- Open access
- Published: 08 July 2020

A critical interpretive synthesis of the roles of midwives in health systems
- Cristina A. Mattison ORCID: orcid.org/0000-0001-7210-0690 1 ,
- John N. Lavis 2 ,
- Michael G. Wilson 2 ,
- Eileen K. Hutton 1 &
- Michelle L. Dion 3
Health Research Policy and Systems volume 18 , Article number: 77 ( 2020 ) Cite this article
9348 Accesses
17 Citations
12 Altmetric
Metrics details
Midwives’ roles in sexual and reproductive health and rights continues to evolve. Understanding the profession’s role and how midwives can be integrated into health systems is essential in creating evidence-informed policies. Our objective was to develop a theoretical framework of how political system factors and health systems arrangements influence the roles of midwives within the health system.
A critical interpretive synthesis was used to develop the theoretical framework. A range of electronic bibliographic databases (CINAHL, EMBASE, Global Health database, HealthSTAR, Health Systems Evidence, MEDLINE and Web of Science) was searched through to 14 May 2020 as were policy and health systems-related and midwifery organisation websites. A coding structure was created to guide the data extraction.
A total of 4533 unique documents were retrieved through electronic searches, of which 4132 were excluded using explicit criteria, leaving 401 potentially relevant records, in addition to the 29 records that were purposively sampled through grey literature. A total of 100 documents were included in the critical interpretive synthesis. The resulting theoretical framework identified the range of political and health system components that can work together to facilitate the integration of midwifery into health systems or act as barriers that restrict the roles of the profession.
Conclusions
Any changes to the roles of midwives in health systems need to take into account the political system where decisions about their integration will be made as well as the nature of the health system in which they are being integrated. The theoretical framework, which can be thought of as a heuristic, identifies the core contextual factors that governments can use to best leverage their position when working to improve sexual and reproductive health and rights.
Peer Review reports
Introduction
Midwives’ roles in sexual and reproductive health and rights (SRHR) continue to evolve and an understanding of the profession’s role in health systems is essential in creating evidence-informed policies. Countries across all income levels face challenges with providing high-quality SRHR and achieving effective coverage [ 1 ]. National or sub-national SRHR policies often do not include the midwifery workforce or account for the professions’ role in the provision of high-quality care [ 1 ]. The lack of conceptual clarity regarding the drivers of midwives’ roles within health systems, ranging from their regulation and scope of practice to their involvement in care, has resulted in significant variability both within and across countries on how the profession is integrated into health systems.
Research on midwifery care has demonstrated that the profession delivers high-quality SRHR services [ 1 , 2 , 3 ]. Care provided by midwives who are trained, licensed and regulated according to international standards is associated with improved health outcomes [ 3 , 4 , 5 , 6 , 7 ]. While midwifery care is associated with positive outcomes, it is an area that is under-researched [ 8 ]. This is particularly true in relation to how political and health system factors influence the profession’s role in health systems. As such, the roles of midwives in health systems are not clearly understood, which continues to challenge the profession’s ability to work effectively in collaborative and interprofessional settings.
Midwifery research is often dichotomised by the development status of the jurisdiction of focus — high-income countries (HICs) compared to low- and middle-income countries (LMICs). In HICs in general, midwives’ roles are focused on primary care to low-risk pregnant people through pregnancy, labour and a limited post-partum period [ 9 ]. In comparison, in LMICs, midwives’ scope of practice can be broader and extends to many aspects of SRHR [ 10 , 11 , 12 , 13 ]. International organisations (e.g. WHO, United Nations Population Fund and the International Confederation of Midwives) support an expanded approach to midwifery roles to include provision of a range of SRHR services (e.g. health counselling and education, prevention of mother-to-child HIV transmission, prevention and treatment of sexually transmitted infections, and provision of safe abortion where legal) [ 4 , 14 ].
Arguably one of the most crucial components of a health system is its health workforce, as highlighted by WHO’s framework of ‘building blocks’ to support health systems strengthening (service delivery, health workforce, health information systems, access to essential medicines, financing and governance) [ 15 ]. While midwifery is recognised as key to SRHR, there is a global shortage of the midwifery workforce [ 2 , 4 ]. Midwives who are educated and regulated according to international standards can provide 87% of a population’s essential SRHR, yet only 36% of the midwifery workforce is made up of such fully trained midwives, with a range of other health workers also delivering midwifery services [ 4 ]. The latter has been made possible by the range of roles that non-midwife health workers play in providing midwifery services [ 4 , 16 ].
The lack of understanding of the roles of midwifery in health systems has led to significant disparities within and across countries. A better understanding of the roles of midwives within the health system is desirable as they are a key component in the delivery of safe and effective SRHR and could possibly improve the cost-effectiveness of the delivery of these services [ 17 , 18 , 19 ]. There is growing recognition that, to strengthen health systems, decisions must be based on the best available research evidence [ 20 , 21 , 22 , 23 ]. Using the available research evidence to understand the roles of midwives across health systems, as well as the political and health system drivers, will yield important insights with the aim of adding to the evidence base that policy-makers can draw from.
The present study asks — across health systems, what are the factors that influence the roles of midwives within the health system? We present a theoretical framework to explain how political and health system factors influence the roles of midwives within the health system. It defines the political system as consisting of three main components, namely institutions, interests and ideas [ 24 ]. ‘Health system arrangements’ are made up of governance, financial and delivery arrangements, and implementation strategies [ 25 ]. Given the lack of theoretical development in the area, this paper, through a critical interpretive synthesis of the available literature, identifies the factors that act as barriers or facilitators to the roles of midwives.
A critical interpretive synthesis was used to develop the theoretical framework, which is an inductive approach to literature analysis. The approach uses conventional systematic review processes while incorporating qualitative inquiries to examine both the empirical and non-empirical literature [ 22 ]. Critical interpretive syntheses are best suited to developing theoretical frameworks that draw on a wide range of relevant sources and are particularly useful when there is a diverse body of literature that is not clearly defined, as is the case with literature related to the roles of midwives in health systems. Conventional systematic reviews have well formulated research questions at the outset, while a critical interpretive synthesis employs a compass question, which is highly iterative and responsive to the findings generated in the review process [ 26 ].
Literature search
The selection of the literature was carried out in phases (Fig. 1 ). The first phase consisted of a systematic search of electronic bibliographic databases. The searches were executed in consultation with a librarian, who provided guidance on developing keywords (along with Boolean operators) and MeSH (Medical Subject Heading), refining the search strategy, identifying additional databases and executing the searches. We searched the following electronic databases through to 14 May 2020: CINAHL, EMBASE, Global Health database, HealthSTAR, Health Systems Evidence, MEDLINE and Web of Science. The search strategy was first developed in the MEDLINE database, using keywords and MeSH. Similar search strings were used across databases, with minor adjustments made to ensure search optimisation. The searches in MEDLINE included midwi* AND (roles OR scope), midwi* AND delivery of health care (MeSH), midwi* AND patient satisfaction (MeSH), midwi* AND quality of health care (MeSH), and midwi* AND standards (MeSH).
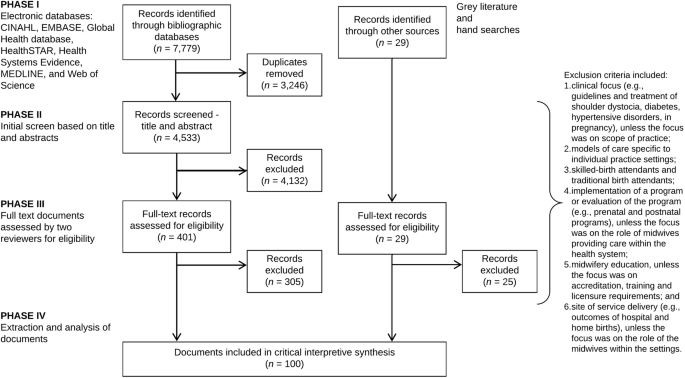
Literature search and study selection flow diagram
The second phase, complementary to the bibliographic database search, was a search of policy and health systems-related SRHR and midwifery organisation websites for relevant documents (e.g. World Health Assembly resolutions and United Nations Population Fund’s State of the World’s Midwifery reports). In addition, hand searches of reference lists from key publications were used to identify further relevant literature (e.g. 2014 Lancet Series on Midwifery). The final step in the literature search process was a purposive search to identify literature to fill the conceptual gaps that emerged.
Article selection
For inclusion, the documents had to relate specifically to trained midwives, with leeway in terms of title (e.g. certified nurse-midwives and certified midwives in the United States). Articles were included, that in addition to providing insight into the compass question, also (1) incorporated a range of perspectives across different countries; (2) integrated different concepts into one document; and (3) included perspectives on the compass question from other disciplines (e.g. geographic information system and other techniques to map the distribution of the midwifery workforce). In order to incorporate a broad range of documents, there were no limits placed on the searches such as regarding language or publication year.
An explicit set of exclusion criteria were developed by the research team to remove the documents that were not relevant to the aims of the study and did not link to the compass question. Exclusion criteria included documents (1) with a clinical focus (e.g. clinical guidelines, pharmacology, diagnostics, devices, surgery and/or treatment of shoulder dystocia, diabetes, hypertensive disorders, in pregnancy), unless the focus was on scope of practice (e.g. midwives working in expanded scopes); (2) focused on models of care that were specific to individual practices or hospitals and included those that were related to health system approaches; (3) relating to unskilled workers providing SRHR (e.g. traditional birth attendants); (4) focused on implementation of a programme or evaluation of the programme (e.g. prenatal and postnatal programmes), unless the focus was on the roles of midwives providing care within the health system; (5) focused on midwifery education, unless the focus was on accreditation, training and licensure requirements; and (6) focused on site of service delivery (e.g. outcomes of hospital and home births), unless the focus was on the roles of midwives within the different practice settings.
Once the series of searches were completed, an Endnote database was created to store and manage the results. All the duplicates were removed from the database and an initial review of the titles and abstracts was performed for each entry by the principal investigator (CAM) and records were classified as ‘possibly include’ or ‘exclude’. In the first stage of screening, records were marked as ‘possibly include’ if they provided insight into the study’s compass question. Full-text copies of the remaining records were retrieved and uploaded to Covidence, an online tool for systematic reviews, for final screening [ 27 ].
The last stage of screening involved two phases and consisted of full-text review by three reviewers (CAM, TD and KMB). Using Covidence, each reviewer examined the records independently to assess inclusion. Any discrepancies were discussed and resolved. The reviewers prioritised the inclusion of empirical articles where possible, including empirical qualitative studies, which are the types of articles most likely to address political and health system components.
Data analysis and synthesis
A coding structure was created to guide the data extraction. The areas of expertise of the authors (health systems and policy, clinical practice and political science) informed the selection of frameworks guiding the data extraction. The political system factors were informed through the 3i framework, which is a broad typology that recognises the complex interplay among institutions, interests, and ideas and provides a way of organising the many factors that can influence policy choices [ 24 , 28 , 29 , 30 ]. Institutions are made up of government structures (e.g. federal versus unitary government), policy legacies (e.g. the roles of past policies) and policy networks (e.g. relationships between actors around a policy issue). Interests can include a range of actors who may face (concentrated or diffuse) benefits and costs with particular courses of action, whereas ideas relate to peoples’ beliefs (including those based on research evidence) and values.
‘Health system arrangements’ were informed through an established taxonomy developed by the McMaster Health Forum that includes (1) governance arrangements (e.g. policy authority, organisational authority and professional authority); (2) financial arrangements (e.g. how systems are financed and health professionals remunerated); (3) delivery arrangements (e.g. how care meets consumers’ needs, who provides the care and where it is provided); and (4) implementation strategy (consumer- or provider-targeted strategies) [ 25 ]. The components of the framework for quality maternal and newborn care (practice categories, organisation of care, values, philosophy and health professionals) were incorporated into the health system arrangements coding structure to yield insights specific to midwifery care [ 3 ].
In addition to the frameworks that guided data extraction, further data was collected on publication year, study design and jurisdiction(s) of focus. A data extraction form was developed based on all of the concepts covered in the frameworks as well as the additional descriptive items.
The critical interpretive synthesis was conducted on the high value articles — those that yielded the most insight into the compass question. The reviewers prioritised the inclusion of empirical articles that were conceptually rich or integrated different concepts, filled disciplinary gaps, captured a breadth of perspectives across different countries or applied approaches outside of health. The articles were read by the principal investigator (CAM) and one- or two-page detailed summaries were created for each article. The summaries were coded using the qualitative software NVivo for Mac, which facilitates the organisation and coding of the data [ 31 ]. Coding was informed by the three key frameworks guiding the analysis and outlined above: 3i framework, ‘health system arrangements’ and components of the framework for quality maternal and newborn care.
Three steps were involved in the analysis for the critical interpretive synthesis. First, the summaries of the articles were coded based on the coding structure outlined in the data extraction form. Using a constant comparative method, emerging data were compared to previously collected data to find similarities and differences [ 32 , 33 ]. The approach included observations on the terms and concepts used to describe midwifery within the health system as well as relationships between the concepts. For example, how the role of midwives within the health system is influenced by policy legacies (i.e. institutions), which is related to problems with collaborative/interprofessional environments (i.e. delivery arrangements, skill mix and interprofessional teams). Second, all the data collected under each code was reviewed and more detailed notes of the concepts that emerged were included in the analysis. Lastly, themes were created for the concepts that emerged throughout the analysis.
Completeness of the findings was ensured through ongoing consultation with members of the research team. Central concepts and emerging themes of the study were discussed as a team and applied to current scholarship within the field of health systems and policy.
Search results and article selection
A total of 7779 records were identified through the searches of electronic bibliographic databases. Once duplicates were removed ( n = 3246), the remaining records ( n = 4533) were screened based on title, abstract and the explicit set of exclusion criteria outlined above, leaving 401 potentially relevant records. In addition to the electronic database search, 29 records were purposively sampled for inclusion through grey literature and hand searches. The remaining 401 documents from the electronic database searches and 29 documents from the grey literature and hand searches were assessed by the reviewers (CAM, TD and KMB) for inclusion using the full text. A total of 100 documents were included in the critical interpretive synthesis (Fig. 1 ).
Over three-quarters (79%) of the documents were published after 2010, with no documents published prior to 2000. Of the 100 documents, the majority were primary research ( n = 78), which were mostly qualitative research ( n = 24) and observational studies ( n = 24), followed by the ‘other’ category ( n = 18) (e.g. geographic information systems research), systematic reviews ( n = 15) and mixed methods ( n = 4), while 1 was a randomised control trial. The remaining documents were categorised as non-research ( n = 22), meaning that the approaches taken in the documents were either not systematic or that the methods were not reported transparently. Of the non-research documents, 8 were theoretical papers, 7 were reviews (non-systematic), 4 were ‘other’ (e.g. World Health Assembly resolutions, toolkits, etc.), and the remaining 3 were editorials. Forty-one of the documents focused on LMIC settings, followed by 35 on HIC settings, and 24 focused on both HIC and LMIC settings.
The results of the critical interpretive synthesis focused on the political and health system factors that influenced the roles of midwives within health systems. Table 1 focuses on the political system factors that emerged from the analysis and presents the relevant themes, relationships with other factors, and key examples from the literature of the factors that acted as either barriers or facilitators to the roles of midwives within the health system. Similarly, Table 2 focuses on the health system factors and presents the relevant themes, relationships with other factors, and key examples from the literature on the ‘health system arrangements’ that either acted as barriers or facilitators to the roles of midwives.
Three main findings emerged from the analysis on political system factors. First, within institutions, the effects of past policies regarding the value of midwives created interpretive effects, shaping the way midwifery care is organised in the health system. The legacies of these policies created barriers, which include SRHR policies that reinforced structural gender inequalities as well as, in a medical model, payment systems privileging physician-provided and hospital-based services [ 11 , 13 , 34 , 41 , 42 , 43 , 44 , 45 , 47 , 48 , 49 , 50 , 51 , 52 , 54 , 55 , 56 , 57 , 58 , 59 , 61 , 62 , 63 , 65 ].
Second, interest groups played an important role in either supporting or opposing the integration of midwifery in the health system. These groups can have direct or indirect influence and policies that provide concentrated benefits and diffuse costs for groups are more likely to move forward [ 24 ]. Interest groups advanced the integration of midwifery in the health system by (1) creating partnerships to improve SRHR [ 45 , 67 ]; (2) promoting regulation and accreditation (e.g. accreditation requirements, setting standards, policies and guidelines) [ 63 , 68 , 69 , 70 ]; (3) capacity-building including midwifery research [ 71 , 72 ]; (4) policy leadership and decision-making [ 43 ]; and (5) lobbying governments and advocacy [ 73 , 74 ]. Strong leadership from midwifery professional associations engaged in policy dialogue and decision-making has helped advance agendas related to universal health coverage and meeting health-related United Nations Sustainable Development Goals [ 8 , 63 , 66 , 71 , 90 ].
Third, the most relevant themes related to ideas that emerged from the analysis pertained to societal values regarding gender (women’s roles within society) as well as the medical model (historical medicalisation of the birth process and associated growth of physician-provided and hospital-based care). We recognise the importance of gender-inclusive language but have use the term ‘women’ in this publication to reflect how gender is referenced in the documents reviewed. Barriers created by societal values included (1) social construction of gender and the status of midwives in a given jurisdiction often reflected the value placed on women within society (i.e. ‘gender penalty’) [ 8 , 11 , 41 , 43 , 46 , 48 , 61 , 71 ]; (2) some cultures and beliefs did not allow women to receive care from men, yet there were few health professionals who were women due to lack of educational opportunities and societal values that restrict women from participating in the paid labour force [ 45 ]; and (3) health system priorities and shifting societal values favoured the medical model [ 41 , 48 , 49 , 50 , 75 , 78 , 99 , 100 , 101 ]. Examples of facilitators included Nordic health systems that value non-medical models and women-dominated professional groups [ 37 ], which respect the right to informed choice [ 86 ].
Within health system factors, the main themes that emerged from the literature are presented according to ‘health system arrangements’. First, within governance arrangements, regulation and accreditation mechanisms to support midwifery education programmes and institutional capacities were central to how midwives are integrated into health systems [ 63 , 70 , 93 , 107 ]. The lack of legislation to support regulatory activities [ 34 , 43 , 48 , 58 , 71 , 82 , 87 , 93 , 94 ] limited recognition and scope [ 38 , 87 ] and the ability for midwives to practice as an autonomous profession [ 80 ]. Globally, there was a general lack of knowledge regarding the International Confederation of Midwives’ Global Standards for Midwifery Education, which was a barrier to the provision of quality midwifery education [ 53 , 66 , 87 , 107 , 108 ]. Within financial arrangements, the literature focused primarily on how systems are financed, on the inclusion of midwifery services within financing systems and on the remuneration of midwives that is reflective of scope of practice [ 1 , 2 , 6 , 10 , 13 , 35 , 38 , 39 , 43 , 50 , 55 , 56 , 57 , 58 , 59 , 61 , 69 , 73 , 74 , 76 , 80 , 84 , 95 , 101 , 104 , 109 , 115 ]. Lastly, the main themes relating to delivery arrangements focused on (1) accessing midwifery care ranging from availability and timely access to workforce supply, distribution and retention; (2) by whom care is provided (e.g. task-sharing and interprofessional teams); and (3) where care is provided (e.g. hospital-based, integration of services and continuity of care) [ 3 , 4 , 6 , 7 , 9 , 10 , 11 , 12 , 13 , 34 , 35 , 36 , 37 , 38 , 39 , 43 , 45 , 46 , 48 , 50 , 51 , 54 , 55 , 58 , 59 , 61 , 62 , 69 , 73 , 74 , 76 , 77 , 79 , 86 , 94 , 96 , 97 , 99 , 100 , 104 , 105 , 110 , 116 , 117 , 118 , 120 , 121 , 122 ].
Theoretical framework
Figure 2 brings together the main findings from the critical interpretive synthesis and presents a theoretical framework, which can be thought of as a heuristic that can be used to map the key elements that influence midwives’ roles in a particular political and health system. The factors presented in the framework are not weighted but rather present the range of variables influencing the level of integration of the profession. The cumulative effects of the barriers presented on the right-hand side of the framework lead to health systems where the profession is disempowered and midwives exist on the margins with very limited capacity. Some of the variables and examples presented in the framework have context specificity to reflect findings from the critical interpretive synthesis (e.g. self-regulated profession, Indigenous self-government, Nordic maternity care systems, and payment systems privileging physician-provided and hospital-based services in some contexts).
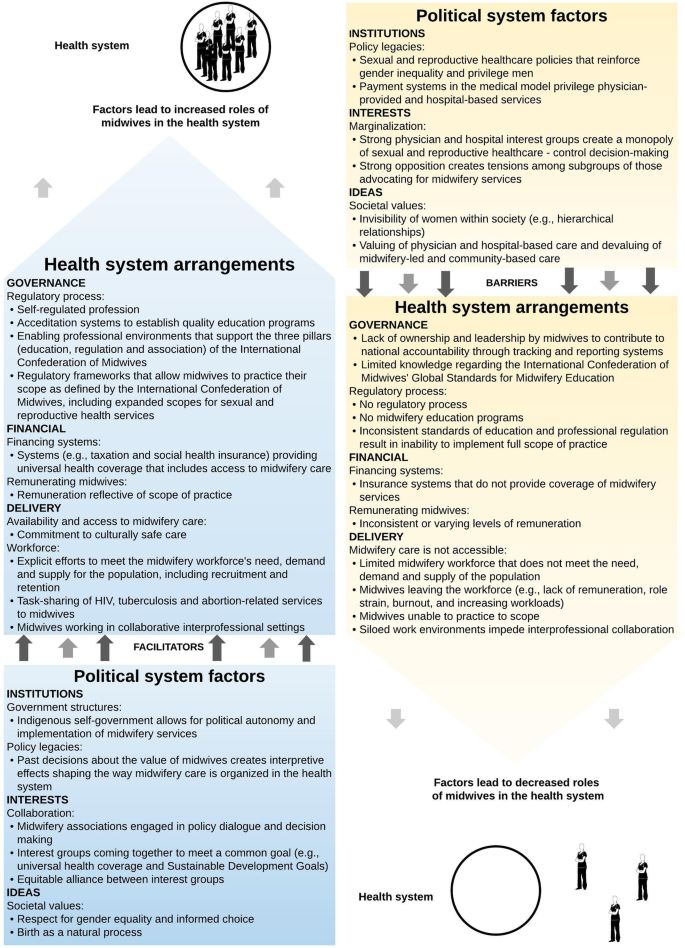
Theoretical framework of the political and health system factors that influence the roles of midwives within the health system
Principal findings
Similar to the concept of WHO’s health system ‘building blocks’, the political system factors presented in the theoretical framework form the bottom building block or the foundation for the ‘health system arrangements’, acting as either a barrier or facilitator. For example, favourable institutional factors (e.g. policy legacies that value midwifery as a profession), interests (e.g. collaborative interest groups coming together to reach a common goal) and ideas (e.g. societal values centring on gender equality and birth as a natural process) act as enablers to ‘health system arrangements’ that build on each other to support the integration of midwifery. Together, supportive political and health system factors lead to health systems where midwives practice to scope (i.e. trained, licensed and regulated according to international standards, working in collaborative/interprofessional settings with an established workforce). On the other hand, health systems that have many political and health system challenges will in turn have a limited midwifery workforce where midwives lack an institutional voice and representation in SRHR decision-making. Significant barriers limit the options available to the midwifery workforce and is most often reflected in siloed work settings with midwives working in the periphery of the health system.
Strengths and limitations of the study
The main strength of the study is the use of a critical interpretive synthesis. This is a relatively new systematic review methodology, which combines a rigorous systematic review of electronic bibliographic databases with iterative and purposive sampling of the literature to fill conceptual gaps. The approach incorporated a range of documents (empirical and non-empirical), which broadened the scope of the literature used to inform the theoretical framework.
The main limitation of the critical interpretive synthesis was that the search strategy may not have fully covered the diverse terminology used to refer to midwifery. However, the principal investigator (CAM) consulted with a librarian and team members to ensure that the search strategy was as inclusive as possible, which is also reflected by the high proportion of articles that were later excluded during the screening process. Meanwhile, the majority of articles retrieved from the searches were published after 2000, which could be related to the release of the Millennium Development Goals and subsequent Sustainable Development Goals, and the wider attention given to SRHR on global agendas.
Implications for policy and practice
Any changes to the roles of midwifery in health systems needs to take into account the political system where decisions about their integration will be made as well as the nature of the health system in which they are being integrated. The theoretical framework is a tool that helps to inform such changes by identifying the drivers of midwives’ roles that facilitate or constrain such integration. The study results have implications for policy-makers as, firstly, the theoretical framework can be used to conduct an assessment of the factors in order to strengthen the profession by identifying the facilitators that can be leveraged as well as the barriers that can be addressed to support change. For example, Sweden has favourable political system conditions (e.g. policy legacies of professionalisation of midwives dating back to the eighteenth century and an equitable alliance between midwifery and physician groups), which is reflected in the health system arrangements where midwives are the primary health professionals for low-risk pregnant people. In contrast, the United States has policy legacies of payment systems valuing physician-provided and hospital-based care, strong physician and hospital interest groups have created a monopoly over sexual and reproductive health services, and existing tensions within the profession between nurse midwives and midwives.
Moving forward, an implication for practice is that changes to further enhance the role of midwives would require different types of policy levers. In looking at growing midwifery in LMICs, governments can use the tool to understand how to best influence the integration of the profession. This information will provide valuable experience and understanding of the contextual factors so that governments can best leverage their position when working with bilateral and multilateral funders to improve SRHR. Conversely, in the example of the United States, the framework presented helps to explain why midwives play such a small role in sexual and reproductive health service delivery in the United States. The tool highlights that funding and regulatory levers would need to be pulled; yet, strong policy legacies and entrenched interests present significant barriers. Change would require spending political capital to modify existing structures within the health system.
While research evidence on the role of midwives in the provision of high-quality SRHR has increased and the 2014 Lancet Series on Midwifery was key to raising the profile of midwifery research, significant gaps in the literature persist. Structural gender inequalities are reflected in the low status of midwifery in some contexts, which leads to poor political and health systems supports to invest in quality midwifery care [ 43 ]. Our findings show that the research evidence related to the roles of midwives within health systems is relatively saturated in terms of delivery arrangements yet surprisingly little is known about governance and financial arrangements and about implementation strategies, which are key to effectively integrating midwifery and pushing the field forward in meaningful ways.
Availability of data and materials
All data generated or analysed during this study are included in this published article and summarised in Tables 1 and 2 .
Abbreviations
High-income countries
Low- and middle-income countries
- Sexual and reproductive health and rights
ten Hoope-Bender P, de Bernis L, Campbell J, Downe S, Fauveau V, Fogstad H, et al. Improvement of maternal and newborn health through midwifery. Lancet. 2014;384(9949):1226–35.
Article PubMed Google Scholar
Homer CS, Friberg IK, Dias MA, ten Hoope-Bender P, Sandall J, Speciale AM, et al. The projected effect of scaling up midwifery. Lancet. 2014;384(9948):1146–57.
Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet. 2014;384(9948):1129–45.
UNFPA. The State of the World’s Midwifery 2014. Geneva: United Nations Population Fund; 2014.
Google Scholar
Hutton EK, Cappelletti A, Reitsma AH, Simioni J, Horne J, McGregor C, et al. Outcomes associated with planned place of birth among women with low-risk pregnancies. CMAJ. 2016;188(5):E80–90.
Malott AM, Davis BM, McDonald H, Hutton E. Midwifery care in eight industrialized countries: how does Canadian midwifery compare? J Obstet Gynaecol Can. 2009;31(10):974–9.
Sandall J, Soltani H, Gates S, Shennan A, Devane D. Midwife-led continuity models versus other models of care for childbearing women. Cochrane Database Syst Rev. 2013;8:CD004667.
Renfrew MJ, Ateva E, Dennis-Antwi JA, Davis D, Dixon L, Johnson P, et al. Midwifery is a vital solution-what is holding back global progress? Birth. 2019;46(3):396–9.
Malott AM, Kaufman K, Thorpe J, Saxell L, Becker G, Paulette L, et al. Models of organization of maternity care by midwives in Canada: a descriptive review. J Obstet Gynaecol Can. 2012;34(10):961–70.
Bartlett L, Weissman E, Gubin R, Patton-Molitors R, Friberg IK. The impact and cost of scaling up midwifery and obstetrics in 58 low- and middle-income countries. PLoS One. 2014;9(6):e98550.
Article PubMed PubMed Central CAS Google Scholar
Fauveau V, Sherratt DR, de Bernis L. Human resources for maternal health: multi-purpose or specialists? Hum Resour Health. 2008;6:21.
Article PubMed PubMed Central Google Scholar
Holcombe SJ, Berhe A, Cherie A. Personal beliefs and professional responsibilities: Ethiopian midwives’ attitudes toward providing abortion services after legal reform. Stud Fam Plan. 2015;46(1):73–95.
Article Google Scholar
Liljestrand J, Sambath MR. Socio-economic improvements and health system strengthening of maternity care are contributing to maternal mortality reduction in Cambodia. Reprod Health Matters. 2012;20(39):62–72.
ICM. International definition of the midwife. The Hague: International Confederation of Midwives; 2017. https://www.internationalmidwives.org/assets/files/definitions-files/2018/06/eng-definition_of_the_midwife-2017.pdf .
World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. Geneva: WHO; 2020. https://www.who.int/healthinfo/systems/WHO_MBHSS_2010_full_web.pdf .
Lopes SC, Titulaer P, Bokosi M, Homer CS, ten Hoope-Bender P. The involvement of midwives associations in policy and planning about the midwifery workforce: a global survey. Midwifery. 2015;31(11):1096–103.
Janssen PA, Mitton C, Aghajanian J. Costs of planned home vs. hospital birth in British Columbia attended by registered midwives and physicians. PLoS One. 2015;10(7):e0133524.
Reinharz D, Blais R, Fraser WD, Contandriopoulos A-P. Cost-effectiveness of midwifery services vs. medical services in Quebec. Can J Public Health. 2000;91(1):I12.
Article CAS PubMed PubMed Central Google Scholar
Schroeder E, Petrou S, Patel N, Hollowell J, Puddicombe D, Redshaw M, et al. Cost effectiveness of alternative planned places of birth in woman at low risk of complications: evidence from the Birthplace in England national prospective cohort study. BMJ. 2012;344:e2292.
Lavis J, Davies H, Oxman A, Denis JL, Golden-Biddle K, Ferlie E. Towards systematic reviews that inform health care management and policy-making. J Health Serv Res Policy. 2005;10(Suppl 1):35–48.
Lavis JN, Guindon GE, Cameron D, Boupha B, Dejman M, Osei EJ, et al. Bridging the gaps between research, policy and practice in low- and middle-income countries: a survey of researchers. CMAJ. 2010;182(9):E350–61.
Moat KA, Lavis JN, Abelson J. How contexts and issues influence the use of policy-relevant research syntheses: a critical interpretive synthesis. Milbank Q. 2013;91(3):604–48.
Wilson MG, Moat KA, Lavis JN. The global stock of research evidence relevant to health systems policymaking. Health Res Policy Syst. 2013;11:32.
Lazar H, Lavis JN, Forest P-G, Church J. Paradigm freeze: why it is so hard to reform health care in Canada. Montreal: McGill-Queen’s University Press; 2013.
Lavis JN, Wilson MG, Moat KA, Hammill AC, Boyko JA, Grimshaw JM, et al. Developing and refining the methods for a ‘one-stop shop’for research evidence about health systems. Health Res Policy Syst. 2015;13:10.
Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Med Res Methodol. 2006;6:35.
Covidence. About us Australia: Covidence; 2017. https://www.covidence.org/about-us .
Hall PA. The role of interests, institutions, and ideas in the comparative political economy of the industrialized nations. In: Comparative politics: rationality, culture, and structure. Cambridge: Cambridge University Press; 1997. p. 174–207.
Oliver MJ, Pemberton H. Learning and change in 20th-century British economic policy. Governance. 2004;17(3):415–41.
Walsh JI. When do ideas matter? Explaining the successes and failures of Thatcherite ideas. Comp Political Stud. 2000;33(4):483–516.
QSR International. NVivo for Mac Australia: QSR International; 2017. http://www.qsrinternational.com/product/nvivo-mac .
Charmaz K. Constructing grounded theory. London: Sage; 2014.
Glaser BG, Strauss A. The discovery of ground theory. Chicago: Aldine; 1967.
Van Wagner V, Epoo B, Nastapoka J, Harney E. Reclaiming birth, health, and community: Midwifery in the Inuit villages of Nunavik, Canada. J Midwifery Womens Health. 2007;52(4):384–91.
Epoo B, Stonier J, Wagner VV, Harney E. Learning midwifery in Nunavik: community-based education for Inuit midwives. J Indigenous Wellbeing. 2012;10(3):283–99.
Wagner V, Osepchook C, Harney E, Crosbie C, Tulugak M. Remote midwifery in Nunavik, Quebec, Canada: outcomes of perinatal care for the Inuulitsivik Health Centre, 2000-2007. Birth Issue Perinat Care. 2012;39(3):230–7.
Wrede S, Benoit C, Einarsdottir T. Equity and dignity in maternity care provision in Canada, Finland and Iceland. Can J Public Health. 2008;99:S16–21.
DeMaria LM, Campero L, Vidler M, Walker D. Non-physician providers of obstetric care in Mexico: perspectives of physicians, obstetric nurses and professional midwives. Hum Resour Health. 2012;10:6.
Van Lerberghe W, Matthews Z, Achadi E, Ancona C, Campbell J, Channon A, et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. Lancet. 2014;384(9949):1215–25.
Bogren M, Erlandsson K. Opportunities, challenges and strategies when building a midwifery profession. Findings from a qualitative study in Bangladesh and Nepal. Sex Reprod Healthc. 2018;16:45–9.
Temmar F, Vissandjee B, Hatem M, Apale A, Kobluk D. Midwives in Morocco: seeking recognition as skilled partners in women-centred maternity care. Reprod Health Matters. 2006;14(27):83–90.
Betron ML, McClair TL, Currie S, Banerjee J. Expanding the agenda for addressing mistreatment in maternity care: a mapping review and gender analysis. Reprod Health. 2018;15(1):143.
Filby A, McConville F, Portela A. What prevents quality midwifery care? A systematic mapping of barriers in low and middle income countries from the provider perspective. PLoS One. 2016;11(5):e0153391.
Witter S, Namakula J, Wurie H, Chirwa Y, So S, Vong S, et al. The gendered health workforce: mixed methods analysis from four fragile and post-conflict contexts. Health Policy Plann. 2017;32(Suppl. 5):v52–62.
Turkmani S, Currie S, Mungia J, Assefi N, Rahmanzai AJ, Azfar P, et al. ‘Midwives are the backbone of our health system’: lessons from Afghanistan to guide expansion of midwifery in challenging settings. Midwifery. 2013;29(10):1166–72.
Beek K, McFadden A, Dawson A. The role and scope of practice of midwives in humanitarian settings: a systematic review and content analysis. Hum Resour Health. 2019;17:5.
Devane D, Murphy-Lawless J, Begley CM. Childbirth policies and practices in Ireland and the journey towards midwifery-led care. Midwifery. 2007;23(1):92–101.
Brodie P. Addressing the barriers to midwifery--Australian midwives speaking out. Aust J Midwifery. 2002;15(3):5–14.
Christiaens W, Nieuwenhuijze MJ, de Vries R. Trends in the medicalisation of childbirth in Flanders and the Netherlands. Midwifery. 2013;29(1):e1–8.
Goodman S. Piercing the veil: the marginalization of midwives in the United States. Soc Sci Med. 2007;65(3):610–21.
Kennedy HP, Rousseau AL, Low LK. An exploratory metasynthesis of midwifery practice in the United States. Midwifery. 2003;19(3):203–14.
Mattison CA, Lavis JN, Hutton EK, Dion ML, Wilson MG. Understanding the conditions that influence the roles of midwives in Ontario, Canada’s health system: an embedded single-case study. BMC Health Serv Res. 2020;20(1):197.
Barger MK, Hackley B, Bharj KK, Luyben A, Thompson JB. Knowledge and use of the ICM global standards for midwifery education. Midwifery. 2019;79:102534.
James S, O'Brien B, Bourret K, Kango N, Gafvels K, Paradis-Pastori J. Meeting the needs of Nunavut families: a community-based midwifery education program. Circumpolar special issue: human health at the ends of the earth. Rural Remote Health. 2010;10(2):1355.
PubMed Google Scholar
Kildea S, Kruske S, Barclay L, Tracy S. ‘Closing the gap’: how maternity services can contribute to reducing poor maternal infant health outcomes for Aboriginal and Torres Strait Islander women. Rural Remote Health. 2010;10(3):1383.
CAS PubMed Google Scholar
Kreiner M. Delivering diversity: newly regulated midwifery returns to Manitoba, Canada, one community at a time. J Midwifery Women Health. 2009;54(1):e1–e10.
National Aboriginal Health Organization. Midwifery and aboriginal midwifery in Canada. Ottawa: National Aboriginal Health Organization; 2004.
Skye AD. Aboriginal midwifery: a model for change. Int J Indigenous Health. 2010;6(1):28–37.
Mavalankar D, Raman PS, Vora K. Midwives of India: missing in action. Midwifery. 2011;27(5):700–6.
Munabi-Babigumira S, Nabudere H, Asiimwe D, Fretheim A, Sandberg K. Implementing the skilled birth attendance strategy in Uganda: a policy analysis. BMC Health Serv Res. 2019;19:655.
Day-Stirk F, Fauveau V. The state of the world’s midwifery: making the invisible visible. Int J Gynecol Obstet. 2012;119:S39–41.
Hogberg U. The decline in maternal mortality in Sweden: the role of community midwifery. Am J Public Health. 2004;94(8):1312–20.
ten Hoope-Bender P, Lopes STC, Nove A, Michel-Schuldt M, Moyo NT, Bokosi M, et al. Midwifery 2030: a woman’s pathway to health. What does this mean? Midwifery. 2016;32:1–6.
Shakibazadeh E, Namadian M, Bohren MA, Vogel JP, Rashidian A, Pileggi VN, et al. Respectful care during childbirth in health facilities globally: a qualitative evidence synthesis. BJOG. 2018;125(8):932–42.
Article CAS PubMed Google Scholar
Oliver K, Parolin Z. Assessing the policy and practice impact of an international policy initiative: the state of the world’s midwifery 2014. BMC Health Serv Res. 2018;18(1):499.
World Health Organization. Nursing and Midwifery in the history of the World Health Organization 1948–2017. Geneva: WHO; 2017.
Spies LA, Garner SL, Faucher MA, Hastings-Tolsma M, Riley C, Millenbruch J, et al. A model for upscaling global partnerships and building nurse and midwifery capacity. Int Nurs Rev. 2017;64(3):331–44.
Chamberlain J, McDonagh R, Lalonde A, Arulkumaran S. The role of professional associations in reducing maternal mortality worldwide. Int J Gynecol Obstet. 2003;83(1):94–102.
Article CAS Google Scholar
Haththotuwa R, Senanayake L, Senarath U, Attygalle D. Models of care that have reduced maternal mortality and morbidity in Sri Lanka. Int J Gynaecol Obstet. 2012;119(Suppl 1):S45–9.
de Bernis L. Implementation of midwifery school accreditation mechanisms in Ivory Coast, Mali and Chad. Sante Publique. 2018;30:57–63.
Homer CSE, Castro Lopes S, Nove A, Michel-Schuldt M, McConville F, Moyo NT, et al. Barriers to and strategies for addressing the availability, accessibility, acceptability and quality of the sexual, reproductive, maternal, newborn and adolescent health workforce: addressing the post-2015 agenda. BMC Pregnancy Childbirth. 2018;18(1):55.
Nabirye RC, Kinengyere AA, Edwards G. Nursing and midwifery research output in Africa: a review of the literature. Int J Childbirth. 2018;8(4):236–41.
Koblinsky M, Matthews Z, Hussein J, Mavalankar D, Mridha MK, Anwar I, et al. Going to scale with professional skilled care... third in a series of five articles. Lancet. 2006;368(9544):1377–86.
World Health Organization. Munich declaration – nurses and midwives: a force for health. Intensive Crit Care Nurs. 2000;16(4):207–8.
Vedam S, Stoll K, MacDorman M, Declercq E, Cramer R, Cheyney M, et al. Mapping integration of midwives across the United States: impact on access, equity, and outcomes. PLoS One. 2018;13(2):e0192523.
Downe S, Finlayson K, Fleming A. Creating a collaborative culture in maternity care. J Midwifery Womens Health. 2010;55(3):250–4.
College of Midwives of Ontario. The Midwifery Scope of Practice: The College of Midwives of Ontario Submission to the Health Professions Regulatory Advisory Council. Toronto: College of Midwives of Ontario; 2008.
Hoope-Bender P, Renfrew MJ. Midwifery – a vital path to quality maternal and newborn care: the story of the Lancet series on midwifery. Midwifery. 2014;30(11):1105–6.
Scholmerich VL, Posthumus AG, Ghorashi H, Waelput AJ, Groenewegen P, Denktas S. Improving interprofessional coordination in Dutch midwifery and obstetrics: a qualitative study. BMC Pregnancy Childbirth. 2014;14:145.
Peterson C. Midwifery and the crowning of health care reform. J Midwifery Womens Health. 2010;55(1):5–8.
Bogren MU, Berg M, Edgren L, Ev T, Wigert H. Shaping the midwifery profession in Nepal - uncovering actors’ connections using a Complex Adaptive Systems framework. Sex Reprod Healthc. 2016;10:48–55.
Bogren MU, van Teijlingen E, Berg M. Where midwives are not yet recognised: a feasibility study of professional midwives in Nepal. Midwifery. 2013;29(10):1103–9.
Klopper HC, Madigan E, Vlasich C, Albien A, Ricciardi R, Catrambone C, et al. Advancement of global health: recommendations from the Global Advisory Panel on the Future of Nursing & Midwifery (GAPFON (R)). J Adv Nurs. 2020;76(2):741–8.
Binfa L, Pantoja L, Ortiz J, Gurovich M, Cavada G. Assessment of the implementation of the model of integrated and humanised midwifery health services in Santiago, Chile. Midwifery. 2013;29(10):1151–7.
Bergevin Y, Fauveau V, McKinnon B. Towards ending preventable maternal deaths by 2035. Semin Reprod Med. 2015;33(1):23–9.
Donnay F. Maternal survival in developing countries: what has been done, what can be achieved in the next decade. Int J Gynecol Obstet. 2000;70(1):89–97.
Castro Lopes S, Nove A, Hoope-Bender P, Bernis LD, Bokosi M, Moyo NT, et al. A descriptive analysis of midwifery education, regulation and association in 73 countries: the baseline for a post-2015 pathway. Hum Resour Health. 2016;14:37.
Bvumbwe T, Mtshali N. Nursing education challenges and solutions in Sub Saharan Africa: an integrative review. BMC Nurs. 2018;17:3.
Yalahow A, Hassan M, Foster AM. Training reproductive health professionals in a post-conflict environment: exploring medical, nursing, and midwifery education in Mogadishu, Somaila. Reprod Health Matters. 2017;25(51):114–23.
Ajuebor O, McCarthy C, Li Y, Al-Blooshi SM, Makhanya N, Cometto G. Are the global strategic directions for strengthening nursing and midwifery 2016–2020 being implemented in countries? Findings from a cross-sectional analysis. Hum Resour Health. 2019;17:54.
Nagle C, McDonald S, Morrow J, Kruger G, Cramer R, Couch S, et al. Informing the development midwifery standards for practice: a literature review for policy development. Midwifery. 2019;76:8–20.
Sandwell R, Bonser D, Hebert E, Kilroy K, Leshabari S, Mwanga F, et al. Stronger together: midwifery twinning between Tanzania and Canada. Glob Health. 2018;14(1):123.
West F, Homer C, Dawson A. Building midwifery educator capacity in teaching in low and lower-middle income countries. A review of the literature. Midwifery. 2016;33:12–23.
Colvin CJ, de Heer J, Winterton L, Mellenkamp M, Glenton C, Noyes J, et al. A systematic review of qualitative evidence on barriers and facilitators to the implementation of task-shifting in midwifery services. Midwifery. 2013;29(10):1211–21.
Sidebotham M, Fenwick J, Rath S, Gamble J. Midwives’ perceptions of their role within the context of maternity service reform: an appreciative inquiry. Women Birth. 2015;28(2):112–20.
McCarthy CF, Voss J, Verani AR, Vidot P, Salmon ME, Riley PL. Nursing and midwifery regulation and HIV scale-up: Establishing a baseline in East, Central and Southern Africa. J Int AIDS Soc. 2013;16:18051.
Jenkins GL. Burning bridges: policy, practice, and the destruction of midwifery in rural Costa Rica. Soc Sci Med. 2003;56(9):1893–909.
Fullerton J, Severino R, Brogan K, Thompson J. The International Confederation of Midwives’ study of essential competencies of midwifery practice. Midwifery. 2003;19(3):174–90.
Amelink-Verburg MP, Buitendijk SE. Pregnancy and labour in the Dutch maternity care system: what is normal? The role division between midwives and obstetricians. J Midwifery Women Health. 2010;55(3):216–25.
Homer CSE, Passant L, Brodie PM, Kildea S, Leap N, Pincombe J, et al. The role of the midwife in Australia: views of women and midwives. Midwifery. 2009;25(6):673–81.
Spendlove Z. Risk and boundary work in contemporary maternity care: tensions and consequences. Health Risk Soc. 2018;20(1–2):63–80.
Summer A, Walker D, Guendelman S. A review of the forces influencing maternal health policies in post-war Guatemala. World Med Health Policy. 2019;11(1):59–82.
Summer A, Walker D. Recommendations for sustainable midwifery in Guatemala. World Med Health Policy. 2018;10(4):356–80.
Kopacz L, Pawelec M, Pietras J, Karmowski A, Palczynski B, Karmowski M, et al. The Polish way to better midwifery or commercialization of maternity services? Adv Clin Exp Med. 2011;20(4):513–20.
Biro MA. What has public health got to do with midwifery? Midwives’ role in securing better health outcomes for mothers and babies. Women Birth. 2011;24(1):17–23.
Homer CSE, Passant L, Kildea S, Pincombe J, Thorogood C, Leap N, et al. The development of national competency standards for the midwife in Australia. Midwifery. 2007;23(4):350–60.
Luyben A, Barger M, Avery M, Bharj KK, O'Connell R, Fleming V, et al. Exploring global recognition of quality midwifery education: vision or fiction? Women Birth. 2017;30(3):184–92.
Zhu X, Yao JS, Lu JY, Pang RY, Lu H. Midwifery policy in contemporary and modern China: from the past to the future. Midwifery. 2018;66:97–102.
McNeill J, Lynn F, Alderdice F. Public health interventions in midwifery: a systematic review of systematic reviews. BMC Public Health. 2012;12:955.
Mainey L, O'Mullan C, Reid-Searl K, Taylor A, Baird K. The role of nurses and midwives in the provision of abortion care: a scoping review. J Clinical Nurs. 2020;29(9–10):1513–26.
Fullerton J, Butler MM, Aman C, Reid T, Dowler M. Abortion-related care and the role of the midwife: a global perspective. Int J Womens Health. 2018;10:751–62.
Massot E, Epaulard O. Midwives’ perceptions of vaccines and their role as vaccinators: the emergence of a new immunization corps. Vaccine. 2018;36(34):5204–9.
Van Hoover C, Holt L. Midwifing the end of life: expanding the scope of modern midwifery practice to reclaim palliative care. J Midwifery Women Health. 2016;61(3):306–14.
Alayande A, Mamman-Daura F, Adedeji O, Muhammad AZ. Midwives as drivers of reproductive health commodity security in Kaduna State, Nigeria. Eur J Contracept Reprod Health Care. 2016;21(3):207–12.
Ir P, Korachais C, Chheng K, Horemans D, Van Damme W, Meessen B. Boosting facility deliveries with results-based financing: a mixed-methods evaluation of the government midwifery incentive scheme in Cambodia. BMC Pregnancy Childbirth. 2015;15:170.
King TL, Laros RK, Parer JT. Interprofessional collaborative practice in obstetrics and midwifery. Obstet Gynecol Clin North Am. 2012;39(3):411–22.
Arias MG, Nove A, Michel-Schuldt M, Bernis L. Current and future availability of and need for human resources for sexual, reproductive, maternal and newborn health in 41 countries in Sub-Saharan Africa. Int J Equity Health. 2017;16(1):69.
Suleiman-Martos N, Albendin-Garcia L, Gomez-Urquiza JL, Vargas-Roman K, Ramirez-Baena L, Ortega-Campos E, et al. Prevalence and predictors of burnout in midwives: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(2):641.
Article PubMed Central Google Scholar
Nove A. The quality of midwifery education in six French-speaking sub-Saharan African countries. Sante Publique. 2018;30:45–55.
Renner RM, Brahmi D, Kapp N. Who can provide effective and safe termination of pregnancy care? A systematic review. BJOG. 2013;120(1):23–31.
Miyake S, Speakman EM, Currie S, Howard N. Community midwifery initiatives in fragile and conflict-affected countries: a scoping review of approaches from recruitment to retention. Health Policy Plan. 2017;32(1):21–33.
Sami S, Amsalu R, Dimiti A, Jackson D, Kenyi S, Meyers J, et al. Understanding health systems to improve community and facility level newborn care among displaced populations in South Sudan: a mixed methods case study. BMC Pregnancy Childbirth. 2018;18(1):325.
Download references
Acknowledgements
The authors would like to thank Kirsty Bourret and Tomasso D’Ovidio for their assistance with assessing documents for eligibility and inclusion in the review.
There are no sources of funding to declare for this research.
Author information
Authors and affiliations.
Department of Obstetrics and Gynecology, McMaster Midwifery Research Centre, 1280 Main St. West, HSC-4H26, Hamilton, ON, L8S 4K1, Canada
Cristina A. Mattison & Eileen K. Hutton
McMaster Health Forum, 1280 Main St West, MML-417, Hamilton, ON, L8S 4L6, Canada
John N. Lavis & Michael G. Wilson
Department of Political Science, McMaster University, 1280 Main St. West, KTH-533, Hamilton, ON, L8S 4M4, Canada
Michelle L. Dion
You can also search for this author in PubMed Google Scholar
Contributions
CAM conceived the study design with her supervisor, JNL, and was responsible for all data collection and analysis. JNL, EKH, MGW and MLD provided content expertise (health systems and health policy, clinical practice and political science) to inform the selection of frameworks guiding the data extraction. All authors contributed to the development of the conceptual framework and approved the final manuscript.
Corresponding author
Correspondence to Cristina A. Mattison .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mattison, C.A., Lavis, J.N., Wilson, M.G. et al. A critical interpretive synthesis of the roles of midwives in health systems. Health Res Policy Sys 18 , 77 (2020). https://doi.org/10.1186/s12961-020-00590-0
Download citation
Received : 27 January 2020
Accepted : 14 June 2020
Published : 08 July 2020
DOI : https://doi.org/10.1186/s12961-020-00590-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Political systems
- Health systems
- Critical interpretive synthesis
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Strengthening Midwifery Research
- First Online: 06 January 2021
Cite this chapter

- Joy Kemp 4 ,
- Gaynor D. Maclean 5 &
- Nester Moyo 6
747 Accesses
1 Citations
Considering research as an integral part of midwifery education and an indispensable tool in evidence-based practice provides the starting point in this chapter. Network theory is considered prior to exploring midwifery research networks and other initiatives in this context. Examples of initiatives to promote research through universities and professional associations are provided. Priority areas for midwifery research are explored, and the importance of high-quality research is considered in the context of providing evidence upon which safe practice can be based. The chapter concludes by considering the place of midwifery research in the wider context of health care and its significance in the development of the profession of midwifery.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Additional Resources for Reflection and Further Study
Visit the website of the Lugina Africa Midwives Research Network (LAMRN) at: http://lamrn.org/ Examine the ambitions and achievements of this network and consider how such a network may be replicated in other regions.
Explore the website of the Journal of Asian Midwifery (JAM) at: https://ecommons.aku.edu/jam/ Reflect on the aims and scope of the journal and consider its role in promoting midwifery research and enhancing evidence-based practice.
Readers may wish to compare and contrast the activities of the two structures described above and consider what strengths could be gleaned from both in order to establish a wider network for undertaking and disseminating midwifery research.
Google Scholar
World Health Organization (2019) Setting the research agenda: read about the current and ongoing research priorities in maternal, newborn and adolescent health at: https://www.who.int/maternal_child_adolescent/research/en/ . Recent research publications are regularly updated here too.
Soltani H, Low LK, Duxbury A et al (2016) Global midwifery research priorities: an international survey. Int J Childbirth 6(1):5–18 Consider these in the context of your own practice and experience
Article Google Scholar
In the context of global research priorities, explore what the National Institute of Health Research (NIHR) Global Health Research Group are doing to address stillbirth and perinatal mortality in Sub-Saharan Africa: https://sites.manchester.ac.uk/stillbirth-prevention-africa/ . Accessed 23 Oct 2019.
Abuya T et al (2015) Exploring the prevalence of disrespect and abuse during childbirth in Kenya. PLoS One 10(4):e0123606. Accessed 3 Oct 2019. https://doi.org/10.1371/journal.pone.0123606
Article CAS PubMed PubMed Central Google Scholar
African Journal of Midwifery (2017) African J Midwifery & Women’s Health. MA Healthcare. http://www.magonlinelibrary.com/toc/ajmw/current . Accessed 12 Mar 2020
American College of Nurse-Midwives (2019) Midwifery Research Interest Groups. American College of Nurse Midwives. http://www.midwife.org/Midwifery-Research-Interest-Groups . Accessed 15 Oct 2019
Australian College of Midwives (2019) Research and innovation: Australian College of Midwives: https://www.midwives.org.au/interest-group/research-and-innovation . Accessed 15 Oct 2019
Azmoud E, Aradmehr M, Dehghani F (2018) Midwives’ attitude and barriers of evidence based practice in maternity care. Malay J Med Sci 25(3):120–128. https://doi.org/10.21315/mjms2018.25.3.12
Barnes S (2019) Empowered midwives could save lives. New Security Beat, Wilson Center, Environmental Change and Security. https://www.newsecuritybeat.org/2019/08/empowered-midwives-save-lives/ . Accessed 16 Oct 2019
Begeley C, Mccarron M, Huntley-Moore S et al (2014) Successful research capacity building in academic nursing and midwifery in Ireland: an exemplar. Nurse Educ Today 34(5):754–760
Bogdan-Lovis E, Sousa A (2006) The contextual influence of professional culture: certified nurse-midwives’ knowledge of and reliance on evidence-based practice. Soc Sci Med 62(11):2681–2693
Bogren M, Doraiswamy S, Erlandsson K (2017) Building a new generation of midwifery faculty members in Bangladesh. J Asian Midwives 4(2):52–58
Bonilla H, Ortiz-Llorens BM et al (2018) Implementation of a programme to develop research projects in a school of midwifery in Santiago. Chile Midwifery 64:60–62
Bowser D, Hill K (2010) Exploring evidence for disrespect and abuse in facility-based childbirth: report of a landscape analysis. USAID-TRAction Project, University Research Corporation, LLC, and Harvard School of Public Health, Bethesda, MD. http://www.tractionproject.org/sites/default/files/Respectful_Care_at_Birth_9-20-101_Final.pdf
Brucker M, Schwarz B (2002) Fact or fiction? International Confederation of Midwives Triennial Conference Proceedings. Austria, Vienna
Burrowes S, Holcombe SJ, Jara D et al (2017) Midwives’ and patients’ perspectives on disrespect and abuse during labor and delivery care in Ethiopia: a qualitative study. BMC Preg Childbirth Open Access 17:263. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-017-1442-1 . Accessed 8 Oct 2019
Directorate General of Nursing and Midwifery (2017) National Guidelines for Midwives, Directorate General of Nursing and Midwifery, Bangladesh. http://dgnm.gov.bd/cmsfiles/files/SOP%20for%20Midwives.pdf . Accessed 23 Oct 2019
Doctoral Midwifery Research Society (2020) DMRS background and membership. https://www.doctoralmidwiferysociety.org/ . Accessed 3 Jun 2020
Einstein A, Shaw GB (2009) Einstein on cosmic religion: and other opinions and other aphorisms. Dover, New York
European Midwives Associations (2019) EU Research. European Midwives Association. http://www.europeanmidwives.com/eu/eu-research . Accessed 15 Oct 2019
Forss K, Maclean G (2007) Evaluation of the Africa midwives research network. A study commissioned by the Swedish International Development Cooperation Agency. Sida, Stockholm
Forss K, Birungi H, Saasa O (2000) Sector wide approaches: from principles to practice. A study commissioned by the Department of Foreign Affairs, Dublin, Ireland. Final report 13/11/2000 Andante – tools for thinking AB. https://www.researchgate.net/publication/252177958_Sector_wide_approaches_from_principles_to_practice . Accessed 26 Oct 2019
Glacken M, Chaney D (2004) Perceived barriers and facilitators to implementing research findings in the Irish practice setting. J Clin Nurs 13(6):731–740. Accessed 3 Jun 2020. https://doi.org/10.1111/j.1365-2702.2004.00941.x
Article PubMed Google Scholar
Goyet S, Sauvegrain P, Schantz C et al (2018) State of midwifery research in France. Midwifery 64(101–109):2018
Granovetter M (1973) The strength of weak ties. Am J Sociol 78:1360–1380
Guyatt GH, Sackett DL, Sinclair JC et al (1995) Users’ Guides to the Medical Literature: IX. A Method for Grading Health Care Recommendations. JAMA 274(22):18001804. Accessed 16 Oct 2019. https://doi.org/10.1001/jama.1995.03530220066035
Hommelstad J, Ruland CM (2004) Norwegian nurses’ perceived barriers and facilitators to research use. Assoc Perioper Reg Nurs J 79(3):621–634. https://doi.org/10.1016/S0001-2092(06)60914-9
Hunter B (2013) Implementing research evidence into practice some reflections on the challenges. Evid Based Midwifery 11(3):76–80
International Confederation of Midwives (2014) Basic and ongoing education for midwives: position statement. strengthening midwifery globally: PS2008_001 V2014. International Confederation of Midwives, The Hague. https://www.internationalmidwives.org/assets/files/statement-files/2019/06/basic-and-ongoing-education-for-midwives-eng-letterhead.pdf . Accessed 15 Oct 2019
International Confederation of Midwives (2018) Research Standing Committee: https://www.internationalmidwives.org/our-work/research/research-standing-committee.html [last accessed 09.11.2020]
International Confederation of Midwives (2019) Research: Midwifery led research. International Confederation of Midwives, The Hague. https://www.internationalmidwives.org/our-work/research/ . Accessed 23 Oct 2019
Iribarren S, Larsen B, Santos F et al (2018) Clinical nursing and midwifery research in Latin American and Caribbean countries: a scoping review. Int J Nurs Pract 24(2):e12623. Accessed 18 Oct 2019. https://doi.org/10.1111/ijn.12623
Article PubMed PubMed Central Google Scholar
Kajermo KN, Boström A-M, Thompson DS et al (2010) The BARRIERS scale—the barriers to research utilization scale: a systematic review. Implement Sci 32(5):1–22. https://doi.org/10.1186/1748-5908-5-32
Kennedy HP, Cheyney M, Dahlen H et al (2018) Asking different questions: research priorities to improve the quality of care for every woman, every child. Lancet Glob Health. Revised May 2018. https://onlinelibrary.wiley.com/doi/pdf/10.1111/birt.12361 . Accessed 28 May 2020
Khammarnia M, Haj Mohammadi M, Amani Z et al (2015) Barriers to implementation of evidence-based practice in Zahedan teaching hospitals, Iran, 2014. Nurs Res Pract:1–5. https://doi.org/10.1155/2015/357140
Kolfenbach M, Birdsall K (2015) (2015) international cooperation: strengthening midwifery in Central Asia. J Asian Midwives 2(2):57–61
Koninklijke Nederlandse Organisatie van Verloskundigen (KNOV) (2013) Midwifery Research Network, Dutch Midwives Association. https://www.knov.nl/vakkennis-en-wetenschap/tekstpagina/117-2/midwifery-research-network/hoofdstuk/45/midwifery-research-network/ . Accessed 15 Oct 2019
Laisser R, Chimwaza A, Omoni G et al (2019) Crisis: an educational game to reduce mortality and morbidity. Afr J Midwifery Women Health 13:1–6. https://doi.org/10.12968/AJMW.2018.0025
Lavender T, Omoni G, Laisser et al (2019) Evaluation of an educational board game to improve use of the partograph in sub-Saharan Africa: a quasi-experimental study. Sex Reprod Healthc (20) 54–59
Lugina African Midwives Research Network (2019) The Lugina Africa Midwives Research Network. http://lamrn.org/ . Accessed 4 Jun 2020
Luyben A, Winjen H, Oblasser C et al (2013) The current state of development of midwifery and midwifery research in four European countries. Midwifery 29(5):417–424. Accessed 1 Jun 2020. https://doi.org/10.1016/j.midw.2012.10.008
Maclean GD, Forss K (2010) An evaluation of the Africa midwives research network. Midwifery 26:e1–e8
Maclean G, Laisser R (2020) The use of educational games in midwifery. Afr J Midwifery Women Health 14(91):1–10
Mills J, Yates K, Harrison H et al (2016) Using a community of inquiry framework to teach a nursing and midwifery research subject: an evaluative study. Nurse Educ Today 43:34–39
Munro J, Spiby H (2001) Evidence into practice for midwifery-led care: part 2. Br J Midwifery 9:771–774
Munro J, Spiby H (2010) The nature and use of evidence in midwifery care: evidence-based midwifery. https://www.researchgate.net/publication/242188203_1_The_Nature_and_Use_of_Evidence_in_Midwifery_Care . Accessed 28 May 2020
Muoni T (2014) Decision-making, intuition and the midwife: understanding heuristics. BJM 20(1). Published Online: 16 Aug 2013. Accessed 26 Oct 2019. https://doi.org/10.12968/bjom.2012.20.1.52
Nanda G, Switlick K, Lule E (2005) Accelerating progress towards achieving the MDG to improve maternal health: a collection of promising approaches. Health, Nutrition & Population Discussion Paper. The International Bank for Reconstruction and Development/The World Bank, Washington, DC, p 20433
National Institute of Health Research (2020) Stillbirth prevention in sub-Saharan Africa. The National Institute of Health Research and University of Manchester. https://sites.manchester.ac.uk/stillbirth-prevention-africa/ . Accessed 4 Jun 2020
Ndwiga C, Maingi G, Serwanga J et al (2017) Exploring provider perspectives on respectful maternity care in Kenya: “Work with what you have”. Reprod Health 14:99. Accessed 8 Oct 2019. https://doi.org/10.1186/s12978-017-0364-8
New Zealand College of Midwives (2019) Research: New Zealand College of Midwives. https://www.midwife.org.nz/midwives/research/ . Accessed 15 Oct 2019
Nohria N, Eccles RG (eds) (1992) Networks and organisations: structure, form and action. Harvard Business School Press, Boston
Olsson A, Adolfsson A (2011) Midwife’s experiences of using intuition as a motivating element in conveying assurance and care. Health 3:453–461. Accessed 26 Oct 2019. https://doi.org/10.4236/health.2011.37075
Perrow C (1986) Complex organisations: a critical essay. Random House, New York
Piore MJ (1990) Fragments of a cognitive theory of technological change and organizational behaviour. In: Nohria N, Eccles RG (eds) Networks and organisations: structure, form and action. Harvard Business School Press, Boston
Porter ME (1990) The competitive advantages of nations. Free Press, New York
Book Google Scholar
Renfrew MJ (1997) The development of evidence-based practice. Br J Midwifery 5(2):100–104
Royal College of Midwives (2019) Evidence-based midwifery. Royal College of Midwives publications. https://www.rcm.org.uk/publications . Accessed 26 Oct 2019
Sackett DL, Rosenberg WM, Gray JA et al (1996) Evidence-based medicine: what it is and what it isn't. Editorial: BMJ. Accessed 16 Oct 2019. https://doi.org/10.1136/bmj.312.7023.71
Siwha J, Roth C (2004) Evidence-based practice. Ch 4. In: Henderson C, Macdonald S (eds) Mayes Midwifery. Bailliėre Tindall, Edinburgh
Soltani H, Low LK, Schuiling KD et al (2016) Global midwifery research priorities: an international survey. Int J Childbirth 6(1):5–1
Sun C, Larson E (2015) Clinical nursing and midwifery research in African countries: a scoping review. Int J Nurs Stud 52(5):1011–1016
Sun C, Dohrn J, Klopper H et al (2015) Clinical nursing and midwifery research priorities in eastern and southern African countries: results from a Delphi survey. Nurs Res 64(6):466–475
Sweileh WM, Al-Jabi SW, Zyoud SH et al (2019) Nursing and midwifery research activity in Arab countries from 1950 to 2017. [Review]. BMC Health Serv Res 19(1):340. Accessed 18 Oct 2019. https://doi.org/10.1186/s12913-019-4178-y
The Partnership for Maternal Newborn & Child Health (2011) A Global Review of the Key Interventions Related to Reproductive, Maternal, Newborn and Child Health (RMNCH). Geneva, Switzerland: PMNCH.
United Nations Population Fund (2014) State of the world’s midwifery: a universal pathway to women’s health. A United Nations publication, New York
van Wagner V (2017) Midwives using research: evidence-based practice and evidence-informed midwifery. Chapter 12. In: Comprehensive midwifery: the role of the midwife in health care practice, education and research. Press Books, Open Library. https://ecampusontario.pressbooks.pub/cmroleofmidwifery/chapter/midwives-using-research-evidence-based-practice-evidence-informed-midwifery/ . Accessed 28 May 2020
Wickham S (2000) Evidence-informed midwifery 3: evaluating midwifery evidence. Midwifery Today Autumn:45–46
World Health Organization (2016a) WHO and partners call for better working conditions for midwives. World Health Organization, Geneva. https://www.who.int/news-room/detail/13-10-2016-who-and-partners-call-for-better-working-conditions-for-midwives . Accessed 16 Oct 2019
World Health Organization (2016b) Midwives’ voices, midwives’ realities. Findings from a global consultation on providing quality midwifery care. Originally published under ISBN 978 92 4 151054 7. World Health Organization, Geneva. https://apps.who.int/iris/bitstream/handle/10665/250376/9789241510547-eng.pdf;jsessionid=6F7EFCDDC808DE4828446A6FF8B7844B?sequence=1 . Accessed 4 Jun 2020
World Health Organization (2018a) Midwives are essential to the provision of quality of care in all settings, globally. World Health Organization, Geneva. International Day of the Midwife 2018: https://www.who.int/news-room/commentaries/detail/midwives-are-essential-to-the-provision-of-quality-of-care-in-all-settings-globally . Accessed 16 Oct 2019
World Health Organization (2018b) World Health Organization Collaborating Centres: fact sheet. https://www.who.int/docs/default-source/documents/about-us/factsheetwhocc2018.pdf?sfvrsn=8c7166ee_2 . Accessed 3 Jun 2020
World Health Organization (2019a) Maternal mental health. Sexual and reproductive health. World Health Organization, Geneva. https://www.who.int/mental_health/maternal-child/maternal_mental_health/en/ . Accessed 12 Apr 2019
World Health Organization (2019b) Comprehensive mental health action plan 2013–2020. World Health Organization, Geneva. https://www.who.int/mental_health/action_plan_2013/en/ . Accessed 12 Apr 2019
World Health Organization (2020) World Health Organization news-room fact sheet: nursing and midwifery. https://www.who.int/news-room/fact-sheets/detail/nursing-and-midwifery . Accessed 3 Jun 2020
Yahui HC, Swaminathan N (2017) Knowledge, attitudes, and barriers towards evidence-based practice among physiotherapists in Malaysia. Hong Kong Physiother J 37:10–18
Download references
Author information
Authors and affiliations.
Global Professional Advisor, The Royal College of Midwives, London, UK
Maternal and Newborn Health, Department of Interprofessional Health, Swansea University, Swansea, UK
Gaynor D. Maclean
Global Midwifery Advisor, The Hague, Zuid-Holland, The Netherlands
Nester Moyo
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Joy Kemp .
Rights and permissions
Reprints and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Kemp, J., Maclean, G.D., Moyo, N. (2021). Strengthening Midwifery Research. In: Global Midwifery: Principles, Policy and Practice. Springer, Cham. https://doi.org/10.1007/978-3-030-46765-4_12
Download citation
DOI : https://doi.org/10.1007/978-3-030-46765-4_12
Published : 06 January 2021
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-46764-7
Online ISBN : 978-3-030-46765-4
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- Open access
- Published: 18 June 2019
Investigating midwives’ barriers and facilitators to multiple health promotion practice behaviours: a qualitative study using the theoretical domains framework
- Julie M. McLellan ORCID: orcid.org/0000-0003-4902-2254 1 ,
- Ronan E. O’Carroll 1 ,
- Helen Cheyne 2 &
- Stephan U. Dombrowski 3
Implementation Science volume 14 , Article number: 64 ( 2019 ) Cite this article
12k Accesses
27 Citations
26 Altmetric
Metrics details
In addition to their more traditional clinical role, midwives are expected to perform various health promotion practice behaviours (HePPBes) such as informing pregnant women about the benefits of physical activity during pregnancy and asking women about their alcohol consumption. There is evidence to suggest several barriers exist to performing HePPBes. The aim of the study was to investigate the barriers and facilitators midwives perceive to undertaking HePPBes.
The research compromised of two studies.
Study 1: midwives based in a community setting ( N = 11) took part in semi-structured interviews underpinned by the theoretical domains framework (TDF). Interviews were analysed using a direct content analysis approach to identify important barriers or facilitators to undertaking HePPBes.
Study 2: midwives ( N = 505) completed an online questionnaire assessing views on their HePPBes including free text responses ( n = 61) which were coded into TDF domains. Study 2 confirmed and supplemented the barriers and facilitators identified in study 1.
Midwives’ perceived a multitude of barriers and facilitators to carrying out HePPBes. Key barriers were requirements to perform an increasing amount of HePPBes on top of existing clinical work load, midwives’ cognitive resources, the quality of relationships with pregnant women, a lack of continuity of care and difficulty accessing appropriate training. Key facilitators included midwives’ motivation to support pregnant women to address their health. Study 1 highlighted strategies that midwives use to overcome the barriers they face in carrying out their HePPBes.
Conclusions
Despite high levels of motivation to carry out their health promotion practice, midwives perceive numerous barriers to carrying out these tasks in a timely and effective manner. Interventions that support midwives by addressing key barriers and facilitators to help pregnant women address their health behaviours are urgently needed.
Peer Review reports
Contributions to the literature
This research systematically examines barriers and facilitators midwives perceive in helping pregnant women with multiple health behaviour change
The theoretical domains framework is used to understand midwives’ multiple health promotion practice behaviours across a range of health topics
The barriers and facilitators health care professionals face in addressing multiple health behaviour change topics will help inform interventions to support the uptake of evidence-based guidelines into routine clinical healthcare practice
Introduction
In many developed countries, the public health focus for midwives has extended from health protection issues, such as reducing maternal and infant mortality and preventing the spread of disease, to health promotion topics, such as smoking cessation, and weight management [ 1 ]. In the United Kingdom (UK), midwives are expected to perform multiple health promotion practice behaviours (HePPBes) for a variety of health promotion topics throughout pregnancy and postnatally. Examples of HePPBes include monitoring carbon monoxide levels, discussing recommended daily fruit and vegetable intake or delivering an alcohol brief intervention (in the UK, the booking appointment takes place between 8 and 12 weeks gestation and is the first routine antenatal appointment).
HePPBes are outlined in the various policies, strategies and guidelines published by government and public-sector bodies, which either directly or indirectly implicate midwives as public health professionals [ 2 , 3 , 4 ]. For example, in the UK, the National Institute of Clinical Excellence (NICE) Smoking: stopping in pregnancy and after childbirth guidelines outline that midwives participate in up to 12 different smoking cessation-related HePPBes during pregnancy, such as measuring carbon monoxide levels, asking the woman if they or anyone in their household smokes and referring to NHS Stop smoking services [ 4 ]. Whilst the NICE Weight management before, during and after pregnancy guidelines [ 5 ] outline various HePPBes including measuring weight and height, asking questions about the pregnant women’s diet and physical activity and giving dietary and physical activity advice. For pregnant women with a BMI ≥ 30, midwives are expected to carry out additional HePPBes such as offering referral to a dietitian. Considering the variety of health promotion topics to be addressed during pregnancy, midwives face a high health promotion workload [ 6 , 7 , 8 , 9 , 10 ].
The factors related to midwives performing multiple HePPBes are poorly understood. Previous studies have examined maternal health care professionals’ behaviour using the theoretical domains framework [TDF; 11 [ 11 ]]. However, these studies examined single health-risk topic such as smoking cessation [ 12 ], weight management and obesity [ 13 ] and physical activity [ 14 ]. The TDF provides a comprehensive grouping of the overlapping constructs within behavioural theories. The original version (TDF v1) summarises the main factors of relevant behaviour change theories into 12 independent domains [ 11 ]. The TDF v1 has been validated through the development of a refined version (TDF v2; [ 15 ]).
Midwives experience several challenges in undertaking multiple HePPBes such as a shortage of resources [ 6 ], a lack of clarity about their public health role [ 7 , 8 ] and lack of self-efficacy [ 8 , 9 ]. However, limited evidence exists on the barriers and facilitators midwives perceive in undertaking multiple HePPBes. This study applies a theoretical approach to investigate potentially relevant factors at a multiple behaviour level.
Research aim
The aim of this study is to investigate midwives’ barriers and facilitators to performing multiple HePPBes across various health promotion topics using the theoretical domains framework in qualitative interviews (study 1) and free text questionnaire responses (study 2).
This study reports two different sources of qualitative data gathered through interviews and questionnaires. Interviews obtained detailed evidence about the barriers and facilitators midwives experience in carrying out their HePPBes. The questionnaires used an open-ended question to capture additional comments on barriers and facilitators that midwives may have had about their HePPBes.
Study design
Qualitative semi-structured interview study.
Participants
Midwives working in a community setting were eligible to participate if they were qualified, practising midwives employed by an NHS health board in central Scotland. Recruitment involved JM, a researcher previously unknown to participants, visiting an out-patient maternity clinic and providing 12 midwives with information about the study. The information provided to midwives included the reason for carrying out the research to inform JM’s PhD to develop an intervention to support midwives in addressing health behaviours with pregnant women. Eleven midwives agreed to take part. One midwife opted not to take part in the study.
Interview topic guide
The interview topic guide (see Additional file 1 ) contained (i) demographic questions (number of years of experience and job title) and (ii) questions based on each of the 12 TDF (v1) domains [ 11 ]. The behavioural category of interest, within the topic guide, was specified as: “supporting pregnant women to change their health behaviour” and the questions were designed to elicit beliefs about the behaviour in relation to each domain.
To remind midwives of the target behaviour of interest, an A4 prompt card was placed in front of them outlining typical examples of women’s health behaviours to be addressed (see the prompt card in Additional file 2 ). The behaviour was specified using terms Target, Action, Context and Time, known as the TACT principle [ 16 ]. TACT summarises the behaviour in terms of doing what, to whom, in a given context and at a specific time [ 17 ]. The behaviour was specified as: “All the things you do in a routine antenatal care consultation, including asking questions, to support pregnant woman change their health behaviours”. The TACT specification complements the general TDF definition used within the topic guide by breaking down of what was meant by “supporting pregnant women to change their health behaviour”.
Face-to-face semi-structured interviews were conducted by JM (a female PhD researcher and Health Psychologist with previous experience of supporting midwives’ behaviour change practice) on two separate occasions in October 2016. Interviews took place within consultation rooms at an out-patient maternity clinic in central Scotland. Information about the study was provided verbally and in written format. Interviews lasted between 27 and 76 min (mean ± SD, 43 ± 14). All interviews were audio recorded and anonymously transcribed verbatim. The demographic data was entered into a Microsoft Excel spread sheet. The consolidated criteria for reporting qualitative research (COREQ; [ 18 ]) was used to ensure all aspects of the qualitative research had been reported (a copy of the checklist is provided in Additional file 3 ).
Transcripts were stored as Microsoft Word documents. Qualitative data analysis was based on recommendations for conducting TDF based qualitative research [ 19 ] and involved the following ten steps:
Interviews were read several times by JM to ensure familiarity with the data.
One interview was jointly coded by JM and SD to develop a coding strategy.
Two interviews were coded by JM using a directed content analysis approach [ 20 ] in which interview content was placed in the most relevant TDF domain(s). Responses which could be attributed to more than one domain were coded into multiple domains.
The coding of the two interviews was checked by SD. Where discrepancies in coding occurred, discussion took place to reach a consensus.
The remaining interviews were coded by JM.
Data saturation was reached as the final three transcripts did not introduce any additional barriers and facilitators than those already identified.
Summaries of domain codings were produced by JM and checked by SD.
Identification of relevant theoretical domains was identified by consensus discussion between JM & SD. Relevance of a domain was based on the following criteria: (i) high frequency of specific beliefs and/or (ii) existence of conflicting beliefs and/or (iii) indication of clear beliefs that may influence the behaviour of interest [ 21 ].
Views were generated for relevant domains by JM and coded as being either generic (views which are made in reference to HePPBes in general) or behaviour specific (views which are in reference to a specific health promotion behaviour).
The views generated were checked by HC (a Professor of Midwifery) to ensure they made sense from a midwifery perspective.
Ethical approval
The University of Stirling Psychology Ethics Committee approved the study. NHS Research and Development approval was granted by Greater Glasgow and Clyde Health Board (R&D reference: GN16OG406).
Online questionnaire study including a qualitative open-ended question.
Individuals registered as a qualified midwife or training to be a midwife, worldwide, were eligible to take part. Recruitment took place online between the February and May 2018. Advertisements were placed on discussion forums, email lists and social media pages. The study was endorsed by the Royal College of Midwives on their Facebook and Twitter pages. Advertisements contained an URL link to the online study platform Qualtrics where the questionnaire was hosted. Overall, 719 participants consented to take part in the study and confirmed they were either a qualified or student midwife. Of those, 214 completed less than 95% of the questionnaire and therefore were excluded from further analysis. Complete responses were obtained from 505 participants.
Questionnaire
The questionnaire examined factors relevant to HePPBes. At the end of the questionnaire, participants were asked: “If you have any other comments on your Public Health role then please include them below”. The current paper reports on the qualitative data obtained from this question.
Midwives accessed the questionnaire by clicking on the URL contained within the online advertisement. Following presentation of study information and eligibility criteria, consent was obtained by the midwife selecting an electronic check box. A screening question: “Are you a qualified or student midwife?” was presented as a method of reducing the likelihood of non-midwives completing the questionnaire. If the response was “no”, then participants were thanked for their interest in the study and exited from the questionnaire. At the end of the questionnaire, midwives were offered the opportunity to be entered into a prize draw to win 1 of 4x £25 shopping vouchers.
Analysis of the qualitative questionnaire data involved the following five steps:
Responses were read several times by JM to ensure familiarity with the data.
Responses were coded by JM using a directed content analysis approach [ 20 ] in which responses were placed in the most relevant TDF domain. If a response could be coded into more than one domain, a decision was made by JM as to the most appropriate domain.
Coding was checked by SD.
The number of responses coded into each domain was calculated by JM.
JM checked how much the barriers identified reflected those in study 1 and if there were any additional barriers or facilitators identified.
The University of Stirling’s General University Ethics Panel approved the study (GUEP316).
All 11 participants were female, employed as community midwives, except one who worked as a Senior Charge Midwife. The mean number of years of experience as a qualified midwife was 22 (range from 3 to 31).
Reviewing of coding
Agreement between coders for two interviews was 76% and 88% for the first and second interview respectively, and disagreement for the same interviews was 17% and 5% respectively. The mean agreement was 82% and mean disagreement was 11%. An additional 7% of codes were suggested by the second coder for each interview.
Relevant theoretical domains
All barriers and facilitators could be identified within the TDF. Nine of the 12 TDF domains were classified as important in understanding the barriers ( b = barrier) and facilitators ( f = facilitator) to undertaking HePPBes. Table 1 lists these domains alongside a domain descriptor.
The identified domains are outlined below and a table containing the associated belief statements are provided in Additional file 4 .
Professional role and identity
Midwives mostly saw HePPBes as part of their professional role (f): “I just see it as my job” (M10) and “I think public health is an essential part our role” (M7). However, some thought that several HePPBes could be addressed prior to conception, especially around weight management (b): “She’s thirty-five and she’s pregnant, so why is it suddenly the midwife that has to look into that?” (M3). Midwives frequently mentioned that the role of the midwife had evolved from providing traditional midwifery care (e.g. measuring the growth of the baby) to having a strong focus on undertaking HePPBes (b): “They seem to keep adding to the list of things we’re expected to do”(M11), and some midwives expressed a feeling that their traditional professional role was being eroded (b): “Our role now, as community midwives, seems to be for referring on … it feels as if your role’s been kind of eroded at” (M10).
Beliefs about consequences
Midwives mentioned several consequences that potentially impact their HePPBes. Contrasting beliefs about how HePPBes impacted on the relationship with the woman were voiced. If performed well, midwives believed it could be useful in gathering information about aspects of the women’s wellbeing (f). However, some stated that performing HePPBes could potentially damage the relationship if they were not carried out carefully, particularly for HePPBes related to weight management (b): “Women get quite offended at that one” (M10).
Similarly, contrasting beliefs about the womens’ receptiveness to HePPBes emerged. Some midwives reported that women expect them to carry out HePPBes (f): “Most women are quite receptive to that because they know they’re pregnant and know it’s not just about their health anymore” (M11). Other midwives said that women were not receptive to HePPBes (b): “It seems to be that everything is piled on to this booking visit and I don’t think it’s fair on the women either” (M3).
The time it takes to perform HePPBes was seen as a clear barrier with appointments over running the allotted time which could impact on other women (b): “You run over and then people are kept waiting.” (M11). Furthermore, midwives held a clear belief that HePPBes had the potential to have positive health benefits for the women and their child (f): “Absolutely, there’s a huge knock-on effect” (M5). Clear views on the short-term impact of HePPBes depended on the behavioural topic. For instance, smoking was perceived as an issue that could be dealt with during pregnancy (f): “This is probably a time, particularly for the smokers, they’ve got that motivation for the baby to change” (M5). Meanwhile, the impact of diet-related HePPBes was considered as unobservable (b): “I’m never going to know whether she’s changed her diet, or even if she did change her diet, whether that’s going to last” (M6). Some midwives expressed a clear belief that it was rewarding for them to observe the benefits of women engaging in health behaviour change attributed to their HePPBes (f): “That is rewarding if you feel like you’ve helped someone make a change in their life.” (M11). Benefits in reducing future workload if HePPBes were carried out effectively were noted (f): “If we do our job well at the booking clinic and women take that on board then we don’t have as much to do” (M2).
Motivation and goals
Midwives frequently reported being highly motivated to undertaking HePPBes to benefit the long-term health of the woman and the baby (f): “I think it’s a huge window of opportunity for midwives” (M5). However, HePPBes were not a priority if there were conflicting clinical risks to the woman and/or baby such as patient safety or adult/child protection issues (b): “I’d say it’s definitely secondary though, obviously check the woman’s blood pressure, making sure she’s well, doing urine analysis, making sure there’s no infections, ruling out pre-eclampsia, listening to baby. That comes first and everything else, I think, would come second to that.” (M11).
Memory/attention and decision processes
Midwives described being prompted by the woman’s maternity notes to cover all HePPB topics (f): “My booking visit would be just going through that book with them because everything I need to tell them is in there, it’s a good thing for me cause it saves me forgetting to stop to talk about things” (M3) which also acted as a prompt to HePPBes at follow-up appointments (f): “I usually always have a wee flick through the notes at the beginning just to check if there’s any kind of outstanding issues to be aware of (M11)”.
If the woman wanted to discuss a particular behaviour, midwives prioritised this (f): “If the woman is worried about her weight, I’m happy to talk about it at every appointment, but if she’s not then I’m not gonna bring it up”, (M6). Some midwives covered a topic in depth if they felt it was of specific relevance (f): “Say I did three bookings yesterday one of them would have had none of these problems, one of them had a BMI was over 35 so that’s the one I concentrated on.” (M5).
Intuition was frequently reported as guiding decision making in relation to HePPBes (f): “If I get vibes from them, that actually they do know” (M5) and “I just have to go with my gut at the time” (M6) . Midwives also based performing HePPBes on the physical health of the woman during the appointment (b): “If they are very sick or they’ve had bleeding, then I’ll just say, ‘we’ll talk about this another time’ because it’s not appropriate to get ahead of ourselves” (M2).
Environmental context and resources
Changes in health care service provision (e.g. changes in timing of booking appointments) were perceived as making it more difficult to carry out HePPBes (b): “… with continuity of care being removed from us we’re not getting the same chance to see the same women again so I find it a bit harder to address things.” (M10).
Some midwives held a belief that accessibility to resources such as training related to HePPB could be improved (b): “It’s quite haphazard how you can get on to these things” (M4). Materials related to HePPBes were generally perceived as high quality (f): “‘Ready Steady Baby’ is I think a fantastic book” (M10). However, some felt the wording of questions within maternity notes made them difficult to ask (b): “That’s a barrier to me asking, because I actually don’t ask the way it’s worded on that because it doesn’t make sense.” (M4). A belief that there were too many HePPBes to undertake in too little time was apparent (b): “We’ve also got to try and work within the time constraints” (M9). Some midwives believed that the woman’s health status at the booking appointment affected the degree to which they could carry out HePPBes (b): “The booking appointment is really difficult for some women to sit there and actually not vomit” (M7). Physical cues were mentioned as prompts to undertake HePPBes (f): “If you pick up a book and it stinks of smoke, you know, you might well say, how you getting on?” (M2).
Social influences
Women were reported as a strong influence on midwives HePPBes and were seen to increasingly inform themselves through online sources. This was perceived as helpful to recommend high-quality information (f): “Get them to use websites because most of them are on computer all the time anyway” (M3) and unhelpful due to the potential to increase stress (b): “A lot of the women have got health anxieties and that’s fuelled by the internet” (M2). Mixed views emerged about how accurately women reported some health behaviours such as alcohol consumption, which impacted on health promotion efforts. Some midwives perceiving accurate accounts (f): and others reporting the opposite (b): “Alcohol, I think, is probably one that’s probably hidden, getting women to be honest is probably very difficult” (M10).
Team working and social support was seen as helpful in resolving issues regarding HePPBes (f): “My kind of closest colleagues, we’d probably have a wee chat and we’ll probably complain about how we’re meant to put this in amongst everything else that people want out of us.” (M10). Intergroup conflict was perceived by some in relation to performing HePPBes (b): “It’s come up in the tearoom and there will be conversations with people saying, ‘Oh public health that’s a load of nonsense’ and I’ll sit there quite openly and say ‘I think it’s one of the best things that’s ever occurred’” (M7).
Midwives described shifting social and group norms useful to normalise addressing health behaviours (f): “There’s very few people that are not happy to answer these questions nowadays because we’ve been doing this for so long they expect it and they do all talk amongst each other” (M7). However, social norms appeared to be unhelpful in normalising obesity (b) “If a lady’s got a BMI of not over 30, I still sort of don’t see it as a huge issue with them” (M7).
Some saw a midwife’s own body mass index (BMI) potentially making it harder to perform weight management HePPBes (b): “I think midwives find it really difficult because if you’re big yourself they’re looking at you thinking: ‘well, she’s got a cheek’, if you’re small they’re looking at you thinking: ‘you have never had a problem in your life’” (M10).
Carrying out HePPBes was associated with a range of positive emotions if these were seen to result in positive outcomes (f): “You feel dead pleased they actually brought it up again” (M9). Some reported concerns about performing specific HePPBes (b): “I do find it causes me anxiety if I know I’m going to tell her today that we’re doing a Social Work referral.” (M10). Carrying out HePPBes was potentially stressful (b): “Sometimes I’m thinking you just want to do the right thing, which is hard sometimes” (M5) and draining (b): “I’m exhausted after a clinic because you feel as if you want to have your senses hyper alert” (M9).
Behavioural regulation
Midwives described using behavioural regulation strategies such as using maternity notes as a prompt to cover all HePPBes, writing notes in SWHMMR as prompt for carrying out HePPBes follow-up appointments, carrying out HePPBes whilst performing clinical tasks, e.g. asking questions about physical activity while taking bloods (f): “I have to say I multi task. I’ll be testing the urine while I’m asking about how they feel in pregnancy and had they had any sickness and how they’re getting on with eating.” (M7). For a list of strategies reported, see Additional file 5 .
Nature of the behaviours
The majority of HePPBes took place at the booking appointment when there is usually the most time to undertake HePPBes (f). Midwives reported HePPBes as being routine practice (f): “We’ve got to tick boxes, we’ve got to tick that we’ve discussed alcohol, we’ve discussed smoking” (M10). The habitual nature of performing HePPBes included the strategies used to regulate health promotion practice as well as the behaviours themselves.
Study 2 results
Forty-seven fully qualified midwives and 14 student midwives provided a statement to the final question. The majority (92%) were based in the UK. The mean number of years of experience as a qualified midwife was 17 (range from 1 month to 40 years).
Responses were coded into seven TDF domains: professional role and identity, beliefs about consequences, motivation and goals, environmental context and resources, social influences, emotion and beliefs about capabilities. The definitions for each domain are the same as those presented in study 1. The domains are presented in terms of (i) the number of responses and (ii) supporting evidence.
Twenty-six responses were coded as environmental context and resources focusing on a need for improved resources, particularly a need for more time, wider access to online materials: “Apps and online mediums for encouraging behaviour change may take the pressure off midwives” and more accessibility to training . Some responses stressed the need for continuity of care.
Nine responses were coded as beliefs about consequences. The potential for weight management HePPBes to impact the midwife-woman relationship was mentioned. Mixed responses about women’s receptiveness to HePPBes emerged .
Nine motivation and goals responses suggested high levels of motivation to carry out HePPBes . Some midwives indicated that the degree to which they were able to support women was not ideal.
Eight responses were coded as social influences and focused on midwives’ own health status in relation to undertaking HePPBes. Some midwives described their own health behaviours and status helping or hindering HePPBes: “My own lifestyle and motivation in public health topics can impact the delivery and communication when approaching topics with women” . Others reported that their health status was irrelevant: “Don’t confuse my welfare with those of the woman and baby I’m caring for... public health roles should not be judged by the delivering midwife”.
Three responses were coded as professional role and identity commenting on a need for health promotion topics to be tackled before pregnancy and the demands placed on midwives to fulfil multiple professional roles.
Three responses coded as emotion focused on the taxing nature of the job and the potential negative health consequences of burn-out.
Beliefs about capabilities
Three responses coded as beliefs about capabilities highlighted that midwives potentially feel more confident in addressing health promotion topics which have greater attention placed on them in health policy and that capability to undertake HePPBes was reliant on resources such as training and time .
Integration of study 1 and 2 findings
Table 2 presents the integration of the findings from both studies by highlighting whether the views demonstrated in study 1 were supported by the responses generated in study 2. The table shows that six of the nine domains identified as important in study 1 were supported by responses from study 2.
Principal findings
Midwives perceived a multitude of barriers and facilitators to carrying out HePPBes. Key barriers were requirements to perform an increasing amount of HePPBes on top of existing clinical work load, which impacted on the time available, midwives’ cognitive resources and the quality of relationships with pregnant women. Organisational issues such as a lack of continuity of care and difficulty accessing appropriate training were also identified. Key facilitators included midwives’ motivation to support pregnant women to address their health. Study 1 also highlighted strategies that midwives use to overcome the barriers they face in carrying out their HePPBes. Some findings were considered both barriers and facilitators as mixed views were expressed about whether certain health promotion topics should be addressed by other health professionals prior to pregnancy, women’s receptiveness to HePPBes during pregnancy and the social influence of midwives’ own health status.
Strengths and limitations
The complimentary nature of the two presented studies is a strength. Study 1 provided detailed insight from a group of midwives working in a community setting which was supplemented in study 2 by free text commentary from a larger sample of midwives, employed within a variety of professional roles.
Limitations include the difficulty to specify target behaviours when simultaneously investigating multiple HePPBes for a variety of health promotion topics at the same time. The use of the TACT principle [ 16 ], and the image within the A4 prompt card provided midwives with a visual aid to remind them of the study focus during the interview. The sample size in study 1 was based on evidence-based guidelines [ 22 ], but is smaller than other qualitative TDF-based studies [ 23 , 24 ]. In addition, the midwives who took part in study 1 were recruited from a single out-patient maternity clinic in Scotland and different and additional barriers and facilitators might have emerged within different contexts.
Study 2 used online recruitment which prevents checking that participating individuals fully met inclusion criteria. The current paper examined HePPBes at a general level but some of the barriers raised were health promotion topics specific (e.g. a lack of dietary services to refer women to). Future research could further explore similarities and differences of HePPBes for different health promotion topics.
Relation to other studies
Limited evidence exists on the psychological factors associated with midwives HePPBes targeting women’s multiple health behaviours. Previously identified barriers to midwives undertaking HePPBes including a lack of time, resources and variability in training quality [ 6 ] were confirmed in the current study and therefore highlight a continued need for midwives to be provided with support. Uncertainty amongst midwives about their public health role [ 7 , 8 ] was also demonstrated through the mixed views midwives expressed regarding whether all HePPBes should fall under the remit of the midwife. Midwives’ use of strategies to overcome the barriers they face in carrying out HePPBes has not been previously reported.
Examining multiple HePPBes increases the complexity of the behavioural influences identified and provides greater understanding of the influences on midwives HePPBes. The complexity of investigating multiple HePPBes is demonstrated by the higher number of barriers identified within the current study compared with studies which have used the TDF to explore midwives’ behaviours in relation to single health risk topics [ 11 , 13 , 14 ].
The TDF [ 10 ] provides an overview of the main psychological constructs explaining health behaviours. However, the theories that these constructs belong to are mainly used to explain single behaviours. Multiple behaviour change processes such as goal facilitation [ 25 ] and goal conflict [ 26 ] and transference [ 27 ] have not been captured by the TDF domain interview questions and therefore might have been missed by the current study.
Possible mechanisms and implications
Barriers such as difficulty to access HePPBe-related training suggest a specific public health component in midwife training or after qualification may be useful. The finding that carrying out HePPBes can be taxing suggests that more support for midwives may be required. Policy makers and key stakeholders commissioning midwives’ continuous professional development opportunities could provide HePPBe support in multiple formats (e.g. through training, handheld materials or peer support).
Given the variations in the type of care that midwives provide, the pressure placed on maternity services by midwives attending training and the limited time that midwives would have to access support, developing handheld (or electronic) materials may be the most feasible option. For example, a leaflet containing examples of the strategies midwives use to carry out their HePPBes, that midwives could refer to during or outwith antenatal consultations, could capitalise on some of the HePPBe facilitators identified within this study.
Unanswered questions and future research
The development of an intervention to support midwives in helping pregnant women address multiple health behaviours is necessary to maximise the effectiveness of public health interventions aimed at behaviour change during pregnancy. Future studies should translate the current findings into acceptable, scalable and effective interventions to support midwives to perform HePPBes.
The findings suggest that despite high levels of motivation to carry out HePPBes, midwives perceive numerous barriers to carrying out these tasks in a timely and effective manner. Interventions that support midwives by addressing key barriers and facilitators to help pregnant women address their health behaviours are urgently needed.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
Consolidated criteria for reporting qualitative research
Health promotion practice behaviours
- Theoretical domains framework
Finlay H. Public health, midwifery and government policy. In: Bowden J, Manning V, editors. Health promotion in midwifery principles and practice. Boca Raton: CRC Press; 2016. p. 1–18.
Google Scholar
National Institute for clinical excellence: CG62—antenatal care for uncomplicated antenatal care for uncomplicated pregnancies, 2008, https://www.nice.org.uk/guidance/cg62
Knight M, Kenyon S, Brocklehurst P, Neilson J, Shakespeare J, Kurinczuk J. On behalf of MBRRACE-UK. Saving lives, improving mothers’ care: lessons learned to inform future maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2009–2012. Oxford: National Perinatal Epidemiology Unit, University of Oxford; 2014.
National Institute for clinical excellence: PH26—smoking: stopping in pregnancy and after childbirth. 2010, https://www.nice.org.uk/guidance/ph26
National Institute for Clinical Excellence: PH27—Weight management before, during and after pregnancy. 2010, https://www.nice.org.uk/guidance/ph27
Sanders J, Hunter B, Warren L. A wall of information? Exploring the public health component of maternity care in England. Midwifery. 2016;34:253–60.
Article Google Scholar
McNeill J, Doran J, Lynn F, Anderson G, Alderdice F. Public health education for midwives and midwifery students: a mixed methods study. BMC Pregnancy Childbirth. 2012;12:142.
McNeill J, Lynn F, Alderdice F. Public health interventions in midwifery: a systematic review of systematic reviews. BMC Public Health. 2012;12:955.
Lavender T, Bennett N, Blundell J, Malpass L. Midwives' views on redefining midwifery 1: health promotion. Br J Midwifery. 2001;9:666–70.
Biro MA. What has public health got to do with midwifery? Midwives’ role in securing better health outcomes for mothers and babies. Women Birth. 2011;24:17–23.
Michie S, Johnston M, Abraham C, Lawton R, Parker D, Walker A. Making psychological theory useful for implementing evidence based practice: a consensus approach. Qual Saf Health Care. 2005;14:26–33.
Article CAS Google Scholar
Beenstock J, Sniehotta FF, White M, Bell R, Milne EM, Araujo-Soares V. What helps and hinders midwives in engaging with pregnant women about stopping smoking? A cross-sectional survey of perceived implementation difficulties among midwives in the north east of England. Implement Sci. 2012;7:36.
Heslehurst N, Newham J, Maniatopoulos G, Fleetwood C, Robalino S, Rankin J. Implementation of pregnancy weight management and obesity guidelines: a meta-synthesis of healthcare professionals' barriers and facilitators using the theoretical domains framework. Obes Rev. 2014;15:462–86.
McParlin C, Bell R, Robson S, MuirHead C, Araujo-Soares V. What helps or hinders midwives to implement physical activity guidelines for obese women? A questionnaire survey using the theoretical domains framework. Midwifery. 2017;49:110–6.
Cane J, O'Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37.
Fishbein M. Attitude and the prediction of behavior. In: Fishbein M, editor. Readings in attitude theory and measurement. Oxford: Wiley; 1967. p. 477–91.
Foy R, Francis JJ, Johnston M, Eccles M, Lecouturier J, Bamford C, Grimshaw J. The development of a theory-based intervention to promote appropriate disclosure of a diagnosis of dementia. BMC Health Serv Res. 2007;7:207.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, Foy R, Duncan EM, Colquhoun H, Grimshaw JM, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12:77.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–88.
Cahir C, Guinan E, Dombrowski SU, Sharp L, Bennett K. Identifying the determinants of adjuvant hormonal therapy medication taking behaviour in women with stages I–III breast cancer: a systematic review and meta-analysis. Patient Educ Couns. 2015;98:1524–39.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field methods. 2006;18:59–82.
Lawton R, Heyhoe J, Louch G, Ingleson E, Glidewell L, Willis TA, McEachan RR, Foy R. Using the theoretical domains framework (TDF) to understand adherence to multiple evidence-based indicators in primary care: a qualitative study. Implement Sci. 2015;11:113.
Patey AM, Islam R, Francis JJ, Bryson GL, Grimshaw JM. Anesthesiologists’ and surgeons’ perceptions about routine pre-operative testing in low-risk patients: application of the theoretical domains framework (TDF) to identify factors that influence physicians’ decisions to order pre-operative tests. Implement Sci. 2012;7:52.
Riediger M, Freund AM. Interference and facilitation among personal goals: differential associations with subjective well-being and persistent goal pursuit. Personal Soc Psychol Bull. 2004;30(12):1511–23.
Presseau J, Boyd E, Francis JJ, Sniehotta FF. Goal conflict and goal facilitation in community-based cardiac rehabilitation: a theory-based interview study. Psychol Health Med. 2015;20(2):227–38.
Fleig L, Ngo J, Roman B, Ntzani E, Satta P, Warner LM, Schwarzer R, Brandi ML. Beyond single behaviour theory: adding cross-behaviour cognitions to the health action process approach. Br J Health Psychol. 2015;20(4):824–41.
Download references
Acknowledgements
The authors are grateful to the Royal College of Midwives and everyone who supported the recruitment of midwives. The authors would like to thank all the midwives who were interviewed and undertook the questionnaire. The authors would also like to thank Angelica Setterington for her support in transcribing the interviews. This work was undertaken by and on behalf of The Scottish Improvement Science Collaborating Centre (SISCC).
This study was funded by the University of Stirling in collaboration with the Scottish Improvement Science Collaborating Centre. The Scottish Improvement Science Collaborating Centre (SISCC) is funded by the Scottish Funding Council (SFC), Chief Scientist’s Office, NHS Education for Scotland and The Health Foundation with in-kind contributions from participating partner universities and health boards. The grant reference number is 242343290 was received from SFC on behalf of all funders.
Author information
Authors and affiliations.
Division of Psychology, Faculty of Natural Sciences, University of Stirling, Stirling, Scotland, UK
Julie M. McLellan & Ronan E. O’Carroll
Nursing Midwifery and Allied Health Professions Research Unit, University of Stirling, Stirling, Scotland, UK
Helen Cheyne
Faculty of Kinesiology, University of New Brunswick, Bathurst, Canada
Stephan U. Dombrowski
You can also search for this author in PubMed Google Scholar
Contributions
JM contributed to the design of the study, carried out data collection and analysis and was primarily responsible for drafting the manuscript. SD contributed to the design of the study, was involved in data analysis and commented on drafts of the manuscript. RO’C and HC were involved in designing the study and commented on drafts of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Julie M. McLellan .
Ethics declarations
Ethics approval and consent to participate.
The University of Stirling Psychology Ethics Committee approved study 1 and NHS Research and Development approval was granted by Greater Glasgow and Clyde Health Board (R&D reference: GN16OG406). The University of Stirling’s General University Ethics Panel approved study 2 (GUEP316). Consent to participate was obtained from all midwives who took part in the studies.
Consent for publication
Consent for publication was obtained from all midwives who took part in the studies.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:.
Study 1 Interview Topic guide. (DOCX 19 kb)
Additional file 2:
Study 1 Prompt card. (DOCX 2283 kb)
Additional file 3:
COREQ checklist. (DOCX 18 kb)
Additional file 4:
Study 1 table of midwives view statements table. (DOCX 18 kb)
Additional file 5:
Study 1 table of midwives HePPBe strategies. (DOCX 16 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
McLellan, J.M., O’Carroll, R.E., Cheyne, H. et al. Investigating midwives’ barriers and facilitators to multiple health promotion practice behaviours: a qualitative study using the theoretical domains framework. Implementation Sci 14 , 64 (2019). https://doi.org/10.1186/s13012-019-0913-3
Download citation
Received : 18 March 2019
Accepted : 03 June 2019
Published : 18 June 2019
DOI : https://doi.org/10.1186/s13012-019-0913-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health promotion
- Multiple health behaviours
Implementation Science
ISSN: 1748-5908
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
What Prevents Quality Midwifery Care? A Systematic Mapping of Barriers in Low and Middle Income Countries from the Provider Perspective
Affiliation National Health Service of England and Wales, The Whittington Hospital, London, United Kingdom
* E-mail: [email protected]
Affiliation Department of Maternal, Newborn, Child and Adolescent Health, World Health Organization, Geneva, Switzerland
- Alex Filby,
- Fran McConville,
- Anayda Portela

- Published: May 2, 2016
- https://doi.org/10.1371/journal.pone.0153391
- Reader Comments
Quality of care is essential for further progress in reducing maternal and newborn deaths. The integration of educated, trained, regulated and licensed midwives into the health system is associated with improved quality of care and sustained decreases in maternal and newborn mortality. To date, research on barriers to quality of care for women and newborns has not given due attention to the care provider’s perspective. This paper addresses this gap by presenting the findings of a systematic mapping of the literature of the social, economic and professional barriers preventing midwifery personnel in low and middle income countries (LMICs) from providing quality of care.
Methods and Findings
A systematic search of five electronic databases for literature published between January 1990 and August 2013. Eligible items included published and unpublished items in all languages. Items were screened against inclusion and exclusion criteria, yielding 82 items from 34 countries. 44% discussed countries or regions in Africa, 38% in Asia, and 5% in the Americas. Nearly half the articles were published since 2011. Data was extracted and presented in a narrative synthesis and tables. Items were organized into three categories; social; economic and professional barriers, based on an analytical framework. Barriers connected to the socially and culturally constructed context of childbirth, although least reported, appear instrumental in preventing quality midwifery care.
Conclusions
Significant social and cultural, economic and professional barriers can prevent the provision of quality midwifery care in LMICs. An analytical framework is proposed to show how the overlaps between the barriers reinforce each other, and that they arise from gender inequality. Links are made between burn out and moral distress, caused by the barriers, and poor quality care. Ongoing mechanisms to improve quality care will need to address the barriers from the midwifery provider perspective, as well as the underlying gender inequality.
Citation: Filby A, McConville F, Portela A (2016) What Prevents Quality Midwifery Care? A Systematic Mapping of Barriers in Low and Middle Income Countries from the Provider Perspective. PLoS ONE 11(5): e0153391. https://doi.org/10.1371/journal.pone.0153391
Editor: Saravana Kumar, University of South Australia, AUSTRALIA
Received: October 29, 2015; Accepted: March 29, 2016; Published: May 2, 2016
Copyright: © 2016 Filby et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: Funding for this project was provided by The United States Agency for International Development (USAID). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Global research has concluded that midwifery care has a pivotal role in the reduction of preventable maternal and newborn mortality and morbidity [ 1 ]. The increased access to skilled attendance at birth in the low and middle income countries (LMICs) that contribute to 99% of the global maternal mortality rate, has not, however, resulted in expected reductions in mortality [ 2 ]. This can be explained by a lack of quality maternity care [ 3 , 4 ]. The evidence indicates that strengthening midwifery is key to improving quality of care and achieving international efforts; yet implementation of educated, trained, regulated and licensed midwives remains inconsistent, resulting in a critical obstacle to progress [ 5 ].
The “three delays” model [1994] identified barriers to accessing care from the perspective of childbearing women; (1) delay in the decision to seek care; (2) delay in arriving at a health facility and (3) delay in the provision of adequate care at the facility [ 6 ]. The perspective of the women who provide that care, however, has remained virtually absent from the discourse [ 7 ]. To initiate the discussions on the possible barriers experienced by midwifery personnel in providing care, the World Health Organization (WHO), in collaboration with the International Confederation of Midwives (ICM) and the White Ribbon Alliance (WRA), convened a session at the 2013 Women Deliver Conference to determine if providers of midwifery care felt empowered , respected and safe [ 8 , 9 ]. The research presented by delegates from Nepal, Papua Guinea and Afghanistan and the ensuing multi-country discussions, highlighted the shortcomings in the education, training, licensure and regulation of professionals, while also detailing the significant personal challenges that women who provide midwifery care face [ 10 ]. This includes: social inequality, inadequate pay to meet the basic cost of living, unsafe working conditions and physical and sexual abuse [ 9 ]. The negative impact of these realities on quality of care was described through the concepts of burn out and moral distress . Burn out is defined as the expenditure of energy, effort and time on work without adequate time or environment to recover physically and emotionally [ 11 ]. Moral distress is defined as the experience of being seriously compromised as a moral agent by being unable to practice in accordance with accepted professional values and standards. This is associated with frustration, anger, guilt, anxiety, perceived lack of control, feeling belittled or unintelligent, and negative physical symptoms [ 12 ].
Analysis of the findings from the Women Deliver session enabled categorisation of the multiple issues faced by the women who provide midwifery care into social, economic and professional barriers, and resulted in the development of an analytical framework ( Fig 1 ). This framework presents burn out and moral distress as a consequence of interactions between all three barriers.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0153391.g001
It has recently been recognised that the complexity of access to quality of care goes beyond a health and development issue and requires a broader human rights approach [ 13 ], thinking beyond the practicalities of health systems to include human relationships, desires and values, roles and norms, and power structures [ 14 ]. Maternal and newborn mortality reduction is described as being hampered by gender inequality on two fronts—the gender discrimination experienced by the woman who provides the care and the additional gender inequality experienced by the childbearing woman [ 15 ]. Midwifery is unique within healthcare, being represented nearly exclusively by women and traversing both domestic and medical domains and cultures [ 16 ]. The recently released Global Strategy for Women’s, Children’s and Adolescent Health (2016–2020) highlights the need for further progress to be based on gender responsive, equity driven and rights based approaches [ 17 ].
Aims and objectives
We conducted a systematic mapping of the literature to describe the literature that answers the question: What are the social , economic and professional barriers preventing midwifery personnel in low and middle income countries (LMICs) from providing quality of care to mothers and newborns ?
The objectives were to develop a map of the literature on barriers to quality midwifery care through a methodical and replicable process and establish the relevance of the analytical framework developed through the Women Deliver session by detailing the barriers found and the type of literature identified.
A systematic mapping allows materials from a range of sources to be identified and does not exclude items based on study design or literature type, while still providing a process that is methodical and replicable [ 18 ]. This approach is particularly helpful in identifying gaps for further reviews and primary research for topics where it is anticipated that effectiveness studies will not be found which can support specific outcome-focused questions. We developed a protocol, which is available from the corresponding author.
An area of anticipated difficulty for the mapping was the definition of midwifery personnel. Midwifery has been described as “commonly misunderstood” [ 5 ] with midwifery care providers lacking a universally protected and acknowledged title. We reviewed different definitions [ 5 , 19 , 20 ]. In order to focus on the wider range of professional groups who are, in many circumstances, providing elements of midwifery care, we adopted the WHO/ICM/FIGO definition of a skilled birth attendant (SBA) to represent midwifery personnel:
An accredited health professional—such as a midwife , doctor or nurse—who has been educated and trained to proficiency in the skills needed to manage normal (uncomplicated) pregnancies , childbirth and the immediate postnatal period , and in the identification , management and referral of complications in women and newborns . [ 20 ]
Although this definition includes doctors, the authors felt that medical professionals are not subject to the same social and economic inequality and misunderstanding over professional title and status as are other midwifery personnel and therefore as indicated further below, medical professionals were not considered in this mapping.
The search was conducted on the 20 th August 2013. The intervening time between the search and article submission was used to analyze the data and draft the paper for submission.
Inclusion/exclusion criteria
All eligible items that discussed barriers to midwifery personnel providing quality care were considered, including published and unpublished material, whether in print or online such as journal articles, news items and project reports from governments and other agencies in all languages. Since the aim is to describe the literature available for the question framed above, items were not assessed for quality or excluded based upon study design. The classification of barriers as social, economic and professional was applied in the analysis stage and did not affect inclusion of articles during the screening process.
Items from LMICs, classified according to the World Bank criteria [ 21 ] were included. This was justified in order to focus on quality of care in the countries that contribute to 99% of the global maternal mortality rate [ 2 ].
Midwifery personnel who met the definition of an SBA as defined above, regardless of professional title were included. Items exclusively discussing medical professionals, including obstetricians and gynaecologists were excluded. Items, however, that discussed obstetricians and gynaecologists collectively with other midwifery personnel were considered, so as not to discard relevant material. The length and content of the professional training was not considered, as long as it resulted in SBA status.
Items that focused on traditional birth attendants were excluded. Items from high income countries and published before January 1990 and after August 2013 were also excluded.
Search strategy
We developed an initial search strategy based on the contributions received from a call for papers from WHO regional offices, midwifery associations, advocacy groups and individual experts. Five relevant references were received, all of which were published items, and were used to pilot electronic searches on Pubmed and CINAHL. The terms developed for barriers were the most challenging aspect of the search design and were largely informed by the analytical framework ( Fig 1 ) and The State of the Worlds’ Midwifery Report 2011 [ 2 ]. The initial piloting process also developed additional terms such as ‘lived experience’, ‘voice’, and ‘opinion’ which returned many relevant items. The LMIC criteria were met by adding a pre-designed filter developed by the WHO.
A systematic search of five bibliographic databases was then conducted. The databases selected were PubMed and The Global Index Medicus, for breadth; The Maternity and Infant Care Index and CINAHL, for a nursing and midwifery focus; and POPLINE, for a reproductive health focus. This selection was intended to capture relevant literature across the disciplines of midwifery, nursing, medicine, social science, health systems, and health policy.
The search strategy was specifically adapted to each electronic database and Medical Subject Headings (MeSH) used where possible. Midwifery personnel terms were searched in combination with approximately 150 terms for ‘barriers’ and a LMIC country filter applied. The search terms are detailed in the Supporting Information ( S1 Table ) accompanying this article.
The search yielded 9126 items across the five databases and the call for papers, which was reduced to 7344 items, once duplicates had been removed. Two of the authors (AF and FM), screened the articles by title and the total was reduced to 1429 items. When a decision could not be reached using the title alone, the item was included for abstract review and full text access as necessary. Two of the authors (AF and FM) reviewed the remaining abstracts independently and met to discuss any discrepancies in judgement. A total of 243 items were selected for full-text access. Two of these items were books, which were also accessed and screened. Of these 243 items, 14 could not be accessed. Items were reviewed by two authors (AF and FM) and discussions were held regarding items that presented difficulty. 147 items failed to meet the inclusion criteria; with a final total of 82 articles included. This screening process is represented in Fig 2 .
https://doi.org/10.1371/journal.pone.0153391.g002
Data was extracted for analysis from all 82 items including: literature type, year of publication, country of origin, midwifery professional title and category of barrier as per the analytical framework ( Fig 1 ). All included items are listed in the Supporting Information ( S2 Table ) accompanying this article.
More than half (60%) of the selected items were published research journal articles. These were all descriptive studies, except for one intervention study. In addition, the mapping identified commentaries without methods (32%), international agency reports (5%), a news item (1%), a press release (1%) and a letter (1%). Only one foreign language item was identified (French) for which an English translation was available.
The terminology adopted for midwifery personnel was midwives (60%), followed by maternity staff (17%) which included midwives with other personnel, (e.g. obstetricians, paediatricians, physicians and neonatal nurses) nurse-midwives/nurses (12%) or SBA s (8%). Only 3.6% of the findings referred to additional cadres who had SBA status, for example, Community Health Extension Workers (CHEWs) in Nigeria.
Of the 82 included items, 71 (87%) were published either in or after 2005, and 34 of these (42% of the total number of items) were published since 2011. Of the included items, 44% discussed countries or regions in Africa, with Ghana, Uganda and South Africa being the most common of these; 38% discussed Asian countries or regions, with Indonesia, Afghanistan, Nepal and India being the most common; only 5% discussed barriers in the Americas region; 13% covered LMICs as a general group rather than specific countries; 1% discussed LMICs within a global context. Countries were classified into regions according to the United Nations Classification of Countries by Major Region and Area of the World [ 22 ].
Most items (93%) fell into the category of professional barriers, followed by economic (42%) and then social (38%). Below we describe the different items in each category, while acknowledging the interaction between categories and clarifying this where possible.
Social barriers
We identified 31 items describing social barriers to the provision of quality midwifery care. We found that many of the social barriers had a strong underlying link to the socially and culturally-constructed context of childbirth as well as gender inequality.
A global policy guidance report concluded that gender inequality and lack of female empowerment was the most significant barrier to the advancement of the midwifery profession [ 23 ]. This assertion was echoed at a national meeting of midwives in Afghanistan [ 24 ]. Interviews with midwives in Anambra state, Nigeria found that deeply embedded gender inequalities predetermine the low social status of the midwifery profession [ 25 ]. This will be further explored in the section below under professional barriers and is associated with professional disrespect and a perceived lack of authority by midwifery personnel [ 23 , 24 ], and in some instances a lack of government commitment [ 26 ].
A global report and items concerning Zimbabwe and Afghanistan, suggested that cultural influences construct a perception of assisting childbirth as low skilled and inherently ‘women’s work’ [ 24 , 26 ]. The association between the low social status of women and attending births was generic, yet culturally specific in its manifestation. For example, research from South Asia described how some Hindu and Muslim families construct a temporary, separate structure for birthing in a dirty area [ 27 ]. Relatives and neighbours may watch and question the attendant's work yet refuse to provide assistance (including a drink of water) for fear of contact with polluted bodily fluids associated with menstruation, childbirth and colostrum [ 27 ]. Research from Pakistan found that women who provide midwifery care were described as “uneducated women of doubtful moral character”, and therefore an unsuitable role for a respectable Muslim woman [ 28 ].
The promotion of evidence-based care by midwifery personnel can be constrained by social barriers. In Mozambique, for example, midwifery personnel hesitated to promote evidence-based skin to skin care at birth. This was due to societal attitudes that the newborn requires cleansing prior to contact, as the childbearing mother’s blood is considered unclean[ 29 , 30 ]. A study from Ghana found that 70% of mothers ignored professional advice regarding care of the umbilical cord, deferring instead to their grandmothers’ guidance [ 31 ]. In Bangladesh, procedures based on best practice may require the consent of the older women in the family [ 27 ]. In Angola efforts by midwifery personnel to increase health facility births were met with resistance due to facility-based practices that do not reflect cultural norms, with only homebirth being acceptable [ 32 ]. Generally across low and middle income countries, and specifically, Indonesia, TBAs were preferred over midwifery personnel as they were seen by women and communities as trustworthy due to their respect for religious beliefs and cultural practices [ 33 , 34 ]. Midwives in Niger and Iran could face social and cultural barriers when providing information about sexual health and contraception in the presence of men, and could be culturally forbidden from using terms related to sexuality [ 35 , 36 ].
Social isolation was reported by midwifery personnel in different contexts [ 29 , 32 , 35 , 37 – 40 ]. Midwifery personnel in rural Nigeria, Niger and Ghana, were typically young and single and rarely had a social connection with the community to which they were deployed. They were often not accepted by the community due to their age, and had little opportunity for marriage or starting a family [ 35 , 37 , 38 ]. In studies from Afghanistan and Burkina Faso, midwives cited not speaking the local language as another reason for social isolation from their assigned communities [ 39 , 40 ].
In some contexts where midwifery has been professionalized, midwifery personnel experienced prejudice for being regarded as too educated and transgressing traditional gender roles [ 39 , 41 , 42 ]. An example from Mali noted that in communities where midwifery personnel were the only educated and salaried females, there can be feelings of jealousy and resentment from local women [ 42 ]. An example from Afghanistan revealed how the professionalization of midwifery could be politically sensitive: the new professional Afghani midwives fulfilled a traditional role, yet also represented educated, independent women [ 39 ]. In a culture where it is generally unacceptable for young women to live away from home for study or work, community midwives were reliant on their families granting them permission to work [ 39 ]. Midwives had to be accompanied by a male relative, and clinics were guarded by security at night due to threats to the midwives’ safety, with one example of a clinic being set on fire [ 22 , 39 , 41 ].
In some contexts, midwifery personnel were extremely vulnerable when attending homes or leaving work late at night, with Ugandan and South African midwives reporting physical attacks [ 43 , 44 ]. In Bangladesh, despite being accompanied by a porter for night calls, female mobility of midwifery personnel after dark was associated with inviting sexual assault [ 27 ]. Young, unmarried women who provide midwifery care, living in rural areas without secure accommodation were concerned for their safety [ 43 , 45 ] and some were unable to provide 24-hour quality care due to the risk of sexual harassment and violence [ 43 ]. This was again linked to the low social status of community midwives underlying the lack of investment in secure accommodation and safe travel to support their services [ 39 ]. Where access to midwifery care is compromised so is quality of care for women and newborns.
Midwifery personnel across LMICs discussed the expectation to fulfil their unpaid domestic and reproductive roles alongside their professional one [ 26 , 45 , 46 , 47 ]. The specific demands of the midwifery role, with excessive working hours outside the home, especially at night, lead to consequent suspicions of infidelity and spousal abandonment [ 30 , 47 ]. A study of midwifery personnel in Malawi suggested that domestic duties, child rearing and accountability to one’s spouse, possibly with a lack of spousal support, could negatively affect job performance and result in a sense of depersonalization and professional inadequacy [ 48 ].
Economic barriers
Economic barriers to the provision of quality of care were described in 34 of the 82 items. Economic issues included low or absent wages, informal payments and a lack of governmental financial commitment. The low wages and economic difficulties described link to the findings below that portray midwifery as an unvalued profession, which in turn refers back to the low social status discussed above.
Items from Afghanistan, Indonesia, Anambra state; Nigeria, Uganda, Koutiala; Mali, as well as Africa-wide and LMICs collectively [ 25 , 30 , 42 , 47 , 49 , 50 , 51 , 52 ] revealed that many midwives were surviving on wages which fail to meet basic living costs, with salaries paid infrequently, or not at all. Midwives in Angola reported that they were often paid three to six months in arrears, and Afghan midwifery personnel indicated they can wait up to six months for their public salary [ 32 , 39 ]. In Mali, on-the-spot fees from women were redistributed as salaries by the local community health committee at unpredictable intervals and amounts [ 42 ]. Midwives in three different maternity units across Luanda, Angola, reported that salaries were too low to provide food, clothes and education for their children [ 32 ]. This was echoed by a global commentary that also noted that wages were inadequate to purchase essential protective equipment, such as gloves, which midwifery personnel were required to provide from their domestic income, if their employer failed to [ 49 ].
Midwifery personnel in several African nations and in Indonesia were required to charge obligatory user fees, or be reimbursed by fee exemption schemes, for their remuneration. This difficult and unreliable process poses another economic barrier. It can also pose a social barrier: The assumption that midwifery personnel will require a cash payment for their services can foster distrust and resentment towards them by the local community and reinforce lack of acceptance [ 30 , 41 , 51 , 52 ]. In Indonesia, midwifery personnel were not always reimbursed for attending women entitled to an official exemption fee and had to prioritize giving care to women that could pay them directly [ 51 ]. In Burkina Faso, midwifery personnel indicated that quality of care could be effected by the financial stress incurred when they had to take out loans to support themselves [ 40 ]. Just to survive, some midwifery personnel had to take on additional, non-midwifery employment [ 46 , 53 ].
For village midwives in Indonesia, and nurse–midwives in Peru, the earning potential of moving to a city outweighed any rural government subsidy and therefore contributed to low rural retention levels [ 52 , 54 ]. In Senegal, midwifery personnel linked their inadequate remuneration with low motivation, low self-esteem and low job satisfaction [ 53 ].
Professional barriers
Professional barriers were identified in 76 of the 82 items. Professional barriers could be grouped into: a lack of investment in quality midwifery education; weak or absent regulation; inadequate numbers of staff; lack of affordable transport; weak facility management and poor working conditions. Whilst the issues described here are not necessarily unique to midwifery care providers, they were found to be intensified due to the low socio-cultural status of the profession and gender inequality. This reflects midwifery personnel largely being women, who are exclusively concerned with women and childbirth.
Midwives interviewed in seven cities across China identified a lack of investment in quality midwifery education and training as one of the most significant barriers to the advancement of the midwifery profession[ 55 ]. Research from Afghanistan, Bangladesh, Bhutan, India, Nepal and Pakistan, China, and Africa in general, concluded that inadequate training was considered to jeopardize professional identity, competence and confidence of midwives as the primary care giver for maternal and newborn health [ 30 , 41 , 55 , 56 , 57 , 58 ].
It is suggested that short-term, unregulated “SBA” courses, ranging from six weeks to one year in length, detracted investments away from midwifery training to international standards [ 25 , 56 ]. While coverage of SBAs was measured through the global Millennium Development Goal 5 indicator, the quality of care provided was not quantified [ 26 ]. Short courses across LMICs and, in South Africa specifically, were reported to underestimate the level of decision making and responsibility required to manage and refer women who need emergency obstetric interventions [ 58 , 59 ]. This was especially noted for those working alone in remote areas without medical support [ 27 , 58 , 57 ]. Short training of multi-purpose health workers was said to also have a negative impact on the quality of care for women and newborns and was considered to be neither cost effective nor sustainable [ 23 , 25 , 26 , 60 , 61 ].
A continuing barrier to improving midwifery training included the lack of investment in faculty who were competent in education, theory and clinical practice [ 26 , 58 , 62 ]. In Jordan, midwifery was commonly being taught by nurse educators or doctors with little knowledge of the midwifery model of care [ 63 ]. Lecturers across LMICs and more specifically, some African countries, were reported to be often disconnected from the clinical areas, with no resources for updating their clinical knowledge, causing students to graduate with outdated practices [ 23 , 26 , 30 , 58 ]. In some countries in Africa, training was typically aimed at highly resourced urban and institutionalized care with medical support, with little adaptation to the national context [ 30 , 58 ], and yet newly qualified midwifery personnel were often deployed to rural posts without prior community practice experience, supervision or support in dealing with emergency situations [ 30 , 58 , 60 , 64 ].
In Afghanistan, poor quality training was found to impact on midwifery personnel through discrimination by other providers, especially doctors, who ridicule their ability [ 41 ]. The strength of the medical hierarchy caused midwifery personnel to defer clinical decision making to inexperienced junior doctors [ 29 , 30 , 65 ], yet midwives in Mozambique noted that at night they were expected to manage care without resource to medical teams [ 29 ]. Examples from the literature of how lack of investment in midwifery training prevents quality midwifery care are presented in Fig 3 .
https://doi.org/10.1371/journal.pone.0153391.g003
Lack of investment in certified registration, effective regulatory bodies or professional associations means that regulatory bodies were unable to enforce the licenses that ensure quality in training and practice [ 25 , 68 ]. In Nepal, this led to midwifery training and professional titles for midwifery practitioners to become diverse and non-indicative of skill level [ 68 ]. Shortfalls in training and poor clinical practice were rarely addressed and midwifery personnel have little support for accountability in their practice and little evidence of professional development [ 39 , 55 , 56 , 58 ].
Where there were midwifery associations, for example in Zimbabwe, members were described as lacking the necessary experience and skills required for leadership and management, as well as basic office facilities [ 70 ]. In Zimbabwe, the finances of the association were found to be completely dependent on membership fees which, due to the low salaries and emigration of midwives, leaves little funding for activities or strategic planning [ 70 ]. In Gujarat, India, where midwifery was found to be represented by a nursing regulatory body, midwifery personnel were neither recognised as autonomous professionals nor deployed as midwives [ 71 ]. Articles from India, Jordan and LMICs generally, suggested that the integration of midwifery and nursing could make the midwifery profession a subsidiary to nursing. This could deny it a unique professional identity and voice and discourage the emergence of strong midwifery leaders [ 57 , 58 , 63 , 71 ]. A study from Anambra State, Nigeria concluded that the lack of a strong unionized voice for midwives diminished the profession’s recognition and reinforced the implementation of programmes for low skilled multipurpose workers [ 25 ]. Fig 4 provides a summary of how the absence of regulatory frameworks and professional associations prevents quality midwifery care.
https://doi.org/10.1371/journal.pone.0153391.g004
Inadequate staffing levels and an increasing workload was an issue across both urban and rural settings [ 50 , 58 , 65 ]. A report concerning African countries stated that inadequate staffing and working excessive overtime was found to compromise safety for women, as well as midwifery personnel [ 30 ]. The impossible demands of their workload could place midwifery personnel in an ethical dilemma of how to prioritize care: Nurse-midwives in Malawi spoke of the daily problem of having to decide whether to care for the newborn or the mother, or even, another mother and another newborn [ 67 ]. In Uganda, the breadth of the midwifery role has been extended beyond care that can be provided with quality, with health centre midwives caring for 50–60 women per day including providing all immunisations, family planning, HIV counselling, as well as, antenatal care and supporting women during childbirth [ 47 ]. The psychological impact of an overwhelming workload and being forced to neglect those under their care was associated with significant low morale, burn out and moral distress [ 50 , 66 , 72 ]. Fig 5 presents examples of how heavy workload prevents quality midwifery care.
https://doi.org/10.1371/journal.pone.0153391.g005
Quality of care can be further compromised by poor working conditions and insufficient basic resources, including scarcity of water, sanitation, drugs and equipment [ 25 , 30 , 45 , 47 , 65 ]. Midwives in rural Uganda described using mobile phones held in their mouths as a light at births because the electricity had been cut off during an attack eight years earlier [ 74 ].
The absence of safe working conditions, such as sharps disposal, water for hand washing, and basic protective supplies such as gloves, as well as limited access to Post Exposure Prophylaxis (PEP) had left midwives highly vulnerable to HIV infection in the workplace [ 45 , 72 , 75 ]. Midwives in one region of Zambia, forty percent of whom were HIV positive, reported withholding information about their infection status and accidents such as needle stick injuries, for fear of stigma or losing their jobs [ 30 ].
Inefficient or absent transport with impassable or dangerous roads was also a recurrent barrier to providing quality midwifery care in both urban and remote areas [ 38 , 40 , 51 ]. Midwifery personnel attended women on foot, by rickshaw, bicycle or horse, carrying minimal supplies through monsoons and floods, and often arrived too late [ 27 , 73 ]. In Nepal, it was estimated that SBAs were able to provide antenatal care to only 7.2% of pregnant women in the hill and mountain districts and attend 1.4% of the expected births within their area [ 76 ]. During the dry season in Bangladesh, midwifery personnel were unable to visit women as they relied on the monsoon season boats for transport [ 27 ]. Night calls were particularly difficult and dangerous to attend, and routine home visits were not possible [ 27 ]. carabao see bubalus bubalis.
Burn out and moral distress
The analytical framework ( Fig 1 ) theorized that the interaction of social, economic and professional barriers resulted in moral distress and burn out. Whilst the expression ‘moral distress’ was not adopted by providers, they did express corresponding feelings of guilt, anger, depersonalization and demoralization that fit the definition [ 29 , 40 , 45 , 53 , 72 ]. This was predominately caused by feelings of inadequacy in the face of an overwhelming maternal and newborn mortality rate [ 30 , 32 ]; not being able to provide best practice or lacking skills to work autonomously [ 29 , 36 , 65 , 77 , 78 ]; and being required to manage complications beyond their competency [ 27 , 30 ]. The term Burn out appeared in the literature to describe the impact of conditions upon midwifery personnel and was associated principally with exhaustion and frustration [ 26 , 48 , 50 , 53 , 72 ]. A study of Malawian midwives suggested that they were at higher risk of burn out than other clinicians [ 48 ]. A global report suggested that the level of burn out amongst midwifery personnel may be due to the predominance of women in the profession and the resulting tension between their professional role and domestic lives [ 26 ]. This is an example of how social barriers interact with professional barriers, with the pressure to fulfill their domestic role as a woman increasing the personal impact of excessive working hours.
Limitations
One particular challenge was to map the concept of barriers to the provision of quality midwifery care . While this was informed by the analytical framework ( Fig 1 ) and The State of the World’s Midwifery Report 2011 [ 2 ], these sources were not exhaustive and some relevant terms may have been omitted. Test searches were used to establish additional terms. This method, while useful, depended upon the authors’ ability to suggest relevant terms to test and was therefore open to omissions. Identification of relevant items and the assignation to a category was discussed at length between the authors but remains a subjective process.
We did not identify any grey literature through our search methods; there is a probability that relevant material has been missed. In addition, 14 items could not be accessed for full text screening and may have been eligible.
Finally, we note that the search concluded in August 2013 due to finite resources. Nonetheless we feel the literature gathered reached the objective of validating the components of the framework.
This first systematic mapping of the literature on barriers to quality midwifery care in LMICs has identified a variety of sources and has established a commonality of barriers. It has consolidated the contributions from the Women Deliver 2013 meeting and explored the relevance of the categories of social, economic and professional barriers [ 8 ].
The social barriers, despite being the least reported in the mapping, were found to be significant in preventing quality midwifery care. As described above, we found that many of the social barriers had a strong underlying link to the socially and culturally-constructed context of childbirth in which midwifery personnel work. These barriers are attributed to childbirth being historically the domain of the home and the responsibility of women [ 16 ]. Midwifery care is therefore bound with the domestic and the feminine.
The concept of women’s triple roles provides an explanation: reproductive (childbearing), productive (economic), and community managing (e.g. unpaid work in support of the community) [ 79 ]. In contrast to the mainly productive role of men, societies expect women to simultaneously undertake their triple roles with neither additional remuneration nor improved social status [ 79 ]. Midwifery personnel not only face this triple responsibility as women, but uniquely face having their productive role as care providers culturally perceived as belonging to the reproductive (childbearing) context, which confuses and undervalues their economic and professional contribution to society [ 79 ]. Additionally, the literature highlights that, in some contexts there is vulnerability to physical and sexual assault when providing care [ 27 , 41 , 44 ], as well as a lack of societal acceptance of trained midwifery personnel [ 41 , 42 ]. A lack of acceptance, especially in societies where the socio-cultural barriers dominate, is likely to limit investment in quality midwifery care.
Economic issues were the second most common barrier discussed in the selected items and included: low or absent wages, the need for additional non-midwifery employment, informal payments and a lack of governmental financial commitment. Although many health workers experience professional and economic barriers, professions disproportionately comprised of women are described as experiencing a “gender penalty” [ 15 ], with men assuming the leadership position and women falling to the bottom of the occupational hierarchy and subsequently earning lower wages, largely because the job related skills are not treated as skills, but qualities of “being a woman” [ 15 ]. For midwifery personnel these professional and economic barriers are reinforced and intensified when they interact with the uniquely feminized profession of midwifery [ 23 – 25 , 26 , 47 ]. The United Nations Research Institute for Social Development states that when care is decently paid and protected, the interest of both the providers and users of care can be met, and has far reaching implications for gender relations and inequalities [ 80 ].
The low status of midwifery personnel, determined by gender inequality, contributes to the lack of financial and political commitment to investing in education, training, regulation and licensing [ 23 26 , 63 ]. This also extends to inadequate investment in secure accommodation, transport and essential resources to enable midwifery personnel to perform their full role [ 43 , 45 ]. These economic barriers reflect and reinforce the socio-cultural and professional perceptions of midwifery as low skilled and domestic work.
Professional barriers were the most frequently discussed, and revealed a lack of shared understanding about what midwifery is, and the level of education, training, support and regulation that is required to enable women and newborns to receive quality midwifery care [ 5 ]. This can extend to a lack of shared political understanding of the role of midwifery, and further limit investment in quality services [ 25 , 26 ]. Professionally, this can be intensified where midwifery is considered as a subsidiary of nursing, preventing a collective midwifery voice and effective leadership [ 58 , 63 , 71 ]. This lack of understanding of midwifery may explain the perception of the role as essentially “women’s work” [ 24 , 26 ] and why gender inequality is described as the primary barrier to the advancement of the midwifery profession [ 25 ].
The authors suggest that moral distress and burn out result in midwifery personnel being disempowered to provide quality of care [ 29 , 45 , 50 , 78 , 79 , 81 ]. This finding is consistent with other research, which has shown burn out to affect the quality of services and patient outcomes through the adoption of negative and unprofessional behaviors [ 82 ]. While there is a potential link with this to the mistreatment of women during childbirth [ 83 ], we are unable to establish this here. The long term impact of burn out and moral distress is poor retention of maternity staff [ 30 , 40 , 50 ]. This outcome worsens the problems facing midwifery personnel, and increases pressure on those that remain [ 30 ].
The findings reveal enhancements that can be made to the original analytical framework, and we propose a revised version ( Fig 6 ). A first enhancement is the adaptation of the social barriers to include cultural barriers, as these are entwined and specific to childbirth. The “social” category is therefore changed to “socio-cultural”. Secondly, the literature mapping revealed the dynamic between the barriers, which reinforce one another. Thirdly, gender inequality is a basis for all three barriers. Lastly, the complex interaction of the barriers along with gender inequality can result in moral distress and burn out and can, consequently, lead to poor quality of care.
https://doi.org/10.1371/journal.pone.0153391.g006
Global strategies to reduce maternal and newborn mortality and morbidity are placing increasing emphasis on quality of care [ 1 ]. Midwifery, provided by educated, trained, regulated, licensed midwives is associated with improved quality of care and rapid and sustained reductions in maternal and newborn mortality [ 84 ]. The findings of this mapping suggest, however, that the provision of quality midwifery care can be prevented by socio-cultural, economic and professional barriers, situated in gender inequality ( Fig 6 ). This can be explained by the low socio-cultural status of midwifery—seen as “women’s work” [ 24 , 26 ]–which reinforces the “gender penalty” [ 15 ] in which women fall to the bottom of the occupational and economic hierarchies. The literature in the mapping describes midwifery as professionally undervalued with a subsequent lack of economic investment due to its socio-cultural feminisation. This dynamic can result in burn out and moral distress, as well as poor quality of care for women and newborns. There could be potential, not established through this mapping, for the barriers detailed here to lead to the mistreatment of women during childbirth.
The issues of social discrimination, work place hierarchy and power structures, lack of safety, basic remuneration and limited leisure time for providers of midwifery care, highlighted throughout the literature, place this issue urgently on the human rights agenda and beyond that of health system management only. We need to better differentiate the impact of barriers faced by midwifery personnel working in hospital facilities and those based in in communities. More needs to be understood about the impact of gender inequality on the provision of quality of care in relation to all three barriers. We need to find out what interventions exist to overcome the barriers and improve quality care.
The new Global Strategy for Women’s, Children’s and Adolescents Health (2016–2030) [ 17 ] builds upon guiding principles that include a gender responsive, equity driven and human rights based approach. We conclude, in light of the findings from the literature and in support of the new Global Strategy, that there is an urgent need for on-going mechanisms to improve quality of care to address the barriers as experienced by providers of midwifery care, as well as the gender inequality and rights issues that underlie them.
Supporting Information
S1 table. table of search terms..
https://doi.org/10.1371/journal.pone.0153391.s001
S2 Table. Table of Included items.
https://doi.org/10.1371/journal.pone.0153391.s002
Acknowledgments
We would like to express our sincere thanks to Mary Ellen Stanton of The United States Agency for International Development in providing encouragement to this process, and to Tomas Allen (WHO) for his support in developing the search strategies. Our thanks also to Pat Brodie, Billie Hunter, Tina Miller Caroline Homer, Marcus Stahlhofer, Rajat Kohsla, Joshua Vogel, Theadora Koller and Joanna Vogel for their input and advice, and to the International Confederation of Midwives for their support at the Women Deliver Conference 2013. Fran McConville and Anayda Portela are staff members of the World Health Organization. The authors alone are responsible for the views expressed in this publication and they do not necessarily represent the decisions or policies of the World Health Organization.
Author Contributions
Conceived and designed the experiments: AF FM AP. Performed the experiments: AF FM. Analyzed the data: AF FM. Wrote the paper: AF FM AP. Developed the protocol: AF. Conducted the search and screening: AF FM. Developed the original analytical framework: FM. Guided the systematic mapping process: AP.
- View Article
- Google Scholar
- 2. United Nations Population Fund. The state of the world’s midwifery 2011: delivering health, saving lives, New York, USA, United Nations Population Fund (UNFPA).2011.
- PubMed/NCBI
- 7. Bowser D, Hill K. Exploring evidence for disrespect and abuse in facility-based childbirth. Report of a landscape analysis. Washington, DC: USAID-TRAction project. 2010. Available: http://www.mhtf.org/wp-content/uploads/sites/17/2013/02/Respectful_Care_at_Birth_9-20-101_Final.pdf .
- 8. Women Deliver 2013 Conference. Available: http://www.womendeliver.org/conferences/2013-conference/ .
- 10. International Confederation of Midwives (ICM). Women Deliver: Celebrate gains as well as challenges. ICM News. 28 May 2013. Available: http://www.internationalmidwives.org/news/?nid=66 . Accessed 27 October 2015.
- 11. Schaufeli WB, Enzmann D. The burnout companion to study and practice: A critical analysis. London. Taylor & Francis. 1998.
- 13. The United Nations Human Rights Council (HRC) Preventable maternal mortality and morbidity and human rights. Report of the Human Rights Council on its eleventh session. HRC resolution 11/8. Geneva: 2009. Available: http://www.who.int/pmnch/events/2010/A_HRC_RES_11_8.pdf .
- 14. The World Health Organization. Strategies toward ending preventable maternal mortality (EPMM). 2015. Available: http://www.everywomaneverychild.org/images/EPMM_final_report_2015.pdf .
- 17. The United Nations. Every Woman. Every Child. Survive. Thrive. Transform. The global strategy for women’s, children’s and adolescents’ health 2016–2030. 2015. Available: http://globalstrategy.everywomaneverychild.org .
- 18. Clapton J, Rutter D, Sharif N. Systematic mapping guidance. London: Social Care Institute for Excellence. 2009.
- 19. International Confederation of Midwives. Definition of the midwife. 2011. Available: http://www.internationalmidwives.org .
- 20. WHO, ICM, FIGO. Making pregnancy safer: the critical role of the skilled attendant. A joint statement, Geneva: World health Organization. 2004.
- 21. World Bank. Country and lending groups. Available: http://data.worldbank.org/about/country-classifications/country-and-lending-groups . Accessed 18 August 2013.
- 22. United Nations. World Population Prospects, the 2012 Revision: Classification of countries by major area and region of the world. 2012. Available: http://esa.un.org/wpp/excel-Data/country-Classification.pdf . Accessed 28 August 2013.
- 23. UNFPA-ICM. Investing in midwives and others with midwifery skills to save the lives of mothers and newborns and improve their health. New York, USA, United Nations Population Fund (UNFPA). 2007.
- 43. Save the Children. Women on the Front Lines of Health Care. State of the World's Mothers 2010, Save the Children. 2010. Available: http://www.savethechildren.org/site/c.8rKLIXMGIpI4E/b.6178267/k.CE3/Women_on_the_Front_Lines_of_Health_Care.htm .
- 45. Hussein J, Phoya A, Ansong Tornui J, Okiwelu T. Midwifery practice in Ghana and Malawi: influences of the health system In: Reid L. editor. Freedom to practise: An international exploration of midwifery practice. Churchill Livingstone Elsevier: London; 2007. pp. 75–99.
- 74. Ford L. Passionate Ugandan midwife takes her message abroad. The Guardian Newspaper. 12 Oct 2011. Available: http://www.theguardian.com/global-development/poverty-matters/2011/oct/12/uganda-midwife-maternal-mortality-campaign . Accessed 28 August 2013.
- 79. Moser C. Gender planning in development: theory, practice and training. London: Routledge; 1993.
- 80. United Nations Research Institute for Social Development (UNRISD) Research and Policy Brief 9. 2010. Available: http://www.unrisd.org/publications/rpb9e .
What do we know about midwives' transition from clinical practice to higher education teaching roles? A scoping review
Affiliations.
- 1 Edith Cowan University, School of Midwifery, ECU Joondalup Campus, 270 Joondalup Drive, WA. Electronic address: [email protected].
- 2 Edith Cowan University, School of Midwifery, ECU Joondalup Campus, 270 Joondalup Drive, WA.
- PMID: 36628886
- DOI: 10.1016/j.nepr.2022.103531
Objective: The aim of this review was to examine the literature to identify what is known about midwives' experiences as academics and their perspectives of transition from clinical practice to university.
Introduction: Literature on health care practitioners, particularly nurses' transition from clinical experts to novice teachers suggests the transition to academia is challenging.Challenges reported by research studies have identified stress, uncertainty, and lack of a supportive and structured transition. There was a dearth of primary research evidence of midwives' perspectives.
Methods: A scoping review using the Johanna Briggs Institute three step approach was employed. First, an initial limited search of Google Scholar and CINAHL was undertaken to identify articles on the topic. Second, the text words contained in the titles and abstracts of relevant articles and the index terms used to describe the articles were used to develop a complete search strategy in databases: EMBASE, MIDIRS, Scopus and PubMed. Finally, a manual search of the reference lists of all included sources of evidence was manually searched for additional studies.
Results: Ten papers that included midwives as the participants were located from Australia, The United Kingdom (UK) and the United States of America (USA) between 2006 and 2022. Analysis of the findings led to three themes: Theme 1: Challenges associated with the transition; Theme 2: Dichotomy of identity; and Theme 3: Fear of losing clinical credibility.
Conclusion: In most studies midwives formed a subset of the sample meaning that the voices of midwifery academics are minimised by the experiences of other health practitioners. However, in depth details were located from four personal reflections which identified that transition from clinical practice to academia can result in a duality of roles while individuals come to terms with their new reality and overcome their fear of losing credibility as clinicians. New academics from health tend to hold onto their identity as clinicians rather than adopting their new persona as academics. Fear of losing credibility stems from the need to maintain competence for continued professional registration as clinicians. Further research is needed which focuses on midwives as the target sample to validate the research evidence from this scoping review.
Keywords: Midwifery; New academics; Transition from clinical practice.
Crown Copyright © 2023. Published by Elsevier Ltd. All rights reserved.
Publication types
- Delivery of Health Care
- Nurse Midwives*
- Qualitative Research
- United Kingdom
- Open access
- Published: 23 February 2024

Strategies used by midwives to enhance knowledge and skill development in midwifery students: an appreciative inquiry study
- Fiona Arundell 1 ,
- Athena Sheehan 1 &
- Kath Peters 2
BMC Nursing volume 23 , Article number: 137 ( 2024 ) Cite this article
1032 Accesses
Metrics details
Midwifery practice experience for midwifery students is an important component of education to enhance knowledge and skill development. Practicing midwives provide student support in the clinical setting, there is minimal literature relating to strategies midwives use to support students.
To explore midwifery student experiences of the strategies used by midwives to facilitate knowledge and skill development in the clinical practice setting.
Qualitative approach based on Appreciative Inquiry. The setting is one University in Australia. Participants, thirteen Graduate Diploma in Midwifery students. Individual interviews followed by thematic analysis.
Data analysis identified six themes, Willingness to share knowledge and develop skills; The positive use of questioning; Moderating support; Teaching through the woman; Learning through problematisation and Providing constructive affirmation.
Conclusions
Midwives incorporated varied strategies to support student development in the clinical setting. For an equitable clinical experience, all midwives need support to develop skills and confidence in facilitating student learning.
Peer Review reports
Midwifery education programs vary internationally; however, they commonly comprise theoretical and clinical practice components. The equal emphasis on theory and midwifery practice experience demonstrates the significance of each component. Midwifery education in Australia is provided as a collaboration between universities and hospitals, and midwifery programs are accredited by the Australian Nursing and Midwifery Accreditation Council (ANMAC). There are two models of midwifery education, postgraduate programs for registered nurses and the Bachelor of Midwifery (BM). This study involved participants undertaking the Graduate Diploma in Midwifery (GDM) a postgraduate midwifery program. This model is for the most part an employed student model where universities provide the theoretical component of the course and hospitals provide employment, clinical education, support and supervision. The midwifery student must meet the standards and clinical skills prescribed by the Australian Nursing and Midwifery Accreditation Council (ANMAC) [ 1 ]. Midwifery practice experience provides students the opportunity to apply theory to practice and knowledge, intuition, and reflexivity as it relates to midwifery [ 2 ]. Most of the responsibility for supporting the development of these standards and clinical skills is undertaken by practicing midwives, who are allocated to midwifery students on a shift by shift basis.
The acquisition of clinical skills is essential to midwifery student education however, students repeatedly provide disenchanted and negative accounts of their clinical learning experience [ 3 , 4 , 5 , 6 ]. This suggests that a midwife with professional experience might not necessarily have the skills to effectively facilitate student learning.
When students are supported in the clinical learning environment, confidence and competence are developed [ 7 , 8 ]. Conversely, midwifery students identify that a lack of commitment and capacity from some midwives to support them in the clinical setting is a source of student stress [ 9 , 10 ]. Skill development is often reliant upon students observing midwives carrying out procedures, usually with minimal explanation [ 11 , 12 ]. Development of clinical skills can be so fragmented that students are not able to envisage a holistic approach to care [ 13 , 14 ]. The lack of support for students in the clinical setting may be linked to midwives being underprepared for role expectations, in Australia the Midwife Standards for Practice state in standard 3.4 that the midwife ‘contributes to a culture that supports learning, teaching, knowledge transfer and critical reflection’ [ 15 ]. Midwives have identified an insecurity in supporting the educational development of students [ 16 ] and have reported teaching using methods by which they were taught [ 11 ]. Midwives however have acknowledged, that if they were adequately educated for the role, student learning would improve [ 13 , 16 , 17 ].
The qualities of an effective clinical teacher include, confidence in their own skills; interest in teaching; providing demonstration-observation-feedback; teaching to suit students’ needs; good communication skills; and awareness of potential learning opportunities [ 11 ]. Students respond most positively to midwives who encourage learning by implementing strategies such as questioning [ 18 ] and in-practice reflection [ 18 , 19 , 20 ].
Although several qualitative studies (3–7; 9–14) have explored the midwifery practice experience of midwifery students, findings primarily highlight the negative aspects of the experience and in particular the relational, social, and emotional experiences of students. While some positive teaching and learning strategies have been identified there is minimal literature detailing the realisation of effective strategies used by midwives to support knowledge and skill development. Therefore, this study sought to explore the midwifery role in the provision of peak experiences for students on midwifery practice experience that had not been explored in previous related studies. The aim of this paper is to report findings that highlight and describe strategies implemented by midwives that students valued as facilitating their knowledge and skill development in the clinical practice setting.
Study design
Previous research has primarily identified the deficits of the midwifery practice experience and in doing so has potentially failed to appreciate supportive practices and behaviours already in place [ 3 , 4 , 5 , 6 ]. When considering the prominence of negative experiences revealed in previous studies, an alternative methodology was sought to optimize the potential of capturing positive experiences for midwifery students on midwifery practice experience. To highlight optimal examples of student skill and knowledge development in the clinical setting, Appreciative Inquiry (AI) was chosen as the methodology because of its focus on the exploration of positive experiences [ 21 ]. AI focuses on what is effective and acknowledges that a solution to improvement already exists [ 22 ]. Consequently, this study aimed to discover the current positive strategies and behaviours of midwives to support clinical skill and knowledge development of midwifery students. AI has four phases, identified as the 4D cycle, the four phases include discovery, dream, design, and destiny [ 21 ]. The process of discovery provides an understanding of the ‘best of what is’ the dream phase to imagine the ‘what might be’, the design phase constructs the ‘what should be’, the design phase to sustain ‘What will be’ [ 21 ].
The focus of this paper was the discovery phase of the study, to provide an understanding of what is being done well [ 22 ]. The discovery phase interviews generated individual student’s peak experiences of the strategies implemented by midwives to facilitate knowledge and skill development in the clinical practice setting. The discovery phase provides new detail and insight into peak midwife strategies and behaviours to support midwifery student knowledge and skill development.
Participant selection and setting
All participants were registered nurses who were enrolled in the GDM and currently on midwifery practice experience at a large tertiary institution in Australia. Participants were personally invited to participate by a midwifery academic not involved in the study or student teaching. Participants were given the option to be interviewed on campus or at a public location of their choosing. All students except one chose to be interviewed on campus on a routine study day, only one student selected to be interviewed at their employing hospital.
Data collection
Each participant was interviewed two to six months after commencement of clinical placement, using an AI interview guide. The interview guide was developed for this study (see supplementary file). In keeping with AI, the questions were designed to have the following qualities, asked in the affirmative; generated from a primary question that draw upon specific past experiences developed from the topic being explored; encouraged storytelling; appreciated ‘what is’; encouraged the uncovering of valuable experiences [ 21 , 23 ]. This method of questioning has been compared to the ‘glass half full’ or positive approach compared to the ‘glass half empty’ or negative approach to questioning [ 22 ]. The duration of interviews ranged between 40 and 80 min. Questions followed a specific format of lead in questions, followed by topic questions, backward questions which focus on past experiences and concluding with inward questions which discovered the attributes and impact of positive support. The format and rationale for the AI interview and the type of questions asked is described in detail in a previous methodological publication [Authors’ own]. All interviews were audio recorded and transcribed. Participants were offered the opportunity to review their transcript and comment or correct if they wished.
Data analysis
Data were analysed using the six stages of Braun and Clarke [ 24 ] thematic analysis framework. First, the transcript of each participant was read and re-read to gain a deep understanding of the data. Each transcript was annotated to identify patterns, repetitions, differences, and similarities. In the next stage, initial coding (level 1 coding) of the whole data set, the codes were then arranged into themes. The entire data set was then reviewed (level 2 coding) identifying further themes and sub-themes. Themes were discussed and refined with all authors and findings were generated and supported with quotes.
Ethical considerations
The study was approved by the Institutional Human Research Ethics Committee (H11484). Students were informed about the purpose of the study and requirements of participation. They were assured that their participation would be strictly confidential and voluntary. Participants chose pseudonyms to ensure data were deidentified for use in dissemination and were aware that they could withdraw from the study without consequence.
Research team and reflexivity
The first author, a midwifery academic, conducted all interviews, but did not have a direct relationship with the study participants at the time. After each interview a reflective journal was completed by the interviewer to reflect on the process and consider whether the interviewer’s preconceptions or the style of questioning during the interview influenced participants’ responses. These reflections were discussed with other authors to ensure rigour in the research process was maintained.
Thirteen students agreed to participate in the study. All were female, aged between 22 and 50 years, with between one and 25 years’ experience as a registered nurse. All participants were enrolled in a 14-month GDM program involving one day per week of on-campus learning and four days per week employment as a midwifery student in a maternity unit.
Analysis of data identified six themes, Willingness to share knowledge and develop skills; The positive use of questioning, Moderating support; Teaching through the woman; Learning through problematisation and Providing constructive affirmation.
Willingness to share knowledge and develop skills
Students recognised that supportive midwives were knowledgeable and skilled practitioners who shared their knowledge. Midwives who were lifelong learners and used evidence to support practice were admired, instilled confidence in the student, and were considered reassuring, Lilac (p.10) described a midwife’s knowledge as ‘comforting’. As well as sharing knowledge, supportive midwives challenged students about their practice and encouraged them to read evidence and decide how research would influence their future practice. Poppy recalled a conversation with midwives discussing perineal support in labour and their subsequent reaction to her thoughts on the topic.
There is actually some research about this,…[they say] you should have a look…every time I ask them something they’re very keen to share…They say, oh, I’ve done this research, or I’ve read an article regarding this. That’s why I feel like I should do it this way. (Poppy, p.5)
Poppy appreciated the opportunity to practice alongside midwives who were enthusiastic about evidence-based practice. The use of evidence in teaching promoted trust in the midwives’ knowledge. Therefore, this knowledge was subsequently transferred to the student and influenced how she envisaged her future practice.
As well as using research evidence, midwives who were willing to expertly explain and demonstrate skills were considered by participants to be more supportive than those who simply role modelled. Students recalled supportive learning experiences that related to both fundamental and complex midwifery skills. Supportive midwives had an appreciation that a fundamental skill might need to be taught more than once therefore building on existing skills. Peony had previously been shown how to undertake a palpation on a woman at term but appreciated being supported to develop the specific skills required for a palpation on a woman at only twenty weeks gestation.
I had a really lovely midwife…go over a proper palp [palpation] with me. It was the first time I’d actually done a proper palp [palpation] on a 20-week antenatal. (Peony, p.5)
Students appreciated being sought out to develop less common midwifery skills. Daisy recalls her experience of a midwife including her in the delivery of care for a stillborn baby and their parents.
Just the practical skills of getting a footprint and a handprint. She was sharing that and things like oh this is good that you’re seeing this as a student. (Daisy, p.17)
Supportive midwives had the ability to share knowledge through advice and tips grounded in years of experience, for example, prevention of perineal trauma.
If you’ve got blanching, you know be careful because it might rip. You might have a tear. This is how you would guard the perineum to prevent that. Warm compresses. (Jasmine, p.7)
Sharing knowledge and skills, also required midwives to consider when and where to do so. Fleur (p.8) recognised that a midwife considered students’ needs by ‘calmly explaining things outside the room’ ensuring the priority in the room was the woman. Similarly, Iris appreciated that the midwife briefed specific aspects of expected care before entering the room.
We did talk about it before we went in there…We’ll do the Syntocinon in the arm, not the leg, because it’s underwater (Iris, p.10).
The outcome of the briefing was that the midwife displayed trust in the student to provide autonomous care. She just left me to it (Iris, p.10).
The positive use of questioning
The use of questioning was seen as helpful by students and fell into two categories, ‘student-led questioning’, and ‘midwife-led questioning’. Midwives who took the time to encourage students to ask questions, or asked students questions, were considered to be invested in student learning.
Student-led questioning
Students who asked questions frequently considered this as taking responsibility for their own learning. Receptive midwives were key to effective student learning because they encouraged and supported the students to ask questions.
She definitely listens…I’m not embarrassed now to ask her questions because I’m thinking I’m an RN, I need to know these things. She tells me “No you’re still learning and you need to ask”.…she makes me feel comfortable (Lilac, p.10).
Supportive midwives let students know they were available to answer questions, with statements such as ‘look if you’re not sure come and ask’ (Peony, p.8) and ‘(the midwife) asked me lots of times, do I have any questions’ (Jasmine, p.6). This provided students with confidence to ask questions.
Midwife-led questioning
Questioning from midwives took several forms including assessing student knowledge on specific topics to establish potential knowledge deficits.
She went through and asked us what’s that drug for? What do we use it for? Any idea what the standard dose is? (Rose, p.9)
Students were receptive to this style of learning. They found it to be to the point, reinforcing that this was expected knowledge in the clinical setting. Midwives would also use questioning to ensure students understood what they were going to do in specific scenarios.
She’d say to me okay this lady now is 28 weeks, what would you be looking at at 28 weeks? (Lilac, p.6)
When questions were asked in a positive way, even in front of women, students felt comfortable because they were not being asked in a way that made the student look inept. Consequently, there was not a negative impact on the student/woman relationship.
They were never questions to degrade me. I always felt that she was asking so the woman can feel confident that I knew what I was doing. (Lilac, p.6)
As students progressed through the course, questioning became more complex, less reliant on recall and more problem based.
…she’d find time to come back to me and be like, so what have you done? Why did you do that? What do you want to do next? (Aster, p.9)
Students reported midwives could pose questions creatively. In one example, the student recalled being overwhelmed by completing a CTG interpretation, she did not think she had the skills to undertake the task. The lack of confidence manifested as student negativity and a resistance to knowledge development. The midwife sensed the student response to the situation and then reframed her questioning.
It was my antenatal rotation and I just said in frustration, and she was right there, and I said I hate CTGs, don’t make me do CTGs I hate them. I mean I walked away I must’ve had a really bad day… She comes around, she plonks herself down and she goes okay, here’s a CTG, tell me what you hate about it. I went okay this is what I hate about it (Lilac, p.11).
The midwife did not accept avoidance but was creative utilising humour to deflect the student’s negative sentiment in order to develop learning.
Moderating support
Students described varying levels of support from midwives in the clinical setting. Supportive midwives were able to moderate the level of support provided to the student depending on need, and usually this moved along a continuum from high to low support. When midwives moderated support, it demonstrated to students that there was not a generic approach to support provided but was considered according to a student‘s need and ability. Knowing that a midwife was in close proximity also encouraged students to undertake skills they would not have attempted when in an unsupported environment. High support required the midwife to be close to the student most of the time, often working in such close proximity that many of the tasks undertaken were shared. As student knowledge and skills developed, and support moved to low support the midwife maintained such proximity to the student to be aware of student care provision and available if required, however at a distance that enabled the student to practice independently.
In the early weeks of placement, students reported high support from midwives to meet their learning needs, which students viewed positively.
I noticed at the beginning when I was with her in clinic days she was sitting right beside me like overviewing everything that I was doing. She was very helpful giving me information, according to the weeks [of gestation] of the woman. (Lilac, p.5).
Aster also described an intense two-week orientation to antenatal ward, expressing that as a result she had increased confidence in this setting. After initial close supervision, Aster perceived that with her growing confidence, the midwife also had increased confidence in her ability. This allowed Aster to take more responsibility with the midwife close at hand if needed.
I found it so helpful… She would go through the ward routine and as we had been working together for a few days she’d allow me to take control of the day and manage my time and everything and just step in say, why are you doing this, like rationale everything that we are doing. (Aster, p.8)
Students recognised that high support and use of positive and encouraging communication pushed them to attempt skills they may have otherwise avoided.
If there’s any questions don’t worry about it, I’m right here, I’ll help you through it. But I am sure you can do it and we’ll do it together. That support from them to say you can do it, I’ll be here. Doesn’t matter if you mess it up. (Fleur, p.9)
As knowledge and skills developed there was a transition from high to low support. This transition was most evident in the antenatal clinic, where the midwife/student dyad had the greatest engagement. Unlike in other clinical areas, the long-term student/midwife exposure in the antenatal clinic enabled midwives to have knowledge of the student’s ability.
When experiencing moderated support, students had the confidence to voice the type of support they needed. The boost of confidence provided by moderated support encouraged students to be more proactive in their development and to initiate care independently knowing support was available if required.
When I work with someone and they will say what are you up to, I’ll say I need this and this and this, I have done this before, but can you just be close by. (Daisy, p.26)
Being able to independently assess, plan and implement care with the back-up of a midwife was described as ‘exciting’ by Daisy.
I think the first high point that comes straight to mind is the birth with one of the recent graduates. It was the first normal that I’ve seen in terms of she wasn’t induced. She didn’t have an epidural. Certainly, I was able to do all the things that I’m meant to do, the palpation, the VE (vaginal examination). I did it first and then she did it and then I had to explain to her and we agreed four centimeters, so that was very exciting. (Daisy (p.7).
For moderating support to be effective a midwife needs to be conscious at all times of a student’s progress through the course and level of capacity.
Teaching through the woman
Students were aware that midwives’ priority was to meet the care needs of women and babies whilst supporting their development. Students frequently recalled midwives converging the women’s need for midwifery care with student learning, by teaching through the woman. This technique did not compromise the woman’s care whilst providing education for the student. The use of teaching through the woman was either protracted as in a clinic setting where the whole visit incorporated teaching through the woman or included in a single skill or action.
Instead of making it a separate little learning thing, they just do it as part of the care that’s being given for the woman. (Rose, p.29)
The practice of teaching through the woman was also seen as being beneficial for women, the focus remained on them while opportunistically providing student education.
They’re teaching me at the same time as well, so they are including me in the conversation with the woman and the woman doesn’t mind that they’re teaching me at the same time. (Bluebell, p.19)
Learning through problematisation
Problematisation occurred when midwives assisted students to recognize problems with clinical practice. There were two types of problematisation. Firstly, a student may have identified a problem themselves but required assistance from the midwife to resolve it. Alternatively, a student may have been unaware that they were facing a clinical problem and needed a midwife to help them identify and resolve it. Students were realistic about their limited knowledge and appreciated midwives’ identification of incorrect knowledge or actions. Regardless of the source of the difficulty students appreciated the positive approach to problem resolution, the midwife would be respectful and kind in their approach. A variety of examples of problematisation were identified.
I happened to notice one deceleration which probably wasn’t a big deal, but I went out and spoke to the midwife who was actually really positive that I’d come out and I’d spoken to her. She went over why there would have been a deceleration at that point in time. Reassured me that I’d done the right thing by alerting her to the situation (Peony, p.6).
Students described instances of misinterpreted information where, if it had not been recognised as a problem by a midwife, they would have provided incorrect care. Commonly, supportive midwives identified problems, addressed them in a way that did not highlight student inadequacy to the woman, and were able to address them in appropriate timeframe. For example,
If… it was the wrong thing I was saying, they would just pipe up and be like or you could try this…Or if I was doing the wrong thing then they would start doing it over the top of me, but then when we left the room, they’d be like you did this wrong… They do rectify it at the time but not in a way that’s…obvious to the woman (Iris, p.14).
Supportive midwives exposed students to clinical experiences that could challenge their decision making and expose the student to new problems for which they needed solutions. Confidence to develop new skills occurred when midwives provided opportunities for exposure to new experiences while providing gentle guidance and correction if necessary. Aster gave an example of this when undertaking a vaginal examination,
If I get it wrong, she is really nice about it. She doesn’t go, no, that’s not right. She will be like, no, but have a feel here. Can you feel more cervix here? She will explain a little bit more what I am feeling. (Aster, p.7)
Although Aster did not expect to get all elements of the vaginal examination correct, she knew the midwife would guide her in developing the required knowledge and skills.
Though a potentially challenging strategy, the consistent message was that the key element of problematisation, was that the midwife involved the student in the process of identifying and resolving the problem.
Providing constructive affirmation
Students reported the importance of receiving positive feedback on clinical performance, which they appreciated, as this was not a common occurrence. Daffodil described positive feedback from a midwife who reassured her that she was where she should be in terms of skills.
You’re doing really well. I didn’t have to do much in there. You’re probably where you should be or a bit further on for where you are in your course. She just gave me good feedback and it just made me feel happy about what I’d done and where I’m going. (Daffodil, p.10)
Students were realistic and accepted that not all feedback on performance would be positive, however as long as it was constructive, receiving feedback was always appreciated.
She’s very good at constructive criticism, she’ll put it in a way where she’s like I’ll help you work on this and we’ll do that. So next time I see you we’ll do this okay… so a really great person to learn off definitely. (Bluebell, p.10)
When there was an educational and developmental approach, students welcomed constructive affirmation.
This study used an AI methodology to discover positive strategies used by midwives to support the development of knowledge and skills of midwifery students on midwifery practice experience. Findings from this study identified that midwives who were invested in student learning used a variety of strategies to support the development of knowledge in midwifery students. Although previous research has found that an effective teacher provides learning opportunities such as demonstration-observation-feedback [ 11 ] questioning and reflection [ 18 , 19 , 20 ], this study provides an understanding of how these strategies are effectively implemented by midwives and the impact on students. This study also identified strategies not previously identified such as Learning through problematisation and Teaching through the woman and Providing constructive affirmation.
Midwives’ willingness to share knowledge and skills, and the use of evidence to support practice, engendered student trust and confidence in the transference of knowledge and that what they were being told was correct. This is important as knowledge development during midwifery practice experience contributes to program completion and confidence and competence as a new graduate midwife [ 13 , 14 ]. The development from a novice student to a beginning practitioner is identified by Benner [ 25 ] as requiring the support of knowledgeable clinicians. Midwives need to be confident in their own practice to be able to support student development, Bäck, Sharma [ 14 ] identify the importance for a midwife to be able to practice with confidence to preserve the ability to provide safe woman-centred care.
Midwives in Australia are expected to contribute to the teaching and knowledge development of midwifery students [ 15 ] yet literature has indicated that midwives do not know how to fulfill this expectation [ 13 , 15 ]. In order to effectively support students, midwives recognised the need to keep up to date with practice knowledge to match students’ theoretical knowledge and did this by reading contemporary literature and undertaking further study [ 17 ]. Although midwives were allocated to support students on a shift by shift basis, students sought additional support from midwives who had a desire and capacity to share their knowledge based on evidence, which is similar to findings from other studies [ 6 , 7 , 18 , 26 ]. The clinical support role of the midwife in relation to supporting the development of midwifery students should be more clearly defined and the knowledge and skills to successfully fulfill this responsibility provided to midwives [ 8 , 27 ].
Students from the current study described a variety of strategies employed by midwives to support skill development. This study builds on previous research by Chamberlain; Hughes and Fraser; Currie [ 11 , 17 , 28 ] on the merit of strategies such as role modelling and questioning, though these studies were unsupported with a detailed understanding of how these strategies are used by midwives. In this study student data has enhanced the understanding of these strategies by detailing the processes employed by midwives and the student impact when sharing knowledge and skills and the positive use of questioning. The benefit of positive role modelling is that this is likely to be modelled by students [ 28 ]. Felstead [ 29 ] contradicts Bandura suggesting that because students need to fit in, they may copy behaviour that contradicts the philosophy of midwifery care. Students in this current study chose to align themselves with midwives whose practice they wanted to emulate. Although questioning is a commonly used strategy there is an art to the construction of questions and when to apply various types of questions in the clinical learning environment, this topic has had minimal discussion in relation to midwifery education. This study expanded the understanding of the types of questioning used by midwives and student response to being encouraged to question and being questioned. Although developed as a model for facilitating nursing student learning on midwifery practice experience a narrative approach to questioning has the potential to be applied to midwifery students to develop more personalised responses and subsequent knowledge development [ 30 ].
The strategy identified as Moderating Support in this study is comparable to a strategy identified by Zwedberg, Barimani [ 17 ] called Fading, a purposeful decrease in the level of support provide to a student, with the goal of independence in practice. Midwives in this study incorporated fading as a strategy in their practice where they withdrew support over time to encourage student independence and initiative. Initially by gaining an understanding of students’ abilities and providing timely and salient learning opportunities, midwives transitioned from providing high to low support. As student competence developed the exposure to complex experiences increased, termed by Spouse [ 31 ] as Scaffolding.
It has been argued that traditional strategies of teaching, may not suit the complex scenarios and patterns presented to students in the clinical learning environment [ 31 ]. Midwives can act as a conduit to enable an understanding of the complexity of midwifery craft knowledge [ 31 , 32 , 33 ]. Participants in this study identified problematisation as an effective teaching strategy used by midwives, in more complex situations. The benefits of problematisation were identified by Titchen [ 33 ] however for successful implementation this complex strategy requires confidence in application [ 32 , 33 ]. This study demonstrated the student benefits of increased confidence to practice knowing that a midwife would solve or identify issues if they occurred.
Teaching through the woman as a creative learning strategy has not been described previously and is a unique finding of this study. In this study, students recognised that for time-poor midwives, this strategy fulfilled the competing requirements of caring for the woman but also supported student learning. What was an effective strategy that enabled midwives to support student learning without compromising care. It could also be hypothesized that the woman also benefitted by becoming more aware of her own care. Incorporation of this strategy by midwives could reduce the burden of the conflicting responsibilities of care provider and educator, it would also reduce the incidence of lost learning opportunities [ 12 ].
In this study students reported appreciating feedback from midwives that provided opportunity to reflect on their development. As found in previous studies students were aware that feedback and subsequent reflection assisted with skill development and linking theory to practice [ 34 , 35 ]. It has been previously reported that the educational relevance of feedback and reflection on practice, needs to be understood to ensure protected reflection time is built into each clinical day [ 6 , 36 ]. Although students in this current study were appreciative of feedback it was not commonly provided. Midwives have previously identified the need to be educated on how to provide feedback to students however they also expressed the desire for student reciprocity in the process [ 16 , 17 ]. In this study midwives used positive language when giving feedback, the midwives use of positive affirmation correlates with a previous study that found that feedback is rewarding to students and encourages repeat behaviour [ 28 ].
Limitations of this study include the small number of participants from one university. Due to the small number of participants transferability of findings could also be limited, as all participants were postgraduate students of midwifery. Another limitation is that all students were postgraduate students and were already registered nurses with previous knowledge of working within a health setting. Students participating in the study are in a paid employment model which adds the complexities of balancing employment and learning demands. These demands are not experienced by undergraduate students in an unpaid model, therefore may have an impact on transferability. The study’s strengths were that participants were placed in several hospitals with a range of acuity from local district to referral hospitals, providing data contributing to further understanding of the effective strategies used by midwives to support students in the clinical leaning environment across a variety of settings.
The use of AI was able to identify positive learning strategies used by midwives in the clinical practice setting. This study offers knowledge about supportive learning strategies identified by students on midwifery practice experience. Ideally, all midwives should be able to impart knowledge and skills to better support students’ professional development in the clinical learning environment. To ensure students experience exposure to consistent support from midwives, midwives need support to ensure they have the capacity and confidence to provide salient and timely learning opportunities.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Appreciative Inquiry
Australian Nursing and Midwifery Accreditation Council
Bachelor of Midwifery
Graduate Diploma in Midwifery
Australian Nursing and Midwifery Accreditation Council. Midwife Accreditation Standards 2021. In: (ANMAC) ANaMAC, editor. Canberra, ACT2021.
Breen A. Supporting the future of midwifery. Br J Midwifery. 2021;29(3):126–7.
Article Google Scholar
Bluff R, Holloway I. The efficacy of midwifery role models. Midwifery. 2008;24(3):301–9.
Article PubMed Google Scholar
Brunstad A, Hjälmhult E. Midwifery students learning experiences in labor wards: a grounded theory. Nurse Educ Today. 2014;34(12):1474–9.
Carolan M, Kruger G. Concerns among first year midwifery students: towards addressing attrition rates. Contemp Nurse. 2011;38(1–2):139–47.
Bradshaw C, Murphy Tighe S, Doody O. Midwifery students’ experience of their clinical internship: a qualitative descriptive study. Nurse Educ Today. 2018;68:213–7.
Licqurish S, Seibold C. Bachelor of midwifery students’ experiences of achieving competencies: the role of the midwife preceptor. Midwifery. 2008;24(4):480–9.
McAra Couper J, Gilkinson A, Fielder A, Donald H. A mixed-method evaluation of a New Zealand based midwifery education development unit. Nurse Educ Pract. 2017;25:57–63.
Cavanagh S, Snape J. Stress in student midwives: an occupational perspective. Br J Midwifery. 1997;5(9):528–33.
Thunes S, Sekse RJT. Midwifery students first encounter with the maternity ward. Nurse Educ Pract. 2015;15(3):243–8.
Chamberlain M. Challenges of clinical learning for student midwives. Midwifery. 1997;13(2):85–91.
Article CAS PubMed Google Scholar
Rahimi M, Haghani F, Kohan S, Shirani M. The clinical learning environment of a maternity ward: a qualitative study. Women Birth. 2019;32:e523–e9.
Adnani Q, Gilkinson A, McAra Couper J. Strengthening midwifery education through clinical experience: findings from a qualitative study in Indonesia. Women Birth. 2022;35(1):87–95.
Bäck L, Sharma B, Karlström A, Tunon K, Hildingsson I. Professional confidence among Swedish final year midwifery students– A cross sectional study. Sex Reproductive Healthc. 2017;14:69–78.
Nursing. and Midwifery Board of Australia. Midwife standards for practice. AHPRA; 2018.
Dewar B, Stultz V, Drayton N, Buliak A, Connolly L, McLaughlin K, et al. Exploring student midwives’ experiences (ESME study): an appreciative inquiry. Prepared on behalf of the Nursing and Midwifery Office New South Wales; 2019.
Zwedberg S, Barimani M, Jonas W. Exploring the internship experiences of Swedish final term student midwives: a cross sectional survey. Sex Reproductive Healthc. 2020;26(100543).
Hughes AJ, Fraser DM. There are guiding hands and there are controlling hands: Student midwives experience of mentorship in the UK. Midwifery. 2011;27(4):477–83.
Embo M, Driessen E, Valcke M, Van der Vleuten C. Relationship between reflection ability and clinical performance: a cross-sectional and retrospective longitudinal correlational cohort study in midwifery. Midwifery. 2015;31(1):90–4.
Longworth M. An exploration of the perceived factors that affect the learning and transfer of skills taught to student midwives. Midwifery. 2013;29:831–7.
Cooperrider D, Whitney DD, Stavros J. The appreciative inquiry handbook: for leaders of change. Berrett-Koehler; 2008.
Whitney D, Trosten-Bloom A. The power of appreciative inquiry a practical guide to positive change. San Francisco, CA: Berrett-Koehler; 2010.
Google Scholar
Watkins JM, Mohr BJ, Kelly R. Appreciative inquiry: change at the speed of imagination. Wiley; 2011.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Benner P. From novice to Expert, Excellence and Power in clinical nursing practice. New Jersey: Prentice Hall; 2001.
Gilmour C, McIntyre M, McLelland G, Hall H, Miles M. Exploring the impact of clinical placement models on undergraduate midwifery students. Women Birth. 2013;26(1):e21–5.
Gray M, Downer T. Midwives’ perspectives of the challenges in mentoring students: a qualitative survey. Collegian. 2021;28:135–42.
Bandura A. Social learning theory. Englewood Cliffs, N.J.: Prentice Hall; 1977.
Felstead I. Role modelling and students’ professional development. Br J Nurs. 2013;22(4):223–7.
Koldestam M, Broström A, Petersson C, Knutsson S. Model for improvements in learning outcomes (MILO): development of a conceptual model grounded in caritative caring aimed to facilitate undergraduate nursing students’ learning during clinical practice (part 1). Nurse Educ Pract. 2021;55:1–9.
Spouse J. Bridging theory and practice in the supervisory relationship: a sociocultural perspective. J Adv Nurs. 2001;33(4):512–22.
Titchen A. Professional Craft knowledge in patient centred nursing and the Facilitation of its development. Ashdale Press: University of Oxford; 2000.
Titchen A, editor. Helping relationships for Practice Development: critical companionship. Oxford: Blackwell; 2004.
Back L, Karlstrom A. Developing confidence during midwifery training: the experience of Swedish final year students. Sex Reproductive Healthc. 2020;25.
Collington V, Hunt S. Reflection in midwifery education and practice– an explanatory analysis. Evid Based Midwifery. 2006;4(3):119–26.
O’Connell R, Bradshaw C. Midwifery education in Ireland– the quest for modernity. Midwifery. 2016;33:34–6.
Download references
The study is not funded.
Author information
Authors and affiliations.
Western Sydney University, School of Nursing and Midwifery, Building EB LG Room 22, Parramatta South Campus, Locked Bag 1797, NSW 2751, Penrith, Australia
Fiona Arundell & Athena Sheehan
Western Sydney University, School of Nursing and Midwifery, Building 7, G Room 55, Campbelltown Campus, Locked Bag 1797, NSW 2751, Penrith, Australia
Kath Peters
You can also search for this author in PubMed Google Scholar
Contributions
F.A. and K.P. Conceptualisation, F.A., K.P. and A.S. Methodology, Formal analysis, F.A. Investigation, Resources, Data curation, Writing– Original draft, F.A., K.P. and A.S. Writing– Review and editing, K.P. and A.S. Supervision.
Corresponding author
Correspondence to Fiona Arundell .
Ethics declarations
Ethics approval and consent to participate.
The research involving human participants in this study was undertaken in accordance with the Declaration of Helsinki. Students were informed about the study, confidentiality and voluntariness of participation, written consent was provided by participants. Participants chose pseudonyms and were aware that they could withdraw from the study without consequence. The study was approved by the Western Sydney University Human Research Ethics Committee (H11484).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Arundell, F., Sheehan, A. & Peters, K. Strategies used by midwives to enhance knowledge and skill development in midwifery students: an appreciative inquiry study. BMC Nurs 23 , 137 (2024). https://doi.org/10.1186/s12912-024-01784-5
Download citation
Received : 01 November 2023
Accepted : 01 February 2024
Published : 23 February 2024
DOI : https://doi.org/10.1186/s12912-024-01784-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Midwifery student
- Clinical practice
- Appreciative inquiry
- Clinical teaching
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Systematic review article, experiences of newly qualified midwives during their transition to practice: a systematic review of qualitative research.

- 1 Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, Shanghai, China
- 2 School of Nursing, Naval Medical University, Shanghai, China
- 3 Department of Obstetrics, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, Shanghai, China
- 4 Department of Nursing, Shanghai First Maternity and Infant Hospital, School of Medicine, Tongji University, Shanghai, China
Objective: To summarize and evaluate the experiences and expectations of newly qualified midwives (NQMs) during their transition from school to clinical practice. One of the main objectives was to provide references for the development of midwifery professional teaching and provide a basis for hospital administrators and instructors of midwifery to develop guidelines and strategies.
Methods: A systemic review of qualitative research using meta-aggregation was conducted. We collected studies from 12 databases between inception and February 2023. All qualitative studies published in English and Chinese that reported on the experiences of NQMs during their transition to practice were included. Two independent reviewers assessed the study quality and the credibility of study findings by using the JBI Qualitative Assessment and Review Instrument. The process of searching followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations.
Results: A total of 14 studies were included, and 84 findings were extracted. The results were grouped into 8 new categories and synthesized into 3 main themes: multi-dimensional challenges, physical and emotional responses, and demands and expectations. The included studies were identified to be of good quality and the results of the methodological quality appraisal were all B grade or higher.
Conclusion: The transition period is a critical career development for NQMs. However, they faced various stress during the period, which had a negative impact on their physical and mental health. Therefore, it’s important to deeply understand their challenges and needs. And effective management strategies should be implemented, such as in-depth cooperation between hospitals and schools, improvement of the clinical transition support system, enhancement of continuing education, and standardization of the management system. This may be beneficial to improve the quality of clinical midwifery and maintain the stability and sustainable development of the midwifery team.
1. Introduction
Improving the health of mothers and newborns is one of the unfinished Millennium Development Goals and remains a priority in the era of sustainable development goals ( 1 ). The Global Strategy for Women, Children, and Adolescents Health (2016–2030) also highlights the significance of ensuring that every woman, child, and adolescent has access to fundamental interventions and a strong team of health professionals ( 2 ). Particularly, midwives play a significant role in improving mother–child dyads’ health. Approximately two-thirds of maternal and neonatal deaths can be prevented with the assistance of well-trained midwives ( 3 ). However, the State of the World’s Midwifery 2021 shows that only 42 percent of people with midwifery skills work in 73 countries where more than 90 percent of all maternal and newborn deaths and stillbirths occur ( 4 ). The survey also reveals that there is a 900,000-midwife deficit worldwide, with a projected 750,000-midwife shortage by 2030 ( 3 , 4 ).
NQMs represent the future of this profession. However, recruitment and retention of midwives is a major challenge, with a high turnover of NQMs. A previous study indicated that the experiences during the transition to practice had an impact on job satisfaction and employee retention, which was a key factor of the global midwifery shortage ( 5 ). The transition period is defined as the period of study and adaptation to work as a registered nurse midwife after completion of a recognized midwifery education program ( 6 ). For many newly qualified practitioners, the transition period from students to qualified health professionals is typically 12 to 18 months ( 7 ). According to the data from the Royal College of Midwives (RCM), the lack of support of NQMs contributes to attrition ranging from 5 to 10% whereby graduates leave during the first year of practice ( 8 ).
To facilitate the retention of valuable midwifery workforce, many countries have developed structured transition support programs to help NQMs successfully transition to practice. However, studies conducted in Australia ( 7 ), Canada ( 9 ), New Zealand ( 10 ), and the United Kingdom ( 11 ) reported that NQMs still faced many challenges during the period, including but not limited to increased customer care responsibilities, problems with healthcare systems, political, managerial and role uncertainty ( 12 ). These challenges caused them to feel insecure, fearful, and stressed ( 13 ). Consequently, the smooth transition into their new roles was interfered and increased personnel losses occurred.
It’s crucial to deeply understand their experiences during the transition period and to explore what factors promote or inhibit the progress. Several qualitative studies have explored the challenges and feelings encountered by NQMs during the transition period but did not provide integrated results. As a result, we conducted a qualitative synthesis that could potentially provide a basis for hospital administrators and instructors of midwifery to develop guidelines and strategies to effectively support NQMs during the transition period.
This qualitative systematic review aimed to understand the experiences of NQMs during their transition to practice and to explore factors that promote or inhibit the progress. In particular, the review may provide hospital administrators and instructors of midwifery a new perspective to formulate guidelines and strategies, consequently, it can provide a better training system and platform for NQMs to help them gain fully play their professional roles and positive working experience.
3.1. Design
A systematic review of qualitative research using meta-aggregation was conducted. The Enhancing Transparency in Reporting the Synthesis of Qualitative Research (ENTREQ) checklist ( Supplementary Table S1 ) was used to report the process and results of synthesis, and enhance transparency ( 14 ).
3.2. Search strategy
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline was adopted in this review. A three-step approach was used to identify the studies: (a) an initial limited search via PubMed, (b) a systematic search of electronic databases, and (c) a manual search of journal references. To find search terms, a preliminary limited search via PubMed was first carried out to examine the index words and the derivatives of terms for studies linked to the experiences of NQMs during their transition from education into practice. Then, we systematically searched 12 electronic databases, including eight English language databases: PubMed, Web of Science Core Collection (via ISI Web of Science), MEDLINE (via ISI Web of Science), Cochrane Library, LWW (via OVID), CINAHL Complete (via EBSCO), Scopus, and ScienceDirect, and four Chinese databases: China National Knowledge Infrastructure (CNKI), Wanfang Database (CECDB), VIP Database, and China Biomedical Database (CBM). For different databases, a separate search strategy is designed and optimized based on the corresponding subject terms and search rules. Results were limited to journal articles written in English or Chinese and published before 15 February 2023. The query included five groups of keywords and MeSH terms combined with Boolean operators: (1) (new graduate midwives) OR (newly graduated midwives) OR (newly qualified midwives) OR (newly qualified nurse midwives) OR (new nurse midwives) OR (new midwives) OR (graduate midwives); (2) (transition) OR (transition period) OR (transition to practice) OR (transition programs) OR (change) OR (culture shock) OR (orientation) OR (standardized training) OR (pre-service training) OR (residency programs) OR (induction program); (3) (perception) OR (feel*) OR (experience*); (4) (qualitative research) OR (qualitative method) OR (qualitative study). Finally, the references of each qualifying articles were searched manually to identify further relevant studies. The sample search strategy for PubMed is presented in Figure 1 .
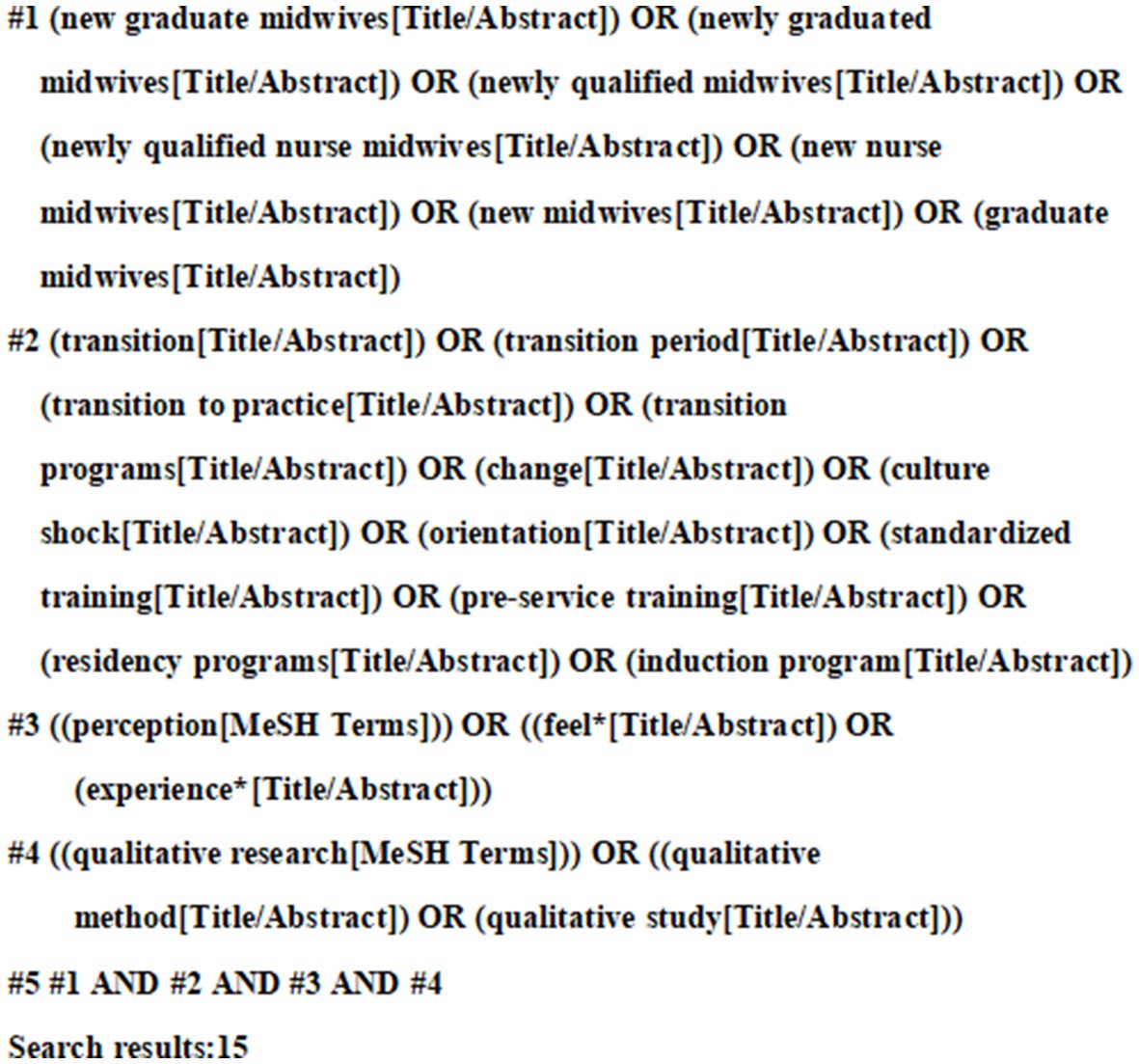
Figure 1 . Search strategy in PubMed.
3.3. Inclusion and exclusion criteria
3.3.1. inclusion criteria.
Studies were included according to the following:
Participant (P): Newly qualified midwives (NQMs) started clinical work for less than three years after graduation.
Interest of phenomena (I): The real experiences of NQMs during their transition from education into practice. The focus was on their stressors, demand, and expectation.
Context (Co): Included studies were those performed during their transition from education into practice.
Study design (S): Qualitative research and mixed-method studies from which the qualitative part could be extracted were included. Studies were included that used any qualitative methodology, including but not limited to phenomenology, grounded theory, case studies, action research, ethnography, and feminist research.
3.3.2. Exclusion criteria
Excluded were studies with qualitative data that were analyzed using quantitative methods; duplicate and unavailable full-text literature; non-English or Chinese literature; research not published in peer-reviewed journals, case reports, conference proceedings, poster abstracts, and theses. Additionally, we looked through their sources to find potential pertinent studies while excluding systematic reviews and other reviews.
3.4. Appraisal of methodological quality
By comparing the evaluation criteria of qualitative research, two researchers (JS, XL) who had undergone qualitative research studies and training in evidence-based methods were selected to conduct the study. Two researchers used the “JBI Evidence-Based Quality Evaluation Criteria for Qualitative Studies in Evidence-Based Health Care Centers” for the final independent evaluation of the included studies. Each item is evaluated by “yes,” “no,” “unclear” and “not applicable.” If all 10 items are “yes,” the possibility of bias is minimal and is A. If the above quality criteria are partially met, the possibility of bias is considered to be B. If all items are If “No,” the possibility of bias is considered high as C. After independent evaluation, the results of the two individuals were compared. Third party re-evaluation or arbitration in case of disagreement. The literature with a quality level of C was finally excluded.
3.5. Data extraction and synthesis
According to the JBI meta-aggregation, qualitative data were extracted in two steps. Firstly, publication details (author’s name, publication year, country or region, research aim, research design, method of data collection, sampling and data analysis, participants) and findings were extracted. Secondly, verbatim statements about the experiences of NQMs during their transition to practice were extracted for a subsequent meta-synthesize across all included studies. Two reviewers (JS, XL) independently evaluated the plausibility of each finding and identified them into three levels: (1) Unequivocal (U): relates to evidence beyond a reasonable doubt, which may include findings that are matter of fact, directly reported/observed and not open to challenge; (2) Equivocal (E): those that are, albeit interpretations, plausible in light of data and the theoretical framework. They can be logically inferred from the data; (3) Not Supported (NS): when 1 nor 2 apply and when most notable findings are not supported by the data. The extracted findings that had similar meanings were aggregated to form new categories. Eventually, these categories were further synthesized to generate more comprehensive findings, called synthesis findings.
4.1. Search results
A total of 509 relevant articles were initially searched from the database. 453 articles were collected in total through NoteExpress after removing duplicates. Two researchers independently read the titles, abstracts and keywords to obtain 20 articles, after reading the full text, 14 articles were included. The detailed search and screening process is showed in Figure 2 .
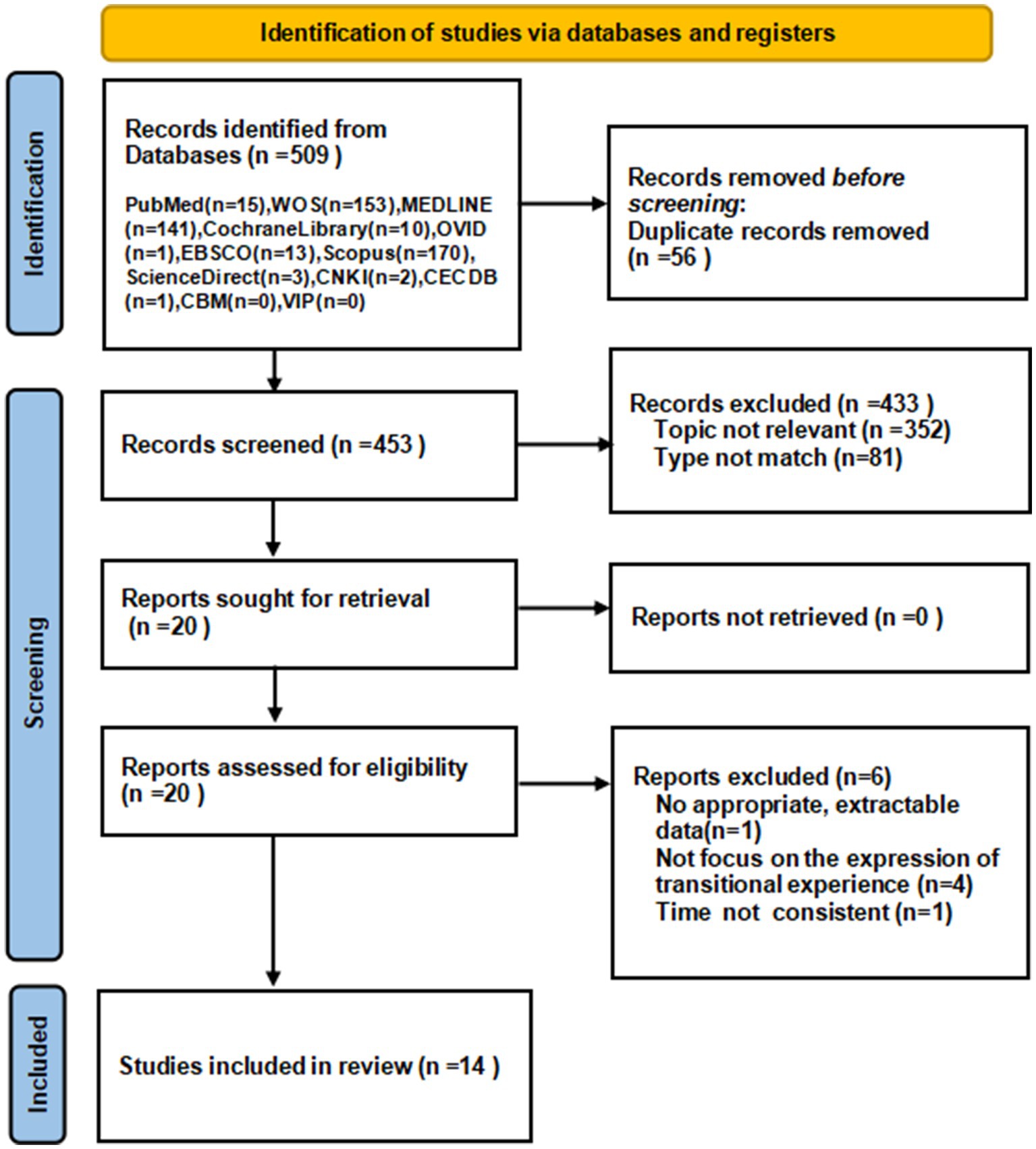
Figure 2 . PRISMA flow diagram for article selection.
4.2. Methodological quality
The quality of the included literature was evaluated and the results were all B grade or higher. The results of the methodological quality appraisal are presented in Table 1 .
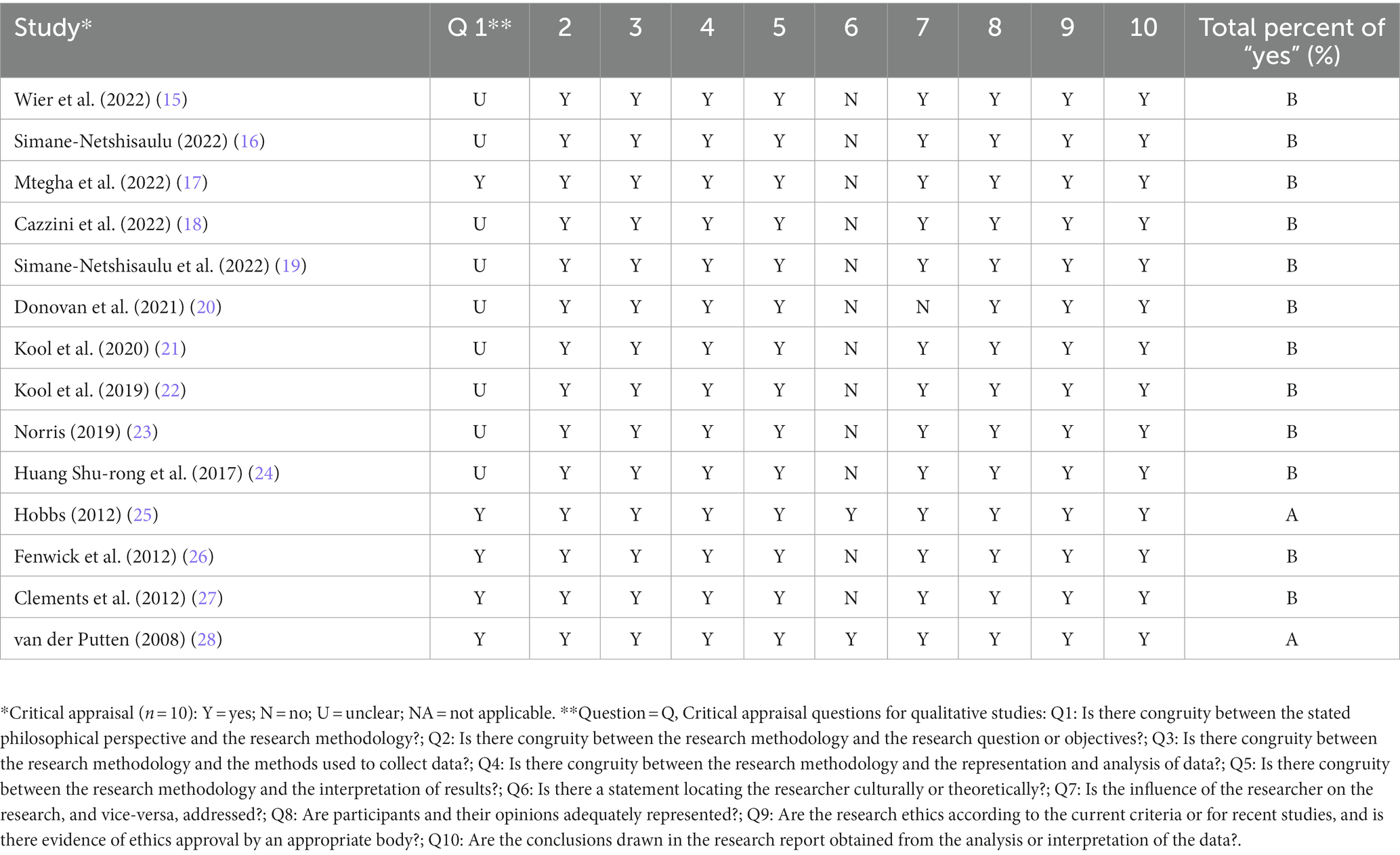
Table 1 . Methodological quality of the 14 included studies.
4.3. Study characteristics
The 14 studies were conducted in the following countries: China ( n = 1), Malawi ( n = 1), South Africa ( n = 2), Netherlands ( n = 2), Ireland ( n = 2), the United Kingdom ( n = 3), and Australia ( n = 3). These studies involved 238 NQMs. Study designs included qualitative action-research approach ( n = 1), phenomenological approach ( n = 4), qualitative descriptive approach ( n = 5), mix-method study ( n = 2), ethnography ( n = 1), and a study described as qualitative without a specific approach ( n = 1). All the studies were published after 2008 and were original articles. Study characteristics are presented in Table 2 .
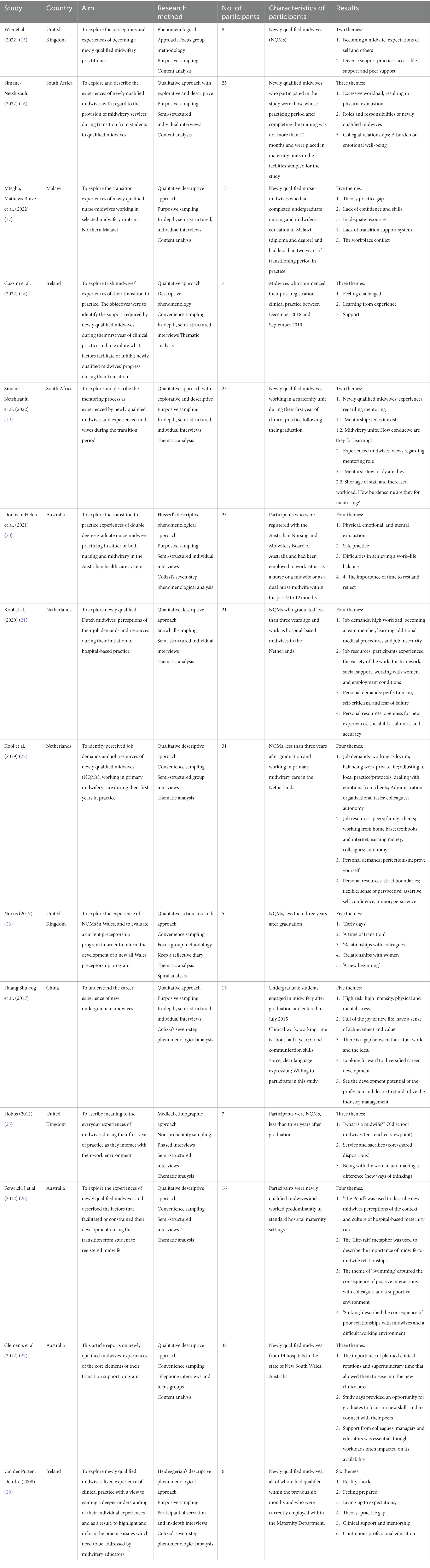
Table 2 . Characteristics of the 14 included qualitative studies.
4.4. Results of meta-synthesis
The researcher extracted 84 findings from 14 articles and summarized into 8 categories. From the 8 categories, three synthesized findings emerged: multi-dimensional challenges, physical, and emotional responses, and demands and expectations. The main findings with illustrations and levels of credibility are presented in Supplementary Table S2 , and the detailed process of synthesis is reported in Supplementary Table S3 .
4.4.1. Synthesized finding 1: multi-dimensional challenges
4.4.1.1. shock from realistic clinical settings.
The real work in the delivery room was challenging for NQMs. First, there was a gap between theoretical knowledge in school and clinical practice. Many participants reported that the theoretical knowledge learned in school was relatively outdated or inconsistent with its application in practice. “Upon reaching the ward, I found that most of the guidelines like HIV guidelines, and some reproductive health standards had changed. There were also new things like CPAP (continuous positive airway pressure). So it was really tough for me as I was referring to old things, yet, the practice had changed on the ground” ( 18 ). In addition, the delivery room was a place of uncertainty, full of challenges and risks directly related to the safety of the mother-infant dyads’ lives. “Getting a baby into the world alive was what everyone worried about” ( 26 ). At the same time, the lack of human resources was a very serious problem, which led to the huge amount of work that individuals need to carry on. “…human resource is a challenge…Despite the nursery ward being one of the busy wards, there are times that you are alone on duty and you are expected to do all the activities…” ( 17 ). In addition, the job was insecure and they always faced the possibility of losing their jobs due to the lack of permanent contracts. “Yes, you know…you have no job security, so you take all the work you can get everywhere…that increases pressure” ( 22 ).
4.4.1.2. High expectations from themselves and others
NQMs were strict with themselves and others also expected more from them. They were eager to prove their abilities quickly, which put a lot of pressure on themselves. “You want to be the best of the best…I probably put too much pressure on myself…I just need to have confidence and take a deep breath…and I’ll be alright…but then every once I have a little panic…” ( 15 ). They viewed them as true midwives and must be responsible for mothers and babies, so they held themselves to a higher standard. “you are more independent as a midwife because you have to make more choices you have to have more clinical judgment…more pressure, more responsibility and being more accountable for what I do” ( 18 ). Experienced colleagues also had high expectations of NQMs because they thought that NQMs were fresh out of school and knowledgeable. “I think are they going to perceive me as: well, you are newly qualified and you need to be able to do this…” ( 15 ). Besides, they were also expected to do more than work, some even beyond their current capabilities. “After three months I was left in charge of the ward as the only midwife and when I questioned it I was told (by the manager) ‘Oh, you can manage … ‘because you have got experience a nurse’…” ( 27 ).
4.4.1.3. Lack of transitional support
Many participants reacted hospitals did not provide a perfect support system during the transition to practice, which increased the difficulty of adapting to new environments and transitioning into new roles. At first, there was a lack of the training about the hospital-related management system. “There are a lot of dynamics in the hospital…And it took me some time to realize which disciplines are involved and which agreements are made per hospital, and about protocols. And even if you have a protocol, the usual way of doing things can be different, and it takes a while before you know this…” ( 21 ). Secondly, the absence of training in clinical skills made NQMs scared. “The situation is not good at all; in some instances, you have to learn through trial and error. I was so scared of resuscitating a new-born baby, until one day in which I had to practice it all by myself” ( 16 ). Thirdly, NQMs were frustrated about the lack of support from experienced mentors. “Do you know in my whole year as a new grad [graduate] I do not think I worked with an [midwifery] educator once” ( 26 ). Finally, NQMs often did not receive a positive response from colleagues when they asked for help. “…however, some are unfriendly. The unfriendly ones give bad and demotivating remarks when we seek for assistance. It’s bad” ( 19 ). “…fter you have had handover and they are like, ‘Oh fine, do not worry.’ Then they go to the desk and they are like: ‘I do not want to come on to work after her, she leaves everything for the night staff” ( 23 ).
4.4.2. Synthesized finding 2: physical and emotional responses
4.4.2.1. physical fatigue.
NQMs suffered physically fatigue because of the high intensity of work. And due to the shift system, their life was irregular and did not get enough rest, which even affected their safe operation. “It’s just exhausting, just physically. Some days you just need to sleep” ( 20 ). “I do not think I will ever get used to shift work! It’s almost debilitating…you just start to doubt yourself and I think ‘Am I safe practicing when I’m this tired or this exhausted?’” ( 20 ).
4.4.2.2. Negative emotion: lack of confidence, fear, and loneliness
NQMs’ negative feelings included lack of confidence, fear, and loneliness. When they entered a new environment, due to unfamiliar with the environment and lack of training, they were not confident in themselves. “When we were students, we were never given any chance to practice managing the unit, but suddenly you are expected to manage the unit including patients, staff members, equipment and supplies. This is not easy. Especially because you do not feel confident enough to delegate duties to some members of staff” ( 16 ). In addition, they often felt fear when facing some clinical problems alone. “I was absolutely terrified just because I had not done it for so long…and I would be like, I do not know if I can do this. I do not know what I’m doing” ( 20 ). For many NQMs who work away from home, they were not accompanied by family and friends and felt very lonely. “Just the loneliness was probably the most emotionally draining thing” ( 20 ). It is very important for them to have time to spend time with their family and friends, and to get their support and company. “It’s really important that you are able to debrief with friends and family because you will say things to friends and family that you would not say to work colleagues” ( 20 ).
4.4.3. Synthesized finding 3: demands and expectations
4.4.3.1. support from peers, colleagues, and managers.
NQMs desperately needed substantial support from peers, colleagues and managers, which was like a light in the dark, making them less nervous and more confident. Support from peers reduced their anxiety. “[having peer support] should be part of the support process…an opportunity for us to feel like our concerns are being listened too…It’s not just us talking amongst ourselves…” ( 15 ). Support from colleagues, especially experienced midwives, helped them smoothly transition, which was essential for them to adapt quickly to their new roles. “…they orientate you, they explain everything to you, the routine, the procedures and practices and they still keep an eye on you, you know make sure you are doing ok and that gives you confidence” ( 28 ). In addition, it was important to have an approachable leader who can provide great clinical and emotional support to NQMs. “The manager on the ward was excellent, she was always checking in with you making sure that you were doing okay” ( 18 ).
4.4.3.2. Improve professional competence
NQMs wanted to improve their professional skills, including clinical decision-making ability, humanistic care, and clinical professional skills. First, NQMs expected independent clinical decision-making capabilities and they needed to have independent autonomy in the care of their patients. “I also dared to make decisions and I dared to pick up [tasks] independently and it is really not that I needed help with anything and everything. I think that I can generally work independently” ( 16 ). Second, almost all the participants hoped to give more humanistic care to women. “My frustration is mainly to do with the women not getting the care that maybe they expected or I expected them to get” ( 25 ). “For me, being with the woman is just a part of my soul…but I do not get a lot of time to do that…I have to do a lot of things rather than actually being with woman…” ( 18 ). By improving humanistic care, in turn inspires them to work better. “When I support a woman…that is why I chose this profession. Then it is easy to get out of my bed in the night. Moreover, I feel that my work is my passion, and my passion is my work” ( 22 ). Finally, NQMs would like to receive more professional training or study in order to adapt faster to the new environment and further strengthen their professional skills. “I hope to continue my study in midwifery and continuously improve my skills in technical operation and clinical thinking” ( 29 ).
4.4.3.3. Standardize the management system
NQMs desired to standardize the industry management and establish an independent midwifery management and training system. “For young midwives, there should be a standardized training system, and they should have standardized training just like clinicians. After all, this line of work requires a high level of competence for midwives, and our work is also related to the safety of mothers and babies” ( 29 ). Besides, there were some shortcomings about the hospital management systems, such as paying too much attention to employee rank, ignoring NQMs’ opinions and feelings, and focusing solely on number rather than quality of the work. “Midwifery is a hierarchical system. It is based on midwifery-in-charge [and] also who has been here the longest or who has the most experience and it’s like you were in a food chain’” ( 26 ). “Midwifery practice requires me to actually give more loyalty to the hospital and do all the tasks that they expect of me in a day to save [them] from being sued or just to say, ‘These jobs have been done’” ( 26 ).
5. Discussion
The systematic review of 14 qualitative studies was rigorously conducted by researchers trained in evidence-based nursing, contributing to a more in-depth and comprehensive understanding of experiences of NQMs during the transition period. The main findings indicated that NQMs faced challenges from multiple sources. These challenges mainly derived from the realistic clinical settings. They felt so stressed as a fresh midwife. At the same time, we also discovered their real needs and expectations. Therefore, to ease their physical and mental stress and further create a friendly work environment, transitional support for NQMs should be strengthened and the training system should be improved, which will play a positive role in reducing the resignation rate of new midwives.
Hospitals and schools should collaborate to facilitate a smooth transition to clinical practice for NQMs. Gap between theory and practice, high risk, high intensity, job insecurity are the main challenges NQMs faced during the transition. Complex interpersonal relationships and high-loaded work cause negative work experience, and affect adversely their physical and mental health ( 30 ). Therefore, it’s urgent to take various measures to help them meet challenges, and enhance their positive career experience. Hospitals and schools need deep cooperation to provide targeted career guidance to students. During the school, midwifery specialists can introduce the nature, significance, professional content and history of the midwifery profession in China and abroad, and share their professional experiences. Besides, the clinical practice is equally important. The midwifery training room should be available for students so that they can have a preliminary understanding and experience of the clinical midwifery work. This may help them identify and internalize their professionalism. Educators should pay attention to the combination of theoretical and practical teaching, cultivate students’ practical ability, so that they can better adapt to clinical after graduation. At the same time, attention should be paid to improve students’ psychological quality and improve their ability to cope with occupational stress.
The clinical transition support system should be improved to promote positive career experience for NQMs. The multifaceted, multi-disciplinary clinical support system has positive implications for the smooth transition of NQMs to new roles. According to studies, the level of clinical support new midwives receive during the clinical transition greatly influences their clinical competence ( 31 ). According to Thunes ( 32 ) and Fenwick ( 33 ), obstetrics students attribute their clinical success to the practitioners they work together every day. On the one hand, improving the support system can reduce the clinical responsibility and pressure of NQMs and prevent them from intentionally narrowing the scope of their practice for fear of taking risks; on the other hand, it can promote NQMs to maximize the professional role and provide maternal-centered midwifery services, so as to further improve the quality of maternal and infant health care.
Strengthen continuing education to ensure the sustainability of the NQMs team. Many NQMs often feel a lack of expertise and competence when face with complex clinical problems, and continuing professional learning becomes the expectation of most of them. And their new level of responsibility inspires the importance of continuous professional education in order to continue to provide safe care for women. Continuing education programs will help healthcare providers improve their professional competence and adapt them to rapidly changing and new roles ( 34 – 36 ). Particularly, midwives are one of the important healthcare providers, and their continuing education can enhance midwives’ ability to improve maternal and child health status ( 37 ).
Standardize the management system and provide a broad career exhibition path for NQMs. They have high expectations for regulated management systems, especially they want independent professional systems and independent professional behavior. At present, in many countries, the midwifery major still belongs to the nursing major ( 38 ), and midwives do not have independent professional title evaluation and promotion sequence, and lack of the corresponding assessment, registration and promotion system (38), which forms certain obstacles to the echelon construction of midwifery talents and the development of professional characteristics. Improving the standard management system of midwifery professional education and midwife registration is conducive to enhancing the sense of responsibility and autonomy of NQMs, providing a richer career development path, so as to promote the development of midwifery profession and the retention of talent resources.
6. Conclusion
This qualitative systematic review expounds the experience and feelings of NQMs during the transition to practice. Studies have shown that NQMs face multifaceted challenges, which have negative effects on their physical and mental health. NQMs are at a critical time in their career development, and properly guiding their role change is a difficult but important task. From the perspective of obstetric educators and clinical managers, this study suggests that hospitals and schools collaborate on guidance and intervention to improve clinical transitional support systems, standardize management systems, and strengthen continuing education. And thus, it helps NQMs make a smooth transition to clinical practice, gain positive career experiences, and provide them with a broad career path. This can contribute to the building and sustainable development of the midwifery workforce and better serve people.
7. Limitations
Although a systematic search was conducted using appropriate search strategies, according to the eligible criteria, only qualitative research or mixed-method studies from which qualitative data could be extracted were included. Gray literature and dissertations were not searched; only articles published in indexed journals in either Chinese or English were included. The omittance may have caused information bias. The included studies were of high quality, but two-thirds of the literature omitted information about the researcher’s theoretical or cultural background, which could have an impact on the results.
Data availability statement
The original contributions presented in the study are included in the article/ Supplementary material , further inquiries can be directed to the corresponding author.
Author contributions
JS and XL: conceptualization, methodology, formal analysis, writing of original draft, and writing – review and editing. YL: conceptualization, methodology, writing of original draft, and writing – review and editing. YL, JL, RZ, and HJ: conceptualization, methodology, formal analysis, and writing – review and editing. All authors contributed to the article and approved the submitted version.
This work was supported by: (1) Technical standard project of Shanghai Municipal 2022 “Action Plan for Science and Technology Innovation” (22DZ2203800), (2) Shanghai Shenkang Hospital Development Center Management Research Project (2022SKMR-18) and (3) Shanghai Shenkang Hospital Development Center Technology Standardization Management and Promotion Project (SHDC22022227).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1242490/full#supplementary-material
1. Nove, A , Friberg, IK , de Bernis, L , McConville, F , Moran, AC , Najjemba, M, et al. Potential impact of midwives in preventing and reducing maternal and neonatal mortality and stillbirths: a lives saved tool modelling study. Lancet Glob Health . (2021) 9:e24–32. doi: 10.1016/S2214-109X(20)30397-1
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Callister, LC . Global strategy for the health of women, children, and adolescents: 2016-2030. MCN Am J Matern Child Nurs . (2016) 41:190. doi: 10.1097/NMC.0000000000000237
3. Boateng, AB , Opoku, DA , Ayisi-Boateng, NK , Sulemana, A , Mohammed, A , Osarfo, J, et al. Factors influencing turnover intention among nurses and midwives in Ghana. Nurs Res Pract . (2022) 2022:4299702–8. doi: 10.1155/2022/4299702
4. The State of the World's Midwifery in 2021.
Google Scholar
5. Clements, V , Davis, D , and Fenwick, J . Continuity of care: supporting new graduates to grow into confident practitioners. Int J Childbirth . (2013):3–12. doi: 10.1891/2156-5287.3.1.3
CrossRef Full Text | Google Scholar
6. Rahmadhena, MP , McIntyre, M , and McLelland, G . New midwives' experiences of transition support during their first year of practice: a qualitative systematic review protocol. JBI Database Syst Rev Implement Rep . (2017) 15:1265–71. doi: 10.11124/JBISRIR-2017-003374
7. Gray, M , Malott, A , Davis, BM , and Sandor, C . A scoping review of how new midwifery practitioners transition to practice in Australia, New Zealand, Canada, United Kingdom and The Netherlands. Midwifery . (2016) 42:74–9. doi: 10.1016/j.midw.2016.09.018
8. Shortage of midwives is the reason for high agency staff costs, says RCM. Pract Midwife . (2015) 18:8.
PubMed Abstract | Google Scholar
9. Nour, V , and Williams, AM . "Theory becoming alive": the learning transition process of newly graduated nurses in Canada. Can J Nurs Res . (2019) 51:6–13. doi: 10.1177/0844562118771832
10. Dixon, L , Calvert, S , Tumilty, E , Kensington, M , Gray, E , Lennox, S, et al. Supporting New Zealand graduate midwives to stay in the profession: an evaluation of the midwifery first year of practice programme. Midwifery . (2015) 31:633–9. doi: 10.1016/j.midw.2015.02.010
11. Lennox, S , Skinner, J , and Foureur, M . Mentorship, preceptorship and clinical supervision: three key processes for supporting midwives. NZ Coll Midwives J . (2008) 39:7–12.
12. Hofler, L , and Thomas, K . Transition of new graduate nurses to the workforce: challenges and solutions in the changing health care environment. N C Med J . (2016) 77:133–6. doi: 10.18043/ncm.77.2.133
13. Labrague, LJ , and McEnroe-Petitte, DM . Job stress in new nurses during the transition period: an integrative review. Int Nurs Rev . (2018) 65:491–504. doi: 10.1111/inr.12425
14. Tong, A , Flemming, K , McInnes, E , Oliver, S , and Craig, J . Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol . (2012) 12:181. doi: 10.1186/1471-2288-12-181
15. Wier, J , and Lake, K . Making the transition: a focus group study which explores third year student and newly qualified midwives' perceptions and experiences of becoming a registrant midwife. Midwifery . (2022) 111:103377. doi: 10.1016/j.midw.2022.103377
16. Simane-Netshisaulu, K , Maputle, M , Netshikweta, LM , and Shilubane, H . Mentorship during transition period: a challenge for newly qualified midwives in Limpopo province of South Africa. Afr Health Sci . (2022) 22:191–9. doi: 10.4314/ahs.v22i1.25
17. Mtegha, MB , Chodzaza, E , Chirwa, E , Kalembo, FW , and Zgambo, M . Challenges experienced by newly qualified nurse-midwives transitioning to practice in selected midwifery settings in Northern Malawi. BMC Nurs . (2022) 21:1–12. doi: 10.1186/s12912-022-01012-y
18. Cazzini, H , Cowman, T , Fleming, J , Fletcher, A , Kuriakos, S , Mulligan, K, et al. An exploration of midwives' experiences of the transition to practice in the Republic of Ireland. Br J Midwifery . (2022) 30:136–43. doi: 10.12968/bjom.2022.30.3.136
19. Simane-Netshisaulu, KG . Student to midwife transition: newly qualified midwives? Experiences in Limpopo province. Health SA Gesondheid . (2022) 27:27. doi: 10.4102/hsag.v27i0.1992
20. Donovan, H , Welch, A , and Williamson, M . Reported levels of exhaustion by the graduate nurse midwife and their perceived potential for unsafe practice: a phenomenological study of Australian double degree nurse midwives. Workplace Health Saf . (2021) 69:73–80. doi: 10.1177/2165079920938000
21. Kool, LE , Schellevis, FG , Jaarsma, D , and Feijen-De, JE . The initiation of Dutch newly qualified hospital-based midwives in practice, a qualitative study. Midwifery . (2020) 83:102648. doi: 10.1016/j.midw.2020.102648
22. Kool, L , Feijen-de Jong, EI , Schellevis, FG , and Jaarsma, D . Perceived job demands and resources of newly qualified midwives working in primary care settings in the Netherlands. Midwifery . (2019) 69:52–8. doi: 10.1016/j.midw.2018.10.012
23. Norris, S . In the wilderness: an action-research study to explore the transition from student to newly qualified midwife. Evid Based Midwifery . (2019) 17:128–34.
24. Huang, S , Yu, Y , Zhou, X , and Cai, W . The occupational experience of the new-recruited undergraduate midwives. Chinese Nursing Education . (2017) 14:692–6.
25. Hobbs, JA . Newly qualified midwives' transition to qualified status and role: assimilating the 'habitus' or reshaping it? Midwifery . (2012) 28:391–9. doi: 10.1016/j.midw.2011.04.007
26. Fenwick, J , Hammond, A , Raymond, J , Smith, R , Gray, J , Foureur, M, et al. Surviving, not thriving: a qualitative study of newly qualified midwives' experience of their transition to practice. J Clin Nurs . (2012) 21:2054–63. doi: 10.1111/j.1365-2702.2012.04090.x
27. Clements, V , Fenwick, J , and Davis, D . Core elements of transition support programs: the experiences of newly qualified Australian midwives. Sex Reprod Healthc . (2012) 3:155–62. doi: 10.1016/j.srhc.2012.08.001
28. van der Putten, D . The lived experience of newly qualified midwives: a qualitative study. Br J Midwifery . (2008) 16:348–58. doi: 10.12968/bjom.2008.16.6.29592
29. Karimyar, JM , Minaei, S , Abdollahifard, S , and Maddahfar, M . The effect of stress management on occupational stress and satisfaction among midwives in obstetrics and gynecology hospital wards in Iran. Glob J Health Sci . (2016) 8:91. doi: 10.5539/gjhs.v8n9p91
30. U-Eun, C , and Hyun-Young, K . The impact of safety climate and fatigue on safety performance of operating room nurses. J Korean Acad Nurs Adm . (2016) 22:471. doi: 10.11111/jkana.2016.22.5.471
31. Thunes, S , and Sekse, RJ . Midwifery students first encounter with the maternity ward. Nurse Educ Pract . (2015) 15:243–8. doi: 10.1016/j.nepr.2015.01.012
32. Power, A , and Grzelak, I . University midwifery societies: support for student midwives, by student midwives. Br J Midwifery . (2016) 24:787–9. doi: 10.12968/bjom.2016.24.11.787
33. Heslehurst, N , Russell, S , McCormack, S , Sedgewick, G , Bell, R , and Rankin, J . Midwives perspectives of their training and education requirements in maternal obesity: a qualitative study. Midwifery . (2013) 29:736–44. doi: 10.1016/j.midw.2012.07.007
34. Elliott, S , Murrell, K , Harper, P , Stephens, T , and Pellowe, C . A comprehensive systematic review of the use of simulation in the continuing education and training of qualified medical, nursing and midwifery staff. JBI Libr Syst Rev . (2011) 9:538–87. doi: 10.11124/01938924-201109170-00001
35. Yolanda, FP , and Magdalena, AC . Factors influencing nursing staff members' participation in continuing education. Rev Lat Am Enferm . (2006) 14:309–15. doi: 10.1590/S0104-11692006000300002
36. Abedian, K , Charati, JY , Samadaee, K , and Shahhosseini, Z . A cross-sectional study of Midwives' perspectives towards their professional educational needs. Mater Sociomed . (2014) 26:182–5. doi: 10.5455/msm.2014.26.182-185
37. O'Connell, MA , and Sosa, G . Midwifery in Abu Dhabi: a descriptive survey of midwives. Women Birth . (2023) 36:e439–44. doi: 10.1016/j.wombi.2023.02.002
38. Ten, HP , Lopes, ST , Nove, A , Michel-Schuldt, M , Moyo, NT , Bokosi, M, et al. Midwifery 2030: a woman's pathway to health. What does this mean? Midwifery . (2016) 32:1–6. doi: 10.1016/j.midw.2015.10.014
Keywords: newly qualified midwives, transition to practice, experience, meta-synthesis, qualitative systematic review
Citation: Shi J, Li X, Li Y, Liu Y, Li J, Zhang R and Jiang H (2023) Experiences of newly qualified midwives during their transition to practice: a systematic review of qualitative research. Front. Med . 10:1242490. doi: 10.3389/fmed.2023.1242490
Received: 20 June 2023; Accepted: 01 August 2023; Published: 16 August 2023.
Reviewed by:
Copyright © 2023 Shi, Li, Li, Liu, Li, Zhang and Jiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hui Jiang, [email protected]
† These authors have contributed equally to this work and share first authorship
This article is part of the Research Topic
Quality of sexual and reproductive health care: strengths, gaps, and challenges for midwifery care
An integrative review of supportive relationships between child‐bearing women and midwives
Hadeer almorbaty.
1 School of Nursing and Midwifery, College of Health Medicine and Well‐Being, The University of Newcastle, University Drive, Callaghan New South Wales, Australia
2 Nursing Department, Prince Sultan Military College of Health Sciences, Dhahran Saudi Arabia
3 Faculty of Health, Southern Cross University, Coffs Harbour New South Wales, Australia
Eileen Dowse
4 School of Nursing and Midwifery, College of Health Medicine and Well‐Being, The University of Newcastle, University Drive, Callaghan New South Wales, Australia
Sally Wai‐Chi Chan
5 Tung Wah College, Dhahran Hong Kong
Associated Data
The data that support the findings of this study are available in [repository name] at [URL/DOI], reference number [reference number]. These data were derived from the following resources available in the public domain: [list resources and URLs].
To review and evaluate the literature on the factors related to developing supportive relationships between women and midwives, including facilitators and barriers.
An integrative review.
The search used CINAHL, MEDLINE, Embase, EMcare, Maternity and Infant Care, PsycINFO, and Google Scholar from January 2009–June 2020. Two reviewers screened the eligible studies, and 2,399 records were identified. Quality was assessed with the mixed methods appraisal tool, and 14 articles were included.
The findings highlight that successful relationships require therapeutic communication, trust, respect, partnership, and shared decision‐making. Supportive relationships improve women′s satisfaction and birth outcomes, and continuity of care model is an enabling factor. Further research is required to understand supportive relationships in non‐continuity of care models and when different cultural backgrounds exist.
What Is Known About This Topic?
- The physical and emotional support midwives provide to child‐bearing women can contribute to positive child‐bearing experiences and birth outcomes.
- Not all women perceive their relationships with midwives as supportive.
- Organizational factors, such as staffing ratios and workload issues, may impede midwives' abilities to build supportive relationships with women.
- Continuity of care models facilitate the development of supportive relationships.
What Does This Paper Add?
- Midwives can facilitate the development of supportive relationships, through effective communication skills, mutual trust, respect, and partnership.
- Workplace culture within maternity units, affects midwives' abilities to develop and maintain supportive relationships with women.
- The socio‐cultural context in which women and midwives live and work further impacts their abilities to develop and maintain supportive relationships.
- There is a lack of knowledge about how supportive relationships are developed in maternity units, especially where continuity of care is not practised.
What Are the Implications for Practices and Policies?
- More research is needed to explore the best approach and most effective strategies for developing supportive relationships, within existing models of care.
- Further research is required to understand how the cultural identities of both women and midwives affect the development of supportive relationships.
1. INTRODUCTION
A key aspect of maternity care is a supportive relationship between the child‐bearing woman and her midwife or maternity nurse—the quality of this relationship is pivotal to safe maternity care and improving the woman′s experience (Agostini et al., 2015 ). Child‐bearing experiences can vary greatly among women. A poor experience can affect a woman′s physiological and psychological wellbeing during the immediate postpartum and long‐term periods (McInnes et al., 2020 ). Understanding how supportive relationships develop, between child‐bearing women and their midwives or maternity nurses during the child‐bearing period can help guide practices and improve maternity care.
2. BACKGROUND
The child‐bearing period can be one of the most significant times in a woman′s life. In this review, the ‘child‐bearing period’ refers to the pregnancy, labour, birth and postpartum period (i.e., up to 6 weeks following the birth) (Qi & Creedy, 2009 , p. 2). During this time, many physiological, psychological and emotional changes can affect the woman′s emotional and physical well‐being as well as the birth outcomes for her baby. A supportive relationship is a fundamental aspect of quality care for patients. In maternity care, supportive relationships between women and their midwives or maternity nurses are founded on mutual respect, shared power, and working in partnership to support women to engage in decision‐making regarding their care (World Health Organization, 2016 ).
The literature has used various terms for healthcare providers supporting child‐bearing women. In this review, “midwives” includes midwives and nurse‐midwives caring for women giving birth and their infants, and preparing them for self‐care and child care at home. It also includes registered or accredited nurses with a significant role in assessing and managing women′s progress in labour, where the provider attends the birthing room when the birth is close or there are serious complications. The exception is the “Results” section, where the original terminology from the reviewed articles is used for clarity.
Research has indicated that the physical and emotional support provided in a therapeutic relationship can contribute to positive child‐bearing experiences and birth outcomes, including reduced oxytocin requirements and perineal lacerations (Sehhatie et al., 2014 ), reduced elective caesarean births, lower healthcare costs (Tracy et al., 2014 ), reduced incidences of postpartum depression and increased levels of satisfaction with care (Backstrom et al., 2016 ; Goodwin et al., 2018 ). Furthermore, an effective supportive relationship can lower a woman′s stress levels and facilitate optimal conditions for the baby′s development (Buckley, 2015 ).
Literature has suggested that certain factors affect the development of supportive relationships, such as ethnic heterogeneity, socioeconomic differences, culture and preferences (Bradfield, Hauck, Duggan, et al., 2019 ; Goodwin et al., 2018 ). Other factors include the healthcare professional′s capacity for empathy, trust, and emotional support, and the hospital′s policies for the maternity care model such as continuity of care (COC) (Bradfield et al., 2019b ). COC is a model of midwifery care where the woman receives COC from a known midwife or known midwifery team throughout the child‐bearing period, and postpartum care may continue in the home (Homer, 2016 ).
The importance of woman–midwife relationships has been the focus of research on models of maternity care that implement COC in their health systems, such as the United Kingdom (UK) and New Zealand (NZ) (Bradfield et al., 2019d ; Homer, 2016 ). However, there is a paucity of summarized evidence focusing on facilitators and barriers to developing supportive relationships. An integrative review is required to synthesize the evidence on developing supportive relationships between child‐bearing women and midwives. Such understanding can help build supportive relationships, and thus improve the quality of maternity care and women′s child‐bearing experiences.
This review aims to evaluate the literature on the factors related to developing supportive relationships between women and midwives, including facilitators and barriers.
4.1. Design
An integrative literature review design was used to understand a particular phenomenon and produce new knowledge in social and behavioural sciences (Torraco, 2016 ). Its flexibility in combining diverse methodologies, and ability to contribute to evidence‐based practice can build knowledge and inform policymakers about a particular phenomenon in practice. This review adopted Whittemore and Knafl′s ( 2005 ) five‐stage process: (1) identifying the research questions; (2) conducting a comprehensive search of the literature; (3) evaluating the studies found; (4) analysing the studies included in the review; and (5) reporting and discussing the findings.
4.1.1. Research questions
- What are the perceived facilitators and barriers to developing supportive relationships during the child‐bearing period from women′s and midwives′ perspectives?
- What cultural factors might affect the process of developing supportive relationships during the child‐bearing period from women′s and midwives′ perspectives?
4.2. Comprehensive literature search
The literature search was limited to publications from January 2009–June 2020. The search included studies from the following databases: CINAHL, MEDLINE, EMbase, Emcare, Maternity and Infant Care, and PsycINFO. Google Scholar was used to find relevant studies. The keywords were: midwife*‐woman relationship, and matern* or midwife*, and facilitators or barriers and experience. Words were combined with AND or OR to focus or limit the search results. Synonyms of each keyword were generated via word expansion (see Table 1 ).
The keywords and synonyms used across all databases
The inclusion criteria included: (1) primary research studies on supportive relationships between women and midwives, or maternity nurses, using any research design; (2) studies published in the English or Arabic languages; and (3) studies published in peer‐review journals. The exclusion criteria included (1) studies not in the English or Arabic languages (due to a lack of translation resources); (2) publications other than primary research studies, such as meta‐analyses, dissertations, books, grey literature, conference abstract papers, reports, and commentaries; (3) studies focused on relationships with healthcare providers other than midwives or nurses; and (4) studies with a focus on a particular maternity or midwifery program, approach or care model.
4.3. Evaluating the studies
The initial search retrieved 2,399 sources. The duplicates were removed ( n = 1,193), and the relevant studies were manually screened. A total of 1,182 articles were excluded because of the study focus, leaving 24 studies for review. One article that aligned with the inclusion criteria was found in the reference list of one of the studies from the search. Therefore, the final review, included 25 studies, which were assessed for relevance, quality, and results concerning the research questions. A second reviewer (a supervisor from the research team) affirmed the eligibility of the included studies. Finally, a total of 14 articles were reviewed. The PRISMA diagram (see Figure 1 ) illustrates the review search steps and outcomes (Moher et al., 2009 ). All reviewers discussed and agreed on the review outcomes.

PRISMA diagram
4.3.1. Quality appraisal
The quality of the included studies was appraised using the mixed‐methods appraisal Tool (MMAT) (Hong et al., 2018 ). The MMAT allows a judgement of the methodological quality of studies for various research designs (qualitative, quantitative, and mixed‐methods studies). One study was judged as being of low quality. However, it was included because of its relevance to the research questions. Table 2 summarizes the included studies using MMAT criteria.
Summary of quality appraisal of qualitative, quantitative and mixed‐methods, using MMAT criteria
Note : S1 and S2 = screening questions (for all types of study design): S1, Are there clear research questions?; S2, Do the collected data allow to address the research questions? 1, 2, 3, 4, and 5 = Methodological quality criteria described below for each design, Qualitative: 1, Is the qualitative approach appropriate to answer the research question?; 2, Are the qualitative data collection methods adequate to address the research question?; 3, Are the findings adequately derived from the data?; 4, Is the interpretation of results sufficiently substantiated by data?; 5, Is there coherence between qualitative data sources, collection, analysis and interpretation? Quantitative, nonrandomized: 1, Are the participants representative of the target population?;2, Are measurements appropriate regarding both the outcome and intervention (or exposure)?; 3, Are there complete outcome data?; 4, Are the confounders accounted for in the design and analysis?; 5, During the study period, is the intervention administered (or exposure occurred) as intended? Mixed‐methods: 1, Is there an adequate rationale for using a mixed methods design to address the research question?; 2, Are the different components of the study effectively integrated to answer the research question?; 3, Are the outputs of the integration of qualitative and quantitative components adequately interpreted?; 4, Are divergences and inconsistencies between quantitative and qualitative results adequately addressed?; 5, Do the different components of the study adhere to the quality criteria of each tradition of the methods involved? (Hong et al., 2018 ).
4.4. Analysing the studies
4.4.1. data extraction.
A data extraction form (see Table 3 ) was used to extract the data from the reviewed articles, including the study description, methods, and results. Thematic analysis was used to analyse the data for factors considered facilitators or barriers to developing supportive relationships. This involved reading the articles, searching for meaningful ideas, creating codes, identifying themes, organizing the themes, and naming them concisely to make sense for the reader (Braun & Clarke, 2006 ). Three main themes and nine sub‐themes were generated (see Table 4 ).
Extracted data of the included articles
Themes and sub‐themes generated
4.5. Reporting and discussing the findings
4.5.1. study characteristics.
Two studies were conducted in the United States of America, three in the UK, two in Sweden, one in Japan, one in East Africa, four in Australia and one in NZ. There were 762 participants in the reviewed studies, including 450 midwives, 78 maternity nurses, 172 child‐bearing women and 101 mothers. Of the participating women (i.e., 273 child‐bearing women and mothers), 22 participated in the studies during pregnancy, 17 were in either the pregnancy or postpartum period, 234 were in the postpartum period and one was in a neonatal intensive care unit (Shimizu & Mori, 2018 ).
5.1. Theme 1: Human interaction factors
Human interaction factors were mentioned in 14 studies. Four sub‐themes emerged: demonstrating trust and respect, recognizing midwives' attitudes and beliefs, developing partnerships and effective communication skills.
5.1.1. Demonstrating trust and respect
Six qualitative studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ; Madula et al., 2018 ; McInnes et al., 2020 ; Menage et al., 2020 ) described trust and respect as a facilitator of developing supportive relationships with women. In this review, ‘respect’ refers to how midwives differentiate the boundaries between professional and personal relationships, including accepting women′s choices (Nursing and Midwifery Board of Australia, 2018). “Trust” is defined as the part of a partnership with a woman that maintains equality and sharing (International Confederation of Midwives, 2017; Nursing and Midwifery Board of Australia, 2018).
Midwives stated that trust promoted the building of supportive relationships with women (Menage et al., 2020 ), and showing respect allowed them to form a strong connection, during a challenging time to engage, such as labour. In a study including 15 child‐bearing women, the importance of respect was reinforced—they experienced positive relationships with maternity nurses when they felt respected (Madula et al., 2018 ).
5.1.2. Recognizing midwives' attitudes and beliefs
“Attitudes” and ‘beliefs’ refer to modes feeling and thinking, which affect behaviour and, therefore, the ability to develop relationships (Bradfield et al., 2019a ; Carlton et al., 2009 ). Three qualitative studies (Backstrom et al., 2016 ; Bradfield et al., 2019a , 2019b ) reported that midwives' negative or positive feelings were important for their attitudes towards developing supportive relationships with women. Eight articles (Aschenbrenner et al., 2016 ; Backstrom et al., 2016 ; Bradfield et al., 2019a , 2019b ; Carlton et al., 2009 ; Goodwin et al., 2018 ; McInnes et al., 2020 ; Menage et al., 2020 ) discussed facilitators or barriers influencing midwives' or maternity nurses' attitudes. These included motivation, personality, preference, experience and knowledge (McInnes et al., 2020 ).
Experience and knowledge can empower midwives to manage challenges while building supportive relationships. The more educated and/or experienced the midwives/maternity nurses, the more their relationships were (Aschenbrenner et al., 2016 ; Bradfield et al., 2019a ; Carlton et al., 2009 ; Menage et al., 2020 ). Further, when a midwife′s and a woman′s personalities do not match, it could impede the supportive relationship (Backstrom et al., 2016 ; Bradfield et al., 2019a ). However, neither study discussed how the personalities might be mismatched.
5.1.3. Developing partnerships
Partnerships were discussed in 10 studies. Carlton et al. ( 2009 ) found that partnerships could be achieved when women and maternity nurses shared power. Partnerships include elements such as shared decision‐making (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ), mutual involvement (Shimizu & Mori, 2018 ) and healthcare professionals advocating for empowering the woman (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; Shimizu & Mori, 2018 ). Empowering child‐bearing women is considered essential in supportive relationships (Menage et al., 2020 ). It is thought to occur when the midwife provides guidance (Crowther & Smythe, 2016 ) and advocates for the woman (Bradfield, Hauck, Duggan, et al., 2019 ). However, there were few details about when to share decision‐making and the relevant aspects of the care.
Two qualitative studies (Bradfield, Hauck, Duggan, et al., 2019 ; Davison et al., 2015 ) asserted that woman‐centred care could enhance positive and supportive relationships with women, facilitate shared decision‐making and improve their birth outcomes, enhancing women′s satisfaction with care and birthing experiences. Seven studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a ; Davison et al., 2015 ; Goodwin et al., 2018 ; McInnes et al., 2020 ; Menage et al., 2020 ; Shimizu & Mori, 2018 ) also reported that woman‐centred care that was tailored to the woman′s preferences facilitated supportive relationships .
Other studies identified positive relationships between women and midwives when women, their family members and significant others were involved in care planning (Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; Goodwin et al., 2018 ; Shimizu & Mori, 2018 ). Shimizu and Mori′s (2018) study was conducted in Japan with a small sample size ( N = 98 ). Although all study participants assessed their relationships with maternity nurses positively, Shimizu and Mori stated that it might not have been positive for those who did not participate. Furthermore, the women′s responses remained positive even when the questions did not apply. Finally, two studies (Bradfield et al., 2019a ; Goodwin et al., 2018 ) reported that some women refused to choose or build any relationships and preferred their own space.
5.1.4. Effective communication skills
Effective communication skills are fundamental in any relationship. Nine articles (Aschenbrenner et al., 2016 ; Backstrom et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Crowther & Smythe, 2016 ; Madula et al., 2018 ; Menage et al., 2020 ; Oscarsson & Stevenson‐Ågren, 2020 ) identified communication as an enabling practice for developing supportive relationships with women. In one study, midwives ( n = 31) described how they used basic communication skills, such as gaining rapport and providing verbal encouragement, to facilitate relationships development with women (Bradfield, Hauck, Duggan, et al., 2019 ). Further, Backstrom et al. ( 2016 ), Oscarsson and Stevenson‐Ågren ( 2020 ) and Menage et al. ( 2020 ) found that active listening skills are essential to developing supportive relationships. However, Madula et al. ( 2018 ) reported that a lack of interpersonal skills in midwives and maternity nurses was a common communication barrier leading to the women feeling frustrated about their unmet needs.
5.2. Theme 2: Cultural factors
Five studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a ; Carlton et al., 2009 ;Goodwin et al., 2018 ; Oscarsson & Stevenson‐Ågren, 2020 ) discussed cultural factors, focusing on individual′s beliefs and, their effects on the expectations and practices of women and midwives.
5.2.1. Women′s health beliefs
Bradfield et al., 2019a described the need for cultural safety, and understanding of women′s cultural backgrounds in the practice of maternity care, which requires trust and respect for other cultures. Two studies found that women and midwives valued supportive relationships, highlighting the importance of keeping this relationship non‐judgmental to facilitate its building, especially in women and midwives with different cultural beliefs (Goodwin et al., 2018 ; Oscarsson & Stevenson‐Ågren, 2020 ). Oscarsson and Stevenson‐Ågren ( 2020 ) reported that women′s health beliefs affected their child‐bearing practices, especially when they differed from midwives′ beliefs, all midwives in Oscarsson and Stevenson‐Ågren′s study were Swedish, which may have affected the results because cultural diversity can affect midwives′ perceptions and experiences. The study also did not report the cultural beliefs of immigrant women, although they were not homogenous. Furthermore, one study in the UK (Goodwin et al., 2018 ) claimed that midwives tended to negatively judge Pakistani women when they were unaware of their cultural practices and beliefs, such as shaving a newborn′s head. Unfamiliarity with women′s beliefs, priorities and expectations was a barrier to developing supportive relationships (Goodwin et al., 2018 ).
5.2.2. Family involvement
Goodwin et al. ( 2018 ) reported that family dynamics in some cultures (e.g., Pakistani) significantly influenced the relationships between maternity nurses and women. Maternity nurses and midwives explained that family members influenced some women′s decisions and the dominant family member was often the decision‐maker (Carlton et al., 2009 ; Goodwin et al., 2018 ; Oscarsson & Stevenson‐Ågren, 2020 ). Extra attention to cultural influence on building supportive relationships was considered as a facilitator (Goodwin et al., 2018 ). Conversely, one study described how some women preferred to handle the labour and birth alone and not involve their partners, preferring to handle the labour and birth alone (Bradfield, Hauck, Duggan, et al., 2019 ).
5.3. Theme 3: Organizational factors
Ten studies identified the organizational factors, such as the model of care, work‐load and resources, for developing supportive relationships with child‐bearing women. Three sub‐themes emerged: COC, time/workload and physical environment.
5.3.1. Continuity of care
Eight studies reported that (COC) facilitates developing supportive relationships with women. Healthcare model differ between countries, influencing the type and extent of COC the maternity team provides. This review included different healthcare systems in which the studies were conducted. Some studies mentioned COC in the health systems in the UK (McInnes et al., 2020 ; Menage et al., 2020 ), Australia (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a ; Davison et al., 2015 ), Sweden (Backstrom et al., 2016 ; Oscarsson & Stevenson‐Ågren, 2020 ), and NZ (Crowther & Smythe, 2016 ). Other studies have reported non‐COC in systems, in the United State of America (Carlton et al., 2009 ) and Australia (Bradfield et al., 2019b ).
Women and midwives in three qualitative studies (Backstrom et al., 2016 ; Bradfield et al., 2019b ; McInnes et al., 2020 ) reported that COC in maternity services facilitates supportive relationships and trust. Additionally, Oscarsson and Stevenson‐Ågren ( 2020 ) and Menage et al. ( 2020 ) suggested that midwives who cared for the same women throughout their pregnancies were more likely to build trusting relationships. However, midwives working in a birthing unit where COC was not practised expressed a feeling of disconnection with women (Bradfield et al., 2019b ). Women in one study (Davison et al., 2015 ) wanted COC and preferred private midwifery care because the relationship with their midwives was as supportive as they needed and they could be involved in shared decisions. This study was conducted in one location in Australia (from 2007–2013) when support for publicly funded home birth was still being developed.
5.3.2. Time and workload
The literature highlighted several work situations as barriers to supportive relationships with child‐bearing women; including lack of adequate time (Aschenbrenner et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Madula et al., 2018 ), heavy workloads (Aschenbrenner et al., 2016 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Menage et al., 2020 ), and staff shortages (Aschenbrenner et al., 2016 ; Carlton et al., 2009 ). Maternity nurses felt distracted by paperwork and technological interventions, such as electronic fetal monitoring and high‐risk protocols for all admitted women (Carlton et al., 2009 ). Carlton et al. ( 2009 ), Bradfield et al., 2019b and Crowther and Smythe ( 2016 ) found that midwives felt overloaded and often had to deal with staff shortages, which affected their abilities to provide care and develop relationships. Maternity nurses also reported a lack of time for developing supportive relationships with women due to their working conditions (Aschenbrenner et al., 2016 ; Carlton et al., 2009 ). Maternity nurses were challenged when they had to balance keeping electronic health records (EHRs) and women′s needs, such as electronic fetal monitoring (a part of HER), resulting in decreased time for building relationships (Aschenbrenner et al., 2016 ; Menage et al., 2020 ).
5.3.3. Physical environment
This sub‐theme refers to organizational facilitators and barriers to providing resources and support for midwives to develop supportive relationships, which midwives considered a significant challenge to staying connected with women (McInnes et al., 2020 ). For example, birthing unit design can influence how women feel. Birthing room environment s have varying levels of privacy, lighting, music or silence and hygiene facilities (Bradfield, Hauck, Duggan, et al., 2019 ). When the design matches a woman′s preferences, promotes a positive relationship between the woman and the midwife (Bradfield, Hauck, Duggan, et al., 2019 ; Menage et al., 2020 ). This can improve women′s physical and psychological comfort, enabling supportive relationships and positively affecting women′s feelings (Aschenbrenner et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Carlton et al., 2009 ; Menage et al., 2020 ).
6. DISCUSSION
This review has provided evidence on the factors related to developing supportive relationships between women and midwives. The findings indicated that midwives' relationships with child‐bearing women are critical and depend on human interaction, cultural and organizational factors. Each factor will be discussed as a facilitator or barrier to developing supportive relationships during the child‐bearing period from women′s and midwives′ perspectives.
6.1. Factors
6.1.1. human interaction.
Developing supportive relationships with child‐bearing women requires mutual trust, respect, partnerships and attitudes and effective communication skills, all of which are interrelated and facilitate relationships. Partnerships allow women to feel empowered to share decision‐making and make their own choices. They require provisions for involvement and advocacy (Bradfield, Hauck, Duggan, et al., 2019 ; Shimizu & Mori, 2018 ). Although some studies (Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; McInnes et al., 2020 ; Shimizu & Mori, 2018 ) identified involvement as a part of partnerships with child‐bearing women, there is insufficient information regarding the process for encouraging such involvement. Some studies focused on partnership as a maternity care approach, a foundational premise in developing supportive relationships (Bradfield et al., 2019a , 2019b ; Carlton et al., 2009 ). However, these studies did not demonstrate the steps necessary to build partnerships with women and thus, facilitate relationships. This area requires further research.
Appropriate shared decision‐making and women′s involvement were not always present in the reviewed studies (Bradfield et al., 2019a , 2019b ; Davison et al., 2015 ; Shimizu & Mori, 2018 ). Thus, there was little information about decision‐making processes, including how, when and the degree to which women were involved in decision‐making, which could be considered a barrier to building supportive relationships. Additionally, there was a lack of information about women′s understanding of empowerment, which may indicate their readiness to make their own decisions. While midwives should employ a woman‐centred care approach, empowering women to participate in joint decision‐making (Nursing and Midwifery Board of Australia, 2018), further research should clarify women′s understanding of empowerment.
Two studies reported described how midwives' or maternity nurses' attitudes, including their personalities, knowledge and experience, affected how they valued developing supportive relationships with women during childbirth (Bradfield et al., 2019a ; Carlton et al., 2009 ). Midwives need to gain women′s trust through positive attitudes and respect for their individual needs and culture.
These human interaction factors will have little success without effective communication skills, which are the basis of relationship development (Aschenbrenner et al., 2016 ; Backstrom et al., 2016 ; Bradfield, Hauck, Duggan, et al., 2019 ; Bradfield et al., 2019b ; Carlton et al., 2009 ; Crowther & Smythe, 2016 ; Madula et al., 2018 ; Menage et al., 2020 ; Oscarsson & Stevenson‐Ågren, 2020 ). Positive communication between healthcare professionals and women facilitates trust, respect and support (Backstrom et al., 2016 ). Therapeutic communication should be supported and practised more often to meet women′s needs and facilitate relationship development (Fenton & Jones, 2015 ; World Health Organization, 2019 ).
6.1.2. Culture
The reviewed studies suggested some cultural factors, such as women′s health beliefs (Carlton et al., 2009 ; Goodwin et al., 2018 ), and family involvement (Oscarsson & Stevenson‐Ågren, 2020 ) that might inhibit the effective communication needed to support the connection between women and midwives. For example, some studies found women had a different view from that of midwives—while midwives often viewed the control of family members as a negatively dominant influence, some women viewed that as a kind of support (Goodwin et al., 2018 ). Such a situation requires that midwives understand cultural influences to maintain supportive relationships in a preferred way.
Further, women from different cultures might present with varying health demands (Tehsin et al., 2018 ), and the cultural barriers can affect supportive relationships. Understanding women′s beliefs and culture can help midwives understand the reasons behind health practices, promote acceptance and facilitate supportive relationships. Therefore, assessing women′s expectations of maternity care can benefit relationship development.
However, the relevant literature included of 14 articles published over the last 10 years, from seven countries, with primarily Western cultures. Few studies focused on cultural factors that affect how supportive relationships develop, indicating a substantial gap in the literature. Country‐specific studies are needed to explore cultural differences, views, expectations and health practices relevant to building relationships with child‐bearing women.
6.1.3. Organization
This review indicates that COC is crucial to meeting women′s. Findings demonstrated that women and midwives prefer to know each other before child birth, preferably meeting during the antenatal period (Bradfield et al., 2019a ), so their care can be continuous throughout the child‐bearing period (McInnes et al., 2020 ). The familiarity between women and midwives has helped midwives understand women′s needs and identify changes in health statuses throughout their visits. Simultaneously, it has helped women feel more comfortable with their midwives and develop trusting and positive relationships (McInnes et al., 2020 ). This finding was supported by recent Cochrane reviews, which established COC as the gold standard for midwifery care and suggested it should be practised much more widely (Homer et al., 2019 ; Sandall et al., 2016 ). However, further studies should address how supportive relationships are enabled within maternity care environments with a non‐COC model.
Findings have shown that midwives and maternity nurses are distracted by workloads due to documentation and technology interventions (Aschenbrenner et al., 2016 ). Developing a successful relationship requires a balance between all support aspects. Therefore, midwives desire enough time to build trust, respect and partnerships with women, particularly those from different cultures. They need extra time before, during and after meeting women to manage their increased workload (Kerr et al., 2014 ). One strategy for managing this challenge is more efficient documentation methods that enable more time and effort strengthening relationships with women (Kent & Morrow, 2014 ). Although the EHR might prompt workflows, several issues have been noted, such as ineffective time management and unexpected deficiencies in patient care and work flow (Abbey et al., 2012 ; Baumann et al., 2018 ). Thus, the effect of EHR on midwives' time needs more attention, suggesting staff training and EHR system modifications to increase the time available for women′s care (Coleman et al., 2021 ; Karp et al., 2019 ).
6.2. Strengths and limitations
This review integrated qualitative and quantitative studies to produce a holistic understanding of developing supportive relationships with child‐bearing women. However, it excluded non‐English and non‐Arabic studies, therefore, relevant data may have been omitted.
6.3. Recommendations
Future research should develop strategies to facilitate supportive relationships, particularly in non‐COC models. This review recommends that strengthening midwives' communication skills is essential. Future research should focus on how midwives share decision‐making power with women throughout the child‐bearing period, which is an important component of supportive relationships. Organizational support is a major factor affecting supportive relationships, and COC models are highly recommended. Further investigations should also address the effect cultural identity on relationship development and how women and midwives manage cultural differences.
7. CONCLUSION
This review highlighted that supportive relationships require therapeutic communication, trust, respect, partnership and shared decision‐making. Developing supportive relationships with women is easier in COC models of maternity care. However, little is known about developing and maintaining supportive relationships in non‐COC models. Further, working with women from different cultural backgrounds can affect developments, with additional considerations required to ensure women feel supported. However, it is unclear how supportive relationships are enabled within maternity care environments with differing cultural identity factors, demonstrating the need for further research.
7.1. Relevance to clinical trial
This study aimed to contribute substantially to evidence‐based decisions about the organizational barriers to building supportive relationships. These findings could be used to review or develop nursing and midwifery education curricula, guidelines and policies to enhance the knowledge, skills and practices used to build supportive relationships with child‐bearing women. Further, birthing outcomes can be improved, reducing health costs and increasing patient satisfaction. The importance of individualized care must be emphasized through the appropriate development of supportive relationships. This, will help midwives and maternity nurses understand and value women′s needs and ensure they have adequate time to build supportive relationships with women, provide woman‐centred care and ultimately improve women′s experiences during the child‐bearing period.
This review highlighted the importance of women′s involvement. Effective supportive relationships between child‐bearing women and midwives, increase women′s involvement and autonomy in caring for themselves and their infants in postpartum and during early childhood. Thus, there is a need to improve midwives′ skills concerning why, what and how to begin women′s involvement, suggesting that reflective supervision methods during home visiting could help maintain boundaries, observe one′s reactions and improving involvement (Tomlin et al., 2016 ).
Continuity of care focuses on building supportive relationships with women, which requires supportive leadership, and enables midwives to stay connected with maternity team (McInnes et al., 2020 ). Thus, further research is needed to examine relationships between all organizational levels in the maternity care. Additionally, there are few details on the strategies midwives and maternity nurses use to build these relationships. Thus, further research should address midwives' and maternity nurses' priorities and the actual time required to develop supportive relationships with child‐bearing women.
AUTHOR CONTRIBUTIONS
All the authors agreed and had a primary contribution to the following: conception and design, data appraisal, extraction, analysis, and reporting of findings. They affirmed their approval of the final version to be published.
FUNDING INFORMATION
This work was completed as a part of PhD research project at The University of Newcastle, University Drive, Callaghan, New South Wales 2308, Australia. Grant number HREC H‐2021‐0217. PhD candidate Hadeer Almorbaty has held a scholarship awarded by Prince Sultan Military College of Health Sciences, Medical Services Division, Armed Forces, Ministry of Defence, Kingdom of Saudi Arabia, for her PhD study at the University of Newcastle, Australia. There are no other funding sources for this project.
CONFLICT OF INTEREST
The authors have declared no conflict of interest.
ACKNOWLEDGEMENTS
We thank Debbie Booth, Senior Research Librarian (The University of Newcastle) for guidance in the literature search.
Almorbaty, H. , Ebert, L. , Dowse, E. , & Chan, S.‐C. (2023). An integrative review of supportive relationships between child‐bearing women and midwives . Nursing Open , 10 , 1327–1339. 10.1002/nop2.1447 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
DATA AVAILABILITY STATEMENT
- Abbey, M. , Chaboyer, W. , & Mitchell, M. (2012). Understanding the work of intensive care nurses: A time and motion study . Australia Critical Care , 25 ( 1 ), 13–22. [ PubMed ] [ Google Scholar ]
- Agostini, F. , Neri, E. , Salvatori, P. , Dellabartola, S. , Bozicevic, L. , & Monti, F. (2015). Antenatal depressive symptoms associated with specific life events and sources of social support among Italian women . Maternal and Child Health Journal , 19 ( 5 ), 1131–1141. 10.1007/s10995-014-1613-x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Aschenbrenner, A. , Hanson, L. , Johnson, T. , & Kelber, S. (2016). Nurses' Own Birth Experiences influence Labor Support attitudes and behaviors . Journal of Obstetric, Gynecologic, & Neonatal Nursing , 45 ( 4 ), 491–501. 10.1016/j.jogn.2016.02.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Backstrom, C. , Martensson, L. , Golsater, M. , & Thorstensson, S. (2016). "It′s like a puzzle": Pregnant women's perceptions of professional support in midwifery care . Women and Birth , 29 ( 6 ), e110–e118. 10.1016/j.wombi.2016.04.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baumann, L. A. , Baker, J. , & Elshaug, A. G. (2018). The impact of electronic health record system on clinical documentation times: A systematic review . Health Policy , 122 ( 8 ), 827–836. [ PubMed ] [ Google Scholar ]
- Bradfield, Z. , Hauck, Y. , Duggan, R. , & Kelly, M. (2019). Midwives' perceptions of being ‘With Woman’: A phenomenological study . BMC Pregnancy & Childbirth , 19 ( 1 ), 787–792. 10.1186/s12884-019-2548-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradfield, Z. , Hauck, Y. , Kelly, M. , & Duggan, R. (2019a). "It's what midwifery is all about": Western Australian midwives’ experiences of being ‘With Woman’ during labour and birth in the known midwife model . BMC Pregnancy & Childbirth , 19 ( 1 ), 29. 10.1186/s12884-018-2144-z [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradfield, Z. , Hauck, Y. , Kelly, M. , & Duggan, R. (2019b). Urgency to build a connection: Midwives' experiences of being ‘With Woman’ in a model where midwives are unknown . Midwifery , 69 , 150–157. 10.1016/j.midw.2018.11.014 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bradfield, Z. , Kelly, N. , Hauck, Y. , & Duggan, R. (2019d). Midwives ‘with Woman’ in the private obstetric model: Where divergent philosophies meet . Women & Birth , 32 ( 2 ), 157–167. [ PubMed ] [ Google Scholar ]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology . Qualitative research in psychology , 3 ( 2 ), 77–101. 10.1191/1478088706qp063oa [ CrossRef ] [ Google Scholar ]
- Buckley, S. (2015). Executive summary of hormonal physiology of childbearing: Evidence and implications for women, babies, and maternity care . The Journal of Perinatal Education , 24 ( 3 ), 145–153. 10.1891/1058-1243.24.3.145 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carlton, T. , Callister, L. , Christiaens, G. , & Walker, D. (2009). Labor and delivery nurses' perceptions of caring for childbearing women in nurse‐managed birthing units . MCN. The American Journal of Maternal/Child Nursing , 34 ( 1 ), 50–56. 10.1097/01.NMC.0000343866.95108.fa [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coleman, C. , Gotz, D. , Eaker, S. , James, E. , Bice, T. , Carson, S. , & Khairat, S. (2021). Analysing EHR navigation patterns and digital workflows among physicians during ICU pre‐rounds . Health Information Management Journal , 50 ( 3 ), 107–117. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Crowther, S. , & Smythe, E. (2016). Open, trusting relationships underpin safety in rural maternity a hermeneutic phenomenology study . BMC Pregnancy & Childbirth , 16 , 370. 10.1186/s12884-016-1164-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Davison, C. , Hauck, Y. , Bayes, S. , Kuliukas, L. , & Wood, J. (2015). The relationship is everything: Women′s reasons for choosing a privately practising midwife in Western Australia . Midwifery , 31 ( 8 ), 772–778. 10.1016/j.midw.2015.04.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fenton, C. , & Jones, L. K. (2015). Achieving cultural safety in Australian indigenous maternity care . International Journal of Health Sciences , 3 ( 1 ), 23–38. 10.15640/ijhs.v3n1a2 [ CrossRef ] [ Google Scholar ]
- Goodwin, L. , Hunter, B. , & Jones, A. (2018). The midwife‐woman relationship in a South Wales community: Experiences of midwives and migrant Pakistani women in early pregnancy . Health Expectations , 21 ( 1 ), 347–357. 10.1111/hex.12629 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Homer, C. S. (2016). Models of maternity care for midwifery continuity of care . Medical Journal of Australia , 205 ( 8 ), 370–374. [ PubMed ] [ Google Scholar ]
- Homer, C. , Brodie, P. , Sandall, J. , & Leap, N. (2019). Midwifery continuity of care: A practical guide . Elsevier Health Sciences. https://books.google.com.sa/books?id=kPaKDwAAQBAJ&lpg=PP1&pg=PP1#v=onepage&q&f=false [ Google Scholar ]
- Hong, Q. N. , Fàbregues, S. , Bartlett, G. , Boardman, F. , Cargo, M. , Dagenais, P. , Gagnon, M.‐P. , Griffiths, F. , Nicolau, B. , & O′Cathain, A. (2018). The mixed methods appraisal tool (MMAT) version 2018 for information pessionals and researchers . Education for Information , 34 ( 4 ), 285–291. 10.3233/EFI-180221 [ CrossRef ] [ Google Scholar ]
- Karp, E. L. , Freeman, R. , Simpson, K. N. , & Simpson, A. N. (2019). Changes in efficiency and quality of nursing electronic health record documentaion after implementaion of an adnission patient history essential data set . CIN: Computers, Informatics, Nursing , 37 ( 5 ), 260–265. [ PubMed ] [ Google Scholar ]
- Kent, P. , & Morrow, K. (2014). Better documentation improves patient care . Nursing Standard , 29 ( 14 ), 44–51. 10.7748/ns.29.14.44.e9267 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kerr, D. , Lu, S. , & McKinlay, L. (2014). Towards patient‐centred care: Perspectives of nurses and midwives regarding shift‐to‐shift bedside Handover . International Journal of Nursing Practice , 20 ( 3 ), 250–257. 10.1111/ijn.12138 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Madula, P. , Kalembo, F. W. , Yu, H. , & Kaminga, A. C. (2018). Healthcare provider‐patient communication: A qualitative study of women's perceptions during childbirth . Reproductive Health , 15 ( 1 ), 135. 10.1186/s12978-018-0580-x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McInnes, R. J. , Aitken‐Arbuckle, A. , Lake, S. , Martin, C. H. , & MacArthur, J. (2020). Implementing continuity of midwife Carer – Just a friendly face? A realist evaluation . BMC Health Services Research , 20 ( 1 ), 1–15. 10.1186/s12913-020-05159-9 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Menage, D. , Bailey, E. , Lees, S. , & Coad, J. (2020). Women's lived experience of compassionate midwifery: Human and professional . Midwifery , 85 , 102662. 10.1016/j.midw.2020.102662 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & Group, P. (2009). Reprint—Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement . Physical Therapy , 89 ( 9 ), 873–880. 10.1093/ptj/89.9.873 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oscarsson, M. G. , & Stevenson‐Ågren, J. (2020). Midwives experiences of caring for immigrant women at antenatal care . Sexual & Reproductive Healthcare , 24 , 100505. 10.1016/j.srhc.2020.100505 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qi, A. M. , & Creedy, D. K. (2009). Central concepts in the midwife‐woman relationship in hospital and community settings . JBI Database of Systematic Reviews and Implementation Reports , 7 ( 34 ), 1–18. 10.11124/jbisrir-2009-587 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sandall, J. , Soltani, H. , Gates, S. , Shennan, A. , & Devane, D. (2016). Midwife‐led continuity models versus other models of care for childbearing women . Cochrane Database of Systematic Reviews(4) , 2016 , CD004667. 10.1002/14651858.CD004667.pub5 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sehhatie, F. , Najjarzadeh, M. , Zamanzadeh, V. , & Seyyedrasooli, A. (2014). The effect of midwifery continuing care on childbirth outcomes . Iranian Journal of Nursing and Midwifery Research , 19 ( 3 ), 233–237. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shimizu, A. , & Mori, A. (2018). Maternal perceptions of family‐centred support and their associations with the mother‐nurse relationship in the neonatal intensive care unit . Journal of Clinical Nursing , 27 ( 7–8 ), e1589–e1599. 10.1111/jocn.14243 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tehsin, F. , Mohammed, A. O. , Lassoued, L. , Ali, S. I. , & al‐Kishi, A. M. (2018). Parturient satisfaction with intrapartum and postpartum care in a maternity referral hospital at Al Ahsa, Saudi Arabia . Journal of the Society of Obstetrics and Gynaecologists of Pakistan , 8 ( 3 ), 169–175. https://jsogp.net/index.php/jsogp/article/view/181/119 [ Google Scholar ]
- Torraco, R. J. (2016). Writing integrative literature reviews: Using the past and present to explore the future . Human Resource Development Review , 15 ( 4 ), 404–428. 10.1177/2F1534484316671606 [ CrossRef ] [ Google Scholar ]
- Tomlin, A. M. , Hines, E. , & Sturm, L. (2016). Relection in home visiting: The what, why, and a beginning step toward how . Infant Mental Health Journal , 37 ( 6 ), 617–627. [ PubMed ] [ Google Scholar ]
- Tracy, S. K. , Welsh, A. , Hall, B. , Hartz, D. , Lainchbury, A. , Bisits, A. , White, J. , & Tracy, M. B. (2014). Caseload midwifery compared to standard or private obstetric care for first time mothers in a ppublic teaching hospital in Australia: Across sectional study of cost and birth outcomes . BMC Pregnancy and Childbirth , 14 ( 1 ), 1–9. 10.1186/1471-2393-14-46 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Whittemore, R. , & Knafl, K. (2005). The integrative review: Updated methodology . Journal of Advanced Nursing , 52 ( 5 ), 546–553. 10.1111/j.1365-2648.2005.03621.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- World Health Organization . (2016). WHO Recommendations on Antenatal Care for a Positive Pregnancy Experience . World Health Organization. https://www.who.int/publications/i/item/9789241549912 [ PubMed ] [ Google Scholar ]
- World Health Organization . (2019). Strengthening quality midwifery education for Universal Health Coverage 2030: Framework for action . World Health Organization. https://www.who.int/publications/i/item/9789241515849 [ Google Scholar ]

COMMENTS
The 2014 Lancet Series on Midwifery showed that interventions provided by the midwifery workforce could reduce maternal and newborn deaths and stillbirths in low-income and middle-income countries (LMICs) by 30-80%, depending on the level of intervention coverage. 2 The Series showed that more efficient use of resources and improved outcomes ...
Midwifery research is often dichotomised by the development status of the jurisdiction of focus — high-income countries (HICs) compared to low- and middle-income countries (LMICs). ... Article PubMed Google Scholar Homer CS, Friberg IK, Dias MA, ten Hoope-Bender P, Sandall J, Speciale AM, et al. The projected effect of scaling up midwifery.
The situation is linked to a shortage of adequate and specialised French journals publishing midwifery topics. ... what strengths could be gleaned from both in order to establish a wider network for undertaking and disseminating midwifery research. Google Scholar World Health Organization (2019) Setting the research agenda: ...
Faculty Academic Quality and Development, Centre for Midwifery and Women's Health Research, Auckland University of Technology, New Zealand. Search for articles by this author. ... Google Scholar]. Once colonisation was underway, and up until the beginning of the 20th century, in Australasia learning about midwifery was based on learning through ...
In this first paper in a series of four papers on midwifery, we aimed to examine, comprehensively and systematically, the contribution midwifery can make to the quality of care of women and infants globally, and the role of midwives and others in providing midwifery care. Drawing on international definitions and current practice, we mapped the scope of midwifery. We then developed a framework ...
In order to develop the search strategy, a preliminary search of PubMed and Google scholar using the terms 'midwifery or midwife-led continuity of care' were used to locate key systematic and scoping reviews on the topic and identify relevant search terms for the systematic search strategy (see S1 Text for the search strategy). We then ...
Introduction. The International Confederation of Midwives' defines a midwife as "…a person who has successfully completed a midwifery education programme that is based on the International Confederation of Midwives (ICM) Essential Competencies for Midwifery Practice" [1].Midwives are educated, qualified professionals able to work within the core scope of practice on graduation ...
Article Google Scholar McNeill J, Lynn F, Alderdice F. Public health interventions in midwifery: a systematic review of systematic reviews. BMC Public Health. 2012;12:955. Article Google Scholar Lavender T, Bennett N, Blundell J, Malpass L. Midwives' views on redefining midwifery 1: health promotion.
In order to develop the search strategy, a preliminary search of PubMed and Google scholar using the terms 'midwifery or midwife-led continuity of care' were used to locate key system-atic and scoping reviews on the topic and identify relevant search terms for the systematic search strategy (see S1 Text for the search strategy).
This study aimed to explore the perceptions of Iranian midwives regarding respectful maternity care during labor and childbirth. This was a qualitative study which was conducted from September-December 2018 in two non-teaching public hospitals in Tehran, Iran. Twenty-four semi-structured interviews were conducted with midwives, who had more ...
Background Quality of care is essential for further progress in reducing maternal and newborn deaths. The integration of educated, trained, regulated and licensed midwives into the health system is associated with improved quality of care and sustained decreases in maternal and newborn mortality. To date, research on barriers to quality of care for women and newborns has not given due ...
Scaling up midwifery to reduce maternal and neonatal deaths has been identified as a global priority.1 Yet, the latest State of the World's Midwifery report outlines how midwifery work remains undervalued.2 Conventionally, professions are granted autonomy and social recognition for the services they provide but midwifery often lacks such status, potentially impeding midwives' success.
There was a dearth of primary research evidence of midwives' perspectives. Methods: A scoping review using the Johanna Briggs Institute three step approach was employed. First, an initial limited search of Google Scholar and CINAHL was undertaken to identify articles on the topic.
Midwives can help to substantially reduce maternal and neonatal mortality and stillbirths in LMICs. However, to realise this potential, midwives need to have skills and competencies in line with recommendations from the International Confederation of Midwives, to be part of a team of sufficient size and skill, and to work in an enabling environment. Our study highlights the potential of ...
Study design. Previous research has primarily identified the deficits of the midwifery practice experience and in doing so has potentially failed to appreciate supportive practices and behaviours already in place [3,4,5,6].When considering the prominence of negative experiences revealed in previous studies, an alternative methodology was sought to optimize the potential of capturing positive ...
Google Scholar] in the University's Bachelor of Midwifery curriculum as it positions the student 'with woman' ... Focus groups are an efficient method of collecting valuable insights into a topic and harnessing the power of a group dynamic to encourage conversation ... 'ISeeYou': a woman-centred care education and research project in ...
Study design. Previous research has primarily identified the deficits of the midwifery practice experience and in doing so has potentially failed to appreciate supportive practices and behaviours already in place [3-6].When considering the prominence of negative experiences revealed in previous studies, an alternative methodology was sought to optimize the potential of capturing positive ...
ObjectiveTo summarize and evaluate the experiences and expectations of newly qualified midwives (NQMs) during their transition from school to clinical practice. One of the main objectives was to provide references for the development of midwifery professional teaching and provide a basis for hospital administrators and instructors of midwifery to develop guidelines and strategies.MethodsA ...
Google Scholar provides a simple way to broadly search for scholarly literature. Search across a wide variety of disciplines and sources: articles, theses, books, abstracts and court opinions.
Midwifery is a research-based profession . ... [Google Scholar] 4. Say L, Souza JP, Pattinson RC. Maternal near miss-towards a standard tool for monitoring quality of maternal health care. ... Dean-Baar S, Pakieser-Reed K. Closing the gap between research and clinical practice. Topics in Stroke Rehabilitation. 2004; 11 (2):60-68. doi: 10. ...
1. INTRODUCTION. A key aspect of maternity care is a supportive relationship between the child‐bearing woman and her midwife or maternity nurse—the quality of this relationship is pivotal to safe maternity care and improving the woman′s experience (Agostini et al., 2015 ). Child‐bearing experiences can vary greatly among women.