- Your Stories
Evidence Based Living
Bridging the gap between research and real life
- In The Media
- The Learning Center
- Cornell Cooperative Extension
- Youth Development
- Health and Wellness

What is translational research?

Cornell’s College of Human Ecology is pursuing a translational research model to better link social and behavioral science research to extension and outreach, creating a more seamless link between science and service. But the question arises: What is “translational research?”
Evidence-Based Living sat down with Wethington to talk about the growing field of translational research.
To start off, what exactly is translational research?
Many definitions have been given for translational research, but the definition I like best is that it is a systematic effort to convert basic research knowledge into practical applications to enhance human health and well being.
Translational research was designed for the medical world. It emerged in response to concern over the long time lag between scientific discoveries and changes in treatments, practices, and health policies that incorporate the new discoveries.
What is applied research, and how does it differ?
Translational research is broader than the traditional term “applied research.” Applied research is any research that may possibly be useful for enhancing health or well-being. It does not necessarily have to have any effort connected with it to take the research to a practical level.
For example, an applied research study might analyze longitudinal data that tracks participants’ health and social relationships. The researchers would report their findings in an academic journal.
But in translational research, the same study would include some “action steps.” The researchers would partner with a community and ask for ideas about how their findings might apply there. Together, they would come up with an intervention plan that would also include scientific evaluation of its effectiveness.
Why are social science researchers slower to adopt these models compared to the medical community?
I think the answer to this question is that researchers have followed where the money has been allocated. The opportunities for social and behavioral scientists have not been established as rapidly.
More recently, three major government institutions have been funding projects that emphasize public health outreach using translational research – the Centers for Disease Control, the National Institutes of Health and the National Institute on Aging. All three have been establishing translational research centers across the country, primarily focused on underserved communities and health disparities.
Thus, social scientists are only now being encouraged to take part. More recently economic stimulus funds dispersed the National Institute of Health funded a number of translational research projects headed by social scientists, including three funded at Cornell. I predict that soon there will be social scientists engaged in translational research across the country, not just at funded centers.
What are the benefits of moving toward translational research?
For researchers, there is benefit to being affiliated with a center that provides seed funding for projects, methodological assistance, advice on developing proposals and experience in getting community input into research projects.
For universities, translational research centers provide a tactical advantage for attracting more funding. Translational research centers also provide a way for universities to meet public service goals in their strategic plans.
For communities, translational research provides opportunities to make a difference in their own communities. As part of one of the Cornell centers, we engaged public service agency directors in events where they could contribute to our research agenda. With a stake in the research, communities feel that they are making a valued and important contribution. We heard over and over from the community members that this was a real source of pride and accomplishment for them.
How can extension programs participate?
One way local extension programs can participate in translational research is to take part in community stakeholder groups that meet with researchers who are designing intervention and prevention research programs. Typically, a wide variety of stakeholders need to be engaged. County Cooperative Extension offices have many collaborative relationships in their counties and can work with researchers to make contacts.
Typically, local extension professionals do not have time to engage in research themselves. Yet they have valuable experience that can be shared. This makes Cooperative Extension an ideal contributor for implementing programs.
Nice reading! Thank you
A remarkable extraordinary read, ideally other huge schools can take an interest in something like this.
Quite the great read, hopefully other large schools are able to participate in something like this.
Speak Your Mind Cancel reply
A project at…, evidence-based blogs.
- Bandolier Evidence-Based Health Care
- British Psychological Society Research Digest
- Economics in Cooperative Extension
- EPB Exchange
- New Voices for Research
- Research Blogging
- Trust the Evidence
Subscribe by e-mail
Please, insert a valid email.
Thank you, your email will be added to the mailing list once you click on the link in the confirmation email.
Spam protection has stopped this request. Please contact site owner for help.
This form is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Return to top of page
Copyright © 2024 · Magazine Theme on Genesis Framework · WordPress · Log in

- Research Overview
- Research Activities
- Research Resources
- Training & Education
- Collaborate With NCATS
- Funding Overview
- Open Funding Opportunities
- Small Business Programs
- Funding Policy & Operating Guidelines
- Grant Information
- Challenges and Prize Competitions
- Scientific Review
- Conference Grant Information
- Resources for You
- Resources for Researchers
- Resources for Trainees
- Resources for Rare Disease Patients and Advocates
- News & Events Overview
- Newsletters
- Scientific Publications
- NCATS Overview
- About Translational Science
- Advisory Committees
- Careers at NCATS
- Director's Corner
- Divisions & Offices
Translational Science Principles
The NCATS Translational Science Principles characterize effective translational science approaches. The Principles were generated by an NCATS committee with expertise across the translational spectrum, and in science, operations and administration.
About Translational Science Principles
Amanda Vogel, Ph.D.

Click the image to view a larger version .
NCATS is making these materials available for download and use via a CC BY 4.0 License.
NCATS’ mission is to turn biomedical research discoveries into health solutions — including diagnostics, treatments, and interventions — through the application of translational science.
Translational science is the field that generates innovations that overcome longstanding challenges along the translational research pipeline. These include scientific, operational, financial and administrative innovations that transform the way that research is done, making it faster, more efficient, and more impactful.
The NCATS Translational Science Principles stem in part from in-depth case studies of three highly successful NCATS-led or -supported initiatives that span the translational continuum and pursue varied scientific goals. These initiatives use diverse scientific and operational strategies to advance translational progress. But the case studies identified underlying principles that characterized the strategies used across these initiatives.
The NCATS Translational Science Principles also build upon scholarship identifying core competencies for translational science. This includes the Core Competencies in Clinical and Translational Research produced by the CTSA Education Core Competency Working Group, and the Characteristics of a Translational Scientist , produced by Translation Together.
These Principles are intentionally broad. They apply to research anywhere along the translational continuum. They do not prescribe particular strategies, but may be helpful to those involved in the translational enterprise to develop strategies that are specific to their own research goals and aligned with these principles. In addition, they are relevant not only to researchers but to everyone who enables, facilitates or supports translation, including those involved in science leadership, management, and administration, and patient and community engagement.
We see the NCATS Translational Principles as a work-in-progress that will continue to be refined to reflect the community’s growing expertise in translational science. This webpage will be updated periodically to reflect these refinements.
Prioritize Initiatives That Address Unmet Needs
Focus on pursuing scientific goals that address unmet scientific, patient or population health needs.
Example approaches:
- Scientific Needs: Contribute to research advances in under-investigated areas of science or on scientific questions that present unique research challenges or disincentives (e.g., currently untreatable diseases; de-risking targets).
- Patient and Population Health Needs: Advance research to develop solutions for unmet patient and population health needs.
Produce Generalizable Solutions for Common and Persistent Challenges
Develop innovations that address persistent challenges to advancing translational progress that are found across multiple research initiatives or projects, or span research on multiple diseases or conditions.
- Across Multiple Projects or Initiatives: Advance research by identifying, developing and/or testing solutions to common bottlenecks or roadblocks that have stymied multiple projects. These may be scientific, operational, or administrative in nature.
- Across Diseases or Conditions: Approach research challenges and develop solutions by seeking commonalities across research projects on a range of diseases or conditions.
- Organizational Environment: Enable development and testing of generalizable solutions through organizational policies, organizational structure, and shared resources.
Emphasize Creativity and Innovation
Leverage creativity and innovation in research design, conduct, and facilitating factors, with the goal of increasing the impact of the research.
- Research Design and Implementation: Pose innovative research questions and develop and implement innovations in research methods, technologies, and approaches that increase the impact of the research, as through pursuit of paradigm-changing goals, or innovations that are generalizable to advancing research across multiple initiatives, diseases and conditions.
- Research Processes and Structures: Develop and implement innovations in research team interactions, leadership and management, partnerships, and operations that facilitate and support the quality and impact of the research.
- Organizational Environment: Enable creativity and innovation through policies that encourage innovations and do not penalize failures.
Leverage Cross-Disciplinary Team Science
Engage team members with expertise across disciplines, fields, and professions to produce research that advances translation along the translational research continuum.
- Leverage Broad Expertise: Engage colleagues from across disciplines, fields, and professions to advance research along the translational continuum. This may involve leveraging scientific, administrative, financial and operational expertise.
- Integrate Knowledge: Integrate concepts, theories, methods, technologies, and approaches from the range of disciplines, fields, and professions that can contribute to advancing the research goals. Leverage knowledge integration to produce more holistic research designs and findings that are therefore more relevant to real-world applications.
- Organizational Environment: Enable team science via organizational policies, team leadership and management, shared instrumentation and space, and recognition and reward systems.
Enhance the Efficiency and Speed of Translational Research
Implement evidence-informed practices and scientific and operational innovations to accelerate the pace of translational research.
- Scientific Efficiencies: Develop and implement innovations in scientific approaches, methods and technologies that accelerate the pace of translational research.
- Collaboration Efficiencies: Implement evidence-informed practices to enhance the speed at which collaborations and teams form, develop a shared vision and goals, effectively communicate, and coordinate work tasks.
- Project Management Efficiencies: Implement milestone-based decision making to enable rapid agreement on go/no-go decisions, to enable resources to be used most efficiently.
- Organizational Environment: Reward efficiency, enable rapid failures and encourage redirection of resources to subsequent attempts.
Utilize Boundary-Crossing Partnerships
Leverage collaborations across agencies and sectors and engage patients and communities in research to advance translational progress.
- Cross-Sectoral Partnerships: Form partnerships across government, universities, and industry to leverage varied expertise and resources to accelerate translational progress. Implement evidence-informed practices for effective cross-sectoral partnerships.
- Patient and Community Engagement: Involve impacted patients and communities as research collaborators to enable research advances across the translational continuum (e.g., via disease registries, clinical trials participation, intervention design). Implement evidence-informed practices for patient- and community-engaged research.
- Organizational Environment: Enable and incentivize boundary-crossing partnerships via leadership, policies, and recognition and reward systems.
Use Bold and Rigorous Research Approaches
Develop ambitious research questions and address them with rigorous and robust methods toward generating reproducible findings that contribute to advancing translation.
- Bold Scientific Approaches: Explore ambitious research goals that have the potential to produce major advances and/or paradigm shifts. These may be in areas of research that have been historically intractable or where there are high risks of failure.
- Rigor and Reproducibility: Employ rigorous and robust approaches to generate reproducible findings and high-quality FAIR (findable, accessible, interoperable, reusable) data that will enable the research to advance translational progress regardless of whether the initial research objective is met (e.g., learning from failures). To the maximum extent possible, disseminate all parameters utilized to conduct the research (e.g., materials, subjects), research methods and conditions, authentication of reagents and biological resources, data sets, metadata, analytic approaches and statistical tools used for experimentation and data interpretation, results and conclusions, to facilitate reproducibility and/or inform future study designs.
- Organizational Environments: Enable rigorous testing of bold, paradigm-challenging ideas, including high-risk high-reward opportunities. Encourage reporting of information necessary for reproducibility toward informing future studies.
Prioritize Diversity, Equity, Inclusion and Accessibility (DEIA)
Leverage diversity, equity, inclusion, and accessibility to produce research outcomes that are relevant to the full diversity of the population.
- Research Priority Setting: Include diverse perspectives in research priority setting, such as through partnerships with diverse collaborators, so research investments represent diverse population and patient health needs.
- Scientific Approaches: Integrate DEIA into the development of research resources and design and implementation of studies, across the translational research continuum.
- Workforce and Operations: Advance DEIA in the scientific workforce to leverage maximum expertise. Implement best practices in outreach, recruitment and hiring, development, and retention to sustain a diverse and talented workforce.
Additional Resources
Publications.
Advancing Education and Training through Application of the Translational Science Principles
Faupel-Badger JM, Vogel AL, Austin CP, Rutter JL. Advancing translational science education . Clin Transl Sci. 2022; 15: 2555-2566.
Translational Science Principles Enabling Team Science in NCATS’ Internal Research Program
Vogel AL, Knebel AR, Faupel-Badger JM, Portilla LM, Simeonov A. A Systems Approach to Enable Effective Team Science from the Internal Research Program of the National Center for Advancing Translational Sciences . Journal of Clinical and Translational Science. Cambridge University Press; 2021;5(1):e163.
Teaching Translational Science Principles
Faupel-Badger JM, Vogel AL, Hussain SF, Austin CP, Hall MD, Ness E, Sanderson P, Terse PS, Xu X, Balakrishnan K, Patnaik S, Marugan JJ, Rudloff U, Ferrer M. Teaching Principles of Translational Science to a Broad Scientific Audience Using a Case Study Approach: A Pilot Course from the National Center for Advancing Translational Sciences . Journal of Clinical and Translational Science . Cambridge University Press; 2022:1–26.
Vogel AL, Hussain SF, Faupel-Badger JM. Evaluation of an online case study-based course in translational science for a broad scientific audience: Impacts on students' knowledge, attitudes, planned scientific activities, and career goals . J Clin Transl Sci. 2022;6(1):e82. Published 2022 Jun 7.
Vogel AL, Haynes BM, Hussain SF, et al. Areas of strength and opportunities for growth in translational science education and training: Results of a scoping review from the NCATS Education Branch . Clin Transl Sci. 2023;16(9):1526-1546.
Case Studies in Translational Science
These video case studies highlight how translational science principles shape NCATS’ research programs and initiatives. The case studies cover drug discovery and development, the Toolkit for Patient-Focused Therapy Development, and the creation and development of tissue chips.
Online Courses
The NCATS Education Branch offers two case study–based courses in translational science principles taught by scientists who have led translational research at NIH, as well as additional experts in translational science.
Last updated on October 4, 2024
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 June 2020
Everyday characterizations of translational research: researchers’ own use of terminology and models in medical research and practice
- Dixi Louise Strand ORCID: orcid.org/0000-0003-0524-2466 1 , 2
Palgrave Communications volume 6 , Article number: 110 ( 2020 ) Cite this article
8933 Accesses
3 Citations
2 Altmetric
Metrics details
- Medical humanities
- Science, technology and society
Biomedical literature and policy are highly concerned with encouraging and improving the clinical application and clinical benefit of new scientific knowledge. Debates, theorizing, and policy initiatives aiming to close the “bench-to-bedside gap” have led to the development of “Translational Research” (TR), an emerging set of research-related discourses and practices within biomedicine. Studies in social science and the humanities have explored and challenged the assumptions underpinning specific TR models and policy initiatives, as well as the socio-material transformations involved. However, only few studies have explored TR as a productive ongoing process of meaning-making taking place as part of the everyday practices of the actual researchers located at the very nexus of science and clinic. This article therefore asks the question of how the discourse and promise of translation is embedded and performed within the practices and perspective of the specific actors involved. The findings are based on material from ethnographic fieldwork among translational researchers situated in a Danish hospital research setting. The analysis draws on the analytical notion of performativity in order to approach statements and models of TR in the light of their performative dimension. This analytical approach thus helps to highlight how the characterizations of TR also contain prescriptions for how the world must change for these characterizations to become true. The analysis provides insights into four different characterizations of TR and reflects on the associated practices where performative success is achieved in practice. With the presentation of these four characterizations, this paper illustrates different uses of the term TR among the actual actors engaged in research-clinic activities and contributes insight into the complex processes of conceptual and material reorganization that form part of the emergence of TR in biomedicine.
Similar content being viewed by others

The translational lag narrative in policy discourse in the United States and the European Union: a comparative study

Wicked problems in a post-truth political economy: a dilemma for knowledge translation
The gains of reduction in translational processes: illness blogs and clinical-ethics cases, introduction.
Translational research has become subject to widespread debates in biomedical literature and politics, evoking high expectations, promises, and concerns. The term “translational research” was first used in a US national cancer program in the 90’s and has since appeared in research programs, research strategies, academic articles and journals, policy reports, and educational programs globally. The main interest underlying the concept in this normative policy oriented debate derives from a perceived series of gaps between life sciences, medical research, clinical practices, and effects in the form of, e.g., measurable health improvements. The rationale and promise of TR is to ensure and encourage that public investments in health science are turned into improved care practice and improved public health. The term TR is used interchangeably with other terms such as translational medicine, translational science, academic medicine, medical knowledge translation etc. TR is closely linked to research policy, funding incentives as well as organizational transformation in Europe, US, Australia, and more recently the Nordic countries, where Academic Health Science Centers (AHSCs) have been established in recent years to encourage translational interaction between research and clinic. As such, TR is important as a pervasive discourse in medical science and as a socio-economic reorganization of research practices. Existing studies have pointed to the multiple meanings of translational research in ongoing academic and policy debates—and to the way in which this concept is tied to a range of varying problems and possible solutions, not only in different medical fields but also in different national contexts (Crabu, 2018 ; Greenhalgh and Wieringa, 2011 ; Krüger et al., 2018 ; van der Laan and Boenink, 2015 ). Very few studies, however, focus empirically on how these expectations and characterizations of TR hold true in the context of actual researcher practices.
This article reports on an ethnographic case study of translational research networks in a Danish university hospital setting. The investigation focused empirically on the nature of these translational activities and on how translational research was “made to work” in a specific research-hospital setting. This article presents a particular sub-set of the data in order to explore how the translational researchers themselves understood and used the concept of translational research (TR). Focus is thus on how actors in a Danish research setting are entangled in wider discourses of TR and how they take part in performing TR discursively and materially. The analysis draws on key ideas from the work of Science and Technology Studies in order to understand TR as a set of performative statements and ideas that generate their own practices and thereby create the world they describe (Mackenzie et al., 2007 ; Mol, 2002 ). As such, the article contributes empirical insights into the researchers’ own descriptions and models regarding the concept, how the concept was performed in the setting studied, how researchers engaged with the concept, and what they made of it.
The article is structured as follows. First, I briefly present the literature on the concept of TR. The next section presents the methodological and theoretical backdrop for the research reported and the areas of investigation, translational research grounded in the fields of psychiatry and oncology. Hereafter, key statements and examples from the data are presented and analyzed. Lastly, the discussion reflects upon TR as a complex process of meaning production and material reorganization.

Translational research
In an important article from 2012, Van der Laan and Boenik “disentangle” the concept and rhetoric of TR and its different meanings, both historically and philosophically (van der Laan and Boenink, 2015 ). They focus on the extensive and exponential use of the concept in biomedical scientific literature during the years 1993–2010 and present different epistemic dimensions regarding the way the concept is interpreted and used. Krueger, Hendriks, and Gauch’s more recent literature survey of the term in biomedical and clinical research also finds a “kaleidoscope” of different dimensions, understandings, and applications related to the term (Krüger et al., 2018 ).
Despite the variances, one focal figure in this literature is the trope of “bench to bedside”. Here, TR is a science-clinic-public relationship conceptualized as a set of translational phases through which knowledge moves from basic biomedical research into diagnosis or treatment, subsequent development into evidence-based protocols, following deployment in clinical practice, and, ultimately, benefits for the individual and society through improvement of public health. The term implies a relocation and translation of knowledge across what are conceived of as somewhat separate domains. Yet, as noted in the existing literature studies, the way in which the specific gaps, models, and problematic barriers are constructed vary greatly. Likewise, the understanding of the very domains involved differs. Basic science, clinical research, clinical practice, the public, society, and politics are also defined and delineated in varying ways.
The social sciences and humanities have entered into and contributed to the biomedical debate on translational research, as recently reviewed by Crabu ( 2018 ). Work in these areas has challenged the transfer notion implicitly found in much of the literature on translational science—as well as the fundamental distinction between basic and applied science. Qualitative empirical studies also bring our attention to the very complex collaborations and recursive pathways of TR, where valuable breakthroughs in science and treatments can emerge by way of the clinical staff and their daily questions and puzzles, from patients or patient groups, commercial activity, or policy demands. The creation of new medical knowledge can thus have many “starting points” in addition to basic science, thus challenging the linearity implied in many discussions and policies on TR. In their study of laboratory and clinical practices related to Huntington Disease, Lewis, Hughes, and Atkinson, for example, point to TR as a complex of clusters and multiple processes of relocation and reconfiguration as objects, knowledge, practices, and resources are circulated between multiple sites (Lewis et al., 2014 ). Based on a study of health care innovation through extended translational networks in Canada, Lander and Atkinson-Grosjean ( 2011 ) likewise describe various hybrid domains of translational science that cut across presumed divides between basic science, clinic, as well as commercial and civic areas. Their study also illustrates how translational pathways flow through the interactions and relations among a complex collection of actors and organizations (Lander and Atkinson-Grosjean, 2011 ). This complexity is less visible in the normative depiction of TR as a unidimensional line from basic research to clinical practice and then to public health.
The study reported on in this paper converges with this line in the literature located in social science and the humanities, both openly exploring the complexities of TR and challenging the foundations and presuppositions of a normative TR agenda. The article focusses on the question of how actors involved in TR in a specific research-hospital setting engage with and use the concept. The exploration asks open questions as to which statements and models of TR circulate among these actors? What does TR mean in the context studied? How do these statements and models participate in shaping research and clinical practice? How does TR relate to other concepts and concerns? In exploring these questions, different understandings have emerged from the data, summarized here as four themes: TR as knowledge flow, TR as a political buzzword, TR as collaboration and exchange, and TR as competency and skills. Each of these understandings is depicted in turn in the analysis section. Based on this analysis, the paper contributes to existing social science and humanities explorations of TR and adds to existing work by illustrating the ways in which the concept of TR circulates in a particular setting and how the concept is adopted and used by actors in this setting as part of their everyday practice. The paper argues that these performative uses of the term are material and productive as they contribute to organizing work, as well as attaching value to specific kinds of work and specific skills.
The study reported here is based on ethnographic fieldwork in Danish hospitals carried out between January 2018 and March 2019. I conducted interviews and observations and collected a broad range of organizational and project documents. Observations included research team meetings, departmental meetings, public presentations of research, two academic conferences, patient testing and treatment, lab visits and informal conversations (~100 h). I took hand written notes during observation and subsequently wrote these out in text files—with concurrent memoing. Observations and informal conversations provided data on daily experiences and were linked to formal interviews that were conducted in parallel (n20). Interviews were conducted with various team members, primarily clinician-scientists (n11) but also research team members such as Ph.D. students (n4), biologists (n2), an engineer (n1), and lastly two department managers (n2). The interviews lasted 1–2 h, were recorded and transcribed with the respondents’ consent. All interviews were conducted at the hospitals and were semi-structured and included questions about the participants’ definitions, understandings, and models regarding the concept of TR. Data was stored, organized, and coded in the qualitative data analysis software NVivo using grounded theory and analytical tools from situational analysis (Clarke, 2005 ). The findings presented in this paper draw on a sub-set of the data regarding the way in which the translational researchers themselves understood and used the concept TR.
Ethical approval and consent were obtained in writing from the principle investigators of the research networks and from the informants. The project was also approved by the hospital management and reported to the regional ethics committee. Throughout the research project, I was simultaneously working as a consultant in a crosscutting research and innovation support unit at the hospitals. This involved weekly visits, meetings, workshops, and communication with staff and management at the hospital departments on issues related to research development and support in the region. This concurring consultancy work gave me a background understanding of the organization and the research infrastructure of the hospitals, but it is not included as a formalized part of the dataset due to research ethics of a dual role of employee and researcher.
Oncology and psychiatry
The setting for the research here is Region Zealand in Denmark and in particular two research networks based in the regional hospitals. These research networks connect different research projects or research protocols within a joint vision of changing and improving diagnosis and/or treatment within two very different medical areas, child and youth psychiatric diagnosis and cancer treatment. The two translational research networks were interdisciplinary, yet anchored in the two domains of oncology and psychiatry, referred to here as the electroporation and autism networks. The electroporation case was an international collaborative network working to develop and improve a new type of treatment for cancer, electroporation. This technique creates an electrostatic field in cancer cells in order to increase the permeability of the cell membrane, allowing chemicals, drugs or DNA to be introduced into the cell. When applied locally, this type of treatment has been found effective in killing the cancer cells of the tumor, and the treatment with this technique combined with administering calcium was found to release patterns into the immune system, possibly hindering a recurrence of the tumor and slowing further spreading of the cancer. A range of related projects sought to refine the technique in relation to specific cancer types and in relation to different types of chemicals, and to explore systemic immune responses of the treatment found clinically as an unexpected outcome of the treatment. This network played an important role in developing and implementing this particular type of cancer treatment internationally. The group was involved in developing European guidelines for clinical practices and in various political and practical implementation efforts to establish the treatment type as part of the standardized treatment program for specific cancer types in Denmark. The researchers were thus deeply engaged in research, but they were also focused on realizing its application in the clinic. Most of the researchers were also responsible for everyday clinical practices of examining patients and determining treatment strategies.
The second research network I studied conducted research on autism disorders in children and youth through a translational research design combining behavioral, psychological, and neurobiological approaches. The project was situated within a broader disciplinary debate regarding the Diagnostic and Statistical Manual (DSM) and concerning controversies as to the way in which to categorize symptoms of mental disorders. Autism in particular presents a contested diagnostic category, appearing clinically in a variety of forms and with varying professional understandings of its nature and appropriate treatments. The research network was concerned with this broader questioning of the very notion of autism as a singular disorder category and was critical of current diagnostic criteria and classification. Furthermore, the research network formed part of a shift in the clinic and the field more generally towards investigating mental disorders such as autism through laboratory practices and technologies like new IT-based cognitive function testing, electroencephalography (EEG), and magnetic resonance imaging (MRI). The researchers’ work was exploratory, seeking to find new ways of understanding autism as both symptoms and pathology, e.g., through a key psychiatric concept of cognitive flexibility that was investigated as part of the project.
Although several of the projects within both of these research networks included industrial partners, the lead researchers themselves stressed that their research was “investigator-initiated” and thus different in nature from clinical trials and medical research driven by industry. The lead researchers themselves framed their research, the research designs and approaches, as “translational”, e.g., in presentations and funding applications (“translational forskning” in Danish).
Analytical framework
Science Studies, Feminist Theory, and Cultural Studies have explored empirically and theoretically the way in which discourse, statements, and representations have productive consequences and effects upon reality (Foucault, 1990 ; Haraway, 1988 ; Latour, 1987 ; Mol, 2002 ). In their book on economics, Mackenzie et al. ( 2007 ) develop the term performativity to examine how economic theory takes part in shaping economic realities—how statements, models, concepts, and formulas over time shape the very worlds they describe. These authors illustrate how reality—socially and materially—over time becomes reshaped to fit with theoretical models and inherent presumptions. This analytical lens is highly relevant for understanding how the language of TR has been, and continually is, an agent for modifying the reality it describes. This analytical lens also leads us to study how actors involved in TR research take part in the actualization and “putting into motion” of TR through their use of TR concepts, models, and research designs. This is the focus in the following analysis where significant examples and excerpts related to the use of TR terminology are presented and discussed. According to Mol ( 2002 ), conversations and interviews are a way of listening to informants as if they were their own ethnographers, telling how their work of TR is understood and carried out. Interviews and conversations are thus analyzed as a way of learning about objects, events, and practices that are material and productive.
The analysis is organized according to four main understandings emerging from the data—TR as knowledge flow, TR as a political buzzword, TR as knowledge collaboration and exchange, and TR as competencies and skills. The quotes and excerpts are anonymized with regard to informant names and field of expertize and only attributed to the research network—named here as the autism and electroporation network, respectively. Throughout the analysis, the two networks also serve as analytical prisms for one another, juxtaposing their similarities and differences.
TR as knowledge flow from theory to practice
During the study, a dominant understanding of TR that appeared during observations, informal conversations, and interview questioning on the topic was TR as knowledge flow from theory to practice . This understanding aligns with the notion and modeling of TR that is pervasive in biomedical literature and the aforementioned bench to bedside trope. TR is conceived of as a set of transfers or flows of knowledge from basic biomedical research into clinical diagnosis and improved health for patients—and also concerns closing the gaps hindering this flow. This understanding was particularly prevalent in the electroporation network. A lead researcher involved in setting up laboratory studies, clinical trials, and implementation efforts in relation to the treatment technique electroporation explains her understanding of translational research to me in an interview:
It is about closing the gap between lab research and the patient’s everyday life. Moving knowledge from the laboratory over into clinical practice, as well as ensuring how we can take the biological tests that afterwards can go back to the researchers… moving from idea, to laboratory research, to clinical research and all the way into guidelines for new treatment. (Electroporation network)
This quote resonates with the dominant understanding of TR as knowledge that flows through a set of otherwise separate contexts and knowledge domains framed as laboratory, clinical practice (with associated guidelines), and the patient’s everyday life. She describes TR as the moving of laboratory research into clinical practice, and how TR also produces the biological data in the clinic to move back into the lab.
At a research event and presentation at the hospital, this researcher presents a timeline of her research on electroporation. She explains how she has been involved in the basic science in order to understand the cells and cell membranes and how they can be briefly destabilized by applying electrical pulses to the area. Based on these insights into cellular behavior, they developed new experimental electro-engineering tools for applying electricity directly to the skin and tumor and then for injecting drugs and chemicals into the area so these can enter into the tumor and cells creating a local and very effective new treatment form. These tools have subsequently been refined and developed and are part of standard treatment regimes for specific types of cancer, such as skin cancer. In addition, the technique and technology are being developed further for other types of cancers. For example, stomach and colon cancer, where the tumor is more difficult to access directly with electrodes. Here, the electrodes were undergoing further development in order for them to work with endoscopic devices.
In a timeline figure, a presentation slide sketches the steps of translation from basic science over into techniques tested on mice in order, for example, to refine how to administer the electricity and chemicals in an appropriate way and with the correct dosages. This led to further experimental treatments on patients, and later on, randomized trials with a larger number of patients proving both the safety and efficacy of this specific type of treatment. In 2013, the UK National Institute for Health and Care Excellence (NICE) guidelines state that sufficient evidence has been established for this particular treatment for cancer spreading in the skin. In conclusion, she notes that this process has been a relatively “rapid process of translation from the first discoveries to a treatment in widespread use.” She moves on to explain their more recent work on using calcium with this type of treatment to determine how this might have effects upon the immune system beyond the local effects of cancer cell death. The timeline and story of electroporation reiterates a temporal TR image of knowledge flow from theory to practice—and back again—over time.
When asked about definitions of the term translational, another researcher, part of the oncology research networks but involved in the study and treatment of other cancer types, similarly notes:
I think translational covers when we turn over basic science into practical science. I see it as research where we get out and onward from the lab. We have an aim that is out of the lab, and it is important for us to do something that potentially can get out and work in society. (Electroporation network)
This quote links up to an understanding of making science applicable and “something that can be used.” Other informants likewise recognized TR as the clinical application of theoretical or experimental knowledge—or “moving new knowledge closer to the clinic, so “it can be used and tested further.” One informant notes that TR in this way consists of a practical achievement that moves theory into clinical practice:
I define translational as the clinical application of theoretical or experimental knowledge. So translational science is that one translates, really a utilitarian term, that you translate something proven ex vivo or proven in a petri dish to something that has clinical consequences for patients.” (Electroporation network)
In the accounts recorded during the study, an understanding of TR as knowledge flow from theory to practice thus is in agreement with the dominant discourse in the literature and “promise of translation” envisioned in the future (Brown et al., 2000 ). The hope is that public investments in health science can and should be paid back in the form of improved care practice and improved public health. “Making a difference” was often mentioned as motivation for the career choice of working with translational hospital-based research, along with the value of participating in research that might be practically applicable to and an improvement of current clinical practice. This applicable-practice motivation was notable in both the electroporation and the autism network.
Following Mackenzie et al. ( 2007 ), the accounts and ideas also speak of actual practices where, in the electroporation network, knowledge artefacts, as well as biological material are relocated and exchanged. There are also accounts of how experimental research is connected to changing procedures for cancer treatment strategies and new standardized treatment programs.
TR as a political buzzword
Several of the informants in both research networks noted the buzzword character of the word, smiling or laughing at my question of their understanding in the interview thereby distancing themselves from the concept and instead locating the concept in a world of politics and funding bodies with interests different from their own. They reiterated statements resembling the objectives discussed above regarding knowledge flow and transfer, but then added that these ideas did not necessarily match the way TR projects actually played out according to their experience. A researcher from the autism network notes:
I know what it means, but that is not how I see it implemented. It is research that supposedly builds bridges between experimental research… over into clinical research, maybe back again. However, when I see translational programs implemented, it does not really get out to the patients, and it does not really get out into the clinic. (Autism network)
Several informants noted that the TR had a political buzzword quality and was about justifying funding for very specific types of research. Therefore, for some there was a discrepancy between the rhetoric of TR and the way it was realized in ongoing projects. Accounts such as the above imply a critical position—that the translational agenda is a way of living up to demands of funders or creating political enthusiasm for research—but that the actual move into clinic and patient benefits could be questioned.
One informant described TR as a specific kind of research funding to expand “the evidence base” rather than research enabling knowledge to flow between basic science and the clinic.
Really, a buzzword is about creating the funding to make the evidence. It is relatively inexpensive to fund the small, experimental studies but gets expensive when you want to test an intervention on a larger group. It is complicated to create the evidence to prove that this really should be part of the standard treatment plan. So it is a way of creating funding for this difficult phase, where promising research needs to create the evidence base for it to get used. (Electroporation network)
Here, TR is a way of creating political support for particular types of research funding—a way of filling an evidence gap that is necessary for something to be legitimate and justifiable as a diagnostic or treatment option in the clinic. Thus, in this understanding TR is understood as a rhetorical device serving particular interests and political agendas. This resonates with the political move to put significant resources into TR to increase the clinical relevance and application of research. Using research relies on the creation of very specific types of “robust” evidence such as randomized controlled trials—and these are a necessary intermediate stage for research findings to reach decision-makers and potentially have societal health impacts. So here, TR is about the political support for specific types of research, for creating particular research infrastructures that can enable credibility, validity, and paths of impacts for medical research.
Conversations and interviews where TR was referred to as a political buzzword can also be seen as part of the actors’ own reflections on a broader knowledge economy where colleagues, or they themselves, attempt to position themselves strategically in relation to political and funding agendas. They adhere to, draw on, but also smile at this—since what they see “play out” sometimes is a different scenario. The actors in both research networks involved were thus attentive to how one as a researcher strategically can link up to political agendas and adjust projects so they match the demands of policy and funding trends. Here, TR is pointed to as rhetorically powerful in justifying specific types of research resonating related analyses of how TR currently is mobilized in other national academic medical settings (Rushforth, 2016 ; Wilson-Kovacs and Hauskeller, 2012 ).
TR as interdisciplinary collaboration and exchange
A third understanding of TR that appeared in both networks was TR as a framing of interdisciplinary collaboration. Models and research designs of TR enabled and encouraged collaborations and exchanges across different medical specializations and across distinct departments and organizations. A researcher from the autism research network replies to the question of how she understands the term translational as follows:
I understand it broadly, that you try to connect knowledge and understanding from different levels—psychological, biological, social etc.—into a joint understanding of a phenomenon… The same phenomenon might really be the result of many different processes. (Autism network)
She moves on to explain how such processes can be captured at different levels and through different investigational methodologies deriving from different disciplines. Methods in her project included preclinical and clinical testing, neurobiological approaches, brain imaging, and at a later stage, if the funding becomes available, possibly also genetic testing. She explains that a translational approach is the next step in developing new knowledge on autism. Here, the promise of TR is to connect different knowledge forms to create radically new understandings.
The idea here is that the translational can dismantle diagnoses, as they are today. If we understand the translational levels, we will understand that the diagnostic system and the psychiatric system should be put together differently. (Autism network)
The research design of the autism project is therefore organized around a translational model that the lead researcher sketches for me on the whiteboard in her office, and later, after the interview, she sends me the model figure used in applications and when presenting the research (Fig. 1 ). Here, different translational levels are depicted along with the examinations, methods, and procedures applied to produce knowledge about these levels. The research project is designed around these translational levels through which the children included in the study move during a series of examinations marked in the figure as “assessments 1–5” under the column with procedures, ranging from standardized clinical screening tests and questionnaires, IT-based cognitive tests and paraclinical methods, including electroencephalography (EEG) and magnetic resonance imaging (MRI). These methods provide knowledge on different translational levels from the “psychosocial down to something increasingly biologically based”, she explains.
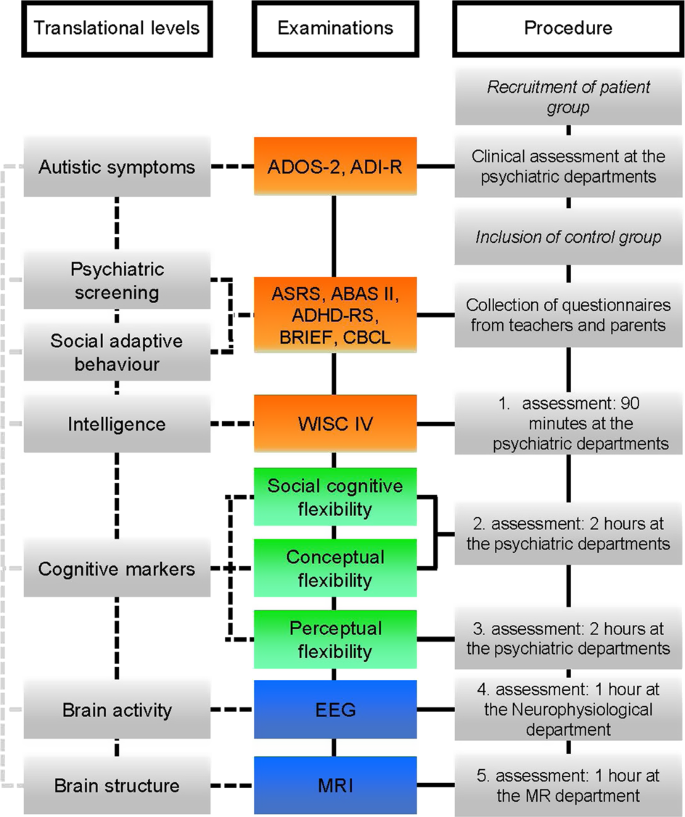
The translational model was shared by an informant in the autism research network and derives from their project description. The model depicts different translational levels along with the examinations, methods, and procedures applied to produce knowledge about these levels. The research project is designed around these translational levels and a series of examinations marked in the figure as “assessments 1–5” under the column with procedures, ranging from standardized clinical screening tests and questionnaires, IT-based cognitive testing, electroencephalography (EEG) to magnetic resonance imaging (MRI).
The model organizes the research project, the series of tests and examinations the patients and control subjects go through in which different kinds of technologies and expertize are involved. The tests take place in the childrens’ homes and in their school settings (using standardized questionnaires filled out by parents and teachers), in the psychiatric clinic (again using standardized screening and new cognitive tests developed as part of the project), in a neurobiology lab at the neurology department and at the department of medical imaging (where the MRI scanning technologies are located). The studies require personnel and expertize from these various disciplines in order to carry out the examinations and analyze the results. The autism research network thus spanned different departments and disciplinary specializations of child and youth psychiatry, psychology, psychophysiology, radiology, neurology, engineering, and screening software/IT development.
“It is like we take a cross-section and look at the same phenomenon at different levels”. (Autism network)
The translational research design brings together different methods and techniques for investigating many different parameters associated with autism. In this sense, the model of the translational research design can be seen as a workable boundary object (Star and Griesemer, 1989 ) enabling collaboration across a complex of scientific inquiry methods and knowledge forms into a joint workable research design. The model helps to make possible collaboration across specializations and departments and facilitates a joint study that combines approaches where autism is framed in different ways: as related to social, behavioral, and clinical symptoms, as a disease with a possible neurological basis, and as a disease with a possible brain structural basis. Through the translational research model, it becomes possible to relocate the phenomenon of autism into different disciplines and as such offers a tool towards collaboration. The language of TR in the autism network can thus be seen as a contact language enabling a joint interdisciplinary project to be planned and agreed upon (Galison, 1999 ).
In the same way, projects within the electroporation network were framed and depicted in translational models and research designs. This network also involved collaboration between a range of disciplines and areas of expertize, requiring collaboration between researchers based in oncology, surgery, dermatology, pathology, biochemistry, molecular biology, immunology, physics, engineering, IT, and palliation. A model (Fig. 2 ) was used in a research presentation to depict and present a subproject taking place within this translational network. The project was set up as a collaboration between the oncology and surgery department at the Danish hospital and included several other partners such as universities, industry, and e.g., a leading immunological research institute in France working to develop new methods to characterize the immune characteristics of cancer tumors, “the cellular landscape of the tumor”. Like the model from the autism network, it looks “across” and combines different types of examination and methodologies in a new way.
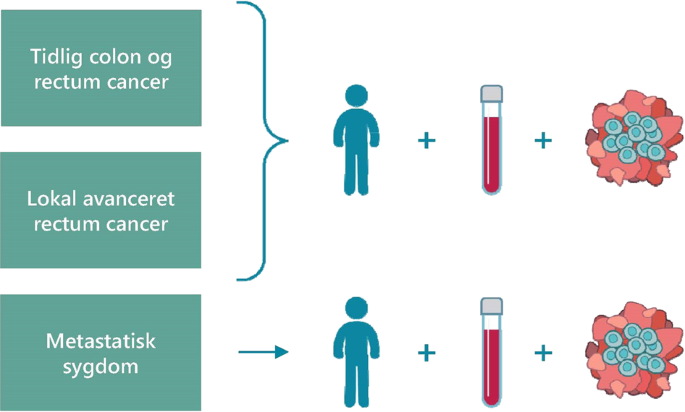
The translational model was shared by an informant in the electropration research network and derives from their project description. The model depicts the translational set-up for the study and different methods for examination that include and “sum up” patient outcomes, blood samples, and tumor biopsies across different stages of cancer—early cancer (Tidlig colon og rectum cancer), advanced cancer (Lokal avanceret rectum cancer), and cancer that has spread in the body (Metastatisk sygdom).
One of the lead researchers explains the translational set-up for the study in which the patient is treated with calcium electroporation before the planned surgical removal of a cancer tumor. The treatment prior to surgery aims to stop the tumor growth and hinder spreading of the cancer. Blood samples and tumor biopsies are taken, and biological data is recorded before and after the surgery to assess the effect of the intervention. In the boxes on the left, the figure presents the different stages of cancer development to be examined—early cancer, advanced cancer, and cancer that has spread in the body (metastasized). The investigations then focus on three ways of “reading” the intervention. Firstly, what happens to the patients? Is it safe? How is the treatment experienced by the patient, e.g., pain? Are the side effects short term and long term? Does the tumor grow or spread (as seen and measured through imaging technologies)? Secondly, what happens as the result of this treatment at the molecular level in the tumor and in the blood, examined through tumor biopsy investigations and blood profiling testing before and after the treatment intervention? These different “readings” of the interventions’ effects are summed up (+). The researcher explains that this can be a new way of producing knowledge about the variation they find clinically, for example of how the same intervention works differently in two patients, by looking at the cellular level and the biological markers to explain and understand the variation and the immunological changes involved. Translation is a way of making the effects of an intervention visible and documentable, as a way of proving a link between treatment and specific effects. As such “translational” is a set of methods and tools that can be used to compare and evaluate treatments with the potentiality of providing a new and different kind of knowledge of what works, and sometimes how it works.
In the electroporation network, several researchers noted that the research is fragmented and separate (e.g., in relation to the different stages of cancers or in relation to different treatments before or after surgery). A researcher explains that not a lot of research focuses on all three phases, but that looking at the immune system as a whole rather than the tumor as an isolated entity to be treated or removed is often neglected. Looking at the effects of the treatment overall requires what he notes as a “helicopter view”. Another researcher in the project similarly refers to this work as grasping the “bigger picture”.
It is about designing the study so you see the bigger picture and get a 360-degree view… If you want to make a difference and do research that moves the way we think, then you have to include all the parts and include the whole spectrum. (Electroporation network)
Ideally, for example, results from patient-reported outcomes, molecular biological examinations of blood samples and immunological investigations of tumor material are linked up in the research project—as are different stages of cancer and phases of cancer treatment like pre, during, and post operation, thereby encompassing the “whole spectrum” by working across disciplines and joining differing techniques and niches of research. For both networks, bringing together these different investigational techniques and methods was where the research had the break-through potential to be a “game changer”, as one researcher puts it—in the sense of a new way of thinking about cancer or an entirely new approach to psychiatric diagnosis. This is where there is a promise and potential to change the foundations for existing classifications, diagnostics, and treatment strategies of illnesses. In both networks, TR is a productive and adaptable way of framing interdisciplinary research and multifaceted research problems. TR holds a promise of not only creating usefulness of research, but also of changing fundamental paradigms of both clinical research and practice.
TR as competencies and skills
A final and fourth understanding reappearing in the data material is TR as competencies and skills. When explaining their TR understandings and research activities it was often noted by the informants that such work required a set of specific competencies and skills. This concerned the ability to develop and use translational tools and methodologies in the research project and at the hospital. In the excerpt below, a lead researcher stresses the aspect of “ability to use”:
“To me, translation is the ability to have a tool to translate an effect of something, a clinical intervention, a clinical problem—to be able to translate that into an effect on the genetic, cellular, or molecular level. So translation to me is using that methodology, that method, to find an effect of something that happens clinically.” (Electroporation network)
As part of the electroporation study, Ph.D. students and young researchers went abroad and participated in research courses, seminars and visits—one in an electro-engineering institute in Slovenia to learn the electrophysics behind the technique, the other in an immunology laboratory in France to learn how to measure immune cells in the tumor with a novel prognostic technique. These kinds of exchanges were vital to developing the skills necessary to realize the TR objectives of the project. One of the Ph.D. students explains this as somewhat different from other kinds of clinical research at the department.
When you are a researcher at a hospital, you stand there with your patient, and then you send off your tests, I have heard jokes about this in the lab, you send off your tests into a black box, and we get a bunch of numbers back. I would like to go into that black box and see what happens, to understand how the tests are practically handled in the lab, because I think that the very numbers I get out of that black box, well I will to a greater degree understand them, if I have been there in the lab, where I see it and have it in my hands. (Electroporation network)
In this quote, the physician in research training points to her own movement between research located in a clinic and in a laboratory. Part of her research plan is to move into the laboratory and acquire the skills to understand laboratory-based analysis, results and possibilities. In order to gain these skills and competencies, and apply them to the clinical focus of her research, she notes how it is necessary to physically “move into the black box” and “have it in my hands”. As such, her training involves a shift from more “traditional” medical research into a new kind of translational research.
Another team member in the project has a background in human biology. She has been hired to support the translational research at the department and highlights that it is the exchanges between the different professional groups in the project that are so necessary and where we “really make the most of the knowledge we have”. She explains her mediating work and role and how her educational background in human biology has equipped her to be a clinical research biologist.
It is really about understanding a little bit of everybody else’s areas or field, so you can be precisely that link between chemists, physicists, and doctors. (Electroporation network)
In the electroporation network, a TR research agenda was thus closely linked with recruiting or educating the “TR agents” that could facilitate research activities and exchanges across disciplinary boundaries. A crucial supporting aim of the TR networks was thus to develop these skills in house—at the department and at the hospital, rendering the opportunities in the technologies and the lab more accessible.
Likewise, Ph.D. students in the autism network were trained thoroughly in the working of the neuro-lab by experts at the hospital and from abroad, setting up and using the physical equipment for carrying out EEG examinations, as well as the technologies and software involved in data analysis of the EEG results. As noted by one of the Ph.D. students, this was really a very different set of “much more technical skills” than those he was trained in as medical doctor in child and youth psychiatry. A key participant in the autism network was for example a trained psychologist and had experience from a previous job with MRI brain scanning techniques. His expertize in both child and youth psychiatry and imaging technologies made it possible to connect the psychiatric research interests with possibilities in the MRI devices for testing and analysis. He could speak the necessary highly specialized language related to diagnostic imaging, such as multi-slicing, pulse-sequences, and fiber tracking etc. He enabled the interactions and exchanges among the psychiatrists and the MRI engineer and imaging professor. Such ability to apply new methodologies across disciplines and to converse and move expertly across more than one discipline is thus a fourth way in which the discourse and promise of translation was embedded within the practices of both research networks.
This article has presented and explored different uses of the TR terminology in two specific settings of biomedical clinic-academic work practices. This type of inquiry is underexplored in the literature, and this empirical contribution thus adds to related efforts into studying how the actors in the field respond to political agendas of TR and changes in the biomedical research-clinic landscapes (Rushforth, 2016 ; Vignola-Gagne, 2014 ; Wilson-Kovacs and Hauskeller, 2012 ). The analysis has put forth a set of performative statements on TR along with the models of translation presented by these actors. Here we see how TR is embedded in the practices and perspectives of a set of particular actors involved in TR.
The first characterization of TR as knowledge flow can be viewed as an adaptation of the normative language of TR debates and policies. The goal and value of bench to bedside work enters into the actors’ own characterizations and meaning-making of their everyday work—as it also productively shapes and organizes these practices. Researchers involved in TR take on and seek to fulfill expectations and visions of the TR discourse and assumptions that circulate among funders, evaluators, management, and in health care prioritization and politics. TR also becomes part of the actors’ own sense-making and vision of how value can be created through their work for patients and for society. This brings our attention to how actors involved in carrying out TR take part in actualizing and putting into motion theories, models, and the very propositions of TR. This characterization places positive value upon specific kinds of work in the hospitals and among the hospital-based researchers. Translational research work that can ensure that research results are used, integrated into practice, and can produce benefits for patients and society is thus also characterized and performed as desirable and good.
The second characterization points to the critical position of TR as associated with a political agenda and something that can be used strategically to secure funding. TR offers an opportunity for researchers to position themselves advantageously in relation to TR policy and funding—thus potentially gaining a privileged professional status as key leaders of change, as noted in related studies (Vignola-Gagne, 2014 ; Wainwright and Williams, 2009 ; Wilson-Kovacs and Hauskeller, 2012 ). The researchers themselves take part in critically reflecting upon political agendas, funding flows and the consequences for their work, their career, and their field of expertize. They thus participate in questioning the very promises and hopes of the TR dominant discourse and the transformations they experience.
In the third characterization presented here, TR as collaboration and exchange, TR becomes a way of seeing and analyzing the subject matter across disciplinary divides. As such, the translational research design combines several different investigational methodologies from different and otherwise somewhat distinct disciplines. In the terms of Latour, these techniques mediate the object studied in different ways, rendering it visible for science in particular ways (Latour, 1987 ), and these different mediations are brought together in the promise of “seeing the bigger picture”—and “changing the game” in radical ways. TR discourse and promises become an organizing factor for research and research activities in the hospital studied. TR serves to facilitate epistemological boundary spanning (Evans and Scarbrough, 2014 ) and is a productive way of framing interdisciplinary research and multifaceted research problems that cannot be solved with traditional research frameworks. In this understanding TR perhaps opens for alternative ways of creating medical knowledge and evidence other than—or in combination with—the gold standard of randomized controlled trials (Timmermans and Berg, 2003 ; Wieringa et al., 2017 ).
Lastly, TR is closely linked to the building and expanding of interdisciplinary and transactional skills in the hospital setting studied. This is discussed under the fourth characterization, TR as competencies and skills. This theme highlights the integration of new knowledge forms into the hospital research setting, as well as the very practical, material, and embodied abilities of TR such as handling the equipment, delivering the electric pulses to the tumor areas as in electroporation, and learning to administer the details of the EEG equipment and devices. New skills must be learned and entered into clinical practice and experimentation. Likewise, medically trained employees move into the lab and learn to work with the biopsies, blood samples, and cells “in their hands”. Scientific investigation of cancers and autism is shifted out of the clinic into the laboratories of for example neurobiology and brain imaging—and the techniques and skills from these disciplines are relocated into clinical and medical practice and achieve new value here.
With the presentation of these four understandings, this article illustrates different uses of the term TR among actors engaged in research-clinic activities in two settings, that of clinical oncology and that of clinical psychiatry. The analysis presented in this article does, of course, not cover all the ways in which actors involved in TR use the term. Rather it illustrates some specific, situated uses—uses that reappeared and were focal in the data material produced in this study. The analysis provides new insights into TR as a”force of example” (Flyvbjerg, 2006 ). Rather than providing a total overview or mapping generalized patterns, the analysis explores specific context-dependent appearances of TR. The study brings out differences and connections for further juxtaposition to other studies in different specializations in different national contexts. It is important to note that the characterizations were not mutually exclusive, but overlapping and entangled in the setting studied. The understandings were mobilized, in turn, to bring out different aspects and values of the hospital-based research work in specific situations. All characterizations circulated in both networks—thus seemingly co-existing within these networks, as well as sometimes in the course of a single interview.
Notable are however also some of the differences in the two research networks. The networks were not analyzed as comparative cases (several cases of the same), but selected due to differences and analyzed in juxtaposition to bring out differences. In the electroporation network, the dominant understanding of TR as knowledge flow was more prevalent than in the autism network. In the electroporation network TR as knowlegde flow appeared as the primary understanding of the term and also as an important guiding rationale of conducting hospital-based translational research. This might be linked to the ways in which the field of cancer research historically has been tied to the political and funding agenda of TR. Historical studies have analyzed how the rise of translational research and a translational agenda, particularly in the US, is closely linked to cancer research and to the promise of cancer cures based on research into new drugs and treatment therapies (Fujimura, 1996 ; Keating and Cambrosio, 2012 ; Löwy, 1996 ). All early publications 1992–1997 using the term are also related to cancer research, in particular research on biomarkers in relation to cancer prevention and the establishment of tissue banks and cancer research centers in this period (van der Laan and Boenink, 2015 ). Historically, TR in this version seems more closely linked to the electroporation network than to that of psychiatry—where the understanding of TR as collaboration and exchange was foregrounded more often. These differences bring our attention to the ways in which TR is situated differently in different disciplines and underscores the contextual nature of the concept.
This article has presented selected findings from an ethnographic study of the everyday practices of TR in a specific setting. The discourse of TR, including the policy initiatives and organizational transformations linked to the TR discourse, can be seen as a paradigmatic shift in medical science. Yet little is known about how such a paradigm shift plays out in concrete settings, what it means to the actors involved, how it changes what constitutes meaningful and valuable research—as well as meaningful and valuable everyday work practices. This article proposes that actors take part in performing the emergence of TR and possible paradigm shifts by foregrounding and valuing specific versions of TR along with specific practices, specific skills. This entails that other practices and skills perhaps are backgrounded and become less visible and less valued. That which the less visible and less-valued practices are composed of (e.g., perspectives of patients or other working groups at the hospitals) constitutes a pressing question for further work beyond the scope of this paper. One of the important points highlighted here is the different ways in which TR discourses, promises, and expectations form an active part of the researchers’ sense-making and practices. The analysis presented in this article also allows us to reflect on how these actors take part in fulfilling a societal obligation, encouraging and improving the clinical application and clinical benefit of new scientific knowledge. They share the concerns found in the TR debates and policy regarding the closing of a “bench-to-bedside gap”, but also rework these orientations in relation to their specific projects and practices. Applying the notion of performativity, statements and models of TR have been approached in the light of their agency and their performative dimension. This analytical approach thus helps to understand how TR characterizations—and statements—also contain a prescription for how the world must change for them to become true. Mackenzie et.al. suggest that performative success is when there is created both a new language and theory, as well as new reality ( 2007 ). This article provides insights into four co-existing characterizations where such performative success was achieved in the setting studied. The analysis also points to a disciplinary difference through the juxtaposition of two different research networks. New languages, theories and realities were successfully in the making in these networks along with changing implications for the way in which research knowledge is produced and applied, as well as cultural shifts in what constitutes good and valuable research. In conclusion, this performative lens is proposed as a potential step forward toward developing a social science and humanities understanding of TR, how usefulness of research is characterized and realized through practice while keeping in sight the complexity and materiality of such processes.
Data availability
The dataset generated and analyzed during the current study is not publicly available due to the sensitive nature of the content and the use/consent agreed with informants. Selected anonymized extracts and summaries are available from the corresponding author on reasonable request and signing of a MOU to ensure the ethical use of data.
Brown N, Rappert B, Webster A (2000) Contested futures: a sociology of prospective techno-science. Ashgate, Farnham
Google Scholar
Clarke AE (2005) Situational analysis: grounded theory after the postmodern turn. Sage Publications, California
Book Google Scholar
Crabu S (2018) Rethinking biomedicine in the age of translational research: organisational, professional, and epistemic encounters. Sociology Compass. https://doi.org/10.1111/soc4.12623
Article Google Scholar
Evans S, Scarbrough, H (2014) Supporting knowledge translation through collaborative translational research initiatives: “bridging” versus “blurring” boundary-spanning approaches in the UK CLAHRC initiative. Soc Sci Med. https://doi.org/10.1016/j.socscimed.2014.01.025
Flyvbjerg B (2006) Five misunderstandings about case-study research. Qual Inq. https://doi.org/10.1177/1077800405284363
Foucault M (1990) The history of sexuality. Volume 1, An introduction. Vintage, New York
Fujimura JH (1996) Crafting science. a sociohistory of the quest for the genetics of cancer. Harvard University Press, Cambridge
Galison P (1999) Trading Zone-coordinating action and belief. In: Biagolo M (ed) The Science Studies Reader. Abingdon-on-Thames, Routledge, pp. 137–160
Greenhalgh T, Wieringa S (2011) Is it time to drop the ‘knowledge translation’ metaphor? A critical literature review. J R Soc Med. https://doi.org/10.1258/jrsm.2011.110285
Haraway D (1988) Situated knowledges: the science question in feminism and the privilege of partial perspective. Fem Stud. https://doi.org/10.2307/3178066
Keating P, Cambrosio A (2012) Cancer on trial: oncology as a new style of practice. University of Chicago Press, Chicago
Krüger AK, Hendriks B, Gauch S (2018) The multiple meanings of translational research. negotiating medical science. https://doi.org/10.31235/OSF.IO/W6XJN
Lander B, Atkinson-Grosjean, J (2011) Translational science and the hidden research system in universities and academic hospitals: a case study. Soc Sci Med. https://doi.org/10.1016/j.socscimed.2010.11.019
Latour B (1987) Science in action: how to follow scientists and engineers through society. Harvard University Press, Cambridge
Lewis J, Hughes J, Atkinson P (2014) Relocation, realignment and standardisation: circuits of translation in Huntington’s disease. Soc Theor Health. https://doi.org/10.1057/sth.2014.13
Löwy I (1996) Between bench and bedside: science, healing, and interleukin-2 in a cancer ward. Harvard University Press, Cambridge
Mackenzie D, Muniesa F, Siu L (2007) Do economists make markets. Do economists make markets? On the Performativity of Economics. Princeton University Press, New Jersey. https://doi.org/10.1086/597458
Mol A (2002) The body multiple: ontology in medical practice. Duke University Press, Durham
Rushforth A (2016) What’s in a slogan? Translational science and the rhetorical work of cancer researchers in a UK university. Nord J Sci Technol Stud. https://doi.org/10.5324/njsts.v4i1.2170
Star SL, Griesemer JR (1989) Institutional ecology, ‘translations’ and boundary objects: amateurs and professionals in Berkeley’s Museum of Vertebrate Zoology, 1907–39. Soc Stud Sci. https://doi.org/10.1177/030631289019003001
Timmermans S, Berg M (2003) The gold standard: the challenge of evidence-based medicine and standardization in health care. Temple University Press, Philadephia
van der Laan AL, Boenink M (2015). Beyond bench and bedside: disentangling the concept of translational research. Health Care Analysis: HCA: J Health Philos Policy. https://doi.org/10.1007/s10728-012-0236-x
Vignola-Gagne E (2014) Argumentative practices in science, technology and innovation policy: the case of clinician-scientists and translational research. Sci Pub Policy. https://doi.org/10.1093/scipol/sct039
Wainwright S, Williams C (2009) Stem cells, translational research and the sociology of science. In: Atkinson P, Glasner P, Lock M. Handbook of genetics and society: mapping the new genomic era. Routledge, Abingdon-on-Thames, pp. 41–58
Wieringa S, Engebretsen E, Heggen K, Greenhalgh T (2017) Has evidence-based medicine ever been modern? A Latour-inspired understanding of a changing EBM. J Eval Clin Practice. https://doi.org/10.1111/jep.12752
Wilson-Kovacs DM, Hauskeller C (2012) The clinician-scientist: professional dynamics in clinical stem cell research. Sociol Health Illn. https://doi.org/10.1111/j.1467-9566.2011.01389.x
Download references
Acknowledgements
This study was funded by Data and Development Support, Region Zealand, and hosted by Department of People and Technology, Roskilde University. The study was carried out with support and supervision from Jesper Grarup, Peter Kjær, and the two research groups Health Promotion Research and Dialogical Communication at Roskilde University. Special thanks are also extended to the participants in the study.
Author information
Authors and affiliations.
Data and Development Support, Region Zealand, Soroe, Denmark
Dixi Louise Strand
Department of People and Technology, Roskilde University, Roskilde, Denmark
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Dixi Louise Strand .
Ethics declarations
Competing interests.
The author declares no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Strand, D.L. Everyday characterizations of translational research: researchers’ own use of terminology and models in medical research and practice. Palgrave Commun 6 , 110 (2020). https://doi.org/10.1057/s41599-020-0489-1
Download citation
Received : 04 December 2019
Accepted : 22 April 2020
Published : 04 June 2020
DOI : https://doi.org/10.1057/s41599-020-0489-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Study at Cambridge
About the university, research at cambridge.
- Undergraduate courses
- Events and open days
- Fees and finance
- Postgraduate courses
- How to apply
- Postgraduate events
- Fees and funding
- International students
- Continuing education
- Executive and professional education
- Courses in education
- How the University and Colleges work
- Term dates and calendars
- Visiting the University
- Annual reports
- Equality and diversity
- A global university
- Public engagement
- Give to Cambridge
- For Cambridge students
- For our researchers
- Business and enterprise
- Colleges & departments
- Email & phone search
- Museums & collections
- Office for Translational Research
- About the OTR overview
- Connections overview
- Industry partnerships
- AIMday overview
- AIMday Cell and Gene Therapy
- Connect: Health Tech
- SAS Institute
- Funding overview
- MRC Confidence in Concept overview
- CiC Expert Panel
- CiC Previous Awards
- CiC Case Studies
- Projects and Programmes overview
- Cambridge-Sunway Collaboration overview
- Sunway Programmes
- Sunway Committees
- RCP-Sunway-Cambridge seminars
- Collaboration Contacts
- Experimental Medicine Initiative overview
- EMI Programme Objectives
- EMI Training Events
- EMI Trainees overview
- Dr Akhilesh Jha
- EMI Case Studies
- EMI Contacts
- EMI How to Apply
- EMI Steering Committee
- Events overview
- Past Events
What is translational research?
- Connections
- Projects and Programmes
Translational research is 'the process of applying ideas, insights, and discoveries generated through basic scientific inquiry to the treatment or prevention of human disease'. The philosophy of 'bench to bedside' underpins the concept of translational medicine, ie. from basic research to patient care.
The translational pathway in medicine can be simplified via the model described within the Cooksey review (2006)*. Though it is not necessarily a linear and uni-directional path, two major gaps in translation were identified and articulated.
translational_pathway_rework.png
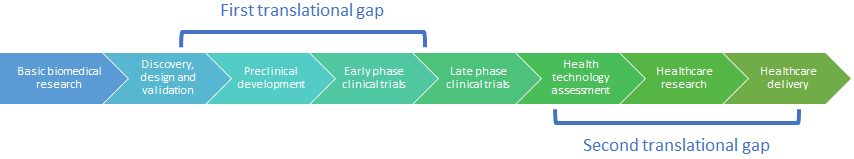
In the context of the University, the OTR mainly addresses the first gap of '…translating ideas from basic and clinical research into the development of new products and approaches to treatment of disease and illness' rather than the second gap of '…implementing those new products and approaches into clinical practice'.
*A Review of UK Health Research Funding (the Cooksey Report) (2006)
© 2024 University of Cambridge
- Contact the University
- Accessibility
- Freedom of information
- Privacy policy and cookies
- Statement on Modern Slavery
- Terms and conditions
- University A-Z
- Undergraduate
- Postgraduate
- Research news
- About research at Cambridge
- Spotlight on...

COMMENTS
Translational research is the conversion of basic research results into practical applications for humans. It involves different stages of translation from laboratory to clinical to community settings, and faces challenges and criticisms.
Translational Research delivers original investigations in the broad fields of laboratory, clinical, and public health research. Published monthly since 1915, it keeps readers up-to-date on significant biomedical research from all subspecialties of medicine.
Translational research is a systematic effort to convert basic research knowledge into practical applications to enhance human health and well being. Learn how Cornell Cooperative Extension engages in translational research and how extension programs can participate in it.
Learn how translational research moves scientific discoveries from the laboratory to real-world practice, leading to improved human health. Explore the different stages and types of translational research, from T1 to T4, and their applications and examples.
Translational research is the process of turning basic science discoveries into health interventions that benefit individuals and the public. Learn about the stages, goals and resources of translational research at TRI, a NCATS-supported center.
Translational research from basic to epidemiologic has been the basis of the seven great advances in pediatrics, including: immunizations to prevent disease, reducing sudden infant death, cure...
Learn how to apply translational science principles to advance biomedical research discoveries into health solutions. The web page outlines six principles that characterize effective translational science approaches and provides examples of how to implement them.
Debates, theorizing, and policy initiatives aiming to close the “bench-to-bedside gap” have led to the development of “Translational Research” (TR), an emerging set of research-related...
Translational Research (formerly The Journal of Laboratory and Clinical Medicine) delivers original investigations in the broad fields of laboratory, clinical, and public health research. Published monthly since 1915, it keeps readers up-to-date on significant biomedical research from all subspecialties of medicine.
Translational research is applying basic scientific discoveries to human disease treatment or prevention. The OTR explains the translational pathway in medicine and the gaps in translation, and its role in developing new products and approaches.