- Patient Care & Health Information
- Diseases & Conditions
- Chronic kidney disease
- What is kidney disease? An expert explains
Learn more from kidney doctor Andrew Bentall, M.D.
I'm Dr. Andrew Bentall, a kidney doctor at Mayo Clinic. I look after patients with kidney disease, either in the early stages, or with more advanced kidney disease considering dialysis and transplantation as treatment options. In this video, we'll cover the basics of chronic kidney disease. What is it? Who gets it? The symptoms, diagnosis and treatment. Whether you are looking for answers for yourself or for someone you love, we're here to give you the best information available.
Chronic kidney disease is a disease characterized by progressive damage and loss of function in the kidneys. It's estimated that chronic kidney disease affects about one in seven American adults. And most of those don't know they have it. Before we get into the disease itself, let's talk a little bit about the kidneys and what they do. Our kidneys play many important roles keeping our bodies in balance. They remove waste and toxins, excess water from the bloodstream, which is carried out of the body in urine. They helped to make hormones to produce red blood cells, and they turn vitamin D into its active form, so it's usable in the body.
There are quite a few things that can cause or put you at higher risk for chronic kidney disease. Some of them are not things that can be avoided. Your risk is simply higher if you have a family history of certain genetic conditions like polycystic kidney disease or some autoimmune diseases like lupus or IgA nephropathy. Defects in the kidney structure can also cause your kidneys to fail, and you have an increased risk as you get older. Sometimes, other common medical conditions can increase your risk. Diabetes is the most common cause of kidney disease. Both type 1 and type 2 diabetes. But also heart disease and obesity can contribute to the damage that causes kidneys to fail. Urinary tract issues and inflammation in different parts of the kidney can also lead to long-term functional decline. There are things that are more under our control: Heavy or long-term use of certain medications, even those that are common over-the-counter. Smoking can also be a contributing factor to chronic kidney disease.
Often there are no outward signs in the earlier stages of chronic kidney disease, which is grouped into stages 1 through 5. Generally, earlier stages are known as 1 to 3. And as kidney disease progresses, you may notice the following symptoms. Nausea and vomiting, muscle cramps, loss of appetite, swelling via feet and ankles, dry, itchy skin, shortness of breath, trouble sleeping, urinating either too much or too little. However, these are usually in the later stages, but they can also happen in other disorders. So don't automatically interpret this as having kidney disease. But if you're experiencing anything that concerns you, you should make an appointment with your doctor.
Even before any symptoms appear, routine blood work can indicate that you might be in the early stages of chronic kidney disease. And the earlier it's detected, the easier it is to treat. This is why regular checkups with your doctor are important. If your doctor suspects the onset of chronic kidney disease, they may schedule a variety of other tests. They may also refer you to a kidney specialist, a nephrologist like myself. Urine tests can reveal abnormalities and give clues to the underlying cause of the chronic kidney disease. And this can also help to determine the underlying issues. Various imaging tests like ultrasounds or CT scans can be done to help your doctor assess the size, the structure, as well as evaluate the visible damage, inflammation or stones of your kidneys. And in some cases, a kidney biopsy may be necessary. And a small amount of tissue is taken with a needle and sent to the pathologist for further analysis.
Treatment is determined by what is causing your kidneys to not function normally. Treating the cause is key, leading to reduced complications and slowing progression of kidney disease. For example, getting better blood pressure control, improved sugar control and diabetes, and reducing weight are often key interventions. However, existing damage is not usually reversible. In some conditions, treatment can reverse the cause of the disease. So seeking medical review is really important. Individual complications vary, but treatment might include high blood pressure medication, diuretics to reduce fluid and swelling, supplements to relieve anemia, statins to lower cholesterol, or medications to protect your bones and prevent blood vessel calcification. A lower-protein diet may also be recommended. It reduces the amount of waste your kidneys need to filter from your blood. These can not only slow the damage of kidney disease, but make you feel better as well. When the damage has progressed to the point that 85 to 90 percent of your kidney function is gone, and they no longer work well enough to keep you alive, it's called end-stage kidney failure. But there are still options. There's dialysis, which uses a machine to filter the toxins and remove water from your body as your kidneys are no longer able to do this. Where possible, the preferred therapy is a kidney transplant. While an organ transplant can sound daunting, it's actually often the better alternative, and the closest thing to a cure, if you qualify for a kidney transplant.
If you have kidney disease, there are lifestyle choices. Namely quit smoking. Consuming alcohol in moderation. If you're overweight or obese, then try to lose weight. Staying active and getting exercise can help not only with your weight, but fatigue and stress. If your condition allows, keep up with your routine, whether that's working, hobbies, social activities, or other things you enjoy. It can be helpful to talk to someone you trust, a friend or relative who's good at listening. Or your doctor could also refer you to a therapist or social worker. It can also be helpful to find a support group and connect with people going through the same thing. Learning you have chronic kidney disease and learning how to live with it can be a challenge. But there are lots of ways to help you to be more comfortable for longer before more drastic measures are needed. And even then, there is plenty of hope. If you'd like to learn even more about chronic kidney disease, watch our other related videos or visit mayoclinic.org. We wish you well.
Chronic kidney disease, also called chronic kidney failure, involves a gradual loss of kidney function. Your kidneys filter wastes and excess fluids from your blood, which are then removed in your urine. Advanced chronic kidney disease can cause dangerous levels of fluid, electrolytes and wastes to build up in your body.
In the early stages of chronic kidney disease, you might have few signs or symptoms. You might not realize that you have kidney disease until the condition is advanced.
Treatment for chronic kidney disease focuses on slowing the progression of kidney damage, usually by controlling the cause. But, even controlling the cause might not keep kidney damage from progressing. Chronic kidney disease can progress to end-stage kidney failure, which is fatal without artificial filtering (dialysis) or a kidney transplant.
- How kidneys work
One of the important jobs of the kidneys is to clean the blood. As blood moves through the body, it picks up extra fluid, chemicals and waste. The kidneys separate this material from the blood. It's carried out of the body in urine. If the kidneys are unable to do this and the condition is untreated, serious health problems result, with eventual loss of life.

Products & Services
- A Book: Mayo Clinic Family Health Book
- A Book: The Body's Keepers
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Signs and symptoms of chronic kidney disease develop over time if kidney damage progresses slowly. Loss of kidney function can cause a buildup of fluid or body waste or electrolyte problems. Depending on how severe it is, loss of kidney function can cause:
- Loss of appetite
- Fatigue and weakness
- Sleep problems
- Urinating more or less
- Decreased mental sharpness
- Muscle cramps
- Swelling of feet and ankles
- Dry, itchy skin
- High blood pressure (hypertension) that's difficult to control
- Shortness of breath, if fluid builds up in the lungs
- Chest pain, if fluid builds up around the lining of the heart
Signs and symptoms of kidney disease are often nonspecific. This means they can also be caused by other illnesses. Because your kidneys are able to make up for lost function, you might not develop signs and symptoms until irreversible damage has occurred.
When to see a doctor
Make an appointment with your doctor if you have signs or symptoms of kidney disease. Early detection might help prevent kidney disease from progressing to kidney failure.
If you have a medical condition that increases your risk of kidney disease, your doctor may monitor your blood pressure and kidney function with urine and blood tests during office visits. Ask your doctor whether these tests are necessary for you.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
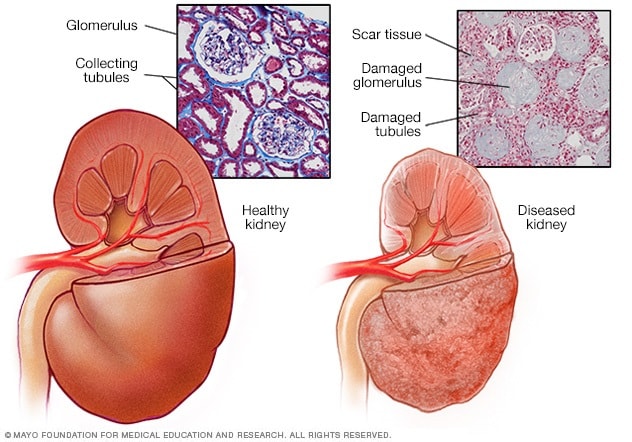
- Healthy kidney vs. diseased kidney
A typical kidney has about 1 million filtering units. Each unit, called a glomerulus, joins a tubule. The tubule collects urine. Conditions such as high blood pressure and diabetes harm kidney function by damaging these filtering units and tubules. The damage causes scarring.
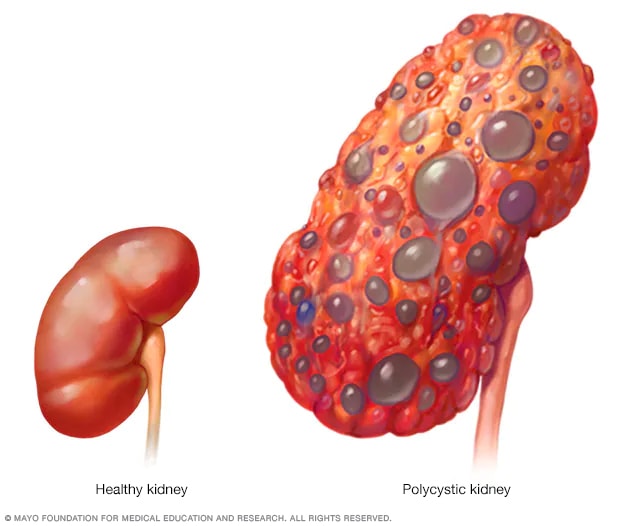
- Polycystic kidney
A healthy kidney (left) removes waste from the blood and maintains the body's chemical balance. With polycystic kidney disease (right), fluid-filled sacs called cysts develop in the kidneys. The kidneys grow larger and slowly lose their ability to work as they should.
Chronic kidney disease occurs when a disease or condition impairs kidney function, causing kidney damage to worsen over several months or years.
Diseases and conditions that cause chronic kidney disease include:
- Type 1 or type 2 diabetes
- High blood pressure
- Glomerulonephritis (gloe-mer-u-low-nuh-FRY-tis), an inflammation of the kidney's filtering units (glomeruli)
- Interstitial nephritis (in-tur-STISH-ul nuh-FRY-tis), an inflammation of the kidney's tubules and surrounding structures
- Polycystic kidney disease or other inherited kidney diseases
- Prolonged obstruction of the urinary tract, from conditions such as enlarged prostate, kidney stones and some cancers
- Vesicoureteral (ves-ih-koe-yoo-REE-tur-ul) reflux, a condition that causes urine to back up into your kidneys
- Recurrent kidney infection, also called pyelonephritis (pie-uh-low-nuh-FRY-tis)
Risk factors
Factors that can increase your risk of chronic kidney disease include:
- Heart (cardiovascular) disease
- Being Black, Native American or Asian American
- Family history of kidney disease
- Abnormal kidney structure
- Frequent use of medications that can damage the kidneys
Complications
Chronic kidney disease can affect almost every part of your body. Potential complications include:
- Fluid retention, which could lead to swelling in your arms and legs, high blood pressure, or fluid in your lungs (pulmonary edema)
- A sudden rise in potassium levels in your blood (hyperkalemia), which could impair your heart's function and can be life-threatening
- Heart disease
- Weak bones and an increased risk of bone fractures
- Decreased sex drive, erectile dysfunction or reduced fertility
- Damage to your central nervous system, which can cause difficulty concentrating, personality changes or seizures
- Decreased immune response, which makes you more vulnerable to infection
- Pericarditis, an inflammation of the saclike membrane that envelops your heart (pericardium)
- Pregnancy complications that carry risks for the mother and the developing fetus
- Irreversible damage to your kidneys (end-stage kidney disease), eventually requiring either dialysis or a kidney transplant for survival
To reduce your risk of developing kidney disease:
- Follow instructions on over-the-counter medications. When using nonprescription pain relievers, such as aspirin, ibuprofen (Advil, Motrin IB, others) and acetaminophen (Tylenol, others), follow the instructions on the package. Taking too many pain relievers for a long time could lead to kidney damage.
- Maintain a healthy weight. If you're at a healthy weight, maintain it by being physically active most days of the week. If you need to lose weight, talk with your doctor about strategies for healthy weight loss.
- Don't smoke. Cigarette smoking can damage your kidneys and make existing kidney damage worse. If you're a smoker, talk to your doctor about strategies for quitting. Support groups, counseling and medications can all help you to stop.
- Manage your medical conditions with your doctor's help. If you have diseases or conditions that increase your risk of kidney disease, work with your doctor to control them. Ask your doctor about tests to look for signs of kidney damage.
Chronic kidney disease care at Mayo Clinic
Living with chronic kidney disease?
Connect with others like you for support and answers to your questions in the Transplants support group on Mayo Clinic Connect, a patient community.
Transplants Discussions

157 Replies Fri, Oct 04, 2024

354 Replies Mon, Sep 23, 2024

13 Replies Sun, Sep 15, 2024
- Goldman L, et al., eds. Chronic kidney disease. In: Goldman-Cecil Medicine. 26th ed. Elsevier; 2020. http://www.clinicalkey.com. Accessed April 27, 2021.
- Chronic kidney disease (CKD). National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/kidney-disease/chronic-kidney-disease-ckd#:~:text=Chronic kidney disease (CKD) means,family history of kidney failure. Accessed April 26, 2021.
- Rosenberg M. Overview of the management of chronic kidney disease in adults. https://www.uptodate.com/contents/search. Accessed April 26, 2021.
- Chronic kidney disease (CKD) symptoms and causes. National Kidney Foundation. https://www.kidney.org/atoz/content/about-chronic-kidney-disease. Accessed April 26, 2021.
- Chronic kidney disease. Merck Manual Professional Version. https://www.merckmanuals.com/professional/genitourinary-disorders/chronic-kidney-disease/chronic-kidney-disease?query=Chronic kidney disease. Accessed April 26, 2021.
- Ammirati AL. Chronic kidney disease. Revista da Associação Médica Brasileira. 2020; doi:10.1590/1806-9282.66.S1.3.
- Chronic kidney disease basics. Centers for Disease Control and Prevention. https://www.cdc.gov/kidneydisease/basics.html. Accessed April 26, 2021.
- Warner KJ. Allscripts EPSi. Mayo Clinic; April 21, 2021.
- Office of Patient Education. Chronic kidney disease treatment options. Mayo Clinic; 2020.
- Chronic kidney disease: Is a clinical trial right for me?
- Eating right for chronic kidney disease
- Effectively managing chronic kidney disease
- Kidney biopsy
- Kidney disease FAQs
- Low-phosphorus diet: Helpful for kidney disease?
- MRI: Is gadolinium safe for people with kidney problems?
- Renal diet for vegetarians
Associated Procedures
- Deceased-donor kidney transplant
- Hemodialysis
- Kidney transplant
- Living-donor kidney transplant
- Nondirected living donor
- Peritoneal dialysis
- Preemptive kidney transplant
News from Mayo Clinic
- Mayo Clinic Q and A: Diagnosed with chronic kidney disease. Now what? Aug. 31, 2024, 11:00 a.m. CDT
- Mayo Clinic Minute: Why Black Americans are at higher risk of chronic kidney disease March 05, 2024, 05:00 p.m. CDT
- Mayo Clinic Minute: Can extra salt hurt your kidneys? Feb. 16, 2024, 04:00 p.m. CDT
- Mayo Clinic Minute: Using AI to predict kidney failure in patients with polycystic kidney disease April 06, 2023, 04:00 p.m. CDT
- Mayo Clinic Q and A: Understanding chronic kidney disease March 23, 2023, 12:35 p.m. CDT
- Mayo Clinic Minute: Game-changing treatment for chronic kidney disease could slow down progression of the disease March 06, 2023, 04:01 p.m. CDT
- Science Saturday: Seeking a cellular therapy for chronic kidney disease Nov. 12, 2022, 12:00 p.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- NEW: Listen to Health Matters Podcast - Mayo Clinic Press NEW: Listen to Health Matters Podcast
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Thank a researcher today
Their crucial work saves lives every day. Let Mayo Clinic researchers know they’re appreciated with a quick message.

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Chronic Kidney Disease (CKD)
Published by Kennedi Warman Modified over 9 years ago
Similar presentations
Presentation on theme: "Chronic Kidney Disease (CKD)"— Presentation transcript:
ABC’s of Nephrology Sobha Malla RD,CSR 9/17/11
William Vega-Ocasio MD. Internal Medicine - Nephrology
+ Understanding Kidney Disease and Renal Dialysis Brooke Grussing Concordia College.
Chronic Kidney Disease Manju Sood GPST3. What is CKD? Chronic renal failure is the progressive loss of nephrons resulting in permanent compromise of renal.
Kidney Physiology Kidney Functions: activate vitamin D (renal 1-alpha hydroxylase)activate vitamin D (renal 1-alpha hydroxylase) produces erythropoietin.
Dinkar Kaw, M.D., Division of Nephrology
Prepared by D. Chaplin Chronic Renal Failure. Prepared by D. Chaplin Chronic Renal Failure Progressive, irreversible damage to the nephrons and glomeruli.
Protein-, Mineral- & Fluid-Modified Diets for Kidney Diseases
Nutrition & Renal Diseases
Uncontrolled secondary hyperparathyroidism in a haemodialysis patient Jordi Bover, MD, PhD Fundació Puigvert Barcelona, Spain © Springer Healthcare, a.

End Stage Renal Disease in Children. End stage kidney disease occurs when the kidneys are no longer able to function at a level that is necessary for.
Chronic Renal Failure (End Stage Renal Disease “ESRD”) Dr. Belal Hijji, RN, PhD April 18 & 23, 2012.
Recent Advances in Management of CRF Yousef Boobess, M.D. Head, Nephrology Division Tawam Hospital.
Chronic Kidney Disease
SLOW- COOKING THE BEANS “OR, HOW TO STOP WORRYING AND APPLY SOME LOVE TO THE KIDNEYS” AN APPROACH TO CKD SARA KATE LEVIN, MD JANUARY 2014.
Calcium & phosphor disturbance CKD- MBD Dr. Atapour.

Kidney Function Tests Contents: Kidney functions Functional units Renal diseases Routine kidney function tests Serum creatinine Creatinine clearance.
This lecture was conducted during the Nephrology Unit Grand Ground by Medical Student rotated under Nephrology Division under the supervision and administration.
Finishing Renal Disease Aging and death. Chronic Renal Failure Results from irreversible, progressive injury to the kidney. Characterized by increased.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Find in topic
RELATED TOPICS
INTRODUCTION
Chronic kidney disease (CKD) is defined by the presence of kidney damage or decreased glomerular filtration rate (GFR) for three or more months, irrespective of the cause ( table 1 ) [ 1 ]. This three-month duration distinguishes chronic from acute kidney disease. Additional details on the definitions and staging are presented at length elsewhere. (See "Definition and staging of chronic kidney disease in adults" and "Definition and staging criteria of acute kidney injury in adults" .)
For patients being evaluated for elevated serum creatinine or reduced estimated glomerular filtration rate (eGFR), it is important to distinguish those who have relatively stable CKD from those who have acute or subacute kidney injury, which may be ongoing and reversible. Acute kidney injury (AKI) is defined by a rise in the serum creatinine level that has developed within hours to days ( table 2 ). Subacute kidney injury (also called acute kidney disease) informally refers to any decline in kidney function that evolves over more than 48 hours but less than three months [ 2 ]. Diagnostic approach to these patients is presented in detail elsewhere. (See "Diagnostic approach to adult patients with subacute kidney injury in an outpatient setting" and "Evaluation of acute kidney injury among hospitalized adult patients" .)
An overview of the presentation and evaluation of patients with newly identified CKD is presented in this topic ( algorithm 1 ). Specific aspects of the evaluation are presented separately:
● Assessment of kidney function by eGFR. Estimation of the GFR requires that the patient is in steady state. (See "Assessment of kidney function" .)
● Careful examination of the urine by both qualitative chemical tests and microscopic examination. The urinary findings narrow the differential. (See "Urinalysis in the diagnosis of kidney disease" .)
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Chronic kidney disease.
Satyanarayana R. Vaidya ; Narothama R. Aeddula .
Affiliations
Last Update: July 31, 2024 .
- Continuing Education Activity
Chronic kidney disease (CKD) is characterized by the presence of kidney damage or an estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73 m², persisting for 3 months or more. CKD involves a progressive loss of kidney function, often leading to the need for renal replacement therapy, such as dialysis or transplantation. The 2012 KDIGO CKD classification considers the underlying cause and categorizes CKD into 6 stages of progression and 3 stages of proteinuria based on glomerular filtration rate and levels of albuminuria. Although the causes of CKD vary, certain disease processes exhibit similar patterns.
The implications of CKD are extensive—it emerges from various disease processes and affects cardiovascular health, cognitive function, bone metabolism, anemia, blood pressure, and many other health indicators. Early recognition of CKD is the first step in treating it, and various methods for measuring eGFR have been described. Both modifiable and non-modifiable risk factors influence the progression of CKD. Management of CKD involves adjusting medication dosages according to the patient's eGFR, preparing for renal replacement therapies, and addressing reversible causes to slow disease progression. This activity reviews the etiology, evaluation, and management of CKD, emphasizing the crucial role of an interprofessional healthcare team in providing comprehensive care. An interprofessional approach focuses on both modifiable and non-modifiable risk factors to manage and mitigate the progression of the disease.
- Identify the early signs and symptoms of chronic kidney disease to facilitate prompt diagnosis and intervention.
- Implement evidence-based guidelines for managing chronic kidney disease, including lifestyle modifications, medication adjustments, and monitoring of disease progression.
- Select appropriate treatment options and renal replacement therapies based on individual patient needs and chronic kidney disease stage.
- Collaborate with an interprofessional team, including nephrologists, dietitians, nurses, and pharmacists, to provide comprehensive care for chronic kidney disease patients.
- Introduction
Chronic kidney disease (CKD) is characterized by the presence of kidney damage or an estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73 m², persisting for 3 months or more, irrespective of the cause. [1] CKD is a state of progressive loss of kidney function, ultimately resulting in the need for renal replacement therapy, such as dialysis or transplantation. Kidney damage refers to pathologic abnormalities suggested by imaging studies or renal biopsy, abnormalities in urinary sediment, or increased urinary albumin excretion rates.
The 2012 Kidney Disease Improving Global Outcomes (KDIGO) CKD classification recommends specifying the cause of CKD and classifies the condition into 6 categories based on GFR (G1 to G5, with G3 split into 3a and 3b). In addition, it also includes staging based on 3 levels of albuminuria (A1, A2, and A3), with each stage of CKD subcategorized according to the urinary albumin-creatinine ratio (ACR; mg/g or mg/mmol) in an early morning "spot" urine sample. [2]
The 6 CKD categories, known as stages 1 through 5, are described below (stage 3 is separated into 3a and 3b):
- G1: GFR 90 mL/min/1.73 m 2 and above with evidence of kidney disease, such as hematuria or proteinuria
- G2: GFR 60 to 89 mL/min/1.73 m 2
- G3a: GFR 45 to 59 mL/min/1.73 m 2
- G3b: GFR 30 to 44 mL/min/1.73 m 2
- G4: GFR 15 to 29 mL/min/1.73 m 2
- G5: GFR less than 15 mL/min/1.73 m 2 or treatment by dialysis
The 3 levels of albuminuria include an ACR:
- A1: ACR less than 30 mg/g (<3.4 mg/mmol)
- A2: ACR 30 to 299 mg/g (3.4-34 mg/mmol)
- A3: ACR greater than 300 mg/g (>34 mg/mmol)
The improved classification of CKD has been beneficial in identifying prognostic indicators related to decreased kidney function and increased albuminuria. However, a downside of this classification system is the potential for overdiagnosis of CKD, particularly in older individuals.
The causes of CKD vary globally, with the most common primary diseases leading to CKD and, ultimately, end-stage renal disease (ESRD) being: [3]
- Type 2 diabetes (30%-50%)
- Type 1 diabetes (3.9%)
- Hypertension (27.2%)
- Primary glomerulonephritis (8.2%)
- Chronic tubulointerstitial nephritis (3.6%)
- Hereditary or cystic diseases (3.1%)
- Secondary glomerulonephritis or vasculitis (2.1%)
- Plasma cell dyscrasias or neoplasm (2.1%)
- Sickle cell nephropathy, which accounts for less than 1% of ESRD patients in the United States. Please see StatPearls' companion resource, " Sickle Cell Nephropathy ," for more information.
CKD may result from disease processes in any of the 3 categories, including prerenal (decreased renal perfusion pressure), intrinsic renal (pathology of the vessels, glomeruli, or tubules-interstitium), or postrenal (obstructive).
Prerenal Disease
Chronic prerenal disease occurs in patients with chronic heart failure or cirrhosis, where persistently decreased renal perfusion increases the risk of intrinsic kidney injury, such as acute tubular necrosis. Over time, this can lead to a progressive loss of renal function.
Intrinsic Renal Disease
Intrinsic renal vascular disease: The most common chronic renal vascular disease is nephrosclerosis, which causes ongoing damage to blood vessels, glomeruli, and the tubulointerstitium. Other renal vascular diseases include renal artery stenosis due to atherosclerosis or fibromuscular dysplasia, which, over months or years, can lead to ischemic nephropathy. This condition is characterized by glomerulosclerosis and tubulointerstitial. [4]
Intrinsic glomerular disease (nephritic or nephrotic): A nephritic pattern is indicated by abnormal urine microscopy showing red blood cell (RBC) casts, dysmorphic red cells, and occasionally white blood cells (WBCs), along with a variable degree of proteinuria. [5] The most common causes are post-infectious glomerulonephritis, infective endocarditis, IgA nephropathy, lupus nephritis, Goodpasture syndrome, and vasculitis. [6]
A nephrotic pattern is associated with proteinuria, usually in the nephrotic range (>3.5 g/24 h), and an inactive urine microscopic analysis with few cells or casts. Common causes include minimal change disease, focal segmental glomerulosclerosis, membranous glomerulonephritis, diabetic nephropathy, and amyloidosis.
Intrinsic tubular and interstitial disease: The most common chronic tubulointerstitial disease is polycystic kidney disease (PKD). Other etiologies include nephrocalcinosis (often due to hypercalcemia and hypercalciuria), sarcoidosis, Sjögren syndrome, and reflux nephropathy in children and young adults. [7]
There is increasing recognition of a relatively high prevalence of CKD of unknown cause among agricultural workers from Central America and parts of Southeast Asia, known as MesoAmerican nephropathy or chronic interstitial nephritis in agricultural communities. Please see StatPearls' companion resources, " Chronic Interstitial Nephritis in Agricultural Communities (CINAC) " and " Reflux Nephropathy ," for more information.
Postrenal (Obstructive Nephropathy)
Chronic obstruction may result from prostatic disease, nephrolithiasis, or an abdominal/pelvic tumor exerting a mass effect on the ureter(s). Congenital abnormalities causing obstruction at the ureteropelvic or ureterovesical junctions are also common. Rare causes of chronic ureteral obstruction include retroperitoneal fibrosis or neurogenic bladder. [8] [9] Please see StatPearls' companion resource, " Obstructive Uropathy ," for further information.
- Epidemiology
The true incidence and prevalence of CKD are challenging to determine due to the asymptomatic nature of early to moderate stages. The prevalence of CKD in the general population is estimated to be around 10% to 14%. Specifically, albuminuria and an eGFR less than 60 mL/min/1.73 m² have prevalences of about 7% and 4%, respectively. [10]
Worldwide, CKD accounted for 2,968,600 (1%) of disability-adjusted life-years and 2,546,700 (1%-3%) life-years lost in 2012. [3] In the United States, CKD affected an estimated 26 million people in 2016. [11] The Kidney Disease Outcomes Quality Initiative (KDOQI) recommends that for diagnosing chronicity and CKD, patients should be tested on 3 separate occasions over a 3-month period, with at least 2 of the 3 results being positive. [12]
Natural History and Progression of Chronic Kidney Disease
CKD diagnosed in the general population (community CKD) typically has a different natural history and progression compared to CKD in patients referred to nephrology practices (referred CKD).
Community CKD primarily affects the older population, who have had lifelong exposure to cardiovascular risk factors, hypertension, and diabetes, all of which can impact kidney function. The average rate of GFR decline in this population is approximately 0.75 to 1 mL/min/year after age 40 to 50. [13] In a large study of community-based CKD by Kshirsagar et al, only 1% and 20% of patients with CKD stages 3 and 4, respectively, required renal replacement therapy. However, 24% and 45% of patients with stages 3 and 4, respectively, died predominantly from cardiovascular disease (CVD), suggesting that cardiac events rather than ESRD are the predominant outcomes in community-based CKD. [14]
In contrast to community CKD, patients with referred CKD often present at an earlier age due to hereditary conditions (eg, autosomal-dominant polycystic kidney disease or ADPKD) or acquired nephropathies (eg, glomerulonephritis, diabetic nephropathy, and tubulointerstitial disease) that cause progressive renal damage and loss of function. The rate of progression in referred CKD varies depending on the specific disease process. Diabetic nephropathy typically shows a rapid decline in GFR, averaging around 10 mL/min/year. In nondiabetic nephropathies, progression is generally faster in patients with chronic proteinuric glomerulonephritis compared to those with lower levels of proteinuria. Patients with ADPKD and CKD stage G3b or higher may experience a faster rate of progression than those with other nephropathies. In patients with hypertensive nephrosclerosis, well-controlled blood pressure and minimal proteinuria are associated with very slow progression.
Risk Factors for Progression of Chronic Kidney Disease
Non-modifiable CKD risk factors: Older age, male gender, and non-White ethnicity, including Black Americans, Afro-Caribbean individuals, Hispanics, and Asians (South Asians and Pacific Asians), all adversely affect CKD progression.
Genetic factors that affect CKD progression have been identified across various kidney diseases. A population-based cohort study found that single nucleotide polymorphisms in the genes TCF7L2 and MTHFS were associated with diabetic nephropathy and CKD progression. The same study also highlighted that polymorphisms in genes involved in renal scarring and the renin-angiotensin-aldosterone system (RAAS) affect CKD progression. [15]
Modifiable CKD risk factors: These include systemic hypertension, proteinuria, and metabolic factors. [16]
Systemic hypertension is a major cause of ESRD worldwide and the second leading cause in the United States, following diabetes. The transmission of systemic hypertension into glomerular capillary beds and the resulting glomerular hypertension is believed to contribute to the progression of glomerulosclerosis. [17] Night-time and 24-hour blood pressure measurements (such as ambulatory blood pressure monitoring or ABPM) are more strongly correlated with CKD progression than standard measurements. Systolic blood pressure, in particular, is a crucial predictor of CKD progression and is associated with complications in CKD.
Multiple studies have demonstrated that significant proteinuria (albuminuria A3) is linked to a faster rate of CKD progression in both diabetic and nondiabetic kidney diseases. Reducing significant proteinuria through RAS blockade or dietary modifications is associated with better renal outcomes. However, large intervention studies, such as the Avoiding Cardiovascular Events Through Combination Therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) and the Ongoing Telmisartan Alone and in Combination with Ramipril Global End Point Trial (ONTARGET), observed notable declines in GFR despite substantial reductions in albuminuria. [18] [19] Therefore, moderate-level albuminuria (A2) is not a reliable surrogate marker for CKD progression.
Multiple studies have linked the RAAS system to the development of hypertension, proteinuria, and renal fibrosis throughout CKD. Consequently, interventions targeting the RAAS have been effective in slowing CKD progression, leading to the widespread use of RAAS blockers in managing proteinuric and diabetic kidney diseases. Obesity and smoking have been associated with the development and progression of CKD. Additionally, metabolic factors such as insulin resistance, dyslipidemia, and hyperuricemia have also been implicated in CKD development and progression. [20] [21]
Recommendations for Chronic Kidney Disease Screening
Screening, primarily targeting high-risk individuals, is being implemented worldwide. The KDOQI guidelines recommend screening high-risk populations, including those with hypertension, diabetes mellitus, and individuals older than 65. Screening should involve urinalysis, measurement of urine ACR, serum creatinine levels, and estimation of GFR, preferably using the CKD Epidemiology Collaboration (CKD-EPI) equation. Currently, evidence to support screening asymptomatic individuals from the general population for CKD does not exist.
- Pathophysiology
Unlike acute kidney injury (AKI), which often results in complete functional recovery, chronic and sustained insults from progressive nephropathies lead to ongoing kidney fibrosis and destruction of normal kidney architecture. This process affects all three compartments of the kidney: the glomeruli, tubules and interstitium, and vessels. Histologically, it manifests as glomerulosclerosis, tubulointerstitial fibrosis, and vascular sclerosis.
The following events leading to scarring and fibrosis are complex, overlapping, and multistage phenomena:
- Infiltration of damaged kidneys with extrinsic inflammatory cells.
- Activation, proliferation, and loss of intrinsic renal cells (through apoptosis, necrosis, mesangiolysis, and podocytopenia).
- Activation and proliferation of extracellular matrix producing cells, including myofibroblasts and fibroblasts.
- Deposition of extracellular matrix, replacing the normal architecture.
Mechanisms of Accelerated Progression of Chronic Kidney Disease
- Systemic and intraglomerular hypertension
- Glomerular hypertrophy
- Intrarenal precipitation of calcium phosphate
- Altered prostanoid metabolism
All these mechanisms lead to a histological entity called glomerulosclerosis. [22]
Clinical risk factors for the accelerated progression of CKD include proteinuria, hypertension, Black race, and hyperglycemia. Environmental exposures, such as lead, smoking, metabolic syndrome, certain analgesic agents, and obesity, have also been linked to the accelerated progression of CKD. [23]
- History and Physical
Early CKD stages are asymptomatic, and symptoms manifest in stages 4 or 5. Some common symptoms and signs at these stages of CKD include:
- Loss of appetite
- Fatigue and weakness
- Sleep disturbance
- Decreased mental sharpness
- Muscle cramps
- Swelling of feet and ankles
- Persistent pruritus
- Chest pain due to uremic pericarditis
- Shortness of breath due to pulmonary edema from fluid overload
- Hypertension
Physical examination is often not helpful, but patients may demonstrate the following symptoms:
- Skin pigmentation
- Scratch marks from pruritus
- Pericardial friction rub due to uremic pericarditis
- Uremic frost, where high levels of blood urea nitrogen (BUN) cause urea in sweat to crystallize into fine, white powder on the skin
- Hyperreflexia or muscle twitches
- Hypertensive fundal changes suggesting chronicity
Establishing Chronicity
When a patient's eGFR is less than 60 mL/min/1.73m 2 , attention must be paid to the previous blood and urine test results and clinical history to determine whether this is a result of AKI or previously undiagnosed CKD. The following factors can help distinguish this:
- A history of long-standing chronic hypertension, proteinuria, microhematuria, or symptoms of prostatic disease can point toward chronicity.
- Physical findings such as skin pigmentation, scratch marks, left ventricular hypertrophy, and hypertensive fundal changes suggest chronicity.
- Blood test results indicating other conditions, such as multiple myeloma and systemic vasculitis, can help aid in diagnosis.
- While low serum calcium and high phosphorus levels have little discriminatory value, normal parathyroid hormone (PTH) levels suggest AKI rather than CKD.
- Patients who suddenly develop AKI are usually symptomatic at similarly elevated BUN/creatinine levels compared to those with CKD.
Assessment of Glomerular Filtration Rate
Kidney function tests should be repeated within 2 weeks of the initial finding of decreased eGFR for patients in whom the distinction between AKI and CKD is unclear. The gold standard for calculating creatinine is measuring the clearance of inulin. However, this is not readily available; therefore, creatinine clearance is used as a surrogate to calculate GFR. Please see StatPearls' companion resources, " Renal Function Tests " and " Creatinine Clearance ," for more information.
Many other compounds are also being examined for use as markers of acute kidney disease and CKD, including cystatin C, kidney injury molecule 1 (KIM-1), soluble urokinase-type plasminogen activator receptor, urinary epithelial growth factor, beta-2 microglobulin, retinol-binding protein, serum neutrophil gelatinase-associated lipocalin (NGAL), L-type fatty acid-binding protein (L-FABP), fibroblast growth factor 23 (FGF23), and beta-trace protein. [24] In addition, the Chronic Renal Insufficiency Cohort (CRIC) study demonstrated that markers such as certain cardiac markers (high-sensitivity troponin T and NTproBNP), the plasma chemokine CXCL12, and urine NGAL were highly associated with the progression of CKD. [25]
Assessment of Proteinuria
The KDIGO guidelines recommend assessing proteinuria by obtaining an early morning urine sample and quantifying the ACR. The degree of albuminuria is graded from A1 to A3, replacing previous terms such as microalbuminuria.
Healthy individuals secrete thousands of different proteins in their urine. The most significant of these are uromodulin (Tamm-Horsfall protein, comprising around 50% of total protein), albumin (comprising about 20%), and immunoglobulins (comprising about 5%). Various quantification and characterization methods, such as chromatography, immunoassays, electrophoresis, mass spectrometry, fluorescence spectroscopy, infrared spectroscopy, and Raman spectroscopy, may be useful. Protein-specific dipstick and immunochemical methods are the fastest and cheapest methods. The most commonly used urine dipstick protein segment measures albumin only because albuminuria is often increased out of proportion to other urine proteins in common proteinuric diseases, but this may not quantify other elevated urine protein levels such as Bence Jones proteins. [26] [27] [28]
If more accurate proteinuria measurements are not available, the KDIGO guidelines suggest estimation: Dipstick protein values of "trace to +" and "+ or greater" can be assigned to albuminuria categories of 30 to 299 mg/g and more than 300 mg/g, respectively. [28]
Imaging of Kidneys
If an ultrasound examination of the kidneys shows small kidneys with reduced cortical thickness, increased echogenicity, scarring, or multiple cysts, this suggests a chronic process. This may also be helpful in diagnosing chronic hydronephrosis from obstructive uropathy and cystic enlargement of the kidney in ADPKD. Renal ultrasound Doppler can be used in suspected renal artery stenosis to evaluate the renal vascular flow.
Computerized tomography can be used to further image kidney size, echogenicity, the collecting duct system, and any possible obstruction. Renal angiography has its role in diagnosing systemic vasculitis or renal artery stenosis, where multiple aneurysms and irregular areas of constriction are seen. Voiding cystourethrography is mainly used when chronic vesicourethral reflux is suspected of causing CKD, [7] which confirms the diagnosis and estimates the severity of reflux.
Renal scans can provide sufficient information about kidney anatomy and function. They are used predominantly in children as they are associated with less radiation exposure compared to CT scans. Radionuclide renal scans can also measure differences in kidney function.
Establishing an Accurate Diagnosis
An accurate diagnosis of CKD is essential, particularly when an underlying treatable condition, such as lupus nephritis or ANCA vasculitis, requires specific management. Certain diseases may have a higher recurrence rate in the kidney after transplantation, and an accurate diagnosis can guide future management. A kidney biopsy is the gold standard for diagnosing the cause of CKD and provides information about the extent of kidney fibrosis.
- Treatment / Management
General Management
- Drug dosages should be adjusted based on the patient's eGFR levels.
- Preparation for renal replacement therapy should include making surgical referrals for the placement of hemodialysis or peritoneal dialysis access and for transplantation when appropriate.
Treatment of Reversible Causes of Renal Failure
Potentially reversible causes of AKI, such as infection, drugs, hypotension, and hypovolemia, should be identified and addressed. Patients with CKD should be carefully evaluated before undergoing intravenous contrast studies, and alternatives should be considered first. Additionally, nephrotoxic agents, including aminoglycoside antibiotics and nonsteroidal anti-inflammatory drugs (NSAIDs), should be avoided.
Slowing the Progression of Chronic Kidney Disease
Factors contributing to the progression of CKD, including hypertension, proteinuria, metabolic acidosis, and hyperlipidemia, should be addressed. Hypertension should be managed according to established blood pressure goals, while proteinuria should be reduced to less than 1 g/d if possible. [29]
Multiple studies have shown that smoking is associated with an increased risk of developing nephrosclerosis, and smoking cessation retards the progression of CKD. [30] Protein restriction has also been shown to slow CKD progression. However, patients with advanced CKD are at risk of malnutrition, making dietician input crucial.
Bicarbonate supplementation for treating chronic metabolic acidosis has been demonstrated to delay CKD progression. [31] Additionally, intensive glucose control in individuals with diabetes has been effective in delaying the onset of albuminuria and preventing the progression from albuminuria to overt proteinuria. [32]
Preparation and Initiation of Renal Replacement Therapy
Once stage 4 CKD progression is noted, patients should be presented with various options for renal replacement therapy, as mentioned below.
- Hemodialysis (home or in-center).
- Peritoneal dialysis (continuous or intermittent).
- Kidney transplantation (living or deceased donor): This is the treatment of choice for ESRD due to its superior long-term outcomes.
- For patients who decline renal replacement therapy, information about conservative and palliative care management should be provided.
- Hemodialysis is performed after establishing stable vascular access in the nondominant arm. Intravenous cannulas should be avoided to preserve the veins in this arm. The preferred vascular access is an AV fistula. Other hemodialysis access options include AV grafts and tunneled hemodialysis catheters. AV fistulas are preferred due to their good patency rates and infrequent infections. They also allow for higher blood flow rates and have a lower risk of recirculation.
- Peritoneal dialysis is performed after placing a peritoneal catheter. [33]
Indications for Renal Replacement Therapy
- Pericarditis or pleuritis (emergent indication).
- Progressive uremic encephalopathy or neuropathy, with signs such as confusion, asterixis, myoclonus, and seizures (emergent indication).
- Clinically significant bleeding diathesis attributable to uremia (emergent indication).
- Hypertension is poorly responsive to antihypertensive medications.
- Fluid overload refractory to diuretics.
- Metabolic disorders that are refractory to medical therapy, such as hyperkalemia, hyponatremia, metabolic acidosis, hypercalcemia, hypocalcemia, and hyperphosphatemia.
- Persistent nausea and vomiting.
- Evidence of malnutrition.
- Any other uremic sign or symptom.
Renal transplantation is the preferred treatment option for ESRD due to its survival benefit compared to long-term dialysis therapy. Patients with CKD are typically eligible for renal transplant evaluation when the eGFR falls below 20 mL/min/1.73 m². If a patient has a living donor who may be able to donate a kidney, referral to a transplant center can be considered even earlier.
Conservative management of ESRD is an option for patients who choose not to pursue renal replacement therapy. This approach includes symptom management, advance care planning, and appropriate palliative care. This strategy is often underutilized and should be considered, particularly for frail patients with poor functional status. To facilitate this discussion, a 6-month mortality score calculator is used, incorporating variables such as age, serum albumin levels, presence of dementia, peripheral vascular disease, and a subjective assessment (a yes/no answer to a question) by the treating nephrologist, "Would I be surprised if this patient died in the next year?"
When to Refer to a Nephrologist
Patients should be referred to a nephrologist at any stage of CKD or for urinary abnormalities, especially when the eGFR falls below 60 mL/min/1.73m 2 . An early referral ensures optimal management. When the eGFR is less than 20 mL/min/1.73 m², preparations for renal replacement therapy should be initiated, including placement of a peritoneal dialysis catheter, establishment of vascular access for hemodialysis, and referral for renal transplantation.
- Differential Diagnosis
When evaluating a patient for CKD, it is crucial to consider other potential diagnoses that may present with similar symptoms and clinical findings. The differential diagnoses include:
- Acute kidney injury
- Alport syndrome
- Antigiomerular basement membrane disease
- Diabetic nephropathy
- Multiple myeloma
- Nephrolithiasis
- Rapidly progressive glomerulonephritis
- Renal artery stenosis
The 6 categories of CKD staging include:
- G1: GFR 90 mL/min/1.73 m 2 and above with urinary abnormalities suggesting kidney disease such as hematuria or proteinuria
- G5: GFR less than 15 mL/min/1.73 m 2 or ESRD
The 3 levels of albuminuria include ACR:
The CRIC study is an observational study that began in 2001 and is still ongoing in the fifth and final phase. The CRIC study examined risk factors for the progression of CKD and CVD among nearly 5500 patients. The study enrolled adults aged 21 to 74 with a broad range of renal disease severity and eGFR between 20 and 70 mL/min/1.73 m 2 . About half the patients had concurrent diabetes. Measures of kidney function and occurrence of new and worsening CVD were primary endpoints, and they have yielded valuable data on a variety of other significant associations. [34] [35]
The CRIC study showed that CKD progression was correlated with cognitive decline, cardiovascular mortality, left ventricular hypertrophy, coronary artery calcification, and clinical depression, among other associations. [35]
- Complications
Systemic Complications of Chronic Kidney Disease
Salt/fluid balance: Salt and fluid balance abnormalities are common in CKD, becoming more apparent in stages 4 and 5. These patients often respond to sodium restriction and loop diuretics. The 2012 KDIGO guidelines recommend sodium intake be restricted to less than 2 g/d for all CKD patients.
Hypertension: Hypertension in CKD can be a manifestation of volume expansion, although patients with CKD do not always have edema to suggest volume expansion. Many patients with CKD benefit from using a loop diuretic before escalating the doses of other antihypertensives. The KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in CKD recommends aiming for a systolic blood pressure below 120 mm Hg for patients not on dialysis. [36]
The 2017 ACC/AHA guidelines set the blood pressure target for patients with diabetes or CKD at less than 130/80 mm Hg. [37] However, other renal societies advocate for more patient-specific goals, suggesting that an office blood pressure between 120 and 140 mm Hg systolic and between 70 and 80 mm Hg diastolic is appropriate. [38] Despite varying guidelines, close monitoring with frequent home blood pressure readings is essential to accurately adjust medications and achieve the desired goals.
Hyperkalemia: Hyperkalemia in CKD can occur particularly in oliguric patients and those with distal renal tubular dysfunction. Contributing factors include dietary potassium intake, tissue breakdown, and aldosterone resistance. Additionally, medications such as angiotensin-converting enzyme (ACE) inhibitors and nonselective beta-blockers can also lead to hyperkalemia.
Metabolic acidosis: Metabolic acidosis is a common complication of advanced CKD due to the retention of acidic compounds. Chronic metabolic acidosis can lead to osteopenia in these patients. Treatment typically involves bicarbonate supplementation to maintain a serum bicarbonate level of 23 mEq/L.
Hyperphosphatemia: Hyperphosphatemia is a common complication of CKD due to a decreased filtered phosphorous load. This leads to increased secretion of PTH and causes secondary hyperparathyroidism. While hyperparathyroidism aims to normalize phosphorus and calcium levels, it often leads to hyperphosphatemia at the expense of bone health. Additionally, FGF23, a protein involved in calcium and phosphorus metabolism, is associated with cardiovascular mortality independently of its bone metabolic effects. [35] Please see StatPearls' companion resource, " Chronic Kidney Disease-Mineral Bone Disorder ," for further information.
Anemia: Anemia of CKD is typically normocytic normochromic and results from reduced erythropoietin production due to decreased functioning renal mass, abnormal iron metabolism, and reduced red blood cell survival. Hemoglobin levels should be checked annually in stage 3 CKD, every 6 months in stages 4 and 5, and monthly in dialysis patients. Erythropoiesis-stimulating agents should be considered when hemoglobin is below 10 g/dL, with iron saturation at least 20% to 30% and ferritin greater than 200 ng/mL. For dialysis patients, the target hemoglobin concentration is 10 to 11.5 g/dL. Please see StatPearls' companion reference, " Anemia of Chronic Renal Disease ," for further information.
Cardiovascular disease: The risk of CVD increases with the severity of CKD. Considerable evidence indicates a significant association between epicardial adipose tissue thickness and the incidence of CVD events in CKD patients. Therefore, assessing epicardial adipose tissue could be a reliable parameter for evaluating cardiovascular risk in CKD patients. [39]
Insulin resistance: Insulin resistance and metabolic syndrome are strongly associated with CKD and contribute to the development of atherosclerotic disease. This association is thought to be mediated by increased inflammatory markers. [11]
Treatment of Complications of End-Stage Renal Disease
Malnutrition in ESRD is often caused by anorexia and inadequate protein intake. The diet for ESRD patients should provide at least 30 to 35 kcal/kg/d. Dietitians play a crucial role in improving the nutritional status and overall health of patients with CKD and ESRD.
Uremic bleeding is a complication resulting from impaired platelet function, which leads to prolonged bleeding times. Asymptomatic patients typically do not require treatment. However, correction of uremic platelet dysfunction is necessary during active bleeding or before surgical procedures. Interventions may include desmopressin (DDAVP), cryoprecipitate, estrogen, and initiation of dialysis.
Complications of Renal Transplantation
Infectious complications are prevalent in posttransplant patients, necessitating appropriate prophylaxis and vaccinations. Other common CKD complications include hypertension, dyslipidemia, coronary artery disease from new-onset diabetes mellitus, arrhythmias, and heart failure. Neurological complications include stroke and posterior reversible encephalopathy syndrome, central nervous system infections, neuromuscular and seizure disorders, and neoplastic disease. Gastrointestinal complications include infection, mucosal injury, mucosal ulceration, perforation, biliary tract disease, pancreatitis, and diverticular disease. Due to immunosuppression, patients with kidney transplants have an increased risk of malignancy, such as posttransplant lymphoproliferative disorder and skin cancer. [40] [41]
- Consultations
As mentioned below, managing CKD often requires input from various specialties to address complex issues and provide comprehensive care.
- Nephrology: Nephrologists should be consulted for all patients with CKD, especially once stages 3 to 5 are reached.
- Urology: A urologist is needed for obstructive uropathy to relieve obstruction using retrograde ureteral catheters or percutaneous nephrostomy.
- Interventional radiology: A consultation with an interventional radiologist can be made for the placement of permanent tunneled hemodialysis catheters.
- Surgery: A surgical consultation is recommended for placing arteriovenous fistulas (AVF) or grafts (AVG), as well as for the insertion of peritoneal dialysis catheters.
- Deterrence and Patient Education
All high-risk patients, including those with diabetes or hypertension, should be screened for CKD and also receive counseling on the symptoms and signs of the condition.
Patients with CKD can benefit from the following home interventions:
- About 85% of CKD patients have hypertension. They should be advised to measure their blood pressure daily and maintain a log of their blood pressure readings and daily weights.
- Patients with hemoglobin levels below 10.0 g/dL might benefit from home administration of subcutaneous erythropoietin-stimulating agents if this is more convenient than office visits.
- Consultation with a nutritionist is recommended for optimal dietary management and to avoid high-potassium foods.
- All patients with advanced CKD should be instructed to monitor their phosphorus levels and take phosphate binders with each meal.
- CKD patients who are pregnant or planning to become pregnant should be informed that pregnancy may exacerbate CKD and that impaired kidney function can negatively impact pregnancy. They should also be made aware that some medications used in CKD, such as ACE inhibitors, are teratogenic.
- Pearls and Other Issues
Key facts to keep in mind regarding CKD include:
- CKD is defined as kidney damage or an eGFR less than 60 mL/min/1.73 m 2 , persisting for 3 months or more, irrespective of the cause.
- CKD is usually asymptomatic until it reaches stages 4 and 5.
- The KDOQI guidelines recommend screening high-risk populations, which include individuals with hypertension, diabetes mellitus, and those aged 65 or older. This screening should involve urinalysis, measurement of urine ACR, serum creatinine, and estimation of GFR, preferably using the CKD Epidemiology Collaboration (CKD-EPI) equation.
- Calcium and phosphorus levels are not useful in distinguishing AKI from CKD. However, normal PTH levels suggest AKI rather than CKD.
- Systemic hypertension, proteinuria, hyperlipidemia, and metabolic acidosis cause the progression of CKD and need to be treated aggressively.
- Bicarbonate supplementation to reach a serum bicarbonate target equal to 23 mEq/L can help delay the progression of CKD.
- All CKD patients need to be evaluated for anemia, hypertension, metabolic acidosis, and bone and mineral disorders.
- Enhancing Healthcare Team Outcomes
CKD has a multitude of manifestations and is optimally managed by an interprofessional team of healthcare professionals. These teams should adhere to guideline-driven kidney care, address complications, recommend lifestyle modifications, and educate patients about various dialysis options. A study comparing standard care with a "healthy transitions" program—where a nurse care manager utilizes a protocol-driven informatics system to provide daily reports on incomplete steps for each patient—demonstrated notable benefits. This approach resulted in reduced hospitalizations, increased use of arteriovenous (AV) fistulas, fewer emergency dialysis procedures, and decreased catheter use, suggesting that such models could potentially lower overall healthcare costs significantly. [42]
Nephrologists play a crucial role in managing CKD by minimizing patient risk factors and optimizing goals for electrolytes and anemia. Primary care providers should focus on educating patients about the importance of quitting smoking, eating a healthy diet, maintaining a healthy weight, and addressing cardiac risk factors. Clinics should include access to a nutritionist, who assesses nutritional status and develops individualized meal plans. Additionally, pharmacists are essential for reviewing medications, screening for nephrotoxic drugs, and adjusting non-nephrotoxic medications based on the patient's renal function.
The nurse practitioner monitors blood pressure and adjusts medications as needed. The dialysis nurse is critical in educating patients on caring for dialysis catheters or AV fistulas. A vascular access nurse assesses suitable patients for hemodialysis access, whereas a renal transplantation nurse provides information on the transplantation procedure and patient selection criteria. An interprofessional approach to managing chronic renal failure reduces redundant testing, is cost-effective, minimizes patient morbidity, and leads to improved outcomes.
- Review Questions
- Access free multiple choice questions on this topic.
- Click here for a simplified version.
- Comment on this article.
Disclosure: Satyanarayana Vaidya declares no relevant financial relationships with ineligible companies.
Disclosure: Narothama Aeddula declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Vaidya SR, Aeddula NR. Chronic Kidney Disease. [Updated 2024 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Chronic Kidney Disease (Nursing). [StatPearls. 2024] Chronic Kidney Disease (Nursing). Vaidya SR, Aeddula NR, Doerr C. StatPearls. 2024 Jan
- Review Chronic kidney disease in adults: assessment and management [ 2015] Review Chronic kidney disease in adults: assessment and management . 2015 Jan
- Review Kidney Disease in Diabetes. [Diabetes in America. 2018] Review Kidney Disease in Diabetes. Pavkov ME, Collins AJ, Coresh J, Nelson RG. Diabetes in America. 2018 Aug
- Improving early detection of chronic kidney disease. [Practitioner. 2015] Improving early detection of chronic kidney disease. Larmour KE, Maxwell AP, Courtney AE. Practitioner. 2015 Feb; 259(1779):19-23, 2-3.
- Health-Related Quality of Life according to Renal Function: Results from a Nationwide Health Interview and Examination Survey. [Kidney Blood Press Res. 2022] Health-Related Quality of Life according to Renal Function: Results from a Nationwide Health Interview and Examination Survey. Faulhaber L, Herget-Rosenthal S, Jacobs H, Hoffmann F. Kidney Blood Press Res. 2022; 47(1):13-22. Epub 2021 Nov 22.
Recent Activity
- Chronic Kidney Disease - StatPearls Chronic Kidney Disease - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Chronic Kidney Disease (CKD)
Last Updated: September 11, 2023
Medically reviewed by NKF Patient Education Team
Table of Contents
About chronic kidney disease (ckd), signs and symptoms, complications, preparing for your appointment, download the nkf fact sheet: newly diagnosed with kidney disease, more resources.
Your kidneys do many important jobs. Some of the ways they keep your whole body in balance include:
- Removing natural waste products and extra water from your body
- Helping make red blood cells
- Balancing important minerals in your body
- Helping maintain your blood pressure
- Keeping your bones healthy
Chronic kidney disease (CKD) is when the kidneys have become damaged over time (for at least 3 months) and have a hard time doing all their important jobs. CKD also increases the risk of other health problems like heart disease and stroke. Developing CKD is usually a very slow process with very few symptoms at first. So, CKD is divided into 5 stages to help guide treatment decisions.
Many people living with CKD do not have any symptoms until the more advanced stages and/or complications develop. If symptoms do happen, they may include:
- Foamy urine
- Urinating (peeing) more often or less often than usual
- Itchy and/or dry skin
- Feeling tired
- Loss of appetite
- Weight loss without trying to lose weight
People who have more advanced stages of CKD may also notice:
- Trouble concentrating
- Numbness or swelling in your arms, legs, ankles, or feet
- Achy muscles or cramping
- Shortness of breath
- Trouble sleeping
- Breath smells like ammonia (also described as urine-like or “fishy”)
Your kidney health is unique. Your path should be too.
Risk factors.
Anyone can develop CKD - at any age. However, some people are at a higher risk than others. The most common CKD risk factors are:
- High blood pressure (hypertension)
- Heart disease and/or heart failure
- Over the age of 60
- Family history of CKD or kidney failure
- Personal history of acute kidney injury (AKI)
- Smoking and/or use of tobacco products
For many people, CKD is not caused by just one reason. Instead, it is a result of many physical, environmental, and social factors . Early detection is important – CKD often begins without causing any noticeable symptoms. Knowing the risk factors can help you know your level of risk and if you should get checked for CKD.
Other causes
CKD can also be caused by many other conditions or circumstances. Some examples include:
- Glomerular diseases: glomerulonephritis , IgA nephropathy (IgAN) , and HIV nephropathy
- Inherited conditions: polycystic kidney disease
- Autoimmune conditions: lupus (lupus nephritis)
- Severe infections: sepsis and hemolytic uremic syndrome (HUS)
- Other causes: kidney cancer , kidney stones , frequent untreated and/or long-lasting urinary tract infections (UTIs) , hydronephrosis , and kidney and urinary tract abnormalities before birth
37 million adults in the United States are living with CKD - and approximately 90% do not even know they have it. Take this one-minute quiz to find out if you are at high risk for CKD.
As CKD worsens, the risk of getting complications goes up. Some examples include:
- Cardiovascular disease (heart disease and/or stroke)
- High blood pressure
- Anemia (low levels of red blood cells)
- Metabolic acidosis (buildup of acid in the blood)
- Mineral and bone disorder (when blood levels of calcium and phosphorus are out of balance leading to bone and/or heart disease)
- Hyperkalemia (high levels of potassium in the blood)
- Kidney failure
Some conditions, like cardiovascular disease and high blood pressure, can also cause or worsen CKD.
Checking for CKD is easy with two simple tests:
- a blood test known as the estimated glomerular filtration rate (eGFR)
- a urine test known as the urine albumin-creatinine ratio (uACR)
Both tests are needed to have a clear picture of your kidney health. Having an eGFR under 60 and/or a uACR over 30 for three months or more is a sign you may have kidney disease.
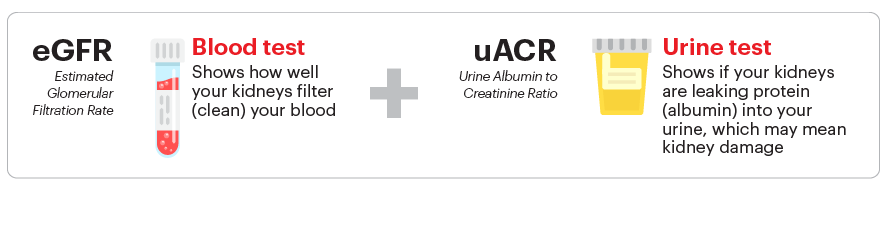
The eGFR is an estimate of how well your kidneys are removing waste products from the blood. It is calculated using your serum creatinine level, age, and sex. It can also be calculated using your cystatin C level. A “normal” eGFR varies according to age – it decreases as you get older. For this test, a higher number is better. Your eGFR number is used to determine your stage of CKD .
The uACR measures the amount of two different substances in your urine – albumin (protein) and creatinine. Healthy kidneys keep the albumin in your blood while filtering the creatinine out into the urine. So, there should be very little or no albumin in your urine. The uACR is calculated by dividing the amount of urine albumin by the amount of urine creatinine to find the ratio. For this test, a lower number is better. Your uACR number is used to test for albuminuria - a significant risk factor for complications.
In some cases, your healthcare professional may order additional tests to get more information about your kidney health. Some examples include a kidney biopsy or medical imaging (CT scan, ultrasound, or MRI).
Understanding my kidney numbers
Watch a playlist of short, animated videos with information about your kidney numbers, including:
- A brief explanation of the uACR and eGFR tests
- Reading the CKD Heat Map and understanding your risk
- Important steps for managing CKD
Managing CKD is focused on four very important goals:
- Managing the disease(s) or condition(s) that are most likely causing the CKD (for example, your diabetes, high blood pressure, or IgA nephropathy)
- Taking steps to slow down the CKD disease process directly (also known as “slowing CKD progression”)
- Lowering your risk of cardiovascular disease (having a heart attack or stroke)
- Treating any complications that you may have because of your CKD
Specific treatment recommendations depend on your stage of CKD and what other health conditions you have (including any CKD complications). Below are recommendations that apply to most people with CKD. No two people are the same, so talk with your healthcare professional about recommendations tailored to you.
Medications
Your healthcare professional may prescribe one or more medicines to help slow down or stop your CKD from getting worse. These medicines can include an ACE inhibitor/ARB , an SGLT2 inhibitor and/or an nsMRA .
Your healthcare professional may also prescribe a statin (cholesterol medicine). Guidelines recommend a statin for people with CKD who also have diabetes, a history of heart disease, or are age 50 or older. Even if you do not have high cholesterol, a statin can help lower your risk of having a heart attack or stroke.
You may also need to take additional medications or supplements to manage any CKD complications you might have (if applicable).
It is important to limit your sodium (salt) intake to less than 2300 mg per day (about 1 teaspoon of salt from all the food and drinks you consume each day). This recommendation is very important if you also have high blood pressure. Your healthcare professional may advise an even lower target depending on your other health conditions. This means a lot more than not using a saltshaker, but also limiting foods with high levels of sodium listed on their nutrition facts label . Some foods that don’t taste salty can have a surprising amount of sodium when you check their nutrition facts label.
Based on the results of your blood tests, your healthcare professional or kidney dietitian may also advise you to change how much potassium , phosphorus , and/or calcium you might be getting through your diet.
Meeting with a dietitian can be especially helpful if you also have other health conditions like high blood pressure, diabetes, or heart failure where it is even more important to integrate a healthy diet into your lifestyle to help prevent complications. It can feel overwhelming to keep track of so many changes, and a dietitian can help you identify what works best for you.
Additional information about eating healthy with kidney disease can be found on the Nutrition and Early Kidney Disease page.
Lifestyle recommendations
Now is a great time to make healthier lifestyle choices:
- If you smoke and/or use tobacco products , stop. Smoking can speed up the kidney disease process and increase your risk of getting kidney failure. It also increases your risk for other serious health problems, including high blood pressure, heart disease, cancers, and stroke.
- Exercise regularly . Remember, it’s okay to start slowly – taking short walks is a great way to begin.
- Sleeping well is important, too. Try to get enough sleep so you are well-rested.
- If you are overweight , losing weight through a balanced diet and physical activity can help improve your health in many ways.
- Find ways to reduce and manage stress in your life.
Other ways to lower your risk
Taking steps to manage other health conditions you may also have can also help your CKD. This includes high blood pressure , diabetes , and high cholesterol .
People with CKD should also avoid certain pain medicines known as non-steroid anti-inflammatory drugs (NSAIDs) . These can be harmful to your kidneys, especially at higher doses and/or with long-term use. Some examples include:
- ibuprofen (Motrin, Advil)
- indomethacin (Indocin)
- naproxen (Aleve, Naprosyn)
- diclofenac tablets or capsules (Cataflam, Zipsor)
- celecoxib (Celebrex)
- meloxicam (Mobic)
- aspirin (only if more than 325 mg per day)
Many of these NSAID medicines are available over-the-counter (OTC) and may be sold under a different name or be mixed with other ingredients (like cough & cold medicines). Sometimes it may not be possible to avoid using these products depending on your other health conditions. Always ask your healthcare professional before using any products with these drug names or if the word “NSAID” is printed on the product’s label. In general, acetaminophen, also called Tylenol, is safe for your kidneys at recommended doses - but check with your healthcare professional first to determine the cause of your pain and the best way to treat it.
If your healthcare professional says you have metabolic acidosis , increasing the amount of fruits and vegetables you eat everyday can help lower the level of acid in your blood. This can also help slow down your CKD progression (worsening).
Check out our online communities to connect, learn more and hear from others going through similar experiences.
Questions to ask.
- What are my eGFR and uACR numbers? What is my CKD stage?
- How high is my level of risk for developing heart disease or a stroke? What can I do to lower my risk?
- When should I have my eGFR and uACR tested again?
- Am I at a healthy weight?
- Is my blood pressure within the recommended goal range?
- Do I have diabetes or prediabetes? If so, is my A1C within the recommended goal range?
- Do I have albuminuria?
- Are there any changes I should make to my diet?
- Should I take any medication(s) to help lower my risk for CKD getting worse?
- Download the NKF fact sheet: Newly diagnosed with kidney disease: English
- Download the NKF fact sheet: Newly diagnosed with kidney disease: Spanish
Stages of Chronic Kidney Disease (CKD)
Learn more information about chronic kidney disease (CKD), including:
- How CKD is detected and classified
- Risk factors for developing CKD
- Information for managing CKD at each stage
- Kidneys and Chronic Kidney Disease
- Kidney Disease and Albuminuria/Proteinuria
- Kidney Numbers and the CKD Heat Map
- Plant Based Diets and Early CKD
- 7 Ways to Help Manage Your Kidney Disease
- NKF Council on Renal Nutrition CKD Kidney Dietitian Directory
How helpful was this content?
Related kidney topics, interstitial cystitis, kidney stones, stage 3b chronic kidney disease (ckd), bk virus: what transplant patients need to know, alport syndrome, childhood nephrotic syndrome, diabetes - a major risk factor for kidney disease, understanding ectopic kidneys, percutaneous nephrolithotomy / nephrolithotripsy, related news and stories.

December 17, 2020
10 Signs You May Have Kidney Disease

January 27, 2016
7 Tips to Protect Your Kidney & Heart Health

September 12, 2024
Surviving the Unexpected: Bacterial Meningitis and Kidney Failure

June 14, 2023
Living with High Potassium (Hyperkalemia): Stories and Advice

December 19, 2018
NKF and Jerry Rice – Making Big Plays for Kidney Health

March 19, 2020
Supporting you during the coronavirus pandemic

April 05, 2017
National Kidney Month 2017 in Review

May 09, 2021
Does a Diagnosis of Lupus Nephritis Also Mean I Have Lupus?

June 25, 2020
On my mind this week: Spikes, inequalities and kids
Related recipes.

Pumpkin Pancakes

Chicken Salad

Cauliflower Au Gratin

Hearty Chicken Baked Pasta


BBQ Pineapple Chicken

Italian Phyllo Cups

Maple-Balsamic Chicken

Love Your Kidneys, Breakfast Cereal

Moroccan Couscous
Chronic Kidney Disease (CKD)
Jul 10, 2014
1.21k likes | 2.13k Views
Chronic Kidney Disease (CKD). Key Concepts Chronic kidney disease (CKD) is classified based on: * the cause of kidney disease, assessment of glomerular filtration rate, and extent of proteinuria .
Share Presentation
- patient education
- intensive blood glucose control
- intensive insulin therapy
- complications
- chronic kidney disease

Presentation Transcript
Key Concepts • Chronic kidney disease (CKD) is classified based on: * the cause of kidney disease, assessment of glomerular filtration rate, and extent of proteinuria. • Frequent complications of advanced CKD include altered sodium and water balance, hyperkalemia, metabolic acidosis, anemia, CKD-related mineral and bone disorder (CKD-MBD), and cardiovascular disease. 3. Key mechanisms responsible for the progression of CKD: Reduction of kidney mass, development of glomerular hypertension, and intratubularproteinuria 4. Anemia of CKD is primarily caused by a deficiency in the production of endogenous erythropoietin by the kidney with iron deficiency as a contributing factor. 5. CKD-MBD includes abnormalities in parathyroid hormone (PTH), calcium, phosphorus, the calcium–phosphorus product, vitamin D, bone turnover, and soft-tissue calcifications and contributes to extravascular calcifications.
Guidelines provide information to assist healthcare providers in clinical decisions and the design of appropriate therapy to manage CKD progression and the associated complications. • Patient education plays a critical role in the appropriate management of patients with CKD and related complications. • ACEIs and ARBs are key pharmacologic treatments of CKD because of their effects on renal hemodynamics and reduction ofBP, which help to limit kidney disease progression. • Management of anemia includes administration of erythropoietic-stimulating agents (ESAs) (epoetinalfa, darbepoetinalfa) and regular iron supplementation (oral or IV administration) to maintain hemoglobin and prevent the need for blood transfusions. There is evidence indicating a higher risk of cardiovascular events when hemoglobin is targeted to greater than 11 g/dL. 10. Management of CKD-MBD includes dietary phosphorus restriction, phosphate-binding agents, vitamin D supplementation, and calcimimetic therapy.
CKD Definition: **Abnormalities in kidney structure or function for ≥ 3 months, with implications for health. • Structural abnormalities include: *Albuminuria of more than 30 mg/day, *Presence of hematuria or red cell casts in urine sediment, *Electrolyte & other abnormalities due to tubular disorders, *Abnormalities detected by histology, *Structural abnormalities detected by imaging, Or *history of kidney transplantation. ** An abnormality in kidney function is usually indicated by a ↓ (GFR).
The prognosis of CKD can vary and depends on: • Cause of kidney disease; (b) GFR at time of diagnosis; (c) Degree of albuminuria; (d) Presence of other comorbid conditions. *Frequent Complications of Advanced CKD: • Altered sodium and water balance, • Hyperkalemia, • Metabolic acidosis, • Anemia, • CKD-related mineral and bone disorder (CKD-MBD), • Cardiovascular disease (CVD).
Epidemiology: • 13% of the U.S. population. • CKD is more likely in: * Those over 60 years of age * Diabetics * Hypertension patients * CVD patients • Rates of ESRD are > in African Americans (3.4 X greater) and Native Americans (0.5 X greater) compared with whites and 1.5 times > in Hispanics than in non-Hispanics.
Etiology of CKD: 1. Susceptibility Factors: • Most of these susceptibility factors are not amenable to pharmacologic or lifestyle, interventions, but are useful for identifying individuals at high risk of CKD. 2. Initiation Factors: • Conditions that directly result in kidney damage & are modifiable by pharmacologic therapy. *Diabetes mellitus: leading cause of CKD & of ESRD in the USA *Hypertension: 2nd leading cause of ESRD *Glomerulonephritis: 3rd leading cause of ESRD
3. Progression Factors: • Result in faster decline in kidney function & cause worsening of CKD. * May be modified by pharmacologic therapy or lifestyle modifications to slow the progression of CKD.
Progression Factors: • Proteinuria: • Marker of glomerular & tubular dysfunction • Degree of proteinuria correlates with progression of CKD. • Microalbuminuria> 30mg/day: linked with vascular injury & ↑ CV mortality
2) Elevated BP * Systemic BP correlates with glomerular pressure • Elevations in both systemic BP & glomerular pressure contribute to glomerular damage • The rate of GFR decline is related to elevated systolic BP
3) Elevated Blood Glucose: • The reaction between glucose & protein in blood produces advanced glycation end products (AGEs), which are metabolized in the proximal tubules. • Hyperglycemia→↑ AGEs synthesis in diabetics (suspected to cause Diabetic kidney disease)
4) Tobacco Smoking: • Induces thickening & hyperplasia of glomerulus • Raises systemic BP • Independent risk factor in developing microalbumiuria in HTN • Independnt & dose-dependent risk factor in developing CKD & microalbuminuria, & progression to ESKD. • Risk is more pronounced in men than in women
Proposed mechanisms for progression of renal disease
Pathophysiology of CKD: 1) Initial kidney damage from initiation factor 2)↓ # functioning nephrons 3) Remaining nephrons hypertrophy to compensate which initially may be adaptive 4) Over time →development of intraglomerular HTN may be mediated by angiotensin II (potent vasoconstrictor of both afferent and efferent arterioles, preferentially affects the efferent arterioles). Angiotensin II may also mediate CKD progression through nonhemodynamiceffects 5) High intraglomerular capillary pressure impairs the size- selective function of the glomerular permeability barrier → ↑urinary excretion of albumin and proteinuria.
Pathophysiology of CKD (cont.): 6) Proteinuria alone may → progressive loss of nephrons by direct cellular damage. (Filtered proteins i.e., albumin, transferrin, complement factors, IGs, cytokines, & angiotensin II in the renal tubule → ↑production of inflammatory & vasoactive cytokines (i.e. endothelinand monocyte chemoattractant protein-1 (MCP-1) → tubular cell toxicity. 7) Proteinuria may also →activation of complement components on the apical membrane of proximal tubules which may be the key mechanism of damage in the progressive proteinuricnephropathies. 8) These events ultimately → a) scarring of the interstitium, b) progressive loss of structural nephron units, c) reduction in GFR.
Assessment: • Screening for CKD should be done in all pts. with↑’d risk for developing CKD. • Assessment for CKD should include: *SCr measurement *Urinalysis *BP *Serum electrolytes &/or*Imaging studies
Proteinuria is the 1⁰ marker for structural kidney damage even with normal GFR. • Clinically significant proteinuria is defined as: * urinary protein execret’n > 300mg/d Or *Spot urine dipstick > 30 mg/dL Microalbuminuria: 30-300 mg urinary albumin/day
Clinical Presentation: • Symptoms • Stages 1& 2 CKD are generally asymptomatic • Stages 3& 4 may be associated with min. symptoms • Stage 5 can be associated with Uremic symptoms (fatigue, weakness, shortness of breath, mental confusion, nausea and vomiting, bleeding, and loss of appetite), itching, cold intolerance, weight gain (from accumulation of fluid), and peripheral neuropathies • Signs: • CV: Worsening HTN, edema, dyslipidemia, LVH, ECG changes, CHF • Muscular: Cramping • Neuropsychiatric: Depression, anxiety, impaired mental cognition • GI: GERD, GI bleeding, abdominal distension • GU: Changes in urine volume & consistency, "foaming" of urine (indicative of proteinuria)
Laboratory tests • All Stages 1-5 CKD: ↑BUN, SCr, ↓GFR • Advanced Stages: • Decreased: bicarbonate (metabolic acidosis), RBCs/Hb/Hct (anemia), iron indices (iron deficiency), vitamin D levels, albumin (malnutrition), glucose (may result from decreased degradation of insulin with impaired kidney function or poor oral intake), and calcium (in early stages). • Increased: potassium, phosphorus, magnesium, PTH, HTN, glucose (uncontrolled diabetes is a cause of CKD), LDL and TG, and calcium (in ESRD). • Other: may be hemoccult-positive if GI bleeding occurs (uremia) Urine may be positive for protein • Other diagnostic tests: Structural abnormalities of kidney may be present on diagnotic test
Treatment: • The 1⁰ goal : To slow & prevent the progression of CKD. • Therefore, it requires early identificat’n of pts @ risk for CKD to initiate interventions early in the course of the dz.
Nonpharmacologic Therapy: • Nutritional Management: • ↓dietary protein intake → slows the progression of kidney dz. • Recommendation: • GFR< 25 ml/min→↓ protein to 0.6g/kg/d • No adequate dietary energy intake → ↑ protein to 0.75 g/kg/d
Malnutrition: common in CKD & may be due to: *↓’d appetite * hypercatabolism * nutrients losses through dialysis • Dialysis CKD pts → 1.2-1.3 g/kg/d • Recommendation: • DM pts with CKD stages 1-4 → limit protein to 0.8 g/kg/d **↓ salt intake to < 2 g/day of sodium ( 5 gNaCl) with hypertension or proteinuria.
Pharmacologic Therapy: • Intensive Blood Glucose Control in DM Pts: • Target HbA1c < 7% to ↓proteinuria with or without diabetic KD • Intensive insulin therapy was effective in delaying development & progression of diabetic KD in types 1 & 2 DM: Insulin 3 or more X/day to maintain preprandial BG 70-120 g/dL & postprandial BG < 180 g/dL
2) Optimal BP Control: Recommendation: ** Goal BP < 130/80 mmHg in CKD <125/75 mmHg in proteinuria • All antihypertensives have similar effects on BP ** ≥ 3 agents are required to achieve the BP < 130/80
3) Reduction of Proteinuria: *ACEIs & ARBs ↓ glomerular capillary pressure & volume due to their effects on Angiotensin II → ↓proteinuria (independent of their ↓ BP) ** ACEIs & ARBs: Antihypertensives of choice for all CKD pts unless contraindicated due to their ability to ↓ proteinuria more than any other antihypertensives (up to 35-40%) • Nonhydropyridine CCBs also↓proteinuria (related to their effects on BP↓)
4) Hyperlipidemia: ** Goals of Tx of dyslipidemia are to: 1st to ↓ atherosclerotic CVD risk 2nd to ↓ proteinuria & decline in kidney function in CKD pts.( prteinuria is associated with ↑d TC, LDL-C, TG) **Statins & Fibric acid derivatives (NOT combined due to ↑d rhabdomyolysis ): First-line therapy unless contraindicated. ** Hyperlipidemia Tx can ↓ proteinuria & CKD progression. **Most statins are affected by enzyme inhibitors EXCEPT Pravastatin & Fluvastatin
5) Smoking Cessation & Exercise: *Smoking cessation is encouraged to slow progression of CKD & to ↓ risk of CVD. *Smoking cessation does not reverse kidney dysfunction in former smokers. *Exercise is recommended for CKD pts @ least 30 minutes 5X/week
6)Anemia: *Anemia→↓O₂ delivery to renal tubules→ release of inflamm. & vasoactive cytokines → CDK progression. • Anemia Tx in CKD pts→ ↓CV effects of anemia & slow CKD progression • Tx will be discussed later
Complications of CKD: • Impaired Na & Water Homeostasis: Pathophysiology: • Na & H₂O balance can be maintained by the FENa & wide range of urine osmolality despite the wide variations in intake with normal kidney function. • As # of functioning nephrons ↓→Remaining nephrons ↑FENa → osmotic diuresis→Impairs the kidneys’ ability to concentrate or dilute the urine →nocturia in stage 3. • As # of functioning nephrons continues to ↓→ Na load overwhelms the remaining nephrons→↓total Na execretion→Naoverload→Fluid retention → ↑Intravascular volume↑systemic BP. • Volume overload can→Pulmonary edema
Clinical Presentation & Diagnosis of Impaired Na & H₂O Homeostasis: • General: • Alterations in Na & H₂O balance in CKD manifests as ↑’d edema • Symptoms: • Nocturia can present in stage 3 CKD • Edema generally presents in stage 4 CKD or later • Signs: • CV: Worsening HTN, edema • GU: Changes in urine volume & consistency • Lab Tests: • ↑’d BP • Na levels remain within normal range • Urine osmolality is generally fixed @ 300mOsm/L
Treatment: • Nonpharmacologic Therapy: • Pts refrain from adding salt to the diet • Na restriction→(-) Na balance →Hypovolemia→↓Renal perfusion→Hastens GFR decline. • Slow changes over several days • Caution in using Saline-containing solutions in CKD pts to avoid volume overload
Fluid restriction unnecessary as long as Na intake is controlled • The intact thirst mechanism maintains total body H₂O & plasma osmolality near normal (fixed usually @≈ 2L/d as urine concentrating ability is lost) • Significant ↑in free H₂Opo or IV intake → volume overload & hyponatremia • Stage 5 CKD pts require RRT to maintain normal volume status • Fluid intake is often limited between hemodialysis • sessions
Pharmacologic Therapy: • Diuretic therapy prevents volume overload in CKD who can still produce urine • Loop diuretics: Mostly used • Thiazides: ineffective in GFR<30ml/min • Metolazone maintains its efficacy @GFR<20ml/min • As CKD progresses: *Higher doses (80-1,000mg/d furosemide) *Continuous IV or *Combination diuretic therapy May be used to ↑ Na & H₂O excretion **AVOID DEHYDRATION
2. Impaired Potassium Homeostasis: • Pathophysiology: • The ↓ in functioning nephrons→ ↑K distal tubular secretion & ↑K GI elim. due to aldosterone stimulation→ maintains serum[K] within normal in stages 1-4 of CKD • Hyperkalemia develops when GFR<20% of normal • Caution with use of ACIs & ARBs in stage 3 CKD or higher
Clinical Presentation & Diagnosis of Hyperkalemia: General: Generally asymptomatic in CKD until [K]>5.5mEq/L when cardiac abnormalities present. Symptoms: Symptoms generally appear in CKD stages 4 or 5 Signs: ECG Changes Lab Tests: ↑[K]
Treatment: • Nonpharmacologic Therapy: • Restrict dietary intake of K to 50-80 mEq/d • Good bowel regimen is important to minimize constipation in hemodialysis pts. to encourage GI k excretion in stage 5 CKD • Severe hyperkalemia is most effectively managed by hemodialysis
Pharmacologic Therapy: • Until Dialysis is started, other therapies should include: 1) * Cagluconate or Ca chloride 1g IV to reverse hyperkalemia-induced life threatening arrhythmias.
2) Temporary measures that could shift K intracellularly within 30-60 min. to stabilize the cell membrane from the effects of excessive serum [K], include: • Reg. Insulin (5-10 U IV)+ Dextrose (5-50%IV) • Nebulized albuterol 10-20 mg • NaHCO₃ is used for shifting only if severe metabolic acidosis (pH<7.2)
3) Sodium Polystyrene Sulfonate (SPS) 15-30g po or rectally: Na-K exchange resin promotes K excretion from GI with OA of 2 hrs & max. effect may take up to 6 hrs (limiting its effect in severe hyperkalemia). 4) Loop diuretics may ↓[K] in normal-mild kidney function but NOT in CKD stage 5
3) Anemia: Epidemiology & Etiology: *Defined as Hgb< 13.5 g/dL in males & < 12g/dL in females *Risk of developing anemia ↑’s as GFR declines • CKD-anemia→↓O₂ delivery & utilization & LVH→ ↑ CV risk & mortality in CKD
Pathophysiology: • The 1⁰ cause of anemia in CKD is ↓in EPO production as # functioning nephrons ↓ →normochromic normocytic anemia *Uremia may also contribute in developing anemia by ↓’ing life span of RBC from 120 days → 60 days in stage 5 CKD. • Other contributing factors include Fe deficiency anemia (from malnutrition , RBC production by EPO-Stimulating Agent) & blood loss (from lab testing & hemodialysis)
- More by User
The Chronic Kidney Disease Client
The Chronic Kidney Disease Client. Valerie Goodnight RN, CNN Missouri Kidney Program Center for Chronic Kidney Disease Education. Goals:. Define Chronic Kidney Disease (CKD) CKD Statistics Renal Anatomy and Physiology Overview Brief Review of Kidney Function Side Effects of Uremia
1.24k views • 39 slides
CHRONIC KIDNEY FAILURE
CHRONIC KIDNEY FAILURE. PRESENTED BY RABIA NAEEM. Objectives. What is Chronic Kidney Disease (CKD) ? What is Vicious Cycle Of CKD L eading to ESRD ? The Facts About Chronic Kidney Disease (CKD) What are the tests for CKD ? What Causes CKD ? What Are the Symptoms of CKD ?
923 views • 20 slides
Chronic Kidney Disease The Recognized Epidemic
Chronic Kidney Disease The Recognized Epidemic. Shagun Chopra m.D. Director of dialysis &Transplant NMcsd Assistant professor of medicine ucsd Assistant professor of medicine usuhs. Outline. ESRD What is CKD? Epidemiology of CKD? What does CKD predict?
1.01k views • 81 slides
Chronic kidney disease (CKD) Cases
Chronic kidney disease (CKD) Cases. Dr. Mohamed Balaha.
1.71k views • 23 slides
Chronic Kidney Disease
Chronic Kidney Disease. CKD Dialysis Renal Transplant. Bones can break, muscles can atrophy, glands can loaf, even the brain can go to sleep without immediate danger to survival. But -- should kidneys fail.... neither bone, muscle, nor brain could carry on. Homer Smith, Ph.D.
1.67k views • 99 slides

Chronic Kidney Disease. What is CKD?. Definition: GFR < 60mL/min/1.73m 2 for > 3 months +/- evidence of kidney damage OR Evidence of kidney damage for > 3 months +/- decreased GFR Microalbuminaemia Proteinuria Glomerular haematuria Pathological abnormalities Anatomical abnormalities.
374 views • 14 slides
Chronic Kidney Disease (CKD). Liz Leen. Patient. Enez Joaquin 24 y/o Pima Indian Diagnosed with T2DM at age 13 Has not been compliant with prescribed treatment Progressive decompensation of kidney function over past 7 years Diagnosed with Stage 3 CKD 2 years ago
905 views • 20 slides
Chronic Kidney Disease. Objectives. Chronic kidney disease (CKD) . Glomerular filtration rate (GFR). Risk factors. Type 1 diabetes . Natural history of chronic kidney disease. Protein, microalbuminuria and macroalbuminuria. Factors affecting albumin excretion. Diabetic renal assessment .
841 views • 31 slides
Chronic Kidney Disease (CKD). BY: DR. NAUSHAD PERVEZ. Chronic Kidney Disease (CKD). Chronic Kidney Disease (CKD). What Kidneys Do? Filter waste from blood Remove excess fluid Adjust the levels of minerals and chemicals Produce hormones regulating blood
544 views • 18 slides
Chronic Kidney Disease. Dr Fenella Mayle Fordbridge Medical Centre 26.11.12. CKD. Chronic renal failure is the progressive loss of nephrons resulting in permanent compromise of renal function. Identification of risk groups. Testing for CKD should be undertaken in the following groups:
765 views • 17 slides
Chronic Kidney Disease. Manju Sood GPST3. What is CKD?. Chronic renal failure is the progressive loss of nephrons resulting in permanent compromise of renal function. defined by evidence of kidney damage and level of renal function
551 views • 16 slides
Chronic Kidney Disease. Dr. Pooran Kumar kohistani FCPS Nephrology. Objectives. CKD Definition Epidemiology Management Treatment to delay progression Treatment to prevent secondary complications. Literature sources. National Kidney Foundation Practice Guidelines for CKD (N/KDOQI)
1.45k views • 65 slides
CHRONIC KIDNEY DISEASE TIMELY REFERRAL
CHRONIC KIDNEY DISEASE TIMELY REFERRAL. Coordinating Care for Improved Renal Disease Outcomes. CKD: Setting a Course for Action. How Many Patients Have CKD? Defining CKD Why do CKD Patients Need Special Care? Does Coordinated Care and Timely Referral Matter? Screening for CKD
766 views • 54 slides
Chronic Kidney Disease. Scott Grogan, DO MAJ, MC Faculty Development Fellow. Objectives. Defined the stages of CKD Calculated GFR Made evidence-based management recommendations Applied knowledge to determine prognosis. Your Priorities. When to refer Medical managm’t
278 views • 11 slides
CHRONIC KIDNEY DISEASE (CKD)
CHRONIC KIDNEY DISEASE (CKD). ETIOLOGY PATHOPHYSIOLOGY CLINIC. Background. CKD is a worldwide public health problem There is a rising incidence and prevalence of kidney failure with poor outcomes and high costs Adverse outcomes of CKD can be prevented or delayed
3.48k views • 42 slides
Chronic Kidney Disease Update
Chronic Kidney Disease Update. Marc McKinley, DO September 21 , 2013. Objectives. Define CKD Discuss patients at risk Identify the stages of CKD Understand the consequences of CKD Learn how to treat the sequelae of CKD Apply above knowledge to daily practice. Definition.
826 views • 67 slides
Chronic Kidney Disease. Jacqueline Annand – CKD Nurse Mary Simpson – CKD Nurse Joyce Mackie – Pre Dialysis/Transplant liaison Sister. What is CKD?. Chronic Kidney Disease (CKD) , is a progressive loss of renal function over a period of months or years.
695 views • 20 slides
Slowing the Progression of Chronic Kidney Disease
Slowing the Progression of Chronic Kidney Disease. Lawrence Fleming, M.D. August 9, 2006. Objectives. Definitions and course of chronic kidney disease (CKD). Statistics- the prevalence of CKD. Diagnosis of CKD. Stratification of CKD. Clinical plan for CKD. Evaluation and treatment.
315 views • 17 slides
Chronic Kidney Disease (CKD). Dr. Sham Sunder. Now we know why the titanic sank !!. < 0.5 %. 5- 10%. CKD – A scary Challenge for Us all !!. CKD – Chronic kidney disease. We have intricate things to learn !!. Practice Guidelines of CKD The National Kidney Foundation (NKF)
1.13k views • 31 slides
CKD – Chronic Kidney Disease - for primary care
CKD – Chronic Kidney Disease - for primary care. Keith Dickerson, MD, MS. Objectives. Definition of CKD and recognition of Risk Factors Why CKD matters Initial Evaluation of CKD: GFR, proteinuria, other workup Appreciate significance of protein in urine Primary Care management of CKD
688 views • 64 slides

Chronic Kidney Disease Market
In 2017, the total prevalent population of Chronic Kidney Disease (CKD) was found to be 122,704,658 in the seven major markets. The prevalent population of Chronic Kidney Disease in the United States was 35,288,932 while Japan had 21,183,442 prevalent cases of CKD in 2017. The market size of Chronic Kidney Disease (CKD) in the 7MM is estimated to be USD 16,897.5 Million by 2030. Advances and future research, increasing prevalence of CKD, opportunities associated with CKD, and early detection & precision medicine are some of key factors expected to drive the CKD market forward in the coming years. Some of the key players in the Chronic Kidney Disease (CKD) market includes GlaxoSmithKline, Akebia Therapeutics, Tricida Pharma, AstraZeneca, FibroGen, Astellas Pharma, Corvidia Therapeutics, Boehringer Ingelheim, Reata Pharmaceuticals and many others. For more details visit: https://www.delveinsight.com/report-store/chronic-kidney-disease-chronic-renal-failure-market
81 views • 1 slides
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches

63 templates
140 templates

33 templates

16 templates

18 templates
fall background
24 templates
Chronic Kidney Disease (CKD)
It seems that you like this template, chronic kidney disease (ckd) presentation, free google slides theme, powerpoint template, and canva presentation template.
Whether for high-profile medical conferences or academic symposiums, equip yourself with this Google Slides and PowerPoint template: It’s simple yet informative, helping you present the facts about chronic kidney disease convincingly. It is fully customizable, enabling you to tailor your presentation to different audiences with ease. Moreover, the AI-generated placeholder texts and medical illustrations can be easily replaced with your study data, research findings, or clinical case discussion. Share vital health messages in an engaging manner!
Features of this template
- 100% editable and easy to modify
- 20 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides, Canva, and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Register for free and start downloading now
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Create your presentation Create personalized presentation content
Writing tone, number of slides.

Premium template
Unlock this template and gain unlimited access

Register for free and start editing online
- Case Report
- Open access
- Published: 24 October 2024
Atypical presentation of PJP: hypercalcemia and kidney injury in an allogeneic stem cell transplant recipient
- Yunus Can Özalp 1 ,
- Hajrij Shehabie 1 ,
- Mehmet Günhan Tekin 2 ,
- Süreyya Yiğit Kaya 3 ,
- Hüseyin Saffet Beköz 3 ,
- Senem Maral 3 ,
- Ömür Gökmen Sevindik 3 &
- Leylagül Kaynar 3
BMC Infectious Diseases volume 24 , Article number: 1201 ( 2024 ) Cite this article
Metrics details
Pneumocystis jirovecii pneumonia (PJP) is an opportunistic infection that primarily affects immunocompromised individuals. Typical symptoms of PJP include the subacute onset of dyspnea, nonproductive cough, and low-grade fever. In hematology patients, particularly those who are allogeneic stem cell transplant recipients, the disease often presents with a more aggressive clinical course. While hypercalcemia has been documented as a manifestation of PJP in some solid organ transplant recipients, it has not been reported in hematology or stem cell transplant patients.
Case presentation
Here, we present a case of PJP in a 56-year-old male allogeneic stem cell transplant recipient, who developed hypercalcemia and renal failure during the late post-transplant period. The patient had a history of allogeneic stem cell transplantation due to acute myeloid leukemia. He presented with symptoms of fatigue and weakness. Laboratory tests revealed hypercalcemia (13.8 mg/dL) and elevated serum creatinine levels (2.3 mg/dL). The patient was hospitalized, and despite initial treatment with hydration and furosemide, the hypercalcemia persisted, leading to the administration of denosumab. During follow-up, hypoxia was detected, and a chest CT scan revealed mosaic attenuation and ground-glass opacities. Bronchoscopy was performed, and PCR testing confirmed the presence of Pneumocystis jirovecii. Other causes of hypercalcemia were ruled out, with PTH measured at 13.8 pg/mL (normal range 15–65 pg/mL), albumin at 3.71 g/dL, 1.25-dihydroxy vitamin D3 at 96 ng/dL (normal range 26–95 ng/dL), and 25-hydroxy vitamin D at 32.5 ng/mL (normal range 20–40 ng/mL). A PET-CT scan demonstrated no pathological FDG uptake, with the exception of findings suggestive of a pulmonary infection. Following treatment with trimethoprim-sulfamethoxazole and denosumab, the patient’s hypercalcemia and infection resolved.
Conclusions
Although rare, PJP can present with hypercalcemia and kidney injury in allogeneic stem cell transplant recipients. Early diagnosis and treatment can improve both PJP and hypercalcemia.
Peer Review reports
Pneumocystis jirovecii pneumonia (PJP) is an opportunistic infection caused by the fungus P. jirovecii, commonly affecting immunocompromised individuals, such as those with HIV, organ transplant recipients, or patients who have undergone allogeneic stem cell transplants. Primary prophylaxis is typically recommended for this high-risk group [ 1 , 2 ].
Notably, patients can develop the condition after discontinuing trimethoprim-sulfamethoxazole prophylaxis or even while receiving prophylactic treatment, therefore it should still be considered in the differential diagnosis if there is a high clinical suspicion [ 3 ].
Typical symptoms of PJP include the subacute onset of dyspnea, nonproductive cough, and low-grade fever. Compared to HIV-positive patients, who tend to have a more indolent clinical course, hematology patients with PJP often experience a sudden onset of hypoxic respiratory failure and dyspnea, frequently requiring intensive care. Hypercalcemia is not commonly associated with PJP; however, it has been reported in many cases involving solid organ transplant recipients, particularly those who have undergone kidney transplants [ 2 , 4 ].
Here, we present a case of PJP in an allogeneic stem cell transplant patient who developed hypercalcemia and renal failure in the late period of transplantation. Denosumab was used in the management of hypercalcemia. According to our literature review, this is the first reported case of PJP presenting with hypercalcemia and kidney injury in allogeneic stem cell transplant recipient.
A 56-year-old male patient with known diagnoses of diabetes mellitus and acute myeloid leukemia (AML) in remission underwent an allogeneic stem cell transplant (allo-HSCT) from a 9/10 HLA-matched unrelated donor, using a myeloablative conditioning regimen (busulfan and fludarabine). There was major and minor blood group incompatibility between the donor and the recipient. Post-transplant cyclophosphamide, cyclosporine, and mycophenolate mofetil were used for graft-versus-host disease (GVHD) prophylaxis. Early post-transplant complications included febrile neutropenia and mucositis. Neutrophil engraftment occurred on day + 16, platelet engraftment on day + 18, and the patient was discharged on day + 24.
The patient was maintained on cyclosporine, mycophenolate mofetil (discontinued on day + 35), valacyclovir (500 mg BID), trimethoprim-sulfamethoxazole (800/160 mg, three times a week), and ursodeoxycholic acid (500 mg BID for the first 90 days). Due to ongoing severe anemia, the patient received one unit of erythrocyte suspension weekly. Full donor chimerism was detected at 1 and 3 months, but a bone marrow biopsy at 3 months revealed pure red cell aplasia on a background of mildly hypocellular bone marrow. Immunosuppressive therapy was discontinued in the fourth month, followed by steroid treatment (prednisolone 1 mg/kg for a week) and then rituximab (375 mg/m 2 , weekly for four doses) due to a lack of response. The patient’s erythrocyte transfusion requirement gradually decreased.
Prophylactic trimethoprim-sulfamethoxazole was discontinued 8 months after transplantation when the lymphocyte count reached 1040/mm 3 . The patient was monitored with hemoglobin levels between 7 and 8 g/dL without the need for transfusions.
In the eleventh month post-transplant (day 325 of transplant), the patient presented with fatigue and weakness for one week. Physical examination revealed no signs of infection or GVHD. Laboratory tests showed hypercalcemia (13.8 mg/dL) and elevated creatinine (2.3 mg/dL), leading to hospitalization. Additional tests revealed WBC 9930/mm 3 , lymphocytes 510/mm 3 , Hb 7.5 g/dL, platelets 515,000/mm 3 , CRP 5 mg/L, LDH 208 U/L (normal range 135–225 U/L), plasma CMV-DNA PCR negative (negative < copies/mL), serum galactomannan 0.150 (normal < 0.5), PTH 13.8 pg/mL (normal range 15–65 pg/ml), albumin 3.71 g/dL, 1.25-dihydroxy vitamin D3 96 ng/dL (normal range 26–95 ng/dL), and 25-hydroxy vitamin D 32.5 ng/mL (normal range 20–40 ng/mL).
Despite intravenous hydration and furosemide treatment, there was no improvement in calcium and creatinine levels. Creatinine clearance was calculated as 38 ml/min. Denosumab (120 mg) was administered on the third day of hospitalization. During follow-up, the patient remained asymptomatic except for subfebrile fever (max fever 37.6 °C ) and low oxygen saturation levels (89–90%) on room air. Chest CT revealed widespread mosaic attenuation and ground-glass opacities suggestive of viral pneumonia (Fig. 1 ). Bronchoscopy and subsequent PCR testing confirmed Pneumocystis jirovecii pneumonia (PJP). Additionally, bronchoalveolar lavage (BAL) for CMV PCR and viral respiratory panel (including Influenza A, Influenza B, Coronavirus 229E, OC43, NL63, HKU1, Parainfluenza 1, 2, 3, 4, Metapneumovirus, Rhinovirus, RSV, Bocavirus, Enterovirus, Parechovirus, Adenovirus, Legionella pneumophila, Mycoplasma pneumoniae, Chlamydia pneumoniae, Haemophilus influenzae, Streptococcus pneumoniae, Bordetella pertussis, Influenza A subtype H1N1/2009, H1, H3), tuberculosis PCR and galactomannan (0.1) were negative.
The patient was started on treatment-dose trimethoprim-sulfamethoxazole and prednisolone (40 mg, once daily for four days). Due to low IgG levels (327 mg/dL), IVIG (0.4 g/kg) was also administered. PET-CT was performed to rule out malignancies, showing areas of increased metabolic activity with ground-glass opacities in both lungs (suggestive of infection). No pathological uptake indicative of malignant involvement was observed in other body areas.
After one week of treatment, calcium (9.2 mg/dL), creatinine (0.96 mg/dL) (Fig. 2 ), and oxygen saturation on room air normalized, and the patient was discharged with a continuation of oral treatment for three weeks.

Mosaic attenuation and ground-glass opacities in Chest CT
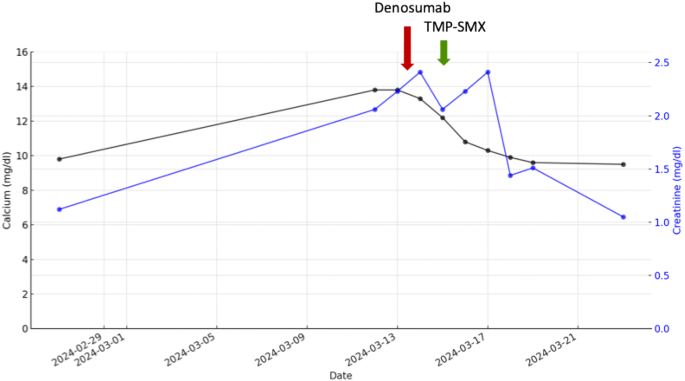
Calcium and creatinine response to Trimethoprim-Sulfamethoxazole (TMP-SMX) and denosumab
At the 18-month follow-up post-transplant, the patient remained without additional complications, and the latest tests showed WBC 6670/mm3, lymphocytes 1140/mm3, Hb 9.6 g/dL, platelets 472,000/mm3, calcium 9.54 mg/dL, and creatinine 1.04 mg/dL.
Discussion and conclusions
We present a case of an allogeneic stem cell transplant recipient who developed hypercalcemia and acute kidney injury in the late post-transplant period, with no symptoms other than fatigue, associated with Pneumocystis jirovecii pneumonia (PJP). After the failure of hydration and furosemide to resolve the hypercalcemia, a single dose of denosumab was administered.
The CIBMTR analysis of Pneumocystis jirovecii pneumonia (PJP) in HSCT patients reported an incidence of 0.63% in allogeneic (allo) recipients. The highest risk period for PJP is considered to be from day 80 to day 270 post-HSCT, with a median time to development of 120 days. Risk factors for PJP include lymphopenia, T-cell dysfunction, immunosuppression, GVHD, and HLA mismatch [ 5 ].
Our patient, who underwent a mismatched unrelated allo-HSCT, was not receiving immunosuppressive therapy (IST) and had no history of GVHD at 11 months post-transplant. However, it was later discovered that the absolute lymphocyte count, which had normalized by month 8, had decreased again, likely due to the delayed effects of rituximab.
PJP typically presents with an abrupt onset, marked by symptoms such as fever, non-productive cough, dyspnea, and diffuse interstitial pneumonia. The disease typically progresses rapidly, especially in cases of non-HIV-associated PJP, with the average time from symptom onset to diagnosis being just a few days. In allogeneic stem cell transplant (ASCT) recipients, PJP may present with an even more sudden onset, leading to rapid clinical deterioration and frequently necessitating admission to the intensive care unit [ 6 , 7 , 8 ].
Hamroun et al. reported that hypercalcemia was detected at the time of diagnosis in 18 out of 49 (37%) kidney transplant patients with PJP. They noted that cases with hypercalcemia had a more indolent clinical course and presented with febrile dyspnea [ 9 ]. While hypercalcemia has been reported in liver transplant patients and other immunosuppressed patients with PJP in case reports, we found no cases in the literature of PJP presenting with hypercalcemia in hematology or stem cell transplant patients [ 10 , 11 , 12 , 13 ].
It has been suggested that the hypercalcemia observed in patients with PJP is due to the extra-renal production of 1,25-dihydroxyvitamin D as a result of a granulomatous response to Pneumocystis [ 12 , 13 ]. Previous research has documented temporary increases in 1,25-dihydroxyvitamin D levels associated with hypercalcemia in PJP cases [ 13 , 14 ]. Similar to other granulomatous diseases, such as tuberculosis and sarcoidosis, granulomatous PJP may lead to the endogenous production of 1-alpha-hydroxylase by activated macrophages. This enzyme catalyzes the conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D, which in turn enhances bone resorption and intestinal calcium absorption. The resolution of mineral metabolism abnormalities following infection treatment further supports the involvement of PJP in the pathogenesis of hypercalcemia [ 12 , 13 , 14 ]. The frequent occurrence of hypercalcemia in PJP patients, coupled with the timing of its onset and resolution in relation to the infection, indicates a direct connection facilitated by increased production of 1,25-dihydroxyvitamin D [ 14 , 15 , 16 ].
Supporting this hypothesis, we observed a slight elevation in 1,25-dihydroxyvitamin D levels in our case, accompanied by suppressed PTH and normal 25-hydroxyvitamin D levels. Given the rapid progression of PJP infection in hematopoietic transplant patients, likely due to their profound immunosuppression, we suggest that there may be insufficient time for granuloma formation, 1,25-dihydroxyvitamin D production, and, consequently, the development of hypercalcemia.
In a pediatric case with refractory hypercalcemia despite treatment with TMP-SMX, hypercalcemia was resolved following the administration of denosumab [ 17 ]. Another case involved the use of pamidronate therapy [ 18 ]. In the review by Hamroun et al., it was noted that in adult renal transplant recipients, bisphosphonate therapy was administered when hypercalcemia was identified prior to the diagnosis of PJP. However, in the majority of cases, the management of PJP resulted in the gradual normalization of hypercalcemia [ 9 ]. In our case, despite early hydration and furosemide treatment, hypercalcemia and acute kidney injury persisted, leading to the administration of denosumab, which subsequently normalized calcium and creatinine levels.
According to our literature review, this case represents a rare instance of PJP manifesting with hypercalcemia and acute kidney injury in an allogeneic stem cell transplant recipient, occurring eleven months post-transplant and six months after rituximab treatment for pure red cell aplasia. Although rare, PJP can present with hypercalcemia and kidney injury in allogeneic stem cell transplant recipients. Early diagnosis and treatment can improve both PJP and hypercalcemia.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
Allogeneic Hematopoietic Stem Cell Transplant
Acute Myeloid Leukemia
Cytomegalovirus
C-Reactive Protein
Graft-Versus-Host Disease
Human Immunodeficiency Virus
Human Leukocyte Antigen
Immunosuppressive Therapy
Intravenous Immunoglobulin
Lactate Dehydrogenase
Pneumocystis jirovecii pneumonia
Polymerase Chain Reaction
Positron Emission Tomography–Computed Tomography
Parathyroid Hormone
Respiratory Syncytial Virus
Trimethoprim-Sulfamethoxazole
Maertens J, Cesaro S, Maschmeyer G, et al. ECIL guidelines for preventing Pneumocystis Jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J Antimicrob Chemother. 2016;71(9):2397–404.
Article CAS PubMed Google Scholar
Bateman M, Oladele R, Kolls JK. Diagnosing pneumocystis jirovecii pneumonia: a review of current methods and novel approaches. Med Mycol. 2020;58(8):1015–28.
Article CAS PubMed PubMed Central Google Scholar
Cordonnier C, Cesaro S, Maschmeyer G, et al. Pneumocystis Jirovecii pneumonia: still a concern in patients with haematological malignancies and stem cell transplant recipients. J Antimicrob Chemother. 2016;71(9):2379–85.
Kofteridis DP, Valachis A, Velegraki M, et al. Predisposing factors, clinical characteristics and outcome of Pneumonocystis Jirovecii pneumonia in HIV-negative patients. J Infect Chemother. 2014;20(7):412–6.
Article PubMed Google Scholar
Williams KM, Ahn KW, Chen M, et al. The incidence, mortality and timing of Pneumocystis Jiroveci pneumonia after hematopoietic cell transplantation: a CIBMTR analysis. Bone Marrow Transpl. 2016;51(4):573–80.
Article CAS Google Scholar
Kato H, Samukawa S, Takahashi H, Nakajima H. Diagnosis and treatment of Pneumocystis Jirovecii pneumonia in HIV-infected or non-HIV-infected patients-difficulties in diagnosis and adverse effects of trimethoprim-sulfamethoxazole. J Infect Chemother. 2019;25(11):920–4.
Salzer HJF, Schäfer G, Hoenigl M, et al. Clinical, diagnostic, and treatment disparities between HIV-Infected and Non-HIV-Infected immunocompromised patients with Pneumocystis Jirovecii Pneumonia. Respiration. 2018;96(1):52–65.
McKinnell JA, Cannella AP, Kunz DF, et al. Pneumocystis pneumonia in hospitalized patients: a detailed examination of symptoms, management, and outcomes in human immunodeficiency virus (HIV)-infected and HIV-uninfected persons. Transpl Infect Dis. 2012;14(5):510–8.
Hamroun A, Lenain R, Bui Nguyen L, et al. Hypercalcemia is common during Pneumocystis pneumonia in kidney transplant recipients. Sci Rep. 2019;9(1):12508.
Article PubMed PubMed Central Google Scholar
Yau AA, Farouk SS. Severe hypercalcemia preceding a diagnosis of Pneumocystis Jirovecii pneumonia in a liver transplant recipient. BMC Infect Dis. 2019;19(1):739.
Mascia G, Argiolas D, Carta E, Michittu MB, P GB. Acute kidney Injury secondary to Hypercalcemia in a kidney transplant patient with Pneumocystis Jirovecii Pneumonia: a Case Report. Transpl Proc. 2019;51(1):220–2.
Chatzikyrkou C, Clajus C, Haubitz M, Hafer C. Hypercalcemia and pneumocystis pneumonia after kidney transplantation: report of an exceptional case and literature review. Transpl Infect Dis. 2011;13(5):496–500.
Ramalho J, Bacelar Marques ID, Aguirre AR, Pierrotti LC, de Paula FJ, Nahas WC, et al. Pneumocystis Jirovecii pneumonia with an atypical granulomatous response after kidney transplantation. Transpl Infect Dis. 2014;16(2):315–9.
Hajji K, Dalle F, Harzallah A, Tanter Y, Rifle G, Mousson C. Vitamin D metabolite-mediated hypercalcemia with suppressed parathormone concentration in Pneumocystis Jirovecii pneumonia after kidney transplantation. Transpl Proc. 2009;41(8):3320–2.
Chen WC, Chang SC, Wu TH, Yang WC, Tarng DC. Hypercalcemia in a renal transplant recipient suffering with pneumocystis carinii pneumonia. Am J Kidney Dis. 2002;39(2):E8.
Bency R, Roger SD, Elder GJ. Hypercalcaemia as a prodromal feature of indolent pneumocystis jivorecii after renal transplantation. Nephrol Dial Transpl. 2011;26(5):1740–2.
Beale F, Gkiourtzis N, Koneru S, O’Brien C, Lalayiannis AD. Denosumab in a pediatric kidney transplant recipient with late, resistant hypercalcemia secondary to Pneumocystis Jirovecii pneumonia. Pediatr Nephrol. 2024;39(8):2355–8.
Hong L, Witton LD, Jolly EC. Pneumocystis Jirovecii pneumonia presenting with severe, refractory hypercalcaemia in an immunosuppressed renal transplant patient: review of the literature and novel biochemical insights. Clin Med (Lond). 2024;24(1):100011.
Download references
Acknowledgements
Not applicable.
This research did not receive any specific grant from funding agencies in the public, commercial, nor not-for-profit sectors.
Author information
Authors and affiliations.
Department of Internal Medicine, School of Medicine, Istanbul Medipol University, Istanbul, Türkiye
Yunus Can Özalp & Hajrij Shehabie
Hematology Department, Çam Sakura City Hospital, Istanbul, Türkiye
Mehmet Günhan Tekin
Department of Hematology, School of Medicine, Istanbul Medipol University, Istanbul, Türkiye
Süreyya Yiğit Kaya, Hüseyin Saffet Beköz, Senem Maral, Ömür Gökmen Sevindik & Leylagül Kaynar
You can also search for this author in PubMed Google Scholar
Contributions
Y.C.Ö., H.S., M.G.T., and H.S.B. were responsible for writing the main manuscript. S.M. and Ö.G.S. collected, analyzed, and interpreted the data. S.Y.K. prepared the figures. H.S.B. and L.K. assessed the patient. All authors revised the manuscript critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work. Additionally, L.K., as the corresponding author, had overall supervision and coordination responsibilities for the study, ensuring its integrity and accuracy.
Corresponding author
Correspondence to Leylagül Kaynar .
Ethics declarations
Ethics approval and consent to participate.
The publication of the case was approved by the Ethics committee of Istanbul Medipol University. Informed consent to participate was obtained from the patient.
Consent for publication
Informed consent for the publication of clinical data, including laboratory and radiology findings, was obtained from the patient.
Clinical trial
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Özalp, Y.C., Shehabie, H., Tekin, M.G. et al. Atypical presentation of PJP: hypercalcemia and kidney injury in an allogeneic stem cell transplant recipient. BMC Infect Dis 24 , 1201 (2024). https://doi.org/10.1186/s12879-024-10074-z
Download citation
Received : 14 August 2024
Accepted : 09 October 2024
Published : 24 October 2024
DOI : https://doi.org/10.1186/s12879-024-10074-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Pneumocystis jirovecii
- Hypercalcemia
- Allogeneic stem cell transplantation
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]

IMAGES
COMMENTS
Kidney failure happens when the damage is so severe that the kidneys do not work well enough to keep you alive. In other words, the kidneys 'fail' to work. If you have kidney failure, you will need to start dialysis or have a kidney transplant to stay alive and live a good quality life. We will talk more about these later.
Early in chronic kidney disease, you might have no signs or symptoms. As chronic kidney disease progresses to end-stage renal disease, signs and symptoms might include: Nausea. Vomiting. Loss of appetite. Fatigue and weakness. Changes in how much you urinate. Chest pain, if fluid builds up around the lining of the heart.
Generally, earlier stages are known as 1 to 3. And as kidney disease progresses, you may notice the following symptoms. Nausea and vomiting, muscle cramps, loss of appetite, swelling via feet and ankles, dry, itchy skin, shortness of breath, trouble sleeping, urinating either too much or too little.
Key Concepts Chronic kidney disease (CKD) is classified based on: * the cause of kidney disease, assessment of glomerular filtration rate, and extent of proteinuria. Frequent complications of advanced CKD include altered sodium and water balance, hyperkalemia, metabolic acidosis, anemia, CKD-related mineral and bone disorder (CKD-MBD), and cardiovascular disease. 3. Key mechanisms responsible ...
Arterio-venous Graft. Surgically constructed connection between an artery and vein using a synthetic piece of material. Same-day procedure with local anesthetic. Usually 1-3 months prior to maturity, though can be ready for use within 2 weeks of getting placed. Image credit: Mayo Foundation for Medical Education and Research.
Presentation Transcript. CKD - new definition 1. Kidney damage for > 3 months with or without decreased GFR, as manifest by either: • Pathological abnormalities, or • Markers of kidney damage (composition of the blood, urine, imaging tests) 2. GFR < 90 ml/min/1,73 m2 for > 3 months with or without kidney damage.
(See "Definition and staging of chronic kidney disease in adults" and "Definition and staging criteria of acute kidney injury in adults".) For patients being evaluated for elevated serum creatinine or reduced estimated glomerular filtration rate (eGFR), it is important to distinguish those who have relatively stable CKD from those who have ...
Chronic kidney disease (CKD) is characterized by the presence of kidney damage or an estimated glomerular filtration rate (eGFR) of less than 60 mL/min/1.73 m², persisting for 3 months or more, irrespective of the cause.[1] CKD is a state of progressive loss of kidney function, ultimately resulting in the need for renal replacement therapy, such as dialysis or transplantation. Kidney damage ...
Kidney disease, also known as chronic kidney disease or CKD, causes more deaths than breast cancer or prostate cancer (NVS 2021 report of 2018 data).1 It is the under-recognized public health crisis. • Kidney disease affects an estimated 37 million people in the U.S. (15% of the adult population; more than 1 in 7 adults).2,3,4
Chronic kidney disease (CKD)—or chronic renal failure (CRF), as it was historically termed—is a term that encompasses all degrees of decreased renal function, from damaged-at risk through mild, moderate, and severe chronic kidney failure. ... Presentation History. Patients with chronic kidney disease (CKD) stages 1-3 (glomerular ...
Free Google Slides theme, PowerPoint template, and Canva presentation template. Kidneys are some of the most important organs, as they take part in various important processes. If you are a physician or urologist, professor or a med student and want to show some details about nephritic conditions and their treatments, use this creative template.
Chronic kidney disease (CKD) is when the kidneys have become damaged over time (for at least 3 months) and have a hard time doing all their important jobs. CKD also increases the risk of other health problems like heart disease and stroke. Developing CKD is usually a very slow process with very few symptoms at first.
Presentation Transcript. Key Concepts • Chronic kidney disease (CKD) is classified based on: * the cause of kidney disease, assessment of glomerular filtration rate, and extent of proteinuria. • Frequent complications of advanced CKD include altered sodium and water balance, hyperkalemia, metabolic acidosis, anemia, CKD-related mineral and ...
Chronic Kidney Disease (CKD) Presentation. Free Google Slides theme, PowerPoint template, and Canva presentation template. Whether for high-profile medical conferences or academic symposiums, equip yourself with this Google Slides and PowerPoint template: It's simple yet informative, helping you present the facts about chronic kidney disease ...
Case presentation. Here, we present a case of PJP in a 56-year-old male allogeneic stem cell transplant recipient, who developed hypercalcemia and renal failure during the late post-transplant period. The patient had a history of allogeneic stem cell transplantation due to acute myeloid leukemia. He presented with symptoms of fatigue and weakness.
Leptospirosis, an acute zoonotic infection caused by spirochetes of the genus Leptospira, poses significant health risks worldwide. Transmission occurs through contact with infected animals' urine, blood, or tissue. This case report examines a 44-year-old man with severe leptospirosis, presenting as Weil's disease, characterized by acute hypoxic respiratory failure and acute kidney injury (AKI ...