This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search

Search menu
Abegaz TM, Shehab A, Gebreyohannes EA, Bhagavathula AS, Elnour AA. Nonadherence to antihypertensive drugs. Medicine (Baltimore). 2017; 96:(4) https://doi.org/10.1097/MD.0000000000005641
Armitage LC, Davidson S, Mahdi A Diagnosing hypertension in primary care: a retrospective cohort study to investigate the importance of night-time blood pressure assessment. Br J Gen Pract. 2023; 73:(726)e16-e23 https://doi.org/10.3399/BJGP.2022.0160
Barratt J. Developing clinical reasoning and effective communication skills in advanced practice. Nurs Stand. 2018; 34:(2)48-53 https://doi.org/10.7748/ns.2018.e11109
Bostock-Cox B. Nurse prescribing for the management of hypertension. British Journal of Cardiac Nursing. 2013; 8:(11)531-536
Bostock-Cox B. Hypertension – the present and the future for diagnosis. Independent Nurse. 2019; 2019:(1)20-24 https://doi.org/10.12968/indn.2019.1.20
Chakrabarti S. What's in a name? Compliance, adherence and concordance in chronic psychiatric disorders. World J Psychiatry. 2014; 4:(2)30-36 https://doi.org/10.5498/wjp.v4.i2.30
De Mauri A, Carrera D, Vidali M Compliance, adherence and concordance differently predict the improvement of uremic and microbial toxins in chronic kidney disease on low protein diet. Nutrients. 2022; 14:(3) https://doi.org/10.3390/nu14030487
Demosthenous N. Consultation skills: a personal reflection on history-taking and assessment in aesthetics. Journal of Aesthetic Nursing. 2017; 6:(9)460-464 https://doi.org/10.12968/joan.2017.6.9.460
Diamond-Fox S. Undertaking consultations and clinical assessments at advanced level. Br J Nurs. 2021; 30:(4)238-243 https://doi.org/10.12968/bjon.2021.30.4.238
Diamond-Fox S, Bone H. Advanced practice: critical thinking and clinical reasoning. Br J Nurs. 2021; 30:(9)526-532 https://doi.org/10.12968/bjon.2021.30.9.526
Donnelly M, Martin D. History taking and physical assessment in holistic palliative care. Br J Nurs. 2016; 25:(22)1250-1255 https://doi.org/10.12968/bjon.2016.25.22.1250
Fawcett J. Thoughts about meanings of compliance, adherence, and concordance. Nurs Sci Q. 2020; 33:(4)358-360 https://doi.org/10.1177/0894318420943136
Fisher NDL, Curfman G. Hypertension—a public health challenge of global proportions. JAMA. 2018; 320:(17)1757-1759 https://doi.org/10.1001/jama.2018.16760
Green S. Assessment and management of acute sore throat. Pract Nurs. 2015; 26:(10)480-486 https://doi.org/10.12968/pnur.2015.26.10.480
Harper C, Ajao A. Pendleton's consultation model: assessing a patient. Br J Community Nurs. 2010; 15:(1)38-43 https://doi.org/10.12968/bjcn.2010.15.1.45784
Hitchings A, Lonsdale D, Burrage D, Baker E. The Top 100 Drugs; Clinical Pharmacology and Practical Prescribing, 2nd edn. Scotland: Elsevier; 2019
Hobden A. Strategies to promote concordance within consultations. Br J Community Nurs. 2006; 11:(7)286-289 https://doi.org/10.12968/bjcn.2006.11.7.21443
Ingram S. Taking a comprehensive health history: learning through practice and reflection. Br J Nurs. 2017; 26:(18)1033-1037 https://doi.org/10.12968/bjon.2017.26.18.1033
James A, Holloway S. Application of concepts of concordance and health beliefs to individuals with pressure ulcers. British Journal of Healthcare Management. 2020; 26:(11)281-288 https://doi.org/10.12968/bjhc.2019.0104
Jamison J. Differential diagnosis for primary care. A handbook for health care practitioners, 2nd edn. China: Churchill Livingstone Elsevier; 2006
History and Physical Examination. 2021. https://patient.info/doctor/history-and-physical-examination (accessed 26 January 2023)
Kumar P, Clark M. Clinical Medicine, 9th edn. The Netherlands: Elsevier; 2017
Matthys J, Elwyn G, Van Nuland M Patients' ideas, concerns, and expectations (ICE) in general practice: impact on prescribing. Br J Gen Pract. 2009; 59:(558)29-36 https://doi.org/10.3399/bjgp09X394833
McKinnon J. The case for concordance: value and application in nursing practice. Br J Nurs. 2013; 22:(13)766-771 https://doi.org/10.12968/bjon.2013.22.13.766
McPhillips H, Wood AF, Harper-McDonald B. Conducting a consultation and clinical assessment of the skin for advanced clinical practitioners. Br J Nurs. 2021; 30:(21)1232-1236 https://doi.org/10.12968/bjon.2021.30.21.1232
Moulton L. The naked consultation; a practical guide to primary care consultation skills.Abingdon: Radcliffe Publishing; 2007
Medicine adherence; involving patients in decisions about prescribed medications and supporting adherence.England: NICE; 2009
National Institute for Health and Care Excellence. How do I control my blood pressure? Lifestyle options and choice of medicines patient decision aid. 2019. https://www.nice.org.uk/guidance/ng136/resources/patient-decision-aid-pdf-6899918221 (accessed 25 January 2023)
National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. NICE guideline NG136. 2022. https://www.nice.org.uk/guidance/ng136 (accessed 15 June 2023)
Nazarko L. Healthwise, Part 4. Hypertension: how to treat it and how to reduce its risks. Br J Healthc Assist. 2021; 15:(10)484-490 https://doi.org/10.12968/bjha.2021.15.10.484
Neighbour R. The inner consultation.London: Radcliffe Publishing Ltd; 1987
The Code. professional standards of practice and behaviour for nurses, midwives and nursing associates.London: NMC; 2018
Nuttall D, Rutt-Howard J. The textbook of non-medical prescribing, 2nd edn. Chichester: Wiley-Blackwell; 2016
O'Donovan K. The role of ACE inhibitors in cardiovascular disease. British Journal of Cardiac Nursing. 2018; 13:(12)600-608 https://doi.org/10.12968/bjca.2018.13.12.600
O'Donovan K. Angiotensin receptor blockers as an alternative to angiotensin converting enzyme inhibitors. British Journal of Cardiac Nursing. 2019; 14:(6)1-12 https://doi.org/10.12968/bjca.2019.0009
Porth CM. Essentials of Pathophysiology, 4th edn. Philadelphia: Wolters Kluwer; 2015
Rae B. Obedience to collaboration: compliance, adherence and concordance. Journal of Prescribing Practice. 2021; 3:(6)235-240 https://doi.org/10.12968/jprp.2021.3.6.235
Rostoft S, van den Bos F, Pedersen R, Hamaker ME. Shared decision-making in older patients with cancer - What does the patient want?. J Geriatr Oncol. 2021; 12:(3)339-342 https://doi.org/10.1016/j.jgo.2020.08.001
Schroeder K. The 10-minute clinical assessment, 2nd edn. Oxford: Wiley Blackwell; 2017
Thomas J, Monaghan T. The Oxford handbook of clinical examination and practical skills, 2nd edn. Oxford: Oxford University Press; 2014
Vincer K, Kaufman G. Balancing shared decision-making with ethical principles in optimising medicines. Nurse Prescribing. 2017; 15:(12)594-599 https://doi.org/10.12968/npre.2017.15.12.594
Waterfield J. ACE inhibitors: use, actions and prescribing rationale. Nurse Prescribing. 2008; 6:(3)110-114 https://doi.org/10.12968/npre.2008.6.3.28858
Weiss M. Concordance, 6th edn. In: Watson J, Cogan LS Poland: Elsevier; 2019
Williams H. An update on hypertension for nurse prescribers. Nurse Prescribing. 2013; 11:(2)70-75 https://doi.org/10.12968/npre.2013.11.2.70
Adherence to long-term therapies, evidence for action.Geneva: WHO; 2003
Young K, Franklin P, Franklin P. Effective consulting and historytaking skills for prescribing practice. Br J Nurs. 2009; 18:(17)1056-1061 https://doi.org/10.12968/bjon.2009.18.17.44160
Newly diagnosed hypertension: case study
Angela Brown
Trainee Advanced Nurse Practitioner, East Belfast GP Federation, Northern Ireland
View articles · Email Angela

The role of an advanced nurse practitioner encompasses the assessment, diagnosis and treatment of a range of conditions. This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as hypertension, but using a concordant approach in practice can optimise patient outcomes. This case study outlines a concordant approach to consultations in clinical practice which can enhance adherence in long-term conditions.
Hypertension is a worldwide problem with substantial consequences ( Fisher and Curfman, 2018 ). It is a progressive condition ( Jamison, 2006 ) requiring lifelong management with pharmacological treatments and lifestyle adjustments. However, adopting these lifestyle changes can be notoriously difficult to implement and sustain ( Fisher and Curfman, 2018 ) and non-adherence to chronic medication regimens is extremely common ( Abegaz et al, 2017 ). This is also recognised by the National Institute for Health and Care Excellence (NICE) (2009) which estimates that between 33.3% and 50% of medications are not taken as recommended. Abegaz et al (2017) furthered this by claiming 83.7% of people with uncontrolled hypertension do not take medications as prescribed. However, leaving hypertension untreated or uncontrolled is the single largest cause of cardiovascular disease ( Fisher and Curfman, 2018 ). Therefore, better adherence to medications is associated with better outcomes ( World Health Organization, 2003 ) in terms of reducing the financial burden associated with the disease process on the health service, improving outcomes for patients ( Chakrabarti, 2014 ) and increasing job satisfaction for professionals ( McKinnon, 2013 ). Therefore, at a time when growing numbers of patients are presenting with hypertension, health professionals must adopt a concordant approach from the initial consultation to optimise adherence.
Great emphasis is placed on optimising adherence to medications ( NICE, 2009 ), but the meaning of the term ‘adherence’ is not clear and it is sometimes used interchangeably with compliance and concordance ( De Mauri et al, 2022 ), although they are not synonyms. Compliance is an outdated term alluding to paternalism, obedience and passivity from the patient ( Rae, 2021 ), whereby the patient's behaviour must conform to the health professional's recommendations. Adherence is defined as ‘the extent to which a person's behaviour, taking medication, following a diet and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider’ ( Chakrabarti, 2014 ). This term is preferred over compliance as it is less paternalistic ( Rae, 2021 ), as the patient is included in the decision-making process and has agreed to the treatment plan. While it is not yet widely embraced or used in practice ( Fawcett, 2020 ), concordance is recognised, not as a behaviour ( Rae, 2021 ) but more an approach or method which focuses on the equal partnership between patient and professional ( McKinnon, 2013 ) and enables effective and agreed treatment plans.
NICE last reviewed its guidance on medication adherence in 2019 and did not replace adherence with concordance within this. This supports the theory that adherence is an outcome of good concordance and the two are not synonyms. NICE (2009) guidelines, which are still valid, show evidence of concordant principles to maximise adherence. Integrating the theoretical principles of concordance into this case study demonstrates how the trainee advanced nurse practitioner aimed to individualise patient-centred care and improve health outcomes through optimising adherence.
Patient introduction and assessment
Jane (a pseudonym has been used to protect the patient's anonymity; Nursing and Midwifery Council (NMC) 2018 ), is a 45-year-old woman who had been referred to the surgery following an attendance at an emergency department. Jane had been role-playing as a patient as part of a teaching session for health professionals when it was noted that her blood pressure was significantly elevated at 170/88 mmHg. She had no other symptoms. Following an initial assessment at the emergency department, Jane was advised to contact her GP surgery for review and follow up. Nazarko (2021) recognised that it is common for individuals with high blood pressure to be asymptomatic, contributing to this being referred to as the ‘silent killer’. Hypertension is generally only detected through opportunistic checking of blood pressure, as seen in Jane's case, which is why adults over the age of 40 years are offered a blood pressure check every 5 years ( Bostock-Cox, 2013 ).
Consultation
Jane presented for a consultation at the surgery. Green (2015) advocates using a model to provide a structured approach to consultations which ensures quality and safety, and improves time management. Young et al (2009) claimed that no single consultation model is perfect, and Diamond-Fox (2021) suggested that, with experience, professionals can combine models to optimise consultation outcomes. Therefore, to effectively consult with Jane and to adapt to her individual personality, different models were intertwined to provide better person-centred care.
The Calgary–Cambridge model is the only consultation model that places emphasis on initiating the session, despite it being recognised that if a consultation gets off to a bad start this can interfere throughout ( Young et al, 2009 ). Being prepared for the consultation is key. Before Jane's consultation, the environment was checked to minimise interruptions, ensuring privacy and dignity ( Green, 2015 ; NMC, 2018 ), the seating arrangements optimised to aid good body language and communication ( Diamond-Fox, 2021 ) and her records were viewed to give some background information to help set the scene and develop a rapport ( Young et al, 2009 ). Being adequately prepared builds the patient's trust and confidence in the professional ( Donnelly and Martin, 2016 ) but equally viewing patient information can lead to the professional forming preconceived ideas ( Donnelly and Martin, 2016 ). Therefore, care was taken by the trainee advanced nurse practitioner to remain open-minded.
During Jane's consultation, a thorough clinical history was taken ( Table 1 ). History taking is common to all consultation models and involves gathering important information ( Diamond-Fox, 2021 ). History-taking needs to be an effective ( Bostock-Cox, 2019 ), holistic process ( Harper and Ajao, 2010 ) in order to be thorough, safe ( Diamond-Fox, 2021 ) and aid in an accurate diagnosis. The key skill for taking history is listening and observing the patient ( Harper and Ajao, 2010 ). Sir William Osler said:‘listen to the patient as they are telling you the diagnosis’, but Knott and Tidy (2021) suggested that patients are barely given 20 seconds before being interrupted, after which they withdraw and do not offer any new information ( Demosthenous, 2017 ). Using this guidance, Jane was given the ‘golden minute’ allowing her to tell her ‘story’ without being interrupted ( Green, 2015 ). This not only showed respect ( Ingram, 2017 ) but interest in the patient and their concerns.
Once Jane shared her story, it was important for the trainee advanced nurse practitioner to guide the questioning ( Green 2015 ). This was achieved using a structured approach to take Jane's history, which optimised efficiency and effectiveness, and ensured that pertinent information was not omitted ( Young et al, 2009 ). Thomas and Monaghan (2014) set out clear headings for this purpose. These included:
- The presenting complaint
- Past medical history
- Drug history
- Social history
- Family history.
McPhillips et al (2021) also emphasised a need for a systemic enquiry of the other body systems to ensure nothing is missed. From taking this history it was discovered that Jane had been feeling well with no associated symptoms or red flags. A blood pressure reading showed that her blood pressure was elevated. Jane had no past medical history or allergies. She was not taking any medications, including prescribed, over the counter, herbal or recreational. Jane confirmed that she did not drink alcohol or smoke. There was no family history to note, which is important to clarify as a genetic link to hypertension could account for 30–50% of cases ( Nazarko, 2021 ). The information gathered was summarised back to Jane, showing good practice ( McPhillips et al, 2021 ), and Jane was able to clarify salient or missing points. Green (2015) suggested that optimising the patient's involvement in this way in the consultation makes her feel listened to which enhances patient satisfaction, develops a therapeutic relationship and demonstrates concordance.
During history taking it is important to explore the patient's ideas, concerns and expectations. Moulton (2007) refers to these as the ‘holy trinity’ and central to upholding person-centredness ( Matthys et al, 2009 ). Giving Jane time to discuss her ideas, concerns and expectations allowed the trainee advanced nurse practitioner to understand that she was concerned about her risk of a stroke and heart attack, and worried about the implications of hypertension on her already stressful job. Using ideas, concerns and expectations helped to understand Jane's experience, attitudes and perceptions, which ultimately will impact on her health behaviours and whether engagement in treatment options is likely ( James and Holloway, 2020 ). Establishing Jane's views demonstrated that she was eager to engage and manage her blood pressure more effectively.
Vincer and Kaufman (2017) demonstrated, through their case study, that a failure to ask their patient's viewpoint at the initial consultation meant a delay in engagement with treatment. They recognised that this delay could have been avoided with the use of additional strategies had ideas, concerns and expectations been implemented. Failure to implement ideas, concerns and expectations is also associated with reattendance or the patient seeking second opinions ( Green, 2015 ) but more positively, when ideas, concerns and expectations is implemented, it can reduce the number of prescriptions while sustaining patient satisfaction ( Matthys et al, 2009 ).
Physical examination
Once a comprehensive history was taken, a physical examination was undertaken to supplement this information ( Nuttall and Rutt-Howard, 2016 ). A physical examination of all the body systems is not required ( Diamond-Fox, 2021 ) as this would be extremely time consuming, but the trainee advanced nurse practitioner needed to carefully select which systems to examine and use good examination technique to yield a correct diagnosis ( Knott and Tidy, 2021 ). With informed consent, clinical observations were recorded along with a full cardiovascular examination. The only abnormality discovered was Jane's blood pressure which was 164/90 mmHg, which could suggest stage 2 hypertension ( NICE, 2019 ; 2022 ). However, it is the trainee advanced nurse practitioner's role to use a hypothetico-deductive approach to arrive at a diagnosis. This requires synthesising all the information from the history taking and physical examination to formulate differential diagnoses ( Green, 2015 ) from which to confirm or refute before arriving at a final diagnosis ( Barratt, 2018 ).
Differential diagnosis
Hypertension can be triggered by secondary causes such as certain drugs (non-steroidal anti-inflammatory drugs, steroids, decongestants, sodium-containing medications or combined oral contraception), foods (liquorice, alcohol or caffeine; Jamison, 2006 ), physiological response (pain, anxiety or stress) or pre-eclampsia ( Jamison, 2006 ; Schroeder, 2017 ). However, Jane had clarified that these were not contributing factors. Other potential differentials which could not be ruled out were the white-coat syndrome, renal disease or hyperthyroidism ( Schroeder, 2017 ). Further tests were required, which included bloods, urine albumin creatinine ratio, electrocardiogram and home blood pressure monitoring, to ensure a correct diagnosis and identify any target organ damage.
Joint decision making
At this point, the trainee advanced nurse practitioner needed to share their knowledge in a meaningful way to enable the patient to participate with and be involved in making decisions about their care ( Rostoft et al, 2021 ). Not all patients wish to be involved in decision making ( Hobden, 2006 ) and this must be respected ( NMC, 2018 ). However, engaging patients in partnership working improves health outcomes ( McKinnon, 2013 ). Explaining the options available requires skill so as not to make the professional seem incompetent and to ensure the patient continues to feel safe ( Rostoft et al, 2021 ).
Information supported by the NICE guidelines was shared with Jane. These guidelines advocated that in order to confirm a diagnosis of hypertension, a clinic blood pressure reading of 140/90 mmHg or higher was required, with either an ambulatory or home blood pressure monitoring result of 135/85 mmHg or higher ( NICE, 2019 ; 2022 ). However, the results from a new retrospective study suggested that the use of home blood pressure monitoring is failing to detect ‘non-dippers’ or ‘reverse dippers’ ( Armitage et al, 2023 ). These are patients whose blood pressure fails to fall during their nighttime sleep. This places them at greater risk of cardiovascular disease and misdiagnosis if home blood pressure monitors are used, but ambulatory blood pressure monitors are less frequently used in primary care and therefore home blood pressure monitors appear to be the new norm ( Armitage et al, 2023 ).
Having discussed this with Jane she was keen to engage with home blood pressure monitoring in order to confirm the potential diagnosis, as starting a medication without a true diagnosis of hypertension could potentially cause harm ( Jamison, 2006 ). An accurate blood pressure measurement is needed to prevent misdiagnosis and unnecessary therapy ( Jamison, 2006 ) and this is dependent on reliable and calibrated equipment and competency in performing the task ( Bostock-Cox, 2013 ). Therefore, Jane was given education and training to ensure the validity and reliability of her blood pressure readings.
For Jane, this consultation was the ideal time to offer health promotion advice ( Green, 2015 ) as she was particularly worried about her elevated blood pressure. Offering health promotion advice is a way of caring, showing support and empowerment ( Ingram, 2017 ). Therefore, Jane was provided with information on a healthy diet, the reduction of salt intake, weight loss, exercise and continuing to abstain from smoking and alcohol ( Williams, 2013 ). These were all modifiable factors which Jane could implement straight away to reduce her blood pressure.
Safety netting
The final stage and bringing this consultation to a close was based on the fourth stage of Neighbour's (1987) model, which is safety netting. Safety netting identifies appropriate follow up and gives details to the patient on what to do if their condition changes ( Weiss, 2019 ). It is important that the patient knows who to contact and when ( Young et al, 2009 ). Therefore, Jane was advised that, should she develop chest pains, shortness of breath, peripheral oedema, reduced urinary output, headaches, visual disturbances or retinal haemorrhages ( Schroeder, 2017 ), she should present immediately to the emergency department, otherwise she would be reviewed in the surgery in 1 week.
Jane was followed up in a second consultation 1 week later with her home blood pressure readings. The average reading from the previous 6 days was calculated ( Bostock-Cox, 2013 ) and Jane's home blood pressure reading was 158/82 mmHg. This reading ruled out white-coat syndrome as Jane's blood pressure remained elevated outside clinic conditions (white-coat syndrome is defined as a difference of more than 20/10 mmHg between clinic blood pressure readings and the average home blood pressure reading; NICE, 2019 ; 2022 ). Subsequently, Jane was diagnosed with stage 2 essential (or primary) hypertension. Stage 2 is defined as a clinic blood pressure of 160/100 mmHg or higher or a home blood pressure of 150/95 mmHg or higher ( NICE, 2019 ; 2022 ).
A diagnosis of hypertension can be difficult for patients as they obtain a ‘sick label’ despite feeling well ( Jamison, 2006 ). This is recognised as a deterrent for their motivation to initiate drug treatment and lifestyle changes ( Williams, 2013 ), presenting a greater challenge to health professionals, which can be addressed through concordance strategies. However, having taken Jane's bloods, electrocardiogram and urine albumin:creatinine ratio in the first consultation, it was evident that there was no target organ damage and her Qrisk3 score was calculated as 3.4%. These results provided reassurance for Jane, but she was keen to engage and prevent any potential complications.
Agreeing treatment
Concordance is only truly practised when the patient's perspectives are valued, shared and used to inform planning ( McKinnon, 2013 ). The trainee advanced nurse practitioner now needed to use the information gained from the consultations to formulate a co-produced and meaningful treatment plan based on the best available evidence ( Diamond-Fox and Bone, 2021 ). Jane understood the risk associated with high blood pressure and was keen to begin medication as soon as possible. NICE guidelines ( 2019 ; 2022 ) advocate the use of an angiotensin-converting enzyme (ACE) inhibitor or angiotensin-receptor blockers in patients under 55 years of age and not of Black African or African-Caribbean origin. However, ACE inhibitors seem to be used as the first-line treatment for hypertensive patients under the age of 55 years ( O'Donovan, 2019 ).
ACE inhibitors directly affect the renin–angiotensin-aldosterone system which plays a central role in regulation of blood pressure ( Porth, 2015 ). Renin is secreted by the juxtaglomerular cells, in the kidneys' nephrons, when there is a decrease in renal perfusion and stimulation of the sympathetic nervous system ( O'Donovan, 2018 ). Renin then combines with angiotensinogen, a circulating plasma globulin from the liver, to form angiotensin I ( Kumar and Clark, 2017 ). Angiotensin I is inactive but, through ACE, an enzyme present in the endothelium of the lungs, it is transformed into angiotensin II ( Kumar and Clark, 2017 ). Angiotensin II is a vasoconstrictor which increases vascular resistance and in turn blood pressure ( Porth, 2015 ) while also stimulating the adrenal gland to produce aldosterone. Aldosterone reduces sodium excretion in the kidneys, thus increasing water reabsorption and therefore blood volume ( Porth, 2015 ). Using an ACE inhibitor prevents angiotensin II formation, which prevents vasoconstriction and stops reabsorption of sodium and water, thus reducing blood pressure.
When any new medication is being considered, providing education is key. This must include what the medication is for, the importance of taking it, any contraindications or interactions with the current medications being taken by the patient and the potential risk of adverse effects ( O'Donovan, 2018 ). Sharing this information with Jane allowed her to weigh up the pros and cons and make an informed choice leading to the creation of an individualised treatment plan.
Jamison (2006) placed great emphasis on sharing information about adverse effects, because patients with hypertension feel well before commencing medications, but taking medication has the potential to cause side effects which can affect adherence. Therefore, the range of side effects were discussed with Jane. These include a persistent, dry non-productive cough, hypotension, hypersensitivity, angioedema and renal impairment with hyperkalaemia ( Hitchings et al, 2019 ). ACE inhibitors have a range of adverse effects and most resolve when treatment is stopped ( Waterfield, 2008 ).
Following discussion with Jane, she proceeded with taking an ACE inhibitor and was encouraged to report any side effects in order to find another more suitable medication and to prevent her hypertension from going untreated. This information was provided verbally and written which is seen as good practice ( Green, 2015 ). Jane was followed up with fortnightly blood pressure recordings and urea and electrolyte checks and her dose of ramipril was increased fortnightly until her blood pressure was under 140/90 mmHg ( NICE, 2019 ; 2022 ).
Conclusions
Adherence to medications can be difficult to establish and maintain, especially for patients with long-term conditions. This can be particularly challenging for patients with hypertension because they are generally asymptomatic, yet acquire a sick label and start lifelong medication and lifestyle adjustments to prevent complications. Through adopting a concordant approach in practice, the outcome of adherence can be increased. This case study demonstrates how concordant strategies were implemented throughout the consultation to create a therapeutic patient–professional relationship. This optimised the creation of an individualised treatment plan which the patient engaged with and adhered to.
- Hypertension is a growing worldwide problem
- Appropriate clinical assessment, diagnosis and management is key to prevent misdiagnosis
- Long-term conditions are associated with high levels of non-adherence to treatments
- Adopting a concordance approach to practice optimises adherence and promotes positive patient outcomes
CPD reflective questions
- How has this article developed your assessment, diagnosis or management of patients presenting with a high blood pressure?
- What measures can you implement in your practice to enhance a concordant approach?
Hypertension

Learn about the nursing care management of patients with hypertension .
Table of Contents
- What is Hypertension?
Classification
Pathophysiology, epidemiology, clinical manifestations, complications, diagnostic tests, pharmacologic therapy.
- Nursing Assessment
- Diagnosis
- Nursing Care Plan and Goals
Nursing Priorities
Nursing interventions, discharge and home care guidelines, documentation guidelines, what is hypertension.
Hypertension is one of the most common lifestyle diseases to date. It affects people from all walks of life. Let us get to know hypertension more by its definitions.
- Hypertension is defined as a systolic blood pressure greater than 140 mmHg and a diastolic pressure of more than 90 mmHg .
- This is based on the average of two or more accurate blood pressure measurements during two or more consultations with the healthcare provider.
- The definition is taken from the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure .
In 2017, the American College of Cardiology and the American Heart Association revised their hypertension guidelines . The previous guidelines set the threshold at 140/90 mm Hg for younger people and 150/80 mm Hg for those ages 65 and older.
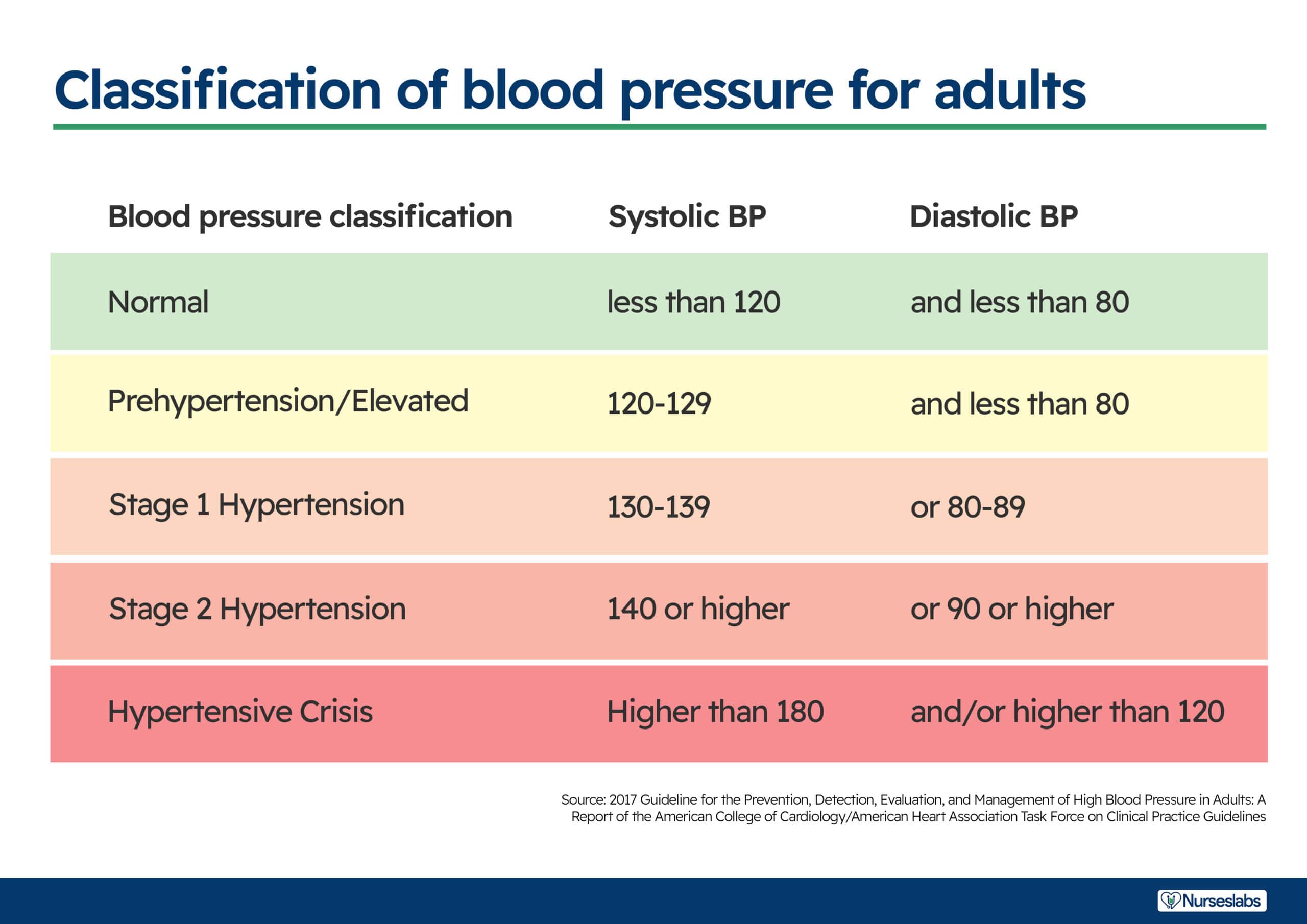
- Normal . The normal range for blood pressure is between, less than 120 mmHg and less than 80 mmHg.
- Elevated . Elevated stage starts from 120 mmHg to 129 mmHg for systolic blood pressure and less than 80 mmHg for diastolic pressure.
- Stage 1 hypertension . Stage 1 starts when the patient has a systolic pressure of 130 to 139 mmHg and a diastolic pressure of 80 to 89 mmHg.
- Stage 2 hypertension . Stage 2 starts when the systolic pressure is already more than or equal than 140 mmHg and the diastolic is more than or equal than 90 mmHg.
In a normal circulation, pressure is transferred from the heart muscle to the blood each time the heart contracts and then pressure is exerted by the blood as it flows through the blood vessels.
The pathophysiology of hypertension follows.
- Hypertension is a multifactorial
- When there is excess sodium intake , renal sodium retention occurs, which increases fluid volume resulting in increased preload and increase in contractility.
- Obesity is also a factor in hypertension because hyperinsulinemia develops and structural hypertrophy results leading to increased peripheral vascular resistance.
- Genetic alteration also plays a role in the development of hypertension because when there is cell membrane alteration, functional constriction may follow and also results in increased peripheral vascular resistance.
Hypertension is slowly rising to the top as one of the primary causes of morbidity in the world . Here are the current statistics of the status of hypertension in some of the leading countries.
- About 31% of the adults in the United States have hypertension.
- African-Americans have the highest prevalence rate of 37%.
- In the total US population of persons with hypertension, 90% to 95% have primary hypertension or high blood pressure from an unidentified cause.
- The remaining 5% to 10% of this group have secondary hypertension or high blood pressure related to identified causes.
- Hypertension is also termed as the “silent killer” because 24% of people who had pressures exceeding 140/90 mmHg were unaware that their blood pressures were elevated.
Hypertension has a lot of causes just like how fever has many causes. The factors that are implicated as causes of hypertension are:
- Increased sympathetic nervous system activity . Sympathetic nervous system activity increases because there is dysfunction in the autonomic nervous system .
- Increase renal reabsorption . There is an increase reabsorption of sodium, chloride, and water which is related to a genetic variation in the pathways by which the kidneys handle sodium.
- Increased RAAS activity . The renin-angiotensin-aldosterone system increases its activity leading to the expansion of extracellular fluid volume and increased systemic vascular resistance.
- Decreased vasodilation of the arterioles . The vascular endothelium is damaged because of the decrease in the vasodilation of the arterioles.
Many people who have hypertension are asymptomatic at first. Physical examination may reveal no abnormalities except for an elevated blood pressure, so one must be prepared to recognize hypertension at its earliest.
- Headache . The red blood cells carrying oxygen is having a hard time reaching the brain because of constricted vessels , causing headache.
- Dizziness occurs due to the low concentration of oxygen that reaches the brain.
- Chest pain . Chest pain occurs also due to decreased oxygen levels .
- Blurred vision. Blurred vision may occur later on because of too much constriction in the blood vessels of the eye that red blood cells carrying oxygen cannot pass through.
Prevention of hypertension mainly relies on a healthy lifestyle and self-discipline.
- Weight reduction . Maintenance of normal body weight can help prevent hypertension.
- Adopt DASH . DASH or the Dietary Approaches to Stop Hypertension includes consummation of a diet rich in fruits, vegetable, and low-fat dairy .
- Dietary sodium retention . Sodium contributes to an elevated blood pressure, so reducing the dietary intake to no more than 2.4 g sodium per day can be really helpful.
- Physical activity . Engage in regular aerobic physical activity for 30 minutes thrice every week.
- Moderation of alcohol consumption . Limit alcohol consumption to no more than 2 drinks per day in men and one drink for women and people who are lighter in weight.
If hypertension is left untreated, it could progress to complications of the different body organs.
- Heart failure . With increased blood pressure, the heart pumps blood faster than normal until the heart muscle goes weak from too much exertion.
- Myocardial infarction . Decreased oxygen due to constriction of blood vessels may lead to MI.
- Impaired vision. Ineffective peripheral perfusion affects the eye, causing problems in vision because of decreased oxygen.
- Renal failure. Blood carrying oxygen and nutrients could not reach the renal system because of the constricted blood vessels .
Assessment and Diagnostic Findings
Assessment of the patient with hypertension must be detailed and thorough. There are also diagnostic tests that can be performed to establish the diagnosis of hypertension.
- Assess the patient’s health history
- Perform physical examination as appropriate.
- The retinas are examined to assess possible organ damage .
- Laboratory tests are also taken to check target organ damage .
- Urinalysis is performed to check the concentration of sodium in the urine though the specific gravity.
- Blood chemistry (e.g. analysis of sodium, potassium , creatinine , fasting glucose , and total and high density lipoprotein cholesterol levels). These tests are done to determine the level of sodium and fat in the body.
- 12-lead ECG . ECG needs to be performed to rule presence of cardiovascular damage .
- Echocardiography . Echocardiography assesses the presence of left ventricular hypertrophy .
- Creatinine clearance . Creatinine clearance is performed to check for the level of BUN and creatinine that can determine if there is renal damage or not.
- Renin level . Renin level should be assessed to determine how RAAS is coping.
- Hemoglobin/hematocrit: Not diagnostic but assesses relationship of cells to fluid volume (viscosity) and may indicate risk factors such as hypercoagulability, anemia .
- Blood urea nitrogen (BUN)/creatinine: Provides information about renal perfusion/function.
- Glucose: Hyperglycemia ( diabetes mellitus is a precipitator of hypertension) may result from elevated catecholamine levels (increases hypertension).
- Serum potassium : Hypokalemia may indicate the presence of primary aldosteronism (cause) or be a side effect of diuretic therapy.
- Serum calcium : Imbalance may contribute to hypertension.
- Lipid panel (total lipids, high-density lipoprotein [HDL], low-density lipoprotein [LDL], cholesterol, triglycerides, phospholipids): Elevated level may indicate predisposition for/presence of atheromatous plaques.
- Thyroid studies: Hyperthyroidism may lead or contribute to vasoconstriction and hypertension.
- Serum/urine aldosterone level: May be done to assess for primary aldosteronism (cause).
- Urinalysis: May show blood, protein, or white blood cells; or glucose suggests renal dysfunction and/or presence of diabetes .
- Creatinine clearance: May be reduced, reflecting renal damage.
- Urine vanillylmandelic acid (VMA) (catecholamine metabolite): Elevation may indicate presence of pheochromocytoma (cause); 24-hour urine VMA may be done for assessment of pheochromocytoma if hypertension is intermittent.
- Uric acid: Hyperuricemia has been implicated as a risk factor for the development of hypertension.
- Renin: Elevated in renovascular and malignant hypertension, salt-wasting disorders.
- Urine steroids: Elevation may indicate hyperadrenalism, pheochromocytoma, pituitary dysfunction, Cushing’s syndrome.
- Intravenous pyelogram (IVP): May identify cause of secondary hypertension, e.g., renal parenchymal disease, renal/ureteral calculi.
- Kidney and renography nuclear scan: Evaluates renal status (TOD).
- Excretory urography: May reveal renal atrophy, indicating chronic renal disease.
- Chest x-ray : May demonstrate obstructing calcification in valve areas; deposits in and/or notching of aorta ; cardiac enlargement.
- Computed tomography (CT) scan: Assesses for cerebral tumor , CVA, or encephalopathy or to rule out pheochromocytoma.
- Electrocardiogram (ECG): May demonstrate enlarged heart, strain patterns, conduction disturbances. Note: Broad, notched P wave is one of the earliest signs of hypertensive heart disease.
Medical Management
Main Topic: Antihypertensive Drugs
The goal of hypertension treatment is to prevent complications and death by achieving and maintaining arterial blood pressure at or below 130/80 mmHg.
- The medications used for treating hypertension decrease peripheral resistance , blood volume , or the strength and rate of myocardial contraction .
- For uncomplicated hypertension, the initial medications recommended are diuretics and beta blockers.
- Only low doses are given, but if blood pressure still exceeds 140/90 mmHg, the dose is increased gradually.
- Thiazide diuretics decrease blood volume , renal blood flow, and cardiac output.
- ARBs are competitive inhibitors of aldosterone binding .
- Beta blockers block the sympathetic nervous system to produce a slower heart rate and a lower blood pressure.
- ACE inhibitors inhibit the conversion of angiotensin I to angiotensin II and lowers peripheral resistance.
Stage 1 Hypertension
- Thiazide diuretic is recommended for most and angiotensin-converting enzyme-1, aldosterone receptor blocker , beta blocker , or calcium channel blocker is considered.
Stage 2 Hypertension
- Two-drug combination is followed, usually including thiazide diuretic and angiotensin-converting enzyme-1, or beta-blocker , or calcium channel blocker.
Nursing Management
The goal of nursing management is to help achieve a normal blood pressure through independent and dependent interventions.
Nursing Assessment
Nursing assessment must involve careful monitoring of the blood pressure at frequent and routinely scheduled intervals.
- If patient is on antihypertensive medications, blood pressure is assessed to determine the effectiveness and detect changes in the blood pressure.
- Complete history should be obtained to assess for signs and symptoms that indicate target organ damage.
- Pay attention to the rate, rhythm, and character of the apical and peripheral pulses.
Based on the assessment data, nursing diagnoses may include the following:
- Deficient knowledge regarding the relation between the treatment regimen and control of the disease process.
- Noncompliance with the therapeutic regimen related to side effects of the prescribed therapy.
- Risk for activity intolerance related to imbalance between oxygen supply and demand.
- Risk- prone health behavior related to condition requiring change in lifestyle.
Nursing Care Plan and Goals
Main article: Hypertension Nursing Care Plans
The major goals for a patient with hypertension are as follows:
- Understanding of the disease process and its treatment.
- Participation in a self-care program.
- Absence of complications.
- BP within acceptable limits for individual.
- Cardiovascular and systemic complications prevented/minimized.
- Disease process/prognosis and therapeutic regimen understood.
- Necessary lifestyle/behavioral changes initiated.
- Plan in place to meet needs after discharge.
- Maintain/enhance cardiovascular functioning.
- Prevent complications.
- Provide information about disease process/prognosis and treatment regimen.
- Support active patient control of condition.
The objective of nursing care focuses on lowering and controlling the blood pressure without adverse effects and without undue cost.
- Encourage the patient to consult a dietitian to help develop a plan for improving nutrient intake or for weight loss .
- Encourage restriction of sodium and fat
- Emphasize increase intake of fruits and vegetables .
- Implement regular physical activity .
- Advise patient to limit alcohol consumption and avoidance of tobacco.
- Assist the patient to develop and adhere to an appropriate exercise regimen.
At the end of the treatment regimen, the following are expected to be achieved:
- Maintain blood pressure at less than 140/90 mmHg with lifestyle modifications, medications, or both.
- Demonstrate no symptoms of angina , palpitations, or visual changes.
- Has stable BUN and serum creatinine levels.
- Has palpable peripheral pulses.
- Adheres to the dietary regimen as prescribed.
- Exercises regularly.
- Takes medications as prescribed and reports side effects.
- Measures blood pressure routinely.
- Abstains from tobacco and alcohol intake.
- Exhibits no complications.
Following discharge, the nurse should promote self-care and independence of the patient.
- The nurse can help the patient achieve blood pressure control through education about managing blood pressure.
- Assist the patient in setting goal blood pressures .
- Provide assistance with social support.
- Encourage the involvement of family members in the education program to support the patient’s efforts to control hypertension.
- Provide written information about expected effects and side effects.
- Encourage and teach patients to measure their blood pressures at home.
- Emphasize strict compliance of follow-up check up .
These are the following data that should be documented for the patient’s record:
- Effects of behavior on health status/condition.
- Plan for adjustments and interventions for achieving the plan and the people involved.
- Client responses to the interventions, teaching, and action plan performed.
- Attainment or progress towards desired outcome.
- Modifications to plan care.
- Individual findings including deviation from prescribed treatment plan.
- Consequences of actions to date.
Posts related to Hypertension:
- Pregnancy Induced Hypertension
- 6 Hypertension Nursing Care Plans
- Antihypertensive Drugs
- Cardiovascular Care Nursing Mnemonics and Tips
6 thoughts on “Hypertension”
I want some NMC questions to solve
Question regarding Stage 1 HTN is incorrect. Stage 1 HTN is BP reading 140-159/90-99.
In new version of Brunner & Suddath’s medical surgical nursing textbook (2022), stage 1 HTN is BP reading 130-139/80-89. (pp: 866, vol 1)
I don’t understand the explanation for the classification of hypertension, the explanation is not matching with the table, why?
“Medical Management Main Topic: Antihypertensive Drugs
The goal of hypertensive treatment I to prevent complications and death by achieving and maintaining the arterial blood pressure at 40/90 mmHg or lower.”
I think need to correct the above sentence as follows;
The goal of hypertensive treatment is to prevent complications and death by achieving and maintaining the arterial blood pressure at 140/90 mmHg or lower.”
please there is a place you wrote BP 40/90,is that correct. Meanwhile, the article is educative.
Leave a Comment Cancel reply

PICO: Form a Focused Clinical Question
- 1. Ask: PICO(T) Question
- 2. Align: Levels of Evidence
- 3a. Acquire: Resource Types
- 3b. Acquire: Searching
- 4. Appraise
- Primary vs. Secondary Sources
- Case Study Example
- Practice PICO
Formulate a Clinical Question from a Case Study
- Case: Hypertension
I: Intervention
C: comparison.
- PICO: Putting It Together
Clinical Scenario
A 68-year-old female patient has recently been diagnosed with high blood pressure. She is otherwise healthy and active. You need to decide whether to prescribe her a beta-blocker or an ACE inhibiter.

Image: "Blood pressure measuring. Doctor and patient. Health care." by agilemktg1 is marked with CC PDM 1.0
► Click on the P: Patient tab to proceed in developing a clinical question.
(Case study from EBM Librarian: Teaching Tools: Scenarios .)
Consider when choosing your patient/problem:
- What are the most important characteristics?
- Relevant demographic factors
- The setting
Patient: adult hypertensive female

Image: "Nurse measuring blood pressure of senior woman at home. Looking at camera, smiling.?" by agilemktg1 is marked with CC PDM 1.0
► Click on the I: Intervention tab to proceed in developing a clinical question.
Consider for your intervention:
- What is the main intervention, treatment, diagnostic test, procedure, or exposure?
- Think of dosage, frequency, duration, and mode of delivery
Intervention: beta-blocker

Image: "Atenolol Blood Pressure Tablets Image 4" by Doctor4U_UK is licensed under CC BY 2.0
► Click on the C: Comparison tab to proceed in developing a clinical question.
Consider for your comparison:
- Inactive control intervention: Placebo, standard care, no treatment
- Active control intervention: A different drug, dose, or kind of therapy
Comparison: ACE inhibiter

Image: "Ramipril Blood Pressure Capsules Image 5" by Doctor4U_UK is licensed under CC BY 2.0
► Click on the O: Outcome tab to proceed in developing a clinical question.
Consider for your outcome:
- Be specific and make it measurable
- It can be something objective or subjective
Outcome: relief of symptoms; controlled blood pressure

Image: "File:BP B6 Connect blood pressure monitor.png" by 百略醫學 is licensed under CC BY-SA 4.0
► Click on the PICO: Putting It Together tab to proceed in developing a clinical question.
Formulate a PICO Question
Answerable PICO Question: In middle-aged adult females with hypertension, are beta blockers more effective than ACE inhibiters in controlling blood pressure?

Image: "Dagstuhl 2008-02-01 - 37" by Nic's events is licensed under CC BY-SA 2.0
Suggested MeSH Terms: Adrenergic beta-Antagonists/therapeutic use; Angiotensin-Converting Enzyme Inhibitors/therapeutic use; hypertension/drug therapy
Tip: Incorporating sex into the search may not be necessary unless there is a significant difference between males and females in relevant studies.
Click "Next" below to practice formulating clinical questions using PICO format.
- << Previous: Primary vs. Secondary Sources
- Next: Practice PICO >>
- Last Updated: Apr 19, 2024 2:46 PM
- URL: https://med-fsu.libguides.com/pico
Maguire Medical Library Florida State University College of Medicine 1115 W. Call St., Tallahassee, FL 32306 Call 850-644-3883 (voicemail) or Text 850-724-4987 Questions? Ask us .
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation
Mr. E.A. is a 40-year-old black male who presented to his Primary Care Provider for a diabetes follow up on October 14th, 2019. The patient complains of a general constant headache that has lasted the past week, with no relieving factors. He also reports an unusual increase in fatigue and general muscle ache without any change in his daily routine. Patient also reports occasional numbness and tingling of face and arms. He is concerned that these symptoms could potentially be a result of his new diabetes medication that he began roughly a week ago. Patient states that he has not had any caffeine or smoked tobacco in the last thirty minutes. During assessment vital signs read BP 165/87, Temp 97.5 , RR 16, O 98%, and HR 86. E.A states he has not lost or gained any weight. After 10 mins, the vital signs were retaken BP 170/90, Temp 97.8, RR 15, O 99% and HR 82. Hg A1c 7.8%, three months prior Hg A1c was 8.0%. Glucose 180 mg/dL (fasting). FAST test done; negative for stroke. CT test, Chem 7 and CBC have been ordered.
Past medical history
Diagnosed with diabetes (type 2) at 32 years old
Overweight, BMI of 31
Had a cholecystomy at 38 years old
Diagnosed with dyslipidemia at 32 years old
Past family history
Mother alive, diagnosed diabetic at 42 years old
Father alive with Hypertension diagnosed at 55 years old
Brother alive and well at 45 years old
Sister alive and obese at 34 years old
Pertinent social history
Social drinker on occasion
Smokes a pack of cigarettes per day
Works full time as an IT technician and is in graduate school
Loading metrics
Open Access
Learning Forum
Learning Forum articles are commissioned by our educational advisors. The section provides a forum for learning about an important clinical problem that is relevant to a general medical audience.
See all article types »
A 21-Year-Old Pregnant Woman with Hypertension and Proteinuria
- Andrea Luk,
* To whom correspondence should be addressed. E-mail: [email protected]
- Ching Wan Lam,
- Wing Hung Tam,
- Anthony W. I Lo,
- Enders K. W Ng,
- Alice P. S Kong,
- Wing Yee So,
- Chun Chung Chow
- Andrea Luk,
- Ronald C. W Ma,
- Ching Wan Lam,
- Wing Hung Tam,
- Anthony W. I Lo,
- Enders K. W Ng,
- Alice P. S Kong,
- Wing Yee So,

Published: February 24, 2009
- https://doi.org/10.1371/journal.pmed.1000037
- Reader Comments
Citation: Luk A, Ma RCW, Lam CW, Tam WH, Lo AWI, Ng EKW, et al. (2009) A 21-Year-Old Pregnant Woman with Hypertension and Proteinuria. PLoS Med 6(2): e1000037. https://doi.org/10.1371/journal.pmed.1000037
Copyright: © 2009 Luk et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The authors received no specific funding for this article.
Competing interests: RCWM is Section Editor of the Learning Forum. The remaining authors have declared that no competing interests exist.
Abbreviations: CT, computer tomography; I, iodine; MIBG, metaiodobenzylguanidine; MRI, magnetic resonance imaging; SDH, succinate dehydrogenase; SDHD, succinate dehydrogenase subunit D
Provenance: Commissioned; externally peer reviewed
Description of Case
A 21-year-old pregnant woman, gravida 2 para 1, presented with hypertension and proteinuria at 20 weeks of gestation. She had a history of pre-eclampsia in her first pregnancy one year ago. During that pregnancy, at 39 weeks of gestation, she developed high blood pressure, proteinuria, and deranged liver function. She eventually delivered by emergency caesarean section following failed induction of labour. Blood pressure returned to normal post-partum and she received no further medical follow-up. Family history was remarkable for her mother's diagnosis of hypertension in her fourth decade. Her father and five siblings, including a twin sister, were healthy. She did not smoke nor drink any alcohol. She was not taking any regular medications, health products, or herbs.
At 20 weeks of gestation, blood pressure was found to be elevated at 145/100 mmHg during a routine antenatal clinic visit. Aside from a mild headache, she reported no other symptoms. On physical examination, she was tachycardic with heart rate 100 beats per minute. Body mass index was 16.9 kg/m 2 and she had no cushingoid features. Heart sounds were normal, and there were no signs suggestive of congestive heart failure. Radial-femoral pulses were congruent, and there were no audible renal bruits.
Baseline laboratory investigations showed normal renal and liver function with normal serum urate concentration. Random glucose was 3.8 mmol/l. Complete blood count revealed microcytic anaemia with haemoglobin level 8.3 g/dl (normal range 11.5–14.3 g/dl) and a slightly raised platelet count of 446 × 10 9 /l (normal range 140–380 × 10 9 /l). Iron-deficient state was subsequently confirmed. Quantitation of urine protein indicated mild proteinuria with protein:creatinine ratio of 40.6 mg/mmol (normal range <30 mg/mmol in pregnancy).
What Were Our Differential Diagnoses?
An important cause of hypertension that occurs during pregnancy is pre-eclampsia. It is a condition unique to the gravid state and is characterised by the onset of raised blood pressure and proteinuria in late pregnancy, at or after 20 weeks of gestation [ 1 ]. Pre-eclampsia may be associated with hyperuricaemia, deranged liver function, and signs of neurologic irritability such as headaches, hyper-reflexia, and seizures. In our patient, hypertension developed at a relatively early stage of pregnancy than is customarily observed in pre-eclampsia. Although she had proteinuria, it should be remembered that this could also reflect underlying renal damage due to chronic untreated hypertension. Additionally, her electrocardiogram showed left ventricular hypertrophy, which was another indicator of chronicity.
While pre-eclampsia might still be a potential cause of hypertension in our case, the possibility of pre-existing hypertension needed to be considered. Box 1 shows the differential diagnoses of chronic hypertension, including essential hypertension, primary hyperaldosteronism related to Conn's adenoma or bilateral adrenal hyperplasia, Cushing's syndrome, phaeochromocytoma, renal artery stenosis, glomerulopathy, and coarctation of the aorta.
Box 1: Causes of Hypertension in Pregnancy
- Pre-eclampsia
- Essential hypertension
- Renal artery stenosis
- Glomerulopathy
- Renal parenchyma disease
- Primary hyperaldosteronism (Conn's adenoma or bilateral adrenal hyperplasia)
- Cushing's syndrome
- Phaeochromocytoma
- Coarctation of aorta
- Obstructive sleep apnoea
Renal causes of hypertension were excluded based on normal serum creatinine and a bland urinalysis. Serology for anti-nuclear antibodies was negative. Doppler ultrasonography of renal arteries showed normal flow and no evidence of stenosis. Cushing's syndrome was unlikely as she had no clinical features indicative of hypercortisolism, such as moon face, buffalo hump, violaceous striae, thin skin, proximal muscle weakness, or hyperglycaemia. Plasma potassium concentration was normal, although normokalaemia does not rule out primary hyperaldosteronism. Progesterone has anti-mineralocorticoid effects, and increased placental production of progesterone may mask hypokalaemia. Besides, measurements of renin activity and aldosterone concentration are difficult to interpret as the renin-angiotensin-aldosterone axis is typically stimulated in pregnancy. Phaeochromocytoma is a rare cause of hypertension in pregnancy that, if unrecognised, is associated with significant maternal and foetal morbidity and mortality. The diagnosis can be established by measuring levels of catecholamines (noradrenaline and adrenaline) and/or their metabolites (normetanephrine and metanephrine) in plasma or urine.
What Was the Diagnosis?
Catecholamine levels in 24-hour urine collections were found to be markedly raised. Urinary noradrenaline excretion was markedly elevated at 5,659 nmol, 8,225 nmol, and 9,601 nmol/day in repeated collections at 21 weeks of gestation (normal range 63–416 nmol/day). Urinary adrenaline excretion was normal. Pregnancy may induce mild elevation of catecholamine levels, but the marked elevation of urinary catecholamine observed was diagnostic of phaeochromocytoma. Conditions that are associated with false positive results, such as acute myocardial infarction, congestive heart failure, acute cerebrovascular event, withdrawal from alcohol, withdrawal from clonidine, and cocaine abuse, were not present in our patient.
The working diagnosis was therefore phaeochromocytoma complicating pregnancy. Magnetic resonance imaging (MRI) of neck to pelvis, without gadolinium enhancement, was performed at 24 weeks of gestation. It showed a 4.2 cm solid lesion in the mid-abdominal aorto-caval region, while both adrenals were unremarkable. There were no ectopic lesions seen in the rest of the examined areas. Based on existing investigation findings, it was concluded that she had extra-adrenal paraganglioma resulting in hypertension.
What Was the Next Step in Management?
At 22 weeks of gestation, the patient was started on phenoxybenzamine titrated to a dose of 30 mg in the morning and 10 mg in the evening. Propranolol was added several days after the commencement of phenoxybenzamine. Apart from mild postural dizziness, the medical therapy was well tolerated during the remainder of the pregnancy. In the third trimester, systolic and diastolic blood pressures were maintained to below 90 mmHg and 60 mmHg, respectively. During this period, she developed mild elevation of alkaline phosphatase ranging from 91 to 188 IU/l (reference 35–85 IU/l). However, liver transaminases were normal and the patient had no seizures. Repeated urinalysis showed resolution of proteinuria. At 38 weeks of gestation, the patient proceeded to elective caesarean section because of previous caesarean section, and a live female baby weighing 3.14 kg was delivered. The delivery was uncomplicated and blood pressure remained stable.
Following the delivery, computer tomography (CT) scan of neck, abdomen, and pelvis was performed as part of pre-operative planning to better delineate the relationship of the tumour to neighbouring structures. In addition to the previously identified extra-adrenal paraganglioma in the abdomen ( Figure 1 ), the CT revealed a 9 mm hypervascular nodule at the left carotid bifurcation, suggestive of a carotid body tumour ( Figure 2 ). The patient subsequently underwent an iodine (I) 131 metaiodobenzylguanidine (MIBG) scan, which demonstrated marked MIBG-avidity of the paraganglioma in the mid-abdomen. The reported left carotid body tumour, however, did not demonstrate any significant uptake. This could indicate either that the MIBG scan had poor sensitivity in detecting a small tumour, or that the carotid body tumour was not functional.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1000037.g001
https://doi.org/10.1371/journal.pmed.1000037.g002
In June 2008, four months after the delivery, the patient had a laparotomy with removal of the abdominal paraganglioma. The operation was uncomplicated. There was no wide fluctuation of blood pressures intra- and postoperatively. Phenoxybenzamine and propranolol were stopped after the operation. Histology of the excised tumour was consistent with paraganglioma with cells staining positive for chromogranin ( Figures 3 and 4 ) and synaptophysin. Adrenal tissues were notably absent.
The tumour is a well-circumscribed fleshy yellowish mass with maximal dimension of 5.5 cm.
https://doi.org/10.1371/journal.pmed.1000037.g003
The tumour cells are polygonal with bland nuclei. The cells are arranged in nests and are immunoreactive to chromogranin (shown here) and synaptophysin.
https://doi.org/10.1371/journal.pmed.1000037.g004
The patient was counselled for genetic testing for hereditary phaeochromocytoma/paraganglioma. She was found to be heterozygous for c.449_453dup mutation of the succinate dehydrogenase subunit D (SDHD) gene ( Figure 5 ). This mutation is a novel frameshift mutation, and leads to SDHD deficiency (GenBank accession number: 1162563). At the latest clinic visit in August 2008, she was asymptomatic and normotensive. Measurements of catecholamine in 24-hour urine collections had normalised. Resection of the left carotid body tumour was planned for a later date. She was to be followed up indefinitely to monitor for recurrences. She was also advised to contact family members for genetic testing. Our patient gave written consent for this case to be published.
https://doi.org/10.1371/journal.pmed.1000037.g005
Phaeochromocytoma in Pregnancy
Hypertension during pregnancy is a frequently encountered obstetric complication that occurs in 6%–8% of pregnancies [ 2 ]. Phaeochromocytoma presenting for the first time in pregnancy is rare, and only several hundred cases have been reported in the English literature. In a recent review of 41 cases that presented during 1988 to 1997, maternal mortality was 4% while the rate of foetal loss was 11% [ 3 ]. Antenatal diagnosis was associated with substantial reduction in maternal mortality but had little impact on foetal mortality. Further, chronic hypertension, regardless of aetiology, increases the risk of pre-eclampsia by 10-fold [ 1 ].
Classically, patients with phaeochromocytoma present with spells of palpitation, headaches, and diaphoresis [ 4 ]. Hypertension may be sustained or sporadic, and is associated with orthostatic blood pressure drop because of hypovolaemia and impaired vasoconstricting response to posture change. During pregnancy, catecholamine surge may be triggered by pressure from the enlarging uterus and foetal movements. In the majority of cases, catecholamine-secreting tumours develop in the adrenal medulla and are termed phaeochromocytoma. Ten percent of tumours arise from extra-adrenal chromaffin tissues located in the abdomen, pelvis, or thorax to form paraganglioma that may or may not be biochemically active. The malignant potential of phaeochromocytoma or paraganglioma cannot be determined from histology and is inferred by finding tumours in areas of the body not known to contain chromaffin tissues. The risk of malignancy is higher in extra-adrenal tumours and in tumours that secrete dopamine.
Making the Correct Diagnosis
The diagnosis of phaeochromocytoma requires a combination of biochemical and anatomical confirmation. Catecholamines and their metabolites, metanephrines, can be easily measured in urine or plasma samples. Day collection of urinary fractionated metanephrine is considered the most sensitive in detecting phaeochromocytoma [ 5 ]. In contrast to sporadic release of catecholamine, secretion of metanephrine is continuous and is less subjective to momentary stress. Localisation of tumour can be accomplished by either CT or MRI of the abdomen [ 6 ]. Sensitivities are comparable, although MRI is preferable in pregnancy because of minimal radiation exposure. Once a tumour is identified, nuclear medicine imaging should be performed to determine its activity, as well as to search for extra-adrenal diseases. I 131 or I 123 MIBG scan is the imaging modality of choice. Metaiodobenzylguanidine structurally resembles noradrenaline and is concentrated in chromaffin cells of phaeochromocytoma or paraganglioma that express noradrenaline transporters. Radionucleotide imaging is contraindicated in pregnancy and should be deferred until after the delivery.
Treatment Approach
Upon confirming the diagnosis, medical therapy should be initiated promptly to block the cardiovascular effects of catecholamine release. Phenoxybenzamine is a long-acting non-selective alpha-blocker commonly used in phaeochromocytoma to control blood pressure and prevent cardiovascular complications [ 7 ]. The main side-effects of phenoxybenzamine are postural hypotension and reflex tachycardia. The latter can be circumvented by the addition of a beta-blocker. It is important to note that beta-blockers should not be used in isolation, since blockade of ß2-adrenoceptors, which have a vasodilatory effect, can cause unopposed vasoconstriction by a1-adrenoceptor stimulation and precipitate severe hypertension. There is little data on the safety of use of phenoxybenzamine in pregnancy, although its use is deemed necessary and probably life-saving in this precarious situation.
The definitive treatment of phaeochromocytoma or paraganglioma is surgical excision. The timing of surgery is critical, and the decision must take into consideration risks to the foetus, technical difficulty regarding access to the tumour in the presence of a gravid uterus, and whether the patient's symptoms can be satisfactorily controlled with medical therapy [ 8 , 9 ]. It has been suggested that surgical resection is reasonable if the diagnosis is confirmed and the tumour identified before 24 weeks of gestation. Otherwise, it may be preferable to allow the pregnancy to progress under adequate alpha- and beta-blockade until foetal maturity is reached. Unprepared delivery is associated with a high risk of phaeochromocytoma crisis, characterised by labile blood pressure, tachycardia, fever, myocardial ischaemia, congestive heart failure, and intracerebral bleeding.
Patients with phaeochromocytoma or paraganglioma should be followed up for life. The rate of recurrence is estimated to be 2%–4% at five years [ 10 ]. Assessment for recurrent disease can be accomplished by periodic blood pressure monitoring and 24-hour urine catecholamine and/or metanephrine measurements.
Genetics of Phaeochromocytoma
Approximately one quarter of patients presenting with phaeochromocytoma may carry germline mutations, even in the absence of apparent family history [ 11 ]. The common syndromes of hereditary phaeochromocytoma/paraganglioma are listed in Box 2 . These include Von Hippel-Lindau syndrome, multiple endocrine neoplasia type 2, neurofibromatosis type 1, and succinate dehydrogenase (SDH) gene mutations. Our patient has a novel frameshift mutation in the SDHD gene located at Chromosome 11q. SDH is a mitochondrial enzyme that is involved in oxidative phosphorylation. Characteristically, SDHD mutation is associated with head or neck non-functional paraganglioma, and infrequently, sympathetic paraganglioma or phaeochromocytoma [ 12 ]. Tumours associated with SDHD mutation are rarely malignant, in contrast to those arisen from mutation of the SDHB gene. Like all other syndromes of hereditary phaeochromocytoma, SDHD mutation is transmitted in an autosomal dominant fashion. However, not all carriers of the SDHD mutation develop tumours, and inheritance is further complicated by maternal imprinting in gene expression. While it may not be practical to screen for genetic alterations in all cases of phaeochromocytoma, most authorities advocate genetic screening for patients with positive family history, young age of tumour onset, co-existence with other neoplasms, bilateral phaeochromocytoma, and extra-adrenal paraganglioma. The confirmation of genetic mutation should prompt evaluation of other family members.
Box 2: Hereditary Phaeochromocytoma/Paraganglioma Syndromes
- Von Hippel-Lindau syndrome
- Multiple endocrine neoplasia type 2A and type 2B
- Neurofibromatosis type 1
- Mutation of SDHB , SDHC , SDHD
- Ataxia-telangiectasia
- Tuberous sclerosis
- Sturge-Weber syndrome
Key Learning Points
- Hypertension complicating pregnancy is a commonly encountered medical condition.
- Pre-existing chronic hypertension must be considered in patients with hypertension presenting in pregnancy, particularly if elevation of blood pressure is detected early during pregnancy or if persists post-partum.
- Secondary causes of chronic hypertension include renal artery stenosis, renal parenchyma disease, primary hyperaldosteronism, phaeochromocytoma, Cushing's syndrome, coarctation of the aorta, and obstructive sleep apnoea.
- Phaeochromocytoma presenting during pregnancy is rare but carries high rates of maternal and foetal morbidity and mortality if unrecognised.
- Successful outcomes depend on early disease identification, prompt initiation of alpha- and beta-blockers, carefully planned delivery, and timely resection of the tumour.
Phaeochromocytoma complicating pregnancy is uncommon. Nonetheless, in view of the potential for catastrophic consequences if unrecognised, a high index of suspicion and careful evaluation for secondary causes of hypertension is of utmost importance. Blood pressure should be monitored in the post-partum period and persistence of hypertension must be thoroughly investigated.
Author Contributions
All authors participated in the management of the patient or writing of the article. AL and RCWM wrote the article, with contributions from all the authors.
- View Article
- Google Scholar
- Search Menu
- Advance articles
- Editor's Choice
- Graphical Abstracts and Tidbit
- Author Guidelines
- Submission Site
- Open Access
- About American Journal of Hypertension
- Editorial Board
- Board of Directors
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- AJH Summer School
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Clinical management and treatment decisions, hypertension in black americans, pharmacologic treatment of hypertension in black americans.
- < Previous
- Article contents
- Figures & tables
- Supplementary Data
Suzanne Oparil, Case study, American Journal of Hypertension , Volume 11, Issue S8, November 1998, Pages 192S–194S, https://doi.org/10.1016/S0895-7061(98)00195-2
- Permissions Icon Permissions
Ms. C is a 42-year-old black American woman with a 7-year history of hypertension first diagnosed during her last pregnancy. Her family history is positive for hypertension, with her mother dying at 56 years of age from hypertension-related cardiovascular disease (CVD). In addition, both her maternal and paternal grandparents had CVD.
At physician visit one, Ms. C presented with complaints of headache and general weakness. She reported that she has been taking many medications for her hypertension in the past, but stopped taking them because of the side effects. She could not recall the names of the medications. Currently she is taking 100 mg/day atenolol and 12.5 mg/day hydrochlorothiazide (HCTZ), which she admits to taking irregularly because “... they bother me, and I forget to renew my prescription.” Despite this antihypertensive regimen, her blood pressure remains elevated, ranging from 150 to 155/110 to 114 mm Hg. In addition, Ms. C admits that she has found it difficult to exercise, stop smoking, and change her eating habits. Findings from a complete history and physical assessment are unremarkable except for the presence of moderate obesity (5 ft 6 in., 150 lbs), minimal retinopathy, and a 25-year history of smoking approximately one pack of cigarettes per day. Initial laboratory data revealed serum sodium 138 mEq/L (135 to 147 mEq/L); potassium 3.4 mEq/L (3.5 to 5 mEq/L); blood urea nitrogen (BUN) 19 mg/dL (10 to 20 mg/dL); creatinine 0.9 mg/dL (0.35 to 0.93 mg/dL); calcium 9.8 mg/dL (8.8 to 10 mg/dL); total cholesterol 268 mg/dL (< 245 mg/dL); triglycerides 230 mg/dL (< 160 mg/dL); and fasting glucose 105 mg/dL (70 to 110 mg/dL). The patient refused a 24-h urine test.
Taking into account the past history of compliance irregularities and the need to take immediate action to lower this patient’s blood pressure, Ms. C’s pharmacologic regimen was changed to a trial of the angiotensin-converting enzyme (ACE) inhibitor enalapril, 5 mg/day; her HCTZ was discontinued. In addition, recommendations for smoking cessation, weight reduction, and diet modification were reviewed as recommended by the Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI). 1
After a 3-month trial of this treatment plan with escalation of the enalapril dose to 20 mg/day, the patient’s blood pressure remained uncontrolled. The patient’s medical status was reviewed, without notation of significant changes, and her antihypertensive therapy was modified. The ACE inhibitor was discontinued, and the patient was started on the angiotensin-II receptor blocker (ARB) losartan, 50 mg/day.
After 2 months of therapy with the ARB the patient experienced a modest, yet encouraging, reduction in blood pressure (140/100 mm Hg). Serum electrolyte laboratory values were within normal limits, and the physical assessment remained unchanged. The treatment plan was to continue the ARB and reevaluate the patient in 1 month. At that time, if blood pressure control remained marginal, low-dose HCTZ (12.5 mg/day) was to be added to the regimen.
Hypertension remains a significant health problem in the United States (US) despite recent advances in antihypertensive therapy. The role of hypertension as a risk factor for cardiovascular morbidity and mortality is well established. 2–7 The age-adjusted prevalence of hypertension in non-Hispanic black Americans is approximately 40% higher than in non-Hispanic whites. 8 Black Americans have an earlier onset of hypertension and greater incidence of stage 3 hypertension than whites, thereby raising the risk for hypertension-related target organ damage. 1 , 8 For example, hypertensive black Americans have a 320% greater incidence of hypertension-related end-stage renal disease (ESRD), 80% higher stroke mortality rate, and 50% higher CVD mortality rate, compared with that of the general population. 1 , 9 In addition, aging is associated with increases in the prevalence and severity of hypertension. 8
Research findings suggest that risk factors for coronary heart disease (CHD) and stroke, particularly the role of blood pressure, may be different for black American and white individuals. 10–12 Some studies indicate that effective treatment of hypertension in black Americans results in a decrease in the incidence of CVD to a level that is similar to that of nonblack American hypertensives. 13 , 14
Data also reveal differences between black American and white individuals in responsiveness to antihypertensive therapy. For instance, studies have shown that diuretics 15 , 16 and the calcium channel blocker diltiazem 16 , 17 are effective in lowering blood pressure in black American patients, whereas β-adrenergic receptor blockers and ACE inhibitors appear less effective. 15 , 16 In addition, recent studies indicate that ARB may also be effective in this patient population.
Angiotensin-II receptor blockers are a relatively new class of agents that are approved for the treatment of hypertension. Currently, four ARB have been approved by the US Food and Drug Administration (FDA): eprosartan, irbesartan, losartan, and valsartan. Recently, a 528-patient, 26-week study compared the efficacy of eprosartan (200 to 300 mg/twice daily) versus enalapril (5 to 20 mg/daily) in patients with essential hypertension (baseline sitting diastolic blood pressure [DBP] 95 to 114 mm Hg). After 3 to 5 weeks of placebo, patients were randomized to receive either eprosartan or enalapril. After 12 weeks of therapy within the titration phase, patients were supplemented with HCTZ as needed. In a prospectively defined subset analysis, black American patients in the eprosartan group (n = 21) achieved comparable reductions in DBP (−13.3 mm Hg with eprosartan; −12.4 mm Hg with enalapril) and greater reductions in systolic blood pressure (SBP) (−23.1 with eprosartan; −13.2 with enalapril), compared with black American patients in the enalapril group (n = 19) ( Fig. 1 ). 18 Additional trials enrolling more patients are clearly necessary, but this early experience with an ARB in black American patients is encouraging.
Efficacy of the angiotensin II receptor blocker eprosartan in black American with mild to moderate hypertension (baseline sitting DBP 95 to 114 mm Hg) in a 26-week study. Eprosartan, 200 to 300 mg twice daily (n = 21, solid bar), enalapril 5 to 20 mg daily (n = 19, diagonal bar). †10 of 21 eprosartan patients and seven of 19 enalapril patients also received HCTZ. Adapted from data in Levine: Subgroup analysis of black hypertensive patients treated with eprosartan or enalapril: results of a 26-week study, in Programs and abstracts from the 1st International Symposium on Angiotensin-II Antagonism, September 28–October 1, 1997, London, UK.
00195-2/2/m_ajh.192S.f1.jpeg?Expires=1719112609&Signature=cvpO6nOV9rurlE9jEgz~8EFmfBlZMmkLnBdQW5bvYyqRvHhRx7M38OoYB63QSNTFir6JYz-NrU5ZSru9g7i-CAAsuY54yxj-Yrc7f8yuJDwf93UghhaPxjy2wb3QxtUezKBjShLhYpqagSXXc2G7aXIXOsp2sEkER2F~jfZ5mgm21qedKErPw5KxlQcQgW4fHR-Bbt5ySRi0tC8Kof3AF4wK09OnHg-0TvgTvwNrmuynf-HpSdFI78JhfZZeDdQqSlub3Sq~-UfCarHvqHEF4u~j32IeHfNjZTfE-cKNgHzMG6va1JqkR1aAFiz0QkfU08WF9RjirZ4zVuMf9ajwTA__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
Approximately 30% of all deaths in hypertensive black American men and 20% of all deaths in hypertensive black American women are attributable to high blood pressure. Black Americans develop high blood pressure at an earlier age, and hypertension is more severe in every decade of life, compared with whites. As a result, black Americans have a 1.3 times greater rate of nonfatal stroke, a 1.8 times greater rate of fatal stroke, a 1.5 times greater rate of heart disease deaths, and a 5 times greater rate of ESRD when compared with whites. 19 Therefore, there is a need for aggressive antihypertensive treatment in this group. Newer, better tolerated antihypertensive drugs, which have the advantages of fewer adverse effects combined with greater antihypertensive efficacy, may be of great benefit to this patient population.
1. Joint National Committee : The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure . Arch Intern Med 1997 ; 24 157 : 2413 – 2446 .
Google Scholar
2. Veterans Administration Cooperative Study Group on Antihypertensive Agents : Effects of treatment on morbidity in hypertension: Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg . JAMA 1967 ; 202 : 116 – 122 .
3. Veterans Administration Cooperative Study Group on Antihypertensive Agents : Effects of treatment on morbidity in hypertension: II. Results in patients with diastolic blood pressures averaging 90 through 114 mm Hg . JAMA 1970 ; 213 : 1143 – 1152 .
4. Pooling Project Research Group : Relationship of blood pressure, serum cholesterol, smoking habit, relative weight and ECG abnormalities to the incidence of major coronary events: Final report of the pooling project . J Chronic Dis 1978 ; 31 : 201 – 306 .
5. Hypertension Detection and Follow-Up Program Cooperative Group : Five-year findings of the hypertension detection and follow-up program: I. Reduction in mortality of persons with high blood pressure, including mild hypertension . JAMA 1979 ; 242 : 2562 – 2577 .
6. Kannel WB , Dawber TR , McGee DL : Perspectives on systolic hypertension: The Framingham Study . Circulation 1980 ; 61 : 1179 – 1182 .
7. Hypertension Detection and Follow-Up Program Cooperative Group : The effect of treatment on mortality in “mild” hypertension: Results of the Hypertension Detection and Follow-Up Program . N Engl J Med 1982 ; 307 : 976 – 980 .
8. Burt VL , Whelton P , Roccella EJ et al. : Prevalence of hypertension in the US adult population: Results from the third National Health and Nutrition Examination Survey, 1988–1991 . Hypertension 1995 ; 25 : 305 – 313 .
9. Klag MJ , Whelton PK , Randall BL et al. : End-stage renal disease in African-American and white men: 16-year MRFIT findings . JAMA 1997 ; 277 : 1293 – 1298 .
10. Neaton JD , Kuller LH , Wentworth D et al. : Total and cardiovascular mortality in relation to cigarette smoking, serum cholesterol concentration, and diastolic blood pressure among black and white males followed up for five years . Am Heart J 1984 ; 3 : 759 – 769 .
11. Gillum RF , Grant CT : Coronary heart disease in black populations II: Risk factors . Heart J 1982 ; 104 : 852 – 864 .
12. M’Buyamba-Kabangu JR , Amery A , Lijnen P : Differences between black and white persons in blood pressure and related biological variables . J Hum Hypertens 1994 ; 8 : 163 – 170 .
13. Hypertension Detection and Follow-up Program Cooperative Group : Five-year findings of the Hypertension Detection and Follow-up Program: mortality by race-sex and blood pressure level: a further analysis . J Community Health 1984 ; 9 : 314 – 327 .
14. Ooi WL , Budner NS , Cohen H et al. : Impact of race on treatment response and cardiovascular disease among hypertensives . Hypertension 1989 ; 14 : 227 – 234 .
15. Weinberger MH : Racial differences in antihypertensive therapy: evidence and implications . Cardiovasc Drugs Ther 1990 ; 4 ( suppl 2 ): 379 – 392 .
16. Materson BJ , Reda DJ , Cushman WC et al. : Single-drug therapy for hypertension in men: A comparison of six antihypertensive agents with placebo . N Engl J Med 1993 ; 328 : 914 – 921 .
17. Materson BJ , Reda DJ , Cushman WC for the Department of Veterans Affairs Cooperative Study Group on Antihypertensive Agents : Department of Veterans Affairs single-drug therapy of hypertension study: Revised figures and new data . Am J Hypertens 1995 ; 8 : 189 – 192 .
18. Levine B : Subgroup analysis of black hypertensive patients treated with eprosartan or enalapril: results of a 26-week study , in Programs and abstracts from the first International Symposium on Angiotensin-II Antagonism , September 28 – October 1 , 1997 , London, UK .
19. American Heart Association: 1997 Heart and Stroke Statistical Update . American Heart Association , Dallas , 1997 .
- hypertension
- blood pressure
- african american
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1941-7225
- Copyright © 2024 American Journal of Hypertension, Ltd.
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Nursing case management for people with hypertension: A randomized controlled trial protocol
Affiliation.
- 1 Department of Urology, People's Hospital of Chengyang District, Qingdao, China.
- PMID: 33350776
- PMCID: PMC7769350
- DOI: 10.1097/MD.0000000000023850
Objective: To explore the effect of management of nursing case on blood pressure control in hypertension patients.
Method: This is a randomized controlled study which will be carried out from May 2021 to May 2022. The experiment was granted through the Research Ethics Committee of the People's Hospital of Chengyang District (03982808). Our research includes 200 patients. Patients who meet the following conditions will be included in this experiment: the patients aged 18 to 60 years; the patients had the diagnosis of hypertension; and the urban residents. While patients with the following conditions will be excluded: having renal failure, liver failure, heart and respiratory failure; and known pregnancy. Primary result is blood pressure, while secondary results are treatment compliance, waist circumference, body mass index (BMI), type and number of antihypertensive agents used, and the existence of metabolic and cardiovascular comorbidities.
Results: Table 1 shows the clinical outcomes between the two groups.
Conclusion: Nursing case management is effective to improve the prognosis of hypertension patients.
Copyright © 2020 the Author(s). Published by Wolters Kluwer Health, Inc.
Publication types
- Clinical Trial Protocol
- Case Management / organization & administration*
- Hypertension* / diagnosis
- Hypertension* / nursing
- Nursing Care / methods*
- Outcome and Process Assessment, Health Care
- Practice Patterns, Nurses'
- Randomized Controlled Trials as Topic

Grants and funding
- 2013-WSZD120/Qingdao Health Bureau project
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
This publication is provided for historical reference only and the information may be out of date.

StatPearls [Internet].
Case study: 60-year-old female presenting with shortness of breath (archive).
Deepa Rawat ; Sandeep Sharma .
Affiliations
Last Update: February 20, 2023 .
- Case Presentation
The patient is a 60-year-old white female presenting to the emergency department with acute onset shortness of breath. Symptoms began approximately 2 days before and had progressively worsened with no associated, aggravating, or relieving factors noted. She had similar symptoms approximately 1 year ago with an acute, chronic obstructive pulmonary disease (COPD) exacerbation requiring hospitalization. She uses BiPAP ventilatory support at night when sleeping and has requested to use this in the emergency department due to shortness of breath and wanting to sleep.
She denies fever, chills, cough, wheezing, sputum production, chest pain, palpitations, pressure, abdominal pain, abdominal distension, nausea, vomiting, and diarrhea.
She reports difficulty breathing at rest, forgetfulness, mild fatigue, feeling chilled, requiring blankets, increased urinary frequency, incontinence, and swelling in her bilateral lower extremities that are new-onset and worsening. Subsequently, she has not ambulated from bed for several days except to use the restroom due to feeling weak, fatigued, and short of breath.
There are no known ill contacts at home. Her family history includes significant heart disease and prostate malignancy in her father. Social history is positive for smoking tobacco use at 30 pack years. She quit smoking 2 years ago due to increasing shortness of breath. She denies all alcohol and illegal drug use. There are no known foods, drugs, or environmental allergies.
Past medical history is significant for coronary artery disease, myocardial infarction, COPD, hypertension, hyperlipidemia, hypothyroidism, diabetes mellitus, peripheral vascular disease, tobacco usage, and obesity. Past surgical history is significant for an appendectomy, cardiac catheterization with stent placement, hysterectomy, and nephrectomy.
Her current medications include fluticasone-vilanterol 100-25 mcg inhaled daily, hydralazine 50 mg by mouth, 3 times per day, hydrochlorothiazide 25 mg by mouth daily, albuterol-ipratropium inhaled every 4 hours PRN, levothyroxine 175 mcg by mouth daily, metformin 500 mg by mouth twice per day, nebivolol 5 mg by mouth daily, aspirin 81 mg by mouth daily, vitamin D3 1000 units by mouth daily, clopidogrel 75 mg by mouth daily, isosorbide mononitrate 60 mg by mouth daily, and rosuvastatin 40 mg by mouth daily.
Physical Exam
Initial physical exam reveals temperature 97.3 F, heart rate 74 bpm, respiratory rate 24, BP 104/54, HT 160 cm, WT 100 kg, BMI 39.1, and O2 saturation 90% on room air.
Constitutional: Extremely obese, acutely ill-appearing female. Well-developed and well-nourished with BiPAP in place. Lying on a hospital stretcher under 3 blankets.
HEENT:
- Head: Normocephalic and atraumatic
- Mouth: Moist mucous membranes
- Macroglossia
- Eyes: Conjunctiva and EOM are normal. Pupils are equal, round, and reactive to light. No scleral icterus. Bilateral periorbital edema present.
- Neck: Neck supple. No JVD present. No masses or surgical scarring.
- Throat: Patent and moist
Cardiovascular: Normal rate, regular rhythm, and normal heart sound with no murmur. 2+ pitting edema bilateral lower extremities and strong pulses in all four extremities.
Pulmonary/Chest: No respiratory status distress at this time, tachypnea present, (+) wheezing noted, bilateral rhonchi, decreased air movement bilaterally. The patient was barely able to finish a full sentence due to shortness of breath.
Abdominal: Soft. Obese. Bowel sounds are normal. No distension and no tenderness
Skin: Skin is very dry
Neurologic: Alert, awake, able to protect her airway. Moving all extremities. No sensation losses
- Initial Evaluation
Initial evaluation to elucidate the source of dyspnea was performed and included CBC to establish if an infectious or anemic source was present, CMP to review electrolyte balance and review renal function, and arterial blood gas to determine the PO2 for hypoxia and any major acid-base derangement, creatinine kinase and troponin I to evaluate the presence of myocardial infarct or rhabdomyolysis, brain natriuretic peptide, ECG, and chest x-ray. Considering that it is winter and influenza is endemic in the community, a rapid influenza assay was obtained as well.
Largely unremarkable and non-contributory to establish a diagnosis.
Showed creatinine elevation above baseline from 1.08 base to 1.81, indicating possible acute injury. EGFR at 28 is consistent with chronic renal disease. Calcium was elevated to 10.2. However, when corrected for albumin, this corrected to 9.8 mg/dL. Mild transaminitis is present as seen in alkaline phosphatase, AST, and ALT measurements which could be due to liver congestion from volume overload.
Initial arterial blood gas with pH 7.491, PCO2 27.6, PO2 53.6, HCO3 20.6, and oxygen saturation 90% on room air, indicating respiratory alkalosis with hypoxic respiratory features.
Creatinine kinase was elevated along with serial elevated troponin I studies. In the setting of her known chronic renal failure and acute injury indicated by the above creatinine value, a differential of rhabdomyolysis is determined.
Influenza A and B: Negative
Normal sinus rhythm with non-specific ST changes in inferior leads. Decreased voltage in leads I, III, aVR, aVL, aVF.
Chest X-ray
Findings: Bibasilar airspace disease that may represent alveolar edema. Cardiomegaly noted. Prominent interstitial markings were noted. Small bilateral pleural effusions
Radiologist Impression: Radiographic changes of congestive failure with bilateral pleural effusions greater on the left compared to the right
- Differential Diagnosis
- Acute on chronic COPD exacerbation
- Acute on chronic renal failure
- Bacterial pneumonia
- Congestive heart failure
- Pericardial effusion
- Hypothyroidism
- Influenza pneumonia
- Pulmonary edema
- Pulmonary embolism
- Confirmatory Evaluation
On the second day of the admission patient’s shortness of breath was not improved, and she was more confused with difficulty arousing on conversation and examination. To further elucidate the etiology of her shortness of breath and confusion, the patient's husband provided further history. He revealed that she is poorly compliant with taking her medications. He reports that she “doesn’t see the need to take so many pills.”
Testing was performed to include TSH, free T4, BNP, repeated arterial blood gas, CT scan of the chest, and echocardiogram. TSH and free T4 evaluate hypothyroidism. BNP evaluates fluid load status and possible congestive heart failure. CT scan of the chest will look for anatomical abnormalities. An echocardiogram is used to evaluate left ventricular ejection fraction, right ventricular function, pulmonary artery pressure, valvular function, pericardial effusion, and any hypokinetic area.
- TSH: 112.717 (H)
- Free T4: 0.56 (L)
- TSH and Free T4 values indicate severe primary hypothyroidism.
BNP can be falsely low in obese patients due to the increased surface area. Additionally, adipose tissue has BNP receptors which augment the true BNP value. Also, African American patients with more excretion may have falsely low values secondary to greater excretion of BNP. This test is not that helpful in renal failure due to the chronic nature of fluid overload. This allows for desensitization of the cardiac tissues with a subsequent decrease in BNP release.
Repeat arterial blood gas on BiPAP ventilation shows pH 7.397, PCO2 35.3, PO2 72.4, HCO3 21.2, and oxygen saturation 90% on 2 L supplemental oxygen.
CT chest without contrast was primarily obtained to evaluate the left hemithorax, especially the retrocardiac area.
Radiologist Impression: Tiny bilateral pleural effusions. Pericardial effusion. Coronary artery calcification. Some left lung base atelectasis with minimal airspace disease.
Echocardiogram
The left ventricular systolic function is normal. The left ventricular cavity is borderline dilated.
The pericardial fluid is collected primarily posteriorly, laterally but not apically. There appeared to be a subtle, early hemodynamic effect of the pericardial fluid on the right-sided chambers by way of an early diastolic collapse of the RA/RV and delayed RV expansion until late diastole. A dedicated tamponade study was not performed.
The estimated ejection fraction appears to be in the range of 66% to 70%. The left ventricular cavity is borderline dilated.
The aortic valve is abnormal in structure and exhibits sclerosis.
The mitral valve is abnormal in structure. Mild mitral annular calcification is present. There is bilateral thickening present. Trace mitral valve regurgitation is present.
- Myxedema coma or severe hypothyroidism
- Pericardial effusion secondary to myxedema coma
- COPD exacerbation
- Acute on chronic hypoxic respiratory failure
- Acute respiratory alkalosis
- Bilateral community-acquired pneumonia
- Small bilateral pleural effusions
- Acute mild rhabdomyolysis
- Acute chronic, stage IV, renal failure
- Elevated troponin I levels, likely secondary to Renal failure
- Diabetes mellitus type 2, non-insulin-dependent
- Extreme obesity
- Hepatic dysfunction
The patient was extremely ill and rapidly decompensating with multisystem organ failure, including respiratory failure, altered mental status, acute on chronic renal failure, and cardiac dysfunction. The primary concerns for the stability of the patient revolved around respiratory failure coupled with altered mental status. In the intensive care unit (ICU), she rapidly began to fail BiPAP therapy. Subsequently, the patient was emergently intubated in the ICU. A systemic review of therapies and hospital course is as follows:
Considering the primary diagnosis of myxedema coma, early supplementation with thyroid hormone is essential. Healthcare providers followed the American Thyroid Association recommendations, which recommend giving combined T3 and T4 supplementation; however, T4 alone may also be used. T3 therapy is given as a bolus of 5 to 20 micrograms intravenously and continued at 2.5 to 10 micrograms every 8 hours. An intravenous loading dose of 300 to 600 micrograms of T4 is followed by a daily intravenous dose of 50 to 100 micrograms. Repeated monitoring of TSH and T4 should be performed every 1 to 2 days to evaluate the effect and to titrate the dose of medication. The goal is to improve mental function. Until coexistent adrenal insufficiency is ruled out using a random serum cortisol measurement, 50 to 100 mg every 8 hours of hydrocortisone should be administered. In this case, clinicians used hydrocortisone 100 mg IV every 8 hours. Dexamethasone 2 to 4 mg every 12 hours is an alternative therapy.
The patient’s mental status rapidly worsened despite therapy. In the setting of her hypothyroidism history, this may be myxedema coma or due to the involvement of another organ system. The thyroid supplementation medications and hydrocortisone were continued. A CT head without contrast was normal.
Respiratory
For worsening metabolic acidosis and airway protection, the patient was emergently intubated. Her airway was deemed high risk due to having a large tongue, short neck, and extreme obesity. As the patient’s heart was preload dependent secondary to pericardial effusion, a 1-liter normal saline bolus was started. Norepinephrine was started at a low dose for vasopressor support, and ketamine with low dose Propofol was used for sedation. Ketamine is a sympathomimetic medication and usually does not cause hypotension as all other sedatives do. The patient was ventilated with AC mode of ventilation, tidal volume of 6 ml/kg ideal body weight, flow 70, initial fio2 100 %, rate 26 per minute (to compensate for metabolic acidosis), PEEP of 8.
Cardiovascular
She was determined to be hemodynamically stable with a pericardial effusion. This patient’s cardiac dysfunction was diastolic in nature, as suggested by an ejection fraction of 66% to 70%. The finding of posterior pericardial effusion further supported this conclusion. The posterior nature of this effusion was not amenable to pericardiocentesis. As such, this patient was preload dependent and showed signs of hypotension. The need for crystalloid fluid resuscitation was balanced against the impact increased intravascular volume would have on congestive heart failure and fluid overload status. Thyroid hormone replacement as above should improve hypotension. However, vasopressor agents may be used to maintain vital organ perfusion targeting a mean arterial pressure of greater than 65 mm Hg as needed. BP improved after fluid bolus, and eventually, the norepinephrine was stopped. Serial echocardiograms were obtained to ensure that the patient did not develop tamponade physiology. Total CK was elevated, which was likely due to Hypothyroidism compounded with chronic renal disease.
Infectious Disease
Blood cultures, urine analysis, and sputum cultures were obtained. The patient's white blood cell count was normal. This is likely secondary to her being immunocompromised due to hypothyroidism and diabetes. In part, the pulmonary findings of diffuse edema and bilateral pleural effusions can be explained by cardiac dysfunction. Thoracentesis of pleural fluid was attempted, and the fluid was analyzed for cytology and gram staining to rule out infectious or malignant causes as both a therapeutic and diagnostic measure. Until these results return, broad-spectrum antibiotics are indicated and may be discontinued once the infection is ruled out completely.
Gastrointestinal
Nasogastric tube feedings were started on the patient after intubation. She tolerated feedings well. AST and ALT were mildly elevated, which was thought to be due to hypothyroidism, and as the TSH and free T4 improved, her AST and ALT improved. Eventually, these values became normal once her TSH level was close to 50.
Her baseline creatinine was found to be close to 1.08 in prior medical records. She presented with a creatinine of 1.8 in the emergency department. Since hypothyroidism causes fluid retention in part because thyroid hormone encourages excretion of free water and partly due to decreased lymphatic function in returning fluid to vascular circulation. Aggressive diuresis was attempted. As a result, her creatinine increased initially but improved on repeated evaluation, and the patient had a new baseline creatinine of 1.6. Overall she had a net change in the fluid status of 10 liters negative by her ten days of admission in the ICU.
Mildly anemic otherwise, WBC and platelet counts were normal. Electrolyte balance should be monitored closely, paying attention to sodium, potassium, chloride, and calcium specifically as these are worsened in both renal failure and myxedema.
Daily sedation vacations were enacted, and the patient's mental status improved and was much better when TSH was around 20. The bilateral pleural effusions improved with aggressive diuresis. Breathing trials were initiated when the patient's fio2 requirements decreased to 60% and a PEEP of 8. She was eventually extubated onto BiPAP and then high-flow nasal cannula while off of BiPAP. Pericardial fluid remained stable, and no cardiac tamponade pathology developed. As a result, it was determined that a pericardial window was unnecessary. Furthermore, she was not a candidate for pericardiocentesis as the pericardial effusion was located posterior to the heart. Her renal failure improved with improved cardiac function, diuretics, and thyroid hormone replacement.
After extubation patient had speech and swallow evaluations and was able to resume an oral diet. The patient was eventually transferred out of the ICU to the general medical floor and eventually to a rehabilitation unit.
Despite the name myxedema coma, most patients will not present in a coma status. This illness is at its core a severe hypothyroidism crisis that leads to systemic multiorgan failure. Thyroid hormones T3, and to a lesser extent, T4 act directly on a cellular level to upregulate all metabolic processes in the body. Therefore, deficiency of this hormone is characterized by systemic decreased metabolism and decreased glucose utilization along with increased production and storage of osmotically active mucopolysaccharide protein complexes into peripheral tissues resulting in diffuse edema and swelling of tissue. [1]
Myxedema coma is an illness that occurs primarily in females at a rate of 4:1 compared to men. It typically impacts the elderly at the age of greater than 60 years old, and approximately 90% of cases occur during the winter months. Myxedema coma is the product of longstanding unidentified or undertreated hypothyroidism of any etiology. Thyroid hormone is necessary throughout the body and acts as a regulatory hormone that affects many organ systems. [2] In cardiac tissues, myxedema coma manifests as decreased contractility with subsequent reduction in stroke volume and overall cardiac output. Bradycardia and hypotension are typically present also. Pericardial effusions occur due to the accumulation of mucopolysaccharides in the pericardial sac, which leads to worsened cardiac function and congestive heart failure from diastolic dysfunction. Capillary permeability is also increased throughout the body leading to worsened edema. Electrocardiogram findings may include bradycardia and low-voltage, non-specific ST waveform changes with possible inverted T waves.
Neurologic tissues are impacted in myxedema coma leading to the pathognomonic altered mental status resulting from hypoxia and decreased cerebral blood flow secondary to cardiac dysfunction as above. Additionally, hypothyroidism leads to decreased glucose uptake and utilization in neurological tissue, thus worsening cognitive function.
The pulmonary system typically manifests this disease process through hypoventilation secondary to the central nervous system (CNS) depression of the respiratory drive with blunting of the response to hypoxia and hypercapnia. Additionally, metabolic dysfunction in the muscles of respiration leads to respiratory fatigue and failure, macroglossia from mucopolysaccharide driven edema of the tongue leads to mechanical obstruction of the airway, and obesity hypoventilation syndrome with the decreased respiratory drive as most hypothyroid patients suffer from obesity.
Renal manifestations include decreased glomerular filtration rate from the reduced cardiac output and increased systemic vascular resistance coupled with acute rhabdomyolysis lead to acute kidney injury. In the case of our patient above who has a pre-existing renal disease status post-nephrectomy, this is further worsened. The net effect is worsened fluid overload status compounding the cardiac dysfunction and edema. [3]
The gastrointestinal tract is marked by mucopolysaccharide-driven edema as well leading to malabsorption of nutrients, gastric ileus, and decreased peristalsis. Ascites is common because of increased capillary permeability in the intestines coupled with coexistent congestive heart failure and congestive hepatic failure. Coagulopathies are common to occur as a result of this hepatic dysfunction.
Evaluation: The diagnosis of myxedema coma, as with all other diseases, is heavily reliant on the history and physical exam. A past medical history including hypothyroidism is highly significant whenever decreased mental status or coma is identified. In the absence of identified hypothyroidism, myxedema coma is a diagnosis of exclusion when all other sources of coma have been ruled out. If myxedema coma is suspected, evaluation of thyroid-stimulating hormone (TSH), free thyroxine (T4), and serum cortisol is warranted. T4 will be extremely low. TSH is variable depending on the etiology of hypothyroidism, with a high TSH indicating primary hypothyroidism and a low or normal TSH indicating secondary etiologies. Cortisol may be low indicating adrenal insufficiency because of hypothyroidism. [4]
Prognosis: Myxedema coma is a medical emergency. With proper and rapid diagnosis and initiation of therapy, the mortality rate is still as high as 25% to 50%. The most common cause of death is due to respiratory failure. The factors which suggest a poorer prognosis include increased age, persistent hypothermia, bradycardia, low score Glasgow Coma Scale, or multi-organ impairment indicated by high APACHE (Acute Physiology and Chronic Health Evaluation) II score. For these reasons, placement in an intensive care unit with a low threshold for intubation and mechanical ventilation can improve mortality outcomes. [3] [5]
- Pearls of Wisdom
- Not every case of shortness of breath is COPD or congestive heart failure (CHF). While less likely, a history of hypothyroidism should raise suspicion of myxedema coma in a patient with any cognitive changes.
- Myxedema is the great imitator illness that impacts all organ systems. It can easily be mistaken for congestive heart failure, COPD exacerbation, pneumonia, renal injury or failure, or neurological insult.
- Initial steps in therapy include aggressive airway management, thyroid hormone replacement, glucocorticoid therapy, and supportive measures.
- These patients should be monitored in an intensive care environment with continuous telemetry. [6]
- Enhancing Healthcare Team Outcomes
This case demonstrates how all interprofessional healthcare team members need to be involved in arriving at a correct diagnosis, particularly in more challenging cases such as this one. Clinicians, specialists, nurses, pharmacists, laboratory technicians all bear responsibility for carrying out the duties pertaining to their particular discipline and sharing any findings with all team members. An incorrect diagnosis will almost inevitably lead to incorrect treatment, so coordinated activity, open communication, and empowerment to voice concerns are all part of the dynamic that needs to drive such cases so patients will attain the best possible outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Case Study of 60 year old female presenting with Shortness of Breath Contributed by Sandeep Sharma, MD
Disclosure: Deepa Rawat declares no relevant financial relationships with ineligible companies.
Disclosure: Sandeep Sharma declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Rawat D, Sharma S. Case Study: 60-Year-Old Female Presenting With Shortness of Breath (Archive) [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Similar articles in PubMed
- Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough (Archive). [StatPearls. 2024] Case Study: 33-Year-Old Female Presents with Chronic SOB and Cough (Archive). Sharma S, Hashmi MF, Rawat D. StatPearls. 2024 Jan
- Acute Exacerbation of COPD. [J Educ Teach Emerg Med. 2023] Acute Exacerbation of COPD. Pappas D, Vempati A. J Educ Teach Emerg Med. 2023 Apr; 8(2):S35-S61. Epub 2023 Apr 30.
- Review Breathlessness with pulmonary metastases: a multimodal approach. [J Adv Pract Oncol. 2013] Review Breathlessness with pulmonary metastases: a multimodal approach. Brant JM. J Adv Pract Oncol. 2013 Nov; 4(6):415-22.
- Stress Cardiomyopathy in the Setting of COPD Exacerbation. [J Investig Med High Impact Cas...] Stress Cardiomyopathy in the Setting of COPD Exacerbation. Landefeld K, Saleh Q, Sander GE. J Investig Med High Impact Case Rep. 2015 Oct-Dec; 3(4):2324709615612847. Epub 2015 Oct 14.
- Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. [J Adv Pract Oncol. 2017] Review Palliative Chemotherapy: Does It Only Provide False Hope? The Role of Palliative Care in a Young Patient With Newly Diagnosed Metastatic Adenocarcinoma. Doverspike L, Kurtz S, Selvaggi K. J Adv Pract Oncol. 2017 May-Jun; 8(4):382-386. Epub 2017 May 1.
Recent Activity
- Case Study: 60-Year-Old Female Presenting With Shortness of Breath (Archive) - S... Case Study: 60-Year-Old Female Presenting With Shortness of Breath (Archive) - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

5 Nursing Case Study Examples + Answer Guide
If you're a nursing student preparing for your nursing license exam , you know how important it is to have access to high-quality study materials.
Sample case study for nursing students can be a valuable tool in your preparation, helping you to develop critical thinking skills and apply your knowledge in real-world scenarios.
That's why we've put together a list of 5 nursing case study examples, complete with answer guides, to help you prepare for the NCLEX -style questions you'll encounter on exam day.
Want more case studies with full-answer rationales tailored to you and your budget? Try Smart’n for free.
Nursing Case Study: Mrs. Johnson's hypertension
Background of mrs. johnson’s hypertension.
Mrs. Johnson is a 62-year-old female who was admitted to the hospital with a complaint of severe headache and dizziness. She has a past medical history of hypertension for the past 5 years, and she has been on antihypertensive medications.
She has a family history of hypertension and heart disease, with her mother and brother both diagnosed with hypertension. Mrs. Johnson is currently working as a school teacher and lives with her husband. She has a sedentary lifestyle and reports occasional non-adherence to her medications due to forgetfulness.
Nurse notes of Mrs. Johnson’s hypertension
Upon admission, Mrs. Johnson's vital signs are as follows: blood pressure (BP) 180/100 mmHg, heart rate (HR) 88 beats per minute (BPM), respiratory rate (RR) 18 breaths per minute, and temperature 98.6°F.
She is alert and oriented but complains of a throbbing headache and lightheadedness. Her skin is warm and dry, and there is no visible edema. Her lungs are clear on auscultation, and her heart sounds are normal with no murmurs. Her abdominal assessment reveals no tenderness or masses. Mrs. Johnson's laboratory results show an elevated fasting blood glucose level of 135 mg/dL, cholesterol level of 240 mg/dL, and serum creatinine level of 1.2 mg/dL. She has a body mass index (BMI) of 30, which indicates obesity.
Questions and answer guide of case study
1. What are the risk factors for hypertension in this case study?
Family history of hypertension and heart disease
Sedentary lifestyle
Non-adherence to medications
2. What are the signs and symptoms of hypertension in Mrs. Johnson?
Severe headache
Elevated blood pressure (180/100 mmHg)
3. What other assessments should the nurse prioritize for Mrs. Johnson?
Regular monitoring of blood pressure
Monitoring of blood glucose and cholesterol levels
Assessment of adherence to medications
Assessment of lifestyle factors, such as physical activity and diet
4. What nursing interventions would be appropriate for Mrs. Johnson's hypertension management?
Administer antihypertensive medications as ordered
Educate Mrs. Johnson and her husband on the importance of medication adherence
Encourage regular physical activity and a healthy diet
Monitor and manage blood glucose and cholesterol levels
Provide education on stress management techniques
Collaborate with the healthcare provider to adjust medications and treatment plans as needed
5. What patient education should the nurse provide to Mrs. Johnson regarding hypertension management?
Importance of adhering to antihypertensive medications as prescribed
Adoption of a healthy lifestyle, including regular exercise and a well-balanced diet
Monitoring and management of blood glucose and cholesterol levels
Strategies for stress management
Importance of regular follow-up appointments with the healthcare provider for monitoring and adjustments to the treatment plan
6. What referrals or consultations should the nurse consider for Mrs. Johnson?
Registered dietitian for nutritional counseling
A social worker for assistance with lifestyle modifications and stress management
Diabetes educator for management of blood glucose levels
Pharmacist for medication review and education
Healthcare provider for possible adjustment of antihypertensive medications or referral to a specialist, such as a cardiologist or endocrinologist.
Want more case studies with answer rationales?
Experience AI-enabled learning support for nurses on Smart ’ n .
Example of realistic NGN-style case study on Smart’n.
Nursing Case Study: Mr. Thompson's diabetic foot ulcer
Background of mr. thompson’s diabetic foot ulcer.
Mr. Thompson is a 68-year-old male with a history of type 2 diabetes for the past 15 years. He has a sedentary lifestyle and a BMI of 32, indicating obesity. Mr. Thompson has a history of poor glycemic control with frequent episodes of hyperglycemia and occasional non-adherence to his diabetic medications due to financial constraints.
He presents to the clinic with a complaint of a non-healing ulcer on his right foot for the past 2 weeks. He reports that he accidentally bumped his foot against a hard object and developed a small blister that has since progressed to a deep, painful ulcer with foul-smelling drainage.
Assessment of Mr. Thompson’s diabetic foot ulcer
Upon assessment, Mr. Thompson's vital signs are stable with a blood pressure (BP) of 132/82 mmHg, heart rate (HR) of 76 beats per minute (BPM), respiratory rate (RR) of 18 breaths per minute, and temperature of 98.2°F.
He appears anxious and in mild distress due to the pain from the foot ulcer. His right foot is swollen, erythematous, and warm to the touch, with a deep, irregularly-shaped ulcer measuring approximately 3 cm x 4 cm on the plantar surface.
There is purulent drainage with a foul odor, and the surrounding skin is macerated. Mr. Thompson has diminished sensation in his right foot and a weak dorsalis pedis pulse. His laboratory results show an elevated fasting blood glucose level of 240 mg/dL and a hemoglobin A1c level of 9.5%.
1. What are the risk factors for the development of diabetic foot ulcer in Mr. Thompson?
History of type 2 diabetes for 15 years
Poor glycemic control with frequent episodes of hyperglycemia
Non-adherence to diabetic medications
Sedentary lifestyle and obesity
Foot injury due to accidental trauma
2. What are the signs and symptoms of the diabetic foot ulcer in Mr. Thompson?
Deep, irregularly-shaped ulcer with foul-smelling drainage
Swollen, erythematous, and warm foot
Macerated skin surrounding the ulcer
Diminished sensation and weak pulse in the affected foot
3. What other assessments should the nurse prioritize for Mr. Thompson's diabetic foot ulcer management?
Assessment of pain level and pain management
Assessment of wound characteristics, including size, depth, drainage, odor, and surrounding skin condition
Neurovascular assessment, including sensation, pulses, and skin temperature
Assessment of glycemic control and diabetes management
Assessment of nutritional status and hydration
4. What nursing interventions would be appropriate for Mr. Thompson's diabetic foot ulcer management?
Administering prescribed analgesics for pain management
Performing wound care, including cleansing, debridement, and dressing changes
Educating Mr. Thompson on proper foot care, including daily inspection, keeping the foot clean and dry, and avoiding trauma
Assisting with glycemic control through medication administration, dietary management, and regular blood glucose monitoring
Facilitating referrals to a wound care specialist, podiatrist, or diabetes educator as needed
Educating Mr. Thompson and his family on the importance of adherence to diabetic medications and lifestyle modifications
5. What patient education should the nurse provide to Mr. Thompson regarding diabetic foot ulcer management?
Proper foot care techniques, including daily foot inspection, keeping the foot clean and dry, and avoiding trauma
Importance of adherence to diabetic medications and lifestyle modifications for glycemic control
Signs and symptoms of infection, such as increased pain, redness, swelling, or drainage, and when to seek medical attention
Appropriate footwear selection and fitting to prevent further foot injury
Importance of regular follow-up appointments with healthcare providers for ongoing monitoring and management of diabetes and foot ulcer
Nutritional recommendations for diabetes management, including a balanced diet and avoiding high-sugar foods and beverages
Importance of maintaining a healthy weight through lifestyle modifications, including regular physical activity and healthy eating habits
Emphasizing the need for strict glycemic control to promote wound healing and prevent complications
Instruction on the proper administration of prescribed medications, including dosages, timing, and potential side effects
Education on the risks and consequences of non-adherence to diabetes management and foot care recommendations
6. What interdisciplinary team members may be involved in Mr. Thompson's diabetic foot ulcer management?
Primary care physician or endocrinologist for diabetes management
Wound care specialist or podiatrist for specialized wound care and management
Diabetes educator for diabetes education and self-management strategies
Pharmacist for medication management and education
Physical therapist for recommendations on appropriate physical activity and exercise
A social worker or financial counselor for assistance with financial constraints related to medication affordability
Nursing Case Study: Mich’s chest pain
Background of mich’s chest pain.
Mich is a 15-year-old male who was brought to the emergency department by his parents due to complaints of chest pain and shortness of breath. Mich has a history of asthma and had been experiencing symptoms for the past two days. Mich's parents reported that he had been compliant with his asthma medications but had recently run out of his inhaler. Upon arrival at the emergency department, Mich was found to have a rapid heart rate and was diagnosed with a severe asthma exacerbation.
Assessment of Mich’s chest pain
On assessment, Mich appeared anxious and in distress, with labored breathing and a respiratory rate of 30 breaths per minute. His oxygen saturation was 88% on room air, and he was immediately started on supplemental oxygen via nasal cannula.
Mich's chest exam was significant for decreased breath sounds and wheezing. His heart rate was 130 beats per minute, and his blood pressure was 120/70 mmHg. Mich's laboratory values were within normal limits, except for an elevated white blood cell count, which was likely due to his asthma exacerbation.
1. What is the priority nursing intervention for Mich?
The priority nursing intervention for Mich is to assess and manage his respiratory distress. This includes providing supplemental oxygen, administering bronchodilator medications, and monitoring his response to treatment.
2. What education should the nurse provide to Mich and his parents?
The nurse should educate Mich and his parents on the proper use of asthma medications, including inhalers and nebulizers. The nurse should also provide education on asthma triggers and how to avoid them, as well as signs and symptoms of an asthma exacerbation and when to seek medical attention.
3. What potential complications should the nurse monitor for in Mich?
The nurse should monitor Mich for potential complications of asthma exacerbation, including respiratory failure, pneumothorax, and cardiac complications such as arrhythmias. The nurse should also monitor for signs of anxiety and provide emotional support to Mich and his family.
4. How can the nurse promote adherence to Mich's asthma treatment regimen?
The nurse can promote adherence to Mich's asthma treatment regimen by providing education and resources, such as written instructions and referrals to support groups. The nurse can also encourage open communication with Mich and his family and address any barriers to adherence, such as cost or access to medications.
5. What discharge planning should the nurse initiate for Mich?
The nurse should initiate discharge planning that includes instructions for Mich and his family on proper asthma management at home. This includes providing education on medication administration, recognizing signs and symptoms of asthma exacerbation, and developing an asthma action plan. The nurse should also ensure that Mich has access to his medications and any necessary equipment, such as a peak flow meter or spacer. Referral to a primary care provider or asthma specialist for ongoing management should also be initiated. Finally, the nurse should provide education on follow-up appointments and any necessary referrals for additional support services, such as social work or mental health resources.
6. How can the nurse promote family-centered care for Mich and his parents?
The nurse can promote family-centered care by involving Mich and his parents in the care planning process and encouraging their participation in decision-making. The nurse can provide emotional support and education to help them feel confident in their role as caregivers, and address any cultural or religious needs of the family to promote a holistic approach to care. The nurse should also encourage family visitation and provide opportunities for Mich and his parents to ask questions and express concerns.
Nursing Case Study: Baby S - Respiratory distress and hypoxemia
Background of baby’s respiratory distress and hypoxemia.
Baby S is a 10-day-old infant who was admitted to the neonatal intensive care unit (NICU) due to respiratory distress and hypoxemia. Baby S was born prematurely at 34 weeks gestation via emergency cesarean section due to fetal distress.
The mother had a history of preeclampsia and received antenatal corticosteroids. Baby S had a birth weight of 2.2 kg and required immediate intubation and mechanical ventilation.
Assessment of baby’s respiratory distress and hypoxemia
On assessment, Baby S appeared to be in moderate respiratory distress, with a respiratory rate of 50 breaths per minute, nasal flaring, and intercostal retractions. Her oxygen saturation was 88% on a fraction of inspired oxygen (FiO2) of 0.5, and her heart rate was 160 beats per minute. Lung auscultation revealed bilateral crackles, and the chest X-ray showed diffuse bilateral infiltrates consistent with respiratory distress syndrome (RDS). Baby S had a central line for parenteral nutrition and was receiving intravenous fluids and medications.
1. What is the pathophysiology of RDS in premature infants?
RDS is a common respiratory disorder in premature infants, caused by a deficiency of pulmonary surfactant, which normally keeps the alveoli open and prevents collapse. In premature infants, the lungs are not fully developed, and surfactant production is inadequate, leading to increased surface tension and collapse of the alveoli. This results in ventilation-perfusion (V/Q) mismatch, hypoxemia, and respiratory distress.
2. What interventions should the nurse implement for Baby S?
The nurse should ensure that Baby S is receiving appropriate respiratory support, including mechanical ventilation, FiO2 titration, and positive end-expiratory pressure (PEEP) as prescribed. The nurse should also monitor Baby S's vital signs, oxygen saturation, and blood gas values closely to optimize oxygenation and ventilation. The nurse should maintain a sterile environment around the central line and monitor for signs of infection. The nurse should also provide enteral or parenteral nutrition as prescribed to meet the infant's metabolic needs and promote growth.
3. What potential complications should the nurse monitor for in Baby S?
The nurse should monitor for potential complications such as infection, barotrauma, bronchopulmonary dysplasia (BPD), and patent ductus arteriosus (PDA). Infection is a common complication in premature infants and can be life-threatening. Barotrauma can occur due to excessive mechanical ventilation and can result in pneumothorax or other complications. BPD is a chronic lung disease that can develop in premature infants who require prolonged mechanical ventilation or oxygen therapy. PDA is a common cardiac complication in premature infants, resulting in abnormal blood flow between the aorta and pulmonary artery.
4. How can the nurse support Baby S's developmental care needs?
The nurse can support Baby S's developmental care needs by providing a quiet and dark environment, minimizing unnecessary handling and stimulation, and promoting restful sleep. The nurse can also encourage skin-to-skin contact with the mother or father to promote bonding and provide comfort. The nurse should also provide appropriate pain management for any procedures or interventions to minimize discomfort and stress.
5. What discharge planning should the nurse initiate for Baby S?
The nurse should initiate discharge planning as early as possible to ensure a smooth transition to home. The nurse should provide education to the parents about the infant's medical needs, including respiratory support, feeding, medication administration, and infection prevention. The nurse should also refer the parents to appropriate community resources, such as home health services, support groups, and developmental follow-up clinics. The nurse should work with the healthcare team to develop a plan for ongoing monitoring and follow-up to ensure that Baby S's medical needs are being met and to monitor for any potential complications or developmental delays.
6. How can the nurse promote family-centered care for Baby S and her parents?
The nurse can do so by involving the parents in the infant's care as much as possible, encouraging their participation in decision-making, and providing emotional support and education to help them feel confident in their role as caregivers. The nurse can also encourage family visitation and provide opportunities for parent-infant bonding, such as skin-to-skin contact and feeding. The nurse should also recognize and address any cultural or religious needs of the family to promote a holistic approach to care.
Nursing Case Study: Mrs. Jones - Postoperative care after total hip replacement surgery
Background of mrs. jones’ hip replacement surgery.
Mrs. Jones is a 72-year-old female who underwent total hip replacement surgery due to severe hip osteoarthritis. She has a history of hypertension and osteoporosis. Mrs. Jones lives alone and has limited mobility due to hip pain and stiffness prior to surgery. She was admitted to the orthopedic surgical unit and is now postoperative day 1 after her surgery.
Assessment of Mrs. Jones’ hip replacement surgery
Mrs. Jones is alert and oriented but reports pain at the surgical site rated 7/10 on the pain scale.
Vital signs: Blood pressure 140/90 mmHg, heart rate 88 bpm, respiratory rate 18 bpm, temperature 98.6°F.
Surgical incision: 15 cm incision over the lateral aspect of the right hip, with moderate serosanguinous drainage.
Limited weight-bearing status on the right leg as per surgeon's orders.
Foley catheter in place for urinary drainage.
Serosanguinous drainage in the surgical drain.
Evaluation of Mrs. Jones’ hip replacement surgery
Mrs. Jones's pain is well managed, with her pain level reduced to 4/10 on the pain scale within 24 hours post-surgery.
Mrs. Jones is able to perform transfers and ambulation with appropriate assistive devices as per the prescribed weight-bearing status.
There are no signs of infection at the surgical site or systemic infection.
Mrs. Jones and her family demonstrate an understanding of the postoperative care plan, including pain management, mobility restrictions, and infection prevention measures.
Mrs. Jones's home environment is assessed to be safe for her discharge, and necessary home health services, medical equipment, or rehabilitation services are arranged.
Questions and answer guide of Case Study
1. What are the priority nursing diagnoses for Mrs. Jones?
Acute Pain related to surgical incision and tissue trauma
Impaired Physical Mobility related to postoperative weight-bearing restrictions
Risk for Infection related to the surgical site and indwelling catheter
2. What are the nursing interventions to address Mrs. Jones's acute pain?
Assess pain level using a numeric pain scale at regular intervals and as needed.
Administer prescribed pain medications, such as acetaminophen and opioids, as ordered and monitor for side effects.
Apply ice or heat to the surgical site as appropriate to help relieve pain and reduce swelling.
Use non-pharmacological pain relief measures, such as relaxation techniques and distraction techniques, to help Mrs. Jones manage her pain.
3. How can the nursing team assist Mrs. Jones with impaired physical mobility?
Assist Mrs. Jones with transferring and ambulation according to the prescribed weight-bearing status and mobility orders.
Educate Mrs. Jones on the proper use of assistive devices, such as crutches or a walker, and provide assistance as needed.
Collaborate with the physical therapy team to develop a plan of care for Mrs. Jones's mobility and ambulation post-surgery.
Encourage Mrs. Jones to perform a range of motion exercises as tolerated to prevent joint stiffness and muscle atrophy.
4. What nursing interventions can be implemented to prevent infection in Mrs. Jones?
Perform frequent hand hygiene and use appropriate personal protective equipment (PPE) when providing care to Mrs. Jones, especially when handling the surgical drain or catheter.
Monitor the surgical incision for signs of infection, such as redness, increased warmth, swelling, or purulent drainage, and report any abnormal findings to the healthcare provider.
Monitor vital signs, including temperature, for signs of systemic infection.
Ensure proper care and maintenance of the indwelling catheter according to the facility's policy and procedure.
5. What should be included in Mrs. Jones's education and discharge planning?
Provide Mrs. Jones and her family with education on the postoperative care plan, including pain management, mobility restrictions, and infection prevention measures.
Provide written materials and verbal instructions on wound care, medication administration, activity restrictions, and follow-up appointments.
Collaborate with the interdisciplinary team, including the physical therapist and social worker, to assess Mrs. Jones's home environment and ensure a safe discharge plan.
Assist with coordinating any necessary home health services, medical equipment, or rehabilitation services for Mrs. Jones's post-discharge care.
6. How will the nursing team evaluate the effectiveness of the care provided to Mrs. Jones?
Monitor Mrs. Jones's pain level and assess for any side effects of pain medications.
Assess Mrs. Jones's ability to perform transfers and ambulation with assistive devices.
Monitor the surgical incision and vital signs for signs of infection.
Evaluate Mrs. Jones's and her family's understanding of the education provided and their ability to implement the postoperative care plan.
Collaborate with the interdisciplinary team to ensure a safe and appropriate discharge plan for Mrs. Jones.
Want more case studies with full-answer rationales?
55 Types Of Nursing Jobs In 2023 + Salaries
Understanding the different types of case studies in 2023.
- Open access
- Published: 17 May 2024
Translation, adaptation, and validation of a Chinese version of the Hypertension Self-Care Activity Level effects (H-SCALE) for patients with hypertension
- Ting-Yu Chen 1 ,
- Chi-Wen Kao ORCID: orcid.org/0000-0003-4003-7564 2 ,
- Shu-Meng Cheng 3 &
- Chieh-Yu Liu 4
BMC Nursing volume 23 , Article number: 334 ( 2024 ) Cite this article
Metrics details
Lifestyle modification is an essential component of prevention and management of hypertension. Existing instruments in Taiwan focus on assessing lifestyle modifications by evaluating medication adherence or confidence in controlling blood pressure. However, other self-care activities, such as diet, physical activity, weight management, smoking, and alcohol consumption are also important. The Hypertension Self-Care Activity Level Effects (H-SCALE) is one such instrument, but there are no similar tools available in Taiwan.
This study aimed to translate the H-SCALE into Chinese and test its validity, and reliability in a sample of adults with hypertension.
The English version of the 31-item H-SCALE was translated into Chinese using the forward-backward method. The content validity index (CVI) of the translated scale was determined by five experts in hypertension. Item analysis was conducted with a pilot sample of 20 patients with hypertension. Cronbach’s α was used to establish the internal consistency reliability for the Chinese version of the H-SCALE (H-SCALE-C). Exploratory factor analysis (EFA) explored the structure of the H-SCALE-C. Additionally, construct validity was examined with confirmatory factor analysis (CFA). Patients with hypertension were recruited by convenience sampling from a cardiovascular outpatient clinic of a medical center in northern Taiwan. A total of 318 patients met the inclusion criteria and participated in factor analysis in the study.
Pilot testing of the scale items indicated most patients could not accurately estimate the number of days of alcohol consumption for the previous week. Therefore, three alcohol-related items were removed. The adaptation resulted in a 28-item H-SCALE-C. EFA revealed a 4-factor solution with 13 items that explained 63.93% of the total variance. CFA indicated a good fit for a 4-factor model and construct validity was acceptable. Internal consistency reliability was acceptable (Cronbach’s alpha for the four subscales ranged from 0.65 to 0.94). Convergent validity was acceptable, and discriminant validity was significant.
Conclusions
The H-SCALE-C is a valid, reliable tool for promptly assessing life-style activities for patients with hypertension in Taiwan. The instrument is suitable for assisting healthcare providers in evaluating self-care activities, which could be used to facilitate lifestyle modifications for patients with hypertension.
Peer Review reports
The World Health Organization (WHO) reported 1.28 million adults were affected by hypertension in 2021, which contributed to premature death and disability worldwide [ 1 ]. In Taiwan, the incidence of hypertension in 2019 was reported to be 25% [ 2 ]. The incidence of hypertension is expected to increase to 65.4% in 2025, with Asian populations contributing significantly to this rise due to their large numbers [ 1 ]. Lifestyle modification is essential for the prevention and management of hypertension, as it not only helps reduce the number and dosage of antihypertensive medications but also lowers the risk of cardiovascular complications [ 2 ]. Multidimensional comprehensive assessment instruments are often used to evaluate lifestyle factors that can influence hypertension, however older scales focus on medication adherence, often excluding other key domains and lacking adequate reliability and validity [ 3 ]. Managing hypertension through self-care activities such as diet, physical activity, weight management, smoking, and alcohol consumption are more effective means of controlling hypertension [ 4 ]. Although self-care assessment instruments are available [ 4 , 5 ], currently there is no available instrument for use in Taiwan.
Self-care is individual actions directed toward self or the environment to regulate individual functioning, which can improve health, reduce risk, avoid related complications, and ensure one’s general well-being [ 4 ]. The Hypertension Self-Care Activity Level Effects (H-SCALE), originally developed by Warren-Findlow and Seymore [ 5 ], is used worldwide to measure self-care activities associated with lifestyle for patients with hypertension [ 6 , 7 , 8 , 9 , 10 ]. The H-SCALE was.
developed following the recommended guidelines of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) [ 5 ]. The scale assesses six lifestyle domains that impact hypertension: medication adherence, a healthy diet, physical activity, body weight, alcohol consumption, and smoking [ 5 , 6 ]. The advantage of the H-SCALE is that the assessments identify domains needing tailored interventions to improve self-care and provide a healthy lifestyle, which can reduce hypertension.
The H-SCALE has been shown to be a valid and reliable measurement of self-care activities and has been translated for application in countries spanning both Eastern and Western regions [ 7 , 8 , 9 , 10 ]. However, to the best of our knowledge, there is no equivalent scale that is tailored to measure self-care activities associated with a healthy lifestyle for patients with hypertension.
The aims of this study were to translate the Hypertension Self-Care Activity Level Effects (H-SCALE) from the English-language version [ 5 ] to a Chinese version (H-SCALE-C), adapt the translated scale for patients with hypertension, and test the reliability and validity of the scale.
Study design and participants
The English version of the H-SCALE was translated into Chinese using a forward-back translation method, described below. Psychometric properties of the translated scale were examined thru a cross-sectional convenience sample of patients with hypertension. To include patients with a broad spectrum of hypertension experiences and management practices, the sample was recruited from a cardiovascular outpatient clinic of a medical center in northern Taiwan. Patients were eligible to participate if they met the following criteria: (1) 20–79 years of age; (2) diagnosed with primary hypertension; and (3) able to read and understand Chinese. Patients were excluded for any of the following criteria: (1) having a diagnosis of cancer, thyroid disease, or a psychiatric disorder; (2) with a history of a permanent pacemaker, heart transplant, or implantable cardioverter defibrillator; (3) currently pregnant; (4) use of antidepressants; or (5) having a history of drug or alcohol abuse.
Original H-SCALE
The original H-SCALE, developed by Warren-Findlow et al. in 2011 and revised in 2013, includes 31 items divided into six domains: medication adherence, dietary quality, physical activity, smoking, weight management, and alcohol consumption [ 5 , 6 ]. Each domain (subscale) represents a component of a patient’s self-care management, which is assessed over a period of a week or a month. The Cronbach’s alphas for the six subscales range from 0.67 to 0.86 [ 6 ]. Details of the six domains are described below.
Medication adherence (items 1–3)
Medication adherence assesses patient’s compliance over one week with taking a prescribed antihypertensive medication using the following three items: (1) take blood pressure medication, (2) takes it at the same time every day, and (3) takes the recommended dosage. Each item is scored from no days (0) up to everyday (7). Total scores range from 0 to 21 points. In this study, a score ≥ 17 (80%) was considered adherent.
Diet quality (items 4–14)
Diet quality was assessed with the revised version of the self-report scale, Dietary Approaches to Stop Hypertension (DASH). The original scale emphasized a low-sodium diet, whereas revised scale focuses on diet quality (DASH-Q) [ 11 ]. The 11-item DASH-Q scale assesses the frequency of following a healthy diet in the past 7 days, which includes avoidance of salty foods as well as the consumption of nutritionally balanced foods, such as fruits, vegetables, alternate forms of protein, and foods with potassium, fiber, and whole grains. Each item is scored from 0 to 7; total scores range from 0 to 77 points. A score greater than 52 points indicates good adherence to a healthy diet.
Physical activity (items 15, 16)
The physical activity subscale is comprised of two items, which assess a patient’s adherence to a recommended combination of aerobic and muscle-strengthening activity for 30 min per day over the last week. Activities include swimming, walking, weightlifting, repeated heavy lifting or pushing/pulling that are not related to housework or employment. Total scores range from 0 to 14; a score greater than 8 points indicates good adherence.
Smoking (items 17, 18)
Smoking exposure was assessed with two questions: “How many of the past 7 days did you smoke a cigarette (even just one puff)?” (item 17, frequency); and “How many of the past 7 days did you stay in a room or ride in an enclosed vehicle while someone was smoking?” (item 18, passive smoking exposure). Items are scored 0 to 7 days. The summed scores for the two items range from 0 to 14; lower scores indicate better adherence to self-care.
Weight management (items 19–28)
The subscale for weight management is comprised of 10 items that assess activities that can help manage body weight, such as reducing portion sizes or making food substitutions. Each item is a statement about the use of a weight management activity over the past 30 days, such as “I have cut out or limited some foods I like but are not good for me” (item 25). Items are scored on a 5-point Likert scale from strongly disagree (1 point) to strongly agree (5 points). Total scores range from 10 to 50; higher scores indicate better weight management practices. Participants who score ≥ 40 (agree or strongly agree on all 10 items) are considered to have good adherence to weight management.
Alcohol consumption (items 29–31)
The alcohol consumption subscale assesses the average intake of alcohol over the last 7 days. Item 29 asks, “On average, how many days a week do you drink alcohol?” A response = 0 indicates good adherence. However, if the response is > 0, the participant must complete items 30 and 31, which are write-in answers. Item 30 asks, “On a typical day when you drink, how many drinks do you have?” Item 31 asks, “What is the maximum number of drinks you had on any given day?” The level of non-adherence is determined by multiplying the numbers given for items 30 and 31 by the number of days reported in item 29. Moderate consumption among men is considered ≤ 2 drinks/day (a score ≤ 14); among women, ≤ 1drink/day is considered moderate (a score ≤ 7).
Translation of the H-SCALE
Permission to translate the English-language H-SCALE was obtained from Dr. Warren-Findlow. The instrument has been translated and validated for use in other languages to measure self-care in patients with hypertension, for instance the Eastern countries of Pakistan [ 7 ] Myanmar [ 8 ], and Iran [ 9 ] and the United States [ 6 , 9 , 11 ].
The forward-backward method of Brislin was used to translate the H-SCALE, which ensures language equivalence (meaning) for cross-cultural translations [ 12 ]. First, a bilingual registered nurse independently translated the H-SCALE into Chinese. A second bilingual registered nurse, blinded to the original version, translated the scale from Chinese back to English. The English-language back-translated version was compared with the original version of the H-SCALE to ensure content equivalence of the translation. To further ensure that the grammar, syntax, and context of the translated scale was equivalent to the original, we conducted a group discussion with bilingual physicians and nurses from the cardiovascular department. Differences in meanings between the two languages were identified and changes were made until group consensus for equivalence of the two versions was reached.
Content validity of the translated Chinese version scale
Five experts in the field of cardiovascular medicine assessed the content validity of the Chinese translation of the scale. Content validity determines if a translated scale is semantically and culturally equivalent to the original scale. Each expert rated the 31 translated items on a 4-point Likert scale from 1 (not at all equivalent) to 4 (completely equivalent). Items with mean scores ≤ 2 (items 3, 7, 12, 15, 16, 17, and 27) were reworded until a score ≥ 3 was obtained, indicating equivalency was achieved. For instance, item 12 included consuming the vegetable “collard greens”, which are not often eaten in Taiwan. Therefore, we replaced collard greens with “sweet potato leaves”, a vegetable similar in nutrition to collard greens and commonly eaten in Taiwan. The overall Content Validity Index (CVI) of the Chinese version of the H-SCALE (H-SCALE-C) was 0.93, which is considered acceptable.
Item analysis
The H-SCALE-C was pilot tested with 20 outpatients with hypertension. After completing the questionnaire, patients were interviewed about clarity of the wording and ability understand the questions. Most patients reported they could not accurately answer the question about the average number of days they drank alcohol in the previous week (item 29). Because scores for non-adherence are the result of multiplying the number of drinks per day (item 30) and maximum number of drinks on a given day (item 31) by the number of days of alcohol consumption (item 29), we felt we would not be able to accurately calculate a score for alcohol consumption and the subscale was removed. Therefore, prior to factor analysis, the H-SCALE-C was comprised of 28 items and five domains.
Data collection
Data were collected in the outpatient clinic from April 2017 to September 2017, after patients provided informed consent. Participants filled out a survey questionnaire about demographic characteristics, such as age, gender, employment. Clinical characteristics, such as duration of hypertension, smoking (yes/no), variables of body mass index (BMI), and comorbidities, were obtained from the patients’ charts, with their permission. They were then provided instructions for completing the H-SCALE-C questionnaire.
Ethical considerations
Approval for conducting this study was obtained from Institutional Review Board of the Tri-Service General Hospital Institutional Review Board. The design and purpose of the study were explained to the patients. They were assured of confidentiality of their data, and the right to refuse to continue with the study at any time and for any reason. All participants provided informed consent and data were coded to maintain anonymity.
Statistical analysis
The SPSS V.23 (IBM Corp, Armonk, New York, USA) was used to perform statistical analysis. Data for continuous variables were described using mean and standard deviation (SD), while categorical variables were presented with frequency and percentage. The level of significance was set to p < .05.
Although the English version of the H-Scale has been demonstrated to be a valid instrument for patients with hypertension, possible differences between Western and Eastern cultures prompted us to view the H-SCALE-C as a new instrument and construct validity of the scale was examined with exploratory factor analysis (EFA). The recommended minimum sample size for EFA is 5–10 participants for each item or 155 to 310 for 31 items indicating the sample of 318 participants in this study was adequate for factor analysis and determining reliability of the H-Scale-C [ 4 , 13 ]. H-SCALE-C data from all 318 participants were used for EFA and subsequent analyses.
The Kaiser-Meyer-Olkin (KMO) measured the sampling adequacy and Bartlett’s test of sphericity determined suitability of the data for factor analysis. A KMO greater than 0.7 and Bartlett’s test of sphericity less than 0.05 are considered adequate to conduct factor analysis.Data extraction was implemented through principal component analysis (PCA). The factors with eigenvalues > 1.0 were retained, and factor loadings greater than 0.40 indicated that items for each factor could be retained [ 14 ].
CFA was conducted using AMOS V.17, version 22.0 (IBM Corp, Armonk, New York, USA). Fit indices for the model were considered acceptable based on the following criteria: Chi-square/degrees of freedom ( df ) < 3; goodness-of-fit index (GFI) > 0.90; adjusted goodness-of-fit index (AGFI) > 0.90; comparative fit index (CFI) > 0.90; standardized root mean square residual (SRMR) ≤ 0.05; and root mean squared error of approximation (RMSEA) ≤ 0.05 [ 15 ]. Convergent validity of the H-SCALE-C was evaluated with values for composite reliability (CR), as a measure of internal consistency, and average variance extracted (AVE), which measures the variance of a construct. Values for CR above 0.70 and AVE ≥ 0.5 are considered acceptable [ 15 ]. Discriminant validity was assessed by comparing the square root of the AVE for each factor with correlations between factors. A value for the square root of the AVE greater than correlation coefficients between factors indicates acceptable discriminant validity [ 15 ].
To ensure that individual items of the translated H-SCALE-C were culturally equivalent to the self-care activities of the original H-SCALE, items were removed if the correlation coefficients between item scores and item-to-total scores were < 0.40, which is more stringent than < 0.30 and results in stronger relationships between items and the total scale [ 16 ]. The internal consistency reliability for the H-SCALE-C was established using Cronbach’s α. A Cronbach’s α greater than 0.7 indicates satisfactory internal consistency [ 17 ].
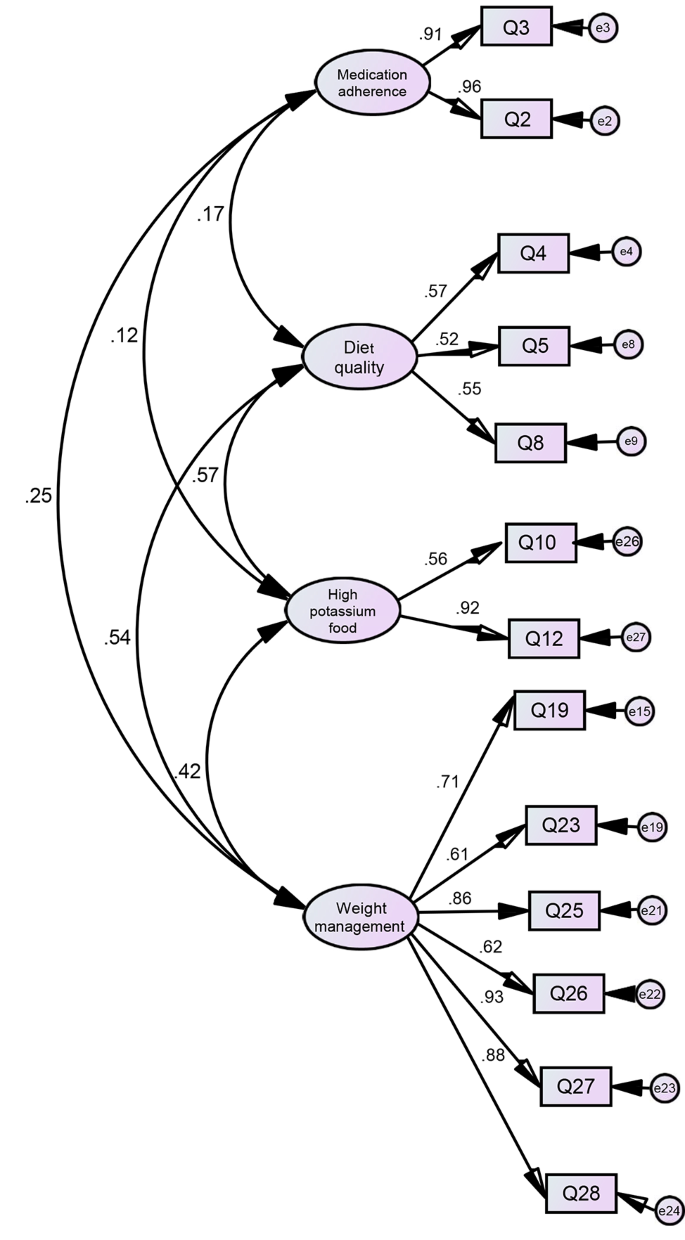
Confirmatory factor analysis of the 13-item Chinese translation of the Hypertension Self-Care Activity Level Effects (H-SCALE-C), based on the four-factor model
Sample characteristics
A total of 318 Taiwanese patients with hypertension were recruited to evaluate the reliability and validity of the translated H-SCALE-C. The mean age of participants was 63.91± 11.80 years (range = 28 to 88 years); slightly over half were male ( n = 170, 53.5%); most ( n = 282, 87.0%) were married; and 37.1% had a college degree or higher. The mean duration of hypertension was 7.53 ± 6.68 years; 65.1% had hypertension for a duration of more than 5 years. The mean BMI was 26.28 ± 4.01 kg/m 2 ; 41.5% ( n = 132) had a BMI ≥ 24 kg/m 2 . Most had one or more comorbidity (67.6%); of those, 44.3% had hyperlipidemia. Other demographic and clinical characteristics of the participants are summarized in Table 1 .
Factor analysis
CFA was first conducted with a maximum likelihood estimate based on the five-factor model of the H-SCALE-C. However, analysis indicated most fit indices did not meet the criteria for acceptability (Table 2 ).
Therefore, EFA was conducted to determine construct validity of the scale. The KMO was 0.85 and Bartlett’s test of sphericity achieved significance ( p < .001), indicating factor analysis was appropriate. Fifteen items were deleted following EFA due to factor loadings below 0.40, which included one item for medication adherence (recommended medication), four for weight management, both items for physical activity, both items for smoking, and six items for diet quality, which included consumption of eggs and high-sodium foods. PCA with Varimax rotation extracted four factors for the 13 items, which were comprised of three of the five original domains plus an additional domain, which we labeled “high potassium food”. All items met the assumption of normality [ 18 ] and multivariate normality was established with Mardia’s coefficient [ 19 ]. There was no cross-loading for any of the factors (Table 3 ). The new factor consisted of two items previously included in the diet quality subscale. The four extracted factors explained 63.93% of the total variance: 34.42% from weight management (six items); 12.32% from medication adherence (two items); 9.36% from diet quality (three items); and 7.84% from high potassium food (two items). Convergent validity was good, as demonstrated by a CR greater than 0.60 and an AVE ≥ 0.40. The overall Cronbach’s alpha value was 0.76. Cronbach’s alpha coefficient for each domain was between 0.65 and 0.94.
Fit indices from CFA of the 13-item 4-factor H-SCALE-C demonstrated an adequate model fit (Table 2 ; Figure 1 ). Table 4 shows the model had good discriminant validity, as demonstrated by the value for the square root of the AVE for the four factors being greater than all correlations among the factors [ 15 ].
The new H-SCALE-C was translated from the H-SCALE developed by Warren-Findlow et al. [ 5 , 6 ], which contains 31 items and six domains. Although the content of the translated 31 items had equivalence with the original items and the CVI was acceptable, item analysis resulted in the removal of the domain of alcohol. EFA with PCA of the 13 remaining items extracted four factors, which eliminated the domains of physical activity and smoking. The final H-SCALE-C is a 13-item instrument with three of the original domains (weight management, medication adherence, diet quality) and a new domain labeled low sodium food.
The primary strength of the original English version of the H-SCALE lies in its coverage of lifestyle domains for patients with hypertension recommended by JNC-7 [ 5 , 6 ], which can enable healthcare providers to swiftly assess the activity levels for reducing hypertension and provide them with timely suggestions relevant to their self-care needs. The participants who completed the H-SCALE-C for factor analysis represented a wide range of characteristics for patients with hypertension. These patients included young and older adults, diagnosed with hypertension recently, living with hypertension for > 10 years, and with and without comorbidities. Therefore, responses to the questionnaire represented a broad range of compliance with self-care management activities to control hypertension. Although only three of the original domains reflected activities our participants employed to manage hypertension, we believe the data provided by this comprehensive group of Taiwanese patients will allow clinicians to reference HSCALE-C assessments when providing patients with individualized self-care strategies that will help them achieve modifications for a healthy lifestyle.
One disadvantage of the H-SCALE-C is the absence of the assessment of alcohol consumption, smoking, and physical activity, all of which are considered important by the JCN-7 guidelines for blood pressure control [ 20 ]. The absence of the domain of smoking as a factor in the HSCALEC may be linked to cultural influences, which might also explain the difficulty the pilot group had when assessing the amount of alcohol consumed. Participants may not have recognized refraining from smoking as an important part of self-care for reducing hypertension. Both alcohol and smoking are important components of societal interactions in Chinese cultures [ 21 , 22 ], where signs of friendliness are frequently demonstrated by proposing a toast with an alcoholic drink or offering someone a cigarette [ 23 ]. The exclusion of the domain for physical activity from the H-SCALE-C might also be the result of cultural influences. Rio and Saligan (2023) reported that both cultural and contextual factors can influence an individual’s attitude towards physical activity. For instance, physical activity may not be considered a health benefit if it is viewed as a leisure activity [ 24 ]. A scale for self-care for Chinese patients with hypertension in Hong Kong developed by Ma et al. (2020) addressed the negative influence of cultural barriers on drinking and smoking by placing items related to these behaviors under the category of ‘habit modification’ [ 23 ]. Hence, modification of the H-SCALE-C by including items related to drinking, smoking and physical activity under the domain of ‘habit modifications’ for self-care will be explored in future studies.
The four domains identified (high potassium foods, weight management, medication adherence, and diet quality) are important self-care activities related to lifestyle in patients with hypertension. Nuclear families remain important in the culture of Taiwan and have a significant influence on the habits of patients in Eastern societies, which differs from Western cultures [ 21 ]. One important component of Asian families is the emphasis on group harmony, which makes dietary options, including cooking methods, not only personal choices but also require considering the expectations of family [ 23 ]. Therefore, when designing strategies to help patients with hypertension modify disease management strategies involving food consumption and daily activities, nurses should also include feedback from family members as to what might be most helpful for improving self-care behaviors. A study on self-care for Korean Americans with diabetes reported that adherence to self-management was positively influenced by support from family members [ 25 ]. The influence of families on patients with diabetes self-care behaviors was also important for individuals who had immigrated from the Middle East to the US [ 26 ].
Limitations
This study had some limitations. First, participants were recruited by convenience sampling from one cardiovascular outpatient clinic of a medical center in northern Taiwan, which restricts the external validity of this study. Therefore, further studies should enroll patients from multiple regions of Taiwan to determine the generalizability, confirm the validity, and strengthen the reliability of the H-SCALE-C. Second, limited time and resources prevented us from evaluating test–retest reliability of the H-SCALE-C, therefore we do not know if the findings are stable over time. We plan to examine this reliability in future studies. Third, the absence of an evaluation of the domains of alcohol consumption, smoking, and physical activity prevent a complete assessment of behaviors known to increase risk of cardiovascular complications for patients with hypertension. Finally, there was no comparison of scores on the H-SCALE-C with another self-care instrument for patients with hypertension, which resulted in a lack of comparative analysis.
The Chinese version of the H-SCALE was demonstrated to be a reliable and valid measure of self-care abilities, which could be applied as a means to facilitate lifestyle modifications to manage hypertension for patients in Taiwan. The higher prevalence of hypertension in Taiwan makes it critically important for access to a suitable instrument to assess self-care activities for patients with hypertension. The H-SCALE-C should be considered for use in clinical practice as an effective means of quickly assessing self-care abilities for patients with hypertension in Taiwan. Scale scores could be used by clinical nurses to provide tailored interventions for lifestyle changes that improve blood pressure control. Healthcare providers could use HSCALEC assessments as a record of quantitative changes in self-care activities, allowing providers to accumulate evidence about the impact of lifestyle changes on blood pressure management for patients with hypertension in Taiwan. Adding an additional domain for ‘habit modification’ that includes alcohol consumption, smoking, and physical activity could further strengthen the applicability of the H-SCALE-C.
Data availability
There are no unpublished data from this study. To access the dataset can contact the.
Abbreviations
Hypertension Self-Care Activity Level Effects
Content validity index
Chinese version of the H-SCALE
Confirmatory factor analysis
Exploratory factor analysis
World Health Organization
Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure
Dietary Approaches to Stop Hypertension-Quality diet
Dietary Approaches to Stop Hypertension diet
Body mass index
Standard deviation
Kaiser-Meyer-Olkin
Principal Component Analysis
Goodness-of-fit index
Adjusted goodness-of-fit index
Comparative fit index
Root mean squared error of approximation
Composite reliability
Average variance extracted
World Health Organization. Hypertension. World Health Organization. 2021. http://www.who.int/news-room/fact-sheets/detail/hypertension . Accessed 30 Jan 2022.
Cheng HM, Lin HJ, Wang TD, Chen CH. Asian management of hypertension: current status, home blood pressure, and specific concerns in Taiwan. J Clin Hypertens (Greenwich). 2020;22(3):511–4. https://doi.org/10.1111/jch.13747 .
Article PubMed Google Scholar
Han HR, Song HJ, Nguyen T, Kim MT. Measuring self-care in patients with hypertension: a systematic review of literature. J Cardiovasc Nurs. 2014;29(1):55–67. https://doi.org/10.1097/JCN.0b013e31827 .
Han HR, Lee H, Commodore-Mensah Y, Kim M. Development and validation of the Hypertension Self-Care Profile: a practical tool to measure hypertension self-care. J Cardiovasc Nurs. 2014;29(3):E11–20. https://doi.org/10.1097/JCN.0b013e3182a3fd46 .
Article PubMed PubMed Central Google Scholar
Warren-Findlow J, Seymour RB. Prevalence rates of hypertension self-care activities among African americans. J Natl Med Assoc. 2011;103(6):503–12. https://doi.org/10.1016/s0027-9684(15)30365-5 .
Warren-Findlow J, Basalik DW, Dulin M, Tapp H, Kuhn L. Preliminary validation of the Hypertension Self-Care Activity Level effects (H-SCALE) and clinical blood pressure among patients with hypertension. J Clin Hypertens. 2013;15(9):637–43. https://doi.org/10.1111/jch.12157 .
Article Google Scholar
Ajani K, Gowani A, Gul R, Petrucka P. Levels and predictors of self-care among patients with hypertension in Pakistan. Int J Gen Med. 2021;25(14):1023–32. https://doi.org/10.2147/IJGM.S297770 .
Huang Z, Hong SA, Tejativaddhana P, Puckpinyo A, Myint MNHA. Multiple self-care behaviors and associated factors in community-dwelling patients with hypertension in Myanmar. Nagoya J Med Sci. 2020;82(2):363–76. https://doi.org/10.18999/nagjms.82.2.363 .
Warren-Findlow J, Krinner LM, Vinoski Thomas E, Coffman MJ, Gordon B, Howden R. Relative and cumulative effects of hypertension self-care behaviors on blood pressure. West J Nurs Res. 2020;42(3):157–64. https://doi.org/10.1177/0193945919851111 .
Zinat Motlagh SF, Chaman R, Sadeghi E, Eslami AA. Self-care behaviors and related factors in hypertensive patients. Iran Red Crescent Med J. 2016;18(6):e35805. https://doi.org/10.5812/ircmj.35805 .
Warren-Findlow J, Reeve CL, Racine EF. Psychometric validation of a brief self-report measure of diet quality: the DASH-Q. J Nutr Educ Behav. 2017;49(2):92–e991. https://doi.org/10.1016/j.jneb.2016.09.004 .
Brislin RW. Back-translation for cross-cultural research. J Cross Cult Psychol. 1970;1(3):185–216. https://doi.org/10.1177/135910457000100301 .
Hair J, Black W, Babin B, Anderson R. Multivariate Data Analysis. 7th ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2010.
Google Scholar
Tabachnick BG, Fidell LS. Using multivariate statistics. 6th ed. Pearson Education; 2013.
Fornell C, Larcker DF. Evaluating structural equation models with unobservable variables and measurement error. J Mark Res. 1981;18(1):39–50. https://doi.org/10.2307/3151312 .
Boateng GO, Neilands TB, Frongillo EA, Melgar-Quinonez HR, Young SL. Best practices for developing and validating scales for health, social, and behavioral research: a primer. Front Public Health. 2018;6:149. https://doi.org/10.3389/fpubh.2019.00149 .
Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;27(2):53–5. https://doi.org/10.5116/ijme.4dfb.8dfd .
Curran PJ, West SG, Finch JF. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol Methods. 1996;1(1):16–29. https://doi.org/10.1037/1082-989X.1.1.16 .
Bollen KA. Structural equations with latent variables. Wiley; 1989. https://doi.org/10.1002/9781118619179 .
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., Jones DW, Materson BJ, Oparil S, Wright JT Jr., Roccella EJ. The Seventh Report of the Joint National Committee on Prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. https://doi.org/10.1001/jama.289.19.2560 .
Article CAS PubMed Google Scholar
Tang Y, Xiang X, Wang X, Cubells JF, Babor TF, Hao W. Alcohol and alcohol-related harm in China: policy changes needed. Bull World Health Organ. 2013;91(4):270–6. https://doi.org/10.2471/BLT.12.107318 .
Huang X, Fu W, ZhangH, et al. Why are male Chinese smokers unwilling to quit? A multicentre cross-sectional study on smoking rationalisation and intention to quit. BMJ Open. 2019;9(2):e025285. https://doi.org/10.1136/bmjopen-2018-025285 .
Ma Y, Cheng HY, Sit JWH, Chien WT. Psychometric evaluation of the Chinese Version of Hypertension Self-Care Profile. J Cardiovasc Nurs. 2021;36(5):420–9. https://doi.org/10.1097/JCN.0000000000000708 .
Rio CJ, Saligan L. Understanding physical activity from a cultural-contextual lens. Front Public Health. 2023;11:1223919. https://doi.org/10.3389/fpubh.2023.1223919 .
Song Y, Song HJ, Han HR, Park SY, Nam S, Kim MT. Unmet needs for social support and effects on diabetes self-care activities in Korean americans with type 2 diabetes. Diabetes Educ. 2012;38(1):77–85. https://doi.org/10.1177/0145721711432456 .
McConatha JT, Kumar VK, Raymond E, Akwarandu A. Cultural dimensions of Diabetes Management: a qualitative study of Middle Eastern immigrants in the U.S. J Cross Cult Gerontol. 2020;35:85–98. https://doi.org/10.1007/s10823-019-09383-7 .
Download references
Acknowledgements
The authors would like to give special thanks to all the patients who participated in this study.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and affiliations.
Department of Nursing, Chang Gung University of Science and Technology, Chiayi, Taiwan
Ting-Yu Chen
School of Nursing, National Defense Medical Center, No.161, Sec. 6, Minquan E. Rd Neihu Dist, Taipei, 11490, Taiwan
Chi-Wen Kao
Division of Cardiology, Department of Internal Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan
Shu-Meng Cheng
Department of Health Care Management, National Taipei University of Nursing and Health Sciences, Taipei, Taiwan
Chieh-Yu Liu
You can also search for this author in PubMed Google Scholar
Contributions
T.-Y.C. designed the study, involved data collection, conducted data analysis, interpreted the results and drafted and revised the manuscript. C.-W.K. designed the study, conducted data analysis, interpreted the results and edited the manuscript. S.-M.C. recruited to participants. C.-Y.L. analyzed the data and interpreted the results.
Corresponding author
Correspondence to Chi-Wen Kao .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations and informed consent was obtained from all participants. The research Ethics approval was obtained from the Tri-Service General Hospital Institutional Review Board (IRB No. 2-104-05-148).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chen, TY., Kao, CW., Cheng, SM. et al. Translation, adaptation, and validation of a Chinese version of the Hypertension Self-Care Activity Level effects (H-SCALE) for patients with hypertension. BMC Nurs 23 , 334 (2024). https://doi.org/10.1186/s12912-024-01993-y
Download citation
Received : 31 August 2023
Accepted : 06 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12912-024-01993-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hypertension
- Translation
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
A 45-year-old woman presented with hypertension, fatigue, and episodic confusion. After medications were administered, the blood pressure decreased but fatigue and confusion persisted. Four ...
Definitions used in these clinical case scenarios. Definitions Stage 1 hypertension Clinic blood pressure is 140/90 mmHg or higher and. subsequent ambulatory blood pressure monitoring (ABPM) daytime average or home blood pressure monitoring (HBPM) average blood pressure is 135/85 mmHg or higher. Stage 2 hypertension Clinic blood pressure is 160 ...
Outline. Mrs. Phillips, a 43-year old African American female, presents to the Emergency Department (ED) complaining of the worst headache of her life. She says it started about 3 hours ago. She reports taking 1,000 mg of Acetaminophen with no relief. Upon further questioning, Mrs. Phillips also reports blurry vision.
This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as ...
1) CASE SUMMARY. Mr. MS is a 58-year-old Malay male who was previously diagnosed with hypertension, gout and triple vessel ischemic heart disease. He first presented with chest pain in March 2010 where he was diagnosed with ischemic heart disease.
First, Nurse Tom recognizes important cues, including temperature 99.4 F or 37.5 C, pulse 75 beats per minute; respirations 16 breaths per minute; blood pressure of 156/89 mmHg, and oxygen saturation 97% on room air. Next, Nurse Tom asks Mahlik about his history.
Abstract. Objective: To explore the effect of management of nursing case on blood pressure control in hypertension patients. Method: This is a randomized controlled study which will be carried out from May 2021 to May 2022. The experiment was granted through the Research Ethics Committee of the People's Hospital of Chengyang District (03982808).
The role of an advanced nurse practitioner encompasses the assessment, diagnosis and treatment of a range of conditions. This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that ...
To synthesize the best available evidence regarding the effectiveness of nursing case management in primary health care, compared to usual care, in improving blood pressure in adults over 18 years with hypertension.Systematic review that includes studies ...
DASH or the Dietary Approaches to Stop Hypertension includes consummation of a diet rich in fruits, vegetable, and low-fat dairy. Dietary sodium retention. Sodium contributes to an elevated blood pressure, so reducing the dietary intake to no more than 2.4 g sodium per day can be really helpful. Physical activity.
This case study presents a patient with newly diagnosed hypertension. It demonstrates effective history taking, physical examination, differential diagnoses and the shared decision making which occurred between the patient and the professional. It is widely acknowledged that adherence to medications is poor in long-term conditions, such as ...
Case Study Example; Practice PICO; Formulate a Clinical Question from a Case Study. Case: Hypertension; P: Patient; I: Intervention; C: Comparison; O: Outcome; PICO: Putting It Together; Clinical Scenario. A 68-year-old female patient has recently been diagnosed with high blood pressure. She is otherwise healthy and active.
Hypertension is one of the chronic medical conditions that is important for nursing students. Studying hypertension case study scenarios can provide students with invaluable insights into management, complications, and preventive strategies and prepare them for the NCLEX exam.. In this article, we delve into three hypertension case studies to uncover the hidden lessons they offer.
Patient Case Presentation. Mr. E.A. is a 40-year-old black male who presented to his Primary Care Provider for a diabetes follow up on October 14th, 2019. The patient complains of a general constant headache that has lasted the past week, with no relieving factors. He also reports an unusual increase in fatigue and general muscle ache without ...
Description of Case. A 21-year-old pregnant woman, gravida 2 para 1, presented with hypertension and proteinuria at 20 weeks of gestation. She had a history of pre-eclampsia in her first pregnancy one year ago. During that pregnancy, at 39 weeks of gestation, she developed high blood pressure, proteinuria, and deranged liver function.
removed from the hypertension register and his QRISK 10 year CVD risk score was calculated to be 9.8%. This gentleman purchased a new, validated blood pressure monitor and now routinely monitors his blood pressure at home as well as attending his surgery for routine blood pressure checks.
History of Present Problem: Mike Kelly is a 51-year-old Caucasian male who is 6 feet tall and weighs 275 pounds (BMI 37) with an abnormal distribution of weight around his abdomen. He does not regularly exercise, does not like to cook, and eats fast food three to five times during the week. He has smoked one pack per day since the age of 20 (31 ...
Case study. Ms. C is a 42-year-old black American woman with a 7-year history of hypertension first diagnosed during her last pregnancy. Her family history is positive for hypertension, with her mother dying at 56 years of age from hypertension-related cardiovascular disease (CVD). In addition, both her maternal and paternal grandparents had CVD.
Abstract. Objective: To explore the effect of management of nursing case on blood pressure control in hypertension patients. Method: This is a randomized controlled study which will be carried out from May 2021 to May 2022. The experiment was granted through the Research Ethics Committee of the People's Hospital of Chengyang District (03982808).
htn case study keith rn lrcc nursing ii clinical 2.9.2017 rapid reasoning case data collection history of present problem: mike kelly is 51 year old caucasian. ... Hypertension - htn case study. htn case study. Course. General Biology (BIOS 101) 75 Documents. Students shared 75 documents in this course. University
Hence, we conduct the randomized controlled study protocol to explore the effect of management of nursing case on blood pressure control in hypertension patients. 2 Materials and methods This is a randomized controlled study which will be carried out from May 2021 to May 2022 at the People's Hospital of Chengyang District.
Sample of 160 people residing in remote hilly area non-Probability Convenience sampling technique was used to select the participants. ... Case study, American Journal of Hypertension, Volume 11 ...
Case Presentation. The patient is a 60-year-old white female presenting to the emergency department with acute onset shortness of breath. Symptoms began approximately 2 days before and had progressively worsened with no associated, aggravating, or relieving factors noted. She had similar symptoms approximately 1 year ago with an acute, chronic ...
Sample case study for nursing students can be a valuable tool in your preparation, helping you to develop critical thinking skills and apply your knowledge in real-world scenarios. That's why we've put together a list of 5 nursing case study examples, complete with answer guides, to help you prepare for the NCLEX -style questions you'll ...
This study aimed to translate the H-SCALE into Chinese and test its validity, and reliability in a sample of adults with hypertension. The English version of the 31-item H-SCALE was translated into Chinese using the forward-backward method. The content validity index (CVI) of the translated scale was determined by five experts in hypertension.