Autism Spectrum Disorder (ASD) Essay
- To find inspiration for your paper and overcome writer’s block
- As a source of information (ensure proper referencing)
- As a template for you assignment

Introduction
Biological and genetic aspects of autism spectrum disorders, asd etiology, prevalence of asd, diagnosis of asd, treatment of asd.
Autism is a serious disorder that has the potential to disrupt the success of people living with it. This report shall set out to explore various aspects regarding this disorder. To this end, an overview of the symptoms, causes, diagnosis and treatment shall be offered. This shall aim at expanding our understanding regarding this disorder so as to enable us to be better prepared to handle it whenever the need arises.
Autism has been noted to be among the most prevalent childhood psychiatric disorder. Kuder (2003) denotes that in the USA, an estimated 2.1% of the population aged between 8 and 17 is affected by autism in its various forms.
Autism is manifested by varied behavior but it is chiefly characterized by inability to communicate, lingual deficits, lack of a sustained attention, low level of activity, temper tantrums, sleep disturbance, aggression inadequate motor control and other non-compliant behavior. These behaviors are detrimental to the social and educational endeavors of the people involved.
Autism spectrum is a medical term that is used to describe children and adults who experience difficulties in motor coordination, socializing, communicating (verbal and non-verbal) and language acquisition (Tager-Flusberg, Paul and Lord, 2005). The authors describe autism as a neurological disorder that stems from the brain’s inability to carryout some functions normally.
The causes of Autism as well as the reasons why it affects lingual and communication skills are not entirely known though there is a close linkage between Autism and genetics.
Studies indicate that Autism Spectrum Disorder (ASD) is inherited between family members. A study conducted by the American Psychiatric Association (2000) indicated that there is a 3-6% chance of getting autism amongst siblings.
However, Korvatska et al (2002) state that the difficulty experienced by scientists in pinpointing the genetic aspects of autism emanates from the lack of extended family histories. In most cases, autistic individual become more detached socially that they rarely marry or have children. As such, finding a family that has detailed genetic information regarding autism is difficult.
On a brighter note, twins have been used to explore the genetics behind autism (Beaudet, 2007). One study indicated an 82% likelihood of an autistic identical twin having the same disorder. This is in contrast to the 10% likelihood indicated by results from fraternal twins. More sophisticated studies have in the recent past concluded that 90% of autism related behavioral phenotypes are as a result of inherited genes (Happé & Ronald, 2008). This shows that there is a strong relationship between autism and genes.
Biologically, the root cause of autism has been difficult due to relative inability to access and study the brain systematically. However, technological innovations and advancements such as MRIs, CT scans and SPECT have made it possible to study the structure and functionality of the brain.
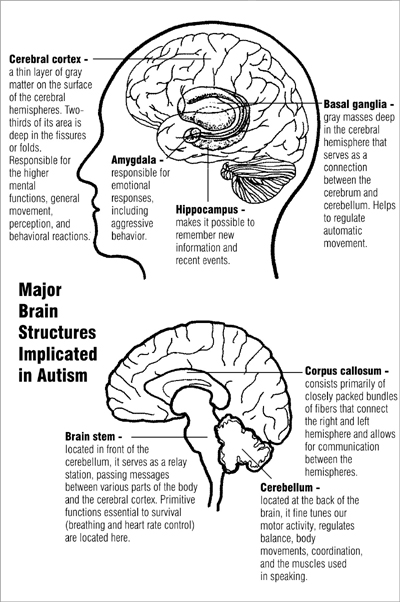
As a result, specialists have been able to deduce that majority of the brain’s structures play a pivotal role in the development of ASD. According to NIMH (2009, p. 1) they include but are not limited to “the cerebellum, cerebral cortex, limbic system, corpus callosum, basal ganglia, and brain stem”.
Similarly, other studies indicate that various neurotransmitters such as serotonin and epinephrine have a strong link to autism. The diagram below shows the biological basis of Autism Spectrum Disorder. It shows various structures of the brain and explains the functions that each play. Various symptoms of ASD are as a result of the structures’ inability to carry out their normal function.
A diagram showing brain structures linked to ASD
As mentioned earlier, the causes of ASD are not well known. However, researches conducted in this regard indicate that genetic, nutritional and environmental factors play a pivotal role in the development of the disorders. Results from numerous studies indicate that genetic factors predominate.
Others indicate that certain foods, infectious diseases, plastic and metallic extracts could cause autism. Similarly, smoking, alcohol, illicit drugs and some (mercury-based) childhood vaccines have also been attributed to causing autism. However, none of these causes are conclusive and more research needs to be conducted. This is to mean that the theory of causation regarding autism is not complete as yet.
The most recent survey conducted by center of disease control (CDC) indicated that autism rates have increased significantly over the past three decades. In most cases, studies indicate that autism is most prevalent among children. According to Rutter (2005), boys are four times more likely to be autistic than their female counterparts.
In addition, the author states that the symptoms of autism exhibit themselves from childbirth until three years of age. Parents are the most likely to discover these symptoms. As a result, they should ensure that they have their children checked at the onset of various abnormal behaviors.
Rutter (2005) asserts that the prevalence of autism disorder has been facilitated by ignorance and assumptions made by caretakers. In some cases, parents assume that their children are ‘slow and that they will develop as they grow up. However, this approach has proven to be costly since autism can best be handled as soon as it is detected.
Delaying makes it difficult to come up with remedies and coping mechanisms for both parents and the individuals having autism disorders. The main symptoms of this disorder include communication (verbal and non-verbal) difficulties, inability to develop and maintain relations with other people, abnormal lingual patterns and repetitive behaviors. Whenever any of these symptoms are discovered, it is highly recommended that medical or psychiatric assistance be sought.
An early diagnosis of ASD is important since it enables the people involved to come up with effective interventions before its too late. Recent studies show that intensive interventions administered in a control environment for a minimum of two years during preschool leads to behavioral and social improvements among children with ASD.
Clinicians base their diagnosis depending on the behavioral traits exhibited by a child. For a diagnosis to be made, NIMH (2009) asserts that at least one of the symptoms associated with ASD must be present. This means that a patient must have abnormal patterns of communication, socialization and restrictive behaviors.
In most cases, the diagnosis is made through a two-stage process. The first stage is “a developmental screening normally conducted during the routine childhood check-ups, while the second one involves a more comprehensive behavioral analysis by a team of experts (NIMH, 2009, p. 1).” Below are the stages that are followed to diagnose ASD.
The American Psychiatric Association (2000) recommends that every parent should ensure that a developmental screening test is carried out for his/her child during the “well child” check-up. The author contends that screening plays a pivotal role in the early identification of ASD symptoms.
Due to its importance, there are various screening instruments that have been developed to facilitate the diagnosis process. They include but are not limited to Checklist of Autism in Toddlers (CHAT) and its modified version; M-CHAT. Similarly, the Screening Tool for Autism in Two-Year-Olds (STAT) as well as the Social Communication Questionnaire (SCQ) have proven to be effective in diagnosing ASD in children aged between two years old and above four years old respectively.
According to Tadevosyan-Leyfer et al (2003), questionnaires given to parents provide important information during the diagnosis process. As such, some instruments rely on such responses while others depend on these responses as well as observations made by the caregiver. However, these screening instruments are not as effective as they should be when it comes to identifying mild ASD or Asperger syndrome. As a result, other screening instruments such as the Autism Spectrum Screening Questionnaire (ASSQ) and the Childhood Asperger Syndrome Test (CAST) among others have been developed so as to diagnose these forms of ASD (NIMH, 2009).
Comprehensive Diagnostic Evaluation
This is the second stage of diagnosis and it relies on the skills of a team of different experts such as psychologists, psychiatrists, neurologists, and therapists among others. This evaluation entails a comprehensive analysis of neural, genetic, cognitive and language testing in order to conclude whether a patient is suffering from autism or other behavioral disorders.
Some of the instruments used at this stage include: Autism Diagnosis Interview-Revised (ADI-R), which is a structured interview designed to test a child’s “communication, social interaction, restrictive behaviors and age-of-onset symptoms, and the Autism Diagnosis Observation Scheduling (ADOS-G), which is designed to identify abnormal, missing or delayed communication and social behaviors (NIMH, 2009, p. 1).”
The teams of experts that conduct this diagnosis determine the strengths and weaknesses of the child and recommend various treatment options that should be undertaken.
According to Freitag (2007) there is no one-shoe-fits-all approach to treating ASD. However, specialists in this area seem to agree on the fact that early interventions are of great importance. Arguably, the best treatment is one that considers the interests of the patient, allows the patient to learn in accordance to his/her ability and causes no harm to the overall well being of the patient. With this in mind, there are specialized programs and treatments that have proven to be effective against ASD symptoms.
For starters, Applied Behavioral Analysis (ABA) is among the most used intervention in treating ASD (SAMHSA, 2011). Similarly, there are dietary and medical interventions that help suppress unwanted behaviors among autistic children (NIMH, 2009). In regard to learning, there are specialized educational programs that seek to enhance the socio-communicative, cognitive and language skills of autistic students.
It can be articulated from this report that Autism is a problem that needs to be focused on. With proper understanding as to what the condition entails, parents and practitioners are better armed to assist patients overcome the weaknesses brought about by the condition and therefore achieve successful lives.
From this study, it can be authoritatively stated that early diagnosis and treatment of Autism spectrum is necessary to increase the chances of success in learning for the child suffering from this disease. Whereas Autism is not curable, it can be managed so as to ensure that it is not disruptive to the life of the individual during his/her future endeavors.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders: DSM-IV-TR (fourth edition, text revision). Washington DC: American Psychiatric Association.
Beaudet, A. L. (2007). Autism: highly heritable but not inherited. Nat Med, 13(5): 534–6.
Freitag, C. M. (2007). The genetics of autistic disorders and its clinical relevance: a review of the literature. Mol Psychiatry. 12(1): 2–22.
Happé, F., & Ronald, A. (2008). The ‘fractionable autism triad’: a review of evidence from behavioral, genetic, cognitive and neural research. Neuropsychol Rev, 18(4): 287–304.
Korvatska, E et al. (2002). Genetic and immunologic considerations in autism. Neurobiology of Disease , 9: 107-125.
Kuder, S. (2003). Teaching Students with Language and Communication Disabilities. USA: Allyn and Bacon.
NIMH. (2009) Autism Spectrum Disorders (Pervasive Developmental Disorders) . Web.
Rutter, M. (2005). Incidence of autism spectrum disorders: changes over time and their meaning. Acta Paediatr. 94(1): 2–15.
SAMHSA. (2011). Autism Spectrum Disorders . Web.
Tadevosyan-Leyfer, O et al. (2003). A principal components analysis of the autism diagnostic interview-revised. Journal of the American Academy of Child and Adolescent Psychiatry, 42(7): 864-872.
Tager-Flusberg, H., & Lord, C. (2005). Language and Communication in Autism. Web.
- Autism Spectrum Disorder in Children and Its Impact on the Family
- Autism Spectrum Disorders: Diagnostic Procedure
- Autism Spectrum Disorder: Diagnosis, Impact, Treatment
- Mental Illnesses History and Treatment
- Psychopathologies: Co-occurring Diagnoses
- The Identification of Bipolar Disorders
- How Do People Labelled With a Mental Illness Deal With Their Stigmatization?
- Attention Deficit Hyperactivity Disorder Causes
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2019, March 24). Autism Spectrum Disorder (ASD). https://ivypanda.com/essays/autism-spectrum-disorder-asd/
"Autism Spectrum Disorder (ASD)." IvyPanda , 24 Mar. 2019, ivypanda.com/essays/autism-spectrum-disorder-asd/.
IvyPanda . (2019) 'Autism Spectrum Disorder (ASD)'. 24 March.
IvyPanda . 2019. "Autism Spectrum Disorder (ASD)." March 24, 2019. https://ivypanda.com/essays/autism-spectrum-disorder-asd/.
1. IvyPanda . "Autism Spectrum Disorder (ASD)." March 24, 2019. https://ivypanda.com/essays/autism-spectrum-disorder-asd/.
Bibliography
IvyPanda . "Autism Spectrum Disorder (ASD)." March 24, 2019. https://ivypanda.com/essays/autism-spectrum-disorder-asd/.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Transl Pediatr
- v.9(Suppl 1); 2020 Feb
Autism spectrum disorder: definition, epidemiology, causes, and clinical evaluation
Holly hodges.
1 Department of Pediatrics, Baylor College of Medicine and Meyer Center for Developmental Pediatrics, Texas Children’s Hospital, Houston, TX, USA;
Casey Fealko
2 Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo, MI, USA;
Neelkamal Soares
3 Department of Pediatric and Adolescent Medicine, Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo, MI, USA
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication and the presence of restricted interests and repetitive behaviors. There have been recent concerns about increased prevalence, and this article seeks to elaborate on factors that may influence prevalence rates, including recent changes to the diagnostic criteria. The authors review evidence that ASD is a neurobiological disorder influenced by both genetic and environmental factors affecting the developing brain, and enumerate factors that correlate with ASD risk. Finally, the article describes how clinical evaluation begins with developmental screening, followed by referral for a definitive diagnosis, and provides guidance on screening for comorbid conditions.
Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication and the presence of restricted interests and repetitive behaviors ( 1 ). In 2013, the Diagnostic and Statistical Manual of Mental Disorders —5 th edition (DSM-5) was published, updating the diagnostic criteria for ASD from the previous 4 th edition (DSM-IV) ( Table 1 ) ( 1 , 2 ).
ASD, autism spectrum disorder; SPCD, social (pragmatic) communication disorder.
In DSM-5, the concept of a “spectrum” ASD diagnosis was created, combining the DSM-IV’s separate pervasive developmental disorder (PDD) diagnoses: autistic disorder, Asperger’s disorder, childhood disintegrative disorder, and pervasive developmental disorder not otherwise specified (PDD-NOS), into one. Rett syndrome is no longer included under ASD in DSM-5 as it is considered a discrete neurological disorder. A separate social (pragmatic) communication disorder (SPCD) was established for those with disabilities in social communication, but lacking repetitive, restricted behaviors. Additionally, severity level descriptors were added to help categorize the level of support needed by an individual with ASD.
This new definition is intended to be more accurate and works toward diagnosing ASD at an earlier age ( 3 ). However, studies estimating the potential impact of moving from the DSM-IV to the DSM-5 have predicted a decrease in ASD prevalence ( 4 , 5 ) and there has been concern that children with a previous PDD-NOS diagnosis would not meet criteria for ASD diagnosis ( 5 - 7 ). There are varying reports estimating the extent of and effects of this change. One study found that with parental report of ASD symptoms alone, the DSM-5 criteria identified 91% of children with clinical DSM-IV PDD diagnoses ( 8 ). However, a systematic review suggests only 50% to 75% of individuals maintain diagnoses ( 9 ) and other studies have also suggested a decreased rate of diagnosis of individuals with ASD under the DSM-5 criteria ( 10 ). Often those who did not meet the requirements were previously classified as high functioning Asperger’s syndrome and PDD-NOS ( 11 , 12 ). Overall, most studies suggest that the DSM-5 provides increased specificity and decreased sensitivity compared to the DSM-IV ( 5 , 13 ); so while those diagnosed with ASD are more likely to have the condition, there is a higher number of children whose ASD diagnosis is missed, particularly older children, adolescents, adults, or those with a former diagnosis of Asperger’s disorder or PDD-NOS ( 14 ). Nevertheless, the number of people who would be diagnosed under the DSM-IV, but not under the new DSM-5 appears to be declining over time, likely due to increased awareness and better documentation of behaviors ( 4 ).
It has yet to be determined how the new diagnosis of SPCD will impact the prevalence of ASD. One study found the new SPCD diagnosis encompasses those individuals who possess subthreshold autistic traits and do not qualify for a diagnosis of ASD, but who still have substantial needs ( 15 ). Furthermore, children who previously met criteria for PDD-NOS under the DSM-IV might now be diagnosed with SPCD.
Epidemiology
The World Health Organization (WHO) estimates the international prevalence of ASD at 0.76%; however, this only accounts for approximately 16% of the global child population ( 16 ). The Centers for Disease Control and Prevention (CDC) estimates about 1.68% of United States (US) children aged 8 years (or 1 in 59 children) are diagnosed with ASD ( 6 , 17 ). In the US, parent-reported ASD diagnoses in 2016 averaged slightly higher at 2.5% ( 18 ). The prevalence of ASD in the US more than doubled between 2000–2002 and 2010–2012 according to Autism and Developmental Disabilities Monitoring Network (ADDM) estimates ( 6 ). Although it may be too early to comment on trends, in the US, the prevalence of ASD has appeared to stabilize with no statistically significant increase from 2014 to 2016 ( 19 ). Changing diagnostic criteria may impact prevalence and the full impact of the DSM-5 diagnostic criteria has yet to be seen ( 17 ).
Insurance mandates requiring commercial plans to cover services for ASD along with improved awareness have likely contributed to the increase in ASD prevalence estimates as well as the increased diagnosis of milder cases of ASD in the US ( 6 , 20 , 21 ). While there was only a modest increase in prevalence immediately after the mandates, there have been additional increases later as health care professionals better understood the regulatory and reimbursement process. The increase in prevalence may also be due to changes in reporting practices. One study in Denmark found the majority of increase in ASD prevalence from 1980–1991 was based on changes of diagnostic criteria and inclusion of outpatient data, rather than a true increase in ASD prevalence ( 21 ).
ASD occurs in all racial, ethnic, and socioeconomic groups, but its diagnosis is far from uniform across these groups. Caucasian children are consistently identified with ASD more often than black or Hispanic children ( 6 ). While the differences appear to be decreasing, the continued discrepancy may be due to stigma, lack of access to healthcare services, and a patient’s primary language being one other than English.
ASD is more common in males ( 22 , 23 ) but in a recent meta-analysis ( 24 ), true male-to-female ratio is closer to 3:1 than the previously reported 4:1, though this study was not done using the DSM-5 criteria. This study also suggested that girls who meet criteria for ASD are at higher risk of not receiving a clinical diagnosis. The female autism phenotype may play a role in girls being misdiagnosed, diagnosed later, or overlooked. Not only are females less likely to present with overt symptoms, they are more likely to mask their social deficits through a process called “camouflaging”, further hindering a timely diagnosis ( 25 ). Likewise, gender biases and stereotypes of ASD as a male disorder could also hamper diagnoses in girls ( 26 ).
Several genetic diagnoses have an increased rate of co-occurring ASD compared to the average population, including fragile X, tuberous sclerosis, Down syndrome, Rett syndrome, among others; however, these known genetic disorders account for a very small amount of overall ASD cases ( 27 - 30 ). Studies of children with sex chromosome aneuploidy describe a specific social functioning profile in males that suggests more vulnerability to autism ( 22 , 23 , 31 , 32 ). With the increased use of chromosomal microarray, several sites (chromosome X, 2, 3, 7, 15, 16, 17, and 22 in particular) have proven to be associated with increased ASD risk ( 28 ).
Other risk factors for ASD include increased parental age and prematurity ( 33 - 35 ). This could be due to the theory that older gametes have a higher probability of carrying mutations which could result in additional obstetrical complications, including prematurity ( 36 ).
ASD is a neurobiological disorder influenced by both genetic and environmental factors affecting the developing brain. Ongoing research continues to deepen our understanding of potential etiologic mechanisms in ASD, but currently no single unifying cause has been elucidated.
Neuropathologic studies are limited, but have revealed differences in cerebellar architecture and connectivity, limbic system abnormalities, and frontal and temporal lobe cortical alterations, along with other subtle malformations ( 28 , 37 , 38 ). A small explorative study of neocortical architecture from young children revealed focal disruption of cortical laminar architecture in the majority of subjects, suggesting problems with cortical layer formation and neuronal differentiation ( 39 ). Brain overgrowth both in terms of cortical size and additionally in terms of increased extra-axial fluid have been described in children with ASD and are areas of ongoing study both in terms of furthering our understanding of its etiology, but also as a potential biomarker ( 40 , 41 ).
Genetic factors play a role in ASD susceptibility, with siblings of patients with ASD carrying an increased risk of diagnosis when compared to population norms, and a much higher, although not absolute, concordance of autism diagnosis in monozygotic twins ( 42 - 44 ).
Genome wide association studies and whole exome sequencing methods have broadened our understanding of ASD susceptibility genes, and learning more regarding the function of these genes can shed light on potential biologic mechanisms ( 45 ). For example candidate genes in ASD include those that play a role in brain development or neurotransmitter function, or genes that affect neuronal excitability ( 46 , 47 ). Many of the genetic defects associated with ASD encode proteins that are relevant at the neuronal synapse or that are involved in activity-dependent changes in neurons, including regulatory proteins such as transcription factors ( 42 , 48 ). Potential “networks” of ASD genetic risk convergence include pathways involved in neurotransmission and neuroinflammation ( 49 ). Transcriptional and splicing dysregulation or alterations in epigenetic mechanisms such as DNA methylation or histone acetylation and modification may play a role ( 42 , 49 - 51 ). A recent study describes 16 newly identified genes associated with ASD that raise new potential mechanisms including cellular cytoskeletal structure and ion transport ( 52 ). Ultimately, ASD remains one of the most genetically heterogeneous neuropsychiatric disorders with rarer de novo and inherited variants in over 700 genes ( 53 ).
While genetics clearly play a role in ASD’s etiology, phenotypic expression of genetic susceptibility remains extremely variable within ASD ( 54 ). Genetic risk may be modulated by prenatal, perinatal, and postnatal environmental factors in some patients ( 35 ). Prenatal exposure to thalidomide and valproic acid have been reported to increase risk, while studies suggest that prenatal supplements of folic acid in patients exposed to antiepileptic drugs may reduce risk ( 55 - 57 ). Research has not confirmed if a small positive trial of folinic acid in autism can be used to recommend supplementation more broadly ( 58 ). Advanced maternal and paternal age have both been shown to have an increased risk of having a child with ASD ( 59 ). Maternal history of autoimmune disease, such as diabetes, thyroid disease, or psoriasis has been postulated, but study results remain mixed ( 60 , 61 ). Maternal infection or immune activation during pregnancy is another area of interest and may be a potential risk factor according to recent investigations ( 62 - 65 ). Both shorter and longer inter-pregnancy intervals have also been reported to increase ASD risk ( 66 ). Infants born prematurely have been demonstrated to carry a higher risk for ASD in addition to other neurodevelopmental disorders ( 34 ). In a prior epidemiologic review, obstetric factors including uterine bleeding, caesarian delivery, low birthweight, preterm delivery, and low Apgar scores were reported to be the few factors more consistently associated with autism ( 67 ). A recent meta-analysis reported several pre, peri and postnatal risk factors that resulted in an elevated relative risk of ASD in offspring ( 35 ), but also revealed significant heterogeneity, resulting in an inability to make true determination regarding the importance of these factors.
Despite the hysteria surrounding the now retracted Lancet article first published in 1998, there is no evidence that vaccines, thimerosal, or mercury is associated with ASD ( 68 - 70 ). In the largest single study to date, there was not an increased risk after measles/mumps/rubella (MMR) vaccination in a nationwide cohort study of Danish children ( 70 ).
Ultimately, research continues to reveal factors that correlate with ASD risk, but no causal determinations have been made. This leaves much room for discovery with investigators continuing to elucidate new variants conveying genetic risk, or new environmental correlates that require further study ( 52 ).
Evaluation in ASD begins with screening of the general pediatric population to identify children at-risk or demonstrating signs suggestive of ASD, following which a diagnostic evaluation is recommended. The American Academy of Pediatrics (AAP) guidelines recommend developmental surveillance at 9, 15 and 30 months well child visits and autism specific screening at 18 months and again at 24 or 30 months ( 28 , 71 ). Early red flags for ASD include poor eye contact, poor response to name, lack of showing and sharing, no gesturing by 12 months, and loss of language or social skills. Screening tools for ASD in this population include the Modified Checklist for Autism in Toddlers, Revised, with Follow-up (M-CHAT-R/F) and Survey of Wellbeing of Young Children (SWYC) ( 72 , 73 ). Red flags in preschoolers may include limited pretend play, odd or intensely focused interests, and rigidity. School age children may demonstrate concrete or literal thinking, have trouble understanding emotions, and may even show an interest in peers but lack conversational skills or appropriate social approach. If there is suspicion of ASD in these groups, screening tools available include the Social Communication Questionnaire (SCQ), Social Responsiveness Scale (SRS), and Autism Spectrum Screening Questionnaire (ASSQ) ( 74 - 76 ).
If concerns are raised at screening, primary care clinicians are recommended to refer the child to early intervention if less than 3 years of age or to the public school system for psychoeducational evaluation in order to establish an individual education program (IEP) if the child is three years of age or older. Clinicians should additionally refer the child to a specialist (pediatric neurologist, developmental-behavioral pediatrician, child psychiatrist, licensed child psychologist) for a definitive diagnosis and comprehensive assessment ( 71 ). A comprehensive assessment should include a complete physical exam, including assessment for dysmorphic features, a full neurologic examination with head circumference, and a Wood’s lamp examination of the skin. A parent interview, collection of any outside informant observations, and a direct clinician observation of the child’s current cognitive, language, and adaptive functioning by a clinician experienced with ASD should be components of this comprehensive assessment. ( 28 , 71 , 77 , 78 ).
Additionally, primary care clinicians need to be aware of (and evaluate for) potential co-occurring conditions in children with ASD. According to a surveillance study of over 2,000 children with ASD, 83% had an additional developmental diagnosis, 10% had at least one psychiatric diagnosis, and 16% at least one neurologic diagnosis ( 79 ). In the past, rates of co-morbid intellectual disability (ID) in patients with ASD were reported from 50% to 70%, with the most recent CDC estimate reported at 31.0% (26.7% to 39.4%) with ID defined as intelligence quotient (IQ) ≤70 ( 6 , 80 ). Other common co-occurring medical conditions include gastrointestinal (GI) disorders, including dietary restrictions and food selectivity, sleep disorders, obesity, and seizures ( 81 - 84 ). Studies using electronic health record (EHR) analysis revealed prevalence of epilepsy ~20% and GI disorders [without inflammatory bowel disease (IBD)] at 10–12% ( 82 ). Epilepsy has been shown to have higher prevalence rates in ASD with comorbid ID and medical disorders of increased risk such as tuberous sclerosis complex (TSC) ( 85 - 87 ). GI disorders or GI symptomatology, including diarrhea, constipation, restrictive eating, or reflux, have been shown to be prominent in ASD across multiple studies ( 81 , 82 , 88 , 89 ). Sleep problems have been reported to occur in anywhere from 50% to 73% of patients with ASD with variation in prevalence dependent on the definition of sleep symptoms or the measurement tool used ( 90 - 92 ). Rates of overweight and obesity in ASD are reported to be roughly 33% and 18% respectively, higher than rates in typically developing children ( 81 - 84 , 93 ).
Other behavioral or psychiatric co-occurring conditions in ASD include anxiety, attention deficit/hyperactivity disorder (ADHD), obsessive compulsive disorder, and mood disorders or other disruptive behavior disorders ( 81 ). Rates of co-occurring ADHD are reported anywhere from 25% to 81% ( 81 , 94 ). A recent meta-analysis of 30 studies measuring rates of anxiety and 29 studies measuring rates of depression reported a high degree of heterogeneity from the current literature, but stated pooled lifetime prevalence for adults with ASD to be 42% for any anxiety disorder and 37% for any depressive disorder, though the use of self-report measures and the presence of ID could influence estimates ( 95 ). In children with ASD seeking treatment, the rate of any anxiety disorder was found to be similar at 42% and in addition this study reported co-morbid oppositional defiant disorder at a rate of 46% and mood disorders at 8%, with 66% of the sample of over 600 patients having more than one co-occurring condition ( 94 ).
Currently no clear ASD biomarkers or diagnostic measures exist, and the diagnosis is made based on fulfillment of descriptive criteria. In light of a relatively high yield in patients with ASD, clinical genetic testing is recommended and can provide information regarding medical interventions or work up that might be necessary and help with family planning ( 96 ). The American College of Medical Genetics and Genomics (ACMGG) guidelines currently recommend chromosomal microarray for all children, fragile X testing in males, and additional gene sequencing, including PTEN and MECP2 , in certain patients as first tier genetic testing in the work up of ASD ( 97 ). High resolution G-banded karyotype, once recommended for all patients with ASD, is no longer routinely indicated based on recent consensus recommendations, but might still be performed in patients with a family or reproductive history suggestive of chromosomal rearrangements or specific syndromes such as sex chromosome anomalies or Trisomy 21 ( 96 - 98 ). Several professional societies recommend genetic testing for ASD, including the American Academy of Neurology, the AAP, ACMGG, and the American Academy of Child and Adolescent Psychiatry, and a child may require further referral to a geneticist and/or genetic counselor, depending on results of testing ( 25 , 28 , 97 , 99 ). As the field of genetics continues to advance rapidly, recent publications suggest whole exome sequencing may become the preferred method for clinical genetic testing in individuals with ASD ( 100 , 101 ).
Aside from genetic testing, no other laboratory work up is routinely recommended for every patient with a diagnosis of ASD. However, further evaluation may be appropriate for patients with particular findings or risk factors. Metabolic work-up should be considered in patients with any of the following concerning symptoms or signs: a history of clear developmental regression including loss or plateau of motor skills; hypotonia; recurrent episodes of vomiting, lethargy or hypoglycemia; microcephaly or poor growth; concern for other organ involvement; coarse features; or concern for seizures or ataxia. Based on the patient’s history and presentation, components of a metabolic laboratory evaluation could include complete blood count (CBC), liver and renal function tests, lactate, pyruvate, carnitine, amino acids, an acylcarnitine profile, urine organic acids and/or urine glycosaminoglycans ( 97 , 102 ). Children with a history of pica should have a lead level measured ( 28 , 103 ). In a child with significantly restricted food intake, one should consider a laboratory evaluation of nutritional status. Sleep symptoms may warrant a referral for a possible sleep study, and if restless sleep symptoms are present, an evaluation for iron deficiency is not unreasonable, particularly if dietary rigidity limits iron intake ( 104 ).
Neuroimaging is not routinely recommended for every patient with ASD ( 28 , 99 ), but may be appropriate in patients with a suspicion for TSC or other neurocutaneous disorders, microcephaly, or an abnormal neurologic exam (spasticity, severe hypotonia, unilateral findings). Patients with suspected seizures should have an electroencephalography (EEG) obtained ( 102 ). If accessible, it might be appropriate to immediately refer children with concern for further genetic, metabolic or neurologic conditions to a specialist who can then obtain and interpret the aforementioned testing. At this time there is inadequate evidence to recommend routine testing for celiac disease, immunologic or neurochemical markers, mitochondrial disorders, allergy testing, hair analysis, intestinal permeability studies, erythrocyte glutathione peroxidase studies, stool analysis, urinary peptides or vitamin and mineral deficiencies without a history of severe food selectivity.
ASD is a neurodevelopmental disorder characterized by deficits in social communication and the presence of restricted interests and repetitive behaviors. Recent changes to the diagnostic criteria occurred with the transition to the new diagnostic manual (DSM-5) and will likely impact prevalence, which currently stands at 1 in 59 children in the US. ASD is a neurobiological disorder influenced by both genetic and environmental factors affecting the developing brain. Research continues to reveal factors that correlate with ASD risk and these findings may guide further etiologic investigation, but no final causal pathway has been elucidated. Clinical evaluation begins with developmental screening of the general pediatric population to identify at-risk children, followed by referral to a specialist for a definitive diagnosis and comprehensive neuropsychological assessment. Children with ASD should also be screened for common co-morbid diagnoses. While no clear biomarkers or diagnostic measures exist, clinical genetic testing is recommended as part of the initial medical evaluation. Further medical work up or subspecialist referrals may be pursued based on specific patient characteristics.
Acknowledgments
Funding: None.
Ethical Statement : The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflicts of Interest : The authors have no conflicts of interest to declare.

Listen Live

BBC World Service
The latest news and information from the world's most respected news source. BBC World Service delivers up-to-the-minute news, expert analysis, commentary, features and interviews.
- Behavioral Health
Autism found me, and then I found my voice
Since my diagnosis with autism in 2015 at age 30, a bolder, more outspoken side of myself has emerged..
- Marta Rusek
(Images courtesy of the author)
‘Coming out’ as autistic
Encouraging greater awareness and advocacy.
WHYY is your source for fact-based, in-depth journalism and information. As a nonprofit organization, we rely on financial support from readers like you. Please give today.
Brought to you by Speak Easy
Thoughtful essays, commentaries, and opinions on current events, ideas, and life in the Philadelphia region.
You may also like
Orna Guralnik on ‘Couples Therapy’
The reality show 'Couples Therapy' puts real-life couples sessions with Dr. Orna Guralnik on camera. Guralnik joins us to talk about relationships and therapy.
Air Date: September 15, 2023 12:00 pm
The Secret Life of Secrets
In The Secret Life of Secrets, Michael Slepian reveals how secrets impact our minds, relationships and more, and gives strategies to make them easier to carry around with us.
Air Date: June 21, 2022 10:00 am

Corona-somnia: Sleep disorders and the global pandemic
Struggling to fall asleep or stay asleep? The stress and uncertainty of COVID-19 increased rates of insomnia, restlessness and something called revenge bedtime procrastination
Air Date: August 26, 2021 10:00 am
About Marta Rusek
Want a digest of WHYY’s programs, events & stories? Sign up for our weekly newsletter.
Together we can reach 100% of WHYY’s fiscal year goal
%20(500%20x%20200%20px).png)
Jackie Schuld Art Therapy Blog
- Feb 17, 2023
The Great List of Autistic Essays
I’m a late-identified autistic who loves writing about autism. How much do I love it? I’ve written over 150 essays on it in the past six months alone.

How do I think of so many autistic topics to write about? I’m an art therapist who specializes in late-identified autistic adults. That means I not only have my personal experience to draw from, but also the hundreds of hours spent listening to my clients.
I share most of my essays here on Medium, which means it has now become quite the library. In an effort to make my essays more accessible to those wanting clear, relatable information about late-identified autism in adults, I’ve sorted my essays into topics below. While I wish I could provide a link to each of them for you… I’ve got to prioritize my time and energy. So if a specific essay interests you, just pop it into the search and it’ll come up
Autism in a Neurotypical World
What Would a World Designed by Autistic People Be Like
The Harm in "They're a Little Autistic"
Autism Does Not Directly Cause Socializing Problems
Please Trust My Lived Autistic Experience
Can Someone Please Create a Neurodivergent Intentional Living Community
What if I Accept that Most Neurotypicals Won't Like Me
How Neuro-Bias Shows Up in Professional Testing
Your Autistic Experience Sounds Just LIke my Neurotypical One
Neurotypical Words that Don't Work for Autistics: Overachiever
But Neurotypicals Experience That, Too!
Neurotypical Norms That Don’t Work for Autistics: Hustle Goals
The Fear of Being a Hypocritical Autistic
Neurodiversity: Us vs Them?
How to Meet an Autistic Adult Exactly Where They're At
Autism Characteristics
The Autistic Mind Loves to Take Detours
4 Reasons Why Autism Symptoms Lists are Confusing
My Autistic Brain: Sunshine and Detours
The Joys of Being Autistic: Part 1
Stop Saying Autistic People Can't Empathize
Redefining Fun for Autistic Adults
9 Reasons Why Autism Looks So Similar to CPTSD
We Need More Depictions of the Interior Experience of Autism
Clarity is What my Autistic Mind Craves
How Trauma and Autism Can be a Confusing Mix to Decipher
Why am I like This? Understanding the Autistic Brain
My Autistic Mind Does What it Wants
The Dissociated Autistic Performance State
The Joys of Being Autistic: Increased Creativity and Innovation
My Autistic Memory Is Not the Same as Others
The Firehouse Dilemma: Autism and Infodumping
The Variability of the Autistic Sensory System
5 Reasons Autistics are Especially Hard on Themselves
The Shame That Often Accompanies Autism
Knowing You’re Different as an Autistic Adult
3 Reasons Autism is Worse After You Learn You're Autistic
Disability and Internalized Ableism
I Had to Dismantle My Fear of Autistic People
Is Autism a Disability?
I’m Ok With Saying I have a Disability, Right?
Dog Training
The Difficulties of Adjusting to a New Dog When You're Autistic
Tips for Adjusting to a New Dog When You're Autistic
5 Tips to Integrate a Dog into Your Autistic Life
Defining and Explaining Autism
What I Wish Others Knew About Autism
Let’s Drop the “Disorder” From Autism Spectrum Disorder
How Low and High Autism Labels are Misleading
We Need All the Autism Theories and Models
Autism Can Be a Murky Thing To Understand
How I Explain Autism to Someone Unfamiliar With It
What is Late Identified Autism
Autistic Statistics are Not Accurate for Late-Identified Autistics
I'm Here for the Autistic Awakening
How It Helps to Know You’re Autistic
Why It Matters to Know You're Neurodivergent
What is Neurodiversity and Why Does it Matter
How Neurodivergent Acceptance Can Improve Our Lived Experiences
How Unidentified Autistics are Taught to Socially Camouflage and Mask
Is There a World Where I can Be Unmasked?
The False Dichotomy of Masked and Unmasked Autism
6 Reasons Why UnMasking Is Harder Than it Sounds
What if You have to Mask Everywhere?
My Personal Experience as an Autistic
Hating Cooking as an Autistic Adult
I Make Giant Lists About Autism for Fun
The Challenges of Writing Publically About Autism
The Risk of Sharing my Autistic Passions with Others
I'm Reclaiming Weird for My Autistic Self
I Expand and Then I Contract
I Stopped Seeing Myself As Broken When I learned I was Autistic
Respecting my Limits as an Autistic Business Owner
I Need to Lessen the Pressure on my Autistic Self
My Autistic Brain Doesn’t Want to Watch TV Right Now
Embracing Who I am as an Autistic Adult
I Used to be a Very Judgemental When I Didn’t Know I was Autistic
A Letter from An Autistic Adult to Trust
Don’t Get So Upset: A Line that Doesn’t Work for This Autist
Why This Autistic Writer Didn't Respond to Your Comment
Relationships
Is Dating Worth it as an Autistic Adult?
Is it Possible to be Happily Partnered as an Autistic Adult?
Not Liking People as an Autistic Adult
Self-Identification
So You Think You Might Be Autistic
Dearly Newly Identified Autistic Person
Am I Actually Autistic?
Dearest Smart, Weird, and Caring Autistic
I Am Deeply Unsure About Autism
How to Self Identify Autism as an Adult
When the Past Makes Sense after a Late-Identification of Autism
Where to Start When You First Learn You’re Autistic
6 Strategies to Harness the Hyperfocus Power of an Autistic Mind
Leave the Gremlin In the Cave: Self-Isolation as a Necessary Autistic Tool
No Plans Days as an Autistic Tool
Making Accommodations for Myself as an Autistic Adult
How Many Accommodations Can We Ask for as Autistic Adults?
Using Art to Help Your Autistic Mind
Dissociation as an Autistic Tool
The Power of the Home Environment for Autistics
Is It Ok to Honor My Autistic Needs?
Recognizing When It's Not Time to Make Decisions as an Autistic
Therapy for Autistics
Dearest Autistic Client of Mine
8 Ways Therapy Can Help With Late Identified Autism
Gaslighting the Autistic Experience
Dearest Therapist Who Knows Barely Anything About Autism
I'm an Autistic Therapist: Sometimes It's Easier Than Everyday Life
Does Your Therapist Know Enough About Autism to Help You?
Questions to Ask a Potential Therapist When You're Autistic
How I Work with Newly Identified Autistic People
What to Ask When You're Seeking Therapy for Late-Identified Autism
12 Ways Therapy Can Enhance Life for Late Identified Autistic Adults
Therapy is Not for Fixing Autism
The Harm I Caused When I Didn't Know about Autism
A Newly Identified Autistic Therapist Working with Newly Identified Autistics
Common Therapy Advice That is Counterproductive for Autistics
A Therapist Told Me Treating Autism is Like Treating Depression
Who Can Diagnose Autism in Adults?
Autistic Adults Deserve Better from the Mental Health Field
Undiagnosed Autism
The Correlation Between Intelligence and Undiagnosed Autism
10 Consequences of a Life with Unidentified Autism
The Gap Between “Diagnosable Autism” and a Lifetime of Unidentified Autism
Autism Diagnosis Criteria are Limiting for Men Too
No Autistic Should Receive a Diagnosis Letter Like Mine
Identifying Autism in Undiagnosed Women Abstract
How I Identify Autism in Undiagnosed Women
Autistic Stereotypes Block People From Knowing They're Autistic
Thank you for reading. If you’d like to read more, sign up for my FUNletter . If you would like to explore your autistic identity with an autistic therapist, you can learn more about my therapy services here .
Recent Posts
My Autistic Sensory System is a Demanding, Bougie Princess
My Autistic Silence Does Not Mean Agreement
This Autistic is Quitting the News
Want to read more on topics that interest you? Subscribe to my FUNletter.
Thanks for submitting!
Home — Essay Samples — Nursing & Health — Autism — Why Autism Awareness is Important
Why Autism Awareness is Important
- Categories: Autism Psychological Disorders
About this sample

Words: 719 |
Published: Aug 24, 2023
Words: 719 | Pages: 2 | 4 min read

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
1 pages / 1411 words
3 pages / 1583 words
1 pages / 1827 words
3 pages / 1364 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Autism
Ziyan (not real name) 7 years old is a boy who studies in Aminiya School. Ziyan lives with his both parents. Moreover he is having an aunt who is taking extra care of him as his parents are not well educated. His mother is a [...]
Autism Spectrum Disorder (ASD) is a complex neurodevelopmental disorder that affects individuals in varying ways. It is characterized by impairments in social interaction, communication, and repetitive behaviors. According to [...]
Autism is a complex neurodevelopmental disorder that affects a person's ability to communicate and interact with others. It is characterized by repetitive behaviors, difficulties in social interaction, and challenges with verbal [...]
In conclusion, "The Reason I Jump" provides a powerful and compelling summary of the world of autism. Through Naoki Higashida's insightful reflections, we gain a deeper understanding of the sensory experiences, social [...]
“I am different, not less.” These simple yet extremely influential words were spoken by Dr. Temple Grandin, one of the most accomplished and well known adults with autism in the world. Dr. Grandin was raised in an era where [...]
The Curious Incident of the Dog in the Night-time by Mark Haddon is the story of Christopher John Francis Boone’s adventures as told by him. The protagonist, Christopher, wrote the book as a murder mystery, describing his [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Dsm 5 Autism Spectrum Disorder
This essay about the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), discusses the significant changes in the classification of Autism Spectrum Disorder (ASD). The shift from multiple distinct categories to a unified spectrum approach reflects a more accurate representation of the diverse manifestations of autism. It highlights how the DSM-5 emphasizes two primary diagnostic criteria: challenges in social communication and repetitive behavioral patterns, including sensory sensitivities. The essay also addresses the implications of these changes for personalized treatment and the broader acceptance of neurodiversity. Concerns about the consistency of diagnoses under the new criteria are discussed, underscoring the need for ongoing adjustments in the diagnostic process to better encompass the full range of autistic experiences. Overall, the essay evaluates how the updated DSM-5 criteria lead to a deeper understanding and improved support for individuals with ASD.
How it works
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) marks a notable advancement in the way mental health professionals understand and approach Autism Spectrum Disorder (ASD). This latest edition has redefined the framework for diagnosing autism, broadening our perspective and enhancing the way support is provided to individuals across the spectrum.
In earlier iterations like the DSM-IV, autism was fragmented into several distinct categories, such as Asperger’s Syndrome and pervasive developmental disorder-not otherwise specified (PDD-NOS). However, the DSM-5 consolidates these into a single category: ASD.
This consolidation is based on the realization that autism manifests through a continuum of symptoms rather than discrete blocks, making a spectrum approach more reflective of the true nature of these experiences.
The criteria for diagnosing ASD in DSM-5 focus heavily on two primary areas: persistent challenges in social communication and interaction across multiple contexts, and patterns of behavior that are restricted and repetitive. This framework acknowledges that while some may face significant challenges in social situations, others might be more affected by sensory sensitivities or inflexible adherence to routines. Including these varied experiences under one category allows for a more nuanced understanding of each individual’s needs.
One significant addition in DSM-5 is the greater emphasis on sensory sensitivities. This new diagnostic element recognizes that sensory experiences—how individuals perceive touch, sound, and light, for example—can greatly impact their social and emotional lives. By considering these factors, the DSM-5 addresses aspects of ASD that were previously underappreciated, allowing for a more comprehensive approach to care.
The adoption of a spectrum-based classification also influences how treatments are designed and implemented. It paves the way for customized support plans that are more closely aligned with the diverse strengths and challenges of individuals with ASD. This tailored approach not only optimizes developmental outcomes but also enhances quality of life, promoting a higher level of inclusion and participation in society.
Despite these improvements, the transition to the DSM-5 criteria has sparked discussions and concerns, particularly regarding the consistency of diagnoses. Some argue that the broader framework might exclude individuals who would have been diagnosed under the more segmented DSM-IV approach. These debates underscore the importance of continued refinement in diagnostic processes, ensuring they capture the full range of autism experiences without narrowing the scope of who receives support.
Reflecting on the changes brought about by the DSM-5, it’s clear that the updated diagnostic criteria represent more than just medical terminology adjustments—they signify a deeper understanding of autism as a diverse and complex experience. This evolution in thought and practice not only helps medical professionals and educators provide better support but also aligns more closely with the advocacy community’s push for recognition and acceptance of neurodiversity.
In sum, the shift to a spectrum-based view in DSM-5 enhances our approach to understanding and supporting individuals with autism. It brings us closer to a society that values and integrates the unique perspectives and abilities of all its members, acknowledging that diversity in human experience enriches us all.
Cite this page
Dsm 5 Autism Spectrum Disorder. (2024, Apr 14). Retrieved from https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/
"Dsm 5 Autism Spectrum Disorder." PapersOwl.com , 14 Apr 2024, https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/
PapersOwl.com. (2024). Dsm 5 Autism Spectrum Disorder . [Online]. Available at: https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/ [Accessed: 31 May. 2024]
"Dsm 5 Autism Spectrum Disorder." PapersOwl.com, Apr 14, 2024. Accessed May 31, 2024. https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/
"Dsm 5 Autism Spectrum Disorder," PapersOwl.com , 14-Apr-2024. [Online]. Available: https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/. [Accessed: 31-May-2024]
PapersOwl.com. (2024). Dsm 5 Autism Spectrum Disorder . [Online]. Available at: https://papersowl.com/examples/dsm-5-autism-spectrum-disorder/ [Accessed: 31-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers

Educating Children with Autism (2001)
Chapter: 16 conclusions and recommendations.
Below is the uncorrected machine-read text of this chapter, intended to provide our own search engines and external engines with highly rich, chapter-representative searchable text of each book. Because it is UNCORRECTED material, please consider the following text as a useful but insufficient proxy for the authoritative book pages.
16 Conclusions and Recommendations This chapter summarizes the committeeâs conclusions about the state of the science in early intervention for children with autistic spectrum disorders and its recommendations for future intervention strategies, pro- grams, policy, and research. The chapter is organized around seven key areas pertaining to educational interventions for young children with autistic spectrum disorders: how the disorders are diagnosed and as- sessed and how prevalent they are; the effect on and role of families; appropriate goals for educational services; characteristics of effective in- terventions and educational programs; public policy approaches to en- suring access to appropriate education; the preparation of educational personnel; and needs for future research. DIAGNOSIS, ASSESSMENT, AND PREVALENCE Conclusions Autism is a developmental disorder of neurobiologic origin that is defined on the basis of behavioral and developmental features. Autism is best characterized as a spectrum of disorders that vary in severity of symptoms, age of onset, and association with other disorders (e.g., mental retardation, specific language delay, epilepsy). The manifestations of au- tism vary considerably across children and within an individual child over time. There is no single behavior that is always typical of autism and no behavior that would automatically exclude an individual child from a 211
212 EDUCATING CHILDREN WITH AUTISM diagnosis of autism, even though there are strong and consistent com- monalities, especially relative to social deficits. The large constellation of behaviors that define autistic spectrum dis- ordersâgenerally representing deficits in social interaction, verbal and nonverbal communication, and restricted patterns of interest or behav- iorsâare clearly and reliably identifiable in very young children to expe- rienced clinicians and educators. However, distinctions among classical autism and atypical autism, pervasive developmental disorder-not other- wise specified (PDD-NOS), and Aspergerâs disorder can be arbitrary and are often associated with the presence or severity of handicaps, such as mental retardation and severe language impairment. Identifying narrow categories within autism is necessary for some research purposes; however, the clinical or educational benefit to subclas- sifying autistic spectrum disorders purely by diagnosis is debated. In contrast, individual differences in language development, verbal and non- verbal communication, sensory or motor skills, adaptive behavior, and cognitive abilities have significant effects on behavioral presentation and outcome, and, consequently, have specific implications for educational goals and strategies. Thus, the most important considerations in pro- gramming have to do with the strengths and weaknesses of the indi- vidual child, the age at diagnosis, and early intervention. With adequate time and training, the diagnosis of autistic spectrum disorders can be made reliably in 2-year-olds by professionals experi- enced in the diagnostic assessment of young children with autistic spec- trum disorders. Many families report becoming concerned about their childrenâs behavior and expressing this concern, usually to health profes- sionals, even before this time. Research is under way to develop reliable methods of identification for even younger ages. Children with autistic spectrum disorders, like children with vision or hearing problems, re- quire early identification and diagnosis to equip them with the skills (e.g., imitation, communication) to benefit from educational services, with some evidence that earlier initiation of specific services for autistic spectrum disorders is associated with greater response to treatment. Thus, well meaning attempts not to label children with formal diagnoses can deprive children of specialized services. There are clear reasons for early identifi- cation of children, even as young as two years of age, within the autism spectrum. Epidemiological studies and service-based reports indicate that the prevalence of autistic spectrum disorders has increased in the last 10 years, in part due to better identification and broader categorization by educators, physicians, and other professionals. There is little doubt that more children are being identified as requiring specific educational inter- ventions for autistic spectrum disorders. This has implications for the provision of services at many levels. Analysis of data from the Office of
CONCLUSIONS AND RECOMMENDATIONS 213 Special Education Programs, gathered for school-age children since the autism category was recognized in 1991, would support investigation of whether the dramatic increases in the numbers of children served with autistic spectrum disorders are offset by commensurate decreases in other categories in which children with autistic spectrum disorders might have previously been misclassified or whether these dramatic increases have come about for other reasons. Although children with autistic spectrum disorders share some char- acteristics with children who have other developmental disorders and may benefit from many of the same educational techniques, they offer unique challenges to families, teachers, and others who work with them. Their deficits in nonverbal and verbal communication require intense effort and skill even in the teaching of basic information. The unique difficulties in social interaction (e.g., in joint attention) may require more individual guidance than for other children in order to attract and sustain their childrenâs attention. Moreover, ordinary social exchanges between peers do not usually occur without deliberate planning and ongoing struc- turing by the adults in the childâs environment. The absence of typical friendships and peer relationships affects childrenâs motivation systems and the meaning of experiences. Appropriate social interactions may be some of the most difficult and important lessons a child with autistic spectrum disorders will learn. In addition, the frequency of behavior problems, such as tantrums and self-stimulatory and aggressive behavior, is high. The need for sys- tematic selection of rewards for many children with autistic spectrum disorders, whose motivation or interests can be limited, requires creativ- ity and continued effort from teachers and parents to maximize the childâs potential. Although general principles of learning and behavior analysis apply to autistic spectrum disorders, familiarity with the specific nature of the disorder should contribute to analysis of the contexts (e.g., commu- nicative and social) of behaviors for individual children and result in more effective programming. For example, conducting a functional as- sessment that considers contexts, and then replacing problem behaviors with more appropriate ways to communicate can be an effective method for reducing problem behaviors. Recommendations 1-1 Because of their shared continuities and their unique social diffi- culties, children with any autistic spectrum disorder (autistic disorder, Aspergerâs disorder, atypical autism, PDD-NOS, child- hood disintegrative disorder), regardless of level of severity or function, should be eligible for special educational services within the category of autistic spectrum disorders, as opposed to other
214 EDUCATING CHILDREN WITH AUTISM terminology used by school systems, such as other health im- paired, social emotionally maladjusted, significantly developmen- tally delayed, or neurologically impaired. 1-2 Identification of autistic spectrum disorders should include a for- mal multidisciplinary evaluation of social behavior, language and nonverbal communication, adaptive behavior, motor skills, atypi- cal behaviors, and cognitive status by a team of professionals experienced with autistic spectrum disorders. An essential part of this evaluation is the systematic gathering of information from parents on their observations and concerns. If the school system cannot carry out such an assessment, the local education author- ity should fund the assessment through external sources. Early diagnosis should be emphasized. Because of variability in early development, younger children with autistic spectrum disorders should receive a follow-up diagnostic and educational assess- ment within one to two years of initial evaluation. 1-3 Professional organizations, with the support of the National Insti- tutes of Health (NIH) and the Department of Educationâs Office of Special Education Programs (OSEP), should disseminate infor- mation concerning the nature and range of autistic spectrum dis- orders in young children to all professionals who have contact with children, particularly those who work with infants, toddlers, and preschool children. This information should include the vari- able presentations and patterns of behavior seen in autistic spec- trum disorders from toddlers to school age children. Members of âchild findâ teams within the early intervention systems, as well as primary care providers, should be trained in identifying the âred flags of autistic spectrum disordersâ and the importance and means of early referral for comprehensive diagnostic evaluation. Advocacy groups and relevant federal agencies, as well as profes- sional organizations, should use effective media resources, in- cluding the Internet, to provide information concerning the range of behaviors in autistic spectrum disorders. ROLE OF FAMILIES Conclusions Having a child with an autistic spectrum disorder is a challenge for any family. Involvement of families in the education of young children with autistic spectrum disorders can occur at multiple levels, including advocacy, parents as participating partners in and agents of education or
CONCLUSIONS AND RECOMMENDATIONS 215 behavior change, and family-centered consideration of the needs and strengths of the family as a unit. Nearly all empirically supported treat- ments reviewed by the committee included a parent component, and most research programs used a parent-training approach. More informa- tion is needed about the benefits of a family-centered orientation or com- bined family-centered and formalized parent training in helping parents. It is well established that parents can learn and successfully apply skills to changing the behavior of their children with autistic spectrum disorders, though little is known about the effects of cultural differences, such as race, ethnicity, and social class, nor about the interactions among family factors, child characteristics, and features of educational interven- tion. For most families, having a child with an autistic spectrum disorder creates added stress. Parentsâ use of effective teaching methods can have a significant effect on that stress, as can support from within the family and the community. Parents need access to balanced information about autistic spectrum disorders and the range of appropriate services and technologies in order to carry out their responsibilities. They also need timely information about assessments, educational plans, and the avail- able resources for their children. This information needs to be conveyed to them in a meaningful way that gives them time to prepare to fulfill their roles and responsibilities. In the last ten years the widespread availability of the Internet and media attention to autistic spectrum disorders have increased parentsâ knowledge but often conveyed perspectives that were not balanced nor well-supported scientifically. Of crucial importance is the question of how to make information available to parents and to ensure their active role in advocacy for their childrenâs education. Recommendations 2-1 Parentsâ concerns and perspectives should actively help to shape educational planning. Specifically: a. In order for a family to be effective members of the Indi- vidualized Education Plan (IEP) team that plans a childâs educa- tion, the local school system should provide to the parents, at the beginning of the assessment process, written information con- cerning the nature of autistic spectrum disorders and eligibility categories, the range of alternatives within best practices in early education of autistic spectrum disorders, sources of funding and support (e.g., a support guide and bibliography), and their childâs rights. b. Prior to the IEP meeting, the local school system should provide to each family the written results of their childâs assess-
216 EDUCATING CHILDREN WITH AUTISM ment, and a contact person to explain the findings if they wish, and should indicate that they will have the opportunity to present their concerns. Early during the IEP meeting, parents should be given an opportunity to voice their questions, concerns, and per- spectives about their childâs development and educational pro- gramming. 2-2 As part of local educational programs and intervention programs for children from birth to age 3, families of children with autistic spectrum disorders should be provided the opportunity to learn techniques for teaching their child new skills and reducing prob- lem behaviors. These opportunities should include not only di- dactic sessions, but also ongoing consultation in which individu- alized problem-solving, including in-home observations or training, occur for a family, as needed, to support improvements at home as well as at school. 2-3 Families that are experiencing stress in raising their children with an autistic spectrum disorder should be provided with mental health support services. Under Part C of the Individuals with Disabilities Education Act (IDEA), which addresses family sup- port and service coordination, including private service provid- ers, services should be extended to include families of children at least up to age 8 years. GOALS FOR EDUCATIONAL SERVICES Conclusions At the root of questions about the most appropriate educational inter- ventions lie differences in assumptions about what is possible and what is important to give students with autistic spectrum disorders through edu- cation. The appropriate goals for educational services are the same as those for other children: personal independence and social responsibility. These goals imply continuous progress in social and cognitive abilities, verbal and nonverbal communication skills, adaptive skills, amelioration of behavioral difficulties, and generalization of abilities across multiple environments. In some cases, reports have suggested that particular treat- ments can foster permanent ârecoveryâ. However, as with other develop- mental disabilities, the core deficits of autistic spectrum disorders have generally been found to persist, to some degree, in most individuals. Research concerning outcomes can be characterized by whether the goal of intervention is broadly defined (e.g., ârecoveryâ or âbest out-
CONCLUSIONS AND RECOMMENDATIONS 217 comeâ) or more specifically defined (e.g., increasing vocabulary or peer- directed social behavior); whether the design involves reporting results in terms of group or individual changes; and whether the goals are short term (i.e., to be achieved in a few weeks or months) or longer term (i.e., over years). A large body of single-subject research has demonstrated substantial progress in individual responses to specific intervention tech- niques in relatively short periods of times (e.g., several months) in many specific areas, including gains in social skills, language acquisition, non- verbal communication, and reductions in challenging behaviors. Studies over longer periods of time have documented joint attention, symbolic play, early language skills, and imitation as core deficits and hallmarks of the disorder that are predictive of longer term outcome in the domains of language, adaptive behaviors, and academic skills. Many treatment studies report postintervention placement as an out- come measure. While successful participation in regular classrooms is an important goal for some children with autistic spectrum disorders, the usefulness of placement in regular education classes as an outcome mea- sure is limited, because placement may be related to many variables other than the characteristics of the child (e.g., prevailing trends in inclusion, availability of other services). The most commonly reported outcome measure in group treatment studies of children with autistic spectrum disorders has been changes in IQ scores, which also have many limita- tions. Studies have reported substantial changes in large numbers of chil- dren in intervention studies and longitudinal studies in which children received a variety of interventions. Even in the treatment studies that have shown the strongest gains, childrenâs outcomes are variable, with some children making substantial progress and others showing very slow gains. The needs and strengths of young children with autistic spectrum disorders are very heterogeneous. Although there is evidence that many interventions lead to improvements and that some children shift in spe- cific diagnosis along the autism spectrum during the preschool years, there does not appear to be a simple relationship between any particular intervention and ârecoveryâ from autistic spectrum disorders. Thus, while substantial evidence exists that treatments can reach short-term specific goals in many areas, gaps remain in addressing larger questions of the relationships between particular techniques, child characteristics, and outcomes. Recommendations The IEP and Individual Family Service Plan (IFSP) should be the vehicles for planning and implementing educational objectives.
218 EDUCATING CHILDREN WITH AUTISM 3-1 Appropriate educational objectives for children with autistic spec- trum disorders should be observable, measurable behaviors and skills. These objectives should be able to be accomplished within 1 year and expected to affect a childâs participation in education, the community, and family life. They should include the devel- opment of: a. Social skills to enhance participation in family, school, and community activities (e.g., imitation, social initiations and re- sponse to adults and peers, parallel and interactive play with peers and siblings); b. Expressive verbal language, receptive language, and non- verbal communication skills; c. A functional symbolic communication system; d. Increased engagement and flexibility in developmentally appropriate tasks and play, including the ability to attend to the environment and respond to an appropriate motivational system; e. Fine and gross motor skills used for age appropriate func- tional activities, as needed; f. Cognitive skills, including symbolic play and basic con- cepts, as well as academic skills; g. Replacement of problem behaviors with more conven- tional and appropriate behaviors; and h. Independent organizational skills and other behaviors that underlie success in regular education classrooms (e.g., complet- ing a task independently, following instructions in a group, ask- ing for help). 3-2 Ongoing measurement of educational objectives must be docu- mented in order to determine whether a child is benefiting from a particular intervention. Every childâs response to the educational program should be assessed after a short period of time. Progress should be monitored frequently and objectives adjusted accord- ingly. CHARACTERISTICS OF EFFECTIVE INTERVENTIONS Conclusions In general, there is consistent agreement across comprehensive inter- vention programs about a number of features, though practical and, some- times, ethical considerations have made well-controlled studies with ran- dom assignment very difficult to conduct without direct evaluation. Characteristics of the most appropriate intervention for a given child must
CONCLUSIONS AND RECOMMENDATIONS 219 be tied to that childâs and familyâs needs. However, without direct evalu- ation, it is difficult to know which features are of greatest importance in a program. Across primarily preschool programs, there is a very strong consensus that the following features are critical: ⢠entry into intervention programs as soon as an autism spectrum diagnosis is seriously considered; ⢠active engagement in intensive instructional programming for a minimum of the equivalent of a full school day, 5 days (at least 25 hours) a week, with full year programming varied according to the childâs choronological age and developmental level; ⢠repeated, planned teaching opportunities generally organized around relatively brief periods of time for the youngest children (e.g., 15- 20 minute intervals), including sufficient amounts of adult attention in one-to-one and very small group instruction to meet individualized goals; ⢠inclusion of a family component, including parent training; ⢠low student/teacher ratios (no more than two young children with autistic spectrum disorders per adult in the classroom); and ⢠mechanisms for ongoing program evaluation and assessments of individual childrenâs progress, with results translated into adjustments in programming. Curricula across different programs differ in a number of ways. They include the ways in which goals are prioritized, affecting the relative time spent on verbal and nonverbal communication, social activities, behav- ioral, academic, motor, and other domains. Strategies from various pro- grams represent a range of techniques, including discrete trials, incidental teaching, structured teaching, âfloor timeâ, and individualized modifica- tions of the environment, including schedules. Some programs adopt a unilateral use of one set of procedures, and others use a combination of approaches. Programs also differ in the relative amount of time spent in homes, centers, or schools, when children are considered ready for inclu- sion into regular classrooms, how the role of peers as intervention agents is supported, and in the use of distraction-free or natural environments. Programs also differ in the credentials that are required of direct support and supervisory staff and the formal and informal roles of collateral staff, such as speech language pathologists and occupational therapists. Overall, many of the programs are more similar than different in terms of levels of organization, staffing, ongoing monitoring, and the use of certain techniques, such as discrete trials, incidental learning, and struc- tured teaching. However, there are real differences in philosophy and practice that provide a range of alternatives for parents and school sys- tems considering various approaches. The key to any childâs educational program lies in the objectives specified in the IEP and the ways they are
220 EDUCATING CHILDREN WITH AUTISM addressed. Much more important than the name of the program attended is how the environment and educational strategies allow implementation of the goals for a child and family. Thus, effective services will and should vary considerably across individual children, depending on a childâs age, cognitive and language levels, behavioral needs, and family priorities. Recommendations The committeeâs recommendations for effective treatment are made on the basis of empirical findings, information from selected representa- tive programs, and findings in the general education and developmental literature. In particular, it is well established that children with autism spend much less time in focused and socially directed activity when in unstructured situations than do other children. Therefore, it becomes crucial to specify time engaged in social and focused activity as part of a program for children with autistic spectrum disorders. 4-1 Based on a set of individualized, specialized objectives and plans that are systematically implemented, educational services should begin as soon as a child is suspected of having an autistic spec- trum disorder. Taking into account the needs and strengths of an individual child and family, the childâs schedule and educational environment, in and out of the classroom, should be adapted as needed in order to implement the IEP. Educational services should include a minimum of 25 hours a week, 12 months a year, in which the child is engaged in systematically planned, develop- mentally appropriate educational activity aimed toward identi- fied objectives. Where this activity takes place and the content of the activity should be determined on an individual basis, de- pending on characteristics of both the child and the family. 4-2 A child must receive sufficient individualized attention on a daily basis so that individual objectives can be effectively implemented; individualized attention should include individual therapies, de- velopmentally appropriate small group instruction, and direct one-to-one contact with teaching staff. 4-3 Assessment of a childâs progress in meeting objectives should be used on an ongoing basis to further refine the IEP. Lack of objec- tively documentable progress over a 3 month period should be taken to indicate a need to increase intensity by lowering stu-
CONCLUSIONS AND RECOMMENDATIONS 221 dent/teacher ratios, increasing programming time, reformulat- ing curricula, or providing additional training and consultation. 4-4 To the extent that it leads to the specified educational goals (e.g., peer interaction skills, independent participation in regular edu- cation), children should receive specialized instruction in settings in which ongoing interactions occur with typically developing children. 4-5 Six kinds of interventions should have priority: a. Functional, spontaneous communication should be the pri- mary focus of early education. For very young children, pro- gramming should be based on the assumption that most children can learn to speak. Effective teaching techniques for both verbal language and alternative modes of functional communication, drawn from the empirical and theoretical literature, should be vigorously applied across settings. b. Social instruction should be delivered throughout the day in various settings, using specific activities and interventions planned to meet age-appropriate, individualized social goals (e.g., with very young children, response to maternal imitation; with preschool children, cooperative activities with peers). c. The teaching of play skills should focus on play with peers, with additional instruction in appropriate use of toys and other materials. d. Other instruction aimed at goals for cognitive develop- ment should also be carried out in the context in which the skills are expected to be used, with generalization and maintenance in natural contexts as important as the acquisition of new skills. Because new skills have to be learned before they can be general- ized, the documentation of rates of acquisition is an important first step. Methods of introduction of new skills may differ from teaching strategies to support generalization and maintenance. e. Intervention strategies that address problem behaviors should incorporate information about the contexts in which the behaviors occur; positive, proactive approaches; and the range of techniques that have empirical support (e.g., functional assess- ment, functional communication training, reinforcement of alter- native behaviors). f. Functional academic skills should be taught when appro- priate to the skills and needs of a child.
222 EDUCATING CHILDREN WITH AUTISM PUBLIC POLICIES Conclusions The Individuals with Disabilities Education Act (IDEA) contains the necessary provisions for ensuring rights to appropriate education for chil- dren with autistic spectrum disorders. However, the implementation and specification of these services are variable. Early intervention for young children with autistic spectrum disorders is expensive, and most local schools need financial help from the state and federal programs to pro- vide appropriate services. The large number of court cases is a symptom of the tension between families and school systems. Case law has yielded an inconsistent pattern of findings that vary according to the characteristics of the individual cases. The number of challenges to decision-making for programming within school systems reflects parentsâ concerns about the adequacy of knowledge and the expertise of school systems in determining their childrenâs education and implementing appropriate techniques. The treatment of autistic spectrum disorders often involves many disciplines and agencies. This confuses lines of financial and intellectual responsibility and complicates assessment and educational planning. When communication between families and school systems goes awry, it can directly affect childrenâs programming and the energy and financial resources that are put into education rather than litigation. Support sys- tems are not generally adequate in undergirding local service delivery programs and maximizing the usefulness of different disciplines and agencies, and transitions between service delivery agencies are often prob- lematic. A number of states have successful models for providing services to children with autism, and mechanisms are becoming increasingly effi- cient and flexible in some states. In most cases, existing agencies at state and federal levels can develop appropriate programs without restructur- ingâwith the possible addition of special task forces or committees de- signed to deal with issues particular to children with autistic spectrum disorders. Recommendations The committee recommends that a variety of steps be taken to ensure that policies are effectively carried out at the state and local levels. 5-1 At the federal level, the National Institutes of Healthâs Autism Coordinating Committee and the Federal Interagency Coordinat- ing Council should jointly appoint a clinical research oversight
CONCLUSIONS AND RECOMMENDATIONS 223 task force of professionals knowledgeable in the field of autistic spectrum disorders, to review and periodically report on basic and applied research programs to the parent agencies and to track program implementation through the State Interagency Coordi- nating Councils or relevant state agencies. Administrative sup- port for these efforts should be provided by the appropriate de- partment of the Secretaryâs office. 5-2 States should have regional resource and training centers with expertise in autistic spectrum disorders to provide training and technical support to local schools. States should also have a mechanism to evaluate the adequacy of current support systems to local schools and recommend ways for improvement. One such mechanism could be an autistic spectrum disorders support systems task force that would examine the relevant provisions for personnel preparation, technical assistance, and demonstration of exemplary programs and would make recommendations as to what would be needed to bring a stateâs support systems into alignment with quality education for children with autistic spec- trum disorders. States should monitor coordination among and transitions between service delivery systems and should develop ways to facilitate these processes. 5-3 Families should have access to consultation and legal knowledge such as provided by an ombudsman who is independent of the school system and who could be a standard part of Individual- ized Educational Plan planning and meetings. The ombudsman should be knowledgeable about autistic spectrum disorders and about relevant law and court decisions. The ombudsmanâs role should include attending IEP meetings, interpreting the school systemâs communications about a child to parents, and propos- ing, at the parentsâ request, alternatives to those presented by the school system. Professional and advocacy groups should work together to provide this service, with the Governorâs Council for Developmental Disabilities or the Autistic Spectrum Disorders Support Systems Task Force responsible for ensuring funding for training and support of this service. 5-4 State and federal agencies should consider ways to work with and support professional and advocacy groups to provide up-to- date, practical, scientifically valid information to parents and practitioners.
224 EDUCATING CHILDREN WITH AUTISM 5-5 States should have clearly defined minimum standards for per- sonnel in educational settings for children with autistic spectrum disorders. For example, at a minimum, teachers should have some special preparation (e.g., preservice course work, equiva- lent inservice training, workshops, and supervised practice in re- search-based practices in autistic spectrum disorders) and should have well-trained, experienced support personnel available to provide ongoing training and additional consultation. 5-6 States should develop a systematic strategy to fund the interven- tions that are necessary for children with autistic spectrum disor- ders in local schools, so that this cost is not borne primarily by the parents or local school systems. State education departments should develop interagency collaborations to pool support for local systems. A state fund for intensive intervention, or more systematic use of Medicaid waivers or other patterns of funding currently in place in some states, should be considered. Families should not be expected to fund or provide the majority of educa- tional programming for their children. 5-7 An updated, accurate summary of case law, consultation services, and mediation mechanisms in autistic spectrum disorders should be made accessible by the Office of Special Education Programs so that schools and parents can understand the options available to them when conflicts arise. 5-8 Since levels of information about autistic spectrum disorders vary greatly within the groups and agencies that make funding and policy decisions about autistic spectrum disorders, including state task forces in education and review panels in federal agencies, it is crucial that persons knowledgeable in the range of needs and interventions associated with autistic spectrum disorders be in- cluded in those decision-making activities. PERSONNEL PREPARATION Conclusions The nature of autistic spectrum disorders and other disabilities that frequently accompany them has significant implications for approaches to education and intervention at school, in the home, and in the commu- nity. Approaches that emphasize the use of specific âpackagesâ of mate- rials and methods associated with comprehensive intervention programs
CONCLUSIONS AND RECOMMENDATIONS 225 may understate the multiple immediate and long-term needs of children for behavior support and for instruction across areas. Teachers are faced with a huge task. They must be familiar with theory and research concerning best practices for children with autistic spectrum disorders, including methods of applied behavior analysis, naturalistic learning, assistive technology, socialization, communication, inclusion, adaptation of the environment, language interventions, assess- ment, and the effective use of data collection systems. Specific problems in generalization and maintenance of behaviors also affect the need for training in methods of teaching children with autistic spectrum disorders. The wide range of IQ scores and verbal skills associated with autistic spectrum disorders, from profound mental retardation and severe lan- guage impairments to superior intelligence, intensify the need for person- nel training. To enable teachers to adequately work with parents and with other professionals to set appropriate goals, teachers need familiar- ity with the course of autistic spectrum disorders and the range of pos- sible outcomes. Teachers learn according to the same principles as their students. Multiple exposures, opportunities to practice, and active involvement in learning are all important aspects of learning for teachers, as well as stu- dents. Many states and community organizations have invested substan- tial funds in teacher preparation through workshops and large-audience lectures by well-known speakers. While such presentations can stimulate enthusiasm, they do not substitute for ongoing consultation and hands- on opportunities to observe and practice skills working with children with autistic spectrum disorders. Personnel preparation remains one of the weakest elements of effec- tive programming for children with autistic spectrum disorders and their families. Ways of building on the knowledge of teachers as they acquire experience with children with autistic spectrum disorders, and ways of keeping skilled personnel within the field, are critical. This is particularly true given recent trends for dependence on relatively inexperienced assis- tants for in-home programs. Providing knowledge about autistic spec- trum disorders to special education and regular education administra- tors, as well as to specialized providers with major roles in early intervention (e.g., speech language pathologists) will be critical in effect- ing change that is proactive. Findings concerning change in educational and other opportunities suggest that administrative attitudes and sup- port are critical in improving schools. Recommendations The committee recommends that relevant state and federal agencies institute an agenda for upgrading personnel preparation for those who
226 EDUCATING CHILDREN WITH AUTISM work with, and are responsible for, children with autistic spectrum disor- ders and their families. These efforts should be part of a larger effort to coordinate and collaborate with the already established infrastructure of special education, regional resource centers, technical assistance pro- grams, personnel preparation, communication sharing, and other relevant aspects of the existing infrastructure. Professionals aware of the special nature of these children are already carrying out many of these recom- mendations in a limited fashion. The committee urges agencies to pro- vide the personnel preparation resources needed for intensified efforts to build a viable support structure for educating children with autistic spec- trum disorders. 6-1 The Office of Special Education Programs should establish a 5- year plan to provide priority funds for preservice and inservice preparation for teachers, paraprofessionals, and other personnel providing services for children with autistic spectrum disorders, including children under age 3 years. 6-2 The need for a team approach involving many professions should be addressed by personnel preparation and practicum work within multidisciplined organizations and teams. 6-3 A special emphasis should be placed on training of trainers. There is a short supply of expertise and experience in the field of educa- tion for children with autistic spectrum disorders, and special attention should be paid to rapidly increase the capabilities of the trainers, who may have experience in special education or related fields, but not in the special skills and practices for children with autistic spectrum disorders. 6-4 The existing support systems that provide short-term training (e.g., technical assistance systems, resource centers, etc.) should include people with special expertise in autistic spectrum disor- ders on their staff. 6-5 The content of the curriculum for children with autistic spectrum disorders should be based on sound research. A continuing pro- gram should be established from such agencies as the National Institute of Mental Health and the National Institute of Child Health and Human Development to translate their research into usable information for practitioners. Work on family research is particularly relevant.
CONCLUSIONS AND RECOMMENDATIONS 227 NEEDED RESEARCH Conclusions There are several distinct and substantial bodies of research relevant to young children with autistic spectrum disorders. One body identifies neurological, behavioral, and developmental characteristics. Another body of research addresses diagnostic practices and related issues of prevalence. Another has examined the effects of comprehensive early treatment programs on the immediate and long-term outcomes of chil- dren and their families. These treatment studies tended to use some form of group experimental design. An additional body of research has ad- dressed individual instructional or intervention approaches, with many studies in this literature using single-subject experimental methodology. Altogether, a large research base exists, but with relatively little integra- tion across bodies of literature. Highly knowledgeable researchers in one area of autistic spectrum disorders may have minimal information from other perspectives, even about studies with direct bearing on their find- ings. Most researchers have not used randomized group comparison de- signs because of the practical and ethical difficulties in randomly assign- ing children and families to treatment groups. In addition, there have been significant controversies over the type of control or contrast group to use and the conditions necessary for demonstrating effectiveness. Al- though a number of comprehensive programs have provided data on their effectiveness, and, in some cases, claims have been made that certain treatments are superior to others, there have been virtually no compari- sons of different comprehensive interventions of equal intensity. Across several of the bodies of literature, the children and families who have participated in studies are often inadequately described. Stan- dardized diagnoses, descriptions of ethnicity, the social class, and associ- ated features of the children (such as mental retardation and language level) are often not specified. Fidelity of treatment implementation has not been consistently assessed. Generalization, particularly across set- tings, and maintenance of treatment effects are not always measured. Though there is little evidence concerning the effectiveness of discipline- specific therapies, there is substantial research supporting the effective- ness of many specific therapeutic techniques. Recommendations 7-1 Funding agencies and professional journals should require minimium standards in design and description of intervention projects. All intervention studies should provide the following information:
228 EDUCATING CHILDREN WITH AUTISM a. Adequate information concerning the children and fami- lies who participated, and who chose not to participate or with- drew from participation, including chronological age, develop- mental assessment data (including verbal and nonverbal IQ levels), standardized diagnoses, gender, race, family characteris- tics, socioeconomic status, and relevant health or other biological impairments; b. description of the intervention in sufficient detail so that an external group could replicate it; detailed documentation is crucial especially if no treatment manual is available; c. fidelity of treatment and degree of implementation; d. specific objective measures of expected outcomes, assessed at regular intervals; and e. measures of outcome that are independent of the interven- tion, in terms of both the evaluators and the measures, and in- clude broad immediate and long-term effects on children and families, particularly generalization and maintenance effects. 7-2 Funders and performers of research should recognize that valu- able information can be provided by a variety of approaches to research in intervention, including group experimental and single-subject designs. 7-3 In order to help educators and consumers make informed deci- sions about appropriate methods of intervention for particular children, federal agencies involved in autistic spectrum disorders initiatives (including the Office of Special Education Programs, the Office of Educational Research and Improvement, the Na- tional Institute of Child Health and Human Development, the National Institute of Mental Health, the National Institute of Neu- rological Disorders and Stroke, and the National Institute on Deaf- ness and Other Communication Disorders) and nonprofit agen- cies with similar national missions (such as Autism Society of America Foundation, Cure Autism Now, and National Alliance for Autism Research) should form a research task force and spe- cifically allocate federal responsibilites for recruiting and funding a comprehensive program of research related to intervention and treatment. This program should include: a. development of more specific, precise measures of impor- tant areas of outcome, such as social functioning, peer relation- ships, spontaneous communication and language, and the acqui- sition of competence in natural contexts (e.g., classroom, home);
CONCLUSIONS AND RECOMMENDATIONS 229 b. definition of appropriate educational skills and sequences in social and cognitive development, informed by normal devel- opmental literature; c. measurement of the effects of the interactions between fam- ily variables (e.g., family structure, family supports, socioeco- nomic status), child factors (such as degree of language impair- ment), and responses to educational interventions (including family-centered, parent training, and other approaches) on out- comes. d. longitudinal treatment studies, where feasible, built on a clinical model with randomly assigned samples of sufficient size to assess the effectiveness of differing modes of treatment. 7-4 Treatment studies should recognize the common components of many comprehensive programs (e.g., standardized curriculum, family training, presence of typically developing peers) and should target and measure, longitudinally when feasible, âactive ingredientsâ and mediating variables that influence the effects of intervention (e.g., communication and interaction opportunities for engagement, levels of interaction and initiation, specific teach- ing techniques, proportion of time in close proximity of peers). The concomitant development of innovative treatments building on these âactive ingredientsâ should be supported. 7-5 In response to amendments in IDEA to make education more outcome oriented, a federal initiative should solicit and fund stud- ies in the following areas, not easily supported under the current review system: a. the development of instruments for measurement of diag- nosis and critical aspects of development, particularly tools for early screening of autistic spectrum disorders and for measure- ment of response to interventions; b. the development and application of sophisticated statisti- cal methods of analysis of change and growth, particularly multi- variate designs and those applicable to small samples; and c. the development and dissemination of novel research de- signs that combine individual and group approaches in ways that minimize biases and maximize the power of small samples. 7-6 Competitively funded initiatives in early education in autistic spectrum disorders should require plans and contain sufficient funding for short- and long-term assessment of child outcomes and measures of program efficacy.
Autism is a word most of us are familiar with. But do we really know what it means?
Children with autism are challenged by the most essential human behaviors. They have difficulty interacting with other people—often failing to see people as people rather than simply objects in their environment. They cannot easily communicate ideas and feelings, have great trouble imagining what others think or feel, and in some cases spend their lives speechless. They frequently find it hard to make friends or even bond with family members. Their behavior can seem bizarre.
Education is the primary form of treatment for this mysterious condition. This means that we place important responsibilities on schools, teachers and children's parents, as well as the other professionals who work with children with autism. With the passage of the Individuals with Disabilities Education Act of 1975, we accepted responsibility for educating children who face special challenges like autism. While we have since amassed a substantial body of research, researchers have not adequately communicated with one another, and their findings have not been integrated into a proven curriculum.
Educating Children with Autism outlines an interdisciplinary approach to education for children with autism. The committee explores what makes education effective for the child with autism and identifies specific characteristics of programs that work. Recommendations are offered for choosing educational content and strategies, introducing interaction with other children, and other key areas.
This book examines some fundamental issues, including:
- How children's specific diagnoses should affect educational assessment and planning
- How we can support the families of children with autism
- Features of effective instructional and comprehensive programs and strategies
- How we can better prepare teachers, school staffs, professionals, and parents to educate children with autism
- What policies at the federal, state, and local levels will best ensure appropriate education, examining strategies and resources needed to address the rights of children with autism to appropriate education.
Children with autism present educators with one of their most difficult challenges. Through a comprehensive examination of the scientific knowledge underlying educational practices, programs, and strategies, Educating Children with Autism presents valuable information for parents, administrators, advocates, researchers, and policy makers.
READ FREE ONLINE
Welcome to OpenBook!
You're looking at OpenBook, NAP.edu's online reading room since 1999. Based on feedback from you, our users, we've made some improvements that make it easier than ever to read thousands of publications on our website.
Do you want to take a quick tour of the OpenBook's features?
Show this book's table of contents , where you can jump to any chapter by name.
...or use these buttons to go back to the previous chapter or skip to the next one.
Jump up to the previous page or down to the next one. Also, you can type in a page number and press Enter to go directly to that page in the book.
To search the entire text of this book, type in your search term here and press Enter .
Share a link to this book page on your preferred social network or via email.
View our suggested citation for this chapter.
Ready to take your reading offline? Click here to buy this book in print or download it as a free PDF, if available.
Get Email Updates
Do you enjoy reading reports from the Academies online for free ? Sign up for email notifications and we'll let you know about new publications in your areas of interest when they're released.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Autism Spectrum Disorder
What is asd.
Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how people interact with others, communicate, learn, and behave. Although autism can be diagnosed at any age, it is described as a “developmental disorder” because symptoms generally appear in the first 2 years of life.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) , a guide created by the American Psychiatric Association that health care providers use to diagnose mental disorders, people with ASD often have:
- Difficulty with communication and interaction with other people
- Restricted interests and repetitive behaviors
- Symptoms that affect their ability to function in school, work, and other areas of life
Autism is known as a “spectrum” disorder because there is wide variation in the type and severity of symptoms people experience.
People of all genders, races, ethnicities, and economic backgrounds can be diagnosed with ASD. Although ASD can be a lifelong disorder, treatments and services can improve a person’s symptoms and daily functioning. The American Academy of Pediatrics recommends that all children receive screening for autism. Caregivers should talk to their child’s health care provider about ASD screening or evaluation.
What are the signs and symptoms of ASD?
The list below gives some examples of common types of behaviors in people diagnosed with ASD. Not all people with ASD will have all behaviors, but most will have several of the behaviors listed below.
Social communication / interaction behaviors may include:
- Making little or inconsistent eye contact
- Appearing not to look at or listen to people who are talking
- Infrequently sharing interest, emotion, or enjoyment of objects or activities (including infrequent pointing at or showing things to others)
- Not responding or being slow to respond to one’s name or to other verbal bids for attention
- Having difficulties with the back and forth of conversation
- Often talking at length about a favorite subject without noticing that others are not interested or without giving others a chance to respond
- Displaying facial expressions, movements, and gestures that do not match what is being said
- Having an unusual tone of voice that may sound sing-song or flat and robot-like
- Having trouble understanding another person’s point of view or being unable to predict or understand other people’s actions
- Difficulties adjusting behaviors to social situations
- Difficulties sharing in imaginative play or in making friends
Restrictive / repetitive behaviors may include:
- Repeating certain behaviors or having unusual behaviors, such as repeating words or phrases (a behavior called echolalia)
- Having a lasting intense interest in specific topics, such as numbers, details, or facts
- Showing overly focused interests, such as with moving objects or parts of objects
- Becoming upset by slight changes in a routine and having difficulty with transitions
- Being more sensitive or less sensitive than other people to sensory input, such as light, sound, clothing, or temperature
People with ASD may also experience sleep problems and irritability.
People on the autism spectrum also may have many strengths, including:
- Being able to learn things in detail and remember information for long periods of time
- Being strong visual and auditory learners
- Excelling in math, science, music, or art
What are the causes and risk factors for ASD?
Researchers don’t know the primary causes of ASD, but studies suggest that a person’s genes can act together with aspects of their environment to affect development in ways that lead to ASD. Some factors that are associated with an increased likelihood of developing ASD include:
- Having a sibling with ASD
- Having older parents
- Having certain genetic conditions (such as Down syndrome or Fragile X syndrome)
- Having a very low birth weight
How is ASD diagnosed?
Health care providers diagnose ASD by evaluating a person’s behavior and development. ASD can usually be reliably diagnosed by age 2. It is important to seek an evaluation as soon as possible. The earlier ASD is diagnosed, the sooner treatments and services can begin.
Diagnosis in young children
Diagnosis in young children is often a two-stage process.
Stage 1: General developmental screening during well-child checkups
Every child should receive well-child check-ups with a pediatrician or an early childhood health care provider. The American Academy of Pediatrics recommends that all children receive screening for developmental delays at their 9-, 18-, and 24- or 30-month well-child visits, with specific autism screenings at their 18- and 24-month well-child visits. A child may receive additional screening if they have a higher likelihood of ASD or developmental problems. Children with a higher likelihood of ASD include those who have a family member with ASD, show some behaviors that are typical of ASD, have older parents, have certain genetic conditions, or who had a very low birth weight.
Considering caregivers’ experiences and concerns is an important part of the screening process for young children. The health care provider may ask questions about the child’s behaviors and evaluate those answers in combination with information from ASD screening tools and clinical observations of the child. Read more about screening instruments on the Centers for Disease Control and Prevention (CDC) website.
If a child shows developmental differences in behavior or functioning during this screening process, the health care provider may refer the child for additional evaluation.
Stage 2: Additional diagnostic evaluation
It is important to accurately detect and diagnose children with ASD as early as possible, as this will shed light on their unique strengths and challenges. Early detection also can help caregivers determine which services, educational programs, and behavioral therapies are most likely to be helpful for their child.
A team of health care providers who have experience diagnosing ASD will conduct the diagnostic evaluation. This team may include child neurologists, developmental pediatricians, speech-language pathologists, child psychologists and psychiatrists, educational specialists, and occupational therapists.
The diagnostic evaluation is likely to include:
- Medical and neurological examinations
- Assessment of the child’s cognitive abilities
- Assessment of the child’s language abilities
- Observation of the child’s behavior
- An in-depth conversation with the child’s caregivers about the child’s behavior and development
- Assessment of age-appropriate skills needed to complete daily activities independently, such as eating, dressing, and toileting
Because ASD is a complex disorder that sometimes occurs with other illnesses or learning disorders, the comprehensive evaluation may include:
- Blood tests
- Hearing test
The evaluation may lead to a formal diagnosis and recommendations for treatment.
Diagnosis in older children and adolescents
Caregivers and teachers are often the first to recognize ASD symptoms in older children and adolescents who attend school. The school’s special education team may perform an initial evaluation and then recommend that a child undergo additional evaluation with their primary health care provider or a health care provider who specialize in ASD.
A child’s caregivers may talk with these health care providers about their child’s social difficulties, including problems with subtle communication. For example, some children may have problems understanding tone of voice, facial expressions, or body language. Older children and adolescents may have trouble understanding figures of speech, humor, or sarcasm. They also may have trouble forming friendships with peers.
Diagnosis in adults
Diagnosing ASD in adults is often more difficult than diagnosing ASD in children. In adults, some ASD symptoms can overlap with symptoms of other mental health disorders, such as anxiety disorder or attention-deficit/hyperactivity disorder (ADHD).
Adults who notice signs of ASD should talk with a health care provider and ask for a referral for an ASD evaluation. Although evaluation for ASD in adults is still being refined, adults may be referred to a neuropsychologist, psychologist, or psychiatrist who has experience with ASD. The expert will ask about:
- Social interaction and communication challenges
- Sensory issues
- Repetitive behaviors
- Restricted interests
The evaluation also may include a conversation with caregivers or other family members to learn about the person’s early developmental history, which can help ensure an accurate diagnosis.
Receiving a correct diagnosis of ASD as an adult can help a person understand past challenges, identify personal strengths, and find the right kind of help. Studies are underway to determine the types of services and supports that are most helpful for improving the functioning and community integration of autistic transition-age youth and adults.
What treatment options are available for ASD?
Treatment for ASD should begin as soon as possible after diagnosis. Early treatment for ASD is important as proper care and services can reduce individuals’ difficulties while helping them build on their strengths and learn new skills.
People with ASD may face a wide range of issues, which means that there is no single best treatment for ASD. Working closely with a health care provider is an important part of finding the right combination of treatment and services.
A health care provider may prescribe medication to treat specific symptoms. With medication, a person with ASD may have fewer problems with:
- Irritability
- Repetitive behavior
- Hyperactivity
- Attention problems
- Anxiety and depression
Read more about the latest medication warnings, patient medication guides, and information on newly approved medications at the Food and Drug Administration (FDA) website .
Behavioral, psychological, and educational interventions
People with ASD may be referred to a health care provider who specializes in providing behavioral, psychological, educational, or skill-building interventions. These programs are often highly structured and intensive, and they may involve caregivers, siblings, and other family members. These programs may help people with ASD:
- Learn social, communication, and language skills
- Reduce behaviors that interfere with daily functioning
- Increase or build upon strengths
- Learn life skills for living independently
Other resources
Many services, programs, and other resources are available to help people with ASD. Here are some tips for finding these additional services:
- Contact your health care provider, local health department, school, or autism advocacy group to learn about special programs or local resources.
- Find an autism support group. Sharing information and experiences can help people with ASD and their caregivers learn about treatment options and ASD-related programs.
- Record conversations and meetings with health care providers and teachers. This information may help when it’s time to decide which programs and services are appropriate.
- Keep copies of health care reports and evaluations. This information may help people with ASD qualify for special programs.
How can I find a clinical trial for ASD?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on ASD : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Where can I learn more about ASD?
Free brochures and shareable resources.
- Autism Spectrum Disorder : This brochure provides information about the symptoms, diagnosis, and treatment of ASD. Also available en español .
- Digital Shareables on Autism Spectrum Disorder : Help support ASD awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about ASD.
Federal resources
- Eunice Kennedy Shriver National Institute of Child Health and Human Development
- National Institute of Neurological Disorders and Stroke
- National Institute on Deafness and Other Communication Disorders
- Centers for Disease Control and Prevention (CDC)
- Interagency Autism Coordinating Committee
- MedlinePlus (also available en español )
Research and statistics
- Science News About Autism Spectrum Disorder : This NIMH webpage provides press releases and announcements about ASD.
- Research Program on Autism Spectrum Disorders : This NIMH program supports research focused on the characterization, pathophysiology, treatment, and outcomes of ASD and related disorders.
- Statistics: Autism Spectrum Disorder : This NIMH webpage provides information on the prevalence of ASD in the U.S.
- Data & Statistics on Autism Spectrum Disorder : This CDC webpage provides data, statistics, and tools about prevalence and demographic characteristics of ASD.
- Autism and Developmental Disabilities Monitoring (ADDM) Network : This CDC-funded program collects data to better understand the population of children with ASD.
- Biomarkers Consortium - The Autism Biomarkers Consortium for Clinical Trials (ABC-CT) : This Foundation for the National Institutes of Health project seeks to establish biomarkers to improve treatments for children with ASD.
Last Reviewed: February 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
- Patient Care & Health Information
- Diseases & Conditions
- Autism spectrum disorder
Autism spectrum disorder is a condition related to brain development that impacts how a person perceives and socializes with others, causing problems in social interaction and communication. The disorder also includes limited and repetitive patterns of behavior. The term "spectrum" in autism spectrum disorder refers to the wide range of symptoms and severity.
Autism spectrum disorder includes conditions that were previously considered separate — autism, Asperger's syndrome, childhood disintegrative disorder and an unspecified form of pervasive developmental disorder. Some people still use the term "Asperger's syndrome," which is generally thought to be at the mild end of autism spectrum disorder.
Autism spectrum disorder begins in early childhood and eventually causes problems functioning in society — socially, in school and at work, for example. Often children show symptoms of autism within the first year. A small number of children appear to develop normally in the first year, and then go through a period of regression between 18 and 24 months of age when they develop autism symptoms.
While there is no cure for autism spectrum disorder, intensive, early treatment can make a big difference in the lives of many children.
Products & Services
- Children’s Book: My Life Beyond Autism
Some children show signs of autism spectrum disorder in early infancy, such as reduced eye contact, lack of response to their name or indifference to caregivers. Other children may develop normally for the first few months or years of life, but then suddenly become withdrawn or aggressive or lose language skills they've already acquired. Signs usually are seen by age 2 years.
Each child with autism spectrum disorder is likely to have a unique pattern of behavior and level of severity — from low functioning to high functioning.
Some children with autism spectrum disorder have difficulty learning, and some have signs of lower than normal intelligence. Other children with the disorder have normal to high intelligence — they learn quickly, yet have trouble communicating and applying what they know in everyday life and adjusting to social situations.
Because of the unique mixture of symptoms in each child, severity can sometimes be difficult to determine. It's generally based on the level of impairments and how they impact the ability to function.
Below are some common signs shown by people who have autism spectrum disorder.
Social communication and interaction
A child or adult with autism spectrum disorder may have problems with social interaction and communication skills, including any of these signs:
- Fails to respond to his or her name or appears not to hear you at times
- Resists cuddling and holding, and seems to prefer playing alone, retreating into his or her own world
- Has poor eye contact and lacks facial expression
- Doesn't speak or has delayed speech, or loses previous ability to say words or sentences
- Can't start a conversation or keep one going, or only starts one to make requests or label items
- Speaks with an abnormal tone or rhythm and may use a singsong voice or robot-like speech
- Repeats words or phrases verbatim, but doesn't understand how to use them
- Doesn't appear to understand simple questions or directions
- Doesn't express emotions or feelings and appears unaware of others' feelings
- Doesn't point at or bring objects to share interest
- Inappropriately approaches a social interaction by being passive, aggressive or disruptive
- Has difficulty recognizing nonverbal cues, such as interpreting other people's facial expressions, body postures or tone of voice
Patterns of behavior
A child or adult with autism spectrum disorder may have limited, repetitive patterns of behavior, interests or activities, including any of these signs:
- Performs repetitive movements, such as rocking, spinning or hand flapping
- Performs activities that could cause self-harm, such as biting or head-banging
- Develops specific routines or rituals and becomes disturbed at the slightest change
- Has problems with coordination or has odd movement patterns, such as clumsiness or walking on toes, and has odd, stiff or exaggerated body language
- Is fascinated by details of an object, such as the spinning wheels of a toy car, but doesn't understand the overall purpose or function of the object
- Is unusually sensitive to light, sound or touch, yet may be indifferent to pain or temperature
- Doesn't engage in imitative or make-believe play
- Fixates on an object or activity with abnormal intensity or focus
- Has specific food preferences, such as eating only a few foods, or refusing foods with a certain texture
As they mature, some children with autism spectrum disorder become more engaged with others and show fewer disturbances in behavior. Some, usually those with the least severe problems, eventually may lead normal or near-normal lives. Others, however, continue to have difficulty with language or social skills, and the teen years can bring worse behavioral and emotional problems.
When to see a doctor
Babies develop at their own pace, and many don't follow exact timelines found in some parenting books. But children with autism spectrum disorder usually show some signs of delayed development before age 2 years.
If you're concerned about your child's development or you suspect that your child may have autism spectrum disorder, discuss your concerns with your doctor. The symptoms associated with the disorder can also be linked with other developmental disorders.
Signs of autism spectrum disorder often appear early in development when there are obvious delays in language skills and social interactions. Your doctor may recommend developmental tests to identify if your child has delays in cognitive, language and social skills, if your child:
- Doesn't respond with a smile or happy expression by 6 months
- Doesn't mimic sounds or facial expressions by 9 months
- Doesn't babble or coo by 12 months
- Doesn't gesture — such as point or wave — by 14 months
- Doesn't say single words by 16 months
- Doesn't play "make-believe" or pretend by 18 months
- Doesn't say two-word phrases by 24 months
- Loses language skills or social skills at any age
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.

From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
Autism spectrum disorder has no single known cause. Given the complexity of the disorder, and the fact that symptoms and severity vary, there are probably many causes. Both genetics and environment may play a role.
- Genetics. Several different genes appear to be involved in autism spectrum disorder. For some children, autism spectrum disorder can be associated with a genetic disorder, such as Rett syndrome or fragile X syndrome. For other children, genetic changes (mutations) may increase the risk of autism spectrum disorder. Still other genes may affect brain development or the way that brain cells communicate, or they may determine the severity of symptoms. Some genetic mutations seem to be inherited, while others occur spontaneously.
- Environmental factors. Researchers are currently exploring whether factors such as viral infections, medications or complications during pregnancy, or air pollutants play a role in triggering autism spectrum disorder.
No link between vaccines and autism spectrum disorder
One of the greatest controversies in autism spectrum disorder centers on whether a link exists between the disorder and childhood vaccines. Despite extensive research, no reliable study has shown a link between autism spectrum disorder and any vaccines. In fact, the original study that ignited the debate years ago has been retracted due to poor design and questionable research methods.
Avoiding childhood vaccinations can place your child and others in danger of catching and spreading serious diseases, including whooping cough (pertussis), measles or mumps.
Risk factors
The number of children diagnosed with autism spectrum disorder is rising. It's not clear whether this is due to better detection and reporting or a real increase in the number of cases, or both.
Autism spectrum disorder affects children of all races and nationalities, but certain factors increase a child's risk. These may include:
- Your child's sex. Boys are about four times more likely to develop autism spectrum disorder than girls are.
- Family history. Families who have one child with autism spectrum disorder have an increased risk of having another child with the disorder. It's also not uncommon for parents or relatives of a child with autism spectrum disorder to have minor problems with social or communication skills themselves or to engage in certain behaviors typical of the disorder.
- Other disorders. Children with certain medical conditions have a higher than normal risk of autism spectrum disorder or autism-like symptoms. Examples include fragile X syndrome, an inherited disorder that causes intellectual problems; tuberous sclerosis, a condition in which benign tumors develop in the brain; and Rett syndrome, a genetic condition occurring almost exclusively in girls, which causes slowing of head growth, intellectual disability and loss of purposeful hand use.
- Extremely preterm babies. Babies born before 26 weeks of gestation may have a greater risk of autism spectrum disorder.
- Parents' ages. There may be a connection between children born to older parents and autism spectrum disorder, but more research is necessary to establish this link.
Complications
Problems with social interactions, communication and behavior can lead to:
- Problems in school and with successful learning
- Employment problems
- Inability to live independently
- Social isolation
- Stress within the family
- Victimization and being bullied
More Information
- Autism spectrum disorder and digestive symptoms
There's no way to prevent autism spectrum disorder, but there are treatment options. Early diagnosis and intervention is most helpful and can improve behavior, skills and language development. However, intervention is helpful at any age. Though children usually don't outgrow autism spectrum disorder symptoms, they may learn to function well.
- Autism spectrum disorder (ASD). Centers for Disease Control and Prevention. https://www.cdc.gov/ncbddd/autism/facts.html. Accessed April 4, 2017.
- Uno Y, et al. Early exposure to the combined measles-mumps-rubella vaccine and thimerosal-containing vaccines and risk of autism spectrum disorder. Vaccine. 2015;33:2511.
- Taylor LE, et al. Vaccines are not associated with autism: An evidence-based meta-analysis of case-control and cohort studies. Vaccine. 2014;32:3623.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Overview of management. https://www.uptodate.com/home. Accessed April 4, 2017.
- Autism spectrum disorder. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://dsm.psychiatryonline.org. Accessed April 4, 2017.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Complementary and alternative therapies. https://www.uptodate.com/home. Accessed April 4, 2017.
- Augustyn M. Autism spectrum disorder: Terminology, epidemiology, and pathogenesis. https://www.uptodate.com/home. Accessed April 4, 2017.
- Bridgemohan C. Autism spectrum disorder: Surveillance and screening in primary care. https://www.uptodate.com/home. Accessed April 4, 2017.
- Levy SE, et al. Complementary and alternative medicine treatments for children with autism spectrum disorder. Child and Adolescent Psychiatric Clinics of North America. 2015;24:117.
- Brondino N, et al. Complementary and alternative therapies for autism spectrum disorder. Evidence-Based Complementary and Alternative Medicine. http://dx.doi.org/10.1155/2015/258589. Accessed April 4, 2017.
- Volkmar F, et al. Practice parameter for the assessment and treatment of children and adolescents with autism spectrum disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53:237.
- Autism spectrum disorder (ASD). Eunice Kennedy Shriver National Institute of Child Health and Human Development. https://www.nichd.nih.gov/health/topics/autism/Pages/default.aspx. Accessed April 4, 2017.
- American Academy of Pediatrics policy statement: Sensory integration therapies for children with developmental and behavioral disorders. Pediatrics. 2012;129:1186.
- James S, et al. Chelation for autism spectrum disorder (ASD). Cochrane Database of Systematic Reviews. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD010766.pub2/abstract;jsessionid=9467860F2028507DFC5B69615F622F78.f04t02. Accessed April 4, 2017.
- Van Schalkwyk GI, et al. Autism spectrum disorders: Challenges and opportunities for transition to adulthood. Child and Adolescent Psychiatric Clinics of North America. 2017;26:329.
- Autism. Natural Medicines. https://naturalmedicines.therapeuticresearch.com. Accessed April 4, 2017.
- Autism: Beware of potentially dangerous therapies and products. U.S. Food and Drug Administration. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm394757.htm?source=govdelivery&utm_medium=email&utm_source=govdelivery. Accessed May 19, 2017.
- Drutz JE. Autism spectrum disorder and chronic disease: No evidence for vaccines or thimerosal as a contributing factor. https://www.uptodate.com/home. Accessed May 19, 2017.
- Weissman L, et al. Autism spectrum disorder in children and adolescents: Behavioral and educational interventions. https://www.uptodate.com/home. Accessed May 19, 2017.
- Huebner AR (expert opinion). Mayo Clinic, Rochester, Minn. June 7, 2017.
Associated Procedures
- Cognitive behavioral therapy
News from Mayo Clinic
- Understanding autism: The path to diagnosis, awareness and support April 28, 2024, 11:00 a.m. CDT
- 10 significant studies from Mayo Clinic's Center for Individualized Medicine in 2023 Dec. 30, 2023, 12:00 p.m. CDT
- Mayo Clinic 'mini-brain' study reveals possible key link to autism spectrum disorder Aug. 10, 2023, 04:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Signs and Symptoms
- Living with Autism Spectrum Disorder
- Frequently Asked Questions (FAQs)
- Data and Statistics on Autism Spectrum Disorder
- Autism Materials and Resources
- Diagnosis ASD
- Information on ASD for Healthcare Providers
- Acceptance Month Partner Toolkit
Related Topics:
- Show All Home
- 2023 Community Report on Autism
- Autism Data Visualization Tool
About Autism Spectrum Disorder
- Autism spectrum disorder (ASD) is a developmental disability caused by differences in the brain.
- Some people with ASD have a known difference, such as a genetic condition. Other causes are not yet known.
- Scientists believe there are multiple causes of ASD that act together to change the most common ways people develop. We still have much to learn about these causes and how they impact people with ASD.
- Early intervention services can greatly improve the development of a child with ASD.

People with ASD may behave, communicate, interact, and learn in ways that are different from most other people. There is often nothing about how they look that sets them apart from other people. The abilities of people with ASD can vary significantly. For example, some people with ASD may have advanced conversation skills whereas others may be nonverbal. Some people with ASD need a lot of help in their daily lives; others can work and live with little to no support.
ASD begins before the age of 3 years and can last throughout a person's life, although symptoms may improve over time. Some children show ASD symptoms within the first 12 months of life. In others, symptoms may not show up until 24 months of age or later. Some children with ASD gain new skills and meet developmental milestones until around 18 to 24 months of age, and then they stop gaining new skills or lose the skills they once had.
As children with ASD become adolescents and young adults, they may have difficulties developing and maintaining friendships, communicating with peers and adults, or understanding what behaviors are expected in school or on the job. They may come to the attention of healthcare providers because they also have conditions such as anxiety, depression, or attention-deficit/hyperactivity disorder (ADHD), which occur more often in people with ASD than in people without ASD.

Signs and symptoms
People with ASD often have problems with social communication and interaction, and restricted or repetitive behaviors or interests. People with ASD may also have different ways of learning, moving, or paying attention. These characteristics can make life very challenging . It is important to note that some people without ASD might also have some of these symptoms.
As a parent, you already have what it takes to help your young child learn and grow. CDC has developed materials to help you track your child's developmental milestones and share that progress, or any concerns, with your child's doctor at every check-up.
Track your child's development
Risk factors.
There is not just one cause of ASD. Many different factors have been identified that may make a child more likely to have ASD, including environmental, biologic, and genetic factors.
Although we know little about specific causes, the available evidence suggests that the following may put children at greater risk for developing ASD:
- Having a sibling with ASD
- Having certain genetic or chromosomal conditions, such as fragile X syndrome or tuberous sclerosis
- Experiencing complications at birth
- Being born to older parents
CDC is currently working on one of the largest US studies to date on ASD. This study, called the Study to Explore Early Development (SEED), was designed to look at the risk factors and behaviors related to ASD. CDC is now conducting a follow-up study of older children who were enrolled in SEED to determine the health, functioning, and needs of people with ASD and other developmental disabilities as they mature.
Screening and diagnosis
Diagnosing ASD can be difficult since there is no medical test, like a blood test, to diagnose the disorder. Doctors look at the child's behavior and development to make a diagnosis.
ASD can sometimes be detected at 18 months of age or younger. By age 2 years, a diagnosis by an experienced professional can be considered reliable. 1 However, many children do not receive a final diagnosis until they are much older. Some people are not diagnosed until they are adolescents or adults. This delay means that people with ASD might not get the early help they need.

Current treatments for ASD seek to reduce symptoms that interfere with daily functioning and quality of life. ASD affects each person differently, meaning that people with ASD have unique strengths and challenges and different treatment needs. 2 Treatment plans usually involve multiple professionals and are catered to the individual.
What CDC is doing
Promoting early identification of asd.
We naturally think of a child's growth as height and weight, but from birth to 5 years, a child should reach milestones in how they play, learn, speak, act, and move. A delay in any of these areas could be a sign of ASD or other developmental disability.
Through the Learn the Signs. Act Early. program, CDC and its partners aim to improve early identification of children with ASD and other developmental disabilities by promoting developmental monitoring , so children and families can get the services and support they need.
Did you know?
Understanding risk factors and causes of asd.
Understanding the risk factors that make a person more likely to develop ASD will help us learn more about the causes. CDC is currently funding and working on one of the largest US studies to date, called Study to Explore Early Development (SEED) .
SEED will help identify factors that may put children at risk for ASD and other developmental disabilities. SEED is a multi-year study being conducted at six sites and a data coordinating center, called the Centers for Autism and Developmental Disabilities Research and Epidemiology (CADDRE) network.
Determining how many people have ASD
There continue to be many children living with ASD who need services and support, both now and as they grow into adolescence and adulthood.
By studying the number of people identified with ASD over time, we can find out if the number is rising, dropping, or staying the same. We can also compare the number of children with ASD in different areas of the country and different groups of people. This information can help us look for causes of ASD.
CDC's Autism and Developmental Disabilities Monitoring (ADDM) Network has been estimating the number of 8-year-old children with ASD in the United States since 2000. ASD occurs in all racial, ethnic, and socioeconomic groups. It is more than 4 times more common among boys than among girls.
If you’re concerned
Research shows that early intervention services can greatly improve a child's development. 3 4 In order to make sure your child reaches their full potential, it is very important to receive services as soon as possible. Contact your child's doctor if you think your child might have ASD or if you have any other concerns about the way your child plays, learns, speaks, or acts.
Referral to a specialist
If you are still concerned, ask the doctor for a referral to a specialist who can do a more in-depth evaluation of your child. Specialists who can do a more in-depth evaluation and make a diagnosis include
- Developmental pediatricians (doctors who have special training in child development and children with special needs)
- Child neurologists (doctors who work on the brain, spine, and nerves)
- Child psychologists or psychiatrists (doctors who know about the human mind)
Free evaluations
At the same time, call your state's public early childhood system to request a free evaluation , sometimes called a Child Find evaluation, to find out if your child qualifies for intervention services. You do not need to wait for a doctor's referral or a medical diagnosis to make this call. Where to call for a free evaluation from the state depends on your child's age.
If your child is not yet 3 years old
- Contact your local early intervention system.
- You can find the right contact information for your state by calling the Early Childhood Technical Assistance Center (ECTA) at 919-962-2001.
- Or visit the ECTA website.
If your child is 3 years old or older
- If your child is 3 years old or older, contact your local public school system.
- Even if your child is not yet old enough for kindergarten or enrolled in a public school, call your local elementary school or board of education and ask to speak with someone who can help you have your child evaluated.
- If you're not sure who to contact, call the ECTA at 919-962-2001.
- Lord C, Risi S, DiLavore PS, Shulman C, Thurm A, Pickles A. Autism from 2 to 9 years of age . Arch Gen Psychiatry . 2006;63(6):694-701.
- Hyman SL, Levy SE, Myers SM; COUNCIL ON CHILDREN WITH DISABILITIES, SECTION ON DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS. Identification, Evaluation, and Management of Children With Autism Spectrum Disorder. Pediatrics . 2020;145(1):e20193447.
- Handleman, Jan S., and Sandra L. Harris, eds. Preschool education programs for children with autism . Austin, TX: Pro-Ed, 2001.
- National Research Council. Educating Children with Autism . National Academies Press, 2001.
Autism Spectrum Disorder (ASD)
Autism spectrum disorder (ASD) is a developmental disability that can cause significant social, communication and behavioral challenges. CDC is committed to continuing to provide essential data on ASD and develop resources that help identify children with ASD as early as possible.
For Everyone
Health care providers, public health.
Prevalence of Autism Spectrum Disorder Among Children and Adolescents in the United States from 2021 to 2022
- Brief Report
- Published: 22 May 2024
Cite this article

- Xiaofang Yan 1 na1 ,
- Yanmei Li 1 na1 ,
- Qishan Li 1 ,
- Qian Li 1 ,
- Guifeng Xu 2 ,
- Jinhua Lu 3 &
- Wenhan Yang ORCID: orcid.org/0000-0002-4786-1516 1
109 Accesses
2 Altmetric
Explore all metrics
The prevalence of autism spectrum disorder (ASD) among children and adolescents seem to be high in countries around the world, and it’s worth understanding the latest prevalence and trends of ASD in children and adolescents. The purpose of this study was to examine the latest prevalence and decade trend of ASD among individuals aged 3–17 years in the United States.
A total of 13,198 individuals aged 3–17 years were included. Annual data were examined from the National Health Interview Survey (2021–2022). Weighted prevalence for each of the selected developmental disabilities were calculated.
This cross-sectional study estimated the weighted prevalence of autism spectrum disorder were 3.05, 3.79, and 3.42% among individuals aged 3–17 years in the US in 2021, 2022, and the 2-year overall, respectively. We also observed a decade-long upward trend even after adjusting for demographic characteristics ( P for trend < .05).
The results of this study showed that the prevalence of ASD among children and adolescents aged 3–17 years in the United States remained high and has increased over the past decade. The further investigation is necessary to evaluate potential modifiable risk factors and causes of ASD.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
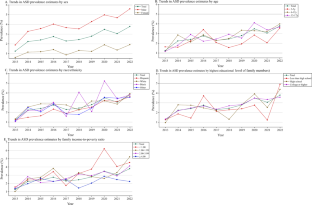
Data Availability
The original contributions presented in the study are publicly available. The datasets analyzed during current study are available at NHIS online website: https://www.cdc.gov/nchs/nhis/index.htm
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5™, 5th edn. https://doi.org/10.1176/appi.books.9780890425596
Barry, C. L., Epstein, A. J., Marcus, S. C., Kennedy-Hendricks, A., Candon, M. K., Xie, M., & Mandell, D. S. (2017). Effects of state insurance mandates on health care use and spending for autism spectrum disorder. Health Affairs (project Hope), 36 (10), 1754–1761. https://doi.org/10.1377/hlthaff.2017.0515
Article PubMed Google Scholar
Boyle, C. A., Boulet, S., Schieve, L. A., Cohen, R. A., Blumberg, S. J., Yeargin-Allsopp, M., Visser, S., & Kogan, M. D. (2011). Trends in the prevalence of developmental disabilities in US children, 1997–2008. Pediatrics, 127 (6), 1034–1042. https://doi.org/10.1542/peds.2010-2989
Buescher, A. V. S., Cidav, Z., Knapp, M., & Mandell, D. S. (2014). Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatrics, 168 (8), 721–728. https://doi.org/10.1001/jamapediatrics.2014.210
Cervantes, P. E., Matheis, M., Estabillo, J., Seag, D. E. M., Nelson, K. L., Peth-Pierce, R., Hoagwood, K. E., & Horwitz, S. M. (2021). Trends over a decade in NIH funding for autism spectrum disorder services research. Journal of Autism and Developmental Disorders, 51 (8), 2751–2763. https://doi.org/10.1007/s10803-020-04746-3
Chatterji, P., Decker, S. L., & Markowitz, S. (2015). The effects of mandated health insurance benefits for autism on out-of-ocket costs and access to treatment. Journal of Policy Analysis and Management [the Journal of the Association for Public Policy Analysis and Management] , 34 (2), 328–353. Retrieved from https://pubmed.ncbi.nlm.nih.gov/25893237
Christensen, D. L., Baio, J., Van Naarden Braun, K., Bilder, D., Charles, J., Constantino, J. N., Daniels, J., Durkin, M. S., Fitzgerald, R. T., Kurzius-Spencer, M., Lee, L.-C., Pettygrove, S., Robinson, C., Schulz, E., Wells, C., Wingate, M. S., Zahorodny, W., & Yeargin-Allsopp, M. (2016). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 Sites, United States, 2012. Morbidity and Mortality Weekly Report: Surveillance Summaries (Washington, DC: 2002) , 65 (3). https://doi.org/10.15585/mmwr.ss6503a1
Durkin, M. S., Maenner, M. J., Baio, J., Christensen, D., Daniels, J., Fitzgerald, R., Imm, P., Lee, L.-C., Schieve, L. A., Van Naarden Braun, K., Wingate, M. S., & Yeargin-Allsopp, M. (2017). Autism spectrum disorder among US children (2002–2010): Socioeconomic, racial, and ethnic disparities. American Journal of Public Health, 107 (11), 1818–1826. https://doi.org/10.2105/AJPH.2017.304032
Article PubMed PubMed Central Google Scholar
Li, Q., Li, Y., Liu, B., Chen, Q., Xing, X., Xu, G., & Yang, W. (2022a). Prevalence of autism spectrum disorder among children and adolescents in the United States from 2019 to 2020. JAMA Pediatrics, 176 (9), 943–945. https://doi.org/10.1001/jamapediatrics.2022.1846
Li, Y.-A., Chen, Z.-J., Li, X.-D., Gu, M.-H., Xia, N., Gong, C., Zhou, Z.-W., Yasin, G., Xie, H.-Y., Wei, X.-P., Liu, Y.-L., Han, X.-H., Lu, M., Xu, J., & Huang, X.-L. (2022b). Epidemiology of autism spectrum disorders: global burden of disease 2019 and bibliometric analysis of risk factors. Frontiers in Pediatrics, 10 , 972809. https://doi.org/10.3389/fped.2022.972809
Lin, J., Costa, M. A., Rezende, V. L., Nascimento, R. R., Ambrósio, P. G., Madeira, K., Pearson, D. A., & Gonçalves, C. L. (2023). Risk factors and clinical profile of autism spectrum disorder in Southern Brazil. Journal of Psychiatric Research, 169 , 105–112. https://doi.org/10.1016/j.jpsychires.2023.11.033
Lyall, K., Croen, L., Daniels, J., Fallin, M. D., Ladd-Acosta, C., Lee, B. K., Park, B. Y., Snyder, N. W., Schendel, D., Volk, H., Windham, G. C., & Newschaffer, C. (2017). The changing epidemiology of autism spectrum disorders. Annual Review of Public Health . https://doi.org/10.1146/annurev-publhealth-031816-044318
Maenner, M. J., Shaw, K. A., Bakian, A. V., Bilder, D. A., Durkin, M. S., Esler, A., Furnier, S. M., Hallas, L., Hall-Lande, J., Hudson, A., Hughes, M. M., Patrick, M., Pierce, K., Poynter, J. N., Salinas, A., Shenouda, J., Vehorn, A., Warren, Z., Constantino, J. N., & Cogswell, M. E. (2021). Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 Sites, United States, 2018. MMWR Surveillance Summary, 70 (11), 1–16. https://doi.org/10.15585/mmwr.ss7011a1
Article Google Scholar
Mandell, D. S., Barry, C. L., Marcus, S. C., Xie, M., Shea, K., Mullan, K., & Epstein, A. J. (2016). Effects of autism spectrum disorder insurance mandates on the treated prevalence of autism spectrum disorder. JAMA Pediatrics, 170 (9), 887–893. https://doi.org/10.1001/jamapediatrics.2016.1049
Moriarity, C., Parsons, V. L., Jonas, K., Schar, B. G., Bose, J., & Bramlett, M. D. (2022). Sample design and estimation structures for the national health interview survey, 2016–2025. Vital Health Stat, 1 (191), 1–30.
Google Scholar
NCHS. National health interview survey: Methods. Retrieved 12 July from https://www.cdc.gov/nchs/nhis/methods.htm
Nevison, C. D. (2014). A comparison of temporal trends in United States autism prevalence to trends in suspected environmental factors. Environmental Health: A Global Access Science Source, 13 , 73. https://doi.org/10.1186/1476-069X-13-73
Nevison, C., Blaxill, M., & Zahorodny, W. (2018). California autism prevalence trends from 1931 to 2014 and comparison to national ASD data from IDEA and ADDM. Journal of Autism and Developmental Disorders, 48 (12), 4103–4117. https://doi.org/10.1007/s10803-018-3670-2
Panda, P. K., Gupta, J., Chowdhury, S. R., Kumar, R., Meena, A. K., Madaan, P., Sharawat, I. K., & Gulati, S. (2021). Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: A systematic review and meta-analysis. Journal of Tropical Pediatrics . https://doi.org/10.1093/tropej/fmaa122
Salari, N., Rasoulpoor, S., Rasoulpoor, S., Shohaimi, S., Jafarpour, S., Abdoli, N., Khaledi-Paveh, B., & Mohammadi, M. (2022). The global prevalence of autism spectrum disorder: A comprehensive systematic review and meta-analysis. Italian Journal of Pediatrics, 48 (1), 112. https://doi.org/10.1186/s13052-022-01310-w
Solmi, M., Song, M., Yon, D. K., Lee, S. W., Fombonne, E., Kim, M. S., Park, S., Lee, M. H., Hwang, J., Keller, R., Koyanagi, A., Jacob, L., Dragioti, E., Smith, L., Correll, C. U., Fusar-Poli, P., Croatto, G., Carvalho, A. F., Oh, J. W., & Cortese, S. (2022). Incidence, prevalence, and global burden of autism spectrum disorder from 1990 to 2019 across 204 countries. Molecular Psychiatry, 27 (10), 4172–4180. https://doi.org/10.1038/s41380-022-01630-7
Wang, X., Weng, X., Pan, N., Li, X., Lin, L., & Jing, J. (2023). Prevalence of autism spectrum disorder in the United States is stable in the COVID-19 era. Journal of Autism and Developmental Disorders, 53 (8), 3309–3312. https://doi.org/10.1007/s10803-023-05915-w
Xu, G., Strathearn, L., Liu, B., & Bao, W. (2018). Prevalence of autism spectrum disorder among us children and adolescents, 2014–2016. JAMA, 319 (1), 81–82. https://doi.org/10.1001/jama.2017.17812
Xu, G., Strathearn, L., Liu, B., O’Brien, M., Kopelman, T. G., Zhu, J., Snetselaar, L. G., & Bao, W. (2019). Prevalence and treatment patterns of autism spectrum disorder in the United States, 2016. JAMA Pediatrics, 173 (2), 153–159. https://doi.org/10.1001/jamapediatrics.2018.4208
Download references
Acknowledgements
The authors would like to acknowledge the support from all the team members and all staff of the National Center for Health Statistics.
This work is supported by the National Natural Science Foundation of China (Grant No. 81973063).
Author information
Xiaofang Yan and Yanmei Li have contributed equally to this work.
Authors and Affiliations
Department of Child and Adolescent Health, School of Public Health, Guangdong Province, Guangdong Pharmaceutical University, Guangzhou, 510006, China
Xiaofang Yan, Yanmei Li, Qishan Li, Qian Li & Wenhan Yang
Department of Pediatrics, The First Affiliated Hospital, University of Science and Technology of China, Hefei, China
Division of Birth Cohort Study, Guangzhou Women and Children’s Medical Center, Guangdong Province, Guangzhou Medical University, Guangzhou, 510623, China
You can also search for this author in PubMed Google Scholar
Contributions
Wenhan Yang and Jinhua Lu have full access to all of the data in this study and assumes responsibility for study supervision. Concept and design: Wenhan Yang, Jinhua Lu, and Guifeng Xu. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: Xiaofang Yan and Yanmei Li. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Xiaofang and Yan Yanmei Li.
Corresponding authors
Correspondence to Jinhua Lu or Wenhan Yang .
Ethics declarations
Conflict of interest.
The authors have no conflict of interest to declare.
Ethical Approval
The NHIS protocols were approved by the National Center for Health Statistics research ethics review board. Written informed consent was obtained for all participants. The Guangdong Pharmaceutical University Academic Review Board determined the present study was exempt from approval because of the use of deidentified data.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Yan, X., Li, Y., Li, Q. et al. Prevalence of Autism Spectrum Disorder Among Children and Adolescents in the United States from 2021 to 2022. J Autism Dev Disord (2024). https://doi.org/10.1007/s10803-024-06390-7
Download citation
Accepted : 01 May 2024
Published : 22 May 2024
DOI : https://doi.org/10.1007/s10803-024-06390-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Autism spectrum disorder
- Children and adolescents
- Find a journal
- Publish with us
- Track your research
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Continuing Education
- Author Guidelines
- Submission Site
- Open Access
- Why publish with this journal?
- About Archives of Clinical Neuropsychology
- About the National Academy of Neuropsychology
- Journals Career Network
- Editorial Board
- Advertising and Corporate Services
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, materials and methods, conflict of interest, appendix a. risk-of-bias assessment, appendix b. narrative summary.
- < Previous
Cognitive Profile in Autism and ADHD: A Meta-Analysis of Performance on the WAIS-IV and WISC-V
- Article contents
- Figures & tables
- Supplementary Data
Alexander C Wilson, Cognitive Profile in Autism and ADHD: A Meta-Analysis of Performance on the WAIS-IV and WISC-V, Archives of Clinical Neuropsychology , Volume 39, Issue 4, June 2024, Pages 498–515, https://doi.org/10.1093/arclin/acad073
- Permissions Icon Permissions
Previous research has suggested that neurodevelopmental conditions may be associated with distinctive cognitive profiles on the Wechsler intelligence tests (of which the most recent editions are the WAIS-IV and WISC-V). However, the extent to which a cognitive profile can be reliably identified for individuals meeting criteria for autism or ADHD remains unclear. The present review investigated this issue.
A search was conducted in PsycInfo, Embase, and Medline in October 2022 for papers reporting the performance of children or adults diagnosed with autism or ADHD on the WAIS-IV or the WISC-V. Test scores were aggregated using meta-analysis.
Scores were analyzed from over 1,800 neurodivergent people reported across 18 data sources. Autistic children and adults performed in the typical range for verbal and nonverbal reasoning, but scored ~1 SD below the mean for processing speed and had slightly reduced scores on working memory. This provides evidence for a “spiky” cognitive profile in autism. Performance of children and adults with ADHD was mostly at age-expected levels, with slightly reduced scores for working memory.
Although the pattern of performance on the Wechsler tests is not sufficiently sensitive or specific to use for diagnostic purposes, autism appears to be associated with a cognitive profile of relative strengths in verbal and nonverbal reasoning and a weakness in processing speed. Attention deficit hyperactivity disorder appears less associated with a particular cognitive profile. Autistic individuals may especially benefit from a cognitive assessment to identify and support with their strengths and difficulties.
When assessing general cognitive ability, psychologists often use the Wechsler series of intelligence tests, which include the Wechsler Adult Intelligence Scale (WAIS; Wechsler, 2008 ) and the Wechsler Intelligence Scale for Children (WISC; Wechsler, 2014 ). Surveys of clinicians indicate that these tests are the most commonly used neuropsychological assessments ( Rabin et al., 2016 ), and have a number of routine uses, including to characterize cognitive functioning in people with neurodevelopmental conditions like autism and attention deficit hyperactivity disorder (ADHD; Aiello et al., 2017 ). In the United Kingdom, the National Institute of Health and Care Excellence ( NICE, 2011 ) recommends that a diagnostic assessment for autism must construct a profile of the person’s strengths and difficulties, potentially including an individual’s intellectual ability and academic skills. Likewise, several policy documents suggest use of cognitive assessment within neurodevelopmental diagnostic services ( Hayes et al., 2018 ). The purpose of this cognitive assessment may be to identify support needs for intervention—however, to assess cognition as part of a neurodevelopmental diagnostic assessment may imply that cognitive assessment is helpful for diagnosis itself. There is some uncertainty about this. On the one hand, research has suggested specific cognitive profiles on the Wechsler scales in autism and ADHD ( Ehlers et al., 1997 ; Kanai et al., 2017 ; Mayes & Calhoun, 2004 ). However, research has not always supported the idea of specific profiles on the Wechsler tests ( Charman et al., 2011 ). Due to this uncertainty, the present review will assess the state of evidence surrounding this question, asking whether autism and ADHD are associated with a distinctive cognitive profile on the Wechsler scales. This is likely to have clinical relevance, as these are the most commonly used cognitive tests ( Aiello et al., 2017 ; Rabin et al., 2016 ).
Autism and ADHD are both neurodevelopmental conditions diagnosed on the basis of behavioral features that emerge in childhood ( American Psychiatric Association, 2013 ). In the case of autism, these include social/communication difficulties and restricted and repetitive behaviors and interests. In the case of ADHD, individuals show a pattern of inattention and/or hyperactivity and impulsivity. These behavioral features are thought to result from differences in genetically mediated brain development, although evidence suggests subtle differences only discernible at the group level. One of the most replicated findings in autism is of accelerated brain growth early in life ( Donovan & Basson, 2017 ), which appears to result in changes in connectivity with reduced long-range connectivity and, potentially, enhanced local connectivity ( O'Reilly et al., 2017 ). In the case of ADHD, there also appear to be alterations in connectivity, specifically affecting cortical attention and inhibitory control networks, alongside subtle structural differences including reduced cortical surface area ( Faraone et al., 2021 ).
In this review, “cognitive profile” is taken to mean a person’s pattern of performance across the different cognitive domains covered in the assessment, including their strengths and weaknesses. There are several versions of the WAIS and WISC, each incorporating a range of subtests targeting different aspects of intellectual functioning. The WAIS-IV is the latest version for adults and consists of 10 core subtests grouped under four cognitive domains ( Wechsler, 2008 ): verbal comprehension, perceptual reasoning, working memory, and processing speed. The latest version for children (WISC-V; Wechsler, 2014 ) measures five cognitive domains: the same as the WAIS-IV, except that visual spatial cognition and fluid reasoning replace perceptual reasoning. Standardized scores can be determined for a person’s performance on each subtest, each domain, and overall intellectual functioning (full-scale IQ, or FSIQ). By reviewing a person’s performance across subtests and indices reflecting different domains, it is possible to identify their profile of strengths and difficulties, relative to both general population norms and the person’s overall ability level. Profiles are therefore inter-individual (comparing across people) as well as intra-individual (comparing skills within a person).
There is a longstanding topic of interest that different neurodevelopmental conditions may be characterized by a distinctive “profile” of performance on the Wechsler scales. In autism, this has been described as an uneven profile with a peak on the Block Design subtest and a particular weakness in the Comprehension subtest (see Happé, 1994 for a review of early research). Happé (1994) linked this pattern to theories of autistic cognition: (1) the strength in Block Design may relate to a cognitive preference for processing local detail and (2) the weakness in Comprehension may relate to differences in a person’s social reasoning. Zayat and colleagues (2011) came to a similar conclusion in their study comparing the verbal profile on the WISC in autism to ADHD; they highlighted that the pattern of performance observed in autistic individuals across verbal subtests (strongest on Similarities, then Vocabulary, then Comprehension) may have been due to autistic difficulties with social reasoning and formulating verbal discourse. Researchers have also been interested in characterizing different profiles within autistic subgroups, in particular differentiating the presentation known as Asperger’s syndrome in DSM-IV from other autistic presentations. A somewhat stronger performance on verbal than nonverbal subtests has been identified as characteristic of Asperger’s, whereas no discrepancy exists for “high-functioning” autism (see Chiang et al., 2014 for a meta-analysis). On the other hand, ADHD may possibly be characterized by lower scores on the working memory and/or processing speed subtests. In over 700 children with ADHD, 90% of the sample received their lowest scores in these domains ( Mayes & Calhoun, 2006 ). The literature also mentions the so-called ACID profile (lower scores on Arithmetic, Coding, Information and Digit Span subtests) and SCAD profile (lower scores on Symbol Search, Coding, Arithmetic and Digit Span subtests), which appear sensitive to ADHD ( Snow & Sapp, 2000 ). All these subtests (except Information) belong to the working memory and processing speed domains, which reinforces the idea that these domains are the most likely areas of difficulty for individuals with ADHD.
There has been some attempt to review evidence of a distinctive cognitive profile in autism, although this research is limited. Takayanagi and coworkers (2022) found that studies tended to identify a strength in Block Design and a weakness in Coding among autistic children. However, this narrative review has several limitations, as it only focuses on certain subtests (neglecting many papers looking at the domain-level index scores), excludes adults, and lacks overall quantitative analysis or comparison with other neurodevelopmental conditions. Chiang and associates (2014) have also reviewed research into intellectual profiles in autism, specifically whether discrepancies between verbal IQ (VIQ) and nonverbal, or performance, IQ (PIQ) distinguish Asperger’s syndrome from other forms of autism. Therefore, Chiang and associates (2014) focus on rather a specific question (which is now less relevant as Asperger’s syndrome is no longer diagnosed under DSM-5), and it would be helpful to understand wider aspects of performance on the Wechsler scales while also investigating whether results are valid for current versions of the Wechsler scales (as this earlier review looked at earlier versions). As for ADHD, there is no existing review of Wechsler profiles in this population.
This meta-analytic review seeks to address the evidence gap, asking whether there are distinctive profiles in autism and ADHD on the latest versions of the Wechsler scales, the WAIS-IV (for adults) and the WISC-V (for children). Restricting attention to the latest versions is likely to be most relevant to current clinical practice, as guidance would be for services to use the latest assessment tools with up-to-date norms and improved psychometric properties. In addition, focusing on more recent research allows us to study neurodevelopmental populations likely to be seen now, which may differ compared to the past due to different diagnostic criteria and much increased diagnostic rates (e.g., Russell et al., 2022 ). This review asks two questions via meta-analysis:
(a) Are autism and ADHD associated with a cognitive profile on the Wechsler scales?
(b) Can we differentiate between autism and ADHD based on Wechsler profile?
This review included peer-reviewed papers published between 2008 (the publication year of the WAIS-IV) and 2022 where they present standardized scores on the WAIS-IV or WISC-V by a sample of children or adults diagnosed with autism or ADHD who underwent a cognitive assessment. Scores needed to be presented for all indexes of the WAIS-IV/WISC-V. A search was conducted using Ovid of databases PsycINFO, Embase and Medline on October 20, 2022 using the following search terms: (attention deficit OR attention-deficit OR hyperactivity OR ADHD* OR autis* OR ASD OR pervasive development* or Asperger*) (in the title) AND (WAIS-IV or WISC-V) (in any element of the source). Reference lists of included papers and the Wechsler manuals were also screened for additional sources.
Papers were screened for inclusion in two steps. In the first step, titles and/or abstracts were screened to ensure the paper reported on original research in a sample of people diagnosed with autism and/or ADHD. In the second step, abstracts and full papers were screened to ensure the paper included index and/or subtest scores on the WAIS-IV/WISC-V. Papers were included if there was a sample of people with a clinical diagnosis of autism or ADHD with standardized scores on all indexes of a fully administered WAIS-IV/WISC-V. Note that some studies administered the WAIS-IV or WISC-V to some/all participants, but only used FSIQ scores to check eligibility for the study, characterize the sample, match clinical participants with control participants, or use as a covariate in analysis. As index scores were not available for these papers, the papers were not included in analysis. Where papers were not published in English, the plan was to translate sections of relevant peer-reviewed papers. This was only required for one paper published in German ( Pauls et al., 2018 ), with support of a German-speaking psychologist.
The following background information was recorded from papers deemed eligible for inclusion: sample size, demographic information about the sample (including age, sex, and race), clinical details about the sample (diagnostic information, age at diagnosis, co-occurring diagnoses, and use of psychostimulants), country of study, purpose of study, method of recruitment/data collection, timing of cognitive assessment in relation to diagnosis, and eligibility criteria for participation. The key study data used in the meta-analysis included means and standard deviations for standardized scores on each index and optionally on each subtest too if subtest-level data were presented by the paper. Index scores were recorded as standard scores (mean = 100; SD = 15) and subtest scores as scaled scores (mean = 10; SD = 3). In addition, any information about WAIS-IV/WISC-V scores and (1) their sensitivity/specificity to neurodevelopmental conditions and (2) their relationships with clinical variables/outcomes was also noted. This data coding process was completed with support of a second rater who coded a random 25% of the data set, with full agreement with the original coding. The risk-of-bias of studies included in the review was also considered, drawing on the Observational Study Quality Evaluation (OSQE; Drukker et al., 2021 ). Using this tool, factors were identified a priori that are most likely to introduce bias: eligibility criteria reducing representativeness, selection bias in recruitment, unsatisfactory neurodevelopmental assessment, and biases in administration/scoring of cognitive assessments. Papers were reviewed in relation to these factors. See Appendix A for a summary of this risk-of-bias assessment.
All papers provided index scores, and these were analyzed through multilevel meta-analyses using R package metafor ( Viechtbauer, 2010 ) in the R computing environment ( R Core Team, 2022 ). For each index (VCI, PRI, VSI, FRI, WMI, PSI, and FSIQ), means were aggregated across four neurodivergent subgroups (autistic children, children with ADHD, autistic adults, and adults with ADHD). As some papers contributed more than one sample, multilevel models were specified with random effects of the sample embedded in paper. Restricted maximum likelihood estimation was used to generate estimates and error terms. These meta-analyses gave an overall mean score for each neurodivergent subgroup for each index. Scores were labeled according to the qualitative descriptors set out by the American Academy of Clinical Neuropsychology ( Guilmette et al., 2020 ); for example, standard scores of 90–110 are “Average.”
Having calculated mean index scores, differences between and within the subgroups were tested in three ways. In each case, the size of effects was quantified according to the guideline by Cohen (1988) , and alpha levels were adjusted for multiple comparisons. The first analysis asked whether mean index scores significantly differed from the normative mean of 100 in the four neurodivergent subgroups (children/adults diagnosed with autism/ADHD). For this analysis, the multilevel meta-analyses were rerun with index scores of all samples centered at zero (by subtracting 100), and the significance of the intercept was tested. As this analysis was carried out for each index in the four subgroups, a correction for multiple comparisons was used for each subgroup. For adult samples, the alpha level was set to .01 (.05 divided by 5, as the WAIS-IV has five indexes), and .008 in child samples (.05 divided by 6, as the WISC-V has six indexes). The second analysis explored whether index scores differed between diagnostic groups. For each index, multilevel meta-analyses were rerun for children and adults across diagnostic groups, including Diagnosis (autism vs. ADHD) as a fixed effect. The significance of this fixed effect allowed testing for group differences between people diagnosed with autism and ADHD. The alpha level was set to the same thresholds as earlier to allow for multiple comparisons. The third analysis shifted from inter-group comparisons to intra-group comparisons. This allows us to assess whether index scores significantly differ from each other within the four neurodivergent subgroups (i.e., to reflect a pattern of relative strengths and difficulties specific to the neurodevelopmental condition). For this analysis, meta-analyses were run within each of the four neurodivergent subgroups, with index as a fixed effect and with a multi-level structure (i.e., random effects clustered indexes within samples). Nonverbal ability was used as a reference level of the fixed effect (PRI or FRI, depending on age), which was compared to each other’s index one at a time. It should be noted that error terms will not be independent in this analysis (as each sample contributed an error term for more than one index). However, the covariance for these error terms is unknown (as papers have no reason to report correlations between indexes in their samples), so cluster robust estimation was used, as suggested by Hedges and colleagues (2010) . For these final meta-analyses, alpha levels were left uncorrected at .05, as these analyses were likely underpowered and more exploratory.
When carrying out the first analysis described previously (quantifying overall means for each index in each neurodivergent subgroup), heterogeneity was assessed across samples contributing to these means. The I 2 value (percent of variance attributable to variance in true effects of samples) was calculated for each multilevel meta-analysis. It was hypothesized that general cognitive ability would influence index scores across samples, so a measure of nonverbal ability (PRI or FRI, depending on age) was included as a moderator in follow-up multilevel meta-analyses, and the I 2 value was recalculated. Analyses were also tested for publication bias by including sample size as a moderator in other follow-up meta-analyses.
In addition to these detailed quantitative analyses of index scores, data were synthesized at the subtest level in the few studies that presented this information. Overall means across studies were computed using random effects meta-analysis, and these summary means (with 95% CIs) are presented in charts showing performance across each subtest. Some papers offered further investigation into cognitive profiles in autism and ADHD, including psychometric properties, ability to discriminate between groups, and correlations with other phenotypic variables. This information is presented as a narrative synthesis in Appendix B .
Participants
A literature search generated 306 sources, of which 16 were eligible for inclusion. Two papers passing initial screening stages were excluded as they included data overlapping with other sources ( Holdnack et al., 2011 ; Theiling et al., 2013 ). One additional paper was identified through review of reference lists of included papers ( Becker et al., 2021 ), and standardization data were included from the WAIS-IV and WISC-V (however, as Dale et al., 2022 used standardization data in their analysis, the WISC-V had effectively already been counted as a data source). This gave a total of 18 sources of cross-sectional data included in the meta-analysis. Figure 1 shows a flow chart presenting this screening process.

Flow chart showing movement of sources through the screening process of the literature search.
Across the 18 sources of data, there were 24 separate samples of individuals, comprising 1,842 individuals in total. Of these, 968 were adults assessed with the WAIS-IV: 437 came from samples focused on autism (mean age = 30 years; 23% female), and 527 came from samples focused on ADHD (mean age = 29 years; 35% female). In addition, there were 856 children aged between 6 and 16 assessed with the WISC-V: 630 came from samples focused on autism (mean age = 10 years; 18% female), and 226 came from samples focused on ADHD (mean age = 11 years; 34% female). Information on race/ethnicity was not consistently available across studies, although most participants were White where this information was given. Tables 1 and 2 present full information on the papers included in this review.
Details of papers included in the review: demographic and clinical variables
Details of studies included in the review: methodological variables
Neurodevelopmental diagnoses were based on DSM-IV, DSM-5, or ICD-10. Among autistic adults, most had a DSM-5 diagnosis ( n = 234); others had a DSM-IV diagnosis of Asperger’s syndrome ( n = 72), autistic disorder ( n = 30), or atypical autism ( n = 16). For some autistic adults, the criteria for diagnosis were not specified in the paper ( n = 85). Autistic adults were largely diagnosed as adults (322 vs. 8 diagnosed as children), although for 107, age of diagnosis was not specified. Most papers excluded autistic adults with co-occurring diagnoses. In the few studies with more relaxed eligibility criteria, papers reported on co-occurring diagnoses (ADHD had been diagnosed in 10 autistic adults). In the samples of adults with ADHD, 103 people were diagnosed with the inattentive subtype, 349 with the combined subtype, and 8 with hyperactive subtype; for 61, information was not available about the subtype. The majority of adults with ADHD were diagnosed as adults (445 vs. 28 diagnosed as children and 44 with age of diagnosis unspecified).
Moving on to the child samples, 183 of the autistic children had a DSM-5 diagnosis, but for many, diagnostic criteria were not specified ( n = 447). For a large number of children, there were no exclusionary criteria regarding co-occurring diagnoses and information was not reported about co-occurring diagnoses. In 183 autistic children for whom this information was available, 21 had co-occurring ADHD. Among children in the ADHD samples, information was not given on subtype, although 178 were diagnosed using ICD-10 criteria and 48 with DSM-5 criteria. Looking across all samples of people with autism or ADHD, the majority of papers excluded individuals with intellectual disability and/or FSIQ below a certain threshold (varying between 60 and 80).
Risk-of-Bias Assessment
See Appendix A for a table showing ratings for risk-of-bias for each paper. A summary of issues is provided here, as all papers showed the same limitations that could introduce systematic bias:
There was no detailed assessment for co-occurring conditions in any paper. Some papers screened for co-occurring conditions, but this was limited to asking if diagnoses had been made, which will not pick up undiagnosed conditions or subthreshold co-occurring traits. This was the case in studies excluding individuals with co-occurring conditions, as well as studies without these exclusion criteria. Across all samples, only 1% of individuals had autism and ADHD diagnoses, which may underestimate true co-occurring traits. Rates of co-occurrence vary widely in the literature (depending on the sample characteristics), but, for the purpose of illustration, a meta-analysis found 40% of autistic people met criteria for ADHD ( Rong et al., 2021 ). However, co-diagnosis of autism and ADHD is a complex task, as both conditions present with traits that may look like the other condition. For instance, attentional differences appear to be an early precursor to core processes affected in autism (including joint attention, arousal regulation, and perceptual processing; Keehn et al., 2013 ). Similar traits may lead to an overestimation of co-occurring autism and ADHD within the wider literature; however, a co-occurrence rate of just 1% in the studies reviewed here seems low. If papers have not fully assessed for co-occurring conditions, it may be difficult to conclude whether a cognitive profile is explained by the condition of interest or other unassessed co-occurring features.
FSIQ thresholds were often used for inclusion, possibly biasing the cognitive profiles present in the samples, especially as some cognitive domains contribute more strongly to FSIQ than other domains. Only one study ( Cicinelli et al., 2022 ) included a significant proportion of individuals meeting criteria for intellectual disability.
Researchers were not blind to the diagnostic status of participants. Where cognitive assessments occurred following diagnosis, this may have biased administration/scoring of assessments if assessors had preconceived ideas about the possible performance of participants.
Quantitative Analyses
Tables 3 and 4 show the key variables included in the meta-analyses that follow. These include the mean scores on the indices of the WAIS-IV or WISC-V for each sample included in the review.
Key study variables: index scores across the WAIS-IV in neurodivergent adults
Note: VCI = Verbal Comprehension Index; PRI = Perceptual Reasoning Index; WMI = Working Memory Index; PSI = Processing Speed Index; FSIQ = Full-Scale Intelligence Quotient.
Key study variables: index scores across the WISC-V in neurodivergent children
Note: VCI = Verbal Comprehension Index; VSI = Visual Spatial Index; FRI = Fluid Reasoning Index; WMI = Working Memory Index; PSI = Processing Speed Index; FSIQ = Full-Scale Intelligence Quotient.
Meta-Analysis 1. Comparing index scores to the normative mean
Table 5 shows mean WAIS-IV index scores generated through meta-analysis across the samples of neurodivergent adults. All mean index scores were in the Average range, except for PSI in autistic adults which was Low Average. Most mean index scores did not differ significantly from the normative mean of 100, indicating that we cannot reliably distinguish adult neurodivergent groups from the general population for most indexes. Among autistic adults, only PSI was significantly lower than the normative mean, p < .001; this was by 13.3 points. Given that 15 points is 1 SD , this represents a large effect size ( Cohen, 1988 ). Among adults with ADHD, WMI was slightly lower than the normative mean, p < .001, although the effect size was small (4.8 points below the normative mean).
Summary scores for neurodivergent adults across the index scores of the WAIS-IV. Scores are shown as standard scores (mean = 100; SD = 15)
There was significant heterogeneity in WAIS-IV index scores in neurodivergent adults. I 2 values varied between 96.2% and 98.3% across the five indexes in autistic adults and between 75.3% and 96.1% in adults with ADHD. It was hypothesized that heterogeneity was likely influenced by general ability in the samples (i.e., samples of higher ability likely performed more highly on all the indexes). Nonverbal ability (PRI) was specified as a moderator, and all meta-analyses (except for the ones modeling PRI and FSIQ) were rerun with PRI as a moderator. This time, I 2 values varied between 53.7% and 88.8% in autistic adults and between 7.5% and 70.4% in adults with ADHD (in adults with ADHD, WMI that had a much lower heterogeneity when controlling for FRI, whereas other I 2 values remained high). Overall, general ability explained some of the heterogeneity among neurodivergent adults, but there was still considerable variability across the samples included in the meta-analyses, suggesting variable patterns of performance across the WAIS-IV in the different samples. The possibility of publication bias was also assessed for these meta-analyses. Sample size was not associated with index scores in neurodivergent adults, all p s > 0.200, indicating no evidence for publication bias.
Table 6 shows mean WISC-V index scores generated in meta-analysis for neurodivergent children. Most mean index scores were in the Average range, except for WMI and PSI in autistic children, which were Low Average. Controlling for multiple comparisons, autistic children scored significantly lower than the normative mean on WMI (by 10.9 points, a medium effect), p < .001, and PSI (by 13.4 points, a large effect), p < .001. This was also the case in children with ADHD, who scored lower than the normative mean on WMI (by 6.3 points, a small effect), p = .006, and PSI (by 7.7 points, a medium effect), p < .001.
Summary scores for neurodivergent children across the index scores of the WISC-IV. Scores are shown as standard scores (mean = 100; SD = 15)
There was significant heterogeneity in WISC-V index scores in neurodivergent children. I 2 values varied between 92.1% and 95.6% for indexes in autistic children and between 0% and 88.7% in children with ADHD. As with the adult samples, it was hypothesized that heterogeneity was likely influenced by general ability in the samples. Nonverbal ability (FRI) was specified as a moderator and all meta-analyses were rerun (except for the ones modeling FRI and FSIQ) with FRI as a moderator. This time, I 2 values were 0% across all child samples for every index. This indicates that, when controlling for general cognitive ability, patterns of index scores were similar across the samples included in this meta-analysis. The possibility of publication bias was also assessed. Sample size was not associated with index scores in autistic children, all p s > 0.600, but was in children with ADHD for all indexes except PSI, p > 0.001. Larger samples were associated with lower scores in children diagnosed with ADHD, so the overall scores may slightly overestimate ability in children with ADHD. This is likely due to a methodological artifact rather than publication bias per se, as one of the two samples contributed by Becker and coworkers (2021) was very small and only consisted of children with no evidence of specific learning difficulties, whereas eligibility criteria in other samples were more inclusive.
Meta-Analysis 2. Comparing index scores between autism and ADHD
There were no significant differences in index scores when comparing people diagnosed with autism to those with ADHD, although we should note that this analysis was not well powered to detect differences due to the relatively small groups and large variances. Among adults, PSI tended to be lower in autistic adults compared to adults with ADHD, 9.6 points [−.4, 19.5]; however, this was not statistically significant, p = .059. Differences in other index scores were more convincingly nonsignificant among adults, all p s > 0.450. Neurodivergent children showed a similar pattern to adults, with similar scores for most indexes, all p s > 0.180, except PSI, which showed a trend for lower scores in autistic children compared to children with ADHD, 5.9 points [−.3, 12.1], p = .062.
Meta-Analysis 3. Comparing index scores within groups
Lastly, index scores were compared within groups to explore whether there was a pattern of relative strengths and difficulties for each group. Among autistic groups, there were difficulties in working memory and processing speed in the context of relative strengths in verbal and nonverbal reasoning. Compared to their PRI, autistic adults had significantly lower WMI, 5.84 points [1.9, 9.8], p = .010, and lower PSI, 9.2 points [6.1, 12.4], p < .001. PRI and VCI did not differ in autistic adults, p = .692. Compared to their FRI, autistic children showed lower WMI, 7.6 points [6.2, 9.0], p < .001, and lower PSI, 10.4 points [6.7, 14.0], p = .003. VCI and VSI did not differ from FRI, p s > 0.250.
ADHD samples showed less marked patterns than autistic groups. Compared to their PRI, adults with ADHD had lower WMI by 4.2 points [1.5, 6.8], p = .015. There was a trend for PSI to be lower by 3.6 points [−1.3, 8.5], but this was nonsignificant, p = .103. PRI and VCI did not differ among adults with ADHD, p = .780. Among children with ADHD, there were no statistical differences between FRI and any other index, all p s > 0.180.
Subtest performance
See Fig. 2a–d for subtest scores. These plots report data from 95 autistic adults, 532 autistic children, 160 adults with ADHD, and 151 children with ADHD.

(a) Plot showing subtest scaled scores of autistic adults on the WAIS-IV. (b) Plot showing subtest scaled scores of adults with ADHD on the WAIS-IV. (c) Plot showing subtest scaled scores of autistic children on the WISC-V. (d) Plot showing subtest scaled scores of children with ADHD on the WISC-V. (a-d) In all plots, the thick black line represents summary means calculated through meta-analysis. The thinner coloured lines represent means from the individual studies. Note : SI = Similarities; VC = Vocabulary; IN = Information; BD = Block Design; VP = Visual Puzzles; MR = Matrix Reasoning; DS = Digit Span; AR = Arithmetic; CD = Coding; SS = Symbol Search; FW = Figure Weights; PS = Picture Span.
There was evidence of a particular cognitive profile on the Wechsler intelligence tests in autistic groups, both in children and adults. This was characterized by verbal and nonverbal reasoning in the Average range, with slightly lower working memory and more significantly reduced processing speed. For both autistic children and adults, mean processing speed was Low Average (i.e., below the 25th percentile). Among individuals with ADHD, there was less robust evidence of a profile. Means of all index scores were in the Average range for people with ADHD, with a pattern of slightly lower working memory in adults and children. Processing speed was possibly slightly reduced in children with ADHD compared to the norm, but not necessarily in relation to their own ability. It remains to be seen whether the differences in groups with ADHD are clinically meaningful. Subtest-level analyses gave a similar pattern of results. There were flat profiles in the typical range for the ADHD samples, and a more uneven profile in the autistic samples, with lowest scores in subtests requiring time-pressured efficient processing of information. However, these results need to be held in mind with several factors. First, the quantitative analyses showed significant variability in performance across samples, as shown by the heterogeneity and large confidence intervals around values. In addition, several papers attempted to use cognitive profile on the Wechsler tests to distinguish individuals with an autism diagnosis from those without a neurodevelopmental diagnosis, but with limited success (e.g., Dale et al., 2021 ; see Appendix B for a narrative review of papers relevant to this issue). Importantly, as highlighted by Stephenson and associates (2021) , there may also be psychometric issues with conducting fine-grained analysis of profiles, as domain-level indexes show poor reliability after accounting for variance associated with FSIQ. This is a key issue that needs to be further researched, as fine-grained analysis of an individual’s performance on a cognitive assessment is commonplace in clinical practice.
Despite these factors, reduced processing speed among autistic people does stand out, given the extent of this reduction compared to the norm. Across samples of autistic children and adults, mean processing speed was ~1 SD lower than the normative mean, and lower than participants’ mean verbal and nonverbal reasoning by ~10 points. Studies reporting subtest-level data also support this picture, as autistic children and adults tended to receive their lowest scores on processing speed tests (especially Coding). This is consistent with previous research, as autistic people have been reported to score low on the Coding subtest in older versions of the Wechsler tests (see Takayanagi et al., 2022 for a review) as well as on other measures of speed including simple reaction time ( Zapparrata et al., 2022 ). Lower processing speed is also consistent with biological accounts of the autistic brain, which indicates reduced long-range connectivity in the brain (in particular, between frontal and posterior regions of cortex; Just et al., 2012 ). However, low processing speed would not be appropriate as a diagnostic marker for autism, as this is found across different neurological and psychiatric conditions ( Rommelse et al., 2020 ). Nonetheless, low processing speed is likely to be common enough in autistic people that it may be useful to screen for these difficulties, as they have real-world impacts. For instance, lower processing speed has been found to correlate with adaptive communication skills ( Oliveras-Rentas et al., 2012 ) and predicts academic underachievement ( Mayes & Calhoun, 2007 ) in autistic children. However, the extent to which low processing speed predicts real-world impacts, independently of other Wechsler indices, is unclear from the literature and would be worth further investigation.
It is worth bearing in mind what “low processing speed” might mean, as it may or may not reflect slower mental processing. The motor demand in tasks may partly explain the differences between autistic and nonautistic groups in PSI, as increasing the motor requirement increases group differences on speeded tasks ( Kenworthy et al., 2013 ) and pure inspection time (without a motor requirement) may represent a relative strength for autistic people ( Barbeau et al., 2013 ). Thus, we should be cautious about necessarily equating lower PSI with lower mental speed. As noted by Rommelse and colleagues (2020) , Wechsler processing speed tests are not pure measures of speed, but tap multiple processes including visual scanning, fine motor skills, short-term memory, interference control, and choice of strategies to optimize speed-accuracy trade-offs—in essence, these tests are measures of complex processing capacity. Another issue is that “processing speed” may or may not be the same construct when measured in autistic compared to neurotypical people using the Wechsler tests, as these tests were not devised with the autistic brain in mind. It is notable, for instance, that the WISC was found to underestimate autistic intelligence in relation to another intelligence test (Raven’s Progressive Matrices) whereas this was not the case in neurotypical controls ( Dawson et al., 2007 ).It would be helpful, therefore, to test the equivalence of the “processing speed” construct between neurodivergent and neurotypical groups to ensure that differences are not due to a measurement bias.
As noted previously, there was less robust evidence of a specific profile in ADHD. WMI was the one index where there was a reliable difference from the norm in both children and adults, but this was a modest effect size (about half an SD or lower). This is similar to existing literature, which has documented working memory difficulties in individuals with ADHD of a similar effect size (e.g., see Ramos et al., 2020 for a review). The lack of a reliable difference in PSI is surprising, as there seems to be a view in the literature that significantly reduced processing speed is common in ADHD. For instance, Cook and coworkers (2018) start from the assumption that processing speed is significantly reduced in ADHD in their review of functional correlates of lower processing speed in ADHD. However, this may not be a key feature in ADHD. Where there are slightly lower scores among groups with ADHD, we also need to be mindful of possible co-occurring specific learning difficulties that may account for scores (e.g., Becker et al., 2021 ). Overall, the rather flat cognitive profiles of the ADHD groups echo previous research that has highlighted the questionable utility of neuropsychological assessment in the diagnosis of ADHD ( Lange et al., 2014 ; Pettersson et al., 2018 ). We might conclude, therefore, that the Wechsler tests are not helpful in diagnosing ADHD, although this is not to underplay that the tests will help identify any individual’s personal strengths and weaknesses, which may support their learning and occupational functioning. For instance, the indexes appear to be associated with various measures of adaptive behavior across different papers reviewed in the narrative synthesis. This can likely be understood in the context of the well-established finding that FSIQ predicts a variety of outcomes ( Nisbett et al., 2012 ). Therefore, a cognitive assessment can tell us something about a person’s functioning whether or not they have a neurodevelopmental condition. One thing that remains unclear is whether an assessment actually improves a person’s functioning (e.g., through building insight into their personal cognitive profile). This has only received limited attention in the research literature, and no studies have evaluated the added value of a cognitive assessment for autistic people ( Donders, 2020 ).
Limitations
There are several limitations to hold in mind about this review. The papers included are all subject to various limitations including (i) use of convenience samples, (ii) poor characterization of co-occurring neurodevelopmental traits, which makes it difficult to be sure that an observed profile is truly related to autism or ADHD and not a co-occurring condition (e.g., dyslexia), and (iii) arbitrary exclusion criteria based on cognitive functioning (i.e., individuals with an IQ below a certain threshold were not included in many studies). These factors may bias estimates in this review. For instance, the FSIQ exclusion criteria may have meant individuals with lower scores on certain indexes were more likely to be excluded (as subtests within the verbal and perceptual domains contribute more strongly to FSIQ than those within the working memory and processing speed domains). These criteria may have biased the results—although the large reduction in processing speed in autistic people found in this review was possibly too large to be simply an artifact of this sampling approach. Certainly, the FSIQ exclusion criteria do mean that a large population of autistic individuals has been undersampled in this review—those with co-occurring intellectual disability. In addition, autistic adults diagnosed as children have been undersampled in this review, as most adults were diagnosed as adults, which is important, as age at diagnosis is likely to influence presentation ( Lai & Baron-Cohen, 2015 ). This review has also undersampled females and individuals with diverse gender identities. Although the ratio of males to females in this review (~3:1) is largely representative of neurodevelopmental conditions ( Bölte et al., 2023 ), the small numbers do make it difficult to know how well the results specifically apply beyond males.
This paper has been restricted to the latest versions of the Wechsler tests (WAIS-IV and WISC-V). The purposes of this were to optimize the relevance of the review for clinicians practicing today, as well as to restrict the amount of research to review—the Wechsler tests are so widely used in research that a review covering all versions would be impractical and overly heterogeneous. There was also the related issue that even when looking at just these two versions of the Wechsler tests, use of the tests is very variable across the research literature, especially when the tests are just used to characterize the sample or apply eligibility criteria (in these cases, it was common for only certain participants to be tested or only certain subtests to be given). This meant it was necessary to approach the review in a principled manner, only including papers where the 10 core subtests were administered and the main indexes reported, which had the positive effect of making the review manageable but with the possible side-effect of reducing overall sample size. This means the overall sample size, while reasonably big, is not well powered for some analyses (such as directly comparing the autistic and ADHD samples).
In addition, an inherent weakness of this type of meta-analysis is the lack of analysis at the individual level. Although the studies showed evidence of cognitive profiles at a group level, it is unclear how common these are on the individual level. In addition, it is plausible that there may be cognitive markers on the individual level that get obscured at the group level (i.e., individuals with neurodevelopmental differences may be more likely to show a variable profile, but this may be distinct to the individual rather than the condition). We know that variability is an element in the cognitive profile of neurodevelopmental conditions (e.g., there is greater variability in reaction time across tasks in people diagnosed with autism and ADHD; Karalunas et al., 2014 ), but we don’t know how this may (or not) present on the Wechsler tests. It is not possible to assess for these issues when only dealing with summary statistics rather than raw data. An interesting suggestion that variability may be a part of the cognitive profile was the heterogeneity analyses among adults diagnosed with autism or ADHD. These analyses showed that patterns of performance across the indices varied across samples. This may have been influenced by variability on the individual level.
Clinical Implications
This review suggests there is no clinically significant cognitive profile that can be detected in ADHD using a WISC-V or WAIS-IV assessment. In the case of autism, processing speed is reduced in both children and adults with a large effect size, which might be important to bear in mind when working with this population. It should be noted that processing speed differences are neither sufficiently sensitive nor specific to use for diagnostic purposes, and there would be a danger of biasing diagnostic decisions if reduced processing speed was considered a cognitive marker of autism. Nonetheless, there is good evidence for a pattern of strengths and difficulties on the Wechsler tests among autistic people, defined by relatively good reasoning skills in the presence of reduced processing speed. This is a pattern that can be supported with appropriate adjustments (e.g., more time for tasks), and the recognition of strengths may improve self-confidence and other people’s understanding of the issues, as well as prompt ideas for person-centered compensatory strategies.
In summary, this review investigated evidence for a distinctive cognitive profile in people with neurodevelopmental conditions on the most recent editions of the Wechsler intelligence tests, the WAIS-IV and WISC-V. Test performance was collated from over 1,800 individuals with a diagnosis of autism or ADHD reported in 18 different sources of data. Among autistic children and adults, there was a consistent pattern of verbal and nonverbal reasoning representing relative strengths, with a significant weakness in processing speed and slight weakness in working memory. People diagnosed with ADHD tended to show slightly weaker working memory than their other abilities, but this was a modest difference. Based on the review, it is unlikely to be helpful to conduct a cognitive assessment for diagnostic purposes, but an assessment may be helpful in determining an individual’s profile of strengths and difficulties, especially among autistic people.
None declared.

Studies are rated for high (-), medium (±), and low (+) risk of bias for the following qualities:
Internal Validity of the Sample I. Are we confident the study recruited individuals meeting criteria for the relevant neurodevelopmental diagnosis?
Internal Validity of the Sample II. Are we confident that co-occurring conditions have been adequately assessed? As this study compares autism and ADHD, it is important to know the extent to which these might co-occur at clinical or subclinical levels in the sample.
External Validity of the Sample I. Are we confident the sample is inclusive of individuals of varying intellectual ability? Given the focus of this study on cognitive abilities, we required studies to be inclusive of individuals regardless of IQ to avoid biasing profiles (although we allowed for exclusion of individuals unable to complete a cognitive assessment).
External Validity of the Sample II. Are we confident that the sample is a relatively random community/clinical sample? For this, we disregarded IQ eligibility criteria as that was considered in (3), and considered issues such as other eligibility criteria, missing data, recruitment pathway, and site of recruitment.
Validity of Assessment. Are we confident that assessors were blinded to avoid bias in profiling the abilities of neurodivergent people?
A few studies investigated aspects of cognitive profile beyond index and subtest means, including whether information from more than one index could distinguish neurodivergent from control participants on the individual level. Dale and associates (2021) found that index scores were only effective in distinguishing autistic children with a co-occurring language impairment, suggesting that the WISC-V was sensitive to language/learning difficulties rather than autism. Shepler & Callan (2022) found that WMI was moderately effective in differentiating adults with ADHD from those with a mental health diagnosis; however, the WAIS-IV was administered during the diagnostic process, so there is a significant risk of bias (i.e., participants scoring lower on the WAIS-IV may have been more likely to receive an ADHD diagnosis). Two studies looked at discrepancies between indexes ( Leung et al., 2019 ; Theiling & Petermann, 2016 ), and both studies’ discrepancies were more common in autistic adults (approximately twice as common as the norm). However, both studies had small samples, and it is unclear whether these were planned analyses, so there is a high risk of type I error. Overall, studies present limited and weak evidence for using a specific profile to distinguish neurodivergent individuals from the general population at the individual level.
Several studies found that Wechsler index scores correlated with adaptive behavior in autistic children ( Audras-Torrent et al., 2021 ) and adults ( Leung et al., 2019 ; Nyrenius & Billstedt, 2020 ). In autistic children, this included moderate correlations between all WISC-V indexes and communication skills (.31 < r < .50) and small correlations between VSI, FRI, and FSIQ and daily living skills ( r = .20 or .21), but no correlations with social skills ( Audras-Torrent et al., 2021 ). In autistic adults, there were moderate correlations between FSIQ, WMI, and PSI and adaptive behavior in the general, conceptual, and practical domains (.40 < r < .49; Nyrenius & Billstedt, 2020 ). Leung and colleagues (2019) found that parent- and self-rated social skills correlated in some cases with WAIS-IV indexes, but many correlations were computed, and so, there is a risk of false positives. In adults with ADHD, Baggio and coworkers (2020) found that lower FSIQ was associated with lower probability of higher education and currently being in work/education and greater probability of repeating a grade at school ( N = 66). Overall, there is evidence that cognitive scores correlate with adaptive skills, but these relationships do not seem specific to any one index.
Stephenson and associates (2021) looked at psychometric properties of the WISC-V in autistic children ( N = 349). They found that the WISC-V did not have the same psychometric structure across autistic and nonautistic groups; specifically, autistic children performed lower on the Digit Span and Coding subtests than would be expected based on their performance across all other subtests. In addition, the researchers found limited reliability of the domain-level indexes after accounting for variance relating to FSIQ. Overall, results from this paper suggest that the WISC-V may detect some autism-specific cognitive differences on particular subtests, but this should be interpreted cautiously on the individual level as such differences may not be psychometrically reliable.
Aiello , R. , Ruble , L. , & Esler , A. ( 2017 ). National study of school psychologists’ use of evidence-based assessment in autism spectrum disorder . Journal of Applied School Psychology , 33 ( 1 ), 67 – 88 . https://doi.org/10.1080/15377903.2016.1236307 .
Google Scholar
American Psychiatric Association . ( 2013 ). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, D.C.: American Psychiatric Publishing. https://doi.org/10.1176/appi.books.9780890425596 .
Google Preview
Audras-Torrent , L. , Miniarikova , E. , Couty , F. , Dellapiazza , F. , Berard , M. , Michelon , C. , et al. ( 2021 ). WISC-V profiles and their correlates in children with autism spectrum disorder without intellectual developmental disorder: Report from the ELENA cohort . Autism Research , 14 ( 5 ), 997 – 1006 . https://doi.org/10.1002/aur.2444 .
Baggio , S. , Hasler , R. , Deiber , M. P. , Heller , P. , Buadze , A. , Giacomini , V. , et al. ( 2020 ). Associations of executive and functional outcomes with full-score intellectual quotient among ADHD adults . Psychiatry Research , 294 , 113521 . https://doi.org/10.1016/j.psychres.2020.113521 .
Barbeau , E. B. , Soulières , I. , Dawson , M. , Zeffiro , T. A. , & Mottron , L. ( 2013 ). The level and nature of autistic intelligence III: Inspection time . Journal of Abnormal Psychology , 122 ( 1 ), 295 – 301 . https://doi.org/10.1037/a0029984 .
Becker , A. , Daseking , M. , & Kerner auch Koerner , J. ( 2021 ). Cognitive profiles in the WISC-V of children with ADHD and specific learning disorders . Sustainability , 13 ( 17 ), 9948 . https://doi.org/10.3390/su13179948 .
Bölte , S. , Neufeld , J. , Marschik , P. B. , Williams , Z. J. , Gallagher , L. , & Lai , M. C. ( 2023 ). Sex and gender in neurodevelopmental conditions . Nature Reviews. Neurology , 19 ( 3 ), 136 – 159 . https://doi.org/10.1038/s41582-023-00774-6 .
Bucaille , A. , Grandgeorge , M. , Degrez , C. , Mallégol , C. , Cam , P. , Botbol , M. , et al. ( 2016 ). Cognitive profile in adults with Asperger syndrome using WAIS-IV: Comparison to typical adults . Research in Autism Spectrum Disorders , 21 , 1 – 9 . https://doi.org/10.1016/j.rasd.2015.09.001 .
Charman , T. , Pickles , A. , Simonoff , E. , Chandler , S. , Loucas , T. , & Baird , G. ( 2011 ). IQ in children with autism spectrum disorders: Data from the special needs and autism project (SNAP) . Psychological Medicine , 41 ( 3 ), 619 – 627 . https://doi.org/10.1017/S0033291710000991 .
Chiang , H. M. , Tsai , L. Y. , Cheung , Y. K. , Brown , A. , & Li , H. ( 2014 ). A meta-analysis of differences in IQ profiles between individuals with Asperger's disorder and high-functioning autism . Journal of Autism and Developmental Disorders , 44 ( 7 ), 1577 – 1596 . https://doi.org/10.1007/s10803-013-2025-2 .
Cicinelli , G. , Nobile , E. , Brighenti , S. , Bari , S. , Tonella , E. , Aresi , A. , et al. ( 2022 ). Wechsler intelligence scale for adults - fourth edition profiles of adults with autism spectrum disorder . Epidemiology and Psychiatric Sciences , 31 , e67. https://doi.org/10.1017/S2045796022000506 .
Cohen , J. ( 1988 ). Statistical power analysis for the behavioral sciences . New York: Routledge .
Cook , N. E. , Braaten , E. B. , & Surman , C. B. H. ( 2018 ). Clinical and functional correlates of processing speed in pediatric attention-deficit/hyperactivity disorder: A systematic review and meta-analysis . Child Neuropsychology , 24 ( 5 ), 598 – 616 . https://doi.org/10.1080/09297049.2017.1307952 .
Dale , B. A. , Finch , W. H. , Shellabarger , K. A. R. , & Davis , A. ( 2021 ). Wechsler intelligence scale for children, fifth edition profiles of children with autism spectrum disorder using a classification and regression trees analysis . Journal of Psychoeducational Assessment , 39 ( 7 ), 783 – 799 . https://doi.org/10.1177/07342829211025924 .
Dale , B. A. , Finch , W. H. , Shellabarger , K. A. R. , & Davis , A. ( 2022 ). Comparison of verbal performance of children with autism spectrum disorder on the WISC-V . Journal of Psychoeducational Assessment , 40 ( 7 ), 811 – 824 . https://doi.org/10.1177/07342829221106592 .
Davids , R. C. D. , Groen , Y. , Berg , I. J. , Tucha , O. , & van Balkom , I. D. C. ( 2020 ). Local-global processing approaches in older autistic adults: A matched control study using RCFT and WAIS-IV . Research in Autism Spectrum Disorders , 78 , 101655 . https://doi.org/10.1016/j.rasd.2020.101655 .
Dawson , M. , Soulières , I. , Gernsbacher , M. A. , & Mottron , L. ( 2007 ). The level and nature of autistic intelligence . Psychological Science , 18 ( 8 ), 657 – 662 . https://doi.org/10.1111/j.1467-9280.2007.01954.x .
Di Sarro , R. , Di Santantonio , A. , Desideri , L. , & Varrucciu , N. ( 2021 ). Profiling planning skills and cognitive flexibility of adults with autism spectrum disorders: Preliminary results from an exploratory service-based study . International Journal of Developmental Disabilities , 68 ( 5 ), 651 – 657 . https://doi.org/10.1080/20473869.2020.1871311 .
Donders , J. ( 2020 ). The incremental value of neuropsychological assessment: A critical review . The Clinical Neuropsychologist , 34 ( 1 ), 56 – 87 . https://doi.org/10.1080/13854046.2019.1575471 .
Donovan , A. P. , & Basson , M. A. ( 2017 ). The neuroanatomy of autism - a developmental perspective . Journal of Anatomy , 230 ( 1 ), 4 – 15 . https://doi.org/10.1111/joa.12542 .
Drukker , M. , Weltens , I. , van Hooijdonk , C. F. M. , Vandenberk , E. , & Bak , M. ( 2021 ). Development of a methodological quality criteria list for observational studies: The observational study quality evaluation . Frontiers in Research Metrics and Analytics , 6 , 675071. https://doi.org/10.3389/frma.2021.675071 .
Ehlers , S. , Nydén , A. , Gillberg , C. , Sandberg , A. D. , Dahlgren , S. O. , Hjelmquist , E. , et al. ( 1997 ). Asperger syndrome, autism and attention disorders: A comparative study of the cognitive profiles of 120 children . Journal of Child Psychology and Psychiatry, and Allied Disciplines , 38 ( 2 ), 207 – 217 . https://doi.org/10.1111/j.1469-7610.1997.tb01855.x .
Faraone , S. V. , Banaschewski , T. , Coghill , D. , Zheng , Y. , Biederman , J. , Bellgrove , M. A. , et al. ( 2021 ). The world federation of ADHD international consensus statement: 208 evidence-based conclusions about the disorder . Neuroscience and Biobehavioral Reviews , 128 , 789 – 818 . https://doi.org/10.1016/j.neubiorev.2021.01.022 .
Guilmette , T. J. , Sweet , J. J. , Hebben , N. , Koltai , D. , Mahone , E. M. , Spiegler , B. J. , et al. ( 2020 ). American Academy of Clinical Neuropsychology consensus conference statement on uniform labeling of performance test scores . The Clinical Neuropsychologist , 34 ( 3 ), 437 – 453 . https://doi.org/10.1080/13854046.2020.1722244 .
Happé , F. G. ( 1994 ). Wechsler IQ profile and theory of mind in autism: A research note . Journal of Child Psychology and Psychiatry, and Allied Disciplines , 35 ( 8 ), 1461 – 1471 . https://doi.org/10.1111/j.1469-7610.1994.tb01287.x .
Hayes , J. , Ford , T. , Rafeeque , H. , & Russell , G. ( 2018 ). Clinical practice guidelines for diagnosis of autism spectrum disorder in adults and children in the UK: A narrative review . BMC Psychiatry , 18 ( 1 ), 222 . https://doi.org/10.1186/s12888-018-1800-1 .
Hedges , L. V. , Tipton , E. , & Johnson , M. C. ( 2010 ). Robust variance estimation in meta-regression with dependent effect size estimates . Research Synthesis Methods , 1 ( 1 ), 39 – 65 . https://doi.org/10.1002/jrsm.5 .
Holdnack , J. , Goldstein , G. , & Drozdick , L. ( 2011 ). Social perception and WAIS-IV performance in adolescents and adults diagnosed with Asperger's syndrome and autism . Assessment , 18 ( 2 ), 192 – 200 . https://doi.org/10.1177/1073191110394771 .
Hong , J. S. , Lee , Y. S. , Hong , M. , Kim , B. , Joung , Y. S. , Yoo , H. K. , et al. ( 2022 ). Cognitive developmental trajectories in adult ADHD patients and controls: A comparative study . Journal of Attention Disorders , 26 ( 3 ), 391 – 407 . https://doi.org/10.1177/1087054720978548 .
Just , M. A. , Keller , T. A. , Malave , V. L. , Kana , R. K. , & Varma , S. ( 2012 ). Autism as a neural systems disorder: A theory of frontal-posterior underconnectivity . Neuroscience and Biobehavioral Reviews , 36 ( 4 ), 1292 – 1313 . https://doi.org/10.1016/j.neubiorev.2012.02.007 .
Kanai , C. , Hashimoto , R. , Itahashi , T. , Tani , M. , Yamada , T. , Ota , H. , et al. ( 2017 ). Cognitive profiles of adults with high-functioning autism spectrum disorder and those with attention-deficit/hyperactivity disorder based on the WAIS-III . Research in Developmental Disabilities , 61 , 108 – 115 . https://doi.org/10.1016/j.ridd.2016.12.008 .
Karalunas , S. L. , Geurts , H. M. , Konrad , K. , Bender , S. , & Nigg , J. T. ( 2014 ). Annual research review: Reaction time variability in ADHD and autism spectrum disorders: Measurement and mechanisms of a proposed trans-diagnostic phenotype . Journal of Child Psychology and Psychiatry, and Allied Disciplines , 55 ( 6 ), 685 – 710 . https://doi.org/10.1111/jcpp.12217 .
Keehn , B. , Müller , R. A. , & Townsend , J. ( 2013 ). Atypical attentional networks and the emergence of autism . Neuroscience and Biobehavioral Reviews , 37 ( 2 ), 164 – 183 . https://doi.org/10.1016/j.neubiorev.2012.11.014 .
Kenny , L. , Hattersley , C. , Molins , B. , Buckley , C. , Povey , C. , & Pellicano , E. ( 2016 ). Which terms should be used to describe autism? Perspectives from the UK autism community . Autism , 20 ( 4 ), 442 – 462 . https://doi.org/10.1177/1362361315588200 .
Kenworthy , L. , Yerys , B. E. , Weinblatt , R. , Abrams , D. N. , & Wallace , G. L. ( 2013 ). Motor demands impact speed of information processing in autism spectrum disorders . Neuropsychology , 27 ( 5 ), 529 – 536 . https://doi.org/10.1037/a0033599 .
Kuenzel , E. , Seguin , D. , Nicolson , R. , & Duerden , E. G. ( 2021 ). Early adversity and positive parenting: Association with cognitive outcomes in children with autism spectrum disorder . Autism Research , 14 ( 12 ), 2654 – 2662 . https://doi.org/10.1002/aur.2613 .
Lai , M. C. , & Baron-Cohen , S. ( 2015 ). Identifying the lost generation of adults with autism spectrum conditions . The Lancet Psychiatry , 2 ( 11 ), 1013 – 1027 . https://doi.org/10.1016/S2215-0366(15)00277-1 .
Lange , K. W. , Hauser , J. , Lange , K. M. , Makulska-Gertruda , E. , Takano , T. , Takeuchi , Y. , et al. ( 2014 ). Utility of cognitive neuropsychological assessment in attention-deficit/hyperactivity disorder . Attention Deficit and Hyperactivity Disorders , 6 ( 4 ), 241 – 248 . https://doi.org/10.1007/s12402-014-0132-3 .
Leung , C. N. W. , Chan , R. W. S. , Fan , J. T. C. , Lam , C. H. Y. , & Yau , S. S. W. ( 2019 ). IQ profiling, autistic traits and social competence in Chinese adults with high-functioning ASD: A comparison between self- and parent-report . The European Journal of Psychiatry , 33 ( 1 ), 24 – 31 . https://doi.org/10.1016/j.ejpsy.2018.10.001 .
Mayes , S. D. , & Calhoun , S. L. ( 2004 ). Similarities and differences in Wechsler Intelligence Scale for Children--Third Edition (WISC-III) profiles: Support for subtest analysis in clinical referrals . The Clinical Neuropsychologist , 18 ( 4 ), 559 – 572 . https://doi.org/10.1080/13854040490888530 .
Mayes , S. D. , & Calhoun , S. L. ( 2006 ). WISC-IV and WISC-III profiles in children with ADHD . Journal of Attention Disorders , 9 ( 3 ), 486 – 493 . https://doi.org/10.1177/1087054705283616 .
Mayes , S. D. , & Calhoun , S. L. ( 2007 ). Learning, attention, writing, and processing speed in typical children and children with ADHD, autism, anxiety, depression, and oppositional-defiant disorder . Child Neuropsychology , 13 ( 6 ), 469 – 493 . https://doi.org/10.1080/09297040601112773 .
National Institute for Health and Care Excellence . ( 2011 ). Autism spectrum disorder in under 19s: Recognition, referral and diagnosis (clinical guideline CG128) . https://www.nice.org.uk/guidance/cg128
Nisbett , R. E. , Aronson , J. , Blair , C. , Dickens , W. , Flynn , J. , Halpern , D. F. , et al. ( 2012 ). Intelligence: New findings and theoretical developments . The American Psychologist , 67 ( 2 ), 130 – 159 . https://doi.org/10.1037/a0026699 .
Nyrenius , J. , & Billstedt , E. ( 2020 ). The functional impact of cognition in adults with autism spectrum disorders . Nordic Journal of Psychiatry , 74 ( 3 ), 220 – 225 . https://doi.org/10.1080/08039488.2019.1694698 .
Oliveras-Rentas , R. E. , Kenworthy , L. , Roberson , R. B. , 3rd , Martin , A. , & Wallace , G. L. ( 2012 ). WISC-IV profile in high-functioning autism spectrum disorders: Impaired processing speed is associated with increased autism communication symptoms and decreased adaptive communication abilities . Journal of Autism and Developmental Disorders , 42 ( 5 ), 655 – 664 . https://doi.org/10.1007/s10803-011-1289-7 .
O'Reilly , C. , Lewis , J. D. , & Elsabbagh , M. ( 2017 ). Is functional brain connectivity atypical in autism? A systematic review of EEG and MEG studies . PLoS One , 12 ( 5 ), e0175870 . https://doi.org/10.1371/journal.pone.0175870 .
Pauls , F. , Daseking , M. , Jacobs , C. , Werpup , L. , & Petermann , F. ( 2018 ). Intelligenzdiagnostik bei Kindern und Jugendlichen mit ADHS: Eine analyse der WISC-V-Leistungsprofile (Measuring intellectual performance of children and adolescents with ADHD: An analysis of WISC-V profiles) . Kindheit und Entwicklung , 27 ( 3 ), 165 – 174 . https://doi.org/10.1026/0942-5403/a000256 .
Pettersson , R. , Söderström , S. , & Nilsson , K. W. ( 2018 ). Diagnosing ADHD in adults: An examination of the discriminative validity of neuropsychological tests and diagnostic assessment instruments . Journal of Attention Disorders , 22 ( 11 ), 1019 – 1031 . https://doi.org/10.1177/1087054715618788 .
R Core Team ( 2022 ). R: A language and environment for statistical computing . Vienna: R Foundation for Statistical Computing . https://www.R-project.org/
Rabin , L. A. , Paolillo , E. , & Barr , W. B. ( 2016 ). Stability in test-usage practices of clinical neuropsychologists in the United States and Canada over a 10-year period: A follow-up survey of INS and NAN members . Archives of Clinical Neuropsychology , 31 ( 3 ), 206 – 230 . https://doi.org/10.1093/arclin/acw007 .
Ramos , A. A. , Hamdan , A. C. , & Machado , L. ( 2020 ). A meta-analysis on verbal working memory in children and adolescents with ADHD . The Clinical Neuropsychologist , 34 ( 5 ), 873 – 898 . https://doi.org/10.1080/13854046.2019.1604998 .
Rommelse , N. , Luman , M. , & Kievit , R. ( 2020 ). Slow processing speed: A cross-disorder phenomenon with significant clinical value, and in need of further methodological scrutiny . European Child & Adolescent Psychiatry , 29 ( 10 ), 1325 – 1327 . https://doi.org/10.1007/s00787-020-01639-9 .
Rong , Y. , Yang , C.-J. , Jin , Y. , & Wang , Y. ( 2021 ). Prevalence of attention-deficit/hyperactivity disorder in individuals with autism spectrum disorder: A meta-analysis . Research in Autism Spectrum Disorders , 83 , 101759 . https://doi.org/10.1016/j.rasd.2021.101759 .
Russell , G. , Stapley , S. , Newlove-Delgado , T. , Salmon , A. , White , R. , Warren , F. , Pearson , A. , & Ford , T. ( 2022 ). Time trends in autism diagnosis over 20 years: A UK population-based cohort study . Journal of Child Psychology and Psychiatry, and Allied Disciplines , 63 (6), 674 –682. https://doi.org/10.1111/jcpp.13505 .
Shepler , D. K. , & Callan , P. D. ( 2022 ). Differences in executive functioning between adults with ADHD and those diagnosed with other psychiatric diagnoses: Utility of the CTMT and the WAIS-IV. Applied Neuropsychology Adult . https://doi.org/10.1080/23279095.2022.2102923
Snow , J. B. , & Sapp , G. L. ( 2000 ). WISC-III subtest patterns of ADHD and normal samples . Psychological Reports , 87 ( 3 Pt 1 ), 759 – 765 . https://doi.org/10.2466/pr0.2000.87.3.759 .
Stephenson , K. G. , Beck , J. S. , South , M. , Norris , M. , & Butter , E. ( 2021 ). Validity of the WISC-V in youth with autism spectrum disorder: Factor structure and measurement invariance . Journal of Clinical Child and Adolescent Psychology , 50 ( 5 ), 669 – 681 . https://doi.org/10.1080/15374416.2020.1846543 .
Takayanagi , M. , Kawasaki , Y. , Shinomiya , M. , Hiroshi , H. , Okada , S. , Ino , T. , et al. ( 2022 ). Review of cognitive characteristics of autism spectrum disorder using performance on six subtests on four versions of the Wechsler Intelligence Scale for Children . Journal of Autism and Developmental Disorders , 52 ( 1 ), 240 – 253 . https://doi.org/10.1007/s10803-021-04932-x .
Theiling , J. , & Petermann , F. ( 2016 ). Neuropsychological profiles on the WAIS-IV of adults with ADHD . Journal of Attention Disorders , 20 ( 11 ), 913 – 924 . https://doi.org/10.1177/1087054713518241 .
Theiling , J. , Petermann , F. , & Daseking , M. ( 2013 ). Zusammenhang zwischen selbsteingeschätzter ADHS-Symptomatik und der Leistungsfähigkeit in der WAIS-IV (Relationship between self-reported ADHD symptoms and WAIS-IV performance) . Gesundheitswesen , 75 ( 11 ), 768 – 774 . https://doi.org/10.1055/s-0033-1357163 .
Tse , V. W. S. , Crabtree , J. , Islam , S. , & Stott , J. ( 2019 ). Comparing intellectual and memory abilities of older autistic adults with typically developing older adults using WAIS-IV and WMS-IV . Journal of Autism and Developmental Disorders , 49 ( 10 ), 4123 – 4133 . https://doi.org/10.1007/s10803-019-04122-w .
Viechtbauer , W. ( 2010 ). Conducting meta-analyses in R with the metafor package . Journal of Statistical Software , 36 ( 3 ), 1 – 48 . https://doi.org/10.18637/jss.v036.i03 .
Wechsler , D. ( 2008 ). Wechsler adult intelligence scale—Fourth edition (WAIS-IV) . San Antonio: Psychological Corporation .
Wechsler , D. ( 2014 ). Wechsler intelligence scale for children—Fifth edition (WISC-V) . Bloomington: Psychological Corporation .
Zapparrata , N. M. , Brooks , P. J. , & Ober , T. M. ( 2022 ). Slower processing speed in autism spectrum disorder: A meta-analytic investigation of time-based tasks . Journal of Autism and Developmental Disorders . https://doi.org/10.1007/s10803-022-05736-3 .
Zayat , M. , Kalb , L. , & Wodka , E. L. ( 2011 ). Brief report: Performance pattern differences between children with autism spectrum disorders and attention deficit-hyperactivity disorder on measures of verbal intelligence . Journal of Autism and Developmental Disorders , 41 ( 12 ), 1743 – 1747 . https://doi.org/10.1007/s10803-011-1207-z .
- attention-deficit/hyperactivity disorder
- autistic disorder
- adult attention deficit hyperactivity disorder
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1873-5843
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Get the best experience and stay connected to your community with our Spectrum News app. Learn More
Continue in Browser
Get hyperlocal forecasts, radar and weather alerts.
Please enter a valid zipcode.

Early genetic testing could help children with autism
One in 36 children are diagnosed with Autism Spectrum Disorder. But of those, very few actually know what specific gene mutation may be behind their diagnosis. National Health Reporter Erin Billups takes a look at how early genetic testing can improve treatment options and quality of life for patients.
“He's happy. He's outgoing. He's more outgoing with adults than he is with children. He loves water play. Loves to swim,” said Genie Egerton-Warbuton, who can’t help but smile herself when she speaks about her 11-year-old son Rowland.
Like many expecting parents, during her pregnancy with Rowland, Egerton-Warbuton underwent prenatal testing.
“I had to have a cesarean section. I'll never forget the doctor saying, you've given birth to a perfect, beautiful baby. Healthy, you know, healthy little boy that we know doesn't have any sort of issues or genetic abnormalities, etc. from this test,” said Egerton-Warbuton.
But from his notched eyelids at birth to missed developmental milestones, Egerton-Warbuton, a former preschool teacher, knew something wasn’t right.
“It's not normal for a child not to walk until they're two. And even his gait wasn't appropriate. And he was able to say some words, but then he was losing the words. He was able to pick up food and kind of feed himself. But then the next day, he needed to be spoon fed. It was just kind of, things did not feel right,” said Egerton-Warbuton.
When Rowland was four, he underwent another round of genetic testing and was finally diagnosed with a form of autism called ADNP syndrome — a deficiency of the activity-dependent neuroprotective protein — a mutation that wasn’t included in the test when Rowland was in utero.
“We know that protein is supposed to play a really important role in brain development,” said Dr. Alexis Kolevzon, director of the Seaver Autism Center at Mount Sinai Hospital in New York City, of the ADNP deficiency. “The hallmarks of ADNP syndrome, like autism, are social communication problems.”
Kolevzon said ADNP is now included on the genetic screening test for autism, along with more than 200 other known gene mutations that cause varying degrees of autism. ADNP accounts for about 0.2% of autism cases, but there may be even more who have it. Kolevzon says it is time for more families to get their kids tested.
“Oftentimes, families don't fully appreciate the value of genetic testing. You know, they have a child, the child that has autism. And it's not clear how knowing what the genetic causes will actually impact the child's life,” said Kolevzon.
The sooner families and doctors know, the better, said Kolevzon. While not every case of autism will have a genetic abnormality, it’s estimated that about 10 to 30 percent will find a known cause through testing.
“For us, there's a kind of a shift towards more personalized medicine. And so, you know, if you know exactly what's wrong with the biology, it gives you an opportunity to develop more targeted treatments,” said Kolevzon.
Rowland was enrolled in a study led by Kolevzon, with nine other kids with ADNP Syndrome.
Each child was given a very low dose of ketamine. Kolevzon said the drug may promote synaptic plasticity or nerve cell growth. That’s what they eventually found, participants saw improvement in sensory sensibilities, hyperactivity and repetitive behaviors. Larger studies are needed to confirm the findings.
“After the infusion, the next day he said, ‘Mommy,’ which was, you know, amazing,” said Egerton-Warbuton. “And we noticed that he was able to navigate a city street without walking into people.”
Rowland continues to work on further developing his speech. He is also learning to use a device that will help him communicate.
Egerton-Warbuton said her hope is that as more people with autism and other brain-based disorders are tested, more resources will go toward finding transformative genetic therapies for ADNP and other disorders.
“So many of these hospitals do want to collaborate and do want to help these children. But it's very hard when you have a small amount of children and adults,” said Egerton-Warbuton. “You just feel kind of stuck.”

IMAGES
VIDEO
COMMENTS
Studies indicate that Autism Spectrum Disorder (ASD) is inherited between family members. A study conducted by the American Psychiatric Association (2000) indicated that there is a 3-6% chance of getting autism amongst siblings. However, Korvatska et al (2002) state that the difficulty experienced by scientists in pinpointing the genetic ...
44 essay samples found. Autism, or Autism Spectrum Disorder (ASD), refers to a broad range of conditions characterized by challenges with social skills, repetitive behaviors, speech, and nonverbal communication. Essays could explore the causes, symptoms, and treatment of autism, the experiences of individuals with autism, and societal ...
Definition. Autism spectrum disorder (ASD) is a neurodevelopmental disorder characterized by deficits in social communication and the presence of restricted interests and repetitive behaviors ( 1 ). In 2013, the Diagnostic and Statistical Manual of Mental Disorders —5 th edition (DSM-5) was published, updating the diagnostic criteria for ASD ...
(A 2012 figure from the CDC says that one in 68 children have been diagnosed with autism spectrum disorder, ... It's taken me over 32 years to write this essay, and if you've read this far, I hope you will finish it with a greater sense of compassion and patience for everyone you meet. Each of us has our own learning style, and we all ...
Autism. PAGES 7 WORDS 2247. Autism is a disorder that starts early in the childhood and stays until adulthood. It has now been known that many conditions are considered co morbid to autism spectrum disorders. These conditions are variable but some of the most common ones include fragile X syndrome and epilepsy.
Autism spectrum disorders (ASD) are a diverse group of conditions. They are characterised by some degree of difficulty with social interaction and communication. Other characteristics are atypical patterns of activities and behaviours, such as difficulty with transition from one activity to another, a focus on details and unusual reactions to sensations.
Autism Essay. Sort By: Page 1 of 50 - About 500 essays. Decent Essays. Autism Between Autism And Autism. 756 Words; 4 Pages; Autism Between Autism And Autism ... Autism Disorder Mohamed Ayoub Community College of Aurora Autism Spectrum Disorder We are living in a time where a remarkable and advanced medical treatments exist. However, scientists ...
Understanding the Autistic Brain. My Autistic Mind Does What it Wants. The Dissociated Autistic Performance State. The Joys of Being Autistic: Increased Creativity and Innovation. My Autistic Memory Is Not the Same as Others. The Firehouse Dilemma: Autism and Infodumping. The Variability of the Autistic Sensory System.
Why Autism Awareness is Important. Autism, a complex neurodevelopmental disorder, affects individuals in diverse ways, shaping their behaviors, communication, and interactions with the world. As society becomes more informed about autism, the importance of raising awareness and promoting understanding has gained prominence.
This essay about the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), discusses the significant changes in the classification of Autism Spectrum Disorder (ASD). The shift from multiple distinct categories to a unified spectrum approach reflects a more accurate representation of the diverse manifestations of autism.
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that involves the reduced ability to emotionally interpret communication, idiosyncratic preoccupations, repetitive motor patterns, sensory sensitivity, and resistance to change. Typically signs such as failure to respond to one's name, or make eye contact with parents lead to the ...
Autism Essay: Autism, also known as autism spectrum disorder (ASD), is a neurodevelopmental disorder. Problems with communications and social interactions, along with repetitive and restricted behaviour, are common in autism. The associated factors of autism include genetics and specific environmental influences. Autism includes a wide range of disorders of which, Asperger syndrome, childhood ...
What policies at the federal, state, and local levels will best ensure appropriate education, examining strategies and resources needed to address the rights of children with autism to appropriate education. Read chapter 16 Conclusions and Recommendations: Autism is a word most of us are familiar with.
Autism is a major, peer-reviewed, international journal, published 8 times a year, publishing research of direct and practical relevance to help improve the quality of life for individuals with autism or autism-related disorders. It is interdisciplinary in nature, focusing on research in many areas, including: intervention; diagnosis; training; education; translational issues related to ...
Autism spectrum disorder (ASD) is a neurological and developmental disorder that affects how people interact with others, communicate, learn, and behave. Although autism can be diagnosed at any age, it is described as a "developmental disorder" because symptoms generally appear in the first 2 years of life.
Autism (Spectrum Disorder) Essays. 56 samples in this category. Essay examples. Essay topics. Autism, also known as Autism Spectrum Disorder (ASD), is a neurological condition. It affects how a person thinks, interacts, and experiences the world around them. Autism is not a disease or something that can be cured.
Autism spectrum disorder is a condition related to brain development that impacts how a person perceives and socializes with others, causing problems in social interaction and communication. The disorder also includes limited and repetitive patterns of behavior. The term "spectrum" in autism spectrum disorder refers to the wide range of ...
Develop an expertise. James, Craft, and Malia all focus on writing about autism, using their experiences to explain life on the spectrum. Garcia has a passion for politics and disability. Schedule down time. Garcia will often take a short nap after work to reset before he settles into book writing in the evening.
Abstract. Autism is a neuropsychiatric disorder characterised by severe and sustained impairment in social interaction, deviance in communication, and patterns of behaviour and interest that are ...
Myth #1: Autism is a disease. Let's start with the most basic misconception, that ASD is a disease. "Autism isn't an illness at all," Dr. Cuffman clarifies. "It's just the way your brain ...
Handbook of Autism and Pervasive Developmental Disorders. New York: Wiley. Autism Spectrum disorders. Introduction Autism awareness in today's society has moved from the shadow of shame and unknown to the forefront of research and education as an increasing number of children and people with Autism Spectrum disorders gain attention in every ...
Autism spectrum disorder (ASD) is a developmental disability caused by differences in the brain. Some people with ASD have a known difference, such as a genetic condition. Other causes are not yet known. Scientists believe there are multiple causes of ASD that act together to change the most common ways people develop. We still have much to ...
Purpose The prevalence of autism spectrum disorder (ASD) among children and adolescents seem to be high in countries around the world, and it's worth understanding the latest prevalence and trends of ASD in children and adolescents. The purpose of this study was to examine the latest prevalence and decade trend of ASD among individuals aged 3-17 years in the United States. Methods A total ...
May 30, 2024. Key takeaways. The study by UCLA scientists is the first to identify potential mechanisms that connect changes occurring in the brain in autism spectrum disorder directly to underlying genetic causes. Identifying these complex molecular mechanisms could eventually help lead to the development of therapeutics to treat autism.
Here, we uniformly processed and integrated bulk DNA methylation and single-nucleotide polymorphism (SNP) genotypes from 1270 postmortem human brain samples, including from donors diagnosed with Alzheimer's disease (n = 300), autism spectrum disorder (ASD) (n = 31), and schizophrenia (n = 186) across the life span (0 to >90 years; Fig. 1).
In the second step, abstracts and full papers were screened to ensure the paper included index and/or subtest scores on the WAIS-IV/WISC-V. Papers were included if there was a sample of people with a clinical diagnosis of autism or ADHD with standardized scores on all indexes of a fully administered WAIS-IV/WISC-V. Note that some studies ...
Kolevzon said ADNP is now included on the genetic screening test for autism, along with more than 200 other known gene mutations that cause varying degrees of autism. ADNP accounts for about 0.2% ...