Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.


How to disseminate your research

Published: 01 January 2019
Version: Version 1.0 - January 2019
This guide is for researchers who are applying for funding or have research in progress. It is designed to help you to plan your dissemination and give your research every chance of being utilised.
What does NIHR mean by dissemination?
Effective dissemination is simply about getting the findings of your research to the people who can make use of them, to maximise the benefit of the research without delay.
Research is of no use unless it gets to the people who need to use it
Professor Chris Whitty, Chief Scientific Adviser for the Department of Health
Principles of good dissemination
Stakeholder engagement: Work out who your primary audience is; engage with them early and keep in touch throughout the project, ideally involving them from the planning of the study to the dissemination of findings. This should create ‘pull’ for your research i.e. a waiting audience for your outputs. You may also have secondary audiences and others who emerge during the study, to consider and engage.
Format: Produce targeted outputs that are in an appropriate format for the user. Consider a range of tailored outputs for decision makers, patients, researchers, clinicians, and the public at national, regional, and/or local levels as appropriate. Use plain English which is accessible to all audiences.
Utilise opportunities: Build partnerships with established networks; use existing conferences and events to exchange knowledge and raise awareness of your work.
Context: Understand the service context of your research, and get influential opinion leaders on board to act as champions. Timing: Dissemination should not be limited to the end of a study. Consider whether any findings can be shared earlier
Remember to contact your funding programme for guidance on reporting outputs .
Your dissemination plan: things to consider
What do you want to achieve, for example, raise awareness and understanding, or change practice? How will you know if you are successful and made an impact? Be realistic and pragmatic.
Identify your audience(s) so that you know who you will need to influence to maximise the uptake of your research e.g. commissioners, patients, clinicians and charities. Think who might benefit from using your findings. Understand how and where your audience looks for/receives information. Gain an insight into what motivates your audience and the barriers they may face.
Remember to feedback study findings to participants, such as patients and clinicians; they may wish to also participate in the dissemination of the research and can provide a powerful voice.
When will dissemination activity occur? Identify and plan critical time points, consider external influences, and utilise existing opportunities, such as upcoming conferences. Build momentum throughout the entire project life-cycle; for example, consider timings for sharing findings.
Think about the expertise you have in your team and whether you need additional help with dissemination. Consider whether your dissemination plan would benefit from liaising with others, for example, NIHR Communications team, your institution’s press office, PPI members. What funds will you need to deliver your planned dissemination activity? Include this in your application (or talk to your funding programme).
Partners / Influencers: think about who you will engage with to amplify your message. Involve stakeholders in research planning from an early stage to ensure that the evidence produced is grounded, relevant, accessible and useful.
Messaging: consider the main message of your research findings. How can you frame this so it will resonate with your target audience? Use the right language and focus on the possible impact of your research on their practice or daily life.
Channels: use the most effective ways to communicate your message to your target audience(s) e.g. social media, websites, conferences, traditional media, journals. Identify and connect with influencers in your audience who can champion your findings.
Coverage and frequency: how many people are you trying to reach? How often do you want to communicate with them to achieve the required impact?
Potential risks and sensitivities: be aware of the relevant current cultural and political climate. Consider how your dissemination might be perceived by different groups.
Think about what the risks are to your dissemination plan e.g. intellectual property issues. Contact your funding programme for advice.
More advice on dissemination
We want to ensure that the research we fund has the maximum benefit for patients, the public and the NHS. Generating meaningful research impact requires engaging with the right people from the very beginning of planning your research idea.
More advice from the NIHR on knowledge mobilisation and dissemination .
What you need to know about research dissemination
Last updated
5 March 2024
Reviewed by
In this article, we'll tell you what you need to know about research dissemination.
- Understanding research dissemination
Research that never gets shared has limited benefits. Research dissemination involves sharing research findings with the relevant audiences so the research’s impact and utility can reach its full potential.
When done effectively, dissemination gets the research into the hands of those it can most positively impact. This may include:
Politicians
Industry professionals
The general public
What it takes to effectively disseminate research will depend greatly on the audience the research is intended for. When planning for research dissemination, it pays to understand some guiding principles and best practices so the right audience can be targeted in the most effective way.
- Core principles of effective dissemination
Effective dissemination of research findings requires careful planning. Before planning can begin, researchers must think about the core principles of research dissemination and how their research and its goals fit into those constructs.
Research dissemination principles can best be described using the 3 Ps of research dissemination.
This pillar of research dissemination is about clarifying the objective. What is the goal of disseminating the information? Is the research meant to:
Persuade policymakers?
Influence public opinion?
Support strategic business decisions?
Contribute to academic discourse?
Knowing the purpose of sharing the information makes it easy to accurately target it and align the language used with the target audience.
The process includes the methods that will be used and the steps taken when it comes time to disseminate the findings. This includes the channels by which the information will be shared, the format it will be shared in, and the timing of the dissemination.
By planning out the process and taking the time to understand the process, researchers will be better prepared and more flexible should changes arise.
The target audience is whom the research is aimed at. Because different audiences require different approaches and language styles, identifying the correct audience is a huge factor in the successful dissemination of findings.
By tailoring the research dissemination to the needs and preferences of a specific audience, researchers increase the chances of the information being received, understood, and used.
- Types of research dissemination
There are many options for researchers to get their findings out to the world. The type of desired dissemination plays a big role in choosing the medium and the tone to take when sharing the information.
Some common types include:
Academic dissemination: Sharing research findings in academic journals, which typically involves a peer-review process.
Policy-oriented dissemination: Creating documents that summarize research findings in a way that's understandable to policymakers.
Public dissemination: Using television and other media outlets to communicate research findings to the public.
Educational dissemination: Developing curricula for education settings that incorporate research findings.
Digital and online dissemination: Using digital platforms to present research findings to a global audience.
Strategic business presentation: Creating a presentation for a business group to use research insights to shape business strategy
- Major components of information dissemination
While the three Ps provide a convenient overview of what needs to be considered when planning research dissemination, they are not a complete picture.
Here’s a more comprehensive list of what goes into the dissemination of research results:
Audience analysis: Identifying the target audience and researching their needs, preferences, and knowledge level so content can be tailored to them.
Content development: Creating the content in a way that accurately reflects the findings and presents them in a way that is relevant to the target audience.
Channel selection: Choosing the channel or channels through which the research will be disseminated and ensuring they align with the preferences and needs of the target audience.
Timing and scheduling: Evaluating factors such as current events, publication schedules, and project milestones to develop a timeline for the dissemination of the findings.
Resource allocation: With the basics mapped out, financial, human, and technological resources can be set aside for the project to facilitate the dissemination process.
Impact assessment and feedback: During the dissemination, methods should be in place to measure how successful the strategy has been in disseminating the information.
Ethical considerations and compliance: Research findings often include sensitive or confidential information. Any legal and ethical guidelines should be followed.
- Crafting a dissemination blueprint
With the three Ps providing a foundation and the components outlined above giving structure to the dissemination, researchers can then dive deeper into the important steps in crafting an impactful and informative presentation.
Let’s take a look at the core steps.
1. Identify your audience
To identify the right audience for research dissemination, researchers must gather as much detail as possible about the different target audience segments.
By gathering detailed information about the preferences, personalities, and information-consumption habits of the target audience, researchers can craft messages that resonate effectively.
As a simple example, academic findings might be highly detailed for scholarly journals and simplified for the general public. Further refinements can be made based on the cultural, educational, and professional background of the target audience.
2. Create the content
Creating compelling content is at the heart of effective research dissemination. Researchers must distill complex findings into a format that's engaging and easy to understand. In addition to the format of the presentation and the language used, content includes the visual or interactive elements that will make up the supporting materials.
Depending on the target audience, this may include complex technical jargon and charts or a more narrative approach with approachable infographics. For non-specialist audiences, the challenge is to provide the required information in a way that's engaging for the layperson.
3. Take a strategic approach to dissemination
There's no single best solution for all research dissemination needs. What’s more, technology and how target audiences interact with it is constantly changing. Developing a strategic approach to sharing research findings requires exploring the various methods and channels that align with the audience's preferences.
Each channel has a unique reach and impact, and a particular set of best practices to get the most out of it. Researchers looking to have the biggest impact should carefully weigh up the strengths and weaknesses of the channels they've decided upon and craft a strategy that best uses that knowledge.
4. Manage the timeline and resources
Time constraints are an inevitable part of research dissemination. Deadlines for publications can be months apart, conferences may only happen once a year, etc. Any avenue used to disseminate the research must be carefully planned around to avoid missed opportunities.
In addition to properly planning and allocating time, there are other resources to consider. The appropriate number of people must be assigned to work on the project, and they must be given adequate financial and technological resources. To best manage these resources, regular reviews and adjustments should be made.
- Tailoring communication of research findings
We’ve already mentioned the importance of tailoring a message to a specific audience. Here are some examples of how to reach some of the most common target audiences of research dissemination.
Making formal presentations
Content should always be professional, well-structured, and supported by data and visuals when making formal presentations. The depth of information provided should match the expertise of the audience, explaining key findings and implications in a way they'll understand. To be persuasive, a clear narrative and confident delivery are required.
Communication with stakeholders
Stakeholders often don't have the same level of expertise that more direct peers do. The content should strike a balance between providing technical accuracy and being accessible enough for everyone. Time should be taken to understand the interests and concerns of the stakeholders and align the message accordingly.
Engaging with the public
Members of the public will have the lowest level of expertise. Not everyone in the public will have a technical enough background to understand the finer points of your message. Try to minimize confusion by using relatable examples and avoiding any jargon. Visual aids are important, as they can help the audience to better understand a topic.
- 10 commandments for impactful research dissemination
In addition to the details above, there are a few tips that researchers can keep in mind to boost the effectiveness of dissemination:
Master the three Ps to ensure clarity, focus, and coherence in your presentation.
Establish and maintain a public profile for all the researchers involved.
When possible, encourage active participation and feedback from the audience.
Use real-time platforms to enable communication and feedback from viewers.
Leverage open-access platforms to reach as many people as possible.
Make use of visual aids and infographics to share information effectively.
Take into account the cultural diversity of your audience.
Rather than considering only one dissemination medium, consider the best tool for a particular job, given the audience and research to be delivered.
Continually assess and refine your dissemination strategies as you gain more experience.
Get started today
Go from raw data to valuable insights with a flexible research platform
Editor’s picks
Last updated: 21 December 2023
Last updated: 16 December 2023
Last updated: 6 October 2023
Last updated: 25 November 2023
Last updated: 12 May 2023
Last updated: 15 February 2024
Last updated: 11 March 2024
Last updated: 12 December 2023
Last updated: 18 May 2023
Last updated: 6 March 2024
Last updated: 10 April 2023
Last updated: 20 December 2023
Latest articles
Related topics, log in or sign up.
Get started for free
- Reserve a study room
- Library Account
- Undergraduate Students
- Graduate Students
- Faculty & Staff
Create a Research Dissemination Plan
Why create a dissemination plan, dissemination planning resources.
- Dissemination Plan Examples
- Dissemination Plan Template
- Guide Background
Questions or Suggestions?

There are a number of reasons to create a dissemination plan:
Applying for a grant and need a research guide? Dissemination plans are required in many grants.
Wanting to share your process or findings with and beyond the academic community.
Connecting with others who share key areas of research interest and those who may enhance your research by providing new ideas.
Enhancing usability of research by other researchers as well as end users.
Sharing research with the public as a part of our mission as a public research university.
Developing and a disseminating a body of work that creates depth in the field, facilitates tenor, allows faculty to be expert source of research area.
Dissemination planning can help expand your thinking about what research you share, how you share it, and who you share it with. Planning can also help expand access to your research, and ultimately, increase its impact.
PHCRIS (Primary Health Care Research & Information Service). Introduction to Research Dissemination.
This guide will introduce the terminology and definitions surrounding research dissemination, as well as provide you with strategies and further resources to aid your dissemination planning.
Dissemination Planning Tool. AHRQ (Agency for Healthcare Research and Quality). Advances in Patient Safety: From Research to Implementation.
This tool was developed to help researchers evaluate their research and develop appropriate dissemination plans, if the research is determined to have "real world" impact. It is designed to prompt your thinking about the processes that you would use to disseminate your findings or products, beyond publishing and presenting in peer-reviewed venues.
CARE (Community Alliance for Research and Engagement). Beyond Scientific Publication: Strategies for Disseminating Research Findings.
This document provides key strategies for dissemination, including practical advice and specific templates you can adapt for your use.
URegina Exchanging Knowledge. A Research Dissemination Toolkit.
This toolkit provides a dissemination plan worksheet, tips for effective dissemination, and further resources to aid your dissemination planning.
Becker Medical Library Model for Assessment of Research Impact
The Becker Medical Library Model for Assessment of Research Impact model is a framework for tracking diffusion of research outputs and activities to locate indicators that demonstrate evidence of biomedical research impact. It is intended to be used as a supplement to publication analysis. Using the Becker Model in tandem with publication analysis provides a more robust and comprehensive perspective of biomedical research impact. The Becker Model also includes guidance for quantifying and documenting research impact as well as resources for locating evidence of impact.
- Next: Dissemination Plan Examples >>
- Last Updated: Nov 20, 2023 11:33 AM
- URL: https://guides.library.vcu.edu/dissemination

Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
16 21. Qualitative research dissemination
Chapter outline.
- Ethical responsibility and cultural respectfulness (8 minute read time)
- Critical considerations (5 minute read time)
- Informing your dissemination plan (11 minute read time)
- Final product taking shape (10 minute read time)
Content warning: Examples in this chapter contain references to research as a potential tool to stigmatize or oppress vulnerable groups, mistreatment and inequalities experienced by Native American tribes, sibling relationships, caregiving, child welfare, criminal justice and recidivism, first generation college students, Covid-19, school culture and race, health (in)equity, physical and sensory abilities, and transgender youth.
Your sweat and hard work has paid off! You’ve planned your study, collected your data, and completed your analysis. But alas, no rest for the weary student researcher. Now you need to share your findings. As researchers, we generally have some ideas where and with whom we desire to share our findings, but these plans may evolve and change during our research process. Communicating our findings with a broader audience is a critical step in the research process, so make sure not to treat this like an afterthought. Remember, research is about making a contribution to collective knowledge-building in the area of study that you are interested in. Indeed, research is of no value if there is no audience to receive it. You worked hard…get those findings out there!
In planning for this phase of research, we can consider a variety of methods for sharing our study findings. Among other options, we may choose to write our findings up as an article in a professional journal, provide a report to an organization, give testimony to a legislative group, or create a presentation for a community event. We will explore these options in a bit more detail below in section 21.4 where we talk more about different types of qualitative research products. We also want to think about our intended audience.
For your research, answer these two key questions as you are planning for dissemination:
- Who are you targeting to communicate your findings to? In other words, who needs to hear the results of your study?
- What do you hope your audience will take away after learning about your study?

21.1 Ethical responsibility and cultural respectfulness
Learning Objectives
Learners will be able to…
- Identify key ethical considerations in developing their qualitative research dissemination plan
- Conceptualize how research dissemination may impact diverse groups, both presently and into the future
Have you ever been misrepresented or portrayed in a negative light? It doesn’t feel good. It especially doesn’t feel good when the person portraying us has power, control and influence. While you might not feel powerful, research can be a powerful tool, and can be used and abused for many ends. Once research is out in the world, it is largely out of our control, so we need to approach dissemination with care. Be thoughtful about how you represent your work and take time to think through the potential implications it may have, both intended and unintended, for the people it represents.
As alluded to in the paragraph above, research comes with hefty responsibilities. You aren’t off the hook if you are conducting quantitative research. While quantitative research deals with numbers, these numbers still represent people and their relationships to social problems. However, with qualitative research, we are often dealing with a smaller sample and trying to learn more from them. As such, our job often carries additional weight as we think about how we will represent our findings and the people they reflect. Furthermore, we probably hope that our research has an impact; that in some way, it leads to change around some issue. This is especially true as social work researchers. Our research often deals with oppressed groups, social problems, and inequality. However, it’s hard to predict the implications that our research may have. This suggests that we need to be especially thoughtful about how we present our research to others.
Two of the core values of social work involve respecting the inherent dignity and worth of each person, practicing with integrity, and behaving in a trustworthy manner [1] . As social work researchers, to uphold these values, we need to consider how we are representing the people we are researching. Our work needs to honestly and accurately reflect our findings, but it also needs to be sensitive and respectful to the people it represents. In Chapter 8 we discussed research ethics and introduced the concept of beneficence or the idea that research needs to support the welfare of participants. Beneficence is particularly important as we think about our findings becoming public and how the public will receive, interpret and use this information. Thus, both as social workers and researchers, we need to be conscientious of how dissemination of our findings takes place.
As you think about the people in your sample and the communities or groups to which they belong, consider some of these questions:
- How are participants being portrayed in my research?
- What characteristics or findings are being shared or highlighted in my research that may directly or indirectly be associated with participants?
- Have the groups that I am researching been stigmatized, stereotyped, and/or misrepresented in the past? If so, how does my research potentially reinforce or challenge these representations?
- How might my research be perceived or interpreted by members of the community or group it represents?
- In what ways does my research honor the dignity and worth of participants?

Qualitative research often has a voyeuristic quality to it, as we are seeking a window into participants’ lives by exploring their experiences, beliefs, and values. As qualitative researchers, we have a role as stewards or caretakers of data. We need to be mindful of how data are gathered, maintained, and most germane to our conversation here, how data are used. We need to craft research products that honor and respect individual participants (micro), our collective sample as a whole (meso), and the communities that our research may represent (macro).
As we prepare to disseminate our findings, our ethical responsibilities as researchers also involve honoring the commitments we have made during the research process. We need to think back to our early phases of the research process, including our initial conversations with research partners and other stakeholders who helped us to coordinate our research activities. If we made any promises along the way about how the findings would be presented or used, we need to uphold them here. Additionally, we need to abide by what we committed to in our informed consent . Part of our informed consent involves letting participants know how findings may be used. We need to present our findings according to these commitments. We of course also have a commitment to represent our research honestly.
As an extension of our ethical responsibilities as researchers, we need to consider the impact that our findings may have, as well as our need to be socially conscientious researchers. As scouts, we were taught to leave our campsite in a better state than when we arrived. I think it is helpful to think of research in these terms. Think about the group(s) that may be represented by your research; what impact might your findings have for the lives of members of this group? Will it leave their lives in a better state than before you conducted your research? As a responsible researcher, you need to be thoughtful, aware and realistic about how your research findings might be interpreted and used by others. As social workers, while we hope that findings will be used to improve the lives of our clients, we can’t ignore that findings can also be used to further oppress or stigmatize vulnerable groups; research is not apolitical and we should not be naive about this. It is worth mentioning the concept of sustainable research here. Sustainable research involves conducting research projects that have a long-term, sustainable impact for the social groups we work with. As researchers, this means that we need to actively plan for how our research will continue to benefit the communities we work with into the future. This can be supported by staying involved with these communities, routinely checking-in and seeking input from community members, and making sure to share our findings in ways that community members can access, understand, and utilize them. Nate Olson provides a very inspiring Ted Talk about the importance of building resilient communities. As you consider your research project, think about it in these terms.
Key Takeaways
- As you think about how best to share your qualitative findings, remember that these findings represent people. As such, we have a responsibility as social work researchers to ensure that our findings are presented in honest, respectful, and culturally sensitive ways.
- Since this phase of research deals with how we are going to share our findings with the public, we need to actively consider the potential implications of our research and how it may be interpreted and used.
Is your work, in some way, helping to contribute to a resilient and sustainable community? It may not be a big tangible project as described in Olson’s Ted Talk , but is it providing a resource for change and growth to a group of people, either directly or indirectly? Does it promote sustainability amongst the social networks that might be impacted by the research you are conducting?
21.2 Critical considerations
- Identify how issues of power and control are present in the dissemination of qualitative research findings
- Begin to examine and account for their own role in the qualitative research process, and address this in their findings
This is the part of our research that is shared with the public and because of this, issues like reciprocity, ownership, and transparency are relevant. We need to think about who will have access to the tangible products of our research and how that research will get used. As researchers, we likely benefit directly from research products; perhaps it helps us to advance our career, obtain a good grade, or secure funding. Our research participants often benefit indirectly by advancing knowledge about a topic that may be relevant or important to them, but often don’t experience the same direct tangible benefits that we do. However, a participatory perspective challenges us to involve community members from the outset in discussions about what changes would be most meaningful to their communities and what research products would be most helpful in accomplishing those changes. This is especially important as it relates to the role of research as a tool to support empowerment.
Ownership of research products is also important as an issue of power and control. We will discuss a range of venues for presenting your qualitative research, some of which are more amenable to shared ownership than others. For instance, if you are publishing your findings in an academic journal, you will need to sign an agreement with that publisher about how the information in that article can be used and who has access to it. Similarly, if you are presenting findings at a national conference, travel and other conference-related expenses and requirements may make access to these research products prohibitive. In these instances, the researcher and the organization(s) they negotiate with (e.g. the publishing company, the conference organizing body) share control. However, disseminating qualitative findings in a public space, public record, or community-owned resource means that more equitable ownership might be negotiated. An equitable or reciprocal arrangement might not always be able to be reached, however. Transparency about who owns the products of research is important if you are working with community partners. To support this, establishing a Memorandum Of Understanding (MOU) or Memorandum of Agreement (MOA) e arly in the research process is important. This document should clearly articulate roles, responsibilities, and a number of other details, such as ownership of research products between the researcher and the partnering group(s).
Resources for learning more about MOUs and MOAs
Center for Community Health and Development, University of Kansas. (n.d.). Community toolbox: Section 9. Understanding and writing contracts and memoranda of agreement [Webpage]. https://ctb.ku.edu/en/table-of-contents/structure/organizational-structure/understanding-writing-contracts-memoranda-agreement/main
Collaborative Center for Health Equity, University of Wisconson Madison. (n.d.). Standard agreement for research with community organizations [Template] https://d1uqjtzsuwlnsf.cloudfront.net/wp-content/uploads/sites/163/2018/08/CCHE-UW-MOU-sample.pdf
Office of Research, UC Davis. (n.d.). Research MOUs [Webpage]. https://research.ucdavis.edu/proposals-grants-contracts/international-agreements/memorandum-understanding/
Office of Research, The University of Texas at Dallas. (n.d.). Types of agreements [Webpage]. https://research.utdallas.edu/researchers/contracts/types-of-agreements
In our discussion about qualitative research, we have also frequently identified the need for the qualitative researcher to account for their role throughout the research process. Part of this accounting can specifically apply to qualitative research products. This is our opportunity to demonstrate to our audience that we have been reflective throughout the course of the study and how this has influenced the work we did. Some qualitative research studies include a positionality statement within the final product. This is often toward the beginning of the report or the presentation and includes information about the researcher(s)’s identity and worldview, particularly details relevant to the topic being studied. This can include why you are invested in the study, what experiences have shaped how you have come to think about the topic, and any positions or assumptions you make with respect to the topic. This is another way to encourage transparency. It can also be a means of relegating or at least acknowledging some of our power in the research process, as it can provide one modest way for us, as the researcher, to be a bit more exposed or vulnerable, although this is a far cry from making the risks of research equitable between the researcher and the researched. However, the positionality statement can be a place to integrate our identities, who we are as an individual, a researcher, and a social work practitioner. Granted, for some of us that might be volumes, but we need to condense this down to a brief but informative statement – don’t let it eclipse the research! It should just be enough to inform the audience and allow them to draw their own conclusions about who is telling the story of this research and how well they can be trusted. This student provides a helpful discussion of the positionality statement that she developed for her study. Reviewing your reflexive journal (discussed in chapter 20 as a tool to enhance qualitative rigor) can help in identifying underlying assumptions and positions you might have grounded in your reactions throughout the research process. These insights can be integrated into your positionality statement. Please take a few minutes to watch this informative video of a student further explaining what a positionality statement is and providing a good example of one.
- The products of qualitative research often benefit the researcher disproportionately when compared to research participants or the communities they represent. Whenever possible, we can seek out ways to disseminate research in ways that addresses this imbalance and supports more tangible and direct benefits to community members.
- Openly positioning ourselves in our dissemination plans can be an important way for qualitative researchers to be transparent and account for our role.
21.3 Informing your dissemination plan
- Appraise important dimensions of planning that will inform their research dissemination plan, including: audience, purpose, context and content
- Apply this appraisal to key decisions they will need to make when designing their qualitative research product(s)
This section will offer you a general overview of points to consider as you form the dissemination plan for your research. We will start with considerations regarding your audience, then turn our attention to the purpose of your research, and finally consider the importance of attending to both content and context as you plan for your final research product(s).
Perhaps the most important consideration you have as you plan how to present your work is your audience. Research is a product that is meant to be consumed, and because of this, we need to be conscious of our consumers. We will speak more extensively about knowing your audience in Chapter 24 , devoted to both sharing and consuming research. Regardless of who your audience is (e.g. community members, classmates, research colleagues, practicing social workers, state legislator), there will be common elements that will be important to convey. While the way you present them will vary greatly according to who is listening, Table 21.1 offers a brief review of the elements that you will want your audience to leave with.
Once we determine who our audience is, we can further tailor our dissemination plan to that specific group. Of course, we may be presenting our findings in more than one venue, and in that case, we will have multiple plans that will meet the needs of each specific audience.
It’s a good idea to pitch your plan first. However you plan to present your findings, you will want to have someone preview before you share with a wider audience. Ideally, whoever previews will be a person from your target audience or at least someone who knows them well. Getting feedback can go a long way in helping us with the clarity with which we convey our ideas and the impact they have on our audience. This might involve giving a practice speech, having someone review your article or report, or practice discussing your research one-on-one, as you would with a poster presentation. Let’s talk about some specific audiences that you may be targeting and their unique needs or expectations.
Below I will go through some brief considerations for each of these different audiences. I have tried to focus this discussion on elements that are relevant specific to qualitative studies since we do revisit this topic in Chapter 24 .

Research community
When presenting your findings to an academic audience or other research-related community, it is probably safe to a make a few assumptions. This audience is likely to have a general understanding of the research process and what it entails. For this reason, you will have to do less explaining of research-related terms and concepts. However, compared to other audiences, you will probably have to provide a bit more detail about what steps you took in your research process, especially as they relate to qualitative rigor, because this group will want to know about how your research was carried out and how you arrived at your decisions throughout the research process. Additionally, you will want to make a clear connection between which qualitative design you chose and your research question; a methodological justification . Researchers will also want to have a good idea about how your study fits within the wider body of scientific knowledge that it is related to and what future studies you feel are needed based on your findings. You are likely to encounter this audience if you are disseminating through a peer-reviewed journal article, presenting at a research conference, or giving an invited talk in an academic setting.
Professional community
We often find ourselves presenting our research to other professionals, such as social workers in the field. While this group may have some working knowledge of research, they are likely to be much more focused on how your research is related to the work they do and the clients they serve. While you will need to convey your design accurately, this audience is most likely to be invested in what you learned and what it means (especially for practice). You will want to set the stage for the discussion by doing a good job expressing your connection to and passion for the topic (a positionality statemen t might be particularly helpful here), what we know about the issue, and why it is important to their professional lives. You will want to give good contextual information for your qualitative findings so that practitioners can know if these findings might apply to people they work with. Also, as since social work practitioners generally place emphasis on person-centered practice, hearing the direct words of participants (quotes) whenever possible, is likely to be impactful as we present qualitative results. Where academics and researchers will want to know about implications for future research, professionals will want to know about implications for how this information could help transform services in the future or understand the clients they serve.
Lay community
The lay community are people who don’t necessarily have specialized training or knowledge of the subject, but may be interested or invested for some other reason; perhaps the issue you are studying affects them or a loved one. Since this is the general public, you should expect to spend the most time explaining scientific knowledge and research processes and terminology in accessible terms. Furthermore, you will want to invest some time establishing a personal connection to the topic (like I talked about for the professional community). They will likely want to know why you are interested and why you are a credible source for this information. While this group may not be experts on research, as potential members of the group(s) that you may be researching, you do want to remember that they are experts in their own community. As such, you will want to be especially mindful of approaching how you present findings with a sense of cultural humility (although hopefully you have this in mind across all audiences). It will be good to discuss what steps you took to ensure that your findings accurately reflect what participants shared with you ( rigor ). You will want to be most clear with this group about what they should take away, without overstating your findings.
Regardless of who your audience is, remember that you are an ambassador. You may represent a topic, a population, an organization, or the whole institution of research, or any combination of these. Make sure to present your findings honestly, ethically, and clearly. Furthermore, I’m assuming that the research you are conducting is important because you have spent a lot of time and energy to arrive at your findings. Make sure that this importance comes through in your dissemination. Tell a compelling story with your research!
Who needs to hear the message of your qualitative research?
- Example. If you are presenting your research about caregiver fatigue to a caregiver support group, you won’t need to spend time describing the role of caregivers because your audience will have lived experience.
- Example. If you are presenting your research findings to a group of academics, you wouldn’t have to explain what a sampling frame is, but if you are sharing it with a group of community members from a local housing coalition, you will need to help them understand what this is (or maybe use a phrase that is more meaningful to them).
- Example. If you are speaking to a group of child welfare workers about your study examining trauma-informed communication strategies, they are probably going to want to know how these strategies might impact the work that they do.
- Example. If you are sharing your findings at a meeting with a council member, it may be especially meaningful to share direct quotes from constituents.
Being clear about the purpose of your research from the outset is immeasurably helpful. What are you hoping to accomplish with your study? We can certainly look to the overarching purpose of qualitative research, that being to develop/expand/challenge/explore understanding of some topic. But, what are you specifically attempting to accomplish with your study? Two of the main reasons we conduct research are to raise awareness about a topic and to create change around some issue. Let’s say you are conducting a study to better understand the experience of recidivism in the criminal justice system. This is an example of a study whose main purpose is to better understand and raise awareness around a particular social phenomenon (recidivism). On the other hand, you could also conduct a study that examines the use of strengths-based strategies by probation officers to reduce recidivism. This would fall into the category of research promoting a specific change (the use of strengths-based strategies among probation officers). I would wager that your research topic falls into one of these two very broad categories. If this is the case, how would you answer the corresponding questions below?
Are you seeking to raise awareness of a particular issue with your research? If so,
- Whose awareness needs raising?
- What will “speak” most effectively to this group?
- How can you frame your research so that it has the most impact?
Are you seeking to create a specific change with your research? If so,
- What will that change look like?
- How can your research best support that change occurring?
- Who has the power to create that change and what will be most compelling in reaching them?
How you answer these questions will help to inform your dissemination plan. For instance, your dissemination plan will likely look very different if you are trying to persuade a group of legislators to pass a bill versus trying to share a new model or theory with academic colleagues. Considering your purposes will help you to convey the message of your research most effectively and efficiently. We invest a lot of ourselves in our research, so make sure to keep your sights focused on what you hope to accomplish with it!
Content and context
As a reminder, qualitative research often has a dual responsibility for conveying both content and context. You can think of content as the actual data that is shared with us or that we obtain, while context is the circumstances under which that data sharing occurs. Content conveys the message and context provides us the clues with which we can decode and make sense of that message.
While quantitative research may provide some contextual information, especially in regards to describing its sample, it rarely receives as much attention or detail as it does in qualitative studies. Because of this, you will want to plan for how you will attend to both the content and context of your study in planning for your dissemination.
- Research is an intentional act; you are trying to accomplish something with it. To be successful, you need to approach dissemination planfully.
- Planning the most effective way of sharing our qualitative findings requires looking beyond what is convenient or even conventional, and requires us to consider a number of factors, including our audience, the purpose or intent of our research and the nature of both the content and the context that we are trying to convey.
21.4 Final product taking shape
- Evaluate the various means of disseminating research and consider their applicability for your research project
- Determine appropriate building blocks for designing your qualitative research product
As we have discussed, qualitative research takes many forms. It should then come as no surprise that qualitative research products also come in many different packages. To help guide you as the final products of your research take shape, we will discuss some of the building blocks or elements that you are likely to include as tools in sharing your qualitative findings. These are the elements that will allow you to flesh out the details of your dissemination plan.
Building blocks
There are many building blocks that are at our disposal as we formulate our qualitative research product(s). Quantitative researchers have charts, graphs, tables, and narrative descriptions of numerical output. These tools allow the quantitative researcher to tell the story of their research with numbers. As qualitative researchers, we are tasked with telling the story of our research findings as well, but our tools look different. While this isn’t an exhaustive list of tools that are at our disposal as qualitative researchers, a number of commonly used elements in sharing qualitative findings are discussed here. Depending on your study design and the type of data you are working with, you may use one or some combination of the building blocks discussed below.
Themes are a very common element when presenting qualitative research findings. They may be called themes, but they may also go by other names: categories, dimensions, main ideas, etc. Themes offer the qualitative researcher a way to share ideas that emerged from your analysis that were shared by multiple participants or across multiple sources of data. They help us to distill the large amounts of qualitative data that we might be working with into more concise and manageable pieces of information that are more consumable for our audience. When integrating themes into your qualitative research product, you will want to offer your audience: the title of the theme (try to make this as specific/meaningful as possible), a brief description or definition of the theme, any accompanying dimensions or sub-themes that may be relevant, and examples (when appropriate).
Quotes offer you the opportunity to share participants’ exact words with your audience. Of course, we can’t only rely on quotes, because we need to knit the information that is shared into one cohesive description of our findings and an endless list of quotes is unlikely to support this. Because of this, you will want to be judicious in selecting your quotes. Choose quotes that can stand on their own, best reflect the sentiment that is being captured by the theme or category of findings that you are discussing, and are likely to speak to and be understood by your audience. Quotes are a great way to help your findings come alive or to give them greater depth and significance. If you are using quotes, be sure to do so in a balanced manner – don’t only use them in some sections but not others, or use a large number to support one theme and only one or two for another. Finally, we often provide some brief demographic information in a parenthetical reference following a quote so our reader knows a little bit about the person who shared the information. This helps to provide some context for the quote.
Kohli and Pizarro (2016) [2] provide a good example of a qualitative study using quotes to exemplify their themes. In their study, they gathered data through short-answer questionnaires and in-depth interviews from racial-justice oriented teachers of Color. Their study explored the experiences and motivations of these teachers and the environments in which they worked. As you might guess, the words of the teacher-participants were especially powerful and the quotes provided in the results section were very informative and important in helping to fulfill the aim of the research study. Take a few minutes to review this article. Note how the authors provide a good amount of detail as to what each of the themes meant and how they used the quotes to demonstrate and support each theme. The quotes help bring the themes to life and anchor the results in the actual words of the participants (suggesting greater trustworthiness in the findings).
Figure 21.1 below offers a more extensive example of a theme being reported along with supporting quotes from a study conducted by Karabanow, Gurman, and Naylor (2012) [3] . This study focused on the role of work activities in the lives of “Guatemalan street youth”. One of the important themes had to do with intersection of work and identity for this group. In this example, brief quotes are used within the body of the description of the theme, and also longer quotes (full sentence(s)) to demonstrate important aspects of the description.
Pictures or videos
If our data collection involves the use of photographs, drawings, videos or other artistic expression of participants or collection of artifacts, we may very well include selections of these in our dissemination of qualitative findings. In fact, if we failed to include these, it would seem a bit inauthentic. For the same reason we include quotes as direct representations of participants’ contributions, it is a good idea to provide direct reference to other visual forms of data that support or demonstrate our findings. We might incorporate narrative descriptions of these elements or quotes from participants that help to interpret their meaning. Integrating pictures and quotes is especially common if we are conducting a study using a Photovoice approach, as we discussed in Chapter 17 , where a main goal of the research technique is to bring together participant generated visuals with collaborative interpretation.
Take some time to explore the website linked here. It is the webpage for The Philidelphia Collaborative for Health Equity’s PhotoVoice Exhibit Gallery and offers a good demonstration of research that brings together pictures and text.
Graphic or figure
Qualitative researchers will often create a graphic or figure to visually reflect how the various pieces of your findings come together or relate to each other. Using a visual representation can be especially compelling for people who are visual learners. When you are using a visual representation, you will want to: label all elements clearly; include all the components or themes that are part of your findings; pay close attention to where you place and how you orient each element (as their spatial arrangement carries meaning); and finally, offer a brief but informative explanation that helps your reader to interpret your representation. A special subcategory of visual representation is process. These are especially helpful to lay out a sequential relationship within your findings or a model that has emerged out of your analysis. A process or model will show the ‘flow’ of ideas or knowledge in our findings, the logic of how one concept proceeds to the next and what each step of the model entails.
Noonan and colleagues (2004) [4] conducted a qualitative study that examined the career development of high achieving women with physical and sensory disabilities. Through the analysis of their interviews, they built a model of career development based on these women’s experiences with a figure that helps to conceptually illustrate the model. They place the ‘dyanmic self’ in the center, surrounded by a dotted (permeable) line, with a number of influences outside the line (i.e. family influences, disability impact, career attitudes and behaviors, sociopoltical context, developmental opportunities and social support) and arrows directed inward and outward between each influence and the dynamic self to demonstrate mutual influence/exchange between them. The image is included in the results section of their study and brings together “core categories” and demonstrates how they work together in the emergent theory or how they relate to each other. Because so many of our findings are dynamic, like Noonan and colleagues, showing interaction and exchange between ideas, figures can be especially helpful in conveying this as we share our results.

Going one step further than the graphic or figure discussed above, qualitative researchers may decide to combine and synthesize findings into one integrated representation. In the case of the graphic or figure, the individual elements still maintain their distinctiveness, but are brought together to reflect how they are related. In a composite however, rather than just showing that they are related (static), the audience actually gets to ‘see’ the elements interacting (dynamic). The integrated and interactive findings of a composite can take many forms. It might be a written narrative, such as a fictionalized case study that reflects of highlights the many aspects that emerged during analysis. It could be a poem, dance, painting or any other performance or medium. Ultimately, a composite offers an audience a meaningful and comprehensive expression of our findings. If you are choosing to utilize a composite, there is an underlying assumption that is conveyed: you are suggesting that the findings of your study are best understood holistically. By discussing each finding individually, they lose some of their potency or significance, so a composite is required to bring them together. As an example of a composite, consider that you are conducting research with a number of First Nations Peoples in Canada. After consulting with a number of Elders and learning about the importance of oral traditions and the significance of storytelling, you collaboratively determine that the best way to disseminate your findings will be to create and share a story as a means of presenting your research findings. The use of composites also assumes that the ‘truths’ revealed in our data can take many forms. The Transgender Youth Project hosted by the Mandala Center for Change , is an example of legislative theatre combining research, artistic expression, and political advocacy and a good example of action-oriented research.
While you haven’t heard much about numbers in our qualitative chapters, I’m going to break with tradition and speak briefly about them here. For many qualitative projects we do include some numeric information in our final product(s), mostly in the way of counts. Counts usually show up in the way of frequency of demographic characteristics of our sample or characteristics regarding our artifacts, if they aren’t people. These may be included as a table or they may be integrated into the narrative we provide, but in either case, our goal in including this information is to offer the reader information so they can better understand who or what our sample is representing. The other time we sometimes include count information is in respect to the frequency and coverage of the themes or categories that are represented in our data. Frequency information about a theme can help the reader to know how often an idea came up in our analysis, while coverage can help them to know how widely dispersed this idea was (e.g. did nearly everyone mention this, or was it a small group of participants).
- There are a wide variety of means by which you can deliver your qualitative research to the public. Choose one that takes into account the various considerations that we have discussed above and also honors the ethical commitments that we outlined early in this chapter.
- Presenting qualitative research requires some amount of creativity. Utilize the building blocks discussed in this chapter to help you consider how to most authentically and effectively convey your message to a wider audience.
What means of delivery will you be choosing for your dissemination plan?
What building blocks will best convey your qualitaitve results to your audience?
- National Association of Social Workers. (2017). NASW code of ethics. Retrieved from https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-Ethics-English ↵
- Kohli, R., & Pizarro, M. (2016). Fighting to educate our own: Teachers of Color, relational accountability, and the struggle for racial justice. Equity & Excellence in Education, 49 (1), 72-84. ↵
- Karabanow, J., Gurman, E., & Naylor, T. (2012). Street youth labor as an Expression of survival and self-worth. Critical Social Work, 13 (2). ↵
- Noonan, B. M., Gallor, S. M., Hensler-McGinnis, N. F., Fassinger, R. E., Wang, S., & Goodman, J. (2004). Challenge and success: A Qualitative study of the career development of highly achieving women with physical and sensory disabilities. Journal of Counseling Psychology, 51 (1), 68. ↵
- Ede, L., & Starrin, B. (2014). Unresolved conflicts and shaming processes: risk factors for long-term sick leave for mental-health reasons. Nordic Journal of Social Research, 5 , 39-54. ↵
how you plan to share your research findings
One of the three values indicated in the Belmont report. An obligation to protect people from harm by maximizing benefits and minimizing risks.
A written agreement between parties that want to participate in a collaborative project.
A research journal that helps the researcher to reflect on and consider their thoughts and reactions to the research process and how it may be shaping the study
Context is the circumstances surrounding an artifact, event, or experience.
Rigor is the process through which we demonstrate, to the best of our ability, that our research is empirically sound and reflects a scientific approach to knowledge building.
Content is the substance of the artifact (e.g. the words, picture, scene). It is what can actually be observed.
Graduate research methods in social work Copyright © 2020 by Matthew DeCarlo, Cory Cummings, Kate Agnelli is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License , except where otherwise noted.
Share This Book
- Systematic review
- Open access
- Published: 15 October 2020
Strategies for effective dissemination of research to United States policymakers: a systematic review
- Laura Ellen Ashcraft ORCID: orcid.org/0000-0001-9957-0617 1 ,
- Deirdre A. Quinn 2 &
- Ross C. Brownson 3 , 4
Implementation Science volume 15 , Article number: 89 ( 2020 ) Cite this article
40k Accesses
52 Citations
41 Altmetric
Metrics details
Research has the potential to influence US social policy; however, existing research in this area lacks a coherent message. The Model for Dissemination of Research provides a framework through which to synthesize lessons learned from research to date on the process of translating research to US policymakers.
The peer-reviewed and grey literature was systematically reviewed to understand common strategies for disseminating social policy research to policymakers in the United States. We searched Academic Search Premier, PolicyFile, SocINDEX, Social Work Abstracts, and Web of Science from January 1980 through December 2019. Articles were independently reviewed and thematically analyzed by two investigators and organized using the Model for Dissemination of Research.
The search resulted in 5225 titles and abstracts for inclusion consideration. 303 full-text articles were reviewed with 27 meeting inclusion criteria. Common sources of research dissemination included government, academic researchers, the peer reviewed literature, and independent organizations. The most frequently disseminated research topics were health-related, and legislators and executive branch administrators were the most common target audience. Print materials and personal communication were the most common channels for disseminating research to policymakers. There was variation in dissemination channels by level of government (e.g., a more formal legislative process at the federal level compared with other levesl). Findings from this work suggest that dissemination is most effective when it starts early, galvanizes support, uses champions and brokers, considers contextual factors, is timely, relevant, and accessible, and knows the players and process.
Conclusions
Effective dissemination of research to US policymakers exists; yet, rigorous quantitative evaluation is rare. A number of cross-cutting strategies appear to enhance the translation of research evidence into policy.
Registration
Not registered.
Peer Review reports
Contributions to the literature
This is one of the first systematic reviews to synthesize how social policy research evidence is disseminated to US policymakers.
Print materials and personal communications were the most commonly used channels to disseminate social policy research to policymakers.
Several cross-cutting strategies (e.g., start early, use evidence “champions,” make research products more timely, relevant, and accessible) were identified that are likely to lead to more effective translate of research evidence into the policy making process in the United States.
In recent years, social scientists have sought to understand how research may influence policy [ 1 , 2 ]. Interest in this area of investigation has grown with the increased availability of funding for policy-specific research (e.g., dissemination and implementation research) [ 3 ]. However, because of variation in the content of public policy, this emerging area of scholarship lacks a coherent message that specifically addresses social policy in the United States (US). While other studies have examined the use of evidence in policymaking globally [ 4 , 5 , 6 , 7 ], the current review focuses on US social policy; for the purposes of this study, social policy includes policies which focus on antipoverty, economic security, health, education, and social services [ 8 , 9 , 10 ].
Significant international research exists on barriers and facilitators to the dissemination and use of research evidence by policymakers [ 4 , 5 ]. Common themes include the importance of personal relationships, the timeliness of evidence, and resource availability [ 4 , 5 ]. Previous work demonstrates the importance of understanding policymakers’ perceptions and how evidence is disseminated. The current review builds on this existing knowledge to examine how research evidence reaches policymakers and to understand what strategies are likely to be effective in overcoming identified barriers.
Theoretical frameworks offer a necessary foundation to identify and assess strategies for disseminating research to policymakers. The Model for Dissemination of Research integrates Diffusion of Innovations Theory and Social Marketing Theory with the Mathematical Theory of Communication [ 11 , 12 ] and the Matrix of Persuasive Communication [ 13 , 14 ] to address the translation gap between research and policy. The purpose of the Model for Dissemination of Research is to highlight the gaps between research and targets audiences (e.g., policymakers) and improve dissemination through the use of a theoretical foundation and review of the literature [ 15 ]. Diffusion of Innovations Theory describes the spread and adoption of novel interventions through an “s-curve,” ordered process, and characteristics of the message and audience [ 16 ]. Additional theoretical contributions for dissemination research come from Social Marketing Theory, which postulates commercial marketing strategies summarized by the four P’s (produce, price, place, and promotion) and the understanding that communication of the message alone will not change behavior [ 17 ].
The Model for Dissemination of Research includes the four key components described by Shannon and Weaver [ 11 , 12 ] and later McGuire [ 13 , 14 ] of the research translation process: the source, message, audience, and channel (Fig. 1 ). The source includes researchers who generate evidence. The message includes relevant information sent by the source on a policy topic. The audience includes those receiving the message via the channel [ 15 ]. The channel is how the message gets from the source to the audience [ 15 ].
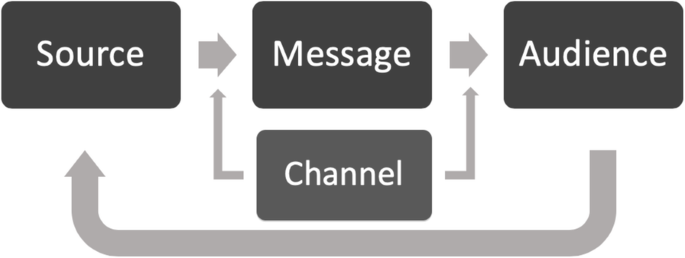
The Model for Dissemination of Research. The Model for Dissemination of Research integrates Diffusion of Innovations Theory, the Mathematical Theory of Communication, and Social Marketing Theory to develop a framework for conceptualizing how information moves from source to audience. Originally published by Brownson et al. in Journal of public health management and practice in 2018
While the Model for Dissemination of Research and its origins (i.e., the Mathematical Theory of Communication and Diffusion of Innovations Theory) appear linear in their presentation, Shannon and Weaver [ 11 , 12 ] and Rogers [ 16 ] clearly acknowledge that the dissemination of information is not a linear process and is effected by the environment within which it occurs. This approach aligns with the system model or knowledge to action approach proposed by Best and Holmes [ 18 ]. The systems model accounts for influence of the environment on a process and accounts for the complexity of the system [ 18 ]. Therefore, while some theoretical depictions appear linear in their presentation; it is important to acknowledge the critical role of systems thinking.
To date, lessons learned from dissemination and implementation science about the ways in which research influences policy are scattered across diverse disciplines and bodies of literature. These disparate lessons highlight the critical need to integrate knowledge across disciplines. The current study aims to make sense of and distill these lessons by conducting a systematic review of scientific literature on the role of research in shaping social policy in the United States. The results of this systematic review are synthesized in a preliminary conceptual model (organized around the Model for Dissemination of Research) with the goal of improving dissemination strategies for the translation of scientific research to policymakers and guiding future research in this area.
This systematic review aims to synthesize existing evidence about how research has been used to influence social policy and is guided by the following research questions:
What are common strategies for using research to influence social policy in the United States?
What is the effectiveness of these strategies?
We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA-P) model [ 19 , 20 ] to examine and distill existing studies on strategies for using research evidence to influence social policy.
Eligibility criteria
Studies were eligible for this review if they met the following inclusion criteria: (1) occurred in the United States; (2) reported in English; (3) systematically evaluated the impact of research on social policy (this typically excluded studies focusing on policymaker dissemination preferences); (4) discussed domestic social policy (as defined above); and (5) were published in the peer reviewed literature or the grey literature (e.g., think tank research briefs, foundation research publications).
We chose to focus our review on the United States to capture the strengths and challenges of its unique, multi-level policy and political environment. The de-centralized structure of government in the United States allows significant decision-making authority at the state and local levels, with wide variation in capacity and the availability of resources across the country [ 21 ]. For example, some states have full-time legislatures while other states have part-time legislatures. In total, these factors create a fitting and complex environment to examine the dissemination of research to policymakers. The influence of lobbying in the United States also differs from other western countries. In the United States, there is more likely to be a “winner-take-all” process where some advocates (often corporations and trade associations) have disproportionate influence [ 22 ]. In addition, the role of evidence differs in the US compared with other countries, where the US tends to take a narrower focus on intervention impact with less emphasis on system-level issues (e.g., implementation, cost) [ 23 ].
Studies were excluded if they were not in English or occurred outside of the United States. We also excluded non-research sources, such as editorials, opinion pieces, and narrative stories that contain descriptions of dissemination strategies without systematic evaluation. Further, studies were excluded if the results focused on practitioners (e.g., case managers, local health department workers) and/or if results for practitioners could not be parsed from results for policymakers.
To identify studies that systematically evaluated the impact of research on social policy, we reviewed the research questions and results of each study to determine whether or not they examined how research evidence reaches policymakers (as opposed to policymaker preferences for disseminated research). For example, we would not include a research study that only describes different types of policy briefs, without also evaluating how the briefs are used by policymakers to inform policy decisions. We used the Model for Dissemination of Research, as defined above, to see if and how the studies describe and test the channels of dissemination. We built on the Model of Dissemination by also considering passive forms of knowledge, such as peer-reviewed literature or research briefs, as potential sources of knowledge and not just as channels in and of themselves.
Information sources
We took a three-pronged approach to develop a comprehensive understanding of existing knowledge in this area. First, we searched the peer reviewed literature using the following databases: Academic Search Premier, PolicyFile, SocINDEX, Social Work Abstracts, and Web of Science. We expanded the inquiry for evidence by searching the grey literature through PolicyFile, and included recommendations from experts in the field of dissemination of research evidence to policymakers resulting in 137 recommended publications.
Search strategy
Our search strategy included the following terms: [research OR study OR studies OR knowledge] AND [policy OR policies OR law OR laws OR legislation] AND [use OR utilization OR utilisation] OR [disseminate OR dissemination OR disseminating] OR [implementation OR implementing OR implement] OR [translate OR translation OR translating]. Our search was limited to studies in the United States between 1980 and 2019. We selected this timeframe based on historical context: the 1950s through the 1970s saw the development of the modern welfare state, which was (relatively) complete by 1980. However, shifting political agendas in the 1980s saw the demand for evidence increase to provide support for social programs [ 24 ]; we hoped to capture this increase in evidence use in policy.
Selection process
All titles and abstracts were screened by the principal investigator (LEA) with 20% reviewed at random by a co-investigator (DAQ) with total agreement post-training. Studies remaining after abstract screening moved to full text review. The full text of each study was considered for inclusion (LEA and DAQ) with conflicts resolved by consensus. The data abstraction form was developed by the principal investigator (LEA) based on previous research [ 25 , 26 ] and with feedback from co-authors. Data were independently abstracted from each reference in duplicate with conflicts resolved by consensus (LEA and DAQ). We completed reliability checks on 20% of the final studies, selected at random, to ensure accurate data abstraction.
Data synthesis
Abstracted data was qualitatively analyzed using thematic analysis (LEA and DAQ) and guided by the Model for Dissemination of Research. The goal of the preliminary conceptual model was to synthesize components of dissemination for studies that evaluate the dissemination of social policy to policymakers.
Descriptive results
The search of the literature resulted in 5675 articles and 137 articles recommended by content experts for review with 5225 titles and abstracts screened after duplicates removed. Of those articles, 4922 were excluded due to not meeting inclusion criteria. Further, 303 full text articles were reviewed with 276 excluded as they did not meet inclusion criteria. Twenty-seven articles met inclusion criteria (see the Fig. 2 for the PRISMA flow diagram).
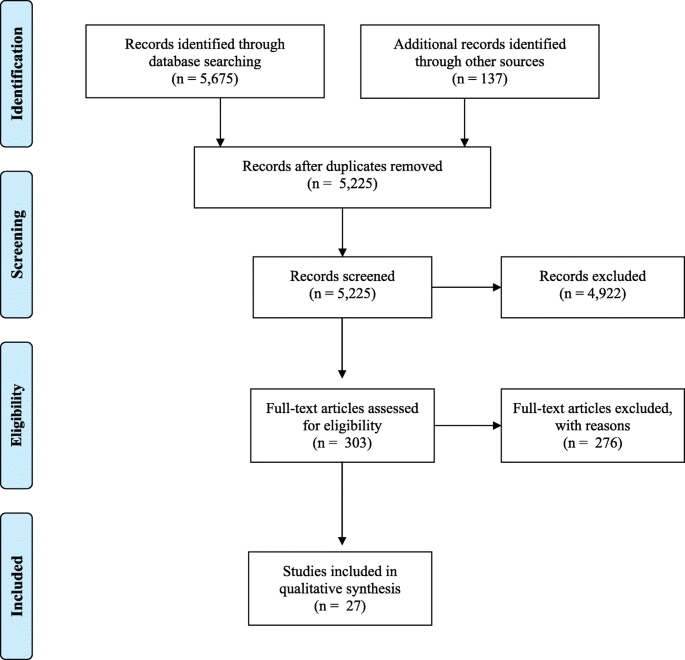
PRISMA flowchart. The preferred reporting items for systematic reviews and meta-analyses (PRISMA) flow diagram reports included and excluded articles in the systematic review
Included studies are listed in Table 1 . The 27 included 6 studies using quantitative methods, 18 that employed qualitative methods, and 3 that used a mixed methods approach. The qualitative studies mostly employed interviews ( n = 10), while others used case studies ( n = 6) or focus groups ( n = 3). Most studies examined state-level policy ( n = 18) and nine studies examined federal-level policy, with some studies looking at multiple levels of government. Included studies focused on the executive and legislative branches with no studies examining the judicial branch.
We examined dissemination based on geographic regions and/or political boundaries (i.e., regions or states). Sixteen of the 27 studies (about 59%) used national samples or multiple states and did not provide geographic-specific results [ 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 ]. Two studies (about 7%) did not specific the geographic region or state in which the study took place [ 43 , 44 ]. Of the remaining studies, four examined policymaking in the Northeastern United States [ 45 , 46 , 47 , 48 ], four in the Western US [ 49 , 50 , 51 , 52 ], and one in the South [ 53 ]. The geographic regional groups used similar channels to disseminate evidence to policymakers including publications and presentations.
We also analyzed whether dissemination at different levels of government (i.e., local, state, and federal) used unique channels. Six of included studies (about 22%) examined multiple levels of government and did not separate results based on specific levels of government [ 27 , 28 , 29 , 30 , 31 , 53 ]. One study did not specifically identify the level of government used [ 46 ]. While there is considerable overlap in dissemination channels used at each level of government, there are some unique characteristics.
Five studies (about 18.5%) examined dissemination at the federal level [ 32 , 33 , 34 , 35 , 36 ]. At the federal level, dissemination channels tended to be more formal such as congressional committee hearings [ 36 ] and legislative development [ 35 ]. Twelve studies (about 44%) evaluated dissemination at the state level [ 38 , 39 , 40 , 41 , 42 , 43 , 44 , 47 , 48 , 50 , 51 , 52 ]. State level dissemination heavily relied on printed materials including from mental health care disparity report cards [ 41 ], policy briefs [ 38 ], and effectiveness reports [ 50 ]. Another common channel was in-person communications such as one-on-one meetings [ 44 ] and presentations to stakeholders [ 51 ]. Three studies (about 11%) focused on local-level government. Dissemination channels at the local level had little consistency across the three studies with channels including public education [ 45 ], reports [ 37 ], and print materials [ 49 ].
Roughly half of studies were atheoretical ( n = 13). Four studies used the Weiss Typology [ 29 , 36 , 54 , 55 ], two studies used the operationalization framework [ 45 , 53 ], and two studies used the advocacy coalition framework [ 53 , 56 ].
Model for dissemination of research
We used the Model for Dissemination of Research to summarize the findings from the included studies into the themes of source, message, audience, and channel (i.e., strategies). We integrated themes from the studies into the Model (see Fig. 3 ).
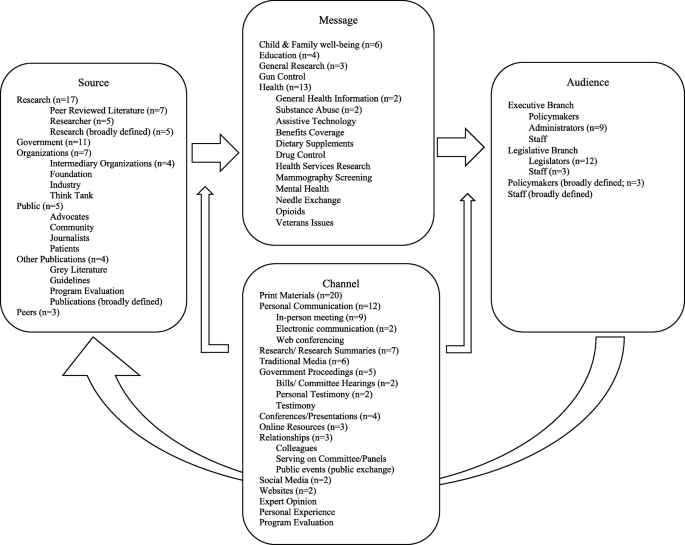
A conceptual model for dissemination of research to policymakers. The populated conceptual model builds on the Model for Dissemination of Research by organizing findings from the current systematic review to build an understanding of how research is disseminated to policymakers in the United States
The sources of knowledge varied across studies with some studies including multiple sources of social policy information. The most common sources of knowledge included research, as in peer-reviewed literature ( n = 7) [ 30 , 33 , 38 , 42 , 43 , 49 , 54 ], researchers ( n = 5) [ 27 , 31 , 32 , 34 , 56 ], and research broadly defined ( n = 5) [ 36 , 39 , 47 , 48 , 55 ], the government ( n = 11) [ 29 , 36 , 41 , 42 , 43 , 44 , 47 , 50 , 54 , 56 , 57 ], and organizations ( n = 7) [ 33 , 36 , 46 , 52 , 53 , 54 , 56 ].
The majority of studies focused on health topics ( n = 12) [ 29 , 30 , 33 , 34 , 38 , 41 , 42 , 45 , 47 , 55 , 56 , 58 ] and child and family well-being ( n = 6) [ 27 , 36 , 46 , 49 , 52 , 57 ]. The remaining studies covered the topics of education ( n = 4) [ 39 , 43 , 53 , 54 ], guns [ 56 ], veterans [ 44 ], and general social research ( n = 3) [ 31 , 32 , 48 ]. Multiple studies offered specific recommendations for message framing, suggesting that the packaging of information is as critical as the information itself [ 27 ]. One study piloted multiple styles of policy briefs and found staffers preferred to use and share narrative or story-based briefs while legislators were more likely to use and share statistical, data-based briefs [ 38 ]. This finding was mirrored in two studies that found testimonial or descriptive evidence to be as effective as data-driven research [ 34 , 52 ], particularly in the context of sympathetic populations [ 52 ]. Three studies highlighted the reliance of effective message delivery on the message’s ability to capture audience interest (e.g., what the research means to the policymaker, specifically and if possible, personally) [ 27 , 34 , 41 ]. Finally, two studies emphasized creating a sense of urgency or even shock-value within the message in order to capture policymakers’ interest [ 36 , 57 ].
The audience included executive branch policymakers [ 49 ], administrators ( n = 9) [ 27 , 31 , 38 , 39 , 41 , 43 , 53 , 55 , 57 ], and staff [ 42 ]. Studies which focused on the legislative branch examined legislators ( n = 12) [ 27 , 32 , 36 , 38 , 44 , 45 , 46 , 47 , 50 , 52 , 53 , 58 ] and staff ( n = 3) [ 32 , 34 , 36 ]. Three studies examined broadly defined policymakers [ 33 , 54 , 56 ] and generalized staff [ 54 ] without indication for specific branch of government.
Included studies examined a variety of channels with many including multiple channels. Print materials was the most commonly used channel, including reports ( n = 10) [ 27 , 30 , 33 , 41 , 46 , 50 , 53 , 55 , 57 , 58 ] and policy briefs ( n = 3) [ 31 , 34 , 38 ]. Researchers examined in-person meetings and communications as a channel to disseminate research ( n = 9) [ 30 , 32 , 33 , 39 , 44 , 48 , 53 , 56 , 57 ]. Research and research summaries were also studied ( n = 7) [ 30 , 31 , 42 , 47 , 49 , 52 , 54 ]. Both traditional ( n = 6) [ 31 , 33 , 47 , 52 , 53 , 54 ] and social media ( n = 2) [ 47 , 53 ] were examined as channels to disseminate research to policymakers. Other channels include conferences and presentations ( n = 4) [ 33 , 34 , 49 , 57 ], electronic communication ( n = 2) [ 27 , 57 ], online resources ( n = 3) [ 34 , 49 , 58 ], and personal testimony ( n =2) [ 42 , 52 ].
Effectiveness and lessons learned
The majority of studies employed qualitative research methods (e.g., interviews, case studies, focus groups) to evaluate the impact of scientific research on domestic social policy. Our review of the literature also identified nine quantitative and mixed-methods studies [ 31 , 32 , 38 , 39 , 42 , 43 , 44 , 49 , 58 ]. We identified a series of cross-cutting dissemination strategies for engaging policymakers including recommendations for and barriers to research-to-policy (see Table 2 ).
Start early
Four studies highlighted the importance for early and ongoing engagement with policymakers throughout the research process in order to maximize interest and applicability. Researchers are encouraged to take the initiative to contact policymakers as early as possible in the research process. Many policymakers may be interested in accessing and using research but uncertain who or how to make connections in the academic or research community [ 27 ]. Involving policymakers when designing projects and framing initial research questions increases the likelihood that key policy stakeholders will remain invested in the work by allowing their individual research interests to shine [ 34 , 41 ]. Early engagement also ensures that research products (e.g., reports, policy briefs, factsheets) will have strategic usefulness for policymakers [ 30 ].
Drum up support
In addition to early policymaker engagement, three studies highlighted the need for researchers to garner outside support for their work, ideally involving a broad pool of experts and cultivating a broader coalition of supporters than typical academic endeavors [ 47 ]. Often, policymakers appear unwilling or uninterested in considering the application of evidence to their work [ 45 , 53 ]; when researchers can demonstrate the value and relevance of their work [ 58 ], policymakers may be more likely to engage.
Use research evidence “champions” or “brokers”
A common strategy for garnering support (as recommended above) is the use of evidence champions or brokers ; these are intermediary individuals or organizations who connect research suppliers (e.g., individual researchers, academic institutions) to research demand (e.g., policymakers) [ 53 ]. These champions can broker important connections; however, researchers and policymakers alike must remember that these intermediaries are not neutral carriers of information, and may spin research in support of personal agendas [ 45 , 52 , 53 ]. Individual biases may also present a barrier in research-to-policy translation, as individuals or organizations are empowered to select the “best” research evidence to share with policymakers [ 29 ]. One study found that nearly half of state policymakers named professional associations as trusted sources for research information, specifically because the organization is perceived not to have a stake in the final policy outcome [ 58 ].
Two studies specifically addressed the role of intermediary organizations or brokers in the translation of research evidence to policy. Hopkins et al. [ 39 ] explored the exchange of research evidence among state education agency (SEA) leaders, while Massell et al. [ 43 ] examined more broadly the origins of research evidence use in three SEAs. Both studies found that external brokers played a role in connecting SEA policymakers to relevant research, as well as in the conceptualization and development of policy.
Focus on context
Multiple studies stressed the importance of research evidence being contextually relevant to the specific policy audience [ 29 , 54 , 55 , 57 ]. For some policymakers, the needs and interests of local constituents will drive the use of research and the specifics of the policy agenda; for others, discussions that integrate research evidence into the broader sociopolitical context will be more effective [ 45 ]. For state- and local-level policymakers, policies may be most effective when based on the evidence-based understanding of local stakeholders, rather than imposed from the federal level without local contextual details [ 29 ].
Ideology of external advisors and brokers (as discussed above) and policymakers’ own personal beliefs and experiences [ 54 ] and the prevailing political ideology of a particular geographic region [ 55 ] are critical components of context. Ideological beliefs, often deeply held and personal, may create a barrier between researchers and policymakers [ 41 ], though differentiating ideology from other factors that affect individual position-taking is difficult in most situations [ 44 ]. McGinty et al. [ 56 ] suggest that in polarized contexts involving strong ideological beliefs, research may add legitimacy to a particular viewpoint, though as with brokers, that research is likely to be carefully curated to support the desired message. Purtle et al. [ 55 ] concur, reporting that some county health officials were wary of the potential to spin research findings to make a case for certain programs over others and noted the need to avoid the challenge of distorting evidence. Two studies recommend positional neutrality as a researcher’s best approach to handling potential ideological differences, suggesting that presenting research findings as simple fact, rather than making specific recommendations for action, may help avoid conflict and also help researchers gain credibility across the ideological spectrum [ 27 , 50 ].
Make research products timely, relevant, and accessible
As with all research endeavors, timeliness and relevance are paramount. However, the typical timeline for academic research (years) is often too long for policymakers whose window for championing a policy action is much shorter (weeks or months) [ 27 , 52 ]. A frequently reported barrier in research-to-policy translation is the complexity of research and concerns about the quality of research evidence [ 29 , 41 , 56 ]; one strategy for combating this concern is the use of clear, careful language [ 27 ], and tailored, audience-specific products that meet the needs of a diverse population of end users [ 27 , 34 , 58 ]. Research that is presented in commonly used, accessible formats (e.g., briefs, factsheets, videos) [ 48 ] may also be more effective, though one study found that use of these formats was dependent on job type, with legislators and staffers preferring different formats [ 58 ].
Multiple studies engaged with policymakers in an effort to determine how they receive research evidence and what strategies or formats are most desirable or effective [ 38 ]. After piloting four different styles of policy briefs (on the same research topic) with state-level policymakers, Brownson et al. [ 38 ] found that while all styles of brief were considered understandable and credible, opinions on the usefulness of the brief varied by the style of the brief and by the level of policymaker (e.g., legislative staff, legislators, and executive branch administrators). These findings suggest that targeted, audience-specific research evidence materials may be more likely to be used by policymakers than generic research evidence. One study explored the usefulness of electronic vs. printed research material and again found differences by type of policymaker—legislators were more likely to read hard copy printed material, while staffers gave higher ratings to online content. Not surprisingly, the age of the policymaker also played a role in the choice to access electronic or printed material, with younger policymakers much more likely to read electronic copy than were their older peers [ 58 ].
A study on state policymakers’ perceptions of comparative effectiveness research (CER) found that the most useful research is that which is consistent and specific to the needs of the policymakers [ 42 ]. The same study identified related barriers to the use of CER in policy decision-making, citing a lack of relevant high quality or conclusive research [ 42 ].
Finally, two studies described pilot projects focused on the delivery of research evidence directly to policymakers. The first cultivated researchers’ capacity to accelerate the translation of research evidence into useable knowledge for policymakers through a rapid response researcher network [ 32 ]. This model was shown to be effective for both researchers (in mobilizing) and policymakers (in eliciting requests for research evidence to bolster a policy conversation or debate) [ 32 ]. The second implementation study reported on a field experiment in which state legislators randomly received relevant research about pending policy proposals [ 44 ]. Findings from this study suggest that having relevant research information increases policymakers’ co-sponsorship of proposals by 60% and highlights the importance of research access in the policy process [ 44 ].
Know the players and the process
Policymakers are as much experts in their arena as researchers are in their academic fields. In order to build lasting working relationships with a target policymaking audience and maximize the relevance of research products for policy work, researchers must first understand the policy process [ 27 , 30 , 34 ]. One study examined the role of researchers themselves in disseminating findings to policymakers and identified individual- and organizational-level facilitators and barriers to the process [ 31 ]. Researchers’ familiarity with the policy process, the relevance of policy dissemination to individual programs of research, and the expectation of dissemination (from higher institutional or funding bodies) facilitated the research-to-policy exchange, while lack of familiarity with effective dissemination strategies and lack of financial and institutional support for dissemination emerged as primary barriers in the research-to-policy exchange [ 31 ].
Public policy, whether legislative, executive, or judicial, affects all areas of daily life in both obvious and subtle ways. The policy process (i.e., the steps from an idea to policy enactment) does not exist in a vacuum; it is influenced by many factors, including public opinion [ 59 , 60 ], special interest groups [ 61 ], personal narratives [ 62 ], expressed needs of constituents [ 1 ], the media [ 63 , 64 , 65 ], and corporations [ 66 , 67 ]. Research may also play a role in shaping policy and has the potential to add objectivity and evidence to these other forces [ 1 , 2 , 68 ]. The current study synthesizes existing knowledge to understand dissemination strategies of social policy research to policymakers in the United States.
Many channels exist to disseminate evidence to policymakers, with the most common being print materials (i.e., reports and policy briefs). This finding is surprising in our current digital age, as print materials are necessarily time-bound and rapidly evolving technology has created more channels (e.g., social media, videos) which may be preferred by policymakers. This shift creates an opportunity to optimize the content of print materials to disseminate in new mediums; it also offers a chance for authors to improve the accessibility of their work for broader audiences (e.g., via more visual presentation formats) [ 15 , 69 , 70 , 71 ].
Our review found strategies to increase effectiveness of research dissemination to policymakers includes starting early, drumming-up support, using champions and brokers, understanding the context, ensuring timeliness, relevance, and accessibility of research products, and knowing the players and the process. These themes align with existing knowledge about policymaker preferences including face-to-face engagement [ 72 , 73 ], contextual considerations (e.g., timeliness and budget) [ 2 , 72 ], and existing barriers and facilitators to research evidence use [ 4 , 5 ]. Our study adds to what we already know about policymakers’ desire for research evidence and their varying preferences as to the context and form of that knowledge [ 2 , 72 , 74 ] and supports existing efforts to bridge the gap between researchers and policymakers.
Many of the barriers and facilitators to research dissemination that we identified in this review mirror those cited by policymakers as barriers and facilitators to evidence use; this overlap reasonably suggests that efforts to expand research dissemination may improve the other. Particularly relevant lessons from the evidence use literature that also emerged from our review include emphasis on the benefit of building personal relationships between researchers and policymakers [ 5 , 75 , 76 ], narrowing the perceived gap between the two groups [ 77 , 78 ], and changing the culture of decision making to increase appreciation for the value of research in policy development [ 5 , 75 , 76 , 77 ]. Considering the multiple pathways through which research evidence is used in policy, from providing direct evidence of a program’s effectiveness to informing or orienting policy makers about relevant issues [ 23 ], these shared lessons around barriers and facilitators may better inform researchers, policymakers, and staff as to best practices for future communication and collaboration.
Our findings also highlight several unique elements of the US policy landscape, wherein significant power is reserved from the federal-level and afforded to state-level government. In some states, this power is further distributed to county and local governments. This system creates major variation across the country in both policy decisions and in resource availability for social policy implementation. Despite our relatively unique government structure, however, many of the effective strategies for dissemination we identified mirror strategies found in other countries [ 79 , 80 ].
Studies that focused on a specific level of government had some unique characteristics such as formality and reliance on print materials. For example, federal dissemination relied more heavily on formal legislative testimony while state level material relied on written policy materials (e.g., policy briefs, report cards). However, these results are limited by small sample sizes and limited evidence about effectiveness.
A wide range of contextual variables may influence policy dissemination in the US at different levels of government. In the federal legislative context alone, multiple committees and subcommittees of both the U.S. House of Representatives and the U.S. Senate may exercise some control over programs and policies related to a single social policy issue (e.g., child and family services) [ 81 ]. At the federal level, the Congressional Research Service (CRS) provides non-partisan research support to legislators in multiple formats including reports on major policy issues, expert testimony, and responses to individual inquiries; the Domestic Social Policy Division offers Congress interdisciplinary research and analysis on social policy issues [ 82 ]. While there may be fewer decision-makers for each issue on the state level, policymaking is further complicated by the extensive rules and reporting requirements attached to state use of federal funding as well as competing priorities or needs at the local level within each state [ 83 , 84 ]. Another dissemination influence may include geographic proximity; for example, geographical proximity may increase the likelihood of university-industry partnerships [ 85 ].
Infrastructure differences may also represent important differences between the US social policy context and that of other developed nations. Each country has a distinct and perhaps unique policy context given available resources, political rules and regulations, and priorities. While models for infrastructure and dissemination interventions may be shared across policy contexts, it may be difficult to directly compare dissemination strategies in one country with dissemination strategies in another country.
Several examples across western countries contribute to a stronger nexus between research evidence and the policy-making process. In the United States, the Wisconsin Family Impact Seminars ( www.wisfamilyimpact.org ) are an example of long-standing initiatives that provide the opportunity for researchers and policymakers to come together to discuss unbiased policy-relevant evidence [ 86 ]. As exemplified by Friese and Bogenschneider [ 27 ], these forums continue to be perceived as objective, relevant, and useful by policymakers and have succeeded at bringing attention to social policy [ 86 ]. Researchers and policymakers in Canada have sought to bridge the research-to-policy gap. For example, the Canadian Foundation for Healthcare Improvement (formerly the Canadian Health Services Research Foundation), funded by the Canadian federal government, brings together researchers and policymakers early and throughout the research development process to discuss, prioritize, and evaluate opportunities for research and dissemination [ 79 ]. In the UK, infrastructure at the national level includes the National Institute for Health Research Policy Research Programme, which funds health research with the explicit goal of informing national policy decisions in health and social care [ 87 ]. These efforts include open calls for research proposals as well as 15 dedicated Policy Research Units located at leading academic institutions around the country. Another resource is the EPPI-Centre at University College London, which provides policymakers support for finding and using research to inform policy decisions through its Research Advisory Service. This allows researchers to work alongside policymakers to reach their goals in addressing educational needs with evidence-informed policy [ 80 ].
Limitations
The current study has several limitations—these illustrate opportunities for future research. First, we attempted to cast a wide net when searching for studies which examined the influence of research on social policy by including a broad search of the peer-reviewed literature, think tanks, and content experts. However, it is possible we missed some studies which examine how research influences policy. Second, we provide a rationale for focusing on US studies and that our findings may not be generalizable to other countries. Third, we were unable to assess the risk of bias for individual studies as current standards note difficulties in assessing quality and bias in qualitative research [ 88 ]. Fourth, many studies examined multiple channels or strategies for how research influences policy, so the parsing of singular strategies (e.g., policy brief, in-person meeting) as an effective approach should be interpreted with caution. Additional investigation is needed to explore and test causal pathways in how these channels can best influence social policy. Fifth, the majority of studies did not use any theory or framework as a foundation or guide for exploration. This gap may indicate a space to use frameworks such as the Model for Dissemination of Research to guide future research. Finally, the dearth of mixed-methods studies that systematically evaluate the impact of research evidence on domestic social policy (this review identified only 3) presents an opportunity for future work in this field to integrate quantitative and qualitative methodologies.
One significant challenge to increasing the rigor in dissemination research studies is the difficulty in choosing and then measuring an outcome. Many of the studies included in this review are either case studies or descriptive, making it difficult to determine what, if any, impact the given research had on policy. Bogenschneider and Corbett discuss this at length as one of the primary challenges to furthering this research [ 72 ], imploring researchers not to focus solely on the outcome of whether or not a piece or legislation passes but rather to examine whether research influenced one of the proposed policy options [ 72 ]. However, this information can be difficult both to operationalize and to collect. That said, some researchers have already begun to think beyond the passage of legislation, as evidenced by Zelizer [ 44 ] who examined bill co-sponsorship rather than passage. A recent review of health policy implementation measurement found that validated quantitative measures are underutilized and recommends further development and testing of such measures [ 89 ]. Difficulties in identifying robust outcomes and high-quality scales to operationalize them present opportunities for additional exploration in this area.
Dissemination and implementation are often described together; not surprisingly, is overlap in effective strategies for each. The current review identified six dissemination strategies and described their reported effectiveness, while the Expert Recommendations for Implementing Change (ERIC) Project identified 73 implementation strategies [ 90 ]. One such similarity is obvious: the dissemination strategy of using champions and brokers mirrors the ERIC implementation strategy of identifying and preparing champions. The difference between the number of implementation strategies and dissemination strategies is striking and highlights the gap in research. Future work should further explore the degree to which dissemination strategies and implementation strategies either overlap or are distinct.
Finally, the dissemination of research to policymakers may raise certain ethical issues. It is imperative for researchers to critically assess when and how to disseminate research findings to policymakers, keeping in mind that promoting a specific policy agenda may result in a perceived or real loss of objectivity [ 91 ]. Syntheses of policy-relevant evidence can be useful, particularly when researchers work in partnership with non-governmental organizations to inform the policy process.
We summarize strategies and illuminate potential barriers to the research-to-policy dissemination process. Key findings are drawn from multiple disciplines and suggest that lessons learned may cut across both research topics and levels of government. The most frequently referenced channel for dissemination to policymakers was print materials, with personal communication (including both in-person and electronic meetings and individual communications) a close second. Corresponding strategies for effective dissemination to policymakers included starting early, drumming-up support, using champions and brokers, understanding the context, ensuring timeliness, relevance, and accessibility of research products, and knowing the players and the process. A shared feature of these strategies is the distillation of complex research findings into accessible pieces of relevant information that can then be delivered via multiple avenues.
Interdisciplinary collaboration is a common practice in scientific research [ 92 ]. Our findings provide leads on how to more effectively to engage with policymakers, leading to a greater likelihood of translating research evidence into policy action. Engaging policymakers early as contributing members of the research team, maintaining communication during the research process, and presenting relevant findings in a clear, concise manner may empower both researchers and policymakers to further apply scientific evidence to improve social policy in the United States.
Availability of data and materials
Raw search results, citations, and abstracts available upon request.
Abbreviations
United States
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Comparative Effectiveness Research
Expert Recommendations for Implementing Change
Dodson EA, Geary NA, Brownson RC. State legislators’ sources and use of information: bridging the gap between research and policy. Health Educ Res. 2015;30:840–8.
PubMed PubMed Central Google Scholar
Purtle J, Dodson EA, Nelson K, Meisel ZF, Brownson RC. Legislators’ sources of behavioral Health research and preferences for dissemination: variations by political party. Psychiatr Serv. 2018; appi.ps.201800153.
Purtle J, Peters R, Brownson RC. A review of policy dissemination and implementation research funded by the National Institutes of Health, 2007-2014. Implement Sci. 2016;11.
Oliver K, Innvar S, Lorenc T, Woodman J, Thomas J. A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res. 2014;14:2.
Article PubMed PubMed Central Google Scholar
Innvær S, Vist G, Trommald M, Oxman A. Health policy-makers’ perceptions of their use of evidence: a systematic review. J Health Serv Res Policy. 2002;7:239–44.
Article PubMed Google Scholar
El-Jardali F, Lavis JN, Ataya N, Jamal D. Use of health systems and policy research evidence in the health policymaking in eastern Mediterranean countries: views and practices of researchers. Implement Sci IS. 2012;7:2.
Campbell DM, Redman S, Rychentnik L, Cooke M, Zwi AB, Jorm L. Increasing the use of evidence in health policy: practice and views of policy makers and researchers. Aust N Z Health Policy CSIRO. 2009;6.
Dean H. Social Policy. Cambridge: Polity; 2012.
Google Scholar
Gilbert N, Terrell P. Dimensions of social welfare policy. 8th ed. Boston: Pearson; 2012.
Marshall TH. Citizenship and social class. Cambridge; 1950.
Shannon CE. A mathematical theory of communication. Bell Syst Tech J. 1948;27:379–423.
Article Google Scholar
Weaver W, Shannon CE. The mathematical theory of communication. Champaign: University of Illinois Press; 1963.
McGuire W. The nature of attitudes and attitude change. Vol. 3. Reading: Addison-Wesley Pub. Co; 1969.
McGuire WJ, Rice R, Atkin C. Input and output variables currently promising for constructing persuasive communications. Public Commun Campaigns. 2001;3:22–48.
Brownson RC, Eyler AA, Harris JK, Moore JB, Tabak RG. Getting the Word Out: New Approaches for Disseminating Public Health Science. J Public Health Manag Pract JPHMP. 2018;24:102–11.
Rogers EM. Diffusion of Innovations, 5th Edition: Simon and Schuster; 2003.
Kotler P, Zaltman G. Social marketing: an approach to planned social change. J Mark. 1971;35:3–12.
Article CAS PubMed Google Scholar
Best A, Holmes B. Systems thinking, knowledge and action: towards better models and methods. Evid Policy J Res Debate Pract Policy Press. 2010;6:145–59.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:g7647.
Political party - Two-party systems. Encycl. Br. 2020 [cited 2020 Aug 10]. Available from: https://www.britannica.com/topic/political-party .
Mahoney C. Why lobbying in America is different [Internet]. POLITICO. 2009 [cited 2020 Aug 10]. Available from: https://www.politico.eu/article/why-lobbying-in-america-is-different/ .
Tseng V, Coburn C. Using evidence in the US. What Works Evid-Inf Policy Pract. Bristol: Policy Press; 2019. p. 351–68.
Stern MJ. Social Policy: History (1950–1980). Encycl Soc Work. 2013; [cited 2020 Apr 17]. Available from: https://oxfordre.com/socialwork/view/10.1093/acrefore/9780199975839.001.0001/acrefore-9780199975839-e-610 .
Ashcraft LE, Asato M, Houtrow AJ, Kavalieratos D, Miller E, Ray KN. Parent empowerment in pediatric healthcare settings: A systematic review of observational studies. Patient Patient Centered Outcomes Res. 2019;12:199–212.
Jacobs LA, Ashcraft LE, Sewall CJR, Folb BL, Mair C. Ecologies of juvenile reoffending: a systematic review of risk factors. J Crim Just. 2020;66:101638.
Friese B, Bogenschneider K. The voice of experience: how social scientists communicate family research to policymakers. Fam Relat. 2009;58:229–43.
Nelson JW, Scammell MK, Altman RG, Webster TF, Ozonoff DM. A new spin on research translation: the Boston Consensus Conference on Human Biomonitoring. Environ Health Perspect. 2009;117:495–9.
Weiss CH, Murphy-Graham E, Petrosino A, Gandhi AG. The fairy godmother—nd her warts. Am J Eval. 2008;29:29–47.
Meisel ZF, Mitchell J, Polsky D, Boualam N, McGeoch E, Weiner J, et al. Strengthening partnerships between substance use researchers and policy makers to take advantage of a window of opportunity. Subst Abuse Treat Prev Policy. 2019;14:12.
McVay AB, Stamatakis KA, Jacobs JA, Tabak RG, Brownson RC. The role of researchers in disseminating evidence to public health practice settings: a cross-sectional study. Health Res Policy Syst. 2016;14:1–9.
Crowley M, Scott JTB, Fishbein D. Translating prevention research for evidence-based policymaking: results from the research-to-policy collaboration pilot. Prev Sci. 2018;19:260–70.
Lane JP, Rogers JD. Engaging national organizations for knowledge translation: Comparative case studies in knowledge value mapping. Implement Sci. 2011;6.
McBride T, Coburn A, MacKinney C, Mueller K, Slifkin R, Wakefield M. Bridging health research and policy: effective dissemination strategies. J Public Health Manag Pract. 2008;14:150–4.
McGinty EE, Siddiqi S, Linden S, Horwitz J, Frattaroli S. Improving the use of evidence in public health policy development, enactment and implementation: a multiple-case study. Health Educ Res. 2019;34:129–44.
Yanovitzky I, Weber M. Analysing use of evidence in public policymaking processes: a theory-grounded content analysis methodology. 2019 [cited 2019 May 8]. Available from: https://www.ingentaconnect.com/content/tpp/ep/pre-prints/content-ppevidpold1700095 .
Purtle J, Lê-Scherban F, Wang XI, Shattuck PT, Proctor EK, Brownson RC. State Legislators’ Support for Behavioral Health Parity Laws: The Influence of Mutable and Fixed Factors at Multiple Levels. Milbank Q. 2019;97:1200–32.
Article PubMed Central Google Scholar
Brownson RC, Dodson EA, Stamatakis KA, Casey CM, Elliott MB, Luke DA, et al. Communicating evidence-based information on cancer prevention to state-level policy makers. J Natl Cancer Inst. 2011;103:306–16.
Hopkins M, Wiley KE, Penuel WR, Farrell CC. Brokering research in science education policy implementation: the case of a professional association. Evid Policy. 2018;14:459–76.
Sorian R, Baugh T. Power of information: closing the gap between research and policy. Health Aff (Millwood). 2002;21:264–73.
Valentine A, DeAngelo D, Alegria M, Cook BL. Translating disparities research to policy: a qualitative study of state mental health policymakers’ perceptions of mental health care disparities report cards. Psychol Serv. 2014;11:377–87.
Weissman JS, Westrich K, Hargraves JL, Pearson SD, Dubois R, Emond S, et al. Translating comparative effectiveness research into Medicaid payment policy: views from medical and pharmacy directors. J Comp Eff Res. 2015;4:79–88.
Massell D, Goertz ME, Barnes CA. State education agencies’ acquisition and use of research knowledge for school improvement. Peabody J Educ. 2012;87:609–26.
Zelizer A. How Responsive Are Legislators to Policy Information? Evidence from a field experiment in a state legislature. Legis Stud Q. 2018;43:595–618.
Allen ST, Ruiz MS, O’Rourke A. The evidence does not speak for itself: The role of research evidence in shaping policy change for the implementation of publicly funded syringe exchange programs in three US cities. Int J Drug Policy. 2015;26:688–95.
Brim OG Jr, Dustan J, Brim OG Jr. Translating research into policy for children: the private foundation experience. Am Psychol. 1983;38:85–90.
Austin SB, Yu K, Tran A, Mayer B. Research-to-policy translation for prevention of disordered weight and shape control behaviors: a case example targeting dietary supplements sold for weight loss and muscle building. Eat Behav. 2017;25:9–14.
Bumbarger B, Campbell E. A state agency-university partnership for translational research and the dissemination of evidence-based prevention and intervention. Adm Policy Ment Health Ment Health Serv Res. 2012;39:268–77.
Garcia AR, Kim M, Palinkas LA, Snowden L, Landsverk J. Socio-contextual determinants of research evidence use in public-youth systems of care. Adm Policy Ment Health Ment Health Serv Res. 2016;43:569–78.
Coffman JM, Hong M-K, Aubry WM, Luft HS, Yelin E. Translating medical effectiveness research into policy: lessons from the California health benefits review program. Milbank Q. 2009;87:863–902.
Jamieson M, Bodonyi JM. Data-driven child welfare policy and practice in the next century. Child Welfare. 1999;78:15–30.
Mosley JE, Courtney ME. Partnership and the politics of care: advocates’ role in passing and implementing California’s law to extend foster care: Chapin Hall Center for Children; 2012.
Jabbar H, Goel La Londe P, Debray E, Scott J, Lubienski C. How Policymakers Define ‘Evidence’: The Politics of Research Use in New Orleans. Policy Futur Educ. 2015;12:286–303.
Nelson SR, Leffler JC, Hansen BA. Toward a research agenda for understanding and improving the use of research evidence. Northwest Reg Educ Lab NWREL. 2009.
Purtle J, Peters R, Kolker J, Diez Roux AV. Uses of population health rankings in local policy contexts: A multisite case study. Med Care Res Rev. 2019;76:478–96.
McGinty B, Siddiqi S, Linden S. Academic research-policy translation strategies to improve the use of evidence in health policy development, enactment and implementation: a 3-part embedded case study. Implement Sci. 2018;13.
Jamieson M, Bodonyi JM. Data-driven child welfare policy and practice in the next century. Fam Foster Care Century. 2001;13.
Sorian R, Baugh T. Power of information: closing the gap between research and policy. Health Aff (Millwood). Health Aff. 2002;21:264–73.
Burstein P. The impact of public opinion on public policy: a review and an agenda. Polit Res Q. 2003;56:29–40.
Pacheco J, Maltby E. The role of public opinion—does it influence the diffusion of ACA decisions? J Health Polit Policy Law. 2017;42:309–40.
Wolton S. Lobbying, Inside and Out: How special interest groups influence policy choices. Rochester, NY: Social Science Research Network; 2017 Mar. Report No.: ID 2190685. Available from: https://papers.ssrn.com/abstract=2190685 .
Stamatakis KA, McBride TD, Brownson RC. Communicating prevention messages to policy makers: the role of stories in promoting physical activity. J Phys Act Health. 2010;7:S99–107.
Otten AL. The influence of the mass media on health policy. Health Aff (Millwood). Health Aff. 1992;11:111–8.
Article CAS Google Scholar
Robinson P. Theorizing the influence of media on world politics: models of media influence on foreign policy. Eur J Commun. 2001;16:523–44.
Shanahan EA, McBeth MK, Hathaway PL. Narrative policy framework: the influence of media policy narratives on public opinion. Polit Policy. 2011;39:373–400.
Salamon LM, Siegfried JJ. Economic power and political influence: the impact of industry structure on public policy. Am Polit Sci Rev. 1977;71:1026–43.
Shelley D, Ogedegbe G, Elbel B. Same strategy different industry: corporate influence on public policy. Am J Public Health. 2014;104:e9–11.
Hird JA. Policy Analysis for What? The effectiveness of nonpartisan policy research organizations. Policy Stud J. 2005;33:83–105.
Trost MJ, Webber EC, Wilson KM. Getting the word out: disseminating scholarly work in the technology age. Acad Pediatr. 2017;17:223–4.
Kapp JM, Hensel B, Schnoring KT. Is Twitter a forum for disseminating research to health policy makers? Ann Epidemiol. 2015;25:883–7.
Dodson EA, Eyler AA, Chalifour S, Wintrode CG. A review of obesity-themed policy briefs. Am J Prev Med. 2012;43:S143–8.
Bogenschneider K, Corbett TJ. Evidence-based policymaking: Insights from policy-minded researchers and research-minded policymakers: Routledge; 2011.
Mitton C, Adair CE, Mckenzie E, Patten SB, Perry BW. Knowledge transfer and exchange: review and synthesis of the literature. Milbank Q. 2007;85:729–68.
Purtle J, Lê-Scherban F, Shattuck P, Proctor EK, Brownson RC. An audience research study to disseminate evidence about comprehensive state mental health parity legislation to US State policymakers: protocol. Implement Sci. 2017;12:1–13.
Van der Arend J. Bridging the research/policy gap: policy officials’ perspectives on the barriers and facilitators to effective links between academic and policy worlds. Policy Stud. 2014;35:611–30.
Langer L, Tripney J, Gough DA. The science of using science: researching the use of research evidence in decision-making: UCL Institute of Education, EPPI-Centre; 2016.
Orton L, Lloyd-Williams F, Taylor-Robinson D, O’Flaherty M, Capewell S. The use of research evidence in public health decision making processes: systematic review. PLoS One. 2011;6:e21704.
Article CAS PubMed PubMed Central Google Scholar
Hennink M, Stephenson R. Using research to inform health policy: barriers and strategies in developing countries. J Health Commun. 2005;10:163–80.
Lomas J. Essay: Using ‘Linkage And Exchange’ To move research into policy at a Canadian Foundation. Health Aff (Millwood). Health Aff. 2000;19:236–40.
EPPI-Centre. Research Advisory Service. 2019 [cited 2020 Aug 4]. Available from: https://eppi.ioe.ac.uk/cms/Default.aspx?tabid=3421 .
Kerner JF, Hall KL. Research dissemination and diffusion: translation within science and society. Res Soc Work Pract. 2009;19:519–30.
Library of Congress. About CRS - congressional research service (Library of Congress). 2020 [cited 2020 Aug 26]. Available from: https://www.loc.gov/crsinfo/about/ .
Edwards C. Complexity in State Government. 2020 [cited 2020 Aug 31]. Available from: https://www.cato.org/blog/complexity-state-government .
Urban Institute. State and Local Expenditures [Internet]. Urban Inst. 2020 [cited 2020 Aug 25]. Available from: https://www.urban.org/policy-centers/cross-center-initiatives/state-and-local-finance-initiative/state-and-local-backgrounders/state-and-local-expenditures .
D’Este P, Guy F, Iammarino S. Shaping the formation of university–industry research collaborations: what type of proximity does really matter? J Econ Geogr. 2013;13:537–58.
Owen JW, Larson AM. Researcher-policymaker partnerships: Strategies for launching and sustaining successful collaborations: Routledge; 2017.
National Institute for Health Research. Policy research. 2020 [cited 2020 Sep 4]. Available from: https://www.nihr.ac.uk/explore-nihr/funding-programmes/policy-research.htm .
Higgins J, Green S. Cochrane Handbook for systematic reviews of interventions. 2011 [cited 2018 Sep 20]. Available from: /handbook.
Allen P, Pilar M, Walsh-Baily C, Hooley C, Mazzucca S, Lewis C, et al. Quantitative measures of health policy implementation determinants and outcomes: a systematic review. Implement Sci. 2020.
Powell BJ, Waltz TJ, Chinman MJ, Damschroder LJ, Smith JL, Matthieu MM, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21.
Brownson RC, Hartge P, Samet JM, Ness RB. From epidemiology to policy: toward more effective practice. Ann Epidemiol. 2010;20:409.
Carroll L, Ali MK, Cuff P, Huffman MD, Kelly BB, Kishore SP, et al. Envisioning a transdisciplinary university. J Law Med Ethics. 2014;42:17–25.
Download references
Acknowledgements
The views expressed herein are those of the authors and do not reflect those of the Department of Veterans Affairs, the Centers for Disease Control and Prevention, or the National Institutes of Health.
LEA is supported by a pre-doctoral Clinical and Translational Science Fellowship (NIH TL1 TR001858 (PI: Kraemer)). DAQ is supported by a postdoctoral fellowship through the Department of Veterans Affairs (VA) Office of Academic Affiliations and the Center for Health Equity Research and Promotion at the VA Pittsburgh Healthcare System. RCB is supported by the National Cancer Institute (P50CA244431) the Centers for Disease Control and Prevention (U48DP006395). The funding entities had no role in the development, data collection, analysis, reporting, or publication of this work. Article processing charges for this article were fully paid by the University Library System, University of Pittsburgh.
Author information
Authors and affiliations.
University of Pittsburgh School of Social Work, 2117 Cathedral of Learning, 4200 Fifth Avenue, Pittsburgh, PA, 15260, USA
Laura Ellen Ashcraft
Center for Health Equity Research and Promotion (CHERP), VA Pittsburgh Healthcare System, University Drive C, Building 30, Pittsburgh, PA, 15240, USA
Deirdre A. Quinn
Prevention Research Center, Brown School, Washington University in St. Louis, One Brookings Drive, Campus Box 1196, St. Louis, MO, 63130, USA
Ross C. Brownson
Department of Surgery, Division of Public Health Sciences, and Alvin J. Siteman Cancer Center, Washington University School of Medicine, 660 South Euclid Avenue, Saint Louis, MO, 63110, USA
You can also search for this author in PubMed Google Scholar
Contributions
Review methodology: LEA, DAQ, RCB; eligibility criteria: LEA, DAQ, RCB; search strings and terms: LEA, DAQ; abstract screening: LEA, DAQ; full text screening: LEA, DAQ; pilot extraction: LEA, DAQ; data extraction: LEA, DAQ; data aggregation: LEA, DAQ; writing: LEA, DAQ; editing: LEA, DAQ, RCB. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Laura Ellen Ashcraft .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.

Consent for publication
Competing interests.
The authors declare they have no conflicting interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
PRISMA Checklist.
Additional File 2.
Search Strategy.
Additional File 3.
Data Abstraction Form.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ashcraft, L.E., Quinn, D.A. & Brownson, R.C. Strategies for effective dissemination of research to United States policymakers: a systematic review. Implementation Sci 15 , 89 (2020). https://doi.org/10.1186/s13012-020-01046-3
Download citation
Received : 18 May 2020
Accepted : 14 September 2020
Published : 15 October 2020
DOI : https://doi.org/10.1186/s13012-020-01046-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Dissemination
- Dissemination science
- Social policy
- Public policy
Implementation Science
ISSN: 1748-5908
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Immigration's Effect on US Wages and Employment Redux
In this article we revive, extend and improve the approach used in a series of influential papers written in the 2000s to estimate how changes in the supply of immigrant workers affected natives' wages in the US. We begin by extending the analysis to include the more recent years 2000-2022. Additionally, we introduce three important improvements. First, we introduce an IV that uses a new skill-based shift-share for immigrants and the demographic evolution for natives, which we show passes validity tests and has reasonably strong power. Second, we provide estimates of the impact of immigration on the employment-population ratio of natives to test for crowding out at the national level. Third, we analyze occupational upgrading of natives in response to immigrants. Using these estimates, we calculate that immigration, thanks to native-immigrant complementarity and college skill content of immigrants, had a positive and significant effect between +1.7 to +2.6\% on wages of less educated native workers, over the period 2000-2019 and no significant wage effect on college educated natives. We also calculate a positive employment rate effect for most native workers. Even simulations for the most recent 2019-2022 period suggest small positive effects on wages of non-college natives and no significant crowding out effects on employment.
We are grateful for Rebecca Brough for her research assistance and suggestions. The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
MARC RIS BibTeΧ
Download Citation Data
Mentioned in the News
More from nber.
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .

- Systematic Review
- Open access
- Published: 26 April 2024
Systematic review on the frequency and quality of reporting patient and public involvement in patient safety research
- Sahar Hammoud ORCID: orcid.org/0000-0003-4682-9001 1 ,
- Laith Alsabek 1 , 2 ,
- Lisa Rogers 1 &
- Eilish McAuliffe 1
BMC Health Services Research volume 24 , Article number: 532 ( 2024 ) Cite this article
230 Accesses
Metrics details
In recent years, patient and public involvement (PPI) in research has significantly increased; however, the reporting of PPI remains poor. The Guidance for Reporting Involvement of Patients and the Public (GRIPP2) was developed to enhance the quality and consistency of PPI reporting. The objective of this systematic review is to identify the frequency and quality of PPI reporting in patient safety (PS) research using the GRIPP2 checklist.
Searches were performed in Ovid MEDLINE, EMBASE, PsycINFO, and CINAHL from 2018 to December, 2023. Studies on PPI in PS research were included. We included empirical qualitative, quantitative, mixed methods, and case studies. Only articles published in peer-reviewed journals in English were included. The quality of PPI reporting was assessed using the short form of the (GRIPP2-SF) checklist.
A total of 8561 studies were retrieved from database searches, updates, and reference checks, of which 82 met the eligibility criteria and were included in this review. Major PS topics were related to medication safety, general PS, and fall prevention. Patient representatives, advocates, patient advisory groups, patients, service users, and health consumers were the most involved. The main involvement across the studies was in commenting on or developing research materials. Only 6.1% ( n = 5) of the studies reported PPI as per the GRIPP2 checklist. Regarding the quality of reporting following the GRIPP2-SF criteria, our findings show sub-optimal reporting mainly due to failures in: critically reflecting on PPI in the study; reporting the aim of PPI in the study; and reporting the extent to which PPI influenced the study overall.
Conclusions
Our review shows a low frequency of PPI reporting in PS research using the GRIPP2 checklist. Furthermore, it reveals a sub-optimal quality in PPI reporting following GRIPP2-SF items. Researchers, funders, publishers, and journals need to promote consistent and transparent PPI reporting following internationally developed reporting guidelines such as the GRIPP2. Evidence-based guidelines for reporting PPI should be encouraged and supported as it helps future researchers to plan and report PPI more effectively.
Trial registration
The review protocol is registered with PROSPERO (CRD42023450715).
Peer Review reports
Patient safety (PS) is defined as “the absence of preventable harm to a patient and reduction of risk of unnecessary harm associated with healthcare to an acceptable minimum” [ 1 ]. It is estimated that one in 10 patients are harmed in healthcare settings due to unsafe care, resulting in over three million deaths annually [ 2 ]. More than 50% of adverse events are preventable, and half of these events are related to medications [ 3 , 4 ]. There are various types of adverse events that patients can experience such as medication errors, patient falls, healthcare-associated infections, diagnostic errors, pressure ulcers, unsafe surgical procedures, patient misidentification, and others [ 1 ].
Over the last few decades, the approach of PS management has shifted toward actively involving patients and their families in managing PS. This innovative approach has surpassed the traditional model where healthcare providers were the sole managers of PS [ 5 ]. Recent research has shown that patients have a vital role in promoting their safety and decreasing the occurrence of adverse events [ 6 ]. Hence, there is a growing recognition of patient and family involvement as a promising method to enhance PS [ 7 ]. This approach includes involving patients in PS policy development, research, and shared decision making [ 1 ].
In the last decade, research involving patients and the public has significantly increased. In the United Kingdom (U.K), the National Institute for Health Research (NIHR) has played a critical role in providing strategic and infrastructure support to integrate Public and Patient Involvement (PPI) throughout publicly funded research [ 8 ]. This has established a context where PPI is recognised as an essential element in research [ 9 ]. In Ireland, the national government agency responsible for the management and delivery of all public health and social services; the National Health Service Executive (HSE) emphasise the importance of PPI in research and provide guidance for researchers on how to involve patients and public in all parts of the research cycle and knowledge translation process [ 10 ]. Similar initiatives are also developing among other European countries, North America, and Australia. However, despite this significant expansion of PPI research, the reporting of PPI in research articles continues to be sub-optimal, inconsistent, and lacks essential information on the context, process, and impact of PPI [ 9 ]. To address this problem, the Guidance for Reporting Involvement of Patients and the Public (GRIPP) was developed in 2011 following the EQUATOR methodology to enhance the quality, consistency, and transparency of PPI reporting. Additionally, to provide guidance for researchers, patients, and the public to advance the quality of the international PPI evidence-base [ 11 ]. The first GRIPP checklist was a significant start in producing higher-quality PPI reporting; however, it was developed following a systematic review, and did not include any input from the international PPI research community. Given the importance of reaching consensus in generating current reporting guidelines, a second version of the GRIPP checklist (GRIPP2) was developed to tackle this problem by involving the international PPI community in its development [ 9 ]. There are two versions of the GRIPP2 checklist, a long form (GRIPP2-LF) for studies with PPI as the primary focus, and a short form (GRIPP2-SF) for studies with PPI as secondary or tertiary focus.
Since the publication of the GRIPP2 checklist, several systematic reviews have been conducted to assess the quality of PPI reporting on various topics. For instance, Bergin et al. in their review to investigate the nature and impact of PPI in cancer research, reported a sub-optimal quality of PPI reporting using the GRIPP2-SF, mainly due to failure to address PPI challenges [ 12 ]. Similarly, Owyang et al. in their systematic review to assess the prevalence, extent, and quality of PPI in orthopaedic practice, described a poor PPI reporting following the GRIPP2-SF checklist criteria [ 13 ]. While a few systematic reviews have been conducted to assess theories, strategies, types of interventions, and barriers and enablers of PPI in PS [ 5 , 14 , 15 , 16 ], no previous review has assessed the quality of PPI reporting in PS research. Thus, our systematic review aims to address this knowledge gap. The objective of this review is to identify the frequency PPI reporting in PS research using the GRIPP2 checklist from 2018 (the year after GRIPP2 was published) and the quality of reporting following the GRIPP2-SF. The GRIPP2 checklist was chosen as the benchmark as it is the first international, evidence-based, community consensus informed guideline for the reporting of PPI in research and more specifically in health and social care research [ 9 ]. Additionally, it is the most recent report-focused framework and the most recommended by several leading journals [ 17 ].
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to plan and report this review [ 18 ]. The review protocol was published on PROSPERO the International Database of Prospectively Registered Systematic Reviews in August 2023 (CRD42023450715).
Search strategy
For this review, we used the PICo framework to define the key elements in our research. These included articles on patients and public (P-Population) involvement (I- phenomenon of Interest) in PS (C-context). Details are presented in Table 1 . Four databases were searched including Ovid MEDLINE, EMBASE, PsycINFO, and CINAHL to identify papers on PPI in PS research. A systematic search strategy was initially developed using MEDLINE. MeSH terms and keywords relevant to specific categories (e.g., patient safety) were combined using the “OR” Boolean term (i.e. patient safety OR adverse event OR medical error OR surgical error) and categories were then combined using the “AND” Boolean term. (i.e. “patient and public involvement” AND “patient safety”). The search strategy was adapted for the other three databases. Full search strategies are provided in Supplementary file 1 . The search was conducted on July 27th, 2023, and was limited to papers published from 2018. As the GRIPP2 tool was published in 2017, this limit ensured the retrieval of relevant studies. An alert system was set on the four databases to receive all new published studies until December 2023, prior to the final analysis. The search was conducted without restrictions on study type, research design, and language. To reduce selection bias, hand searching was carried out on the reference lists of all the eligible articles in the later stages of the review. This was done by the first author. The search strategy was developed by the first author and confirmed by the research team and a Librarian. The database search was conducted by the first author.
Inclusion and exclusion criteria
Studies on PPI in PS research with a focus on health/healthcare were included in this review. We defined PPI as active involvement which is in line with the NIHR INVOLVE definition as “research being carried out ‘with’ or ‘by’ members of the public rather than ‘to’, ‘about’ or ‘for’ them” [ 19 ]. This includes any PPI including, being a co-applicant on a research project or grant application, identifying research priorities, being a member of an advisory or steering group, participating in developing research materials or giving feedback on them, conducting interviews with study participants, participating in recruitment, data collection, data analysis, drafting manuscripts and/or dissemination of results. Accordingly, we excluded studies where patients or the public were only involved as research participants.
We defined patients and public to include patients, relatives, carers, caregivers and community, which is also in line with the NIHR PPI involvement in National Health Service [ 19 ].
Patient safety included topics on medication safety, adverse events, communication, safety culture, diagnostic errors, and others. A full list of the used terms for PPI and PS is provided in Supplementary file 1 . Regarding the research type and design, we included empirical qualitative, quantitative, mixed methods, and case studies. Only articles published in peer-reviewed journals and in English were included.
Any article that did not meet the inclusion criteria was excluded. Studies not reporting outcomes were excluded. Furthermore, review papers, conference abstracts, letters to editor, commentary, viewpoints, and short communications were excluded. Finally, papers published prior to 2018 were excluded.
Study selection
The selection of eligible studies was done by the first and the second authors independently, starting with title and abstracts screening to eliminate papers that failed to meet our inclusion criteria. Then, full text screening was conducted to decide on the final included papers in this review. Covidence, an online data management system supported the review process, ensuring reviewers were blinded to each other’s decisions. Disagreements between reviewers were discussed first, in cases where the disagreement was not resolved, the fourth author was consulted.
Data extraction and analysis
A data extraction sheet was developed using excel then piloted, discussed with the research team and modified as appropriate. The following data were extracted: citation and year of publication, objective of the study, country, PS topic, design, setting, PPI participants, PPI stages (identifying research priorities, being a member of an advisory or steering group, etc.…), frequency of PPI reporting as per the GRIPP2 checklist, and the availability of a plain language summary. Additionally, data against the five items of GRIPP2-SF (aim of PPI in the study, methods used for PPI, outcomes of PPI including the results and the extent to which PPI influenced the study overall, and reflections on PPI) were extracted. To avoid multiple publication bias and missing outcomes, data extraction was done by the first and the second authors independently and then compared. Disagreements between reviewers were first discussed, and then resolved by the third and fourth authors if needed.
Quality assessment
The quality of PPI reporting was assessed using GRIPP2-SF developed by Staniszewska et al. [ 9 ] as it is developed to improve the quality, consistency, and reporting of PPI in social and healthcare research. Additionally the GRIPP2-SF is suitable for all studies regardless of whether PPI is the primary, secondary, or tertiary focus, whereas the GRIPP2-LF is not suitable for studies where PPI serves as a secondary or tertiary focus. The checklist includes five items (mentioned above) that authors should include in their studies. It is important to mention that Staniszewska et al. noted that “while GRIPP2-SF aims to guide consistent reporting, it is not possible to be prescriptive about the exact content of each item, as the current evidence-base is not advanced enough to make this possible” ([ 9 ] p5). For that reason, we had to develop criteria for scoring the five reporting items. We used three scoring as Yes, No, and partial for each of the five items of the GRIPP2-SF. Yes, was given when authors presented PPI information on the item clearly in the paper. No, when no information was provided, and partial when the information partially met the item requirement. For example, as per GRIPP2-SF authors should provide a clear description of the methods used for PPI in the study. In the example given by Staniszewska et al., information on patient/public partners and how many of them were provided, as well as the stages of the study they were involved in (i.e. refining the focus of the research questions, developing the search strategy, interpreting results). Thus, in our evaluation of the included studies, we gave a yes if information on PPI participants (i.e. patient partners, community partners, or family members etc..) and how many of them were involved was provided, and information on the stages or actions of their involvement in the study was provided. However, we gave a “partial” if information was not fully provided (i.e. information on patient/public partners and how many were involved in the study without describing in what stages or actions they were involved, and vice versa), and a “No” if no information was presented at all.
The quality of PPI reporting was done by the first and the second authors independently and then compared. Disagreements between reviewers were first discussed, and then resolved by the third and fourth author when needed.
Assessing the quality or risk of bias of the included studies was omitted, as the focus in this review was on appraising the quality of PPI reporting rather than assessing the quality of each research article.
Data synthesis
After data extraction, a table summarising the included studies was developed. Studies were compared according to the main outcomes of the review; frequency of PPI reporting following the GRIPP2 checklist and the quality of reporting as per GRIPP2-SF five items, and the availability of a plain language summary.
Search results and study selection
The database searches yielded a total of 8491 studies. First, 2496 were removed as duplicates. Then, after title and abstract screening, 5785 articles were excluded leaving 210 articles eligible for the full text review. After a careful examination, 68 of these studies were included in this review. A further 38 studies were identified from the alert system that was set on the four databases and 32 studies from the reference check of the included studies. Of these 70 articles, 56 were further excluded and 14 were added to the previous 68 included studies. Thus, 82 studies met the inclusion criteria and were included in this review. A summary of the database search results and the study selection process are presented in Fig. 1 .
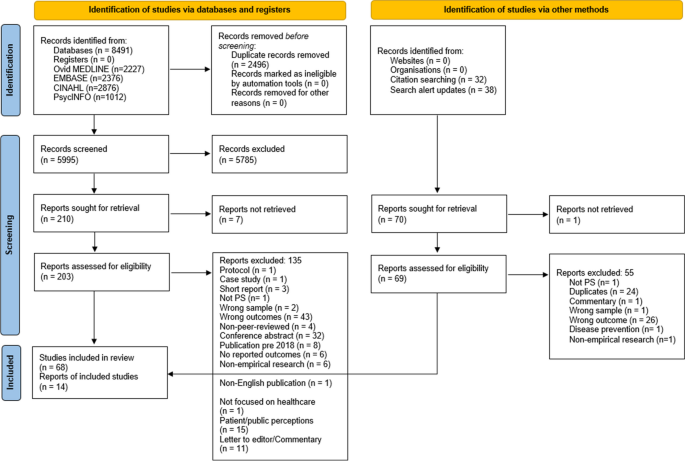
PRISMA flow diagram of the study selection process. The PRISMA flow diagram details the review search results and selection process
Overview of included studies
Details of the study characteristics including first author and year of publication, objective, country, study design, setting, PS topic, PPI participants and involvement stages are presented in Supplementary file 2 . The majority of the studies were conducted in the U.K ( n = 24) and the United States of America ( n = 18), with the remaining 39 conducted in other high income countries, the exception being one study in Haiti. A range of study designs were identified, the most common being qualitative ( n = 31), mixed methods ( n = 13), interventional ( n = 5), and quality improvement projects ( n = 4). Most PS topics concerned medication safety ( n = 17), PS in general (e.g., developing a PS survey or PS management application) ( n = 14), fall prevention ( n = 13), communication ( n = 11), and adverse events ( n = 10), with the remaining PS topics listed in Supplementary file 2 .
Patient representatives, advocates, and patient advisory groups ( n = 33) and patients, service users, and health consumers ( n = 32) were the main groups involved. The remaining, included community members/ organisations. Concerning PPI stages, the main involvement across the studies was in commenting on or developing research materials ( n = 74) including, patient leaflets, interventional tools, mobile applications, and survey instruments. Following this stage, involvement in data analysis, drafting manuscripts, and disseminating results ( n = 30), and being a member of a project advisory or steering group ( n = 18) were the most common PPI evident in included studies. Whereas the least involvement was in identifying research priorities ( n = 5), and being a co-applicant on a research project or grant application ( n = 6).
Regarding plain language summary, only one out of the 82 studies (1.22%) provided a plain language summary in their paper [ 20 ].
Frequency and quality of PPI reporting
The frequency of PPI reporting following the GRIPP2 checklist was 6.1%, where only five of the 82 included studies reported PPI in their papers following the GRIPP2 checklist. The quality of PPI reporting in those studies is presented in Table 2 . Of these five studies, one study (20%) did not report the aim of PPI in the study and one (20%) did not comment on the extent to which PPI influenced the study overall.
The quality of PPI reporting of the remaining 77 studies is presented in Table 3 . The aim of PPI in the study was reported in 62.3% of articles ( n = 48), while 3.9% ( n = 3) partially reported this. A clear description of the methods used for PPI in the study was reported in 79.2% of papers ( n = 61) and partially in 20.8% ( n = 16). Concerning the outcomes, 81.8% of papers ( n = 63) reported the results of PPI in the study, while 10.4% ( n = 8) partially did. Of the 77 studies, 68.8% ( n = 53) reported the extent to which PPI influenced the study overall and 3.9% ( n = 3) partially reported this. Finally, 57.1% ( n = 44) of papers critically reflected on the things that went well and those that did not and 2.6% ( n = 2) partially reflected on this.
Summary of main findings
This systematic review assessed the frequency of reporting PPI in PS research using the GRIPP2 checklist and quality of reporting using the GRIPP2-SF. In total, 82 studies were included in this review. Major PS topics were related to medication safety, general PS, and fall prevention. Patient representatives, advocates, patient advisory groups, patients, service users, and health consumers were the most involved. The main involvement across the studies was in commenting on or developing research materials such as educational and interventional tools, survey instruments, and applications while the least was in identifying research priorities and being a co-applicant on a research project or grant application. Thus, significant effort is still needed to involve patients and the public in the earlier stages of the research process given the fundamental impact of PS on their lives.
Overall completeness and applicability of evidence
A low frequency of reporting PPI in PS research following the GRIPP2 guidelines was revealed in this review, where only five of the 82 studies included mentioned that PPI was reported as per the GRIPP2 checklist. This is despite it being the most recent report-focused framework and the most recommended by several leading journals [ 17 ]. This was not surprising as similar results were reported in recent reviews in other healthcare topics. For instance, Musbahi et al. in their systematic review on PPI reporting in bariatric research reported that none of the 90 papers identified in their review mentioned or utilised the GRIPP2 checklist [ 102 ]. Similarly, a study on PPI in orthodontic research found that none of the 363 included articles reported PPI against the GRIPP2 checklist [ 103 ].
In relation to the quality of reporting following the GRIPP2-SF criteria, our findings show sub-optimal reporting within the 77 studies that did not use GRIPP2 as a guide/checklist to report their PPI. Similarly, Bergin et al. in their systematic review to investigate the nature and impact of PPI in cancer research concluded that substandard reporting was evident [ 12 ]. In our review, this was mainly due to failure to meet three criteria. First, the lowest percentage of reporting (57.1%, n = 44) was related to critical reflection on PPI in the study (i.e., what went well and what did not). In total, 31 studies (42.9%) did not provide any information on this, and two studies were scored as partial. The first study mentioned that only involving one patient was a limitation [ 27 ] and the other stated that including three patients in the design of the tool was a strength [ 83 ]. Both studies did not critically comment or reflect on these points so that future researchers are able to avoid such problems and enhance PPI opportunities. For instance, providing the reasons/challenges behind the exclusive inclusion of a single patient and explaining how this limits the study findings and conclusion would help future researchers to address these challenges. Likewise, commenting on why incorporating three patients in the design of the study tool could be seen as a strength would have been beneficial. This could be, fostering diverse perspectives and generating novel ideas for developing the tool. Similar to our findings, Bergin et al. in their systematic review reported that 40% of the studies failed to meet this criterion [ 12 ].
Second, only 48 out of 77 articles (62.3%) reported the aim of PPI in their study, which is unlike the results of Bergin et al. where most of the studies (93.1%) in their review met this criterion [ 12 ]. Of the 29 studies which did not meet this criterion in our review, few mentioned in their objective developing a consensus-based instrument [ 41 ], reaching a consensus on the patient-reported outcomes [ 32 ], obtaining international consensus on a set of core outcome measures [ 98 ], and facilitating a multi-stakeholder dialogue [ 71 ] yet, without indicating anything in relation to patients, patient representatives, community members, or any other PPI participants. Thus, the lack of reporting the aim of PPI was clearly evident in this review. Reporting the aim of PPI in the study is crucial for promoting transparency, methodological rigor, reproducibility, and impact assessment of the PPI.
Third, 68.8% ( n = 53) of the studies reported the extent to which PPI influenced the study overall including positive and negative effects if any. This was again similar to the findings of Bergin et al., where 38% of the studies did not meet this criterion mainly due to a failure to address PPI challenges in their respective studies [ 12 ]. Additionally, Owyang et al. in their review on the extent, and quality of PPI in orthopaedic practice, also described a poor reporting of PPI impact on research [ 13 ]. As per the GRIPP2 guidelines, both positive and negative effects of PPI on the study should be reported when applicable. Providing such information is essential as it enhances future research on PPI in terms of both practice and reporting.
Reporting a clear description of the methods used for PPI in the study was acceptable, with 79.2% of the papers meeting this criterion. Most studies provided information in the methods section of their papers on the PPI participants, their number, stages of their involvement and how they were involved. Providing clear information on the methods used for PPI is vital to give the reader a clear understanding of the steps taken to involve patients, and for other researchers to replicate these methods in future research. Additionally, reporting the results of PPI in the study was also acceptable with 81.8% of the papers reporting the outcomes of PPI in the results section. Reporting the results of PPI is important for enhancing methodological transparency, providing a more accurate interpretation for the study findings, contributing to the overall accountability and credibility of the research, and informing decision making.
Out of the 82 studies included in this review, only one study provided a plain language summary. We understand that PS research or health and medical research in general is difficult for patients and the public to understand given their diverse health literacy and educational backgrounds. However, if we expect patients and the public to be involved in research then, it is crucial to translate this research that has a huge impact on their lives into an easily accessible format. Failing to translate the benefits that such research may have on patient and public lives may result in them underestimating the value of this research and losing interest in being involved in the planning or implementation of future research [ 103 ]. Thus, providing a plain language summary for research is one way to tackle this problem. To our knowledge, only a few health and social care journals (i.e. Cochrane and BMC Research Involvement and Engagement) necessitate a plain language summary as a submission requirement. Having this as a requirement for submission is crucial in bringing the importance of this issue to researchers’ attention.
Research from recent years suggests that poor PPI reporting in articles relates to a lack of submission requirements for PPI reporting in journals and difficulties with word limits for submitted manuscripts [ 13 ]. Price et al. assessed the frequency of PPI reporting in published papers before and after the introduction of PPI reporting obligations by the British Medical Journal (BMJ) [ 104 ]. The authors identified an increase in PPI reporting in papers published by BMJ from 0.5% to 11% between the periods of 2013–2014 and 2015–2016. The study findings demonstrate the impact of journal guidelines in shaping higher quality research outputs [ 13 ]. In our review, we found a low frequency of PPI reporting in PS research using the GRIPP2 checklist, alongside sub-optimal quality of reporting following GRIPP2-SF. This could potentially be attributed to the absence of submission requirements for PPI reporting in journals following the GRIPP2 checklist, as well as challenges posed by word limits.
Strengths and limitations
This systematic review presents an overview on the frequency of PPI reporting in PS research using the GRIPP2 checklist, as well as an evaluation of the quality of reporting following the GRIPP2-SF. As the first review to focus on PS research, it provides useful knowledge on the status of PPI reporting in this field, and the extent to which researchers are adopting and adhering to PPI reporting guidelines. Despite these strengths, our review has some limitations that should be mentioned. First, only English language papers were included in this review due to being the main language of the researchers. Thus, there is a possibility that relevant articles on PPI in PS research may have been omitted. Another limitation is related to our search which was limited to papers published starting 2018 as the GRIPP2 guidelines were published in 2017. Thus it is probable that the protocols of some of these studies were developed earlier than the publication of the GRIPP2 checklist, meaning that PPI reporting following GRIPP2 was not common practice and thus not adopted by these studies. This might limit the conclusions we can draw from this review. Finally, the use of GRIPP2 to assess the quality of PPI reporting might be a limitation as usability testing has not yet been conducted to understand how the checklist works in practice with various types of research designs. However, the GRIPP2 is the first international, evidence-based, community consensus informed guideline for the reporting of PPI in health and social care research. Reflections and comments from researchers using the GRIPP2 will help improve its use in future studies.
Implications for research and practice
Lack of PPI reporting not only affects the quality of research but also implies that others cannot learn from previous research experience. Additionally, without consistent and transparent reporting it is difficult to evaluate the impact of various PPI in research [ 9 ]: “if it is not reported it cannot be assessed” ([ 105 ] p19). Enhanced PPI reporting will result in a wider range and richer high-quality evidence-based PPI research, leading to a better understanding of PPI use and effectiveness [ 103 ]. GRIPP2 reporting guidelines were developed to provide guidance for researchers, patients, and the public to enhance the quality of PPI reporting and improve the quality of the international PPI evidence-base. The guidance can be used prospectively to plan PPI or retrospectively to guide the structure or PPI reporting in research [ 9 ]. To enhance PPI reporting, we recommend the following;
Publishers and journals
First, we encourage publishers and journals to require researchers to report PPI following the GRIPP2 checklist. Utilising the short or the long version should depend on the primary focus of the study (i.e., if PPI is within the primary focus of the research then the GRIPP2-LF is recommended). Second, we recommend that journals and editorial members advise reviewers to evaluate PPI reporting within research articles following the GRIPP2 tool and make suggestions accordingly. Finally, we encourage journals to add a plain language summary as a submission requirement to increase research dissemination and improve the accessibility of research for patients and the public.
Researchers
Though there is greater evidence of PPI in research, it is still primarily the researchers that are setting the research agenda and deciding on the research questions to be addressed. Thus, significant effort is still needed to involve patients and the public in the earlier stages of the research process given the fundamental impact of PS on their lives. To enhance future PPI reporting, perhaps adding a criterion following the GRIPP2 tool to existing EQUATOR checklists for reporting research papers such as STROBE, PRISMA, CONSORT, may support higher quality research. Additionally, currently, there is no detailed explanation paper for the GRIPP2 where each criterion is explained in detail with examples. Addressing this gap would be of great benefit to guide the structure of PPI reporting and to explore the applicability of each criterion in relation to different stages of PPI in research. For instance, having a detailed explanation for each criterion across different research studies having various PPI stages would be of high value to improve future PPI reporting given the growing interest in PPI research in recent years and the relatively small PPI evidence base in health and medical research.
Funding bodies can also enhance PPI reporting by adding a requirement for researchers to report PPI following the GRIPP2 checklist. In Ireland, the National HSE has already initiated this by requiring all PPI in HSE research in Ireland to be reported following the GRIPP2 guidelines [ 10 ].
This study represents the first systematic review on the frequency and quality of PPI reporting in PS research using the GRIPP2 checklist. Most PS topics were related to medication safety, general PS, and fall prevention. The main involvement across the studies was in commenting on or developing research materials. Thus, efforts are still needed to involve patients and the public across all aspects of the research process, especially earlier stages of the research cycle. The frequency of PPI reporting following the GRIPP2 guidelines was low, and the quality of reporting following the GRIPP2-SF criteria was sub-optimal. The lowest percentages of reporting were on critically reflecting on PPI in the study so future research can learn from this experience and work to improve it, reporting the aim of the PPI in the study, and reporting the extent to which PPI influenced the study overall including positive and negative effects. Researchers, funders, publishers, journals, editorial members and reviewers have a responsibility to promote consistent and transparent PPI reporting following internationally developed reporting guidelines such as the GRIPP2. Evidence-based guidelines for reporting PPI should be supported to help future researchers plan and report PPI more effectively, which may ultimately improve the quality and relevance of research.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its Supplementary information files.
Abbreviations
- Patient safety
United Kingdom
National Institute for Health Research
Public and Patient Involvement
Health Service Executive
Guidance for Reporting Involvement of Patients and the Public
Second version of the GRIPP checklist
Long form of GRIPP2
Short form of GRIPP2
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
The International Database of Prospectively Registered Systematic Reviews
British Medical Journal
Patient saftey: World Health Organisation. 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety . Updated 11 Sept 2023.
Slawomirski L, Klazinga N. The economics of patient safety: from analysis to action. Paris: Organisation for Economic Co-operation and Development; 2020.
Google Scholar
Panagioti M, Khan K, Keers RN, Abuzour A, Phipps D, Kontopantelis E, et al. Prevalence, severity, and nature of preventable patient harm across medical care settings: systematic review and meta-analysis. Bmj-Brit Med J. 2019;366:l4185.
Article Google Scholar
Hodkinson A, Tyler N, Ashcroft DM, Keers RN, Khan K, Phipps D, et al. Preventable medication harm across health care settings: a systematic review and meta-analysis. Bmc Medicine. 2020;18(1):313.
Article PubMed PubMed Central Google Scholar
Park M, Giap TTT. Patient and family engagement as a potential approach for improving patient safety: A systematic review. J Adv Nurs. 2020;76(1):62–80.
Article PubMed Google Scholar
Chegini Z, Janati A, Bababie J, Pouraghaei M. The role of patients in the delivery of safe care in hospital: Study protocol. J Adv Nurs. 2019;75(9):2015–23.
Chegini Z, Arab-Zozani M, Islam SMS, Tobiano G, Rahimi SA. Barriers and facilitators to patient engagement in patient safety from patients and healthcare professionals’ perspectives: A systematic review and meta-synthesis. Nurs Forum. 2021;56(4):938–49.
Going the extra mile: improving the nation’s health and wellbeing through public involvement in research. London: National Institute for Health; 2015.
Staniszewska S, Brett J, Simera I, Seers K, Mockford C, Goodlad S, et al. GRIPP2 reporting checklists: tools to improve reporting of patient and public involvement in research. Bmj-Brit Med J. 2017;358:j3453.
Article CAS Google Scholar
Minogue V. Knowledge translation, dissemination, and impact: a practical guide for researchers. Guide No 8: patient and public involvement in HSE research. Ireland: Health Service Executive Research and Development; 2021.
Staniszewska S, Brett J, Mockford C, Barber R. The GRIPP checklist: Strengthening the quality of patient and public involvement reporting in research. Int J Technol Assess Health Care. 2011;27(4):391–9.
Bergin RJ, Short CE, Davis N, Marker J, Dawson MT, Milton S, et al. The nature and impact of patient and public involvement in cancer prevention, screening and early detection research: A systematic review. Prev Med. 2023;167:107412.
Owyang D, Bakhsh A, Brewer D, Boughton OR, Cobb JP. Patient and public involvement within orthopaedic research a systematic review. J Bone Joint Surg Am. 2021;103(13):e51.
Busch IM, Saxena A, Wu AW. Putting the patient in patient safety investigations: barriers and strategies for involvement. J Patient Saf. 2021;17(5):358–62.
Lee M, Lee NJ, Seo HJ, Jang H, Kim SM. Interventions to engage patients and families in patient safety: a systematic review. West J Nurs Res. 2021;43(10):972–83.
Ocloo J, Garfield S, Franklin BD, Dawson S. Exploring the theory, barriers and enablers for patient and public involvement across health, social care and patient safety: a systematic review of reviews. Health Res Policy Syst. 2021;19(1):8.
Greenhalgh T, Hinton L, Finlay T, Macfarlane A, Fahy N, Clyde B, et al. Frameworks for supporting patient and public involvement in research: Systematic review and co-design pilot. Health Expect. 2019;22(4):785–801.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Plos Medicine. 2021;18(3):372.
INVOLVE. What is public involvement in research? NIHR; 2019. Available from: https://www.invo.org.uk/find-out-more/what-is-public-involvement-in-research-2/ .
Shahid A, Sept B, Kupsch S, Brundin-Mather R, Piskulic D, Soo A, et al. Development and pilot implementation of a patient-oriented discharge summary for critically Ill patients. World J Crit Care Med. 2022;11(4):255–68.
Bisset CN, Dames N, Oliphant R, Alasadi A, Anderson D, Parson S, et al. Exploring shared surgical decision-making from the patient’s perspective: is the personality of the surgeon important? Colorectal Dis. 2020;22(12):2214–21.
Article CAS PubMed Google Scholar
Morris RL, Ruddock A, Gallacher K, Rolfe C, Giles S, Campbell S. Developing a patient safety guide for primary care: A co-design approach involving patients, carers and clinicians. Health Expect. 2021;24(1):42–52.
Tobiano G, Marshall AP, Gardiner T, Jenkinson K, Shapiro M, Ireland M. Development and psychometric testing of the patient participation in bedside handover survey. Health Expect. 2022;25(5):2492–502.
Francis-Coad J, Farlie MK, Haines T, Black L, Weselman T, Cummings P, et al. Revising and evaluating falls prevention education for older adults in hospital. Health Educ J. 2023;82(8):878–91.
Troya MI, Chew-Graham CA, Babatunde O, Bartlam B, Higginbottom A, Dikomitis L. Patient and public involvement and engagement in a doctoral research project exploring self-harm in older adults. Health Expect. 2019;22(4):617–31.
Aharaz A, Kejser CL, Poulsen MW, Jeftic S, Ulstrup-Hansen AI, Jorgensen LM, et al. Optimization of the Danish National Electronic Prescribing System to improve patient safety: Development of a user-friendly prototype of the digital platform shared medication record. Pharmacy (Basel, Switzerland). 2023;11(2):41.
PubMed Google Scholar
Aho-Glele U, Bouabida K, Kooijman A, Popescu IC, Pomey MP, Hawthornthwaite L, et al. Developing the first pan-Canadian survey on patient engagement in patient safety. BMC Health Serv Res. 2021;21(1):1099.
Albutt A, O’Hara J, Conner M, Lawton R. Involving patients in recognising clinical deterioration in hospital using the patient wellness questionnaire: A mixed-methods study. J Res Nurs. 2020;25(1):68–86.
Bell SK, Bourgeois F, DesRoches CM, Dong J, Harcourt K, Liu SK, et al. Filling a gap in safety metrics: development of a patient-centred framework to identify and categorise patient-reported breakdowns related to the diagnostic process in ambulatory care. BMJ Qual Saf. 2022;31(7):526–40.
Boet S, Etherington N, Lam S, Lê M, Proulx L, Britton M, et al. Implementation of the Operating Room Black Box research program at the Ottawa Hospital through patient, clinical, and organizational engagement: Case study. J Med Internet Res. 2021;23(3):e15443.
Carter J, Tribe RM, Shennan AH, Sandall J. Threatened preterm labour: Women’s experiences of risk and care management: A qualitative study. Midwifery. 2018;64:85–92.
Da Silva Lopes AM, Colomer-Lahiguera S, Mederos Alfonso N, Aedo-Lopez V, Spurrier-Bernard G, Tolstrup LK, et al. Patient-reported outcomes for monitoring symptomatic toxicities in cancer patients treated with immune-checkpoint inhibitors: A Delphi study. Eur J Cancer. 2021;157:225–37.
de Jong LD, Lavender AP, Wortham C, Skelton DA, Haines TP, Hill AM. Exploring purpose-designed audio-visual falls prevention messages on older people’s capability and motivation to prevent falls. Health Soc Care Community. 2019;27(4):e471–82.
Doucette L, Kiely BT, Gierisch JM, Marion E, Nadler L, Heflin MT, et al. Participatory research to improve medication reconciliation for older adults in the community. J Am Geriatr Soc. 2023;71(2):620–31.
Elrod CS, Pappa ST, Heyn PC, Wong RA. Using an academic-community partnership model to deliver evidence-based falls prevention programs in a metropolitan setting: A community case study. Front Public Health. 2023;11:1073520.
Feldman E, Pos FJ, Smeenk RJ, van der Poel H, van Leeuwen P, de Feijter JM, et al. Selecting a PRO-CTCAE-based subset for patient-reported symptom monitoring in prostate cancer patients: a modified Delphi procedure. ESMO Open. 2023;8(1):100775.
Article CAS PubMed PubMed Central Google Scholar
Francis-Coad J, Watts T, Bulsara C, Hill A-M. Designing and evaluating falls prevention education with residents and staff in aged care homes: a feasibility study. Health Educ (0965-4283). 2022;122(5):546–63.
Fuller TE, Pong DD, Piniella N, Pardo M, Bessa N, Yoon C, et al. Interactive digital health tools to engage patients and caregivers in discharge preparation: implementation study. J Med Internet Res. 2020;22(4):e15573.
Gibson B, Butler J, Schnock K, Bates D, Classen D. Design of a safety dashboard for patients. Patient Educ Couns. 2020;103(4):741–7.
Giles SJ, Lewis PJ, Phipps DL, Mann F, Avery AJ, Ashcroft DM. Capturing patients’ perspectives on medication safety: the development of a patient-centered medication safety framework. J Patient Saf. 2020;16(4):e324–39.
Gnagi R, Zuniga F, Brunkert T, Meyer-Massetti C. Development of a medication literacy assessment instrument (MELIA) for older people receiving home care. J Adv Nurs. 2022;78(12):4210–20.
Goodsmith N, Zhang L, Ong MK, Ngo VK, Miranda J, Hirsch S, et al. Implementation of a community-partnered research suicide-risk management protocol: case study from community partners in care. Psychiatr Serv (Washington, DC). 2021;72(3):281–7.
Gorman LS, Littlewood DL, Quinlivan L, Monaghan E, Smith J, Barlow S, et al. Family involvement, patient safety and suicide prevention in mental healthcare: ethnographic study. BJPsych open. 2023;9(2):e54.
Green MM, Meyer C, Hutchinson AM, Sutherland F, Lowthian JA. Co‐designing being your best program—a holistic approach to frailty in older community dwelling australians. Health Soc Care Community. 2021;30(5):e2022–32.
Guo X, Wang Y, Wang L, Yang X, Yang W, Lu Z, et al. Effect of a fall prevention strategy for the older patients: A quasi-experimental study. Nurs Open. 2023;10(2):1116–24.
Hahn-Goldberg S, Chaput A, Rosenberg-Yunger Z, Lunsky Y, Okrainec K, Guilcher S, et al. Tool development to improve medication information transfer to patients during transitions of care: A participatory action research and design thinking methodology approach. Res Social Adm Pharm. 2022;18(1):2170–7.
Harrington A, Darke H, Ennis G, Sundram S. Evaluation of an alternative model for the management of clinical risk in an adult acute psychiatric inpatient unit. Int J Ment Health Nurs. 2019;28(5):1099–109.
Harris K, Softeland E, Moi AL, Harthug S, Ravnoy M, Storesund A, et al. Development and validation of patients’ surgical safety checklist. BMC Health Serv Res. 2022;22(1):259.
Hawley-Hague H, Tacconi C, Mellone S, Martinez E, Ford C, Chiari L, et al. Smartphone apps to support falls rehabilitation exercise: app development and usability and acceptability study. JMIR Mhealth Uhealth. 2020;8(9):e15460.
Holmqvist M, Ros A, Lindenfalk B, Thor J, Johansson L. How older persons and health care professionals co-designed a medication plan prototype remotely to promote patient safety: case study. JMIR aging. 2023;6:e41950.
Jayesinghe R, Moriarty F, Khatter A, Durbaba S, Ashworth M, Redmond P. Cost outcomes of potentially inappropriate prescribing in middle-aged adults: A Delphi consensus and cross-sectional study. Br J Clin Pharmacol. 2022;88(7):3404–20.
Johannessen T, Ree E, Stromme T, Aase I, Bal R, Wiig S. Designing and pilot testing of a leadership intervention to improve quality and safety in nursing homes and home care (the SAFE-LEAD intervention). BMJ Open. 2019;9(6):e027790.
Joseph K, Newman B, Manias E, Walpola R, Seale H, Walton M, et al. Engaging with ethnic minority consumers to improve safety in cancer services: A national stakeholder analysis. Patient Educ Couns. 2022;105(8):2778–84.
Khan A, Spector ND, Baird JD, Ashland M, Starmer AJ, Rosenbluth G, et al. Patient safety after implementation of a coproduced family centered communication programme: multicenter before and after intervention study. BMJ. 2018;363:k4764.
Khazen M, Mirica M, Carlile N, Groisser A, Schiff GD. Developing a framework and electronic tool for communicating diagnostic uncertainty in primary care: a qualitative study. JAMA Network Open. 2023;6(3):e232218-e.
Knight SW, Trinkle J, Tschannen D. Hospital-to-homecare videoconference handoff: improved communication, coordination of care, and patient/family engagement. Home Healthc Now. 2019;37(4):198–207.
Lawrence V, Kimona K, Howard RJ, Serfaty MA, Wetherell JL, Livingston G, et al. Optimising the acceptability and feasibility of acceptance and commitment therapy for treatment-resistant generalised anxiety disorder in older adults. Age Ageing. 2019;48(5):741–50.
Louch G, Reynolds C, Moore S, Marsh C, Heyhoe J, Albutt A, et al. Validation of revised patient measures of safety: PMOS-30 and PMOS-10. BMJ Open. 2019;9(11):e031355.
MacDonald T, Jackson S, Charles M-C, Periel M, Jean-Baptiste M-V, Salomon A, et al. The fourth delay and community-driven solutions to reduce maternal mortality in rural Haiti: a community-based action research study. BMC Pregnancy Childbirth. 2018;18(1):254.
Mackintosh N, Sandall J, Collison C, Carter W, Harris J. Employing the arts for knowledge production and translation: Visualizing new possibilities for women speaking up about safety concerns in maternity. Health Expect. 2018;21(3):647–58.
Marchand K, Turuba R, Katan C, Brasset C, Fogarty O, Tallon C, et al. Becoming our young people’s case managers: caregivers’ experiences, needs, and ideas for improving opioid use treatments for young people using opioids. Subst Abuse Treat Prev Policy. 2022;17(1):1–15.
Mazuz K, Biswas S. Co-designing technology and aging in a service setting: Developing an interpretive framework of how to interact with older age users. Gerontechnology. 2022;21(1):1–13.
McCahon D, Duncan P, Payne R, Horwood J. Patient perceptions and experiences of medication review: qualitative study in general practice. BMC Prim Care. 2022;23(1):293.
McMullen S, Panagioti M, Planner C, Giles S, Angelakis I, Keers RN, et al. Supporting carers to improve patient safety and maintain their well-being in transitions from mental health hospitals to the community: A prioritisation nominal group technique. Health Expect. 2023;26(5):2064–74.
Morris RL, Giles S, Campbell S. Involving patients and carers in patient safety in primary care: A qualitative study of a co-designed patient safety guide. Health Expect. 2023;26(2):630–9.
Morris RL, Stocks SJ, Alam R, Taylor S, Rolfe C, Glover SW, et al. Identifying primary care patient safety research priorities in the UK: a James Lind Alliance Priority Setting Partnership. BMJ Open. 2018;8(2):e020870.
Nether KG, Thomas EJ, Khan A, Ottosen MJ, Yager L. Implementing a robust process improvement program in the neonatal intensive care unit to reduce harm. J Healthc Qual. 2022;44(1):23–30.
Powell C, Ismail H, Cleverley R, Taylor A, Breen L, Fylan B, et al. Patients as qualitative data analysts: Developing a method for a process evaluation of the “Improving the Safety and Continuity of Medicines management at care Transitions” (ISCOMAT) cluster randomised control trial. Health Expect. 2021;24(4):1254–62.
Article PubMed Central Google Scholar
Powell C, Ismail H, Davis M, Taylor A, Breen L, Fylan B, et al. Experiences of patients with heart failure with medicines at transition intervention: Findings from the process evaluation of the Improving the Safety and Continuity of Medicines management at Transitions of care (ISCOMAT) programme. Health Expect. 2022;25(5):2503–14.
Radecki B, Keen A, Miller J, McClure JK, Kara A. Innovating fall safety: engaging patients as experts. J Nurs Care Qual. 2020;35(3):220–6.
Rosgen BK, Plotnikoff KM, Krewulak KD, Shahid A, Hernandez L, Sept BG, et al. Co-development of a transitions in care bundle for patient transitions from the intensive care unit: a mixed-methods analysis of a stakeholder consensus meeting. BMC Health Serv Res. 2022;22(1):10.
Schenk EC, Bryant RA, Van Son CR, Odom-Maryon T. Developing an intervention to reduce harm in hospitalized patients: patients and families in research. J Nurs Care Qual. 2019;34(3):273–8.
Spazzapan M, Vijayakumar B, Stewart CE. A bit about me: Bedside boards to create a culture of patient-centered care in pediatric intensive care units (PICUs). J Healthc Risk Manag. 2020;39(3):11–9.
Stoll JA, Ranahan M, Richbart MT, Brennan-Taylor MK, Taylor JS, Brady L, et al. Development of video animations to encourage patient-driven deprescribing: A team alice study. Patient Educ Couns. 2021;104(11):2716–23.
Subbe CP, Tomos H, Jones GM, Barach P. Express check-in: developing a personal health record for patients admitted to hospital with medical emergencies: a mixed-method feasibility study. Int J Qual Health Care. 2021;33(3):121.
Tai D, Li E, Liu-Ambrose T, Bansback N, Sadatsafavi M, Davis JC. Patient-Reported Outcome Measures (PROMs) to support adherence to falls prevention clinic recommendations: a qualitative study. Patient Prefer Adherence. 2020;14:2105–21.
Thakur T, Chewning B, Zetes N, Lee JTY. Involving caregivers in design and assessment of opioid risk and safety communication intervention in children. Patient Educ Couns. 2021;104(10):2432–6.
Thomas J, Dahm MR, Li J, Georgiou A. Can patients contribute to enhancing the safety and effectiveness of test-result follow-up? Qualitative outcomes from a health consumer workshop. Health Expect. 2021;24(2):222–33.
Tremblay MC, Bradette-Laplante M, Witteman HO, Dogba MJ, Breault P, Paquette JS, et al. Providing culturally safe care to indigenous people living with diabetes: Identifying barriers and enablers from different perspectives. Health Expect. 2021;24(2):296–306.
Troya MI, Dikomitis L, Babatunde OO, Bartlam B, Chew-Graham CA. Understanding self-harm in older adults: A qualitative study. EClinicalMedicine. 2019;12:52–61.
Tyler N, Giles S, Daker-White G, McManus BC, Panagioti M. A patient and public involvement workshop using visual art and priority setting to provide patients with a voice to describe quality and safety concerns: Vitamin B12 deficiency and pernicious anaemia. Health Expect. 2021;24(1):87–94.
Tyler N, Planner C, Shears B, Hernan A, Panagioti M, Giles S. Developing the Resident Measure of Safety in Care Homes (RMOS): A Delphi and think aloud study. Health Expect. 2023;26(3):1149–58.
Van den Bulck SA, Vankrunkelsven P, Goderis G, Van Pottelbergh G, Swerts J, Panis K, et al. Developing quality indicators for Chronic Kidney Disease in primary care, extractable from the Electronic Medical Record. A Rand-modified Delphi method. BMC Nephrol. 2020;21(1):161.
Van Strien-Knippenberg IS, Boshuizen MCS, Determann D, de Boer JH, Damman OC. Cocreation with Dutch patients of decision-relevant information to support shared decision-making about adjuvant treatment in breast cancer care. Health Expect. 2022;25(4):1664–77.
Wilson NA, Reich AJ, Graham J, Bhatt DL, Nguyen LL, Weissman JS. Patient perspectives on the need for implanted device information: Implications for a post-procedural communication framework. Health Expect. 2021;24(4):1391–402.
Winterberg AV, Lane B, Hill LM, Varughese AM. Optimizing Pediatric Induction Experiences Using Human-centered Design. J Perianesth Nurs. 2022;37(1):48–52.
Yang R, Donaldson GW, Edelman LS, Cloyes KG, Sanders NA, Pepper GA. Fear of older adult falling questionnaire for caregivers (FOAFQ-CG): Evidence from content validity and item-response theory graded-response modelling. J Adv Nurs. 2020;76(10):2768–80.
Young A, Menon D, Street J, Al-Hertani W, Stafinski T. A checklist for managed access programmes for reimbursement co-designed by Canadian patients and caregivers. Health Expect. 2018;21(6):973–80.
Yuen EYN, Street M, Abdelrazek M, Blencowe P, Etienne G, Liskaser R, et al. Evaluating the efficacy of a digital App to enhance patient-centred nursing handover: A simulation study. J Clin Nurs. 2023;32(19–20):7626–37.
Jo S, Nabatchi T. Coproducing healthcare: individual-level impacts of engaging citizens to develop recommendations for reducing diagnostic error. Public Manag Rev. 2019;21(3):354–75.
O’Hara JK, Reynolds C, Moore S, Armitage G, Sheard L, Marsh C, et al. What can patients tell us about the quality and safety of hospital care? Findings from a UK multicentre survey study. BMJ Qual Saf. 2018;27(9):673–82.
de Jong LD, Francis-Coad J, Wortham C, Haines TP, Skelton DA, Weselman T, et al. Evaluating audio-visual falls prevention messages with community-dwelling older people using a World Cafe forum approach. BMC Geriatrics. 2019;19(1):345.
O’Donnell D, Shé ÉN, McCarthy M, Thornton S, Doran T, Smith F, et al. Enabling public, patient and practitioner involvement in co-designing frailty pathways in the acute care setting. BMC Health Serv Res. 2019;19(1):797.
Russ S, Latif Z, Hazell A, Ogunmuyiwa H, Tapper J, Wachuku-King S, et al. A Smartphone app designed to empower patients to contribute toward safer surgical care: community-based evaluation using a participatory approach. Jmir Mhealth Uhealth. 2020;8(1):e12859.
Mazuz K, Biswas S, Lindner U. Developing self-management application of fall prevention among older adults: a content and usability evaluation. Front Digital Health. 2020;2:11.
Hjelmfors L, Strömberg A, Friedrichsen M, Sandgren A, Mårtensson J, Jaarsma T. Using co-design to develop an intervention to improve communication about the heart failure trajectory and end-of-life care. Bmc Palliat Care. 2018;17:17.
Horgan S, Hegarty J, Andrews E, Hooton C, Drennan J. Impact of a quality improvement intervention on the incidence of surgical site infection in patients undergoing colorectal surgery: Pre-test-post-test design. J Clin Nurs. 2023;32(15–16):4932–46.
Tyler N, Wright N, Grundy A, Waring J. Developing a core outcome set for interventions to improve discharge from mental health inpatient services: a survey, Delphi and consensus meeting with key stakeholder groups. BMJ Open. 2020;10(5):e034215.
Ward ME, De Brún A, Beirne D, Conway C, Cunningham U, English A, et al. Using Co-Design to Develop a Collective Leadership Intervention for Healthcare Teams to Improve Safety Culture. Int J Environ Res Public Health. 2018;15(6):1182.
Berthelsen DB, Simon LS, Ioannidis JPA, Voshaar M, Richards P, Goel N, et al. Stakeholder endorsement advancing the implementation of a patient-reported domain for harms in rheumatology clinical trials: outcome of the OMERACT safety working group. Semin Arthritis Rheum. 2023;63:152288.
Okkenhaug A, Tritter JQ, Landstad BJ. Developing a research tool to detect iatrogenic adverse events in psychiatric health care by involving service users and health professionals. J Psychiatr Ment Health Nurs. 2023;00:1–12.
Musbahi A, Clyde D, Small P, Courtney M, Mahawar K, Lamb PJ, et al. A systematic review of patient and public involvement (PPI) in bariatric research trials: the need for more work. Obes Surg. 2022;32(11):3740–51.
Patel VA, Shelswell J, Hillyard N, Pavitt S, Barber SK. A study of the reporting of patient and public involvement and engagement (PPIE) in orthodontic research. J Orthod. 2021;48(1):42–51.
Price A, Schroter S, Snow R, Hicks M, Harmston R, Staniszewska S, et al. Frequency of reporting on patient and public involvement (PPI) in research studies published in a general medical journal: a descriptive study. BMJ Open. 2018;8:e020452.
Amadea T, Anne-Marie B, Louise L. A researcher’s guide to patient and public involvement. 2017.
Download references
Acknowledgements
This research is funded as part of the Collective Leadership and Safety Cultures (Co-Lead) research programme which is funded by the Irish Health Research Board, grant reference number RL-2015–1588 and the Health Service Executive. The funders had no role in the study conceptualisation, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
UCD Centre for Interdisciplinary Research, Education and Innovation in Health Systems (UCD IRIS), School of Nursing, Midwifery and Health Systems, Health Sciences Centre, University College Dublin, Dublin, Ireland
Sahar Hammoud, Laith Alsabek, Lisa Rogers & Eilish McAuliffe
Department of Oral and Maxillofacial Surgery, University Hospital Galway, Galway, Ireland
Laith Alsabek
You can also search for this author in PubMed Google Scholar
Contributions
S.H and E.M.A designed the study. S.H developed the search strategies with feedback from L.A, L.R, and E.M.A. S.H conducted all searches. S.H and L.A screened the studies, extracted the data, and assessed the quality of PPI reporting. S.H analysed the data with feedback from E.M.A. S.H drafted the manuscript. All authors revised and approved the submitted manuscript. All authors agreed to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Authors’ information
Corresponding author.
Correspondence to Sahar Hammoud .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hammoud, S., Alsabek, L., Rogers, L. et al. Systematic review on the frequency and quality of reporting patient and public involvement in patient safety research. BMC Health Serv Res 24 , 532 (2024). https://doi.org/10.1186/s12913-024-11021-z
Download citation
Received : 10 January 2024
Accepted : 21 April 2024
Published : 26 April 2024
DOI : https://doi.org/10.1186/s12913-024-11021-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient and public involvement
- Patient participation
- Research reporting
- Research involvement
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Strategic Plan: Fiscal Years 2024-2028
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Introduction to the strategic plan, structure of the strategic plan.
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) Strategic Plan: Fiscal Years 2024–2028 describes research goals, themes, and programs that support the NIAAA mission. These goals also support the NIH-Wide Strategic Plan for Diversity, Equity, Inclusion, and Accessibility: Fiscal Years 2023–2027 , as well as complement other National Institutes of Health (NIH) strategic plans and U.S. Department of Health and Human Services initiatives.
Four research goals represent long-standing pillars of NIAAA-supported research. Cross-cutting research themes represent high-priority concepts and emergent research opportunities that cut across the four research goals. Cross-cutting research programs describe coordinated programs with elements that span the four research goals. In addition to conducting and funding research, NIAAA has established capacity and operational priorities toward sustaining robust research capabilities, practicing good scientific stewardship, and strengthening the reach and impact of NIAAA-supported research.
National Institute on Alcohol Abuse and Alcoholism Mission
NIAAA’s mission is to generate and disseminate fundamental knowledge about the adverse effects of alcohol on health and well-being and to apply that knowledge to improve diagnosis, prevention, and treatment of alcohol-related problems, including alcohol use disorder (AUD) , across the life span.
Today, NIAAA is the world’s largest funder of alcohol research. NIAAA provides leadership in the national effort to reduce alcohol-related problems by:
- Conducting and supporting alcohol-related research in a wide range of scientific areas, including neuroscience and behavior, epidemiology and prevention, treatment and recovery, and metabolism and health effects
- Coordinating and collaborating with other research institutes and federal programs on alcohol-related issues
- Collaborating with institutions (including international, national, state, and local), organizations, agencies, and programs engaged in alcohol-related work
- Translating and disseminating research findings to health care providers, researchers, policymakers, and the public
Statutory Authority
As established by the Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act of 1970 , NIAAA’s mission is to “develop and conduct comprehensive health, education, training, research, and planning programs for the prevention and treatment of alcohol abuse and alcoholism.” Visit the History of NIAAA webpage to learn more about NIAAA’s major milestones.
Institute Organization
NIAAA is one of the 27 Institutes and Centers of NIH, a component of HHS. NIH is the foremost federal agency for funding biomedical research in the United States.
NIAAA’s organizational structure includes the Office of the Director , which sets research, programmatic, and institute-wide priorities in collaboration with NIAAA offices and research divisions. NIAAA offices include the Office of Extramural Activities , the Office of Science Policy and Communications , and the Office of Resource Management . NIAAA’s intramural research division, the Division of Intramural Clinical and Biological Research , conducts cutting-edge alcohol research and promotes research training. NIAAA’s four extramural research division—the Division of Epidemiology and Prevention Research , the Division of Metabolism and Health Effects , the Division of Neuroscience and Behavior , and the Division of Treatment and Recovery —develop, plan, and coordinate multidisciplinary research and research training in a wide range of scientific areas essential to NIAAA’s mission.
Strategic Planning Process
NIAAA’s strategic planning process considers the long-term priorities of the field while remaining flexible to adapt to emerging public health needs and scientific opportunities. It also considers a dynamic balance of basic, translational, and clinical research relevant to NIAAA’s broad mission. Although NIAAA engages in formal strategic planning, the institute continually assesses and refines priorities as the science and public health landscape evolves.

To initiate its strategic planning process, NIAAA formed a strategic plan working group comprising staff from the NIAAA Office of Science Policy and Communications in 2020. This group convened meetings with NIAAA leadership and all NIAAA offices and divisions to develop an overall framework for the new strategic plan. Additionally, two listening sessions were held with extramural and intramural staff to provide input on the process and utility of the strategic plan. These sessions were followed by meetings with each NIAAA research division, which was asked to identify research needs and opportunities related to its scientific areas. Their feedback, with input from NIAAA leadership, formed the basis of an outline representing the draft strategic plan framework.
A request for information (RFI) inviting public comment on the draft framework was issued in 2021. RFI responses were received from researchers, advocacy groups, professional societies, and others. The results were summarized in a report to the National Advisory Council on Alcohol Abuse and Alcoholism in September 2021. The outline was refined based on the RFI feedback and Council input and was followed by writing of the strategic plan in consultation with NIAAA leadership, offices, and research divisions.
The final NIAAA Strategic Plan: Fiscal Years 2024–2028 represents a collaborative effort of NIAAA leadership, NIAAA staff across the institute, and the National Advisory Council on Alcohol Abuse and Alcoholism.
Strategic Plan Implementation and Monitoring
Over the next five years, NIAAA will monitor progress on its goals and research priorities. NIAAA’s ability to pursue its research goals and priorities is supported by its commitment to building a robust research capacity and serving as a responsible steward of the public’s investment. This strategic plan is a living document that is responsive to public health challenges as well as to changes in the scientific landscape.
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
In Tight Presidential Race, Voters Are Broadly Critical of Both Biden and Trump
About half of voters say that, if given the chance, they would replace both candidates on the ballot, table of contents.
- The state of the 2024 presidential race
- Other findings: Biden’s job approval ticks up, Trump’s election-related criminal charges
- Educational differences in candidate support
- What are 2020 voters’ preferences today?
- How Biden’s supporters view his personal traits
- How Trump’s supporters view his personal traits
- Views of Biden’s presidency and retrospective evaluations of Trump’s time in office
- Attention to the candidates
- Does it matter who wins?
- What if voters could change the presidential ballot?
- How important is it for the losing candidate to publicly acknowledge the winner?
- 4. Joe Biden’s approval ratings
- Acknowledgments
- The American Trends Panel survey methodology
- Validated voters
Pew Research Center conducted this study to understand voters’ views on the 2024 presidential election, as well how the public views President Joe Biden. For this analysis, we surveyed 8,709 adults – including 7,166 registered voters – from April 8 to April 14, 2024. Everyone who took part in this survey is a member of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Here are the questions used for this report , along with responses, and the survey methodology .
As the 2024 presidential race heats up, American voters face a similar set of choices as they did four years ago – and many are not happy about it.
With the election still more than six months away, a new Pew Research Center survey finds that the presidential race is virtually tied : 49% of registered voters favor Donald Trump or lean toward voting for him, while 48% support or lean toward Joe Biden.
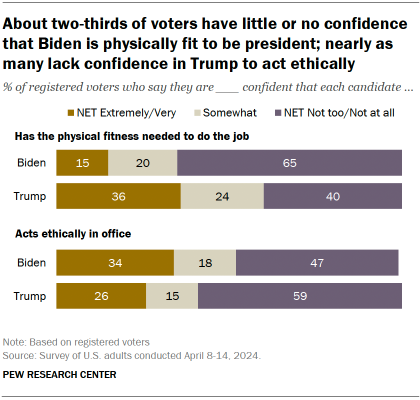
A defining characteristic of the contest is that voters overall have little confidence in either candidate across a range of key traits, including fitness for office, personal ethics and respect for democratic values.
Where Trump has the advantage: More than a third of voters say they are extremely or very confident that Trump has the physical fitness (36%) and mental fitness (38%) needed to do the job of president.
Far fewer say the same of Biden (15% are at least very confident in his physical fitness; 21% are extremely or very confident in his mental fitness). Majorities say they are not too or not at all confident in Biden’s physical and mental fitness.
Where Biden has the advantage: More voters are extremely or very confident in Biden (34%) than in Trump (26%) to act ethically in office. And while 38% say they are at least very confident in Biden to respect the country’s democratic values, fewer (34%) express that level of confidence in Trump. The survey was conducted before the start of Trump’s “hush money” trial in New York City .
( Read more about voters’ views of Biden and Trump in Chapter 2. )
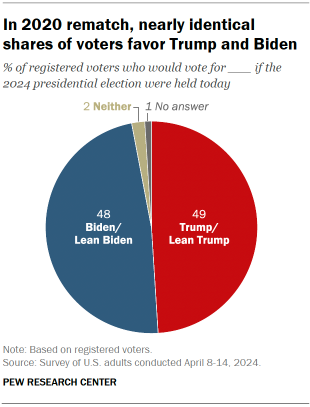
The new Center survey of 8,709 adults – including 7,166 registered voters – conducted April 8-14, 2024, finds large divides in voters’ candidate preference by age, education, and race and ethnicity. As was the case in 2020, younger voters and those with a four-year college degree are more likely to favor Biden than Trump.
Older voters and those with no college degree favor Trump by large margins.
Among racial and ethnic groups:
- White voters favor Trump (56%) over Biden (42%) by a wide margin.
- Roughly three-quarters of Black voters (77%) support Biden, while 18% back Trump.
- Hispanic voters are more evenly divided – 52% favor Biden, while 44% back Trump.
- Asian voters favor Biden (59%) over Trump (36%).
( Read more about voters’ candidate preferences in Chapter 1. )
Most voters who turned out in 2020 favor the same candidate in 2024. Among validated 2020 voters, overwhelming majorities of those who cast ballots for Biden (91%) and Trump (94%) support the same candidate this year. Registered voters who did not vote in 2020 are about evenly divided: 48% back Trump, while 46% support Biden.
A majority of voters say “it really matters who wins” the 2024 race. Today, 69% of voters say it really matters which candidate wins the presidential contest this November. This is somewhat smaller than the share who said this in April 2020 about that year’s election (74%). Nearly identical shares of Biden’s and Trump’s supporters say the outcome of the presidential race really matters.
About half of voters would replace both Biden and Trump on the 2024 ballot
Reflecting their dissatisfaction with the Biden-Trump matchup, nearly half of registered voters (49%) say that, if they had the ability to decide the major party candidates for the 2024 election, they would replace both Biden and Trump on the ballot .
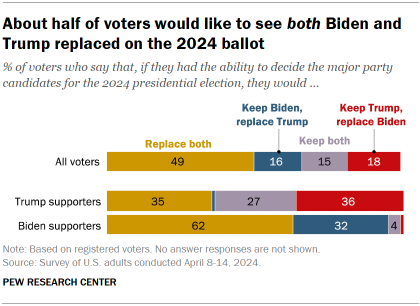
Biden’s supporters are especially likely to say they would replace both candidates if they had the chance. Roughly six-in-ten (62%) express this view, compared with 35% of Trump supporters.
There also are stark age differences in these views: 66% of voters under 30 say they would replace both candidates if they had the chance, compared with 54% of those ages 30 to 49 and fewer than half (43%) of those 50 and older.
( Read more about voters’ feelings toward the upcoming election in Chapter 3. )
Evaluations of the Biden and Trump presidencies
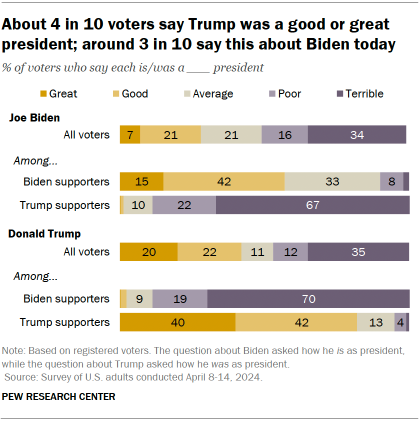
- 42% of voters overall say Trump was a good or great president, while 11% say he was average. This is a modest improvement since March 2021, two months after he left office.
- 28% of voters say Biden is a good or great president, while 21% say he is average. These views are mostly on par with June 2020 assessments of the kind of president Biden would be – but today, a smaller share of voters say he is average.
( Read more about ratings of Biden’s and Trump’s presidencies in Chapter 1. )
- Biden’s approval among the general public: Today, Biden’s approval rating sits at 35% – roughly on par with his rating in January (33%). His job rating has climbed slightly among Democrats over that period, however. Today, 65% of Democrats approve of him – up 4 percentage points since January. ( Read more about Biden’s approval rating in Chapter 4. )
- Conceding the presidential election: A majority of voters say it is important that the losing candidate in November publicly acknowledge the winner as the legitimate president. But Trump’s supporters are far less likely than Biden’s to say it is very important (44% vs. 77%). ( Read more about voters’ views on election concession in Chapter 3. )
Trump’s criminal charges related to the 2020 election
As Trump faces charges that he sought to overturn the outcome of the 2020 election, 45% of Americans say they think Trump’s actions broke the law. This compares with 38% who say his actions did not break the law – including 15% who say his actions were wrong but not illegal, and 23% who say he did nothing wrong. Nearly two-in-ten are not sure.
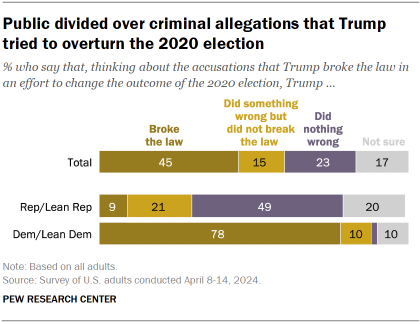
Democrats mostly say Trump broke the law; Republicans are more divided. An overwhelming majority of Democrats and Democratic-leaning independents (78%) say Trump’s actions in seeking to change the outcome of the 2020 election broke the law.
Among Republicans and Republican leaners:
- 49% say Trump did nothing wrong.
- 21% say he did something wrong but did not break the law.
- 9% say Trump broke the law.
- 20% are not sure.
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Donald Trump
- Election 2024
- Partisanship & Issues
- Presidential Approval
- Voter Demographics
- Voter Participation
Voters’ views of Trump and Biden differ sharply by religion
Changing partisan coalitions in a politically divided nation, about 1 in 4 americans have unfavorable views of both biden and trump, 2024 presidential primary season was one of the shortest in the modern political era, americans more upbeat on the economy; biden’s job rating remains very low, most popular, report materials.
- April 2024 Biden Job Approval Detailed Tables
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Age & Generations
- Coronavirus (COVID-19)
- Economy & Work
- Family & Relationships
- Gender & LGBTQ
- Immigration & Migration
- International Affairs
- Internet & Technology
- Methodological Research
- News Habits & Media
- Non-U.S. Governments
- Other Topics
- Politics & Policy
- Race & Ethnicity
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Terms & Conditions
Privacy Policy
Cookie Settings
Reprints, Permissions & Use Policy
The Federal Register
The daily journal of the united states government, request access.
Due to aggressive automated scraping of FederalRegister.gov and eCFR.gov, programmatic access to these sites is limited to access to our extensive developer APIs.
If you are human user receiving this message, we can add your IP address to a set of IPs that can access FederalRegister.gov & eCFR.gov; complete the CAPTCHA (bot test) below and click "Request Access". This process will be necessary for each IP address you wish to access the site from, requests are valid for approximately one quarter (three months) after which the process may need to be repeated.
An official website of the United States government.
If you want to request a wider IP range, first request access for your current IP, and then use the "Site Feedback" button found in the lower left-hand side to make the request.

IMAGES
VIDEO
COMMENTS
Some researchers have even decided to make all of their research findings public in real time by keeping open notebooks [5,6]. In particular, ... Create a dissemination plan. Many funded research projects require a dissemination plan. However, even if not, the formal exercise of creating a plan at the outset that organises dissemination around ...
Principles of good dissemination. Stakeholder engagement: Work out who your primary audience is; engage with them early and keep in touch throughout the project, ideally involving them from the planning of the study to the dissemination of findings. This should create 'pull' for your research i.e. a waiting audience for your outputs.
4. Manage the timeline and resources. Time constraints are an inevitable part of research dissemination. Deadlines for publications can be months apart, conferences may only happen once a year, etc. Any avenue used to disseminate the research must be carefully planned around to avoid missed opportunities.
Research Dissemination; Dissemination Plan Examples; Dissemination Plan Template. Dissemination Plan Template; Guide Background; Dissemination Plan Template. What kinds of research findings do you want to share (data, videos, images, etc.)? Does your research contain sensitive or protected data? Will you need to place conditions or restrictions ...
Introduction. Dissemination refers to the process of sharing research findings with stakeholders and wider audiences. Dissemination is essential for uptake, and uptake and use of research findings is crucial for the success and sustainability of practice-based research networks (PBRNs) in the long term.
Create a Research Dissemination Plan. ... Dissemination Plan Template; Guide Background; Dissemination Plan Examples. The Community Voice: A Photovoice Project Identifying Barriers and Facilitators to Health ... Given the large number of participants, and rich phenotypic data, we are eager to disseminate the data and project findings in an ...
A dissemination plan is a plan for disseminating research findings or products to those who will use the information in practice and is something that you should be thinking about early on. It is what will help you get the message out whether it is results of research or a successful intervention.
Case studies - click for examples of effective dissemination. »Case study 1: Using blogs, podcasts and social media to increase reach. »Case study 2: Making use of press releases and infographics. »Case study 3: BITES and Signals to showcase findings. »Case study 4: New ways of utilising steering groups for dissemination.
dissemination plan. These might seem a bit obvious or laborious but are critical first steps towards strategically planning a project. Define objectives The motivation to disseminate research can come in many forms. You might want to share your findings with wider nonacademic audiences to raise awareness of particular issues or
We define dissemination as a planned process that involves consideration of target audiences and the settings in which research findings are to be received and, where appropriate, communicating and interacting with wider policy and health service audiences in ways that will facilitate research uptake in decision-making processes and practice.
This tool was developed to help researchers evaluate their research and develop appropriate dissemination plans, if the research is determined to have "real world" impact. It is designed to prompt your thinking about the processes that you would use to disseminate your findings or products, beyond publishing and presenting in peer-reviewed venues.
AHRQ is increasingly interested in research that has "real world" impact in the practice of health care. This tool will help you, the Patient Safety Researcher, develop a plan for disseminating your research findings and products to potential users in the health care system. This tool is designed to prompt your thinking about the processes ...
External dissemination of findings via a poster or oral presentation is a vital component of any dissemination plan. When preparing for this mechanism of external dissemination, there are several important considerations. Table 2 lists key questions that should be addressed to aid in identifying the optimal venue for dissemination.
In fact, many. people view the appropriate distribution of research findings as an ethical obligation of researchers and research institutes. Developing a dissemination plan is a step-by-step process that starts with identifying the message and audience. Specific goals and objectives for dissemination must be determined and carefully described ...
Background Addressing deficiencies in the dissemination and transfer of research-based knowledge into routine clinical practice is high on the policy agenda both in the UK and internationally. However, there is lack of clarity between funding agencies as to what represents dissemination. Moreover, the expectations and guidance provided to researchers vary from one agency to another. Against ...
To help guide you as the final products of your research take shape, we will discuss some of the building blocks or elements that you are likely to include as tools in sharing your qualitative findings. These are the elements that will allow you to flesh out the details of your dissemination plan.
Additional Materials Available for Download. The training materials included within each of the above-listed, four focus areas are consolidated and streamlined versions of ten, expert-led, on-line trainings, originally presented live to over 100 hospitals as they worked in real time to implement proven strategies for increasing patient participation in their CR programs.
Treasury FY 2025 Annual Evaluation Plan 3 Overview of Planned FY 2025 Evaluation Projects Title I of the Evidence Act requires that agencies share specific information for selected significant evaluation projects to help anticipate the completion of and plan for the appropriate dissemination of the findings for use in agency decision-making.
The Agency's dissemination framework includes an array of symposium presentations, peer reviewed journal publications, and NASA internal and external council discussions. Agency evaluations that provide promising and effective findings are systematically and broadly disseminated to potential beneficiaries and to federal agency partners.
Research has the potential to influence US social policy; however, existing research in this area lacks a coherent message. The Model for Dissemination of Research provides a framework through which to synthesize lessons learned from research to date on the process of translating research to US policymakers. The peer-reviewed and grey literature was systematically reviewed to understand common ...
Founded in 1920, the NBER is a private, non-profit, non-partisan organization dedicated to conducting economic research and to disseminating research findings among academics, public policy makers, and business professionals.
Background In recent years, patient and public involvement (PPI) in research has significantly increased; however, the reporting of PPI remains poor. The Guidance for Reporting Involvement of Patients and the Public (GRIPP2) was developed to enhance the quality and consistency of PPI reporting. The objective of this systematic review is to identify the frequency and quality of PPI reporting in ...
Structure of the Strategic Plan The National Institute on Alcohol Abuse and Alcoholism (NIAAA) Strategic Plan: Fiscal Years 2024-2028 describes research goals, themes, and programs that support the NIAAA mission. These goals also support the NIH-Wide Strategic Plan for Diversity, Equity, Inclusion, and Accessibility: Fiscal Years 2023-2027, as well as complement other National Institutes ...
Pew Research Center conducted this study to understand voters' views on the 2024 presidential election, as well how the public views President Joe Biden. For this analysis, we surveyed 8,709 adults - including 7,166 registered voters - from April 8 to April 14, 2024. ... Other findings: Biden's job approval ticks up, Trump's election ...
This PDF is the current document as it appeared on Public Inspection on 04/26/2024 at 8:45 am. It was viewed 198 times while on Public Inspection. If you are using public inspection listings for legal research, you should verify the contents of the documents against a final, official edition of the Federal Register.