Editorial Policy
Authors Info
Current Issue
Special Issue
Editorial Board

Welcome to IJCRR
IC Value (2018): 90.90
SJIF (2021): 6.66
IPI Factor : 4.02
Impact Factor (CiteFactor) (2020-21): 1.84
ISI Impact Factor (2021-2022): 2.176
IC Value (2019): 90.81
IC Value (2020): 91.47
SJIF (2020) = 7.893
IJCRR DOI Prefix (CrossRef): 10.31782/2231-2196
Information Matrix for the Analysis of Journals (ICDS = 9.6)
Peer Reviewed::Scientific
Frequency: Fortnightly
Language: English
Indexed and Abstracted in : Crossref, CAS Abstracts, Publons, Google Scholar, Open J-Gate, ROAD, Indian Citation Index (ICI), ResearchGATE, Ulrich's Periodicals Directory, WorldCat (World's largest network of library content and services)
Search Articles
Track manuscript
Readers around the world

Advertisement

International Journal of Current Research and Review (IJCRR) is one of the popular fortnightly published Healthcare and Life Sciences journal. IJCRR is a peer-reviewed indexed journal that is available online and in print format. IJCRR is a fortnightly indexed international journal publishing the finest peer-reviewed research and review articles in fields of Healthcare and Life Sciences.
Aim and Scope:
To publish quality articles, IJCRR follows stringent guidelines to select the manuscripts based on its originality, importance, timeliness, accessibility, grace, and astonishing conclusions in Healthcare (Nursing, Nutrition, Dentistry, Medicine, Pharmacy, Alternative Medicine, Psychology, Social care, Complimentary medicine, Traditional Medicine, Anatomy, Immunology, Dietetics) and Life Sciences (Botany, Zoology, Genetics, Biochemistry, Molecular Biology, Cytology, Ethology, Ecology, Astrobiology, Cell biology, Bioinformatics, Physiology, Microbiology). Scope of the journal limited to Healthcare and Life Sciences.
Vision Statement:
To set a landmark by encouraging and awarding publication of high-quality, authentic research and review in streams of Healthcare and Life Sciences.
Affiliation and Ownership:
International Journal of Current Research and Review (IJCRR) is the official publication of Radiance Research Academy which is governed by Swadesh Bahu-uddeshiya Kalyankari Shikshan Sanstha, Nagpur (Registered under Society’s Act 1860, XXI, Regd. No. 868/11 Ngp and Bombay Trust Act 1950 Regd. No. F-287/4 Ngp). Journal’s publication activities are administered through Radiance Research Academy.
IJCRR Award for Best Article:
IJCRR editorial team MONTHLY selects one 'Best Article' for the award among published articles.
The articles in IJCRR are open access articles licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
IJCRR’s Good Publishing Practices:
To achieve a high standard of publication, we adopt Good Publishing Practices (updated in 2022) which are inspired by guidelines provided by Committee on Publication Ethics ( COPE ), Open Access Scholarly Publishers Association ( OASPA ) and International Committee of Medical Journal Editors ( ICMJE ).
Principles of Transparency and Best Practices at IJCRR
As per the recent guidelines by Committee on Publication Ethics ( COPE ), the Directory of Open Access Journals ( DOAJ ), the Open Access Scholarly Publishers Association ( OASPA ), and the World Association of Medical Editors ( WAME ), International Journal of Current Research and Review (IJCRR) voluntarily adopts the following mechanism as Best Practices to maintain the Principles of Transparency.
1. Website:
Domain name selected for website i.e. is unique and abbreviation of the journal’s name. Information given on the journal’s website is detailed. Care has been taken to ensure high ethical and professional standards. Necessary information for authors, reviewers, editors, and other stakeholders has been provided in detail. The aim, scope, and readership of the journal are clearly defined.
Official e-mail ID for communication: All official communications are done using e-mail ID – [email protected] and [email protected]. Authors are requested to use [email protected] or [email protected] for communication with IJCRR. Researchers should note that NO other e-mail ID is used by IJCRR for official communication with authors.
2. Name of journal:
The name of the journal- International Journal of Current Research and Review (IJCRR) is unique and it matches the content published in the journal. Manuscripts are published as per the aim and scope of the journal.
3. Peer review process:
A double-blinded peer-review process is adopted at IJCRR. Journal Management Software, Artificial Intelligence technique is used to select reviewers from the concerned area of expertise to review the manuscript. Policies related to the ‘Manuscript Review Process’ are clearly described on the journal website. IJCRR does not guarantee acceptance of manuscript or short peer-review times.
4. Ownership and management:
International Journal of Current Research and Review (IJCRR) is owned by Radiance Research Academy, its office address is- 148, IMSR Building, Ayurvedic Layout, Sakkardara, Nagpur, PIN-440024, Maharashtra, India. Radiance Research Academy is governed by Swadesh Bahu-uddeshiya Kalyanakari Shikshan Sanstha (Registered under Indian Society’s Act 1860 and Bombay Trust Act ).
5. Governing body:
Journal editorial board consists of eminent experts in the subject areas included within the journal’s scope. The Journal management team is responsible for the overall daily administration of the official activities of the journal. Details of the editorial board and journal management team along with their roles and responsibilities are displayed on the journal’s website.
6. Editorial team / contact information:
IJCRR’s Editorial Board members are eminent experts in the subject areas included within the journal’s scope. They are identified from different countries. The average experience of editorial board members is 18 years. Mostly, subject experts from academia from different universities around the world are identified as editorial board members. Full names, affiliation, and contact details of editorial board members are displayed in the ‘Editorial Board’ section of the journal’s website.
7. Copyright and Licensing:
The policy for copyright is clearly stated in the author’s guidelines, a sample copy of the copyright form is available on IJCRR’s website . The new policy of including the name of the copyright holder on all published articles is initiated from Vol. 12 Issue 15. Licensing information is also clearly described in guidelines on the website; licensing terms including Creative Commons license is indicated on all published articles, both HTML and PDFs from Vol. 12 Issue 15. Policies on posting of final accepted versions or published articles on third party repositories are clearly stated.
Copyright Form
8. Author fees:
Journal does not charge submission fees. A nominal fee INR 5000 (USD 120) is charged from authors of accepted articles.
9. Process for identification of and dealing with allegations of research misconduct:
Following mechanism adopted at IJCRR to identify and prevent the publication of papers where research misconduct has occurred including plagiarism, citation manipulation, and data falsification/fabrication.
All manuscripts are processed through licensed plagiarism detection software before acceptance of the manuscript for publication. Reviewers who are experts in the subject areas are selected automatically using artificial intelligence techniques based on the topic and keywords of the manuscript for review. Reviewers identified by IJCRR are trained to identify citation manipulation and data falsification/fabrication. Author (s) if identified for such misconduct or allegations are dealing as per the guidelines given by COPE and mentioned in IJCRR's Good Publishing Practices. 10. Publication Ethics:
IJCRR has policies on publishing ethics, it includes-
Journal policies on authorship and contribution Policies on handling the complaints and appeals Journal policies on conflicts of interest / competing interests Journal policies on data sharing and reproducibility Journal’s policy on ethical oversight Journal’s policy on intellectual property Journal’s options for post-publication discussions and corrections. These policies are discussed in detail in IJCRR's Good Publishing Policies (click here)
11. Publishing schedule:
International Journal of Current Research and Review is published fortnightly. Its publication schedule is maintained for the last thirteen years. Theme based issues are published at regular intervals as ‘Special Issues’.
12. Access:
International Journal of Current Research and Review is open access journal under Creative Commons license. Readers can freely access the journal and individual articles from the journal website without its subscription. The print version of the journal is available for subscription to institutional libraries.
13. Archiving:
IJCRR has its own mechanism for electronic backup and preservation. The self repository is used to archive the articles as per DOI identification number. IJCRR also archives published articles via indexing agencies including several library repository agencies. Currently, the journal is working on the preservation of articles using PubMed Central, CLOCKSS, and related such electronic backup services.
14. Revenue sources:
Administrative and other expenses are met through revenue generated via author fees, subscriptions, reprints, and institutional support. Several schemes and Research incentives are given to encourage research and publication culture among readers and authors. Details of these schemes and research incentives are detailed on IJCRR’s website www.ijcrr.com
15. Advertising:
IJCRR do not advertise widely. Publication of journal issue is notified to authors and readers through e-mail and official social media including Facebook and Twitter. The Journal management team takes a decision on popularizing the notifications.
16. Direct marketing:
IJCRR do not use direct marketing as a tool for advertising purpose.
17. Flow Charts
a) Governing Board
b) Manuscript Handling Process
c) Roles and Responsibility of Publishers
d) Article Retraction flow chart
18. COPE Guidelines for peer reviewers.
Announcements
Dr. Pramod Kumar Manjhi joined Editor-in-Chief since July 2021 onwards
COPE guidelines for Reviewers
SCOPUS indexing: 2014, 2019 to 2021
Awards, Research and Publication incentive Schemes by IJCRR
Best Article Award:
One article from every issue is selected for the ‘Best Article Award’. Authors of selected ‘Best Article’ are rewarded with a certificate. IJCRR Editorial Board members select one ‘Best Article’ from the published issue based on originality, novelty, social usefulness of the work. The corresponding author of selected ‘Best Article Award’ is communicated and information of award is displayed on IJCRR’s website. Drop a mail to [email protected] for more details.
Women Researcher Award:
This award is instituted to encourage women researchers to publish her work in IJCRR. Women researcher, who intends to publish her research work in IJCRR as the first author is eligible to apply for this award. Editorial Board members decide on the selection of women researchers based on the originality, novelty, and social contribution of the research work. The corresponding author of the selected manuscript is communicated and information is displayed on IJCRR’s website. Under this award selected women, the author is eligible for publication incentives. Drop a mail to [email protected] for more details.
Emerging Researcher Award:
‘Emerging Researcher Award’ is instituted to encourage student researchers to publish their work in IJCRR. Student researchers, who intend to publish their research or review work in IJCRR as the first author are eligible to apply for this award. Editorial Board members decide on the selection of student researchers for the said award based on originality, novelty, and social applicability of the research work. Under this award selected student researcher is eligible for publication incentives. Drop a mail to [email protected] for more details.
Best Article Award
List of Awardees
A Study by Ese Anibor et al. " Evaluation of Temporomandibular Joint Disorders Among Delta State University Students in Abraka, Nigeria " from Vol 13 issue 16 received Emerging Researcher Award
A Study by Alkhansa Mahmoud et al. entitled " mRNA Expression of Somatostatin Receptors (1-5) in MCF7 and MDA-MB231 Breast Cancer Cells " from Vol 13 issue 06 received Emerging Researcher Award
Indexed and Abstracted in

Antiplagiarism Policy: IJCRR strongly condemn and discourage practice of plagiarism. All received manuscripts have to pass through "Plagiarism Detection Software" test before Toto Macau forwarding for peer review. We consider "Plagiarism is a crime"
IJCRR Code of Conduct: To achieve a high standard of publication, we adopt Good Publishing Practices (updated in 2022) which are inspired by guidelines provided by Committee on Publication Ethics (COPE) , Open Access Scholarly Publishers Association (OASPA) and International Committee of Medical Journal Editors (ICMJE)
Disclaimer: International Journal of Current Research and Review (IJCRR) provides platform for researchers to publish and discuss their original research and review work. IJCRR can not be held responsible for views, opinions and written statements of researchers published in this journal.
International Journal of Current Research and Review (IJCRR) provides platform for researchers to publish and discuss their original research and review work. IJCRR can not be held responsible for views, opinions and written statements of researchers published in this journal

Useful links
148, IMSR Building, Ayurvedic Layout, Near NIT Complex, Sakkardara, Nagpur-24, Maharashtra State, India

Copyright © 2024 IJCRR. Specialized online journals by ubijournal .Website by Ubitech solutions
International Journal of Current Research and Review
Discontinued in Scopus as of 2021
Subject Area and Category
- Biochemistry, Genetics and Molecular Biology (miscellaneous)
- Dentistry (miscellaneous)
- Health Professions (miscellaneous)
Radiance Research Academy
Publication type
09755241, 22312196
2014, 2019-2021
The set of journals have been ranked according to their SJR and divided into four equal groups, four quartiles. Q1 (green) comprises the quarter of the journals with the highest values, Q2 (yellow) the second highest values, Q3 (orange) the third highest values and Q4 (red) the lowest values.
The SJR is a size-independent prestige indicator that ranks journals by their 'average prestige per article'. It is based on the idea that 'all citations are not created equal'. SJR is a measure of scientific influence of journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from It measures the scientific influence of the average article in a journal, it expresses how central to the global scientific discussion an average article of the journal is.
Evolution of the number of published documents. All types of documents are considered, including citable and non citable documents.
This indicator counts the number of citations received by documents from a journal and divides them by the total number of documents published in that journal. The chart shows the evolution of the average number of times documents published in a journal in the past two, three and four years have been cited in the current year. The two years line is equivalent to journal impact factor ™ (Thomson Reuters) metric.
Evolution of the total number of citations and journal's self-citations received by a journal's published documents during the three previous years. Journal Self-citation is defined as the number of citation from a journal citing article to articles published by the same journal.
Evolution of the number of total citation per document and external citation per document (i.e. journal self-citations removed) received by a journal's published documents during the three previous years. External citations are calculated by subtracting the number of self-citations from the total number of citations received by the journal’s documents.
International Collaboration accounts for the articles that have been produced by researchers from several countries. The chart shows the ratio of a journal's documents signed by researchers from more than one country; that is including more than one country address.
Not every article in a journal is considered primary research and therefore "citable", this chart shows the ratio of a journal's articles including substantial research (research articles, conference papers and reviews) in three year windows vs. those documents other than research articles, reviews and conference papers.
Ratio of a journal's items, grouped in three years windows, that have been cited at least once vs. those not cited during the following year.
Evolution of the percentage of female authors.
Evolution of the number of documents cited by public policy documents according to Overton database.
Evoution of the number of documents related to Sustainable Development Goals defined by United Nations. Available from 2018 onwards.
Leave a comment
Name * Required
Email (will not be published) * Required
* Required Cancel
The users of Scimago Journal & Country Rank have the possibility to dialogue through comments linked to a specific journal. The purpose is to have a forum in which general doubts about the processes of publication in the journal, experiences and other issues derived from the publication of papers are resolved. For topics on particular articles, maintain the dialogue through the usual channels with your editor.
Follow us on @ScimagoJR Scimago Lab , Copyright 2007-2024. Data Source: Scopus®
Cookie settings
Cookie Policy
Legal Notice
Privacy Policy
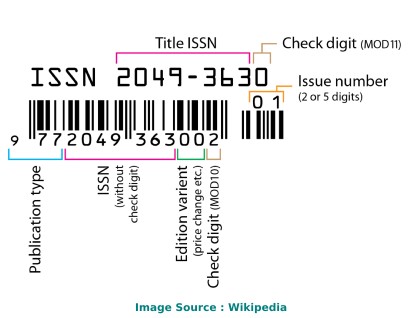
Identifiers
Linking ISSN (ISSN-L): 0975-5241
URL http://www.ijcrr.com
Google https://www.google.com/search?q=ISSN+%220975-5241%22
Bing https://www.bing.com/search?q=ISSN+%220975-5241%22
Yahoo https://search.yahoo.com/search?p=ISSN%20%220975-5241%22
National Library of India http://nationallibraryopac.nvli.in/cgi-bin/koha/opac-search.pl?advsearch=1&idx=ns&q=0975-5241&weight_search=1&do=Search&sort_by=relevance
Resource information
Title proper: International journal of current research and review.
Country: India
Medium: Online
Record information
Last modification date: 29/05/2023
Type of record: Confirmed
ISSN Center responsible of the record: ISSN National Centre for India
downloads requested
Discover all the features of the complete ISSN records
Display mode x.
Labelled view
MARC21 view
UNIMARC view
International Journal of Current Research and Review - Impact Score, Ranking, SJR, h-index, Citescore, Rating, Publisher, ISSN, and Other Important Details
Published By: Radiance Research Academy
Abbreviation: Int. J. Curr. Res. Rev.
Impact Score The impact Score or journal impact score (JIS) is equivalent to Impact Factor. The impact factor (IF) or journal impact factor (JIF) of an academic journal is a scientometric index calculated by Clarivate that reflects the yearly mean number of citations of articles published in the last two years in a given journal, as indexed by Clarivate's Web of Science. On the other hand, Impact Score is based on Scopus data.
Important details, about international journal of current research and review.
International Journal of Current Research and Review is a journal published by Radiance Research Academy . This journal covers the area[s] related to A, Biochemistry, Genetics and Molecular Biology (miscellane, Dentistry (miscellane, Health Professions (miscellane, etc . The coverage history of this journal is as follows: 2014, 2019-2021. The rank of this journal is 27475 . This journal's impact score, h-index, and SJR are 0.39, 9, and , respectively. The ISSN of this journal is/are as follows: 09755241, 22312196 . The best quartile of International Journal of Current Research and Review is - . This journal has received a total of 237 citations during the last three years (Preceding 2021).
International Journal of Current Research and Review Impact Score 2021-2022
The impact score (IS), also denoted as the Journal impact score (JIS), of an academic journal is a measure of the yearly average number of citations to recent articles published in that journal. It is based on Scopus data.
Prediction of International Journal of Current Research and Review Impact Score 2022
Impact Score 2021 of International Journal of Current Research and Review is 0.39 . If a similar upward trend continues, IS may increase in 2022 as well.
Impact Score Graph
Check below the impact score trends of international journal of current research and review. this is based on scopus data., international journal of current research and review h-index.
The h-index of International Journal of Current Research and Review is 9 . By definition of the h-index, this journal has at least 9 published articles with more than 9 citations.
What is h-index?
The h-index (also known as the Hirsch index or Hirsh index) is a scientometric parameter used to evaluate the scientific impact of the publications and journals. It is defined as the maximum value of h such that the given Journal has published at least h papers and each has at least h citations.
International Journal of Current Research and Review ISSN
The International Standard Serial Number (ISSN) of International Journal of Current Research and Review is/are as follows: 09755241, 22312196 .
The ISSN is a unique 8-digit identifier for a specific publication like Magazine or Journal. The ISSN is used in the postal system and in the publishing world to identify the articles that are published in journals, magazines, newsletters, etc. This is the number assigned to your article by the publisher, and it is the one you will use to reference your article within the library catalogues.
ISSN code (also called as "ISSN structure" or "ISSN syntax") can be expressed as follows: NNNN-NNNC Here, N is in the set {0,1,2,3...,9}, a digit character, and C is in {0,1,2,3,...,9,X}
International Journal of Current Research and Review Ranking and SCImago Journal Rank (SJR)
SCImago Journal Rank is an indicator, which measures the scientific influence of journals. It considers the number of citations received by a journal and the importance of the journals from where these citations come.
International Journal of Current Research and Review Publisher
The publisher of International Journal of Current Research and Review is Radiance Research Academy . The publishing house of this journal is located in the India . Its coverage history is as follows: 2014, 2019-2021 .
Call For Papers (CFPs)
Please check the official website of this journal to find out the complete details and Call For Papers (CFPs).
Abbreviation
The International Organization for Standardization 4 (ISO 4) abbreviation of International Journal of Current Research and Review is Int. J. Curr. Res. Rev. . ISO 4 is an international standard which defines a uniform and consistent system for the abbreviation of serial publication titles, which are published regularly. The primary use of ISO 4 is to abbreviate or shorten the names of scientific journals using the technique of List of Title Word Abbreviations (LTWA).
As ISO 4 is an international standard, the abbreviation ('Int. J. Curr. Res. Rev.') can be used for citing, indexing, abstraction, and referencing purposes.
How to publish in International Journal of Current Research and Review
If your area of research or discipline is related to A, Biochemistry, Genetics and Molecular Biology (miscellane, Dentistry (miscellane, Health Professions (miscellane, etc. , please check the journal's official website to understand the complete publication process.
Acceptance Rate
- Interest/demand of researchers/scientists for publishing in a specific journal/conference.
- The complexity of the peer review process and timeline.
- Time taken from draft submission to final publication.
- Number of submissions received and acceptance slots
- And Many More.
The simplest way to find out the acceptance rate or rejection rate of a Journal/Conference is to check with the journal's/conference's editorial team through emails or through the official website.
Frequently Asked Questions (FAQ)
What is the impact score of international journal of current research and review.
The latest impact score of International Journal of Current Research and Review is 0.39. It is computed in the year 2022.
What is the h-index of International Journal of Current Research and Review?
The latest h-index of International Journal of Current Research and Review is 9. It is evaluated in the year 2022.
What is the SCImago Journal Rank (SJR) of International Journal of Current Research and Review?
The latest SCImago Journal Rank (SJR) of International Journal of Current Research and Review is . It is calculated in the year 2022.
What is the ranking of International Journal of Current Research and Review?
The latest ranking of International Journal of Current Research and Review is 27475. This ranking is among 27955 Journals, Conferences, and Book Series. It is computed in the year 2022.
Who is the publisher of International Journal of Current Research and Review?
International Journal of Current Research and Review is published by Radiance Research Academy. The publication country of this journal is India.
What is the abbreviation of International Journal of Current Research and Review?
This standard abbreviation of International Journal of Current Research and Review is Int. J. Curr. Res. Rev..
Is "International Journal of Current Research and Review" a Journal, Conference or Book Series?
International Journal of Current Research and Review is a journal published by Radiance Research Academy.
What is the scope of International Journal of Current Research and Review?
- Biochemistry, Genetics and Molecular Biology (miscellane
- Dentistry (miscellane
- Health Professions (miscellane
For detailed scope of International Journal of Current Research and Review, check the official website of this journal.
What is the ISSN of International Journal of Current Research and Review?
The International Standard Serial Number (ISSN) of International Journal of Current Research and Review is/are as follows: 09755241, 22312196.
What is the best quartile for International Journal of Current Research and Review?
The best quartile for International Journal of Current Research and Review is -.
What is the coverage history of International Journal of Current Research and Review?
The coverage history of International Journal of Current Research and Review is as follows 2014, 2019-2021.
Credits and Sources
- Scimago Journal & Country Rank (SJR), https://www.scimagojr.com/
- Journal Impact Factor, https://clarivate.com/
- Issn.org, https://www.issn.org/
- Scopus, https://www.scopus.com/
Note: The impact score shown here is equivalent to the average number of times documents published in a journal/conference in the past two years have been cited in the current year (i.e., Cites / Doc. (2 years)). It is based on Scopus data and can be a little higher or different compared to the impact factor (IF) produced by Journal Citation Report. Please refer to the Web of Science data source to check the exact journal impact factor ™ (Thomson Reuters) metric.
Impact Score, SJR, h-Index, and Other Important metrics of These Journals, Conferences, and Book Series
Check complete list
International Journal of Current Research and Review Impact Score (IS) Trend
Top journals/conferences in a, top journals/conferences in biochemistry, genetics and molecular biology (miscellane, top journals/conferences in dentistry (miscellane, top journals/conferences in health professions (miscellane.

- Paper Archives
- Journal Indexing
- Research Conference
- Add Journal
Searching By
- Search More ...

Description
Last modified: 2010-08-30 09:46:26
- No Archives
Advertisement
- Our Profile
- Virtual Events-Sponsor
- Conference with Publication
- Upcoming Medical Conferences
- For Institutions
- For Individuals

About Bioleagues
International journal of current research and review (ijcrr).
ISSN: 0975-5241
INDEXED IN SCOPUS
Medicine, Alternative Medicine, Traditional Medicine, Complementary medicine, Nursing, Nutrition, Dentistry, Pharmacy, Social care, Anatomy, Immunology, Dietetics, Genetics, Botany, Zoology, Biochemistry, Molecular Biology, Cytology, Ethology, Ecology, Astrobiology, Cell biology, Bioinformatics, Physiology, and Microbiology.
Agricultural and Biological Sciences
General Agricultural and Biological Sciences
Biochemistry
Genetics and Molecular Biology
General Biochemistry
Veterinary: General Veterinary

For Individuals ×

EDITORIAL BOARD
- INSTRUCTION TO AUTHOR
- Current Issue
- February 2024
- January 2024
- December 2023
- November, 2023
- October 2023
- September 2023
- August 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- February 2022
- January 2022
- December 2021
- November, 2021
- October, 2021
- September, 2021
- August, 2021
- February 2021
- January 2021
- CALL FOR PAPERS 2022
- Certificate
- Reviewers Form
- Indexing & Abstracting
- Editorial Board
- Submit Manuscript
- Instruction to Author
- Past Issues
- Call for papers/May 2024
- Ethics and Malpractice
- Conflict of Interest Statement
- Statement of Informed Consent
- Final Proof Correction and Submission
- Publication Ethics
- Peer review process
- Cover images -April-2024
- Quick Response - Contact Us
CERTIFICATE
Author Information
- Copyright Form
- Join Editor & Peer Reviewers
- Paper Submission
- Impact Factor
- Policy of Screening
IMPACT FACTOR 2021

Subject Area
- Life Sciences / Biology
- Architecture / Building Management
- Asian Studies
- Business & Management
- Computer Science
- Economics & Finance
- Engineering / Acoustics
- Environmental Science
- Agricultural Sciences
- Pharmaceutical Sciences
- General Sciences
- Materials Science
- Mathematics
- Nanotechnology & Nanoscience
- Nonlinear Science
- Chaos & Dynamical Systems
- Social Sciences & Humanities
Why Us? >>
- Open Access
- Peer Reviewed
- Rapid Publication
- Life time hosting
- Free promotion service
- Free indexing service
- More citations
- Search engine friendly
ABOUT THE JOURNAL
People Contact Editorial Board Policies Focus and Scope Section Policies Open Access Policy Memberships Submissions Online Submissions Author Guidelines Conferences Books Other Site Map Editorial and Publishing Process Statistics
CALL FOR PAPERS
Online paypal payment, ijmce recommendation.

Monthly archive
- November 2023
- November 2021
Advantages of IJCR
- Rapid Publishing
- Professional publishing practices
- Indexing in leading database
- High level of citation
- High Qualitiy reader base
- High level author suport
Plagiarism Detection
IJCR is following an instant policy on rejection those received papers with plagiarism rate of more than 20% . So, All of authors and contributors must check their papers before submission to making assurance of following our anti-plagiarism policies.


International Journal of Current Research and Review Impact Factor & Key Scientometrics
International journal of current research and review overview, impact factor.
I. Basic Journal Info

Journal ISSN: 09755241, 22312196
Publisher: radiance research academy, history: 2014, 2019-2021, journal hompage: link, how to get published:, research categories, scope/description:.
--------------------------------
Best Academic Tools
- Academic Writing Tools
- Proofreading Tools
- Academic Search Engines
- Project Management Tools
- Survey Tools for Research
- Transcription Tools
- Reference Management Software
- AI-Based Summary Generators
- Academic Social Network Sites
- Plagiarism Checkers
- Science Communication Tools
- Jasper AI Review
II. Science Citation Report (SCR)
International journal of current research and review scr impact factor, international journal of current research and review scr journal ranking, international journal of current research and review scimago sjr rank.
SCImago Journal Rank (SJR indicator) is a measure of scientific influence of scholarly journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from.
International Journal of Current Research and Review Scopus 2-Year Impact Factor Trend
International journal of current research and review scopus 3-year impact factor trend, international journal of current research and review scopus 4-year impact factor trend, international journal of current research and review impact factor history.
- 2022 Impact Factor NA NA NA
- 2021 Impact Factor 0.389 0.389 0.389
- 2020 Impact Factor 0.22 0.22 0.22
- 2019 Impact Factor 0 0 0
- 2018 Impact Factor NA NA NA
- 2017 Impact Factor NA NA NA
- 2016 Impact Factor NA NA NA
- 2015 Impact Factor NA NA NA
- 2014 Impact Factor 0 NA NA
- 2013 Impact Factor NA NA NA
- 2012 Impact Factor NA NA NA
- 2011 Impact Factor NA NA NA
- 2010 Impact Factor NA NA NA
- 2009 Impact Factor NA NA NA
- 2008 Impact Factor NA NA NA
- 2007 Impact Factor NA NA NA
- 2006 Impact Factor NA NA NA
- 2005 Impact Factor NA NA NA
- 2004 Impact Factor NA NA NA
- 2003 Impact Factor NA NA NA
- 2002 Impact Factor NA NA NA
- 2001 Impact Factor NA NA NA
- 2000 Impact Factor NA NA NA
See what other people are reading
HIGHEST PAID JOBS
- Highest Paying Nursing Jobs
- Highest Paying Non-Physician Jobs
- Highest Paying Immunology Jobs
- Highest Paying Microbiology Jobs
LATEX TUTORIALS
- LaTeX Installation Guide – Easy to Follow Steps to Install LaTeX
- 6 Easy Steps to Create Your First LaTeX Document
- How to Use LaTeX Paragraphs and Sections
- How to Use LaTeX Packages with Examples
MUST-READ BOOKS
- Multidisciplinary
- Health Science
Impact factor (IF) is a scientometric factor based on the yearly average number of citations on articles published by a particular journal in the last two years. A journal impact factor is frequently used as a proxy for the relative importance of a journal within its field. Find out more: What is a good impact factor?
III. Other Science Influence Indicators
Any impact factor or scientometric indicator alone will not give you the full picture of a science journal. There are also other factors such as H-Index, Self-Citation Ratio, SJR, SNIP, etc. Researchers may also consider the practical aspect of a journal such as publication fees, acceptance rate, review speed. ( Learn More )
International Journal of Current Research and Review H-Index
The h-index is an author-level metric that attempts to measure both the productivity and citation impact of the publications of a scientist or scholar. The index is based on the set of the scientist's most cited papers and the number of citations that they have received in other publications
International Journal of Current Research and Review H-Index History

scijournal.org is a platform dedicated to making the search and use of impact factors of science journals easier.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
NLM Catalog
Collections of the national library of medicine.
- Create alert
Result Filters
- Summary (text)
- Full (text)
- NLM ID List
Send to: jQuery(document).ready( function () { jQuery("#send_to_menu input[type='radio']").click( function () { var selectedValue = jQuery(this).val().toLowerCase(); var selectedDiv = jQuery("#send_to_menu div." + selectedValue); if(selectedDiv.is(":hidden")){ jQuery("#send_to_menu div.submenu:visible").slideUp(); selectedDiv.slideDown(); } }); }); jQuery("#sendto").bind("ncbipopperclose", function(){ jQuery("#send_to_menu div.submenu:visible").css("display","none"); jQuery("#send_to_menu input[type='radio']:checked").attr("checked",false); });
- Collections
- Format Summary (text) Full (text) XML NLM ID List
- Search: 0975-833x
- Format Summary Summary (text) Full Full (text) XML NLM ID List
International journal of current research
Supplemental content.

Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
International Journal of Research and Review
International Journal of Research and Review (IJRR)
Issn: 2349-9788 (online) issn: 2454-2237 (print).
International Journal of Research and Review (E-ISSN: 2349-9788; P-ISSN: 2454-2237)is a double-blind, Indexed peer-reviewed, open access international journal dedicated to promotion of research in multidisciplinary areas. We define Open Access-journals as journals that use a funding model that does not charge readers or their institutions for access. From the BOAI definition of "Open Access" users shall have the right to "read, download, copy, distribute, print, search, or link" to the full texts of articles. The journal publishes original research article from broad areas like Accountancy, Agriculture, Anthropology, Anatomy, Architecture, Arts, Biochemistry, Bioinformatics, Biology, Bioscience, Biostatistics, Biotechnology, Botany, Chemistry, Commerce, Computer Science, Dairy Technology, Dentistry, Ecology, Economics, Education, Engineering, Environmental Science, Food & Nutrition, Forensic Science, Forestry, Geology, Geography, Health Sciences, History, Home Science, Journalism & Mass Communication, Language, Law, Life Science, Literature, Management, Marine Science, Mathematics, Medical Science, Microbiology, Pathology, Paramedical Science, Pharmacy, Philosophy, Physical Education, Physiotherapy, Physics, Political Science, Public Health, Psychology, Science, Social Science, Sociology, Sports Medicine, Statistics, Tourism, Veterinary Science & Animal Husbandry, Yoga, Zoology etc.
The International Journal of Research and Review (IJRR) provides rapid publication of articles in all areas of research.
Frequency: Monthly Language: English
Scope of Journal
International Journal of Research and Review (IJRR) is a double-blind Indexed peer-reviewed open access journal which publishes original articles, reviews and short communications that are not under consideration for publication elsewhere. The journal publishes papers based on original research that are judged by critical reviews, to make a substantial contribution in the field. It aims at rapid publication of high quality research results while maintaining rigorous review process. The Journal welcomes the submission of manuscripts that meet the general criteria of significance and academic excellence. Papers are published approximately one month after acceptance.
IJRR is dedicated to promote high quality research work in multidisciplinary field.
Index Copernicus Value (ICV) for 2022: 100.00; ICV 2021: 100.00; ICV 2020: 100.00; ICV 2019: 96.58; ICV 2018: 95.79; ICV 2017: 85.08; ICV 2016: 67.22; ICV 2015: 73.64; ICV 2014: 52.85
Salient features of our journal.
✵ Journal is indexed with Index Copernicus and other indexing agencies.
✵ Print version (hard copy) with P-ISSN number is available.
✵ Fast Publication Process.
✵ Free e-Certificate of Publication on author's request.
How to Submit Manuscript:
Thesis publication, research articles.
Nitin V Vichare, Rakesh Maggon
Smita Deshkar, Niranjan Patil, Pranali Balmiki
Ashish Choudhary, Riyaz Farooq, Aamir Rashid Purra, Fayaz Ahmed Ahangar
Joshi Medhavi H., Desai Devangi S, Singh Lalli M, Joshi Vaibhavi A
Jasvir Singh
Mariya Thomas Chacko, Tima Babu, Jenin Vincent Parambi, Irene T. Ivan, Sheik Haja Sherief
Click Here to Read more...
Anwar Sholeh, Alwi Thamrin Nasution, Radar Radius Tarigan
Arnaldi Fernando, Dairion Gatot, Yan Indra Fajar Sitepu
Iji Clement O, Age Terungwa James
Varsha S. Dhage, Pratibha Chougule
Uzma Khan, Arindam Ghosh
Dr. Uzma Khan, Dr. Arindam Ghosh, Dr. John Pramod
Our Journals
Visit Website
International Journal of Science and Healthcare Research
Galore International Journal of Health Sciences and Research
Galore International Journal of Applied Sciences and Humanities
National Academy of Agricultural Sciences (NAAS) : NAAS Score: *3.92 (2024)[Effective from January 1, 2024] For more details click here
Ijcrar is now doi (crossref) registered research journal. the dois are assigned to all published ijcrar articles., ijcrar impact factor: 5.2*, volume 12-issue 4 april 2024 published, aim & scope.
The International Journal of Current Research and Academic Review (ISSN 2347 - 3215) aims at the publication of original research, reviews and short communications on the latest developments in all fields of Science & Humanities and Engineering technology. The journal publishes original papers in English which contribute to the understanding of science and Humanities and also developments of the engineering technology and education. Papers may be theoretical, experimental or both. The contribution should be unpublished before and not under consideration for publication elsewhere. The Journal is a peer reviewed international journal publishing high-quality articles dedicated to all aspects of Science and Humanities and Engineering technology. The Journal considers only manuscripts that have not been published (or submitted simultaneously), at any language, elsewhere. The Journal is issued only in electronic form.
Subject areas for suitable for publications include:
Life sciences.
•Biological Sciences, •Biochemistry, •Genetics, •Environmental Science, •Immunology and Microbiology, •Cellular Microbiology, •Environmental Microbiology, •Medical Microbiology, •Industrial Microbiology, •Soil and Agricultural, •Microbial Genetics, •Microbial Ecology, •Vermitechnology, •Medicinal Plants, •Biotechnology, •Pharmacology Science, •Botany, •Cellbiology, •Conservation biology, •Developmental biology, •Ecology, •Evolutionary biology, •Evolutionary genetics, •Food science, •Genetics, •Genomics, •Immunology, •Marine biology, •Molecular biology, •Parasitology, •Pathology, •Pharmacogenomics, •Pharmacology, •Physiology, •Population dynamics, •Proteomics, •Structural biology, •Systems biology, •Zoology.
Physical Sciences
•Chemical Engineering, •Chemistry, •Computer Science, •Earth and Planetary Science, •Energy, •Mathematics, •Physics and Astronomy, Engineering, •Material Science, •Statistics, •Comparison of chemistry and physics, •Natural and physical sciences, •Earth science, •Biophysics, •Mathematics and Computer Science Research, •Pure and Applied Chemistry, •Geology and Mining Research, •Environmental Chemistry and Ecotoxicology, •Internet and Information Systems, •Oceanography and Marine Science,•Petroleum Technology and Alternative Fuels
Health Science
•Medicine and Dentistry, •Nursing and Health Professions, •Pharmacology and Toxicology, •Pharmaceutical Science •Veterinary Science •Veterinary Medicine, •Nutrition and Metabolism, •Cancer Research and Experimental Oncology, •Clinical Pathology and Forensic, Medicine, •Diabetes and Endocrinology, •Infectious Diseases and Immunity, •Medical Laboratory and Diagnosis, •Neuroscience and Behavioral Health, •Public Health and Epidemiology, •Medical Case Studies, •Medical Practice and Reviews
Social Science and Humanities
•Arts and Humanities, •Business Management, •Management Accounting, •Decision, •Economics, •Econometrics, •Finance, Anthropology, •Communication studies, •Human geography, •History, •Political science, •Public administration, •Psychology, •Sociology, •Geography and Regional Planning, •Hospitality Management and Tourism, •Sociology and Anthropology, •Public Administration and Policy Research, •Social Psychology, •Social Sciences by publishing original research work, short communications and review articles.
Agriculture Science
•Agricultural Economics •Agricultural Engineering •Agricultural Extension •Agronomy •Water Resource Management •Agricultural Biotechnology •Agricultural Microbiology •Agricultural Botany •Soil Science •Organic Farming •Sustainable Agricultural Practices •Plant Breeding •Plant and Agricultural Technology •Entomology •Integrated Pest Management •Biological Pest Control •Crop Improvement •Horticulture •Plant Pathology •Weed Management •Forestry and All the Fields of Allied Agricultural Sciences.
Animal Husbandry, Veterinary and Allied Sciences
•Animal Anatomy •Animal Breeding •Animal Nutrition •Animal Therapy •Veterinary Pathology •Fodder Crops •Veterinary Medicine •Livestock Production •Transgenics •Pet Animals •Vaccination •Aquaculture •Feed Science •Sericulture •Poultry Science
Plant Biology
•Angiosperm Taxonomy •Adaptation •Allelopathy in Plants •Biosystematics •Ethnobotany •Ethnopharmacology •Traditional Medicinal Plants •Plant Physiology •Plant Stress Biology •New Records of Flora •Plant Tissue Culture •Gene Transfer Studies •Plant Ecology •Economic Botany •Ecophysiology •Plant-microbe interactions •Mycology •Phycology •Lichens • Endemic and Endangered Plants •Embryology and Seed Science •Palaeobotany •Medicinal Botany, etc.
Ecology and Environmental Sciences
•Animal Behaviour •Biodiversity and Conservation •Biological Invasion •Biological Interaction •Climate Change •Carbon Sequestration •Ecosystem •Ecobiology •Environmental Biology •Ecotoxicology •Extreme Environment •Environmental Safety •Environmental Microbiology •Environmental Monitoring •Evolutionary Biology •Evolutionary Genetics •Pollution Studies •Population Biology •Vermitechnology •Waste Management
•Medicine and Dentistry •Nursing and Health Professions •Pharmaceutical Science •Nutrition and Metabolism •Cancer Research and Experimental Oncology •Clinical Pathology and Forensic Medicine •Diabetes and Endocrinology •Infectious Diseases and Immunity •Medical Laboratory and Diagnosis •Neuroscience and Behavioral Health •Public Health and Epidemiology •Medical Case Studies •Medical Practice and Reviews
•Chemical Engineering, •Chemistry, •Computer Science, •Earth and Planetary Science, •Energy, •Mathematics, •Physics and Astronomy, Engineering, •Material Science, •Statistics, •Comparison of chemistry and physics, •Natural and physical sciences, •Earth science, •Biophysics, •Mathematics and Computer Science Research, •Pure and Applied Chemistry, •Geology and Mining Research, •Environmental Chemistry and Ecotoxicology, •Internet and Information Systems, •Oceanography and Marine Science,•Petroleum Technology and Alternative Fuels.
•Arts and Humanities, •Business Management, •Management Accounting, •Decision, •Economics, •Econometrics, •Finance, Anthropology, •Communication studies, •Human geography, •History, •Political science, •Public administration, •Psychology, •Sociology, •Geography and Regional Planning, •Hospitality Management and Tourism, •Sociology and Anthropology, •Public Administration and Policy Research, •Social Psychology, •Social Sciences by publishing original research work, short communications and review articles.
Engineering and Technology
•Computer Science and Engineering, •Electrical Engineering, •Civil Engineering, •Infrastructure Engineering, •Electronics & Communication Engineering, •Industrial Engineering, •Mechanical Engineering, •Manufacturing Engineering, •Graphics and Multimedia, •Software Engineering, •Biological Engineering, •Chemical Engineering, •Agricultural engineering, •Remote sensing and information system. The Journal accepts various types of articles defined as follows: Types of articles include
- Original research papers,
- Mini-reviews,
- Short research communications,
- Letters to the editor.
IJCRAR is designed for the prompt publication of peer-reviewed articles in all areas of the subject. The journal articles will be accessed freely online. All manuscripts are pre-reviewed by the editor, and if appropriate, sent for blind peer review. Contributions must be original, not previously or simultaneously published elsewhere, and are critically reviewed before they are published. Manuscripts submitted to the IJCRAR are peer reviewing, initially reviewed according to the flow diagram reviewing and then reach to the technical reviewer. A minimum of three reviews related to subject is required for each Journal manuscript. IJCRAR publishes original articles, short communications to editor and reviews monthly. IJCRAR is currently accepting manuscripts; you can support this journal (IJCRAR) by sending your manuscripts to us at [email protected] A manuscript number will be emailed to the corresponding author within 48 hours.
- Editorial Member Login
Quick Navigation
- Call for Papers
- Processing Charges
- Join with us
- Editorial Board
2024-Issues
- Volume 12-1 January
- Volume 12-2 February
- Volume 12-3 March
- Volume 12-4 April
2023-Issues
- Volume 11-1 January
- Volume 11-2 February
- Volume 11-3 March
- Volume 11-4 April
- Volume 11-5 May
- Volume 11-6 June
- Volume 11-7 July
- Volume 11-8 August
- Volume 11-9 September
- Volume 11-10 October
- Volume 11-11 November
- Volume 11-12 December
2022-Issues
- Volume 10-1 January
- Volume 10-2 February
- Volume 10-3 March
- Volume 10-4 April
- Volume 10-5 May
- Volume 10-6 June
- Volume 10-7 July
- Volume 10-8 August
- Volume 10-9 September
- Volume 10-10 October
- Volume 10-11 November
- Volume 10-12 December
2021-Issues
- Volume 9-1 January
- Volume 9-2 February
- Volume 9-3 March
- Volume 9-4 April
- Volume 9-5 May
- Volume 9-6 June
- Volume 9-7 July
- Volume 9-8 August
- Volume 9-9 September
- Volume 9-10 October
- Volume 9-11 November
- Volume 9-12 December
2020-Issues
- Volume 8-1 January
- Volume 8-2 February
- Volume 8-3 March
- Volume 8-4 April
- Volume 8-5 May
- Volume 8-6 June
- Volume 8-7 July
- Volume 8-8 August
- Volume 8-9 September
- Volume 8-10 October
- Volume 8-11 November
- Volume 8-12 December
- View All Archives
- Advertise(IJCRAR)
- Terms of Use
- Copyright Form
© Copyright 2013-2016 all rights reserved by IJCRAR. Powered by 7Cube Technologies
- Editorial Board
- Current Issue
- Special Issue
- Submit Article
IJCMAS operates peer review process based on the guidelines of Committee on Publication Ethics
Call Us: +91 9566 45 2355

- Volume-13, Issue-4 Published
- Call for paper-Vol-13, Issue 5- May 2024
Invite Research Articles for Special Issue-3 Publication in the National Conference on “Contemporary Advances in Biotechnology and Bioinformatics frontline”
- Abstracting and Indexing
- Aims and Scope
- Article Processing Charges
- Editorial Review Policy
- Plagiarism Prevention Policy
- Author Guidelines
Aim & Scope
International Journal of Current Microbiology and Applied Sciences ISSN:2319-7692(Print), ISSN:2319-7706(Online) is a multidisciplinary peer-reviewed journal with reputable academics and experts as members of its Editorial Board. The Current Microbiology aims to publish all the latest and outstanding research articles. Review and letters in all areas of major importance to techniques of microbiology and applied research with publishes high quality of review and research articles on novel aspects of Microbiology including Environmental, Food, Agricultural, Medical, Pharmaceutical, Veterinary, Soil, Water and Biodeterioration.
The Applied Sciences aims to publish Research articles in Biological Sciences, Biodiversity, Biotechnology, Clinical Sciences, Agricultural Sciences, Chemical Sciences, and Environmental Sciences.
Subject areas for suitable for publications include:
All manuscripts are pre-reviewed by the editor, and if appropriate, sent for blind peer review. Contributions must be original, not previously or simultaneously published elsewhere, and are critically reviewed before they are published. Manuscripts submitted to the IJCMAS are peer reviewing, initially reviewed according to the flow diagram reviewing and then reach to the technical reviewer. A minimum of three reviews related to subject is required for each Journal manuscript. IJCMAS publishes original articles, short communications to editor and reviews monthly .
IJCMAS is currently accepting manuscripts; you can support this journal (IJCMAS) by sending your manuscripts to us at [email protected]
A manuscript number will be emailed to the corresponding author within 48 hours.
About the Journal
International Journal of Current Microbiology and Applied Sciences ISSN:2319-7692(Print), ISSN:2319-7706(Online) is a fully open access peer reviewed international journal dedicated to publish scientific articles from all areas of Microbiology. and Applied Sciences to share the current research to a broader audience all over the world.
Journal Metrics - Google Scholar based
- Submit a Manuscript
- Advanced search

American Journal of Neuroradiology
Advanced Search
The ASNR International Collaborations Committee: Cultivating a Global Learning Community
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Noushin Yahyavi-Firouz-Abadi
- ORCID record for Amy F. Juliano
- ORCID record for Bruno A. Policeni
- Figures & Data
- Supplemental
- Info & Metrics
The American Society of Neuroradiology has expanded its global presence, driven by the efforts of the International Collaborations Committee. This committee is actively involved in training radiologists and fostering collaborations worldwide in the fields of education, research, and community service. This article explores key initiatives of the committee, such as the Anne G. Osborn ASNR International Outreach Professor Program, the International Imaging Series, and Virtual Reading Rooms. Additionally, we provide insight into recent developments related to the pandemic and outline future opportunities.
- ABBREVIATIONS:
Our American Society of Neuroradiology (ASNR) has thrived, now comprising >5800 members, with >600 residing beyond the North American borders. Figure 1 illustrates our membership statistics across different regions of the world beyond North America as of December 2023, highlighting countries that have hosted prior outreach professors.
- Download figure
- Open in new tab
- Download powerpoint
ASNR membership across different regions of the world: Asia, Middle East, Africa, South America, and Australia. Red dots highlight countries that have hosted ASNR outreach professors in the past.
ASNR engages in collaborations with neuroradiology partners worldwide, extending its benefits to neuroradiologists in every corner of the globe. The American Journal of Neuroradiology ( AJNR ), the official journal of the ASNR and the leading global research publication in clinical neuroradiology, provides complimentary or affordable access to individuals in developing nations through the World Health Organization’s Health InterNetwork Access to Research Initiative program. 1 The society has also transformed into a global entity, propelling the advancement of neuroradiologic science and practice across the world by entrusting the ASNR International Collaborations Committee (ICC) with the execution of these international initiatives. This perspective summarizes the recent trends and future directions of the ICC.
While the coronavirus 2019 (COVID-19) pandemic temporarily paused our in-person programs, it sparked a vibrant era of virtual collaborations, including virtual case conferences, virtual didactic lectures, and participation in the ASNR neuroradiology webinar series.
Currently, the Committee’s main activities consist of the Anne G. Osborn ASNR International Outreach Professor Program, the International Imaging Series, and Virtual Reading Rooms.
Anne G. Osborn ASNR International Outreach Professor Program
The ASNR International Outreach Professor Program started in 2015 and was named after Professor Anne G. Osborn, MD, in 2017. This is a voluntary opportunity open to ASNR senior members who wish to engage in teaching activities in developing nations. This program distinguishes itself from traditional visiting professor initiatives by operating as an outreach program, with expenses shared among the ASNR outreach Professor, the ASNR organization, and the host institution in the recipient country. The program was temporarily halted in 2021 and 2022 due to the COVID-19 pandemic but resumed in 2023. The Online Supplemental Data illustrate the host countries and outreach professors since the inception. For the 2024 program, 7 countries are participating: Argentina, Brazil (including 2 programs in Brazil), Ghana, Tanzania, Ethiopia, South Africa, and Colombia. Additional countries are likely to join in 2025.
The Anne G. Osborn ASNR International Outreach Professor Program aims to promote knowledge exchange and teaching in developing countries. The selected outreach professors are dedicated educators, adaptable to different teaching environments and audience demographics, and conduct various teaching activities during a minimum 1-week professorship. These include lectures, case reviews, teaching files, or “Workstation” sessions. The program is flexible to the needs of the host country. As an example, Dr Carlos Torres worked with a large group of radiologists and radiology residents from 3 different residency programs in his 1-week visit to Yangon, Myanmar. He gave an average of 5 didactic lectures and 1 or 2 case-based presentations in a day. Dr Majid Khan gave 5 hours of talks each day followed by 2 hours of case reviews in his 1-week visit to Ghana. His lectures were in a hybrid format and attended by about 40 radiology residents and a few specialists in person, in addition to about 100 virtual attendees including other radiology residents, radiologists, head and neck surgeons, and neurosurgeons. Figure 2 illustrates Dr Bruno Soares among radiology residents and radiologists in his visit to Ghana in 2017. Reports from prior outreach professors with details of their visits can be found on the ASNR website. 2 The ASNR supports up to 10 placements per year, with applications opening in late summer. The application emphasizes teaching skills and experience, with a preference for first-time outreach professors. Many of the outreach professors have maintained contact with the host program and are actively engaged in ongoing collaborations or mentoring of trainees and radiologists. An example is Dr Gregory Obala, who became a neuroradiology fellow at Oregon Health & Science University after meeting Dr Joshua Nickerson, Section Chief of Neuroradiology, during his visit to Kenya in 2018.
Dr Bruno Soares with his audience during his visit to Accra, Ghana in 2017.
International Imaging Series
The International Imaging Series comprises educational events lasting 2–3 days held by a host country, addressing a range of neuroradiology subjects. 3 This series was inaugurated in 2016 and typically convenes 1–2 times annually. The Imaging Series transitioned to a virtual format during the COVID-19 pandemic. Most speakers are senior ASNR members selected for their topic expertise and teaching abilities. They are often accompanied by local experts. ASNR members can take advantage of reduced registration fees when attending these symposia.
Previous ASNR International Imaging Series were held in the following locations:
2016: Bangkok, Thailand
2017: Singapore and Bangkok, Thailand
2018: Hong Kong and Cape Town, South Africa
2019: Fortaleza, Brazil and Kyiv, Ukraine
2021: (Virtual) Australia and Argentina.
For example, the inaugural 2016 International Imaging Series was held in Bangkok and included 18 talks by faculty volunteers who were invited speakers in the preceding International Society for Magnetic Resonance in Medicine meeting in Singapore. Topics included state-of-the-art imaging of stroke, traumatic brain injury, brain tumors, white matter injuries, and dementia.
ASNR Virtual Reading Rooms
The ASNR Virtual Reading Room program was launched during the COVID-19 pandemic. The concept behind this effort is to simulate a reading room environment for the host country participants, incorporating a selected ASNR representative as a guest attending in that Virtual Reading Room, free to conduct readouts of cases of the host country’s selection, review challenging cases, delve into the thought process behind image interpretation, and deliver teaching points and/or didactic lectures as desired by the host country. The professor selects focus reading material and submits it to the host country 4–5 weeks before the virtual event. The host country requests that the audience submit relevant cases and questions to the selected professor 2–3 weeks ahead of the virtual session. The virtual session length is 1 hour to 1 hour 30 minutes.
In February 2021, the ASNR ICC and the Mongolian Society of Neuro, Head and Neck Imaging organized a successful Virtual Reading Room led by Dr Amy Juliano and moderated by Dr Bruno Policeni. More than 70 members of the Mongolian Society benefited from Dr Juliano’s expertise through this interactive virtual program.
In July 2021, Drs Caroline Robson and Mai-Lan Ho presented Pediatric Epilepsy Imaging and Pediatric Head and Neck Tumors to members of the Ghana neuroradiological community.
Future Directions
The impact of the ICC extends beyond outreach programs and lectures. Numerous program participants have gone on to forge ongoing collaborations, leading to long-term projects and publications. 4 Furthermore, several subspecialty societies, such as the American Societies of Head and Neck Radiology (ASHNR), Functional Neuroradiology (ASFNR), and Pediatric Neuroradiology (ASPNR) have either hosted or initiated international events. For instance, the ASHNR International Relations Committee in collaboration with its European counterpart has hosted quarterly webinars, including didactic and case-based lectures. It has also held a Zoom social hour with the Australian and New Zealand Society of Neuroradiology. Our international connections go beyond a common interest in neuroradiology and extend to global health and humanitarian endeavors such as helping war victims. The ASNR made a statement in support of radiology colleagues and health care workers in Ukraine and urged its members to donate to a charity to assist with medical care to Ukrainian war victims.
In addition, the ICC looks forward to building long-term virtual collaborations beyond the activities mentioned above. The ASNR evaluates international collaboration requests from both host organizations and individual volunteers through the ASNR ICC website. 5 Collaborative educational initiatives, including virtual case conferences, virtual didactic lectures, and virtual neuroradiology mentorship programs, can be explored for potential partnerships between ASNR and host organizations. The ICC also looks forward to collaborating with the growing number of global health radiology programs with the aim of improving access and knowledge of imaging using both in-person and virtual formats. Engaging radiology trainees in these opportunities can help shape their careers and create future global health leaders. 6
Disclosure forms provided by the authors are available with the full text and PDF of this article at www.ajnr.org .
- 1. ↵ WHO HINARI program for free/low cost journal access . https://www.asnr.org/ajnr-access-for-who-hinari-nations/ . Accessed September 25, 2023
- 2. ↵ Feedback from outreach participants . https://www.asnr.org/international-collaboration/anne-g-osborn-asnr-international-outreach-professor-program/feedback-from-outreach-participants/ . Accessed September 25, 2023
- 3. ↵ ASNR International Imaging Series . https://www.asnr.org/international-collaboration/anne-g-osborn-asnr-international-outreach-professor-program/asnr-international-imaging-series-upcoming-symposia/ Accessed Sep 25, 2023
- Coelho Neto CAF , et al
- 5. ↵ Virtual International Collaboration Requests . https://www.asnr.org/international-collaboration/asnr-international-virtual-activities/virtual-international-collaboration-requests/ . Accessed Sep 25, 2023
- England RW ,
- Lugossy AM ,
- Received November 3, 2023.
- Accepted after revision January 4, 2024.
- © 2024 by American Journal of Neuroradiology
Thank you for your interest in spreading the word on American Journal of Neuroradiology.
NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. We do not capture any email address.
Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager

- Tweet Widget
- Facebook Like
- Google Plus One
Jump to section
Related articles.
- Google Scholar
Cited By...
- No citing articles found.
This article has not yet been cited by articles in journals that are participating in Crossref Cited-by Linking.
More in this TOC Section
- Shift Volume Directly Impacts Neuroradiology Error Rate at a Large Academic Medical Center: The Case for Volume Limits
- Patient Engagement in Neuroradiology: A Narrative Review and Case Studies
Similar Articles
- Open access
- Published: 11 May 2024
Inotuzumab ozogamicin for the treatment of adult acute lymphoblastic leukemia: past progress, current research and future directions
- Nicholas J. Short 1 ,
- Elias Jabbour 1 ,
- Nitin Jain 1 &
- Hagop Kantarjian 1
Journal of Hematology & Oncology volume 17 , Article number: 32 ( 2024 ) Cite this article
554 Accesses
24 Altmetric
Metrics details
Inotuzumab ozogamicin (INO) is an anti-CD22 antibody-drug conjugate that was first evaluated in B-cell lymphomas but was subsequently shown to be highly effective in acute lymphoblastic leukemia (ALL). INO improved response rates and survival in a randomized study in adults with relapsed/refractory B-cell ALL, leading to its regulatory approval in the United States in 2017. While the formal approval for INO is as monotherapy in relapsed/refractory ALL, subsequent studies with INO administered in combination with chemotherapy and/or blinatumomab both in the frontline and salvage settings have yielded promising results. In this review, we discuss the clinical development of INO in ALL, highlighting lessons learned from the initial clinical trials of INO, as well as the many ongoing studies that are seeking to expand the role of INO in ALL.
Introduction
The anti-CD22 antibody drug conjugate inotuzumab ozogamicin (INO) was developed in the early 2000s based on initial preclinical data showing promising activity in B-cell lymphoid diseases. These laboratory observations were then followed by several early phase clinical trials that showed significant efficacy of INO in acute lymphoblastic leukemia (ALL), ultimately prompting to its evaluation in a large, randomized trial in adults with relapsed/refractory CD22-positive B-cell ALL. In the pivotal INO-VATE study, INO significantly improved response rates and overall survival (OS) compared with conventional chemotherapy, leading to its approval by the Food and Drug Administration (FDA) in August 2017 [ 1 ]. Figure 1 shows a timeline of its clinical development. In this review, we discuss the lessons learned during its development and how these are being applied to current research efforts. We will also discuss the new research that is attempting to expand the potential applications of INO in B-cell ALL, including using it in combination with chemotherapy and/or other immunotherapies, in the frontline treatment of ALL, and in treatment of measurable residual disease (MRD).
Timeline of the clinical development of inotuzumab ozogamicin in acute lymphoblastic leukemia. For context, approval dates for other novel immunotherapies in adult B-cell acute lymphoblastic leukemia are also shown
Drug mechanism and preclinical development
INO is an IgG anti-CD22 monoclonal antibody drug conjugate that was developed by Celltech (a British biotechnology company) and Wyeth (a pharmaceutical company, later purchased by Pfizer in 2009). It is covalently linked to calicheamicin dimethyl hydrazide with acid-labile 4-(4’-acetylphenoxy) butanoic acid liner [ 2 ]. INO has sub-nanomolar binding affinity to CD22 and is rapidly internalized upon binding, after which it delivers the calicheamicin toxin intracellularly where it binds to the minor DNA groove and leads to double-strand cleavage and subsequent apoptosis. INO was first shown in preclinical studies to be active against B-cell lymphoma cell lines [ 2 ]. Subsequent studies were performed in mouse models of aggressive B-cell lymphomas, showing both monotherapy activity as well as synergy with rituximab or chemotherapy, including CVD and CHOP [ 3 , 4 , 5 ]. Given the clear preclinical activity in B-cell lymphoma models, INO was also tested in CD22-positive ALL models, where it induced complete tumor regression and cures in mice, warranting its clinical development in ALL [ 5 , 6 ].
Phase I and II studies
The first study of INO in humans was a phase I study in adults with relapsed or refractory CD22-positive B-cell non-Hodgkin’s lymphoma [ 7 ]. Seventy-nine patients were treated, and the maximum tolerated dose (MTD) was 1.8 mg/m 2 administered as a single dose every 3–4 weeks. Thrombocytopenia was the dose-limiting toxicity, with 90% of patients experiencing thrombocytopenia of any grade, which was grade ≥ 3 in 63%. Encouraging activity was observed, and the overall response rate was 39% among all patients, with response rates in follicular lymphoma and diffuse large B-cell lymphoma of 69% and 15%, respectively, at the MTD. Investigator-initiated pilot studies at MD Anderson Cancer Center were ongoing simultaneously, though the chosen regulatory approval path by the company was initially in lymphomas. Fortunately, by the time the phase III pivotal trial in lymphoma had failed to meet the primary study endpoint in 2014 [ 8 , 9 ], the pilot studies in ALL had shown encouraging results, thus shifting the regulatory focus to ALL.
The investigator-initiated phase II study at MD Anderson Cancer Center evaluated INO in children and adults with CD22-positive relapsed or refractory ALL (Table 1 ). In the initial publication, 49 patients received INO at a dose of 1.3 mg/m 2 to 1.8 mg/m 2 administered once every 3–4 weeks [ 10 ]. The population was heavily pretreated, with 73% of patients being treated as second or later salvage. The complete remission (CR)/CR with incomplete hematologic recovery (CRi) rate was 57%, and the median OS was 5.1 months. The most common adverse events were fever (59%), transaminase elevation (57%), and hyperbilirubinemia (29%). An important observation was that allogeneic hematopoietic stem cell transplantation (HSCT) increased the risk of toxicity. Among the 26 patients who underwent HSCT following INO, the 1-year OS rate was only 20%, driven by higher rates of non-relapse mortality (NRM) and 5 deaths due to sinusoidal obstruction syndrome (SOS) / veno-occlusive disease (VOD). To improve upon the safety/efficacy profile of INO, the study was then amended to fractionate the dose of INO and administer a dose of 0.8 mg/m 2 on day 1 and 0.5 mg/m 2 on day 8 and 15, given every 3–4 weeks, with the rationale that lower dose and more frequent schedules of INO may improve anti-ALL efficacy (which is determined primarily by the area under the curve) while reducing toxicities (which is determined primarily by the peak level of INO). In a subsequent analysis after treating 90 total patients (49 at the original schedule and 41 at the new schedule), the response rates and survival outcomes were similar [ 11 ]. However, the new dosing schedule appeared safer and resulted in lower rates of fever, hypotension and hyperbilirubinemia. The rate of SOS/VOD was also lower with the new schedule (7% versus 17% with the previous schedule), which may have been driven by the fractionated dosing as well as better understanding of the SOS/VOD risk with INO, leading to a reduced use of alkylating agents in HSCT preparative regimens.
The safety and efficacy of INO was later confirmed with a phase I/II multicenter study that evaluated INO in a similar population of adults with relapsed or refractory ALL (Table 1 ) [ 12 ]. This study also evaluated divided, weekly doses of INO (ranging from 1.2 mg/m 2 to 1.8 mg/m 2 per cycle) given for up to 6 cycles. The recommended phase II dose was 1.8 mg/m 2 per cycle, with the dose reduced to 1.6 mg/m 2 once CR/CRi was achieved. Seventy-two patients were treated, including 78% in salvage 2 or beyond and approximately one-third who had undergone previous allogeneic HSCT. The CR/CRi rate was 68% (including CR in 32%), and the median OS was 7.4 months. One-third of patients received a subsequent allogeneic HSCT, and there were 4 cases of SOS/VOD (6% total).
Phase III study (INO-VATE)
Efficacy and safety outcomes.
Based on the promising safety and efficacy data from the 2 prior clinical studies of INO in B-cell ALL, the INO-VATE study was designed as pivotal trial to compare INO to conventional chemotherapy in adults with relapsed or refractory CD22-positive B-cell ALL (Table 1 ) [ 1 ]. Three hundred and twenty-six patients were randomized 1:1 to INO or combination chemotherapy (either fludarabine, cytarabine and granulocyte-stimulating factor [FLAG], cytarabine plus mitoxantrone, or high-dose cytarabine). Given the superior safety observed with weekly dosing, INO was given at a dose of 0.8 mg/m 2 on day 1 and 0.5 mg/m 2 on days 8 and 15, for up to 6 cycles. The median age was 47 years in both arms, and 32% of patients in the INO arm and 36% in the control arm were in second salvage. INO resulted in a significantly higher rate of CR/CRi than did conventional chemotherapy (80.7% [95% confidence interval (CI), 72.1–87.7%] vs. 29.4% [95% CI, 21.0–38.8%], respectively; P < 0.001). Superior responses with INO were observed across all subgroups, with the exception of patients with t(4;11), although the number of patients was small. Among responders, INO was also associated with significantly higher rates of MRD negativity by multiparameter flow cytometry (78.4% vs. 28.1%, respectively; P < 0.001) and higher rates of subsequent HSCT (41% vs. 11%, respectively; P < 0.001). Driven by the higher rates of response and HSCT realization, INO resulted in significantly better median OS (7.7 months [95% CI, 6.0 to 9.2] vs. 6.7 months [95% CI, 4.9 to 8.3]; P = 0.04). While the numerical improvement in median OS was marginal, the greatest benefit to INO was observed in the long-term survival outcomes, where INO more than doubled the 2-year OS rate compared with chemotherapy (23% vs. 10%, respectively). Febrile neutropenia and thrombocytopenia were more common in the control group, while liver-related adverse events were more common with INO. The SOS/VOD rate with INO and chemotherapy were 11% and 1%, respectively. Based on the substantial improvement in both response rates and OS, the FDA approved INO in August 2017 for the treatment of adults with relapsed/refractory B-cell ALL.
Subgroups analyses, including transplant outcomes
Following the initial publication of the INO-VATE study, several subgroup analyses of the trial population have been published. These analyses have highlighted important considerations for the use of INO, including its good activity irrespective of bone marrow blast percentage, extramedullary involvement, or CD22 expression, and its activity in Philadelphia chromosome (Ph)-positive ALL [ 13 , 14 , 15 ]. INO is associated with a higher rate of HSCT realization, which is the most significant predictor of OS following INO therapy by multivariate analysis [ 16 ]. Among patients in the INO-VATE study who received INO and achieved CR/CRi, those who underwent subsequent allogeneic had the best outcomes (median OS 12.6 months and 2-year OS rate 39% versus median OS 7.1 months and 2-year OS rate 13% in non-transplanted). However, subsequent transplant is associated with higher risk of SOS/VOD after INO (23% versus 9% in non-transplanted patients), which contributes to INO-related non-relapse mortality. Proper patient selection for INO and mitigation strategies are therefore imperative to prevent this important potential copmlication. Similar post-transplant findings were observed in a pooled analysis of 2 INO studies, where patients who underwent allogeneic HSCT following INO had a post-HSCT median OS of 9.2 months and 2-year post-HSCT OS rate of 41% [ 17 ]. The overall rate of SOS/VOD among transplanted patients across these 2 studies was 18%.
Pooled analyses from multiple INO studies have been used to better understand the risk for SOS/VOD, which is a severe and potential toxicity with INO treatment. Across these studies, the predictors for the development of SOS/VOD include: older age, the use of double alkylator preparative regimens for HSCT, elevated pretreatment transaminases and/or bilirubin, more cycles and higher cumulative doses of INO, and multiple prior ALL therapies, especially prior HSCT [ 1 , 18 , 19 , 20 ]. Subsequent consensus guidelines have been developed to mitigate these risks. Important considerations to prevent the risk of SOS/VOD in patients receiving INO include: proper selection of patients (e.g. avoiding in patients were severe underlying hepatic dysfunction, avoiding dual alkylator conditioning regimens in transplanted patients, limiting INO to a cumulative dose of 2.7 to 3.6 mg/m 2 in patients proceeding to allogeneic HSCT, use of high dose steroids at the first sign of liver dysfunction, and distancing the last dose of INO from time of HSCT [ 21 ]. Ursodiol prophylaxis 300 mg three times daily should be considered for all patients receiving INO, although there is no clear role for defibrotide as prophylaxis, even for high-risk patients [ 22 ].
Combination therapies with INO for relapsed/refractory ALL
While single-agent INO therapy represents a therapeutic advance for patients with relapsed/refractory ALL, it is not curative for most patients when given as monotherapy, with < 20% of patients achieving long-term survival [ 16 ]. Research efforts have therefore been focused on combination therapies of INO with chemotherapy and/or other novel agents such as blinatumomab, with the goal of deepening response and further improving survival outcomes (Table 2 ). At MD Anderson Cancer Center, a regimen of mini-hyper-CVD (dose-reduced hyperfractionated cyclophosphamide, vincristine and dexamethasone alternating with dose-reduced methotrexate and cytarabine) in combination with INO was studied in relapsed/refractory Ph-negative B-cell ALL. Figure 2 shows the evolution of this regimen over the past decade. INO was originally given on day 3 of cycles 1–4 at a dose of 1.8 mg/m 2 in cycle 1 and 1.3 mg/m 2 in cycles 2–4 (cumulative dose of 5.7 mg/m 2 ) and then was later reduced to 1.3 mg/m 2 in cycle 1 and 1 mg/m 2 in cycles 2–4 (cumulative dose of 4.3 mg/m 2 ) in an effort to reduce the risk of SOS/VOD (Fig. 2 A) [ 23 ]. Among 59 patients treated, the overall response rate was 78%, with 82% of responders achieving MRD negativity by flow cytometry. Response rates were particularly encouraging in first salvage, where the overall response rate was 91%. The SOS/VOD rate was 15% using this single-dose regimen, which was similar to the 17% rate observed in the initial phase II study using a similar dosing strategy [ 10 ]. The median OS was 11 months, and the 1-year OS rate was 46%. The survival outcomes were compared to historical data with INO monotherapy using an inverse probability of treatment weighing analysis, which suggested that the combination therapy was superior to expectations with INO monotherapy.
Evolution of the hyper-CVD and inotuzumab ozogamicin ± blinatumomab regimen at MD Anderson Cancer Center. A .) Hyper-CVD plus inotuzumab ozogamicin, B .) Hyper-CVD plus inotuzumab ozogamicin with sequential blinatumomab, C .) “Dose dense” hyper-CVD, inotuzumab ozogamicin and blinatumomab
This study was then amended to further reduce and fractionate the dose of INO, add blinatumomab, and mandate ursodiol prophylaxis (Fig. 2 B) [ 24 ]. The purpose of these changes was two-fold: to deepen response with the addition of blinatumomab and to mitigate the risk of SOS/VOD by reducing the dose of INO and by increasing the interval between the last dose of INO and allogeneic HSCT. In this new design, patients received 4 cycles of mini-hyper-CVD plus INO, followed by 4 cycles of blinatumomab, and then a maintenance phase of blocks of POMP (6-mercaptopurine, vincristine, methotrexate, and prednisone) alternating with blinatumomab. INO was reduced to 0.6 mg/m 2 on day 2 and 0.3 mg/m 2 on day 8 in cycle 1 and 0.3 mg/m 2 on days 2 and 8 in cycles 2–4 (cumulative dose of 2.7 mg/m 2 ). In the most recent published analysis of the mini-hyper-CVD, INO ± blinatumomab regimen (with blinatumomab given to patients #68+), 110 patients have been treated [ 25 ]. The overall response rate was 83%, and 82% of responders achieved MRD negativity by flow cytometry. The median OS was 17 months, and the 3-year OS rate was 40%. Outcomes were best for those treated in first salvage, where the median OS was 31 months, and the 3-year OS rate was 49%. In a landmark analysis, there was no benefit for receipt of subsequent allogeneic HSCT (3-year OS 54% for both groups). The SOS/VOD rate was also observed to be lower after the amendment to reduce and fractionate INO and add blinatumomab (2% vs. 13% with the previous design; P = 0.05). These data highlight that SOS/VOD can be substantially mitigated with use of lower doses of INO without compromising efficacy.
The mini-hyper-CVD, INO and blinatumomab regimen has now been amended to administer to deliver all agents beginning in cycle 1 (Fig. 2 C). In the latest study design, 6 cycles of “dose-dense” mini-hyper-CVD, INO and blinatumomab are given, followed by POMP/blinatumomab maintenance in non-transplanted patients. In each cycle, blinatumomab is started on day 4 (i.e. once the mini-hyper-CVD chemotherapy has been delivered) and continues through day 21 of each cycle, followed by a 7-day break before beginning the next cycle. To date, 15 patients with relapsed/refractory ALL have been treated with this regimen. All patients responded, with 92% achieving flow MRD negativity (77% after 1 cycle) [ 26 ]. High rates of early response have also been observed in a retrospective analysis of this regimen in both newly diagnosed and relapsed/refractory patients [ 27 ]. Among patients with newly diagnosed or MRD-positive ALL, 10/11 (91%) achieved MRD negativity at a level of 10 − 6 by next-generation sequencing, an endpoint shown to be associated with superior outcomes in ALL [ 28 , 29 ]. The deep and rapid MRD negative responses with the dose-dose mini-hyper-CVD, INO and blinatumomab regimen are encouraging, and this regimen is also now being evaluated in older adults with newly diagnosed B-cell ALL.

Combination therapies with INO for newly diagnosed ALL
Older adults.
Several studies are also evaluating INO in patients with newly diagnosed ALL. Most of these efforts have focused on its use in older adults, a group with poor tolerance to conventional chemotherapy and with historical long-term OS rates of only 20% [ 31 , 32 ]. Ongoing trials exploring INO in the frontline setting are shown in Table 3 , and a summary of available trial data of INO-based regimens in older adults with ALL is shown in Table 4 . At MD Anderson Cancer Center, the same mini-hyper-CVD plus INO regimen previously described was also studied in patients ≥ 60 years of age with newly diagnosed Ph-negative B-cell ALL [ 32 ]. Initially, 52 patients with a median age of 68 years were treated. The overall response rate was 98%, with 96% of patients achieving MRD negativity by flow cytometry. These high rates of response translated to encouraging long-term survival with 3-year progression-free survival (PFS) and OS rates of 49% and 56%, respectively. As with the relapsed/refractory study, this regimen was later amended to use lower, fractionated doses of INO (cumulative dose 2.7 mg/m 2 ), add blinatumomab and mandate ursodiol prophylaxis. A total of 80 older patients have been treated with the mini-hyper-CVD, INO ± blinatumomab regimen (patients #50 + treated with the updated regimen) [ 33 ]. Twelve patients (15%) have relapsed, and the 5-year PFS and OS rates are 44% and 46%, respectively. These outcomes compare favorably to the historical 5-year OS rate of approximately 20% when chemotherapy alone is used. The superiority of the mini-hyper-CVD, INO and blinatumomab regimen as compared with dose-reduced hyper-CVAD in a similar older population was confirmed in a propensity score analysis [ 34 ].
Despite the improvement over historical expectations, toxicity is still a significant concern with this regimen. Overall, 35 patients (44%) died in remission (including 9 from myelodysplastic syndrome or acute myeloid leukemia, 8 from infection and 5 from SOS/VOD). The risk of death in remission was higher in patients ≥ 70 years of age (accounting for 85% of deaths in remission), resulting in age-dependent survival outcomes (median OS 75 months, 47 months, and 35 months for patients 60–64, 65–69 and ≥ 70 years of age, respectively). Due to the specific risks related to the chemotherapy backbone (e.g. secondary myeloid malignancy and infection), patients ≥ 70 years of age will now receive INO and blinatumomab only, without the mini-hyper-CVD backbone. A similar approach has been evaluated in the Alliance A041703 study [ 35 ]. In this trial, patients ≥ 60 years of age with newly diagnosed Ph-negative B-cell ALL received induction with fractionated INO at 1.8 mg/m 2 in cycle 1 and 1.5 mg/m 2 in cycle 2, followed by consolidation with blinatumomab for 4–5 cycles. Among 33 patients treated, the overall response rate was 96% (85% after INO induction), and the 1-year OS rate was 84%. Longer term follow-up will be needed to confirm the durability of these responses.
Several other INO-based frontline regimens are being evaluated in older adults with newly diagnosed ALL. In the INITIAL-1 study, patients > 55 years of age with newly diagnosed Ph-negative B-cell ALL received induction with 3 cycles of dexamethasone plus INO (1.8 mg/m 2 in cycle 1 and 1.5 mg/m 2 in cycles 2–3), followed by 6 cycles of age-adjusted chemotherapy as consolidation/maintenance. 37 Forty-three patients were treated with a median age of 64 years (range, 56–80 years). All patients achieved CR/CRi, with 71% achieving MRD negativity at a sensitivity of 10 − 4 after the 3 cycles of INO induction. The 3-year event-free survival (EFS) and OS rates were 55% and 73%, respectively, and there was only 1 case of non-fatal SOS/VOD. The EWALL-INO study also enrolled a similar population of patients and treated them with 2 cycles of induction consisting of INO, vincristine and dexamethasone (induction 1) and INO, cyclophosphamide and dexamethasone (induction 2), followed by 6 cycles of age-adjusted consolidation and then POMP maintenance [ 37 ]. Overall, 131 patients were treated, and the CR/CRi rate after 2 cycles of induction was 90%. The estimated 2-year OS rate was 54%. Taken together, these studies show that frontline INO-based therapy is safe and effective in older adults with B-cell ALL. Building on the promising experience with the mini-hyper-CVD and INO regimen from MD Anderson, the Alliance A042001 is a randomized phase II study evaluating mini-hyper-CVD plus INO versus dose-adjusted hyper-CVAD in older adults (≥ 50 years of age) with newly diagnosed B-cell ALL [ 38 ]. No data are yet available, and this study is ongoing.
Younger adults
Combination approaches using INO are also being explored in younger adults with newly diagnosed ALL. At MD Anderson, we developed a protocol of hyper-CVAD plus blinatumomab, which has now been amended to add INO. The hyper-CVAD plus blinatumomab regimen consists of 4 cycles of hyper-CVAD, followed by 4 cycles of blinatumomab, and then POMP and blinatumomab maintenance. In the first 38 patients treated, all patients responded, with 97% becoming MRD negative by flow cytometry. This translated to encouraging 3-year relapse-free survival (RFS) and OS rates of 73% and 81%, respectively [ 39 ]. An additional 37 patients have now been treated with the addition of INO (0.3 mg/m 2 on day 1 and 8 of cycles 2, 4, 6 and 8; cumulative dose of 2.4 mg/m 2 ) [ 41 ]. With a median follow-up of 22 months, only 3 relapses have been observed. The estimated 2-year RFS and OS rates of 88% and 100%, respectively. The initial data with the addition of INO are encouraging and suggest a potential benefit with the routine use of INO in younger patients with newly diagnosed Ph-negative B-cell ALL.
Of note, the Alliance A041501 was a randomized study that also evaluated the addition of INO to standard chemotherapy (CALGB 10,403 backbone) in newly diagnosed B-cell ALL. This study was suspended due to toxicity concerns with the combination regimen, possibly related to the use of multiple hepatoxic agents in this regimen (e.g. INO and asparaginase). The lack of success of this study highlights the need for rationale combinations with INO and to avoid overlapping toxicities.
Other investigational applications of INO in ALL
Ino for mrd-positive disease.
In the INO-VATE study, INO was associated with a flow MRD negativity rate of 63% among responders [ 41 ] and provided support for the evaluation of INO for MRD-positive B-cell ALL. In a phase II study, 26 patients with MRD-positive ALL were enrolled and treated with INO at a dose of 0.6 mg/m 2 and 0.3 mg/m 2 on days 1 and 8, respectively, of cycle 1 and 0.3 mg/m 2 on day 1 and 8 of cycles 2-6 [ 42 ]. Sixteen patients (62%) had Ph-positive ALL and also received a BCR::ABL1 TKI (predominantly ponatinib). The MRD negativity response at a sensitivity of 10 − 4 was 69%, which translated to a 2-year OS rate of 60%. In another study from GIMEMA, INO was evaluated in 20 patients with MRD-positive B-cell ALL. Eleven of 20 patients (55%) achieved MRD response < 10 − 4 [ 44 ]. These encouraging data support the further of evaluation of INO as an MRD-directed therapy in ALL and also provide support for its continued evaluation in the frontline setting to induce deep, MRD-negative remissions.
INO for Ph + ALL
INO is active in relapsed/refractory Ph-positive ALL and achieves a CR/CRi rate of 73% and median OS of 8.7 months, which are similar to the findings from the broader population of the INO-VATE study [ 14 ]. In a phase I/II study, INO was combined with bosutinib in patients with relapsed/refractory Ph-positive ALL who did not harbor a T315I mutation [ 44 ]. Among 18 patients (16 with Ph-positive ALL and 2 with CML in lymphoid blast phase), the CR/CRi rate was 83%, with 56% achieving a complete molecular response. The median OS was 13.5 months, which appears superior to expectations with INO as monotherapy.
INO as post-transplant maintenance
INO has been evaluated as post-transplant maintenance in a phase I study of patients with CD22-positive ALL and high-risk for relapse [ 45 ]. INO doses of 0.3 mg/m 2 to 0.6 mg/m 2 were administered once per cycle for up to 12 cycles. The MTD was 0.6 mg/m 2 . Among 18 treated patients, no cases of SOS/VOD were observed. With a median follow-up of 18.1 months, only 2 relapses were observed, and the 1-year PFS and OS rates were 89% and 94%, respectively. This study suggests that low-dose INO can be safely administered in the peri-transplant setting and may also be helpful in preventing relapse in high-risk patients.
Sequencing of INO with CAR T-cell therapy
In clinical practice, INO is commonly given prior to CAR T-cell therapy, either as a salvage regimen and as bridging therapy. However, the data are mixed regarding whether prior INO exposure impacts the effectiveness of CAR T-cells [ 46 , 47 , 48 ]. Some studies in children have suggested that prior INO—including INO as bridging therapy—did not impact response rates or long-term outcomes following tisagenlecleucel, as compared with historical expectations [ 46 , 47 ]. However, in the ZUMA-3 study of brexucabtagene autoleucel in adult patients, those with prior INO exposure had numerically lower CR/CRi rates (59% with prior INO exposure versus 77% without prior INO exposure) and inferior OS (median OS 8.8 months and 47.0 months, respectively) [ 48 ]. Future studies evaluating the optimal sequencing of INO with other available therapies—including blinatumomab and CD19 CAR T-cells—and the use of INO as bridging therapy prior to CAR T-cell therapy are needed.
Conclusions
Along with the blinatumomab and CAR T-cells, the clinical development of INO has been a major contributor to improving outcomes of adult ALL over the past decade [ 49 ]. While INO has been shown to be more effective than conventional cytotoxic chemotherapy in relapsed/refractory B-cell ALL, its greatest potential is as combination therapy in both the frontline and salvage settings. When used along with low-dose chemotherapy and blinatumomab in relapsed/refractory ALL, a 3-year OS rate > 50% has been observed, even in non-transplanted patients. Similarly, very encouraging outcomes have been observed with INO in newly diagnosed B-cell ALL, whether combined with chemotherapy, blinatumomab or both. Over the course of these studies, the INO dose has been modified, with some studies suggesting that lower, fractionated doses of INO can be highly effective and may also reduce the risk of SOS/VOD, which is one of the feared potential toxicities of INO. Studies continue to expand the potential applications of INO, including its use for MRD-positive disease, combination with BCR::ABL1 tyrosine kinase inhibitors, and its use in low doses as post-transplant maintenance. Many of these ongoing research efforts seek to explore alternative dosing strategies of INO. New translational research is also seeking to understand the mechanisms of resistance to INO, which may help to inform future rational drug combinations [ 50 , 51 , 52 , 53 ]. The FDA approval of INO in 2017 marked a major milestone that paved the way for these important studies, but it is imperative to note that this was just one step in the clinical development of INO. The research that has followed in the years since the INO-VATE study highlight a truism in oncology: that regulatory approval of a drug is often only the beginning of its true clinical development and innovation.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
Acute lymphoblastic leukemia
Confidence interval
Chronic myeloid leukemia
Complete remission
Complete remission with incomplete hematologic recovery
Event-free survival
Food and Drug Administration
Hematopoietic stem cell transplantation
Inotuzumab ozogamicin
Dose-attenuated hyperfractionated cyclophosphamide, vincristine and dexamethasone alternating with methotrexate and cytarabine
Measurable residual disease
Maximum tolerated dose
Non-relapse mortality
Overall survival
Progression-free survival
Philadelphia chromosome
6-mercaptopurine, vincristine, methotrexate, and prednisone
Relapse-free survival
Sinusoidal obstruction syndrome
Tyrosine kinase inhibitor
Veno-occlusive disease
Kantarjian HM, DeAngelo DJ, Stelljes M, et al. Inotuzumab Ozogamicin versus Standard Therapy for Acute Lymphoblastic Leukemia. N Engl J Med. 2016;375:740–53.
Article CAS PubMed PubMed Central Google Scholar
DiJoseph JF, Armellino DC, Boghaert ER, et al. Antibody-targeted chemotherapy with CMC-544: a CD22-targeted immunoconjugate of calicheamicin for the treatment of B-lymphoid malignancies. Blood. 2004;103:1807–14.
Article CAS PubMed Google Scholar
DiJoseph JF, Goad ME, Dougher MM, et al. Potent and specific antitumor efficacy of CMC-544, a CD22-targeted immunoconjugate of calicheamicin, against systemically disseminated B-cell lymphoma. Clin Cancer Res. 2004;10:8620–9.
DiJoseph JF, Dougher MM, Kalyandrug LB, et al. Antitumor efficacy of a combination of CMC-544 (inotuzumab ozogamicin), a CD22-targeted cytotoxic immunoconjugate of calicheamicin, and rituximab against Non-hodgkin’s B-cell lymphoma. Clin Cancer Res. 2006;12:242–9.
de Vries JF, Zwaan CM, De Bie M, et al. The novel calicheamicin-conjugated CD22 antibody inotuzumab ozogamicin (CMC-544) effectively kills primary pediatric acute lymphoblastic leukemia cells. Leukemia. 2012;26:255–64.
Article PubMed Google Scholar
Dijoseph JF, Dougher MM, Armellino DC, Evans DY, Damle NK. Therapeutic potential of CD22-specific antibody-targeted chemotherapy using inotuzumab ozogamicin (CMC-544) for the treatment of acute lymphoblastic leukemia. Leukemia. 2007;21:2240–5.
Advani A, Coiffier B, Czuczman MS, et al. Safety, pharmacokinetics, and preliminary clinical activity of inotuzumab ozogamicin, a novel immunoconjugate for the treatment of B-cell non-hodgkin’s lymphoma: results of a phase I study. J Clin Oncol. 2010;28:2085–93.
Dang NH, Ogura M, Castaigne S, et al. Randomized, phase 3 trial of inotuzumab ozogamicin plus rituximab versus chemotherapy plus rituximab for relapsed/refractory aggressive B-cell non-hodgkin lymphoma. Br J Haematol. 2018;182:583–6.
Dang NH, Ogura M, Castaigne S, et al. Randomized, phase 3 trial of inotuzumab ozogamicin plus rituximab (R-InO) versus chemotherapy for relapsed/refractory aggressive B-cell non-hodgkin lymphoma (B-NHL). J Clin Oncol. 2014;32:8529.
Article Google Scholar
Kantarjian H, Thomas D, Jorgensen J, et al. Inotuzumab ozogamicin, an anti-CD22–calecheamicin conjugate, for refractory and relapsed acute lymphocytic leukaemia: a phase 2 study. Lancet Oncol. 2012;13:403–11.
Kantarjian H, Thomas D, Jorgensen J, et al. Results of inotuzumab ozogamicin, a CD22 monoclonal antibody, in refractory and relapsed acute lymphocytic leukemia. Cancer. 2013;119:2728–36.
DeAngelo DJ, Stock W, Stein AS, et al. Inotuzumab ozogamicin in adults with relapsed or refractory CD22-positive acute lymphoblastic leukemia: a phase 1/2 study. Blood Adv. 2017;1:1167–80.
DeAngelo DJ, Advani AS, Marks DI, et al. Inotuzumab ozogamicin for relapsed/refractory acute lymphoblastic leukemia: outcomes by disease burden. Blood Cancer J. 2020;10:81.
Article PubMed PubMed Central Google Scholar
Stock W, Martinelli G, Stelljes M, et al. Efficacy of inotuzumab ozogamicin in patients with Philadelphia chromosome-positive relapsed/refractory acute lymphoblastic leukemia. Cancer. 2021;127:905–13.
Kantarjian HM, Stock W, Cassaday RD, et al. Inotuzumab Ozogamicin for Relapsed/Refractory Acute Lymphoblastic Leukemia in the INO-VATE trial: CD22 Pharmacodynamics, Efficacy, and Safety by Baseline CD22. Clin Cancer Res. 2021;27:2742–54.
Kantarjian HM, DeAngelo DJ, Stelljes M, et al. Inotuzumab ozogamicin versus standard of care in relapsed or refractory acute lymphoblastic leukemia: final report and long-term survival follow-up from the randomized, phase 3 INO-VATE study. Cancer. 2019;125:2474–87.
Marks DI, Kebriaei P, Stelljes M, et al. Outcomes of allogeneic stem cell transplantation after Inotuzumab Ozogamicin treatment for relapsed or refractory Acute Lymphoblastic Leukemia. Biol Blood Marrow Transpl. 2019;25:1720–9.
Article CAS Google Scholar
Kantarjian HM, DeAngelo DJ, Advani AS, et al. Hepatic adverse event profile of inotuzumab ozogamicin in adult patients with relapsed or refractory acute lymphoblastic leukaemia: results from the open-label, randomised, phase 3 INO-VATE study. Lancet Haematol. 2017;4:e387–98.
Mohty M, Malard F, Abecassis M, et al. Sinusoidal obstruction syndrome/veno-occlusive disease: current situation and perspectives-a position statement from the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transpl. 2015;50:781–9.
Kebriaei PSR, Wallis W, et al. P739: predictive factors for developing veno-occlusive disease in patients with acute lymphoblastic leukemia treated with inotuzumab ozogamicin followed by allogeneic hematopoietic stem cell transplantation. Haematologica. 2017;102:299.
Google Scholar
Kebriaei P, Cutler C, de Lima M, et al. Management of important adverse events associated with inotuzumab ozogamicin: expert panel review. Bone Marrow Transpl. 2018;53:449–56.
Giglio F, Xue E, Greco R, et al. Defibrotide Prophylaxis of Sinusoidal obstruction syndrome in adults treated with Inotuzumab Ozogamicin prior to hematopoietic stem cell transplantation. Front Oncol. 2022;12:933317.
Jabbour E, Ravandi F, Kebriaei P, et al. Salvage Chemoimmunotherapy with Inotuzumab Ozogamicin Combined with Mini-Hyper-CVD for patients with relapsed or refractory Philadelphia chromosome-negative Acute Lymphoblastic Leukemia: a phase 2 clinical trial. JAMA Oncol. 2018;4:230–4.
Jabbour E, Sasaki K, Short NJ, et al. Long-term follow-up of salvage therapy using a combination of inotuzumab ozogamicin and mini-hyper-CVD with or without blinatumomab in relapsed/refractory Philadelphia chromosome-negative acute lymphoblastic leukemia. Cancer. 2021;127:2025–38.
Kantarjian H, Haddad FG, Jain N, et al. Results of salvage therapy with mini-hyper-CVD and inotuzumab ozogamicin with or without blinatumomab in pre-B acute lymphoblastic leukemia. J Hematol Oncol. 2023;16:44.
Haddad F, Jabbour E, Nasnas C et al. S119: COMBINATION OF MINI-HYPER-CVD AND INOTUZUMAB (INO) FOLLOWED BY BLINATUMOMAB (BLINA) CONSOLIDATION IN PATIENTS WITH RELAPSED/REFRACTORY (R/R) ACUTE LYMPHOBLASTIC LEUKEMIA (ALL): A PHASE II TRIAL. Hemasphere 2023;7.
Short NJ, Jabbour E, Jamison T et al. Dose-dense Mini-Hyper-CVD, Inotuzumab Ozogamicin and Blinatumomab achieves Rapid MRD-Negativity in Philadelphia chromosome-negative B-cell Acute Lymphoblastic Leukemia. Clinical Lymphoma, Myeloma and Leukemia.
Short NJ, Kantarjian H, Ravandi F, et al. High-sensitivity next-generation sequencing MRD assessment in ALL identifies patients at very low risk of relapse. Blood Adv. 2022;6:4006–14.
Kotrová M, Koopmann J, Trautmann H, et al. Prognostic value of low-level MRD in adult acute lymphoblastic leukemia detected by low- and high-throughput methods. Blood Adv. 2022;6:3006–10.
Sive JI, Buck G, Fielding A, et al. Outcomes in older adults with acute lymphoblastic leukaemia (ALL): results from the international MRC UKALL XII/ECOG2993 trial. Br J Haematol. 2012;157:463–71.
O’Brien S, Thomas DA, Ravandi F, Faderl S, Pierce S, Kantarjian H. Results of the hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone regimen in elderly patients with acute lymphocytic leukemia. Cancer. 2008;113:2097–101.
Kantarjian H, Ravandi F, Short NJ, et al. Inotuzumab ozogamicin in combination with low-intensity chemotherapy for older patients with Philadelphia chromosome-negative acute lymphoblastic leukaemia: a single-arm, phase 2 study. Lancet Oncol. 2018;19:240–8.
Jabbour E, Short NJ, Senapati J, et al. Mini-hyper-CVD plus inotuzumab ozogamicin, with or without blinatumomab, in the subgroup of older patients with newly diagnosed Philadelphia chromosome-negative B-cell acute lymphocytic leukaemia: long-term results of an open-label phase 2 trial. Lancet Haematol. 2023;10:e433–44.
Jabbour EJ, Sasaki K, Ravandi F, et al. Inotuzumab ozogamicin in combination with low-intensity chemotherapy (mini-HCVD) with or without blinatumomab versus standard intensive chemotherapy (HCVAD) as frontline therapy for older patients with Philadelphia chromosome-negative acute lymphoblastic leukemia: a propensity score analysis. Cancer. 2019;125:2579–86.
Wieduwilt MJ, Yin J, Kour O, et al. Chemotherapy-free treatment with inotuzumab ozogamicin and blinatumomab for older adults with newly diagnosed, Ph-negative, CD22-positive, B-cell acute lymphoblastic leukemia: Alliance A041703. J Clin Oncol. 2023;41:7006.
Stelljes M, Raffel S, Alakel N et al. Inotuzumab Ozogamicin as induction therapy for patients older than 55 years with Philadelphia chromosome-negative B-Precursor ALL. J Clin Oncol 2023:Jco2300546.
Chevallier P, Leguay T, KIM R, et al. Fractionated Inotuzumab Ozogamicin combined with low-intensity chemotherapy in older patients with newly diagnosed CD22 + Philadelphia chromosome (Ph)-Negative B-Cell precursor (BCP) Acute Lymphoblastic Leukemia (ALL): results of the EWALL-INO Study. Blood. 2022;140:6114–6.
Muffly L. ALLIANCE A042001: a Randomized Clinical Trial to determine whether inotuzumab + Mini-HyperCVD will replace HyperCVAD as Frontline Treatment in older adult ALL. The Hematologist 2023;20.
Jabbour E, Short NJ, Jain N, et al. Hyper-CVAD and sequential blinatumomab for newly diagnosed Philadelphia chromosome-negative B-cell acute lymphocytic leukaemia: a single-arm, single-centre, phase 2 trial. Lancet Haematol. 2022;9:e878–85.
Nguyen D, Kantarjian HM, Short NJ, et al. Updated results from a phase II study of Hyper-CVAD, with or without Inotuzumab Ozogamicin, and sequential blinatumomab in patients with newly diagnosed B-Cell Acute Lymphoblastic Leukemia. Blood. 2023;142:4245.
Jabbour E, Gökbuget N, Advani A, et al. Impact of minimal residual disease status in patients with relapsed/refractory acute lymphoblastic leukemia treated with inotuzumab ozogamicin in the phase III INO-VATE trial. Leuk Res. 2020;88:106283.
Jabbour EJ, Haddad FG, Short NJ et al. Phase II study of inotuzumab ozogamicin for measurable residual disease in acute lymphoblastic leukemia in remission. Blood. 2024;143(5):417–21.
Marconi G, Piciocchi A, Chiaretti S, et al. Gimema ALL2418: interim analysis of a phase Iia Study of Feasibility and Effectiveness of Inotuzumab Ozogamicin in Adult patients with B-Cell Acute Lymphoblastic Leukemia with positive minimal residual disease before any hematopoietic stem cell transplantation. Blood. 2022;140:6119–21.
Jain N, Maiti A, Ravandi F, et al. Inotuzumab ozogamicin with bosutinib for relapsed or refractory Philadelphia chromosome positive acute lymphoblastic leukemia or lymphoid blast phase of chronic myeloid leukemia. Am J Hematol. 2021;96:1000–7.
Metheny L, Sobecks RM, Cho C et al. A multicenter study of posttransplant low-dose inotuzumab ozogamicin to prevent relapse of acute lymphoblastic leukemia. Blood Adv 2024.
Rubinstein JD, Breese EH, Krupski MC et al. The Choice of Either Conventional Chemotherapy or Inotuzumab Ozogamicin as Bridging Regimen Does Not Appear To Impact Clinical Response to CD19-Directed CAR-T Therapy in Pediatric B-ALL. Transplantation and Cellular Therapy, Official Publication of the American Society for Transplantation and Cellular Therapy. 2023;29:311.e1-.e7.
Ceolin V, Brivio E, van Tinteren H, et al. Outcome of chimeric antigen receptor T-cell therapy following treatment with inotuzumab ozogamicin in children with relapsed or refractory acute lymphoblastic leukemia. Leukemia. 2023;37:53–60.
Shah BD, Cassaday RD, Park JH, et al. Impact of prior therapies and subsequent transplantation on outcomes in adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia treated with brexucabtagene autoleucel in ZUMA-3. J Immunother Cancer. 2023;11:e007118.
Jabbour E, Short NJ, Jain N, et al. The evolution of acute lymphoblastic leukemia research and therapy at MD Anderson over four decades. J Hematol Oncol. 2023;16:22.
Wintering A, Ishiyama K, Tamaki S, et al. CD22low/Bcl-2high expression identifies poor response to inotuzumab ozogamicin in relapsed/refractory acute lymphoblastic leukemia. Blood Adv. 2023;7:251–5.
Ryland GL, Barraclough A, Fong CY, et al. Inotuzumab ozogamicin resistance associated with a novel CD22 truncating mutation in a case of B-acute lymphoblastic leukaemia. Br J Haematol. 2020;191:123–6.
Zhao Y, Short NJ, Kantarjian HM et al. Genomic determinants of response and resistance to inotuzumab ozogamicin in B-cell ALL. Blood. 2024. (In press)
Luskin MR, Shimony S, Keating J, et al. A phase I study of Venetoclax in Combination with Inotuzumab Ozogamicin for Relapsed or Refractory ALL in adults. Blood. 2023;142:1509.
Download references
Acknowledgements
The authors wish to thank Lewis Nasr MD and Omer Karrar MD for their assistance with creation of tables and formatting of the manuscript.
This research is supported in part by the MD Anderson Cancer Center Leukemia SPORE CA100632, and the NIH/NCI Cancer Center Support Grant P30 CA016672.
Author information
Authors and affiliations.
Department of Leukemia, The University of Texas MD Anderson Cancer Center, Unit 428, 1515 Holcombe Boulevard, Houston, TX, 77030, USA
Nicholas J. Short, Elias Jabbour, Nitin Jain & Hagop Kantarjian
You can also search for this author in PubMed Google Scholar
Contributions
N.J.S. wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approve of the final version.
Corresponding author
Correspondence to Nicholas J. Short .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
N.J.S. has served as consultant for Pfizer Inc., GSK, NKARTA, Autolus, and Sanofi, reports receiving research grants from Takeda Oncology, Astellas Pharma Inc., Xencor, Stemline Therapeutics, and NextCure, and has received honoraria from Adaptive Biotechnologies, Novartis, Amgen, Takeda Oncology, Pfizer Inc., Astellas Pharma Inc., Sanofi and BeiGene. E.J. reports receiving research grants and consultancy fees from AbbVie, Adaptive Biotechnologies, Amgen, Ascentage, Bristol Myers Squibb, Genentech, Incyte, Pfizer, and Takeda. N.J. reports receiving research grants from Pharmacyclics, AbbVie, Genentech, AstraZeneca, BMS, Pfizer, ADC Therapeutics, Cellectis, Adaptive Biotechnologies, Precision Biosciences, Fate Therapeutics, Kite/Gilead, Mingsight, Takeda, Medisix, Loxo Oncology, Novalgen, Dialectic Therapeutics, Newave, TransThera Sciences, Novartis, Carna Biosciences, Sana Biotechnology, Kisoji Biotechnology, and has received honoraria from Pharmacyclics, Janssen, AbbVie, Genentech, AstraZeneca, BMS, Adaptive Biotechnologies, Kite/Gilead, Precision Biosciences, Beigene, Cellectis, MEI Pharma, Ipsen, CareDX, MingSight, and Novalgen. H.K. reports receiving research grants from AbbVie, Agios, Amgen, Ariad, Astex, BMS, Cyclacel, Daiichi-Sankyo, Immunogen, Jazz Pharma, Novartis, Pfizer, Actinium, and Takeda.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Short, N.J., Jabbour, E., Jain, N. et al. Inotuzumab ozogamicin for the treatment of adult acute lymphoblastic leukemia: past progress, current research and future directions. J Hematol Oncol 17 , 32 (2024). https://doi.org/10.1186/s13045-024-01552-7
Download citation
Received : 26 January 2024
Accepted : 29 April 2024
Published : 11 May 2024
DOI : https://doi.org/10.1186/s13045-024-01552-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Antibody-drug conjugate
- Clinical trials
- Lymphoid diseases
- Immunotherapy
Journal of Hematology & Oncology
ISSN: 1756-8722
- General enquiries: [email protected]
Reference management. Clean and simple.
Journal abbreviation: International journal of research
The abbreviation of the journal title " International journal of research " is " Int. J. Res. ". It is the recommended abbreviation to be used for abstracting, indexing and referencing purposes and meets all criteria of the ISO 4 standard for abbreviating names of scientific journals.
Abbreviation rules
The table below outlines in detail the ISO 4 rules and matches to the ISSN maintained list of title word abbreviations ( TWA ) to derive the abbreviation.
Abbreviation systems
ISO 4 abbreviation is a uniform system created by the International Organization for Standardization to abbreviate journal titles in a consistent manner. It serves to facilitate effective communication and reference within the academic community.
ISO, standing for International Organization for Standardization, is a universal abbreviation system for journal titles across disciplines. NLM, or National Library of Medicine, is specific to biomedical sciences, and CASSI, the CAS Source Index, caters to chemistry-related disciplines.
About the journal
Other journal abbreviations.
- Archives of clinical infectious diseases
- Wuhan University journal of natural sciences
- Open access
- Published: 08 May 2024
Advances and challenges of the cell-based therapies among diabetic patients
- Ramin Raoufinia 1 , 2 ,
- Hamid Reza Rahimi 2 ,
- Ehsan Saburi 2 &
- Meysam Moghbeli ORCID: orcid.org/0000-0001-9680-0309 2
Journal of Translational Medicine volume 22 , Article number: 435 ( 2024 ) Cite this article
407 Accesses
Metrics details
Diabetes mellitus is a significant global public health challenge, with a rising prevalence and associated morbidity and mortality. Cell therapy has evolved over time and holds great potential in diabetes treatment. In the present review, we discussed the recent progresses in cell-based therapies for diabetes that provides an overview of islet and stem cell transplantation technologies used in clinical settings, highlighting their strengths and limitations. We also discussed immunomodulatory strategies employed in cell therapies. Therefore, this review highlights key progresses that pave the way to design transformative treatments to improve the life quality among diabetic patients.
Diabetes mellitus poses a formidable global public health challenge due to its rapid growing prevalence and associated morbidity, disability, and mortality [ 1 ]. According to the International Diabetes Federation, over 537 million adults aged 20–79 had diabetes worldwide in 2021 that is expected to rise to around 783 million cases by 2045 [ 2 ]. Obesity, unhealthy diets, physical inactivity as well as genetic and epigenetic predispositions are important risk factors of diabetes [ 3 , 4 , 5 ]. Diabetes is typically classified into type 1 diabetes mellitus (T1DM), gestational diabetes mellitus (GDM), and type 2 diabetes mellitus (T2DM) [ 2 ]. T1DM primarily arises from autoimmune-related damage of insulin-secreting beta cells, resulting in severe hyperglycemia and ketoacidosis [ 6 ]. In contrast, T2DM generally has a more gradual onset characterized by insulin resistance along with diminished compensatory insulin secretion from pancreatic beta cell dysfunction [ 7 ]. Diabetes is associated with macrovascular complications such as heart disease and stroke, as well as microvascular issues in eyes, kidneys, and nervous system [ 8 ]. Cancer is also a leading cause of diabetes-related death, and dementia-associated mortality has risen in recent decades [ 9 , 10 , 11 , 12 ]. Cell therapy involves transferring autologous or allogenic cellular material into patients [ 13 ]. The global market size of cell therapy is estimated to grow from $9.5 billion in 2021 to $23 billion by 2028 [ 14 ]. It combines stem and non-stem cell therapies consisting of unicellular or multicellular preparations. Cell therapies typically use autologous or allogenic cells via injection and infusion [ 15 ]. In the present review, we discussed the recent advances in cell-based therapy of diabetes, from foundational islet transplantation to regenerative strategies to highlight key developments that improve the effective treatments for diabetic patients.
Cell replacement therapy for diabetes
Pancreatic transplantation was firstly used in 1966 to treat type 1 diabetes using whole organ transplants. During the 1970s–80s, segmental pancreatic grafts were combined with techniques to divert digestive secretions away from transplanted cells. Three main techniques emerged; simultaneous pancreas-kidney transplants, pancreas transplants following kidney transplants, and pancreatic transplants. International collaboration on tracking outcomes began in 1980 with the formation of several pancreatic transplant registries and associations. However, whole organ transplantation was faced with several challenges including organ rejection, vascular complications, limited organ availability, and the effects of lifelong immunosuppression [ 16 , 17 ]. Islet cell transplantation was explored as an alternative, however isolating and transplanting pancreatic islets proved difficult due to donor availability, rejection, and immunosuppression side effects. Recent research has focused on stem cell sources that could reconstitute immune tolerance and preserve beta cell function such as mesenchymal stem cells, bone marrow cells, and embryonic stem cells [ 18 ]. A novel stem cell therapy called VX-880 was developed using proprietary technology to grow insulin-producing beta cells from allogeneic stem cells. Clinical trials began in 2021 after FDA approval to deliver the cells intrahepatically under immune suppression. A second approach called VX-264 encapsulates the same cells, avoiding immunosuppression but requiring surgical implantation [ 17 ]. In 2023, FDA approved the first allogeneic pancreatic islet cell therapy called Lantidra for adults with type 1 diabetes experiencing severe hypoglycemia. Approval was based on two studies where 21–30% of participants no longer required insulin one year post-treatment, with benefits lasting over five years in some cases. However, this treatment have mild and serious adverse events that are associated with treatment dose and the methods of islet cell infusion [ 19 , 20 ].
Emerging strategies for cell delivery via microencapsulation and biological devices in clinical trials
Alginate capsules as cell delivery systems.
A seminal investigation conducted in 1994 demonstrated the successful transplantation of alginate-encapsulated islets into the peritoneum of kidney transplant patients who were receiving immunosuppression therapy. Remarkably, these patients achieved insulin independence for up to nine months [ 21 ]. However, subsequent trials conducted without immunosuppression yielded inconsistent outcomes. In a study conducted in 2006, islets were encapsulated in triple-layer alginate capsules and implanted intraperitoneally in type 1 diabetes (T1D) patients. There was a positive correlation between the encapsulation and insulin production that reduced exogenous insulin requirements during one year. Despite this progress, the entry of cytokines remained a potential concern [ 22 ]. Another study employed the single-layer barium-alginate capsules that sustained insulin production for up to 2.5 years [ 23 ]. It has been reported that the microneedle, comprising a calcium alginate frame with polydopamine-coated poly-lactic-co-glycolic acid microspheres encapsulating insulin, enables light-triggered insulin release. Microneedle provided a suitable insulin dose to maintain blood glucose levels in line with daily fluctuations. These results established the efficacy and safety of the developed microneedle for diabetes treatment [ 24 ]. Another therapeutic approach explored the encapsulation of pancreatic islets with mesenchymal stem cells (MSCs) and decellularized pancreatic extracellular matrix (ECM). ECM derived from the pancreas supported islet cell growth and maintenance to enhance insulin expression [ 25 ]. Sodium alginate and hyaluronic acid were incorporated due to their roles in collagen production, wound healing, and physical crosslinking. The 3D porous membranes allowed optimal water and oxygen transfer while diverting excess exudate from diabetic wounds. Hydrogel accelerated re-epithelization, while decreased inflammation, indicating potential as the diabetic wound dressings [ 26 ]. Additionally, the incorporation of specific ECM components, such as collagen IV and RGD, into alginate-based microcapsules significantly improved the survival, insulin secretion, and longevity of microencapsulated islets [ 27 ].
Encaptra® device from ViaCyte
In contrast to microencapsulation techniques, ViaCyte developed a semipermeable pouch method named Encaptra, which contains pancreatic precursor cells derived from the embryonic stem cells [ 28 ]. In the initial trial conducted in 2014, the “VC-01” device was implanted in T1D individuals without the use of immunosuppression [ 29 ]. The trial confirmed the safety of the device; however, the occurrence of hypoxia induced cellular necrosis [ 30 ]. The device was modified as “VC-02” with larger pores, and two trials (NCT03162926, NCT03163511) demonstrated promising outcomes, including increased fasting C-peptide levels and a 20% reduction in insulin requirements during one year in the majority of participants [ 31 ]. In order to eliminate the necessity for immunosuppressants, ViaCyte collaborated with Gore to develop an expanded polytetrafluoroethylene (ePTFE) device with both immuno-isolating and pro-angiogenic properties [ 32 ]. This device (NCT04678557) aimed to prevent immune cell attachment and T-cell activation [ 33 ]. Additionally, ViaCyte is exploring the integration of CRISPR technology to modify stem cells, specifically by eliminating β2-microglobulin expression and PD-L1 up regulation. It is hypothesized that these genetic modifications will further hinder immune cell attachment and T-cell activation [ 30 , 34 ].
Semipermeable device from Semma therapeutics
Semma Therapeutics, which has been acquired by Vertex, pioneered the utilization of differentiated stem cell-derived islet cell clusters in clinical trials. Semma houses these cells between two semipermeable polyvinylidene fluoride membranes and is designed for subcutaneous implantation (NCT04786262) [ 31 , 35 ]. Vertex reported a significant breakthrough by infusing differentiated beta cells via the portal vein in a participant who was receiving immunosuppressants. This approach led to substantial C-peptide production and improved glycemic control during 90 days [ 36 ].
βAir device from Beta O2
Beta O2’s innovative βAir device utilizes an alginate-PTFE membrane complex to encapsulate islets, providing partial immunoisolation while ensuring a continuous supply of oxygen, which is crucial for optimal islet function [ 37 , 38 ]. The βAir device that was seeded with human islets was subcutaneously implanted in T1D individuals (NCT02064309). Although, low insulin levels were produced for up to eight weeks, there was not any reduction in the required exogenous insulin [ 37 ]. While, increasing the number of islets could potentially enhance their function, it is important to note that the continuous reliance on oxygen poses a risk of infection, despite efforts to optimize the survival of encapsulated islets [ 39 , 40 ].
Cell pouch™ device from Sernova
Sernova has developed the Cell Pouch device, which offers pre-vascularized polypropylene chambers for islet transplantation without the need for immunoprotection. The device consists of multiple cylindrical chambers that are prefilled with PTFE plugs, which are then removed after implantation to create the empty space [ 41 ]. In a 2012 trial (NCT01652911), islets were placed in the vascularized pouches of three recipients who were also receiving immunosuppression that resulted in a transient increase in C-peptide levels [ 41 ]. In a 2018 trial (NCT03513939), immunosuppression was administered after implantation and islet introduction. This trial reported sustained C-peptide production for up to nine months in two recipients, along with improved glycemic control [ 42 ]. Regarding the limitations of immunosuppression, Sernova is exploring the possibility of encapsulating islets in hydrogel as an alternative approach [ 43 ].
Shielded living therapeutics™ from Sigilon Therapeutics
Sigilon has developed the Shielded Living Therapeutics sphere, which consists of cell clusters enclosed within an alginate-TMTD coating [ 44 ]. Preclinical studies demonstrated that murine islet transplants encapsulated within these spheres maintained normoglycemia for a period of six months [ 45 ]. In a 2020 trial conducted for hemophilia (NCT04541628), the spheres were evaluated for their ability to express Factor VIII [ 46 ]. However, the trial was paused due to the development of antibodies in the third recipient receiving the highest cell doses. While, preclinical studies have shown promising efficacy, there are safety concerns regarding the TMTD coating that need to be addressed before these spheres can be used for human islet transplantation as a treatment for diabetes [ 31 ]. Emerging technologies have been investigated in clinical trials for delivering insulin-producing islets or stem cell-derived beta cells via microencapsulation or use of implantable biological devices (Table 1). Optimizing encapsulation and developing alternative implantable devices moves the field toward delivering safe and effective islet replacement without chronic immunosuppression dependency that represented an important new frontier for the cell-based treatment of diabetes. However, continued refining will be required to fully realize this promising vision and using these preclinical concepts in clinic.
Immunoengineering strategies: biomaterials for modulating immune responses
Islet encapsulation aims to prevent immune responses toward transplant antigens. However, foreign body response (FBR) against biomaterials induces inflammation around encapsulated islets that obstructs oxygen/nutrient access and causes graft failure [ 31 ]. Extensive research revealed biomaterial properties profoundly influence FBR severity, with high purity/biocompatibility moderating inflammation [ 47 ]. Deeper understanding of biomaterial immunobiology enabled developing immune-modulating constructs to steer host interactions. By altering topology/chemistry to hinder nonspecific binding and cell adhesion, these “immune-evasive biomaterials” intended to attenuate xenograft rejection at inception [ 44 ]. Both innate and adaptive immune responses have crucial roles in the context of pancreatic islet transplantation. These responses encompass the activation of tissue macrophages and neutrophils following injury, leading to the release of inflammatory cytokines that subsequently activate antigen-presenting cells (APCs), CD8 + T cells, CD4 + T cells, and cytotoxic T lymphocytes (Fig. 1 ). Zwitterionic polymers conferred anti-fouling attributes but crosslinking limitations constrained their application [ 48 ]. Novel mild zwitterionization introduced alginate modifications that prolonged prevention of fibrotic overgrowth by mitigating initial responses [ 49 , 50 , 51 ]. The prevention of graft rejection following islet cell transplantation necessitates the systemic administration of immunosuppressive agents. While, these agents effectively suppress immune responses, their continuous use exposes patients to an increased risk of infection and cancer. To mitigate these concerns, an alternative approach involving the localized delivery of immunosuppressants at the transplantation site has emerged. This localized delivery system offers several advantages, including targeted drug delivery, reduced systemic exposure, and potentially reduces the immunosuppressants doses [ 52 ]. Polymeric carriers dispersed cyclosporine A continuously at the graft site to dynamically tamp down proinflammatory cascades and T-cell activation [ 53 , 54 ]. TGF-β/IL-10 co-delivery at the microencapsulation interface hindered innate antigen presentation, obstructing adaptive response priming [ 55 , 56 ]. Regulatory T-cells emerged as the potent immunomodulators when coated on islets to improve insulin production in vitro [ 57 ]. Similarly, recombinant Jagged-1 surface patterning increased regulatory lymphocytes in vitro while enhancing glycemic oversight in vivo [ 58 ]. Targeting proinflammatory effector T-cells or presenting their Fas ligand death receptor improved long-term viability when combined with rapamycin prophylaxis [ 52 , 59 ]. Immobilizing thrombomodulin or urokinase mitigated local inflammation, with the latter conferring lifelong xenotransplant survival [ 60 ]. Peptides recognizing IL-1 receptors provided robust protection from destabilizing proinflammatory cytokines [ 61 ]. Leukemia inhibiting factor improved islet performance over polyethylene glycol encapsulation alone by inducing regulatory T-cell lineages [ 62 ]. Silk scaffolds facilitated IL-4/dexamethasone emancipation that meaningfully decreased immune reactions to grafts [ 63 ]. Therefore, the localized delivery of immunosuppressants at the transplantation site represents a promising strategy for islet cell transplantation. Compared to systemic administration, local delivery can achieve targeted immune modulation only at the graft location while reducing drug exposure throughout the body. This localized approach aims to sufficiently suppress the immune response to prevent rejection, while limiting negative side effects that may occur from systemic immunosuppression. A variety of biomaterials and surface modification strategies have been developed and investigated for the local delivery of immunosuppressive agents and immunomodulatory cytokines [ 64 , 65 , 66 ]. Understanding how biomaterial properties influence the immune response is critical to design biomaterials that can modulate inflammation and improve islet graft survival through localized immunomodulation.
Cell-based therapy through the integration of additive manufacturing techniques
Additive manufacturing utilizes computer modeling to fabricate complex 3D structures on-site with minimal post-processing. Common methods for the biomedical application are fused filament fabrication (FFF), stereolithography (SLA), and bioprinting [ 67 ]. FFF is a layer-by-layer technique that extrudes heated thermoplastics [ 68 ]. Commonly used feedstocks include acrylonitrile butadiene styrene (ABS) and polylactic acid (PLA). Other thermoplastics that have been utilized with FDM include thermoplastic polyurethane (TPU), polycarbonate (PC), polystyrene (PS), polyetherimide (PEI), polycaprolactone (PCL), polyaryletherketone (PAEK), and polyetheretherketone (PEEK), with the latter demonstrating high strength and heat tolerance. A major advantage of FDM is its ability to fabricate multi-material objects through continuous printing and alteration of the build material. In addition to typical polymers like PC and polystyrene (PS), FDM can print composites reinforced with glass, metals, ceramics, and bioresorbable polymers via integration of the constituent powders with a binding matrix. This enables enhanced control over the experimental component fabrication. While, ceramic and metal filaments traditionally contain the corresponding powder mixed with a binder, FDM provides versatility in the functional prototype construction from a wide range of thermoplastic feedstocks using precise and additive layer manufacture [ 68 , 69 , 70 , 71 , 72 ]. It provides geometric reproducibility and reduced variability compared to traditional techniques. FFF prints served as scaffolds for the transplanted cells [ 67 ]. However, minimum feature size is limited to ? ∼ 250 μm by nozzle diameter [ 68 ]. SLA employs light-curable liquid resins and achieves higher 50–150 μm resolution than FFF but with restricted material choices. Bone grafts and surgical guides are common applications [ 67 ]. Incorporating biomaterials like hydroxyapatite has expanded utility, though processing is required to mitigate cytotoxicity. Additive manufacturing can address limitations in oxygen transport, cell/material placement control and vasculature formation, and clinically translatable insulin-secreting implants [ 67 ]. Therefore, additive manufacturing technologies have the potential to enhance various aspects of the cell-based transplant design, from improving nutrient transport through optimized implant geometry to achieving precision integration of therapeutic agents (Table 2).
Enhancing nutrient transport through optimization of implant geometry
Tissue engineering for the islet transplantation requires maximizing nutrient transport [ 73 , 74 ]. Traditional scaffold fabrication introduces macroporosity but lacks precision that results in inflammation [ 67 ]. Cell encapsulation provides immunoprotection by limiting interactions between transplanted cells and the host immune system. However, this protective barrier also poses challenges for the efficient transport of essential nutrients, including oxygen, to the encapsulated cells. Modifying the geometries of encapsulation devices using conventional methods to enhance oxygen delivery has proven to be inconsistently challenging [ 67 ], so that novel approaches are required to address these challenges. Additive manufacturing allows customizing biomaterial scaffolds with defined geometries and micropore sizes to improve transport [ 75 , 76 , 77 , 78 , 79 ]. The 3D printed PLA scaffolds with islets have successful vascularization and cellular survival after subcutaneous transplantation [ 80 , 81 ]. Interlocking toroidal hydrogel-elastomer constructs also increased surface area and cell viability [ 82 , 83 , 84 ].
Enhancing vascularization and engraftment
Rich host vascularization of transplant devices is essential to support long-term islet survival through efficient nutrient delivery and insulin kinetics. Early platforms modified bulk material properties to promote vessel infiltration and anastomoses [ 85 , 86 , 87 , 88 , 89 ]. Additive manufacturing can further optimize microscale geometry to both accelerate host vessel connections and control intra-device vasculature homogeneity beyond traditional fabrication. Initial work reproduced macroscale vessels but scales were diverged from cell-based therapies [ 73 , 90 , 91 , 92 ]. Leveraging Additive manufacturing designed structures guided vessel formation in vitro and in vivo [ 80 , 89 , 93 ]. Shifting to bioprinting complex branching conduits in supportive hydrogels facilitated clinical translation for diverse cell therapies [ 94 , 95 , 96 , 97 , 98 ]. Researchers focused on developing a 3D scaffold platform to improve the transplantation outcomes of islet cells in T1D. The scaffold featured a heparinized surface and immobilized vascular endothelial growth factor (VEGF) to enhance vascularization. Scaffold effectively promoted angiogenesis and facilitated the growth of new blood vessels. Additionally, encapsulated islets within the scaffold had functional responses to glucose stimuli. These findings suggested that the developed scaffold platform holds potential for successful extra-hepatic islet transplantation, offering new possibilities for T1D treatment [ 99 ]. Research on vascularization of islets via additive manufacturing techniques has primarily focused on the fundamental discoveries. In one study, engineered pseudo islets (EPIs) were created by combining the mouse insulin-secreting beta cells with rat heart microvascular endothelial cells. EPIs demonstrated extensive outgrowth of capillaries into the surrounding matrix. Although, EPIs containing both cell types that underwent capillarization maintained viability and function over time in culture, non-vascularized EPIs lacking endothelial cells could not sustain viability or functionality long-term. This supported the potential for inducing angiogenesis within bioengineered islet constructs. Future work may combine patient-specific stem cell-derived human beta cells with endothelial cells using this approach to promote long-term graft survival for treating type 1 diabetes [ 98 ]. While, large-scale 3D printed vascularized structures are currently limited for the islet transplantation, advancements in leveraging additive manufacturing for the optimization vascularization conditions through the pore sizes and material choices, may facilitate translation to β-cell therapy in type 1 diabetes.
Precision placement of cells and matrix for enhanced control
Beyond distributing biomaterials, additive manufacturing enables micro-level cell and protein control. For islet transplantation, optimal cellular distribution and supportive extracellular matrix niche reduce rapid dysfunction and apoptosis [ 100 , 101 , 102 ]. Traditional techniques heterogeneously load cells after fabrication or struggle with incomplete encapsulation [ 103 , 104 ]. Bioprinting allows in situ encapsulation and printing of multiple cell types and matrix components while dictating 3D placement and dimensions [ 105 , 106 ]. Islet transplant research prints hydrogel-encapsulated clusters surrounded by supportive cells and doped with immune modulators to improve the transplant environment [ 107 ]. Progress in bioprinting offers consistency and defines physical/chemical graft properties beyond traditional fabrication.
Achieving controlled integration of therapeutic agents for enhanced efficacy
In addition to the cell and matrix placement, additive manufacturing enables precision therapeutic integration. Incorporating therapeutics aims to recapitulate the in vivo environment through angiogenesis, islet health promotion, and immunomodulation [ 67 , 108 ]. Growth factors promote vessel formation and insulin secretion while decrease apoptosis [ 108 , 109 , 110 , 111 ]. Local immunomodulators regulate the immune system in a specific site of the body. They decrease inflammation and promote the successful integration of transplanted cells or tissues by minimizing the need for widespread immune suppression in whole body [ 67 ]. Traditional homogeneous delivery methods restrict the ability to customize the spatial distribution of substances and pose a risk of harmful effects on transplants or hosts [ 112 ]. The use of discreet gradients in bioprinting can offer precise physiological signals. By combining traditional drug release methods with AM, it becomes possible to create tissues that exhibit distinct therapeutic localization. Bioprinted composites have the ability to release factors with gradients throughout the entire construct that enables a more comprehensive and targeted approach in tissue engineering [ 112 , 113 , 114 ].
Cell based gene therapy
Gene therapy holds great promise for diabetes management, offering innovative approaches to deliver and manipulate the insulin gene in various tissues. Viral methods, such as lentivirus, adenovirus, and adeno-associated virus (AAV), along with non-viral techniques like liposomes and naked DNA, have been utilized to deliver the insulin gene to target tissues [ 115 ]. This section aims to provide an overview of important studies in the field of gene therapy for diabetes management, emphasizing advancements in insulin gene delivery and manipulation (Table 3).
Enteroendocrine K-cells and pancreatic β-cells
Enteroendocrine K-cells in the intestines and pancreatic β-cells share similarities in their production of glucose-dependent insulinotropic polypeptide (GIP) and their regulatory mechanisms. Understanding these similarities offers insights into T2D management and improving glucose homeostasis. However, attempts to reverse diabetes effectively through K-cell transplantation have been unsuccessful. Nevertheless, research on gene editing techniques has shown promising results in management of the diabetes mellitus [ 116 , 117 ]. AAV vectors have been employed to co-express insulin and glucokinase genes in skeletal muscles, demonstrating long-term effectiveness in achieving normo-glycemia without exogenous insulin [ 118 , 119 ].
Gene editing techniques
Gene editing techniques using AAV vectors effectively improved normo-glycemia in animal models. Co-expression of insulin and glucokinase in transgenic mice increased glucose absorption and regulated insulin production. Duodenal homeobox 1 (PDX1) gene transfer via AAV2 in a humanized liver mouse model also led to insulin secretion and glycemic control [ 120 ]. Adenovirus-mediated transfection of hepatic cells with neurogenin 3 (NGN3) resulted in insulin production and trans-differentiation of oval cell populations [ 121 , 122 ]. Targeting specific promoters in liver cells such as phosphoenolpyruvate carboxykinase (PEPCK), glucose 6-phosphatase (G6Pase), albumin, and insulin-like growth factor binding protein-1 (IGFBP-1) enhanced hepatic insulin gene therapy [ 123 , 124 ]. AAV-mediated overexpression of SIRT1 reduced inflammation, hypoxia, apoptosis and improved neural function in the retina of diabetic db/db mice [ 125 ]. Another study developed a plasmid expressing a single-strand insulin analogue for intramuscular injection using a specialized gene delivery technique. A single administration provided sustained insulin expression for 1.5 months and effectively regulated blood glucose levels without immune responses or tissue damage in diabetic mice.
Non-viral gene delivery methods
Non-viral approaches have also key roles in achieving glycemic control. The combination of insulin fragments with DNA plasmid, administered via intravenous injection improved normo-glycemia for extended periods. DNA transposon facilitated gene integration into the host chromosome that addressed the short-term liver expression. Additionally, the co-injection of DNA plasmid containing insulin with furin significantly enhanced insulin production within muscles [ 126 ]. Non-viral plasmids were engineered to carry proinsulin and pancreatic regenerating genes to ameliorate streptozotocin-induced T1DM [ 127 ]. The pVAX plasmid vectors prolonged therapeutic effects in achieving normo-glycemia without the need for further treatment [ 127 ]. Bioreducible cationic polymers, such as poly-(cystamine bisacrylamide-diamino hexane) (p(CBA-DAH)), have been employed to deliver RAE-1 to pancreatic islets, resulting in improved insulin levels [ 128 ]. Furthermore, ex vivo gene transfer and autologous grafts have shown promising outcomes in animal models. The introduction of the human insulin gene into pancreatic or liver cells followed by autologous grafts improved insulin secretion, glycemic control, and alleviated the diabetic complications in pigs. However, gene silencing eventually occurred, necessitating a deeper understanding of the underlying mechanisms [ 128 , 129 ].
Stem cell based therapy in diabetes
Efforts are ongoing to develop standardized processes for donor and recipient selection/allocation to increase pancreas utilization [ 130 , 131 , 132 , 133 ]. Techniques for isolating pancreatic islets are being optimized to become more standardized and consistent. Noninvasive imaging technologies allow the monitoring of the transplanted islets without surgery [ 134 , 135 ]. Biomarkers could also evaluate how immunomodulation strategies are working [ 136 , 137 , 138 ]. Researchers are also exploring alternative transplant sites in the body beyond just the liver, to see if the other locations may better support islet graft survival and function. Together, these areas of refinement aim to improve the safety and reliability of islet transplantation procedures as a potential therapy for diabetes [ 139 ]. Bioengineering approaches are being developed to optimize the islet transplantation microenvironment using biomaterials which enhance islet engraftment and function through engineered extracellular niches [ 140 , 141 ]. For example, encapsulation techniques aim to protect pancreatic islets against immune reponse by enclosing them within semipermeable hydrogel polymer capsules [ 142 , 143 ]. This localized immunoisolation strategy utilizes biomaterials like alginate to create a physical barrier preventing immune cell contact while still allowing nutrient and oxygen diffusion. Researchers concurrently seek alternative unlimited cellular sources to address limited islet availability. Mesenchymal stem cells possess immunomodulatory properties and their adjuvant delivery, either early in disease onset or simultaneously with islet transplantation, has shown promising signs of improving outcomes in preclinical investigations. By dampening inflammatory responses and favoring regenerative processes, stem cells may help to establish a more tolerogenic transplant environment. These bioengineering and cell therapy approaches offer potential pathways towards eliminating the exogenous insulin requirement [ 144 , 145 ]. A variety of stem cell types have therapeutic potential for diabetes (Fig. 2 ). Pluripotent stem cells possess immense promise for overcoming the limitations of islet transplantation. Human embryonic stem cells and induced pluripotent stem cells are especially attractive candidates due to their unique ability to both self-renew indefinitely and differentiate into any cell type. This makes them an ideal source of replacement pancreatic beta cells. Significant research effort across academic and industrial laboratories has led to advancement in differentiation protocols that can convert pluripotent stem cells into functional beta-like cells in vitro. However, establishing consistent, well-characterized cellular production methods that comply with stringent safety and efficacy standards remains a priority for clinical translation. Ongoing work aims to generate therapeutic stem cell-derived beta cell replacements exhibiting stable, glucose-responsive insulin secretion comparable to primary islets. Although, technological and regulatory hurdles still must be cleared, pluripotent stem cells have the greatest potential to finally solve the problem of limited cell availability and provide an unlimited source of transplantable tissue suitable for widespread treatment of diabetes [ 145 , 146 , 147 , 148 ]. There are currently six registered clinical trials evaluating the use of human pluripotent stem cells for the T1D treatment. All trials except one use PEC-01 cells, which consist of a mixture of pancreatic endoderm and polyhormonal cell population derived from CyT49 stem cells that are fully committed to endocrine differentiation upon implantation [ 149 ]. The initial trial implanted PEC-01 cells within an encapsulation device, hypothesizing no need for immunosuppression. While, well-tolerated with minor adverse effects, insufficient engraftment occurred due to foreign body responses that eliminated the cells [ 150 ]. The trial transitioned in 2017 to use an open encapsulation device that required immunosuppression. Subcutaneous engraftment, differentiation of cells into islet-like clusters, and glucose-responsive insulin production provided the first evidence that pancreatic progenitor cells can survive, mature, and function as the endocrine cells in humans. Potential benefits on stimulated C-peptide levels and glycemic control were observed in one patient [ 151 , 152 ]. Two reports in late 2021 described results in 17 patients receiving PEC-01 cells in an open device. Engraftment and insulin expression occurred in the majority, glucose-responsive secretion in over one-third, and various glycemic improvements were observed at six months. Explanted tissues contained heterogeneous pancreatic compositions including mature beta cells, with no teratoma formation and mild adverse effects related to surgery/immunosuppression. VX-880 uses fully differentiated insulin-producing stem cell-derived islet cells in phase 1/2 trial evaluating portal infusion and different doses requiring immunosuppression. Preliminary results suggest early engraftment and insulin secretion. The manin challenge was controlling immune rejection without systemic immunosuppression [ 149 ]. Several strategies are being explored to address the challenges of immune rejection in stem cell therapies for diabetes. They include generating stem cell lines that are universally compatible through HLA silencing, developing milder regimens of immunosuppression, and refining encapsulation and containment approaches to protect transplanted cells toward immune response. Establishing standardized stem cell banks is also an area of investigation [ 153 , 154 ]. Xenotransplantation using gene-edited porcine islets remains an exciting avenue of research given advances to improve engraftment and reduce immunogenicity in preclinical studies [ 155 ]. Novel approaches continue to emerge as well, such as decellularization techniques, 3D bioprinting of tissue constructs, and creating interspecies chimeras. Rapid evolution of cell-based therapies across both academic and commercial sectors is promising to restore normoglycemic control in diabetic cases. Refinement of existing methods and development of new strategies hold potential to perform a safe and effective cell replacement without reliance on systemic immunosuppression. Stem cell and regenerative therapies may ultimately manage diabetes through restored endogenous insulin production [ 156 ]. Recently a meta analysis evaluated the safety and efficacy of MSC-based therapy for diabetes in humans. This comprehensive analysis was conducted on 262 patients across six trials that met the inclusion criteria within the last five years. The results reveal that treatment with MSCs significantly reduced the dosage of anti-diabetic drugs over a 12-months. Following treatment, HbAc1 levels decreased by an average of 32%, fasting blood glucose levels decreased by an average of 45%, and C-peptide levels showed a decrease of 38% in two trials and an increase of 36% in four trials. Notably, no severe adverse events were reported across all trials. Therefore, it can be concluded that MSC therapy for type 2 diabetes is safe and effective [ 157 ].
Advances in islet transplantation and stem cell-derived Beta cells
Limited number of the islet transplantation donors highlights the importance of cell therapy in diabetes. Although, higher islet numbers from multiple donors increase the success, limited pancreas availability restricts widespread use [ 158 ]. Using multiple donors also increases rejection risk, while isolation of the islets can cause tissue damage [ 159 ]. To overcome these challenges, researchers have explored the differentiation of stem cells into beta cells in vitro to generate an unlimited supply of insulin-producing cells with standardized and characterized products. Genetic engineering techniques have also been investigated to confer advantages such as stress resistance or immune evasion [ 158 ]. ViaCyte has developed a stem cell-derived pancreatic progenitor called PEC-01, which has the ability to mature into endocrine cells in rodent models. To protect the transplanted cells from immune response, retrieval encapsulation devices were also created [ 160 , 161 , 162 ]. In an initial human clinical trial conducted in 2014 (NCT02239354), the Encaptra device was utilized with the aim of providing complete immunoprotection of transplanted cells through the use of a cell-impermeable membrane. Although, the PEC-Encap product showed reliable tolerance and minimal adverse effects, the trial was stopped due to the inadequate engraftment of functional products. While, a few endocrine cells were observed, fibrosis around the capsule led to graft loss and supression of the insulin secretion. To address this challenge, a more recent development called the PEC-Direct device was introduced, which featured openings in the membrane to facilitate vascularization, thereby improving nutrient exchange and supporting cell viability. However, since host cells could infiltrate the device, immunosuppression was necessary following the transplantation [ 163 , 164 , 165 ]. Protocols were developed to generate clusters of stem cell-derived beta cells that secreted glucose-responsive insulin. These clusters, referred to SC-islets, also contained other endocrine cells, including glucagon-producing cells. SC-islets improved glycemic control in diabetic mice and nonhuman primates [ 146 , 166 , 167 , 168 ]. In a trial conducted in 2017 (NCT03163511), the transplantation of progenitor cells resulted in the maturation of endocrine cells, and glucose-responsive C-peptide secretion was observed 6–9 months post-transplantation. Notably, the majority of these mature endocrine cells exhibited glucagon-positive characteristics. The porous regions housing the endocrine cells allowed for the infiltration of host vessels to facilitate vascularization. However, non-cellular regions were isolated by the presence of fibrosis [ 164 , 165 ]. Although, there was not a sufficient levels of circulating C-peptide in these trials, the findings underscored the significance of promoting vascularization and minimizing fibrotic reactions [ 164 , 169 ]. Vertex conducted a human trial in 2021 (NCT04786262) involving the transplantation of half-dose VX-880 cells (SC-islets) without a device to avoid previous problems, which necessitated immunosuppression. Preliminary results reported improved glycemic control, although it took longer to achieve the same outcome compared to rodent models [ 158 ]. Overall, progresses in islet transplantation and stem cell-derived beta cells pave the way for overcoming the limitations of traditional approaches. Further research and refinements are also required to achieve consistent and clinically significant outcomes in the treatment of diabetes.
Chalenges and limitations
Cell-based therapies have been significantly progressed for diabetes; however, there are still several challenges that need to be overcome. Clinical trials investigating encapsulation devices and islet transplantation techniques have provided valuable insights but face several obstacles including oxygenation, host immune responses, and insufficient long-term engraftment success. Immunoengineering of biomaterials and additive manufacturing for the development of 3D islet structures aim to modulate inflammation and promote graft revascularization. Nevertheless, achieving consistent normalization of blood glucose levels without exogenous insulin remains a challenge in human studies. In the field of gene therapy and stem cell differentiation, research focuses on genetically-modified or progenitor-derived insulin-secreting β-like cells to optimize protocols that ensure safety and functionality. The main challenge is to establish stable and functional cells capable of permanently restoring normoglycemia without the need for external intervention. One major barrier is the immune response, which targets allogeneic and xenogeneic islet grafts. Although, local immunotherapy minimizes the systemic effects, evading graft destruction through biomaterials without the requirement of immune suppression remains a significant challenge. The translation of precision 3D islet constructs and genetically reprogrammed cells also necessitates scalable manufacturing processes to ensure consistent function and long-term safety across batches. When critically appraising progress in the field of cell-based diabetes treatments, it is imperative to consider the regulatory, ethical, economic, and safety factors that shape translational applications. At the regulatory level, oversight bodies play a pivotal role in establishing standards to ensure patient welfare while enabling therapeutic innovation. FDA oversees clinical trials and product approvals in the United States (US), while in Europe the EMA provides parallel regulatory guidance. Within the US, organizations like the United Network for Organ Sharing (UNOS) and Organ Procurement and Transplantation Network (OPTN) govern organ and cell allocation protocols [ 17 , 170 ]. However, as regenerative approaches diverge from traditional organ transplantation, regulatory pathways require ongoing harmonization between the agencies and jurisdictions. Continual dialogue between researchers, oversight boards, and policymakers will be crucial to streamline guidelines in a patient-centric manner that balances safety, efficacy, and timely access to cutting-edge therapies. For instance, as stem cell-derived beta cells and 3D bioprinted tissue constructs emerge, traditional drug and device frameworks may not adequately address product characterization and manufacturing complexities for these advanced therapeutic products [ 67 ]. Within clinics, maintaining compliance with evolving regulations impacts research directives and ultimately patients’ access to the novel treatments. Addressing informed consent, clinical trial design, and privacy protections for sensitive health data are also paramount from an ethical perspective [ 128 , 129 ]. Autonomy and agency of research participants in decision-making related to experimental therapies demand prudency. Equitable accessibility of new treatment options also warrants attention to avoid certain populations facing undue barriers. Cell sourcing presents ethical issues depending on derivation from embryonic, fetal or adult tissues. Logistical matters like shipping and processing stem cell-derived islets prior to transplantation necessitate scrutiny. Tumorigenic potential of the undifferentiated pluripotent stem cells should be optimized through rigorous preclinical testing. Transitioning therapies between animal and early human investigations necessitates well-characterized cellular products showing consistent safety and glucose-responsive insulin secretion profiles comparable to pancreatic islets. Long-term animal model data substantiating lack of malignant transformation following transplantation aids allaying ethical safety concerns as the therapies progress clinically. Researchers carefully screen new concepts to prevent side effects in participants while pursuing curative goals. In terms of economic costs, islet and stem cell transplant procedures remain prohibitively expensive for broad applicability despite promising clinical signals. The field requires sustained study to validate techniques, track long-term outcomes, assess healthcare costs offsets from mitigating diabetes’ debilitating complications, and establish cost-benefit ratios for national reimbursement paradigms. Public-private partnerships may accelerate large, interventional trials and longitudinal research to precisely quantify the cellular therapies’ safety profiles and real-world efficacies compared to intensive management versus costs of intensive diabetes care. Ongoing developments like 3D bioprinting offer catalytic manufacturing potential fundamentally recalibrating economics by enhancing yields, standardizing procedures, and reducing costs through scale. By thoroughly and sensitively examining regulatory frameworks, informed consent processes, risks and benefits, as well as financial considerations at both micro and macro levels, researchers, oversight boards and broader stakeholder networks can advance cell-based therapies towards delivering life-changing benefits for all communities. A multidisciplinary, conscientious approach balances progress against patient welfare. A combination of multiple strategies may help to overcome these limitations. For instance, gene-modified islets integrated within vascularized biomaterial implants or sequenced therapies have promising results to prime grafts in pro-regenerative environments before transplantation. Collaboration across disciplines offers hope that refined individualized therapies may eventually achieve durable insulin independence through functional pancreatic cell or tissue engraftment, not only for diabetes but also for chronic pancreatitis. Regarding, ongoing progresses in unraveling these barriers, cell replacement approaches have the potential to improve diabetes management.
Conclusions
This review provides a comprehensive overview of the advances, challenges, and future directions in various cell-based therapeutic approaches for the treatment of diabetes. Significant progresses have been achieved in microencapsulation design, immunomodulation, tissue constructs, genetic and cellular reprogramming techniques, as well as initial clinical translation. However, the complete restoration of normoglycemia without the need for lifelong immunosuppression is still considered as a significant therapeutic challenge. Therefore, addressing the transplant environment of the hostile nature, developing minimally invasive delivery methods, and overcoming limitations in engraftment efficiency and longevity are crucial issues for the future researches. Through the sustained multidisciplinary efforts for the improvement of existing strategies and establishing novel paradigms, achieving durable insulin independence can be a realistic goal for all diabetic cases through the personalized cell replacement or regeneration.
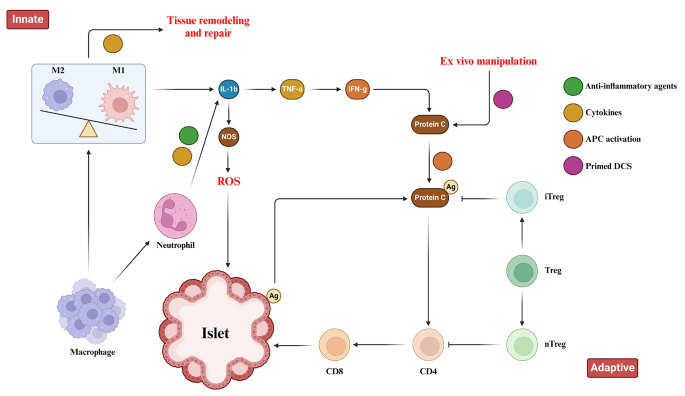
Immune Responses toward pancreatic islets following transplantation. This figure illustrates the immune responses, including the innate and adaptive immunity that are triggered upon pancreatic islet transplantation. Immune response begins with the activation of tissue macrophages and neutrophils in response to injury. Subsequent, release of inflammatory cytokines stimulates antigen-presenting cells (APCs), CD4 + T cells, CD8 + T cells, and cytotoxic T lymphocytes to orchestrate the immune response
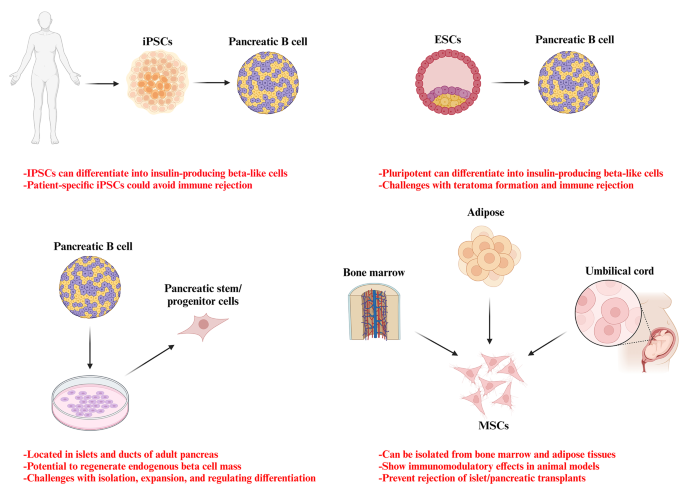
Potential stem cell sources for the treatment of diabetes
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Acrylonitrile butadiene styrene
Activate antigen-presenting cells
Adeno-associated virus
Duodenal homeobox 1
Engineered pseudo islets
Expanded polytetrafluoroethylene
Extracellular matrix
Foreign body response
Fused filament fabrication
Gestational diabetes mellitus
Glucose 6-phosphatase
Insulin-like growth factor binding protein-1
Mesenchymal stem cells
Neurogenin 3
Organ Procurement and Transplantation Network
Phosphoenolpyruvate carboxykinase
Polyaryletherketone
Polycaprolactone
Polycarbonate
Polyetheretherketone
Polyetherimide
Poly-lactic acid
Polystyrene
Stereolithography
Thermoplastic polyurethane
Type 1 diabetes
Type 1 diabetes mellitus
Type 2 diabetes mellitus
United Network for Organ Sharing
United States
Vascular endothelial growth factor
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the global burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22.
Article Google Scholar
Cho NH, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
Article CAS PubMed Google Scholar
Moghbeli M, Naghibzadeh B, Ghahraman M, Fatemi S, Taghavi M, Vakili R, et al. Mutations in HNF1A gene are not a Common cause of familial young-onset diabetes in Iran. Indian J Clin Biochem. 2018;33(1):91–5.
Akhlaghipour I, Bina AR, Mogharrabi MR, Fanoodi A, Ebrahimian AR, Khojasteh Kaffash S, et al. Single-nucleotide polymorphisms as important risk factors of diabetes among Middle East population. Hum Genomics. 2022;16(1):11.
Article CAS PubMed PubMed Central Google Scholar
Moghbeli M, Khedmatgozar H, Yadegari M, Avan A, Ferns GA, Ghayour Mobarhan M. Cytokines and the immune response in obesity-related disorders. Adv Clin Chem. 2021;101:135–68.
Eizirik DL, Pasquali L, Cnop M. Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure. Nat Reviews Endocrinol. 2020;16(7):349–62.
Article CAS Google Scholar
Siqueira ISLd, Alves Guimarães R, Mamed SN, Santos TAP, Rocha SD, Pagotto V, et al. Prevalence and risk factors for self-report diabetes mellitus: a population-based study. Int J Environ Res Public Health. 2020;17(18):6497.
Free radical research.
Zhu B, Qu S. The relationship between diabetes mellitus and cancers and its underlying mechanisms. Front Endocrinol. 2022;13:800995.
Mojarrad M, Moghbeli M. Genetic and molecular biology of bladder cancer among Iranian patients. Mol Genet Genomic Med. 2020;8(6):e1233.
Article PubMed PubMed Central Google Scholar
Moghbeli M. Genetic and molecular biology of breast cancer among Iranian patients. J Transl Med. 2019;17(1):218.
Abbaszadegan MR, Moghbeli M. Genetic and molecular origins of colorectal Cancer among the iranians: an update. Diagn Pathol. 2018;13(1):97.
Kim I. A brief overview of cell therapy and its product. J Korean Association Oral Maxillofacial Surg. 2013;39(5):201.
Mount NM, Ward SJ, Kefalas P, Hyllner J. Cell-based therapy technology classifications and translational challenges. Philosophical Trans Royal Soc B: Biol Sci. 2015;370(1680):20150017.
El-Kadiry AE-H, Rafei M, Shammaa R. Cell therapy: types, regulation, and clinical benefits. Front Med. 2021;8:756029.
Squifflet J-P, Gruessner R, Sutherland D. The history of pancreas transplantation: past, present and future. Acta Chir Belg. 2008;108(3):367–78.
Article PubMed Google Scholar
Parums DV. First Regulatory approval for allogeneic pancreatic islet Beta cell infusion for adult patients with type 1 diabetes Mellitus. Med Sci Monitor: Int Med J Experimental Clin Res. 2023;29:e941918–1.
Yang L, Hu Z-M, Jiang F-X, Wang W. Stem cell therapy for insulin-dependent diabetes: are we still on the road? World J Stem Cells. 2022;14(7):503.
Affan M, Dar MS. Donislecel-the first approved pancreatic islet cell therapy medication for type 1 diabetes: a letter to the editor. Ir J Med Sci (1971-). 2023:1–2.
Harris E. FDA greenlights first cell therapy for adults with type 1 diabetes. JAMA. 2023.
Soon-Shiong P, Heintz R, Merideth N, Yao Q, Yao Z, Zheng T, et al. Insulin independence in a type 1 diabetic patient after encapsulated islet transplantation. Lancet (London England). 1994;343(8903):950–1.
Calafiore R, Basta G, Luca G, Lemmi A, Montanucci MP, Calabrese G, et al. Microencapsulated pancreatic islet allografts into nonimmunosuppressed patients with type 1 diabetes: first two cases. Diabetes Care. 2006;29(1):137–8.
Tuch BE, Keogh GW, Williams LJ, Wu W, Foster JL, Vaithilingam V, et al. Safety and viability of microencapsulated human islets transplanted into diabetic humans. Diabetes Care. 2009;32(10):1887–9.
Weng L, Wang X, Liu H, Yu Z, Liu S. Light-responsive microneedle array with tunable insulin release function for painless and on-demand anti-diabetic therapy. Mater Lett. 2023:135684.
Okcu A, Yazir Y, Şimşek T, Mert S, Duruksu G, Öztürk A, et al. Investigation of the effect of pancreatic decellularized matrix on encapsulated islets of Langerhans with mesenchymal stem cells. Tissue Cell. 2023;82:102110.
Khaliq T, Sohail M, Minhas MU, Mahmood A, Munir A, Qalawlus AHM, et al. Hyaluronic acid/alginate-based biomimetic hydrogel membranes for accelerated diabetic wound repair. Int J Pharm. 2023;643:123244.
Kuwabara R, Qin T, Llacua LA, Hu S, Boekschoten MV, de Haan BJ, et al. Extracellular matrix inclusion in immunoisolating alginate-based microcapsules promotes longevity, reduces fibrosis, and supports function of islet allografts in vivo. Acta Biomater. 2023;158:151–62.
Kirk K, Hao E, Lahmy R, Itkin-Ansari P. Human embryonic stem cell derived islet progenitors mature inside an encapsulation device without evidence of increased biomass or cell escape. Stem cell Res. 2014;12(3):807–14.
Dufrane D, van Steenberghe M, Goebbels R-M, Saliez A, Guiot Y, Gianello P. The influence of implantation site on the biocompatibility and survival of alginate encapsulated pig islets in rats. Biomaterials. 2006;27(17):3201–8.
Pullen LC. Stem cell–derived pancreatic progenitor cells have now been transplanted into patients: report from IPITA 2018. Wiley Online Library; 2018. pp. 1581–2.
Dang HP, Chen H, Dargaville TR, Tuch BE. Cell delivery systems: toward the next generation of cell therapies for type 1 diabetes. J Cell Mol Med. 2022;26(18):4756–67.
Viacyte. ViaCyte and gore enter clinical phase agreement based on novel membrane technology for PEC-encap product candidate. 2020.
Viacyte. viacyte announces initiation of phase 2 study of encapsulated cell therapy for type 1 diabetes patients 2021 2021. https://viacyte.com/press-releases/viacyte‐announces‐initiation‐of‐phase‐2‐study‐of‐encapsulated‐cell‐ther‐apy‐for‐type‐1‐diabetes‐patients/ .
Hodgson J. Drug pipeline 3Q23—ERT, bispecifics and CRISPR in sickle cell disease. Nat Biotechnol. 2023;41(11):1498–500.
Pagliuca F. Pre-clinical proof-of-Concept in two lead programs in type 1 diabetes. International Socety for Stem Cell Research; 2019.
Jones PM, Persaud SJ. β-cell replacement therapy for type 1 diabetes: closer and closer. Diabet Med. 2022;39(6).
Carlsson P-O, Espes D, Sedigh A, Rotem A, Zimerman B, Grinberg H, et al. Transplantation of macroencapsulated human islets within the bioartificial pancreas βAir to patients with type 1 diabetes mellitus. Am J Transplant. 2018;18(7):1735–44.
Ludwig B, Zimerman B, Steffen A, Yavriants K, Azarov D, Reichel A, et al. A novel device for islet transplantation providing immune protection and oxygen supply. Horm Metab Res. 2010;42(13):918–22.
Evron Y, Colton CK, Ludwig B, Weir GC, Zimermann B, Maimon S, et al. Long-term viability and function of transplanted islets macroencapsulated at high density are achieved by enhanced oxygen supply. Sci Rep. 2018;8(1):6508.
Cao R, Avgoustiniatos E, Papas K, de Vos P, Lakey JR. Mathematical predictions of oxygen availability in micro-and macro‐encapsulated human and porcine pancreatic islets. J Biomedical Mater Res Part B: Appl Biomaterials. 2020;108(2):343–52.
Gala-Lopez B, Pepper A, Dinyari P, Malcolm A, Kin T, Pawlick L, et al. Subcutaneous clinical islet transplantation in a prevascularized subcutaneous pouch–preliminary experience. CellR4. 2016;4(5):e2132.
Google Scholar
Sernova Corp Presents Positive Preliminary. Safety and Efficacy Data in its Phase I/II Clinical Trial for Type-1 Diabetes: Biospace. https://www.biospace.com/article/sernova‐corp‐presents‐positive‐preliminary‐safety‐and‐efficacy‐data‐in‐its‐phase‐i‐ii‐clinical‐trial‐for‐type‐1‐diabetes/ .
Bachul PJ, Perez-Gutierrez A, Juengel B, Golab K, Basto L, Perea L et al. 306-OR: modified approach for improved isllotransplantation into prevascularized sernova cell pouch device: preliminary results of the phase i/ii clinical trial at University of Chicago. Diabetes. 2022;71(Supplement_1).
Vegas AJ, Veiseh O, Doloff JC, Ma M, Tam HH, Bratlie K, et al. Combinatorial hydrogel library enables identification of materials that mitigate the foreign body response in primates. Nat Biotechnol. 2016;34(3):345–52.
Vegas AJ, Veiseh O, Gürtler M, Millman JR, Pagliuca FW, Bader AR, et al. Long-term glycemic control using polymer-encapsulated human stem cell–derived beta cells in immune-competent mice. Nat Med. 2016;22(3):306–11.
Shapiro AD, Konkle BA, Croteau SE, Miesbach WA, Hay CRM, Kazmi R, et al. First-in-human phase 1/2 clinical trial of SIG-001, an innovative shielded cell therapy platform, for hemophilia Α. Blood. 2020;136:8.
Taraballi F, Sushnitha M, Tsao C, Bauza G, Liverani C, Shi A, et al. Biomimetic tissue engineering: tuning the immune and inflammatory response to implantable biomaterials. Adv Healthc Mater. 2018;7(17):1800490.
Yesilyurt V, Veiseh O, Doloff JC, Li J, Bose S, Xie X, et al. A facile and versatile method to endow biomaterial devices with zwitterionic surface coatings. Adv Healthc Mater. 2017;6(4):1601091.
Liu Q, Chiu A, Wang L-H, An D, Zhong M, Smink AM, et al. Zwitterionically modified alginates mitigate cellular overgrowth for cell encapsulation. Nat Commun. 2019;10(1):5262.
Noverraz F, Montanari E, Pimenta J, Szabó L, Ortiz D, Gonelle-Gispert C, et al. Antifibrotic effect of ketoprofen-grafted alginate microcapsules in the transplantation of insulin producing cells. Bioconjug Chem. 2018;29(6):1932–41.
Jeon SI, Jeong J-H, Kim JE, Haque MR, Kim J, Byun Y, et al. Synthesis of PEG-dendron for surface modification of pancreatic islets and suppression of the immune response. J Mater Chem B. 2021;9(11):2631–40.
Derakhshankhah H, Sajadimajd S, Jahanshahi F, Samsonchi Z, Karimi H, Hajizadeh-Saffar E, et al. Immunoengineering Biomaterials in Cell-based therapy for type 1 diabetes. Tissue Eng Part B: Reviews. 2022;28(5):1053–66.
Piemonti L, Maffi P, Nano R, Bertuzzi F, Melzi R, Mercalli A, et al. Treating diabetes with islet transplantation: lessons from the Milan experience. Transplantation, Bioengineering, and regeneration of the endocrine pancreas. Elsevier; 2020. pp. 645–58.
Azzi J, Tang L, Moore R, Tong R, El Haddad N, Akiyoshi T, et al. Polylactide-cyclosporin A nanoparticles for targeted immunosuppression. FASEB J. 2010;24(10):3927.
Chen X, Liu H, Li H, Cheng Y, Yang L, Liu Y. In vitro expansion and differentiation of rat pancreatic duct-derived stem cells into insulin secreting cells using a dynamic three-dimensional cell culture system. Genet Mol Res. 2016;15(2).
Becker MW, Simonovich JA, Phelps EA. Engineered microenvironments and microdevices for modeling the pathophysiology of type 1 diabetes. Biomaterials. 2019;198:49–62.
Graham JG, Zhang X, Goodman A, Pothoven K, Houlihan J, Wang S, et al. PLG scaffold delivered antigen-specific regulatory T cells induce systemic tolerance in autoimmune diabetes. Tissue Eng Part A. 2013;19(11–12):1465–75.
Izadi Z, Hajizadeh-Saffar E, Hadjati J, Habibi-Anbouhi M, Ghanian MH, Sadeghi-Abandansari H, et al. Tolerance induction by surface immobilization of Jagged-1 for immunoprotection of pancreatic islets. Biomaterials. 2018;182:191–201.
McHugh MD, Park J, Uhrich R, Gao W, Horwitz DA, Fahmy TM. Paracrine co-delivery of TGF-β and IL-2 using CD4-targeted nanoparticles for induction and maintenance of regulatory T cells. Biomaterials. 2015;59:172–81.
Chen H, Teramura Y, Iwata H. Co-immobilization of urokinase and thrombomodulin on islet surfaces by poly (ethylene glycol)-conjugated phospholipid. J Controlled Release. 2011;150(2):229–34.
Su J, Hu B-H, Lowe WL Jr, Kaufman DB, Messersmith PB. Anti-inflammatory peptide-functionalized hydrogels for insulin-secreting cell encapsulation. Biomaterials. 2010;31(2):308–14.
Dong H, Fahmy TM, Metcalfe SM, Morton SL, Dong X, Inverardi L, et al. Immuno-isolation of pancreatic islet allografts using pegylated nanotherapy leads to long-term normoglycemia in full MHC mismatch recipient mice. PLoS ONE. 2012;7(12):e50265.
Kumar M, Nandi SK, Kaplan DL, Mandal BB. Localized immunomodulatory silk macrocapsules for islet-like spheroid formation and sustained insulin production. ACS Biomaterials Sci Eng. 2017;3(10):2443–56.
Hotaling NA, Tang L, Irvine DJ, Babensee JE. Biomaterial Strategies for Immunomodulation. Annu Rev Biomed Eng. 2015;17:317–49.
Shi Y, Zhao YZ, Jiang Z, Wang Z, Wang Q, Kou L, et al. Immune-Protective formulations and process strategies for improved survival and function of transplanted islets. Front Immunol. 2022;13:923241.
Zhang S, Yang H, Wang M, Mantovani D, Yang K, Witte F, et al. Immunomodulatory biomaterials against bacterial infections: Progress, challenges, and future perspectives. Innovation. 2023;4(6):100503.
CAS PubMed PubMed Central Google Scholar
Accolla RP, Simmons AM, Stabler CL. Integrating Additive Manufacturing techniques to improve cell-based implants for the treatment of type 1 diabetes. Adv Healthc Mater. 2022;11(13):e2200243.
Gross BC, Erkal JL, Lockwood SY, Chen C, Spence DM. Evaluation of 3D printing and its potential impact on biotechnology and the chemical sciences. ACS; 2014.
Bol RJ, Šavija B. Micromechanical models for FDM 3D-Printed polymers: a review. Polymers. 2023;15(23):4497.
Paul S. Finite element analysis in fused deposition modeling research: a literature review. Measurement. 2021;178:109320.
Monaldo E, Ricci M, Marfia S. Mechanical properties of 3D printed polylactic acid elements: experimental and numerical insights. Mech Mater. 2023;177:104551.
Anoop M, Senthil P. Microscale representative volume element based numerical analysis on mechanical properties of fused deposition modelling components. Materials Today: Proceedings. 2021;39:563 – 71.
McGuigan AP, Sefton MV. Vascularized organoid engineered by modular assembly enables blood perfusion. Proceedings of the National Academy of Sciences. 2006;103(31):11461-6.
Pedraza E, Coronel MM, Fraker CA, Ricordi C, Stabler CL. Preventing hypoxia-induced cell death in beta cells and islets via hydrolytically activated, oxygen-generating biomaterials. Proceedings of the National Academy of Sciences. 2012;109(11):4245-50.
Espona-Noguera A, Ciriza J, Cañibano-Hernández A, Orive G, Hernández RM, del Saenz L, et al. Review of advanced hydrogel-based cell encapsulation systems for insulin delivery in type 1 diabetes mellitus. Pharmaceutics. 2019;11(11):597.
Dimitrioglou N, Kanelli M, Papageorgiou E, Karatzas T, Hatziavramidis D. Paving the way for successful islet encapsulation. Drug Discovery Today. 2019;24(3):737–48.
Omer A, Duvivier-Kali V, Fernandes J, Tchipashvili V, Colton CK, Weir GC. Long-term normoglycemia in rats receiving transplants with encapsulated islets. Transplantation. 2005;79(1):52–8.
Song S, Roy S. Progress and challenges in macroencapsulation approaches for type 1 diabetes (T1D) treatment: cells, biomaterials, and devices. Biotechnol Bioeng. 2016;113(7):1381–402.
Zhi ZL, Kerby A, King AJF, Jones PM, Pickup JC. Nano-scale encapsulation enhances allograft survival and function of islets transplanted in a mouse model of diabetes. Diabetologia. 2012;55(4):1081–90.
Farina M, Chua CYX, Ballerini A, Thekkedath U, Alexander JF, Rhudy JR, et al. Transcutaneously refillable, 3D-printed biopolymeric encapsulation system for the transplantation of endocrine cells. Biomaterials. 2018;177:125–38.
Farina M, Ballerini A, Fraga DW, Nicolov E, Hogan M, Demarchi D et al. 3D printed vascularized device for Subcutaneous Transplantation of Human islets. Biotechnol J. 2017;12(9).
Lei D, Yang Y, Liu Z, Yang B, Gong W, Chen S, et al. 3D printing of biomimetic vasculature for tissue regeneration. Mater Horiz. 2019;6(6):1197–206.
Melchels FP, Domingos MA, Klein TJ, Malda J, Bartolo PJ, Hutmacher DW. Additive manufacturing of tissues and organs. Prog Polym Sci. 2012;37(8):1079–104.
Ernst AU, Wang LH, Ma M. Interconnected toroidal hydrogels for islet encapsulation. Adv Healthc Mater. 2019;8(12):1900423.
Liang J-P, Accolla RP, Jiang K, Li Y, Stabler CL. Controlled release of anti-inflammatory and proangiogenic factors from macroporous scaffolds. Tissue Eng Part A. 2021;27(19–20):1275–89.
Pedraza E, Brady A-C, Fraker CA, Molano RD, Sukert S, Berman DM, et al. Macroporous three-dimensional PDMS scaffolds for extrahepatic islet transplantation. Cell Transplant. 2013;22(7):1123–35.
Chiu Y-C, Cheng M-H, Engel H, Kao S-W, Larson JC, Gupta S, et al. The role of pore size on vascularization and tissue remodeling in PEG hydrogels. Biomaterials. 2011;32(26):6045–51.
Kuss MA, Wu S, Wang Y, Untrauer JB, Li W, Lim JY, et al. Prevascularization of 3D printed bone scaffolds by bioactive hydrogels and cell co-culture. J Biomedical Mater Res Part B: Appl Biomaterials. 2018;106(5):1788–98.
Liu X, Jakus AE, Kural M, Qian H, Engler A, Ghaedi M, et al. Vascularization of natural and synthetic bone scaffolds. Cell Transplant. 2018;27(8):1269–80.
Costa-Almeida R, Gomez-Lazaro M, Ramalho C, Granja PL, Soares R, Guerreiro SG. Fibroblast-endothelial partners for vascularization strategies in tissue engineering. Tissue Eng Part A. 2015;21(5–6):1055–65.
Newman AC, Nakatsu MN, Chou W, Gershon PD, Hughes CC. The requirement for fibroblasts in angiogenesis: fibroblast-derived matrix proteins are essential for endothelial cell lumen formation. Mol Biol Cell. 2011;22(20):3791–800.
Vlahos AE, Cober N, Sefton MV. Modular tissue engineering for the vascularization of subcutaneously transplanted pancreatic islets. Proceedings of the National Academy of Sciences. 2017;114(35):9337-42.
Farina M, Ballerini A, Fraga DW, Nicolov E, Hogan M, Demarchi D, et al. 3D printed vascularized device for subcutaneous transplantation of human islets. Biotechnol J. 2017;12(9):1700169.
Bertassoni LE, Cecconi M, Manoharan V, Nikkhah M, Hjortnaes J, Cristino AL, et al. Hydrogel bioprinted microchannel networks for vascularization of tissue engineering constructs. Lab Chip. 2014;14(13):2202–11.
Jia W, Gungor-Ozkerim PS, Zhang YS, Yue K, Zhu K, Liu W, et al. Direct 3D bioprinting of perfusable vascular constructs using a blend bioink. Biomaterials. 2016;106:58–68.
Gao Q, Liu Z, Lin Z, Qiu J, Liu Y, Liu A, et al. 3D bioprinting of vessel-like structures with multilevel fluidic channels. ACS Biomaterials Sci Eng. 2017;3(3):399–408.
Noor N, Shapira A, Edri R, Gal I, Wertheim L, Dvir T. 3D printing of personalized thick and perfusable cardiac patches and hearts. Adv Sci. 2019;6(11):1900344.
Hospodiuk M, Dey M, Ayan B, Sosnoski D, Moncal KK, Wu Y, et al. Sprouting angiogenesis in engineered pseudo islets. Biofabrication. 2018;10(3):035003.
Marchioli G, Luca AD, de Koning E, Engelse M, Van Blitterswijk CA, Karperien M, et al. Hybrid polycaprolactone/alginate scaffolds functionalized with VEGF to promote de novo vessel formation for the transplantation of islets of Langerhans. Adv Healthc Mater. 2016;5(13):1606–16.
Dionne KE, Colton CK, Lyarmush M. Effect of hypoxia on insulin secretion by isolated rat and canine islets of Langerhans. Diabetes. 1993;42(1):12–21.
de Groot M, Schuurs TA, Keizer PP, Fekken S, Leuvenink HG, Van Schilfgaarde R. Response of encapsulated rat pancreatic islets to hypoxia. Cell Transplant. 2003;12(8):867–75.
Thomas F, Wu J, Contreras JL, Smyth C, Bilbao G, He J, et al. A tripartite anoikis-like mechanism causes early isolated islet apoptosis. Surgery. 2001;130(2):333–8.
Barkai U, Rotem A, de Vos P. Survival of encapsulated islets: more than a membrane story. World J Transplantation. 2016;6(1):69.
Jiang K, Chaimov D, Patel SN, Liang JP, Wiggins SC, Samojlik MM, et al. 3-D physiomimetic extracellular matrix hydrogels provide a supportive microenvironment for rodent and human islet culture. Biomaterials. 2019;198:37–48.
Pati F, Jang J, Ha D, Won Kim S, Rhie J, Shim J, et al. Printing three-dimensional tissue analogues with decellularized extracellular matrix bioink. Nat Commun. 2014;5:3935.
Kim BS, Kwon YW, Kong J-S, Park GT, Gao G, Han W, et al. 3D cell printing of in vitro stabilized skin model and in vivo pre-vascularized skin patch using tissue-specific extracellular matrix bioink: a step towards advanced skin tissue engineering. Biomaterials. 2018;168:38–53.
Hu S, Martinez-Garcia FD, Moeun BN, Burgess JK, Harmsen MC, Hoesli C, et al. An immune regulatory 3D-printed alginate-pectin construct for immunoisolation of insulin producing β-cells. Mater Sci Engineering: C. 2021;123:112009.
Phelps EA, Templeman KL, Thulé PM, García AJ. Engineered VEGF-releasing PEG–MAL hydrogel for pancreatic islet vascularization. Drug Delivery Translational Res. 2015;5:125–36.
Kooptiwut S, Kaewin S, Semprasert N, Sujjitjoon J, Junking M, Suksri K, et al. Estradiol prevents high glucose-induced β-cell apoptosis by decreased BTG2 expression. Sci Rep. 2018;8(1):12256.
Dang TT, Thai AV, Cohen J, Slosberg JE, Siniakowicz K, Doloff JC, et al. Enhanced function of immuno-isolated islets in diabetes therapy by co-encapsulation with an anti-inflammatory drug. Biomaterials. 2013;34(23):5792–801.
Wang Y, He D, Ni C, Zhou H, Wu S, Xue Z, et al. Vitamin D induces autophagy of pancreatic β-cells and enhances insulin secretion. Mol Med Rep. 2016;14(3):2644–50.
Tarafder S, Koch A, Jun Y, Chou C, Awadallah MR, Lee CH. Micro-precise spatiotemporal delivery system embedded in 3D printing for complex tissue regeneration. Biofabrication. 2016;8(2):025003.
Liu YY, Yu HC, Liu Y, Liang G, Zhang T, Hu QX. Dual drug spatiotemporal release from functional gradient scaffolds prepared using 3 D bioprinting and electrospinning. Polym Eng Sci. 2016;56(2):170–7.
Freeman FE, Pitacco P, van Dommelen LH, Nulty J, Browe DC, Shin J-Y, et al. 3D bioprinting spatiotemporally defined patterns of growth factors to tightly control tissue regeneration. Sci Adv. 2020;6(33):eabb5093.
Wong MS, Hawthorne WJ, Manolios N. Gene therapy in diabetes. Self Nonself. 2010;1(3):165.
Ahmad Z, Rasouli M, Azman AZF, Omar AR. Evaluation of insulin expression and secretion in genetically engineered gut K and L-cells. BMC Biotechnol. 2012;12:1–9.
Tudurí E, Bruin JE, Kieffer TJ. Restoring insulin production for type 1 diabetes. J Diabetes. 2012;4(4):319–31.
Romer AI, Sussel L. Pancreatic islet cell development and regeneration. Current opinion in endocrinology, diabetes, and obesity. 2015;22(4):255.
Jaén ML, Vilà L, Elias I, Jimenez V, Rodó J, Maggioni L, et al. Long-term efficacy and safety of insulin and glucokinase gene therapy for diabetes: 8-year follow-up in dogs. Mol therapy-methods Clin Dev. 2017;6:1–7.
Li H, Li X, Lam KS, Tam S, Xiao W, Xu R. Adeno-associated virus-mediated pancreatic and duodenal homeobox gene-1 expression enhanced differentiation of hepatic oval stem cells to insulin-producing cells in diabetic rats. J Biomed Sci. 2008;15:487–97.
Schwitzgebel VM, Scheel DW, Conners JR, Kalamaras J, Lee JE, Anderson DJ, et al. Expression of neurogenin3 reveals an islet cell precursor population in the pancreas. Development. 2000;127(16):3533–42.
Abed A, Critchlow C, Flatt PR, McClenaghan NH, Kelly C. Directed differentiation of progenitor cells towards an islet-cell phenotype. Am J Stem Cells. 2012;1(3):196.
PubMed PubMed Central Google Scholar
Zhao M, Amiel SA, Ajami S, Jiang J, Rela M, Heaton N, et al. Amelioration of streptozotocin-induced diabetes in mice with cells derived from human marrow stromal cells. PLoS ONE. 2008;3(7):e2666.
Handorf AM, Sollinger HW, Alam T. Genetic engineering of surrogate β cells for treatment of type 1 diabetes mellitus. J Diabetes Mellitus. 2015;5(04):295–312.
Grant MB, Adu-Agyeiwaah Y, Vieira CP, Asare-Bediako B, Hammer SS, Calzi SL, et al. Intravitreal administration of AAV2-SIRT1 reverses diabetic retinopathy (DR) in a murine model of type 2 diabetes (T2D). Investig Ophthalmol Vis Sci. 2022;63(7):2310.
Yoon J-W, Jun H-S. Recent advances in insulin gene therapy for type 1 diabetes. Trends Mol Med. 2002;8(2):62–8.
Hou W-R, Xie S-N, Wang H-J, Su Y-Y, Lu J-L, Li L-L, et al. Intramuscular delivery of a naked DNA plasmid encoding proinsulin and pancreatic regenerating III protein ameliorates type 1 diabetes mellitus. Pharmacol Res. 2011;63(4):320–7.
Joo WS, Jeong JH, Nam K, Blevins KS, Salama ME, Kim SW. Polymeric delivery of therapeutic RAE-1 plasmid to the pancreatic islets for the prevention of type 1 diabetes. J Controlled Release. 2012;162(3):606–11.
Dezashibi HM, Shabani A. A Mini-review of Current Treatment approaches and Gene Therapy as potential interventions for diabetes Mellitus types 1. Adv Biomed Res. 2023;12:219.
Vantyghem M-C, de Koning EJ, Pattou F, Rickels MR. Advances in β-cell replacement therapy for the treatment of type 1 diabetes. Lancet. 2019;394(10205):1274–85.
Hudson A, Bradbury L, Johnson R, Fuggle S, Shaw J, Casey J, et al. The UK pancreas allocation scheme for whole organ and islet transplantation. Am J Transplant. 2015;15(9):2443–55.
Cornateanu SM, O’Neill S, Dholakia S, Counter CJ, Sherif AE, Casey JJ, et al. Pancreas utilization rates in the UK–an 11-year analysis. Transpl Int. 2021;34(7):1306–18.
Nordheim E, Lindahl JP, Carlsen RK, Åsberg A, Birkeland KI, Horneland R, et al. Patient selection for islet or solid organ pancreas transplantation: experiences from a multidisciplinary outpatient-clinic approach. Endocr Connections. 2021;10(2):230–9.
Arifin DR, Bulte JW. In vivo imaging of pancreatic islet grafts in diabetes treatment. Front Endocrinol. 2021;12:640117.
Murakami T, Fujimoto H, Inagaki N. Non-invasive beta-cell imaging: visualization, quantification, and beyond. Front Endocrinol. 2021;12:714348.
Piemonti L, Everly MJ, Maffi P, Scavini M, Poli F, Nano R, et al. Alloantibody and autoantibody monitoring predicts islet transplantation outcome in human type 1 diabetes. Diabetes. 2013;62(5):1656–64.
Anteby R, Lucander A, Bachul PJ, Pyda J, Grybowski D, Basto L, et al. Evaluating the prognostic value of islet autoantibody monitoring in islet transplant recipients with long-standing type 1 diabetes mellitus. J Clin Med. 2021;10(12):2708.
Buron F, Reffet S, Badet L, Morelon E, Thaunat O. Immunological monitoring in beta cell replacement: towards a pathophysiology-guided implementation of biomarkers. Curr Diab Rep. 2021;21:1–11.
Cantarelli E, Piemonti L. Alternative transplantation sites for pancreatic islet grafts. Curr Diab Rep. 2011;11:364–74.
Tremmel DM, Odorico JS. Rebuilding a better home for transplanted islets. Organogenesis. 2018;14(4):163–8.
Citro A, Moser PT, Dugnani E, Rajab TK, Ren X, Evangelista-Leite D, et al. Biofabrication of a vascularized islet organ for type 1 diabetes. Biomaterials. 2019;199:40–51.
Basta G, Montanucci P, Calafiore R. Microencapsulation of cells and molecular therapy of type 1 diabetes mellitus: the actual state and future perspectives between promise and progress. J Diabetes Invest. 2021;12(3):301–9.
Samojlik MM, Stabler CL. Designing biomaterials for the modulation of allogeneic and autoimmune responses to cellular implants in type 1 diabetes. Acta Biomater. 2021;133:87–101.
Carlsson P-O, Schwarcz E, Korsgren O, Le Blanc K. Preserved β-cell function in type 1 diabetes by mesenchymal stromal cells. Diabetes. 2015;64(2):587–92.
Madani S, Setudeh A, Aghayan HR, Alavi-Moghadam S, Rouhifard M, Rezaei N, et al. Placenta derived mesenchymal stem cells transplantation in type 1 diabetes: preliminary report of phase 1 clinical trial. J Diabetes Metabolic Disorders. 2021;20:1179–89.
Pagliuca FW, Millman JR, Gürtler M, Segel M, Van Dervort A, Ryu JH, et al. Generation of functional human pancreatic β cells in vitro. Cell. 2014;159(2):428–39.
Russ HA, Parent AV, Ringler JJ, Hennings TG, Nair GG, Shveygert M, et al. Controlled induction of human pancreatic progenitors produces functional beta-like cells in vitro. EMBO J. 2015;34(13):1759–72.
Sambathkumar R, Migliorini A, Nostro MC. Pluripotent stem cell-derived pancreatic progenitors and β-like cells for type 1 diabetes treatment. Physiology. 2018;33(6):394–402.
Sordi V, Monaco L, Piemonti L. Cell therapy for type 1 diabetes: from islet transplantation to stem cells. Hormone Res Paediatrics. 2022;96(6):658–69.
Henry RR, Pettus J, Wilensky J, SHAPIRO AJ, Senior PA, Roep B et al. Initial clinical evaluation of VC-01TM combination product—a stem cell–derived islet replacement for type 1 diabetes (T1D). Diabetes. 2018;67(Supplement_1).
Shapiro A, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus JH et al. Insulin expression and glucose-responsive circulating C-peptide in type 1 diabetes patients implanted subcutaneously with pluripotent stem cell-derived pancreatic endoderm cells in a macro-device. David and Donner, Thomas W and Bellin, Melena D and Hsueh, Willa and Pettus, Jeremy H and Wilensky, Jon S and Daniels, Mark and Wang, Richard M and Kroon, Evert J and Brandon, Eugene Paul and D’Amour, Kevin A and Foyt, Howard, Insulin Expression and Glucose-Responsive Circulating C-Peptide in Type. 2019;1.
Keymeulen B, Jacobs-Tulleneers-Thevissen D, Kroon EJ, Jaiman MS, Daniels M, Wang R et al. 196-LB: stem cell–derived islet replacement therapy (VC-02) demonstrates production of C-peptide in patients with type 1 diabetes (T1D) and hypoglycemia unawareness. Diabetes. 2021;70(Supplement_1).
Piemonti L. Felix dies natalis, insulin… ceterum autem censeo beta is better. Acta Diabetol. 2021;58(10):1287–306.
Sordi V, Pellegrini S, Piemonti L. Immunological issues after stem cell-based β cell replacement. Curr Diab Rep. 2017;17:1–8.
Coe TM, Markmann JF, Rickert CG. Current status of porcine islet xenotransplantation. Curr Opin Organ Transpl. 2020;25(5):449–56.
Edgar L, Pu T, Porter B, Aziz J, La Pointe C, Asthana A, et al. Regenerative medicine, organ bioengineering and transplantation. J Br Surg. 2020;107(7):793–800.
Mathur A, Taurin S, Alshammary S. The safety and efficacy of mesenchymal stem cells in the treatment of type 2 Diabetes- A literature review. Diabetes Metab Syndr Obes. 2023;16:769–77.
Hogrebe NJ, Ishahak M, Millman JR. Developments in stem cell-derived islet replacement therapy for treating type 1 diabetes. Cell Stem Cell. 2023;30(5):530–48.
Paraskevas S, Maysinger D, Wang R, Duguid WP, Rosenberg L. Cell loss in isolated human islets occurs by apoptosis. Pancreas. 2000;20(3):270–6.
Kelly OG, Chan MY, Martinson LA, Kadoya K, Ostertag TM, Ross KG, et al. Cell-surface markers for the isolation of pancreatic cell types derived from human embryonic stem cells. Nat Biotechnol. 2011;29(8):750–6.
Rezania A, Bruin JE, Riedel MJ, Mojibian M, Asadi A, Xu J, et al. Maturation of human embryonic stem cell–derived pancreatic progenitors into functional islets capable of treating pre-existing diabetes in mice. Diabetes. 2012;61(8):2016–29.
Kroon E, Martinson LA, Kadoya K, Bang AG, Kelly OG, Eliazer S, et al. Pancreatic endoderm derived from human embryonic stem cells generates glucose-responsive insulin-secreting cells in vivo. Nat Biotechnol. 2008;26(4):443–52.
Agulnick AD, Ambruzs DM, Moorman MA, Bhoumik A, Cesario RM, Payne JK, et al. Insulin-producing endocrine cells differentiated in vitro from human embryonic stem cells function in macroencapsulation devices in vivo. Stem Cells Translational Med. 2015;4(10):1214–22.
Ramzy A, Thompson DM, Ward-Hartstonge KA, Ivison S, Cook L, Garcia RV, et al. Implanted pluripotent stem-cell-derived pancreatic endoderm cells secrete glucose-responsive C-peptide in patients with type 1 diabetes. Cell Stem Cell. 2021;28(12):2047–61. e5.
Dolgin E, Diabetes. Encapsulating the problem. Nature. 2016;540(7632):S60–2.
Rezania A, Bruin JE, Arora P, Rubin A, Batushansky I, Asadi A, et al. Reversal of diabetes with insulin-producing cells derived in vitro from human pluripotent stem cells. Nat Biotechnol. 2014;32(11):1121–33.
Hogrebe NJ, Augsornworawat P, Maxwell KG, Velazco-Cruz L, Millman JR. Targeting the cytoskeleton to direct pancreatic differentiation of human pluripotent stem cells. Nat Biotechnol. 2020;38(4):460–70.
Nair GG, Liu JS, Russ HA, Tran S, Saxton MS, Chen R, et al. Recapitulating endocrine cell clustering in culture promotes maturation of human stem-cell-derived β cells. Nat Cell Biol. 2019;21(2):263–74.
Shapiro AJ, Thompson D, Donner TW, Bellin MD, Hsueh W, Pettus J et al. Insulin expression and C-peptide in type 1 diabetes subjects implanted with stem cell-derived pancreatic endoderm cells in an encapsulation device. Cell Rep Med. 2021;2(12).
Witkowski P, Anteby R, Olaitan OK, Forbes RC, Niederhaus S, Ricordi C, et al. Pancreatic islets Quality and Potency cannot be verified as required for drugs: reflection on the FDA Review of a biological license application for human islets. Transplantation. 2021;105(12):e409–10.
Download references
Acknowledgements
Author information, authors and affiliations.
Noncommunicable Diseases Research Center, Neyshabur University of Medical Sciences, Neyshabur, Iran
Ramin Raoufinia
Department of Medical Genetics and Molecular Medicine, School of Medicine, Mashhad University of Medical Sciences, Mashhad, Iran
Ramin Raoufinia, Hamid Reza Rahimi, Ehsan Saburi & Meysam Moghbeli
You can also search for this author in PubMed Google Scholar
Contributions
RR, HRR, and ES were involved in search strategy and drafting. MM revised, designed, and supervised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Meysam Moghbeli .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Raoufinia, R., Rahimi, H.R., Saburi, E. et al. Advances and challenges of the cell-based therapies among diabetic patients. J Transl Med 22 , 435 (2024). https://doi.org/10.1186/s12967-024-05226-3
Download citation
Received : 14 February 2024
Accepted : 22 April 2024
Published : 08 May 2024
DOI : https://doi.org/10.1186/s12967-024-05226-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cell therapy
- Translplantation
- Immunosuppression
Journal of Translational Medicine
ISSN: 1479-5876
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 13 May 2024
The impact of the world’s first regulatory, multi-setting intervention on sedentary behaviour among children and adolescents (ENERGISE): a natural experiment evaluation
- Bai Li ORCID: orcid.org/0000-0003-2706-9799 1 ,
- Selene Valerino-Perea 2 ,
- Weiwen Zhou 3 ,
- Yihong Xie 4 ,
- Keith Syrett 5 ,
- Remco Peters 1 ,
- Zouyan He 4 ,
- Yunfeng Zou 4 ,
- Frank de Vocht 6 , 7 &
- Charlie Foster 1
International Journal of Behavioral Nutrition and Physical Activity volume 21 , Article number: 53 ( 2024 ) Cite this article
507 Accesses
122 Altmetric
Metrics details
Regulatory actions are increasingly used to tackle issues such as excessive alcohol or sugar intake, but such actions to reduce sedentary behaviour remain scarce. World Health Organization (WHO) guidelines on sedentary behaviour call for system-wide policies. The Chinese government introduced the world’s first nation-wide multi-setting regulation on multiple types of sedentary behaviour in children and adolescents in July 2021. This regulation restricts when (and for how long) online gaming businesses can provide access to pupils; the amount of homework teachers can assign to pupils according to their year groups; and when tutoring businesses can provide lessons to pupils. We evaluated the effect of this regulation on sedentary behaviour safeguarding pupils.
With a natural experiment evaluation design, we used representative surveillance data from 9- to 18-year-old pupils before and after the introduction of the regulation, for longitudinal ( n = 7,054, matched individuals, primary analysis) and repeated cross-sectional ( n = 99,947, exploratory analysis) analyses. We analysed pre-post differences for self-reported sedentary behaviour outcomes (total sedentary behaviour time, screen viewing time, electronic device use time, homework time, and out-of-campus learning time) using multilevel models, and explored differences by sex, education stage, residency, and baseline weight status.
Longitudinal analyses indicated that pupils had reduced their mean total daily sedentary behaviour time by 13.8% (95% confidence interval [CI]: -15.9 to -11.7%, approximately 46 min) and were 1.20 times as likely to meet international daily screen time recommendations (95% CI: 1.01 to 1.32) one month after the introduction of the regulation compared to the reference group (before its introduction). They were on average 2.79 times as likely to meet the regulatory requirement on homework time (95% CI: 2.47 to 3.14) than the reference group and reduced their daily total screen-viewing time by 6.4% (95% CI: -9.6 to -3.3%, approximately 10 min). The positive effects were more pronounced among high-risk groups (secondary school and urban pupils who generally spend more time in sedentary behaviour) than in low-risk groups (primary school and rural pupils who generally spend less time in sedentary behaviour). The exploratory analyses showed comparable findings.
Conclusions
This regulatory intervention has been effective in reducing total and specific types of sedentary behaviour among Chinese children and adolescents, with the potential to reduce health inequalities. International researchers and policy makers may explore the feasibility and acceptability of implementing regulatory interventions on sedentary behaviour elsewhere.
The growing prevalence of sedentary behaviour in school-aged children and adolescents bears significant social, economic and health burdens in China and globally [ 1 ]–[ 3 ]. Sedentary behaviour refers to any waking behaviour characterised by an energy expenditure equal or lower than 1.5 metabolic equivalents (METs) while sitting, reclining, or lying [ 3 ]. Evidence from systematic reviews, meta-analyses and longitudinal studies have shown that excessive sedentary behaviour, in particular recreational screen-based sedentary behaviour, affect multiple dimensions of children and adolescents’ wellbeing, spanning across mental health [ 4 ], cognitive functions/developmental health/academic performance [ 5 ], [ 6 ], quality of life [ 7 ], and physical health [ 8 ]. In China, over 60% of school pupils use part of their sleep time to play mobile phones/digital games and watch TV programmes, and 27% use their sleep time to do homework or other learning activities [ 9 ]. Screen-based, sedentary entertainment has become the leading cause for going to bed late, which is linked to detrimental consequences for children’s physical and mental health [ 10 ]. Notably, academic-related activities such as post-school homework and off campus tutoring also contribute to the increasing amounts of sedentary behaviour. According to the Organisation for Economic Co-operation and Development (OECD) report, China is the leading country in time spent on homework by adolescents (14 h/week on average) [ 11 ].
The COVID-19 pandemic exacerbated this global challenge, with children and adolescents reported to have been the most affected group [ 12 ]. Schools are a frequently targeted setting for interventions to reduce sedentary behaviour [ 13 ]. However, school-based interventions have had limited success when delivered under real-world conditions or at scale [ 14 ]. School-based interventions alone have also been unsuccessful in mitigating the trend of increasing sedentary behaviour that is driven by a complex system of interdependent factors across multiple sectors [ 13 ]. Even for parents and carers who intend to restrict screen-based sedentary behaviour and for children who wish to reduce screen-based sedentary behaviour, social factors including peer pressure often form barriers to changing behaviour [ 15 ]. In multiple public health fields such as tobacco control and healthy eating promotion, there has been a notable shift away from downstream (e.g., health education) towards an upstream intervention approach (e.g., sugar taxation). However, regulatory actions for sedentary behaviour are scarce [ 16 ]. World Health Organization (WHO) 2020 guidelines on sedentary behaviour encourage sustainable and scalable approaches for limiting sedentary behaviour and call for more system-wide policies to improve this global challenge [ 8 ]. Up-stream interventions can act on sedentary behaviour more holistically and have the potential to maximise reach and health impact [ 13 ]. In response to this pressing issue, and to widespread demands from many parents/carers, the Chinese government introduced nationwide regulations in 2021 to restrict (i) the amount of homework that teachers can assign, (ii) when (and for how long) online gaming businesses can provide access to young people, and (iii) when tutoring businesses can provide lessons [ 17 ], [ 18 ]. Consultations with WHO officials and reviewers of international health policy interventions confirmed that this is currently the only government-led, multi-setting regulatory intervention on multiple types of sedentary behaviour among school-aged children and adolescents. A detailed description of this programme is available in the Additional File 1 .
We evaluated the impact of this regulatory intervention on sedentary behaviour in Chinese school-aged children and adolescents. We also investigated whether and how intervention effects differed by sex, education stage, geographical area, and baseline weight status.
Study design
The introduction of the nationwide regulation provided a unique opportunity for a natural experiment evaluation where the pre-regulation comparator group data (Wave 1) was compared to the post-regulation group data (Wave 2). Multiple components of the intervention (see Additional File 1 ) were introduced in phases from July 2021 with all components being fully in place by September 2021 [ 17 ], [ 18 ]. This paper follows the STROBE reporting guidance [ 19 ], [ 20 ].
Data source, study population and sampling
We obtained regionally representative data on 99,947 pupils who are resident in the Chinese province of Guangxi as part of Guangxi Centre for Disease Control and Prevention’s (CDC) routine surveillance. The data, available from participants in grade 4 (aged between 9 and 10 years) and higher, were collected using a multi-stage random sampling design (Fig. 1 ) through school visits by trained health professionals following standardised protocols (see Supplementary Fig. 1 , Additional File 1 ). In Wave 1 (data collected from September to November 2020), pupils were randomly selected from schools in 31 urban/rural counties from 14 cities in Guangxi. At least eight schools, including primary, secondary, high schools, and ‘vocational high schools’, were selected from urban counties. Five schools were selected from rural counties. Approximately 80 students were randomly selected from each grade at the schools selected. The same schools were invited to participate in Wave 2 (data collected from September to November 2021), and new schools were invited to replace Wave 1 schools that no longer participated. Children with available data at both Wave 1 and Wave 2 represented approximately 10% of the sample ( n = 7,587). Paper-based questionnaires were administrated to students by trained personnel or teachers. The questionnaires were designed and validated by China National Health Commission, and have been utilised in routine surveillance throughout the country.
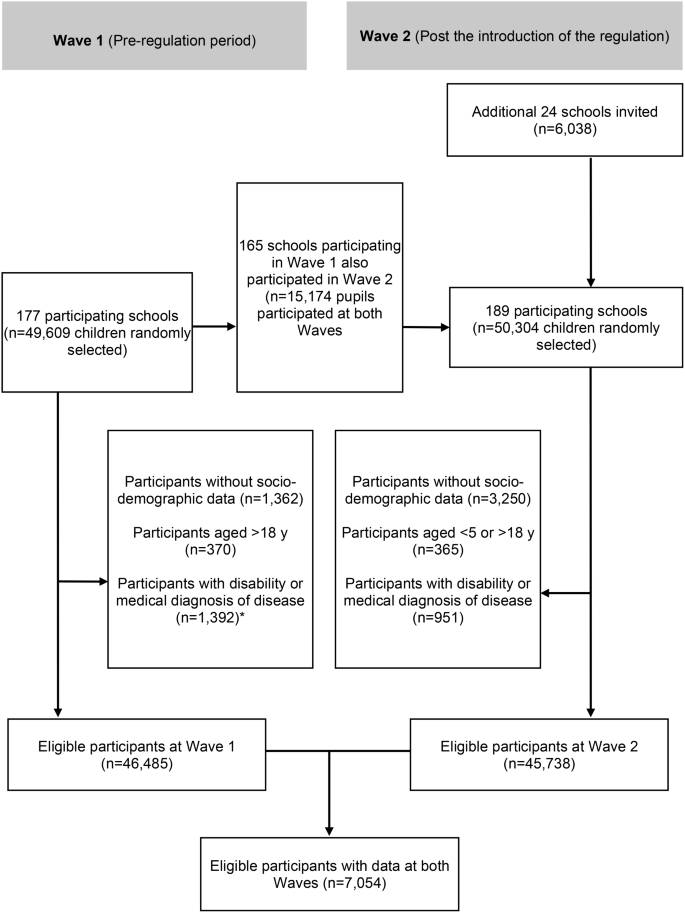
Flow diagram of participants included in the ENERGISE study
We used data from the age groups 7–18 years for most analyses. For specific analyses of homework and out-of-campus tutoring, we excluded high school pupils (16–18 years) because the homework and out-of-campus tutoring regulations apply to primary (7–12 years) and middle (13–15 years) school pupils only. Furthermore, participants without socio-demographic data or those who reported medical history of disease, or a physical disability were excluded. This gave us a total sample of 7,054 eligible school-aged children and adolescents with matching data (longitudinal sample).
Outcomes and subgroups
Guangxi CDC used purposively designed questions for surveillance purposes to assess sedentary behaviour outcomes (Table 1 ).
The primary outcomes of interest included: (1) total sedentary behaviour time, (2) homework time, (3) out-of-campus learning (private tutoring) time, and (4) electronic device use time (Table 1 ). We considered electronic device use time, including mobile phones, handheld game consoles, and tablets, the most suitable estimator of online game time (estimand) in the surveillance programme since these are the main devices used for online gaming in China [ 23 ]. Secondary outcomes were: (1) total screen-viewing time, (2) internet-use time, (3) likelihood of meeting international screen-viewing time recommendations, and (4) likelihood of meeting the regulation on homework time (Table 1 ).
We calculated total sedentary behaviour time as the sum of total screen-viewing time (secondary outcome), homework time, and out-of-campus learning time (Table 1 ). Total screen-viewing time represents the sum of electronic device use time per day, TV/video game use time per day, and computer use time per day (Table 1 ). Total screen-viewing time was considered as an alternative estimator of online game time (estimand) since TV/videogame console use time and computer time could also capture the small proportion of children who use these devices for online gaming (Table 1 ). The international screen-viewing time recommendations were based on the American Academy of Paediatrics guidelines [ 21 ]. We did not include internet use time (secondary outcome) in total screen-viewing time, and total sedentary behaviour time, because this measure likely overlaps with other variables.
We defined subgroups by demographic characteristics, including the child’s sex (at birth: girls or boys), date of birth, education stage [primary school or secondary school [including middle school, high school, and ‘occupational schools’]), children’s residency (urban versus rural) and children’s baseline weight status (non-overweight versus overweight/obesity). Each sampling site selected for the survey was classified by the surveillance personnel as urban/rural and as lower-, medium-, or higher-economic level based on the area’s gross domestic product (GDP) per capita. The area’s GDP per capita was measured by the Chinese Centre for Disease Control and Prevention (CDC). Trained personnel also measured height, and weight using calibrated stadiometers and scales. Children’s weight/height were measured with light clothing and no shoes. Measurements during both waves were undertaken when students lived a normal life (no lockdowns, school were opened normally). We classified weight status (normal weight vs. overweight/obesity) according to the Chinese national reference charts [ 24 ].
Statistical analyses
We treated sedentary behaviour values that exceeded 24-hours per day as missing. We did not exclude extreme values for body mass index from the analyses 25 . Additional information, justifications, and results of implausible and missing values can be found in the Supplementary Table 1 , Additional File 1 .
The assumptions for normality and heteroscedasticity were assessed visually by inspecting residuals. We assessed multicollinearity via variance inflation factors. The outcome variables for linear regression outcomes were transformed using square roots to meet assumptions. We reported descriptive demographic characteristics (age, sex, area of residence, socioeconomic status), weight status, and outcome variables using means (or medians for non-normally distributed data) and proportions [ 26 ]
We ran multilevel models with random effects nested at the school and child levels to compare the outcomes in Wave 1 against Wave 2. We developed separate models for each sedentary behaviour outcome variable. We treated the introduction of the nationwide regulation as the independent binary variable (0 for Wave 1 and 1 for Wave 2). We ran linear models for continuous outcomes, logistic models for binary outcomes, and ordered logistic models for ordinal outcomes in a complete case analysis estimating population average treatment effects [ 27 ]. For the main analysis, in which participants had measurements in both Waves (longitudinal sample), only those with non-missing data at both time points were included.
We estimated marginal effects for each sedentary behaviour outcome. With a self-developed directed acyclic graph (DAG) we identified age (continuous), sex (male/female), area of residence (urban/rural), and socioeconomic status (high/medium/low) as confounders (see Supplementary Figs. 2–4, Additional File 1 ).
We evaluated subgroup effects defined by child’s sex at birth (boys versus girls), child’s stage of education (primary school versus secondary school [including middle school, high school, and ‘occupational schools’]), children’s residency (rural versus urban), and children’s baseline weight status (non-overweight versus overweight/obesity). We also repeated the covariate-adjusted model with interaction terms (between Wave and sex; Wave and child stage of education; Wave and residency; and Wave and weight status). We adjusted for multiple testing using Bonferroni correction ( p 0.05 divided by the number of performed tests for an outcome). The resulting cut-off point of p < 0.005 was used to determine the presence of any interaction effects.
We also conducted exploratory analyses (including subgroup analyses) by evaluating the same models with a representative, cross-sectional sample of 99,947 pupils. This cross-sectional sample included different schools and children at Wave 1 and Wave 2. We therefore used propensity score (PS) weighting to account for sample imbalances in the socio-demographic characteristics. Propensity scores were calculated by conducting a logistic regression, which calculated the likelihood of each individual to be in Wave 2 (dependent variable). Individual’s age, sex, area of residence and the GDP per area were treated as independent variables. Subsequently, inverse probability of treatment weighting was applied to balance the demographic characteristics in the sample in Wave 1 (unexposed to the regulatory intervention) and Wave 2 (exposed to the regulatory intervention). The sample weight for individuals in Wave 1 were calculated using the Eq. 1/ (1-propensity score). The sample weight for individuals in Wave 2 were calculated using the Eq. 1/propensity score [ 28 ].
We only ran linear models for continuous outcomes since it was not possible to run PS-weighted multilevel models with this sample size in Stata. We conducted all statistical analyses in Stata version 16.0.
Participant sample
In our primary, longitudinal analyses, we analysed data from 7,054 children and adolescents. The mean age was 12.3 years (SD, 2.4) and 3,477 (49.3%) were girls (Table 2 ). More detailed information on characteristics of subgroups in the longitudinal sample are presented in the Supplementary Tables 2–5, Additional File 2 .
Primary outcomes
Children and adolescents reported a reduction in their daily mean total sedentary behaviour time by 13.8% (95% CI: -15.9 to -11.7), or 46 min, on average between Waves 1 and 2. Participants were also less likely to report having increased their time spent on homework (adjusted odd ratio/AOR: 0.39; 95% CI: 0.35–0.43) and in out-of-campus learning (AOR: 0.53; 95% CI: 0.47 to 0.59) in Wave 2 in comparison to Wave 1, respectively (Tables 3 and 4 ). We did not find any changes in electronic device use time.
Secondary outcomes
Participants reported reducing their mean daily screen-viewing time by 6.4% (95% CI: -9.6 to -3.3%), or 10 min, on average (Tables 3 and 4 ). Participants were also 20% as likely to meet international screen time recommendations (AOR: 1.20; 95% CI: 1.09 to 1.32) and were 2.79 times as likely to meet the regulatory requirement on homework time (95% CI: 2.47 to 3.14) compared to the reference group (before the introduction of the regulation).
Subgroup analyses
Most screen- and study-related sedentary behaviour outcomes differed by education stage ( p < 0.005) (see Supplementary Tables 6–13, Additional File 2 ), with the reductions being larger in secondary school pupils than in primary school pupils (Tables 3 and 4 , and Table 5 ). Only secondary school pupils reduced their total screen-viewing time (-8.4%; 95% CI: -12.4 to -4.3) and were also 1.41 times as likely to meet screen-viewing recommendations (AOR: 1.41; 95% CI: 1.23 to 1.61) at Wave 2 compared to Wave 1.
Conversely, at Wave 2, primary school pupils reported a lower likelihood of spending more time doing homework (AOR: 0.30; 95%: 0.26 to 0.34) than secondary school pupils (AOR: 0.58; 95% CI: 0.50 to 0.67) compared to their counterparts at Wave 1. At Wave 2, primary school pupils also had a higher likelihood of reporting meeting homework time recommendations (AOR: 3.61; 95% CI: 3.09 to 4.22) than secondary school pupils (middle- and high school) (AOR: 2.11; 95% CI: 1.74 to 2.56) compared to their counterparts at Wave 1 (Table 5 ). There was also a residence interaction effect ( p < 0.001) in total sedentary behaviour time, with participants in urban areas reporting larger reductions (-15.3%; 95% CI: -17.8 to -12.7) than those in rural areas (-11.2%; 95% CI: -15.0 to -7.4). There was no evidence of modifying effects by children’s sex or baseline weight status (Tables 4 and 5 ).
Findings from the exploratory repeated cross-sectional analyses were similar to the findings of the main longitudinal analyses including total sedentary behaviour time, electronic device use time, total screen-viewing time and internet use time (see Supplementary Tables 14–23, Additional File 2 ).
Principal findings
Our study evaluated the impact of the world’s first regulatory, multi-setting intervention on multiple types of sedentary behaviour among school-aged children and adolescents in China. We found that children and adolescents reduced their total sedentary behaviour time, screen-viewing time, homework time and out-of-campus learning time following its implementation. The positive intervention effects on total screen-viewing time (-8.4 vs. -2.3%), and the likelihood of meeting recommendations on screen-viewing time (1.41 vs. 1.02 AOR) were more pronounced in secondary school pupils compared with primary school pupils. Intervention effects on total sedentary behaviour time (-15.3 vs. -11.2%) were more pronounced among pupils living in the urban area (compared to pupils living in the rural area). These subgroup differences imply that the regulatory intervention benefit more the groups known to have a higher rate of sedentary behaviour [ 29 ].
Interestingly, the observed reduction in electronic device use itself did not reach statistical significance following implementation of regulation. This could be viewed as a positive outcome if this is correctly inferred and not the result of reporting bias or measurement error. International data indicated that average sedentary and total screen time have increased among children due to the COVID-19 pandemic [ 12 ]. However, such interesting finding might be explained by the absence of lockdowns in Guangxi during both surveillance waves when most school-aged students outside China were affected by pandemic mitigation measures such as online learning.
Strengths and weaknesses
Our study has several notable strengths. This is the first study to evaluate the impact of multi-setting nationwide regulations on multiple types of sedentary behaviour in a large and regionally representative sample of children and adolescents. Still, to gain a more comprehensive view of the regulatory intervention on sedentary behaviour across China, similar evaluation research should be conducted in other regions of China. Furthermore, access to a rich longitudinal dataset allowed for more robust claims of causality. The available data also allowed us to measure the effect of the intervention on multiple sedentary behaviours including recreational screen-time and academic-related behaviours. Lastly, the large data set allowed us to explore whether the effect of the regulatory intervention varied across important subgroups, suggesting areas for further research and development.
Some limitations need to be taken into consideration when interpreting our findings. First, a common limitation in non-controlled/non-randomised intervention studies is residual confounding. We aimed to limit this by adjusting our analysis for confounders known to impact the variables of interest, but it is impossible to know whether important confounding may still have been present. With maturation bias, it is possible that secular trends are the cause for any observed effects. However, this seems unlikely in our study as older children may spend more time doing homework [ 23 ] and engage more in screen-viewing activities [ 30 ]. In this study, we observed reductions in these outcomes. The use of self-reported outcomes (social desirability bias) was a limitation and might have led to the intervention effects being over-estimated [ 13 ]. However, since our data were collected as part of a routine surveillance programme, pupils were unaware of the evaluation. This might mitigate reporting bias. In addition, the data were collected in Guangxi which might not representative of the whole population in China. Another limitation is using electronic device use time as a proxy measure of online gaming time. It is possible that electronic devices can be used for other purposes. However, mobile phones, handheld game consoles and tablets are the main devices used for online gaming. In this study, electronic device use time provided a practical means of assessing the broad effects of regulatory measures on screen time behaviours, including online gaming, in a large (province level) surveillance programme. In the future, instruments specifically designed to capture online gaming behaviour should be used in surveillance and research work.
Comparisons with other studies
Neither China nor other countries globally have previously implemented and evaluated multi-setting regulatory interventions on multiple types of sedentary behaviour, which makes comparative discussions challenging. In general, results of health behaviour research over the past decades have shown that interventions that address structural and environmental determinants of multiple behaviours to be more effective in comparison with individual-focussed interventions [ 31 ]. Furthermore, the continuous and universal elements of regulatory interventions may be particularly important explanations for the observed reductions in sedentary behaviour. Standalone school and other institution-led interventions may struggle with financial and logistic costs which threaten long-term implementation [ 13 ]. In contrast, the universality element of regulatory intervention can reduce or remove peer pressures and potential stigmatisation among children and teachers that are often associated with more selective/targeted interventions [ 24 ]. Our findings support WHO guidelines for physical activity and sedentary behaviour that encourage sustainable and scalable approaches for limiting sedentary behaviour and call for more system-wide policies to improve this global challenge[ 8 ].
Implications for future policy and research
Our study has important implications for future research and practice both nationally and internationally. Within China, future research should focus on optimising the implementation of the regulatory intervention through implementation research and assess long-term effects of the regulation on both behavioral and health outcomes. Internationally, our findings also provide a promising policy avenue for other countries and communities outside of China to explore the opportunities and barriers to implement such programmes on sedentary behaviour. This exploratory process could start with assessing how key stakeholders (including school-aged children, parents/carers, schoolteachers, health professionals, and policy makers) within different country contexts perceive regulatory actions as an intervention approach for improving health and wellbeing in young people, and how they can be tailored to fit their own contexts. Within public health domains, including healthy eating promotion, tobacco and alcohol control, regulatory intervention approaches (e.g., smoking bans and sugar taxation) have been adopted. However, regulatory actions for sedentary behaviour are scarce [ 19 ]. Within the education sector, some countries recently banned mobile phone use in schools for academic purpose [ 25 ]. While this implies potential feasibility and desirability of such interventions internationally, there is little research on the demand for, and acceptability of, multi-faceted sedentary behaviour regulatory interventions for the purpose of improving health and wellbeing. It will be particularly important to identify and understand any differences in perceptions and feasibility both within (e.g., public versus policy makers) and across countries of differing socio-cultural-political environments.
This natural experiment evaluation indicates that a multi-setting, regulatory intervention on sedentary behaviour has been effective in reducing total sedentary behaviour, and multiple types of sedentary behaviour among Chinese school-aged children and adolescents. Contextually appropriate, regulatory interventions on sedentary behaviour could be explored and considered by researchers and policy makers in other countries.
Data availability
Access to anonymised data used in this study can be requested through the corresponding author BL, subject to approval by the Guangxi CDC. WZ and SVP have full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Abbreviations
Centre for disease control and prevention
Directed acyclic graph
Gross domestic product
Metabolic equivalents
Organisation for Economic Co-operation and Development
Bao R, Chen S-T, Wang Y, Xu J, Wang L, Zou L, Cai Y. Sedentary Behavior Research in the Chinese Population: a systematic scoping review. Int J Environ Res Public Health 2020, 17(10).
Nguyen P, Le LK-D, Ananthapavan J, Gao L, Dunstan DW, Moodie M. Economics of sedentary behaviour: a systematic review of cost of illness, cost-effectiveness, and return on investment studies. Prev Med. 2022;156:106964.
Article PubMed Google Scholar
World Health Organization. WHO guidelines on physical activity and sedentary behaviour. In. Geneva: World Health Organization; 2020.
Zhang J, Yang SX, Wang L, Han LH, Wu XY. The influence of sedentary behaviour on mental health among children and adolescents: a systematic review and meta-analysis of longitudinal studies. J Affect Disord. 2022;306:90–114.
Madigan S, Browne D, Racine N, Mori C, Tough S. Association between Screen Time and children’s performance on a Developmental Screening Test. JAMA Pediatr. 2019;173(3):244–50.
Article PubMed PubMed Central Google Scholar
Pagani LS, Fitzpatrick C, Barnett TA, Dubow E. Prospective Associations between Early Childhood Television Exposure and academic, psychosocial, and Physical Well-being by Middle Childhood. Arch Pediatr Adolesc Med. 2010;164(5):425–31.
Boberska M, Szczuka Z, Kruk M, Knoll N, Keller J, Hohl DH, Luszczynska A. Sedentary behaviours and health-related quality of life. A systematic review and meta-analysis. Health Psychol Rev. 2018;12(2):195–210.
Fiona CB, Salih SA-A, Stuart B, Katja B, Matthew PB, Greet C, Catherine C, Jean-Philippe C, Sebastien C, Roger C et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. British Journal of Sports Medicine 2020, 54(24):1451.
China Sleep Research Association. Sleep White Paper of Chine People’s Health. In. Beijing, China; 2022.
Chaput J-P, Gray CE, Poitras VJ, Carson V, Gruber R, Olds T, Weiss SK, Gorber SC, Kho ME, Sampson M, et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S266–82. (Suppl. 3)).
OECD. Does Homework Perpetuate inequities in Education? OECD Publishing 2014(46):4.
Trott M, Driscoll R, Iraldo E, Pardhan S. Changes and correlates of screen time in adults and children during the COVID-19 pandemic: a systematic review and meta-analysis. eClinicalMedicine 2022, 48.
van Sluijs EMF, Ekelund U, Crochemore-Silva I, Guthold R, Ha A, Lubans D, Oyeyemi AL, Ding D, Katzmarzyk PT. Physical activity behaviours in adolescence: current evidence and opportunities for intervention. Lancet. 2021;398(10298):429–42.
Cassar S, Salmon J, Timperio A, Naylor P-J, van Nassau F, Contardo Ayala AM, Koorts H. Adoption, implementation and sustainability of school-based physical activity and sedentary behaviour interventions in real-world settings: a systematic review. Int J Behav Nutr Phys Activity. 2019;16(1):120.
Article Google Scholar
Martins J, Costa J, Sarmento H, Marques A, Farias C, Onofre M, Valeiro MG. Adolescents’ perspectives on the barriers and facilitators of physical activity: an updated systematic review of qualitative studies. Int J Environ Res Public Health 2021, 18(9).
Gelius P, Messing S, Tcymbal A, Whiting S, Breda J, Abu-Omar K. Policy Instruments for Health Promotion: a comparison of WHO Policy Guidance for Tobacco, Alcohol, Nutrition and Physical Activity. Int J Health Policy Manage. 2022;11(9):1863–73.
Google Scholar
The General Office of the CPC Central Committee and the General Office of the State. Council issued the opinions on further reducing the Burden of Homework and off-campus training for students in the stage of Compulsory Education. https://www.gov.cn/zhengce/2021-07/24/content_5627132.htm .
Notice of the State Press and Publication Administration on Further Strict. Management to Effectively Prevent Minors from Being Addicted to Online Games. https://www.gov.cn/zhengce/zhengceku/2021-09/01/content_5634661.htm .
Craig P, Cooper C, Gunnell D, Haw S, Lawson K, Macintyre S, Ogilvie D, Petticrew M, Reeves B, Sutton M, et al. Using natural experiments to evaluate population health interventions: new Medical Research Council guidance. J Epidemiol Commun Health. 2012;66(12):1182–6.
Craig P, Campbell M, Bauman A, Deidda M, Dundas R, Fitzgerald N, Green J, Katikireddi SV, Lewsey J, Ogilvie D, et al. Making better use of natural experimental evaluation in population health. BMJ. 2022;379:e070872.
American Academy of Pediatrics. Children, adolescents, and television. Pediatrics. 2001;107(2):423–6.
Bauer CP. Applied Causal Analysis (with R). In. Bookdown; 2020.
Matthay EC, Hagan E, Gottlieb LM, Tan ML, Vlahov D, Adler NE, Glymour MM. Alternative causal inference methods in population health research: evaluating tradeoffs and triangulating evidence. SSM - Popul Health. 2020;10:100526.
Greenberg MT, Abenavoli R. Universal interventions: fully exploring their impacts and potential to produce Population-Level impacts. J Res Educational Eff. 2017;10(1):40–67.
Selwyn N, Aagaard J. Banning mobile phones from classrooms—An opportunity to advance understandings of technology addiction, distraction and cyberbullying. Br J Edu Technol. 2021;52(1):8–19.
Boushey CJ, Harris J, Bruemmer B, Archer SL. Publishing nutrition research: A review of sampling, sample size, statistical analysis, and other key elements of manuscript preparation, Part 2. J Acad Nutr Dietet. 2008;108(4):679–688.
Matthay EC, Hagan E, Gottlieb LM, Tan ML, Vlahov D, Adler NE, Glymour MM. Alternative causal inference methds in population health research:Evaluating tradeoffs nd triangulating evidence. SSM - Population Health. 2020;10:100526.
Chesnaye NC, Stel VS, Tripepi G, Dekker FW, Fu EL, Zoccali C, Jager KJ. An introduction to inverse probability of treatment weighting in observation research. Clin Kid J. 2021;15(1):14–20.
Song C, Gong W, Ding C, Yuan F, Zhang Y, Feng G, Chen Z, Liu A. Physical activity and sedentary behaviour among Chinese children agd 6-17 years: a cross-sectional analysis of 2010-2012 China National Nutrition and Health Survey. BMC Public Health. 2019;19(1):936.
Zhu X, Haegele JA, Tang Y, Wu X. Physical activity and sedentary behaviors of urban chinese children: grade level prevalence and academic burden associations. BioMed Res Int. 2017;2017:7540147.
Rutter H, Bes-Rastrollo M, de Henauw S, Lathi-Koski M, Lehtinen-Jacks S, Mullerova D, Rasmussen F, Rissanen A, Visscher TLS, Lissner L. Balancing upstream and downstream measures to tackle the obesity epidemic: a position statement from the european association for the study of obesity. Obesity Facts. 2017;10(11):61–63.
Download references
Acknowledgements
We would like to acknowledge Dr Peter Green and Dr Ruth Salway for providing feedback on the initial data analysis plan, and Dr Hugo Pedder and Lauren Scott who provided feedback on the statistical analyses.
This work was funded by the Wellcome Trust through the Global Public Health Research Strand, Elizabeth Blackwell Institute for Health Research. The funder of our study had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and affiliations.
Centre for Exercise, Nutrition and Health Sciences, School for Policy Studies, University of Bristol, Bristol, UK
Bai Li, Remco Peters & Charlie Foster
Public Health Wales, Cardiff, UK
Selene Valerino-Perea
Department of Nutrition and School Health, Guangxi Center for Disease Control and Prevention, Nanning, Guangxi, China
Weiwen Zhou
School of Public Health, Guangxi Medical University, Nanning, Guangxi, China
Yihong Xie, Zouyan He & Yunfeng Zou
Centre for Health, Law, and Society, School of Law, University of Bristol, Bristol, UK
Keith Syrett
Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
Frank de Vocht
NIHR Applied Research Collaboration West (ARC West), Bristol, UK
You can also search for this author in PubMed Google Scholar
Contributions
BL conceived the study idea and obtained the funding with support from WZ, CF, KS, YX, YZ, ZH and RP. BL, CF, FdV and KS designed the study. WZ led data collection and provided access to the data. YX, SVP and ZH cleaned the data. SVP analysed the data with guidance from BL, FdV and CF. BL, SVP and RP drafted the paper which was revised by other authors. All authors read and approved the final manuscript for submission.
Corresponding author
Correspondence to Bai Li .
Ethics declarations
Ethical approval and consent to participate.
Ethics approvals were granted by the School for Policy Studies Research Ethics Committee at the University of Bristol (reference number SPSREC/20–21/168) and the Research Ethics Committee at Guangxi Medical University (reference number 0136). Written informed consent was obtained from each participant, and a parent or guardian for participants aged < 20 years.
Consent for publication
The co-authors gave consent for publication.
Competing interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential competing interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Li, B., Valerino-Perea, S., Zhou, W. et al. The impact of the world’s first regulatory, multi-setting intervention on sedentary behaviour among children and adolescents (ENERGISE): a natural experiment evaluation. Int J Behav Nutr Phys Act 21 , 53 (2024). https://doi.org/10.1186/s12966-024-01591-w
Download citation
Received : 20 December 2023
Accepted : 04 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12966-024-01591-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sedentary behaviour
- Physical activity
- Regulatory intervention
- Health policy
- Screen time
- Natural experiment
- Mental health
- Health promotion
- Child health
International Journal of Behavioral Nutrition and Physical Activity
ISSN: 1479-5868
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 11 May 2024
Surgical choice for the treatment of partial intestinal ischemic necrosis caused by acute type a aortic dissection combined with malperfusion of superior mesenteric artery
- Wenbo Yu 1 ,
- Yuan Liang 1 ,
- Jianfeng Gao 1 ,
- Dilin Xie 1 &
- Jianxian Xiong 2
Journal of Cardiothoracic Surgery volume 19 , Article number: 286 ( 2024 ) Cite this article
106 Accesses
Metrics details
Acute type A aortic dissection is a severe cardiovascular disease characterized by rapid onset and high mortality. Traditionally, urgent open aortic repair is performed after admission to prevent aortic rupture and death. However, when combined with malperfusion syndrome, the low perfusion of the superior mesenteric artery can further lead to intestinal necrosis, significantly impacting the surgery’s prognosis and potentially resulting in adverse consequences, bringing. This presents great significant challenges in treatment. Based on recent domestic and international research literature, this paper reviews the mechanism, current treatment approaches, and selection of surgical methods for poor organ perfusion caused by acute type A aortic dissection. The literature review findings suggest that central aortic repair can be employed for the treatment of acute type A aortic dissection with inadequate perfusion of the superior mesenteric artery. The superior mesenteric artery can be windowed and (/or) stented, followed by delayed aortic repair. Priority should be given to revascularization of the superior mesenteric artery, followed by central aortic repair. During central aortic repair, direct blood perfusion should be performed on the distal true lumen of the superior mesenteric artery, leading to resulting in favorable therapeutic outcomes. The research results indicate that even after surgical aortic repair, intestinal ischemic necrosis may still occur. In such cases, prompt laparotomy and necessary necrotic bowel resection are crucial for saving the patient’s life.
Peer Review reports
Introduction
Acute type A aortic dissection (ATAAD) is a life-threatening disease, with a rapidly deteriorating patient condition. The mortality rate increases by 1% within 1 h after onset, and if medical intervention is not performed in time, the mortality rate within 48 h can be as high as 30-50% [ 1 ]. Approximately 40% of patients with ATAAD experience malperfusion syndrome (MPS) [ 2 ], resulting in a total mortality rate of up to 45% [ 3 ]. Malperfusion is reported as a complication associated with ATAAD in 3.7% of cases [ 4 ]. The combination of acute aortic dissection and dissection-related MPS can lead to organ ischemic necrosis and functional failure, significantly impacting patient prognosis and potentially causing adverse consequences. Due to the lack of clear treatment strategies for malperfusion, the mortality rate of malperfusion caused by acute aortic dissection (AAD) is higher than that of AAD without malperfusion [ 5 , 6 , 7 ]. AAD complicated with malperfusion syndrome is defined as the loss of blood supply to important organs caused by the loss of perfusion of the branch arteries secondary to the dissection [ 8 ]. Malperfusion syndrome can affect any mesentery with inadequate blood flow, but mesenteric malperfusion (MMP) presents the greatest challenge, leading to a 3 to 4-fold increase in mortality in cases of acute type A and type B aortic dissection. The incidence of MMP has been reported to range between 66% and 100% in various studies [ 9 ]. Mesenteric ischemia malperfusion is a significant and often overlooked complication of ATAAD [ 10 ], It has been reported that the incidence of mesenteric ischemia in large multicenter registries is approximately 4–6% [ 11 ]. It significantly increases the mortality rate of ATAAD by 3–4 times. Even after complete revascularization, there is still a risk of postoperative death due to ischemia/reperfusion injury [ 12 ]. Therefore, mesenteric malperfusion deserves particular attention. Preoperative mesenteric malperfusion was associated with a mortality rate of 63.2% [ 13 , 14 ]. Even with early intervention, the mortality rate for these patients remains as high as 42% [ 15 ]. Consequently, the control of malperfusion is the key to improving the outcomes of surgery for ATAAD [ 16 ]. Timely surgical relief of major organ ischemia is very important to save lives [ 17 ]. Accurate and timely diagnosis and appropriate intervention are needed before aortic repair surgery to prevent irreversible organ damage [ 18 ].
The mechanism of organ malperfusion caused by ATAAD
Aortic branch vessel involvement is defined as the extension of the dissection to the coronary, cerebral, and splanchnic arteries on computed tomography (CT) [ 19 ], Hypoperfusion syndrome can occur in all branches from the coronary artery to the bifurcation of the abdominal aorta. Therefore, when AAD is complicated with MPS. It affects almost all branches of the aorta (including the central nervous system, coronary artery involvement, liver and kidney dysfunction, and gastrointestinal ischemic necrosis). The incidence and severity of malperfusion of each organ are different. The mechanism behind the low perfusion of branch vessels is mainly due to the compression of the true lumen by the false lumen of the branch vessel dissection. Additionally, the false lumen of the branch vessel intima is perfused with blood flow [ 20 ]. An AAD can cause mesenteric ischemia by two mechanisms: first, by occluded or narrowed SMA arteries by directly progressive dissection into the vessel, and second, by occlusion of the vessel origin by a dissection flap within the aortic lumen [ 21 , 22 ], known as aortic type and branch type [ 23 ]. For cases of aortic malperfusion with dynamic obstruction, central aortic surgery or fenestration is recommended, where there is an obstruction at the origin of the vessel due to a dissecting flap within the aortic lumen. Conversely, for cases of branch-type malperfusion with static obstruction, stenting or bypass grafting is preferred [ 24 ]. In cases of static obstruction, anatomic flaps track the false lumen into branch vessels, and using self-expanding stents in the true lumen is the preferred method. For dynamic occlusion, the anatomic plane maintains branch origins, blocks flow to branch vessels, and the recommended treatment involves aortic fenestration along with deploying self-expanding stents in the true lumen [ 25 ].
Diagnosis of ATAAD combined with malperfusion of the superior mesenteric artery
Clinical manifestation.
ATAAD is characterized by sudden tear-like pain in the chest, back, or abdomen. As the dissection progresses, the pain may spread to either the distal or proximal end. Severe pain was reported as the most common initial symptom (92.3%). The majority of patients experienced back pain (79.3%), while approximately 30.2% of patients complained of chest pain [ 26 ]. When combined with malperfusion of the superior mesenteric artery, the progression of the disease can result in intestinal ischemic necrosis. This can lead to symptoms such as progressive abdominal distension, abdominal pain, disappearance of bowel sounds, abdominal tenderness, and rebound pain.
Imaging examinations
Computed tomography angiography (CTA) has emerged as the primary imaging modality for diagnosing AAD due to its high sensitivity and specificity. In clinical practice, CTA is the preferred method for both diagnosing and differentiating AAD. It enables visualization of the intimal flap and inwards movement of the stripping intima, which leads to the formation of the true and false lumen, as well as the presence of intramural hematoma. These criteria serve as important diagnostic indicators [ 27 ]. Structures such as the thoracic cavity and pericardial cavity should be clearly displayed, along with an evaluation of the involvement of branch vessels. After diagnosing AAD, clinicians must immediately consider the possibility of malperfusion [ 28 ]. CT is considered the gold standard for diagnosing acute mesenteric ischemia. CT images reveal excessive expansion of the intestinal wall, thickening of the intestinal wall, mesenteric edema, intestinal effusion, and increased fuzzy density of the surrounding fat gap [ 29 ]. Due to the difficulty in diagnosing mesenteric infarction and its potential fatality if delayed, laparoscopic or exploratory laparotomy may be performed for patients [ 30 ]. To overcome this challenge and even identify the early stages of ischemia, fluorescein-assisted laparoscopy can be used [ 31 ].
Treatment status of ATAAD with organ malperfusion
Organ malperfusion in aortic dissection refers to the inadequate blood supply to organs caused by obstruction of visceral arteries, leading to organ dysfunction and MPS. This syndrome is characterized by cell death, tissue necrosis, and organ failure [ 32 ]. The impact of organ malperfusion on the outcomes of AAD surgery, both in the early and late stages, is significant. Acute occlusion of the coronary, carotid, or visceral arteries sometimes leads to irreversible organ damage after aortic surgery [ 11 , 33 , 34 ]. Therefore, treating ATAAD with MPS remains challenging [ 35 ]. Managing poor preoperative perfusion is a major hurdle in reducing mortality associated with surgical treatment of AAD [ 36 ]. For patients with acute type A dissection, surgical replacement of diseased vessels is the best treatment option [ 37 , 38 ]. To restore the perfusion of vital organs before the progression of organ dysfunction, surgical aortic surgery is often prioritized [ 39 ]. Central aortic repair should be considered for all patients with malperfusion [ 40 ]. Poor mesenteric perfusion is a relatively serious complication, and the risk of in-hospital death is high, because it is difficult to diagnose mesenteric ischemia before necrosis changes, and when it occurs, the patient’s condition has deteriorated [ 41 ]. Diagnosis of acute mesenteric ischemia in patients with AAD may be difficult as abdominal pain is a nonspecific symptom during diagnosis [ 22 ]. The occurrence of ischemia can occur at any stage of dissection treatment. When ischemia occurs, it disrupts the oxygen supply, leading to intestinal mucosal necrosis within 3 h. If left untreated, full-thickness necrosis of the intestinal wall can occur within 6 h. Therefore, diagnosing this condition during these critical hours is crucial for successful treatment [ 42 ]. Currently, for patients with ATAAD who may have low perfusion of the superior mesenteric artery, emergency central aortic repair should be prioritized after admission, unless there is persistent or severe visceral ischemia with intestinal necrosis [ 43 ]. This approach not only saves the dissecting aneurysm from rupture but also aims to restore blood supply and pressure to the true lumen, ensuring that branch vessels can be reopened and reperfused. Postoperation, further treatment depends on the recovery of blood supply in the branch vessels and the extent of organ ischemia.
Selection of surgical methods for ATAAD with mesenteric hypoperfusion
Central aortic repair surgery.
Aortic repair is typically performed through surgery to address malperfusion of the aortic root, coronary artery orifice, and distal end of the dissection, including brain and visceral perfusion [ 44 ]. In cases of ATAAD, central aortic repair, specifically total aortic arch replacement with stented elephant trunk implantation (Sun’s Procedure), is commonly employed to halt the progression of dissection after admission. This approach helps prevent aortic rupture, which can be life-threatening, and restore proper blood supply to branch vessels, thereby resolving the issue of poor tissue and organ perfusion. This type of surgery typically necessitates prolonged extracorporeal circulation, which can worsen the already compromised blood flow to organ tissues during the procedure. As a result, in cases where there is inadequate blood flow to the superior mesenteric artery prior to the operation, emergency central aortic repair may lead to an increased risk of malperfused intestinal necrosis post-operation. While repair of the proximal aorta often leads to the subsidence of the false lumen and improvement in tissue and organ hypoperfusion, as well as the alleviation of mesenteric ischemia symptoms, without the need for further intervention [ 45 ], there are cases where AAD involving the superior mesenteric artery can cause hypoperfusion tissue ischemia at any point before, during, or after surgery. Complete occlusion of the superior mesenteric artery can result in irreversible intestinal mucosal ischemic injury within six hours of occlusion [ 46 ]. Therefore, if central aortic repair cannot be completed within this limited time, ischemic intestinal necrosis may still occur postsurgery, significantly impacting patient prognosis and hospitalization duration. In such situations, emergency laparotomy is often necessary. If intestinal necrosis has been confirmed before surgery, central aortic repair cannot effectively improve the intestinal necrotic tissue, and exploratory laparotomy and intestinal necrosis resection are necessary.
The superior mesenteric artery was first fenestrated and/or stented, and then the aorta was repaired by delayed opening
In patients with stable ATAAD and MPS, percutaneous or surgical revascularization is the initial intervention before proximal aortic repair [ 47 , 48 ]. Intravascular fenestration and/or stent implantation have emerged as more favorable strategies for addressing malperfusion and delayed open aortic repair [ 49 ]. For patients diagnosed with MPS, fenestration, with or without stent implantation, can be performed prior to open surgery to repair the diseased aorta and reperfuse and stabilize the ischemic organ [ 50 ]. In 1996, the University of Michigan introduced a new treatment model for patients with ATAAD and MPS, surgical treatment options vary depending on whether the patient is hemodynamically stable or unstable (Fig. 1 ) [ 51 ]. This involved performing fenestration and/or stent implantation on abdominal organs experiencing severe malperfusion, followed by delayed open repair of the proximal aorta of the dissection to enable early percutaneous intravascular revascularization [ 52 ]. At Michigan Medical Center, patients with visceral and limb MPS have been treated with endovascular fenestration/stent implantation and delayed open aortic repair for 20 years, resulting in positive short-term and long-term outcomes [ 52 , 53 , 54 ]. Yang B.‘s study on 82 patients with acute A-type aortic dissection complicated by mesenteric hypoperfusion after endovascular fenestration/stent implantation revealed that 38% of the patients died due to organ failure or aortic rupture before undergoing open aortic repair. The remaining patients either survived through open aortic repair or were discharged without requiring it [ 53 ]. When considering central aortic repair, caution should be exercised in performing preoperative fenestration or stent implantation of the ischemic mesenteric artery. Even if the stent is implanted in the true lumen of the mesenteric artery, it remains a low-pressure cavity, and the blood supply may still not be fully restored. On the other hand, performing intima fenestration allows for blood flow to be drained from the high-pressure false lumen to the low-pressure true lumen, partially restoring blood supply. However, if central aortic repair is performed again, the pressure between the true lumen and the false lumen is reversed, and intima fenestration may lead to new hemodynamic problems due to changes in intima morphology.
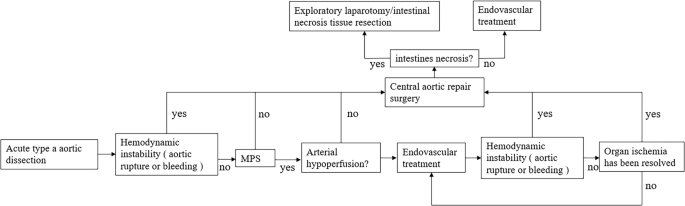
Surgical treatment options vary depending on whether the patient is hemodynamically stable or unstable
Superior mesenteric artery revascularization was given priority, and then aortic central repair was performed
Most patients with ATAAD typically undergo simple central aortic repair as the initial treatment. It is important to address mesenteric artery occlusion and intestinal ischemia through central aortic repair, which aims to restore blood supply to the true lumen and improve perfusion to branch vessels [ 55 ]. Preoperative CTA examination clearly confirmed the involvement of branch vessels. It is very important to restore true lumen blood supply as soon as possible through central aortic repair, solve the problem of low perfusion of branch vessels and reduce the time of low perfusion of tissues and organs. Research suggests that central aortic surgery or fenestration is effective for aortic malperfusion, while branch type may require stent implantation or bypass grafting [ 24 ]. A case study reported successful results in a patient with ATAAD and mesenteric ischemia who underwent a right common iliac artery to superior mesenteric artery bypass prior to aortic repair [ 56 ]. In the case reports, the patient’s intestinal necrosis was removed and the common iliac artery was bypassed to the superior mesenteric artery. Subsequently, after confirming the improvement of acidosis, ascending aortic replacement was performed on the same day, successfully saving the patient’s life [ 56 , 57 , 58 , 59 , 60 ]. These findings suggest that in cases where patients with ATAAD have malperfusion of the superior mesenteric artery, considering a bypass graft before central aortic repair can also be an effective treatment option. However, it is crucial to ensure stable hemodynamics and persistent mesenteric ischemia before opting for this approach.
According to Kamman et al., surgical delay in patients with malperfusion was found to be significantly associated with lower mortality. They recommend a treatment approach where branch vessel occlusion is addressed first, followed by emergency aortic repair after resolving MPS and its complications [ 34 ]. Tsagakis et al. introduced the concept of a hybrid operating room, emphasizing the revascularization of malperfusion as a priority [ 61 ]. Consequently, the strategy of prioritizing revascularization for ATAAD combined with poor mesenteric perfusion is also deemed acceptable and may yield positive outcomes [ 41 ]. The findings of these studies lean towards the conclusion that the optimal treatment strategy for emergency aortic dissection with poor mesenteric perfusion involves immediate revascularization of the superior mesenteric artery, followed by central aortic repair once the low perfusion of the superior mesenteric artery improves. The literature recognizes the catastrophic consequences of acute superior mesenteric artery occlusion and the need for emergency revascularization in patients with type A aortic dissection before central aortic repair [ 62 ].
Direct perfusion of the distal true lumen of the superior mesenteric artery was performed while the central aorta was repaired
ATAAD can lead to various types of superior mesenteric artery hypoperfusion ischemia, each requiring different treatment measures. The aortic type involves direct compression of the superior mesenteric artery by the aortic false lumen. Remission can be achieved through simple central aortic repair in this case. On the other hand, the branch vascular type necessitates direct intervention in the superior mesenteric artery. In some patients with ATAAD, urgent central aortic repair becomes necessary due to the presence of a ruptured aorta and coronary artery ischemia after admission. In such cases, a transverse incision can be made on the superior mesenteric artery to enable direct blood perfusion. Wataru Kato et al. reported two cases of ATAAD with superior mesenteric artery ischemia, where direct blood perfusion was performed on the distal true lumen of the superior mesenteric artery during central aortic repair for the patient [ 63 ]. This approach yielded positive therapeutic outcomes and successfully avoided the need for intestinal resection.
Conclusion and foresight
For patients with ATAAD, it is crucial to determine the blood supply of each branch before surgery, assess the level of ischemia, and choose an individualized treatment plan based on the specific conditions. In cases where there is poor blood flow to the superior mesenteric artery, central aortic repair can still be performed to effectively address the blockage caused by ATAAD and promptly restore blood supply to the branch vessels. However, if the patient experiences worsening abdominal pain postsurgery and auxiliary examinations reveal signs of intestinal necrosis, prompt consideration should be given to the possibility of intestinal ischemic necrosis. In such cases, emergency laparotomy should be performed to remove the necrotic bowel, which is an effective remedial treatment measure.
Data availability
Not applicable.
Abbreviations
Acute type A aortic dissection
- Malperfusion syndrome
Acute aortic dissection
Computed tomography
Computed tomography angiography
Total aortic arch replacement with stented elephant trunk implantation
Zheng Z, Yang L, Zhang Z, et al. Early and late outcomes of non-total aortic arch replacement for repair of acute Stanford Type A aortic dissection. Am J Transl Res. 2021;13(6):7047–52.
PubMed PubMed Central Google Scholar
Ahmad RA, Orelaru F, Graham N, et al. Progression of distal aorta after endovascular fenestration/stenting in acute type a aortic dissection with malperfusion syndrome. JTCVS Open. 2023;14:1–13.
Article PubMed PubMed Central Google Scholar
Juraszek A, Czerny M, Rylski B. Update in aortic dissection. Trends Cardiovasc Med. 2022;32(7):456–61.
Article PubMed Google Scholar
Di Eusanio M, Trimarchi S, Patel HJ, et al. Clinical presentation, management, and short-term outcome of patients with type a acute dissection complicated by mesenteric malperfusion: observations from the International Registry of Acute Aortic Dissection. J Thorac Cardiovasc Surg. 2013;145(2):385–90. e381.
Pape LA, Awais M, Woznicki EM, et al. Presentation, diagnosis, and outcomes of Acute Aortic dissection: 17-Year trends from the International Registry of Acute Aortic Dissection. J Am Coll Cardiol. 2015;66(4):350–8.
Yagdi T, Atay Y, Engin C, et al. Impact of organ malperfusion on mortality and morbidity in acute type a aortic dissections. J Card Surg. 2006;21(4):363–9.
Patel HJ, Williams DM, Dasika NL, et al. Operative delay for peripheral malperfusion syndrome in acute type a aortic dissection: a long-term analysis. J Thorac Cardiovasc Surg. 2008;135(6):1288–95. discussion 1295 – 1286.
Rodiere M, Thony F, Michoud M, et al. [Acute visceral ischaemia, early complication of the aortic syndrome: how to detect and manage it?]. Presse Med. 2011;40(1 Pt 1):54–61.
Velayudhan BV, Idhrees AM, Mukesh K, et al. Mesenteric malperfusion in Acute Aortic dissection: challenges and frontiers. Semin Thorac Cardiovasc Surg. 2019;31(4):668–73.
Berretta P, Trimarchi S, Patel HJ, et al. Malperfusion syndromes in type A aortic dissection: what we have learned from IRAD. J Vis Surg. 2018;4:65.
Czerny M, Schoenhoff F, Etz C, et al. The impact of pre-operative malperfusion on Outcome in Acute Type A aortic dissection: results from the GERAADA Registry. J Am Coll Cardiol. 2015;65(24):2628–35.
Ren Y, Zhang J, Zhou H, et al. Experience in curing refractory gastrointestinal bleeding due to type A aortic dissection combined with mesenteric artery malperfusion: a case report. Ann Palliat Med. 2021;10(9):10102–7.
Di Eusanio M, Patel HJ, Nienaber CA, et al. Patients with type a acute aortic dissection presenting with major brain injury: should we operate on them? J Thorac Cardiovasc Surg. 2013;145(3 Suppl):S213–e221211.
Gudbjartsson T, Ahlsson A, Geirsson A, et al. Acute type a aortic dissection - a review. Scand Cardiovasc J. 2020;54(1):1–13.
Sabe AA, Percy ED, Kaneko T, et al. When to consider deferral of surgery in Acute Type A aortic dissection: a review. Ann Thorac Surg. 2021;111(6):1754–62.
Uchida K, Karube N, Kasama K, et al. Early reperfusion strategy improves the outcomes of surgery for type a acute aortic dissection with malperfusion. J Thorac Cardiovasc Surg. 2018;156(2):483–9.
Yamashiro S, Kuniyoshi Y, Miyagi K, et al. Successful management in the case of mesenteric ischemia complicated with acute type a dissection. Ann Thorac Cardiovasc Surg. 2002;8(4):231–5.
PubMed Google Scholar
Okita Y, Okada K. Treatment strategies for malperfusion syndrome secondary to acute aortic dissection. J Card Surg. 2021;36(5):1745–52.
Hashimoto O, Saito Y, Nakayama T, et al. Prognostic impact of Branch Vessel involvement on computed tomography versus clinical presentation of Malperfusion in patients with type a Acute Aortic Dissection. Am J Cardiol. 2021;152:158–63.
Orihashi K. Mesenteric ischemia in acute aortic dissection. Gen Thorac Cardiovasc Surg. 2018;66(10):557–64.
Morisaki A, Kato Y, Motoki M, et al. Delayed intestinal ischemia after surgery for type a Acute Aortic Dissection. Ann Vasc Dis. 2015;8(3):255–7.
Geana RC, Pavel P, Nayyerani R, et al. Successfully superior mesenteric artery stenting in operated type a aortic dissection complicated with delayed mesenteric malperfusion. SAGE Open Med Case Rep. 2021;9:2050313X211021184.
Mochida Y, Morinaga H, Shimizu Y, et al. Critical Malperfusion caused by Central Aortic Repair for Acute Aortic dissection: a Case Report. Ann Vasc Dis. 2019;12(3):404–7.
Shiiya N, Matsuzaki K, Kunihara T, et al. Management of vital organ malperfusion in acute aortic dissection: proposal of a mechanism-specific approach. Gen Thorac Cardiovasc Surg. 2007;55(3):85–90.
Khayat M, Cooper KJ, Khaja MS, et al. Endovascular management of acute aortic dissection. Cardiovasc Diagn Ther. 2018;8(Suppl 1):S97–107.
Duan WX, Wang WG, Xia L, et al. Clinical profiles and outcomes of acute type a aortic dissection and intramural hematoma in the current era: lessons from the first registry of aortic dissection in China. Chin Med J (Engl). 2021;134(8):927–34.
Sueyoshi E, Murakami T, He X, et al. CT findings of type a acute aortic dissection that did and did not result in prehospital death. Med (Baltim). 2022;101(4):e28657.
Article Google Scholar
Jaffar-Karballai M, Tran TT, Oremakinde O, et al. Malperfusion in Acute Type A aortic dissection: management strategies. Vasc Endovascular Surg. 2021;55(7):721–9.
Yu H, Kirkpatrick IDC. An update on Acute Mesenteric Ischemia. Can Assoc Radiol J. 2023;74(1):160–71.
Shiiya N, Sawada A, Tanaka E, et al. Percutaneous mesenteric stenting followed by laparoscopic exploration for visceral malperfusion in acute type B aortic dissection. Ann Vasc Surg. 2006;20(4):521–4.
Paral J, Ferko A, Plodr M, et al. Laparoscopic diagnostics of acute bowel ischemia using ultraviolet light and fluorescein dye: an experimental study. Surg Laparosc Endosc Percutan Tech. 2007;17(4):291–5.
van Bakel PAJ, Henry M, Kim KM, et al. Imaging features of renal malperfusion in aortic dissection. Eur J Cardiothorac Surg. 2022;61(4):805–13.
Pacini D, Leone A, Belotti LM, et al. Acute type a aortic dissection: significance of multiorgan malperfusion. Eur J Cardiothorac Surg. 2013;43(4):820–6.
Kamman AV, Yang B, Kim KM, et al. Visceral malperfusion in aortic dissection: the Michigan experience. Semin Thorac Cardiovasc Surg. 2017;29(2):173–8.
Inoue Y, Inoue M, Koga M et al. Novel brain computed tomography perfusion for cerebral malperfusion secondary to acute type a aortic dissection. Interact Cardiovasc Thorac Surg. 2022;35(1).
Zindovic I, Gudbjartsson T, Ahlsson A, et al. Malperfusion in acute type a aortic dissection: an update from the Nordic Consortium for Acute Type A aortic dissection. J Thorac Cardiovasc Surg. 2019;157(4):1324–e13331326.
Yanase Y, Ohkawa A, Inoue S, et al. Stanford Type A Acute Aortic dissection with Intimal Intussusception. Ann Thorac Cardiovasc Surg. 2020;26(1):51–4.
Koga M, Iguchi Y, Ohara T, et al. Acute ischemic stroke as a complication of Stanford type A acute aortic dissection: a review and proposed clinical recommendations for urgent diagnosis. Gen Thorac Cardiovasc Surg. 2018;66(8):439–45.
Meriggi F, Alloni A, Gramigna P, et al. Acute aortic dissection with intestinal ischemia: what to do first. Ann Thorac Cardiovasc Surg. 2011;17(6):631–3.
Williams IM, Idhrees M, Velayudhan B, et al. Malperfusion syndrome in acute type a aortic dissection: it’s not what you know, it’s what you can prove! J Card Surg. 2022;37(11):3835–7.
Sugiyama K, Watanuki H, Okada M, et al. Revascularization-first strategy in acute aortic dissection with mesenteric malperfusion. J Card Surg. 2020;35(11):3004–9.
Alemanno G, Somigli R, Prosperi P, et al. Combination of diagnostic laparoscopy and intraoperative indocyanine green fluorescence angiography for the early detection of intestinal ischemia not detectable at CT scan. Int J Surg Case Rep. 2016;26:77–80.
Zhao MM, Guo ZJ, Lu JK, et al. Research progress of acute type a aortic dissection complicated with poor perfusion syndrome. J Cardiopulm Vascular Disease. 2019;38(10):1071–3.
Google Scholar
Song SB, Wu XJ, Sun Y, et al. A modified frozen elephant trunk technique for acute Stanford type A aortic dissection. J Cardiothorac Surg. 2020;15(1):322.
Doenges JE, Reed AB, Huddleston S, et al. Persistent malperfusion after central aortic repair in acute type I aortic dissections. J Vasc Surg. 2023;77(6):1618–24.
Klar E, Rahmanian PB, Bucker A, et al. Acute mesenteric ischemia: a vascular emergency. Dtsch Arztebl Int. 2012;109(14):249–56.
Leshnower BG, Keeling WB, Duwayri YM, et al. The thoracic endovascular aortic repair-first strategy for acute type a dissection with mesenteric malperfusion: initial results compared with conventional algorithms. J Thorac Cardiovasc Surg. 2019;158(6):1516–24.
Malaisrie SC, Szeto WY, Halas M, et al. 2021 the American Association for Thoracic Surgery expert consensus document: Surgical treatment of acute type a aortic dissection. J Thorac Cardiovasc Surg. 2021;162(3):735–e758732.
Norton EL, Farhat L, Wu X, et al. Managing Malperfusion Syndrome in Acute Type A aortic dissection with previous cardiac surgery. Ann Thorac Surg. 2021;111(1):52–60.
Moorthy PSK, Sakijan AS. Malperfusion in acute type a aortic dissection: how we handle the challenge? Indian J Thorac Cardiovasc Surg. 2022;38(Suppl 1):122–31.
Deeb GM, Williams DM, Bolling SF, et al. Surgical delay for acute type a dissection with malperfusion. Ann Thorac Surg. 1997;64(6):1669–75. discussion 1675 – 1667.
Article CAS PubMed Google Scholar
Yang B, Rosati CM, Norton EL, et al. Endovascular Fenestration/Stenting first followed by delayed Open Aortic Repair for Acute Type A Aortic Dissection with Malperfusion Syndrome. Circulation. 2018;138(19):2091–103.
Yang B, Norton EL, Rosati CM, et al. Managing patients with acute type a aortic dissection and mesenteric malperfusion syndrome: a 20-year experience. J Thorac Cardiovasc Surg. 2019;158(3):675–e687674.
Norton EL, Khaja MS, Williams DM, et al. Type a aortic dissection complicated by malperfusion syndrome. Curr Opin Cardiol. 2019;34(6):610–5.
Abe T, Usui A. [Management of Acute Type A Dissection complicated with Acute Mesenteric Ischemia]. Kyobu Geka. 2017;70(8):605–11.
Emmoto T. [Successful two-stage Surgical Treatment of Acute Type A aortic dissection with mesenteric ischemia]. Kyobu Geka. 2016;69(4):286–91.
Sakaki K, Onishi Y, Toyoda M, et al. [Stanford Type A Acute aortic dissection complicated with intestinal ischemia preceded by Superior Mesenteric Artery Bypass:report of a case]. Kyobu Geka. 2023;76(5):375–8.
Kondo T, Isomura T, Hoshino J, et al. [Acute Type A aortic dissection with superior mesenteric arterial dissection; report of a case]. Kyobu Geka. 2013;66(3):234–6.
Fujii H, Koizumi S, Koyama T. [Superior Mesenteric Artery Bypass Grafting from the Ascending Aorta using a Saphenous Vein Graft for treatment of Acute Aortic dissection with abdominal malperfusion:report of a case]. Kyobu Geka. 2021;74(5):388–91.
Kunihara T, Matsui Y, Murashita T, et al. [Acute type a aortic dissection associated with intestinal necrosis]. Kyobu Geka. 2005;58(5):356–60.
Tsagakis K, Janosi RA, Frey UH, et al. True Lumen stabilization to Overcome Malperfusion in Acute Type I aortic dissection. Semin Thorac Cardiovasc Surg. 2019;31(4):740–8.
Mukherjee D, Collins DT, Ryan L. Retrograde stenting of the superior mesenteric artery is the procedure of choice for dissection of the aorta with mesenteric compromise. J Vasc Surg Cases Innov Tech. 2019;5(4):431–4.
Kato W, Fujita T, Uchida K, et al. Superior mesenteric artery plasty for type a acute aortic dissection with visceral ischemia. Gen Thorac Cardiovasc Surg. 2016;64(7):422–4.
Download references
Acknowledgements
This research received no external funding.
Author information
Authors and affiliations.
The First Clinical Medical College of Gannan Medical University, Ganzhou, 341000, China
Wenbo Yu, Yuan Liang, Jianfeng Gao & Dilin Xie
First Affiliated Hospital of Gannan Medical University, Ganzhou, 341000, China
Jianxian Xiong
You can also search for this author in PubMed Google Scholar
Contributions
WY and YL reviewed the literature and drafted the manuscript. JG and DX reviewed the literature. JX edited and revised the manuscript. All authors contributed to and approved the submitted manuscript.
Corresponding author
Correspondence to Jianxian Xiong .
Ethics declarations
Ethics approval and consent to participate, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yu, W., Liang, Y., Gao, J. et al. Surgical choice for the treatment of partial intestinal ischemic necrosis caused by acute type a aortic dissection combined with malperfusion of superior mesenteric artery. J Cardiothorac Surg 19 , 286 (2024). https://doi.org/10.1186/s13019-024-02790-z
Download citation
Received : 30 September 2023
Accepted : 03 May 2024
Published : 11 May 2024
DOI : https://doi.org/10.1186/s13019-024-02790-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Acute type a aortic dissection
- Mesenteric hypoperfusion
- Intestinal necrosis
- Treatment strategy
Journal of Cardiothoracic Surgery
ISSN: 1749-8090
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Abbreviation of International Journal of Current Research and Review. The ISO4 abbreviation of International Journal of Current Research and Review is - . It is the standardised abbreviation to be used for abstracting, indexing and referencing purposes and meets all criteria of the ISO 4 standard for abbreviating names of scientific journals.
International Journal of Current Research and Review (IJCRR) is the official publication of Radiance Research Academy which is governed by Swadesh Bahu-uddeshiya Kalyankari Shikshan Sanstha, Nagpur (Registered under Society's Act 1860, XXI, Regd. No. 868/11 Ngp and Bombay Trust Act 1950 Regd. No. F-287/4 Ngp).
The SJR is a size-independent prestige indicator that ranks journals by their 'average prestige per article'. It is based on the idea that 'all citations are not created equal'. SJR is a measure of scientific influence of journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals ...
International Journal of Current Research and Review (IJCRR) is one of the popular monthly international interdisciplinary science journals. IJCRR is a peer reviewed indexed journal which is available online and in print format as well. References have shown that within short span of time, citations for IJCRR are increasing with noticeable pace.
The abbreviation of the journal title " International journal of current research " is " Int. J. Curr. Res. ". It is the recommended abbreviation to be used for abstracting, indexing and referencing purposes and meets all criteria of the ISO 4 standard for abbreviating names of scientific journals. Organize your papers in one place.
The Impact IF 2021 of International Journal of Current Research and Review is 0.39, which is computed in 2022 as per its definition. International Journal of Current Research and Review IF is increased by a factor of 0.15 and approximate percentage change is 62.5% when compared to preceding year 2020, which shows a rising trend. The impact IF, also denoted as Journal impact score (JIS), of an ...
ISSN 2347-3215 (Online) | International journal of current research and academic ... International journal of current research and academic review. Identifiers. ISSN : 2347-3215. Linking ISSN (ISSN-L): 2347-3215. Resource information. Title proper: International journal of current research and academic review. Abbreviated key-title: Int. j ...
ISSN 0975-5241 (Online) | International journal of current research and review. Skip to main content. Leave this field blank . Log In; Automatic login IP; PUBLISHERS' AREA DISCOVER ISSN SERVICES SEARCH OPEN ... International journal of current research and review. Identifiers. ISSN : 0975-5241. Linking ISSN (ISSN-L): 0975-5241.
The latest impact score (IS) of the International Journal of Current Research and Review is .39.It is computed in the year 2022 as per its definition and based on Scopus data. 0.39 It is increased by a factor of around 0.15, and the percentage change is 62.5% compared to the preceding year 2020, indicating a rising trend.The impact score (IS), also denoted as the Journal impact score (JIS ...
Description. International Journal of Current Research (ISSN: 0975-833X) is an peer-review' and 'refereed' journal. Review boards in the field of expertise examining the journal articles before acceptance for publication. It is the process through which experts in the field of study assess the quality of articles that are submitted to a journal ...
The International Journal of Current Research (IJCR) is a multidisciplinary journal aimed at attracting contributions from multidisciplinary. Authors are cordially invited to submit full length paper, Original and unpublished research articles, based on theoretical or experimental works, are solicited for publication in the journal.
Send in your manuscripts for publication at the International Journal of Current and Research and Review. On the hunt for a widely recognized peer reviewed journal or other open access journals to have your research published in? Send in your manuscripts for publication at the International Journal of Current and Research and Review ...
Editorial and Publishing Process. Statistics. Rapid Publishing. Professional publishing practices. Indexing in leading database. High level of citation. High Qualitiy reader base. High level author suport.
International Journal of Current Research and ReviewSCImago SJR Rank. SCImago Journal Rank (SJR indicator) is a measure of scientific influence of scholarly journals that accounts for both the number of citations received by a journal and the importance or prestige of the journals where such citations come from.
The International Journal of Current Research and Academic Review ISSN: 2347 - 3215 ... Review can be made by authors in the current topics and intensive areas. ... K.Tim, Chennai, Magazine or personal communication, Newsletter). Journal names are abbreviated according to Chemical Abstracts. Authors are fully responsible for the accuracy of the ...
NLM Title Abbreviation: Int J Curr Res Title(s): International journal of current research. Other Title(s): IJCR Publication Start Year: 2010 Country of Publication: India Publisher: [India?] : International Journal of Current Research Description: 1 online resource Language: English ISSN: 0975-833X (Electronic) 0975-833X (Linking) LCCN: 2012261060
ISSN: 2454-2237 (Print) International Journal of Research and Review (E-ISSN: 2349-9788; P-ISSN: 2454-2237)is a double-blind, Indexed peer-reviewed, open access international journal dedicated to promotion of research in multidisciplinary areas. We define Open Access-journals as journals that use a funding model that does not charge readers or ...
Aim & Scope. The International Journal of Current Research and Academic Review (ISSN 2347 - 3215) aims at the publication of original research, reviews and short communications on the latest developments in all fields of Science & Humanities and Engineering technology. The journal publishes original papers in English which contribute to the ...
International Journal of Current Microbiology and Applied Sciences ISSN:2319-7692(Print), ISSN:2319-7706(Online) is a multidisciplinary peer-reviewed journal with reputable academics and experts as members of its Editorial Board. The Current Microbiology aims to publish all the latest and outstanding research articles. Review and letters in all areas of major importance to techniques of ...
The American Society of Neuroradiology has expanded its global presence, driven by the efforts of the International Collaborations Committee. This committee is actively involved in training radiologists and fostering collaborations worldwide in the fields of education, research, and community service. This article explores key initiatives of the committee, such as the Anne G. Osborn ASNR ...
Social media has become more popular in the last few years. It has been used in public health development and healthcare settings to promote healthier lifestyles. Given its important role in today's culture, it is necessary to understand its current trends and future directions in public health. This review aims to describe and summarize how public health professionals have been using social ...
Inotuzumab ozogamicin (INO) is an anti-CD22 antibody-drug conjugate that was first evaluated in B-cell lymphomas but was subsequently shown to be highly effective in acute lymphoblastic leukemia (ALL). INO improved response rates and survival in a randomized study in adults with relapsed/refractory B-cell ALL, leading to its regulatory approval in the United States in 2017. While the formal ...
Journal abbreviation: International journal of research. The abbreviation of the journal title " International journal of research " is " Int. J. Res. ". It is the recommended abbreviation to be used for abstracting, indexing and referencing purposes and meets all criteria of the ISO 4 standard for abbreviating names of scientific journals.
Diabetes mellitus is a significant global public health challenge, with a rising prevalence and associated morbidity and mortality. Cell therapy has evolved over time and holds great potential in diabetes treatment. In the present review, we discussed the recent progresses in cell-based therapies for diabetes that provides an overview of islet and stem cell transplantation technologies used in ...
1 Department of Molecular and Medical Virology, Ruhr University Bochum, Bochum, Germany. 2 Schaller Research Group, Department of Infectious Diseases, Virology, University Hospital Heidelberg, Heidelberg, Germany. 3 Heidelberg Biosciences International Graduate School (HBIGS), Heidelberg, Germany. 4 Center of Structural and Cell Biology in Medicine, Institute of Biochemistry, University of ...
Regulatory actions are increasingly used to tackle issues such as excessive alcohol or sugar intake, but such actions to reduce sedentary behaviour remain scarce. World Health Organization (WHO) guidelines on sedentary behaviour call for system-wide policies. The Chinese government introduced the world's first nation-wide multi-setting regulation on multiple types of sedentary behaviour in ...
Acute type A aortic dissection is a severe cardiovascular disease characterized by rapid onset and high mortality. Traditionally, urgent open aortic repair is performed after admission to prevent aortic rupture and death. However, when combined with malperfusion syndrome, the low perfusion of the superior mesenteric artery can further lead to intestinal necrosis, significantly impacting the ...