Midwifery Practice and Education: Current Challenges and Opportunities
- PMID: 26812270
Midwifery clinical practice and education has changed significantly since Mary Breckinridge first introduced nurse-midwives to the United States in 1925. This article discusses current challenges in midwifery clinical practice and education and proposes possible solutions. Midwifery clinical challenges include restrictive legislation and business-related barriers, including but not limited to physician supervision restrictions, prescriptive authority, out-of-hospital birth legislation, and third party reimbursement. Educational challenges highlighted include the current healthcare climate's influence on midwifery education, the contribution of clinical sites and preceptors, and the benefits of midwifery education.
- Midwifery / education*
- Midwifery / legislation & jurisprudence
- Nurse Midwives / education*
- Nurse Midwives / legislation & jurisprudence
- Professional Autonomy*
- Professional Practice / legislation & jurisprudence
- Professional Practice / trends*
- United States

Progress and problems in midwifery education: some conclusions from published research
Cite this chapter.

- Sarah Robinson
42 Accesses
Midwifery education is at a particularly challenging juncture in its history. Both the programmes leading to qualification as a midwife are now firmly linked to higher education, with courses offered at diploma and, increasingly, at degree level. Mergers with colleges of nursing and with institutions of higher education have presented opportunities for extending the knowledge base of midwifery and for increasing academic rigour (Roch, 1993). On the other hand difficulties have arisen over midwifery losing its unique identity in these larger institutions and in the often increased distance between educational facilities and the practice setting (Hall, 1994; Warwick, 1992). Those responsible for midwifery education are rising to the challenge of preparing students for the more independent role envisaged by the Expert Maternity Group (Department of Health, 1993). At the same time, midwife teachers are subject to an increasing range of pressures. They are required to attain graduate status, to maintain a credible clinical profile when often far removed from practice settings, and organize educational programmes within the complexities of the purchaser—provider system implemented by the NHS and Community Care Act of 1990.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
Similar content being viewed by others

Experiences of a new cadre of midwives in Bangladesh: findings from a mixed method study

Development and initiation of a preceptor program to improve midwifery and nursing clinical education in sub-saharan Africa: protocol for a mixed methods study
Norwegian midwives’ opinion of their midwifery education – a mixed methods study.
Association of Radical Midwives (1986) The Vision: Proposals for the Future of the Maternity Services . Association of Radical Midwives, London.
Google Scholar
Balch, B. (1982) Teacher training for midwives: an investigation of the midwife teacher’s diploma course 1975–79 at the Royal College of Midwives, London, with special reference to teaching practice. In Thomson, A.M. (ed), Research and the Midwife Conference Proceedings for 1981 . Department of Nursing, University of Manchester.
Barriball, K.L., While, A. and Norman, I. (1991) Continuing professional education for qualified nurses: a review of the literature. Journal of Advanced Nursing , 17 , 1129–40.
Article Google Scholar
Bedford, H., Phillips, T., Robinson, J. and Schostak, J. (1993) Assessing Competencies in Nursing and Midwifery Education . English National Board, London.
Chamberlain, M. (1992) Factors affecting students becoming competent in midwifery skills. In Thomson, A., Robinson, S. and Tickner, V. (eds), Research and the Midwife Conference Proceedings for 1991 . Department of Nursing, University of Manchester.
Clarke, J. and Rees, C. (1989) The midwife and continuing education. Midwives Chronicle and Nursing Notes , 102 (1220), 228–290.
Davies, R. (1991) Perspectives on midwifery: students’ beginnings. In Robinson, S., Thomson, A. and Tickner, V. (eds), Research and the Midwife Conference Proceedings for 1990 . Department of Nursing, University of Manchester.
Department of Health (1993) Changing Childbirth: Report of the Expert Maternity Group Parts 1 and 2 (Cumberledge Report) . HMSO, London.
English National Board (1993) Project Specification: An Outcome Evaluation of the Effectiveness of Pre-registration Midwifery Programmes of Education . English National Board, London.
Flanders, N. (1970) Analysing Teaching Behaviour . Addison Wesley, Massachusetts.
Fraser, D.M., Murphy, R.J.L., Worth-Butler, M. (1994) Evaluation of the effectiveness of pre-registration midwifery programmes of education. A joint project between the Faculty of midwifery, Mid Trent College of Nursing and Midwifery, and the school of Education, University of Nottingham. Interim report to the English National Board Research and Development Group. English National Board, London.
Garcia, J. and Garforth, S. (1991) Midwifery policies and policy-making. In Robinson, S. and Thomson, A.M. (eds), Midwives , Research and Childbirth , Vol. 2 Chapman, and Hall, London.
Green, J., Kitzinger, J. and Coupland, V. (1986) The Division of Labour: Implications of Medical Staffing Structures for Doctors and Midwives on the Labour Ward . Child Care and Development Group, University of Cambridge.
Golden, J. (1980) Midwifery training: the views of newly qualified midwives. Midwives Chronicle and Nursing Notes , 93 (1109), 190–94.
PubMed CAS Google Scholar
Hall, J. (1994) Midwifery education: where is it going. MIDIRS Midwifery Digest , 4 (4), 384–6.
Hicks, C. (1993) A survey of midwives’ attitudes to, and involvement in, research: the first stage in identifying needs for staff development programmes Midwifery , 9 (2), 51–62.
Article PubMed CAS Google Scholar
Hicks, C. (1994) Bridging the gap between research and practice: an assessment of the value of a study day in development of critical research reading skills in midwives. Midwifery , 10 (1). 18 -25.
House of Commons Health Committee (1992) Second Report , Session 1991–92. Maternity Services (Winterton Report) . HMSO, London.
Kent, J., MacKeith, N. and Maggs, C. (1994a) Direct but Different: Volume 1 - The Discussion . Maggs Research Associates, Bath.
Kent, J., MacKeith, N. and Maggs, C. (1994b) Direct but Different: Volume 2 - The Evidence . Maggs Research Associates, Bath.
Kilty, J.M. and Potter, F.W. (1975) The midwife teacher’s diploma project. University of Surrey, Guildford.
Leong, W. (1989) The introduction of computer-assisted learning in a school of midwifery using the Wessex Care Plan Program. Nurse Education Today , 9 , 114–123.
Maggs, C. (1994) Mentorship in nursing and midwifery education: issues for research. Nurse Education Today , 14 (1), 22–29.
Mander, R. (1984) Stop and consider: student midwife wastage in training. In Thomson, A. and Robinson, S. (eds), Research and the Midwife Conference Proceedings for 1983 . Department of Nursing, University of Manchester.
Mander, R. (1986) Refresher course: unfulfilled potential. Midwives Chronicle , 99 (1176), 4–5.
Mander, R. (1989a) Who continues? A preliminary examination of data on continuation of employment in midwifery. Midwifery , 5 (1), 26–35.
Mander, R. (1989b) The best laid schemes: An evaluation of the extension of midwifery training in Scotland. International Journal of Nursing Studies , 26 (1), 27–41.
Mander, R. (1993) Midwifery training and employment decisions. In Robinson, S. and Thomson, A.M. (eds), Midwives , Research and Childbirth , Vol. 3, Chapman, and Hall, London.
McCrea, H. (1989) Motivation for continuing education in midwifery. Midwifery , 5 (3), 134–5.
McCrea, H.,Thompson, K., Carswell, L. and Whittington, D. (1994) Student midwives’ learning experiences on the wards. Journal of Clinical Nursing , 3 , 97–102.
Maclean, G. (1980) A Study of the Educational Needs of Midwives in Wales and How They Might be Met . West Glamorgan Health Authority.
Midgley, C. (1993) Continuing education for non-practising midwives. In Robinson, S., Thomson, A. and Tickner, V. (eds), Research and the Midwife Conference Proceedings for 1992 . Department of Nursing, University of Manchester.
Mitchell, M. (1994) The views of students and teachers on the use of portfolios as a learning and assessment tool in midwifery education. Nursing Education Today , 14 (1), 38–43.
Article CAS Google Scholar
Mountford, B. in collaboration with Fraser, D.M., Murphy R.J.L. and Worth-Butler, M. (1995) An Interpretative Comment on 23 Pre-registration Midwifery Education Curricula Documents . EME project, English National Board, London.
Murphy-Black, T. (1991) Antenatal Education: Evaluation of a Post-basic Training Course . In Robinson, S. and Thomson, A.M. (eds), Midwives , Research and Childbirth , Vol. 2. Chapman, and Hall, London.
Opoku, D. and Davis, K. (1988) Exploring other perspectives in the midwifery curriculum. In Robinson, S. and Thomson, A.M. (eds), Research and the Midwife Conference Proceedings for 1987 . Department of Nursing, University of Manchester.
Parnaby, C. (1987) Surveying the opinions of midwives regarding the curriculum content of refresher courses. Midwifery , 3 (3), 133–42.
Phillips,. R. (1993) Choice or chance? An exploratory study describing the criteria and processes used to select midwifery students. In Robinson, S., Thomson, A.,and Tickner, V. (eds), Research and the Midwife Conference Proceedings for 1992 . Department of Nursing, University of Manchester.
Pollock, M. (1992) Establishment of a Midwifery Education Research and Development Unit . Department of Education Studies, University of Surrey.
Pope, V. (1986) Midwifery training in Scotland: An opinion survey. Midwives Chronicle , 99 (1184), 198–200.
Radford, N. and Thompson, A. (1988) Direct Entry: A Preparation for Midwifery Practice . ENB, London.
Radford, N. and Thompson, A. (1994) A study of issues concerning the implementation of direct entry midwifery education. In Robinson, S. and Thomson, A.M. (eds), Midwives , Research and Childbirth , Vol. 3. Chapman, and Hall, London.
Raymond, R. and Ananda-Rajan, K. (1993) Learning practice. Nursing Times , 89 (31), 36.-7.
Robinson, S. (1980) Are there enough midwives? Nursing Times , 76 (17), 726–30.
Robinson, S. (1986a) Midwifery training: the views of newly qualified midwives. Nurse Education Today , 6 (2), 49–59.
Robinson, S. (1986b) Career intentions of newly qualified midwives Midwifery 2 (1), 25–36.
Robinson, S. (1989) Caring for childbearing women: the inter-relationship between midwifery and medical responsibilities. In Robinson, S. and Thomson, A.M. (eds), Midwives, Research and Childbirth , Vol. 1. Chapman, and Hall, London.
Chapter Google Scholar
Robinson, S. (1991) Preparation for practice: the educational experiences and career intentions of newly qualified midwives. In Robinson, S. and Thomson, A.M. (eds)
Midwives, Research and Childbirth,Vol. 2. Chapman , and Hall, London.
Robinson, S. (1994) Professional development in midwifery: findings from a longitudinal study of midwives’ careers. Nurse Education Today , 14 , 161–76.
Robinson, S., Golden, J. and Bradley, S. (1983) A study of the Role and Responsibilities of the Midwife . NERU Report No 1, Nursing Education Research Unit, King’s College, London.
Robinson, S. and Owen, H. (1994) Retention in midwifery: findings from a longitudinal study of midwives’ careers. In Robinson, S. and Thomson, A.M. (eds), Midwives , Research and Childbirth , Vol. 3. Chapman, and Hall, London.
Robinson, S., Owen, H. and Jacka, K. (1992) The Midwives’ Career Patterns Project . Report to Department of Health, Nursing Research Unit, London University.
Robinson, S., Thomson, A.M. and Tickner, V. (1989) Midwives’ views on directions and developments in midwifery research. In Robinson S. and Thomson, A.M. (eds), Research and the Midwife Conference Proceedings for 1988 . Nursing Research Unit, London University.
Roch, S. (1993) Excellence in midwifery education. Modern Midwife , March—April, 36–8.
Royal College of Midwives (1987) The Role and Education of the Future Midwife in the United Kingdom . Royal College of Midwives, London.
Sims, C., McHaffie, H., Renfrew, M. and Ashurst, H. (1994) The Midwifery Research Database MIRIAD . Books for midwives Press, Hale.
Sleep, J. and Clark, E. (1993) Major new survey to identify and prioritize research issues for midwifery practice. Midwives Chronicle 106 (1265) 217–218.
Standon-Batt, M. (1979) Where are the tutors? Midwives Chronicle and Nursing Notes , 92 (1,100), 304.
Stewart, A. (1981) The present state of midwifery training. Midwife , Health Visitor and Community Nurse , 17 (7), 270–72.
CAS Google Scholar
Sugarman, E. (1988) The case of the disappearing midwives. Nursing Times , 84 (8), 35–6.
Sweet, B. (1994) A critical review of research related to midwifery education. In Thomson, A., Robinson, S. and Tickner, V. (eds), Research and the Midwife Conference Proceedings for 1993 . Department of Nursing, University of Manchester.
Walker, J. (1976) Midwife or obstetric nurse? Some perceptions of midwives and obstetricians of the role of the midwife. Journal of Advanced Nursing , 1 (2), 129–38.
Walker, P. (1990) How midwives prepare to teach. Nursing , 4 (14), 22–4.
Warwick, C. (1992) Reflections on the current management of midwifery education. MIDIRS Midwifery Digest , 2 (3), 251–4.
West, S., Thomson, A.M. (1995) Midwifery Competencies Why 40 deliveries. In Robinson, S., Thomson, A.M., Silverton, L. (eds) Research and the Midwife Conference Proceedings for 1994. Department of Nursing Studies, University of Manchester.
While, A. (1994) Competence versus performance: which is more important? Journal of Advanced Nursing , 20 , 525–31.
Worth-Butler, M., Murphy, R.J.L. and Fraser, D.M. (1994) Towards an integrated model of competence in midwifery. Midwifery , 10 (4), 225–31.
Worth-Butler, M., Murphy, R.J.L., Fraser, D.M. (1995) The need to define competence in midwifery. British Journal of Midwifery 3 (5): 259–62.
UKCC (1994) Midwifery programmes of education: changes in terminology. Registrar’s letter. UKCC, London.
Download references
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Nursing Research Unit, King’s College, London, UK
Sarah Robinson ( Senior Research Fellow ) ( Senior Research Fellow )
School of Nursing Studies, Health Care Research Unit, Manchester College of Midwifery and Nursing, University of Manchester, UK
Ann M. Thomson ( Senior Lecturer in Midwifery, Director ) ( Senior Lecturer in Midwifery, Director )
Rights and permissions
Reprints and permissions
Copyright information
© 1995 Springer Science+Business Media Dordrecht
About this chapter
Robinson, S. (1995). Progress and problems in midwifery education: some conclusions from published research. In: Robinson, S., Thomson, A.M. (eds) Midwives, Research and Childbirth. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-6956-9_7
Download citation
DOI : https://doi.org/10.1007/978-1-4899-6956-9_7
Publisher Name : Springer, Boston, MA
Print ISBN : 978-0-412-45840-8
Online ISBN : 978-1-4899-6956-9
eBook Packages : Springer Book Archive
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Midwifery.. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2016; 20 https://doi.org/10.1016/S1751-4851(16)30144-1
Coates D, Foureur M. The Role and Competence of Midwives in Supporting Women with Mental Health Concerns during the Perinatal Period: A Scoping Review.. Health and Social Care in the Community. 2019; 27:(4) https://doi.org/10.1111/hsc.12740
Midwifery Myth: Health Insurance Does Not Cover Midwife Care.. 2018. http://www.uihc.org/health-topics/midwifery-myth-health-insurance-does-not-cover-midwife-care (accessed 20 November 2020)
Homer CSE, Davies-Tuck M, Dahlen HG, Scarf VL. The Impact of Planning for COVID-19 on Private Practising Midwives in Australia.. Women and Birth. 2020; https://doi.org/10.1016/j.wombi.2020.09.013
Howard LM, Khalifeh H. Perinatal Mental Health: a Review of Progress and Challenges.. World Psychiatry. 2020; 19 https://doi.org/10.1002/wps.20769
Phillippi JC, King TL. Defining and Redefining Midwifery Practice.. Journal of Midwifery and Women′s Health. 2019; https://doi.org/10.1111/jmwh.12995
Seng JS, D′Andrea W, Ford JD. Complex mental health sequelae of psychological trauma among women in prenatal care.. Psychological Trauma: Theory, Research, Practice and Policy. 2014; 6:(1)41-49 https://doi.org/10.1037/a0031467
Wu Y, Zhang C, Liu H Perinatal depressive and anxiety symptoms of pregnant women during the coronavirus disease 2019 outbreak in China.. Am J Obstet Gynecol. 2020; 223:(2)e1-240 https://doi.org/10.1016/j.ajog.2020.05.009
Challenges currently faced in midwifery careers
Sydney Kerolo
Freelance writer
View articles

For generations, the practice of midwifery has shown the world a way of personalised pregnancy and childbirth that is dedicated to the mother and her child. Midwives are dedicated to their practice, giving full attention to their duties, which include becoming a caretaker, providing primary care, and allowing their patients to receive individualised care for new mothers ( Association of Women′s Health, Obstetric and Neonatal Nurses, 2016 ). A midwife develops a bond with their patients, they go through challenging life changes with them: pregnancy, labor and life after birth. But, as with many practices in life, there have been challenges and complications that come with it.
Many families go through a period where their mental health is tested during pregnancy. They may experience postpartum depression ( Seng et al, 2014 ) or, even more recently, an increase in perinatal depression and anxiety ( Wu et al, 2020 ). In these situations, the family requires extra help, not only to ensure that their child will be safe, but to help the mother establish a healthy mental state throughout the entire experience. According to Coates and Foureur (2019) , ‘Perinatal mental health problems impact on women themselves, their families and communities, and also affect the mental, physical, emotional and psychosocial development of infants’. With this information, Coates and Foureur have advanced their research to show how necessary it is for midwives to consider the mental health of their patients, both throughout the pregnancy and afterwards. If a mother's mental state is unhealthy throughout the pregnancy, there can be life long effects for both parties.
‘Furthermore, mental health problems during the antenatal period are associated with obstetric complications, such as preterm birth, low neonatal birth weight, gestational hypertension, and perinatal infant and mother mortality.’
( Coates and Foureur, 2019 )
To combat this challenge, midwives should develop a strong understanding of depression, anxiety and any other mental health disorder that can occur during a pregnancy. The presence of mental health disorders in pregnant women is not an entirely new scenario, but it has become more recognised and easier to deal with in recent years ( Howard and Khalifeh, 2020 ).
For years, midwives have provided care for families during pregnancy, through a natural and holistic process that focuses on individualised care for mother and baby ( Association of Women′s Health, Obstetric and Neonatal Nurses, 2016 ).
‘Over time, our clinical practice has expanded from a specific focus on pregnancy and birth to include skills in the realms of family planning, gynecologic care, and primary care.’
( Phillippi and King, 2019 )
A midwife's job is complex, as they are needed to provide care in a number of settings. They are needed within the home, the birthing centre, the clinic, the office and in hospital. Their practices go hand in hand with an obstetric nurse, but with an individualised approach that makes the family feel comfortable ( Association of Women′s Health, Obstetric and Neonatal Nurses, 2016 ). But, unlike an obstetric nurse, a midwife undertakes their own education, certification, licensing and more on their own, rather than within a nursing programme.
Medical insurance is used all around the globe, and every provider offers different regulations. In Australia, there are midwives who practice privately and need to be certified by a specific board to practice. According to Homer et al (2020) , 0.3% of Australian babies are born in the home and a majority of these home births are done by privately practicing midwives, who are all self-employed. Laura Dellos (2018) stated that while it may be rare for an insurance provider not to cover midwifery services, there are instances where this occurs.
Along with issues regarding insurance, there has recently been an uptick in the need for midwives because of the current global coronavirus pandemic. According to Homer et al (2020) , more people are turning to a home birth because it decreases the chance of becoming exposed to the virus, since there are fewer people around. But this requires more midwives and a method that ensures that all midwives are following proper procedures and protocols when they are in their patients' homes.
‘Maternity services in all countries have been impacted by the COVID-19 response, including the implementation of Telehealth, social distancing, use of personal protective equipment for clinical care and reduced visitors and support people.’
( Homer et al, 2020 )
While hospitals were able to acquire personal protective equipment, a lot of midwives who were working privately had to provide for themselves and were affected by common shortages of items including masks, gowns and gloves ( Homer et al, 2020 ). Many midwives also stated that they changed the way they communicated with their patients by limiting consultations to 15 minutes or less, spacing out their appointments, conducting telephone consultations and ensuring that they changed their clothes after every meeting and sanitized all equipment after each use ( Homer et al, 2020 ).
With new regulations, treatments and needs, a midwife′s career path has gained complications, but the role of a midwife has become more important now than ever. These challenges can be addressed with more training for every midwife, so they can learn how to properly handle the mental wellbeing of their patients during their pregnancy and afterwards. This is especially important now, while we are in the midst of a global pandemic. A midwife is counted on for more than just the safe delivery of a baby, they are needed to encourage mental wellbeing, to provide proper safety protocols, and to ensure that no matter what the situation, both mother and child are happy and healthy in the end.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Clinical placements as a challenging opportunity in midwifery education: A qualitative study
Maryam modarres, mehrnaz geranmayeh, mitra amini, monireh toosi.
- Author information
- Article notes
- Copyright and License information
Correspondence , Monireh Toosi, Department of Midwifery, Fatemeh (P.B.U.H) School of Nursing and Midwifery, Nemazee Square, Zand St., Shiraz, Iran. Email: [email protected]
Corresponding author.
Revised 2021 Sep 8; Received 2021 Jan 20; Accepted 2021 Nov 16; Collection date 2022 Mar.
This is an open access article under the terms of the http://creativecommons.org/licenses/by/4.0/ License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited.
The aim of this qualitative study was to explore some of the existing statuses of clinical education and examine the strengths and weaknesses of the clinical faculty programme.
A qualitative study.
This qualitative study was designed through the directed content analysis approach, which was completed according to the Context, Input, Process, and Product evaluation model. The purposeful sampling method of maximum variation was employed to select 33 participants, and the data were collected through in‐depth individual interviews and focus group discussion.
After the interview transcripts were analysed, the participants' opinions of the clinical faculty programme and the relevant challenges, dimensions and factors were classified into four categories and sixteen subcategories. The categories were compiled in the CIPP evaluation model, including context, input, process and product. Based on the content analysis results, appropriate planning was recommended for teaching effective clinical skills to students.
Keywords: clinical education, midwifery students, qualitative study
1. INTRODUCTION
Midwifery education is a part of the higher education system that deals with human life, and attention to its quantitative and qualitative aspects is of special importance (Fasihi et al., 2004 ).
Midwifery training is done in different ways in different countries. In Iran, midwifery students are admitted to a four‐year university course via a national examination. The Ministry of Health and Medical Education has designed the midwifery training programme in a single curriculum for all universities across the country.
A statistically significant part of the midwifery course is devoted to acquiring clinical skills, during which students develop skills in groups of four to eight in clinical settings. To complete the midwifery course, students must participate in at least 60 natural deliveries, and in order to graduate, they must successfully pass a comprehensive midwifery examination.
The clinical training course is an opportunity to learn, acquire and develop clinical skills, during which students acquire the necessary practical skills for professional midwifery activities (Thompson et al., 2011 ). Clinical education provides an opportunity for students to translate theoretical knowledge into the necessary mental, psychological and motor skills for patient care (Omidvar et al., 2005 ). Graduates of this field must have acquired the minimum professional skills required for midwifery tasks (Wiegers et al., 2010 ).
Clinical education is considered one of the most important educational strategies in order to prepare students to enter clinical settings, take responsibilities, develop skills and improve the ability to decide on health issues (Birks et al., 2017 ).
In this regard, midwifery schools are responsible for graduating students who can provide midwifery services in accordance with the latest scientific advances (Cheraghi et al., 2019 ). On the other hand, pre‐planned improvement of clinical skills and knowledge of midwifery graduates can significantly enhance the quality of services provided at all levels of the health system. In addition to guiding students in practical and clinical fields, acquisition of clinical skills improves their knowledge and substantially enhances the quality of clinical education (Donough & Van Der Heever, 2018 ; Ekstedt et al., 2019 ; Graham et al., 2016 ).
However, the results of many studies in Iran have shown a relatively deep gap in midwifery students' theoretical and clinical education. Accordingly, existing clinical education does not convey to students the ability to achieve appropriate clinical competency (Sharghi et al., 2015 ). Evidence has also indicated that students' professional skills have decreased compared with the previous decade (Delaram et al., 2013 ; Mousavi & Montazeri, 2013 ). Accordingly, despite having theoretical knowledge, new graduates do not have sufficient skills and efficiency in clinical settings (Saleh et al., 2014 ). In other words, clinical education has not successfully achieved its goals of training skilled people and improving the quality‐of‐care services (Seyedamini et al., 2018 ).
In this context, various studies have demonstrated that multiple problems in clinical settings have prevented the achievement of educational goals (Valiee et al., 2013 ). Therefore, it seems that midwifery education needs fundamental changes in clinical education (Haghani & Hojat, 2013 ). In 2004, the standard programme for the midwifery profession stated that the training provided in the midwifery curriculum should ensure that midwifery students are prepared to practice the trade under the standards.
According to these standards, midwifery students must be able to provide clinical services on patients' bedsides. The educational goals were seen in the curriculum, and the theoretical and practical training must ensure these capabilities. In addition, midwifery students must have the necessary self‐efficacy to perform the assigned tasks (Bellack et al., 1998 ). Hence, the necessary skills have been developed in different countries to train midwifery students. The International Confederation of Midwives published the Minimum Standards for Clinical Midwifery Education in 2006 and 2008 (Butler et al., 2008 ). In the United Kingdom, the Nursing and Midwifery Organization has published professional standards for midwifery based on what midwives can do in their clinical careers (Leap et al., 2002 ).
Standard institutions in the United States have also extracted a list of essential clinical skills for midwives, including all the skills available in the midwifery curriculum, in particular pregnancy, obstetrics and gynaecology (Bellack et al., 1998 ).
Iran has also taken steps to coordinate and improve the quality of clinical education, including launching a clinical midwifery faculty programme. In this regard, since 2014, the plan to revive clinical education and establish faculty members in the midwifery department in hospitals and clinical settings was announced by the Ministry of Health and Medical Education to universities across the country.
The purpose of the midwifery clinical faculty programme is to return the midwife to her original position in performing natural delivery and to determine the position of midwifery professors and students in teaching hospitals. In this programme, midwifery faculty members who have the knowledge and skills of midwifery attend educational and medical centres and give scientific and high‐quality care for pregnant mothers (24‐hr stay in midwifery clinics in morning, evening and night shifts) and give clinical education for students in order to empower them in the fields of care, education and research.
The clinical midwifery faculty programme, as a new educational programme, needs continuous control and quality improvement. Evaluation and even revision of educational programmes fall into the field of educational evaluation. Since any educational programme is formed and developed through evaluation, a pivotal role must be given to the educational evaluation process.
Therefore, a constructive and effective evaluation model is expected to help decision‐makers and planners to make the right decisions throughout the development stages of an educational programme, including ideation, planning, design and execution (Fitzpatrick, 2011 ). The CIPP model is one of the models that can systematically evaluate an educational system. This model can be used to design and develop educational programmes and systems of management and accountability. Developed by Daniel Stufflebeam and colleagues in the 1960s, the CIPP evaluation model requires the evaluation of context, input, process and product in judging a programme's value (Stufflebeam & Zhang, 2017 ).
Emphasizing the constructive evaluation of the development stages of a programme (ideation, planning, design and execution), the CIPP evaluation model helps decision‐makers and planners to make the right decisions (Fitzpatrick, 2011 ). Considering the significance of promoting midwifery clinical education to achieve international standards, there is a need for studies to thoroughly evaluate the quality of midwifery clinical faculty programmes.
Since the clinical midwifery faculty programme has recently been performed in some Iranian universities of medical sciences, it seems that the authorities need to systematically eliminate the challenges of this clinical programme in qualitative studies in order to design optimal educational programmes to improve the quality of midwifery services provided for pregnant mothers. Hence, the researchers have decided to conduct this qualitative study on the clinical midwifery faculty programme based on the CIPP evaluation model to identify the challenges and propose solutions for promoting this programme and, ultimately, public health.
Since there has been no study on Iranian universities' clinical midwifery faculty programme, this study aimed to explore the themes related to the perception of the clinical midwifery faculty programme to provide helpful Information to policymakers that promote clinical education experiences.
2.1. Aim and design
This is a qualitative study with a content analysis methods study, which aimed to explore some of the existing problems of clinical education and examine the strengths and weaknesses of the clinical faculty programme. The purposeful sampling method of maximum variation was employed to select 33 participants, and the data were collected through in‐depth individual interviews and focus group discussion.
To achieve the maximum variation, participants included all those who were somehow involved in the clinical faculty programme, age and different education were selected.
The study was conducted in the School of Nursing and Midwifery, Shiraz University of Medical Sciences, from August 2019–February 2020. This university ( https://www.sums.ac.ir/en/home ) enrols about 120 midwifery students and graduates about 30 midwifery students annually. Directed content analysis was used in this qualitative research to obtain rich and deep Information from the phenomenon under investigation (Speziale et al., 2011 ). Since qualitative research emphasizes trust, transparency, verifiability and flexibility, it is considered an excellent method to develop insight and interpretation in midwifery education (Polit & Beck, 2009 ).
2.2. Study participants
The present qualitative study with a content analysis approach was conducted using individual interviews and focus group discussion. Participants in the individual interviews included all those who were somehow involved in the clinical faculty programme at Shiraz University of Medical Sciences and included 11 midwifery instructors, eight midwifery staff, six obstetrics–gynaecology residents, five midwifery graduate students and three midwifery board officials who were selected based on purposeful sampling and were required to sign an informed consent form to enter the study. The inclusion criteria included participants who were somehow involved in the clinical faculty programme. The exclusion criteria included participants who did not participate in the midwifery clinical faculty programme or were not willing to participate in the study.
2.3. Data collection procedure
In order to determine the challenges of midwifery clinical education in dealing with the clinical setting, individual interviews and focus group discussions were used. Individual interviews with the participants were carried out in a face‐to‐face manner and in a convenient place at the School of Nursing and Midwifery, Shiraz University of Medical Sciences. Focus group discussions with midwifery students were also performed to achieve a deeper understanding of this phenomenon (Traynor, 2015 ). The participants were invited to take part in the research by telephone or email. The individual and group interviews were begun by asking the participants a general and open question about the description of their encounter with the clinical setting. Then, some other questions were asked based on the participants' statements and responses (Speziale et al., 2011 ).
The semi‐structured interviews and open‐ended guide questions were developed by the researchers based on the literature review and experts' opinions and included: “how do you feel about the clinical faculty programme in general,” “would you like to talk about those clinical experiences which you found most anxiety‐producing,” “what are the best and worst things that you think can happen during the clinical experience,” “how do you think clinical experiences can be improved,” “what is your expectation from clinical experiences” and “what are the benefits and disadvantages of clinical experiences in your opinion.” For clarification of the explanations, further probing questions were then asked (“could you give me an example” or “would you explain more”). The first two questions were general questions, which were used as icebreakers to stimulate discussion and put the participants at ease to encourage them to interact normally with the interviewer. The author conducted the interviews in Persian and then was translated them into English after all the analysis was finished.
After obtaining permission from the Ethics Committee of Tehran University of Medical Sciences, all interviews were conducted at the School of Nursing and Midwifery, Shiraz University of Medical Sciences. The participants were interviewed by the face‐to‐face method in the Persian language, and each interview was carried out in one session. In the focus group discussion, the students were encouraged to talk to one another, ask questions, exchange anecdotes and comment on each other's experiences and perspectives. Each interview lasted for 40–60 min. The focus group discussion also lasted for 85 min. Each of the interviews was digitally recorded and immediately transcribed after the end of the interview sessions. The interviews were continued with the participants until the data were saturated. In qualitative studies, data saturation indicates the completion of interviews, which means no new data are generated (Traynor, 2015 ).
2.4. Ethical considerations
The Ethics Committee approved the present study of Tehran University of Medical Sciences (IR.TUMS.FNM.REC.1398.057). After introducing herself to the participants, the researcher explained the study objectives to them and assured them about their information confidentiality and their authority to reject the invitation or remain in the study. She also requested the participants to sign written informed consent forms.
2.5. Data analysis
Data management was performed using MAXQDA 10 software. After each interview, the data were analysed through a directed content analysis approach proposed by Zhang and Wildemuth (Wildemuth, 2016 ). Directed content analysis was used in this research in order to identify and understand the midwifery students' challenges in dealing with the clinical setting. The qualitative data will be analysed using the content analysis method proposed by Zhang and Wildemuth ( 2016 ) in eight steps as follows. In the first step, the data will be prepared for qualitative content analysis. The recorded interviews will be transcribed, and the non‐verbal messages of the participants, such as tone of speech, silence and cry noted during the interview, will be added to the transcripts because the hidden concepts and patterns should be extracted from data.
The second step pertains to the analysis unit. The analysis or semantic unit is actually the most basic part of the text that is categorized and coded during content analysis. Therefore, the identification of these units is one of the most important and basic decisions of content analysis. In qualitative content analysis, personal themes including words, sentences and paragraphs are usually used. Therefore, one should seek the text for the phrases or expressions from which the themes are extracted.
The third step is to inductively categorize and code the themes through continuous comparison of the categories extracted from data. Similar codes will be grouped under a single subcategory, and then, the subcategories form the categories according to their relationship. The categories will be then organized in a way to achieve internal consistency and external inconsistency.
In the fourth step, the coding will be tested on a sample text. To this end, the researcher codes an excerpt, and then, two members of the research team will control the coding consistency. In the fifth step, after the agreement between the researcher and the two members of the research team on the coding consistency, a replicable process of coding will be generalized to the whole text.
The sixth step is to achieve coding consistency. To this end, the initial codes and their allocation to categories will be controlled once again by two other members of the research team and experts in qualitative research. This aims to eliminate any human error caused by fatigue or misunderstanding and changes in participants' perception of categories and coding rules over time that may lead to inconsistency because new themes and concepts may be extracted from the text.
The seventh step is to conclude the categorized and coded data. The features and dimensions of the categories will be detected, the connections between categories will be determined, the hidden patterns will be revealed, and the categories will be examined on a wide range of data so that the categories, subcategories and transcripts will be compared and the inputs and outputs will be extracted and investigated to show whether the main categories and themes represent the data. Finally, in the eighth stage, the formed categories will be reported (Wildemuth, 2016 ). Rethinking about the codes and the subclasses resulted in the extraction of four categories and sixteen subcategories. It should be emphasized that before the data were submitted to content analysis, the interview transcripts were sent to the participants to approve. All participants were satisfied with the interview transcripts and confirmed the results.
2.6. Trustworthiness of data
Credibility, dependability, conformability, transferability and authenticity were considered for the trustworthiness of the results (Polit & Beck, 2009 ). The credibility of the research results was strengthened by spending sufficient time on data collection, diversity of participants and member checking in which the transcripts and codes were returned to the participants for the clarification of any ambiguous codes. Dependability and conformability were enhanced through external checking and peer debriefing.
Therefore, the research team, including two expert qualitative researchers and two external supervisors, reviewed and rechecked the transcripts, codes and categories to find any conflicts in the coding process. Moreover, purposeful sampling was employed with maximum variation for transferability. Furthermore, authenticity was confirmed through member checking, and the participants compared the research team's results to their views. The interviews were conducted in Persian and were then translated into English for publication. Two different individuals translated the interviews into English, and a third person confirmed the translated versions.
The study participants included 11 midwifery instructors, eight hospital midwifery staff, six residents, five midwifery graduate students and three midwifery board officials. Almost 70 midwifery students also participated in seven focus group sessions. Due to the lack of time, one person refused to participate in the study (Table 1 ).
Demographic characteristics of the study participants
After analysing the interviews with the participants about the challenges of midwifery students in dealing with clinical education, 1250 codes were extracted from the interview texts and were classified into the following four categories and sixteen subcategories. The categories were compiled in the form of the CIPP evaluation model and included context, input, process and product (Table 2 ).
The categories and subcategories extracted from the data
3.1. Context
The context of the educational programme is to determine the effective elements in an educational environment and to identify the problems, needs and opportunities in an educational context. In the field of the educational programme, factors such as needs, facilities and problems in an educational environment are examined (Stufflebeam & Zhang, 2017 ). From the participant's perspective, the context included the necessity to implement the programme and failure to achieve goals and implement regulations.
3.1.1. Necessity to implement the programme
According to the participants, the implementation of the clinical faculty programme was necessary in order to solve the existing problems in the clinical environment and integrate clinical skills. Regarding the necessity to implement the faculty programme, one of the participants said: “The presence of the professor can provide students with proper training. This means that the professor gives scientific training to students. During this program and with the presence of the professor, the students are more orderly and learn more scientifically. They learn more, and the implementation of this program has been essential for the scientific education of students” (45‐year‐old midwife, maternity hospital staff, individual interview).
3.1.2. Failure to achieve goals and implement regulations
The success rate of any training programme is measured by the extent to which the programme achieves its goals. There are obstacles and problems in the faculty programme that have hindered the achievement of the educational goals of the programme. The study participants reported failures in achieving the goals and implementation of the regulations, such as poor information about the objectives of the training programme and incomplete implementation of the regulations. In this regard, one of the students stated: “Before entering the program, we were not taught anything about the goals. We read a series of theoretical articles and then went to the ward, but we do not know the goals of the program. We have not specified the educational goals of the program, and we do not know them exactly” (23‐year‐old midwifery student, 7th semester of midwifery, focus group discussion).
The input of the clinical programmes includes all the factors that enter the training programme and pave the way for the implementation of the programme and achieving the goals of the programme. Input means all individuals and human resources, including students, professors, administrators, financial resources and scientific resources, that are included in an educational programme (Stufflebeam & Zhang, 2017 ). The five subcategories of the input of the clinical faculty programme from the perspective of the participants included inadequacy in educational content, heterogeneity of students in clinical skills, lack of facilities and equipment, professional competence of professors and inappropriate educational environment.
3.2.1. Inadequacy in the educational content
In any educational programme, one of the most important educational indicators is the existence of desirable and effective educational content for teaching specific scientific or practical content. The results of the study showed that there was no desirable educational content in the clinical faculty curriculum. In this respect, one of the participants maintained: “We did not have written content, and the training of the instructors were not the same. For example, each instructor said something and taught the procedure in a different way; some instructors taught the procedures differently, and this would cause problems and confusion for us. The instructors themselves were challenged by this difference” (25‐year‐old student, 8th semester of midwifery, focus group discussion).
3.2.2. Heterogeneity of students in clinical skills
Some participants believed that the students were not the same in performing clinical skills. In this regard, one of the participants stated: “Students' initial abilities vary when they enter the program; some students have better abilities, and some have lower abilities. We also have a student who is poor at performing clinical procedures. We should not evaluate all students together. In the end, all of them will reach an appropriate level of competence and acquire the necessary clinical skills during the training program” (Midwifery instructor, 36 years old, individual interview).
3.2.3. Lack of facilities and equipment
One of the requirements of optimal education is the adequacy of educational and welfare facilities. An environment that is equipped with advanced educational facilities and desirable welfare ultimately leads to effective education and increases the students' interest. The results of the present study showed that the educational facilities of the programme were not at the desired level and that the lack of appropriate educational and welfare facilities had caused a decrease in the quality of the clinical education from the perspective of both students and educators. In this regard, one participant stated: “Well, we do not have a room for conferences. It means that the conference room space is not really suitable. Furthermore, we have a room where professors have to rest, for example, where there is a monitor and a small library. Educational equipment has affected and distorted education. The facilities are not enough to teach, and we do not even have a model for teaching students. We do not even have a video projector or something in the room that the students could work with” (Midwifery instructor, 39 years old, individual interview).
3.2.4. Professional competence of instructors
Clinical instructors are one of the most important components of any clinical education and can have a profound impact on students' learning. Clinical instructors must have specific skills in communication and functional skills, clearly know how to apply these skills and be able to transfer them to students. In the current study, one of the strengths of the programme from the participants' viewpoints was the professional ability of the programme's instructors. In this regard, one of the participants said: “The professors had the required clinical skills and could transfer the skills to us. They also had the appropriate clinical ability and skills. They also had the necessary knowledge to provide scientific and practical materials related to midwifery. Their training was very useful to me” (26‐year‐old student, 8th semester of midwifery, focus group discussion).
3.2.5. Inappropriate educational environment
One of the influential factors in any educational programme is the appropriate educational environment and background of that programme, which can have a statistically significant impact on the students' desires and interests. Regarding the inappropriate educational environment and context in the faculty programme, one of the participants mentioned: "From the beginning, we were supposed to have an independent ward with independent staff to teach students according to the midwifery rules, but until the ward is not separated and the medical environment is prevailing, the situation continues, and we do not have an independent environment for midwifery students. Working in the medical environment is very difficult, and midwifery students cannot be independent. It is not a suitable environment for education" (Midwifery instructor, 53 years old, individual interview).
3.3. Process
In the process dimension, implementation of educational programmes and determination of the impact of the educational programme on learners are discussed. In this area, the teaching‐learning activities and the management‐supervisory process are examined. Process refers to all the activities that take place during the implementation of educational programmes (Stufflebeam & Zhang, 2017 ). Based on the present study results, the process of the clinical midwifery faculty programme consisted of active and interactive teaching classes, teaching midwifery professional requirements, prominent presence of the teacher in education, showing professional identity to students, restrictions on performing legal duties, poor interactions of medical staff and failure in the management‐regulatory process.
3.3.1. Active and interactive teaching
Active and interactive teaching is one of the essential skills in education, which is mainly related to teachers' educational skills. Students described active and interactive teaching as one of the pillars of an effective learning environment compared to teacher‐centred training. In this regard, one of the participants stated: “Clinical training methods actually depend on the instructor, but the program has the flexibility that each instructor can use different training methods according to the needs s/he sees. We have a computer system and an Internet search engine that can easily teach theory. We also have a good time with students to teach. In fact, there is the potential in the program that we meet the educational needs of the students according to their wishes and desires. According to the students' own opinions, we put the items that need more explanation in the educational planning and teach them in that field” (Midwifery instructor, 35 years old, individual interview).
3.3.2. Training of professional midwifery requirements
Professional requirement training is an essential principle of midwifery care. Teaching ethics, midwifery rules and regulations, emergency care training and teamwork training are some of the highlights of the clinical faculty programme mentioned by the participants. In this regard, one participant said: “Yes, we were taught to respect the rights of the patients; i.e., maintaining patients' privacy, asking for permission from the patients, our behaviors towards non‐Iranian patients like Afghans, and following the ethical fundamentals regardless of the patients' nationalities or beliefs” (23‐year‐old student, 7th semester of midwifery, focus group discussion).
With regard to teaching midwifery rules and regulations in the programme, one of the participants mentioned: “I learned this training from the teacher, and I try to work legally. For example, I know that if I give medicine and I do not register it, there are consequences. They taught me the accurate process of registration. This program had a good thing, and the professors taught us the rules and regulations of midwifery in practice, we learned in practice that we had to follow the rules of midwifery” (24‐year‐old student, 8th semester of midwifery, focus group discussion).
3.3.3. Prominent presence of the instructor
The instructor plays an educational role and a supportive role. This relationship leads to the formation of professional identity in students. The study participants noted the impact of the teacher's prominent role in clinical education. In this regard, one participant stated: “Instructors in this program focus in a very specific way on a student to teach her a specific skill, and this focus of the teacher on a student definitely affects her learning. Because the teaching involves an individual‐to‐individual process, I felt I had to learn this because I thought she was just teaching me, and I had to learn this. The subject was very important to me” (25‐year‐old student, 7th semester of midwifery, focus group discussion).
3.3.4. Induction of professional identity to students
Professional identity includes the values and beliefs that guide individuals' thinking, actions and interactions with other people and plays a key role in the socialization of individuals. With the help of professional identity, a person establishes one's existence in one's profession and reaches excellence in the profession. Professional identity is formed by one's experiences in clinical settings. Regarding the induction of professional identity to students in the programme, one of the participants said: “Using new methods such as having a leader in the program has increased the students' motivation. They plan and run the program themselves; this participation is effective in increasing motivation in the program and gives students more motivation to work and study. In fact, the students find their job identity in this program” (Midwifery instructor, 39 years old, individual interview).
Regarding the increase of students' self‐confidence in the programme, one of the participants maintained: “The psychological support of the instructor in the program increases the students' self‐confidence, and we see that when students enter this program, their self‐confidence increases over time. They should and will gain higher self‐confidence during this program” (Midwifery instructor, 40 years old, individual interview).
3.3.5. Restrictions on performing legal duties
Clinical environments are, in fact, the practical areas for students. In the present study, the participants noted barriers in the clinical settings that created constraints on the students' legal duties. In this regard, a participant maintained: “The personnel and residents intervene in performance of the procedures, which makes our work difficult and deprives us of our independence. Staff and residents come, and because of their haste in emptying the ward, they interfere with our legal duties and prevent us from doing our legal duties properly” (30‐year‐old midwifery instructor, individual interview).
3.3.6. Poor interactions among the medical staff
Proper communication is one of the essential principles of midwifery and nursing care. The ability to interact appropriately is central to all nursing and midwifery activities. These interactions can be between the midwifery group and colleagues as well as between the midwifery group and patients. In this regard, the participants pointed out the weak interactions between the medical staff and the students. One of the participants said: “The work pressure of the staff was transferred to the students, and the staff did not do any work other than recording the birth events. The entire workload of nursing and midwifery is on the students, and the staff gave us all the unnecessary work not related to education. The staff did not cooperate with us well. They did not participate in teaching and did not answer our scientific questions. They also interfered with our teaching by giving unnecessary tasks to the students” (32‐year‐old student, 8th semester of midwifery, focus group discussion).
3.3.7. Failure in the management–supervisory process
The management–supervisory process is one of the effective factors in promoting training programmes. In addition, continuous monitoring of training programmes identifies the weaknesses and enhances the strengths of each training programme. In the present study, the participants pointed out shortcomings in the management–supervisory process of the programme. In this respect, one of the participants said: “I did not see them coming from an office to oversee the program. When there was a problem, the faculty members came to discuss the problem in the program. However, I did not see them coming from any other ministry or organization for supervision. The supervision in this training program is not done seriously and academically” (34‐year‐old midwifery instructor, individual interview).
3.4. Product
The product of the clinical programme is related to evaluating and determining the effects of the educational programme on the graduates, the results of an educational programme compared to its goals, and the relationship between expectations and actual results. Output means all graduates, produced knowledge, and achievements of the training programme (Stufflebeam & Zhang, 2017 ). From the perspective of the current study participants, the product included experienced graduates and a ground for the promotion of the community's health.
3.4.1. Experienced graduates
Clinical education is a dynamic process aimed at educating professionally qualified graduates. These graduates should be able to work independently and skilfully and apply the learned skills adequately in clinical settings. Regarding the professional competence of the graduates of the programme, one of the participants said: “I worked for a program, and I had the necessary ability when I entered the ward. I visited all the emergency cases, and the staff and the head of the ward were satisfied with my performance. The head of the department was satisfied with me at the beginning of the project and had a good view of me. I was even her substitute in the ward for a while when she was not the head nurse” (24‐year‐old graduate student, individual interview).
3.4.2. A ground for promotion of community's health
Considering the impact of the programme on the community's health and creating a suitable environment for promoting the community's health, one of the participants maintained: “This program has an impact on increasing the level of women's health and, consequently, community's health. The continuous presence of students and instructors makes pregnant mothers calm. Students and instructors are involved in maternity care, and the services they provide are more accurate and can definitely improve the community's health” (26‐year‐old graduate student, individual interview).
4. DISCUSSION
Clinical education is a sensitive and important period in midwifery education for which there are different educational models used around the world. Identifying the problems associated with clinical, educational programmes and then resolving these problems will help us achieve educational goals, train skilful midwives, provide suitable care services and promote the quality of midwifery education. One of the requirements of optimal education is having an appropriate educational environment in terms of the equipment, professors (Mc Carthy et al., 2018 ).
Educational researchers believe that setting realistic goals that are fitted to facilities, especially at the beginning of the educational programme, is very effective in improving the quality of clinical education (Ghafourifard, 2016 ). Expressing goals facilitates the proper implementation of teaching–learning activities (Tavakoli et al., 2014 ).
In order to achieve the educational goals, it is necessary for teachers to clearly and accurately explain the goals of clinical internships to students and other educational groups at the beginning of their educational activities (Ghafourifard, 2016 ). The qualitative results of the present study showed that the participants believed that the programme was ineffective in achieving the goals and implementing the curriculum regulations.
Given the importance of achieving educational goals, it seems that the expression of goals and planning and implementation of programmes related to clinical education needs to be reconsidered (Fotoukian et al., 2013 ) because proper educational planning can increase the quality of clinical education and lead to the achievement of clinical education goals(Sharif & Masoumi, 2005 ).
In the current study, the majority of the students participating in the focus group discussions stated that the educational goals were not matched with the expectations of the ward staff. According to the researchers, formulating realistic goals and explaining these goals to the groups participating in educational programmes is very effective in improving the quality of clinical education and should be considered in developing clinical education programmes (Raisler et al., 2003 ).
One of the requirements of desirable education is the appropriateness of the educational environment in terms of physical space, facilities and equipment, professors and staff. In an environment where there is proper cooperation among different clinical groups, the realization of educational goals and ultimately the conditions for more effective education are provided (Elcigil & Sarı, 2007 ). The present study results demonstrated that the physical condition of the clinical education facilities was not optimal and that the lack of adequate facilities had reduced the quality of clinical education from the perspective of the students and their instructors.
Limited resources were also reported as a challenge in midwifery clinical training. Clinical training settings have always faced shortcomings. Admission of midwifery students based on the clinical capacity of the university, providing and improving welfare facilities appropriate to the educational needs of the departments and providing facilities for students to improve the quality of education is essential. Midwifery clinical training requires facilities and resources to be provided, which is consistent with the findings of similar studies conducted on the issue (Boelens et al., 2018 ).
In this context, identifying and resolving the shortcomings and deficiencies and preventing discrimination in the allocation of resources and facilities to medical and non‐medical students appear to be the main mission of academic training systems. Lack of independence of midwifery students in providing childbirth services and making decisions for low‐risk deliveries, lack of explanation about the position of midwifery students and description of midwifery duties in the clinical environment, disregarding students' opinions in clinical decisions, unnecessary interventions of female residents in natural childbirth and students' dissatisfaction with the method of clinical evaluation have also been mentioned as other weaknesses of clinical education.
Other Iranian studies have reported problems in clinical settings, as well. These studies indicated that the students were not satisfied with or had negative attitudes towards the facilities and equipment of clinical environments (Jooibari & Sanaghoo, 2010 ; Ramezani & Kermanshahi, 2011 ).
The participants in a qualitative study cited that such factors as insufficient facilities, educational centres burnout, the prevailing atmosphere on the patients' bedsides and students' lack of interest in their field hindered clinical learning. On the other hand, the availability of educational facilities caused students to acquire the necessary clinical competencies and to perform faster in emergencies. Since the clinical environment is a key place for nursing and midwifery students and is one of the factors affecting clinical education, it is very important to pay attention to it (Lambert & Glacken, 2004 ).
Moreover, providing clinical guidance, including internship objectives, departmental regulations, job descriptions of students and clinical instructors, time and method of evaluation and the resources needed by students at the beginning of clinical education, can promote the students' responsibility, knowledge of tasks and integration of theoretical learning with skills. From the perspective of the participants in the present study, the lack of clinical guidance in the educational programme has caused differences in the way of teaching clinical procedures, ultimately confusing the students in learning these procedures. Hence, the curriculum in this field of study should be developed in such a way that the objectives expected by the health system are met. In fact, ensuring the quality of the midwifery training programmes is crucial for the clinical training system.
The training needs of medical students and the professional goals of the training are considered components of the training based on the needs of the system (Olafsdottir et al., 2018 ). One of the effective factors in clinical education is the atmosphere of the educational environment, which includes the way of communication and the attitudes of the personnel and those involved in the educational environment (Atack et al., 2000 ).
One solution to this problem is to select experienced, expert and knowledgeable trainers (Rowe et al., 2012 ). Identifying the challenges of midwifery clinical training is the first step towards achieving midwives' educational and training goals.
The present study showed the clinical instructors efficient in improving midwifery clinical training as their most important responsibility. Therefore, the instructors should have or acquire the skills required for responding to the educational needs of the students (Raofi et al., 2009 ). From the participants' viewpoints, one of the strengths of this programme was that the trainers benefitted from appropriate clinical abilities.
In fact, by having characteristics such as effective communication, instructors transferred their knowledge and experiences to the students and were the bridge between theoretical and clinical education. In other words, the implementation of the teaching‐learning process through competent and efficient instructors could enable the students to make the most of their abilities. Clinical educators also have a tremendous effect on increasing the quality of clinical education and can make clinical experiences enjoyable for students (Peyman et al., 2011 ).
Instructors' motivation is mainly affected by professional autonomy in the areas of duties and professional support. The autonomy of midwifery instructors is necessary for developing trust, respect, skills and competency (Basaran Acil & Dinç, 2018 ). The factors reported affecting professional autonomy include transparency in the definition of the concept of professional autonomy, receiving support from managers, midwifery teamwork based on evidence and regular study, and using a comprehensive theory of professional autonomy (Balhara & Mathur, 2013 ; Laschinger et al., 2014 ).
In the present investigation, most of the participants were dissatisfied with the inappropriate treatment of the nursing staff, assignment of unrelated tasks to students and unnecessary interventions of female residents in natural childbirth. The way staff and other medical groups interact with students plays a key role in the students' clinical learning and can be a key factor in accelerating their learning process (Tang et al., 2005 ).
The majority of the participants in the current research reported the unfriendly behaviours of the physicians, staff and sometimes instructors towards the midwifery students. Unfriendly behaviours included verbal abuse, bullying and disrespect, and threatening of the students' health in clinical training settings (Dinmohammadi et al., 2014 ). Additionally, the clinical setting did not support the students and was referred to as the phenomenon of “vertical violence against students” (Hajihosseini et al., 2018 ).
The gap between theory and practice and the negative attitude of clinical staff towards clinical trainers may also be among the causes of inadequate clinical training.
Lukasse et al. showed that much clinical staff has a negative view of midwifery trainers who have not been in clinical practice for years or have not been updated. The old and outdated method of teaching leads to a gap between theory and practice (Lukasse et al., 2017 ).
A study in Ghana showed that environmental factors and interpersonal and academic relationships could negatively affect midwifery students, with interpersonal stressors being the strongest (Lukasse et al., 2017 ).
Midwifery students experience specific problems during their academic and clinical education, leading to uncertainty, dissatisfaction and failure to adapt to their profession (Carolan‐Olah et al., 2014 ).
Most of these problems stem from a wide range of potential issues in the clinical learning environment and interpersonal relationships that can affect student learning. While midwifery students usually have extensive knowledge, they do not have sufficient clinical skills and fail to apply their theoretical knowledge in a stressful environment (Cooper et al., 2012 ; Gönenç & Sezer, 2019 ).
Developing a safe environment and friendly behaviours in clinical settings can develop a sense of value in midwifery students and improve education and learning conditions. Induction of professional identity to the students was another concept identified in the present study. Having a professional identity is considered a pre‐requisite for achieving success in different fields of study. The steps required to be taken to reform the policies and clinical training programmes and eliminate or add new fields of study include the recognition of different factors associated with the students' attitudes towards their fields of study (Fida et al., 2018 ; Harris et al., 2013 ).
Mutual interaction with other medical groups shared understanding, and shared objectives are essential for creating positive student experiences in a learning environment (Thunes & Sekse, 2015 ). Another study seeking students' evaluation of certain factors in the clinical learning environment at a Slovakian university revealed that a positive attitude and an appropriate collaborative atmosphere improved the students' learning (Gurková et al., 2016 ).
Thus, the authorities in charge of the midwifery clinical training are expected to develop strategies to institutionalize beliefs and values according to the field of study and appropriate expectations to modify the physical conditions of the clinical environment in order to attract students and promote self‐esteem, motivation, professional identity and positive educational attitudes among midwifery students. Poor interaction among the medical staff was another concept identified in the present study. Educational support is one of the important components of clinical education in nursing and midwifery courses, which requires the interaction and cooperation of educational instructors and clinical nurses (Seidi et al., 2014 ).
The existence of appropriate professional interactions between students and medical staff helps the transition of students and leads to the formation of professional identity (Apker et al., 2006 ). Appropriate professional interactions also play an essential role in motivating students to learn, leading to a positive self‐concept and increasing their learning motivation (Andrews et al., 2006 ). Elo's study of students 'experiences in the clinical environment showed that poor communication between staff and students could lead to students' lack of interest in learning and their negative attitudes (Mikkonen et al., 2016 ).
In the present research, an inappropriate educational environment was reported as a challenge in midwifery training. It has been reported that the facilitating role of staff and physicians' cooperation with students contributes to the effectiveness of clinical education. Several Iranian researchers have referred to disrespect among the staff and the lack of coordination between the treatment and educational systems of the university (Reising et al., 2018 ).
The supportive behaviour of the staff can contribute to professional growth and affect the teaching–learning process (Jasemi et al., 2018 ). The supportive behaviour of the staff towards midwifery students and the intra‐organizational coordination among the faculties and hospitals appear to improve the status of the midwifery clinical training (Arimoto et al., 2012 ).
In the present study, the lack of a specific tool and method for evaluation was proposed as a problem in clinical education. The students had called for a revision of the method of evaluation. The existence of the same and specific evaluation method and its uniform application seems necessary for all students. In another study, Helminen found that the evaluation process of students' clinical practice lacked consistency. High diversity in assessment quality and differences in the mentors' perceptions of assessment forms were among the student assessment challenges (Helminen et al., 2016 ). According to researchers, one of the main challenges for educators in clinical education is evaluating students in clinical settings (McCutchan, 2015 ). Because evaluation can be a way to determine the achievement of goals and provide students with proper feedback, it seems necessary to modify and review the evaluation methods of the clinical faculty programme.
The present study revealed active and interactive teaching as a strength of midwifery training since efficient teaching methods are crucial for developing the skills required for students. As an objective of clinical training, developing basic skills involving problem‐solving and efficient communication can improve the quality of clinical training. In this context, the instructors' knowledge of modern teaching methods and the students' ability to make decisions was reported as the main clinical training strengths from the students' perspectives. Using active teaching methods in midwifery training can result in more profound learning and improve the students' clinical skills. Given the complexity of midwifery, using modern clinical training methods can enhance the level of clinical training. The present study identified a more comprehensive view of the problems in clinical education. In addition, the students emphasized their professional future, professional discrimination and the need for employing experienced instructors.
4.1. Limitations
As this study was qualitative, the obtained results cannot be generalized to other clinical education programmes. Lack of sufficient motivation among some of the participants to interview was one of the limitations of this study, and due to the limited resources, time and location and wide distribution of midwifery graduates, this study was unable to cover large groups of graduates.
5. CONCLUSION
Based on the results of the present study, the lack of appropriate physical and welfare space in the ward, lack of facilities for scientific conferences, intervention in clinical education, unnecessary intervention in the process of natural childbirth, lack of uniformity in clinical procedures and lack of a systematic evaluation system were among the essential problems of clinical education. Therefore, fundamental changes in clinical environments are necessary to improve clinical skills and achieve clinical education goals. The results of this study would help educators to design strategies for more effective clinical teaching. Hence, the findings should be considered by midwifery education professionals. Given the complexity of the field of midwifery, using modern clinical training methods, such as the clinical faculty programme, may enhance the efficiency of clinical training in Iran.
CONFLICT OF INTEREST
The authors have no conflicts of interest relevant to this article.
AUTHOR CONTRIBUTIONS
Maryam Modarres, Mehrnaz Geranmayeh, Mitra Amini and Monireh Toosi performed conceptualization of the study, coordination, acquisition of data and drafting of the manuscript. All authors read and approved the final manuscript.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Written informed consent forms were obtained from all participants. This study was approved by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (code: IR.TUMS.FNM.REC.1398.057).
ACKNOWLEDGEMENT
The authors would like to thank Ms. A. Keivanshekouh at the Research Improvement Center of Shiraz University of Medical Sciences for improving the use of English in the manuscript.
Modarres, M. , Geranmayeh, M. , Amini, M. , & Toosi, M. (2022). Clinical placements as a challenging opportunity in midwifery education: A qualitative study. Nursing Open, 9, 1015–1027. 10.1002/nop2.1139
DATA AVAILABILITY STATEMENT
The data are available on request from the corresponding author.
- Andrews, G. J. , Brodie, D. A. , Andrews, J. P. , Hillan, E. , Gail Thomas, B. , Wong, J. , & Rixon, L. (2006). Professional roles and communications in clinical placements: A qualitative study of nursing students' perceptions and some models for practice. International Journal of Nursing Studies, 43(7), 861–874. [ DOI ] [ PubMed ] [ Google Scholar ]
- Apker, J. , Propp, K. M. , Zabava Ford, W. S. , & Hofmeister, N. (2006). Collaboration, credibility, compassion, and coordination: Professional nurse communication skill sets in health care team interactions. Journal of Professional Nursing, 22(3), 180–189. [ DOI ] [ PubMed ] [ Google Scholar ]
- Arimoto, A. , Gregg, M. F. , Nagata, S. , Miki, Y. , & Murashima, S. (2012). Evaluation of doctoral nursing programs in Japan by faculty members and their educational and research activities. Nurse Education Today, 32(5), e1–e7. [ DOI ] [ PubMed ] [ Google Scholar ]
- Atack, L. , Comacu, M. , Kenny, R. , LaBelle, N. , & Miller, D. (2000). Student and staff relationships in a clinical practice model: Impact on learning. Journal of Nursing Education, 39(9), 387–392. [ DOI ] [ PubMed ] [ Google Scholar ]
- Balhara, Y. P. S. , & Mathur, S. (2013). A comparative study of attitudes toward psychiatry among nursing students across successive training years. Indian Journal of Psychological Medicine, 35(2), 159. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Basaran Acil, S. , & Dinç, L. (2018). Turkish adaptation and psychometric characteristics of the Nursing Authority and Autonomy Scale. Journal of Nursing Management, 26(6), 735–743. [ DOI ] [ PubMed ] [ Google Scholar ]
- Bellack, J. P. , Graber, D. , O’Neil, E. H. , & Musham, C. (1998). Curriculum trends in nurse‐midwifery education: Views of program directors. Journal of Nurse‐Midwifery, 43(5), 341–350. [ DOI ] [ PubMed ] [ Google Scholar ]
- Birks, M. , Bagley, T. , Park, T. , Burkot, C. , & Mills, J. (2017). The impact of clinical placement model on learning in nursing: A descriptive exploratory study. Australian Journal of Advanced Nursing, 34(3), 16. [ Google Scholar ]
- Boelens, R. , Voet, M. , & De Wever, B. (2018). The design of blended learning in response to student diversity in higher education: Instructors' views and use of differentiated instruction in blended learning. Computers & Education, 120, 197–212. [ Google Scholar ]
- Butler, M. M. , Fraser, D. M. , & Murphy, R. J. (2008). What are the essential competencies required of a midwife at the point of registration? Midwifery, 24(3), 260–269. [ DOI ] [ PubMed ] [ Google Scholar ]
- Carolan‐Olah, M. , Kruger, G. , Walter, R. , & Mazzarino, M. (2014). Final year students' experiences of the Bachelor of Midwifery course. Midwifery, 30(5), 519–525. [ DOI ] [ PubMed ] [ Google Scholar ]
- Cheraghi, R. , Jasemi, M. , & Namadi, F. (2019). Effectiveness of the clinical teaching associate model in clinical nursing education. Nursing and Midwifery Studies, 8(3), 132–136. [ Google Scholar ]
- Cooper, S. , Bulle, B. , Biro, M. A. , Jones, J. , Miles, M. , Gilmour, C. , Buykx, P. , Boland, R. , Kinsman, L. , Scholes, J. , & Endacott, R. (2012). Managing women with acute physiological deterioration: Student midwives performance in a simulated setting. Women and Birth, 25(3), e27–e36. [ DOI ] [ PubMed ] [ Google Scholar ]
- Delaram, M. , Safdari Dahcheshme, F. , Sh, B. , Kazemian, A. , Sereshti, M. , Raeisi, Z. , & Asefi, F. (2013). Midwifery students' self assessment of their ability in practical skills. Education Strategies in Medical Sciences, 6(3), 177–182. [ Google Scholar ]
- Dinmohammadi, M. , Peyrovi, H. , & Mehrdad, N. (2014). Undergraduate student nurses' experiences in clinical environment: Vertical violence. Iran Journal of Nursing, 27(90), 83–93. [ Google Scholar ]
- Donough, G. , & Van Der Heever, M. (2018). Undergraduate nursing students' experience of clinical supervision. Curationis, 41(1), 1–8. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ekstedt, M. , Lindblad, M. , & Löfmark, A. (2019). Nursing students' perception of the clinical learning environment and supervision in relation to two different supervision models–a comparative cross‐sectional study. BMC Nursing, 18(1), 49. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Elcigil, A. , & Sarı, H. Y. (2007). Determining problems experienced by student nurses in their work with clinical educators in Turkey. Nurse Education Today, 27(5), 491–498. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fasihi, H. T. , Soltani, A. S. , Tahami, S. , & Mohammad, A. S. (2004). Viewpoints of medical students about the quality of clinical education. [ Google Scholar ]
- Fida, R. , Laschinger, H. K. S. , & Leiter, M. P. (2018). The protective role of self‐efficacy against workplace incivility and burnout in nursing: A time‐lagged study. Health Care Management Review, 43(1), 21–29. [ DOI ] [ PubMed ] [ Google Scholar ]
- Fitzpatrick, J. L. (2011). Program evaluation alternative approaches and practical guidelines. [ Google Scholar ]
- Fotoukian, Z. , Hosseini, S. J. , Beheshti, Z. , Zabihi, A. , Aziznejad, P. , & Ghaffari, F. (2013). Clinical education status according to the nursing students' point of view, Babol medical sciences university. Biannual Journal of Medical Education Development Center (edc) Babol University of Medical Sciences, 1(1), 26–33. [ Google Scholar ]
- Ghafourifard, M. (2016). The status of clinical education in teaching hospitals affiliated with Zanjan university of medical sciences from the viewpoints of nursing and midwifery students. Journal of Medical Education Development, 8(20), 9–20. [ Google Scholar ]
- Gönenç, İ. M. , & Sezer, N. Y. (2019). Evaluation of the effectiveness of four different training techniques in the development of non‐stress testing application skills: A randomised controlled trial. Nurse Education Today, 76, 118–124. [ DOI ] [ PubMed ] [ Google Scholar ]
- Graham, C. L. , Phillips, S. M. , Newman, S. D. , & Atz, T. W. (2016). Baccalaureate minority nursing students perceived barriers and facilitators to clinical education practices: An integrative review. Nursing Education Perspectives, 37(3), 130–137. [ DOI ] [ PubMed ] [ Google Scholar ]
- Gurková, E. , Žiaková, K. , Cibríková, S. , Magurová, D. , Hudáková, A. , & Mrosková, S. (2016). Factors influencing the effectiveness of clinical learning environment in nursing education. Central European Journal of Nursing and Midwifery, 7(3), 470–475. [ Google Scholar ]
- Haghani, F. , & Hojat, M. (2013). Challenges of clinical education in health system. Education & Ethic in Nursing, 2(3), 9–19. [ Google Scholar ]
- Hajihosseini, F. , Tafreshi, M. Z. , Hosseini, M. , & Baghestani, A. R. (2018). Postgraduate nursing students' expectations of their supervisors in Iran: A qualitative study. Iranian Journal of Nursing and Midwifery Research, 23(2), 98. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Harris, R. C. , Rosenberg, L. , & Grace O’Rourke, M. E. (2013). Addressing the challenges of nursing student attrition. Journal of Nursing Education, 53(1), 31–37. [ DOI ] [ PubMed ] [ Google Scholar ]
- Helminen, K. , Coco, K. , Johnson, M. , Turunen, H. , & Tossavainen, K. (2016). Summative assessment of clinical practice of student nurses: A review of the literature. International Journal of Nursing Studies, 53, 308–319. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jasemi, M. , Whitehead, B. , Habibzadeh, H. , Zabihi, R. E. , & Rezaie, S. A. (2018). Challenges in the clinical education of the nursing profession in Iran: A qualitative study. Nurse Education Today, 67, 21–26. [ DOI ] [ PubMed ] [ Google Scholar ]
- Jooibari, L. , & Sanaghoo, A. (2010). Effective instructor: Depth looks at the experiences and views of students and instructors. Strides Development Medical Education: Journal of Medical Education Development Center Kerman University of Medical Sciences, 6(2), 119–128. [ Google Scholar ]
- Lambert, V. , & Glacken, M. (2004). Clinical support roles: A review of the literature. Nurse Education in Practice, 4(3), 177–183. [ DOI ] [ PubMed ] [ Google Scholar ]
- Leap, N. , Barclay, L. , Nagy, E. , Sheehan, A. , Brodie, P. , & Tracy, S. (2002). Midwifery education: Literature review and additional material. Final Report: Department of education, science and training. [ Google Scholar ]
- Lukasse, M. , Lilleengen, A. M. , Fylkesnes, A. M. , & Henriksen, L. (2017). Norwegian midwives' opinion of their midwifery education–a mixed methods study. BMC Medical Education, 17(1), 1–12. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mc Carthy, J. , Graham, M. M. , Tuohy, D. , O'Brien, B. , Fahy, A. , Hennessy, T. , O'Sullivan, D. , & Markey, K. (2018). Potential and challenges for learning during acute medical/surgical placement for intellectual disability, mental health and midwifery students. Nurse Education in Practice, 28, 135–140. [ DOI ] [ PubMed ] [ Google Scholar ]
- McCutchan, J. A. (2015). The experience of baccalaureate degree seeking nursing students undergoing the process of clinical evaluation appraisal. [ Google Scholar ]
- Mikkonen, K. , Elo, S. , Kuivila, H.‐M. , Tuomikoski, A.‐M. , & Kääriäinen, M. (2016). Culturally and linguistically diverse healthcare students' experiences of learning in a clinical environment: A systematic review of qualitative studies. International Journal of Nursing Studies, 54, 173–187. [ DOI ] [ PubMed ] [ Google Scholar ]
- Mousavi, P. , & Montazeri, S. (2013). Evaluating the achieving rate of learning minimums in clinic and gynecology units and their performance obstacles from midwifery students' viewpoint of nursing and midwifery school in Ahvaz. [ Google Scholar ]
- Olafsdottir, O. A. , Kristjansdottir, H. , Halfdansdottir, B. , & Gottfredsdottir, H. (2018). Midwifery in Iceland: From vocational training to university education. Midwifery, 62, 104–106. [ DOI ] [ PubMed ] [ Google Scholar ]
- Omidvar, S. , Bakouei, F. , & Salmalian, H. (2005). Clinical education problems: The viewpoints of midwifery students in Babol Medical University. [ Google Scholar ]
- Peyman, H. , Darash, M. , Sadeghifar, J. , Yaghoubi, M. , Yamani, N. , & Alizadeh, M. (2011). Evaluating the viewpoints of nursing and midwifery students about their clinical educational status. Iranian Journal of Medical Education, 10(5), 1121‐1130. [ Google Scholar ]
- Polit, D. F. , & Beck, C. T. (2009). Essentials of nursing research: Appraising evidence for nursing practice. Lippincott Williams & Wilkins. [ Google Scholar ]
- Raisler, J. , O'Grady, M. , & Lori, J. (2003). Clinical teaching and learning in midwifery and women's health. Journal of Midwifery & Women's Health, 48(6), 398–406. [ DOI ] [ PubMed ] [ Google Scholar ]
- Ramezani, M. , & Kermanshahi, S. (2011). A survey of the quality of clinical education in nursing. Journal of Jahrom University of Medical Sciences, 9, 14. [ Google Scholar ]
- Raofi, R. , Talaghani, F. , Hojat, M. , & Shahriari, M. (2009). A review of the literature: The situation of continuing nursing education in Iran. Nursing, 4, 8. [ Google Scholar ]
- Reising, D. L. , James, B. , & Morse, B. (2018). Student perceptions of clinical instructor characteristics affecting clinical experiences. Nursing Education Perspectives, 39(1), 4–9. [ DOI ] [ PubMed ] [ Google Scholar ]
- Rowe, M. , Frantz, J. , & Bozalek, V. (2012). The role of blended learning in the clinical education of healthcare students: A systematic review. Medical Teacher, 34(4), e216–e221. [ DOI ] [ PubMed ] [ Google Scholar ]
- Saleh, A. S. , Golafrooz, S. M. , Nasrollahi, S. , Akbarzadeh, M. , & Mirchouli, N. (2014). Clinical education problems and ways of enhancing its quality from the perspective of clinical instructors and students of nursing and midwifery at sabzevar university medical sciences in 2008. [ Google Scholar ]
- Seidi, J. , Alhani, F. , & Salsali, M. (2014). Professional support as a facilitator to the development of Iranian nurses' clinical judgment: A content analysis. Iranian Journal of Nursing and Midwifery Research, 19(7) (Suppl 1), S13. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Seyedamini, B. , Mahmoudifar, Y. , & Esmaeillou, Y. (2018). Effective stressors in clinical education. International Archives of Health Sciences, 5(3), 104. [ Google Scholar ]
- Sharghi, N. R. , Alami, A. , Khosravan, S. , Mansoorian, M. R. , & Ekrami, A. (2015). Academic training and clinical placement problems to achieve nursing competency. Journal of Advances in Medical Education & Professionalism, 3(1), 15. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sharif, F. , & Masoumi, S. (2005). A qualitative study of nursing student experiences of clinical practice. BMC Nursing, 4(1), 6. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spence Laschinger, H. K. , Nosko, A. , Wilk, P. , & Finegan, J. (2014). Effects of unit empowerment and perceived support for professional nursing practice on unit effectiveness and individual nurse well‐being: A time‐lagged study. International Journal of Nursing Studies, 51(12), 1615–1623. [ DOI ] [ PubMed ] [ Google Scholar ]
- Speziale, H. S. , Streubert, H. J. , & Carpenter, D. R. (2011). Qualitative research in nursing: Advancing the humanistic imperative. Lippincott Williams & Wilkins. [ Google Scholar ]
- Stufflebeam, D. L. , & Zhang, G. (2017). The CIPP evaluation model: How to evaluate for improvement and accountability. Guilford Publications. [ Google Scholar ]
- Tang, F.‐I. , Chou, S.‐M. , & Chiang, H.‐H. (2005). Students' perceptions of effective and ineffective clinical instructors. Journal of Nursing Education, 44(4), 187–192. [ DOI ] [ PubMed ] [ Google Scholar ]
- Tavakoli, M. , Khazaei, T. , Tolyat, M. , & Ghorbani, S. (2014). The quality of clinical education from the viewpoints of students and instructors of paramedical and nursing‐obstetrics schools of Birjand University of Medical Sciences. [ Google Scholar ]
- Thompson, J. B. , Fullerton, J. T. , & Sawyer, A. J. (2011). The international confederation of midwives: Global standards for midwifery education (2010) with companion guidelines. Midwifery, 27(4), 409–416. [ DOI ] [ PubMed ] [ Google Scholar ]
- Thunes, S. , & Sekse, R. J. T. (2015). Midwifery students first encounter with the maternity ward. Nurse Education in Practice, 15(3), 243–248. [ DOI ] [ PubMed ] [ Google Scholar ]
- Traynor, M. (2015). Focus group research. Nursing Standard, 29(37), 44–48. [ DOI ] [ PubMed ] [ Google Scholar ]
- Valiee, S. , Moridi, G. , & Khaledi, S. (2013). Barriers to and facilitators of clinical education from Sanandaj nursing students' viewpoints, 2010‐2011. [ Google Scholar ]
- Wiegers, T. , Boerma, W. , & de Haan, O. (2010). Maternity care and birth preparedness in rural Kyrgyzstan and Tajikistan. Sexual & Reproductive Healthcare, 1(4), 189–194. [ DOI ] [ PubMed ] [ Google Scholar ]
- Wildemuth, B. M. (2016). Applications of social research methods to questions in information and library science. ABC‐CLIO. [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
- View on publisher site
- PDF (487.4 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

Addressing Challenges in Midwifery Education
Challenges in midwifery education.
The field of midwifery is dynamic and continually evolving, requiring midwives to stay updated with the latest knowledge, skills, and best practices. Continuing education is not just a requirement for maintaining certification; it’s a commitment to providing the highest standard of care for mothers and babies. Here’s why continuing education is so important for midwives.

1. Staying Current with Medical Advancements
(keeping up with new research and techniques).
Medical research constantly brings new insights into maternal and newborn health . Continuing education helps midwives stay informed about:
- Latest Research: Understanding new findings in prenatal care, labor and delivery, postpartum care, and neonatal health.
- Innovative Techniques: Learning new procedures and practices that improve patient outcomes.
- Updated Guidelines: Adhering to the latest guidelines and standards set by professional organizations and healthcare authorities.
2. Enhancing Clinical Skills (Improving Hands-On Expertise)
Continuing education offers opportunities to refine and enhance clinical skills through:
- Workshops and Seminars: Practical sessions that provide hands-on experience with new equipment or techniques.
- Simulation Training: Using advanced simulation tools to practice complex scenarios in a safe environment.
- Certifications and Specializations: Gaining additional certifications or specializations in areas such as lactation consulting, perinatal mental health, or high-risk pregnancies.
3. Providing Culturally Competent Care (Understanding and Respecting Diversity)
Midwives work with diverse populations, and cultural competence is crucial for providing respectful and personalized care. Continuing education helps midwives:
- Cultural Sensitivity: Understand different cultural practices and beliefs related to childbirth and maternal care.
- Effective Communication: Learn strategies to communicate effectively with clients from various backgrounds.
- Inclusive Practices: Implement care practices that respect and accommodate cultural differences.
4. Promoting Leadership and Advocacy (Developing Skills Beyond Clinical Care)
Midwives often take on roles that involve leadership and advocacy. Continuing education supports this by:
- Leadership Training: Building skills needed to lead teams, manage practices, or take on administrative roles.
- Advocacy Skills: Equipping midwives with the tools to advocate for policy changes and improvements in maternal and newborn health.
- Community Engagement: Learning how to engage with the community and build strong support networks.
5. Ensuring Professional Growth and Fulfillment (Fostering Lifelong Learning and Career Advancement)
Continuing education is a pathway to professional growth and personal fulfillment. It provides:
- Career Advancement: Opportunities to advance in the profession, take on new roles, or open a private practice.
- Personal Satisfaction: The satisfaction of mastering new skills and knowledge, which enhances confidence and competence.
- Networking Opportunities: Connecting with other professionals, sharing experiences, and learning from peers.
6. Improving Patient Outcomes (Delivering High-Quality, Evidence-Based Care)
The ultimate goal of continuing education is to improve patient outcomes by:
- Providing Evidence-Based Care: Ensuring that practices are based on the latest and most reliable evidence.
- Enhancing Patient Safety: Reducing risks and complications through up-to-date knowledge and skills.
- Increasing Patient Satisfaction: Offering high-quality, compassionate care that meets the needs and expectations of patients.
7. Adapting to Healthcare Changes (Navigating a Changing Healthcare Landscape)
The healthcare environment is constantly changing due to new laws, technologies, and societal needs. Continuing education helps midwives:
- Adapt to Regulations: Stay compliant with new regulations and standards.
- Embrace Technology: Learn how to use new technologies that enhance care, such as electronic health records or telehealth services.
- Respond to Emerging Needs: Be prepared to address emerging healthcare needs and challenges, such as managing pandemics or addressing mental health crises.
Continuing education is essential for midwives to provide the best care possible, stay competitive in their field, and advance their careers. It ensures that midwives remain knowledgeable, skilled, and capable of delivering high-quality, evidence-based, and culturally competent care. By committing to lifelong learning, midwives can continually enhance their practice, improve patient outcomes, and contribute to the advancement of the midwifery profession.
Join the Learning Journey
Navigating the challenges in midwifery education demands continuous adaptation and resilience. From limited resources and varied curriculums to evolving healthcare needs, midwifery programs must equip students with not just medical skills but also cultural competence and empathy.
Addressing these challenges ensures that future midwives are well-prepared to provide comprehensive and compassionate care. The journey, though tough, is crucial for the advancement of midwifery and the health of communities worldwide. Always aim to learn, adapt, and grow in the face of adversity
Are you a midwife committed to challenges in midwifery education? Explore available courses , workshops , and resources to stay updated and enhance your skills. Together, we can ensure a brighter future for maternal and newborn health.
Related Posts


Midwifery State Regulations

Tips For Increasing Access to Midwifery Services
Leave a comment cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
EMPOWERING MIDWIFERY EDUCATION
[email protected], copyright © 2024 empowering midwifery education - all rights reserved..
- Open access
- Published: 17 September 2020
Midwives’ challenges and factors that motivate them to remain in their workplace in the Democratic Republic of Congo—an interview study
- Malin Bogren ORCID: orcid.org/0000-0003-2432-8097 1 ,
- Malin Grahn 1 , 2 ,
- Berthollet Bwira Kaboru 3 &
- Marie Berg 1 , 2
Human Resources for Health volume 18 , Article number: 65 ( 2020 ) Cite this article
23k Accesses
18 Citations
23 Altmetric
Metrics details
The Democratic Republic of Congo (DRC) has high maternal mortality and a low number of midwives, which undermines the achievement of goal 3 of the Sustainable Development Goals (SDGs) for 2030, specifically the health of the mother and newborn. Scaling up the midwifery workforce in relation to number, quality of healthcare, and retention in service is therefore critical. The aim of this study was to investigate midwives’ challenges and factors that motivate them to remain in their workplace in the DRC.
Data were collected in two out of 26 provinces in the DRC through ten focus group discussions with a total of 63 midwives working at ten different healthcare facilities. Transcribed discussions were inductively analysed using content analysis.
The midwives’ challenges and the factors motivating them to remain in their workplace in the DRC are summarised in one main category— Loving one’s work makes it worthwhile to remain in one’s workplace, despite a difficult work environment and low professional status —consisting of three generic categories: Midwifery is not just a profession; it’s a calling is described in the subcategories Saving lives through midwifery skills, Building relationships with the women and the community, and Professional pride; Unsupportive organisational system is expressed in the subcategories Insufficient work-related security and No equitable remuneration system, within Hierarchical management structures; and Inadequate pre-conditions in the work environment includes the subcategories Lack of resources and equipment and Insufficient competence for difficult working conditions.
Midwives in the DRC are driven by a strong professional conscience to provide the best possible care for women during childbirth, despite a difficult work environment and low professional status. To attract and retain midwives and ensure that they are working to their full scope of practice, we suggest coordinated actions at the regional and national levels in the DRC and in other low-income countries with similar challenges, including (i) conducting midwifery education programmes following international standards, (ii) prioritising and enforcing policies to include adequate remuneration for midwives, (iii) involving midwives’ associations in policy and planning about the midwifery workforce, and (iv) ensuring that midwives’ working environments are safe and well equipped.
Peer Review reports
Healthcare provided by midwives who are educated and regulated according to global professional standards is defined as a core strategy for decreasing maternal mortality rates and improving reproductive, maternal, and newborn health [ 1 , 2 , 3 ]. However, a shortage of professional midwives informed by international standards is detrimental to the need for universal access to high-quality care [ 1 ]. This is especially a challenge in Sub-Saharan Africa, for instance, in the Democratic Republic of Congo (DRC), which reports a maternal mortality rate of 846 per 100,000 live births [ 4 ] and a fertility rate of 6.2 [ 5 ]. These numbers can be explained by, among other things, poor healthcare quality [ 6 ], which in turn is partially due to a severely strained health system afflicted by many years of political conflict [ 7 ]. With only one midwife per 20,000 persons, the midwifery workforce in the DRC is far from the minimum required for meeting the predicted need for midwives within maternity care [ 8 ], and for reaching Sustainable Development Goal (SDG) 3 on health aiming at a maternal mortality rate of fewer than 70 per 100,000 live births by 2030 [ 9 ].
However, scaling up midwifery healthcare implies not only increasing the quantity of midwives, but also customising evidence-based healthcare to fit local conditions and necessities [ 10 , 11 ]. Thus, investigating what enables midwives to provide quality care is crucial [ 5 ].
In the DRC, the midwifery profession has received increased attention only in recent years [ 9 ]. Since the country’s educational reform in 2013, two paths of midwifery education are offered at the higher education institutes for applied medical sciences (ISTM). Both lead to an advanced diploma. The first, a 3-year direct-entry full-time programme, is currently offered at 16 ISTMs located in 12 of the country’s 26 provinces. The second is a 12-month programme for nurses educated within a 3-year programme at a higher academic level. Both programmes consist of 60% theory and 40% clinical practice. This programme, while too short to fulfil international standards, is currently offered at three ISTMs located in three provinces [ 12 ]. As of 2019, a total of 3646 midwives had been schooled in the new midwifery educational programmes. However, despite the educational reform in 2013, the midwifery educational system faces several challenges. These include a low academic level among the tutors within the programmes, including the midwifery educators and clinical preceptors. Furthermore, the midwifery profession is not yet regulated and is thus not allowed to work as an autonomous profession within a defined area of practice and competence [ 9 , 13 ]. This means that after completing an education programme, midwives are often obliged to work in areas that are not related to the midwifery area of practice [ 9 ].
This situation for midwives in the DRC echoes findings from a global consultation with 2470 midwives in 93 countries (not including the DRC). Hierarchies of power and gender discrimination were identified as barriers to providing high-quality, respectful care for women, newborns, and their families [ 14 ]. In low- and middle-income countries, such barriers have been identified to include economic, social, and professional areas [ 15 , 16 , 17 ]. Contributing factors include gender inequalities with a lack of power for women [ 15 , 17 ], low professional autonomy [ 14 , 16 ], and unmanageable workloads [ 16 ], the last of which is also identified as a significant barrier in high-income countries [ 18 ].
In a conceptual model on how health worker motivation is influenced and how health sector reform can positively affect worker motivation, it has been concluded that motivating factors have a high impact on health worker performance and on general health outcomes in health workers and that the factors cover both individual, organisational, and cultural dimensions [ 19 ]. Creating a motivating work environment in alignment with midwives’ preferences and well-being is identified as crucial for avoiding the unnecessary resignation of midwives, and thereby increasing the possibility to achieve universal access to sexual, reproductive, maternal, and newborn care [ 11 , 20 , 21 ].
To secure high-quality care before, during, and after childbirth, it is essential to understand not only what challenges midwives face but also what motivates them to remain in their profession [ 14 , 15 ]. In accordance with the recommendations by the United Nations Population Fund in East and Southern Africa [ 13 ], there is a need to understand what encourages midwives in their work and enables them to provide quality care. There is abundant research from high-income settings on what challenges midwives face and factors that force them to leave the profession, but similar research from low- and middle-income settings is much more limited. The aim of this study was to investigate midwives’ challenges and the factors motivating them to remain in their workplace in the DRC, in order to identify strategies that enable the DRC to use professional midwives in an optimal way in its strive to reach the 2030 SDGs associated with maternal and newborn health.
Study design and setting
A qualitative study including focus group discussions (FGDs) with midwives was conducted. This method is appropriate to use when seeking a contextualised understanding within a topic on which little is known [ 22 ].
The healthcare system in the DRC is divided into health zones and offers care at three levels: the primary level at healthcare centres, some of which include maternity wards; the secondary level at district hospitals with the capacity to perform caesarean sections; and the tertiary level at referral hospitals. Our study was conducted at selected healthcare facilities, including both public and private settings, in the two provinces of Maniema in eastern DRC and Kasai in the central part of the country, which have a high incidence of maternal and newborn death and are part of a larger health-strengthening project—BOMOYI—with a focus on maternal and newborn health, managed by the local organisation Soins de Santé Primaires en Milieu Rural (SANRU Asbl).
One of the weaknesses of the public health system in the DRC is a poorly structured remuneration system for public servants. The pay structures for midwives in the DRC vary. The public sector pay is commonly composed of different elements, with a basic salary as a small component of the overall pay. In order to be on the public service payroll, a civil service number is required, which many midwives do not have. However, according to anecdotal information, a majority of midwives who do have a civil service number nonetheless do not receive regular payment. The monthly salary (as of 2020) ranges from 80,000 to 150,000 Congolese Francs (US$ 40–75). Allowances, taken from resources levied through patient fees, contribute more to a midwife’s total income than salary does. More than 40% of healthcare expenditures in the DRC are basically supported by households [ 23 ]. The cost of normal childbirth varies depending on the level of care, place of residence, whether the care is provided at a private or public facility, and whether the healthcare facility receives external funding. In general, at the primary level, the cost of normal birth is US$ 10–20 and at the secondary level US$ 15–25, while at referral hospitals, the estimated cost is US$ 20–35.
Participants and data collection
Managers at the selected healthcare facilities representing all three levels were informed about the study. All of them approved the study and provided contact information for midwives working at different maternity units, who were then invited to participate by SANRU focal staff. Interested midwives were given verbal and written information about the study, including the fact that participation was voluntary and that withdrawal was allowed at any time without explanation. Midwives agreeing to participate signed an informed consent.
Ten FGDs were conducted in October 2019, at ten healthcare facilities near the midwives’ workplaces. Six to eight midwives participated in each FGD, totalling 63 midwives who worked at different healthcare facilities representing both governmental and private sectors, all of which were integrated into the DRC’s public healthcare system. For details about the study participants, see Table 1 . Two of the authors (MBo and MBe) conducted the FGDs, together with a representative from the national midwifery association who acted as an observer. The FGDs were audio-recorded and lasted 30–45 min, with a mean of 40 min. MBe led the discussion in French based on an interview guide (see Additional file 1 ) and translated continuously during the FGD into Swedish to MBo, who made field notes and asked clarifying questions. The audio-recorded FGDs were transcribed from French into Swedish text.
Data analysis
The data were analysed through an inductive approach according to content [ 24 ]. First, the text was read through several times to become familiar with the data. Next, in new readings, meaning units were marked, compared, and sorted into codes, which were then compared and clustered into subcategories, generic categories, and one main category. After several analysis refinements moving from text details to wholeness, the results were finalised. An example of the analysis process is shown in Table 2 .
The midwives’ challenges, and the factors motivating them to remain in their workplace in the DRC, are summarised in one main category—Loving one’s work makes it worthwhile to remain in one’s workplace, despite a difficult work environment and low professional status—consisting of three generic categories: Midwifery is not just a profession; it’s a calling , comprising the three subcategories (1) Saving lives through midwifery skills, (2) Building relationships with the women and the community, and (3) Professional pride; Unsupportive organisational system , comprising the three subcategories (1) Insufficient work-related security, (2) No equitable remuneration system, and (3) Hierarchical management structures; and Inadequate pre-conditions in the work environment , comprising the two subcategories (1) Lack of resources and equipment and (2) Insufficient competence for difficult working conditions (Table 3 ).
Midwifery is not just a profession; it’s a calling
The generic category Midwifery is not just a profession; it’s a calling concerns the midwives’ motivation in their work, which included saving lives through midwifery skills, building relationships with the women and the community, and having professional pride.
Saving lives through midwifery skills
Saving the lives of mothers and newborns was a strong motivating factor. Specifically, it was motivational to have skills within the midwifery domain, such as managing the full continuum of care during pregnancy and labour, supporting women in having normal physiologic births, or being able to handle complications:
I feel very good when I can handle the complications during a birth and afterwards; for example, if a woman comes in unconscious and I can handle it. (FGD1)
The midwives felt that their main role was to save lives and thereby contribute to decreasing the country’s high maternal mortality rate. Saving a woman’s life was valued as a measurement of high-quality care. This was a driving force in their daily work and made them feel motivated, as their work made a difference for the survival of women in the DRC:
I have given my life to save lives (FGD3) // We have decided to always be at the women’s side, to save their lives. We cannot break this promise to save their lives. (FGD2) //I want to continue working at my workplace to be able to make a difference and decrease the maternal mortality. (FGD4)
Building relationships with the women and the community
Building relationships with the women and playing a significant role in the community were central to and valued by the midwives. They repeatedly expressed having strong feelings of love for the women and for the community and experienced their work as important and meaningful:
It’s the love for the sick that motivates us. (FGD7) // I want to continue this work because of the love for our country and the population. (FGD1)
Mutual trust and a duty to the community characterised the midwives’ perceptions of their relationships with the women. They felt appreciated and trusted by both the women and the community. They emphasised that they wanted to continue their work in order to be loyal to their patients and to society as a whole:
I feel good when the woman has trust in us … she surrenders herself in confidence to us. (FGD6) // We have built trust with the women and made them feel safe. (FGD5) // If we abandon our work, we leave a people that will suffer. (FGD2)
Professional pride
The midwives radiated professional pride; they had a profession that they enjoyed and believed in. Their position in society to help women also gave them feelings of satisfaction and accomplishment:
We have studied to work as midwives. We are proud of our profession, to help women. (FGD4) // The greatest motivation is that we are midwives and we love the profession. (FGD1)
The midwives felt that their role as midwives was essential because of their ability to help women. This resulted in feelings of commitment, duty, and resilience, despite their difficult working conditions, which in turn characterised their sense of professional identity and gave them motivation. Sacrificing themselves for the belief in their profession was motivational, in the sense of making a difference for the women:
Because we are midwives, we have to continue helping the women. We are midwives whether or not we are motivated. (FGD2) // It is our profession! We have chosen our profession and must continue. We have committed ourselves and will continue to be midwives, regardless of the situation. This is our calling; we exist to work as midwives. (FGD6)
Unsupportive organisational system
The generic category Unsupportive organisational system describes how midwives were challenged by insufficient work-related security, hierarchical management structures, and the lack of an equitable remuneration system.
Insufficient work-related security
The midwives’ work environment was surrounded by insecurity. Especially during night shifts, due to the darkness, they often felt frightened on their way to and from work. Many years of conflict and continuous unstable security in society had installed fear in them, and they were afraid of being a victim of aggression, including rape. Practical constraints increased their insecurity, such as the lack of transportation to and from work and the inability to pay for secure transport such as a taxi or a motorbike, or not having a flashlight or money to pay for batteries, further amplified their feelings of insecurity and fear:
Working at night makes us insecure… we are always afraid in the dark. (FGD3) // We are all scared of the military, scared of being raped… The conflict was in 2018 and there were two doctors and midwives who were killed then. (FGD2)
A professional identity card could protect them, but not all midwives had received such a card from their employer:
We bring ID card to work. When the military comes and we can show our ID card, there are no approaches from the military. (FGD1)
No equitable remuneration system
There was no equitable remuneration system in place, and the midwives stressed the lack of regular payment or compensation for their employment. There was no fixed amount of money for their services that was paid on a monthly basis. Some expressed that their salary was too low and was not sustainable for them to live on, while others described having more of a monetary incentive, equal to US$ 5, than any actual salary. At some facilities, they were dependent on the patient fees in order to get paid. This meant that sometimes the midwives had to take up a second job in order to meet their everyday needs, which resulted in feelings of increased everyday stress and being underappreciated:
We cannot live on our salary. We work shifts and then have to work in the fields on our days off. (FGD6) // We don’t receive any income from the state, only through patient fees. Our work is voluntary work, we don’t even get soap. (FGD9)
Hierarchical management structures
Another challenge involved hierarchical management structures within the healthcare facility. Several midwives expressed feeling insecure and uncertain in their employment and their relationships with their supervisors. Many midwives had no employment contract, while others could be punished for, for example, being late to work by losing their job or being sent home for 3 months without work or payment. Not feeling safe in their job caused the midwives to feel uncertain in their everyday work situation:
We cannot complain, we lose our job if we complain… We have never signed anything when we started our employment here, we don’t have any contracts. (FGD4) // If you question the supervisor you can be let go without pay for three months… So I don’t say anything, because then I won’t get paid. (FGD1) // I am afraid that I won’t get to work on time, which can be due to not being able to find a motorbike or not being able to pay for it. (FGD4)
A few midwives who worked at a private healthcare facility did not have such an unsecured working condition. They could even question work routines without being afraid of losing their job.
Many midwives reported being placed at departments where their specific midwifery professional competence was not useful, such as surgery/internal medicine wards, the pharmacy, or the administration office. They could be moved around according to their supervisor’s preferences rather than their specific domain. Not being allowed to practise their profession and not receiving recognition for their work made it very demanding to continue their job, leading the midwives to feel frustrated and undervalued. A need for support from the local midwifery association was expressed:
They don’t make use of our potential as midwives; we have to work in other departments like medicine, paediatrics, surgery… I feel like I’m used as an object. (FGD4) // We want the state to care about midwives. (FGD6)
Inadequate pre-conditions in the work environment
The generic category Inadequate pre-conditions in the work environment describes how the midwives were challenged by inadequate pre-conditions at work, including a lack of resources and equipment as well as insufficient competence for difficult working conditions. The midwives simply lacked the means to carry out their work and provide quality care.
Lack of resources and equipment
For the midwives, a lack of resources and equipment to perform their daily work duties posed a significant challenge. This problem concerned several areas, such as space and function and a shortage of the basic, essential clinical equipment needed to provide care during labour, birth, and after. This could include a lack of birth sets, syringes, caesarean kits, blood pressure cuffs, oxygen, medicines, and vacuum extractors. There was also a shortage of personal protective equipment like work uniforms, visors, gloves, boots, soap, birth caps, and disinfectant. This caused the midwives to feel worried about being infected with communicable diseases. Working without sufficient resources impaired not only the safety of their work environment but also their sheer ability to carry out work of sufficient quality:
We have not received any external support to rebuild the hospital after the war… We’re working under tough conditions. We only have one birthing set… one vacuum extractor, but it does not work. (FGD7) // I feel bad when we have learned different techniques like vacuum extraction and revival, but cannot perform these due to a lack of material… We want work clothes; we have to pay for them ourselves. We need boots to protect us, and medicines. (FGD3)
The facilities were described as inadequate for meeting the needs of the number of patients coming to the clinics. A lack of birthing beds could mean that two to three women had to share one bed. There was often a shortage of electricity, which led to a lack of lighting and the incubator and revival machines not functioning. Lacking materials and having inadequate facilities to work in served as a constant source of frustration for the midwives, and was a major challenge to their ability to provide care.
Insufficient competence for difficult working conditions
The midwives expressed having insufficient competence in providing care in critical conditions, such as resuscitation of mother and child, the third stage of labour, and the postpartum period. They described thanking God if things went well, or hoping for good outcomes, rather than trusting their competence to handle the possible complications. Another tough working condition was when poor, dirty women, for instance, sex slaves, came to the hospital seeking care. This often caused the midwives to feel frustrated, wishing they had more resources to help these women. The working conditions led to the midwives often feeling tired after work and not having the time or means to eat. Insufficient competence, in combination with difficult working conditions, resulted in their undertaking an overwhelming personal responsibility and feeling inadequate at work. The midwives often brought these feelings home, which led to negative effects on their general well-being:
I feel bad when mother and child die… or when a birth ends with excessive bleeding… If I can’t see that I have done enough I blame myself. This effects how I feel at home, can disrupt my sleep. (FGD5)
To manage the difficult situations described above, the midwives stressed needing additional competence through proper, sufficient education and continual professional development. They felt that they needed more education and training in all areas in order to increase their general competence, as their skills were insufficient. This would result in increased confidence as midwives, and better outcomes in their work. Due to the education reform of 2013, they felt an increased need to update their knowledge. However, training was not incorporated in all working environments and, when it was provided, it often did not include everyone, which led to unequal conditions and stagnation of the midwives’ competence:
We have the old education system and because of the new education reform we need to be updated in the new educational programme. We lack competence in how to support during labour, how to avoid bleeding… (FGD8) // We really need further education in order to increase our professional capacity. We do not receive continual training. (FGD2)
In this qualitative interview study with midwives working in two of the 26 provinces of the DRC, the results show that the main force motivating and driving the midwives to work is a strong feeling of love for their work. Their working conditions are extremely difficult. However, they regard midwifery as not just a profession but a calling, which makes the job worthwhile. In tune with what was recently found in the global consultation mentioned earlier, they are generally very committed to providing care to women and newborns due to a high professional conscience and loyalty to their patients, despite their tough working environments [ 14 ].
The DRC midwives in our study were motivated to continue working and building relationships with the women and the community, driven by feeling a strong professional pride and having the skills to save lives. On the other hand, they faced challenges in the remaining of their work due to factors such as an unsupportive organisational system, with inadequate pre-conditions in the work environment. This is in line with a conceptual framework on health worker motivation presented by Franco et al. [ 19 ], which defines key determinants influencing workers motivation at individual, organisational, and cultural and community levels.
Among the challenging work factors that the DRC midwives in our study experienced was an unsupportive organisational system, which was linked to insufficient work-related security, a lack of a proper remuneration system, and hierarchical management structures. Filby et al. have concluded that such factors are the result of the lack of status of, and respect for, the midwifery profession. This in turn puts midwives’ occupational health and safety at risk [ 15 ].
The lack of an equitable remuneration system and insufficient security when going to and from work that was experienced by the DRC midwives in our study has also been confirmed to be highly problematic in other studies in low- and middle-income settings [ 15 , 16 ], leading to serious challenges in managing daily life and accentuating the profession’s low status. In settings where salaries are extremely low or unpredictable, proper remuneration is seen as crucial to worker motivation [ 25 , 26 , 27 ].
The World Health Organization (WHO) emphasises work security, proper remuneration, and professional health and safety as core dimensions of strengthening the health workforce and ensuring decent employment terms. This can serve as guidance for health systems in general, in order to build more reliable and supportive organisational systems [ 28 ].
With regard to remuneration in particular, the midwifery workforce in the DRC, as was also found in the global consultation of midwives, suffer from insufficient and irregular remuneration [ 14 ]. This corresponds to staff within weaker professions in the DRC who also work without being on a payroll, and thus depend on fees levied by health facilities on patients. In contrast, it has been reported that there are many cases of ghost workers, i.e. people who are paid but are non-existent in the health services [ 29 ]. According to a recent study by WHO, this could be detected and prevented through increased transparency and accountability in payroll processes, improved recordkeeping and strong record management systems, monitoring of human resources for health, and the use of specific technology tools [ 30 ]. Removing such ghost workers could result in substantial savings that could be used to improve the remunerations of working healthcare professionals.
For midwives in the DRC and elsewhere, to be able to provide their full scope of midwifery practice informed by the International Confederation of Midwives [ 31 ], and thereby contribute to improved health outcomes for women, newborn, and families [ 1 ], it is of critical importance that they are deployed within their specific professional area, i.e. sexual, reproductive, and maternal healthcare. The midwives in our study described being moved around by management to different departments far from their competence area, which resulted in their competence not being fully used. It also made them feel devalued and underappreciated. This is not unique to midwives in the DRC; however; midwives in many parts of the world experience that there is a poor understanding and use of their professional competence, and they often feel undervalued [ 14 , 15 , 16 ].
Strengthening the midwifery association has been identified as one way to improve the status of the midwifery profession. This was also mentioned by the midwives in our study. It is known that ensuring strong midwifery associations, and thereby establishing autonomy and recognition for the profession, is imperative for raising midwives’ status and enabling them to provide quality care [ 14 ]. Thus, in accordance with a global study conducted by Lopes et al. [ 32 ] including 73 midwives’ associations representing 67 countries, it is also necessary for the DRC to strengthen the country’s midwifery association and to include midwives in policy discussions concerning the profession—which, although it is stable and recognised by the government, still struggles to ensure education, regulation, and respect for the autonomous profession [ 9 ].
Inadequate pre-conditions in the DRC midwives’ work environment was another challenge found in our study. The midwives lacked both functioning healthcare facilities and materials, which added to their already difficult work situation. Constantly having a shortage of resources and equipment prevented them from working safely and jeopardised their provision of quality care. Lacking safety equipment is known to make midwives more vulnerable to infectious diseases [ 15 ], and having appropriate facilities and sufficient resources is regarded as necessary for worker motivation and performance [ 28 ]. Therefore, it is important that health systems improve the availability of resources and functioning facilities to fit the care services, in order to enable midwives to provide care of high quality.
The midwives in this study expressed a need for additional professional competence as part of their continuing professional development. The education system for midwives in the DRC is known to need significant improvement [ 9 ] and if reformed could increase both the capabilities and status of the profession. Already burdened by a high maternal mortality rate and heavy workloads, and with inadequate competence, time, and resources to do more than the absolute necessary work, the midwives in this study were left feeling frustrated and less motivated. These findings correspond to the global consultation [ 14 ], in which midwives experienced difficult work situations due to heavy workloads and shortage of staff, high levels of maternal and newborn mortality rates, and a lack of sufficient competence to autonomously manage work tasks, which made them feel frustrated, guilty, and inadequate. As such, this can contribute to distress and burnout, which in turn prevents midwives from being able to provide quality care and can eventually cause them to leave the profession [ 15 ]. This phenomenon does not seem to differ between settings in high-, middle-, and low-income countries [ 16 , 18 ]. Therefore, in order to retain midwives in their work positions and enable them to provide quality care, it is crucial to create supportive work environments by ensuring sufficient pre-conditions [ 33 ]. Hence, midwives need to take the power to influence their own situation [ 15 ]. When midwives are included in customising their work environments, it has proven to result in improved quality of care for women and newborns around the globe [ 14 ], and it is suggested that the DRC also embraces this.
Methodological considerations
This study has limitations. Two that particularly stand out are common criticisms of FGDs when it comes to obtaining valid data: (i) the possibility that the participants may not have expressed their honest and personal opinions about the topic under discussion and (ii) compared to individual interviews, there is no guarantee of depth in the topic being discussed [ 34 ]. However, we chose to conduct FGDs to encourage a discussion among the participants that would enable them to be inspired by each other and continue with reflections stimulated by each other’s statements. Our conviction is that this methodology favoured openness as it enhanced a sense of community, sharing common problems. We therefore ensured that everyone could express their opinions through the open questions and by being attentive to allow everyone the opportunity to talk. The number of participants per group—six to eight—enabled a good discussion climate and ensured that everyone’s views were heard. A strength was that the participants represented different healthcare facilities, both public and private, and different regions, and thereby offered deeper and more varied experiences and reflections. Despite that the interviews were conducted in only two out of 26 provinces, we find them valuable as a predominant strength of the study is that the working environment of the midwives in the DRC has not been made visible in earlier studies. In general, there is a shortage of recent studies on what motivates midwives in their work globally, which this study addresses. It is worth noting that the findings regarding the challenges and motivating factors for remaining in their workplace mentioned by the midwives in this study are context-specific and that different countries and settings must interpret these in light of their own context. The first and last authors (MBo and MBe) are Swedish researchers and midwifery experts and are both familiar with the DRC context and with conducting research in low-income settings. In this study, being a foreigner proved to be a strength in the sense that the participants were keen to explain their challenges and factors that motivate them to remain in their workplace in the DRC to someone who was not from there. The third author (BK), who grew up in the DRC and is a researcher and an expert on systems strengthening, took part in the steps of the research process and acted as an outsider in the interpretation of the results.
The findings of this investigation of challenges and factors motivating DRC midwives to remain in their workplace should be of serious concern to the profession and its leaders. Midwives in the DRC are driven by a strong professional conscience, and their provision of care for women in childbirth depends on their feeling that their professional work is a calling. To overcome an unsupportive organisational system and inadequate pre-conditions in the working environment, which hinders midwives in providing high-quality care, in accordance with the 2020 Triad Statement made by the International Council of Nurses, the International Confederation of Midwives, and the World Health Organization [ 35 ], it is suggested that policymakers, employers, and regulators in the DRC and settings with similar conditions coordinate actions in the following:
✓ Increasing funding to educate midwives, informed by international standards
✓ Prioritising and enforcing policies to include adequate remuneration to attract and retain midwives within midwifery practice
✓ Involving midwives’ associations in policy and planning concerning the midwifery workforce
✓ Ensuring that midwives are working to their full scope of practice
✓ Ensuring that midwives’ working environments are safe and well equipped (functional facility with water, supplies and commodities, communication and transportation for referral)
✓ Providing an enabling environment for midwifery care to improve conducive working conditions that enable midwives to provide respectful care
Availability of data and materials
Available upon request.
Abbreviations
- Democratic Republic of Congo
Sustainable Development Goal
International Confederation of Midwives
Soins de Santé Primaires en Milieu Rural
Focus group discussion
World Health Organization
Homer CS, Friberg IK, Dias MA, ten Hoope-Bender P, Sandall J, Speciale AM, et al. The projected effect of scaling up midwifery. Lancet (London, England). 2014;384(9948):1146–57.
Article Google Scholar
Renfrew MJ, McFadden A, Bastos MH, Campbell J, Channon AA, Cheung NF, et al. Midwifery and quality care: findings from a new evidence-informed framework for maternal and newborn care. Lancet (London, England). 2014;384(9948):1129–45.
UNFPA WHO, ICM. The state of the world’s midwifery 2014: a universal pathway. New York: A woman’s right to health; 2014.
Google Scholar
Ministère du Plan et Suivi de la Mise en œuvre de la Révolution de la Modernité (MPSMRM) MdlSPMaII. Democratic Republic of Congo Demographic and Health Survey 2013-14: key findings. Rockville, Maryland; 2014.
United Nations Population Fund. Country programme document for the Democratic Republic of the Congo. New York: New York; 2020.
Miller S, Abalos E, Chamillard M, Ciapponi A, Colaci D, Comandé D, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. The Lancet. 2016;388(10056):2176–92.
World Health Organization. Democratic Republic of the Congo: improving aid coordination in the health sector. Geneva; 2015.
Van Lerberghe W, Matthews Z, Achadi E, Ancona C, Campbell J, Channon A, et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. Lancet (London, England). 2014;384(9949):1215–25.
Bogren M, Ndela B, Toko C, Berg M. Midwifery education, regulation and association in the Democratic Republic of Congo (DRC) - current state and challenges. Global Health Action. 2020;13(1):1717409.
World Health Organization. Strategies toward ending preventable maternal mortality. Geneva; 2015.
Koblinsky M, Moyer CA, Calvert C, Campbell J, Campbell OM, Feigl AB, et al. Quality maternity care for every woman, everywhere: a call to action. Lancet (London, England). 2016;388(10057):2307–20.
Bogren M, Kaboru BB, Berg M. Barriers to delivering quality midwifery education programmes in the Democratic Republic of Congo—an interview study with educators and clinical preceptors. Women and Birth. 2020.
United Nations Population Fund East and Southern Africa Regional Office. The state of the world’s midwifery: analysis of the sexual, reproductive, maternal, newborn and adolescent health workforce in East & Southern Africa. Johannesburg; 2017.
World Health Organization, International Confederation of Midwives, White Ribbon Alliance. Midwives’ voices, midwives’ realities: findings from a global consultation on providing quality midwifery care. Geneva; 2016.
Filby A, McConville F, Portela A. What prevents quality midwifery care? A systematic mapping of barriers in low and middle income countries from the provider perspective. PloS one. 2016;11(5):e0153391.
Bogren M, Erlandsson K, Byrskog U. What prevents midwifery quality care in Bangladesh? A focus group enquiry with midwifery students. BMC Health Services Research. 2018;18(1):639.
Byrskog U, Akther HA, Khatoon Z, Bogren M, Erlandsson K. Social, economic and professional barriers influencing midwives’ realities in Bangladesh: a qualitative study of midwifery educators preparing midwifery students for clinical reality. Evidence Based Midwifery. 2019;17(1):19–26.
Suleiman-Martos N, Albendín-García L, Gómez-Urquiza JL, Vargas-Román K, Ramirez-Baena L, Ortega-Campos E, et al. Prevalence and predictors of burnout in midwives: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(2):641.
Franco LM, Bennett S, Kanfer R. Health sector reform and public sector health worker motivation: a conceptual framework. Social Science & Medicine. 2002;54(8):1255–66.
Campbell J. The route to effective coverage is through the health worker: there are no shortcuts. The Lancet. 2013;381(9868):725.
Cramer E, Hunter B. Relationships between working conditions and emotional wellbeing in midwives. Women and Birth. 2019;32(6):521–32.
Polit DF, Beck CT. Essentials of nursing research: appraising evidence for nursing practice. 8th ed. Philadelphia: Lippincott Williams & Wilkins; 2014.
Ministry of Public Health. DRC: National Health Accounts 2019. Kinshasa; 2019.
Elo S, Kyngas H. The qualitative content analysis process. Journal of Advanced Nursing. 2008;62(1):107–15.
Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution. The Lancet Global Health. 2018;6(11):e1196–e252.
Mathauer I, Imhoff I. Health worker motivation in Africa: the role of non-financial incentives and human resource management tools. Human Resources for Health. 2006;4:24.
Willis-Shattuck M, Bidwell P, Thomas S, Wyness L, Blaauw D, Ditlopo P. Motivation and retention of health workers in developing countries: a systematic review. BMC Health Services Research. 2008;8:247.
World Health Organization. Global strategy on human resources for health: workforce 2030. Geneva; 2016.
DFID. Ghost workers: the politics, incentives and impact of staff inflation. DFID DRC Evidence, Analysis and Coordination Programme (EACP). Unpublished; 2017.
WHO. Findings from a rapid review of literature on ghost workers in the health sector: towards improving detection and prevention. Geneva; 2020.
International Confederation of Midwives. International definition of the midwife: ICM; 2017 [Available from: https://internationalmidwives.org/assets/files/definitions-files/2018/06/eng-definition_of_the_midwife-2017.pdf ].
Lopes SC, Titulaer P, Bokosi M, Homer CSE, ten Hoope-Bender P. The involvement of midwives associations in policy and planning about the midwifery workforce: a global survey. Midwifery. 2015;31(11):1096–103.
International Confederation of Midwives. Strengthening midwifery globally: strategy 2017-2020 The Hague: International Confederation of Midwives; 2017 [Available from: https://www.internationalmidwives.org/assets/files/general-files/2018/04/final-copy-icm-strategy-2017-20-online.pdf ].
Barbour RS. Focus groups. In: Bourgeault I, Dingwall R, Vries Rd, editors. The SAGE handbook of qualitative methods in health research. London: Sage; 2010. p. 327-352.
Duff E. INTERNATIONAL NEWS - September 2020. Midwifery. 2020;88:102811.
Download references
Acknowledgements
We would like to express our sincere appreciation to all the midwives who participated in this study. We also want to thank SANRU Asbl, who provided logistical support throughout our data collection in the DRC, and Philemon Mulongo, who provided us with information to help us understand the remuneration system for midwives and the cost of facility-based childbirth in the DRC.
The study was conducted with financial assistance from the Swedish International Development Cooperation Agency, administrated by SANRU Asbl in the DRC. Open access funding provided by University of Gothenburg.
Author information
Authors and affiliations.
Institute of Health and Care Sciences, Sahlgrenska Academy, University of Gothenburg, Arvid Wallgrens backe 1, 413 46, Gothenburg, Sweden
Malin Bogren, Malin Grahn & Marie Berg
Department of Obstetrics, Sahlgrenska University Hospital, Region Västra Götaland, Diagnosvägen 15, 416 50, Gothenburg, Sweden
Malin Grahn & Marie Berg
Swedish Embassy in Kinshasa, Democratic Republic of Congo, 93 Avenue Roi Baudouin, Kinshasa-Gombe, Democratic Republic of Congo
Berthollet Bwira Kaboru
You can also search for this author in PubMed Google Scholar
Contributions
MBo and MBe designed the study and collected the data. The data analysis and presentation of results were completed by MG in collaboration with MBo and were validated by MBe. MG and MBo prepared the first draft of the paper, to which all authors contributed important revisions. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Malin Bogren .
Ethics declarations
Ethics approval and consent to participate.
All study participants provided written informed consent. Ethical approval was obtained from the Research Ethics Committee at the Congo Protestant University, 13 August 2019 (reference number CEUPC 0059).
Consent for publication
Not applicable.
Competing interests
One author (BK) is employed by the funder. The authors alone are responsible for the views expressed in this publication, which do not necessarily represent the decisions or policies of the funder.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:..
Interview guide.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bogren, M., Grahn, M., Kaboru, B.B. et al. Midwives’ challenges and factors that motivate them to remain in their workplace in the Democratic Republic of Congo—an interview study. Hum Resour Health 18 , 65 (2020). https://doi.org/10.1186/s12960-020-00510-x
Download citation
Received : 14 July 2020
Accepted : 07 September 2020
Published : 17 September 2020
DOI : https://doi.org/10.1186/s12960-020-00510-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Midwifery profession
- Health workforce
- Quality care
- Low- and middle-income countries
Human Resources for Health
ISSN: 1478-4491
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 24 October 2024
Pioneering point-of-care obstetric ultrasound integration in midwifery education – the MEPOCUS study
- Julia Groos 1 ,
- Adeline Walter 1 ,
- Ruben Plöger 1 ,
- Brigitte Strizek 1 ,
- Ulrich Gembruch 1 ,
- Agnes Wittek 1 na1 &
- Florian Recker 1 na1
BMC Medical Education volume 24 , Article number: 1209 ( 2024 ) Cite this article
Metrics details
Ultrasound technology is indispensable in perinatal care due to its non-invasive and painless nature, offering vital insights into foetal development and childbirth. With the academisation of midwifery in Germany, there is a growing necessity to incorporate ultrasound training into midwifery education. This paper discusses the development and implementation of an introductory obstetric ultrasound curriculum tailored for midwifery students, focusing on fundamental ultrasound techniques in obstetrics.
Materials and methods
We used Kern’s six-step approach of curricular development comprising [ 1 ] problem identification and general needs assessment [ 2 ], needs assessment of the targeted learners [ 3 ], goals and objectives [ 4 ], educational strategies [ 5 ], implementation, and [ 6 ] evaluation and feedback. The individual components of the curriculum were meticulously designed based on comprehensive literature reviews, thorough consultations with experienced ultrasound experts and evaluated needs of participants prior to the course instruction.
Twenty-seven ultrasound-naive midwifery students participated in the newly developed obstetric ultrasound course. Structured as a modular and integrated framework, the course aimed to provide theoretical and practical instruction in basic obstetric ultrasound, with intrapartum sonography and focused assessment with abdominal sonography for trauma (FAST) as key supplementary specialisations. The results demonstrated a significant increase in the students’ overall knowledge and practical skills, as evidenced by the median post-course total score rising from 20 to 60 out of 75 ( p < 0.001) in the objective structured clinical examination (OSCE) and from 9 to 19 out of 20 ( p = 0.001) in the knowledge test. Additionally, students reported high satisfaction with the course and noted substantial personal benefits.
The integration of basic obstetric ultrasound training within the midwifery curriculum is feasible and effective to teach fundamental knowledge and skills of obstetric ultrasound examinations to midwifery students. Expansion, standardisation and regulatory structures are critical components for a continued improvement and realistic integration into midwifery educational frameworks and thus the further development of the midwifery profession.
Peer Review reports
The widespread utilisation of ultrasound as a diagnostic tool in pregnancy care has become increasingly prominent in recent years [ 1 ]. Its painlessness, radiation-free nature, and non-invasive character contribute to its high value, enabling the monitoring of foetal development and the well-being of both mother and child [ 2 , 3 , 4 ]. Especially, employing Point-of-Care Ultrasound (PoCUS) allows for flexible, precise, and rapid decision-making, hence its useful integration into daily practice within the delivery ward [ 1 ]. Here, the intrapartum usage of ultrasound enables diagnosing foetal head position and station and monitoring of head descent within the birth canal, thus providing assurance of favourable labour progress [ 5 ]. As a result, ultrasound technology assumes a pivotal role as an adjunctive tool to conventional diagnostic methods in both prenatal care and the delivery ward, thereby proving invaluable for midwives as well [ 4 , 6 ].
Midwives, as key providers of prenatal care, shoulder significant responsibilities in providing care for pregnant women and their infants. Considering the value of midwives in obstetric care and the significance of ultrasound within this domain, it is prudent to universally integrate ultrasound training into midwifery education [ 7 , 8 ]. From a global perspective, standardised ultrasound training for midwives has the potential to counteract the shortage of skilled ultrasound personnel, particularly prevalent in low- and middle-income countries (LMICs) [ 8 ]. This endeavour could help to better implement specific recommendations of the World Health Organization (WHO), by promoting access to early ultrasound examinations for pregnant women [ 9 , 10 ]. In contrast to Germany, obstetric ultrasound has already become an integral component of midwifery practice in nations like Norway, where midwives obtain specialised qualifications as “midwife sonographers”, empowering them to perform ultrasound examinations independently [ 11 ]. However, with the implementation of the Midwifery Reform Act in 2020, the field of midwifery in Germany has experienced substantial changes, with a crucial step towards the academisation of midwifery. The ongoing academisation and elevation of qualification levels contribute to the development of midwifery work [ 12 ].
This trend positions ultrasound as an increasingly crucial element, with the potential to enhance the scope of midwifery practice, thereby facilitating the provision of comprehensive obstetric care. Although the foundation for the academic advancement of the midwifery profession is in place, consensus is still lacking on how to integrate and implement ultrasound training within midwifery education programmes. Therefore, our initiative seeks to initiate first steps towards the didactic incorporation of ultrasound training into midwifery education. The aim of the study was to establish a modular ultrasound course specifically designed for bachelor’s degree midwifery students and to assess the educational outcomes of this curriculum.
The objective of this study was to develop an innovative ultrasound curriculum, utilising Kern’s six-step approach, for midwifery students of the bachelor’s degree programme in Midwifery Science at the Rhenish Friedrich-Wilhelms-University of Bonn, and to evaluate the course after its implementation [ 13 ]. The degree programme is structured as a dual bachelor’s programme with a standard duration of eight semesters. The ultrasound course is being implemented for the first time within the degree programme, aiming to equip third year midwifery students with both theoretical knowledge and practical skills through informative lectures and hands-on patient practice. Given the minimal inclusion of ultrasound training in the curriculum, most midwifery students possess little to no familiarity with ultrasound techniques, categorising them as novices in this area. Consequently, we utilised Kern’s six-step approach, which encompasses problem identification, needs assessment for targeted learners, setting goals and objectives, formulating educational strategies, implementation, and evaluation with feedback. Data acquisition and analysis were performed in compliance with protocols approved by the Ethical Committee of the University of Bonn (No. 179/23-EP). A declaration of consent was obtained from each study participant.
Problem identification
In order to identify the most appropriate content for a comprehensive obstetric ultrasound curriculum for midwifery students, we undertook a detailed examination of several main sources, including the German Association of Midwives (Deutscher Hebammenverband, DHV), the European Midwives Association (EMA), the Global Midwives’ Hub, the International Confederation of Midwives (ICM) and the International Society for Ultrasound in Obstetrics and Gynecology (ISUOG). Additionally, we examined the published literature to research essential ultrasound competencies or algorithms deemed vital for midwives and to identify any potential ultrasound curricula already proposed for midwifery students.
Needs assessment of targeted learners
Through a systematic literature review, we conducted an in-depth examination of international published literature to identify the specific needs of targeted learners within the relevant educational context [ 14 ]. Following this analysis, we discussed the identified content-specific, technical, and implementation-related needs with core group members, aligning them with the competencies proposed by DHV and ICM and tailoring them to our targeted learners. To ensure an adequate needs assessment, participating students were surveyed about their requirements before the course started, identifying a clear need that was also confirmed during the course’s implementation and taken into account accordingly. Additionally, a post-course survey was conducted to thoroughly assess the learners’ specific needs, enabling to effectively adapt and prioritise the content of potential subsequent courses.
Goals and objectives
Identified content-specific, technical, and implementation-related needs were operationalised with regard to their technical, physiological, and pathological properties. As a result, goals and objectives were formulated through a synthesis of literature review, survey results, as well as the clinical expertise and previous evaluation of ultrasound curricula of panel members. We established a scientific Delphi process to develop the curriculum content and define learning objectives. This process involved clinical members possessing qualification levels I–III of the German Society for Ultrasound in Medicine (Deutsche Gesellschaft für Ultraschall in der Medizin, DEGUM) from the relevant specialty. These experts were integral to the Delphi methodology, which was conducted over two rounds. The process utilised multilevel, self-completed questionnaires based on a 9-point Likert scale, coupled with individual feedback sessions. The author collaborated with an additional ten members to facilitate this iterative method, ensuring a comprehensive and consensus-driven approach to curriculum development.
Educational strategies
In order to address the defined learning goals and objectives, encompassing both theoretical knowledge and practical skills, various educational strategies were integrated in the curriculum. Within the selection process and with regard to the course content and structure, different educational methods were thoroughly analysed, compared and discussed. We used methods developed, used, and evaluated by the DEGUM for ultrasound training: lectures for the theoretical knowledge and supervised hands-on training for the practical scanning [ 15 ]. Furthermore, and in addition to traditional lectures, theoretical knowledge was delivered through a blended learning concept, allowing participants to access the teaching content digitally. The combined approach within the curriculum thus ensured comprehensive coverage of all areas and aspects.
Implementation
The curriculum was delivered in two periods: from October 2023 to January 2024, and from April 2024 to July 2024, corresponding to the fifth and sixth semesters of the first academic year. Students were assigned to each semester in alphabetical order. As part of the curriculum development process, core group members participated in medical didactic training programmes to ensure they were well-prepared for the demands of implementing the curriculum. Board-certified experts in ultrasound and didactics, who had experience in ultrasound teaching, also contributed to the development and implementation of the curriculum [ 16 ]. Furthermore, the necessary infrastructure for the ultrasound curriculum was quickly established.
Evaluation and feedback
To evaluate the attainment of predefined learning objectives and consequently gauge the success of the MEPOCUS curriculum, complementary methodologies were implemented at the start and completion of each course period, with an interval of three months between the respective evaluation points. These included an objective structured clinical examination (OSCE), administered in both semesters, as well as a theoretical single-choice test and a questionnaire, used in the second semester. All three evaluation methods were specifically developed for the purpose of this study. The knowledge test was designed in digital format and comprised a total of 20 questions covering key content of the seven modules of the course. For each question, students were required to choose the correct answer from four available options, with each correct answer earning one point, and a total possible score of 20 points. The OSCE consisted of three stations with clinical, case-based tasks solvable using course-acquired knowledge and skills, each worth 25 points, resulting in a total possible score of 75 points. Task sheets, assessment forms and instructions were tailored to defined objectives. Practical assessments in each room involved ultrasound examinations on a volunteer pregnant woman, evaluated by an obstetrics ultrasound specialist. Both the test and OSCE were applied in identical format before and after the course, with statistical analyses used to identify performance variances. Furthermore, a digital questionnaire was developed to collect students’ perspectives, self-reflection and feedback anonymously before the initial and after the final OSCE. The questionnaire included both Likert scale and open-ended questions. A 4-point Likert scale was used to evaluate students’ perspectives in the first part (1 = strongly disagree, 4 = strongly agree) and their self-assessment in the second part (1 = very unconfident, 4 = very confident). The questions were the same in both the pre- and post-course versions. As a third part, Likert styled questions were used in the pre-course questionnaire to gather midwives’ previous experiences with ultrasound (1 = strongly disagree, 4 = strongly agree) and in the post-course questionnaire to obtain course evaluations in combination with open-ended questions. All students and voluntary pregnant participants were comprehensively informed about the procedures prior to their participation, and informed consent was obtained from each individual.
Statistical analysis
Statistical analysis was performed using Microsoft Excel software, version 2016 and SPSS (IBM SPSS Statistics for Windows, version 29.0.2.0). The results that were analysed, comprised the students’ performance on final OSCE, written test and questionnaire, compared to their initial assessments. Specifically, the students’ scores for each OSCE station and the total scores of pre- and post-course OSCE and test were reported as medians, mean values and standard deviations, with their 95% confidence interval. The normality of data distribution for the scores was evaluated using the Shapiro-Wilk test and histograms. Given the absence of normality in the data distribution, significant changes in pre- and post-course scores for all students with matched pre- and post-course scores were calculated using Wilcoxon signed-rank test. P values less than 0.05 were considered statistically significant.
An ultrasound curriculum specifically tailored for students of the inaugural Bachelor’s programme in Midwifery Sciences has been developed. The course’s emphasis on competency and quality is maintained by aligning with international and national guidelines, as well as engaging board-certified ultrasound experts and acclaimed didactic specialists. As a local initiative, our course represents an initial step in study-integrated ultrasound teaching for midwives.
In absence of specific recommendations for ultrasound training tailored to midwives, several main sources increasingly adjust ultrasound proficiency to the essential competencies for basic midwifery practice. Accordingly, the International Confederation of Midwives (ICM) included the use of ultrasound to confirm pregnancy, estimate gestational age, and assess the well-being of both mother and child in its competency profile for midwives [ 17 ]. Similarly, the German Association of Midwives (Deutscher Hebammenverband, DHV) is dedicated to ensuring that graduates of the German midwifery degree programme attain proficiency in ultrasound application as an integral component of their academic training and has meticulously articulated this requirement within a carefully developed competency profile [ 18 ]. However, given the emergent nature of the topic in Germany, there is currently no standardised ultrasound curriculum integrated into the midwifery curriculum in Germany. Consequently, there exists a necessity for standardised ultrasound training programmes for midwifery students in Germany to achieve the competencies outlined by the ICM and DHV.
Needs assessment of target learners
Following an extensive review of the international literature, alongside in-depth surveys, discussions, and meticulous adjustments, we systematically elucidated the needs of the participants in our ultrasound course. Accordingly, it was determined that midwifery students require an integrated educational approach that combines theoretical teaching with practical demonstration in group settings, as well as opportunities for independent application. Given their demanding schedules, it was also deemed essential that students have the ability to access course materials and engage with content independently, outside of the designated in-person events. Theoretical instruction was seen as a fundamental component, covering key topics such as ultrasound physics and technology, basic antepartum examinations like key biometric parameters, foetal presentation and foetal count, through to the evaluation of placental positioning and amniotic fluid volume [ 19 ]. Additionally, it was recognised that inclusion of essential intrapartum sonography elements and the focused assessment with sonography for trauma (FAST), according the FAST protocol, which includes the four standard exam views (the right upper quadrant, left upper quadrant, subcostal cardiac, and pelvis) presents a crucial element [ 20 , 21 ]. In general, focusing on the fundamentals of ultrasound examination was deemed more effective than delving into detailed specifics. Hands-on training of theoretical content, guided by experienced ultrasound experts, was seen as a core component, necessitating a sufficient timeframe. Instruction and direct application on pregnant women were particularly valued for providing specific hands-on experience while fostering communicative skills and professional conduct. Furthermore, independent and autonomous ultrasound examinations in simulated scenarios were recognised as a vital component. The targeted needs assessment provided us with essential insights into prevailing pedagogical approaches, instructional content, and identified deficiencies that were taken into consideration during the implementation of our curriculum.
The needs assessment informed the structuring of the ultrasound curriculum into seven sequential modules. Each module was developed with specific knowledge-based and practical objectives that students are expected to achieve by the course’s conclusion. Figure 1 illustrates the learning objectives of each module, which cover fundamentals, as well as the specific topics of our course, the intrapartum sonography and FAST.
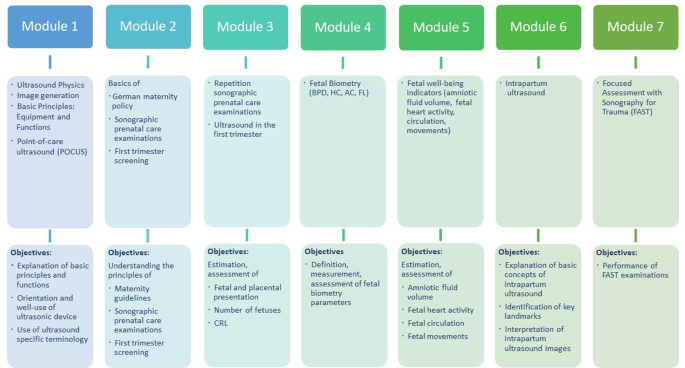
Modules and learning objectives of the obstetric ultrasound course. AC: abdominal circumference, BPD: biparietal diameter, CRL: crown rump length, FL: femur length, HC: head circumference
The seven modules of our ultrasound course encompassed both theoretical knowledge and practical competencies, necessitating the integration of diverse appropriate educational strategies (see Fig. 1 ). Theoretical knowledge is conveyed through a blended learning concept, consisting of classroom-based and online components. The initial two modules are exclusively provided online on the university’s learning platform, enabling asynchronous access that supports flexible study of fundamentals at their own pace and thus offers ideal preparation for application in class. The theoretical content of the remaining modules is delivered through traditional lectures at the beginning of each course day in-person, each conducted by a pair of team members who are both clinicians and experts in ultrasound. Following the course, the material from these modules remained accessible to students on the online platform. Additionally, they received an access code to a special e-learning system, where they could practise image recognition and interpretation at will and independently repeat the content learned in the course. In this practice-oriented course, the practical phase follows the theoretical lectures on each course day with a greater allocation of time and is conducted as supervised hands-on training sessions on voluntary pregnant women. During this phase of the course, students developed practical skills through a “See one, do one” approach, where ultrasound experts first demonstrated module-related content and then provided support and assistance to the students in carrying it out independently. The students were thus prepared to carry out independent, case-based ultrasound examinations in the final practical examination.
Our obstetric ultrasound curriculum for midwifery students was introduced by the local obstetrics department in 2023. The participating third-year students were divided into two cohorts. The first group, consisting of 14 students, attended the course in the winter semester of 2023/2024, while the second group, comprising 13 students, participated in the summer semester of 2024. The course scheduling was strategically planned to align with the students’ demanding timetables and the clinical commitments of the involved clinicians, ensuring the most suitable period for its execution. Key faculty members and essential stakeholders were engaged from the beginning of the project and the required infrastructure to sustain the curriculum was subsequently established. Each course day consisted of 60 min theoretical lectures and two hours practical training. Within the practical phases, students were divided into small groups of four to five persons, each supervised and supported by a tutor [ 16 ]. This division enabled each student to practise the module-related content and directly discuss the procedure and the images with the tutor. While practical exercises for module 7, covering the FAST domain, were conducted reciprocally among the students, pregnant women voluntarily participated in individual course sessions for all preceding modules, with their needs consistently taken into account.
Within our obstetric ultrasound curriculum, a multifaceted assessment strategy was implemented, encompassing a pre-and post-course OSCE conducted over the entire project duration of two semesters, as well as a theoretical single-choice test and a questionnaire administered in the second semester. Each assessment approach was newly developed and administered both prior to and following the completion of the course, to effectively monitor the learning progress of knowledge, practical skills, and self-efficacy in conducting ultrasound examinations. The results of the different evaluation formats are detailed separately in the following sections.
The pre-, post-course knowledge test
A single-choice knowledge test was conducted both before and after the course, using identical questions to ensure comparability. With a clear focus on evaluating the theoretical components of the course, two to three subject-specific questions were posed for each module. The questions consequently addressed the fundamentals of ultrasound knobology and handling, maternity guidelines, and foetal biometry, as well as foetal well-being monitoring, the utility of intrapartum ultrasound and the FAST examination. The comparative analysis of scores, with a maximum score of 20 points, shows that students’ total score levels were significantly lower in the pre-course knowledge test (Mdn = 9) than in the post-course knowledge test (Mdn = 19), z = -3.192, p = 0.001, r = -0.626 (see Table 1 ).
The pre-, post-course objective structured clinical examination
The OSCE was successfully conducted both prior to and subsequent to the course using identical case-based tasks and assessment criteria to facilitate a direct performance comparison. Tasks were carried out with the involvement of three pregnant volunteers, each allocated to one station. Each station evaluated content from one of three course days in presence, with basic elements from modules 1 and 2 also included in every station’s evaluation (see Fig. 2 ). Due to absences in either the first or second OSCE, 23 of the 27 midwifery students could be included in the analysis. The comparative analysis of scores, with a maximum score of 75 points, shows that students’ total score levels were significantly lower on pre-course OSCE (Mdn = 20) than on post-course OSCE (Mdn = 60), z = -4.200, p < 0.001, r = -0.619. At the first station, akin to the subsequent two, participants underwent assessment on fundamental ultrasound operation techniques with the primary emphasis on the visualisation and localisation of the placenta and foetus. The results from this OSCE station show a significant rise in score from pre- (Mdn = 10) to post-course OSCE (Mdn = 23), z=-4.204, p < 0.001, r = -0,620. The second OSCE station focused on determining the gestational age using biometric parameters and indicators of foetal well-being, such as the amount of amniotic fluid in particular. The outcomes from this OSCE station also demonstrate a marked increase in score from pre- (Mdn = 6) to post-course OSCE (Mdn = 18), z = -4.202, p < 0.001, r = -0,620. At the third station, which focused on proficiency in intrapartum ultrasound and competencies in the FAST examination, results also indicate a significant increase in score from pre- (Mdn = 4) to post-course OSCE (Mdn = 23), z = -4.110, p < 0.001, r = -0,606. Correspondent differences of station-related pre- and post-course OSCE scores are illustrated in Table 2 . The most significant improvement in scores between the pre- and post-course OSCE can be seen at station 3, indicating the greatest enhancement in knowledge and skills related to intrapartum sonography and FAST.

Evaluation criteria of Objective Structured Clinical Examination (OSCE)
The pre-, post-course questionnaire
A digital questionnaire assessing participant perspectives, self-assessment, and satisfaction was administered to all 13 students (100%) of the second semester before and after the course. The pre-course questionnaire examined the students’ prior ultrasound experience and their perspectives on its application in midwifery, while the post-course version revisited these perspectives and included a course evaluation. Identical self-assessment questions in both questionnaires highlighted potential performance improvements, evaluating perceived confidence in using ultrasound technology and performing specific examinations. These covered proficiency in handling the ultrasound probe and knobology, visualising the foetus, placenta and uterine artery, measuring biometric parameters and amniotic fluid volume, conducting the FAST examination. The questionnaire results indicate that the majority ( n = 12, 92.3%) had no prior experience with ultrasound. Nevertheless, all students initially either agreed ( n = 6, 46.2%) or strongly agreed ( n = 7, 53.8%) that they were interested in integrating ultrasound in their clinical practice. Pre-course self-evaluation shows all students had low or very low confidence in all application areas, particularly they reported very low confidence in knobology ( n = 13, 100%), measuring foetal head and abdominal circumference ( n = 12, 92.3%), measuring femur length ( n = 11, 84.6%), and conducting the FAST examination ( n = 13, 100%). Post-course results indicate an overall increase in confidence. Especially, students felt confident or very confident in handling the ultrasound transducer ( n = 9, 69.2%), visualising the foetus ( n = 11, 84.6%), measuring amniotic fluid volume ( n = 9, 69.2%), and conducting the FAST examination ( n = 8, 61.6%). However, few students still felt very unconfident in knobology ( n = 3, 23.1%) and measuring femur length ( n = 3, 23.1%). The course evaluations indicate that participants found the course helpful in improving their ultrasound skills and confidence, and that they found the focus of the training on the basics appropriate. Students found comprehensive device operation, including knobology, the orientation in the image and measuring femur length particularly challenging. Many emphasised the importance of hands-on training and expressed a desire for more sessions to better apply and consolidate their learning.
As a response to the evolving demands of the midwifery profession, this study represents the inaugural effort to develop and implement a comprehensive obstetric ultrasound curriculum within a midwifery degree programme in Germany. Our study shows that incorporating ultrasound instruction within midwifery education is practicable and significantly improves students’ theoretical knowledge and practical skills. Successes were assessed using an OSCE, a knowledge-based single-choice test, and a self-assessment questionnaire, all administered both before and after the course.
Several other studies have been published on training courses for midwives in the field of obstetric ultrasound, demonstrating comparable successes [ 9 , 22 , 23 ]. For instance, Bentley et al. reported on a one-week ultrasound curriculum for midwives in Liberia, which resulted in a notable increase in the midwives’ knowledge and practical skills, as well as in self-rated comfort [ 24 ]. In the spectrum of existing comparable initiatives, our research significantly contributes to the field, as most existing studies, identified in our systematic literature review, have been conducted in low- and middle-income countries, where intentions, frameworks, and resource availability differ significantly from those in industrialised nations and thus contribute to significant challenges in course instruction [ 14 ]. Our ultrasound course benefited from advanced infrastructure and abundant resources, allowing for a different approach with broad implications for midwifery education. Our project targets midwives in training and integrates seamlessly into their curriculum, unlike most studies that include practising midwives, often leading to conflicts with their professional responsibilities [ 9 , 25 ]. We are therefore following the recommendation of Hall et al., which suggests to establish dedicated timeslots for attending practical sessions to ensure they do not overlap with other commitments [ 22 ].
To ensure the success of ultrasound courses, the implementation necessitates several considerations, with a key one being a needs assessment to identify participants’ requirements, which in turn shapes the learning objectives, content, and course structure [ 13 ]. Our needs assessment led to a blended learning approach with fundamental theoretical and practical content, supplemented by online materials and autonomous ultrasound examinations in simulated scenarios [ 14 ]. Each of these aspects, particularly the combination of didactic and hands-on elements, has proven effective in previous projects [ 23 , 26 , 27 ]. This blend of learning methods facilitated a modular structure of the course, leading to effective content organisation and the inclusion of both online and face-to-face course days. Unlike Shaw-Battista et al., we used online modules only to introduce basic knowledge, reserving face-to-face sessions for advanced and practical content [ 28 ]. Our emphasis on foundational instruction, encompassing ultrasound machine operation and fundamental obstetric examination techniques, has been well-regarded in the literature and highly valued by our participants [ 9 , 29 ]. Additionally, we uniquely included instruction in FAST and intrapartum sonography, equipping participants with crucial skills for obstetric scenarios [ 30 , 31 ]. In this context, transabdominal intrapartum sonography is particularly notable for its relative ease of learning compared to conventional clinical methods for determining foetal position during labour [ 32 ]. As a highly valued aspect noted by Shaw-Battista et al., the practical instruction included supervised hands-on practice with experienced ultrasound professionals [ 28 ]. Finally, the combination of test, practical examination, and questionnaire, an approach that had already been successfully applied in further researches, enabled a comprehensive evaluation of the students’ learning progress [ 9 , 24 ].
Despite the successful implementation, our study has several limitations, particularly the constrained timeframe due to integrating teaching units into the extensive bachelor’s programme curriculum, which limited topic coverage, repetition, and time for developing practical skills. Similar to findings by Shah et al., students highlighted this deficit, suggesting extended or more frequent sessions would have been beneficial [ 23 , 33 ]. Evaluations were conducted three months apart, covering a large amount of material in a short period, making it challenging to achieve high proficiency in all areas. Skills with high redundancy, such as device operation, image orientation, and foetal location, are likely to be retained longer than less frequently covered but essential topics like biometric measurements. While our study demonstrates comprehensive knowledge gains, it remains unclear how well these skills will be retained and applied long term, particularly outside the structured learning environment, highlighting the need for long-term observation studies. Especially, first trimester ultrasound, as a comprehensive core procedure, may require advanced expertise and extended focused training to ensure thorough and safe coverage. Although students will have gained an insight into first trimester ultrasound within two modules, it seems unlikely that they have achieved the necessary competence to perform these examinations independently. Additionally, learning outcomes during the practical exercises varied due to the randomised assignment of groups and pregnant participants, limiting exposure to diverse clinical scenarios, which may affect recognition in actual patients post-course. Staff shortages also led to different raters in the pre- and post-course OSCE, potentially impact interrater reliability.
Although midwifery education and associated ultrasound training at German universities are still in their infancy, policy interventions are needed to expand academisation and enhance access to advanced educational opportunities [ 14 ]. In addition to firmly integrating ultrasound training into the curricula with sufficient time to cover foundational topics, early establishment of alignments and basic standards is essential for ensuring consistent competency, improving educational methods, and developing the midwifery practice [ 12 , 14 ]. Furthermore, regulatory measures, including financing teaching costs, setting guidelines for role allocations, and funding ultrasound examinations by midwives, are crucial [ 14 ].
Ultrasound proficiency is gaining increasing significance for midwifery students from both registration and workplace perspectives. In many regions, regulatory bodies and professional standards for midwives increasingly recognise ultrasound as part of a midwife’s scope of practice. While not universally required as a core competency, there is a growing expectation for midwives to possess foundational knowledge in ultrasound, particularly in placental location, foetal positioning, and amniotic fluid assessment. From a registration perspective, ultrasound competency can elevate professional qualifications, aligning with the evolving needs of healthcare systems, and as the use of ultrasound technology in routine antenatal care increases, midwifery students skilled in ultrasound techniques may experience better job prospects. Employers often prefer candidates who offer a broader range of services, such as ultrasound, allowing for more comprehensive diagnostics and fewer referrals. In the workplace, ultrasound allows midwives to provide more comprehensive antenatal and emergency care, enabling quicker clinical decisions, earlier interventions and more personalised birth planning. However, with transitions of students into clinical practice, it is essential to conduct long-term observations to assess the practical application of ultrasound skills, how these responsibilities are coordinated with other professional groups such as physicians, and how ultrasound education for midwives can be adapted accordingly.
Our study represents the inaugural initiative to introduce a comprehensive obstetric ultrasound curriculum into a midwifery degree programme in Germany, demonstrating its viability and effectiveness in training midwifery students. Statistical analyses reveal significant enhancements in the students’ knowledge and skills across all areas of the course, suggesting that the curriculum serves as a valuable teaching approach and provides well-tailored educational strategies that meet the specific needs of the students. Establishing early standards and developing comprehensive financial and regulatory frameworks are crucial to further improve and realise the firm integration of ultrasound teaching in midwifery education. Finally, the incorporation of ultrasound training may constitute an important component in the ongoing process of professionalising and academising the field of midwifery.
Data availability
Data available on request from the authors.
Abramowicz JS. Obstetric ultrasound: where are we and where are we going? Ultrasonography. 2021;40(1):57–74.
Article Google Scholar
Van Adrichem A, Faes E, Kinget K, Jacquemyn Y. Intrapartum ultrasound: viewpoint of midwives and parturient women and reproducibility. Int J Womens Health. 2018;10:251–6.
Herbst MK, Tafti D, Shanahan MM. Obstetric Ultrasound. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 Apr 2]. http://www.ncbi.nlm.nih.gov/books/NBK470450/
Dębska M, Kretowicz P, Dębski R. Intrapartum sonography – eccentricity or necessity? J Ultrason. 2015;15(61):125–36.
Wilkinson M, Usman S, Barton H, Lees CC. The views of pregnant women, midwives, and a women’s panel on intrapartum ultrasound research: a pilot study. Australas J Ultrasound Med. 2019;22(3):186–90.
Malvasi A, Vimercati A. Is it time for midwives to do intrapartum ultrasound in the delivery ward? J Matern Fetal Neonatal Med. 2022;35(25):9568–9.
Casmod Y, Armstrong SJ. Obstetric ultrasound training programmes for midwives: a scoping review. Health SA Gesondheid. 2023;28:2163.
Mubuuke AG, Nassanga R. Point of care obstetric ultrasound knowledge retention among mid-wives following a training program: a prospective cohort pilot study. BMC Pregnancy Childbirth. 2023;23(1):104.
Viner AC, Membe-Gadama G, Whyte S, Kayambo D, Masamba M, Makwakwa E, et al. Training in Ultrasound to Determine Gestational Age (TUDA): evaluation of a Novel Education Package to teach Ultrasound-Naive midwives Basic Obstetric Ultrasound in Malawi. Front Glob Womens Health. 2022;3:880615.
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience [Internet]. Geneva: World Health Organization. 2016 [cited 2024 Aug 1]. 152 p. https://iris.who.int/handle/10665/250796
Reiso M, Langli B, Sommerseth E, Johannessen A. A qualitative study of the work experiences of midwives performing obstetric ultrasound in Norway. BMC Pregnancy Childbirth. 2020;20:641.
Plappert CF, Bauer NH, Dietze-Schwonberg K, Grieshop M, Kluge-Bischoff A, Zyriax BC, et al. Academic education of midwives in Germany (part 1): requirements for bachelor of science programmes in midwifery education. Position paper of the Midwifery Science Committee (AHW) in the DACH Association for Medical Education (GMA). GMS J Med Educ. 2024;41(3):Doc33.
Google Scholar
Kern DE. Curriculum Development for Medical Education: a Six Step Approach. JHU; 1998. p. 202.
Groos J, Walter A, Wittek A, Strizek B, Gembruch U, Recker F. Shaping ultrasound in midwifery: towards an evidence-based training framework for enhanced prenatal care. Arch Gynecol Obstet. 2024;310(1):23–43.
Dietrich CF, Sirli RL, Barth G, Blaivas M, Daum N, Dong Y et al. Student ultrasound education - current views and controversies. Ultraschall Med Stuttg Ger. 1980. 2024;45(4):389–94.
Barth G, Prosch H, Blaivas M, Gschmack AM, Hari R, Hoffmann B et al. Student Ultrasound Education, Current Views and Controversies; Who Should be Teaching? Z Für Gastroenterol [Internet]. 2024 Jul 29 [cited 2024 Aug 7]; https://www.thieme-connect.de/products/ejournals/abstract/ https://doi.org/10.1055/a-2356-7906
International Confederation of Midwives. Essential competencies for midwifery practice [Internet]. 2019 [cited 2024 Jul 19]. https://www.internationalmidwives.org/wp-content/uploads/icm-competencies-en-print-october-2019_final_18-oct-5db05248843e8.pdf
Deutscher Hebammenverband e.V. (DHV). Kompetenzen von Hebammen - Anhang 1 zur Stellungnahme HebStPrV [Internet]. 2019 [cited 2024 Apr 20]. https://hebammenverband.de/wp-content/uploads/2021/02/2019-09-13_DHV_Kompetenzen_von_Hebammen_Anhang_1_zur_Stellungnahme_HebStPrV.pdf
Salomon Lj, Alfirevic Z, Da Silva Costa F, Deter Rl, Figueras F, Ghi T, et al. ISUOG Practice guidelines: ultrasound assessment of fetal biometry and growth. Ultrasound Obstet Gynecol. 2019;53(6):715–23.
Ghi T, Eggebø T, Lees C, Kalache K, Rozenberg P, Youssef A, et al. ISUOG Practice guidelines: intrapartum ultrasound. Ultrasound Obstet Gynecol. 2018;52(1):128–39.
Savoia P, Jayanthi SK, Chammas MC. Focused Assessment with Sonography for Trauma (FAST). J Med Ultrasound. 2023;31(2):101–6.
Hall EA, Matilsky D, Zang R, Hase N, Habibu Ali A, Henwood PC, et al. Analysis of an obstetrics point-of-care ultrasound training program for healthcare practitioners in Zanzibar, Tanzania. Ultrasound J. 2021;13:18.
Bidner A, Bezak E, Parange N. Evaluation of antenatal point-of-care ultrasound training workshops for rural/remote healthcare clinicians: a prospective single cohort study. BMC Med Educ. 2022;22:906.
Bentley S, Hexom B, Nelson BP. Evaluation of an Obstetric Ultrasound Curriculum for midwives in Liberia. J Ultrasound Med. 2015;34(9):1563–8.
Vinayak S, Sande J, Nisenbaum H, Nolsøe CP. Training midwives to perform Basic Obstetric Point-of-care Ultrasound in Rural areas using a tablet platform and mobile phone Transmission Technology—A WFUMB COE Project. Ultrasound Med Biol. 2017;43(10):2125–32.
Johnston BK. Evaluation of Point of Care Ultrasound Training for Midwives [Internet] [Thesis]. 2021 [cited 2024 Aug 1]. http://hdl.handle.net/11375/26969
Gueneuc A, De Garnier J, Dommergues M, Rivière M, Ville Y, Chalouhi GE. Impact de l’intégration de la simulation en échographie obstétricale dans le cursus des étudiants sages-femmes. Gynécologie Obstétrique Fertil Sénologie. 2019;47(11):776–82.
Shaw-Battista J, Young-Lin N, Bearman S, Dau K, Vargas J. Interprofessional Obstetric Ultrasound Education: successful development of Online Learning modules; Case-based seminars; and Skills Labs for registered and Advanced Practice Nurses, midwives, Physicians, and trainees. J Midwifery Womens Health. 2015;60(6):727–34.
Nathan RO, Swanson JO, Swanson DL, McClure EM, Bolamba VL, Lokangaka A, et al. Evaluation of focused Obstetric Ultrasound examinations by Health Care Personnel in the Democratic Republic of Congo, Guatemala, Kenya, Pakistan, and Zambia. Curr Probl Diagn Radiol. 2017;46(3):210–5.
Santana EFM, Castello RG, Passos MET, Ribeiro GCF, Araujo Júnior E. How to Reach the best Ultrasound performance in the delivery room. Rev Bras Ginecol E Obstetrícia. 2023;44:1070–7.
Ghose I, Chelliah A, Gordon R, Andrade EH, Refuerzo J, Blackwell SC, et al. 1136 the FAST exam in obstetrics: a feasibility study. Am J Obstet Gynecol. 2021;224(2):S700–1.
Rozenberg P, Porcher R, Salomon LJ, Boirot F, Morin C, Ville Y. Comparison of the learning curves of digital examination and transabdominal sonography for the determination of fetal head position during labor. Ultrasound Obstet Gynecol. 2008;31(3):332–7.
Shah S, Santos N, Kisa R, Mike Maxwell O, Mulowooza J, Walker D, et al. Efficacy of an ultrasound training program for nurse midwives to assess high-risk conditions at labor triage in rural Uganda. PLoS ONE. 2020;15(6):e0235269.
Download references
Open Access funding enabled and organized by Projekt DEAL.
Author information
Agnes Wittek and Florian Recker contributed equally to this work.
Authors and Affiliations
Department of Obstetrics and Prenatal Medicine, University Hospital Bonn, Venusberg Campus 1, 53127, Bonn, Germany
Julia Groos, Adeline Walter, Ruben Plöger, Brigitte Strizek, Ulrich Gembruch, Agnes Wittek & Florian Recker
You can also search for this author in PubMed Google Scholar
Contributions
JG: Conceptualization, Methodology, Writing - Original Draft, Writing - Review & Editing. AW: Conceptualization, Resources, Writing - Review & Editing. RP: Resources, Writing - Review & Editing. BS: Writing - Review & Editing, Resources. UG: Writing - Review & Editing, Resources. AWi: Writing - Original Draft, Writing - Review & Editing, Resources. FR: Conceptualization, Methodology, Formal analysis, Writing - Original Draft, Writing - Review & Editing.
Corresponding author
Correspondence to Florian Recker .
Ethics declarations
Ethical approval.
An ethic approval was obtained from the ethical committee of the University of Bonn (No. 179/23-EP).
Informed consent
Informed consent was obtained from all participants involved in the study.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Groos, J., Walter, A., Plöger, R. et al. Pioneering point-of-care obstetric ultrasound integration in midwifery education – the MEPOCUS study. BMC Med Educ 24 , 1209 (2024). https://doi.org/10.1186/s12909-024-06221-4
Download citation
Received : 09 August 2024
Accepted : 18 October 2024
Published : 24 October 2024
DOI : https://doi.org/10.1186/s12909-024-06221-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ultrasound curriculum
- Point-of-care ultrasound
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]

COMMENTS
Midwifery clinical practice and education has changed significantly since Mary Breckinridge first introduced nurse-midwives to the United States in 1925. This article discusses current challenges in midwifery clinical practice and education and proposes possible solutions. Midwifery clinical challenges include restrictive legislation and business-related barriers, including but not limited to ...
Abstract. Midwifery clinical practice and education has changed significantly since Mary Breckinridge first introduced nurse-midwives to the United States in 1925. This article discusses current challenges in midwifery clinical practice and education and proposes possible solutions. Midwifery clinical challenges include restrictive legislation ...
In 2021, midwives attended 12% of births in the U.S. We found that the number of midwives and midwifery students in the U.S. has increased—although the extent of care they can provide varies by state. Also, some students may have trouble with the cost of education and the limited number of clinical training opportunities available.
In 2022, according to the International Confederation of Midwives (ICM) Essential Competencies for Midwifery Practice and the framework of the ICM Global Standards for Midwifery Education [1], a midwife is defined as having successfully completed a midwifery education programme that is based on those standards.
Midwifery education is a key solution to the challenge of providing universal and quality maternal and newborn care to meet our Sustainable Development Goals. While improving access to care is critical, ensuring good quality of care has an even greater impact in terms of lives saved.
Clinical learning is an indispensable part of nursing and midwifery education programme and an integration of theoretical and practical learning experiences which plays an important role in the acquisition of professional abilities (Ironside et al., 2014; Jonsén et al., 2013; Aghamohammadi-Kalkhoran et al., 2011).An optimal clinical learning environment (CLE) brings a positive impact on ...
Midwives in this study reported a range of ethical challenges and minimal classroom education related to ethics. Midwifery educators should consider the purposeful and explicit inclusion of midwifery-specific ethics content in their curricula and in interprofessional ethics education.
Midwifery education is viewed as a process of lifelong learning, for maintaining competence and as a means of acquiring a body of midwifery knowledge. This chapter concludes by examining how to maximise the opportunities, address challenges and consider the implications for policy, research and practice.
Some aspects of midwifery history are uncomfortable to reckon with (eg, midwives' role in moral guardianship). 5 Yet, other histories reveal midwives improving midwifery education, and thus outcomes for mothers and babies, before obstetrics and gynaecology became a medical specialty. Although conflict between male doctors and female midwives has received much attention, there is a need to ...
The third global State of the World's Midwifery report (SoWMy 2021) provides an updated evidence base on the sexual, reproductive, maternal, newborn and adolescent health (SRMNAH) workforce. For the first time, SoWMy includes high-income countries (HICs) as well as low- and middle-income countries. This paper describes the similarities and differences between regions and income groups, and ...
Midwifery education is at a particularly challenging juncture in its history. Both the programmes leading to qualification as a midwife are now firmly linked to higher education, with courses offered at diploma and, increasingly, at degree level. ... Maggs, C. (1994) Mentorship in nursing and midwifery education: issues for research. Nurse ...
Looking back over the past 25 years of midwifery education enables us to learn from old ways of working and the related events that took place, to help plan for a future where the women is at the centre of personalised safe care ... Reflecting on the past 25 years of midwifery education provides insights into the challenges of midwifery ...
Integral to quality midwifery practice is the education of midwives. Like other countries, Australia faces ongoing challenges in delivering midwifery education programs. Reasons include escalating program costs, challenges in securing meaningful clinical experiences, subsumption of midwifery with nursing, and associated loss of identity in some institutions.
Given the anticipated challenges presenting the profession, since the completion of this study, the Chief Nursing Officers across the UK commissioned the Midwifery 2020 Programme, 2010b to develop a vision for the midwifery workforce in practice and education and the findings of this study reinforce some of its key messages.
In 2016, the authors interviewed 8 persons (5 NL, 3 IS) on national issues around midwifery education. The participants were national key figures in midwifery education, professional organisations and policy development. All acknowledged that midwifery education faces challenges in keeping up-to-date with the changes going on in maternity care ...
midwifery education programs generally increased in recent years. According to stakeholders GAO interviewed, students may face challenges accessing midwifery education, including educational costs and limited availability of clinical training placements. Agencies within the Department of Health and Human
Challenges currently faced in midwifery careers. 02 December 2020. Career Special. Sydney Kerolo. 02 December 2020. Volume 28 · Issue 12. ISSN (print): 0969-4900. ISSN (online): 2052-4307. Download File.
In order to determine the challenges of midwifery clinical education in dealing with the clinical setting, individual interviews and focus group discussions were used. Individual interviews with the participants were carried out in a face‐to‐face manner and in a convenient place at the School of Nursing and Midwifery, Shiraz University of ...
Respond to Emerging Needs: Be prepared to address emerging healthcare needs and challenges, such as managing pandemics or addressing mental health crises. Continuing education is essential for midwives to provide the best care possible, stay competitive in their field, and advance their careers.
The midwives' challenges, and the factors motivating them to remain in their workplace in the DRC, are summarised in one main category—Loving one's work makes it worthwhile to remain in one's workplace, despite a difficult work environment and low professional status—consisting of three generic categories: Midwifery is not just a profession; it's a calling, comprising the three ...
Background Ultrasound technology is indispensable in perinatal care due to its non-invasive and painless nature, offering vital insights into foetal development and childbirth. With the academisation of midwifery in Germany, there is a growing necessity to incorporate ultrasound training into midwifery education. This paper discusses the development and implementation of an introductory ...