- College Essay
- Argumentative Essay
- Expository Essay
- Narrative Essay
- Descriptive Essay
- Scholarship Essay
- Admission Essay
- Reflective Essay
- Nursing Essay
- Economics Essay
Assignments
- Term Papers
- Research Papers
- Case Studies
- Dissertation
- Presentation
- Editing Help
- Cheap Essay Writing
- How to Order
Persuasive Essay Guide
Persuasive Essay About Covid19

How to Write a Persuasive Essay About Covid19 | Examples & Tips
14 min read

People also read
A Comprehensive Guide to Writing an Effective Persuasive Essay
A Catalogue of 300 Best Persuasive Essay Topics for Students
Persuasive Essay Outline - A Complete Guide
30+ Persuasive Essay Examples To Get You Started
Read Excellent Examples of Persuasive Essay About Gun Control
How To Write A Persuasive Essay On Abortion
Learn to Write a Persuasive Essay About Business With 5 Best Examples
Check Out 14 Persuasive Essays About Online Education Examples
Persuasive Essay About Smoking - Making a Powerful Argument with Examples
Are you looking to write a persuasive essay about the Covid-19 pandemic?
Writing a compelling and informative essay about this global crisis can be challenging. It requires researching the latest information, understanding the facts, and presenting your argument persuasively.
But don’t worry! with some guidance from experts, you’ll be able to write an effective and persuasive essay about Covid-19.
In this blog post, we’ll outline the basics of writing a persuasive essay . We’ll provide clear examples, helpful tips, and essential information for crafting your own persuasive piece on Covid-19.
Read on to get started on your essay.
- 1. Steps to Write a Persuasive Essay About Covid-19
- 2. Examples of Persuasive Essay About COVID-19
- 3. Examples of Persuasive Essay About COVID-19 Vaccine
- 4. Examples of Persuasive Essay About COVID-19 Integration
- 5. Examples of Argumentative Essay About Covid 19
- 6. Examples of Persuasive Speeches About Covid-19
- 7. Tips to Write a Persuasive Essay About Covid-19
- 8. Common Topics for a Persuasive Essay on COVID-19
Steps to Write a Persuasive Essay About Covid-19
Here are the steps to help you write a persuasive essay on this topic, along with an example essay:
Step 1: Choose a Specific Thesis Statement
Your thesis statement should clearly state your position on a specific aspect of COVID-19. It should be debatable and clear. For example:
Step 2: Research and Gather Information
Collect reliable and up-to-date information from reputable sources to support your thesis statement. This may include statistics, expert opinions, and scientific studies. For instance:
- COVID-19 vaccination effectiveness data
- Information on vaccine mandates in different countries
- Expert statements from health organizations like the WHO or CDC
Step 3: Outline Your Essay
Create a clear and organized outline to structure your essay. A persuasive essay typically follows this structure:
- Introduction
- Background Information
- Body Paragraphs (with supporting evidence)
- Counterarguments (addressing opposing views)
Step 4: Write the Introduction
In the introduction, grab your reader's attention and present your thesis statement. For example:
Step 5: Provide Background Information
Offer context and background information to help your readers understand the issue better. For instance:
Step 6: Develop Body Paragraphs
Each body paragraph should present a single point or piece of evidence that supports your thesis statement. Use clear topic sentences , evidence, and analysis. Here's an example:
Step 7: Address Counterarguments
Acknowledge opposing viewpoints and refute them with strong counterarguments. This demonstrates that you've considered different perspectives. For example:
Step 8: Write the Conclusion
Summarize your main points and restate your thesis statement in the conclusion. End with a strong call to action or thought-provoking statement. For instance:
Step 9: Revise and Proofread
Edit your essay for clarity, coherence, grammar, and spelling errors. Ensure that your argument flows logically.
Step 10: Cite Your Sources
Include proper citations and a bibliography page to give credit to your sources.
Remember to adjust your approach and arguments based on your target audience and the specific angle you want to take in your persuasive essay about COVID-19.
Paper Due? Why Suffer? That's our Job!
Examples of Persuasive Essay About COVID-19
When writing a persuasive essay about the COVID-19 pandemic, it’s important to consider how you want to present your argument. To help you get started, here are some example essays for you to read:
Here is another example explaining How COVID-19 has changed our lives essay:
Let’s look at another sample essay:
Check out some more PDF examples below:
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
If you're in search of a compelling persuasive essay on business, don't miss out on our “ persuasive essay about business ” blog!
Examples of Persuasive Essay About COVID-19 Vaccine
Covid19 vaccines are one of the ways to prevent the spread of COVID-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your thoughts and persuading others.
A persuasive essay about the COVID-19 vaccine could consider the benefits of getting vaccinated as well as the potential side effects.
Below are some examples of persuasive essays on getting vaccinated for Covid-19.
Covid19 Vaccine Persuasive Essay
Persuasive Essay on Covid Vaccines
Interested in thought-provoking discussions on abortion? Read our persuasive essay about abortion blog to eplore arguments!
Examples of Persuasive Essay About COVID-19 Integration
Covid19 has drastically changed the way people interact in schools, markets, and workplaces. In short, it has affected all aspects of life. However, people have started to learn to live with Covid19.
Writing a persuasive essay about it shouldn't be stressful. Read the sample essay below to get an idea for your own essay about Covid19 integration.
Persuasive Essay About Working From Home During Covid19
Searching for the topic of Online Education? Our persuasive essay about online education is a must-read.
Examples of Argumentative Essay About Covid 19
Covid-19 has been an ever-evolving issue, with new developments and discoveries being made on a daily basis.
Writing an argumentative essay about such an issue is both interesting and challenging. It allows you to evaluate different aspects of the pandemic, as well as consider potential solutions.
Here are some examples of argumentative essays on Covid19.
Argumentative Essay About Covid19 Sample
Argumentative Essay About Covid19 With Introduction Body and Conclusion
Looking for a persuasive take on the topic of smoking? You'll find it all related arguments in out Persuasive Essay About Smoking blog!
Examples of Persuasive Speeches About Covid-19
Do you need to prepare a speech about Covid19 and need examples? We have them for you!
Persuasive speeches about Covid-19 can provide the audience with valuable insights on how to best handle the pandemic. They can be used to advocate for specific changes in policies or simply raise awareness about the virus.
Check out some examples of persuasive speeches on Covid-19:
Persuasive Speech About Covid-19 Example
Persuasive Speech About Vaccine For Covid-19
You can also read persuasive essay examples on other topics to master your persuasive techniques!
Tips to Write a Persuasive Essay About Covid-19
Writing a persuasive essay about COVID-19 requires a thoughtful approach to present your arguments effectively.
Here are some tips to help you craft a compelling persuasive essay on this topic:
- Choose a Specific Angle: Narrow your focus to a specific aspect of COVID-19, like vaccination or public health measures.
- Provide Credible Sources: Support your arguments with reliable sources like scientific studies and government reports.
- Use Persuasive Language: Employ ethos, pathos, and logos , and use vivid examples to make your points relatable.
- Organize Your Essay: Create a solid persuasive essay outline and ensure a logical flow, with each paragraph focusing on a single point.
- Emphasize Benefits: Highlight how your suggestions can improve public health, safety, or well-being.
- Use Visuals: Incorporate graphs, charts, and statistics to reinforce your arguments.
- Call to Action: End your essay conclusion with a strong call to action, encouraging readers to take a specific step.
- Revise and Edit: Proofread for grammar, spelling, and clarity, ensuring smooth writing flow.
- Seek Feedback: Have someone else review your essay for valuable insights and improvements.
Tough Essay Due? Hire Tough Writers!
Common Topics for a Persuasive Essay on COVID-19
Here are some persuasive essay topics on COVID-19:
- The Importance of Vaccination Mandates for COVID-19 Control
- Balancing Public Health and Personal Freedom During a Pandemic
- The Economic Impact of Lockdowns vs. Public Health Benefits
- The Role of Misinformation in Fueling Vaccine Hesitancy
- Remote Learning vs. In-Person Education: What's Best for Students?
- The Ethics of Vaccine Distribution: Prioritizing Vulnerable Populations
- The Mental Health Crisis Amidst the COVID-19 Pandemic
- The Long-Term Effects of COVID-19 on Healthcare Systems
- Global Cooperation vs. Vaccine Nationalism in Fighting the Pandemic
- The Future of Telemedicine: Expanding Healthcare Access Post-COVID-19
In search of more inspiring topics for your next persuasive essay? Our persuasive essay topics blog has plenty of ideas!
To sum it up,
You’ve explored great sample essays and picked up some useful tips. You now have the tools you need to write a persuasive essay about Covid-19. So don’t let doubts hold you back—start writing!
If you’re feeling stuck or need a bit of extra help, don’t worry! MyPerfectWords.com offers a professional persuasive essay writing service that can assist you. Our experienced essay writers are ready to help you craft a well-structured, insightful paper on Covid-19.
Just place your “ do my essay for me ” request today, and let us take care of the rest!
Frequently Asked Questions
What is a good title for a covid-19 essay.
A good title for a COVID-19 essay should be clear, engaging, and reflective of the essay's content. Examples include:
- "The Impact of COVID-19 on Global Health"
- "How COVID-19 Has Transformed Our Daily Lives"
- "COVID-19: Lessons Learned and Future Implications"
How do I write an informative essay about COVID-19?
To write an informative essay about COVID-19, follow these steps:
- Choose a specific focus: Select a particular aspect of COVID-19, such as its transmission, symptoms, or vaccines.
- Research thoroughly: Gather information from credible sources like scientific journals and official health organizations.
- Organize your content: Structure your essay with an introduction, body paragraphs, and a conclusion.
- Present facts clearly: Use clear, concise language to convey information accurately.
- Include visuals: Use charts or graphs to illustrate data and make your essay more engaging.
How do I write an expository essay about COVID-19?
To write an expository essay about COVID-19, follow these steps:
- Select a clear topic: Focus on a specific question or issue related to COVID-19.
- Conduct thorough research: Use reliable sources to gather information.
- Create an outline: Organize your essay with an introduction, body paragraphs, and a conclusion.
- Explain the topic: Use facts and examples to explain the chosen aspect of COVID-19 in detail.
- Maintain objectivity: Present information in a neutral and unbiased manner.
- Edit and revise: Proofread your essay for clarity, coherence, and accuracy.

Write Essay Within 60 Seconds!

Caleb S. has been providing writing services for over five years and has a Masters degree from Oxford University. He is an expert in his craft and takes great pride in helping students achieve their academic goals. Caleb is a dedicated professional who always puts his clients first.
Struggling With Your Paper?
Get a custom paper written at
With a FREE Turnitin report, and a 100% money-back guarantee
LIMITED TIME ONLY!
Keep reading

OFFER EXPIRES SOON!
Persuasive Essay Writing
Persuasive Essay About Covid 19

Top Examples of Persuasive Essay about Covid-19
Published on: Jan 10, 2023
Last updated on: Oct 18, 2024

People also read
How to Write a Persuasive Essay: A Step-by-Step Guide
Easy and Unique Persuasive Essay Topics with Tips
The Basics of Crafting an Outstanding Persuasive Essay Outline
Ace Your Next Essay With These Persuasive Essay Examples!
Persuasive Essay About Gun Control - Best Examples for Students
Learn How To Write An Impressive Persuasive Essay About Business
Learn How to Craft a Compelling Persuasive Essay About Abortion With Examples!
Make Your Point: Tips and Examples for Writing a Persuasive Essay About Online Education
Learn How To Craft a Powerful Persuasive Essay About Bullying
Craft an Engaging Persuasive Essay About Smoking: Examples & Tips
Learn How to Write a Persuasive Essay About Social Media With Examples
Craft an Effective Argument: Examples of Persuasive Essay About Death Penalty
Share this article
In these recent years, covid-19 has emerged as a major global challenge. It has caused immense global economic, social, and health problems.
Writing a persuasive essay on COVID-19 can be tricky with all the information and misinformation.
But don't worry! We have compiled a list of persuasive essay examples during this pandemic to help you get started.
Here are some examples and tips to help you create an effective persuasive essay about this pandemic.
On This Page On This Page -->
Examples of Persuasive Essay About Covid-19
The coronavirus pandemic has everyone on edge. You can expect your teachers to give you an essay about covid-19. You might be overwhelmed about what to write in an essay.
Worry no more!
Here are a few examples to help get you started.
Persuasive Essay About Covid-19 Pandemic
Sample Of Persuasive Essay About Covid-19
Persuasive Essay About Covid-19 In The Philippines - Example
Check out some more persuasive essay examples to get more inspiration and guidance.
Examples of Persuasive Essay About the Covid-19 Vaccine
With so much uncertainty surrounding the Covid-19 vaccine, it can be challenging for students to write a persuasive essay about getting vaccinated.
Here are a few examples of persuasive essays about vaccination against covid-19.
Check these out to learn more.
Persuasive essay on the covid-19 vaccine
Tough Essay Due? Hire a Writer!

Examples of Persuasive Essay About Covid-19 Integration
Writing a persuasive essay on Covid-19 integration doesn't have to be stressful or overwhelming.
With the right approach and preparation, you can write an essay that will get them top marks!
Here are a few samples of compelling persuasive essays. Give them a look and get inspiration for your next essay.
Integration of Covid-19 Persuasive essay
Integration of Covid-19 Persuasive essay sample
Examples of Argumentative Essay About Covid-19
Writing an argumentative essay can be a daunting task, especially when the topic is as broad as the novel coronavirus pandemic.
Read the following examples of how to make a compelling argument on covid-19.
Argumentative essay on Covid-19
Argumentative Essay On Covid-19
Examples of Persuasive Speeches About Covid-19
Writing a persuasive speech about anything can seem daunting. However, writing a persuasive speech about something as important as the Covid-19 pandemic doesnât have to be difficult.
So let's explore some examples of perfectly written persuasive essays.
Persuasive Speech About Covid-19 Example
Tips to Write a Persuasive Essay
Here are seven tips that can help you create a strong argument on the topic of covid-19.
Check out this informative video to learn more about effective tips and tricks for writing persuasive essays.
1. Start with an attention-grabbing hook:
Use a quote, statistic, or interesting fact related to your argument at the beginning of your essay to draw the reader in.
2. Make sure you have a clear thesis statement:
A thesis statement is one sentence that expresses the main idea of your essay. It should clearly state your stance on the topic and provide a strong foundation for the rest of your content.
3. Support each point with evidence:
To make an effective argument, you must back up each point with credible evidence from reputable sources. This will help build credibility and validate your claims throughout your paper.
4. Use emotional language and tone:
Emotional appeals are powerful tools to help make your argument more convincing. Use appropriate language for the audience and evokes emotion to draw them in and get them on board with your claims.
5. Anticipate counterarguments:
Use proper counterarguments to effectively address all point of views.
Acknowledge opposing viewpoints and address them directly by providing evidence or reasoning why they are wrong.
6. Stay focused:
Keep your main idea in mind throughout the essay, making sure all of your arguments support it. Donât stray off-topic or introduce unnecessary information that will distract from the purpose of your paper.
7. Conclude strongly:
Make sure you end on a strong note. Reemphasize your main points, restate your thesis statement, and challenge the reader to respond or take action in some way. This will leave a lasting impression in their minds and make them more likely to agree with you.
Writing an effective persuasive essay is a piece of cake with our guide and examples. Check them out to learn more!

Tough Essay Due? Hire Tough Writers!
We hope that you have found the inspiration to write your next persuasive essay about covid-19.
However, If you're overwhelmed by the task, don't worry - our professional essay writing service is here to help.
Our expert and experienced persuasive essay writer can help you write a persuasive essay on covid-19 that gets your readers' attention.
Our professional essay writer can provide you with all the resources and support you need to craft a well-written, well-researched essay. Our essay writing service offers top-notch quality and guaranteed results.
Frequently Asked Questions
How do you begin a persuasive essay.
To begin a persuasive essay, you must choose a topic you feel strongly about and formulate an argument or position. Start by researching your topic thoroughly and then formulating your thesis statement.
What are good topics for persuasive essays?
Good topics for persuasive essays include healthcare reform, gender issues, racial inequalities, animal rights, environmental protection, and political change. Other popular topics are social media addiction, internet censorship, gun control legislation, and education reform.
What impact does COVID-19 have on society?
The COVID-19 pandemic has had a major impact on society worldwide. It has changed the way we interact with one another. The pandemic has also caused economic disruption, forcing many businesses to close or downsize their operations.
Cathy A. (Literature, Education)
For more than five years now, Cathy has been one of our most hardworking authors on the platform. With a Masters degree in mass communication, she knows the ins and outs of professional writing. Clients often leave her glowing reviews for being an amazing writer who takes her work very seriously.
Need Help With Your Essay?
Also get FREE title page, Turnitin report, unlimited revisions, and more!
Keep reading

OFF ON CUSTOM ESSAYS
Legal & Policies
- Privacy Policy
- Cookies Policy
- Terms of Use
- Refunds & Cancellations
- Our Writers
- Success Stories
- Our Guarantees
- Affiliate Program
- Referral Program
- AI Essay Writer
Disclaimer: All client orders are completed by our team of highly qualified human writers. The essays and papers provided by us are not to be used for submission but rather as learning models only.
- Share full article
Advertisement
Supported by
The Morning Newsletter
Vaccine Persuasion
Many vaccine skeptics have changed their minds.

By David Leonhardt
When the Kaiser Family Foundation conducted a poll at the start of the year and asked American adults whether they planned to get vaccinated, 23 percent said no.
But a significant portion of that group — about one quarter of it — has since decided to receive a shot. The Kaiser pollsters recently followed up and asked these converts what led them to change their minds . The answers are important, because they offer insight into how the millions of still unvaccinated Americans might be persuaded to get shots, too.
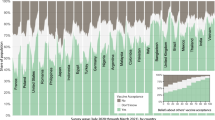
First, a little background: A few weeks ago, it seemed plausible that Covid-19 might be in permanent retreat, at least in communities with high vaccination rates. But the Delta variant has changed the situation. The number of cases is rising in all 50 states .
Although vaccinated people remain almost guaranteed to avoid serious symptoms, Delta has put the unvaccinated at greater risk of contracting the virus — and, by extension, of hospitalization and death. The Covid death rate in recent days has been significantly higher in states with low vaccination rates than in those with higher rates:
(For more detailed state-level charts, see this piece by my colleagues Lauren Leatherby and Amy Schoenfeld Walker. The same pattern is evident at the county level, as the health policy expert Charles Gaba has been explaining on Twitter.)
Nationwide, more than 99 percent of recent deaths have occurred among unvaccinated people, and more than 97 percent of recent hospitalizations have occurred among the unvaccinated, according to the C.D.C. “Look,” President Biden said on Friday, “the only pandemic we have is among the unvaccinated.”
The three themes
What helps move people from vaccine skeptical to vaccinated? The Kaiser polls point to three main themes.
(The themes apply to both the 23 percent of people who said they would not get a shot, as well as to the 28 percent who described their attitude in January as “wait and see.” About half of the “wait and see” group has since gotten a shot.)
1. Seeing that millions of other Americans have been safely vaccinated.
Consider these quotes from Kaiser’s interviews :
“It was clearly safe. No one was dying.” — a 32-year-old white Republican man in South Carolina “I went to visit my family members in another state and everyone there had been vaccinated with no problems.” — a 63-year-old Black independent man in Texas “Almost all of my friends were vaccinated with no side effects.” — a 64-year-old Black Democratic woman in Tennessee
This suggests that emphasizing the safety of the vaccines — rather than just the danger of Covid, as many experts (and this newsletter) typically do — may help persuade more people to get a shot.
A poll of vaccine skeptics by Echelon Insights, a Republican firm, points to a similar conclusion. One of the most persuasive messages, the skeptics said, was hearing that people have been getting the vaccine for months and it is “working very well without any major issues.”
2. Hearing pro-vaccine messages from doctors, friends and relatives.
For many people who got vaccinated, messages from politicians, national experts and the mass media were persuasive. But many other Americans — especially those without a college degree — don’t trust mainstream institutions. For them, hearing directly from people they know can have a bigger impact.
“Hearing from experts,” as Mollyann Brodie, who oversees the Kaiser polls, told me, “isn’t the same as watching those around you or in your house actually go through the vaccination process.”
Here are more Kaiser interviews:
“My daughter is a doctor and she got vaccinated, which was reassuring that it was OK to get vaccinated.” — a 64-year-old Asian Democratic woman in Texas “Friends and family talked me into it, as did my place of employment.” — a 28-year-old white independent man in Virginia “My husband bugged me to get it and I gave in.” — a 42-year-old white Republican woman in Indiana “I was told by my doctor that she strongly recommend I get the vaccine because I have diabetes.” — a 47-year-old white Republican woman in Florida
These comments suggest that continued grass-roots campaigns may have a bigger effect at this stage than public-service ad campaigns. The one exception to that may be prominent figures from groups that still have higher vaccine skepticism, like Republican politicians and Black community leaders.
3. Learning that not being vaccinated will prevent people from doing some things.
There is now a roiling debate over vaccine mandates , with some hospitals, colleges, cruise-ship companies and others implementing them — and some state legislators trying to ban mandates. The Kaiser poll suggests that these requirements can influence a meaningful number of skeptics to get shots, sometimes just for logistical reasons.
“Hearing that the travel quarantine restrictions would be lifted for those people that are vaccinated was a major reason for my change of thought.” — a 43-year-old Black Democratic man in Virginia “To see events or visit some restaurants, it was easier to be vaccinated.” — a 39-year-old white independent man in New Jersey “Bahamas trip required a COVID shot.” — a 43-year-old Hispanic independent man in Pennsylvania
More on the virus:
Indonesia is the pandemic’s new epicenter , with the highest count of new infections.
After Los Angeles County reinstated indoor mask requirements, the sheriff said the rules were “not backed by science” and refused to enforce them.
The American tennis star Coco Gauff tested positive and will not participate in the Tokyo Olympics.
THE LATEST NEWS
Remote voting in Congress has become a personal and political convenience for House members of both parties.
The Times’s Mark Leibovich profiled Ron Klain , Biden’s chief of staff, whom some Republicans call “Prime Minister Klain.”
Flooding in Western Europe killed at least 183 people, with hundreds still missing . “The German language has no words, I think, for the devastation,” Chancellor Angela Merkel said.
Burned-out landscapes and dwindling water supplies are threatening Napa Valley, the heart of America’s wine industry .
Here’s the latest on the extreme heat and wildfires in the West.
Other Big Stories
A Japanese court sentenced two Americans to prison for helping the former Nissan leader Carlos Ghosn escape from Japan in a box.
Although the Me Too movement heightened awareness of the prevalence of sexual assault, the struggle to prosecute cases has endured.
Mat George, co-host of the podcast “She Rates Dogs,” died after a hit-and-run in Los Angeles. He was 26 .
The green economy is shaping up to be filled with grueling work schedules, few unions, middling wages and limited benefits, The Times’s Noam Scheiber reports .
Several governments use a cyberespionage tool to target rights activists, dissidents and journalists, leaked data suggests.
Tadej Pogacar, a 22-year-old cycling phenom from Slovenia, won his second straight Tour de France .
Bret Stephens and Gail Collins discuss big government .
MORNING READS
Into the woods: Smartphones are steering novice hikers onto trails they can’t handle .
Driven: Maureen Dowd meets Dara Khosrowshahi, Uber’s “weirdly normal” C.E.O.
The Games: Has the world had enough of the Olympics ?
A Times classic: Try this science-based 7-minute workout .
Quiz time: The average score on our most recent news quiz is 8.1 out of 11. See if you can do better .
Lives Lived: Gloria Richardson famously brushed aside a National Guardsman’s bayonet as she led a campaign for civil rights in Cambridge, Md. She died at 99 .
ARTS AND IDEAS
What matters in a name sign.
Shortly after the 2020 presidential election, five women teamed up to assign Vice President-elect Kamala Harris a name sign — the equivalent of a person’s name in American Sign Language.
The women — Ebony Gooden, Kavita Pipalia, Smita Kothari, Candace Jones and Arlene Ngalle-Paryani — are members of the “capital D Deaf community,” a term some deaf people use to indicate they embrace deafness as a cultural identity and communicate primarily through ASL.
Through social media, people submitted suggestions and put the entries to a vote. The result: A name sign that draws inspiration, among other things, from the sign for “lotus flower” — the translation of “Kamala” in Sanskrit — and the number three, highlighting Harris’s trifecta as the first Black, Indian and female vice president.
“Name signs given to political leaders are usually created by white men, but for this one we wanted to not only represent women, but diversity — Black women, Indian women,” Kothari said. Read more about it, and see videos of the signs . — Sanam Yar, a Morning writer
PLAY, WATCH, EAT
What to cook.
Debate ham and pineapple pizza all you want. There’s no denying the goodness of caramelized pineapple with sausages .
What to Watch
Based on books by R.L. Stine, the “Fear Street” trilogy on Netflix offers gore and nostalgia.
“ Skipped History ,” a comedy web series, explores overlooked people and events that shaped America.
Now Time to Play
The pangram from Friday’s Spelling Bee was lengthened . Here is today’s puzzle — or you can play online .
Here’s today’s Mini Crossword , and a clue: Hot tub nozzles (four letters).
If you’re in the mood to play more, find all our games here .
Thanks for spending part of your morning with The Times. See you tomorrow. — David
P.S. Ashley Wu , who has worked for Apple and New York magazine, has joined The Times as a graphics editor for newsletters. You’ll see her work in The Morning soon.
Here’s today’s print front page .
“ The Daily ” is about booster shots. On the Book Review podcast , S.A. Cosby talks about his new novel.
Lalena Fisher, Claire Moses, Ian Prasad Philbrick, Tom Wright-Piersanti and Sanam Yar contributed to The Morning. You can reach the team at [email protected] .
Sign up here to get this newsletter in your inbox .
David Leonhardt writes The Morning, The Times's main daily newsletter. Previously at The Times, he was the Washington bureau chief, the founding editor of The Upshot, an Op-Ed columnist, and the head of The 2020 Project, on the future of the Times newsroom. He won the 2011 Pulitzer Prize for commentary. More about David Leonhardt
Lessons learned: What makes vaccine messages persuasive

You’re reading Lessons Learned, which distills practical takeaways from standout campaigns and peer-reviewed research in health and science communication. Want more Lessons Learned? Subscribe to our Call to Action newsletter .
Vaccine hesitancy threatened public health’s response to the COVID-19 pandemic. Scientists at the University of Maryland recently reviewed 47 randomized controlled trials to determine how COVID-19 communications persuaded—or failed to persuade—people to take the vaccine. ( Health Communication , 2023 DOI: 10.1080/10410236.2023.2218145 ).
What they learned: Simply communicating about the vaccine’s safety or efficacy persuaded people to get vaccinated. Urging people to follow the lead of others, by highlighting how many millions were already vaccinated or even trying to induce embarrassment, was also persuasive.
Why it matters: Understanding which message strategies are likely to be persuasive is crucial.
➡️ Idea worth stealing: The authors found that a message’s source didn’t significantly influence its persuasiveness. But messages were more persuasive when source and receivers shared an identity, such as political affiliation.
What to watch: How other formats, such as interactive chatbots and videos, might influence persuasiveness. And whether message tailoring could persuade specific population subgroups.
News from the School

Nurturing student entrepreneurs

40 years after Bhopal disaster, suffering continues

Meet the Dean

Making health care more affordable

Coronavirus Disease 2019
The 7 best tactics to persuade the vaccine-hesitant, trying to convince someone to get vaccinated here are science’s best answers..
Posted June 23, 2021 | Reviewed by Ekua Hagan
- Take our Your Mental Health Today Test
- Find a therapist near me
- Some of the most effective tactics for persuading the vaccine-hesitant were identified by researchers Stacy Wood and Kevin Schulman.
- Ways to convince someone who is hesitant to get vaccinated include sharing positive anecdotes and reminding them of the grim alternatives.
- Those who resist all vaccines need to be approached differently than others if they are to change their minds.
Like many, you might still be trying to convince a friend or family member to get vaccinated. In fact, I had this very issue myself. However, after using advice prescribed by this article from The New England Journal of Medicine , I was able to convince an older conservative male (one of the most vaccine-hesitant populations) to get his vaccine.
Researchers Stacy Wood and Kevin Schulman reviewed much of the behavioral research in the field to identify some of the most effective strategies for persuading the vaccine-hesitant. And although each person’s circumstance will dictate which approach will be most effective — and how it's implemented — these different strategies are some of the best science can offer.
1. Use Analogies to Explain the Vaccine
The vaccine can seem confusing or dangerous to people. So, comparing key aspects of the vaccine to examples they can understand (i.e., analogies) can be very effective.
For example, if someone doesn’t understand how the vaccine works, you can describe mRNA as “giving blueprints” to your immune cells so they know how to defeat the virus. Or, if the person is concerned about side effects, you can point out that vaccinated people have a better chance of being struck by lightning than dying from COVID-19.
2. Promote Control Through Compromise
Nobody likes to be forced into making a decision — which is how some people feel about getting this vaccine. However, research shows that if you can reduce the external pressure to do something, people actually become more likely to do it.
To help alleviate these feelings, try to emphasize how the person has control over which vaccine they’d like to get. Or even consider making a deal with the person: If they get vaccinated, you’ll do something they think is good for you that you’ve resisted. Helping to make the person’s decision feel less forced upon them can actually make them more willing to get it!
3. Find a Common Enemy With the Person
Sometimes, there is no truer saying than “the enemy of my enemy is my friend.” And in the case of the COVID-19 vaccine, you can use this to your advantage. For example, considering how much damage this pandemic has done to the economy, you can point out how this person and the vaccine are on the same side — they’re both trying to get the economy back in action. Or, if there’s another country this person feels “in competition ” with, you can frame this person’s vaccination as national support in the vaccination race against this other country.
4. Combat Anecdotal Evidence With Your Own
For some individuals, their negativity toward vaccinations is based more on their feelings and emotions rather than any thoughts or reasons. For example, maybe they heard about someone who had a bad reaction to the vaccine. Rather than try to convince this person with statistics, it can actually be more effective to share positive anecdotes of your own. For example, you can share instances of people who had mild to no side effects from the vaccines, or stories about vaccinated people who didn’t catch COVID-19 in groups where it was otherwise spread.
5. Increase Awareness of Others Who Are Vaccinated
A classic finding from persuasion research is the power of the crowd. If most people are doing something, it is very compelling information that this person should do it, too. To that effect, try to point out respected friends or family members who have been vaccinated. Or similarly, if there is a public individual or aspirational role model the person likes, try to find one (or more) who have been vaccinated. Showing this individual that people they respect (e.g., top leaders from their preferred political party) are vaccinated can be very convincing.
6. Remind Them of Possible Regrets
Although a little grim, sometimes you need to remind people of the serious consequences of catching COVID-19. Activating these potential futures (e.g., where they have permanent organ damage because of COVID-19, or they feel guilt from spreading the disease to vulnerable family members) can be a powerful motivator. Of course, you don’t want to guilt-trip the person too much, but reminding them of their possible regret could help them understand the severity and value of getting vaccinated.
7. Point Out Events They Could Miss (Create FOMO)
On a lighter note, rather than focusing on all the negative events that could occur from catching COVID-19, focus on the positive events they would miss out on by not being vaccinated.
For example, you could remind them of the various bars and events that are only open to those who are vaccinated. Or, if it’s someone close to you, you could even create a great experience for them if they do get vaccinated. For example, you could tell them that you’ll take them for a night out, pamper them for a day, or offer any other kind of incentive if they’re willing to get vaccinated.

Now, of course, these aren’t all the strategies one could potentially employ, but they are some of the most proven. In implementing any of them, though, it’s important to remember that each person is different. So the advice above might require tweaking for who it’s being used on.
And of course, there will be some people who deny vaccines altogether (and they require different approaches than even these). However, for people who aren’t staunchly anti-vaccine — just maybe toward this COVID-19 one — hopefully something above will help you reach them.
Wood, S., & Schulman, K. (2021). Beyond Politics—Promoting Covid-19 Vaccination in the United States. The New England Journal of Medicine. 384 (23). DOI: 10.1056/NEJMms2033790

Jake Teeny , Ph.D. , is an assistant professor of marketing in the Kellogg School of Management at Northwestern University, where he researches persuasion, metacognition, and consumer behavior.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

It’s increasingly common for someone to be diagnosed with a condition such as ADHD or autism as an adult. A diagnosis often brings relief, but it can also come with as many questions as answers.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

COVID vaccine hesitancy: spell out the personal rather than collective benefits to persuade people — new research
Professor of Clinical Psychology, University of Oxford
Disclosure statement
Daniel Freeman receives funding from the National Institute for Health Research and the Medical Research Council. The current research was funded by the NIHR Oxford Biomedical Research Centre (BRC) and the NIHR Oxford Health BRC.
University of Oxford provides funding as a member of The Conversation UK.
View all partners
Approximately 10% of UK adults say they will never get vaccinated against COVID-19 or will avoid doing so for as long as possible. Scientists call this group the “vaccine hesitant”, though hesitancy may not seem the right term to describe views often held with clear conviction. People who are vaccine hesitant have often thought long and hard about whether to take a COVID-19 vaccine.
How can such views be shifted? Ideally, one would sit down with people, listen and discuss. In reality, public health campaigners have only mass messaging at their disposal: information disseminated through billboards, TV slots and social media. These are crude tools for tackling sometimes deeply ingrained personal beliefs. What messages delivered through them might really make a difference?
Over the past year, the Oxford Coronavirus Explanations, Attitudes and Narratives Surveys (OCEANS) team has tried to answer this question. We’ve worked to form a psychological explanation for vaccine hesitancy by canvassing the views of people for, against and undecided about vaccines.
We’ve found that hesitancy emerges from a nexus of beliefs , the most important being scepticism about the collective benefits of vaccination. The hesitant don’t accept that taking a vaccine means we’re all better off. They also tend to believe that COVID-19 isn’t a big danger to their health. And they worry that vaccines may be ineffective or downright harmful. The rapid development of COVID-19 vaccines reinforces these concerns.
Behind these specific ideas often lies mistrust. People who are hesitant tend to be suspicious of authority . But while it’s wise to make judgements based on evidence rather than blithely accepting what we’re told, in many cases we’ve found that the vaccine hesitant are susceptible to misinformation.
Fuelling this may be a sense of marginalisation. Vaccine-hesitant people are a little more likely to believe that they’re of lower social status . Feeling that society doesn’t care about them, they are unwilling to trust what they’re told by politicians and scientists.
Getting personal
Equipped with these insights, we decided to see whether we could craft messages that might shift negative attitudes. If people don’t appreciate the collective benefits of vaccination, let’s persuasively set out the case. Let’s explain that vaccines make it less likely we’ll pass on the virus, helping to protect others, particularly those especially vulnerable to the virus. And let’s make it clear that by reducing the risk of getting severely ill, we can help the country bounce back as quickly as possible. That should help shift attitudes, right?
To find out, in early February we surveyed nearly 19,000 UK adults, carefully selected to be representative for age, gender, ethnicity, income and region. Participants were then randomly asked to read one of ten texts about COVID-19 vaccines.

Some texts focused the collective benefits of vaccination, some on the personal benefits, some on safety and some a combination of messages. One text contained only basic information about the vaccine and didn’t provide any detail on benefits, and was used as a control. After reading their allocated text, participants completed a questionnaire on their willingness to be vaccinated for COVID-19.
The results were surprising. Previous surveys had suggested beliefs about the collective benefits of vaccination were pivotal to driving uptake. The extent to which people bought into this narrative seemed to determine their willingness to take a vaccine.
But the text that was most likely to change the minds of the vaccine hesitant (when compared to the control) emphasised not the collective but the personal benefits of vaccination. It pointed out that you can’t be sure that you won’t get seriously ill or struggle with long-term COVID-related problems, and that vaccination will minimise your chances of falling ill.
Months of media coverage in the UK has instead focused on collective responsibility – that we owe it to our fellow citizens to get vaccinated. But for the sceptical 10%, this hasn’t cut through, which is perhaps to be expected. If you think vaccines are unsafe, then you’ll be worried about what getting the jab will do to you. Your decision making then becomes dominated by personal risk.
The best way to counter these concerns, therefore, is to highlight the opposite: personal benefits – and our new research suggests this could well work. It’s also probable that for a group that’s more likely to feel socially excluded, messages that focus on the personal rather than collective ramifications of COVID-19 will be more compelling.

What about the view that the vaccines have been developed too quickly? It’s an understandable fear: these vaccines have been produced with unparalleled speed . In response to this, one text in our study explained that the speed of development reflects the exceptional commitment, investment and cooperation of scientists, governments, public health organisations and pharmaceutical companies – as well as of the tens of thousands of members of the public who volunteered to test the vaccines.
This text noted too that side-effects that affect a significant proportion of people don’t suddenly appear months and years after vaccination. Because of the way vaccines work – quickly training the body’s immune system to fight off a virus – any issues arise within a month and usually much sooner. Happily, this information did seem to reassure people and helped reduce hesitancy.
COVID-19 is unlikely to disappear in the foreseeable future, which means vaccination messaging will remain of critical importance. When it comes to persuading the vaccine hesitant, our research shows that we need to listen, understand concerns and address them seriously. No message will be truly effective if the messenger has not earned trust, nor if it doesn’t account for the desires and worries of those receiving it.
- Coronavirus
- Vaccine hesitancy
- Coronavirus insights

Editorial Internship

Research Fellow in Dark Matter Particle Phenomenology

Integrated Management of Invasive Pampas Grass for Enhanced Land Rehabilitation

Deputy Vice-Chancellor (Indigenous Strategy and Services)
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 14 May 2021

Public attitudes toward COVID-19 vaccination: The role of vaccine attributes, incentives, and misinformation
- Sarah Kreps 1 ,
- Nabarun Dasgupta 2 ,
- John S. Brownstein 3 , 4 ,
- Yulin Hswen 5 &
- Douglas L. Kriner ORCID: orcid.org/0000-0002-9353-2334 1
npj Vaccines volume 6 , Article number: 73 ( 2021 ) Cite this article
20k Accesses
82 Citations
43 Altmetric
Metrics details
- Health care
- Translational research
While efficacious vaccines have been developed to inoculate against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; also known as COVID-19), public vaccine hesitancy could still undermine efforts to combat the pandemic. Employing a survey of 1096 adult Americans recruited via the Lucid platform, we examined the relationships between vaccine attributes, proposed policy interventions such as financial incentives, and misinformation on public vaccination preferences. Higher degrees of vaccine efficacy significantly increased individuals’ willingness to receive a COVID-19 vaccine, while a high incidence of minor side effects, a co-pay, and Emergency Use Authorization to fast-track the vaccine decreased willingness. The vaccine manufacturer had no influence on public willingness to vaccinate. We also found no evidence that belief in misinformation about COVID-19 treatments was positively associated with vaccine hesitancy. The findings have implications for public health strategies intending to increase levels of community vaccination.
Similar content being viewed by others
Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA
Vaccine hesitancy and monetary incentives
Providing normative information increases intentions to accept a COVID-19 vaccine
Introduction.
In less than a year, an array of vaccines was developed to bring an end to the SARS-CoV-2 pandemic. As impressive as the speed of development was the efficacy of vaccines such as Moderna and Pfizer, which are over 90%. Despite the growing availability and efficacy, however, vaccine hesitancy remains a potential impediment to widespread community uptake. While previous surveys indicate that overall levels of vaccine acceptance may be around 70% in the United States 1 , the case of Israel may offer a cautionary tale about self-reported preferences and vaccination in practice. Prospective studies 2 of vaccine acceptance in Israel showed that about 75% of the Israeli population would vaccinate, but Israel’s initial vaccination surge stalled around 42%. The government, which then augmented its vaccination efforts with incentive programs, attributed unexpected resistance to online misinformation 3 .
Research on vaccine hesitancy in the context of viruses such as influenza and measles, mumps, and rubella, suggests that misinformation surrounding vaccines is prevalent 4 , 5 . Emerging research on COVID-19 vaccine preferences, however, points to vaccine attributes as dominant determinants of attitudes toward vaccination. Higher efficacy is associated with greater likelihood of vaccinating 6 , 7 , whereas an FDA Emergency Use Authorization 6 or politicized approval timing 8 is associated with more hesitancy. Whether COVID-19 misinformation contributes to vaccine preferences or whether these attributes or policy interventions such as incentives play a larger role has not been studied. Further, while previous research has focused on a set of attributes that was relevant at one particular point in time, the evidence and context about the available vaccines has continued to shift in ways that could shape public willingness to accept the vaccine. For example, governments, employers, and economists have begun to think about or even devise ways to incentivize monetarily COVID-19 vaccine uptake, but researchers have not yet studied whether paying people to receive the COVID-19 vaccine would actually affect likely behavior. As supply problems wane and hesitancy becomes a limiting factor, understanding whether financial incentives can overcome hesitancy becomes a crucial question for public health. Further, as new vaccines such as Johnson and Johnson are authorized, knowing whether the vaccine manufacturer name elicits or deters interest in individuals is also important, as are the corresponding efficacy rates of different vaccines and the extent to which those affect vaccine preferences. The purpose of this study is to examine how information about vaccine attributes such as efficacy rates, the incidence of side effects, the nature of the governmental approval process, identity of the manufacturers, and policy interventions, including economic incentives, affect intention to vaccinate, and to examine the association between belief in an important category of misinformation—false claims concerning COVID-19 treatments—and willingness to vaccinate.
General characteristics of study population
Table 1 presents sample demographics, which largely reflect those of the US population as a whole. Of the 1335 US adults recruited for the study, a convenience sample of 1100 participants consented to begin the survey, and 1096 completed the full questionnaire. The sample was 51% female; 75% white; and had a median age of 43 with an interquartile range of 31–58. Comparisons of the sample demographics to those of other prominent social science surveys and U.S. Census figures are shown in Supplementary Table 1 .
Vaccination preferences
Each subject was asked to evaluate a series of seven hypothetical vaccines. For each hypothetical vaccine, our conjoint experiment randomly assigned values of five different vaccine attributes—efficacy, the incidence of minor side effects, government approval process, manufacturer, and cost/financial inducement. Descriptions of each attribute and the specific levels used in the experiment are summarized in Table 2 . After seeing the profile of each vaccine, the subject was asked whether she would choose to receive the vaccine described, or whether she would choose not to be vaccinated. Finally, subjects were asked to indicate how likely they would be to take the vaccine on a seven-point likert scale.
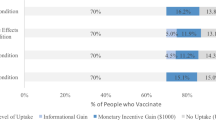
Across all choice sets, in 4419 cases (58%) subjects said they would choose the vaccine described in the profile rather than not being vaccinated. As shown in Fig. 1 , several characteristics of the vaccine significantly influenced willingness to vaccinate.
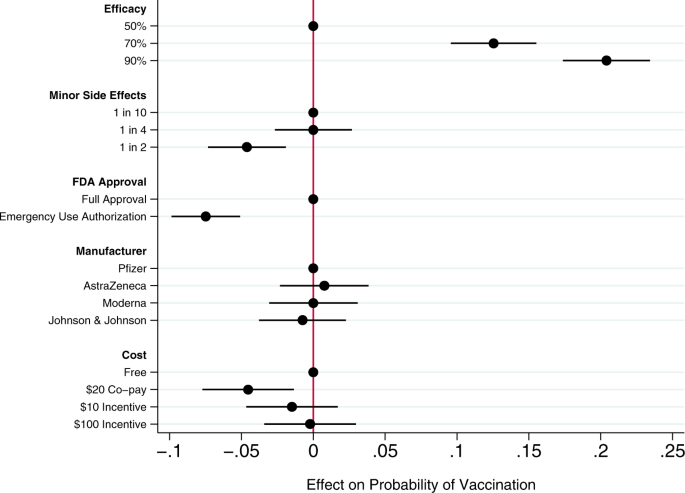
Circles present the estimated effect of each attribute level on the probability of a subject accepting vaccination from the attribute’s baseline level. Horizontal lines through points indicate 95% confidence intervals. Points without error bars denote the baseline value for each attribute. The average marginal component effects (AMCEs) are the regression coefficients reported in model 1 of Table 3 .
Efficacy had the largest effect on individual vaccine preferences. An efficacy rate of 90% increased uptake by about 20% relative to the baseline at 50% efficacy. Even a high incidence of minor side effects (1 in 2) had only a modest negative effect (about 5%) on willingness to vaccinate. Whether the vaccine went through full FDA approval or received an Emergency Use Authorization (EUA), an authority that allows the Food and Drug Administration mechanisms to accelerate the availability and use of treatments or medicines during medical emergencies 9 , significantly influenced willingness to vaccinate. An EUA decreased the likelihood of vaccination by 7% compared to a full FDA authorization; such a decline would translate into about 23 million Americans. While a $20 co-pay reduced the likelihood of vaccination relative to a no-cost baseline, financial incentives did not increase willingness to vaccinate. Lastly, the manufacturer had no effect on vaccination attitudes, despite the public pause of the AstraZeneca trial and prominence of Johnson & Johnson as a household name (our experiment was fielded before the pause in the administration of the Johnson & Johnson shot in the United States).
Model 2 of Table 3 presents an expanded model specification to investigate the association between misinformation and willingness to vaccinate. The primary additional independent variable of interest is a misinformation index that captures the extent to which each subject believes or rejects eight claims (five false; three true) about COVID-19 treatments. Additional analyses using alternate operationalizations of the misinformation index yield substantively similar results (Supplementary Table 4 ). This model also includes a number of demographic control variables, including indicators for political partisanship, gender, educational attainment, age, and race/ethnicity, all of which are also associated with belief in misinformation about the vaccine (Supplementary Table 2 ). Finally, the model also controls for subjects’ health insurance status, past experience vaccinating against seasonal influenza, attitudes toward the pharmaceutical industry, and beliefs about vaccine safety generally.
Greater levels of belief in misinformation about COVID-19 treatments were not associated with greater vaccine hesitancy. Instead, the relevant coefficient is positive and statistically significant, indicating that, all else being equal, individuals who scored higher on our index of misinformation about COVID-19 treatments were more willing to vaccinate than those who were less susceptible to believing false claims.
Strong beliefs that vaccines are safe generally was positively associated with willingness to accept a COVID-19 vaccine, as were past histories of frequent influenza vaccination and favorable attitudes toward the pharmaceutical industry. Women and older subjects were significantly less likely to report willingness to vaccinate than men and younger subjects, all else equal. Education was positively associated with willingness to vaccinate.
This research offers a comprehensive examination of attitudes toward COVID-19 vaccination, particularly the role of vaccine attributes, potential policy interventions, and misinformation. Several previous studies have analyzed the effects of vaccine characteristics on willingness to vaccinate, but the modal approach is to gauge willingness to accept a generic COVID-19 vaccine 10 , 11 . Large volumes of research show, however, that vaccine preferences hinge on specific vaccine attributes. Recent research considering the influence of attributes such as efficacy, side effects, and country of origin take a step toward understanding how properties affect individuals’ intentions to vaccinate 6 , 7 , 8 , 12 , 13 , but evidence about the attributes of actual vaccines, debates about how to promote vaccination within the population, and questions about the influence of misinformation have moved quickly 14 .
Our conjoint experiment therefore examined the influence of five vaccine attributes on vaccination willingness. The first category of attributes involved aspects of the vaccine itself. Since efficacy is one of the most common determinants of vaccine acceptance, we considered different levels of efficacy, 50%, 70%, and 90%, levels that are common in the literature 7 , 15 . Evidence from Phase III trials suggests that even the 90% efficacy level in our design, which is well above the 50% threshold from the FDA Guidance for minimal effectiveness for Emergency Use Authorization 16 , has been exceeded by both Pfizer’s and Moderna’s vaccines 17 , 18 . The 70% efficacy threshold is closer to the initial reports of the efficacy of the Johnson & Johnson vaccine, whose efficacy varied across regions 19 . Our analysis suggests that efficacy levels associated with recent mRNA vaccine trials increases public vaccine uptake by 20% over a baseline of a vaccine with 50% efficacy. A 70% efficacy rate increases public willingness to vaccinate by 13% over a baseline vaccine with 50% efficacy.
An additional set of epidemiological attributes consisted of the frequency of minor side effects. While severe side effects were plausible going into early clinical trials, evidence clearly suggests that minor side effects are more common, ranging from 10% to 100% of people vaccinated depending on the number of doses and the dose group (25–250 mcg) 20 . Since the 100 mcg dose was supported in Phase III trials 21 , we include the highest adverse event probability—approximating 60% as 1 in 2—and 1 in 10 as the lowest likelihood, approximating the number of people who experienced mild arthralgia 20 . Our findings suggest that a the prevalence of minor side effects associated with recent trials (i.e. a 1 in 2 chance), intention to vaccinate decreased by about 5% versus a 1 in 10 chance of minor side effects baseline. However, at a 25% rate of minor side effects, respondents did not indicate any lower likelihood of vaccination compared to the 10% baseline. Public communications about how to reduce well-known side effects, such as pain at the injection site, could contribute to improved acceptance of the vaccine, as it is unlikely that development of vaccine-related minor side effects will change.
We then considered the effect of EUA versus full FDA approval. The influenza H1N1 virus brought the process of EUA into public discourse 22 , and the COVID-19 virus has again raised the debate about whether and how to use EUA. Compared to recent studies also employing conjoint experimental designs that showed just a 3% decline in support conditional on EUA 6 , we found decreases in support of more than twice that with an EUA compared to full FDA approval. Statements made by the Trump administration promising an intensely rapid roll-out or isolated adverse events from vaccination in the UK may have exacerbated concerns about EUA versus full approval 8 , 23 , 24 , 25 . This negative effect is even greater among some subsets of the population. As shown in additional analyses reported in the Supplementary Information (Supplementary Fig. 5 ), the negative effects are greatest among those who believe vaccines are generally safe. Among those who believe vaccines generally are extremely safe, the EUA decreased willingness to vaccinate by 11%, all else equal. This suggests that outreach campaigns seeking to assure those troubled by the authorization process used for currently available vaccines should target their efforts on those who are generally predisposed to believe vaccines are safe.
Next, we compared receptiveness as a function of the manufacturer: Moderna, Pfizer, Johnson and Johnson, and AstraZeneca, all firms at advanced stages of vaccine development. Vaccine manufacturers in the US have not yet attempted to use trade names to differentiate their vaccines, instead relying on the association with manufacturer reputation. In other countries, vaccine brand names have been more intentionally publicized, such as Bharat Biotech’s Covaxin in India and Gamaleya Research Institute of Epidemiology and Microbiology Sputnik V in Russia. We found that manufacturer names had no impact on willingness to vaccinate. As with hepatitis and H. influenzae vaccines 26 , 27 , interchangeability has been an active topic of debate with coronavirus mRNA vaccines which require a second shot for full immunity. Our research suggests that at least as far as public receptiveness goes, interchangeability would not introduce concerns. We found no significant differences in vaccination uptake across any of the manufacturer treatments. Future research should investigate if a manufacturer preference develops as new evidence about efficacy and side effects becomes available, particularly depending on whether future booster shots, if needed, are deemed interchangeable with the initial vaccination.
Taking up the question of how cost and financial incentives shape behavior, we looked at paying and being paid to vaccinate. While existing research suggests that individuals are often willing to pay for vaccines 28 , 29 , some economists have proposed that the government pay individuals up to $1,000 to take the COVID-19 vaccine 30 . However, because a cost of $300 billion to vaccinate the population may be prohibitive, we posed a more modest $100 incentive. We also compared this with a $10 incentive, which previous studies suggest is sufficient for actions that do not require individuals to change behavior on a sustained basis 31 . While having to pay a $20 co-pay for the vaccine did deter individuals, the additional economic incentives had no positive effect although they did not discourage vaccination 32 . Consistent with past research 31 , 33 , further analysis shows that the negative effect of the $20 co-pay was concentrated among low-income earners (Supplementary Fig. 7 ). Financial incentives failed to increase vaccination willingness across income levels.
Our study also yields important insights into the relationship between one prominent category of COVID-19 misinformation and vaccination preferences. We find that susceptibility to misinformation about COVID-19 treatments—based on whether individuals can distinguish between factual and false information about efforts to combat COVID-19—is considerable. A quarter of subjects scored no higher on our misinformation index than random guessing or uniform abstention/unsure responses (for the full distribution, see Supplementary Fig. 2 ). However, subjects who scored higher on our misinformation index did not exhibit greater vaccination hesitancy. These subjects actually were more likely to believe in vaccine safety more generally and to accept a COVID-19 vaccine, all else being equal. These results run counter to recent findings of public opinion in France where greater conspiracy beliefs were negatively correlated with willingness to vaccinate against COVID-19 34 and in Korea where greater misinformation exposure and belief were negatively correlated with taking preventative actions 35 . Nevertheless, the results are robust to alternate operationalizations of belief in misinformation (i.e., constructing the index only using false claims, or measuring misinformation beliefs as the number of false claims believed: see Supplementary Table 4 ).
We recommend further study to understand the observed positive relationship between beliefs in COVID-19 misinformation about fake treatments and willingness to receive the COVID-19 vaccine. To be clear, we do not posit a causal relationship between the two. Rather, we suspect that belief in misinformation may be correlated with an omitted factor related to concerns about contracting COVID-19. For example, those who believe COVID-19 misinformation may have a higher perception of risk of COVID-19, and therefore be more willing to take a vaccine, all else equal 36 . Additional analyses reported in the Supplementary Information (Supplementary Fig. 6 ) show that the negative effect of an EUA on willingness to vaccinate was concentrated among those who scored low on the misinformation index. An EUA had little effect on the vaccination preferences of subjects most susceptible to misinformation. This pattern is consistent with the possibility that these subjects were more concerned with the disease and therefore more likely to vaccinate, regardless of the process through which the vaccine was brought to market.
We also observe that skepticism toward vaccines in general does not correlate perfectly with skepticism toward the COVID-19 vaccine. Therefore, it is important not to conflate people who are wary of the COVID-19 vaccine and those who are anti-vaccination, as even medically informed individuals may be hesitant because of the speed at which the COVID-19 vaccine was developed. For example, older people are more likely to believe vaccines are safe but less willing to receive the COVID-19 vaccine in our survey, perhaps following the high rates of vaccine skepticism among medical staff expressing concerns regarding the safety of a rapidly-developed vaccine 2 . This inverse relationship between age and willingness to vaccinate is also surprising. Most opinion surveys find older adults are more likely to vaccinate than younger adults 37 . However, most of these survey questions ask about willingness to take a generic vaccine. Two prior studies, both recruiting subjects from the Lucid platform and employing conjoint experiments to examine the effects of vaccine attributes on public willingness to vaccinate, also find greater vaccine hesitancy among older Americans 6 , 7 . Future research could explore whether these divergent results are a product of the characteristics of the sample or of the methodological design in which subjects have much more information about the vaccines when indicating their vaccination preferences.
An important limitation of our study is that it necessarily offers a snapshot in time, specifically prior to both the election and vaccine roll-out. We recommend further study to understand more how vaccine perceptions evolve both in terms of the perceived political ownership of the vaccine—now that President Biden is in office—and as evidence has emerged from the millions of people who have been vaccinated. Similarly, researchers should consider analyzing vaccine preferences in the context of online vaccine controversies that have been framed in terms of patient autonomy and right to refuse 38 , 39 . Vaccination mandates may evoke feelings of powerlessness, which may be exacerbated by misinformation about the vaccines themselves. Further, researchers should more fully consider how individual attributes such as political ideology and race intersect with vaccine preferences. Our study registered increased vaccine hesitancy among Blacks, but did not find that skepticism was directly related to misinformation. Perceptions and realities of race-based maltreatment could also be moderating factors worth exploring in future analyses 40 , 41 .
Overall, we found that the most important factor influencing vaccine preferences is vaccine efficacy, consistent with a number of previous studies about attitudes toward a range of vaccines 6 , 42 , 43 . Other attributes offer potential cautionary flags and opportunities for public outreach. The prospect of a 50% likelihood of mild side effects, consistent with the evidence about current COVID-19 vaccines being employed, dampens likelihood of uptake. Public health officials should reinforce the relatively mild nature of the side effects—pain at the injection site and fatigue being the most common 44 —and especially the temporary nature of these effects to assuage public concerns. Additionally, in considering policy interventions, public health authorities should recognize that a $20 co-pay will likely discourage uptake while financial incentives are unlikely to have a significant positive effect. Lastly, belief in misinformation about COVID-19 does not appear to be a strong predictor of vaccine hesitancy; belief in misinformation and willingness to vaccinate were positively correlated in our data. Future research should explore the possibility that exposure to and belief in misinformation is correlated with other factors associated with vaccine preferences.
Survey sample and procedures
This study was approved by the Cornell Institutional Review Board for Human Participant Research (protocol ID 2004009569). We conducted the study on October 29–30, 2020, prior to vaccine approval, which means we captured sentiments prospectively rather than based on information emerging from an ongoing vaccination campaign. We recruited a sample of 1096 adult Americans via the Lucid platform, which uses quota sampling to produce samples matched to the demographics of the U.S. population on age, gender, ethnicity, and geographic region. Research has shown that experimental effects observed in Lucid samples largely mirror those found using probability-based samples 45 . Supplementary Table 1 presents the demographics of our sample and comparisons to both the U.S. Census American Community Survey and the demographics of prominent social science surveys.
After providing informed consent on the first screen of the online survey, participants turned to a choice-based conjoint experiment that varied five attributes of the COVID-19 vaccine. Conjoint analyses are often used in marketing to research how different aspects of a product or service affect consumer choice. We build on public health studies that have analyzed the influence of vaccine characteristics on uptake within the population 42 , 46 .
Conjoint experiment
We first designed a choice-based conjoint experiment that allowed us to evaluate the relative influence of a range of vaccine attributes on respondents’ vaccine preferences. We examined five attributes summarized in Table 2 . Past research has shown that the first two attributes, efficacy and the incidence of side effects, are significant drivers of public preferences on a range of vaccines 47 , 48 , 49 , including COVID-19 6 , 7 , 13 , 50 . In this study, we increased the expected incidence of minor side effects from previous research 6 to reflect emerging evidence from Phase III trials. The third attribute, whether the vaccine received full FDA approval or an EUA, examines whether the speed of the approval process affects public vaccination preferences 6 . The fourth attribute, the manufacturer of the vaccine, allows us to examine whether the highly public pause in the AstraZeneca trial following an adverse event, and the significant differences in brand familiarity between smaller and less broadly known companies like Moderna and household name Johnson & Johnson affects public willingness to vaccinate. The fifth attribute examines the influence of a policy tool—offsetting the costs of vaccination or even incentivizing it financially—on public willingness to vaccinate.
Attribute levels and attribute order were randomly assigned across participants. A sample choice set is presented in Supplementary Fig. 1 . After viewing each profile individually, subjects were asked: “If you had to choose, would you choose to get this vaccine, or would you choose not to be vaccinated?” Subjects then made a binary choice, responding either that they “would choose to get this vaccine” or that they “would choose not to be vaccinated.” This is the dependent variable for the regression analyses in Table 3 . After making a binary choice to take the vaccine or not be vaccinated, we also asked subjects “how likely or unlikely would you be to get the vaccine described above?” Subjects indicated their vaccination preference on a seven-point scale ranging from “extremely likely” to “extremely unlikely.” Additional analyses using this ordinal dependent variable reported in Supplementary Table 3 yield substantively similar results to those presented in Table 3 .
To determine the effect of each attribute-level on willingness to vaccinate, we followed Hainmueller, Hopkins, and Yamamoto and employed an ordinary least squares (OLS) regression with standard errors clustered on respondent to estimate the average marginal component effects (AMCEs) for each attribute 51 . The AMCE represents the average difference in a subject choosing a vaccine when comparing two different attribute values—for example, 50% efficacy vs. 90% efficacy—averaged across all possible combinations of the other vaccine attribute values. The AMCEs are nonparametrically identified under a modest set of assumptions, many of which (such as randomization of attribute levels) are guaranteed by design. Model 1 in Table 3 estimates the AMCEs for each attribute. These AMCEs are illustrated in Fig. 1 .
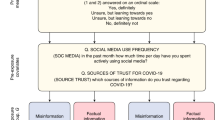
Analyzing additional correlates of vaccine acceptance
To explore the association between respondents’ embrace of misinformation about COVID-19 treatments and vaccination willingness, the survey included an additional question battery. To measure the extent of belief in COVID-19 misinformation, we constructed a list of both accurate and inaccurate headlines about the coronavirus. We focused on treatments, relying on the World Health Organization’s list of myths, such as “Hand dryers are effective in killing the new coronavirus” and true headlines such as “Avoiding shaking hands can help limit the spread of the new coronavirus 52 .” Complete wording for each claim is provided in Supplementary Appendix 1 . Individuals read three true headlines and five myths, and then responded whether they believed each headline was true or false, or whether they were unsure. We coded responses to each headline so that an incorrect accuracy assessment yielded a 1; a correct accuracy assessment a -1; and a response of unsure was coded as 0. From this, we created an additive index of belief in misinformation that ranged from -8 to 8. The distribution of the misinformation index is presented in Supplementary Fig. 2 . A possible limitation of this measure is that because the survey was conducted online, some individuals could have searched for the answers to the questions before responding. However, the median misinformation index score for subjects in the top quartile in terms of time spent taking the survey was identical to the median for all other respondents. This may suggest that systematic searching for correct answers is unlikely.
To ensure that any association observed between belief in misinformation and willingness to vaccinate is not an artifact of how we operationalized susceptibility to misinformation, we also constructed two alternate measures of belief in misinformation. These measures are described in detail in the Supplementary Information (see Supplementary Figs. 3 and 4 ). Additional regression analyses using these alternate measures of misinformation beliefs yield substantively similar results (see Supplementary Table 4 ). Additional analyses examining whether belief in misinformation moderates the effect of efficacy and an FDA EUA on vaccine acceptance are presented in Supplementary Fig. 6 .
Finally, model 2 of Table 3 includes a range of additional control variables. Following past research, it includes a number of demographic variables, including indicator variables identifying subjects who identify as Democrats or Republicans; an indicator variable identifying females; a continuous variable measuring age (alternate analyses employing a categorical variable yield substantively similar results); an eight-point measure of educational attainment; and indicator variables identifying subjects who self-identify as Black or Latinx. Following previous research 6 , the model also controlled for three additional factors often associated with willingness to vaccinate: an indicator variable identifying whether each subject had health insurance; a variable measuring past frequency of influenza vaccination on a four-point scale ranging from “never” to “every year”; beliefs about the general safety of vaccines measured on a four-point scale ranging from “not at all safe” to “extremely safe”; and a measure of attitudes toward the pharmaceutical industry ranging from “very positive” to “very negative.”
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
All data and statistical code to reproduce the tables and figures in the manuscript and Supplementary Information are published at the Harvard Dataverse via this link: 10.7910/DVN/ZYU6CO.
Hamel, L., Kirzinger, A., Munana, C. & Brodie, M. KFF COVID-19 Vaccine Monitor: December 2020 | KFF (2020).
Dror, A. A. et al. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur. J. Epidemiol. 35 , 775–779 (2020).
Article CAS PubMed Google Scholar
Scharf, I. & Ben Zion, I. As Vaccinations Lag, Israel Combats Online Misinformation. AP2 (21AD).
Nyhan, B. & Reifler, J. Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine 33 , 459–464 (2015).
Article PubMed Google Scholar
Hussain, A., Ali, S., Ahmed, M. & Hussain, S. The anti-vaccination movement: a regression in modern medicine. Cureus 10 , e2919 (2018).
PubMed PubMed Central Google Scholar
Kreps, S. et al. Factors Associated With US Adults’ Likelihood of Accepting COVID-19 Vaccination. JAMA Netw. open 3 , (2020).
Motta, M. Can a COVID-19 vaccine live up to Americans’ expectations? A conjoint analysis of how vaccine characteristics influence vaccination intentions. Soc. Sci. Med . 113642, https://doi.org/10.1016/j.socscimed.2020.113642 (2021).
Bokemper, S. E., Huber, G. A., Gerber, A. S., James, E. K. & Omer, S. B. Timing of COVID-19 vaccine approval and endorsement by public figures. Vaccine , https://doi.org/10.1016/j.vaccine.2020.12.048 (2021).
Quinn, S. C., Jamison, A. M. & Freimuth, V. Communicating effectively about emergency use authorization and vaccines in the COVID-19 pandemic. Am. J. Public Health e1–e4 (2020).
Malik, A. A., McFadden, S. A. M., Elharake, J. & Omer, S. B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 26 , 100495 (2020).
Article PubMed PubMed Central Google Scholar
Fisher, K. A. et al. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of U.S. adults. Ann. Intern. Med. 173 , 964–973 (2020).
Lazarus, J. V. et al . A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med . 1–4 (2020).
Schwarzinger, M., Watson, V., Arwidson, P., Alla, F. & Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Heal ., https://doi.org/10.1016/s2468-2667(21)00012-8 (2021).
Wood, S. & Schulman, K. Beyond politics—promoting Covid-19 vaccination in the United States. N. Engl. J. Med . NEJMms2033790, https://doi.org/10.1056/NEJMms2033790 (2021).
Marshall, H. S., Chen, G., Clarke, M. & Ratcliffe, J. Adolescent, parent and societal preferences and willingness to pay for meningococcal B vaccine: a discrete choice experiment. Vaccine 34 , 671–677 (2016).
Administration, F. and D. Development and Licensure of Vaccines to Prevent COVID-19: Guidance for Industry . (2020).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med. 383 , 2603–2615 (2020).
Baden, L. R. et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med ., https://doi.org/10.1056/nejmoa2035389 (2020).
Johnson & Johnson. Johnson & Johnson Announces Single-Shot Janssen COVID-19 Vaccine Candidate Met Primary Endpoints in Interim Analysis of its Phase 3 ENSEMBLE Trial. (2020). Available at: https://www.jnj.com/johnson-johnson-announces-single-shot-janssen-covid-19-vaccine-candidate-met-primary-endpoints-in-interim-analysis-of-its-phase-3-ensemble-trial . (Accessed 28 Feb 2021).
Jackson, L. A. et al. An mRNA vaccine against SARS-CoV-2—preliminary report. N. Engl. J. Med. 383 , 1920–1931 (2020).
Anderson, E. J. et al. Safety and immunogenicity of SARS-CoV-2 mRNA-1273 vaccine in older adults. N. Engl. J. Med. 383 , 2427–2438 (2020).
Quinn, S. C., Kumar, S., Freimuth, V. S., Kidwell, K. & Musa, D. Public willingness to take a vaccine or drug under emergency use authorization during the 2009 H1N1 pandemic. Biosecurity Bioterrorism 7 , 275–290 (2009).
Holden Thorp, H. A dangerous rush for vaccines. Science 369 , 885 (2020).
Limaye, R. J., Sauer, M. & Truelove, S. A. Politicizing public health: the powder keg of rushing COVID-19 vaccines. Hum. Vaccines Immunother ., https://doi.org/10.1080/21645515.2020.1846400 (2020).
Feuer, W. Trump Says ‘No President’s Ever Pushed’ the FDA Like Jim, Vaccine Coming ‘Very Shortly’. CNBC (2020).
Soysal, A., Gokçe, I., Pehlivan, T. & Bakir, M. Interchangeability of a hepatitis A vaccine second dose: Avaxim 80 following a first dose of Vaqta 25 or Havrix 720 in children in Turkey. Eur. J. Pediatr. 166 , 533–539 (2007).
Greenberg, D. P. & Feldman, S. Vaccine interchangeability. Clin. Pediatrics 42 , 93–99 (2003).
Article Google Scholar
Bishai, D., Brice, R., Girod, I., Saleh, A. & Ehreth, J. Conjoint analysis of French and German parents’ willingness to pay for meningococcal vaccine. PharmacoEconomics 25 , 143–154 (2007).
Cameron, M. P., Newman, P. A., Roungprakhon, S. & Scarpa, R. The marginal willingness-to-pay for attributes of a hypothetical HIV vaccine. Vaccine 31 , 3712–3717 (2013).
Litan, R. Want herd immunity? Pay people to take the vaccine. Brookings (2020).
Kane, R. L., Johnson, P. E., Town, R. J. & Butler, M. A structured review of the effect of economic incentives on consumers’ preventive behavior. Am. J. Preventive Med. 27 , 327–352 (2004).
Volpp, K. G., Loewenstein, G. & Buttenheim, A. M. Behaviorally informed strategies for a National COVID-19 vaccine promotion program. JAMA - J. Am. Med. Assoc. 325 , 125–126 (2020).
Google Scholar
Nowalk, M. P. et al. Improving influenza vaccination rates in the workplace. A randomized trial. Am. J. Prev. Med. 38 , 237–246 (2010).
Bertin, P., Nera, K. & Delouvée, S. Conspiracy beliefs, rejection of vaccination, and support for hydroxychloroquine: a conceptual replication-extension in the COVID-19 pandemic context. Front. Psychol. 11 , 2471 (2020).
Lee, J. J. et al. Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: cross-sectional online study. J. Med. Internet Res. 22 , e22205 (2020).
Reyna, V. F. Risk perception and communication in vaccination decisions: a fuzzy-trace theory approach. Vaccine 30 , 3790–3797 (2012).
Lin, C., Tu, P. & Beitsch, L. M. Confidence and receptivity for covid‐19 vaccines: a rapid systematic review. Vaccines 9 , 1–32 (2021).
Broniatowski, D. A. et al. Facebook pages, the ‘Disneyland’ measles outbreak, and promotion of vaccine refusal as a civil right, 2009–2019. Am. J. Public Health 110 , S312–S318 (2020).
Moon, K., Riege, A., Gourdon-Kanhukamwe, A. & Vallée-Tourangeau, G. The Moderating Effect of Autonomy on Promotional Health Messages Encouraging Flu Vaccination Uptake Among Healthcare Professionals . (PsyArXiv, 2020), https://doi.org/10.31234/OSF.IO/AJV4Q .
Ferdinand, K. C., Nedunchezhian, S. & Reddy, T. K. The COVID-19 and influenza “Twindemic”: barriers to influenza vaccination and potential acceptance of SARS-CoV2 vaccination in African Americans. J. Natl. Med. Assoc. 112 , 681–687 (2020).
PubMed Google Scholar
Jaiswal, J., LoSchiavo, C. & Perlman, D. C. Disinformation, misinformation and inequality-driven mistrust in the time of COVID-19: lessons unlearned from AIDS denialism. AIDS Behav. 24 , 2776–2780 (2020).
Determann, D. et al. Acceptance of vaccinations in pandemic outbreaks: a discrete choice experiment. PLoS ONE 9 , e102505 (2014).
Simpson, C. R., Ritchie, L. D., Robertson, C., Sheikh, A. & McMenamin, J. Effectiveness of H1N1 vaccine for the prevention of pandemic influenza in Scotland, UK: A retrospective observational cohort study. Lancet Infect. Dis. 12 , 696–702 (2012).
Remmel, A. COVID vaccines and safety: what the research says. Nature 590 , 538–540 (2021).
Coppock, A. & McClellan, O. A. Validating the demographic, political, psychological, and experimental results obtained from a new source of online survey respondents. Res. Polit. 6 , 1–14 (2019).
de Bekker-Grob, E. W. et al. The impact of vaccination and patient characteristics on influenza vaccination uptake of elderly people: A discrete choice experiment. Vaccine 36 , 1467–1476 (2018).
Determann, D. et al. Public preferences for vaccination programmes during pandemics caused by pathogens transmitted through respiratory droplets–A discrete choice experiment in four European countries, 2013. Eurosurveillance 21 , 1–13 (2016).
de Bekker-Grob, E. W. et al. Girls’ preferences for HPV vaccination: A discrete choice experiment. Vaccine 28 , 6692–6697 (2010).
Guo, N., Zhang, G., Zhu, D., Wang, J. & Shi, L. The effects of convenience and quality on the demand for vaccination: results from a discrete choice experiment. Vaccine 35 , 2848–2854 (2017).
Kaplan, R. M. & Milstein, A. Influence of a COVID-19 vaccine’s effectiveness and safety profile on vaccination acceptance. Proc. Natl. Acad. Sci. USA 118 , 2021726118 (2021).
Hainmueller, J., Hopkins, D. J. & Yamamoto, T. Causal inference in conjoint analysis: Understanding multidimensional choices via stated preference experiments. Polit. Anal. 22 , 1–30 (2014).
Organization, W. H. Coronavirus disease (COVID-19) advice for the public: Mythbusters. (2020). Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/myth-busters . (Accessed 14 Jan 2021).
Download references
Acknowledgements
S.K. and D.K. would like to thank the Cornell Atkinson Center for Sustainability for financial support.
Author information
Authors and affiliations.
Department of Government, Cornell University, Ithaca, NY, USA
Sarah Kreps & Douglas L. Kriner
Injury Prevention Research Center, University of North Carolina, Chapel Hill, NC, USA
Nabarun Dasgupta
Department of Pediatrics, Harvard Medical School, Boston, MA, USA
John S. Brownstein
Computational Epidemiology Lab, Boston Children’s Hospital, Boston, MA, USA
Epidemiology and Biostatistics, University of California, San Francisco, CA, USA
Yulin Hswen
You can also search for this author in PubMed Google Scholar
Contributions
S.K. and D.K. designed the experiment/survey instrument and conducted the statistical analysis. S.K., N.D., J.B., Y.H., and D.K. all contributed to the conceptual design of the research and to the writing of the paper.
Corresponding author
Correspondence to Douglas L. Kriner .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Kreps, S., Dasgupta, N., Brownstein, J.S. et al. Public attitudes toward COVID-19 vaccination: The role of vaccine attributes, incentives, and misinformation. npj Vaccines 6 , 73 (2021). https://doi.org/10.1038/s41541-021-00335-2
Download citation
Received : 25 January 2021
Accepted : 06 April 2021
Published : 14 May 2021
DOI : https://doi.org/10.1038/s41541-021-00335-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Public perspectives on covid-19 public health and social measures in japan and the united kingdom: a qualitative study.
- Saki Kawamitsu
- Tin Zar Win
- Chris Smith
BMC Public Health (2024)
Public and health care provider attitudes, understanding, and behaviors regarding emergency use authorizations: a scoping literature review
- Caroline Rains
- Kathryn J. Aikin
- Sandra Crouse Quinn
Progress with COVID vaccine development and implementation
- Richard W. Titball
- David I. Bernstein
- Alan D. T. Barrett
npj Vaccines (2024)
COVID-19 vaccine refusal is driven by deliberate ignorance and cognitive distortions
- Kamil Fuławka
- Ralph Hertwig
- Thorsten Pachur
Knowledge, attitudes and demographic drivers for COVID-19 vaccine hesitancy in Malawi
- Yamikani Ndasauka
- Halima Sumayya Twabi
- Catherine Makhumula-Mtimuni
Scientific Reports (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Persuasive Effects of Message Framing and Narrative Format on Promoting COVID-19 Vaccination: A Study on Chinese College Students
- Author information
- Article notes
- Copyright and License information
Correspondence: [email protected] ; Tel.: +86-755-2603-5185
Received 2021 Aug 14; Accepted 2021 Sep 3; Collection date 2021 Sep.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( https://creativecommons.org/licenses/by/4.0/ ).
During a public health crisis, the provision and dissemination of health-related information are important for the relevant authorities to keep the public informed. By using different types of message framing, the authorities can effectively guide and persuade people to adopt health-related behaviors (such as vaccination). In this study, a web-based experiment using a 2 × 2 (message framing: gain framing versus loss framing) × (message presentation: narrative versus non-narrative) design was conducted to investigate the effects of different message frames on vaccination promotion. In total, 298 college students were recruited to participate in this study. The results suggest that, for message framing, loss-framed (vs. gain-framed) messages lead to higher intentions to get vaccinated. Furthermore, compared with non-narrative messages, narrative messages are more persuasive in promoting vaccination behavior. However, the interaction effect between gain–loss message framing and narrative framing is not significant. Additionally, perceived severity, perceived benefits, and perceived costs mediate the effect of narrative framing on behavioral intentions. In other words, compared with non-narrative messages, narrative messages lead to higher levels of perceived severity and perceived benefits, and a lower level of perceived costs, which in turn increase intentions to get vaccinated. This paper provides insightful implications for both researchers and practitioners.
Keywords: COVID-19, message framing, narrative framing, health belief model, health behavior, vaccination
1. Introduction
During a public health crisis, the provision and dissemination of health-related information are important for the relevant authorities to keep the public informed. By using different types of message framing, the authorities can effectively guide and persuade people to adopt health-related behaviors (such as vaccination).
Previous studies in the field of health communication focused more on analyzing the effectiveness of specific information contexts and less on the relationships between message framing and behavioral intentions [ 1 , 2 , 3 , 4 , 5 ]. The way people process health-related information is not completely rational [ 6 , 7 ]; this indicates that the sole examination of media presentations cannot precisely measure the real persuasive effects of messages [ 8 , 9 ]. People’s decision-making preferences are also affected by how information is presented [ 10 , 11 , 12 ]. According to framing effect theory, different presentations of health-related information can affect individuals’ decision-making preferences. Therefore, grasping the process of interaction between information and people and designing effective information to influence people’s decision-making processes can produce a positive impact when communicating during a public health crisis.
Due to the asymmetries between people’s responses to and preferences for information expressions and their different attitudes toward various options during the decision-making process [ 13 , 14 , 15 , 16 ], the effects of gain framing and loss framing have been primarily discussed and compared in previous studies. The research proposed that whether the information was presented with benefits or risks would have significant and different impacts on people’s behavioral preferences [ 16 ]. Under the definition of gain–loss framing effect, both “benefit” and “risk” are expressed as a subjective view and personal feeling of possible or assumed consequences. Specifically, health information with the gain frame will focus on defining the gains obtained by people from accepting a specific behavior. The information with loss frame, on the other hand, will highlight the risks associated with the rejection of such a health behavior [ 17 , 18 ]. Then, gain- and loss-framed messages have emerged as the essential tool to examine the framing effect in health communication studies [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 ]. Many studies also found that more attention should be paid to research contexts when examining the effectiveness of message frameworks, and combining framed messages with specific contexts is a necessary aspect to be considered [ 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 ].
Moreover, different types of health behaviors have also been introduced as moderators in analyzing the relationships between the framing effect and behavioral intentions [ 17 , 18 ]. Specifically, loss-framed messages have proven to be more persuasive in encouraging detection behaviors [ 19 , 20 , 21 ]; conversely, messages presented in gains are more persuasive in encouraging prevention behaviors [ 22 , 23 , 24 ]. Thus, gain framing may be more effective in promoting vaccination, which has been considered one type of prevention behavior [ 23 , 24 , 25 ]. However, regarding the global COVID-19 pandemic that continues to influence daily life significantly worldwide, it is unknown whether a gain-framed message will be more effective than a loss-framed message in promoting vaccination against COVID-19.
According to exemplification theory, many studies have argued that people pay more attention to information represented with vivid and lucid cases, and, compared with messages expressed with statistical descriptions, those expressed with anecdotes play a greater role in persuasion [ 26 , 27 , 28 , 29 ]. The explorations and findings related to exemplification theory have also contributed to the study of the relationships between narratives and persuasive effects. Narratives are defined as one type of message format associated with a series of events and characters, and compared with non-narratives, narratives tell stories from the first-person perspective [ 29 , 30 ]. Many empirical studies have proven that narrative messages, compared with non-narrative messages, have a greater persuasive effect on promoting health behaviors [ 31 , 32 , 33 ]. In this case, the fictional and fascinating stories presented in narrative messages play a good role in transporting health information to their audiences by providing a sense of familiarity and imaginability and will largely reduce people’s perceptions of fear and uncertainty [ 33 , 34 ]. Based on this, it is also meaningful to examine the effectiveness of narrative messages in the promotion of COVID-19 vaccination.
People’s decisions are closely related to various psychological factors, including cognitions, emotions, attitudes, and intentions [ 35 , 36 , 37 , 38 ]. Some theoretical frameworks, including the Elaboration Likelihood Model (ELM) and the Health Belief Model (HBM), have been used to analyze and predict people’s health behaviors [ 39 , 40 , 41 ]. The ELM provides a general framework for organizing, categorizing, and understanding the fundamental processes underlying the effectiveness of persuasive communications [ 39 ]. As a critical variable in the ELM model, issue involvement is used to measure the importance or relevance of the information to individuals. Thus, some studies combined the theory of the framing effect with the ELM and introduced issue involvement as a mediator to analyze the framing effect on people’s behavioral intentions [ 39 , 42 ]. The HBM has always been seen as one of the most widely used mainstream theoretical frameworks. It is also the earliest theoretical model for exploring people’s attitudes and individual decision preferences. The HBM asserts that individuals’ attitudes and intention to adopt health-related behaviors depend on their health beliefs [ 40 , 41 , 43 ]. The HBM proposes that people’s intentions are caused by their perceived threats of specific diseases and their evaluation of the recommended preventive measures [ 41 , 43 ]. Specifically, four main health beliefs, namely, perceived severity, perceived susceptibility, perceived benefits, and perceived costs, have been extensively discussed [ 44 , 45 , 46 , 47 , 48 ]. Moreover, previous studies have also examined and proven the mediating effects of health beliefs on message framing [ 49 , 50 , 51 ]. Conversely, it has also been proposed that health beliefs significantly mediate the interaction between framed messages and behavioral intentions.
According to the latest Ipsos survey conducted by the World Economic Forum, among more than 18,000 adults from 15 countries, about 73% agreed to get vaccinated against COVID-19; however, perhaps due to concerns about possible side effects resulting from the short clinical trials, 27% disagreed. As a result, the analysis of people’s attitudes and intentions toward COVID-19 vaccination is quite meaningful. Among different groups of people, many studies have focused on understanding the persuasive effects of messages in the promotion of the vaccination behavior of young adults. Specifically, a variety of studies have examined the effects of framing on promoting undergraduate students’ intentions to get the HPV vaccine [ 35 , 52 , 53 ]. For COVID-19 vaccination, increasingly more vaccines are being approved for young adults. However, promoting COVID-19 vaccination among young adults may be challenging, as they believe they are less at risk compared with older adults. Persuading young adults to get vaccinated is meaningful for the vaccination campaign as a whole and is also the key to achieving herd immunity. In addition, according to the latest report released by China’s Ministry of Education, as of 2020, the total enrollment in higher education in China was 41.83 million, with an enrollment rate of 54.4%. Because college students are considered important human resources for social development, their health conditions are associated with the future of the entire nation. Furthermore, the determination of how to improve the persuasiveness of health information to affect college students’ behavioral intentions via the manipulation of different message strategies helps to achieve health education on a larger scale [ 54 ]. Thus, the examination of the effect of framing on the promotion of health behavior intentions makes both academic and practical contributions. Therefore, the present research aims to explore how different message framings affect their persuasiveness in promoting COVID-19 vaccination for young adults.
To inform and examine the effectiveness of framed messages, this research seeks to understand how intentions to get vaccinated are influenced by message framing and message presentation. Furthermore, this research investigates the mediating effects of health beliefs on the relationship between framing and intentions. Specifically, this study aims to answer the following research questions. (1) Do gain-framed and loss-framed messages have different persuasive effects on COVID-19 vaccination intention? (2) Do narrative messages and non-narrative messages have different persuasive effects on COVID-19 vaccination intention? (3) Do message frames interact with narrative framing to influence COVID-19 vaccination intention? (4) How do narrative and non-narrative messages affect respondents’ health beliefs? (5) Are the effects on vaccination intention mediated by health beliefs?
2. Materials and Methods
2.1. study design and participants.
A web-based experiment using a 2 × 2 (message framing: gain framing versus loss framing) × (message presentation: narrative versus non-narrative) design was conducted. College students were recruited from an online panel run by Wenjuanxing (available online: https://www.wjx.cn/ (accessed on 19 March 2021)), which is like Amazon’s Mechanical Turk and Prolific. Students who have never received any COVID-19 vaccine were included in this study. The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Discipline and Ethics Committee of Peking University HSBC Business School (PHBS0401, 21 April 2021). Following Simmons, Nelson, and Simonsohn’s recommendations [ 55 ], we planned to target at least 50 per cell in online studies. As the final sample, 298 students ( M age = 21.44; 46.3% female; 63.7% undergraduate students and 36.3% graduate students (including 0.7% Ph.D. students) were recruited to participate in this study. The participants were invited to browse a web page, where they were shown a brief introduction and asked to sign an informed consent form. Once they agreed to participate, they were randomly assigned to one of the four experimental conditions. The participants were primarily asked to report their basic knowledge about COVID-19 and the associated vaccines. Then, the participants were presented with one piece of health messaging promoting COVID-19 vaccination. The message framing was manipulated; the message was either gain-framed or loss-framed. The message presentation was also manipulated; the message was presented in either a narrative or non-narrative format. After reading the message stimuli, the participants were asked to answer a series of questions. A set of Likert scales was used to measure several variables, including the behavioral intention to get the COVID-19 vaccine and health beliefs toward vaccination. Participants were finally asked to report demographic information, including their age, gender, location, education level, and income level.
The final sample was composed of 298 college students. The participants in this experiment lived in 29 provinces in China, accounting for 85% of the total number of provinces in the country. Based on the ratio of the geographical distribution of participants, the participants were evenly distributed between east-west and north-south. Thus, the participants could represent the basic characteristics of Chinese college students, and the bias caused by regions could be effectively avoided. A brief survey was conducted to test the students’ basic knowledge and cognition related to both COVID-19 and the COVID-19 vaccines. This survey found that no participants in the selected sample had been infected with COVID-19, 84.3% said that they had previously heard of the COVID-19 vaccine, and 15.7% said that they had not previously heard of it. Most participants believed that they had a good understanding of the mechanism of the COVID-19 vaccine and believed that accepting vaccination is quite beneficial to human health; however, only half of the Chinese population believe that their daily life is closely related to the COVID-19 vaccine.
2.2. Message Stimuli
The health messages were presented as newsletters, which provided basic information regarding COVID-19 and the COVID-19 vaccines. Then, two features of the message were designed, including message framing and message presentation. Following prior studies [ 56 , 57 ], the gain-framed messages conveyed the benefits of getting vaccinated, while the loss-framed messages focused on the potential detriments of not getting vaccinated. In addition, following previous research [ 35 , 54 ], the narrative messages were manipulated by presenting a personal story from the first-person perspective. In the non-narrative messages, no specific characters were involved, and the messages conveyed an objective conclusion. The message stimuli are reported in Table 1 .
Message stimuli in experiment conditions.
2.3. Measurements
Unless indicated otherwise, the responses to items were given on 5-point Likert scales. The Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) as endpoints and the average mean values of related items were considered as indexes for the related variables. Before measuring all related variables, this study conducted the manipulation checks to examine the efficiency and reliability of the design of message stimuli. This study then measured the dependent variable, that is, intention to get the COVID-19 vaccine. Then, the present study continued to measure four main health beliefs as mediators, which include perceived severity, perceived susceptibility, perceived benefits, and perceived costs. Finally, this study measured demographical variables, including the participants’ age, gender, education level, and Internet literacy.
2.3.1. Manipulation Checks
The present study conducted a set of manipulation checks of the framed messages before measuring all related variables. The purpose of this is to test the effectiveness and accuracy of the message designs. The manipulation checks contained two dimensions of measurement: one is to measure how much participants think this is a piece of positive or negative message, and the other is to measure how much participants think this message is a narrative or non-narrative one. This study asked participants to complete the scoring of the following questions based on their feelings after reading the assigned health message, and the Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) was also used in the questionnaire. Specifically, six items were included: “This information emphasizes the benefits of getting COVID-19 vaccination”; “This information emphasizes the risk of not getting COVID-19 vaccination”; “This information emphasizes that getting COVID-19 vaccination will bring you positive effects”; “This information emphasizes that getting COVID-19 vaccination will bring you negative effects”; “This information is written in a person’s narrative”; “This information is written in an objective style”.
2.3.2. Intention to Get the COVID-19 Vaccine
The measurement of the intention to get the COVID-19 vaccine was adapted from past studies [ 54 ] that measured people’s intentions to get a vaccination in both the short term and the long term. Participants were asked to respond to three questions (e.g., “How likely would you be to get the COVID-19 vaccine sometime soon?”; Cronbach’s α = 0.77, M = 3.71, SD = 1.14). Higher scores indicated participants’ stronger intention to get vaccinated.
2.3.3. Health Beliefs
Scales adapted from previous studies [ 57 , 58 ] were used to measure the four specific health beliefs. Three items assessed perceived susceptibility by measuring the perception of risks associated with COVID-19 and the possibility of infection (e.g., “I may get COVID-19”; Cronbach’s α = 0.89, M = 3.26, SD = 1.41). Three items assessed perceived severity by measuring the perception of the negative consequences caused by COVID-19 (e.g., “I believe that COVID-19 will result in severe health problems”; Cronbach’s α = 0.71, M = 3.72, SD = 1.07). Another three questions were posed to test perceived benefits by measuring the evaluation of vaccine efficacy in preventing COVID-19 (e.g., “I believe if I get the COVID-19 vaccine, I will be less likely to get COVID-19”; Cronbach’s α = 0.76, M = 3.74, SD = 1.15). Furthermore, three items were used to assess perceived costs by measuring the perception of barriers from getting vaccinated (i.e., “I worry about the short-term side effects of the COVID-19 vaccine”; “I worry that the COVID-19 vaccine might negatively affect my body”; “I worry that the COVID-19 vaccine might have unknown long-term side effects”; Cronbach’s α = 0.83, M = 2.39, SD = 1.26). Higher scores indicated stronger health beliefs.
2.3.4. Control Variables
The choice of college students as research participants may have led to greater similarity between groups. The age, gender, education level, and Internet literacy of the participants were therefore included in the analyses as control variables.
2.4. Data Analysis Strategies
To test the research questions, series of analyses of variance (ANOVAs) and analyses of mediation were conducted. Via ANOVA, the differences between experimental groups were compared while controlling for demographic variables. The main effects of message framing and message presentation were first examined, after which the interaction effect between message framing and message presentation was tested. The PROCESS macro (version 3.5, Andrew F. Hayes, Columbus, OH, USA) for SPSS 27 (IBM, Armonk, NY, USA) was used for mediation analysis (Model 4) because it adopts a bootstrap method to estimate the mediating effect [ 59 ]. Via mediation analyses, the mediating effects of the four health beliefs on the relationship between narrative message presentation and the intention to get the COVID-19 vaccine were examined.
3.1. Manipulation Checks Results
Manipulation checks were conducted on message framing (gain framing versus loss framing) and message format (narrative versus non-narrative) using a series of independent t-tests. The results showed that participants in the gain-framed message condition perceived the message to focus more on expressing the positive information related to vaccination ( M = 3.966, SD = 0.519) as compared to those in the loss-framed message condition ( M = 3.3226, SD = 1.2709), t = 5.647, p < 0.001. Moreover, participants in the narrative message condition were more likely to perceive the message to be presented from the personal perspective ( M = 4.1769, SD = 0.7375) than were those in the non-narrative message condition ( M = 2.0204, SD = 0.8148), t = 23.7902, p < 0.001. Therefore, both manipulations were successful.
3.2. Main Effects
To answer RQ1, whether gain-framed and loss-framed messages have different persuasive effects on COVID-19 vaccination intention, the results show that for message framing, the loss-framed message, compared with the gain-framed message, promoted the intention to get the COVID-19 vaccine. A one-way ANOVA was conducted on the COVID-19 vaccination intention, and message framing was entered as the independent variable. As shown in Table 2 , the results indicate that the main effects of message framing on vaccination intention were statistically significant, F (1, 296) = 9.855, p = 0.002. Specifically, the loss-framed message led to stronger behavioral intention ( M loss-framed = 3.895 versus M gain-framed = 3.563). Furthermore, another one-way ANOVA was performed to answer RQ2, which is whether narrative and non-narrative messages have different persuasive effects. The message format was introduced as the independent variable, and vaccination intention was considered as the dependent variable. The results indicate that the main effects of the message format on vaccination intention were statistically significant, F (1, 296) = 11.334, p = 0.001. Specifically, the narrative message promoted the intention to get the COVID-19 vaccine ( M narrative = 3.908 versus M non-narrative = 3.552). The interaction between the loss-gain framing and narrative framing was examined, and the interaction effect on vaccination intention was not found to be statistically significant. Thus, for RQ3, whether gain–loss framing interacts with narrative framing on COVID-19 vaccination intention, the interaction was not statistically significant.
Means and standard deviation related to research questions 1–2.
3.3. Mediation Effects
RQ4 tried to investigate whether and how narrative and non-narrative messages affect college students’ health beliefs, including perceived susceptibility, perceived severity, perceived benefits, and perceived costs. To address this question, an analysis of mediation was conducted by using the PROCESS macro in SPSS, and the model 4 was selected. Using a bootstrap method, this study selected a sample size of 5000. Narrative message presentation was entered as the independent variable, vaccination intention was introduced as the dependent variable, and health beliefs were included as mediators. As shown in Table 3 , the results indicate that the mediation effects of health beliefs on narrative framing were partially significant. When testing the mediation effects of perceived severity, perceived benefits, and perceived costs, their confidence intervals of the bootstrap did not include zero, which means that those three variables had significant mediating effects on narrative framing. Specifically, the mediating effects of perceived severity (BootLLCI = 0.0186, BootULCI = 0.0868), perceived benefits (BootLLCI = 0.0137, BootULCI = 0.1030), and perceived costs ( BootLLCI = 0.0046, BootULCI = 0.0660) were statistically significant in the 95% bias-corrected bootstrap confidence interval. Therefore, perceived severity, perceived benefits, and perceived costs mediate the relationship between narrative framing and behavioral intention. RQ5 then investigated whether the health beliefs mediate the relationship between narrative framing and intentions to get the vaccination. To address this research question, the coefficients of the mediating models were examined to analyze the directions of the mediating effects and the results were shown in Figure 1 . Specifically, compared with non-narrative messages, narrative messages led to a higher level of the perceived severity of COVID-19 and the perceived benefits of the COVID-19 vaccine. Furthermore, compared with the non-narrative messages, the narrative messages led to a lower level of perceived costs. In conclusion, narrative messages were found to lead to higher levels of perceived severity and perceived benefits, while they led to a lower level of perceived costs, and therefore were ultimately found to promote the intention to get the COVID-19 vaccine.
Mediation effects related to research questions 4–5.
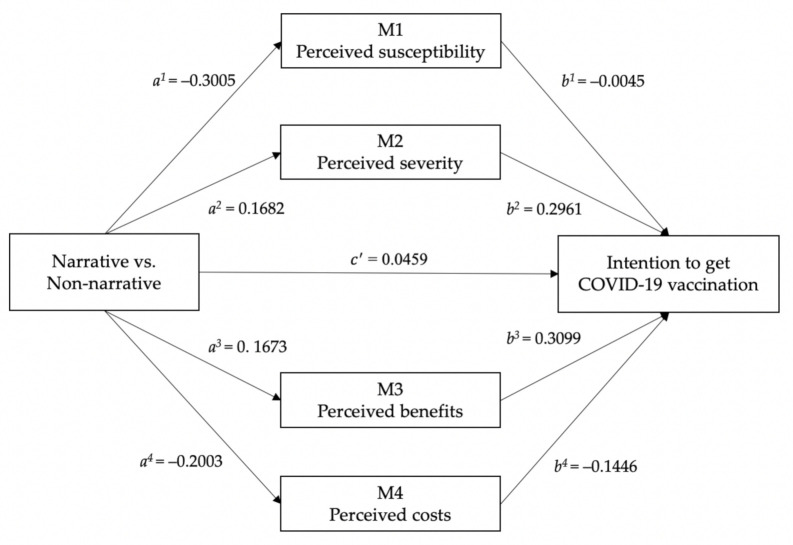
Mediating model on narrative framing.
4. Discussion
This present research is one of the first few studies to investigate the effects of message framing and narrative message presentation on promoting COVID-19 vaccination. Specifically, the persuasiveness of gain-framed versus loss-framed messages was compared, as was the persuasiveness of narrative versus non-narrative messages. Because the research targets were Chinese college students, it is difficult to compare the results of the present research with those of previous studies due to the lack of surveys conducted among the same group. This research, however, revealed some notable findings in the prediction of the intention to get the COVID-19 vaccine.
A central thesis of this research is that vaccination, unlike other preventative health-related behaviors, is associated with higher risks due to side effects and other safety concerns. Moreover, under the influence of public opinion, the anxiety of the public will spread, causing a large portion of the population to be reluctant to get vaccinated even if they believe that vaccination is a beneficial behavior. Drawing upon prospect theory [ 16 , 53 , 60 ], people will prefer less risky behavior when those risks are expressed salient. Because people will exhibit greater aversion to the risks caused by vaccination, loss-framed messages are more likely to enhance their intention to get the COVID-19 vaccine. The results of the controlled experiment were found to be largely consistent with the research questions, and the findings are consistent with the results of some previous studies conducted in other contexts [ 33 , 34 , 53 , 54 ].
Similarly, this research also posited that narrative messages are more persuasive than non-narrative messages to promote COVID-19 vaccination behavior. Narrative descriptions associated with fictional and fascinating stories will benefit people to build a more specific and concrete understanding of the issue [ 28 , 29 , 30 , 60 ]. Furthermore, compared with didactic and objective arguments, messages in narrative format provide people with more familiarity and imaginability, and will therefore be more persuasive in promoting behavioral intentions. Consistent with the prediction, the results showed that narrative messages, both gain-framed and loss-framed, are more persuasive than non-narrative messages in promoting vaccination. These findings are consistent with those of previous studies that have suggested the greater effectiveness of narrative messages in promoting vaccination [ 33 , 34 , 61 ].
In addition to examining the effects of message framing and presentation, this research examined the mediating roles of various health beliefs on the interaction between narrative framing and vaccination intention. Drawing upon the HBM, people’s decision-making processes can be influenced by their evaluations of potential threats and efficacy [ 41 , 42 , 62 ]; thus, many studies have introduced health beliefs into a framing effect model to examine their mediating effects [ 34 , 48 , 49 ]. In the present research, it was found that health beliefs significantly mediate framing effects; this is consistent with the findings of some previous studies [ 33 , 62 , 63 , 64 ], even though they were focused on other types of health behaviors or other framing effects. Specifically, narrative (versus non-narrative) messages will lead to higher levels of perceived severity and perceived benefits and will simultaneously lead to a lower level of perceived costs; thus, they will promote the intention to get the COVID-19 vaccine. Messages conveyed in narrative format will enhance people’s perceived threats of COVID-19 and the perceived efficacy of the vaccines. Furthermore, messages presented as narratives will help people to better understand and avoid the well-demonstrated risks, and, conversely, will lessen their concerns about vaccine side effects and other safety barriers.
Of course, all the conclusions of this research must be evaluated in consideration of several limitations. This research failed to introduce discrete emotions as mediators in analyzing the interactions between framing effects and intentions. Although the research fully measured and investigated people’s health beliefs, people’s emotions, including fear, sadness, guilt, and relief, can also lead to different behavioral responses [ 30 , 62 , 65 , 66 , 67 , 68 , 69 , 70 ]. Future research may seek to examine the mediating roles of emotions on framing effects, especially the mediating role of fear. People with fear tend to retreat from loss-framed stimuli and will avoid any behavior to address them [ 65 , 71 , 72 ]. In other words, people can be too afraid to make any possible attempt, even if they clearly know that such an attempt is beneficial to them. Additionally, future research can introduce the Extended Parallel Process Model (EPPM) into the discussion. Compared with the HBM, the EPPM can better measure people’s perceived threats and efficacy and can therefore be used to comprehensively examine the effect of framing on the persuasion of people’s behavioral intentions [ 56 ]. Finally, the present study did not examine the roles of individual affective and cognitive orientations on promoting behavioral intentions. This study merely focused on analyzing the persuasiveness of messages with different expressions. However, people’s affective and cognitive attitudes should also be introduced into the model. According to the theory of matching effect, if the framed message matches an individual’s affective and cognitive orientations, it will enhance the effectiveness of persuasion [ 73 ]. In other words, matches between people’s psychological states and the message will make it more persuasive [ 74 , 75 , 76 ]. Those related theories do give great inspiration for future research. According to the findings in this study, loss framing, compared with gain framing, is more persuasive. Additionally, narratives also have a more significant persuasive effect compared with non-narratives. However, this study did not take affective orientation and cognitive orientations into consideration. What type of framed messages can significantly match individual’s psychological states and will better trigger their behavioral intentions? In future research, it may be necessary to add more variables to measure the dimensions of personal psychological characteristics to better measure the influence of emotion and cognition orientations on persuasiveness.
5. Conclusions
In conclusion, the results of this study emphasize that the persuasive effects of various message expressions are significantly different. First, the difference between gain framing and loss framing in the promotion of vaccination intention was proven to be significant. Specifically, loss-framed messages are more persuasive than gain-framed messages in promoting COVID-19 vaccination. Because vaccination is one type of health behavior associated with risk, according to prospect theory, loss-framed messages are more persuasive. Second, the difference between narrative and non-narrative messages in encouraging vaccination was also proven to be significant. In other words, narrative messages are more effective than messages presented in a non-narrative format, as narrative messages allow people to better understand the potential risks of rejecting vaccination against COVID-19 or the benefits of getting the vaccine. Furthermore, narrative descriptions will enhance people’s familiarity with the framed message and more strongly trigger their intention to get the COVID-19 vaccine. Moreover, the mediating effects of health beliefs, including perceived severity, perceived benefits, and perceived costs, were proven to be significant. Specifically, messages conveyed in a narrative format will increase people’s perceptions of the severity of COVID-19 and the benefits obtained from getting the vaccine. Additionally, perceived costs will play a negative mediating role, i.e., narrative messages will result in a lower level of perceived costs and will make people more likely to get the COVID-19 vaccine.
Author Contributions
Conceptualization, W.Y. and Q.L.; data curation, Q.L.; methodology, Q.L. and S.Y.; supervision, W.Y. and S.Y.; writing—original draft, Q.L.; writing—review & editing, W.Y. and S.Y. All authors have read and agreed to the published version of the manuscript.
This research was supported by The National Social Science Fund of China (“Research on Algorithm-mediated Online Platform Labor”, grant number 19BXW098).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Discipline and Ethics Committee of Peking University HSBC Business School (PHBS0401, 21 April 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
- 1. Frey K.P., Eagly A.H. Vividness can undermine the persuasiveness of messages. J. Pers. Soc. Psychol. 1993;65:32–44. doi: 10.1037/0022-3514.65.1.32. [ DOI ] [ Google Scholar ]
- 2. Joyce N., Harwood J. Context and identification in persuasive mass communication. J. Media Psychol. 2014;26:50. doi: 10.1027/1864-1105/a000110. [ DOI ] [ Google Scholar ]
- 3. Nabi R.L., Moyer-Gusé E., Byrne S. All joking aside: A serious investigation into the persuasive effect of funny social issue messages. Commun. Monogr. 2007;74:29–54. doi: 10.1080/03637750701196896. [ DOI ] [ Google Scholar ]
- 4. Oinaskukkonen H., Harjumaa M. A systematic framework for designing and evaluating persuasive systems. Lect. Notes Comput. Sci. 2008;5033:164–176. [ Google Scholar ]
- 5. Nabi R.L., Green M.C. The role of a narrative’s emotional flow in promoting persuasive outcomes. Media Psychol. 2015;18:137–162. doi: 10.1080/15213269.2014.912585. [ DOI ] [ Google Scholar ]
- 6. Pacini R., Epstein S. The relation of rational and experiential information processing styles to personality, basic beliefs, and the ratio-bias phenomenon. J. Pers. Soc. Psychol. 1999;76:972. doi: 10.1037/0022-3514.76.6.972. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Krauss D.A., Lieberman J.D., Olson J. The effects of rational and experiential information processing of expert testimony in death penalty cases. Behav. Sci. Law. 2004;22:801–822. doi: 10.1002/bsl.621. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Reyna V.F., Farley F. Risk and rationality in adolescent decision making implications for theory, practice, and public policy. Psychol. Sci. Public Interest. 2006;7:1–44. doi: 10.1111/j.1529-1006.2006.00026.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Mccaughey D., Bruning N.S. Rationality versus reality: The challenges of evidence-based decision making for health policy makers. Implement. Sci. 2010;5:1–13. doi: 10.1186/1748-5908-5-39. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Voss R.P., Corser R., Mccormick M. Influencing health decision-making: A study of colour and message framing. J. Health Psychol. 2018;33:941–954. doi: 10.1080/08870446.2018.1453509. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Bartels R.D., Kelly K.M., Rothman A.J. Moving beyond the function of the health behaviour: The effect of message frame on behavioural decision-making. J. Health Psychol. 2010;25:821–838. doi: 10.1080/08870440902893708. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Vidal G., Machín L., Aschemann-Witzel J. Does message framing matter for promoting the use of nutritional warnings in decision making? Public Health Nutr. 2019;22:1–10. doi: 10.1017/S1368980019002507. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Rozin P., Royzman E.B. Negativity bias, negativity dominance, and contagion. Pers. Soc. Psychol. Rev. 2001;5:296–320. doi: 10.1207/S15327957PSPR0504_2. [ DOI ] [ Google Scholar ]
- 14. Dijksterhuis A., Aarts H. On wildebeests and humans: The preferential detection of negative stimuli. Psychol. Sci. 2003;14:14–18. doi: 10.1111/1467-9280.t01-1-01412. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Taylor S.E. Asymmetrical effects of positive and negative events: The mobilization-minimization hypothesis. Psychol. Bull. 1991;110:67. doi: 10.1037/0033-2909.110.1.67. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Tversky A., Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211:453–458. doi: 10.1126/science.7455683. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Rothman A.J., Salovey P. Shaping perceptions to motivate healthy behavior: The role of message framing. Psychol. Bull. 1997;121:3. doi: 10.1037/0033-2909.121.1.3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Rothman A.J., Martino S.C., Bedell B.T. The systematic influence of gain-and loss-framed messages on interest in and use of different types of health behavior. Pers. Soc. Psychol. Bull. 1999;25:1355–1369. doi: 10.1177/0146167299259003. [ DOI ] [ Google Scholar ]
- 19. Banks S.M., Salovey P., Greener S. The effects of message framing on mammography utilization. J. Health Psychol. 1995;14:178. doi: 10.1037/0278-6133.14.2.178. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Meyerowitz B.E., Chaiken S. The effect of message framing on breast self-examination attitudes, intentions, and behavior. J. Pers. Soc. Psychol. 1987;52:500. doi: 10.1037/0022-3514.52.3.500. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Schneider T.R., Salovey P., Apanovitch A.M. The effects of message framing and ethnic targeting on mammography use among low-income women. J. Health Psychol. 2001;20:256. doi: 10.1037/0278-6133.20.4.256. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Cox D., Cox A.D. Communicating the consequences of early detection: The role of evidence and framing. J. Mark. 2001;65:91–103. doi: 10.1509/jmkg.65.3.91.18336. [ DOI ] [ Google Scholar ]
- 23. Rothman A.J., Salovey P., Antone C. The influence of message framing on intentions to perform health behaviors. J. Exp. Soc. Psychol. 1993;29:408–433. doi: 10.1006/jesp.1993.1019. [ DOI ] [ Google Scholar ]
- 24. Robberson M.R., Rogers R.W. Beyond fear appeals: Negative and positive persuasive appeals to health and self-esteem. J. Appl. Soc. Psychol. 1988;13:277–287. doi: 10.1111/j.1559-1816.1988.tb00017.x. [ DOI ] [ Google Scholar ]
- 25. Detweiler J.B., Bedell B.T., Salovey P., Pronin E., Rothman A.J. Message framing and sunscreen use: Gain-framed messages motivate beachgoers. Health Psychol. 1999;18:189–196. doi: 10.1037/0278-6133.18.2.189. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Yu N., Ahern L.A., Connolly-Ahern C., Shen F. Communicating the risks of fetal alcohol spectrum disorder: Effects of message framing and exemplification. Health Commun. 2010;25:692–699. doi: 10.1080/10410236.2010.521910. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Zillmann D., Perkins J.W., Sundar S.S. Impression-formation effects of printed news varying in descriptive precision and exemplification. J. Media Psychol. 1992;4:168–185. [ Google Scholar ]
- 28. Kreuter M.W., Green M.C., Cappella J.N. Narrative communication in cancer prevention and control: A framework to guide research and application. Ann. Behav. Med. 2007;33:221–235. doi: 10.1007/BF02879904. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Green M.C., Brock T.C. The role of transportation in the persuasiveness of public narratives. J. Pers. Soc. Psychol. 2000;79:701. doi: 10.1037/0022-3514.79.5.701. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Slater M.D., Rouner D. Entertainment—education and elaboration likelihood: Understanding the processing of narrative persuasion. Commun. Theory. 2002;12:173–191. [ Google Scholar ]
- 31. Baesler E.J., Burgoon J.K. The temporal effects of story and statistical evidence on belief change. Commun. Res. 1994;21:582–602. doi: 10.1177/009365094021005002. [ DOI ] [ Google Scholar ]
- 32. Green M.C. Narratives and cancer communication. J. Commun. 2006;56:163–183. doi: 10.1111/j.1460-2466.2006.00288.x. [ DOI ] [ Google Scholar ]
- 33. Liu S., Yang J.Z., Chu H. Now or future? Analyzing the effects of message frame and format in motivating Chinese females to get HPV vaccines for their children. Patient Educ. Couns. 2019;102:61–67. doi: 10.1016/j.pec.2018.09.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Kim H.K., Lee T.K. Conditional effects of gain–loss-framed narratives among current smokers at different stages of change. J. Health Commun. 2017;22:990–998. doi: 10.1080/10810730.2017.1396629. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Becker M.H., Maiman L.A. Sociobehavioral determinants of compliance with health and medical care recommendations. Med. Care. 1975;13:10–24. doi: 10.1097/00005650-197501000-00002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Weinstein N.D., Rothman A.J. Commentary: Revitalizing research on health behavior theories. Health Educ. Res. 2005;20:294–297. doi: 10.1093/her/cyg125. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Fishbein M., Ajzen I. Belief, attitude, intention, and behavior: An introduction to theory and research. Philos. Rhetor. 1977;10:177–189. [ Google Scholar ]
- 38. Rosenstock I.M., Strecher V.J., Becker M.H. Social learning theory and the health belief model. Health Educ. Q. 1988;15:175–183. doi: 10.1177/109019818801500203. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Angst C.M., Agarwal R. Adoption of electronic health records in the presence of privacy concerns: The elaboration likelihood model and individual persuasion. Manag. Inf. Syst. Q. 2009;33:339–370. doi: 10.2307/20650295. [ DOI ] [ Google Scholar ]
- 40. Carpenter C.J. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010;25:661–669. doi: 10.1080/10410236.2010.521906. [ DOI ] [ PubMed ] [ Google Scholar ]
- 41. Janz N.K., Becker M.H. The health belief model: A decade later. Health Educ. Behav. 1984;11:1–47. doi: 10.1177/109019818401100101. [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Chen M.S., Land K.C. Testing the health belief model: LISREL analysis of alternative models of causal relationships between health beliefs and preventive dental behavior. Soc. Psychol. Q. 1986;49:45–60. doi: 10.2307/2786856. [ DOI ] [ Google Scholar ]
- 43. Harrison J.A., Mullen P.D., Green L.W. A meta-analysis of studies of the health belief model with adults. Health Educ. Res. 1992;7:107–116. doi: 10.1093/her/7.1.107. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Jones L.W., Sinclair R.C., Courneya K.S. The effects of source credibility and message framing on exercise intentions, behaviors, and attitudes: An integration of the elaboration likelihood model and prospect theory. J. Appl. Soc. Psychol. 2003;33:179–196. doi: 10.1111/j.1559-1816.2003.tb02078.x. [ DOI ] [ Google Scholar ]
- 45. Stein J.A., Fox S.A., Murata P.J. Mammography usage and the health belief model. Health Educ. Res. 1992;19:447–462. doi: 10.1177/109019819201900409. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Becker M.H., Maiman L.A., Kirscht J.P. The health belief model and prediction of dietary compliance: A field experiment. J. Health Soc. Behav. 1977;18:348–366. doi: 10.2307/2955344. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Bush P.J., Iannotti R.J. A children’s health belief model. Med. Care. 1990;28:69–86. doi: 10.1097/00005650-199001000-00008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 48. Gerend M.A., Shepherd J.E. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Ann. Behav. Med. 2012;44:171–180. doi: 10.1007/s12160-012-9366-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Nan X., Kim J. Predicting H1N1 vaccine uptake and H1N1-related health beliefs: The role of individual difference in consideration of future consequences. J. Health Commun. 2014;19:376–388. doi: 10.1080/10810730.2013.821552. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Woodward N.J., Wallston B.S. Age and health care beliefs: Self-efficacy as a mediator of low desire for control. Psychol. Aging. 1987;2:3. doi: 10.1037/0882-7974.2.1.3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Cho J., Chun J.W., Lee M.J. Impacts of message framing and social distance in health campaign for promoting regular physical exercise. J. Health Commun. 2018;23:824–835. doi: 10.1080/10810730.2018.1527872. [ DOI ] [ PubMed ] [ Google Scholar ]
- 52. Nan X. Relative persuasiveness of gain-versus loss-framed human papillomavirus vaccination messages for the present-and future-minded. Hum. Commun. Res. 2012;38:72–94. doi: 10.1111/j.1468-2958.2011.01419.x. [ DOI ] [ Google Scholar ]
- 53. Noar S.M., Zimmerman R.S. Health behavior theory and cumulative knowledge regarding health behaviors: Are we moving in the right direction? Health Educ. Res. 2005;20:275–290. doi: 10.1093/her/cyg113. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Gerend M.A., Shepherd J.E. Using message framing to promote acceptance of the human papillomavirus vaccine. J. Health Psychol. 2007;26:745. doi: 10.1037/0278-6133.26.6.745. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Simmons J.P., Nelson L.D., Simonsohn U. False-positive psychology: Undisclosed flexibility in data collection and analysis allows presenting anything as significant. Psychol. Sci. 2011;22:1359–1366. doi: 10.1177/0956797611417632. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Witte K. Putting the fear back into fear appeals: The extended parallel process model. Commun. Monogr. 1992;59:329–349. [ Google Scholar ]
- 57. Kirscht J.P., Haefner D.P., Kegeles S.S. A national study of health beliefs. J. Health Soc. Behav. 1966:248–254. doi: 10.2307/2948771. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Nan X., Zhao X., Yang B. Effectiveness of cigarette warning labels: Examining the impact of graphics, message framing, and temporal framing. J. Health Commun. 2015;30:81–89. doi: 10.1080/10410236.2013.841531. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Hayes A.F. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Commun. Monogr. 2009;76:408–420. doi: 10.1080/03637750903310360. [ DOI ] [ Google Scholar ]
- 60. Dahlstrom M.F. Using narratives and storytelling to communicate science with nonexpert audiences. Proc. Natl. Acad. Sci. USA. 2014;111:13614–13620. doi: 10.1073/pnas.1320645111. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 61. Moyer-Gusé E., Nabi R.L. Comparing the effects of entertainment and educational television programming on risky sexual behavior. J. Health Commun. 2011;26:416–426. doi: 10.1080/10410236.2011.552481. [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. Murphy S.T., Frank L.B., Moran M.B. Involved, transported, or emotional? Exploring the determinants of change in knowledge, attitudes, and behavior in entertainment-education. J. Commun. 2011;61:407–431. doi: 10.1111/j.1460-2466.2011.01554.x. [ DOI ] [ Google Scholar ]
- 63. Murphy S.T., Frank L.B., Chatterjee J.S. Narrative versus nonnarrative: The role of identification, transportation, and emotion in reducing health disparities. J. Commun. 2013;63:116–137. doi: 10.1111/jcom.12007. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 64. McGregor L.M., von Wagner C., Vart G. The impact of supplementary narrative-based information on colorectal cancer screening beliefs and intention. BMC Cancer. 2015;15:1–9. doi: 10.1186/s12885-015-1167-3. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 65. Lazarus R.S. Cognition and motivation in emotion. Am. Psychol. 1991;46:352. doi: 10.1037/0003-066X.46.4.352. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Nabi R. Anger, fear, uncertainty, and attitudes: A test of the cognitive-functional model. Commun. Monogr. 2002;69:204–216. doi: 10.1080/03637750216541. [ DOI ] [ Google Scholar ]
- 67. DeSteno D., Gross J.J., Kubzansky L. Affective science and health: The importance of emotion and emotion regulation. Health Psychol. 2013;32:474. doi: 10.1037/a0030259. [ DOI ] [ PubMed ] [ Google Scholar ]
- 68. Oatley K. Why fiction may be twice as true as fact: Fiction as cognitive and emotional simulation. Rev. Gen. Psychol. 1999;3:101–117. doi: 10.1037/1089-2680.3.2.101. [ DOI ] [ Google Scholar ]
- 69. Scannell N., Villani A., Mantzioris E. Understanding the self-perceived barriers and enablers toward adopting a mediterranean diet in Australia: An application of the theory of planned behaviour framework. Int. J. Environ. Res. Public Health. 2020;17:9321. doi: 10.3390/ijerph17249321. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 70. Shayganfard M., Mahdavi F., Haghighi M. Health anxiety predicts postponing or cancelling routine medical health care appointments among women in perinatal stage during the Covid-19 lockdown. Int. J. Environ. Res. Public Health. 2020;17:8272. doi: 10.3390/ijerph17218272. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Witte K. Fear control and danger control: A test of the extended parallel process model (EPPM) Commun. Monogr. 1994;61:113–134. doi: 10.1080/03637759409376328. [ DOI ] [ Google Scholar ]
- 72. Dillard J.P. Rethinkin the study of fear appeals: An emotional perspective. Commun. Theory. 1994;4:295–323. doi: 10.1111/j.1468-2885.1994.tb00094.x. [ DOI ] [ Google Scholar ]
- 73. Mayer N.D., Tormala Z.L. “Think” versus “feel” framing effects in persuasion. Pers. Soc. Psychol. Bull. 2010;36:443–454. doi: 10.1177/0146167210362981. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Petty R.E., Wegener D.T. Matching versus mismatching attitude functions: Implications for scrutiny of persuasive messages. Pers. Soc. Psychol. Bull. 1998;24:227–240. doi: 10.1177/0146167298243001. [ DOI ] [ Google Scholar ]
- 75. Tormala Z.L., Rucker D.D., Seger C.R. When increased confidence yields increased thought: A confidence-matching hypothesis. J. Exp. Soc. Psychol. 2008;44:141–147. doi: 10.1016/j.jesp.2006.11.002. [ DOI ] [ Google Scholar ]
- 76. Mackie D.M., Worth L.T., Asuncion A.G. Processing of persuasive in-group messages. J. Pers. Soc. Psychol. 1990;58:812. doi: 10.1037/0022-3514.58.5.812. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
- View on publisher site
- PDF (1.8 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
These are the pro-vaccine messages people want to hear
Successful strategies showcase celebrities such as dolly parton and tyler perry, but also local doctors, pastors and neighbors.
With all Americans 16 and over now eligible to receive a coronavirus vaccine, health-care workers and public health officials are turning their attention to the approximately one-third of Americans who say that they are on the fence or that they do not want to get vaccinated.
No single message will persuade everyone, but experts say a combination of strategies is already convincing reluctant people that getting vaccinated is for them.
Here are some of those strategies, from the broadest to the most personal.
Make vaccination visible
For any strategy to work, people first have to perceive vaccination as a normal part of life.
That is why public health officials, nonprofit groups and major brands are collaborating on nationwide public service campaigns and partnering with celebrities to make vaccination more visible.
The model for the celebrity shot dates to 1956, when few teenagers were getting the year-old polio vaccine. Two critical things happened that fall to reverse the trend.
First, 21-year-old Elvis Presley got the shot in front of cameras before “The Ed Sullivan Show.” Second, the March of Dimes launched a wildly successful peer-to-peer campaign among teen social groups. In short, it leveraged the cool kids, but it may not have gotten the cool kids without the King.
The wide range of celebs touting coronavirus vaccines includes musicians and actors (such as Elton John , Britney Spears and Lin-Manuel Miranda ), sports personalities ( Patrick Mahomes, Richard Petty , Kareem Abdul-Jabbar ), WWE stars and Fox News personalities. “Don’t be such a chicken-squat,” chided country music icon Dolly Parton in a video as she got an injection of the Moderna vaccine, which she helped finance. “Afterwards, I felt like superwoman,” Oprah Winfrey wrote.
[ Could Beyoncé do for coronavirus vaccine what Elvis did for polio? ]
Tyler Perry was vaccinated live on a BET special. TV shows as varied as “South Park” and “This Is Us” have incorporated vaccinations into their story lines.
Broad public service announcements, however, inevitably turn some people off. One person may find Google’s “ Get back to what you love ” message poignant, while another finds it manipulative.
“No national ad campaign is ever going to be as effective … as people who look like you and come from your community saying: ‘This is important. It’s the right thing for us,’” said Kelly Moore of the vaccine education group Immunization Action Coalition.
It’s why the polio campaign needed both Elvis and the teens next door.
Have nationally trusted messengers recommend it
The opinions of our leaders matter, whether that is the president or a prominent public health official such as Anthony S. Fauci , the nation’s top infectious-disease expert.
“When the people in the front of the room — political leaders and so on, people in charge of vaccination — speak up in favor of vaccination, confidence rises and stays high,” said University of North Carolina researcher Noel Brewer, who studies the intersection of public health and human behavior. “When the government and the folks in charge of vaccination do not speak in favor of it, confidence falls.”
Both of those scenarios have played out since the first vaccine became available in December .
Although President Donald Trump led the initiative that sped vaccines to the market, he was vaccinated privately in January before leaving office and did not disclose it or encourage his supporters to get a shot until March . (Vice President Mike Pence and his wife were vaccinated on television in December.)
It was a puzzling missed opportunity to celebrate a big achievement, Brewer said, “and we see the remnants of that in today’s society.” According to an Economist-YouGov poll released this week, 30 percent of Republicans said they would not get vaccinated, compared with 22 percent of adults overall.
President Biden , Vice President Harris and all other living former presidents have rolled up their sleeves in public.
While politicians’ cheerleading can be useful for some, it won’t convince everyone. A focus group of vaccine-hesitant Trump voters last month said pitches from politicians — Trump included — were not persuasive.
It is the medical professionals who can best convey the possible risks of both the vaccines and the disease to a jittery public, Moore said.
This is why many are still listening to Fauci.
“He established trust by saying things people didn’t want to hear when they needed to be said, then also saying encouraging things,” Moore said. “There is nothing more easily lost in this process and nothing more precious in the process than that real trust.”
But not everyone likes what he has to say, either. This week in a different focus group, vaccine-hesitant Trump voters said they do not want to hear from Fauci.
[ ‘We want to be educated, not indoctrinated,’ say Trump voters wary of coronavirus vaccination ]
Make vaccination come with privileges
Of the many strategies Brewer and his colleagues explored in a 2017 study on the psychology of vaccine uptake, one of the most effective was simply requiring it.
For some people, being allowed to travel to see the grandkids, to take a cruise or to return to the office or school is enough of an incentive to persuade them to get vaccinated. According to a Kaiser Family Foundation poll conducted in late March, 7 percent of respondents said that they would get a vaccine “only if required.”
However, that step cannot occur before people believe vaccinations are safe.
“If there’s not some community-wide level of confidence in the vaccine,” Brewer said, “policymakers cannot implement all of these super-effective approaches without receiving a great deal of blowback from the general public.”
In the Economist-YouGov poll, 61 percent of respondents thought the Moderna vaccine was very safe or somewhat safe, compared with 59 percent for the Pfizer-BioNTech vaccine and 42 percent for the Johnson & Johnson vaccine.
Pushback against “vaccine passports” has already begun in the United States, even though the Biden administration has said it does not plan to create them . But private businesses such as cruise lines, sports teams and others are already beginning to require proof of vaccinations.
[ 'Vaccine passports' are on the way, but developing them won't be easy ]
“Being confident in the vaccine and deciding to get vaccinated — those need to be voluntary, personal decisions,” said Elisabeth Wilhelm, a vaccine confidence strategist with the Centers for Disease Control and Prevention. “We ask people to think very, very carefully when they talk about incentives, whether it’s a bag of rice for your kid getting vaccinated in Nigeria or getting a coronavirus vaccine in your workplace in the United States. It is a lever that can be used — it just should not be the first that you pull on.”
[ Everything travelers need to know about vaccine passports ]
Tailor the message to the audience
Traditionally, public health messages — from smoking cessation to seat-belt campaigns — have been broadcast widely, on billboards, in public service announcements and on popular TV shows. That one-size-fits-all approach doesn’t work well for vaccines, experts say, because pregnant women, for example, probably have concerns very different from those of Republican men or Latino immigrants.
“When it comes to vaccine hesitancy, it is more like personalized medicine,” said Christopher Graves, founder of the Ogilvy Center for Behavioral Science at Ogilvy Consulting, “more customized to specific worldviews and cultural filters.”
And unlike conventional vaccine messaging, which aims to persuade parents to get children vaccinated, the coronavirus messages are aimed at persuading adults to get their shots.
“Respecting their autonomy is important,” Moore said.
As is adapting the message to the recipient.
People who say they prize individual choice are more likely to be convinced by messages emphasizing that getting vaccinated increases your freedom to get together with friends and colleagues, experts say.
Gabriel Salguero, founder of the National Latino Evangelical Coalition , said he is using biblical references in his sermons to quell the fears of some Christians who falsely believe the vaccines contain microchips or fetal tissue or are an ominous sign of the End Times.
Successful messaging isn’t only about finding the right words. Olajide Williams, a Columbia University neurologist, uses music and art in the Hip Hop Public Health program to reach communities of color.
And for those who are skeptical of the science, data can make a real difference: 95 percent of doctors who have been offered a vaccine have taken it — a figure that helped turn around 19 vaccine-hesitant Trump voters who took part in a two-hour virtual focus group .
“The one group everyone trusts is doctors,” said Claire Hannan, executive director of the Association of Immunization Managers , a nonprofit that coordinates with states to control vaccine-preventable diseases.
Have friendly faces in familiar places
While many people are eager to sign up for mass vaccination sites, others are unable or unwilling to take a place in line, for reasons such as a lack of transportation or worries about showing up at sites where staffers are often dressed in uniform.
[ Lack of health services and transportation impede access to vaccine in communities of color ]
When it comes to relieving those worries, nothing beats a friendly face in a familiar place, say experts who have documented the value of enlisting primary-care physicians, community leaders and pastors. It’s better still if the shot can be given right there, in their office or sanctuary.
“It’s one thing for a pastor to say it, another to have a pop-up vaccination site in the church,” Wilhelm said.
In Maryland, the Health Advocates In-Reach and Research Initiative (HAIR) is using barbershops and beauty salons to debunk misinformation within the Black community.
Ideally — and particularly if an easily stored, single-shot vaccine were widely available — doctors could offer shots during regular appointments, just as they do the flu shot.
“It is done as a matter of routine, rather than a big issue,” said former CDC director Tom Frieden, who has advocated for primary-care physicians to play a bigger role.
Messengers need to be honest about risks, communicating how they compare with the benefits, said Moore, who advocates for transparency with issues such as the rare but worrisome clotting associated with the AstraZeneca and Johnson & Johnson vaccines. Federal officials paused the use of the Johnson & Johnson vaccine last week.
“If you hedge, you can undermine the entire vaccination campaign in a moment if you appear to be covering up,” Moore said.
And trusted spaces exist on social media, where small groups can engage in Q&A sessions or Facebook live streams.
Meeting people where they are could even involve going door-to-door, as in a political campaign or with the census.
The key to getting more people vaccinated, said UNC’s Brewer, is “to make it easier.”
Make vaccination routine in peer groups and social networks
Seeing Elvis or Fauci getting vaccinated is helpful. But most people who are considering getting the shot want the answer to a straightforward question.
“Are people like me taking this vaccine, and how are they doing?” said Bruce Gellin, president of global immunization at the Sabin Vaccine Institute .
You are more likely to roll up your sleeve, Gellin and other experts say, if you’ve talked to your neighbor, co-worker, cousin or golf buddy about having done so.
That’s why the Philadelphia Department of Health began building connections with vaccine role models people may spot in their neighborhoods rather than on TV or at the ballpark, looking to block captains, pastors and barbers to lead the way.
“They are people where someone will say: ‘I know this guy. I’ve seen them on the block,’” said James Garrow, the department’s communications director.
Vaccine experts leverage the peer pressure with other tools, giving out “I’m vaccinated” stickers and buttons, offering selfie opportunities at mass vaccination sites and encouraging people to post their just-vaxxed pictures online to create a sense of solidarity. “Vaxxies” have become one of the defining social media images of 2021.
It’s all about creating links with people where they are — online or in person.
“Don’t mute your crazy uncle,” said the CDC’s Wilhelm. Instead, she said, share your experience with family and friends and talk to them about the advantages of getting a shot — such as new opportunities to get together safely.
The bottom line, Wilhelm said, is that vaccination is contagious.
Scott Clement contributed to this report.
About this story
Design, development and animation by Chloe Meister. Graphics by Tim Meko. Illustrations by The Washington Post using images from iStock, AP (Presley, Parton), Jabin Botsford/The Washington Post (Fauci) and IAC (vaccine button).
Coronavirus: What you need to read
Coronavirus maps: Cases and deaths in the U.S. | Cases and deaths worldwide
Vaccines: J&J vaccine pause | Tracker by state | Guidance for vaccinated people | How long does immunity last? | County-level vaccine data
What you need to know: Variants | Symptoms guide | Masks FAQ | Your life at home | Personal finance guide | Follow all of our coverage and sign up for our free newsletter
Got a pandemic question? We answer one every day in our coronavirus newsletter
Are you planning a long-awaited reunion after you get vaccinated? We want to hear from you
Motivating COVID-19 Vaccination through Persuasive Communication: A Systematic Review of Randomized Controlled Trials
Affiliation.
- 1 Department of Communication, University of Maryland.
- PMID: 37254940
- DOI: 10.1080/10410236.2023.2218145
Vaccination is a vital defense against COVID-19 infections and outbreaks, yet vaccine hesitancy poses a significant threat to pandemic response and recovery. We conducted a systematic review of published randomized controlled trials ( N = 47) assessing the persuasive effects of COVID-19 communication on COVID-19 vaccine acceptance. Individual vs. collective appeals and gain vs. loss frames are among the most frequently assessed message features, but they generally do not make a difference in persuasion. Normative messages that highlight higher (vs. lower) prevalence of vaccine acceptance are more persuasive. Message sources overall have limited impact on COVID-19 vaccine acceptance, but sources that have a shared identity with the message receivers tend to be persuasive. More engaging message channels such as interactive chatbots and videos are promising communication tools but are generally under-utilized and under-studied. Compared to no communication or irrelevant communication, COVID-19 vaccine messages generally have a small advantage in increasing COVID-19 vaccine acceptance. Messages that include 1) vaccine safety and/or efficacy information; 2) collective appeals combined with embarrassment appeals; and 3) political leaders' vaccine endorsement are among the most effective messaging strategies. There is no evidence of any backfire effects of COVID-19 vaccine messages. We discuss the implications of our findings for persuasive message design in pandemic vaccine communication.
Publication types
- Systematic Review
- COVID-19 Vaccines* / administration & dosage
- COVID-19* / prevention & control
- Health Communication / methods
- Motivation*
- Persuasive Communication*
- Randomized Controlled Trials as Topic*
- Vaccination / psychology
- Vaccination Hesitancy / psychology
- COVID-19 Vaccines

STUDENT ESSAY: Is Compulsory COVID-19 Vaccination a Violation of Human Rights?
In response to the COVID-19 pandemic, the UK Government passed the Coronavirus Act 2020 (CA), which implemented a number of emergency powers, allowing public officials to take action in specific situations in order to contain and slow down the spread of the virus as well as ease the burden on frontline staff. [1] Examples of these emergency powers include: the capability for public officials to test, isolate, and detain a person where they have reasonable grounds to think that the person is infected; restrict or prohibit gatherings or events; and require the temporary closure of a school or registered childcare provider. [2]
In its efforts to support the public health benefit, the CA has arguably led to interference with individuals’ right to liberty under Article 5(1) of the European Convention on Human Rights (ECHR). [3] Pugh’s 2020 article on the CA discusses how individuals may be deprived of their liberty to prevent the spread of infectious diseases, if that deprivation is “necessary and proportionate” and is in accordance with a procedure prescribed by law. [4] Pugh refers to this as “the public health exception”. [5] The importance of this approach directly relates to the consideration of a compulsory COVID-19 vaccine, specifically whether limitations on specific rights can be justified.
This essay analyzes whether a compulsory COVID-19 vaccine would be a violation of human rights law in the UK. For a comprehensive understanding of the implications of this topic, I provide background information and discuss perspectives regarding compulsory vaccinations in general. This discussion is followed by an outline of the specific rights under the ECHR that may be affected if a compulsory vaccination was to be implemented in the UK. I then discuss various interpretations of the elements required for state interference upon these rights and expand on them in regard to their application to compulsory vaccination. Through this analysis, it is concluded that a compulsory COVID-19 vaccination would not be a violation of human rights in the UK if the government sets out explicit parameters whereby a compulsory vaccination would be “necessary and proportionate” in the interests of health and safety, and if it was to ensure that the state is fulfilling its positive obligation to protect the right to life. [6]
Background on vaccinations and vaccine hesitancy
The topic of vaccination has been vastly studied across the world, affirming that high rates of vaccination coverage in childhood are important in preventing infectious diseases and contributing to a decline in mortality. [7] Despite the fact that vaccinations have proven to decrease rates of common childhood diseases and in some cases result in the complete termination of diseases, there is a rising trend of parents refusing to vaccinate their children. [8] This trend is commonly referred to as the anti-vaccination movement or Anti-Vaxx. The basis for these views revolves around arguments that vaccinations cause sickness, use unethical practices, and overall hold a lot of uncertainty, which causes hesitancy. [9] In addition, wide use of social media has allowed the Anti-Vaxx trend to become more widespread, and in a number of cases has led to vaccination rates dropping below the levels needed for herd immunity. Herd immunity occurs when a high enough percentage of the population is vaccinated that there are then too few people available to become hosts, so transmission of the disease or virus stops. [10] One of the most important characteristics of herd immunity is that it not only protects those who receive vaccination, but helps to protect individuals who are not vaccinated for whatever reason. [11]
Looking further into vaccine hesitancy, Kestenbaum and Feester identified some of the common factors contributing to this trend, including knowledge and information sources, experience or lack of experience with vaccine-preventable diseases, the role of recommendations by health professionals, social norms, and parental responsibility, trust, and religious beliefs. [12] They found many factors contribute to this trend, with uncertainty and the rapid transfer of information leading to the refusal of vaccination by families and individuals. The rise in the Anti-Vaxx movement has been shown to significantly impair health protection. A number of studies found that from 2006-2011, decreases in MMR (measles, mumps, and rubella) vaccination rates in the UK, Ireland, France, Italy, and the United States, had a direct correlation with measles outbreaks in those areas. [13] In response to these changes, both Italy and France passed legislation that made specific vaccinations, including MMR, compulsory for children. [14]
Religious beliefs and conscientious objection, which would fall under Article 9 of the ECHR, also contribute to decisions not to vaccinate. [15] There are a number of governments that have implemented compulsory vaccination for children in public and private schools, as well as childcare centres. In conjunction with these policies, governments allow for exemption from vaccination on medical and non-medical grounds. In this context, the non-medical grounds often relate to religion and conscientious objection. But religion has not been found to contribute much to decisions not to vaccinate. A North American study published in the Journal of the American Academy of Pediatricians found that over 70% of 512 doctors who had patients who had refused vaccines, claimed that parents had denied vaccination for their children because they felt the vaccine was unnecessary. [16] In addition, the Vanderbilt University Medical Centre states that “most religions have no prohibition against vaccinations” but the two common objecting religions are ‘Christian Scientists’ and ‘Dutch Reformed Congregations’. [17] These studies suggest that in the United States most non-medical exemptions fall under the category of conscientious objection rather than religion and that this trend is one of the primary reasons why some US jurisdictions have chosen to ban non-medical exemptions for compulsory vaccinations. [18]
State obligations under ECHR and compulsory vaccination
Regarding the potential implementation of a compulsory vaccination, the primary source of law to be considered is the ECHR, which was incorporated into UK law through the Human Rights Act 1998. [19] Article 2 of the ECHR concerning the right to life is of upmost importance in this context as it places positive and negative obligations on the state. Interpretation of this Article is summarized by the ECtHR in L.C.B. v The United Kingdom (1998), stating that “the state must not only refrain from the intentional and unlawful taking of life, but also take appropriate steps to safeguard the lives of those within its jurisdiction.” [20] Specifically regarding the positive obligation, states have a “primary duty to put in place a legislative and administrative framework designed to provide effective deterrence against threats to the right to life.” [21] As suggested by Camilleri, the positive obligation deriving from Article 2 may lead to claims that, in the context of a public health emergency, a vaccine should be made mandatory for those who are able to receive it, in order to protect those who rely on herd immunity for protection against such diseases. [22] However, when considering a narrower compulsory vaccination claim, the case of Calvelli and Ciglio (2002) is highly relevant as the court applied the positive obligation principle of Article 2 specifically to “the public health sphere”, stating that the obligation “requires states to make regulations compelling hospitals, whether public or private, to adopt appropriate measures for the protection of their patients’ lives.” [23]
This concept is demonstrated through a number of examples where the MMR vaccine, among others, has been made a legal requirement for healthcare professionals. Countries such as Canada, Australia, and several Caribbean countries, as well as some countries in Europe, have polices whereby certain vaccinations are a requirement by law for those directly in the healthcare sector, one of them being the UK. [24] In addition, there are a number of governments that have adopted similar policies with specific focus on the education sector. For example, in Italy, France, three provinces of Canada, as well as the United States, there is a requirement for children to be vaccinated in order to attend public or private schools. [25] An important element of this requirement is that they allow for medical, religious, and philosophical exemptions, aside from Mississippi, West Virginia, and California, which now only allow for medical exemptions. [26] In countries such as Australia, although vaccinations for children are not mandatory, the government offers financial incentives to have their children vaccinated. This is through non-taxable payments for each child who meets the requirements for immunization. [27]
One of the key outcomes of the implementation of these mandatory vaccination policies is that the government has not only taken positive action to protect the right to life of individuals within their jurisdiction, but they have ensured that individuals who rely on herd immunity are able to fully enjoy their human rights and fundamental freedoms the same way every other individual is able to, without putting their own lives at risk.
State interference and limitations on rights
From a public health perspective, a compulsory vaccination would be beneficial and it is clear that states have an obligation to protect the life of those within its jurisdiction. However, consideration should be given as to whether forcing individuals to receive a vaccination would interfere with any of their rights, and if so, would such an interference be lawful in the circumstances. Camilleri brings forward two specific ECHR articles with which compulsory vaccination would likely interfere: (i) Article 8-right to respect for private and family life, and (ii) Article 9-freedom of thought, conscience and religion. [28] The primary argument behind a violation of these rights relates to the idea that individuals should have reasonable control over the actions in which they partake, particularly when it considers an individual’s human body. As we can see in the case of Herczegfalvy (1992), the forceful administration of food was considered under Article 8, but was held to be compatible with respect for the claimant’s private life, as medical treatment was a necessity under the principles of psychiatry at that time. [29] Although the claimant was unsuccessful in this element, the violation would have been deemed unlawful if the court found that it was either not necessary, proportionate, or for a legitimate aim.
Regarding Article 8 specifically, the state holds a primary negative obligation to ensure that public authorities do not interfere with individuals’ right to private and family life. [30] As confirmed in the case of Kroon and others (1994), private life includes both the physical and psychological integrity of the individual. [31] Therefore, the physical aspect of the individual is an important element which may be conflicted with if that individual is required to be vaccinated by law. That said, Article 8(2) sets out that a state may interfere with the enjoyment of this right in certain circumstances. Similarly, Article 9 follows an analogous provision where states have an obligation to not interfere unless specific criteria can be satisfied. The “Guide on Article 8 of the ECHR”, which is again similar to that of Article 9, says that for interference to be lawful, it must be: (1) in accordance with the law; (2) in the interests of national security, public safety, or the economic well-being of the country, for the prevention of the disorder of crime, for the protection of health or morals, or for the protection of the rights and freedoms of others; and (3) that such interference is necessary in a democratic society. [32]
Regarding the first element, the court has been consistent in ensuring that any interference with these rights by a public authority must be in accordance with the law. This requirement revolves around the rule of law, as an interference must not only comply with domestic law but should be equally enforced among all individuals and entities that fall under its jurisdiction. [33] An interpretation of this element is found in Silver and Others (1983), stating that the national law must be clear, foreseeable, and adequately accessible. [34] As mentioned in Piechowicz (2012) the clarity requirement relates to “the scope of discretion exercised by public authorities” which is to ensure that individuals are provided with a “minimum degree of protection” from the relevant authorities and the authorities are therefore working within the rule of law. [35]
The second element relates to the question of whether the interference is in line with a legitimate aim set out in paragraph 2 of the relevant Article. [36] The court has often shown that as long as the aim of the interference falls within one of the objects set out in the provision, they will not hesitate to confirm satisfaction of this requirement. This can be observed in S.A.S. v France (2014) , where the sensitive action of banning full face veils in public places did in fact serve a legitimate aim to ensure individuals can enjoy their right to live in spaces of socialization without having any barrier to social interaction. [37] That said, it would be fairly clear that a compulsory vaccination would work directly in line with an aim to protect the interests of public health and safety, as well as for the protection of the rights and freedoms of others through the effective implementation of herd immunity.
The third element is perhaps the most critical, as “necessary” is a requirement that relies heavily on the specific circumstances. In the case of Olssen v Sweden (1988), “necessary” was said to imply the existence of a pressing social need and that it must be proportionate to the legitimate aim pursued. [38] This is a direct understanding that was incorporated into the ECtHR’s “Guide on Article 8”. [39] An important interpretation of this element is again found in Piechowicz , where it is stated that although the respondent state in the case must “demonstrate the existence of a pressing social need behind the interference”, it is the court who must consider the margin of appreciation left to the state authorities. [40] This margin of appreciation varies depending on the circumstances in question, and therefore, allows the court to resolve practical differences in the implementation of provisions within the convention. [41] Upon the elements of necessity and proportionality, it would be very difficult to justify that a compulsory vaccination applying to all individuals within the UK jurisdiction would be justified.
In the case of Biblical Centre of the Chuvash Republic v Russia (2014), the relevant authorities had to show that no other measures were available to achieve the same end that would interfere less seriously with the fundamental right concerned. [42] This was a burden that existed in order to prove that the interference was in fact necessary and proportionate. Specifically in relation to a compulsory COVID-19 vaccination, it is important to consider that there are alternatives that could be applied that would follow the same legitimate aim, yet would likely be less intrusive on individual rights. One of the more feasible options would be to continue, or even further the restrictions that have been implemented by the Coronavirus Act 2020, and that would apply to the UK population as a whole. In addition, while considering the elements of interference above, due to the variety of individual characteristics, activities, and needs across the population of the UK, it would be fair to say that certain population groups would find a compulsory vaccine significantly less necessary and proportionate than others.
In considering each of the three essential elements relating to the lawful interference of Article 8, the recent decision in Vavřička and Others v. the Czech Republic is highly significant as the ECtHR provided a ruling specifically in respect of compulsory vaccinations for MMR, as well as other diseases such as poliomyelitis, hepatitis B, and tetanus. [43] The applicants in Vavřička challenged the lawfulness of the sanctions imposed as a result of failing to fully vaccinate their children under Czech law, specifically the Public Health Protection Act. [44] The sanctions imposed consisted of a fine equivalent to €110 for Mr. Vavřička, and denial of admission to nursery schools for the children of the other applicants. [45] In determining whether the interfering sanctions entailed a violation of Article 8, the court was required to assess whether it was justified under Article 8(2), by applying the three prong test: (1) whether it was in accordance with the law, (2) whether it pursued one or more legitimate aims, and (3) whether it was necessary in a democratic society. [46] Without going into extensive detail, the court was satisfied that the state met each of these three requirements as the law existed to protect against diseases posing a serious health risk, to prevent decline in vaccination rates among children, and to support the state’s positive obligation to protect the lives and health of those within its jurisdiction. [47] Furthermore, the ECtHR decided that the interference was proportionate in light of the aim pursued, therefore it concluded that there was no violation of Article 8. [48]
Vavřička is a case that very clearly considers all of the elements required in determining the lawfulness of compulsory vaccination under Article 8. That being said, although the ECtHR determined that compulsory vaccination in this case was lawful, it does not necessarily mean that this decision is the sole precedent for a challenge to a compulsory COVID-19 vaccination. Firstly, this is due to the fact that the court in Vavřička explicitly states that “the present case relates to the standard and routine vaccination of children against diseases that are well known to medical science.” [49] It would be extremely difficult to claim that medical professionals have reached the same level of understanding of COVID-19 as the diseases concerned in the case of Vavřička . Furthermore, the court made it clear that while vaccination was a legal duty in the Czech Republic, there were no provisions that allowed forceable vaccination. Therefore, this decision is one that was made based on the specific facts involved and cannot be assumed to dictate the ruling in a case of compulsory COVID-19 vaccination. Given this decision, the lawfulness of efforts to enforce a compulsory COVID-19 vaccination may depend on the degree of the consequence for noncompliance, while also considering what might be deemed an exception for noncompliance, specifically medical or religious reasons.
The history of compulsory vaccination across the globe shows a trend of specific areas where compulsory vaccinations are lawfully implemented and therefore considered legitimate, necessary, and proportionate. There is a compelling argument supporting the implementation of such a vaccine to those in the public and private education sectors, as well as those who work in the healthcare system. These are typically environments where large numbers of people occupy relatively small areas. This leads to conditions where viruses can easily be transferred and therefore health matters within these areas are of high concern. Supporting the argument for the need for increased protection in these areas, a study from the Usher Institute showed that the reopening of schools (without any regard to vaccination) increases transmission of the virus by 24%. [50] Furthermore, a study conducted by the University College London Hospitals (UCLH) NHS Foundation Trust found that about 45% of the healthcare workers at the UCLH showed evidence of being infected with COVID-19 between the months of April and May 2020. [51] When applying the criteria for interference under Article 8(2) and Article 9(2), specifically to the education and healthcare sectors, the argument supporting necessity and proportionality appears to be considerably stronger than that of a compulsory vaccine directed at the general public.
The purpose of this essay is simply to state whether a compulsory COVID-19 vaccination would be a violation of human rights law. From the above analysis, primarily regarding the elements of the relevant articles of the ECHR and the interpretation of those elements by the court, it is evident that a compulsory vaccination would be lawful if the government were to implement such a policy within explicit parameters whereby a compulsory vaccination would be necessary and proportionate in the interest of public health and safety and for the protection of the rights and freedoms of others. The Joint Committee on Vaccination and Immunisation (JCVI) is the independent expert advisory committee that advises the UK health departments on immunisation, making recommendations concerning vaccination schedules and vaccine safety. In December 2020, JCVI provided a document to the UK Government with advice to facilitate the development of policy on COVID-19 vaccination. [52] This document set out the recommendations regarding prioritization of the administration of COVID-19 vaccines in the UK population based on a comprehensive review of COVID-19, demographic data, clinical risk factors for mortality and hospitalisation, as well as the mathematical modelling on the potential impact of different vaccination programs. [53] If at some point there is a decision to make a COVID-19 vaccination compulsory in the UK, who would be subject to this compulsory vaccination would likely be a decision made in line with further advice from JCVI through enforcement by the UK Government. However, imposing such a requirement upon specific groups of people raises a number of significant concerns, considering the potential challenges that can be brought forward by ethicists and/or representatives of various religions. These questions and concerns are highly complicated matters which are essentially outside the scope of this specific discussion.
As COVID-19 continues to develop, the questions about vaccination become more significant. When considering the case law on the legality of interference with specific provisions of the ECHR, it seems possible that a compulsory COVID-19 vaccination can be enforced while still complying with human rights law. Only time will tell if compulsory vaccination will be adopted, but when it comes to the state’s protection of the greater good under such unprecedented circumstances, enforcement of a compulsory vaccination appears to be one of the most effective and beneficial protective measures.
Aaron Chia is a law graduate from the School of Law, University of Stirling, Scotland and currently a student associate at Yeghoyan & Jacula Law Firm, Ontario, Canada.
[1] UK Public General Acts, Coronavirus Act 2020 , c.7 (March 25, 2020).
[2] Ibid, s.51; s.52; s.38-39.
[3] European Convention on Human Rights, European Treaty Series No. 5 (1950), art. 5. Available at http://www.conventions.coe.int/Treaty/en/Treaties/Word/005.doc .
[4] J. Pugh, “The United Kingdom’s Coronavirus Act, deprivations of liberty, and the right to liberty and security of the person,” Journal of the Law and the Biosciences 7/1 (2020), pp. 1-14.
[6] Enhorn v. Sweden App no. 56529/00 (ECtHR, January 25, 2005); European Convention on Human Rights (see note 2), art. 2.
[7] Centers for Disease Control and Prevention, “Impact of vaccines universally recommended for children–United States, 1990-1998,” Morbidity and Mortality Weekly Report 48/12 (1999), pp. 243-248.
[8] Hussain et al., “The Anti-vaccination Movement: A Regression in Modern Medicine,” Cureus Journal of Medical Science 10/7 (2018), e2919.
[9] R. Pierik, “Mandatory Vaccination: An Unqualified Defence” Journal of Applied Philosophy 35/2 (2016), pp. 381-398.
[10] M. Mallory, L.Lindesmith, and R. Baric, “Vaccination-induced herd immunity: Success and challenges,” Journal of Allergy and Clinical Immunology 142/1 (2018), pp. 64-66.
[11] M. Sadarangani, Oxford Vaccine Group, Herd Immunity: How does it work? (2016). Available at https://www.ovg.ox.ac.uk/news/herd-immunity-how-does-it-work .
[12] L. Kestenbaum, and K. Feemster, “Identifying and Addressing Vaccine Hesitancy” Pedatric annals 44/4 (2015), pp. e71-e75.
[13] D. Antona et al., “Measles Elimination Efforts and 2008-2011 Outbreak, France,” Emerging Infectious Diseases 19/3 (2013), pp. 357-364; M. Pepys, “Science and serendipity,” Clinical Medicine 7/6 (2007), pp. 562-578.
[14] G. Rezza, “Mandatory vaccination for infants and children: the Italian experience,” Pathogens and Global Health 113/7 (2019), pp. 291-296; D. Lévy-Bruhl et al. “Extension of French vaccination mandates: from the recommendation of the Steering Committee of the Citizen Consultation on Vaccination to the law,” Eurosurveillance 23/17 (2018), 18-00048.
[15] European Convention on Human Rights (see note 2), art. 9.
[16] C. Hough-Telford et al. “Vaccine Delays, Refusals, and Patient Dismissals: A Survey of Pediatricians,” Journal of the American Academy of Pediatrics 138/3 (2016), e20162127.
[17] Vanderbilt Occupational Health Clinic, Immunizations and Religion (2013). Available at https://www.vumc.org/health-wellness/news-resource-articles/immunizations-and-religion ; J. Grabenstein, “What the world’s religions teach, applied to vaccines and immune globulins,” Vaccine 31/16 (2013), pp. 2011-2023.
[18] E. Walkinshaw, “Mandatory vaccinations: The international landscape,” Canadian Medical Association Journal 183/16 (2011), pp. e1167-e1168.
[19] UK Public General Acts, Human Rights Act 1998 , c.42 (November 9, 1998).
[20] L.C.B. v The United Kingdom App no. 14/1997/798/1001 (ECtHR, June 9, 1998), para. 36.
[21] O¨neryildiz v Turkey App no. 48939/99 (ECtHR, November 30, 2004), para. 89.
[22] F. Camilleri, “Compulsory vaccinations for children: Balancing the competing human rights at stake,” Netherlands Quarterly of Human Rights 37/3 (2019), pp. 245-267.
[23] Calvelli and Ciglio v Italy App no. 32967/96 (ECtHR, January 17, 2002), para. 49.
[24] A. Fiebelkorn, J. Seward, and W. Orenstein, “A Global Perspective of Vaccination of Healthcare Personnel against Measles: Systematic Review,” Vaccine 32/38 (2015), 4823.
[25] F. D’Ancona, “The law on compulsory vaccination in Italy: an update 2 years after the introduction,” Eurosurveillance 24/26 (2019), 1900371; Lévy-Bruhl et al. (see note 13); E. Walkinshaw, “Mandatory vaccination: The Canadian picture,” Canadian Medical Association Journal 183/16 (2011), pp. e1165-e1166; Walkinshaw (see note 17), pp. e1167.
[27] K. Ward, B. Hull, and J. Leask, “Financial incentives for childhood immunisation – a unique but changing Australian initiative,” Medical Journal of Australia 198/11 (2013), pp. 590-592.
[28] Camilleri (see note 21), pp. 251-252.
[29] Herczegfalvy v Austria App no. 10533/83 (ECtHR, September 24, 1992).
[30] European Convention on Human Rights (see note 2), art. 8.
[31] Kroon and Others v. the Netherlands App no. 18535/91 (ECtHR, October 27, 1994), para. 31.
[32] European Court of Human Rights, “Guide on Article 8 of the European Convention on Human Rights – Right to respect for private and family life,” (December 31, 2016). Available at https://www.echr.coe.int/documents/guide_art_8_eng.pdf.
[33] Halford v The United Kingdom App no. 20605/92 (ECtHR, June 25, 1997).
[34] Silver and others v The United Kingdom App no. 5947/72; 6205/73; 7052/75; 7061/75; 7107/75; 7113/75; 7136/75 (ECtHR, March 25 1983).
[35] Piechowicz v Poland App no, 20071/07 (ECtHR, April 17, 2012).
[36] European Court of Human Rights, “Freedom of thought, conscience and religion: A guide to the implementation of Article 9 of the European Convention on Human Rights,” (June, 2007). Available at https://www.echr.coe.int/Documents/Guide_Art_9_ENG.pdf .
[37] S.A.S. v France App no. 43835/11 (ECtHR, July 1, 2014).
[38] Olsson v Sweden App no. 10465/83 (ECtHR), March 24, 1988), para. 67; Dudgeon v. The United Kingdom App no. 7525/76 (ECtHR, October 22, 1981).
[39] Also see Z v Finland App no. 22009/93 (ECtHR, February 25, 1997).
[40] Piechowicz (see note 34).
[41] Paradiso and Campanelli v Italy App no. 25358 (ECtHR, January 24, 2017), para. 182.
[42] Biblical Centre of the Chuvash Republic v Russia App no. 33203/08 (ECtHR, June 12, 2014).
[43] Vavřička and Others v. the Czech Republic App no. 47621/13 and 5 others (ECtHR, April 8, 2021).
[44] Act No. 258/2000 on protection of public health as consolidated to Act No. 471/2005.
[45] Vavřička (see note 42), para. 293.
[46] Vavřička (see note 42), para. 265.
[47] Vavřička (see note 42), para. 272; para. 284; para. 282.
[48] Vavřička (see note 42), paras. 290-309; para. 311.
[49] Vavřička (see note 42), para. 158.
[50] Y. Li et al. “The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: a modelling study across 131 countries,” The Lanclet Infectious Diseases 22/2 (2021), pp.139-202.
[51] University College London Hospitals NHS Foundation Trust, “Pandemic peak SARS-CoV-2 infection and seroconversion rates in London frontline health-care workers,” Elsevier Public Health Emergency Collection 396 (2020) pp. e6-e7.
[52] Department of Health and Social Care, “Joint Committee on Vaccination and Immunisation: advice on priority groups for COVID-19 vaccination,” (December 30, 2020). Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/950113/jcvi-advice-on-priority-groups-for-covid-19-vaccination-30-dec-2020-revised.pdf .
[53] Ibid, pp. 1.
Here Are Arguments That Can Help Overcome COVID-19 Vaccine Hesitancy

October 2024

Related Content
Oral anticoagulants underused in atrial fibrillation patients with high stroke risk, cardiovascular disease deaths rose during early covid-19 pandemic, tight glycemic control increases fracture risk in men with diabetes, mixed success with lipid control across ethnic/racial groups.

- Advertising Contacts
- Editorial Staff
- Professional Organizations
- Submitting a Manuscript
- Privacy Policy
- Classifieds

COMMENTS
Examples of Persuasive Essay About COVID-19 Vaccine. Covid19 vaccines are one of the ways to prevent the spread of COVID-19, but they have been a source of controversy. Different sides argue about the benefits or dangers of the new vaccines. Whatever your point of view is, writing a persuasive essay about it is a good way of organizing your ...
Vaccination stands as a monumental achievement in medicine, offering protection against various infectious diseases and significantly improving public health. The journey from the development of the smallpox vaccine to the rapid response to COVID-19 vaccines highlights the importance and versatility of vaccination in addressing health challenges.
Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective action problem and highlighting the prosocial benefit of vaccination or the ...
Examples of Persuasive Essay About the Covid-19 Vaccine. With so much uncertainty surrounding the Covid-19 vaccine, it can be challenging for students to write a persuasive essay about getting vaccinated. Here are a few examples of persuasive essays about vaccination against covid-19. Check these out to learn more.
2. Hearing pro-vaccine messages from doctors, friends and relatives. For many people who got vaccinated, messages from politicians, national experts and the mass media were persuasive.
COVID-19 vaccination should be mandatory - at least for certain groups. This means there would be penalties for failure to vaccinate, such as fines or limitations on freedom of movement. The ...
The subsequent paragraphs are going to provide detailed explanations of the reasons why it is necessary for the COVID-19 vaccine to be taken. Firstly, the COVID-19 vaccine is necessary because it helps build protection against the virus. COVID-19 is a terrifying and dangerous communicable disease. The virus affects the respiratory organ of the ...
Vaccine hesitancy threatened public health's response to the COVID-19 pandemic. Scientists at the University of Maryland recently reviewed 47 randomized controlled trials to determine how COVID-19 communications persuaded—or failed to persuade—people to take the vaccine. (Health Communication, 2023 DOI: 10.1080/10410236.2023.2218145).
Helping to make the person's decision feel less forced upon them can actually make them more willing to get it! 3. Find a Common Enemy With the Person. Sometimes, there is no truer saying than ...
This article is part of a series of explainers on vaccine development and distribution. Learn more about vaccines - from how they work and how they're made to ensuring safety and equitable access - in WHO's Vaccines Explained series.. Vaccines are a critical tool in the battle against COVID-19, and getting vaccinated is one of the best ways to protect yourself and others from COVID-19.
Participants were then randomly asked to read one of ten texts about COVID-19 vaccines. A potentially persuasive personal benefit of taking a vaccine is avoiding long COVID.
Without high rates of uptake, however, the pandemic is likely to be prolonged. Here we use two survey experiments to study how persuasive messaging affects COVID-19 vaccine uptake intentions. In the first experiment, we test a large number of treatment messages. One subgroup of messages draws on the idea that mass vaccination is a collective ...
While efficacious vaccines have been developed to inoculate against severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2; also known as COVID-19), public vaccine hesitancy could still ...
Introduction. The COVID-19 pandemic has sparked global efforts to develop countermeasures against SARS-CoV-2. One such measure lies with the rapid research and development of effective COVID-19 vaccines1 which are critical to achieve impactful COVID-19 vaccination campaigns.2 Although credible vaccine information from official sources is abundantly available,3-6 vaccine-hesitant individuals ...
To answer RQ1, whether gain-framed and loss-framed messages have different persuasive effects on COVID-19 vaccination intention, the results show that for message framing, the loss-framed message, compared with the gain-framed message, promoted the intention to get the COVID-19 vaccine. A one-way ANOVA was conducted on the COVID-19 vaccination ...
April 22, 2021. With all Americans 16 and over now eligible to receive a coronavirus vaccine, health-care workers and public health officials are turning their attention to the approximately one ...
Vaccination is a vital defense against COVID-19 infections and outbreaks, yet vaccine hesitancy poses a significant threat to pandemic response and recovery. We conducted a systematic review of published randomized controlled trials (N = 47) assessing the persuasive effects of COVID-19 communication on COVID-19 vaccine acceptance. Individual vs ...
Our analyses indicate that vaccine effectiveness generally decreases over time against SARS-CoV-2 infections, hospitalisations, and mortality. The baseline vaccine effectiveness levels for the omicron variant were notably lower than for other variants. Therefore, other preventive measures (eg, face-mask wearing and physical distancing) might be necessary to manage the pandemic in the long term.
Aaron Chia. In response to the COVID-19 pandemic, the UK Government passed the Coronavirus Act 2020 (CA), which implemented a number of emergency powers, allowing public officials to take action in specific situations in order to contain and slow down the spread of the virus as well as ease the burden on frontline staff. Examples of these emergency powers include: the capability for public ...
Here are statements found to be most convincing for vaccination acceptance, according to the poll: • "At 95 percent efficacy, this vaccine is extraordinarily effective at protecting you from the virus". • "Vaccines will help bring this pandemic to an end". • "Getting vaccinated will help keep you, your family, your community, and ...