Urinary Tract Infection Case Study (45 min)
Watch More! Unlock the full videos with a FREE trial

Included In This Lesson
Study tools.
Access More! View the full outline and transcript with a FREE trial
Mrs. Phillips is an 84 year old female who arrived to the Emergency Department from a nursing home, where caregivers report she has altered mental status, confusion, and weakness that they just noticed this morning. The nurse inserts 2 large bore PIV’s and draws blood for a chemistry and complete blood count, as ordered by the Provider, who is concerned she may be having a stroke.
What initial nursing assessments should be performed??
- Assess for stroke symptoms, last known well, NIHSS, etc.
- Full set of vital signs
- Heart and Lung assessment, plus peripheral perfusion (pulses, skin, etc.)
What diagnostic testing do you anticipate for Mrs. Phillips?
- CT scan to rule out hemorrhagic stroke
- Neurologic exam by neurologist
- Possible further blood testing if stroke negative
Mrs. Phillips’s vitals are as follows:
HR 122 RR 24
BP 92/58 SpO 2 92%
Temp 103.6°F
Her NIHSS score is 2, CT scan is negative for an intracranial bleed, and the neurologist believes she is NOT having a stroke. The nurse is called into the room by the caregivers as the patient has wet herself. The nurse notes a foul, sour odor to the urine. Mrs. Phillips’ blood pressure is now 88/52. The nurse notifies the Provider.
What orders do you anticipate from the provider?
- The high heart rate and low blood pressure indicate Mrs. Phillips may be dehydrated, or possibly at risk for Septic Shock – she will need IV fluids
- We need to check a urine culture and urinalysis
- Should check blood cultures as well, in case of sepsis
- Will also likely need IV antibiotics – broad spectrum until specific bacteria identified
What may be going on with Mrs. Phillips physiologically?
- She likely has a urinary tract infection, as evidenced by her altered mental status, fever, and foul-smelling urine
The provider places orders for the following:
Keep SpO 2 > 92%
Blood Cultures x 2
Urine Culture
500 mL NS IV bolus STAT
100 mL/hr NS IV continuous infusion
Vancomycin 1,000 mg IV x 1 dose NOW.
Which order should be implemented first? Why?
- Urine and blood cultures should always be obtained before antibiotics
- Since the patient has peripheral IV’s already, it would be most appropriate to start the STAT IV fluid bolus before obtaining blood cultures. **Note – most facilities do NOT allow blood cultures to be obtained from existing IV lines due to risk for contamination**
- However, if no IV access was available – inserting IV’s and obtaining blood cultures with insertion would be the #1 priority.
The nurse obtains 2 sets of blood cultures and the UAP obtains a sterile urine sample via I&O cath. The UAP reports cloudy, foul-smelling urine. The nurse initiates the IV fluid bolus and requests the Vancomycin from the Pharmacy. Mrs. Phillips’ caregiver asks why she is so confused?
Why is Mrs. Phillips presenting with Altered Mental Status?
- The brain is very sensitive to changes in circulating bacteria, oxygen levels, and glucose levels. This is especially true in older patients. The presence of an infectious / inflammatory process in the system causes stress to the brain cells – leading to confusion and an altered mental state.
After 3 days of treatment with IV antibiotics, Mrs. Phillips is awake and oriented x 2-3 (she has dementia at baseline and occasionally thinks it’s 1946). She is calm, conversing with staff, and able to ambulate the halls. She will be discharged home with PO antibiotics tomorrow.
What discharge teaching should be provided to Mrs. Phillips and to the caregivers at Mrs. Phillips’ nursing home?
- Medication instructions – take as prescribed and take the full course
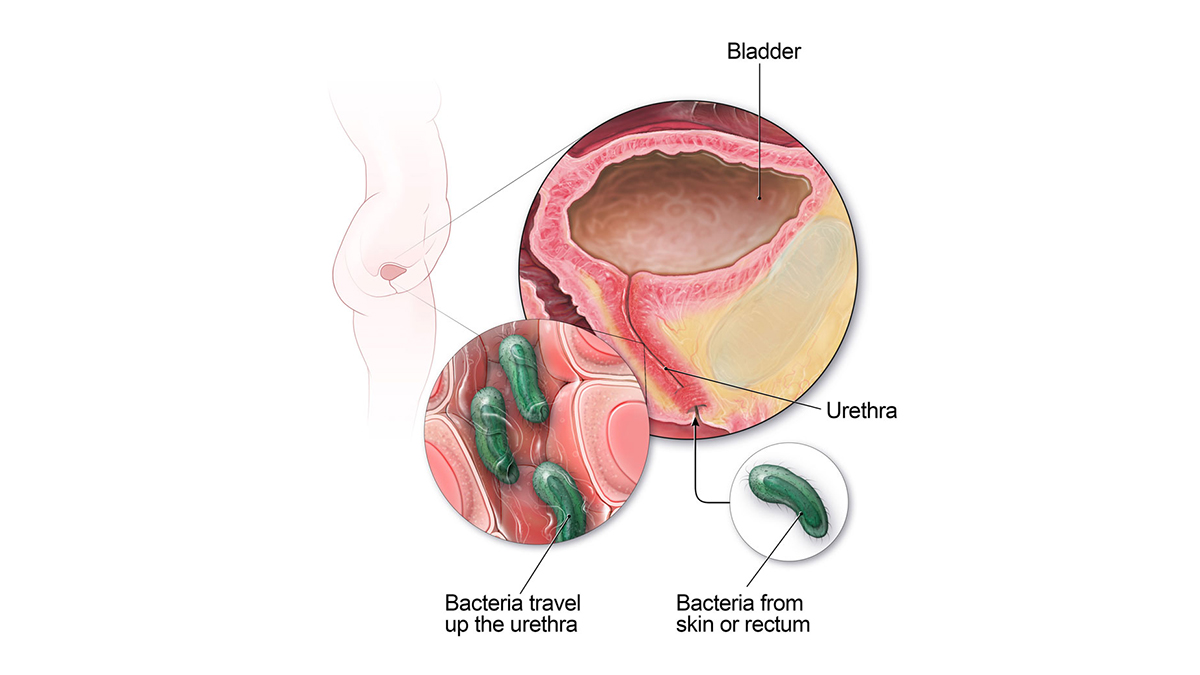
- Perform excellent perineal care, wiping front to back, to avoid a future UTI
- Notify provider of any foul-smelling urine or fevers right away
View the FULL Outline
When you start a FREE trial you gain access to the full outline as well as:
- SIMCLEX (NCLEX Simulator)
- 6,500+ Practice NCLEX Questions
- 2,000+ HD Videos
- 300+ Nursing Cheatsheets
“Would suggest to all nursing students . . . Guaranteed to ease the stress!”
Nursing Case Studies

This nursing case study course is designed to help nursing students build critical thinking. Each case study was written by experienced nurses with first hand knowledge of the “real-world” disease process. To help you increase your nursing clinical judgement (critical thinking), each unfolding nursing case study includes answers laid out by Blooms Taxonomy to help you see that you are progressing to clinical analysis.We encourage you to read the case study and really through the “critical thinking checks” as this is where the real learning occurs. If you get tripped up by a specific question, no worries, just dig into an associated lesson on the topic and reinforce your understanding. In the end, that is what nursing case studies are all about – growing in your clinical judgement.
Nursing Case Studies Introduction
Cardiac nursing case studies.
- 6 Questions
- 7 Questions
- 5 Questions
- 4 Questions
GI/GU Nursing Case Studies
- 2 Questions
- 8 Questions
Obstetrics Nursing Case Studies
Respiratory nursing case studies.
- 10 Questions
Pediatrics Nursing Case Studies
- 3 Questions
- 12 Questions
Neuro Nursing Case Studies
Mental health nursing case studies.
- 9 Questions
Metabolic/Endocrine Nursing Case Studies
Other nursing case studies.
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Presentation
Ms. Smith is a 27-year-old woman who presents to her PCP after just finishing a course of antibiotics for an upper respiratory infection with complaints of dysuria and foul-smelling urine. She also complains of frequency to void, but only able to get out a few drops at a time. She has had 4/10 abdominal discomfort for the past 5 days, endorses lower back pain, and denies any hematuria with urination. She denies nausea/vomiting and denies having a fever.
Past Medical History
- Type I diabetic
- Recent use of antibiotics for URI
- History of chlamydia at age 19
Pertinent Surgical History
- No surgical history
Pertinent Family History
- Mother healthy and alive at 56 years
- Father healthy and alive at 59 years
- Sister alive and type I diabetic at age 24 years old
- Healthy 3 year old son
Pertinent Social History
- Married to husband for 5 years
- Sexually active
- Spermicide as a contraceptive method
- Physically active and attends spinning class 5 times a week

VICTORIA J. SHARP, MD, DANIEL K. LEE, MD, AND ERIC J. ASKELAND, MD
A more recent article on office-based urinalysis is available.
Am Fam Physician. 2014;90(8):542-547
Author disclosure: No relevant financial affiliations.
Urinalysis is useful in diagnosing systemic and genitourinary conditions. In patients with suspected microscopic hematuria, urine dipstick testing may suggest the presence of blood, but results should be confirmed with a microscopic examination. In the absence of obvious causes, the evaluation of microscopic hematuria should include renal function testing, urinary tract imaging, and cystoscopy. In a patient with a ureteral stent, urinalysis alone cannot establish the diagnosis of urinary tract infection. Plain radiography of the kidneys, ureters, and bladder can identify a stent and is preferred over computed tomography. Asymptomatic bacteriuria is the isolation of bacteria in an appropriately collected urine specimen obtained from a person without symptoms of a urinary tract infection. Treatment of asymptomatic bacteriuria is not recommended in nonpregnant adults, including those with prolonged urinary catheter use.
Urinalysis with microscopy has proven to be an invaluable tool for the clinician. Urine dipstick testing and microscopy are useful for the diagnosis of several genitourinary and systemic conditions. 1 , 2 In 2005, a comprehensive review of urinalysis was published in this journal. 3 This article presents a series of case scenarios that illustrate how primary care physicians can utilize the urinalysis in common clinical situations.
Microscopic Hematuria: Case 1
Microscopic hematuria is common and has a broad differential diagnosis, ranging from completely benign causes to potentially invasive malignancy. Causes of hematuria can be classified as glomerular, renal, or urologic 3 – 5 ( Table 1 6 ) . The prevalence of asymptomatic microscopic hematuria varies among populations from 0.18% to 16.1%. 4 The American Urological Association (AUA) defines asymptomatic microscopic hematuria as three or more red blood cells per high-power field in a properly collected specimen in the absence of obvious causes such as infection, menstruation, vigorous exercise, medical renal disease, viral illness, trauma, or a recent urologic procedure. 5 Microscopic confirmation of a positive dipstick test for microscopic hematuria is required. 5 , 7
DIAGNOSTIC APPROACH
Case 1: microscopic hematuria.
A 58-year-old truck driver with a 30-year history of smoking one pack of cigarettes per day presents for a physical examination. He reports increased frequency of urination and nocturia, but does not have gross hematuria. Physical examination reveals an enlarged prostate. Results of his urinalysis with microscopy are shown in Table 2 .
Based on this patient's history, symptoms, and urinalysis findings, which one of the following is the most appropriate next step?
A. Repeat urinalysis in six months.
B. Obtain blood urea nitrogen and creatinine levels, perform computed tomographic urography, and refer for cystoscopy.
C. Treat with an antibiotic and repeat the urinalysis with microscopy.
D. Inform him that his enlarged prostate is causing microscopic hematuria, and that he can follow up as needed.
E. Perform urine cytology to evaluate for bladder cancer.
The correct answer is B .
For the patient in case 1 , because of his age, clinical history, and lack of other clear causes, the most appropriate course of action is to obtain blood urea nitrogen and creatinine levels, perform computed tomographic urography, and refer the patient for cystoscopy. 5 An algorithm for diagnosis, evaluation, and follow-up of patients with asymptomatic microscopic hematuria is presented in Figure 1 . 5 The AUA does not recommend repeating urinalysis with microscopy before the workup, especially in patients who smoke, because tobacco use is a risk factor for urothelial cancer ( Table 3 ) . 5
A previous article in American Family Physician reviewed the American College of Radiology's Appropriateness Criteria for radiologic evaluation of microscopic hematuria. 8 Computed tomographic urography is the preferred imaging modality for the evaluation of patients with asymptomatic microscopic hematuria. 5 , 8 It has three phases that can detect various causes of hematuria. The non–contrast-enhanced phase is optimal for detecting stones in the urinary tract; the nephrographic phase is useful for detecting renal masses, such as renal cell carcinoma; and the delayed phase outlines the collecting system of the urinary tract and can help detect urothelial malignancies of the upper urinary tract. 9 Although the delayed phase can detect some bladder masses, it should not replace cystoscopy in the evaluation for bladder malignancy. 9 After a negative microscopic hematuria workup, the patient should continue to be followed with yearly urinalysis until at least two consecutive normal results are obtained. 5
In patients with microscopic hematuria, repeating urinalysis in six months or treating empirically with antibiotics could delay treatment of potentially curable diseases. It is unwise to assume that benign prostatic hyperplasia is the explanation for hematuria, particularly because patients with this condition typically have risk factors for malignancy. Although urine cytology is typically part of the urologic workup, it should be performed at the time of cystoscopy; the AUA does not recommend urine cytology as the initial test. 5
Dysuria and Flank Pain After Lithotripsy: Case 2
After ureteroscopy with lithotripsy, a ureteral stent is often placed to maintain adequate urinary drainage. 10 The stent has one coil that lies in the bladder and another that lies in the renal pelvis. Patients with ureteral stents may experience urinary frequency, urgency, dysuria, flank pain, and hematuria. 10 They may have dull flank pain that becomes sharp with voiding. This phenomenon occurs because the ureteral stent bypasses the normal nonrefluxing uretero-vesical junction, resulting in transmission of pressure to the renal pelvis with voiding. Approximately 80% of patients with a ureteral stent experience stent-related pain that affects their daily activities. 11
POTENTIALLY MISLEADING URINALYSIS
Case 2: dysuria and flank pain after lithotripsy.
A 33-year-old woman with a history of nephrolithiasis presents with a four-week history of urinary frequency, urgency, urge incontinence, and dysuria. She recently had ureteroscopy with lithotripsy of a 9-mm obstructing left ureteral stone; she does not know if a ureteral stent was placed. She has constant dull left flank pain that becomes sharp with voiding. Results of her urinalysis with microscopy are shown in Table 4 .
A. Treat with three days of ciprofloxacin (Cipro), and tailor further antibiotic therapy according to culture results.
B. Treat with 14 days of ciprofloxacin, and tailor further antibiotic therapy according to culture results.
C. Obtain a urine culture and perform plain radiography of the kidneys, ureters, and bladder.
D. Perform a 24-hour urine collection for a metabolic stone workup.
E. Perform computed tomography.
The correct answer is C .
The presence of a ureteral stent causes mucosal irritation and inflammation; thus, findings of leukocyte esterase with white and red blood cells are not diagnostic for urinary tract infection, and a urine culture is required. In this setting, plain radiography of the kidneys, ureters, and bladder would be useful to determine the presence of a stent. If a primary care physician identifies a neglected ureteral stent, prompt urologic referral is indicated for removal. Retained ureteral stents may become encrusted, and resultant stone formation may lead to obstruction. 10
Flank discomfort and recent history of urinary tract manipulation suggest that this is not an uncomplicated urinary tract infection; therefore, a three-day course of antibiotics is inadequate. Although flank pain and urinalysis suggest possible pyelonephritis, this patient should not be treated for simple pyelonephritis in the absence of radiography to identify a stent. A metabolic stone workup may be useful for prevention of future kidney stones, but it is not indicated in the acute setting. Finally, although computed tomography would detect a ureteral stent, it is not preferred over radiography because it exposes the patient to unnecessary radiation. Typically, microscopic hematuria requires follow-up to ensure that there is not an underlying treatable etiology. In this case , the patient's recent ureteroscopy with lithotripsy is likely the etiology.
Urinalysis in a Patient Performing Clean Intermittent Catheterization: Case 3
Case 3: urinalysis in a patient performing clean intermittent catheterization.
A 49-year-old man who has a history of neurogenic bladder due to a spinal cord injury and who performs clean intermittent catheterization visits your clinic for evaluation. He reports that he often has strong-smelling urine, but has no dysuria, urge incontinence, fever, or suprapubic pain. Results of his urinalysis with microscopy are shown in Table 5 .
A. Inform the patient that he has a urinary tract infection, obtain a urine culture, and treat with antibiotics.
B. Refer him to a urologist for evaluation of a complicated urinary tract infection.
C. Perform computed tomography of the abdomen and pelvis to evaluate for kidney or bladder stones.
D. Inform him that no treatment is needed.
E. Obtain a serum creatinine level to evaluate for chronic kidney disease.
The correct answer is D .
Although the urinalysis results are consistent with a urinary tract infection, the clinical history suggests asymptomatic bacteriuria. Asymptomatic bacteriuria is the isolation of bacteria in an appropriately collected urine specimen obtained from a person without symptoms of a urinary tract infection. 12 The presence of bacteria in the urine after prolonged catheterization has been well described; one study of 605 consecutive weekly urine specimens from 20 chronically catheterized patients found that 98% contained high concentrations of bacteria, and 77% were polymicrobial. 13
Similar results have been reported in patients who perform clean intermittent catheterization; another study of 1,413 urine cultures obtained from 407 patients undergoing clean intermittent catheterization found that 50.6% contained bacteria. 14 Guidelines from the Infectious Diseases Society of America recommend against treatment of asymptomatic bacteriuria in nonpregnant patients with spinal cord injury who are undergoing clean intermittent catheterization or in those using a chronic indwelling catheter. 12
In the absence of symptoms of a urinary tract infection or nephrolithiasis, there is no need to culture the urine, treat with antibiotics, refer to a urologist, or perform imaging of the abdomen and pelvis. There is no reason to suspect acute kidney injury in this setting; thus, measurement of the serum creatinine level is also unnecessary.
Data Sources : Literature searches were performed in PubMed using the terms urinalysis review, urinalysis interpretation, microscopic hematuria, CT urogram, urinary crystals, indwelling ureteral stent, asymptomatic bacteriuria, and bacteriuria with catheterization. Guidelines from the American Urological Association were also reviewed. Search dates: October 2012 and June 2013.
Wu X. Urinalysis: a review of methods and procedures. Crit Care Nurs Clin North Am. 2010;22(1):121-128.
Hardy PE. Urinalysis interpretation. Neonatal Netw. 2010;29(1):45-49.
Simerville JA, Maxted WC, Pahira JJ. Urinalysis: a comprehensive review [published correction appears in Am Fam Physician . 2006;74(7):1096]. Am Fam Physician. 2005;71(6):1153-1162.
Cohen RA, Brown RS. Clinical practice. Microscopic hematuria. N Engl J Med. 2003;348(23):2330-2338.
American Urological Association. Diagnosis, evaluation and follow-up of asymptomatic microhematuria (AMH) in adults. http://www.auanet.org/education/asymptomatic-microhematuria.cfm . Accessed June 6, 2014.
Ahmed Z, Lee J. Asymptomatic urinary abnormalities. Hematuria and proteinuria. Med Clin North Am. 1997;81(3):641-652.
Rao PK, Jones JS. How to evaluate ‘dipstick hematuria’: what to do before you refer. Cleve Clin J Med. 2008;75(3):227-233.
Choyke PL. Radiologic evaluation of hematuria: guidelines from the American College of Radiology's Appropriateness Criteria. Am Fam Physician. 2008;78(3):347-352.
Sadow CA, Wheeler SC, Kim J, Ohno-Machado L, Silverman SG. Positive predictive value of CT urography in the evaluation of upper tract urothelial cancer. AJR Am J Roentgenol. 2010;195(5):W337-W343.
Haleblian G, Kijvikai K, de la Rosette J, Preminger G. Ureteral stenting and urinary stone management: a systematic review. J Urol. 2008;179(2):424-430.
Joshi HB, Stainthorpe A, MacDonagh RP, Keeley FX, Timoney AG, Barry MJ. Indwelling ureteral stents: evaluation of symptoms, quality of life and utility. J Urol. 2003;169(3):1065-1069.
Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM Infectious Diseases Society of America; American Society of Nephrology; American Geriatric Society. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults [published correction appears in Clin Infect Dis . 2005;40(10):1556]. Clin Infect Dis. 2005;40(5):643-654.
Warren JW, Tenney JH, Hoopes JM, Muncie HL, Anthony WC. A prospective microbiologic study of bacteriuria in patients with chronic indwelling urethral catheters. J Infect Dis. 1982;146(6):719-723.
Bakke A, Digranes A. Bacteriuria in patients treated with clean intermittent catheterization. Scand J Infect Dis. 1991;23(5):577-582.
Continue Reading

More in AFP
More in pubmed.
Copyright © 2014 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

19.1: Case Study: Waste Management
- Last updated
- Save as PDF
- Page ID 16837

- Suzanne Wakim & Mandeep Grewal
- Butte College
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Case Study: Drink and Flush
“Wow, this line for the restroom is long!” Bintou says to Maeva, anxiously bobbing from side to side to ease the pressure in her bladder. Maeva nods and says, “It’s always like this at parties. It’s the alcohol.”
Bintou and Maeva are 21-year-old college students at a party. They and many other people have been drinking alcoholic beverages over the course of the evening. As the night has gotten later, the line for the restroom has gotten longer and longer. You may have noticed this phenomenon if you have been to places where large numbers of people are drinking alcohol, like at the ballpark below.

Bintou says, “I wonder why alcohol makes you have to pee?” Maeva learned about this in her Human Biology class and tells Bintou that alcohol inhibits a hormone that helps you retain water. So instead of your body retaining water, you urinate more out. This could lead to dehydration, so she suggests that after their trip to the restroom, they start drinking water instead of alcohol.
For people who drink occasionally or moderately, this effect of alcohol on the excretory system—the system that removes wastes such as urine—is usually temporary. However, in people who drink excessively, alcohol can have serious, long-term effects on the excretory system. For example, heavy drinking on a regular basis can cause liver and kidney disease.
As you will learn in this chapter, the liver and kidneys are important organs of the excretory system, and impairment of the functioning of these organs can cause serious health consequences. At the end of the chapter, you will learn which hormone Maeva was referring to, and some of the ways alcohol can affect the excretory system, both after the occasional drink and in cases of excessive alcohol use and abuse.
Chapter Overview: Excretory System
In this chapter, you will learn about the excretory system, which rids the body of toxic waste products and helps maintain homeostasis. Specifically, you will learn about:
- The organs of the excretory system, which include the skin, liver, large intestine, lungs, and kidneys, eliminate waste and excess water from the body.
- How wastes are eliminated through sweat, feces, urine, and exhaled gases; and how toxic substances in the blood are broken down by the liver.
- The urinary system, which includes the kidneys, ureters, bladder, and urethra.
- The main function of the urinary system, which is to filter the blood and eliminate wastes, mineral ions, and excess water from the body in the form of urine.
- How the kidneys filter the blood, retain needed substances, produce urine, and help maintain homeostasis, such as proper ion and water balance.
- How urine is stored, transported, and released from the body.
- Disorders of the urinary system, including bladder infections, kidney stones, polycystic kidney disease, urinary incontinence, and kidney damage due to factors such as uncontrolled diabetes and high blood pressure.
As you read the chapter, think about the following questions:
- Which hormone do you think Maeva was referring to? Remember that this hormone causes the urinary system to retain water and excrete less water out in the urine.
- How and where does this hormone work?
- Long-term, excessive use of alcohol can affect the liver and kidneys. How do these two organs of excretion interact and work together?
Attributions
- Gotta Pee (from QUACK design, Oslo based design agency that make interiors from recycled materials) by Jon-Eric Melsæter , CC BY 2.0 via Flickr.com
- Line at ballpark by Dorothy, CC BY 2.0 via Flickr.com
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0
Urinary Disorders NCLEX Practice Quiz (150 Questions)

Here are your NCLEX practice questions for urinary system disorders. In this nursing test bank , test your nursing knowledge on the nursing care management of patients with renal disorders.
Urinary Disorders Nursing Test Bank
This nursing test bank set includes 150 NCLEX -style practice questions for urinary system disorders. Included topics are kidney transplant, acute kidney disease, chronic renal failure , acute glomerulonephritis , peritoneal dialysis, prostatectomy, renal calculi, urinary tract infection , and more. All questions on this set are updated to give you the most challenging questions, along with insightful rationales to reinforce learning .
Quiz Guidelines
Before you start, here are some examination guidelines and reminders you must read:
- Practice Exams : Engage with our Practice Exams to hone your skills in a supportive, low-pressure environment. These exams provide immediate feedback and explanations, helping you grasp core concepts, identify improvement areas, and build confidence in your knowledge and abilities.
- You’re given 2 minutes per item.
- For Challenge Exams, click on the “Start Quiz” button to start the quiz.
- Complete the quiz : Ensure that you answer the entire quiz. Only after you’ve answered every item will the score and rationales be shown.
- Learn from the rationales : After each quiz, click on the “View Questions” button to understand the explanation for each answer.
- Free access : Guess what? Our test banks are 100% FREE. Skip the hassle – no sign-ups or registrations here. A sincere promise from Nurseslabs: we have not and won’t ever request your credit card details or personal info for our practice questions. We’re dedicated to keeping this service accessible and cost-free, especially for our amazing students and nurses. So, take the leap and elevate your career hassle-free!
- Share your thoughts : We’d love your feedback, scores, and questions! Please share them in the comments below.
Quizzes included in this guide are:
Recommended Resources
Recommended books and resources for your NCLEX success:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Saunders Comprehensive Review for the NCLEX-RN Saunders Comprehensive Review for the NCLEX-RN Examination is often referred to as the best nursing exam review book ever. More than 5,700 practice questions are available in the text. Detailed test-taking strategies are provided for each question, with hints for analyzing and uncovering the correct answer option.

Strategies for Student Success on the Next Generation NCLEX® (NGN) Test Items Next Generation NCLEX®-style practice questions of all types are illustrated through stand-alone case studies and unfolding case studies. NCSBN Clinical Judgment Measurement Model (NCJMM) is included throughout with case scenarios that integrate the six clinical judgment cognitive skills.

Saunders Q & A Review for the NCLEX-RN® Examination This edition contains over 6,000 practice questions with each question containing a test-taking strategy and justifications for correct and incorrect answers to enhance review. Questions are organized according to the most recent NCLEX-RN test blueprint Client Needs and Integrated Processes. Questions are written at higher cognitive levels (applying, analyzing, synthesizing, evaluating, and creating) than those on the test itself.

NCLEX-RN Prep Plus by Kaplan The NCLEX-RN Prep Plus from Kaplan employs expert critical thinking techniques and targeted sample questions. This edition identifies seven types of NGN questions and explains in detail how to approach and answer each type. In addition, it provides 10 critical thinking pathways for analyzing exam questions.

Illustrated Study Guide for the NCLEX-RN® Exam The 10th edition of the Illustrated Study Guide for the NCLEX-RN Exam, 10th Edition. This study guide gives you a robust, visual, less-intimidating way to remember key facts. 2,500 review questions are now included on the Evolve companion website. 25 additional illustrations and mnemonics make the book more appealing than ever.

NCLEX RN Examination Prep Flashcards (2023 Edition) NCLEX RN Exam Review FlashCards Study Guide with Practice Test Questions [Full-Color Cards] from Test Prep Books. These flashcards are ready for use, allowing you to begin studying immediately. Each flash card is color-coded for easy subject identification.

Recommended Links
An investment in knowledge pays the best interest. Keep up the pace and continue learning with these practice quizzes:
- Nursing Test Bank: Free Practice Questions UPDATED ! Our most comprehenisve and updated nursing test bank that includes over 3,500 practice questions covering a wide range of nursing topics that are absolutely free!
- NCLEX Questions Nursing Test Bank and Review UPDATED! Over 1,000+ comprehensive NCLEX practice questions covering different nursing topics. We’ve made a significant effort to provide you with the most challenging questions along with insightful rationales for each question to reinforce learning.
11 thoughts on “Urinary Disorders NCLEX Practice Quiz (150 Questions)”
Nurseslabs has real NCLEX questions with good rationales, and has shown me concepts I had not looked at during my review of particular topics. Thank you
Question 28 asks about the 2nd stage of AKI which they refer to be the diuretic stage. Was the 1st stage, onset, left out or is it not accounted for when counting the stages?
I came to the comment section once I got to this exact question. The second stage should be oliguria less than 400/mL day
It is counted as one of the stages.
Question 28 is incorrect. There is the onset stage, oliguric, diuretic and recovery. Sometimes the oliguric stage is skipped, however, but the 4 stages are as I listed.
I think this one is incorrect. There are 4 stages: initiation, oliguria, diuresis and recovery. Situation in the question is 3rd stage, duresis.
The initiation/onset stage is often not considered. so most questions will refer to the oliguric stage as stage 1
question 41’s explanation can be confusing due to definition of oliguria is less than 400 ml in 24 hours not 50 ml
Hello Grace, Thanks for the feedback! Glad you liked the urinary system disorders quiz. If there’s a specific area you’re curious about or if you need more quizzes or info, just let me know. Always happy to help!
Leave a Comment Cancel reply
- Skip to Content
- Skip to Main Navigation
- Skip to Information Links
- Skip to Site Search
- Skip to Footer
- Skip to Accessibility Information
This site is intended for healthcare professionals
Information Links
Main navigation.
- GP Training
Case Study - Patient with urinary symptoms
20 May 2010
In this case, symptoms continued after a provisional diagnosis of UTI. By Dr Lizzie Croton
A 56-year-old man presented to surgery with new-onset urinary tract symptoms over the preceding week. These consisted of urgency and frequency associated with suprapubic pain. There was no frank haematuria. He had no significant past medical history and no history of STIs.
Clinically he was afebrile and his abdomen was soft with no palpable bladder. There were no testicular abnormalities. A provisional diagnosis of UTI was made and the patient was prescribed a seven-day course of ciprofloxacin 500mg daily.
His symptoms improved over the week and the urine microscopy report revealed no growth but large quantities of white and red blood cells.
Review The patient was reviewed at 10 days and was asymptomatic. A repeat urine microscopy was normal. At the review appointment, digital rectal examination revealed a non-tender benign prostatic enlargement.
Biochemical tests including a PSA, glomerular filtration rate and U+Es were normal.
Three weeks later he presented with frank haematuria and incontinence with lower abdominal and left-sided loin pain. He had a palpable bladder and a large stone trapped at the urethral entrance. He was admitted as a surgical emergency and underwent a meatotomy and stone removal under anaesthetic. A cystoscopy was normal and there was no evidence of further calculi in the renal tract.
The stone was calcium oxalate and thought to have originated from the ureter. A coexistent UTI had caused urethral impaction secondary to epithelial slough and an element of BPH.
He has been well since.
Renal calculi The overall prevalence of renal calculi in the UK is 3 per cent. Males are more affected with peak age incidences in the mid-twenties and mid-fifties.
The majority arise in the upper urinary tract and most are radio opaque. Smaller stones are more likely to migrate causing pain while larger stones may remain within the kidney.
Many calculi form in the absence of obvious precipitating factors but recognised causative factors include:
- An excess of a normal constituent in blood or urine, for example hypercalcaemia or hyperuricaemia.
- Impaired drainage causing chronic urethral obstruction, for example, benign prostatic hypertrophy.
- The presence of abnormal constituents, for example coexistent urinary infection.
Clinical features Kidney stones cause flank pain that spreads around the abdomen as the stone migrates.
There is often associated microor macroscopic haematuria.
There may be an associated UTI with pyrexia and septicaemia. An acute pyelonephritis associated with urinary obstruction requires emergency urological review.
Ureteric stones present with colicky pain radiating from the flank into the scrotum or the labia majora. There is commonly associated haematuria and symptoms of urinary infection. Abdominal examination may elicit tenderness along the course of the ureter but this is usually milder than the pain reported.
In the lower urinary tract stones may cause pain in the lower abdomen or genitalia.
This may be worse on standing or at the end of micturition if the stone is lying on the trigone.
Management Around 90 per cent of stones will pass spontaneously. The patient should be kept hydrated and appropriate analgesia given.
If the patient is unwell, febrile or in severe pain, hospital admission is indicated with consideration of IV fluids and antibiotics to treat associated infection.
When the stone is passed, it is important to retain it for further histological examination.
Larger stones may require surgical management. Open surgery has now been largely replaced by endoscopic and percutaneous techniques to remove stones. Lithotripsy is also readily used.
Once the acute phase has passed, the patient should remain under urological follow-up to ensure there are no further residual stones.
- Dr Croton is a GP in Birmingham

Related Drug Categories
Urinary tract infections, have you registered with us yet.
Register now to enjoy more articles and free email bulletins
Already registered?
The voice for today's GP. News, insights and clinical education.
- Register today for further access to articles and daily updates on the issues that matter to you.
Register Now
Stay signed in
Forgotten password?

- Registered Nurse Omnihealth New Zealand (Opportunities Available Nationwide)
- Salaried GP Role, North Aberdeenshire Prospect Health Banff
- Salaried GP Prospect Health Uttoxeter
- General Practitioner Omnihealth New Zealand (Opportunities Available Nationwide)
- GP Tuakau Health Centre New Zealand (Tuakau - Franklin Region)
Just published

GPs threaten mass resignation from NHS in landmark LMCs vote
LMCs have backed the profession's leaders to threaten mass resignation from the NHS...

GP forced to use foodbank due to long COVID and loss of earnings
A GP unable to work due to long COVID was forced to use a food bank for Christmas...

Medical practitioner stabbed at south-east London GP practice
A man has been arrested on suspicion of attempted murder after a medical practitioner...

UK LMCs conference 2024: full coverage
GP representatives from LMCs across the UK are meeting in Newport, Wales on 23 and...

GP registrars fear unemployment when they qualify this summer
GP registrars fear they will struggle to find work when they qualify this summer...

LMCs voice fears over physician associates replacing GPs
GP leaders have voiced growing concern over the use of physician associates in general...
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Can Urol Assoc J
- v.7(9-10 Suppl 4); Sep-Oct 2013
Painful bladder: Case studies
As part of the program at the 3 rd Annual Canadian Urology Forum (2013), participants engaged in interactive discussions of difficult cases throughout the event. The following is a summary of discussions pertaining to two cases illustrating the difficulties in diagnosis and management of bladder pain symptoms.
An 18-year-old female with recurrent “urinary tract infection”/cystitis
The patient is an 18-year-old female, with a two-year history of “recurrent urinary tract infection” (UTI)/cystitis. She has had two positive cultures and 10 negative. Courses of antibiotics have provided some relief at times, but other times have had no effect.
She presents for an ongoing episode over the past two weeks in which she has been experiencing frequency (every 30–60 minutes during the day), a constant urge, voiding five times prior to falling asleep and waking three times each night. She experiences significant dysuria and suprapubic (SP) pain with bladder fullness. She has not experienced any episodes of incontinence. Although she describes this as a “flare,” she has had similar but slightly less intense symptoms on a daily basis for the past two years. She is accompanied at this visit by her mother, who is demanding answers about what is wrong with her daughter.
She has been sexually active for the past two years and says that she finds sexual activity uncomfortable. She is a smoker (approximately two packs per week), but has no other chronic conditions or remarkable medical history.
Physical examination finds a tender SP region and anterior vaginal wall.
Urinalysis shows 1 to 3 red blood cells and 5 to 10 white blood cells per high-power field. Culture and sensitivity are negative.
The participants at the 2013 Urology Forum made several observations and recommendations with respect to the diagnosis and management of this patient. The opinions regarding appropriate investigations and interventions at this point were varied.
Smoking cessation was deemed to be of paramount importance, and should be a major focus of patient education initiatives. It was agreed that education in general (about painful bladder syndrome, how it is treated) is a critical component of care, particularly with such a young patient.
In a situation like this, much will depend on the patient’s level of awareness and knowledge of their condition. Many patients will already have researched their condition on the Internet and have already tried conservative measures (e.g., avoiding irritants, dietary modification, exercise, stress reduction). Such patients may be ready to move on to other treatment options such as pelvic-floor physiotherapy, oral or intravesical therapy, or cystoscopy with hydrodistention (note that if the patient had not yet been sexually active, cystoscopy may be less appropriate). Other participants advocated further work-up with local cystoscopy and pelvic examination to investigate for potential causes of her pain and, if negative, to reassure the patient that the bladder is normal, at least in the anatomical aspect.
The discussion of treatment options in this session seemed to reflect the nature of the evidence available for interventions for painful bladder syndrome. There is no clear, compelling evidence that any therapy is superior to others. Among the participants, there were advocates of every different potential therapeutic approach to this patient, including hydrodistention, oral therapy, intravesical therapy or combinations of these approaches.
The possibility of an extended course of antibiotics (e.g., nitro-furantoin + pyridium for 2–3 weeks) therapy was also discussed as a means of ruling out an infectious etiology (given that her symptoms are episodic). Participants also felt that multimodality (addressing the LUTS, pain, emotional health, etc) management was recommended but is not always feasible given local resources.
A 32-year-old woman with a seven-year history of severe suprapubic pain
This patient has a seven-year history of severe suprapubic pain, with urethral burning, and urinary frequency. She describes her pain as “achy, burny and gripping.” Her daytime frequency is 14 to 18, with nocturia averaging four voids. She says she has constant urgency, hesitancy, slow flow, and experiences significant dyspareunia. Cultures have always been negative.
Before this referral, she had already been to see two different urologists and two different gynecologists. Her treatment history includes seven hydrodistentions, which have provided some benefit lasting anywhere from two weeks to three months.
She has failed courses of therapy with antimuscarinics, tricyclic antidepressants, pentosan polysulfate, intravesical lidocaine, and heparin therapy. She is currently using oxycodone as needed to manage her pain. She is highly distressed and frustrated about the inability to manage her symptoms.
Cystoscopy, which the patient has trouble tolerating due to pain, shows a small capacity (150 mL) and normal mucosa. Urodynamics show early sensation, maximum cystometric capacity of 90 mL, no detrusor overactivity, poor bladder contraction, slow flow and complete emptying.
The participants agreed that this is a very challenging case, for which there is no easy and standard answer. Prior to embarking on surgical intervention, it was agreed that all means of conservative management modalities be exhausted, in particular achieving better pain management. This patient might benefit from involvement by a pain specialist, physiotherapist and psychologist. It was, however, mentioned that there are substantial practical barriers to implementing this strategy, including access to therapists who are trained in this sub-specialty and cost.
This patient has not yet been offered a trial of sacral nerve stimulation or botulinum toxin injection. These would also be reasonable options to try at this point. Bladder augmentation is not advised given the significant vaginal and urethral pain, and potential self-catheterization may not be successful for that reason. Urinary diversion would be the absolute last option and is not recommended at this point in time.
Competing interests: This article is part of a CUAJ supplement sponsored by Astellas Pharma Canada, Inc. Dr. Bailly has received speaker fees, educational grants, and/or travel assistance from Allergan, Astellas, Eli Lilly, and Pfizer.
Textbook Resources
- Preview Chapter
- Study on the Fly
- Biology and A&P Prep Sites
- Get Body Smart
- A&P Revealed
- Lab Exercises
- Case Studies
- Student Study Outlines
- Supplemental Lab Exercises (Hole)
- Boxed Readings
Chapter Activities
- Student Study Outline Answers
- Student PPT
- Learning Outcomes
- Flashcards/Vocabulary
- Concentration Games
- Interactive Art Quizzes
- Fluid Exchange Across the Walls of Capillaries
- Introducing Connect
- Table of Contents
- About the Authors
- Sample Chapter
- Prep-Step Correlation Guide
- Feature Summary
- New To This Edition
- High School Lab Manual Answer Key
- High School Lab Manual Correlation
- Presentation Tools
- Student Study Guide Answers
- Case Study Answers
- Practice Question Answers
- Chapter Assessment Answers
- Integrative Assessment Answers
- Teacher's Manual
- Detailed Lecture Outlines
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Health Department HAI/AR Programs
- Cleaning in Global Healthcare Settings
- Infection Control Guidance
- Introduction to the Patient Notification Toolkit
HAI Prevention and Control for Healthcare
- Public Health and Policy Strategies
- HAI Prevention, Control and Outbreak Response for Public Health and Healthcare
- Prevention Epicenters
- Healthcare-Associated Infections - Community Interface Activity (HAIC)
HAIs: Reports and Data
- Preventing MDROs
- Laboratory Resources
- Antibiotic Prescribing and Use
- Antimicrobial Resistance
- Infection Control for Healthcare Providers
- Safe Injection Practices and Your Health
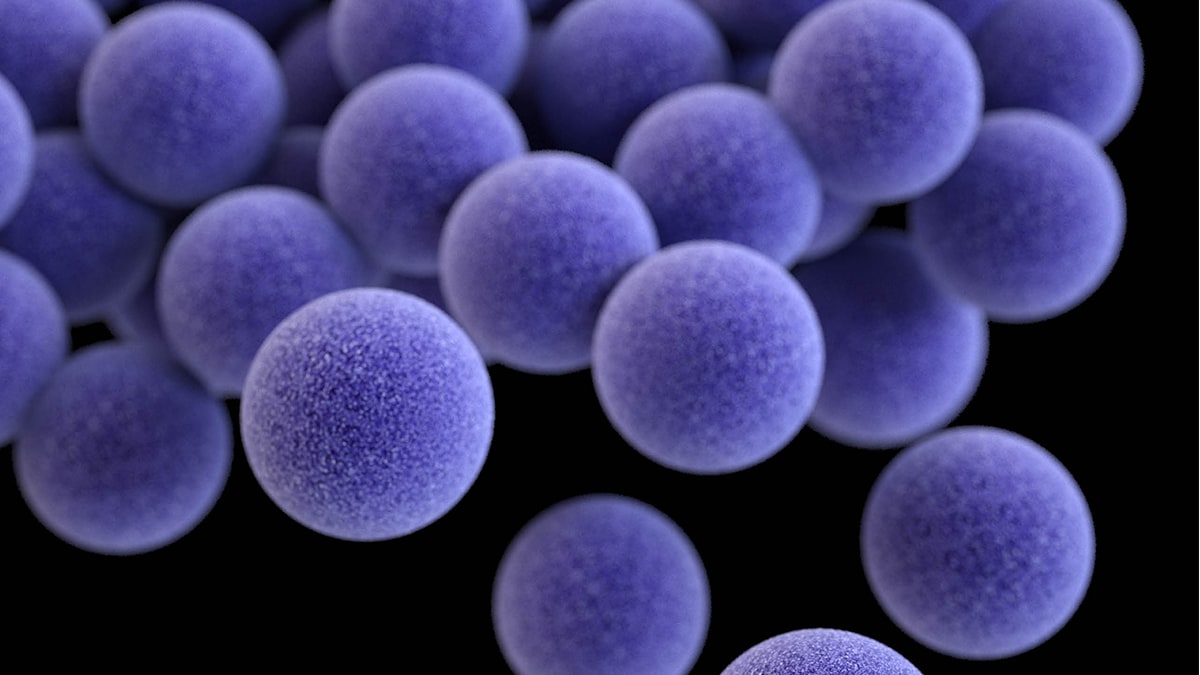
Methicillin-resistant Staphylococcus aureus (MRSA) Basics
Healthcare-Associated Infections (HAIs)

Laboratory Resources for HAIs

Research Gaps in Patient and Healthcare Personnel Safety
Related organisms & infections

About Acinetobacter
About Burkholderia cepacia complex
About Carbapenem-resistant Enterobacterales
Catheter-associated Urinary Tract Infection Basics

Central Line-associated Bloodstream Infection (CLABSI) Basics
About Clostridium sordellii
About ESBL-producing Enterobacterales
About Gram-negative Bacteria
About Klebsiella
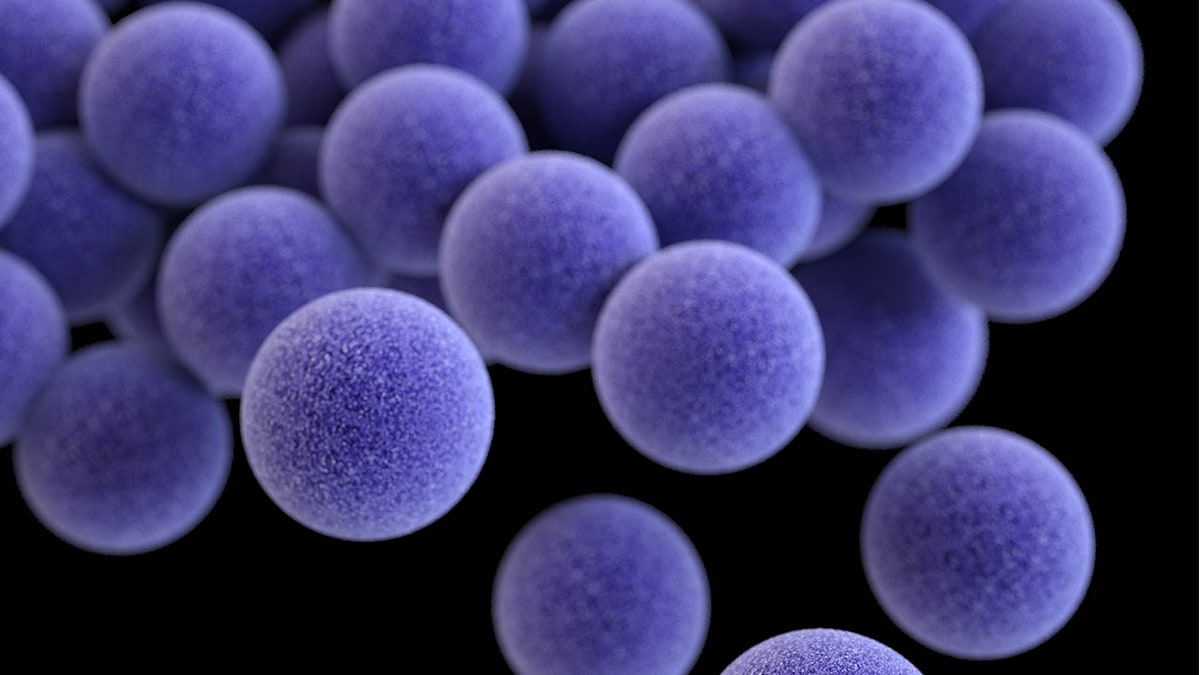
Staphylococcus aureus Basics
About Nontuberculous Mycobacteria (NTM) Infections

About Pseudomonas aeruginosa

Surgical Site Infection Basics

Ventilator-associated Pneumonia Basics
HAIs are associated with medical devices, complications following surgery, transmission between patients and healthcare workers, antibiotic overuse, and more.
For Everyone
Health care providers, public health.

IMAGES
VIDEO
COMMENTS
Human A & P II Urinary System Case Study Answer Sheet. Please submit your answers to the case study utilizing this document. Please do not submit as a .pages or .png file. (color) The color of urine is directly associated with how diluted or concentrated the urine is. The more concentrated the urine is, the darker it is because more substances ...
Max's Maximum: A Case Study on the Urinary System. 8 terms. Madison_Cunha4. Preview. Biology, The Digestive System, Enzymes and Cell membrane, Middle school. 6 terms. Serafina287. ... Choose the right answers from the pull-down menus. 10 terms. Veronika_2284. Preview. CNS (pt 2) 29 terms. quizlette85267000. Preview. Anatomy practical ...
Max's Maximum: A Case Study on the Urinary System. It took the diagnosis of high blood pressure (hypertension) at the age of 45 to shock Max into taking better care of himself. ... Explain your answer. Immediately after exercise. He was losing water via sweat and exhalation to cool his body during exercise and was unable to effectively ...
Max's Maximum: A Case Study on the Urinary System. What does the color of Max's urine tell Tracey about how concentrated or dilute it is? How does Max's urine color/concentration compare to the urine specific gravity at the same time? The darker the pigment of urine, the higher the concentration will be. Max's urine pigment also correlates with ...
A. Staphylococcus Saprophyticus is the second most common bacteria found in a urinary tract infection. B. Klebsiella and D. Pseudomonas are less common. 2.) Your patient was recently diagnosed with a UTI. As the nurse practitioner, you are assessing whether the patient has any improvement with their symptoms of hematuria.
Module 3 Urinary System Case Study. A 27-year-old patient presents at her obstetrician's office for her first prenatal visit at 26 weeks gestation. She has no medical history and has had an uncomplicated pregnancy. Her examination is normal other than glycosuria noted on the urine dipstick. A 1-hour glucose challenge test is performed along ...
Mrs. Phillips's vitals are as follows: HR 122 RR 24. BP 92/58 SpO2 92%. Temp 103.6°F. Her NIHSS score is 2, CT scan is negative for an intracranial bleed, and the neurologist believes she is NOT having a stroke. The nurse is called into the room by the caregivers as the patient has wet herself. The nurse notes a foul, sour odor to the urine.
Patient Presentation. Ms. Smith is a 27-year-old woman who presents to her PCP after just finishing a course of antibiotics for an upper respiratory infection with complaints of dysuria and foul-smelling urine. She also complains of frequency to void, but only able to get out a few drops at a time. She has had 4/10 abdominal discomfort for the ...
For the patient in case 1, because of his age, clinical history, and lack of other clear causes, the most appropriate course of action is to obtain blood urea nitrogen and creatinine levels ...
Case Study: Drink and Flush "Wow, this line for the restroom is long!" Bintou says to Maeva, anxiously bobbing from side to side to ease the pressure in her bladder. ... Disorders of the urinary system, including bladder infections, kidney stones, polycystic kidney disease, urinary incontinence, and kidney damage due to factors such as ...
This nursing test bank set includes 150 NCLEX-style practice questions for urinary system disorders. Included topics are kidney transplant, acute kidney disease, chronic renal failure, acute glomerulonephritis, peritoneal dialysis, prostatectomy, renal calculi, urinary tract infection, and more. All questions on this set are updated to give you ...
Urinary case study. Term. 1 / 61. What are the functions of the urinary system? Click the card to flip 👆. Definition. 1 / 61. Eliminates wastes, filters blood, produces urine and maintains homeostasis.
This is a review of a case study that I use in my Human Anatomy and Physiology courses. This is for educational use.Medical and Health Disclaimer:This Video...
Case Study - Patient with urinary symptoms. In this case, symptoms continued after a provisional diagnosis of UTI. By Dr Lizzie Croton.
This patient has a seven-year history of severe suprapubic pain, with urethral burning, and urinary frequency. She describes her pain as "achy, burny and gripping.". Her daytime frequency is 14 to 18, with nocturia averaging four voids. She says she has constant urgency, hesitancy, slow flow, and experiences significant dyspareunia.
what would be the result of primary hyperparathyroidism? high calcium levels. 1. increase osteoclast activity. 2. increase activation of vit. 3. increase Ca2+ reabsorption at the DCT. Study with Quizlet and memorize flashcards containing terms like What is filtration?, what is reabsorption?, What is secretion? and more.
Chapter 17: Urinary System In this Chapter: Textbook Resources. Animation Activities; Get Body Smart; Human Body Case Studies; APR Link; Atlases; Blood Testing Lab (Lab 49) Clinical Terms ... Human Body Case Studies; APR Link; Atlases; Blood Testing Lab (Lab 49) Clinical Terms; Study on the Fly;
Chapter 20: Urinary System In this Chapter: Textbook Resources. Preview Chapter; Study on the Fly; Biology and A&P Prep Sites ... Case Studies; Student Study Outlines; Supplemental Lab Exercises (Hole) Boxed Readings; Chapter Activities
Study with Quizlet and memorize flashcards containing terms like Diverticulum, Cystitis, Dysuria and more.
HAIs: Reports and Data. CDC publishes data reports to help track progress and target areas that need assistance. HAI Prevention and Control for Healthcare. HAI Prevention, Control and Outbreak Response for Public Health and Healthcare. Introduction to the Patient Notification Toolkit.