- Case Report
- Open access
- Published: 25 November 2008

A case of PTSD presenting with psychotic symptomatology: a case report
- Georgios D Floros 1 ,
- Ioanna Charatsidou 1 &
- Grigorios Lavrentiadis 1
Cases Journal volume 1 , Article number: 352 ( 2008 ) Cite this article
30k Accesses
4 Citations
1 Altmetric
Metrics details
A male patient aged 43 presented with psychotic symptomatology after a traumatic event involving accidental mutilation of the fingers. Initial presentation was uncommon although the patient responded well to pharmacotherapy. The theoretical framework, management plan and details of the treatment are presented.
Recent studies have shown that psychotic symptoms can be a hallmark of post-traumatic stress disorder [ 1 , 2 ]. The vast majority of the cases reported concerned war veterans although there were sporadic incidents involving non-combat related trauma (somatic or psychic). There is a biological theoretical framework for the disease [ 3 ] as well as several psychological theories attempting to explain cognitive aspects [ 4 ].
Case presentation
A male patient, aged 43, presented for treatment with complaints tracing back a year ago to a traumatic work-related event involving mutilation of the distal phalanges of his right-hand fingers. Main complaints included mixed hallucinations, irritability, inability to perform everyday tasks and depressive mood. No psychic symptomatology was evident before the event to him or his social milieu.
Mental state examination
The patient was a well-groomed male of short stature, sturdy build and average weight. He was restless but not agitated, with a guarded attitude towards the interviewer. His speech pattern was slow and sparse, his voice low. He described his current mood as 'anxious' without being able to provide with a reason. Patient appeared dysphoric and with blunted affect. He was able to maintain a linear train of thought with no apparent disorganization or irrational connections when expressing himself. Thought content centred on his amputated fingers with a semi-compulsive tendency to gaze to his (gloved) hand. The patient was typically lost in ruminations about his accident with a focus on the precise moment which he experienced as intrusive and affectively charged in a negative and painful way. He could remember wishing for his fingers to re-attach to his hand almost as the accident took place. A trigger in his intrusive thoughts was the painful sensation of neuropathic pain from his half-mutilated fingers, an artefact of surgery.
He denied and thoughts of harming himself and demonstrated no signs of aggression towards others. Hallucinations had a predominantly depressive and ego-dystonic character. He denied any perceptual disturbances at the time of the examination. Their appearance was typically during nighttime especially in the twilight. Initially they were visual only, involving shapes and rocks tumbling down towards the patient, gradually becoming more complex and laden with significance. A mixed visual and tactile hallucination of burning rain came afterwards while in the time of examination a tall stranger clad in black and raiding a tall steed would threaten and ridicule the patient. He scored 21 on a MMSE with trouble in the attention, calculation and recall categories. The patient appeared reliable and candid to the extent of his self-disclosure, gradually opening up to the interviewer but displayed a marked difficulty on describing his emotions and memories of the accident, apparently independent of his conscious will. His judgement was adequate and he had some limited Insight into his difficulties, hesitantly attributing them to his accident.
He was married and a father of three (two boys and a girl aged 7–12) He had no prior medical history for mental or somatic problems and received no medication. He admitted to occasional alcohol consumption although his relatives confirmed that he did not present addiction symptoms. He had some trouble making ends meet for the past five years. Due to rampant unemployment in his hometown, he was periodically employed in various jobs, mostly in the construction sector. One of his children has a congenital deformity, underwent several surgical procedures with mixed results and, before the time of the patient's accident, it was likely that more surgery would be forthcoming. The patient's father was a proud man who worked hard but reportedly was victimized by his brothers, they reaping the benefits of his work in the fields by manipulating his own father. He suffered a nervous breakdown attributed to his low economic status after a failed economic endeavour ending in him being robbed of the profits, seven years before the accident. There was no other relevant family history.
Before the accident the patient was a lively man, heavily involved as a participant and organizer in important local social events from a young age. He was respected by his fellow villagers and felt his involvement as a unique source of pride in an otherwise average existence. Prior to his accident, the patient was repeatedly promised a permanent job as a labourer and fate would have it that his appointment was supposedly approved immediately after the accident only to be subsequently revoked. He viewed himself as an exploited man in his previous jobs, much the same way his father was, while he harboured an extreme bitterness over the unavailability of support for his long-standing problems. His financial status was poor, being in sick-leave from his previous job for the last four months following the accident and hoping to receive some compensation. Although his injuries were considered insufficient for disability pension he could not work to his full capacity since the hand affected was his primary one and he was a manual labourer.
Given that the patient clearly suffered a high level of distress as a result of his hallucinatory experiences he was voluntary admitted to the 2nd Psychiatric Department of the Aristotle University of Thessaloniki for further assessment, observation and treatment. A routine blood workup was ordered with no abnormalities. A Rorschach Inkblot Test was administered in order to gain some insight into patient's dynamics, interpersonal relations and underlying personality characteristics while ruling out any malingering or factitious components in the presentation as suggested in Wilson and Keane [ 5 ]. Results pointed to inadequate reality testing with slight disturbances in perception and a difficulty in separating reality from fantasy, leading to mistaken impressions and a tendency to act without forethought in the face of stress. Uncertainty in particular was unbearable and adjustment to a novel environment hard. Cognitive functions (concentration, attention, information processing, executive functions) were impaired possibly due to cognitive inability or neurological disease. Emotion was controlled with a tendency for impulsive behaviour; however there was difficulty in processing and expressing emotions in an adaptive manner. There were distinct patterns of aggression and anger towards others but expressing those patterns was avoided, switching to passivity and denial rather than succumbing to destructive urges or mature competitiveness. Self-esteem was low with feelings of inferiority and inefficiency.
A neurological examination revealed a left VI cranial nerve paresis, reportedly congenital, resulting in diplopia while gazing to the extreme left, which did not significantly affect the patient. The patient had a chronic complaint of occasional vertigo, to which he partly attributed his accident, although the symptoms were not of a persisting nature.
Initial diagnosis at this stage was 'Psychotic disorder NOS' and pharmacological treatment was initiated. An MRI scan of the brain with gadolinium contrast was ordered to rule out any focal neurological lesions. It was performed fifteen days later and revealed no abnormalities.
Patient was placed on ziprasidone 40 mg bid and lorazepam 1 mg bid. He reported an immediate improvement but when the attending physician enquired as to the nature of the improvement the patient replied that in his hallucinations he told the tall raider that he now had a tall doctor who would help him and the raider promptly left (sic). Apparently, the random assignment of a strikingly tall physician had an unexpected positive effect. Ziprasidone gradually increased to 80 mg bid within three days with no notable effect to the perceptual disturbances but with the development of akathisia for which biperiden was added, 1 mg tid. Duloxetine was added, 60 mg once-daily, in a hope that it could have a positive effect to his mood but also to this neuropathic pain which was frequent and demoralising. The patient had a tough time accommodating to the hospital milieu, although the grounds were extended and there was plenty of opportunity for walks and other activities. He preferred to stay in bed sometimes in obvious agony and with marked insomnia. He presented a strong fear for the welfare of his children, which he could not reason for. Due to the apparent inability of ziprasidone to make a dent in the psychotic symptomatology, medication was switched to amisulpride 400 mg bid and the patient was given a leave for the weekend to visit his home. On his return an improvement in his symptoms was reported by him and close relatives, although he still had excessive anxiety in the hospital setting. It was decided that his leave was to be extended and the patient would return for evaluation every third day. After three appointments he had a marked improvement, denied any psychotic symptoms while his sleep pattern improved. A good working relationship was established with his physician and the patient was with a schedule of follow-up appointments initially every fifteen days and following two months, every thirty days. His exit diagnosis was "Psychotic disorder Not Otherwise Specified – PTSD". He remained asymptomatic for five months and started making in-roads in a cognitively-oriented psychotherapeutic approach but unfortunately further trouble befell him, his wife losing a baby and his claim to an injury compensation rejected. He experienced a mood loss and duloxetine was increased to 120 mg per day to some positive effect. His status remains tenuous but he retains a strong will to make his appointments and work with his physician. A case conceptualization following a cognitive framework [ 6 ] is presented in Figure 1 .
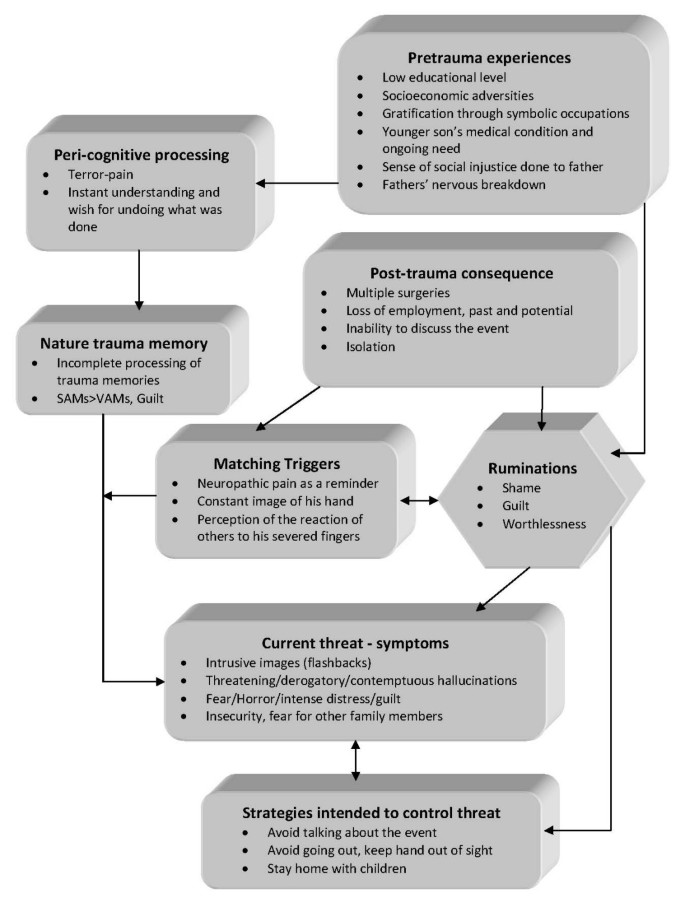
Case formulation – (Persistent PTSD, adapted from Ehlers and Clark [ 6 ] ) . Case formulation following the persistent PTSD model of Ehlers and Clark [ 6 ]. It is suggested that the patient is processing the traumatic information in a way which a sense of immediate threat is perpetuated through negative appraisals of trauma or its consequences and through the nature of the traumatic experience itself. Peri-traumatic influences that operate at encoding, affect the nature of the trauma memory. The memory of the event is poorly elaborated, not given a complete context in time and place, and inadequately integrated into the general database of autobiographical knowledge. Triggers and ruminations serve to re-enact the traumatic information while symptoms and maladaptive coping strategies form a vicious circle. Memories are encoded in the SAM rather than the VAM system, thus preventing cognitive re-appraisal and eventual overcoming of traumatic experience [ 4 ].
The value of a specialized formulation is made clear in complex cases as this one. There is a relationship between the pre-existing cognitive schemas of the individual, thought patterns emerging after the traumatic event and biological triggers. This relationship, best described as a maladaptive cognitive processing style, culminates into feelings of shame, guilt and worthlessness which are unrelated to similar feelings, which emerge during trauma recollection, but nonetheless acts in a positive feedback loop to enhance symptom severity and keep the subject in a constant state of psychotic turmoil. Its central role is addressed in our case formulation under the heading "ruminations" which best describes its ongoing and unrelenting character. The "what if" character of those ruminations may serve as an escape through fantasy from an unbearably stressful cognition. Past experience is relived as current threat and the maladaptive coping strategies serve as negative re-enforcers, perpetuating the emotional suffering.
The psychosocial element in this case report, the patient's involvement with a highly symbolic activity, demonstrates the importance of individualising the case formulation. Apparently the patient had a chronic difficulty in expressing his emotions and integrating into his social surroundings, a difficulty counter-balanced somewhat with his involvement in the local social events which gave him not only a creative way out from any emotional impasse but also status and recognition. His perceived inability to continue with his symbolic activities was not only an indicator of the severity of his troubles but also a stressor in its own right.
Complex cases of PTSD presenting with hallucinatory experiences can be effectively treated with pharmacotherapy and supportive psychotherapy provided a good doctor-patient relationship is established and adverse medication effects rapidly dealt with. A cognitive framework and a Rorschach test can be valuable in deepening the understanding of individuals and obtaining a personalized view of their functioning and character dynamics. A biopsychosocial approach is essential in integrating all aspects of the patients' history in a meaningful way in order to provide adequate help.
Patient's perspective
"My life situation can't seem to get any better. I haven't had any support from anyone in all my life. Leaving home to go anywhere nowadays is hard and I can't seem to be able to stay anyplace else for a long time either. Just getting to the hospital [where the follow-up appointments are held] makes me very nervous, especially the minute I walk in. Can't seem to stay in place at all, just keep pacing while waiting for my appointment. I am only able to open up somewhat to my doctor, whom I thank for his support. Staying in hospital was close to impossible; I was very stressed and particularly concerned for my children, not being able to be close to them. I still need to have them near-by. Getting the MRI scan was also a stressful experience, confined in a small space with all that noise for so long. I succeeded only after getting extra medication.
I hope that things will get better. I don't trust anyone for any help any more; they should have helped me earlier."
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
stands for 'Post Traumatic Stress Disorder'
for 'Verbally Accessible Memory'
for 'Situationally Accessible Memory'
Butler RW, Mueser KT, Sprock J, Braff DL: Positive symptoms of psychosis in posttraumatic stress disorder. Biological Psychiatry. 1996, 39: 839-844. 10.1016/0006-3223(95)00314-2.
Article CAS PubMed Google Scholar
Seedat S, Stein MB, Oosthuizen PP, Emsley RA, Stein DJ: Linking Posttraumatic Stress Disorder and Psychosis: A Look at Epidemiology, Phenomenology, and Treatment. The Journal of Nervous and Mental Disease. 2003, 191: 675-10.1097/01.nmd.0000092177.97317.26.
Article PubMed Google Scholar
Nutt DJ: The psychobiology of posttraumatic stress disorder. J Clin Psychiatry. 2000, 61: 24-29.
CAS PubMed Google Scholar
Brewin CR, Holmes EA: Psychological theories of posttraumatic stress disorder. Clinical Psychology Review. 2003, 23: 339-376. 10.1016/S0272-7358(03)00033-3.
Wilson JP, Keane TM: Assessing Psychological Trauma and PTSD. 2004, The Guilford Press
Google Scholar
Ehlers A, Clark DM: A cognitive model of posttraumatic stress disorder. Behaviour Research and Therapy. 2000, 38: 319-345. 10.1016/S0005-7967(99)00123-0.
Download references
Acknowledgements
The authors wish to acknowledge the valuable support and direction offered by the department's chair, Professor Ioannis Giouzepas who places the utmost importance in creating a suitable therapeutic environment for our patients and a superb learning environment for the SHO's and registrars in his department.
Author information
Authors and affiliations.
2nd Department of Psychiatry, Psychiatric Hospital of Thessaloniki, 196 Langada str., 564 29, Thessaloniki, Greece
Georgios D Floros, Ioanna Charatsidou & Grigorios Lavrentiadis
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Georgios D Floros .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors' contributions
GF was the attending SHO and the major contributor in writing the manuscript. IC performed the psychological evaluation and Rorschach testing and interpretation. GL provided valuable guidance in diagnosis and handling of the patient. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Authors’ original file for figure 1
Rights and permissions.
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Reprints and permissions
About this article
Cite this article.
Floros, G.D., Charatsidou, I. & Lavrentiadis, G. A case of PTSD presenting with psychotic symptomatology: a case report. Cases Journal 1 , 352 (2008). https://doi.org/10.1186/1757-1626-1-352
Download citation
Received : 12 September 2008
Accepted : 25 November 2008
Published : 25 November 2008
DOI : https://doi.org/10.1186/1757-1626-1-352

Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ziprasidone
- Psychotic Disorder
- Amisulpride
- Hallucinatory Experience
Cases Journal
ISSN: 1757-1626
- Advanced search

Advanced Search
PTSD as a Criminal Defense: A Review of Case Law
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- Figures & Data
- Info & Metrics
Posttraumatic stress disorder (PTSD) has been offered as a basis for criminal defenses, including insanity, unconsciousness, self-defense, diminished capacity, and sentencing mitigation. Examination of case law (e.g., appellate decisions) involving PTSD reveals that when offered as a criminal defense, PTSD has received mixed treatment in the judicial system. Courts have often recognized testimony about PTSD as scientifically reliable. In addition, PTSD has been recognized by appellate courts in U.S. jurisdictions as a valid basis for insanity, unconsciousness, and self-defense. However, the courts have not always found the presentation of PTSD testimony to be relevant, admissible, or compelling in such cases, particularly when expert testimony failed to show how PTSD met the standard for the given defense. In cases that did not meet the standard for one of the complete defenses, PTSD has been presented as a partial defense or mitigating circumstance, again with mixed success.
Even before posttraumatic stress disorder (PTSD) became an official diagnosis, traumatic stress syndromes, such as traumatic neurosis of war, were successfully offered as bases for criminal defenses. 1 Soon after its introduction in the Diagnostic and Statistical Manual of Mental Disorders, Third Edition (DSM-III), in 1980, 2 the PTSD diagnosis also made its way into the criminal courts as a basis for several types of criminal defenses for both violent and nonviolent crimes. 1 , 3 , 4 In addition, other trauma-related syndromes not included in the DSM, such as battered-wife syndrome and battered-child syndrome, have been offered as bases for criminal defenses. 3 , 5 , 6 However, these related syndromes have generally been presented as special types of PTSD. 4 , 5
Initially, the introduction of PTSD raised concern about its potential misuse in the criminal courts. 1 , 3 Skepticism was further heightened by cases in which malingered PTSD was used as a criminal defense. 3 In addition, shortly after the introduction of PTSD as a diagnosis, widespread reform of insanity defense statutes took place after the insanity acquittal of John Hinkley in 1984. These trends most likely made the successful use of PTSD as a criminal defense more difficult. 1 , 3 Appelbaum et al . 7 examined the frequency and rate of success of the insanity defense based on PTSD in several states and found that defendants had no more success with PTSD than with other mental disorders and that insanity pleas based on PTSD made up a small fraction of all insanity pleas, suggesting that fears about abuse of the diagnosis in the courts were largely unfounded.
Various PTSD phenomena have been presented in courts as bases for criminal defenses, including dissociative flashbacks, hyperarousal symptoms, survivor guilt, and sensation-seeking behaviors. 1 , 3 , 4 , 8 , – , 10 It has been suggested by some that dissociative flashbacks should be the only legitimate basis for insanity and other exculpating defenses and that other PTSD phenomena are insufficient to warrant exculpation. However, there has not been consensus on this proposal in the field. 1 , 3 , 4 Furthermore, although there has been some psychiatric research examining the role of certain PTSD phenomena in violent and criminal behavior, this body of research is yet to elucidate the relevance of such phenomena to criminal defenses. 8 , 9 Correlations between a diagnosis of PTSD and interpersonal violence, as well as between a diagnosis of PTSD and criminal behavior, have been described in the psychiatric literature, lending some empirical support for the use of PTSD as a criminal defense. 11 , – , 14 However, there has been little empirical research examining the role of specific PTSD symptoms in criminal behavior. The relevance of PTSD and specific PTSD symptoms to criminal defenses may therefore be best understood by examining how the criminal justice system has addressed the question.
In this article, we review United States criminal case law involving PTSD as a criminal defense. Case law is based on published legal decisions, which are typically at the appellate level. The significance of these cases is that they establish precedents for courts to follow in subsequent cases. Verdicts at the trial court level are usually not published, unless they are appealed. In addition, most pretrial decisions, such as whether a criminal defense based on PTSD can be presented at trial, are not published, unless they are appealed. As a result, research on appellate cases preferentially involves cases in which a criminal defense based on PTSD was barred or failed at the trial court level. On the other hand, cases in which a criminal defense based on PTSD was allowed at trial or was successfully presented at trial are largely not included in this review. This review will not address trends at the pretrial or trial court level; however, it will address the precedents that trial judges follow in rendering decisions about the use of PTSD as a basis for criminal defenses.
A systematic review of case law was conducted using the legal database LexisNexis. Federal and state appellate cases through 2010 were sought by using the search terms PTSD, posttraumatic stress disorder, post-traumatic stress disorder, or post traumatic stress disorder occurring in the summary, syllabus, or overview sections of cases, along with the terms criminal, insanity, diminished capacity, mens rea , self-defense, mitigation, or unconsciousness occurring in the same sections. The search was restricted to those criteria so that cases were selected in which PTSD played a prominent role.
A search for relevant law review articles was conducted on LexisNexis with the criterion that the term PTSD or a variation thereof appeared more than 10 times in the article. PubMed was searched using the terms PTSD, insanity, and criminal behavior. Identified law review and PubMed articles were searched for cited legal cases.
The search of LexisNexis yielded 194 cases, of which 47 involved a criminal defense based on PTSD. In 39 of these 47 cases, the defense was addressed by the appellate court in some way, whereas in the remaining 8 cases the issue appealed was not related to the use of PTSD as a criminal defense. Twenty-nine of the cases in which the use of PTSD as a criminal defense was addressed on appeal will be further described later in the text. The 10 cases that are not described in this article were excluded because they were redundant with other cases, in that the issues addressed by the appellate court were the same as those in other cases that are discussed. The search of law review articles and the psychiatric literature for cited legal cases yielded two published cases in which trauma-related disorders that preceded the DSM diagnosis of PTSD were the bases for criminal defenses. It also yielded three unpublished trial court cases in which PTSD was the basis for criminal defenses. These cases will be described later.
Table 1 lists the published cases that we identified, including the two cases that involved trauma-related disorders that preceded PTSD. The table lists the jurisdiction, legal issue, and outcome of each appellate case. Table 2 lists the three unpublished cases that we identified, along with the jurisdiction, legal issue, and verdict in each case.
- View inline
Published Cases in Which PTSD Was Presented as a Criminal Defense
Unpublished Cases in Which PTSD Was Successfully Presented as the Basis for an Insanity Defense
Admissibility of PTSD Expert Witness Testimony
In a series of landmark decisions commonly called the Daubert trio, the Supreme Court established criteria for the admissibility of expert witness testimony in federal court. 59 , – , 61 The Daubert standard requires that trial courts establish the reliability and relevance to the case at hand of proffered expert witness testimony. Some elements identified as relevant to this determination include the reliability of the techniques underlying a proposed testimony, peer-reviewed publications supporting it, and the general acceptance of it in the relevant field. 59 With a large and growing research base supporting the diagnosis of PTSD, along with its widespread acceptance in the mental health professions and its inclusion in the DSM, the diagnosis certainly meets the reliability prong of the Daubert standard, as has been well established in case law. 5
Given its widespread acceptance in the mental health professions, PTSD has also met the Frye standard of admissibility, which preceded the Daubert standard in the federal courts and is still the standard in some state jurisdictions. 62 For example, in Doe v. Superior Court , 16 a 1995 California appellate court case, the defendant was charged with capital murder. In pretrial motions, she petitioned the court to appoint experts of her choosing to assist in presenting a defense based on PTSD and battered-woman syndrome. The trial court denied her motion and instead appointed a panel expert without such expertise. The defendant appealed this decision, which the appellate court reversed, holding that“Expert testimony on Battered Woman Syndrome and PTSD is routinely admitted in criminal trials in California and other states and no one suggests they are not recognized psychiatric conditions” (Ref. 16 , p 541). The court cited several cases supporting its opinion.
With respect to the relevance prong of the Daubert and other admissibility standards, courts have ruled more variably on PTSD's relevance to various criminal defenses. However, in some cases PTSD has been found to be relevant to the criminal defenses of insanity, unconsciousness, self-defense, diminished capacity, and sentencing mitigation. A more detailed discussion of each follows.
PTSD and the Insanity Defense
Even before the addition of PTSD to the DSM, traumatic stress disorders were offered as the basis for insanity defenses. In Houston v. State , 17 a 1979 Alaska Supreme Court case, the defendant, an army sergeant, shot and killed a man he perceived to be reaching for a weapon. At trial, a defense expert testified that Mr. Houston had traumatic neurosis of war and severe alcoholism and that the shooting took place while he was in a dissociative state. The trial court denied his request for a bifurcated trial with an insanity phase, and he was found guilty of second-degree murder. The appeals court reversed and remanded, finding that he had provided substantial evidence to support an insanity defense.
Shortly after its introduction into DSM-III in 1980, 2 PTSD itself became the basis for successful insanity defenses. In State of New Jersey v. Cocuzza , the defendant, a Vietnam veteran who assaulted a police officer was found to be not guilty by reason of insanity. 57 Mr. Cocuzza maintained that he believed he was attacking enemy soldiers, and his claim was supported by the testimony of a police officer that Mr. Cocuzza was holding a stick as if it were a rifle. In another case, State v. Heads , 56 the defendant, also a Vietnam veteran, was charged with the shooting death of his sister-in-law's husband, after he entered the victim's residence in search of his estranged wife and began to fire a gun. Although he was found guilty in the first trial, the conviction was reversed on several grounds. In a subsequent trial, he was found not guilty by reason of insanity after testimony about PTSD was offered. The expert gave testimony that Mr. Heads had PTSD, that he had experienced at least one prior dissociative episode, and that there was a resemblance between the scene of the shooting and Vietnam. 63 In the case State v. Wood , 58 a 1982 Illinois Circuit Court case, the defendant, again a Vietnam veteran, was found not guilty by reason of insanity in the shooting of the foreman in the factory where he worked. The shooting took place shortly after Mr. Wood was confronted about his alcohol use by the foreman in front of several witnesses. The defense presented expert testimony about PTSD, about Mr. Wood's combat exposures, and about the ways in which the factory environment was reminiscent of combat, contending that the shooting took place while Mr. Wood was in a dissociative state. In yet another case, Commonwealth v. Tracy , 22 a 1989 Massachusetts case, Mr. Tracy, a Vietnam veteran who was charged with armed robbery, was found not guilty by reason of insanity based on PTSD. The defense contended that he was in a dissociative state during the robbery, which was triggered by stress and by the sight of a funeral parlor, which was a reminder of his Vietnam experience. Of note, Massachusetts employs the American Law Institute standard for insanity, in which a defendant is not considered criminally responsible if, as a result of mental disease or defect, the defendant lacked the capacity either to appreciate the criminality of his conduct or to conform his conduct to the requirements of the law. 62 Given that most jury verdicts are unpublished, it is not possible to determine how PTSD testimony has fared overall as a basis for the insanity defense. However, analysis of this selection of jury verdicts indicates that the PTSD phenomenon of dissociation has been successfully presented as a basis for insanity, at least when the American Law Institute standard for insanity was used.
At the appellate level, over the three decades of its existence as a diagnosis, PTSD has received mixed treatment when offered as a basis for insanity. This disparity was particularly noticeable after the widespread reform of insanity defense statutes in 1984, where, in both the federal system and in many states, insanity defense statutes were amended to require the presence of a severe mental disorder, proof of insanity under the M'Naughten standard or its variant, and proof of insanity by the defense at the clear-and-convincing level. Under the more stringent M'Naughten standard, a defendant is not considered criminally responsible if, as a result of mental disease or defect, the defendant lacked the capacity to understand the nature and quality or the wrongfulness of his conduct. 62 The placement of the burden of proof on the defendant constituted a significant shift in many jurisdictions. In the past, the defendant had been required only to present evidence in support of insanity, with the prosecution bearing the burden of showing that the standard for insanity was not met.
With respect to admissibility as a qualifying mental disorder for the insanity defense, in several jurisdictions, a PTSD defense was met with skepticism, particularly after the changes in insanity defense statutes. For example, in United States v. Duggan , 19 a 1984 federal case, the district court denied the defendants' pretrial motion for an insanity plea, finding that they failed to offer evidence or clinical findings in support of insanity, and the court questioned whether PTSD is a diagnosis that could ever lead to insanity. The defendants were found guilty of various firearms and explosives charges, which they appealed. The court of appeals upheld the conviction and agreed with the trial court's finding that an insanity plea based on PTSD was not supported. In United States v. Whitehead , 23 a 1990 federal case, Mr. Whitehead, a Vietnam veteran, was charged with bank robbery. He mounted an insanity defense based on PTSD and presented the expert testimony of a psychologist. The district court found that there was insufficient evidence to support a jury instruction on insanity, and Mr. Whitehead was found guilty of his charges. The court of appeals upheld the trial court's decision on the insanity defense, finding that, based on the testimony and evidence presented by the defense, no fact finder found that Mr. Whitehead could not appreciate the nature or wrongfulness of his actions or that his actions were a result of a severe mental illness at the clear-and-convincing standard. In its decision, the court did not specifically address whether PTSD could ever be a qualifying mental disorder for insanity. In United States v. Cartagena-Carrasquillo , 28 a 1995 federal case, the defendants were charged with cocaine-related offenses. At trial, one defendant gave notice and sought to present PTSD testimony as part of an insanity defense. The district court, after reviewing the expert's report, denied the defense, finding that the report did not show how the defendant, whether he had PTSD or not, did not know right from wrong. The defendants were convicted, and on appeal, the court of appeals affirmed the conviction, as well as the district court's decision to exclude the PTSD testimony, also finding that it was insufficient to support an insanity defense. Finally, in United States v. Long Crow , 27 a 1994 federal case, the defendant was charged with assault with a deadly weapon for firing a gun at a party after a confrontation with another individual. He claimed insanity based on PTSD and presented the testimony of a psychiatrist who observed him in court but did not evaluate him. The trial court refused to instruct the jury on the insanity defense, and he was found guilty of several charges. The court of appeals affirmed the conviction and agreed with the district court that there was insufficient evidence to support an insanity defense based on PTSD. In its decision, the court stated that it was unable to find cases in which PTSD was successfully presented as a basis for insanity, although it did not reject the possibility that PTSD could lead to insanity. Taken together, the appellate decisions in these federal cases suggest that the primary reason for the rejection of an insanity defense based on PTSD resulted from a lack of showing by the defense of how PTSD could lead to insanity. It does not appear that the federal courts of appeals found that PTSD was categorically disqualified as a basis for insanity, even after the Insanity Defense Reform Act of 1984.
In fact, some courts explicitly found PTSD to be a qualifying mental disorder that could lead to a defense of insanity. For example, in United States v. Rezaq , 29 a District of Columbia district court case, the defendant was charged with aircraft piracy, for which he intended to present an insanity defense based on PTSD. In support of this defense, he offered the opinions of three psychiatrists who diagnosed PTSD. The government sought to exclude this testimony, stating that the defendant's PTSD was not a sufficient basis for insanity. The district court denied the motion, finding that the reports by the defendant's experts“clearly indicate that defendant's diagnosis of PTSD meets the test of insanity as set out” in federal statutes (Ref. 29 , p 467). In addition, in several cases that will be discussed later in the article, insanity defenses based on PTSD were found to be compelling by appellate courts in both state and federal jurisdictions. It appears that as a matter of law, some courts have found PTSD to be a sufficiently severe mental disorder that could lead to insanity, but based on the facts of specific cases, it has sometimes been rejected.
In cases in which an insanity defense based on PTSD was allowed, but in which the defendant was convicted and the case was appealed, appellate courts have in some cases upheld the rejection of the insanity defense by juries. This has been the case in jurisdictions that use the M'Naughten standard for insanity and in those that use the American Law Institute standard. For example, in Gentry v. State , 20 a 1984 Tennessee Court of Criminal Appeals case, Mr. Gentry was charged with the first-degree murder of his girlfriend. He claimed insanity based on PTSD, contending that, after accidentally shooting his girlfriend, he lost touch with reality and shot her again. Mr. Gentry was diagnosed with PTSD by both defense and prosecution experts, but prosecution experts opined that the disorder was not sufficiently severe to render him incapable of understanding the wrongfulness of his acts or of conforming his conduct to the requirements of the law. The jury found him guilty of first-degree murder, rejecting his insanity defense. The court of appeals upheld the conviction, finding that he did not have a mental disorder sufficient to render him insane under Tennessee's American Law Institute insanity standard. In State v. Wilson , 24 a 1991 Louisiana Court of Appeal case, Mr. Wilson was accused of the attempted murder of a couple he knew, after he shot them in their home. The defendant, a Vietnam veteran, claimed insanity based on a PTSD flashback induced by jets flying overhead. He presented the testimony of three psychiatrists who diagnosed PTSD and who opined that he committed the shooting in the context of a flashback. In rebuttal, the prosecution presented the testimony of psychiatrists who evaluated the defendant's competency to stand trial. They were asked questions based on hypotheticals and in response opined that the defendant was able to tell right from wrong. The jury convicted Mr. Wilson, rejecting his insanity defense under Louisiana's M'Naughten insanity standard. On appeal, Mr. Wilson asserted that the jury had erred in failing to find him not guilty by reason of insanity. The court of appeal disagreed and affirmed the conviction, finding that there was sufficient evidence for the jury to reject the insanity defense, given that the burden of proof was the defendant's. In State v. Angel , 25 a North Carolina Supreme Court case, Mr. Angel was accused of the first-degree murder of his estranged wife. He pleaded not guilty by reason of insanity due to dissociation caused by PTSD and presented lay and expert testimony in support of his defense. In rebuttal, the prosecution in part presented hearsay testimony that the victim feared for her life from the defendant. The defendant was convicted. He appealed on the basis that the hearsay testimony should not have been admitted. The court of appeals affirmed, finding that even if the admission of the testimony was an error, there was sufficient evidence to reject his insanity defense under North Carolina's M'Naughten insanity standard. Finally, in People v. Rodriguez , 26 a 1993 New York appellate division court case, the defendant appealed his conviction of five counts of armed robbery on the basis that the jury erred in failing to find him not guilty by reason of insanity related to chronic PTSD under New York's American Law Institute insanity standard. The appellate court affirmed the conviction, finding that there was conflicting but credible expert witness testimony, and it was within the purview of the jury to determine which expert's testimony should be given more weight. These cases demonstrate that in the presence of conflicting expert witness testimony as to a defendant's PTSD diagnosis and sanity, juries' rejections of the insanity defense based on PTSD have often been affirmed by appellate courts.
However, in some cases, appellate courts have found an insanity defense based on PTSD to be compelling and at times to be grounds for reversal. For example, in State v. Percy , 21 a 1988 Supreme Court of Vermont case, a Vietnam veteran was accused of sexual assault and kidnapping, among other charges. At trial, he did not dispute committing the acts, but he claimed insanity based on having a PTSD flashback during the incident. Defense and prosecution experts all diagnosed PTSD, but disagreed on whether it was related to Mr. Percy's offenses. Defense experts opined that Mr. Percy was experiencing an unconscious flashback during the commission of his crimes and that as a result he was not in control of his thinking and behavior. Under Vermont's American Law Institute insanity standard, Mr. Percy was found guilty by the trial court, and he appealed. The Vermont Supreme Court determined that in reaching its verdict, the trial court improperly considered Mr. Percy's silence after he received the Miranda warning. The court reversed and remanded for a new trial, concluding that it was not possible to determine what verdict the trial court would have reached absent the error, as there was conflicting expert witness testimony as to the defendant's sanity.
In summary, in some cases in which the insanity defense based on PTSD was successful or was found by appellate courts to be viable, the defense theory involved dissociative phenomena leading to a break with reality. As has been suggested elsewhere, this is probably the sole PTSD phenomenon that could meet the strict insanity standards in most current jurisdictions that use the M'Naughten standard or its variant, with a clear-and-convincing standard of proof. 1 , 3 , 4 However, even dissociative phenomena have been rejected as a valid basis for insanity in some if not most cases.
PTSD and the Unconsciousness Defense
Another exculpating defense in which PTSD has had relevance is that of unconsciousness. In that defense, the defendant claims not to have been conscious during the commission of the criminal act. Therefore, the act was not voluntary, and there was no criminal liability. Unlike insanity, unconsciousness is a complete defense, resulting in exoneration but not in a hospital commitment. 62 Traumatic disorders were the basis for successful unconsciousness defenses even before the introduction of PTSD as a diagnosis. 4 , 8
For example, in People v. Lisnow , 32 a 1978 California Supreme Court Appellate Department case, Mr. Lisnow was convicted of battery in an apparently unprovoked assault that he engaged in while dining in a restaurant. He claimed unconsciousness, and a defense expert testified that the defendant was unconscious at the time of the incident as a result of a fugue state brought on by a continuing traumatic neurosis related to his service in Vietnam. The trial court struck the expert witness's testimony, resulting in a conviction. The appeals court reversed the judgment, holding that the evidence of Mr. Lisnow's unconsciousness at the time of the incident was admissible and compelling.
In another case, State v. Fields , 33 Mr. Fields was charged and convicted of the first-degree murder of his sister's boyfriend, who was allegedly abusive toward the defendant's sister. The defendant presented lay and expert witness testimony that suggested he had PTSD and was in a dissociated state when the homicide took place. The trial court refused to instruct the jury on the unconsciousness defense, and Mr. Fields was found guilty. On appeal, the court found that the evidence presented by the defense tended to show that the defendant was unconscious just before and during the homicide and that the jury should have received instructions on the unconsciousness defense. The court reversed and remanded for a new trial. These cases illustrate that, in addition to relevance to the insanity defense, the PTSD phenomenon of dissociation has been used as a basis for the unconsciousness defense.
PTSD and Self-Defense
Since its introduction, PTSD and related syndromes, such as battered-woman syndrome, have been used in the justification defense of self-defense. The basic elements of self-defense are that the defendant is not the aggressor, the defendant reasonably fears imminent death or great bodily harm that necessitates the use of force to save his life, and the amount of force used by the defendant is reasonably necessary to avert the danger and not more than exigency demands. Self-defense is precluded if a defendant uses excessive force. In perfect self-defense, all elements of self-defense are met and complete exoneration results. In imperfect self-defense, only some of the elements are met, and typically a conviction of a lesser included offense (e.g., manslaughter as opposed to first-degree murder) results. 62
Expert testimony about PTSD has been used to establish the necessary state-of-mind element of self-defense (namely that the defendant reasonably feared imminent death or great bodily harm). Such testimony has been most relevant in jurisdictions that have a subjective test of imminent danger, where the trier of fact must determine whether the defendant believed that there was an imminent risk that necessitated the use of force. In most jurisdictions, an additional objective test is used to determine whether a reasonable person under the same circumstances would have believed that there was imminent risk that necessitated the use of force. 62 The relevance of PTSD in jurisdictions that use an objective test is more limited, although some courts have considered PTSD to be an aspect of the circumstances to be considered in the objective test.
At the appellate level in different jurisdictions, expert witness testimony on PTSD and related syndromes has been deemed relevant to claims of self-defense, particularly in cases that involved the homicide or attempted homicide of an abuser (i.e., the perpetrator of trauma leading to PTSD). For example, in State v. Kelly , 34 a 1984 New Jersey Supreme Court case, Ms. Kelly was charged with the first-degree murder of her husband. She admitted to the killing, but claimed to have acted in self-defense. In support of this claim, the defense sought to introduce expert witness testimony on battered-spouse syndrome (but not PTSD), given past abuse of the defendant at the hands of her husband, including at the time of the homicide. First described by Dr. Lenore Walker, 1 , 4 , – , 6 , 34 battered-spouse syndrome is a psychological construct that describes and explains behavior patterns typical of battered spouses. The trial court excluded this testimony as irrelevant, and Ms. Kelly was convicted of manslaughter. On appeal, the court held that the testimony sought by the defense on battered-spouse syndrome was in fact relevant to self-defense. The court reasoned that the testimony was relevant to bolster the credibility of the defendant that she subjectively feared for her life and to aid the jury in determining whether, in the defendant's circumstances, a reasonable person would have feared for her life. The court therefore reversed the conviction and remanded. At the same time, the appellate court allowed the trial court to determine whether the expert testimony on battered-spouse syndrome was sufficiently reliable to admit, given its recent emergence as a syndrome.
In Rogers v. State , 36 a 1993 Florida Court of Appeal case, the defendant was convicted of the first-degree murder of her boyfriend. At trial, she sought to present expert witness testimony about battered-woman syndrome, which included characterizing the disorder as a form of PTSD. The trial court excluded the testimony as not meeting the standard for admission. On appeal, the court disagreed and found the testimony to be relevant and to meet the standard for admission, noting that PTSD is commonly accepted in the mental health community and that expert testimony on PTSD has been recognized as admissible by Florida courts. The conviction was reversed, and the case was remanded for a new trial.
In State v. Hines , 40 a 1997 Superior Court of New Jersey, Appellate Division case, the defendant was charged with the intentional murder and robbery of her father and was convicted of the lesser included charges of manslaughter and theft. At trial, Ms. Hines claimed self-defense, contending that she was sexually abused by her father as a child and that on the day of the offense he made sexual advances toward her and threatened her. She contended that she feared for her safety and as a result struck him repeatedly with a hammer, killing him. To support her defense, Ms. Hines sought to admit expert testimony on PTSD. The trial court excluded the testimony. On appeal, the court found that the exclusion of PTSD testimony was an error, as this testimony would have been relevant to the defendant's claim of self-defense. The conviction was reversed and the case was remanded for a new trial. These cases demonstrate that some appellate courts have viewed testimony on PTSD as relevant to self-defense claims involving the homicide or attempted homicide of abusers.
PTSD testimony has also been proffered by the defense in cases involving the homicide of nonabusers, but it has enjoyed less acceptance by courts in such cases. For example, in Perryman v. State , 41 a 1999 Oklahoma Court of Criminal Appeals case, the defendant was convicted of the first-degree murder of a man who he claimed attempted to assault him sexually and then threatened to shoot him when he fought back. The defendant sought to introduce PTSD testimony related to alleged childhood sexual abuse. The trial court excluded the testimony on the grounds of irrelevance. On appeal, the court affirmed the conviction and the exclusion of PTSD testimony, reasoning that the relevance of PTSD to self-defense involving a nonabuser (as opposed to an abuser) is questionable.
Other courts have found testimony on PTSD to be relevant to self-defense claims for the homicide or attempted homicide of nonabusers. For example, in State v. Mizell , 42 a 2000 Florida Court of Appeal case, the defendant, a Vietnam veteran, was charged with attempted second-degree murder after he got into a fight with another man at the home of a third person. Mr. Mizell claimed that the victim threatened him and ran his hand over his pocket, at which point he picked up a stick and hit the victim several times. Mr. Mizell sought to introduce testimony about PTSD, which the court allowed. The state appealed the decision to allow such testimony. The court of appeal held that PTSD evidence is admissible and relevant to the question of self-defense.
In cases in which PTSD or related syndrome testimony was allowed, courts have at times refused to instruct juries on self-defense, questioning whether the defense theory based on PTSD was compelling. On appeal of some of those cases, courts have reversed, suggesting that self-defense based on PTSD is a recognized phenomenon in case law. For example, in State v. Janes , 37 a 1993 Washington Supreme Court case, 17-year-old Mr. Janes shot and killed his mother's boyfriend, who reportedly had abused Mr. Janes, his mother, and his siblings over a period of 10 years. An argument between the defendant's mother and the victim took place the night before the shooting, but reportedly there was no confrontation between the defendant and the victim at the time of the shooting. At trial, Mr. Janes presented two defenses, self-defense based on the history of abuse and diminished capacity. He presented expert witness testimony that he had PTSD, which led him to believe he was in imminent danger from the victim. The trial court refused to issue self-defense instructions to the jury, because it did not believe that Mr. Janes was in imminent danger of abuse. Mr. Janes was convicted of second-degree murder. On appeal, the lower appellate court reversed the conviction, which the state appealed to the Supreme Court of Washington. In its decision, the court held that testimony on PTSD and battered-child syndrome was admissible and that the trial court erred in failing to consider the subjective element of self-defense in the context of the expert testimony given. The court remanded the case to the trial court to reconsider the self-defense jury instructions.
Appellate courts had similar findings in cases of self-defense claims involving nonabusers. In State v. Sullivan , 39 a 1997 Maine Supreme Judicial Court case, Mr. Sullivan was charged with attempted murder and aggravated assault related to his shooting into a crowd in a bar after an altercation with a bar patron. Mr. Sullivan claimed self-defense, which in part involved PTSD. The trial court refused to instruct the jury on self-defense, and Mr. Sullivan was convicted of all three charges of aggravated assault. On the basis of expert witness testimony, the appeals court vacated the convictions, holding that a jury could have reasonably found that Mr. Sullivan acted in self-defense.
A review of appealed jury verdicts in cases in which self-defense based on PTSD was claimed reveals that conviction of a lesser included offense is another potential outcome of such cases. Such outcomes often occurred in jurisdictions that allow imperfect self-defense. For example, in Harwood v. State , 38 a 1997 Texas Court of Appeals case, 16-year-old Mr. Harwood was charged with the murder of a man who had molested him. He claimed self-defense and introduced the testimony of his therapist, who had diagnosed PTSD and testified to his opinion that the shooting was in self-defense. Mr. Harwood was convicted of the lesser included offense of manslaughter. On appeal, the verdict was affirmed, as the court found that the jury most likely believed the defendant's version of events but did not believe it should result in complete exoneration.
In summary, appellate courts have found expert testimony on PTSD to be relevant in cases of self-defense. This finding has been true for offenses of abusers as well as nonabusers, although for the latter, some courts have excluded PTSD testimony. Self-defense claims based on PTSD have been offered primarily in jurisdictions that use a subjective test of reasonableness. Finally, in jurisdictions that allow an imperfect self-defense, in which conviction of a lesser included charge is possible, PTSD has been relevant and successfully presented as an element of the defense. Detailed review of these cases indicates that expert testimony on PTSD as it relates to self-defense was focused on the PTSD phenomena of hyperarousal symptoms, increased impulsivity, re-experiencing of psychological distress when confronted with an abuser or reminders of past traumas, and the overestimation of danger.
PTSD and Refuting Mens Rea
In the criminal courts, expert witness testimony on PTSD has also been introduced to refute the requisite state of mind, or mens rea , for certain criminal charges. Most U.S. jurisdictions allow mental health expert testimony to refute mens rea , whereas some jurisdictions restrict such testimony to the insanity defense. 62 In jurisdictions that allow such testimony, appellate courts have in some cases found testimony about PTSD to be admissible for such purposes and to be compelling. For example, in United States v. Cebian , 44 a 1985 federal case, the defendant was charged with cocaine-related offenses. Her defense was that she lacked the ability to form the requisite state of mind for the charged crime as a result of PTSD related to abuse by her spouse, a cocaine dealer. Expert witness testimony to this effect was presented by the defense and was admitted. Although the jury ultimately found the defendant guilty on the basis of prosecution evidence countering the defense claims, the admissibility of such testimony was not questioned on appeal.
In State v. Warden , 45 a 1997 Washington Supreme Court case, Ms. Warden, a 41-year-old woman, was charged with the first-degree murder of an 81-year-old woman who had formerly employed her as a housekeeper. She presented the defense of diminished capacity due to PTSD from long-standing abuse by her son. A psychiatric expert testified that the defendant had PTSD with dissociative states and that she lacked the capacity to form specific intent with respect to the charged crime. The judge instructed the jury on first- and second-degree murder, but not on manslaughter. On appeal, the supreme court reversed, finding that there was substantial evidence to support a conviction of the lesser charge of manslaughter on the basis of the expert witness testimony offered. In State v. Bottrell , 46 a 2000 Washington Court of Appeals case, Ms. Bottrell was charged with the premeditated murder of an elderly man who had made sexual overtures toward her. The trial court excluded expert testimony on PTSD that the defendant sought to present to support her defense of diminished capacity. She was convicted, but the appeals court reversed, ruling that the exclusion of PTSD testimony was an error. In its decision, the court held that,“Washington case law acknowledges that PTSD is recognized within the scientific and psychiatric communities and can affect the intent of the actor resulting in diminished capacity” (Ref. 46 , p 715). In summary, PTSD testimony has been allowed and has been found to be relevant and compelling by some appellate courts when offered in conjunction with a diminished capacity or related mens rea defense.
PTSD as a Mitigating Circumstance
In the federal jurisdiction, a mental illness can be a basis for downward departure in sentencing if the defendant committed the offense while in a significantly reduced mental state and if the reduced mental state contributed substantially to the commission of the offense. 62 In some state jurisdictions, the presence of a mental illness as a factor in a crime can similarly mitigate sentencing. Courts have found PTSD to be a relevant diagnosis for such mitigation, and, in some cases, sentences have been reversed because of the exclusion or oversight of such testimony. For example, in In re Nunez , 51 a 2009 California Court of Appeal case, the defendant, a juvenile, was convicted of charges related to an attempted kidnapping and firing at police during a high-speed chase. The defendant was sentenced to life imprisonment without the possibility of parole. On appeal, the court found that PTSD evidence should have been considered in sentencing and should have mitigated the sentence, which was excessive. Mr. Nunez's diagnosis was PTSD related to past traumas, including childhood abuse by his father, being the victim of a shooting, and witnessing the shooting death of his brother only months before the offense. An expert opined that PTSD contributed substantially to his offense, an opinion that the court found compelling. The court therefore vacated the sentence and remanded to the trial court for resentencing.
In Gilley v. Morrow , 49 a 2007 federal case, the defendant was convicted of the murder of his parents and sister. No mitigating evidence was introduced during the sentencing phase of his trial. Mr. Gilley filed a petition for a writ of habeas corpus for ineffective assistance of counsel, which was granted by the federal district court. The court of appeals affirmed the district court's granting of his petition in the sentencing phase, but not in the trial phase. The court found that evidence about the defendant's PTSD from childhood abuse would have been relevant in sentencing, so that trial counsel rendered ineffective assistance when he failed to present such evidence.
In some cases, courts have chosen not to reduce sentencing on the basis of the presence of PTSD as a factor in the crime, and their rulings have been upheld on appeal. For example, in United States v. Cope , 50 a 2008 federal case, the defendant received the maximum sentence for methamphetamine-related charges. The defendant contended that his military service in Vietnam and his related PTSD should have mitigated the sentence, but the trial court opined that“even individuals with this disorder have to take responsibility for their actions ” (Ref. 50 , p 371). The court of appeals affirmed the sentence, holding that the trial court had the discretion of not considering the presence of PTSD to be a mitigating factor in the sentence.
Finally, in some cases, courts did not find the purported connection between PTSD and the offense to be compelling, thus denying a downward deviation of sentencing. For example, in United States v. Johnson , 47 a 1995 federal case, Mr. Johnson was convicted of two cocaine sales charges. He appealed his sentence, in part because he argued that the district court should have reduced his sentence because of his diminished mental capacity related to PTSD. The court of appeals upheld the district court's rejection of Mr. Johnson's diminished mental capacity claim, finding that he failed to show a direct connection between PTSD and the offense. Similarly, in Hall v. Lee , 52 a 2009 Georgia Supreme Court case, Mr. Hall and an accomplice broke into a gun store and stole several guns. The defendant then drove to his father's house, planning to kill him; however, his father was not home and the defendant shot his father's girlfriend. Following conviction, sentencing, and appeal, he filed a habeas petition for ineffective assistance of counsel, contending that his trial counsel did not sufficiently investigate mitigating circumstances. In support of his argument, he presented expert testimony that he had PTSD. The habeas court denied his petition, holding that he had failed to show how PTSD was related to his offense.
In summary, in cases in which PTSD played a role in an offense but did not meet the standard for an exculpating defense, courts have found it to be a mitigating circumstance that permits a reduction in sentencing. In such cases, a wide range of PTSD phenomena have been found to be applicable, including hyperarousal symptoms, impaired impulse control, overestimation of danger, and dissociative phenomena. However, in most jurisdictions, a showing of a direct connection between PTSD and the offense is required.
In this article we reviewed U.S. case law relating to the use of PTSD as a criminal defense. Since its introduction in DSM-III, 2 PTSD has been offered as the basis for defenses, including insanity, unconsciousness, self-defense, and diminished capacity and as a mitigating circumstance in sentencing. The diagnosis has received both positive and negative treatment by appellate courts when presented as the basis for each of these defenses. An analysis of the reviewed cases yielded the following conclusions.
Appellate courts in some jurisdictions have found testimony on PTSD to meet both the Daubert and Frye standards for admissibility. In assessing expert testimony, courts have favorably regarded the direct evaluation of the defendant by the expert, confirmation of the traumatic exposure via collateral information, and the existence of documented PTSD symptomatology and treatment before the occurrence of the criminal act in question.
Appellate courts have found criminal defenses based on PTSD to be viable and compelling when a clear and direct connection between the defendant's PTSD symptoms and the criminal incident was found by the expert. The PTSD phenomena that appellate courts have found to be most relevant to criminal defenses include dissociations, hyperarousal symptoms, hypervigilance symptoms, and the overestimation of danger. Although other PTSD phenomena, such as survivor guilt, a sense of a foreshortened future, and thrill seeking, have been proposed in the literature and in expert testimony as relevant, the case law reviewed in this article suggests that courts have not agreed. 3 , 4 , 8
In the rare instances of crimes committed in the context of dissociative episodes, the exculpating defenses of insanity and unconsciousness have been successfully presented. In such cases, the mental health expert has been called on to determine whether the defendant was indeed in the midst of a PTSD dissociation while committing the offense. PTSD dissociations have been the basis for successfully presented arguments of self-defense, diminished capacity, and other mens rea defenses. These defenses have also been successfully based on the PTSD phenomena of overascertainment of danger and hyperarousal symptoms. Finally, for crimes in which PTSD played a role but did not amount to one of these defenses, some courts have found it to be a mitigating circumstance in sentencing.
Several authors have offered recommendations for the forensic expert evaluating PTSD as a potential criminal defense, although these have largely not been research based. For example, in describing two cases of malingered PTSD offered as a basis for criminal defense, Sparr and Atkinson 3 discussed the importance of assessing the veracity of the trauma that is presented as reason for the diagnosis. Recommendations included the use of confirmatory records and being alert to signs of an exaggerated or factitious trauma, such as grandiose stories, esoteric terminology that is difficult to understand, or contradictory stories. Colbach 64 proposed similar recommendations in a paper describing a case of malingered PTSD that was successfully used as a basis for an insanity defense but that was later exposed in a civil suit. In reviewing PTSD as a criminal defense, Sparr 4 proposed characteristics of authentic PTSD dissociations that cause criminal acts. These included the absence of a motive or explanation for the crime, lack of premeditation, similarities between the circumstances of the crime and the trauma causing PTSD, a random or fortuitous victim, and no criminal history. Sparr and Atkinson 3 , 4 and others 8 have also proposed certain interview techniques in the evaluation of PTSD as a criminal defense, such as beginning with open-ended questions before inquiring about specific PTSD symptoms. The utility of neuropsychological tests in diagnosing PTSD has also been discussed and reviewed by others. Finally, although not yet an aspect of clinical or forensic practices, physiological testing, reviewed elsewhere, 8 has been studied as a potentially useful adjunctive tool to aid in the diagnosis of PTSD.
Analysis of the cases reviewed in this article supports some of the above recommendations. First, accurately diagnosing PTSD is fundamental for the acceptance of expert testimony as reliable by courts. Second, forensic experts should specifically determine whether and how specific PTSD phenomena played a role in the criminal act in question. Particular attention should be directed to whether PTSD phenomena that have been recognized by courts as relevant to criminal defenses were present. The forensic expert should elucidate as clearly as possible how the PTSD phenomena that were present contributed to the act. In doing so, the forensic expert should keep in mind the relevant criminal defenses involved, including insanity, self-defense, and diminished capacity. In numerous cases reviewed in this article, expert testimony has been excluded or deemed irrelevant because of a failure to identify a clear and direct connection between the defendant's PTSD symptoms and the criminal act.
This review has several limitations. First, it is limited to U.S. case law, which is likely to be only partially relevant in other countries. However, as has been suggested by Friel et al. , 8 the prevalence of PTSD-based criminal defenses in U.S. courts has very likely been higher than in other countries as a result of the Vietnam War. Because of that, U.S. case law in this area is likely to serve as an important reference point for other jurisdictions. Second, and as discussed earlier, because this review is based on published cases, it cannot address trends in PTSD-based criminal defenses in jury trials. Furthermore, the published decisions examined often contained only short exerpts or brief synopses of expert testimony, such that the complete examination of expert testimonies offered was not possible. Finally, this review describes the extent to which appellate courts have found PTSD and specific phenomena of the disorder to be valid bases for criminal defenses. These findings may differ from those in future empirical research, regarding the validity of PTSD phenomena and their role in criminal behavior.
Disclosures of financial or other potential conflicts of interest: None.
- © 2012 American Academy of Psychiatry and the Law
- Jordan HW ,
- Gelsomino J ,
- American Psychiatric Association
- Atkinson RM
- Garcia-Rill E
- Hafemeister TL ,
- Appelbaum PS ,
- Moskowitz A
- Aprilakis C
- Zatzick DF ,
- Marmar CR ,
- Bekham JC ,
- Feldman ME ,
- Churchill CM ,
- Collins JJ ,
- 15. Shepard v. State, 847 P.2d 75 (Alaska Ct. App. 1993) .
- 16. ↵ Doe v. Superior Court, 39 Cal. App. 4th 538 (Cal. Ct. App. 1995) .
- 17. ↵ Houston v. State, 602 P.2d 784 (Alaska 1979) .
- 18. State v. Felde, 422 So. 2d 370 (La. 1982) .
- 19. ↵ United States v. Duggan, 743 F.2d 59, 81 (2d Cir. 1984) .
- 20. ↵ Gentry v. State, 1984 Tenn. Crim. App. LEXIS 2738 (Tenn. Crim. App. 1984) .
- 21. ↵ State v. Percy, 548 A.2d 408 (Vt. 1988) .
- 22. ↵ Commonwealth v. Tracy, 539 N.E.2d 1043 (Mass. App. Ct. 1989) .
- 23. ↵ United States v. Whitehead, 896 F.2d 432 (9th Cir. 1990) .
- 24. ↵ State v. Wilson, 581 So.2d 394 (La. Ct. App. 1991) .
- 25. ↵ State v. Angel, 408 S.E.2d 724 (N.C. 1991) .
- 26. ↵ People v. Rodriguez, 192 A.D.2d 465 (N.Y. App. Div. 1993) .
- 27. ↵ United States v. Long Crow, 37 F.3d 1319, 1324 (8th Cir. 1994) .
- 28. ↵ United States v. Cartagena-Carrasquillo, 70 F.3d 706 (1st Cir. 1995) .
- 29. ↵ United States v. Rezaq, 918 F. Supp. 463 (D.D.C. 1996) .
- 30. State v. Page, 488 S.E.2d 225 (N.C. 1997) .
- 31. United States v. Calvano, Federal court (2009) .
- 32. ↵ People v. Lisnow, 151 Cal. Rptr. 621 (Cal. App. Dep't Super. Ct. 1978) .
- 33. ↵ State v. Fields, 376 S.E.2d 740 (N.C. 1989) .
- 34. ↵ State v. Kelly, 478 A.2d 364, 382 (N.J. 1984) .
- 35. United States v. Simmonds, 931 F.2d 685 (10th Cir. 1991) .
- 36. ↵ Rogers v. State, 616 So.2d 1098 (Fla. Dist. Ct. App. 1993) .
- 37. ↵ State v. Janes, 850 P.2d 495 (Wash. 1993) .
- 38. ↵ Harwood v. State, 961 S.W.2d 531 (Tex. Ct. App. 1997) .
- 39. ↵ State v. Sullivan, 695 A.2d 115 (Me. 1997) .
- 40. ↵ State v. Hines, 696 A.2d 780 (N.J. Super. Ct. App. Div. 1997) .
- 41. ↵ Perryman v. State, 990 P.2d 900 (Okla. Crim. App. 1999) .
- 42. ↵ State v. Mizell, 773 So.2d 618, 619 (Fla. Dist. Ct. App. 2000) .
- 43. State v. Stuart, 143 P.3d 595 (Wash. 2006) .
- 44. ↵ United States v. Cebian, 774 F.2d 446 (11th Cir. 1985) .
- 45. ↵ State v. Warden, 947 P.2d 708 (Wash. 1997) .
- 46. ↵ State v. Bottrell, 14 P.3d 164 (Wash. Ct. App. 2000) .
- 47. ↵ United States v. Johnson, 49 F.3d 766 (D.C. Cir. 1995) .
- 48. United States v. Kim, 313 F.Supp.2d 295 (S.D.N.Y. 2004) .
- 49. ↵ Gilley v. Morrow, 246 Fed. Appx. 519 (9th Cir. 2007) .
- 50. ↵ United States v. Cope, 282 Fed. Appx. 369 (6th Cir. 2008) .
- 51. ↵ In re Nunez, 93 Cal. Rptr. 3d 242 (Cal. Ct. App. 2009) .
- 52. ↵ Hall v. Lee, 684 S.E.2d 868 (Ga. 2009) .
- 53. Dever v. Kansas State Penitentiary, 788 F.Supp. 496 (D. Kan. 1992) .
- 54. Seidel v. Merkle, 146 F.3d 750 (9th Cir. 1998) .
- 55. Aguirre v. Alameida, 120 Fed. Appx. 721 (9th Cir. Cal. 2005) .
- 56. ↵ State v. Heads, 385 So.2d 230, 231 (La. 1980) .
- 57. ↵ State v. Cocuzza, No. 1484-79 (N.J. Super. Ct. 1981) .
- 58. ↵ State v. Wood, No. 80-7410 (Ill. Cir. Ct. May 5, 1982) .
- 59. ↵ Daubert v. Merrell Dow Pharmaceuticals, Inc., 509 U.S. 579 (1993) .
- 60. ↵ General Electric Co. v. Joiner, 522 U.S. 136 (1997) .
- 61. ↵ Kumho Tire Co. v. Carmichael, 526 U.S. 137 (1999) .
- Erlinder EC
In this issue
- Table of Contents
- Index by author
Thank you for your interest in recommending The Journal of the American Academy of Psychiatry and the Law site.
NOTE: We only request your email address so that the person you are recommending the page to knows that you wanted them to see it, and that it is not junk mail. We do not capture any email address.
Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager

- Tweet Widget
- Facebook Like
- Google Plus One
Jump to section
Related articles, cited by..., more in this toc section.
- Mental Health Service Referral and Treatment Following Screening and Assessment in Juvenile Detention
- Clinical and Legal Considerations When Optimizing Trauma Narratives in Immigration Law Evaluations
- When a Patient Is at Foreseeable Risk of Losing Decisional and Functional Capacity
Similar Articles

IMAGES
VIDEO
COMMENTS
This is a case example for the treatment of PTSD using Cognitive Behavioral Therapy. It is strongly recommended by the APA Clinical Practice Guideline for the Treatment of PTSD. Download case example (PDF, 108KB).
This is a case example for the treatment of PTSD using Eye Movement Desensitization and Reprocessing (EMDR) therapy. EMDR is conditionally recommended by the APA Clinical Practice Guideline for the Treatment of PTSD.
CASE STUDY. “Tom” is a 23-year-old, single, white male who present- ed for treatment approximately 1 year after a traumatic event that occurred during his military service in Iraq. Tom received CPT while on active duty in the Army. Tom was born the third of four children to his parents.
This article presents an overview of complex trauma and a case study describing the evidence-informed treatment of a 25-year-old woman with chronic complex trauma symptoms resulting from childhood sexual, physical, and psychological abuse from a caregiver.
Complex cases of PTSD presenting with hallucinatory experiences can be effectively treated with pharmacotherapy and supportive psychotherapy provided a good doctor-patient relationship is established and adverse medication effects rapidly dealt with.
Examination of case law (e.g., appellate decisions) involving PTSD reveals that when offered as a criminal defense, PTSD has received mixed treatment in the judicial system. Courts have often recognized testimony about PTSD as scientifically reliable.