(3)497-529 https://doi.org/10.1037/0033-2909.117.3.497
Benner P From novice to expert. Excellence and power in clinical nursing practice.Menlo Park (CA): Addison-Wesley; 1984
Carlin A, Duffy K Newly qualified staff's perceptions of senior charge nurse roles. Nurs Manage. 2013; 20:(7)24-30 https://doi.org/10.7748/nm2013.11.20.7.24.e1142
Chang E, Hancock K Role stress and role ambiguity in new nursing graduates in Australia. Nurs Health Sci. 2003; 5:(2)155-163 https://doi.org/10.1046/j.1442-2018.2003.00147.x
Chesser-Smyth PA, Long T Understanding the influences on self-confidence among first-year undergraduate nursing students in Ireland. J Adv Nurs. 2013; 69:(1)145-157 https://doi.org/10.1111/j.1365-2648.2012.06001.x
Christiansen A, Robson L, Griffith-Evans C Creating an improvement culture for enhanced patient safety: service improvement learning in pre-registration education. J Nurs Manag. 2010; 18:(7)782-788 https://doi.org/10.1111/j.1365-2834.2010.01114.x
Coventry TH, Maslin-Prothero SE, Smith G Organizational impact of nurse supply and workload on nurses continuing professional development opportunities: an integrative review. J Adv Nurs. 2015; 71:(12)2715-2727 https://doi.org/10.1111/jan.12724
Craig L Service improvement in health care: a literature review. Br J Nurs. 2018; 27:(15)893-896 https://doi.org/10.12968/bjon.2018.27.15.893
Davis L, Taylor H, Reyes H Lifelong learning in nursing: A Delphi study. Nurse Educ Today. 2014; 34:(3)441-445 https://doi.org/10.1016/j.nedt.2013.04.014
Dinmohammadi M, Peyrovi H, Mehrdad N Concept analysis of professional socialization in nursing. Nurs Forum. 2013; 48:(1)26-34 https://doi.org/10.1111/nuf.12006
Draucker BC The critique of Heideggerian hermeneutic nursing research. J Adv Nurs. 1999; 30:(2)360-373 https://doi.org/10.1046/j.1365-2648.1999.01091.x
Duchscher JB A process of becoming: the stages of new nursing graduate professional role transition. J Contin Educ Nurs. 2008; 39:(10)441-450 https://doi.org/10.3928/00220124-20081001-03
Duchscher JEB Transition shock: the initial stage of role adaptation for newly graduated Registered Nurses. J Adv Nurs. 2009; 65:(5)1103-1113 https://doi.org/10.1111/j.1365-2648.2008.04898.x
Feng RF, Tsai YF Socialisation of new graduate nurses to practising nurses. J Clin Nurs. 2012; 21:(13-14)2064-2071 https://doi.org/10.1111/j.1365-2702.2011.03992.x
Fretwell JE Ward teaching and learning.London: Royal College of Nursing; 1982
Gadamer H-G Truth and method, 2nd edn. London: Sheed and Ward; 1979
Gignac-Caille AM, Oermann MH Student and faculty perceptions of effective clinical instructors in ADN programs. J Nurs Educ. 2001; 40:(8)347-353
Gollop R, Whitby E, Buchanan D, Ketley D Influencing sceptical staff to become supporters of service improvement: a qualitative study of doctors' and managers' views. Qual Saf Health Care. 2004; 13:(2)108-114 https://doi.org/10.1136/qshc.2003.007450
Gray M, Smith LN The professional socialization of diploma of higher education in nursing students (Project 2000): a longitudinal qualitative study. J Adv Nurs. 1999; 29:(3)639-647 https://doi.org/10.1046/j.1365-2648.1999.00932.x
Gray PD, Thomas D Critical analysis of ‘culture’ in nursing literature: implications for nursing education in the United States. In: Oermann MH, Heinrich KT (eds). NewYork (NY): Springer Publishing Company; 2005
Guba EG, Lincoln YS Competing paradigms in qualitative research. In: Denzin NK, Lincoln YS (eds.). Thousand Oaks (CA): Sage; 1994
Hatlevik IKR The theory-practice relationship: reflective skills and theoretical knowledge as key factors in bridging the gap between theory and practice in initial nursing education. J Adv Nurs. 2012; 68:(4)868-877 https://doi.org/10.1111/j.1365-2648.2011.05789.x
Houghton CE ‘Newcomer adaptation’: a lens through which to understand how nursing students fit in with the real world of practice. J Clin Nurs. 2014; 23:(15-16)2367-2375 https://doi.org/10.1111/jocn.12451
Huybrecht S, Loeckx W, Quaeyhaegens Y, De Tobel D, Mistiaen W Mentoring in nursing education: perceived characteristics of mentors and the consequences of mentorship. Nurse Educ Today. 2011; 31:(3)274-278 https://doi.org/10.1016/j.nedt.2010.10.022
Jackson D, Firtko A, Edenborough M Personal resilience as a strategy for surviving and thriving in the face of workplace adversity: a literature review. J Adv Nurs. 2007; 60:(1)1-9 https://doi.org/10.1111/j.1365-2648.2007.04412.x
James B, Beattie M, Shepherd A, Armstrong L, Wilkinson J Time, fear and transformation: student nurses' experiences of doing a practicum (quality improvement project) in practice. Nurse Educ Pract. 2016; 19:70-78 https://doi.org/10.1016/j.nepr.2016.05.004
Johnson N., Penny J., Robinson D., Cooke M. W., Fowler-Davis S., Janes G., Lister S. Introducing service improvement to the initial training of clinical staff Retrieved 05.04.2012, 2012. 2010; https://doi.org/10.1136/qshc.2007.024984
Lindseth A, Norberg A A phenomenological hermeneutical method for researching lived experience. Scand J Caring Sci. 2004; 18:(2)145-153 https://doi.org/10.1111/j.1471-6712.2004.00258.x
Machin AI, Jones D Interprofessional service improvement learning and patient safety: A content analysis of pre-registration students' assessments. Nurse Educ Today. 2014; 34:(2)218-224 https://doi.org/10.1016/j.nedt.2013.06.022
Mackintosh C Caring: The socialisation of pre-registration student nurses: A longitudinal qualitative descriptive study. Int J Nurs Stud. 2006; 43:(8)953-962 https://doi.org/10.1016/j.ijnurstu.2005.11.006
Madden MA Empowering nurses at the bedside: what is the benefit?. Aust Crit Care. 2007; 20:(2)49-52 https://doi.org/10.1016/j.aucc.2007.02.002
Maben J, Latter S, Clark JM The theory–practice gap: impact of professional–bureaucratic work conflict on newly-qualified nurses. J Adv Nurs. 2006; 55:(4)465-477 https://doi.org/10.1111/j.1365-2648.2006.03939.x
Maslow AH Toward a psychology of being.Chichester: John Wiley and Sons; 1998
McGowan B Who do they think they are? Undergraduate perceptions of the definition of supernumerary status and how it works in practice. J Clin Nurs. 2006; 15:(9)1099-1105 https://doi.org/10.1111/j.1365-2702.2005.01478.x
NHS Improvement. Patient Safety Measurement Unit. 2017. https://tinyurl.com/y8pagbwq
NHS website. High impact actions for nursing and midwifery—the essential collection. 2010. https://tinyurl.com/yawpgcjy
NHS website. Releasing time to care, the NHS Productive Series. 2020. https://www.england.nhs.uk/improvement-hub/productives
Future nurse: Standards of proficiency for registered nurses.London: NMC; 2018
Ogier M An ‘ideal’ sister—seven years on. Nurs Times. 1986; 82:(5)54-57
Ó Lúanaigh P Becoming a professional: what is the influence of registered nurses on nursing students' learning in the clinical environment?. Nurse Educ Pract. 2015; 15:(6)450-456 https://doi.org/10.1016/j.nepr.2015.04.005
Orton H Ward learning climate: a study of the role of the ward sister in relation to student nurse learning on the ward.London: Royal College of Nursing; 1981
Potter J Representing reality: discourse, rhetoric and social construction.London: Sage; 1996
Potter P, Perry A Fundamentals of nursing, 5th edn. St Louis (Mo): Elsevier; 2001
Robson C Real world research, 3rd edn. Chichester: John Wiley and Sons; 2011
Salmon J The use of phenomenology in nursing research. Nurse Res. 2012; 19:(3)4-5 https://doi.org/10.7748/nr.19.3.4.s2
Schoessler M, Waldo M The first 18 months in practice: a developmental transition model for the newly graduated nurse. Journal for Nurses in Staff Development (JNSD). 2006; 22:(2)47-52 https://doi.org/10.1097/00124645-200603000-00001
Shafer L, Aziz MG Shaping a unit's culture through effective nurse-led quality improvement. Medsurg nursing. 2013; 22:(4)229-236
Smith N, Lister S Turning students' ideas into service improvements. Learning Disability Practice. 2011; 14:(2)12-16 https://doi.org/10.7748/ldp2011.03.14.2.12.c8377
Smith J, Pearson L, Adams J Incorporating a service improvement project into an undergraduate nursing programme: a pilot study. Int J Nurs Pract. 2014; 20:(6)623-628 https://doi.org/10.1111/ijn.12217
Standing M A new critical framework for applying hermeneutic phenomenology. Nurse Res. 2009; 16:(4)20-30 https://doi.org/10.7748/nr2009.07.16.4.20.c7158
Strouse SM, Nickerson CJ Professional culture brokers: nursing faculty perceptions of nursing culture and their role in student formation. Nurse Educ Pract. 2016; 18:10-15 https://doi.org/10.1016/j.nepr.2016.02.008
Thomas LJ, Revell SH Resilience in nursing students: an integrative review. Nurse Educ Today. 2016; 36:457-462 https://doi.org/10.1016/j.nedt.2015.10.016
van Manen M Researching lived experience. Human science for an action sensitive pedagogy.New York (NY): State University of New York Press; 1990
Welsh I, Swann C Partners in learning. A guide to support and assessment in nurse education.Cornwall: Radcliffe Medical Press Ltd; 2002
Wilcock P, Carr E Improving teaching about improving practice. Qual Saf Health Care. 2001; 10:(4)201-202 https://doi.org/10.1136/qhc.0100201w
Developing and sustaining nurses' service improvement capability: a phenomenological study
Subject Lead, Adult Nursing, and Senior Lecturer, Northumbria University, Newcastle upon Tyne
View articles
Alison Machin
Professor of Nursing and Interprofessional Education, Northumbria University/Executive Member (workforce), Council of Deans of Health
View articles · Email Alison
Background:
Service improvement to enhance care quality is a key nursing responsibility and developing sustainable skills and knowledge to become confident, capable service improvement practitioners is important for nurses in order to continually improve practice. How this happens is an under-researched area.
A hermeneutic, longitudinal study in Northern England aimed to better understand the service improvement lived experiences of participants as they progressed from undergraduate adult nursing students to registrants.
Twenty year 3 student adult nurses were purposively selected to participate in individual semi-structured interviews just prior to graduation and up to 12 months post-registration. Hermeneutic circle data analysis were used.
Themes identified were service improvement learning in nursing; socialisation in nursing practice; power and powerlessness in the clinical setting; and overcoming service improvement challenges. At the end of the study, participants developed seven positive adaptive behaviours to support their service improvement practice and the ‘model of self-efficacy in service improvement enablement’ was developed.
Conclusion:
This study provides a model to enable student and registered nurses to develop and sustain service improvement capability.
Embedding a nursing service improvement culture has been a focus of successive UK policy initiatives ( Craig, 2018 ), such as the NHS Safety Thermometers scheme ( NHS Improvement, 2017 ), the 2012 nurse-led quality framework Energise for Excellence, High Impact Actions for Nursing and Midwifery ( NHS website, 2010 ) and the NHS Productive Series ( NHS website, 2020 ). However, information about how nurses develop and sustain service improvement skills beyond their initial education is lacking.
Service improvement can be defined as ‘the combined efforts of everyone to make changes, leading to better patient outcomes (health), better system performance (care) and better professional development (learning) regardless of the theoretical concept or tool utilised’ ( Batalden and Davidoff, 2007:2 ).
In 2007, a national initiative to embed this learning in undergraduate programmes created many opportunities for pre-registration nursing students to develop these skills ( Johnson et al, 2010 ). Students involved in the initiative evaluated it very positively and subsequent studies suggest it enhanced their understanding of the practicalities of implementing service improvement activity ( Machin and Jones 2014 ). Johnson et al's (2010) study suggested that resistance from staff, lack of time and student status were barriers to the success of students' service improvement efforts. Despite challenges, service improvement learning and the opportunity to improve the patient care experience is valued by pre-registration students ( Smith and Lister, 2011 ), with classroom-based sessions seen as beneficial for learning ( Baillie et al, 2014 ; Smith et al, 2014 ). Educational programmes encompassing service improvement have helped prepare student nurses to make changes in practice when qualified ( Machin and Jones, 2014 ; James et al, 2016 ). However, little is known about the sustainability of this learning.
This study aimed to understand service improvement experiences of undergraduate adult nursing students in their final year of university and up to 12 months into their graduate practice. The following research questions were posed:
- What are student adult nurses' experiences of service improvement in education and its application in the practice learning setting?
- What are registered adult nurses' experiences of service improvement in their first year of clinical practice?
A longitudinal hermeneutic phenomenological design was used to explore participants' perceptions of their pre- and post-qualification experiences of service improvement in nursing. Phenomenology was appropriate as a research methodology because it seeks to understand particular phenomenon as it is lived by participants.
Sampling from five to 25 participants is often suggested for qualitative research methodologies, which include phenomenology. A longitudinal hermeneutic study carried out by Standing (2009) explored the experiences of transition from student to registered nurse. Following the post-qualifying period, there was 50% attrition. This helped inform the decision to include 20 participants in the present study, a sufficient number to enable rich data collection and allow for potential attrition during phase 2 (there were 15 participants for phase 2, an attrition of 5).
Participants had completed a service improvement module as part of their second-year education programme, where they engaged with service improvement, explored theoretical improvement methodologies and appraised via a written assessment of their experiences.
All participants' placements were in the NHS trust that was likely to be the location of their first staff nurse job. This was important to enable post-graduate follow-up. The 20 students gave consent to be individually interviewed twice, once as a student and again in their first year of being qualified.
An interview schedule was developed to facilitate semi-structured interviews in both phases of the study. Robson (2011) suggested that interview schedules should incorporate an introduction, a focused lead question and several key questions or prompts:
- What does service improvement mean to you?
- What do you understand about service improvement?
- What experience have you had of service improvement learning?
- What experience have you had of service improvement in practice?
- Has there been anything in your service improvement experience that has changed the way you feel about it or the way you facilitate it?
- Is there anything else you want to tell me about your role in service improvement?
Each participant was asked the same opening question and the same final question.
Forty interviews lasting 30-45 minutes were undertaken by the lead researcher (LC) at the university, digitally recorded and transcribed verbatim. Digital and written data were stored in line with data protection policy. Data were analysed using a phenomenological, hermeneutic circle approach ( van Manen, 1990 ), comprising three stages ( Lindseth and Norberg, 2004 ), and the process was informed by re-reading the relevant literature:
- Transcripts were read and recordings listened to in order to understand the context of each participant
- Key themes across the transcripts were identified and clustered into overarching themes
- These themes were then interpreted to develop in-depth understanding of participant experiences of service improvement learning and practice.
Researcher understanding of participants' experiences was checked with them throughout data collection. Member checking occurred with participants concurrently as part of each interview during both phases.
A transparent audit trail of researcher decision-making ensured that the study and its results were trustworthy ( Guba and Lincoln, 1994 ).
Ethical permission
Ethical permission was given by the university's ethical approval committee and the research development department at the participating NHS trust.
van Manen's (1990) six-step approach was used because it was congruent with the research methodology and is conducive to analysing hermeneutic phenomenological data. Although there are six steps, the process undertaken was not linear and the lead researcher (LC) frequently returned to the hermeneutic circle for naive reading, re-reading and interpretation of the transcripts throughout each stage of analysis ( Table 1 ). Gadamer (1979) supports this approach, suggesting that movement between the six activities, forward and backward, allows researchers the time to consider, reconsider and reflect on the parts and the whole. It is through these activities that the researcher can fully engage in the hermeneutic circle and enabled them to identify convergent and divergent viewpoints.
Four overarching themes emerged from the hermeneutic data analysis of the participants' ( Figure 1 ):
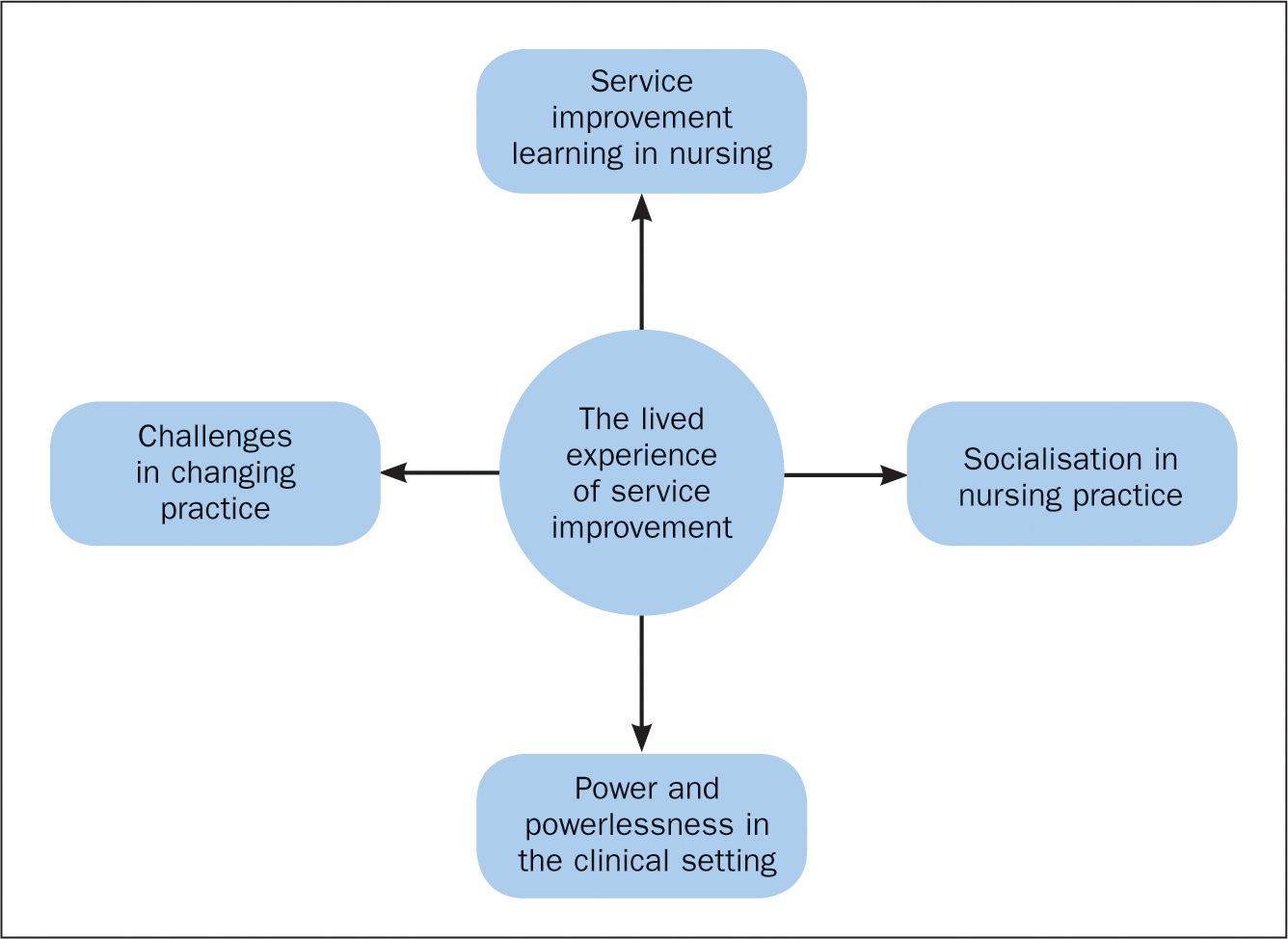
Service improvement learning in nursing
Socialisation in nursing practice, power and powerlessness in the clinical setting.
- Challenges in changing practice.
Service improvement in nursing was an overarching theme incorporating subthemes, such as a personal understanding of service improvement, seeing a need for service improvement, micro and macro perspectives of service improvement and linking theory to practice. It was evident in the findings that all participants had socially constructed an understanding of service improvement and were able to give a definition of what this meant to them. The findings illustrated that participants had experienced service improvement both in university and in their clinical practice.
As students, they conveyed their understanding of service improvement, citing their rationale, and applied theoretical models and different approaches for the process:
‘[Service improvement] means trying to improve and change the service so patients have a better experience, an overall experience’
Another participant also identified a patient-focused rationale for service improvement:
‘[Service improvement is] changing any service or [a] service that you give to patients, so it could be an intervention or some other way care is given or organised’
This understanding stayed with the newly qualified participants; however, they talked about their nursing role in service improvement in a more personalised way, recognising the scope of the contribution they could make as individual newly qualified practitioners:
‘Looking back, you gain knowledge and skills as your career progresses. You don't want to go in with a huge service improvement, just start little and build up. I have used some of the theory about change and PDSA [plan, do, study, act]. I am always reflecting and learning’
Another talked about the importance of having service improvement confidence, despite being newly qualified and still on a learning journey:
‘I am still learning, but if you have a good idea about something, having the confidence to go with it, giving reasons and rationale as to how and why you want to do it, to improve the patients service’
Several participants described service improvement opportunities within the preceptorship period as consolidating their learning:
‘As part of preceptorship I did service improvement. We have the knowledge and skills framework, which we have to work towards. Without learning, you would never be getting to best practice. I think, if you don't look for how you can improve your service, you don't improve things for your patients’
Several of the new registrants recognised that, as lifelong learners, there may be a time when they would need to refresh their understanding of service improvement learning theory, for example:
‘If I was doing some service improvement, I would look back at the theories behind it. I would have a good read and re-educate myself’
It was apparent that socialisation and learning in nursing practice was an important feature for participants, both when they were students and as registered nurses. Socialisation is a process that starts during nurse education and continues throughout a nurse's career ( Dinmohammadi et al, 2013 ; Strouse and Nickerson, 2016 ). Socialisation in nursing occurs through social interactions with colleagues in clinical practice and can have both positive and negative consequences concerning the development of nurses ( Gray and Smith, 1999 ; Mackintosh, 2006 ).
Service improvement confidence was not always experienced by student participants who, arguably, had not yet been fully socialised into the nursing community of practice. One student participant felt they did not really belong to the clinical area team within which they were trying to make improvements:
‘As a student, I think it is difficult to fit in, you haven't been properly socialised into the team’
Another expressed the same feelings, describing having to ‘fit in’ as a prerequisite to making changes of any kind:
‘You don't feel you belong. It doesn't matter what you do. You have to just learn to fit in. You're not part of the social scene. I felt not supported [in service improvement activity]’
Several suggested that they tried to join conversations to develop relationships with work colleagues, but were ignored:
‘They did not like the idea of me coming in as an outsider and changing [service improvements]. You don't fit in. You would go to lunch and try and join the conversation, and they would blank you. It wasn't sociable’
At a time when retention of nursing students on their course is a national priority, this perceived lack of support on placement is of concern. However, this perception changed after the nurses became qualified and were employed in their first job. Fitting in and having supportive relationships was perceived as important:
‘As a student you weren't embedded in a culture or in a team quite yet. You were an outsider with outside views which is sometimes good, but when you are working here all the time it is easier to pick up the things that need a little bit of help’
This sense of becoming an ‘insider’ is an indication of the participants' socialisation into the nursing profession post-qualification. Another newly qualified participant also reflected on how different she had felt as a student:
‘When I look back to being a student, I don't think I was ever really part of the team. Compared to now’
As students, and later as registered nurses, the participants discussed an awareness of power in the context of making changes through service improvements. They were aware of power as a dynamic in the clinical environment and that this influenced how they approached and undertook service improvements in practice. Power and powerlessness emerged as an important feature in how they experienced service improvements in nursing.
Nursing occurs in a social environment, where power impacts nurses in context of their working situation ( Gray and Thomas, 2005 ). Power pervades social norms and sustains power-imbalanced relationships ( Potter, 1996 ; Gray and Thomas, 2005 ). In this context, this theme had three related subthemes: personal influence, fear of failure and professional responsibility. Student participants were aware of the power imbalance in the clinical environment and this influenced how they approached their service improvements projects. Some felt powerless because of their student nurse status:
‘There was nothing, nothing [service improvement] I could do as a lowly student nurse’
Another, who had also felt powerless, suggested that common assumptions were that service improvements were implemented ‘top-down’, driven by people more ‘senior’ with more organisational power:
‘I am still in my little white student nurse uniform, not higher up. I have no power. I think a lot of people expect service improvement to come from higher up’
This perception reflects a lack of confidence as a student for engaging in ‘bottom-up’ improvements and change. As registered nurses participants noted a tangible change in their power, status, responsibility and authority in making improvements once they had qualified:
‘It's completely different, looking back. [As a staff nurse] I am aware of it [service improvement] in everything I do. I am aware of small things every day that you can do to improve the service. You can see where the flaws are. We have the power now to say, “maybe we can change this’ ”
Another participant felt empowered in her newly qualified status, and able to suggest changes proactively:
‘Now, when qualified, you do have a say [in service improvement] and it's important that I do speak up … you do have the power to say how things are done’
Another recently qualified participant described the transition phase between student and becoming a registered nurse as being an optimum time to engage in service improvement:
‘Looking back, you are in the best place. You just come in from university with new eyes and want to improve’
This suggests that harnessing service improvement enthusiasm in the important preceptorship period and empowering graduates might be a way of maintaining the sustainability of service improvement learning and practice.
Challenges in changing practice
There were several subthemes associated with challenges to change: mentors and staff as practice-based support, ward manager as change agent, resistance to change and ritual and routine. Positive relationships in clinical practice were key enablers for overcoming challenges in implementing service improvement. For students, perhaps understandably, it was the positive, effective mentors they had encountered who helped them to feel good about their service improvement efforts:
‘It depends who you work with. You can have some mentors who are quite good at facilitating change and asking for ideas, and they have some respect for the student. You are not just another body’
‘My mentor was brilliant, she respected student nurses … She was a role model for me [in service improvement]’
Some of the newly qualified nurse participants reflected on their student experiences. They were able to make comparisons between their experiences then and now, in trying to overcome service improvement challenges. They also identified relationships within teams as factor influencing nurses' ability and opportunity to challenge and improve practice:
‘As a student, you don't have the confidence to implement anything. I guess it's how well you get on in the team, but moving from placement to placement all the time makes it really difficult. As a qualified member of the team you get on well with everyone. You fit in and you wouldn't be afraid to say to someone, “maybe we can do it this way” ’
Having colleagues on the ward with a research role seemed to be something that could enhance the receptivity of staff to new ideas and try them out:
‘I would go and see the other nurses and see what they thought, if there was enough “oomph” behind it. We have a lot of research nurses … They are a great support’
People-focused ward managers were key enablers in empowering qualified participants to make improvements:
‘Definitely our ward manager supports change and values your ideas, and always listens to what you have to say’
‘She [the sister] was really receptive. She was a great help to me’
Strong leadership skills were identified by another as pivotal to embedding a service improvement culture where challenges could be overcome:
‘They [the ward manager] is confident, they are a strong leader. They are supportive, open to staff opinions; not only listening to senior staff member, but to everybody’
Self-determination was identified as a way of overcoming the challenges of implementing service improvement. One student participant said:
‘I just got on with it [service improvement]. I got a bit more confident. Sometimes you can't please everyone, you just have to get on with things’
Several participants, once qualified, discussed how, despite challenges, they would persevere, believing that they had an important role to play in improving care for patients:
‘If you don't look at how you can improve your services, you don't improve things for your patients. There are not going to be any advances, you are not going to use any evidenced-based practice’
One participant suggested that continuous improvement and change were essential to ensure that patients received the best, contemporary, evidence-based nursing care:
‘If you are stuck in your ways and set in a certain pattern, you are not always going to meet everybody's needs, and it could be detrimental to patients’
Summary of findings and further theoretical development
In keeping with hermeneutic phenomenology, the four key themes and related subthemes have been presented supported by literature to inform the analysis of the findings ( Draucker, 1999 ). Through further theoretical analysis of each key theme, there was evidence that a range of contextual, professional and behavioural factors were influencing the lived experience of the participants engaging in service improvement ( Figure 2 ). These factors and the four themes identified were synthesised into three overarching processes experienced by participants: professional transformation, developing resilience and becoming empowered in making service improvements. This helped to develop further understanding of the participants' lived experiences.
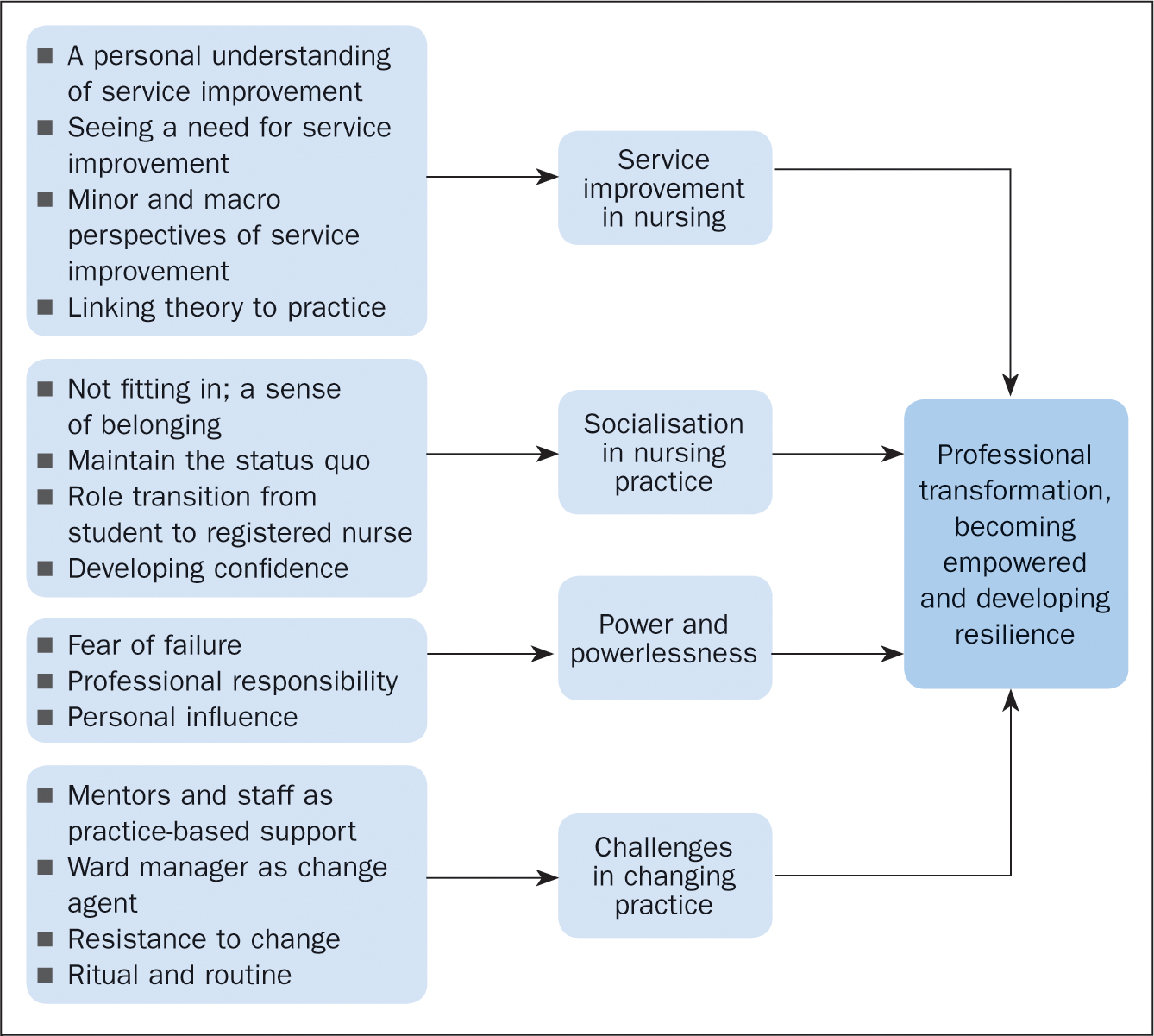
This study aimed to better understand the service improvement experiences of participants as student nurses and throughout their first year of post-registration practice. Across the themes identified common behaviours helped participants engage in service improvement, sustaining their knowledge and enthusiasm post-qualification. Participants were revealing behaviours they had developed in response to their learning and experiences of service improvement in nursing. These ‘positive adaptive behaviours’ are consistent with Bandura (2002) , who found that effective problem solvers are motivated to improve their own practice. The adaptive behaviours identified included ( Figure 3 ):
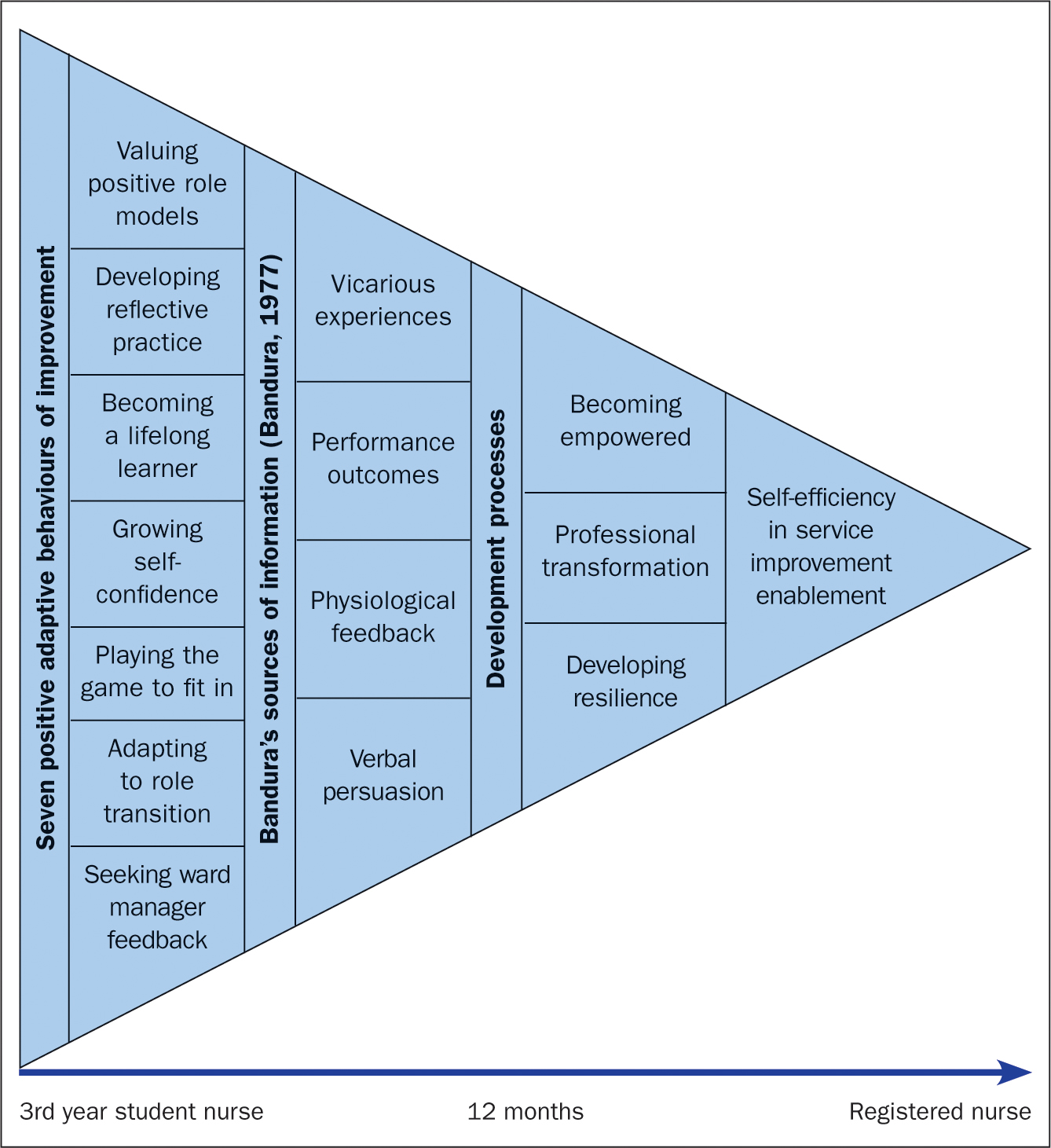
Valuing positive role models
Developing reflective practice, becoming a lifelong learner, growing in self-confidence, playing the game to fit in, adapting to role transition.
- Seeking ward manager feedback and support.
Several participants (P9, P14, P17, P19, P20) talked about role model mentors and colleagues. They described how their sense of self-efficacy had grown from watching and learning from them as students to seeking to emulate them as qualified nurses. Positive role modelling in nursing usually occurs through a process of mentorship, and helping students to fit in and develop the skills necessary for professional practice (Gignac-Caille and Oermann, 2010; Huybrecht et al, 2011 ; Houghton, 2014 ; Ó Lúanaigh, 2015 ). This study identified that service improvement role models are also important for students and new registrants.
Many participants (P2, P8, P7, P13, P20) reflected on their service improvement experiences. In keeping with other research ( Hatlevik, 2012 ), they perceived that reflection helped bridge the service improvement theory–implementation gap, facilitating development of their identity and knowledge as service improvers. Through reflection, participants developed resilience, as has been reported in other studies ( Jackson et al, 2007 ; Thomas and Revell, 2016 ). Reflection also helped them to identify strategies to overcome service improvement challenges, believing passionately in the positive impact service improvement has on patient care. Bandura (1977) found that learners model their behaviours through being self-reflective and self-reactive.
Two participants (P2, P15) discussed preceptorship and lifelong learning as being integral to the nursing role ( Benner, 1984 ; Nursing and MIdwifery Council, 2018 ). Other studies have shown that professional development that starts in the pre-qualifying period continues throughout a nursing career through lifelong learning ( Davis et al, 2014 ; Coventry et al, 2015 ). In this study, the preceptorship period was crucial for sustaining and further developing service improvement learning. A service improvement mindset was synonymous with a lifelong learning philosophy mindset. Where confidence dipped, participants would return to study the theory underpinning their practice.
Effective ward managers were viewed as those willing to listen and learn from students, as well as qualified staff, where new learning could improve patient care. Effective integration of lifelong service improvement learning into a clinical practice setting culture will also have positive benefits for future students.
Participants (P2, P4, P5, P6, P14, P19) who felt supported in practice developed more self-confidence as service improvers. Conversely, a lack of support from mentors and colleagues impacted negatively on participants' confidence as change agents. Other research has also indicated that student nurses develop self-confidence in practice through positive mentoring experiences, peer support and being successful in practice ( Bahn, 2001 ; Chesser-Smyth and Long, 2013 ). Self-confidence is linked to self-efficacy and reflects an individual's perception of their own ability to perform a goal or task ( Bandura, 1997 ; Potter and Perry, 2001 . Once qualified, participants described growing service improvement self-confidence and self-efficacy through reflective practice and colleague support.
Several participants (P20, P7, P13, P8) described developing what might be called ‘belongingness’ in social psychological terms; through social contact, working on incremental acceptance and becoming an integral component of the group in the clinical practice area ( Baumeister and Leary, 1995 ; Maslow, 2014). Studies suggest that nursing socialisation starts during training, through social interactions in practice placements, and continues throughout a nursing career ( Gray and Smith, 1999 ; Mackintosh, 2006 ; Dinmohammadi et al, 2013 ; Strouse and Nickerson, 2016 ).
As students, participants perceived that their lack of confidence in making service improvements was linked to feelings of not fitting in or lack of belonging, and this was exacerbated by the short length of time spent in any one area. They described the adaptive behaviours they adopted to fit in, such as using previous work and personal stories to start conversations. Some participants perceived that these casual, non-threatening conversations could help them get their service improvement ideas accepted.
Role transition was an important point in participants' service improvement experiences. As students, some of them felt powerless to make service improvements. Research suggests that social norms in nursing sustain power-imbalanced relationships: where this is negative, it can affect practice efficacy ( Potter, 1996 ; Gray and Thomas, 2005 ). Some participants described a feeling akin to ‘transition shock’ ( Duchscher, 2009 ) in the newly qualified period, finding it hard to cope with the competing demands of clinical practice and ongoing learning, including service improvement learning.
This is in keeping with other research suggesting that role transition is complex and challenging ( Maben et al, 2006 ; Feng and Tsai, 2012 ; Hatlevik, 2012 ). In this context, some participants also found it hard to make service improvements during role transition unless it was part of their preceptorship programme expectations ( Chang and Hancock, 2003 ; Schoessler and Waldo, 2006 ; Duchscher, 2008 ; Duchscher, 2009 ; Feng and Tsai, 2012 ; Hatlevik, 2012 ). Nevertheless, through professional transformation, some participants (P1, P2, P4, P16) recognised an increased accountability and responsibility for making service improvements now that they were qualified.
Seeking ward manager feedback and support
Most participants (P2, P4, P5, P12, P9, P16) described ward managers as important in fostering a culture of service improvement and change. The significance of the ward manager in creating ward learning cultures is well documented ( Orton, 1981 ; Fretwell, 1982 ; Ogier, 1986 ; Welsh and Swann, 2002 ; McGowan, 2006 ; Carlin and Duffy, 2013 ). Whether student participants felt empowered to make service improvements depended mainly on ward manager leadership. This leadership was also identified as important by the new registrants. Active engagement from those in senior positions is critical to successful service improvement ( Gollop et al, 2004 ). Nurses can experience high levels of empowerment when ward managers nurture perceptions of autonomy and confidence ( Madden, 2007 ). This study confirms that ward manager leadership is integral to nurse-led service improvement models ( Shafer and Aziz, 2013 ).
A proposed model of self-efficacy in service improvement enablement
The seven positive adaptive behaviours identified ( Figure 3 ) underpinned a process of participant professional transformation towards self-efficacy ( Bandura, 1997 ). With increasing resilience, they felt more empowered to make service improvements as they transitioned from student to registered nurse. The ‘model of self-efficacy in service improvement enablement’ brings together these positive adaptive behaviours as a way of understanding how participants' education and practice were interrelated to influence their service improvement learning and practice.
Although the model is presented as a linear process, the rate of service improvement engagement and development differed between participants, and was influenced by the context of their learning and practice. However, by the time they had made the transition from student to registered nurse they had all achieved a degree of empowerment, resilience and transformation, enabling them to move forward with service improvements in their own work context. This model offers an explanation for other research, which found that nurse-led service improvement requires knowledge and skills that must be continually practised and refined in order to be successful ( Wilcock and Carr, 2001 ; Christiansen et al, 2010 ).
Nursing undergraduate and preceptorship programmes should focus on developing these positive adaptive behaviours towards sustainable service improvement knowledge and skills. Policymakers at local level need to ensure that students and new registrants are supported by ward managers in their implementation of service improvement projects in order to develop their service improvement self-efficacy. Further research with other professional groups and in different healthcare contexts is needed to refine and test the model.
Limitations
This study took place in one university and NHS foundation trust; it is therefore context specific. Participants were in adult nursing only, which reduces transferability of the findings.
This study explored service improvement experiences of adult nurses as students and as qualified practitioners. It showed that they used positive adaptive behaviours to navigate their service improvement learning and practice contexts. The process of becoming service improvement practitioners has been explained through the ‘model of self-efficacy in service improvement enablement’. This provides a framework for understanding how nurses undergo concurrent processes of professional transformation, empowerment and resilience building, through service improvement experiences.
Ward management leadership approaches, supportive colleagues and an opportunity to practise service improvement skills pre-qualifying and in the preceptorship period were identified as essential to develop and sustain service improvement capability. This was important for participants as students but also as qualified nurses, at which time they believed that service improvement practice could be sustained through reflection and lifelong learning.
For all participants the central motivation to push past challenges encountered was a commitment to improving care for the patients they were caring for. This study's findings can inform the practice of nurse educators, practitioners, policy makers and healthcare delivery organisations, thereby potentially making a contribution to global efforts to embed a service improvement culture for the ongoing benefit of all.
- Looking for ways to continually improve the experience of those they care for is a professional responsibility of all nurses in all settings
- Service improvement learning in pre-registration programmes enables the development of nurses' ability to facilitate positive changes in practice
- The positive adaptive behaviours developed through service improvement learning can be sustained through lifelong learning, reflective practice and a supportive work environment, where a commitment to high-quality patient care delivery is prioritised
CPD reflective questions
- How do I view service improvement in practice?
- What skills and knowledge do I have to help me make service improvements in practice?
- How can I meet the gaps in my knowledge and practice?
- How do I support learners in practice in identifying and making service improvements?
- How can I make service improvement central to nursing activity?
Implementing service improvement projects within pre-registration nursing education: a multi-method case study evaluation
Affiliations.
- 1 Faculty of Health and Social Care, London South Bank University London, United Kingdom; University College London Hospitals, London, United Kingdom. Electronic address: [email protected].
- 2 Faculty of Health and Social Sciences, University of Bedfordshire, United Kingdom. Electronic address: [email protected].
- 3 Faculty of Health and Social Sciences, University of Bedfordshire, United Kingdom. Electronic address: [email protected].
- 4 University of Surrey, Guildford, Surrey, United Kingdom. Electronic address: [email protected].
- 5 University of Bedfordshire, United Kingdom. Electronic address: [email protected].
- PMID: 23867284
- DOI: 10.1016/j.nepr.2013.06.006
Background: Preparing healthcare students for quality and service improvement is important internationally. A United Kingdom (UK) initiative aims to embed service improvement in pre-registration education. A UK university implemented service improvement teaching for all nursing students. In addition, the degree pathway students conducted service improvement projects as the basis for their dissertations.
Aim: The study aimed to evaluate the implementation of service improvement projects within a pre-registration nursing curriculum.
Method: A multi-method case study was conducted, using student questionnaires, focus groups with students and academic staff, and observation of action learning sets. Questionnaire data were analysed using SPSS v19. Qualitative data were analysed using Ritchie and Spencer's (1994) Framework Approach.
Results: Students were very positive about service improvement. The degree students, who conducted service improvement projects in practice, felt more knowledgeable than advanced diploma students. Selecting the project focus was a key issue and students encountered some challenges in practice. Support for student service improvement projects came from action learning sets, placement staff, and academic staff.
Conclusion: Service improvement projects had a positive effect on students' learning. An effective partnership between the university and partner healthcare organisations, and support for students in practice, is essential.
Keywords: Clinical practice; Dissertation; Evaluation; Service improvement projects; Student nurses.
Copyright © 2013 Elsevier Ltd. All rights reserved.
Publication types
- Research Support, Non-U.S. Gov't
- Education, Nursing, Baccalaureate / standards*
- Education, Nursing, Baccalaureate / trends
- Focus Groups
- Mentors / psychology*
- Models, Educational
- Qualitative Research
- Quality Assurance, Health Care / methods
- Quality Assurance, Health Care / standards*
- Quality Improvement / standards
- Students, Nursing / psychology*
- Surveys and Questionnaires
- United Kingdom
- Login / Register

‘Let’s hear it for the midwives and everything they do’
STEVE FORD, EDITOR
- You are here: Archive
Changing practice 1: assessing the need for service improvement
22 February, 2016

Before implementing a change in practice, nurses require a systematic, evidence-based approach to identifying gaps in services and the need for change
In order to ensure the service they offer is of an appropriate standard, nurses need to know how to assess its quality, identify the need for change, and implement and evaluate that change. This two-part series offers practical guidance on how to bring about an evidence-based change in practice, and how to demonstrate the success, or otherwise, of that change. It uses the example of an initiative undertaken to improve medicines management in a hospice to illustrate the process. The article also illustrates how work undertaken in changing practice can form part of the evidence submitted in the nurse revalidation process. Part 1 considers how to determine when a change in practice is needed, how to assess and measure current practice, and identify gaps or weaknesses. Part 2 will discuss how to find out why the current practice is falling short of the desired level, and how to go about implementing improvements and measuring the effect of changes.
Citation: Carter H, Price L (2016) Changing practice 1: assessing the need for service improvement. Nursing Times ; 112: 8, 15-17.
Authors: Helen Carter is an independent healthcare advisor; Lynda Price is a clinical governance and infection control facilitator, Helen & Douglas House, Oxford.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here
- Read part 2 of this series here
Introduction
Nurses have a responsibility to preserve safety; this is made clear in the revised code of conduct for nurses (Nursing and Midwifery Council, 2015a). The Code states that nurses must “take account of current evidence, knowledge and developments in reducing mistakes and the effect of them and the impact of human factors and system failures”.
Preserving safety involves protecting vulnerable people and ensuring patient safety by reducing errors, rectifying mistakes and reporting concerns immediately. This requires nurses to identify problems and their causes, and put in place changes that will improve safety and the quality of care; it can involve participating in clinical audits and reviews, and any other activity that results in changing practice. This two-part series provides practical advice for nurses wishing to make changes to practice, as well as suggestions for documenting and evaluating the resulting changes.
When nurse revalidation begins in April 2016, the NMC will expect nurses to provide evidence of how they practise effectively. This will involve written information, including personal reflections and feedback from colleagues and patients, and evidence of having undertaken continuing professional development (CPD). Bringing together the expectations from The Code (Nursing and Midwifery Council, 2015a) and How to revalidate with the NMC (NMC, 2015b), the article also aims to help nurses consider ways to use the evidence collated in service-improvement projects as part of the material submitted in their revalidation evidence.
Importance of reflective practice
The Royal College of Nursing (2010) has developed a set of eight principles to enable nurses to reflect on their own practice. Principle F highlights the need for evidence-based practice, where “nurses and nursing staff have up-to-date knowledge and skills, and use these with intelligence, insight and understanding in line with the needs of each individual in their care” (Gordon and Watts, 2011). More recently, in the Shape of Caring review, Lord Willis stated that: “Registered nurses and care assistants are required at all levels to adapt, support and lead research and innovation to deliver high-quality care” (Willis, 2015). His recommendations were influenced by the need to celebrate good care and build on the expertise and evidence base of existing clinical practice.
Evidence-based practice has been defined as: “the integration of best research evidence with clinical expertise and patient values” (Sackett et al, 2000). Implementing a change in practice involves collating a variety of information and analysing the findings against national guidance, service provision and patients’ views of their care.
Identifying the need for change
Nursing practice is continually changing and it is important to identify improvements and deterioration in practice, particularly if they affect patient safety. Identifying issues in practice relies on nurses using their clinical judgement and knowledge to collate relevant information, thoroughly analyse appropriate data and provide robust evidence for the success, or otherwise, of change (Benner, 2000).
Once the need for change has been noticed, the process of bringing about change can be thought of as a series of steps:
- What are we trying to achieve? A review of the relevant evidence-based practice for the particular area of healthcare.
- Are we achieving it? How does current practice measure up to local and national standards?
- Why are we not achieving it? A review of current systems and processes to discover why current practice is falling short.
- What can be done to improve things? Recommendations, timescales and strategies to bring about a change in practice.
- Have things been improved?
Re-audit of current practice and ongoing review to see whetherm change has been successful.
This article explains steps 1 and 2. Steps 3 to 5 will be discussed in part 2 .
What are we trying to achieve?
It is essential to assess current practice within national and local guidance, standards and expectations; this will help to reveal potential gaps in practice and give an indication of what needs to be the main focus of an audit. A range of tools, advice and standards is available that can be used as a baseline or framework for measuring practice. While it is not within the scope of this article to address these in depth, they may include:
- National Institute for Health and Care Excellence (NICE) guidelines;
- Scottish Intercollegiate Guidelines Network;
- National social care standards;
- The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 (part 3);
- NHS Commissioning Board Special Health Authority (responsible for patient safety);
- Professional-body standards and guidelines.
Measuring gaps in practice
Regular audits of the structure, processes and outcomes of service provision are key in measuring whether or not established criteria and standards are being met (Chambers et al, 2006). Even in the best services there is likely to be a gap between what is happening in clinical practice and what has been identified as good practice in national and local guidance.
Carey et al (2009) suggested that closing the gap between best evidence and current clinical practice has the potential to improve health outcomes. If a nurse identifies a gap in practice, evidence such as incident forms, complaints, observations made by staff, patients or the public may show whether it is more than an isolated case. Nurses should therefore explore all available evidence, and discussions with colleagues will help to confirm any gap or poor practice
Once clinical issues needing to be addressed have been identified, it is important to select the most appropriate method to measure the quality and standard that should be available to patients; each will have its advantages and disadvantages. The method used to gather information will depend on the aim of the project. Depending on the time, resources and level of support available, clinical leads may choose to use some or all of the following methods:
- Clinical audit;
- Service review;
- Seeking patient and staff feedback;
- Observation of practice;
- Literature review;
- Complaints review;
- Patterns of incident reporting;
- Primary and/or secondary research.
This series uses a case study of some of the processes used by a nurse who undertook a medicines-management audit in a hospice, outlined in Box 1. Clinical audit is “a quality improvement process that seeks to improve patient care and outcomes through a systematic review of care against explicit criteria and the implementation of change” (NICE, 2002). Based on the audit cycle, Fig 1 (attached) outlines the processes that can be followed to maintain a robust approach to any project. Since the process is a cycle, once an audit has been undertaken and the relevant changes made, a re-audit should be carried out to close the loop and evaluate how the service is performing after making changes.
Box 1. Case study: Investigating medication errors in a hospice
A nurse working in a hospice was studying for an infection prevention and control qualification. The assignment for a module on quality and clinical governance was to identify an area of practice in which the standards of care could be improved. This involved using clinical governance tools and techniques, such as clinical audit, risk management, change management and evidence-based practice.
Within the organisation was a steady flow of incident reports concerning medication errors. The nurse decided to look into the issue to see if she could find any patterns, causes or contributing factors that might reveal why the errors were occurring. With this information the nurse would be able to recommend a change in practice that would improve the quality of care patients received.
The nurse began by auditing incident forms from the previous 12 months. These were benchmarked against criteria in the National Patient Safety Agency (NPSA) patient safety incident reports. Using this information, the nurse analysed the current position of the organisation to identify any underlying causes for the errors.
The nurse felt supported by senior staff and undertook the audit with the full backing of the hospice, which viewed medication errors as valuable opportunities for learning on an organisational and personal level. The World Health Organization (2004) suggested that this response to reporting incidents is more likely to improve patient care than the reporting process.
With information gathered about the causes of errors, and collated evidence of best practice, the nurse would be able to make recommendations to reduce the risk or prevent further errors.
Are we achieving it?
Having identified the issue(s) to be audited, the next step in the process (Fig 1, attached) is to assess whether or not the organisation or an identified clinical area is achieving its aims, in this case, the safe administration of medication. It is imperative to analyse the existing situation; a number of tools such as those mentioned above can be used to determine whether the organisation is achieving a high standard of care and, if not, the reasons for this.
A strengths, weaknesses, opportunities and threats (SWOT) analysis can be undertaken to identify barriers and opportunities for change. This is an integral part of the planning stage, and can save time and frustration at later stages of the project. A SWOT analysis is easy to do, and provides an assessment of internal and external factors that can influence changes in practice. It can be used to support short-term clinical or organisational goals (NICE, 2007).
Table 1 (attached) illustrates a SWOT analysis reviewing potential organisational influences on the prevalence of medication errors in the hospice. In this case, the analysis demonstrated that the organisation was open, trusting, willing to learn from mistakes and share good practice. This attitude is reflected in nursing practice and the willingness of staff to report incidents.
Defining the scope
After the need for change has been identified, the project’s scope and aim need to be described. The scope highlights the area to be included and excluded from the review or audit, while the aim can be an overarching statement to determine the areas of interest. Examples of reflective questions to ask when defining the scope include:
- What is being measured?
- Is this an audit or review?
- What are the risks to patients, staff and the organisation?
- What is the benchmark?
- Are there any standards to indicate what should be achieved?
- Is a baseline audit required?
The rationale for the project needs to be clearly articulated. The hospice nurse identified the aim as being to reduce the risk of preventable medication errors, thus improving the quality and safety of care.
Documenting change
Records are a vital component throughout the process of change, in order to provide evidence of how issues were identified and why service aims were not being achieved; recommendations to improve practice; and to show that the service has improved. The nature of this cyclical process means that monitoring and ongoing reviews determine whether the change has had an impact on practice or not.
Having identified where practice is not meeting the required national and local standards, the next step it to find out why this is happening and what could be done to improve practice. This will be discussed in part 2 .
- Nurses are required to have up-to-date skills
- Evidence-based practice is a cornerstone of all healthcare
- As part of revalidation, nurses will need to provide evidence to support practice
- Regular audits of service provision will measure standards
- Audit/review cycle ensures high standards
Related files
240216_assessing-the-need-for-service-improvement.pdf, fig 1 the cycle of audit and reevaluation.pdf, table 1 swot analysis of the hospice.pdf.
- Add to Bookmarks
Have your say
Sign in or Register a new account to join the discussion.
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
Learning Zone Previous Next
Using service improvement methodology to change practice, william gage lead nurse for practice development and innovation, imperial college healthcare nhs trust, london..
This article discusses the role of service improvement methodology in changing the quality of care delivered. It outlines the six-stage framework for quality improvement recommended by the NHS Institute for Innovation and Improvement. The reader is encouraged to complete a series of activities to plan and deliver a service improvement project. Potential challenges to the successful delivery of a service improvement project are also considered. The article concludes with an example of the use of the six-stage framework to improve the quality of urinary catheter care in one acute NHS trust.
Nursing Standard . 27, 23, 51-57. doi: 10.7748/ns2013.02.27.23.51.e7241R1
This article has been subject to double blind peer review
Received: 03 October 2012
Accepted: 16 November 2012
management - leadership - quality - change management - quality improvement - service improvement
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

06 February 2013 / Vol 27 issue 23
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: Using service improvement methodology to change practice
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
Service improvement in health care: a literature review
- Nursing, Midwifery and Health
Research output : Contribution to journal › Article › peer-review
Access to Document
- 10.12968/bjon.2018.27.15.893
Fingerprint
- Nursing Nursing and Health Professions 100%
- Enalapril Maleate Nursing and Health Professions 100%
- Nurse Nursing and Health Professions 100%
- Service Development Nursing and Health Professions 100%
- Literature Review Nursing and Health Professions 100%
- Error Nursing and Health Professions 100%
- Treatment Outcome Nursing and Health Professions 100%
- Cost Control Nursing and Health Professions 100%
T1 - Service improvement in health care
T2 - a literature review
AU - Craig, Lynn
PY - 2018/8/9
Y1 - 2018/8/9
N2 - Service improvements in health care can improve provision, make cost savings, streamline services and reduce clinical errors. However, on its own it may not be adequate for improving patient outcomes and quality of care. The complexity of healthcare provision makes service improvement a challenge, and there is little evidence on whether improvement initiatives change healthcare practices and improve care. To understand the concept of service development within health care, it is necessary to explore the national context and how the NHS has adopted improvement initiatives. To equip the nursing workforce with the skills necessary to make positive change, higher education institutions have developed courses that include the topic within their pre-registration programmes. However, service improvement is a learned skill that nurses need to practise in order to become competent.
AB - Service improvements in health care can improve provision, make cost savings, streamline services and reduce clinical errors. However, on its own it may not be adequate for improving patient outcomes and quality of care. The complexity of healthcare provision makes service improvement a challenge, and there is little evidence on whether improvement initiatives change healthcare practices and improve care. To understand the concept of service development within health care, it is necessary to explore the national context and how the NHS has adopted improvement initiatives. To equip the nursing workforce with the skills necessary to make positive change, higher education institutions have developed courses that include the topic within their pre-registration programmes. However, service improvement is a learned skill that nurses need to practise in order to become competent.
KW - Service improvement
KW - Nursing, practice development
KW - Quality improvement
U2 - 10.12968/bjon.2018.27.15.893
DO - 10.12968/bjon.2018.27.15.893
M3 - Article
SN - 0966-0461
JO - British Journal of Nursing
JF - British Journal of Nursing
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- 10 Essential Public Health Services
- Cooperative Agreements, Grants & Partnerships
- Public Health Professional: Programs
- Health Assessment: Index
- Research Summary
- COVID-19 Health Disparities Grant Success Stories Resources
- Communication Resources
Performance Management and Quality Improvement: Definitions and Concepts
At a glance.
In the public health field, many initiatives and organizations focus on improving public health practice, using different terms. This page provides common definitions for public health performance management.
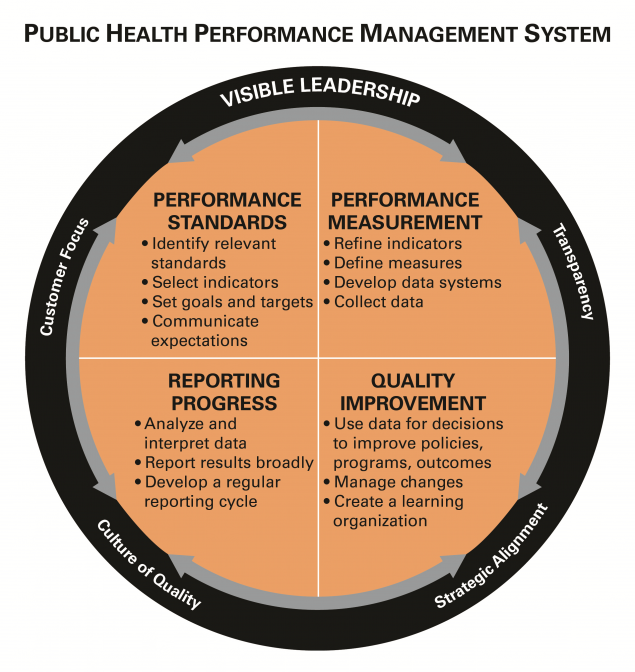
Definitions and concepts
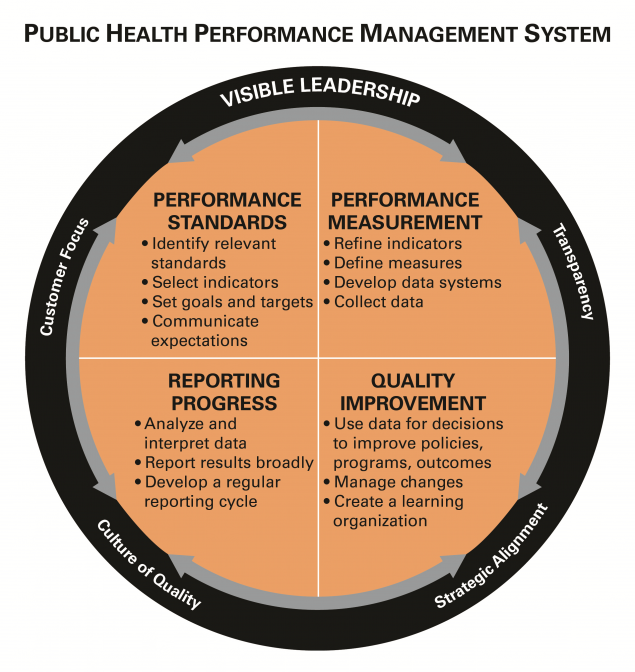
There has been a rapidly growing interest in performance and quality improvement within the public health community, and different names and labels are often used to describe similar concepts or activities. Other sectors, such as industry and hospitals, have embraced a diverse and evolving set of terms but which generally have the same principles at heart (i.e., continuous quality improvement, quality improvement, performance improvement, six sigma, and total quality management).
In the public health field, an array of initiatives has set the stage for attention to improving public health practice, using assorted terms. The Turning Point Collaborative focused on performance management, the National Public Health Performance Standards Program created a framework to assess and improve public health systems, while the US Department of Health and Human Services has provided recommendations on how to achieve quality in healthcare . In 2011, the Public Health Accreditation Board launched a national voluntary accreditation program that catalyzes quality improvement but also acknowledges the importance of performance management within public health agencies. Regardless of the terminology, a common thread has emerged—one that focuses on continuous improvement and operational excellence within public health programs, agencies, and the public health system.
To anchor common thinking, below are links to some of the definitions that are frequently used throughout these pages.

Key definitions
- Riley et al, "Defining Quality Improvement in Public Health", JPHMP, 2010, 16(10), 5-7.
- Public Health Accreditation Board Acronyms and Glossary of Terms, Version 2022 [PDF]
Public Health Gateway
CDC's National Center for State, Tribal, Local, and Territorial Public Health Infrastructure and Workforce helps drive public health forward and helps HDs deliver services to communities.

Message placeholder

- A. V. Khutorskoy Key competencies and educational standards , Internet magazine “Eidos”. (2002), URL: http://eidos.ru/journal/2002/0423.htm 194 (data of access: 05.10.2017) [Google Scholar]
- A. V. Khutorskoy Design technology of key and subject competences , Internet magazine “Eidos”. (2005), URL : http://www.eidos.ru/yournal/2006/0505.htm 195 (data of access: 25.09.2017) [Google Scholar]
- V.I. Zvonnikov, M.B. Chelyshkova Evaluation of the quality of learning outcomes in attestation: competence approach (Logos, Moscow, 2012) [Google Scholar]
- A. A. Ozerina Professional identity of undergraduate students. PhD dissertation. (Yaroslavl, 2012) [Google Scholar]
- Y. P. Povarenkov, Siberian psychological journal. 24 , 53–58, (2006) [Google Scholar]
- E. V. Voevoda Theory and practice of professional language training of international specialists in Russia PhD dissertation (Moscow, 2011) [Google Scholar]
- A. S. Nekrasov The development of professional identity of the cadet military school. PhD dissertation (Krasnodar, 2005) [Google Scholar]
- M. V. Panfilova Professional and personal identification as a factor in the formation of the future tourism Manager . Extended abstract of PhD dissertation. (Krasnodar, 2008) [Google Scholar]
- V.L. Zhvetkov, Y. V. Slobodchikov, Psychopedagogy in law enforcement 1(52) , 30–32, (2013) [Google Scholar]
- J. Mohtashami, H. Rahnama, F. Farzinfard, A. Talebi, F. Atashzadeh-Shoorideh, M. A. Ghalenoee Open Journal of Nursing 5 , 765–772, [Google Scholar]
- S. L. Rubinstein Principles and ways of development of psychology (AN SSSR, Moscow, 1959) [Google Scholar]
Current usage metrics show cumulative count of Article Views (full-text article views including HTML views, PDF and ePub downloads, according to the available data) and Abstracts Views on Vision4Press platform.
Data correspond to usage on the plateform after 2015. The current usage metrics is available 48-96 hours after online publication and is updated daily on week days.
Initial download of the metrics may take a while.

Theses and Dissertations Collection
Open Access Repository of University of Idaho Graduate ETD
Description
An open access repository of theses and dissertations from University of Idaho graduate students. The collection includes the complete electronic theses and dissertations submitted since approximately 2014, as well as, select digitized copies of earlier documents dating back to 1910.
Top Subjects
computer science ecology electrical engineering natural resource management mechanical engineering plant sciences water resources management education civil engineering environmental science animal sciences forestry engineering materials science agriculture biology chemical engineering wildlife management
Top Programs
natural resources education mechanical engineering computer science electrical and computer engineering plant, soil and entomological sciences civil engineering environmental science english water resources movement & leisure sciences animal and veterinary science anthropology chemical and materials science engineering geology curriculum & instruction bioinformatics & computational biology chemistry
1910 to 2023 View Timeline
1893 PDFs 395 Records 147 Embargoed ETDs View table
Collection as Data (click to download)
Metadata CSV Metadata JSON Subjects JSON Subjects CSV Timeline JSON Facets JSON Source Code
On the Problem of Cooperation of the Reaction of Hands: I. Cooperation of Hand Reaction to Sound and Light Stimuli in Healthy Subjects
- Published: November 2002
- Volume 28 , pages 698–701, ( 2002 )
Cite this article

- S. M. Blinkov 1 &
- M. G. Nikandrov 1
44 Accesses
Explore all metrics
Coordinated reaction of hands was analyzed during examination of healthy subjects and patients with focal lesions of the central nervous system in order to find the morphological structures responsible for such cooperation. Results of investigation of coordinated hand reaction in healthy subjects to sound and light stimuli with a warning signal are presented. The degree of cooperation was estimated by the correlation coefficient between the values of the reaction time of the right and left hands under conditions of their simultaneous response. In healthy subjects, there exists a strong positive correlation, whose variability in repeated examinations is determined by constitutional features of the subject.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Manual asymmetry for temporal and spatial parameters in sensorimotor synchronization.

Physical Analysis of Handshaking Between Humans: Mutual Synchronisation and Social Context

Normal and Impaired Cooperative Hand Movements: Role of Neural Coupling
Blinkov, S.M., On a Method of Revealing Brain Mechanisms (Simple Motor Reaction), A.R. Luriya i sovremennaya psikhologiya (A.R. Luria and Modern Psychology), Moscow: Mosk. Gos. Univ., 1982, p. 224.
Google Scholar
Nikandrov, M.G. and Blinkov, S.M., Simple Motor Reaction Time and Respiration. I. The Influence of a Warning Signal, Fiziol. Chel. , 1982, vol. 8, no. 4, p. 665.
Moskatova, A.K., Quantitative Estimation of Symptoms of an Injury of the Sensorimotor Area of Human Brain by the Simple Motor Reaction Time, Cand. Sc. (Biol.) Dissertation , Moscow, 1967.
Yakovlev, A.I., The Time of Reaction to Passive Movement, Cand. Sc. (Biol.) Dissertation , Moscow, 1978.
Nikandrov, M.G., Early Diagnostics of Primary Brainstem Lesions by Temporal Parameters of a Simple Motor Reaction, Diagnostika i khirurgicheskoe lechenie opukholei i sosudistykh zabolevanii golovnogo mozga (Diagnostics and Surgery of Brain Tumors and Vascular Diseases), Moscow: Akad. Med. Nauk SSSR, 1983, p. 51.
Nikandrov, M.G., Quantitative Estimation of Brainstem Lesions. Reaction Time, Cand. Sc. (Med.) Dissertation ,Moscow, 1996.
Blinkov, S.M. and El'ner, A.M., Vremya reaktsii pri povyshennoi vozbudimosti segmentarnogo apparata spinnogo mozga (Reaction Time under Conditions of Increased Excitability of Spinal Segmental Apparatus), Available from VINITI, Moscow, 1982, no. 5628-82.
Luk'yanov, V.I., Loginov, O.E., Dan'kov, V.B., et al. ,Information-Instrumentation System for Investigation of Human Motor Reaction Time, Mikroprotsessornye sredstva i sistemy , 1989, no. 5, p. 68.
Download references
Author information
Authors and affiliations.
Burdenko Scientific Research Institute of Neurosurgery, Russian Academy of Medical Sciences, ul. 4-ya Tverskaya-Yamskaya 16, Moscow, 125047, Russia
S. M. Blinkov & M. G. Nikandrov
You can also search for this author in PubMed Google Scholar
Rights and permissions
Reprints and permissions
About this article
Blinkov, S.M., Nikandrov, M.G. On the Problem of Cooperation of the Reaction of Hands: I. Cooperation of Hand Reaction to Sound and Light Stimuli in Healthy Subjects. Human Physiology 28 , 698–701 (2002). https://doi.org/10.1023/A:1021104407031
Download citation
Issue Date : November 2002
DOI : https://doi.org/10.1023/A:1021104407031
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nervous System
- Central Nervous System
- Reaction Time
- Healthy Subject
- Strong Positive Correlation
- Find a journal
- Publish with us
- Track your research

- News & Events
Nursing Research News: April 2024
Each month, the Center for Research and Scholarship at the Frances Payne Bolton School of Nursing sends an internal research newsletter to faculty, staff, students and researchers. A recap is posted here.
Message from the Associate Dean for Research
The National Institutes of Health (NIH), through Deputy Director of Extramural Research, Dr. Mike Lauer, and Director of the NIH Center for Scientific Review, Dr. Noni Byrnes, has announced significant changes to the peer review process and application forms for fellowship applications (e.g., F30, F31, F32, F33, and F99/K00), effective January 25, 2025.
These changes aim to address concerns raised by the extramural community regarding potential biases in the current fellowship review process. The revisions to the NIH fellowship application and review process are designed to increase the likelihood of identifying the most promising fellowship candidates consistently.
Key changes include reorganizing and refining the current five scored criteria into three:
- Candidate’s Goals, Preparedness, and Potential
- Research Training Plan, and
- Commitment to Candidate.
The Center for Research and Scholarship will provide more information about the changes in the fellowship application forms and the review process as it becomes available.
-Ronald Hickman, PhD, RN, ACNP-BC, FNAP, FAAN
Scholarship Awards and Grants
Derry Ann Moritz Scholarship
Colleen Carroll, PhD candidate, is the inaugural recipient of the Derry Ann Moritz Scholarship , which supports PhD candidates at the Frances Payne Bolton School of Nursing whose dissertations focus on topics regarding palliative and end-of-life care.
An oncology palliative care nurse practitioner at University Hospitals Seidman Cancer Center since 2022, Carroll was looking for opportunities to elevate her experience in the field. Last year, she had the opportunity to be the primary author of a medical manuscript. Toward the end of the writing process, she connected with Susan Mazanec, a nurse scientist at University Hospitals Seidman Cancer Center and associate professor at the School of Nursing. Carroll and Mazanec stayed in touch, and Dr. Mazanec ended up recommending Carroll for the Moritz Scholarship. Congratulations, Colleen!
Sigma Spring 2024 Call for Research Grants
The Alpha Mu Chapter of Sigma Global Nursing (STTI) is funding two grants, each up to $1,000: one for student applicants with at least a master's degree in nursing or are enrolled in a nursing doctoral program, and have Sigma membership, and the other grant is open to all STTI members. Allocation of funds is based on the quality of the proposed research, the future promise of the applicant, and the applicant's research budget. Applications from novice researchers who have received no other national research funds are encouraged. Funds for these grants do not cover expenses incurred prior to the funding date, travel, conference registrations, and computer software or hardware. Submission deadline is May 1, 2024. See this "call for grants" document for more details .
Stielau Award for Early-Stage PhD Research
The Joyce M. Stielau Award is available to current PhD candidates at the Frances Payne Bolton School of Nursing. This funding is intended for early-career investigators currently conducting early-stage research. Applicants can request up to $2,000 for funding of their current IRB-approved research. All fields and areas of study will be considered.
The late Joyce M. Stielau was a nurse anesthesiologist, devoted hospital volunteer, philanthropist, and former president of the Greater Cleveland chapter of Mended Hearts, a support group for cardiac patients. A veteran of the United States Air Force, Mrs. Stielau earned her nursing degree from the University of Cincinnati. The foundation named for her and her late husband Herbert supports scholarships and research in the field of nursing, among other important causes. Details about the Stielau Award and how to apply can be found on the School of Nursing website .
Algase Dissertation Award for Eldercare Research
Research funding is available through the Donna Algase Dissertation Award to current PhD candidates at the Frances Payne Bolton School of Nursing. Provided by the generous support of the Donna Algase Dissertation Award Endowed Fund, this award will grant two early career investigators up to $1,350 each for their early-stage research in the field of eldercare.
CWRU alumna Donna L. (Muszynski) Algase (GRS '88, nursing), began her nursing career in pediatric and pediatric intensive care, but found her passion for gerontological nursing and research while completing her bachelor's degree at the University of Toledo.
Widely published on nursing theory, gerontological nursing, and dementia research, Dr. Algase developed her nursing knowledge into an entrepreneurial opportunity and, along with a colleague, began an educational consulting business to deliver in-service and continuing education programs for long-term care facilities. An established authority on end-of-life care and research, she received the Distinguished Alumni Award in 2004.
Details about the Donna Algase Dissertation Award and how to apply can be found on this page of the School of Nursing website.
Research and Scholarly News
Faculty Co-Edit Interprofessional Leadership Textbook
FPB School of Nursing faculty members Carol Savrin, associate professor, and Jesse Honsky, assistant professor, collaborated to edit Interprofessional Leadership for Nurses: Mastering Knowledge, Skills, and Attitudes for Success, 1st Edition , recently published by Cognella Academic Publishing.
Savrin and Honsky developed this book as a supplementary text for entry-level and advanced nursing courses and programs to help entry-level and advanced nursing students recognize and build on their leadership and teamwork skills. The text integrates knowledge, skills, and attitudes from multiple disciplines, and links students to the American Association of Colleges of Nursing Essentials for nursing education.
The book provides students with salient advice from the field to help them develop into competent and effective healthcare professionals with leadership skills.
Other News and Information
New Name for VA Medical Center
The Louis Stokes Cleveland Department of Veterans Affairs (VA) Medical Center has asked CWRU to now identify the hospital as "VA Northeast Ohio Healthcare System" going forward.
Guidance for working with the VA is on the RADAR Canvas site. The Form 2 for memorandums of understanding between the VA and CWRU has been updated to reflect the new name. Additionally, VA Guidelines have been updated, including information regarding rules for the utilization of an independent physician association (IPA). The current indirect cost (IDC) rate agreement has been extended through June 30, 2025, and is also on the Canvas site.
CWRU Human Research Protection Program Renewed
CWRU's Human Research Protection Program (CWRU HRPP) recently received a 5-year renewal of its Association for the Accreditation of Human Research Protection Programs (AAHRPP) full accreditation status.
It was originally accredited in 2016, with a renewal in 2019. The CWRU HRPP is responsible for monitoring the rights and welfare of CWRU research participants while ensuring the university’s commitment to high-quality research. AAHRPP, seen as the gold standard of HRPP accreditation, serves to ensure “ethically sound and scientifically valuable research through the accreditation of high-quality human research protection programs.” CWRU’s accreditation is critically important to our researchers’ ability to receive federal and nonfederal funding, as well as to collaborate with other AAHRPP-accredited national and international organizations.
NIH News and Updates
Changes Coming to Applications and Peer Review
The National Institutes of Health (NIH) is implementing multiple changes that will impact the preparation and peer review of most grant applications submitted for due dates on or after Jan. 25, 2025. Although each of these initiatives have specific goals, they are all meant to simplify, clarify, or ensure greater fairness. NIH has released a guide notice ( NOT-OD-24-084 ) that provides an overview of each change to help the research community contextualize them as details are released over the next few months.
Where’s the Public Access Policy?
There is a new location for NIH public access policy content and resources . As of March 12, 2024, NIH Public Access Policy content and resources have been consolidated into the NIH Sharing Site.
Recent School of Nursing Publications
Dolansky, M. A., Davey, C. H., & Moore, S. M. (2024). Research and Practice in Quality Improvement and Implementation Science: The Synergy for Change Model. Journal of Nursing Care Quality , 10-1097.
Ruksakulpiwat, S., Thorngthip, S., Niyomyart, A., Benjasirisan, C., Phianhasin, L., Aldossary, H., Ahmed, B. H., & Samai, T. (2024). A Systematic Review of the Application of Artificial Intelligence in Nursing Care: Where Are We, and What’s Next? Journal of Multidisciplinary Healthcare , 1604-1605.
This paper is in the following e-collection/theme issue:
Published on 16.5.2024 in Vol 26 (2024)
Implementation of Inpatient Electronic Consultations During the COVID-19 Crisis and Its Sustainability Beyond the Pandemic: Quality Improvement Study
Authors of this article:

Original Paper
- Anna S Aledia, BS ;
- Amish A Dangodara, MD ;
- Aanya A Amin ;
- Alpesh N Amin, MD, MBA
Department of Medicine & Hospital Medicine, University of California, Irvine, Orange, CA, United States
Corresponding Author:
Alpesh N Amin, MD, MBA
Department of Medicine & Hospital Medicine
University of California, Irvine
333 City Boulevard West
Orange, CA, 92868
United States
Phone: 1 714 456 3785
Fax:1 714 456 3871
Email: [email protected]
Background: Limiting in-person contact was a key strategy for controlling the spread of the highly infectious novel coronavirus (COVID-19). To protect patients and staff from the risk of infection while providing continued access to necessary health care services, we implemented a new electronic consultation (e-consult) service that allowed referring providers to receive subspecialty consultations for patients who are hospitalized and do not require in-person evaluation by the specialist.
Objective: We aimed to assess the impact of implementing e-consults in the inpatient setting to reduce avoidable face-to-face referrals during the COVID-19 pandemic.
Methods: This quality improvement study evaluated all inpatient e-consults ordered from July 2020 to December 2022 at the University of California Irvine Medical Center. The impact of e-consults was assessed by evaluating use (eg, number of e-consults ordered), e-consult response times, and outcome of the e-consult requests (eg, resolved electronically or converted to the in-person evaluation of patient).
Results: There were 1543 inpatient e-consults ordered across 11 participating specialties. A total of 53.5% (n=826) of requests were addressed electronically, without the need for a formal in-person evaluation of the patient. The median time between ordering an e-consult and a specialist documenting recommendations in an e-consult note was 3.7 (IQR 1.3-8.2) hours across all specialties, contrasted with 7.3 (IQR 3.6-22.0) hours when converted to an in-person consult ( P <.001). The monthly volume of e-consult requests increased, coinciding with surges of COVID-19 cases in California. After the peaks of the COVID-19 crisis subsided, the use of inpatient e-consults persisted at a rate well above the precrisis levels.
Conclusions: An inpatient e-consult service was successfully implemented, resulting in fewer unnecessary face-to-face consultations and significant reductions in the response times for consults requested on patients who are hospitalized and do not require an in-person evaluation. Thus, e-consults provided timely, efficient delivery of inpatient consultation services for appropriate problems while minimizing the risk of direct transmission of the COVID-19 virus between health care providers and patients. The service also demonstrated its value as a tool for effective inpatient care coordination beyond the peaks of the pandemic leading to the sustainability of service and value.
Introduction
When the novel coronavirus (COVID-19), the disease caused by SARS-CoV-2, began to quickly spread around the world, the high transmissibility of this disease urged health care systems to explore alternatives to face-to-face interactions that would reduce the risk of exposure for both the patient and the provider. Electronic consultations (e-consults) are asynchronous, non–face-to-face, provider-to-provider exchanges that have been shown to improve patient access to specialty care for appropriate referral problems that do not require an in-person evaluation of the patient by the specialist [ 1 - 3 ]. The rapid rise in COVID-19 cases induced a demand for the adoption of e-consult services and triggered an increase in the use of e-consults [ 4 ]. Although its use in the outpatient setting is well established [ 5 , 6 ], e-consults in the inpatient arena are relatively new.
As the only academic health system in the sixth largest county in the United States, University of California Irvine (UCI) Health has been a leader in the advancement of telehealth technologies that expand access to care and improve health care efficiency and resource use [ 7 ]. UCI already has a well-developed e-consults program in the ambulatory setting [ 8 ], and to complement this existing service, we expanded e-consults to patients who were hospitalized to further help reduce in-person contacts between consulting providers and patients, thereby minimizing disease transmission and conserving scarce personal protective equipment (PPE) during the COVID-19 crisis. Other health systems have implemented similar e-consult services for inpatients, but provider use of e-consults was temporary in response to the pandemic, favoring in-person consultative care instead [ 9 ]; inpatient e-consults were offered by only a single specialty consulting service [ 10 , 11 ]; and use cases involved early inpatient e-consult models [ 12 , 13 ]. In this study, we describe our rapid implementation of inpatient e-consults in multiple specialties and its sustained use beyond the peaks of the pandemic.
The inpatient e-consult service was implemented at the UCI Medical Center, a 478-bed acute care hospital providing tertiary and quaternary care, ambulatory and specialty medical clinics, behavioral health care, and rehabilitation services. Located in Orange County, California, it serves a diverse population of close to 4 million persons with broad health care needs. With more than 500 specialty and primary care physicians, UCI offers a full scope of acute and general care services. It is also the primary teaching location for UCI medical and nursing students, medical residents, and fellows, and it is home to Orange County’s only adult level 1 and pediatric level 2 trauma centers, a National Cancer Institute–designated comprehensive cancer center, a regional burn center, the county’s only hematopoietic stem cell and bone marrow transplant program, and the region’s only high-risk perinatal and neonatal program and maternal-fetal transport system. In winter 2020, UCI Medical Center opened a temporary mobile field hospital that added up to 50 acute care beds in response to a surge of patients with COVID-19.
Implementation
The design and implementation of inpatient e-consults were guided by a steering committee, which included the Chair of the Department of Medicine and Executive Director of Hospital Medicine (who was the lead to design and develop e-consults at the UCI), a clinical informaticist, specialty physician leads, an IT build team, representatives from the Compliance and Privacy Office and Physicians Billing Group, and a project manager. Early on, members of this committee engaged UCI leadership to affirm support for the new service and obtain the IT resources needed to build the inpatient e-consults workflow. Regular steering committee meetings were established to discuss the design of the inpatient e-consults workflow and develop a process for provider reimbursement or credit. Prior to the go-live, the inpatient e-consult service was publicized by members of the steering committee through email communications with house staff. Steering committee members also hosted Zoom training (Zoom Technologies) and orientation sessions with participating consulting services, and they distributed tip sheets summarizing the steps to complete the requesting provider and responding consultant workflows.
Our IT team was able to efficiently implement our inpatient e-consult service by designing workflows similar to those for traditional in-person consults. Thus, the processes for requesting and responding to inpatient e-consults were not unfamiliar to providers ( Figure 1 ). To request an e-consult, the inpatient service or team places a consult order in the electronic health record (EHR), indicating that the request is for an e-consult. The patient is then added to the physician e-consults system list of the appropriate specialty. A follow-up call or page is also sent to the specialty by the requesting team to alert the inpatient consulting team of the e-consult and, if necessary, provide them with any additional details. To respond to the e-consult request, the inpatient consulting team reviews the relevant clinical information available in the EHR and documents their assessment and recommendations in a consult note. If the case is deemed too complex to be addressed electronically, the consulting team converts the e-consult to a traditional in-person consultation and the patient is examined before documenting guidance in the EHR. The requesting provider and responding consultant are each credited with 0.7 work relative value units (a measure of the provider’s time and effort required to perform the service) for every completed e-consult that does not result in an in-person evaluation of the patient by the consulting service, while usual billing or relative value unit credit applies for in-person consultations.

Measurement and Analysis
We conducted a retrospective evaluation of all inpatient e-consults ordered at the UCI Medical Center from implementation in July 2020 to December 2022 to assess use, outcomes, and response times. Use was tracked by examining the volume of e-consults ordered per specialty over the 2.5-year period and comparing it with the volume of traditional in-person consults ordered for the specialties offering inpatient e-consults. To assess outcomes, we categorized the result of each e-consult order as either “resolved electronically” if the consulting team addressed the request without a face-to-face evaluation of the patient or “converted to in-person” if the consulting team deemed the case too complex and the patient required a physical examination. The response time was defined as the interval between the documented consult order in the EHR and the consulting team filing recommendations in a consult note. We calculated the median response time and the IQR in hours for each specialty and performed nonparametric Mann-Whitney U tests in SPSS (version 28; IBM Corp) to compare the median response times of requests resolved electronically and converted to in person. All P values were 2-tailed, and P <.05 was considered statistically significant.
Ethical Considerations
Our implementation and retrospective analysis of the inpatient e-consults service constituted as quality improvement activities and not human subjects research. Thus, our study did not require institutional review board review. This study followed the Standards for Quality Improvement Reporting Excellence guidelines.
UCI’s e-consults service was launched in 11 total specialties (allergy and immunology, cardiology, dermatology, endocrinology, infectious diseases, nephrology, palliative care, pediatric endocrinology, pulmonary and critical care, radiation oncology, and rheumatology). Over a 2.5-year period, 1543 e-consults were requested out of 14,974 total consult orders (e-consult and traditional in-person consults) across the 11 participating specialties ( Figure 2 ). Thus, the average proportion of consult orders requested as e-consults is 10.3%, although this proportion varied widely among participating specialties. The specialty with the lowest e-consult proportion was pulmonary and critical care, which had 1.5% (13/850) of total consult orders requested as e-consults, while the specialty with the highest e-consult proportion was pediatric endocrinology, which had 48% (12/25) of total consult orders requested as e-consults. However, with only 25 total consult orders, pediatric endocrinology had the fewest number of total consult orders of all participating specialties.
The most requested e-consult specialties were infectious diseases (which received 574/1543, 37.2% of the e-consult requests), cardiology (261/1543, 16.9% of the e-consult requests), endocrinology (229/1543, 14.8% of the e-consult requests), and dermatology (226/1543, 14.6% of the e-consult requests; Table 1 ). A total of 53.5% (826/1543) of e-consult requests across all participating specialties were addressed without the need for an in-person evaluation of the patient by the consulting team. The specialty with the fewest e-consult requests resolved electronically was pulmonary and critical care, which completed 0% (0/13) of requests electronically, while the specialty with the most e-consult requests resolved electronically was pediatric endocrinology, which completed 100% (12/12) of e-consult requests, without needing to physically examine the patient. However, both specialties had the smallest volumes of e-consult requests of all participating specialties.
We found that the overall median response time of e-consult requests resolved electronically was significantly lower than requests converted to an in-person consultation ( Figure 3 ). The median time between ordering an e-consult and a specialist documenting recommendations in a consult note was 3.7 (IQR 1.3-8.2) hours across all specialties when resolved electronically, contrasted with 7.3 (IQR 3.6-22.0) hours when converted to an in-person consult ( P <.001). Over half (6/11, 55%) of the participating specialties had significantly faster median e-consult response times for requests resolved electronically compared to requests converted to an in-person consultation. The specialties with the fastest e-consult response times were dermatology and radiation oncology, which had median response times of 1.3 (IQR 0.4-3.0) hours and 0.9 (IQR 0.3-1.5) hours when resolved electronically, respectively. However, radiation oncology had one of the smallest volumes of e-consult requests among participating specialties.
The overall response times of e-consult requests were much faster than the turnaround goal mandated by our institutional guidelines, which require a same-day response by 8 PM if the consult is ordered before noon or a response by the following morning if ordered after noon. For reference, the overall median response time for completion of a traditional in-person consult by the same 11 specialties during the same 2.5-year period is 25.8 (IQR 10.8-65.7) hours ( Multimedia Appendix 1 ). Thus, regardless of whether an e-consult request was resolved electronically or converted to an in-person consult, e-consults significantly improved the turnaround times for inpatient consultations.
The average volume of requests was 19 inpatient e-consults per month during the first 5 months that inpatient e-consults were live ( Figure 4 ). Then, California experienced surges of COVID-19 cases throughout the pandemic and we saw corresponding increases in inpatient e-consults use. During the winter 2020 surge, the average volume of requests increased to 52 inpatient e-consults per month. Then, the Delta variant wave arrived in summer 2021, and the average volume of requests increased to 61 inpatient e-consults per month. When the Omicron variant wave emerged in winter 2021, the average volume of requests peaked at 75 inpatient e-consults per month. During a sustained wave in spring-summer 2022 driven by Omicron subvariants, the average volume of requests was 62 inpatient e-consults per month. After these surges subsided and COVID-19 cases declined, the use of inpatient e-consults remained at a high-level baseline with an average of 53 inpatient e-consults per month. Interestingly, similar patterns of increased e-consults use were observed in the ambulatory setting.

Principal Findings
In response to the COVID-19 crisis, we successfully implemented an inpatient e-consult service that offered providers the option of requesting a subspecialty consultation for patients who are hospitalized and do not require an in-person evaluation by the specialist. Strong engagement by the clinical champions and technology partners in our steering committee, along with support from UCI’s leadership which provided us with dedicated IT, compliance, and billing teams, contributed to the successful design and implementation of our inpatient e-consults service. In addition, we were able to rapidly launch the service by leveraging our experiences with implementing e-consults in the ambulatory setting and capitalizing on existing infrastructure for inpatient consults. Instead of creating unique e-consult orders, configuring our existing inpatient consult order reduced the build components for our IT team, allowing us to quickly and effectively launch the inpatient e-consults service. Because we used workflows similar to those for traditional in-person consults, the processes for requesting and responding to inpatient e-consults were not new for providers. This strategy, along with provider familiarity with our well-established e-consults service in the ambulatory setting, likely helped to foster the adoption of inpatient e-consults. Although the COVID-19 crisis provided the key stimulus, these factors may have also contributed to the more rapid adoption of inpatient e-consults in comparison to the initial uptake of our ambulatory e-consults.
We found that the e-consult services helped to significantly reduce the response time for consults requested on patients who are hospitalized and do not require an in-person evaluation. In fact, the overall median response time of e-consult requests resolved electronically was approximately half of the response time for requests converted to an in-person consultation and nearly 7 times faster than the response time for traditional in-person consults. This time saving was critical during surges of COVID-19 cases when emergency departments and inpatient units were overwhelmed, leading to prolonged wait times for patients who were hospitalized to receive consultative care. e-Consults helped to streamline the inpatient consultation process and enabled the consulting team to promptly and efficiently provide recommendations on patients not needing a physical examination.
Although some diagnoses require in-person evaluation of the patient, lower complexity problems can be managed effectively using e-consults. Indeed, we found that over half of e-consult requests were addressed electronically without the need for an in-person evaluation of the patient by the consulting team. By reducing unnecessary in-person consultations, e-consults likely helped to limit the use of scarce PPE; minimize disease transmission; and free up specialists for other activities, such as examining patients with more complicated conditions and performing procedures. This improved resource use may also translate to potential cost savings associated with avoided in-person consultations and increased productivity. Future work should aim to analyze the cost-effectiveness of inpatient e-consults.
After the peaks of the COVID-19 crisis subsided in California, we discovered that provider use of inpatient e-consults persisted at a rate well above the precrisis levels. This sustained use implies positive provider experiences with the service and suggests a preference for e-consults when addressing lower complexity problems. Developing workflows for the inpatient e-consults service that were familiar to providers and significantly improving the turnaround times for inpatient consultations also likely helped to facilitate this sustainability. Thus, while case numbers and death rates associated with the COVID-19 pandemic have declined, e-consults continued to be an important part of our health care delivery.
Although relatively new, there have been a few reports of e-consults in the inpatient setting. The earliest examples involved the unexpected use of the ambulatory e-consult platform in the inpatient setting [ 13 ] and the design of an inpatient e-consult protocol that provided subspecialty consultations to inpatients at a remote hospital that lacked access to these clinical services [ 12 ]. Other reports described the feasibility and use of inpatient e-consults for only 1 specific specialty consulting service [ 10 , 11 ]. While 1 health system reported their implementation of an inpatient e-consult program in several specialties, provider adoption was temporary in response to the COVID-19 crisis [ 9 ]. Our experience with inpatient e-consults uniquely contrasts with these other health systems because we not only successfully implemented inpatient e-consults in multiple specialties but also demonstrated its sustained use beyond the pandemic.
Limitations
Although anecdotal provider feedback has been positive, limitations to this study include the absence of a formal assessment of user experiences with the inpatient e-consults service. In addition, the volumes of e-consult requests and total consult orders were low for some specialties; thus, caution must be applied in the interpretation of results from these low-volume specialties. Nevertheless, we believe our unique development of inpatient e-consults is easily translatable to other institutions interested in implementing it and will lead to a positive user experience and greater use since we fit the e-consult process into already existing and common workflows of requesting a consultation. Additionally, although the implementation of our inpatient e-consults service was in a single academic health system, we successfully demonstrated that the use of e-consults in the inpatient setting is a promising approach to expediting patient care and reporting our experience in designing and implementing inpatient e-consults may provide guidance to other health systems considering similar telehealth models.
Conclusions
Our implementation of e-consults in the inpatient setting highlighted an innovative use for e-consults in the era of COVID-19. It allowed for timely, efficient delivery of inpatient consultation services while reducing the unnecessary exposure of health care workers to potential infection. Consequently, inpatient e-consults likely helped to conserve precious PPE, minimize disease transmission, and enhance our ability to deal with surges in COVID-19 cases by expediting rapid assessment and management of lower complexity referrals. Although the COVID-19 emergency served as motivation to expand our ambulatory e-consults program to the inpatient setting, the service has become a vital component of our regular practices and will remain an essential part of our health care delivery, both in the ambulatory and inpatient settings, beyond the current pandemic, achieving sustainability and value.
Acknowledgments
The authors thank our steering committee members (Dr Byron Allen and Dr Nathan Rojek) and IT build team (Donna Jackson, Brian Lambertson, Elizabeth Burrows, Jaymee Zillgitt, and Tanya Sickles) for their contributions to the design and implementation of our inpatient e-consults. We also thank additional team members Kathy LaPierre, Jennifer Rios, and Debra Webb Torres for their guidance with compliance and billing issues.
Conflicts of Interest
ANA has been a principal investigator or coinvestigator of clinical trials sponsored by the National Institutes of Health/National Institute of Allergy and Infectious Diseases, NeuroRx Pharma, Pulmotect, Blade Therapeutics, Novartis, Takeda, Humanigen, Eli Lilly, PTC Therapeutics, OctaPharma, Fulcrum Therapeutics, and Alexion, as well as a speaker and consultant for BMS, Pfizer, BI, Portola, Sunovion, Mylan, Salix, Alexion, AstraZeneca, Novartis, Nabriva, Paratek, Bayer, Tetraphase, Achogen LaJolla, Ferring, Seres, Spero, Eli Lilly, Gilead, Millenium, HeartRite, Aseptiscope, and Sprightly; these relationships were unrelated to the current work. ASA, AAD, and AAA have no conflicts of interest to report.
Median (IQR) response times by specialty for traditional in-person consults, compared with median (IQR) response times for e-consults converted to in-person and e-consults resolved electronically.
- Chen AH, Kushel MB, Grumbach K, Yee HF. Practice profile. A safety-net system gains efficiencies through 'eReferrals' to specialists. Health Aff (Millwood). 2010;29(5):969-971. [ CrossRef ] [ Medline ]
- Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemed J E Health. 2013;19(10):733-738. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Malagrino GD, Chaudhry R, Gardner M, Kahn M, Speer L, Spurrier BR, et al. A study of 6,000 electronic specialty consultations for person-centered care at The Mayo Clinic. Int J Pers Cent Med. 2012;2(3):458-466. [ CrossRef ]
- Arora A, Fekieta R, Nouri Z, Carder D, Colgan MM, Fuhlbrigge A, et al. Trends in utilization of electronic consultations associated with patient payer and language among US academic medical centers during the COVID-19 pandemic. JAMA Netw Open. 2022;5(7):e2224628. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Liddy C, Moroz I, Mihan A, Nawar N, Keely E. A systematic review of asynchronous, provider-to-provider, electronic consultation services to improve access to specialty care available worldwide. Telemed J E Health. 2019;25(3):184-198. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vimalananda VG, Gupte G, Seraj SM, Orlander J, Berlowitz D, Fincke BG, et al. Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare. 2015;21(6):323-330. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kuo S, Aledia A, O'Connell R, Rudkin S, Dangodara AA, Amin AN. Implementation and impact on length of stay of a post-discharge remote patient monitoring program for acutely hospitalized COVID-19 pneumonia patients. JAMIA Open. 2022;5(3):ooac060. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Amin AN, Aledia A. An eConsults program to improve patient access to specialty care in an academic health system. J Clin Outcomes Manag. 2020;27(3):115-122. [ CrossRef ]
- Rikin S, Epstein EJ, Gendlina I. Rapid implementation of inpatient eConsult programme addresses new challenges for patient care during COVID-19 pandemic. BMJ Innov. 2021;7(2):271-277. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mustafa SS, Staicu ML, Yang L, Baumeister T, Vadamalai K, Ramsey A. Inpatient electronic consultations (E-consults) in allergy/immunology. J Allergy Clin Immunol Pract. 2020;8(9):2968-2973. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yagnik KJ, Saad HA, King HL, Bedimo RJ, Lehmann CU, Medford RJ. Characteristics and outcomes of infectious diseases electronic COVID-19 consultations at a multisite academic health system. Cureus. 2021;13(11):e19203. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Najafi N, Harrison JD, Duong J, Greenberg A, Cheng HQ. It all just clicks: development of an inpatient e-consult program. J Hosp Med. 2017;12(5):332-334. [ CrossRef ] [ Medline ]
- Gupte G, Vimalananda V, Simon SR, DeVito K, Clark J, Orlander JD. Disruptive innovation: implementation of electronic consultations in a veterans affairs health care system. JMIR Med Inform. 2016;4(1):e6. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by T de Azevedo Cardoso, S He; submitted 19.12.23; peer-reviewed by J Chen, I Moroz; comments to author 14.02.24; revised version received 06.03.24; accepted 27.03.24; published 16.05.24.
©Anna S Aledia, Amish A Dangodara, Aanya A Amin, Alpesh N Amin. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 16.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.
Artificial intelligence is being used in healthcare for everything from answering patient questions to assisting with surgeries and developing new pharmaceuticals.
According to Statista , the artificial intelligence (AI) healthcare market, which is valued at $11 billion in 2021, is projected to be worth $187 billion in 2030. That massive increase means we will likely continue to see considerable changes in how medical providers, hospitals, pharmaceutical and biotechnology companies, and others in the healthcare industry operate.
Better machine learning (ML) algorithms, more access to data, cheaper hardware, and the availability of 5G have contributed to the increasing application of AI in the healthcare industry, accelerating the pace of change. AI and ML technologies can sift through enormous volumes of health data—from health records and clinical studies to genetic information—and analyze it much faster than humans.
Healthcare organizations are using AI to improve the efficiency of all kinds of processes, from back-office tasks to patient care. The following are some examples of how AI might be used to benefit staff and patients:
- Administrative workflow: Healthcare workers spend a lot of time doing paperwork and other administrative tasks. AI and automation can help perform many of those mundane tasks, freeing up employee time for other activities and giving them more face-to-face time with patients. For example, generative AI can help clinicians with note-taking and content summarization that can help keep medical records as thoroughly as possible. AI might also help with accurate coding and sharing of information between departments and billing.
- Virtual nursing assistants: One study found that 64% of patients are comfortable with the use of AI for around-the-clock access to answers that support nurses provide. AI virtual nurse assistants—which are AI-powered chatbots, apps, or other interfaces—can be used to help answer questions about medications, forward reports to doctors or surgeons and help patients schedule a visit with a physician. These sorts of routine tasks can help take work off the hands of clinical staff, who can then spend more time directly on patient care, where human judgment and interaction matter most.
- Dosage error reduction: AI can be used to help identify errors in how a patient self-administers medication. One example comes from a study in Nature Medicine , which found that up to 70% of patients don’t take insulin as prescribed. An AI-powered tool that sits in the patient’s background (much like a wifi router) might be used to flag errors in how the patient administers an insulin pen or inhaler.
- Less invasive surgeries: AI-enabled robots might be used to work around sensitive organs and tissues to help reduce blood loss, infection risk and post-surgery pain.
- Fraud prevention: Fraud in the healthcare industry is enormous, at $380 billion/year, and raises the cost of consumers’ medical premiums and out-of-pocket expenses. Implementing AI can help recognize unusual or suspicious patterns in insurance claims, such as billing for costly services or procedures that are not performed, unbundling (which is billing for the individual steps of a procedure as though they were separate procedures), and performing unnecessary tests to take advantage of insurance payments.
A recent study found that 83% of patients report poor communication as the worst part of their experience, demonstrating a strong need for clearer communication between patients and providers. AI technologies like natural language processing (NLP), predictive analytics, and speech recognition might help healthcare providers have more effective communication with patients. AI might, for instance, deliver more specific information about a patient’s treatment options, allowing the healthcare provider to have more meaningful conversations with the patient for shared decision-making.
According to Harvard’s School of Public Health , although it’s early days for this use, using AI to make diagnoses may reduce treatment costs by up to 50% and improve health outcomes by 40%.
One use case example is out of the University of Hawaii , where a research team found that deploying deep learning AI technology can improve breast cancer risk prediction. More research is needed, but the lead researcher pointed out that an AI algorithm can be trained on a much larger set of images than a radiologist—as many as a million or more radiology images. Also, that algorithm can be replicated at no cost except for hardware.
An MIT group developed an ML algorithm to determine when a human expert is needed. In some instances, such as identifying cardiomegaly in chest X-rays, they found that a hybrid human-AI model produced the best results.
Another published study found that AI recognized skin cancer better than experienced doctors. US, German and French researchers used deep learning on more than 100,000 images to identify skin cancer. Comparing the results of AI to those of 58 international dermatologists, they found AI did better.
As health and fitness monitors become more popular and more people use apps that track and analyze details about their health. They can share these real-time data sets with their doctors to monitor health issues and provide alerts in case of problems.
AI solutions—such as big data applications, machine learning algorithms and deep learning algorithms—might also be used to help humans analyze large data sets to help clinical and other decision-making. AI might also be used to help detect and track infectious diseases, such as COVID-19, tuberculosis, and malaria.
One benefit the use of AI brings to health systems is making gathering and sharing information easier. AI can help providers keep track of patient data more efficiently.
One example is diabetes. According to the Centers for Disease Control and Prevention , 10% of the US population has diabetes. Patients can now use wearable and other monitoring devices that provide feedback about their glucose levels to themselves and their medical team. AI can help providers gather that information, store, and analyze it, and provide data-driven insights from vast numbers of people. Using this information can help healthcare professionals determine how to better treat and manage diseases.
Organizations are also starting to use AI to help improve drug safety. The company SELTA SQUARE, for example, is innovating the pharmacovigilance (PV) process , a legally mandated discipline for detecting and reporting adverse effects from drugs, then assessing, understanding, and preventing those effects. PV demands significant effort and diligence from pharma producers because it’s performed from the clinical trials phase all the way through the drug’s lifetime availability. Selta Square uses a combination of AI and automation to make the PV process faster and more accurate, which helps make medicines safer for people worldwide.
Sometimes, AI might reduce the need to test potential drug compounds physically, which is an enormous cost-savings. High-fidelity molecular simulations can run on computers without incurring the high costs of traditional discovery methods.
AI also has the potential to help humans predict toxicity, bioactivity, and other characteristics of molecules or create previously unknown drug molecules from scratch.
As AI becomes more important in healthcare delivery and more AI medical applications are developed, ethical, and regulatory governance must be established. Issues that raise concern include the possibility of bias, lack of transparency, privacy concerns regarding data used for training AI models, and safety and liability issues.
“AI governance is necessary, especially for clinical applications of the technology,” said Laura Craft, VP Analyst at Gartner . “However, because new AI techniques are largely new territory for most [health delivery organizations], there is a lack of common rules, processes, and guidelines for eager entrepreneurs to follow as they design their pilots.”
The World Health Organization (WHO) spent 18 months deliberating with leading experts in ethics, digital technology, law, and human rights and various Ministries of Health members to produce a report that is called Ethics & Governance of Artificial Intelligence for Health . This report identifies ethical challenges to using AI in healthcare, identifies risks, and outlines six consensus principles to ensure AI works for the public’s benefit:
- Protecting autonomy
- Promoting human safety and well-being
- Ensuring transparency
- Fostering accountability
- Ensuring equity
- Promoting tools that are responsive and sustainable
The WHO report also provides recommendations that ensure governing AI for healthcare both maximizes the technology’s promise and holds healthcare workers accountable and responsive to the communities and people they work with.
AI provides opportunities to help reduce human error, assist medical professionals and staff, and provide patient services 24/7. As AI tools continue to develop, there is potential to use AI even more in reading medical images, X-rays and scans, diagnosing medical problems and creating treatment plans.
AI applications continue to help streamline various tasks, from answering phones to analyzing population health trends (and likely, applications yet to be considered). For instance, future AI tools may automate or augment more of the work of clinicians and staff members. That will free up humans to spend more time on more effective and compassionate face-to-face professional care.
When patients need help, they don’t want to (or can’t) wait on hold. Healthcare facilities’ resources are finite, so help isn’t always available instantaneously or 24/7—and even slight delays can create frustration and feelings of isolation or cause certain conditions to worsen.
IBM® watsonx Assistant™ AI healthcare chatbots can help providers do two things: keep their time focused where it needs to be and empower patients who call in to get quick answers to simple questions.
IBM watsonx Assistant is built on deep learning, machine learning and natural language processing (NLP) models to understand questions, search for the best answers and complete transactions by using conversational AI.
Get email updates about AI advancements, strategies, how-tos, expert perspective and more.
See IBM watsonx Assistant in action and request a demo
Get our newsletters and topic updates that deliver the latest thought leadership and insights on emerging trends.
World Bank Supports Improvement of Quality and Access to Early Childhood Education and Care Services in Kosovo
WASHINGTON, May 14, 2024 —The World Bank’s Board of Executive Directors approved today the Early Childhood Education and Care for Kosovo's Human Capital Project , which aims to improve the quality and equitable access to early childhood education and care services in Kosovo.
Kosovo has the lowest Early Childhood Education and Care (ECEC) enrollment in the Western Balkans, with more barriers for children from low-income families. Only 19.5 percent of children aged 0-6 were enrolled in all early childhood education and care services during 2021/2022. Insufficient number and inadequate distribution of early childhood education and care centers affect access to services. This contributes to low levels of foundational literacy and numeracy skills, which can trigger a life-long struggle to catch up and access productive career opportunities. Also, the poor access to child and eldercare contributes to exceptionally low employment and workforce participation of women in Kosovo.
“ In prioritizing early childhood education and care, Kosovo is demonstrating a commitment to enhancing educational outcomes of small boys and girls and nurturing the country's human capital to effectively address the challenges of the future economy ”, said Massimiliano Paolucci, World Bank Country Manager for Kosovo, and North Macedonia . “ The World Bank will continue to support Kosovo in strengthening its Human Capital, enhancing social inclusion, and fostering economic growth .”
The project will support activities which aim to improve the quality of ECEC services through improvements to the regulatory framework, institutional capacity building, and training of teachers and healthcare professionals. It also aims to enhance child development outcomes by fostering collaboration across diverse sectors. The project will also improve access to ECEC services through the creation of additional spaces, provision of essential equipment, and facilitation of teaching and learning materials. Furthermore, a voucher program will be implemented to safeguard access for vulnerable children and families. The project is expected to reach 3,800 children, 1,500 ECEC teachers and education professionals, and 1,500 healthcare professionals who would benefit from training, renovations, repurposing, adaptation, and construction of new facilities, a voucher program, and training opportunities. Expanded provision of childcare is also expected to increase the participation of women in the workforce.
The approved financial support for this project is EUR 18.6 million (US$20 million equivalent), a concessional credit from World Bank’s International Development Association (IDA). The credit repayment period for this operation is 25 years, which includes a 5-year grace period. The project will also be financed with an additional US$2 million grant from the Early Learning Partnership Trust Fund. It pioneers the introduction of performance-based financing to optimize the impact of social programs in the country. The Government of Kosovo and the World Bank will sign a project financing agreement, which needs to be ratified by the Parliament of Kosovo for the project funds to become available for disbursement for the benefit of the citizens of Kosovo. The Ministry of Education, Science, Technology, and Innovations of Kosovo will be responsible for project implementation.
This site uses cookies to optimize functionality and give you the best possible experience. If you continue to navigate this website beyond this page, cookies will be placed on your browser. To learn more about cookies, click here .

COMMENTS
Service Improvement Project. Adam Breen. Paper completed for my Nursing degree dissertation. It discusses the implementation of a patients DNACPR status and its identification on a patients wristband. The text follows a hypothetical project to implement the service improvement within an NHS trust; including research, stakeholder engagement and ...
Embedding a nursing service improvement culture has been a focus of successive UK policy initiatives (Craig, 2018), such as the NHS Safety Thermometers scheme (NHS Improvement, 2017), the 2012 nurse-led quality framework Energise for Excellence, High Impact Actions for Nursing and Midwifery (NHS website, 2010) and the NHS Productive Series (NHS website, 2020).
Abstract. Service improvements in health care can improve provision, make cost savings, streamline services and reduce clinical errors. However, on its own it may not be adequate for improving patient outcomes and quality of care. The complexity of healthcare provision makes service improvement a challenge, and there is little evidence on ...
This extract from NHS 2010-2015: from good to great: preventative, people-centred, productive indicates that the quality of care remains an enduring concern in the organisation and management of health care.Indeed in the English National Health Service there has been a major policy drive to address the twin challenges of service quality and patient safety.
Background: Service improvement to enhance care quality is a key nursing responsibility and developing sustainable skills and knowledge to become confident, capable service improvement practitioners is important for nurses in order to continually improve practice. How this happens is an under-researched area. Aim: A hermeneutic, longitudinal study in Northern England aimed to better understand ...
Dr Lynn Craig. Professor Alison Machin. Abstract: Background: Service improvement to enhance care quality is a key nursing responsibility. Developing sustainable skills and knowledge to become ...
A UK university implemented service improvement teaching for all nursing students. In addition, the degree pathway students conducted service improvement projects as the basis for their dissertations. Aim: The study aimed to evaluate the implementation of service improvement projects within a pre-registration nursing curriculum.
Service improvements in health care can improve provision, make cost savings, streamline services and reduce clinical errors. However, on its own it may not be adequate for improving patient outcomes and quality of care. The complexity of healthcare provision makes service improvement a challenge, and there is little evidence on whether improvement initiatives change healthcare practices and ...
In order to explore service improvement in nursing, hermeneutic phenomenology was used to gain an understanding of the lived experiences from student to registered nurse. A purposive sample of twenty participants were selected from an adult pre-registration nursing programme, during their third year. ...
N2 - Background: Service improvement to enhance care quality is a key nursing responsibility. Developing sustainable skills and knowledge to become confident, capable service improvement practitioners is important for nurses in order to continually improve practice. How this happens is under researched.
tice, and demonstrate how to use service delivery evaluation and audit findings to bring about continuous improvement. Platform 7: Co-ordinating care 7.12 demonstrate understanding of the processes involved in developing a basic business case for additional care funding by applying knowledge of finance, resources and safe staffing levels.
Citation: Carter H, Price L (2016) Changing practice 1: assessing the need for service improvement. Nursing Times; 112: 8, 15-17. Authors: Helen Carter is an independent healthcare advisor; Lynda Price is a clinical governance and infection control facilitator, Helen & Douglas House, Oxford. This article has been double-blind peer reviewed
A UK university implemented service improvement teaching for all nursing students. In addition, the degree pathway students conducted service improvement projects as the basis for their dissertations. ... Academics considered that personal tutors, who acted as dissertation supervisors, would need to adjust to supporting students with service ...
Successful leadership of health care improvement combines service specific knowledge from clinical experts, improvement know-how and change ... TAR_7_010 1.Dissertation 7 Both 60 A 12,000 word dissertation on either a research/work-based project such as service evaluation or audit. 2. A 12,000 word
Potential challenges to the successful delivery of a service improvement project are also considered. The article concludes with an example of the use of the six-stage framework to improve the quality of urinary catheter care in one acute NHS trust. Nursing Standard. 27, 23, 51-57. doi: 10.7748/ns2013.02.27.23.51.e7241R1. Peer review
T1 - Service improvement in health care. T2 - a literature review. AU - Craig, Lynn. PY - 2018/8/9. Y1 - 2018/8/9. N2 - Service improvements in health care can improve provision, make cost savings, streamline services and reduce clinical errors. However, on its own it may not be adequate for improving patient outcomes and quality of care.
Report application Quality Improvement (QI) methods/ approaches to identifying and understanding an improvement issue(s) and gaining agreement to pursue it/ them. Report explicit engagement of patients/carers in all stages of the project. Report developing a preliminary plan for their project that demonstrates it fell within a service ...
"It was an amazing day of sharing ideas and discussion," said Coral Drane, Lecturer in Adult Nursing at UEA. "We are so proud of our final year student nurses, both in terms of the quality of their service improvement posters and their professionalism." The event was attended by NNUH staff, who were also impressed by what they saw.
This chapter aims to introduce a service improvement and the application to the role of the nurse when implementing a change in practice. Service improvement is defined by the British Journal of Nursing (Craig, L., 2018) as a systematic approach that aims to improve service provision, reduce errors within the clinical area and save money.
School of Nursing University of Pittsburgh 3500 Victoria Street Victoria Building Pittsburgh, PA 15261. 412-624-4586 1-888-747-0794 [email protected] Contact Us
The Turning Point Collaborative focused on performance management, the National Public Health Performance Standards Program created a framework to assess and improve public health systems, while the US Department of Health and Human Services has provided recommendations on how to achieve quality in healthcare.
E. V. Voevoda Theory and practice of professional language training of international specialists in Russia PhD dissertation (Moscow, 2011) [Google Scholar] A. S. Nekrasov The development of professional identity of the cadet military school.
To determine the generalised process quality, it is recommended to apply one of the means (arithmetic, geometry, harmonised), which allow linking together the separate estimates. According to Figure. 1. , the values on the additional scale change - 3 ≤ x ≤ 3 and estimates on the dimensionless scale correspond to.
An open access repository of theses and dissertations from University of Idaho graduate students. The collection includes the complete electronic theses and dissertations submitted since approximately 2014, as well as, select digitized copies of earlier documents dating back to 1910.
Coordinated reaction of hands was analyzed during examination of healthy subjects and patients with focal lesions of the central nervous system in order to find the morphological structures responsible for such cooperation. Results of investigation of coordinated hand reaction in healthy subjects to sound and light stimuli with a warning signal are presented. The degree of cooperation was ...
The Joyce M. Stielau Award is available to current PhD candidates at the Frances Payne Bolton School of Nursing. This funding is intended for early-career investigators currently conducting early-stage research. Applicants can request up to $2,000 for funding of their current IRB-approved research. All fields and areas of study will be considered.
Background: Limiting in-person contact was a key strategy for controlling the spread of the highly infectious novel coronavirus (COVID-19). To protect patients and staff from the risk of infection while providing continued access to necessary health care services, we implemented a new electronic consultation (e-consult) service that allowed referring providers to receive subspecialty ...
AI can help providers gather that information, store, and analyze it, and provide data-driven insights from vast numbers of people. Using this information can help healthcare professionals determine how to better treat and manage diseases. Organizations are also starting to use AI to help improve drug safety.
WASHINGTON, May 14, 2024—The World Bank's Board of Executive Directors approved today the Early Childhood Education and Care for Kosovo's Human Capital Project, which aims to improve the quality and equitable access to early childhood education and care services in Kosovo.. Kosovo has the lowest Early Childhood Education and Care (ECEC) enrollment in the Western Balkans, with more barriers ...