An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.


StatPearls [Internet].
Right heart failure.
Stacy A. Mandras ; Sapna Desai .
Affiliations
Last Update: July 17, 2023 .
- Continuing Education Activity
Heart failure is a condition in which the heart loses its ability to pump blood efficiently to the rest of the body. Right heart failure is most commonly a result of left ventricular failure via volume and pressure overload. Clinically, patients will present with signs and symptoms of chest discomfort, breathlessness, palpitations, and body swelling. This condition is evaluated using non-invasive techniques such as echocardiography, nuclear angiography, MRI, 64-slice CT, as well as invasive hemodynamic measurements. Management is aimed at increasing right ventricular contractility, reducing right ventricular afterload and optimizing volume status. This activity reviews the evaluation and management of right heart failure and highlights the role of the interprofessional team in improving care for affected patients.
- Review the presentation of a patient with right heart failure.
- Describe the workup of a patient with right heart failure.
- Identify the treatment options for right heart failure.
- Outline the importance of collaboration and communication among the interprofessional team members to recognize the clinical signs of heart failure and evaluate it using non-invasive and invasive measures which will enhance the delivery of care for the affected patients.
- Introduction
When addressing heart failure, most commonly, the left ventricle (LV) is the topic of discussion, and the right heart overlooked. However, the right ventricle (RV) is unique in structure and function and is affected by a set of disease processes that rival that of the LV. This article will review the normal structure and function of the RV, describe the pathophysiology of RV failure (RVF), and detail the medical and surgical management of the various disease processes during which RVF occurs. [1] [2]
Right ventricular failure (RVF) is most commonly a result of left ventricular failure (LVF), via pressure and volume overload. [3]
In addition to LVF, there are other conditions of pressure overload that lead to RVF. These include transient processes such as:
- Pulmonary embolism (PE)
- Mechanical ventilation
- Acute respiratory distress syndrome (ARDS)
Furthermore, chronic conditions of pressure overload may lead to RVF. These include:
- Primary pulmonary arterial hypertension (PAH) and secondary pulmonary hypertension (PH) as seen in chronic-obstructive pulmonary disease (COPD) or pulmonary fibrosis)
- Congenital heart disease (pulmonic stenosis, right ventricular outflow tract obstruction, or a systemic RV).
The following conditions result in volume overload causing RVF:
- Valvular insufficiency (tricuspid or pulmonic)
- Congenital heart disease with a shunt (atrial septal defect (ASD) or anomalous pulmonary venous return (APVR)).
Another important mechanism that leads to RVF is intrinsic RV myocardial disease. This includes:
- RV ischemia or infarct
- Infiltrative diseases such as amyloidosis or sarcoidosis
- Arrhythmogenic right ventricular dysplasia (ARVD)
- Cardiomyopathy
- Microvascular disease.
Lastly, RVF may be caused by impaired filling which is seen in the following conditions:
- Constrictive pericarditis
- Tricuspid stenosis
- Systemic vasodilatory shock
- Cardiac tamponade
- Superior vena cava syndrome
- Hypovolemia.
- Epidemiology
RVF is most often a result of LVF, and patients with biventricular failure have a 2-year survival of 23% versus 71% in patients with LVF alone. [4] [5]
In the CHARITEM registry, RVF accounted for 2.2% of heart failure admissions and was secondary to LVF in more than one-fifth of cases. In the Egyptian Heart Failure-LT registry, 4.5% of patients presenting with acutely decompensated heart failure had RVF versus 3% in other regions of the European Society of Cardiology. It has been proposed that this difference is due to the increased prevalence of rheumatic heart disease in this region.
- Pathophysiology
During fetal development, the RV accounts for approximately 66% of the cardiac output, and via the ductus arteriosus and foramen ovale, shunts blood to the lower body and placenta. At birth, exposure to oxygen and nitric oxide, as well as lung expansion, leads to a rapid decrease in pulmonary vascular resistance (PVR). The lungs, which were bypassed in utero, become a low-pressure, highly distensible circuit. The thick-walled fetal RV becomes thinner. [6]
Anatomically the structures and resulting function of the RV and the LV are vastly different. For example:
- The LV is elliptical and made of thick muscle fibers wrapped in two anti-parallel layers separated by a circumferential band. This results in a complex contraction that involves torsion, thickening, and shortening.
- The RV, in contrast, takes a triangular and crescentic shape and is made up of both a superficial layer that runs circumferentially and parallels to the atrioventricular groove and a deeper layer that runs longitudinally from the base to the apex. Because of its structure, the contraction of the RV is limited to longitudinal shortening of the tricuspid annulus towards the apex. The RV free wall is displaced inward toward the septum and traction is created by the septum as it moves toward the LV in systole.
- The RV is more heavily trabeculated and contains a circumferential moderator band at the apex.
- The tricuspid valve (TV) is unique in that it has a large annulus and is tethered by greater than three papillary muscles which make it vulnerable to structural deformation under sustained increased pressure or volume loading.
- Because the RV is substantially thinner than the LV with lower elastance, the RV is much more susceptible to increases in afterload. A modest change in PVR may result in a marked decrease in RV stroke volume. This is evident in patients with pulmonary arterial hypertension (PAH), pulmonary embolism (PE), mitral valve disease with secondary pulmonary hypertension (PH), and the adult respiratory distress syndrome (ARDS). The thinner RV is also more sensitive to the pericardial constraint.
Like the LV, contraction of the RV is preload dependent at normal physiologic filling pressures, and excessive RV filling can result in a shift of the septum towards the LV and ventricular interdependence causing impaired LV function.
Because of lower right-sided pressures and wall stress, the oxygen requirement of the RV is lower than that of the LV. Coronary blood flow to the RV is lower, as is oxygen extraction. For this reason, the RV is less susceptible to ischemic insults, and increases in oxygen demand are met via increases in coronary flow as is the case in PAH or increased oxygen extraction which occurs with exercise.
RV function is affected by atrial contraction, heart rate, and synchronicity. Each of these has important clinical implications, and RVF for any reason is a strong prognostic indicator.
The response of the RV to a pathologic load is complex. The nature, severity, chronicity, and timing (in utero, childhood or adulthood) each play a role in how the RV responds to an increased load. For example, in childhood, when confronted with congenital pulmonic stenosis, fetal right ventricular hypertrophy (RVH) persists and allows the RV to compensate for the increase in afterload.
In adulthood, however, the ability of RV to tolerate a chronic increase in afterload, such as that seen in PAH, is poor. In the early stages of PAH, the RV responds to elevated pulmonary arterial pressures (PAP) by increasing contractility, with little to no change in RV size. As PAP continue to rise, the RV myocardium begins to hypertrophy, and RV stroke volume (SV) is maintained. This, however, is not enough to normalize wall stress, and subsequently, dilatation occurs. This is accompanied by rising filling pressures, decreased contractility, loss of synchronicity as the RV becomes more spherical, and dilatation of the TV annulus resulting in poor coaptation of the valve leaflets and functional tricuspid regurgitation (TR). The TR worsens the RV volume overload, RV enlargement (RVE), wall stress, contractility and cardiac output.
This differs from the response of the RV to an acute increase in afterload, such as that seen with an acute PE. In this case, the RV responds with an increase in contractility and end-diastolic volume, but does not have time for the adaptations that are seen in chronic RVF to occur, and quickly fails when unable to generate enough pressure to maintain flow.
- History and Physical
As with all disease states, the initial assessment of RVF begins with a thorough history and physical examination. The acuity, severity, and etiology should be determined so that an appropriate treatment plan may be put in place.
Clinically, patients present with the signs and symptoms of hypoxemia and systemic venous congestion. These include:
- Breathlessness
- Chest discomfort
- Palpitations
Common findings on the exam include:
- Jugular venous distension
- Hepatojugular reflux
- Peripheral edema
- Hepatosplenomegaly/hepatic pulsation
- Signs of concomitant LVF
- Paradoxical pulse.
When severe, presyncope or syncope may occur when the RV is unable to maintain cardiac output. This is accompanied on the exam by the following:
- Hypotension
- Tachycardia
- Cool extremities
- Delayed capillary refill
- Central nervous system depression
- Oliguria.
After the history and physical, the evaluation continues with an electrocardiogram, arterial blood gas, blood lactate, and chest x-ray. Blood work should include markers of end-organ function (renal and hepatic panel) to assess severity. A D-Dimer is useful in the diagnostic workup of suspected PE. There are no biomarkers specific for RVF, however B-type natriuretic peptide and cardiac troponin are highly sensitive for early detection of RVF and myocardial injury. When elevated, these are associated with poor prognosis in RVF due to PAH. [7] [8]
Noninvasive Measures
Echocardiography
The assessment of RV function can be challenging because of its location, shape and afterload dependence. Two-dimensional echocardiography (2DE) is the first-line and most commonly used non-invasive imaging modality to assess RV size, hemodynamics, and function. Images are acquired in multiple cross-sectional planes, and and the following measurements obtained:
- Quantification of RV enlargement (RVE) and right atrial enlargement (RAE): Because of its shape, quantitative assessment of RV function is difficult and is often described qualitatively in comparison with LV function. A normal RV should not be more than two-thirds the size of the LV. RVE is a strong prognostic indicator.
- TAPSE: Used to quantify the movement of tricuspid annulus toward the apex and estimates RV function. This has been a good predictor in patients with PAH and LVF, however, in patients with congenital heart disease or after cardiac surgery, it is less reliable.
- Right ventricular strain: Another useful tool to assess RV function. The strain is a composite measurement of RV loading and dysfunction- abnormal strain patterns have been associated with disease progression, higher diuretic doses, and mortality in PAH. The strain has also been shown to predict RVF after implantation with a left ventricular assist device (LVAD) and predicts clinical outcomes in those referred for heart transplantation.
- Fractional area of change (FAC): An important quantitative measurement of RV systolic function derived either by 2DE or magnetic resonance imaging (MRI). It has been shown to be an independent predictor of HF, sudden death, stroke and mortality in PE and in myocardial infarction.
- Myocardial performance index (MPI): Estimates global ventricular function and is calculated by adding the isovolumic contraction and relaxation times divided by the ejection time. In RVF, MPI increases as the isovolumic times increase and contraction times decrease. MPI has been shown to predict PAH in connective tissue disease and is an independent prognostic indicator in PAH.
- Eccentricity index: A useful measurement of RVE. Acquired in the short-axis view, at end-systole and end-diastole, the eccentricity index is a ratio of the length of two perpendicular minor-axis diameters, one of which bisects and is perpendicular to the interventricular septum. This allows for a quantitative measurement of septal-flattening and distinguishes between pressure and volume overload.
- All of the hemodynamic variables measured during invasive right heart catheterization (RHC) may be estimated using echocardiography. For example, the diameter and collapsibility of the inferior vena cava (IVC) in the subcostal view may be used to estimate RA filling pressure. A normal IVC collapses more than 50% with inspiration and is associated with a RA pressure less than 10 mmHg. By measuring the maximum TR velocity and using a modified Bernoulli equation, the systolic PAP may be estimated. The diastolic PAP may be estimated by using the same equation on the pulmonic regurgitant jet or by transposing the pulmonary opening time on the tricuspid regurgitant velocity curve and calculating the pressure gradient between the RA and the RV.
Three-dimensional echocardiography has also been used more recently to quantify RV volumes and ejection fraction using a modified Simpson’s method (summation of disks). This has been validated to correlate well with the gold standard MRI, but is time-consuming and less feasible given the proximity of the RV to the sternum and its trabeculations.
Nuclear Angiography
First-pass radionuclide ventriculography was for a long time the gold standard to measure RV ejection fraction (RVEF). A bolus of the 99m-Tc tracer is injected, and a sequence of cardiac cycles is acquired as the bolus passes through the heart. A normal RVEF is 52% plus or minus 6% with 40% considered the lower limit of normal. Nuclear angiography is limited by its inability to measure RV volumes and sensitivity to cardiac arrhythmia.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI), as mentioned previously, is now the gold-standard for the measure of RV volumes and function. In addition to measuring RV mass, volumes and chamber dimensions, MRI can calculate and quantify regurgitant volumes, delayed enhancement, scar burden, strain, perfusion, and pulmonary pulsatility. Also, changes in the global function of the RV after medical therapy have been shown to have a direct correlation to the functional class and survival in patients with PAH.
MRI is limited by its temporal resolution, its contraindication in those with implantable cardiac devices, and the time required for data acquisition and analysis.
64-Slice Computed Tomography
Computed tomography (CT) may be used to measure RVEF and RV volumes. However, acquisition of RV parameters cannot be obtained simultaneously with LV parameters or CT angiography. This results in the need for additional radiation exposure which is not negligible, and therefore CT is not routinely used for this purpose.
Invasive Hemodynamic Measurement
Right heart catheterization (RHC) or pulmonary artery catheterization (PAC) is often very useful in making the diagnosis and tailoring management in RVF. Though it is an invasive procedure, RHC is considered safe with a low complication rate, especially in experienced centers. Current practice guidelines recommend the use of RHC for unexplained diagnostic or treatment-resistant cases, for the continuous and accurate measurement of right and left-sided filling pressures, cardiac output, and PVR.
The hemodynamic variables obtained in a RHC have important prognostic significance. A high RA pressure and low cardiac output have repeatedly been shown to be associated with poor outcomes in PAH. In addition, a PVR greater than three Woods units and pulmonary vascular compliance (SV/pulmonary pulse pressure) have both been associated with poor outcomes in LVF as well as PAH.
- Treatment / Management
Management of Acute Right Ventricular Failure
Medical Management
Management of acute RVF starts with an assessment the severity of the patient’s condition and the decision to admit the patient to the intensive care unit (ICU) or intermediate care unit when appropriate. Rapid identification and management of triggering factors (i.e., sepsis, arrhythmias, drug withdrawal) are necessary. In the case of an RV infarct, rapid revascularization is essential, as is reperfusion therapy in a patient with a high-risk PE. As infection portends a very poor prognosis in acute RVF, preventative measures and prompt detection and treatment of infection are important. [9] [10]
The mainstay of treatment focuses on three tenants: optimizing volume status, increasing RV contractility, and reducing RV afterload.
Volume loading may be appropriate if the patient is hypotensive and has low or normal filling pressures. Placement of a PAC or central venous pressure monitoring is often helpful as while the RV is preload dependent. Volume loading may over distend the RV and result in a further decline in cardiac output. If volume overload is present, IV diuresis is indicated, or renal replacement therapy if volume removal cannot be accomplished with medication. In addition to improving symptoms, diuresis has the additional benefits of reducing TR, restoring synchronous RV contraction, and reducing ventricular interdependence. Sodium restriction, daily weights, and strict monitoring of fluid intake and urine output is advised to aid in maintaining euvolemia.
Efforts should also be made to restore sinus rhythm in patients with atrial arrhythmias given the contribution of atrial contraction to cardiac output in RVF. In addition, hemodynamically significant tachy- and bradyarrhythmias should be treated. Digoxin has been shown to be of some benefit in patients with severe PAH. However, care must be taken in the critically ill patient given its narrow therapeutic window and possible side effects.
When hemodynamic instability is present, vasopressors are indicated. Norepinephrine is the pressor of choice to improve systemic hypotension and restore cerebral, cardiac and end-organ perfusion. Inotropes, including dobutamine, levosimendan, and the phosphodiesterase-3 inhibitor milrinone are also helpful in that they improve contractility and cardiac output. Dobutamine is the inotrope of choice in RVF, as it leads to increased myocardial contractility via the beta receptor and vasodilatation/decreased afterload via the beta receptor. Caution should be taken however with dobutamine and milrinone as both may reduce systemic pressure. If this occurs, the addition of a vasopressor may be required.
If pressure overload is the etiology of the RVF, as is the case in PAH, afterload reduction with pulmonary vasodilators is the primary therapy. These drugs target three therapeutic pathways, nitric oxide (NO), endothelin and prostacyclin. It has been demonstrated that regardless of the class of drug used; acute responsiveness has prognostic significance in acute RVF. In addition to lowering afterload, some of these agents, such as the endothelin receptor antagonist (ERA) bosentan and the phosphodiesterase-5 (PDE5) inhibitor sildenafil, have also been shown to directly increase RV contractility. The pulmonary vasodilators used to treat acute RVF include:
- Inhaled nitric oxide (iNO) acts via the cyclic guanosine monophosphate (cGMP) pathway to cause pulmonary vasodilatation. It is rapidly inactivated by hemoglobin in the capillaries of the lung, thereby preventing systemic hypotension. The iNO acts only in ventilated areas of the lung, lowering PAP and PVR and improving oxygenation, without worsening hypoxia due to the ventilation-perfusion mismatch or shunting that can be seen with the systemic vasodilators. The iNO has been well studied in patients with acute RVF and has been shown in combination with dobutamine to improve CO, oxygenation, and PVR. Caution must be taken to avoid methemoglobinemia, and iNO must be withdrawn slowly to avoid hemodynamic decompensation from rebound PH.
- The intravenous (IV) prostacyclins epoprostenol and treprostinil act via the cyclic adenosine monophosphate pathway to result in potent pulmonary vasodilatation, systemic vasodilatation, and inhibition of platelet aggregation. Epoprostenol is the prostacyclin of choice for critically ill patients with acute RVF given its 6-minute half-life. Epoprostenol is started at 1 ng/kg/min to -2 ng/kg/min and up-titrated as tolerated, with caution in patients with comorbidities, hypoxemia or hemodynamic instability. Like iNO, the prostacyclins decrease PAP and PVR and increase cardiac output, however dose-dependent side effects (hypotension, nausea/vomiting/diarrhea, and headache) often limit titration. Prospective data demonstrating treatment benefit of IV prostacyclins in acute RVF is limited.
- Iloprost and treprostinil: inhaled prostacyclins. Both reduce PVR and improve cardiac output, with less systemic side effects. While treprostinil may also be given subcutaneously, it is inferior in critically ill, hemodynamically unstable patients due to its unpredictable absorption and longer half-life.
- ERAs and PDE5-inhibitors: oral, pulmonary vasodilators that reduce PAP, reduce PVR, and improve cardiac output in patients with RVF. ERAs block the endothelin-A and endothelin-B receptors in endothelial and vascular smooth muscle cells, reducing the vasoconstrictive, proliferative and proinflammatory effects of endothelin. The use of ERAs in the ICU is limited by their longer half-life and hepatotoxicity (bosentan). PDE5-inhibitors block degradation of cGMP. In addition to the previously mentioned hemodynamic effects, PDE5i have been shown to reduce hypoxic pulmonary vasoconstriction (HPV) and the up-regulation of pro-inflammatory cytokines induced by HPV. The limited data for the use of PDE5-inhibitors in the ICU suggest a potential benefit in patients with RVF after mitral valve repair, coronary artery bypass grafting, or LVAD placement, and to reduce rebound PH in PAH patients weaning from iNO.
Caution must be taken with patients requiring mechanical ventilation, as excessive tidal volumes (V) and positive end-expiratory pressure (PEEP) increase PAP, RAP and RV afterload. Also, PEEP may worsen the picture by reducing venous return in the preload-dependent RV. While permissive hypercapnia leads to vasoconstriction, thereby increasing PAP and worsening RVF, hyperventilation acutely reduces PAP and acidosis-induced vasoconstriction. Care must be taken to avoid high V in this setting. The optimal ventilator setting for the patient with RVF is that which delivers adequate oxygenation and ventilation with the lowest V, plateau pressure, and PEEP.
Surgical Management and Interventional Therapies
For patients with reversible RVF refractory to medical therapy, surgical options are indicated either as a bridge to recovery or transplantation. Surgery may also be indicated for patients with RVF in the setting of valvular heart disease, congenital heart disease, and chronic thromboembolic pulmonary hypertension (CTEPH). Adequate preoperative diuresis is imperative, and the use of pulmonary vasodilators and inotropes peri-operatively may be needed. In addition, the irreversible end-organ damage is a contraindication for surgical management.
Veno-arterial (VA) extracorporeal membrane oxygenation (ECMO) may be indicated as salvage therapy in patients with massive PE and refractory cardiogenic shock following systemic thrombolysis. ECMO may also be used as a bridge to lung or heart-lung transplantation in patients with severe RVF due to end-staged PAH.
Mechanical support with a right ventricular-assist device (RVAD) may be an option for the patient with isolated RVF awaiting transplant. However, ECMO may be a better treatment option for unloading the RV in the setting of severely increased PVR as pumping blood into the PA may worsen PH and cause lung injury.
Patients with RVF due to LVF may benefit from LVAD implantation, with improved PAP before heart transplantation and possibly improved post-transplant survival. However, LVADs may worsen or lead to new RVF due to alterations in RV geometry and flow/pressure dynamics and biventricular support may be required.
Pulmonary thromboendarterectomy (PTE) is the treatment of choice for patients with CTEPH and is often curative. PTE has been shown to improve functional status, exercise tolerance, quality of life, gas exchange, hemodynamics, RV function, and survival, particularly in patients with proximal lesions and minimal small vessel disease. , PTE is not recommended for patients with massively elevated PVR (greater than 1000 dyn/cm to 1200 dyn/cm). Outcomes with PTE have been shown to directly correlate with the surgeon and center experience, concordance between the anatomic disease and PVR, preoperative PVR, the absence of comorbidities (particularly splenectomy and ventricular-atrial shunt) and post-operative PVR. Operative mortality in an experienced center is between 4% to 7%, and PTE should not be delayed in operative candidates in favor of treatment with pulmonary vasodilator therapy.
Surgical embolectomy or percutaneous embolectomy may be used for acute RVF in the setting of massive PE, but data comparing embolectomy with thrombolysis are limited.
Balloon atrial septostomy (BAS) is indicated for PAH patients with syncope or refractory RVF to decompress the RA and RV and improve CO via the creation of a right-to-left shunt. BAS may be used as a bridge to transplantation or as palliative therapy in advanced RVF/PAH and has a role in third world countries in which pulmonary vasodilators are not available. Mortality associated with BAS is low (approximately 5%), particularly in experienced centers, however spontaneous closure of the defect often necessitates repeating the procedure. Contraindications of BAS include high RAP (greater than 20 mmHg), oxygen saturation less than 90% on room air, severe RVF requiring cardiorespiratory support, PVRI greater than 55 U/m and LV end-diastolic pressure greater than 18 mmHg.
Cardiac resynchronization therapy (CRT) restores mechanical synchrony in the failing LV, leading to improved hemodynamics and reverse remodeling and improved morbidity and mortality in LVF. Animal studies and small case series suggest that RV pacing results in acute hemodynamic improvement in patients with RVF in the setting of PAH, however, no data show long-term clinical benefit in this population.
Ultimately, heart, lung, or combined heart-lung transplantation (HLT) is the treatment of last-resort for end-staged RVF. In patients with RVF due to PAH, RAP greater than 15 and CI less than 2.0 are poor prognostic indicators and referral for transplantation is indicated. It remains unclear at which point the RV is beyond recovery, however, in general, the RV is resilient, and most often lung transplant alone is sufficient with estimated 1-year-survival of 65% to 75% and 10-year survival of 45% to 66%.
Congenital patients with RVF in the setting of Eisenmenger syndrome may undergo lung transplantation with repair of simple shunts (ASDs) at the time of surgery or combined HLT, which has demonstrated a survival benefit in this population.
- Differential Diagnosis
- Community-Acquired pneumonia (CAP)
- Goodpasture syndrome
- Idiopathic pulmonary fibrosis (IPF)
- Interstitial (Nonidiopathic) Pulmonary fibrosis
- Myocardial infarction
- Nephrotic syndrome
- Neurogenic pulmonary edema
- Pneumothorax imaging
- Respiratory failure
- Venous insufficiency
- Viral pneumonia
- Enhancing Healthcare Team Outcomes
Right heart failure is a systemic disorder that can affect many organs and hence is best managed by an interprofessional team. The outcomes of patients with RVF is worse than those with LVF, but it does depend on the cause and other comorbidities. Patients with persistently elevated pulmonary artery pressures have the worst outcomes. Many of these patients require repeat admissions and also have prolonged stays. Despite the various therapies for RVF, the outcomes have not greatly improved over the past two decades. While heart transplant is the ideal treatment for patients with no lung pathology, the shortage of donors is a limiting factor. [11] (Level V)
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Stacy Mandras declares no relevant financial relationships with ineligible companies.
Disclosure: Sapna Desai declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Mandras SA, Desai S. Right Heart Failure. [Updated 2023 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Right Heart Failure - StatPearls Right Heart Failure - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic
RELATED TOPICS
INTRODUCTION
This topic will address unique aspects of pathophysiology, clinical manifestation, and diagnosis of RHF. Evaluation of the cause and management of RHF are discussed separately. (See "Right heart failure: Causes and management" .)
Other aspects of HF are discussed separately, including the diagnosis and evaluation of HF, management of HF with reduced ejection fraction (HFrEF), and management of HF with preserved ejection fraction (HFpEF). (See "Heart failure: Clinical manifestations and diagnosis in adults" and "Determining the etiology and severity of heart failure or cardiomyopathy" and "Overview of the management of heart failure with reduced ejection fraction in adults" and "Heart failure with preserved ejection fraction: Clinical manifestations and diagnosis" and "Treatment and prognosis of heart failure with preserved ejection fraction" .)
PREVALENCE AND DEMOGRAPHICS

Evaluation and Management of Right-Sided Heart Failure
- There are diverse causes of right-sided heart failure (RHF) with associated increased morbidity and mortality.
- This paper reviews those causes and the epidemiology of right ventricular dysfunction and the pathophysiology of acute and chronic RHF.
- This scientific statement provides guidance on the assessment and management of RHF.
AHA Scientific Statement: Evaluation and Management of Right sided Heart Failure
Larry Allen interviews Marvin Konstam and Michael Kiernan about this new AHA Scientific Statement.
Supporting Materials
- Commentary: Taking the Good With the Bad – Assigning Value and Blame to the Right Heart in Cardiovascular Disease by Jason N. Katz, MD, MHS
- Top Things to Know: Evaluation and Management of Right-Sided Heart Failure
Recommended Reading
- 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure
- Chronic Heart Failure in Congenital Heart Disease
- 2013 ACCF/AHA Guideline for the Management of Heart Failure
- Recommendations for the Use of Mechanical Circulatory Support: Device Strategies and Patient Selection
- Forecasting the Impact of Heart Failure in the United States
Related Resources
- Guidelines & Statements
- Patient Care & Health Information
- Diseases & Conditions
- Heart failure
Heart failure occurs when the heart muscle doesn't pump blood as well as it should. When this happens, blood often backs up and fluid can build up in the lungs, causing shortness of breath.
Certain heart conditions gradually leave the heart too weak or stiff to fill and pump blood properly. These conditions include narrowed arteries in the heart and high blood pressure.
Proper treatment may improve the symptoms of heart failure and may help some people live longer. Lifestyle changes can improve quality of life. Try to lose weight, exercise, use less salt and manage stress.
But heart failure can be life-threatening. People with heart failure may have severe symptoms. Some may need a heart transplant or a device to help the heart pump blood.
Heart failure is sometimes called congestive heart failure.
Products & Services
- A Book: Future Care
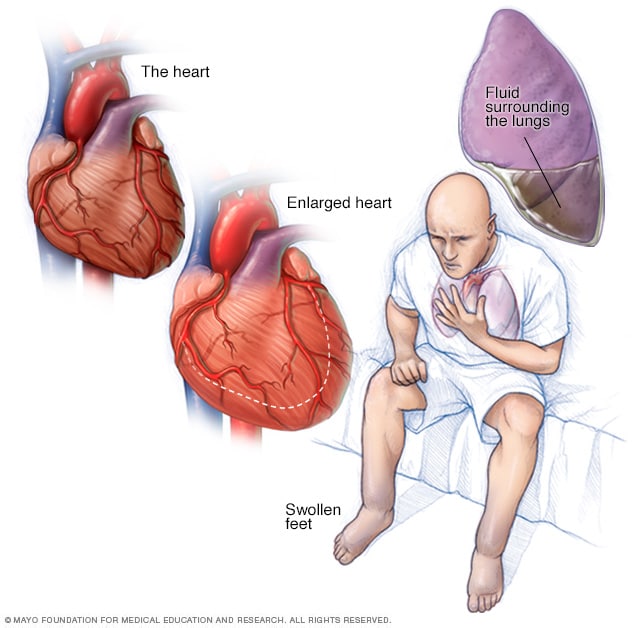
Heart failure occurs when the heart muscle doesn't pump blood as well as it should. Blood often backs up and causes fluid to build up in the lungs and in the legs. The fluid buildup can cause shortness of breath and swelling of the legs and feet. Poor blood flow may cause the skin to appear blue or gray. Depending on your skin color, these color changes may be harder or easier to see. Some types of heart failure can lead to an enlarged heart.
If you have heart failure, your heart can't supply enough blood to meet your body's needs.
Symptoms may develop slowly. Sometimes, heart failure symptoms start suddenly. Heart failure symptoms may include:
- Shortness of breath with activity or when lying down.
- Fatigue and weakness.
- Swelling in the legs, ankles and feet.
- Rapid or irregular heartbeat.
- Reduced ability to exercise.
- A cough that doesn't go away or a cough that brings up white or pink mucus with spots of blood.
- Swelling of the belly area.
- Very rapid weight gain from fluid buildup.
- Nausea and lack of appetite.
- Difficulty concentrating or decreased alertness.
- Chest pain if heart failure is caused by a heart attack.
When to see a doctor
See your health care provider if you think you might have symptoms of heart failure. Call 911 or emergency medical help if you have any of the following:
- Chest pain.
- Fainting or severe weakness.
- Rapid or irregular heartbeat with shortness of breath, chest pain or fainting.
- Sudden, severe shortness of breath and coughing up white or pink, foamy mucus.
These symptoms may be due to heart failure. But there are many other possible causes. Don't try to diagnose yourself.
At the emergency room, health care providers do tests to learn if your symptoms are due to heart failure or something else.
Call your health care provider right away if you have heart failure and:
- Your symptoms suddenly become worse.
- You develop a new symptom.
- You gain 5 pounds (2.3 kilograms) or more within a few days.
Such changes could mean that existing heart failure is getting worse or that treatment isn't working.
More Information
Heart failure care at Mayo Clinic
- Cardiac asthma: What causes it?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
Get the latest heart transplant-related health information from Mayo Clinic.
Sign up for free, and receive heart transplant and heart failure content, plus expertise on heart health.
Error Select a location
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing
You will receive the first heart failure and transplantation email in your inbox shortly. When seeking answers, people often look to experts for clear and accurate information. By subscribing to heart failure content from Mayo Clinic, you have taken an important first step in gaining knowledge and using it for your overall health and well-being.
If you don't receive our email within 5 minutes, check your SPAM folder, then contact us at [email protected] .
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
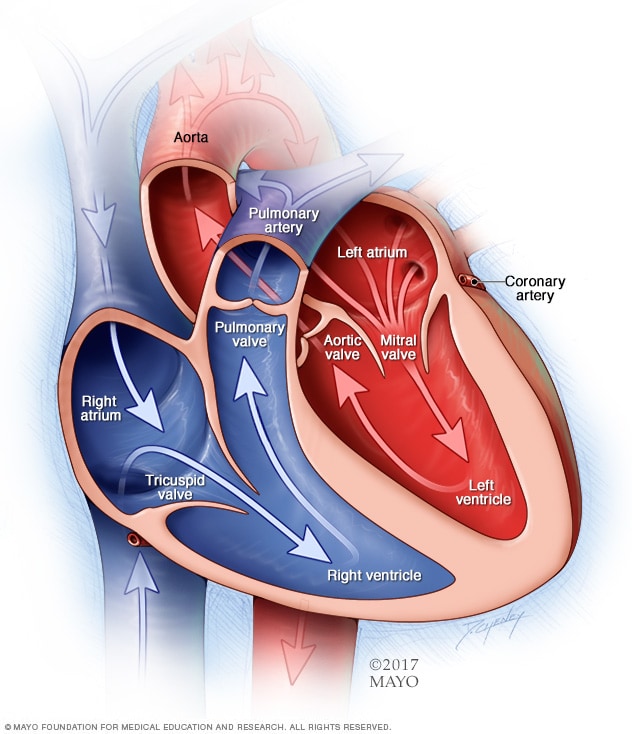
Chambers and valves of the heart
A typical heart has two upper and two lower chambers. The upper chambers, the right and left atria, receive incoming blood. The lower chambers, the more muscular right and left ventricles, pump blood out of the heart. The heart valves, which keep blood flowing in the right direction, are gates at the chamber openings.
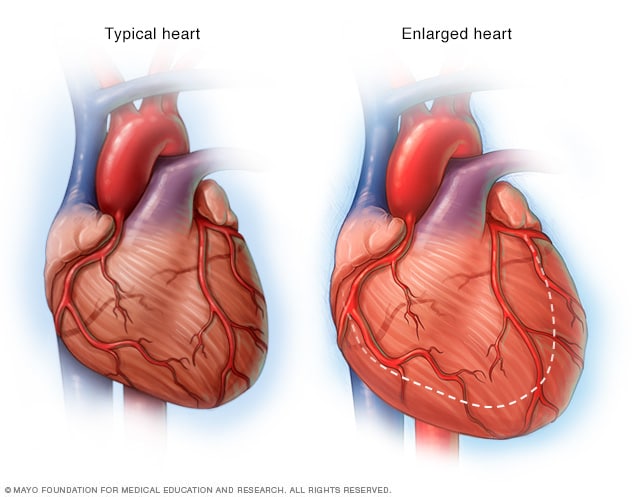
Enlarged heart, in heart failure
If the heart weakens, as it can with heart failure, it begins to enlarge. This forces the heart to work harder to pump blood to the rest of the body.
Heart failure can be caused by a weakened, damaged or stiff heart.
- If the heart is damaged or weakened, the heart chambers may stretch and get bigger. The heart can't pump out the needed amount of blood.
- If the main pumping chambers of the heart, called the ventricles, are stiff, they can't fill with enough blood between beats.
The heart muscle can be damaged by certain infections, heavy alcohol use, illegal drug use and some chemotherapy medicines. Your genes also can play a role.
Any of the following conditions also can damage or weaken the heart and cause heart failure.
Coronary artery disease and heart attack. Coronary artery disease is the most common cause of heart failure. The disease results from the buildup of fatty deposits in the arteries. The deposits narrow the arteries. This reduces blood flow and can lead to heart attack.
A heart attack occurs suddenly when an artery feeding the heart becomes completely blocked. Damage to the heart muscle from a heart attack may mean that the heart can no longer pump as well as it should.
- High blood pressure. Also called hypertension, this condition forces the heart to work harder than it should to pump blood through the body. Over time, the extra work can make the heart muscle too stiff or too weak to properly pump blood.
- Heart valve disease. The valves of the heart keep blood flowing the right way. If a valve isn't working properly, the heart must work harder to pump blood. This can weaken the heart over time. Treating some types of heart valve problems may reverse heart failure.
- Inflammation of the heart muscle, also called myocarditis. Myocarditis is most commonly caused by a virus, including the COVID-19 virus, and can lead to left-sided heart failure.
- A heart problem that you're born with, also called a congenital heart defect. If the heart and its chambers or valves haven't formed correctly, the other parts of the heart have to work harder to pump blood. This may lead to heart failure.
- Irregular heart rhythms, called arrhythmias. Irregular heart rhythms may cause the heart to beat too fast, creating extra work for the heart. A slow heartbeat also may lead to heart failure. Treating an irregular heart rhythm may reverse heart failure in some people.
- Other diseases. Some long-term diseases may contribute to chronic heart failure. Examples are diabetes, HIV infection, an overactive or underactive thyroid, or a buildup of iron or protein.
Causes of sudden heart failure also include:
- Allergic reactions.
- Any illness that affects the whole body.
- Blood clots in the lungs.
- Severe infections.
- Use of certain medicines.
- Viruses that attack the heart muscle.
Heart failure usually begins with the lower left heart chamber, called the left ventricle. This is the heart's main pumping chamber. But heart failure also can affect the right side. The lower right heart chamber is called the right ventricle. Sometimes heart failure affects both sides of the heart.
Risk factors
Diseases and conditions that increase the risk of heart failure include:
- Coronary artery disease. Narrowed arteries may limit the heart's supply of oxygen-rich blood, resulting in weakened heart muscle.
- Heart attack. A heart attack is a form of coronary artery disease that occurs suddenly. Damage to the heart muscle from a heart attack may mean the heart can no longer pump as well as it should.
- Heart valve disease. Having a heart valve that doesn't work properly raises the risk of heart failure.
- High blood pressure. The heart works harder than it has to when blood pressure is high.
- Irregular heartbeats. Irregular heartbeats, especially if they are very frequent and fast, can weaken the heart muscle and cause heart failure.
- Congenital heart disease. Some people who develop heart failure were born with problems that affect the structure or function of their heart.
- Diabetes. Having diabetes increases the risk of high blood pressure and coronary artery disease.
- Sleep apnea. This inability to breathe properly during sleep results in low blood-oxygen levels and an increased risk of irregular heartbeats. Both of these problems can weaken the heart.
- Obesity. People who have obesity have a higher risk of developing heart failure.
- Viral infections. Some viral infections can damage to the heart muscle.
Medicines that may increase the risk of heart failure include:
- Some diabetes medicines. The diabetes drugs rosiglitazone (Avandia) and pioglitazone (Actos) have been found to increase the risk of heart failure in some people. Don't stop taking these medicines without first talking to your health care provider.
- Some other medicines. Other medicines that may lead to heart failure or heart problems include nonsteroidal anti-inflammatory drugs (NSAIDs) and some medicines used to treat high blood pressure, cancer, blood conditions, irregular heartbeats, nervous system diseases, mental health conditions, lung and urinary problems, and infections.
Other risk factors for heart failure include:
- Aging. The heart's ability to work decreases with age, even in healthy people.
- Alcohol use. Drinking too much alcohol may weaken the heart muscle and lead to heart failure.
- Smoking or using tobacco. If you smoke, quit. Using tobacco increases the risk of heart disease and heart failure.
Complications
If you have health failure, it's important to have regular health checkups, even if symptoms improve. Your health care provider can examine you and run tests to check for complications.
Complications of heart failure depend on your age, overall health and the severity of heart disease. They may include:
- Kidney damage or failure. Heart failure can reduce the blood flow to the kidneys. Untreated, this can cause kidney failure. Kidney damage from heart failure can require dialysis for treatment.
- Other heart problems. Heart failure can cause changes in the heart's size and function. These changes may damage heart valves and cause irregular heartbeats.
- Liver damage. Heart failure can cause fluid buildup that puts too much pressure on the liver. This fluid backup can lead to scarring, which makes it more difficult for the liver to work properly.
- Sudden cardiac death. If the heart is weak, there is a risk of dying suddenly due to a dangerous irregular heart rhythm.
One way to prevent heart failure is to treat and control the conditions that can cause it. These conditions include coronary artery disease, high blood pressure, diabetes and obesity.
Some of the same lifestyle changes used to manage heart failure also may help prevent it. Try these heart-healthy tips:
- Don't smoke.
- Get plenty of exercise.
- Eat healthy foods.
- Maintain a healthy weight.
- Reduce and manage stress.
- Take medicines as directed.
- Heart failure. National Heart, Lung, and Blood Institute. https://www.nhlbi.nih.gov/health-topics/heart-failure. Accessed Nov. 30, 2022.
- Ferri FF. Heart failure. In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Nov. 30, 2022.
- Colucci WS. Determining the etiology and severity of heart failure or cardiomyopathy. https://www.uptodate.com/contents/search. Accessed Nov. 30, 2022.
- Colucci WS. Evaluation of the patient with suspected heart failure. https://www.uptodate.com/contents/search. Accessed Nov. 30, 2022.
- Heart failure (HF). Merck Manual Professional Version. https://www.merckmanuals.com/professional/cardiovascular-disorders/heart-failure/heart-failure-hf. Accessed Nov. 28, 2022.
- Vasan RS, et al. Epidemiology and causes of heart failure. https://www.uptodate.com/contents/search. Accessed Nov. 28, 2022.
- Goldman L, et al., eds. Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Nov. 28, 2022.
- AskMayoExpert. Heart failure with reduced ejection fraction (HFrEF) (adult). Mayo Clinic; 2022.
- Rakel D, ed. Heart failure. In: Integrative Medicine. 4th ed. Elsevier; 2018. https://www.clinicalkey.com. Accessed Nov. 28, 2022.
- AskMayoExpert. Heart failure with preserved ejection fraction (HFpEF) (adult). Mayo Clinic; 2022.
- Allen L. Palliative care for patients with advanced heart failure: Decision support, symptom management, and psychosocial assistance. https://www.uptodate.com/contents/search. Accessed Nov. 28, 2022.
- The dying patient. Merck Manual Professional Version. http://www.merckmanuals.com/professional/special-subjects/the-dying-patient/the-dying-patient. Accessed Nov. 28, 2022.
- Ami TR. Allscripts EPSi. Mayo Clinic. Oct. 4, 2022.
- Mancini D. Heart transplantation in adults: Indications and contraindications. https://www.uptodate.com/contents/search. Accessed Nov. 28, 2022.
- Sawalha K, et al. Systematic review of COVID-19 related myocarditis: Insights on management and outcome. Cardiovascular Revascularization Medicine. 2021; doi:10.1016/j.carrev.2020.08.028.
- Armstrong PW, et al. Vericiguat in patients with heart failure and reduced ejection fraction. The New England Journal of Medicine. 2020; doi:10.1056/NEJMoa1915928.
- Armstrong PW, et al. A multicenter, randomized, double-blind, placebo-controlled trial of the efficacy and safety of the oral soluble guanylate cyclase stimulator. Journal of the American College of Cardiology: Heart Failure. 2018; doi:10.1016/j.jchf.2017.08.013.
- Verquvo (approval letter). New Drug Application 214377. U.S. Food and Drug Administration. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=214377. Accessed Nov. 28, 2022.
- Heidenreich PA, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022; doi:10.1161/CIR.0000000000001063.
- Clarke JD, et al. Effect of inotropes on patient-reported health status in end-stage heart failure: A review of published clinical trials. Circulation: Heart Failure. 2021; doi:10.1161/CIRCHEARTFAILURE.120.007759.
- Lopez-Jimenez F (expert opinion). Mayo Clinic. Dec. 2, 2021.
- Types of heart failure. American Heart Association. https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/types-of-heart-failure. Accessed Nov. 28, 2022.
- Zannad F, et al. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: a meta-analysis of the EMPEROR-Reduced and DAPA-HF trials. Lancet. 2020; doi:10.1016/S0140-6736(20)31824-9.
- Sodium-glucose cotransporter-2 (SGLT2) inhibitors. U.S. Food and Drug Administration. https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/sodium-glucose-cotransporter-2-sglt2-inhibitors. Accessed Jan. 10, 2022.
- Lee MCH, et al. Clinical efficacy of SGLT2 inhibitors with different SGLT1/SGLT2 selectivity in cardiovascular outcomes among patients with and without heart failure: A systematic review and meta-analysis of randomized trials. Medicine (Baltimore). 2022; doi:10.1097/MD.0000000000032489.
- Mankad R (expert opinion). Mayo Clinic. Jan. 12, 2023.
- ACC, AHA, HFSA issue heart failure guideline. American Heart Association. https://newsroom.heart.org/news/acc-aha-hfsa-issue-heart-failure-guideline. Accessed Jan. 31, 2023.
- Heart failure action plan
- Heart failure and sex: Is it safe?
- Holiday Heart
Associated Procedures
- Cardiac catheterization
- Chest X-rays
- Coronary angiogram
- Coronary artery bypass surgery
- Echocardiogram
- Electrocardiogram (ECG or EKG)
- Heart transplant
- Implantable cardioverter-defibrillators (ICDs)
- Palliative care
- Stress test
- Ventricular assist device

News from Mayo Clinic
- Hope beyond heart failure: Innovative treatment allows woman to change the course of her heart failure April 17, 2023, 04:30 p.m. CDT
- Heart failure induces cardiac and stem cell aging, Mayo Clinic study finds March 22, 2023, 02:30 p.m. CDT
- AI transforms smartwatch ECG signals into a diagnostic tool for heart failure Nov. 14, 2022, 05:26 p.m. CDT
- Mayo Clinic Q&A podcast: Reducing the risk of heart failure Oct. 07, 2022, 12:30 p.m. CDT
- Mayo Clinic Healthcare expert shares heart failure signs, risk factors people may not be aware of Aug. 10, 2022, 02:00 p.m. CDT
- Mayo Clinic Minute: Left ventricular failure -- the silent condition that could be fatal May 02, 2022, 04:45 p.m. CDT
- Mayo researchers use AI to detect weak heart pump via patients' Apple Watch ECGs May 02, 2022, 04:00 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Cardiology & Heart Surgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
EMCrit RACC
Online Medical Education on Emergency Department (ED) Critical Care, Trauma, and Resuscitation
EMCrit 272 – Right Heart Failure with Sara Crager
April 29, 2020 by Scott Weingart, MD FCCM 25 Comments

Additional New Information
More on emcrit.
Right Ventricular failure (Opens in a new browser tab)
Eight pearls for the crashing patient with massive PE (Opens in a new browser tab)
Additional Resources
You Need an EMCrit Membership to see this content . Login here if you already have one.
- Recent Posts
- EMCrit 372 – FoundStab Intubation SOP - April 5, 2024
- EMCrit RACC-Lit Review – March 2024 - March 28, 2024
- EMCrit 371 – Iodinated Contrast Issues: Part 2 – Contrast Reactions - March 24, 2024
Share this:
Cite this post as:.
Scott Weingart, MD FCCM. EMCrit 272 – Right Heart Failure with Sara Crager. EMCrit Blog . Published on April 29, 2020. Accessed on April 9th 2024. Available at [https://emcrit.org/emcrit/right-heart-sara-crager/ ].
Financial Disclosures:
Dr. Scott Weingart, Course Director, reports no relevant financial relationships with ineligible companies. This episode’s speaker(s), (listed above), report no relevant financial relationships with ineligible companies.
Original Release: April 29, 2020 Date of Most Recent Review: Jan 1, 2022 Termination Date: Jan 1, 2025
You finished the 'cast, Now Join EMCrit!
As a member, you can....
- Get CME hours
- Get the On Deeper Reflection Podcast
- Support the show
- Write it off on your taxes or get reimbursed by your department
Get the EMCrit Newsletter
If you enjoyed this post, you will almost certainly enjoy our others. Subscribe to our email list to keep informed on all of the Resuscitation and Critical Care goodness.
This Post was by the EMCrit Crew , published 4 years ago. We never spam; we hate spammers! Spammers probably work for the Joint Commission.
Magic, crystal clear and very upbeat! Thank you. I think the sales of Flolan and nitric oxide will fall after this presentation!
Wow, so insightful and engaging. great listen
Dr. Crager needs to be in charge of all PowerPoint presentations for everything…ever! Thank you for breaking down a complex topic.
Wow great presentation Dr Crager. I’m speaking as an ED physician from the UK- that’s the best explanation I have ever heard about these patients in 15 years of my practice! Thank you.
Probably one of the best episode/presentation on EMCrit.
I’m blown away – perhaps the best presentation ever?
Absolutely amazing presentation! More Sara Crager! Please make her join the EMCrit team.
Thank-you Sara, Such a helpful & clear breakdown of a (usually) complex topic.
Great talk and great slides! Can’t wait for part two!
Fantastic talk. One question about vasopressors: in paediatrics we use phenylephrine to treat hypercyanotic (tet) spells, as it increases SVR more than PVR, thereby reducing the amount of right-to-left shunt. However, in this talk the opposite is suggested: that phenylephrine increases PVR more than SVR. Is this a physiologic difference between paeds and adults, or is there some other effect going on?
The choice of phenylephrine has more to do with it’s lack of inotropy. It increases SVR more than PVR, but also hypothetically will not cause infundibular spasm that can be caused by vasopressors with inotrpoic effects (epi, norepi).
https://emcrit.org/ibcc/pressors/
Great talk! Very informative and well explained!
Amazing lecture. Makes so much sense. Thank you for posting it.
is there anyway to watch the slide show in time with the podcast? i tried to do it manually but kept getting lost 🙁
Sara Crager is a legend. Where can I find more of her content?
Really wonderful talk. However one “criticism” I have would be with repeated references to “pressure that the RV must overcome.” The pressure is not an entity that is something that exists by itself and that anything needs to overcome in these scenarios, it is rather the PVR that is such a thing (whether by pulmonary vasoconstriction or resistance to flow due to elevated LAP). The pressure seen in the PA is a PRODUCT of the RV contractility producing CO and the PVR. That is why you can have high PAP with crummy (but not critically low) flow in chronic pulmonary … Read more »
Thanks for this excellent lecture. Other than ECMO, are there any tips on resuscitation once the patient is in cardiac arrest?
Never in my life, i thought i would be on the edge of my seat while listening to a story about an RV princess. 😉 Very engaging ! Thank you for the amazing talk.
I am wondering why this paragraph in the UpToDate article “Clinical presentation, evaluation, and diagnosis of the nonpregnant adult with suspected acute pulmonary embolism” contains a casual recommendation to give fluids in suspected PE with haemodynamic instability then… is there another reason a patient could be unstable besides right heart strain?
![Screenshot_2020-10-15 Clinical presentation, evaluation, and diagnosis of the nonpregnant adult with suspected acute pulmon[...].png Screenshot_2020-10-15 Clinical presentation, evaluation, and diagnosis of the nonpregnant adult with suspected acute pulmon[...].png](https://i0.wp.com/emcrit.org/wp-content/uploads/2020/10/Screenshot_2020-10-15-Clinical-presentation-evaluation-and-diagnosis-of-the-nonpregnant-adult-with-suspected-acute-pulmon-1602772756.84.png?fit=500%2C357&ssl=1)
Excellent lecture. I have gone back to it time and time again. Each pass educates a bit more.
Here is a link to a recently updated version of this talk with video and slides!
https://www.emrap.org/hd/playlist/latest/episode/rescuingthe
Great pearls I should have known before. Thanks Sara and Scott for filling the gap
Listened again for the second time. Best Right Heart lecture I have ever heard!
This lecture is phenomenal. Dr. Crager nailed it.
We are the EMCrit Project , a team of independent medical bloggers and podcasters joined together by our common love of cutting-edge care, iconoclastic ramblings, and FOAM.
Subscribe by Email
Insert/edit link.
Enter the destination URL
Or link to existing content
New Onset Heart Failure: Which Side Is It, Right or Left?
- First Online: 28 March 2020
Cite this chapter
- Christopher P. Blomberg 6 ,
- Wajih A. Syed 7 &
- Lana Tsao 8
Part of the book series: Clinical Cases in Cardiology ((CCC))
759 Accesses
Distinguishing between right and left heart failure is often difficult. Fatigue, elevated neck veins, and lower extremity edema in the setting of clear lungs should prompt suspicion for primarily right heart failure (RHF); however, these signs and symptoms are neither sensitive nor specific for RHF. The diagnosis of RHF is typically made after left-sided pathologies have been excluded, and the underlying cause of a patient’s symptoms has been identified. Unfortunately, no generalizable therapies have been proven to augment right ventricular function, rather we are limited to a few targeted interventions for specific disease processes. Maintenance of euvolemia is typically the primary goal in the treatment of RHF. Chronic RHF can also be associated with cardiorenal syndrome, congestive hepatopathy, and gastric abnormalities. RHF portends a poor prognosis and is associated with increased mortality.
- Right heart failure
- Carvallo sign
- Right ventricular heave
- Ventricular interdependence
- Cardiorenal syndrome
- Cardiohepatic syndrome
- Pulmonary vasodilators
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Gan C, Lankhaar J, Marcus J, Westerhof N, Marques K, Bronzwaer J, et al. Impaired left ventricular filling due to right-to-left ventricular interaction in patients with pulmonary arterial hypertension. Am J Physiol Heart Circ Physiol. 2006;290(4):H1528–33. https://doi.org/10.1152/ajpheart.01031.2005 .
Article CAS PubMed Google Scholar
Samsky M, Patel C, DeWald T, Smith A, Felker G, Rogers J, Hernandez A. Cardiohepatic interactions in heart failure: an overview and clinical implications. J Am Coll Cardiol. 2013;61(24):2397–405. https://doi.org/10.1016/j.jacc.2013.03.042 .
Article PubMed Google Scholar
Konstam M, Kiernan M, Bernstein D, Bozkurt B, Jacob M, Kapur N, American Heart Association Council on Clinical Cardiology, Council on Cardiovascular Disease in the Young, and Council on Cardiovascular Surgery and Anesthesia, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation. 2018;137(20):e578–622. https://doi.org/10.1161/CIR.0000000000000560 .
Mullens W, Abrahams Z. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol. 2009;53:589–96. https://doi.org/10.1016/j.jacc.2008.05.068 .
Article PubMed PubMed Central Google Scholar
Wilfried Mullens ZA. Elevated intra-abdominal pressure in acute decompensated heart failure. J Am Coll Cardiol. 2008;51(3):300–6. https://doi.org/10.1016/j.jacc.2007.09.043 .
Dixon DL, Mayne GC. Chronic elevation of pulmonary microvascular pressure in chronic heart failure reduces bi-directional pulmonary fluid flux. Eur J Heart Fail. 2013;15(4):368–75. https://doi.org/10.1093/eurjhf/hfs201 .
Townsley MI, Fu Z, Mathieu-Costello O. Pulmonary microvascular permeability. Responses to high vascular pressure after induction of pacing-induced heart failure in dogs. Circ Res. 1995;77(2):317–25. https://doi.org/10.1161/01.RES.77.2.317 .
Huang W, Kingsbury M, Turner M, Donnelly J, Sheridan DJ, Flores NA. Capillary filtration is reduced in lungs adapted to chronic heart failure: morphological and haemodynamic correlates. Cardiovasc Res. 2001;49(1):207–17. https://doi.org/10.1016/S0008-6363(00)00223-6 .
Rizkallah J, Jack M, Saeed M, Shafer L, Vo M, Tam J. Non-invasive bedside assessment of central venous pressure: scanning into the future. PLoS One. 2014;9(10):e109215. https://doi.org/10.1371/journal.pone.0109215 .
Article CAS PubMed PubMed Central Google Scholar
Dunn G, Hayes P, Breen K, Schenker S. The liver in congestive heart failure: a review. Am J Med Sci. 1973;265(3):174–89. https://doi.org/10.1097/00000441-197303000-00001 .
Myers RP, Cerini R, Sayegh R, Moreau R, Degott C, Lebrec D, Lee SS. Cardiac hepatopathy: clinical, hemodynamic, and histologic characteristics and correlations. Hepatology. 2003;37(2):393–400. https://doi.org/10.1053/jhep.2003.50062 .
Møller S, Bernardi M. Interactions of the heart and the liver. Eur Heart J. 2013;34(36):2804–11. https://doi.org/10.1093/eurheartj/eht246 .
Anton Vonk Noordegraaf BE. The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol. 2017;69(2):236–43. https://doi.org/10.1016/j.jacc.2016.10.047 .
Ryan J, Huston J, Kutty S, Hatton N, Bowman L, Tian L, et al. Right ventricular adaptation and failure in pulmonary arterial hypertension. Can J Cardiol. 2015;31(4):391–406. https://doi.org/10.1016/j.cjca.2015.01.023 .
Ronco C, Haapio M, House A, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52(19):1527–39. https://doi.org/10.1016/j.jacc.2008.07.051 .
Groenveld H, Januzzi J, Damman K, van Wijngaarden J, Hillege H, van Veldhuisen D, van der Meer P. Anemia and mortality in heart failure patients a systematic review and meta-analysis. J Am Coll Cardiol. 2008;52(10):818–27. https://doi.org/10.1016/j.jacc.2008.04.061 .
Alvarez A, Mukherjee D. Liver abnormalities in cardiac diseases and heart failure. Int J Angiol. 2011;20(3):135–42. https://doi.org/10.1055/s-0031-1284434 .
Poelzl G, Ess M, Mussner-Seeber C, Pachinger O, Frick M, Ulmer H. Liver dysfunction in chronic heart failure: prevalence, characteristics and prognostic significance. Eur J Clin Investig. 2012;42(2):153–63. https://doi.org/10.1111/j.1365-2362.2011.02573.x .
Article CAS Google Scholar
Hiew C, Collins N. Successful surgical treatment of protein-losing enteropathy complicating rheumatic tricuspid regurgitation. Heart Lung Circ. 2008;17(1):73–5. https://doi.org/10.1016/j.hlc.2006.11.004 .
Hasse M, Müller C, Damman K, Murray P, Kellum J, Ronco C, McCullough P. Pathogenesis of cardiorenal syndrome type 1 in acute decompensated heart failure: workgroup statements from the eleventh consensus conference of the Acute Dialysis Quality Initiative (ADQI). Contrib Nephrol. 2013;182:99–116. https://doi.org/10.1159/000349969 .
Article Google Scholar
Harjola V, et al. Contemporary management of acute right ventricular failure: a statement from the Heart Failure Association and the Working Group on Pulmonary Circulation and Right Ventricular Function of the European Society of Cardiology. Eur J Heart Fail. 2016;18(3):226–41. https://doi.org/10.1002/ejhf.478 .
Troughton R, Prior D, Pereira J, Martin M, Fogarty A, Morehead A, et al. Plasma B-type natriuretic peptide levels in systolic heart failure: importance of left ventricular diastolic function and right ventricular systolic function. J Am Coll Cardiol. 2004;43(3):416–22. https://doi.org/10.1016/j.jacc.2003.08.046 .
Mariano-Goulart D, Eberlé M, Boudousg V, Hejazi-Moughari A, Piot C, Caderas de Kerleau C, et al. Major increase in brain natriuretic peptide indicates right ventricular systolic dysfunction in patients with heart failure. Eur J Heart Fail. 2003;5(4):481–8. https://doi.org/10.1016/s1388-9842(03)00041-2 .
Benza R, Gomberg-Maitland M, Miller D, Frost A, Frantz R, Foreman A, et al. The REVEAL Registry risk score calculator in patients newly diagnosed with pulmonary arterial hypertension. Chest. 2012;141(2):354–62. https://doi.org/10.1378/chest.11-0676 .
Yancy C, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62(16):e147–239. https://doi.org/10.1016/j.jacc.2013.05.019 .
Forfia PR, Fisher MR, Mathai SC, Housten-Harris T, Hemnes AR, Borlaug BA, et al. Tricuspid annular displacement predicts survival in pulmonary hypertension. Am J Respir Crit Care Med. 2006;174(9):1034–41. https://doi.org/10.1164/rccm.200604-547OC .
Galea N, Carbone I. Right ventricular cardiovascular magnetic resonance imaging: normal anatomy and spectrum of pathological findings. Insights Imaging. 2013;4(2):213–23. https://doi.org/10.1007/s13244-013-0222-3 .
Ameri P, Bertero E, Meliota G, Cheli M, Canepa M, Brunelli C, Balbi M. Neurohormonal activation and pharmacological inhibition in pulmonary arterial hypertension and related right ventricular failure. Heart Fail Rev. 2016;21(5):539–47. https://doi.org/10.1007/s10741-016-9566-3 .
Vaillancourt M, Chia P, Sarji S, Nguyen J, Hoffman N, Ruffenach G, et al. Autonomic nervous system involvement in pulmonary arterial hypertension. Respir Res. 2017;18(1):201. https://doi.org/10.1186/s12931-017-0679-6 .
Alajaji W, Baydoun A, Al-Kindi S, Henry L, Hanna M, Oliveira G. Digoxin therapy for cor pulmonale: a systematic review. Int J Cardiol. 2016;223:320–4. https://doi.org/10.1016/j.ijcard.2016.08.018 .
Nishimura RA, Otto CM, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease. J Am Coll Cardiol. 2014;63(22):57–185. Retrieved 2019.
Download references
Author information
Authors and affiliations.
Division of Cardiovascular Medicine, Southern Maine Health Care - MaineHealth, Biddeford, ME, USA
Christopher P. Blomberg
Division of Cardiovascular Medicine, Kaiser Permanente, Roseville, CA, USA
Wajih A. Syed
Division of Cardiovascular Medicine, Steward St. Elizabeth’s Medical Center/Tufts University School of Medicine, Boston, MA, USA
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Lana Tsao .
Editor information
Editors and affiliations.
St. Elizabeth’s Medical Center, Boston, MA, USA
Maine Medical Center, Portland, ME, USA
Maxwell E. Afari
Rights and permissions
Reprints and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Blomberg, C.P., Syed, W.A., Tsao, L. (2020). New Onset Heart Failure: Which Side Is It, Right or Left?. In: Tsao, L., Afari, M. (eds) Clinical Cases in Right Heart Failure. Clinical Cases in Cardiology. Springer, Cham. https://doi.org/10.1007/978-3-030-38662-7_2
Download citation
DOI : https://doi.org/10.1007/978-3-030-38662-7_2
Published : 28 March 2020
Publisher Name : Springer, Cham
Print ISBN : 978-3-030-38661-0
Online ISBN : 978-3-030-38662-7
eBook Packages : Medicine Medicine (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
When addressing heart failure, most commonly, the left ventricle (LV) is the topic of discussion, and the right heart overlooked. However, the right ventricle (RV) is unique in structure and function and is affected by a set of disease processes that rival that of the LV. This article will review the normal structure and function of the RV, describe the pathophysiology of RV failure (RVF), and ...
INTRODUCTION. Right heart failure (RHF) is a clinical syndrome in which symptoms and signs are caused by dysfunction of the right heart structures (predominantly the right ventricle [RV], but also the tricuspid valve apparatus and right atrium) or impaired vena cava flow, resulting in impaired ability of the right heart to perfuse the lungs at ...
INTRODUCTION. Right heart failure (RHF) is a clinical syndrome in which symptoms and signs are caused by dysfunction of the right heart structures (predominantly the right ventricle [RV] but also the tricuspid valve apparatus and right atrium) or pericardium, resulting in impaired ability of the right heart to perfuse the lungs at normal ...
Right-Sided Heart Failure. In right-sided heart failure, the heart's right ventricle is too weak to pump enough blood to the lungs. As blood builds up in the veins, fluid gets pushed out into the tissues in the body. Right-sided heart failure symptoms include swelling and shortness of breath. Treatment focuses on stopping progression of the ...
The authors discuss the mechanisms, clinical presentation, and evaluation of right ventricular failure, ... Bernstein D, et al. Evaluation and management of right-sided heart failure: a scientific ...
Left sided heart failure is the primary cause of right sided heart failure. When the left ventricle is not working as effectively, fluid pressure increases and ends up moving back through the lungs.
Background and Purpose: The diverse causes of right-sided heart failure (RHF) include, among others, primary cardiomyopathies with right ventricular (RV) involvement, RV ischemia and infarction, volume loading caused by cardiac lesions associated with congenital heart disease and valvular pathologies, and pressure loading resulting from pulmonic stenosis or pulmonary hypertension from a ...
Right heart failure accounts for significant morbidity and mortality in the world. The list of conditions that cause right ventricular (RV) dysfunction that can progress to significant right heart failure are many, and these causes are often different from the conditions that cause classic, predominantly left-sided heart failure. Solid-organ replacement by heart or heart-lung transplantation ...
In older children, left-sided venous congestion causes tachypnea, respiratory distress, and wheezing (cardiac asthma). Right-sided congestion may result in hepatosplenomegaly, jugular venous distention, edema, ascites, and/or pleural effusions. Uncompensated heart failure in older children may cause fatigue or lower-than-usual energy levels.
Right-sided HF, which can cause or worsen pulmonary hypertension and left-sided HF, is defined as a structural or functional abnormality of the right heart circulatory sys-tem that impedes blood delivery to the pul-monary system or elevates venous pressures at rest or with exercise. Right ventricular dysfunc-tion is the terminology used when a ...
Causes of right heart failure. The causes of RHF can be divided broadly into three categories: secondary to pulmonary hypertension; RV and tricuspid valve pathology; and diseases of the pericardium. Pulmonary hypertension (PH) is the most common cause of RHF (Table 1). The commonest cause of pulmonary hypertension is left-sided heart failure.
There are diverse causes of right-sided heart failure (RHF) with associated increased morbidity and mortality. This paper reviews those causes and the epidemiology of right ventricular dysfunction and the pathophysiology of acute and chronic RHF. This scientific statement provides guidance on the assessment and management of RHF.
Heart failure usually begins with the lower left heart chamber, called the left ventricle. This is the heart's main pumping chamber. But heart failure also can affect the right side. The lower right heart chamber is called the right ventricle. Sometimes heart failure affects both sides of the heart.
Pleural effu- sions are frequent in the presence of severe HF, particu- larly when pulmonary and systemic venous pressures are both elevated. Konstam et al Evaluation and Management of Right-Sided Heart Failure. Circulation.2018;137:e578-e622. DOI: 10.1161/CIR.0000000000000560 May 15, 2018e597.
Right-sided heart failure (RHF) and tricuspid regurgitation (TR) ... Clinical presentation and course. Right HF and TR are debilitating conditions strongly affecting quality of life, hospitalization rates and survival. 38 They can be considered as parts of a multi-organ syndrome involving cardiac ...
We did an amazing episode on EMCrit with Susan Wilcox on Right Heart Failure. However, this oft neglected ventricle deserves even more coverage giving how pesky it can be when it fails. So we brought Sara Crager, MD to Stony Brook to give Grand Rounds. You are going to love this lecture. Part 2 is a Q&A and will be released as a separate episode.
Overview. Right-sided heart failure means that the right side of the heart is not pumping blood to the lungs as well as normal. Most people develop heart failure because of a problem with the left ventricle. But reduced function of the right ventricle can also occur in heart failure. Right-sided heart failure can happen if there is high blood ...
Left sided heart failure is more common, and right sided heart failure usually occurs as a result of left sided heart failure. Certain conditions, such as CAD and high blood pressure, have close ...
Clinical Pearls. Right heart failure is most commonly caused by left heart disease. The right ventricle can adapt to volume overload better than pressure overload. Assessment of right ventricular failure requires a careful history and physical examination as well as a high index of suspicion.