- Publications
- Conferences & Events
- Professional Learning
- Science Standards
- Awards & Competitions
- Instructional Materials
- Free Resources
- American Rescue Plan
- For Preservice Teachers
- NCCSTS Case Collection
- Partner Jobs in Education
- Interactive eBooks+
- Digital Catalog
- Regional Product Representatives
- e-Newsletters
- Bestselling Books
- Latest Books
- Popular Book Series
- Prospective Authors
- Web Seminars
- Exhibits & Sponsorship
- Conference Reviewers
- National Conference • Denver 24
- Leaders Institute 2024
- National Conference • New Orleans 24
- Submit a Proposal
- Latest Resources
- Professional Learning Units & Courses
- For Districts
- Online Course Providers
- Schools & Districts
- College Professors & Students
- The Standards
- Teachers and Admin
- eCYBERMISSION
- Toshiba/NSTA ExploraVision
- Junior Science & Humanities Symposium
- Teaching Awards
- Climate Change
- Earth & Space Science
- New Science Teachers
- Early Childhood
- Middle School
- High School
- Postsecondary
- Informal Education
- Journal Articles
- Lesson Plans
- e-newsletters
- Science & Children
- Science Scope
- The Science Teacher
- Journal of College Sci. Teaching
- Connected Science Learning
- NSTA Reports
- Next-Gen Navigator
- Science Update
- Teacher Tip Tuesday
- Trans. Sci. Learning

MyNSTA Community
- My Collections
Asthma Attack!
By Hollie L. Leavitt
Share Start a Discussion
This interrupted case study follows the progress of a pediatric patient who experiences an acute asthma exacerbation brought on by an environmental trigger. Students completing the case will synthesize their understanding of respiratory system anatomy and physiology with the clinical treatment of an obstructive lung disorder. Topics reviewed include bronchoconstriction and dilation, pulmonary ventilation, air flow, gas exchange, respiratory volumes, the oxygen-hemoglobin dissociation curve, pCO2, pO2, and the effects of medications used to treat asthma. Students should have an understanding of the respiratory system before starting the case and thus it is best used at the end of the respiratory system unit as a way for students to apply what they have learned to a real-world situation. The case was developed for an anatomy and physiology class for majors taught through the “flipped” method at a community college, but would also work well for students in a pathophysiology course or in pre-professional programs in health care. It may also be suitable for high school students in an advanced or honors anatomy and physiology program.
Download Case
Date Posted
- Describe the anatomy of the respiratory passageways.
- Understand respiratory system function including air flow and gas exchange.
- Determine the effects of bronchoconstriction and bronchodilation on air flow.
- Describe the pressure gradients required for pulmonary ventilation.
- Understand respiratory volumes and how they are used clinically to assess disease.
- Know how to use the oxygen-hemoglobin dissociation curve.
- Predict how pCO2 and pO2 are affected by an obstructive lung disease.
- Describe pathological changes in the airways and environmental factors that can lead to an acute asthma exacerbation.
- Understand the effects of some of the medications used to treat asthma.
asthma; respiratory anatomy; respiratory physiology; respiratory system; lung pathology; respiratory volumes; oxygen-hemoglobin dissociation;
Subject Headings
EDUCATIONAL LEVEL
High school, Undergraduate lower division, Undergraduate upper division, Professional (degree program)
TOPICAL AREAS
TYPE/METHODS
Teaching Notes & Answer Key
Teaching notes.
Case teaching notes are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Teaching notes are intended to help teachers select and adopt a case. They typically include a summary of the case, teaching objectives, information about the intended audience, details about how the case may be taught, and a list of references and resources.
Download Notes
Answer Keys are protected and access to them is limited to paid subscribed instructors. To become a paid subscriber, purchase a subscription here .
Download Answer Key
Materials & Media
Supplemental materials.
Normal 0 false false false EN-US X-NONE X-NONE MicrosoftInternetExplorer4
The PowerPoint presentation below includes optional slides for in-class review before presenting the case.
- asthma_attack_sup.ppt (~634 KB)
- How Does Asthma Work? This animated video gives an overview of asthma, including why people get it, and how it can be deadly. Running time: 5:09 min. Produced by TED-Ed, 2017.
You may also like
Web Seminar
Join us on Tuesday, June 4, 2024, from 7:00 PM to 8:30 PM ET, to learn about the free lesson plans and storyline units designed for high school studen...
Join us on Thursday, October 24, 2024, from 7:00 PM to 8:00 PM ET, to learn about all NSTA Teacher Awards available and how to apply.Did you come up w...
Join us on Thursday, September 19, 2024, from 7:00 PM to 8:00 PM ET, to learn about NSTA election process for new and interested members of the Board ...
- No category
Respiratory Case Study - Asthma Attack - Student handout

Related documents
Study collections
Add this document to collection(s).
You can add this document to your study collection(s)
Add this document to saved
You can add this document to your saved list
Suggest us how to improve StudyLib
(For complaints, use another form )
Input it if you want to receive answer
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 16 October 2014
A woman with asthma: a whole systems approach to supporting self-management
- Hilary Pinnock 1 ,
- Elisabeth Ehrlich 1 ,
- Gaylor Hoskins 2 &
- Ron Tomlins 3
npj Primary Care Respiratory Medicine volume 24 , Article number: 14063 ( 2014 ) Cite this article
16k Accesses
2 Citations
6 Altmetric
Metrics details
- Health care
A 35-year-old lady attends for review of her asthma following an acute exacerbation. There is an extensive evidence base for supported self-management for people living with asthma, and international and national guidelines emphasise the importance of providing a written asthma action plan. Effective implementation of this recommendation for the lady in this case study is considered from the perspective of a patient, healthcare professional, and the organisation. The patient emphasises the importance of developing a partnership based on honesty and trust, the need for adherence to monitoring and regular treatment, and involvement of family support. The professional considers the provision of asthma self-management in the context of a structured review, with a focus on a self-management discussion which elicits the patient’s goals and preferences. The organisation has a crucial role in promoting, enabling and providing resources to support professionals to provide self-management. The patient’s asthma control was assessed and management optimised in two structured reviews. Her goal was to avoid disruption to her work and her personalised action plan focused on achieving that goal.
Similar content being viewed by others

Determinants of behaviour and their efficacy as targets of behavioural change interventions

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Key recommendations for primary care from the 2022 Global Initiative for Asthma (GINA) update
A 35-year-old sales representative attends the practice for an asthma review. Her medical record notes that she has had asthma since childhood, and although for many months of the year her asthma is well controlled (when she often reduces or stops her inhaled steroids), she experiences one or two exacerbations a year requiring oral steroids. These are usually triggered by a viral upper respiratory infection, though last summer when the pollen count was particularly high she became tight chested and wheezy for a couple of weeks.
Her regular prescription is for fluticasone 100 mcg twice a day, and salbutamol as required. She has a young family and a busy lifestyle so does not often manage to find time to attend the asthma clinic. A few weeks previously, an asthma attack had interfered with some important work-related travel, and she has attended the clinic on this occasion to ask about how this can be managed better in the future. There is no record of her having been given an asthma action plan.
What do we know about asthma self-management? The academic perspective
Supported self-management reduces asthma morbidity.
The lady in this case study is struggling to maintain control of her asthma within the context of her busy professional and domestic life. The recent unfortunate experience which triggered this consultation offers a rare opportunity to engage with her and discuss how she can manage her asthma better. It behoves the clinician whom she is seeing (regardless of whether this is in a dedicated asthma clinic or an appointment in a routine general practice surgery) to grasp the opportunity and discuss self-management and provide her with a (written) personalised asthma action plan (PAAP).
The healthcare professional advising the lady is likely to be aware that international and national guidelines emphasise the importance of supporting self-management. 1 – 4 There is an extensive evidence base for asthma self-management: a recent synthesis identified 22 systematic reviews summarising data from 260 randomised controlled trials encompassing a broad range of demographic, clinical and healthcare contexts, which concluded that asthma self-management reduces emergency use of healthcare resources, including emergency department visits, hospital admissions and unscheduled consultations and improves markers of asthma control, including reduced symptoms and days off work, and improves quality of life. 1 , 2 , 5 – 12 Health economic analysis suggests that it is not only clinically effective, but also a cost-effective intervention. 13
Personalised asthma action plans
Key features of effective self-management approaches are:
Self-management education should be reinforced by provision of a (written) PAAP which reminds patients of their regular treatment, how to monitor and recognise that control is deteriorating and the action they should take. 14 – 16 As an adult, our patient can choose whether she wishes to monitor her control with symptoms or by recording peak flows (or a combination of both). 6 , 8 , 9 , 14 Symptom-based monitoring is generally better in children. 15 , 16
Plans should have between two and three action points including emergency doses of reliever medication; increasing low dose (or recommencing) inhaled steroids; or starting a course of oral steroids according to severity of the exacerbation. 14
Personalisation of the action plan is crucial. Focussing specifically on what actions she could take to prevent a repetition of the recent attack is likely to engage her interest. Not all patients will wish to start oral steroids without advice from a healthcare professional, though with her busy lifestyle and travel our patient is likely to be keen to have an emergency supply of prednisolone. Mobile technology has the potential to support self-management, 17 , 18 though a recent systematic review concluded that none of the currently available smart phone ‘apps’ were fit for purpose. 19
Identification and avoidance of her triggers is important. As pollen seems to be a trigger, management of allergic rhinitis needs to be discussed (and included in her action plan): she may benefit from regular use of a nasal steroid spray during the season. 20
Self-management as recommended by guidelines, 1 , 2 focuses narrowly on adherence to medication/monitoring and the early recognition/remediation of exacerbations, summarised in (written) PAAPs. Patients, however, may want to discuss how to reduce the impact of asthma on their life more generally, 21 including non-pharmacological approaches.
Supported self-management
The impact is greater if self-management education is delivered within a comprehensive programme of accessible, proactive asthma care, 22 and needs to be supported by ongoing regular review. 6 With her busy lifestyle, our patient may be reluctant to attend follow-up appointments, and once her asthma is controlled it may be possible to make convenient arrangements for professional review perhaps by telephone, 23 , 24 or e-mail. Flexible access to professional advice (e.g., utilising diverse modes of consultation) is an important component of supporting self-management. 25
The challenge of implementation
Implementation of self-management, however, remains poor in routine clinical practice. A recent Asthma UK web-survey estimated that only 24% of people with asthma in the UK currently have a PAAP, 26 with similar figures from Sweden 27 and Australia. 28 The general practitioner may feel that they do not have time to discuss self-management in a routine surgery appointment, or may not have a supply of paper-based PAAPs readily available. 29 However, as our patient rarely finds time to attend the practice, inviting her to make an appointment for a future clinic is likely to be unsuccessful and the opportunity to provide the help she needs will be missed.
The solution will need a whole systems approach
A systematic meta-review of implementing supported self-management in long-term conditions (including asthma) concluded that effective implementation was multifaceted and multidisciplinary; engaging patients, training and motivating professionals within the context of an organisation which actively supported self-management. 5 This whole systems approach considers that although patient education, professional training and organisational support are all essential components of successful support, they are rarely effective in isolation. 30 A systematic review of interventions that promote provision/use of PAAPs highlighted the importance of organisational systems (e.g., sending blank PAAPs with recall reminders). 31 A patient offers her perspective ( Box 1 ), a healthcare professional considers the clinical challenge, and the challenges are discussed from an organisational perspective.
Box 1: What self-management help should this lady expect from her general practitioner or asthma nurse? The patient’s perspective
The first priority is that the patient is reassured that her condition can be managed successfully both in the short and the long term. A good working relationship with the health professional is essential to achieve this outcome. Developing trust between patient and healthcare professional is more likely to lead to the patient following the PAAP on a long-term basis.
A review of all medication and possible alternative treatments should be discussed. The patient needs to understand why any changes are being made and when she can expect to see improvements in her condition. Be honest, as sometimes it will be necessary to adjust dosages before benefits are experienced. Be positive. ‘There are a number of things we can do to try to reduce the impact of asthma on your daily life’. ‘Preventer treatment can protect against the effect of pollen in the hay fever season’. If possible, the same healthcare professional should see the patient at all follow-up appointments as this builds trust and a feeling of working together to achieve the aim of better self-management.
Is the healthcare professional sure that the patient knows how to take her medication and that it is taken at the same time each day? The patient needs to understand the benefit of such a routine. Medication taken regularly at the same time each day is part of any self-management regime. If the patient is unused to taking medication at the same time each day then keeping a record on paper or with an electronic device could help. Possibly the patient could be encouraged to set up a system of reminders by text or smartphone.
Some people find having a peak flow meter useful. Knowing one's usual reading means that any fall can act as an early warning to put the PAAP into action. Patients need to be proactive here and take responsibility.
Ongoing support is essential for this patient to ensure that she takes her medication appropriately. Someone needs to be available to answer questions and provide encouragement. This could be a doctor or a nurse or a pharmacist. Again, this is an example of the partnership needed to achieve good asthma control.
It would also be useful at a future appointment to discuss the patient’s lifestyle and work with her to reduce her stress. Feeling better would allow her to take simple steps such as taking exercise. It would also be helpful if all members of her family understood how to help her. Even young children can do this.
From personal experience some people know how beneficial it is to feel they are in a partnership with their local practice and pharmacy. Being proactive produces dividends in asthma control.
What are the clinical challenges for the healthcare professional in providing self-management support?
Due to the variable nature of asthma, a long-standing history may mean that the frequency and severity of symptoms, as well as what triggers them, may have changed over time. 32 Exacerbations requiring oral steroids, interrupting periods of ‘stability’, indicate the need for re-assessment of the patient’s clinical as well as educational needs. The patient’s perception of stability may be at odds with the clinical definition 1 , 33 —a check on the number of short-acting bronchodilator inhalers the patient has used over a specific period of time is a good indication of control. 34 Assessment of asthma control should be carried out using objective tools such as the Asthma Control Test or the Royal College of Physicians three questions. 35 , 36 However, it is important to remember that these assessment tools are not an end in themselves but should be a springboard for further discussion on the nature and pattern of symptoms. Balancing work with family can often make it difficult to find the time to attend a review of asthma particularly when the patient feels well. The practice should consider utilising other means of communication to maintain contact with patients, encouraging them to come in when a problem is highlighted. 37 , 38 Asthma guidelines advocate a structured approach to ensure the patient is reviewed regularly and recommend a detailed assessment to enable development of an appropriate patient-centred (self)management strategy. 1 – 4
Although self-management plans have been shown to be successful for reducing the impact of asthma, 21 , 39 the complexity of managing such a fluctuating disease on a day-to-day basis is challenging. During an asthma review, there is an opportunity to work with the patient to try to identify what triggers their symptoms and any actions that may help improve or maintain control. 38 An integral part of personalised self-management education is the written PAAP, which gives the patient the knowledge to respond to the changes in symptoms and ensures they maintain control of their asthma within predetermined parameters. 9 , 40 The PAAP should include details on how to monitor asthma, recognise symptoms, how to alter medication and what to do if the symptoms do not improve. The plan should include details on the treatment to be taken when asthma is well controlled, and how to adjust it when the symptoms are mild, moderate or severe. These action plans need to be developed between the doctor, nurse or asthma educator and the patient during the review and should be frequently reviewed and updated in partnership (see Box 1). Patient preference as well as clinical features such as whether she under- or over-perceives her symptoms should be taken into account when deciding whether the action plan is peak flow or symptom-driven. Our patient has a lot to gain from having an action plan. She has poorly controlled asthma and her lifestyle means that she will probably see different doctors (depending who is available) when she needs help. Being empowered to self-manage could make a big difference to her asthma control and the impact it has on her life.
The practice should have protocols in place, underpinned by specific training to support asthma self-management. As well as ensuring that healthcare professionals have appropriate skills, this should include training for reception staff so that they know what action to take if a patient telephones to say they are having an asthma attack.
However, focusing solely on symptom management strategies (actions) to follow in the presence of deteriorating symptoms fails to incorporate the patients’ wider views of asthma, its management within the context of her/his life, and their personal asthma management strategies. 41 This may result in a failure to use plans to maximise their health potential. 21 , 42 A self-management strategy leading to improved outcomes requires a high level of patient self-efficacy, 43 a meaningful partnership between the patient and the supporting health professional, 42 , 44 and a focused self-management discussion. 14
Central to both the effectiveness and personalisation of action plans, 43 , 45 in particular the likelihood that the plan will lead to changes in patients’ day-to-day self-management behaviours, 45 is the identification of goals. Goals are more likely to be achieved when they are specific, important to patients, collaboratively set and there is a belief that these can be achieved. Success depends on motivation 44 , 46 to engage in a specific behaviour to achieve a valued outcome (goal) and the ability to translate the behavioural intention into action. 47 Action and coping planning increases the likelihood that patient behaviour will actually change. 44 , 46 , 47 Our patient has a goal: she wants to avoid having her work disrupted by her asthma. Her personalised action plan needs to explicitly focus on achieving that goal.
As providers of self-management support, health professionals must work with patients to identify goals (valued outcomes) that are important to patients, that may be achievable and with which they can engage. The identification of specific, personalised goals and associated feasible behaviours is a prerequisite for the creation of asthma self-management plans. Divergent perceptions of asthma and how to manage it, and a mismatch between what patients want/need from these plans and what is provided by professionals are barriers to success. 41 , 42
What are the challenges for the healthcare organisation in providing self-management support?
A number of studies have demonstrated the challenges for primary care physicians in providing ongoing support for people with asthma. 31 , 48 , 49 In some countries, nurses and other allied health professionals have been trained as asthma educators and monitor people with stable asthma. These resources are not always available. In addition, some primary care services are delivered in constrained systems where only a few minutes are available to the practitioner in a consultation, or where only a limited range of asthma medicines are available or affordable. 50
There is recognition that the delivery of quality care depends on the competence of the doctor (and supporting health professionals), the relationship between the care providers and care recipients, and the quality of the environment in which care is delivered. 51 This includes societal expectations, health literacy and financial drivers.
In 2001, the Australian Government adopted a programme developed by the General Practitioner Asthma Group of the National Asthma Council Australia that provided a structured approach to the implementation of asthma management guidelines in a primary care setting. 52 Patients with moderate-to-severe asthma were eligible to participate. The 3+ visit plan required confirmation of asthma diagnosis, spirometry if appropriate, assessment of trigger factors, consideration of medication and patient self-management education including provision of a written PAAP. These elements, including regular medical review, were delivered over three visits. Evaluation demonstrated that the programme was beneficial but that it was difficult to complete the third visit in the programme. 53 – 55 Accordingly, the programme, renamed the Asthma Cycle of Care, was modified to incorporate two visits. 56 Financial incentives are provided to practices for each patient who receives this service each year.
Concurrently, other programmes were implemented which support practice-based care. Since 2002, the National Asthma Council has provided best-practice asthma and respiratory management education to health professionals, 57 and this programme will be continuing to 2017. The general practitioner and allied health professional trainers travel the country to provide asthma and COPD updates to groups of doctors, nurses and community pharmacists. A number of online modules are also provided. The PACE (Physician Asthma Care Education) programme developed by Noreen Clark has also been adapted to the Australian healthcare system. 58 In addition, a pharmacy-based intervention has been trialled and implemented. 59
To support these programmes, the National Asthma Council ( www.nationalasthma.org.au ) has developed resources for use in practices. A strong emphasis has been on the availability of a range of PAAPs (including plans for using adjustable maintenance dosing with ICS/LABA combination inhalers), plans for indigenous Australians, paediatric plans and plans translated into nine languages. PAAPs embedded in practice computer systems are readily available in consultations, and there are easily accessible online paediatric PAAPs ( http://digitalmedia.sahealth.sa.gov.au/public/asthma/ ). A software package, developed in the UK, can be downloaded and used to generate a pictorial PAAP within the consultation. 60
One of the strongest drivers towards the provision of written asthma action plans in Australia has been the Asthma Friendly Schools programme. 61 , 62 Established with Australian Government funding and the co-operation of Education Departments of each state, the Asthma Friendly Schools programme engages schools to address and satisfy a set of criteria that establishes an asthma-friendly environment. As part of accreditation, the school requires that each child with asthma should have a written PAAP prepared by their doctor to assist (trained) staff in managing a child with asthma at school.
The case study continues...
The initial presentation some weeks ago was during an exacerbation of asthma, which may not be the best time to educate a patient. It is, however, a splendid time to build on their motivation to feel better. She agreed to return after her asthma had settled to look more closely at her asthma control, and an appointment was made for a routine review.
At this follow-up consultation, the patient’s diagnosis was reviewed and confirmed and her trigger factors discussed. For this lady, respiratory tract infections are the usual trigger but allergic factors during times of high pollen count may also be relevant. Assessment of her nasal airway suggested that she would benefit from better control of allergic rhinitis. Other factors were discussed, as many patients are unaware that changes in air temperature, exercise and pets can also trigger asthma exacerbations. In addition, use of the Asthma Control Test was useful as an objective assessment of control as well as helping her realise what her life could be like! Many people with long-term asthma live their life within the constraints of their illness, accepting that is all that they can do.
After assessing the level of asthma control, a discussion about management options—trigger avoidance, exercise and medicines—led to the development of a written PAAP. Asthma can affect the whole family, and ways were explored that could help her family understand why it is important that she finds time in the busy domestic schedules to take her regular medication. Family and friends can also help by understanding what triggers her asthma so that they can avoid exposing her to perfumes, pollens or pets that risk triggering her symptoms. Information from the national patient organisation was provided to reinforce the messages.
The patient agreed to return in a couple of weeks, and a recall reminder was set up. At the second consultation, the level of control since the last visit will be explored including repeat spirometry, if appropriate. Further education about the pathophysiology of asthma and how to recognise early warning signs of loss of control can be given. Device use will be reassessed and the PAAP reviewed. Our patient’s goal is to avoid disruption to her work and her PAAP will focus on achieving that goal. Finally, agreement will be reached with the patient about future routine reviews, which, now that she has a written PAAP, could be scheduled by telephone if all is well, or face-to-face if a change in her clinical condition necessitates a more comprehensive review.
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, 2012. Available from: http://www.ginasthma.org (accessed July 2013).
British Thoracic Society/Scottish Intercollegiate Guideline Network British Guideline on the Management of Asthma. Thorax 2008; 63 (Suppl 4 iv1–121, updated version available from: http://www.sign.ac.uk (accessed January 2014).
Article Google Scholar
National Asthma Council Australia. Australian Asthma Handbook. Available from: http://www.nationalasthma.org.au/handbook (accessed May 2014).
National Asthma Education and Prevention Program (NAEPP) Coordinating Committee. Expert Panel Report 3 (EPR3): Guidelines for the Diagnosis and Management of Asthma. Available from: https://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm (accessed May 2014).
Taylor SJC, Pinnock H, Epiphaniou E, Pearce G, Parke H . A rapid synthesis of the evidence on interventions supporting self-management for people with long-term conditions. (PRISMS Practical Systematic Review of Self-Management Support for long-term conditions). Health Serv Deliv Res (in press).
Gibson PG, Powell H, Wilson A, Abramson MJ, Haywood P, Bauman A et al. Self-management education and regular practitioner review for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No. CD001117.
Tapp S, Lasserson TJ, Rowe BH . Education interventions for adults who attend the emergency room for acute asthma. Cochrane Database Syst Rev 2007: (Issue 3) Art No. CD003000.
Powell H, Gibson PG . Options for self-management education for adults with asthma. Cochrane Database Syst Rev 2002: (Issue 3) Art No: CD004107.
Toelle B, Ram FSF . Written individualised management plans for asthma in children and adults. Cochrane Database Syst Rev 2004: (Issue 1) Art No. CD002171.
Lefevre F, Piper M, Weiss K, Mark D, Clark N, Aronson N . Do written action plans improve patient outcomes in asthma? An evidence-based analysis. J Fam Pract 2002; 51 : 842–848.
PubMed Google Scholar
Boyd M, Lasserson TJ, McKean MC, Gibson PG, Ducharme FM, Haby M . Interventions for educating children who are at risk of asthma-related emergency department attendance. Cochrane Database Syst Rev 2009: (Issue 2) Art No.CD001290.
Bravata DM, Gienger AL, Holty JE, Sundaram V, Khazeni N, Wise PH et al. Quality improvement strategies for children with asthma: a systematic review. Arch Pediatr Adolesc Med 2009; 163 : 572–581.
Bower P, Murray E, Kennedy A, Newman S, Richardson G, Rogers A . Self-management support interventions to reduce health care utilisation without compromising outcomes: a rapid synthesis of the evidence. Available from: http://www.nets.nihr.ac.uk/projects/hsdr/11101406 (accessed April 2014).
Gibson PG, Powell H . Written action plans for asthma: an evidence-based review of the key components. Thorax 2004; 59 : 94–99.
Article CAS Google Scholar
Bhogal SK, Zemek RL, Ducharme F . Written action plans for asthma in children. Cochrane Database Syst Rev 2006: (Issue 3) Art No. CD005306.
Zemek RL, Bhogal SK, Ducharme FM . Systematic review of randomized controlled trials examining written action plans in children: what is the plan?. Arch Pediatr Adolesc Med 2008; 162 : 157–163.
Pinnock H, Slack R, Pagliari C, Price D, Sheikh A . Understanding the potential role of mobile phone based monitoring on asthma self-management: qualitative study. Clin Exp Allergy 2007; 37 : 794–802.
de Jongh T, Gurol-Urganci I, Vodopivec-Jamsek V, Car J, Atun R . Mobile phone messaging for facilitating self-management of long-term illnesses. Cochrane Database Syst Rev 2012: (Issue 12) Art No. CD007459.
Huckvale K, Car M, Morrison C, Car J . Apps for asthma self-management: a systematic assessment of content and tools. BMC Med 2012; 10 : 144.
Allergic Rhinitis and its Impact on Asthma. Management of Allergic Rhinitis and its Impact on Asthma: Pocket Guide. ARIA 2008. Available from: http://www.whiar.org (accessed May 2014).
Ring N, Jepson R, Hoskins G, Wilson C, Pinnock H, Sheikh A et al. Understanding what helps or hinders asthma action plan use: a systematic review and synthesis of the qualitative literature. Patient Educ Couns 2011; 85 : e131–e143.
Moullec G, Gour-Provencal G, Bacon SL, Campbell TS, Lavoie KL . Efficacy of interventions to improve adherence to inhaled corticosteroids in adult asthmatics: Impact of using components of the chronic care model. Respir Med 2012; 106 : 1211–1225.
Pinnock H, Bawden R, Proctor S, Wolfe S, Scullion J, Price D et al. Accessibility, acceptability and effectiveness of telephone reviews for asthma in primary care: randomised controlled trial. BMJ 2003; 326 : 477–479.
Pinnock H, Adlem L, Gaskin S, Harris J, Snellgrove C, Sheikh A . Accessibility, clinical effectiveness and practice costs of providing a telephone option for routine asthma reviews: phase IV controlled implementation study. Br J Gen Pract 2007; 57 : 714–722.
PubMed PubMed Central Google Scholar
Kielmann T, Huby G, Powell A, Sheikh A, Price D, Williams S et al. From support to boundary: a qualitative study of the border between self care and professional care. Patient Educ Couns 2010; 79 : 55–61.
Asthma UK . Compare your care report. Asthma UK, 2013. Available from: http://www.asthma.org.uk (accessed January 2014).
Stallberg B, Lisspers K, Hasselgren M, Janson C, Johansson G, Svardsudd K . Asthma control in primary care in Sweden: a comparison between 2001 and 2005. Prim Care Respir J 2009; 18 : 279–286.
Reddel H, Peters M, Everett P, Flood P, Sawyer S . Ownership of written asthma action plans in a large Australian survey. Eur Respir J 2013; 42 . Abstract 2011.
Wiener-Ogilvie S, Pinnock H, Huby G, Sheikh A, Partridge MR, Gillies J . Do practices comply with key recommendations of the British Asthma Guideline? If not, why not? Prim Care Respir J 2007; 16 : 369–377.
Kennedy A, Rogers A, Bower P . Support for self care for patients with chronic disease. BMJ 2007; 335 : 968–970.
Ring N, Malcolm C, Wyke S, Macgillivray S, Dixon D, Hoskins G et al. Promoting the Use of Personal Asthma Action Plans: A Systematic Review. Prim Care Respir J 2007; 16 : 271–283.
Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, Casale TB et al. A new perspective on concepts of asthma severity and control. Eur Respir J 2008; 32 : 545–554.
Horne R . Compliance, adherence, and concordance: implications for asthma treatment. Chest 2006; 130 (suppl): 65S–72S.
Reddel HK, Taylor DR, Bateman ED, Boulet L-P, Boushey HA, Busse WW et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med 2009; 180 : 59–99.
Thomas M, Kay S, Pike J, Rosenzweig JR, Hillyer EV, Price D . The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Prim Care Respir J 2009; 18 : 41–49.
Hoskins G, Williams B, Jackson C, Norman P, Donnan P . Assessing asthma control in UK primary care: use of routinely collected prospective observational consultation data to determine appropriateness of a variety of control assessment models. BMC Fam Pract 2011; 12 : 105.
Pinnock H, Fletcher M, Holmes S, Keeley D, Leyshon J, Price D et al. Setting the standard for routine asthma consultations: a discussion of the aims, process and outcomes of reviewing people with asthma in primary care. Prim Care Respir J 2010; 19 : 75–83.
McKinstry B, Hammersley V, Burton C, Pinnock H, Elton RA, Dowell J et al. The quality, safety and content of telephone and face-to-face consultations: a comparative study. Qual Saf Health Care 2010; 19 : 298–303.
Gordon C, Galloway T . Review of Findings on Chronic Disease Self-Management Program (CDSMP) Outcomes: Physical, Emotional & Health-Related Quality of Life, Healthcare Utilization and Costs . Centers for Disease Control and Prevention and National Council on Aging: Atlanta, GA, USA, 2008.
Beasley R, Crane J . Reducing asthma mortality with the self-management plan system of care. Am J Respir Crit Care Med 2001; 163 : 3–4.
Ring N, Jepson R, Pinnock H, Wilson C, Hoskins G, Sheikh A et al. Encouraging the promotion and use of asthma action plans: a cross study synthesis of qualitative and quantitative evidence. Trials 2012; 13 : 21.
Jones A, Pill R, Adams S . Qualitative study of views of health professionals and patients on guided self-management plans for asthma. BMJ 2000; 321 : 1507–1510.
Bandura A . Self-efficacy: toward a unifying theory of behavioural change. Psychol Rev 1977; 84 : 191–215.
Gollwitzer PM, Sheeran P . Implementation intentions and goal achievement: a meta-analysis of effects and processes. Adv Exp Soc Psychol 2006; 38 : 69–119.
Google Scholar
Hardeman W, Johnston M, Johnston DW, Bonetti D, Wareham NJ, Kinmonth AL . Application of the theory of planned behaviour change interventions: a systematic review. Psychol Health 2002; 17 : 123–158.
Schwarzer R . Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol 2008; 57 : 1–29.
Sniehotta F . Towards a theory of intentional behaviour change: plans, planning, and self-regulation. Br J Health Psychol 2009; 14 : 261–273.
Okelo SO, Butz AM, Sharma R, Diette GB, Pitts SI, King TM et al. Interventions to modify health care provider adherence to asthma guidelines: a systematic review. Pediatrics 2013; 132 : 517–534.
Grol R, Grimshaw RJ . From best evidence to best practice: effective implementation of change in patients care. Lancet 2003; 362 : 1225–1230.
Jusef L, Hsieh C-T, Abad L, Chaiyote W, Chin WS, Choi Y-J et al. Primary care challenges in treating paediatric asthma in the Asia-Pacific region. Prim Care Respir J 2013; 22 : 360–362.
Donabedian A . Evaluating the quality of medical care. Milbank Q 2005; 83 : 691–729.
Fardy HJ . Moving towards organized care of chronic disease. The 3+ visit plan. Aust Fam Physician 2001; 30 : 121–125.
CAS PubMed Google Scholar
Glasgow NJ, Ponsonby AL, Yates R, Beilby J, Dugdale P . Proactive asthma care in childhood: general practice based randomised controlled trial. BMJ 2003; 327 : 659.
Douglass JA, Goemann DP, Abramson MJ . Asthma 3+ visit plan: a qualitative evaluation. Intern Med J 2005; 35 : 457–462.
Beilby J, Holton C . Chronic disease management in Australia; evidence and policy mismatch, with asthma as an example. Chronic Illn 2005; 1 : 73–80.
The Department of Health. Asthma Cycle of Care. Accessed on 14 May 2014 at http://www.health.gov.au/internet/main/publishing.nsf/Content/asthma-cycle .
National Asthma Council Australia. Asthma and Respiratory Education Program. Accessed on 14 May 2014 at http://www.nationalasthma.org.au/health-professionals/education-training/asthma-respiratory-education-program .
Patel MR, Shah S, Cabana MD, Sawyer SM, Toelle B, Mellis C et al. Translation of an evidence-based asthma intervention: Physician Asthma Care Education (PACE) in the United States and Australia. Prim Care Respir J 2013; 22 : 29–34.
Armour C, Bosnic-Anticevich S, Brilliant M, Burton D, Emmerton L, Krass I et al. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax 2007; 62 : 496–502.
Roberts NJ, Mohamed Z, Wong PS, Johnson M, Loh LC, Partridge MR . The development and comprehensibility of a pictorial asthma action plan. Patient Educ Couns 2009; 74 : 12–18.
Henry RL, Gibson PG, Vimpani GV, Francis JL, Hazell J . Randomised controlled trial of a teacher-led asthma education program. Pediatr Pulmonol 2004; 38 : 434–442.
National Asthma Council Australia. Asthma Friendly Schools program. Accessed on 14 May 2014 at http://www.asthmaaustralia.org.au/Asthma-Friendly-Schools.aspx .
Download references
Author information
Authors and affiliations.
Asthma UK Centre for Applied Research, Centre for Population Health Sciences, The University of Edinburgh, Edinburgh, UK,
Hilary Pinnock & Elisabeth Ehrlich
NMAHP-RU, University of Stirling, Stirling, UK,
Gaylor Hoskins
Discipline of General Practice, University of Sydney, Sydney, NSW, Australia
Ron Tomlins
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hilary Pinnock .
Ethics declarations
Competing interests.
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
Reprints and permissions
About this article
Cite this article.
Pinnock, H., Ehrlich, E., Hoskins, G. et al. A woman with asthma: a whole systems approach to supporting self-management. npj Prim Care Resp Med 24 , 14063 (2014). https://doi.org/10.1038/npjpcrm.2014.63
Download citation
Received : 23 June 2014
Revised : 15 July 2014
Accepted : 15 July 2014
Published : 16 October 2014
DOI : https://doi.org/10.1038/npjpcrm.2014.63
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Case Study: Managing Severe Asthma in an Adult
—he follows his treatment plan, but this 40-year-old male athlete has asthma that is not well-controlled. what’s the next step.
By Kirstin Bass, MD, PhD Reviewed by Michael E. Wechsler, MD, MMSc
This case presents a patient with poorly controlled asthma that remains refractory to treatment despite use of standard-of-care therapeutic options. For patients such as this, one needs to embark on an extensive work-up to confirm the diagnosis, assess for comorbidities, and finally, to consider different therapeutic options.

Case presentation and patient history
Mr. T is a 40-year-old recreational athlete with a medical history significant for asthma, for which he has been using an albuterol rescue inhaler approximately 3 times per week for the past year. During this time, he has also been waking up with asthma symptoms approximately twice a month, and has had three unscheduled asthma visits for mild flares. Based on the National Asthma Education and Prevention Program guidelines , Mr. T has asthma that is not well controlled. 1
As a result of these symptoms, spirometry was performed revealing a forced expiratory volume in the first second (FEV1) of 78% predicted. Mr. T then was prescribed treatment with a low-dose corticosteroid, fluticasone 44 mcg at two puffs twice per day. However, he remained symptomatic and continued to use his rescue inhaler 3 times per week. Therefore, he was switched to a combination inhaled steroid and long-acting beta-agonist (LABA) (fluticasone propionate 250 mcg and salmeterol 50 mcg, one puff twice a day) by his primary care doctor.
Initial pulmonary assessment Even with this step up in his medication, Mr. T continued to be symptomatic and require rescue inhaler use. Therefore, he was referred to a pulmonologist, who performed the initial work-up shown here:
- Spirometry, pre-albuterol: FEV1 79%, post-albuterol: 12% improvement
- Methacholine challenge: PC 20 : 1.0 mg/mL
- Chest X-ray: Within normal limits
Continued pulmonary assessment His dose of inhaled corticosteroid (ICS) and LABA was increased to fluticasone 500 mcg/salmeterol 50 mcg, one puff twice daily. However, he continued to have symptoms and returned to the pulmonologist for further work-up, shown here:
- Chest computed tomography (CT): Normal lung parenchyma with no scarring or bronchiectasis
- Sinus CT: Mild mucosal thickening
- Complete blood count (CBC): Within normal limits, white blood cells (WBC) 10.0 K/mcL, 3% eosinophils
- Immunoglobulin E (IgE): 25 IU/mL
- Allergy-skin test: Positive for dust, trees
- Exhaled NO: Fractional exhaled nitric oxide (FeNO) 53 parts per billion (pbb)
Assessment for comorbidities contributing to asthma symptoms After this work-up, tiotropium was added to his medication regimen. However, he remained symptomatic and had two more flares over the next 3 months. He was assessed for comorbid conditions that might be affecting his symptoms, and results showed:
- Esophagram/barium swallow: Negative
- Esophageal manometry: Negative
- Esophageal impedance: Within normal limits
- ECG: Within normal limits
- Genetic testing: Negative for cystic fibrosis, alpha1 anti-trypsin deficiency
The ear, nose, and throat specialist to whom he was referred recommended only nasal inhaled steroids for his mild sinus disease and noted that he had a normal vocal cord evaluation.
Following this extensive work-up that transpired over the course of a year, Mr. T continued to have symptoms. He returned to the pulmonologist to discuss further treatment options for his refractory asthma.
Diagnosis Mr. T has refractory asthma. Work-up for this condition should include consideration of other causes for the symptoms, including allergies, gastroesophageal reflux disease, cardiac disease, sinus disease, vocal cord dysfunction, or genetic diseases, such as cystic fibrosis or alpha1 antitrypsin deficiency, as was performed for Mr. T by his pulmonary team.
Treatment options When a patient has refractory asthma, treatment options to consider include anticholinergics (tiotropium, aclidinium), leukotriene modifiers (montelukast, zafirlukast), theophylline, anti-immunoglobulin E (IgE) antibody therapy with omalizumab, antibiotics, bronchial thermoplasty, or enrollment in a clinical trial evaluating the use of agents that modulate the cell signaling and immunologic responses seen in asthma.
Treatment outcome Mr. T underwent bronchial thermoplasty for his asthma. One year after the procedure, he reports feeling great. He has not taken systemic steroids for the past year, and his asthma remains controlled on a moderate dose of ICS and a LABA. He has also been able to resume exercising on a regular basis.
Approximately 10% to 15% of asthma patients have severe asthma refractory to the commonly available medications. 2 One key aspect of care for this patient population is a careful workup to exclude other comorbidities that could be contributing to their symptoms. Following this, there are several treatment options to consider, as in recent years there have been several advances in the development of asthma therapeutics. 2
Treatment options for refractory asthma There are a number of currently approved therapies for severe, refractory asthma. In addition to therapy with ICS or combination therapies with ICS and LABAs, leukotriene antagonists have good efficacy in asthma, especially in patients with prominent allergic or exercise symptoms. 2 The anticholinergics, such as tiotropium, which was approved for asthma in 2015, enhance bronchodilation and are useful adjuncts to ICS. 3-5 Omalizumab is a monoclonal antibody against IgE recommended for use in severe treatment-refractory allergic asthma in patients with atopy. 2 A nonmedication therapeutic option to consider is bronchial thermoplasty, a bronchoscopic procedure that uses thermal energy to disrupt bronchial smooth muscle. 6,7
Personalizing treatment for each patient It is important to personalize treatment based on individual characteristics or phenotypes that predict the patient's likely response to treatment, as well as the patient's preferences and practical issues, such as adherence and cost. 8
In this case, tiotropium had already been added to Mr. T's medications and his symptoms continued. Although addition of a leukotriene modifier was an option for him, he did not wish to add another medication to his care regimen. Omalizumab was not added partly for this reason, and also because of his low IgE level. As his bronchoscopy was negative, it was determined that a course of antibiotics would not be an effective treatment option for this patient. While vitamin D insufficiency has been associated with adverse outcomes in asthma, T's vitamin D level was tested and found to be sufficient.
We discussed the possibility of Mr. T's enrollment in a clinical trial. However, because this did not guarantee placement within a treatment arm and thus there was the possibility of receiving placebo, he opted to undergo bronchial thermoplasty.
Bronchial thermoplasty Bronchial thermoplasty is effective for many patients with severe persistent asthma, such as Mr. T. This procedure may provide additional benefits to, but does not replace, standard asthma medications. During the procedure, thermal energy is delivered to the airways via a bronchoscope to reduce excess airway smooth muscle and limit its ability to constrict the airways. It is an outpatient procedure performed over three sessions by a trained physician. 9
The effects of bronchial thermoplasty have been studied in several trials. The first large-scale multicenter randomized controlled study was the Asthma Intervention Research (AIR) Trial , which enrolled patients with moderate to severe asthma. 10 In this trial, patients who underwent the procedure had a significant improvement in asthma symptoms as measured by symptom-free days and scores on asthma control and quality of life questionnaires, as well as reductions in mild exacerbations and increases in morning peak expiratory flow. 10 Shortly after the AIR trial, the Research in Severe Asthma (RISA) trial was conducted to evaluate bronchial thermoplasty in patients with more severe, symptomatic asthma. 11 In this population, bronchial thermoplasty resulted in a transient worsening of asthma symptoms, with a higher rate of hospitalizations during the treatment period. 11 Hospitalization rate equalized between the treatment and control groups in the posttreatment period, however, and the treatment group showed significant improvements in rescue medication use, prebronchodilator forced expiratory volume in the first second (FEV1) % predicted, and asthma control questionnaire scores. 11
The AIR-2 trial followed, which was a multicenter, randomized, double-blind, sham-controlled study of 288 patients with severe asthma. 6 Similar to the RISA trial, patients in the treatment arm of this trial experienced an increase in adverse respiratory effects during the treatment period, the most common being airway irritation (including wheezing, chest discomfort, cough, and chest pain) and upper respiratory tract infections. 6
The majority of adverse effects occurred within 1 day of the procedure and resolved within 7 days. 6 In this study, bronchial thermoplasty was found to significantly improve quality of life, as well as reduce the rate of severe exacerbations by 32%. 6 Patients who underwent the procedure also reported fewer adverse respiratory effects, fewer days lost from work, school, or other activities due to asthma, and an 84% risk reduction in emergency department visits. 6
Long-term (5-year) follow-up studies have been conducted for patients in both the AIR and the AIR-2 trials. In patients who underwent bronchial thermoplasty in either study, the rate of adverse respiratory effects remained stable in years 2 to 5 following the procedure, with no increase in hospitalizations or emergency department visits. 7,12 Additionally, FEV1 remained stable throughout the 5-year follow-up period. 7,12 This finding was maintained in patients enrolled in the AIR-2 trial despite decreased use of daily ICS. 7
Bronchial thermoplasty is an important addition to the asthma treatment armamentarium. 7 This treatment is currently approved for individuals with severe persistent asthma who remain uncontrolled despite the use of an ICS and LABA. Several clinical trials with long-term follow-up have now demonstrated its safety and ability to improve quality of life in patients with severe asthma, such as Mr. T.
Severe asthma can be a challenge to manage. Patients with this condition require an extensive workup, but there are several treatments currently available to help manage these patients, and new treatments are continuing to emerge. Managing severe asthma thus requires knowledge of the options available as well as consideration of a patient's personal situation-both in terms of disease phenotype and individual preference. In this case, the patient expressed a strong desire to not add any additional medications to his asthma regimen, which explained the rationale for choosing to treat with bronchial thermoplasty. Personalized treatment necessitates exploring which of the available or emerging options is best for each individual patient.
Published: April 16, 2018
- 1. National Asthma Education and Prevention Program: Asthma Care Quick Reference.
- 2. Olin JT, Wechsler ME. Asthma: pathogenesis and novel drugs for treatment. BMJ . 2014;349:g5517.
- 3. Boehringer Ingelheim. Asthma: U.S. FDA approves new indication for SPIRIVA Respimat [press release]. September 16, 2015.
- 4. Peters SP, Kunselman SJ, Icitovic N, et al. Tiotropium bromide step-up therapy for adults with uncontrolled asthma. N Engl J Med . 2010;363:1715-1726.
- 5. Kerstjens HA, Engel M, Dahl R. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med . 2012;367:1198-1207.
- 6. Castro M, Rubin AS, Laviolette M, et al. Effectiveness and safety of bronchial thermoplasty in the treatment of severe asthma: a multicenter, randomized, double-blind, sham-controlled clinical trial. Am J Respir Crit Care Med . 2010;181:116-124.
- 7. Wechsler ME, Laviolette M, Rubin AS, et al. Bronchial thermoplasty: long-term safety and effectiveness in patients with severe persistent asthma. J Allergy Clin Immunol . 2013;132:1295-1302.
- 8. Global Initiative for Asthma: Pocket Guide for Asthma Management and Prevention (for Adults and Children Older than 5 Years).
- 10. Cox G, Thomson NC, Rubin AS, et al. Asthma control during the year after bronchial thermoplasty. N Engl J Med . 2007;356:1327-1337.
- 11. Pavord ID, Cox G, Thomson NC, et al. Safety and efficacy of bronchial thermoplasty in symptomatic, severe asthma. Am J Respir Crit Care Med . 2007;176:1185-1191.
- 12. Thomson NC, Rubin AS, Niven RM, et al. Long-term (5 year) safety of bronchial thermoplasty: Asthma Intervention Research (AIR) trial. BMC Pulm Med . 2011;11:8.
Treatable traits and future exacerbation risk in severe asthma, baker’s asthma, the long-term trajectory of mild asthma, age, gender, & systemic corticosteroid comorbidities, ask the expert: william busse, md, challenges the current definition of the atopic march, considering the curveballs in asthma treatment, do mucus plugs play a bigger role in chronic severe asthma than previously thought, an emerging subtype of copd is associated with early respiratory disease.

- Search Menu
- Advance Articles
- Supplements
- Author Guidelines
- Submission Site
- Open Access
- Self-Archiving Policy
- Advertising & Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- Journals Career Network
- About Paediatrics & Child Health
- About The Canadian Paediatric Society
- Editorial Board
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Case 1 diagnosis: allergy bullying, clinical pearls.
- < Previous
Case 1: A 12-year-old girl with food allergies and an acute asthma exacerbation
- Article contents
- Figures & tables
- Supplementary Data
Lopamudra Das, Michelle GK Ward, Case 1: A 12-year-old girl with food allergies and an acute asthma exacerbation, Paediatrics & Child Health , Volume 19, Issue 2, February 2014, Pages 69–70, https://doi.org/10.1093/pch/19.2.69
- Permissions Icon Permissions
A 12-year-old girl with a history of asthma presented to the emergency department with a three-day history of increased work of breathing, cough and wheezing. She reported no clear trigger for her respiratory symptoms, although she had noted some symptoms of a mild upper respiratory tract infection. With this episode, the patient had been using a short-acting bronchodilator more frequently than she had in the past, without the expected resolution of symptoms.
On the day of presentation, the patient awoke feeling ‘suffocated’ and her mother noted her lips to be blue. In the emergency department, her oxygen saturation was 85% and her respiratory rate was 40 breaths/min. She had significantly increased work of breathing and poor air entry bilaterally to both lung bases, with wheezing in the upper lung zones. She was treated with salbutamol/ipratropium and received intravenous steroids and magnesium sulfate. Her chest x-ray showed hyperinflation and no focal findings.
Her medical history revealed that she was followed by a respirologist for her asthma, had good medication adherence and had not experienced a significant exacerbation for six months. She also had a history of wheezing, dyspnea and pruritis with exposure to peanuts, chickpeas and lentils; she had been prescribed an injectible epinephrine device for this. However, her device had expired at the time of presentation. In the past, her wheezing episodes had been seasonal and related to exposure to grass and pollens; this presentation occurred during the winter. Further history revealed the probable cause of her presentation.
Although reluctant to disclose the information, our patient later revealed that she had been experiencing significant bullying at school, which was primarily related to her food allergies. Three days before her admission, classmates had smeared peanut butter on one of her schoolbooks. She developed pruritis immediately after opening the book and she started wheezing and coughing later that day. This event followed several months of being taunted with peanut products at school. The patient was experiencing low mood and reported new symptoms of anxiety related to school. The review of systems was otherwise negative, with no substance use.
The patient's asthma exacerbation resolved with conventional asthma treatment. Her pulmonary function tests were nonconcerning (forced expiratory volume in 1 s 94% and 99% of predicted) after her recovery. The trigger for her asthma exacerbation was likely multifactorial, related to exposure to the food allergen as well as the upper respiratory infection. A psychologist was consulted to assess the symptoms of anxiety and depression that had occurred as a result of the bullying. During the hospitalization, the medical team contacted the patient's school to provide education on allergy bullying, treatment of severe allergic reactions and its potential for life-threatening reactions with exposure to allergens. The medical team also recommended community resources for further education of students and staff about allergy bullying and its prevention.
Allergy bullying is a form of bullying with potentially severe medical outcomes. In recent years, it has gained increasing notoriety in schools and in the media. Population-based studies have shown that 20% to 35% of children with allergies experience bullying. In many cases (31% in one recent study [ 1 ]), this bullying is related directly to the food allergy. From a medical perspective, there are little published data regarding allergy bullying, and many health care providers may not be aware of the issue.
Allergy bullying can include teasing a child about their allergy, throwing food at a child, or even forcing them to touch or eat allergenic foods. Most episodes of allergy bullying occur at school, and can include episodes perpetrated by teachers and/or staff ( 2 ).
Allergy bullying can lead to allergic reactions, which may be mild or severe (eg, urticaria, wheezing, anaphylaxis), but may also lead to negative emotional consequences (sadness, depression) ( 2 ) and an overall decrease in quality of life measures ( 1 ). Adolescents commonly resist using medical devices, such as injectible epinephrine devices, and bullying may be a contributing factor for this ( 3 ). Attempting to conceal symptoms in a bullying situation may place children at risk for a worse outcome.
Physicians can play a key role in detecting allergy bullying and its health consequences. In many cases, children have not discussed this issue with their parents ( 1 ). Given the prevalence of bullying, its potential to lead to severe harm, including death, and the lack of awareness of this issue, clinicians should specifically ask about bullying in all children and teens with allergies. Physicians can also work with families and schools to support these children, educate their peers and school staff, and help prevent negative health outcomes from allergy bullying.
Online resources
www.anaphylaxis.ca − A national charity that aims to inform, support, educate and advocate for the needs of individuals and families living with anaphylaxis, and to support and participate in research. This website includes education modules for schools and links to local support groups throughout Canada.
www.whyriskit.ca/pages/en/live/bullying.php − A website for teenagers with food allergies; includes a segment that addresses food bullying.
www.foodallergy.org − Contains numerous resources for children and their families, including a significant discussion on bullying and ways to prevent it.
Allergy bullying is common but is often unrecognized as a factor in clinical presentations of allergic reactions.
Physicians should make a point of asking about bullying in patients with allergies and become familiar with resources for dealing with allergy bullying.
Physicians can play roles as advocates, educators and collaborators with the school system to help make the school environment safer for children with allergies who may be at risk for allergy bullying.
Google Scholar
Email alerts
Citing articles via, looking for your next opportunity.
- About Paediatrics & Child Health
- Recommend to Your Librarian
- Advertising and Corporate Services
Affiliations
- Online ISSN 1918-1485
- Print ISSN 1205-7088
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.

Case of Acute Severe Asthma
Kane guthrie.
- Dec 2, 2022
A 25-year-old lady Miss. Poor Compliance is rushed into your Emergency Department as a Priority 1. She is a brittle asthmatic and has been given 3x 5mg salbutamol nebs, and 0.5mg of adrenaline IM prehospital. On arrival Miss PC is sitting forward in the tripod position , using her accessory muscles to breath. She is tachypnoeic, agitated and unable to talk.
Vital signs: Pulse 143, BP 138/95, RR 42, Sp02 91% on neb, GCS 14/15.
Past Medical and Medication History
- Smoker. Severe asthmatic. Intubated twice in past 2 years
- Currently taking seritide 250/50mg, salbutamol MDI PRN and prednisolone 50mg PRN
Asthma Epidemiology
- Over 2.2 million Australians have currently diagnosed asthma
- 406 deaths attributed to asthma in 2006
- Highest risk of dying from asthma is in the elderly over 70
- The emergency clinician’s goal in treating acute severe asthma is preventing intubation
- Severe/Critical asthma is a life threatening condition
Asthma Pathophysiology
- Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role, in particular, mast cells, eosinophils, T lymphocytes, macrophages, neutrophils, and epithelial cells.
- Smooth muscle hypertrophy and hyperplasia
- Inflammatory cell infiltration and oedema
- Goblet cell and mucous gland hyperplasia with mucous hypersecretion
- Protein deposition including collagen
- Epithelial desquamation
- Most common, responsible for 80-85% of all fatal events is characterised by eosinophilic inflammation associated with gradual deterioration over days-weeks occurring in patients with severe or poorly controlled asthma, and is slow to respond to therapy.
- The second phenotype, with neutrophilic inflammation, has both rapid onset and response to therapy.
Markers of severe asthma:
- Inability to speak in full sentences
- Use of accessory muscles or tracheal tugging
- Cyanosis and sweating
- Pulsus paradoxus (>15mmHg decreased with inspiration). With severe muscle fatigue might be absent
- Quiet chest on auscultation (The “Silent Chest”)
- Confusion or decreased level of consciousness
- Hypotension or bradycardia
- FEV 1<40% predicted
- PEF <40% of predicted or best (<25% in life threatening asthma)
- Oxygen saturation <90-92%
- PaO2 <60mmHg
- PaCO2 >45mmHg
Complications of Asthma :
- Pneumothorax, Pneumomediastinum, Pneumopericardium and Pneumoretroperitoneum
- Cardiac Arrhythmias, Myocardial ischaemia or infarction
- Electrolyte disturbances (hypokalaemia, hypomagnesaemia, hypophosphataemia)
- Lactic Acidosis
- Hyperglycaemia

Conditions that may mimic acute asthma:
- Upper airway obstruction
- Foreign-body aspiration
- Vocal cord dysfunction syndrome
- Pulmonary oedema
- Acute exacerbations of COPD
- Hysterical conversion reaction
- Munchausen syndrome
Diagnostic Test:
- Hyperinflation 5-10%
- Infiltrate 5%
- Pneumothorax <1%
- Pneumomediastinum <1%
- Respiratory alkalosis typical
- Inaccurate predictor of outcome
- Will seldom alter your treatment plan
- An objective measure of lung function
- Useful to assess response to treatment
- Impossible to obtain in the dying patient
- <25% Severe
- 25-50% Moderate
- 50-70% Mild
- >70% Discharge Goal
- Simple, and less painful than ABG
- Provides continuous oxygenation measurements
- Needs to placed on well-perfused site, difficult to obtain readings if global hypoperfusion or peripheral vasoconstriction present.
- Aim to keep sp02 >92%
Management of Acute Severe Asthma
- Hypoxia is the main cause of death in asthma
- Oxygen should be given to keep Sp02 above 92%
- A slight Pco2 rise may occur with oxygen therapy but this is of no clinical significance.
Beta-agonists:
- Rapid acting inhaled beta-agonists (bronchodilators) are the first line therapy for acute asthma.
- Nebulisers should generally be used in acute severe asthma, as provide easier delivery of medication to patient, multi dose inhalers have a role in mild to moderate asthma.
- IV salbutamol gives you the advantage of hitting the beta 2 receptors from the back door, while continuing nebulizer treatment, and should be trialed in patients not responding to nebulisers.
- Continuous nebuliser therapy appears to be more effective than intermittent nebulisers for delivering beta-agonist drugs to relieve airway spasm in acute severe asthma. (Cochrane Review, 2009)
- Salbutamol toxicity can caused a lactic acidosis which is often unrecognized in asthma patients, the lactic acidosis has been hypothesized to adversely affect ventilation by increasing ventilatory demand, increasing dead space ventilation, worsening dynamic hyperinflation and intrinsic PEEP. Management is to discontinue salbutamol at the earliest opportunity.
- Dose: Salbutamol Nebuliser Ampoule 5mg
- Dose: Salbutamol IV 5mg in 500mL of 0.9% sodium chloride or 5% dextrose start at 30mL/hr titrating up to 120mL/hr
Anticholinergics:
- Anticholinergics agents block muscarinic receptors in airway smooth muscles, inhibit vagal cholinergic tone and result in bronchodilation.
- Dose: Ipratropium bromide (Atrovent) 500ug to second dose of salbutamol via neb, can be repeated every 4hours
- Use of corticosteroids within 1 hour of presentation to an ED significantly reduces the need for hospital admission in patients with acute asthma. Benefits appear greatest in patients with more severe asthma, and those not currently receiving steroids
- Dose: Prednisolone 50mg PO
- Dose: IV Hydrocortisone 100-200mg
- Note: Parenteral route is indicated in ventilated patient or patient unable to swallow, eg. Vomiting
Adrenaline:
- Can be give either intravenously or via nebulizer
- Bronchoconstriction is the major pathology in asthma; airway oedema might also make a significant contribution. Both the a-agonist and B-agonist effects of adrenaline might be beneficial, with the alpha effect decreasing oedema and the beta effect responsible for bronchodilation.
- Dose: IV 6mg in 100mls 5% dextrose start at 1-15mLs/hour
- Dose: Nebulizer 1mg in 3ml normal saline
Aminophylline:
- The popularity of aminophylline in asthma exacerbations has diminished in recent years.
- Systematic reviews have shown that IV aminophylline in severe acute asthma does not produce additional bronchodilation above that achieved with beta-agonist and corticosteroids.
- Side effects; cardiac arrhythmia’s, vomiting, toxicity.
- Dose : 5mg/kg over 20min followed by infusion of 500mg aminophyline n 500mL of 5% dextrose at 0.5mg/kg per hour
Magnesium Sulphate:
- Magnesium potential role is asthma may involve a combination of smooth muscle relaxation, inhibition of histamine release and acetylcholine release from nerve endings.
- Most evidence to support the use of magnesium in asthma is in the acute severe asthmatic were it has been shown to be safe and beneficial.
- Dose : IV 2-4g over 30-60mins
- Heliox Mixture 80% helium/20% oxygen
- There is evidence that helium and oxygen mixtures (heliox) may provide additional benefits to patients with acute asthma.
- Heliox mixtures have the potential to decrease airway resistance, and therefore decrease the work of breathing for the severe acute asthma patient.
Antibiotics:
- Antibiotics are not indicated in the management of severe acute asthma.
- Antibiotics should only be used in the setting of an underlying pneumonia, respiratory tract infection or to aid in the prevention of ventilator-associated pneumonia in ICU.
Airway Management
Non-Invasive Positive Pressure Ventilation:
Good quality evidence and trails to support the use of NPPV in asthma are lacking, however it is worth trying when intubation is not immediately indicated. Remember the goal of the emergency clinician’s in treating asthma is to prevent intubation.
- Positive pressure is generally less than 15cmH2O
- Benefit between CPAP vs BiPAP is unknown
- Tachypnea caused by severe asthma can make it difficult for the patient to coordinate they’re breathing with machine making BiPAP uncomfortable
- Need a large randomised control trial to determine the effectives properly of NIV, in acute severe asthma.
“Asthmatic on BiPAP before being Intubated”
Mechanical Ventilation:
1-3% of acute severe asthma requires intubation. Prevention of intubation and mechanical ventilation are the goals of managing acute severe asthma, this can be achieved by maximising pre-intubation therapy, however you don’t want to wait too long or let the severe asthmatic tire before trying to intubate them. Once an asthmatic is intubated and ventilated their morbidity and mortality increasing dramatically, and it can be difficult to wean from the ventilator.
Criteria for Intubation:
- Cardiac or Respiratory arrest
- Altered mental status
- Progressive exhaustion
- Severe hypoxia despite maximal oxygen delivery
- Failure to reverse severe respiratory acidosis despite intensive therapy
- pH <7.2, carbon dioxide pressure increasing by more than 5mmHg/hr or greater than 55 to 70mm/Hg, or oxygen pressure of less than 60mm/Hg.
Challenges:
- Effective pre-oxygenation impossible
- No margin for error or delay
- Need to be intubated by most experienced person available
- High intrathoracic pressure after RSI
Recommendations:
- Fluid bolus before intubation if possible
- RSI preferred
- Ketamine for bronchodilator effects
- Permissive hypercapnea essential
Initial Ventilator settings in paralysed patients:
- FiO2 1.0, then titrate to keep SpO2 >94%
- Tidal Volume 5-6ml/kg
- Ventilator rate 6-8 breaths/min
- Long expiratory time (I:E ratio >1:2)
- Minimal PEEP < 5cmH2O
- Limit peak inspiratory pressure to <40cmH2O
- Target plateau pressure <20cmH2O
- Ensure effective humidification
- Brenner, B. Corbridge, T. & Kazzi, A. (2009). Intubation and mechanical ventilation of the asthmatic patient in respiratory failure. The Journal of Emergency Medicine. 37(2s), s23-s34.
- Camargo, C. Rachelefsky, G. & Schatz, M. (2009). Managing Asthma Exacerbation in the Emergency Department: Summary of the National Asthma Education and Prevention Program Expert Panel Report 3 Guidelines for the Management of Asthma Exacerbation.The Journal of Emergency Medicine. 37 (2S), S6-S17.
- Camargo, C. Spooner, C. & Rowe, B. (2009). Continuous versus intermittent beta-agonist for acute asthma (Review). http://www.thecochranelibrary.com.
- Chua, F. & Lai, D. (2007). Acute severe asthma: Triage, treatment and thereafter. Current Anaesthesia & Critical Care. 18, 61-68.
- Creagh-Brown, B. & Ball, J. (2007). An under-recognized complication of treatment of acute severe asthma. American Journal of Emergency Medicine. 26, 513-515.
- Hodder, R. et al. (2009). Management of acute asthma in adults in the emergency department: nonventilatory management. CMAJ. 182(2), E55-E67.
- Holley, A. & Boots, R.(2009). Review article: Management of acute severe and near-fatal asthma. Emergency Medicine Australasia, (21) 259-268.
- Jones, L. & Goodacre, S. (2009). Magnesium sulphate in the treatment of acute asthma: evaluation of current practice in adult emergency departments. Emergency Medicine Journal. 26, 783-785.
- Melnick, E. & Cottral, J. (2010). Current Guidelines for Management of Asthma in the Emergency Department. http://www.ebmedicine.net. 2(2). 1-13.
- Morris, F. & Fletcher, A. (Ed). (2009). ABC of Emergency Differential Diagnosis. Oxford: Blackwell Publishing
- National Asthma Council of Australia. Asthma management handbook: 2006. Accessed http://www.nationalasthma.org.au/cms/images/stories/amh2006_web_5.pdf, 12/02/2010
- Nowak, R. Corbridge, T. & Brenner, B. (2009). Noninvasive Ventilation. The Journal of Emergency Medicine. 37(2S), S18-S22.
- Peters, S. (2007). Continuous Bronchodilator Therapy. Chest. 131(1),1-5.
- Phipps, P. & Garrard, C. (2003). The pulmonary physician in critical care. 12: Acute severe asthma in the intensive care unit. Thorax. 58, 81-88.
- Ram, F. Wellington, S. Rowe, B. & Wedzicha, J. (2009). Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma (Review)
- Rodrigo, G. Pollack, C. Rodrigo, C. Rowe, B. (2010). Heliox for non-intubated acute asthma patents (Review).
- Rowe, B. Spooner, C. Ducharme, F. Bretzlaff, J. Bota, G. (2008). Early emergency department treatment of acute asthma with systemic corticosteroids (Review). http://www.thecochranelibrary.com.
- Rowe, B. et al. (2009). Magnesium sulfate for treating exacerbations of acute asthma in the emergency department (Review). http://www.thecochranelibrary.com.
Emergency nurse with ultra-keen interest in the realms of toxicology, sepsis, eLearning and the management of critical care in the Emergency Department | LinkedIn |
Leave a Reply Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Allergy Rhinol (Providence)
- v.2(2); Apr-Jun 2011
A case of uncontrolled asthma
Ömür aydin.
From the 1 Department of Chest Diseases, Division of Immunology and Allergy,
Cabir Yüksel
2 Department of Thoracic Surgery,
Aylin Okçu Heper
3 Department of Pathology, Ankara University School of Medicine, Ankara, Turkey
Șevket Kavukc̦u
Zeynep misirligil.
A 48-year-old female patient with uncontrolled severe asthma was referred to our hospital for anti-IgE therapy. She was suffering with persistent wheezing and dyspnea after a severe asthma attack that had taken place 5 months previously. Her asthma had not been controlled with adequate asthma treatment, including budesonide at 320 μg + formoterol at 9 μg b.i.d. combination, montelukast at 10 mg/day, and oral steroids (30–40 mg/day of prednisolone), during this period. She was hospitalized for evaluation for anti-IgE therapy. Chest radiography revealed a left-sided hilar opacity. Fiberoptic bronchoscopy was performed and showed an endobronchial lesion obstructing the left lower bronchus lumen. Computed tomography also revealed a nodular lesion at the same location. The patient underwent left lower lobectomy and mediastinal lymph node dissection. Pathological examination concluded the diagnosis of typical carcinoid tumor. After surgery, her symptoms disappeared and she has had no recurrence. In conclusion, a diagnosis of severe asthma requires confirmation of asthma. Uncontrolled symptoms that linger despite aggressive therapy warrant evaluation to rule out other etiologies, such as a carcinoid tumor, before selecting new treatment options.
CASE PRESENTATION
A 48-year-old white woman, a housewife, was admitted to our tertiary clinic complaining of wheezing and dyspnea. She had been diagnosed with asthma 12 years previously and was well controlled using budesonide at 160 μg + formoterol at 4.5 μg b.i.d. combination therapy until 5 months before her visit to our clinic. She had had a severe asthma attack at that time, during which her wheezing was not well correlated with physical exercise and had persisted for several months. She was treated unsuccessfully with budesonide at 320 μg + formoterol at 9 μg b.i.d. combination, montelukast at 10 mg/day, and oral steroids (30–40 mg/day of prednisolone) during that period, and because her asthma had failed to come back under control, was referred to our clinic and hospitalized for evaluation for anti-IgE therapy. Her medical history was significant for appendectomy and hemorrhoidectomy. She was taking thyroid hormone for Hashimoto's thyroiditis and calcium tablets for osteoporosis.
Her vitals were stable with a heart rate of 76 bpm, a temperature of 36.5°C, blood pressure of 110/70 mmHg, and respiratory rate of 18/min on physical examination. Her examination was normal with the exception of decreased auscultation in the left lung. Her routine blood count was hematocrit, 38.2%; leukocyte, 9300; and erythrocyte sedimentation rate 13, mm/hr. Spirometry showed an obstructive pattern (forced expiratory volume in 1 second [FEV 1 ], 2.20 L [82%]; forced vital capacity [FVC], 3.45 L [110%]; FEV 1 /FVC, 60%). We were unable to show spirometric reversibility but were able to learn that during a previous hospitalization at another clinic, she had had a reversible airway obstruction. (prebronchodilator FEV 1 , 1.70 L [64%]; postbronchodilator FEV 1 , 2.01 L [75%]; reversibility, 17%). Her skin-prick test was positive for house-dust mites. Total IgE level was 115 kU/L. All data about the patient seemed to indicate that she could be a candidate for anti-IgE therapy. Chest radiography revealed a left-sided hilar opacity. For further evaluation, computerized tomography was performed and showed a 15-mm nodular lesion located in the left lower lobe bronchus ( Fig. 1 ). These radiological findings changed our management plan and diagnosis from asthma to a chest mass. A fiberoptic bronchoscopy was performed, which revealed an endobronchial lesion obstructing the left lower bronchus lumen ( Fig. 2 ). Biopsy was not performed because the lesion was highly vascularized and there was a risk of bleeding. Bronchial lavage fluid was removed from the left bronchus. Cytological examination of the lavage fluid was normal. The patient was transferred to the thoracic surgery ward for surgical treatment. She underwent left lower lobectomy and mediastinal lymph node dissection.

Thorax CT scan of the patient.

Bronchoscopic imaging of the carcinoid tumor.
Histopathological evaluation revealed an intrabronchial tumor, made up of monotonous cells with oval or round, finely granular nuclei and eosinophilic cytoplasm. No mitotic figures or necrosis was detected. The stroma was vascular and scant. Focal tumoral invasion of the lung parenchyma through the bronchial wall was also noted. Immunohistochemical staining indicated epithelial and neuroendocrine differentiation of the tumor cells with cytoplasmic positivity of pancytokeratin, chromogranin A, synaptophysin, and CD56. These findings established the diagnosis of a typical carcinoid (TC) tumor ( Figs. 3 and and4). 4 ). The dissected peribronchial and regional lymph nodes showed no metastasis.

The tumor made up of uniform polygonal cells with finely granular chromatin in round nuclei and moderate amount of eosinophilic cytoplasm. There were no nuclear atypia, mitosis and necrosis, H&Ex400.

The cytoplasmic positivity of chromogranin-A in tumor cells, Chromogranin-Ax400.
After surgical resection, she was asymptomatic with budesonide at 160 μg + formoterol at 4.5 μg combination therapy and had a better pulmonary function (FEV 1 , 2.53 L [95%], FVC, 4.29 L [138%]; FEV 1 /FVC, 59%). Eight months after the operation, she had another asthma attack. She was hospitalized for asthma treatment and further evaluation of recurrent tumor. There was the presence of reversible airway obstruction, particularly in the small airways, on spirometric evaluation (FEV 1 , 2.24 L [85%] with 10% reversibility and forced expiratory flow at 25–75%, 1.63 L [49%] with 17% reversibility). Computerized tomography of the thorax, abdomen, and pelvis revealed no pathological finding. Bronchoscopy was performed and cytological examination of the lavage fluid result was normal. She had no recurrence for 2 years and her asthma is presently well controlled.
Today, achieving asthma control is indicated as the main goal of asthma management by international guidelines. Although most asthma patients can be treated and controlled with inhaled steroids, some patients remain uncontrolled despite adequate asthma therapy. In our country, nearly one-half of patients with asthma were found uncontrolled in a multicenter survey. 1 A systematic review should be conducted during the management of uncontrolled asthmatic patients, and it is imperative that this include first reconfirming that a diagnosis of asthma is appropriate and then evaluating for other coexisting diseases that may influence one's asthma control. Here, we report a case of uncontrolled asthma that was, after further evaluation, revealed to be a carcinoid tumor.
Pulmonary carcinoid tumors are the most frequently encountered benign tumors of the tracheobronchial tree and constitute 2–5% of all lung cancers. 2 , 3 TCs and atypical carcinoids (ACs) are subgroups of neuroendocrine tumors that are determined as low-grade and intermediate-grade tumors according to biological aggressiveness, respectively. TCs account for 90% of all carcinoids and 80% show up in a peripheral location. 4 Although TCs are low-grade tumors, regional lymph node metastasis can be seen in 10–23% of cases; this rate, however, is 40–50% for ACs. 5 This accounts for the higher 5-year survival rates seen in TCs when compared with ACs. 5 – 7
The most common symptoms of pulmonary carcinoid tumors are hemoptysis (caused by high vascularization), lower respiratory tract infections, cough, wheezing, and shortness of breath. 8 , 9 Some patients may be asymptomatic. There is usually a time gap from the onset of symptoms until diagnosis, and patients are often misdiagnosed with asthma. 6 , 10 – 13 There are a limited number of cases diagnosed as carcinoid tumor who had also received a true diagnosis of coexisting asthma. The patient we present here had already received a diagnosis of asthma proven by reversible bronchial obstruction, and it was for this reason that her symptoms of dyspnea and wheezing were first attributed to asthma. The differential diagnosis was expanded after her poor response to standard therapy; thus, it is not surprising that a further treatment choice of anti-IgE was considered for this patient.
Anti-IgE (omalizumab) is an approved treatment for patients with severe asthma that acts on decreasing serum IgE levels. Several published studies have documented the effectiveness of this molecule in effectively treating asthma. We have been prescribing anti-IgE therapy in our tertiary clinic since 2006. In light of our experience, we believe that several factors impact a good response to anti-IgE treatment. First, proper determination of the correct indications for medicine use is vital, closely followed by the proper selection of patients. The most important issue, in our opinion, in achieving this is confirming diagnosis and excluding comorbid diseases. Therefore, the patient described in this study was evaluated accordingly. Clinical symptoms and reversible airway obstruction in spirometry led us to believe her asthma diagnosis was valid initially even though another disease state did in fact exist. Also, because an asthma attack occurred 8 months after the surgery we were convinced that she did have real asthma, retrospectively. In the literature, the associated factors with worsening asthma control included poor adherence, rhinitis, gastroesophageal reflux disease, nasal polyps, vocal cord dysfunction, bronchiectasis, allergic bronchopulmonary aspergillosis, Churg-Strauss syndrome, drugs, airway malignancy, respiratory tract infections, and thyrotoxicosis. 14 – 16 Our patient had already been evaluated for upper airway disease and gastroesophageal reflux disease by an ear–nose–throat physician and a gastroenterologist, respectively, and no pathology was determined at the first hospital to which she was admitted. During the hospitalization period, she was adherent to her asthma therapy. There were no other diagnostic criteria supporting allergic bronchopulmonary aspergillosis and Churg-Strauss syndrome. She was not taking any kind of medication ( e.g. , β-blocker, angiotensin-converting enzyme inhibitor, or nonsteroidal anti-inflammatory drug) that could exacerbate asthma. No clinical or laboratory finding of thyrotoxicosis or infection was present. We decided to make the differential diagnosis of a possible chest mass based on the left hilar opacity observable from chest radiography. In the light of computerized tomography, we performed a fiberoptic bronchoscopy and made the diagnosis of carcinoid tumor by bronchoscopic biopsy specimen.
Pulmonary carcinoids are generally located centrally in the main or lobar bronchi. 17 , 18 Available specimens for pathological examination can generally be provided from fiberoptic bronchoscopy and histopathological diagnosis is easily achieved. In this case, the tumor was located in the left lower bronchus and could easily be seen during fiberoptic bronchoscopic examination. A biopsy specimen was not taken because carcinoid tumors are highly vascularized and there is a risk for hemorrhage in nearly one-fourth of cases. 4 , 19 Furthermore, some authors advise against performing biopsies with flexible bronchoscopes. 20
Because treatment options differ according to tumor type, determining a tumor's histological type is important. In this case, the microscopic, morphological, and immunohistochemical features were characteristic for pulmonary carcinoid tumor. Pulmonary carcinoid tumors are divided into low-grade TCs and intermediate-grade ACs based on histopathological criteria. A typical pulmonary carcinoid tumor shows no focal necrosis and rare mitosis whereas an atypical pulmonary carcinoid tumor shows either focal necrosis or mitosis numbering between 2 and 10/mm 2 . 21 , 22 In our case, the absence of mitosis and necrosis with the characteristic morphological and immunohistochemical features were compatible with a low-grade typical pulmonary carcinoid tumor.
Surgery is the main choice for treatment of carcinoid tumors. In general, radical excision with detailed lymph node sampling is recommended. 8 In patients with a centrally located typical pulmonary carcinoid, bronchial sleeve resection or sleeve lobectomy is preferred. Despite its having a low recurrence rate, peripherally located TCs should be thought of as low-malignant tumors and resected anatomically. A more extensive surgical approach is recommended in AC tumors. 18 Our patient was treated with left lower lobectomy and mediastinal lymph node dissection and had experienced no recurrence for 30 months.
This case is an example of the importance of making a good differential diagnosis and confirming a diagnosis of asthma. Asthma unresponsive to treatment should alert clinicians to the possibility of differential diagnoses of other reasons for airway obstruction. Consequently, we strongly support the view that diagnosis confirmation is essential in patients with uncontrolled asthma before trying more expensive treatments.
The authors have no conflicts of interest to declare pertaining to this article
- Join our Mailing List
Working locally in primary care and collaborating globally to improve respiratory health
Clinical case study - asthma, clinical case study - asthma, resource information.
- Disease management
A Robot-assisted real case-handling approach to improving students’ learning performances in vocational training
- Published: 14 May 2024

Cite this article

- Chun-Chun Chang 1 &
- Gwo-Jen Hwang ORCID: orcid.org/0000-0001-5155-276X 2 , 3
In vocational education, cultivating students’ ability to deal with real cases is a crucial training objective. The BSFE (i.e., Brainstorming, Screening, Formation, Examination) model is a commonly adopted training procedure. Each stage is designed for guiding students to analyze and find solutions to handle real cases. However, as one teacher is generally responsible for several dozen students, it becomes challenging for the teacher to adequately address each student’s questions and individual needs. Therefore, this study proposed the robot teaching assistant-supported learning (RTAL) mode following the BSFE model to cope with this problem. This investigation assessed its efficacy through an experiment within an Acute Asthma Attack curriculum. The research involved 103 nursing students in their third year from two distinct classes at a vocational university. Fifty-three students from a class constituted the experimental group that implemented the RTAL approach, whereas the other class, comprising 50 students, was the control group utilizing the standard technology-supported learning (CTL) approach. Findings indicated that the experimental group surpassed the control group in various aspects, including learning outcomes, learning attitudes, problem-solving tedencies, critical thinking awareness, acceptance of technology, and satisfaction with the learning experience. The interview findings also revealed that the RTAL mode could cater to individualized learning needs, facilitate interaction, and serve as an auxiliary instructional tool.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
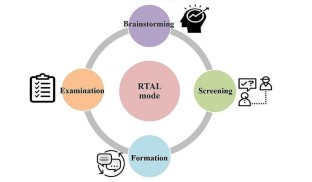
Similar content being viewed by others

Developing a gamified artificial intelligence educational robot to promote learning effectiveness and behavior in laboratory safety courses for undergraduate students
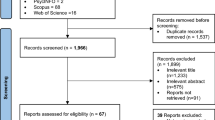
Barriers and Facilitators of Robot-Assisted Education in Higher Education: A Systematic Mixed-Studies Review
“hand-it-on”: an innovative simulation on the relation of non-technical skills to healthcare, data availability.
The data and materials are available upon request to the corresponding author.
Code availability
Not applicable.
Aralihond, A., Shanta, Z., Pullattayil, A., & Powell, C. V. E. (2020). Treating acute severe asthma attacks in children: Using aminophylline. Breathe , 16 (4). https://doi.org/10.1183/20734735.0081-2020 .
Banaeian, H., & Gilanlioglu, I. (2021). Influence of the NAO robot as a teaching assistant on university students’ vocabulary learning and attitudes. Australasian Journal of Educational Technology , 37 (3), 71–87. https://doi.org/10.14742/ajet.6130 .
Article Google Scholar
Bell, D. (1996). The formation of concepts and the structure of thoughts. Philosophy and Phenomenological Research , 56 (3), 583–596.
Belpaeme, T., Kennedy, J., Ramachandran, A., Scassellati, B., & Tanaka, F. (2018). Social robots for education: A review. Science Robotics , 3 (21), eaat5954. https://doi.org/10.1126/scirobotics.aat5954 .
Chen, H., Park, H. W., & Breazeal, C. (2020). Teaching and learning with children: Impact of reciprocal peer learning with a social robot on children’s learning and emotive engagement. Computers & Education , 150 , 103836. https://doi.org/10.1016/j.compedu.2020.103836 .
Chen, B., Hwang, G. H., & Wang, S. H. (2021). Gender differences in cognitive load when applying game-based learning with Intelligent Robots. Educational Technology & Society , 24 (3), 102–115.
Google Scholar
Chen, X., Cheng, G., Zou, D., Zhong, B., & Xie, H. (2023). Artificial intelligent robots for precision education. Educational Technology & Society , 26 (1), 171–186.
Chookaew, S., & Panjaburee, P. (2022). Implementation of a robotic-transformed five-phase inquiry learning to foster students’ computational thinking and engagement: A mobile learning perspective. International Journal of Mobile Learning and Organisation , 16 (2), 198–220.
Chu, H. C., Hwang, G. J., Tsai, C. C., & Tseng, J. C. R. (2010). A two-tier test approach to developing location-aware mobile learning systems for natural science courses. Computers & Education , 55 (4), 1618–1627. https://doi.org/10.1016/j.compedu.2010.07.004 .
Dubovi, I., Levy, S. T., & Dagan, E. (2017). Now I know how! The learning process of medication administration among nursing students with non-immersive desktop virtual reality simulation. Computers & Education , 113 , 16–27. https://doi.org/10.1016/j.compedu.2017.05.009 .
Engwall, O., & Lopes, J. (2020). Interaction and collaboration in robot-assisted language learning for adults. Computer Assisted Language Learning , 1–37. https://doi.org/10.1080/09588221.2020.1799821 .
Fildes, E. E., Campell, N. J., & Garcia, R. (2021). International nursing collaboration to establish the Philippine quit line using a conceptual model for partnership and sustainability in global health. Journal of Addictions Nursing , 32 (1), 27–31. https://doi.org/10.1097/JAN.0000000000000382 .
Galvão, E. C. F., & Püschel, V. A. A. (2012). Multimedia application in mobile platform for teaching the measurement of central venous pressure. Revista da Escola de Enfermagem da Usp, 46 , 107–115. https://doi.org/10.1590/S0080-62342012000700016 .
Hong, Z. W., Huang, Y. M., Hsu, M., & Shen, W. W. (2016). Authoring robot-assisted instructional materials for improving learning performance and motivation in EFL classrooms. Educational Technology & Society , 19 (1), 337–349.
Hsieh, J. C., & Lee, J. S. (2021). Digital storytelling outcomes, emotions, grit, and perceptions among EFL middle school learners: Robot-assisted versus Power Point-assisted presentations. Computer Assisted Language Learning . https://doi.org/10.1080/09588221.2021.1969410 .
Hwang, G. J., Yang, T. C., Tsai, C. C., & Yang, S. J. H. (2009). A context-aware ubiquitous learning environment for conducting complex science experiments. Computers & Education , 53 (2), 402–413. https://doi.org/10.1016/j.compedu.2009.02.016 .
Hwang, G. J., Yang, L. H., & Wang, S. Y. (2013). A concept map-embedded educational computer game for improving students’ learning performance in natural science courses. Computers & Education , 69 , 121–130. https://doi.org/10.1016/j.compedu.2013.07.008 .
Jahan, A., Ismail, M. Y., Sapuan, S. M., & Mustapha, F. (2010). Material screening and choosing methods–a review. Materials & Design , 31 (2), 696–705. https://doi.org/10.1016/j.matdes.2009.08.013 .
Johnson, D. W., & Johnson, R. T. (2018). Cooperative learning: The foundation for active learning. IntechOpen , 1–12. https://doi.org/10.5772/intechopen.81086 .
Jones, H., Lawton, A., & Gupta, A. (2022). Asthma attacks in children—challenges and opportunities. Indian Journal of Pediatrics , 89 (4), 373–377.
Kanero, J., et al. (2018). Social robots for early language learning: Current evidence and future directions. Child Development Perspectives , 12 (3), 146–151. https://doi.org/10.1111/cdep.12277 .
Kennedy, J., Baxter, P., Senft, E., & Belpaeme, T. (2016, March). Social robot tutoring for child second language learning. 2016 11th ACM/IEEE International Conference on Human-Robot Interaction (HRI) (pp. 231–238). IEEE.
Kim, R. H., & Mellinger, J. D. (2020). Educational strategies to foster bedside teaching. Surgery , 167 (3), 532–534. https://doi.org/10.1016/j.surg.2019.06.007 .
Konijn, E. A., & Hoorn, J. F. (2020). Robot tutor and pupils’ educational ability: Teaching the times tables. Computers & Education , 157 , 103970. https://doi.org/10.1016/j.compedu.2020.103970 .
Kubilinskiene, S., Zilinskiene, I., Dagiene, V., & Sinkevicius, V. (2017). Applying robotics in school education: A systematic review. Baltic Journal of Modern Computing , 5 (1), 50–69. https://doi.org/10.22364/bjmc.2017.5.1.04 .
Lai, C. L., & Hwang, G. J. (2014). Effects of mobile learning time on students’ conception of collaboration, communication, complex problem-solving, meta-cognitive awareness and creativity. International Journal of Mobile Learning and Organization , 8 (3), 276–291. https://doi.org/10.1504/IJMLO.2014.067029 .
Article MathSciNet Google Scholar
Lei, X., & Rau, P. L. P. (2021). Effect of Robot Tutor’s feedback Valence and Attributional Style on Learners. International Journal of Social Robotics , 1–19.
Li, D., & Chen, X. (2020). Study on the Application and Challenges of Educational Robots in Future Education Paper presented at the 2020 International Conference on Artificial Intelligence and Education (ICAIE). Lin, C. Y., & Wang, T. H. (2017). Implementation of personalized e-assessment for remedial teaching in an e-learning environment. Eurasia Journal of Mathematics, Science and Technology Education, 13 (4), 1045–1058. https://doi.org/10.12973/eurasia.2017.00657a .
Liao, Y. J., Jao, Y. L., Boltz, M., Adekeye, O. T., Berish, D., Yuan, F., & Zhao, X. (2023). Use of a Humanoid Robot in supporting Dementia Care: A qualitative analysis. SAGE Open Nursing , 9 , 23779608231179528.
Lin, H. C., Hwang, G. J., & Hsu, Y. D. (2019). Effects of ASQ-based flipped learning on nurse practitioner learners’ nursing skills, learning achievement and learning perceptions. Computers & Education , 139 , 207–221. https://doi.org/10.1016/j.compedu.2019.05.014 .
Mater, E. A. M., Ahmed, E. I., ElSayed, A. A., Shaikh, M. A. E., & Farag, M. K. (2014). The impact of the objective structured clinical examination approach for clinical evaluation skills on the student’s performance in nursing college. World Journal of Medical Sciences , 11 (4), 609–613. https://doi.org/10.5829/idosi.wjms.2014.11.4.91139 .
Mazzoni, E., & Benvenuti, M. (2015). A robot-partner for preschool children learning English using socio-cognitive conflict. Educational Technology & Society , 18 (4), 474–485.
Obafemi, K. E. (2024). Enhancing pupils’ academic performance in mathematics using brainstorming instructional strategy. ASEAN Journal of Science and Engineering Education , 4 (2), 99–106.
Papadopoulos, I., Lazzarino, R., Miah, S., & Weaver, T. (2020). A systematic review of the literature regarding socially assistive robots in pre-tertiary education. Computers & Education , 155 , 103924. https://doi.org/10.1016/j.compedu.2020.103924 .
Park, H. W., Grover, I., Spaulding, S., Gomez, L., & Breazeal, C. (2019, July). A model-free affective reinforcement learning approach to personalization of an autonomous social robot companion for early literacy education. In Proceedings of the AAAI Conference on Artificial Intelligence, 33 (l), 687–694. https://doi.org/10.1609/aaai.v33i01.3301687 .
Pfadenhauer, M., & Dukat, C. (2015). Robot caregiver or robot-supported caregiving? The performative deployment of the social robot PARO in dementia care. International Journal of Social Robotics , 7 , 393–406.
Pueyo-Garrigues, M., Whitehead, D., Pardavila-Belio, M. I., Canga-Armayor, A., Pueyo-Garrigues, S., & Canga-Armayor, N. (2019). Health education: A rogerian concept analysis. International Journal of Nursing Studies , 94 , 131–138. https://doi.org/10.1016/j.ijnurstu.2019.03.005 .
Randall, N. (2019). A Survey of Robot-assisted Language Learning (RALL). ACM transactions on Human-Robot Interaction , ( 9 ) 1.7:1–736. https://doi.org/10.1145/3345506 .
Rezasoltani, A., Saffari, E., Konjani, S., Ramezanian, H., & Zam, M. (2022). Exploring the viability of robot-supported flipped classes in English for medical purposes reading com-prehension. arXiv Preprint arXiv:2208 07442 . https://doi.org/10.48550/arXiv.2208.07442 .
Richert, A., Schiffmann, M., & Yuan, C. (2020). A nursing robot for social interactions and health assessment. In Advances in Human Factors in Robots and Unmanned Systems: Proceedings of the AHFE 2019 International Conference on Human Factors in Robots and Unmanned Systems, July 24–28, 2019, Washington DC, USA 10 (pp. 83–91). Springer International Publishing.
Rowe, B. H., Sevcik, W., & Villa-Roe, C. (2011). Management of severe acute asthma in the emergency department. Current Opinion in Critical Care , 17 (4), 335–341. https://doi.org/10.1097/MCC.0b013e328348bf09 .
Shimada, M., Kanda, T., & Koizumi, S. (2012). How can a social robot facilitate children’s collaboration? In Social Robotics: 4th International Conference, ICSR 2012, Chengdu, China, October 29–31, 2012. Proceedings 4 (pp. 98–107). Springer Berlin Heidelberg. https://doi.org/10.1007/978-3642-34103-810 .
Su, C. H., He, Y. H., & Peng, Y. H. (2012). Respiratory care for a patient undergoing extracorporeal life support for Status Asthmaticus. Journal of Respiratory Therapy , 11 (1), 45–55. https://doi.org/10.6269/JRT.2012.11.1.05 .
Trollvik, A., Nordbach, R., Silen, C., & Ringsberg, K. C. (2011). Children’s experiences of living with asthma: Fear of exacerbations and being ostracized. Journal of Pediatric Nursing , 26 (4), 295–303. https://doi.org/10.1016/j.pedn.2010.05.003 .
Varney, M. W., Janoudi, A., Aslam, D. M., & Graham, D. (2012). Building young engineers: TASEM for third graders in woodcreek magnet elementary school. IEEE Transactions on Education , 55 (1), 78–82. https://doi.org/10.1109/TE.2011.2131143 .
Yang, K. H., & Lu, B. C. (2021). Towards the successful game-based learning: Detection and feedback to misconceptions is the key. Computers & Education , 160 , 104033. https://doi.org/10.1016/j.compedu.2020.104033 .
Yueka, L. (2019). Current situation, d ynamic and problems of AI + t eacher education . Journal of Modern Education Technology , 29 (11), 114–120. Zhong, S.
Download references
This study is supported in part by the National Science and Technology Council of Taiwan under contract numbers NSTC 112-2410-H-011-012-MY3 and MOST 111-2410-H-011 -007 -MY3. The study is also supported by the “Empower Vocational Education Research Center” of National Taiwan University of Science and Technology (NTUST) from the Featured Areas Research Center Program within the framework of the Higher Education Sprout Project by the Ministry of Education (MOE) in Taiwan.
Author information
Authors and affiliations.
Department of Nursing, Chang Gung University of Science and Technology, Taoyuan City, Taiwan
Chun-Chun Chang
Graduate Institute of Educational Information and Measurement, National Taichung University of Education, Taichung City, Taiwan
Gwo-Jen Hwang
Graduate Institute of Digital Learning and Education, National Taiwan University of Science and Technology, Taipei City, Taiwan
You can also search for this author in PubMed Google Scholar
Contributions
The authors contributed to the conceptualization and design of the study. Material preparation, data collection, analysis, project management and methodology were performed by Chun-Chun Chang. Methodology and supervision were performed Gwo-Jen Hwang.
Corresponding author
Correspondence to Gwo-Jen Hwang .
Ethics declarations
Ethical approval.
The study has been evaluated and approved by the research ethics committee of Chang Gung with the IRB number 202300304B0C101.
Consent to participate
The participants all agreed to take part in this study.
Consent for publication
The publication of this study has been approved by all authors.
Conflicts of interest
There is no potential conflict of interest in this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Chang, CC., Hwang, GJ. A Robot-assisted real case-handling approach to improving students’ learning performances in vocational training. Educ Inf Technol (2024). https://doi.org/10.1007/s10639-024-12778-w
Download citation
Received : 13 March 2024
Accepted : 07 May 2024
Published : 14 May 2024
DOI : https://doi.org/10.1007/s10639-024-12778-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vocational education
- Nursing education
- Professional training
- Find a journal
- Publish with us
- Track your research
- International edition
- Australia edition
- Europe edition

Wednesday briefing: The study that says semaglutide can do much more than help you lose weight
In today’s newsletter: A new study suggests semaglutides reduce not just obesity but risks to your heart too. What will that mean for their availability on the NHS?
Sign up here for our daily newsletter, First Edition
Good morning. If you hear brand names like Ozempic and Wegovy and think of suddenly gaunt A-listers posing on the red carpet, it is surely now time to think again. There has already been substantial evidence that as well as in their initial role as a diabetes treatment, semaglutides – the kind of drug in question – can have a real impact on obesity for people for whom nothing else works. Now a new study has found that they don’t just help those people lose weight – they have a major effect on their heart health , regardless of how much weight they lose.
Obesity affects more than a quarter of adults, and nearly as many children – and those numbers are only going up , which brings serious consequences for public health, especially among the most deprived. So this is hugely significant news, which study author Prof John Deanfield says heralds a class of drugs as powerful as statins, “that could equally transform many chronic diseases of ageing”.
Today’s newsletter, with obesity expert and lecturer in physiology at Anglia Ruskin university Dr Simon Cork, is about what we’ve just learned, why it changes our understanding of semaglutides and whether it will mean they become more widely available. Here are the headlines.
Five big stories
Georgia | Tbilisi has been warned by the US not to turn towards Russia as its parliament defied mass street protests to pass a “Kremlin-inspired” law . A US official said that the “foreign agents” bill, which takes aim at civil society groups with funding from abroad, could jeopardise support from Washington for the former Soviet state “if we are now regarded as an adversary”.
France | Elite French police are searching for gunmen who attacked a prison van in Normandy, killing at least two prison officers and freeing the high-security inmate being transported . The fugitive prisoner was named as Mohamed Amra, who was convicted last week of aggravated robbery and charged in a case of abduction leading to death.
Education | There is no evidence of widespread abuse of the UK’s graduate visa route, a major report has concluded , despite claims from Conservatives that it is being exploited to enter the jobs market. The government is expected to decide next week whether to remove the scheme, a move which would mean financial turmoil for the sector.
US | Donald Trump’s ex-lawyer Michael Cohen has testified in Manhattan court that he submitted phoney invoices for legal services to cover up what were reimbursements for hush money paid to Stormy Daniels . In a second day of evidence, Cohen repeatedly identified Trump as the driver of the Daniels payoff scheme.
Manchester | After a series of humiliating setbacks, the £450m Co-op Live music venue finally opened its doors on Tuesday , with a concert by Elbow that had been meant to be the 15th event on its schedule. The venue’s boss, Tim Leiweke, claimed that it would be “the greatest arena ever built”.
In depth: ‘These drugs aren’t going to solve obesity, but they have a huge amount of promise’

Ozempic and Wegovy are brand names for a snappily named class of drugs called glucagon-like peptide receptor agonists, or GLP-1 agonists. They were first authorised as diabetes treatments, and have proven very effective. The specific GLP-1 agonist in them is semaglutide. It works by mimicking a naturally occurring hormone, GLP-1, which is released by the gut after we eat and makes us feel full.
They don’t work in the same way for everyone, as this set of Guardian reader accounts from last year suggests: sustained healthy weight loss and a liberating release from cravings at one end of the spectrum, total failure and horrible side effects at the other. But overall, studies have shown that semaglutide is more effective than earlier generations of GLP-1 drugs, helping overweight and obese people lose about 15% of their body weight when combined with diet and exercise – much more than those who used diet and exercise alone.
“The existing studies around weight loss cover two years,” Simon Cork said. “We know that the vast majority of patients lose a significant amount of weight, and that that weight loss is associated with a drop in blood pressure and blood glucose” – both linked to heart health. “They don’t cause you to lose weight in and of themselves – to get that effect you have to have an overarching change in your lifestyle.”
It’s also worth noting that users will typically need to maintain their dose for the effects to last. When people stop using semaglutides, studies have shown, “almost everyone regains two-thirds to three-quarters of the weight back – and with that the associated health risks also return”.
What the new study tells us
The previous research on semaglutide as a weight loss treatment has largely focused on that primary role. The evidence about heart health has only been of the impact you would expect to be associated with the corresponding weight loss. But the new study , led by researchers at University College London, sets out evidence that could have a significant impact on how we think about the drug’s potential importance.
The study, which is yet to be published but has been presented at a conference, looked at more than 17,000 overweight or obese adults aged over 45 who had previously experienced a cardiovascular event such as a heart attack, and divided them into two groups – one receiving semaglutide, the other getting a placebo.
It found that those receiving semaglutide were 20% less likely to have a heart attack. Crucially, Cork said, “you can separate out the decrease in cardiovascular risk from the weight changes. We had assumed it was a consequence of losing weight – but this seems to suggest there’s a separate pathway.” We don’t know how those effects would play out in patients at a healthy weight, because they weren’t part of the study – so it doesn’t mean that semaglutides should be considered as a treatment for anyone with heart issues regardless of their weight.
At the same time as the UCL study was released, another study of a new drug, retatrutide, found that it could be even more effective – with participants losing 24% of their body weight over 48 weeks, partly because it has an impact on metabolism as well as appetite. “That can be hugely significant for someone with obesity,” Cork said. But he noted that it also demonstrated how important it is to have such drugs available under proper clinical guidance: “Someone of normal weight or who’s underweight with body dysmorphia using that could be very dangerous.”
What it could mean for availability on the NHS

At the moment, guidance published by the National Institute for Care and Excellence (Nice) says that Wegovy should be prescribed for a maximum of two years – even though the evidence suggests that when it stops being used, the benefits stop too. So another important aspect of the study, Cork said, “is that it was carried out over four years – it’s the first beyond a two-year period. It shows that the health impact is prolonged over four years, and also safe over that period. Obesity is a lifelong condition – we wouldn’t end prescriptions for patients with hypertension or asthma. So that has to change.”
Another barrier: the Nice guidelines also say that Wegovy should only be prescribed by specialist weight management services – but those are badly oversubscribed. “There has been some talk that GPs should be able to prescribe, which would reduce the burden,” Cork said.
Wegovy’s use for weight loss has already caused issues with availability for diabetes patients – and the cost of the drug is also potentially prohibitive. But even from a solely economic perspective, Cork pointed out, obesity “ costs the NHS more than £6bn a year because of the associated risks – heart attacks, diabetes, stroke. So anything we can do to mitigate that has to be helpful in the long run.”
There is no instant fix to the supply issues, although these are primarily the result of private prescriptions rather than those on the NHS. “But if you look at the drugs coming down the line that are in late stage trials, I think it’s very likely that we’re going to see increased availability as they hit the market – and that will have a positive effect on the price, as well.”
What the long-term impact might be
The really remarkable thing about the new study is the hard evidence that it provides of benefits for cardiovascular health that go beyond weight loss alone. One possible impact of that is a shift in the way drugs like Ozempic and Wegovy are discussed: because of the way they came to prominence through stories of celebrities using them to squeeze into outfits, and their usage becoming commonplace among wealthy Americans who want to look good on the beach, they are now caught between being treated as miracle cures and as shortcuts to cosmetic benefits for the terminally lazy.
“That tone is very visible – you only have to look in the comments section on articles or social media,” Cork said. “People simply think the answer is eat less and exercise more – but for obesity that’s not really true.
“We can have a separate conversation about policy to prevent people becoming overweight or obese, whether it’s the affordability of healthy foods or access to green spaces – but the bottom line is that there are people who are overweight and obese because of their genetic makeup, and we have to find effective ways to help those people.”
In that context, and given the new evidence about cardiovascular impact, Cork hopes to see much wider use in the years ahead. “We have no other real way of managing obesity other than ineffective instructions about diet and exercise. These drugs aren’t going to solve the problem, but they have a huge amount of promise.”
after newsletter promotion
What else we’ve been reading

As the debate over assisted dying in the UK shifts towards a majority view that the ban is an immoral anachronism, it’s really worth reading Anna Moore’s interview with the actor Liz Carr , who’s made a BBC documentary that presents an alternative argument through the prism of her own disability. This line will stay with me: “The biggest catastrophe is that we’d choose it ourselves because there was no more choice for us.” Frances Ryan gives the film five stars . Archie
Hannah Grace Deller and Esther Addley beautifully captured the journeys that NHS nurses have taken since quitting their job after the pandemic in this picture essay. Nimo
Suella Braverman has joined the long list of charities and experts who say that the two-child benefits limit should be scrapped – and on this issue, she’s to the left of Labour. By outflanking the Tories on so many subjects, Gaby Hinsliff writes , Keir Starmer has left “his party defending a frankly implausible swathe of political territory, and not just from an attack by the left”. Archie
This week’s TechScape newsletter is about the Online Safety Act , which Alex Hern describes as “quietly one of the most important pieces of legislation to have come out of this government”. Nimo
Over 100 musicians share their stories with Alfie Packham about the punishing financial landscape that has left many out of pocket and unable to pursue their musical ambitions. Nimo

Football | Erling Haaland scored twice to give Manchester City a 2-0 win at Tottenham to reclaim top spot in the Premier League heading into the last day of the season. Because Tottenham fans are unenthusiastic about Arsenal winning the league, “there was a sense around the crowd of some necessary duty being discharged,” Barney Ronay wrote – but the final result was “a serial champion simply stretching away in the straight”.
Formula One | The More than Equal initiative, a global development programme created to assist women’s progress toward Formula One and in motor racing, has announced its first selection of female drivers . The six teenagers selected will now work with a team of experienced driving coaches in an attempt to address the gender imbalance in the sport.
Rugby | Saracens have confirmed that Billy and Mako Vunipola will leave the club at the end of the season while Gloucester have also announced that Jonny May is making his exit. All three have been England regulars over the past decade but are set to join the growing number of recent Test players in moving abroad in the summer.
The front pages

The Guardian print edition leads this morning with “US warns Georgia not to side with Russia against the west”. The i has “New weight loss jab ‘gold rush’ offers obesity hope to millions”. “Anglo reveal break up plan to thwart BHP takeover” is the top story in the Financial Times ; in the Metro it’s “UK’s record 3m food parcels”. The Times reports “Don’t teach pupils about gender ID, schools told” while the Daily Telegraph splashes on “Tories tell police: Bring back stop and search”. “Sex education to be banned for under 9s – and no more gender dogma” says the Daily Mail . “‘Fighting chance’ migration will fall to 150,000 a year” – that’s the Daily Express. “Mummy’s a legend … I’m a mess” – that’s the Daily Mirror , which covers TV host Ant McPartlin having a baby with his wife, Anne-Marie.
Today in Focus

The ‘foreign agents’ law that has set off mass protests in Georgia
The bill requires any civil society organisation that receives more than 20% of its funds from abroad to register as being under foreign influence. Daniel Boffey reports
Cartoon of the day | Martin Rowson

A bit of good news to remind you that the world’s not all bad

Ncazelo Ncube-Mlilo, a Zimbabwean psychologist, has spent much of her professional career developing “culturally sensitive” therapeutic tools – the most famous is COURRAGE. Each letter in the acronym a theme in an eight-week group counselling program that encourages participants to reframe trauma as stories of survival and strength.
The program is spearheaded by her charity, Phola, which reaches more than 10,000 women, men and children in townships around Johannesburg, South Africa every year. Her method has been adopted in 40 countries including the UK, and participants have gone on to create their own support networks. “Now we are there for each other,” one participant says. “If one of us is going through something, we are just a call away.”
Sign up here for a weekly roundup of The Upside, sent to you every Sunday
Bored at work?
And finally, the Guardian’s puzzles are here to keep you entertained throughout the day. Until tomorrow.
Quick crossword
Cryptic crossword
- First Edition newsletter
- Medical research
- Heart attack
- UCL (University College London)
- newsletters
Most viewed
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 15, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
written by researcher(s)
Why is whooping cough surging in the UK? Falling vaccination rates may be the answer
by Michael Head, The Conversation

A large outbreak of pertussis (more commonly known as whooping cough) has been ongoing in the UK since the beginning of 2024. There have been 2,793 confirmed cases so far this year. Sadly, five infant deaths due to whooping cough have been confirmed, with unconfirmed reports that a sixth infant may have died in the last week of the bacterial infection.
This is a stark reminder that whooping cough is a very nasty infection. While the symptoms are usually mild in healthy older children and adults, it can be lethal for babies.
Globally, there are an estimated 24 million cases of whooping cough each year and around 160,000 deaths.
Whooping cough is caused by a bacteria called Bordetella pertussis . Pertussis often begins like most other respiratory infections, with typical symptoms including a runny nose and a fever. The distinctive "whoop" cough may only appear after a week or so of illness—though it does not occur in all cases. As such, confirming cases of whooping cough may require a laboratory test.
Whooping cough is very infectious. On average, a single case of pertussis can transmit infection on to about 15–17 other people . This infection rate is similar to measles and higher than the COVID variants .
The reason whooping cough is so infectious is in part due to pertussis having a very long infectious period of up to five weeks—where infected people can pass the bacteria on to others. Prompt treatment can greatly reduce transmission—antibiotics shown to reduce contagiousness just five days after starting treatment.
But prior to treatment, there are plenty of opportunities for transmission to occur and for an outbreak to be maintained. Both confirmed and asymptomatic cases can be responsible for onward transmission of whooping cough.
Why have cases spiked?
One slightly curious aspect of whooping cough is that there are big outbreaks typically every few years. The last sizeable outbreak in the UK was in 2016 with almost 6,000 confirmed cases . The reasons for these cycles are not fully understood, but a key factor is probably waning immunity at the population level .
The immunity from the pertussis vaccine is initially very protective, but it does decline a few years after the initial vaccination. This is why a consistently high vaccine uptake across the population is vital.
The vaccine is very safe and effective . Vaccinating young children and pregnant women —some of the most vulnerable groups within the population—is particularly crucial for preventing infection and illness.
Children who are fully vaccinated are 84% less likely to get a confirmed whooping cough infection compared to those who weren't vaccinated. Vaccines not only prevent young children from becoming unwell—vaccines also lower the risk of children transmitting the infection onto young siblings, family members and friends.
Immunization during pregnancy is also particularly important as the antibodies the mother gets from the vaccine protects the newborn in their first few weeks of life—before the baby is themselves old enough to receive their first pertussis vaccine dose. A dose during pregnancy prevents around 78% of pertussis cases in newborn babies.
But vaccine coverage has dropped in recent years. Maternal vaccine uptake was 70% in 2017, but only 58% in 2023.
The percentage of children vaccinated by their first birthday dropped slightly from around 93% just prior to the pandemic to 92% in 2022–2023. A similar drop (from 85% to 83% ) is seen with the booster dose children can have prior to their fifth birthday. This drop in coverage may be contributing to the current outbreak.
While one publication has suggested the outbreak is probably a " surge fueled by lockdown ," there's no evidence to support this assertion.
This kind of messaging isn't helpful as it doesn't raise awareness or educate the public on the things they can do to prevent the spread of whooping cough. Given that people's health-related behavior can be significantly impacted by the news they read , high-profile media sources have a responsibility to report accurate information .
The sheer extent of the pandemic may have affected access to health care and vaccination rates, resulting in a drop of the population-wide immunity needed to prevent severe outbreaks. Geographical variations in vaccine uptake might also be a contributing factor—though, at the time of writing, there isn't any data available on case numbers by UK region.
To control the current outbreak, widespread use of antibiotics to treat or prevent pertussis infections will probably be used. If anyone suspects they have whooping cough, they should speak to their doctor as soon as possible—not only because of the severity of the illness, but because prompt treatment reduces person's infectious period.
While UK guidance does not routinely recommend a pertussis vaccine in adults, an extra dose is known to be safe and effective. This may be advised for people who have come in close contact with someone who has whooping cough. It may also be important for people who could be vulnerable to a severe infection—such as the elderly.
Ultimately, whooping cough is an infection that can be prevented by vaccines. The grim news of infant fatalities in the UK reminds us all that there are very good reasons why immunization is recommended. And, in the longer-term, outbreaks can be minimized in both the number of cases and the severity of cases by maintaining a high vaccine coverage.
Access to vaccination, as well as accurate information about the small risks and significant benefits, is going to be key in bringing the outbreak under control.
Explore further
Feedback to editors

Fruit fly study reveals brain-cell circuitry that could underlie how creatures large and small see wavelengths of light
15 minutes ago

Climate change is likely to aggravate brain conditions, study finds
10 hours ago

Researchers develop innovative platform for modeling human muscle diseases in worms
12 hours ago

Pre- and post-surgical immunotherapy improves outcomes for patients with operable lung cancer, Phase III study finds

Study finds reduced risk of breast cancer following bariatric surgery in women with hyperinsulinemia

Treatment-resistant depression linked to body mass index: Study

Chiropractic associated with lower likelihood of tramadol prescription in adults with sciatica

Study finds two genes of the germline are essential for the development of brain tumors in Drosophila

Study reveals immunotherapy's potential in boosting immune systems of older individuals

Alzheimer's disease processes without symptoms. How is that possible?
13 hours ago
Related Stories

Whooping cough is surging in Australia: Why, and how it can protect itself
Apr 5, 2024

For baby's sake, moms-to-be need the whooping cough vaccine: CDC
Feb 8, 2023

Babies better protected against whooping cough if mom is vaccinated during pregnancy, study finds
Oct 10, 2023

Four children die in Serbia whooping cough outbreak
Jan 31, 2024

Croatia struggles to contain whooping cough epidemic
Nov 29, 2023

Do you know who to talk to about your child's routine vaccinations?
Feb 14, 2023
Recommended for you

Wearing face masks did not reduce risk of COVID infection after first omicron wave, research suggests
15 hours ago

Study finds H5N1 virus from 2022 mink outbreak capable of inefficient airborne transmission
14 hours ago

Researchers develop method to monitor patients with spinal muscular atrophy using sound waves

Researchers find microplastics in canine and human testicular tissue

New study identifies mechanism of immune evasion of SARS-CoV-2 and variants
19 hours ago
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter

IMAGES
VIDEO
COMMENTS
1. a. Tidal volume is the volume of air inhaled or exhaled during normal quiet breathing. b. Inspiratory reserve volume is the amount of air that can be inhaled after a normal tidal volume. How do you think that each of these lung volumes (tidal, inspiratory reserve, and expiratory reserve) would change for someone experiencing an asthma attack ...
Abstract. This interrupted case study follows the progress of a pediatric patient who experiences an acute asthma exacerbation brought on by an environmental trigger. Students completing the case will synthesize their understanding of respiratory system anatomy and physiology with the clinical treatment of an obstructive lung disorder.
Figure 1. The respiratory passageways in a non-asthmatic (L) bronchoconstriction can severely decrease the diameter of the. and asthmatic (R) lung. Credit: BruceBlaus, cc by 3.0. already swollen, mucus-producing airways, making it very. difficult to move air into and out of the lungs. The decrease in air flow can range from mild to life ...
may cause a great deal of anxiety for someone actively suffering from an acute asthma exacerbation, or asthma attack. Questions You may need to use the internet or another source to help answer some of the questions in this case study. 1. According to the passage above, what are the three factors involving the airways that lead to an asthma ...
Supported self-management reduces asthma morbidity. The lady in this case study is struggling to maintain control of her asthma within the context of her busy professional and domestic life.
Case presentation. The patient, a 66-year-old asthmatic man, had a 3-day history of worsening cough, wheeze and shortness of breath that was not relieved by his salbutamol inhaler. ... In a prospective study 7 of 18 patients with acute exacerbation of asthma, attending the emergency department, the change in lactate levels after administering ...
The majority of adverse effects occurred within 1 day of the procedure and resolved within 7 days. 6. In this study, bronchial thermoplasty was found to significantly improve quality of life, as ...
In recent years, it has gained increasing notoriety in schools and in the media. Population-based studies have shown that 20% to 35% of children with allergies experience bullying. In many cases (31% in one recent study ), this bullying is related directly to the food allergy. From a medical perspective, there are little published data ...
Airflow obstruction in asthma is the result of contraction of the airway smooth muscle and swelling of the airway wall due to: Smooth muscle hypertrophy and hyperplasia. Inflammatory cell infiltration and oedema. Goblet cell and mucous gland hyperplasia with mucous hypersecretion. Protein deposition including collagen.
SNC4U snc4m case study: asthma attack! national center for case study teaching in science asthma attack! hollie leavitt department of biology college of. Skip to document. University; High School. ... You may need to use the internet or another source to help answer some of the questions in this case study.
Case Study - Asthma. a 17 yr old student experienced reversible, periodic attacks of chest tightness with coughing, wheezing, and hyperpnea. She states that expiration is more difficult than inspiration, and that she is most comfortable sitting forward with arms leaning on some support. CXR revealed mild overinflation of the chest.
Asthma - Page 1. Review structure and functions of the respiratory system in the Case Study Workbook and through the following videos. All of these videos are on the same page. Scroll down to find each video: Respiratory System - Respiration - The Mechanics of Breathing. Sixteen-year-old Ben Mason was warming up for a high school soccer ...
Case Presentation. The patient is a 60-year-old white female presenting to the emergency department with acute onset shortness of breath. Symptoms began approximately 2 days before and had progressively worsened with no associated, aggravating, or relieving factors noted. She had similar symptoms approximately 1 year ago with an acute, chronic ...
Case Study course: training and development chapter the asthma attack case study professor: darlene friesen student: sarah jolicoeur date may 31st, 2021 run the. ... Chapter 3 - The Asthma Attack Case Study Professor: Darlene Friesen Student: Sarah Jolicoeur Date May 31. st, 2021. 1. Run the asthma attack incident through the need's ...
Quick-Relief Medication for All Patients: SABA as needed for symptoms. Intensity of treatment depends on severity of symptoms: up to 3 treatments at 20-minute intervals as needed. Short course of systemic oral corticosteroids may be needed. Caution: Increasing of b-agonist or use >2x/week for symptoms control indicates.
Asthma Attack - Assignment Training & Development Sarah Glass Hi Laurie, "Asthma Attack" Case Study: In March of 2013, a teenage boy visiting a Tim Hortons franchise in London, Ontario, suffered an asthma attack. The 17-year-old boy was having difficulty breathing and was gasping for air as he tried to get the attention of ...
A 48-year-old female patient with uncontrolled severe asthma was referred to our hospital for anti-IgE therapy. She was suffering with persistent wheezing and dyspnea after a severe asthma attack that had taken place 5 months previously. Her asthma had not been controlled with adequate asthma treatment, including budesonide at 320 μg ...
Asthma affects about 6.1 million children in the US under 18 years of age, making it one of the most common chronic childhood disorders (American Lung Association, 2021). Asthma occurs as a result of a stimulus which can range from allergens, cigarette smoke, changes in temperature, stress, or exercise. In this case we'll experience an asthma ...
Clinical case study - asthma . 2019 . Clinical Case Study - Asthma. pdf. Clinical Case Study - Asthma. 6.34 MB. Resource information. Respiratory conditions. Asthma; Respiratory topics. Disease management; Diagnosis; Type of resource. Presentation . Author(s) Jaime Correia de Sousa Ioanna Tsiligianni Miguel Román Rodriguez
For example, C02 (C: Control group; 02: the second student in the group) stated that the case study learning sheets increased the opportunity for her to think and synthesize learning outcomes when writing the answers. C08 also mentioned that he knew that the Acute Asthma Attack course was professional and important.
Chapter 28 :: Patient With Asthma Case Study. Asthma is a chronic inflammatory disorder of the airways. There are 3 components of asthma: inflammation, increased mucous production, and bronchospasm. These components lead to recurrent episodes of wheezing, breathlessness, chest tightness, and cough, particularly at night or in the early morning.
But overall, studies have shown that semaglutide is more effective than earlier generations of GLP-1 drugs, helping overweight and obese people lose about 15% of their body weight when combined ...
This is a stark reminder that whooping cough is a very nasty infection. While the symptoms are usually mild in healthy older children and adults, it can be lethal for babies.. Globally, there are ...