Login Create an NNLM User Account

What Is Health Literacy?
According to the U.S. Department of Health and Human Services’ (HHS) Healthy People 2030 initiative , health literacy involves the information and services that people need to make well-informed health decisions. There are many aspects of health literacy:
- Personal health literacy is the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others. Examples of personal health literacy include understanding prescription drug instructions, understanding doctor’s directions and consent forms, and the ability to navigate the complex healthcare system.
- Organizational health literacy is the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others. Examples of organizational health literacy include simplifying the process to schedule appointments, using the Teach-Back method to ensure patient comprehension, and providing communications in the appropriate language, reading level and format.
- Digital health literacy, as defined by the World Health Organization , is the ability to seek, find, understand, and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem. Examples of digital health literacy include accessing your electronic health record, communicating electronically with your health care team, ability to discern reliable online health information, and using health and wellness apps.
- Numeracy , also known as quantitative literacy, refers to a set of mathematical and advanced problem-solving skills that are necessary to succeed in a society increasingly driven by data, as defined by the National Association of Secondary School Principals . Examples of Numeracy include understanding nutrition information, interpreting blood sugar readings, taking correct dosage of medication (ex. take one capsule twice a day), evaluating treatment benefits and risks, and understanding insurance costs and coverage.
Who Has Limited Health Literacy Skills?
Nearly 9 out of 10 adults struggle with health literacy. Even people with high literacy skills may have low health literacy skills in certain situations. For example, someone who is stressed and sick when they’re accessing health information may have trouble remembering, understanding, and using that information.
Why Is Health Literacy Important?
Health literacy involves more than reading — it also includes specific skills, like calculating the right dose of a medicine, following directions for fasting before a surgery, or checking a nutrition label to make sure an item is safe for someone with a food allergy. People with low health literacy skills may have trouble doing these things.
People with low health literacy skills are more likely to:
- Have poor health outcomes, including hospital stays and emergency room visits
- Make medication errors
- Have trouble managing chronic diseases
- Skip preventive services, like flu shots
People with higher health literacy skills are more likely to make informed health decisions. That means they’re more likely to be healthy — and even to live longer.
How Can We Address Health Literacy?
Communicating clearly with people helps them find and understand health information. And when people understand health information, they can make well-informed health decisions.
We can also consider taking these steps to address health literacy:
- Ensure that people in the community can easily access the health information they need
- Create and provide plain language health materials in different languages
- Provide trainings to teach health professionals and others who provide health information about health literacy best practices
- Create clearinghouses of information about health literacy for health professionals
- Review health materials (like insurance forms and medication instructions) with community members to help make sure they understand the information — and what actions they need to take
You can find more information about Health Literacy in MedlinePlus . To find journal articles about Health Literacy, you can use the MEDLINE/PubMed health literacy search to retrieve citations to English language journal literature.
How does NNLM support Health Literacy?
Training. The Network of the National Library of Medicine offers training for those who provide health information to the public such as our On Demand Health Literacy Class . Many of our trainings support the understanding of health literacy and its effects on health while others help professionals gain needed skills to address health literacy in their communities.
Resources. NNLM creates and promotes resources that can support network members in improving the health literacy of their communities. These resources include:
- Clinical Conversations is a training program for clinicians about health literacy and related concepts. This program allows clinical trainers or managers to offer brief trainings embedded into existing meetings or trainings as a way to offer continuing education that does not take time out of already busy schedules.
- Project SHARE is a program developed by the University of Maryland Health Sciences and Human Services Library and funded by the National Library of Medicine. Project SHARE aims to build high school students' skills to reduce health disparities at the personal, family and community level. Module II of the curriculum focuses on health literacy.
- Digital Health Literacy Tools from NNLM and All of Us in partnership with the Public Library Association (PLA) and Wisconsin Health Literacy aim to reach people on the other side of the digital divide. These tools help people gain the digital literacy skills needed to access and evaluate health information online and to participate in the All of Us Research Program (All of Us).
- Evaluating Internet Health Information: A Tutorial from the National Library of Medicine and MedlinePlus teaches people how to evaluate a variety of sources on the internet to determine how to find reliable sources. This also teaches people how to make proactive decisions about their health.
Funding. NNLM’s Regional Medical Libraries offer grant funding in their respective regions. Funded projects often address health literacy by linking members of the community with quality health information resources and providing training on their use. Other projects address health literacy by offering training to information professionals, healthcare providers or other health professionals about how to support and address health literacy in their communities. Select projects are highlighted in the videos below. More information about funding, including additional previously funded projects is available on NNLM’s funding page.
Promotores de Salud (Tucson, AZ)
NLM Outreach - Wash and Learn (St Paul, MN)
Technology Outreach to Reduce Health Disparities and Stigma
Health Literacy Projects
Browse NNLM's past funded projects to gain inspiration for your health literacy project.
Health Literacy in Healthy People 2030
Health literacy is a central focus of Healthy People 2030. One of the initiative’s overarching goals demonstrates this focus: “Eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all.”
Watch this video to learn more about health literacy:
Which Healthy People 2030 objectives are related to health literacy?
Six Healthy People objectives — developed by the Health Communication and Health Information Technology Workgroup — are related to health literacy:
- Increase the proportion of adults whose health care provider checked their understanding — HC/HIT‑01
- Decrease the proportion of adults who report poor communication with their health care provider — HC/HIT‑02
- Increase the proportion of adults whose health care providers involved them in decisions as much as they wanted — HC/HIT‑03
- Increase the proportion of people who say their online medical record is easy to understand — HC/HIT‑D10
- Increase the proportion of adults with limited English proficiency who say their providers explain things clearly — HC/HIT‑D11
- Increase the health literacy of the population — HC/HIT‑R01
How does Healthy People define health literacy?
Healthy People 2030 addresses both personal health literacy and organizational health literacy and provides the following definitions:
- Personal health literacy is the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.
- Organizational health literacy is the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.
These definitions are a change from the health literacy definition used in Healthy People 2010 and Healthy People 2020: “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions.” The new definitions:
- Emphasize people’s ability to use health information rather than just understand it
- Focus on the ability to make “well-informed” decisions rather than “appropriate” ones
- Incorporate a public health perspective
- Acknowledge that organizations have a responsibility to address health literacy
Learn more about the history of Healthy People’s health literacy definitions .
Personal health literacy
Healthy People 2030’s definition of personal health literacy is aligned with the concept that people’s health literacy can be assessed at a given point in time. Such a definition is important for conducting both population studies and research on interventions aimed at ensuring equal access to information and services for people with limited literacy skills.
The new definition — with its emphasis on the use of health information and its public health perspective — may also prompt new ways of studying and promoting personal health literacy. In addition, it encourages efforts to address the skills that help people move from understanding to action and from a focus on their own health to a focus on the health of their communities.
Organizational health literacy
By adopting a definition for organizational health literacy, Healthy People acknowledges that personal health literacy is contextual and that producers of health information and services have a role in improving health literacy. The definition also emphasizes organizations’ responsibility to equitably address health literacy, in line with Healthy People 2030’s overarching goals.
In addition, including a definition for organizational health literacy in Healthy People aligns with the HHS National Action Plan to Improve Health Literacy .
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
Patient education and health literacy
Affiliations.
- 1 Research Group Lifestyle and Health, Utrecht University of Applied Sciences, Heidelberglaan 7, 3584 CS, Utrecht, The Netherlands. Electronic address: [email protected].
- 2 Research Group Lifestyle and Health, Utrecht University of Applied Sciences, Heidelberglaan 7, 3584 CS, Utrecht, The Netherlands.
- PMID: 30017902
- DOI: 10.1016/j.msksp.2018.06.004
Introduction: Patient education is a relatively new science within the field of health care. In the past it consisted mainly of the transfer of knowledge and mostly biomedically based advice. Research has shown this to not be effective and sometimes counterproductive. As health care has moved away from applying a traditional paternalistic approach of 'doctor knows best' to a patient-centred care approach, patient education must be tailored to meet persons' individual needs.
Purpose: The purpose of this master paper is to increase awareness of patients' health literacy levels. Health literacy is linked to literacy and entails people's knowledge, motivation and competences to access, understand, appraise and apply health information in order to make judgements and take decisions in everyday life concerning health care, disease prevention and health promotion to maintain or improve quality of life during the life course. Many patients have low health literacy skills, and have difficulty with reading, writing, numeracy, communication, and, increasingly, the use of electronic technology, which impede access to and understanding of health care information.
Implications: Multiple professional organizations recommend using universal health literacy precautions to provide understandable and accessible information to all patients, regardless of their literacy or education levels. This includes avoiding medical jargon, breaking down information or instructions into small concrete steps, limiting the focus of a visit to three key points or tasks, and assessing for comprehension by using the teach back cycle. Printed information should be written at or below sixth-grade reading level. Visual aids can enhance patient understanding.
Keywords: Biopsychosocial; Health literacy; Patient centred care; Patient education.
Copyright © 2018 Elsevier Ltd. All rights reserved.
- Aged, 80 and over
- Health Knowledge, Attitudes, Practice*
- Health Literacy*
- Middle Aged
- Patient Education as Topic / methods*
- Patient-Centered Care / methods*
- MEMBER DIRECTORY
- Member Login
- Publications
- Clinician Well-Being
- Culture of Health and Health Equity
- Fellowships and Leadership Programs
- Future of Nursing
- U.S. Health Policy and System Improvement
- Healthy Longevity
- Human Gene Editing
- U.S. Opioid Epidemic
- Staff Directory
- Opportunities
- Action Collaborative on Decarbonizing the U.S. Health Sector
- Climate Communities Network
- Communicating About Climate Change & Health
- Research and Innovation
- Culture of Health
- Fellowships
- Emerging Leaders in Health & Medicine
- Culture & Inclusiveness
- Digital Health
- Evidence Mobilization
- Value Incentives & Systems
- Substance Use & Opioid Crises
- Reproductive Health, Equity, & Society
- Credible Sources of Health Information
- Emerging Science, Technology, & Innovation
- Pandemic & Seasonal Influenza Vaccine Preparedness and Response
- Preventing Firearm-Related Injuries and Deaths
- Vital Directions for Health & Health Care
- NAM Perspectives
- All Publications
- Upcoming Events
- Past Events
- MEMBER HOME

Health Literacy and Health Education in Schools: Collaboration for Action

Introduction
This NAM Perspectives paper provides an overview of health education in schools and challenges encountered in enacting evidence-based health education; timely policy-related opportunities for strengthening school health education curricula, including incorporation of essential health literacy concepts and skills; and case studies demonstrating the successful integration of school health education and health literacy in chronic disease management. The authors of this manuscript conclude with a call to action to identify upstream, systems-level changes that will strengthen the integration of both health literacy and school health education to improve the health of future generations. The COVID-19 epidemic [10] dramatically demonstrates the need for children, as well as adults, to develop new and specific health knowledge and behaviors and calls for increased integration of health education with schools and communities.
Enhancing the education and health of school-age children is a critical issue for the continued well-being of our nation. The 2004 Institute of Medicine (IOM, now the National Academies of Sciences, Engineering, and Medicine [NASEM]) report, Health Literacy: A Prescription to End Confusion [27] noted the education system as one major pathway for improving health literacy by integrating health knowledge and skills into the existing curricula of kindergarten through 12th-grade classes. The NASEM Roundtable on Health Literacy has held multiple workshops and forums to “inform, inspire, and activate a wide variety of stakeholders to support the development, implementation, and sharing of evidence-based health literacy practices and policies” [37]. This paper strives to present current evidence and examples of how the collaboration between health education and health literacy disciplines can strengthen K–12 education, promote improved health, and foster dialogue among school officials, public health officials, teachers, parents, students, and other stakeholders.
This discussion also expands on a previous NAM Perspectives paper, which identified commonalities and differences in the fields of health education, health literacy, and health communication and called for collaboration across the disciplines to “engage learners in both formal and informal health educational settings across the life span” [1]. To improve overall health literacy, i.e., “the capacity of individuals to obtain, process, and understand basic health information and services needed to make appropriate health decisions” [42], it is important to start with youth, when life-long health habits are first being formed.
Another recent NAM Perspectives paper proposed the expansion of the definition of health literacy to include broader contextual factors, including issues that impact K–12 health education efforts like state rather than federal control of education priorities and administration, and subsequent state- or local-level laws that impact specific school policies and practices [39]. In addition to addressing individual needs and abilities, socio-ecological factors can impact a student’s health. For example, the Centers for Disease Control and Prevention (CDC) uses a four-level social-ecological model to describe “the complex interplay” of (1) individuals (biological and personal history factors), (2) relationships (close peers, family members), (3) community (settings such as neighborhoods, schools, after-school locations), and (4) societal factors (cultural norms, policies related to health and education, or inequalities between groups in societies) that put one at risk or prevent him/her from experiencing negative health outcomes [11]. Also worth examining are protective factors that help children and adolescents avoid behaviors that place them at risk for adverse health and educational outcomes (e.g., self-efficacy, self-esteem, parental support, adult mentors, and youth programs) [21,59].
Recognizing the influence of this larger social context on learning and health can help catalyze both individual and community-based solutions. For example, students with chronic illnesses such as asthma, which can affect their school attendance, can be educated about the impact of air quality or housing (e.g., mold, mites) in exacerbating their condition. Students in varied locations and at a range of ages continue, often with the guidance of adults, to take health-related social action. Various local, national, and international examples illustrate high schoolers taking social action related to health issues such as tobacco, gun safety, and climate change [18,21,57].
By employing a broad approach to K–12 education (i.e., using combined principles of health education and health literacy), the authors of this manuscript foresee a template for the integration of skills and abilities needed by both school health professionals and children and parents to increase health knowledge for a lifetime of improved health [1,29,31].
The right measurements to evaluate success and areas that need improvement must be clearly identifed because in all matters related to health education and health literacy, it is vital to document the linkages between informed decisions and actions. Often, individuals are presumed to be making informed decisions when actually broader socio-ecological factors are predominant behavioral influences (e.g., an individual who is overweight but has never learned about food labeling and lives in a community where there are no safe places to be physically active).
Health Education in Schools
Standardized and broadly adopted strategies for how health education is implemented in schools—and by whom and on what schedule—is a continuing challenge. Although the principles of health literacy are inherently important to any instruction in schools and in community settings, the most effective way to incorporate those principles in existing and differing systems becomes a key to successful health education for children and young people.
The concept of incorporating health education into the formal education system dates to the Renaissance. However, it did not emerge in the United States until several centuries later [26]. In the early 19th century, Horace Mann advocated for school-based health instruction, while William Alcott also underscored the contributions of health services and the school environment to children’s health and well-being [17]. Public health pioneer Lemuel Shattuck wrote in 1850 that “every child should be taught early in life, that to preserve his own life and his own health and the lives of others, is one of the most important and abiding duties” [43]. During this same time, Harvard University and other higher education institutions with teacher preparation programs began including hygiene (health) education in their curricula.
Despite such early historical recognition, in the mid-1960s, the School Health Education Study documented serious disarray in the organization and administration of school health education programs [45]. A renewed call to action, several decades later, introduced the concepts of comprehensive school health programs and school health education [26].
From 1998 through 2014, the CDC and other organizations began using the term “coordinated school health programs” to encompass eight components affecting children’s health in schools, including nutrition, health services, and health instruction. Unfortunately, the term was not broadly embraced by the educational sector, and in 2014, CDC and ASCD (formerly the Association for Supervision and Curriculum Development) unveiled the Whole School, Whole Community, Whole Child (WSCC) framework [36]. This framework has ten components, including health education, which aims to ensure that each student is healthy, safe, engaged, supported, and challenged. Among the foundational tenets of the framework is ensuring that every student enters school healthy and, while there, learns about and practices a healthy lifestyle.
At its core, health education is defined as “any combination of planned learning experiences using evidence-based practices and/or sound theories that provide the opportunity to acquire knowledge, attitudes, and skills needed to adopt and maintain healthy behaviors” [3]. Included are a variety of physical, social, emotional, and other components focused on reducing health-risk behaviors and promoting healthy decision making. Health education curricula emphasize a skills-based approach to help students practice and advocate for their health needs, as well as the needs of their families and their communities. These skills help children and adolescents find and evaluate health information needed for making informed health decisions and ultimately provide the foundation of how to advocate for their own well-being throughout their lives.
In the last 40 years, many studies have documented the relationship between student health and academic outcomes [29,40,41]. Health-related problems can diminish a student’s motivation and ability to learn [4]. Complications with vision, hearing, asthma, occurrences of teen pregnancy, aggression and violence, lack of physical activity, and low cognitive and emotional ability can reduce academic success [4].
To date, there have been no long-term sequential studies of the impact of K–12 health education curricula on health literacy or health outcomes. However, research shows that students who participate in health education curricula in combination with other interventions as part of the coordinated school health model (i.e., physical activity, improved nutrition, and/or family engagement) have reduced rates of obesity and/ or improved health-promoting behaviors [25,30,34]. In addition, school health education has been shown to prevent tobacco and alcohol use and prevent dating aggression and violence. Teaching social and emotional skills improves the academic behaviors of students, increases motivation to do well in school, enhances performance on achievement tests and grades, and improves high school graduation rates.
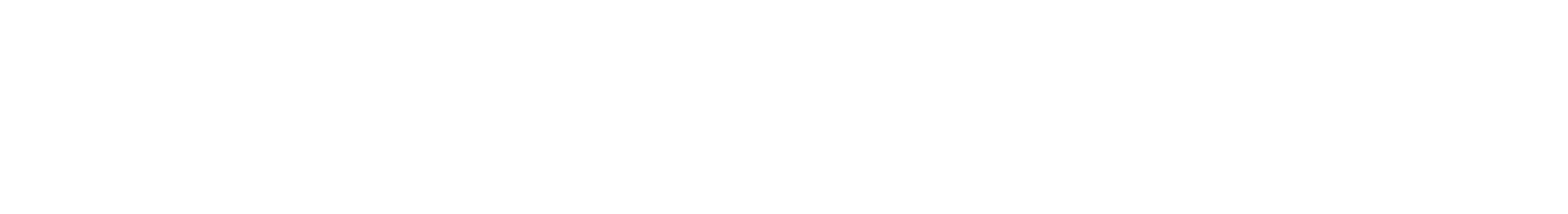
As with other content areas, it is up to the state and/or local government to determine what should be taught, under the 10th Amendment to the US Constitution [48]. However, both public and private organizations have produced seminal documents to help guide states and local governments in selecting health education curricula. First published in 1995 and updated in 2004, the National Health Education Standards (NHES) framework comprises eight health education foundations for what students in kindergarten through 12th grade should know and be able to do to promote personal, family, and community health (see Table 1 ) [12]. The NHES framework serves as a reference for school administrators, teachers, and others addressing health literacy in developing or selecting curricula, allotting instructional resources, and assessing student achievement and progress. The NHES framework contains written expectations for what students should know and be able to do by grades 2, 5, 8, and 12 to promote personal, family, and community health.
The Coordinated Approach to Child Health (CATCH) model, which was first developed in the late 1980s with funds by the National Heart, Lung, and Blood Institute, serves to implement the NHES framework and was the largest school-based health promotion study ever conducted in the United States. CATCH has 25 years of continuous research and development of its programs [24] and aligns with the WSCC framework. Individualized programs like the CATCH model develop programming based on the NHES framework at the local level, so that local control still exists, but the mix and depth of topics can vary based on need and composition of the community.
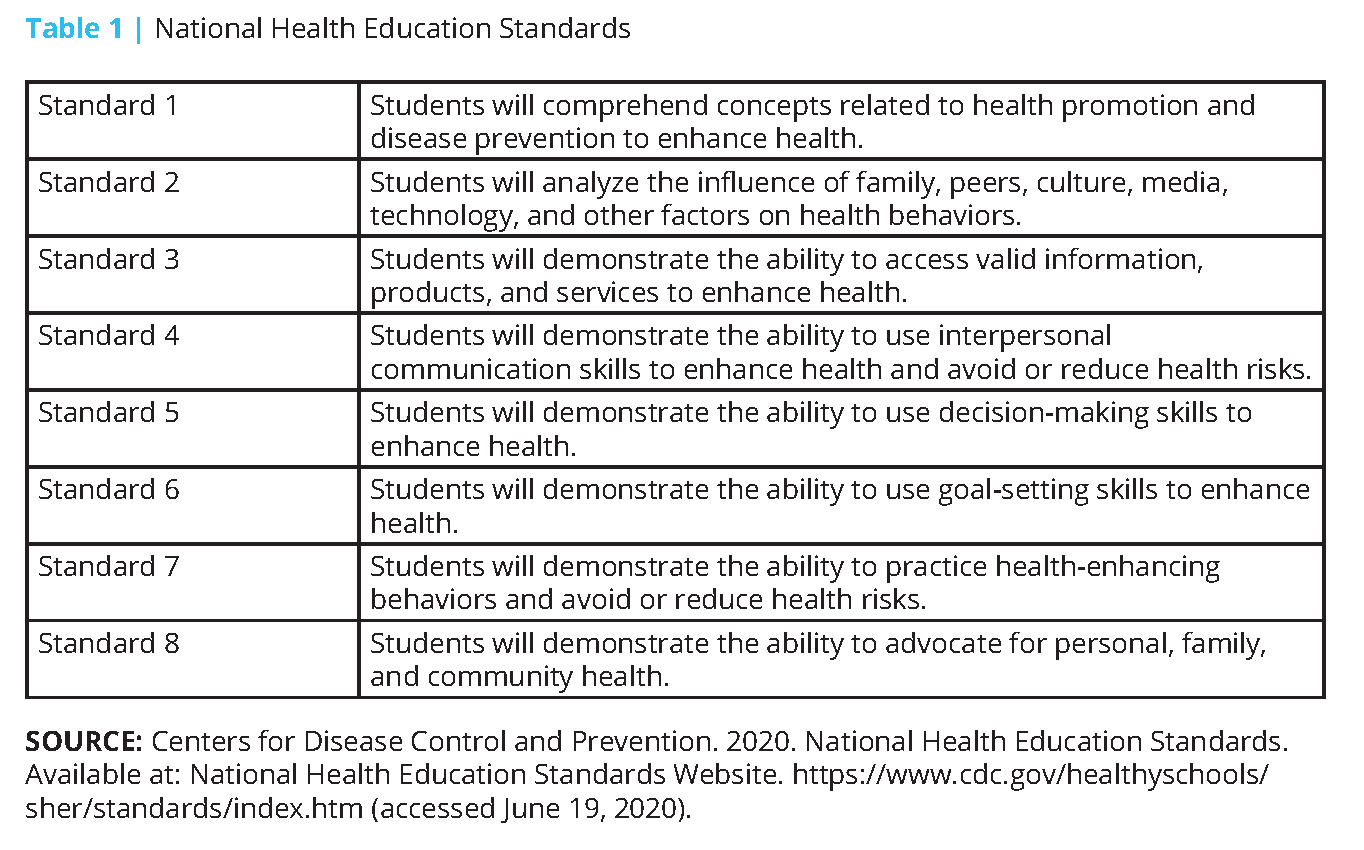
Based on reviews of effective programs and curricula and experts in the field of health education, CDC recommends that today’s state-of-the-art health education curricula emphasize four core elements: “Teaching functional health information (essential knowledge); shaping personal values and beliefs that support healthy behaviors; shaping group norms that value a healthy lifestyle; and developing the essential health skills necessary to adopt, practice, and maintain health enhancing behavior” [13]. In addition to the 15 characteristics presented in Box 1 , the CDC website has more detailed explanations and examples of how the statements could be put into practice in the classroom. For example, a curriculum that “builds personal competence, social competence, and self-efficacy by addressing skills” would be expected to guide students through a series of developmental steps that discuss the importance of the skill, its relevance, and relationship to other learned skills; present steps for developing the skill; model the skill; practice and rehearse the skill using real-life scenarios; and provide feedback and reinforcement.
In addition, CDC has developed a Health Education Curriculum Analysis Tool [14] to help schools conduct an analysis of health education curricula based on the NHES framework and the Characteristics of an Effective Health Education Curriculum.
Despite CDC’s extensive efforts during the past 40 years to help schools implement effective school health education and other components of the broader school health program, the integration of health education into schools has continued to fall short in most US states and cities. According to the CDC’s 2016 School Health Profiles report, the percentage of schools that required any health education instruction for students in any of grades 6 through 12 declined. For example, 8 in 10 US school districts only required teaching about violence prevention in elementary schools and violence prevention plus tobacco use prevention in middle schools, while instruction in only seven health topics was required in most high schools [6].
Although 8 of every 10 districts required schools to follow either national, state, or district health education standards, just over a third assessed attainment of health standards at the elementary level while only half did so at the middle and high school levels [6]. No Child Left Behind legislation, enacted in 2002, emphasized testing of core subjects, such as reading, science, and math, which resulted in marginalization of other subjects, including health education [22,31]. Academic subjects that are not considered “core” are at risk of being eliminated as public school principals and administrators struggle to meet adequate yearly progress for core subjects, now required to maintain federal funding.
In addition to the quality and quantity of health education taught in schools, there are numerous problems related to those considered qualified to provide instruction [5,7]. Many school and university administrators lack an understanding of the distinction between health education and physical education (PE) [9,16,19] and consider PE teachers to be qualified to teach health education. Yet the two disciplines differ regarding national standards, student learning outcomes, instructional content and methods, and student assessment [5]. Kolbe notes that making gains in school health education will require more interdisciplinary collaboration in higher education (e.g., those training the public health workforce, the education workforce, school nurses, pediatricians) [29]. Yet faculty who train various school health professionals usually work within one university college, focus on one school health component, and affiliate with one national professional organization. In addition, Kolbe notes that health education teachers in today’s workforce often lack support and resources for in-service professional development.
Promising Opportunities for Strengthening School Health Education
Comprehensive health education can increase health literacy, which has been estimated to cost the nation $1.6 to $3.6 trillion dollars annually [54]. The National Action Plan to Improve Health Literacy by the US Department of Health and Human Services (HHS) includes the goal to “Incorporate accurate, standards-based, and developmentally appropriate health and science information and curricula in childcare and education through the university level” [49].
HHS’s Healthy People Framework presents another significant opportunity for tracking health in education as well as health literacy. The Healthy People initiative launched officially in 1979 with the publication of Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention [50]. This national effort establishes 10-year goals and objectives to improve the health and well-being of people in the United States. Since its inception, Healthy People has undertaken extensive efforts to collect data, assess progress, and engage multi-stakeholder feedback to set objectives for the next ten years. The Healthy People 2020 objectives were self-described as having input from public health and prevention experts, a wide range of federal, state, and local government officials, a consortium of more than 2,000 organizations, and perhaps most importantly, the public” [51]. In addition to other childhood and adolescent objectives (e.g., nutrition, physical activity, vaccinations), Healthy People 2020 specified social determinants as a major topic for the first time. A leading health indicator for social determinants was “students graduating from high school within 4 years of starting 9th grade (AH-5.1)” [52]. The Secretary’s Advisory Committee report on the Healthy People 2030 objectives includes the goal to “eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all” [53]. The national objectives are expected to be released in summer 2020 and will help catalyze “leadership, key constituents, and the public across multiple sectors to take action and design policies that improve the health and well-being of all” [53].
In terms of supports in federal legislation, the Every Student Succeeds Act (ESSA) of 2015 recognized health education as a distinct discipline for the first time and designated it as a “well-rounded” education subject [2,22]. According to Department of Education guidelines, each state must submit a plan that includes four academic indicators that include proficiency in math, English, and English-language proficiency. High schools also must use their graduation rates as their fourth indicator, while elementary and middle schools may use another academic indicator. In addition, states must specify at least one nonacademic indicator to measure school quality or school success, such as health education. Under the law, federal funding also is available for in-service instruction for teachers in well-rounded education subjects such as health education. These two items open additional pathways for both identifying existing or added programs and having the capacity to collect data.
While several states have chosen access to physical education, physical fitness, or school climate as their nonacademic indicators of school success, the majority (36 states and the District of Columbia) have elected to use chronic absenteeism [2]. Given the underlying causal connection between student health and chronic absenteeism, absenteeism as an indicator represents a significant opportunity to raise awareness of chronic health conditions or other issues (e.g., student social/emotional concerns around bullying, school safety) that contribute to absenteeism. It also represents a significant opportunity for schools to work with stakeholders to prevent and manage such health conditions through school health education and other WSCC strategies to improve school health. Educators are more likely to support comprehensive health education if they are made aware of its immediate benefits related to student learning (e.g., less disruptive behavior, improved attention) and maintaining safe social and emotional school climates [31].
In an assessment of how states are addressing WSCC, Child Trends reported that health education is either encouraged or required for all grades in all states’ laws, with nutrition (40 states) and personal health (44 states) as the most prominent topics [15]. However, the depth and breadth of such instruction in schools is not known, nor if health education is being taught by qualified teachers. In 25 states, laws address or otherwise incorporate the NHES as part of the state health education curriculum.
The authors’ review of state 2017–2018 ESSA plans, analyzed by the organization Cairn, showed nine states that have specifically identified health education as one of its required well-rounded subjects (Florida, Georgia, Indiana, Louisiana, Maine, Maryland, Nevada, North Dakota, and Tennessee) [8]. Cairn recommends that most states include health education and physical education in state accountability systems, school report card indicators, school improvement plans, professional development plans, needs assessment tools, and/or prioritized funding under Title IV, Part A.
In 2019, representatives of the National Committee on the Future of School Health Education, sponsored by the Society for Public Health Education (SOPHE) and the American School Health Association (ASHA), published a dozen recommendations for strengthening school health education [5,31,55]. The recommendations addressed issues such as developing and adopting standardized measures of health literacy in children and including them in state accountability systems; changing policies, practices, and systems for quality school health education (e.g., establishing Director of School Health Education positions in all state and territory education agencies tasked with championing health education best practices, and holding schools accountable for improving student health and wellbeing); and strengthening certification, professional preparation, and ongoing professional development in health education for teachers at both the elementary and secondary levels. Recommendations also call for stronger alignment and coordination between the public health and education sectors. The committee is now moving ahead on prioritizing the recommendations and developing action steps to address them.
Integrating Youth Health Education and Health Literacy: Success Stories
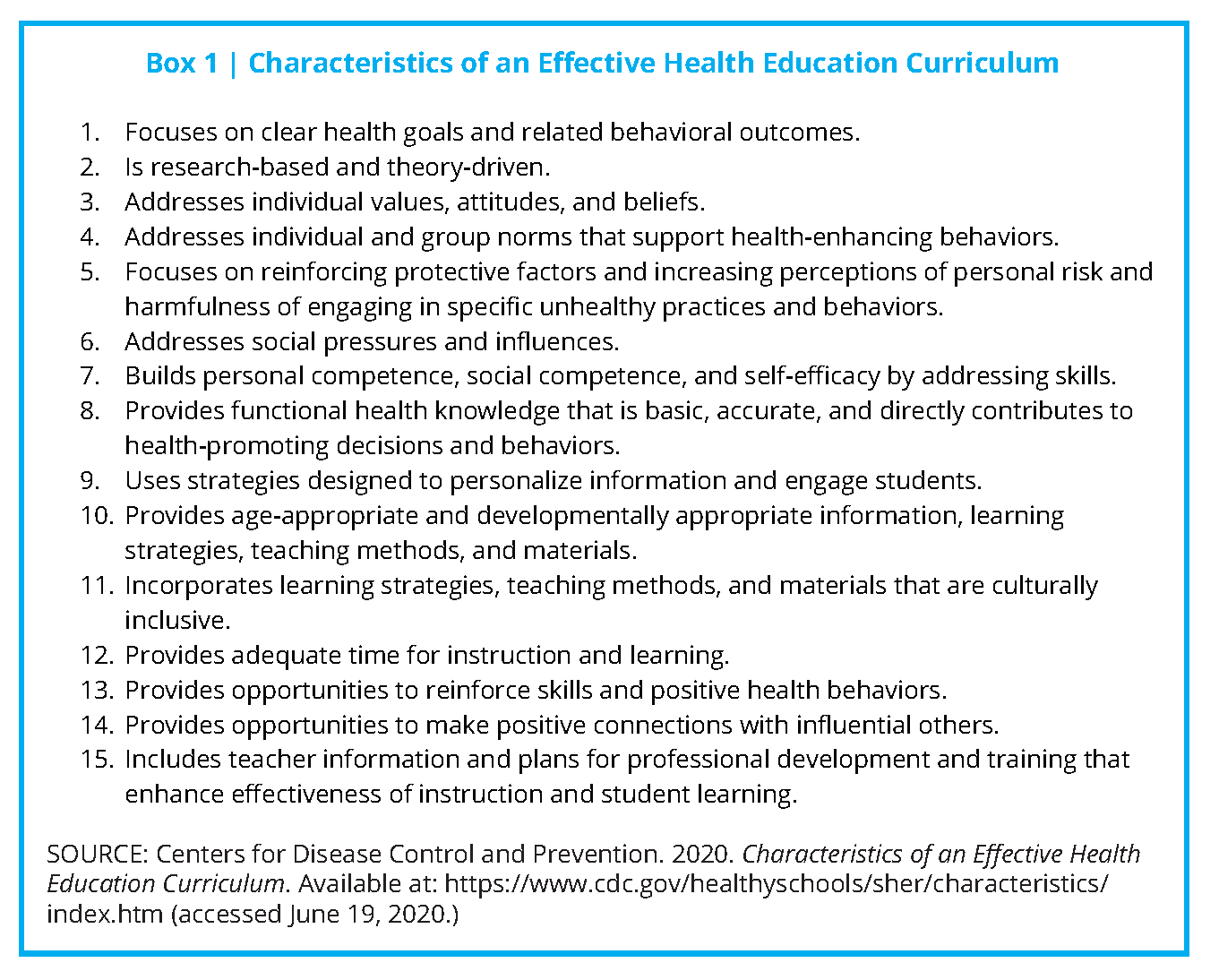
Minnesota statewide model: integrating school health education and health literacy through broad partnership.
The Roundtable on Health Literacy held a workshop on health literacy and public health in 2014, with examples of how state health departments are addressing health literacy in their states [28]. One recent example of a strong collaboration between K–12 education and public health agencies is the Statewide Health Improvement Partnership (SHIP) within the Minnesota Department of Health’s Office of Statewide Health Initiative [35].
SHIP was created by a landmark 2008 Minnesota health reform law. The law was intended to improve the health of Minnesotans by reducing the risk factors that lead to chronic disease. The program funds grantees in all of the state’s 87 counties and 10 tribal nations to support the creation of locally driven policies, systems, and environmental changes to increase health equity, improve access to healthy foods, provide opportunities for physical activity, and ensure a tobacco-free environment [35]. Local public health agencies collaborate with partners including schools, childcare settings, workplaces, multiunit housing facilities, and health care centers through SHIP.
SHIP models the integration of (1) law, (2) policy, (3) goal-setting, and (4) resource building and forging some 2,000 collaborative partnerships and measuring outcomes. SHIP sets a helpful example for others attempting to create synergies across the intersections of state government, health education, local communities, and private organizations. The principles of health literacy are within these collaborations.
Grantees throughout the state have received technical assistance and training to improve school nutrition and physical activity strategies (see Figure 1 ). SHIP grantees and their local school partner sites set goals and adopt best practices for physical education and physical activity inside and outside the classroom. They improve access to healthy food environments through locally sourced produce, lunchrooms with healthier food options, and school-based agriculture. In 2017, SHIP grantees partnered with 995 local schools and accounted for 622 policy, systems, and environmental changes.
Minnesota has also undertaken a broad approach to health literacy by educating stakeholders and decision-makers (i.e., administrators, food service and other staff, students, community partners, and parents) about various health-related social and environmental issues to reduce students’ chronic disease risks.
SHIP grantees assist in either convening or organizing an established school health/wellness council that is required by USDA for each local education agency participating in the National School Lunch Program and/or School Breakfast Program [46,47]. A local school wellness policy is required to address the problem of childhood obesity by focusing on nutrition and physical activity. SHIP also requires schools to complete an assessment that aligns with the WSCC model and provides annual updates. Once the assessment is completed by a broad representation of stakeholders, SHIP grantees assist schools in prioritizing and working toward annual goals. The goal-setting and assessment and goal-setting cycle is continuous.
The Bigger Picture: A Case Study of Community Integration of Health Education and Health Literacy
Improving the health literacy of young people not only influences their personal health behaviors but also can influence the health actions of their peers, their families, and their communities. According to the SEARCH for Diabetes in Youth study funded by the CDC and the National Institutes of Health’s National Institute of Diabetes, Digestive, and Kidney Diseases, from 2002 to 2012, the national rate of new diagnosed cases of Type 2 diabetes increased 4.8% [32]. Among youth ages 10-19, the rate of new diagnosed cases of Type 2 diabetes rose most sharply in Native Americans (8.9%) (although not generalizable to all Native American youth because of small sample size), compared to Asian Americans/Pacific Islanders (8.5%), non-Hispanic blacks (6.3%), Hispanics (3.1%), and non-Hispanic whites (0.6%).
Since 2011, Dean Schillinger, Professor of Medicine in Residence at the University of California San Francisco and Chief of the Diabetes Prevention and Control Program for the California Department of Public Health, has led a capacity-building effort to address Type 2 diabetes [23,28,44].
This initiative called The Bigger Picture (TBP) has mobilized collaborators to create resources by and for young adults focused on forestalling and, hopefully, reversing the distressing increase in pediatric Type 2 diabetes by exposing the environmental and social conditions that lead to its spread. Type 2 diabetes is increasingly affecting young people of color, and TBP is specifically developed by and directed to them.
TBP seeks to increase the number of well-informed young people who can participate in determining their own lifelong health behaviors and influencing those of their friends, families, communities, and their own children. The project aims to create a movement that changes the conversation about diabetes from blame-and-shame to the social drivers of the epidemic [23].
TPB is described by the team that created it as a “counter-marketing campaign using youth-created, spoken-word public services announcements to reframe the epidemic as a socio-environmental phenomenon requiring communal action, civic engagement, and norm change” [44]. The research team provides a description of questionnaire responses to nine of the public service announcements in the context of campaign messages, film genre and accompanying youth value, participant understanding of fi lm’s public health message, and the participant’s expression of the public health message. The investigators also correlate the responses with dimensions of health literacy such as conceptual foundations, functional health literacy, interactive health literacy, critical skills, and civic orientation.
One of the campaign partners, Youth Speaks, has created a toolkit to equip and empower students and communities to become change agents in their respective environments, raising their voices and joining the conversation about combating the spread of Type 2 diabetes [56].
In a discussion of qualitative evaluations of TBP and what low-income youth “see,” Schillinger et al. note that “TBP model is unique in how it nurtures and supports the talent, authenticity, and creativity of new health messengers: youth whose lived experience can be expressed in powerful ways” [44].
COVID-19: Health Crisis Affecting Children and their Families and a Need for Health Education and Health Literacy in K-12
In a recent op-ed, Rebecca Winthrop, co-director of the Center for Universal Education and Senior Fellow of Global and Economic Development of the Brookings Institution asked, “COVID-19 is a health crisis. So why is health education missing from school work?” [58] She notes that “helping sustain education amid crises in over 20 countries, I’ve learned that one of the first things you do, after finding creative ways to continue educational activities, is to incorporate life-saving health and safety messages.” Her call is impassioned for age-appropriate, immediately available resources on COVID-19 that can be easily incorporated into distance lesson plans for both children and families. Many organizations, such as Child Trends, are curating collections of such resources. Framing these materials using principles of health literacy and incorporating them into health education messages and resources may be an ideal model for incorporating new pathways for public health K–12 learning.
Call to Action for Collaboration
Strategic and dedicated efforts are needed to bridge health education and health literacy. These efforts would foster the expertise to provide students with the information needed to access and assess useful health information, and to develop the necessary skills for an emerging understanding of health.
Starting with students in school settings, learning to be health literate helps overcome the increased incidence of chronic diseases such as Type 2 diabetes, and imbues a sense of self-efficacy and empowerment through health education. It also sets the course for lifelong habits, skills, and decision making, which can also influence community health.
Pursuing institutional changes to reduce disparities and improve the health of future generations will require significant collaboration and quality improvement among leaders within health education and health literacy. Recommendations provided in previous reports such as IOM’s 1997 report, Schools and Health: Our Nation’s Investment [26]; the 2004 IOM report on Health Literacy [27]; and the 2010 National Action Plan to Improve Health Literacy [49] should be revisited. More recently, a November 2019 Health Literacy Roundtable Workshop (1) explored the necessity of developing health literacy skills in youth, (2) examined the research on developmentally appropriate health literacy milestones and transitions and measuring health literacy in youth, (3) described programs and policies that represent best practices for developing health literacy skills in youth, and (4) explored potential collaborations across disciplines for developing health literacy skills in youth [38]. With its resulting report, the information provided in the workshop should provide additional insights into collaborations needed to reduce institutional barriers to youth health literacy and empowerment.
At the national level, representatives from public sector health and education levels (e.g., HHS’s Office of Disease Prevention and Health Promotion, CDC, Department of Education) can collaborate with school-based nongovernmental organizations (e.g., SOPHE, ASCD, ASHA, National Association of State Boards of Education, School Superintendents Association, Council of Chief State School Officers, Society of State Leaders of Health and Physical Education) to provide data and lead reform efforts. Leaders of higher education (e.g., Association of American Colleges and Universities, Association of Schools and Programs of Public Health) can join with philanthropies and educational scholars to pursue curricular reforms and needed research to further health education and health literacy as an integral component of higher education.
Among the approaches needed are (1) careful incorporation of key principles of leadership within systems; (2) the training and evaluation of professionals; (3) finding and sharing replicable, effective examples of constructive efforts; and (4) including young people in the development of information and materials to ensure their accessibility, appeal, and utility. Uniting the wisdom, passion, commitment, and vision of the leaders in health literacy and health education, we can forge a path to a healthier generation.
Join the conversation!
Download the graphics below and share them on social media!
- Allen, M., E. Auld, R. Logan, J. Henry Montes, and S. Rosen. 2017. Improving collaboration among health communication, health education, and health literacy. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201707c
- Alliance for a Healthier Generation. 2018. Every Student Succeeds Act Frequently Asked Questions. Available at: https://www.healthiergeneration.org/sites/default/files/documents/20180814/3beb1de8/ESSA-FAQ.pdf (accessed May 3, 2020).
- American Association for Health Education. 2012. Report of the 2011 Joint Committee on Health Education and Promotion Terminology. American Journal of Health Education 43:sup2, 1-19. https://doi.org/10.1080/19325037.2012.11008225
- Basch, C. E. 2011. Healthier students are better learners: A missing link in school reforms to close the achievement gap. Journal of School Health 81:593-598. Available at: https://healthyschoolscampaign.org/wp-content/uploads/2017/03/AMissing-Link-in-School-Reforms-to-Closethe-Achievement-Gap.pdf (accessed May 18, 2020).
- Birch, D. A., S. Goekler, M. E. Auld, D. K. Lohrmann, and A. Lyde. 2019. Quality assurance in teaching K–12 health education: Paving a new path forward. Health Promotion Practice 20(6):845-857. https://doi.org/10.1177/1524839919868167
- Brener, N. D., Z. Demissie, T. McManus, S. L. Shanklin, B. Queen, and L. Kann. 2017. School Health Profiles 2016: Characteristics of Health Programs Among Secondary Schools. Atlanta, GA: Centers for Disease Control and Prevention. Available at: https://www.cdc.gov/healthyyouth/data/profiles/pdf/2016/2016_Profiles_Report.pdf (accessed May 18, 2020).
- McCormack Brown, K. R. 2013. Health education in higher education: What is the future? American Journal of Health Education 44(5):245-251. https://doi.org/10.1080/19325037.2013.807755
- Cairn. 2020. State ESSA Plans . Available at: http://www.cairnguidance.com/essa-plans/ (accessed May 3, 2020).
- Cardina, C. 2014. Academic majors and subject-area certifications of health education teachers in the United States, 2011-2012. Journal of Health Education Teaching 5(1):35-43. Available at: https://eric.ed.gov/?id=EJ1085288 (accessed May 18, 2020).
- Centers for Disease Control and Prevention (CDC). 2020. Coronavirus Disease 2019 (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/ (accessed June 17, 2020).
- Centers for Disease Control and Prevention (CDC). 2015. Principles of community engagement, 2nd ed. Atlanta, GA: CDC/ATSDR Committee on Community Engagement. Available at: https://www.atsdr.cdc.gov/communityengagement/index.html (accessed May 18, 2020).
- Centers for Disease Control and Prevention (CDC). 2019a. National Health Education Standards Website. Available at: https://www.cdc.gov/healthyschools/sher/standards/index.htm (accessed May 18, 2020).
- Centers for Disease Control and Prevention (CDC). 2019b. Characteristics of an Effective Health Education Curriculum Website. Available at: https://www.cdc.gov/healthyschools/sher/characteristics/index.htm (accessed May 18, 2020).
- Centers for Disease Control and Prevention. 2019c. Health Education Curriculum Analysis Tool (HECAT). Available at: https://www.cdc.gov/healthyyouth/hecat/index.htm (accessed May 18, 2020).
- Child Trends. 2019. State statutes and regulations for healthy schools: Health education. Available at: https://www.childtrends.org/wp-content/uploads/2019/01/WSCC-State-Policy-Health-Education.pdf (accessed May 28, 2019).
- Cobb, R. S. 1981. Health Education…A separate and unique discipline. Journal of School Health 51(9):603-604. https://doi.org/10.1111/j.1746-1561.1981.tb02243.x.
- Cottrell, R. R., J. T. Girvan, J. F. McKenzie, and D. Seabert. 2018. Principles and Foundations of Health Promotion and Education, 7th ed. Pearson: New York.
- Dubb, S. 2019. Parkland Students Outline Gun Safety Vision in Comprehensive Plan. Nonprofit Quarterly. Available at: https://nonprofi tquarterly.org/parkland-students-outline-gun-safety-vision-in-comprehensive-plan/ (accessed May 18, 2020).
- Goodwin, S. C. 1993. Health and physical education—Agonists or antagonists? Journal of Physical Education, Recreation and Dance 64(7):74-78. https://doi.org/10.1080/07303084.1993.1060679
- Gould, L., E. Mogford, and A. DeVoght. 2010. Successes and Challenges of Teaching the Social Determinants of Health in Secondary Schools: Case Examples in Seattle, Washington. Health Promotion Practice 11(3):26S-33S. https://doi.org/10.1177/1524839909360172
- Guhne, J. 2001. Students send magazines’ tobacco ads back to publishers in “Don’t Buy” effort. Baltimore Sun. Available at: https://www.baltimoresun.com/news/bs-xpm-2001-04-12-0104120141-story.html (accessed May 18, 2020).
- Hampton, C., A. Alikhani, M. E. Auld, and V. White. 2017. Advocating for Health Education in Schools (Policy brief). Society for Public Health Education: Washington, DC. Available at: https://www.sophe.org/wp-content/uploads/2017/01/ESSAPolicy-Brief.pdf (accessed May 18, 2020).
- Hoffman, A. 2016. In San Francisco, the fight against diabetes gets personal: A local doctor tries to raise awareness about the social causes of Type 2 diabetes, in his community and others. CityLab. Available at: https://www.citylab.com/life/2014/11/in-san-francisco-the-fight-against-diabetes-getspersonal/382275/ (accessed May 18, 2020).
- Hoelscher, D. M., H. A. Feldman, C. C. Johnson, L. A. Lytle, S. K. Osganian, G. S. Parcel, S. H. Kelder, E. J. Stone, and P. R. Nader. 2004. School-based health education programs can be maintained over time: Results from the CATCH Institutionalization study. Preventive Medicine 38(5):594-606. Available at: https://www.sciencedirect.com/science/article/pii/S0091743503003311 (accessed May 18, 2020).
- Hoelscher, D. M., A. E. Springer, N. Ranjit, C. L. Perry, A. E. Evans, M. Stigler, and S. H. Kelder. 2010. Reductions in child obesity among disadvantaged school children with community involvement: The Travis County CATCH Trial. Obesity 18(1):36-44. https://doi.org/ 10.1038/oby.2009.430.
- Institute of Medicine (IOM). 1997. Schools and Health: Our Nation’s Investment. Washington, DC: The National Academies Press. https://doi.org/10.17226/5153.
- Institute of Medicine (IOM). 2004. Health Literacy: A Prescription to End Confusion. Washington, DC: The National Academies Press. https://doi.org/10.17226/10883.
- Institute of Medicine. 2014. Implications of Health Literacy for Public Health: Workshop Summary. Washington, DC: The National Academies Press. https://doi.org/10.17226/18756.
- Kolbe, L. 2019. School health as both a strategy to improve both public health and education. Annual Review of Public Health 40:443-463. https://doi.org/10.1146/annurev-publhealth-040218-043727.
- Luepker, R. V., C. L. Perry, S. M. McKinlay, P. R. Nader, G. S. Parcel, E. J. Stone, L. S. Webber, J. P. Elder, H. A. Feldman, C. C. Johnson, S. H. Kelder, M. Wu, P. Nader, J. Elder, T. McKenzie, K. Bachman, S. Broyles, E. Busch, S. Danna, T. Galati, K. Haye, C. Hayes, M. McGreevy, B. J. Williston, M. Zive, C. Perry, L. Lytle, R. Luepker, B. Davidann, P. Brothen, V. Dahlstrom, M. Dammen, S. Ehlinger, T. Greene, B. Hann, J. Heberle, T. Hoffl ander, C. Kelder, P. Kelliher, T. Kunz, B. Manning, D. McDuffi e, T. Morrow, M. Miller, J. Mrosala, G. Newman, M. Pusateri, M. Reinhardt, R. Sieving, J. Smisson, M. Smyth, P. Snyder, M. Staufacker, J. Traut, T. Wick, G. Parcel, S. Kelder, D. Montgomery, M. Nichaman, W. Taylor, K. Wambsgans Cook, E. Barrera, L. Berry, J. Carbonneau, K. Chemycz, P. Cribb, S. Evans, R. Gordon, J. Gwinn, S. Luton, B. Scaife, S. Sharkey, S. Snider, S. Spigner, K. Wilson, S. Woods, J. Wilmore, L. Webber, C. Johnson, T. Nicklas, V. Anthony, N. Baker, K. Barnwell, S. Belou, G. Berenson, S. Bonura, K. Bordelon, S. Cameron, A. Clesi, L. Crochet, A. Cunningham, D. Franklin, A. Haque, D. Harsha, J. Joy, S. M. Hunter, D. Kuras, P. Lambie, A. Layman, S. Little-Christian, S. Pedersen, J. Reeds-Epping, R. Rice, K. Romero, C. Pitcher-Smith, P. Strikmiller, M. White, S. McKinlay, S. Osganian, H. Feldman, H. Mitchell, S. Budman, P. Connell, M. Koehler, P. Mitchell, C. Kannler, G. Rennie, D. Sellers, M. Walsh, M. Yang, J. Dwyer, M. K. Ebzery, A. Garceau, L. Hewes, C. Hosmer, D. Raizman, L. Bausserman, E. Stone, M. Evans, J. Cutler, R. Lauer, T. Coates, W. Haskell, C. A. Johnson, R. Prineas, L. Van Horn, and J. Verter. 1996. Outcomes of a field trial to improve children’s dietary patterns and physical activity: The child and adolescent trial for cardiovascular health. Journal of the American Medical Association 275(10):768-776. https://doi.org/10.1001/jama.1996.03530340032026
- Mann, M. J., and D. K. Lohrmann. 2019. Addressing challenges to the reliable, large-scale implementation of effective school health education. Health Promotion Practice 20(6):834-844. https://doi.org/10.1177/1524839919870196.
- Mayer-Davis, E. J., J. M. Lawrence, D. Dabelea, J. Divers, S. Isom, L. Dolan, G. Imperatore, B. Linder, S. Marcovina, D. J. Pettitt, C. Pihoker, and S. Saydah. 2017. Incidence trends of Type 1 and Type 2 diabetes among youths, 2002-2012. New England Journal of Medicine 376(15):1419-1429. https://doi.org/10.1056/NEJMoa1610187.
- Means, R. K. 1975. A History of Health Education. Philadelphia, PA: Lea & Febiger.
- Melnyk, B. M., D. Jacobson, S. Kelly, M. Belyea, G. Shaibi, L. Small, J. O’Haver, and F. F. Marsiglia. 2013. Promoting healthy lifestyles in adolescents: A randomized control trial. American Journal of Preventive Medicine 45(4):407-415. https://doi.org/10.1016/j.amepre.2013.05.013
- Minnesota Department of Health. Office of Statewide Health Improvement Initiatives. 2012. Statewide Health Improvement Partnership Evaluation Data. Reported by SHIP grantees using the REDCap system.
- Morse L. L. and D. D. Allensworth. 2015. Placing students at the center: The Whole School, Whole Community, Whole Child model. Journal of School Health 85:785-794. https://doi.org/10.1111/josh.12313.
- National Academies of Sciences, Engineering, and Medicine. Health and Medicine Division. Roundtable on Health Literacy. Available at: http://www.nationalacademies.org/hmd/Activities/PublicHealth/HealthLiteracy.aspx#home (accessed May 3, 2020).
- National Academies of Sciences, Engineering, and Medicine. 2019. Developing health literacy skills in youth and young adults. Proceedings of a workshop. Washington, DC: The National Academies Press.
- Pleasant, A., R. E. Rudd, C. O’Leary, M. K. Paasche-Orlow, M. P. Allen, W. Alvarado-Little, L. Myers, K. Parson, and S. Rosen. 2016. Considerations for a New Definition of Health Literacy. NAM Perspectives. Discussion Paper, National Academy of Medicine, Washington, DC. https://doi.org/10.31478/201604a.
- Rasberry, C. N., G. F. Tiu, L. Kann, T. McManus, S. L. Michael, C. L. Merlo, S. M. Lee, M. K. Bohm, F. Annor, and K. A. Ethier. 2017. Health-related behaviors and academic achievement among high school students—United States, 2015. Morbidity and Mortality Weekly Report 66(35):921-927. https://doi.org/10.15585/mmwr.mm6635a1
- Rasberry, C. N., S. Slade, D. K. Lohrmann, and R. F. Valois. 2015. Lessons learned from the Whole Child and Coordinated School Health Approaches. Journal of School Health 85(11):759-765. https://doi.org/10.1111/josh.12307.
- Ratzan, S. C., and R. M. Parker. 2000. Introduction. In National Library of Medicine current bibliographies in medicine: Health literacy . NLM Pub. No. CBM 2000-1, edited by C. R. Selden, M. Zorn, S. C. Ratzan, and R. M. Parker. Bethesda, MD: National Institutes of Health, US Department of Health and Human Services.
- Shattuck, L. 1850. Report of the Sanitary Commission of Massachusetts. Sanitary Commission; London School of Hygiene and Tropical Medicine; London School of Hygiene and Tropical Medicine. Reprinted from Cambridge: Harvard University Press, 1948, p. 178.
- Schillinger, D., J. Tran, and S. Fine. 2018. Do low income youth of color see “The Bigger Picture” when discussing Type 2 diabetes: A qualitative evaluation of a public health literacy campaign. International Journal of Environmental Research and Public Health 15(5):840. https://doi.org/10.3390/ijerph15050840
- Sliepcevich, E. M. 1968. The school health education study: A foundation for community health education. Journal of School Health 38:45-50. https://doi.org/10.1111/j.1746-1561.1968.tb04941.x
- US Department of Agriculture. Food and Nutrition Service. 2020a. National School Lunch program. Available at: https://www.fns.usda.gov/nslp (accessed May 18, 2020).
- US Department of Agriculture. Food and Nutrition Service. 2020b. National Breakfast Program. Starting the school day right with a healthy breakfast. Available at: https://www.fns.usda.gov/sbp/schoolbreakfast-program (accessed May 18, 2020).
- US Department of Education. 2020. The Federal Role in Education. Available at: https://www2.ed.gov/about/overview/fed/role.html (accessed May 18, 2020).
- US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. 2010. National Action Plan to Improve Health Literacy. Washington, DC. Available at: https://health.gov/our-work/health-literacy/national-action-planimprove-health-literacy (accessed May 18, 2020).
- US Department of Health, Education, & Welfare. 1979. Healthy People: The Surgeon General’s Report on Health Promotion and Disease Prevention. DHEW (PHS) Publ. No. 79-55071. Washington, DC: Public Health Service.
- US Department of Health and Human Services. 2010. Healthy People 2020. Available at: https://www.healthypeople.gov/sites/default/files/DefaultPressRelease_1.pdf (accessed May 3, 2020).
- US Department of Health and Human Services. 2010. Healthy People 2020 Leading Health Indicator Topics: Social Determinants. Available at: https://www.healthypeople.gov/2020/leading-healthindicators/2020-lhi-topics/Social-Determinants (accessed May 3, 2020).
- US Department of Health and Human Services. 2017. Secretary’s Advisory Committee Report on Approaches to Healthy People 2030. Healthy People 2030 Draft Framework. Available at: https://www.healthypeople.gov/2020/about-healthy-people/development-healthy-people-2030/draft-framework (accessed May 15, 2020).
- Vernon, J. A., A. Trujillo, S. Rosenbaum, and B. De-Buono. 2007. Low health literacy: Implications for national policy. Available at: http://www.gwumc.edu/sphhs/ departments/healthpolicy/chsrp/downloads/LowHealthLiteracyReport10_4_07.pdf (accessed May 18, 2020).
- Videto, D. M. and J. A. Dake. 2019. Promoting health literacy through defining and measuring quality school health education. Health Promotion Practice 20(6):824-833. https://doi.org/10.1177/1524839919870194.
- Youth Speaks. 2018. The Bigger Picture Toolkit. Available at: http://youthspeaks.org/wp-content/uploads/The%20Bigger%20Picture%20Tool%20Kit.pdf (accessed May 18, 2020).
- Weise, E. and J. Wilson. 2019. “The eyes of future generations are on you,” Thunberg tells UN Climate Summit. USA TODAY. Available at: https://www.usatoday.com/story/news/2019/09/23/howdare-you-look-away-greta-thunberg-tells-un-climate-change-summit/2418058001 (accessed May 18, 2020).
- Winthrop, R. 2020. Covid-19 is a health crisis: So why is health education missing from school work? Available at: https://www.edsurge.com/news/2020-04-03-covid-19-is-a-health-crisis-sowhy-is-health-education-missing-from-schoolwork (accessed May 18, 2020).
- Zimmerman, M. A. 2013. Resiliency theory: A strengths-based approach to research and practice for adolescent health. Health Education & Behavior 40(4):381-383. https://doi.org/10.1177/1090198113493782
https://doi.org/10.31478/202007b
Suggested Citation
Auld, M. E., M. P. Allen, C. Hampton, J. H. Montes, C. Sherry, A. D. Mickalide, R. Logan, W. Alvarado-Little, and K. Parson. 2020. Health Literacy and Health Education in Schools: Collaboration for Action. NAM Perspectives. Discussion Paper. National Academy of Medicine. Washington, DC. https//doi.org/10.31478/202007b
Author Information
M. Elaine Auld, MPH, MCHES is Chief Executive Officer, Society for Public Health Education. Marin P. Allen, PhD, is Deputy Associate Director, Office of Communications and Public Liaison and Director of Public Information, Office of the Director, National Institutes of Health (retired). Cicily Hampton, PhD, MPA, is Adjunct Assistant Research Professor, University of North Carolina at Charlotte. J. Henry Montes, MPH, is former Chair, Public Health Education and Promotion Section, American Public Health Association. Cherylee Sherry, MPH, MCHES is Healthy Systems Supervisor, Office of Statewide Health Improvement Initiatives, Minnesota Department of Health. Angela D. Mickalide, PhD, MCHES, is Vice President, Programs and Education, American College of Preventive Medicine. Robert A. Logan, PhD, is Senior Staff, U.S. National Library of Medicine (retired) and Professor emeritus, University of Missouri-Columbia. Wilma Alvarado-Little, MA, MSW, is Associate Commissioner, New York State Department of Health and Director, Office of Minority Health and Health Disparities Prevention. Kim Parson, BA, is Principal, KPCG LLC.
Acknowledgments
The authors would like to express our gratitude to Melissa French and Alexis Wojtowicz for their support in the development of this paper.
Conflict-of-Interest Disclosures
Wilma Alvarado-Little has no relevant financial or nonfinancial relationships to disclose. She contributed to this article based on her experience in the field of health literacy and cultural competency and the opinions and conclusions of the article do not represent the official position of the New York State Department of Health. Cherylee Sherry discloses that she works for the Minnesota Department of Health in the Office of Statewide Health Improvement Initiatives which oversees the Statewide Health Improvement Partnership Program funded by the State of Minnesota.
Correspondence
Questions or comments about this manuscript should be directed to M. Elaine Auld at [email protected].
The views expressed in this paper are those of the authors and not necessarily of the authors’ organizations, the National Academy of Medicine (NAM), or the National Academies of Sciences, Engineering, and Medicine (the National Academies). The paper is intended to help inform and stimulate discussion. It is not a report of the NAM or the National Academies. Copyright by the National Academy of Sciences. All rights reserved.
Join Our Community
Sign up for nam email updates.
Texas A&M-McAllen Students Lead Mental Health-Focused Events In Rio Grande Valley Colonias

This spring, Texas A&M University Higher Education Center at McAllen (HECM) Public Health professor Dr. Krystal Flores-Chavez was awarded $5,000 from the HECM’s High Impact Teaching Grant to support a service-learning project for her Project Management in Public Health course.
She separated her students into two groups and awarded each team $2,500 to implement a “real world” project addressing mental health in a colonia in the Rio Grande Valley.
“I really wanted to create a fun, engaging course project where students could work collaboratively with community partners. The course uses high impact teaching methodologies in the form of service – learning pedagogy and collaborative projects. This type of learning is preferred as it provides students with the opportunity to actively apply concepts learned in the classroom to address a community identified need,” Flores-Chavez said. “Mental health was selected as the public health issue students would address based on information provided by focus groups conducted by the Texas A&M University Colonias Program . Their findings reflected residents’ desire for mental health services and increased awareness surrounding the issue.”
The teams collaborated with the Colonias Program and Puentes de Cristo to select the colonia community and launch their respective events. The organizations selected the South Tower Colonias in Alamo, Texas, and the La Piñata colonia in Donna, Texas, as the sites for the team projects.


Clean Environment + Happy, Healthy Minds
In early April, the Donna team invited students of all majors at the HECM to volunteer and help clean a colonia. Students united to help create a cleaner, greener environment by picking up trash, assisting with minor landscaping and distributing freshly potted plants to residents. Each student wore a white shirt with the message: “A clean environment promotes a happy and healthy mind.”
Then last weekend, the Alamo team invited the community to attend a free Mental Health Awareness Fair at the Alamo Community Resource Center and Park for free services from local clinics and non-profit organizations. The students also partnered with Denise Martinez, a doctoral student and community health worker from the Texas A&M University School of Public Health in College Station to prepare a mental health-themed game of loteria (Bingo) and prizes for participants. The organizations at the community event included Nuestra Clinica Del Valle, South Texas Health Systems Clinics, South Texas Health Systems Behavioral, South Texas Research Institute, HOPE Family Health Center, Mujeres Unidas/Women Together, Puentes De Cristo and the Texas A&M Colonias Program.
Lesly Mata ‘25, one of Flores-Chavez’s students, assisted her team with the planning process and gathering the necessary tools to make the community clean-up a success. “We got to see concepts from the course reflected in real life along the way,” Mata said. “It was a very rewarding and valuable experience helping transform the residents’ neighborhood.”
Adamari De La Cerda ‘25 was also determined to help her team provide valuable mental health resources to colonia residents at the Mental Health Awareness Fair. “My team and I started working with local stakeholders and ultimately decided that hosting a community fair along with a loteria would allow us to personally connect with community members,” said De La Cerda. “We understand how pursuing mental well-being is often stigmatized to be a sign of ‘weakness’ that often forces one to avoid any sort of help. Our goal was to spread awareness about the importance of preserving mental health and destigmatize negative perceptions by personally connecting with community members and offering resources.”
Despite the heavy lifting needed for such projects, it can truly be a fulfilling experience for all involved. “Implementing service learning in courses is often difficult and very time-consuming for both faculty and students. It involves several steps and takes a considerable amount of effort. However, it is incredibly rewarding to be able to witness the growth experienced by students as they navigate the course and challenges associated with developing a ‘real world’ project. Witnessing students gain confidence in their abilities as future public health professionals is one of my favorite aspects of being a professor,” Flores-Chavez said.
Related Stories

Texas A&M AgriLife Turfgrass Program Leads Through Innovation
From backyards to football fields and golf courses, science is reshaping the turfgrass experience.

How To Help Your Cat Breathe Easy With Feline Asthma
Wheezing is often a strong indication of asthma, but there are also other signs that can be used to help make a diagnosis.
Researchers Solve Mystery Of How Phages Disarm Bacteria
New Texas A&M AgriLife research that clarifies how bacteria-infecting viruses disarm pathogens could lead to new treatment methods for bacterial infections.
Recent Stories

Take Control Of Your Money During Financial Literacy Month
An instructor from Texas A&M’s Financial Planning Program says it’s more important than ever for young adults to manage their personal finances wisely. Here’s how.

Former President Of France Speaks At Texas A&M, Honors Bush School Professor
François Hollande delivered a talk on global security and terrorism before presenting Dr. Richard Golsan with one of France’s highest academic honors.

Subscribe to the Texas A&M Today newsletter for the latest news and stories every week.
eHealth Literacy
‹ View Table of Contents
Defining health literacy and eHealth literacy
Assessing health literacy in eHealth studies
Factors associated with use of eHealth
Understanding use of eHealth: Tailoring for success
An important role for health and communication professionals
According to Pew Research Center external icon , approximately 52% of American adults in 2000 said they used the Internet compared to 89% in early 2018; a trend that is likely to continue rising.
Yet individuals are not the only ones using the Internet more. Organizations have also mobilized the Internet to deliver health services. The World Health Organization pdf icon external icon (WHO) reports 58% of Member States surveyed reported they have an eHealth strategy, signaling a global movement. WHO defines electronic health (eHealth) services as the cost-effective and secure use of information communication technologies to support health and health-related fields. Examples include electronic communication between patients and providers, electronic medical records, patient portals, and personal health records. A category of eHealth is mobile health (mHealth) including phones, tablets, and computers to use applications (apps), wearable tracking devices, and texting services. The research referenced on this page may include mHealth when referring to eHealth.
As more people and health organizations use eHealth services and products, we need to understand how a person’s level of health literacy influences the interaction. Equally important is how health professionals and communication specialists can provide support.
In Healthy People 2030, the U.S. Department of Health and Human Services (HHS) updated the definition of health literacy to include personal health literacy as well as organizational health literacy. HHS provides the following definitions:
- Personal health literacy is the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others.
- Organizational health literacy is the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others
Norman and Skinner (2006) external icon define eHealth literacy as the ability to appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem.
Readers are cautioned not to substitute eHealth literacy for health literacy as noted by Monkman and colleagues (2017) external icon . The authors analyzed participant responses (N=36) on the Newest Vital Sign to measure health literacy, and used the eHealth Literacy Scale (eHEALS) to assess eHealth literacy. Their findings suggest assessing health literacy and eHealth literacy separately.
In 2021, Sanders and colleagues published the results of a randomized controlled trial in which they examined the impact of a six-week, peer-led intervention on eHealth literacy, general health literacy, HIV-related health literacy, and numeracy among people living with HIV (PLWH). The investigators used the Electronic Health Literacy Scale to measure eHealth literacy, the Rapid Estimate of Adult Literacy to measure general health literacy, the Brief Estimate of Health Knowledge and Action-HIV to measure HIV-related health literacy, and the Newest Vital Sign to measure numeracy. At the end of the intervention and six months later, the intervention group had statistically significant improvements in eHealth literacy and HIV-related health literacy compared to the control group. Neither the control group nor the intervention group showed any statistically significant improvement in general health literacy or numeracy.
(For more on numeracy, see Numeracy Research Summaries and Understanding Literacy & Numeracy . Read more about health literacy and PLWH too.)

As more people and health organizations use eHealth services, we need to understand how a person’s level of health literacy influences the interaction.
Kim & Xie (2017) external icon conducted a literature review (N=74) to assess how people with limited health literacy use online health services. Only nine studies reported interventions focused on improving health literacy. The review indicates that six of those nine reported positive effects on knowledge, skills, and confidence using eHealth. Measures: Thirty-three studies reported measuring participants’ health literacy level. Five studies used the Short Test of Functional Health Literacy in Adults (S-TOFHLA) and four studies used the Rapid Estimate of Adult Literacy in Medicine (REALM). Eight of the 33 studies used the eHealth Literacy Scale (eHEALS), which as noted previously may not accurately capture health literacy but rather a sub-category—eHealth literacy. Recommendations: When designing websites, the authors suggest improving readability in web-based apps and mobile apps (sixth grade reading level or below), increasing content available for people with limited English proficiency, using plain language strategies such as shorter sentences, use of bullets, and incorporating more consistent design with icons and pictures.
Most studies in this review reported a mean participant age between 46-66 years. However, in an intervention study by Horvath & Bauermeister (2017) that focused on a population of men self-identifying as having sex with men, the mean age of participants was of 21 years. Researchers assessed participants’ eHealth literacy and randomized them into tailored and non-tailored message groups for an HIV/STI (sexually transmitted infection) online intervention. Participants with low eHealth literacy in the non-tailored group were less likely to educate others about HIV/STIs and less likely to report deciding to get tested at 30-day follow-up. Findings from this study suggest that tailoring and eHealth literacy may influence behavior change.
Visit Health Literacy Online external icon to access research-based guidance for better web and digital tool design.
Wearable digital devices (also known as fitness trackers) have become popular tools for providing users with information about their health. However, a variety of barriers to their use lead to disparities among populations. Holko and colleagues (2022) identified those barriers by surveying more than 1,000 adult patients in six Federally Qualified Health Centers (FQHCs) across the United States. FQHCs are community-based health care providers that receive federal funds to deliver primary care services in areas with limited access to medical care.
Of the five hindering factors to device ownership, three were related to health literacy: language barriers, lack of access to devices due to cost, and the need for information on how to use the devices. Of the six helping factors to ownership, three were related to health literacy: the belief that the devices could provide relevant health information, the desire to learn how the devices could provide health information, and the desire to have access to the devices (thus making the information they provide accessible). The authors also noted the importance of using culturally appropriate language when referring to these devices. When the researchers used the term “fitness tracker,” some Spanish-speaking participants were concerned that the devices could track their movements. The authors also provide recommendations for overcoming barriers to the use of wearable digital health devices.
As more people use the internet and social media platforms to access health information, more organizations are using these digital channels to share their health information. A study published in 2022 by Arshanapally et al indicated that a paid digital marketing campaign increased the rate at which parents of newborns through preschoolers downloaded a mobile health app that tracks childhood milestones. The authors found that messages—in English and Spanish—that included animated GIFs and simple, direct calls to action prompted more readers to click through to the app. The authors also discuss the features and limitations of the digital marketing platforms they used.
A cross-sectional study published in 2021 assessed whether health literacy, access to technology, and sociodemographic factors are associated with online health information-seeking behavior. Questions from the Health Information National Trends Survey were used to measure health-related information seeking. Health literacy was assessed using three health literacy items from the 2016 Behavioral Risk Factor Surveillance System Questionnaire . The data showed that people with higher health literacy scores and greater access to technology devices were more likely to use the internet for health information compared to people with lower health literacy scores or less access to technology.
The authors also found that
- Health-related internet use among adults increased with age until about 38 years, decreased between 38 and 71 years, and increased again after 71 years.
- People who reported poor or fair health status had higher health-related internet use scores than people who reported good, very good, or excellent health status.
- Nearly half of respondents used the internet to communicate with their health care provider.
- More than half of respondents searched for online information about diet, weight, and physical activity.
- More than half of respondents went online to search for health-related information about someone else.
In a survey conducted by Escoffery’s (2017) external icon , more than 70% of the 400 participants reported they owned laptops and smartphones, and nearly half reported using the Internet several times a day. Female participants reported higher use of health apps and were more likely to have apps related to exercise and diet compared to males. However, males were more likely to report looking for information for themselves the last time they searched the Internet compared to females.
Spooner and colleagues (2016) external icon surveyed adults (N=3677) and found that Hispanic people, people the authors categorized as non-Hispanic others, and people from higher income households were more likely to have communicated with a provider via text, phone app, or social media. Those who preferred non-Internet sources of information such as books, primary care provider, or brochures were more likely to be people over 65 years, Hispanic people, and people with less than a high school education.
Trust and confidence
In addition to socio-demographics, we must also consider the possible association between eHealth literacy and perceived trust in source, self-efficacy (confidence), and other factors. Paige and colleagues (2017) external icon surveyed participants (N=402) to assess use of internet health resources in the last 12 months. While 75% of respondents said they had skills to evaluate online health resources, only 60% reported confidence in evaluating the quality or these resources and making health decisions based on that information. Females with lower eHealth literacy reported higher trust in online sources compared to men with low eHealth literacy and compared to females with higher eHealth literacy. Researchers also learned that older adults with low eHealth literacy were more likely to trust online channels compared to younger adults. Compared to Caucasian (White) participants with high eHealth literacy, Black/African American participants with high eHealth literacy were more likely to report higher trust in online information from government, charitable, and religious organizations.
A growing number of studies are exploring the use of eHealth resources and self-management of chronic conditions. Stellefson and colleagues (2017) external icon surveyed (N=1270) patients with chronic obstructive pulmonary disease (COPD). Higher eHealth literacy was associated with higher COPD knowledge and use of web-based resources. Most participants were laptop and desktop users, and 25% reported use of wireless devices including phones. Greater COPD self-efficacy was significantly associated with finding helpful resources online, knowing how to use them to make health decisions, and feeling able to distinguish quality of materials. Escoffery (2017) external icon , referenced earlier, also reported similar findings related to self-efficacy. Participants in that study reported high trust in doctors, the Internet, and government agencies.
Other factors
As a follow-up to a failed attempt to enroll participants for a trial, Thies and colleagues (2017) external icon conducted interviews (N=22) and learned about the various aspects of readiness to use eHealth resources among patients and health professionals. The authors suggest a health team needs to assess patients’ eHealth literacy including proficiency with technology and whether patients have phones that support apps. It is equally important to assess patients’ motivation for behavior change and the degree to which their health condition is under control. The authors learned that barriers that prevented health professionals from adopting the app in this trial included: not having enough time in a twenty-minute visit to explain and download the app, lack of integration to an electronic health record, and no dedicated staff to support the trial.
In the Spooner and colleagues (2016) external icon study described earlier, 65%-85% of participants reported interest in exchanging information with providers electronically, but 68% said they had no online patient-provider communication. Researchers posited that access offered by the provider and the individual’s personal health information online access behavior predict occurrence of patient-provider communication.
From these few studies we know adults use eHealth resources. We also know that health literacy and eHealth literacy are influential factors in successful use of eHealth resources. What we are still learning is how greater emphasis on eHealth may disproportionately affect groups with limited health literacy. In light of what is known,

Ask patients about their preferred and available communication options.
Health professionals can
- Assess how confident a person feels about managing their own health.
- Identify a patient’s knowledge or skill gaps and together create a plan that is understandable .
- Identify a health team member who can teach patients how to evaluate web content external icon and who can suggest top web sources external icon for patient health information.
- Ask patients about their preferred and available communication options, e.g., telephone, teleconference, email, apps, patient portal, or another preference.
Communication professionals can
- Use plain language strategies external icon – shorter sentences, bulleted lists.
- Assess readability of all materials.
- Use Health Literacy Online external icon recommendations.
- Incorporate images and graphics that complement and reinforce text.
- Design materials for populations with limited English skills.
- Consider demographic characteristics when determining the channel and source for different audience segments.
Health Literacy Topics
- Research Summaries
- Communication Strategies
- Patient Engagement
- › eHealth Literacy
- Food Literacy
- Heart Disease
- Other Conditions
- Medications
To receive email updates about this page, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Lit Res Pract
- v.5(3); 2021 Jul

Social Determinants, Health Literacy, and Disparities: Intersections and Controversies
This article synthesizes what is known about the relationship between social disadvantage and measures of health literacy (HL), and reviews the research examining whether low HL is an explanatory factor connecting social disadvantage, health outcomes, and health disparities. Written from a United States perspective, this article offers a novel conceptual framework that presents how the social determinants of health might interact with HL to result in health disparities. The framework articulates relationships that reflect public health pathways and health care pathways, which include their related health literacies. The article continues with several cautionary statements based on the inherent limitations of current HL research, including problems and concerns specific to the attribution of HL as an explanatory factor for extant socioeconomic and racial/ethnic health disparities. The article closes with recommendations regarding future research directions. [ HLRP: Health Literacy Research and Practice . 2021;5(3):e233–e243.]
Plain Language Summary:
Socially disadvantaged populations have worse health and health literacy compared to privileged populations. Scientists, health care providers, and policymakers are interested in the possible role health literacy plays in explaining health differences. The article reviews our current understandings of whether and how population characteristics and related exposures to risk interact with low health literacy to generate worse health to inform interventions.
Despite 30 years of active research, how social disadvantage and health literacy (HL) interact, and whether HL can explain some of the observed relationships between social determinants of health, health outcomes, and health disparities remain critical questions for the fields of clinical medicine and public health. This narrative review, written from a United States perspective, describes how social determinants of health might relate to low HL to result in health disparities. It further presents a novel conceptual framework that reflects both health care pathways (including health literate health care organizations) as well as public health pathways (e.g., the socioecological model, differential exposures, and life course perspectives) and their related HLs. This article also provides relevant caveats related to the attribution of HL as an explanatory factor for extant socioeconomic and racial/ethnic health disparities. Finally, this review article provides research recommendations and suggests future directions to help close gaps in our understanding of complex relationships between social determinants of health, HL, and health.
Limited Health Literacy and Social Disadvantage
Vulnerable populations represent subgroups of the larger population that, because of social, economic, political, structural, geographic, and historical forces, are exposed to a greater risk of risks, and are thereby at a disadvantage with respect to their health and health care ( Paasche-Orlow et al., 2005 ). Vulnerable populations are exposed to contextual conditions that distinguish them from the rest of the population. It is estimated that one-third to one-half of the U.S. adult population has low HL, which is defined by the U.S. Institute of Medicine as a limited capacity to obtain, process, and understand the basic health information and services needed to make informed health decisions ( National Academies Press, 2004 ). Although low HL affects people across the spectrum of sociodemo-graphics, low HL disproportionally affects vulnerable populations ( Kutner et al., 2006 ). Vulnerable populations include the older adults, people with disabilities, people with lower socioeconomic status, racial/ethnic minorities, people with limited English proficiency (LEP), and people with limited education ( Fleary & Ettienne, 2019 ). The most comprehensive assessment of variation in HL skills across different social groups occurred as a part of the National Assessment of Adult Literacy (NAAL) ( Kutner et al., 2006 ). Assessments were performed in person; they had to be age 16 years or older and speak English or Spanish fluently. Results of the NAAL suggested significant differences in the distribution of HL skills by race and ethnicity; educational attainment; income; and language spoken before starting school. A more recent study using data from the 2013 Health Information National Trends Survey confirmed these findings ( DeWalt et al., 2004 ).
Low HL can be a marker for (or manifestation of) many life circumstances, including but not restricted to limited access to education, access to poor quality education, LEP, learning differences and disabilities, and cognitive impairment. People with low HL are more likely to have poor health, higher rates of chronic disease, and a nearly 2-fold higher mortality rate as compared to people with adequate HL ( Cavanaugh et al., 2008 ). As such, compared to those with adequate HL, persons with low HL also are more likely to experience disparities in health and health care access, and have lower rates of receiving screening and preventive services. Patients with low HL exhibit patterns of utilization of care reflecting a greater degree of unmet needs, such as excess emergency department (ED) visits and hospitalizations, even when comorbid conditions and health insurance status are statistically held constant. Patients with low HL are more likely to have poorer knowledge of their disease processes, medication regimens, and exhibit worse medication adherence and inadequate skills and methods for managing their disease ( Logan, 2017 ; Vernon et al., 2007 ). Low HL also has a negative effect on doctor-patient communication. Patients with low HL tend to be more passive in their visits with clinicians, have visits that are less interactive, are less likely to engage in decision-making, and are more likely to report that interactions with their physicians are not helpful or empowering. A study conducted over a decade ago estimated that low HL leads to excess health expenditures of greater than $100 billion annually ( Mantwill et al., 2015 ).
Evidence Connecting Health Literacy with Health Disparities
The problem of health disparities experienced within vulnerable populations is largely one of the differential exposures and associated behaviors. This framing eliminates some of the “shame and blame” often associated with the higher burden of disease among people who are socially disadvantaged. As such, social vulnerability is not necessarily an attribute that is intrinsic to people or subpopulations; instead, vulnerability status is determined by how society and its institutions are constructed. Low HL is tightly and simultaneously linked to several social determinants of health. Some investigators and health policy experts have even considered low HL itself to be a social determinant of health ( Pelikan et al., 2018 ). Others suggest that HL is key to improving control over modifiable social determinants of health ( Rowlands et al., 2017 ), describing it as a mediator or effect modifier. Wherever one falls in this debate, the high burden of low HL among vulnerable populations has led many to believe that low HL is a contributor to both health and health care disparities. In turn, an ensuing set of questions include (1) Might HL partially explain the health and health care disparities associated with the social determinants of health? (2) Might HL lead to differential effects of exposures or interventions on specific subgroups of the general population? Although these questions are of paramount importance, relatively little research has provided an empirically rigorous answer ( Cooper & Schillinger, 2011 ).
In public health practice in the U.S., racial/ethnic minorities, immigrants with LEP, and those of lower socioeconomic status (having low income, having obtained a high school diploma or less), are generally regarded as vulnerable groups. Recent research, including a systematic review, focuses on race/ethnicity and educational attainment with respect to the question of whether HL explains some of the relationships between social circumstances and health outcomes ( Bennett et al., 2009 ). In addition, the extant research is varied regarding the HL assessments used and health-related outcomes examined. In general, multivariable modeling has been used to determine independent effects of predictors and mediating variables on specific health outcomes. Some evidence has reported a mediating function of HL on health and health care outcomes across racial/ethnic and educational disparities. Some evidence suggests the potential effect of HL and numeracy on racial/ethnic disparities in health behaviors and knowledge. In all research with positive associations, the effect of the mediation was partial; HL did not fully explain broader relationships.
More specific research about health disparities related to educational attainment, health disparities related to race/ethnicity, health disparities between ethnic and linguistic subgroups, and prospective studies are outlined below.
Health Disparities Related to Educational Attainment
Although several cross-sectional studies have explored HL as a meditating factor in the relationships between socioeconomic disparities and health outcomes, the following research specifically evaluates the relationship among HL, other variables, and educational attainment. An assessment by Bennett et al. ( 2009 ) (a population of nearly 3,000 adults older than age 65 years who participated in the NAAL) found that HL mediated the relationship between educational attainment and self-rated health, as well as indicators of health care access and utilization, including receipt of flu vaccines, receipt of mammograms, and dental care.
In contrast, another study (of more than 3,000 seniors who participated in the Prudential Health Insurance Study) found that HL explained the relationship between education and physical and mental health scores, but not preventive care use, such as flu vaccine, mammograms, and dental care ( Howard et al., 2006 ). A study by Yin et al. ( 2009 ) (of parents who participated in NAAL) found that HL mediated the relationship between educational attainment and HL-related tasks regarding child health, dosing medications, and pediatrician appointments.
Sentell and Halpin ( 2006 ) studied approximately 24,000 community-dwelling participants in the NAAL (performed in the 1990s) and found that HL mediated the relationship between education and the presence of chronic illness and a health condition that limited ability to function in society ( Schillinger et al., 2006 ). Similarly, in a study of more than 14,000 persons with diabetes in a large, pre-paid integrated health plan, Sarkar et al. ( 2010 ) found that HL mediated the relationship between educational attainment and patient's use of an electronic patient portal, which was associated with better health outcomes ( Bailey et al., 2009 ). Finally, Schillinger et al. ( 2006 ) studied a diverse sample of more than 400 public hospital patients with diabetes and found that HL mediated the relationship between education and hemoglobin A1c (a standard measure of diabetes control) ( Osborn et al., 2009 ).
Health Disparities Related to Race/Ethnicity
As to whether HL explains racial and ethnic disparities in health or health care outcomes, several cross-sectional studies—some already mentioned, some additional—have looked at the explanatory power of HL with respect to Black/White differences in health outcomes; few studies have assessed other racial or ethnic differences. Bennett et al. ( 2009 ) found that HL mediated the relationship between race and self-rated health as well as flu vaccine receipt, but not mammography or dental care ( Sentell & Halpin, 2006 ). Howard et al. ( 2006 ), studying the NAAL participants, found that HL mediated the relationship between race and mental health but not physical health, and not the receipt of preventive care ( Sarkar et al., 2010 ).
Sentell and Halpin in their study of approximately 24,000 community-dwelling participants found that HL mediated the relationship between race and long-term illness and a limiting health condition, just as HL did with education ( Schillinger et al., 2006 ). In a study of 373 parents, Bailey et al. ( 2009 ) found that HL mediated the relationship between race and misunderstandings about liquid medication dosing ( Wolf et al., 2006 ). Osborn et al. ( 2011 ) found that diabetes-related numeracy mediated the relationship between race and hemoglobin A1c (a measure of blood sugar control), an effect seen primarily in patients with diabetes who used insulin ( Osborn et al., 2011 ). In patients with prostate cancer, Wolf et al. ( 2006 ) found that HL mediated the relationship between race and the level of prostate-specific-antigen at the time of presentation with prostate cancer ( Curtis et al., 2012 ). Osborn et al. ( 2009 ) found that HL mediated the relationship between HL and diabetes medication adherence ( Gwynn et al., 2016 ). Another study suggested that, although HL reduced the effect of race/ethnicity in Black and Hispanic people on asthma-related quality of life and asthma control (and for Black people only on ED visits), differences between Black and White people for asthma-related hospitalizations persisted ( Smith et al., 2012 ). Finally, a study of more than 225 mostly Black and White patients demonstrated that HL mediated the relationship between race and a measure of patient activation ( Sentell et al., 2013 ).
Health Disparities Between Ethnic and Linguistic Subgroups
Relatively few studies have explored the effects of HL in health disparities experienced by Hispanic or Asian subgroups, and still fewer have examined HL's role in explaining health disparities associated with LEP. A study comparing Spanish to English speakers in an ED suggested only the former were less likely to show up for follow-up appointments if they had low HL ( Sentell & Braun, 2012 ). A study of Asian Americans found that low HL was not significantly associated with meeting colorectal cancer screening guidelines, but LEP was associated ( Schenker et al., 2011 ). However, the combination of LEP and low HL had synergistic effects among Asian Americans. A large study ( Sentell & Braun, 2012 ) that featured diverse participants found that low HL was only significantly related to health status in White people and unknown races, but not within any Asian group. However, the study found the highest odds of poor health status occurred among Chinese, Vietnamese, and Hispanics with low HL and LEP. ( Sentell & Braun, 2012 ). Similar synergistic effects were observed on patient-reported interpersonal communication outcomes in a large sample of English- and Spanish-speaking primary care patients ( Sudore et al., 2009 ). Low HL and LEP each was associated with worse communication within the receptive, expressive, and interactive domains of interpersonal communication, whereas the combination was associated with the worst communication.
Prospective Studies
Only five prospective studies have examined the question of whether HL functions as a mediator or moderator of health disparities. In a longitudinal cohort study with 342 Black, Hispanic, and White adults with persistent asthma, HL mediated the relationship between race/ethnicity and asthma-related hospitalizations and ED visits ( Sperber et al., 2013 ). In a before and after trial, Volandes et al. ( 2008 ) found that HL mediated the relationship between race and changes in advanced care preferences ( Karter et al., 2015 ). After viewing a video, patient preferences, particularly among those with low HL, changed to preferring less aggressive care, an effect that was more pronounced among Black patients. An experiment of the differential effects between Black and White people and HL that studied response to a telephone-based osteoarthritis self-management support intervention found a significant interaction between HL and race/ethnicity on change in pain; Black people with low HL had the highest improvement in pain in the intervention compared to the usual care group ( Sperber et al., 2013 ). Finally, a natural experiment (involving more than 8,000 ethnically diverse patients with diabetes to enhance medication adherence, implementation of an intervention to promote mail-order pharmacy use that was not tailored for patients with low HL) reported a differential up-take of the intervention that further disadvantaged patients with low HL, especially among Hispanic and lower income subgroups ( Karter et al., 2015 ). A trial of literacy-appropriate, easy-to-understand video narratives and testimonials (presented in English and Spanish to encourage advance care planning demonstrated improvements across HL levels) yielded benefits for Spanish speakers, although the interaction between study arms and language was not statistically significant ( Sudore et al., 2018 ).
The Need for a Novel Model That Incorporates The Public Health Perspective
In reviewing this literature, it is important to note that many studies applied clinical epidemiologic approaches to address the larger question whether low HL can explain health disparities by either exploring the interactions among HL and a particular social determinant (e.g., effect modification by race or education) on health outcomes or performing formal meditational analyses. In so doing, investigators attempted to answer whether HL had differential effects on health outcomes based on a person's race or educational attainment or whether HL explained observed differences in outcomes by race or education.
Yet, from a public health perspective, given the disproportionately high prevalence of low HL among vulnerable populations, these types of analytic approaches may be overly reductionist. Insofar as low HL is more prevalent in socially disadvantaged populations, and as low HL appears to be an explanatory factor in the development of illness or its complications across populations, interventions to effectively address low HL are likely to result in a reduction in health disparities. Yet, this effect may be because low HL is unequally distributed across the U.S. population more than a unique explanatory power of low HL, meaning that HL-appropriate interventions could yield population-wide impacts that could reduce health and health care disparities even if HL is not a mediator. This suggests the need for a socioecologically oriented model.
Conceptual Framework for the Relationships Among Social Determinants of Health, Health Literacy, and Health Disparities
To advance our understanding of the inter-relationships among social determinants of health, health literacy and health disparities, I present a novel conceptual framework ( Figure Figure1 1 ) that integrates a socioecological framework with the more traditional causal frameworks associated with HL. Socioecological models emphasize multiple levels of influence on health (such as individual, interpersonal, organizational, community and public policy) and embrace the idea that behaviors both shape and are shaped by their surrounding social environment. The proposed conceptual model synthesizes research from multiple disciplines (such as clinical epidemiology, health services research, economics, political science, anthropology, health communication science, and public health) to better explain the potential pathways by which the social determinants of health, HL, and health disparities interact. The framework, and its explication, elucidate pathways; the associated factors additionally provide potential targets for intervention in the effort to reduce health disparities. The model acknowledges that HL is not necessarily a fixed attribute. Rather, HL can be improved directly through interventions that enable experience and build skills, or indirectly through interventions that reduce HL demands or alter the environment by shifting the balance in favor of health-promoting resources vs. unhealthy exposures.

Conceptual framework for the pathways that connect social determinants of health, health literacy, and health disparities. Pathways on the right represent health care pathways; those on the left represent public health pathways.
Figure Figure1 1 illustrates the two predominant pathways through which social determinants of health and social disadvantage can interact with low HL to result in health disparities. The first is the public health pathway that suggests the structural factors that reflect the maldistribution of health-promoting resources and unhealthy life course exposures across the general population in the U.S. The second is the health care pathway that suggests the organizational factors that reflect the responsiveness of health systems to the needs of clinical populations in the U.S., with respect to access to and quality of care. Differences in resources and exposures in public health and community settings, as well as differences in access and quality in clinical settings, both generate consequences that contribute to worse health outcomes and health disparities. To aid in understanding, several of the constructs and variables within Figure Figure1 1 are described below.
Social Determinants of Health
The top box (and construct) in Figure Figure1 1 is the starting point for all pathways and reflects the unequal distribution of health-promoting resources and unhealthy life course exposures resulting from differences in social status, often instigated, reinforced, or perpetuated by social policy and practice. This construct focuses on subpopulations of low income/poverty status; low educational attainment; racial and ethnic minority populations subject to marginalization and oppression; and those with LEP/linguistic isolation.
Structural Resources and Life Course Exposures
In Figure Figure1 1 , the triangle and diamond on the left and below represent the factors within the public health pathway that are protective to health and those that jeopardize health, that together often shape health behaviors. These factors, so-called “structural determinants,” flow from historical and current institutional, local, state, and federal policies and practices and generate facts on the ground that can profoundly affect people, families, and neighborhoods. Exposure to these structural determinants is a function of the social status and flows from the determinants of health, such as lower socioeconomic status and racial and ethnic minority status. The balance between health-promoting resources and risk exposures over the life course are a major determinant of the health of people and communities. Some of these structural factors include air quality/pollution; safe and green spaces for physical activity and recreation; features of the built environment and associated zoning regulations; transportation infrastructure; housing/segregation; the retail food environment/food deserts; commercial marketing environments (such as advertisements on billboards for unhealthy products); employment opportunities and occupational hazards; community stress and trauma; presence or absence of public health-promoting regulations; social support; social cohesion; and social investment.
Mediating and Moderating Related Health Literacy Domains (Public Health Pathway)
Within the public health pathway, HL is depicted as both a product of the social determinants of health as well as a potential asset that can positively influence the balance between health-promoting resources and unhealthy risk exposures, and/or mitigate the ill effects of unhealthy exposures. Health exposures can be influenced by environmental HL ( Finn & O'Fallon, 2017 ), occupational HL, nutritional HL ( Rauscher & Myers, 2014 ), mental HL ( Jorm, 2012 ), and the larger construct of “public health literacy” ( Freedman et al., 2009 ). Public HL can be an attribute of an individual, a community, or an entire population. Public HL refers to the degree to which people and groups can obtain, process, understand, evaluate, and act upon information needed to make public health decisions that benefit the community. Public HL aims to engage more stakeholders in public health efforts and address determinants of health. It requires an understanding of conceptual foundations related to the socioecological model of health, critical skills, and a civic orientation. Although advocacy and policy change are its currency, improving the health of the public is its ultimate objective.
The Consequences
The depiction of the maldistribution of resources and exposures between populations, compounded by a disproportionately high rate of low HL of the types described above among vulnerable populations, has real consequences for health behavior and health status. These include higher rates of chronic diseases such as obesity, type 2 diabetes, cardiovascular disease and stroke, asthma, cancer, chronic pain, and disability from both physical and mental health problems ( Köppen et al., 2018 ; Lincoln et al., 2008 ; Sudore et al., 2006 ; Wolf et al., 2005 ).
Health Literate Health Care Organizations
The triangle on the right side of Figure Figure1 1 represents the next step in the health care pathway connecting social determinants of health, HL, and health disparities. Brach et al. ( 2012 ) defined health literate health care organizations (HLHCOs) as those that ensure HL is deeply and explicitly integrated into all of their activities and that HL informs both strategic and operational planning. Appropriate measures to evaluate specific HL initiatives are developed and used. More importantly, the measurement of overall organizational performance assesses success with vulnerable populations. However, because of inadequacies and bias in health policy, health care financing, health care regulation, health professions training, health care innovation, and health care practice, there is significant variation in the degree to which U.S. health care systems are responsive to the needs of socioeconomically and ethnically diverse patients with varying levels of HL. As such, the extent to which health systems demonstrate the attributes of HLHCOs reflects a structural determinant of health.
Health Care Access and Quality
The depiction of Figure Figure1 1 underscores a basic tenet of the U.S. health care system, whereby the patients who maximally benefit from health care often have the greatest capacity and resources, including but not limited to HL. The health care system's weaknesses are undergirded by issues related to unequal access to care, including incomplete and/or unequal health insurance coverage; unnecessary barriers to obtaining public insurance; overly complex health insurance practices; insufficient provider workforce for specific (underserved) populations; lack of a diverse health care workforce; under-valuing or under-resourcing primary care; and segregation of health care (including an obligatory over-reliance on overex-tended safety net health systems among vulnerable populations). There are additional features within many U.S. health systems that further undermine the quality of care that are particularly salient for vulnerable populations and patients with low HL. These include inadequate preparation, training and maldistribution of the clinical workforce ( Institute of Medicine, 2000 ), and associated poor provider performance (especially with respect to interpersonal processes of care) ( Institute of Medicine, 2004 ); insufficient caregiver involvement and support; lack of ethnic and linguistic diversity in the workforce ( McCabe & Healey, 2018 ); lack of involvement of vulnerable populations in the design of health care services and its associated innovations; lack of peer and lay health educator models; lack of HL-appropriate digital health/e-health innovations; lack of resources and integrated interventions to assess and address social needs; fragmentation of health care; lack of inter-visit communication; incomplete trust in the provider; and insufficient or inappropriate policies, regulatory standards, oversight, measurement and/or incentives to reduce disparities and promote health care equity ( Grumbach & Mendoza, 2008 ; Schillinger et al., 2004 ; Stepanikova et al., 2016 ).
Mediating and Moderating Health Literacy Domains (Health Care Pathway)
Within the depicted health care pathway, HL is a product of HLHCOs as well as a potential asset that can positively influence the balance between HL-related demands health care systems place on patients and the HL-related skills of patients and families. The latter can mitigate the effects of receiving care in systems that are unresponsive to the needs of persons with low HL. Much has been studied and written about the patient-related HL skills required to optimally function within U.S. health care settings. These skills include communicative HL capabilities, such as speaking, listening, reading, and increasingly writing (e.g., secure messages in electronic patient portals) of health-related content, quantitative skills (e.g., health numeracy), and health insurance literacy (e.g., the ability to navigate bureaucratic procedures and advocate for oneself) ( Dubbin et al., 2013 ; Schillinger et al., 2017 ).
Overall, the lack of evolution and diffusion of the model of HLHCOs, combined with the fragmentation, overextension, and under-resourcing characteristic of many safety net health care systems (further compounded by a disproportionately high rate of low HL of the types described above among vulnerable patients), yields consequences for health care disparities, with respect to access, processes of care, and outcomes. The latter include presenting late to medical attention, often with more advanced disease, demonstrating more missed appointments ( Baskaradoss, 2016 ), poorer self-management skills, lesser degrees of patient activation, suboptimal clinician-patient communication, less shared decision-making, lower trust, worse quality of care, and greater rates of medical error and patient safety events. The consequences of the depicted health care pathway, together with the public health pathway (which leads vulnerable populations to be even more reliant on health care because of a higher burden of disease) includes greater complication rates, worse health outcomes, higher costs of care and utilization of services, and greater premature morbidity and mortality.
Caveats Regarding Health Literacy as an Explanatory Factor in Health Disparities
The scientific endeavor combines unbiased experimentation with objective observations of the natural world to accumulate knowledge to approximate truth. However, although medicine is largely seen as a force for good, clinical science has a checkered record. At times, its tools and its authority have been used to promote or perpetuate inhumane policies and practices ranging from unethical research and medical practices that have harmed lower income and racial/ethnic and religious minority populations, subjecting them to “racial hygiene” (a eugenics-based approach, institutionalized by Nazi Germany, based on medical beliefs of the day regarding racial hierarchies, marked by efforts to avoid the “contamination” of “higher races” with “lower ones”) that led to race-based genocide ( Proctor, 2002 ).
When examining the question of whether and how HL affects health, researchers need to be mindful that literacy represents a resource which, for racial/ethnic minority subgroups, historically has been withheld to oppress, or has been measured and then used to judge groups as inferior or ineligible to participate as citizens, or as an alternate means to oppress ( Goldman, 2004 ). There are several related challenges in HL research that researchers, policymakers, and practitioners must be aware of that temper confidence in the validity of the research and its synthesis just presented, and which support the need to carry out additional, complementary research to better approximate truth and not perpetuate mistruths. The specific challenges of measurement and attribution are discussed in the remainder of this section.
To begin, there are diverse challenges in this field associated with research measurement ( Schillinger & Sarkar, 2009 ). How best to measure patient HL, and whether or not HL measures are detecting true differences in capacities and skills in marginalized populations, can be problematic and controversial. A recent review of all HL research measures ( Health Literacy Tool Shed, 2021 ) found that 200 unique measures have been created and employed, including 14 in Spanish, with most (52%) requiring paper and pencil responses, and some measures (12%) requiring more than 15 minutes to administer. Of the 200, 128 (64%) measured general HL, 76 (38%) measured disease or content-specific HL, and only 1 (0.5%) measured a public health literacy domain (water environmental literacy). Thirty-one (15.5%) assessed pronunciation, 25 (12.5%) assessed conceptual knowledge, and 43 (21.5%) assessed comprehension.
As previously described, health disparities are produced and perpetuated by multilevel forces operating at the individual, family, health system, community, and public policy levels that mutually reinforce each other to produce injustice and perpetuate inequity. Because conventional literacy assessments are bounded by cultural and linguistic assumptions derived from the majority population, more research is needed to assess patient HL in a comprehensive, holistic, and unbiased manner, and to expand the assessment of reliability and validity across subgroups of interest to avoid misattributing health disparities solely to limited HL.
A clear, but by no means isolated example of this challenge is the use of HL measures that require proper pronunciation of medical terms to assess HL, such as the REALM (Rapid Estimate of Adult Literacy in Medicine). It is not hard to imagine that biased measurement may occur for a measure in which a White researcher scores a patient's HL by determining whether a patient has read and pronounced a medical term “correctly.” This can be true for some Black patients whose pronunciation of some words in the English language may differ from the “mainstream” linguistic culture ( Goldman, 2004 ). The problem of cultural hegemony in literacy assessment, and the untoward downstream effects of related mismeasurement, has been well elucidated in the social psychology field ( Harris, 2010 ).
A second research challenge is attribution. The critique here is both general to social epidemiology and specific to HL research. For example, do the observations that low HL is more common in marginalized populations, and that in some cases observed social disparities in health outcomes appear to be statistically mediated by low HL suggest that the relationship indeed is causal? There are alternative hypothesized mechanisms by which low HL may be associated with health care quality and health outcomes in research exploring the causes of health disparities among vulnerable populations that are not causal ( Harris, 2010 ). These mechanisms include:
- Confounds: low HL may simply be a marker for or a result of sociodemographic and behavioral factors or life course exposures or experiences that by themselves directly or indirectly lead to morbidity and mortality. Although most studies attempt to account for confounds using multivariable analytic methods, it is widely recognized that socioeconomic variables obtained at one point in time (such as income) only incompletely capture income over the life course, or that income does not necessarily signify assets and wealth. As such, residual confounding is not only possible, but is almost certain to exist. Similarly, although variables such as race or immigration status are often collected, these measures do not begin to capture the experience of being Black or an immigrant in the U.S.
- Reverse or cyclical causation: low HL may be a consequence of high disease burden or poor disease control, and thus associated with worse health trajectories (cyclical effect). As an example, people with longstanding diabetes that is poorly controlled have been shown to experience worse cognitive function as a complication of the disease. In turn, this may contribute to the downward trajectory in self-management due to poor understanding, but it may be captured as low HL within a cross-sectional HL assessment, all occurring in a patient whose clinical course has already been largely determined.
- Attention bias: What we choose to measure and what we choose not to measure inevitably influences inferences regarding cause and effect. Low HL may affect outcomes through a demand-capacity mismatch, with the health care system placing inappropriate communication demands on patients; or communication resources are poorly distributed for the population with the greatest needs. The latter hypothesis suggests changes at the health system level provide intervention targets to mitigate health disparities related to low HL. Whereas greater attention is finally being paid to the communication attributes of clinicians and health care organizations as they relate to patient HL, there has been little work to operationalize a measure of clinician or systems responsiveness to the needs of population with low HL ( Brach et al., 2014 ). This has hindered progress in reducing HL and racial and ethnic disparities in health care.
- Attribution bias: Finally, insofar as literacy skills, be they HL or otherwise, reflect a resource that results from privilege and power, the absence of literacy reflects a particular manifestation of oppression and marginalization, be it historical or ongoing. Following this argument, those with low HL have inexorably been exposed to other forms of systematic deprivation, including forms of intergenerational oppression that are difficult or impossible to measure at the individual level. In this case, low HL, despite consistently demonstrating statistically significant meditational relationships, may present itself as an overly simplistic, stereotype-laden, and potentially dangerously false explanation for observed health disparities.
Future Directions
When it comes to shedding light on the fundamental causes of health disparities, articulating mechanisms leading to health disparities, and intervening to promote health equity, HL research needs to evolve in many ways to achieve its promise. First, future research should focus on developing alternative HL measures that are not subject to bias and mismeasurement in marginalized populations and should attend to ensuring the reliability and validity of these measures across population subgroups. Second, more attention needs to be paid to comprehensively measure confounding variables, with a particular emphasis to avoid attribution bias. Second, because most HL research has focused on patients' HL deficits, much more work needs to be done to operationalize a measure of clinician or systems' responsiveness to the needs of populations with low HL, including the communication attributes of clinicians and health care organizations ( Brach et al., 2014 ; Crossley et al., 2020 ; Institute of Medicine, 2012 ; Schillinger, 2007 ).
Third, while making significant advances during the last 20 years, the field of HL research in the U.S. has involved a relative paucity of investigators from under-represented minority (URM) groups, groups that otherwise are active in the field of health disparities research. This may be due, in part, to the inherent assumptions, biases, and limitations that are in HL research. Although there is a growing body of community-based participatory research in the field of HL, there remains a critical need to extend and enhance HL research by including the experience, voices, and intellectual capacity of a multidisciplinary cohort of URM researchers. Only by expanding inclusivity in this way will the field of HL be able to be optimally harnessed to reduce health and health care disparities.
Fourth, descriptive research must be designed and powered to enable the simultaneous disentanglement of socioeconomic status, race/ethnicity (representative of all major ethnic subgroups) and LEP from HL, and to enable valid and informative meditational analyses, with a particular emphasis on longitudinal studies. Fifth, investment in interventional research must increase to (1) ensure an ability to stratify effectiveness results by sociodemographic characteristics as well as by HL level to identify effect modification; (2) enable formal exploration of mediational effects, including the impacts of HL relative to other explanatory factors; and (3) include public HL interventions. Relatedly, a lack of differential effectiveness should not prevent the dissemination, uptake, and adoption of effective HL-appropriate interventions. Rather, given the disproportionate burden of low HL in vulnerable populations, such interventions should be seen as an important means to reduce health disparities.
Conclusions
Low HL is more common in populations that are socially disadvantaged, and there is a growing body of research to suggest that HL may be an explanatory factor in pathways that generate health disparities, especially those associated with social determinants of health such as lower educational attainment and racial/ethnic status. To better understand the potential mechanisms whereby HL can mediate health disparities associated with the social determinants of health, this article presents a novel conceptual framework that can inform research, policy, and practice for those interested in promoting health equity in the U.S. and potentially beyond. The framework describes two primary pathways that generate consequences for health outcomes based, in part, on HL. The first operates through multilevel factors related to the unequal distribution of resources and exposures and their related environmental and public health literacies. The second operates through underdeveloped (and arguably discriminatory) institutional capacities of the health care systems, and the related individual communicative literacies of the patients that rely on these systems. Both pathways emerge within a complex society characterized by competing forces that reflect both a history of marginalization and oppression of vulnerable subgroups as well as a tradition of civic engagement and advocacy for progressive change that is the foundation of democracy. The field of HL represents a progressive force whose objectives and early achievements can help reverse deeply ingrained policies, structures, and practices at the health care and broader societal levels that create, perpetuate, or even amplify health disparities ( Paasche-Orlow et al., 2018 ). HL research—both descriptive and interventional—is still somewhat nascent; it needs to further evolve and expand to accurately situate HL as a target to reduce health disparities.
- Bailey , S. C. , Pandit , A. U. , Yin , S. , Federman , A. , Davis , T. C. , Parker , R. M. , & Wolf , M. S. ( 2009. ). Predictors of misunderstanding pediatric liquid medication instructions . Family Medicine , 41 ( 10 ), 715 – 721 PMID: [ PubMed ] [ Google Scholar ]
- Baskaradoss , J. K. ( 2016. ). The association between oral health literacy and missed dental appointments . The Journal of the American Dental Association , 147 ( 11 ), 867 – 874 . 10.1016/j.adaj.2016.05.011 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Bennett , I. M. , Chen , J. , Soroui , J. S. , & White , S. ( 2009. ). The contribution of health literacy to disparities in self-rated health status and preventive health behaviors in older adults . Annals of Family Medicine , 7 ( 3 ), 204 – 211 . 10.1370/afm.940 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brach , C. ( 2017. ). The Journey to become a health literate organization: a snapshot of health system improvement . Studies in Health Technology and Informatics , 240 , 203 – 237 PMID: [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brach , C. , Dreyer , B. P. , & Schillinger , D. ( 2014. ). Physicians' roles in creating health literate organizations: A call to action . Journal of General Internal Medicine , 29 ( 2 ), 273 – 275 . 10.1007/s11606-013-2619-6 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brach , C. , Keller , D. , Hernandez , L. M. , Baur , C. , Parker , R. , Dreyer , B. , Schyve , P. , Lemerise , A. J. , & Schillinger , D . ( 2012. ). Ten attributes of health literate health care organizations . https://nam.edu/wp-content/uploads/2015/06/BPH_Ten_HLit_Attributes.pdf [ Google Scholar ]
- Cavanaugh , K. , Huizinga , M. M. , Wallston , K. A. , Gebretsadik , T. , Shin-tani , A. , Davis , D. , Gregory , R. P. , Fuchs , L. , Malone , R. , Cherrington , A. , Pignone , M. , DeWalt , D. A. , Elasy , T. A. , & Rothman , R. L. ( 2008. ). Association of numeracy and diabetes control . Annals of Internal Medicine , 148 ( 10 ), 737 – 746 . 10.7326/0003-4819-148-10-200805200-00006 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cooper , L. , & Schillinger , D . ( 2011. ). The role of health literacy in health disparities research. In Innovations in health literacy research: workshop summary (pp. 7 – 12 ). Institute of Medicine of the National Academies; . [ Google Scholar ]
- Crossley , S. A. , Balyan , R. , Liu , J. , Karter , A. J. , McNamara , D. , & Schillinger , D. ( 2020. ). Predicting the readability of physicians' secure messages to improve health communication using novel linguistic features: The ECLIPPSE study . Journal of Communication in Healthcare , 13 , 344 – 356 . 10.1080/17538068.2020.1822726 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Curtis , L. M. , Wolf , M. S. , Weiss , K. B. , & Grammer , L. C. ( 2012. ). The impact of health literacy and socioeconomic status on asthma disparities . The Journal of Asthma , 49 ( 2 ), 178 – 183 . 10.3109/02770903.2011.648297 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- DeWalt , D. A. , Berkman , N. D. , Sheridan , S. , Lohr , K. N. , & Pignone , M. P. ( 2004. ). Literacy and health outcomes . Gen Intern Med , 19 ( 12 ): 1228 – 1239 . 10.1111/j.1525-1497.2004.40153.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dubbin , L. A. , Chang , J. S. , & Shim , J. K. ( 2013. ). Cultural health capital and the interactional dynamics of patient-centered care . Social Science & Medicine , 93 , 113 – 120 . 10.1016/j.socscimed.2013.06.014 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Finn , S. , & O'Fallon , L. ( 2017. ). The emergence of environmental health literacy--From its roots to its future potential . Environmental Health Perspectives , 125 ( 4 ), 495 – 501 . 10.1289/ehp.1409337 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fleary , S. A. , & Ettienne , R. ( 2019. ). Social disparities in health literacy in the United States . Health Literacy Research and Practice , 3 ( 1 ), e47 – e52 . 10.3928/24748307-20190131-01 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Freedman , D. A. , Bess , K. D. , Tucker , H. A. , Boyd , D. L. , Tuchman , A. M. , & Wallston , K. A. ( 2009. ). Public health literacy defined . American Journal of Preventive Medicine , 36 ( 5 ), 446 – 451 . 10.1016/j.amepre.2009.02.001 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goldman , D. ( 2004. ). The modern-day literacy test: Felon disenfranchisement and race discrimination . Stanford Law Review , 57 , 611 . [ Google Scholar ]
- Grumbach , K. , & Mendoza , R. ( 2008. ). Disparities in human resources: Addressing the lack of diversity in the health professions . Health Affairs (Project Hope) , 27 ( 2 ), 413 – 422 . 10.1377/hlthaff.27.2.413 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gwynn , K. B. , Winter , M. R. , Cabral , H. J. , Wolf , M. S. , Hanchate , A. D. , Henault , L. , Waite , K. , Bickmore , T. W. , & Paasche-Orlow , M. K. ( 2016. ). Racial disparities in patient activation: Evaluating the mediating role of health literacy with path analyses . Patient Education and Counseling , 99 ( 6 ), 1033 – 1037 . 10.1016/j.pec.2015.12.020 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Harris , V. J. ( 2010. ). African-American conceptions of literacy: A historical perspective . Theory into Practice , 31 ( 4 ), 276 – 286 . 10.1080/00405849209543554 [ CrossRef ] [ Google Scholar ]
- Health Literacy Tool Shed . ( 2021. ). Health literacy tool shed. Find the right health literacy measurement tool for your research . https://healthliteracy.bu.edu/ [ Google Scholar ]
- Howard , D. H. , Sentell , T. , & Gazmararian , J. A. ( 2006. ). Impact of health literacy on socioeconomic and racial differences in health in an elderly population . Journal of General Internal Medicine , 21 , 857 – 861 . 10.1111/j.1525-1497.2006.00530.x PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Institute of Medicine . ( 2000. ). America's health care safety net: Intact but endangered . https://www.ncbi.nlm.nih.gov/books/NBK224521/ [ PubMed ] [ Google Scholar ]
- Institute of Medicine . ( 2004. ). Health literacy: A prescription to end confusion . https://pubmed.ncbi.nlm.nih.gov/25009856/ [ Google Scholar ]
- Institute of Medicine . ( 2012. ). How can health care organizations become more health literate? https://www.nap.edu/catalog/13402/how-can-health-care-organizations-become-more-health-literate-workshop#toc [ Google Scholar ]
- Jorm , A. F. ( 2012. ). Mental health literacy: Empowering the community to take action for better mental health . The American Psychologist , 67 ( 3 ), 231 – 243 . 10.1037/a0025957 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Karter , A. J. , Parker , M. M. , Duru , O. K. , Schillinger , D. , Adler , N. E. , Moffet , H. H. , Adams , A. S. , Chan , J. , Herman , W. H. , & Schmittdiel , J. A. ( 2015. ). Impact of a pharmacy benefit change on new use of mail order pharmacy among diabetes patients: The Diabetes Study of Northern California (DISTANCE) . Health Services Research , 50 ( 2 ), 537 – 559 . 10.1111/1475-6773.12223 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Köppen , P. J. , Dorner , T. E. , Stein , K. V. , Simon , J. , & Crevenna , R. ( 2018. ). Health literacy, pain intensity and pain perception in patients with chronic pain . Wiener Klinische Wochenschrift , 130 ( 1–2 ), 23 – 30 . 10.1007/s00508-017-1309-5 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kutner , M. , Greenburg , E. , Ying , J. , & Paulsen , C . ( 2006. ). The health literacy of America's adults: Results from the 2003 national assessment of adult Literacy. NCES 2006-483 . https://eric.ed.gov/?id=ED493284
- Lincoln , A. , Espejo , D. , Johnson , P. , Paasche-Orlow , M. , Speckman , J. L. , Webber , T. L. , & White , R. F. ( 2008. ). Limited literacy and psychiatric disorders among users of an urban safety-net hospital's mental health outpatient clinic . The Journal of Nervous and Mental Disease , 196 ( 9 ), 687 – 693 . 10.1097/NMD.0b013e31817d0181 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Logan , R. A. ( 2017. ). Seeking an expanded, multidimensional conceptual approach to health literacy and health disparities research . Studies in Health Technology and Informatics , 240 , 96 – 123 . 10.3233/ISU-160809 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mantwill , S. , Monestel-Umaña , S. , & Schulz , P. J. ( 2015. ). The relationship between health literacy and health disparities: A systematic review . PLoS One , 10 , e0145455 Advance online publication. 10.1371/journal.pone.0145455 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McCabe , R. , & Healey , P. G. T. ( 2018. ). Miscommunication in doctor-patient communication . Topics in Cognitive Science , 10 , 409 – 424 . 10.1111/tops.12337 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- National Academies Press . ( 2004. ). Health literacy: A prescription to end confusion . https://pubmed.ncbi.nlm.nih.gov/25009856/ [ PubMed ] [ Google Scholar ]
- Osborn , C. Y. , Cavanaugh , K. , Wallston , K. A. , Kripalani , S. , Elasy , T. A. , Rothman , R. L. , & White , R. O. ( 2011. ). Health literacy explains racial disparities in diabetes medication adherence . Journal of Health Communication , 16 ( Suppl. 3 ), 268 – 278 . 10.1080/10810730.2011.604388 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Osborn , C. Y. , Cavanaugh , K. , Wallston , K. A. , White , R. O. , & Rothman , R. L. ( 2009. ). Diabetes numeracy: An overlooked factor in understanding racial disparities in glycemic control . Diabetes Care , 32 ( 9 ), 1614 – 1619 . 10.2337/dc09-0425 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paasche-Orlow , M. K. , Parker , R. M. , Gazmararian , J. A. , Nielsen-Bohlman , L. T. , & Rudd , R. R. ( 2005. ). The prevalence of limited health literacy . Journal of General Internal Medicine , 20 ( 2 ), 175 – 184 . 10.1111/j.1525-1497.2005.40245.x PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Paasche-Orlow , M. K. , Schillinger , D. , Weiss , B. D. , Bickmore , T. , Cabral , H. , Chang , P. , Bailey , S. C. , Dewalt , D. A. , Fernandez , A. , Fransen , M. , Leung , A. , McCaffery , K. , Meade , C. D. , McCormack , L. A. , Protheroe , J. , Parker , R. , Rothman , R. , Rubin , D. , Rudd , R. , Ownby , R. L. ( 2018. ). Health literacy and power . HLRP: Health Literacy Research and Practice , 2 ( 3 ), e132 – e133 . 10.3928/24748307-20180629-01 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pelikan , J. M. , Ganahl , K. , & Roethlin , F. ( 2018. ). Health literacy as a determinant, mediator and/or moderator of health: Empirical models using the European Health Literacy Survey dataset . Global Health Promotion , 25 ( 4 ), 1757975918788300 10.1177/1757975918788300 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Proctor , R. N. ( 2002. ). Medicine under the Nazis . Harvard University Press; . [ Google Scholar ]
- Rauscher , K. J. , & Myers , D. J. ( 2014. ). Occupational health literacy and work-related injury among U.S. adolescents . International Journal of Injury Control and Safety Promotion , 21 ( 1 ), 81 – 89 . 10.1080/17457300.2013.792288 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Rowlands , G. , Shaw , A. , Jaswal , S. , Smith , S. , & Harpham , T. ( 2017. ). Health literacy and the social determinants of health: A qualitative model from adult learners . Health Promotion International , 32 ( 1 ), 130 – 138 . 10.1093/heapro/dav093 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sarkar , U. , Karter , A. J. , Liu , J. Y. , Adler , N. E. , Nguyen , R. , López , A. , & Schil-linger , D. ( 2010. ). The literacy divide: Health literacy and the use of an internet-based patient portal in an integrated health system-results from the diabetes study of northern California (DISTANCE) . Journal of Health Communication , 15 ( Suppl. 2 ), 183 – 196 . 10.1080/10810730.2010.499988 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schenker , Y. , Fernandez , A. , Sudore , R. , & Schillinger , D. ( 2011. ). Interventions to improve patient comprehension in informed consent for medical and surgical procedures: A systematic review . Medical Decision Making , 31 , 151 – 173 . 10.1177/0272989X10364247 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schillinger , D. ( 2007. ). Literacy and health communication: Reversing the ‘inverse care law’ . The American Journal of Bioethics , 7 , 15 – 18 . 10.1080/15265160701638553 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schillinger , D. , Barton , L. R. , Karter , A. J. , Wang , F. , & Adler , N. ( 2006. ). Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes . Public Health Reports , 121 , 245 – 254 . 10.1177/003335490612100305 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schillinger , D. , Bindman , A. , Wang , F. , Stewart , A. , & Piette , J. ( 2004. ). Functional health literacy and the quality of physician-patient communication among diabetes patients . Patient Education and Counseling , 52 ( 3 ), 315 – 323 . 10.1016/S0738-3991(03)00107-1 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schillinger , D. , McNamara , D. , Crossley , S. , Lyles , C. , Moffet , H. H. , Sarkar , U. , Duran , N. , Allen , J. , Liu , J. , Oryn , D. , Ratanawongsa , N. , & Karter , A. J. ( 2017. ). The next frontier in communication and the ECLIPPSE Study: Bridging the linguistic divide in secure messaging . Journal of Diabetes Research , 2017 , 1348242 10.1155/2017/1348242 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schillinger , D. , & Sarkar , U. ( 2009. ). Numbers don't lie, but do they tell the whole story? Diabetes Care , 32 ( 9 ), 1746 – 1747 doi: 10.2337/dc09=1071 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Schillinger , D. , Tran , J. , & Fine , S. ( 2018. ). Do low income youth of color see “the bigger picture” when discussing type 2 diabetes: A qualitative evaluation of a public health literacy campaign . International Journal of Environmental Research and Public Health , 15 , E840 Advance online publication. 10.3390/ijerph15050840 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Seibert , R. G. , Winter , M. R. , Cabral , H. J. , Wolf , M. S. , Curtis , L. M. , & Paasche-Orlow , M. K. ( 2019. ). Health literacy and income mediate racial/ethnic asthma disparities . HLRP: Health Literacy Research and Practice , 3 ( 1 ), e9 – e18 . 10.3928/24748307-20181113-01 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sentell , T. , Braun , K. L. , Davis , J. , & Davis , T. ( 2013. ). Colorectal cancer screening: Low health literacy and limited English proficiency among Asians and Whites in California . Journal of Health Communication , 18 ( Suppl. 1 ), 242 – 255 . 10.1080/10810730.2013.825669 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sentell T , Braun KL . ( 2012. ). Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California . Journal of Health Communication , 17 ( Suppl. 3 ), 82 – 99 . 10.1080/10810730.2012.712621 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sentell , T. L. , & Halpin , H. A. ( 2006. ). Importance of adult literacy in understanding health disparities . Journal of General Internal Medicine , 21 ( 8 ), 862 – 866 . 10.1111/j.1525-1497.2006.00538.x PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Smith , P. C. , Brice , J. H. , & Lee , J. ( 2012. ). The relationship between functional health literacy and adherence to emergency department discharge instructions among Spanish-speaking patients . Journal of the National Medical Association , 104 ( 11–12 ), 521 – 527 . 10.1016/S0027-9684(15)30218-2 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sperber , N. R. , Bosworth , H. B. , Coffman , C. J. , Lindquist , J. H. , Oddone , E. Z. , Weinberger , M. , & Allen , K. D. ( 2013. ). Differences in osteoarthritis self-management support intervention outcomes according to race and health literacy . Health Education Research , 28 ( 3 ), 502 – 511 . 10.1093/her/cyt043 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stepanikova , I. , Mollborn , S. , Cook , K. S. , Thom , D. H. , & Kramer , R. M. ( 2006. ). Patients' race, ethnicity, language, and trust in a physician . Journal of Health and Social Behavior , 47 , 390 – 405 . 10.1177/002214650604700406 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sudore , R. L. , Landefeld , C. S. , Pérez-Stable , E. J. , Bibbins-Domingo , K. , Williams , B. A. , Schillinger , D. ( 2009. ). Unraveling the relationship between literacy, language proficiency, and patient-physician communication . Patient Education and Counseling , 75 ( 3 ), 398 – 402 doi: 10.1016/j.pec.2009.02.019 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sudore , R. L. , Mehta , K. M. , Simonsick , E. M. , Harris , T. B. , Newman , A. B. , Satterfield , S. , Rosano , C. , Rooks , R. N. , Rubin , S. M. , Ayonayon , H. N. , & Yaffe , K. ( 2006. ). Limited literacy in older people and disparities in health and healthcare access . Journal of the American Geriatrics Society , 54 , 770 – 776 . 10.1111/j.1532-5415.2006.00691.x PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sudore , R. L. , Schillinger , D. , Katen , M. T. , Shi , Y. , Boscardin , W. J. , Osua , S. , & Barnes , D. E. ( 2018. ). Engaging diverse English and Spanish-speaking older adults in advance care planning . JAMA Internal Medicine , 178 ( 12 ), 1616 – 1625 . 10.1001/jamainternmed.2018.4657 PMID: [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Vernon , J. A. , Trujilo , A. , Rosenbaum , S. J. , & DeBuono , B . ( 2007. ). Low health hiteracy: Implications for National Health Policy . https://hsrc.himmelfarb.gwu.edu/sphhs_policy_facpubs/172/ [ Google Scholar ]
- Volandes , A. E. , Paasche-Orlow , M. , Gillick , M. R. , Cook , E. F. , Shaykevich , S. , Abbo , E. D. , & Lehmann , L. ( 2008. ). Health literacy not race predicts end-of-life care preferences . Journal of Palliative Medicine , 11 , 754 – 762 . 10.1089/jpm.2007.0224 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wolf , M. S. , Gazmararian , J. A. , & Baker , D. W. ( 2005. ). Health literacy and functional health status among older adults . Archives of Internal Medicine , 165 ( 17 ), 1946 – 1952 . 10.1001/archinte.165.17.1946 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wolf , M. S. , Knight , S. J. , Lyons , E. A. , Durazo-Arvizu , R. , Pickard , S. A. , Arseven , A. , Arozullah , A. , Colella , K. , Ray , P. , & Bennett , C. L. ( 2006. ). Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer . Urology , 68 ( 1 ), 89 – 93 . 10.1016/j.urology.2006.01.064 PMID: [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yin , H. S. , Johnson , M. , Mendelsohn , A. L. , Abrams , M. A. , Sanders , L. M. , & Dreyer , B. P. ( 2009. ). The health literacy of parents in the United States: A nationally pepresentative study . Pediatrics , 124 ( Suppl. 3 ), S289 – S298 . 10.1542/peds.2009-1162E [ PubMed ] [ CrossRef ] [ Google Scholar ]
More From Forbes
How social media affects our financial health - the good, bad and ugly.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Social media application on the smartphone screen
Social media is everywhere and covers everything. People use social media for connecting, shopping, content, entertainment and sharing information. While some scrolling is harmless, the dangers of social media is becoming more and more evident. This is especially true when it comes to our financial health.
Lifestyle inflation, the tendency to increase spending as your income increases, is nothing new. However, James Curry, Senior Vice President, Director of Wealth Management at Greenleaf Trust , explains that social media has made it easier to fall prey to the allure of lifestyle inflation. “Social media constantly exposes us to the glamorous lives of others. Carefully curated snapshots of lavish lifestyles fill our feeds as we scroll through the social media platforms, flashing images of luxurious vacations, designer wardrobes, and extravagant dining experiences.” This leads us to an unrealistic, inflated and inaccurate perception of wealth. Curry believes this constant exposure to excess can subconsciously influence us to adjust our spending habits to match the experiences we are seeing online.
“As individuals strive to maintain appearances consistent with the inflated standards set by social media, debt often becomes a consequence. The pressure to live up to unrealistic standards can drive individuals into debt traps.” The result, Curry says, is often high-interest credit cards and loans used to sustain a lifestyle that is unsustainable in the long run, jeopardizing their financial stability and future goals.
JPMorgan Joins Goldman Sachs In Serious Bitcoin Halving Price Warning
Google makes a major new sale offer to pixel 8 buyers, drugs like ozempic and mounjaro could treat other conditions here s what scientists are looking at.
To avoid these traps and the financial pressures brought on by social media, Curry recommends establishing clear financial goals and balancing your short-term enjoyment without harming your long-term goals.
In addition to the dangers of lifestyle inflation, social media also poses a threat with the massive amount of financial content and advice found online. A recent survey commissioned by Forbes Advisor and conducted by market research company Prolific show 79% of Americans representing the millennial or Gen Z age groups have gotten financial advice from social media
While there are plenty of ‘finfluencers’ giving great advice, educating users and making a positive impact, you should always consider the source and motivation before making any financial decisions. Things to watch out for are:
- Anyone selling or promoting a financial product. This isn’t to say that the product is a bad idea, but do your research before buying anything. Look up the posters credentials and check if they receive a commission.
- ‘Hacks’ for getting out of debt or ‘Get rich quick’ schemes. Unfortunately there are very few short cuts in finance. And, if someone had a way that actually made them ‘rich quick’ - why would they monetize it?
- ‘Guaranteed’ returns or results. With a few exceptions, there are no investment guarantees. The nature of investing is risk. The bigger the risk, the bigger the potential reward (and loss).
- Financial Courses. Again, there are some really valuable ones out there. But before you pay for ‘expert’ advice, make sure they are an expert.
But it’s not all bad and ugly - social media has done a lot of good when it comes to our financial lives. Financial influencers are normalizing talking about money. They are making finance relatable to everyone and even (dare I say) ‘cool’ for younger generations. This is a huge leap from how Millennials and older generations were raised, when talking about money was seen as taboo. Gen Z and Alpha are exposed to all types of financial concepts, are more savvy, and recognize the importance of financial education and accountability. The same survey shows 76% believe financial content on social media has made it less taboo to talk about money and 62% feel empowered by their access to financial advice on social media.
Although there are always bad apples, there are plenty of finfluencers who are inspiring people by motivating them to take control of their financial world and make changes to be financially healthy.
- Editorial Standards
- Reprints & Permissions

IMAGES
VIDEO
COMMENTS
In 2006, the U.S. Department of Education published the only national data on health literacy skills. The study found that adults who self-report the worst health also have the most limited literacy, numeracy, and health literacy skills. See The Health Literacy Of America's Adults: Results from the 2003 National Assessment of Adult Literacy.
Although studies have found clear relationships between (a) education and health literacy, (b) education and health, and (c) health literacy and health, this study is among the first to actually examine the possible contribution of health literacy in explaining the relationship between education and health (Bennett et al., 2009; Howard et al ...
Organizational health literacy is the degree to which organizations equitably enable individuals to find, understand, and use information and services to inform health-related decisions and actions for themselves and others. These definitions are a change from the health literacy definition used in Healthy People 2010 and Healthy People 2020 ...
This paper strives to present current evidence and examples of how the collaboration between health education and health literacy disciplines can strengthen K-12 education, promote improved health, and foster dialogue among school officials, public health officials, teachers, parents, students, and other stakeholders.
health literacy cost the US economy up to $238 billion every year, or 17 percent of all personal health-care expenditure (Vernon, 2007). Health literacy is an intermediate social determinant of health in a model where individual-level characteristics interact with context-dependent determinants and
June 13, 2017 - Patient education and health literacy are two key concepts in patient engagement and chronic care management. Healthcare experts strive to improve patient health knowledge, asserting that knowledgeable patients are more engaged in shared decision-making and self-management. Because patient education and health literacy are so ...
The construct of health literacy covers three broad elements: (1) knowledge of health, healthcare and health systems; (2) processing and using information in various formats in relation to health and healthcare; and (3) ability to maintain health through self-management and working in partnerships with health providers.
Health literacy enables pupils to understand themselves, others and the world in a way that will enable them to make informed health decisions and work on (and change) the factors that constitute their own and others' health chances. Five broader health literacy competencies are covered (see left column of Table 1).
Literature Summary. Healthy People 2030 has elevated the importance of health literacy by declaring it a foundational principle and overarching goal, and by adopting two definitions that together constitute health literacy. Personal health literacy is the degree to which individuals have the ability to find, understand, and use information and ...
Along with updated definitions, ODPHP has also made health literacy a central focus of Healthy People 2030 with an overarching goal to "Eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all.". In advancing that goal, we've identified three core health literacy ...
Welcome to CDC's health literacy website. This site is for health communicators, public health professionals, and community leaders who seek information and tools on health literacy research, practice, and evaluation. We aim to bring you timely information about the work of CDC and other organizations to improve health literacy.
What Is Health Literacy? According to the U.S. Department of Health and Human Services' (HHS) Healthy People 2030 initiative, health literacy involves the information and services that people need to make well-informed health decisions.There are many aspects of health literacy: Personal health literacy is the degree to which individuals have the ability to find, understand, and use ...
that clarifies the relationship between health literacy, health promotion, determinants of health and healthy public policy and health outcomes. It is targeted at health promotion and education professionals and professionals in related disciplines. HED theoretical concepts COVER - print - 1 May 2012.indd 1 5/3/2012 8:38:08 AM
The present study aims to study whether health literacy could be a pathway by which level of education affects health status. Health literacy was measured by the Health Activities and Literacy Scale, using data from a subsample of 5,136 adults between the ages of 25 and 65 years, gathered within the context of the 2007 Dutch Adult Literacy and ...
Health literacy is a central focus of Healthy People 2030. One of the initiative's overarching goals demonstrates this focus: "Eliminate health disparities, achieve health equity, and attain health literacy to improve the health and well-being of all.". Watch this video to learn more about health literacy: 5 Things to Know About Health ...
Health literacy has a mediating role between education and health. Health literacy is known as a complex concept, it has multiple definitions, underlying meanings and conceptual models. Diversity of health literacy can be a challenging motivator for health education. In-depth study of scientific literature was carried out to highlight the link ...
As health care has moved away from applying a traditional paternalistic approach of 'doctor knows best' to a patient-centred care approach, patient education must be tailored to meet persons' individual needs. Purpose: The purpose of this master paper is to increase awareness of patients' health literacy levels. Health literacy is linked to ...
The National Health and Family Planning Commission worked closely with Ministry of Education to add health literacy as a key curriculum area for primary, secondary and tertiary schools. Through continuous interventions, the national health literacy surveillance data showed that the national health literacy level amongst Chinese residents rose ...
COVID-19: Health Crisis Affecting Children and their Families and a Need for Health Education and Health Literacy in K-12 . In a recent op-ed, Rebecca Winthrop, co-director of the Center for Universal Education and Senior Fellow of Global and Economic Development of the Brookings Institution asked, "COVID-19 is a health crisis.
In the health literacy questionnaire, scores' domain was defined as 0-132. Based on the distribution of 50%, 75%, and 100%, if an individual's score was 0-66, he/she had inadequate health literacy, the score 67-100 was identified to possess marginal health literacy, and a health literacy score of 100-132 was considered adequate.
What comes out is health literacy. Effectively, Health Education is the activity aimed at achieving good knowledge and an attitude to value Health by improving individual behavior and the practice ...
News from Texas A&M University. This spring, Texas A&M University Higher Education Center at McAllen (HECM) Public Health professor Dr. Krystal Flores-Chavez was awarded $5,000 from the HECM's High Impact Teaching Grant to support a service-learning project for her Project Management in Public Health course.
Washington — A new report finding that many mental health patients must go out of network to find care is disturbing and points to the necessity for insurance reform to ensure access to those in need, according to the American Psychological Association. "The findings of this report, while not surprising, are gravely disappointing," said APA CEO Arthur C. Evans Jr., PhD.
Assessing health literacy in eHealth studies. In 2021, Sanders and colleagues published the results of a randomized controlled trial in which they examined the impact of a six-week, peer-led intervention on eHealth literacy, general health literacy, HIV-related health literacy, and numeracy among people living with HIV (PLWH). The investigators used the Electronic Health Literacy Scale to ...
The Bibb County School District received a $1 million grant from the Georgia Department of Education which will expand health care access in the community, school officials announced Tuesday at a ...
Abstract. This article synthesizes what is known about the relationship between social disadvantage and measures of health literacy (HL), and reviews the research examining whether low HL is an explanatory factor connecting social disadvantage, health outcomes, and health disparities. Written from a United States perspective, this article ...
To avoid these traps and the financial pressures brought on by social media, Curry recommends establishing clear financial goals and balancing your short-term enjoyment without harming your long ...