

Essay on Vitamins
Students are often asked to write an essay on Vitamins in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Vitamins
What are vitamins.
Vitamins are tiny helpers in our body that make sure we stay healthy. They help our body grow, heal, and even turn food into energy. We need to eat foods that have vitamins because our body cannot make enough of them on its own.
Types of Vitamins
There are two main types of vitamins: fat-soluble and water-soluble. Fat-soluble vitamins, like A, D, E, and K, get stored in our body’s fat. Water-soluble vitamins, like C and all the B vitamins, need to be taken in every day because our body doesn’t store them.
Why Vitamins Matter
Vitamins are essential for keeping our body working properly. They help us see in the dark, fight off colds, and keep our bones strong. Without enough vitamins, our body can get sick and not work the way it should.
250 Words Essay on Vitamins
What are vitamins.
Vitamins are a group of nutrients that our body needs to function properly. They help us to utilize the food we eat, turn food into energy, keep our immune system healthy, and protect cells from being damaged. Vitamins are classified as either water-soluble or fat-soluble. Water-soluble vitamins (vitamin C and B vitamins) are not stored in the body and need to be consumed daily. Fat-soluble vitamins (vitamins A, D, E, and K) are stored in the liver and fat tissues and can be stored for long periods.
Where can we find Vitamins?
Vitamins can be found in a variety of foods like fruits, vegetables, whole grains, meat, and fish. Different vitamins are found in different foods, so it is essential to eat a variety of foods to make sure we get all the vitamins our body needs. If we don’t get enough vitamins from our diet, we can take vitamin supplements. However, it is usually better to get vitamins from food because it is more natural and less likely to cause side effects.
What happens if we don’t get enough Vitamins?
If we don’t get enough vitamins, we can develop vitamin deficiency diseases. For example, vitamin C deficiency can cause scurvy, vitamin D deficiency can cause rickets, and vitamin A deficiency can cause night blindness. Vitamin deficiency diseases can be serious, so it is essential to make sure we get enough vitamins from our diet.
Vitamins are essential nutrients that our body needs to function properly. We can get vitamins from a variety of foods, and it is essential to eat a variety of foods to make sure we get all the vitamins our body needs.
500 Words Essay on Vitamins
Vitamins are substances that our bodies need to function properly. They help us grow, develop, and stay healthy. Vitamins can be found in the foods we eat. There are two main types of vitamins: water-soluble vitamins and fat-soluble vitamins.
Water-Soluble Vitamins
Water-soluble vitamins are vitamins that dissolve in water. They include vitamin C and the B vitamins. Water-soluble vitamins are not stored in the body, so we need to eat foods that contain them every day.
Fat-Soluble Vitamins
Fat-soluble vitamins are vitamins that dissolve in fat. They include vitamins A, D, E, and K. Fat-soluble vitamins are stored in the body, so we do not need to eat foods that contain them every day.
Functions of Vitamins
Vitamins have many different functions in the body. Some vitamins help us to see, while others help us to fight infection. Some vitamins help us to grow, while others help us to produce energy. Vitamins are essential for good health, and a deficiency of any vitamin can lead to health problems.
Sources of Vitamins
The best way to get vitamins is to eat a healthy diet that includes a variety of foods. Fruits, vegetables, and whole grains are all good sources of vitamins. Meat, fish, and eggs are also good sources of vitamins.
Vitamin Deficiency
A vitamin deficiency is a condition that occurs when the body does not get enough of a particular vitamin. Vitamin deficiencies can be caused by a number of factors, including a poor diet, certain medical conditions, and medications. Vitamin deficiencies can lead to a variety of health problems, including fatigue, weakness, and skin problems.
Vitamins are essential for good health. We can get the vitamins we need by eating a healthy diet that includes a variety of foods.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Visit To A Strange Place
- Essay on Visit To A Beach
- Essay on Vision In Life As A Student
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Vitamins and Dietary Supplement Essay
Examples of vitamins examples of minerals, works cited.
This is the time of when it pays to be health conscious. In the pre-modern age there was no need to be extra careful in what one eats. But in the 21 st century a less vigilant person can be in deep trouble because changes in the atmosphere and the availability of food an easily make a person sick. This is because his system is already in need of vitamins and minerals that are no longer available in his or her diet. The solution of course is to eat vegetables, fruits and meat sources such as beef, chicken, fish and lamb that can supply the required daily allowance needed for optimum growth and repair of body tissues. But before this can be done there is a need to understand what the difference between vitamins and dietary supplements.
According to one report, “Vitamins do not share a common chemistry, but they do share certain characteristics. They are all organic nutrients that are necessary in small amounts for normal metabolism and good health” (Nidus, par. 1). Still there is still confusion when asked to compare Vitamins and dietary supplements. The capsules taken in as dietary supplements are similar looking to the vitamins in capsule forms that are also readily available in drugstores and pharmacies. Moreover, the nutritious component of fruits, vegetables and meat products are also called vitamins. It is common to hear someone say that carrots are rich in Vitamin A and that citrus fruits are rich in Vitamin C.
In order to clarify this matter there is a need to break down related concepts into the following:
- There are naturally occurring vitamins found in plant and animal sources;
- Dietary supplements are products containing vitamins, minerals, herbs etc.
According to the Dietary Supplement Health Act of 1994 dietary supplements it must be one or any combination of the following substances:
- an herb or other botanical;
- an amino acid;
- enzymes or tissues from organs or glands;
- a concentrate, metabolite, constituent or extract.
- Vitamin B 6
- VitaminB 12
There are two kinds of vitamins and dietary supplements. As far as human consumption is concerned there are two kinds of vitamins, the first type are those that can be found as naturally occurring organic nutrients that can be found in plants and animals. The second type of vitamins are those that can be manufactured by the human body such as Vitamin D, K, and B). When it comes to dietary supplements there can be also two types. The first one contains only one vitamin and the second type contains multiple ingredients that may include a vitamin, a mineral or enzymes.
Vitamins and dietary supplements can be understood from the point of view of human consumption and what is needed for healthy living. When it comes to vitamins there are those that can be manufactured by the human body. Therefore those vitamins that cannot be manufactured by the body must be acquired through the eating of fruits, vegetables and meat products. The consumption of these types of food is called the diet. Therefore those essential vitamins and minerals that are not included in the diet must be acquired using dietary supplements.
As the name implies dietary supplements is needed to supplement the diet. Whatever is missing in the daily food intake must be supplemented by dietary supplements. Depending on the need of the person the dietary supplement can contain one vitamin or a combination of vitamins, minerals, herbs, etc. This is the basic description of what constitutes a vitamin and a dietary supplement.
Nidus Information Services, Inc. “What Are Vitamins, Carotenoids and Pythochemicals?” New York City.
Nidus Information Services, Inc. “Report #39: Vitamins.” New York City.
Office of Dietary Supplements. “Vitamin and Mineral Supplement Fact Sheets.” National Institute of Health . 2009. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 10). Vitamins and Dietary Supplement. https://ivypanda.com/essays/vitamins-and-dietary-supplement/
"Vitamins and Dietary Supplement." IvyPanda , 10 Mar. 2024, ivypanda.com/essays/vitamins-and-dietary-supplement/.
IvyPanda . (2024) 'Vitamins and Dietary Supplement'. 10 March.
IvyPanda . 2024. "Vitamins and Dietary Supplement." March 10, 2024. https://ivypanda.com/essays/vitamins-and-dietary-supplement/.
1. IvyPanda . "Vitamins and Dietary Supplement." March 10, 2024. https://ivypanda.com/essays/vitamins-and-dietary-supplement/.
Bibliography
IvyPanda . "Vitamins and Dietary Supplement." March 10, 2024. https://ivypanda.com/essays/vitamins-and-dietary-supplement/.
- Dietary Supplements: Benefits, Risks, Regulation
- Dietary Supplement Smarts in the US
- The Impact of Health Supplements and Vitamins
- Healthy Nutrition: Supplements or Herbs
- Vitamin and Supplement Treatments: Good or Bad?
- Root Problems of Dietary Supplements
- Weight and Muscle Gain: Different Ways Comparison
- Chromium Dietary Supplement: Benefits, Side Effects, and Restrictions
- The Documentary "Supplements and Safety"
- Iron Supplement and Performance of Endurance Athlete
- Gas Versus Charcoal Barbeque Comparison
- Nutrition or Climate Change
- The Common Factors That Causes Bad Eating Habits
- Nutrition Education: Its Importance and Promotion
- Influence of Modelling in Teenager’s Eating Disorders
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 23 November 2021
The health effects of vitamin D supplementation: evidence from human studies
- Roger Bouillon ORCID: orcid.org/0000-0002-6446-3763 1 ,
- Despoina Manousaki 2 ,
- Cliff Rosen ORCID: orcid.org/0000-0003-3436-8199 3 ,
- Katerina Trajanoska 4 ,
- Fernando Rivadeneira ORCID: orcid.org/0000-0001-9435-9441 5 &
- J. Brent Richards 6 , 7
Nature Reviews Endocrinology volume 18 , pages 96–110 ( 2022 ) Cite this article
115k Accesses
177 Citations
237 Altmetric
Metrics details
- Endocrine system
- Endocrine system and metabolic diseases
Vitamin D supplementation can prevent and cure nutritional rickets in infants and children. Preclinical and observational data suggest that the vitamin D endocrine system has a wide spectrum of skeletal and extra-skeletal activities. There is consensus that severe vitamin D deficiency (serum 25-hydroxyvitamin D (25OHD) concentration <30 nmol/l) should be corrected, whereas most guidelines recommend serum 25OHD concentrations of >50 nmol/l for optimal bone health in older adults. However, the causal link between vitamin D and many extra-skeletal outcomes remains unclear. The VITAL, ViDA and D2d randomized clinical trials (combined number of participants >30,000) indicated that vitamin D supplementation of vitamin D-replete adults (baseline serum 25OHD >50 nmol/l) does not prevent cancer, cardiovascular events, falls or progression to type 2 diabetes mellitus. Post hoc analysis has suggested some extra-skeletal benefits for individuals with vitamin D deficiency. Over 60 Mendelian randomization studies, designed to minimize bias from confounding, have evaluated the consequences of lifelong genetically lowered serum 25OHD concentrations on various outcomes and most studies have found null effects. Four Mendelian randomization studies found an increased risk of multiple sclerosis in individuals with genetically lowered serum 25OHD concentrations. In conclusion, supplementation of vitamin D-replete individuals does not provide demonstrable health benefits. This conclusion does not contradict older guidelines that severe vitamin D deficiency should be prevented or corrected.
Vitamin D and calcium supplementation can cure nutritional rickets and can modestly decrease the risk of major fractures in older adults with poor vitamin D status or calcium intake.
Large supplementation trials recruiting vitamin D-replete adults (serum 25OHD concentration >50 nmol/l) have demonstrated no effects on the incidence of cancer, cardiovascular events or type 2 diabetes mellitus (T2DM) and no benefits in terms of bone density and the risk of falls.
Post-hoc analysis of large supplementation trials has suggested that supplementation of individuals with vitamin D deficiency modestly delays age-related bone loss and progression to T2DM, and improves lung function.
A meta-analysis suggested that vitamin D supplementation results in a modest decrease in cancer mortality.
Over 60 Mendelian randomization studies have examined causal links between genetically lower vitamin D levels and health outcomes; most studies generated null effects except four studies that demonstrated an increased risk of multiple sclerosis.
In conclusion, supplementation of vitamin D-replete individuals does not generate overall health benefits; however, correction of severe vitamin D deficiency remains essential.
Similar content being viewed by others

Vitamin D deficiency 2.0: an update on the current status worldwide
Karin Amrein, Mario Scherkl, … Oliver Malle
Absence of causal association between Vitamin D and bone mineral density across the lifespan: a Mendelian randomization study
Yanchao Tang, Feng Wei, … Xiaoguang Liu
Targeted 25-hydroxyvitamin D concentration measurements and vitamin D3 supplementation can have important patient and public health benefits
William B. Grant, Fatme Al Anouti & Meis Moukayed
Introduction
There is consensus that daily intake of 400 IU of vitamin D can prevent nutritional rickets in infants and children 1 . However, the skeletal effects of vitamin D deficiency in adults and older adults (aged >65 years), and the potential extra-skeletal effects of vitamin D are more controversial. Some people consider that vitamin D supplementation is futile 2 . By contrast, others have suggested that the vitamin D intake requirement is much higher than currently achieved by the general population and that people should aim to achieve 25-hydroxyvitamin D (25OHD, the major marker of vitamin D status) concentrations similar to those found in certain tribes in equatorial Africa with a sun exposure lifestyle that might be similar to that of early humans 3 , 4 , 5 , 6 , 7 .
The potential extra-skeletal effects of the vitamin D endocrine system (which refers to vitamin D in its active form, its precursors and metabolites, and vitamin D receptor) are based on several arguments. For example, the vitamin D receptor (VDR) and CYP27B1 (the enzyme primarily responsible for producing the active form of vitamin D, 1,25-dihydroxyvitamin D or 1,25(OH) 2 D 3 ) are widely expressed, including in tissues that are not involved in calcium or phosphate transport (Fig. 1 ). In addition, ~3% of the human and mouse genomes are under the direct or indirect control of 1,25(OH) 2 D 3 (refs 8 , 9 ). Finally, many diseases and illnesses in humans are associated with a poor vitamin D status, as measured by low serum levels of 25OHD. Therefore, one of the major clinical questions in the field is whether poor vitamin D status plays a causal role in the diseases and conditions associated with low 25OHD levels, such as cancer, impaired muscle strength and falls, and immune, metabolic or cardiovascular diseases. Furthermore, if the link is causal, the threshold serum level of 25OHD below which the risk of these diseases is increased must be identified 8 .

The potential skeletal and extra-skeletal target tissues and effects of the vitamin D endocrine system (vitamin D and vitamin D receptor) as based on preclinical and observational studies, Mendelian randomization studies and randomized controlled trials (RCTs). In vitro studies have identified many molecular and genetic targets of vitamin D action. Animal models have confirmed a variety of skeletal and extra-skeletal actions. Human observational data are largely in line with preclinical data. However, Mendelian randomization studies and RCTs have not confirmed such a widespread action profile in vitamin D-replete adults. Therefore, the health consequences of poor vitamin D status remain controversial. The strength of the relationship between the vitamin D endocrine system and health effects are indicated by the arrow thickness. FGF23, fibroblast growth factor 23; PTH, parathyroid hormone.
Up to about a decade ago, there was tremendous uncertainty about vitamin D supplementation for the maintenance of adequate health levels. Large, randomized placebo-controlled trials with clinically important outcomes and/or surrogates had yet to be performed and only a few meta-analyses of randomized controlled trials (RCTs) were available. On the other hand, many observational studies had been conducted that were confounded by multiple variables. The Institute of Medicine (IOM) guidelines were developed to provide an answer based on the best available evidence at that time 10 . The IOM Committee established minimal dosing to maintain adequate serum levels of 25OHD in young and older individuals and established the tolerable upper limits of supplementation. The Committee also examined the totality of evidence relating vitamin D supplementation to numerous outcomes, and concluded that large randomized trials were needed to establish efficacy and safety. Other societies, such as the Endocrine Society 11 , and governmental organizations also generated a variety of guidelines 12 . The minimal serum level of 25OHD that was considered to provide vitamin D sufficiency varied from 30 nmol/l (UK Scientific Advisory Committee on Nutrition 13 ), to 50 nmol/l (IOM and many other governmental guidelines) 12 , 14 , 75 nmol/l (Endocrine Society and some other societies) 11 and even >100 nmol/l (refs 12 , 14 ). Of note, serum levels of >100 nmol/l are found in people living in Africa under conditions of sun exposure supposed to be similar to that of early humans.
In this Review, we summarize the results of recent (2017–2020) RCTs as well as Mendelian randomization studies, while not reviewing observational studies, which have been well-documented previously 9 . We have chosen these two study designs because they are both types of causal inference studies and can help provide insights into the role of vitamin D in the aetiology of common diseases. The reviewed studies do not provide evidence that vitamin D supplementation prevents negative health outcomes in vitamin D-replete adults. However, all these studies reveal new suggestions for potential effects of vitamin D supplementation. Note that throughout the text vitamin D refers to vitamin D 3 unless otherwise specified.
RCTs: 2017–2020
Many small-scale RCTs have been published over the past few years. In addition, several large studies have generated a wealth of new data (Table 1 ; Supplementary Box 1 ). The new major RCTs deal with more than 35,000 study participants who have a generally better health profile than participants in older studies. These studies used higher dosages than previous studies and the volunteers were mostly vitamin D-replete at baseline. These differences might explain why these large RCTs generated mostly null results in the intention-to-treat (ITT) analysis.
The largest trial to date is the VITAL study 15 that recruited more than 25,000 adults from 44 centres in the USA and evaluated daily doses (2,000 IU) of vitamin D for a mean duration of 5.3 years. The Vitamin D Assessment Study (ViDA study) 16 evaluated the effects of monthly high-dose vitamin D supplementation in more than 5,000 adults in New Zealand followed for a mean duration of 3.3 years. The primary aim of the D2d study of 2,423 US participants was to evaluate the effects of a daily dose of vitamin D (4,000 IU per day) for a mean duration of 2.5 years on the conversion of prediabetes to type 2 diabetes mellitus (T2DM) 17 . The DO-HEALTH study evaluated the effects of vitamin D (2,000 IU per day) in 2,157 older adults in Europe for a duration of 3 years 18 . The Calgary study was not really a megatrial, as it included only 311 Canadian adults and explored the effects on bone structure and quality and the safety of daily high-dose vitamin D (4,000 and 10,000 IU versus 400 IU) for 3 years 18 , 19 , 20 .
Mendelian randomization studies
Mendelian randomization is an established genetic epidemiological method, which can be used to test whether genetically decreased 25OHD levels are associated with increased risk of disease. To do this, Mendelian randomization uses single nucleotide polymorphisms (SNPs) that are associated with 25OHD levels in genome-wide association studies (GWAS) as instruments to infer 25OHD levels. Depending on their number, these SNPs can explain from 2% to 10% of the variance in 25OHD levels. This approach offers an alternative analytical technique able to reduce bias from confounding and reverse causation present in observational studies and re-estimates observations in a framework enabling causal inference (Supplementary Box 2 ). The very large number of Mendelian randomization studies of vitamin D have also generated mostly null results; however, they have been handicapped by the low power to predict decreased serum 25OHD concentrations.
Effects of vitamin D on health outcomes
Many observational studies suggest a link between low vitamin D status and T2DM 9 .
Evidence from RCTs
In the large D2d RCT of patients with prediabetes (Table 1 ), vitamin D supplementation only showed a non-significant trend to slow down the progression of prediabetes into T2DM. The study design intentionally included people with a high risk of progression to T2DM, who received vitamin D (4,000 IU per day). In the ITT analysis, the hazard ratio for the development of T2DM in the group receiving vitamin D was 0.88 (95% CI 0.75–1.04; P = 0.12) compared with the placebo group. In a post hoc analysis, however, a significant effect was observed in individuals with a baseline BMI below 30 mg/m 2 , severe vitamin D deficiency at baseline, perfect adherence to treatment during the study or serum 25OHD above 100 nmol/l throughout the study 21 (Tables 2 , 3 ). Analysis of the combined data from the D2d trial and two other trials specifically designed and conducted to investigate the effectiveness of vitamin D supplementation in preventing T2DM showed that vitamin D supplementation (when compared with placebo) reduced the risk of developing T2DM from 23% to 13% (a 10% reduction) in persons with prediabetes not selected for vitamin D deficiency 22 . This finding is in line with two meta analyses published in 2020 dealing with eight 23 and seven 24 RCTs in people with prediabetes. These meta-analyses concluded that vitamin D supplementation decreased the risk to progress to T2DM by about 10%, especially when using doses above 1,000 IU per day and in participants without obesity. Participant-level meta-analysis of these trials might provide a better estimate of risk reduction and identify populations of patients with prediabetes who are likely to benefit the most from vitamin D supplementation.
Evidence from Mendelian randomization
Since 2015, seven large Mendelian randomization studies have investigated the causal effect of genetically altered 25OHD levels on risk of T2DM and related traits (Supplementary Box 3 ). These Mendelian randomization studies included very large numbers of participants and mostly recruited white individuals and Chinese individuals. One study 25 generated conflicting results, as part of the study using only two SNPs concluded that high predicted serum levels of 25OHD protected against T2DM (OR 0.86 of T2DM for a 25 nmol/l higher 25OHD concentration than that seen in the general population). However, in a slightly larger group of the same study that included two additional SNPs, the odds ratio became insignificant (Supplementary Box 3 ). All the other Mendelian randomization studies, including more than 500,000 volunteers, did not find a significant odds ratio for the relationship between predicted 25OHD and risk of T2DM.
Vitamin D and T2DM — summary
Although observational data have consistently confirmed lower serum 25OHD concentrations in patients with T2DM or the metabolic syndrome 9 , most Mendelian randomization studies have not supported these conclusions. Importantly, the large D2d RCT only showed a non-significant trend to slow down the progression of prediabetes into T2DM. In a small subgroup of individuals with overweight (rather than obesity) and prediabetes, supplementation provided some modest benefit, albeit lower than lifestyle modifications or metformin 26 . Furthermore, analysis of the combined results of the D2d trial and two other trials showed that vitamin D supplementation reduced the risk of developing T2DM in people with prediabetes not selected for vitamin D deficiency 22 . Additional studies or more in-depth analysis of the existing studies are needed to validate these findings. In summary, the evidence from large-scale Mendelian randomization studies and RCTs are convergent and do not support the use of vitamin D supplementation for the prevention of T2DM.
Strong preclinical data exist that link vitamin D with cell cycle control and cancer. Furthermore, many observational studies have associated poor vitamin D status with increased risk of cancer or poor prognosis 27 .
The largest RCT (VITAL) did not find an effect of daily vitamin D supplementation on invasive cancer incidence (HR 0.96, 95% CI 0.88–1.06) in US adults during a 5.3-year follow-up 15 . Further subanalysis (not statistically corrected for multiple comparisons) revealed a significant reduction in cancer risk in individuals with a normal BMI (<25 kg/m 2 ) and a trend for decreased cancer risk in African Americans. Baseline serum 25OHD concentrations did not influence cancer incidence or mortality but the number of participants with vitamin D deficiency at baseline (<50 nmol/l) was low (~10% of the total cohort) 28 . In the ViDA trial in New Zealand adults, monthly vitamin D supplementation did not modify cancer incidence (overall or specific types of cancer, excluding non-melanoma skin cancers) with an overall hazard ratio of 1.01 (95% CI 0.81–1.25) 16 .
Cancer mortality, as evaluated in a Cochrane systematic review 29 , was modestly decreased by vitamin D supplementation in four RCTs (44,492 participants), with a relative risk (RR) for cancer mortality of 0.88 (95% CI 0.78–0.98) in individuals receiving a mean daily dose of 1,146 IU (compared with no supplementation) during a mean follow-up of 6.3 years. Cancer mortality was also evaluated in several large RCTs (Supplementary Box 4 ). In the ITT analysis of the VITAL trial, a non-significant trend of reduction in total cancer mortality (HR 0.83, 95% CI 0.67–1.02) was observed in the vitamin D supplementation group. When excluding cancer deaths during the first year, or the first and second year after randomization, a significant reduction in cancer mortality was observed in the vitamin D supplementation group compared with no supplementation (HR 0.75, 95% CI 0.59–0.96). In a Kaplan–Meier plot, the cumulative increased risk of cancer mortality was visible from year 4 of follow-up onwards 28 . In the ViDA trial, however, the number of cancer deaths was not influenced by vitamin D supplementation (HR 0.97), even after exclusion of cancer deaths registered in the first year after randomization (HR 0.95) 16 . This discrepancy might be related to the short duration of follow-up. The ViDA trial lasted <4 years, whereas the effect of vitamin D supplementation in the VITAL study was only significant 4 years after randomization. An updated summary from the VITAL study 28 confirmed a small but significant effect on cancer death in vitamin D-supplemented individuals (HR 0.87, 95% CI 0.79–0.96; P = 0.005). As the final serum concentration of 25OHD in the VITAL trial (~110 nmol/l) and the ViDA trial (~125 nmol/l or 50 ng/ml) were in the high normal range it is unlikely that higher doses would be more effective.
The Ovarian Cancer Association Consortium (10,065 patients with ovarian cancer, 21,654 control individuals) 30 found a 27% increase in the risk of epithelial ovarian cancer per 20 nmol/l decrease in genetically determined 25OHD serum concentration (OR 1.27, 95% CI 1.06–1.51). However, the results were not corroborated by another Mendelian randomization study 31 which also showed no evidence of an association between 25OHD and risk of colorectal, breast, prostate, lung and pancreatic cancer or neuroblastoma. Similar findings were reported in a separate study 32 in relation to total incident cancer and cancer subtypes such as breast, colorectal and lung cancer in 23,294 women. A null effect of genetically determined 25OHD on colorectal carcinoma was confirmed in men and women after including two additional SNPs 33 . Similarly, a large-scale two-sample Mendelian randomization study (122,977 patients with breast cancer and 79,148 patients with prostate cancer) did not show any effects of genetically predicted 25OHD concentrations on these cancers (Supplementary Box 5 ). Evidence from Mendelian randomization also refutes a link between 25OHD concentrations with risk of oesophageal adenocarcinoma 34 , melanoma and non-melanoma skin cancer 35 (Supplementary Box 5 ).
Vitamin D and cancer — summary
No effects of vitamin D supplementation on cancer risk were observed in the large VITAL and ViDA trials. In line with prior studies and Mendelian randomization results, it thus seems clear that vitamin D supplementation in vitamin D-replete adults does not change cancer risk. However, a subanalysis of the VITAL trial showed that vitamin D supplementation might have some minor benefits in individuals with a normal BMI, but this finding was not corrected for multiple end point analysis 15 . In addition, several independent trials have suggested, in post hoc analysis, potential benefits of vitamin D supplementation on cancer mortality, especially when the follow-up is longer than 4 years 28 (Supplementary Box 4 ). Therefore, a link between vitamin D status and cancer incidence or mortality cannot be excluded, but will be very difficult to verify. Small changes in vitamin D status are unlikely to affect cancer incidence based on several Mendelian randomization studies.
Cardiovascular events
Major cardiovascular events.
The results of any observational studies in humans are in line with preclinical data and have demonstrated a consistent association between low vitamin D status and increased risk of cardiovascular diseases, hypertension and cardiovascular events, including ischaemic cardiac events, cardiomyopathy, congestive heart failure, stroke and even cardiovascular mortality. In a meta-analysis of nearly 850,000 individuals, low serum 25OHD concentrations were associated with an increased risk of cardiovascular events (RR 1.43, comparing individuals with the lowest vitamin D status with individuals with a better vitamin D status) 36 .
Two large RCTs (VITAL and ViDA) were designed to include cardiovascular events as one of their primary end points 15 , 37 . During the 5.3 years of follow-up in the VITAL trial, the hazard ratio for the expanded composite end point of major cardiovascular events including coronary revascularization was 0.97 (95% CI 0.85–1.12) in the vitamin D supplementation group, compared with placebo. A similar hazard ratio was found for cardiovascular death (HR 1.11, 95% CI 0.88–1.40), or death from any cause. Exclusion of cardiovascular events or deaths during the first 2 years of follow-up did not change the overall results. Similarly, in the ViDA study, the primary outcome of major cardiovascular events was not influenced by monthly vitamin D supplementation over 3.3 years 37 . The adjusted hazard ratio for a combination of major cardiovascular events in the vitamin D supplementation group was 1.02 (95% CI 0.87–1.20) compared with placebo, and such null findings also applied for a large list of secondary end points (myocardial infarction, heart failure, stroke and hypertension, among others), or cardiovascular deaths. Findings were not dependent on the baseline serum 25OHD concentration or previous cardiovascular status. When the results of these two major trials (including together more than 30,000 participants) were combined with those of previous studies evaluating the potential effects of vitamin D supplementation, a similar general conclusion of no effect of vitamin D supplementation was reached. An analysis of 21 RCTs including more than 80,000 participants showed that major cardiovascular events were not influenced by vitamin D supplementation 38 . The hazard ratios for myocardial infarction, stroke or cardiovascular death were all close to 1 and the 95% confidence intervals included the null. The results are uniformly concordant despite variation in target groups, baseline vitamin D status and vitamin dosage or regimens. Furthermore, vitamin D supplementation of largely vitamin D-replete participants did not significantly reduce first or recurrent hospitalization rates for heart failure compared with no supplementation in the VITAL Heart Failure study (HR 0.93, 95% CI 0.78–1.11; non-significant).
To date, six Mendelian randomization studies have investigated the effect of genetically altered 25OHD levels on cardiovascular events and related outcomes (Supplementary Box 6 ). These studies evaluated the effects of genetically altered 25OHD concentrations (based on two to six SNPs) in more than a million European and Chinese adults and found no significant effects on any cardiovascular event or mortality 39 , 40 , 41 , 42 . A 2020 study 43 , using a substantially larger number of SNPs (242 SNPs associated with 25OHD levels adjusted for BMI, and 232 SNPs associated to 25OHD levels without adjustment for BMI), showed a non-significant odds ratio for coronary artery disease in people with genetically lowered 25OHD levels of 0.98 (95% CI −0.06–0.02) compared with those with normal or high 25OHD level in a sample of 417,580 white British individuals from the UK Biobank.
Hypertension
Observational data also link hypertension with low vitamin D status but this apparent association could have been due to many other confounding factors (for example, related to lifestyle). Causal inference studies, such as RCTs and Mendelian randomization studies, should provide insights that reduce the risk of confounding. The data on blood pressure effects of vitamin D supplementation in the VITAL trial (VITAL Hypertension) are not yet available (NCT01653678; as of October 2021). The ViDA trial, however, studied extensively the effects of vitamin D supplementation in a subgroup of participants using a state of the art invasive technology (suprasystolic oscillometry) 44 . After a mean follow-up of 1.1 years, vitamin D supplementation generated null effects. In participants with vitamin D deficiency at baseline (<50 nmol/l), brachial systolic and diastolic blood pressure decreased by 3 mmHg to 5 mmHg (not statistically significant); however, aortic systolic blood pressure (−7.5 mmHg, P = 0.03) and other parameters (augmentation index, pulse wave velocity, peak reservoir pressure and backward pressure amplitude) improved on correction of baseline vitamin D deficiency 44 . The DO-HEALTH trial in European older adults did not find any effect of vitamin D supplementation on systolic or diastolic blood pressure 18 .
The evidence from Mendelian randomization studies on the effects of predicted serum 25OHD levels on hypertension, systolic and diastolic blood pressure is consistent across five large studies, and overall does not support any of these outcomes (Supplementary Box 6 ). Specifically, a study in 146,581 European individuals 45 , using two SNPs in the two vitamin D synthesis genes showed a marginal decrease in diastolic blood pressure of 0.29 mmHg per 10% increase in 25OHD level. There was no significant effect on systolic blood pressure, and the Mendelian randomization odds ratio for hypertension was 0.92 per 10% increase in 25OHD level (95% CI 0.87–0.97). A 2019 study, using six 25OHD-related SNPs 46 , failed to show any evidence of a causal association between 25OHD levels and systolic blood pressure, diastolic blood pressure or hypertension. Finally, using up to 252 SNPs as instruments for estimating levels of 25OHD, the most recent Mendelian randomization study in this field published in 2020 (ref. 43 ) showed a marginal effect of 25OHD levels on risk of hypertension (Mendelian randomization OR 0.97 per unit increase in rank-based inverse normal-transformed 25OHD level, 95% CI 0.94–1.0) in 417,580 White British individuals from UK Biobank. After adjusting for BMI, this association became non-significant. In non-European populations, Mendelian randomization results thus far are consistent with those in Europeans. Specifically, a Mendelian randomization study 47 on 2,591 Korean adults failed to show any causal effect of 25OHD levels on systolic blood pressure, diastolic blood pressure or risk of hypertension. A Mendelian randomization study 48 in 10,655 Chinese individuals showed equally a null effect of 25OHD on systolic and diastolic blood pressure.
Vitamin D and cardiovascular disease — summary
In summary, convergent evidence from Mendelian randomization studies and RCTs demonstrates that vitamin D supplementation does not decrease the risk of cardiovascular disease. The link between vitamin D status and a variety of cardiovascular events or risk factors was tested previously in mostly small-scale studies. The 2017–2020 megatrials (Table 1 ) and Mendelian randomization studies clearly confirm the lack of benefit of vitamin D supplementation in vitamin D-replete adults. This conclusion most likely also applies to people with vitamin D deficiency as based on subgroup analyses of the VITAL and ViDA trials. Unfortunately, both studies recruited very few participants with severe vitamin D deficiency. A dedicated detailed analysis of the ViDA trial suggested some modest benefits on central (but not peripheral) blood pressure, but the implications of this observations are limited in view of the small scale of this ViDA substudy 44 .
Musculoskeletal effects and falls
Vitamin d and bone health.
Severe vitamin D deficiency is the leading cause of nutritional rickets 1 . The importance of more modest vitamin D deficiency than seen in nutritional rickets for the skeleton of adults and older adults is disputed. Supplementation with vitamin D only is unlikely to be able to reduce fracture risk in older adults; 2 , 49 however, a combination of calcium and vitamin D supplementation can modestly reduce hip and non-vertebral fracture incidence in this population 2 , 50 , 51 . This conclusion is in line with a 2019 overview and meta-analysis on vitamin D and calcium supplementation and fractures 52 , which concluded from observational data (39,0141 participants) that a 25 nmol/l increase in the serum 25OHD concentration reduces the risk of any fracture or hip fracture by 7% and 20%, respectively (both statistically significant). A similar conclusion was reached in another meta-analysis 53 .
Several large RCTs have generated new results regarding the effects of vitamin D supplementation on the adult skeleton. The VITAL Bone Health study is an ancillary study of the VITAL trial, including a subcohort of 771 participants (men aged ≥50 years and women aged ≥55 years; not taking bone active medications) evaluated at baseline and after 2 years (89% retention), and aims to evaluate the effects of vitamin D on bone structure and architecture. Supplemental vitamin D (compared with placebo) had no effect on 2-year changes in areal bone mineral density (BMD) at the spine, femoral neck, total hip or whole body, or on measures of bone structure. This conclusion remained valid in a subgroup analysis, including individuals with the lowest vitamin D status (as measured by total 25OHD) at baseline. New technology allows the direct measurement of free (non-protein-bound) 25OHD as an alternative strategy to define vitamin D status 54 . In participants of the VITAL trial with the lowest directly measured free 25OHD concentrations, vitamin D supplementation generated a slight increase in spine areal BMD (0.75% in the vitamin D group versus 0% in the placebo group; P = 0.043) and attenuation in loss of total hip areal BMD (−0.42% in the vitamin D group versus −0.98% in the placebo group; P = 0.044), yet such results might not survive multiple testing correction 55 . The ViDA trial did not find an effect of monthly vitamin D supplementation on the incidence of non-vertebral fractures (RR 1.19, 95% CI 0.94–1.50; non-significant) compared with no supplementation 56 . In participants with baseline vitamin D deficiency (<50 nmol/l), the HR for non-vertebral fractures was 0.94 compared with that in vitamin D-replete participants (95% CI 0.58–1.52). This conclusion was confirmed in the DO-HEALTH trial 18 .
A well-validated risk factor for fracture, such as BMD, might provide more information on the possible effects of vitamin D supplementation. In a subgroup of participants in the ViDA trial ( n = 452) 57 , the loss of BMD during follow-up was about 0.5% lower in the vitamin D group compared with the control group. This difference was statistically significant for the femoral neck and total hip but not for the lumbar spine or total body BMD. However, in the small ( n = 30) group of participants with a baseline serum 25OHD concentration of <30 nmol/l, BMD of the lumbar spine increased significantly by 3.1% compared with that in controls. These data indicate that correction of severe vitamin D deficiency might improve bone density, but not when given to vitamin D-replete people. A smaller RCT in Scottish adults confirmed that vitamin D supplementation (daily dose of 1,000 IU) increased BMD in individuals with a baseline serum 25OHD concentration of <30 nmol/l but not in people with a better vitamin D status at baseline 58 . These results are also in line with a RCT in US adults randomized to receive placebo, 800 IU of vitamin D or high-dose vitamin D (50,000 IU per day for 2 weeks followed by 50,000 IU per 2 weeks for 1 year), which concluded that neither low-dose nor high-dose vitamin D improved bone density in participants with a mean baseline serum 25OHD of 50 nmol/l (ref. 59 ). The same conclusion was drawn from a RCT of vitamin D supplementation in Black American women, as increasing baseline serum 25OHD concentrations of 55 nmol/l to concentrations above 75 nmol/l by vitamin D supplementation did not change the rate of bone loss during 3 years of follow-up 60 . Similarly, Finnish children below the age of 2 years who received 1,200 IU of vitamin D per day for ~2 years did not have better bone density (measured by peripheral quantitative CT (pQCT)) compared with children receiving the standard dose of 400 IU per day 61 . This finding is not totally unexpected, as the baseline serum 25OHD concentration was higher (80 nmol/l) than expected in this study due to the introduction of vitamin D supplementation of food in Finland.
The Calgary study was designed to evaluate the effect of long-term high-dose vitamin D on bone mass and quality. A daily dose of 400 IU, 4,000 IU or 10,000 IU of vitamin D for 3 years in Canadian adults did not increase BMD, but rather slightly decreased BMD, as measured by the best available methodology (high-resolution pQCT) 19 . Indeed, BMD at the radius and tibia significantly decreased by 3.5% and 1.7 %, respectively in the 10,000 IU per day group compared with the 400 IU per day group, whereas the decrease at both sites was not statistically significant in the 4,000 IU per day group compared with the 400 IU per day group. This study does demonstrate that vitamin D supplementation in vitamin D-replete adults (baseline serum 25OHD concentration of about 75 nmol/l) does not improve bone mass or quality. Moreover, very high doses might even have negative effects, as a small percentage of participants developed hypercalciuria or hypercalcaemia, which quickly resolved after adjustment of dosing. Of course, this finding might imply that regular follow-up is desirable when using such dosages 19 , 62 .
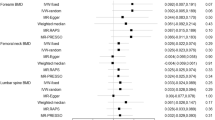
Many Mendelian randomization studies showed no causal effect of vitamin D status on a variety of bone traits in populations of European and non-European ancestry. An early Mendelian randomization study 63 found that genetically predicted one standard deviation increase in 25OHD was not associated with increased femoral neck BMD, lumbar spine BMD or estimated BMD change. Similar results were observed in relation to total body BMD 64 . A more powered Mendelian randomization analysis 65 (37,857 patients with fracture and 227,116 control individuals) also did not support a causal effect of 25OHD on fracture risk. However, a Mendelian randomization study in children 66 showed that haplotypes associating with low 25OHD were associated with low pQCT parameters (BMD, cross-sectional area and cortical density) in 2-year-old children. Finally, evidence from Mendelian randomization studies 67 refutes causal associations between predicted serum 25OHD concentrations and either BMD or bone metabolism markers found in 1,824 postmenopausal Chinese women (Supplementary Box 6 ).
Vitamin D and muscle function or falls
In mice, total deletion of VDR generates structural and functional consequences for skeletal and cardiac muscle 9 . Furthermore, humans with congenital CYP27B1 mutations or patients with severe combined deficiency of 25OHD and 1,25(OH) 2 D due to chronic renal failure develop severe muscle weakness that rapidly improves after treatment with 1,25(OH) 2 D 9 . Several meta-analyses have come to different conclusions regarding the consequences of vitamin D supplementation on muscle strength, with both positive 68 and null effects 69 . In addition, ample literature is available supporting a link between poor vitamin D status and increased risk of falls, but hesitance remains regarding causality 70 . High boluses of vitamin D, however, might transiently increase the risk of falls in older women 71 . High-dose continuous vitamin D supplementation to increase serum 25OHD concentrations to above 112 nmol/l might also induce an increased risk of falls in older men and women 72 , 73 , 74 . However, the large ViDA trial showed that monthly 100,000 IU doses of vitamin D did not reduce or increase the risk of falls. The hazard ratio for falls was 0.99 (95% CI 0.92–1.07) in the overall cohort who were treated with vitamin D compared with those receiving placebo and 1.07 (95% CI 0.91–1.25) in vitamin D-supplemented participants with baseline serum 25OHD concentrations below 50 nmol/l (ref. 56 ). The VITAL trial also looked at the effects of daily vitamin D supplementation on physical disability and falls in the SRURDY study 75 and found a non-significant (OR 0.97, 95% CI 0.91–1.25) effect of vitamin D supplementation on the risk of two falls or injurious falls requiring support from a doctor or hospital 76 . In further exploratory analysis, the same conclusion was reached when the baseline serum concentration of 25OHD was taken into account.
To our knowledge, no Mendelian randomization studies so far have examined the causal association between genetically estimated 25OHD levels and muscle traits or falls.
Vitamin D and musculoskeletal effects — summary
Of note, the 2017–2020 megatrials did not address the question of vitamin D supplementation and rickets, as there is consensus in all vitamin D guidelines from the past decade that serum 25OHD concentrations below 30 nmol/l are a risk factor for rickets or osteomalacia 12 . A daily vitamin D dose of 400 IU can prevent rickets and osteomalacia and increase serum concentrations of 25OHD well above 30 nmol/l (12 ng/ml) 77 . However, ~7% of the world population lives with severe vitamin D deficiency, with this percentage being much higher in the Middle East, North Africa and many countries in Asia 78 .
The role of vitamin D in the skeleton of adults and older adults is more disputed. The 2017–2020 megatrials were not designed to primarily evaluate the effect of vitamin D supplementation on fracture risk in older adults. These trials 15 , 16 recruited mostly vitamin D-replete adults with a fairly low risk of fracture. Even the DO-HEALTH trial in older, less vitamin D-replete, adults (compared with the other megatrials) did not find an effect on non-vertebral fractures 18 . However, the ViDA trial demonstrated that correction of severe vitamin D deficiency (<30 nmol/l) prevents age-related bone loss in adults. By contrast, the 2017–2020 megatrials demonstrate that vitamin D supplementation in vitamin D-replete adults does not improve bone mass, density or quality 16 .
Taken together, the findings indicate that supplementation with vitamin D only does not have a beneficial effect on fracture risk in vitamin D-replete, mostly white adults. However, combined calcium and vitamin D supplementation in older adults, especially those with poor vitamin D status and poor calcium intake, might decrease the risk of hip fractures and other major fractures by about 20% 51 . Therefore, most recent guidelines recommend a daily vitamin D supplement of about 800 IU of vitamin D combined with a good calcium intake (above 1,000 mg per day) in all older adults with a high risk or documented vitamin D deficiency. Of note, the Calgary study demonstrated that high daily doses of vitamin D (4,000 and especially 10,000 IU per day) might decrease BMD and bone quality 19 , 20 . Therefore, the optimal dose in vitamin D-deficient older adults should be at least 800 IU per day but not more than 4,000 IU per day.
Meta-analyses of older studies suggested a modest decrease in the risk of falls in older, mostly vitamin D-deficient, adults 79 . However, the ViDA trial did not confirm this finding as vitamin D supplementation did not change the risk of falls. The New Zealand population was younger and had a better vitamin D status than the participants in the older studies. There might also be a U-shaped relationship as very high vitamin status, especially due to high bolus doses, might increase the risk of falls 72 , 73 , 74 .
Lung function and respiratory effects
Vitamin d and respiratory infections or lung function.
The lung is increasingly recognized as an important target tissue for vitamin D. Observational data link poor vitamin D status with several inflammatory lung diseases or impaired lung function 80 , 81 , 82 . The most recent analysis published in 2019 (ref. 83 ) evaluated 10,933 participants in 25 RCTs and found a significant overall reduction in acute respiratory infections following vitamin D supplementation (OR 0.88, 95% CI 0.81–0.96) compared with no supplementation. The number needed to treat for benefit was 33. Subgroup analysis revealed that the greatest benefits were found in people with severe vitamin D deficiency (<25 nmol/l) at baseline (OR 0.58, 95% CI 0.40–0.82). Subgroup analysis revealed that intermittent (monthly or less frequent) doses of vitamin D did not generate protection, whereas daily or weekly vitamin D supplementation was more effective for preventing acute respiratory infections (OR 0.81, 95% CI 0.072–0.91). In the ViDA trial, however, no effects of vitamin D supplementation were found on acute respiratory infections in older adults 84 . This finding is not a total surprise as the lack of effects might be due to the intermittent dosing and/or adequate vitamin D status at baseline, and therefore might not contradict the findings of the 2019 meta-analysis 83 . In addition, the European DO-HEALTH trial did not show an effect on infections in general nor on upper respiratory infections 18 .
Several small-scale studies (eight RCTs) did not find an improvement in lung function (as measured in terms of forced expiratory volume in 1 s (FEV1)) in patients with chronic obstructive pulmonary disease (COPD) who were randomized to receive vitamin D supplementation 85 . A substudy of the ViDA trial, however, evaluated the effects of monthly vitamin D supplementation 86 in 442 adults treated for 1.1 years. Overall, in the ITT analysis, no significant effects were observed on FEV1. However, subgroup analysis revealed some beneficial effects, especially in subjects with existing lung problems such as asthma, COPD or a history of smoking (Table 2 ). To date, no Mendelian randomization studies have been performed that examined 25OHD levels, COPD and lung function.
Vitamin D and COVID-19
In view of the enormous health implications of the coronavirus disease 19 (COVID-19) pandemic caused by the worldwide spread of severe acute respiratory syndrome coronavirus 2, a possible link with poor vitamin D status and the risk or severity of COVID-19 has received great attention. Seven studies so far compared serum 25OHD concentrations in patients with COVID-19 compared with individuals without COVID-19 (ref. 87 ) and found a lower level (mean difference of about 12 nmol/l) in patients with COVID-19; however, in many studies the sampling did not take place at the same time in both groups. In addition, these studies were unable to control for confounding factors, a major problem due to the large number of similarities in the risk factors for vitamin D deficiency and COVID-19. About 31 studies looked at a possible link between vitamin D status and severity of the outcome of COVID-19. Lower serum concentrations of 25OHD were associated with greater mortality, greater need for intensive care treatment or increased severity of illness in general compared with better vitamin D status. However, this finding was based on observational studies. One placebo-controlled intervention study using a bolus dose of vitamin D (200,000 IU) did not reveal a beneficial effect in patients hospitalized with COVID-19 with a mean baseline 25OHD concentration of 50 nmol/l (ref. 88 ). However, one pilot study (which was not placebo-controlled) showed a marked reduction in the need for intensive care treatment in patients hospitalized for COVID-19 and treated with a high dose of 25OHD (calcifediol) at the time of admission 89 . Therefore, the link between vitamin D status and COVID-19 is unsettled so far, but many trials are ongoing that might clarify this question.
In 2021, a Mendelian randomization study assessed the causal role of serum 25OHD levels on COVID-19 susceptibility and disease severity 90 . Using data from 11,181 patients with COVID-19 and 116,456 control individuals from the Host Genetics Initiative, and six vitamin D SNPs that explain 2.5% of the variance in serum 25OHD levels, this study did not show any association between genetically decreased 25OHD and COVID-19 susceptibility or severity. These results were confirmed in a separate Mendelian randomization study using 81 25OHD SNPs that explain 4.3% of the variance in serum 25OHD levels, which also showed no effect of genetically determined 25OHD levels on risk of COVID-19-related hospitalization 91 .
Vitamin D and asthma
Research investigating the potential effects of vitamin D status on asthma has largely focused on a possible link between prenatal or maternal vitamin D status and wheezing or asthma in the offspring. A meta-analysis of four prospective studies and three RCTs concluded that vitamin D intake (~800 IU per day) by women during pregnancy is inversely related to wheezing or asthma in their offspring during up to 3 years of follow-up 92 . However, a longer follow-up did not confirm this conclusion: vitamin D supplementation during the prenatal period alone did not influence the 6-year incidence of asthma and recurrent wheeze among children who were at risk of asthma 93 . Two Mendelian randomization studies have investigated the causal association between vitamin D and asthma. A large study (n > 160,000 children and adults) 94 found odds ratios of 1.03 (95% CI 0.90–1.19) for asthma and 0.95 (95% CI 0.69–1.31) for childhood-onset asthma per standard deviation of log-transformed decrease in serum 25OHD (Supplementary Box 6 ). These findings suggest that vitamin D levels probably do not have clinically relevant effects on the risk of asthma.
Vitamin D and respiratory effects — summary
The vitamin D endocrine system influences all cells and most cytokines of the immune system 9 . The innate immune system is stimulated by 1,25(OH) 2 D and this is in line with a decreased risk of upper respiratory infections with vitamin D supplementation in individuals with vitamin D deficiency 83 . Meta-analysis of intervention studies suggested a benefit of vitamin D supplementation of participants with severe vitamin D deficiency and COPD, asthma, or similar lung diseases, and on reducing the risk of acute upper respiratory infections in severely deficient individuals 83 . However, where tested, these findings have not been supported by Mendelian randomization studies 90 . According to the results of the LUNG-ViDA trial, vitamin D supplementation might modestly improve expiratory lung function 85 . If confirmed, such data would imply that the lung is a clinically relevant target issue for vitamin D. Of note, currently there are insufficient RCTs to evaluate the potential benefit of vitamin D or calcifediol supplementation on the risk or severity of COVID-19.
Autoimmune diseases
Observational studies have, in line with preclinical data, made a link between poor vitamin D status and increased risk of infection or risk of autoimmune diseases (such as multiple sclerosis (MS), inflammatory bowel diseases or type 1 diabetes mellitus) 95 . RCTs in humans dealing with infections have mainly focused on upper respiratory infections and an overview is presented in the previous section. Unfortunately, no major RCTs have addressed the possible primary or secondary prevention of the major human autoimmune diseases. So far, the 2017–2020 megatrials (Table 1 ) have not shown results related to autoimmune diseases.
Currently, strong evidence exists that supports a causal association between genetically low serum 25OHD levels and increased risk of MS 96 , 97 , 98 , 99 . The most recent Mendelian randomization study from 2020 evaluated data from The International Multiple Sclerosis Genetics Consortium discovery phase GWAS (14,802 MS and 26,703 controls from the USA, Europe, Australia and some Asian countries) 97 using six SNPs associated with serum levels of 25OHD and found that each genetically determined unit increase in log-transformed 25(OH)D 3 was associated with an odds ratio for MS of 0.57 (95% CI 0.41–0.81; P = 0.001) (Table 4 ). This effect applies to adult-onset and childhood-onset MS.
Earlier Mendelian randomization evidence 100 did not support causality of predicted serum 25OHD levels in systemic lupus erythematosus or rheumatoid arthritis. Consistent null effects on rheumatoid arthritis were found in a 2020 Mendelian randomization study in participants from the UK Biobank, using ~220 vitamin D-associated SNPs as instruments 43 . Null effects of predicted serum 25OHD levels were also shown in Mendelian randomization studies on Crohn’s disease (odds ratio for 10 nmol/l higher 25OHD of 1.04, 95% CI 0.93–1.16) and ulcerative colitis (OR 1.13, 95% CI 1.06–1.21) 101 . Similarly, no effect on ulcerative colitis was found in participants from the UK Biobank 43 . The UK Biobank study also did not support a causal role of vitamin D on allergic rhinitis. Finally, Mendelian randomization 94 does not support causal effects of 25OHD on atopic dermatitis. A 2021 Mendelian randomization study on type 1 diabetes mellitus did not support causal effects of genetically lowered 25OHD levels on the risk of this disease 102 .
In summary, the adaptive immune system is downregulated by 1,25(OH) 2 D and therefore vitamin D deficiency might predispose to autoimmune diseases 9 . Observational studies have suggested this effect might apply to humans, but too few intervention studies have been conducted to evaluate this statement. Four independent Mendelian randomization studies agree, however, that individuals with genetically driven lower serum 25OHD concentrations have an increased risk of developing MS, either during adolescence or adulthood (Table 4 ).
Intervention studies as summarized in a Cochrane review from 2016 (ref. 103 ) dealing with 22 RCTs including 3,725 pregnant women, concluded that vitamin D supplementation significantly reduced the risk of pre-eclampsia (RR 0.48), gestational diabetes mellitus (RR 0.51) and low birthweight (<2,500 g; RR 0.55) compared with no supplementation. An update of these data 104 largely confirmed these observations. However, a large RCT in pregnant Bangladeshi women with severe vitamin D deficiency (baseline mean serum 25OHD about 25 nmol/l) supplemented from week 17–24 onwards with placebo or vitamin D (three groups receiving 4,200, 16,800 or 28,000 IU per week) until birth did not find a beneficial effect on fetal or neonatal parameters of length, weight or head circumference, either at birth or at one year of age ( n = 1,164 infants) 105 .
To date only one Mendelian randomization study 106 has examined the causal effect of predicted serum 25OHD levels on gestational hypertension and pre-eclampsia. Overall, the evidence was weak supporting a causal effect of vitamin D status on gestational hypertension (OR 0.90, 95% CI 0.78–1.03) or pre-eclampsia (OR 0.98, 95% CI: 0.89–1.07) per 10% decrease in serum 25OHD (Supplementary Box 5 ).
In summary, pregnant women more frequently have a poor vitamin D status than non-pregnant women of the same age but the absolute and relative values vary from country to country. Several meta-analyses have suggested that vitamin D supplementation might modestly decrease maternal morbidity and improve the health of their offspring 103 , 104 . However, a 2018 large RCT in Bangladeshi women with severe vitamin D deficiency did not confirm this observation 105 . Therefore, the effects of poor vitamin D status during pregnancy on pregnancy outcomes for mother and infant remains unsettled.
Patients in intensive care
Patients with severe acute illness requiring intensive care frequently have low serum concentrations of 25OHD and this poor vitamin D status is linked with increased morbidity and mortality 107 , 108 . Two major RCTs so far in patients in intensive care units (ICU) have generated conflicting results. In the VITdAL-ICU trial, patients in the ICU were randomized to either placebo ( n = 243) or high-dose oral vitamin D ( n = 249) (starting dose 540,000 IU followed by monthly maintenance doses of 90,000 IU for 5 months). Mean baseline serum 25OHD concentrations were low (33 nmol/l) and increased to ~82 nmol/l at day 3. Length of stay in the ICU or hospital, mortality in the ICU, in-hospital mortality and mortality at 6 months did not improve with the intervention. In a predefined subgroup with severe vitamin D deficiency who received the intervention (<30 nmol/l), hospital mortality (HR 0.56, 95% CI, 0.35–0.90) and 6-month mortality (HR 0.60, 95% CI, 0.39–0.93) were significantly decreased compared with patients with severe vitamin D deficiency who received placebo 107 . In the much larger Amrein ICU trial 108 , 1,059 patients in the ICU with vitamin D deficiency (<50 nmol/l) received either placebo or a single oral high dose of vitamin D (540,000 IU). This dose increased mean serum 25OHD concentration at day 3 to a mean concentration of 117 ± 58 nmol/l in comparison with the control group (mean concentration 28 ± 14 nmol/ml). The primary end point (90-day mortality) and other non-fatal outcomes were similar in the two groups. Although all patients in both studies were admitted to ICUs, the US patients in the VITdAL-ICU trial were probably less sick than those in the Amrein trial 107 as indicated by the percentage of patients requiring mechanical ventilation (32% in the US trial).
Effects of vitamin D supplementation on safety outcomes
In all vitamin D supplementation RCTs, some safety end points have been reported in addition to mortality (see next section). No effects were found on serum calcium or calciuria unless very high doses were used, such as 4,000–10,000 IU per day in the Calgary study. Even in these circumstances, hypercalcaemia was infrequent and occurred transiently after changes in treatment modality 19 , 62 . A modestly increased risk of kidney stones was observed in the WHI trial 109 , but this effect was not seen in the more recent 2017–2020 megatrials (that is, ViDA, VITAL and D2d; Table 1 ). Furthermore, no changes in kidney function were found in these large trials. Skeletal consequences were either null effects, slight (beneficial) increases in BMD in subgroups with poor vitamin D status at baseline, or a modest but significant decrease in BMD during high-dose (10,000 IU per day) therapy in the Calgary study 19 . An increased risk of fractures in patients receiving high intermittent bolus doses has been reported 71 , 110 . Similarly, an increased risk of falls has been reported when either high intermittent doses 71 or high continuous doses were used 72 , 73 . Importantly, the 2017–2020 megatrials (that is, ViDA, VITAL and D2d), with detailed evaluation of about 30,000 participants for 2–5 years, did not discover notable adverse effects. These findings indicate that a daily dose (or dose equivalent) of 2,000–4,000 IU can be considered as safe in an adult (even vitamin D-replete) population. High-dose vitamin D also did not modify arterial calcifications during a 3-year follow up in the Calgary study 111 .
Effects of vitamin D supplementation on mortality
Observational data have repeatedly linked poor vitamin D status with increased mortality. This effect was extensively documented in several NHANES studies based on representative samples of the US population and confirmed after validation of serum 25OHD concentrations according to standards generated by the US National Institute of Standards and Technology 112 . To decrease the possible effect of reverse causation, people who died within the first 3 years after 25OHD measurements were excluded from the analysis; however, the same association between poor vitamin D status and increased mortality remained 112 . Using a combination of several European prospective studies, mortality was also higher in the population with the poorest vitamin D status compared with the vitamin D-replete population 113 . A 2019 large long-term (>10 years) Finnish study concluded that people with the highest tertile of 25OHD concentrations (>50 nmol/l) had a mortality odds ratio of 0.77 (95% CI 0.71–0.84) compared with people with the lowest tertile of 25OHD concentrations, even in a multivariate model with correction of multiple co-variables 114 .
As nearly all long-term vitamin D supplementation trials include data on mortality, several meta-analyses have shown the effects of vitamin D supplementation on mortality. Extensive meta-analyses published in 2014 showed a modest decrease in overall mortality in participants randomized to vitamin D supplementation; based on 22 RCTs, the risk of death decreased by 11% 36 . A 2014 Cochrane analysis 29 evaluated 56 RCTs including 95,286 participants (mostly healthy women older than 70 years) with a mean follow-up of 4.4 years. Vitamin D supplementation significantly reduced all-cause mortality (RR 0.94, 95% CI 0.91–0.98; P = 0.002) compared with no supplementation. This finding implies that vitamin D supplementation of 150 women for 5 years prevented one additional death. Vitamin D supplementation also decreased cancer mortality (RR 0.88, 95% CI 0.78–0.98; P = 0.02) compared with no supplementation 29 .
In the 2017–2020 megatrials (that is, VITAL, ViDA and D2d), overall mortality was much lower than shown in the previous meta-analyses 29 , 36 and did not show an effect of vitamin D supplementation on overall mortality 15 . A new meta-analysis of 52 RCTs including a total of 75,454 participants concluded that vitamin D (either vitamin D 3 or D 2 ) supplementation did not change mortality (RR 0.98, 95% CI 0.95–1.02) compared with no supplementation 115 . A subanalysis, however, found that vitamin D 3 (instead of D 2 ) supplementation trials tended to reduce mortality (RR 0.95, 95% CI 1.90–1.00; P = 0.06), whereas this was not the case for vitamin D 2 supplementation trials. These new findings conflict with the 2014 reports 112 . The difference could be partly because the 2019 meta-analysis did not include ten RCTs including ~50,000 participants using a combination of vitamin D and calcium supplementation. However, the 2019 meta-analysis did include two megatrials (VITAL and ViDA) that evaluated the effects of vitamin D supplementation in a younger population of mostly vitamin D-replete participants 115 .
In a large-scale population Mendelian randomization study (10,349 deaths in 95,766 total participants) 116 , the odds ratios for a genetically determined lower 25OHD concentration was 1.30 (95% CI 1.05–1.61) for all-cause mortality, 0.77 (95% CI 0.55–1.08) for cardiovascular mortality, 1.43 (95% CI 1.02–1.99) for cancer mortality and 1.44 (95% CI 1.01–2.04) for other types of mortality. Similar point estimates and effect sizes, whose 95% confidence intervals included the null, were found for all-cause mortality in two follow-up Mendelian randomization studies 46 , 117 . Nevertheless, both studies may have been underpowered to detect existing causal associations. Finally, evidence from Mendelian randomization 118 did not support an association between 25OHD concentrations and cancer mortality in a sample of 6,998 deaths from cancer. These data provide some evidence that genetically lowered vitamin D levels might increase overall mortality risks, but the results have not been consistent across studies, or across causes of mortality.
If vitamin D supplementation exerts beneficial effects on extra-skeletal health outcomes and major diseases, then it is likely to have some effects on mortality, especially in older adults with poor vitamin D status. Large meta-analyses dealing mostly with women older than 70 years 29 , 36 showed a 6–11% reduction in mortality; however, adding the newest 2017–2020 megatrials eliminated this effect, possible because these new trials recruited a younger population.
Discordance between studies
Preclinical data are mostly in line with the very large number of observational studies linking very poor vitamin D status with skeletal and extra-skeletal health effects (Fig. 1 ). However, Mendelian randomization studies and the majority of RCTs do not confirm the causality of these associations. Several possible reasons exist for this discrepancy. Most importantly, serum 25OHD levels are a highly confounded variable. Specifically, serum 25OHD levels are affected by a host of health behaviours, the presence of obesity, socioeconomic status and education levels. Although most observational studies have attempted to control for such confounding through multivariable adjustment, such approaches depend upon the degree of accuracy of measurement of the confounders, knowledge that such confounding takes place, and most often that the nature of the confounding relationship (linear versus nonlinear) is known. Furthermore, statistical adjustment for confounding variables can only be accomplished if the confounding variables are known.
The concordance between 25OHD Mendelian randomization studies and RCTs is striking and suggests that Mendelian randomization might be a more relevant way to begin to understand the effect of 25OHD levels on risk of disease than observational studies. Perhaps the vitamin D endocrine system only has a role in these extra-skeletal effects in people with prolonged and very severe vitamin D deficiency. Studies in countries or population groups with severe vitamin D deficiency who need improved vitamin D status anyway might be the ideal approach to better understand the effect of vitamin D supplementation in individuals with severe vitamin D deficiency. Most RCTs and Mendelian randomization studies have been undertaken in individuals from the general population in which the rates of severe vitamin D deficiency are low.
Of note, the available Mendelian randomization studies were not able to predict large variations in serum 25OHD concentrations (usually only about 5% difference or less). However, this low degree of variance would affect the statistical power of a study but not introduce bias. New techniques will soon enable us to use a much larger number of SNPs than used in current studies (usually based on less than six SNPs), thereby allowing much larger variations in serum 25OHD concentrations to be predicted. Most RCTs did not last longer than 3–5 years. In such short-term scenarios, answering the question of causality is extremely difficult. This fact implies that only very long-term improvements in vitamin D status might generate beneficial effects. However, Mendelian randomization studies provide estimates of the effect of a lifetime of genetically lowered vitamin D levels and such Mendelian randomization studies have generally produced null findings.
Reverse causality remains a valid rationale to explain the discordance between observational and intervention studies. The most plausible hypothesis states that individuals with any health problems are less likely to regularly engage in outdoor activity and less exposure to sunlight results in lower vitamin D status. Another mechanism of reverse causality might be that the activity of hepatic 25-hydroxylase is decreased in many major diseases and this decrease could cause low serum 25OHD concentrations. Indeed, data in mice demonstrate that diet-induced obesity, type 1 diabetes mellitus or T2DM, fasting and exposure to glucocorticoids substantially decrease the gene and protein expression of CYP2R1, thereby decreasing the overall 25-hydroxylase activity 119 , 120 , 121 . This finding implies that decreased 25OHD concentrations are the consequence of disease, rather than involved in the origin of these metabolic diseases. Of course, these data from mice need confirmation in humans. Finally, many diseases other than those described in this Review (including brain-related diseases) are linked with poor vitamin D status; however, causality is doubtful without adequate Mendelian randomization studies or RCTs.
Future Mendelian randomization studies
Improved understanding of the genetic determinants of 25OHD has helped re-assess the role of vitamin D in the aetiology of complex diseases through Mendelian randomization. Taken together, the evidence from over 60 Mendelian randomization studies published to date assessing the role vitamin D does not support a causal role for the large majority of studied outcomes. Despite this null data, in the few cases where the evidence from Mendelian randomization supported a causal role of vitamin D status, such as in the example of MS, these results had important clinical implications. For instance, clinical care guidelines for the use of vitamin D in preventing MS in those at risk were published by the MS Society of Canada 122 .
The earlier Mendelian randomization studies used, as instruments for 25OHD levels, SNPs within the four genes related to 25OHD synthesis and metabolism ( DHCR7 , CYP2R1 , GC and CYP24A1 ), which together explained 2.4% of the variance in 25OHD levels 123 . Later Mendelian randomization studies combined the aforementioned four SNPs with two SNPs in SEC23A and AMDHD1 (both genes without clear role in the vitamin D metabolic pathway), and thereby explained ~5.3% of the variance in 25OHD levels. The identification of over 150 25OHD-associated genetic variants in 2020, which explain a considerable portion of the variance in 25OHD levels (~10.5%) 43 , has enabled a deeper understanding of the genetic determinants contributing to variation in circulating 25OHD levels. These newly identified SNPs will probably enable improved instrumentation of vitamin D in Mendelian randomization studies. Moreover, with the emergence of large-scale GWAS in densely phenotyped biobanks, we anticipate that more powerful vitamin D Mendelian randomization studies will be published that utilize the optimized set of genetic instruments. Such new studies should revisit previously studied diseases and investigate new disease outcomes, to further aid causal effect estimation.
Conclusions
In conclusion, the data generated by the 2017–2020 megatrials of vitamin D supplementation in largely vitamin D-replete adults (Table 1 ) demonstrate that increasing the serum 25OHD concentration into the high normal range (based on the IOM and most recent guidelines published over the past decade 12 , in the range of 50–125 nmol/l or 20–50 ng/ml) does not generate benefits for global health or major diseases or medical events such as cancer, cardiovascular events, T2DM, falls or fractures. Therefore, no reason exists at present to recommend vitamin D supplementation of already vitamin D-replete individuals. These data do not contradict the causal link between severe vitamin D deficiency and rickets, or the need to correct severe deficiency at any age. Similarly, the 2017–2020 trials do not contradict the probable beneficial effects of combined supplementation of calcium and vitamin D in older adults with poor vitamin D and calcium status on their risks of fracture or falls.
A few hints have emerged that vitamin D supplementation might have some extra-skeletal benefits, especially in people with severe vitamin D deficiency (such as reduced progression to T2DM, decreased numbers of infections, increased lung function and decreased cancer or overall mortality) (Tables 2 , 3 ). These suggestions are largely based on subgroup or post hoc analyses and thus should not result in the systematic recommendation of vitamin D supplements in such populations but might guide the correct design of future studies.
Arguments have been put forward that daily doses of ≥4,000 IU of vitamin D convey some risks other than simple hypercalcaemia or hypercalciuria. Such doses, or the equivalent of serum 25OHD concentrations well above 112 nmol/l or 45 ng/ml bring no benefits, but might be harmful in some people (for example, in causing loss of BMD or increasing the risk of falls). The same is true for intermittent high-dose boluses of vitamin D. Unfortunately, about 3% of the US population as screened by NHANES use such high dose vitamin D supplements.
Over the past few decades, vitamin D has been a hot topic for scientists and lay people alike, who frequently suggest that vitamin D supplementation might generate a wide variety of health benefits. The data discussed in the present Review might well dampen such enthusiasm. However, a large number of intervention studies (and most probably Mendelian randomization studies) are still ongoing, and these might help provide a better understanding of who would benefit from vitamin D supplementation.
In conclusion, it seems that far too many people with severe vitamin D deficiency (~7% of the world population) do not take or even have access to normal doses of vitamin D. About a third of the world population lives with suboptimal (below 20 ng/ml) serum 25OHD concentrations 78 . However, many vitamin D-replete people take vitamin D supplements without clear benefits. In addition, a small percentage of the population takes higher doses than the upper limit of safe intake. Therefore, we recommend that vitamin D be used wisely and “giveth to those who needeth” 7 .
Munns, C. F. et al. Global consensus recommendations on prevention and management of nutritional rickets. J. Clin. Endocrinol. Metab. 101 , 394–415 (2016).
Article CAS PubMed PubMed Central Google Scholar
Bolland, M. J., Grey, A. & Avenell, A. Effects of vitamin D supplementation on musculoskeletal health: a systematic review, meta-analysis, and trial sequential analysis. Lancet Diabetes Endocrinol. 6 , 847–858 (2018).
Article CAS PubMed Google Scholar
Luxwolda, M. F., Kuipers, R. S., Kema, I. P., Dijck-Brouwer, D. A. & Muskiet, F. A. Traditionally living populations in East Africa have a mean serum 25-hydroxyvitamin D concentration of 115 nmol/l. Br. J. Nutr. 108 , 1557–1561 (2012).
Luxwolda, M. F. et al. Vitamin D status indicators in indigenous populations in East Africa. Eur. J. Nutr. 52 , 1115–1125 (2013).
Holick, M. F. & Grant, W. B. Vitamin D status and ill health. Lancet Diabetes Endocrinol. 2 , 273–274 (2014).
Article PubMed Google Scholar
Bouillon, R., Lips, P. & Bilezikian, J. P. Vitamin D supplementation and musculoskeletal health. Lancet Diabetes Endocrinol. 7 , 85–86 (2019).
Lips, P., Bilezikian, J. P. & Bouillon, R. Vitamin D: giveth to those who needeth. JBMR 4 , e10232 (2020).
CAS Google Scholar
Ebeling, P. R. et al. Management of endocrine disease: therapeutics of vitamin D. Eur. J. Endocrinol. 179 , R239–R259 (2018).
Bouillon, R. et al. Skeletal and extraskeletal actions of vitamin D: current evidence and outstanding questions. Endocr. Rev. 40 , 1109–1151 (2019).
Institute of Medicine. Dietary Reference Intakes for Calcium and Vitamin D (National Academies Press, 2011)
Holick, M. F. et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 96 , 1911–1930 (2011).
Bouillon, R. Comparative analysis of nutritional guidelines for vitamin D. Nat. Rev. Endocrinol. 13 , 466–479 (2017).
Scientific Advisory Committee on Nutrition (SACN). Vitamin D and health. GOV.UK https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report (2016).
Lips, P. et al. Current vitamin D status in European and Middle East countries and strategies to prevent vitamin D deficiency; a position statement of the European Calcified Tissue Society. Eur. J. Endocrinol. 180 , 23–54 (2019).
Article Google Scholar
Manson, J. E. et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N. Engl. J. Med. 380 , 33–44 (2019).
Scragg, R. et al. Monthly high-dose vitamin D supplementation and cancer risk: a post hoc analysis of the vitamin D assessment randomized clinical trial. JAMA Oncol. 4 , e182178 (2018).
Article PubMed PubMed Central Google Scholar
Pittas, A. G. et al. Vitamin D supplementation and prevention of type 2 diabetes. N. Engl. J. Med. 381 , 520–530 (2019).
Bischoff-Ferrari, H. A. et al. Effect of vitamin D supplementation, omega-3 fatty acid supplementation, or a strength-training exercise program on clinical outcomes in older adults: the DO-HEALTH Randomized Clinical Trial. JAMA 324 , 1855–1868 (2020).
Burt, L. A. et al. Effect of high-dose vitamin D supplementation on volumetric bone density and bone strength: a randomized clinical trial. JAMA 322 , 736–745 (2019).
Billington, E. O. et al. Safety of high-dose vitamin D supplementation: secondary analysis of a randomized controlled trial. J. Clin. Endocrinol. Metab. 105 , 1261–1273 (2020).
Dawson-Hughes, B. et al. Intratrial exposure to vitamin D and new-onset diabetes among adults with prediabetes: a secondary analysis from the Vitamin D and Type 2 Diabetes (D2d) Study. Diabetes Care 43 , 2916–2922 (2020).
Pittas, A. G., Jorde, R., Kawahara, T. & Dawson-Hughes, B. Vitamin D supplementation for prevention of type 2 diabetes mellitus: to D or not to D? J. Clin. Endocrinol. Metab. 105 , 3721–3733 (2020).
Article PubMed Central Google Scholar
Zhang, Y. et al. Effects of Vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: a systematic review and meta-analysis. Diabetes Care 43 , 1650–1658 (2020).
Barbarawi, M. et al. Effect of vitamin D supplementation on the incidence of diabetes mellitus. J. Clin. Endocrinol. Metab. 105 , 2857–2868 (2020).
Lu, L. et al. Association of vitamin D with risk of type 2 diabetes: a Mendelian randomisation study in European and Chinese adults. PLoS Med. 15 , e1002566 (2018).
Diabetes Prevention Program Research Group. Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol. 3 , 866–875 (2015).
Feldman, D., Krishnan, A. V., Swami, S., Giovannucci, E. & Feldman, B. J. The role of vitamin D in reducing cancer risk and progression. Nat. Rev. Cancer 14 , 342–357 (2014).
Manson, J. E., Bassuk, S. S., Buring, J. E. & Group, V. R. Principal results of the VITamin D and OmegA-3 TriaL (VITAL) and updated meta-analyses of relevant vitamin D trials. J. Steroid Biochem. Mol. Biol. 198 , 105522 (2020).
Bjelakovic, G. et al. Vitamin D supplementation for prevention of cancer in adults. Cochrane Database Syst. Rev. 6 , CD007469 (2014).
Google Scholar
Ong, J. S. et al. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. Int. J. Epidemiol. 45 , 1619–1630 (2016).
Dimitrakopoulou, V. I. et al. Circulating vitamin D concentration and risk of seven cancers: Mendelian randomisation study. BMJ 359 , j4761 (2017).
Chandler, P. D. et al. Association between vitamin D genetic risk score and cancer risk in a large cohort of U.S. women. Nutrients 10 , 55 (2018).
He, Y. et al. Exploring causality in the association between circulating 25-hydroxyvitamin D and colorectal cancer risk: a large Mendelian randomisation study. BMC Med. 16 , 142 (2018).
Dong, J. et al. No association between vitamin D status and risk of Barrett’s esophagus or esophageal adenocarcinoma: a Mendelian randomization study. Clin. Gastroenterol. Hepatol. 17 , 2227–2235.e1 (2019).
Winslow, U. C., Nordestgaard, B. G. & Afzal, S. High plasma 25-hydroxyvitamin D and high risk of nonmelanoma skin cancer: a Mendelian randomization study of 97 849 individuals. Br. J. Dermatol. 178 , 1388–1395 (2018).
Chowdhury, R. et al. Vitamin D and risk of cause specific death: systematic review and meta-analysis of observational cohort and randomised intervention studies. BMJ 348 , g1903 (2014).
Scragg, R. et al. Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the Vitamin D Assessment Study: a randomized clinical trial. JAMA Cardiol. 2 , 608–616 (2017).
Barbarawi, M. et al. Vitamin D supplementation and cardiovascular disease risks in more than 83000 individuals in 21 randomized clinical trials: a meta-analysis. JAMA Cardiol. 4 , 765–776 (2019).
Afzal, S., Brondum-Jacobsen, P., Bojesen, S. E. & Nordestgaard, B. G. Genetically low vitamin D concentrations and increased mortality: Mendelian randomisation analysis in three large cohorts. BMJ 349 , g6330 (2014).
Manousaki, D., Mokry, L. E., Ross, S., Goltzman, D. & Richards, J. B. Mendelian randomization studies do not support a role for vitamin D in coronary artery disease. Circ. Cardiovasc. Genet. 9 , 349–356 (2016).
Larsson, S. C. et al. Serum 25-hydroxyvitamin D concentrations and ischemic stroke and its subtypes. Stroke 49 , 2508–2511 (2018).
Huang, T. et al. Vitamin D and cause-specific vascular disease and mortality: a Mendelian randomisation study involving 99,012 Chinese and 106,911 European adults. BMC Med. 17 , 160 (2019).
Revez, J. A. et al. Genome-wide association study identifies 143 loci associated with 25 hydroxyvitamin D concentration. Nat. Commun. 11 , 1647 (2020).
Sluyter, J. D. et al. Effect of monthly, high-dose, long-term vitamin D supplementation on central blood pressure parameters: a randomized controlled trial substudy. J. Am. Heart Assoc. 6 , e006802 (2017).
Vimaleswaran, K. S. et al. Association of vitamin D status with arterial blood pressure and hypertension risk: a Mendelian randomisation study. Lancet Diabetes Endocrinol. 2 , 719–729 (2014).
Meng, X. et al. Phenome-wide Mendelian-randomization study of genetically determined vitamin D on multiple health outcomes using the UK Biobank study. Int. J. Epidemiol. 48 , 1425–1434 (2019).
Kwak, S. Y., Cho, Y., Oh, H. & Shin, M. J. Association of circulating 25-hydroxyvitamin D levels with hypertension and blood pressure values in Korean adults: a Mendelian randomization study on a subset of the Korea National Health and Nutrition Survey 2011-2012 population. Nutr. Res. Pract. 13 , 498–508 (2019).
Chen, C. et al. Association of 25-hydroxyvitamin D with cardiometabolic risk factors and metabolic syndrome: a Mendelian randomization study. Nutr. J. 18 , 61 (2019).
Boonen, S. et al. Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials. J. Clin. Endocrinol. Metab. 92 , 1415–1423 (2007).
Bolland, M. J., Grey, A., Gamble, G. D. & Reid, I. R. The effect of vitamin D supplementation on skeletal, vascular, or cancer outcomes: a trial sequential meta-analysis. Lancet Diabetes Endocrinol. 2 , 307–320 (2014).
Avenell, A., Mak, J. C. & O’Connell, D. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men. Cochrane Database Syst. Rev. 4 , CD000227 (2014).
Yao, P. et al. Vitamin D and calcium for the prevention of fracture: a systematic review and meta-analysis. JAMA Netw. Open 2 , e1917789 (2019).
Chakhtoura, M., Chamoun, N., Rahme, M. & Fuleihan, G. E. Impact of vitamin D supplementation on falls and fractures–a critical appraisal of the quality of the evidence and an overview of the available guidelines. Bone 131 , 115112 (2020).
Bikle, D., Bouillon, R., Thadhani, R. & Schoenmakers, I. Vitamin D metabolites in captivity? Should we measure free or total 25(OH)D to assess vitamin D status? J. Steroid Biochem. Mol. Biol. 173 , 105–116 (2017).
LeBoff, M. S. et al. Effects of supplemental vitamin D on bone health outcomes in women and men in the VITamin D and OmegA-3 TriaL (VITAL). J. Bone Miner. Res. 35 , 883–893 (2020).
Khaw, K. T. et al. Effect of monthly high-dose vitamin D supplementation on falls and non-vertebral fractures: secondary and post-hoc outcomes from the randomised, double-blind, placebo-controlled ViDA trial. Lancet Diabetes Endocrinol. 5 , 438–447 (2017).
Reid, I. R. et al. Effect of monthly high-dose vitamin D on bone density in community-dwelling older adults substudy of a randomized controlled trial. J. Intern. Med. 282 , 452–460 (2017).
Macdonald, H. M. et al. 25-hydroxyvitamin D threshold for the effects of vitamin D supplements on bone density: secondary analysis of a randomized controlled trial. J. Bone Miner. Res. 33 , 1464–1469 (2018).
Hansen, K. E. et al. Treatment of vitamin D insufficiency in postmenopausal women: a randomized clinical trial. JAMA Intern. Med. 175 , 1612–1621 (2015).
Aloia, J. et al. Vitamin D supplementation in elderly black women does not prevent bone loss: a randomized controlled trial. J. Bone Miner. Res. 33 , 1916–1922 (2018).
Rosendahl, J. et al. Effect of higher vs standard dosage of vitamin D3 supplementation on bone strength and infection in healthy infants: a randomized clinical trial. JAMA Pediatrics 172 , 646–654 (2018).
Bouillon, R. Safety of high-dose vitamin D supplementation. J. Clin. Endocrinol. Metab. 105 , 1290–1291 (2020).
Larsson, S. C., Melhus, H. & Michaelsson, K. Circulating serum 25-hydroxyvitamin D levels and bone mineral density: Mendelian randomization study. J. Bone Miner. Res. 33 , 840–844 (2018).
Sun, J. Y. et al. Circulating serum vitamin D levels and total body bone mineral density: a Mendelian randomization study. J. Cell Mol. Med. 23 , 2268–2271 (2019).
Trajanoska, K. et al. Assessment of the genetic and clinical determinants of fracture risk: genome wide association and Mendelian randomisation study. BMJ 362 , k3225 (2018).
Kampe, A. et al. Genetic variation in GC and CYP2R1 affects 25-hydroxyvitamin D concentration and skeletal parameters: a genome-wide association study in 24-month-old Finnish children. PLoS Genet. 15 , e1008530 (2019).
Li, S. S. et al. Genetically low vitamin D Levels, bone mineral density, and bone metabolism markers: a Mendelian randomisation study. Sci. Rep. 6 , 33202 (2016).
Beaudart, C. et al. The effects of vitamin D on skeletal muscle strength, muscle mass, and muscle power: a systematic review and meta-analysis of randomized controlled trials. J. Clin. Endocrinol. Metab. 99 , 4336–4345 (2014).
Tabrizi, R. et al. The effects of vitamin D supplementation on muscle function among postmenopausal women: a systematic review and meta-analysis of randomized controlled trials. EXCLI J. 18 , 591–603 (2019).
PubMed PubMed Central Google Scholar
Girgis, C. M., Clifton-Bligh, R. J., Hamrick, M. W., Holick, M. F. & Gunton, J. E. The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr. Rev. 34 , 33–83 (2013).
Sanders, K. M. et al. Annual high-dose oral vitamin D and falls and fractures in older women: a randomized controlled trial. JAMA 303 , 1815–1822 (2010).
Bischoff-Ferrari, H. A. et al. Monthly high-dose vitamin D treatment for the prevention of functional decline: a randomized clinical trial. JAMA Intern. Med. 176 , 175–183 (2016).
Gallagher, J. C. Vitamin D and falls–the dosage conundrum. Nat. Rev. Endocrinol. 12 , 680–684 (2016).
Smith, L. M., Gallagher, J. C. & Suiter, C. Medium doses of daily vitamin D decrease falls and higher doses of daily vitamin D3 increase falls: a randomized clinical trial. J. Steroid Biochem. Mol. Biol. 173 , 317–322 (2017).
Michos, E. D. et al. Rationale and design of the Study To Understand Fall Reduction and Vitamin D in You (STURDY): a randomized clinical trial of vitamin D supplement doses for the prevention of falls in older adults. Contemp. Clin. trials 73 , 111–122 (2018).
LeBoff, M. S. et al. VITamin D and OmegA-3 TriaL (VITAL): effects of vitamin D supplements on risk of falls in the US population. J. Clin. Endocrinol. Metab. 105 , 2929–2938 (2020).
Cashman, K. D., Ritz, C., Kiely, M. & Odin, C. Improved dietary guidelines for vitamin D: application of individual participant data (IPD)-level meta-regression analyses. Nutrients 9 , 469 (2017).
Bouillon, R. Vitamin D status in Africa is worse than in other continents. Lancet Glob. Health 8 , e20–e21 (2020).
Bischoff-Ferrari, H. A. et al. Effect of vitamin D on falls: a meta-analysis. JAMA 291 , 1999–2006 (2004).
Lange, N. E., Sparrow, D., Vokonas, P. & Litonjua, A. A. Vitamin D deficiency, smoking, and lung function in the Normative Aging Study. Am. J. Respir. Crit. Care Med. 186 , 616–621 (2012).
Janssens, W. et al. Vitamin D deficiency is highly prevalent in COPD and correlates with variants in the vitamin D-binding gene. Thorax 65 , 215–220 (2010).
Maes, K., Serre, J., Mathyssen, C., Janssens, W. & Gayan-Ramirez, G. Targeting vitamin D deficiency to limit exacerbations in respiratory diseases: utopia or strategy with potential? Calcif. Tissue Int. 106 , 76–87 (2020).
Martineau, A. R. et al. Vitamin D supplementation to prevent acute respiratory infections: individual participant data meta-analysis. Health Technol. Assess. 23 , 1–44 (2019).
Camargo, C. A. et al. Effect of monthly high-dose vitamin D supplementation on acute respiratory infections in older adults: a randomized controlled trial. Clin. Infect. Dis. 71 , 311–317 (2019).
Chen, F. Y., Xiao, M., Ling, B., Liu, L. & Chen, L. Vitamin D does not improve lung function decline in COPD: a meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 23 , 8637–8644 (2019).
PubMed Google Scholar
Sluyter, J. D. et al. Effect of monthly, high-dose, long-term vitamin D on lung function: a randomized controlled trial. Nutrients 9 , 1353 (2017).
Bassatne, A. et al. The link between COVID-19 and vitamin D (VIVID): a systematic review and meta-analysis. Metabolism 119 , 15475 (2021).
Murai, I. H. et al. Effect of a single high dose of vitamin D3 on hospital length of stay in patients with moderate to severe COVID-19: a randomized clinical trial. JAMA 325 , 1053–1060 (2021).
Entrenas Castillo, M. et al. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: a pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 203 , 105751 (2020).
Amin, H. & Drenos, F. No evidence that vitamin D is able to prevent or affect the severity of COVID-19 in individuals with European ancestry: a Mendelian randomisation study of open data. BMJ Nutr. Prev. Health 4 , 42–48 (2021).
Butler-Laporte, G. et al. Vitamin D and COVID-19 susceptibility and severity in the COVID-19 Host Genetics Initiative: a Mendelian randomization study. PLoS Med. 18 , e1003605 (2021).
Li, W. et al. Vitamin D supplementation during pregnancy and the risk of wheezing in offspring: a systematic review and dose-response meta-analysis. J. Asthma 56 , 1266–1273 (2019).
Litonjua, A. A. et al. Six-year follow-up of a trial of antenatal vitamin D for asthma reduction. N. Engl. J. Med. 382 , 525–533 (2020).
Manousaki, D. et al. Vitamin D levels and susceptibility to asthma, elevated immunoglobulin E levels, and atopic dermatitis: a Mendelian randomization study. PLoS Med. 14 , e1002294 (2017).
Murdaca, G. et al. Emerging role of vitamin D in autoimmune diseases: an update on evidence and therapeutic implications. Autoimmun. Rev. 18 , 102350 (2019).
Mokry, L. E. et al. Vitamin D and risk of multiple sclerosis: a mendelian randomization study. PLoS Med. 12 , e1001866 (2015).
Jacobs, B. M., Noyce, A. J., Giovannoni, G. & Dobson, R. BMI and low vitamin D are causal factors for multiple sclerosis: a Mendelian randomization study. Neurol. Neuroimmunol. Neuroinflamm 7 , e662 (2020).
Gianfrancesco, M. A. et al. Evidence for a causal relationship between low vitamin D, high BMI, and pediatric-onset MS. Neurology 88 , 1623–1629 (2017).
Rhead, B. et al. Mendelian randomization shows a causal effect of low vitamin D on multiple sclerosis risk. Neurol. Genet. 2 , e97 (2016).
Bae, S. C. & Lee, Y. H. Vitamin D level and risk of systemic lupus erythematosus and rheumatoid arthritis: a Mendelian randomization. Clin. Rheumatol. 37 , 2415–2421 (2018).
Lund-Nielsen, J. et al. Vitamin D and inflammatory bowel disease: Mendelian randomization analyses in the Copenhagen studies and UK biobank. J. Clin. Endocrinol. Metab. 103 , 3267–3277 (2018).
Manousaki, D. et al. Vitamin D levels and risk of type 1 diabetes: a Mendelian randomization study. PLoS Med. 18 , e1003536 (2021).
Palacios, C., De-Regil, L. M., Lombardo, L. K. & Pena-Rosas, J. P. Vitamin D supplementation during pregnancy: updated meta-analysis on maternal outcomes. J. Steroid Biochem. Mol. Biol. 164 , 148–155 (2016).
Palacios, C., Kostiuk, L. K. & Pena-Rosas, J. P. Vitamin D supplementation for women during pregnancy. Cochrane Database Syst. Rev. 7 , CD008873 (2019).
Roth, D. E. et al. Vitamin D supplementation in pregnancy and lactation and infant growth. N. Engl. J. Med. 379 , 535–546 (2018).
Magnus, M. C. et al. Vitamin D and risk of pregnancy related hypertensive disorders: Mendelian randomisation study. BMJ 361 , k2167 (2018).
Amrein, K. et al. Effect of high-dose vitamin D3 on hospital length of stay in critically ill patients with vitamin D deficiency: the VITdAL-ICU randomized clinical trial. JAMA 312 , 1520–1530 (2014).
National Heart, L. et al. Early high-dose vitamin D3 for critically ill, vitamin D-deficient patients. N. Engl. J. Med. 381 , 2529–2540 (2019).
Wactawski-Wende, J. et al. Calcium plus vitamin D supplementation and the risk of colorectal cancer. N. Engl. J. Med. 354 , 684–696 (2006).
Smith, H. et al. Effect of annual intramuscular vitamin D on fracture risk in elderly men and women–a population-based, randomized, double-blind, placebo-controlled trial. Rheumatology 46 , 1852–1857 (2007).
Billington, E. O. et al. Effect of high-dose vitamin D supplementation on peripheral arterial calcification: secondary analysis of a randomized controlled trial. Osteoporos. Int. 31 , 2141–2150 (2020).
Durazo-Arvizu, R. A. et al. The reverse J-shaped association between serum total 25-Hydroxyvitamin D concentration and all-cause mortality: the impact of assay standardization. Am. J. Epidemiol. 185 , 720–726 (2017).
Gaksch, M. et al. Vitamin D and mortality: individual participant data meta-analysis of standardized 25-hydroxyvitamin D in 26916 individuals from a European consortium. PLoS ONE 12 , e0170791 (2017).
Mattila, T. et al. Airway obstruction, serum vitamin D and mortality in a 33-year follow-up study. Eur. J. Clin. Nutr. 73 , 1024–1032 (2019).
Zhang, Y. et al. Association between vitamin D supplementation and mortality: systematic review and meta-analysis. BMJ 366 , l4673 (2019).
Ordonez-Mena, J. M. et al. Genetic variants in the vitamin D pathway, 25(OH)D levels, and mortality in a large population-based cohort study. J. Clin. Endocrinol. Metab. 102 , 470–477 (2016).
Aspelund, T. et al. Effect of genetically low 25-hydroxyvitamin D on mortality risk: Mendelian randomization analysis in 3 large European cohorts. Nutrients 11 , 74 (2019).
Article CAS PubMed Central Google Scholar
Ong, J. S. et al. Vitamin D and overall cancer risk and cancer mortality: a mendelian randomization study. Hum. Mol. Genet. 27 , 4315–4322 (2018).
CAS PubMed Google Scholar
Bouillon, R. & Bikle, D. Vitamin D metabolism revised: fall of dogmas. J. Bone Miner. Res. 34 , 1985–1992 (2019).
Aatsinki, S. M. et al. Fasting-induced transcription factors repress vitamin D bioactivation, a mechanism for vitamin D deficiency in diabetes. Diabetes 68 , 918–931 (2019).
Roizen, J. D. et al. Obesity decreases hepatic 25-hydroxylase activity causing low serum 25-hydroxyvitamin D. J. Bone Miner. Res. 34 , 1068–1073 (2019).
Atkinson, S. A. Recommendations on vitamin D needs in multiple sclerosis from the MS Society of Canada. Public Health Nutr. 23 , 1278–1279 (2020).
Wang, T. J. et al. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet 376 , 180–188 (2010).
Wu, H. X. et al. Effects of vitamin D supplementation on the outcomes of patients with pulmonary tuberculosis: a systematic review and meta-analysis. BMC Pulm. Med. 18 , 108 (2018).
Download references
Author information
Authors and affiliations.
Clinical and Experimental Endocrinology, Department of Chronic Diseases and Metabolism, KU Leuven, Leuven, Belgium
Roger Bouillon
Research Center of the Sainte-Justine University Hospital, University of Montreal, Montreal, Quebec, Canada
Despoina Manousaki
Maine Medical Center Research Institute, Scarborough, ME, USA
Cliff Rosen
Department of Internal Medicine, Erasmus MC University Medical Center, Rotterdam, Netherlands
Katerina Trajanoska
Translational Skeletal Genomics, Department of Internal Medicine, Erasmus MC University Medical Center, Rotterdam, Netherlands
Fernando Rivadeneira
Centre for Clinical Epidemiology, Lady Davis Institute for Medical Research, Jewish General Hospital, Montreal, Quebec, Canada
J. Brent Richards
Departments of Medicine, Human Genetics, Epidemiology and Biostatistics, McGill University, Montreal, Quebec, Canada
You can also search for this author in PubMed Google Scholar
Contributions
R.B., D.M. and K.T. researched data for the article. All authors contributed substantially to discussion of the content. R.B. and D.M. wrote the article. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Correspondence to Roger Bouillon .
Ethics declarations
Competing interests.
R.B. received modest speaking or consultancy fees from Fresenius, Abiogen, FAES Farma, Ceres and Proctor and Gamble. J.B.R. has worked as a consultant to GlaxoSmithKline and Deerfield Capital. The other authors declare no competing interests
Additional information
Peer review information.
Nature Reviews Endocrinology thanks D. Bikle, C. Carlberg, G. Jones and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions.
Reprints and permissions
About this article
Cite this article.
Bouillon, R., Manousaki, D., Rosen, C. et al. The health effects of vitamin D supplementation: evidence from human studies. Nat Rev Endocrinol 18 , 96–110 (2022). https://doi.org/10.1038/s41574-021-00593-z
Download citation
Accepted : 25 October 2021
Published : 23 November 2021
Issue Date : February 2022
DOI : https://doi.org/10.1038/s41574-021-00593-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Clinical data mining: challenges, opportunities, and recommendations for translational applications.
- Huimin Qiao
- Yijing Chen
Journal of Translational Medicine (2024)
Journal Club
- Anna Maria Meyer
Zeitschrift für Gerontologie und Geriatrie (2024)
New insights into the vitamin D/PTH axis in endocrine-driven metabolic bone diseases
- Luigi di Filippo
- John P. Bilezikian
- Andrea Giustina
Endocrine (2024)
Tremendous Fidelity of Vitamin D3 in Age-related Neurological Disorders
- Manjari SKV
- Sharon Mariam Abraham
- Pragya Komal
Molecular Neurobiology (2024)
Vitamin D and human health: evidence from Mendelian randomization studies
- Aiping Fang
- Edward L. Giovannucci
European Journal of Epidemiology (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Weight Management
- Nutrition Facts
- Nutrition Basics
- Meal Delivery Services
- Fitness Gear
- Apparel & Accessories
- Recipe Nutrition Calculator
- Weight Loss Calorie Goal
- BMI Calculator
- Body Fat Percentage Calculator
- Calories Burned by Activity
- Daily Calories Burned
- Pace Calculator
- Editorial Process
- Meet Our Review Board
- Benefits and Risks
- Who May Benefit
- Purchasing Tips
- Which To Take
- What To Skip
- What To Buy
Benefits and Risks of Dietary Supplements
Shereen Lehman, MS, is a former writer for Verywell Fit and Reuters Health. She's a healthcare journalist who writes about healthy eating and offers evidence-based advice for regular people.
:max_bytes(150000):strip_icc():format(webp)/shereen-1f60ac63296d45eb89b4c7a7d782067e-5608c06027ba4ebeb5c54ccdc47f9d42-124899b94c76488b9fb1896447b45474.jpg)
Elena Klimenko, MD, is a board-certified doctor in internal medicine and is licensed in medical acupuncture and homeopathy.
:max_bytes(150000):strip_icc():format(webp)/Elena-Klimenko-1000-da1728dd626c4b90945406ebd9498103.jpg)
Potential Problems
- Next in Supplements Guide Why Aren't Dietary Supplements Regulated?
Dietary supplements are products designed to augment your daily intake of nutrients, including vitamins and minerals. Many are safe and offer significant health benefits, but there are some that pose health risks, especially if overused. Dietary supplements include amino acids, fatty acids, enzymes, probiotics , herbals, botanicals, and animal extracts.
In addition to vitamins and essential minerals , popular supplements include:
- Chondroitin
- Glucosamine
- St. John’s wort
- Saw palmetto
Normally, most people should be able to get all the nutrients they need from a balanced diet . However, supplements can provide you with extra nutrients when your diet is lacking or certain health conditions (such as cancer, diabetes, or chronic diarrhea) trigger a deficiency. Supplements for runners , for example, can provide certain nutrients that can be harder to get enough of on a plant-based diet.
In most cases, a multivitamin/mineral supplement will provide all the micronutrients your body needs. They are generally safe because they contain only small amounts of each nutrient (as measured by the daily value , or DV).
Individual nutrients are available as supplements, usually in doses larger than your typical multivitamin. They can be used to treat a deficiency, such as an iron deficiency, or reduce the risk of a medical condition, such as hypertension.
For example, large doses of vitamin B3 (niacin) may help raise "good" high-density lipoprotein (HDL) cholesterol, while folic acid has long been used to reduce the risk of a birth defect called spina bifida. Antioxidants, such as vitamin C and vitamin E, may reduce the toxic effect of chemotherapy drugs (allowing patients to tolerate larger doses of chemo). Turmeric supplements can be helpful for those with inflammation-related conditions.
Unless a specific deficiency is identified, a supplement is usually not necessary if you eat and exercise properly. When it comes to vitamins for women , specific formulations are often recommended for certain stages of life, such as childbearing years and menopause. The appropriate use of supplements can help you avoid side effects and toxicities associated with overuse.
In the United States, dietary supplements are not regulated as strictly as pharmaceutical drugs. Manufacturers do not have to prove that they are either safe or effective. The U.S. Food and Drug Administration (FDA) doesn't even determine whether dietary supplements are effective before they are shipped to market shelves.
The FDA does maintain a list of tainted or potentially harmful products marketed as dietary supplements. The worst offenders are usually weight loss aids, "natural" sexual enhancement pills , and supplements targeted at bodybuilders.
Supplement manufacturers have to follow certain labeling guidelines, including what they can say and not about the purported benefits. That doesn't stop manufacturers from claiming, often misleadingly, that their product can "boost the immune system" or "treat arthritis" even if there is little scientific evidence to support the claims. Generally speaking, the FDA only acts on the most serious infractions.
Large doses of certain nutrients can have adverse effects. You can even overdose on certain supplements, risking serious harm and death. Among some of the harmful interactions or dosing concerns:
- Vitamin K can reduce the effectiveness of blood thinners like Coumadin (warfarin).
- Vitamin E can increase the action of blood thinners, leading to easy bruising and nosebleeds.
- St. John’s wort can accelerate the breakdown of many drugs, including antidepressants and birth control pills, thereby reducing their effectiveness.
- Vitamin B6 (pyridoxine), when used for a year or more at high doses, can cause severe nerve damage. Vitamin B6 can also reduce the effectiveness of the anti-seizure drug Dilantin (phenytoin) and levodopa (used to treat Parkinson's disease).
- Vitamin A used with retinoid acne medications such as Accutane (isotretinoin) and Soriatane (acitretin) can cause vitamin A toxicity.
- Iron and calcium supplements can reduce the effectiveness of antibiotics, namely tetracyclines and fluoroquinolones, by as much as 40%.
- Vitamin C can cause diarrhea when taken in doses higher than the gut can absorb (but some patients can tolerate 5,000mg to 25,000mg per day).
- Selenium , boron, and iron supplements can be toxic if taken in large amounts.
Speak with a healthcare provider about any supplements you plan to take as well as any medications you are currently taking, whether they be pharmaceutical, over-the-counter, herbal, traditional, or homeopathic.
For the utmost safety and quality, choose supplements tested and approved by a certifying body such as the U.S. Pharmacopeia (USP). Never use expired supplements .
U.S. Food and Drug Administration. Tips for older dietary supplement users .
Afolayan AJ, Wintola OA. Dietary supplements in the management of hypertension and diabetes - a review . Afr J Tradit Complement Altern Med . 2014;11(3):248-258. doi:10.4314/ajtcam.v11i3.35
National Institutes of Health Office of Dietary Supplements. Niacin fact sheet for health professionals .
Centers for Disease Control and Prevention. Folic acid helps prevent some birth defects .
Singh K, Bhori M, Kasu YA, Bhat G, Marar T. Antioxidants as precision weapons in war against cancer chemotherapy induced toxicity: Exploring the armoury of obscurity . Saudi Pharm J . 2018;26(2):177-190. doi:10.1016/j.jsps.2017.12.013
U.S. Food and Drug Administration. Tainted products marketed as dietary supplements .
U.S. Food and Drug Administration. Center for Biologics Evaluation and Research 2003 .
U.S. Food and Drug Administration. Fortify your knowledge about vitamins .
National Institutes of Health Office of Dietary Supplements. Dietary supplements: What you need to know .
Sulli MM. Ezzo D. Drug interactions with vitamins and minerals . US Pharm. 2007;1:42-55.
By Shereen Lehman, MS Shereen Lehman, MS, is a former writer for Verywell Fit and Reuters Health. She's a healthcare journalist who writes about healthy eating and offers evidence-based advice for regular people.
Healthy Eating
Healthy food for kids, healthy eating and diet tips for women.
- Organic Foods: What You Need to Know
Cooking for One
Eating well on a budget, mindful eating, cooking at home.
- Online Therapy: Is it Right for You?
- Mental Health
- Health & Wellness
- Children & Family
- Relationships
Are you or someone you know in crisis?
- Bipolar Disorder
- Eating Disorders
- Grief & Loss
- Personality Disorders
- PTSD & Trauma
- Schizophrenia
- Therapy & Medication
- Exercise & Fitness
- Well-being & Happiness
- Weight Loss
- Work & Career
- Illness & Disability
- Heart Health
- Childhood Issues
- Learning Disabilities
- Family Caregiving
- Teen Issues
- Communication
- Emotional Intelligence
- Love & Friendship
- Domestic Abuse
- Healthy Aging
- Aging Issues
- Alzheimer’s Disease & Dementia
- Senior Housing
- End of Life
- Meet Our Team
Are you getting the vitamins and minerals you need?
Essential nutrients for your body, micronutrients with a big role in the body, a closer look at water-soluble vitamins, a closer look at fat-soluble vitamins, a closer look at major minerals, a closer look at trace minerals, a closer look at antioxidants, vitamins and minerals.
There so many different vitamins and mineral supplements available, it can feel overwhelming trying to decide what you should take. Here’s how to ensure you’re getting the right amounts of everything you need.

Adapted with permission from Making Sense of Vitamins and Minerals , a special health report published by Harvard Health Publishing.
Vitamins and minerals are essential nutrients because they perform hundreds of roles in the body. There is a fine line between getting enough of these nutrients (which is healthy) and getting too much (which can end up harming you). Eating a healthy diet remains the best way to get sufficient amounts of the vitamins and minerals you need.
Every day, your body produces skin, muscle, and bone. It churns out rich red blood that carries nutrients and oxygen to remote outposts, and it sends nerve signals skipping along thousands of miles of brain and body pathways. It also formulates chemical messengers that shuttle from one organ to another, issuing the instructions that help sustain your life.
But to do all this, your body requires some raw materials. These include at least 30 vitamins, minerals, and dietary components that your body needs but cannot manufacture on its own in sufficient amounts.
Vitamins and minerals are considered essential nutrients—because acting in concert, they perform hundreds of roles in the body. They help shore up bones, heal wounds, and bolster your immune system. They also convert food into energy, and repair cellular damage.
But trying to keep track of what all these vitamins and minerals do can be confusing. Read enough articles on the topic, and your eyes may swim with the alphabet-soup references to these nutrients, which are known mainly be their initials (such as vitamins A, B, C, D, E, and K—to name just a few).
In this article, you’ll gain a better understanding of what these vitamins and minerals actually do in the body and why you want to make sure you’re getting enough of them.
Vitamins and minerals are often called micronutrients because your body needs only tiny amounts of them. Yet failing to get even those small quantities virtually guarantees disease. Here are a few examples of diseases that can result from vitamin deficiencies:
- Scurvy. Old-time sailors learned that living for months without fresh fruits or vegetables—the main sources of vitamin C—causes the bleeding gums and listlessness of scurvy.
- Blindness. In some developing countries, people still become blind from vitamin A deficiency.
- Rickets. A deficiency in vitamin D can cause rickets, a condition marked by soft, weak bones that can lead to skeletal deformities such as bowed legs. Partly to combat rickets, the U.S. has fortified milk with vitamin D since the 1930s.
Just as a lack of key micronutrients can cause substantial harm to your body, getting sufficient quantities can provide a substantial benefit. Some examples of these benefits:
- Strong bones. A combination of calcium, vitamin D, vitamin K, magnesium, and phosphorus protects your bones against fractures.
- Prevents birth defects. Taking folic acid supplements early in pregnancy helps prevent brain and spinal birth defects in offspring.
- Healthy teeth. The mineral fluoride not only helps bone formation but also keeps dental cavities from starting or worsening.
The difference between vitamins and minerals
Although they are all considered micronutrients, vitamins and minerals differ in basic ways. Vitamins are organic and can be broken down by heat, air, or acid. Minerals are inorganic and hold on to their chemical structure.
So why does this matter? It means the minerals in soil and water easily find their way into your body through the plants, fish, animals, and fluids you consume. But it’s tougher to shuttle vitamins from food and other sources into your body because cooking, storage, and simple exposure to air can inactivate these more fragile compounds.
Interacting—in good ways and bad
Many micronutrients interact. Vitamin D enables your body to pluck calcium from food sources passing through your digestive tract rather than harvesting it from your bones. Vitamin C helps you absorb iron.
The interplay of micronutrients isn’t always cooperative, however. For example, vitamin C blocks your body’s ability to assimilate the essential mineral copper. And even a minor overload of the mineral manganese can worsen iron deficiency.
Speak to a Licensed Therapist
BetterHelp is an online therapy service that matches you to licensed, accredited therapists who can help with depression, anxiety, relationships, and more. Take the assessment and get matched with a therapist in as little as 48 hours.
Water-soluble vitamins are packed into the watery portions of the foods you eat. They are absorbed directly into the bloodstream as food is broken down during digestion or as a supplement dissolves.
Because much of your body consists of water, many of the water-soluble vitamins circulate easily in your body. Your kidneys continuously regulate levels of water-soluble vitamins, shunting excesses out of the body in your urine.
Water-soluble vitamins
B vitamins:
- Biotin (vitamin B7)
- Folic acid (folate, vitamin B9)
- Niacin (vitamin B3)
- Pantothenic acid (vitamin B5
- Riboflavin (vitamin B2)
- Thiamin (vitamin B1)
- Vitamin B12
What they do
Although water-soluble vitamins have many tasks in the body, one of the most important is helping to free the energy found in the food you eat. Others help keep tissues healthy. Here are some examples of how different vitamins help you maintain health:
- Release energy. Several B vitamins are key components of certain coenzymes (molecules that aid enzymes) that help release energy from food.
- Produce energy. Thiamin, riboflavin, niacin, pantothenic acid, and biotin engage in energy production.
- Build proteins and cells. Vitamins B6, B12, and folic acid metabolize amino acids (the building blocks of proteins) and help cells multiply.
- Make collagen. One of many roles played by vitamin C is to help make collagen, which knits together wounds, supports blood vessel walls, and forms a base for teeth and bones.
Words to the wise
Contrary to popular belief, some water-soluble vitamins can stay in the body for long periods of time. You probably have several years’ supply of vitamin B12 in your liver. And even folic acid and vitamin C stores can last more than a couple of days.
Generally, though, water-soluble vitamins should be replenished every few days.
Just be aware that there is a small risk that consuming large amounts of some of these micronutrients through supplements may be quite harmful. For example, very high doses of B6—many times the recommended amount of 1.3 milligrams (mg) per day for adults—can damage nerves, causing numbness and muscle weakness.
Rather than slipping easily into the bloodstream like most water-soluble vitamins, fat-soluble vitamins gain entry to the blood via lymph channels in the intestinal wall (see illustration). Many fat-soluble vitamins travel through the body only under escort by proteins that act as carriers.
Absorption of fat-soluble vitamins
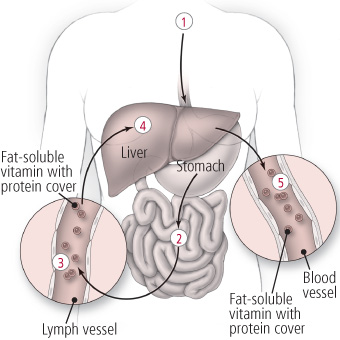
- Food containing fat-soluble vitamins is ingested.
- The food is digested by stomach acid and then travels to the small intestine, where it is digested further. Bile is needed for the absorption of fat-soluble vitamins. This substance, which is produced in the liver, flows into the small intestine, where it breaks down fats. Nutrients are then absorbed through the wall of the small intestine.
- Upon absorption, the fat-soluble vitamins enter the lymph vessels before making their way into the bloodstream. In most cases, fat-soluble vitamins must be coupled with a protein in order to travel through the body.
- These vitamins are used throughout the body, but excesses are stored in the liver and fat tissues.
- As additional amounts of these vitamins are needed, your body taps into the reserves, releasing them into the bloodstream from the liver.
Fatty foods and oils are reservoirs for the four fat-soluble vitamins. Within your body, fat tissues and the liver act as the main holding pens for these vitamins and release them as needed.
To some extent, you can think of these vitamins as time-release micronutrients. It’s possible to consume them every now and again, perhaps in doses weeks or months apart rather than daily, and still get your fill. Your body squirrels away the excess and doles it out gradually to meet your needs.
Fat-soluble vitamins
Together this vitamin quartet helps keep your eyes, skin, lungs, gastrointestinal tract, and nervous system in good repair. Here are some of the other essential roles these vitamins play:
- Build bones. Bone formation would be impossible without vitamins A, D, and K.
- Protect vision. Vitamin A also helps keep cells healthy and protects your vision.
- Interact favorably. Without vitamin E, your body would have difficulty absorbing and storing vitamin A.
- Protect the body. Vitamin E also acts as an antioxidant (a compound that helps protect the body against damage from unstable molecules).
Because fat-soluble vitamins are stored in your body for long periods, toxic levels can build up. This is most likely to happen if you take supplements. It’s very rare to get too much of a vitamin just from food.
The body needs, and stores, fairly large amounts of the major minerals. These minerals are no more important to your health than the trace minerals; they’re just present in your body in greater amounts.
Major minerals travel through the body in various ways. Potassium, for example, is quickly absorbed into the bloodstream, where it circulates freely and is excreted by the kidneys, much like a water-soluble vitamin. Calcium is more like a fat-soluble vitamin because it requires a carrier for absorption and transport.

Major minerals
One of the key tasks of major minerals is to maintain the proper balance of water in the body. Sodium, chloride, and potassium take the lead in doing this. Three other major minerals—calcium, phosphorus, and magnesium—are important for healthy bones. Sulfur helps stabilize protein structures, including some of those that make up hair, skin, and nails.
Having too much of one major mineral can result in a deficiency of another. These sorts of imbalances are usually caused by overloads from supplements, not food sources. Here are two examples:
- Salt overload. Calcium binds with excess sodium in the body and is excreted when the body senses that sodium levels must be lowered. That means that if you ingest too much sodium through table salt or processed foods, you could end up losing needed calcium as your body rids itself of the surplus sodium.
- Excess phosphorus. Likewise, too much phosphorus can hamper your ability to absorb magnesium.
A thimble could easily contain the distillation of all the trace minerals normally found in your body. Yet their contributions are just as essential as those of major minerals such as calcium and phosphorus, which each account for more than a pound of your body weight.
Trace minerals
Trace minerals carry out a diverse set of tasks. Here are a few examples:
- Iron is best known for ferrying oxygen throughout the body.
- Fluoride strengthens bones and wards off tooth decay.
- Zinc helps blood clot, is essential for taste and smell, and bolsters the immune response.
- Copper helps form several enzymes, one of which assists with iron metabolism and the creation of hemoglobin, which carries oxygen in the blood.
The other trace minerals perform equally vital jobs, such as helping to block damage to body cells and forming parts of key enzymes or enhancing their activity.
Trace minerals interact with one another, sometimes in ways that can trigger imbalances. Too much of one can cause or contribute to a deficiency of another. Here are some examples:
- A minor overload of manganese can exacerbate iron deficiency. Having too little can also cause problems.
- When the body has too little iodine, thyroid hormone production slows, causing sluggishness and weight gain as well as other health concerns. The problem worsens if the body also has too little selenium.
The difference between “just enough” and “too much” of the trace minerals is often tiny. Generally, food is a safe source of trace minerals, but if you take supplements, it’s important to make sure you’re not exceeding safe levels.
Antioxidant is a catchall term for any compound that can counteract unstable molecules such as free radicals that damage DNA, cell membranes, and other parts of cells.
Your body cells naturally produce plenty of antioxidants to put on patrol. The foods you eat—and, perhaps, some of the supplements you take—are another source of antioxidant compounds. Carotenoids (such as lycopene in tomatoes and lutein in kale) and flavonoids (such as anthocyanins in blueberries, quercetin in apples and onions, and catechins in green tea) are antioxidants. The vitamins C and E and the mineral selenium also have antioxidant properties.
Why free radicals may be harmful
Free radicals are a natural byproduct of energy metabolism and are also generated by ultraviolet rays, tobacco smoke, and air pollution. They lack a full complement of electrons, which makes them unstable, so they steal electrons from other molecules, damaging those molecules in the process.
Free radicals have a well-deserved reputation for causing cellular damage. But they can be helpful, too. When immune system cells muster to fight intruders, the oxygen they use spins off an army of free radicals that destroys viruses, bacteria, and damaged body cells in an oxidative burst. Vitamin C can then disarm the free radicals.
How antioxidants may help
Antioxidants are able to neutralize marauders such as free radicals by giving up some of their own electrons. When a vitamin C or E molecule makes this sacrifice, it may allow a crucial protein, gene, or cell membrane to escape damage. This helps break a chain reaction that can affect many other cells.
It is important to recognize that the term “antioxidant” reflects a chemical property rather than a specific nutritional property. Each of the nutrients that has antioxidant properties also has numerous other aspects and should be considered individually. The context is also important—in some settings, for example, vitamin C is an antioxidant, and in others it can be a pro-oxidant.
Articles and advertisements have touted antioxidants as a way to help slow aging, fend off heart disease, improve flagging vision, and curb cancer. And laboratory studies and many large-scale observational trials (the type that query people about their eating habits and supplement use and then track their disease patterns) have noted benefits from diets rich in certain antioxidants and, in some cases, from antioxidant supplements.
But results from randomized controlled trials (in which people are assigned to take specific nutrients or a placebo) have failed to back up many of these claims. One study that pooled results from 68 randomized trials with over 230,000 participants found that people who were given vitamin E, beta carotene, and vitamin A had a higher risk of death than those who took a placebo. There appeared to be no effect from vitamin C pills and a small reduction in mortality from selenium, but further research on these nutrients is needed.
These findings suggest little overall benefit of the antioxidants in pill form. On the other hand, many studies show that people who consume higher levels of these antioxidants in food have a lower risk of many diseases.
The bottom line? Eating a healthy diet is the best way to get your antioxidants.
More in Healthy Eating
Simple ways to plan, enjoy, and stick to a healthy diet

Easy tips to help your children and teens eat healthier

Eating right to look and feel your best at every stage of your life

Organic Foods
The benefits of organic food and how to keep it affordable

Improve your health by cooking for yourself

Tips to help you and your family eat delicious, healthy food on a tight budget

How focusing on the experience of eating can improve your diet

How to get started in preparing more home-cooked meals

Professional therapy, done online
BetterHelp makes starting therapy easy. Take the assessment and get matched with a professional, licensed therapist.
Help us help others
Millions of readers rely on HelpGuide.org for free, evidence-based resources to understand and navigate mental health challenges. Please donate today to help us save, support, and change lives.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Health effects of...
Health effects of vitamin and mineral supplements
Read our food for thought 2020 collection.
- Related content
- Peer review
- Fang Fang Zhang , associate professor 1 ,
- Susan I Barr , professor 2 ,
- Helene McNulty , professor 3 ,
- Duo Li , professor 4 ,
- Jeffrey B Blumberg , professor 1
- 1 Friedman School of Nutrition Science and Policy, Tufts University, Boston, USA
- 2 University of British Columbia, Vancouver, Canada
- 3 Nutrition Innovation Centre for Food and Health, Ulster University, Coleraine, UK
- 4 Institute of Nutrition and Health, Qingdao University, Qingdao, China
- Correspondence to: F F Zhang fang_fang.zhang{at}tufts.edu
Growing numbers of healthy people are taking dietary supplements but there is little evidence that they protect against non-communicable diseases, say Fang Fang Zhang and colleagues
Vitamin and mineral supplements are the most commonly used dietary supplements by populations worldwide. 1 2 3 4 The amount of micronutrients they provide ranges from less than recommended intakes to much more, making them important contributors to total intakes. While supplements can be used to correct micronutrient deficiency or maintain an adequate intake, over-the-counter supplements are most often taken by people with no clinical signs or symptoms of deficiency. However, the effect of vitamin and mineral supplements on the risk of non-communicable diseases in “generally healthy” populations is controversial. We examine patterns of supplement use and the evidence on their effects from randomised trials.
Who uses supplements?
Vitamin and mineral supplements have a large worldwide market, but we will focus on their use in North America and Europe, where there is most evidence on patterns of use and health outcomes. The use of vitamin, mineral, and fish oil supplements 5 is common among adults in North America ( fig 1 ). 6 The prevalence of use has increased for some individual nutrients—for example, there was a fourfold increase in use of vitamin D supplements among US adults from 1999 to 2012, excluding intake obtained from multivitamin and mineral. 7 The use of omega-3 fatty acid supplements also increased sevenfold. 7

Proportion of US adults taking commonly vitamin, mineral, and fish oil supplements, National Health and Nutrition Examination Survey 1999-2014 6
- Download figure
- Open in new tab
- Download powerpoint
Supplement use is generally less prevalent in other countries than in the US and Canada but varies widely (eg, Denmark 51%, South Korea 34%, Australia 43%, UK 36%, Spain 6%, Greece 2%). 2 3 4 Different methods for assessing supplement use may contribute to the different prevalence in high income countries. National survey data for supplement use in the general population remain scarce for low and middle income countries.
Supplement use varies considerably among population subgroups within North America and Europe. In the US, >70% of adults aged ≥65 years use supplements 8 compared with a third of children and adolescents. 9 More women than men use supplements. 6 Supplement use correlates positively with educational and socioeconomic status. 10 It also clusters with healthy lifestyle factors such as not being a smoker or heavy drinker, not being overweight or obese, and being physically active. 6 Importantly, people who use supplements tend to have a better overall diet quality than those who don’t use them and their nutrient intake from foods mostly meets recommended intake levels. 11 12
Are supplements needed?
Use of supplements contributes substantially to total vitamin and mineral intakes at the population level. 13 Intake of vitamin B 6 , thiamin, and riboflavin among US adults is at least five times higher from supplements than from foods, and intakes are 15 to 20 times higher for supplements for vitamins B 12 and E. 6 Consequently, supplement use considerably reduces the proportion of the general population with inadequate nutrient intake ( box 1 ).
Population nutrient intake—definitions
Estimated average requirement is the daily level of nutrient intake estimated to meet the requirement of half of healthy people in a population
Inadequate nutrient intake —The population prevalence of inadequate intake is estimated as the percentage of the population with nutrient intake below the estimated average requirement
Tolerable upper intake is the highest daily nutrient intake that is likely to pose no risk of adverse health effects to almost all healthy people in a population. As intake increases above the upper level, the potential risk of adverse effects increases.
Excess intake —The population prevalence of excess intake is estimated as the percentage of the population with nutrient intake above the upper level
This is especially true for vitamins and minerals identified as “shortfall” nutrients such as calcium and vitamin D ( fig 2 ). 14 Despite the high use of supplements, inadequate intakes of micronutrients are still common in high income countries, where dietary patterns are typically energy rich but nutrient poor.

Prevalence of inadequate and excess nutrient intake among US Adults, National Health and Nutrition Examination Survey 1999-2014 6
In low and middle income countries, where specific micronutrient deficiencies are prevalent (eg, of iodine, iron, zinc, and vitamin A), supplementation is recommended when food based approaches such as dietary modification, fortification, or food provision are unable to achieve inadequate intake. 15 In the US and other countries, food fortification and enrichment such as the addition of iodine to salt, vitamin D to milk, and B 1 and B 3 vitamins to refined flour have contributed to the virtual elimination of their syndromes of deficiency (goitre, rickets, beriberi, and pellagra, respectively). 16 17
The widespread use of vitamin and mineral supplements in high income countries seems to contribute to an increase in population prevalence of intake above the upper tolerable level ( box 1 ). 6 Although the overall proportion of US adults with intakes above the upper level is below 5% for most nutrients ( fig 2 ), some population subgroups may have high rates of excess intake. For example, in a Canadian national survey, over 80% of children aged 1-3 years who took dietary supplements consumed vitamin A and niacin at levels above the upper limit. 18 In the US, excessive intake was noted for vitamin A (97%) and zinc (68%) among toddlers who were given supplements. 19 High quality evidence is lacking on the long term adverse effects of excess intake for several nutrients so it is unclear whether this is a cause for concern.
Do supplements protect against non-communicable diseases?
It remains controversial whether supplements are effective in reducing the risk of non-communicable diseases. In contrast to results of observational studies, the accumulated evidence from randomised controlled trials does not support benefits of supplements in reducing risks of cardiovascular disease, cancer, or type 2 diabetes in healthy people with no clinical nutritional deficiencies.
Cardiovascular disease
An updated systematic review of 15 randomised trials published after the 2013 US Preventive Service Task Force (USPSTF) review 20 confirmed the lack of benefits of supplements on cardiovascular events, mostly among patients with risk factors. 21 Although randomised trials of folic acid, alone or in combination with vitamins B 12 or B 6 , found significant reductions in plasma homocysteine levels, total cardiovascular events were not reduced. Another systematic review reported a reduced risk of stroke in association with supplementation of homocysteine lowering B vitamins, 22 but the result was largely driven by one large trial in China. 23 Overall, there is no consistent evidence to support the use of antioxidant supplements for reducing cardiovascular risk. 22 24
The Vitamin D and Omega-3 Trial (VITAL), one of the few randomised trials of supplements for primary prevention of cardiovascular disease, found no effect of vitamin D supplementation (2000 IU/day) on its primary endpoint (myocardial infarction, stroke, or cardiovascular death) in healthy people. 25 Previous large scale trials such as the Women’s Health Initiative Calcium and Vitamin D Supplementation Study 26 and the Vitamin D Assessment Study 27 also showed vitamin D supplements, alone or in combination with calcium, had no effect on cardiovascular risk.
Supplementation with omega-3 fatty acids (1 g/day) did not reduce the risk of major cardiovascular events among healthy people in the VITAL trial. 28 However, benefits were found for some secondary endpoints such as total myocardial infarctions. This result is largely consistent with findings from meta-analyses that fish oil supplementation did not have substantial effects on the primary or secondary prevention of cardiovascular disease. 29 30 However, a meta-analysis including the most recent trials reported a significant reduction in risk of myocardial infarction. 31 Further studies are needed to determine whether fish oil supplementation has a greater effect on risk of heart disease than of stroke. 32
Current evidence does not support a role of vitamin and mineral supplements in reducing cancer risk, with some evidence suggesting potential harm. β-Carotene supplementation increased the risk of lung cancer among high risk individuals in two randomised trials. The α-Tocopherol, β-Carotene Cancer Prevention Study reported an 18% increase in relative risk among smokers randomised to β-carotene (20 mg/day) compared with those who did not. 33 The β-Carotene and Retinol Efficacy Trial found that β-carotene (30 mg/day) plus vitamin A as retinol (25 000 IU/day) increased risk by 28% among smokers and workers with occupational exposure to asbestos. 34 The Selenium and Vitamin E Cancer Prevention Trial found that vitamin E (400 IU/day) supplementation was associated with a 17% increase in prostate cancer risk among men. 35
Although maternal folic acid supplementation has been proved to reduce the risk of neural tube defects, concerns have been raised that high folic acid exposure may promote cancer progression, especially in countries with mandatory fortification. 36 Most notably, folic acid supplementation at ≥1 mg/day may promote the growth of undiagnosed colorectal adenomas. 37 However, a meta-analysis of 11 randomised trials concluded that folic acid supplementation neither increased nor decreased site specific cancer risk within the first five years of supplementation. 38
Randomised trials have failed to detect a benefit of vitamin D supplementation, alone or combined with calcium, on cancer risk at either high or low doses 25 39 despite some evidence suggesting reduced total cancer mortality. 25 40 The limited evidence on fish oil supplementation suggests it does not reduce cancer risk. 28 41
Type 2 diabetes
Current evidence does not support the use of supplements with vitamins C or E, β-carotene, or fish oil to reduce the risk of type 2 diabetes, although the overall evidence from randomised trials is limited. 42 43 A recent placebo controlled trial of vitamin D supplementation (4000 IU/day) failed to reduce the risk of type 2 diabetes despite significantly increasing serum 25-hydroxyvitamin D concentrations. 44
Osteoporosis
Recent evidence regarding the effects of vitamin D and calcium supplementation is inconsistent. A meta-analysis of trials in community living older adults found that vitamin D or calcium supplementation did not reduce the risk of hip fracture or total fracture, 45 whereas another meta-analysis reported that while vitamin D alone did not reduce fracture risk, combined calcium and vitamin D supplementation decreased the relative risk of hip fracture (16%) and all fractures (6%) among older adults. 46 Ongoing research is assessing the effect of high dose vitamin D supplements on several health outcomes, including fractures, 46 but a recent three year trial of 400, 4000, or 10 000 IU/day reported that the higher doses reduced volumetric bone density, suggesting potential for harm. 47 In the absence of clear evidence on supplementation, it is prudent to ensure that dietary recommendations on calcium and vitamin D intakes are met through food and supplementation.
To date, randomised trials have largely shown no benefit of vitamin, mineral, and fish oil supplements on the risk of major non-communicable diseases in people without clinical nutritional deficiency. These results contrast with findings from observational studies, where supplemental nutrient intakes are often associated with a reduced risk of these diseases. The apparent associations from observational studies may result from unknown or unmeasured confounding factors such as socioeconomic status and lifestyle factors, including a better overall diet.
Although randomisation reduces confounding, relying exclusively on the results of randomised trials also has limitations. Trials are often conducted among high risk populations with pre-existing conditions, so the findings may not be applicable to healthy individuals. Supplements may also have health benefits for population subgroups, such as people with inadequate nutrient intake from foods, but randomised trials are not usually designed to evaluate subgroup differences. Furthermore, financial and practical constraints mean that most trials are able to investigate only a single dose, which may result in selection of a dose that is either too low (no efficacy) or too high (untoward outcomes).
Nutrients obtained from foods and supplements may confer different health effects. The Cancer Prevention Study (CPS)-II Nutrition Cohort found that supplemental calcium intake at ≥1000 mg/day was associated with an increased risk of all-cause mortality in men whereas high levels of calcium intake from foods had no harm. 48 Among US adults in the National Health and Nutrition Examination Survey, adequate intake of nutrients from foods, but not supplements, was associated with a lower risk of all-cause mortality. 6 The benefits of nutrient intake from foods may reflect synergistic interactions among multiple nutrients and other bioactive substances in foods.
The effect of supplements in specific populations warrants further investigation. Older adults are at an increased risk of malnutrition because of reduced nutrient intake and age related decreases in the bioavailability of some micronutrients. Vitamin D supplementation is recommended for breastfed infants before the introduction of whole milk and solid foods. Supplements may be more effective in reducing the risk of non-communicable disease in specific ethnic groups or people with low micronutrient intake from foods. 28 With a recent increase in the proportion of people reporting that they follow restricted dietary patterns such as ketogenic, Palaeolithic, vegan, and vegetarian diets, the value of supplements to meet the needs of these specific populations requires evaluation. In addition, potential nutrient-gene interactions have rarely been examined in studies of dietary supplements. Future studies on the role of nutrigenetics should help refine and personalise targeted recommendations for supplement use ( box 2 ).
Areas for research in vitamin and mineral supplementation
Differing health effects of nutrients obtained from foods versus supplements
Synergistic interactions among multiple nutrients and with other bioactive substances
Subpopulation studies (eg, elderly people, ethnic groups, vegans)
Nutrigenetics and “omics” sciences
Personalised supplementation
Specific needs in low and middle income countries
It is also important to recognise that the need for nutrient supplements is different in countries where nutrition deficiency is common. Ensuring adequate nutrition through food fortification and nutrient supplementation can be crucial to prevent serious adverse outcomes of nutrient deficiencies in low and middle income countries, especially among children <5 years, for whom malnutrition contributes to more than half their deaths. 15
In summary, current evidence does not support recommending vitamin or fish oil supplements to reduce the risk of non-communicable diseases among populations without clinical nutritional deficiency. Continuing efforts are warranted to further understand the potentially different roles of nutrients from foods versus supplements in health promotion among a generally healthy population as well as individuals or groups with specific nutritional needs, including those living in low and middle income countries. These efforts, coupled with the integration of new research approaches, will better inform clinical practice and public health policies.
Key messages
Randomised trial evidence does not support use of vitamin, mineral, and fish oil supplements to reduce the risk of non-communicable diseases
People using supplements tend to be older, female, and have higher education, income, and healthier lifestyles than people who do not use them
Use of supplements appreciably reduces the prevalence of inadequate intake for most nutrients but also increases the prevalence of excess intake for some nutrients
Further research is needed to assess the long term effects of supplements on the health of the general population and in individuals with specific nutritional needs, including those from low and middle income countries
Contributors and sources: All authors contributed to drafting the manuscript, with FFZ taking a lead role and serving as the guarantor. Sources of information for this manuscript included published articles based on national surveys, systematic reviews, and primary research of randomised controlled trials and prospective cohort studies. All authors contributed to critical revision of the manuscript for important intellectual content and approved the final manuscript.
Competing interests: All authors have read and understood BMJ policy on declaration of interests and declared the following: FFZ declares funding from the National Institutes of Health, NIMHD (R01 MD 011501) and the Bristol Mayer Squibb Foundation (Bridging Cancer Care Programme). DL declares funding from the National Natural Science Foundation of China (NSFC 81773433) and Key Scientific Research Projects in Shandong Providence China (2017YYSP007). JBB declares funding from Danone. HM declares funding from DSM Nutritional Products, Switzerland. The funders had no role in the design or conduct of the study, collection, management, analysis, or the interpretation of the data. JBB reports service on scientific advisory boards of AdvoCare International, California Prune Board, California Walnut Commission, Church and Dwight, Cranberry Marketing Committee, Guiding Stars, Quaker Oats, Segterra, and SmartyPants, not related to this work.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of series commissioned by The BMJ. Open access fees are paid by Swiss Re, which had no input into the commissioning or peer review of the articles. T he BMJ thanks the series advisers, Nita Forouhi, Dariush Mozaffarian, and Anna Lartey for valuable advice and guiding selection of topics in the series.
This is an Open Access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
- MacLennan GS ,
- Avenell A ,
- Bolland M ,
- RECORD Trial Group
- Braaten T ,
- Hjartåker A ,
- O’Brien SK ,
- Malacova E ,
- Sherriff JL ,
- Clarke TC ,
- Barnes PM ,
- Stussman BJ ,
- Blumberg JB ,
- Kantor ED ,
- Giovannucci EL
- Fulgoni VL ,
- Weaver CM ,
- Alexander GC ,
- Guadamuz JS ,
- Bailey RL ,
- Fulgoni VL 3rd . ,
- Harrison RA ,
- Pattison DJ ,
- Murphy SP ,
- West KP Jr . ,
- Institute of Medicine Committee on Use of Dietary Reference Intakes in Nutrition Labeling
- Shakur YA ,
- Tarasuk V ,
- O’Connor DL
- Briefel R ,
- US Preventive Services Task Force
- Jenkins DJA ,
- Spence JD ,
- Giovannucci EL ,
- Martí-Carvajal AJ ,
- Lathyris D ,
- CSPPT Investigators
- Buring JE ,
- Christen WG ,
- Manson JE ,
- VITAL Research Group
- Women’s Health Initiative Investigators
- Stewart AW ,
- Abdelhamid AS ,
- Brainard JS ,
- Kromhout D ,
- Omega-3 Treatment Trialists’ Collaboration
- Bassuk SS ,
- Alpha-Tocopherol, Beta Carotene Cancer Prevention Study Group
- Goodman GE ,
- Thornquist MD ,
- Thompson IM Jr . ,
- Tangen CM ,
- Sandler RS ,
- Polyp Prevention Study Group
- Vollset SE ,
- Lewington S ,
- B-Vitamin Treatment Trialists’ Collaboration
- Travers-Gustafson D ,
- Colmers IN ,
- Albert CM ,
- Van Denburgh M ,
- Pittas AG ,
- Dawson-Hughes B ,
- Sheehan P ,
- D2d Research Group
- Bennett D ,
- Billington EO ,
- Raymond DA ,
- Hanley DA ,
- Campbell PT ,
- Gapstur SM ,
3 pervasive myths about supplements, as explained by an expert
They act kind of like drugs, but they aren't regulated like them.

Americans seem to have quite a positive view of dietary supplements . According to a 2023 survey, 74% of U.S. adults take vitamins, prebiotics and the like .
The business of supplements is booming , and with all the hype around them, it's easy to forget what they actually are: substances that can powerfully affect the body and your health, yet aren't regulated like drugs are. They're regulated more like food .
Thanks in large part to a 1994 law, the Food and Drug Administration is essentially toothless when it comes to supplements. As the agency acknowledges : “FDA does not have the authority to approve dietary supplements before they are marketed. Companies can sell supplements without going through any sort of approval process, or even having to share safety evidence.”
As a research faculty member in graduate medical education , I'm responsible for teaching resident physicians how to understand and critically engage with health research. I also write about health , wellness and supplements for a broader audience. As a result, I spend a lot of time thinking about supplements.
It's important to consider why so many people believe supplements can help them lead a healthier life. While there are many reasons, how supplements are marketed is undeniably an important one . In my years following the industry, I've found that three mistaken assumptions appear over and over in supplement marketing.
1. The appeal to nature fallacy
The appeal to nature fallacy occurs when you assume that because something is "natural" it must be good. The word natural is used a lot in the marketing of supplements. In the context of health, it often feels right to want natural medicine, remedies, prevention techniques and so forth.
For example, if I say "vitamin C," what do you immediately think of? Probably oranges or citrus in general and flu prevention. But if I say "the flu shot," what immediately comes to mind? Probably doctor's offices, a little bit of pain and pharmaceutical companies. One of these is clinically proven to prevent flu infections and lessen the severity of illness. The other has been marketed as though it does those same things, but there's no clinical evidence to support this.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
The supplement industry is awash with brand names that incorporate the word "nature," invoking the appeal to nature fallacy. Also, look at websites and advertisements that urge customers to forgo "artificial" products in favor of "pure" and "natural nutrition." Using the word artificial to describe other products and natural to describe a specific supplement is intended to make you feel like that product will be superior to the competition and that you need it to be healthy.
To be clear, "natural" does not equate to "better," but that's what the marketing wants you to think.
2. The belief that more of a good thing is always better
There's another assumption that piggybacks on the appeal to nature fallacy: If something is natural, it must be good, and more of it must also always be better. If a little vitamin C is good for us, then a lot of it must be great!

The truth is that our bodies tightly regulate levels of the vitamins and minerals we consume. If you don't have a deficiency, consuming more of a particular vitamin or mineral through a supplement won't necessarily lead to health benefits . That's why supplement skeptics sometimes say, "You're just paying for expensive pee" — since your body will excrete the excess.
For an example of the more-is-better myth, look at basically any vitamin C supplement . The packaging often prominently displays dosages that can reach 750 or 1,000 milligrams. But adults need only about 75 to 120 milligrams of vitamin C per day . Similarly, look at vitamin D supplements that can come in dosages of 5,000 IU, or international units — a fact also often prominently displayed on packaging. But adults should have no more than 4,000 IU daily . Again, it's easy to exceed what we need.
3. The action bias
Finally, the supplement industry likes to capitalize on the idea that doing something is better than doing nothing. This is the action bias . Taking action makes people feel like they have more control of a situation, which is especially powerful when it comes to health. "Even if I don't need the extra vitamin C," they might think, "I'll take it just to be sure. What’s the harm?"
The examples in the last section show that supplements often contain many times the recommended daily intake of a particular vitamin or mineral. This assumes that taking that much of any of those particular substances is safe.
— Best protein powder for women 2024: Boost your protein intake with female-friendly supplements
— Most melatonin gummies have higher doses than what's on the label
— Best multivitamin for women 2024: Support your daily routine at every life stage
It is possible to have too much of a good thing. Too much vitamin C can lead to diarrhea, nausea, stomach cramps and more . Too much vitamin D can lead to conditions including nausea, vomiting and kidney stones . Supplements can also interact with prescribed medications. For example, St. John's wort is famous for interacting with contraceptives, immunosuppressive drugs, statins and chemotherapy by exacerbating or dulling their effects. When it comes to supplements, taking them isn't necessarily better than not.
Be on the lookout for these marketing messages — they aren't necessarily correct or good for your health. And talk with your doctor before taking any supplements.
This edited article is republished from The Conversation under a Creative Commons license. Read the original article .

I am non-clinical faculty in graduate medical education for HCA Healthcare where I am a regional director of research. I develop and teach research curriculum to medical residents and fellows as well as mentor and oversee their research projects during residency and fellowship.
Scientists may have pinpointed the true origin of the Hope Diamond and other pristine gemstones
NASA reveals 'glass-smooth lake of cooling lava' on surface of Jupiter's moon Io
Space photo of the week: Bizarre 'Helix Galaxy' is unlike any other in the universe. Can you see why?
Most Popular
- 2 Scientists are one step closer to knowing the mass of ghostly neutrinos — possibly paving the way to new physics
- 3 Giant, 82-foot lizard fish discovered on UK beach could be largest marine reptile ever found
- 4 See the explosive 'devil comet' get its tail ripped off by a solar storm days before its close approach to the sun
- 5 Global 'time signals' subtly shifted as the total solar eclipse reshaped Earth's upper atmosphere, new data shows
- 2 Enormous dinosaur dubbed Shiva 'The Destroyer' is one of the biggest ever discovered
- 3 2,500-year-old skeletons with legs chopped off may be elites who received 'cruel' punishment in ancient China
- 4 Rare 'porcelain gallbladder' found in 100-year-old unmarked grave at Mississippi mental asylum cemetery
- 5 What's the largest waterfall in the world?
To revisit this article, visit My Profile, then View saved stories .
- Backchannel
- Newsletters
- WIRED Insider
- WIRED Consulting
Amanda Hoover
Students Are Likely Writing Millions of Papers With AI
Students have submitted more than 22 million papers that may have used generative AI in the past year, new data released by plagiarism detection company Turnitin shows.
A year ago, Turnitin rolled out an AI writing detection tool that was trained on its trove of papers written by students as well as other AI-generated texts. Since then, more than 200 million papers have been reviewed by the detector, predominantly written by high school and college students. Turnitin found that 11 percent may contain AI-written language in 20 percent of its content, with 3 percent of the total papers reviewed getting flagged for having 80 percent or more AI writing. (Turnitin is owned by Advance, which also owns Condé Nast, publisher of WIRED.) Turnitin says its detector has a false positive rate of less than 1 percent when analyzing full documents.
ChatGPT’s launch was met with knee-jerk fears that the English class essay would die . The chatbot can synthesize information and distill it near-instantly—but that doesn’t mean it always gets it right. Generative AI has been known to hallucinate , creating its own facts and citing academic references that don’t actually exist. Generative AI chatbots have also been caught spitting out biased text on gender and race . Despite those flaws, students have used chatbots for research, organizing ideas, and as a ghostwriter . Traces of chatbots have even been found in peer-reviewed, published academic writing .
Teachers understandably want to hold students accountable for using generative AI without permission or disclosure. But that requires a reliable way to prove AI was used in a given assignment. Instructors have tried at times to find their own solutions to detecting AI in writing, using messy, untested methods to enforce rules , and distressing students. Further complicating the issue, some teachers are even using generative AI in their grading processes.
Detecting the use of gen AI is tricky. It’s not as easy as flagging plagiarism, because generated text is still original text. Plus, there’s nuance to how students use gen AI; some may ask chatbots to write their papers for them in large chunks or in full, while others may use the tools as an aid or a brainstorm partner.
Students also aren't tempted by only ChatGPT and similar large language models. So-called word spinners are another type of AI software that rewrites text, and may make it less obvious to a teacher that work was plagiarized or generated by AI. Turnitin’s AI detector has also been updated to detect word spinners, says Annie Chechitelli, the company’s chief product officer. It can also flag work that was rewritten by services like spell checker Grammarly, which now has its own generative AI tool . As familiar software increasingly adds generative AI components, what students can and can’t use becomes more muddled.
Detection tools themselves have a risk of bias. English language learners may be more likely to set them off; a 2023 study found a 61.3 percent false positive rate when evaluating Test of English as a Foreign Language (TOEFL) exams with seven different AI detectors. The study did not examine Turnitin’s version. The company says it has trained its detector on writing from English language learners as well as native English speakers. A study published in October found that Turnitin was among the most accurate of 16 AI language detectors in a test that had the tool examine undergraduate papers and AI-generated papers.

Emily Mullin

Joel Khalili

C. Brandon Ogbunu
Schools that use Turnitin had access to the AI detection software for a free pilot period, which ended at the start of this year. Chechitelli says a majority of the service’s clients have opted to purchase the AI detection. But the risks of false positives and bias against English learners have led some universities to ditch the tools for now. Montclair State University in New Jersey announced in November that it would pause use of Turnitin’s AI detector. Vanderbilt University and Northwestern University did the same last summer.
“This is hard. I understand why people want a tool,” says Emily Isaacs, executive director of the Office of Faculty Excellence at Montclair State. But Isaacs says the university is concerned about potentially biased results from AI detectors, as well as the fact that the tools can’t provide confirmation the way they can with plagiarism. Plus, Montclair State doesn’t want to put a blanket ban on AI, which will have some place in academia. With time and more trust in the tools, the policies could change. “It’s not a forever decision, it’s a now decision,” Isaacs says.
Chechitelli says the Turnitin tool shouldn’t be the only consideration in passing or failing a student. Instead, it’s a chance for teachers to start conversations with students that touch on all of the nuance in using generative AI. “People don’t really know where that line should be,” she says.
You Might Also Like …
In your inbox: The best and weirdest stories from WIRED’s archive
Jeffrey Epstein’s island visitors exposed by data broker
8 Google employees invented modern AI. Here’s the inside story
The crypto fraud kingpin who almost got away
Listen up! These are the best podcasts , no matter what you’re into

Stephen Ornes

Will Knight
Estelle Erasmus
Kate Knibbs

Steven Levy

Matt Burgess
Reece Rogers

Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
How Pew Research Center will report on generations moving forward
Journalists, researchers and the public often look at society through the lens of generation, using terms like Millennial or Gen Z to describe groups of similarly aged people. This approach can help readers see themselves in the data and assess where we are and where we’re headed as a country.
Pew Research Center has been at the forefront of generational research over the years, telling the story of Millennials as they came of age politically and as they moved more firmly into adult life . In recent years, we’ve also been eager to learn about Gen Z as the leading edge of this generation moves into adulthood.
But generational research has become a crowded arena. The field has been flooded with content that’s often sold as research but is more like clickbait or marketing mythology. There’s also been a growing chorus of criticism about generational research and generational labels in particular.
Recently, as we were preparing to embark on a major research project related to Gen Z, we decided to take a step back and consider how we can study generations in a way that aligns with our values of accuracy, rigor and providing a foundation of facts that enriches the public dialogue.
A typical generation spans 15 to 18 years. As many critics of generational research point out, there is great diversity of thought, experience and behavior within generations.
We set out on a yearlong process of assessing the landscape of generational research. We spoke with experts from outside Pew Research Center, including those who have been publicly critical of our generational analysis, to get their take on the pros and cons of this type of work. We invested in methodological testing to determine whether we could compare findings from our earlier telephone surveys to the online ones we’re conducting now. And we experimented with higher-level statistical analyses that would allow us to isolate the effect of generation.
What emerged from this process was a set of clear guidelines that will help frame our approach going forward. Many of these are principles we’ve always adhered to , but others will require us to change the way we’ve been doing things in recent years.
Here’s a short overview of how we’ll approach generational research in the future:
We’ll only do generational analysis when we have historical data that allows us to compare generations at similar stages of life. When comparing generations, it’s crucial to control for age. In other words, researchers need to look at each generation or age cohort at a similar point in the life cycle. (“Age cohort” is a fancy way of referring to a group of people who were born around the same time.)
When doing this kind of research, the question isn’t whether young adults today are different from middle-aged or older adults today. The question is whether young adults today are different from young adults at some specific point in the past.
To answer this question, it’s necessary to have data that’s been collected over a considerable amount of time – think decades. Standard surveys don’t allow for this type of analysis. We can look at differences across age groups, but we can’t compare age groups over time.
Another complication is that the surveys we conducted 20 or 30 years ago aren’t usually comparable enough to the surveys we’re doing today. Our earlier surveys were done over the phone, and we’ve since transitioned to our nationally representative online survey panel , the American Trends Panel . Our internal testing showed that on many topics, respondents answer questions differently depending on the way they’re being interviewed. So we can’t use most of our surveys from the late 1980s and early 2000s to compare Gen Z with Millennials and Gen Xers at a similar stage of life.
This means that most generational analysis we do will use datasets that have employed similar methodologies over a long period of time, such as surveys from the U.S. Census Bureau. A good example is our 2020 report on Millennial families , which used census data going back to the late 1960s. The report showed that Millennials are marrying and forming families at a much different pace than the generations that came before them.
Even when we have historical data, we will attempt to control for other factors beyond age in making generational comparisons. If we accept that there are real differences across generations, we’re basically saying that people who were born around the same time share certain attitudes or beliefs – and that their views have been influenced by external forces that uniquely shaped them during their formative years. Those forces may have been social changes, economic circumstances, technological advances or political movements.
When we see that younger adults have different views than their older counterparts, it may be driven by their demographic traits rather than the fact that they belong to a particular generation.
The tricky part is isolating those forces from events or circumstances that have affected all age groups, not just one generation. These are often called “period effects.” An example of a period effect is the Watergate scandal, which drove down trust in government among all age groups. Differences in trust across age groups in the wake of Watergate shouldn’t be attributed to the outsize impact that event had on one age group or another, because the change occurred across the board.
Changing demographics also may play a role in patterns that might at first seem like generational differences. We know that the United States has become more racially and ethnically diverse in recent decades, and that race and ethnicity are linked with certain key social and political views. When we see that younger adults have different views than their older counterparts, it may be driven by their demographic traits rather than the fact that they belong to a particular generation.
Controlling for these factors can involve complicated statistical analysis that helps determine whether the differences we see across age groups are indeed due to generation or not. This additional step adds rigor to the process. Unfortunately, it’s often absent from current discussions about Gen Z, Millennials and other generations.
When we can’t do generational analysis, we still see value in looking at differences by age and will do so where it makes sense. Age is one of the most common predictors of differences in attitudes and behaviors. And even if age gaps aren’t rooted in generational differences, they can still be illuminating. They help us understand how people across the age spectrum are responding to key trends, technological breakthroughs and historical events.
Each stage of life comes with a unique set of experiences. Young adults are often at the leading edge of changing attitudes on emerging social trends. Take views on same-sex marriage , for example, or attitudes about gender identity .
Many middle-aged adults, in turn, face the challenge of raising children while also providing care and support to their aging parents. And older adults have their own obstacles and opportunities. All of these stories – rooted in the life cycle, not in generations – are important and compelling, and we can tell them by analyzing our surveys at any given point in time.
When we do have the data to study groups of similarly aged people over time, we won’t always default to using the standard generational definitions and labels. While generational labels are simple and catchy, there are other ways to analyze age cohorts. For example, some observers have suggested grouping people by the decade in which they were born. This would create narrower cohorts in which the members may share more in common. People could also be grouped relative to their age during key historical events (such as the Great Recession or the COVID-19 pandemic) or technological innovations (like the invention of the iPhone).
By choosing not to use the standard generational labels when they’re not appropriate, we can avoid reinforcing harmful stereotypes or oversimplifying people’s complex lived experiences.
Existing generational definitions also may be too broad and arbitrary to capture differences that exist among narrower cohorts. A typical generation spans 15 to 18 years. As many critics of generational research point out, there is great diversity of thought, experience and behavior within generations. The key is to pick a lens that’s most appropriate for the research question that’s being studied. If we’re looking at political views and how they’ve shifted over time, for example, we might group people together according to the first presidential election in which they were eligible to vote.
With these considerations in mind, our audiences should not expect to see a lot of new research coming out of Pew Research Center that uses the generational lens. We’ll only talk about generations when it adds value, advances important national debates and highlights meaningful societal trends.
- Age & Generations
- Demographic Research
- Generation X
- Generation Z
- Generations
- Greatest Generation
- Methodological Research
- Millennials
- Silent Generation

How Teens and Parents Approach Screen Time
Who are you the art and science of measuring identity, u.s. centenarian population is projected to quadruple over the next 30 years, older workers are growing in number and earning higher wages, teens, social media and technology 2023, most popular.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
AI Index: State of AI in 13 Charts
In the new report, foundation models dominate, benchmarks fall, prices skyrocket, and on the global stage, the U.S. overshadows.

This year’s AI Index — a 500-page report tracking 2023’s worldwide trends in AI — is out.
The index is an independent initiative at the Stanford Institute for Human-Centered Artificial Intelligence (HAI), led by the AI Index Steering Committee, an interdisciplinary group of experts from across academia and industry. This year’s report covers the rise of multimodal foundation models, major cash investments into generative AI, new performance benchmarks, shifting global opinions, and new major regulations.
Don’t have an afternoon to pore through the findings? Check out the high level here.
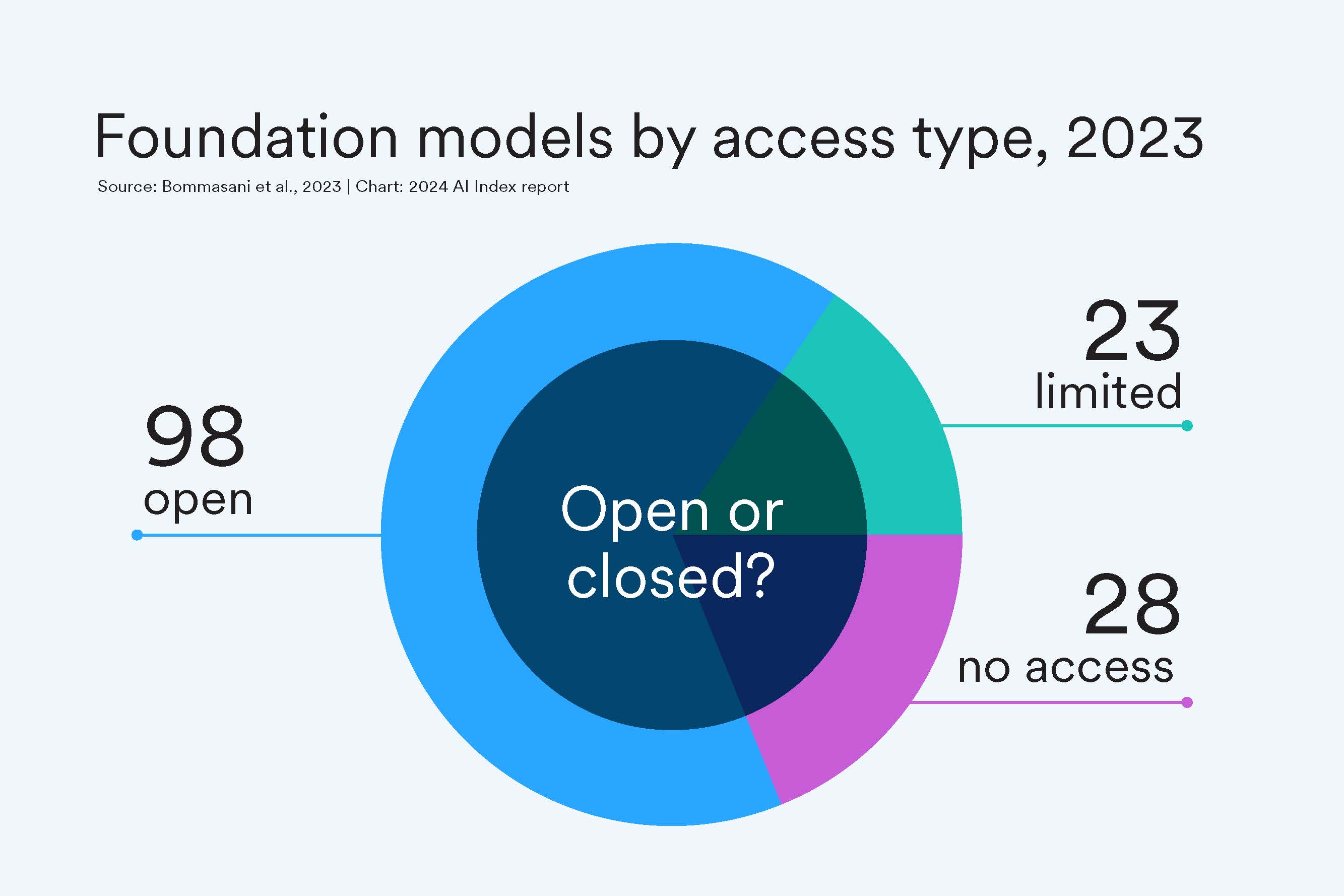
A Move Toward Open-Sourced
This past year, organizations released 149 foundation models, more than double the number released in 2022. Of these newly released models, 65.7% were open-source (meaning they can be freely used and modified by anyone), compared with only 44.4% in 2022 and 33.3% in 2021.
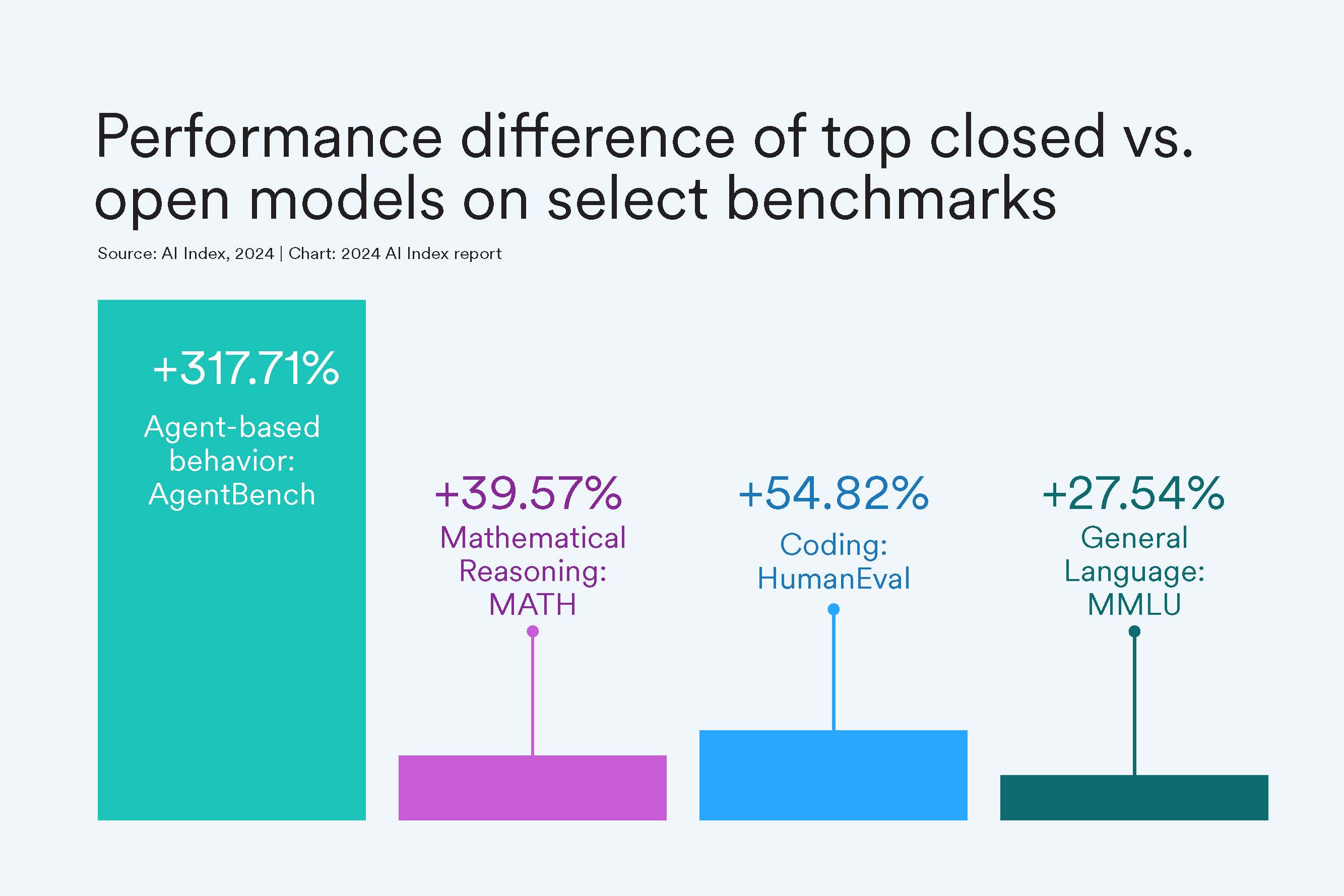
But At a Cost of Performance?
Closed-source models still outperform their open-sourced counterparts. On 10 selected benchmarks, closed models achieved a median performance advantage of 24.2%, with differences ranging from as little as 4.0% on mathematical tasks like GSM8K to as much as 317.7% on agentic tasks like AgentBench.
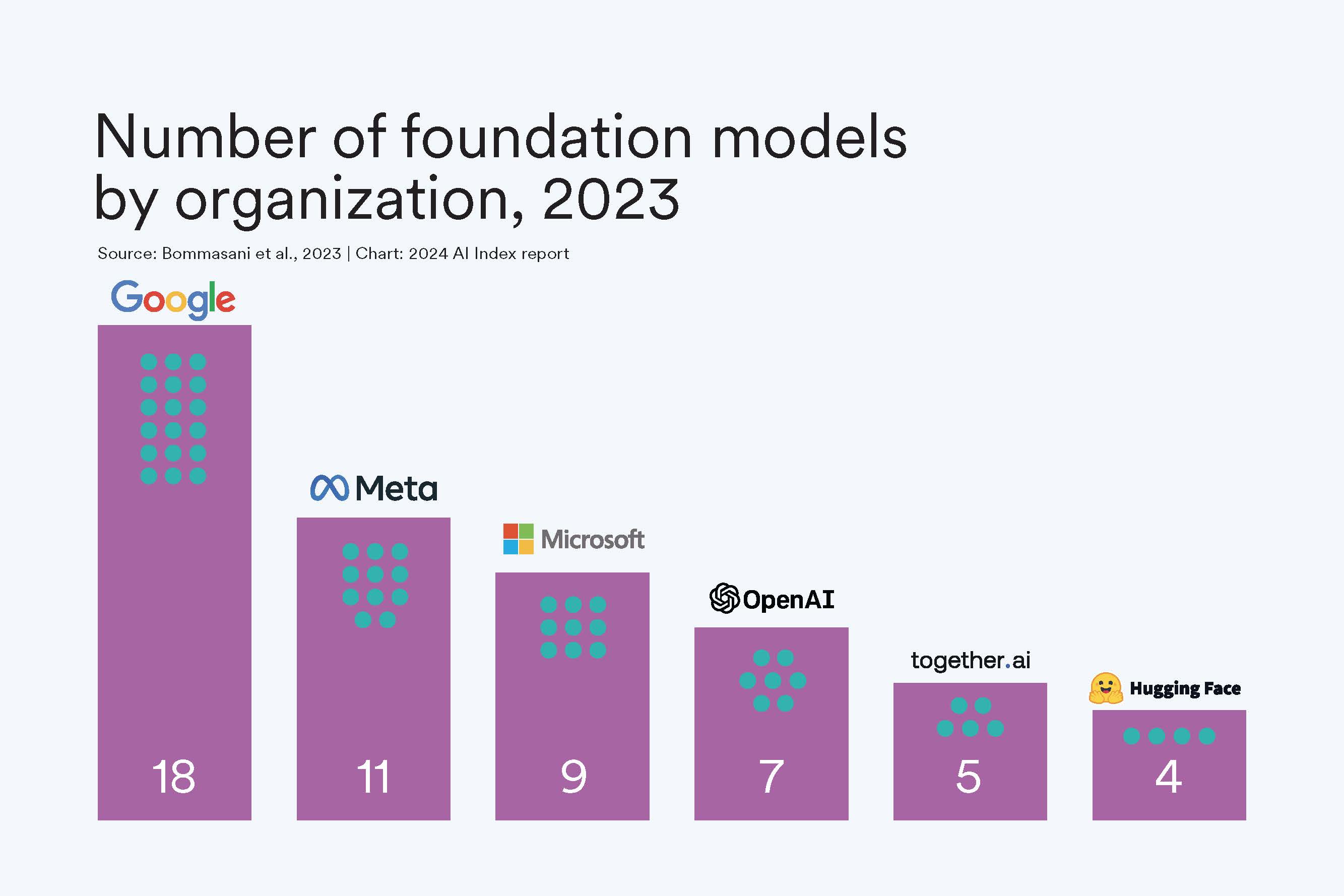
Biggest Players
Industry dominates AI, especially in building and releasing foundation models. This past year Google edged out other industry players in releasing the most models, including Gemini and RT-2. In fact, since 2019, Google has led in releasing the most foundation models, with a total of 40, followed by OpenAI with 20. Academia trails industry: This past year, UC Berkeley released three models and Stanford two.
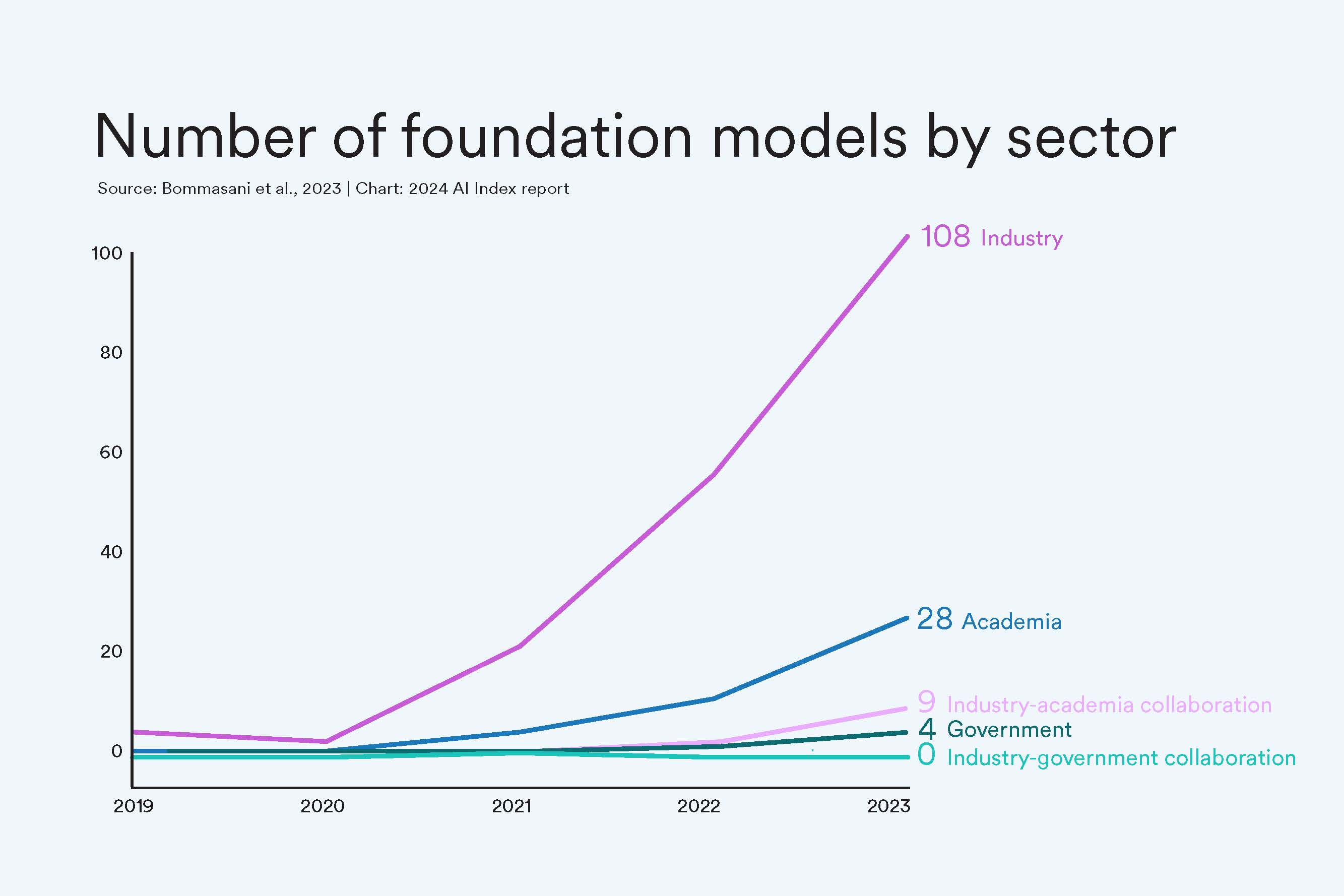
Industry Dwarfs All
If you needed more striking evidence that corporate AI is the only player in the room right now, this should do it. In 2023, industry accounted for 72% of all new foundation models.
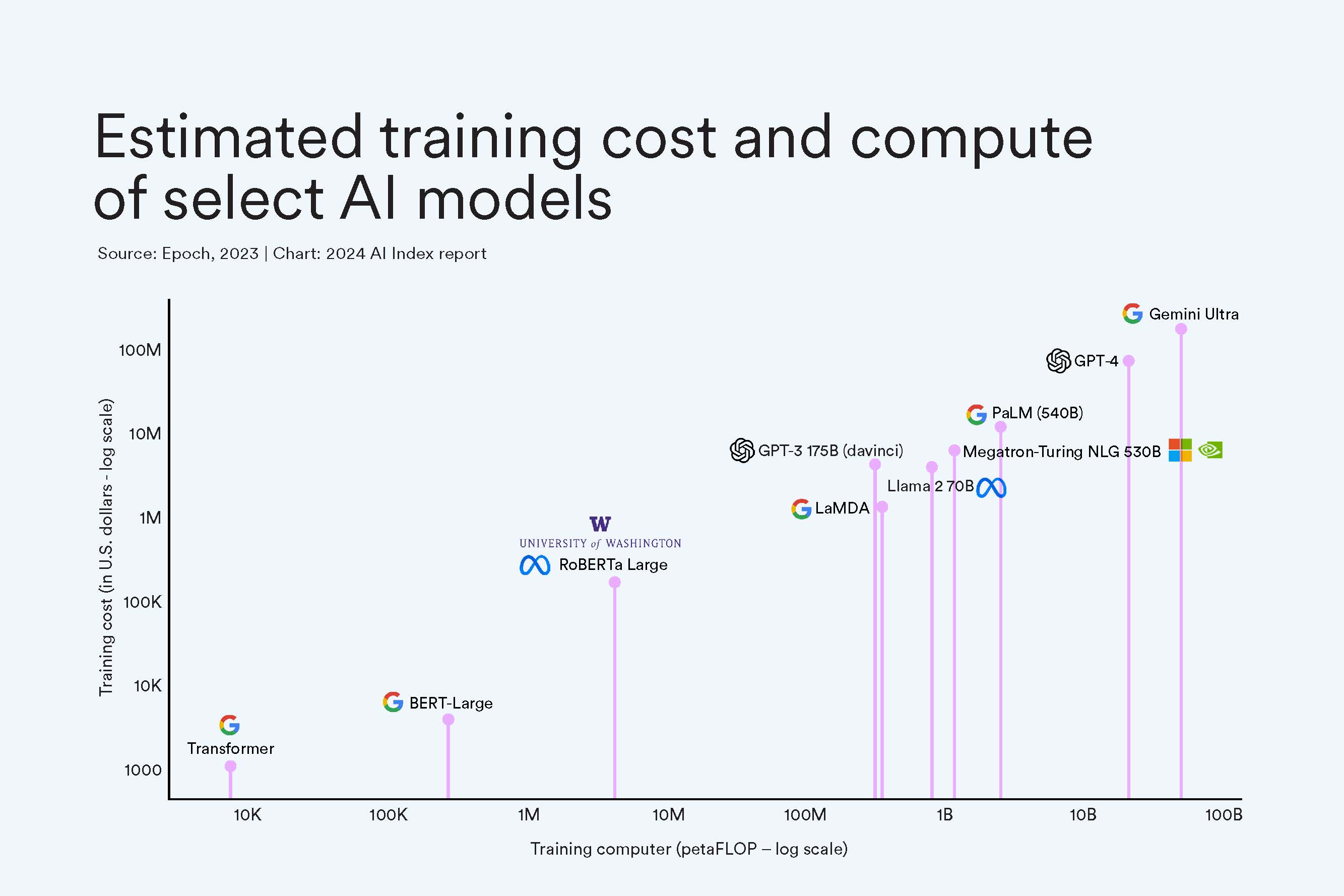
Prices Skyrocket
One of the reasons academia and government have been edged out of the AI race: the exponential increase in cost of training these giant models. Google’s Gemini Ultra cost an estimated $191 million worth of compute to train, while OpenAI’s GPT-4 cost an estimated $78 million. In comparison, in 2017, the original Transformer model, which introduced the architecture that underpins virtually every modern LLM, cost around $900.
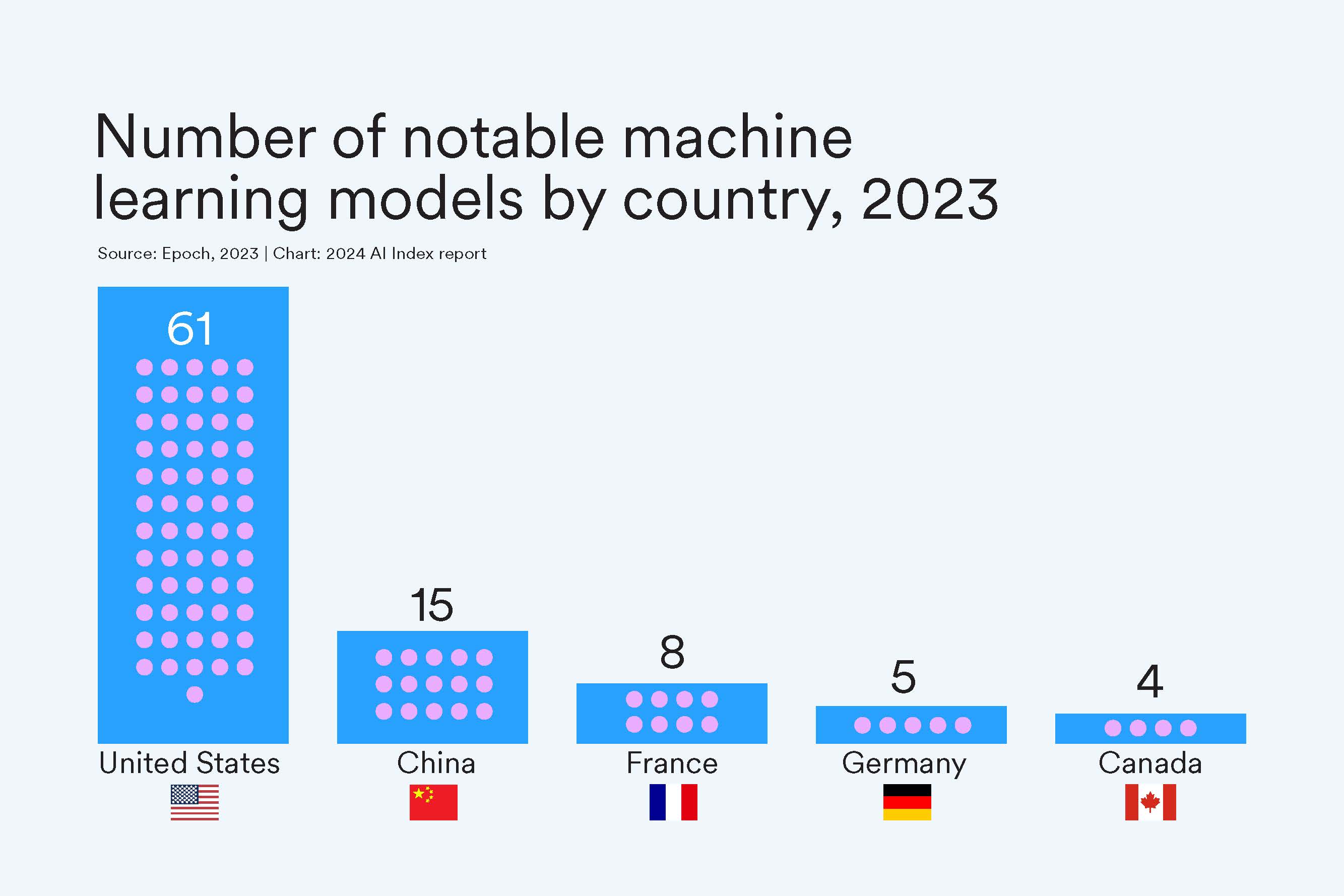
What AI Race?
At least in terms of notable machine learning models, the United States vastly outpaced other countries in 2023, developing a total of 61 models in 2023. Since 2019, the U.S. has consistently led in originating the majority of notable models, followed by China and the UK.
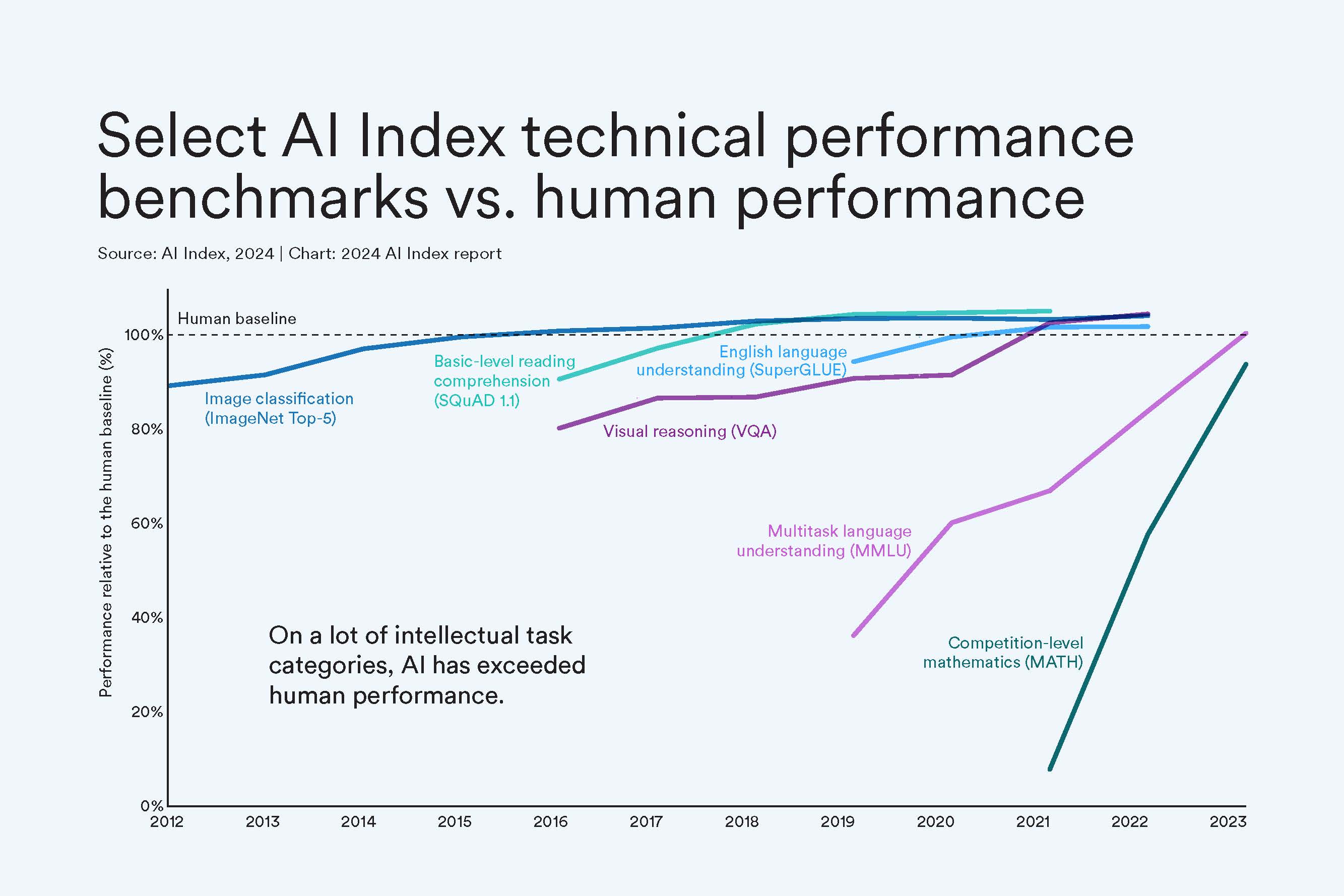
Move Over, Human
As of 2023, AI has hit human-level performance on many significant AI benchmarks, from those testing reading comprehension to visual reasoning. Still, it falls just short on some benchmarks like competition-level math. Because AI has been blasting past so many standard benchmarks, AI scholars have had to create new and more difficult challenges. This year’s index also tracked several of these new benchmarks, including those for tasks in coding, advanced reasoning, and agentic behavior.
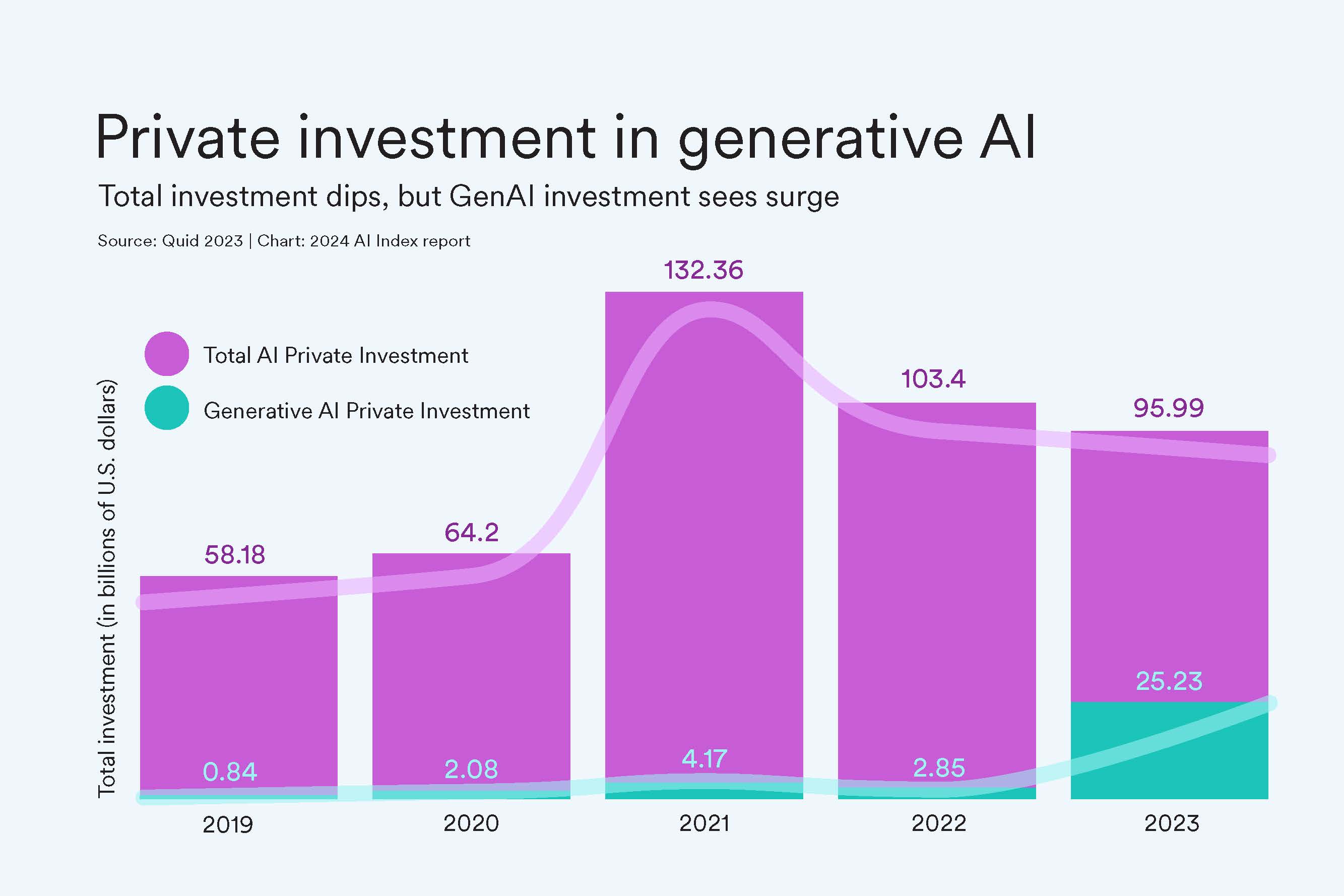
Private Investment Drops (But We See You, GenAI)
While AI private investment has steadily dropped since 2021, generative AI is gaining steam. In 2023, the sector attracted $25.2 billion, nearly ninefold the investment of 2022 and about 30 times the amount from 2019 (call it the ChatGPT effect). Generative AI accounted for over a quarter of all AI-related private investments in 2023.
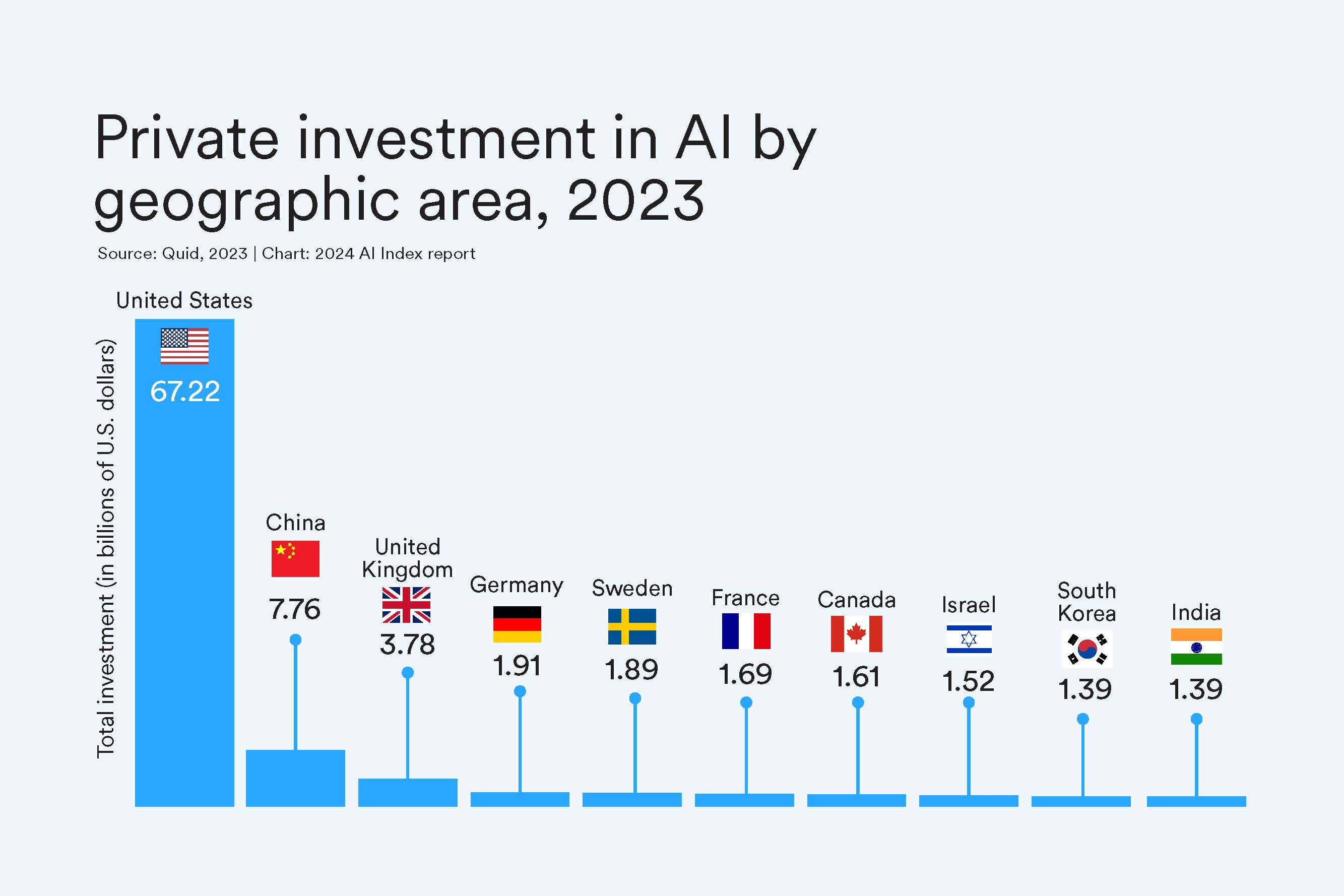
U.S. Wins $$ Race
And again, in 2023 the United States dominates in AI private investment. In 2023, the $67.2 billion invested in the U.S. was roughly 8.7 times greater than the amount invested in the next highest country, China, and 17.8 times the amount invested in the United Kingdom. That lineup looks the same when zooming out: Cumulatively since 2013, the United States leads investments at $335.2 billion, followed by China with $103.7 billion, and the United Kingdom at $22.3 billion.
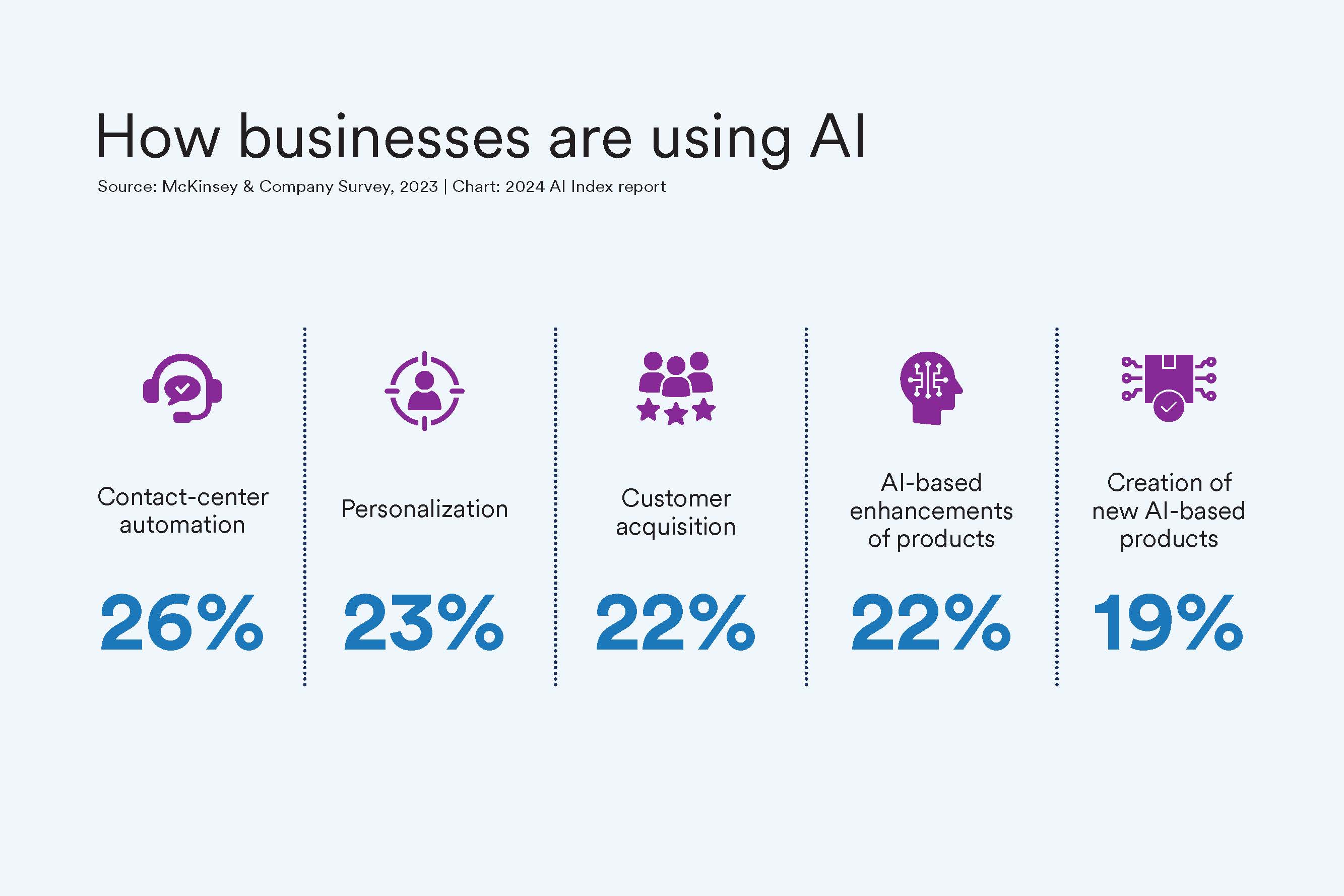
Where is Corporate Adoption?
More companies are implementing AI in some part of their business: In surveys, 55% of organizations said they were using AI in 2023, up from 50% in 2022 and 20% in 2017. Businesses report using AI to automate contact centers, personalize content, and acquire new customers.
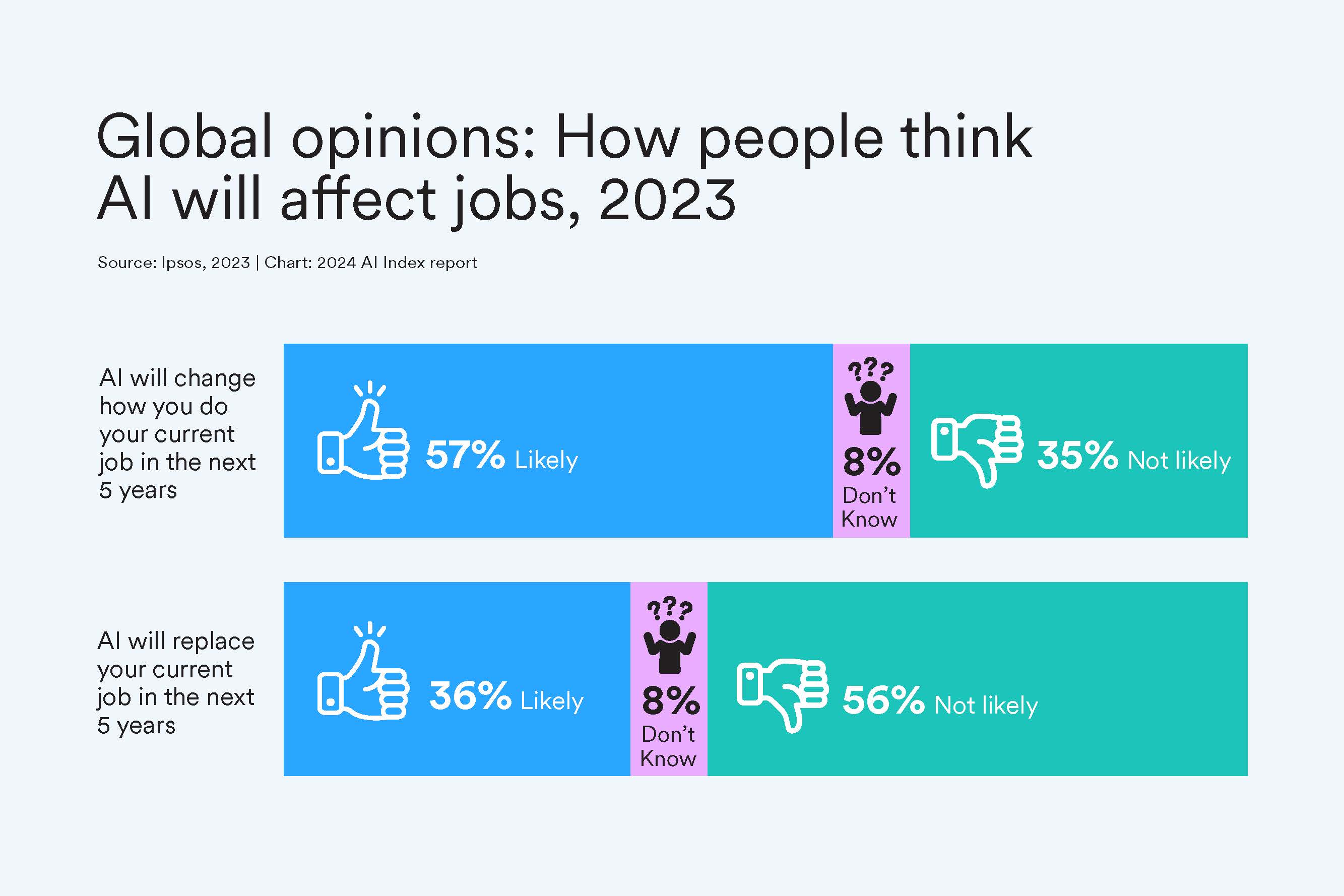
Younger and Wealthier People Worry About Jobs
Globally, most people expect AI to change their jobs, and more than a third expect AI to replace them. Younger generations — Gen Z and millennials — anticipate more substantial effects from AI compared with older generations like Gen X and baby boomers. Specifically, 66% of Gen Z compared with 46% of boomer respondents believe AI will significantly affect their current jobs. Meanwhile, individuals with higher incomes, more education, and decision-making roles foresee AI having a great impact on their employment.
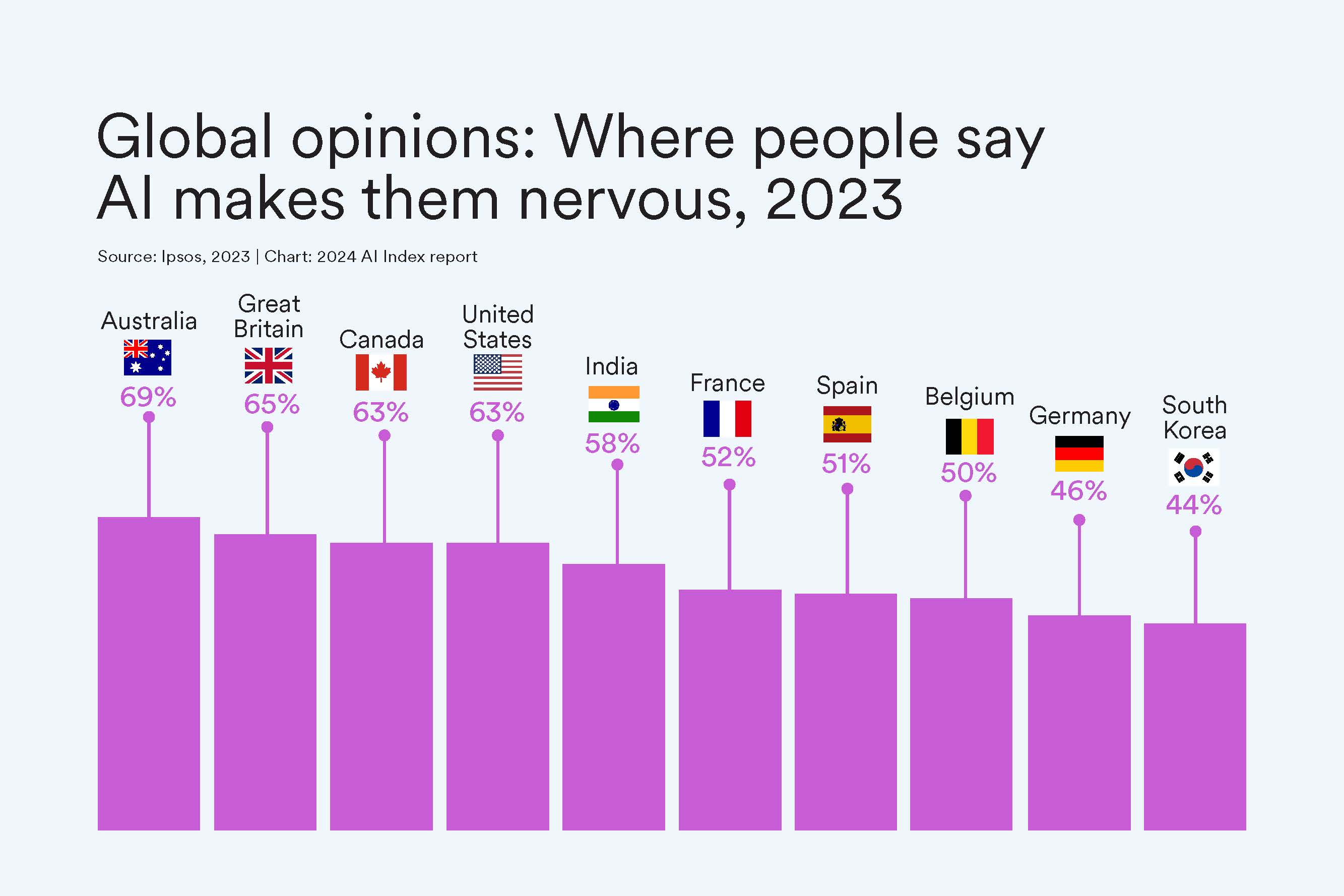
While the Commonwealth Worries About AI Products
When asked in a survey about whether AI products and services make you nervous, 69% of Aussies and 65% of Brits said yes. Japan is the least worried about their AI products at 23%.
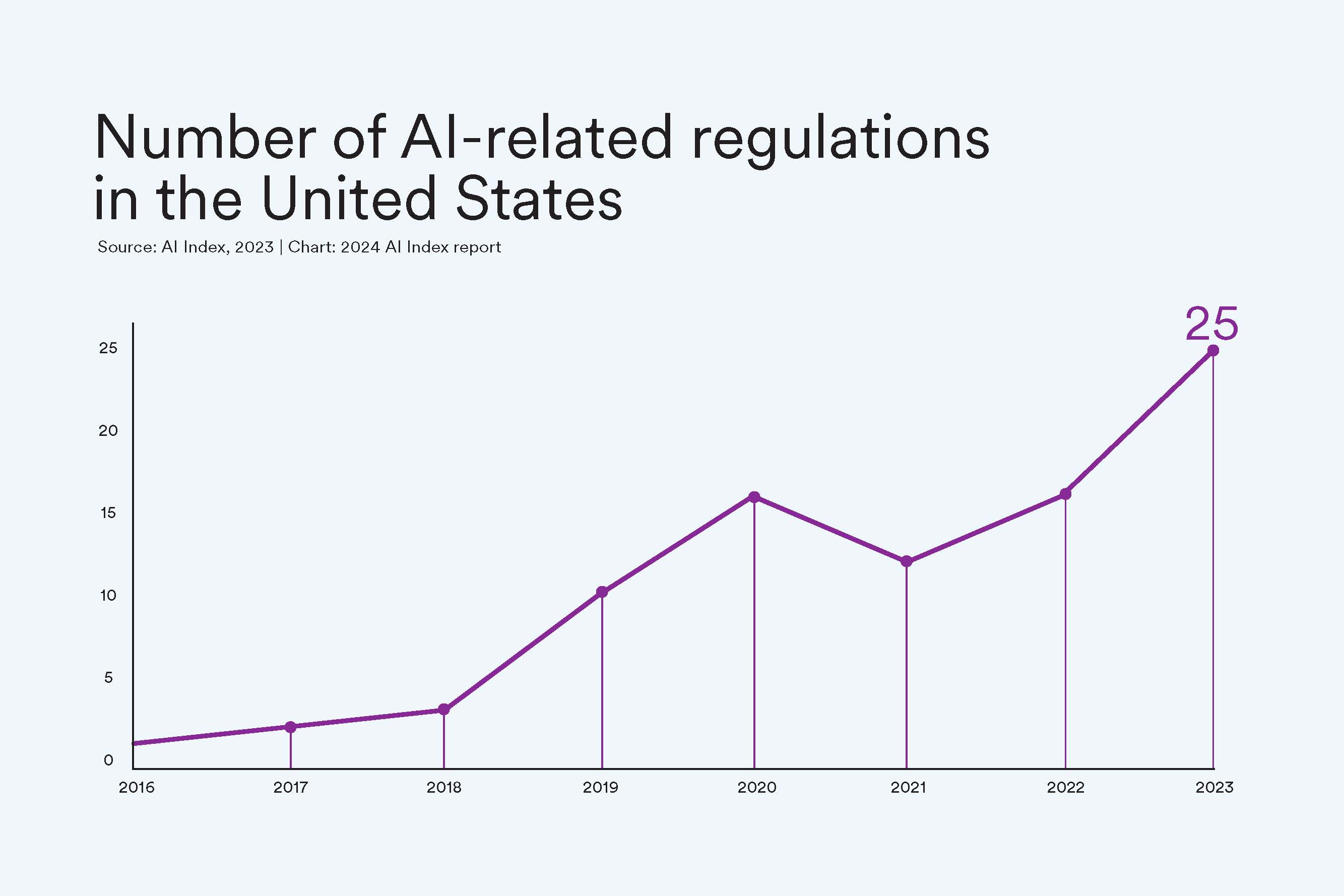
Regulation Rallies
More American regulatory agencies are passing regulations to protect citizens and govern the use of AI tools and data. For example, the Copyright Office and the Library of Congress passed copyright registration guidance concerning works that contained material generated by AI, while the Securities and Exchange Commission developed a cybersecurity risk management strategy, governance, and incident disclosure plan. The agencies to pass the most regulation were the Executive Office of the President and the Commerce Department.
The AI Index was first created to track AI development. The index collaborates with such organizations as LinkedIn, Quid, McKinsey, Studyportals, the Schwartz Reisman Institute, and the International Federation of Robotics to gather the most current research and feature important insights on the AI ecosystem.
More News Topics
Israeli Weapon Damaged Iranian Air Defenses Without Being Detected, Officials Say
- Share full article

Strike was meant to show Iran that Israel could paralyze its defenses, Western officials say.
An Israeli airstrike on Iran on Friday damaged an air defense system, according to Western and Iranian officials, and appeared calculated to deliver a message that Israel could bypass Iran’s defensive systems undetected and paralyze them.
The strike damaged a defensive battery near Natanz, a city in central Iran that is critical to the country’s nuclear weapons program, according to the officials.
Even though the Israeli attack was in retaliation for Iran’s aerial barrage last week, it used a fraction of the firepower Tehran deployed. That attack, intercepted by Israel and its allies, caused minimal damage.
The strike on Friday was the latest salvo in a series of tit-for-tat attacks between the two countries this month that have heightened fears of a broader regional conflict. The relatively limited scope of Israel’s strike and the muted response from Iranian officials, however, seem to have eased tensions.
The two Iranian officials said the strike on Friday had damaged an S-300 antiaircraft system at a military base in the nearby province of Isfahan. The officials’ account is supported by satellite imagery analyzed by The New York Times , which showed damage to the radar of an S-300 system at the Eighth Shekari Air Base in Isfahan.
It was unclear what sort of weapon struck the Iranian air defense system. Three Western and two Iranian officials confirmed on Friday that Israel had deployed aerial drones and at least one missile fired from a warplane. Previously, Iranian officials said the attack on the military base had been conducted by small drones, most likely launched from inside Iranian territory.
A missile, two Western officials said, was fired from a warplane far from Israeli or Iranian airspace and included technology that enabled it to evade Iran’s radar defenses. Neither the missile nor the aircraft that fired it entered Jordanian airspace, the Western officials said, a gesture meant to keep the kingdom out of the conflict after it helped shoot down Iranian weapons last week.
The two Iranian officials said that Iran’s military had not detected anything entering Iran’s airspace on Friday, including drones, missiles and aircraft. Iran’s state news agency, IRNA, reported that no missile attacks had occurred and that Iran’s air defense system had not been activated.
Israel, the two Western officials said, had scrapped an earlier plan to fire back on Iran with a large-scale attack. That plan, they said, was replaced with a strike intended to send a quiet but decisive message with the aim of ending the cycle of reprisal.
Israel’s use of drones launched from inside Iran and a missile that it could not detect, the Western officials said, was intended to give Iran a taste of what a larger-scale attack might look like. The attack, they said, was calibrated to make Iran think twice before launching a direct attack on Israel in the future.
Officials from both Iran and Israel refrained from speaking publicly about Friday’s attack, a move that appeared aimed at de-escalating a conflict some fear could spiral into a broader regional war. Israel’s silence on the attack, an Iranian official said, would allow Tehran to treat the strike as it had previous clandestine attacks in the countries’ long-running shadow war and not prompt an immediate response.
Eric Schmitt contributed reporting.
— Farnaz Fassihi and Ronen Bergman
Deadly Israeli airstrikes again hit Rafah.
Israeli airstrikes on the southern Gaza city of Rafah on Saturday killed several civilians, including women and children, according to Palestinian state media, sending more fear through an area where over one million displaced Palestinians are crowded into tents and temporary quarters.
For many weeks, Palestinians have been bracing for an announced Israeli ground offensive on Rafah, the southernmost part of Gaza, where more than half of the strip’s 2.2 million residents fled after being forced from their homes by more than six months of Israeli bombardment and a ground invasion.
The airstrikes hit two family homes, killing 10 residents, and missiles and artillery also struck other areas of Rafah and the surrounding area, according to the Wafa news agency.
The Israeli military would not immediately comment on the strikes. It has said the goal of its offensive in Gaza is to eradicate Hamas, the armed group that has controlled the Gaza Strip for nearly two decades.
“It was like an earthquake,” Mohammad al-Masri, a 31-year-old accountant who is sheltering with his family in a tent in a large Rafah encampment, said of the shaking from the strikes.
The first strike hit at a little past midnight, shaking the earth and lighting up the night sky, and a second one came soon after, he said. “When we hear these strikes we don’t know what to do,” he said. “Everyone is saying the same thing, ‘Where can we go?’”
President Biden and other world leaders have urged Israel not to invade Rafah because it would make an already dire humanitarian crisis even worse.
But Prime Minister Benjamin Netanyahu has not heeded those calls and claims a ground offensive is necessary to “complete the elimination of Hamas’s battalions” and to destroy its tunnel networks.
Saturday’s strikes stoked fears for Palestinians in Rafah that an invasion could be imminent.
In a briefing to the Security Council this week, Secretary-General António Guterres said that Israel’s military offensive in Rafah would “compound this humanitarian catastrophe.”
Rahaf Al-Madhoun, 17, was streaming live on TikTok to talk about the living conditions in Rafah, when the first airstrike hit very close, she said. She stopped to collect herself before continuing. Then she described the terror sown by the strikes and the ever-present buzz of surveillance drones overhead.
“We’re at a loss, I swear,” she said. “The fear itself is killing us.”
Rawan Sheikh Ahmad contributed reporting.
— Raja Abdulrahim
Israeli raid on a refugee camp in the West Bank kills at least 10 people.
Israeli soldiers killed at least 10 people during a raid on a refugee camp in the West Bank on Saturday, Israel’s military said. It’s the latest deadly assault in the long-running conflict there that has only become worse during the six-month war between Israel and Hamas in the Gaza Strip.
The latest violence prompted the Fatah party, which dominates the Palestinian Authority, to declare a general strike across the West Bank on Sunday in protest, with support from the Palestinian teachers and transit worker unions. The region’s government services, schools and educational facilities are expected to shutter for the day.
The Israeli military said that 10 Palestinians had been killed and eight people were arrested during what it called a “counterterrorism operation” at the Nur Shams refugee camp in Tulkarem. Soldiers also raided a compound where explosives were stored and then destroyed or confiscated weapons, the military said. The Israeli military said the 10 killed were militants, a claim that could not be immediately verified.
The Palestinian Health Ministry in the West Bank confirmed that at least 13 people including a 15-year-old, have been killed with several more wounded during the clashes in the area, which have been going on since Thursday evening.
Violence in the occupied West Bank has sharply escalated since the Hamas-led attacks on Israel on Oct. 7. Across the West Bank and in East Jerusalem, more than 400 Palestinians have been killed by Israeli forces since the start of the war, according to the United Nations. Many were killed during near-daily Israeli military raids in Palestinian cities and towns, while others had carried out or attempted attacks on Israelis.
There were clashes elsewhere on the West Bank on Saturday.
Yesh Din, an Israeli rights group that tracks Jewish extremist violence in the West Bank, reported that a Palestinian Red Crescent ambulance had been fired at while responding to armed settler attacks in another town farther south, Al-Sawiya.
It was unclear who fired at the ambulance, but the 50-year-old paramedic who was driving the vehicle, Mohammed Awad Allan, was killed while treating injured people, the Palestinian Health Ministry and the Palestinian Red Crescent said.
Mustafa Taqatqa, the Palestinian Authority governor in the Tulkarem area, said residents there were “seeing violence and destruction like there is in Gaza.” He said that Israeli military patrols had also deployed outside the Nur Shams refugee camp — the focus of the raid.
“There are very few people out in the streets, and a feeling of danger is everywhere,” Mr. Taqatqa said.
Israeli tractors and heavy vehicles had torn some streets in and around the refugee camp, he said. Municipal officials had just finished repaving a major road damaged in another recent Israeli raid, only for Israeli tractors to damage it once again when the military operation began on Thursday night, Mr. Taqatqa said.
The Palestinian Authority has also sought to crack down on armed militants and has worked closely with Israeli security forces to arrest them, a policy known as security coordination. Mr. Taqatqa said that shortly before the raid, militants and Palestinian security forces had clashed in the city of Tulkarem over what he called a “misunderstanding.” He declined to provide further details.
“But in Nur Shams, it’s not just militants,” he said. “There are civilians in the line of fire, all the residents of this refugee camp. We feel that everyone is facing an unrestrained assault.”
— Gaya Gupta and Aaron Boxerman
The House, with a bipartisan vote, approves an aid package for Israel.
The House voted resoundingly on Saturday to approve billions of dollars in aid for Israel as part of a larger package that would also fund Ukraine and Taiwan.
In four back-to-back votes, overwhelming bipartisan coalitions of lawmakers approved the new rounds of funding for the three U.S. allies.
The legislation allocates $26 billion for Israel and for humanitarian aid for civilians in conflict zones, including Gaza; $60 billion for Kyiv; and $8 billion for the Indo-Pacific region.
The House approved assistance to Israel by a vote of 366 to 58. Representative Rashida Tlaib, Democrat of Michigan and a vocal supporter of the Palestinian cause, voted “present.”
Thirty-seven liberal Democrats opposed the aid package for Israel because the legislation placed no conditions on how Israel could use American aid, even though there have been thousands of civilian casualties and Gaza faces the risk of famine.
That was a relatively small sliver of opposition given that left-wing lawmakers had pressed their colleagues to vote “no” on the bill to send a message to President Biden about the depth of anger within his political coalition over his backing for Israel’s tactics in the war.
“Sending more weapons to the Netanyahu government will make the U.S. even more responsible for atrocities and the horrific humanitarian crisis in Gaza, which is now in a season of famine,” said Representative Jonathan L. Jackson, Democrat of Illinois, speaking of Prime Minister Benjamin Netanyahu of Israel. “The United States Congress must be the moral compass. I continue to call for the release of all prisoners and hostages. I continue to pray and work for peace, security and stability.”
The Senate is expected to pass the legislation as early as Tuesday and send it to Mr. Biden’s desk, capping a tortured journey through Congress .
— Catie Edmondson
The Palestinian Authority’s president threatens to reconsider relations with the United States.
The Palestinian Authority’s president, Mahmoud Abbas, said the Ramallah-based government would reconsider its relationship with the United States after Washington earlier this week vetoed a resolution before the U.N. Security Council that would have urged the General Assembly to recognize Palestinian statehood, a longstanding goal of Palestinian leaders.
Mr. Abbas told the news agency Wafa on Saturday that the United States had prompted “unprecedented anger” among the Palestinian people by vetoing the U.N. Security Council measure. He added that the United States had pushed the region toward “further instability, chaos and terrorism.”
The resolution had recommended to the U.N. General Assembly that “the State of Palestine be admitted to membership of the United Nations,” according to diplomats. It is currently considered a “nonmember observer state.”
The Palestinian envoy to the United Nations, Riyad Mansour, said that the resolution was part of an effort to assert its right to self-determination. The United States, the only nation among the council’s 15 members that wielded its veto power, said the recognition of a Palestinian state must come as part of a negotiated settlement with Israel to end the 75-year-old conflict. Britain and Switzerland abstained from the vote.
Mr. Abbas also accused the United States of abandoning its promises to work toward a two-state solution and of funding Israel’s war in Gaza, which Gazan health officials say has killed more than 34,000 Palestinians, most of them civilians, and destroyed much of the enclave’s infrastructure.
— Gaya Gupta
At a meeting in Turkey, Hamas’s political leader and Erdogan discussed how to achieve a ‘fair and permanent peace in the region.’
Ismail Haniyeh, the political leader of Hamas, was in Turkey on Saturday to meet with its president, Recep Tayyip Erdogan, one of Hamas’s staunchest supporters in NATO and a fierce critic of Prime Minister Benjamin Netanyahu of Israel.
Since the war in Gaza began in October, Mr. Erdogan has forcefully defended Hamas and condemned Israel, despite its diplomatic ties to Turkey. In the week before Saturday’s meeting, he described Mr. Haniyeh as “the leader of the Palestinian cause.”
After the meeting, Mr. Erdogan told reporters he would use every opportunity to draw attention to the suffering in Gaza, for which he hoped Israel would be held accountable.
“Israel will certainly pay the price of the atrocities it has been inflicting on Palestinians one day,” Mr. Erdogan told reporters.
Turkey’s relationship with Israel has been turbulent during Mr. Erdogan’s two decades as the country’s dominant politician, but it has sharply deteriorated over the last six months during the war in Gaza. Mr. Erdogan has strongly backed the Palestinian cause, which has widespread public support in Turkey, and has said that Hamas was not a terrorist organization, a position contrary to that held by most Western countries.
On Saturday, Mr. Erdogan’s office said he and Mr. Haniyeh had discussed Israel’s attacks against “Palestinian land, primarily against Gaza.” They also talked about what needed to be done for adequate humanitarian aid to reach Gaza and how to achieve “a fair and permanent peace in the region.”
Three weeks after the Oct. 7 Hamas attacks in Israel ignited the war, and which Israeli officials say killed roughly 1,200 people, Mr. Erdogan gave a televised address excoriating Israel and defending Hamas.
He said Israel’s goal in Gaza was “not self-defense, but savagery, to commit the premeditated act of crime against humanity.” He defended Hamas as “not a terror organization.”
“It is an organization of liberation,” he said, “of mujahedeen, who fight to protect their land and citizens.”
Israel’s Foreign Ministry said it “wholeheartedly rejected” Mr. Erdogan’s comments.
Since then, Mr. Erdogan has strongly condemned Israel and its leaders. He has compared Mr. Netanyahu to Hitler and called Israel a terrorist state . He has said Turkey would provide evidence in the case accusing Israel of genocide before the United Nations’s high court and has restricted Turkish exports to Israel.
In January, Israel’s foreign minister, Israel Katz, struck back, saying that Mr. Erdogan came “from a country with the Armenian genocide in its past” and “now boasts of targeting Israel with unfounded claims.”
“Israel stands in defense, not destruction, against your barbarian allies,” he added, in reference to Hamas.
Turkey was once Israel’s closest friend in the Muslim world, and even under Mr. Erdogan the two countries have maintained significant trade ties despite their political differences. But Turkey cut diplomatic ties with Israel after a confrontation in 2010 between Israeli commandos and activists on a Turkish ship that was trying to breach Israel’s naval blockade of Gaza. Nine Turks were killed, including one who also had American citizenship.
The countries restored full diplomatic ties in April 2022, after President Isaac Herzog of Israel made a state visit to Turkey , the highest-level meeting with an Israeli leader in the country in 14 years.
— Liam Stack and Safak Timur
An explosion damages a military base in Iraq used by an Iran-backed armed group.
Iraq’s joint military command says one person was killed and eight were injured in an explosion early Saturday at a base used by an Iranian-backed armed group, Harakat al Nujaba, in Iraq’s Babylon Province.
In a carefully worded statement, Iraq’s military did not attribute the explosion to an air attack with a missile or a drone. “Air Defense Command confirmed that there was no drone or jet fighter in the airspace of Babylon Province before and during the explosion,” the statement said.
Privately, however, military officials say it appears that at least one projectile had hit inside the Kalsu base’s perimeter. A video taken shortly after the event and posted on social media showed damaged buildings and a large rubble-filled crater. A second video showed several parts of the base on fire.
According to Iraq’s joint command, the base is used by several elements of the Iraqi security forces including the Iraqi army and police as well as the Popular Mobilization Forces , or P.M.F., an umbrella organization.
The P.M.F. includes some brigades that are backed by Iran. The one stationed at this base, Harakat al Nujaba, has participated in attacks on U.S. installations in Iraq and Syria. More recently it has joined with other Iranian-backed forces in Syria and Lebanon to attack Israeli territory.
There was no immediate claim of responsibility for the strike.
The U.S. military, which has carried out strikes on Iranian-backed armed groups in Iraq in the past, said in a statement released shortly after the attack that it had not participated in strikes on locations in Iraq. The Israeli military declined to comment.
The explosion came a day after Israel attacked a military air base near the city of Isfahan in central Iran, according to two Israeli and three Iranian officials who spoke on the condition of anonymity because they were not authorized to discuss the matter publicly. That attack, on Friday, appeared to be Israel’s first military response to Iran’s massive drone and missile attack on Israeli soil nearly a week ago.
Falih Hassan contributed from Baghdad .
— Alissa J. Rubin
Satellite imagery shows that a precision attack damaged an air defense system at an Iranian base.
The Israeli attack on an Iranian air base in Isfahan hit a crucial part of an air defense system, a New York Times analysis of satellite imagery found.
Images showed that the precision attack at the Eighth Shekari Air Base damaged or destroyed the “flap-lid” radar , which is used in S-300 air defense systems to track incoming targets.
The Times used several satellite images in its analysis; the location of the damaged area was first pointed out on the social media platform X by Aurora Intel , and the findings have also been confirmed by a former U.S. government imagery analyst, Chris Biggers.
The radar is typically surrounded by several vehicles, including four trucks carrying missiles. Before the strike, the missiles were seen positioned next to the radar. After the strike, they had been moved and did not appear visibly damaged. It was not clear why the missiles had been moved. However, the fact that they appear undamaged indicated that the attack had a very precise target, according to Mr. Biggers.
Other areas of the air base and adjacent airport also appeared to be undamaged. The precision of the strike, deep within Iran and with several sensitive sites close by, suggested Israel chose the specific and narrow target, the air defense system.
According to the Missile Defense Project of the Washington think tank Center for Strategic and International Studies, Iran has acquired Russian-made S-300 air defense systems to deter Israeli and other airstrikes.
— Christoph Koettl and Christiaan Triebert
Advertisement
Gig workers are writing essays for AI to learn from
- Companies are hiring highly educated gig workers to write training content for AI models .
- The shift toward more sophisticated trainers comes as tech giants scramble for new data sources.
- AI could run out of data to learn from by 2026, one research institute has warned.

As artificial intelligence models run out of data to train themselves on, AI companies are increasingly turning to actual humans to write training content.
For years, companies have used gig workers to help train AI models on simple tasks like photo identification , data annotation, and labelling. But the rapidly advancing technology now requires more advanced people to train it.
Companies such as Scale AI and Surge AI are hiring part-timers with graduate degrees to write essays and creative prompts for the bots to gobble up, The New York Times reported . Scale AI, for example, posted a job last year looking for people with Master's degrees or PhDs, who are fluent in either English, Hindi, or Japanese and have professional writing experience in fields like poetry, journalism, and publishing.
Related stories
Their mission? To help AI bots "become better writers," Scale AI wrote in the posting.
And an army of workers are needed to do this kind of work. Scale AI has as many as tens of thousands of contractors working on its platform at a time, per the Times.
"What really makes the A.I. useful to its users is the human layer of data, and that really needs to be done by smart humans and skilled humans and humans with a particular degree of expertise and a creative bent," Willow Primack, the vice president of data operations at Scale AI, told the New York Times. "We have been focusing on contractors, particularly within North America, as a result."
The shift toward more sophisticated gig trainers comes as tech giants scramble to find new data to train their technology on. That's because the programs learn so incredibly fast that they're already running out of available resources to learn from. The vast trove of online information — everything from scientific papers to news articles to Wikipedia pages — is drying up.
Epoch, an AI research institute, has warned that AI could run out of data by 2026.
So, companies are finding more and more creative ways to make sure their systems never stop learning. Google has considered accessing its customers' data in Google Docs , Sheets, and Slides while Meta even thought about buying publishing house Simon & Schuster to harvest its book collection, Business Insider previously reported.
Watch: Nearly 50,000 tech workers have been laid off — but there's a hack to avoid layoffs
- Main content

How Big Tech and Silicon Valley are Transforming the Military-Industrial Complex

America’s military-industrial complex has been rapidly expanding from the Capital Beltway to Silicon Valley. Although much of the Pentagon’s budget is spent on conventional weapons systems, the Defense Department has increasingly sought to adopt AI-enabled systems. Big tech companies, venture capital, and private equity firms benefit from multi-billion dollar Defense contracts, and smaller defense tech startups that “move fast and break things” also receive increased Defense funding. This report illustrates how a growing portion of the Defense Department’s spending is going to large, well-known tech firms, including some of the most highly valued corporations in the world.
Given the often-classified nature of large defense and intelligence contracts, a lack of transparency makes it difficult to discern the true amount of U.S. spending diverted to Big Tech. Yet, research reveals that the amount is substantial, and growing. According to the nonprofit research organization Tech Inquiry , three of the world’s biggest tech corporations were awarded approximately $28 billion from 2018 to 2022, including Microsoft ($13.5 billion), Amazon ($10.2 billion), and Alphabet, which is Google’s parent company ($4.3 billion). This paper found that the top five contracts to major tech firms between 2019 and 2022 had contract ceilings totaling at least $53 billion combined.
From 2021 through 2023, venture capital firms reportedly pumped nearly $100 billion into defense tech startup companies — an amount 40 percent higher than the previous seven years combined. This report examines how Silicon Valley startups, big tech, and venture capital who benefit from classified Defense contracts will create costly, high-tech defense products that are ineffective, unpredictable, and unsafe – all on the American taxpayer’s dime.
READ FULL PAPER >
Executive Summary >
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List

The Evolving Role of Multivitamin/Multimineral Supplement Use among Adults in the Age of Personalized Nutrition
Jeffrey b. blumberg.
1 Friedman School of Nutrition Science and Policy, Tufts University, 711 Washington Street, Boston, MA 02111, USA
Regan L. Bailey
2 Department of Nutrition Science, Purdue University, 700 West State Street, West Lafayette, IN 47907, USA; ude.eudrup@yeliabnager
Howard D. Sesso
3 Brigham and Women’s Hospital and Harvard Medical School, 900 Commonwealth Avenue East, 3rd Floor, Boston, MA 02215, USA; ude.dravrah.hpsh@ossesh
Cornelia M. Ulrich
4 Huntsman Cancer Institute and Department of Population Health Sciences, University of Utah, 2000 Circle of Hope, Salt Lake City, UT 84112, USA; [email protected]
Micronutrient deficiencies occur in segments of the adult population in the United States. Multivitamin/multimineral supplements (MVMS) are widely used by this population, which reduces inadequacies in micronutrient intake, but the potential for exceeding tolerable upper intake levels in others should be considered. There are concerns associated with the excessive intake of certain nutrients, particularly folic acid, and potential untoward consequences. The advent of nutrigenomics and the enhanced ability to directly study the interactions between nutrition and genetic variants and expression will allow for the conduct of more targeted studies with specific endpoints and may ultimately lead to progress in the field of personalized nutrition. The role of MVMS in health maintenance and chronic disease prevention remains controversial. Conducting studies in this area has been hampered by, among other factors, inconsistent definitions of MVMS, ranging from as few as three vitamins to broad-spectrum products containing more than two dozen vitamins and minerals. Results from some observational studies and large-scale, randomized, controlled trials suggest that MVMS may reduce the risk of some forms of cancer and, potentially, cardiovascular disease. The ongoing COcoa Supplement and Multivitamin Outcomes Study (COSMOS) is expected to build on this research and provide additional insights into these areas.
1. Introduction
The World Health Organization has estimated that more than 2 billion people worldwide experience deficiencies in the intake of essential vitamins and minerals [ 1 ]. In the United States (US), a number of shortfall nutrients have been identified in the general population as described by the Dietary Guidelines Advisory Committee to the US Departments of Health and Human Services and Agriculture, which include vitamins A, C, D, and E and choline, calcium, magnesium, iron, and potassium [ 2 ]. Further, deficiencies in calcium, potassium, dietary fiber, and vitamin D are considered to be of public health concern based on their demonstrated role in health maintenance combined with their known low intake levels. Indeed, consistent with earlier reports, a recent analysis of National Health and Nutrition Examination Survey (NHANES) data indicates that a substantial number of individuals have intakes of these nutrients from dietary sources that fall below the Estimated Average Requirement (EAR) [ 3 , 4 , 5 ]. These dietary shortfalls occur despite the wide use of dietary supplements [ 6 , 7 , 8 ]. However, dietary supplements are often used by individuals who already have nutrient-rich diets. In particular among older women, multiple supplements can be used, which can increase the potential for oversupplementation and excessive nutrient intake [ 7 , 9 ]. Multivitamin/multimineral supplements (MVMS) are the most commonly utilized supplements among US adults, although their use overall has declined in recent years, from 37–40% in 1999–2006 to 31% in 2011–2012 [ 6 ].
The objective of this review is to summarize presentations on the patterns of MVMS use among adults from a scientific session of the American Society for Nutrition at the Experimental Biology 2017 Conference in Chicago, IL, USA. The session reviewed the role of MVMS and described evidence from observational studies and randomized, controlled trials that evaluated the effects of MVMS on chronic disease outcomes. The evolving field of nutrigenomics and its influence on the application of personalized nutrition was also discussed.
2. Role of MVMS in the US Diet
Approximately half of all US adults take some form of dietary supplement, with vitamin and mineral supplements accounting for a substantial portion of total use [ 6 , 9 ]. Despite a recent apparent decrease in MVMS use overall, the most recent NHANES data (2011–2014) suggest that 34–49% of older adults regularly take an MVMS [ 10 ]. As of April 2017, the Dietary Supplement Label Database of the US National Institutes of Health Office of Dietary Supplements and National Library of Medicine listed 1404 different vitamin/mineral products containing the word “multi” [ 11 ].
Estimating the use and evaluating the benefits and risks of MVMS in observational studies and controlled trials is complicated by a lack of a consistent scientific or regulatory definition of these over-the-counter products [ 12 ]. Definitions of MVMS vary according to investigators, professional organizations, and manufacturers. For example, different NHANES analyses have included MVMS products containing ≥3 vitamins, ≥3 vitamins plus ≥1 mineral, and ≥9 or ≥10 total micronutrients [ 4 , 6 , 9 , 13 , 14 ]. The Older Americans Act Amendment of 2006 proposed that an MVMS should contain at least two-thirds of vitamins and essential minerals and provide 100% of the Daily Value (DV) for the intended life stage [ 15 ], but official definitions of MVMS continue to evolve [ 16 ]. Some MVMS are formulated to contain approximately 100% of the DV for as many as 30 vitamins and essential minerals [ 17 , 18 , 19 ], while other products have been designed to address a particular health problem, such as those used for maintaining eye health in older adults [ 20 ]. Notably, the health claims of dietary supplements are regulated as foods, not as pharmaceuticals, by the US Food and Drug Administration (FDA) [ 21 ]. These definitions also do not generally account for micronutrient inadequacies or needs based on factors such as age, health status, or dietary pattern, which are each pertinent considerations when formulating an MVMS in the context of personalized nutrition.
In reports analyzing NHANES data, the most common reasons cited by consumers for using an MVMS were to maintain or improve overall health, prevent health problems, and promote bone or heart health [ 10 , 22 ]. In these two studies, only 22% of individuals reported using these products specifically to supplement their diets. Importantly, individuals with healthier lifestyles were shown to be more likely to use MVMS [ 22 ], and analyses of NHANES data from 2003 to 2006 found that supplement users had comparatively higher intakes of most vitamins and minerals from their dietary choices alone than did those who reported not using supplements [ 7 , 8 ]. These factors can lead to intakes exceeding the tolerable upper intake level (UL) in some users, while those who are not reaching adequate intake levels from their diets are also less likely to be using dietary supplements to reach those levels.
Given the potential of micronutrient inadequacies or deficiencies in certain segments of the adult US population [ 3 , 4 , 5 ], approaches to addressing these issues, beyond general nutrition education, should be considered. Deficiencies in micronutrient intake are related to the socioeconomic status, with a significant association being observed between income and micronutrient intake, as well as dietary supplement use [ 23 ]. Adults in higher income brackets had a lower prevalence of inadequate intakes compared with those in lower income brackets. Therefore, strategies to enhance nutrient intakes across certain segments of the US population may be necessary, while also considering the risk of exceeding ULs in those already achieving an adequate intake from their diets and/or taking multiple dietary supplements. For individuals at risk of inadequate consumption, dietary supplements may be used to fill gaps in nutrient intake without increasing caloric intake.
Evidence that dietary supplement use increases micronutrient intake includes analyses of NHANES data collected between 2009 and 2012. These analyses revealed that MVMS use by individuals ≥19 years of age significantly reduced the proportion of subjects with intakes below the EAR for 15 of the 17 micronutrients evaluated, including for 7 of the 10 nutrients that are deemed “underconsumed” in the 2015–2020 Dietary Guidelines for Americans ( Figure 1 ) [ 3 ].

Proportion of subjects ≥19 years of age achieving an intake of shortfall nutrients below the EAR from food or from food + MVMS. Reprinted from Blumberg, J.B., et al. [ 3 ]. Abbreviations: EAR: Estimated Average Requirement; MVMS: multivitamin/multimineral supplement. * p < 0.01 versus food only.
The greatest decrease in individuals with intakes below the EAR was observed in those whose frequency of MVMS use was ≥21 days/month ( Figure 2 ).

Proportion of subjects ≥19 years of age achieving an intake of shortfall nutrients below the EAR from food + MVMS by frequency of intake. Reprinted from Blumberg, J.B., et al. [ 3 ]. Abbreviations: EAR: Estimated Average Requirement; MVMS: multivitamin/multimineral supplement. * p < 0.01 versus 0 days per month; a,b,c Values by frequency of MVMS use with different superscripts are significantly different ( p < 0.01).
It is noteworthy that MVMS use in this specific analysis significantly increased the prevalence of intake above the UL in ≤4% of the population for seven nutrients. However, further research is warranted to determine whether any untoward outcomes are associated with even this low level of overconsumption. In addition to dietary supplements, the nutritional status can also be improved by consuming micronutrient-fortified foods; NHANES data have shown that the consumption of highly fortified breakfast cereals can fill many gaps in micronutrient intake [ 24 ].
In summary, accurately assessing the role of MVMS is complicated by the lack of a consistent definition for this product category, but data clearly suggest that using an MVMS can improve the nutritional status. However, the future of supplementation may involve developing new, targeted formulations such as those designed to provide more personalized nutrition (e.g., those that focus on the interactions between risk factors for chronic disease, life stage, nutrient intake, and genetics). Determining the presupplementation levels of dietary nutrient intake should also be considered to ensure that individuals are not exceeding the UL.
3. Micronutrient Intake/Status and Gene Expression
The sequencing of the human genome has allowed for identifying interactions between nutrient intake and the activity of specific genes related to health, which has given rise to the field of nutrigenomics [ 25 , 26 ]. Nutrigenetics and nutrigenomics are the terms that are used to describe the science that evaluates the impact that genetic variants have on the dietary response and determines the effect that nutrients and bioactive food compounds may have on gene expression, respectively [ 27 ]. Multiple single-nucleotide polymorphisms (SNPs) appear to affect the synthesis and function of key proteins, with implications for the modification of nutrient requirements and metabolism [ 26 ]. This interaction between nutrition, gene expression, and health has been well established for lactose intolerance and phenylketonuria [ 26 ], but emerging research suggests an array of other targets, including the risk for developing chronic diseases. Although controversy exists regarding the current applicability of genetic-based personalized nutrition [ 28 ], it is important to note that clinical trials suggest that behavioral coaching informed by personal data may improve the adherence to dietary advice and clinical biomarkers [ 29 , 30 ], and businesses are now offering relevant services to practitioners [ 31 ]. Some studies have investigated genome-wide predictors of nutrient levels in plasma or serum. Although statistically significant genetic polymorphisms have been identified as predictors, they have explained little variation in nutrient levels thus far [ 32 ]. For example, vitamin D heritability is only 7.5%, and of that, only 38% can be explained by known genetic variants; this represents only 3% of the total variability in circulating 25-OH-D levels [ 33 ].
Folic acid has been well studied with regard to nutrigenomic interactions involving the one-carbon metabolism pathway central to DNA methylation and nucleotide synthesis [ 34 , 35 , 36 , 37 ]. Furthermore, the link between folate deficiencies or inadequacies and the occurrence of neural tube defects (NTDs) and, conversely, folic acid supplementation during pregnancy and reduction in the occurrence and reoccurrence of NTDs has been firmly established. As a result, folic acid supplementation has become routine during pregnancy [ 38 , 39 , 40 ]. However, folate may also play a role in the pathogenesis of a number of other health problems, including cardiovascular disease (CVD), cancer, and neurodegenerative conditions such as dementia and Alzheimer’s disease [ 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 ].
Methylenetetrahydrofolate reductase (MTHFR) catalyzes the conversion of 5,10-methylenetetrahydrofolate to 5-methylenetetrahydrofolate, an irreversible step in folate metabolism [ 51 , 52 , 53 , 54 ]. Molecular epidemiology studies have found that the C677T polymorphism in the MTHFR gene may modulate the risk of colorectal cancer [ 51 , 52 , 53 , 54 ]. The direction and magnitude of this risk modification is influenced by folate status [ 53 , 54 ], as well as by alcohol consumption [ 52 ] and the supply of methyl group donors [ 51 ]. A study conducted in women found that the C677T polymorphism was further associated with a 62% increased risk of breast cancer; however, this risk was ameliorated by the intake of nutrients involved in one-carbon metabolism, including folate and related B vitamins, as well as the amino acid methionine [ 55 ].
Despite the promising evidence related to folate status and positive health outcomes, there are also data suggesting that folic acid supplementation in some individuals can cause adverse health outcomes. Results from the Aspirin/Folate Polyp Prevention Study revealed a trend toward an increased risk of advanced colorectal lesions and adenoma multiplicity among subjects randomized to receive folic acid supplementation [ 56 ]. Another study also found that folic acid supplementation was associated with a significant increase in the risk of prostate cancer (hazard ratio (HR): 2.63; 95% confidence interval (CI): 1.23–5.65) [ 57 ]. Further, in the Women’s Health Initiative (WHI) study, women with high folate status during the period prior to routine folic acid fortification had lower levels of DNA methylation than in the postfortification period. These results suggest that the relationship between folate status and DNA methylation is not linear and that fortification in otherwise well-nourished individuals may attenuate the positive effects of folate and cause adverse health outcomes [ 58 ]. Other evidence also supports the possibility that folic acid supplementation in the presence of fortification may cause excess dietary intake and increase the risk of developing some forms of cancer [ 56 , 57 , 59 ]. Overall, a dual role of folate in carcinogenesis has been proposed and substantiated by mathematical modeling [ 59 , 60 ]. Variants in genes other than MTHFR associated with folate and one-carbon metabolism have been linked to both increases and decreases in the risk of colorectal cancer, depending on folate status [ 37 ]. Therefore, clinicians must evaluate potential risks as well as benefits when considering folic acid supplementation in individuals who may be at risk for certain types of cancer.
In addition to the effects of folate status on DNA methylation and the development of some types of cancer, there are also data implicating folate status in a number of other biological processes and disease outcomes. A study investigating predictors of long interspersed nucleotide element (LINE) methylation noted that folate status seemed to modify the associations, in particular, those observed between sex hormones and DNA methylation [ 61 ]. Unmetabolized folic acid has been linked to reduced natural killer cell cytotoxicity in both humans and mice [ 62 , 63 ]. Other studies have suggested a role for folate–gene interactions in inflammation, diabetes, and the health of newborns [ 64 , 65 , 66 ].
Interactions between MTHFR polymorphisms and other genes with folate and vitamin B 12 status may also affect the development of Alzheimer’s disease [ 67 ]. In one study, high dietary folate levels were not found to be beneficial to memory in community-dwelling, elderly subjects with a del/del 19-bp polymorphism in the DHFR gene, which codes dihydrofolate reductase [ 68 ]. Indeed, higher dietary folate levels may cause adverse effects on cognitive functioning. Variants in the MAT1A gene, which is responsible for coding methionine adenosyl transferase, have also been linked to hypertension and stroke; however, depending on the individual’s genotype, improving vitamin B 6 status might decrease this risk [ 69 ].
Other nutrient–gene interactions relevant to health outcomes have also been identified. For example, vitamin D inadequacy has been linked to increased cancer risk and/or tumor development through regulation of gene expression relating to cell cycle progression, apoptosis, cellular adhesion, oxidative metabolism, immune function, and steroid metabolism [ 70 , 71 ]. Vitamin D has also been implicated in the transcriptional activation of tryptophan hydroxylase-2, which catalyzes serotonin synthesis and thus may have relevance to some neurological conditions, such as attention deficit hyperactivity disorder, bipolar disorder, schizophrenia, depression, impulsive behavior, and autism [ 72 , 73 ]. However, clinical benefits have not been demonstrated in controlled trials of the impact of vitamin D supplementation (alone or with calcium) on neurological conditions [ 74 , 75 ]. Evidence is also available for other gene–nutrient interactions, which, despite being limited, warrant mentioning. For example, polymorphisms in the vitamin C co-transporter gene have been shown to be associated with an increased risk of primary open-angle glaucoma [ 76 ]. Additionally, the ability of vitamin E supplementation to prevent respiratory tract infections in the elderly has been suggested to be dependent on interleukin-10 SNPs for immunoregulatory genes [ 77 ]. Interactions have also been observed between vitamin E and polymorphisms controlling the production of other cytokines, including tumor necrosis factor-α, which may impact the immunomodulatory effects of vitamin E supplementation [ 78 ].
As knowledge of nutrient–gene interactions and their relationship to intermediary disease biomarkers evolves, nutrigenomics has the potential to substantially inform personalized nutrition and help individualize recommendations for the use of dietary supplements. Using a targeted approach in this field will allow for the conduct of clinical trials focused on those populations most likely to experience significant benefits on specific endpoints based on their genotype. Such studies will also help identify likely “nonresponders,” as well as those susceptible to untoward outcomes from supplementation with specific nutrients.
In addition to the impact of genetic factors on the nutritional status, in numerous other individuals, common factors also impact the absorption, metabolism, distribution, utilization, storage, and excretion of nutrients obtained from MVMS. Nonmodifiable factors that may alter the nutrient status include age, sex, and environmental toxicants [ 79 ]. Modifiable factors that have previously been demonstrated to alter nutrient absorption include smoking [ 80 ], medication use (i.e., drug–nutrient interactions) [ 81 , 82 , 83 ], nutrient intake (i.e., nutrient–nutrient interactions), inflammation [ 84 ], life-stage (e.g., pregnancy, lactation), and presence of disease. Furthermore, the increasing body weight is a significant public health challenge [ 85 ], and a growing body of scientific literature suggests that a suboptimal weight status is associated with a poor micronutrient status [ 80 , 86 ]. For example, obesity is associated with poor vitamin D status [ 87 ], and obese women of childbearing potential are at higher risk for poor folate status [ 88 ]. Additionally, obese adults are less likely to use dietary supplements than those within their recommended body mass index range [ 9 , 22 ].
4. Emerging Evidence on MVMS in Chronic Disease Outcomes
Observational studies and randomized clinical trials of MVMS offer optimal settings in which to examine important nutrient–gene interactions and other promising areas of nutrigenomics to enable the personalization of recommendations for MVMS use across a range of populations and chronic disease outcomes. However, no observational studies or randomized clinical trials of MVMS have considered either confounding or effect modification by genetic variation, which may be an important consideration in the results from observational studies on MVMS described below. While a well-conducted clinical trial offers the key advantage of eliminating unmeasured confounding, there may be important modifying effects by genetic variation that build upon one-carbon metabolism and other important mechanistic pathways related to nutrigenomics.
4.1. Observational Studies
The outcomes of observational studies have revealed inconsistent results regarding the benefits of MVMS in the prevention of chronic diseases. For example, the Cancer Prevention Study II, conducted in a population of more than 1 million Americans, reported a reduction in the risk of cardiovascular (CV) mortality in users of MVMS and vitamin A, C, or E supplements [ 89 ]. However, the same study reported an increase in the risk of cancer mortality among male supplement users who smoked. The Stockholm Heart Epidemiology Program found a reduction in nonfatal myocardial infarction in both occasional and regular users of dietary supplements (including MVMS and single-nutrient supplements) compared with nonusers [ 90 ], which was supported by similar results among women in the Swedish Mammography Cohort [ 91 ]. The WHI reported no overall association between the use of MVMS and the risk of CVD in postmenopausal women [ 92 ]. However, in a prospective analysis of NHANES data, a protective association was observed between MVMS use over an 18 year follow-up period and CVD-related mortality in a population of women [ 93 ].
Observational studies that have evaluated MVMS in cancer risk have primarily reported null results. As observed for CVD, the WHI found no association between MVMS use and the risk of cancer at several common sites [ 92 ]. The Multiethnic Cohort Study also found no significant relationship between MVMS use and cancer risk, either overall or at specific sites [ 94 ]. However, a prospective analysis of the Cancer Prevention Study II cohort found an 11% reduction (relative risk (RR): 0.89; 95% CI: 0.80–0.99) in colorectal cancer among individuals taking an MVMS that was presumed to contain folic acid [ 95 ].
All observational studies of MVMS have several inherent limitations that preclude making definitive conclusions about the risk of various chronic disease endpoints, including inconsistent definitions of MVMS, imprecision regarding the frequency and duration of MVMS use, and residual confounding. Further, many observational studies of MVMS use lack data on baseline micronutrient status, changes in dietary patterns during the follow-up period, as well as the potential reasons for these changes (i.e., the development of new comorbidities). It is also possible, as suggested by the long-term follow-up of the Physicians’ Health Study (PHS) I that evaluated CVD outcomes [ 96 ], that MVMS use may need to be of sufficient duration to observe a significant health benefit.
4.2. Randomized, Controlled Trials
In addition to these observational data, a number of randomized, controlled clinical trials that evaluated MVMS have been conducted; some key studies are summarized in Table 1 [ 17 , 18 , 19 , 20 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 ].
Randomized, controlled trials of MVMS.
Abbreviations: AMD: age-related macular degeneration; AREDS: Age-Related Eye Disease Study; BMI: body mass index; CI: confidence interval; CV: cardiovascular; DHA: docosahexaenoic acid; EPA: eicosapentaenoic acid; HDL: high-density lipoprotein; LDL: low-density lipoprotein; MACE: major cardiovascular event; MVMS: multivitamin/multimineral supplement; NA: not applicable; OR: odds ratio; PHS: Physicians’ Health Study; SU.VI.MAX: Supplémentation en Vitamines et Minéraux Antioxydants; TACT: Trial to Assess Chelation Therapy; US: United States. * MVMS containing 26–30 different vitamins, minerals, and bioactives at amounts that primarily meet or slightly exceed daily values based on the study population [ 18 , 19 , 98 ].
The Linxian trial was conducted in subjects with a diagnosis of esophageal dysplasia and found no overall reduction in the risk of cancer for those randomized to receive MVMS or placebo. However, a nonsignificant 8% reduction in esophageal/cardia cancer mortality (RR: 0.92; 95% CI: 0.67–1.28) and a nonsignificant 38% reduction in cerebrovascular mortality (RR: 0.62; 95% CI: 0.37–1.06) were observed [ 98 ]. In the Supplémentation en Vitamines et Minéraux Antioxydants (SU.VI.MAX) study, which randomized men and women to receive a combination of antioxidants, including ascorbic acid, vitamin E, β-carotene, selenium, and zinc, or placebo, there was a significant reduction in the risk of cancer in men (RR: 0.69; 95% CI: 0.53–0.91) [ 101 ]. After a median of 7.54 years of follow-up, there were no differences in the incidence of all-cause cancer or ischemic CVD; however, interestingly, a post hoc analysis of the SU.VI.MAX study revealed that 5 years after the end of the trial, MVMS use among men was associated with a significantly greater probability of healthy aging (RR: 1.16; 95% CI: 1.04–1.29) [ 106 ]. After a median follow-up of 11.2 years, the randomized, double-blind, placebo-controlled PHS II observed a significant 8% reduction in total cancer in subjects who received MVMS compared with those who received the placebo (HR: 0.92; 95% CI: 0.86–0.998) [ 100 ]. Additionally, MVMS use was associated with a reduction in cancer risk of 18% in those ≥70 years of age (HR: 0.82; 95% CI: 0.72–0.93) and a reduction of 27% among those with histories of cancer (HR: 0.73; 95% CI: 0.56–0.96; p = 0.02) [ 100 ].
In contrast to the results related to cancer risk, the PHS II study found no impact of MVMS use on the risk of major CV events (HR: 1.01; 95% CI: 0.91–1.10) [ 18 ]. There was, however, a significant reduction in myocardial infarction-related death (HR: 0.56; 95% CI: 0.33–0.95), but this finding may be the result of chance, as a total of only 70 events were observed [ 18 ]. In secondary analyses of the PHS II trial results on MVMS use, men aged ≥70 years who consumed a healthy diet (based on Alternative Healthy Eating Index and Alternate Mediterranean Diet Score) appeared to benefit from taking an MVMS on the basis of the observed reduction in the incidence of myocardial infarction [ 107 ]. A smaller short-term clinical trial also demonstrated a positive effect of MVMS on changes in CV risk factors in obese women [ 17 , 19 ], but larger studies are needed to further investigate additional outcomes related to CV health. The results of these studies highlight the potential for targeted nutrition strategies that may or may not include an MVMS that is tailored to an individual’s life stage, chronic disease history, or nutritional status.
There do not appear to be any major safety concerns associated with the long-term use of broad-spectrum MVMS because their use does not significantly increase the risk of exceeding the UL [ 3 , 108 ]. A systematic review of 15 MVMS studies reported that only mild gastrointestinal adverse events were observed [ 108 ]. In the randomized, controlled PHS II, MVMS use did not produce significant effects on gastrointestinal side effects, fatigue, drowsiness, skin discoloration, or migraine [ 18 ]. However, MVMS use was associated with a modest increase in skin rashes, as well as some inconsistent effects on minor bleeding that were considered to be more likely a function of chance than effect [ 18 ].
Meta-analyses have provided additional ambiguity regarding the role of MVMS for health promotion. A meta-analysis of randomized, controlled trials by MacPherson et al. [ 109 ] indicated that using an MVMS had no effect on overall mortality (RR: 0.98; 95% CI: 0.94–1.02), but in the primary prevention studies there was a modest trend toward a reduction in the risk of all-cause mortality (RR: 0.94; 95% CI: 0.89–1.00). A key weakness of this analysis, however, was the wide variability in the definitions of MVMS that were combined across a wide array of studies included in the meta-analysis; any vitamin/mineral product with three or more ingredients (excluding B vitamin-only combinations) was analyzed [ 109 ]. As a result, the US Preventive Services Task Force indicated that there is insufficient evidence to recommend using an MVMS in the prevention of cancer, CVD, or mortality [ 110 ]. Table 1 illustrates this heterogeneity in the design of MVMS studies, with different definitions of MVMS, subject inclusion criteria, and length of follow-up. Therefore, interpreting the total body of evidence from randomized, controlled trials conducted with MVMS remains difficult.
Because of the limited number of long-term randomized, controlled trials of MVMS but given the potential benefits suggested by the PHS II [ 99 , 100 ] and several large scale, prospective observational studies, additional research is warranted. The forthcoming randomized, controlled COcoa Supplement and Multivitamin Outcomes Study (COSMOS) has been designed to evaluate an MVMS and a cocoa extract (containing 600 mg cocoa flavanols) on the incidence of major CV outcomes and invasive cancer [ 111 ]. COSMOS plans to enroll 12,000 women ≥65 years of age and 6000 men ≥60 years of age who are free of CVD or were not recently diagnosed with cancer. Subjects will be randomized in a 2 × 2 factorial design to receive the cocoa extract (600 mg) or a placebo and an MVMS (including 30 essential vitamins, minerals, and bioactives) or a placebo. The primary clinical endpoints of COSMOS are major CV events (myocardial infarction, stroke, CVD-related death, and coronary revascularization) and invasive cancer [ 111 ].
5. Conclusions
The use of dietary MVMS is common among adults in the US, and using an MVMS has been shown to reduce the prevalence of inadequate micronutrient intake (i.e., intakes below the EAR) and status. Exceeding the UL, however, should be considered in vulnerable subgroups such as children and older adults and those already taking multiple dietary supplements. High dietary intakes from supplements with certain nutrients, in particular, folic acid, may have negative health outcomes such as increasing the progression of precancerous lesions and tumors. Nutrigenomic approaches should provide new insights into the pursuit of providing personalized nutrition, as ongoing research continues to elucidate the role of nutrition in gene expression and disease. Evidence from some large prospective, cohort studies and randomized, controlled trials suggests that MVMS may contribute to a reduction in the risk of some chronic diseases such as CVD and cancer, but additional long-term clinical trials are necessary. Agreement on the standardization of MVMS products by the FDA would provide a helpful contribution to future research studies testing these products. Forthcoming studies assessing the health benefits and risks of MVMS and other dietary supplements should involve specific objectives and methods relevant to individualizing outcomes and informing the practice of personalized nutrition.
Acknowledgments
The Scientific Session, “Multivitamin/Mineral Supplements in the Age of Personalized Nutrition,” held at Experimental Biology 2017 in Chicago, IL, USA, was sponsored through an unrestricted gift from Pfizer Consumer Healthcare to the American Society of Nutrition (ASN). The session speakers received travel and honoraria for their scientific presentations, but did not receive funding for the preparation or publication of this article. Medical writing support was provided by James Street and Dennis Stancavish of Peloton Advantage, LLC, funded by Pfizer.
Author Contributions
All authors contributed to the analysis and interpretation of data and to the critical revision and review of this manuscript. All authors have approved the final draft for submission.
Conflicts of Interest
The authors declare no conflict of interest. JBB acts as a consultant to companies that manufacture or market dietary supplements, including service on the Nutrition Advisory Committee at Pfizer Consumer Healthcare. HDS declares that he has received investigator-initiated grant support from the Council for Responsible Nutrition Foundation and from Mars Symbioscience and Pfizer Inc. (including donations of study pills) for the COcoa Supplement and Multivitamin Outcomes Study (COSMOS). CMU and RLB declare no conflict of interest. The funding sponsors had no role in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish.

IMAGES
VIDEO
COMMENTS
The use of vitamin, mineral, and fish oil supplements 5 is common among adults in North America (fig 1). 6 The prevalence of use has increased for some individual nutrients—for example, there was a fourfold increase in use of vitamin D supplements among US adults from 1999 to 2012, excluding intake obtained from multivitamin and mineral. 7 ...
For instance, vitamin D and calcium can be included in the health supplements to keep the bones of the user stronger. Equine Nutrition: Calcium, Phosphorus and Vitamin D Importance. Horses require calcium, phosphorus, and vitamin D as macronutrients that are important in the formation and the growth of bones.
Vitamin B2. Chemical name: riboflavin. It is water-soluble. Function: It is essential for the growth and development of body cells and helps metabolize food. Deficiency: Symptoms include ...
Vitamins are a group of nutrients that our body needs to function properly. They help us to utilize the food we eat, turn food into energy, keep our immune system healthy, and protect cells from being damaged. Vitamins are classified as either water-soluble or fat-soluble. Water-soluble vitamins (vitamin C and B vitamins) are not stored in the ...
Four crystalline D vitamins are isolated and at least 10 pro-vitamins D are known. For humans, most of the vitamin D supply comes from animal sources or synthe- sized following sun exposure.
Vitamins are a group of organic compounds essential to physiological functions in the body. This Special Issue features systematic review and original research articles of vitamins in health and disease. Among other topics, the association of endogenous vitamin levels with disease risk, the therapeutic role of vitamin supplementation in various ...
vitamin B 1. component of a coenzyme in carbohydrate metabolism; supports normal nerve function. impairment of the nerves and heart muscle wasting. riboflavin. vitamin B 2. component of coenzymes required for energy production and lipid, vitamin, mineral, and drug metabolism; antioxidant. inflammation of the skin, tongue, and lips; ocular ...
Calcium. Chromium. Folate. Iron. Magnesium. Selenium. Zinc. There are two kinds of vitamins and dietary supplements. As far as human consumption is concerned there are two kinds of vitamins, the first type are those that can be found as naturally occurring organic nutrients that can be found in plants and animals.
The reasons why Americans may be taking vitamin supplements unnecessarily include misinformation, trend, and clever marketing making some vitamins "in vogue," (Nierenberg, 2014). Taking vitamin supplements may be necessary in some cases, as when a patient cannot absorb a certain vitamin or mineral due to a preexisting condition or dietary allergen.
Unfortunately, about 3% of the US population as screened by NHANES use such high dose vitamin D supplements. Over the past few decades, vitamin D has been a hot topic for scientists and lay people ...
Vitamin K can reduce the effectiveness of blood thinners like Coumadin (warfarin).; Vitamin E can increase the action of blood thinners, leading to easy bruising and nosebleeds.; St. John's wort can accelerate the breakdown of many drugs, including antidepressants and birth control pills, thereby reducing their effectiveness.; Vitamin B6 (pyridoxine), when used for a year or more at high ...
Summary. Vitamin C is a vital nutrient for health. Vitamin C benefits include helping form and maintain bones, cartilage, skin, and blood vessels. As an antioxidant, it also supports the immune ...
Some examples of these benefits: Strong bones. A combination of calcium, vitamin D, vitamin K, magnesium, and phosphorus protects your bones against fractures. Prevents birth defects. Taking folic acid supplements early in pregnancy helps prevent brain and spinal birth defects in offspring. Healthy teeth.
Essay # 3. Vitamins Acting on Different Body Systems: The following is a brief summary of the various vitamins acting on different tissues and systems, it must be remembered that, like the endocrines, vitamins also act in close co-operation with one another. The functions of a particular vitamin are not independent, but depend upon the proper ...
These vitamins prevent blood clotting and helps blood cells as well as muscle tissue. Other types of vitamins are seen to promote development in the body. Vitamin D is important for bone development; this helps with bone development and prevents an individual from developing rickets. Vitamin B12 and Folic acids prevent anemia in a human being.
Growing numbers of healthy people are taking dietary supplements but there is little evidence that they protect against non-communicable diseases, say Fang Fang Zhang and colleagues Vitamin and mineral supplements are the most commonly used dietary supplements by populations worldwide.1234 The amount of micronutrients they provide ranges from less than recommended intakes to much more, making ...
Americans seem to have quite a positive view of dietary supplements. According to a 2023 survey, 74% of U.S. adults take vitamins, prebiotics and the like. The business of supplements is booming ...
Though the effects are most severe in children, vitamin D deficiencies can also cause a softening of adult bones called osteomalacia, and increase the risk of osteoporosis, where bones become weak, brittle and more prone to fractures.Though experts debate what exactly constitutes a vitamin D deficiency — and know that healthy levels may vary from person to person — everyone agrees that ...
Students have submitted more than 22 million papers that may have used generative AI in the past year, new data released by plagiarism detection company Turnitin shows. A year ago, Turnitin rolled ...
About 1 in 5 U.S. teens who've heard of ChatGPT have used it for schoolwork. By. Olivia Sidoti and Jeffrey Gottfried. (Maskot/Getty Images) Roughly one-in-five teenagers who have heard of ChatGPT say they have used it to help them do their schoolwork, according to a new Pew Research Center survey of U.S. teens ages 13 to 17.
This means that most generational analysis we do will use datasets that have employed similar methodologies over a long period of time, such as surveys from the U.S. Census Bureau. A good example is our 2020 report on Millennial families, which used census data going back to the late 1960s. The report showed that Millennials are marrying and ...
fabrication; properties. This research examines the production, characteristics, and possible uses of biodegradable polymer nanocomposites in the field of sustainable agriculture. By doing a thorough examination of the experimental data, significant discoveries have been clarified. The composition analysis showed differences in polymer type and ...
While AI private investment has steadily dropped since 2021, generative AI is gaining steam. In 2023, the sector attracted $25.2 billion, nearly ninefold the investment of 2022 and about 30 times the amount from 2019 (call it the ChatGPT effect). Generative AI accounted for over a quarter of all AI-related private investments in 2023.
Israeli soldiers killed at least 10 people during a raid on a refugee camp in the West Bank on Saturday, Israel's military said, the latest deadly assault in the long-running conflict there that ...
Companies are hiring highly educated gig workers to write training content for AI models. The shift toward more sophisticated trainers comes as tech giants scramble for new data sources. AI could ...
From 2021 through 2023, venture capital firms reportedly pumped nearly $100 billion into defense tech startup companies — an amount 40 percent higher than the previous seven years combined. This report examines how Silicon Valley startups, big tech, and venture capital who benefit from classified Defense contracts will create costly, high ...
2. Role of MVMS in the US Diet. Approximately half of all US adults take some form of dietary supplement, with vitamin and mineral supplements accounting for a substantial portion of total use [6,9].Despite a recent apparent decrease in MVMS use overall, the most recent NHANES data (2011-2014) suggest that 34-49% of older adults regularly take an MVMS [].