What Is Medicare Assignment?
Written by: Rachael Zimlich, RN, BSN
Reviewed by: Eboni Onayo, Licensed Insurance Agent

Key Takeaways
Medicare assignment describes the fee structure that your doctor and Medicare have agreed to use.
If your doctor agrees to accept Medicare assignment, they agree to be paid whatever amount Medicare has approved for a service.
You may still see doctors who don’t accept Medicare assignment, but you may have to pay for your visit up front and submit a claim to Medicare for reimbursement.
You may have to pay more to see doctors who don’t accept Medicare assignment.
How Does Medicare Assignment Work?
What is Medicare assignment ?
Medicare assignment simply means that your provider has agreed to stick to a Medicare fee schedule when it comes to what they charge for tests and services. Medicare regularly updates fee schedules, setting specific limits for what it will cover for things like office visits and lab testing.
When a provider agrees to accept Medicare assignment, they cannot charge more than the Medicare-approved amount. For you, this means your out-of-pocket costs may be lower than if you saw a provider who did not accept Medicare assignment. The provider acknowledges that the amount Medicare set for a particular service is the maximum amount that will be paid.
You may still have to pay a Medicare deductible and coinsurance, but your provider will have to submit a claim to Medicare directly and wait for payment before passing any share of the costs onto you. Doctors who accept Medicare assignment cannot charge you to submit these claims.
Find the Medicare Advantage plan that meets your needs.
How Do I Know if a Provider Accepts Medicare Assignment?
There are a few levels of commitment when it comes to Medicare assignment.
- Providers who have agreed to accept Medicare assignment sign a contract with Medicare.
- Those who have not signed a contract with Medicare can still accept assignment amounts for services of their choice. They do not have to accept assignment for every service provided. These are called non-participating providers.
- Some providers opt out of Medicare altogether. Doctors who have opted out of Medicare completely or who use private contracts will not be paid anything by Medicare, even if it’s for a covered service within the fee limits. You will have to pay the full cost of any services provided by these doctors yourself.
You can check to see if your provider accepts Medicare assignment on Medicare’s website .
Billing Arrangement Options for Providers Who Accept Medicare
Doctors that take Medicare can sign a contract to accept assignment for all Medicare services, or be a non-participating provider that accepts assignment for some services but not all.
A medical provider that accepts Medicare assignment must submit claims directly to Medicare on your behalf. They will be paid the agreed upon amount by Medicare, and you will pay any copayments or deductibles dictated by your plan.
If your doctor is non-participating, they may accept Medicare assignment for some services but not others. Even if they do agree to accept Medicare’s fee for some services, Medicare will only pay then 95% of the set assignment cost for a particular service.
If your provider does plan to work with Medicare, either the provider or you can submit a claim to Medicare, but you may have to pay the entire cost of the visit up front and wait for reimbursement. They can’t charge you for more than the amount approved by Medicare, but they can charge you above the Medicare-approved amount. This is called the limiting charge, and can be up to 15% more than Medicare-approved amount for non-participating providers.
What Does It Mean When a Provider Does Not Accept Medicare Assignment?
Providers who refuse Medicare assignment can still choose to accept Medicare’s set fees for certain services. These are called non-participating providers.
There are a number of providers who opt out of participating in Medicare altogether; they are referred to as “opt-out doctors”. This means they have signed an opt-out agreement with Medicare and can’t be paid by Medicare at all — even for services normally covered by Medicare. Opt-out contracts last for at least two years. Some of these providers may only offer services to patients who sign contracts.
You do not need to sign a contract with a private provider or use an opt-out provider. There are many options for alternative providers who accept Medicare. If you do choose an opt-out or private contract provider, you will have to pay the full cost of services on your own.
What Medicare coverage is right for my specific situation?
Do providers have to accept Medicare assignment?
No. Providers can choose to accept a full Medicare assignment, or accept assignment rates for some services as a non-participating provider. Doctors can also opt out of participating in Medicare altogether.
How much will I have to pay if my provider doesn't accept Medicare assignment?
Some providers that don’t accept assignment as a whole will accept assignment for some services. These are called non-participating providers. For these providers and providers who have completely opted out of Medicare, you will pay the majority of or the full amount for your care.
How do I submit a claim?
If you need to submit your own claim to Medicare, you can call 1-800-MEDICARE or use Form CMS-1490S .
Can my provider charge to submit a claim?
No. Providers are not allowed to charge to submit a claim to Medicare on your behalf.
Lower Costs with Assignment. Medicare.gov.
Fee Schedules . CMS.gov.
This website is operated by GoHealth, LLC., a licensed health insurance company. The website and its contents are for informational and educational purposes; helping people understand Medicare in a simple way. The purpose of this website is the solicitation of insurance. Contact will be made by a licensed insurance agent/producer or insurance company. Medicare Supplement insurance plans are not connected with or endorsed by the U.S. government or the federal Medicare program. Our mission is to help every American get better health insurance and save money. Any information we provide is limited to those plans we do offer in your area. Please contact Medicare.gov or 1-800-MEDICARE to get information on all of your options.
Let's see if you're missing out on Medicare savings.
We just need a few details.
Related Articles

What Is Medicare IRMAA?
What Is an IRMAA in Medicare?

Do All Doctors Accept Medicare?
What Does It Mean for a Doctor to Accept Medicare Assignment?

How to Report Medicare Fraud
Medicare Fraud Examples & How to Report Abuse

How to Change Your Address with Medicare
Reporting a Change of Address to Medicare

Can I Get Medicare if I’ve Never Worked?
Can You Get Medicare if You've Never Worked?

Why Are Some Medicare Advantage Plans Free?
Why Are Some Medicare Advantage Plans Free? $0 Premium Plans Explained

Am I Enrolled in Medicare?

When and How Do I Enroll?
When and How Do I Enroll in Medicare?

Medicare Frequently Asked Questions
Let’s see if you qualify for Medicare savings today!
Medicare Interactive Medicare answers at your fingertips -->
Participating, non-participating, and opt-out providers, outpatient provider services.
You must be logged in to bookmark pages.
Email Address * Required
Password * Required
Lost your password?
If you have Original Medicare , your Part B costs once you have met your deductible can vary depending on the type of provider you see. For cost purposes, there are three types of provider, meaning three different relationships a provider can have with Medicare . A provider’s type determines how much you will pay for Part B -covered services.
- These providers are required to submit a bill (file a claim ) to Medicare for care you receive. Medicare will process the bill and pay your provider directly for your care. If your provider does not file a claim for your care, there are troubleshooting steps to help resolve the problem .
- If you see a participating provider , you are responsible for paying a 20% coinsurance for Medicare-covered services.
- Certain providers, such as clinical social workers and physician assistants, must always take assignment if they accept Medicare.
- Non-participating providers can charge up to 15% more than Medicare’s approved amount for the cost of services you receive (known as the limiting charge ). This means you are responsible for up to 35% (20% coinsurance + 15% limiting charge) of Medicare’s approved amount for covered services.
- Some states may restrict the limiting charge when you see non-participating providers. For example, New York State’s limiting charge is set at 5%, instead of 15%, for most services. For more information, contact your State Health Insurance Assistance Program (SHIP) .
- If you pay the full cost of your care up front, your provider should still submit a bill to Medicare. Afterward, you should receive from Medicare a Medicare Summary Notice (MSN) and reimbursement for 80% of the Medicare-approved amount .
- The limiting charge rules do not apply to durable medical equipment (DME) suppliers . Be sure to learn about the different rules that apply when receiving services from a DME supplier .
- Medicare will not pay for care you receive from an opt-out provider (except in emergencies). You are responsible for the entire cost of your care.
- The provider must give you a private contract describing their charges and confirming that you understand you are responsible for the full cost of your care and that Medicare will not reimburse you.
- Opt-out providers do not bill Medicare for services you receive.
- Many psychiatrists opt out of Medicare.
Providers who take assignment should submit a bill to a Medicare Administrative Contractor (MAC) within one calendar year of the date you received care. If your provider misses the filing deadline, they cannot bill Medicare for the care they provided to you. However, they can still charge you a 20% coinsurance and any applicable deductible amount.
Be sure to ask your provider if they are participating, non-participating, or opt-out. You can also check by using Medicare’s Physician Compare tool .
Update your browser to view this website correctly. Update my browser now
Medicare Assignment: Understanding How It Works

Medicare assignment is a term used to describe how a healthcare provider agrees to accept the Medicare-approved amount. Depending on how you get your Medicare coverage, it could be essential to understand what it means and how it can affect you.
What is Medicare assignment?
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment.
You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare . You can see any doctor nationwide that accepts Medicare.
Understanding the differences between your cost and the difference between accepting Medicare and accepting Medicare assignment could be worth thousands of dollars.
Doctors that accept Medicare
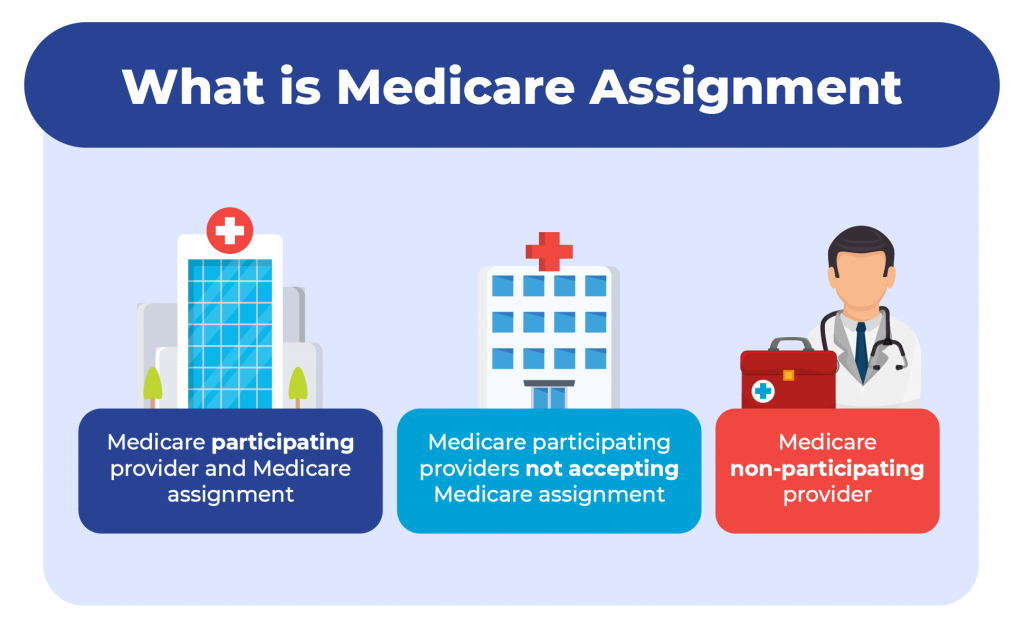
Your healthcare provider can fall into one of three categories:
Medicare participating provider and Medicare assignment
Medicare participating providers not accepting medicare assignment, medicare non-participating provider.
More than 97% of healthcare providers nationwide accept Medicare. Because of this, you can see almost any provider throughout the United States without needing referrals.
Let’s discuss the three categories the healthcare providers fall into.
Participating providers are doctors or healthcare providers who accept assignment. This means they will never charge more than the Medicare-approved amount.
Some non-participating providers accept Medicare but not Medicare assignment. This means you can see them the same way a provider accepts assignment.
You need to understand that since they don’t take the assigned amount, they can charge up to 15% more than the Medicare-approved amount.
Since Medicare will only pay the Medicare-approved amount, you’ll be responsible for these charges. The 15% overcharge is called an excess charge. A few states don’t allow or limit the amount or services of the excess charges. Only about 5% of providers charge excess charges.
Opt-out providers don’t accept Original Medicare, and these healthcare providers are in the minority in the United States. If healthcare providers don’t accept Medicare, they won’t be paid by Medicare.
This means choosing to see a provider that doesn’t accept Medicare will leave you responsible for 100% of what they charge you. These providers may be in-network for a Medicare Advantage plan in some cases.
Avoiding excess charges
Excess charges could be large or small depending on the service and the Medicare-approved amount. Avoiding these is easy. The simplest way is to ask your provider if they accept assignment before service.
If they say yes, they don’t issue excess charges. Or, on Medicare.gov , a provider search tool will allow you to look up your healthcare provider and show if they accept Medicare assignment or not.
Medicare Supplement and Medicare assignment
Medigap plans are additional insurance that helps cover your Medicare cost-share . If you are on specific plans, they’ll pay any extra costs from healthcare providers that accept Medicare but not Medicare assigned amount. Most Medicare Supplement plans don’t cover the excess charges.
The top three Medicare Supplement plans cover excess charges if you use a provider that accepts Medicare but not Medicare assignment.
Medicare Advantage and Medicare assignment
Medicare assignment does not affect Medicare Advantage plans since Medicare Advantage is just another way to receive your Medicare benefits. Since your Medicare Advantage plan handles your healthcare benefits, they set the terms.
Most Medicare Advantage plans require you to use network providers. If you go out of the network, you may pay more. If you’re on an HMO, you’d be responsible for the entire charge of the provider not being in the network.
Do all doctors accept Medicare Supplement plans?
All doctors that accept Original Medicare accept Medicare Supplement plans. Some doctors don’t accept Medicare. In this case, those doctors won’t accept Medicare Supplements.
Where can I find doctors who accept Medicare assignment?
Medicare has a physician finder tool that will show if a healthcare provider participates in Medicare and accepts Medicare assignments. Most doctors nationwide do accept assignment and therefore don’t charge the Part B excess charges.
Why do some doctors not accept Medicare?
Some doctors are called concierge doctors. These doctors don’t accept any insurance and require cash payments.
What is a Medicare assignment?
Accepting Medicare assignment means that the healthcare provider has agreed only to charge the approved amount for procedures and services.
What does it mean if a doctor does not accept Medicare assignment?
The doctor can change more than the Medicare-approved amount for procedures and services. You could be responsible for up to a 15% excess charge.
How many doctors accept Medicare assignment?
About 97% of doctors agree to accept assignment nationwide.
Is accepting Medicare the same as accepting Medicare assignment?
No. If a doctor accepts Medicare and accepts Medicare assigned amount, they’ll take what Medicare approves as payment in full.
If they accept Medicare but not Medicare assignment, they can charge an excess charge of up to 15% above the Medicare-approved amount. You could be responsible for this excess charge.
What is the Medicare-approved amount?
The Medicare-approved amount is Medicare’s charge as the maximum for any given medical service or procedure. Medicare has set forth an approved amount for every covered item or service.
Can doctors balance bill patients?
Yes, if that doctor is a Medicare participating provider not accepting Medicare assigned amount. The provider may bill up to 15% more than the Medicare-approved amount.

What happens if a doctor does not accept Medicare?
Doctors that don’t accept Medicare will require you to pay their full cost when using their services. Since these providers are non-participating, Medicare will not pay or reimburse for any services rendered.
Get help avoiding Medicare Part B excess charges
Whether it’s Medicare assignment, or anything related to Medicare, we have licensed agents that specialize in this field standing by to assist.
Give us a call, or fill out our online request form . We are happy to help answer questions, review options, and guide you through the process.
Related Articles
- What are Medicare Part B Excess Charges?
- How to File a Medicare Reimbursement Claim?
- Medicare Defined Coinsurance: How it Works?
- Welcome to Medicare Visit
- Guide to the Medicare Program

CALL NOW (833) 972-1339
- Individuals myGov is a simple and secure way to access online government services.
- PRODA Log in to access HPOS, Business Hub, Aged Care Provider Portal and a range of other government online services.
- Centrelink Business Online
- Child Support Business Online
Assignment of benefit
Signature requirements when a patient assigns their Medicare benefit to the servicing provider as full payment for health services.
on this page
Responsible person, patient unable to sign - sensitive issue, patient unable to sign - deceased, email agreement.
If a patient is unable to sign an assignment of benefit form , you can get a signature from any of the following:
- the patient’s parent
- the patient’s guardian
- another responsible person.
In the absence of a parent, guardian or responsible person, leave the ‘patient signature’ section blank.
Where the signature space is either left blank or another person signs on the patient’s behalf, the assignment of benefit form must include the following:
- the notation ‘Patient unable to sign’
- in the ‘Practitioner’s Use’ section, the reason why the patient was unable to sign. For example, use ‘unconscious’, ‘injured hand’ or ‘verbal consent obtained’.
For Medicare Easyclaim , consent from the patient, the patient’s parent, guardian or other responsible person is acceptable. Press the OK or YES button on the EFTPOS terminal.
‘Responsible person’ refers to an adult person accompanying the patient or in whose care the patient has been placed.
A responsible person can include someone who is any of the following:
- the parent or guardian
- holds power of attorney
- holds a guardianship order
- the next of kin.
This does not include the:
- health professional who rendered the service
- health professional’s staff
- hospital proprietor or staff
- aged care home proprietor or staff.
If you assess the reason a patient is unable to sign is of a highly sensitive nature, write in the ‘Practitioner’s Use’ section either:
- ‘due to medical condition’
- ‘due to sensitive condition’.
Only do this if revealing the reason would:
- mean an unacceptable breach of patient confidentiality
- unduly embarrass or distress the recipient of the patient’s copy of the assignment of benefit form.
This should not be routine practice. You can’t use ‘extenuating circumstances’ as a reason for no patient signature.
You and the patient must have entered into a bulk bill agreement at the time of service. This must include having the patient sign the assignment of benefit form.
If the patient has not signed the form, a signature from a responsible person is acceptable.
A responsible person can be either:
- the executor of the will
- an appointed administrator.
You must not write ‘patient deceased’ as a reason for not getting a signature on the assignment of benefit form.
Follow the steps in the table below when a patient assigns their right to a Medicare benefit to you by email.
For privacy reasons, don’t include the Medicare card number and provider number in the email.
This process complies with section 10 of the Electronic Transactions Act 1999 . This act outlines the steps to be taken for an electronic signature to be recognised.
It also meets the legal requirement of needing a patient signature to assign a Medicare benefit.
Example email
Dear Mr Jones (patient)
Details of the telehealth consultation to be claimed with Medicare:
Item number: 91822
Benefit amount: $78.05
Date and time of consultation: 01.07.2022 10:30 am
Patient name: Peter Jones
Health professional name: Jane Smith
If you (the patient) agree to the assignment of the Medicare benefit directly to the health professional (bulk bill), reply to this email including the following wording:
- ‘Yes, I agree to the assignment of the Medicare benefit directly to the health professional.’
- your (the patient’s) name or the name of parent or guardian (where a child is the patient and unable to sign).
Regards Dr Jane Smith
Privacy note: Your personal information is protected by law, including the Privacy Act 1988, and is collected by Services Australia for the assessment and administration of payments and services. This information is required to process your application or claim. Your information may be used by the agency, or given to other parties where you have agreed to that, or where it is required or authorised by law (including for the purpose of research or conducting investigations). You can get more information about the way in which the agency will manage your personal information, including our privacy policy .
Read more about Assignment of benefit and signature requirements for telehealth services .
This information was printed 20 May 2024 from https://www.servicesaustralia.gov.au/assignment-benefit-signature-requirements-and-exemptions . It may not include all of the relevant information on this topic. Please consider any relevant site notices at https://www.servicesaustralia.gov.au/site-notices when using this material.
Printed link references
Accessibility Report
[Enter personal and organization information through the Preferences > Identity dialog.]
The checker found no problems in this document.
- Needs manual check: 2
- Passed manually: 0
- Failed manually: 0
Detailed Report
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Balance Billing in Health Insurance
- How It Works
- When It Happens
- What to Do If You Get a Bill
- If You Know in Advance
Balance billing happens after you’ve paid your deductible , coinsurance or copayment and your insurance company has also paid everything it’s obligated to pay toward your medical bill. If there is still a balance owed on that bill and the healthcare provider or hospital expects you to pay that balance, you’re being balance billed.
This article will explain how balance billing works, and the rules designed to protect consumers from some instances of balance billing.
Is Balance Billing Legal or Not?
Sometimes it’s legal, and sometimes it isn’t; it depends on the circumstances.
Balance billing is generally illegal :
- When you have Medicare and you’re using a healthcare provider that accepts Medicare assignment .
- When you have Medicaid and your healthcare provider has an agreement with Medicaid.
- When your healthcare provider or hospital has a contract with your health plan and is billing you more than that contract allows.
- In emergencies (with the exception of ground ambulance charges), or situations in which you go to an in-network hospital but unknowingly receive services from an out-of-network provider.
In the first three cases, the agreement between the healthcare provider and Medicare, Medicaid, or your insurance company includes a clause that prohibits balance billing.
For example, when a hospital signs up with Medicare to see Medicare patients, it must agree to accept the Medicare negotiated rate, including your deductible and/or coinsurance payment, as payment in full. This is called accepting Medicare assignment .
And for the fourth case, the No Surprises Act , which took effect in 2022, protects you from "surprise" balance billing.
Balance billing is usually legal :
- When you choose to use a healthcare provider that doesn’t have a relationship or contract with your insurer (including ground ambulance charges, even after implementation of the No Surprises Act).
- When you’re getting services that aren’t covered by your health insurance policy, even if you’re getting those services from a provider that has a contract with your health plan.
The first case (a provider not having an insurer relationship) is common if you choose to seek care outside of your health insurance plan's network.
Depending on how your plan is structured, it may cover some out-of-network costs on your behalf. But the out-of-network provider is not obligated to accept your insurer's payment as payment in full. They can send you a bill for the remainder of the charges, even if it's more than your plan's out-of-network copay or deductible.
(Some health plans, particularly HMOs and EPOs , simply don't cover non-emergency out-of-network services at all, which means they would not cover even a portion of the bill if you choose to go outside the plan's network.)
Getting services that are not covered is a situation that may arise, for example, if you obtain cosmetic procedures that aren’t considered medically necessary, or fill a prescription for a drug that isn't on your health plan's formulary . You’ll be responsible for the entire bill, and your insurer will not require the medical provider to write off any portion of the bill—the claim would simply be rejected.
Prior to 2022, it was common for people to be balance billed in emergencies or by out-of-network providers that worked at in-network hospitals. In some states, state laws protected people from these types of surprise balance billing if they had state-regulated health plans.
But not all states had these protections. And the majority of people with employer-sponsored health insurance are covered under self-insured plans, which are not subject to state regulations. This is why the No Surprises Act was so necessary.
How Balance Billing Works
When you get care from a doctor, hospital, or other healthcare provider that isn’t part of your insurer’s provider network (or, if you have Medicare, from a provider that has opted out of Medicare altogether , which is rare but does apply in some cases ), that healthcare provider can charge you whatever they want to charge you (with the exception of emergencies or situations where you receive services from an out-of-network provider while you're at an in-network hospital).
Since your insurance company hasn’t negotiated any rates with that provider, they aren't bound by a contract with your health plan.
Medicare Limiting Charge
If you have Medicare and your healthcare provider is a nonparticipating provider but hasn't entirely opted out of Medicare, you can be charged up to 15% more than the allowable Medicare amount for the service you receive (some states impose a lower limit).
This 15% cap is known as the limiting charge, and it serves as a restriction on balance billing in some cases. If your healthcare provider has opted out of Medicare entirely, they cannot bill Medicare at all and you'll be responsible for the full cost of your visit.
If your health insurance company agrees to pay a percentage of your out-of-network care, the health plan doesn’t pay a percentage of what’s actually billed . Instead, it pays a percentage of what it says should have been billed, otherwise known as a reasonable and customary amount.
As you might guess, the reasonable and customary amount is usually lower than the amount you’re actually billed. The balance bill comes from the gap between what your insurer says is reasonable and customary, and what the healthcare provider or hospital actually charges.
Let's take a look at an example in which a person's health plan has 20% coinsurance for in-network hospitalization and 40% coinsurance for out-of-network hospitalization. And we're going to assume that the No Surprises Act does not apply (ie, that the person chooses to go to an out-of-network hospital, and it's not an emergency situation).
In this scenario, we'll assume that the person already met their $1,000 in-network deductible and $2,000 out-of-network deductible earlier in the year (so the example is only looking at coinsurance).
And we'll also assume that the health plan has a $6,000 maximum out-of-pocket for in-network care, but no cap on out-of-pocket costs for out-of-network care:
When Does Balance Billing Happen?
In the United States, balance billing usually happens when you get care from a healthcare provider or hospital that isn’t part of your health insurance company’s provider network or doesn’t accept Medicare or Medicaid rates as payment in full.
If you have Medicare and your healthcare provider has opted out of Medicare entirely, you're responsible for paying the entire bill yourself. But if your healthcare provider hasn't opted out but just doesn't accept assignment with Medicare (ie, doesn't accept the amount Medicare pays as payment in full), you could be balance billed up to 15% more than Medicare's allowable charge, in addition to your regular deductible and/or coinsurance payment.
Surprise Balance Billing
Receiving care from an out-of-network provider can happen unexpectedly, even when you try to stay in-network. This can happen in emergency situations—when you may simply have no say in where you're treated or no time to get to an in-network facility—or when you're treated by out-of-network providers who work at in-network facilities.
For example, you go to an in-network hospital, but the radiologist who reads your X-rays isn’t in-network. The bill from the hospital reflects the in-network rate and isn't subject to balance billing, but the radiologist doesn’t have a contract with your insurer, so they can charge you whatever they want. And prior to 2022, they were allowed to send you a balance bill unless state law prohibited it.
Similar situations could arise with:
- Anesthesiologists
- Pathologists (laboratory doctors)
- Neonatologists (doctors for newborns)
- Intensivists (doctors who specialize in ICU patients)
- Hospitalists (doctors who specialize in hospitalized patients)
- Radiologists (doctors who interpret X-rays and scans)
- Ambulance services to get you to the hospital, especially air ambulance services, where balance billing was frighteningly common
- Durable medical equipment suppliers (companies that provide the crutches, braces, wheelchairs, etc. that people need after a medical procedure)
These "surprise" balance billing situations were particularly infuriating for patients, who tended to believe that as long as they had selected an in-network medical facility, all of their care would be covered under the in-network terms of their health plan.
To address this situation, many states enacted consumer protection rules that limited surprise balance billing prior to 2022. But as noted above, these state rules don't protect people with self-insured employer-sponsored health plans, which cover the majority of people who have employer-sponsored coverage.
There had long been broad bipartisan support for the idea that patients shouldn't have to pay additional, unexpected charges just because they needed emergency care or inadvertently received care from a provider outside their network, despite the fact that they had purposely chosen an in-network medical facility. There was disagreement, however, in terms of how these situations should be handled—should the insurer have to pay more, or should the out-of-network provider have to accept lower payments? This disagreement derailed numerous attempts at federal legislation to address surprise balance billing.
But the Consolidated Appropriations Act, 2021, which was enacted in December 2020, included broad provisions (known as the No Surprises Act) to protect consumers from surprise balance billing as of 2022. The law applies to both self-insured and fully-insured plans, including grandfathered plans, employer-sponsored plans, and individual market plans.
It protects consumers from surprise balance billing charges in nearly all emergency situations and situations when out-of-network providers offer services at in-network facilities, but there's a notable exception for ground ambulance charges.
This is still a concern, as ground ambulances are among the medical providers most likely to balance bill patients and least likely to be in-network, and patients typically have no say in what ambulance provider comes to their rescue in an emergency situation. But other than ground ambulances, patients are no longer subject to surprise balance bills as of 2022.
The No Surprises Act did call for the creation of a committee to study ground ambulance charges and make recommendations for future legislation to protect consumers. The Biden Administration announced the members of that committee in late 2022, and the committee began holding meetings in May 2023.
Balance billing continues to be allowed in other situations (for example, the patient simply chooses to use an out-of-network provider). Balance billing can also still occur when you’re using an in-network provider, but you’re getting a service that isn’t covered by your health insurance. Since an insurer doesn’t negotiate rates for services it doesn’t cover, you’re not protected by that insurer-negotiated discount. The provider can charge whatever they want, and you’re responsible for the entire bill.
It is important to note that while the No Surprises Act prohibits balance bills from out-of-network working at in-network facilities, the final rule for implementation of the law defines facilities as "hospitals, hospital outpatient departments, critical access hospitals, and ambulatory surgical centers." Other medical facilities are not covered by the consumer protections in the No Surprises Act.
Balance billing doesn’t usually happen with in-network providers or providers that accept Medicare assignment . That's because if they balance bill you, they’re violating the terms of their contract with your insurer or Medicare. They could lose the contract, face fines, suffer severe penalties, and even face criminal charges in some cases.
If You Get an Unexpected Balance Bill
Receiving a balance bill is a stressful experience, especially if you weren't expecting it. You've already paid your deductible and coinsurance and then you receive a substantial additional bill—what do you do next?
First, you'll want to try to figure out whether the balance bill is legal or not. If the medical provider is in-network with your insurance company, or you have Medicare or Medicaid and your provider accepts that coverage, it's possible that the balance bill was a mistake (or, in rare cases, outright fraud).
And if your situation is covered under the No Surprises Act (ie, an emergency, or an out-of-network provider who treated you at an in-network facility), you should not be subject to a balance bill. So be sure you understand what charges you're actually responsible for before paying any medical bills.
If you think that the balance bill was an error, contact the medical provider's billing office and ask questions. Keep a record of what they tell you so that you can appeal to your state's insurance department if necessary.
If the medical provider's office clarifies that the balance bill was not an error and that you do indeed owe the money, consider the situation—did you make a mistake and select an out-of-network healthcare provider? Or was the service not covered by your health plan?
If you went to an in-network facility for a non-emergency, did you waive your rights under the No Surprises Act (NSA) and then receive a balance bill from an out-of-network provider? This is still possible in limited circumstances, but you would have had to sign a document indicating that you had waived your NSA protections.
Negotiate With the Medical Office
If you've received a legitimate balance bill, you can ask the medical office to cut you some slack. They may be willing to agree to a payment plan and not send your bill to collections as long as you continue to make payments.
Or they may be willing to reduce your total bill if you agree to pay a certain amount upfront. Be respectful and polite, but explain that the bill caught you off guard. And if it's causing you significant financial hardship, explain that too.
The healthcare provider's office would rather receive at least a portion of the billed amount rather than having to wait while the bill is sent to collections. So the sooner you reach out to them, the better.
Negotiate With Your Insurance Company
You can also negotiate with your insurer. If your insurer has already paid the out-of-network rate on the reasonable and customary charge, you’ll have difficulty filing a formal appeal since the insurer didn’t actually deny your claim . It paid your claim, but at the out-of-network rate.
Instead, request a reconsideration. You want your insurance company to reconsider the decision to cover this as out-of-network care , and instead cover it as in-network care. You’ll have more luck with this approach if you had a compelling medical or logistical reason for choosing an out-of-network provider .
If you feel like you’ve been treated unfairly by your insurance company, follow your health plan’s internal complaint resolution process.
You can get information about your insurer’s complaint resolution process in your benefits handbook or from your human resources department. If this doesn’t resolve the problem, you can complain to your state’s insurance department.
- Learn more about your internal and external appeal rights.
- Find contact information for your Department of Insurance using this resource .
If your health plan is self-funded , meaning your employer is the entity actually paying the medical bills even though an insurance company may administer the plan, then your health plan won't fall under the jurisdiction of your state’s department of insurance.
Self-funded plans are instead regulated by the Department of Labor’s Employee Benefit Services Administration. Get more information from the EBSA’s consumer assistance web page or by calling an EBSA benefits advisor at 1-866-444-3272.
If You Know You’ll Be Legally Balance Billed
If you know in advance that you’ll be using an out-of-network provider or a provider that doesn’t accept Medicare assignment, you have some options. However, none of them are easy and all require some negotiating.
Ask for an estimate of the provider’s charges. Next, ask your insurer what they consider the reasonable and customary charge for this service to be. Getting an answer to this might be tough, but be persistent.
Once you have estimates of what your provider will charge and what your insurance company will pay, you’ll know how far apart the numbers are and what your financial risk is. With this information, you can narrow the gap. There are only two ways to do this: Get your provider to charge less or get your insurer to pay more.
Ask the provider if he or she will accept your insurance company’s reasonable and customary rate as payment in full. If so, get the agreement in writing, including a no-balance-billing clause.
If your provider won’t accept the reasonable and customary rate as payment in full, start working on your insurer. Ask your insurer to increase the amount they’re calling reasonable and customary for this particular case.
Present a convincing argument by pointing out why your case is more complicated, difficult, or time-consuming to treat than the average case the insurer bases its reasonable and customary charge on.
Single-Case Contract
Another option is to ask your insurer to negotiate a single-case contract with your out-of-network provider for this specific service.
A single-case contract is more likely to be approved if the provider is offering specialized services that aren't available from locally-available in-network providers, or if the provider can make a case to the insurer that the services they're providing will end up being less expensive in the long-run for the insurance company.
Sometimes they can agree upon a single-case contract for the amount your insurer usually pays its in-network providers. Sometimes they’ll agree on a single-case contract at the discount rate your healthcare provider accepts from the insurance companies she’s already in-network with.
Or, sometimes they can agree on a single-case contract for a percentage of the provider’s billed charges. Whatever the agreement, make sure it includes a no-balance-billing clause.
Ask for the In-Network Coinsurance Rate
If all of these options fail, you can ask your insurer to cover this out-of-network care using your in-network coinsurance rate. While this won’t prevent balance billing, at least your insurer will be paying a higher percentage of the bill since your coinsurance for in-network care is lower than for out-of-network care.
If you pursue this option, have a convincing argument as to why the insurer should treat this as in-network. For example, there are no local in-network surgeons experienced in your particular surgical procedure, or the complication rates of the in-network surgeons are significantly higher than those of your out-of-network surgeon.
Balance billing refers to the additional bill that an out-of-network medical provider can send to a patient, in addition to the person's normal cost-sharing and the payments (if any) made by their health plan. The No Surprises Act provides broad consumer protections against "surprise" balance billing as of 2022.
A Word From Verywell
Try to prevent balance billing by staying in-network, making sure your insurance company covers the services you’re getting, and complying with any pre-authorization requirements. But rest assured that the No Surprises Act provides broad protections against surprise balance billing.
This means you won't be subject to balance bills in emergencies (except for ground ambulance charges, which can still generate surprise balance bills) or in situations where you go to an in-network hospital but unknowingly receive care from an out-of-network provider.
Congress.gov. H.R.133—Consolidated Appropriations Act, 2021 . Enacted December 27, 2021.
Kona M. The Commonwealth Fund. State balance billing protections . April 20, 2020.
Data.CMS.gov. Opt Out Affidavits .
Chhabra, Karan; Schulman, Kevin A.; Richman, Barak D. Health Affairs. Are Air Ambulances Truly Flying Out Of Reach? Surprise-Billing Policy And The Airline Deregulation Act . October 17, 2019.
Kaiser Family Foundation. 2022 Employer Health Benefits Survey .
Centers for Medicare and Medicaid Services. Members of New Federal Advisory Committee Named to Help Improve Ground Ambulance Disclosure and Billing Practices for Consumers . December 13, 2022.
Centers for Medicare and Medicaid Services. Advisory Committee on Ground Ambulance and Patient Billing (GAPB) .
Internal Revenue Service; Employee Benefits Security Administration; Health and Human Services Department. Requirements Related to Surprise Billing . August 26, 2022.
National Conference of State Legislatures. States Tackling "Balance Billing" Issue . July 2017.
By Elizabeth Davis, RN Elizabeth Davis, RN, is a health insurance expert and patient liaison. She's held board certifications in emergency nursing and infusion nursing.

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
What should I do if I get a call claiming there is a problem with my Social Security number or account?
Sign up for Medicare
Medicare is our country’s health insurance program for people age 65 or older. You’ll sign up for Medicare Part A and Part B through Social Security, so you can make both retirement and Medicare choices and withhold any premiums from your benefit payments.
If you’re under age 65, you may be eligible for Medicare if you have permanent kidney failure or if you receive Disability benefits. Supplemental Security Income (SSI) does not qualify you for Medicare on its own. Even if you receive SSI, you must meet one of the other requirements to qualify.
Information you'll need to provide
Basic information about yourself
- Social Security number
- Where you were born (city, state, country)
Health insurance information
- Start and end dates for any current group health plans
- Start and end dates for any group health plans after age 65
For Part B only
- Valid email address
- Your existing Medicare number
If you're 65 or older, you can enroll online for Parts A and B, or Part A only. You can delay Part B if you're already covered through an employer group health plan.
The application is for retirement benefits and Medicare, or Medicare only.
- Apply online
Sign up for Part B only
If you've previously declined or never signed up for Part B, you can sign up for Part B only.
- Get started
Sign up for other parts of Medicare
Review and sign up for Medicare Advantage and drug plans on Medicare.gov.
Sign up if you have end-stage renal disease (ESRD)
You can get Medicare if you have ESRD. Call 800-772-1213 and tell the representative you want to apply for Medicare because you have ESRD.
Other ways to complete this task
Call +1 800-772-1213
Tell the representative you want to sign up for Medicare Parts A and B, or Part A only.
Call TTY +1 800-325-0778 if you're deaf or hard of hearing.
After you submit a request
Check the status of your application.
The Federal Register
The daily journal of the united states government, request access.
Due to aggressive automated scraping of FederalRegister.gov and eCFR.gov, programmatic access to these sites is limited to access to our extensive developer APIs.
If you are human user receiving this message, we can add your IP address to a set of IPs that can access FederalRegister.gov & eCFR.gov; complete the CAPTCHA (bot test) below and click "Request Access". This process will be necessary for each IP address you wish to access the site from, requests are valid for approximately one quarter (three months) after which the process may need to be repeated.
An official website of the United States government.
If you want to request a wider IP range, first request access for your current IP, and then use the "Site Feedback" button found in the lower left-hand side to make the request.

IMAGES
VIDEO
COMMENTS
All providers who accept assignment must submit claims directly to Medicare, which pays 80 percent of the approved cost for the service and will bill you the remaining 20 percent. You can get some preventive services and screenings, such as mammograms and colonoscopies, without paying a deductible or coinsurance if the provider accepts assignment.
The assignment of benefits is when the insured authorizes Medicare to reimburse the provider directly. In return, the provider agrees to accept the Medicare charge as the full charge for services. Non-participating providers can accept assignments on an individual claims basis.
If your doctor, provider, or supplier doesn't accept assignment: You might have to pay the full amount at the time of service. They should submit a claim to Medicare for any Medicare-covered services they give you, and they can't charge you for submitting a claim. If they refuse to submit a Medicare claim, you can submit your own claim to ...
What is Medicare Assignment. Medicare assignment is an agreement by your doctor or other healthcare providers to accept the Medicare-approved amount as the full cost for a covered service. Providers who "accept assignment" bill Medicare directly for Part B-covered services and cannot charge you more than the applicable deductible and ...
A Medicare assignment provider agrees to charge no more than the Medicare-approved price for a specific service. The doctor or other provider also agrees to bill Medicare directly, rather than charging the patient on the day of service. This means that if you go to a Medicare-participating provider, you won't usually have to pay anything at the time of service.
Summary: Medicare Assignment is an agreement between healthcare providers and Medicare, where providers accept the Medicare-approved amount as full payment, preventing them from charging beneficiaries extra. This benefits Medicare beneficiaries by controlling their costs and ensuring they only pay deductibles and copayments.
Doctors that take Medicare can sign a contract to accept assignment for all Medicare services, or be a non-participating provider that accepts assignment for some services but not all. A medical provider that accepts Medicare assignment must submit claims directly to Medicare on your behalf. They will be paid the agreed upon amount by Medicare ...
Participating providers accept Medicare and always take assignment. Taking assignment means that the provider accepts Medicare's approved amount for health care services as full payment. These providers are required to submit a bill (file a claim) to Medicare for care you receive. Medicare will process the bill and pay your provider directly ...
1. Participating providers, or those who accept Medicare assignment. These providers have an agreement with Medicare to accept the Medicare-approved amount as full payment for their services. You don't have to pay anything other than a copay or coinsurance (depending on your plan) at the time of your visit.
"Your Medicare Benefits" isn't a legal document. Official Medicare Program legal guidance is contained in the relevant statutes, regulations, and rulings. 3 ... Assignment is an agreement by your doctor, provider, or other supplier to be paid directly by Medicare, to accept the payment amount Medicare approves ...
Non-assignment of Benefits. Non-assigned is the method of reimbursement a physician/supplier has when choosing to not accept assignment of benefits. Under this method, a non-participating provider is the only provider that can file a claim as non-assigned. When the provider does not accept assignment, the Medicare payment will be made directly ...
In addition, the beneficiary does not need to assign benefits in any circumstance where assignment is mandatory. Thus, in most cases, a signed assignment of benefits is not needed. Resource. CMS Internet Only Manual, Publication 100-04, Medicare Claims Processing Manual, Chapter 1, Section 50.1.6
Medicare assignment, or Medicare assignment of benefits, is the process in which a Medicare beneficiary authorizes Medicare to directly reimburse health care providers for services. To ensure all services are charged at Medicare-determined rates, recipients should verify whether their primary physicians fall under the accept assignment ...
Medicare sets a fixed cost to pay for every benefit they cover. This amount is called Medicare assignment. You have the largest healthcare provider network with over 800,000 providers nationwide on Original Medicare. You can see any doctor nationwide that accepts Medicare. Understanding the differences between your cost and the difference ...
Participating physicians/practitioners and suppliers sign an agreement with Medicare to accept assignment of Medicare benefits for all Medicare patients. A claim for which a beneficiary elects to assign his/her benefits under a Medigap policy to a participating physician/practitioner and supplier is called a "mandated Medigap transfer."
Medicare assignment of benefits is a way to identify providers who accept Medicare benefits and those who do not. These providers can be individual physicians, whole hospitals or various suppliers such as physical therapists who work independently.
You must not write 'patient deceased' as a reason for not getting a signature on the assignment of benefit form. Email agreement. Follow the steps in the table below when a patient assigns their right to a Medicare benefit to you by email. For privacy reasons, don't include the Medicare card number and provider number in the email.
terminate a reassignment of Medicare benefits after enrollment in the Medicare program or make a change in their reassignment of Medicare benefit information using either: • The Internet-based Provider Enrollment, Chain and Ownership System (PECOS), or • The paper CMS-855R application. Be sure you are using the most current version.
Processing the CMS-855R Medicare Enrollment Application - Reassignment of Benefits Page 1 . Processing the CMS-855R Medicare Enrollment Application - Reassignment of Benefits. Disclaimer: The information contained in this guide is to assist providers/suppliers in completing the CMS -855R application and MACs in processing the CMS-855R application.
Visit Medicare.gov, or call 1-800-MEDICARE (1-800-633-4227) to get the most current information. TTY users can call 1-877-486-2048. "Medicare & Your Mental Health Benefits" isn't a legal document. Oficial Medicare Program legal guidance is contained in the relevant statutes, regulations, and rulings.
But if your healthcare provider hasn't opted out but just doesn't accept assignment with Medicare (ie, doesn't accept the amount Medicare pays as payment in full), you could be balance billed up to 15% more than Medicare's allowable charge, in addition to your regular deductible and/or coinsurance payment. ... Employee Benefits Security ...
Part D, which covers prescription drug costs, also has a monthly charge that varies depending on which plan you choose; the average Part D total premium for 2024 will be about $55.50 per month in ...
Accepting assignment on a Medicare claim can be a definite advantage to both the physician/supplier and the beneficiary. The Medicare claim itself constitutes a legal agreement between the physician/supplier and the beneficiary which carries specific terms with it that must be observed. ... Assignment of benefits applies to all participating ...
1. Participating providers, or those who accept Medicare assignment. These providers have an agreement with Medicare to accept the Medicare-approved amount as full payment for their services. You don't have to pay anything other than a copay or coinsurance (depending on your plan) at the time of your visit.
Medicare is our country's health insurance program for people age 65 or older. You'll sign up for Medicare Part A and Part B through Social Security, so you can make both retirement and Medicare choices and withhold any premiums from your benefit payments.
Joe Biden sounded more like a professional wrestler than a president when he issued a vertical video social media debate challenge to his rival Wednesday morning.
A federal government website managed and paid for by the U.S. Centers for Medicare and Medicaid Services. 7500 Security Boulevard, Baltimore, MD 21244
Medicare Part B coverage includes the surgeon's fees for performing the kidney transplant procedure and perioperative care. Medicare Part B also covers physician services for the living kidney donor without regard to whether the service would otherwise be covered by Start Printed Page 43528 Medicare. Part A and Part B share responsibility for ...