Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Natural Hazards - Impacts, Adjustments and Resilience

Disaster Management: A State-of-the-Art Review
Submitted: 17 June 2020 Reviewed: 13 October 2020 Published: 12 November 2020
DOI: 10.5772/intechopen.94489
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Natural Hazards - Impacts, Adjustments and Resilience
Edited by Ehsan Noroozinejad Farsangi
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
1,333 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Overall attention for this chapters
Disaster management involves the pillars of emergency management: planning and preparation, mitigation, response, and recovery. Emergencies are serious events that threaten health, life, and property and can be managed within the capabilities of the affected organization. Disasters, on the other hand, are hypercomplex emergencies, requiring resources not immediately available. Disaster management follows the principles of emergency management, and emphasizes flexibility, collaboration, and teamwork. Lack of resources will challenge people and organizations both in effects of disasters and the ability to manage them. Poverty, climate change, governance, and education are foundations to improve capacity. Hospitals play an important role in disaster response and can prepare accordingly. Plans, to be effective, must be implemented through appropriately-targeted exercises. Building on an all-hazards approach, to more hazard-specific considerations can improve disaster preparedness as well as day-to-day efficiency. Disaster management is complex and crucial. These principles are explored through the fictional tale of Tucci1, a coastal city in the worst flood anyone can remember. Well, almost anyone…
- natural disasters
- emergency management
- disaster management
- disaster training
Author Information
Jared bly *.
- University of Alberta, Canada
- Royal Roads University, Canada
Louis Hugo Francescutti
Danielle weiss.
- Northern Alberta Institute of Technology, Canada
*Address all correspondence to: [email protected]
1. Introduction
“Well, this is a disaster” said Jojo, the 19 year old apprentice to his mentor, Raj. They were pulling in the fishing nets near the usually beautiful seaside village of Tucci, now dull and grey and partly under water. The nets were heavy with debris from the churning sea. Raj grunted a mirthless laugh. “No. This is just a hard day of work. Tomorrow will be the disaster.”
Then the old man added, “unless it stops raining, the bridge stays above water, the power line’s fixed, and we have enough sandbags for everyone to keep their houses from washing away.”
It wasn’t totally exaggerated. The rain had been the worst in decades. Many homes in the low-lying village were already flooded. Those that were a little higher than the rest were already overcrowded with friends and relatives who’s houses were in a foot or two of water. And the bridge, the only land access to the village, was visible only as rail posts marking a dotted line through the sea between the village and the green foothills.
Disasters require both a potentially harmful event and a component of vulnerability [ 1 ]. If an event overwhelms local response capacity, whether by insufficient material resources or by inadequate social systems or structure, outside help is needed. This is a disaster. Thus the magnitude of an event that causes a disaster will vary by organizational capacity. Many of the natural events described elsewhere in this textbook (earthquakes, tsunamis, etc.) create disasters. An earthquake in a remote, uninhabited area might be called a natural disaster, but it is not truly a disaster if people are not severely impacted. Disasters occur at the interface of nature and civilization [ 2 ].
Emergency management is usually described in terms of planning, mitigation, response, and recovery. As we move along the spectrum of severity, from emergency to disaster, the same principles apply, with an emphasis on adaptability and collaboration. Specific to hospital disaster management, contextual issues such as triage, decontamination, and patient care are built upon a general and pervasive approach to disaster readiness. In resource-poor environments, the challenge is magnified as the impacts of natural disasters are greater, and the ability to respond and recover less. Education and training will be most effective if methods match the objectives. With all the uncertainty therein, training for disaster must include establishing relationships between organizations and allowing for flexibility in the face of events that can be predicted but never fully anticipated.
Not every windstorm, earth-tremor, or rush of water is a catastrophe…So long as the ship rides out the storm, so long as the city resists the earth-shocks, so long as the levees hold, there is no disaster. It is the collapse of the cultural protections that constitutes the disaster proper. ([ 3 ], p. 211)
2. Definitions
From crisis to catastrophe, emergency to disaster, there is a spectrum of events that may threaten people and organizations. Not just the event, but the characteristics of the affected population define disaster. Risk and resilience are opposing forces that must be considered with disaster management.
2.1 Emergencies
Disasters and emergencies differ in quality and magnitude but are often and inaccurately used synonymously. “Disasters are not just ‘big emergencies’” ([ 4 ], p. 293). Emergencies are time-sensitive, potentially harmful events that put life and well-being at risk. Resources are available at the local level to prevent, mitigate, or minimize the harm, and a single responding organization is responsible [ 5 , 6 ]. Local resources, as a variable in the equation, can affect what constitutes an emergency, and what goes beyond. An event of the same magnitude, in locations or situations with different capabilities and resources, may be managed within the organization (emergency) or need outside help (disaster). An example in a health care context might be a car crash involving one or two seriously injured people requiring prompt medical investigations and treatment, assuming the facility is equipped to deal with such an event.
2.2 Disasters
Disasters are sometimes considered “hypercomplex emergencies” or “major emergencies” involving multiple people at risk of harm, multiple jurisdictions responding, and resources that are not immediately available locally ([ 5 ], p. 8; [ 7 ]). Coordination between agencies, many of whom have no prior relationships, becomes a challenge [ 5 ]. Plans for resource utilization must change when those resources are overwhelmed [ 8 ]. Preparations, planning, and training at the local level, within the abilities and available resources of a single agency, do little to prepare for disaster.
Crisis is a more generic description. A crisis is a “critical event or point of decision which, if not handled in an appropriate and timely manner (or if not handled at all), may turn into a disaster or catastrophe” [ 9 ]. We use the word crisis , then, nonspecifically, as an emergency event that has potential to evolve; emergency as time-sensitive event with potential harm; and disaster as an event larger and more harmful than an emergency, with many people at risk, and where management requires resources outside of the responding organization or department.
2.4 Catastrophe
The word catastrophe , more severe than a disaster, completes the spectrum [ 5 ]. Many variations of the definition exist, but all suggest a magnitude of harm and inadequacy of response capabilities beyond what would be considered disaster [ 1 ] ( Figure 1 ).

Spectrum of crises.
The school gymnasium was packed with wet bodies. A kind of bored panic filled the air. After all, what more could they do but wait for the worst the storm threw at them and then pick up the pieces when it blew itself out?
“Thanks for being here, I know it’s been hard for everyone. And there’s still lots of work to do to clean up after yesterday’s catastrophe” said Ros, the town’s mayor, referring to the wind that had blown off parts of a few roofs, and torn off a main limb of the biggest cedar in town, crushing a corner of J. Z.’s corner store.
Ian spoke up, “we can’t worry about yesterday’s fiasco. We gotta think about the crisis we’re gonna be in tomorrow if the power’s not back. Then it will be a real emergency!”
Our first thought when we think of a hazard will often be an event—earthquake, flood, or fire. But only thinking in terms of characteristics of the event — windspeed, the size of tsunami wave, the magnitude of an earthquake, etc. — is to neglect a critical component. To become relevant to disaster management, nature must collide with human activity [ 10 ]. Hazards can be quantified simplistically as the probability of an event occurring, causing harm [ 11 ]. And there is no separating hazard from risk and resilience [ 12 ]. So the hazard is the oncoming storm and the potential for harm to the village it approaches ( Figure 2 ).

Hazard, risk, and vulnerability illustrated.
Risk is connected choice and probability [ 11 ]. Choice by the decisions we make. We build in flood zones, we develop seaside resorts, and we ignore all but the most active fault lines when looking at real estate. We buy fire insurance or not. We upgrade the old building to comply with seismic billing codes or not. We run disaster drills or not.
Probability is the other face of risk. Risk is an abstract concept, forever in the future, always uncertain.
Risk is a complex and, at the same time, curious concept. It represents something unreal, related to random chance and possibility, with something that still has not happened. It is imaginary, difficult to grasp and can never exist in the present, only in the future. ([ 11 ], p. 47).
2.7 Vulnerability
Vulnerability will create harm from the hazard. A predisposition to be harmed, intrinsic to the organization or organism is its vulnerability [ 11 ]. Poverty, age, gender, racial identification, geography, and many social, economic, and political factors are all parts. The vulnerability can accumulate until recovery is complete [ 12 ].
2.8 Resilience
The ability to adapt is central to an organization’s ability to resist and rebound from disaster [ 13 ]. Resilience is woven through all aspects of disaster management—from preparation through mitigation, response, and recovery [ 12 , 14 ]. Resilience alters the disaster threshold. The more resilient a system, the more harm can be absorbed before the system is overcome [ 13 ]. More resilience means less susceptibility to disaster.
3. Emergency management
Preparation and planning, mitigation, response, and recovery are the basic principles of emergency management [ 15 ]. It is called emergency management, but should really be called disaster management. Necessarily limited to first responders, the title emergency management gives an illusion of control that makes it both “a misnomer and an oxymoron” ([ 16 ], p. 5). Regardless of the size of the event’s magnitude, management includes all those efforts before, during, and after to minimize physical, social, and economic damages. Both planned and improvised actions should be included [ 16 ].
Preparation occurs before the disaster and includes preventative measures [ 17 ]. Disaster preparation, then, can also raise the disaster threshold if the disaster is thus avoided. At least, effects are minimized through planned measures. In our example settlement, prevention of a storm may not have been possible, but prevention of harm was through city planning, weather warning systems, and flood-resistant housing and infrastructure. Food and fuel stores could only be built up before the flooding.
Mitigation also includes a component of prevention but is closer to the event than planning. Anything to minimize harms that are not prevented could be considered mitigation. This can be through the reduction of the effects of the hazard, vulnerability of those affected in harm’s way. In Tucci, they could build up walls of sandbags to protect their homes. They could moor their boats securely. They could evacuate, or they may have been able to if they had made adequate plans and preparations. Clearly, all these components are intricately connected.
The response may be what we typically think of when we envision a disaster. This is the responders—firefighters, paramedics, police, military, municipal forces, and volunteers—dousing the flames, treating the wounded, rescuing the stranded, and searching for victims.
Recovery entails returning, rebuilding, restoring. It is regaining a sense of normalcy, if not returning exactly to the pre-disaster state. Tucci will never be the same. The coastline will be altered. Attitudes may change forever. Lives may be lost. Houses will have to be repaired or rebuilt. Few residents will rebuild their houses exactly as they were before the storm. Recovery should focus on learning from the disaster and improving those liabilities made apparent by the wind and waves. This applies not only to the repairs to physical structures but to emotional health and economic stability.
3.1 From emergency management to disaster management
Preparation, planning, mitigation, and recovery are all important management principles for crises of any magnitude. As complexity increases towards disasters, we focus on the response at the front lines. This is because this phase sees the most variation and inconsistency [ 18 ]. On the front and back ends, in planning and recovery, the skies are clear. There is time to think. Not so in response. The response is the result of planning and facilitates recovery. To be prepared for an emergency should be routine. Preparedness for a disaster does not automatically follow.
By definition, local resources are sufficient to respond to an emergency. When these resources are overwhelmed, either by supply (nature of the event) or demand (response capabilities), the situation is a disaster ([ 19 ], Ch1). Outside help is needed. Intra-agency communication and coordination are required, usually without the benefit of established relationships and protocols. As complexity increases, more emphasis must be placed on flexibility and coordination between teams.
When the crisis moves from emergency to disaster, flexibility becomes increasingly important in planning, preparation, and response. In disaster planning, people should be prepared not to respond to specific circumstances, but to be able to adapt to the unanticipated. Training for disaster, then, ideally trains flexibility, communication, and the ability to work across organizational boundaries [ 20 , 21 ]. Some structure is necessary to create the ability to adapt the structure to the situation. Brandrud’s [ 22 ] description of their successful system is excellent: “…[the] written preparedness and response plan was structured just enough to remind the health professional of their role and task, yet flexible enough to enable them to release their creativity to improvise solutions” (p. 811).
“Anyone got a charger?” The question was becoming a little repetitive. At first, the people that asked this were given sympathetic smiles and apologies. Now, if anyone dared ask, it was only met with grunts and grumbles. Part of ‘the plan’ involved keeping in touch with people by cell phone. There were only a handful of people who still had any battery life left on their phones, and no one had reception.
All but a few of the townspeople were crammed into the school for the night. It was loud. Fifty quiet conversations, a few crying babies, the howling wind, and the incessant rain added up. And the air was thick with sweat and sewer (the toilets had all overflowed). A dozen people were standing in a circle in the middle of the gym, sorting through a pile of walky-talkies.
The side door flew open with the outside coming inside, and a group of bodies in rain gear, dripping from head to toe. It was a crew from Uah, an even smaller town down the coast. They had got their whole village out last week and came here on a few all-terrain vehicles to lend a hand. Apparently, there was a team coming from the city to take everyone out. If the rain ever stopped…
Crisis standards of care are a reflection of the flexibility needed to respond when resources are lacking for the situation’s need [ 23 ]. The same standards employed in day to day operations, or even in an emergency (when an organization has the capability to manage it), will consume valuable assets (time, supplies, personnel, cognition) when the system is asked to perform beyond capacity. Awareness of the difference between disaster standards and the standards applied to usual operations will facilitate effective disaster planning and response ( Figure 3 ).

Principles in management when emergency becomes disaster.
3.2 Disaster management: resource poor environment
Natural hazards alone do not result in disaster, but rather the vulnerability of the populations of countries impacted [ 24 ]. The complexity and chaos of disasters make management challenging in many ways. Even the best plans will be unable to address each difficulty encountered in a disaster [ 25 ].
Resources are defined as the organization’s fundamental financial, physical, individual and organizational capital attributes [ 26 , 27 ]. In resource-poor environments, the challenge is greatly magnified. The environments most often impacted by a lack of resources are those of a lower socioeconomic status. Poverty and disasters are strongly associated [ 19 ]. Developing countries are repeatedly subject to disasters resulting in reduced or negative development [ 19 ].
There was a lot of talk about fixing houses, repairing roads, upgrading the bridge. People didn’t want to talk about the deeper issues. Most would never be able to afford anything more than patching the holes. Someone brought up the idea of building up on the hillside where the waves couldn’t reach. But that was so utterly inconceivable. How would they build a new town if they couldn’t even build new houses? Some would have to leave. Hard to live in a fishing village if your boat got washed away and you got no other way to make a living.
More impoverished communities are more vulnerable to natural disasters due to a mixture of social, political, cultural and economic factors [ 28 ]. Residents within these poorer communities tend to live in environments more prone to hazards such as rural areas with limited access to resources. The reduction in resources results in a more extended reconstruction period and can further delay developmental lag [ 19 ]. For example, in 2001, both El Salvador and the United States were hit by earthquakes, resulting in $2 billion in damages [ 19 ]. Although the same monetary value, the impact on each country’s economy varied drastically. This $2 billion in damages had minimal impact on the U. S. economy, whereas, in El Salvador it resulted in 15% of the countries GDP [ 19 ]. These financial setbacks to developing countries can create a cyclical impact of further delayed development lag and economic growth.
Beyond the economic impacts, developing countries also face higher casualty rates. Over 96% of disaster-related deaths in recent years have taken place in developing countries [ 29 ]. Disasters may bring about harm to poor, developing countries in many ways beyond death, injury and destruction [ 19 ]. Some of the numerous examples include an increase in crime due to poverty and desperation, damage to schools leading to longterm impacts on education and further employment, destruction to hospitals which increase the vulnerability of disease, and the impact to vital infrastructure such as roads, bridges and airports, which may take years to rebuild and further impact resource access [ 19 ].
For meaningful disaster preparedness, the focus must be on improving availability and access to resources. This improvement should be a continual improvement effort to implement these resources to the area permanently. This implementation will help to support improvement to the quality of life to those impacted and decrease the inequity of resources and support when faced by disasters. Improved governance, combined approaches on all government levels, empowering communities, assessing vulnerability, ensuring access to quality information, and increasing the resilience of livelihood and infrastructure within these environments will reduce poverty and increase the quality of life [ 29 ].
Climate change and sustainable development both also influence the frequency and severity of disasters, particularly in resource-poor countries. Climate change, and irresponsible use of natural resources such as deforestation, make the environment more susceptible to hazards and disaster [ 30 ]. Disasters related to natural hazards, such as floods, storms and earthquakes, have significantly risen over recent years [ 30 ]. Such an increase in disasters is likely to further the frequency and severity of the impacts on the resource poor countries. Sustainable development is crucial to help reduce this burden.
3.3 Hospital disaster management
Disasters are easily forgotten. The unfortunate truth is that the longer the distance in time and space from disasters, the less influence they have on preparedness and planning [ 31 ]. This is especially relevant to hospitals because of a number of other interactions. Perception of disaster preparedness is often quite different between planners and frontline workers, the latter decidedly less optimistic about the facility’s state of readiness [ 31 ]. And the pressures and problems of everyday operations can easily push aside concerns for an unforeseeable event. The attitude of disaster preparedness needs to pervade all aspects of the organization in the face of so many unseen but real hazards [ 32 ].
Specific hospital management principles include, but are definitely not limited to, vulnerability analysis, communications, triage, surge capacity, psychosocial effects, and medicolegal issues [ 31 ]. Hospitals must consider the disaster and its effects not only on a massive influx of patients but on existing patients, as well as health care workers in and out of hospital [ 33 ]. Patient care may be complicated and compromised by issues of security, chemical or biological exposure, and capacity for definitive care [ 29 , 34 ].
Typically, an ‘all-hazards’ approach is employed as a basis of preparation for crises of any nature. More advanced preparedness will be tailored to specific hazards [ 30 , 35 ]. We cannot plan for every possibility, especially not every extreme and infrequent event covered in this textbook. Plans must be broad enough to allow adaptation as needed [ 22 ]. If plans are too narrowly focused the preparation may be ineffective. Flexibility is key.
Good thing we made it out when we did, although, an hour earlier would have been ideal. The leak that had been dripping constantly in the west corner of the gym turned into a stream, then a river, then the storm outside as the tiles gave way. The sick and the injured were evacuated first, down to Mayor Ros. Raj and me came on the last load. The hospital at Alec wasn’t used to a hundred people at all, much less all within a couple hours. It was hard to tell who was who - doctors, nurses, housekeepers — might have been the president of the hospital — who were finding blankets, mopping up the incessant streams of muddy water, handing out bottles of clean water, looking at cuts and bruises and sore throats.
Hospital disaster planning has important ramifications for capacity-building. That is, the threshold for disaster, an event that overwhelms local abilities, is intricately connected to capacity. “If a disaster is defined as an event that outstrips the organization’s ability to deliver healthcare, preparedness is a method of “vaccination,” raising the threshold not only in disaster periods but also in normal day-to-day function” ([ 31 ], p. xi). Disaster preparation is capacity-building.
Disaster preparedness is also about building networks. Again it comes back to the definition of disaster that requires help outside the immediately-affected organization. Coordination and communication between agencies are important in the success or deficiency of disaster response [ 23 , 31 , 36 ]. Establishing and enhancing relationships between organizations cannot be done in the moment of need. This should be a high priority for any organization in this time of global connectedness. Whether for a hospital, a nation, or a single-family, Alexander’s [ 32 ] words for current and future emergency managers applies here: “Nothing can substitute for personal relationships” ([ 32 , 37 ], p. 10).
The worst possible outcome of preparedness activities is to engender complacency. A “paper plan syndrome” refers to passively placing confidence in a document detailing a facility’s readiness ([ 35 ], p. 3). Written plans do not obviate problems [ 33 , 38 ]. To be effective, training needs to be continuous, team-centred, and at least as far as disasters go, focused on the non-technical aspects of working in teams [ 22 ]. They have to use existing resources and include the possibility of the loss of these resources. The loss of electrical power is particularly important to consider. Our increasing reliance on technology is a modern blessing in times of peace and a serious susceptibility when things are bad [ 12 ].
4. Training
Plans are only ‘fantasy documents’ if they have no real implementation through training ([ 39 ], p. 2). Exercises also may only be preparation in fantasy if not implemented conscientiously. When planning disaster training exercises, we should consider our purposes. Is the intent to expose participants to the disaster response plan or their roles in the organizational structure? Is it to test the implantation of the response plan, to expose its weaknesses and oversights? This is often the objective, intended or not ([ 40 ], p. 277). Evaluation and improvement of disaster plans may be a useful objective if that is the need [ 31 ]. But simply observing shortcomings does not itself remedy them. Lessons “identified” does not mean lessons “learned” ([ 40 ], p. 280) Is the intent to learn from or improve collaboration with other agencies? Is the intent to improve decision-making and specific skills? These are all valid objectives and need to be determined to meet the organization’s needs, lest any coincidental success be wrongly attributed to ineffective plans [ 41 ]. Disaster training should focus on adaptability. “Exercises and training on how to be creative and imaginative under such circumstances would be more useful than detailed disaster plans” ([ 25 ], p. 376).
A month later…
“We just need to stick to the plan next time,” Jan said, the last part sounding like a question. The storm was a memory like a bad dream. The town meeting, those who were left, was about getting ready for the next one.
The plan was new to almost everyone. Ros dug up some dusty old binder a few days ago. Too bad it made it, untouched, through the storm. It was full of detailed instructions about houses reporting to block leaders, block leaders reporting to councillors, councillors to the mayor, the mayor to the assistance team that was supposed to come from Alec, the capital city. Only thing was, households were all rearranged, trying to find somewhere dry to sleep. The block leaders didn’t even know who they were, the mayor didn’t have any councillors, and the team, well, not sure there ever was one.
4.1 Barriers to effective exercises
Disaster exercises may not accomplish what is intended during their design [ 20 ]. Excessive complexity, targeting the wrong audience, and unforeseen social psychological effects are some of the problems that can impair the efficacy of disaster education.
Complexity. More complex does not mean better when it comes to training exercises [ 21 ]. Thinking that testing more skills will improve more skills, stressing more processes will improve more processes, and designing more complex scenarios will enhance a greater repertoire of individual and systemic responses is flawed. The opposite can occur. Complexity can obscure the purpose of the exercise, lead to passivity among participants, and decrease collaboration [ 42 ]. Complexity can also interfere with learning [ 20 ]. Complex responses may be better trained by simple exercises. The goal is internal complexity with external simplicity (Loveluck cited in [ 21 ], p. 423).
Leaders versus participants. Many exercises benefit the designers and facilitators more than the participants [ 20 , 21 ]. This may be effective when that is the goal. Some exercises explicitly target leaders and not participants [ 43 ]. But often, the intent is to train participants. Even when that is the stated objective, participants may not see it that way [ 44 ]. Facilities and educators may not be training who they hope to train. It is important to consider who the exercise is for, and who is actually benefitting.
Social psychological. Recognizing that crisis simulations are meant to evoke some stress in individuals and organizations, some researchers have examined the adverse social and psychological effects of exercises [ 20 , 43 ]. Sometimes “unintended consequences” of these effects can appear as a failure to participate when trainees fear evaluation from superiors ([ 20 ], p. 422). Supervisors giving feedback can reinforce incorrect behaviors if hierarchical relationships are ignored [ 20 ].
4.2 Benefits
There is no doubt that planning and training is key to disaster preparedness [ 41 ]. Disaster exercises are beneficial when objectives are clear, and debriefing is effective. When objectives are appropriate and align with needs, response capacities improve. Debriefing helps with this and with all aspects of learning and growth. The debrief is one of the most important parts of effective exercise.
Clearly defined objectives. Objectives should identify whether the purpose of the exercise is evaluation or training, individual skills or collaboration, crisis or emergency response. Experts commonly identify the need for objectives to guide disaster exercises [ 20 , 45 ]. Yet hospital exercises often do not include specific objectives [ 46 ] or have not clearly defined them [ 47 ]. Objectives help operationalize disaster training. That means we can identify what we wish to improve, measure to see if we have improved, and actually improve in the desired area [ 20 , 21 , 43 , 46 ]. In many cases, the method of training and objectives of an exercise is not complementary and do not create the conditions for improvement in operational capacities [ 46 , 48 ].
Disaster vs emergency, stability vs flexibility, training vs drills. Disasters and emergencies are different events and require different responses [ 21 ]. Training for emergencies requires drills, practicing being able to perform planned responses to anticipated events [ 20 , 42 , 51 ]. In a disaster, responses outside an organization’s policies and protocols are required [ 20 , 44 ]. Training for disaster ideally trains flexibility, communication, and the ability to work across organizational boundaries [ 20 , 21 ].
Collaboration. Disasters require interactions across and within organizations that is outside of usual lines of communication [ 20 ]. Collaboration, then, is key. Collaborative communication can help organizations recognize crises in the first place [ 49 ] and throughout the event. If there are barriers to effective communication across organizational boundaries, the response will be less timely, flexible, and effective [ 51 ]. We should prepare for the need to collaborate through practice working within new relationships and organizational structures [ 25 ].
Debriefing. “… the only reason for running a simulation is so that an exercise can be debriefed” (Thiagarjan cited in [ 20 ], p. 421). Debriefing is essential in order for learning to occur [ 20 , 49 ]. Debriefing helps accomplish objectives, be they developing plans, training existing skills, or learning new things [ 50 ]. Learning from an exercise increases with reflection individually and collectively [ 21 , 44 , 51 ]. The utility of an effective and adequate debrief cannot be underemphasized ( Table 1 ).
Questions to ask to make disaster training effective.
Seems like a dream. A dream I’d like to forget. I said as much to Raj, adding “won’t see another one like that for a hundred years.”
He was just shaking his head. “Forget this dream and it might as well be three days till the next one. Be the same dream all over again unless you keep this one in mind.”
5. Conclusion
Disaster management is challenged by the difficulty we have as people and organizations to think about future, uncertain events. The complexity and chaos of disasters further complicate the tasks of planning, preparing, and responding. The more complex the event, the more an organization must adapt and collaborate with other organizations. This frameworks of resource management in disasters will guide organizations in their disaster preparedness activities. We have touched on some applications of these principles to hospitals and resource-poor environments. From an accurate understanding of what constitutes a disaster, education and training will more likely be effective — directed to the right people, developing the right skills in the right places.
- 1. Blanchard BW. Guide to emergency management and related terms, definitions, concepts, acronyms, organizations, programs, guidance, executive orders & legislation: A tutorial on emergency management, broadly defined, past and present. In United States Federal Emergency Management Agency 2008 Oct 27. Available from https://training.fema.gov/hiedu/docs/terms and definitions/terms and definitions.pdf
- 2. De Smet H, Lagadec P, Leysen J. Disasters out of the box: A new ballgame? JCCM. 2007; 20 (3):138-148. DOI: 10.1111/j.1468-5973.2012.00666.x
- 3. Carr LJ. Disaster and the sequence-pattern concept of social change. The American Journal of Sociology. 1932; 38 (2):207-218. DOI: 10.1086/216030
- 4. Tierney KJ. Businesses and Disasters: Vulnerability, impacts, and recovery. In handbook of disaster research. Handbooks of Sociology and Social Research. 2007. https://doi.org10.1007/978-0-387-32353-4_16
- 5. Oliver C. Catastrophic Disaster Planning and Response. CRC Press; 2010
- 6. United Nations (2019). UN-SPIDER. Space Based Information for Disaster Management and Emergency Response. Retrieved from http://www.un-spider.org/
- 7. McMaster R, Baber C. Multi-agency operations: Cooperation during flooding. Applied ergonomics. 2012 Jan 1; 43 (1):38-47. DOI: 10.1016/j.apergo.2011.03.006
- 8. Cannava P, Cicillini D, Higgins M, McGrath A, O'Leary J. Response to H1N1 influenza outbreak in a pediatric children's hospital: Challenges faced and lessons learned. Journal of Pediatric Nursing. 2010 Oct 1; 25 (5):375-381. DOI: 10.1016/j.pedn.2010.03.001
- 9. Business dictionary. http://www.businessdictionary.com/definition/crisis.html
- 10. World Health Organization. WHO/EHA Panafrican Emergency Training Centre, Addis Ababa. 2002. Retrieved from http://apps.who.int/disasters/repo/7656.pdf
- 11. Cardona OD. The need for rethinking the concepts of vulnerability and risk from a holistic perspective: A necessary review and criticism for effective risk management. In: Hilhorst D, Frerks G, Bankoff G, editors. Mapping Vulnerability: Disasters, Development and People. London: Earthscan Publications; 2003. pp. 37-51 Retrieved from http://www.academia.edu/download/54365737/Rethinking_Risk_Cardona.pdf
- 12. Etkin D. Disaster Theory: An Interdisciplinary Approach to Concepts and Causes. Butterworth-Heinemann; 2014
- 13. Hufschmidt G. A comparative analysis of several vulnerability concepts. Natural hazards. 2011 Aug 1; 58 (2):621-643. DOI: 10.1007/s11069-011-9823-7
- 14. Murphy BL, Etkin D. Introuction. In Etkin D, Murphy BL, editors. Disaster and emergency management in Canada . Canadian risk and hazards Network 2011. p. 1-16. Retrieved from https://www.crhnet.ca/sites/default/files/library/Introduction%20Formatted.pdf
- 15. Public Safety Canada. An Emergency Management Framework for Canada (Third Ed.) Government of Canada. 2017
- 16. McEntire DA. The status of emergency management theory: Issues, barriers, and recommendations for improved scholarship. University of North Texas. Department of Public Administration. Emergency administration and Planning 2004. Retrieved from http://precisionmi.com/precisionmi/Materials/ManagementMat/Status%20of%20Emergency%20Management%20Theory.pdf
- 17. Public Safety Canada. Disaster prevention and mitigation. 2015. Available from https://www.publicsafety.gc.ca/cnt/mrgnc-mngmnt/dsstr-prvntn-mtgtn/index-en.aspx
- 18. Van Wart M, Kapucu N. Crisis management competencies: The case of emergency managers in the USA. Public Management Review. 2011 May 1; 13 (4):489-511. DOI: 10.1080/14719037.2010.525034
- 19. Coppola, D. P. (2015). Introduction to international disaster management. Retrieved from https://ebookcentral-proquest-com.ezproxy.royalroads.ca
- 20. Borodzicz EP. The missing ingredient is the value of flexibility. Simulation & Gaming. 2004 Sep; 35 (3):414-426. DOI: 10.1177/1046878104266221
- 21. Borodzicz E, Van Haperen K. Individual and group learning in crisis simulations. Journal of contingencies and crisis management. 2002 Sep; 10 (3):139-147. DOI: 10.1111/1468-5973.00190
- 22. Brandrud AS, Bretthauer M, Brattebø G, Pedersen MJ, Håpnes K, Møller K, et al. Local emergency medical response after a terrorist attack in Norway: A qualitative study. BMJ Quality & Safety. 2017 Oct 1; 26 (10):806-816. DOI: 10.1136/bmjqs-2017-006517
- 23. Timbie JW, Ringel JS, Fox DS, Pillemer F, Waxman DA, Moore M, et al. Systematic review of strategies to manage and allocate scarce resources during mass casualty events. Annals of emergency medicine. 2013 Jun 1; 61 (6):677-689. DOI: 10.1016/j.annemergmed.2013.02.005
- 24. UNDP. Disaster Risk Reduction Governance & Mainstreaming. October, 2010. Retrieved from https://www.preventionweb.net/files/17429_4disasterriskreductiongovernance1.pdf '
- 25. Quarantelli EL. Disaster crisis management: A summary of research findings. Journal of management studies. 1988 Jul; 25 (4):373-385. DOI: 10.1111/j.1467-6486.1988.tb00043.x
- 26. Hill CW, Jones GR, Schilling MA. Strategic Management: Theory: An Integrated Approach. Boston: Houghton-Mifflin; 2001
- 27. Hitt MA, Ireland RD, Hoskisson RE. Strategic Management: Competitiveness and Globalization, 2nd Ed. 1997. West, St Paul, MN
- 28. Benson C, Twigg J, Myers M. NGO initiatives in risk reduction: An overview. Disasters. 2001 Sep; 25 (3):199-215. DOI: 10.1111/1467-7717.00172
- 29. OECD. Poverty and climate change: Reducing the vulnerability of the poor through adaptation. Available from www.oecd.org/env/cc/2502872.pdf
- 30. De Smet H, Lagadec P, Leysen J. Disasters out of the box: A new ballgame? Journal of Contingencies and Crisis Management. 2012 Sep; 20 (3):138-148. DOI: 10.1111/j.1468-5973.2012.00666.x
- 31. Kollek D, editor. Disaster preparedness for health care facilities. In: PMPH-USA. 2013
- 32. Health Standards Organization. Emergency and disaster management [guideline]. 2020. Available from www.healthstandards.org
- 33. Francescutti LH, Sauve M, Prasad AS. Natural disasters and healthcare: Lessons to be learned. In Healthcare management forum. 2017 Jan.; 30 (1):53-55. DOI: 10.1177/0840470416679338
- 34. Baker MS. Creating order from chaos: Part I: Triage, initial care, and tactical considerations in mass casualty and disaster response. Military medicine. 2007 Mar 1; 172 (3):232-236. DOI: 10.7205/MILMED.172.3.232
- 35. McCann, DGC. Introduction to disasters and disaster planning. in Kollek, D, editor. Disaster Preparedness for Health Care Facilities. PMPH-USA. 2013. p. 1-9
- 36. Hu Q , Knox CC, Kapucu N. What have we learned since September 11, 2001? A network study of the Boston marathon bombings response. Public Administration Review. 2014 Nov; 74 (6):698-712. DOI: 10.1111/puar.12284
- 37. Alexander DE. 2030: Adapting to complexity. Haznet 2020;14(1). http://haznet.ca/haznet-magazine-spring-2020-issue/
- 38. Juffermans J, Bierens JJ. Recurrent medical response problems during five recent disasters in the Netherlands. Prehospital and disaster medicine. 2010 Apr 1; 25 (2):127 http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.176.1952&rep=rep1&type=pdf
- 39. Clarke L. Mission Improbable: Using Fantasy Documents to Tame Disaster. University of Chicago Press; 1999 May 15
- 40. Skryabina E, Reedy G, Amlot R, Jaye P, Riley P. What is the value of health emergency preparedness exercises? A scoping review study. International journal of disaster risk reduction. 2017 Mar 1; 21 :274-283. DOI: 10.1016/j.ijdrr.2016.12.010
- 41. Steigenberger N. Organizing for the big one: A review of case studies and a research agenda for multi-agency disaster response. Journal of Contingencies and Crisis Management. 2016 Jun; 24 (2):60-72. DOI: 10.1111/1468-5973.12106
- 42. Berlin JM, Carlström ED. Collaboration exercises—The lack of collaborative benefits. International Journal of Disaster Risk Science. 2014; 5 (3):192-205. DOI: 10.1007/s13753-014-0025-2
- 43. Peterson DM, Perry RW. The impacts of disaster exercises on participants. Disaster Prevention and Management: An International Journal. 1999; 8 (4):241-255. DOI: 10.1108/09653569910283879
- 44. Berlin JM, Carlström ED. Collaboration exercises: What do they contribute? –a study of learning and usefulness. Journal of Contingencies and Crisis Management. 2015 Mar; 23 (1):11-23. DOI: 10.1111/1468-5973.12064
- 45. Hsu EB, Jenckes MW, Catlett CL, Robinson KA, Feuerstein C, Cosgrove SE, et al. Effectiveness of hospital staff mass-casualty incident training methods: A systematic literature review. Prehospital and disaster medicine. 2004 Sep; 19 (3):191-199. DOI: 10.1017/S1049023X00001771
- 46. Verheul ML, Dückers ML. Defining and operationalizing disaster preparedness in hospitals: A systematic literature review. Prehospital and disaster medicine. 2020 Feb; 35 (1):61-68. DOI: 10.1017/S1049023X19004187
- 47. Jamieson T. Disastrous measures: Conceptualizing and measuring disaster risk reduction. International Journal of Disaster Risk Reduction. 2016 Oct 1; 19 :399-412. DOI: 10.1016/j.ijdrr.2016.09.010
- 48. Beerens RJ, Tehler H. Scoping the field of disaster exercise evaluation-a literature overview and analysis. International Journal of Disaster Risk Reduction. 2016 Oct 1; 19 :413-446. DOI: 10.1016/j.ijdrr.2016.09.001
- 49. Lagadec P. Learning processes for crisis management in complex organizations. Journal of Contingencies and Crisis management. 1997 Mar; 5 (1):24-31. DOI: 10.1111/1468-5973.00034
- 50. Hermann MG. In conclusion: The multiple pay-offs of crisis simulations. Journal of Contingencies and Crisis Management. 1997 Dec; 5 (4):241-243. DOI: https://doi.org/10.1111/1468-5973.00062
- 51. Berlin JM, Carlström ED. The three-level collaboration exercise–impact of learning and usefulness. Journal of Contingencies and Crisis Management. 2015 Dec; 23 (4):257-265. DOI: https://doi.org/10.1111/1468-5973.12070
- I went with a fictional disaster to demonstrate the principles of disaster management for a number of reasons. 1. Any current disaster would soon be overshadowed by one more recent. 2. There are many people that would have a much greater understanding than me of any historical event. 3. Any real event risks being ‘foreign’ to people in other places. The story of Tucci belongs to no one, and so applies to anyone. I agree with Robert Fulghum who wrote" …myth is more potent than history" (The storyteller’s creed in All I needed to know I learned in kindergarten). JB
© 2020 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Natural hazards.
Published: 30 June 2021
By Frank Jerome Glago
2869 downloads
By Md. Shahin, Sanjida Akter, Prome Debnath and A.K.M...
671 downloads
By Diana Dimitrova
567 downloads
IntechOpen Author/Editor? To get your discount, log in .
Discounts available on purchase of multiple copies. View rates
Local taxes (VAT) are calculated in later steps, if applicable.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- My Bibliography
- Collections
- Citation manager
Save citation to file
Email citation, add to collections.
- Create a new collection
- Add to an existing collection
Add to My Bibliography
Your saved search, create a file for external citation management software, your rss feed.
- Search in PubMed
- Search in NLM Catalog
- Add to Search
Seven Decades of Disasters: A Systematic Review of the Literature
Affiliations.
- 1 1Edith Cowan University,School of Medical and Health Sciences,Joondalup,Western Australia.
- 2 3Harvard Humanitarian Initiative,Harvard Universityand Harvard T.C. Chan School of Public Health,Cambridge,MassachusettsUSA.
- 3 2James Cook University,College of Public Health,Medical,and Veterinary Sciences,Division of Tropical Health and Medicine,Cairns,Australia.
- 4 5School of Public Health, Faculty of Health,Queensland University of Technology,Brisbane,Australia.
- PMID: 30129914
- DOI: 10.1017/S1049023X18000638
IntroductionThe impact of disasters and large-scale crises continues to increase around the world. To mitigate the potential disasters that confront humanity in the new millennium, an evidence-informed approach to disaster management is needed. This study provides the platform for such an evidence-informed approach by identifying peer-reviewed disaster management publications from 1947 through July 2017.
Methods: Peer-reviewed disaster management publications were identified using a comprehensive search of: MEDLINE (US National Library of Medicine, National Institutes of Health; Bethesda, Maryland USA); CINAHL (EBSCO Information Services; Ipswich, Massachusetts USA); EMBASE (Elsevier; Amsterdam, Netherlands); PsychInfo (American Psychological Association; Washington DC, USA); and the Cochrane Library (The Cochrane Collaboration; Oxford, United Kingdom).
Results: A total of 9,433 publications were identified. The publications were overwhelmingly descriptive (74%) while 18% of publications reported the use of a quantitative methodology and eight percent used qualitative methodologies. Only eight percent of these publications were classified as being high-level evidence. The publications were published in 918 multi-disciplinary journals. The journal Prehospital and Disaster Medicine (World Association for Disaster and Emergency Medicine; Madison, Wisconsin USA) published the greatest number of disaster-management-related publications (9%). Hurricane Katrina (2005; Gulf Coast USA) had the greatest number of disaster-specific publications, followed by the September 11, 2001 terrorist attacks (New York, Virginia, and Pennsylvania USA). Publications reporting on the application of objective evaluation tools or frameworks were growing in number.
Conclusion: The "science" of disaster management is spread across more than 900 different multi-disciplinary journals. The existing evidence-base is overwhelmingly descriptive and lacking in objective, post-disaster evaluations. SmithEC, BurkleFMJr, AitkenP, LeggattP. Seven decades of disasters: a systematic review of the literature. Prehosp Disaster Med. 2018;33(4):418-423.
Keywords: CRED Center for Research on the Epidemiology of Disasters; PPRR Prevention/Preparedness/Response/Recovery; disaster; evidence-based practice; literature review.
PubMed Disclaimer
Similar articles
- Three decades of disasters: a review of disaster-specific literature from 1977-2009. Smith E, Wasiak J, Sen A, Archer F, Burkle FM Jr. Smith E, et al. Prehosp Disaster Med. 2009 Jul-Aug;24(4):306-11. doi: 10.1017/s1049023x00007020. Prehosp Disaster Med. 2009. PMID: 19806554 Review.
- No Calm After the Storm: A Systematic Review of Human Health Following Flood and Storm Disasters. Saulnier DD, Brolin Ribacke K, von Schreeb J. Saulnier DD, et al. Prehosp Disaster Med. 2017 Oct;32(5):568-579. doi: 10.1017/S1049023X17006574. Epub 2017 Jun 13. Prehosp Disaster Med. 2017. PMID: 28606191 Review.
- Quality Indicators for Evaluating Prehospital Emergency Care: A Scoping Review. Howard I, Cameron P, Wallis L, Castren M, Lindstrom V. Howard I, et al. Prehosp Disaster Med. 2018 Feb;33(1):43-52. doi: 10.1017/S1049023X17007014. Epub 2017 Dec 10. Prehosp Disaster Med. 2018. PMID: 29223193 Review.
- Categorization and Analysis of Disaster Health Publications: An Inventory. Birnbaum ML, Adibhatla S, Dudek O, Ramsel-Miller J. Birnbaum ML, et al. Prehosp Disaster Med. 2017 Oct;32(5):473-482. doi: 10.1017/S1049023X17006525. Epub 2017 May 31. Prehosp Disaster Med. 2017. PMID: 28560942
- Trend analysis of disaster health articles in peer-reviewed publications pre- and post-9/11. Kelen G, Sauer LM. Kelen G, et al. Am J Disaster Med. 2008 Nov-Dec;3(6):369-76. Am J Disaster Med. 2008. PMID: 19202890 Review.
- Hospitals as disaster victims: Lessons not learned? Melnychuk E, Sallade TD, Kraus CK. Melnychuk E, et al. J Am Coll Emerg Physicians Open. 2022 Jan 11;3(1):e12632. doi: 10.1002/emp2.12632. eCollection 2022 Feb. J Am Coll Emerg Physicians Open. 2022. PMID: 35036993 Free PMC article. Review.
- Absorptive capacity facilitates adaptation to novel environmental disasters. Cheong SM, Assenova VA. Cheong SM, et al. PLoS One. 2021 Nov 17;16(11):e0259368. doi: 10.1371/journal.pone.0259368. eCollection 2021. PLoS One. 2021. PMID: 34788322 Free PMC article.
- Disaster Medicine in Taiwan . Lin CH. Lin CH. J Acute Med. 2019 Sep 1;9(3):83-109. doi: 10.6705/j.jacme.201909_9(3).0002. J Acute Med. 2019. PMID: 32995238 Free PMC article. Review.
- Factors Associated with Food Insecurity Following Hurricane Harvey in Texas. Clay LA, Ross AD. Clay LA, et al. Int J Environ Res Public Health. 2020 Jan 25;17(3):762. doi: 10.3390/ijerph17030762. Int J Environ Res Public Health. 2020. PMID: 31991735 Free PMC article.
- Mitigating the impact of disasters and emergencies on clinical trials site conduct: A site perspective following major and minor unforeseen events. Lunt H, Heenan H. Lunt H, et al. Contemp Clin Trials Commun. 2019 Nov 12;16:100487. doi: 10.1016/j.conctc.2019.100487. eCollection 2019 Dec. Contemp Clin Trials Commun. 2019. PMID: 31872156 Free PMC article.
Publication types
- Search in MeSH
Related information
- Cited in Books
LinkOut - more resources
Full text sources.
- Cambridge University Press
Other Literature Sources
- scite Smart Citations
- MedlinePlus Health Information
- Citation Manager
NCBI Literature Resources
MeSH PMC Bookshelf Disclaimer
The PubMed wordmark and PubMed logo are registered trademarks of the U.S. Department of Health and Human Services (HHS). Unauthorized use of these marks is strictly prohibited.
To read this content please select one of the options below:
Please note you do not have access to teaching notes, a systematic literature review of community disaster resilience: main and related research areas and agendas.
Continuity & Resilience Review
ISSN : 2516-7502
Article publication date: 7 September 2021
Issue publication date: 14 September 2021
This study aims to characterize the main research areas of published works, identify the disciplines that associated with the works and propose research agendas for future inquiries, based on a systematic literature review that encompasses 89 research papers from 2010 to 2020.
Design/methodology/approach
This review commenced with the definition of the three research questions, and subsequently three steps were followed: (1) defining criteria for research paper selection; (2) specifying the data bases and selecting the papers based on the criteria and (3) data analysis, conclusion and discussion of selected papers. The search was limited to the selection of research papers in English, focusing on “community disaster resilience” which is the subject of this review and referred to as keywords which were used for the online search for papers. All these three words must be present in the title of the selected papers.
The area “resilience management” and “disaster resilience assessment” accounted for 43% of the studies, and it indicates that research has emphasized the description of how community disaster resilience has been managed and assessed. Three disciplines relating to disaster resilience are disaster risk science, public health and environment, and it indicates that research has fostered core areas of community disaster resilience. Three key research agenda include a growing trend to describe successful efforts to avert a potentially catastrophic disaster through solution-based case studies; a paradigmatic shift and implementation of how communities could help the disaster victims recuperate from disasters.
Research limitations/implications
This review is limited to the numbers of chosen papers, as only full papers were chosen. However, in order to establish more rigorous and inclusive results of the study, the numbers of citations of published papers to be chosen for future inquiry should be taken into account.
Originality/value
This present review originally investigated how the concept of disaster resilience has been applied at the community level and in related areas. As resilience is a multidisciplinary concept that has been investigated by several different disciplines, such as sustainability, psychology, economy and sociology, this study looked into how disciplines related to community disaster resilience to provide agenda for future inquiries. This study therefore characterized the main research areas of published works, identified the disciplines that associated with the works and proposed a research agenda for future inquiries.
- Community disaster resilience
- Resilience management
- Disaster resilience
Upadhyay, A. and Sa-ngiamwibool, A. (2021), "A systematic literature review of community disaster resilience: main and related research areas and agendas", Continuity & Resilience Review , Vol. 3 No. 2, pp. 192-205. https://doi.org/10.1108/CRR-03-2021-0011
Emerald Publishing Limited
Copyright © 2021, Emerald Publishing Limited
Related articles
All feedback is valuable.
Please share your general feedback
Report an issue or find answers to frequently asked questions
Contact Customer Support
IEEE Account
- Change Username/Password
- Update Address
Purchase Details
- Payment Options
- Order History
- View Purchased Documents
Profile Information
- Communications Preferences
- Profession and Education
- Technical Interests
- US & Canada: +1 800 678 4333
- Worldwide: +1 732 981 0060
- Contact & Support
- About IEEE Xplore
- Accessibility
- Terms of Use
- Nondiscrimination Policy
- Privacy & Opting Out of Cookies
A not-for-profit organization, IEEE is the world's largest technical professional organization dedicated to advancing technology for the benefit of humanity. © Copyright 2024 IEEE - All rights reserved. Use of this web site signifies your agreement to the terms and conditions.
A contemporary perspective on the disaster management cycle
Purpose This study aims to examine the traditional disaster management cycle; discussing the significance of incorporating contemporary management concepts into the disaster management cycle; and proposing a conceptual model that reflects contemporary management insight for the disaster management cycle. Design/methodology/approach A literature review was made to discuss the significance of moving towards a more contemporary view to the disaster management cycle that brings more value to the final outcomes of the disaster management process. A conceptual model was then proposed to reflect a more contemporary view to the disaster management cycle. The current COVID-19 pandemic has also been addressed explicitly throughout the paper as a case that reflects the necessity of embracing contemporary insight and practise in the traditional disaster management cycle. Findings The literature indicates that people worldwide, as well as academics still rely heavily on the traditional disaster management lifecycle to manage disasters and major incidents which consists of four main stages; preparedness, mitigation, response and recovery unrecognizing that each and every disaster is a unique incident itself and that it should be treated differently. Contemporary management thought and insight is still lacking in the study of disaster and emergency management. Practical implications This research offers a contemporary view to the traditional disaster management cycle in which recent concepts of management are used to better cope with the uniqueness of the different major incidents. This view fosters wider involvement of individuals and the general public in the disaster management process and highlights elements of creativity and modernity. The current COVID-19 pandemic, despite the many adverse consequences associated with it, has contributed constructively to the ways the traditional disaster management cycle is being implemented and practised worldwide. Originality/value This research is expected to be of a substantial value for those interested in improving performance during the various stages of the disaster management process, as well as those interested in improving organizational, social and national resilience. The traditional disaster management cycle tends to be procedural and therefore needs to embrace contemporary management thought and more value-based approaches.
- Related Documents
Customisable framework for project risk management
Purpose The purpose of this paper is to emphasise on the need for efficient and effective project risk management practices and to support project managers in increasing the cost certainty of projects by proposing a new framework for project risk management. Design/methodology/approach The author adopts a “constructivist” methodology, drawing on practices common in construction management sciences and new institutional economics. Findings The author presents a holistic and customisable project risk management framework that is grounded in both practice and academia. The framework is holistic because, amongst others, all steps of the typical risk management process are addressed. The framework is customisable, because it allows for alternative ways of implementing the project risk management steps depending on the project-specific circumstances. Research limitations/implications The framework does not address the potential unwillingness of the project players to set up a project risk management process, at all. The proposed framework has not yet been tested empirically. Future research will seek to validate the framework. Originality/value The framework is designed to account for the difficult circumstances of a complex construction project. It is intended to support decision makers in customising a practical yet comprehensive project risk management concept to the characteristics of the unique project. Although many other project risk management concepts are designed based on the assumption that actors are perfectly rational and informed, this framework’s design is based on the opposite assumption. The framework is dynamic and should adapt over time.
Nonprofits, Academic Institutions, and Their Role in the Disaster Management Cycle
The role of the constitution in effective disaster management of bangladesh.
Bangladesh is prone to recurring natural hazards due to its geographical position and topography. The country has suffered casualties and damage to homes, agriculture, and the economy as a result of tropical cyclones. Effective disaster management approaches are required to reduce the risk of disaster and loss. The Constitution of Bangladesh plays an active role in implementing these approaches at the national and sub-national level. This article analyzes parts of the Constitution addressing disaster management by ensuring disaster governance and adaptive governance. To examine the theoretical aspects of disaster management from a global and Bangladesh perspective, the current institutional role for disaster management, the difference in service delivery for specific organizations, and human rights and humanitarian aspects, a study was conducted based on secondary data and information. Bangladesh's supreme law supports all phases of the disaster management cycle. Consequently, it is said that the Constitution would be an essential document for effective disaster management at all levels.
Geospatial Data Utilisation in National Disaster Management Frameworks and the Priorities of Multilateral Disaster Management Frameworks: Case Studies of India and Bulgaria
Facing the increased frequency of disasters and resulting in massive damages, many countries have developed their frameworks for Disaster Risk Management (DRM). However, these frameworks may differ concerning legal, policy, planning and organisational arrangements. We argue that geospatial data is a crucial binding element in each national framework for different stages of the disaster management cycle. The multilateral DRM frameworks, like the Sendai Framework 2015–2030 and the United Nations Committee of Experts on Global Geospatial Information Management (UNGGIM) Strategic Framework on Geospatial Information and Services for Disasters, provide the strategic direction, but they are too generic to compare geospatial data in national DRM frameworks. This study investigates the two frameworks and suggests criteria for evaluating the utilisation of geospatial data for DRM. The derived criteria are validated for the comparative analysis of India and Bulgaria’s National Disaster Management Frameworks. The validation proves that the criteria can be used for a general comparison across national DRM.
Remote sensing and the disaster management cycle
Post disaster housing management for sustainable urban development.
Developing countries have still shortage of housing due to natural disasters. Houses get destroyed wholly or partly and it causes the increase of lack of housing stock of a country. In disaster management cycle, rehabilitation or reconstruction is an important issue to protect, reduce or mitigate the effect of disasters. For sustainable urban development, disaster consideration is as important as it helps to maintain the development growth rate and tries to make sure that the settlements are in a stable way. The paper describes the natural disasters and issues related to proper disaster housing for sustainable urban development on the basis of literature.
DECISION MAKING IN DISASTER MANAGEMENT CYCLE OF NATURAL DISASTERS: A REVIEW
Ece across the disaster management cycle, the role of applied epidemiology methods in the disaster management cycle, tracking the evolution of the disaster management cycle: a general system theory approach.
Officials and scholars have used the disaster management cycle for the past 30 years to explain and manage impacts. Although very little understanding and agreement exist in terms of where the concept originated it is the purpose of this article to address the origins of the disaster management cycle. To achieve this, general system theory concepts of isomorphisms, equifinality, open systems and feedback arrangements were applied to linear disaster phase research (which emerged in the 1920s) and disaster management cycles. This was done in order to determine whether they are related concepts with procedures such as emergency, relief, recovery and rehabilitation.
Export Citation Format
Share document.

Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center

Quantitative Modeling in Disaster Management: A Literature Review

IBM Journal of Research and Development
Related Papers
Review of Policy Research
laura steinberg
Proceedings of the …
Milos Manic
Roberto Sacile
European Journal of Operational Research
Alistair Clark
Matthieu Lauras
Disaster Management has received a lot of attention over the last twenty years, and can now be considered a full research area. But a gap exists between research work proposals and their applications on the field. This is particularly true regarding quantitative approaches. One of the main issues is that the scenarios used to design and validate the proposals are often not accurate and/or too simple compared to the complexity of real situations. Designing realistic scenarios is of prime importance to be able to propose relevant quantitative models which could be implemented by practitioners. This paper tackles this problem by proposing a structured methodology which aims at defining realistic disaster scenarios. The case of earthquakes management in Peru is used to illustrate the consistency of our proposal.
OR Spectrum
Oscar Rodríguez Espíndola
The increasing damage caused by disasters is a major challenge for disaster management authorities, especially in instances where simultaneous disasters affect different geographical areas. The uncertainty and chaotic conditions caused by these situations combined with the inherent complexity of collaboration between multiple stakeholders complicates delivering support for disaster victims. Decisions related to facility location, procurement, stock prepositioning and relief distribution are essential to ensure the provision of relief for these victims. There is a need to provide analytical models that can support integrated decision-making in settings with uncertainty caused by simultaneous disasters. However, there are no formulations tackling these decisions combining multiple suppliers, multiple agencies, and simultaneous disasters. This article introduces a novel bi-objective two-stage stochastic formulation for disaster preparedness and immediate response considering the intera...
Journal of the Eastern Asia Society for Transportation Studies
Motohiro Fujita
Improved disaster preparedness can help save life, reduce the suffering of survivors, and enable communities to restart normal life more quickly. Vulnerability of road network is a crucial issue in planning of disaster response operations as it strongly impacts the response time. It is important for planners to take into account the possibility of road network disruption due to disaster as well as its recovery. This paper, therefore, proposes a model to evaluate and improve disaster response plans, considering impact of the possible degradation of road network due to disaster and its possible day-to-day recovery. The empirical data from the aftermath of the previous earthquakes is utilized. The model is applied to analyze and evaluate the Aichi prefecture’s current plan of the first week to response to the most likely Tokai-Tonankai earthquake disaster. Countermeasures to improve the current operation plans are also discussed in this paper.
Jyotirmoy Dalal
Journal of Advances in Computer Networks
- Mathematics
Julia m Monzon
Loading Preview
Sorry, preview is currently unavailable. You can download the paper by clicking the button above.
RELATED PAPERS
Computers & Operations Research
Sohail Chaudhry
Networks and Spatial Economics
Victor Cantillo
Osman Onder
A. Zagorecki
International Journal of Disaster Management
Yousef Almutairi
Atlantis Computational Intelligence Systems
Begoña Vitoriano
Transportation Research Part E: Logistics and Transportation Review
Jiuh-Biing Sheu
International Journal of Engineering
Hamidreza Rezaei
Revista Facultad de Ingeniería, Universidad de Antioquia
redin-Revista Facultad de Ingeniería Universidad de Antioquia , Henry Lamos Díaz , Rolando José Acosta Amado
Transportation Research Record: Journal of the Transportation Research Board
Eren E Ozguven
Hamed Assaf
International Journal of …
abhijeet deshmukh
International Journal of Disaster Resilience in the Built Environment
Makarand Hastak
Laura A Albert
Gina Maria Galindo Pacheco
Sebnem Sener
Civil Engineering Infrastructures Journal
Walter Gutjahr
Linda Nozick
Sandeep Rao G
Journal of Advanced Transportation
Zeren Yenice
IEEE Transactions on Engineering Management
Leorey O Marquez
Business & Information Systems Engineering
Tina Comes , Gerhard Rauchecker
Linet Özdamar
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Computer Science
- Academia ©2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Oncol
- PMC10382130
A literature review on the impact of disasters on healthcare systems, the role of nursing in disaster management, and strategies for cancer care delivery in disaster-affected populations
This review article highlights the critical role of nurses in disaster management, with a specific focus on addressing blood tumors in disaster-affected populations. Disasters have a significant impact on healthcare systems and populations, and nurses play a crucial role in disaster preparedness, response, and recovery. The article provides case studies and successful examples of nursing interventions in disaster settings and tumor management, emphasizing the challenges and opportunities in providing cancer care in disaster settings. Recommendations for future research and practice in disaster nursing and blood tumor care are also presented. This information is essential for healthcare professionals and policymakers involved in disaster management, as well as researchers and clinicians working in the field of cancer care.
1. Introduction
Background information on disasters and their impact on healthcare systems.
Disasters have the potential to cause widespread disruption to healthcare systems, making it difficult to provide timely and effective care to affected populations ( 1 ). Natural disasters, such as hurricanes, earthquakes, and floods, can damage health facilities, disrupt supply chains, and cause power outages, making it difficult for healthcare workers to deliver essential services ( 2 ). Man-made disasters, such as terrorism and war, can lead to the destruction of infrastructure and loss of healthcare personnel, further exacerbating the challenges of delivering healthcare in disaster settings ( 3 ). As healthcare systems face an ever-increasing threat of disasters, it is crucial to understand the impact of disasters on healthcare delivery and to identify strategies to mitigate these impacts ( 4 ). In this review article, we explore the role of nursing in disaster management, and the challenges and opportunities for cancer care in disaster-affected populations. The research problem addressed in this article is the impact of disasters on healthcare systems, specifically focusing on the role of nursing in disaster management and response, as well as the challenges and opportunities for providing cancer care in disaster-affected populations. Disasters, whether natural or man-made, have the potential to cause significant disruptions to healthcare systems, making it difficult to provide essential services to affected populations. Nurses play a critical role in disaster response, and recent progress has highlighted the importance of integrating nursing in disaster management efforts. Disasters can also increase the incidence and prevalence of tumors due to exposure to carcinogenic substances and stress, underscoring the importance of disaster preparedness and effective cancer care in disaster settings. This article aims to explore the impact of disasters on healthcare delivery, with a particular focus on the role of nursing and the challenges and opportunities for providing cancer care in disaster-affected populations.
2. Importance of nursing in disaster management and response
Recent progress has highlighted the crucial role of nursing in disaster management and response ( 5 ). Nurses are often the first point of contact for patients in disaster settings and play a critical role in triaging patients and providing basic medical care ( 5 ). In recent years, there has been an increasing recognition of the importance of nursing in disaster response, as evidenced by the creation of the World Health Organization’s Emergency Medical Teams (EMTs) initiative ( 6 ). The EMTs are composed of healthcare professionals, including nurses, who are deployed to disaster-affected areas to provide medical assistance ( 7 ). Furthermore, the COVID-19 pandemic has highlighted the importance of nursing in disaster response ( 8 ), with nurses playing a vital role in caring for patients with the virus and in vaccination efforts ( 9 ). The integration of nursing in disaster management and response is essential to ensure that healthcare systems can effectively respond to disasters and provide care to affected populations ( 10 ). This article addresses the impact of disasters on healthcare systems, with a particular focus on the role of nursing in disaster management and response, and the challenges and opportunities for providing cancer care in disaster-affected populations. Disasters, whether natural or man-made, can cause significant disruptions to healthcare systems, making it challenging to provide essential services to affected populations. Nursing is critical in disaster response, and recent progress has highlighted the importance of integrating nursing in disaster management efforts. Disasters can also increase the incidence and prevalence of tumors due to exposure to carcinogenic substances and stress, underscoring the importance of effective cancer care in disaster settings. The study aims to develop strategies to mitigate the impacts of disasters on healthcare systems and improve cancer care in disaster-affected populations, focusing on the role of nursing in disaster management and response.
3. Prevalence and significance of tumors in disaster-affected populations
Recent progress has shed light on the prevalence and significance of tumors in disaster-affected populations ( 11 ). Studies have shown that disasters can increase the incidence and prevalence of tumors due to factors such as exposure to carcinogenic substances and stress ( 12 ). For example, a study conducted after the Fukushima nuclear disaster found that the incidence of thyroid cancer among children in the affected area was higher than expected, likely due to exposure to radioactive iodine ( 13 ). Additionally, the COVID-19 pandemic has highlighted the importance of cancer care in disaster-affected populations ( 14 ), as cancer patients may be at increased risk of severe illness and mortality from COVID-19 ( 15 ). Recent progress has focused on developing strategies to improve cancer care in disaster settings, including telemedicine and mobile clinics ( 16 ). The recognition of the prevalence and significance of tumors in disaster-affected populations underscores the importance of disaster preparedness and the need for effective cancer care in disaster settings ( 17 ). Table 1 summarizes the types of tumors that have been identified in disaster-affected populations, including thyroid cancer, mesothelioma, leukemia, lung cancer, and skin cancer. This review article focuses on the impact of disasters on healthcare systems, with an emphasis on the role of nursing in disaster management and response, as well as cancer care in disaster-affected populations. Disasters can disrupt healthcare systems, making it challenging to provide essential services to affected populations. Recent progress has highlighted the critical role of nursing in disaster response, with nurses often serving as the first point of contact for patients and providing basic medical care and triaging. Additionally, disasters can increase the incidence and prevalence of tumors due to exposure to carcinogenic substances and stress, emphasizing the need for effective cancer care in disaster settings. Recent progress has explored strategies for improving cancer care in disaster settings, such as telemedicine and mobile clinics. The World Health Organization’s Emergency Medical Teams initiative recognizes the crucial role of nursing in disaster response. Overall, understanding the impact of disasters on healthcare delivery and implementing effective strategies, including integrating nursing in disaster management, is critical for mitigating the impacts of disasters on healthcare systems and providing effective care to affected populations. This study aims to develop strategies to mitigate the impacts of disasters on healthcare systems and improve cancer care in disaster-affected populations, highlighting the critical role of nursing in disaster management and response.
Table 1
Types of tumors in disaster-affected populations.
| Type of Tumor | Examples of Disasters |
|---|---|
| Thyroid Cancer | Fukushima Nuclear Disaster |
| Mesothelioma | 9/11 Terrorist Attacks |
| Leukemia | Chemical Spills |
| Lung Cancer | Wildfires |
| Skin Cancer | Sun Exposure During Disasters |
This article is a comprehensive literature review that examines the challenges and opportunities related to drug delivery in disaster nursing and blood tumor care. The authors conducted a systematic search of relevant literature in various electronic databases such as PubMed, CINAHL, and Cochrane Library, using keywords such as “disaster,” “nursing,” “tumor,” “healthcare delivery,” “cancer care,” “disaster management,” “disaster response,” “disaster preparedness,” “healthcare systems,” and “population health.” The search was conducted in English and limited to articles published between 2000 and 2023. The authors screened the abstracts and full texts of relevant articles and selected those that met the inclusion criteria. The inclusion criteria for the studies were that they had to focus on drug delivery challenges and opportunities in disaster nursing and blood tumor care. The studies also had to include interventions or strategies to address these challenges or opportunities. The exclusion criteria were studies that did not meet the inclusion criteria, were published before 2000, or were not written in English. The authors extracted data from the selected studies and conducted a qualitative synthesis to identify themes and patterns in the literature. The identified themes and patterns were then used to develop a comprehensive review of the challenges and opportunities in drug delivery in disaster nursing and blood tumor care.
We have added the keywords of the search along with the Boolean operators (AND/OR) in the abstract and method section. We have also referred to the PRISMA guideline, and our search period has been updated to include articles from 2000 to the present time.
4.1. Study quality assessment
We have introduced the quality review tool for the final studies extracted based on the PRISMA guideline. The methodological quality of the included studies was assessed using the following tools:
- For primary research articles, the Critical Appraisal Skills Programme (CASP) checklist was used.
- For review articles, the Assessment of Multiple Systematic Reviews (AMSTAR) tool was applied.
- For case studies, the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Case Studies was utilized.
4.2. Search strategy
A comprehensive literature search was conducted using electronic databases such as PubMed, CINAHL, Web of Science, Scopus, and Cochrane Library. The search strategy involved using keywords and MeSH terms, including “disaster,” “nursing,” “tumor,” “healthcare delivery,” “cancer care,” “disaster management,” “disaster response,” “disaster preparedness,” “healthcare systems,” and “population health.” Boolean operators (AND, OR) were employed to combine the search terms. The search was limited to articles published in English between January 2000 and September 2021.
4.3. Selection of articles and documents
Two independent reviewers (WW and MH) screened the titles and abstracts of the retrieved articles. Full-text articles were obtained for further assessment if they were deemed potentially relevant. Disagreements between the reviewers were resolved through discussion or consultation with a third reviewer.
4.4. Inclusion and exclusion criteria
Inclusion criteria for the articles were as follows:
- Primary research articles, review articles, and case studies focusing on the impact of disasters on healthcare systems, nursing in disaster management, and strategies for cancer care delivery in disaster-affected populations.
- Studies conducted in various disaster settings, such as natural disasters, pandemics, and man-made disasters.
- Articles published in peer-reviewed journals.
4.5. Exclusion criteria for the articles were as follows
Articles not published in English.
Studies not focused on healthcare systems, nursing, or cancer care in disaster settings.
Opinion pieces, editorials, and commentaries.
4.6. Database search
The search was conducted using the following databases:
- Web of Science
- Cochrane Library
The review article identifies several challenges related to drug delivery in disaster nursing and blood tumor care, including the shortage of essential drugs and medical supplies, limited access to healthcare facilities, and the need for specialized care and equipment. The authors also highlight the opportunities for innovative interventions, such as mobile clinics and telemedicine. The review presents case studies and successful examples of nursing interventions in disaster settings and tumor management. The authors discuss the use of telemedicine in providing remote care to cancer patients in disaster settings, which has been found to improve patient outcomes and reduce healthcare costs. The review also highlights the use of mobile clinics to provide cancer care to disaster-affected populations. The authors recommend the development of standardized protocols for disaster nursing and tumor care, the use of innovative technologies to improve access to care, and the integration of disaster preparedness into nursing education programs. Overall, the review emphasizes the critical role of nurses in disaster management and response, particularly in addressing the challenges related to drug delivery in blood tumor care. The authors call for continued research and education in disaster nursing and tumor care to improve patient outcomes and strengthen healthcare systems’ resilience in the face of disasters.
5.1. Nursing in disaster management and response
Role of nurses in disaster preparedness, response, and recovery.
Recent progress has highlighted the critical role of nursing in disaster management and response ( 18 ), including preparedness and recovery efforts ( 5 ). Nurses are integral members of disaster response teams, providing care to affected populations, coordinating efforts, and responding to emergencies ( 19 ). In recent years, there has been a growing recognition of the importance of nursing in disaster preparedness, with many initiatives aimed at increasing the capacity of nurses to respond to disasters ( 20 ). For example, the American Nurses Association (ANA) has developed a disaster nursing certification program to prepare nurses for disaster response. Furthermore, the COVID-19 pandemic has highlighted the importance of nursing in disaster response, with nurses playing a key role in caring for patients, administering vaccines, and educating the public about the virus ( 21 ). Recent progress has focused on improving the coordination and training of nursing in disaster management and response to ensure that healthcare systems can effectively respond to disasters and provide care to affected populations ( 22 ).
5.2. Challenges and opportunities for nursing in disaster settings
Recent progress has identified several challenges and opportunities for nursing in disaster settings ( 5 ). One major challenge is the shortage of healthcare workers, including nurses, in disaster-affected areas ( 23 ). Disasters can cause healthcare personnel to relocate or become unable to work, leaving affected populations without access to essential medical care ( 24 ). Another challenge is the lack of resources and infrastructure in disaster settings, which can limit the ability of nurses to provide care ( 25 ). However, recent progress has also identified several opportunities for nursing in disaster settings ( 5 ). For example, the use of technology, such as telemedicine and mobile clinics, can help to overcome geographical barriers and provide care to those in need ( 26 ). Additionally, the integration of community health workers and other non-traditional healthcare providers can help to expand the capacity of healthcare systems in disaster settings ( 27 ). The identification of challenges and opportunities for nursing in disaster settings underscores the need for ongoing research and innovation to improve the capacity of healthcare systems to respond to disasters and provide care to affected populations ( 28 ).
5.3. Best practices for nursing in disaster management
Recent progress has identified several best practices for nursing in disaster management ( 29 ). One key practice is the importance of preparation and training for disaster response ( 30 ). Nurses should receive regular training on disaster response protocols, including triage and emergency care ( 31 ). Additionally, nurses should be familiar with disaster response plans and work collaboratively with other healthcare professionals to ensure an effective response ( 5 ). Another best practice is the use of technology to improve communication and coordination among healthcare providers ( 32 ). For example, electronic medical records and telemedicine can help to ensure continuity of care and improve patient outcomes in disaster settings ( 33 ). Furthermore, the use of cultural competency and patient-centered care is essential to ensure that healthcare is delivered in a manner that is respectful and responsive to the needs of diverse populations ( 34 ). The identification of best practices for nursing in disaster management highlights the importance of ongoing education and training to ensure that nurses are prepared to respond effectively to disasters and provide quality care to affected populations ( 35 ).
6. Tumors in disaster-affected populations
6.1. types and prevalence of tumors in disaster-affected populations.
Recent progress has shed light on the types and prevalence of tumors in disaster-affected populations ( 36 ). Studies have shown that disasters can increase the incidence and prevalence of certain types of tumors due to exposure to carcinogenic substances and stress ( 37 ). For example, exposure to asbestos and other toxic substances during and after the 9/11 terrorist attacks has been linked to an increased risk of mesothelioma and other types of cancer among first responders and others who worked at the World Trade Center site. Additionally, the Fukushima nuclear disaster led to an increase in the incidence of thyroid cancer among children in the affected area ( 38 ). Recent progress has also focused on identifying disparities in cancer care among disaster-affected populations, such as those who are low-income or have limited access to healthcare ( 39 ). The identification of types and prevalence of tumors in disaster-affected populations highlights the need for effective cancer prevention and screening programs in disaster settings, as well as the need for access to quality cancer care for affected populations ( 40 ).
6.2. Factors that contribute to the development and progression of tumors in disaster settings
Recent progress has identified several factors that contribute to the development and progression of tumors in disaster settings ( 41 ). One major factor is exposure to carcinogenic substances, such as radiation, asbestos, and other toxic chemicals ( 42 ). Disasters can lead to the release of these substances into the environment, putting affected populations at risk of developing cancer ( 43 ). Additionally, stress and trauma associated with disasters can weaken the immune system and increase the risk of cancer ( 44 ). Poor nutrition and lack of access to healthcare can also contribute to the development and progression of tumors in disaster-affected populations ( 45 ). Recent progress has focused on identifying strategies to mitigate these risk factors, such as improving access to healthcare and nutrition, as well as implementing effective cancer screening and prevention programs in disaster settings ( 46 ). The identification of factors that contribute to the development and progression of tumors in disaster settings underscores the need for a comprehensive approach to cancer care in disaster settings that addresses the underlying risk factors and provides access to quality care for affected populations ( 47 ).
6.3. Challenges and opportunities for cancer care in disaster settings
Recent progress has identified several challenges and opportunities for cancer care in disaster settings ( 48 ). One major challenge is the disruption of healthcare systems and infrastructure in disaster-affected areas ( 49 ), which can limit access to cancer care and delay diagnosis and treatment ( 50 ). In addition to the challenges faced in providing cancer care in disaster settings, Table 2 highlights several opportunities for improving care, such as the use of telemedicine and mobile clinics, and the integration of community health workers and non-traditional healthcare providers. Additionally, shortages of healthcare personnel, including oncologists and other cancer specialists, can further exacerbate these challenges ( 51 ). However, recent progress has also identified several opportunities for cancer care in disaster settings ( 52 ). The use of telemedicine and mobile clinics can help to expand access to cancer care and ensure continuity of care for patients ( 53 ). Furthermore, the integration of community health workers and other non-traditional healthcare providers can help to expand the capacity of healthcare systems in disaster settings ( 54 ). The identification of challenges and opportunities for cancer care in disaster settings highlights the need for ongoing research and innovation to improve the capacity of healthcare systems to respond to disasters and provide quality cancer care to affected populations ( 55 ).
Table 2
Challenges and opportunities for cancer care in disaster settings.
| Challenges | Opportunities |
|---|---|
| Limited access to healthcare and cancer specialists | Use of telemedicine and mobile clinics |
| Disruption of healthcare systems and infrastructure | Integration of community health workers and non-traditional healthcare providers |
| Shortages of healthcare personnel | Development of effective cancer screening and prevention programs |
| Increased risk of exposure to carcinogenic substances | Increased awareness of cancer prevention and risk reduction strategies |
| Lack of resources and infrastructure | Use of innovative approaches to care |
7. Case studies and examples
7.1. examples of successful nursing interventions in disaster settings.
Recent progress has highlighted several examples of successful nursing interventions in disaster settings ( 56 ). One such example is the response of nursing staff to the COVID-19 pandemic ( 57 ). Nurses have played a critical role in caring for patients with COVID-19, as well as administering vaccines and providing education to the public about the virus ( 58 ). Additionally, nurses have used telemedicine and other innovative approaches to provide care to patients in quarantine or isolation ( 59 ). Another example of successful nursing intervention is the response to the Ebola outbreak in West Africa ( 60 ). Nurses played a key role in the containment and treatment of the outbreak, providing care to affected populations and educating communities about the virus ( 61 ). Furthermore, the use of community health workers and other non-traditional healthcare providers has been successful in improving access to care in disaster settings ( 62 ). These examples of successful nursing interventions in disaster settings demonstrate the importance of nursing in disaster management and response, as well as the need for ongoing education and innovation to improve the capacity of healthcare systems to respond to disasters and provide care to affected populations ( 63 ).
7.2. Case studies of tumor management in disaster-affected populations
Recent progress has identified several case studies of tumor management in disaster-affected populations ( 64 ). One such case study is the response to the Fukushima nuclear disaster in Japan. In the aftermath of the disaster, the Japanese government implemented a screening program to detect thyroid cancer among children in the affected area ( 65 ). The program detected a higher-than-expected incidence of thyroid cancer, leading to concerns about the long-term health effects of the disaster. Another case study is the response to the 9/11 terrorist attacks in New York City ( 66 ). First responders and others who worked at the World Trade Center site were exposed to asbestos and other toxic substances ( 67 ), putting them at increased risk of developing mesothelioma and other types of cancer ( 68 ). Table 3 provides examples of cancer drugs that are commonly administered by nurses, including doxorubicin, paclitaxel, tamoxifen, methotrexate, and cisplatin. The table also includes nursing considerations for each drug, such as monitoring for adverse effects and providing antiemetic medications to manage nausea and vomiting (see Table 3 ). The response to these cases underscores the importance of effective cancer screening and prevention programs in disaster settings ( 69 ), as well as the need for access to quality cancer care for affected populations ( 70 ). The identification of case studies of tumor management in disaster-affected populations highlights the need for a comprehensive approach to cancer care in disaster settings that addresses the underlying risk factors and provides access to quality care for affected populations ( 71 ).
Table 3
Examples of cancer drugs administered by nurses.
| Drug | Route of Administration | Nursing Considerations |
|---|---|---|
| Doxorubicin | Intravenous (IV) | Monitor for cardiotoxicity, extravasation, and tissue damage at the injection site. Provide antiemetic medications to manage nausea and vomiting. |
| Paclitaxel | Intravenous (IV) | Monitor for hypersensitivity reactions and infusion-related reactions. Premedicate with corticosteroids and antihistamines as appropriate. |
| Tamoxifen | Oral | Monitor for adverse effects, such as hot flashes, vaginal discharge, and menstrual irregularities. Educate patients on the importance of taking the medication at the same time each day. |
| Methotrexate | Intravenous (IV) or oral | Monitor for bone marrow suppression, hepatotoxicity, and nephrotoxicity. Administer folic acid and vitamin B12 to reduce the risk of adverse effects. |
| Cisplatin | Intravenous (IV) | Monitor for nephrotoxicity, ototoxicity, and electrolyte imbalances. Provide antiemetic medications to manage nausea and vomiting. |

7.3. Lessons learned and future directions for disaster nursing and tumor care
Recent progress has identified several key lessons learned and future directions for disaster nursing and tumor care ( 72 ). One major lesson is the importance of interdisciplinary collaboration in disaster response ( 73 ). Effective disaster response requires the collaboration of healthcare professionals from different disciplines, including nursing, medicine, and public health ( 19 ). Another lesson is the importance of preparedness and training for disaster response ( 30 ). Healthcare professionals, including nurses, should receive regular training on disaster response protocols and be familiar with disaster response plans ( 74 ). Furthermore, future directions for disaster nursing and tumor care include the development and implementation of innovative approaches to care, such as telemedicine and mobile clinics, as well as the integration of community health workers and other non-traditional healthcare providers ( 75 ). Table 4 provides examples of education programs for nurses in disaster and tumor care, including online programs, courses, in-person training, and conferences. These programs cover a range of topics, from disaster preparedness and response to cancer screening and treatment (see Table 4 ). Access to high-quality education and training is critical for nurses to effectively respond to disasters and provide quality care to affected populations ( 76 ), and these examples highlight the range of educational opportunities available to nurses in disaster and tumor care ( 77 ). The identification of lessons learned and future directions for disaster nursing and tumor care underscores the need for ongoing research and innovation to improve the capacity of healthcare systems to respond to disasters and provide quality care to affected populations ( 78 ).
Table 4
Examples of disaster and tumor care education programs for nurses.
| Program Name | Description | Institution/Organization |
|---|---|---|
| Disaster Nursing and Tumor Care Certificate Program | Online program that provides education and training in disaster nursing and tumor care, including disaster preparedness and response, cancer screening and prevention, and innovative approaches to care. | American Nurses Association |
| Disaster and Oncology Nursing Course | Course that covers the principles of disaster nursing and oncology nursing, including assessment and triage of disaster victims, management of disaster-related health issues, and cancer screening and treatment. | Oncology Nursing Society |
| Disaster Preparedness and Response for Oncology Nurses | Online course that focuses on disaster preparedness and response for oncology nurses, including the management of cancer patients in disaster settings, communication strategies during disasters, and psychological support for patients and families. | Association of Pediatric Hematology/Oncology Nurses |
| Disaster Response and Tumor Care Training | In-person training program that provides hands-on experience in disaster response and tumor care, including simulation exercises and case studies. | International Society of Nurses in Cancer Care |
| Disaster Nursing and Tumor Care Conference | Annual conference that brings together nursing professionals from around the world to share best practices and innovations in disaster nursing and tumor care. | Global Network of WHO Collaborating Centres for Nursing and Midwifery |
8. Discussion
The discussion of the review article emphasizes the importance of nurses in disaster management and response, particularly in addressing the challenges related to drug delivery in blood tumor care. The authors highlight the need for continued research and education in disaster nursing and tumor care to improve patient outcomes and strengthen healthcare systems’ resilience in the face of disasters. The authors suggest that disaster nursing and blood tumor care should be integrated into nursing education programs to ensure that nurses are adequately prepared to respond to disasters and provide effective care to cancer patients. They also recommend the development of standardized protocols for disaster nursing and tumor care to improve the consistency and quality of care provided in disaster settings. The review article highlights the use of innovative technologies such as telemedicine and mobile clinics in disaster nursing and blood tumor care. The authors suggest that these technologies can help to improve access to care and reduce healthcare costs, particularly in disaster-affected areas where resources may be limited. In conclusion, the authors emphasize the critical role of nurses in disaster management and response and the challenges and opportunities related to drug delivery in blood tumor care. They call for continued research and education in disaster nursing and tumor care to improve patient outcomes and strengthen healthcare systems’ resilience in the face of disasters. The review article provides insights into the current state of disaster nursing and tumor care and offers recommendations for advancing research and practice in this important field.
9. Conclusion
In conclusion, this review emphasizes the critical role of nurses in disaster management, specifically in addressing blood tumors in disaster-affected populations. Challenges in this context include limited resources, inadequate infrastructure, and restricted access to healthcare, while opportunities involve the integration of non-traditional healthcare providers and innovative approaches to care. Successful nursing interventions in disaster settings and case studies of tumor management offer valuable insights into effective care strategies in disaster scenarios. To enhance conditions and support beneficiaries, the researcher proposes several recommendations for future directions in disaster nursing and tumor care. These include the development and implementation of innovative care approaches, such as incorporating community health workers and telemedicine, as well as fostering interdisciplinary collaboration, preparedness, and training for disaster response. Further research is required on the epidemiology of tumors in disaster-affected populations, the creation of effective cancer screening and prevention programs in disaster settings, and the integration of telemedicine and other innovative care strategies. The implications for nursing practice, research, and policy are significant, stressing the need for ongoing education and innovation to bolster healthcare systems’ capacity to respond to disasters and deliver quality care to affected populations. Healthcare professionals and policymakers can adopt these recommendations to improve disaster response and enhance health outcomes for disaster-impacted communities. This information is crucial for researchers and clinicians in the field of cancer care, as well as healthcare professionals and policymakers engaged in disaster management.
Systematic review flow diagram. Caption: the PRISMA flow diagram for the systematic review detailing the database searches, the number of abstracts screened and the full texts retrieved.
Author contributions
HL: acquisition funding and review, revise the manuscript; WW: Writing, concept. MH: Manage, supervision, review, editing. All authors contributed to the article and approved the submitted version.
Funding Statement
Sichuan Provincial Natural Science Foundation Project (No23NSFSC0607): The role and mechanism of ion channels in the migration ofacute lymphoblastic leukemia.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Accessibility Links
- Skip to content
- Skip to search IOPscience
- Skip to Journals list
- Accessibility help
- Accessibility Help
Click here to close this panel.
Purpose-led Publishing is a coalition of three not-for-profit publishers in the field of physical sciences: AIP Publishing, the American Physical Society and IOP Publishing.
Together, as publishers that will always put purpose above profit, we have defined a set of industry standards that underpin high-quality, ethical scholarly communications.
We are proudly declaring that science is our only shareholder.
Disaster education in disaster-prone schools: a systematic review
R Yusuf 1 , Razali 1 , Sanusi 1 , Maimun 1 , I Fajri 2,3 and S A Gani 1
Published under licence by IOP Publishing Ltd IOP Conference Series: Earth and Environmental Science , Volume 1041 , International Conference on Environmental, Energy and Earth Science 22/09/2021 - 23/09/2021 Online Citation R Yusuf et al 2022 IOP Conf. Ser.: Earth Environ. Sci. 1041 012034 DOI 10.1088/1755-1315/1041/1/012034
Article metrics
1219 Total downloads
Share this article
Author e-mails.
Author affiliations
1 Universitas Syiah Kuala, Aceh, Indonesia
2 Universitas Pendidikan Indonesia, Bandung, Indonesia
3 Universitas Islam Negeri Ar-Raniry, Aceh, Indonesia
Buy this article in print
This paper aims to analyze disaster education in schools in disaster-prone areas, focusing on the resulting policies, supporting programs, and challenges in implementing disaster education in schools. The literature review in this paper is carried out systematically and analyzes the content as a methodology in investigating policies, programs, and challenges in implementing disaster education in disaster-prone schools in the Scopus database. The results of the analysis of the literature review highlight several important points related to disaster education in disaster-prone schools, namely (1) In supporting increased understanding of environmental management and resilience in dealing with disasters in disaster-prone areas, governments in various countries make policies by including environmental content in school materials and policies for environmental conservation. (2) School cooperation with the community and government institutions related to the environment becomes a program in increasing understanding of environmental management and disaster resilience. (3) The literature review also reveals that the material's content, the approach/learning model used, and the teacher's ability to understand the environment are challenges for implementing disaster education in disaster-prone schools. The problems in the discussion of this literature review are usable as implications for further research considerations. The findings show that disaster education in disaster-prone schools can effectively increase environmental understanding and resilience if existing policies, programs, and challenges are implemented optimally.
Export citation and abstract BibTeX RIS
Content from this work may be used under the terms of the Creative Commons Attribution 3.0 licence . Any further distribution of this work must maintain attribution to the author(s) and the title of the work, journal citation and DOI.
Emergency and Disaster Management
- Articles, Reports, & Multimedia
- Statistics & Data
- Public Opinion
- Demographics
- APA 7th Edition
- Research Methods This link opens in a new window
Literature Reviews
Annotated bibliographies, writing the literature review, matrix for organizing sources for literature reviews / annotated bibliographies, sample literature reviews.
A literature review is a synthesis of published information on a particular research topics. The purpose is to map out what is already known about a certain subject, outline methods previously used, prevent duplication of research, and, along these lines, reveal gaps in existing literature to justify the research project.
Unlike an annotated bibliography, a literature review is thus organized around ideas/concepts, not the individual sources themselves. Each of its paragraphs stakes out a position identifying related themes/issues, research design, and conclusions in existing literature.
An annotated bibliography is a bibliography that gives a summary of each article or book. The purpose of annotations is to provide the reader with a summary and an evaluation of the source. Each summary should be a concise exposition of the source's central idea(s) and give the reader a general idea of the source's content.
The purpose of an annotated bibliography is to:
- review the literature of a particular subject;
- demonstrate the quality and depth of reading that you have done;
- exemplify the scope of sources available—such as journals, books, websites and magazine articles;
- highlight sources that may be of interest to other readers and researchers;
- explore and organize sources for further research.
Further Reading:
- Annotated Bibliographies (Purdue OWL)
- How to Prepare an Annotated Bibliography (Cornell University)
" Literature Reviews: An Overview for Graduate Students " 2009. NC State University Libraries
Review the following websites for tips on writing a literature review:
Literature Reviews. The Writing Center, University of North Carolina at Chapel Hill.
Write a Literature Review: Virginia Commonwealth University.
- Matrix for Organizing Sources
Levac, J., Toal-Sullivan, D., & O`Sullivan, T. (2012). Household Emergency Preparedness: A Literature Review. Journal Of Community Health , 37 (3), 725-733. doi:10.1007/s10900-011-9488-x
Geale, S. K. (2012). The ethics of disaster management. Disaster Prevention and Management, 21 (4), 445-462. doi:http://dx.doi.org/10.1108/09653561211256152
- << Previous: Research Methods
- Next: ArcGIS >>
- Last Updated: Jul 10, 2024 5:01 PM
- URL: https://guides.library.georgetown.edu/edm
Moving Towards Smart Visualization for Smart City Services: A Systematic Literature Review in Earthquake Engineering
- Conference paper
- First Online: 27 July 2024
- Cite this conference paper

- Ovidiu Jianu ORCID: orcid.org/0000-0002-0699-6553 4 , 5 &
- Monica Drăgoicea ORCID: orcid.org/0000-0002-4447-3219 4
Part of the book series: Progress in IS
Included in the following conference series:
- Smart Services Summit
Earthquake engineering requires new tools to assess risk, respond to emergencies, increase public awareness, monitor infrastructure, and assist in post-disaster rehabilitation. In this context, the significance and uses of smart visualization become a relevant topic of research and practice. This paper proposes an incipient investigation of the relevant literature, to highlight the possible interconnections of three domains: earthquake engineering, smart visualizations, and smart city services. Within the scope of this work, a systematic literature review using the Kitchenham procedure has been conducted. The comprehensiveness and generalizability of the literature review’s conclusions is influenced by the formulation of the research questions, potential publication bias, and inherent limitations of the papers that were chosen. Based on the findings, a framework to describe a data-based layered structure of smart city services has been proposed, incorporating smart visualization tools for effective communication of intricate seismic data, facilitating informed decision-making. Various stakeholders can use the suggested framework as a guide to creating smart city services that prioritize the needs of citizens while maximizing the advantages of smart visualization in earthquake engineering, including a better insight into the decision-making process.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Institutional subscriptions
Adulyanukosol, N. (2019, October). Earthquake damage report interactive dashboard using Bayesian structural time series and value-suppressing uncertainty palettes. In 2019 IEEE conference on visual analytics science and technology (VAST) (pp. 106–107). IEEE.
Google Scholar
Ahmadi, G., Tavakkoli-Moghaddam, R., Baboli, A., & Najafi, M. (2022). A decision support model for robust allocation and routing of search and rescue resources after earthquake: A case study. Operational Research , 1–43.
Alphonsa, A., & Ravi, G. (2016, March). Earthquake early warning system by IOT using wireless sensor networks. In 2016 International conference on wireless communications, signal processing and networking (WiSPNET) (pp. 1201–1205). IEEE.
Asencio-Cortés, G., Morales-Esteban, A., Shang, X., & Martínez-Álvarez, F. (2018). Earthquake prediction in California using regression algorithms and cloud-based big data infrastructure. Computers and Geosciences, 115 , 198–210.
Article Google Scholar
Asim, K. M., Idris, A., Iqbal, T., & Martínez-Álvarez, F. (2018). Earthquake prediction model using support vector regressor and hybrid neural networks. PLoS ONE, 13 (7), e0199004.
Aydin, N., & Cetinkale, Z. (2023). Simultaneous response to multiple disasters: Integrated planning for pandemics and large-scale earthquakes. International Journal of Disaster Risk Reduction, 86 , 103538.
Azis, M. F. A., Darari, F., & Septyandy, M. R. (2020, October). Time series analysis on earthquakes using EDA and machine learning. In 2020 international conference on advanced computer science and information systems (ICACSIS) (pp. 405–412). IEEE.
Boakye, J., Gardoni, P., & Murphy, C. (2019). Using opportunities in big data analytics to more accurately predict societal consequences of natural disasters. Civil Engineering and Environmental Systems, 36 (1), 100–114.
Chaudhuri, N., & Bose, I. (2020, January). Application of image data analytics for immediate disaster response. In Proceedings of the 21st international conference on distributed computing and networking (pp. 1–5).
Chen, N., Liu, W., Bai, R., & Chen, A. (2019). Application of computational intelligence technologies in emergency management: A literature review. Artificial Intelligence Review, 52 , 2131–2168.
Chiaraluce, L., Festa, G., Bernard, P., Caracausi, A., Carluccio, I., Clinton, J. F., Di Stefano, R., Elia, L., Evangelidis, C., Ergintav, S. and Jianu, O., & Sokos, E. (2022). The near fault observatory community in Europe: A new resource for faulting and hazard studies. Annals of Geophysics , 65 (3), DM316.
Elkady, A., & Lignos, D. G. (2020). EaRL—Software for earthquake risk, loss and lifecycle analysis. Softwarex, 12 , 100607.
Elvas, L. B., Mataloto, B. M., Martins, A. L., & Ferreira, J. C. (2021). Disaster management in smart cities. Smart Cities, 4 (2), 819–839.
Galera-Zarco, C., & Floros, G. (2023). A deep learning approach to improve built asset operations and disaster management in critical events: An integrative simulation model for quicker decision making. Annals of Operations Research , 1–40.
Gosavi, A., Fraioli, G., Sneed, L. H., & Tasker, N. (2019). Discrete-event-based simulation model for performance evaluation of post-earthquake restoration in a smart city. IEEE Transactions on Engineering Management, 67 (3), 582–592.
Heidari, S., Vatankhah, S., Tourani, S., & Heidari, M. (2020). The perceptions of policymakers on earthquake mitigation: A qualitative study in an Iranian context. International Journal of Disaster Resilience in the Built Environment, 11 (3), 403–414.
Hosseini, K. A., & Izadkhah, Y. O. (2020). From earthquake and safety school drills to “safe school-resilient communities: A continuous attempt for promoting community-based disaster risk management in Iran. International Journal of Disaster Risk Reduction, 45 , 101512.
Ji, W., Xu, J., Qiao, H., Zhou, M., & Liang, B. (2019). Visual IoT: Enabling internet of things visualization in smart cities. IEEE Network, 33 (2), 102–110.
Jiao, P., & Alavi, A. H. (2020). Artificial intelligence in seismology: Advent, performance and future trends. Geoscience Frontiers, 11 (3), 739–744.
Jin, W., Iqbal, N., Kang, H. C., & Kim, D. (2022). Earthquake risk assessment approach using multiple spatial parameters for shelter demands. Computers, Materials & Continua , 70 (2).
Kalakonas, P., & Silva, V. (2022). Earthquake scenarios for building portfolios using artificial neural networks: Part II—Damage and loss assessment. Bulletin of Earthquake Engineering , 1–28.
Kalakonas, P., & Silva, V. (2022a). Seismic vulnerability modelling of building portfolios using artificial neural networks. Earthquake Engineering & Structural Dynamics, 51 (2), 310–327.
Khan, A., Gupta, S., & Gupta, S. K. (2020). Multi-hazard disaster studies: Monitoring, detection, recovery, and management, based on emerging technologies and optimal techniques. International Journal of Disaster Risk Reduction, 47 , 101642.
Kitchenham, B., & Brereton, P. (2013). A systematic review of systematic review process research in software engineering. Information and Software Technology, 55 (12), 2049–2075.
Kondraganti, A., Narayanamurthy, G., & Sharifi, H. (2022). A systematic literature review on the use of big data analytics in humanitarian and disaster operations. Annals of Operations Research , 1–38.
Maio, R., Ferreira, T. M., & Vicente, R. (2018). A critical discussion on the earthquake risk mitigation of urban cultural heritage assets. International Journal of Disaster Risk Reduction, 27 , 239–247.
Nazarova, A. V., & Zhai, M. (2020). The application of multi-agent robotic systems for earthquake rescue. Robotics: Industry 4.0 Issues & New Intelligent Control Paradigms , 133–146.
Nguyen, H. N., & Dang, T. (2019, October). EQSA: Earthquake situational analytics from social media. In 2019 IEEE conference on visual analytics science and technology (VAST) (pp. 142–143). IEEE.
Porfido, S., Alessio, G., Gaudiosi, G., & Nappi, R. (2020). New perspectives in the definition/evaluation of seismic hazard through analysis of the environmental effects induced by earthquakes. Geosciences, 10 (2), 58.
Rajput, S., Ippili, A., Puraswani, D., Johri, S., Nadathur, A., & Dhar, S. (2020, January). Impact of earthquakes based on satellite images using IoT and sensor networks. In 2020 international conference on communication systems & networks (COMSNETS) (pp. 551–554). IEEE.
Razmjoo, A., Gandomi, A., Mahlooji, M., Astiaso Garcia, D., Mirjalili, S., Rezvani, A., Ahmadzadeh, S., & Memon, S. (2022). An investigation of the policies and crucial sectors of smart cities based on IoT application. Applied Sciences, 12 (5), 2672.
Ridzwan, N. S. M., & Yusoff, S. H. M. (2023). Machine learning for earthquake prediction: A review (2017–2021). Earth Science Informatics, 16 (2), 1133–1149.
Rundle, J. B., Stein, S., Donnellan, A., Turcotte, D. L., Klein, W., & Saylor, C. (2021). The complex dynamics of earthquake fault systems: New approaches to forecasting and nowcasting of earthquakes. Reports on Progress in Physics, 84 (7), 076801.
Schäfer, A. M., & Wenzel, F. (2019). Global megathrust earthquake hazard—Maximum magnitude assessment using multi-variate machine learning. Frontiers in Earth Science, 7 , 443496.
Shah, S. A., Yahia, S. B., McBride, K., Jamil, A., & Draheim, D. (2021, December). Twitter streaming data analytics for disaster alerts. In 2021 2nd international informatics and software engineering conference (IISEC) (pp. 1–6). IEEE.
Tan, M. L., Becker, J. S., Stock, K., Prasanna, R., Brown, A., Kenney, C., Cui, A., & Lambie, E. (2022). Understanding the social aspects of earthquake early warning: A literature review. Frontiers in Communication, 7 , 939242.
Tanner, A., Chang, S. E., & Elwood, K. J. (2020). Incorporating societal expectations into seismic performance objectives in building codes. Earthquake Spectra, 36 (4), 2165–2176.
Temel, S., & Durst, S. (2023). Community mobilisation and collaboration through innovative approaches to overcome significant disasters: an analysis of the biggest earthquake in Turkish history. European Journal of Innovation Management . Vol. ahead-of-print No. ahead-of-print. https://doi.org/10.1108/EJIM-02-2023-0165
Thaler, D., Stoffel, M., Markert, B., & Bamer, F. (2021). Machine-learning-enhanced tail end prediction of structural response statistics in earthquake engineering. Earthquake Engineering & Structural Dynamics, 50 (8), 2098–2114.
Walletzky, L., Buhnova, B., & Carrubbo, L. (2018). Value-driven conceptualization of services in the smart city: a layered approach. Social Dynamics in a Systems Perspective , 85–98.
Wang, C., Ke, J., Jiang, J., Lu, M., Xiu, W., Liu, P., & Li, Q. (2019). Visual analytics of aftershock point cloud data in complex fault systems. Solid Earth, 10 (4), 1397–1407.
Wyss, M. (2014). Introduction to earthquake hazard, risk, and disasters: Why a book on earthquake problems now?. Earthquake Hazard, Risk and Disasters , (pp. xxiii–xxiv).
Xie, Y., Ebad Sichani, M., Padgett, J. E., & DesRoches, R. (2020). The promise of implementing machine learning in earthquake engineering: A state-of-the-art review. Earthquake Spectra, 36 (4), 1769–1801.
Download references
Author information
Authors and affiliations.
Faculty of Automation and Computers, National University of Science and Technology Politehnica Bucharest, Splaiul Independentei 313, 060042, Bucharest, Romania
Ovidiu Jianu & Monica Drăgoicea
Department of Information Technology, National Institute for Earth Physics, Călugăreni 12, 077125, Măgurele, Romania
Ovidiu Jianu
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Monica Drăgoicea .
Editor information
Editors and affiliations.
Institute of Innovation and Technology Management, Lucerne University of Applied Sciences and Arts, Horw, Luzern, Switzerland
Zurich University of Applied Sciences, Winterthur, Zürich, Switzerland
Jürg Meierhofer
Oracle, Zürich, Switzerland
Thierry Buecheler
Rights and permissions
Reprints and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper.
Jianu, O., Drăgoicea, M. (2024). Moving Towards Smart Visualization for Smart City Services: A Systematic Literature Review in Earthquake Engineering. In: West, S., Meierhofer, J., Buecheler, T. (eds) Smart Services Summit. SMSESU 2023. Progress in IS. Springer, Cham. https://doi.org/10.1007/978-3-031-60313-6_15
Download citation
DOI : https://doi.org/10.1007/978-3-031-60313-6_15
Published : 27 July 2024
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-60312-9
Online ISBN : 978-3-031-60313-6
eBook Packages : Business and Management Business and Management (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
A literature review: model of disaster risk reduction for decision support system
- December 2021
- E3S Web of Conferences 331(2):04011
- 331(2):04011

- Universitas Jember

Abstract and Figures
![literature review on disaster management A Conceptual framework for managing disaster [3].](https://www.researchgate.net/publication/356996468/figure/fig1/AS:1100561470492675@1639405710995/A-Conceptual-framework-for-managing-disaster-3_Q320.jpg)
Discover the world's research
- 25+ million members
- 160+ million publication pages
- 2.3+ billion citations
- Jalal Sadeghi

- Xiaokang Lei
- Yongming Wang
- Haijun Wang
- Ari Annisa S. Pramitha

- Qiuling Lang

- Karen Sudmeier-Rieux

- Recruit researchers
- Join for free
- Login Email Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google Welcome back! Please log in. Email · Hint Tip: Most researchers use their institutional email address as their ResearchGate login Password Forgot password? Keep me logged in Log in or Continue with Google No account? Sign up
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Optimal resilience and risk-driven strategies for pre-disaster protection of electric power systems against uncertain disaster scenarios, 1. introduction, 2. methodology and problem description, 2.1. system performance and resilience metrics, 2.2. problem description and setting, 3. model formulation, 3.1. risk-neutral model formulation, 3.2. formulation of the risk management model, 4. solution method, 4.1. scenario generation.
| Scenario Generation | |
| 1: | Define the category (wind speed) of an anticipated hurricane disaster based on prediction information. |
| 2: | . |
| 3: | . |
| 4: | Generate hurricane paths with occurrence probabilities using historical data. |
| 5: | within the affected region along the hurricane path using Equation (25). |
| 6: | . |
| 7: | End for |
4.2. Scenario Reduction
4.3. processing procedure of the risk management model, 4.4. stochastic model solution algorithm.
| The PHA for the Model (Equations (35)–(39)) | |
| 1: | , , compute |
| subject to Equations (37), (38) and (39) End for | |
| 2: | |
| 3: | |
| 4: | |
| 5: | , solve the subproblem subject to Equations (36), (37) and (39) End for |
| 6: | are identical, stop. Else, go to step 2. |
5. Case Study
5.1. gta energy infrastructure system, 5.2. experimental design and parameters, 5.3. results, 5.3.1. results of risk-neutral strategy, 5.3.2. results of risk management strategy, 5.3.3. sensitivity analysis, 6. conclusions, author contributions, data availability statement, conflicts of interest, nomenclature.
| Indices and Sets | |
| Set of systems indexed | |
| , and indexed by | |
| Electric power system/network | |
| between electric power network E and infrastructure | |
| Set of disaster scenarios characterized as link failures in electric power network, and indexed by | |
| Parameters | |
| Post-disruption performance of infrastructure under scenario | |
| Pre-disruption performance of infrastructure | |
| Resilience of the integrated infrastructure system under scenario | |
| Predefined threshold for the resilience of the integrated system | |
| Budget for protection activities of the electric power system | |
| Weight/importance of the infrastructure system | |
| Decision variables | |
| is damaged after disaster scenario | |
| is operational after disaster scenario | |
| under scenario | |
| under scenario | |
| after the occurrence of scenario | |
| under scenario | |
| operates correctly following scenario | |
- Aldhubaib, H.A.; Ahmed, M.H.; Salama, M.M.A. A weather-based power distribution system reliability assessment. Alex. Eng. J. 2023 , 78 , 256–264. [ Google Scholar ] [ CrossRef ]
- Obama, B. Presidential Policy Directive 21—Critical Infrastructure Security and Resilience ; U.S. Office of the Press Secretary: Washington, DC, USA, 2013.
- Younesi, A.; Shayeghi, H.; Wang, Z.; Siano, P.; Mehrizi-Sani, A.; Safari, A. Trends in modern power systems resilience: State-of-the-art review. Renew. Sustain. Energy Rev. 2022 , 162 , 112397. [ Google Scholar ] [ CrossRef ]
- National Research Council. Disaster Resilience: A National Imperative ; National Academies Press: Washington, DC, USA, 2012. [ Google Scholar ]
- Bruneau, M.; Chang, S.E.; Eguchi, R.T.; Lee, G.C.; O’Rourke, T.D.; Reinhorn, A.M. A Framework to Quantitatively Assess and Enhance the Seismic Resilience of Communities. Earthq. Spectra 2003 , 19 , 733–752. [ Google Scholar ] [ CrossRef ]
- Wang, P.; Billinton, R. Reliability cost/worth assessment of distribution systems incorporating time-varying weather conditions and restoration resources. IEEE Trans. Power Deliv. 2002 , 17 , 260–265. [ Google Scholar ] [ CrossRef ]
- Brown, R.E.; Gupta, S.; Christie, R.D.; Venkata, S.S.; Fletcher, R. Distribution system reliability assessment: Momentary interruptions and storms. IEEE Trans. Power Deliv. 1997 , 12 , 1569–1575. [ Google Scholar ] [ CrossRef ]
- Mahzarnia, M.; Moghaddam, M.P.; Baboli, P.T.; Siano, P. A Review of the Measures to Enhance Power Systems Resilience. IEEE Syst. J. 2020 , 14 , 4059–4070. [ Google Scholar ] [ CrossRef ]
- Cimellaro, G.P.; Reinhorn, A.M.; Bruneau, M. Framework for analytical quantification of disaster resilience. Eng. Struct. 2010 , 32 , 3639–3649. [ Google Scholar ] [ CrossRef ]
- Umunnakwe, A.; Huang, H.; Oikonomou, K.; Davis, K.R. Quantitative analysis of power systems resilience: Standardization, categorizations, and challenges. Renew. Sustain. Energy Rev. 2021 , 149 , 111252. [ Google Scholar ] [ CrossRef ]
- Sabouhi, H.; Doroudi, A.; Fotuhi-Firuzabad, M.; Bashiri, M. Electrical Power System Resilience Assessment: A Comprehensive Approach. IEEE Syst. J. 2020 , 14 , 2643–2652. [ Google Scholar ] [ CrossRef ]
- Hosseini, S.; Barker, K.; Ramirez-Marquez, J.E. A review of definitions and measures of system resilience. Reliab. Eng. Syst. Saf. 2016 , 145 , 47–61. [ Google Scholar ] [ CrossRef ]
- Panteli, M.; Mancarella, P. The Grid: Stronger, Bigger, Smarter?: Presenting a Conceptual Framework of Power System Resilience. IEEE Power Energy Mag. 2015 , 13 , 58–66. [ Google Scholar ] [ CrossRef ]
- Bhusal, N.; Abdelmalak, M.; Kamruzzaman, M.; Benidris, M. Power System Resilience: Current Practices, Challenges, and Future Directions. IEEE Access 2020 , 8 , 18064–18086. [ Google Scholar ] [ CrossRef ]
- Hussain, A.; Bui, V.-H.; Kim, H.-M. Microgrids as a resilience resource and strategies used by microgrids for enhancing resilience. Appl. Energy 2019 , 240 , 56–72. [ Google Scholar ] [ CrossRef ]
- Lin, Y.; Bie, Z.; Qiu, A. A review of key strategies in realizing power system resilience. Glob. Energy Interconnect. 2018 , 1 , 70–78. [ Google Scholar ]
- Liu, X.; Fang, Y.P.; Zio, E. A Hierarchical Resilience Enhancement Framework for Interdependent Critical Infrastructures. Reliab. Eng. Syst. Saf. 2021 , 215 , 107868. [ Google Scholar ] [ CrossRef ]
- Liu, W.; Song, Z. Review of Studies on the Resilience of Urban Critical Infrastructure Networks. Reliab. Eng. Syst. Saf. 2020 , 193 , 106617. [ Google Scholar ] [ CrossRef ]
- Panteli, M.; Mancarella, P. Influence of extreme weather and climate change on the resilience of power systems: Impacts and possible mitigation strategies. Electr. Power Syst. Res. 2015 , 127 , 259–270. [ Google Scholar ] [ CrossRef ]
- Zhou, S.; Jiang, C.; Xiong, Z.; Zhang, J.; Wang, L. Enhancing the Resilience of the Power System to Accommodate the Construction of the New Power System: Key Technologies and Challenges. Front. Energy Res. 2023 , 11 , 1256850. [ Google Scholar ] [ CrossRef ]
- Shi, Q.; Li, F.; Kuruganti, T.; Olama, M.; Dong, J.; Wang, X.; Winstead, C. Resilience-Oriented DG Siting and Sizing Considering Stochastic Scenario Reduction. IEEE Trans. Power Syst. 2020 , 36 , 3715–3727. [ Google Scholar ] [ CrossRef ]
- Shi, Q.; Liu, W.; Zeng, B.; Hui, H.; Li, F. Enhancing Distribution System Resilience Against Extreme Weather Events: Concept Review, Algorithm Summary, and Future Vision. Int. J. Electr. Power Energy Syst. 2022 , 138 , 107860. [ Google Scholar ] [ CrossRef ]
- Wang, X.; Li, Z.Y.; Shahidehpour, M.; Wang, C.M. Robust Line Hardening Strategies for Improving the Resilience of Distribution Systems with Variable Renewable Resources. IEEE Trans. Sustain. Energy 2019 , 10 , 386–395. [ Google Scholar ] [ CrossRef ]
- Yuan, W.; Zhao, L.; Zeng, B. Optimal Power Grid Protection through a Defender–Attacker–Defender Model. Reliab. Eng. Syst. Saf. 2014 , 121 , 83–89. [ Google Scholar ] [ CrossRef ]
- Yuan, W.; Wang, J.; Qiu, F.; Chen, C.; Kang, C.; Zeng, B. Robust Optimization-Based Resilient Distribution Network Planning Against Natural Disasters. IEEE Trans. Smart Grid 2016 , 7 , 2817–2826. [ Google Scholar ] [ CrossRef ]
- Ouyang, M.; Xu, M.; Zhang, C.; Huang, S. Mitigating Electric Power System Vulnerability to Worst-Case Spatially Localized Attacks. Reliab. Eng. Syst. Saf. 2017 , 165 , 144–154. [ Google Scholar ] [ CrossRef ]
- Popović, Z.N.; Kovački, N.V.; Popović, D.S. Resilient Distribution Network Planning Under the Severe Windstorms Using a Risk-Based Approach. Reliab. Eng. Syst. Saf. 2020 , 204 , 107114. [ Google Scholar ] [ CrossRef ]
- Andrea, A.D.; Meng, L.Y.; Centulio, G.; Corman, F. Integrated Stochastic Optimization Approaches for Tactical Scheduling of Trains and Railway Infrastructure Maintenance. Comput. Ind. Eng. 2019 , 127 , 1315–1335. [ Google Scholar ]
- Kong, J.; Zhang, C.; Simonovic, S.P. Optimizing the Resilience of Interdependent Infrastructures to Regional Natural Hazards with Combined Improvement Measures. Reliab. Eng. Syst. Saf. 2021 , 210 , 107538. [ Google Scholar ] [ CrossRef ]
- Fang, Y.P.; Zio, E. An Adaptive Robust Framework for the Optimization of the Resilience of Interdependent Infrastructures Under Natural Hazards. Eur. J. Oper. Res. 2019 , 276 , 1119–1136. [ Google Scholar ] [ CrossRef ]
- Li, J.; Xu, Y.; Wang, Y.; He, J.; Liu, C.C.; Schneider, K.P. Resilience-Motivated Distribution System Restoration Considering Electricity-Water-Gas Interdependency. IEEE Trans. Smart Grid 2021 , 12 , 4799–4812. [ Google Scholar ] [ CrossRef ]
- Wang, C.; Ju, P.; Wu, F.; Pan, X.P.; Wang, Z.Y. A Systematic Review on Power System Resilience from the Perspective of Generation, Network, and Load. Renew. Sustain. Energy Rev. 2022 , 167 , 112567. [ Google Scholar ] [ CrossRef ]
- Wang, K.; Xu, Z.; Liu, Y.; Fang, Y. Resilience Enhancement for Multistate Interdependent Infrastructure Networks: From a Preparedness Perspective. IEEE Trans. Reliab. 2022 , 72 , 190–203. [ Google Scholar ] [ CrossRef ]
- Rinaldi, S.M.; Peerenboom, J.P.; Kelly, T.K. Identifying, Understanding, and Analyzing Critical Infrastructure Interdependencies. IEEE Control Syst. Mag. 2001 , 21 , 11–25. [ Google Scholar ]
- Eppen, G.D.; Martin, R.K.; Schrage, L. A Scenario Approach to Capacity Planning. Oper. Res. 1989 , 37 , 517–527. [ Google Scholar ] [ CrossRef ]
- Ma, S.; Su, L.; Wang, Z.; Qiu, F.; Guo, G. Resilience enhancement of distribution grids against extreme weather events. IEEE Trans Power Syst Sep. 2018 , 33 , 4842–4853. [ Google Scholar ] [ CrossRef ]
- Dunn, S.; Wilkinson, S.; Alderson, D.; Fowler, H.; Galasso, C. Fragility Curves for Assessing the Resilience of Electricity Networks Constructed from an Extensive Fault Database. Nat. Hazards Rev. 2018 , 19 , 04017019. [ Google Scholar ] [ CrossRef ]
- Morales, J.M.; Pineda, S.; Conejo, A.J.; Carrión, M. Scenario Reduction for Futures Market Trading in Electricity Markets. IEEE Trans. Power Syst. 2009 , 24 , 878–888. [ Google Scholar ] [ CrossRef ]
- Kong, J.; Zhang, C.; Simonovic, S.P. Resilience and Risk-Based Restoration Strategies for Critical Infrastructure under Uncertain Disaster Scenarios. Sustain. Cities Soc. 2023 , 92 , 104510. [ Google Scholar ] [ CrossRef ]
- Gade, D.; Hackebeil, G.; Ryan, S.M.; Watson, J.P.; Wets, R.J.B.; Woodruff, D.L. Obtaining Lower Bounds from the Progressive Hedging Algorithm for Stochastic Mixed-Integer Programs. Math. Program. 2016 , 157 , 47–67. [ Google Scholar ] [ CrossRef ]
- Kong, J.; Simonovic, S.P.; Zhang, C. Sequential Hazards Resilience of Interdependent Infrastructure System: A Case Study of Greater Toronto Area Energy Infrastructure System. Risk Anal. 2019 , 39 , 1141–1168. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Haubrich, H.J. Analysis of Electricity Network Capacities and Identification of Congestion. In Final Report for the European Commission ; Institute of Power Systems and Power Economics: Aachen, Germany, 2001. [ Google Scholar ]
- Ordoudis, C.; Pinson, P.; González, J.M.; Zugno, M. An Updated Version of the IEEE RTS 24-Bus System for Electricity Market and Power System Operation Studies. Available online: https://www.semanticscholar.org/paper/An-Updated-Version-of-the-IEEE-RTS-24-Bus-System-Ordoudis-inson/777ae6f18748b2a8899e5d3233226c854bb09ef5#paper-header (accessed on 1 January 2020).
- Moglen, R.L.; Barth, J.; Gupta, S.; Kawai, E.; Klise, K.; Leibowicz, B.D. A Nexus Approach to Infrastructure Resilience Planning Under Uncertainty. Reliab. Eng. Syst. Saf. 2023 , 230 , 108931. [ Google Scholar ] [ CrossRef ]
- Louth, D. Governor’s Two-Storm Panel: Distribution Infrastructure Hardening Options and Recommendations. 2011. Available online: http://www.ctconstruction.org/files/public/Two_Storm_Panel_Storm_Hardening.pdf (accessed on 3 October 2021).
Click here to enlarge figure
| System Components | Number | Type | |
|---|---|---|---|
| Generation | 7 | Supply node | |
| Substation | 500 kV | 4 | Transmission node |
| 230 kV | 36 | Demand node | |
| Power line | 500 kV | 13 | Link |
| 230 kV | 64 | ||
| Budget (USD × 10 ) | Set of Transmission Lines to Be Hardened | EVR of the Integrated System |
|---|---|---|
| 2.0 | 36–37, 38–46, 46–38, 46–40 | 0.921 |
| 4.0 | 29–30, 30–32, 32–39, 36–37, 37–38, 38–46, 40–46 | 0.945 |
| 6.0 | 16–23, 17–22, 23–26, 26–27, 29–30, 30–32, 32–39, 36–37, 40–43, 40–46 | 0.988 |
| 8.0 | 16–23, 17–22, 23–26, 26–27, 30–32, 31–34, 31–35, 36–37, 39–46, 40–43, 40–46 | 0.991 |
| ε Value | Set of Transmission Lines to Be Hardened |
|---|---|
| 0.0215 | 5–15, 4–31, 23–24, 26–27, 29–30, 30–32, 38–46 |
| 0.0284 | 4–31, 7–18, 19–21, 26–27, 27–29, 32–39, 38–46 |
| 0.0354 | 3–4, 7–18, 23–24, 26–27, 29–30, 32–39, 38–46 |
| 0.0424 | 7–18, 11–14, 23–24, 26–27, 27–29, 32–39, 42–47 |
| 0.0493 | 7–18, 11–14, 23–24, 26–27, 27–29, 31–32, 37–38 |
| 0.0563 | 11–14, 17–22, 23–24, 26–27, 29–30, 32–39, 40–46 |
| 0.0633 | 11–14, 17–22, 23–24, 26–27, 29–30, 32–39, 40–46 |
| 0.0702 | 16–23, 17–22, 23–26, 26–27, 29–30, 32–39, 36–37 |
| 0.0772 | 16–23, 17–22, 30–32, 36–37, 37–38, 38–46, 40–46 |
| 0.0842 | 29–30, 30–32, 32–39, 36–37, 37–38, 38–46, 40–46 |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Wang, C.; Zhang, C.; Luo, L.; Qi, X.; Kong, J. Optimal Resilience and Risk-Driven Strategies for Pre-Disaster Protection of Electric Power Systems against Uncertain Disaster Scenarios. Energies 2024 , 17 , 3619. https://doi.org/10.3390/en17153619
Wang C, Zhang C, Luo L, Qi X, Kong J. Optimal Resilience and Risk-Driven Strategies for Pre-Disaster Protection of Electric Power Systems against Uncertain Disaster Scenarios. Energies . 2024; 17(15):3619. https://doi.org/10.3390/en17153619
Wang, Chen, Chao Zhang, Ling Luo, Xiaoman Qi, and Jingjing Kong. 2024. "Optimal Resilience and Risk-Driven Strategies for Pre-Disaster Protection of Electric Power Systems against Uncertain Disaster Scenarios" Energies 17, no. 15: 3619. https://doi.org/10.3390/en17153619
Article Metrics
Article access statistics, further information, mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals

- Advanced Search
Management of a post-disaster emergency scenario through unmanned aerial vehicles: : Multi-Depot Multi-Trip Vehicle Routing with Total Completion Time Minimization
New citation alert added.
This alert has been successfully added and will be sent to:
You will be notified whenever a record that you have chosen has been cited.
To manage your alert preferences, click on the button below.
New Citation Alert!
Please log in to your account
Information & Contributors
Bibliometrics & citations, view options, recommendations, a matheuristic for multi-depot multi-trip vehicle routing problems.
Starting from a real-life application, in this short paper, we propose the original Multi-Depot Multi-Trip Vehicle Routing Problem with Total Completion Times minimization (MDMT-VRP-TCT) . For it, we propose a mathematical formulation as a MILP, ...
Autonomous Landing Allocation of Multiple Unmanned Aerial Vehicles on Multiple Unmanned Surface Vessels Subject to Energy Consumption
This paper proposes a distributed energy-based landing allocation method of multiple unmanned aerial vehicles (UAVs) on multiple unmanned surface vessels (USVs). First, an optimization function is established, which consists of the limited energy ...
Trajectory Planning for Emergency Landing of VTOL Fixed-Wing Unmanned Aerial Vehicles
In recent years, inspired by technological progress and the outstanding performance of Unmanned Aerial Vehicles (UAVs) in several local wars, the UAV industry has witnessed explosive development, widely used in communication relay, logistics, surveying ...
Information
Published in.
Pergamon Press, Inc.
United States
Publication History
Author tags.
- Multi-depot
- Completion time
- Matheuristic
- Unmanned aerial vehicles (UAVs)
- Research-article
Contributors
Other metrics, bibliometrics, article metrics.
- 0 Total Citations
- 0 Total Downloads
- Downloads (Last 12 months) 0
- Downloads (Last 6 weeks) 0
View options
Login options.
Check if you have access through your login credentials or your institution to get full access on this article.
Full Access
Share this publication link.
Copying failed.
Share on social media
Affiliations, export citations.
- Please download or close your previous search result export first before starting a new bulk export. Preview is not available. By clicking download, a status dialog will open to start the export process. The process may take a few minutes but once it finishes a file will be downloadable from your browser. You may continue to browse the DL while the export process is in progress. Download
- Download citation
- Copy citation
We are preparing your search results for download ...
We will inform you here when the file is ready.
Your file of search results citations is now ready.
Your search export query has expired. Please try again.
- Open access
- Published: 25 July 2024
Strategies to strengthen the resilience of primary health care in the COVID-19 pandemic: a scoping review
- Ali Mohammad Mosadeghrad 1 ,
- Mahnaz Afshari 2 ,
- Parvaneh Isfahani 3 ,
- Farahnaz Ezzati 4 ,
- Mahdi Abbasi 4 ,
- Shahrzad Akhavan Farahani 4 ,
- Maryam Zahmatkesh 5 &
- Leila Eslambolchi 4
BMC Health Services Research volume 24 , Article number: 841 ( 2024 ) Cite this article
Metrics details
Primary Health Care (PHC) systems are pivotal in delivering essential health services during crises, as demonstrated during the COVID-19 pandemic. With varied global strategies to reinforce PHC systems, this scoping review consolidates these efforts, identifying and categorizing key resilience-building strategies.
Adopting Arksey and O'Malley's scoping review framework, this study synthesized literature across five databases and Google Scholar, encompassing studies up to December 31st, 2022. We focused on English and Persian studies that addressed interventions to strengthen PHC amidst COVID-19. Data were analyzed through thematic framework analysis employing MAXQDA 10 software.
Our review encapsulated 167 studies from 48 countries, revealing 194 interventions to strengthen PHC resilience, categorized into governance and leadership, financing, workforce, infrastructures, information systems, and service delivery. Notable strategies included telemedicine, workforce training, psychological support, and enhanced health information systems. The diversity of the interventions reflects a robust global response, emphasizing the adaptability of strategies across different health systems.
Conclusions
The study underscored the need for well-resourced, managed, and adaptable PHC systems, capable of maintaining continuity in health services during emergencies. The identified interventions suggested a roadmap for integrating resilience into PHC, essential for global health security. This collective knowledge offered a strategic framework to enhance PHC systems' readiness for future health challenges, contributing to the overall sustainability and effectiveness of global health systems.
Peer Review reports
The health system is a complex network that encompasses individuals, groups, and organizations engaged in policymaking, financing, resource generation, and service provision. These efforts collectively aim to safeguard and enhance people health, meet their expectations, and provide financial protection [ 1 ]. The World Health Organization's (WHO) framework outlines six foundational building blocks for a robust health system: governance and leadership, financing, workforce, infrastructure along with technologies and medicine, information systems, and service delivery. Strengthening these elements is essential for health systems to realize their objectives of advancing and preserving public health [ 2 ].
Effective governance in health systems encompasses the organization of structures, processes, and authority, ensuring resource stewardship and aligning stakeholders’ behaviors with health goals [ 3 ]. Financial mechanisms are designed to provide health services without imposing financial hardship, achieved through strategic fund collection, management and allocation [ 4 , 5 ]. An equitable, competent, and well-distributed health workforce is crucial in delivering healthcare services and fulfilling health system objectives [ 2 ]. Access to vital medical supplies, technologies, and medicines is a cornerstone of effective health services, while health information systems play a pivotal role in generating, processing, and utilizing health data, informing policy decisions [ 2 , 5 ]. Collectively, these components interact to offer quality health services that are safe, effective, timely, affordable, and patient-centered [ 2 ]
The WHO, at the 1978 Alma-Ata conference, introduced primary health care (PHC) as the fundamental strategy to attain global health equity [ 6 ]. Subsequent declarations, such as the one in Astana in 2018, have reaffirmed the pivotal role of PHC in delivering high-quality health care for all [ 7 ]. PHC represents the first level of contact within the health system, offering comprehensive, accessible, community-based care that is culturally sensitive and supported by appropriate technology [ 8 ]. Essential care through PHC encompasses health education, proper nutrition, access to clean water and sanitation, maternal and child healthcare, immunizations, treatment of common diseases, and the provision of essential drugs [ 6 ]. PHC aims to provide protective, preventive, curative, and rehabilitative services that are as close to the community as possible [ 9 ].
Global health systems, however, have faced significant disruptions from various shocks and crises [ 10 ], with the COVID-19 pandemic being a recent and profound example. The pandemic has stressed health systems worldwide, infecting over 775 million and claiming more than 7.04 million lives as of April 13th, 2024 [ 11 ]. Despite the pandemic highlighting the critical role of hospitals and intensive care, it also revealed the limitations of specialized medicine when not complemented by a robust PHC system [ 12 ].
The pandemic brought to light the vulnerabilities of PHC systems, noting a significant decrease in the use of primary care for non-emergency conditions. Routine health services, including immunizations, prenatal care, and chronic disease management, were severely impacted [ 13 ]. The challenges—quarantine restrictions, fears of infection, staffing and resource shortages, suspended non-emergency services, and financial barriers—reduced essential service utilization [ 14 ]. This led to an avoidance of healthcare, further exacerbating health inequalities and emphasizing the need for more resilient PHC systems [ 15 , 16 , 17 ].
Resilient PHC systems are designed to predict, prevent, prepare, absorb, adapt, and transform when facing crises, ensuring the continuity of routine health services [ 18 ]. Investing in the development of such systems can not only enhance crisis response but also foster post-crisis transformation and improvement. This study focuses on identifying global interventions and strategies to cultivate resilient PHC systems, aiding policymakers and managers in making informed decisions in times of crisis.
In 2023, we conducted a scoping review to collect and synthesize evidence from a broad spectrum of studies addressing the COVID-19 pandemic. A scoping review allows for the assessment of literature's volume, nature, and comprehensiveness, and is uniquely inclusive of both peer-reviewed articles and gray literature—such as reports, white papers, and policy documents. Unlike systematic reviews, it typically does not require a quality assessment of the included literature, making it well-suited for rapidly gathering a wide scope of evidence [ 19 ]. Our goal was to uncover the breadth of solutions aimed at bolstering the resilience of the PHC system throughout the COVID-19 crisis. The outcomes of this review are intended to inform the development of a model that ensures the PHC system's ability to continue delivering not just emergency services but also essential care during times of crisis.
We employed Arksey and O'Malley's methodological framework, which consists of six steps: formulating the research question, identifying relevant studies, selecting the pertinent studies, extracting data, synthesizing and reporting the findings, and, where applicable, consulting with stakeholders to inform and validate the results [ 20 ]. This comprehensive approach is designed to capture a wide range of interventions and strategies, with the ultimate aim of crafting a robust PHC system that can withstand the pressures of a global health emergency
Stage 1: identifying the research question
Our scoping review was guided by the central question: "Which strategies and interventions have been implemented to enhance the resilience of primary healthcare systems in response to the COVID-19 pandemic?" This question aimed to capture a comprehensive array of responses to understand the full scope of resilience-building activities within PHC systems.
Stage 2: identifying relevant studies
To ensure a thorough review, we conducted systematic searches across multiple databases, specifically targeting literature up to December 31st, 2022. The databases included PubMed, Web of Science, Scopus, Magiran, and SID. We also leveraged the expansive reach of Google Scholar. Our search strategy incorporated a bilingual approach, utilizing both English and Persian keywords that encompassed "PHC," "resilience," "strategies," and "policies," along with the logical operators AND/OR to refine the search. Additionally, we employed Medical Subject Headings (MeSH) terms to enhance the precision of our search. The results were meticulously organized and managed using the Endnote X8 citation manager, facilitating the systematic selection and review of pertinent literature.
Stage 3: selecting studies
In the third stage, we meticulously vetted our search results to exclude duplicate entries by comparing bibliographic details such as titles, authors, publication dates, and journal names. This task was performed independently by two of our authors, LE and MA, who rigorously screened titles and abstracts. Discrepancies encountered during this process were brought to the attention of a third author, AMM, for resolution through consensus.
Subsequently, full-text articles were evaluated by four team members—LE, MA, PI, and SHZ—to ascertain their relevance to our research question. The selection hinged on identifying articles that discussed strategies aimed at bolstering the resilience of PHC systems amidst the COVID-19 pandemic Table 1 .
We have articulated the specific inclusion and exclusion criteria that guided our selection process in Table 2 , ensuring transparency and replicability of our review methodology
Stage 4: charting the data
Data extraction was conducted by a team of six researchers (LE, MA, PI, MA, FE, and SHZ), utilizing a structured data extraction form. For each selected study, we collated details including the article title, the first author’s name, the year of publication, the country where the study was conducted, the employed research methodology, the sample size, the type of document, and the PHC strengthening strategies described.
In pursuit of maintaining rigorous credibility in our study, we adopted a dual-review process. Each article was independently reviewed by pairs of researchers to mitigate bias and ensure a thorough analysis. Discrepancies between reviewers were addressed through discussion to reach consensus. In instances where consensus could not be reached, the matter was escalated to a third, neutral reviewer. Additionally, to guarantee thoroughness, either LE or MA conducted a final review of the complete data extraction for each study.
Stage 5: collating, summarizing and reporting the results
In this stage, authors LE, MZ, and MA worked independently to synthesize the data derived from the selected studies. Differences in interpretation were collaboratively discussed until a consensus was reached, with AMM providing arbitration where required.
We employed a framework thematic analysis, underpinned by the WHO's health system building blocks model, to structure our findings. This model categorizes health system components into six foundational elements: governance and leadership; health financing; health workforce; medical products, vaccines, and technologies; health information systems; and service delivery [ 2 ]. Using MAXQDA 10 software, we coded the identified PHC strengthening strategies within these six thematic areas.
Summary of search results and study selection
In total, 4315 articles were found by initial search. After removing 397 duplicates, 3918 titles and abstracts were screened and 3606 irrelevant ones were deleted. Finally, 167 articles of 312 reviewed full texts were included in data synthesis (Fig. 1 ). Main characteristics of included studies are presented in Appendix 1.

PRISMA Flowchart of search process and results
Characteristics of studies
These studies were published in 2020 (18.6%), 2021 (36.5%) and 2022 (44.9%). They were conducted in 48 countries, mostly in the US (39 studies), the UK (16 studies), Canada (11 studies), Iran (10 studies) and Brazil (7 studies) as shown in Fig. 2 .

Distribution of reviewed studies by country
Although the majority of the reviewed publications were original articles (55.1 %) and review papers (21 %), other types of documents such as reports, policy briefs, analysis, etc., were also included in this review (Fig. 3 ).
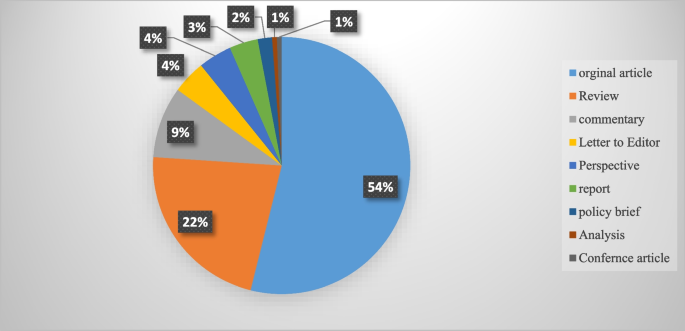
An overview of the publication types
Strengthening interventions to build a resilient PHC system
In total, 194 interventions were identified for strengthening the resilience of PHC systems to respond to the COVID-19 pandemic. They were grouped into six themes of PHC governance and leadership (46 interventions), PHC financing (21 interventions), PHC workforce (37 interventions), PHC infrastructures, equipment, medicines and vaccines (30 interventions), PHC information system (21 interventions) and PHC service delivery (39 interventions). These strategies are shown in Table 3 .
This scoping review aimed to identify and categorize the range of interventions employed globally to strengthen the resilience of primary healthcare (PHC) systems in the face of the COVID-19 pandemic. Our comprehensive search yielded 194 distinct interventions across 48 countries, affirming the significant international efforts to sustain healthcare services during this unprecedented crisis. These interventions have been classified according to the WHO’s six building block model of health systems, providing a framework for analyzing their breadth and depth. This review complements and expands upon the findings from Pradhan et al., who identified 28 interventions specifically within low and middle-income countries, signaling the universality of the challenge and the myriad of innovative responses it has provoked globally [ 178 ].
The review highlights the critical role of governance and leadership in PHC resilience. Effective organizational structure changes, legal reforms, and policy development were crucial in creating adaptive healthcare systems capable of meeting the dynamic challenges posed by the pandemic. These findings resonate with the two strategies of effective leadership and coordination emphasized by Pradhan et al. (2023), and underscore the need for clear vision, evidence-based policy, and active community engagement in governance [ 178 ]. The COVID-19 pandemic posed significant challenges for PHC systems globally. A pivotal response to these challenges was the active involvement of key stakeholders in the decision-making process. This inclusivity spanned across the spectrum of general practitioners, health professionals, health managers, and patients. By engaging these vital contributors, it became possible to address their specific needs and to design and implement people-centered services effectively [ 41 , 42 , 43 ].
The development and implementation of collaborative, evidence-informed policies and national healthcare plans were imperative. Such strategies required robust leadership, bolstered by political commitment, to ensure that the necessary changes could be enacted swiftly and efficiently [ 41 , 45 ]. Leaders within the health system were called upon to foster an environment of good governance. This entailed promoting increased participation from all sectors of the healthcare community, enhancing transparency in decision-making processes, and upholding the principles of legitimacy, accountability, and responsibility within the health system [ 10 ]. The collective aim was to create a more resilient, responsive, and equitable healthcare system in the face of the pandemic's demands.
In the wake of the COVID-19 pandemic, governments were compelled to implement new laws and regulations. These were designed to address a range of issues from professional accreditation and ethical concerns to supporting the families of healthcare workers. Additionally, these legal frameworks facilitated the integration of emerging services such as telemedicine into the healthcare system, ensuring that these services were regulated and standardized [ 38 , 40 , 61 ]. A key aspect of managing the pandemic was the establishment of effective and transparent communication systems for patients, public health authorities, and the healthcare system at large [ 60 , 61 ]. To disseminate vital information regarding the pandemic, vaccination programs, and healthcare services, authorities leveraged various channels. Public media, local online platforms, and neighborhood networks were instrumental in keeping the public informed about the ongoing situation and available services [ 53 , 60 , 86 ]. For health professionals, digital communication tools such as emails and WhatsApp groups, as well as regular meetings, were utilized to distribute clinical guidelines, government directives, and to address any queries they might have had. This ensured that healthcare workers were kept up-to-date with the evolving landscape of the pandemic and could adapt their practices accordingly [ 60 , 144 ].
Healthcare facilities function as complex socio-technical entities, combining multiple specialties and adapting to the ever-changing landscape of healthcare needs and environments [ 179 ]. To navigate this dynamic, policy makers must take into account an array of determinants—political, economic, social, and environmental—that influence health outcomes. Effective management of a health crisis necessitates robust collaboration across various sectors, including government bodies, public health organizations, primary healthcare systems, and hospitals. Such collaboration is not only pivotal during crisis management but also during the development of preparedness plans [ 63 ]. Within the health system, horizontal collaboration among departments and vertical collaboration between the Ministry of Health and other governmental departments are vital. These cooperative efforts are key to reinforce the resilience of the primary healthcare system. Moreover, a strong alliance between national pandemic response teams and primary healthcare authorities is essential to identifying and resolving issues within the PHC system [ 29 ]. On an international scale, collaborations and communications are integral to the procurement of essential medical supplies, such as medicines, equipment, and vaccines. These international partnerships are fundamental to ensuring that health systems remain equipped to face health emergencies [ 63 ].
To ensure the PHC system's preparedness and response capacity was at its best, regular and effective monitoring and evaluation programs were put in place. These included rigorous quarterly stress tests at the district level, which scrutinized the infrastructure and technology to pinpoint the system’s strengths and areas for improvement [ 43 ]. Furthermore, clinical audits were conducted to assess the structure, processes, and outcomes of healthcare programs, thereby enhancing the quality and effectiveness of the services provided [ 63 ]. These evaluation measures were crucial for maintaining a high standard of care and for adapting to the ever-evolving challenges faced by the PHC system.
Financial strategies played a critical role in enabling access to essential health services without imposing undue financial hardship. Various revenue-raising, pooling, and purchasing strategies were implemented to expand PHC financing during the pandemic, illustrating the multifaceted approach needed to sustain healthcare operations under strained circumstances [ 9 , 19 ].
In response to the COVID-19 pandemic, the Indian government took decisive action to bolster the country's healthcare infrastructure. By enhancing the financial capacity of states, the government was able to inject more funds into the Primary Health Care (PHC) system. This influx of resources made it possible to introduce schemes providing free medications and diagnostic services [ 50 ]. The benefits of increased financial resources were also felt beyond India's borders, enabling the compensation of health services in various forms. In Greece, it facilitated the monitoring and treatment of COVID-19 through in-person, home-based, and remote health services provided by physicians in private practice. Similarly, in Iran, the financial boost supported the acquisition of basic and para-clinical services from the private sector [ 21 , 65 ]. These measures reflect a broader international effort to adapt and sustain health services during a global health crisis.
The COVID-19 pandemic presented a formidable challenge to the PHC workforce worldwide. Healthcare workers were subjected to overwhelming workloads and faced significant threats to both their physical and mental well-being. To build resilience in the face of this crisis, a suite of interventions was implemented. These included recruitment strategies, training and development programs, enhanced teamwork, improved protective measures, comprehensive performance appraisals, and appropriate compensation mechanisms, as documented in Table 3 . To address staffing needs within PHC centers, a range of professionals including general practitioners, nurses, community health workers, and technical staff were either newly employed or redeployed from other healthcare facilities [ 63 ]. Expert practitioners were positioned on the frontlines, providing both in-person services and telephone consultations, acting as gatekeepers in the health system [ 49 , 63 ]. Support staff with technological expertise played a crucial role as well, assisting patients in navigating patient portals, utilizing new digital services, and conducting video visits [ 102 ]. Furthermore, the acute shortage of healthcare workers was mitigated by recruiting individuals who were retired, not currently practicing, or in training as students, as well as by enlisting volunteers. This strategy was key to bolstering the workforce and ensuring continuity of care during the pandemic [ 109 ].
During the pandemic, new training programs were developed to prepare healthcare staff for the evolving demands of their roles. These comprehensive courses covered a wide array of critical topics, including the correct use of personal protective equipment (PPE), the operation of ventilators, patient safety protocols, infection prevention, teamwork, problem-solving, self-care techniques, mental health support, strategies for managing stress, navigating and applying reliable web-based information, emergency response tactics, telemedicine, and direct care for COVID-19 patients [ 74 , 95 , 100 , 108 , 110 , 112 , 117 ].
Acknowledging the psychological and professional pressures faced by the primary healthcare workforce, health managers took active measures to safeguard both the physical and mental well-being of their employees during this challenging period [ 124 ]. Efforts to protect physical health included monitoring health status, ensuring vaccination against COVID-19, and providing adequate PPE [ 63 , 72 ]. To address mental health, a variety of interventions were deployed to mitigate anxiety and related issues among frontline workers. In Egypt, for instance, healthcare workers benefited from psychotherapy services and adaptable work schedules to alleviate stress [ 126 ]. Singapore employed complementary strategies, such as yoga, meditation, and the encouragement of religious practices, to promote relaxation among staff [ 133 ]. In the United States, the Wellness Hub application was utilized as a tool for employees to enhance their mental health [ 132 ]. In addition to health and wellness initiatives, there were financial incentives aimed at motivating employees. Payment protocols were revised, and new incentives, including scholarship opportunities and career development programs, were introduced to foster job satisfaction and motivation among healthcare workers [ 63 ].
The resilience of PHC systems during the pandemic hinged on several key improvements. Enhancing health facilities, supplying medicines and diagnostic kits, distributing vaccines, providing medical equipment, and building robust digital infrastructure were all fundamental elements that contributed to the strength of PHC systems, as outlined in Table 3 . Safe and accessible primary healthcare was facilitated through various means. Wheelchair routes were created for patients to ensure their mobility within healthcare facilities. , dedicated COVID-19 clinics were established, mass vaccination centers were opened to expedite immunization, and mobile screening stations were launched to extend testing capabilities [ 23 , 33 , 63 , 140 ].
In Iran, the distribution and availability of basic medicines were managed in collaboration with the Food and Drug Organization, ensuring that essential medications reached those in need [ 89 ]. During the outbreak, personal protective equipment (PPE) was among the most critical supplies. Access to PPE was prioritized, particularly for vulnerable groups and healthcare workers, to provide a layer of safety against the virus [ 63 ]. Vaccines were made available at no cost, with governments taking active measures to monitor their safety and side effects, to enhance their quality, and to secure international approvals. Furthermore, effective communication strategies were employed to keep the public informed about vaccine-related developments [ 32 , 83 ].
These comprehensive efforts underscored the commitment to maintaining a resilient PHC system in the face of a global health every individual in the community could access healthcare services. To facilitate this, free high-speed Wi-Fi hotspots were established, enabling patients to engage in video consultations and utilize a range of e-services without the barrier of internet costs crisis. Significant enhancements were made to the digital infrastructure. This expansion was critical in ensuring that [ 30 , 54 ]. Complementing these measures, a variety of digital health tools were deployed to further modernize care delivery. Countries like Nigeria and Germany, for instance, saw the introduction of portable electrocardiograms and telemedical stethoscopes. These innovations allowed for more comprehensive remote assessments and diagnostics, helping to bridge the gap between traditional in-person consultations and the emerging needs for telemedicine [ 141 , 180 ].
Throughout the COVID-19 pandemic, targeted interventions were implemented to bolster information systems and research efforts, as outlined in Table 3 . Key among these was the advancement of a modern, secure public health information system to ensure access to health data was not only reliable and timely but also transparent and accurate [ 33 , 45 , 49 ]. The "Open Notes" initiative in the United States exemplified this effort, guaranteeing patient access to, and editorial control over, their health records [ 141 ]. Management strategies also promoted the "one-health" approach, facilitating the exchange of health data across various departments and sectors to enhance public health outcomes [ 10 ].
In addition to these information system upgrades, active patient surveillance and early warning systems were instituted in collaboration with public health agencies. These systems played a pivotal role in detecting outbreaks, providing precise reports on the incidents, characterizing the epidemiology of pathogens, tracking their spread, and evaluating the efficacy of control strategies. They were instrumental in pinpointing areas of concern, informing smart lockdowns, and improving contact tracing methods [ 33 , 63 , 72 ]. The reinforcement of these surveillance and warning systems had a profound impact on shaping and implementing a responsive strategy to the health crisis [ 10 ].
To further reinforce the response to the pandemic, enhancing primary healthcare (PHC) research capacity became crucial. This enabled healthcare professionals and policymakers to discern both facilitators and barriers within the system and to devise fitting strategies to address emerging challenges. To this end, formal advisory groups and multidisciplinary expert panels, which included specialists from epidemiology, clinical services, social care, sociology, policy-making, and management, were convened. These groups harnessed the best available evidence to inform decision-making processes [ 30 ]. Consequently, research units were established to carry out regular telephone surveys and to collect data on effective practices, as well as new diagnostic and therapeutic approaches [ 31 , 89 ]. The valuable insights gained from these research endeavors were then disseminated through trusted channels to both the public and policymakers, ensuring informed decisions at all levels [ 36 ].
The COVID-19 pandemic acted as a catalyst for the swift integration of telemedicine into healthcare systems globally. This period saw healthcare providers leverage telecommunication technologies to offer an array of remote services, addressing medical needs such as consultations, diagnosis, monitoring, and prescriptions. This transition was instrumental in ensuring care continuity and mitigating infection risks for both patients and healthcare workers, highlighting an innovative evolution in healthcare delivery [ 170 , 181 ].
Countries adapted to this new model of healthcare with varied applications: Armenia established telephone follow-ups and video consultations for remote patient care, while e-pharmacies and mobile health tools provided immediate access to medical information and services [ 29 ]. In France and the United States, tele-mental health services and online group support became a means to support healthy living during the pandemic [ 147 , 158 ] . New Zealand introduced the Aroha chatbot, an initiative to assist with mental health management [ 139 ].
The implementation and effectiveness of these telehealth services were not limited by economic barriers, as underscored by Pradhan et al. (2023), who noted the key role of telemedicine in low and middle-income countries. These countries embraced the technology to maintain health service operations, proving its global applicability and utility [ 178 ]. The widespread adoption of telemedicine, therefore, represents a significant and perhaps lasting shift in healthcare practice, one that has redefined patient care in the face of a global health crisis and may continue to shape the future of healthcare delivery [ 170 , 178 , 181 ].
The study highlighted PHC strengthening strategies in COVID-19 time . Notably, the adaptations and reforms spanned across governance, financing, workforce management, information system, infrastructural readiness, and service delivery enhancements. These interventions collectively contributed to the robustness of health systems against the sudden surge in demand and the multifaceted challenges imposed by the pandemic and resulted.
Significantly, the findings have broader implications for health policy and system design worldwide. The pandemic has highlighted the critical need for resilient health systems that are capable of not only responding to health emergencies but also maintaining continuity in essential services. The strategies documented in this review serve as a template for countries to fortify their health systems by embedding resilience into their PHC frameworks (Fig. 4 ). Future health crises can be better managed by learning from these evidenced responses, which emphasize the necessity of integrated, well-supported, and dynamically adaptable health care structures.
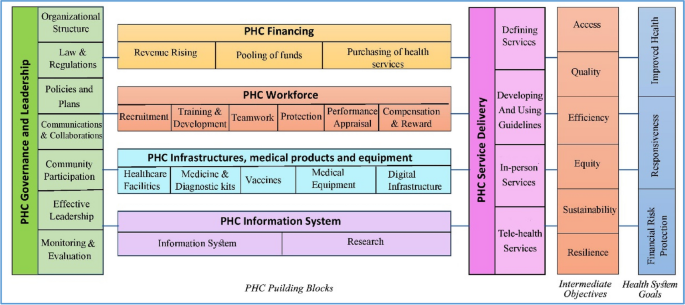
A model for strengthening the resilience of the primary health care system
Looking ahead, realist reviews could play a pivotal role in refining PHC resilience strategies. By understanding the context in which specific interventions succeed or fail, realist reviews can help policymakers and practitioners design more effective health system reforms, as echoed in the need for evidence-based planning in health system governance [ 9 ] . These reviews offer a methodological advantage by focusing on the causality between interventions and outcomes, aligning with the importance of effective health system leadership and management [ 50 , 182 ] . They take into account the underlying mechanisms and contextual factors, thus providing a nuanced understanding that is crucial for tailoring interventions to meet local needs effectively [ 28 , 86 ] , ultimately leading to more sustainable health systems globally. This shift towards a more analytical and context-sensitive approach in evaluating health interventions, as supported by WHO's framework for action [ 2 , 10 ] , will be crucial for developing strategies that are not only effective in theory but also practical and sustainable in diverse real-world settings.
Limitations and future research
In our comprehensive scoping review, we analyzed 167 articles out of a dataset of 4,315, classifying 194 interventions that build resilience in primary healthcare systems across the globe in response to pandemics like COVID-19. While the review's extensive search provides a sweeping overview of various strategies, it may not capture the full diversity of interventions across all regions and economies. Future research should focus on meta-analyses to evaluate the effectiveness of these interventions in greater detail and employ qualitative studies to delve into the specific challenges and successes, thus gaining a more nuanced understanding of the context. As the review includes articles only up to December 31, 2022, it may overlook more recent studies. Regular updates, a broader linguistic range, and the inclusion of a more diverse array of databases are recommended to maintain relevance and expand the breadth of literature, ultimately guiding more focused research that could significantly enhance the resilience of PHC systems worldwide.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
Primary Health Care
World Health Organization
Sustainable Development Goals
Universal Health Coverage
Personal Protective Equipment
General Practitioner
Mosadeghrad AM. A practical model for health policy making and analysis. Payesh. 2022;21(1):7–24 ([in Persian]).
Article Google Scholar
World Health Organization. Everybody’s Business: Strengthening Health Systems to Improve Health Outcomes. WHO’s Framework for Action. Geneva: World Health Organization; 2007.
Google Scholar
Khosravi MF, Mosadeghrad AM, Arab M. Health System Governance Evaluation: A Scoping Review. Iran J Public Health. 2023;52(2):265.
PubMed PubMed Central Google Scholar
Mosadeghrad AM, Abbasi M, Abbasi M, Heidari M. Sustainable health financing methods in developing countries: a scoping review. J of School Public Health Inst Public Health Res. 2023;20(4):358–78 ([in Persian]).
Mosadeghrad AM. Health strengthening plan, a supplement to Iran health transformation plan: letter to the editor. Tehran Univ Med J. 2019;77(8):537–8 ([in Persian]).
World Health Organization. Declaration of alma-ata. Copenhagen: Regional Office for Europe; 1978. p. 1–4.
Rasanathan K, Evans TG. Primary health care, the Declaration of Astana and COVID-19. Bull World Health Organ. 2020;98(11):801.
Article PubMed PubMed Central Google Scholar
World Health Organization, UNICEF. Operational framework for primary health care: transforming vision into action. Geneva: World Health Organization and the United Nations Children’s Fund; 2020.
Mosadeghrad AM, Heydari M, Esfahani P. Primary health care strengthening strategies in Iran: a realistic review. J School Public Health Inst Public Health Res. 2022;19(3):237–58 ([in Persian]).
Sagan A, Webb E, Azzopardi-Muscat N, de la Mata I, McKee M, Figueras J. Health systems resilience during COVID-19: Lessons for building back better. Regional Office for Europe: World Health Organization; 2021.
World Health Organization, Coronavirus (COVID-19) map. Available at https://covid19.who.int/ /. Access date 14/04/2024.
Plagg B, Piccoliori G, Oschmann J, Engl A, Eisendle K. Primary health care and hospital management during COVID-19: lessons from lombardy. Risk Manag Healthc Policy. 2021:3987–92.
World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. World Health Organization; 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
Mosadeghrad AM, Jajarmizadeh A. Continuity of essential health services during the COVID-19 pandemic. Tehran Univ Med J. 2021;79(10):831–2 ([in Persian]).
Splinter MJ, Velek P, Ikram MK, Kieboom BC, Peeters RP, Bindels PJ, Ikram MA, Wolters FJ, Leening MJ, de Schepper EI, Licher S. Prevalence and determinants of healthcare avoidance during the COVID-19 pandemic: A population-based cross-sectional study. PLoS Med. 2021;18(11):e1003854.
Article CAS PubMed PubMed Central Google Scholar
Wangmo S, Sarkar S, Islam T, Rahman MH, Landry M. Maintaining essential health services during the pandemic in Bangladesh: the role of primary health care supported by routine health information system. WHO South East Asia J Public Health. 2021;10(3):93.
Kumpunen S, Webb E, Permanand G, Zheleznyakov E, Edwards N, van Ginneken E, Jakab M. Transformations in the landscape of primary health care during COVID-19: Themes from the European region. Health Policy. 2022;126(5):391–7.
Article PubMed Google Scholar
Ezzati F, Mosadeghrad AM, Jaafaripooyan E. Resiliency of the Iranian healthcare facilities against the Covid-19 pandemic: challenges and solutions. BMC Health Serv Res. 2023;23(207):1–16.
Mosadeghrad AM, Isfahani P, Eslambolchi L, Zahmatkesh M, Afshari M. Strategies to strengthen a climate-resilient health system: a scoping review. Global Health. 2023;19(1):62.
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodol. 2005;8(1):19–32.
Akrami F, Riazi-Isfahani S, Mahdavi hezaveh A, Ghanbari Motlagh A, Najmi M, Afkar M, et al. Iran’s Status of NCDs Prevention and Management Services during COVID-19 Pandemic at PHC Level. SJKU. 2021;26(5):50–68.
Etienne CF, Fitzgerald J, Almeida G, Birmingham ME, Brana M, Bascolo E, Cid C, Pescetto C. COVID-19: transformative actions for more equitable, resilient, sustainable societies and health systems in the Americas. BMJ Global Health. 2020;5(8):e003509.
Tabrizi JS, Raeisi A, Namaki S. Primary health care and COVID-19 Pandemic in the Islamic Republic of Iran. Depict Health. 2022;13(Suppl 1):S1-10.
Danhieux K, Buffel V, Pairon A, Benkheil A, Remmen R, Wouters E, Van Olmen J. The impact of COVID-19 on chronic care according to providers: a qualitative study among primary care practices in Belgium. BMC Fam Pract. 2020;21:1–6.
Goodyear-Smith F, Kidd M, Oseni TIA, Nashat N, Mash R, Akman M, Phillips RL, van Weel C. Internationalexamples of primary care COVID-19 preparedness and response: a comparison of four countries. Fam MedCommunity Health. 2022;10(2):e001608.
Kinder K, Bazemore A, Taylor M, Mannie C, Strydom S, George J, Goodyear-Smith F. Integrating primary care and public health to enhance response to a pandemic. Prim Health Care Res Dev. 2021;22:e27.
De Maeseneer J. Prim Health Care Res Dev. 2021;22:e73.
Westfall JM, Liaw W, Griswold K, Stange K, Green LA, Phillips R, Bazemore A, Jaén CR, Hughes LS, DeVoe J, Gullett H. Uniting public health and primary care for healthy communities in the COVID-19 era and beyond. J Am Board Fam Med. 2021;34(Supplement):S203-9.
Johansen AS, Shriwise A, Lopez-Acuna D, Vracko P. Strengthening the primary health care response to COVID-19: an operational tool for policymakers. Prim Health Care ResDev. 2021;22:e81.
Reath J, Lau P, Lo W, Trankle S, Brooks M, Shahab Y, Abbott P. Strengthening learning and research in health equity–opportunities for university departments of primary health care and general practice. Aust J Prim Health. 2022;29(2):131–6.
Ferenčina J, Tomšič V. COVID-19 clinic as a basis of quality primary health care in the light of the pandemic - an observational study. Med Glas (Zenica). 2022;19(1). https://doi.org/10.17392/1437-21 .
Mosadeghrad AH. Promote COVID-19 vaccination uptake: a letter to editor. Tehran Univ Med Sci J. 2022;80(2):159–60.
Chaiban L, Benyaich A, Yaacoub S, Rawi H, Truppa C, Bardus M. Access to primary and secondary health care services for people living with diabetes and lower-limb amputation during the COVID-19 pandemic in Lebanon: a qualitative study. BMC Health Serv Res. 2022;22(1):593.
Džakula A, Banadinović M, Lovrenčić IL, Vajagić M, Dimova A, Rohova M, Minev M, Scintee SG, Vladescu C, Farcasanu D, Robinson S. A comparison of health system responses to COVID-19 in Bulgaria, Croatia and Romania in 2020. Health Policy. 2022;126(5):456–64.
Ghazi Saeedi M, Tanhapour M. Telemedicine System: A Mandatory Requirement in Today’s World. Payavard. 2022;15(5):490–507.
Ferorelli D, Nardelli L, Spagnolo L, Corradi S, Silvestre M, Misceo F, Marrone M, Zotti F, Mandarelli G, Solarino B, Dell’Erba A. Medical legal aspects of telemedicine in Italy: application fields, professional liability and focus on care services during the COVID-19 health emergency. J Prim CareCommun Health. 2020;11:2150132720985055.
CAS Google Scholar
Fulmer T, Reuben DB, Auerbach J, Fick DM, Galambos C, Johnson KS. Actualizing better health and health care for older adults: commentary describes six vital directions to improve the care and quality of life for all older Americans. Health Aff. 2021;40(2):219–25.
Hernández Rincón EH, Pimentel González JP, Aramendiz Narváez MF, Araujo Tabares RA, Roa González JM. Description and analysis of primary care-based COVID-19 interventions in Colombia. Medwave. 2021;21(3):e8147.
Giannopoulou I, Tsobanoglou GO. COVID-19 pandemic: challenges and opportunities for the Greek health care system. Irish J Psychol Med. 2020;37(3):226–30.
Chow C, Goh SK, Tan CS, Wu HK, Shahdadpuri R. Enhancing frontline workforce volunteerism through exploration of motivations and impact during the COVID-19 pandemic. Int J Disaster Risk Reduct. 2021;1(66):102605.
Alboksmaty A, Kumar S, Parekh R, Aylin P. Management and patient safety of complex elderly patients in primary care during the COVID-19 pandemic in the UK—Qualitative assessment. PLoS One. 2021;16(3):e0248387.
Savoy A, Patel H, Shahid U, Offner AD, Singh H, Giardina TD, Meyer AN. Electronic Co-design (ECO-design) Workshop for Increasing Clinician Participation in the Design of Health Services Interventions: Participatory Design Approach. JMIR Hum Fact. 2022;9(3):e37313.
Tumusiime P, Karamagi H, Titi-Ofei R, Amri M, Seydi AB, Kipruto H, Droti B, Zombre S, Yoti Z, Zawaira F, Cabore J. Building health system resilience in the context of primary health care revitalization for attainment of UHC: proceedings from the Fifth Health Sector Directors’ Policy and Planning Meeting for the WHO African Region. BMC Proc. 2020;14:1–8 (BioMed Central).
Atoofi MK, Rezaei N, Kompani F, Shirzad F, Sh D. Requirements of mental health services during the COVID-19 outbreak: a systematic review. Iran J Psychiatry Clin Psychol. 2020;26(3):264–79.
Mosadeghrad AM, Taherkhani T, Shojaei S, Jafari M, Mohammadi S, Emamzadeh A, Akhavan S. Strengthening primary health care system resilience in COVID-19 pandemic: a scoping review. sjsph 2022;20(1):13-24.
Fotokian Z, Mohammadkhah F. Primary health care as a strategy to fight COVID-19 pandemic: letter to the editor. J Isfahan Med School. 2021;39(630):470–4. https://doi.org/10.22122/jims.v39i630.14016 .
Li D, Howe AC, Astier-Peña MP. Primary health care response in the management of pandemics: Learnings from the COVID-19 pandemic. Atención Primaria. 2021;1(53):102226.
Chua AQ, Tan MMJ, Verma M, Han EKL, Hsu LY, Cook AR, et al. BMJ Global Health. 2020;5(9):e003317.
Eisele M, Pohontsch NJ, Scherer M. Strategies in primary care to face the SARS-CoV-2/COVID-19 pandemic: an online survey. Front Med. 2021;2(8):613537.
Lamberti-Castronuovo A, Valente M, Barone-Adesi F, Hubloue I, Ragazzoni L. Primary health care disaster preparedness: a review of the literature and the proposal of a new framework. Int J Dis Risk Reduct. 2022;2:103278.
Piché-Renaud PP, Ji C, Farrar DS, Friedman JN, Science M, Kitai I, Burey S, Feldman M, Morris SK. Impact of the COVID-19 pandemic on the provision of routine childhood immunizations in Ontario Canada. Vaccine. 2021;39(31):4373–82.
Saxenian H, Alkenbrack S, Freitas Attaran M, Barcarolo J, Brenzel L, Brooks A, Ekeman E, Griffiths UK, Rozario S, Vande Maele N, Ranson MK. Sustainable financing for Immunization Agenda 2030. Vaccine. 2024;42 Suppl 1:S73-S81. https://doi.org/10.1016/j.vaccine.2022.11.037 .
Saso A, Skirrow H, Kampmann B. Impact of COVID-19 on immunization services for maternal and infant vaccines: results of a survey conducted by imprint—the immunising pregnant women and infants network. Vaccines. 2020;8(3):556.
Sagan A, Thomas S, McKee M, Karanikolos M, Azzopardi-Muscat N, de la Mata I, Figueras J, World Health Organization. COVID-19 and health systems resilience: lessons going forwards. Eurohealth. 2020;26(2):20–4.
Celuppi IC, Meirelles BH, Lanzoni GM, Geremia DS, Metelski FK. Management in the care of people with HIV in primary health care in times of the new coronavirus. Revista de Saúde Pública. 2022;1(56):13.
Denis JL, Potvin L, Rochon J, Fournier P, Gauvin L. On redesigning public health in Québec: lessons learned from the pandemic. Can J Public Health= Revue Canadienne de Sante Publique. 2020;111(6):912.
PubMed Google Scholar
Wilson G, Windner Z, Dowell A, Toop L, Savage R, Hudson B. Navigating the health system during COVID-19: primary care perspectives on delayed patient care. N Z Med J. 2021;134(1546):17–27 (PMID: 34855730).
Zhang N, Yang S, Jia P. Cultivating resilience during the COVID-19 pandemic: a socioecological perspective. Annu Rev Psychol. 2022;4(73):575–98. https://doi.org/10.1146/annurev-psych-030221-031857 . (Epub 2021 Sep 27 PMID: 34579547).
Al Ghafri T, Al Ajmi F, Al Balushi L, Kurup PM, Al Ghamari A, Al Balushi Z, Al Fahdi F, Al Lawati H, Al Hashmi S, Al Manji A, Al Sharji A. Responses to the pandemic covid-19 in primary health care in oman: muscat experience. Oman Med J. 2021;36(1):e216.
Adler L, Vinker S, Heymann AD, Van Poel E, Willems S, Zacay G. The effect of the COVID-19 pandemic on primary care physicians in Israel, with comparison to an international cohort: a cross-sectional study. Israel J Health Policy Res. 2022;11(1):1.
Haldane V, Zhang Z, Abbas RF, Dodd W, Lau LL, Kidd MR, Rouleau K, Zou G, Chao Z, Upshur RE, Walley J. National primary care responses to COVID-19: a rapid review of the literature. BMJ Open. 2020;10(12):e041622.
Hussein ES, Al-Shenqiti AM, Ramadan RM. Applications of medical digital technologies for noncommunicable diseases for follow-up during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19(19):12682.
Desborough J, Dykgraaf SH, Phillips C, Wright M, Maddox R, Davis S, Kidd M. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Fam Pract. 2021;38(6):811–25.
Sandhu HS, Smith RW, Jarvis T, O’Neill M, Di Ruggiero E, Schwartz R, Rosella LC, Allin S, Pinto AD. Early impacts of the COVID-19 pandemic on public health systems and practice in 3 Canadian provinces from the perspective of public health leaders: a qualitative study. J Public Health Manag Pract. 2022;28(6):702–11.
Farsalinos K, Poulas K, Kouretas D, Vantarakis A, Leotsinidis M, Kouvelas D, Docea AO, Kostoff R, Gerotziafas, Antoniou MN, Polosa R. Improved strategies to counter the COVID-19 pandemic: Lockdowns vs. primary and community healthcare. Toxicol Rep. 2021;8:1–9.
Article CAS PubMed Google Scholar
Fitzpatrick K, Sehgal A, Montesanti S, Pianarosa E, Barnabe C, Heyd A, Kleissen T, Crowshoe L. Examining the role of Indigenous primary healthcare across the globe in supporting populations during public health crises. Global Public Health. 2022;24:1–29.
Liaw ST, Kuziemsky C, Schreiber R, Jonnagaddala J, Liyanage H, Chittalia A, Bahniwal R, He JW, Ryan BL, Lizotte DJ, Kueper JK. Primary care informatics response to Covid-19 pandemic: adaptation, progress, and lessons from four countries with high ICT development. Yearbook Med Inform. 2021;30(01):044–55.
Djalante R, Shaw R, DeWit A. Progress in disaster. Science. 2020;6:100080.
Fatima R, Akhtar N, Yaqoob A, Harries AD, Khan MS. Building better tuberculosis control systems in a post-COVID world: learning from Pakistan during the COVID-19 pandemic. Int J Infect Dis. 2021;1(113):S88-90.
Shin WY, Kim C, Lee SY, Lee W, Kim JH. Role of primary care and challenges for public–private cooperation during the coronavirus disease 2019 pandemic: An expert Delphi study in South Korea. Yonsei Med J. 2021;62(7):660.
Thompson RN, et al. Key questions for modelling COVID-19exit strategies. Proc R Soc B. 2020;287:20201405. https://doi.org/10.1098/rspb.2020.1405 .
Baral P. Health systems and services during COVID-19: lessons and evidence from previous crises: a rapid scoping review to inform the United Nations research roadmap for the COVID-19 recovery. Int J Health Serv. 2021;51(4):474–93.
Daou M, Helou S, El Helou J, El Hachem C, El Helou E. Ensuring care continuity in extreme crises: A participatory action research approach. InMEDINFO 2021: One World, One Health–Global Partnership for Digital Innovation 2022 (pp. 937-941). IOS Press.
Besigye IK, Namatovu J, Mulowooza M. Coronavirus disease-2019 epidemic response in Uganda: the need to strengthen and engage primary healthcare. Afr J Prim Health Care Fam Med. 2020;12(1):1–3.
Silva MJ, Santos P. The impact of health literacy on knowledge and attitudes towards preventive strategies against COVID-19: a cross-sectional study. Int J Environ Res Public Health. 2021;18(10):5421. https://doi.org/10.3390/ijerph18105421 . (PMID:34069438;PMCID:PMC8159089).
Sultana A, Bhattacharya S, Hossain MM. COVID-19 and primary care: a critical need for strengthening emergency preparedness across health systems. J Fam Med Primary Care. 2021;10(1):584–5.
Xu RH, Shi LS, Xia Y, Wang D. Associations among eHealth literacy, social support, individual resilience, and emotional status in primary care providers during the outbreak of the SARS-CoV-2 Delta variant. Digit Health. 2022;25(8):20552076221089788. https://doi.org/10.1177/20552076221089789 . (PMID:35355807;PMCID:PMC8958311).
Bajgain BB, Jackson J, Aghajafari F, Bolo C, Santana MJ. Immigrant Healthcare Experiences and Impacts During COVID-19: A Cross-Sectional Study in Alberta Canada. J Patient Exp. 2022;9:23743735221112708.
Kim AY, Choi WS. Considerations on the implementation of the telemedicine system encountered with stakeholders’ resistance in COVID-19 pandemic. Telemed e-Health. 2021;27(5):475–80.
Tayade MC. Strategies to tackle by primary care physicians to mental health issues in India in COVId-19 pandemic. J Fam Med Prim Care. 2020;9(11):5814–5.
Thomas C. Resilient health and care: Learning the lessons of Covid-19 in the English NHS, IPPR. 2020. http://www.ippr.org/research/publications/resilient-health-and-care .
Saab MM, O’Driscoll M, FitzGerald S, Sahm LJ, Leahy-Warren P, Noonan B, Kilty C, Lyons N, Burns HE, Kennedy U, Lyng Á. Primary healthcare professionals’ perspectives on patient help-seeking for lung cancer warning signs and symptoms: a qualitative study. BMC Prim Care. 2022;23(1):1–5.
Ma L, Han X, Ma Y, Yang Y, Xu Y, Liu D, Yang W, Feng L. Decreased influenza vaccination coverage among Chinese healthcare workers during the COVID-19 pandemic. Infect Dis Pov. 2022;11(05):63–73.
Ismail SA, Lam ST, Bell S, Fouad FM, Blanchet K, Borghi J. Strengthening vaccination delivery system resilience in the context of protracted humanitarian crisis: a realist-informed systematic review. BMC Health Serv Res. 2022;22(1):1–21.
Litke N, Weis A, Koetsenruijter J, Fehrer V, Koeppen M, Kuemmel S, Szecsenyi J, Wensing M. Building resilience in German primary care practices: a qualitative study. BMC Prim Care. 2022;23(1):1–4.
Den Broeder L, South J, Rothoff A, Bagnall AM, Azarhoosh F, Van Der Linden G, Bharadwa M, Wagemakers A. Community engagement in deprived neighbourhoods during the COVID-19 crisis: perspectives for more resilient and healthier communities. Health promotion international. 2022;37(2):daab098.
Sundararaman T, Muraleedharan VR, Ranjan A. Pandemic resilience and health systems preparedness: lessons from COVID-19 for the twenty-first century. J Soc Econ Dev. 2021;23(Suppl 2):1–11. https://doi.org/10.1007/s40847-020-00133-x . (Epub ahead of print. PMID: 34720480; PMCID: PMC7786882).
Ferreira NN, Garibaldi PM, Moraes GR, Moura JC, Klein TM, Machado LE, Scofoni LF, Haddad SK, Calado RT, Covas DT, Fonseca BA. The impact of an enhanced health surveillance system for COVID-19 management in Serrana, Brazil. Public Health Pract. 2022;1(4):100301.
Harzheim E, Martins C, Wollmann L, Pedebos LA, Faller LD, Marques MD, Minei TS, Cunha CR, Telles LF, Moura LJ, Leal MH. Federal actions to support and strengthen local efforts to combat COVID-19: Primary Health Care (PHC) in the driver’s seat. Ciência Saúde Coletiva. 2020;5(25):2493–7.
Smaggus A, Long J, Ellis LA, Clay-Williams R, Braithwaite J. Government actions and their relation to resilience in healthcare during the COVID-19 pandemic in New South Wales, Australia and Ontario, Canada. Int J Health Policy Manag. 2022;11(9):1682–94. https://doi.org/10.34172/ijhpm.2021.67 .
Tselebis A, Pachi A. Primary mental health care in a New Era. Healthcare (Basel). 2022;10(10):2025. https://doi.org/10.3390/healthcare10102025 . (PMID:36292472;PMCID:PMC9601948).
Rieckert A, Schuit E, Bleijenberg N, Ten Cate D, de Lange W, de Man-van Ginkel JM, Mathijssen E, Smit LC, Stalpers D, Schoonhoven L, Veldhuizen JD, Trappenburg JC. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11(1):e043718. https://doi.org/10.1136/bmjopen-2020-043718 .
Basu P, Alhomoud S, Taghavi K, Carvalho AL, Lucas E, Baussano I. Cancer screening in the coronavirus pandemic era: adjusting to a new situation. JCO Global Oncol. 2021;7(1):416–24.
Rieckert A, Schuit E, Bleijenberg N, et al. How can we build and maintain the resilience of our health care professionals during COVID-19? Recommendations based on a scoping review. BMJ Open. 2021;11:e043718. https://doi.org/10.1136/bmjopen-2020-043718 .
Shaikh BT. Strengthening health system building blocks: configuring post-COVID-19 scenario in Pakistan. Prim Health Care Res Dev. 2021;22:e9 Cambridge University Press.
Franzosa E, Gorbenko K, Brody AA, Leff B, Ritchie CS, Kinosian B, Ornstein KA, Federman AD. “At home, with care”: lessons from New York City home-based primary care practices managing COVID-19. J Am Geriatr Soc. 2021;69(2):300–6.
Adhikari B, Mishra SR, Schwarz R. Transforming Nepal’s primary health care delivery system in global health era: addressing historical and current implementation challenges. Global Health. 2022;18(1):1–2.
Mas Bermejo P, Sánchez Valdés L, Somarriba López L, Valdivia Onega NC, Vidal Ledo MJ, Alfonso Sánchez I, et al. Equity and the Cuban National Health System's response to COVID-19. Rev Panam Salud Publica. 2021;45:e80. https://doi.org/10.26633/RPSP.2021.80 .
Gong F, Hu G, Lin H, Sun X, Wang W. Integrated Healthcare Systems Response Strategies Based on the Luohu Model During the COVID-19 Epidemic in Shenzhen, China. Int J Integr Care. 2021;21(1):1. https://doi.org/10.5334/ijic.5628 .
Gomez T, Anaya YB, Shih KJ, Tarn DM. A qualitative study of primary care physicians’ experiences with telemedicine during COVID-19. J Am Board Fam Med. 2021;34(Supplement):S61-70.
Teng K, Russo F, Kanuch S, Caron A. Virtual Care Adoption-Challenges and Opportunities From the Lens of Academic Primary Care Practitioners. J Public Health Manag Pract. 2022;28(6):599–602. https://doi.org/10.1097/PHH.0000000000001548 . (Epub 2022 Aug 27. PMID: 36037465; PMCID: PMC9555588).
Anaya YB, Mota AB, Hernandez GD, Osorio A, Hayes-Bautista DE. Post-pandemic telehealth policy for primary care: an equity perspective. J Am Board Fam Med. 2022;35(3):588–92.
Florea M, Lazea C, Gaga R, Sur G, Lotrean L, Puia A, Stanescu AM, Lupsor-Platon M, Florea H, Sur ML. Lights and shadows of the perception of the use of telemedicine by Romanian family doctors during the COVID-19 pandemic. Int J Gen Med. 2021;14:1575.
Selick A, Durbin J, Hamdani Y, Rayner J, Lunsky Y. Accessibility of Virtual Primary Care for Adults With Intellectual and Developmental Disabilities During the COVID-19 Pandemic: Qualitative Study. JMIR Form Res 2022;6(8):e38916. https://formative.jmir.org/2022/8/e38916 . https://doi.org/10.2196/38916 .
Frost R, Nimmons D, Davies N. Using remote interventions in promoting the health of frail older persons following the COVID-19 lockdown: challenges and solutions. J Am Med Direct Assoc. 2020;21(7):992.
Suija K, Mard LA, Laidoja R, et al. Experiences and expectation with the use of health data: a qualitative interview study in primary care. BMC Prim Care. 2022;23:159. https://doi.org/10.1186/s12875-022-01764-1 .
Sullivan EE, McKinstry D, Adamson J, Hunt L, Phillips RS, Linzer M. Burnout Among Missouri Primary Care Clinicians in 2021: Roadmap for Recovery? Mo Med. 2022;119(4):397–400 (PMID: 36118800; PMCID: PMC9462904).
Tang C, Chen X, Guan C, Fang P. Attitudes and Response Capacities for Public Health Emergencies of Healthcare Workers in Primary Healthcare Institutions: A Cross-Sectional Investigation Conducted in Wuhan, China, in 2020. Int Environ Res Public Health. 2022;19(19):12204. https://doi.org/10.3390/ijerph191912204 .
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, Perez T. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80.
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, Perez T, Tan SM, Bartos M, Mabuchi S, Bonk M, McNab C, Werner GK, Panjabi R, Nordström A, Legido-Quigley H. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964-80. https://doi.org/10.1038/s41591-021-01381-y .
Berger Z, De Jesus VA, Assoumou SA, Greenhalgh T. Long COVID and health inequities: the role of primary care. Milbank Q. 2021;99(2):519.
Haldane V, Dodd W, Kipp A, Ferrolino H, Wilson K, Servano D, Lau LL, Wei X. Extending health systems resilience into communities: a qualitative study with community-based actors providing health services during the COVID-19 pandemic in the Philippines. BMC Health Serv Res. 2022;22(1):1–2.
Haun JN, Cotner BA, Melillo C, Panaite V, Messina W, Patel-Teague S, Zilka B. Proactive integrated virtual healthcare resource use in primary care. BMC Health Serv Res. 2021;21(1):1–4.
Kelly F, Uys M, Bezuidenhout D, Mullane SL, Bristol C. Improving Healthcare Worker Resilience and Well-Being During COVID-19 Using a Self-Directed E-Learning Intervention. Front Psychol. 2021;12:748133. https://doi.org/10.3389/fpsyg.2021.748133 .
Thekkur P, Fernando M, Nair D, Kumar AMV, Satyanarayana S, Chandraratne N, Chandrasiri A, Attygalle DE, Higashi H, Bandara J, Berger SD, Harries AD. Primary Health Care System Strengthening Project in Sri Lanka: Status and Challenges with Human Resources, Information Systems, Drugs and Laboratory Services. Healthcare. 2022;10(11):2251. https://doi.org/10.3390/healthcare10112251 .
Balogun M, Banke-Thomas A, Gwacham-Anisiobi U, Yesufu V, Ubani O, Afolabi BB. Actions and AdaptationsImplemented for Maternal, Newborn and Child Health Service Provision During the Early Phase of the COVID-19 Pandemic in Lagos, Nigeria: Qualitative Study of Health Facility Leaders. Ann Glob Health. 2022;88(1):13. https://doi.org/10.5334/aogh.3529 .
Llamas S, MP AP, Felipe P. Patient safety training and a safe teaching in primary care. Aten Primaria. 2021;53 Suppl 1(Suppl 1):102199.
Eze-Emiri C, Patrick F, Igwe E, Owhonda G. Retrospective study of COVID-19 outcomes among healthcare workers in Rivers State, Nigeria. BMJ Open. 2022;12(11):e061826.
Golechha M, Bohra T, Patel M, Khetrapal S. Healthcare worker resilience during the COVID-19 pandemic: a qualitative study of primary care providers in India. World Med Health Policy. 2022;14(1):6–18.
Gómez-Restrepo C, Cepeda M, Torrey WC, Suarez-Obando F, Uribe-Restrepo JM, Park S, Acosta MP, Camblor PM, Castro SM, Aguilera-Cruz J, González L. Perceived access to general and mental healthcare in primary care in Colombia during COVID-19: A cross-sectional study. Frontiers in Public Health. 2022;10:896318.
Nejat N, Borzabadi Farahani Z. COVID-19 pandemic: opportunities for continuing nursing professional development. J Med Educ Dev. 2022;14(44):1–2.
DeVoe JE, Cheng A, Krist A. JAMA Health Forum. 2020;1(4):e200423.
Hoeft TJ, Hessler D, Francis D, Gottlieb LM. Applying lessons from behavioral health integration to social care integration in primary care. Ann Fam Med. 2021;19(4):356–61.
Silsand L, Severinsen GH, Berntsen G. Preservation of Person-Centered care through videoconferencing for patient follow-up during the COVID-19 pandemic: case study of a multidisciplinary care team. JMIR Format Res. 2021;5(3):e25220.
Sullivan E, Phillips R.S. Sustaining primary care teams in the midst of a pandemic. Isr J Health Policy Res. 2020; 9. 77. https://doi.org/10.1186/s13584-020-00434-w .
Abd El Kader AI, Faramawy MA. COVID-19 anxiety and organizational commitment among front line nurses: Perceived role of nurse managers' caring behavior. Nurs Pract Today. 2022;9(1):X.
Croghan IT, Chesak SS, Adusumalli J, Fischer KM, Beck EW, Patel SR, Ghosh K, Schroeder DR, Bhagra A. Stress, resilience, and coping of healthcare workers during the COVID-19 pandemic. J Prim Care Commun Health. 2021;12:21501327211008450.
Aragonès E, del Cura-González I, Hernández-Rivas L, Polentinos-Castro E, Fernández-San-Martín MI, López-Rodríguez JA, Molina-Aragonés JM, Amigo F, Alayo I, Mortier P, Ferrer M. Psychological impact of the COVID-19 pandemic on primary care workers: a cross-sectional study. Br J Gen Pract. 2022;72(720):e501-10.
Franck E, Goossens E, Haegdorens F, Geuens N, Portzky M, Tytens T, Dilles T, Beeckman K, Timmermans O, Slootmans S, Van Rompaey B. Role of resilience in healthcare workers’ distress and somatization during the COVID-19 pandemic: a cross-sectional study across Flanders Belgium. Nurs Open. 2022;9(2):1181–9.
DeTore NR, Sylvia L, Park ER, Burke A, Levison JH, Shannon A, et al. J Psychiatr Res. 2022;146:228–33.
Shi LS, Xu RH, Xia Y, Chen DX, Wang D. The impact of COVID-19-related work stress on the mental health of primary healthcare workers: the mediating effects of social support and resilience. Front Psychol. 2022;21(12):800183. https://doi.org/10.3389/fpsyg.2021.800183 . (PMID:35126252;PMCID:PMC8814425).
Golden EA, Zweig M, Danieletto M, Landell K, Nadkarni G, Bottinger E, Katz L, Somarriba R, Sharma V, Katz CL, Marin DB. A resilience-building app to support the mental health of health care workers in the COVID-19 era: Design process, distribution, and evaluation. JMIR Format Res. 2021;5(5):e26590.
Chan AY, Ting C, Chan LG, Hildon ZJ. “The emotions were like a roller-coaster”: a qualitative analysis of e-diary data on healthcare worker resilience and adaptation during the COVID-19 outbreak in Singapore. Hum Resour Health. 2022;20(1):60.
Ashley C, James S, Williams A, Calma K, Mcinnes S, Mursa R, Stephen C, Halcomb E. The psychological well-being of primary healthcare nurses during COVID-19: a qualitative study. J Adv Nurs. 2021;77(9):3820–8.
Carmona LE, Nielfa MD, Alvarado AL. The Covid-19 pandemic seen from the frontline. Int Braz J Urol. 2020;27(46):181–94.
Delobelle PA, Abbas M, Datay I, De Sa A, Levitt N, Schouw D, Reid S. Non-communicable disease care and management in two sites of the Cape Town Metro during the first wave of COVID-19: A rapid appraisal. Afr J Prim Health Care Fam Med. 2022;14(1):e1-e7. https://doi.org/10.4102/phcfm.v14i1.3215 .
Luciani S, Agurto I, Caixeta R, Hennis A. Prioritizing noncommunicable diseases in the Americas region in the era of COVID-19. Rev Panam Salud Publica. 2022;46:e83. https://doi.org/10.26633/RPSP.2022.83 .
Cabral IE, Pestana-Santos M, Ciuffo LL, Nunes YDR, Lomba MLLF. Child health vulnerabilities during the COVID-19 pandemic in Brazil and Portugal. Rev Lat Am Enfermagem. 2021;29:e3422. https://doi.org/10.1590/1518-8345.4805.3422 . (Published 2021 Jul 2).
Ludin N, Holt-Quick C, Hopkins S, Stasiak K, Hetrick S, Warren J, Cargo T. A Chatbot to support young people during the COVID-19 Pandemic in New Zealand: evaluation of the real-world rollout of an open trial. J Med Internet Res. 2022;24(11):e38743.
Breton M, Deville-Stoetzel N, Gaboury I, Smithman MA, Kaczorowski J, Lussier MT, Haggerty J, Motulsky A, Nugus P, Layani G, Paré G. Telehealth in primary healthcare: a portrait of its rapid implementation during the COVID-19 pandemic. Healthcare Policy. 2021;17(1):73.
Knop M, Mueller M, Niehaves B. Investigating the use of telemedicine for digitally mediated delegation in team-based primary care: mixed methods study. J Med Internet Res. 2021;23(8):e28151.
Zamiela C, Hossain NUI, Jaradat R. Enablers of resilience in the healthcare supply chain: A case study of U.S healthcare industry during COVID-19 pandemic. Res Transport Econ. 2022;93:101174. https://doi.org/10.1016/j.retrec.2021.101174 . Epub 2021 Dec 24. PMCID: PMC9675944.
Lukong AM, Jafaru Y. Covid-19 pandemic challenges, coping strategies and resilience among healthcare workers: a multiple linear regression analysis. Afr J Health Nurs Midwifery. 2021;4:16–27.
Hearnshaw S, Serban S, Mohammed I, Zubair A, Jaswal D, Grant S. A local dental network approach to the COVID-19 pandemic: innovation through collaboration. Prim Dental J. 2021;10(1):33–9.
Haase CB, Bearman M, Brodersen J, Hoeyer K, Risor T. ‘You should see a doctor’, said the robot: Reflections on a digital diagnostic device in a pandemic age. Scand J Public Health. 2021;49(1):33–6.
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A, Yaya S. Introduction of mobilehealth tools to support COVID-19 training and surveillance in Ogun State Nigeria. Frontiers in Sustainable Cities. 2021;3:638278:1-9.
Ibragimov K, Palma M, Keane G, Ousley J, Crowe M, Carreño C, Casas G, Mills C, Llosa A. Shifting to Tele-Mental Health in humanitarian and crisis settings: an evaluation of Médecins Sans Frontières experience during the COVID-19 pandemic. Conflict Health. 2022;16(1):1–5.
Wherton J, Greenhalgh T, Hughes G, Shaw SE. The role of information infrastructures in scaling up video consultations during COVID-19: mixed methods case study into opportunity, disruption, and exposure. J Med Internet Res. 2022;24(11):e42431. https://doi.org/10.2196/42431 . (PMID:36282978;PMCID:PMC9651004).
Jonnagaddala J, Godinho MA, Liaw ST. From telehealth to virtual primary care in Australia? a rapid scoping review. Int J Med Inform. 2021;1(151):104470.
Tanemura N, Chiba T. The usefulness of a checklist approach-based confirmation scheme in identifying unreliable COVID-19-related health information: a case study in Japan. Humanit Soc Sci Commun. 2022;9(1):270. https://doi.org/10.1057/s41599-022-01293-3 . (Epub 2022 Aug 15. PMID: 35990766; PMCID: PMC9376898).
Zaroushani V. Occupational safety and health and response to COVID-19 using the fourth industrial revolution technologies. J Health Saf Work. 2020;10(4):329–48.
Binagwaho A, Hirwe D, Mathewos K. Health System Resilience: Withstanding Shocks and Maintaining Progress. Glob Health Sci Pract. 2022;10(Suppl 1):e2200076. https://doi.org/10.9745/GHSP-D-22-00076 .
Freed SL, Thiele D, Gardner M, Myers E. COVID-19 evaluation and testing strategies in a federally qualified health center. Am J Public Health. 2022;112(S3):S284-7.
Levy P, McGlynn E, Hill AB, Zhang L, Korzeniewski SJ, Foster B, Criswell J, O’Brien C, Dawood K, Baird L, Shanley CJ. From pandemic response to portable population health: a formative evaluation of the Detroit mobile health unit program. Plos One. 2021;16(11):e0256908.
Corwin C, Sinnwell E, Culp K. A mobile primary care clinic mitigates an early COVID-19 outbreak among migrant farmworkers in Iowa. J Agromed. 2021;26(3):346–51.
Mills WR, Buccola JM, Sender S, Lichtefeld J, Romano N, Reynolds K, Price M, Phipps J, White L, Howard S. Home-based primary care led-outbreak mitigation in assisted living facilities in the first 100 days of coronavirus disease 2019. J Am Med Direct Assoc. 2020;21(7):951–3.
Sigurdsson EL, Blondal AB, Jonsson JS, Tomasdottir MO, Hrafnkelsson H, Linnet K, Sigurdsson JA. How primary healthcare in Iceland swiftly changed its strategy in response to the COVID-19 pandemic. BMJ Open. 2020;10(12):e043151. https://doi.org/10.1136/bmjopen-2020-043151 . (PMID:33293329;PMCID:PMC7722808).
Mirsky JB, Thorndike AN. Virtual group visits: hope for improving chronic disease management in primary care during and after the COVID-19 pandemic. Am J Health Promot. 2021;35(7):904–7.
Lauriola P, Martín-Olmedo P, Leonardi GS, Bouland C, Verheij R, Dückers ML, Van Tongeren M, Laghi F, Van Den Hazel P, Gokdemir O, Segredo E. On the importance of primary and community healthcare in relation to global health and environmental threats: lessons from the COVID-19 crisis. BMJ Global Health. 2021;6(3):e004111.
Stengel S, Roth C, Breckner A, et al. Resilience of the primary health care system – German primary care practitioners’ perspectives during the early COVID-19 pandemic. BMC Prim Care. 2022;23:203. https://doi.org/10.1186/s12875-022-01786-9 .
Adu PA, Stallwood L, Adebola SO, Abah T, Okpani AI. The direct and indirect impact of COVID-19 pandemic on maternal and child health services in Africa: a scoping review. Global Health Res Policy. 2022;7(1):1–4.
Segal M, Giuffrida P, Possanza L, Bucciferro D. The critical role of health information technology in the safe integration of behavioral health and primary care to improve patient care. J Behav Health Serv Res. 2022;49(2):221–30. https://doi.org/10.1007/s11414-021-09774-0 . (Epub 2021 Oct 19. PMID: 34668115; PMCID: PMC8525847).
Gallardo-Rincón H, Gascon JL, Martínez-Juárez LA, Montoya A, Saucedo-Martínez R, Rosales RM, Tapia-Conyer R. MIDO COVID: A digital public health strategy designed to tackle chronic disease and the COVID-19 pandemic in Mexico. Plos One. 2022;17(11):e0277014.
Shah SS, Safa A, Johal K, et al. A prospective observational real world feasibility study assessing the role of app-based remote patient monitoring in reducing primary care clinician workload during the COVID pandemic. BMC Fam Pract. 2021;22:248. https://doi.org/10.1186/s12875-021-01594-7 .
Lu M, Liao X. Access to care through telehealth among US Medicare beneficiaries in the wake of the COVID-pandemic. Front Public Health. 2022;10:946944.
Reges O, Feldhamer I, Wolff Sagy Y, Lavie G. Factors associated with using telemedicine in the primary care clinics during the COVID-19 pandemic in Israel. Int J Environ Res Public Health. 2022;19(20):13207.
Neves AL, Li E, Gupta PP, Fontana G, Darzi A. Virtual primary care in high-income countries during the COVID-19 pandemic: Policy responses and lessons for the future. Eur J Gen Pract. 2021;27(1):241–7.
Fadul N, Regan N, Kaddoura L, Swindells S. A midwestern academic HIV clinic operation during the COVID-19 pandemic: implementation strategy and preliminary outcomes. J International Assoc Provid AIDS Care (JIAPAC). 2021;2(20):23259582211041424.
Gray C, Ambady L, Chao S PharmD, Smith W MPH, Yoon J. Virtual Management of Chronic Conditions During the COVID-19 Pandemic: Insights From Primary Care Providers and Clinical Pharmacists. Mil Med. 2023;188(7-8):e2615-e2620. https://doi.org/10.1093/milmed/usac277 .
Hincapié MA, Gallego JC, Gempeler A, Piñeros JA, Nasner D, Escobar MF. Implementation and usefulness of telemedicine during the COVID-19 pandemic: a scoping review. J Prim Care Commun Health. 2020;11:2150132720980612.
Calvo-Paniagua J, Díaz-Arribas MJ, Valera-Calero JA, et al. A tele-health primary care rehabilitation program improves self-perceived exertion in COVID-19 survivors experiencing Post-COVID fatigue and dyspnea: A quasi-experimental study. PLoS One. 2022;17(8):e0271802. https://doi.org/10.1371/journal.pone.0271802 . (Published 2022 Aug 4).
Chen K, Davoodi NM, Strauss DH, Li M, Jiménez FN, Guthrie KM, et al. J Appl Gerontol. 2022;41(11):2282–95.
Murphy M, Scott LJ, Salisbury C, Turner A, Scott A, Denholm R, Lewis R, Iyer G, Macleod J, Horwood J. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract. 2021;71(704):e166-77.
Maria AR, Serra H, Heleno B. Teleconsultations and their implications for health care: a qualitative study on patients’ and physicians’ perceptions. Int J Med Inform. 2022;1(162):104751.
Liddy C, Singh J, Mitchell R, Guglani S, Keely E. How one eConsult service is addressing emerging COVID-19 questions. J Am Board Fam Med. 2022;35(3):601–4.
Schow DC, Thomson A, Trusty WT, Buchi-Fotre L. Use of a research as intervention approach to explore telebehavioral health services during the COVID-19 pandemic in Southeastern Idaho. J Prim Care Commun Health. 2022;13:21501319211073000.
Bruns BE, Lorenzo-Castro SA, Hale GM. Controlling blood pressure during a pandemic: The impact of telepharmacy for primary care patients. J Pharm Pract. 2022;27:08971900221136629.
Pradhan NA, Samnani AA, Abbas K, Rizvi N. Resilience of primary healthcare system across low-and middle-income countries during COVID-19 pandemic: a scoping review. Health Res Policy Syst. 2023;21(1):98.
Esfahani P, Mosadeghrad AM, Akbarisari A. The success of strategic planning in health care organizations of Iran. Int J Health Care Qual Assur. 2018;31(6):563–74.
Otu A, Okuzu O, Ebenso B, Effa E, Nihalani N, Olayinka A, Yaya S. Introduction of mobile health tools to support COVID-19 training and surveillance in Ogun State Nigeria. Front Sustain Cities. 2021;5(3):638278.
Ndayishimiye C, Lopes H, Middleton J. A systematic scoping review of digital health technologies during COVID-19: a new normal in primary health care delivery. Health Technol. 2023;13(2):273–84.
Ghiasipour M, Mosadeghrad AM, Arab M, Jaafaripooyan E. Leadership challenges in health care organizations: The case of Iranian hospitals. Med J Islam Repub Iran. 2017;31(1):560–7.
Download references
Acknowledgments
We would like to thank Dr. Arshad Altaf for his invaluable comments on the earlier drafts of this work.
Funding for this project was provided by the World Health Organization Eastern Mediterranean Region.
Author information
Authors and affiliations.
Health policy and management, Health Economics and Management Department, Tehran University of Medical Sciences, Tehran, Iran
Ali Mohammad Mosadeghrad
Health policy, School of Nursing and Midwifery, Saveh University of Medical Sciences, Saveh, Iran
Mahnaz Afshari
Health management, School of Public Health, Zabol University of Medical Sciences, Zabol, Iran
Parvaneh Isfahani
Health services management, Health Economics and Management Department, Tehran University of Medical Sciences, Tehran, Iran
Farahnaz Ezzati, Mahdi Abbasi, Shahrzad Akhavan Farahani & Leila Eslambolchi
Health Management, School of Business and Management, Royal Holloway University of London, London, UK
Maryam Zahmatkesh
You can also search for this author in PubMed Google Scholar
Contributions
LE, MA, MZ and AMM participated in the design of the study. LE, AMM, MA, MZ, PI, FE, MA and SHA undertook the literature review process. All authors drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Leila Eslambolchi .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was obtained from the Tehran University of Medical Science (Approval ID: IR.TUMS.SPH.REC.1401.0979).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mosadeghrad, A.M., Afshari, M., Isfahani, P. et al. Strategies to strengthen the resilience of primary health care in the COVID-19 pandemic: a scoping review. BMC Health Serv Res 24 , 841 (2024). https://doi.org/10.1186/s12913-024-11278-4
Download citation
Received : 14 January 2024
Accepted : 03 July 2024
Published : 25 July 2024
DOI : https://doi.org/10.1186/s12913-024-11278-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Primary health care system
- Strengthening strategies
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Disaster management is a critical area that requires efficient methods and techniques to address various challenges. This comprehensive assessment offers an in-depth overview of disaster management systems, methods, obstacles, and potential future paths. Specifically, it focuses on flood control, a significant and recurrent category of natural disasters. The analysis begins by exploring ...
For this literature review, ∼150 academic papers from 2012 to 2017 1 were identified from Google Scholar. This selection was based ... (VGI) and crowdsourcing in disaster management: a systematic literature review. Google Scholar. Howard, A., T. Blakemore, and M. Bevis. 2017. "Older People as Assets in Disaster Preparedness, Response and ...
In this systematic review, we reflect on the above concerns by sorting through 20 years of crisis and disaster literature (from 2001 to 2020) and charting the steps that have been taken to identify important trends and developments. ... Governance, and Public Management Review. Search terms were CRISIS or DISASTER, and the search engine used ...
Disaster management involves the pillars of emergency management: planning and preparation, mitigation, response, and recovery. ... Cosgrove SE, et al. Effectiveness of hospital staff mass-casualty incident training methods: A systematic literature review. Prehospital and disaster medicine. 2004 Sep; 19 (3):191-199. DOI: 10.1017 ...
Conclusion: The "science" of disaster management is spread across more than 900 different multi-disciplinary journals. The existing evidence-base is overwhelmingly descriptive and lacking in objective, post-disaster evaluations. SmithEC, BurkleFMJr, AitkenP, LeggattP. Seven decades of disasters: a systematic review of the literature.
Disaster management is a critical area that requires efficient methods and techniques to address various challenges. This comprehensive assessment offers an in-depth overview of disaster ...
Goldschmidt K. H., Kumar S. 2016. Humanitarian operations and crisis/disaster management: A retrospective review of the literature and framework for development. International Journal of Disaster Risk Reduction, 20: 1‐13.
Disaster Prevention and Management: A Critical Review of The. Literature. Nazaruddin Ali Basyah *, Muhamm ad Syukri, Irham Fahmi, Ismail Ali, Zulf adhli Rusli, Elva Se sioria. Putri. 1 Department ...
Disaster management agencies invest differing levels of resources into guiding communities to get ready for a range of hazards, and are increasingly turning to community engagement as a way of increasing preparedness. ... Personal Disaster Preparedness: an Integrative Review of the Literature. Disaster Medicine and Public Health Preparedness ...
In a recently published study, a systematic literature review was completed of more than 10,000 peer-reviewed English language studies since 2000, within the context of threat assessment, sense making, and ... the study was unrelated to ethical decision making in disaster management. The literature retrieved via this study was high in ...
Emmanuel Raju. Sonja Ayeb-Karlsson. This article analyses the suite of policies and measures enacted by the Indian Union Government in response to the COVID-19 pandemic through apparatuses of ...
The technique could enable disaster management professionals to identify relative levels of urgency and deploy recovery aid with more precision regarding the spatial and ... Social media applications and emergency management: a literature review and research agenda. Int. J. Disaster Risk Reduc., 28 (2018), pp. 565-577. View PDF View article ...
A literature review was made to discuss the significance of moving towards a more contemporary view to the disaster management cycle that brings more value to the final outcomes of the disaster management process. A conceptual model was then proposed to reflect a more contemporary view to the disaster management cycle.
A systematic literature review of community disaster resilience: main and related research areas and agendas - Author: Arvind Upadhyay, Amporn Sa-ngiamwibool ... All these three words must be present in the title of the selected papers.,The area "resilience management" and "disaster resilience assessment" accounted for 43% of the ...
The number, magnitude, complexity, and impact of natural disasters have been steadily increasing in various parts of the world. When preparing for, responding to, and recovering from a disaster, multiple organizations make decisions and take actions considering the needs, available resources, and priorities of the affected communities, emergency supply chains, and infrastructures. Most of the ...
Design/methodology/approach A literature review was made to discuss the significance of moving towards a more contemporary view to the disaster management cycle that brings more value to the final outcomes of the disaster management process. A conceptual model was then proposed to reflect a more contemporary view to the disaster management cycle.
Citation information: DOI 10.1147/JRD.2019.2960356, IBM Journal of Research and Development IBM J. Res. & Dev.; Baxter et al.: Quantitative Modeling in Disaster Management: A Literature Review Quantitative Modeling in Disaster Management: A Literature Review A. Baxter 1, H. Wilborn Lagerman1, P. Keskinocak The number, magnitude, complexity, and ...
1 BACKGROUND. A disaster is a condition that requires national or international assistance, causing physical, economic, social, or environmental losses that the affected group or society cannot cope with using their own resources (Genc et al., 2022).Disasters may lead to large-scale physical and economic losses and significant social and psychological destruction (Altun, 2018).
The paper identifies and develops a categorization of community-related knowledge management in disaster preparedness using a systematic literature review. Subsequently, the categorization is utilized in a case study to determine if community-related knowledge management in the preparedness phase can improve communities' responses in the ...
2. Importance of nursing in disaster management and response. Recent progress has highlighted the crucial role of nursing in disaster management and response ().Nurses are often the first point of contact for patients in disaster settings and play a critical role in triaging patients and providing basic medical care ().In recent years, there has been an increasing recognition of the importance ...
LOCAL GOVERNMENT'S PROBLEM WITH DISASTER MANAGEMENT: A LITERATURE REVIEW AND STRUCTURAL ANALYSIS 1. Robert P. Wolensky, Robert P. Wolensky. Professor of Sociology and co-director of the Center for the Small City at the University of Wisconsin-Stevens Point. Since 1973 he has conducted research on the political repercussions and dynamics ...
The results of the analysis of the literature review highlight several important points related to disaster education in disaster-prone schools, namely (1) In supporting increased understanding of environmental management and resilience in dealing with disasters in disaster-prone areas, governments in various countries make policies by ...
A literature review is a synthesis of published information on a particular research topics. The purpose is to map out what is already known about a certain subject, outline methods previously used, prevent duplication of research, and, along these lines, reveal gaps in existing literature to justify the research project.
Application of computational intelligence technologies in emergency management: A literature review. Artificial Intelligence Review, 52, 2131-2168. Article ... (2023). A deep learning approach to improve built asset operations and disaster management in critical events: An integrative simulation model for quicker decision making. Annals of ...
A literature review: model of disaster risk reduction for. decision support system. Soetjipto Jojok Widodo1, Hidayah Entin. 1. , and Sholikhah Faizatus. 1. 1 Program of Civil Engineering, Jember ...
Pre-disaster protection strategies are essential for enhancing the resilience of electric power systems against natural disasters. Considering the budgets for protection strategies, the dependency of other infrastructure systems on electricity, and the uncertainty of disaster scenarios, this paper develops risk-neutral and risk management models of strategies for pre-disaster protection. The ...
In this paper, we foster the interface of Operational Research with computer science in general and sensor networking in particular by focusing on managing a post-disaster emergency scenario where the use of a fleet of UAVs helps rescue teams identify people needing help inside an affected area.
In 2023, we conducted a scoping review to collect and synthesize evidence from a broad spectrum of studies addressing the COVID-19 pandemic. A scoping review allows for the assessment of literature's volume, nature, and comprehensiveness, and is uniquely inclusive of both peer-reviewed articles and gray literature—such as reports, white papers, and policy documents.
The communication and miscommunication of emotion by email. The Academy of Management Review, 33(2), 309-327. ... , D., Bonaretti, D. (2022). A systematic literature review on information systems for disaster management and proposals for its future research agenda. ... An application of a model-based framework to disaster management in Brazil