

ORAL CASE PRESENTATION
Oct 15, 2017 | Clinical Teaching
- Oral case presentations are the fundamental way in which we communicate in medicine. To do this effectively, the content should be organized, clear, succinct, and with sufficient repetition to ensure understanding.
- Experts build OCPs by first considering the diagnoses they have in mind, then distilling the narrative in a way that implicitly highlights information relevant to the diagnoses under consideration.
- OCPs follow the same organization as a written H&P, and effective transition sentences ensure that listeners remain oriented to each relevant section.
- The OCP assessment is an opportunity to highlight important findings, using repetition to ensure understanding among listeners.
Additional Resources
- Oral Case Presentation (PDF)
Recent Posts
- Virtual Simulation in Medical Education
- CLIME Conversation Café Recording: The Jazz of Educational Design: Maximizing the Power of the Arts in Medical Education
- 2024 CALL FOR SMALL GRANT PROPOSALS
- CLIME Conversation Café Recording: The Power of Film in Medical Education
- CLIME Conversation Café Recording: Ethics in Medicine
How to make an oral case presentation to healthcare colleagues
The content and delivery of a patient case for education and evidence-based care discussions in clinical practice.

BSIP SA / Alamy Stock Photo
A case presentation is a detailed narrative describing a specific problem experienced by one or more patients. Pharmacists usually focus on the medicines aspect , for example, where there is potential harm to a patient or proven benefit to the patient from medication, or where a medication error has occurred. Case presentations can be used as a pedagogical tool, as a method of appraising the presenter’s knowledge and as an opportunity for presenters to reflect on their clinical practice [1] .
The aim of an oral presentation is to disseminate information about a patient for the purpose of education, to update other members of the healthcare team on a patient’s progress, and to ensure the best, evidence-based care is being considered for their management.
Within a hospital, pharmacists are likely to present patients on a teaching or daily ward round or to a senior pharmacist or colleague for the purpose of asking advice on, for example, treatment options or complex drug-drug interactions, or for referral.
Content of a case presentation
As a general structure, an oral case presentation may be divided into three phases [2] :
- Reporting important patient information and clinical data;
- Analysing and synthesising identified issues (this is likely to include producing a list of these issues, generally termed a problem list);
- Managing the case by developing a therapeutic plan.

Specifically, the following information should be included [3] :
Patient and complaint details
Patient details: name, sex, age, ethnicity.
Presenting complaint: the reason the patient presented to the hospital (symptom/event).
History of presenting complaint: highlighting relevant events in chronological order, often presented as how many days ago they occurred. This should include prior admission to hospital for the same complaint.
Review of organ systems: listing positive or negative findings found from the doctor’s assessment that are relevant to the presenting complaint.
Past medical and surgical history
Social history: including occupation, exposures, smoking and alcohol history, and any recreational drug use.
Medication history, including any drug allergies: this should include any prescribed medicines, medicines purchased over-the-counter, any topical preparations used (including eye drops, nose drops, inhalers and nasal sprays) and any herbal or traditional remedies taken.
Sexual history: if this is relevant to the presenting complaint.
Details from a physical examination: this includes any relevant findings to the presenting complaint and should include relevant observations.
Laboratory investigation and imaging results: abnormal findings are presented.
Assessment: including differential diagnosis.
Plan: including any pharmaceutical care issues raised and how these should be resolved, ongoing management and discharge planning.
Any discrepancies between the current management of the patient’s conditions and evidence-based recommendations should be highlighted and reasons given for not adhering to evidence-based medicine ( see ‘Locating the evidence’ ).
Locating the evidence
The evidence base for the therapeutic options available should always be considered. There may be local guidance available within the hospital trust directing the management of the patient’s presenting condition. Pharmacists often contribute to the development of such guidelines, especially if medication is involved. If no local guidelines are available, the next step is to refer to national guidance. This is developed by a steering group of experts, for example, the British HIV Association or the National Institute for Health and Care Excellence . If the presenting condition is unusual or rare, for example, acute porphyria, and there are no local or national guidelines available, a literature search may help locate articles or case studies similar to the case.
Giving a case presentation
Currently, there are no available acknowledged guidelines or systematic descriptions of the structure, language and function of the oral case presentation [4] and therefore there is no standard on how the skills required to prepare or present a case are taught. Most individuals are introduced to this concept at undergraduate level and then build on their skills through practice-based learning.
A case presentation is a narrative of a patient’s care, so it is vital the presenter has familiarity with the patient, the case and its progression. The preparation for the presentation will depend on what information is to be included.
Generally, oral case presentations are brief and should be limited to 5–10 minutes. This may be extended if the case is being presented as part of an assessment compared with routine everyday working ( see ‘Case-based discussion’ ). The audience should be interested in what is being said so the presenter should maintain this engagement through eye contact, clear speech and enthusiasm for the case.
It is important to stick to the facts by presenting the case as a factual timeline and not describing how things should have happened instead. Importantly, the case should always be concluded and should include an outcome of the patient’s care [5] .
An example of an oral case presentation, given by a pharmacist to a doctor, is available here .
A successful oral case presentation allows the audience to garner the right amount of patient information in the most efficient way, enabling a clinically appropriate plan to be developed. The challenge lies with the fact that the content and delivery of this will vary depending on the service, and clinical and audience setting [3] . A practitioner with less experience may find understanding the balance between sufficient information and efficiency of communication difficult, but regular use of the oral case presentation tool will improve this skill.
Tailoring case presentations to your audience
Most case presentations are not tailored to a specific audience because the same type of information will usually need to be conveyed in each case.
However, case presentations can be adapted to meet the identified learning needs of the target audience, if required for training purposes. This method involves varying the content of the presentation or choosing specific cases to present that will help achieve a set of objectives [6] . For example, if a requirement to learn about the management of acute myocardial infarction has been identified by the target audience, then the presenter may identify a case from the cardiology ward to present to the group, as opposed to presenting a patient reviewed by that person during their normal working practice.
Alternatively, a presenter could focus on a particular condition within a case, which will dictate what information is included. For example, if a case on asthma is being presented, the focus may be on recent use of bronchodilator therapy, respiratory function tests (including peak expiratory flow rate), symptoms related to exacerbation of airways disease, anxiety levels, ability to talk in full sentences, triggers to worsening of symptoms, and recent exposure to allergens. These may not be considered relevant if presenting the case on an unrelated condition that the same patient has, for example, if this patient was admitted with a hip fracture and their asthma was well controlled.
Case-based discussion
The oral case presentation may also act as the basis of workplace-based assessment in the form of a case-based discussion. In the UK, this forms part of many healthcare professional bodies’ assessment of clinical practice, for example, medical professional colleges.
For pharmacists, a case-based discussion forms part of the Royal Pharmaceutical Society (RPS) Foundation and Advanced Practice assessments . Mastery of the oral case presentation skill could provide useful preparation for this assessment process.
A case-based discussion would include a pharmaceutical needs assessment, which involves identifying and prioritising pharmaceutical problems for a particular patient. Evidence-based guidelines relevant to the specific medical condition should be used to make treatment recommendations, and a plan to monitor the patient once therapy has started should be developed. Professionalism is an important aspect of case-based discussion — issues must be prioritised appropriately and ethical and legal frameworks must be referred to [7] . A case-based discussion would include broadly similar content to the oral case presentation, but would involve further questioning of the presenter by the assessor to determine the extent of the presenter’s knowledge of the specific case, condition and therapeutic strategies. The criteria used for assessment would depend on the level of practice of the presenter but, for pharmacists, this may include assessment against the RPS Foundation or Pharmacy Frameworks .
Acknowledgement
With thanks to Aamer Safdar for providing the script for the audio case presentation.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal . You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
[1] Onishi H. The role of case presentation for teaching and learning activities. Kaohsiung J Med Sci 2008;24:356–360. doi: 10.1016/s1607-551x(08)70132–3
[2] Edwards JC, Brannan JR, Burgess L et al . Case presentation format and clinical reasoning: a strategy for teaching medical students. Medical Teacher 1987;9:285–292. doi: 10.3109/01421598709034790
[3] Goldberg C. A practical guide to clinical medicine: overview and general information about oral presentation. 2009. University of California, San Diego. Available from: https://meded.ecsd.edu/clinicalmed.oral.htm (accessed 5 December 2015)
[4] Chan MY. The oral case presentation: toward a performance-based rhetorical model for teaching and learning. Medical Education Online 2015;20. doi: 10.3402/meo.v20.28565
[5] McGee S. Medicine student programs: oral presentation guidelines. Learning & Scholarly Technologies, University of Washington. Available from: https://catalyst.uw.edu/workspace/medsp/30311/202905 (accessed 7 December 2015)
[6] Hays R. Teaching and Learning in Clinical Settings. 2006;425. Oxford: Radcliffe Publishing Ltd.
[7] Royal Pharmaceutical Society. Tips for assessors for completing case-based discussions. 2015. Available from: http://www.rpharms.com/help/case_based_discussion.htm (accessed 30 December 2015)
You might also be interested in…

How to demonstrate empathy and compassion in a pharmacy setting

Be more proactive to convince medics, pharmacists urged

How pharmacists can encourage patient adherence to medicines
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- How to present patient...
How to present patient cases
- Related content
- Peer review
- Mary Ni Lochlainn , foundation year 2 doctor 1 ,
- Ibrahim Balogun , healthcare of older people/stroke medicine consultant 1
- 1 East Kent Foundation Trust, UK
A guide on how to structure a case presentation
This article contains...
-History of presenting problem
-Medical and surgical history
-Drugs, including allergies to drugs
-Family history
-Social history
-Review of systems
-Findings on examination, including vital signs and observations
-Differential diagnosis/impression
-Investigations
-Management
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1
The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the patient’s condition and further management can be planned accordingly. 2 To give a high quality presentation you need to take a thorough history. Consultants make decisions about patient care based on information presented to them by junior members of the team, so the importance of accurately presenting your patient cannot be overemphasised.
As a medical student, you are likely to be asked to present in numerous settings. A formal case presentation may take place at a teaching session or even at a conference or scientific meeting. These presentations are usually thorough and have an accompanying PowerPoint presentation or poster. More often, case presentations take place on the wards or over the phone and tend to be brief, using only memory or short, handwritten notes as an aid.
Everyone has their own presenting style, and the context of the presentation will determine how much detail you need to put in. You should anticipate what information your senior colleagues will need to know about the patient’s history and the care he or she has received since admission, to enable them to make further management decisions. In this article, I use a fictitious case to show how you can structure case presentations, which can be adapted to different clinical and teaching settings (box 1).
Box 1: Structure for presenting patient cases
Presenting problem, history of presenting problem, medical and surgical history.
Drugs, including allergies to drugs
Family history
Social history, review of systems.
Findings on examination, including vital signs and observations
Differential diagnosis/impression
Investigations
Case: tom murphy.
You should start with a sentence that includes the patient’s name, sex (Mr/Ms), age, and presenting symptoms. In your presentation, you may want to include the patient’s main diagnosis if known—for example, “admitted with shortness of breath on a background of COPD [chronic obstructive pulmonary disease].” You should include any additional information that might give the presentation of symptoms further context, such as the patient’s profession, ethnic origin, recent travel, or chronic conditions.
“ Mr Tom Murphy is a 56 year old ex-smoker admitted with sudden onset central crushing chest pain that radiated down his left arm.”
In this section you should expand on the presenting problem. Use the SOCRATES mnemonic to help describe the pain (see box 2). If the patient has multiple problems, describe each in turn, covering one system at a time.
Box 2: SOCRATES—mnemonic for pain
Associations
Time course
Exacerbating/relieving factors
“ The pain started suddenly at 1 pm, when Mr Murphy was at his desk. The pain was dull in nature, and radiated down his left arm. He experienced shortness of breath and felt sweaty and clammy. His colleague phoned an ambulance. He rated the pain 9/10 in severity. In the ambulance he was given GTN [glyceryl trinitrate] spray under the tongue, which relieved the pain to 5/10. The pain lasted 30 minutes in total. No exacerbating factors were noted. Of note: Mr Murphy is an ex-smoker with a 20 pack year history”
Some patients have multiple comorbidities, and the most life threatening conditions should be mentioned first. They can also be categorised by organ system—for example, “has a long history of cardiovascular disease, having had a stroke, two TIAs [transient ischaemic attacks], and previous ACS [acute coronary syndrome].” For some conditions it can be worth stating whether a general practitioner or a specialist manages it, as this gives an indication of its severity.
In a surgical case, colleagues will be interested in exercise tolerance and any comorbidity that could affect the patient’s fitness for surgery and anaesthesia. If the patient has had any previous surgical procedures, mention whether there were any complications or reactions to anaesthesia.
“Mr Murphy has a history of type 2 diabetes, well controlled on metformin. He also has hypertension, managed with ramipril, and gout. Of note: he has no history of ischaemic heart disease (relevant negative) (see box 3).”
Box 3: Relevant negatives
Mention any relevant negatives that will help narrow down the differential diagnosis or could be important in the management of the patient, 3 such as any risk factors you know for the condition and any associations that you are aware of. For example, if the differential diagnosis includes a condition that you know can be hereditary, a relevant negative could be the lack of a family history. If the differential diagnosis includes cardiovascular disease, mention the cardiovascular risk factors such as body mass index, smoking, and high cholesterol.
Highlight any recent changes to the patient’s drugs because these could be a factor in the presenting problem. Mention any allergies to drugs or the patient’s non-compliance to a previously prescribed drug regimen.
To link the medical history and the drugs you might comment on them together, either here or in the medical history. “Mrs Walsh’s drugs include regular azathioprine for her rheumatoid arthritis.”Or, “His regular drugs are ramipril 5 mg once a day, metformin 1g three times a day, and allopurinol 200 mg once a day. He has no known drug allergies.”
If the family history is unrelated to the presenting problem, it is sufficient to say “no relevant family history noted.” For hereditary conditions more detail is needed.
“ Mr Murphy’s father experienced a fatal myocardial infarction aged 50.”
Social history should include the patient’s occupation; their smoking, alcohol, and illicit drug status; who they live with; their relationship status; and their sexual history, baseline mobility, and travel history. In an older patient, more detail is usually required, including whether or not they have carers, how often the carers help, and if they need to use walking aids.
“He works as an accountant and is an ex-smoker since five years ago with a 20 pack year history. He drinks about 14 units of alcohol a week. He denies any illicit drug use. He lives with his wife in a two storey house and is independent in all activities of daily living.”
Do not dwell on this section. If something comes up that is relevant to the presenting problem, it should be mentioned in the history of the presenting problem rather than here.
“Systems review showed long standing occasional lower back pain, responsive to paracetamol.”
Findings on examination
Initially, it can be useful to practise presenting the full examination to make sure you don’t leave anything out, but it is rare that you would need to present all the normal findings. Instead, focus on the most important main findings and any abnormalities.
“On examination the patient was comfortable at rest, heart sounds one and two were heard with no additional murmurs, heaves, or thrills. Jugular venous pressure was not raised. No peripheral oedema was noted and calves were soft and non-tender. Chest was clear on auscultation. Abdomen was soft and non-tender and normal bowel sounds were heard. GCS [Glasgow coma scale] was 15, pupils were equal and reactive to light [PEARL], cranial nerves 1-12 were intact, and he was moving all four limbs. Observations showed an early warning score of 1 for a tachycardia of 105 beats/ min. Blood pressure was 150/90 mm Hg, respiratory rate 18 breaths/min, saturations were 98% on room air, and he was apyrexial with a temperature of 36.8 ºC.”
Differential diagnoses
Mentioning one or two of the most likely diagnoses is sufficient. A useful phrase you can use is, “I would like to rule out,” especially when you suspect a more serious cause is in the differential diagnosis. “History and examination were in keeping with diverticular disease; however, I would like to rule out colorectal cancer in this patient.”
Remember common things are common, so try not to mention rare conditions first. Sometimes it is acceptable to report investigations you would do first, and then base your differential diagnosis on what the history and investigation findings tell you.
“My impression is acute coronary syndrome. The differential diagnosis includes other cardiovascular causes such as acute pericarditis, myocarditis, aortic stenosis, aortic dissection, and pulmonary embolism. Possible respiratory causes include pneumonia or pneumothorax. Gastrointestinal causes include oesophageal spasm, oesophagitis, gastro-oesophageal reflux disease, gastritis, cholecystitis, and acute pancreatitis. I would also consider a musculoskeletal cause for the pain.”
This section can include a summary of the investigations already performed and further investigations that you would like to request. “On the basis of these differentials, I would like to carry out the following investigations: 12 lead electrocardiography and blood tests, including full blood count, urea and electrolytes, clotting screen, troponin levels, lipid profile, and glycated haemoglobin levels. I would also book a chest radiograph and check the patient’s point of care blood glucose level.”
You should consider recommending investigations in a structured way, prioritising them by how long they take to perform and how easy it is to get them done and how long it takes for the results to come back. Put the quickest and easiest first: so bedside tests, electrocardiography, followed by blood tests, plain radiology, then special tests. You should always be able to explain why you would like to request a test. Mention the patient’s baseline test values if they are available, especially if the patient has a chronic condition—for example, give the patient’s creatinine levels if he or she has chronic kidney disease This shows the change over time and indicates the severity of the patient’s current condition.
“To further investigate these differentials, 12 lead electrocardiography was carried out, which showed ST segment depression in the anterior leads. Results of laboratory tests showed an initial troponin level of 85 µg/L, which increased to 1250 µg/L when repeated at six hours. Blood test results showed raised total cholesterol at 7.6 mmol /L and nil else. A chest radiograph showed clear lung fields. Blood glucose level was 6.3 mmol/L; a glycated haemoglobin test result is pending.”
Dependent on the case, you may need to describe the management plan so far or what further management you would recommend.“My management plan for this patient includes ACS [acute coronary syndrome] protocol, echocardiography, cardiology review, and treatment with high dose statins. If you are unsure what the management should be, you should say that you would discuss further with senior colleagues and the patient. At this point, check to see if there is a treatment escalation plan or a “do not attempt to resuscitate” order in place.
“Mr Murphy was given ACS protocol in the emergency department. An echocardiogram has been requested and he has been discussed with cardiology, who are going to come and see him. He has also been started on atorvastatin 80 mg nightly. Mr Murphy and his family are happy with this plan.”
The summary can be a concise recap of what you have presented beforehand or it can sometimes form a standalone presentation. Pick out salient points, such as positive findings—but also draw conclusions from what you highlight. Finish with a brief synopsis of the current situation (“currently pain free”) and next step (“awaiting cardiology review”). Do not trail off at the end, and state the diagnosis if you are confident you know what it is. If you are not sure what the diagnosis is then communicate this uncertainty and do not pretend to be more confident than you are. When possible, you should include the patient’s thoughts about the diagnosis, how they are feeling generally, and if they are happy with the management plan.
“In summary, Mr Murphy is a 56 year old man admitted with central crushing chest pain, radiating down his left arm, of 30 minutes’ duration. His cardiac risk factors include 20 pack year smoking history, positive family history, type 2 diabetes, and hypertension. Examination was normal other than tachycardia. However, 12 lead electrocardiography showed ST segment depression in the anterior leads and troponin rise from 85 to 250 µg/L. Acute coronary syndrome protocol was initiated and a diagnosis of NSTEMI [non-ST elevation myocardial infarction] was made. Mr Murphy is currently pain free and awaiting cardiology review.”
Originally published as: Student BMJ 2017;25:i4406
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed
- ↵ Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med 2009 ; 24 : 370 - 3 . doi:10.1007/s11606-008-0900-x pmid:19139965 . OpenUrl CrossRef PubMed Web of Science
- ↵ Olaitan A, Okunade O, Corne J. How to present clinical cases. Student BMJ 2010;18:c1539.
- ↵ Gaillard F. The secret art of relevant negatives, Radiopedia 2016; http://radiopaedia.org/blog/the-secret-art-of-relevant-negatives .

- © 2019
Presenting Your Case
A Concise Guide for Medical Students
- Clifford D. Packer 0
Professor of Medicinem, Department of Medicine, Case Western Reserve University School of Medicine, Louis Stokes Cleveland VA Medical Center, Cleveland, USA
You can also search for this author in PubMed Google Scholar
- Provides a comprehensive guide to case presentation and related activities
- Covers various types of oral case presentations on the wards, including the traditional new patient presentation, transfers, night float admissions, and brief SOAP presentations on daily rounds
- Prepares medical students for their clerkship evaluations, which depend largely on the quality of their oral presentations
11k Accesses
1 Citations
1 Altmetric
- Table of contents
About this book
Authors and affiliations, about the author, bibliographic information.
- Publish with us
Buying options
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Other ways to access
This is a preview of subscription content, log in via an institution to check for access.
Table of contents (14 chapters)
Front matter, the importance of a good case presentation and why students struggle with it.
Clifford D. Packer
Organization of the Oral Case Presentation
Variations on the oral case presentation, the hpi: a timeline, not a time machine, pertinent positives and negatives, the diagnostic power of description, the assessment and plan, approaches to differential diagnosis, searching and citing the literature, adding value to the oral presentation, teaching rounds: speaking up, getting involved, and learning to accept uncertainty, the art of the 5-minute talk, future directions of the oral case presentation, back matter.
Medical students often struggle when presenting new patients to the attending physicians on the ward. Case presentation is either poorly taught or not taught at all in the first two years of medical school. As a result, students are thrust into the spotlight with only sketchy ideas about how to present, prioritize, edit, and focus their case presentations. They also struggle with producing a broad differential diagnosis and defending their leading diagnosis. This text provides a comprehensive guide to give well-prepared, focused and concise presentations. It also allows students to discuss differential diagnosis, incorporate high-value care, educate their colleagues, and participate actively in the care of their patients.
Linking in-depth discussion of the oral presentation with differential diagnosis and high value care, Presenting Your Case is a valuable resource for medical students, clerkship directors and others who educatestudents on the wards and in the clinic.
- Oral case presentation
- Differential Diagnosis
- Five-Minute-Talk
Clifford D. Packer, MD
Professor of Medicine
Department of Medicine
Case Western Reserve University School of Medicine
Louis Stokes Cleveland VA Medical Center
Cleveland, OH, USA
Book Title : Presenting Your Case
Book Subtitle : A Concise Guide for Medical Students
Authors : Clifford D. Packer
DOI : https://doi.org/10.1007/978-3-030-13792-2
Publisher : Springer Cham
eBook Packages : Medicine , Medicine (R0)
Copyright Information : Springer Nature Switzerland AG 2019
Softcover ISBN : 978-3-030-13791-5 Published: 14 May 2019
eBook ISBN : 978-3-030-13792-2 Published: 29 April 2019
Edition Number : 1
Number of Pages : XIV, 196
Number of Illustrations : 8 b/w illustrations, 9 illustrations in colour
Topics : General Practice / Family Medicine
Policies and ethics
- Find a journal
- Track your research

- Research & Collections
- Borrow & Request
- Computing & Technology

PBL Information Resources and Tools for the First Year: Oral Presentation Resources
- Clinical Resources
- Background Info Resources
- Drug Info Resources
- Current Case
- PBL Case Archive
- Search Tips & Tutorials
- APA Examples
- Numbered Style Example
- What About Citations in Slides?
- Reference : Normal Lab Values
- Oral Presentation Resources
- Write-Ups: Word & PowerPoint Tips
Books Worth Checking Out
Have a resource to share or need something more? Let Karen know .
Oral Presentations
Dr. Konop's Tips
The oral case presentation requires a bit of effort and benefits from repeated practice. You may have questions about what to include and the following resources will help you keep in mind the salient points to cover. Some presentations will be brief - when fewer points will be covered - and some will be longer - where you can cover all of the key points.
- Dr. Goldberg's Tips Don't forget the tips at the end.
- Michigan's State's PBL List (concise) A list with brief details on some points.
- Cornell's Tips for 3rd Year A bit specific to the wards, but some good guidelines to use.
- Drexel's Tip (lots of detail) Including examples, mnemonics & common mistakes. They advise, "an oral case presentation is NOT a simple recitation of your write-up. It is a concise, edited presentation of the most essential information."
Dr. Gates Tip
Dr. Gates found a great form to use as a reminder of what to cover. For those of you that like notes, this will work well, and those of you who just want some structure, it will provide that.
- Oral Presentation as PDF A fill in the blanks form.
- Oral Presentation as Word file A fill in the blanks form where you can enter the patient info.
Quick Reminder:
Don't bury the lead!
In other words, state up front the Chief Complaint . Knowing that will give your listeners the chance to put all the pieces of info that you have to say together in a way that helps them.
For an Alternative Perspective
- BMJ Article on How to Present a Case A bit more detailed (good for clerkship maybe?) but some good tips. Requires a free account to BMJ Student.
- << Previous: Reference : Normal Lab Values
- Next: Write-Ups: Word & PowerPoint Tips >>
- Last Updated: Mar 14, 2024 2:18 PM
- URL: https://ucsd.libguides.com/Foundations
Featured Clinical Reviews
- Screening for Atrial Fibrillation: US Preventive Services Task Force Recommendation Statement JAMA Recommendation Statement January 25, 2022
- Evaluating the Patient With a Pulmonary Nodule: A Review JAMA Review January 18, 2022
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
The Oral Case Presentation : A Key Tool for Assessment and Teaching in Competency-Based Medical Education
- 1 Wilson Centre, University of Toronto, Toronto, Ontario, Canada
- 2 Department of Medicine, University of Toronto, Toronto, Ontario, Canada
- 3 HoPingKong Centre, University Health Network, Toronto, Ontario, Canada
Oral case presentations by trainees to supervisors are core activities in academic hospitals across all disciplines and form a key milestone in US and Canadian educational frameworks. Yet despite their widespread use, there has been limited attention devoted to developing case presentations as tools for structured teaching and assessment. In this Viewpoint, we discuss the challenges in using oral case presentations in medical education, including lack of standardization, high cognitive demands, and the role of trust between supervisor and trainee. We also articulate how, by addressing these tensions, case presentations can play an important role in competency-based education, both for assessment of clinical competence and for teaching clinical reasoning.
Read More About
Melvin L , Cavalcanti RB. The Oral Case Presentation : A Key Tool for Assessment and Teaching in Competency-Based Medical Education . JAMA. 2016;316(21):2187–2188. doi:10.1001/jama.2016.16415
Manage citations:
© 2024
Artificial Intelligence Resource Center
Cardiology in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.115(1); Jan-Feb 2018

Implementation of Oral Case Presentations in an Immunology Course
Implementation of oral case presentations (OCP) in the Immunology course at A.T. Still University–Kirksville College of Osteopathic Medicine has significantly improved written examination scores and student satisfaction with the course by enhancing its clinical relevance. With six faculty facilitators, an average class size of 172 students can complete the exercise in a single day. The exercise requires small group meeting rooms, each equipped with a computer and wall-mounted monitor, but no other physical resources.
Introduction
The oral case presentation (OCP) is an effective tool for teaching and evaluating medical students as they develop competence in communication skills, medical knowledge, and clinical reasoning. 1 – 3 Although approaches to the OCP may vary, most incorporate elements represented by the mnemonic “SNAPPS,” which refers to summarizing the patient’s history and physical findings, narrowing the differential, analyzing the differential by comparing and contrasting the possible diagnoses, probing for additional information about uncertainties, planning management of the patient’s medical issues, and selecting a case-related issue for self-directed learning. 4 The OCP can be adapted to all stages of medical training, from the pre-clinical years 5 through residency programs. 4 , 6 In this paper, I describe implementation of an OCP exercise in an Immunology course taken by first- or second-year osteopathic medical students at A.T. Still University–Kirksville College of Osteopathic Medicine (ATSU–KCOM).
The OCP exercise was introduced into the Immunology course in 2011. At that time, Immunology consisted of 21 contact hours, and was by far the shortest course in an academic term that totaled 283 contact hours. Perhaps due in part to its small footprint, Immunology compared unfavorably in student evaluations to larger courses taught during the same term, the largest of which comprised 90 contact hours. To emphasize the importance of Immunology in medical education despite the brevity of the course, the Immunology OCP was implemented with three major goals in mind: 1) to enhance the clinical relevance of material presented during traditional lectures, 2) to improve written examination scores, and 3) to increase student satisfaction with the course. The Immunology OCP exercise was modeled after similar exercises performed in our Medical Microbiology and Infectious Diseases courses, which have been highly successful in achieving the same goals. 5 Now in its seventh year, the Immunology OCP has a proven record of producing high-yield results while using few faculty and physical resources.
Study Participants
This study received exempt status from the ATSU–KCOM Institutional Review Board. ATSU–KCOM osteopathic medical students participating in the study fell into three experimental groups. Group I students (n=352) took Immunology as a single, comprehensive 21-hour course in Quarter 2 of the curriculum; they did not participate in the Immunology OCP exercise. Group II students (n=335) also took Immunology as a single 21-hour course, but these students participated in the OCP exercise. For Group III students (n=513), curricular changes led to the division of Immunology into an 11-hour foundational course in Semester 1, followed by a 10-hour clinical course in Semester 3. Group III students participated in the OCP exercise during the Semester 3 clinical course. Groups I and II each comprised two classes of students, whereas Group III included students from three classes.
Clinical Cases
All clinical immunology cases were adapted by the author from printed texts, e-books, or reputable on-line resources that describe case studies. 7 – 10 The cases were developed around the chief complaints of abdominal pain, bowel upset, breathing difficulty, cough, diarrhea, joint pain, numbness, and skin lesions. Differential diagnoses included immunodeficiencies, autoimmune diseases, and hypersensitivities. Case packets were created using the template developed by Chamberlain et al. 5 Each packet consisted of 1–3 printed pages containing one or more photographs of the patient; the patient’s chief complaint and associated symptoms; the patient’s history, vital signs and physical examination results; and laboratory and medical procedure data that required interpretation by the student.
Case Presentations
Groups of 5 students and one facilitator were assigned to small group meeting rooms equipped with a computer and wall-mounted monitor. Each student in the group randomly received a unique paper case and had 10 minutes to read and take notes over the data. Students were not allowed to consult reference materials or their peers during the reading period. After returning the case packets to the facilitator, each student gave a 3-minute oral presentation that summarized the main issues of the case, explained the lab and medical procedure data, and explained why each diagnosis in a list of five choices should be ruled in or ruled out. The student was aided during the oral presentation by a PowerPoint slide containing case exhibits, and by the hand-written notes taken during review of the case packet. After the presenting the case and defending the diagnosis, the student spent the next three minutes fielding questions from his or her peers and the facilitator. For each group of five students, the entire exercise required 50 min to complete. Typically, six groups were run simultaneously, allowing 30 students to complete the exercise each hour, and an average class size of 172 students to complete the exercise in a single day.
Student performance was evaluated using a rubric that assessed six microskills: 1) behaving and speaking in a professional manner; 2) adding value to the discussion by asking probing questions of the presenter; 3) covering important aspects of the patient’s signs, symptoms, history and physical; 4) thoroughly explaining laboratory and medical procedure data; 5) justifying why each answer choice in the differential diagnosis list should be ruled in or ruled out; and 6) correctly answering a basic science question associated with the case. The basic science question varied, but often involved asking the presenter to identify the molecular defect causing an immunodeficiency, the molecular target of an autoimmune disease, or the mode of action of an immunotherapeutic treatment. New cases were introduced at planned intervals to minimize the advantage gained by students in later sessions who might unfairly discuss the cases with classmates who completed the exercise earlier in the day.
The OCP exercise was scheduled to take place three to seven days before the last unit examination in the Immunology course. Because the course ends long before the academic term is over, students completed the OCP exercise an average of 4 weeks before they took the Immunology comprehensive final examination at the end of the academic term.
Statistical Analysis of Final Exam Scores and Likert Scale Data
To determine whether the Immunology OCP exercise impacted student learning, scores earned by students on the Immunology comprehensive final examination before (Group I) and after (Groups II and III) implementation of the OCP were compared by one-way ANOVA (P<0.05). Post hoc comparisons were done using the Bonferroni correction to the p-value (P<0.05). The questions on the comprehensive final examinations taken by students in Groups I and II were consistent except for minor changes made for clarity. The comprehensive final exams taken by Group III students largely omitted the basic science questions found on Group I and II final exams, but contained the same clinical questions as before, plus additional clinical questions.
Student satisfaction with the Immunology course before and after implementation of the OCP was evaluated using the 4-point Likert item, “Achievement in this course advances me toward being a physician,” where 1=strongly agree, 2=agree, 3=disagree, and 4=strongly disagree. Likert scores were compared between groups by one-way ANOVA (P<0.05), followed by post hoc comparisons done with the Bonferroni correction to the p-value (P<0.05).
Anonymous Student Comments Regarding the Immunology OCP
Students had the opportunity to express their opinions about the Immunology OCP through anonymous written comments submitted via the on-line Immunology course evaluation. Course evaluations were completed after students had taken the Immunology comprehensive final examination at the end of the academic term.
Students who participated in the Immunology OCP (Groups II and III) scored significantly higher on the Immunology comprehensive final examination than Group I students, who did not participate in the exercise (one-way ANOVA, P<0.001; Bonferroni post hoc test, P<0.001) ( Table 1 ). Among students who took Immunology as a single 21-hour course, the mean final exam score improved from 76.5% (Group I) to 81.8% (Group II) upon implementation of the Immunology OCP. Between the two groups of students who participated in the OCP, those who took the 10-hour clinical Immunology course in Semester 3 (Group III) scored significantly higher on the comprehensive final exam than those who took Immunology as a single, 21-hour course in Quarter 2 or 3 (Group II) (one-way ANOVA, P<0.001; Bonferroni post hoc test, P<0.001) ( Table 1 ). Final exam scores earned by Group II and Group III were 81.8% and 87.0%, respectively.
Comparison of mean comprehensive final examination scores in Immunology before (Group I) and after (Groups II and III) implementation of Immunology Case Presentations.
Student satisfaction with the Immunology course, as assessed using the Likert item, “Achievement in this course advances me toward being a physician,” also significantly improved upon implementation of the OCP ( Table 2 ). Students who participated in the OCP (Groups II and III) strongly agreed with the statement, reflected by Likert scores of 1.21 and 1.18, respectively. Both scores were significantly better than the 1.78 rating conferred by Group I students, who did not participate in the OCP (one-way ANOVA, P<0.001; Bonferroni post hoc test, P<0.001). There was no significant difference in Likert scores between Groups II and III (one-way ANOVA, P<0.001; Bonferroni post hoc test, P=0.94).
Comparison of mean Likert scores far the statement, “Achievement in this course advances me toward being a physician,” before (Group I) and after (Groups II and III) implementation of Immunology Case Presentations. a
In general, anonymous student comments submitted as part of the Immunology course evaluation were positive toward the OCP exercise ( Table 3 ). Negative comments focused on the perception that some facilitators tended to give lower scores than others, and that cases or case-associated basic science questions were not uniform in difficulty.
A sampling of anonymous student comments written about the Immunology OCP, reprinted from Immunology course evaluations.
Since introducing the oral case presentations exercise into the Immunology course at ATSU–KCOM, comprehensive final examination scores and student satisfaction with the course have improved significantly. Final exam scores have risen from the mid-70 percent range earned by students who did not participate in the Immunology OCP, to the low- or mid-80 percent range earned by students who did participate in the exercise. With implementation of the OCP, concurrence with the statement, “Achievement in this course advances me toward being a physician,” has improved from “agree” to “strongly agree” in student ratings. Students report that the OCP allows them to integrate basic science knowledge into a clinical setting and helps them think like physicians. Such statements are taken as evidence that the OCP enhances the clinical relevance of the lecture-based material that comprises the bulk of the Immunology course.
As expected, students reported that the OCP made them feel better prepared for the unit exam that came three to seven days after the OCP exercise. Somewhat surprising was the persistence of the exercise’s beneficial effect through the end of the academic term, resulting in higher scores on the Immunology comprehensive final exam taken one month after completion of the OCP exercise than in years prior to OCP implementation. The lasting impact of the OCP on student learning was also reflected in student perceptions of preparedness for the COMLEX Level 1 board examination, which is taken at the end of the second year of osteopathic medical education. Since implementing the Immunology OCP, 94% to 99% of students have reported feeling adequately to extremely well-prepared in Immunology for the COMLEX Level 1 exam, up from a low of 68% before the OCP exercise was introduced. Graffam 11 notes that intentional engagement and active learning change the nature of learning in such a way that knowledge gain and recall abilities are improved, an assertion supported by our experience with the Immunology OCP exercise.
It should be noted that the Immunology final exams given to students in Groups I and II varied little from year to year, enabling direct comparison of exam scores between these two groups. However, the curricular changes that divided Immunology into separate foundational and clinical courses necessitated changes to the final exam taken by students in Group III. For all three groups, the same core clinical questions were asked on the final exam, but the Group III exam contained additional clinical questions and omitted questions covering basic immunological concepts. Fewer lectures were covered on the Group III exam, resulting in less material to study. A more important advantage enjoyed by Group III students was the timing of the Immunology final exam, which came later in their medical education. Exposure to additional coursework allowed Group III students to make connections between knowledge gained in Immunology with knowledge gained from the Pathology and Medicine courses. Inshort, the improvement seen in Group III Immunology comprehensive final examination scores most likely derived from a combination of factors, including the Immunology OCP.
Onishi 12 distinguishes between OCP exercises that have short (1–2 minutes) and long (5–10 minutes) formats. To improve clinical reasoning, the short presentation offers the advantages of requiring abstraction of information, time efficiency, and fostering informal interactions with the audience. 12 Long presentations allow educators to be more involved in the diagnostic reasoning process as they listen to detailed descriptions of the patient’s signs and symptoms. 12 A frequently used short-format case presentation is the One-Minute Preceptor (OMP), which employs six microskills. 4 These include requiring the student to commit to a diagnosis, probing for supporting evidence, teaching general rules, reinforcing what is right, correcting mistakes, and identifying the next learning steps. 4 The Immunology OCP used a mixed approach, falling between the short and long case presentation formats while blending elements of SNAPPS and the OMP, with good results.
Although students expressed concern that some facilitators graded more harshly than others during the OCP, steps were taken to minimize inter-rater variability. In all three courses where we use OCP exercises, we have found that a useful method for reducing inconsistencies is to enter the data for each case into a spread sheet, so that the scores assigned to each item in the grading rubric can be compared across facilitators by a single evaluator. Adjustments are made if discrepancies are found in the number of points deducted by different facilitators for the same infraction. Using this method, the mean scores across all facilitators typically differ by less than 5%. Although the perfect evaluation instrument for the OCP has yet to be developed, 13 – 15 our simplified rubric, in conjunction with written comments made by the facilitators, provides valuable feedback to the students as they develop oral case presentation skills.

Conclusions
Introduction of the oral case presentations exercise into the Immunology course at ATSU–KCOM has enhanced the clinical relevance of material presented during traditional lectures, improved retention of basic science and medical knowledge, and increased student satisfaction with their educational experience. The Immunology OCP complements similar exercises we conduct in our Medical Microbiology and Infectious Diseases courses. Together, these three courses have fostered development of oral communication and clinical reasoning skills that will serve our students well during their third and fourth years of medical training.
Acknowledgments
The oral case presentations exercise would not be possible without the cooperation and dedication of the entire Department of Microbiology/Immunology faculty and staff at ATSU–KCOM. Additional thanks go to Shalini Bhatia, Biostatistician, for advice on statistics, and to Patricia Sexton, DHEd, Associate Dean for Curriculum, and Neal Chamberlain, PhD, Professor of Microbiology/Immunology, for critical reading of the manuscript.
Melissa K. Stuart, PhD, Department of Microbiology/Immunology, is at Kirksville College of Osteopathic Medicine, A.T. Still University, Kirksville, Missouri.
Contact: ude.usta@trautsm

None reported.
- Open access
- Published: 24 May 2023
Comparing oral case presentation formats on internal medicine inpatient rounds: a survey study
- Brendan Appold 1 ,
- Sanjay Saint 1 , 2 ,
- David Ratz 2 &
- Ashwin Gupta 1 , 2
BMC Medical Education volume 23 , Article number: 377 ( 2023 ) Cite this article
2672 Accesses
11 Altmetric
Metrics details
Oral case presentations – structured verbal reports of clinical cases – are fundamental to patient care and learner education. Despite their continued importance in a modernized medical landscape, their structure has remained largely unchanged since the 1960s, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed for medical records. We developed a problem-based alternative known as Events, Assessment, Plan (EAP) to understand the perceived efficacy of EAP compared to SOAP among learners.
We surveyed (Qualtrics, via email) all third- and fourth-year medical students and internal medicine residents at a large, academic, tertiary care hospital and associated Veterans Affairs medical center. The primary outcome was trainee preference in oral case presentation format. The secondary outcome was comparing EAP and SOAP on 10 functionality domains assessed via a 5-point Likert scale. We used descriptive statistics (proportion and mean) to describe the results.
The response rate was 21% (118/563). Of the 59 respondents with exposure to both the EAP and SOAP formats, 69% ( n = 41) preferred the EAP format as compared to 19% ( n = 11) who preferred SOAP ( p < 0.001). EAP outperformed SOAP in 8 out of 10 of the domains assessed, including advancing patient care, learning from patients, and time efficiency.
Conclusions
Our findings suggest that trainees prefer the EAP format over SOAP and that EAP may facilitate clearer and more efficient communication on rounds, which in turn may enhance patient care and learner education. A broader, multi-center study of the EAP oral case presentation will help to better understand preferences, outcomes, and barriers to implementation.
Peer Review reports
Excellent inter-physician communication is fundamental to both providing high-quality patient care and promoting learner education [ 1 ], and has been recognized as an important educational goal by the Clerkship Directors in Internal Medicine, the Association of American Medical Colleges, and the Accreditation Council for Graduate Medical Education [ 2 ]. Oral case presentations, structured verbal reports of clinical cases [ 3 ], have been referred to as the “currency with which clinicians communicate” [ 4 ]. Oral case presentations are a key element of experiential learning in clinical medicine, requiring learners to synthesize, assess, and convey pertinent patient information and to formulate care plans. Furthermore, oral case presentations allow supervising clinicians to identify gaps in knowledge or clinical reasoning and enable team members to learn from one another. Despite modernization in much of medicine, oral case presentation formats have remained largely unchanged, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed by Dr. Lawrence Weed in his Problem Oriented Medical Record in 1968 [ 5 ].
Given that the goals of a medical record are different than those of oral case presentations, it should not be assumed that they should share the same format. While Dr. Weed sought to make the medical record as “complete as possible,” [ 6 ] internal medicine education leaders have expressed desire for oral case presentations that are succinct, with an emphasis on select relevant details [ 2 ]. Using a common SOAP format between the medical record and oral case presentations risks conflating the distinct goals for each of these communication methods. Indeed, in studying how learners gain oral case presentation skills, Haber and Lingard [ 7 ] found differences in understanding of the fundamental purpose of oral case presentations between medical students and experienced physicians. While students believed the purpose of oral case presentations was to organize the large amount of data they collected about their patients, experienced physicians saw oral case presentations as a method of telling a story to make an argument for a particular conclusion [ 7 ].
In accordance with Dr. Weed’s “problem-oriented approach to data organization,” [ 6 ] but with an eye toward optimizing for oral case presentations, we developed an alternative to SOAP known as the Events, Assessment, Plan (EAP) format. The EAP format is used for patients who are already known to the inpatient team, and may also be utilized for newly admitted patients for whom the attending physician already has context (e.g., via handoff or review of an admission note). As the EAP approach is utilized by a subset of attending physicians at our academic hospital, we sought to understand the perceived effectiveness of the EAP format in comparison to the traditional SOAP format among learners (i.e., medical students and resident physicians).
EAP is a problem-based format used at the discretion of the attending physician. In line with suggested best practices [ 8 ], the EAP structure aims to facilitate transmission of data integrated within the context of clinical problem solving. In this format, significant interval events are discussed first (e.g., a fall, new-onset abdominal pain), followed by a prioritized assessment and plan for each relevant active problem. Subjective and objective findings are integrated into the assessment and plan as relevant to a particular problem. This integration of subjective and objective findings by problem is distinct from SOAP, where subjective and objective findings are presented separately as their own sections, with each section often containing information that is relevant to several problems (Fig. 1 , Additional file 1 : Appendix A).
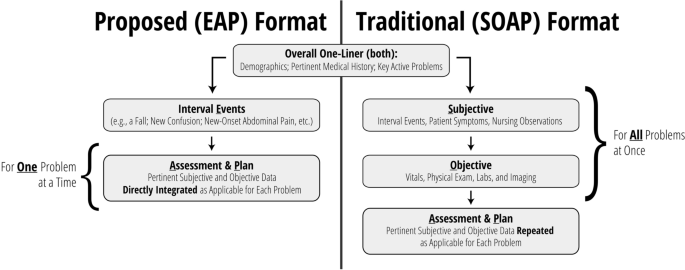
Overview: comparing EAP to SOAP
Settings and participants
We surveyed third- and fourth-year medical students, and first- through fourth-year internal medicine and internal medicine-pediatrics residents, caring for patients at a large, academic, tertiary care hospital and an affiliated Veterans Affairs medical center. Internal medicine is a 12-week core clerkship for all medical students in their second year, with 8 weeks spent on the inpatient wards. All student participants had completed their internal medicine clerkship rotation at the time of the survey. We did not conduct a sample size calculation at the outset of this study.
Data collection methods and processes
An anonymous, electronic survey (Qualtrics, Provo, UT) was created to assess student and resident experience with and preference between EAP and SOAP oral case presentation formats during inpatient internal medicine rounds (Additional file 2 : Appendix B). Ten domains were assessed via 5-point Likert scale (1 [strongly disagree] to 5 [strongly agree]), including the ability of the format to incorporate the patient’s subjective experience, the extent to which the format encouraged distillation and integration of information, the extent to which the format focused on the assessment and plan, the format’s ability to help trainees learn from their own patients and those of their peers, time efficiency, and ease of use. Duration of exposure to each format was also assessed, as were basic demographic data for the purposes of understanding outcome differences among respondents (e.g., students versus residents). For those who had experienced both formats, preference between formats was recorded as a binary choice. Participants additionally had the opportunity to provide explanation via free text. For participants with experience in both formats, the order of evaluation of EAP and SOAP formats were randomized by participant. For questions comparing EAP and SOAP formats directly, choice order was randomized.
The survey was distributed via official medical school email in October 2021 and was available to be completed for 20 days. Email reminders were distributed approximately one week after distribution and again 48 h prior to survey conclusion.
The primary outcome was trainee preference in oral case presentation format. Secondary outcomes included comparison between EAP and SOAP on content inclusion/focus, data integration, learning, time efficiency, and ease of use.
Statistical analyses
Descriptive statistics were used to describe the results (proportion and mean). For comparative analysis between EAP and SOAP, responses from respondents who had experience with both formats were compared using the Wilcoxon Signed Rank Test to evaluate differences. All statistical analyses were done using SAS V9.4 (SAS Institute, Cary, NC). We considered p < 0.05 to be statistically significant.
The overall response rate was 21% (118/563). The response rate was 14% ( n = 62/441) among medical students and 46% ( n = 56/122) among residents. Respondents were 61% ( n = 72) female. A total of 98% ( n = 116) and 52% ( n = 61) of respondents reported experience with SOAP and EAP formats, respectively. Among medical students, 60% ( n = 37) reported experience with SOAP only while 39% ( n = 24) had experience with both formats. Among residents, 36% ( n = 20) and 63% ( n = 35) had experience with SOAP only and both formats, respectively (Table 1 ). Most students (93%) and residents (96%) reported > 8 weeks of exposure to the SOAP format. Duration of exposure to the EAP format varied (0 to 2 weeks [32% of students, 17% of residents], 2 to 4 weeks [36% of students, 47% of residents], 4 to 8 weeks [16% of students, 25% of residents], and > 8 weeks [16% of students, 11% of residents]).
Of the 59 respondents with exposure to both the SOAP and EAP formats, 69% ( n = 41) preferred the EAP format as compared to 19% ( n = 11) preferring SOAP ( p < 0.001). The remainder ( n = 7, 12%) indicated either no preference between formats or indicated another preference. Among residents, 66% ( n = 23) favored EAP, whereas 20% ( n = 7) and 14% ( n = 5) preferred SOAP or had no preference, respectively ( p < 0.001). Among students, 75% ( n = 18) favored EAP, whereas 17% ( n = 4) and 8% ( n = 2) favored SOAP or had no preference, respectively ( p < 0.001).
Likert scale ratings for domains assessed by trainees who had experience in either format are shown in Table 2 . In general, scores for each domain were higher for EAP than SOAP, with the exception of perceived ease of use among students. Among those with experience using both formats, EAP outperformed SOAP most prominently in time efficiency (mean 4.39 vs 2.59, p < 0.001) and encouragement to: focus on assessment and plan (4.64 vs 3.05, p < 0.001), distill pertinent information (4.63 vs 3.17, p < 0.001), and integrate data (4.58 vs 3.31, p < 0.001) (Table 3 ). Respondents also ranked EAP higher in its effectiveness at advancing patient care (4.31 vs 3.71, p < 0.001), its capacity to convey one’s thinking (4.53 vs 3.95, p < 0.001), and its ability to facilitate learning from peers (4.10 vs 3.58, p < 0.001) and one’s own patients (4.24 vs 3.78, p = 0.003). There were no significant differences in the amount of time allotted for discussing the patient’s subjective experience or in ease of use.
Evaluation of trainee free text responses regarding oral case presentation preference revealed several general themes (Table 4 ). First, respondents generally felt that EAP was more time efficient and less repetitive, allowing for additional time to be spent discussing pertinent patient care decisions. Second, several respondents indicated that EAP aligns well with how trainees consider problems naturally (as a single problem in completion). Finally, respondents generally believed that EAP allowed learners to effectively communicate their thinking and demonstrate their knowledge. Those preferring SOAP most often cited format familiarity and the difficulty in switching between formats in describing their preference, though some also believed SOAP was more effective in describing a patient’s current status.
Our single site survey comparing 2 oral case presentation formats revealed a preference among respondents for EAP over SOAP for those medical students and internal medicine residents who had experience with both formats. Furthermore, EAP outperformed SOAP in 8 out of 10 of the functionality domains assessed, including areas such as advancing patient care, learning from patients, and, particularly, time efficiency. Such a constellation of findings implies that EAP may not only be a more effective means to accomplish the key goals of oral case presentations, but it may also provide an opportunity to save time in the process. In line with SOAP’s current de facto status as an oral case presentation format, almost all respondents reported exposure to the SOAP format. Still, indicative of EAP’s growing presence at our academic system, more than one third of medical students and more than one half of residents also reported having experience with the EAP format.
While limited data exist that compare alternative oral case presentations to SOAP on inpatient medicine rounds, such alternatives have been previously trialed in other clinical venues. One such format, the multiple mini-SOAP, developed for complex outpatient visits, encourages each problem to be addressed “in its entirety” before presenting subsequent problems, and emphasizes prioritization by problem pertinency [ 9 ]. The creators suggest that this approach encourages more active trainee participation in formulating the assessment and plan for each problem, by helping the trainee to avoid getting lost in an “undifferentiated jumble of problems and possibilities” [ 9 ] that accumulate when multiple problems are presented all at once. On the receiving end, the multiple mini-SOAP enables faculty to assess student understanding of specific clinical problems one at a time and facilitates focused teaching accordingly.
Another approach has been assessed in the emergency department. Specifically, Maddow and colleagues explored assessment-oriented oral case presentations to increase efficiency in communication between residents and faculty at the University of Chicago [ 10 ]. In the assessment-oriented format, instead of being presented in a stylized order, pertinent information was integrated into the analysis. The authors found that assessment-oriented oral case presentations were about 40% faster than traditional presentations without significant differences in case presentation effectiveness.
Prior to our study, the nature of the format for inpatient medicine oral case presentations had thus far escaped scrutiny. This is despite the fact that oral case presentations are time (and therefore resource) intensive, and that they play an integral role in patient care and learner education. Our study demonstrates that learners favor the EAP format, which has the potential to increase both the effectiveness and efficiency of rounding.
Still, it should be noted that a transition to EAP does present challenges. Implementing this problem-based presentation format requires a conscious effort to ensure a continued holistic approach to patient care: active problems should be defined and addressed in accordance with patient preferences, and the patient’s subjective experience should be meaningfully incorporated into the assessment and plan for each problem. During initial implementation, attending physicians and learners must internalize this new format, often through trial and error.
From there, on an ongoing basis, EAP may require more upfront preparation by attending physicians as compared to SOAP. While chart review by attendings in advance of rounding is useful regardless of the format utilized, this practice is especially important for the EAP format, where trainees are empowered to interpret and distill – rather than simply report a complete set of – information. Therefore, the attending physician must be aware of pertinent data prior to rounds to ensure that key information is not neglected. Specifically, attendings should pre-orient themselves with laboratory values, imaging, and other studies completed, and new suggestions from consultants. More extensive pre-work may be required if teams wish to employ the EAP format for newly admitted patients, as attending physicians must also familiarize themselves with a patient’s medical history and their current presentation prior to initial team rounds.
Our findings should be interpreted within the context of specific limitations. First, low response rates may have led to selection bias within our surveyed population. For instance, learners who desired change in the oral case presentation format may have been more motivated to engage with our survey. Second, there could be unmeasured confounding variables that could have skewed our results in favor of the EAP format. For example, attendings who utilized the EAP format may have been more likely to innovate in other ways to create a more positive experience for learners, which may have influenced the scoring of the oral case presentation format. Third, our findings were largely based on subjective experience. Objective measurement (e.g., duration of rounds, patient care outcomes) may lend additional credibility to our findings. Lastly, our study included only a single site, limiting our ability to generalize our findings.
Our study also had several strengths. Our learner participant pool was broad and included all third- and fourth-year medical students and all internal medicine residents at a major academic hospital. Participation was encouraged regardless of the nature of a participant’s prior exposure to different oral case presentation formats. Our survey was anonymous with randomization to mitigate order bias, and we focused our comparison analysis on those who had exposure to both the EAP and SOAP formats. We collected data to compare EAP with SOAP in 2 distinct ways: head-to-head preference and numeric ratings amongst key domains. Both of these methods demonstrated a significant preference for EAP among learners in aggregate, as well as for students and residents analyzed independently.
Our findings suggest a preference for the EAP format over SOAP, and that EAP may facilitate clearer and more efficient communication on rounds. These improvements may in turn enhance patient care and learner education. While our preliminary data are compelling, a broader, multi-center study of the EAP oral case presentation is necessary to better understand preferences, outcomes, and barriers to implementation. Further studies should seek to improve response rates, for the data to represent a larger proportion of trainees. One potential strategy to improve response rates among medical students and residents is to survey them directly at the end of each internal medicine clerkship period or rotation, respectively. Ultimately, EAP may prove to be a much-needed update to the “currency with which clinicians communicate.”
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, AG, upon reasonable request.
Kihm JT, Brown JT, Divine GW, Linzer M. Quantitative analysis of the outpatient oral case presentation: piloting a method. J Gen Intern Med. 1991;6(3):233–6.
Article Google Scholar
Green EH, Durning SJ, DeCherrie L, Fagan MJ, Sharpe B, Hershman W. Expectations for oral case presentations for clinical clerks: opinions of internal medicine clerkship directors. J Gen Intern Med. 2009;24(3):370–3.
Daniel M, Rencic J, Durning SJ, Holmboe E, Santen SA, Lang V, et al. Clinical Reasoning Assessment Methods: A Scoping Review and Practical Guidance. Acad Med. 2019;94(6):902–12.
Lewin LO, Beraho L, Dolan S, Millstein L, Bowman D. Interrater reliability of an oral case presentation rating tool in a pediatric clerkship. Teach Learn Med. 2013;25(1):31–8.
Wright A, Sittig DF, McGowan J, Ash JS, Weed LL. Bringing science to medicine: an interview with Larry Weed, inventor of the problem-oriented medical record. J Am Med Inform Assoc. 2014;21(6):964–8.
Weed LL. Medical records that guide and teach. New Engl J Med. 1968;278(12):652–7.
Haber RJ, Lingard LA. Learning oral presentation skills: a rhetorical analysis with pedagogical and professional implications. J Gen Intern Med. 2001;16(5):308–14.
Wiese J, Saint S, Tierney LM. Using clinical reasoning to improve skills in oral case presentation. Semin Med Pract. 2002;5(3):29–36.
Google Scholar
Schillinger E, LeBaron S. The multiple mini-SOAP format for student presentations of complex patients. Fam Med. 2003;35(1):13–4.
Maddow CL, Shah MN, Olsen J, Cook S, Howes DS. Efficient communication: assessment-oriented oral case presentation. Acad Emerg Med. 2003;10(8):842–7.
Download references
Acknowledgements
The authors would like to thank Jason M. Engle, MPH, who helped edit, prepare, format, and submit this manuscript and supporting files.
Author information
Authors and affiliations.
University of Michigan Medical School, Ann Arbor, MI, USA
Brendan Appold, Sanjay Saint & Ashwin Gupta
VA Ann Arbor Healthcare System, 2215 Fuller Road, Ann Arbor, MI, 48105, USA
Sanjay Saint, David Ratz & Ashwin Gupta
You can also search for this author in PubMed Google Scholar
Contributions
Conceptualization: BA SS AG. Data curation: BA DR AG. Formal Analysis: BA SS DR AG. Funding acquisition: SS AG. Investigation: BA SS AG. Methodology: BA SS AG. Project administration: BA SS AG. Resources: SS AG. Software: DR. Supervision: SS AG. Validation: BA SS DR AG. Visualization: BA SS DR AG. Writing – original draft: BA AG. Writing – review & editing: BA SS DR AG. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Ashwin Gupta .
Ethics declarations
Ethics approval and consent to participate.
All methods were carried out in accordance with relevant guidelines and regulations. The need for ethical approval was waived by the ethics committee/Institutional Review Board of the University of Michigan Medical School. The need for informed consent was waived by the ethics committee/Institutional Review Board of the University of Michigan Medical School.
Consent for publication
Not applicable.
Competing interests
Dr. Saint, Mr. Ratz, and Dr. Gupta are employed by the US Department of Veterans Affairs. Dr. Saint reports receiving grants from the Department of Veterans Affairs and personal fees from ISMIE Mutual Insurance Company, Jvion, and Doximity. Dr. Appold, Mr. Ratz, and Dr. Gupta report no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:.
Appendix A. Exemplar Transcripts (EAP, SOAP).
Additional file 2:
Appendix B. Survey Instrument.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Appold, B., Saint, S., Ratz, D. et al. Comparing oral case presentation formats on internal medicine inpatient rounds: a survey study. BMC Med Educ 23 , 377 (2023). https://doi.org/10.1186/s12909-023-04292-3
Download citation
Received : 24 August 2022
Accepted : 22 April 2023
Published : 24 May 2023
DOI : https://doi.org/10.1186/s12909-023-04292-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical education
- Oral case presentations
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Oral medicine
Mar 11, 2019
450 likes | 815 Views
Oral medicine. Done by Abdulaziz m. ghannam 0610052. Personal data. Name/A.S.G Age/16 Sex/ male Nationality/Saudi Occupation/student. Patient history. Chief complain: He wants to check his teeth. Medical history: Not significant. Family history: Not significant.
Share Presentation
- nestin expression
- investigate nestin expression
- odontogenic fibroma expressed nestin

Presentation Transcript
Oral medicine Done by Abdulaziz m. ghannam 0610052
Personal data • Name/A.S.G • Age/16 • Sex/ male • Nationality/Saudi • Occupation/student
Patient history • Chief complain: He wants to check his teeth. • Medical history: Not significant. • Family history: Not significant. • dental history & habits: Not significant.
Clinical examination • Extra oral examination: Not significant.
Clinical examination • Intra oral examination: Not significant, except for the impacted left lower canine
radiographs
radiographs • Radiograph interpretation report: An OPG showing a mixed lesion localized at the left region of the mandible extending from the distal of the lower lateral to the mesial side of the first left premolar, the lesion is large rounded and appear as RO with RL rim of fibrous capsule and extend from the apical third of the lateral to near the inferior of the mandible displacing the left impacted canine with some root resorption, the teeth #37,38 and 48 are congenitally missing. Small multilocular RL lesion at the region of the teeth # 37 & 38 may be O.K.C or early stage of amiloblastoma
definitive diagnosis • Odontoma(complex)
odontoma • Def/An odontoma in which the various odontogenic tissues appear in a haphazard arrangement that bears no resemblence to teeth. • Def/a non-neoplastic malformation, a hamartoma, consisting of a mixture of enamel, dentine and cementum. • Hamartoma: a benign tumor-like nodule composed of an overgrowth of mature cells and tissues that normally occur in the effected part, but with disorganization and often with one element predominating.
Treatment plan • The treatment of choice is the Surgical treatment and the biopsy can be done during surgery. ….but
Cont. • The patient refuse the surgery because of his financial status ,so we well proceed with a follow up approach.
Related topic Nestin expression in odontoblasts and odontogenic ectomesenchymal tissue of odontogenic tumours
Background: Nestin, one of the intermediate filaments constituting the cytoskeleton, is a marker of neural stem cells or progenitor cells. Its expression is also related to tooth development and repair of dentine.
:Aims The aim of this study was to investigate nestin expression in various odontogenic tumours and evaluate its usefulness for histopathological diagnosis.
Methods They studied formalin fixed, paraffin embedded specimens from 129 cases of odontogenic tumours and 9 of mandibular intraosseous myxoma.
After characterisation of odontogenic ectomesenchymal tissues in these tumours using antibodies to vimentin, desmin, neurofilament, and glial fibrillary acidic protein, we immunohistochemically examined nestin expression.
Results No differentiation towards muscle and nervous tissues was found in the odontogenic ectomesenchymal tissues. Although almost all the ameloblastomas and malignant ameloblastomas were negative for nestin, odontogenic ectomesenchyme in the odontogenic mixed tumours demonstrated nestin immunolocalisation, particularly in the region adjacent to the odontogenic epithelium.
Odontoblasts and their processes, pulp cells near the positive odontoblasts, and flat cells adhering to the dentine showed immunoreaction with nestin in the odontomas and odontoma‐like component in the ameloblastic fibro‐odontomas. Neoplastic cells in almost half cases of jaw myxoma and one case of odontogenic fibroma expressed nestin.
Parenchyma and stoma cells of ameloblastoma showed no nestinimmunoreactivity.
Odontoma showed nestin expression in the odontoblasts and their processes in the dental tubules. Pulp cells adjacent to the odontoblasts gave a positive reaction (arrows).
Conclusions The distribution of nestin in the odontogenic mixed tumours suggests that nestin expression in the odontogenic ectomesenchyme is upregulated by stimulation from odontogenic epithelium. In addition, nestin may also be involved in the differentiation from pulp cells to odontoblasts in odontogenic tumours. Therefore, nestin is a useful marker for the odontogenic ectomesenchyme and odontoblasts in odontogenic tumours.
Nestin, one of the intermediate filaments constituting the cytoskeleton, is a marker of neural stem cells or progenitor cells. Its expression is also related to tooth development and repair of dentine.
Referances 1-Martine S, Michael G : benign tumors of the oral cavity , Burket’s oral medicine, 11th edition (2008). 2-1. Lendahl U, Zimmerman L B, McKay R D. CNS stem cells express a new class of intermediate filament protein. Cell 1999. 60585–595.
- More by User
Oral Diagnosis Oral Medicine Oral Radiology
Oral Diagnosis Oral Medicine Oral Radiology Naval Postgraduate Dental School National Naval Dental Center Bethesda, MD Oral Diagnosis, Oral Medicine, Oral Radiology 2-year residency program Accredited by the American Board of Oral Medicine (ABOM)
1.75k views • 7 slides
Feline dentistry and oral medicine
Feline dentistry and oral medicine. CATS. Several oral diseases and lesions are specific to cats Buccal bone expansion Tooth resorptions/Resorptive lesions Viral-induced oral disease Lymphocytic-Plasmacytic Gingivostomatitis Eosinophilic granuloma complex Often idiopathic
1.31k views • 35 slides
Oral Diagnosis and Oral Medicine Competency
Oral Diagnosis and Oral Medicine Competency. Collette Lucas Patient Number 487-9-07 Pictures – 09-13-2010. The Patient . 55 year old white male Patient was diagnosed with epilepsy at age 6 after contracting measles and was in a coma for a month
481 views • 15 slides
Oral Diagnosis and Oral Medicine Competency Case
Oral Diagnosis and Oral Medicine Competency Case . Jessica Rudd Team 3 Case #: 543-6-66 Photos taken-8/2/10. Patient History. 56 year old white female Smokes cigarettes (pack/day) Is not on any medications Has no known health complications Seeking regular dental care.
307 views • 14 slides
Oral Diagnosis and Oral Medicine
Laura E. Davies FS 2010 – November 8, 2010 Team 1 Competency Case #508-4-81. Oral Diagnosis and Oral Medicine. Patient History. 76 year old female Maxillary Complete Denture and Mandibular Partial Denture Medications – Darvocet , Lexapro , Morphine, Soma
279 views • 10 slides
Oral Diagnosis & Oral Medicine Competency Case
Oral Diagnosis & Oral Medicine Competency Case. Megan Lieberenz 11/8/10. The Patient. 68 year old A frican A merican female patient. Patient presents with controlled high blood pressure, asthma, and rheumatoid arthritis. Patient chart number #471-8-97. The lesion.
298 views • 7 slides
Oral Medicine and Oral Diagnosis Competency Case
Oral Medicine and Oral Diagnosis Competency Case. David Rainwater Fall 2010. Patient Information . Pt ID: 546-5-48 10 year old M iddle Eastern male No significant health history and no medications Pt presents with a high caries rate and poor oral hygiene/home care. Presentation .
345 views • 11 slides
Oral Diagnosis and Oral Medicine Competency Case. Brad Green Pt. Chart 436-8-71. The Patient. 15 y ear old black male. Patient is in good health, taking no medications.
288 views • 8 slides

Oral Medicine Competency
Oral Medicine Competency. Brett Cotham 11/15/2010. Patient. Unknown patient with two conditions of interest. Lesion 1. Widespread red plaque like lesions on the dorsum and lateral borders of the tongue.
571 views • 18 slides
Oral Diagnosis & Oral Medicine Competency Case. Jay Joshi October 19, 2010 Team 2 Case # 547591. The Patient. 63 year old white male from Bentonville, AR
375 views • 8 slides

Oral Diagnosis & Oral Medicine Competency
Oral Diagnosis & Oral Medicine Competency. Tim Dixon Pt # 546-5-60 Pics taken 10/19/10. Patient History. 58 Year old Caucasian Male Seeking regular dental care Pt presents with type II diabetes (well controlled) Cardiovascular problems (triple bypass) Previous tobacco user
288 views • 7 slides
Oral Medicine and Diagnosis Competency Case
Oral Medicine and Diagnosis Competency Case. Jon Kinderknecht Patient 542-7-10. Patient History and Chief Complaint. 28 year old, White Female Hx of Ovarian Cysts CC Evaluation of 3 rd Molar Impactions, Displacement of Tooth #9 Patient had previous orthodontic tx during her teens.
210 views • 11 slides
Eric Tolliver 11-1-10. Oral Diagnosis & Oral Medicine Competency Case. Patient. Chart # 542-6-08 78 year old white female Patient presented with white lesion existing at least for 4 years. After questioning, the patient recalled occasional burning and sensitivity in that area .
352 views • 10 slides
Tobacco –Related Lesions Oral Medicine Block
Tobacco –Related Lesions Oral Medicine Block. Nicholas Quach Sean Young Sanaz Hamzehpour. Smoker’s Melanosis. Background Constituent of tobacco smoke stimulates increased melanin production. Common in men & women More intense in female smokers who also take conraceptive pills.
786 views • 27 slides
An Overview of Oral Medicine
An Overview of Oral Medicine. WHAT IS ORAL MEDICINE?. “The specialty of dentistry concerned with the oral health care of patients with chronic, recurrent and medically related disorders of the oral and maxillofacial region, and with their diagnosis and non-surgical management.”.
1.19k views • 91 slides
Oral Diagnosis and Medicine Competency Case
Oral Diagnosis and Medicine Competency Case. Seth Rush Team 2 UMKC SOD 2012 Chart #: 546-6-24. Patient History. 78 year old Caucasian female Pt. came if for routine dental care Pt. has a history of: broken jaw, broken ankle rectal abscess degenerative arthritis w/ pain back
275 views • 10 slides
Dermatosis Papulosa Nigra and Linear Epidermal Nevus Kirandeep Arora Team 3 Competency case # 494-1-84. Oral Diagnosis and Oral Medicine. Patient’s History. 66 year old , African American female
358 views • 14 slides
Oral Diagnosis and Oral Medicine Competency. Mary Augustyn Chart #547-8-40. Patient Description. 52 year-old white female Hypothyroidism, bipolar, osteoarthritis
258 views • 8 slides
Oral Diagnosis & Medicine
Oral Diagnosis & Medicine. Tyler Slaughter Team 2 11/15/10 Competency Case # 434-2-87. Patient History. 78 year old Hispanic Female. Occasional high blood pressure. Type II Diabetes controlled with diet and exercise. Pt. has arthritis and the beginnings of osteoporosis.
370 views • 10 slides
Oral Diagnosis and Medicine Competency Case. Team 3 Jacob Smith #433-5-01. Patient Medical History. 78 year old, white, female Stable Angina-nitro as needed Emphysema Glaucoma Cataracts Angular Cheilitis, vertical dimension too far closed. Patient Information.
217 views • 9 slides
Oral Medicine Competency. Student: Kevin Duniven Team 2 Patient: Shirley Gorrell (352-8-25). Patient: Shirley Gorrell (352-8-25). Diagnosis and Photos Taken June 17 th , 2010 Pathology Consult: Dr. Joseph Craig Whitt Lesion: Multiple Traumatic Ulcers on Large Palatal Torus.
260 views • 13 slides
Oral Diagnosis and Oral Medicine. 9/28/10 Kyle Palmer Team 3 Competency Case # 515-3-57. Patient History. 21 year old male No medical conditions No medications. Lesion Description.
293 views • 10 slides
Watch CBS News
The legal battle over the abortion pill has reached the Supreme Court. Here's what to know.
By Melissa Quinn
Updated on: March 26, 2024 / 11:25 PM EDT / CBS News
The following preview was published before the Supreme Court heard arguments in the case known as FDA v. Alliance for Hippocratic Medicine. Read coverage of the arguments here .
Washington — Twenty months after the Supreme Court ruled to return abortion policy to the states, the issue will be before the justices again on Tuesday, when they weigh a case that threatens to curtail access to a commonly used drug taken in a medication abortion .
The dispute involves a series of actions that the Food and Drug Administration took beginning in 2016 that made the pill, mifepristone, easier to obtain. A group of medical associations that oppose abortion rights have argued the agency acted unlawfully when it relaxed the rules surrounding mifepristone's use.
The justices will first have to consider a procedural issue — whether the doctors and their associations have legal standing to challenge the FDA's efforts in federal court — before deciding whether the FDA's changes complied with the law.
Hanging in the balance is the availability of the pill nationwide. States that restrict abortion access and those that protect it would all be impacted by a decision that rolls back the FDA's recent moves.
"We know that reversing the changes made in 2016 and 2021 to access mifepristone will make reproductive care more resource-intensive and less safe," said Marsha Henderson, former FDA associate commissioner for women's health, during a call with reporters. "It will also undermine FDA's congressionally granted authority and confuse patients.
Mifepristone, she said, has been regulated "more strictly and studied more intensely" than more other drugs.
The rise of medication abortions

Medication abortions made up more than half of all abortions in the U.S. in 2023, according to new research from the Guttmacher Institute, an organization that supports abortion rights. The group found that abortions done by pills accounted for 63% of all that took place within the health care system last year, a jump from 2020, when more than 5 in 10 abortions were medication abortions.
The increase in medication abortions in the three-year span followed efforts by the FDA to make mifepristone easier to obtain, namely by allowing it to be sent through the mail. The agency temporarily lifted a requirement that the drug be dispensed in-person during the COVID-19 pandemic, and made the change permanent in late 2021.
The Supreme Court is now reviewing whether the FDA acted lawfully when it made that move, along with several other steps the agency took in 2016 surrounding mifepristone's use. As part of the 2016 actions, the FDA allowed mifepristone to be taken later in a pregnancy, increasing the gestational age limit from seven to 10 weeks. It also reduced the number of in-person visits required by a patient undergoing a medication abortion from three to one, and allowed more health care providers to prescribe the drug.
"This isn't just any method of abortion," said Mary Ziegler, a University of California, Davis, law professor who is a leading historian on the abortion debate in the U.S. Not only is it the most popular, but medication abortion is "one that is uniquely important at a time when abortion is a crime in a lot of places," she continued.
Twenty-one states have either banned or restricted abortion since the Supreme Court overturned Roe v. Wade in June 2022.
How the case arrived at the Supreme Court
The FDA first approved mifepristone in 2000. It's taken with a second drug, misoprostol, to terminate an early pregnancy. In the more than 20 years since mifepristone became available in the U.S., more than 5 million women have taken the drug, according to the agency .
Serious adverse events as a result of mifepristone are "exceedingly rare," the FDA said, and studies show that hospitalization of women who have taken the drug occurs in less than 1% of cases.
But in November 2022 — more than two decades after the FDA green-lighted mifepristone — a group of medical associations that oppose abortion rights filed a lawsuit in federal district court in Texas challenging both the 2000 approval and the more recent changes. The organizations claimed the FDA did not have the authority to approve mifepristone for sale and failed to adequately consider the drug's safety and effectiveness.
The federal judge overseeing the case, U.S. District Judge Matthew Kacsmaryk, agreed that the FDA's 2000 approval and subsequent actions were likely unlawful. He blocked the FDA's initial action allowing the drug to be sold in the U.S.
But Kacsmaryk put his ruling on hold for a week, setting off a frenetic series of decisions from a federal appeals court and the Supreme Court. In April 2023, the high court preserved access to mifepristone while legal proceedings continued.
Months after the Supreme Court issued its emergency relief, the U.S. Court of Appeals for the 5th Circuit upheld the FDA's 2000 approval of the abortion pill, but said the agency violated the law with its more recent changes to the rules for its use.
The 5th Circuit made clear that its decision was preempted by the Supreme Court's earlier order protecting access, which remains in effect until the justices issue a ruling in the case.
The Justice Department and Danco Laboratories — the maker of Mifeprex, the brand-name version of mifepristone — asked the Supreme Court to review the 5th Circuit's ruling, and it agreed to do so in December. A ruling is expected by the end of June.
The arguments in the mifepristone case

Before considering whether the FDA went too far with its 2016 and 2021 changes, the Supreme Court will first weigh whether the medical associations and their members sufficiently showed that they may be injured by the agency's actions, and that those alleged injuries can be traced to the FDA's relaxing of the rules for mifepristone.
The Justice Department argued in filings that the doctors involved in the legal challenge do not prescribe the drug and haven't identified a single case where a member has been forced to complete an abortion for a woman who shows up at an emergency room with an ongoing pregnancy.
The associations' theory of how one of their members may be harmed rests on a "long and speculative chain of contingencies," Solicitor General Elizabeth Prelogar wrote. Under their theory, a woman who takes mifepristone must suffer an "exceedingly rare serious adverse event" that requires emergency care. Instead of returning to the provider who prescribed the drug, the woman must then seek care from one of the association members or show up in an emergency room where a member physician is working.
The doctor would only be forced to complete the abortion if another physician wasn't available to help, or if the member couldn't invoke federal conscience protections for some reason, Prelogar reasoned.
But lawyers for the Alliance for Hippocratic Medicine told the court that their members object not only to abortion, but also to "complicity in the process." Even completing a medication abortion when the fetus is no longer alive harms doctors who consider abortion objectionable, said the group, which is represented by the conservative legal organization Alliance Defending Freedom.
"FDA has spent decades directing women harmed by abortion drugs to emergency rooms. Many of them have sought treatment from respondent doctors," the lawyers wrote. "Now that FDA is called to account for the harm caused, the agency cannot insist that the very treatment option it directed is somehow speculative."

If the Supreme Court finds that the doctors failed to show they would suffer a concrete injury, the justices would order the case to be dismissed without deciding whether the FDA acted lawfully when it relaxed the rules for mifepristone's use.
But if they reach the key legal issues in the case, the Justice Department and Danco told the justices that the FDA's changes were lawful.
The agency relied on a "voluminous body of medical evidence" on mifepristone's use over decades when it determined that the 2016 changes would be safe, Prelogar wrote. In any event, the district court was wrong to second-guess the determinations that Congress empowered the FDA to make, she said.
"To the government's knowledge, this case marks the first time any court has restricted access to an FDA-approved drug by second-guessing FDA's expert judgment about the conditions required to assure that drug's safe use," Prelogar wrote.
Lawyers for the physicians countered that the FDA failed to give a "satisfactory explanation" for its decision to lift the in-person dispensing requirement and called the studies the agency relied on "deeply problematic."
Withdrawing the in-person visit requirement in 2021 eliminated the opportunity for health care workers to screen for ectopic pregnancies and other conditions, the associations argued. In 2016, the FDA removed "interrelated safeguards without studies" that examined the changes as a whole, they continued.
Warnings of chaos
The prospect of the Supreme Court allowing the 5th Circuit's decision to stand has raised concerns not only about the impact to medication abortion in the future, but also about what would happen to the mifepristone that's already available.
"One of the possibilities would be that mifepristone access would be limited or potentially eliminated nationwide, and that would create a lot of chaos," Ziegler said. "Even if the court did what the 5th Circuit is doing or wanted to do, that would cause a lot of issues too because all of the mifepristone on the market would be misbranded and mislabeled, and that would require both Danco and the FDA to take steps to comply with whatever the Supreme Court says."
Elisa Wells, the founder of Plan C, a website that provides information about how and where to get abortion pills, agreed that if the doctors prevail, it could cause "chaos, fear and harm" to those seeking medication abortions. But she said international telehealth providers and online vendors could help reduce the impact of a decision that unwinds the FDA's more recent changes.
"There will be an increase in demand and alternate routes of access," she told CBS News.
One of those organizations, Aid Access, is a major telemedicine provider of mifepristone, and has provided the pills to women across the U.S. Its founder, Dr. Rebecca Gomperts, said new shield laws in six states have allowed her group's prescribing to be done by domestic providers.
The shield laws offer protections to licensed health care providers in those states who prescribe and send abortion pills to patients living in states where abortion is restricted or banned.
"Doctors have the right to prescribe medication outside of the label, so in that sense, it really doesn't matter what the Supreme Court says, because that is the discretion of medical providers," Gomperts told CBS News. "We are just going to continue no matter what the decision is. It won't affect our work."
As a backup, Gomperts said Aid Access could always go back to its initial model, in which Gomperts herself prescribed mifepristone remotely from Europe.
"The reality is the pills are not going to go away," she said. "Women will always get them, and we will do whatever it takes to get them to them."
Controversy surrounding the case
Separate from concerns about the ramifications of a decision against the FDA, the dispute over mifepristone has been surrounded by controversy since the Alliance for Hippocratic Medicine brought the case 16 months ago.
The lawsuit was filed in Amarillo, Texas, where Kacsmaryk is the lone district judge and was effectively guaranteed to oversee the case. Appointed to the federal bench by former President Donald Trump in 2019, Kacsmaryk had written critically about abortion and Roe v. Wade.
The decision by the medical groups to file their case in Amarillo sparked accusations they engaged in "forum-shopping," a practice in which a party pursues a claim in the court that's most favorable to them.
The Judicial Conference of the United States, the policy-making arm of the federal judiciary, announced a new practice earlier this month in which civil cases with statewide and nationwide implications will be assigned at random. The change is meant to curb judge-shopping, according to U.S. Senior District Judge Robert Conrad, secretary of the Judicial Conference.
Studies cited by Kacsmaryk and the 5th Circuit in their rulings in favor of the Alliance for Hippocratic Medicine have also faced scrutiny. The American Civil Liberties Union warned the Supreme Court in a filing that the lower court decisions relied on "patently unreliable witnesses" and "ideologically tainted junk science."
The group said doctors who submitted declarations during an earlier stage in the case have been criticized by judges in other cases involving abortion restrictions. Also, one study referenced by Kacsmaryk about the mental health impacts of medication abortion relied on 98 anonymous blog posts from women who shared their purported experiences with medication abortion between 2007 and 2018.
Additionally, the publisher of an academic journal retracted two studies from 2021 and 2022 that were cited by Kacsmaryk after a reader raised concerns about the data and whether the authors' affiliations with organizations that oppose abortion rights presented a conflict of interest.
Two experts reviewed the articles, and they identified issues that "demonstrate a lack of scientific rigor and invalidate the authors' conclusions in whole or in part," according to the publisher, Sage Journals.
Haley Ott contributed to this report.
Melissa Quinn is a politics reporter for CBSNews.com. She has written for outlets including the Washington Examiner, Daily Signal and Alexandria Times. Melissa covers U.S. politics, with a focus on the Supreme Court and federal courts.
More from CBS News

More than 300 tried to evade airport security in the last year, TSA says

No Labels abandons plans for "unity" ticket in 2024 presidential race

Alabama hospital to stop IVF services at end of the year

More than 500 New Yorkers set to be considered as jurors for Trump trial

IMAGES
VIDEO
COMMENTS
Oral Case Presentation Guidelines for 3rd year Medicine Clerkship. A. Purpose of case presentation - to concisely summarize 4 parts of your patient's presentation: (1) history, (2) physical examination, (3) laboratory results, and (4) your understanding of these findings (i.e., clinical reasoning). The oral case presentation is a story that ...
The ability to deliver oral case presentations is a core skill for any physician. Effective oral case presentations help facilitate information transfer among physicians and are essential to delivering quality patient care. Oral case presentations are also a key component of how medical students and residents are assessed during their training.
Oral case presentations are the fundamental way in which we communicate in medicine. To do this effectively, the content should be organized, clear, succinct, and with sufficient repetition to ensure understanding. Experts build OCPs by first considering the diagnoses they have in mind, then distilling the narrative in a way that implicitly ...
The preparation for the presentation will depend on what information is to be included. Generally, oral case presentations are brief and should be limited to 5-10 minutes. This may be extended if the case is being presented as part of an assessment compared with routine everyday working ( see 'Case-based discussion' ).
Presenting patient cases is a key part of everyday clinical practice. A well delivered presentation has the potential to facilitate patient care and improve efficiency on ward rounds, as well as a means of teaching and assessing clinical competence. 1 The purpose of a case presentation is to communicate your diagnostic reasoning to the listener, so that he or she has a clear picture of the ...
Oral Medicine and Diagnosis Competency Case Jon Kinderknecht Patient 542-7-10. Patient History and Chief Complaint • 28 year old, White Female • Hx of Ovarian Cysts • CC Evaluation of 3rd Molar Impactions, Displacement of Tooth #9 • Patient had previous orthodontic tx during her teens. Lesion Description • Patient presented with slight mobility of anterior teeth • Radiographic ...
CONCLUSION. The oral case presentation is an art and a skill that has endured through the technological transformation of medicine and takes practice to master. Its most important function is for listeners to absorb key information to determine if the inferences and plans need modification. It is also a stressful experience for early learners ...
Oral communication between physicians plays a vital role in patient care. 1, 2 The oral case presentation (OCP) is a common vehicle for such communication, and its importance has been recognized by the Clerkship Directors in Internal Medicine, 3, 4 the Association of American Medical Colleges, 5 and the Accreditation Council for Graduate Medical Education. 6 The published literature, however ...
This text provides a comprehensive guide to give well-prepared, focused and concise presentations. It also allows students to discuss differential diagnosis, incorporate high-value care, educate their colleagues, and participate actively in the care of their patients. Linking in-depth discussion of the oral presentation with differential ...
PBL Information Resources and Tools for the First Year: Oral Presentation Resources This guide provides resources and strategies for finding background, clinical and drug information, including evidence-based medicine strategies and specific information for problem-based learning exercises.
The Patient Presentation Rating (PPR) tool can be used to evaluate oral case presentations, and was developed using focus groups of medical school educators from several medical disciplines including pediatrics, internal medicine, psychiatry, surgery, and neurology. Methods: The PPR includes 18 items, comprising six sections and an overall ...
Oral Diagnosis and Oral Medicine Competency Case. Oral Diagnosis and Oral Medicine Competency Case . Jessica Rudd Team 3 Case #: 543-6-66 Photos taken-8/2/10. Patient History. 56 year old white female Smokes cigarettes (pack/day) Is not on any medications Has no known health complications Seeking regular dental care. 307 views • 14 slides
Oral lichen planus (OLP) belongs to inflammatory chronic skin and/or oral pathology [ 1 ]. Studies have revealed the malignant potential of the OLP lesions, but the results are controversial, since the reported rate of OLP malignant transformation varies between 0% and 10% [ 2 ]. Microscopically, OLP lesions are characterized by the presence of ...
Oral case presentations by trainees to supervisors are core activities in academic hospitals across all disciplines and form a key milestone in US and Canadian educational frameworks. Yet despite their widespread use, there has been limited attention devoted to developing case presentations as tools for structured teaching and assessment.
The oral case presentation (OCP) is a key genre in medical communication among medical practitioners. ... The oral case presentation: what internal medicine clinician-teachers expect from clinical clerks. Teach Learn Med. 2011; 23: 58-61. Google Scholar. Haber RJ , Lingard LA . Learning oral presentation skills: a rhetorical analysis with ...
Presentation Transcript. Oral Medicine and Oral Diagnosis Competency Case David Rainwater Fall 2010. Patient Information • Pt ID: 546-5-48 • 10 year oldMiddle Eastern male • No significant health history and no medications • Pt presents with a high caries rateandpoor oral hygiene/home care. Presentation • Patient presents with a ...
Abstract. Implementation of oral case presentations (OCP) in the Immunology course at A.T. Still University-Kirksville College of Osteopathic Medicine has significantly improved written examination scores and student satisfaction with the course by enhancing its clinical relevance. With six faculty facilitators, an average class size of 172 ...
Background Oral case presentations - structured verbal reports of clinical cases - are fundamental to patient care and learner education. Despite their continued importance in a modernized medical landscape, their structure has remained largely unchanged since the 1960s, based on the traditional Subjective, Objective, Assessment, Plan (SOAP) format developed for medical records. We ...
Oral Diagnosis and Oral Medicine Competency Case. Oral Diagnosis and Oral Medicine Competency Case . Jessica Rudd Team 3 Case #: 543-6-66 Photos taken-8/2/10. Patient History. 56 year old white female Smokes cigarettes (pack/day) Is not on any medications Has no known health complications Seeking regular dental care. 307 views • 14 slides
The Supreme Court heard arguments Tuesday in a case challenging a series of actions the FDA took in 2016 and 2021 that made the abortion pill mifepristone easier to obtain.