

‘You have to suffer for your PhD’: poor mental health among doctoral researchers – new research
Lecturer in Social Sciences, University of Westminster
Disclosure statement
Cassie Hazell has received funding from the Office for Students.
University of Westminster provides funding as a member of The Conversation UK.
View all partners
PhD students are the future of research, innovation and teaching at universities and beyond – but this future is at risk. There are already indications from previous research that there is a mental health crisis brewing among PhD researchers.
My colleagues and I studied the mental health of PhD researchers in the UK and discovered that, compared with working professionals, PhD students were more likely to meet the criteria for clinical levels of depression and anxiety. They were also more likely to have significantly more severe symptoms than the working-professional control group.
We surveyed 3,352 PhD students, as well as 1,256 working professionals who served as a matched comparison group . We used the questionnaires used by NHS mental health services to assess several mental health symptoms.
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety.
The groups reported an equally high risk of suicide. Between 33% and 35% of both PhD students and working professionals met the criteria for “suicide risk”. The figures for suicide risk might be so high because of the high rates of depression found in our sample.
We also asked PhD students what they thought about their own and their peers’ mental health. More than 40% of PhD students believed that experiencing a mental health problem during your PhD is the norm. A similar number (41%) told us that most of their PhD colleagues had mental health problems.
Just over a third of PhD students had considered ending their studies altogether for mental health reasons.
There is clearly a high prevalence of mental health problems among PhD students, beyond those rates seen in the general public. Our results indicate a problem with the current system of PhD study – or perhaps with academic more widely. Academia notoriously encourages a culture of overwork and under-appreciation.
This mindset is present among PhD students. In our focus groups and surveys for other research , PhD students reported wearing their suffering as a badge of honour and a marker that they are working hard enough rather than too much. One student told us :
“There is a common belief … you have to suffer for the sake of your PhD, if you aren’t anxious or suffering from impostor syndrome, then you aren’t doing it "properly”.
We explored the potential risk factors that could lead to poor mental health among PhD students and the things that could protect their mental health.
Financial insecurity was one risk factor. Not all researchers receive funding to cover their course and personal expenses, and once their PhD is complete, there is no guarantee of a job. The number of people studying for a PhD is increasing without an equivalent increase in postdoctoral positions .
Another risk factor was conflict in their relationship with their academic supervisor . An analogy offered by one of our PhD student collaborators likened the academic supervisor to a “sword” that you can use to defeat the “PhD monster”. If your weapon is ineffective, then it makes tackling the monster a difficult – if not impossible – task. Supervisor difficulties can take many forms. These can include a supervisor being inaccessible, overly critical or lacking expertise.
A lack of interests or relationships outside PhD study, or the presence of stressors in students’ personal lives were also risk factors.
We have also found an association between poor mental health and high levels of perfectionism, impostor syndrome (feeling like you don’t belong or deserve to be studying for your PhD) and the sense of being isolated .
Better conversations
Doctoral research is not all doom and gloom. There are many students who find studying for a PhD to be both enjoyable and fulfilling , and there are many examples of cooperative and nurturing research environments across academia.
Studying for a PhD is an opportunity for researchers to spend several years learning and exploring a topic they are passionate about. It is a training programme intended to equip students with the skills and expertise to further the world’s knowledge. These examples of good practice provide opportunities for us to learn about what works well and disseminate them more widely.
The wellbeing and mental health of PhD students is a subject that we must continue to talk about and reflect on. However, these conversations need to happen in a way that considers the evidence, offers balance, and avoids perpetuating unhelpful myths.
Indeed, in our own study, we found that the percentage of PhD students who believed their peers had mental health problems and that poor mental health was the norm, exceeded the rates of students who actually met diagnostic criteria for a common mental health problem . That is, PhD students may be overestimating the already high number of their peers who experienced mental health problems.
We therefore need to be careful about the messages we put out on this topic, as we may inadvertently make the situation worse. If messages are too negative, we may add to the myth that all PhD students experience mental health problems and help maintain the toxicity of academic culture.
- Mental health
- Academic life
- PhD research

Data Manager

Director, Social Policy

Coordinator, Academic Advising

Head, School of Psychology

Senior Research Fellow - Women's Health Services
- Open access
- Published: 26 August 2020
Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis
- Cassie M. Hazell ORCID: orcid.org/0000-0001-5868-9902 1 ,
- Laura Chapman 2 ,
- Sophie F. Valeix 3 ,
- Paul Roberts 4 ,
- Jeremy E. Niven 5 &
- Clio Berry 6
Systematic Reviews volume 9 , Article number: 197 ( 2020 ) Cite this article
14k Accesses
60 Citations
82 Altmetric
Metrics details
Data from studies with undergraduate and postgraduate taught students suggest that they are at an increased risk of having mental health problems, compared to the general population. By contrast, the literature on doctoral researchers (DRs) is far more disparate and unclear. There is a need to bring together current findings and identify what questions still need to be answered.
We conducted a mixed methods systematic review to summarise the research on doctoral researchers’ (DRs) mental health. Our search revealed 52 articles that were included in this review.
The results of our meta-analysis found that DRs reported significantly higher stress levels compared with population norm data. Using meta-analyses and meta-synthesis techniques, we found the risk factors with the strongest evidence base were isolation and identifying as female. Social support, viewing the PhD as a process, a positive student-supervisor relationship and engaging in self-care were the most well-established protective factors.
Conclusions
We have identified a critical need for researchers to better coordinate data collection to aid future reviews and allow for clinically meaningful conclusions to be drawn.
Systematic review registration
PROSPERO registration CRD42018092867
Peer Review reports
Student mental health has become a regular feature across media outlets in the United Kingdom (UK), with frequent warnings in the media that the sector is facing a ‘mental health crisis’ [ 1 ]. These claims are largely based on the work of regulatory authorities and ‘grey’ literature. Such sources corroborate an increase in the prevalence of mental health difficulties amongst students. In 2013, 1 in 5 students reported having a mental health problem [ 2 ]. Only 3 years later, however, this figure increased to 1 in 4 [ 3 ]. In real terms, this equates to 21,435 students disclosing mental health problems in 2013 rising to 49,265 in 2017 [ 4 ]. Data from the Higher Education Statistics Agency (HESA) demonstrates a 210% increase in the number of students terminating their studies reportedly due to poor mental health [ 5 ], while the number of students dying by suicide has consistently increased in the past decade [ 6 ].
This issue is not isolated to the UK. In the United States (US), the prevalence of student mental health problems and use of counselling services has steadily risen over the past 6 years [ 7 ]. A large international survey of more than 14,000 students across 8 countries (Australia, Belgium, Germany, Mexico, Northern Ireland, South Africa, Spain and the United States) found that 35% of students met the diagnostic criteria for at least one common mental health condition, with highest rates found in Australia and Germany [ 8 ].
The above figures all pertain to undergraduate students. Finding equivalent information for postgraduate students is more difficult, and where available tends to combine data for postgraduate taught students and doctoral researchers (DRs; also known as PhD students or postgraduate researchers) (e.g. [ 4 ]). The latest trend analysis based on data from 36 countries suggests that approximately 2.3% of people will enrol in a PhD programme during their lifetime [ 9 ]. The countries with the highest number of DRs are the US, Germany and the UK [ 10 ]. At present, there are more than 281,360 DRs currently registered across these three countries alone [ 11 , 12 ], making them a significant part of the university population. The aim of this systematic review is to bring attention specifically to the mental health of DRs by summarising the available evidence on this issue.
Using a mixed methods approach, including meta-analysis and meta-synthesis, this review seeks to answer three research questions: (1) What is the prevalence of mental health difficulties amongst DRs? (2) What are the risk factors associated with poor mental health in DRs? And (3) what are the protective factors associated with good mental health in DRs?
Literature search
We conducted a search of the titles and abstracts of all article types within the following databases: AMED, BNI, CINAHL, Embase, HBE, HMIC, Medline, PsycInfo, PubMed, Scopus and Web of Science. The same search terms were used within all of the databases, and the search was completed on the 13th April 2018. Our search terms were selected to capture the variable terms used to describe DRs, as well as the terms used to describe mental health, mental health problems and related constructs. We also reviewed the reference lists of all the papers included in this review. Full details of the search strategy are provided in the supplementary material .
Inclusion criteria
Articles meeting the following criteria were considered eligible for inclusion: (1) the full text was available in English; (2) the article presented empirical data; (3) all study participants, or a clearly delineated sub-set, were studying at the doctoral level for a research degree (DRs or equivalent); and (4) the data collected related to mental health constructs. The last of these criteria was operationalised (a) for quantitative studies as having at least one mental health-related outcome measure, and (b) for qualitative studies as having a discussion guide that included questions related to mental health. We included university-published theses and dissertations as these are subjected to a minimum level of peer-review by examiners.
Exclusion criteria
In order to reduce heterogeneity and focus the review on doctoral research as opposed to practice-based training, we excluded articles where participants were studying at the doctoral level, but their training did not focus on research (e.g. PsyD doctorate in Clinical Psychology).
Screening articles
Papers were screened by one of the present authors at the level of title, then abstract, and finally at full text (Fig. 1 ). Duplicates were removed after screening at abstract. At each level of screening, a random 20% sub-set of articles were double screened by another author, and levels of agreement were calculated (Cohen’s kappa [ 13 ]). Where disagreements occurred between authors, a third author was consulted to decide whether the paper should or should not be included. All kappa values evidence at least moderate agreement between authors [ 14 ]—see Fig. 1 for exact kappa values.
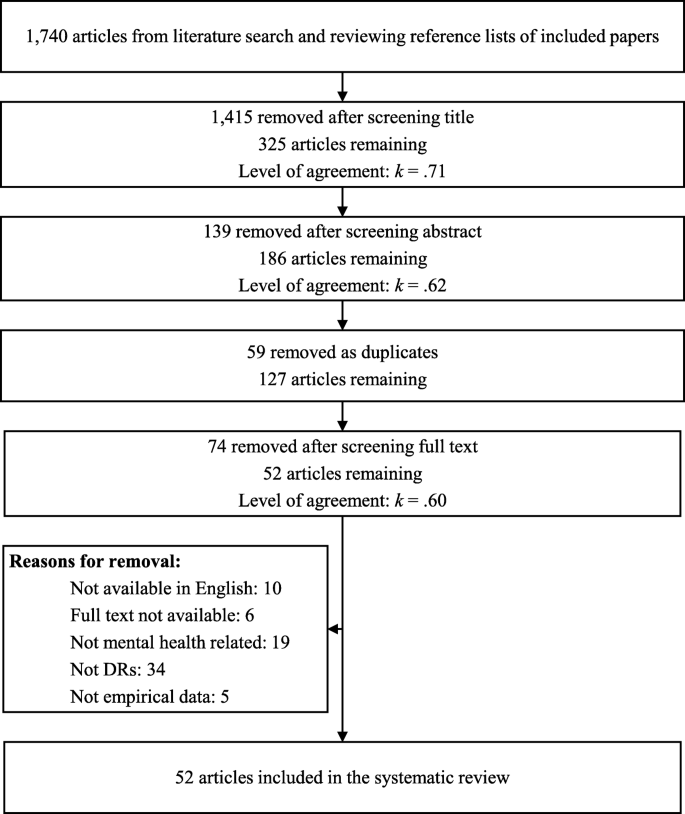
PRISMA diagram of literature review process
Data extraction
This review reports on both quantitative and qualitative findings, and separate extraction methods were used for each. Data extraction was performed by authors CH, CB, SV and LC.
Quantitative data extraction
The articles in this review used varying methods and measures. To accommodate this heterogeneity, multiple approaches were used to extract quantitative data. Where available, we extracted (a) descriptive statistics, (b) correlations and (c) a list of key findings. For all mental health outcome measures, we extracted the means and standard deviations for the DR participants, and where available for the control group (descriptive statistics). For studies utilising a within-subjects study design, we extracted data where a mental health outcome measure was correlated with another construct (correlations). Finally, to ensure that we did not lose important findings that did not use descriptive statistics or correlations, we extracted the key findings from the results sections of each paper (list of key findings). Key findings were identified as any type of statistical analysis that included at least one mental health outcome.
Qualitative data extraction
In line with the meta-ethnographic method [ 15 ] and our interest in the empirical data as well as the authors’ interpretations thereof, i.e. the findings of each article [ 16 ], the data extracted from the articles comprised both results/findings and discussion/conclusion sections. For articles reporting qualitative findings, we extracted the results and discussion sections from articles verbatim. Where articles used mixed methods, only the qualitative section of the results was extracted. Methodological and setting details from each article were also extracted and provided (see Appendix A) in order to contextualise the studies.
Data analysis
Quantitative data analysis, descriptive statistics.
We present frequencies and percentages of the constructs measured, the tools used and whether basic descriptive statistics ( M and SD ) were reported. The full data file is available from the first author upon request.
Effect sizes
Where studies had a control group, we calculated a between-group effect size (Cohen’s d ) using the formula reported by Wilson [ 17 ], and interpreted using the standard criteria [ 13 ]. For all other studies, we sought to compare results with normative data where the following criteria were satisfied: (a) at least three studies reported data using the same mental health assessment tool; (b) empirical normative data were available; and (c) the scale mean/total had been calculated following original authors’ instructions. Only the Perceived Stress Scale (PSS) 10- [ 18 ] and 14-item versions [ 19 ] met these criteria. Normative data were available from a sample of adults living in the United States: collected in 2009 for the 10-item version ( n = 2000; M = 15.21; SD = 7.28) [ 20 ] and in 1983 for the 14-item version ( n = 2355; M = 19.62; SD = 7.49) [ 18 ].
The meta-analysis of PSS data was conducted using MedCalc [ 21 ], and based on a random effects model, as recommended by [ 22 ]. The between-group effect sizes (DRs versus US norms) were calculated comparing PSS means and standard deviations in the respective groups. The effect sizes were weighted using the variable variances [ 23 ].
Correlations
Where at least three studies reported data reflecting a bivariate association between a mental health and another variable, we summarised this data into a meta-analysis using the reported r coefficients and sample sizes. Again, we used MedCalc [ 21 ] to conduct the analysis using a random effects model, based on the procedure outlined by Borenstein, Hedges, Higgins and Rothstein [ 24 ]. This analysis approach involves converting correlation coefficients into Fisher’s z values [ 25 ], calculating the summary of Fisher’s z , and then converting this to a summary correlation coefficient ( r ). The effect sizes were weighted in line with the Hedges and Ollkin [ 23 ] method. Heterogeneity was assessed using the Q statistic, and I 2 value—both were interpreted according to the GRADE criteria [ 26 ]. Where correlations could not be summarised within a meta-analysis, we have reported these descriptively.
Due to the heterogenous nature of the studies, the above methods could not capture all of the quantitative data. Therefore, additional data (e.g. frequencies, statistical tests) reported in the identified articles was collated into a single document, coded as relating to prevalence, risk or protective factors and reported as a narrative review.
Qualitative data analysis
We used thematic analytic methods to analyse the qualitative data. We followed the thematic synthesis method [ 16 , 27 ] and were informed by a thematic analysis approach [ 28 , 29 ]. We took a critical realist epistemological stance [ 30 , 31 ] and aimed to bring together an analysis reflecting meaningful patterns amongst the data [ 29 ] or demi-regularities, and identifying potential social mechanisms that might influence the experience of such phenomena [ 31 ]. The focus of the meta-synthesis is interpretative rather than aggregative [ 32 ].
Coding was line by line, open and complete. Following line-by-line coding of all articles, a thematic map was created. Codes were entered on an article-by-article basis and then grouped and re-grouped into meaningful patterns. Comparisons were made across studies to attempt to identify demi-regularities or patterns and contradictions or points of departure. The thematic map was reviewed in consultation with other authors to inductively create and refine themes. Thematic summaries were created and brought together into a first draft of the thematic structure. At this point, each theme was compared against the line-by-line codes and the original articles in order to check its fit and to populate the written account with illustrative quotations.
Research rigour
The qualitative analysis was informed by independent coding by authors CB and SV, and analytic discussions with CH, SV and LC. Our objective was not to capture or achieve inter-rater reliability, rather the analysis was strengthened through involvement of authors from diverse backgrounds including past and recent PhD completion, experiences of mental health problems during PhD completion, PhD supervision experience, experience as employees in a UK university doctoral school and different nationalities. In order to enhance reflexivity, CB used a journal throughout the analytic process to help notice and bracket personal reflections on the data and the ways in which these personal reflections might impact on the interpretation [ 29 , 33 ]. The ENTREQ checklist [ 34 ] was consulted in the preparation of this report to improve the quality of reporting.
Quality assessment
Quantitative data.
The quality of the quantitative papers was assessed using the STROBE combined checklist [ 35 ]. A random 20% sub-sample of these studies were double-coded and inter-rater agreement was 0.70, indicating ‘substantial’ agreement [ 14 ]. The maximum possible quality score was 23, with a higher score indicating greater quality, with the mean average of 15.97, and a range from 0 to 22. The most frequently low-scoring criteria were incomplete reporting regarding the management of missing data, and lack of reported efforts to address potential causes of bias.
Qualitative data
There appeared to be no discernible pattern in the perceived quality of studies; the highest [ 36 , 37 , 38 , 39 , 40 ] and lowest scoring [ 41 , 42 , 43 , 44 , 45 , 46 ] studies reflected both theses and journal publications, a variety of locations and settings and different methodologies. The most frequent low-scoring criteria were relating to the authors’ positions and reflections thereof (i.e. ‘Qualitative approach and research paradigm’, ‘Researcher characteristics and reflexivity’, ‘Techniques to enhance trustworthiness’, ‘Limitations’, ‘Conflict of interest and Funding’). Discussions of ethical issues and approval processes was also frequently absent. We identified that we foregrounded higher quality studies in our synthesis in that these studies appeared to have greater contributions reflected in the shape and content of the themes developed and were more likely to be the sources of the selected illustrative quotes.
Mixed methods approach
The goal of this review is to answer the review questions by synthesising the findings from both quantitative and/or qualitative studies. To achieve our goal, we adopted an integrated approach [ 47 ], whereby we used both quantitative and qualitative methods to answer the same review question, and draw a synthesised conclusion. Different analysis approaches were used for the quantitative and qualitative data and are therefore initially reported separately within the methods. A separate synthesised summary of the findings is then provided.
Overview of literature
Of the 52 papers included in this review (Table 1 ), 7 were qualitative, 29 were quantitative and 16 mixed methods. Most articles (35) were peer-reviewed papers, and the minority were theses (17). Only four of the articles included a control group; in three instances comprising students (but not DRs) and in the other drawn from the general population.
Quantitative results
Thirty-five papers reported quantitative data, providing 52 reported sets of mental health related data (an average of 1.49 measures per study): 24 (68.57%) measured stress, 10 (28.57%) anxiety, 9 (25.71%) general wellbeing, 5 (14.29%) social support, 3 (8.57%) depression and 1 (2.86%) self-esteem. Five studies (9.62%) used an unvalidated scale created for the purposes of the study. Fifteen studies (28.85%) did not report descriptive statistics.
Of the four studies that included a control group, only two of these reported descriptive statistics for both groups on a mental health outcome [ 66 , 69 ]. There is a small (Cohen’s d = 0.27) and large between-group effect (Cohen’s d = 1.15) when DRs were compared to undergraduate and postgraduate clinical psychology students respectively in terms of self-reported stress.
The meta-analysis of DR scores on the PSS (both 10- and 14-item versions) compared to population normative data produced a large and significant between-group effect size ( d = 1.12, 95% CI [0.52, 1.73]) in favour of DRs scoring higher on the PSS than the general population (Fig. 2 ), suggesting DRs experience significantly elevated stress. However, these findings should be interpreted in light of the significant between-study heterogeneity that can be classified as ‘considerable’ [ 26 ].
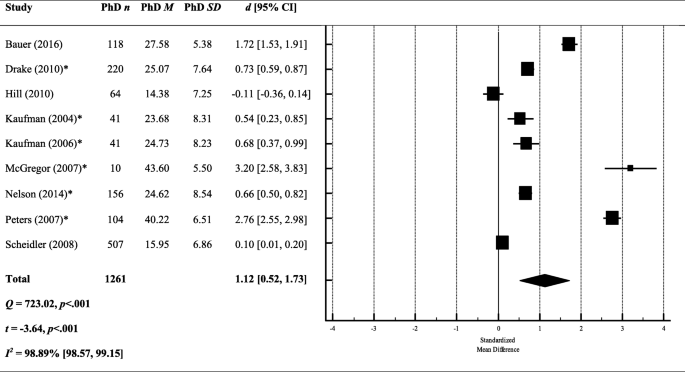
A meta-analysis of between-group effect sizes (Cohen’s d ) comparing PSS scores (both 10- and 14-item versions) from DRs and normative population data. *Studies using the 14 item version of the PSS; a positive effect size indicates DRs had a higher score on the PSS; a negative effect size indicates that the normative data produced a higher score on the PSS; black diamond = total effect size (based on random effects model); d = Cohen’s d ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
To explore this heterogeneity, we re-ran the meta-analysis separately for the 10- and 14-item versions. The effect size remained large and significant when looking only at the studies using the 14-item version ( k = 6; d = 1.41, 95% CI [0.63, 2.19]), but was reduced and no longer significant when looking at the 10-item version only ( k = 3; d = 0.57, 95% CI [− 0.51, 1.64]). However, both effect sizes were still marred by significant heterogeneity between studies (10-item: Q = 232.02, p < .001; 14-item: Q = 356.76, p < .001).
Studies reported sufficient correlations for two separate meta-analyses; the first assessing the relationship between stress (PSS [ 18 , 19 ]) and perceived support, and the second between stress (PSS) and academic performance.
Stress x support
We included all measures related to support irrespective of whom that support came from (e.g. partner support, peer support, mentor support). The overall effect size suggests a small and significant negative correlation between stress and support ( r = − .24, 95% CI [− 0.34, − 0.13]) (see Fig. 3 ), meaning that low support is associated with greater perceived stress. However, the results should be interpreted in light of the significant heterogeneity between studies. The I 2 value quantifies this heterogeneity as almost 90% of the variance being explained by between-study heterogeneity, which is classified as ‘substantial’ (26).
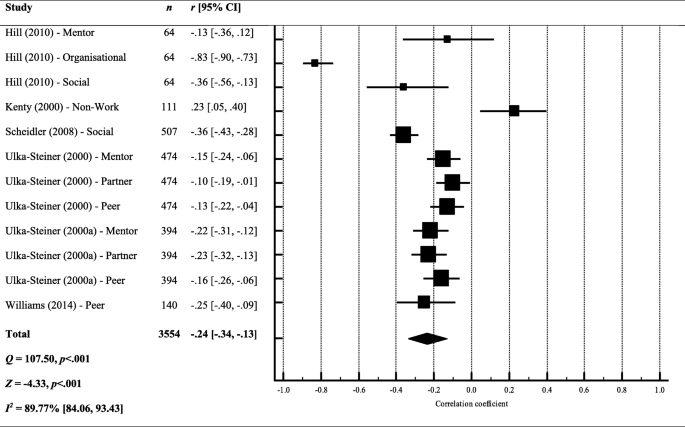
Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and perceived support. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
Stress x performance
The overall effect size suggests that there is no relationship between stress and performance in their studies ( r = − .07, 95% CI [− 0.19, 0.05]) (see Fig. 4 ), meaning that DRs perception of their progress was not associated with their perceived stress This finding suggests that the amount of progress that DRs were making during their studies was not associated with stress levels.
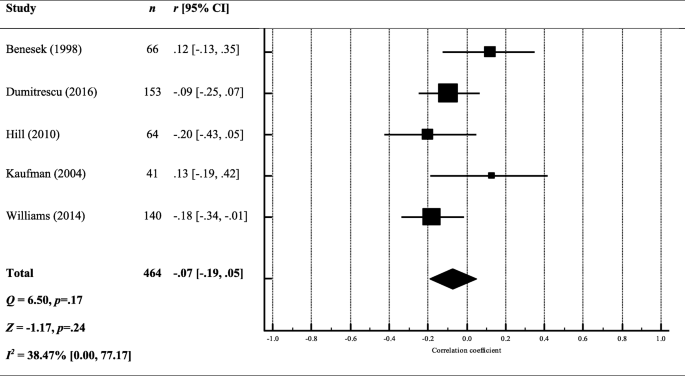
Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and performance. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
Other correlations
Correlations reported in less than three studies are summarised in Fig. 5 . Again, stress was the most commonly tested mental health variable. Self-care and positive feelings towards the thesis were consistently found to negatively correlate with mental health constructs. Negative writing habits (e.g. perfectionism, blocks and procrastination) were consistently found to positively correlate with mental health constructs. The strongest correlations were found between stress, and health related quality of life ( r = − .62) or neuroticism ( r = .59), meaning that lower stress was associated with greater quality of life and reduced neuroticism. The weakest relationships ( r < .10) were found between mental health outcomes and: faculty concern, writing as knowledge transformation, innate writing ability (stress and anxiety), years married, locus of control, number of children and openness (stress only).
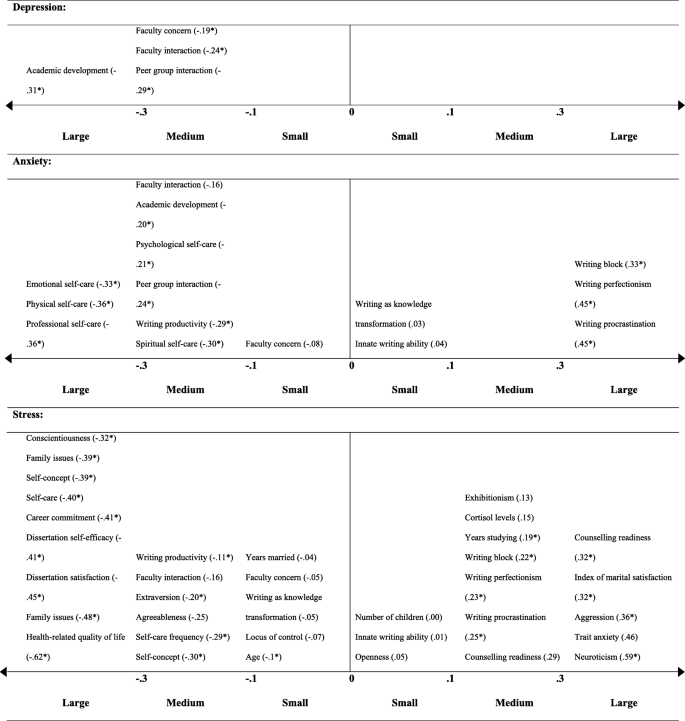
Correlation coefficients testing the relationship between a mental health outcome and other construct. Correlation coefficients are given in brackets ( r ); * p < .05; each correlation coefficient reflects the results from a single study
Several studies reported DR mental health problem prevalence and this ranged from 36.30% [ 54 ] to 55.9% [ 67 ]. Using clinical cut-offs, 32% were experiencing a common psychiatric disorder [ 64 ]; with another study finding that 53.7% met the questionnaire cut-off criteria for depression, and 41.9% for anxiety [ 67 ]. One study compared prevalence amongst DRs and the general population, employees and other higher education students; in all instances, DRs had higher levels of psychological distress (non-clinical), and met criteria for a clinical psychiatric disorder more frequently [ 64 ].
Risk factors
Demographics Two studies reported no significant difference between males and females in terms of reported stress [ 57 , 73 ], but the majority suggested female DRs report greater clinical [ 80 ], and non-clinical problems with their mental health [ 37 , 64 , 79 , 83 , 89 ].
Several studies explored how mental health difficulties differed in relation to demographic variables other than gender, suggesting that being single or not having children was associated with poorer mental health [ 64 ] as was a lower socioeconomic status [ 71 ]. One study found that mental health difficulties did not differ depending on DRs’ ethnicity [ 51 ], but another found that Black students attending ‘historically Black universities’ were significantly more anxious [ 87 ]. The majority of the studies were conducted in the US, but only one study tested for cross-cultural differences: reporting that DRs in France were more psychologically distressed than those studying in the UK [ 67 ].
Work-life balance Year of study did not appear to be associated with greater subjective stress in a study involving clinical psychology DRs (Platt and Schaefer [ 75 ]), although other studies suggested greater stress reported by those in the latter part of their studies [ 89 ], who viewed their studies as a burden [ 81 ], or had external contracts, i.e. not employed by their university [ 85 ]. Regression analyses revealed that a common predictor of poor mental health was uncertainty in DR studies; whether in relation to uncertain funding [ 64 ] or uncertain progress [ 80 ]. More than two-thirds of DRs reported general academic pressure as a cause of stress, and a lack of time as preventing them from looking after themselves [ 58 ]. Being isolated was also a strong predictor of stress [ 84 ].
Protective factors
DRs who more strongly endorsed all of the five-factor personality traits (openness, conscientiousness, extraversion, agreeableness and neuroticism) [ 66 ], self-reported higher academic achievement [ 40 ] and viewed their studies as a learning process (rather than a means to an end) [ 82 ] reported fewer mental health problems. DRs were able to mitigate poor mental health by engaging in self-care [ 72 ], having a supervisor with an inspirational leadership style [ 64 ] and building coping strategies [ 56 ]. The most frequently reported coping strategy was seeking support from other people [ 37 , 58 ].
Qualitative results
Meta-synthesis.
Four higher-order themes were identified: (1) Always alone in the struggle, (2) Death of personhood, (3) The system is sick and (4) Seeing, being and becoming. The first two themes reflect individual risk/vulnerability factors and the processes implicated in the experience of mental distress, the third represents systemic risk and vulnerability factors and the final theme reflects individual and systemic protective mechanisms and transformative influences. See Table 2 for details of the full thematic structure with illustrative quotes.
Always alone in the struggle
‘Always alone in the struggle’ reflects the isolated nature of the PhD experience. Two subthemes reflect different aspects of being alone; ‘Invisible, isolated and abandoned’ represents DRs’ sense of physical and psychological separation from others and ‘It’s not you, it’s me’ represents DRs’ sense of being solely responsible for their PhD process and experience.
Invisible, isolated and abandoned
Feeling invisible and isolated both within and outside of the academic environment appears a core DR experience [ 39 , 43 , 81 ]. Isolation from academic peers seemed especially salient for DRs with less of a physical presence on campus, e.g. part-time and distance students, those engaging in extensive fieldwork, outside employment and those with no peer research or lab group [ 36 , 52 , 68 ]. Where DRs reported relationships with DR peers, these were characterised as low quality or ‘not proper friendships’ and this appeared linked to a sense of essential and obvious competition amongst DRs with respect to current and future resources, support and opportunities [ 39 ], in which a minority of individuals were seen to receive the majority share [ 36 , 74 ]. Intimate sharing with peers thus appeared to feel unsafe. This reflected the competitive environment but also a sense of peer relationships being predicated on too shared an experience [ 39 ].
In addition to poor peer relations, a mismatch between the expected and observed depth of supervisor interest, engagement and was evident [ 40 , 81 ]. This mismatch was clearly associated with disappointment and anger, and a sense of abandonment, which appeared to impact negatively on DR mental health and wellbeing [ 42 ] (p. 182). Moreover, DRs perceived academic departments as complicit in their isolation; failing to offer adequate opportunities for academic and social belonging and connections [ 42 , 81 ] and including PGRs only in a fleeting or ‘hollow’ sense [ 37 ]. DRs identified this isolation as sending a broader message about academia as a solitary and unsupported pursuit; a message that could lead some DRs to self-select out of planning for future in academia [ 37 , 42 ]. DRs appeared to make sense of their lack of belonging in their department as related to their sense of being different, and that this difference might suggest they did not ‘fit in’ with academia more broadly [ 74 ]. In the short-term, DRs might expend more effort to try and achieve a social and/or professional connection and equitable access to support, opportunities and resources [ 74 ]. However, over the longer-term, the continuing perception of being professionally ‘other’ also seemed to undermine DRs’ sense of meaning and purpose [ 81 ] and could lead to opting out of an academic career [ 62 , 74 ].
Isolation within the PhD was compounded by isolation from one’s personal relationships. This personal isolation was first physical, in which the laborious nature of the PhD acted as a catalyst for the breakdown of pre-existing relationships [ 76 ]. Moreover, DRs also experienced a sense of psychological detachment [ 45 , 74 ]. Thus, the experience of isolation appeared to be extremely pervasive, with DRs feeling excluded and isolated physically and psychologically and across both their professional and personal lives.
It’s not you, it’s me
‘It’s not you, it’s me’ reflects DRs’ perfectionism as a central challenge of their PhD experience and a contributor to their sense of psychological isolation from other people. DRs’ perfectionism manifested in four key ways; firstly, in the overwhelming sense of responsibility experienced by DRs; secondly, in the tendency to position themselves as inadequate and inferior; thirdly, in cycles of perfectionist paralysis; and finally, in the tendency to find evidence which confirms their assumed inferiority.
DRs positioned themselves as solely responsible for their PhD and for the creation of a positive relationship with their supervisor [ 36 , 52 , 81 ]. DRs expressed a perceived need to capture their supervisors’ interest and attention [ 36 , 52 , 74 ], feeling that they needed to identify and sell to their supervisors some shared characteristic or interest in order to scaffold a meaningful relationship. DRs appeared to feel it necessary to assume sole responsibility for their personal lives and to prohibit any intrusion of the personal in to the professional, even in incredibly distressing circumstances [ 42 ].
DRs appeared to compare themselves against an ideal or archetypal DR and this comparison was typically unfavourable [ 37 ], with DRs contrasting the expected ideal self with their actual imperfect and fallible self [ 37 , 42 , 52 ]. DRs’ sense of inadequacy appeared acutely and frequently reflected back to them by supervisors in the form of negative or seemingly disdainful feedback and interactions [ 41 , 76 ]. DRs framed negative supervisor responses as a cue to work harder, meaning they were continually striving, but never reaching, the DR ideal [ 76 ]. This ideal-actual self-discrepancy was associated with a tendency towards punitive self-talk with clear negative valence [ 38 ].
DRs appear to commonly use self-castigation as a necessary (albeit insufficient) means to motivate themselves to improve their performance in line with perfectionistic standards [ 38 , 41 ]. The oscillation between expectation and actuality ultimately resulted in increased stress and anxiety and reduced enjoyment and motivation. Low motivation and enjoyment appeared to cause procrastination and avoidance, which lead to a greater discrepancy between the ideal and actual self; in turn, this caused more stress and anxiety and further reduced enjoyment and motivation leading to a sense of stuckness [ 76 ].
The internalisation of perceived failure was such that DRs appeared to make sense of their place, progress and possible futures through a lens of inferiority, for example, positioning themselves as less talented and successful compared to their peers [ 37 ]. Thus, instances such as not being offered a job, not receiving funding, not feeling connected to supervisors, feeling excluded by academics and peers were all made sense of in relation to DRs’ perceived relative inadequacy [ 36 ].
Death of personhood
The higher-order theme ‘Death of personhood’ reflects DRs’ identity conflict during the PhD process; a sense that DRs’ engage in a ‘Sacrifice of personal identity’ in which they feel they must give up their pre-existing self-identity, begin to conceive of themselves as purely ‘takers’ personally and professionally, thus experiencing the ‘Self as parasitic’, and ultimately experience a ‘Death of self-agency’ in relation to the thesis, the supervisor and other life roles and activities.
A sacrifice of personal identity
The sacrifice of personal identity first manifests as an enmeshment with the PhD and consequent diminishment of other roles, relationships and activities that once were integral to the DRs’ sense of self [ 59 , 76 ]. DRs tended to prioritise PhD activities to the extent that they engaged in behaviours that were potentially damaging to their personal relationships [ 76 ]. DRs reported a sense of never being truly free; almost physically burdened by the weight of their PhD and carrying with them a constant ambient guilt [ 37 , 38 , 44 , 76 ]. Time spent on non-PhD activities was positioned as selfish or indulgent, even very basic activities of living [ 76 ].
The seeming incompatibility of aspects of prior personal identity and the PhD appears to result in a sense of internal conflict or identity ‘collision’ [ 59 ]. Friends and relatives often provided an uncomfortable reflection of the DR’s changing identity, leaving DRs feeling hyper-visible and carrying the burden of intellect or trailblazer status [ 74 ]; providing further evidence for the incompatibility of their personal and current and future professional identities. Some DRs more purposefully pruned their relationships and social activities; to avoid identity dissonance, to conserve precious time and energy for their PhD work, or as an acceptance of total enmeshment with academic work as necessary (although not necessarily sufficient) for successful continuation in academia [ 40 , 52 , 77 ]. Nevertheless, the diminishment of the personal identity did not appear balanced by the development of a positive professional identity. The professional DR identity was perceived as unclear and confusing, and the adoption of an academic identity appeared to require DRs to have a greater degree of self-assurance or self-belief than was often the case [ 37 , 81 ].
Self as parasitic
Another change in identity manifested as DRs beginning to conceive of themselves as parasitic. DRs spoke of becoming ‘takers’, feeling that they were unable to provide or give anything to anyone. For some DRs, being ‘parasitic’ reflected them being on the bottom rung of the professional ladder or the ‘bottom of the pile’; thus, professionally only able to receive support and assistance rather than to provide for others. Other DRs reported more purposefully withdrawing from activities in which they were a ‘giver’, for example voluntary work, as providing or caring for others required time or energy that they no longer had [ 38 , 44 ]. Furthermore, DRs appeared to conceive of themselves as also causing difficulty or harm to others [ 81 ], as problems in relation to their PhD could lead them to unwillingly punishing close others, for example, through reducing the duration or quality of time spent together [ 38 ].
Feeling that close others were offering support appeared to heighten the awareness of the toll of the PhD on the individual and their close relationships, emphasising the huge undertaking and the often seemingly slow progress, and actually contributing to the sense of ambient guilt, shame, anger and failure [ 38 ]. Moreover, DRs spoke of feeling extreme guilt in perceiving that they had possibly sacrificed their own, and possibly family members’, current wellbeing and future financial security [ 49 ].
Death of self-agency
In addition to their sense of having to sacrifice their personal identity, DRs also expressed a loss of their sense of themselves as agentic beings. DRs expressed feeling powerless in various domains of their lives. First, DRs positioned the thesis as a powerful force able to overwhelm or swallow them [ 46 , 52 , 59 ]. Secondly, DRs expressed a sense of futility in trying to retain any sense of personal power in the climate of academia. An acute feeling of powerlessness especially in relation to supervisors was evident, with many examples provided of being treated as means to an end, as opposed to ends in themselves [ 39 , 42 , 62 ]. Supervisors did not interact with DRs in a holistic way that recognised their personhood and instead were perceived as prioritising their own will, or the will of other academics, above that of the DR [ 39 , 62 ].
Furthermore, DRs reported feeling as if they were used as a means for research production or furthering their supervisors’ reputations or careers [ 62 ]. DRs perceived that holding on to a sense of personal agency sometimes felt incompatible with having a positive supervisor relationship [ 42 ]. Thus whilst emotional distress, anger, disappointment, sadness, jealousy and resentment were clearly evident in relation to feeling excluded, used or over-powered by supervisors [ 37 , 42 , 52 , 62 ], DRs usually felt unable to change supervisor irrespective of how seriously this relationship had degraded [ 37 , 62 ]. Instead, DRs appeared to take on a position of resignation or defensive pessimism, in which they perceived their supervisors as thwarting their personhood, personal goals and preferences, but typically felt compelled to accept this as the status quo and focus on finishing their PhDs [ 42 ]. DRs resignation was such that they internalised this culture of silence and silenced themselves; tending to share litanies of problems with supervisors whilst prefacing or ending the statements with some contradictory or undermining phrase such as ‘but that’s okay’ [ 42 , 52 ].
The apparent lack of self-agency extended outward from the PhD into DRs not feeling able to curate positive life circumstances more generally [ 76 ]. A lack of time was perhaps the key struggle across both personal and professional domains, yet DRs paradoxically reported spending a lot of time procrastinating and rarely (if ever) mentioned time management as a necessary or desired coping strategy for the problem of having too little time [ 46 ]. The lack of self-agency was not only current but also felt in reference to a bleak and uncertain future; DRs lack of surety in a future in academia and the resultant sense of futility further undermined their motivation to engage currently with PhD tasks [ 38 , 40 ].
The system is sick
The higher-order theme ‘The system is sick’ represents systemic influences on DR mental health. First, ‘Most everyone’s mad here’ reflects the perceived ubiquity mental health problems amongst DRs. ‘Emperor’s new clothes’ reflects the DR experience of engaging in a performative piece in which they attempt to live in accordance with systemic rather than personal values. Finally, ‘Beware the invisible and visible walls’ reflects concerns with being caught between ephemeral but very real institutional divides.
Most everyone’s mad here
No studies focused explicitly on experiences of DRs who had been given diagnoses of mental health problems. Some study participants self-disclosed mental health problems and emphasised their pervasive impact [ 50 ]. Further lived experiences of mental distress in the absence of explicit disclosure were also clearly identifiable. The ‘typical’ presentation of DRs with respect to mental health appeared characterised as almost unanimous [ 39 ] accounts of chronic stress, anxiety and depression, emotional distress including frustration, anger and irritability, lack of mental and physical energy, somatic problems including appetite problems, headaches, physical pain, nausea and problems with drug and alcohol abuse [ 39 , 46 , 59 , 76 ]. Health anxiety, concerns regarding perceived new and unusual bodily sensations and perceived risks of developing stress-related illnesses were also common [ 46 , 59 , 76 ]. A PhD-specific numbness and hypervigilance was also reported, in which DRs might be less responsive to personal life stressors but develop an extreme sensitivity and reactivity to PhD-relevant stimuli [ 39 ].
An interplay of trait and state factors were suggested to underlie the perceived ubiquity of mental health problems amongst DRs. Etiological factors associated with undertaking a PhD specifically included the high workload, high academic standards, competing personal and professional demands, social isolation, poor resources in the university, poor living conditions and poverty, future and career uncertainty [ 36 , 41 , 43 , 46 , 49 , 76 ]. The ‘nexus’ of these factors was such that the PhD itself acted as a crucible; a process of such intensity that developing mental health problems was perhaps inevitable [ 39 ].
The perceived inevitability of mental health problems was such that DRs described people who did not experience mental health problems during a PhD as ‘lucky’ [ 39 ]. Supervisors and the wider academic system were seen to promote an expectation of suffering, for example, with academics reportedly normalising drug and alcohol problems and encouraging unhealthy working practices [ 39 ]. Furthermore, DRs felt that academics were uncaring with respect to the mental challenge of doing a PhD [ 39 ]. Nevertheless, academics were suggested to deny any culpability or accountability for mental health problems amongst DRs [ 39 , 59 , 74 ]. The cycle of indigenousness was further maintained by a lack of mental health literacy and issues with awareness, availability and access to help-seeking and treatment options amongst DRs and academics more widely [ 39 ]. Thus, DRs appeared to feel they were being let down by a system that was almost set up to cause mental distress, but within which there was a widespread denial of the size and scope of the problem and little effort put into identifying and providing solutions [ 39 , 59 ]. DRs ultimately felt that the systemic encouragement of unhealthy lifestyles in pursuit of academic success was tantamount to abuse [ 62 ].
A performance of optimum suffering
Against a backdrop of expected mental distress, DRs expressed their PhD as a performative piece. DRs first had to show just the right amount of struggle and difficulty; feeling that if they did not exhibit enough stress, distress and ill-health, their supervisors or the wider department might not believe they were taking their PhD seriously enough [ 40 ]. At the same time, DRs felt that their ‘researcher mettle’ was constantly being tested and they must rise to this challenge. This included first guarding against presenting oneself as intellectually inferior [ 36 ]. Yet it also seemed imperative not to show vulnerability more broadly [ 74 ]. Disclosing mental or physical health problems might lead not only to changed perceptions of the DR but to material disadvantage [ 74 ]. The poor response to mental health disclosures suggested to some DRs that universities might be purposefully trying to dissuade or discourage DRs with mental health problems or learning disabilities from continuing [ 74 ]. The performative piece is thus multi-layered, in that DRs must experience extreme internal psychological struggles, exhibit some lower-level signs of stress and fatigue for peer and faculty observance, yet avoid expressing any real academic or interpersonal weakness or the disclosure of any diagnosable disability or disease.
Emperor’s new clothes
DRs described feeling beholden to the prevailing culture in which it was expected to prioritise above all else developing into a competitive, self-promoting researcher in a high-performing research-active institution [ 39 , 42 ]. Supervisors often appeared the conduit for transmission of this academic ideal [ 74 ]. DRs felt reticent to act in any way which suggested that they did not personally value the pursuit of a leading research career above all else. For example, DRs felt that valuing teaching was non-conformist and could endanger their continuing success within their current institution [ 55 ]. Many DRs thus exhibited a sense of dissonance as their personal values often did not align with the institutional values they identified [ 74 ]. Yet DRs expressed a sense of powerlessness and a feeling of being ‘caught up’ in the values of the institution even when such values were personally incongruent [ 74 ]. The psychological toll of this sense of inauthenticity seemed high [ 55 ]. Where DRs acted in ways which ostensibly suggested values other than prioritising a research career, for example becoming pregnant, they sensed disapproval [ 76 ]. DRs also felt unable to challenge other ‘institutional myths’ for example, the perceived institutional denial of the duration of and financial struggle involved in completing a PhD [ 49 ]. There was a perceived tendency of academics to locate problems within DRs as opposed to acknowledging institutional or systemic inequalities [ 49 ]. DRs expressed strongly a sense in which there is inequity in support, resources and opportunities, yet universities were perceived as ignoring such inequity or labelling such divisions as based on meritocracy [ 36 , 74 ].
Beware the invisible and visible walls
DRs described the reality of working in academia as needing to negotiate a maze of invisible and visible walls. In the former case, ‘invisible walls’ reflect ephemeral norms and rules that govern academia. DRs felt that a big part of their continuing success rested upon being able to negotiate such rules [ 39 ]. Where rules were violated and explicit or implicit conflicts occurred, DRs were seen to be vulnerable to being caught in the ‘crossfire’ [ 36 ]. DRs identified academic groups and departments as being poor in explicitly identifying, discussing and resolving conflicts [ 37 ]. The intangibility of the ‘invisible walls’ gave rise to a sense of ambient anxiety about inadvertently transgressing norms and divides, such that some DRs reported behaving in ways that surprised even themselves [ 37 ].
Gendered and racial micropolitics of academic institutions were seen to manifest as more visible walls between people, with institutions privileging those with ‘insider’ status [ 36 ]. Women and people of colour typically felt excluded or disadvantaged in a myriad of observable and unobservable ways, with individuals able to experience both insider and outsider statuses simultaneously [ 36 , 37 ], for example when a male person of colour [ 36 ]. Female DRs suggested that not only must women prove themselves to a greater extent than men to receive equal access to resources, opportunities and acclaim but also are typically under additional pressure in both their professional and personal lives [ 37 , 52 , 76 ]. Women also felt that they had to take on more additional roles and responsibilities and encountered more conflicts in their personal lives compared to men [ 52 ]. Examples of professionally successful women in DRs’ departments were described as those who had crossed the divide and adopted a more traditionally male role [ 40 ]. Thus, being female or non-White were considered visible characteristics that would disadvantage people in the competitive academic environment and could give rise to a feeling of increased stress, pressure, role conflicts, and a feeling of being unsafe.
Seeing, being and becoming
The higher-order theme of ‘Seeing, being and becoming’ reflects protective and transformative influences on DR mental health. ‘De-programming’ refers to the DRs disentangling their personal beliefs and values from systemic values and also from their own tendency towards perfectionism. ‘The power of being seen’ reflects the positive impact on DR mental health afforded by feeling visible to personal and professional others. ‘Finding hope, meaning and authenticity’ refers to processes by which DRs can find or re-locate their own self-agency, purpose and re/establish a sense of living in accordance with their values. ‘The importance of multiple goals, roles and groups’ represents the beneficial aspects of accruing and sustaining multiple aspects to one’s identity and connections with others and activities outside the PhD. Finally, ‘The PhD as a process of transcendence’ reflects how the struggles involved in completing a PhD can be transformative and self-actualising.
De-programming
DRs reported being able to protect their mental health by ‘de-programming’ and disentangling their attitudes and practices from social and systemic values and norms. This disentangling helped negate DRs’ adopting unhealthy working practices and offered some protection against experiencing inauthenticity and dissonance between personal and systemic values.
First, DRs spoke of rejecting the belief that they should sacrifice or neglect personal relationships, outside interests and their self-identity in pursuit of academic achievement. DRs could opt-out entirely by choosing a ‘user-friendly’ programme [ 44 ] which encouraged balance between personal and professional goals, or else could psychologically reject the prevailing institutional discourse [ 40 ]. Rather than halting success, de-programming from the prioritisation of academia above all else was seen to be associated not only with reduced stress but greater confidence, career commitment and motivation [ 40 , 50 ]. It was also suggested possible to ‘de-programme’ in the sense of choosing not to be preoccupied by the ‘invisible walls’ of academia and psychologically ‘opt out’ of being concerned by potential conflicts, norms and rules governing academic workplace conduct [ 36 ]. Interaction with people outside of academia was seen to scaffold de-programming, by helping DRs to stay ‘grounded’ and offering a model what ‘normal’ life looks like. People outside of academia could also help DRs to see the truth by providing unbiased opinions regarding systemic practices [ 39 ].
A further way in which de-programming manifested was in DRs challenging their perfectionist beliefs. This include re-framing the goal as not trying to be the archetype of a perfect DR, and accepting that multiple demands placed on one individual invariably requires compromise [ 40 , 76 ]. DRs spoke of the need to conceptualise the PhD as a process, rather than just a product [ 46 , 82 ]. The process orientation facilitated framing of the PhD as just one-step in the broader process of becoming an academic as opposed to providing discrete evidence of worth [ 82 ]. Within this perspective, uncertainty itself could be conceived as a privilege [ 81 ]. The PhD was then seen as an opportunity rather than a test [ 37 , 46 ]. Moreover, the process orientation facilitated viewing the PhD as a means of growing into a contributing member of the research community, as opposed to needing to prove oneself to be accepted [ 82 ]. Remembering the temporary nature of the PhD was advised [ 45 ] as was holding on to a sense that not completing the PhD was also a viable life choice [ 76 ]. DRs also expressed, implicitly or explicitly, a decision to change their conceptualisation of themselves and their progress; choosing not to perceive themselves as stuck, but planning, learning and progressing [ 38 , 39 , 81 , 82 ]. This new perspective appeared to be helpful in reducing mental distress.
The power of being seen
DRs described powerful benefits to feeling seen by other people, including a sense of belonging and mattering, increased self-confidence and a sense of positive progress [ 37 ]. Being seen by others seems to provoke the genesis of an academic identity; it brings DRs into existence as academics. Being seen within the academic institution also supports mental health and can buffer emotional exhaustion [ 37 , 52 , 55 , 81 ]. DRs expressed a need to feel that supervisors, academics and peers were interested in them as people, their values, goals, struggles and successes; yet they also needed to feel that they and their research mattered and made a difference within and outside of the institution [ 42 , 52 , 81 ]. It was clear that DRs could find in their disciplinary communities the sense of belonging that often eluded them within their immediate departments [ 42 ]. Feeling a sense of belonging to the academic community seemed to buffer disengagement and amotivation during the PhD [ 81 ]. Positive engagement with the broader community was scaffolded by a sense of trust in the supervisor [ 81 ]. DRs often felt seen and supported by postdocs, especially where supervisors appeared absent or unsupportive [ 50 ].
Spending time with peers could be beneficial when there was a sense of shared experience and walking alongside each other [ 39 ]. Friendship was seen to buffer stress and protect against mental health problems through the provision of social and emotional support and help in identifying struggles [ 39 , 43 ]. In addition to relational aspects, the provision of designated physical spaces on campus or in university buildings also seemed important to being seen [ 37 ]. Peers in the university could provide DRs with further physical embodiments of being seen, for example, gift-giving in response to their birthdays or returning from leave [ 37 , 50 ]. Outside of the academic institution, DRs described how being seen by close others could support DRs to be their authentic selves, providing an antidote to the invisible walls of academia [ 50 ]. Good quality friendships within or outside academia could be life-changing, providing a visceral sense of connection, belonging and authenticity that can scaffold positive mental health outcomes during the PhD [ 39 ]. Pets could also serve to help DRs feel seen but without needing to extend too much energy into maintaining social relationships [ 50 ].
Finally, DRs also needed to see themselves, i.e. to begin to see themselves as burgeoning academics as opposed to ‘just students’ [ 81 ]. Feeling that the supervisor and broader academic community were supportive, developing one’s own network of process collaborators and successfully obtaining grant funding seemed tangible markers that helped DRs to see themselves as academics [ 37 , 81 ]. Seeing their own work published was also helpful in providing a boost in confidence and being a joyful experience [ 42 ]. Moreover, with sufficient self-agency, DRs can not only see themselves but render themselves visible to other people [ 37 ].
Multiple goals, roles and groups
In antidote to the diminished personal identity and enmeshment with the PhD, DRs benefitted from accruing and sustaining multiple goals, roles, occupations, activities and social group memberships. Although ‘costly’ in terms of increased stress and role conflicts, sustaining multiple roles and activities appeared essential for protecting against mental health problems [ 50 , 68 ].
Leisure activities appeared to support mental health through promoting physical health, buffering stress, providing an uplift to DRs’ mood and through the provision of another identity other than as an academic [ 44 , 50 , 76 ]. Furthermore, engagement in activities helped DRs to find a sense of freedom, allowing them to carve up leisure and work time and psychologically detach from their PhD [ 68 , 76 ]. Competing roles, especially family, forced DRs to distance themselves from the PhD physically which reinforced psychological separation [ 50 , 59 ]. Engaging in self-care and enjoyable activities provided a sense of balance and normalcy [ 39 , 44 , 68 ]. This normalcy was a needed antidote to abnormal pressure [ 59 ]. Even in the absence of fiercely competing roles and priorities, DRs still appeared to benefit from treating their PhD as if it is only one aspect of life [ 59 ]. Additional roles and activities reduced enmeshment with the PhD to the extent that considering not completing the PhD was less averse [ 40 ]. This position appeared to help DRs to be less overwhelmed and less sensitive to perceived and anticipated failures.
Finding hope, meaning and authenticity
Finding hopefulness and meaning within the PhD can scaffold a sense of living a purposeful, enjoyable, important and authentic life. Hopefulness is predicated on the ability to identify a goal, i.e. to visualise and focus on the desired outcome and to experience both self-agency and potential pathways towards the goal. Hopefulness was enhanced by the ability to break down tasks into smaller goals and progress in to ‘baby steps’ [ 38 , 59 ]. In addition, DRs benefitted from finding explicit milestones against which they can compare their progress [ 59 ], as this appeared to feed back into the cycle of hopeful thinking and spur further self-agency and goal pursuit.
The experience of meaning manifested in two main ways; first as the more immediate lived experience of passion in action [ 76 ]. Secondly, DRs found meaning in feeling that in their PhD and lives more broadly they were living in accordance with their values, for example, experiencing their own commitment in action through continuing to work on their PhD even when it was difficult to do so [ 76 ]. DRs who were able to locate their PhD within a broader sense of purpose appeared to derive wellbeing benefits. There was a need to ensure that values were in alignment, for example, finding homeostasis between emotional, intellectual, social and spiritual parts of the self [ 46 , 59 , 90 ].
The processes of finding hopefulness and meaning appear to be largely relational. Frequent contact with supervisors in person and social and academic contact with other DRs were basic scaffolds for hope and meaning [ 52 ]. DRs spoke of how a sense that their supervisors believed in them inspired their self-agency and motivation [ 42 , 62 , 76 ]. Partners, friends and family could also inspire motivation for continuing in PhD tasks [ 44 , 76 ]. Other people also could help instil a sense of motivation to progress and complete the PhD; a sense of being seen is to be beholden to finish [ 39 ]. Meaning appeared to be scaffolded by a sense of contribution, belonging and mattering [ 81 ] and could arise from the perception of putting something into the collective pot, inspiring hopefulness and helping others [ 39 , 42 ]. Moreover, hopefulness, meaning and authenticity also appeared mutually reinforcing [ 81 ]. Finding meaning and working on a project which is in accordance with personal values, preferences and interests is also helpful in completing the PhD and provides a feedback loop into hope, motivation and agentic thinking [ 39 , 81 ]. Furthermore, DRs could use agentic action to source a community of people who share their values, enabling them to engage in collective authenticity [ 39 ].
The PhD as a process of transcendence
The immense challenge of the PhD could be a catalyst for growth, change and self-actualisation, involving empowerment through knowledge, self-discovery, and developing increased confidence, maturity, capacity for self-direction and use of one’s own autonomy [ 44 , 82 ]. The PhD acted as a forge in which DRs were tested and became remoulded into something greater than they had been before [ 44 , 82 , 90 ]. The struggles endured during the PhD caused DRs to reconsider their sense of their own capacities, believing themselves to be more able than they previously would have thought [ 50 ]. The struggles endured added to the sense of accomplishment. A trusted and trusting supervisor appears to aid in the PhD being a process of transcendence [ 62 ].
More broadly, the PhD also helped DRs to transcend personal tragedy, allowing immersion in a meaningful activity which begins as a means of coping and becomes something completely [ 39 ]. The PhD could also serve as a transformative selection process for DRs’ social relationships, with some relationships cast aside and yet others formed anew [ 39 ]. Overall, therefore, the very aspects of the PhD which were challenging, and distressing could allow DRs to transcend their former selves and, through the struggle, become something more.
Summation of results
The findings regarding the risk and protective factors associated with DR mental health have been summarised in Table 3 in relation to (1) the type of research evidencing the factor (i.e. whether the evidence is quantitative only, part of the meta-synthesis only, or evident in both results sections); and (2) the volume of evidence (i.e. whether the factor was found in a single study or across multiple studies). The factors in the far-right column (i.e. the factors found across multiple research studies utilising both qualitative and quantitative methods) are the ones with the strongest evidence at present.
This systematic review summarises a heterogeneous research area, with the aim of understanding the mental health of DRs, including possible risk and protective factors. The qualitative and quantitative findings presented here suggest that poor mental health is a pertinent problem facing DRs; stress appears to be a key issue and significantly in excess of that experienced in the general population. Several risk and protective factors at the individual, interpersonal and systemic levels emerged as being important in determining the mental health of DRs. The factors with the strongest evidence-base (i.e. those supported by multiple studies using qualitative and quantitative findings) denote that being female and isolated increases the risk of the mental health problems, whereas seeing the PhD as a process, feeling socially supported, having a positive supervisor relationship and engaging in self-care is protective.
Results in context
Stress can be defined as (1) the extent to which a stimulus exerts pressure on an individual, and their propensity to bear the load; (2) the duration of the response to an aversive stimuli, from initial alert to exhaustion; or (3) a dynamic (im)balance between the demands and personal resource to manage those demands [ 91 ]. The Perceived Stress Scale (PSS) [ 18 , 19 ] used in our meta-analysis is aligned with the third of these definitions. As elaborated upon within the Transactional Model of Stress [ 92 ], stress is conceptualised as a persons’ appraisal of the internal and external demands put upon them, and whether these exceed their available resources. Thus, our results suggest that, when compared to the general population, PhD students experience a greater maladaptive imbalance between their available resources and the demands placed upon them. Stress in itself is not a diagnosable mental health problem, yet chronic stress is a common precipitant to mental health difficulties such as depression and posttraumatic stress disorder [ 93 , 94 ]. Therefore, interventions should seek to bolster DRs’ resources and limit demands placed on them to minimise the risks associated with acute stress and limit its chronicity.
Individual factors
Female DRs were identified as being at particular risk of developing mental health difficulties. This may result from additional hurdles when studying in a male-dominated profession [ 95 , 96 , 97 ], and the expectation that in addition to their doctoral studies, females should retain sole or majority responsibility for the domestic and/or caring duties within their family [ 52 , 76 ]. It may also be that females are more willing to disclose and seek help for mental health difficulties [ 98 ]. Nevertheless, the World Health Organisation (WHO) mental health survey results indicate that whilst anxiety and mood disorders are more prevalent amongst females, externalising disorders are more common in males [ 99 ]. As the vast majority of studies in this review focussed on internalising problems (e.g. stress, anxiety and depression) [ 37 , 64 , 79 , 80 , 83 , 89 ], this may explain the gender differences found in this review. Further research is needed to explore which perspective, if any, may explain gender gap in our results.
Perhaps unsurprisingly, self-care was associated with reduced mental health problems. The quantitative findings suggest that all types of self-care are likely to be protective of mental health (i.e. physical, emotional, professional and spiritual self-care). Self-care affords DRs the opportunity to take time away from their studies and nurture their non-PhD identities. However, the results from our meta-synthesis suggest that DRs are not attending to their most basic needs much less engaging in self-care behaviours that correspond to psychological and/or self-fulfilment needs [ 100 ]. Consequently, an important area for future enquiry will be identifying the barriers preventing DRs from engaging in self-care.
Interpersonal factors
Across both quantitative and qualitative studies, interpersonal factors emerged as the most salient correlate of DR mental health. That is, isolation was a risk factor, whereas connectedness to others was a protective factor. There was some variability in how these constructs were conceptualised across studies, i.e. (1) isolation: a lack of social support, having fewer social connections, feeling isolated or being physically separate from others; and (2) social connectedness: multiple group membership, academic relationships or non-academic relationships; but there was no indication that effects varied between concepts. The relationship between isolation and negative health consequences is well-established, for example both physical and mental health problems [ 101 ], and even increased mortality [ 102 ]. Conversely, social support is associated with reduced stress in the workplace [ 103 , 104 ]. Reducing isolation is therefore a promising interventional target for improving DRs’ mental health.
The findings regarding isolation are even more alarming when considered alongside the findings from several studies that PhD studies are consistently reported to dominate the lives of DRs, resulting in poor ‘work-life balance’ and losing non-PhD aspects of their identities. The negative impact of having fewer identities [ 105 ] can be mitigated by having a strong support network [ 106 ], and increasing multiple group memberships [ 107 ]. But for DRs, it is perhaps the absence of this social support, combined with identity impoverishment, which can explain the higher than average prevalence of stress found in our meta-analysis.
Systemic factors
DRs’ attitudes towards their studies may be a product of top-down systemic issues in academia more broadly. Experiencing mental health problems was reported as being the ‘norm’, but also appeared to be understood as a sign of weakness. The meta-synthesis results suggest that DRs believed their respective universities prioritise academic success over workplace wellbeing and encourage unhealthy working habits. Working in an unsupportive and pressured environment is strongly associated with negative psychological outcomes, including increased depression, anxiety and burnout [ 108 ]. The supervisory relationship appeared a particularly important aspect of the workplace environment. The quantitative analysis found a negative correlation between inspirational supervision and mental health problems. Meta-synthetic finding suggested toxic DR-supervisor relationships characterised by powerlessness and neglect, as well as relationships where DRs felt valued and respected—the former of these being associated with poor mental health, and the latter being protective. The association between DR-supervisor relationship characteristics needs to be verified using quantitative methods. Furthermore, DRs’ sense that they needed to exhibit ‘optimum suffering’, which appears to reflect a PhD-specific aspect of a broader academic performativity [ 109 ], is an important area for consideration. An accepted narrative around DRs needing to experience a certain level of dis/stress would likely contribute to poor mental health and as an impediment to the uptake and effectiveness of proffered interventions. Although further research is needed, it is apparent that individual interventions alone are not sufficient to improve DR mental health, and that a widespread culture shift is needed in order to prevent the transmission of unhealthy work attitudes and practices.
Limitations of the literature
Although we found a respectable number of articles in this area, the focus and measures used varied to the extent that typical review analysis procedures could not be used. That is, there was much heterogeneity in terms of how mental health was conceptualised and measured, as well as the range of risk and protective factors explored. Similarly, the quality of the studies was hugely variable. Common flaws amongst the literature include small sample sizes, the use of unvalidated tools and the incomplete reporting of results. Furthermore, for qualitative studies specifically, there appeared to be a focus on breadth instead of depth, particularly in relation to studies using mixed methods.
The generalisability of our findings is limited largely due to the lack of research conducted outside of the US, but also because we limited our review to papers written in English only. The nature of doctoral studies varies in important ways between studies. For example, in Europe, PhD studies usually apply for funding to complete their thesis within 3–4 years and must know their topic of interest at the application stage. Whereas in the US, PhD studies usually take between 5 and 6 years, involve taking classes and completing assignments, and the thesis topic evolves over the course of the PhD. These factors, as well as any differences in the academic culture, are likely to affect the prevalence of mental health problems amongst DRs and the associated risk and protective factors. More research is needed outside of the US.
‘Mental health’ in this review was largely conceptualised as a type of general wellbeing rather than a clinically meaningful construct. None of the studies were ostensibly focused on sampling DRs who were currently experiencing or had previously experienced mental health problems per se, meaning the relevance of the risk, vulnerability and protective factors identified in the meta-synthesis may be more limited in this group. Few studies used clinically meaningful measures. Where clinical measures were used, they captured data on common mental health problems only (i.e. anxiety and depression). Due to these limitations, we are unable to make any assertions about the prevalence of clinical-level mental health problems amongst DRs.
Limitations of this review
As a result of the heterogeneity in this research area, some of the results presented within this review are based on single studies (e.g. correlation data; see Fig. 5 ) rather than the amalgamation of several studies (e.g. meta-analysis/synthesis). To aid clarity when interpreting the results of this review, we have (Table 3 ) summarised the volume of evidence supporting risk and protective factors. Moreover, due to the small number of studies eligible for inclusion in this review, we were unable to test whether any of our findings are related to the study characteristics (e.g. year of publication, country of origin, methodology).
We were able to conduct three meta-analyses, one of which aimed to calculate the between-group effect size on the PSS [ 18 , 19 ] between DRs and normative population data. Comparing these data allowed us to draw some initial conclusions about the prevalence of stress amongst DRs, yet we were unable to control for other group differences which might moderate stress levels. For example, the population data was from people in the United States (US) in 1 year, whereas the DR data was multi-national at a variety of time points; and self-reported stress levels may vary with nationality [ 110 ] or by generation [ 111 , 112 ]. Moreover, two of the three meta-analyses showed significant heterogeneity. This heterogeneity could be explained by differences in the sample characteristics (e.g. demographics, country of origin), doctoral programme characteristics (e.g. area of study, funding status, duration of course) or research characteristics (e.g. study design, questionnaires used). However, due to the small number of studies included in these meta-analyses, we were unable to test any of these hypotheses and are therefore unable to determine the cause of this heterogeneity. As more research is conducted on the mental health of DRs, we will be able to conduct larger and more robust meta-analyses that have sufficient power and variance to statistically explore the causes of this heterogeneity. At present, our findings should be interpreted in light of this limitation.
Practice recommendations
Although further research is clearly needed, we assert that this review has identified sufficient evidence in support of several risk and protective factors to the extent that they could inform prevention and intervention strategies. Several studies have evidenced that isolation is toxic for DRs, and that social support can protect against poor mental health. Initiatives that provide DRs with the opportunity to network and socialise both in and outside of their studies are likely to be beneficial. Moreover, there is support for psychoeducation programmes that introduce DRs to a variety of self-care strategies, allow them to find the strategies that work for them and encourage DRs to make time to regularly enact their chosen strategies. Finally, the supervisory relationship was identified as an important correlate of DR mental health. Positive supervision was characterised as inspirational and inclusive, whereas negative supervision productised DRs or neglected them altogether. Supervisor training programmes should be reviewed in light of these findings to inform how institutions shape supervisory practices. Moreover, the initial findings reported here evidence a culture of normalising and even celebrating suffering in academia. It is imperative therefore that efforts to improve and protect the mental health of DRs are endorsed by the whole institution.
Research recommendations
First, we encourage further large-scale mental health prevalence studies that include a non-PhD comparison group and use validated clinical tools. None of the existing studies focused on the presence of serious mental health problems—this should be a priority for future studies in this area. Mixed-methods explorations of the experiences of DRs who have mental health problems, including serious problems, and in accessing mental health support services would be a welcome addition to the literature. More qualitative studies involving in-depth data collection, for example interview and focus group techniques, would be useful in further supplementing findings from qualitative surveys. Our review highlights a need for better communication and collaboration amongst researchers in this field with the goal of creating a level of consistency across studies to strengthen any future reviews on this subject.
The results from this systematic review, meta-analysis and meta-synthesis suggest that DRs reported greater levels of stress than the general population. Research regarding the risk and protective factors associated with the mental health of DRs is heterogenous and disparate. Based on available evidence, robust risk factors appear to include being isolated and being female, and robust protective factors include social support, viewing the PhD as a process, a positive DR-supervisor relationship and engaging in self-care. Further high-quality, controlled research is needed before any firm statements can be made regarding the prevalence of clinically relevant mental health problems in this population.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Confidence intervals
Doctoral researchers
Higher Education Statistics Agency
Perceived Stress Scale
Standard deviation
United Kingdom
United States
Baron E. Eleven sketches inspired by the university mental health crisis—in pictures. The Guardian. 2017. Available from: https://www.theguardian.com/education/gallery/2017/jun/27/eleven-sketches-university-mental-health-crisis . Cited 2017 Oct 6.
Google Scholar
National Union of Students. 20 per cent of students consider themselves to have a mental health problem: National Union of Students; 2013. Available from: https://www.nus.org.uk/en/news/20-per-cent-of-students-consider-themselves-to-have-a-mental-health-problem/ . Cited 2017 Oct 6.
YouGov. One in four students suffer from mental health problems. 2016. Available from: https://d25d2506sfb94s.cloudfront.net/cumulus_uploads/document/obtomdatp4/Survey_Results.pdf . Cited 2017 Oct 6.
Universities UK. Minding Our Future: starting a conversation about the support of student mental health. London: Universities UK; 2017. Available from: https://www.universitiesuk.ac.uk/minding-our-future .
The Guardian. Number of university dropouts due to mental health problems trebles. The Guardian. 2017. Available from: https://www.theguardian.com/society/2017/may/23/number-university-dropouts-due-to-mental-health-problems-trebles . Cited 2017 Oct 6.
Thorley C. Not By Degrees: Improving student mental health in the UK’s universities. London; 2017. Available from: www.ippr.org . Cited 2017 Oct 6.
Oswalt SB, Lederer AM, Chestnut-Steich K, Day C, Halbritter A, Ortiz D. Trends in college students’ mental health diagnoses and utilization of services, 2009–2015. J Am Coll Health. 2018;68:41–51.
Auerbach RP, Mortier P, Bruffaerts R, Alonso J, Benjet C, Cuijpers P, et al. WHO world mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018;127(7):623–38.
PubMed PubMed Central Google Scholar
OECD. Education at a Glance 2019. Education at a Glance: OECD Indicators: OECD; 2019. (Education at a Glance). Available from: http://gpseducation.oecd.org/Content/EAGCountryNotes/BRA.pdf . Cited 2020 Mar 26.
OECD. OECD Science, Technology and Innovation Outlook 2016. OECD Science, technology and innovation outlook 2016. 2016. Available from: http://www.oecd.org/sti/STIO 10 key technology trends for the future.pdf. Cited 2020 Mar 26.
Higher Education Statistics Agency (HESA). Higher education student statistics: UK, 2016/17: HESA; 2018. Available from: https://www.hesa.ac.uk/news/11-01-2018/sfr247-higher-education-student-statistics/numbers .
NCES. Number of doctoral degrees earned in the United States from 1949/50 to 2028/29, by gender. 2019. Available from: https://www.statista.com/statistics/185167/number-of-doctoral-degrees-by-gender-since-1950/ .
Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46 Available from: http://psycnet.apa.org/index.cfm?fa=search.displayRecord&uid=1960-06759-001 .
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159 Available from: http://www.jstor.org/stable/2529310?origin=crossref . Cited 2017 Mar 8.
CAS PubMed Google Scholar
Noblit GW, Hare RD. Meta-ethnography: Synthesizing qualitative studies: Sage Publications; 1988. p. 88.
Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45.
Wilson DB. Meta-analysis stuff. 2011. Available from: http://mason.gmu.edu/~dwilsonb/ma.html . Cited 2017 Dec 3.
Cohen S, Williamson GM. Perceived stress in a probability sample of the U.S. In: Spacapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on Applied Social Psychology. Newbury Park, CA: Sage; 1988.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Cohen S, Janicki-Deverts D. Who’s Stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol. 2012;42(6):1320–34.
MedCalc Software bvba. MedCalc Statistical Software. Belgium: Ostend; 2016.
Viechtbauer W. Bias and efficiency of Meta-analytic variance estimators in the random-effects model. J Educ Behav Stat. 2005;30(3):261–93 Available from: http://jeb.sagepub.com/cgi/doi/10.3102/10769986030003261 . Cited 2017 Mar 8.
Hedges LV, Ollkin L. Statistical methods for meta-analysis. New York: Academic Press; 1985. Available from:. https://doi.org/10.1002/9780470743386.refs .
Book Google Scholar
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to meta-analysis. Chichester: Wiley; 2009. Cited 2019 Jan 10. Available from. https://doi.org/10.1002/9780470743386 .
Fisher RA. Frequency distribution of the values of the correlation coefficient in samples from an indefinitely large population. Biometrika. 1915;10(4):507–21 Available from: https://www.statista.com/statistics/185167/number-of-doctoral-degrees-by-gender-since-1950/ .
Schünemann H, Brożek J, Guyatt G, Oxman A. Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach: GRADE Working Group; 2013. Available from: gdt.guidelinedevelopment.org/app/handbook/handbook.html .
Lachal J, Revah-Levy A, Orri M, Moro MR. Metasynthesis: an original method to synthesize qualitative literature in psychiatry. Front Psychiatry. 2017;8:269.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. London: Sage Publications Ltd; 2013.
Bhaskar R. The possibility of naturalism: a philosophical critique of the contemporary human sciences. London: Routledge; 2014.
Fletcher AJ. Applying critical realism in qualitative research: methodology meets method. Int J Soc Res Methodol. 2017;20(2):181–94.
Walsh D, Downe S. Meta-synthesis method for qualitative research: a literature review. J Adv Nurs. 2005;50(2):204–11.
PubMed Google Scholar
Maton K. Reflexivity, relationism, & research: Pierre Bourdieu and the epistemic conditions of social scientific knowledge. Sp Cult. 2003;6(1):52–65.
Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol. 2012;12(1):181.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for Reporting Observational Studies. Ann Intern Med. 2007;147(8):573. Cited 2019 Sep 27. Available from. https://doi.org/10.7326/0003-4819-147-8-200710160-00010 .
Article Google Scholar
Acker S, Haque E. The struggle to make sense of doctoral study. High Educ Res Dev. 2015;34(2):229–41. Available from. https://doi.org/10.1080/07294360.2014.956699 .
Appel ML, Dahlgren LG. Swedish doctoral students’ experiences on their journey towards a PhD: obstacles and opportunities inside and outside the academic building. Scand J Educ Res. 2003;47(1):89–110. Available from. https://doi.org/10.1080/00313830308608 .
Devonport TJ, Lane AM. In it together: Dyadic coping among doctoral students and partners. J Hosp Leis Sport Tour Educ. 2014;15:124–34. Available from. https://doi.org/10.1016/j.jhlste.2014.08.002 .
Enzor J. Friendship, mental health, and doctoral education: a generic qualitative thematic analysis: Capella University; 2017.
Kurtz-Costes B, Helmke LA, Ülkü-Steiner B. Gender and doctoral studies: the perceptions of Ph.D. students in an American university. Gend Educ. 2006;18(2):137–55.
Bazrafkan L, Shokrpour N, Yousefi A, Yamani N. Management of stress and anxiety among PhD students during thesis writing: a qualitative study. The Health Care Manager. 2016;35:231–40.
Cotterall S. More than just a brain: emotions and the doctoral experience. High Educ Res Dev. 2013;32(2):174–87.
Kaufman JA. Personal perceptions of stress and self-perceived need for social support among doctoral psychology students in a distance education university sample: Capella University; 2004.
Kenty JR. Stress management strategies for women doctoral students. Nurse Educ. 2000;25(5):251–4 Available from: http://pesquisa.bvsalud.org/portal/resource/pt/mdl-16646205 .
Scrubb MM. An examination of the doctoral student stress survey (DSSS) as an instrument for measuring the effects of stress as perceived by doctoral students in a distance learning university: Walden University; 1997.
Usman Yousaf S, Akram M, Usman B. Exploring the causes of stress and coping with it amongst doctoral level students: highlighting the importance of information collection and management. Pakistan J Inf Manag Libr. 2016;18(2):12–25 Available from: https://search.proquest.com/openview/68246cbba8a9da0ec067d56631b479f1/1?pq-origsite=gscholar&cbl=54989 .
Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis Studies. Res Sch. 2006;13(1):29 Available from: http://www.ncbi.nlm.nih.gov/pubmed/20098638%0A http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2809982 .
Bauer J. Personality factors, self-care, and perceived stress levels on counselor education and counseling psychology doctoral students. Dissertations: Western Michigan University; 2016.
Begun AL, Carter JR. Career Implications of Doctoral Social Work Student Debt Load. J Soc Work Educ. 2017;53(2):161–73. Available from. https://doi.org/10.1080/10437797.2016.1243500 .
Benjamin S, Williams J, Maher MA. Focusing the lens to share the story: using photographs and interviews to explore doctoral students’ sense of well-being. Int J Dr Stud. 2017;12:197–217.
Benesek JP. Stress and coping among psychology doctoral students: a comparison of self-reported stress levels and coping styles of PhD and PsyD students: University of Hartford; 1998.
Bireda AD. Challenges to the doctoral journey: a case of female doctoral students from Ethiopia. Open Prax. 2015;7(4):287–97.
Bolliger DU, Halupa C. Student perceptions of satisfaction and anxiety in an online doctoral program. Distance Educ. 2012;33(1):81–98.
Cole LJ. Academic worry and frequent mental distress among online doctoral students: Walden University; 2008.
Devine K, Hunter KH. PhD student emotional exhaustion: the role of supportive supervision and self-presentation behaviours. Innov Educ Teach Int. 2017;54(4):335–44.
Drake KL. Psychology graduate student well-being: the relationship between stress, coping, and health outcomes: University of Cincinnati; 2010.
Dumitrescu GA. Self-efficacy, locus of control , perceived stress and student satisfaction as correlates of dissertation completion: Andrews University; 2016.
El-Ghoroury NH, Galper DI, Sawaqdeh A, Bufka LF. Stress, coping, and barriers to wellness among psychology graduate students. Train Educ Prof Psychol. 2012;6(2):122–34.
Haynes C, Bulosan M, Citty J, Grant-Harris M, Hudson J, Koro-Ljungberg M. My world is not my doctoral program…Or is it?: Female students’ perceptions of well-being. Int J Dr Stud. 2012;7:001–17.
Hill LM. Perceived stress, academic support, social support, and professional support factors as predictors of student success in distributed-learning doctoral education: Fielding Graduate University; 2010.
Holahan CK. Stress experienced by women doctoral students, need for support, and occupational sex typing: An interactional view. Sex Roles. 1979;5(4):425–36.
Hunter KH, Devine K. Doctoral students’ emotional exhaustion and intentions to leave academia. Int J Doctoral Stud. 2016;11.
Kaufman JA. Stress and social support among online doctoral psychology students. J College Stud Psychother. 2006;20(3):79–88 Available from: http://search.proquest.com/docview/57185202?accountid=12253%5Cn http://man-fe.hosted.exlibrisgroup.com/openurl/44MAN/44MAN_services_page?url_ver=Z39.88-2004&rft_val_fmt=journal&genre=unknown&sid=ProQ:ProQ%3Aeducation&atitle=Stress+and+Social+Support+among +.
Levecque K, Anseel F, De Beuckelaer A, Van Der Heyden J, Gisle L. Work organization and mental health problems in PhD students. Res Policy. 2017;46:868–79.
Lonka K, Chow A, Keskinen J, Hakkarainen K, Sandström N, Pyhältö K. How to measure PhD students’ conceptions of academic writing - and are they related to wellbeing? J Writ Res. 2014;5(3):245–69.
Lowe RL. The relationship between personality, self-care, stress, and perceived wellness in psychology doctoral students: Tennessee University; 2015.
Marais GAB, Shankland R, Haag P, Fiault R, Juniper B. A survey and a positive psychology intervention on French PhD student well-being. Int J Dr Stud. 2018;13:109–38.
Martinez E, Ordu C, Sala MRD, McFarlane A. Striving to obtain a school-work-life balance: The full-time doctoral student. Int J Dr Stud. 2013;8:39–59.
McGregor BA, Antoni MH, Ceballos R, communication BBBS. very low CD19+ B-lymphocyte percentage is associated with high levels of academic stress among healthy graduate students. Stress Heal. 2008;24(5):413–8.
Nelson K. Academic progress in doctoral students: Levels of hope, subjective well-being, and stress: Walden University; 2014. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc12&NEWS=N&AN=2015-99151-189 .
Nottingham K. A predictive analysis of the psychosocial outcomes of doctoral students: Capella University; 2017.
Orozco AB. Self-care effects on anxiety in doctoral students: Fielding Graduate University; 2014. p. 35–61.
Peters BM. The relationships among physiological and perceived stress, quality of life, self-care and impairment in doctoral students: State University of New York at Buffalo; 2007.
Pifer MJ, Baker VL. “It could be just because I’m different”: Otherness and its outcomes in doctoral education. J Divers High Educ. 2014;7(1):14–30.
Platt J, Schaefer C. Clinical psychological students’ subjective stress ratings during their doctoral training. Psychol Rep. 1995;76:994 Available from: http://www.ncbi.nlm.nih.gov/pubmed/7568619 .
Pychyl TA. Personal projects, subjective well-being and the lives of doctoral students. Ottawa: Carleton University; 1995.
Pychyl TA, Little BR. Dimensional specificity in the prediction of subjective well-being: Personal projects in pursuit of the PhD. Soc Indic Res. 1998;45(1–3):423–73 Available from: file://d/d/Texte/Guenter/Literatu/Original/Journals/SIR98-45-423-473.pdf.
Rocha-Singh IA. Perceived stress among graduate students: development and validation of the Graduate Stress Inventory. Educ Psychol Meas. 1994;54(3):714–27.
Scheidler JA. Effects of perceived stress and perceived social support on marital satisfaction in doctoral students: Walden University. 2008;20.
Sekas G, Wile MZ. Stress-related illnesses and sources of stress: comparing M.D., Ph.D., M.D. and Ph.D. students. J Med Educ. 1980;55:440–6 Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L10000589%5Cn http://sfx.library.uu.nl/utrecht?sid=EMBASE&issn=00222577&id=doi:&atitle=Stress-related+illnesses+and+sources+of+stress%3A+comparing+M.D.-Ph.D.%2C+M.D.+and+Ph.D.+student .
Stubb J, Pyhältö K, Lonka K. Balancing between inspiration and exhaustion: PhD students’ experienced socio-psychological well-being. Stud Contin Educ. 2011;33(1):33–50.
Stubb J, Pyhältö K, Lonka K. The experienced meaning of working with a PhD thesis. Scand J Educ Res. 2012;56(4):439–56.
Ülkü-Steiner B, Kurtz-Costes B, Kinlaw CR. Doctoral student experiences in gender-balanced and male-dominated graduate programs. J Educ Psychol. 2000;92(2):296–307.
Volkert D, Candela L, Bernacki M. Student motivation, stressors, and intent to leave nursing doctoral study: a national study using path analysis. Nurse Educ Today. 2018;61:210–5. Available from. https://doi.org/10.1016/j.nedt.2017.11.033 .
Article PubMed Google Scholar
Waaijer CJF, Heyer A, Kuli S. Effects of appointment types on the availability of research infrastructure, work pressure, stress, and career attitudes of PhD candidates of a Dutch university. Res Eval. 2016;25(4):349–57.
Wang C-H, Chen Y-W, Wu T-Y. Self-guided bibliotherapy: a case study of a Taiwanese doctoral student. Int J Humanties. 2010;8(1):413–22.
Williams MD. HBCU vs. PWI: institutional integration at PWIs and Black doctoral student depression, anxiety, and stress: University of Minnesota; 2014.
Wright T. Issues in brief counselling with postgraduate research students. Couns Psychol Q. 2006;19(4):357–72.
Scrubb MM. An examination of the Doctoral Student Stress Survey (DSSS) as an instrument for measuring the effects of stress as perceived by doctoral students in a distance learning university, vol. 58: Walden University; 1998. p. 3041. Dissertation Abstracts International Section A: Humanities and Social Sciences. Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=psyc3&NEWS=N&AN=1998-95003-070 .
Hadden BW, Smith CV. I gotta say, today was a good (and meaningful) day: daily meaning in life as a potential basic psychological need. J Happiness Stud. 2017:1–18.
Butler G. Definitions of stress. Occas Pap R Coll Gen Pract. 1993;(61):1–5 Available from: http://www.ncbi.nlm.nih.gov/pubmed/8199583%0A http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2560943 .
Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York: Springer Publishing Company; 1984.
Siegrist J. Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. Eur Arch Psychiatry Clin Neurosci. 2008;258(SUPPL. 5):115–9.
Marin MF, Lord C, Andrews J, Juster RP, Sindi S, Arsenault-Lapierre G, et al. Chronic stress, cognitive functioning and mental health. Neurobiol Learn Mem. 2011;96(4):583–95. Available from. https://doi.org/10.1016/j.nlm.2011.02.016 .
Ward M. The gender salary gap in British academia. Appl Econ. 2001;33(13):1669–81. Cited 2019 May 23. Available from. https://doi.org/10.1080/00036840010014445 .
Howe-Walsh L, Turnbull S. Barriers to women leaders in academia: tales from science and technology. Stud High Educ. 2016;41(3):415–28. Cited 2019 May 23. Available from. https://doi.org/10.1080/03075079.2014.929102 .
Gardiner M, Tiggemann M. Gender differences in leadership style, job stress and mental health in male- and female-dominated industries. J Occup Organ Psychol. 1999;72(3):301–15.
Mackenzie CS, Gekoski WL, Knox VJ. Age, gender, and the underutilization of mental health services: the influence of help-seeking attitudes. Aging Ment Health. 2006;10(6):574–82 Cited 2017 May 12. Available from: http://www.tandfonline.com/action/journalInformation?journalCode=camh20 .
Seedat S, Scott KM, Sampson NA, Williams D, Kessler RC. Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Pschiatry. 2013;66(7):785–95.
Maslow AH. A theory of human motivation. Psychol Rev. 1943;50(4):370–96 Available from: http://content.apa.org/journals/rev/50/4/370 . Cited 2019 Jun 10.
Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health. 2017;152:157–71 Available from: https://doi.org/10.1016/j.puhe.2017.07.035 .
Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality. Perspect Psychol Sci. 2015;10(2):227–37. Available from. https://doi.org/10.1177/1745691614568352 .
Viswesvaran C, Sanchez JI, Fisher J. The role of social support in the process of work stress: a meta-analysis. J Vocat Behav. 1999;54(2):314–34.
Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med. 2003;60(1):3–9.
CAS PubMed PubMed Central Google Scholar
Brook AT, Garcia J, Fleming M. The effects of multiple identities on psychological well-being. Personal Soc Psychol Bull. 2008;34(12):1588–600.
Thoits PA. Self, Identity, Stress, and Mental Health. In: Aneshensel CS, Phelan JC, Bierman A, editors. Handbook of the Sociology of Mental Health. Dordrecht: Springer; 2012. p. 357–77.
Haslam C, Jetten J, Cruwys T, Dingle G, Haslam A. The new psychology of health: Unlocking the social cure. New York: Routledge; 2018.
Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: a meta-analysis. Occup Environ Med. 2005;62(2):105–12.
Macfarlane B. Student performativity in higher education: converting learning as a private space into a public performance. High Educ Res Dev. 2015;34(2):338–50.
Daniels K. Perceived risk from occupational stress: a survey of 15 European countries. Occup Environ Med. 2004;61(5):467–70.
American Psychiatric Association (APA). Stress in America: missing the health care connection. Washington: American Psychiatric Association (APA). 2013.
Twenge JM. Time period and birth cohort differences in depressive symptoms in the U.S., 1982–2013. Soc Indic Res. 2015;121(2):437–54.
Download references
Acknowledgements
Thank you to the Office for Students for their funding to support this work; and thank you to the University of Sussex Doctoral school and our steering group for championing and guiding the ‘Understanding the mental health of Doctoral Researchers (U-DOC)’ project.
The present project was supported by the Office for Students Catalyst Award. The funder had no involvement in the design of the study, the collection, analysis or interpretation of the data, nor the writing of this manuscript.
Author information
Authors and affiliations.
School of Social Sciences, University of Westminster, 115 New Cavendish Street, London, W1W 6UW, UK
Cassie M. Hazell
School of Psychology, University of Sussex, Falmer, Brighton, BN1 9QJ, UK
Laura Chapman
Research and Enterprise, University of Sussex, Falmer, Brighton, BN1 9RH, UK
Sophie F. Valeix
Centre for Higher Education and Equity Research, University of Sussex, Falmer, Brighton, BN1 9RH, UK
Paul Roberts
School of Life Sciences, University of Sussex, Falmer, Brighton, BN1 9QG, UK
Jeremy E. Niven
Primary Care and Public Health, Brighton and Sussex Medical School and School of Psychology, University of Sussex, Falmer, Brighton, BN1 9PH, UK
You can also search for this author in PubMed Google Scholar
Contributions
CH contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. LC contributed to the data curation, investigation, project administration, validation and writing—review and editing of this paper. SV contributed to the data curation, formal analysis, investigation, project administration, validation and writing—review and editing of this paper. PR contributed to the funding acquisition, project administration, supervision and writing—review and editing of this paper. JN contributed to the conceptualisation, funding acquisition, methodology, project administration, supervision, validation, writing—original draft preparation and writing—review and editing of this paper. CB contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Clio Berry .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval was not needed for the present study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hazell, C.M., Chapman, L., Valeix, S.F. et al. Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis. Syst Rev 9 , 197 (2020). https://doi.org/10.1186/s13643-020-01443-1
Download citation
Received : 15 June 2020
Accepted : 31 July 2020
Published : 26 August 2020
DOI : https://doi.org/10.1186/s13643-020-01443-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- PhD students
- doctoral researchers
- Postgraduate researchers
- Systematic review
Systematic Reviews
ISSN: 2046-4053
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
The most important aspect of your PhD: supervisor-student relationship
There are many variables when applying for a PhD programme (country, system, length, funding, project, etc.). In regards to choosing a supervisor, I did my best to make an educated choice, and I really lucked out in terms of the people that I am working with. In the past 3.5 years, I have received scientific and professional support, mentorship, networking opportunities, creative encouragement, and much more from my supervisors.
Similarly to how Leo Tolstoy’s ‘ Anna Karenina ’ starts, we can think of doctoral students: ‘ Happy PhD students are all alike; every unhappy PhD student is unhappy in their own way ’. That statement is definitely something I have observed within my peers. While there are many aspects to a fulfilling PhD, the relationship with the supervisor(s) is one of the main variables contributing to PhD success [1] . In my opinion, the prospective supervisor(s) is an important variable at an individual level for PhD applicants, and a key factor when institutions design the training programmes for the next generation of scientists and thinkers .
Happy PhD students are all alike; every unhappy PhD student is unhappy in their own way
Let us look at how I will use the phrase ‘successful PhD’ in this blog entry. Conventionally, a successful PhD is not only a completed degree to the requirements of each institution, but also a PhD that has publishable outcomes in peer-reviewed scientific journals. Unsurprisingly, I happen to disagree with the second part. Beyond passing the degree requirements, success during a PhD is up to the internal definition of the candidate . For some people ‘success’ could mean publishing papers, while for some others it might mean pivoting their career into a different field, living in another country, or an opportunity to do some cool science just for fun. In order to accomplish your goals during your PhD you absolutely need to be on the same page as your supervisor(s) in your definition of ‘success’ and to have their support.
There is strong evidence pointing out that the success within academia is heavily influenced by PhD mentors (see literature review in [1- 3] ). The first mentor is the project supervisor(s). They are the ones who set you up for early success (or not) in the way they shape the PhD project, support you attending conferences, introduce you to their academic peers, and recommend you for committees/panels etc. Later in the PhD, it is the supervisor(s) who helps you navigate the publication process, and most importantly, recommends you for jobs in academia and/or industry in a formal and/or informal manner.
Surveys of PhD students indicate that they experience depression and anxiety at higher rates than the general population (references in [4- 5] ). Amongst the many factors contributing to the ill mental health of PhD students is their relationship with their supervisor. In some cases, the supervisor can be the primary cause for an overall unsatisfactory PhD experience and ill mental health through bullying and harassment [6] , unprofessionalism and poor management skills (e.g., [6] ) or just general disinterest in the project and/or student. In other instances, the student-supervisor relationship can turn toxic if the supervisor shows lack of understanding and/or support when life outside the PhD happens (and yes, it does) and the student needs to access medical or maternity leave, vacation time, peer support networks, or financial help.
Most importantly, your PhD supervisor(s) will be the key and main scientific influence in your early career from a scholarly point of view. While becoming a scientist is about forming one’s independent thinking, I think it’s fair to say that early career researchers are heavily influenced by the approach of their supervisors. I find this aspect quite thrilling; being a PhD student sometimes makes me feel like Michaelangelo’s apprentice: learning the craft while looking for my own style and contributing to the bigger legacy of the research groups I am part of. However, the nature of this individualised style of training new generations has offered a shield for institutions to guard faculty members from mandatory management training, implicit bias training, and overall accountability in students’ experience. While some students (like me) have supervisors who are both brilliant scientists and wonderful mentors, many other students do not achieve their goals during their degree and might have an awful time on top of it due to the nature of their relationship with their supervisor [2] . I find it a flaw in the educational system that sometimes these two categories of students share the same building .
Thus, on an individual level, in my opinion, prospective PhD students should assign more decisional weight to the supervisors’ managerial and leadership qualities, compared to how catchy a project sounds or the prestige of an institution/programme. I know this is hard and overwhelming for prospective applicants, and one can not control into which PhD programmes you get accepted into. However, I do think prospective students can make educated choices when signing up to one PhD over another. Some common practices done by applicants include: informal lab visits or video calls, informal chats with current or past members of the research group, and informal talk with collaborators or other people from the sub-field.

As I sat down at the microscope, I couldn’t help but wonder: how would I have navigated this pandemic without my supervisors???
The realisation of how powerful the supervisor-student relationship is for an individual and for training the next generation of scientists has major implications at institutional level. Many of the resources included here contain excellent recommendations for institutions ( [1] , [2] , [5] and references therein), but since this is The Internet, here are my 2 cents. Institutions really ought to pay attention to the matters raised by their student body, and implement meaningful changes in liaison with faculty. Students always end up with so many surveys to fill, elect representatives, create working groups, table discussions for matters affecting us within departments and scientific societies, and yet, the relationship with their supervisor remains the ‘elephant in the room’ with no action taken to improve student-supervisor relationships.
The classical institutional matryoshka of committees leads to change on geological timescales and heavily impacts efforts of diversity, equality, and inclusion within STEM . In my ideal world, institutions would design PhD programmes with at least two supervisors. This approach could promote scientific interdisciplinarity, relationship balance, and wider support for the student. Having to manage multiple scientific work relationships is also more relevant in mirroring the collaborative aspect of scientific research. Furthermore, all institutions should set-up mentorship and career networks based on gender and race, such that the student would be exposed to a variety of working styles and approaches.
Institutions should facilitate students raising issues in their relationship with their supervisor in a safe manner, and — hot take — implement a neutral and standardised way for students to provide feedback to their supervisors . In fact, the current lack of a feedback loop between supervisors and students can be inferred from reports of differences in what supervisors think they have communicated vs what the students received (e.g., [1] ). A lot of the dissatisfaction of PhD students is related to the little time they receive from (most likely overworked) supervisors [6] , so of course in my ideal institution, I would hire more faculty members, unload existing faculty, facilitate management and communications workshops, and promote good supervision examples within the department. While there has been an increase in institutional awareness of toxicity in academia and related mental health problems, the truth is, one extra departmental yoga class or mindfulness podcast is not a long-term fix for work-related issues faced by students or supervisors.
The PhD student-supervisor relationship remains the ‘elephant in the room’, with no action taken to improve it
I think there is broad agreement that PhDs are not easy, and completing one comes with personal, emotional, and financial investments. However, the intellectual difficulty of a PhD degree should not be a shield to perpetuate toxic, abusive, or unprofessional behaviours . In the past 3.5 years I have witnessed many students navigate the ups and downs of their PhDs. To circle back to ‘ Anna Karenina ’, all the students I know are unhappy in their own way: life happens, experiments are not working, papers are rejected, or there are difficult (work) relationships. However, all the happy-ish* and satisfied PhD students have one thing in common: the privilege of excellent supervisor(s) .
*I am yet to encounter a fully-happy PhD student
On each first Monday of the month, The PhD Chronicles blog series gives a special place for PhD researchers to share their successes, challenges, and failures. Would you like to share your story? Contact us here .
Related Posts
Leave a Reply Cancel Reply
Your email address will not be published. Required fields are marked *
You may use these HTML tags and attributes: <a href="" title=""> <abbr title=""> <acronym title=""> <b> <blockquote cite=""> <cite> <code> <del datetime=""> <em> <i> <q cite=""> <s> <strike> <strong>
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 11 November 2021
Sleeplessness and anxiety: PhD supervisors on toll of COVID pandemic
You can also search for this author in PubMed Google Scholar
Around one-third of scientists who supervise doctoral students say they have lost sleep during the pandemic because of their role, according to a poll of almost 3,500 research supervisors in the United Kingdom. Two-thirds said that their supervision responsibilities had increased over this time, with many wanting more support to address the well-being and mental health of their PhD students.
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
185,98 € per year
only 3,65 € per issue
Rent or buy this article
Prices vary by article type
Prices may be subject to local taxes which are calculated during checkout
doi: https://doi.org/10.1038/d41586-021-03374-w
Reprints and permissions
Related Articles

Brazil’s plummeting graduate enrolments hint at declining interest in academic science careers
Career News 21 MAY 24

Reading between the lines: application essays predict university success
Research Highlight 17 MAY 24

How to stop students cramming for exams? Send them to sea
News & Views 30 APR 24

I had my white colleagues walk in a Black student’s shoes for a day
Career Q&A 28 MAY 24

Changemakers — Nature’s new series celebrates champions of inclusion in science
Editorial 28 MAY 24

Researcher parents are paying a high price for conference travel — here’s how to fix it
Career Column 27 MAY 24
Trials that infected people with common colds can inform today’s COVID-19 challenge trials
Correspondence 21 MAY 24

A global pandemic treaty is in sight: don’t scupper it
Editorial 21 MAY 24

US halts funding to controversial virus-hunting group: what researchers think
News 16 MAY 24
Faculty Positions at Great Bay University, China
We are now seeking outstanding candidates in Physics, Chemistry and Physical Sciences.
Dongguan, Guangdong, China
Great Bay University, China (GBU)
Postdoctoral Associate- Medical Image Analysis
Houston, Texas (US)
Baylor College of Medicine (BCM)
Postdoctoral Associate- Optogenetics, Voltage Imaging, and All-Optical Electrophysiology
Postdoctoral and visiting scholar positions in immunology, stem cells, and cancer.
Postdoctoral Research Fellow and Visiting Scholar positions in immunology, stem cells and cancer are immediately available at UConn in USA
Storrs Mansfield, Connecticut
University of Connecticut-Lai's Lab
Zhejiang Provincial Hospital of Chinese Medicine on Open Recruitment of Medical Talents and Postdocs
Director of Clinical Department, Professor, Researcher, Post-doctor
Hangzhou, Zhejiang, China
The First Affiliated Hospital of Zhejiang Chinese Medical University
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

Understanding the mental health of doctoral researchers: a mixed methods systematic review with meta-analysis and meta-synthesis
Cassie m. hazell.
1 School of Social Sciences, University of Westminster, 115 New Cavendish Street, London, W1W 6UW UK
Laura Chapman
2 School of Psychology, University of Sussex, Falmer, Brighton, BN1 9QJ UK
Sophie F. Valeix
3 Research and Enterprise, University of Sussex, Falmer, Brighton, BN1 9RH UK
Paul Roberts
4 Centre for Higher Education and Equity Research, University of Sussex, Falmer, Brighton, BN1 9RH UK
Jeremy E. Niven
5 School of Life Sciences, University of Sussex, Falmer, Brighton, BN1 9QG UK
6 Primary Care and Public Health, Brighton and Sussex Medical School and School of Psychology, University of Sussex, Falmer, Brighton, BN1 9PH UK
Associated Data
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Data from studies with undergraduate and postgraduate taught students suggest that they are at an increased risk of having mental health problems, compared to the general population. By contrast, the literature on doctoral researchers (DRs) is far more disparate and unclear. There is a need to bring together current findings and identify what questions still need to be answered.
We conducted a mixed methods systematic review to summarise the research on doctoral researchers’ (DRs) mental health. Our search revealed 52 articles that were included in this review.
The results of our meta-analysis found that DRs reported significantly higher stress levels compared with population norm data. Using meta-analyses and meta-synthesis techniques, we found the risk factors with the strongest evidence base were isolation and identifying as female. Social support, viewing the PhD as a process, a positive student-supervisor relationship and engaging in self-care were the most well-established protective factors.
Conclusions
We have identified a critical need for researchers to better coordinate data collection to aid future reviews and allow for clinically meaningful conclusions to be drawn.
Systematic review registration
PROSPERO registration CRD42018092867
Student mental health has become a regular feature across media outlets in the United Kingdom (UK), with frequent warnings in the media that the sector is facing a ‘mental health crisis’ [ 1 ]. These claims are largely based on the work of regulatory authorities and ‘grey’ literature. Such sources corroborate an increase in the prevalence of mental health difficulties amongst students. In 2013, 1 in 5 students reported having a mental health problem [ 2 ]. Only 3 years later, however, this figure increased to 1 in 4 [ 3 ]. In real terms, this equates to 21,435 students disclosing mental health problems in 2013 rising to 49,265 in 2017 [ 4 ]. Data from the Higher Education Statistics Agency (HESA) demonstrates a 210% increase in the number of students terminating their studies reportedly due to poor mental health [ 5 ], while the number of students dying by suicide has consistently increased in the past decade [ 6 ].
This issue is not isolated to the UK. In the United States (US), the prevalence of student mental health problems and use of counselling services has steadily risen over the past 6 years [ 7 ]. A large international survey of more than 14,000 students across 8 countries (Australia, Belgium, Germany, Mexico, Northern Ireland, South Africa, Spain and the United States) found that 35% of students met the diagnostic criteria for at least one common mental health condition, with highest rates found in Australia and Germany [ 8 ].
The above figures all pertain to undergraduate students. Finding equivalent information for postgraduate students is more difficult, and where available tends to combine data for postgraduate taught students and doctoral researchers (DRs; also known as PhD students or postgraduate researchers) (e.g. [ 4 ]). The latest trend analysis based on data from 36 countries suggests that approximately 2.3% of people will enrol in a PhD programme during their lifetime [ 9 ]. The countries with the highest number of DRs are the US, Germany and the UK [ 10 ]. At present, there are more than 281,360 DRs currently registered across these three countries alone [ 11 , 12 ], making them a significant part of the university population. The aim of this systematic review is to bring attention specifically to the mental health of DRs by summarising the available evidence on this issue.
Using a mixed methods approach, including meta-analysis and meta-synthesis, this review seeks to answer three research questions: (1) What is the prevalence of mental health difficulties amongst DRs? (2) What are the risk factors associated with poor mental health in DRs? And (3) what are the protective factors associated with good mental health in DRs?
Literature search
We conducted a search of the titles and abstracts of all article types within the following databases: AMED, BNI, CINAHL, Embase, HBE, HMIC, Medline, PsycInfo, PubMed, Scopus and Web of Science. The same search terms were used within all of the databases, and the search was completed on the 13th April 2018. Our search terms were selected to capture the variable terms used to describe DRs, as well as the terms used to describe mental health, mental health problems and related constructs. We also reviewed the reference lists of all the papers included in this review. Full details of the search strategy are provided in the supplementary material .
Inclusion criteria
Articles meeting the following criteria were considered eligible for inclusion: (1) the full text was available in English; (2) the article presented empirical data; (3) all study participants, or a clearly delineated sub-set, were studying at the doctoral level for a research degree (DRs or equivalent); and (4) the data collected related to mental health constructs. The last of these criteria was operationalised (a) for quantitative studies as having at least one mental health-related outcome measure, and (b) for qualitative studies as having a discussion guide that included questions related to mental health. We included university-published theses and dissertations as these are subjected to a minimum level of peer-review by examiners.
Exclusion criteria
In order to reduce heterogeneity and focus the review on doctoral research as opposed to practice-based training, we excluded articles where participants were studying at the doctoral level, but their training did not focus on research (e.g. PsyD doctorate in Clinical Psychology).
Screening articles
Papers were screened by one of the present authors at the level of title, then abstract, and finally at full text (Fig. (Fig.1). 1 ). Duplicates were removed after screening at abstract. At each level of screening, a random 20% sub-set of articles were double screened by another author, and levels of agreement were calculated (Cohen’s kappa [ 13 ]). Where disagreements occurred between authors, a third author was consulted to decide whether the paper should or should not be included. All kappa values evidence at least moderate agreement between authors [ 14 ]—see Fig. Fig.1 1 for exact kappa values.

PRISMA diagram of literature review process
Data extraction
This review reports on both quantitative and qualitative findings, and separate extraction methods were used for each. Data extraction was performed by authors CH, CB, SV and LC.
Quantitative data extraction
The articles in this review used varying methods and measures. To accommodate this heterogeneity, multiple approaches were used to extract quantitative data. Where available, we extracted (a) descriptive statistics, (b) correlations and (c) a list of key findings. For all mental health outcome measures, we extracted the means and standard deviations for the DR participants, and where available for the control group (descriptive statistics). For studies utilising a within-subjects study design, we extracted data where a mental health outcome measure was correlated with another construct (correlations). Finally, to ensure that we did not lose important findings that did not use descriptive statistics or correlations, we extracted the key findings from the results sections of each paper (list of key findings). Key findings were identified as any type of statistical analysis that included at least one mental health outcome.
Qualitative data extraction
In line with the meta-ethnographic method [ 15 ] and our interest in the empirical data as well as the authors’ interpretations thereof, i.e. the findings of each article [ 16 ], the data extracted from the articles comprised both results/findings and discussion/conclusion sections. For articles reporting qualitative findings, we extracted the results and discussion sections from articles verbatim. Where articles used mixed methods, only the qualitative section of the results was extracted. Methodological and setting details from each article were also extracted and provided (see Appendix A) in order to contextualise the studies.
Data analysis
Quantitative data analysis, descriptive statistics.
We present frequencies and percentages of the constructs measured, the tools used and whether basic descriptive statistics ( M and SD ) were reported. The full data file is available from the first author upon request.
Effect sizes
Where studies had a control group, we calculated a between-group effect size (Cohen’s d ) using the formula reported by Wilson [ 17 ], and interpreted using the standard criteria [ 13 ]. For all other studies, we sought to compare results with normative data where the following criteria were satisfied: (a) at least three studies reported data using the same mental health assessment tool; (b) empirical normative data were available; and (c) the scale mean/total had been calculated following original authors’ instructions. Only the Perceived Stress Scale (PSS) 10- [ 18 ] and 14-item versions [ 19 ] met these criteria. Normative data were available from a sample of adults living in the United States: collected in 2009 for the 10-item version ( n = 2000; M = 15.21; SD = 7.28) [ 20 ] and in 1983 for the 14-item version ( n = 2355; M = 19.62; SD = 7.49) [ 18 ].
The meta-analysis of PSS data was conducted using MedCalc [ 21 ], and based on a random effects model, as recommended by [ 22 ]. The between-group effect sizes (DRs versus US norms) were calculated comparing PSS means and standard deviations in the respective groups. The effect sizes were weighted using the variable variances [ 23 ].
Correlations
Where at least three studies reported data reflecting a bivariate association between a mental health and another variable, we summarised this data into a meta-analysis using the reported r coefficients and sample sizes. Again, we used MedCalc [ 21 ] to conduct the analysis using a random effects model, based on the procedure outlined by Borenstein, Hedges, Higgins and Rothstein [ 24 ]. This analysis approach involves converting correlation coefficients into Fisher’s z values [ 25 ], calculating the summary of Fisher’s z , and then converting this to a summary correlation coefficient ( r ). The effect sizes were weighted in line with the Hedges and Ollkin [ 23 ] method. Heterogeneity was assessed using the Q statistic, and I 2 value—both were interpreted according to the GRADE criteria [ 26 ]. Where correlations could not be summarised within a meta-analysis, we have reported these descriptively.
Due to the heterogenous nature of the studies, the above methods could not capture all of the quantitative data. Therefore, additional data (e.g. frequencies, statistical tests) reported in the identified articles was collated into a single document, coded as relating to prevalence, risk or protective factors and reported as a narrative review.
Qualitative data analysis
We used thematic analytic methods to analyse the qualitative data. We followed the thematic synthesis method [ 16 , 27 ] and were informed by a thematic analysis approach [ 28 , 29 ]. We took a critical realist epistemological stance [ 30 , 31 ] and aimed to bring together an analysis reflecting meaningful patterns amongst the data [ 29 ] or demi-regularities, and identifying potential social mechanisms that might influence the experience of such phenomena [ 31 ]. The focus of the meta-synthesis is interpretative rather than aggregative [ 32 ].
Coding was line by line, open and complete. Following line-by-line coding of all articles, a thematic map was created. Codes were entered on an article-by-article basis and then grouped and re-grouped into meaningful patterns. Comparisons were made across studies to attempt to identify demi-regularities or patterns and contradictions or points of departure. The thematic map was reviewed in consultation with other authors to inductively create and refine themes. Thematic summaries were created and brought together into a first draft of the thematic structure. At this point, each theme was compared against the line-by-line codes and the original articles in order to check its fit and to populate the written account with illustrative quotations.
Research rigour
The qualitative analysis was informed by independent coding by authors CB and SV, and analytic discussions with CH, SV and LC. Our objective was not to capture or achieve inter-rater reliability, rather the analysis was strengthened through involvement of authors from diverse backgrounds including past and recent PhD completion, experiences of mental health problems during PhD completion, PhD supervision experience, experience as employees in a UK university doctoral school and different nationalities. In order to enhance reflexivity, CB used a journal throughout the analytic process to help notice and bracket personal reflections on the data and the ways in which these personal reflections might impact on the interpretation [ 29 , 33 ]. The ENTREQ checklist [ 34 ] was consulted in the preparation of this report to improve the quality of reporting.
Quality assessment
Quantitative data.
The quality of the quantitative papers was assessed using the STROBE combined checklist [ 35 ]. A random 20% sub-sample of these studies were double-coded and inter-rater agreement was 0.70, indicating ‘substantial’ agreement [ 14 ]. The maximum possible quality score was 23, with a higher score indicating greater quality, with the mean average of 15.97, and a range from 0 to 22. The most frequently low-scoring criteria were incomplete reporting regarding the management of missing data, and lack of reported efforts to address potential causes of bias.
Qualitative data
There appeared to be no discernible pattern in the perceived quality of studies; the highest [ 36 – 40 ] and lowest scoring [ 41 – 46 ] studies reflected both theses and journal publications, a variety of locations and settings and different methodologies. The most frequent low-scoring criteria were relating to the authors’ positions and reflections thereof (i.e. ‘Qualitative approach and research paradigm’, ‘Researcher characteristics and reflexivity’, ‘Techniques to enhance trustworthiness’, ‘Limitations’, ‘Conflict of interest and Funding’). Discussions of ethical issues and approval processes was also frequently absent. We identified that we foregrounded higher quality studies in our synthesis in that these studies appeared to have greater contributions reflected in the shape and content of the themes developed and were more likely to be the sources of the selected illustrative quotes.
Mixed methods approach
The goal of this review is to answer the review questions by synthesising the findings from both quantitative and/or qualitative studies. To achieve our goal, we adopted an integrated approach [ 47 ], whereby we used both quantitative and qualitative methods to answer the same review question, and draw a synthesised conclusion. Different analysis approaches were used for the quantitative and qualitative data and are therefore initially reported separately within the methods. A separate synthesised summary of the findings is then provided.
Overview of literature
Of the 52 papers included in this review (Table (Table1), 1 ), 7 were qualitative, 29 were quantitative and 16 mixed methods. Most articles (35) were peer-reviewed papers, and the minority were theses (17). Only four of the articles included a control group; in three instances comprising students (but not DRs) and in the other drawn from the general population.
List of studies included in this review
M and SD rounded to whole figures; D dissertation, P peer reviewed paper, N / A not applicable, – = not reported, USA United Stated of America, UK United Kingdom; *Study used mixed methods, but only qualitative data were used in this review as quantitative data did not pertain to mental health
Quantitative results
Thirty-five papers reported quantitative data, providing 52 reported sets of mental health related data (an average of 1.49 measures per study): 24 (68.57%) measured stress, 10 (28.57%) anxiety, 9 (25.71%) general wellbeing, 5 (14.29%) social support, 3 (8.57%) depression and 1 (2.86%) self-esteem. Five studies (9.62%) used an unvalidated scale created for the purposes of the study. Fifteen studies (28.85%) did not report descriptive statistics.
Of the four studies that included a control group, only two of these reported descriptive statistics for both groups on a mental health outcome [ 66 , 69 ]. There is a small (Cohen’s d = 0.27) and large between-group effect (Cohen’s d = 1.15) when DRs were compared to undergraduate and postgraduate clinical psychology students respectively in terms of self-reported stress.
The meta-analysis of DR scores on the PSS (both 10- and 14-item versions) compared to population normative data produced a large and significant between-group effect size ( d = 1.12, 95% CI [0.52, 1.73]) in favour of DRs scoring higher on the PSS than the general population (Fig. (Fig.2), 2 ), suggesting DRs experience significantly elevated stress. However, these findings should be interpreted in light of the significant between-study heterogeneity that can be classified as ‘considerable’ [ 26 ].

A meta-analysis of between-group effect sizes (Cohen’s d ) comparing PSS scores (both 10- and 14-item versions) from DRs and normative population data. *Studies using the 14 item version of the PSS; a positive effect size indicates DRs had a higher score on the PSS; a negative effect size indicates that the normative data produced a higher score on the PSS; black diamond = total effect size (based on random effects model); d = Cohen’s d ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
To explore this heterogeneity, we re-ran the meta-analysis separately for the 10- and 14-item versions. The effect size remained large and significant when looking only at the studies using the 14-item version ( k = 6; d = 1.41, 95% CI [0.63, 2.19]), but was reduced and no longer significant when looking at the 10-item version only ( k = 3; d = 0.57, 95% CI [− 0.51, 1.64]). However, both effect sizes were still marred by significant heterogeneity between studies (10-item: Q = 232.02, p < .001; 14-item: Q = 356.76, p < .001).
Studies reported sufficient correlations for two separate meta-analyses; the first assessing the relationship between stress (PSS [ 18 , 19 ]) and perceived support, and the second between stress (PSS) and academic performance.
Stress x support
We included all measures related to support irrespective of whom that support came from (e.g. partner support, peer support, mentor support). The overall effect size suggests a small and significant negative correlation between stress and support ( r = − .24, 95% CI [− 0.34, − 0.13]) (see Fig. Fig.3), 3 ), meaning that low support is associated with greater perceived stress. However, the results should be interpreted in light of the significant heterogeneity between studies. The I 2 value quantifies this heterogeneity as almost 90% of the variance being explained by between-study heterogeneity, which is classified as ‘substantial’ (26).

Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and perceived support. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value

Stress x performance
The overall effect size suggests that there is no relationship between stress and performance in their studies ( r = − .07, 95% CI [− 0.19, 0.05]) (see Fig. Fig.4), 4 ), meaning that DRs perception of their progress was not associated with their perceived stress This finding suggests that the amount of progress that DRs were making during their studies was not associated with stress levels.

Forest plot and meta-analysis of correlation coefficients testing the relationship between stress and performance. Black diamond = total effect size (based on random effects model); r = Pearson’s r ; Q = heterogeneity; Z = z score; I 2 = proportion of variance due to between-study heterogeneity; p = exact p value
Other correlations
Correlations reported in less than three studies are summarised in Fig. Fig.5. 5 . Again, stress was the most commonly tested mental health variable. Self-care and positive feelings towards the thesis were consistently found to negatively correlate with mental health constructs. Negative writing habits (e.g. perfectionism, blocks and procrastination) were consistently found to positively correlate with mental health constructs. The strongest correlations were found between stress, and health related quality of life ( r = − .62) or neuroticism ( r = .59), meaning that lower stress was associated with greater quality of life and reduced neuroticism. The weakest relationships ( r < .10) were found between mental health outcomes and: faculty concern, writing as knowledge transformation, innate writing ability (stress and anxiety), years married, locus of control, number of children and openness (stress only).

Correlation coefficients testing the relationship between a mental health outcome and other construct. Correlation coefficients are given in brackets ( r ); * p < .05; each correlation coefficient reflects the results from a single study
Several studies reported DR mental health problem prevalence and this ranged from 36.30% [ 54 ] to 55.9% [ 67 ]. Using clinical cut-offs, 32% were experiencing a common psychiatric disorder [ 64 ]; with another study finding that 53.7% met the questionnaire cut-off criteria for depression, and 41.9% for anxiety [ 67 ]. One study compared prevalence amongst DRs and the general population, employees and other higher education students; in all instances, DRs had higher levels of psychological distress (non-clinical), and met criteria for a clinical psychiatric disorder more frequently [ 64 ].
Risk factors
Demographics Two studies reported no significant difference between males and females in terms of reported stress [ 57 , 73 ], but the majority suggested female DRs report greater clinical [ 80 ], and non-clinical problems with their mental health [ 37 , 64 , 79 , 83 , 89 ].
Several studies explored how mental health difficulties differed in relation to demographic variables other than gender, suggesting that being single or not having children was associated with poorer mental health [ 64 ] as was a lower socioeconomic status [ 71 ]. One study found that mental health difficulties did not differ depending on DRs’ ethnicity [ 51 ], but another found that Black students attending ‘historically Black universities’ were significantly more anxious [ 87 ]. The majority of the studies were conducted in the US, but only one study tested for cross-cultural differences: reporting that DRs in France were more psychologically distressed than those studying in the UK [ 67 ].
Work-life balance Year of study did not appear to be associated with greater subjective stress in a study involving clinical psychology DRs (Platt and Schaefer [ 75 ]), although other studies suggested greater stress reported by those in the latter part of their studies [ 89 ], who viewed their studies as a burden [ 81 ], or had external contracts, i.e. not employed by their university [ 85 ]. Regression analyses revealed that a common predictor of poor mental health was uncertainty in DR studies; whether in relation to uncertain funding [ 64 ] or uncertain progress [ 80 ]. More than two-thirds of DRs reported general academic pressure as a cause of stress, and a lack of time as preventing them from looking after themselves [ 58 ]. Being isolated was also a strong predictor of stress [ 84 ].
Protective factors
DRs who more strongly endorsed all of the five-factor personality traits (openness, conscientiousness, extraversion, agreeableness and neuroticism) [ 66 ], self-reported higher academic achievement [ 40 ] and viewed their studies as a learning process (rather than a means to an end) [ 82 ] reported fewer mental health problems. DRs were able to mitigate poor mental health by engaging in self-care [ 72 ], having a supervisor with an inspirational leadership style [ 64 ] and building coping strategies [ 56 ]. The most frequently reported coping strategy was seeking support from other people [ 37 , 58 ].
Qualitative results
Meta-synthesis.
Four higher-order themes were identified: (1) Always alone in the struggle, (2) Death of personhood, (3) The system is sick and (4) Seeing, being and becoming. The first two themes reflect individual risk/vulnerability factors and the processes implicated in the experience of mental distress, the third represents systemic risk and vulnerability factors and the final theme reflects individual and systemic protective mechanisms and transformative influences. See Table Table2 2 for details of the full thematic structure with illustrative quotes.
Thematic structure with illustrative quotes
Always alone in the struggle
‘Always alone in the struggle’ reflects the isolated nature of the PhD experience. Two subthemes reflect different aspects of being alone; ‘Invisible, isolated and abandoned’ represents DRs’ sense of physical and psychological separation from others and ‘It’s not you, it’s me’ represents DRs’ sense of being solely responsible for their PhD process and experience.
Invisible, isolated and abandoned
Feeling invisible and isolated both within and outside of the academic environment appears a core DR experience [ 39 , 43 , 81 ]. Isolation from academic peers seemed especially salient for DRs with less of a physical presence on campus, e.g. part-time and distance students, those engaging in extensive fieldwork, outside employment and those with no peer research or lab group [ 36 , 52 , 68 ]. Where DRs reported relationships with DR peers, these were characterised as low quality or ‘not proper friendships’ and this appeared linked to a sense of essential and obvious competition amongst DRs with respect to current and future resources, support and opportunities [ 39 ], in which a minority of individuals were seen to receive the majority share [ 36 , 74 ]. Intimate sharing with peers thus appeared to feel unsafe. This reflected the competitive environment but also a sense of peer relationships being predicated on too shared an experience [ 39 ].
In addition to poor peer relations, a mismatch between the expected and observed depth of supervisor interest, engagement and was evident [ 40 , 81 ]. This mismatch was clearly associated with disappointment and anger, and a sense of abandonment, which appeared to impact negatively on DR mental health and wellbeing [ 42 ] (p. 182). Moreover, DRs perceived academic departments as complicit in their isolation; failing to offer adequate opportunities for academic and social belonging and connections [ 42 , 81 ] and including PGRs only in a fleeting or ‘hollow’ sense [ 37 ]. DRs identified this isolation as sending a broader message about academia as a solitary and unsupported pursuit; a message that could lead some DRs to self-select out of planning for future in academia [ 37 , 42 ]. DRs appeared to make sense of their lack of belonging in their department as related to their sense of being different, and that this difference might suggest they did not ‘fit in’ with academia more broadly [ 74 ]. In the short-term, DRs might expend more effort to try and achieve a social and/or professional connection and equitable access to support, opportunities and resources [ 74 ]. However, over the longer-term, the continuing perception of being professionally ‘other’ also seemed to undermine DRs’ sense of meaning and purpose [ 81 ] and could lead to opting out of an academic career [ 62 , 74 ].
Isolation within the PhD was compounded by isolation from one’s personal relationships. This personal isolation was first physical, in which the laborious nature of the PhD acted as a catalyst for the breakdown of pre-existing relationships [ 76 ]. Moreover, DRs also experienced a sense of psychological detachment [ 45 , 74 ]. Thus, the experience of isolation appeared to be extremely pervasive, with DRs feeling excluded and isolated physically and psychologically and across both their professional and personal lives.
It’s not you, it’s me
‘It’s not you, it’s me’ reflects DRs’ perfectionism as a central challenge of their PhD experience and a contributor to their sense of psychological isolation from other people. DRs’ perfectionism manifested in four key ways; firstly, in the overwhelming sense of responsibility experienced by DRs; secondly, in the tendency to position themselves as inadequate and inferior; thirdly, in cycles of perfectionist paralysis; and finally, in the tendency to find evidence which confirms their assumed inferiority.
DRs positioned themselves as solely responsible for their PhD and for the creation of a positive relationship with their supervisor [ 36 , 52 , 81 ]. DRs expressed a perceived need to capture their supervisors’ interest and attention [ 36 , 52 , 74 ], feeling that they needed to identify and sell to their supervisors some shared characteristic or interest in order to scaffold a meaningful relationship. DRs appeared to feel it necessary to assume sole responsibility for their personal lives and to prohibit any intrusion of the personal in to the professional, even in incredibly distressing circumstances [ 42 ].
DRs appeared to compare themselves against an ideal or archetypal DR and this comparison was typically unfavourable [ 37 ], with DRs contrasting the expected ideal self with their actual imperfect and fallible self [ 37 , 42 , 52 ]. DRs’ sense of inadequacy appeared acutely and frequently reflected back to them by supervisors in the form of negative or seemingly disdainful feedback and interactions [ 41 , 76 ]. DRs framed negative supervisor responses as a cue to work harder, meaning they were continually striving, but never reaching, the DR ideal [ 76 ]. This ideal-actual self-discrepancy was associated with a tendency towards punitive self-talk with clear negative valence [ 38 ].
DRs appear to commonly use self-castigation as a necessary (albeit insufficient) means to motivate themselves to improve their performance in line with perfectionistic standards [ 38 , 41 ]. The oscillation between expectation and actuality ultimately resulted in increased stress and anxiety and reduced enjoyment and motivation. Low motivation and enjoyment appeared to cause procrastination and avoidance, which lead to a greater discrepancy between the ideal and actual self; in turn, this caused more stress and anxiety and further reduced enjoyment and motivation leading to a sense of stuckness [ 76 ].
The internalisation of perceived failure was such that DRs appeared to make sense of their place, progress and possible futures through a lens of inferiority, for example, positioning themselves as less talented and successful compared to their peers [ 37 ]. Thus, instances such as not being offered a job, not receiving funding, not feeling connected to supervisors, feeling excluded by academics and peers were all made sense of in relation to DRs’ perceived relative inadequacy [ 36 ].
Death of personhood
The higher-order theme ‘Death of personhood’ reflects DRs’ identity conflict during the PhD process; a sense that DRs’ engage in a ‘Sacrifice of personal identity’ in which they feel they must give up their pre-existing self-identity, begin to conceive of themselves as purely ‘takers’ personally and professionally, thus experiencing the ‘Self as parasitic’, and ultimately experience a ‘Death of self-agency’ in relation to the thesis, the supervisor and other life roles and activities.
A sacrifice of personal identity
The sacrifice of personal identity first manifests as an enmeshment with the PhD and consequent diminishment of other roles, relationships and activities that once were integral to the DRs’ sense of self [ 59 , 76 ]. DRs tended to prioritise PhD activities to the extent that they engaged in behaviours that were potentially damaging to their personal relationships [ 76 ]. DRs reported a sense of never being truly free; almost physically burdened by the weight of their PhD and carrying with them a constant ambient guilt [ 37 , 38 , 44 , 76 ]. Time spent on non-PhD activities was positioned as selfish or indulgent, even very basic activities of living [ 76 ].
The seeming incompatibility of aspects of prior personal identity and the PhD appears to result in a sense of internal conflict or identity ‘collision’ [ 59 ]. Friends and relatives often provided an uncomfortable reflection of the DR’s changing identity, leaving DRs feeling hyper-visible and carrying the burden of intellect or trailblazer status [ 74 ]; providing further evidence for the incompatibility of their personal and current and future professional identities. Some DRs more purposefully pruned their relationships and social activities; to avoid identity dissonance, to conserve precious time and energy for their PhD work, or as an acceptance of total enmeshment with academic work as necessary (although not necessarily sufficient) for successful continuation in academia [ 40 , 52 , 77 ]. Nevertheless, the diminishment of the personal identity did not appear balanced by the development of a positive professional identity. The professional DR identity was perceived as unclear and confusing, and the adoption of an academic identity appeared to require DRs to have a greater degree of self-assurance or self-belief than was often the case [ 37 , 81 ].
Self as parasitic
Another change in identity manifested as DRs beginning to conceive of themselves as parasitic. DRs spoke of becoming ‘takers’, feeling that they were unable to provide or give anything to anyone. For some DRs, being ‘parasitic’ reflected them being on the bottom rung of the professional ladder or the ‘bottom of the pile’; thus, professionally only able to receive support and assistance rather than to provide for others. Other DRs reported more purposefully withdrawing from activities in which they were a ‘giver’, for example voluntary work, as providing or caring for others required time or energy that they no longer had [ 38 , 44 ]. Furthermore, DRs appeared to conceive of themselves as also causing difficulty or harm to others [ 81 ], as problems in relation to their PhD could lead them to unwillingly punishing close others, for example, through reducing the duration or quality of time spent together [ 38 ].
Feeling that close others were offering support appeared to heighten the awareness of the toll of the PhD on the individual and their close relationships, emphasising the huge undertaking and the often seemingly slow progress, and actually contributing to the sense of ambient guilt, shame, anger and failure [ 38 ]. Moreover, DRs spoke of feeling extreme guilt in perceiving that they had possibly sacrificed their own, and possibly family members’, current wellbeing and future financial security [ 49 ].
Death of self-agency
In addition to their sense of having to sacrifice their personal identity, DRs also expressed a loss of their sense of themselves as agentic beings. DRs expressed feeling powerless in various domains of their lives. First, DRs positioned the thesis as a powerful force able to overwhelm or swallow them [ 46 , 52 , 59 ]. Secondly, DRs expressed a sense of futility in trying to retain any sense of personal power in the climate of academia. An acute feeling of powerlessness especially in relation to supervisors was evident, with many examples provided of being treated as means to an end, as opposed to ends in themselves [ 39 , 42 , 62 ]. Supervisors did not interact with DRs in a holistic way that recognised their personhood and instead were perceived as prioritising their own will, or the will of other academics, above that of the DR [ 39 , 62 ].
Furthermore, DRs reported feeling as if they were used as a means for research production or furthering their supervisors’ reputations or careers [ 62 ]. DRs perceived that holding on to a sense of personal agency sometimes felt incompatible with having a positive supervisor relationship [ 42 ]. Thus whilst emotional distress, anger, disappointment, sadness, jealousy and resentment were clearly evident in relation to feeling excluded, used or over-powered by supervisors [ 37 , 42 , 52 , 62 ], DRs usually felt unable to change supervisor irrespective of how seriously this relationship had degraded [ 37 , 62 ]. Instead, DRs appeared to take on a position of resignation or defensive pessimism, in which they perceived their supervisors as thwarting their personhood, personal goals and preferences, but typically felt compelled to accept this as the status quo and focus on finishing their PhDs [ 42 ]. DRs resignation was such that they internalised this culture of silence and silenced themselves; tending to share litanies of problems with supervisors whilst prefacing or ending the statements with some contradictory or undermining phrase such as ‘but that’s okay’ [ 42 , 52 ].
The apparent lack of self-agency extended outward from the PhD into DRs not feeling able to curate positive life circumstances more generally [ 76 ]. A lack of time was perhaps the key struggle across both personal and professional domains, yet DRs paradoxically reported spending a lot of time procrastinating and rarely (if ever) mentioned time management as a necessary or desired coping strategy for the problem of having too little time [ 46 ]. The lack of self-agency was not only current but also felt in reference to a bleak and uncertain future; DRs lack of surety in a future in academia and the resultant sense of futility further undermined their motivation to engage currently with PhD tasks [ 38 , 40 ].
The system is sick
The higher-order theme ‘The system is sick’ represents systemic influences on DR mental health. First, ‘Most everyone’s mad here’ reflects the perceived ubiquity mental health problems amongst DRs. ‘Emperor’s new clothes’ reflects the DR experience of engaging in a performative piece in which they attempt to live in accordance with systemic rather than personal values. Finally, ‘Beware the invisible and visible walls’ reflects concerns with being caught between ephemeral but very real institutional divides.
Most everyone’s mad here
No studies focused explicitly on experiences of DRs who had been given diagnoses of mental health problems. Some study participants self-disclosed mental health problems and emphasised their pervasive impact [ 50 ]. Further lived experiences of mental distress in the absence of explicit disclosure were also clearly identifiable. The ‘typical’ presentation of DRs with respect to mental health appeared characterised as almost unanimous [ 39 ] accounts of chronic stress, anxiety and depression, emotional distress including frustration, anger and irritability, lack of mental and physical energy, somatic problems including appetite problems, headaches, physical pain, nausea and problems with drug and alcohol abuse [ 39 , 46 , 59 , 76 ]. Health anxiety, concerns regarding perceived new and unusual bodily sensations and perceived risks of developing stress-related illnesses were also common [ 46 , 59 , 76 ]. A PhD-specific numbness and hypervigilance was also reported, in which DRs might be less responsive to personal life stressors but develop an extreme sensitivity and reactivity to PhD-relevant stimuli [ 39 ].
An interplay of trait and state factors were suggested to underlie the perceived ubiquity of mental health problems amongst DRs. Etiological factors associated with undertaking a PhD specifically included the high workload, high academic standards, competing personal and professional demands, social isolation, poor resources in the university, poor living conditions and poverty, future and career uncertainty [ 36 , 41 , 43 , 46 , 49 , 76 ]. The ‘nexus’ of these factors was such that the PhD itself acted as a crucible; a process of such intensity that developing mental health problems was perhaps inevitable [ 39 ].
The perceived inevitability of mental health problems was such that DRs described people who did not experience mental health problems during a PhD as ‘lucky’ [ 39 ]. Supervisors and the wider academic system were seen to promote an expectation of suffering, for example, with academics reportedly normalising drug and alcohol problems and encouraging unhealthy working practices [ 39 ]. Furthermore, DRs felt that academics were uncaring with respect to the mental challenge of doing a PhD [ 39 ]. Nevertheless, academics were suggested to deny any culpability or accountability for mental health problems amongst DRs [ 39 , 59 , 74 ]. The cycle of indigenousness was further maintained by a lack of mental health literacy and issues with awareness, availability and access to help-seeking and treatment options amongst DRs and academics more widely [ 39 ]. Thus, DRs appeared to feel they were being let down by a system that was almost set up to cause mental distress, but within which there was a widespread denial of the size and scope of the problem and little effort put into identifying and providing solutions [ 39 , 59 ]. DRs ultimately felt that the systemic encouragement of unhealthy lifestyles in pursuit of academic success was tantamount to abuse [ 62 ].
A performance of optimum suffering
Against a backdrop of expected mental distress, DRs expressed their PhD as a performative piece. DRs first had to show just the right amount of struggle and difficulty; feeling that if they did not exhibit enough stress, distress and ill-health, their supervisors or the wider department might not believe they were taking their PhD seriously enough [ 40 ]. At the same time, DRs felt that their ‘researcher mettle’ was constantly being tested and they must rise to this challenge. This included first guarding against presenting oneself as intellectually inferior [ 36 ]. Yet it also seemed imperative not to show vulnerability more broadly [ 74 ]. Disclosing mental or physical health problems might lead not only to changed perceptions of the DR but to material disadvantage [ 74 ]. The poor response to mental health disclosures suggested to some DRs that universities might be purposefully trying to dissuade or discourage DRs with mental health problems or learning disabilities from continuing [ 74 ]. The performative piece is thus multi-layered, in that DRs must experience extreme internal psychological struggles, exhibit some lower-level signs of stress and fatigue for peer and faculty observance, yet avoid expressing any real academic or interpersonal weakness or the disclosure of any diagnosable disability or disease.
Emperor’s new clothes
DRs described feeling beholden to the prevailing culture in which it was expected to prioritise above all else developing into a competitive, self-promoting researcher in a high-performing research-active institution [ 39 , 42 ]. Supervisors often appeared the conduit for transmission of this academic ideal [ 74 ]. DRs felt reticent to act in any way which suggested that they did not personally value the pursuit of a leading research career above all else. For example, DRs felt that valuing teaching was non-conformist and could endanger their continuing success within their current institution [ 55 ]. Many DRs thus exhibited a sense of dissonance as their personal values often did not align with the institutional values they identified [ 74 ]. Yet DRs expressed a sense of powerlessness and a feeling of being ‘caught up’ in the values of the institution even when such values were personally incongruent [ 74 ]. The psychological toll of this sense of inauthenticity seemed high [ 55 ]. Where DRs acted in ways which ostensibly suggested values other than prioritising a research career, for example becoming pregnant, they sensed disapproval [ 76 ]. DRs also felt unable to challenge other ‘institutional myths’ for example, the perceived institutional denial of the duration of and financial struggle involved in completing a PhD [ 49 ]. There was a perceived tendency of academics to locate problems within DRs as opposed to acknowledging institutional or systemic inequalities [ 49 ]. DRs expressed strongly a sense in which there is inequity in support, resources and opportunities, yet universities were perceived as ignoring such inequity or labelling such divisions as based on meritocracy [ 36 , 74 ].
Beware the invisible and visible walls
DRs described the reality of working in academia as needing to negotiate a maze of invisible and visible walls. In the former case, ‘invisible walls’ reflect ephemeral norms and rules that govern academia. DRs felt that a big part of their continuing success rested upon being able to negotiate such rules [ 39 ]. Where rules were violated and explicit or implicit conflicts occurred, DRs were seen to be vulnerable to being caught in the ‘crossfire’ [ 36 ]. DRs identified academic groups and departments as being poor in explicitly identifying, discussing and resolving conflicts [ 37 ]. The intangibility of the ‘invisible walls’ gave rise to a sense of ambient anxiety about inadvertently transgressing norms and divides, such that some DRs reported behaving in ways that surprised even themselves [ 37 ].
Gendered and racial micropolitics of academic institutions were seen to manifest as more visible walls between people, with institutions privileging those with ‘insider’ status [ 36 ]. Women and people of colour typically felt excluded or disadvantaged in a myriad of observable and unobservable ways, with individuals able to experience both insider and outsider statuses simultaneously [ 36 , 37 ], for example when a male person of colour [ 36 ]. Female DRs suggested that not only must women prove themselves to a greater extent than men to receive equal access to resources, opportunities and acclaim but also are typically under additional pressure in both their professional and personal lives [ 37 , 52 , 76 ]. Women also felt that they had to take on more additional roles and responsibilities and encountered more conflicts in their personal lives compared to men [ 52 ]. Examples of professionally successful women in DRs’ departments were described as those who had crossed the divide and adopted a more traditionally male role [ 40 ]. Thus, being female or non-White were considered visible characteristics that would disadvantage people in the competitive academic environment and could give rise to a feeling of increased stress, pressure, role conflicts, and a feeling of being unsafe.
Seeing, being and becoming
The higher-order theme of ‘Seeing, being and becoming’ reflects protective and transformative influences on DR mental health. ‘De-programming’ refers to the DRs disentangling their personal beliefs and values from systemic values and also from their own tendency towards perfectionism. ‘The power of being seen’ reflects the positive impact on DR mental health afforded by feeling visible to personal and professional others. ‘Finding hope, meaning and authenticity’ refers to processes by which DRs can find or re-locate their own self-agency, purpose and re/establish a sense of living in accordance with their values. ‘The importance of multiple goals, roles and groups’ represents the beneficial aspects of accruing and sustaining multiple aspects to one’s identity and connections with others and activities outside the PhD. Finally, ‘The PhD as a process of transcendence’ reflects how the struggles involved in completing a PhD can be transformative and self-actualising.
De-programming
DRs reported being able to protect their mental health by ‘de-programming’ and disentangling their attitudes and practices from social and systemic values and norms. This disentangling helped negate DRs’ adopting unhealthy working practices and offered some protection against experiencing inauthenticity and dissonance between personal and systemic values.
First, DRs spoke of rejecting the belief that they should sacrifice or neglect personal relationships, outside interests and their self-identity in pursuit of academic achievement. DRs could opt-out entirely by choosing a ‘user-friendly’ programme [ 44 ] which encouraged balance between personal and professional goals, or else could psychologically reject the prevailing institutional discourse [ 40 ]. Rather than halting success, de-programming from the prioritisation of academia above all else was seen to be associated not only with reduced stress but greater confidence, career commitment and motivation [ 40 , 50 ]. It was also suggested possible to ‘de-programme’ in the sense of choosing not to be preoccupied by the ‘invisible walls’ of academia and psychologically ‘opt out’ of being concerned by potential conflicts, norms and rules governing academic workplace conduct [ 36 ]. Interaction with people outside of academia was seen to scaffold de-programming, by helping DRs to stay ‘grounded’ and offering a model what ‘normal’ life looks like. People outside of academia could also help DRs to see the truth by providing unbiased opinions regarding systemic practices [ 39 ].
A further way in which de-programming manifested was in DRs challenging their perfectionist beliefs. This include re-framing the goal as not trying to be the archetype of a perfect DR, and accepting that multiple demands placed on one individual invariably requires compromise [ 40 , 76 ]. DRs spoke of the need to conceptualise the PhD as a process, rather than just a product [ 46 , 82 ]. The process orientation facilitated framing of the PhD as just one-step in the broader process of becoming an academic as opposed to providing discrete evidence of worth [ 82 ]. Within this perspective, uncertainty itself could be conceived as a privilege [ 81 ]. The PhD was then seen as an opportunity rather than a test [ 37 , 46 ]. Moreover, the process orientation facilitated viewing the PhD as a means of growing into a contributing member of the research community, as opposed to needing to prove oneself to be accepted [ 82 ]. Remembering the temporary nature of the PhD was advised [ 45 ] as was holding on to a sense that not completing the PhD was also a viable life choice [ 76 ]. DRs also expressed, implicitly or explicitly, a decision to change their conceptualisation of themselves and their progress; choosing not to perceive themselves as stuck, but planning, learning and progressing [ 38 , 39 , 81 , 82 ]. This new perspective appeared to be helpful in reducing mental distress.
The power of being seen
DRs described powerful benefits to feeling seen by other people, including a sense of belonging and mattering, increased self-confidence and a sense of positive progress [ 37 ]. Being seen by others seems to provoke the genesis of an academic identity; it brings DRs into existence as academics. Being seen within the academic institution also supports mental health and can buffer emotional exhaustion [ 37 , 52 , 55 , 81 ]. DRs expressed a need to feel that supervisors, academics and peers were interested in them as people, their values, goals, struggles and successes; yet they also needed to feel that they and their research mattered and made a difference within and outside of the institution [ 42 , 52 , 81 ]. It was clear that DRs could find in their disciplinary communities the sense of belonging that often eluded them within their immediate departments [ 42 ]. Feeling a sense of belonging to the academic community seemed to buffer disengagement and amotivation during the PhD [ 81 ]. Positive engagement with the broader community was scaffolded by a sense of trust in the supervisor [ 81 ]. DRs often felt seen and supported by postdocs, especially where supervisors appeared absent or unsupportive [ 50 ].
Spending time with peers could be beneficial when there was a sense of shared experience and walking alongside each other [ 39 ]. Friendship was seen to buffer stress and protect against mental health problems through the provision of social and emotional support and help in identifying struggles [ 39 , 43 ]. In addition to relational aspects, the provision of designated physical spaces on campus or in university buildings also seemed important to being seen [ 37 ]. Peers in the university could provide DRs with further physical embodiments of being seen, for example, gift-giving in response to their birthdays or returning from leave [ 37 , 50 ]. Outside of the academic institution, DRs described how being seen by close others could support DRs to be their authentic selves, providing an antidote to the invisible walls of academia [ 50 ]. Good quality friendships within or outside academia could be life-changing, providing a visceral sense of connection, belonging and authenticity that can scaffold positive mental health outcomes during the PhD [ 39 ]. Pets could also serve to help DRs feel seen but without needing to extend too much energy into maintaining social relationships [ 50 ].
Finally, DRs also needed to see themselves, i.e. to begin to see themselves as burgeoning academics as opposed to ‘just students’ [ 81 ]. Feeling that the supervisor and broader academic community were supportive, developing one’s own network of process collaborators and successfully obtaining grant funding seemed tangible markers that helped DRs to see themselves as academics [ 37 , 81 ]. Seeing their own work published was also helpful in providing a boost in confidence and being a joyful experience [ 42 ]. Moreover, with sufficient self-agency, DRs can not only see themselves but render themselves visible to other people [ 37 ].
Multiple goals, roles and groups
In antidote to the diminished personal identity and enmeshment with the PhD, DRs benefitted from accruing and sustaining multiple goals, roles, occupations, activities and social group memberships. Although ‘costly’ in terms of increased stress and role conflicts, sustaining multiple roles and activities appeared essential for protecting against mental health problems [ 50 , 68 ].
Leisure activities appeared to support mental health through promoting physical health, buffering stress, providing an uplift to DRs’ mood and through the provision of another identity other than as an academic [ 44 , 50 , 76 ]. Furthermore, engagement in activities helped DRs to find a sense of freedom, allowing them to carve up leisure and work time and psychologically detach from their PhD [ 68 , 76 ]. Competing roles, especially family, forced DRs to distance themselves from the PhD physically which reinforced psychological separation [ 50 , 59 ]. Engaging in self-care and enjoyable activities provided a sense of balance and normalcy [ 39 , 44 , 68 ]. This normalcy was a needed antidote to abnormal pressure [ 59 ]. Even in the absence of fiercely competing roles and priorities, DRs still appeared to benefit from treating their PhD as if it is only one aspect of life [ 59 ]. Additional roles and activities reduced enmeshment with the PhD to the extent that considering not completing the PhD was less averse [ 40 ]. This position appeared to help DRs to be less overwhelmed and less sensitive to perceived and anticipated failures.
Finding hope, meaning and authenticity
Finding hopefulness and meaning within the PhD can scaffold a sense of living a purposeful, enjoyable, important and authentic life. Hopefulness is predicated on the ability to identify a goal, i.e. to visualise and focus on the desired outcome and to experience both self-agency and potential pathways towards the goal. Hopefulness was enhanced by the ability to break down tasks into smaller goals and progress in to ‘baby steps’ [ 38 , 59 ]. In addition, DRs benefitted from finding explicit milestones against which they can compare their progress [ 59 ], as this appeared to feed back into the cycle of hopeful thinking and spur further self-agency and goal pursuit.
The experience of meaning manifested in two main ways; first as the more immediate lived experience of passion in action [ 76 ]. Secondly, DRs found meaning in feeling that in their PhD and lives more broadly they were living in accordance with their values, for example, experiencing their own commitment in action through continuing to work on their PhD even when it was difficult to do so [ 76 ]. DRs who were able to locate their PhD within a broader sense of purpose appeared to derive wellbeing benefits. There was a need to ensure that values were in alignment, for example, finding homeostasis between emotional, intellectual, social and spiritual parts of the self [ 46 , 59 , 90 ].
The processes of finding hopefulness and meaning appear to be largely relational. Frequent contact with supervisors in person and social and academic contact with other DRs were basic scaffolds for hope and meaning [ 52 ]. DRs spoke of how a sense that their supervisors believed in them inspired their self-agency and motivation [ 42 , 62 , 76 ]. Partners, friends and family could also inspire motivation for continuing in PhD tasks [ 44 , 76 ]. Other people also could help instil a sense of motivation to progress and complete the PhD; a sense of being seen is to be beholden to finish [ 39 ]. Meaning appeared to be scaffolded by a sense of contribution, belonging and mattering [ 81 ] and could arise from the perception of putting something into the collective pot, inspiring hopefulness and helping others [ 39 , 42 ]. Moreover, hopefulness, meaning and authenticity also appeared mutually reinforcing [ 81 ]. Finding meaning and working on a project which is in accordance with personal values, preferences and interests is also helpful in completing the PhD and provides a feedback loop into hope, motivation and agentic thinking [ 39 , 81 ]. Furthermore, DRs could use agentic action to source a community of people who share their values, enabling them to engage in collective authenticity [ 39 ].
The PhD as a process of transcendence
The immense challenge of the PhD could be a catalyst for growth, change and self-actualisation, involving empowerment through knowledge, self-discovery, and developing increased confidence, maturity, capacity for self-direction and use of one’s own autonomy [ 44 , 82 ]. The PhD acted as a forge in which DRs were tested and became remoulded into something greater than they had been before [ 44 , 82 , 90 ]. The struggles endured during the PhD caused DRs to reconsider their sense of their own capacities, believing themselves to be more able than they previously would have thought [ 50 ]. The struggles endured added to the sense of accomplishment. A trusted and trusting supervisor appears to aid in the PhD being a process of transcendence [ 62 ].
More broadly, the PhD also helped DRs to transcend personal tragedy, allowing immersion in a meaningful activity which begins as a means of coping and becomes something completely [ 39 ]. The PhD could also serve as a transformative selection process for DRs’ social relationships, with some relationships cast aside and yet others formed anew [ 39 ]. Overall, therefore, the very aspects of the PhD which were challenging, and distressing could allow DRs to transcend their former selves and, through the struggle, become something more.
Summation of results
The findings regarding the risk and protective factors associated with DR mental health have been summarised in Table Table3 3 in relation to (1) the type of research evidencing the factor (i.e. whether the evidence is quantitative only, part of the meta-synthesis only, or evident in both results sections); and (2) the volume of evidence (i.e. whether the factor was found in a single study or across multiple studies). The factors in the far-right column (i.e. the factors found across multiple research studies utilising both qualitative and quantitative methods) are the ones with the strongest evidence at present.
Risk and protective factors associated with DR mental health in terms of the type and volume of evidence
Single = evidenced in a single study; multiple = evidenced across more than one study
This systematic review summarises a heterogeneous research area, with the aim of understanding the mental health of DRs, including possible risk and protective factors. The qualitative and quantitative findings presented here suggest that poor mental health is a pertinent problem facing DRs; stress appears to be a key issue and significantly in excess of that experienced in the general population. Several risk and protective factors at the individual, interpersonal and systemic levels emerged as being important in determining the mental health of DRs. The factors with the strongest evidence-base (i.e. those supported by multiple studies using qualitative and quantitative findings) denote that being female and isolated increases the risk of the mental health problems, whereas seeing the PhD as a process, feeling socially supported, having a positive supervisor relationship and engaging in self-care is protective.
Results in context
Stress can be defined as (1) the extent to which a stimulus exerts pressure on an individual, and their propensity to bear the load; (2) the duration of the response to an aversive stimuli, from initial alert to exhaustion; or (3) a dynamic (im)balance between the demands and personal resource to manage those demands [ 91 ]. The Perceived Stress Scale (PSS) [ 18 , 19 ] used in our meta-analysis is aligned with the third of these definitions. As elaborated upon within the Transactional Model of Stress [ 92 ], stress is conceptualised as a persons’ appraisal of the internal and external demands put upon them, and whether these exceed their available resources. Thus, our results suggest that, when compared to the general population, PhD students experience a greater maladaptive imbalance between their available resources and the demands placed upon them. Stress in itself is not a diagnosable mental health problem, yet chronic stress is a common precipitant to mental health difficulties such as depression and posttraumatic stress disorder [ 93 , 94 ]. Therefore, interventions should seek to bolster DRs’ resources and limit demands placed on them to minimise the risks associated with acute stress and limit its chronicity.
Individual factors
Female DRs were identified as being at particular risk of developing mental health difficulties. This may result from additional hurdles when studying in a male-dominated profession [ 95 – 97 ], and the expectation that in addition to their doctoral studies, females should retain sole or majority responsibility for the domestic and/or caring duties within their family [ 52 , 76 ]. It may also be that females are more willing to disclose and seek help for mental health difficulties [ 98 ]. Nevertheless, the World Health Organisation (WHO) mental health survey results indicate that whilst anxiety and mood disorders are more prevalent amongst females, externalising disorders are more common in males [ 99 ]. As the vast majority of studies in this review focussed on internalising problems (e.g. stress, anxiety and depression) [ 37 , 64 , 79 , 80 , 83 , 89 ], this may explain the gender differences found in this review. Further research is needed to explore which perspective, if any, may explain gender gap in our results.
Perhaps unsurprisingly, self-care was associated with reduced mental health problems. The quantitative findings suggest that all types of self-care are likely to be protective of mental health (i.e. physical, emotional, professional and spiritual self-care). Self-care affords DRs the opportunity to take time away from their studies and nurture their non-PhD identities. However, the results from our meta-synthesis suggest that DRs are not attending to their most basic needs much less engaging in self-care behaviours that correspond to psychological and/or self-fulfilment needs [ 100 ]. Consequently, an important area for future enquiry will be identifying the barriers preventing DRs from engaging in self-care.
Interpersonal factors
Across both quantitative and qualitative studies, interpersonal factors emerged as the most salient correlate of DR mental health. That is, isolation was a risk factor, whereas connectedness to others was a protective factor. There was some variability in how these constructs were conceptualised across studies, i.e. (1) isolation: a lack of social support, having fewer social connections, feeling isolated or being physically separate from others; and (2) social connectedness: multiple group membership, academic relationships or non-academic relationships; but there was no indication that effects varied between concepts. The relationship between isolation and negative health consequences is well-established, for example both physical and mental health problems [ 101 ], and even increased mortality [ 102 ]. Conversely, social support is associated with reduced stress in the workplace [ 103 , 104 ]. Reducing isolation is therefore a promising interventional target for improving DRs’ mental health.
The findings regarding isolation are even more alarming when considered alongside the findings from several studies that PhD studies are consistently reported to dominate the lives of DRs, resulting in poor ‘work-life balance’ and losing non-PhD aspects of their identities. The negative impact of having fewer identities [ 105 ] can be mitigated by having a strong support network [ 106 ], and increasing multiple group memberships [ 107 ]. But for DRs, it is perhaps the absence of this social support, combined with identity impoverishment, which can explain the higher than average prevalence of stress found in our meta-analysis.
Systemic factors
DRs’ attitudes towards their studies may be a product of top-down systemic issues in academia more broadly. Experiencing mental health problems was reported as being the ‘norm’, but also appeared to be understood as a sign of weakness. The meta-synthesis results suggest that DRs believed their respective universities prioritise academic success over workplace wellbeing and encourage unhealthy working habits. Working in an unsupportive and pressured environment is strongly associated with negative psychological outcomes, including increased depression, anxiety and burnout [ 108 ]. The supervisory relationship appeared a particularly important aspect of the workplace environment. The quantitative analysis found a negative correlation between inspirational supervision and mental health problems. Meta-synthetic finding suggested toxic DR-supervisor relationships characterised by powerlessness and neglect, as well as relationships where DRs felt valued and respected—the former of these being associated with poor mental health, and the latter being protective. The association between DR-supervisor relationship characteristics needs to be verified using quantitative methods. Furthermore, DRs’ sense that they needed to exhibit ‘optimum suffering’, which appears to reflect a PhD-specific aspect of a broader academic performativity [ 109 ], is an important area for consideration. An accepted narrative around DRs needing to experience a certain level of dis/stress would likely contribute to poor mental health and as an impediment to the uptake and effectiveness of proffered interventions. Although further research is needed, it is apparent that individual interventions alone are not sufficient to improve DR mental health, and that a widespread culture shift is needed in order to prevent the transmission of unhealthy work attitudes and practices.
Limitations of the literature
Although we found a respectable number of articles in this area, the focus and measures used varied to the extent that typical review analysis procedures could not be used. That is, there was much heterogeneity in terms of how mental health was conceptualised and measured, as well as the range of risk and protective factors explored. Similarly, the quality of the studies was hugely variable. Common flaws amongst the literature include small sample sizes, the use of unvalidated tools and the incomplete reporting of results. Furthermore, for qualitative studies specifically, there appeared to be a focus on breadth instead of depth, particularly in relation to studies using mixed methods.
The generalisability of our findings is limited largely due to the lack of research conducted outside of the US, but also because we limited our review to papers written in English only. The nature of doctoral studies varies in important ways between studies. For example, in Europe, PhD studies usually apply for funding to complete their thesis within 3–4 years and must know their topic of interest at the application stage. Whereas in the US, PhD studies usually take between 5 and 6 years, involve taking classes and completing assignments, and the thesis topic evolves over the course of the PhD. These factors, as well as any differences in the academic culture, are likely to affect the prevalence of mental health problems amongst DRs and the associated risk and protective factors. More research is needed outside of the US.
‘Mental health’ in this review was largely conceptualised as a type of general wellbeing rather than a clinically meaningful construct. None of the studies were ostensibly focused on sampling DRs who were currently experiencing or had previously experienced mental health problems per se, meaning the relevance of the risk, vulnerability and protective factors identified in the meta-synthesis may be more limited in this group. Few studies used clinically meaningful measures. Where clinical measures were used, they captured data on common mental health problems only (i.e. anxiety and depression). Due to these limitations, we are unable to make any assertions about the prevalence of clinical-level mental health problems amongst DRs.
Limitations of this review
As a result of the heterogeneity in this research area, some of the results presented within this review are based on single studies (e.g. correlation data; see Fig. Fig.5) 5 ) rather than the amalgamation of several studies (e.g. meta-analysis/synthesis). To aid clarity when interpreting the results of this review, we have (Table (Table3) 3 ) summarised the volume of evidence supporting risk and protective factors. Moreover, due to the small number of studies eligible for inclusion in this review, we were unable to test whether any of our findings are related to the study characteristics (e.g. year of publication, country of origin, methodology).
We were able to conduct three meta-analyses, one of which aimed to calculate the between-group effect size on the PSS [ 18 , 19 ] between DRs and normative population data. Comparing these data allowed us to draw some initial conclusions about the prevalence of stress amongst DRs, yet we were unable to control for other group differences which might moderate stress levels. For example, the population data was from people in the United States (US) in 1 year, whereas the DR data was multi-national at a variety of time points; and self-reported stress levels may vary with nationality [ 110 ] or by generation [ 111 , 112 ]. Moreover, two of the three meta-analyses showed significant heterogeneity. This heterogeneity could be explained by differences in the sample characteristics (e.g. demographics, country of origin), doctoral programme characteristics (e.g. area of study, funding status, duration of course) or research characteristics (e.g. study design, questionnaires used). However, due to the small number of studies included in these meta-analyses, we were unable to test any of these hypotheses and are therefore unable to determine the cause of this heterogeneity. As more research is conducted on the mental health of DRs, we will be able to conduct larger and more robust meta-analyses that have sufficient power and variance to statistically explore the causes of this heterogeneity. At present, our findings should be interpreted in light of this limitation.
Practice recommendations
Although further research is clearly needed, we assert that this review has identified sufficient evidence in support of several risk and protective factors to the extent that they could inform prevention and intervention strategies. Several studies have evidenced that isolation is toxic for DRs, and that social support can protect against poor mental health. Initiatives that provide DRs with the opportunity to network and socialise both in and outside of their studies are likely to be beneficial. Moreover, there is support for psychoeducation programmes that introduce DRs to a variety of self-care strategies, allow them to find the strategies that work for them and encourage DRs to make time to regularly enact their chosen strategies. Finally, the supervisory relationship was identified as an important correlate of DR mental health. Positive supervision was characterised as inspirational and inclusive, whereas negative supervision productised DRs or neglected them altogether. Supervisor training programmes should be reviewed in light of these findings to inform how institutions shape supervisory practices. Moreover, the initial findings reported here evidence a culture of normalising and even celebrating suffering in academia. It is imperative therefore that efforts to improve and protect the mental health of DRs are endorsed by the whole institution.
Research recommendations
First, we encourage further large-scale mental health prevalence studies that include a non-PhD comparison group and use validated clinical tools. None of the existing studies focused on the presence of serious mental health problems—this should be a priority for future studies in this area. Mixed-methods explorations of the experiences of DRs who have mental health problems, including serious problems, and in accessing mental health support services would be a welcome addition to the literature. More qualitative studies involving in-depth data collection, for example interview and focus group techniques, would be useful in further supplementing findings from qualitative surveys. Our review highlights a need for better communication and collaboration amongst researchers in this field with the goal of creating a level of consistency across studies to strengthen any future reviews on this subject.
The results from this systematic review, meta-analysis and meta-synthesis suggest that DRs reported greater levels of stress than the general population. Research regarding the risk and protective factors associated with the mental health of DRs is heterogenous and disparate. Based on available evidence, robust risk factors appear to include being isolated and being female, and robust protective factors include social support, viewing the PhD as a process, a positive DR-supervisor relationship and engaging in self-care. Further high-quality, controlled research is needed before any firm statements can be made regarding the prevalence of clinically relevant mental health problems in this population.
Supplementary information
Acknowledgements.
Thank you to the Office for Students for their funding to support this work; and thank you to the University of Sussex Doctoral school and our steering group for championing and guiding the ‘Understanding the mental health of Doctoral Researchers (U-DOC)’ project.
Abbreviations
Authors’ contributions.
CH contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. LC contributed to the data curation, investigation, project administration, validation and writing—review and editing of this paper. SV contributed to the data curation, formal analysis, investigation, project administration, validation and writing—review and editing of this paper. PR contributed to the funding acquisition, project administration, supervision and writing—review and editing of this paper. JN contributed to the conceptualisation, funding acquisition, methodology, project administration, supervision, validation, writing—original draft preparation and writing—review and editing of this paper. CB contributed to the conceptualisation, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, validation, visualisation, writing—original draft preparation and writing—review and editing of this paper. The author(s) read and approved the final manuscript.
The present project was supported by the Office for Students Catalyst Award. The funder had no involvement in the design of the study, the collection, analysis or interpretation of the data, nor the writing of this manuscript.
Availability of data and materials
Ethics approval and consent to participate.
Ethical approval was not needed for the present study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Cassie M. Hazell, Email: [email protected] .
Laura Chapman, Email: [email protected] .
Sophie F. Valeix, Email: [email protected] .
Paul Roberts, Email: [email protected] .
Jeremy E. Niven, Email: [email protected] .
Clio Berry, Email: [email protected] .
Supplementary information accompanies this paper at 10.1186/s13643-020-01443-1.
- Admission & Aid
- Student Life
Online Ph.D. in Counselor Education and Supervision
Learn the theory and practice of educating and supervising future counselors in clinical settings and in your own higher education classroom.

Programs & Requirements
- Mission & Goals
- Career Outcomes
- Request Info
Expand your impact. Empower others. Teach the next generation of counselors.
Learn the theory and practice of educating and supervising future counselors in clinical settings and your own higher education classroom.
Expand your impact. Empower others. Teach the next generation of counselors. Are you ready to apply your counseling expertise to a new challenge? Earning a PhD in Counselor Education and Supervision could be how you take your career to the next level, whether in the classroom or in a leadership capacity. Your courses will cover the advanced leadership skills needed to drive change as an administrator in behavioral health agencies and beyond. Coursework in areas like research design, counselor education, and inferential statistics will also help you prepare to contribute original knowledge to the counseling field.
By the numbers
Phd in counselor education and supervision.
The fully accredited online PhD in Counselor Education and Supervision from University of the Cumberlands teaches the knowledge and skills you need to launch a career in research and postsecondary teaching in counseling programs across the United States. Our program also covers the advanced leadership skills needed to drive change as an administrator in behavioral health agencies and beyond.
Our curriculum covers the five major domains of contemporary counselor education curriculum: advanced clinical work, supervision, teaching, research and scholarship, and leadership and advocacy. The program breaks down into three essential components: core CES coursework, professional research and field experience coursework. In total, you’ll complete 66 post-master’s credit hours, including courses such as:
- Advanced Counseling Theories and Skills
- Theories and Techniques of Clinical Supervision
- Leadership & Advocacy in Professional Counseling
- Online Teaching & Learning in Counselor Education
- Advanced Educational Research
Finally, you’ll work in collaboration with graduate faculty members to research, write and defend an original dissertation that advances knowledge in the counseling profession. You’ll graduate equipped with:
- Mastery that prepares you for a teaching career in higher education environments
- Administrative expertise preparing you for leadership in clinical and educational settings
- Advanced clinical skills aimed to maximize proficiency in an independent practice milieu
- Independent research skills preparing you to make original contributions to your field
Course Requirements
- CES 700 Program Orientation (0 Hours)
- CES 704 Professional Writing
- CES 705 Introduction to CES: Professional Identity
- CES 715 Online Counseling and Supervision
- CES 730 Andragogy in Counselor Education and Supervision
- CES 731 Multicultural Issues in Counselor Education and Supervision
- CES 733 Ethical and Legal Issues in Counselor Education and Supervision
- CES 735 Advanced Counseling Theories and Skills
- CES 831 Theories and Techniques of Clinical Supervision
- CES 833 Leadership & Advocacy in Professional Counseling
- CES 835 Online Teaching & Learning in Counselor Education
- CES 837 Neuroanatomy & Behavioral Medicine for Professional Counseling
And one elective from the following:
- CES 737 Trauma Counseling: Etiology, Treatment, and Interventions
- CES 710 Mindfulness Based Cognitive Behavioral Interventions in Mental Health Counseling
- COUN 538 Intro to Play Therapy
- COUN 540 Human Sexuality in Counseling
*CES 738 or CES 851 may also be used to fulfill elective credits
- CES 931 Advanced Practicum
- CES 953 Advanced Internship
- CES 955 Advanced Internship II
Nine hours of the degree are earned through a series of courses focusing on research methods and research activities. The research courses culminate in the completion of a dissertation. Both CES 734 and CES 850 are required for all students. Each student will select either CES 851 or CES 738 depending on the methodology you intend to pursue with your dissertation research. Students may take both advanced research design courses and count one as their elective.
- CES 734 Quantitative Research Design
- CES 850 Qualitative Research Design
- CES 851 Advanced Qualitative Research Design or CES 738 Advanced Quantitative Research Design
Department of Counseling Sample Syllabi *The syllabi in this folder are samples and may not reflect the most current syllabus content
- CES 838 CES Comprehensive Exam (0 Hours)
- CES 736 Dissertation Seminar
- CES 839 Advanced Educational Research
Students must be enrolled in a minimum of two semesters of dissertation coursework for a total of six (6) credit hours.
- CES 950 Dissertation
- CES 951 Dissertation
NOTE ON DISSERTATION CREDITS AND PROCEDURES: The candidate must file an Intent to Graduate at the beginning of term of intended completion; must schedule Oral Dissertation Defense at least two weeks prior to Intended Date; and must file approved dissertation with Program Director prior to graduation.
Take the Next Step
- Schedule a Visit
Request Information
Mission and goals.
The mission of UC's PhD in Counselor Education and Supervision online program is to develop counselor educators and supervisors who are innovative in their contributions to the profession through research, leadership, advocacy, and clinical excellence.
Counselor Education and Supervision Careers & Outcomes
All stats from U.S. Bureau of Labor Statistics
Licensed Professional Counselor Supervisor: $101,340
As a Licensed Professional Counselor Supervisor, you’ll provide an opportunity for your supervisees to discuss any work-related issues and difficulties they may have and help determine possible ways for them to be resolved.
Psychologist: $81,040
Psychologists study cognitive, emotional, and social processes and behavior by observing, interpreting, and recording how individuals relate to one another and to their environments.
Mental Health Program Manager: $101,340
Mental Health Program Managers plan, direct, and coordinate the business activities of their mental health facility.
Educational or Career Counselor: $60,140
Advise and assist students and provide educational and vocational guidance services.
Compliance Manager: $71,690
Examine, evaluate, and investigate eligibility for or conformity with laws and regulations governing contract compliance of licenses and permits, and perform other compliance and enforcement inspection and analysis activities not classified elsewhere.
Postsecondary Teacher: $79,640
Postsecondary teachers instruct students in a variety of academic subjects beyond the high school level.
Common Questions
All programs at University of the Cumberlands are offered at some of the lowest rates in the nation – and we even include free textbooks through our One Price Promise! For more information on how affordable this program would be for you, visit our Financial Aid page.
A Ph.D. in Counselor Education and Supervision is a doctoral degree that equips counseling professionals to teach in higher education classrooms. As a graduate counseling student at Cumberlands, you’ll learn the theory and practice of educating and supervising future counselors in clinical settings, as well as leadership skills you can apply in education, behavioral health, and human services settings.
With your Ph.D. in Counselor Education and supervision, you’ll be able to choose from a variety of counseling career paths, including: counselor educator, licensed professional counselor supervisor, clinical director, regulatory affairs director, quality assurance director, compliance manager, compliance operations manager, risk manager, academic leadership, or assistant professor in a related field.
As it turns out, University of the Cumberlands is one of the only higher education institutions to offer synchronous, CACREP-accredited programs online! When a PhD in Counselor Education and Supervision online program is available online, it provides a flexible, synchronous format to make it possible to pursue your studies even while working as a counselor. Admissions requirements typically include a CACREP-accredited master’s degree in counseling or the equivalent, as well as an active professional counseling license.
When considering pursuing an online PhD in Counselor Education and Supervision it is important to remember that a PhD is the same as a doctorate, and degree programs at this level are typically research-intensive and require an original dissertation. As a PhD in Counselor Education and Supervision online student, you’ll be taking courses in areas like research design, counselor education, and inferential statistics to help you prepare to contribute original knowledge to the field of counseling.
Pursuing your doctoral degree in counseling education and supervision could be one way to enhance your career and drive change on a larger scale. Some reasons you may find it worthwhile to further your education with a PhD in Counselor Education and Supervision program are that postsecondary education roles in the field of mental health are expected to increase by 12 percent between 2021 and 2030; a PhD in Counselor Education and Supervision offers the chance to build on your past education and experience while preparing to take your career in a new direction; and the median annual salary for postsecondary counseling professors was $77,500 in 2021, nearly $30,000 more than most other counseling professions.
Faculty Experts
Get to know your future CES professors.

Dr. Lekesha Davis
Contact information.

Dr. Christian J. Dean

Dr. Marina Gilberti Bunch
Cacrep assessment.
The CACREP Council accredits the Clinical Mental Health Counseling program, Addiction Counseling program, PhD in Counselor Education & Supervision, and the related Doctorate of Educational Leadership Online (EdD) Program. CACREP is a specialized accrediting body recognized by the Council for Higher Education Accreditation (CHEA) that accredits counselor-preparation graduate degree programs. For more information, visit https://www.cacrep.org .
CACREP Outcomes for the Department of Counseling at University of Cumberlands:
Vital Statistics: 2017 , 2018 , 2019 , 2020
Program Evaluation Outcomes Report: 2015-2018 , 2021 , 2022
Interested in learning more about how our PhD in Counselor Education and Supervision program can help you achieve your professional goals? We're ready to talk.
Enter a Search Term
Mental health counseling, phd.
- Westchester
This PhD in Mental Health Counseling program is accredited by the Council for Accreditation of Counseling and Related Educational Programs (CACREP).
Next Generation Leaders
This program is designed to train mental health counselors in advanced clinical and supervisory skills, prepare counselors to conduct research that will further the profession’s knowledge base, and foster the next generation of leaders who will be teachers and advocates for the mental health counseling profession across the country.
Advance your education
- Students emerge as highly skilled professionals in therapeutic practice and research, well-positioned to be leaders in the field and advocates for their clients and the profession.
- Master-level students gain advanced professional training, opportunities for intensive research, and opportunities to significantly advance the field of mental health.
- Specializations include grief counseling, substance abuse counseling, and positive psychotherapy and counseling.
Take Courses Like…
Throughout the curriculum, you’ll receive intensive training focused on advanced clinical issues, counseling education, supervision, and research focused on the promotion of mental health and the counseling profession.
Graduates leave the program equipped with a solid foundation in counseling built upon a combination of coursework, fieldwork, seminars, and guided research.
- MHC 731 Theories and Methods of Counselor
- MHC 732 Theories and Methods of Counselor Supervision
- MHC 831 Doctoral Dissertation Seminar I
Add Opportunities And Experiences
A small and selective program—accepting approximately 10 students per academic year—means small classes, in which students are exposed to evidence-based counseling approaches for demographically and clinically diverse populations.
Students work closely with faculty to develop and carry out independent research projects culminating in a doctoral dissertation. These activities are designed to integrate counseling intervention and research skills training, preparing graduates for a variety of counseling, policy-based, advocacy, teaching, and research careers.
The Department of Psychology’s strong community of faculty, professionals, and alumni in the field of mental health equip doctoral students with an established network of support. Both faculty and alumni hold key leadership positions in the New York Mental Health Counselors Association (NYMHCA).
Each semester, the department offers a speaker series inviting leading researchers and professionals to talk about current and pertinent issues in the field.
“This unique doctoral program will provide mental health professionals with the opportunity to take their training and knowledge to the next level in a way that will help them stand apart from the crowd. In essence, we are seeking to develop the next wave of leaders in counseling that will help significantly advance the study and treatment of mental health.” –Paul Griffin, PhD, Department Chair
Professional Associations
Students and faculty can interact, join, and present at regional, state, and national association conferences. This includes developing partnerships to conduct critical research on topics impacting individuals seeking mental health counseling services and beyond. Faculty have a longstanding and collaborative relationship with the following key organizations, allowing them to guide students in establishing professional connections during their time in the program.
- American Counseling Association (ACA)
- American Counseling Association-New York (ACA-NY)
- American Mental Health Counselors Association (AMHCA)
- New York Mental Health Counselors Association (NYMHCA)
- Association for Counselor Education and Supervision (ACES)
- North Atlantic Region Association for Counselor Education and Supervision (NARACES)
- New York Association for Counselor Education and Supervision (ACES)
Choose Your Career
Career options.
The PhD program prepares candidates for a multitude of growing careers, including:
- Community mental health
- Mental health policymaking
- Private practice
- University teaching
What You Need to Know
Students who substantially meet the following requirements will be invited to an interview with the departmental admission screening committee:
- An earned master’s degree in mental health counseling with a curriculum equivalent to that of Pace University’s 60-credit graduate master of science program in mental health counseling.
- Earned graduate-level GPA of 3.6 or higher.
- Submitted letters of recommendation, personal statement, and official academic transcripts.
- Students are required to complete 100 clinical hours in a supervised clinical setting for MHC 710: Doctoral Practicum in Mental Health Counseling
- Students are required to complete 600 internship hours of supervised experiences in at least three of the five doctoral core areas (counseling, teaching, supervision, research and scholarship, leadership and advocacy) for MHC 725 & MHC 726: Doctoral Internship I & II
- Be eligible for New York State limited permit in mental health counseling.
- Obtained a limited permit in New York State.
- Be licensed in mental health counseling in New York State.
- Be licensed in mental health counseling in a state other than New York.
CACREP Annual Assessment Reports
MS and PhD Programs in Mental Health Counseling-Field Placement Site Supervisor Training (PDF) Please read and review the PowerPoint Training and the MS and/or corresponding PhD Field Placement Practicum and Internship Handbook as part of our CACREP Accreditation Requirement.
MS and PhD Programs in Mental Health Counseling Field Placement Site Supervisor Training Verification (PDF) Site supervisors are required to complete this form each semester that they sponsor MS and/or PhD Practicum or Internship students as part of our CACREP Accreditation Requirement.
- Meet Program Faculty
- PhD Student Handbook
- PhD Field Placement Practicum and Internship Handbook
- PhD Program of Study Curriculum Worksheet
- Dissertation Template
The following is Pace University’s Doctor of Philosophy (PhD) Program Objectives (POs) Assessment Report for the program's annual review. This plan includes input from the various stakeholders including: aggregate student assessment data that addresses student knowledge, skills, and professional dispositions; demographic and other characteristics of applicants, students, and graduates; and data from systematic follow-up studies of graduates, site supervisors, and employers of program graduates.
The assessment data compiled and analyzed is based on a five-point scale which is constituted as:
- Ineffective
- Somewhat Ineffective
- Very Effective
Program goals are baselined at a minimum standard of 80% to designate “meeting standard” or above. Our students continued to receive high quality academic instruction, strong clinical practicum experiences, and internship professional roles among five doctoral core areas, including:
- Supervision
- Research and scholarship
- Leadership and advocacy.
99% of our stakeholders indicated that the program was Effective or Very Effective in meeting the program objectives. Again, 99% of our stakeholders indicated that the program was Adequate, Effective, or Very Effective in meeting the program objectives.
View complete Program Objectives (PO) Annual Assessment Report for 2022–2023 (PDF)
99% of our stakeholders indicated that the program was Effective or Very Effective in meeting the program objectives. 100% of our stakeholders indicated that the program was Adequate, Effective, or Very Effective in meeting the program objectives.
View complete Program Objectives (PO) Annual Assessment Report for 2021-2022 (PDF)
The following is Pace University’s Doctor of Philosophy (PhD) Program Objectives (POs) Assessment Report for the program’s annual review. This plan includes input from the various stakeholders including: aggregate student assessment data that addresses student knowledge, skills, and professional dispositions; demographic and other characteristics of applicants, students, and graduates; and data from systematic follow-up studies of graduates, site supervisors, and employers of program graduates.
- Somewhat Effective
Our previous program goals have been baselined at a minimum standard of 85% to designate “meeting standard” or above. As a result of the COVID-19 pandemic, while students continued to receive high quality academic instruction, strong clinical practicum experiences, and internship professional roles among five doctoral core areas, including: (1) counseling; (2) supervision; (3) teaching; (4) research and scholarship; (5) leadership and advocacy, all transitioned to remote platforms. The results of our annual Program Objectives assessment were impacted due to classes and field placements transitioning to remote platforms. This resulted in all of our constituencies adapting to multiple modalities, including academic instruction, clinical telehealth services and provisions, and remote supervision. Several of our students needed to secure new practicum placements and/or professional roles for internship as their original sites either fully paused services or could not support the requirements associated with CACREP standards and/or New York State Office of the Professions regulations. As such, we have adjusted our baseline minimum standard from 85% to 80% for this academic year to reflect these adjustments. Additionally, we have also included Adequate, Effective, and Very Effective in the five-point scale to calculate our aggregate outcome. While this baseline adjustment has been made, the program will continue to document, review and report any changes based on the 85% original baseline.
97% of our stakeholders indicated that the program was Adequate, Effective or Very Effective in meeting the program objectives.
View complete Program Objectives (PO) Annual Assessment Report for 2020-21 (PDF)
The assessment data compiled and analyzed is based on a five point scale which is constituted as:
- Very Effective.
Program goals are baselined at a minimum standard of 85% to designate “meeting standard” or above.
97% of our stakeholders indicated that the program was Effective or Very Effective in meeting the program objectives.
View complete Program Objectives (PO) Annual Assessment Report for 2019-20 (PDF)
Part I: Narrative
During the 2018-2019 academic year, the faculty and staff of the Doctor of Philosophy programs in Mental Health Counseling at Pace University conducted an annual review of the program. The program’s core objectives remain focused on fostering student development in advanced clinical and supervisory skills, training them to become proficient researchers that will advance knowledge on issues pertaining to mental health and counseling, and to promote future leaders of the profession who will serve as both educators and advocates. Past and current students’ dissertations have examined key issues in clinical mental health counseling and counselor education. To assist them in their studies, graduate assistantships and adjunct teaching assignments continue to be offered to doctoral students in the department. Based on the feedback that we received during the CACREP Site Visit in May 2018, the changes outlined below were implemented:
- MHC 707: Qualitative Methods in Counseling Research (4 credits)
- MHC 710: Doctoral Practicum in Mental Health Counseling (4 credits)
- MHC 726: Doctoral Internship II in Mental Health Counseling (0 credits)
- MHC 734: Advanced Theory & Practice of Counseling (4 credits)
Additionally, the department modified the following course curriculum to include Leadership and Advocacy (CACREP Section 6 Standard B 5.d.-Accreditation): MHC 733: Leadership & Advocacy in Mental Health Counseling
Further, the MHC 710: Doctoral Practicum in Mental Health Counseling course at the master’s level is now a significant preparation for our program. Michael Tursi, Ph.D. (from the counselor education doctoral program at the University of Rochester) continues to advance our practicum and internship courses, including MHC 725: Doctoral Internship I in Mental Health Counseling and MHC 726: Doctoral Internship II in Mental Health Counseling. Both courses are significantly structured and students’ progress is documented throughout.
Part II: Graduates and Pass, Completion, and Job Placement Rates
- Number of Graduates: 6
- Program Completion Rate: 100% for the 2018-2019 academic year
- Estimate of Job Placement Rates: Many of our students enter our program either as licensed and/or certified counselors, limited permit holders, and/or apply for permits in mental health counseling while enrolled. The graduates who complete their doctorate in May 2019, are employed either full time or part in mental health counseling settings, school setting, and/or teach as adjuncts in counseling or related areas.
View complete Program Objectives (PO) Annual Assessment Report for 2018-19 (PDF)
During the 2017-2018 academic year, the faculty and staff of the Master of Science in Mental Health Counseling at Pace University conducted an annual review of the program.
We focused on following up on emphasizing ethical standards in the key practice courses within the program. We have included this focus as it relates to internships, practicum experiences, as well as other courses. We stress the importance of ethics and multicultural diversity in the foundations course, the introductory counseling courses, as well as the group counseling, family counseling, social and cultural foundations, and the elective LGBTQA+ course.
In the past year, the practicum course has evolved into a robust preparation for the internship courses. Dr. Michael Tursi, a new addition to our department with a doctorate in counselor education from the University of Rochester, has brought fresh perspectives into this course as well as into the doctoral-level internship course.
Finally, the department determined that additional faculty in the field of mental health counseling was needed. We have hired two new full-time faculty in the counselor education field to start in the Fall 2018 semester.
- Number of Graduates: 27
- # tested: 5
- # passed: 3
- # passed: 5
- Program Completion Rate: 100% for 2017-18 Academic Year
- Estimate of Job Placement Rates: Approximately 60% of our graduates are currently employed in a counseling or a counseling-related capacity.
View complete Program Objectives (PO) Annual Assessment Report for 2017-18 (PDF)
supportive. informative. community.
Join the community for just $5/month, jun 20 should i tell my advisor about my mental health.
At the end of my first year of my PhD program, I was completely, utterly, and magnificently burned out. I had one final seminar paper left to turn in, and it was due at noon that day. My anxiety was so out of control that I couldn't bring myself to start the paper until the day before it was due, and I pulled an all nighter (my first) to finish it. I finished it, went to campus to print it, only to find that my endnote software had crashed and I had to redo the bibliography by hand. it was late, my professor noticed, and commented. I felt no relief, only more anxiety. I walked across campus to the campus counseling center, past the undergrads relaxing on the Diag feeling the joy I wished to feel, and requested a same day, emergency appointment. Within a week, I was seeing a therapist off campus (my condition was "more severe" than the short-term counseling services felt comfortable handling) for appointments two days a week. Outside of my partner, who lived with me and was blessedly not an academic, I told no one and attempted to keep up with the work load of my summer research job, exam list preparation, and archival research trips. This was, in retrospect, not the most effective way to manage my own health and kept me from important sources of support. But through continued work with professionals, I eventually learned how to speak about my own mental health in a way that felt safe and professional.
One of the hardest parts of my graduate school career centered around the issue of disclosure. I never felt entirely confident that I was telling people what they needed to know, or that I was safe in disclosing information about my health, mental and otherwise. Some studies estimate that as many as a third of all graduate students are dealing with mental health issues at some point during their graduate studies. As the conversation on campuses about mental health continues to grow, and more and more people call for policies and protections for students and faculty both, but unlike undergraduate students, grad students walk the line between colleague and direct report, often without explicit cues that the roles are switching. So how do you know if you need to disclose a mental health condition to your advisor? Here are my general guidelines, with the explicit acknowledgment that my thoughts are not meant to be prescriptive, but to give you a starting place for thinking through your own relationships.
If your health - mental, physical, emotional - is in jeopardy because of a work deadline or situation, find advocates to help you facilitate the conversation with your advisor. In crisis or acute situations, there are often third parties available on campus to help facilitate these conversations - check your on campus counseling centers, Dean of Students office, or Services for Students with Disabilities office. Just as you might accept documentation for a student in your class of an acute crisis, so too can you offer that same documentation. Even if the conversation is less formal or does not involve documentation, talking to a mental health professional about how to disclose a crisis or acute situation can be a helpful step before talking to your advisor, giving you a script or language to fall back on if the situation is emotional or tense.
You do not need to justify your mental state with details, symptoms, or diagnoses to "prove" the legitimacy of your situation. I often felt the pressure to share more details about a crisis or diagnosis to "prove" that I wasn't suffering from "regular" anxiety and therefore "deserved" the deadline extension or other accommodation. A great rule of thumb is that if you wouldn't share that level of detail for a physical health situation that you are having, you do not need to share it for a mental health situation. If for some reason your advisor or department is pushing for detail that you are not comfortable providing, you can look into obtaining documentation from your health care provider that verifies that you are seeking care without containing details you want to keep private.
Consider building a team beyond your advisor to support your work, especially for long term projects and deadlines. Graduate student advisors are, as we all are, busy people, and very few have the bandwidth available to coach students through the day to day process of producing work. If you only check in with your advisor when major milestones are hit, it might be helpful to build in smaller deadlines with accountability checks to writing groups, writing partners, other committee members, or an outside coach. When the system for enforcing deadlines shrinks to the student-advisor dyad, the temptation to procrastinate, avoid, or ignore work grows, and the relationship can feel adversarial rather than supportive. Having more structure in place to spread out that accountability can help lessen the pressure of the "final" deadline and encourage smaller, more consistent work sessions. You can then keep the day to day challenges of working out of the conversation with your advisor, and seek support from others with less weighted relationships.
Communication (following boundaries that you feel comfortable with) is key. If it becomes clear that a deadline is no longer workable, or that you are in a situation that significantly impacts your work, being in control of the conversation and communication can help to alleviate some of the anxiety of disclosure. Rather than waiting until a deadline or other milestone has been missed to offer an explanation, take the initiative to disclose your situation, and then offer a plan that is workable for you. Email is an amazing tool here - it lets you control the information that you give without the pressure of an in person conversation. Communicating early, and offering solutions that work for you, shows that you are taking responsibility for your work rather than being "caught" when the crisis has already occurred.
Just because you shared details of your mental health in a previous situation does not mean that you are obligated to do so in the future. Being open with other graduate students or peers does not mean that you have to be as open with faculty members. Each situation, and each conversation, is unique. As I was still learning to cope with my anxiety disorder and the pressure of graduate school, I gave more detail than I would later feel comfortable doing. A therapist told me that no one is entitled to details of my mental health just as no one is entitled to details of my physical health. It is my responsibility to take ownership of my own work, my deadlines, and my contributions to the work of the department (teaching, etc) but it is not my responsibility to keep everyone "up to date" on my health unless I felt comfortable doing so. It is appropriate to have different boundaries with different people - openness with some does not obligate you to openness with all. Mental health challenges is, whether it appears so or not, an increasingly common aspect of graduate school. The more that these conversations happen in safe, productive ways, the more normalized the situation becomes. However, your health, your boundaries, and your needs come first. Hopefully some of these thoughts will help you to formulate your own game plan for how to balance all the aspects of yourself in your professional relationships.
Jun 26 How to bullet journal!
Jun 15 this book taught me how to write a dissertation..
Counselor Education & Supervision (Ph.D.)
Find Your Program
Clicking the 'Get Started' button below constitutes your expressed written consent to be called and/or texted by representatives of University of the Cumberlands at the phone number(s) you provided above, including my mobile phone, regarding furthering your education. You understand that these calls may be generated using an automated technology. I understand that my consent is not a requirement for enrollment.
Program Quick Facts

Credit Hours
If you’re passionate about enhancing learning experiences for aspiring behavioral health counselors, University of the Cumberlands Ph.D. in Counselor Education & Supervision is for you. Your program will help you pursue leadership roles in academia or as a high-level administrator in clinical settings, such as a behavioral health agency.
Through this online counseling education Ph.D. program, you’ll have the opportunity to:
- Gain a comprehensive understanding of counseling and educational theory
- Master relevant research areas and how they can be applied to strategic problem-solving
- Fortify your commitment to professional service, grounded in ethical decision-making
As a graduate of the program, you’ll be prepared for leadership roles with the comprehensive knowledge base needed to:
- Teach counselor education and assure students graduate with advanced clinical expertise
- Lead and manage counseling groups
- Strongly advocate for the professional counseling vocation
- Use state-of-the-art tech to facilitate effective instruction in counseling
- Grow your skills as a researcher, scholar or professional writer in the field of counseling
Plus, this education leadership Ph.D. program is accredited by the Council for Accreditation of Counseling & Related Educational Programs (CACREP).
Are you ready for a terminal degree in Educational Leadership? One focused on helping you help future counseling professionals be their best? One that is 100 percent online to fit your busy life? And one that is fully accredited by the top counseling education accreditation agency in the U.S?
Then we have your online Ph.D. in Counselor Education & Supervision program. Fill out the form today and we’ll get you the information you need to get started on your career-changing program.
Program Outcomes
Participate in an immersive, expert-led curriculum in a convenient online format.
Broaden your skillset and establish yourself as one of the best in your profession., enhance your professional connections as you prepare to become a leader in your field..
Commitment to Quality
Convenient Online Curriculum
Affordability
Real-World Learning
- Future Students
- Parents/Families
- Alumni/Friends
- Current Students
- Faculty/Staff
- MyOHIO Student Center
- Visit Athens Campus
- Regional Campuses
- OHIO Online
- Faculty/Staff Directory
Counseling and Higher Education
- History and Legacy
- Mission & Vision
- Academic Departments
- Centers and Offices
- Office of the Dean
- Accreditation and Assessment
- Strategic Plan
- Academic Programs
- Honor Programs
- Schedule a Tour
- Brothers Rise Initiative
- Holmes Scholars (Graduate Students)
- International Student Resources
- Transfer Students
- Financial Aid & Scholarships
- Graduate Assistantships
- Professional Development Institute for Alternate Licensure
- Undergraduate Advising
- Group Study Rooms
- Patton College Forms
- Military and Veteran Services
- Career Network
- Clinical Practice in Education
- Student of the Month Nominations
- Dean's Circle of Engagement
- Emeriti Faculty and Staff
- Alumni of the Month Nominations
- Give to The Patton College
- Faculty and Staff Directory
- Faculty Resources
- Patton College Faculty-Staff Awards
Helpful Links
Navigate OHIO
Connect With Us
Doctorate of Philosophy in Counselor Education & Supervision
Program code: ph6265.
Apply Now for Fall 2024 Join our program where our mission is to provide advanced preparation for counselors in the areas of counseling, supervision, teaching, research and scholarship, and leadership and advocacy. Our graduates serve as counselor education faculty in colleges and universities, and counseling leaders in public and private educational, human services, and mental health settings.
Apply on or before January 15, 2024.
Doctoral study in Counselor Education and Supervision (CES) at Ohio University is designed to provide advanced preparation for counselors in the areas of counseling, supervision, teaching, research and scholarship, and leadership and advocacy. Graduates of the program serve as counselor education faculty in colleges and universities and counseling leaders in public and private educational, human services, and mental health settings. The first Ph.D. degree from the Ohio University Counselor Education program was granted in 1962 and the CES program was one of the first accredited by the Council for Accreditation of Counseling & Related Educational Programs ( CACREP ) in 1986. The CES program is accredited through October 31, 2024 .
The program has a history of leadership and advocacy in the counseling field. Professor Emeritus Dr. Tom Sweeney launched Chi Sigma Iota, Counseling Academic and Professional Honor Society at Ohio University in 1985 along with other leaders in the counseling profession. Thanks to Dr. Sweeney’s vision, we are proud to be the home of the Alpha Chapter of Chi Sigma Iota. Professors Emeriti Tom Davis, Luther Hasely, and Mel Witmer are other prominent leaders who led our profession forward.
Our current faculty and students are in leadership roles. To mention a few, Dr. Christine Suniti Bhat is the President-Elect of ACA and Dr. Tamarine Foreman is President of OACES. Among doctoral students, Ibrahim Akmese is a CSI Intern (2023-2024), Sarah Hatch is the President of Ohio SAIGE, and many of our students are graduates of the Ohio Counseling Association Emerging Leader Academy. The doctoral program received the Innovative Doctoral Program award from NCACES in 2021.
Students and faculty in the Ohio University Counselor Education program are guided by the American Counseling Association (ACA, 2014) Code of Ethics and are committed to the ethical practice of counseling. In the classroom, fieldwork, and extra-curricular activities, we acknowledge and value the diverse backgrounds and perspectives of our students, faculty, site supervisors, and clients. We believe that an emphasis on diversity, inclusion, and advocacy strengthens the learning experiences of all. Please review the Counselor Education program's commitment to diversity and inclusion to learn more about our values.
Program Overview and Information
CES doctoral students seek to improve their scholarly, instructional, clinical, and research skills to acquire advanced training in counselor education. The program is based on the philosophy that each student enters with unique strengths, abilities, and professional goals. Therefore, beyond the required courses, each student is expected to build a program of study based on prior academic preparation, previous work experience, and career goals. All doctoral students complete: (a) core coursework in counselor education and supervision, (b) coursework in quantitative and qualitative research, (c) a 100-hour counseling practicum, (d) a 600-hour internship, (e) a written comprehensive exam and oral defense, and (f) a doctoral dissertation. Please see the graduate catalog for a full description of program requirements . To learn more about CES, prospective and current students can contact the CES coordinator, Tamarine Foreman ( [email protected] ).
Students admitted to the doctoral program possess a Master’s degree in Counseling or a closely related field. Doctoral students must have master’s coursework and demonstrated knowledge in the core counseling areas for entry-level counselors and meet requirements for the Clinical Mental Health Counseling (CMHC) specialty to be eligible for licensure as an Ohio Licensed Professional Counselor ( LPC ). Doctoral students who have not met core counseling and/or CMHC requirements are required to complete requisite coursework in addition to their doctoral studies.
Program Outcomes
Doctoral graduates typically become (1) counselor education faculty members in academia; (2) counselors, administrators, consultants, and trainers in mental health settings; or (3) practitioners in private practice. Prospective s tudents can learn more about counselor education and supervision by visiting the Association for Counselor Education and Supervision ( ACES ) website and ACES resources for graduate students . Our 2021-2022 academic program and student outcomes are available at: https://www.ohio.edu/education/counseling-higher-education/accreditation .
For more information, contact:
Tamarine Foreman Counselor Education Program Coordinator Patton Hall 432L 740.593.4395 [email protected]
Approximately 6-10 doctoral students are admitted to the Counselor Education program annually. Review of applications begins on January 15, 2023, for the Fall 2023 admission term. Prospective students can apply by selecting the following program code: PH6265. Required application materials include:
- Transcripts showing a Master’s degree in Counseling or a closely-related field with a grade point average (GPA) of 3.4 on a 4.0 scale. Applicants that do not meet the GPA criteria may still apply but should address past academic performance and aptitude for doctoral study in the Personal Statement. The review committee will consider additional information provided by the applicant and references on an individual basis.
- Résumé/CV highlighting the professional experience of a nature and extent appropriate to doctoral study in Counselor Education. Include information on counseling, teaching, research, writing, and participation in professional organizations.
- Three letters of recommendation written by current or former professors/supervisors, or others in the field who can address the applicant’s suitability for doctoral-level work in Counselor Education and Supervision.
- What are your career goals?
- What qualities and skills do you possess that you believe enable you to become an effective counselor educator?
- Describe your personal characteristics that will be assets and challenges to your study in counselor education?
- Doctoral students typically work as supervisors and co-instructors. Describe how you will work with faculty and students in these roles.
- How will you manage your personal and professional boundaries through a demanding doctoral program?
- Describe your culturally relevant interpersonal experiences with individuals or groups who differ from you (e.g., race, gender, sexual orientation, age, spiritual beliefs, ability).
- What distinguishes you from other candidates for the counselor education program?
- Describe anything else you would like the program faculty to consider with your application.
Admissions Process:
- Applications will be reviewed by faculty immediately following January 15th.
- Applicants who are short-listed by faculty will be invited for an interview.
- Following the interview, the faculty will submit admissions recommendations to the Graduate College.
- Official notices of admission are sent via email from the Graduate College. Applicants must respond in a timely manner and inform the Graduate College whether or not they accept the offer of admission.
- Students who accept an offer of admission and then change their minds about attending must inform the Program Coordinator and Graduate College immediately.
- Accepted students will receive communication from the program coordinator about their assigned faculty advisor, orientation, and course registration.
The Counselor Education program continues to accept applications beyond the January 15th priority deadline. Interested applicants for the doctoral program are encouraged to apply as soon as possible. Prospective students interested in applying after the January 15th date must contact the Program Coordinator directly. Applications will only be considered if all positions have not been filled. Students are admitted for the Fall semester each year and may begin taking elective coursework in the preceding Summer session.
Counselor Education doctoral students are expected to review program handbooks, policies, and procedures and be familiar with the handbooks and forms provided by the Patton College of Education and Graduate College .
- Counselor Education Program Commitment to Diversity and Inclusion
- Counselor Education Graduate Program Handbook

Doctoral students in the Counselor Education program at Ohio University are encouraged and expected to become involved in counseling professional organizations during their program. Belonging to a professional organization encourages collaboration and advocacy, promotes professionalism and leadership and gives students the opportunity to work with colleagues and leaders in the profession throughout the state and nation. Students are encouraged to explore the following professional organizations that focus on counseling and counselor education:
- American Counseling Association (ACA) and its divisions
- Association for Counselor Education and Supervision (ACES)
- Chi Sigma Iota (CSI), Alpha Chapter
- National Council on Rehabilitation Education (NCRE)
- National Rehabilitation Association (NRA)
- North Central Association for Counselor Education and Supervision (NCACES)
- Ohio Association for Counselor Education and Supervision (OACES)
- Ohio Counseling Association (OCA)
- Ohio Rehabilitation Association (ORA)

BRAIN at 10: A View from the National Institute of Mental Health

The BRAIN Initiative is marking a milestone—10 years of advancing neuroscience and neurotechnology research by funding innovative projects. As part of a rotating series of blog posts, the Directors of the BRAIN Initiative-partnering Institutes and Centers share their voice and perspectives on the impact BRAIN has made on their respective missions—and vice versa.
By Joshua A. Gordon, MD, PhD, Director, NIMH
For 75 years, the National Institute of Mental Health (NIMH) has vigorously pursued its mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure. Basic neuroscience research is a key component of our broad portfolio that seeks to build a foundation for translation into novel approaches to treatment and prevention.
For the last decade, the B rain Research Through Advancing Innovative Neurotechnology® Initiative, or The BRAIN Initiative ® , has dramatically accelerated our basic neuroscience research efforts and progress, and we’re already starting to see the return on these crucial investments with translational successes.
Q . How has the BRAIN Initiative advanced or shaped the NIMH mission?
NIMH’s involvement in the BRAIN Initiative has provided critical resources to help us understand the biological underpinnings of mental illnesses, which is a central component of our mission. Importantly, scientists are using tools, technologies, and resources developed through the BRAIN Initiative to improve on existing treatments. For example, scientists are using novel brain modulation tools, including ultrasound and deep brain stimulation, to treat people living with treatment-resistant depression, anxiety, and other mental illnesses.
Q. How has NIMH participated in the BRAIN Initiative?
NIMH co-leads the BRAIN Initiative along with the National Institute of Neurological Disorders and Stroke. Eight other NIH institutes and centers are also part of this NIH-wide endeavor. In particular, our institute co-leads two focal areas of the BRAIN Initiative: Tools and Technologies for Cells and Circuits and Data Science and Informatics .
The Tools and Technologies for Cells and Circuits research program aims to define, characterize, and access the many diverse cell types of the brain. The Cell Census and Cell Atlas networks, which are part of this program, have already shown amazing success — recently releasing detailed cellular maps of the human, nonhuman primate , and mouse brains. These incredibly detailed resources enable neuroscience researchers to advance knowledge about the cellular basis of brain function and dysfunction, helping pave the way for a new generation of precision therapeutics for people with mental illnesses and other brain disorders. Researchers are building on these detailed knowledge scaffolds to map the impact of risk factors for mental illnesses.
The recently launched Armamentarium for Precision Brain Cell Access transformative project, also part of the Tools and Technologies for Cells and Circuits program , is particularly exciting. The project aims to identify and validate regulatory regions of genes that researchers can exploit to probe the functions of specific cell types in both model organisms and humans. Although early progress uncovered circuits involved in cognition and emotion, the real payoff will come when this revolutionary project is complete. Scientists at NIMH and elsewhere will be able to use these tools to rapidly expand our understanding of complex behavior and, we hope, develop truly transformative therapies tailored to an individual’s unique biology.
The second area that NIMH manages directly is the BRAIN Initiative Data Science and Informatics program, which has developed and maintained nine data archives for storing, managing, and sharing all BRAIN Initiative data. The archives are domain-specific, covering diverse data types including neuroimaging, neurophysiology, multi-omics, light microscopic imaging, electron microscopic imaging, behavior, and more. The program has also developed a variety of community standards, which allow for consistent data collection, description, formatting, organization, and analysis — in keeping with the BRAIN Initiative’s commitment to open science. Through this program, NIMH has also developed many informatics or software tools for integrating, visualizing, and analyzing multi-modality data. NIMH scientists are already using these datasets to make new discoveries relevant to our understanding of mental illnesses.
Q. Why do you think it’s important for NIMH to participate in the NIH BRAIN Initiative?
The brain is the most complex organ in the body—made up of billions of cells linked through trillions of networked connections. If we want to fully understand and treat mental illnesses, we must understand these cells and connections.
The BRAIN Initiative brings together a diverse research community. Projects are conducted not only by neuroscientists, but also by physicists, engineers, mathematicians, chemists, and physician scientists who employ innovative strategies to develop and validate tools with a common goal: advancing neuroscience research to understand the human brain. This level of collaboration across expertise domains is critical to making groundbreaking discoveries in brain cell structure, function, development, and organization necessary for supporting future prevention, treatments, and cures for mental illnesses.
NIMH is excited about the work that has already been accomplished through our participation in the BRAIN Initiative, and we are eager for the many scientific discoveries on the horizon from this transformational research effort.
Image: Joshua A. Gordon, MD, PhD, Director, NIMH
Latest from The BRAIN Blog
The BRAIN Blog covers updates and announcements on BRAIN Initiative research, events, and news.
Hear from BRAIN Initiative trainees, learn about new scientific advancements, and find out about recent funding opportunities by visiting The BRAIN Blog.

Advertisement
Exploring the Relationship Between Supervisor Support and Anxiety of Graduate Students in China: The Mediating Role of Scientific Research Efficacy
- Regular Article
- Published: 12 April 2023
- Volume 33 , pages 321–329, ( 2024 )
Cite this article

- Lichao Ma ORCID: orcid.org/0000-0002-3401-9696 1 ,
- Hao Yao ORCID: orcid.org/0000-0002-5794-7129 2 &
- Jiaqi Hou 1
671 Accesses
1 Altmetric
Explore all metrics
This study examined the relationship among supervisor support, scientific research efficacy and anxiety of graduate students in the Chinese context. A quantitative survey method was applied, and seven hypothesized relationships were tested with a sample of 1,095 graduate students from China. The results showed that instrumental and emotional support from supervisors were significantly and positively related to scientific research efficacy of graduate students, and negatively correlated with their anxiety. The scientific research efficacy was significantly and negatively associated with anxiety among graduate students, and mediated the relationships between supervisor support and anxiety. The present study provides valuable theoretical implications for enriching the analytical framework of anxiety, and has practical implications for intervention of the mental health of graduate students.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
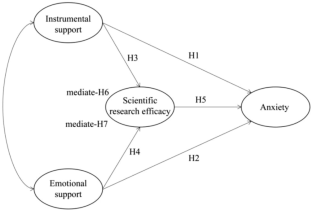
Similar content being viewed by others
Supportive Chinese supervisor, innovative international students: a social exchange theory perspective

How to improve academic well-being: an analysis of the leveraging factors based on the Italian case

How does the servant supervisor influence the employability of postgraduates? Exploring the mechanisms of self-efficacy and academic engagement
Data availability.
The data that support this study are available from the corresponding author, upon reasonable request.
Allen, H. K., Lilly, F., Green, K. M., Zanjani, F., Vincent, K. B., & Arria, A. M. (2020). Graduate student burnout: Substance use, mental health, and the moderating role of advisor satisfaction. International Journal of Mental Health and Addiction, 20 , 1130–1146. https://doi.org/10.1007/s11469-020-00431-9
Article PubMed PubMed Central Google Scholar
Andriopoulou, P., & Prowse, A. (2020). Towards an effective supervisory relationship in research degree supervision: Insights from attachment theory. Teaching in Higher Education, 25 (5), 648–661. https://doi.org/10.1080/13562517.2020.1731449
Article Google Scholar
Azizli, N., Atkinson, B. E., Baughman, H. M., & Giammarco, E. A. (2015). Relationships between general self-efficacy, planning for the future, and life satisfaction. Personality and Individual Differences, 82 , 58–60. https://doi.org/10.1016/j.paid.2015.03.006
Bandura, A. (1986). Social Foundations of thought and Action: A Socio-Cognitive Theory . Prentice Hall.
Google Scholar
Bandura, A. (1991). Social cognitive theory of self-regulation. Organizational Behavior and Human Decision Processes, 50 (2), 248–287. https://doi.org/10.1016/0749-5978(91)90022-L
Bandura, A., Caprara, G. V., Barbaranelli, C., & Gerbino, M. (2003). Role of affective self-regulatory efficacy in diverse spheres of psychosocial functioning. Child Development, 74 (3), 769–782. https://doi.org/10.1111/1467-8624.00567
Article PubMed Google Scholar
Bandura, A., Freeman, W. H., & Lightsey, R. (1997). Self-efficacy: The exercise of control. Journal of Cognitive Psychotherapy, 50 (3), 801–804. https://doi.org/10.1891/0889-8391.13.2.158
Bernstein, E. E., Leblanc, N. J., Bentley, K. H., Barreira, P. J., & Mcnally, R. J. (2021). A single-session workshop to enhance emotional awareness and emotion regulation for graduate students: A pilot study. Cognitive and Behavioral Practice, 28 (3), 393–409. https://doi.org/10.1016/j.cbpra.2020.09.008
Bieschke, K. J., Bishop, R. M., & Garcia, V. L. (1996). The Utility of the Research Self-Efficacy Scale. Journal of Career Assessment, 4 (1), 59–75. https://doi.org/10.1177/106907279600400104
Butler-Rees, A., & Robinsonb, N. (2020). Encountering precarity, uncertainty and everyday anxiety as part of the postgraduate research journey. Emotion, Space and Society, 37 , 100743. https://doi.org/10.1016/j.emospa.2020.100743
Byrom, N. C., Dinu, L., Kirkman, A., & Hughes, G. (2020). Predicting stress and mental wellbeing among doctoral researchers. Journal of Mental Health. Advance online publication . https://doi.org/10.1080/09638237.2020.1818196
Chapell, M. S., Blanding, Z. B., Silverstein, M. E., Takahashi, M., Newman, B., Gubi, A., & McCann, N. (2005). Test anxiety and academic performance in undergraduate and graduate students. Journal of Educational Psychology, 97 (2), 268–274. https://doi.org/10.1037/0022-0663.97.2.268
Corner, S., Pyhalto, K., Peltonen, J., & Bengtsen, S. S. E. (2018). Similar or different? Researcher community and supervisory support experiences among Danish and Finnish social sciences and humanities PhD student. Studies in Graduate and Postdoctoral Education, 9 (2), 274–295. https://doi.org/10.1108/SGPE-D-18-00003
Cowie, M. E., Nealis, L. J., Sherry, S. B., Hewitt, P. L., & Flett, G. L. (2018). Perfectionism and academic difficulties in graduate students: Testing incremental prediction and gender moderation. Personality and Individual Differences, 123 , 223–228. https://doi.org/10.1016/j.paid.2017.11.027
Crisp, G., & Cruz, I. (2009). Mentoring college students: A critical review of the literature between 1990 and 2007. Research in Higher Education, 50 (6), 525–545. https://doi.org/10.1007/s11162-009-9130-2
Curtin, N., Malley, J., & Stewart, A. J. (2016). Mentoring the next generation of faculty: Supporting academic career aspirations among doctoral students. Research in Higher Education, 57 (6), 714–738. https://doi.org/10.1007/s11162-015-9403-x
Denicolo, P. (2004). Doctoral supervision of colleagues: Peeling off the veneer of satisfaction and competence. Studies in Higher Education, 29 (6), 693–707. https://doi.org/10.1080/0307507042000287203
Dericks, G., Thompson, E., Roberts, M., & Phua, F. (2019). Determinants of phd student satisfaction: The roles of supervisor, department, and peer qualities. Assessment & Evaluation in Higher Education, 44 (7), 1053–1068. https://doi.org/10.1080/02602938.2019.1570484
Evans, T. M., Bira, L., Gastelum, J. B., Weiss, L. T., & Vanderford, N. L. (2018). Evidence for a mental health crisis in graduate education. Nature Biotechnology, 36 (3), 282–284. https://doi.org/10.1038/nbt.4089
Article PubMed CAS Google Scholar
Franke, A., & Arvidsson, B. (2011). Research supervisors’ different ways of experiencing supervision of doctoral students. Studies in Higher Education, 36 (1), 7–19. https://doi.org/10.1080/03075070903402151
Godskesen, M., & Kobayashi, S. (2015). Coaching doctoral students—A means to enhance progress and support self-organisation in doctoral education. Studies in Continuing Education, 38 (2), 145–161. https://doi.org/10.1080/0158037X.2015.1055464
Grady, R. K., Touche, R. L., Oslawski-Lopez, J., Powers, A., & Simacek, K. (2014). Betwixt and between: The social position and stress experiences of graduate students. Teaching Sociology, 42 (1), 5–16. https://doi.org/10.1177/0092055X13502182
Grewal, R., Cote, J. A., & Baumgartner, H. (2004). Multicollinearity and measurement error in structural equation models: Implications for theory testing. Marketing Science, 23 (4), 519–529. https://doi.org/10.1287/mksc.1040.0070
Hemmings, B., & Kay, R. (2015). The relationship between research self-efficacy, research disposition and publication output. Educational Psychology, 36 (2), 347–361. https://doi.org/10.1080/01443410.2015.1025704
Hilsenroth, M. J., Segal, D. L., & Hersen, M. (2004). Comprehensive Handbook of Psychological Assessment, Personality Assessment . John Wiley & Sons Inc.
Huerta, M., Goodson, P., Beigi, M., & Chlup, D. (2017). Graduate students as academic writers: Writing anxiety, self-efficacy and emotional intelligence. Higher Education Research and Development, 36 (4), 716–729. https://doi.org/10.1080/07294360.2016.1238881
Hutchings, M. (2017). Improving doctoral support through group supervision: Analysing face-to-face and technology-mediated strategies for nurturing and sustaining scholarship. Studies in Higher Education, 42 (3), 533–550. https://doi.org/10.1080/03075079.2015.1058352
Jiao, Q. G., Onwuegbuzie, A. J., & Bostick, S. L. (2006). The relationship between race and library anxiety among graduate students: A replication study. Information Processing and Management, 42 (3), 843–851. https://doi.org/10.1016/j.ipm.2005.03.018
Jones-White, D. R., Soria, K. M., Tower, E. K. B., & Horner, O. G. (2021). Factors associated with anxiety and depression among U.S. doctoral students: Evidence from the gradSERU survey. Journal of American College Health, 1 , 1–12. https://doi.org/10.1080/07448481.2020.1865975
Kang, X. S., & Gong, Z. J. (2011). The connotation and perfection of tutor responsibility system based on scientific research. Academic Degrees and Graduate Education, 3 , 18–21. https://doi.org/10.16750/j.adge.2011.03.008
Lambie, G. W., Hayes, B. G., Griffith, C., Limberg, D., & Mullen, P. R. (2014). An exploratory investigation of the research self-efficacy, interest in research, and research knowledge of Ph D in education students. Innovative Higher Education, 39 (2), 139–153. https://doi.org/10.1007/s10755-013-9264-1
Le, T. P., Hsu, T., & Raposa, E. B. (2021). Effects of natural mentoring relationships on college students’ mental health: The role of emotion regulation. American Journal of Community Psychology, 68 (1–2), 167–176. https://doi.org/10.1002/ajcp.12504
Levecque, K., Anseel, F., Beuckelaer, A. D., Heyden, J. V. D., & Gisle, L. (2017). Work organization and mental health problems in PhD students. Research Policy, 46 (04), 868–879. https://doi.org/10.1016/j.respol.2017.02.008
Li, F., Wang, C., & Yue, X. (2022). Impact of doctoral student training process fit on doctoral students’ mental health. International Journal of Mental Health Promotion, 24 (2), 169–187. https://doi.org/10.32604/ijmhp.2022.020034
Article ADS MathSciNet Google Scholar
Li, Z. B., Peng, C., Chen, S. M., & Rong, Y. (2019). Abusive supervision and scientific creativity:the role of academic anxiety and gender congruence. Chinese Journal of Clinical Psychology, 27 (01), 158–162. https://doi.org/10.16128/j.cnki.1005-3611.2019.01.032
Liu, C., Wang, L., Qi, R., Wang, W., Jia, S., Shang, D., Shao, Y., Yu, M., Zhu, X., Yan, S., Chang, Q., & Zhao, Y. (2019). Prevalence and associated factors of depression and anxiety among doctoral students: The mediating effect of mentoring relationships on the association between research self-efficacy and depression/anxiety. Psychology Research and Behavior Management, 12 , 195–208. https://doi.org/10.2147/PRBM.S195131
Loeb, C., Stempel, C., & Isaksson, K. (2016). Social and emotional self-efficacy at work. Scandinavian Journal of Psychology, 57 (2), 152–161. https://doi.org/10.1111/sjop.12274
Mackie, S. A., & Bates, G. W. (2018). Contribution of the doctoral education environment to phd candidates’ mental health problems: A scoping review. Higher Education Research and Development, 38 (3), 565–578. https://doi.org/10.1080/07294360.2018.1556620
Mohamed, F., & Nordin, R. (2013). Research efficacy among engineering and science undergraduates. Procedia—Social and Behavioral Sciences, 102 , 164–168. https://doi.org/10.1016/j.sbspro.2013.10.729
Muoz, L. R. (2021). Graduate student self-efficacy: Implications of a concept analysis. Journal of Professional Nursing, 37 (1), 112–121. https://doi.org/10.1016/j.profnurs.2020.07.001
Mustafa, M. B., Nasir, R., & Yusooff, F. (2010). Parental support, personality, self-efficacy and depression among medical students. Procedia—Social and Behavioral Sciences, 7 (1), 419–424. https://doi.org/10.1016/j.sbspro.2010.10.057
Ng, A., & Lovibond, P. F. (2019). Self-efficacy moderates the relationship between avoidance intentions and anxiety. Emotion, 20 (6), 1098–1103. https://doi.org/10.1037/emo0000594
Overall, N. C., Deane, K. L., & Peterson, E. R. (2011). Promoting doctoral students’ research self-efficacy: Combining academic guidance with autonomy support. Higher Education Research & Development, 30 (6), 791–805. https://doi.org/10.1080/07294360.2010.535508
Pasupathy, R., & Siwatu, K. O. (2014). An investigation of research self-efficacy beliefs and research productivity among faculty members at an emerging research university in the USA. Higher Education Research & Development, 33 (4), 728–741. https://doi.org/10.1080/07294360.2013.863843
Raposa, E. B., & Hurd, N. M. (2018). Understanding networks of natural mentoring support among underrepresented college students. Applied Developmental Science, 25 (1), 38–50. https://doi.org/10.1080/10888691.2018.1526635
Russo, G. (2011). Graduate students: Aspirations and anxieties. Nature, 475 (7357), 533–535. https://doi.org/10.1038/nj7357-533a
Ryan, R. M., & Deci, E. L. (2006). Self-regulation and the problem of human autonomy: Does psychology need choice, self-determination, and will? Journal of Personality, 74 (6), 1557–1585. https://doi.org/10.1111/j.1467-6494.2006.00420.x
Schmidt, M., & Hansson, E. (2018). Doctoral students’ well-being: A literature review. International Journal of Qualitative Studies on Health & Well Being, 13 (1), 1508171. https://doi.org/10.1080/17482631.2018.1508171
Schwarzer, R., Mueller, J., & Greenglass, E. (1999). Assessment of perceived general self-efficacy on the internet: Data collection in cyberspace. Anxiety Stress & Coping, 12 (2), 145–161. https://doi.org/10.1080/10615809908248327
Selian, S. N., Hutagalung, F. D., & Rosli, N. A. (2020). Academic stress, coping and social cultural adaptation of psychological well-being among Indonesian postgraduate students. Pertanika Journal of Social Science and Humanities, 28 (4), 2505–2527. https://doi.org/10.47836/pjssh.28.4.02
Shu, F., Sugimoto, C. R., & Lariviere, V. (2021). The institutionalized stratification of the Chinese higher education system. Quantitaive Science Studies, 2 (1), 327–334. https://doi.org/10.1162/qss_a_00104
Tai, T. E., & Tang, C. W. (2021). The role of graduate students’ learning strategies in reducing their English medium instruction avoidance: The mediation effect of language anxiety. Asia Pacific Journal of Education, 41 (2), 368–384. https://doi.org/10.1080/02188791.2020.1777937
Tenenbaum, H. R., Crosby, F. J., & Gliner, M. D. (2001). Mentoring relationships in graduate school. Journal of Vocational Behavior, 59 (3), 326–341. https://doi.org/10.1006/jvbe.2001.1804
Vernon, N. A., Evans, M. M., & Frissen, I. (2016). The relationship between dimensions of personality and library anxiety in graduate students. Education for Information, 32 (4), 397–410. https://doi.org/10.3233/EFI-160083
Waight, E., & Giordano, A. (2018). Doctoral students’ access to non-academic support for mental health. Journal of Higher Education Policy & Management, 40 (4), 390–412. https://doi.org/10.1080/1360080X.2018.1478613
William, W. K. Z. (1971). A rating instrument for anxiety disorders. Psychosom, 12 (6), 371–379. https://doi.org/10.1016/S0033-3182(71)71479-0
Winter, T., Riordan, B., Hunter, J. A., Tustin, K., Gollop, M., Taylor, N., Kokaua, J., Poulton, R., & Scarf, D. (2021). A longitudinal study of mental wellbeing in students in Aotearoa New Zealand who transitioned into PhD study. Frontiers in Psychology, 12 , 659163. https://doi.org/10.3389/fpsyg.2021.659163
Woolston, C. (2019). PhDs: The Tortuous Truth. Nature, 575 (7782), 403–406. https://doi.org/10.1038/d41586-019-03459-7
Article ADS PubMed CAS Google Scholar
Zhao, L. L., & Jiang, B. J. (2020). The influence of tutor support on academic adaptation of academic doctoral students: Based on the investigation of 16 universities in Jiangsu, Zhejiang, Shanghai and Anhui. China Higher Education Research . https://doi.org/10.16298/j.cnki.1004-3667.2020.08.10
Zhou, W. H., Zhang, A. X., Liu, J. Q., & Zhao, Q. H. (2010). Investigation on the status quo of the relationship between postgraduates and tutors in chinese universities. Academic Degrees & Graduate Education, 09 , 7–14. https://doi.org/10.16750/j.adge.2010.09.002
Download references
Acknowledgements
We highly acknowledge the valuable suggestions from Professor Hamish Coates in the research process.
East China Normal University, YBNLTS2021-018, Hao Yao, Shanghai Municipal Education Commission, A2021008, Hao Yao
Author information
Authors and affiliations.
Institute of Education, Tsinghua University, Beijing, China
Lichao Ma & Jiaqi Hou
Institute of Higher Education, Tongji University, Shanghai, China
You can also search for this author in PubMed Google Scholar
Contributions
LM, male, Ph.D candidate of Institute of Education, Tsinghua University. He mainly focuses on the fields of higher education management, engineering education, and college students development. HY, male, assistant professor of Institute of Higher Education, Tongji University. He mainly focuses on the fields of educational economics, educational empirical research methods.. JH, female, master student of Institute of Education, Tsinghua University. She mainly focuses on the fields of higher education.
Corresponding author
Correspondence to Hao Yao .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Ma, L., Yao, H. & Hou, J. Exploring the Relationship Between Supervisor Support and Anxiety of Graduate Students in China: The Mediating Role of Scientific Research Efficacy. Asia-Pacific Edu Res 33 , 321–329 (2024). https://doi.org/10.1007/s40299-023-00730-4
Download citation
Accepted : 01 April 2023
Published : 12 April 2023
Issue Date : April 2024
DOI : https://doi.org/10.1007/s40299-023-00730-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Instrumental support
- Emotional support
- Scientific research efficacy
- Graduate students
- Find a journal
- Publish with us
- Track your research
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Mental health in the workplace: a conversation bridging research and practice
How can we promote mental health in the workplace .
This is a question that Zhiqing (Albert) Zhou , PhD, and Lawanda Lewis are constantly asking themselves in their work, just from different perspectives. As an associate professor in the Department of Mental Health, Dr. Zhou researches how employees’ work-related experiences impact their health, well-being, and safety. As an HR Business Partner who oversees multiple academic departments at the Bloomberg School, Ms. Lewis has firsthand experience with assessing the mental health needs of employees and the effectiveness of workplace mental health and wellness programs.
This Mental Health Awareness Month, we brought them together for a wide-ranging conversation about research, practice, program implementation, and what still needs to be learned to help workplaces manage and support the mental health of their employees.
This conversation has been edited and condensed for length and clarity.
Lawanda Lewis: Post-COVID, we’re seeing different work modalities, from fully remote work to hybrid work to a mix. Hybrid work seems to be the way of the world now. What approaches can organizations take to better promote mental wellness in a hybrid workforce?
Albert Zhou: There is consistent evidence of the benefits of hybrid work, such as more flexibility, more autonomy, reducing commuting time, and better work-life balance. Meanwhile, there are reports of remote or hybrid workers feeling lonely or isolated, dealing with the added stress of shared spaces and family responsibilities, and feeling pressure to always appear available and present. We published a study in 2022 in the International Journal of Human Resource Management that found that workers’ mental health was negatively impacted when they felt too closely monitored by their managers.
One way to deal with this is to make sure managers are trained to prepare, support, and better communicate expectations and guidelines for hybrid and remote workers, while giving workers flexibility and more control over their time. Social and emotional support from coworkers and supervisors is also instrumental to building a healthy work life. People should be able to ask questions, connect with their colleagues, and access resources regardless of when and where they’re working. My collaborators and I are trying to understand how hybrid or remote work can be better managed so that workers can enjoy the benefits and reduce the negative consequences for their mental health.
LL: What has recent research revealed about the mental health benefits of transitioning to a four-day work week with no pay reduction?
AZ: We still need to do more research on the four-day work week, and we don’t yet have consistent solutions, even though this topic has been discussed for over 50 years. But there have been pilots and case studies in several countries that have shown evidence of increased productivity. Workers in these studies reported that they are more satisfied with their work, have better work life balance, and experience less stress and burnout. However, one issue that came up is scheduling problems. For example, I’m working for four days, but my clients are not, so how can we align our work? When we studied weekly work cycles , we found that Monday is already the most stressful day. Since working on Friday is off the table, how do I make sure too much work doesn’t pile up on Monday?
It’s important to note that these pilot programs were tested with a small number of organizations who voluntarily participated, which means they were already open to the idea of a four-day work week. It's unclear, then, whether their practices can be generalized to other workplaces. The transition to a four-day work week may be easier for office workers, but it would be harder for people in industries where people’s work schedules are less flexible, like blue collar workers or healthcare workers. Again, more research is needed, especially with HR professionals like you, since a lot of these changes will be implemented through HR functions. You are at the front line of making sure that it works as planned, taking feedback, and continuously shaping the practice.
I’m learning a lot about HR practices, and I was wondering if you could give examples of programs you have implemented to promote workplace mental health.
LL: One of our most important programs is the Johns Hopkins Employee Assistance Program (JHEAP), which provides confidential counseling, resources, and referrals to employees and their families for personal and work-related issues. And we’ve implemented flexible work arrangements. Hybrid or modified hybrid schedules allow employees to meet the needs of their roles and divisions while still managing their personal and work lives.
We also provide programs that can help employees manage their physical, emotional, social, and financial well-being, like meditation and yoga classes; premium memberships to tools that reduce stress and improve focus, like the Calm app; and the Healthy at Hopkins Wellness Initiative hub for resources and benefits.
Our leadership trainings raise awareness of mental health and unconscious bias and help supervisors recognize and manage employee stress. To reduce the stigma of talking about mental health, we regularly coach managers on how to create open dialogue with their employees about issues like stress and workloads. Through these kinds of initiatives, we want to help managers create a psychologically safe work environment.
AZ: Offering a variety of programs is great for addressing individuals’ different needs and creating psychologically safe relationships, while also caring about the overall work environment. Of all these different programs, what has worked well?
LL: Our Employee Assistance Program has evolved over the years. The University has been good at adapting it as work set-ups change and employee needs change, so that flexibility has led to a lot of reinventions over the years. Being flexible with our employees’ work arrangements has also worked really well. Everyone is dealing with day-to-day issues and unpredictable situations, so we want managers to balance knowing what needs to be done with caring for their employees.
JHU’s supervisor trainings have helped managers lead fairly, create open communication, and provide timely feedback so that employees always know where they stand. We also think it’s important to show employees appreciation and recognition for their hard work.
AZ: Definitely. We’ve seen in research that lack of recognition negatively affects productivity, performance, and mental well-being. It’s always good to see appreciation and recognition coming from the top down. Are there other workplace mental health topics that HR professionals like you are interested in right now?
LL: I'm interested in learning more about efforts to reduce stigma and promote open dialogue, especially when it comes to relationships between supervisors and their subordinates. What should organizations look out for when managing that relationship?
AZ: That's a great question because supervisors play an important role in employee mental health. From the research perspective, we develop specific, reliable, and valid measures to assess supervisor behaviors. The commonly used approach is asking workers to answer questions about the frequency of certain supervisor behaviors, such as rudeness or inattention. Those kinds of behaviors are subtle and sometimes low intensity but can affect people’s well-being if experienced regularly.
It's important to note that sometimes employees’ perceptions might not correspond to the actual behavior of the supervisor. The supervisor might not intentionally be rude, but their behaviors can still be perceived as rudeness or incivility. That's why when we study supervisor behaviors, it's important to calibrate across multiple direct reports of the same supervisor. That's an indication of a pattern of behavior and that action needs to be taken in terms of interventions or training. So, I think it’s important for organizations to continuously gather employees’ perceptions and combine data from multiple sources to get a more accurate reflection of supervisor behaviors. To prevent incivility in the workplace, it's important to build an environment where people are aware of their behavior and are mindful of their impact and talk about mental health.
LL: Reducing mental health stigma is a major theme. We want to raise awareness of resources and make sure that people get the support they need. But when we start talking about illnesses, we start to trickle into the lines of protected health information and figuring out how to handle that information. We have an office that supports employees who need accommodations, but we are still learning.
AZ: It’s great that HR is thinking about and prioritizing workplace mental health because that’s not the case everywhere. The research on workplace mental health is also still evolving. I’m doing a review piece with a student about disclosure of mental health conditions and how we can foster more open communication so support can be provided. But there’s still a long way to go. As a researcher, I want to keep providing evidence to help teams like yours who are doing actual implementation and supporting employee health and well-being.
Related Content

Global Mental Health NOW

Activity, Sleep & Dementia

Rev. Pamula Yerby-Hammack Breaking the Stigma of Mental Health

Inside the Movement to Transform Mental Health in Sierra Leone

Autism and Suicidal Thinking: ‘Alarming’ New Insights
- Communities
- Monday Business
- Police Logs
- Court News and Tickets
- Agribusiness
- MN State News
- National News
- International News
- Public Records
- Local Sports
- MN State Sports
- National Sports
- Lifestyle Columns
- Lifestyle Feature
- Engagements
- CORONAVIRUS
- Classifieds
- Garage Sales
- New Ulm Community Guide
- Open Routes
- Statement of Values
- Terms of Service
- Submit News
- Browse Notices
- Place Notice
- Today's Paper
Subscribe Today
Commissioners hear of mental health challenges, bridge on center members happy to return after pandemic.
NEW ULM — Brown County commissioners learned of the challenges of mental health programs from county human services behavioral staff Tuesday.
Brown County Behavioral Health Supervisor Julie Hogen said provider shortages continue to affect access to outpatient mental health services.
She said after Southern Minnesota Behavioral Health of New Ulm closed its doors last year, several independent providers opened in New Ulm and Sleepy Eye, reducing client wait lists for individual therapy, diagnostic assessments and medication management.
Hogen said adult rehabilitative mental health and children’s therapeutic and support services are experienced staffing shortages, largely due to high staff turnover. She said lack of capacity continues to create patient back logs, especially hospitalization for aggressive clients.
Hogen said utilization of the New Ulm Medical Center (NUMC) behavioral health unit has been running at 100% with high child and adult mental health traffic. More aggressive clients are often transferred to larger Allina behavioral units in the Twin Cities.
Brown County Human Services has a contract with Brown County Public Health to provide medication management services to clients who don’t have any other payment source.
A variety of transportation services are available through county human services. Choices include public providers Heartland and Hermann Express, TRUE Transit, private providers and volunteer drivers.
TRUE Transit will pick up in New Ulm when someone schedules ride and transport to any location in Blue Earth, Nicollet or Le Sueur Counties. Their rate is $5 per ride. They don’t bill insurance companies.
Brown County Children’s Mental Health Case Manager Abby Schwab said the Brown County Local Advisory Council (LAC) boosts mental health awareness and education by providing recommendations, reviews and evaluations of community mental health services.
Local organizations and individuals are invited to speak on their community work at quarterly LAC meetings at Brown County Human Services.
Schwab said a number of people were put on a LAC volunteer list at a recent mental health conference at the Sleepy Eye Event Center. Call 507-359-6500 for more information.
The Bridge on Center (Street) Clubhouse, located next to county human services, is a safe place for individuals with mental illness to socialize, participate in games and other activities. It remained open throughout 2023 with on group limitations. Members who were sick or exposed to illness were asked to stay home or mask according to Centers for Disease Control and Prevention (CDC) guidelines.
Additional funding this year was used to buy a gaming system, Smart TV, outdoor gas grill and new flooring.
“Our members tell us they really enjoy having a meal with friends at the clubhouse. Sitting at a table like a family is very comforting in a world where they sometimes feel alone,” said Hogen.
Members are encouraged to help shop and cook for shared meals with coordinator Jackie Nelson.
The clubhouse started a ‘Pay It Forward’ group that gave fleece tie blankets to the fire department, delivered puzzles to nursing homes and assisted living facilities and participated in backpack and lunchbox projects for school children, and Salvation Army bell ringing, among other things,” said Hogen.
Favorite group activities of Bridge on Center members include bowling, baking, painting, arts and crafts, yard games, walking at the track, birthday parties, bingo, puzzles, coffee and musical events.
Commissioner Brian Braun thanked Hogen and Brown County Children’s Mental Health Case Manager Abby Schwab for their mental health work he said makes a positive difference in Brown County.
Today's breaking news and more in your inbox
- Daily Newsletter
- Breaking News
NEW ULM — Brown County commissioners learned of the challenges of mental health programs from county human ...

Demolition begins on Lincoln Park pickleball courts

George’s Ballroom project moves forward

Popping good time once again on Broadway
3 incumbents file to run in county and city elections.
NEW ULM — There is one week remaining for candidates to file to appear on the Nov. 5 election ballot for ...
Mobile crisis team reaching out to Brown County
NEW ULM — In an effort to increase recognition that May is mental health awareness month, Horizon Homes, Inc. ...
Starting at $4.38/week.

County looks to buy Vista's Green Oak Ranch for future mental health hub, residents push back
G reen Oak Ranch, a coveted piece of property in southern Vista , is up for sale, and the County of San Diego is looking to buy it. The sprawling land is a total of 138 acres, but only 110 acres are for sale.
“It’s a unique and extraordinary opportunity for a future regional behavioral health site in San Diego County,” said County Supervisor Jim Desmond at the Board of Supervisors meeting on April 30.
The County voted unanimously to enter negotiations with the real estate trust that owns the acreage for sale, while also laying down $300,000 in an earnest money deposit.
“We can see the needs in our streets, our sidewalks, our hospitals and parks and underpasses for more facilities for treatment and mental health services,” said Desmond.
Desmond’s vision for the property, which over past decades has been host to popular summer camps for kids and RV parking for low-income families, would be a $335 million dollar transformation into a mental health hub .
“Immediately I was shocked,” said Tim Troncone, a homeowner who lives nearby.
He found out about the County’s proposal three weeks ago and quickly galvanized neighbors in a Facebook group to oppose it.
“We’ve heard a thousand beds possible, we’ve heard 200 beds,” said Troncone. “The story’s changed on what exactly is going to happen, so we don’t know.”
CBS 8 called Supervisor Desmond’s office and staff told us they’d have a maximum of 200 beds on the property in what they’re calling a “regional campus for healing.”
“I have small kids,” said Troncone. “My neighborhood is a family neighborhood. We all have kids, and we all have concerns.”
Desmond’s initial plan calls for a referral-only sober-living recovery program as well as psychiatric care with 24/7 supervision and security, and no walk-ins allowed.
“Once the County of San Diego would become the owners of this property, all land use control would be in the hands of the County,” said Vista’s Mayor John Franklin.
For many decades, Green Oak Ranch Ministries has operated a faith-based drug and alcohol recovery program for 50 people at a time. The program’s facilities are located on the 28 acres not for sale, so it will remain where it is regardless of what happens with the sale.
Mayor Franklin raised concerns to CBS 8 about patients being released into the City of Vista from a large county-run facility at Green Oak.
“‘Where will they go? How will they get back to the places that they came from before they came to Vista?’ We simply don’t have the resources to manage that problem if it spills out onto the city streets of Vista,” said Mayor Franklin.
Others also interested in buying the property are Solutions for Change , a Vista-based nonprofit that provides homeless services to families, and the City of Vista, which hasn’t released their potential vision for the site.
“The City of Vista needs to buy this land and build a sports complex, more fields for our community and our kids,” said Troncone. “The Vista firefighters need a training facility. We would love to have a training facility built here for our firefighters.”
The Vista City Council will be discussing the possibilities in a closed session meeting Tuesday. A large group of neighbors is expected to show up and speak out at the public meeting at 5:30 p.m. , though this item is not on the agenda.
WATCH RELATED: Vista mechanic rolls out a special gift for a deserving high schooler


IMAGES
VIDEO
COMMENTS
More than 40% of PhD students met the criteria for moderate to severe depression or anxiety. In contrast, 32% of working professionals met these criteria for depression, and 26% for anxiety. The ...
Your PhD supervisor will strongly influence the success and quality of your degree as well as your general well-being throughout the program. It is therefore vital to choose the right supervisor for you. ... Evidence for a mental health crisis in graduate education. Nat Biotechnol. 2018; 36:282-4. doi: 10.1038/nbt.4089 ...
The factors with the strongest evidence-base (i.e. those supported by multiple studies using qualitative and quantitative findings) denote that being female and isolated increases the risk of the mental health problems, whereas seeing the PhD as a process, feeling socially supported, having a positive supervisor relationship and engaging in ...
A good supervisor can lift you up when you are low, push you to be a better researcher, and continue to advocate for your success way beyond your PhD. Yet at the opposite end of the spectrum, a poor PhD Supervisor can bully you, gaslight you, and lead to a truly miserable few years of PhD study. In fact, in Nature's 2019 PhD student survey 24 ...
PhD supervision is associated with a variety of expectations and responsibilities, from both the student and the supervisor, but there is also not a single approach to the supervisor relationship. ... Others have recently developed resources to facilitate peer support of student mental health that should be considered for wider use (e.g., Homer ...
Amongst the many factors contributing to the ill mental health of PhD students is their relationship with their supervisor. In some cases, the supervisor can be the primary cause for an overall unsatisfactory PhD experience and ill mental health through bullying and harassment [6] , unprofessionalism and poor management skills (e.g., [6] ) or ...
The book goes beyond typical mental health discussions (where the focus for improving mental health is placed on PhD students to become "more resilient") and explores some of the often unspoken environmental factors that can impact mental health. These include the PhD student-supervisor relationship, the pressure to publish, and deep ...
Two-thirds said that their supervision responsibilities had increased over this time, with many wanting more support to address the well-being and mental health of their PhD students.
The factors with the strongest evidence-base (i.e. those supported by multiple studies using qualitative and quantitative findings) denote that being female and isolated increases the risk of the mental health problems, whereas seeing the PhD as a process, feeling socially supported, having a positive supervisor relationship and engaging in ...
Looking back at the statistic that ~1 in 2 PhD students experience mental health concerns from Chap. 1, the 2014 report by UC Berkeley (one of the most cited reports to date) found that 47% of graduate students from a range of disciplines met the threshold to be considered depressed [].This work was expanded upon by Evans et al. (2018), finding that graduate students are more than six times as ...
Some reasons you may find it worthwhile to further your education with a PhD in Counselor Education and Supervision program are that postsecondary education roles in the field of mental health are expected to increase by 12 percent between 2021 and 2030; a PhD in Counselor Education and Supervision offers the chance to build on your past ...
The programme provides an interdisciplinary training. PhD supervisors have been selected across departments from King's campuses, for their expertise in core areas of relevance to mental health.. Collectively, the supervisors provide knowledge in translational neuroscience, digital mental health and social science and policy.
The PhD degree is a research-oriented doctoral degree. In the first two years, students take core courses in the Departments of Mental Health, Biostatistics, and Epidemiology, in research ethics, and attend weekly department seminars. Students must complete a written comprehensive exam (in January of their second year), a preliminary exam, two ...
May be of interest: PhD supervisor wants me to quit after break - Snijderfrey. Aug 10, 2023 at 20:23. ... known to be a good point of first contact for undergraduate and graduate students suffering from depression and other mental health issues, so I get to hear from a lot of students about their struggles. I am not a therapist, so the only ...
Mental Health and Your PhD: Resources and Support. Mental health is a serious issue that impacts students at any level. PhD students face unique stressors and pressure that can impact mental health. Use the resources in this guide to find the support you need. Author: Angela Myers. Editor: PhDs Editing Staff.
An earned master's degree in mental health counseling with a curriculum equivalent to that of Pace University's 60-credit graduate master of science program in mental health counseling. Earned graduate-level GPA of 3.6 or higher. Submitted letters of recommendation, personal statement, and official academic transcripts. Degree conferral ...
Even if the conversation is less formal or does not involve documentation, talking to a mental health professional about how to disclose a crisis or acute situation can be a helpful step before talking to your advisor, giving you a script or language to fall back on if the situation is emotional or tense. You do not need to justify your mental ...
Completion Time: 4 years. Earned Credits: 54. Graduates of Saybrook's Ph.D. in Counselor Education and Supervision program will be prepared to hold full-time faculty positions within counseling programs. As counselor educators they will hold advanced knowledge and skills in teaching, clinical supervision, research, advocacy and leadership.
Location. If you're passionate about enhancing learning experiences for aspiring behavioral health counselors, University of the Cumberlands Ph.D. in Counselor Education & Supervision is for you. Your program will help you pursue leadership roles in academia or as a high-level administrator in clinical settings, such as a behavioral health ...
Counselor Education Program Coordinator. Patton Hall 432L. 740.593.4395. [email protected]. Program Code: PH6265 Apply Now for Fall 2024 Join our program where our mission is to provide advanced preparation for counselors in the areas of counseling, supervision, teaching, research and scholarship, and leadership and advocacy.
With a PhD in Counselor Education and Supervision with a specialization in Clinical Mental Health Counseling, you'll be ready to train future clinical mental health counselors or broaden your private-practice credentials. Ideal for students with a nonclinical mental health master's degree, this specialization takes a deep dive into ...
The mental health services here are underfunded and overcrowded (the school had ~5 suicides this past year). - stressedout. Jul 3, 2015 at 15:45 ... (as many PhD students are, at least in Europe), once you need an extension, although employers are ethically and often also legally obligated not to discriminate on grounds of health.
By Joshua A. Gordon, MD, PhD, Director, NIMH For 75 years, the National Institute of Mental Health (NIMH) has vigorously pursued its mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure.
This study examined the relationship among supervisor support, scientific research efficacy and anxiety of graduate students in the Chinese context. ... Mackie, S. A., & Bates, G. W. (2018). Contribution of the doctoral education environment to phd candidates' mental health problems: A scoping review. Higher Education Research and Development ...
How can we promote mental health in the workplace? This is a question that Zhiqing (Albert) Zhou, PhD, and Lawanda Lewis are constantly asking themselves in their work, just from different perspectives.As an associate professor in the Department of Mental Health, Dr. Zhou researches how employees' work-related experiences impact their health, well-being, and safety.
In Memoriam: Elena H. Chartoff, PhD. May 29, 2024. It is with great sadness that we share with you the unexpected death of longtime colleague Elena H. Chartoff, PhD, director, Neurobiology of Motivated Behavior Laboratory, and associate professor of psychiatry at Harvard Medical School. Chartoff was well-known throughout the McLean community ...
May 30, 2024. Fritz Busch. Staff Writer. [email protected]. NEW ULM — Brown County commissioners learned of the challenges of mental health programs from county human services behavioral ...
Mental Health Supervisor Registry. Act 117 (2022) requires OPR to maintain a registry of licensed mental health professionals who are available to serve as supervisors for mental health professionals in training ("Mental Health Supervisor Registry" or "Registry"). Licensees who are available to be a supervisor may request to be listed on the Mental Health Supervisor Registry.
The County's initial plan calls for a referral-only sober-living recovery program and psychiatric care with 24/7 supervision and security, and no walk-ins allowed. Health Real Estate
Overview. Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources. DHS Executive Leadership.