Fetal Position And Presentation Quiz Questions And Answers

Hey, are you studying maternal and child health nursing concepts? Try these fetal position and presentation quiz questions and answers that we have prepared below and test your knowledge on this topic? This test consists of well-researched and intensive questions and answers that will keep you engaged till the end. You will also get to know your final score by the end of the quiz. So, if you're someone who is studying this subject or have studied it earlier, you should play this quiz and freshen up your memory!
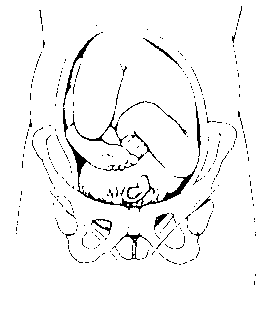

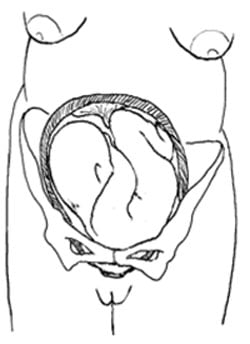
Determine the fetal position presented in the picture above.
Right occipitotransverse
Left occipitotransverse
Right occipitoposterior
Left occipitoposterior
Rate this question:
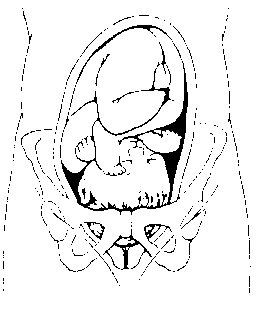
Identify the fetal position presented above.
Left occipitoanterior
Right occipitoanterior
Determine the fetal position above.
Determine the fetal position provided in the picture above.

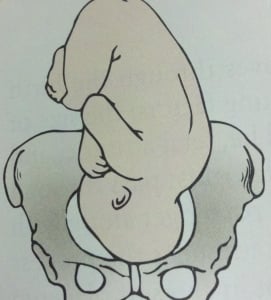
Determine the fetal presentation presented in this picture.
Shoulder presentation
Frank breech
Single footling breech
Compete breech
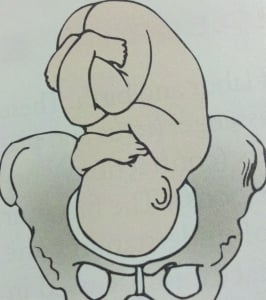
Determine the fetal presentation shown in this image.
Complete breech
Shoulder breech
Determine the fetal presentation presented above by using the Leopold maneuvers.

Determine thefetal position that is presented above.
Single or (double) footling breech
A student nurse is differentiating TRUE labor from FALSE labor to a 39th-week pregnant woman admitted to the labor and delivery department last night. The student nurse needs further teaching if she mentioned which of the following?
"True labor usually begins in your lower back and it may extend to your abdomen"
"There will be thinning or disappearance of the cervix during true labor"
"Ambulation will relieve your abdominal pain when you're in true labor"
"There are no cervical changes in false labor"
What are the prodromal labor signs? Select all that apply.
Braxton Hicks contraction
Left occipital anterior position of the fetus for delivery
Cervical softening
Slight effacement
Bloody show or expulsion of the mucus plug
The nurse practitioner described to the patient that she is 3 cm effacement. The mother was shy to ask questions to the nurse practitioner. When you went to the room and gave her towels, she asked you what effacement means. As an LPN you know that effacement means:
"It is the degree of cervical dilation which is usually 0-10 centimeters "
"it is the thinning or disappearance of the cervix during cervical dilation or labor"
"The nurse practitioner is pertaining to the fetal location in relation to the ischial spine located in your hip bone"
"The nurse practitioner is just hungry at that time, she doesn't know what she's talking about, don't worry about what she said."
What anatomical part of the fetus is the BEST part to hear the fetal heart rate (FHR)?
The back of the fetus
The apical pulse located in the heart
Brachial artery
The popliteal
The patient in labor is hyperventilating with a respiratory rate of 29. You are expecting that the client will have an acid-base imbalance and is in a respiratory alkalosis condition because she is releasing too much carbon dioxide outside her body. As an LPN, you would notice the patient to have which of the following presenting manifestations? Select all that apply.
Productive and persistent coughing
Tingling in the fingers
When should a laboring mother begin to voluntarily push the fetus?
When the cervix is at 10 cm dilation
When the cervix is at 3 cm dilation
When the fetal station is at -2
When the fetal station is engaged
What are the FIVE symptoms of respiratory distress in the newborn? Select all that apply.
Tachycardia
Pallor or dusky color
Flaring of the nares
Chest retraction
Decreased blood pressure
Smiling and crying
What medication should be given to the newly born child to prevent ophthalmia neonatorum from gonorrheal exposure through the birth canal in a vaginal delivery?
Silver nitrate
Butorphanol
What are the CARDINAL MOVEMENTS of the fetus during delivery? Select all that apply.
Internal rotation
Restitution
External rotation
When should we administer a pudendal block?
First stage of labor
Second stage of labor
Third stage of labor
Fourth stage of labor
What are the FIRST signs of regional block effectiveness?
Warmth and tingling sensation of the big toe
Cool and tingling sensation of the big toe
Tingling sensation in the lateral portion of the mouth and slight dizziness
Tingling sensation in the arms and chest pain
The nurse is applying Erythromycin on the newborn to prevent ophthalmia neonatorum. She is aware that to apply this medication correctly to the newborn, she must consider which nursing implication?
Instruct the parents that can wipe the excess medications around the baby's eye after 1 minute
Place a thin line of ointment along the entire lower lid in conjunctival sac
Irrigate the neonate's eye first with normal saline and instill Erythromycin from inner to outer portion of the lower eyelid
Inject the medication in the newborn's eye until it bleeds
When is the appropriate time to give oxytocin to the patient?
After the placenta is delivered
Before the placenta is delivered
Before laboring
If pain does not go away during laboring
What are the normal Puerperium changes relating to the body of the postpartal woman? Select all that apply.
Rugae in the vagina reappears within 3 weeks
Pulse may decrease to 50
The fundus is at the level of the umbilicus after delivery
25,000 WBC count
Palmar erythema declines quickly
Pelvic muscle regain tone in 6 weeks unless diastasis recti
Abdominal muscle regain tone in 3-6 weeks
Bowel movement is expected for 2 to 3 days
Colostrum is expressed first, and then milk
30000 mL/day of urine is normal after delivery because of 40% gain during pregnancy
Chloasma and hyperpigmentation decreases
Coagulation factors postpartally increases
ESR value is elevated for the first 10 days postpartum
Hematocrit decreases because of hemodilution
They are risk for UTI
What is the most common cause of uterine atony in the first 24 hours postpartum?
Decreased lochial flow
Full bladder
Retained placenta
Too late administration of morphine sulfate
What are the objective manifestations of positive maternal-infant bonding? Select all that apply.
Eye contact between mother and infant
Exploration of infant from head to toe
Stroking, kissing, and fondling the neonate
Smiling, talking,singing and kicking the neonate
Use of exclaiming expressions
Naming the newborn as alien's child
Taking out the clothes of the infant and letting the child cry
A postpartum mother feels unexplained tearfulness, feeling down and "not feeling to eat well". As a nurse, your correct response would be:
"I understand how you feel, this is normal especially if you have a bad looking child"
This is called the postpartum blues, they are normal behaviors of the postpartum mother especially 5 days following delivery"
"You don't feel well?, take a walk with your husband in the hallway with the newborn child."
"I completely understand how you feel, let me refer you to a psychiatrist, this signifies that you have dementia."
A woman who just delivered twenty four hours ago with a full term infant sleeps the whole day and needs assistance in doing activities of daily living. The nurse identified this as normal especially during the first 24 to 48 hours postpartum. According to Riva Rubin, what stage of maternal psychological adaptation is the postpartum mother in?
Taking-in stage
Taking-hold stage
Letting-go stage
Let-down stage
What are the interventions necessary for episiotomy wounds? Select all that apply.
Provide good perineal care
Lavage the perineum with several squirts of warm water
Blot dry the perineal area without touching the anal area
Carefully wiping the perineal area from back to front to avoid contamination of the vaginal area
Drink at least 3 liters of fluids (at least 4-6 glasses of water) daily
Quiz Review Timeline +
Our quizzes are rigorously reviewed, monitored and continuously updated by our expert board to maintain accuracy, relevance, and timeliness.
- Current Version
- Aug 22, 2024 Quiz Edited by ProProfs Editorial Team
- May 24, 2012 Quiz Created by Nursejbv21
Related Topics
- Breastfeeding
Recent Quizzes
Featured Quizzes
Popular Topics
- ACLS Quizzes
- AHS Quizzes
- CEN Quizzes
- CMA Quizzes
- CPR Quizzes
- EMT Quizzes
- GPAT Quizzes
- MLT Quizzes
- NBME Quizzes
- NCCT Quizzes
- NCLEX Quizzes
- RMT Quizzes
- USMLE Quizzes

Related Quizzes
Wait! Here's an interesting quiz for you.
Registered Nurse RN
Registered Nurse, Free Care Plans, Free NCLEX Review, Nurse Salary, and much more. Join the nursing revolution.
Fetal Station Maternity Nursing Review
This review will cover fetal station in preparation for maternity nursing exams.
For exams, you want to be familiar with how to interpret fetal station measurements and the meaning of the measurement. In this review you will learn:
- What is fetal station?
- How it’s measured?
- How to identify and interpret fetal station
Fetal Station Lecture for Maternity Nursing
Fetal station review.
Fetal means baby and station means location or position.
Therefore, fetal station is where the baby’s presenting part is located in the pelvis.
What is a presenting part? The presenting part is usually the head, but can be other parts of the baby like the foot etc. In a nutshell, it is whatever part of the baby that is closest to the exit of the uterus, which is the internal os of the cervix. This structure is the “doorway” that allows the baby to leave the uterus.
How is fetal station measured?

- This measurement gives us an idea of how much the baby has descended down into the pelvis. Example: whether the baby is engaged (lightening has occurred…meaning the head or presenting part has entered into the pelvic inlet and is at the ischial spines…meaning fetal station is 0).
- It also helps the healthcare team be prepared for the delivery of the baby.
- It will look at the amount of cm from the top of the ischial spine line and bottom of the ischial spine line. Therefore, we are assessing 5 cm from the top of the ischial spine line to 5 cm below the ischial spine line
- However, fetal station is not referred to in centimeters but as minus or plus numbers.
- If the baby’s presenting part is at 5 cm above the ischial spines…the fetal station would be –5 .
- If the baby’s presenting part is at 2 cm above the ischial spines…the fetal station would be -2 .
- If the baby’s presenting part is at the ischial spines …the fetal station would be 0 . Remember this is referred to as the engagement of the baby and tends to happen around 38 weeks for first time moms, but later for women who’ve had other babies.
- If the baby’s presenting part is at 1 cm below the ischial spines…the fetal station would be +1.
- When fetal station is 4 cm (+4) or 5 cm (+5) baby’s birth is very near so be prepared for delivery.
Test your knowledge: Fetal Station Quiz
References:
Labor and birth | Womenshealth.gov. Retrieved 7 February 2020, from https://www.womenshealth.gov/pregnancy/childbirth-and-beyond/labor-and-birth
Your baby in the birth canal: MedlinePlus Medical Encyclopedia. Retrieved 7 February 2020, from https://medlineplus.gov/ency/article/002060.htm
Please Share:
- Click to print (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to share on Pocket (Opens in new window)
- Click to share on Telegram (Opens in new window)
Disclosure and Privacy Policy
Important links, follow us on social media.
- Facebook Nursing
- Instagram Nursing
- TikTok Nurse
- Twitter Nursing
- YouTube Nursing
Copyright Notice
Recent Lessons
- Show all results for " "

MPN CH 6 Nursing Care of Mother and Infant During
More actions.
- PDF Questions
- Make a copy
Podcast Beta
Questions and answers, which term refers to the process of the cervix opening during labor.
- Dilation (correct)
What is the term used to describe the thick mucus plug that is expelled from the cervix as a sign of impending labor?
- Leopold's maneuver
- Bloody show (correct)
What is the term used to describe the process of the baby's head appearing at the vaginal opening during labor?
- Crowning (correct)
- Acceleration
- Deceleration
What is the term used to describe the rhythmic contractions of the uterus during labor?
<p>Powers</p> Signup and view all the answers
Which fetal presentation is the most common and favorable for a vaginal birth?
<p>Vertex presentation</p> Signup and view all the answers
Which fetal presentation is characterized by the head being fully extended and the face presenting?
<p>Face presentation</p> Signup and view all the answers
Which fetal presentation is characterized by the head being neither flexed nor extended?
<p>Military presentation</p> Signup and view all the answers
Which fetal presentation is characterized by the buttocks presenting at the cervix?
<p>Frank breech</p> Signup and view all the answers
During labor, contractions cause the cervix to efface and dilate. Effacement is determined by a vaginal examination and is described as a percentage of the original cervical length. What is the cervix like when it is 100% effaced?
<p>Thin and slick</p> Signup and view all the answers
What is the average duration of a contraction?
<p>45 to 50 seconds</p> Signup and view all the answers
How is the intensity of a contraction described?
<p>Mild, moderate, or strong</p> Signup and view all the answers
What is the interval in relation to contractions?
<p>The amount of time between contractions</p> Signup and view all the answers
Which part of the pelvis is directly involved in childbirth?
<p>The true pelvis</p> Signup and view all the answers
Which fontanelle is formed by the intersection of four sutures?
<p>The anterior fontanelle</p> Signup and view all the answers
What can reduce or eliminate the natural urge to push during childbirth?
<p>Epidural analgesia</p> Signup and view all the answers
What can excessive anxiety or fear during labor cause?
<p>All of the above</p> Signup and view all the answers
Which of the following birth settings allows the mother and infant to remain in the same room until discharge?
<p>Labor, delivery, recovery, and postpartum room</p> Signup and view all the answers
What is a disadvantage of giving birth at home?
<p>Limited choice of birth attendants</p> Signup and view all the answers
What are the two powers of labor?
<p>Uterine contractions and the mother's pushing efforts</p> Signup and view all the answers
What are some advantages of freestanding birth centers?
<p>Homelike setting for the low-risk woman</p> Signup and view all the answers
Which of the following is a traditional birth practice that may vary depending on cultural background?
<p>Presence of a support person during labor and delivery</p> Signup and view all the answers
What is the term for a vaginal birth after a previous cesarean section?
<p>Trial of labor after cesarean</p> Signup and view all the answers
In which settings can a woman choose to deliver her child?
What is the role of the bedside nurse in the labor and delivery unit.
<p>To protect the privacy and rights of the mother</p> Signup and view all the answers
Which fetal presentation is considered most favorable for normal labor?
<p>ROA</p> Signup and view all the answers
Which presentation is associated with a longer, 'back labor' birth process?
<p>RMP</p> Signup and view all the answers
Which presentation is associated with the occiput facing the posterior section of the woman's pelvis?
Which presentation involves the mentum facing anteriorly on the left side.
<p>LMA</p> Signup and view all the answers
Which presentation involves the sacrum facing posteriorly on the right side?
<p>RSP</p> Signup and view all the answers

Which presentations are not included in the given text because they occur infrequently?
<p>Brow, military, and shoulder presentations</p> Signup and view all the answers
Which of the following birth settings is commonly referred to as a labor, delivery, and recovery (LDR) room?
<p>Hospital birthing room</p> Signup and view all the answers
What is the term used to describe the process of the cervix opening during labor?
<p>Dilation</p> Signup and view all the answers
<p>Contractions</p> Signup and view all the answers
Which term refers to the bluish discoloration of the hands and feet of a newborn shortly after birth?
<p>Acrocyanosis</p> Signup and view all the answers
What is the term used to describe the thinning and shortening of the cervix during labor?
<p>Effacement</p> Signup and view all the answers
What is the term used to describe the process of the baby's head becoming visible at the vaginal opening during labor?
<p>Crowning</p> Signup and view all the answers
What is the term used to describe the stretching and shaping of the baby's head to fit through the birth canal?
<p>Molding</p> Signup and view all the answers
<p>Outlet</p> Signup and view all the answers
<p>Labor</p> Signup and view all the answers
During labor, contractions cause the cervix to efface and dilate. What is effacement?
<p>The cervix becomes thinner and shorter</p> Signup and view all the answers
What is the term used to describe the average time from the beginning of one contraction to the beginning of the next?
<p>Frequency</p> Signup and view all the answers
What is the approximate strength of a mild contraction?
<p>Fundus is easily indented with the fingertips</p> Signup and view all the answers
When the woman's cervix is fully dilated, she adds voluntary pushing to involuntary uterine contractions. What is this stage of labor called?
<p>Stage 2</p> Signup and view all the answers
Which fetal presentation involves the head being fully extended and the face presenting?
Which fetal presentation involves the buttocks presenting at the cervix, which term is used to describe how the head is oriented if the fetus is in a cephalic vertex presentation.
<p>Occiput</p> Signup and view all the answers
Which of the following birth settings is often operated by full-service hospitals and attended by certified nurse-midwives?
<p>Freestanding birth center</p> Signup and view all the answers
What are the two primary powers of labor?
<p>Uterine contractions and maternal pushing efforts</p> Signup and view all the answers
What are some advantages of hospital-based birth settings?
<p>Preregistration, easy access to specialized services, and family-centered care</p> Signup and view all the answers
<p>LSA</p> Signup and view all the answers
<p>VBAC</p> Signup and view all the answers
<p>RSA</p> Signup and view all the answers
<p>Slower progress</p> Signup and view all the answers
<p>Footling breech</p> Signup and view all the answers
<p>Dilate</p> Signup and view all the answers
<p>The outlet</p> Signup and view all the answers
<p>Brow presentation</p> Signup and view all the answers
<p>Right sacrum posterior</p> Signup and view all the answers
<p>Uterine contractions</p> Signup and view all the answers
<p>The process of the cervix thinning</p> Signup and view all the answers
What is the term used to describe the period of increasing strength during a contraction?
<p>Increment</p> Signup and view all the answers
What is the approximate strength of a moderate contraction described as?
<p>Fundus can be indented with the fingertips but with more difficulty; the fundus of the uterus feels similar to the chin</p> Signup and view all the answers
What is the average time from the beginning of one contraction to the beginning of the next called?
<p>Hospital-based birth setting</p> Signup and view all the answers
<p>Low costs due to lack of expensive departments</p> Signup and view all the answers
What are the primary powers of labor?
What are some disadvantages of giving birth at home, which term refers to a test used to determine the ph level of vaginal fluid during pregnancy.
<p>Nitrazine test</p> Signup and view all the answers
What is the term used to describe the condition where the umbilical cord is wrapped around the fetus's neck?
<p>Nuchal cord</p> Signup and view all the answers
What is the term for an infection of the eyes in a newborn, usually caused by exposure to a mother's sexually transmitted infection during delivery?
<p>Ophthalmia neonatorum</p> Signup and view all the answers
What is the term for the condition where the fetal heart rate shows temporary decreases during labor?
<p>Prolonged decelerations</p> Signup and view all the answers
<p>Left mentum anterior</p> Signup and view all the answers
<p>Left occiput anterior</p> Signup and view all the answers
<p>Sacrum</p> Signup and view all the answers
<p>Tachysystole</p> Signup and view all the answers
<p>Breech presentation</p> Signup and view all the answers
<p>Contractions and pushing</p> Signup and view all the answers
How is effacement of the cervix determined?
<p>Through vaginal examination</p> Signup and view all the answers
What is the average dilation for a fully dilated cervix?
<p>10 cm</p> Signup and view all the answers
What is the approximate strength of a firm contraction described as?
<p>Similar to the forehead</p> Signup and view all the answers
What is the term used to describe the bluish discoloration of the hands and feet of a newborn?
What is the term used to describe the rupture of the amniotic sac during labor.
<p>Amniotomy</p> Signup and view all the answers
What is the term used to describe the process of the cervix thinning and shortening during labor?
<p>Efface</p> Signup and view all the answers
Which fetal presentation is characterized by the head being fully flexed and the smallest possible diameter of the head entering the pelvis?
What are the advantages of hospital-based birth settings.
<p>Preregistration, access to specialized personnel, family-centered care</p> Signup and view all the answers
What are the advantages of freestanding birth centers?
<p>Homelike setting, lower costs, certified nurse-midwives</p> Signup and view all the answers
What are the advantages of a home birth?
<p>Control over who is present, low risk of acquiring pathogens, low-technology birth</p> Signup and view all the answers
Which fetal presentation is most favorable for normal labor?
<p>LOA</p> Signup and view all the answers
What is the term for the presentation where the occiput faces the posterior section of the woman's pelvis?
What are the abbreviations for the right occiput transverse and left occiput transverse presentations, respectively.
<p>LOT, RSP</p> Signup and view all the answers
<p>OP</p> Signup and view all the answers
Which term refers to the process of the cervix thinning and shortening during labor?
<p>30 to 45 seconds</p> Signup and view all the answers
<p>Similar to the tip of the nose</p> Signup and view all the answers
What is the most common presentation in childbirth?
What is the term used to describe how the head is oriented if the fetus is in a cephalic vertex presentation.
<p>Right occiput posterior</p> Signup and view all the answers
What is the term used to describe the process of the baby's head changing shape as it passes through the pelvis?
Which fontanelle is formed by the intersection of four sutures and has a diamond shape, what is the most common orientation of the fetus to the mother's spine.
<p>Longitudinal lie</p> Signup and view all the answers
Which of the following birth settings is operated by full-service hospitals and often attended by certified nurse-midwives?
<p>Freestanding birth centers</p> Signup and view all the answers
What is the main advantage of hospital-based birth settings?
<p>Preregistration</p> Signup and view all the answers
Which of the following is a disadvantage of giving birth at home?
Which fetal presentation is associated with a longer, 'back labor' birth process.
<p>OA</p> Signup and view all the answers
True or false: Vertex presentations include LOA, ROA, ROT, and LOT positions.
<p>True</p> Signup and view all the answers
True or false: Face presentations include LMA, RMA, LMP, and RMP positions.
True or false: breech presentations include lsa, rsa, lsp, and rsp positions., true or false: brow, military, and shoulder presentations occur frequently..
<p>False</p> Signup and view all the answers
True or false: The occiput facing the posterior section of the woman's pelvis is associated with a longer, 'back labor' birth process.
True or false: the roa or loa position is most favorable for normal labor., true or false: abbreviations for brow, military, and shoulder presentations are included in the text., true or false: the vertex presentation involves the head being fully extended and the face presenting., true or false: the right occiput transverse and left occiput transverse presentations are not included in the text., true or false: the sacrum facing posteriorly on the right side is associated with a longer, 'back labor' birth process., more like this.

Labor and Birth Process Nursing Management Quiz
Labor and Birth Nursing Interventions
1.1 NURSING CARE DURING LABOR AND BIRTH
2.1 Nursing Management of Pain During Labor and Birth
Share this lesson.
Upgrade to continue
Today's Special Offer
Save an additional 20% with coupon: SAVE20
Upgrade to a paid plan to continue
Trusted by top students and educators worldwide
Please submit any issues or feature requests here. For billing support, please use the Help Center.
Create your free account
By continuing, you agree to Quizgecko's Terms of Service and Privacy Policy .
Appointments at Mayo Clinic
- Pregnancy week by week
- Fetal presentation before birth
The way a baby is positioned in the uterus just before birth can have a big effect on labor and delivery. This positioning is called fetal presentation.
Babies twist, stretch and tumble quite a bit during pregnancy. Before labor starts, however, they usually come to rest in a way that allows them to be delivered through the birth canal headfirst. This position is called cephalic presentation. But there are other ways a baby may settle just before labor begins.
Following are some of the possible ways a baby may be positioned at the end of pregnancy.
Head down, face down
When a baby is head down, face down, the medical term for it is the cephalic occiput anterior position. This the most common position for a baby to be born in. With the face down and turned slightly to the side, the smallest part of the baby's head leads the way through the birth canal. It is the easiest way for a baby to be born.

Head down, face up
When a baby is head down, face up, the medical term for it is the cephalic occiput posterior position. In this position, it might be harder for a baby's head to go under the pubic bone during delivery. That can make labor take longer.
Most babies who begin labor in this position eventually turn to be face down. If that doesn't happen, and the second stage of labor is taking a long time, a member of the health care team may reach through the vagina to help the baby turn. This is called manual rotation.
In some cases, a baby can be born in the head-down, face-up position. Use of forceps or a vacuum device to help with delivery is more common when a baby is in this position than in the head-down, face-down position. In some cases, a C-section delivery may be needed.

Frank breech
When a baby's feet or buttocks are in place to come out first during birth, it's called a breech presentation. This happens in about 3% to 4% of babies close to the time of birth. The baby shown below is in a frank breech presentation. That's when the knees aren't bent, and the feet are close to the baby's head. This is the most common type of breech presentation.
If you are more than 36 weeks into your pregnancy and your baby is in a frank breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Most babies in a frank breech position are born by planned C-section.

Complete and incomplete breech
A complete breech presentation, as shown below, is when the baby has both knees bent and both legs pulled close to the body. In an incomplete breech, one or both of the legs are not pulled close to the body, and one or both of the feet or knees are below the baby's buttocks. If a baby is in either of these positions, you might feel kicking in the lower part of your belly.
If you are more than 36 weeks into your pregnancy and your baby is in a complete or incomplete breech presentation, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. It involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a breech position, talk with a member of your health care team about the choices you have for delivery. Many babies in a complete or incomplete breech position are born by planned C-section.

When a baby is sideways — lying horizontal across the uterus, rather than vertical — it's called a transverse lie. In this position, the baby's back might be:
- Down, with the back facing the birth canal.
- Sideways, with one shoulder pointing toward the birth canal.
- Up, with the hands and feet facing the birth canal.
Although many babies are sideways early in pregnancy, few stay this way when labor begins.
If your baby is in a transverse lie during week 37 of your pregnancy, your health care professional may try to move the baby into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of your health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
If the procedure isn't successful, or if the baby moves back into a transverse lie, talk with a member of your health care team about the choices you have for delivery. Many babies who are in a transverse lie are born by C-section.

If you're pregnant with twins and only the twin that's lower in the uterus is head down, as shown below, your health care provider may first deliver that baby vaginally.
Then, in some cases, your health care team may suggest delivering the second twin in the breech position. Or they may try to move the second twin into a head-down position. This is done using a procedure called external cephalic version. External cephalic version involves one or two members of the health care team putting pressure on your belly with their hands to get the baby to roll into a head-down position.
Your health care team may suggest delivery by C-section for the second twin if:
- An attempt to deliver the baby in the breech position is not successful.
- You do not want to try to have the baby delivered vaginally in the breech position.
- An attempt to move the baby into a head-down position is not successful.
- You do not want to try to move the baby to a head-down position.
In some cases, your health care team may advise that you have both twins delivered by C-section. That might happen if the lower twin is not head down, the second twin has low or high birth weight as compared to the first twin, or if preterm labor starts.

- Landon MB, et al., eds. Normal labor and delivery. In: Gabbe's Obstetrics: Normal and Problem Pregnancies. 8th ed. Elsevier; 2021. https://www.clinicalkey.com. Accessed May 19, 2023.
- Holcroft Argani C, et al. Occiput posterior position. https://www.updtodate.com/contents/search. Accessed May 19, 2023.
- Frequently asked questions: If your baby is breech. American College of Obstetricians and Gynecologists https://www.acog.org/womens-health/faqs/if-your-baby-is-breech. Accessed May 22, 2023.
- Hofmeyr GJ. Overview of breech presentation. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Strauss RA, et al. Transverse fetal lie. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Chasen ST, et al. Twin pregnancy: Labor and delivery. https://www.updtodate.com/contents/search. Accessed May 22, 2023.
- Cohen R, et al. Is vaginal delivery of a breech second twin safe? A comparison between delivery of vertex and non-vertex second twins. The Journal of Maternal-Fetal & Neonatal Medicine. 2021; doi:10.1080/14767058.2021.2005569.
- Marnach ML (expert opinion). Mayo Clinic. May 31, 2023.
Products and Services
- A Book: Mayo Clinic Guide to a Healthy Pregnancy
- 3rd trimester pregnancy
- Fetal development: The 3rd trimester
- Overdue pregnancy
- Pregnancy due date calculator
- Prenatal care: Third trimester
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- NEW: Listen to Health Matters Podcast - Mayo Clinic Press NEW: Listen to Health Matters Podcast
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Fetal position and presentation — Printable Worksheet
Download and print this quiz as a worksheet.
You can move the markers directly in the worksheet.
Page 1 of 2
This is a printable worksheet made from a PurposeGames Quiz.
To play the game online, visit Fetal position and presentation
Download Printable Worksheet
Please note! You can modify the printable worksheet to your liking before downloading.
About this Worksheet
This is a free printable worksheet in PDF format and holds a printable version of the quiz Fetal position and presentation . By printing out this quiz and taking it with pen and paper creates for a good variation to only playing it online.
Other Quizzes Available as Worksheets

Worksheet Settings
Before you print this worksheet you can modify it to your liking using the settings below.
Marker Options
Note! You can move markers around in the worksheet, should they be overlapping.
Save Settings Settings Saved!
Worksheet Stats
Play it online.
If you are looking for the online quiz that this printable worksheet is based on, visit Fetal position and presentation .

IMAGES
VIDEO
COMMENTS
Fetal Position And Presentation Quiz Questions And Answers . Approved & Edited by ProProfs Editorial Team. The editorial team at ProProfs Quizzes consists of a select group of subject experts, trivia writers, and quiz masters who have authored over 10,000 quizzes taken by more than 100 million users. This team includes our in-house seasoned ...
Test your knowledge of fetal station, a maternity nursing concept that measures the baby's presenting part in the pelvis. Take a quiz with six questions and answers, and learn how to interpret fetal station for labor and delivery.
Study with Quizlet and memorize flashcards containing terms like LOA, LOT, LOP and more.
This online quiz is called Fetal Position and Presentation. It was created by member Kathryn Montgomery and has 15 questions.
Study with Quizlet and memorize flashcards containing terms like describe fetal presentation, Mentum Anterior, Mentum Posterior and more. ... Test #1 OBGYN . 178 terms. maddiemeyer01. Preview. module 33 reproduction- exam 1 concept/ antepartum/ intrapartum. 58 terms. Garcal22. Preview. idk . 12 terms. alue15. Preview. Fetal Circulation.
Diagnostic Ultrasound Fetal presentation Learn with flashcards, games, and more — for free.
Fetal positions — Quiz Information. This is an online quiz called Fetal positions . You can use it as Fetal positions practice, completely free to play. ... Fetal Position and Presentation. by Kathryn Montgomery. 175 plays. 15p Image Quiz. Fetal positions . by Kathryn Montgomery. 525 plays. 8p Image Quiz.
This online quiz is called Fetal position and presentation. It was created by member Jane Yao and has 13 questions.
This quiz covers key concepts related to fetal presentation, positioning, and the challenges of dystocia during labor. Understand the alignment of fetal lie, the significance of fetal presentation types, and the contributing factors to labor difficulties. Explore how the four P's—Powers, Passenger, Passage, and Psyche—impact the labor process.
Quiz yourself with questions and answers for fetal chest and presentation quiz , so you can be ready for test day. Explore quizzes and practice tests created by teachers and students or create one from your course material.
Learn how to measure and interpret fetal station, the location of the baby's presenting part in the pelvis, for maternity nursing exams. Fetal station is measured in minus or plus numbers from the ischial spines and indicates how much the baby has descended into the pelvis.
Identification of fetal positions done through assessment of the face and breech presentations. In breech presentations, both buttocks can be palpated, and potential staining with meconium indicates passage through the anus. Factors Favoring Cesarean Delivery for Breech Fetuses. Lack of operator experience with vaginal delivery of breech.
Test your knowledge on fetal attitude and presentation with this quiz. Learn about the normal fetal attitude of flexion and its implications during labor, as well as the concept of presentation and the different fetal parts that enter the pelvis first.
Study with Quizlet and memorize flashcards containing terms like The fetus has both a _____ and a _____, Presentation refers to, Presentation is also referred to as and more.
This is a printable worksheet called Fetal Position and Presentation and was based on a quiz created by member Kathryn Montgomery. ... This is a printable worksheet made from a PurposeGames Quiz. To play the game online, visit ...
Learn about the different ways your baby can be situated in your womb at birth, such as head-down, breech, posterior, transverse, and oblique. Find out how fetal presentation and position can affect your labor and delivery, and what interventions may be needed.
Study with Quizlet and memorize flashcards containing terms like Fetal Position, Fetal Position: 1st Letter, Fetal Position: 2nd Letter and more. ... nursing test unfinished. 10 terms. britt3596. Preview. MS exam 4. 25 terms. anib0404. Preview. CBN EXAM 2. 86 terms. geen_rocks. ... which indicate the land mark of the fetal presentation. Fetal ...
Learn about the different ways a baby may be positioned in the uterus just before birth, such as cephalic, breech, transverse and oblique. Find out how fetal presentation can affect labor and delivery, and what options you have if your baby is in a non-cephalic position.
This is a printable worksheet called Fetal position and presentation and was based on a quiz created by member Jane Yao. ... This is a free printable worksheet in PDF format and holds a printable version of the quiz Fetal position and presentation. By printing out this quiz and taking it with pen and paper creates for a good variation to only ...
Study with Quizlet and memorize flashcards containing terms like fetal attitude, fetal lie, fetal presentation and more. ... Quiz ICD-10-CM Chapter 15 Pregnancy, Childbirth and the Puerperium (O00-O9A) 9 terms. leeharp92. Preview. PSYCH 2.5, 2.6 PART 2 Childbirth and Newborn. 10 terms.