- Patient Care & Health Information
- Diseases & Conditions
- Depression (major depressive disorder)
- What is depression? A Mayo Clinic expert explains.
Learn more about depression from Craig Sawchuk, Ph.D., L.P., clinical psychologist at Mayo Clinic.
Hi, I'm Dr. Craig Sawchuk, a clinical psychologist at Mayo Clinic. And I'm here to talk with you about depression. Whether you're looking for answers for yourself, a friend, or loved one, understanding the basics of depression can help you take the next step.
Depression is a mood disorder that causes feelings of sadness that won't go away. Unfortunately, there's a lot of stigma around depression. Depression isn't a weakness or a character flaw. It's not about being in a bad mood, and people who experience depression can't just snap out of it. Depression is a common, serious, and treatable condition. If you're experiencing depression, you're not alone. It honestly affects people of all ages and races and biological sexes, income levels and educational backgrounds. Approximately one in six people will experience a major depressive episode at some point in their lifetime, while up to 16 million adults each year suffer from clinical depression. There are many types of symptoms that make up depression. Emotionally, you may feel sad or down or irritable or even apathetic. Physically, the body really slows down. You feel tired. Your sleep is often disrupted. It's really hard to get yourself motivated. Your thinking also changes. It can just be hard to concentrate. Your thoughts tend to be much more negative. You can be really hard on yourself, feel hopeless and helpless about things. And even in some cases, have thoughts of not wanting to live. Behaviorally, you just want to pull back and withdraw from others, activities, and day-to-day responsibilities. These symptoms all work together to keep you trapped in a cycle of depression. Symptoms of depression are different for everyone. Some symptoms may be a sign of another disorder or medical condition. That's why it's important to get an accurate diagnosis.
While there's no single cause of depression, most experts believe there's a combination of biological, social, and psychological factors that contribute to depression risk. Biologically, we think about genetics or a family history of depression, health conditions such as diabetes, heart disease or thyroid disorders, and even hormonal changes that happen over the lifespan, such as pregnancy and menopause. Changes in brain chemistry, especially disruptions in neurotransmitters like serotonin, that play an important role in regulating many bodily functions, including mood, sleep, and appetite, are thought to play a particularly important role in depression. Socially stressful and traumatic life events, limited access to resources such as food, housing, and health care, and a lack of social support all contribute to depression risk. Psychologically, we think of how negative thoughts and problematic coping behaviors, such as avoidance and substance use, increase our vulnerability to depression.
The good news is that treatment helps. Effective treatments for depression exist and you do have options to see what works best for you. Lifestyle changes that improve sleep habits, exercise, and address underlying health conditions can be an important first step. Medications such as antidepressants can be helpful in alleviating depressive symptoms. Therapy, especially cognitive behavioral therapy, teaches skills to better manage negative thoughts and improve coping behaviors to help break you out of cycles of depression. Whatever the cause, remember that depression is not your fault and it can be treated.
To help diagnose depression, your health care provider may use a physical exam, lab tests, or a mental health evaluation. These results will help identify various treatment options that best fit your situation.
Help is available. You don't have to deal with depression by yourself. Take the next step and reach out. If you're hesitant to talk to a health care provider, talk to a friend or loved one about how to get help. Living with depression isn't easy and you're not alone in your struggles. Always remember that effective treatments and supports are available to help you start feeling better. Want to learn more about depression? Visit mayoclinic.org. Do take care.
Depression is a mood disorder that causes a persistent feeling of sadness and loss of interest. Also called major depressive disorder or clinical depression, it affects how you feel, think and behave and can lead to a variety of emotional and physical problems. You may have trouble doing normal day-to-day activities, and sometimes you may feel as if life isn't worth living.
More than just a bout of the blues, depression isn't a weakness and you can't simply "snap out" of it. Depression may require long-term treatment. But don't get discouraged. Most people with depression feel better with medication, psychotherapy or both.
Depression care at Mayo Clinic

Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Begin Exploring Women's Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Although depression may occur only once during your life, people typically have multiple episodes. During these episodes, symptoms occur most of the day, nearly every day and may include:
- Feelings of sadness, tearfulness, emptiness or hopelessness
- Angry outbursts, irritability or frustration, even over small matters
- Loss of interest or pleasure in most or all normal activities, such as sex, hobbies or sports
- Sleep disturbances, including insomnia or sleeping too much
- Tiredness and lack of energy, so even small tasks take extra effort
- Reduced appetite and weight loss or increased cravings for food and weight gain
- Anxiety, agitation or restlessness
- Slowed thinking, speaking or body movements
- Feelings of worthlessness or guilt, fixating on past failures or self-blame
- Trouble thinking, concentrating, making decisions and remembering things
- Frequent or recurrent thoughts of death, suicidal thoughts, suicide attempts or suicide
- Unexplained physical problems, such as back pain or headaches
For many people with depression, symptoms usually are severe enough to cause noticeable problems in day-to-day activities, such as work, school, social activities or relationships with others. Some people may feel generally miserable or unhappy without really knowing why.
Depression symptoms in children and teens
Common signs and symptoms of depression in children and teenagers are similar to those of adults, but there can be some differences.
- In younger children, symptoms of depression may include sadness, irritability, clinginess, worry, aches and pains, refusing to go to school, or being underweight.
- In teens, symptoms may include sadness, irritability, feeling negative and worthless, anger, poor performance or poor attendance at school, feeling misunderstood and extremely sensitive, using recreational drugs or alcohol, eating or sleeping too much, self-harm, loss of interest in normal activities, and avoidance of social interaction.
Depression symptoms in older adults
Depression is not a normal part of growing older, and it should never be taken lightly. Unfortunately, depression often goes undiagnosed and untreated in older adults, and they may feel reluctant to seek help. Symptoms of depression may be different or less obvious in older adults, such as:
- Memory difficulties or personality changes
- Physical aches or pain
- Fatigue, loss of appetite, sleep problems or loss of interest in sex — not caused by a medical condition or medication
- Often wanting to stay at home, rather than going out to socialize or doing new things
- Suicidal thinking or feelings, especially in older men
When to see a doctor
If you feel depressed, make an appointment to see your doctor or mental health professional as soon as you can. If you're reluctant to seek treatment, talk to a friend or loved one, any health care professional, a faith leader, or someone else you trust.
When to get emergency help
If you think you may hurt yourself or attempt suicide, call 911 in the U.S. or your local emergency number immediately.
Also consider these options if you're having suicidal thoughts:
- Call your doctor or mental health professional.
- Contact a suicide hotline.
- In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat . Services are free and confidential.
- U.S. veterans or service members who are in crisis can call 988 and then press “1” for the Veterans Crisis Line . Or text 838255. Or chat online .
- The Suicide & Crisis Lifeline in the U.S. has a Spanish language phone line at 1-888-628-9454 (toll-free).
- Reach out to a close friend or loved one.
- Contact a minister, spiritual leader or someone else in your faith community.
If you have a loved one who is in danger of suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
More Information
Depression (major depressive disorder) care at Mayo Clinic
- Male depression: Understanding the issues
- Nervous breakdown: What does it mean?
- Pain and depression: Is there a link?
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
It's not known exactly what causes depression. As with many mental disorders, a variety of factors may be involved, such as:
- Biological differences. People with depression appear to have physical changes in their brains. The significance of these changes is still uncertain, but may eventually help pinpoint causes.
- Brain chemistry. Neurotransmitters are naturally occurring brain chemicals that likely play a role in depression. Recent research indicates that changes in the function and effect of these neurotransmitters and how they interact with neurocircuits involved in maintaining mood stability may play a significant role in depression and its treatment.
- Hormones. Changes in the body's balance of hormones may be involved in causing or triggering depression. Hormone changes can result with pregnancy and during the weeks or months after delivery (postpartum) and from thyroid problems, menopause or a number of other conditions.
- Inherited traits. Depression is more common in people whose blood relatives also have this condition. Researchers are trying to find genes that may be involved in causing depression.
- Marijuana and depression
- Vitamin B-12 and depression
Risk factors
Depression often begins in the teens, 20s or 30s, but it can happen at any age. More women than men are diagnosed with depression, but this may be due in part because women are more likely to seek treatment.
Factors that seem to increase the risk of developing or triggering depression include:
- Certain personality traits, such as low self-esteem and being too dependent, self-critical or pessimistic
- Traumatic or stressful events, such as physical or sexual abuse, the death or loss of a loved one, a difficult relationship, or financial problems
- Blood relatives with a history of depression, bipolar disorder, alcoholism or suicide
- Being lesbian, gay, bisexual or transgender, or having variations in the development of genital organs that aren't clearly male or female (intersex) in an unsupportive situation
- History of other mental health disorders, such as anxiety disorder, eating disorders or post-traumatic stress disorder
- Abuse of alcohol or recreational drugs
- Serious or chronic illness, including cancer, stroke, chronic pain or heart disease
- Certain medications, such as some high blood pressure medications or sleeping pills (talk to your doctor before stopping any medication)
Complications
Depression is a serious disorder that can take a terrible toll on you and your family. Depression often gets worse if it isn't treated, resulting in emotional, behavioral and health problems that affect every area of your life.
Examples of complications associated with depression include:
- Excess weight or obesity, which can lead to heart disease and diabetes
- Pain or physical illness
- Alcohol or drug misuse
- Anxiety, panic disorder or social phobia
- Family conflicts, relationship difficulties, and work or school problems
- Social isolation
- Suicidal feelings, suicide attempts or suicide
- Self-mutilation, such as cutting
- Premature death from medical conditions
- Depression and anxiety: Can I have both?
There's no sure way to prevent depression. However, these strategies may help.
- Take steps to control stress, to increase your resilience and boost your self-esteem.
- Reach out to family and friends, especially in times of crisis, to help you weather rough spells.
- Get treatment at the earliest sign of a problem to help prevent depression from worsening.
- Consider getting long-term maintenance treatment to help prevent a relapse of symptoms.
- Brown AY. Allscripts EPSi. Mayo Clinic, Rochester, Minn. Nov. 17, 2016.
- Research report: Psychiatry and psychology, 2016-2017. Mayo Clinic. http://www.mayo.edu/research/departments-divisions/department-psychiatry-psychology/overview?_ga=1.199925222.939187614.1464371889. Accessed Jan. 23, 2017.
- Depressive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Depression. National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/depression/index.shtml. Accessed Jan. 23, 2017.
- Depression. National Alliance on Mental Illness. http://www.nami.org/Learn-More/Mental-Health-Conditions/Depression/Overview. Accessed Jan. 23, 2017.
- Depression: What you need to know. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/depression-what-you-need-to-know/index.shtml. Accessed Jan. 23, 2017.
- What is depression? American Psychiatric Association. https://www.psychiatry.org/patients-families/depression/what-is-depression. Accessed Jan. 23, 2017.
- Depression. NIH Senior Health. https://nihseniorhealth.gov/depression/aboutdepression/01.html. Accessed Jan. 23, 2017.
- Children’s mental health: Anxiety and depression. Centers for Disease Control and Prevention. https://www.cdc.gov/childrensmentalhealth/depression.html#depression. Accessed. Jan. 23, 2017.
- Depression and complementary health approaches: What the science says. National Center for Complementary and Integrative Health. https://nccih.nih.gov/health/providers/digest/depression-science. Accessed Jan. 23, 2017.
- Depression. Natural Medicines. https://naturalmedicines.therapeuticresearch.com/databases/medical-conditions/d/depression.aspx. Accessed Jan. 23, 2017.
- Natural medicines in the clinical management of depression. Natural Medicines. http://naturaldatabase.therapeuticresearch.com/ce/CECourse.aspx?cs=naturalstandard&s=ND&pm=5&pc=15-111. Accessed Jan. 23, 2017.
- The road to resilience. American Psychological Association. http://www.apa.org/helpcenter/road-resilience.aspx. Accessed Jan. 23, 2017.
- Simon G, et al. Unipolar depression in adults: Choosing initial treatment. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Stewart D, et al. Risks of antidepressants during pregnancy: Selective serotonin reuptake inhibitors (SSRIs). http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Kimmel MC, et al. Safety of infant exposure to antidepressants and benzodiazepines through breastfeeding. http://www.uptodate.com/home. Accessed Jan. 23, 2017.
- Bipolar and related disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. Arlington, Va.: American Psychiatric Association; 2013. http://www.psychiatryonline.org. Accessed Jan. 23, 2017.
- Hirsch M, et al. Monoamine oxidase inhibitors (MAOIs) for treating depressed adults. http://www.uptodate.com/home. Accessed Jan. 24, 2017.
- Hall-Flavin DK (expert opinion). Mayo Clinic, Rochester, Minn. Jan. 31, 2017.
- Krieger CA (expert opinion). Mayo Clinic, Rochester, Minn. Feb. 2, 2017.
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Antidepressants: Which cause the fewest sexual side effects?
- Atypical antidepressants
- Clinical depression: What does that mean?
- Depression in women: Understanding the gender gap
- Depression, anxiety and exercise
- Depression: Supporting a family member or friend
- MAOIs and diet: Is it necessary to restrict tyramine?
- Monoamine oxidase inhibitors (MAOIs)
- Natural remedies for depression: Are they effective?
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
Associated Procedures
- Complete blood count (CBC)
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
News from Mayo Clinic
- Mayo Clinic Q and A: How to support a loved one with depression Oct. 23, 2022, 11:00 a.m. CDT
- Mayo study lays foundation to predict antidepressant response in people with suicide attempts Oct. 03, 2022, 03:30 p.m. CDT
- Science Saturday: Researchers validate threshold for determining effectiveness of antidepressant treatment Aug. 27, 2022, 11:00 a.m. CDT
- Mayo Clinic expert explains differences between adult and teen depression May 24, 2022, 12:19 p.m. CDT
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Make twice the impact
Your gift can go twice as far to advance cancer research and care!
What Is Depression?
Reviewed by Psychology Today Staff
"The grey drizzle of horror," author William Styron memorably called depression. The mood disorder may descend seemingly out of the blue, or it may come on the heels of a defeat or personal loss, producing persistent feelings of sadness, worthlessness, hopelessness, helplessness, pessimism , or guilt . Depression also interferes with concentration , motivation , and other aspects of everyday functioning.
According to the World Health Organization, depression is the leading cause of disability worldwide. Globally, more than 300 million people of all ages suffer from the disorder. And the incidence of the disorder is increasing everywhere. Americans are highly concerned with happiness , yet they are increasingly depressed: Some 15 million Americans battle the disorder, and increasing numbers of them are young people.
Depression comes in forms ranging from major depression to dysthymia and seasonal affective disorder. Depressive episodes are also a feature of bipolar disorder .
Depression is a complex condition, involving many systems of the body, including the immune system, either as cause or effect. It disrupts sleep and it interferes with appetite ; in some cases, it causes weight loss; in others, it contributes to weight gain. Depression is also often accompanied by anxiety . Research indicates that not only do the two conditions co-occur but that they overlap in vulnerability patterns.
Because of its complexity, a full understanding of depression has been elusive. There is mounting evidence that depression may actually be a necessary defense strategy of the body, a kind of shutdown or immobilization in response to danger or defeat , that is actually meant to preserve your energy and help you survive.
Researchers have some evidence that depression susceptibility is related to diet , both directly—through inadequate consumption of nutrients such as omega-3 fats—and indirectly, through the variety of bacteria that populate the gut. But depression involves mood and thoughts as well as the body, and it causes pain for both those living with the disorder and those who care about them. Depression is also increasingly common in children.
Even in the most severe cases, depression is highly treatable. The condition is often cyclical, and early treatment may prevent or forestall recurrent episodes. Many studies show that the most effective treatment is cognitive behavioral therapy , which addresses problematic thought patterns, with or without the use of antidepressant drugs. In addition, evidence is quickly accumulating that regular mindfulness meditation , on its own or combined with cognitive therapy , can stop depression before it starts by diminishing reactivity to distressing experiences, effectively enabling disengagement of attention from the repetitive negative thoughts that often set the downward spiral of mood in motion.
For more on causes, symptoms, and treatments of depressive disorders, see our Diagnosis Dictionary .

Not everyone who is depressed experiences every symptom. Some people experience a few symptoms, some many. The severity of symptoms varies among individuals and over time.
Depression often involves persistent sad, anxious, or empty mood; feelings of hopelessness or pessimism ; and feelings of guilt , worthlessness, or helplessness. It can also involve loss of interest or pleasure in hobbies and activities that were once enjoyed, including sex . Decreased energy, fatigue, or a sense of being "slowed down" are also common, as are restlessness, irritability, and difficulty concentrating, remembering, or making decisions. Many with depression have thoughts of death or suicide.
People with depression may experience disruptions in sleep ( insomnia , early morning awakening or oversleeping) and in eating behavior ( appetite changes, weight loss or gain). Persistent physical symptoms may include headaches, digestive disorders, and chronic pain .
For more see Signs and Symptoms of Depression.

There is no single known cause of depression. Rather, it likely results from a combination of genetic, biologic, environmental, and psychological factors. Major negative experiences— trauma , loss of a loved one, a difficult relationship, or any stressful situation that overwhelms the ability to cope—may trigger a depressive episode. Subsequent depressive episodes may occur with or without an obvious trigger.
Depression is not an inevitable consequence of negative life events, however. Research increasingly suggests that it is only when such events set in motion excessive rumination and negative thought patterns, especially about oneself, that mood enters a downward spiral.
Research utilizing brain-imaging technologies such as magnetic resonance imaging (MRI) shows that the brains of people who have depression look different than those of people who do not. Specifically, the parts of the brain responsible for regulating mood, thinking, sleep, appetite, and behavior appear to function abnormally. It is not clear which changes seen in the brain may be the cause of depression and which may be the effect.
Some types of depression tend to run in families, suggesting there may be some genetic vulnerability to the disorder.
For more see Causes of Depression .

Depression, even the most severe cases, is a highly treatable disorder. As with many illnesses, the earlier treatment begins, the more effective it can be and the greater the likelihood that recurrence can be prevented.
Appropriate treatment for depression starts with an examination by a physician. Certain medications, as well as some medical conditions such as viral infections or a thyroid disorder, can cause the same symptoms as depression and should be ruled out. The doctor should ask about alcohol and drug use, and whether the patient has thoughts about death or suicide.
Once diagnosed, a person with depression can be treated a number of ways. The most common treatments are medication and psychotherapy . Many studies show that cognitive behavioral psychotherapy is highly effective, alone or in combination with drug therapy.
Psychotherapy addresses the thinking patterns that precipitate depression, and studies show that it prevents recurrence. Drug therapy is often helpful in relieving symptoms, such as severe anxiety , so that people can engage in meaningful psychotherapy.
For more see Treatment of Depression and Therapy for Depression .

Depression requires active treatment, because the disorder can have enduring effects on brain function that make future episodes more likely. The longer a depression episode lasts, the more likely a future episode.
However, there are many ways to treat depression, and some of the most effective, especially in cases of mild to moderate disorder, do not require a prescription or medical-type intervention of any kind.
Depression can be seen as a kind of cave , and it takes some time and effort to get out of the cave. But it is possible, usually by learning some new patterns of thinking and doing. Nutrition plays a role as well.
For more see Natural Approaches to Depression.

Mental anguish is hard on your health: People suffering from depression have three times the risk of experiencing a cardiac event. In fact, depression affects the entire body. It weakens the immune system, increasing susceptibility to viral infections and, over time, possibly even some kinds of cancer—a strong argument for early treatment. It also interferes with sleep, adding to feelings of lethargy, compounding problems of focus and concentration , and generally undermining health.
Those suffering from depression also experience higher rates of diabetes and osteoporosis. Sometimes depression manifests as a persistent low mood, a condition known as dysthymia which is usually marked by years-long periods of low energy, low self-esteem , and little ability to experience pleasure.
For more see Depression and Physical Health .

Everyone experiences an occasional blue mood. Yet clinical depression is a more pervasive experience of repetitive negative rumination, bleak outlook, and lack of energy. It is not a sign of personal weakness or a condition that can be willed or wished away. People with depression cannot merely "pull themselves together" to get better.
It doesn't help that modern-day living carries growing pressures. There is an emphasis on early childhood achievement at the expense of free play, a cultural shift away from direct social contact in favor of electronic connection, and a focus on material wealth at the expense of rich experiences and social contact. All play a part.
However, there is some evidence that, painful as depression is, it may serve a positive purpose, bringing with it ways of thinking that force those who suffer to focus on problems as a prelude to solving them. In effect, some researchers hypothesize that depression can help prod a person into much needed self-awareness.
For more see How to Prevent and Manage Depression .

What most people mean when they talk about depression is unipolar depression—an unremitting state of sadness, apathy, hopelessness, and loss of energy. It is also called major depression.
Depressive episodes also occur in bipolar disorder , a condition marked by periods of depression interspersed with periods of high-energy mania . People swing between the two poles of mood states, sometimes over the course of days, and sometimes over years, often with stable periods in between.
The birth of a baby can trigger mood swings or crying spells in the days or weeks that follow, the so-called baby blues. When the reaction is more severe and prolonged, it is considered postpartum depression , a condition requiring treatment because it can interfere with a parent's ability to care for their newborn.
Depression can also occur seasonally, primarily in the winter months when sunlight is in short supply. Known as seasonal affective disorder, or SAD, it is often ameliorated by daily exposure to specific types of artificial light.
For more see Types of Depression .

Depression makes deep inroads on biology to bring about the many symptoms of depression, from sleep disruption and inability to experience pleasure to lack of motivation and feelings of guilt. Because of its complexity—and because the disorder contributes so much to human suffering—the biology of depression is a major subject of ongoing research.
Overexcitability of the stress response system, shifts in activity of various neurochemicals in the brain, diminished efficiency of nerve circuitry and nerve generation, disturbances in energy use in nerve cells, the intrusion of inflammatory substances in the brain, upsets in the brain’s 24-hour (circadian) clock—all play a role in depression onset or progression and influence the kind and severity of symptoms.
For more see The Biology of Depression

Most suicides are linked to some form of psychiatric illness, particularly depression, and the more severe the depression, the greater the risk. Still, most people with major depression do not die by their own hand.
Studies show that about 5 percent of depressed persons may have thoughts about suicide— suicidal ideation. Only a small percentage of them actively make plans to end their lives.
The clearest warning sign of suicide is talk about wanting to die . And the best way to determine whether suicide is a risk is to ask.
For more see Depression and Suicide .

Mental health conditions such as depression are increasingly afflicting the young, including preschoolers. Especially in the young, depression requires active treatment—it can interfere with normal development.
Depression can show up in children much as it does in adults, signified by sadness, lethargy, and disinterest. But especially among children it manifests as irritability. Other times it manifests as anger and acting out.
Depression in children can have many causes. It can be a response to bullying . There is ample evidence that social media plays a role in depression among young people. Another source may be the decline of free play, an arena in which children traditionally work out their concerns and a great source of pleasure.
For more see Children and Depression .

Incels, like everyone, want love and connection, but if they do not have the tools to get their sexual needs met legally, they remain at risk of becoming sex offenders.

Because of the way open heart meditation practices influence neural connections, they may be the perfect practice to balance the brain and improve mood.
A new memoir concerns the treatment of prolonged grief in one of America’s most influential psychiatric hospitals.

When our minds get stuck, it can be an incredibly painful experience. Here are four strategies to break free.

Bewildered and grieving widows and widowers, mothers and fathers, as well as best friends have asked me, "What did I miss?"

The challenges of coping with a friend’s suicide.

What to expect from your first treatment: side effects, planning for treatment, and understanding the risks.

We'll all experience grief at some point in our lives. But what exactly is grief?

According to a 2019 study, over 11% of young people have a diagnosable mental disorder. These disorders accounted for about 20% of all disease-related disability in this age group.

The secret to success is not concealing the effort it takes.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Teletherapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Therapy Center NEW
- Diagnosis Dictionary
- Types of Therapy

Understanding what emotional intelligence looks like and the steps needed to improve it could light a path to a more emotionally adept world.
- Coronavirus Disease 2019
- Affective Forecasting
- Neuroscience

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Stakeholder Engagement
- Connect with NIMH
- Digital Shareables
- Science Education
- Upcoming Observances and Related Events
Digital Shareables on Depression
Use these resources to raise awareness about depression.

Depression is a common but serious mood disorder. It causes severe symptoms that affect how someone feels, thinks, and handles daily activities, such as sleeping, eating, or working. For more information on depression, visit the health topic page or view the available brochures .
Help raise awareness about depression by sharing information and materials based on the latest research.
Share these graphics and social media messages
Download and share these messages to help spread the word about depression. You can copy and paste the text and graphic into a tweet, email, or post. We encourage you to use the hashtag #shareNIMH in your social media posts to connect with people and organizations with similar goals. For more ideas on how to use these resources, visit our help page .

Let's Talk About Depression
Help raise awareness about depression, which is one of the most common mental disorders in the U.S., by sharing informational materials based on the latest research. Share science. Share hope. https://go.nih.gov/anhTIQn #shareNIMH
Copy post to clipboard

Depression: What You Need to Know
Disponible en español
Everyone feels sad or low, but these feelings usually pass. Depression is different and has severe symptoms that affect how people feel, think, and act. Learn the signs and symptoms of depression, how it is diagnosed, treatments, and ways to get help. https://go.nih.gov/0uqAIBh #shareNIMH

Depression is Common But Treatable
Not everyone who is depressed experiences every symptom. Some people experience only a few symptoms while others may experience many. Learn more about the signs and symptoms: https://go.nih.gov/whGyYK2 #shareNIMH

Depression is Different
Depression is a common but serious mood disorder. It causes severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working. Learn more about depression by visiting https://go.nih.gov/whGyYK2 #shareNIMH

Depression is not a Sign of Weakness
Well-meaning friends or family members may try to tell someone with depression to “snap out of it,” or “just be positive.” But depression is not a sign of weakness or a character flaw. Most people with depression need treatment to get better. Start by visiting https://go.nih.gov/whGyYK2 . #shareNIMH
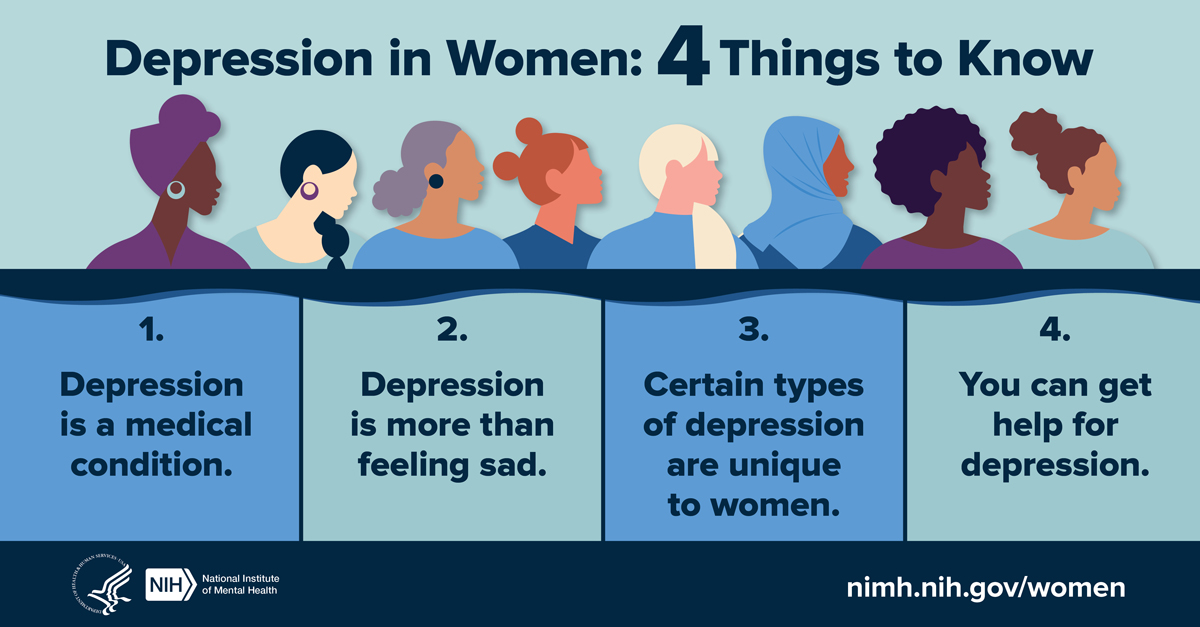
Women and Depression
Depression is a serious mood disorder with unique impacts on women. Here's 4 things to know about depression in women: https://go.nih.gov/irI3sCf #shareNIMH

Depression and Older Adults
Depression may sometimes be undiagnosed or misdiagnosed in some older adults because sadness may not be their main symptom. Depression has many symptoms, including physical ones. Know the signs: https://go.nih.gov/whGyYK2 #shareNIMH
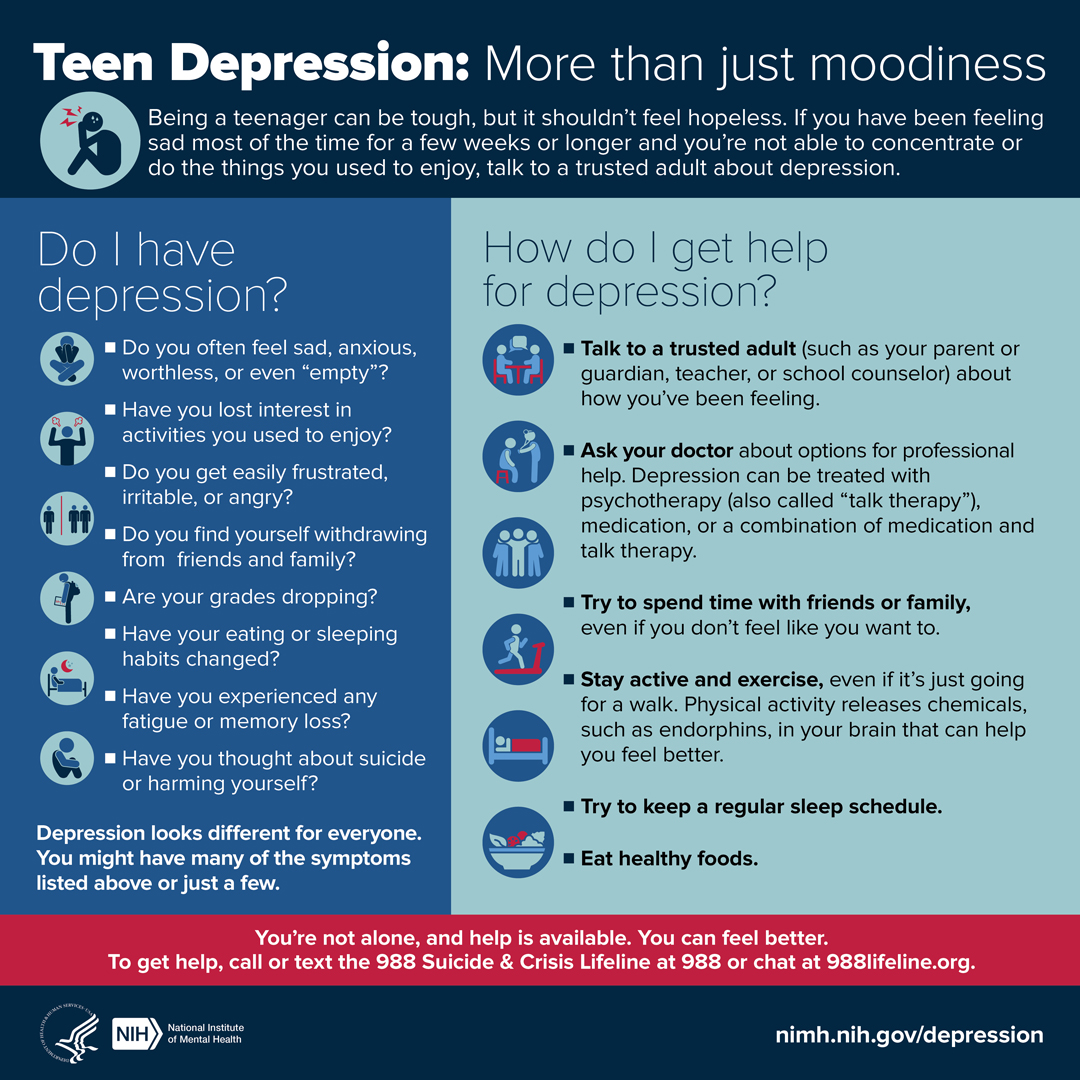
Teen Depression
Being a teenager can be tough, but it shouldn’t feel hopeless. Check your symptoms, and find out what you can do if you think you might have depression. https://go.nih.gov/dGGEwYi #shareNIMH
Perinatal Depression
Perinatal depression can cause feelings of extreme sadness, anxiety, and fatigue that may make it difficult to carry out daily tasks. Spouses, partners, family members, and friends may be the first to recognize symptoms. https://go.nih.gov/06k2QSH #shareNIMH

Seasonal Affective Disorder
Is it just the 'winter blues' or seasonal affective disorder (SAD)? This infographic may help guide you on when to seek professional help. https://go.nih.gov/i4nN2C4 #shareNIMH


Chronic Illness and Mental Health
Depression is common among people with chronic illnesses such as heart disease. Fortunately, depression is treatable even when you have another medical illness or condition. Learn more about chronic illness and mental health: https://go.nih.gov/LNA4CG1 #shareNIMH

Mental Health Matters
Your mental health matters. Mental health is just as important as physical health. Good mental health helps you cope with stress and can improve your quality of life. Get tips and resources from NIMH to help take care of your mental health. https://go.nih.gov/wwSau0W #shareNIMH
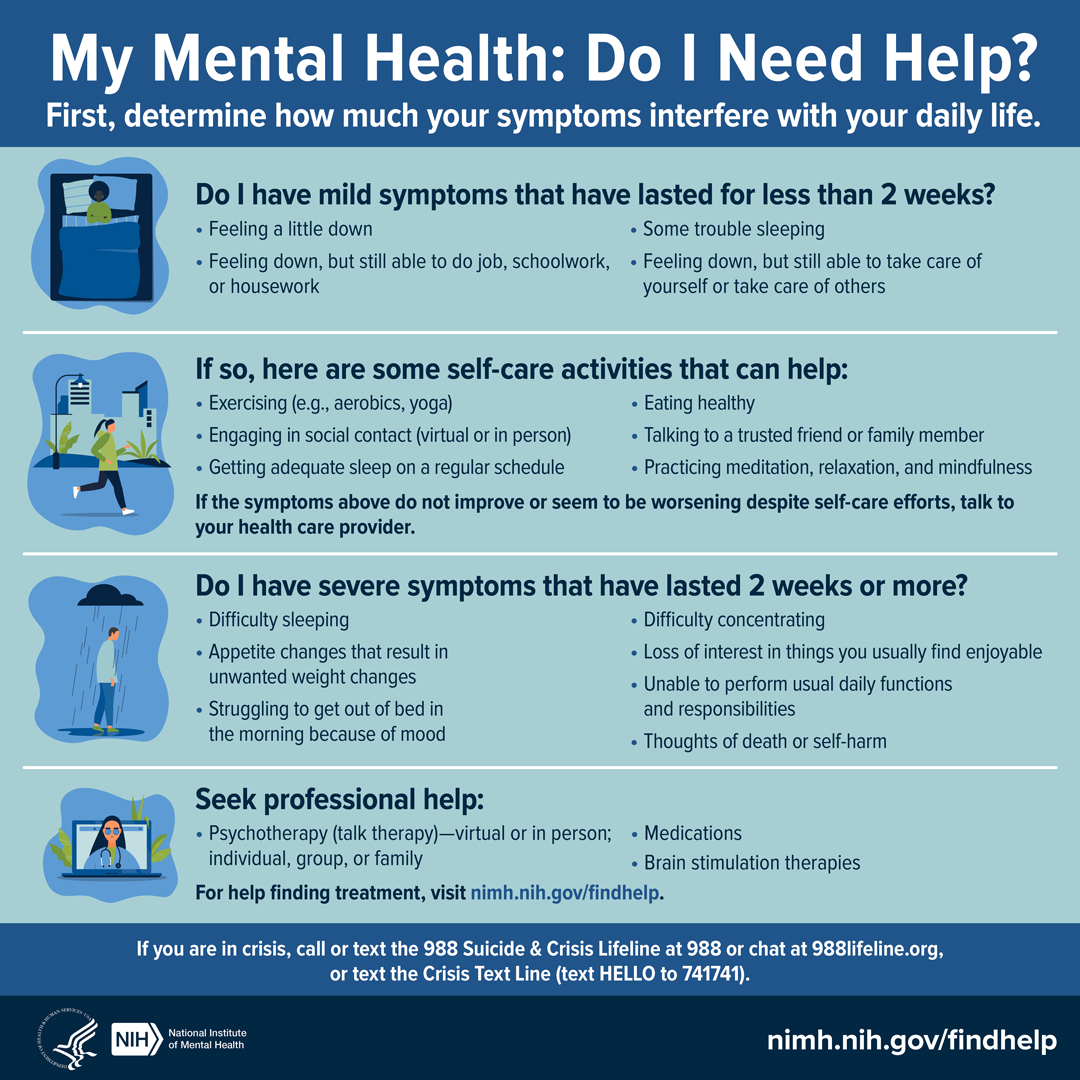
My Mental Health: Do I Need Help?
Do you need help with your mental health? If you don't know where to start, this infographic may help guide you. https://go.nih.gov/1VtK7eA #shareNIMH
What is Telemental Health?
Research suggests that telemental health services can be effective for many people, including, but not limited to those with ADHD, PTSD, depression, and anxiety. Learn about factors to consider when using telemental health. https://go.nih.gov/FldCw5O . #shareNIMH
Help for Mental Illnesses
If you or someone you know has a mental illness, is struggling emotionally, or has concerns about their mental health, use these resources to find help for yourself, a friend, or a family member: https://go.nih.gov/Fx6cHCZ . #shareNIMH
Use videos to educate others
Click “Copy link” to copy the video URL and post these videos on social media, or embed them on your website.
Mental Health Minute: Depression: Got 60 seconds? Take a mental health minute to learn about depression.
NIMH Experts Discuss the Menopause Transition and Depression: Learn about the signs, symptoms, treatments, and latest research on the menopause transition and depression.
Discover NIMH: Personalized and Targeted Brain Stimulation Therapies: Learn more about how brain stimulation therapies can be effective treatments for people with depression and other mental disorders.
NIMH Expert Discusses Seasonal Affective Disorder (SAD): Learn about the signs, symptoms, treatments, and latest research on SAD.
The Evolution of Brain Stimulation Therapy: Listen to NIMH expert talk about brain stimulation and learn how seizure therapies can help with depression.
Depression: The Case for Ketamine: Hear from NIMH expert about the history behind the development of ketamine and how it can help with depression.
Learn more about depression
more information about depression, brochures and fact sheets, statistics, 988 suicide & crisis lifeline .
Last Reviewed: March 2024
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Psychiatry
DSM-5 Criteria and Depression Severity: Implications for Clinical Practice
Background: Depression diagnosis requires five or more symptoms (Diagnostic and Statistical Manual of Mental Disorders-DSM-5). One of them must be either Depressed mood or Anhedonia, named main criteria. Although the secondary symptoms can be divided into somatic and non-somatic clusters, the DSM-5 identify depression in all or none fashion. In contrast, depression severity is a continuous variable. Therefore, it is commonly assessed with scales such as the Hamilton Depression Rating Scale (HAMD). Previously, we reported that patients with moderate depression (MD) exhibit greater impairments in cardiac-autonomic modulation than severely depressed (SD) patients. However, clinicians usually do not use scales.
Objective: To verify whether the DSM-5 symptoms would be able to discriminate SD from MD and MD from non-depressed (ND) subjects.
Material and Methods: Depression was diagnosed based on the Structured Clinical Interview for DSM-5® Disorders. The HAMD evaluated depression severity. In depressed subjects, MD and SD were defined considering the HAMD scores. ND was defined considering both the absence of DSM-5 criteria for depression and the HAMD score. Among 782 outpatients, 46 SD were found. MD and ND subjects were randomly sampled to match the demographic variables of the SD group.
Results: Discriminant analysis showed that Depressed Mood was the most reliable symptom to discriminate ND from MD. Anhedonia discriminated SD from MD. Among the secondary DSM-5 criteria, the somatic cluster discriminated ND from MD and the non-somatic cluster SD from MD patients.
Discussion: The presence of the somatic cluster in MD may indicate decreased vagal tone and/or increased sympathetic tone, leading to higher cardiovascular risk. As SD is associated with the non-somatic cluster, these patients are at risk of committing suicide. The DSM-5 symptoms exhibited by the patient may help the choice of adequate pharmacological treatment. This would avoid the use of antidepressants that unnecessarily increase cardiac risk in MD. When the symptom cluster suggests SD, the treatment must focus on the prevention of suicide.
Conclusions: Depression severity may be inferred based on the DSM-5 criteria. The presence of the Anhedonia main criterium accompanied by non-somatic criteria indicate SD. The Depressive Mood criterium followed by somatic criteria suggest MD.
Introduction
Depression is a common psychiatric disorder, with an estimated lifetime prevalence of 10% in the general population ( 1 , 2 ). In clinical settings, its prevalence may reach as high as 20% ( 1 , 3 ). According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the diagnosis of a Major Depression Episode (MDE) requires five or more symptoms to be present within a 2-week period ( 4 ). One of the symptoms should, at least, be either a depressed mood (DM) or anhedonia (loss of interest or pleasure- LI). The secondary symptoms of MDE are appetite or weight changes (AW), sleep difficulties (insomnia or hypersomnia), psychomotor agitation or retardation (PAR), fatigue or loss of energy (FE), diminished ability to think or concentrate (C), feelings of worthlessness or excessive guilt (FW), and suicidality (SU). These symptoms are rated in an all or none (0 or 1) fashion.
According to the DSM-5 criteria, the symptoms are summed to determine the presence or the absence of a major depression episode ( 4 ). Consequently, the DSM assumes that the depression construct may be considered unidimensional. However, several studies have described different subtypes of depression ( 1 , 5 , 6 ). Furthermore, the unidimensional model of depression has been challenged by studies on the factor structure of the DSM symptom criteria ( 7 – 9 ). Elhai et al. ( 10 ) have reported that a two-factor model fits better than the one-factor unidimensional mode. They found that major depression symptoms are best represented by somatic and non-somatic factors. The somatic items included sleep difficulties (SD), appetite or weight changes, poor concentration, fatigue, and psychomotor agitation/retardation. The non-somatic factor consisted of affective items such as depressed mood, anhedonia, feelings of worthless, and thoughts of death.
Previous investigations have reported that cognitive dysfunction, age, psychosis, unemployment, suicide ideation are associated with depression severity ( 11 – 13 ). However, to our knowledge, there is a lack of a systematic study on the relationship between DMS-5 symptoms and depression severity. There is no consensus if the number of symptoms is indicative of depression severity or even if the degree of each symptom can be used as an index to classify depression as mild, moderate, or severe. Consequently, the severity of depression is commonly assessed with the aid of rating depression scales, such as the Hamilton Depression Rating Scale (HAMD) ( 14 ). HAMD has been the most frequently used rating scale for depression ( 14 – 17 ).
Almas et al. ( 18 ) reported that moderately depressed persons showed a higher risk for cardiovascular disease (CVD) compared to severely depressed patients. Recently, Tolentino and Schmidt ( 19 ) have shown that cardiac autonomic regulation is associated with depression severity, as measured by the HAMD, in an intriguing way: moderately depressed patients showed greater impairment in autonomic modulation as compared to either severely depressed patients or non-depressed subjects. Then, subjects with moderate depression who do not seek treatment are at higher risk of CVD. However, some antidepressants such as the tricyclics increase the risk of cardiac arrhythmia and sudden cardiac death ( 20 – 23 ). Therefore, structured and unstructured clinical interviews need to be supplemented by ratings based on appropriated scales ( 24 ). As sometimes the use of extensive scales is not possible, there is a practical interest to verify whether depression severity could be assessed using the DSM5 symptoms.
The present study aimed to verify whether the DSM-5 criteria for depression would be able to discriminate moderate from severe depression as assessed with the aid of the HAMD. A clinical sample was selected because of the highest prevalence of depression in this population ( 1 , 2 ). Based on the effects of moderate depression on cardiac autonomic modulation ( 16 ), we hypothesized that specific somatic DSM-5 symptoms might be closely related to moderate depression. Symptom expressions such as sleep difficulties, appetite or weight changes, and psychomotor agitation/retardation would be maximized in moderately depressed patients as compared to non-depressive subjects. In addition, patients with severe depression would be characterized by thoughts of death and feelings of worthlessness.
Materials and methods
Study sample.
The participants were selected from a primary care practice located at Rio de Janeiro, Brazil (Gaffrée and Guinle University Hospital). The research protocol was administered by well-trained raters. The initial sample consisted of 904 outpatients. The exclusion criteria were: age below 18 years; patients with neurological diseases; alcohol and substance use-related disorders; dementia and other cognitive disorders (Mini-Mental State Examination score below 24 points); presence of psychotic symptoms; uncontrolled clinical diseases, such as hypothyroidism, diabetes, or hypertension; and who were taking antidepressants within the last 3 months. After applying the exclusion criteria, 782 eligible patients were recruited to participate in first part of this study. Based on the Structured Clinical Interview for DSM-5® Disorders-Clinician Version (SCID-5-CV) ( 25 ), 189 patients were found to exhibit MDE at the time of the interview. After the analysis of the HAMD scores ( n = 782), 46 severely depressed (SD) patients were found. The participants in the Non-depressed and Moderately depressed groups were selected based on matching demographic characteristics with the Severely depressed group. Then, 46 controls and 46 moderately depressed patients were randomly selected to be analyzed (Figure (Figure1). 1 ). The non-depressed group was composed of patients without criteria for depression through SCID-5-CV and HAMD.

Design of the study (timeline). The initial sample consisted of 904 outpatients. After applying the exclusion criteria, 782 eligible patients were recruited to participate in first part of this study. Based on the DSM-5 criteria, 189 patients exhibited a major depressive episode at the time of the Structured Clinical Interview for DSM-5® Disorders-Clinician Version. The Hamilton Depression Rating Scale (HAMD) were administered in the depressed outpatients and the non-depressed group ( n = 593). Based on the HAMD cut-off scores, three groups were selected: Non-depressed (ND), Moderately Depressed (MD), and Severely Depressed (SD). After the analysis of the HAMD scores ( n = 782), 46 severely depressed patients were found. Age, percentage of females, years of education, and mini-mental state exam scores were calculated for the SD group. These demographic values were used to sample the other two groups (ND and MD). Then, from the total number of subjects in the other two groups (ND and MD), 92 subjects (46 MD and 46 ND) were randomly selected to be included in the analyses.
The Mini-Mental State Examination ( 26 ) was used to assess cognitive function in each general outpatients clinic ( n = 904). Psychiatric assessments were done in 782 subjects included in the study, through the application of SCID-5-CV to MDE diagnosis and the 17-items of the Hamilton Depression Rating Scale (17-item HAMD) to measure depression severity ( 14 , 17 , 27 , 28 ). The SCID-5-CV that was applied for the MDE diagnosis is a semi-structured interview for making DSM-5 diagnoses ( 25 ). It was administered by trained physicians that are familiar with the DSM-5 diagnostic criteria.
The 17-item, clinician-administered Hamilton Rating Scale for Depression was administered in the depressive outpatients ( n = 189) and the non-depressed group ( n = 583). Two trained raters independently scored each patient at the same interview. Only patients who received equal scores from the two raters were included in the sample. It should be mentioned that high interrater reliability has been described previously ( 16 , 28 , 29 ). The total score on the 17-item HAMD ranges from 0 to 52, with higher scores representing greater severity of depression. In this study, the 17-item HAMD cut-off points were defined as follows: >24 = severe; 17–23 = moderate; 8–16 = mild; and none (non-depressed) = 0–7 ( 17 ). Based on these HAMD cut-off scores, three groups were selected: Non-depressed (ND), Moderately Depressed (MD), and Severely Depressed (SD).
Ethical approval
The study is consistent with the declaration of Helsinki, and it was approved by Gaffrée and Guinle University Hospital Ethics committee. All subjects gave written informed consent in accordance with the Declaration of Helsinki.
Statistical analysis
Quantitative variables are reported as absolute and relative frequencies, means ( M ), and standard deviations. Across the demographic variables, group differences were tested using T- tests for the continuous variables and chi-square tests (χ 2 ) for the categorical variables (Table (Table1 1 ).
Comparison of matched groups variables according to the Hamilton Depression Rating Scale.
ND, Non-depressed group; MD, Moderately depressed group; SD, Severely depressed group; p, proof value .
Discriminant analysis was performed to examine if the DSM-5 criteria accurately distinguished between Non-depressed, Moderately Depressed and Severely Depressed groups as defined by the 17-item HAMD scores. Results will be presented for Non-depressed vs. Moderately Depressed, and Severely Depressed vs. Moderately Depressed.
Initially, the equality of the group means was tested using Wilk's λ. It should be mentioned that the smaller the λ, the more important is the independent variable to the discriminant function. Then, the assumptions of the discriminant analyses were tested (linearity, normality, multilinearity, equal variances, and multivariate normal distribution of the predictors). Box's M -tests were performed to test the assumption of the homogeneity of covariance matrices. It should be mentioned that discriminant analysis is robust when the homogeneity of variances assumption is not met, provided the data do not contain important outliers. For our data, the Box's M -test was interpreted in conjunction with the inspection of the log determinants. Considering our sample size and the absence of outliers, we concluded that the small deviations from homogeneity groups did not violate the assumptions of the discriminant analysis.
For each case (Non-depressed vs. Moderately Depressed and Severely Depressed vs. Moderately Depressed), the discriminant was created as a linear combination of the nine independent variables. The standardized canonical coefficients of the discriminant function analysis were used to identify the most reliable variable for discriminating between Severely Depressed and Moderately Depressed groups as well as between Non-depressed and Moderately Depressed groups. The Pearson correlations between predictors and standardized canonical discriminant functions were calculated and loadings <0.30 were removed from the model. Then, the canonical discriminant function coefficients were calculated to obtain the Discriminant Function (DF). Canonical correlations (λs) were calculated to measure how well each DF separate cases into the two groups (Moderately Depressed vs. Non-depressed, and Moderately Depressed vs. Severely Depressed). For each case, the correspondent chi-squared was calculated to verify if the DF did better than the chance level of separating the two groups. With the aid of the DF, the accuracy of the classification was measured for each case.
SPSS Statistics for Windows, version 22.0 (SPSS Inc., Chicago, IL) was used for analysis, and the significance level was set at p < 0.0.5.
The age ranged from 21 to 82 years ( M = 45.9; standard deviation = 14.6) in the sample selected to participate in the first part of the study (eligible outpatients; n = 782). Most participants were female sex (65.3%). The mean years of schooling and the Mini-Mental State Examination (MMSE) scores were 9.1 (standard deviation = 4.1) and 28.1 (standard deviation = 2.6), respectively. The prevalence of MDE in this clinical sample was 24.2% ( n = 189), and the mean score on the HAMD was 9.7 (standard deviation = 2.8).
In the whole sample, 46 depressive patients were found to be severely depressed. Severe depression was found to be more frequent in women (71.7%). Logistic regression showed that female sex was associated with severe depression (odds ratio = 3.74; 95% confidence interval = 1.66–8.42). In contrast, there was not an association between sex and moderate depression.
The Non-depressed and the Moderately Depressed groups were matched considering the demographic variables of the Severely Depressed group (Table (Table1). 1 ). There was no statistically significant differences according to race (Caucasians and non-Caucasians) among the three groups. The human development index in our sample ranged from 0.782 to 0.842 and no differences were found among the three groups. The relative frequency distributions of the nine DSM-5 criteria for each group indicated that patients with severe depression exhibited more non-somatic DSM-5 symptoms than moderately depressed patients, especially for anhedonia, feelings of worthlessness/excessive guilt, and suicidality (Table (Table2). 2 ). As expected, all the DSM-5 symptoms were found to be more frequent in Severely Depressed and Moderately Depressed groups as compared to the control (Non-depressed) group.
The relative frequencies of the DSM-5 criteria for major depressive episode among the groups.
DM, depressed mood; LI, loss of interest or pleasure; AW, appetite or weight disturbance; SD, sleep difficulties (insomnia or hypersomnia); PAR, psychomotor agitation or retardation; FE, fatigue or loss of energy; FW, feelings of worthlessness or excessive guilt; C, diminished ability to think or concentrate; SU, suicidality. Note the markedly differences among Severely Depressed group and the other two groups for LI, FW, and SU (bold) .
Non-depressed group vs. moderately depressed group
Group means were found to be significantly different for all DSM-5 criteria. The smallest Wilk's λ was found for depressed mood followed by sleep difficulties (insomnia or hypersomnia). Depressed mood was the most reliable variable for discriminating between groups, followed by sleep difficulties and poor concentration. The smallest discriminant ability was found for suicidality. The pooled within-groups correlations (Table (Table3) 3 ) identified the large correlations with the full discriminant model: Depressed mood, sleep difficulties, poor concentration, and fatigue. The lowest was suicidality followed by feelings of worthlessness/excessive guilt. After excluding loadings <0.30, the following discriminant function (DF) was deduced from the analysis: DF = −3.290 + (2.120 * DM) + (2.40 * SD) + (0.764 * FE) + (1.327 * C).The canonical discriminate function reached an eigenvalue of 6.931 (χ 2 = 182.23, d.f = 4, p < 0.001). Therefore, the DF significantly separated the two groups. Based on the DF formula, subjects with DF > 0 were classified as moderately depressed, and subjects with DF < 0 were classified as controls with 98% accuracy.
Pooled within-groups correlations between discriminating variables and standardized canonical discriminant function: Non-depression vs. moderate depression, and Moderate depression vs. Severe depression.
Correlations < 0.30 were excluded from the discriminant equation .
Moderately depressed group vs. severely depressed group
Group means were found to be significantly different for depressed mood, loss of interest or pleasure (anhedonia), feelings of worthlessness/excessive guilt, and suicidality. The smallest Wilk's λ was found for suicidality followed by anhedonia. The highest value was fatigue. The analysis of the standardized canonical coefficients indicated that suicidality was the most reliable variable for discriminating between the groups, followed by anhedonia. The smallest discriminant ability was found for fatigue. The pooled within-groups correlations (Table (Table3) 3 ) identified the large correlations with the DF (suicidality, loss of interest or pleasure, feelings of worthlessness/excessive guilt, and depressed mood). The lowest was fatigue.
The following discriminant function (DF) was deduced from the analysis: DF = −3.078 + (1.147 * LI) + (0.596 * FW) + (1.404 * SU) + (1.222 * DM).
The canonical discriminate function reached an eigenvalue of 0.261(χ 2 = 20.44, d.f = 4, p < 0.001). Therefore, the DF significantly separated the two groups. Based on the DF formula, subjects with DF > 0 were classified as Severely Depressed and subjects with DF < 0 were classified as Moderately Depressed with 72.7% accuracy.
Taken together, the somatic DSM-5 items discriminated Moderately Depressed from Non-depressed and all the affective items discriminated Moderately Depressed from Severely Depressed groups (Figure (Figure2 2 ).

Summary of the results. Depressed mood is the most reliable DSM-5 symptom to discriminate moderately depressed (MD) group from non-depressed (ND) group. Loss of interest or pleasure discriminates severely depressed (SD) group from MD. Considering the secondary DSM-5 criteria, the somatic items discriminate MD from ND groups. All the non-somatic DSM-5 criteria separate MD from SD groups. The ellipses represent the non-somatic DSM-5 items and the rectangles the somatic DSM-5 items, according to the factor structure described by Elhai et al. ( 10 ). DM, depressed mood; LI, loss of interest or pleasure; SD, sleep difficulties (insomnia or hypersomnia); C, diminished ability to think or concentrate; FE, fatigue or loss of energy; FW, feelings of worthlessness or excessive guilt; SU, suicidality; AW, appetite or weight disturbance; PAR, psychomotor agitation or retardation.
The two main diagnostic criteria for depression (depressed mood and loss of interest or pleasure) differ regarding their discrimination ability when the level of depression is considered: depressed mood is the most reliable DSM-5 symptom to discriminate moderate depression from non-depression whereas anhedonia emerges as an important criterion when depression becomes more severe. Among the secondary DSM criteria, the somatic cluster shows high discriminant ability to separate non-depression from moderate depression. For the discrimination of severe from moderate depression, the most reliable DSM-5 symptom is suicidality, followed by anhedonia, feelings of worthlessness and depressed mood. In summary, the non-somatic DSM-5 criteria are found to distinguish moderate from severe depression reliably, while the somatic factors are useful for the discrimination between moderate and non-depression groups.
The present data support a two-factor model of depression proposed by Elhai et al. ( 10 ). Among the secondary DSM-5 symptoms, the somatic factors are related to moderate depression, whereas the non-somatic or cognitive-affective factors are related to severe depression. The finding that the two main criteria for depression (depressed mood and anhedonia) exhibit distinct discrimination ability may reflect the possible differences between these two symptoms. Depressive mood is often associated with the presence of stressors ( 30 ), often loss situations (death, economic reversal, separation, illness, etc.). Thus, it is possible to speculate that depressed mood may be considered a compound factor indicating either a response to stressful situations (somatic factor) or a sadness feeling (affective factor). Anhedonia may indicate either loss of interest (motivational anhedonia or absence of an anticipatory pleasure from future activities) or loss of pleasure in response to stimuli that were previously perceived as rewarding (consummatory anhedonia) ( 31 ). Therefore, anhedonia is fully related to the affective factor while depressed mood might be related to both affective and somatic factors (stressful situations). This might explain why depressed mood is a good discriminator of moderate from non-depressed groups. However, another interpretation is that HAMD simply gives more importance to depressed mood items than to anhedonia ( 14 , 16 , 17 ).
Depression has been closely associated with autonomic nervous system dysfunction, with reduced parasympathetic and/or increased sympathetic activity leading to increased cardiovascular risk in depressed patients ( 32 – 34 ). In line with these findings, increased inter-lead QT interval differences on 12-lead electrocardiography (QT dispersion) or reduced heart rate variability (HRV) has been reported in depressed patients ( 19 , 35 – 41 ). Either reduced HRV or augmented QT dispersion reflects excessive sympathetic modulation and/or inadequate cardiac vagal control ( 19 , 35 – 44 ). Thus, both conditions may predispose individuals with depression to ventricular tachycardia, ventricular fibrillation, myocardial ischemia, and sudden cardiac death ( 44 – 46 ). However, research on depression and HRV has been typically conducted in patients with cardiovascular disease ( 46 – 50 ). Our findings are in agreement with the recent report by Benvenuti et al. ( 51 ) who showed that somatic depressive symptoms are related to reduced HRV in medically healthy individuals with dysphoria. Here we demonstrated that moderately and severely depressed patients may express symptoms of low mood or distress through two distinct clusters of DSM-5 criteria. The present study report that moderate depression is associated with the somatic cluster is in agreement with the previous finding of highest autonomic dysfunction in moderate depression as compared to all other groups, including control and severely depressed patients ( 19 ).
The somatic symptoms may be related to autonomic disturbances in depressed patients without known cardiovascular disease ( 52 , 53 ). Likewise, the Mental Stress-Induced Myocardial Ischemia has already been described in a patient with normal coronary arteries and generalized anxiety disorder ( 51 ). In this case, anxiety might be considered a somatic component of depression ( 54 – 57 ). Decreasing serotonin may cause a decrease in parasympathetic activity ( 58 ), and emotional response capabilities are marked peripherally by vagal efference to the heart ( 40 , 59 ). Specifically, high parasympathetic tone helps to maintain heart stability and protect against possible adverse cardiac events ( 32 , 34 ). Conversely, increased sympathetic tone increases the risk of malignant arrhythmias and sudden cardiac death ( 60 ). Thus, a high degree of HRV provides cardioprotective effect whereas the reduction in HRV is associated with higher cardiovascular risk in depressed patients ( 43 , 51 , 52 ).
Although medication-free depressed patients already exhibit reductions in HRV ( 52 ), the use of specific antidepressants (e.g., tricyclics) further decreases HRV ( 50 , 61 – 65 ). This poses an additional risk for the depressed patients. The finding that the somatic cluster is related to moderate depression indicates a decrease in parasympathetic activity leading to higher cardiovascular risk. Therefore, the present data suggest that the cluster of DSM-5 symptoms exhibited by the patient may guide the choice of the adequate antidepressant drug treatment.
In addition, severe depression was found to be linked to increased suicidality, highlighting the importance of needing clear markers of severe depression for clinicians to identify the patients are at risk for committing suicide ( 63 ). In our study, the presence of the anhedonia main criterium indicates severe depression, especially when accompanied by feelings of worthless or excessive guilt, and thoughts of death. It is known that the anhedonia, suicidality, and the feelings of worthlessness/excessive guilt criteria may be mainly related to a decrease in central norepinephrine levels ( 65 ). Although serotonin has been the most studied neurotransmitter in depression, norepinephrine is also of importance in depressive disorders. An association of specific features and symptoms of depression and a deficiency or dysfunction of certain neurotransmitters has been proposed ( 65 – 67 ): a serotonin deficiency is related to problems such as anxiety, obsessions, and compulsions whereas dysfunctional dopaminergic activity is implicated in problems of motivation and pleasure ( 66 – 68 ). Accordingly, norepinephrine deficiency is associated with increased suicide risk ( 50 , 65 , 67 ).
A limitation of this study is the use of a clinical sample. We choose a clinical sample because it maximizes the prevalence of depression. Although the DSM criteria do not require distinguishing between clinical and non-clinical populations, it is possible to speculate that specific clinical problems may bias both the Hamilton Depression Rating Scale (e.g., irritable bowel syndrome) ( 69 , 70 ) and the DSM-5 criteria (e.g., fibromyalgia) ( 71 , 72 ). In addition, the study was done from a sample in Brazil, and some cultural factors could influence the symptoms. Therefore, it would be useful to add other scales to measure depression such as something that the patients could fill out to show if there is a relationship among the multiple instruments ( 73 – 75 ). Another limitation is the lack of power to study sex differences. Although the DSM criteria do not distinguish men from women, men's experiences of depression may be different from women, such as higher rates of anger attacks and aggression in men compared to women ( 76 ). It would be of interest to perform a confirmatory analysis using the equations derived from the present data controlling gender and using non- clinical samples.
From a clinical point of view, the present study suggests that somatic rather than cognitive-affective DSM-5 criteria are linked to moderate depression. As moderate depression is associated with adverse cardiovascular outcomes ( 18 , 19 ), the presence of these somatic symptoms would guide the choice of antidepressants which do not increase cardiac risk. It should be stressed that this recommendation is also important for depressed patients without cardiovascular disease because some antidepressants increase the cardiac risk in individuals without previous cardiac disease ( 18 , 40 , 49 , 50 ). As cognitive-affective symptoms are associated with severe depression, the presence of these symptoms increases the need to use antidepressants to prevent suicide ( 63 , 77 ).
In conclusion, the presence of anhedonia criterium indicates severe depression, especially when accompanied by non-somatic secondary criteria whiles the somatic factors are related to moderate depression. The present study may help the clinical practitioner to infer about depression severity based only on the DSM-5 criteria. The clusters of DSM-5 symptoms exhibited by the patient may help the choice of adequate pharmacological treatments. The correct choice of antidepressants would avoid the use of antidepressants that unnecessarily increase cardiac risk in moderate depression. In addition, when the symptom cluster suggests severe depression, the treatment must focus on the prevention of suicide.
Author contributions
SS and JT contributed to the overall conception and design of the study. Both authors materially participated in the research and article preparation. JT did the data extraction. SS did the statistical analyses. All authors contributed to interpretation of results and drafting of this manuscript. All authors read and approved the final manuscript.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to gratefully acknowledge the collaboration of all participants in this study.
Abbreviations
Ohio State nav bar
The Ohio State University
- BuckeyeLink
- Find People
- Search Ohio State
Patient Case Presentation

Figure 1. Blue and silver stethoscope (Pixabay, N.D.)
Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness. She also noticed other changes about herself, including decreased appetite, insomnia, fatigue, and poor ability to concentrate. The things that used to bring Ms. S.W. joy, such as gardening and listening to podcasts, are no longer bringing her the same happiness they used to. She became especially concerned as within the past two weeks she also started experiencing feelings of worthlessness, the perception that she is a burden to others, and fleeting thoughts of death/suicide.
Ms. S.W. acknowledges that she has numerous stressors in her life. She reports that her daughter’s grades have been steadily declining over the past two semesters and she is unsure if her daughter will be attending college anymore. Her relationship with her son is somewhat strained as she and his father are not on good terms and her son feels Ms. S.W. is at fault for this. She feels her career has been unfulfilling and though she’d like to go back to school, this isn’t possible given the family’s tight finances/the patient raising a family on a single income.
Ms. S.W. has experienced symptoms of depression previously, but she does not think the symptoms have ever been as severe as they are currently. She has taken antidepressants in the past and was generally adherent to them, but she believes that therapy was more helpful than the medications. She denies ever having history of manic or hypomanic episodes. She has been unable to connect to a mental health agency in several years due to lack of time and feeling that she could manage the symptoms on her own. She now feels that this is her last option and is looking for ongoing outpatient mental health treatment.
Past Medical History
- Hypertension, diagnosed at age 41
Past Surgical History
- Wisdom teeth extraction, age 22
Pertinent Family History
- Mother with history of Major Depressive Disorder, treated with antidepressants
- Maternal grandmother with history of Major Depressive Disorder, Generalized Anxiety Disorder
- Brother with history of suicide attempt and subsequent inpatient psychiatric hospitalization,
- Brother with history of Alcohol Use Disorder
- Father died from lung cancer (2012)
Pertinent Social History
- Works full-time as an enrollment specialist for Columbus City Schools since 2006
- Has two children, a daughter age 17 and a son age 14
- Divorced in 2015, currently single
- History of some emotional abuse and neglect from mother during childhood, otherwise denies history of trauma, including physical and sexual abuse
- Smoking 1/2 PPD of cigarettes
- Occasional alcohol use (approximately 1-2 glasses of wine 1-2 times weekly; patient had not had any alcohol consumption for the past year until two weeks ago)
Got any suggestions?
We want to hear from you! Send us a message and help improve Slidesgo
Top searches
Trending searches
49 templates
18 templates
40 templates
american football
16 templates

41 templates
tropical rainforest
29 templates
Depression: Dysthymic Disorder
Depression: dysthymic disorder presentation, free google slides theme and powerpoint template.
Dysthymia, also known as persistent depressive disorder, is a type of depression that often goes unnoticed. Why is that? Because the patient believes that the symptoms (mainly those from depression) are just part of their own nature, making them believe that there's nothing wrong with them. It's best if we leave the actual definitions to true psychologists, like you! This sober template can be useful to raise awareness about this condition, or to inform about its existence and its signs. Notice the use of shadows on the backgrounds and the neutral color palette to underline the serious side of the matter.
Features of this template
- 100% editable and easy to modify
- 20 different slides to impress your audience
- Contains easy-to-edit graphics such as graphs, maps, tables, timelines and mockups
- Includes 500+ icons and Flaticon’s extension for customizing your slides
- Designed to be used in Google Slides and Microsoft PowerPoint
- 16:9 widescreen format suitable for all types of screens
- Includes information about fonts, colors, and credits of the resources used
How can I use the template?
Am I free to use the templates?
How to attribute?
Attribution required If you are a free user, you must attribute Slidesgo by keeping the slide where the credits appear. How to attribute?
Related posts on our blog.

How to Add, Duplicate, Move, Delete or Hide Slides in Google Slides

How to Change Layouts in PowerPoint

How to Change the Slide Size in Google Slides
Related presentations.

Premium template
Unlock this template and gain unlimited access


IMAGES
VIDEO
COMMENTS
Depression is a mood disorder that causes feelings of sadness that won't go away. Unfortunately, there's a lot of stigma around depression. Depression isn't a weakness or a character flaw. It's not about being in a bad mood, and people who experience depression can't just snap out of it. Depression is a common, serious, and treatable condition.
Depression Presentation templates Depression is a serious topic, but that doesn't mean we can't make it more approachable! We've put together a collection of Google Slides & PPT presentation templates about depression that we think are perfect for this subject. These templates are designed to help you start tough conversations about mental ...
Identifying depression • Depression means that there is a considerable impairment in a person's ability to function in daily life. • Some people may experience a persistent depressed mood but they are able to continue functioning in daily life. Therefore, their symptoms do not amount to depression and can be managed
Depression. Depression is a common mental health condition that causes a persistent feeling of sadness and changes in how you think, sleep, eat and act. There are several different types. Depression is treatable — usually with talk therapy, medication or both. Seeking medical help as soon as you have symptoms is essential.
Depression (also called major depressive disorder or clinical depression) is diferent. It can cause severe symptoms that afect how you feel, think, and handle daily activities, such as sleeping, eating, or working. It is an illness that can afect anyone— regardless of age, race, income, culture, or education.
2 What is depression? It is a medical illness that involves the mind and body. It is more than feeling blue, down in the dumps, or sad about a particular issue or situation. It interferes with a person's function in daily living, relationship, and work life. It is a condition that requires diagnosis and treatment by a trained healthcare provider.
Depression (also known as major depression, major depressive disorder, or clinical depression) is a common but serious mood disorder. It causes severe symptoms that affect how a person feels, thinks, and handles daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least 2 ...
- they can make depression worse. • If you feel suicidal, contact someone you trust for help, or ring the emergency services. Depression: what you should know If you think that you might have depression, read on… REMEMBER: With the right support, you can get better - so if you think you might be depressed, seek help.
Depression with symptoms of psychosis is a severe form of depression in which a person experiences psychosis symptoms, such as delusions or hallucinations. Bipolar disorder involves depressive episodes, as well as manic episodes (or less severe hypomanic episodes) with unusually elevated mood, greater irritability, or increased activity level.
Depression is a common mental health problem that involves a low mood and a loss of interest in activities. Learn more about the symptoms, different types, and treatment options.
Depressive disorder (also known as depression) is a common mental disorder. It involves a depressed mood or loss of pleasure or interest in activities for long periods of time. Depression is different from regular mood changes and feelings about everyday life. It can affect all aspects of life, including relationships with family, friends and ...
Depression Symptoms: Physical. 3 /23. Depression is sometimes linked to physical symptoms. These include: Fatigue and decreased energy. Insomnia, especially early-morning waking. Excessive sleep ...
Depression (major depressive disorder) is a common and serious medical illness that negatively affects how you feel, the way you think and how you act. Fortunately, it is also treatable. Depression causes feelings of sadness and/or a loss of interest in activities you once enjoyed. It can lead to a variety of emotional and physical problems and ...
Free Google Slides theme, PowerPoint template, and Canva presentation template. Do you want to overcome depression? Then this template is here to help! It's designed to be clear and concise with illustrated visuals that make it easy to understand and follow. Professional and friendly, it covers everything you need to know about dealing with ...
Depression is a complex condition, involving many systems of the body, including the immune system, either as cause or effect. It disrupts sleep and it interferes with appetite; in some cases, it ...
Digital Shareables on Depression. Use these resources to raise awareness about depression. Depression is a common but serious mood disorder. It causes severe symptoms that affect how someone feels, thinks, and handles daily activities, such as sleeping, eating, or working. For more information on depression, visit the health topic page or view ...
Depression is a very common disorder encountered by the nurse practitioner, primary care provider, psychiatrist, and mental health worker, coordinating as an interprofessional healthcare team. The disorder has extremely high morbidity including the risk of suicide. All healthcare workers should be knowledgeable about this disorder and refer the ...
PK !-¿aƒB O [Content_Types].xml ¢ ( ÌœÛnÚ@ †ï+õ o+0>6B¢ª‡« "%}€½€[Ÿä]rxû®M "10cý¾ 1öìü Ì7kükÏ/ï³tt++• ùÌr&Sk$ó¨ˆ"|1³~ß| ŸY#¥E ‹´ÈåÌz ʺ¼xûæüæ¡"jd¢s5³-Z— m[EK™ 5)J™›=ó¢Ê„6›ÕÂ.EôO,¤íN§¡ ¹-¹ ëz ëâü‹œ‹UªG_ïÍÛk%e¾°FŸ×ÇÕ©fV'ÕñõûöÞˆ¿¥Ü ÒìØ SÉTí¤ e™&'Ц öm ...
Premium Google Slides theme and PowerPoint template. If your research led you to new discoveries on depression, you can share all the details with this presentation. It's very cool and contains waves in the background. Explain your objectives, methodology, results analysis and edit its graphs and infographics.
Introduction. Depression is a common psychiatric disorder, with an estimated lifetime prevalence of 10% in the general population (1, 2).In clinical settings, its prevalence may reach as high as 20% (1, 3).According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the diagnosis of a Major Depression Episode (MDE) requires five or more symptoms to be present ...
Patient Case Presentation. Figure 1. Blue and silver stethoscope (Pixabay, N.D.) Ms. S.W. is a 48-year-old white female who presented to an outpatient community mental health agency for evaluation of depressive symptoms. Over the past eight weeks she has experienced sad mood every day, which she describes as a feeling of hopelessness and emptiness.
Depression: Dysthymic Disorder Presentation . Medical . Free Google Slides theme and PowerPoint template . Dysthymia, also known as persistent depressive disorder, is a type of depression that often goes unnoticed. Why is that? Because the patient believes that the symptoms (mainly those from depression) are just part of their own nature ...