Psychology: Research and Review
- Open access
- Published: 04 June 2018

Behavioral problems of school children: impact of social vulnerability, chronic adversity, and maternal depression
- Ana Karina Braguim Martineli ORCID: orcid.org/0000-0003-2549-5583 1 ,
- Fernanda Aguiar Pizeta 1 &
- Sonia Regina Loureiro 1
Psicologia: Reflexão e Crítica volume 31 , Article number: 11 ( 2018 ) Cite this article
29k Accesses
8 Citations
19 Altmetric
Metrics details
This study’s objective was to identify the predictive effect of indicators concerning social vulnerability, chronic adversity, and maternal depression on behavioral problems among school-aged children, according to the perceptions of mothers and teachers, considering the presence or absence of difficulties in the contexts of family and school. A total of 85 pairs of mothers and school children were distributed into three groups according to the behavioral problems identified. A General Questionnaire, the PHQ-9, the Chronic Adversity Scale, and the (Strengths and Difficulties Questionnaire) SDQ were applied to the mothers; the Raven’s Colored Progressive Matrices were applied to the children; and the SDQ was applied to the teachers. Data were analyzed with descriptive, predictive, and comparative statistical procedures ( p ≤ 0.05). The results reveal the presence of cumulative risks for children with behavioral problems; mothers more frequently identified behavioral problems than teachers; and maternal depression was a predictor for behavioral problems. Such findings are relevant for devising mental health programs.
The behavior of school-aged children is an important indicator of adaptation in this stage of development; however, not all children are successful and may present externalizing or internalizing behavioral problems, expressed within the family and/or school contexts (Achenbach, Ivanova, Rescorla, Turner, & Althoff, 2016 ; Linhares & Martins, 2015 ; Marturano, 2013 ).
Families present structural and internal dynamics that may contribute to either risk or protective outcomes in terms of child development (Macana & Comim, 2015 ; Walsh, 2016 ) so that adaptive difficulties associated with behavioral problems are frequent among children (Pizato, Marturano, & Fontaine, 2014 ). Considering the relevance of the influence exerted by the family context on school children, various studies have addressed the association of cumulative adversity present in the family context and the outcomes of behavioral problems among children (Duncombe, Havighurst, Holland, & Frankling, 2012 ; Leis, Heron, Stuart, & Mendelson, 2014 ; Pizeta, Silva, Cartafina, & Loureiro, 2013 ).
When analyzing the potential risk factors for the development of psychopathologies in 252 children and adolescents who are victims of domestic violence, Hildebrand, Celeri, Morcillo, and Zanolli ( 2015 ) verified that 92.8% of the participants were exposed to at least one risk factor. The authors also noticed that the association of two or more risk factors were present in 53.2% of the sample, namely family conflicts, mental health problems within the family, gender violence between parents, family involvement with drug trafficking and criminal behavior, and the abusive consumption of alcohol by parents or legal guardians, among others.
Therefore, among the events listed as conditions that predispose children to behavioral problems, we highlight indicators of chronic adversity and mental health conditions affecting the parents, especially maternal depression, as risk conditions acknowledged to have a negative impact on children. Additionally, the presence of variables related to social vulnerability is also identified based on conditions or events of life that may interfere in the course of developmental outcomes for children, contributing to the maladaptation of children in typical developmental tasks when experiencing risk conditions.
Considering social vulnerability in the population in general, low socioeconomic status and unemployment among mothers were identified as predictors of behavioral problems among children in situations of poverty, according to a study conducted by Bele, Bodhare, Valsangkar, and Saraf ( 2013 ) of children in India. In the Brazilian context, Correia, Saur, and Loureiro ( 2014 ) conducted a cohort study and identified an association of behavioral problems with low socioeconomic status for boys and low maternal education and larger families for girls. In the same direction, Pizato et al. ( 2014 ) verified association between improved socioeconomic conditions with fewer behavioral problems and more social skills in school-aged children; Saur and Loureiro ( 2015 ) identified associations between behavioral problems among 10-year-old children with low maternal educational level and low socioeconomic status and families with more than four members. It is also considered that the family socioeconomic condition can influence the cognitive performance of children, being this condition strongly related to other environmental aspects such as maternal depression (Piccolo et al., 2012 ).
In regard to the parents’ mental health, maternal depression, especially given its high prevalence and recurrence (World Health Organization [WHO], 2017a , 2017b ), stands out as a form of adversity in different periods of child development, impacting the behavior of school-aged children (Bagner, Pettit, Lewinsohn, & Seeley, 2010 ; Callender, Olson, Choe, & Sameroff, 2012 ; Edwards & Hans, 2015 ; Loosli, Pizeta, & Loureiro, 2016 ). Such a psychopathology, however, is associated with other adverse contextual conditions, favoring cumulative risk in the family context (Kessler, 2012 ). Note that the condition of cumulative risk has been acknowledged in the literature as having a greater impact for outcomes among children compared to the presence of a single risk (Evans, Li, & Whipple, 2013 ). Thus, this justifies the relevance of studying potential associations between maternal depression and behavioral problems, including other variables in the family environment, as proposed in this paper.
Indicators of social vulnerability and clinical characteristics of maternal depression have been identified as relevant factors to understanding risk conditions for child development. Barker, Copeland, Maughan, Jaffee, and Uher ( 2012 ) monitored children from their first year of life up to the age of 7 and verified that, in comparison to children of mothers without depression, children of mothers with depression were more frequently exposed to 10 out of the 11 risk factors assessed in the study, among which, low socioeconomic status, single parent, physical abuse, low maternal education, and drug and alcohol consumption. The frequency of exposure was at a significant level. Indicators concerning the severity of depression and anxiety were examined by Leis et al. ( 2014 ), in a sample of 2891 mother-child pairs, taking into account the perspectives of mothers and teachers. The authors found an association between severe depressive symptoms during pregnancy and more frequent behavioral problems at the age of 10 and 11 years old, according to the reports of teachers. Conners-Burrow et al. ( 2016 ), who took into account the assessment of mothers, determined that early contact with maternal mild depressive symptoms increased the risk of children presenting internalizing and externalizing behavioral problems during school-age years.
Still considering chronic risk and adversity and their influence on child behavior, we highlight the study by Wang, Christ, Mills-Koonce, Garrett-Peters, and Cox ( 2013 ), who found associations between externalizing problems among 4- to 12-year-old children and the use of more rigid control and low maternal educational levels. The study by Bouvette-Turcot et al. ( 2017 ) reports that exposure to more adversity and low family income during childhood was associated with the development of depressive symptoms in adulthood.
When addressing behavioral problems, one issue that arises refers to the source of assessments, considering that children and adolescents may present problems in a specific context but not in another, for instance, family versus school, indicating a need to obtain assessments from multiple informants, especially from parents or legal guardians and teachers (Martoni, Trevisan, Dias, & Seabra, 2016 ; Miller, Martinez, Shumka, & Baker, 2014 ). In this direction, some studies draw attention to the low to moderate level of agreement obtained between informants and to the relevance of such information to implementing clinical practices intended to address specific contexts in which children present problems (De Los Reyes et al., 2015 ; Martel, Markon, & Smith, 2017 ). Despite disagreement among the various informants, different observers provide different perspectives of the same problem (Miller et al., 2014 ). Each observer, though, can provide potentially valuable data in regard to the same patient (De Los Reyes, Thomas, Goodman, & Kundey, 2013 ; Clark, Durbin, Hicks, Iacono, & McGue, 2017 ), taking into consideration different contexts.
With school-aged children in mind, mothers and teachers have a privileged opportunity to observe the behavior of children, since the family and school are the primary contexts of development where competence in specific tasks inherent to this period is acquired (Achenbach et al., 2008 ), as previously mentioned. Some studies addressing the behavior of children according to the assessments of parents and teachers highlight the discrepancy between such assessments. Johnson, Hollis, Marlow, Simms, and Wolke ( 2014 ) used the Strengths and Difficulties Questionnaire (SDQ) to assess 219 children aged 11 years old who were born prematurely. The authors verified that the parents considered their children to present more emotional, attention, and relationship problems compared to the assessments provided by teachers. The informants agreed only in regard to the assessment of problems related to hyperactivity, which indicates the importance of using combined assessments. Kovess et al. ( 2015 ) conducted a study with 9084 children between 6 and 9 years of age, from seven countries (Italy, the Netherlands, Germany, Romania, Bulgaria, Lithuania, and Turkey), in which both teachers and parents were informants. The objective was to identify risks to the mental health of students. They verified that the teachers found the children to present more externalizing problems and fewer internalizing problems when compared to the parents’ assessments.
Even though assessments provided by multiple informants are considered relevant, the literature still lacks data. This study seeks to fill this gap and is intended to produce new data concerning the behavior of school children assessed by mothers and teachers, considering conditions in which children live with maternal depression and other adversities. Therefore, this study is intended to fill the gaps pointed out by De Los Reyes et al. ( 2015 ) concerning the need for further research using the assessments of multiple informants and addressing the specifics of contexts in which behavioral problems manifest, as a way to improve understanding regarding such problems, focusing on maternal depression. According to Goodman et al. ( 2011 ), there is a need for studies focusing on the multiple adversities presented in the family environment, taking into account the influence of maternal mental health when assessing the behavior of children, as indicated by Leis et al. ( 2014 ).
Therefore, the objective was to identify the behavioral profile of school children and associations between the evaluation of mothers and teachers, identifying the level of agreement among the informants. In addition, we aimed to evaluate the predictive effect of indicators concerning social vulnerability, chronic adversity, and maternal depression on behavioral problems presented by school children, according to the perspectives of mothers and teachers, considering the presence or absence of difficulties in both family and school contexts. The hypothesis guiding this study was that social vulnerability, chronic adversity, and maternal depression predict more frequent behavioral problems among school children in both developmental contexts, family and school, assessed by mothers and teachers, respectively.
A cross-sectional, correlational, predictive, comparative design was adopted using data obtained with different techniques from different sources, namely mothers, teachers, and children. The study was approved by the Institutional Review Board (no. 36415514.5.0000.5407) and complied with the ethical recommendations proposed by the Declaration of Helsinki.
Participants
A total of 85 mother-child pairs and 16 teachers from a public school located in the state of São Paulo, Brazil, took part in this study. The participants were assigned to three groups, according to the children’s indicators of behavioral problems assessed by their mothers and teachers, namely G1 = 18 children with behavioral problems according to their mothers and teachers, G2 = 39 children with behavioral problems according to their mothers or teachers, and G3 = 28 children without behavioral problems according to their mothers and teachers.
According to the inclusion criteria, mothers were aged between 25 and 45 years old, 34.5 years old on average (SD = 5.51), and all were literate. The children were aged between 7 and 10 years old, 8.8 years old on average (SD = 1.06) and were homogeneously distributed into three groups. In regard to the children’s sex, 39 were girls and 46 were boys, making a balanced distribution according to sex impossible: G1 presented significantly more boys than girls when compared to the G2 and G3 ( p = 0.05; p = 0.02, respectively). In order to assess the weight of this variable for the presence or absence of behavioral problems among children, as assessed by both their mothers and their teachers, an ordinal regression analysis was performed considering the sex of the children, which revealed a model that did not present the minimum criteria regarding slope homogeneity [chi-square (1) = 5.285; p = 0.022; D (1) = 5.524; p = 0.019], that is, it is not a model that fits data under analysis.
The inclusion criteria are that the children live with their biological mothers, rather than adoptive mothers, and have attended at least 1 year of primary school. Institutionalized children or those with apparent physical or mental disabilities were excluded. The assessment of children was initiated after consent was obtained from their mothers, and only one child per family was included in the study. In regard to the teachers, only those who had had at least 3 months of contact with the children and taught the children whose mothers explicitly consented to the assessment of their children at school were included. In accordance with the principles of good research practices, the participation of mothers and teachers was voluntary, without incentive payment mechanisms that stimulated the involvement with the research. A lecture was offered to the school on the behavior and learning of school children.
Instruments
Raven’s colored progressive matrices (raven).
The Raven is an instrument standardized by Angelini, Alves, Custódio, Duarte, and Duarte ( 1999 ), to assess the intellectual level of Brazilian children between 5 and 11 years old. It is a psychological test of non-verbal intelligence; the objective of which is to assess one’s analogical reasoning as a general factor, composed of three series: A, AB, and B, each with 12 problems. It presents good psychometric qualities, inferred by construct validity, internal consistency, with item-total correlation between 0.30 and 0.80 for most items, as well as precision, inter-item coefficient of correlation for the total sample equal to 0.92 (Angelini et al., 1999 ). Children presenting potential cognitive deficits, who presented percentiles lower than 25, were excluded from the study (Muniz, Gomes, & Pasian, 2016 ), balancing groups according to the percentiles obtained by the children.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is a module directly based on the diagnostic criteria for major depression disorder from the DSM-IV, proposed and validated by Spitzer, Kroenke, and Williams ( 1999 ) and by Kroenke, Spitzer, and Williams ( 2001 ). The questionnaire enables both screening for signs and symptoms of current major depression, as well as classifying levels of severity, from mild to moderate or severe; the greater the score, the more indicators of problems the individual presents. It is composed of nine items assessed by an ordinal scale that measures the frequency of signs and symptoms of depression in the last 2 weeks. According to the instrument’s technical instructions, the total score was used so that scores greater than or equal to 10 indicate the presence of depressive symptoms, while scores lower than 10 indicate an absence of such symptoms. The Brazilian version used in this study was translated by Pfizer (Copyright © 2005 Pfizer Inc., New York, NY), the reliability of which was verified by Osório, Mendes, Crippa, and Loureiro ( 2009 ), presenting satisfactory psychometric indicators.
Strengths and Difficulties Questionnaire (SDQ)
The SDQ was developed by Goodman ( 1997 ) and is intended to assess the behavior of children and adolescents, aged between 4 and 16 years old, by screening their behavioral strengths and difficulties. There is a version for children and adolescents between 11 and 16 years of age, a version for parents, and another for teachers. The SDQ is composed of 25 items subdivided into five subscales: emotional symptoms, conduct problems, hyperactivity, peer relationship problems, and pro-social behavior, with five items each. It provides raw scores and cutoff points for each of the subscales, as well as a total score for difficulty that is obtained by totaling the four behavioral problem scales. Scores are classified as normal, borderline, and abnormal. It was translated to Portuguese and adapted for Brazilian sociocultural characteristics by Fleitlich, Cortázar, and Goodman ( 2000 ), while psychometric data, concerning validity and reliability, were described by Woerner et al. ( 2004 ), presenting good indicators. In this study, based on individual scores and cutoff points established for the Brazilian population, we considered the outcome variable for children classified as normal or borderline, according to the SDQ, to be “without difficulties,” while those who were classified as abnormal to be “with difficulties.” These outcomes were grouped with the assessments performed by the mothers and teachers, according to the distribution in the groups.
Chronic Adversity Scale (CAS)
The CAS was proposed by Marturano ( 1999 ) and is intended to identify recurrent adverse events that may have taken place in a child’s life and happened repeated times or lasted 1 year or longer. It is composed of 18 items addressing issues concerning chronic adversity regarding the child’s or the parents’ health, parents’ temperament, and potential family or marital conflicts. The scale is completed by the mothers based on a list of adverse conditions that may have developed in the lives of children since birth, specifying the duration in years and the child’s period of life at the time. Each item is scored either 0 (absence of recurrence or chronic nature of the event in the child’s life) or 1 (the event was recurrent or has a chronic nature); the sum of all 18 items results in the total score, which is used to identify the existence of chronic events.
General Questionnaire
This questionnaire addresses sociodemographic data and specific information concerning the mothers’ age, marital status, and educational level; the families’ monthly income and socioeconomic status; and the age, sex, and education of the children included in the study. The items from the Brazil Economic Classification Criteria, developed by the Brazilian Association of Survey Companies ( 2015 ), were used to assess socioeconomic conditions. Such information was used to characterize the participants and groups, as well as to identify social vulnerability indicators, including low maternal and paternal education, single-parent families, low socioeconomic status, and low family income, as well as being recipients of governmental financial support.
Data collection procedures
Preferably, data were collected at school in a private room, or in the families’ homes when requested by the mothers, in which case we sought to preserve the respondents’ privacy and convenience. All interviews were held by the first researcher, who is a psychologist and properly trained in the application of instruments.
Initially, 427 families received an invitation letter, which was delivered to the children in their classrooms. The 260 families who responded to the invitation were contacted by phone with the objective to provide clarification about the study’s objectives and schedule an assessment. A total of 154 families accepted the invitation to cooperate with the study, but nine of these were excluded because the grandmothers were the primary caregivers of these families’ children. Of the 145 mothers scheduled for assessment, 43 did not attend the interviews, resulting in 102 families. Seventeen of these did not meet the inclusion criteria: adolescent mothers or mothers older than 45 years of age, children exclusively living with their fathers, and children with characteristics that were not homogeneous with those presented by the groups. Thus, a total of 85 mother-child pairs were included and assessed.
Of the 427 families initially invited to participate in this research, 316 refused to collaborate with the survey and 26 were excluded because they did not meet the inclusion criteria.
The instruments were individually and in-person applied to mothers in a single section according to the following order: General Questionnaire, PHQ-9, CAS, and SDQ, with an average duration of 60 min. The researcher read the instruments and checked the responses while the mothers had a copy of the instruments to accompany the reading. This procedure was adopted to deal with potential difficulties or fatigue that the reading could produce in the mothers, given their level of education or potential depressive symptoms, though the mothers presented a minimum level of literacy that enabled them to understand the questions posed by the instruments.
The children were assessed at school in individual sessions that lasted an average of 15 min. After briefly establishing rapport, the Raven’s Colored Progressive Matrices was applied. The three groups were compared according to the percentiles children obtained in order to balance the groups in regard to this variable. Note that there were no significant statistical differences between them in regard to the children’s cognitive performances (G1: \( \overline{x} \) = 75.1; σ = 19.12; G2: \( \overline{x} \) = 76.0; σ = 13.44; G3: \( \overline{x} \) = 66.9; σ = 14.97).
The 16 teachers collectively completed the SDQ, focusing on the behavior of 85 children who had been previously assessed by their mothers, at the regular time scheduled for a meeting concerning collective teaching work. Each teacher was supposed to assess up to five students per meeting, with an average duration of 50 min and approximately 10 min per child. The teachers filled in the questionnaire, and the researcher remained in the room during the assessment to clarify potential doubts.
Data treatment and analysis
The PHQ-9, Raven, SDQ, and CAS were coded according to the purpose of each instrument. The assessments concerning the behaviors of children performed by the mothers and teachers using the SDQ were used as distinct sources in paired samples, in order to assign the participants to one of the three groups.
Coded data were typed in an Excel® spreadsheet and checked by independent reviewers. The statistical analyses were performed using IBM SPSS Statistics (v. 23; IBM SPSS, Chicago, IL), and a significance level of 0.05 was adopted.
The reliability of the PHQ-9 was verified for this sample using Cronbach’s alpha, which presented good psychometric quality ( α = 0.87). The reliability of the SDQ ( n = 85) for the totality of items regarding difficulties was based on the mothers’ ( α = 0.77) and teachers’ answers ( α = 0.89), as well as items of the pro-social behavior scale answered by mothers ( α = 0.71) and teachers.
Normality tests (Kolmogorov-Smirnov, with Lilliefors significance correlation, and Shapiro-Wilk) were performed to guide decision-making regarding the statistical tests used for each set of variables.
The behavioral profile of children, obtained through the assessments of mothers and teachers and represented by the raw scores obtained on the scales addressing problems and pro-social resources and the total scale of difficulties in the SDQ, was analyzed using descriptive and comparative statistics by means of the Wilcoxon test. Indicators of the presence and absence of behavioral problems among children, assessed by the mothers and teachers using the SDQ, were compared using the McNemar test. Inter-observer agreement was also verified using the Kappa coefficient, while the criterion proposed by Landis and Koch ( 1977 ) was adopted.
The sociodemographic data and profiles of social vulnerability and chronic adversity were analyzed using descriptive statistics, while the groups were compared using chi-square and Kruskal-Wallis tests. After the univariate analysis, the predictive effect of cumulative adverse conditions on school children’s behavioral problems was assessed using ordinal regression analysis (Maroco, 2014 ), adopting criteria proposed by Field ( 2013 ) for the inclusion of predictive variables.
The weight of contextual adverse cumulative variables for the children’s behavioral problems was tested using ordinal regression analysis based on the significant variables identified in the comparison between groups. The predictive variables were included in the model (family income, mother’s education, and maternal depression were included as factors, and the score of chronic adversity was included as a covariant), independently tested, and combined with the sex of children, because the distribution of children in the groups according to sex was not homogeneous. Additionally, the contextual variables of cumulative risk were jointly tested in a multivariate model.
The analysis of the social vulnerability indicators (income and maternal education) and maternal depression, in one analysis disregarding the sex of children and then one considering the sex of children, showed that the models did not fit the data. The analysis of the models that included chronic adversity, as a single variable or associated with the sex of children, revealed statistically significant models, with very small effect sizes, in which independent variables did not predict the behavioral outcome among children, thus did not present relevant results. Afterwards, the multivariate model including maternal depression, social vulnerability indicators, and chronic adversity was tested and presented goodness of fit and is the model presented here.
Based on the objectives proposed, the results are presented taking into account the analyses concerning the children’s behavioral profiles according to the assessments of mothers and teachers as distinct sources, comparisons between G1, G2, and G3 regarding profile of social vulnerability, maternal depression, and chronic adversity, as well as the predictive effect of significant variables on the children’s behavioral problems assessed by mothers and professors, as combined sources of information.
The children’s behavioral profiles
Table 1 presents the behavioral profiles of the children assessed, according to the SDQ, by mothers and teachers as two different sources, adopting the presence or absence of behavioral problems verified by the SDQ and total difficulties as the outcome of the development of school children.
Significant statistical differences were found when comparing mothers and teachers in regard to the four specific scales of difficulties and total difficulties. Note that the mothers considered their children to present more emotional symptoms, conduct problems, hyperactivity, peer relationship problems, and total difficulties than the teachers. In regard to pro-social behavior, no statistically significant differences were found in regard to the comparisons between mothers and teachers.
In regard to the level of agreement obtained between assessments (mothers and teachers), note that reasonable agreement levels were found for conduct problems (kappa = 0.29 p = 0.003) and total behavioral problems (kappa = 0.21; p = 0.007), in addition to minimum indexes for hyperactivity (kappa = 0.19; p = 0.035).
Similarly, the same differences were found for continuous scores. The means of the mothers were greater than those presented by the teachers for the total difficulties score (mothers: \( \overline{x} \) = 17.5; σ = 6.98; teachers: \( \overline{x} \) = 9.33; σ = 7.28; p < 0.001) and for the four scales concerning symptoms: emotional symptoms (mothers: \( \overline{x} \) = 3.19; σ = 2.52; teachers: \( \overline{x} \) = 2.26; σ = 1.89; p < 0.001), conduct problems (mothers: \( \overline{x} \) = 3.32; σ = 2.56; teachers: \( \overline{x} \) = 1.59; σ = 2.23; p < 0.001), hyperactivity (mothers: \( \overline{x} \) = 6.79; σ = 2.76; teachers: \( \overline{x} \) = 4.04; σ = 3.23; p < 0.001), and peer relationships (mothers: \( \overline{x} \) = 2.20; σ = 2.20; teachers: \( \overline{x} \) = 1.42; σ = 1.90; p < 0.001).
The profiles of families in terms of vulnerability and risk variables
Table 2 presents comparisons concerning social vulnerability, maternal depression, and chronic adversities presented in the family context of children according to their distribution in the three groups.
Statistically significant differences were found between G1, G2, and G3 in regard to maternal education, family income, maternal depression, and chronic adversity. The comparison concerning maternal education revealed significant differences between G1 and G3 ( χ 2 = 5.660, p = 0.017) and between G2 and G3 ( χ 2 = 12.075, p < 0.001). Significant differences were also found in terms of family income between G1 and G2 ( χ 2 = 4.349, p < 0.037) and between G1 and G3 ( χ 2 = 5.841, p = 0.016). No differences were found between groups in terms of paternal education, marital status, socioeconomic status, or receiving governmental financial aid. Considering the variable maternal depression, however, statistically significant differences were found between G1 and G2 ( χ 2 = 13.876, p < 0.000) and between G1 and G3 ( χ 2 = 22.489, p < 0.001). G1 was the group in which mothers more frequently presented current symptoms of depression in comparison to the other two groups, while no differences were found between G2 and G3.
Comparisons concerning chronic adversities revealed significant differences between G2 and G3 ( F = 363.000, p = 0.016), but no differences were found between G1 and G2 or between G1 and G3.
The predictive effect of adverse cumulative variables on child behavior
Table 3 presents the weight of adverse cumulative contextual variables on child behavior, including data concerning coefficients and significance of the adjusted ordinal model.
Data suggest that the adjusted model is significantly better than the null model [ G 2 (4) = 24,792, p < 0.001). Additionally, the multivariate model was statistically significant [chi-square (58) = 50,367, p = 0.752; D (58) = 57,402, p = 0.497] and showed moderate effect size (R 2 MF = 0.253; R 2 N = 0.288; R 2 CS = 0.139). According to the model, children are more likely to present behavioral problems when their mothers present indicators of depression, according to the assessments of both mothers and teachers ( b = 1.955, p = 0.001).
This study was intended to verify associations between indicators of social vulnerability, chronic adversity, and maternal depression, and the weight of such associations, with behavioral problems among school children, as assessed by their mothers and teachers. In this study, mothers and teachers were considered distinct sources of information, and the information they provided on the children’s behaviors was combined considering the presence or absence of difficulties manifested in the two developmental contexts of family and school. The hypothesis guiding this study that social vulnerabilities, chronic adversity, and maternal depression impact behavioral problems among school children was partially confirmed, as data analysis revealed peculiarities regarding such variables, which deserve to be highlighted.
The assessments of the children’s behavior from the perspectives of mothers and teachers in general showed that mothers identified more behavioral problems in children than did the teachers. This finding is in agreement with those reported in the studies conducted by De Los Reyes et al. ( 2015 ) and Martel et al. ( 2017 ), which indicate low to moderate agreement among informants. In this same direction, Clark et al. ( 2017 ) consider that agreement between assessments of parents, teachers, and children is rarely high, however, emphasizing that varied information enriches the understanding of the associations between academic conditions, personality, psychosocial functioning, behavioral aspects, mental health, and social adjustment of school children. According to the mothers’ assessments, a larger number of children experienced difficulties concerning emotional symptoms, while the teachers identified a larger number of children with externalizing problems expressed through conduct problems and hyperactivity. Such results are similar to those reported by Kovess et al. ( 2015 ), who note that externalizing problems are more visible to teachers than internalizing problems.
Analysis of this discrepancy between assessments should take into account that the interaction of mothers and teachers with children occurs in contexts that exhibit different demands, in addition to the fact that observers are guided by different criteria. In the family context, mothers have a more detailed picture of their children’s behavior due to the large range of daily situations, which are not always structured (Leis et al., 2014 ). In the case of the mothers, the parameter is one specific child. In the classroom, in contrast, teachers have more structured situations to assess children and the teachers’ references include comparing the behavior of a set of children with similar demographic parameters. In this sense, when the assessments of mothers and teachers were combined, we accessed a larger set of information concerning the behavior of children, focusing on aspects of contextual comparisons and individual and collective parameters, as proposed by Miller et al. ( 2014 ) and De Los Reyes et al. ( 2015 ).
The literature has recognized the relevance of assessments performed by teachers; however, few studies address behavioral difficulties of children using multiple informants and combined data as a strategy to identify the presence of problems in more than one context of life. The predominance of the mother as the only informant may compromise the results of assessments, especially when a mother presents a psychopathological disorder (Leis et al., 2014 ), such as depression. Such a disorder may influence the individual’s perception of child behavior, and avoiding this influence justifies the use of distinct and combined sources of information. Therefore, we note that one of the contributions of this study, in addition to including multiple informants, is the combined analysis of children’s behavioral outcomes, which enabled verifying problems in two contexts, family and school, to estimate how many children face these sorts of difficulties, information that is relevant for practices in the mental health field.
Another aspect to be analyzed involves social vulnerability, which was assessed considering different social and economic factors, among which are low maternal educational level and income. These are relevant social determinants associated with the presence of behavioral problems among children, according to the assessments by mothers and/or children, indicating aspects to be considered when planning preventive practices. Note that these findings are consistent with those reported by Correia et al. ( 2014 ), who identified association between child behavioral problems and low socioeconomic status and low maternal educational level, indicating a potential profile of cumulative vulnerability favoring behavioral problems among children. Families with low socioeconomic status generally have high rates of divorce, unemployment, and a larger number of members, while parents with a high socioeconomic level have a higher educational level and invest more in their children’s education (Carneiro, Meghir, & Parey, 2013 ; Piccolo et al., 2012 ).
The associations between mental health conditions and vulnerability indicators have been widely recognized by the World Health Organization (WHO, 2017a , 2017b ), which highlights low schooling, lower income, worse material and economic conditions, and less social support, as possible determinants that negatively influence health mental health of adults and children, favoring the accumulation of vulnerability and risk conditions. This developmental scenario focuses on the relevance of the present study, which encompasses diverse and competing contextual variables that influence children’s developmental outcomes in the perception of different informants.
The presence of current depressive symptoms among the mothers was associated with behavioral problems among the children, as indicated by the mothers and/or teachers, characterizing problems in two contexts, family and school. Such an association was also verified by Leis et al. ( 2014 ) and Conners-Burrow et al. ( 2016 ), who noted an increase in behavioral problems among children who had early experience with maternal depression. In this sense, when we considered the behavior of children from the perspectives of mothers and teachers together, we verified that, regardless of the informant, children living with maternal depression more frequently experienced behavioral problems, including in the school context, characterizing the need for specific mental health practices directed to this group, which was identified as the most vulnerable.
The presence of chronic adversities was also verified to identify variables with a potential negative impact on school-aged children. This study reveals that children facing behavioral difficulties, according to the combined assessments of mothers and teachers, lived in family environments that presented more chronic adversities, indicating cumulative and recurrent adversity in these children’s contexts of life. These findings corroborate the study conducted by Hildebrand et al. ( 2015 ), who identified an association of two or more risk factors for more than half of the sample under study.
The identification of differences among groups, especially for children facing problems in the family and school contexts (G1) in regard to social vulnerability, current maternal depression, and chronic adversity, characterizes a group that requires greater attention, as it is exposed to multiple risks. This information highlights the relevance of investigating the presence of cumulative risk in the family context to understand developmental outcomes among children (Evans et al., 2013 ; Goodman et al., 2011 ).
In regard to the identification of the predictive effect of cumulative risk variables and vulnerability, as potential predictors of behavioral problems among children, only maternal depression appears as an explanatory variable for the presence of behavioral problems among children in the context of multiple adverse conditions. These findings are in agreement with Bagner et al. ( 2010 ), who stress that living with maternal depression increases a child’s likelihood of presenting externalizing and internalizing behavioral problems up to the age of 12 years old. Therefore, maternal depression was the only adverse condition with the power to predict the behavioral problem outcome, confirming the relevance of considering such a variable when addressing child behavior, especially considering the high prevalence of depression among women of childbearing age (World Health Organization [WHO], 2017a , 2017b ).
As the positive aspects of this study, we highlight the presence of multiple informants, the methodological care adopted in the systematic assessment of the participants, and the use of validated instruments, in addition to the inclusion of diverse variables to identify, in the same sample, vulnerability indicators that potentially impact the behavior of school children. It is highlighted as the main strength of the study the inclusion of children in the groups considering the presence or absence of behavioral problems in the two main development contexts for the school period, namely, family and school, thus highlighting relevant variables associated with vulnerability and to developmental resources in both contexts, which may favor preventive care and target groups with potential risks.
This study’s limitations include the sample size, lack of a homogeneous distribution between groups in regard to the sex of children, and the identification of depressive symptoms using a screening instrument, which limit the generalization of results. Further studies adopting longitudinal designs, considering the influence of contextual risks over the course of a child’s development, including other sources of information, in addition to the reports of mothers, are needed, as well as observational measures. The relevance of inclusion in new studies of parents’/stepfathers’ evaluations, as well as studies that address the characteristics of the various family configurations in which children are inserted as conditions that can influence the behavior of the school-aged children, is also highlighted. Another relevant point to be considered in new studies is the inclusion of variables that may function as protective factors, which in a cumulative way to vulnerability and risk conditions may favor a more complete and complex analysis of the mechanisms that favor or hinder children’s behavioral problems.
Conclusions
In this study, low maternal educational level, low family income, the presence of more chronic adversity, and living with current maternal depression are factors associated with the outcome of behavioral problems among children in both family and school contexts, showing the importance of including such factors in assessment protocols intended to address the mental health of school-aged children. Note, however, that among these indicators, current maternal depression emerged as the most relevant variable in comparison to the remaining adversities analyzed here. Therefore, this condition requires specific care when implementing mental health actions.
Finally, these results can contribute to and have implications for the planning of mental health programs, confirming the relevance of identifying maternal depressive symptoms and multiple adversities, including social vulnerability indicators as conditions or events that demand attention.
Achenbach, T. M., Becker, A., Döpfner, M., Heiervang, E., Roessner, V., Steinhausen, H.-C., & Rothenberger, A. (2008). Multicultural assessment of child and adolescent psychopathology with ASEBA and SDQ instruments: Research findings, applications, and future directions. Journal of Child Psychology and Psychiatry , 49 (3), 251–275. https://doi.org/10.1111/j.1469-7610.2007.01867.x .
PubMed Google Scholar
Achenbach, T. M., Ivanova, M. Y., Rescorla, L. A., Turner, L. V., & Althoff, R. R. (2016). Internalizing/externalizing problems: Review and recommendations for clinical and research applications. Journal of the American Academy of Child & Adolescent Psychiatry , 55 (8), 647–656. https://doi.org/10.1016/j.jaac.2016.05.012 .
Google Scholar
Angelini, A. L., Alves, I. C., Custódio, E. M., Duarte, W. F., & Duarte, J. L. (1999). Manual das Matrizes Progressivas Coloridas de Raven: escala especial. Manual . São Paulo: Centro Editor de Testes e Pesquisas em Psicologia.
Associação Brasileira de Empresas de Pesquisa. (2015). Critério Padrão de Classificação Econômica Brasil. Recuperado de http://www.abep.org/ .
Bagner, D. M., Pettit, J. W., Lewinsohn, P. M., & Seeley, J. R. (2010). Effect of maternal depression on child behavior: A sensitive period? Journal of the American Academy of Child & Adolescent Psychiatry , 49 (7), 699–707. https://doi.org/10.1016/j.jaac.2010.03.012 .
Barker, E. D., Copeland, W., Maughan, B., Jaffee, S. R., & Uher, R. (2012). The relative impact of maternal depression and associated risk factors on offspring psychopathology. The British Journal of Psychiatry , 200 (2), 124–129. https://doi.org/10.1192/bjp.bp.111.092346 .
PubMed PubMed Central Google Scholar
Bele, S. D., Bodhare, T. N., Valsangkar, S., & Saraf, A. (2013). An epidemiological study of emotional and behavioral disorders among children in an urban slum. Psychology, Health & Medicine , 18 (2), 223–232. https://doi.org/10.1080/13548506.2012.701751 .
Bouvette-Turcot, A.-A., Unternaehrer, E., Gaudreau, H., Lydon, J. E., Steiner, M., & Meaney, M. J. (2017). The joint contribution of maternal history of early adversity and adulthood depression to socioeconomic status and potential relevance for offspring development. Journal of Affective Disorders , 207 , 26–31. https://doi.org/10.1016/j.jad.2016.08.012 .
Callender, K. A., Olson, S. L., Choe, D. E., & Sameroff, A. J. (2012). The effects of parental depressive symptoms, appraisals, and physical punishment on later child externalizing behavior. Journal of Abnormal Child Psychology , 40 (3), 471–483. https://doi.org/10.1007/s10802-011-9572-9 .
Carneiro, P., Meghir, C., & Parey, M. (2013). Maternal education, home environments, and the development of children and adolescents. Journal of the European Economic Association , 1 , 123–160. https://doi.org/10.1111/j.1542-4774.2012.01096.x .
Clark, D. A., Durbin, C. E., Hicks, B. M., Iacono, W. G., & McGue, M. (2017). Personality in the age of industry: Structure, heritability, and correlates of personality in middle childhood from the perspective of parents, teachers, and children. Journal of Research in Personality , 67 , 132–143. https://doi.org/10.1016/j.jrp.2016.06.013 .
Conners-Burrow, N. A., McKelvey, L., Perry, D., Whiteside-Mansell, L., Kraleti, S., Mesman, G., … Kyzer, A. (2016). Low-level symptoms of depression in mothers of young children are associated with behavior problems in middle childhood. Maternal and Child Health Journal , 20 (3), 516–524. https://doi.org/10.1007/s10995-015-1849-0 .
Correia, S. K. B., Saur, A. M., & Loureiro, S. R. (2014). Behavior of school children stratified by birth weight and gestational age. Psicologia: Teoria e Pesquisa , 30 (2), 179–188. https://doi.org/10.1590/S0102-37722014000200007 .
De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D. A., Burgers, D. E., & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin , 141 (4), 858–900. https://doi.org/10.1037/a0038498 .
Duncombe, M. E., Havighurst, S. S., Holland, K. A., & Frankling, E. J. (2012). The contribution of parenting practices and parent emotion factors in children at risk for disruptive behavior disorders. Child Psychiatry & Human Development , 43 (5), 715–733. https://doi.org/10.1007/s10578-012-0290-5 .
Edwards, R. C., & Hans, S. L. (2015). Infant risk factors associated with internalizing, externalizing, and co-occurring behavior problems in young children. Developmental Psychology , 51 (4), 489. https://doi.org/10.1037/a0038800 .
Evans, G. W., Li, D., & Whipple, S. S. (2013). Cumulative risk and child development. Psychological Bulletin , 139 (6), 1342–1396. https://doi.org/10.1037/a0031808 .
Field, A. (2013). Discovering statistics using IBM SPSS Statistics. 4th edition. SAGE Publications, London. ISBN 978-1-4462-4971-8.
Fleitlich, B. W., Cortázar, P. G., & Goodman, R. (2000). Questionário de Capacidades e Dificuldades (SDQ). Infanto - Revista de Neuropsiquiatria da Infância e da Adolescência , 8 (1), 44–50.
Goodman, R. (1997). The strengths and difficulties questionnaire: a research note. Journal of Child Psychology and Psychiatry, 38, 581–586. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x .
Goodman, S. H., Rouse, M. H., Connell, A. M., Broth, M. R., Hall, C. M., & Heyward, D. (2011). Maternal depression and child psychopathology: A meta-analytic review. Clinical Child and Family Psychology Review , 14 (1), 1–27. https://doi.org/10.1007/s10567-010-0080-1 .
Hildebrand, N. A., Celeri, E. H. R. V., Morcillo, A. M., & Zanolli, M. D. L. (2015). Domestic violence and risk for mental health in childhood and adolescence. Psicologia: Reflexão e Crítica , 28 (2), 213–221. https://doi.org/10.1590/1678-7153.201528201 .
Johnson, S., Hollis, C., Marlow, N., Simms, V., & Wolke, D. (2014). Screening for childhood mental health disorders using the Strengths and Difficulties Questionnaire: The validity of multi-informant reports. Developmental Medicine & Child Neurology , 56 (5), 453–459. https://doi.org/10.1111/dmcn.12360 .
Kessler, R. C. (2012). The costs of depression. The Psychiatric Clinics of North America , 35 (1), 1–14. https://doi.org/10.1016/j.psc.2011.11.005 .
Kovess, V., Carta, M. G., Pez, O., Bitfoi, A., Koç, C., Goelitz, D., … Otten, R. (2015). The school children mental health in Europe (SCMHE) project: Design and first results. Clinical Practice & Epidemiology in Mental Health , 11 (1), 113–123. https://doi.org/10.2174/1745017901511010113 .
Kroenke, K., Spitser, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine , 16 (9), 606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x .
Landis, J. R., & Koch, G. G. (1977). The measurement of observer agreement for categorical data. Biometrics, 33(1), 159–174. https://doi.org/10.2307/2529310 .
Leis, J. A., Heron, J., Stuart, E. A., & Mendelson, T. (2014). Associations between maternal mental health and child emotional and behavioral problems: Does prenatal mental health matter? Journal of Abnormal Child Psychology , 42 (1), 161–171. https://doi.org/10.1007/s10802-013-9766-4 .
Linhares, M. B. M., & Martins, C. B. S. (2015). The self-regulation process on child development. Estudos de Psicologia (Campinas) , 32 (2), 281–293. https://doi.org/10.1590/0103-166X2015000200012 .
Loosli, L., Pizeta, F. A., & Loureiro, S. R. (2016). School-age children who live with recurrent maternal depression: Differences between the sexes. Psicologia: Teoria e Pesquisa , 32 (3), 1–10. https://doi.org/10.1590/0102-3772e32322 .
De Los Reyes, A., Thomas, S. A., Goodman, K. L., & Kundey, S. M. (2013). Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology , 9 , 123–149 Recuperado de https://pdfs.semanticscholar.org/4508/6bb381dbf14491e656a95f0d6f57e635adfc.pdf .
Macana, E. C., & Comim, F. (2015). O papel das práticas e estilos parentais no desenvolvimento da primeira infância. In G. A. Pluciennik, M. C. Larazzari, & M. F. Chicaro (Eds.), Fundamentos da família como promotora do desenvolvimento infantil: parentalidade em foco , (pp. 34–47). São Paulo: Fundação Maria Cecília Souto Vidigal Recuperado de http://agendaprimeirainfancia.org.br/arquivos/Fundamentos_Familia.pdf .
Maroco, J. (2014). Análise estatística com o SPSS Statistics . Pêro Pinheiro: Report Number.
Martel, M. M., Markon, K., & Smith, G. T. (2017). Research review: Multi-informant integration in child and adolescent psychopathology diagnosis. Journal of Child Psychology and Psychiatry , 58 (2), 116–128. https://doi.org/10.1111/jcpp.12611 .
Martoni, A. T., Trevisan, B. T., Dias, N. M., & Seabra, A. G. (2016). Funções executivas: relação entre relatos de pais, de professores e desempenho de crianças. Temas em Psicologia , 24 (1), 173–188. https://doi.org/10.9788/TP2016.1-12 .
Marturano, E. M. (1999). Recursos no ambiente familiar e dificuldades de aprendizagem na escola. Psicologia: Teoria e Pesquisa , 15 (2), 135–142 Recuperado de http://dx.doi.org/10.1590/S0102-37721999000200006 .
Marturano, E. M. (2013). A criança, a família, a escola e a transição para o ensino fundamental. In E. C. Konkiewitz (Ed.), Aprendizagem, comportamento e emoções na infância e adolescência: uma visão transdisciplinar , (pp. 47–68). Dourados: UFGD.
Miller, L. D., Martinez, Y. J., Shumka, E., & Baker, H. (2014). Multiple informant agreement of child, parent, and teacher ratings of child anxiety within community samples. The Canadian Journal of Psychiatry , 59 (1), 34–39. https://doi.org/10.1177/070674371405900107 .
Muniz, M., Gomes, C. M. A., & Pasian, S. R. (2016). Factor structure of Raven’s Coloured Progressive Matrices. Psico-USF , 21 (2), 259–272. https://doi.org/10.1590/1413-82712016210204 .
Osório, F. L., Mendes, A. V., Crippa, J. A., & Loureiro, S. R. (2009). Study of the discriminative validity of the PHQ-9 and PHQ-2 in a sample of Brazilian women in the context of primary health care. Perspectives in Psychiatric Care , 45 (3), 216–227. https://doi.org/10.1111/j.1744-6163.2009.00224.x .
Piccolo, L. R., Falceto, O. G., Fernandes, C. L., Levandowski, D. C., Grassi-Oliveira, R., & Salles, J. F. (2012). Psychosocial variables and reading performance of children with low socioeconomic status. Psicologia: Teoria e Pesquisa , 28 (4). https://doi.org/10.1590/S0102-37722012000400004 .
Pizato, E. C. G., Marturano, E. M., & Fontaine, A. M. G. V. (2014). Trajectories of social skills and behavior problems in primary school: Influence of early childhood education. Psicologia: Reflexão e Crítica , 27 (1), 189–197. https://doi.org/10.1590/S0102-79722014000100021 .
Pizeta, F. A., Silva, T. B. F., Cartafina, M. I. B., & Loureiro, S. R. (2013). Maternal depression and risks for children s behavior and mental health: A review. Estudos de Psicologia (Natal) , 18 (3), 429–437. https://doi.org/10.1590/S1413-294X2013000300003 .
Saur, A. M., & Loureiro, S. R. (2015). Mental health of small children for normal gestational age: A cohort study from Southeastern Brazil. Psicologia: Reflexão e Crítica , 28 (1), 204–212. https://doi.org/10.1590/1678-7153.201528122 .
Spitzer, R. L., Kroenke, K., & Williams, J.B.W. (1999). The Patient Health Questionnaire Primary Care Study Group, Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Journal of American Medicine Association, 282(18), 1737–1744. https://doi.org/10.1001/jama.282.18.1737 .
Walsh, F. (2016). Processos normativos da família: diversidade e complexidade . Porto Alegre: Artmed.
Wang, F., Christ, S. L., Mills-Koonce, W. R., Garrett-Peters, P., & Cox, M. J. (2013). Association between maternal sensitivity and externalizing behavior from preschool to preadolescence. Journal of Applied Developmental Psychology , 34 (2), 89–100. https://doi.org/10.1016/j.appdev.2012.11.003 .
Woerner, W., Fleitlich-Bilyk, B., Martinussen, R., Fletcher, J., Cucchiaro, G., Dalgalarrondo, P., … Tannock, R. (2004). The Strengths and Difficulties Questionnaire overseas: Evaluations and applications of the SDQ beyond Europe. European Child & Adolescent Psychiatry , 13 (2), 47–54. https://doi.org/10.1007/s00787-004-2008-0 .
World Health Organization [WHO]. (2017a). Depression and other common mental disordes: global health estimates. World Health Organization . Recuperado de http://apps.who.int/iris/bitstream/handle/10665/254610/WHO-MSD-MER-2017.2-eng.pdf;jsessionid=D941E8D6BCD7068FF960F8ACF5312F39?sequence=1 . Accessed Jan 2018
World Health Organization [WHO]. (2017b). Policy options on mental health . Recuperado de http://apps.who.int/iris/bitstream/10665/259406/1/9789241513296-eng.pdf?ua=1 . Accessed Jan 2018
Download references
Acknowledgements
Not applicable in this section
To the development of this research, we counted on the financial support of the National Council for Scientific and Technological Development (CNPq/Brazil) under number 307394/2014-0.
Availability of data and materials
All data necessary to understand the results and analyses presented are found throughout the manuscript, and no additional files were submitted.
Author information
Authors and affiliations.
Universidade de São Paulo (USP), Rua Tenente Catão Roxo, 2650, Ribeirão Preto, SP, CEP: 14051-140, Brazil
Ana Karina Braguim Martineli, Fernanda Aguiar Pizeta & Sonia Regina Loureiro
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the preparation of this manuscript, approved the submission of their current version, and show their agreement with the publication fee, which will be charged if the manuscript obtains final acceptance. All authors contributed to the conceptualization of the research, to the formal analysis. The first author has a master’s degree and was responsible for data collection.
Corresponding author
Correspondence to Ana Karina Braguim Martineli .
Ethics declarations
Ethics approval and consent to participate.
All the ethical aspects described by the Helsinki Declaration were considered in this manuscript and during the data collection, all the participants signed a consent term, and the study was approved by the Research Ethics Committee of the Faculty of Philosophy, Sciences and Letters of Ribeirão Preto (USP) under number 36415514.5.0000.5407.
Consent for publication
The manuscript was not submitted to another journal, and everyone involved in this research agreed that the work was submitted for publication. If the article is accepted for publication, the copyright will be transferred to Psychology: Reflection and Critical.
Competing interests
The authors declare that they have no competing interests and that this manuscript was not submitted for publication to any other periodical or means of publication.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Reprints and permissions
About this article
Cite this article.
Martineli, A.K.B., Pizeta, F.A. & Loureiro, S.R. Behavioral problems of school children: impact of social vulnerability, chronic adversity, and maternal depression. Psicol. Refl. Crít. 31 , 11 (2018). https://doi.org/10.1186/s41155-018-0089-9
Download citation
Received : 20 July 2017
Accepted : 02 March 2018
Published : 04 June 2018
DOI : https://doi.org/10.1186/s41155-018-0089-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- School children
- Adversities
- Maternal depression
- Social vulnerability
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Introduction
Evidence-based treatments, systemic barriers, recommendations, lead authors, council on early childhood executive committee, 2015–2016, committee on psychosocial aspects of child and family health, 2015–2016, section on developmental and behavioral pediatrics executive committee, 2015–2016, addressing early childhood emotional and behavioral problems.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
COUNCIL ON EARLY CHILDHOOD , COMMITTEE ON PSYCHOSOCIAL ASPECTS OF CHILD AND FAMILY HEALTH , SECTION ON DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS , Dina Lieser , Beth DelConte , Elaine Donoghue , Marian Earls , Danette Glassy , Terri McFadden , Alan Mendelsohn , Seth Scholer , Jennifer Takagishi , Douglas Vanderbilt , Patricia Gail Williams , Michael Yogman , Nerissa Bauer , Thresia B. Gambon , Arthur Lavin , Keith M. Lemmon , Gerri Mattson , Jason Richard Rafferty , EdM , Lawrence Sagin Wissow , Carol Cohen Weitzman , Nerissa S. Bauer , David Omer Childers , Jack M. Levine , Ada Myriam Peralta-Carcelen , Peter Joseph Smith , Nathan J. Blum; Addressing Early Childhood Emotional and Behavioral Problems. Pediatrics December 2016; 138 (6): e20163023. 10.1542/peds.2016-3023
Download citation file:
- Ris (Zotero)
- Reference Manager
Emotional, behavioral, and relationship problems can develop in very young children, especially those living in high-risk families or communities. These early problems interfere with the normative activities of young children and their families and predict long-lasting problems across multiple domains. A growing evidence base demonstrates the efficacy of specific family-focused therapies in reducing the symptoms of emotional, behavioral, and relationship symptoms, with effects lasting years after the therapy has ended. Pediatricians are usually the primary health care providers for children with emotional or behavioral difficulties, and awareness of emerging research about evidence-based treatments will enhance this care. In most communities, access to these interventions is insufficient. Pediatricians can improve the care of young children with emotional, behavioral, and relationship problems by calling for the following: increased access to care; increased research identifying alternative approaches, including primary care delivery of treatments; adequate payment for pediatric providers who serve these young children; and improved education for pediatric providers about the principles of evidence-based interventions.
Emotional, relationship, and behavioral problems affect nearly as many preschoolers as older children, with prevalence rates of 7% to 10%. 1 , – 3 Emotional, behavioral, and relationship problems, including disorders of attachment, disruptive behavior disorders, attention-deficit/hyperactivity disorder (ADHD), anxiety and mood disorders, and disorders of self-regulation of sleep and feeding in children younger than 6 years, interfere with development across multiple domains, including social interactions, parent–child relationships, physical safety, ability to participate in child care, and school readiness. 4 , – 6 Importantly, if untreated, these problems can persist and have long-lasting effects, including measurable abnormalities in brain functioning and persistent emotional and behavioral problems. 7 , – 10 In short, early emotional, behavioral, and relationship problems in preschool-aged children interfere with their current well-being, jeopardize the foundations of emotional and behavioral health, and have the potential for long-term consequences. 11
Pediatricians and other child health care providers can reduce the risk of childhood emotional and behavioral problems by reducing exposure to toxic stress, promoting protective factors, and systematically screening for risk factors for emerging clinical problems. 12 , 13 Existing policy statements address universal approaches, early identification, and strategies for children at risk. The present policy statement focuses on clinical interventions for children with clinical disorders that warrant targeted treatment. Treatment planning is guided by a comprehensive assessment of the clinical presentation with attention to the child, the parent–child relationships, and community stressors. Beyond assessment, effective treatment of clinical disorders requires the following: (1) access to evidence-based treatments; and (2) primary care providers’ sufficient familiarity with evidence-based treatments to implement first-line approaches, make informed and effective referrals, and collaborate with specialty providers who have expertise in early childhood emotional and behavioral well-being. 14 Currently, most young children with an emotional, relationship, or behavioral problem receive no interventions for their disorder. This policy statement provides a summary of empirically supported approaches, describes readily identifiable barriers to accessing quality evidence-based interventions, and proposes recommendations to enhance the care of young children. This statement has been endorsed by Zero to Three and the American Academy of Child and Adolescent Psychiatry.
Awareness of the relative levels of evidence supporting pharmacologic and nonpharmacologic therapies for emotional, behavioral, and relationship problems can guide clinical decisions in the primary care setting. The evidence base related to psychopharmacologic agents in children younger than 6 years is limited and has only addressed ADHD. 15 Only 2 rigorous trials have examined the safety and efficacy of medications in this age group. Both the trial of methylphenidate and the study of atomoxetine for moderate to severe ADHD demonstrated that the trial medication was more effective than placebo but was less effective for younger children than for older children and produced higher rates of adverse effects in younger children. 16 , 17 Other medications have been less rigorously evaluated in preschool-aged children, although the rates of prescriptions for atypical antipsychotic agents, with their potential for substantial metabolic morbidity, have increased steadily in this age group. 18 , – 20
Nonpharmacologic treatments have more durable effects than medications, with documented effects lasting for years. 21 , – 23 A first step in reducing the barriers to evidence-based treatments is to ensure that primary care pediatricians are familiar with these approaches, which should be available to young children with emotional, behavioral, or relationship problems. 24
For infants and toddlers with clinical-level emotional, behavioral, or relationship concerns, dyadic interventions promote attachment security and child emotional regulation and can promote regulation of stress hormones. Examples of these interventions include infant–parent psychotherapy, video feedback to promote positive parenting, and attachment biobehavioral catch-up. These interventions often use real-time infant–parent interactions to support positive interactions, enhance parents’ capacity to reflect on their parenting patterns, and promote sensitivity and an understanding of the infant’s needs. 25
For preschool-aged children, parent management training models, including parent–child interaction therapy (PCIT), the Incredible Years series, the New Forest Program, Triple P (Positive Parenting Program), and Helping the Noncompliant Child, 26 are effective in decreasing symptoms of ADHD and disruptive behavior disorders. Parents are actively involved in all of these interventions, sometimes without the child and sometimes in parent–child interactions. All share similar behavioral principles, most consistently engaging parents as partners to: (1) reinforce positive behaviors; (2) ignore low-level provocative behaviors; and (3) provide clear, consistent, safe responses to unacceptable behaviors. Table 1 presents some of the characteristics of the best-supported programs for disruptive behavior disorders and ADHD. 25 , 27
Characteristics of the Best-Supported Programs for Disruptive Behavior Disorders and ADHD
Posttraumatic stress disorder can be treated effectively with cognitive behavioral therapy and child–parent psychotherapy in very young children. In cognitive behavioral therapy for posttraumatic stress disorder, preschool-aged children learn relaxation techniques and are gradually exposed to their frightening memories while using these techniques. Child–parent psychotherapy focuses on supporting parents to create a safe, consistent relationship with the child through helping them understand the child’s emotional experiences and needs. 33 Cognitive behavioral therapy is also effective for other common anxiety disorders, and recent promising studies report effectiveness of modified PCIT for selective mutism and depression. 34 , – 36 Adaptations for use in primary care, including Triple P, the Incredible Years series, and PCIT, similarly show positive outcomes, although further research is warranted. 37 , – 39
Ensuring that parents have access to appropriate support or clinical care is often an important component of clinical intervention for children. Effective parental treatment (eg, for depression) may reduce child symptoms substantially. 40
Despite the strong empirical support for these interventions, most young children with emotional, behavioral, and relationship problems do not receive nonpharmacologic treatments. 41 Physical separation, challenges coordinating across systems, stigma, parental beliefs, and provider beliefs about mental health services may interfere with identification of concerns and success of referrals. New models such as co-located care, in which mental health professionals work together with medical care providers in the same space, improve care coordination and referral success, decrease stigma, and reduce symptoms compared with traditional referrals. 42 , – 44 There are insufficient numbers of skilled providers to meet the emotional, behavioral, and relationship needs of children (and young children in particular) who require developmentally specialized interventions. 45 , 46 Therefore, when a primary care pediatrician identifies an emotional, relationship, or behavioral problem in a young child, it is often difficult to identify a professional (eg, social worker, psychologist, child and adolescent psychiatrist, developmental-behavioral pediatrician) with expertise in early childhood to accept the referral and provide evidence-based treatments.
Mental health coverage systems may also reduce access to care. 47 Although mental health parity regulations took effect in 2014, there are still “carved out” mental health programs that prohibit payment to primary care pediatricians for care of a child with an emotional, relationship, or behavioral health diagnosis and may limit access to trained specialists. 48 Even when a trained provider of an evidence-based treatment is identified, communication, coordination of care with primary care pediatricians, and adequate payment can be challenges. 14 , 49 Many health care systems do not pay for, or underpay for, necessary components of early childhood care such as care conferences, school observations, discussions with additional caregivers, same-day services, care coordination, and appointments that do not include face-to-face treatment of the child.
In the context of the focus of the American Academy of Pediatrics on early child and brain development, pediatricians have the opportunity to advocate for legislative and research approaches that will increase access to evidence-based treatments for very young children with emotional, behavioral, and relationship problems.
1a. At the legislative level, pediatricians should advocate for: (1) funding programs that increase dissemination and implementation of evidence-based treatments, especially in areas with limited resources; (2) addressing the early childhood mental health workforce shortage by providing incentives for training in these professions; (3) decreasing third-party payer barriers to accessing mental health services to very young children; and (4) promoting accountable care organization regulations that protect early childhood mental health services.
1b. In collaboration with other child-focused organizations, pediatricians should advocate for prioritization of research that will enhance the evidence base for treatment of very young children with emotional, behavioral, and relationship problems. Comparative effectiveness studies between psychopharmacologic and psychotherapeutic interventions and comparison of mental health service delivery approaches (eg, co-located models, community-based consultation, targeted referrals to specialists) are needed to guide management and policy decisions. In addition, studies that examine moderators of treatment effects, including family, social, and biological factors, are warranted. Studies of interventions adapted to treat young children with mild symptoms in the primary care setting could decrease barriers to care.
At the community and organizational levels, pediatricians should collaborate with local governmental and private agencies to identify local and national clinical services that can serve young children and explore opportunities for innovative service delivery models such as consultation or co-location.
Primary care pediatricians and developmental-behavioral pediatricians, together with early childhood mental health providers, including child and adolescent psychiatrists, and developmental specialists, can create educational materials for trainees and providers to enhance the care young children receive.
Without adequate payment for screening and assessment by primary care providers and management by specialty providers with expertise in early childhood mental health, treatment of very young children with emotional and behavioral problems will likely remain inaccessible for many children. Given existing knowledge regarding the importance of early childhood brain development on lifelong health, adequate payment for early childhood preventive services will benefit not only the patients but society as well and should be supported. Mental health carve-outs should be eliminated because they provide a significant barrier to access to mental health care for children. Additional steps toward equal access to mental health and physical health care include efficient prior authorization processes; adequate panels of early childhood mental health providers; payment to all providers, including primary care providers, for mental health diagnoses; sustainable payment for co-located mental health providers and care coordination; payment for evidence-based approaches focused on parents; and payment for the necessary collection of information from children’s many caregivers and for same-day services. Advocacy for true mental health parity must continue.
To ensure that all providers caring for children are knowledgeable participants and partners in the care of young children with emotional, behavioral, and relationship problems, graduate medical education and continuing medical education should include opportunities for training that ensure that pediatric providers: (1) are competent to identify young children with emotional, behavioral, and relationship problems as well as risk and protective factors; (2) are aware that common early childhood emotional, behavioral, and relationship problems can be treated with evidence-based treatments; (3) recognize the limitations in the data supporting use of medications in very young children, even for ADHD; (4) are prepared to identify and address parental factors that influence early child development; and (5) can collaborate and refer across disciplines and specialties, including developmental-behavioral pediatrics, child and adolescent psychiatry, psychology, and other mental health services.
attention-deficit/hyperactivity disorder
parent–child interaction therapy
This document is copyrighted and is property of the American Academy of Pediatrics and its Board of Directors. All authors have filed conflict of interest statements with the American Academy of Pediatrics. Any conflicts have been resolved through a process approved by the Board of Directors. The American Academy of Pediatrics has neither solicited nor accepted any commercial involvement in the development of the content of this publication.
The guidance in this statement does not indicate an exclusive course of treatment or serve as a standard of medical care. Variations, taking into account individual circumstances, may be appropriate.
All policy statements from the American Academy of Pediatrics automatically expire 5 years after publication unless reaffirmed, revised, or retired at or before that time.
Mary Margaret Gleason, MD, FAAP
Edward Goldson, MD, FAAP
Michael W. Yogman, MD, FAAP
Dina Lieser, MD, FAAP, Chairperson
Beth DelConte, MD, FAAP
Elaine Donoghue, MD, FAAP
Marian Earls, MD, FAAP
Danette Glassy, MD, FAAP
Terri McFadden, MD, FAAP
Alan Mendelsohn, MD, FAAP
Seth Scholer, MD, FAAP
Jennifer Takagishi, MD, FAAP
Douglas Vanderbilt, MD, FAAP
Patricia Gail Williams, MD, FAAP
Lynette M. Fraga, PhD – Child Care Aware
Abbey Alkon, RN, PNP, PhD, MPH – National Association of Pediatric Nurse Practitioners
Barbara U. Hamilton, MA – Maternal and Child Health Bureau
David Willis, MD, FAAP – Maternal and Child Health Bureau
Claire Lerner, LCSW – Zero to Three
Charlotte Zia, MPH, CHES
Michael Yogman, MD, FAAP, Chairperson
Nerissa Bauer, MD, MPH, FAAP
Thresia B. Gambon, MD, FAAP
Arthur Lavin, MD, FAAP
Keith M. Lemmon, MD, FAAP
Gerri Mattson, MD, FAAP
Jason Richard Rafferty, MD, MPH, EdM
Lawrence Sagin Wissow, MD, MPH, FAAP
Sharon Berry, PhD, LP – Society of Pediatric Psychology
Terry Carmichael, MSW – National Association of Social Workers
Edward Christophersen, PhD, FAAP – Society of Pediatric Psychology
Norah Johnson, PhD, RN, CPNP-BC – National Association of Pediatric Nurse Practitioners
Leonard Read Sulik, MD, FAAP – American Academy of Child and Adolescent Psychiatry
George J. Cohen, MD, FAAP
Stephanie Domain, MS, CHES
Nathan J. Blum, MD, FAAP, Chairperson
Michelle M. Macias, MD, FAAP, Immediate Past Chairperson
Nerissa S. Bauer, MD, MPH, FAAP
Carolyn Bridgemohan, MD, FAAP
Peter J. Smith, MD, MA, FAAP
Carol Cohen Weitzman, MD, FAAP
Stephen H. Contompasis, MD, FAAP, Web site Editor
Damon R. Korb, MD, FAAP, Discussion Board Moderator
Michael I. Reiff, MD, FAAP, Newsletter Editor
Robert G. Voigt, MD, FAAP, Program Chairperson
Beth Ellen Davis, MD, MPH, FAAP – Council on Children with Disabilities
Pamela C. High, MD, MS, FAAP – Society for Developmental and Behavioral Pediatrics
Linda Paul, MPH
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 26 February 2020
Parental and social factors in relation to child psychopathology, behavior, and cognitive function
- Han Zhang ORCID: orcid.org/0000-0002-9348-6104 1 ,
- Zu Xuan Lee 1 ,
- Tonya White 2 &
- Anqi Qiu ORCID: orcid.org/0000-0002-0215-6338 1
Translational Psychiatry volume 10 , Article number: 80 ( 2020 ) Cite this article
14k Accesses
25 Citations
11 Altmetric
Metrics details
- Human behaviour
- Predictive markers
Parental and social factors have long-term impact on the neurodevelopment of offspring, but tend to highly covary with each other. Thus, it is difficult to parse out which parental and social factor contributes most to neurodevelopmental outcomes. This study aimed to assess clusters of parental and social factors associated with child psychopathology, behavioral problems, and cognition. This study employed the data of 11,875 children (9 to 11 years) from the Adolescent Brain Cognitive Development (ABCD) study. Principal component analysis (PCA) was performed on 39 environmental measures and 30 child behavior and cognitive measures separately to identify clusters of parental and social factors and clusters of child psychopathology, behaviour, and cognition. Regression analysis was used to examine independent effects of each cluster of parental and social factors on child psychopathology, behavioral problems, and cognition. Greater Parent Psychopathology cluster was associated with greater Child Psychopathology cluster. Moreover, greater Socioeconomic Status cluster was associated with greater child General Cognition and Executive Function but less Behavioral Inhibition clusters. Greater Proximal Social Environment and Interaction cluster were associated with less child Impulsive Behavior and Behavioral Inhibition , but greater Behavioral Activation cluster. The environmental clusters related to birth outcomes, maternal tobacco, and drug use were not significantly related to child psychopathology, behavior, and cognition. Our findings suggest that socioeconomic status, parental psychopathology, and social environment and interactions are the strongest risks for behavioral problems and cognitive performance in a general child population. Intervention programs should target modifiable factors within these domains.
Similar content being viewed by others

Association between parental age, brain structure, and behavioral and cognitive problems in children

Pathways link environmental and genetic factors with structural brain networks and psychopathology in youth

Delineating and validating higher-order dimensions of psychopathology in the Adolescent Brain Cognitive Development (ABCD) study
Introduction.
Parental, socioeconomic, and social factors, such as parent psychopathology, pregnancy complications, household income, parental education, and family environment, can have long-term impact on the neurodevelopment of offspring 1 , 2 , 3 , 4 . However, most of existing studies typically assess parental, socioeconomic, and social factors, and their influences on child psychopathology, behavior, and cognition, separately. These environmental factors not only play an important role in neurodevelopment, but also tend to covary highly with each other, which makes it difficult to parse out which parental and social factor contributes most to neurodevelopmental outcomes, or whether the risk is additive 5 , 6 .
The Adolescent Brain Cognitive Development (ABCD) study (version 2.0) acquired comprehensive information on prenatal and postnatal parental, socioeconomic, and social environment as well as child outcomes in 11,875 children aged at 9 to 11 years 7 . It provided a unique opportunity to assess each aspect of parental, socioeconomic, and psychosocial factors in relation with child psychopathology, behavioral problems, and cognition when considering the interplay of different aspects of parental and social factors. For this, we employed principal component analysis to identify clusters within a wide spectrum of parental, socioeconomic, and social environmental factors and clusters within a wide spectrum of child psychopathology, behavioral problems, and cognition. Such an approach provides a comprehensive map for understanding the contribution of individual aspects of parental, socioeconomic and social factors to child psychopathology, behavioral problems, and cognition, which potentially provides the guidance of future intervention on improving child neurodevelopment in a general population.
Participants
Participant data were obtained from the open baseline from the ongoing Adolescent Brain Cognitive Development (ABCD) study (release 2.0; https://abcdstudy.org/ ). Youth ( n = 11,875) 9–11 years of age were recruited for this study and formed a similar proportion of males and females living in the United States. The sample selection criteria were targeted to reflect the sociodemographic proportion of the U.S. population as described in the ABCD study design 7 . All participants were administered assessments to obtain data on the respective youth’s brain morphology, cognitive function, substance use, demographics, and environment 8 . Written informed consent was obtained from all parents, and all children provided assent to a research protocol approved by the institutional review board at each data collection site ( https://abcdstudy.org/study-sites/ ) 9 .
Of the 11,875 participants, we excluded 23 subjects with missing values of demographics, 3219 subjects with one or more missing values of the parental and social environmental measures, 914 subjects with one or more missing values of the questionnaires/tasks of the child psychopathology, behavior, and cognitive measures, and 283 subjects with missing values in either of these two data. Therefore, our study employed 11,875 participants and 8002 participants (67.4% of full sample) for statistical analysis, separately. Supplementary Table S1 in the Supplementary Material lists the subject id whose data were not included in this study.
Parental and social environmental measures
This study included 39 parental, socioeconomic, and social environmental measures, including10 measures of parent psychopathology, 6 maternal substance use measures, 5 developmental adversity measures, 7 social demographics, 5 proximal environmental measures, and 6 social interaction measures 8 , 10 .
Parent psychopathology
Parent psychopathology symptoms were assessed using the Adult Self Report (ASR) and Family History Assessment Module Screener (FHAM-S) questionnaires. The ASRprovides 8 empirically-based syndrome scales (anxious/depressed, withdrawn, somatic complaints, thought problems, attention problems, aggressive behaviour, rule-breaking behavior, and intrusive) 11 . FHAM-S reports the presence/absence of symptoms associated with alcohol and drug use, depression, and mania in all 1st and 2nd degree “blood relatives” of the youth 12 . The presence of alcohol and drug use problems of the child’s relatives was defined as the family psychopathology risk of substance use disorders. Similarly, the accumulated presence of depression and mania was scored as the family psychopathology risk of mental disorders.
Maternal substance use
The parent-reported Developmental History Questionnaire was used to assess maternal consumption of tobacco, alcohol, and marijuana before and after the mothers knew that they were pregnancy 13 , 14 , 15 .
Developmental adversity
The developmental History Questionnaire 8 was used to assess prematurity, birth weight, pregnancy and birth complications and the Modified Ohio State University Traumatic Brain Injury Screen-Short Version 16 was employed to assess the parent-report overall brain injury/concussion during the child’s development.
Social demographics
The parent-report demographics battery from the PhenX toolkit measured social demographics of the parental highest education, household annual income, and marriage status 17 . Economic insecurity 18 , the grand total Uniform Crime Reports, Area Deprivation Index by the scaled weighted sum, and the estimated lead risk in census tract of primary residential address 19 , 20 were also employed to provide additional information about socioeconomic influences.
Proximal environment
The “Safety from Crime” items from the PhenX Toolkit was used to assess neighborhood safety and crime reports 21 , 22 . Additionally, children reported their school risk and protective factors via a 12-item Inventory for School Risk and Protective Factors of the PhenX toolkit 23 . Three measures was selected to assess a child’s connectedness to his/her school, including school teacher and classroom environment, personal involvement in school, and alienation from academic goals.
Social interaction
The child-reported parental monitoring and acceptance, as well as the child- and parent-reported prosocial tendency and family conflicts were included to measure social interactions. Parent monitoring was accessed by a 5-item summary score of the Parental Monitoring Scale 24 . Parent acceptance was evaluated by the Acceptance Scale, a subscale of the Child Report of Behavior Inventory (CRPBI) 25 . Prosocial behavior (e.g., being nice, helping, caring) was assessed using the Prosocial Behavior Scale, a subscale from the “Strengths and Difficulties Questionnaire” (SDQ) 26 . Both parents and youth reported on the youth’s prosocial behavior (e.g., being considerate of other people’s feelings, often offering to help others). In order to assess the family conflicts, the ABCD protocol utilized a 9-item Family Conflict subscale of the Moos Family Environment Scale (FES) for the baseline protocol 27 .
For the parental and environmental measures related to psychopathology, maternal substance use, and developmental adversity, higher scores represents more severe psychiatric symptoms, worse substance use, and developmental adversity. For the measures of social demographics, proximal environment, and social interactions, higher scores represent better socioeconomic status, proximal environment, and social interactions. For the ease of interpretation, a few scores were inverted to align the direction in their same category as mentioned above. Figure 1 marks these inverted measures in parenthesis.
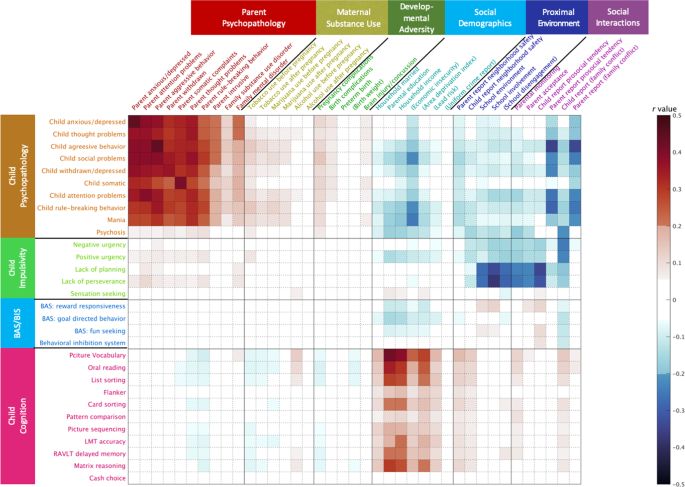
The value in the color bar corresponds to Pearson correlation coefficient. Significant correlations are shown in non-white color at Bonferroni corrected p < 0.001. The scores of the variables in (•) were inversed in order to align their direction with the variables in each domain.
Child psychopathology, behavior, and cognition
This study employed 30 child psychopathology, behavior, and cognitive measures, including 10 child psychopathology measures, 9 behavior measures, and 11 cognitive measures 8 , 28 . To provide converging evidence about the youth’s behavior, we also utilized the available data ( n = 2440) with the teach-reported total behavior problems which were evaluated by the Brief Problem Monitor-Teacher Form 11 .
Child psychopathology
Child Psychopathology was assessed based on the parent report of Child Behavior Checklist (CBCL) 11 , the ten-item Mania Scale derived from the Parent General Behavior Inventory for Children and Adolescents 29 , and the Prodromal Questionnaire Brief Version 30 . This study included 8 empirically-based syndrome scales from CBCL (aggressive behavior, anxious/depressed, attention problems, rule-breaking behavior, somatic complaints, social problems, thought problems, and withdrawn/depressed scales), a risk score of bipolar variability in mood and behaviour, and a severity score of psychosis risk symptoms.
Child behavior
The 20-item Children-Short Form (UPPS-P) was used to assess five facets of impulsivity 31 , including negative and positive urgency, lack of planning, lack of perseverance, and sensation seeking. The 24-item Behavioral Inhibition/Activation Scales (BIS/BAS) were also utilized: BIS (e.g., worry, fearfulness), BAS drive (intensity of goal directed behavior), BAS reward responsiveness (excitement over reinforcing outcomes), and BAS fun seeking (enjoyment for its own sake, spontaneity) 32 .
Child cognition
The neurocognitive battery comprised of 11 tasks 28 and was administered using an iPad with one-on-one monitoring by a research assistant. Among the 11 cognitive tasks, there were 7 from the NIH Toolbox ( http://www.nihtoolbox . org), including flanker (inhibitory control), dimensional change card sort (cognitive flexibility), list sorting working memory (working memory), picture sequence memory (episodic memory), pattern comparison processing speed (processing speed), picture vocabulary (vocabulary comprehension), and oral reading recognition tasks (reading decoding). ABCD also administered Matrix Reasoning Task from the Wechsler Intelligence Test for Children-V (fluid Reasoning) 33 , Little Man Task (LMT, visual-spatial processing), Rey Auditory Verbal Learning Test (RAVLT, auditory learning, memory, and recognition), and Cash Choice Task (a single-item delayed gratification measure with dichotomous scoring). Notably, we employed the response accuracy of LMT, the delayed recall accuracy of RAVLT, and the total scaled score of Matrix Reasoning.
For measures related to child psychopathology and behavior, a higher score represented worse psychopathology and behavioral problems. For measures of child cognition, a higher score represented better cognitive ability.
Statistical analysis
Each score of 39 environmental measures and 30 child characteristics was first standardized with zero mean and unit variance using rank-based inverse Gaussian transformation 33 , 34 . Pearson’s correlation coefficients were used to explore the associations of individual parental and social environment variables with individual child measures. Bonferroni correction was used to determine the significance of multiple correlations (the number of tests: 1170) at p < 0.001.
For multivariate analysis, principal component analyses (PCA) was first performed within all environmental measures and within the child characteristics, respectively 33 . Varimax rotation was applied to factor loadings of the PCs with eigenvalues greater than 1. The component scores were further computed based on the varimax rotated loadings beyond 0.35. This procedure ensured statistical independence of the PCs within the environmental measures and within the child characteristics.
Mixed effect models were used to examine associations of all environmental PCs with each child characteristic PCs. Age, sex and ethnicity were covariates. The information of twins, non-twin siblings, and 21 different research sites was entered as random effects. Bonferroni correction was used to determine the significance of statistical tests ( n = 48) at p < 0.001.
This study included 8022 out of 11,875 children (mean[SD] age, 9.9 [0.6] years; 47.8% girls; 57.0% white ethnicity) with the complete environmental and child characteristic data. Table 1 lists the 39 environmental measures and 30 child characteristics of subjects with the complete data ( n = 8002) and all 11,875 subjects. The sample with the complete data ( n = 8022) did not differ from the whole sample ( n = 11,875) in most of measures. However, some environmental measures (i.e., household married percentage, parental education, lead risk, and parent report neighborhood safety) and cognitive measures (i.e., picture vocabulary, oral reading, list sorting, card sorting, picture sequencing, RAVLT delayed memory and matrix reasoning) were better in the sample with the complete data than the whole sample (see p -values in Table 1 ). The severity of child psychopathology (i.e., child aggressive behavior, child attention problems, and child rule-breaking behavior from CBCL, and the mania score). was slightly lower in the sample with the complete data than in the whole sample data (see p -values in Table 1 ).
Figure 1 illustrates significant correlations between 39 parental and social environment measures and 30 child outcomes (Bonferroni corrected p < 0.001). This suggested strong correlations between parental and child psychopathology, between socioeconomic status and cognition, between social interactions and child psychopathology, and between proximal social environment and interactions and child impulsive behaviors.
Figure 2 shows 8 PCs for environmental factors (48.7% variance explained) and 6 PCs for child characteristics (51.6% variance explained). The 8 PC environmental factors included (1) Parent Psychopathology (14.3% variance explained), Socioeconomic Status (7.5% variance explained), (3) Proximal social environment and interaction (7.3% variance explained), Birth Outcomes (5.1% variance explained), (5) Maternal Tobacco Use (4.7% variance explained), (6) Neighbourhood Safety (3.5% variance explained), (7) Family Psychopathology (3.3% variance explained), and (8) Maternal Marijuana Use (3.0% variance explained). The 6 PC child characteristic components included (1) Child Psychopathology (17.9% variance explained), General Cognition (11.6% variance explained), (3) Behavioral Activation (8.3% variance explained), Impulsive Behavioral Problems (5.6% variance explained), (5) Executive Function (4.3% variance explained), and (6) Behavioral Inhibition (3.9% variance explained).
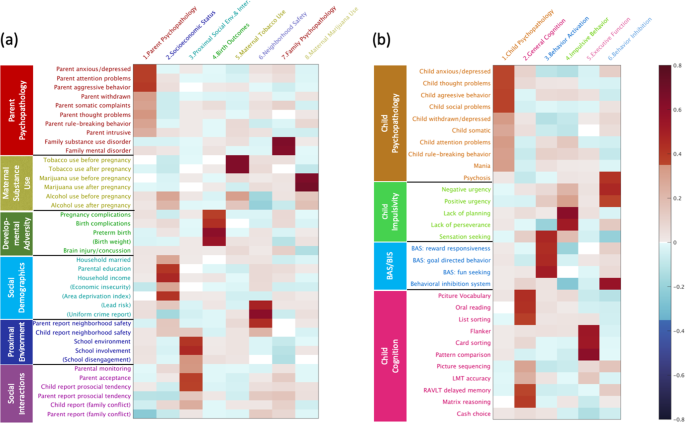
a Parental, socioeconomic, and social environmental factors have 8 components retained. b Child characteristics have 6 components retained. BAS, behavioral activation system; BIS, behavioral inhibition system.
After controlling for age, gender, ethnicity, and the other environmental PC factors, greater Parent Psychopathology (standardized β = 0.56, [0.54, 0.58], p < 0.001) was associated with greater Child Psychopathology (Fig. 3a ). Using available reports on the Teacher Report Form on child behaviors ( n = 2440), the associations between Parent Psychopathology and teacher-reported child behavioral problems remained significant (standardized β = 0.06, [0.02, 0.11], p = 0.002). Moreover, greater Socioeconomic Status was associated with greater child General Cognition (standardized β = 0.37, [0.34, 0.39], p < 0.001) and Executive Function (standardized β = 0.11, [0.08, 0.14], p < 0.001, Fig. 3b ) but with less Behavioral Inhibition (standardized β = −0.13, [−0.16, −0.10], p < 0.001; Fig. 3a ). Greater Proximal Social Environment and Interaction were associated with less child Impulsive Behavioral Problems (standardized β = −0.50, [−0.52, −0.48], p < 0.001) and Behavioral Inhibition (standardized β = −0.21, [−0.24, −0.19], p < 0.001), but greater Behavioral Activation (standardized β = 0.09, [0.07, 0.12], p < 0.001; Fig. 3a ). The environmental PCs related to birth outcomes, maternal alcohol, tobacco, and drug use were not significantly related to child psychopathology, behavior, and cognition (Tables 2 , 3 ).
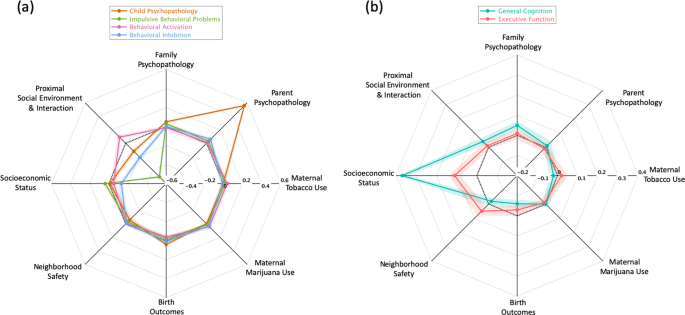
a The standardized regression coefficients of eight parental, socioeconomic, and social environmental components on each child psychopathology and the behavioral components. b The standardized regression coefficients of eight parental, socioeconomic, and social environmental components on child general cognition and executive function. In each panel, the colorful rings represent the child characteristic components, and the verteces represent the eight parental, socioeconomic, and social environmental components. From the center to the periphery, the regression coefficients are from negative to positive, and zero is highlighted by the black dash ring. The shade around each colorful ring shows the 95% confidence interval of the corresponding regression coefficient.
Our repeated analyses using the full study sample ( n = 11,875) and mean imputation for missingness showed the similar findings as stated above (in Supplementary Figs. S1 and S2 of the Supplementary Material ).
This study showed the distinctive influences of the parental, socioeconomic, and social environmental factors on child psychopathology, behavioral problems, and cognition. As expected, strong relationships were found between Parent Psychopathology and Child Psychopathology , between Socioeconomic Status and child Cognition , and between Proximal Social Environment and Interaction and child Impulsive behaviors . What was unexpected, however, was our lack of identifying relationships between birth outcomes, maternal tobacco and drug use with child psychopathology, behavioral problems, and cognition.
Consistent with previous findings 35 , 36 , we found strong association between the psychopathology in parents and their children. Child psychopathology was assessed by parents and thus there is a tendency that parents with greater psychopathology will also rate their child as having greater psychopathology. When we utilized teacher reported behavioral problems of the child and parent self-report, the association remained significant, albeit less strong. Our findings provide further support for a potential genetic contribution for the transgenerational transmission of psychopathology from parents to behavioral characteristics of children.
This study also identified the associations of Socioeconomic Status with child General Cognition and Executive Function . This is congruent with previous findings, suggesting that lower Socioeconomic Status strongly predicts lower IQ and executive functions 3 , 37 . Most of previous studies employ household income and/or parental education or both as the representation of Socioeconomic Status 20 . In contrast, we quantified Socioeconomic Status using a broad construct that incorporated variation not only from household income and parental education, but also from a regional deprivation index. From this aspect, our study provided evidence supporting the idea of a reduction of poverty and increasing education at the level of both family and neighbourhood may help improve child cognitive development.
Unlike previous studies 38 , 39 , our findings did not support strong associations of birth outcomes, maternal tobacco, and drug use with child psychopathology, behavior, and cognition in this general child population. Nevertheless, when analyzing the association between maternal marijuana use and psychosis, we showed the similar result ( p = 0.014 in Table 2 ) as that presented in 15 . The lack of such associations among the PC scores is partly because our findings were obtained after controlling for Parental Psychopathology , Socioeconomic Status , and etc, suggesting that Parental Psychopathology and Socioeconomic Status had a greater effect on child neurodevelopmental outcomes. Most of existing studies generally focus only on a case-control or imbalanced designs and do not assess the comprehensive profile of parental, socioeconomic, and social factors and hence may not quantify true effects of maternal tobacco and drug use as well as birth outcomes on child neurodevelopment in a general population 40 .
One of the strengths of our study is that we employed a large population-based sample of children who are all participating in the ABCD baseline wave of data collection. Thus, we were able to incorporate a comprehensive assessment of parental, socioeconomic, and social environmental factors as well as child characteristics. Nevertheless, the reliance on cross-sectional data precludes any determination of causality. Moreover, the ABCD study sampled from the United States, which may limit the generalizability of our findings. Further research is necessary to explore across other ethnicities and cultures to enhance the potential generalization of our findings.
Our findings suggest that parental psychopathology, socioeconomic status, and social environment and interactions are the strongest risks for behavioral problems and cognitive performance in a general child population. These children should be targeted for intervention programs, with the possibility for including both primary and secondary prevention.
Wang, Q. et al. Sex-dependent associations among maternal depressive dymptoms, child reward network, and behaviors in early childhood. Cereb. Cortex https://doi.org/10.1093/cercor/bhz135 (2019).
Clark, C. A., Woodward, L. J., Horwood, L. J. & Moor, S. Development of emotional and behavioral regulation in children born extremely preterm and very preterm: biological and social influences. Child Dev. 79 , 1444–1462 (2008).
Article Google Scholar
Noble, K. G. et al. Family income, parental education and brain structure in children and adolescents. Nat. Neurosci. 18 , 773–778 (2015).
Article CAS Google Scholar
Almas, A. N. et al. The impact of caregiving disruptions of previously institutionalized children on multiple outcomes in late childhood. Child Dev. 91 , 96–109 (2020).
Potijk, M. R., Kerstjens, J. M., Bos, A. F., Reijneveld, S. A. & de Winter, A. F. Developmental delay in moderately preterm-born children with low socioeconomic status: risks multiply. J. Pediatr. 163 , 1289–1295 (2013).
Harnish, J. D., Dodge, K. A. & Valente, E. Mother-child interaction quality as a partial mediator of the roles of maternal depressive symptomatology and socioeconomic status in the development of child behavior problems. Conduct problems prevention research group. Child Dev. 66 , 739–753 (1995).
CAS PubMed Google Scholar
Garavan, H. et al. Recruiting the ABCD sample: design considerations and procedures. Dev. Cogn. Neurosci. 32 , 16–22 (2018).
Barch, D. M. et al. Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Dev. Cogn. Neurosci. 32 , 55–66 (2018).
Clark, D. B. et al. Biomedical ethics and clinical oversight in multisite observational neuroimaging studies with children and adolescents: The ABCD experience. Dev. Cogn. Neurosci. 32 , 143–154 (2018).
Zucker, R. A. et al. Assessment of culture and environment in the Adolescent Brain and Cognitive Development Study: Rationale, description of measures, and early data. Dev. Cogn. Neurosci. 32 , 107–120 (2018).
Achenbach, T. Achenbach System of Empirically Based Assessment (ASEBA): Development, Findings, Theory, and Applications. Encyclopedia of Autism Spectrum Disorders .
Rice, J. P. et al. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol. Clin. Exp. Res. 19 , 1018–1023 (1995).
Kessler, R. C. et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A). Int. J. Methods Psychiatr. Res. 18 , 69–83 (2009).
Kessler, R. C. et al. National comorbidity survey replication adolescent supplement (NCS-A): II. Overview and design. J. Am. Acad. Child Adolesc. Psychiatry 48 , 380–385 (2009).
Fine, J. D. et al. Association of prenatal cannabis exposure with psychosis proneness among children in the Adolescent Brain Cognitive Development (ABCD) Study. JAMA Psychiatry 4–6 https://doi.org/10.1001/jamapsychiatry.2019.0076 (2019).
Bogner, J. A. et al. Test-retest reliability of traumatic brain injury outcome measures. J. Head. Trauma Rehabil. 32 , E1–E16 (2017).
Hamilton, C. M. et al. The PhenX Toolkit: get the most from your measures. Am. J. Epidemiol. 174 , 253–260 (2011).
Diemer, M. A., Mistry, R. S., Wadsworth, M. E., López, I. & Reimers, F. Best practices in conceptualizing and measuring social class in psychological research Anal. Soc. Issues Public Policy 13 , 77–113 (2013).
Kind, A. J. H. et al. Neighborhood socioeconomic disadvantage and 30-day rehospitalization. Ann. Intern. Med. 161 , 765 (2014).
Farah, M. J. The neuroscience of socioeconomic status: correlates, causes, and consequences. Neuron 96 , 56–71 (2017).
Echeverria, S. E. Reliability of self-reported neighborhood characteristics. J. Urban Heal. Bull. N. Y. Acad. Med. 81 , 682–701 (2004).
Google Scholar
Mujahid, M. S., Diez Roux, A. V., Morenoff, J. D. & Raghunathan, T. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am. J. Epidemiol. 165 , 858–867 (2007).
Stover, P. J., Harlan, W. R., Hammond, J. A., Hendershot, T. & Hamilton, C. M. PhenX: A toolkit for interdisciplinary genetics research. Curr. Opin. Lipidol. 21 , 136–140 (2010).
Chilcoat, H. D. & Anthony, J. C. Impact of parent monitoring on initiation of drug use through late childhood. J. Am. Acad. Child Adolesc. Psychiatry 35 , 91–100 (1996).
Schaefer, E. S. A configurational analysis of children’s reports of parent behavior. J. Consult. Psychol. 29 , 552–557 (1965).
Goodman, R., Meltzer, H. & Bailey, V. The strengths and difficulties questionnaire: a pilot study on the validity of the self-report version. Int. Rev. Psychiatry 15 , 173–177 (2003).
Moos, R. H. & Moos, B. S. Family Environment Scale manual . (Consulting Psychologists Press, Palo Alto, CA, 1986).
Luciana, M. et al. Adolescent neurocognitive development and impacts of substance use: Overview of the adolescent brain cognitive development (ABCD) baseline neurocognition battery. Dev. Cogn. Neurosci. 32 , 67–79 (2018).
Youngstrom, E. A., Frazier, T. W., Demeter, C., Calabrese, J. R. & Findling, R. L. Developing a 10-Item mania scale from the parent general behavior inventory for children and adolescents. J. Clin. Psychiatry 69 , 831–839 (2008).
Loewy, R. L., Therman, S., Manninen, M., Huttunen, M. O. & Cannon, T. D. Prodromal psychosis screening in adolescent psychiatry clinics. Early Interv. Psychiatry 6 , 69–75 (2012).
Zapolski, T. C. B., Stairs, A. M., Settles, R. F., Combs, J. L. & Smith, G. T. The measurement of dispositions to rash action in children. Assessment 17 , 116–125 (2010).
Carver, C. S. & White, T. L. Behavioral inhibition, behavioral activation, and affective responses to impending reward and punishment: The BIS/BAS Scales. J. Pers. Soc. Psychol. 67 , 319–333 (1994).
Thompson, W. K. et al. The structure of cognition in 9 and 10 year-old children and associations with problem behaviors: Findings from the ABCD study’s baseline neurocognitive battery. Dev. Cogn. Neurosci. 36 , 100606 (2019).
Miller, K. L. et al. Multimodal population brain imaging in the UK Biobank prospective epidemiological study. Nat. Neurosci. 19 , 1523–1536 (2016).
Befera, Mschulte & Barkley, R. A. Hyperactive and normal girls and boys: mother-child interaction, parent psychiatric status and child psychopathology. J. Child Psychol. Psychiatry 26 , 439–452 (1985).
Gunlicks, M. L. & Weissman, M. M. Change in child psychopathology with improvement in parental depression: a systematic review. J. Am. Acad. Child Adolesc. Psychiatry 47 , 379–389 (2008).
Turkheimer, E., Haley, A., Waldron, M., D’Onofrio, B. & Gottesman, I. I. Socioeconomic status modifies heritability of IQ in young children. Psychol. Sci. 14 , 623–628 (2003).
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M. & Anand, K. J. S. Cognitive and behavioral outcomes of school-aged children who were born preterm. JAMA 288 , 728 (2002).
Huizink, A. C. & Mulder, E. J. H. Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neurosci. Biobehav. Rev. 30 , 24–41 (2006).
Huizink, A. C. Prenatal cannabis exposure and infant outcomes: overview of studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 52 , 45–52 (2014).
Download references
Acknowledgements
This research is supported by the Singapore Ministry of Education (Academic research fund tier 1; NUHSRO/2017/052/T1-SRP-Partnership/01), and NUS Institute of Data Science, Singapore. Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study ( https://abcdstudy.org ), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under awards U01DA041022, U01DA041025, U01DA041028, U01DA041048, U01DA041089, U01DA041093, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners/ . A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/study-sites/ . ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from https://doi.org/10.15154/1517592 .
Author information
Authors and affiliations.
Department of Biomedical Engineering, National University of Singapore, Singapore, Singapore
Han Zhang, Zu Xuan Lee & Anqi Qiu
Department of Child and Adolescent Psychiatry, Erasmus University Medical Center - Sophia, Children’s Hospital, Rotterdam, The Netherlands
Tonya White
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Anqi Qiu .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.

Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary material, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhang, H., Lee, Z.X., White, T. et al. Parental and social factors in relation to child psychopathology, behavior, and cognitive function. Transl Psychiatry 10 , 80 (2020). https://doi.org/10.1038/s41398-020-0761-6
Download citation
Received : 22 October 2019
Accepted : 07 February 2020
Published : 26 February 2020
DOI : https://doi.org/10.1038/s41398-020-0761-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Brain volumes, behavioral inhibition, and anxiety disorders in children: results from the adolescent brain cognitive development study.
- Rawan A. Hammoud
- Lara Abou Ammar
- Martine Elbejjani
BMC Psychiatry (2024)
Parental Deprivation- and Threat-Based Factors Associated with Youth Emotion-Based Neurocircuitry and Externalizing Behavior: A Systematic Review
- Kathleen Feeney
- Rosario Pintos Lobo
- Erica D. Musser
Research on Child and Adolescent Psychopathology (2024)
Sleep duration in preschool age and later behavioral and cognitive outcomes: an individual participant data meta-analysis in five European cohorts
- Kathrin Guerlich
- Demetris Avraam
- Sabine Plancoulaine
European Child & Adolescent Psychiatry (2024)
Early life stress, prenatal secondhand smoke exposure, and the development of internalizing symptoms across childhood
- Mariah DeSerisy
- Jacob W. Cohen
- Amy E. Margolis
Environmental Health (2023)
- Chaoqiang Liu
Neuropsychopharmacology (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
- We're Hiring!
- Help Center
Child Behavior
- Most Cited Papers
- Most Downloaded Papers
- Newest Papers
- Save to Library
- Last »
- Intensive In-Home Therapy Follow Following
- Family Functioning Follow Following
- Psychological aspects of diabetes Follow Following
- Conducta Prosocial Follow Following
- Child Behavior Problems Follow Following
- Offender Follow Following
- Sexual Abuse, Risk Assessment, Child Pornography Follow Following
- Self Disclosure Follow Following
- Child Sexual Abuse Disclosure Follow Following
- Communication of Feedback in the Teaching Practice Follow Following
Enter the email address you signed up with and we'll email you a reset link.
- Academia.edu Publishing
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
Understanding how behavior problems are related to child abuse and neglect

Do abuse and neglect cause behavior problems among children or do behavior problems among children cause abuse and neglect? A new study from researchers in the Penn State College of Health and Human Development confirmed that the former happens much more often than the latter.
Anneke Olson , graduate student in human development and family studies , and her adviser, Chad Shenk , professor of human development and family studies and of pediatrics and Social Science Research Institute cofunded faculty member, led research demonstrating abuse and neglect during childhood lead to both problematic internalizing behaviors — including depression and worry — and externalizing behaviors — including delinquency and noncompliance with parents. The study was published today (May 14) in Pediatrics .
“The central question of this research was: does child maltreatment lead to behavior problems or vice versa?” Shenk said. “Short term or cross-sectional studies can’t capture this information, so we combined a unique dataset with a novel statistical approach to show that children who were maltreated were more likely to display subsequent behavior problems at multiple ages throughout childhood and adolescence.”
The researchers used data from the Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) , which were collected every two years from when children were four until they turned 18. Using seven waves of data from 1,354 children and their caregivers between the ages of four and 16, the researchers identified whether the children had a documented experience of maltreatment. Then, they simultaneously examined the relationship between maltreatment exposure and externalizing and internalizing behaviors.
The researchers employed a random-intercept, cross-lagged panel model, which they said helped them understand how exposure to maltreatment, or changes in internalizing and externalizing behaviors, influence one another over time. At the majority of timepoints throughout childhood and adolescence, children who had experienced maltreatment displayed an otherwise unexplained increase in behavior problems during the next wave of data collection.
When looking at the data in the other direction — examining whether children who displayed behavior problems were more likely to be maltreated within the next two years — they found that children were generally not more likely to be maltreated if they displayed increases in problem behaviors. The one exception to this trend was that children who displayed increases in externalizing behaviors at age 10, like noncompliance or delinquency, were more likely to experience maltreatment two years later.
Olson said this could be a significant finding for understanding how abuse and behavior problems are related.
“The ages of 10 to 12 are when children start to transition to adolescence,” Olson said. “As this happens, peers become more important to them, and individuals begin to think more for themselves, which can result in more externalizing behaviors. This is the only period during the study when an increase in externalizing behavior problems led to increased maltreatment. At the same time, exposure to maltreatment during this period also led to an increase in behavior problems.”
The researchers said that modeling this two-way relationship between behavior problems and maltreatment simultaneously may represent a unique opportunity for enhanced screening and the type and timing of interventions.
“Screening for maltreatment exposure and behavior problems in pediatrician offices is an important take away from this study," Shenk said. "Screening during the ages of 10 to 12 is especially important given maltreatment and externalizing behaviors were related to one another at this point in development. There are brief, scientifically valid screenings that pediatricians can use for maltreatment and behavior problems. Additionally, when pediatricians identify children who have experienced maltreatment or demonstrated increased behavior problems, there are interventions that can work to decrease both.”
The researchers pointed to parent-child interaction therapy — which was developed to address externalizing behaviors in a family context — as an excellent potential tool for reducing problem behaviors prior to age 10. They said the therapy teaches children to manage their behavior and often results in significant reductions in behavior problems. It has also been shown to prevent future abuse because caregivers learn new behaviors and strategies for promoting family relationships and addressing externalizing behaviors without resorting to violent words or actions.
Shenk, who has a joint appointment in the Penn State College of Medicine Department of Pediatrics, expressed excitement about the potential of this research to guide better evaluation and intervention by pediatricians.
Olson said she was surprised at how robust and clear the results were.
“Everyone in Dr. Shenk’s lab wants to ask questions that will move the needle on our understanding of child maltreatment,” Olson explained. “On this study, we found that child maltreatment robustly predicts subsequent behavior problems at multiple ages, but we also learned that there is little evidence that behavior problems increase the risk for subsequent maltreatment.”
John Felt of the Penn State Center for Healthy Aging, Emily Dunning of the Penn State Department of Human Development and Family Studies, Zhenyu Zhang of the Penn State Department of Psychology, Metzli A. Lombera of the Penn State Department of Psychology, Camille Moeckel of the Penn State College of Medicine, Manal U. Mustafa of the Penn State College of Medicine's Department of Pediatrics, Brian Allen of the Penn State College of Medicine's Department of Pediatrics and Department of Psychiatry and Behavioral Health, and Lori Frasier of the Penn State College of Medicine Department of Pediatrics also contributed to this research.
The National Institutes of Health and the U.S. National Science Foundation funded this research.
Related News
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Environ Res Public Health

The Use of Social Media in Children and Adolescents: Scoping Review on the Potential Risks
Elena bozzola.
1 Pediatric Unit, IRCCS Bambino Gesù Children Hospital, 00100 Rome, Italy
2 The Italian Pediatric Society, 00100 Rome, Italy
Giulia Spina
Rino agostiniani.
3 Department of Pediatrics, San Jacopo Hospital, 51100 Pistoia, Italy
Sarah Barni
Rocco russo, elena scarpato.
4 Department of Translational Medical Sciences-Section of Pediatric, University Federico II, 80100 Naples, Italy
Antonio Di Mauro
Antonella vita di stefano, cinthia caruso, giovanni corsello.
5 Department of Health Promotion, Mother and Child Care, Internal Medicine and Medical Specialties “G. D’Alessandro”, University of Palermo, 90100 Palermo, Italy
Annamaria Staiano
Associated data.
Data available at Dr Bozzola’s study.
In recent years, social media has become part of our lives, even among children. From the beginning of COVID-19 pandemic period, media device and Internet access rapidly increased. Adolescents connected Internet alone, consulting social media, mostly Instagram, TikTok, and YouTube. During “lockdown”, the Internet usage allowed communication with peers and the continuity activities such as school teaching. However, we have to keep in mind that media usage may be related to some adverse consequences especially in the most vulnerable people, such as the young. Aim of the review is to focus on risks correlated to social media use by children and adolescents, identifying spies of rising problems and engaging in preventive recommendations. The scoping review was performed according to PRISMA guidelines, searching on PubMed the terms “social media” or “social network”, “health”, and “pediatrics”. Excluding articles not pertinent, we found 68 reports. Out of them, 19 were dealing with depression, 15 with diet, and 15 with psychological problems, which appeared to be the most reported risk of social media use. Other identified associated problems were sleep, addiction, anxiety, sex related issues, behavioral problems, body image, physical activity, online grooming, sight, headache, and dental caries. Public and medical awareness must rise over this topic and new prevention measures must be found, starting with health practitioners, caregivers, and websites/application developers. Pediatricians should be aware of the risks associated to a problematic social media use for the young’s health and identify sentinel signs in children as well as prevent negative outcomes in accordance with the family.
1. Introduction
Media device use is increasing year by year in Italy as well as in many other countries. An ISTAT report referred that in 2019, 85.8% of Italian adolescents aged 11–17 years regularly used smartphones, and over 72% accessed Internet via smartphones [ 1 ]. Almost 95% of Italian families with a child had a broadband internet connection [ 2 ]. Internet connection was mostly used to communicate with friends and to use social networks [ 1 ]. In 2020, COVID-19 pandemic represented one of the greatest disruptions for everybody’s everyday life, in Italy as well as all around the world. From the beginning of the pandemic period, media device and Internet access rapidly increased. In line, a 2021 CENSIS report revealed an even progressive increment of smartphone use by adolescents, which reached 95% [ 3 ]. In particular, the majority of adolescents (59%) admitted they use smartphone even more frequently than in the past with a daily use of more than 3 h in 46% of cases. Adolescents connected Internet alone (59%), consulting social media, mostly Instagram (72%), TikTok (62%), and YouTube (58%) [ 4 ]. In this context, social interaction over the Internet or simply social network consulting may play an important part in the lives of many young people, influencing them and their relationship with self-esteem and well-being [ 5 ]. Not being guided and monitored in Internet fruition, the young may be exposed to several risks, including cyberbullying which affects 7% of children aged 11–13 years and 5.2% of 14–17 years old adolescents or stalking which affects more than 600 minors in Italy. On social media, the young are more vulnerable and may display risk behavior, including pertaining substance abuse, sexual behaviors, or violence [ 6 ].
On the other hand, media and social networks are, actually, present in almost any house and are considered a great resource for anybody, including children and adolescents. Especially during “lockdown”, the Internet usage allowed communication with peers and the continuity activities such as school teaching. Social media services enable various form of communication verbally or visually by internet-based networking, bringing people together, facilitating instant connection and interaction, such as a like or a comment on something [ 7 ]. There was also a “school” use of smartphones and social media during lockdown which represented a tool of information and education [ 8 ].
In line, websites and applications that enable users to create and share content or to participate in social networking may be currently use as a definition of a social media. Facebook launched in 2004 and Twitter in 2006 were the first social media introduced, rapidly followed by many others [ 9 ]. Actually, Facebook with 2.9 billion monthly active users, YouTube with 2 billion, Instagram with 1.5 billion, and TikTok with 1 billion are the most accessed social media in the world [ 10 ]. As social media are spreading in every day’s life, regulatory models are required to address a broad range of challenges social media pose to the community, including privacy and protection of sensitive data.
Media usage is related to some adverse consequences especially in the most vulnerable people. The health emergency had a strong impact on the mental and psychological health of adolescents causing changing in their routine and daily activities. Forced isolation increased anxiety and stress especially in the most fragile individuals, such as children and adolescents, leading to a change in habitual lifestyles. The greatest risk was that of taking refuge in excessive use of smartphones, electronic devices, and social networks, running into a “digital overdose” [ 11 ].
A recent survey conducted by the Italian Society of Pediatrics in collaboration with State Police and Skuola.net investigated the relationship with media devices in times of pandemic, investigating the habits of adolescents on the use of media and social networks, underlined that 15% of them declared they “cannot stay without” their own media device [ 1 ].
The aim of the review is to focus on risks correlated to social media use by the young, identifying spies of rising problems, and engaging in preventive recommendations.
2. Materials and Methods
This scoping review has been conducted by The Italian Pediatric Society Scientific Communication Group in order to provide an overview of a complex research area. The aim is reviewing international literature disguising about social media and their effect on the pediatric age, including minors less than 18 years, to underline possible risks found so far, identifying the signs of a dangerous use, and to eventually give new recommendation based on these findings.
We define a risk as the possibility of something unfavorable happens, as an effect or an implication of social media usage and which may potentially affect human health. This scoping review has been performed according to the PRISMA Extension guidelines for Scoping Reviews [ 12 ].
An electronic search was undertaken on PubMed database on 23 January 2022. To avoid missing results that may be of note for our revision study, constructing our search in PubMed, we used all of the important concepts from our basic clinical question, avoiding unnecessary filters.
So, the search terms “social media”, “health”, and “pediatrics” in text or title/abstract were used, with the time span set as “all years”. The search on the selected database has produced n 651 among articles and reviews. Another research was made using “social network”, “health” and “pediatrics” as search terms in text or title/abstract, with the time span always set as “all years”. It resulted in 354 articles/reviews.
The two research were downloaded from PubMed and then uploaded to the web application “Rayyan” [ 13 ], a website used to screen and analyze articles, specific for writing reviews. Additional articles for potential inclusion were identified in a second stage by hand searching the reference lists in relevant articles.
Studies were considered eligible for this scoping review if they met the following inclusion criteria:
- - Full-length articles or reviews.
- - Pertaining to children and adolescents up to 18 years old.
- - Negative impact on a pediatric population using social media.
- - Social media meant as forms of electronic communication.
The exclusion criteria were:
- - Reports not in English.
- - Duplications.
- - Not pertinent field of investigation (e.g., use of the social media to promote healthcare, benefits of social media, social media used to debate on health-related issues, and social network meant as real social interactions).
- - The population analyzed was adult (>18 years).
- - The population had previous pathologies.
To reduce errors and bias, two researchers independently, two researchers conducted the screening process to identify articles that met all inclusion criteria. Using the web application “Rayyan” [ 13 ], duplicates were removed, then titles and abstracts were analyzed to exclude distinctly irrelevant articles. Finally, the eligibility of the articles was confirmed by evaluating the full text. Disagreements regarding inclusion/exclusion were settled by discussion between the researchers.
Relevant articles were selected on the web application “Rayyan” and grouped together based on the issue they were dealing with. Afterwards, data were compiled in a Microsoft Excel spreadsheet to calculate frequencies and percentages of the problems related to social media use, found in the research.
All the 1005 documents have been reviewed for relevance and eligibility.
As shown in the Figure 1 , through the help of the web application “Rayyan” [ 13 ] we removed before screening 9 duplicates, 25 foreign language works, and 49 publications dated before 2004. We excluded paper published before 2004, the year of Facebook foundation, because before that year “social networks” was a term used to mean “social interactions in real life”, as they were not pertinent to our research.

Flow chart of the selection process. * automation tools were used: 6 records were excluded by automation tools and 3 were excluded by authors. Twenty-five records were excluded because they were not written in English, these were identified using automation tools, but then checked by authors. ** 49 records were removed because they were published before 2004, and no social network existed before that year.
According to PRISMA guidelines [ 12 ], of the 922 works identified, all abstracts were analyzed, and 832 records were excluded. Around 66% of the excluded records were dealing with other topics (e.g., vaccines, promoting health by social media, social networks meant as real social interactions, and social lockdown during SARS-CoV-2 period), a percentage of 28% of the records corresponded to a wrong population: mostly parents, pregnant women, young adults, or children with pathologies (e.g., ADHD). About 6% of the excluded studies used social media tools to recruit people in their studies or to deliver questionnaires.
In conclusion, 90 were the records to be analyzed reading their full-length articles. The whole article of four of them has not been found (“reports not retrieved”), arriving at 86 reports assessed for eligibility. Figure 1 presents the flow chart of the selection process, adapted from PRISMA guideline [ 14 ].
Of the 86 reports attained, we read the whole length articles and then excluded 20 studies.
Of these twenty, 6 were excluded because not leading to any conclusion; 13 were dealing with wrong topics, such as: doctors’ social media knowledge; social lock down during the pandemic; social media marketing; underage and privacy; survey on how social media is perceived by adolescents; time consumed on social media; predictor factors of problematic social media use. Finally, one was not included because it focused on parents and families.
Searching through the cited studies in the included reports, two reviews which were not initially included in the research were added.
With 68 included reports analyzed, there were 15 reviews; of these two were systematic reviews, one validation study, and one editorial. Cross-sectional studies and longitudinal studies have been considered, eight and nine, respectively.
Many articles reported more than one issue correlated to social media use. The most frequent problems involved mental health, followed by diet and weight problems. Table 1 shows the problematic topics found to be related to social media use in children and adolescents and their prevalence, expressed as percentage, over the 68 reports analyzed.
Social media health related problems in a pediatric population. This table shows the issues found in this scoping review. Depression was argued in 19 reports, being the main topic found (27.9% of the whole study). Diet associated problems were discussed in 15 reports, cyberbullying in 15, psychological problems in 14, sleep related problems in 13, addiction in 10, anxiety in 10, sex related problems in 9, behavioral problems in 7, body images distortion in 6, reduced physical activity and related problems has been reported in 5 reports, online grooming in 3 reports, sight problems in 3, also headache in 3, and dental caries in total of 2 articles.
The most frequent problems found are related to mental health: depression, anxiety, and addiction.
Other problems are related to sleep, diet and nutrition, cyberbullying, psychological aspects, behavioral problems, sex, body image perception, physical activity, online grooming, sight, headache, and dental caries.
4. Discussion
4.1. social media and depression.
We identified 19 publications reporting a relationship between social media use and depression [ 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 ]. Table 2 summarized the main finding regarding each article. Out of them, four investigated the impact of COVID 19 pandemic on both social media use and depression ( Table 2 ).
Social media and depression.
4.1.1. Before COVID-19 Pandemic
Investigating the impact of social media on adolescents’ wellbeing is a priority due to a progressive increase in mental health problems or addiction and access to Emergency Department [ 15 ]. As Chiu and Rutter stated, there is a positive relationship between internalizing symptoms, such as depression and anxiety, and social media use [ 15 , 16 ]. Depression is connected to a rapidly increased of digital communication and virtual spaces, which substitute face-to-face contact by excessive smartphone use and online chatting. The more time adolescents spend on social device the higher levels of depression are found out. In this sense, social media are representing a risk factor for depression in the young. Depression, anxiety, and behavioral disorders are among the leading causes of illness and disability among adolescents [ 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 ]. Key findings which correlate to depression regarding social media exposure are repeated activities such as checking messages, investment, and addition [ 23 ]. The findings were similar all over the world.
For example, in Sweden, spending more than 2 h on social media was associated with higher odds of feeling [ 20 ]. In Egypt, as well, students who have problematic Internet use, have higher psychiatric comorbidities, such as depression, anxiety, and suicidal tendency [ 24 ].
Social media addiction and more precisely Facebook addiction was linked not only to depression but even to dysthymia, so that the expression “Facebook depression” was coined to identify a relationship between depression and social networking activity [ 15 , 25 , 26 ]. Individuals suffering from Facebook depression may be at an increased risk of social isolation and may be more vulnerable to drugs or behavioral problems [ 26 ].
Internet penetrance and connectivity are also connected to cyberbullying which can lead to depression and suicidality [ 27 , 28 , 29 ].
On the other side, physical activity may decrease depression and anxiety, potentially protecting the young against the harmful effect of social media abuse [ 16 ].
At last, even if a positive correlation between internalizing symptoms and media use device is noted, Hoge states that there is also evidence that social media communication may improve mood and promote health strategies in some occasions [ 18 ].
Finally, even if evidence revealed that social media use is linked to poor mental health, the relationship between social media and depression in adolescents is still to be completely understood. It is still unclear whether social media use leads to more depression or if these depressive symptoms cause individuals to seek out more social media, which could feed into a vicious cycle [ 16 ]. Keles’s conclusion as well suggest defining the relationship between internalizing symptoms and social media use as an association and not a causative effect [ 23 ].
4.1.2. After COVID 19 Pandemic
During COVID-19 pandemic, the state of emergency and social isolation determined an increase in time on screen not only as a source of online education, but to continuously access social media. According to recent data, a percentage of 48% of adolescents spent a mean of 5 h per day on social media and 12% spent more than 10 h. Moreover, with that increase in virtual time depression arose [ 30 ].
The degree of social media usage in children is a significant predictor of depression, which increases with each additional hour of social media use [ 31 ].
During the pandemic, depressive symptoms may have been reactive to the context of being afraid of the virus and necessitating social isolation [ 32 ].
However, in this peculiar period, schoolchildren who increased time spent on either smartphones, social media, or gaming had significantly elevated psychological distress, such as depressive symptoms, than those with decreased time spent on these internet-related activities [ 33 ].
4.2. Social Media and Diet
Out of the reports, 15 dealt with the association of social media use and diet [ 21 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 ]. The problems were related to junk food marketing (9 reports) [ 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 ] obesity (4 reports) [ 21 , 41 , 42 , 43 ], unhealthy eating behaviors (3 reports) [ 44 , 45 , 46 ], and alcohol marketing (2 reports) [ 21 , 47 ]. In Table 3 the retrieved articles dealing with social media and diet, and their major findings are presented ( Table 3 ).
Social media and diet.
4.2.1. Before COVID-19 Pandemic
Junk food marketing.
Reports found that children are exposed to the marketing of unhealthy foods on social media and to their persuasive techniques. Digital marketing represents a major threat for children and adolescents in Mexico, because of its persuasive techniques. Cola and soft drinks, sweetened juices and in general the so-called junk food have high followers on Facebook and Twitter. [ 34 ]. This may cause an increase in children’s immediate consumption of the promoted product, unhealthy behaviors and may led to obesity, as confirmed by several studies [ 34 , 35 , 36 ]. Reports agree on the youth major vulnerability to unhealthy food advertisement, including digital marketing, sponsored content, influencers, and persuasive design [ 34 , 35 , 36 ]. This contributes to the obesity epidemic [ 36 ].
Major social media platforms do not have comprehensive policies in place to restrict the marketing of unhealthy foods on their platforms [ 36 , 37 ]. Therefore, exposure to the marketing of unhealthy products, on social media may be considered a risk factor for related unhealthy behaviors.
Analysis of the advertising policies of the 16 largest social media platforms proved them ineffective in protecting children and adolescents from exposure to the digital marketing of unhealthy food [ 37 ].
Among social media, YouTube is particularly worrying considering the affinity of the young toward the platform. Unhealthy food advertisements predominate in YouTube content aimed towards children. In fact, analysis of advertisements encountered in YouTube videos targeted at children revealed that food and beverage ads appeared most frequently, with more than half of these promoting unhealthy foods [ 38 ].
As confirmed by an Irish study, adolescents are very attracted to junk food advertisements and are likely to share comments on their network: generalized linear mixed models showed that advertisements for unhealthy food evoked significantly more positive responses, compared to non-food and healthy food. Of all the advertising, they see in social media, they view unhealthy food advertising posts for longer [ 39 ]. This confirms the vulnerability of children towards ad and digital marketing.
Moreover, it has been demonstrated that adolescent heavy social media users (>3 h/day) are more willing to engage with food ads compared to light social media users, and are more willing to “like” Instagram food ads featuring many “likes” versus few “likes”, demonstrating the power of social norms in shaping behaviors. Adolescents interact with brands in ways that mimic interactions with friends on social media, which is concerning when brands promote unhealthy product. [ 40 ]. There is a need of more strict policies to limit digital marketing, which is becoming more and more intense, especially towards children and adolescents.
4.2.2. After COVID-19 Pandemic
During the COVID-19 pandemic, this phenomenon even increased. In fact, the combination of staying at home, online education and social media usage have all caused screen time to surge and the food industry has been quick to identify this change in their target audience and has intensified online advertising and focused on children. The COVID-19 experience led to an increase in risk and severity of inappropriate behavioral eating habits, affecting the health and weight [ 41 ].
4.2.3. Before COVID-19 Pandemic
Social media is the first independent risk factor for obesity in primary school children and the second for high school students. In both primary school and high school models, children’s social media use has the highest impact on child’s BMI [ 42 ]. In addition, heavy media use during preschool years is associated with small but significant increases in BMI, especially if used ≥ 2 h of media per day [ 21 ].
4.2.4. After COVID-19 Pandemic
Obesity and social media correlated through junk food advertisements [ 41 , 43 ]. During COVID 19 pandemic poor quality food, energy-dense, and nutrient-poor products consumption increased, leading to the risk of overweight and obesity. The phenomenon has been called “Covibesity” [ 41 ].
4.3. Unhealthy Eating Behavior
Some social media contents promote pro-anorexia messages [ 44 , 45 , 46 ]. These messages are no longer limited to websites that can be easily monitored, but instead have been transferred to constantly changing media such as Snapchat, Twitter, Facebook, Pinterest, and Tumblr. Consequently, pro-eating disorder content has become more easily accessible by the users. Pro-anorexia website use is correlated with a higher drive for thinness, lower evaluations of their appearance, and higher levels of perfectionism, and all correlates with eating disturbances [ 44 , 46 ].
In detail, there is a real bombardment of unhealthy messages on media promoting low-nutrition aliments and sugar-sweetened drinks [ 45 ].
It is likely that the suboptimal quality of online information on social media platform contributes to the development of unhealthy eating attitudes and behaviors in young adolescent internet users seeking nutritional information. They look for nutritional information on internet sources such as commercial websites or social media in order to lose weight. In this occasion, they may be exposed to higher risk of eating disorders due to the high quantity of misinformation. Moreover, they may find dangerous methods to rapidly lose weight with possible harm for their health [ 46 ].
Literature agrees on the risk of time spent on social media as well as on the poor quality and reliability of weight loss information on media [ 44 , 45 , 46 ].
4.4. Alcohol Marketing
Adolescents identify drinking brands to peculiar images of ideal adults. Brands know well this underlying psychological mechanism and promote that identity adolescents seek, with specific advertisement on social media [ 47 ].
Studies have shown that exposure to alcohol in TV or movies is associated with initiation of this behavior. The major alcohol brands have a strong advertising presence on social media, including Facebook, Twitter, and YouTube. Several studies underlined risky health behaviors, such as illegal alcohol use or overuse. Evidence suggests that peer viewers of this content are likely to consider these behaviors as normative and desirable. Therefore, targeted advertising via social media has a significant effect on adolescent behavior [ 21 ].
4.5. Social Media and Cyberbullying
We identified 15 publications reporting a relationship between social media use and cyberbullying [ 21 , 22 , 25 , 26 , 27 , 28 , 29 , 45 , 48 , 49 , 50 , 51 , 52 , 53 , 54 ]. Table 4 summarized the main finding regarding each article ( Table 4 ).
Social media and cyberbullying.
Cyberbullying may be defined as any behavior performed through electronic or digital media by individuals or groups that repeatedly communicate hostile or aggressive messages intended to inflict harm or discomfort on others. Compared to bullying, cyberbullying may be even more dangerous as victims can be reached anytime and in any place. Moreover, anonymity amplifies aggression as the perpetrator feels out of reach.
Moreover, the ability to hide behind fake names provides bullies the opportunity to communicate in content and language they would not use in front of people [ 26 , 48 , 49 ]. As confirmed by Shah et al., the anonymity of cyberbullying increases the risk for inappropriate behaviors among adolescents [ 50 ].
In literature, cyberbullying has been identified in phone calls, text messages, pictures/video clips, emails, and messaging apps. This is a great public health concern: in Italy, 2015 ISTAT data showed that 19.8% of 11–17 years old internet users report being cyberbullied [ 49 ].
This phenomenon is increasing. In fact, the number of adolescents being cyberbullied at least once in their life increased from 20.8% in 2010 to 33.8% in 2016 [ 50 ].
Victims of bullies exhibit increased depressive symptoms, anxiety, internalizing behaviors, externalizing behaviors, and greater academic distractions [ 21 , 22 , 25 , 27 , 28 , 29 , 51 ].
Cyberbullying has been associated with higher risks of depression, paranoia, anxiety, and suicide than the traditional form of bullying [ 21 , 22 ]. According to a metanalysis of 34 studies, traditional bullying increased suicide ideation by a factor of 2.16, whereas cyberbullying increased it by a factor of 3.12 [ 39 ].
In adolescence, social media intense or problematic use and frequent online contact with strangers are all independently associated with cyberbullying [ 45 , 52 , 53 ]. In this contest, social media represent a risk factor for cyberbullying and for inappropriate behavior related to it. In fact, problematic social media use is an important driver of cyberbullying victimization and perpetration, especially among girls [ 50 , 53 ]. The highest percentage is observed in adolescents, aged 13 to 15 years as suggested by literature reviews and, in particular, by Marengo and Uludasdemir [ 53 , 54 ]. However, Marengo also suggests that in presence of social support, the phenomenon is attenuated [ 53 ].
Moreover, having daily access to the Internet and the sharing of gender on social media increased the likelihood of cyber victimization among adolescents aged 12–17 years. Those who use Tumblr and Snapchat were found to become victims even more frequently [ 54 ].
4.6. Psychological Problems and Social Media
We identified 14 publications reporting a relationship between social media use and psychological problems [ 17 , 23 , 33 , 45 , 49 , 52 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 ]. Table 5 summarized the main finding regarding each article ( Table 5 ).
Social media and psychological problems.
4.6.1. Before COVID-19 Pandemic
A high use of screen device has been correlated to a low psychological well-being among children and adolescents, especially among females [ 17 ].
For examples, in Canadians adolescents, the prevalence of loneliness was higher for daily computer-mediated communication users than non-daily users [ 55 ]. As well as for cyberbullying, adolescents may benefit from social support, family communication, and interaction to ameliorate feelings of loneliness [ 53 , 55 ]. Boer et al. confirmed that intense user reported more frequent psychological complaints than non-intense user as well as less family and friend support [ 56 ]. In line with this finding, in Lithuania a problematic social media use has been associated with two times higher odds for lower life satisfaction [ 57 ].
Moreover, an intense social media use correlated to either low school well-being and reduced social well-being (decreased family and friends support and relations) [ 56 ].
A relationship between poor life satisfaction, problematic social media use, and lack of social support was found not only in adolescents, but also in children [ 52 , 57 , 58 , 59 , 60 ].
Social media use is also correlated with conduct and emotional problems, attention deficit, peer problems, school impairments, and psychological distress [ 23 , 45 , 61 , 62 ].
Social networks and media device use correlate to low academic outcomes, reduced concentration, and procrastination. In fact, problematic smartphone use correlates to a surface approach to learning rather than to a deep approach, leading to reduced creativity, organization skills, own thinking, and comprehension of information [ 49 ].
4.6.2. After COVID-19 Pandemic
During this COVID-19 pandemic, primary school children reported significantly higher psychological distress than the period prior to the COVID-19 outbreak. Studies showed that schoolchildren who increased time spent on either smartphones, social media, or gaming had significantly elevated psychological distress than those with decreased time spent on these internet-related activities [ 33 ].
4.7. Social Media and Sleep
Extended use of digital media screen time correlates with sleep impairment [ 18 , 21 , 22 , 26 , 31 , 43 , 47 , 49 , 57 , 61 , 63 , 64 , 65 ]. Table 6 summarizes the evidence in literature ( Table 6 ). Exposure to screen-based devices, online social networking sites, and video-sharing platforms is significantly associated with sleep-onset difficulties in adolescents [ 18 , 49 ]. Findings from a meta-analysis of 20 cross-sectional studies show 53% higher odds of poor sleep quality among adolescents with consistent bedtime media use [ 63 ]. Moreover, the use of computers and smartphones among adolescents is associated with daytime sleepiness and fatigue, shorter sleep duration, later bedtime, and unfavorable changes in sleep habits over time [ 22 ]. Smartphones may be easily carried around and even taken to bed. Several sleep disorders correlate to both overall and night phone use among adolescents. It has been demonstrated that social media addiction in school students decreases students’ sleep efficiency [ 61 ]. Use of cellphones, particularly for nighttime texting, and consulting social media were associated with insufficient sleep [ 63 ]. A 5 or more hours daily of media devices use has been related to a higher risk of sleep problems when compared to a 1 h use daily [ 49 ]. This finding is confirmed by Buda who correlates problematic social media with about two times higher odds for a bad sleep quality [ 57 ]. Varghese as well associated social media use with sleep difficulties. Furthermore, YouTube user had two-times higher odds for sleep-onset difficulties [ 63 ].
Social media and sleep.
In addition, it seems that girls suffer more than boys from these sleep problems [ 57 ].
Sleeping problems, especially sleep duration, have been then associated with time spent on screen, problematic behaviors, and higher internalizing and externalizing symptoms [ 64 ].
Even among children, there is a problem with extended use of social media sites, which result in sleep deprivation due to delayed bedtimes and reduced total sleep duration and quality of rest [ 31 , 65 ]. The report by Hadjipanayis as well confirms that sleeping disturbances may be associated with the disruption of circadian rhythms due to the blue light emission from the electronic screen-based media devices [ 26 ]. Negative outcomes including poor school performance, childhood overweight and obesity, and emotional issues have all been associated with sleep deprivation [ 21 , 26 , 43 , 47 ]. Inadequate sleep quality or quantity associated to social media use represents a risk factor for metabolic conditions such as for diabetes, cardiovascular disease and for mental problem, such as depression or substance abuse [ 49 ].
4.8. Social Media and Addiction
Ten reports found correlations between social media use and risk of different types of addictions: with internet [ 17 , 24 , 49 , 51 , 52 , 66 ], with substance abuse [ 15 , 67 ], with alcohol addiction and gaming [ 67 ], with gambling [ 68 ], and with tobacco use [ 69 ]. In Table 7 , the major findings of the related reports are presented ( Table 7 ).
Social media and addiction.
Investigating the impact of social media on adolescents’ wellbeing is a priority due to a progressive increase in mental health problems and access to Emergency Department [ 15 ]. Chiu reported that mental health or addiction related emergency department access increased by almost 90% in ten years mainly among adolescents aged 14–21 years. The increment well correlates to an increase availability of social media [ 15 ].
High screen use associated with internet addiction is also confirmed by O’Keeffe who states that technology is influencing children’s lives from a very young age [ 51 ].
More than 7% of youth have problematic social media use, indicated by symptoms of addiction to social media [ 52 ]. Warning signs of internet addiction can be skipping activities, meals, and homework for social media; weight loss or gain; a reduction in school grades [ 41 ]. In detail: concern, loss of controlling tolerance, withdrawal, instability and impulsiveness, mood modification, lies, and loss of interest have been identified as risk factors for smartphone addiction. Females have almost three times more risk for smartphone addiction than males and it may be related to a stronger desire for social relationships [ 66 ]. Main problems correlated to addiction are low self-esteem, stress, anxiety, depression, insecurity, solitude, and poor scholastic outcomes. Smartphone addiction correlates to both fear of missing out (FOMO) and boredom. FOMO is the apprehension of losing experiences and the consequent wish to remain constantly connected with others, continuously checking social applications. Boredom is defined as an unpleasant emotional state, related to lack of psychological involvement and interest associated with dissatisfaction, to cope with boredom adolescents may seek additional stimulation and compulsively use smartphones [ 49 ].
As well as O’Keeffe, Hawi found out that children are starting to use digital devices at a very young age, and so should be screened for the risk of digital addiction. New scales of early identifications have been developed such as the Digital Addiction Scale for Children, validated to assess the behavior of children 9 to 12 years old in association with digital devices usage. Out of the sample size, 12.4% were identified as at risk of addiction and most of them (62.4%) were male. Nevertheless, results demonstrated that weekday device use among females causes more conflicts [ 66 ].
Different grading scales can test addictions. A study assessed 700 adolescents aged from 14 to 18 years and found out that 65.6% were having internet addiction, 61.3% were gaming addicts, and 92.8% Facebook addicts. Internet addict students had statistically significant higher age, higher socioeconomic scale score, male gender, and lower last year grades in comparison to non-addicts. Depression, dysthymia, suicide, social anxiety, and phobias were common comorbidities in addicted adolescents [ 24 ].
In undergraduate students, disordered online social networking use is associated with higher levels of alcohol craving and in pupils aged from 11 to 13, it is associated with a higher likelihood of being substance users [ 67 ]. In addition, excessive video gaming is associated with increased substance use [ 15 , 67 ].
One report showed greater risk for children and adolescents to develop gambling problems. In fact, the prevalence of adolescent gambling has increased in recent years. Across Europe, self-reported rates of adolescent gambling in 2019 ranged from 36% in Italy to 78% in Iceland. Adolescent problem gambling prevalence ranges from 1.6 to 5.6%. Not only adolescents but also children are widely exposed to gambling advertisements on television and via social media. In recent years, there has been an expansion in sports betting online, and this has been heavily promoted by advertising and marketing attractive to adolescents. Gambling is also promoted to children via social media: children are sharing and re-tweeting messages from gambling companies, they are active in conversations around gambling, and regularly consume and share visual gambling adverts. Lastly, there is also a strong relationship between gaming and gambling: in video games, children pretend to gamble and some video games would ask real money to play [ 68 ].
Finally, there might be a relationship between youth using tobacco and tobacco social media posts. It is not clear if the relationship can be cause-effect or only a correlation. Adolescents who participate in conversations about tobacco in social media by posting positive messages about tobacco are more likely to be past-month tobacco users. Posting even only one positive tobacco-related tweet was associated with greater odds of using cigarettes, e-cigarettes, or any tobacco product, compared to those who did not post positive messages about tobacco [ 69 ].
Finally, social media has been associated to social media use and may represent a risk factor for the young as it interferes with dailies activities leading to unhealthy habits. The easy access to social media by smartphone undoubtedly facilitates addiction.
4.9. Social Media and Anxiety
We identified 10 publications reporting a relationship between social media use and anxiety. Out of them, three investigated the impact of COVID 19 pandemic on social media use and anxiety [ 15 , 16 , 17 , 18 , 22 , 23 , 31 , 32 , 33 , 70 ]. Table 8 summarized the main findings ( Table 8 ).
Social media and anxiety.
4.9.1. Before COVID-19 Pandemic
Evidence agrees that the degree of social media usage in children is a significant predictor of anxiety and perceived stress levels and that it increases with each additional hour of social media use [ 17 , 23 , 31 ]. Anxiety may represent a risk factor for children and adolescents’ health as it influences the way they see their body, the way they feel, and it may impact on social acceptance and relations with peers.
The excessive use of at least one type of screen, including television, computer, social media, and video gaming, has been connected with anxiety symptoms in the pediatric age [ 22 , 23 , 31 ]. Furthermore, in Rutter’s study a significant association between depression and anxiety with social media use has been detached [ 16 ]. Nevertheless, it is still unclear if social media use provoke anxiety or if anxiety is the cause of excessive use of social media [ 16 ]. Emergency department visits for mental health, including anxiety problems, has arisen since 2009, likely linked to the increased use and the harmful effect of social media [ 15 ]. On the contrary, physical activity may protect the young against the harmful effect of social media, preventing depression and anxiety [ 16 ].
In a scientific report, Muzaffar confirmed that an association between anxiety and social media is of note. In detail, increased adolescent generalized anxiety symptoms were associated with increased Facebook use and repetitive Facebook habits. Anxious adolescents may not be able to control their discomfort to the point that they need to regularly go back to check their previous posting on Facebook [ 70 ].
The constant connection to social networks through digital devices, on its side, potentially contributes to feelings of anxiety. Adolescents and children suffering from social anxiety may prefer to interact with texting, instant messaging, and emailing than over face-to-face interactions. However, the behavior may increase risk in individuals vulnerable to social anxiety disorder because substituting digital media for interpersonal communication to avoid feared situations may be reinforced over time, making the person even more avoidant and worsening the symptoms and severity of social anxiety disorder [ 18 ].
However, in some studies, not just overexposure but also underexposure to social media was associated with adolescent anxiety, depression, and suicidal ideation [ 22 ].
4.9.2. After COVID-19 Pandemic
Screen time and social media use have increased during the pandemic. Social media has been helpful during lockdown to keep social relationships and not to discontinuate school activities. However, an excessive Internet use may negatively affect children and adolescents’ well being. So, during social lockdown, an elevated psychological distress and anxious symptoms have been described in schoolchildren who increased time spent on screen [ 32 , 33 ]. Children who increased by 15 or 30 min daily the time spent on internet presented a high level of psychological distress.
4.10. Social Media and Sex Related Problems
Studies have found social media use related to sexual problematic behaviors such as early sexual activity, exposure to pornography, and sexting. [ 21 , 22 , 26 , 50 , 51 , 71 , 72 , 73 , 74 ]. Table 9 summarizes the results ( Table 9 ).
Social media and sex related problems.
The prevalence of sex related problems cannot be accurately recorded as for a wide range of definition and sampling methods and the comparison among reports is difficult.
Especially for girls, higher social media use, associated with lower family affluence and poorer body image, are key to early sexual activity [ 71 ].
Social media use was found to be significantly associated with risky sexual behavior among pre-college students in Ethiopia. Facebook, Instagram, YouTube, and other platforms have been identified as a factor that alters adolescent’s perception and influences them to engage in risky sexual behavior. Those who view sexually suggestive Facebook photos have a higher chance of having unprotected sexual intercourse and sex with strangers [ 72 ].
Moreover, youth can be exposed to unwanted sexual material online, including unwanted nude pictures or sexually explicit videos through means such as pop-up windows or spam e-mails [ 73 ].
Children exposed to inappropriate sexual content are prone to high-risk behaviors in subsequent sexual encounters. [ 22 ] Sexting activities may also affect emotional and social wellbeing of adolescents; it is correlated to depression and risky health behaviors, such as substance use, alcohol consumption, and suicide [ 26 , 50 ]. The odds of risky sexual behavior were 1.23 higher in social media user than in other students [ 72 ]. Furthermore, on the internet, pornography is readily accessible by media device, so that Wana found out that 7% of students use social media for pornography. In most cases, adolescents admit they intentionally viewed materials [ 74 ]. Pornographic media depict a fantasy world in which unrealistic encounters result in immediate sexual gratification, and intimate relationships are nonexistent. Repeated exposure of the adolescent brain to the world of online pornography can make it difficult for adolescents to develop mature healthy sexual relationships [ 22 ].
Internet pornography usage has been documented in adolescents before the age of 18. Online pornography is often the first source of sex education for many adolescents, and exposure to violent pornography increases the odds of sexually aggressive behavior [ 50 ]. Peer advice as well as substance abuse are significant predictor for risky sexual behavior [ 72 ].
Finally, among adolescents 10–19 years of age, the rate of sexting ranges from 5 to 22% [ 50 , 72 , 74 ].
Sexting is the use of media to send nude or sexualized contents such as texts, photos, or videos. An extensive sharing of these contents through technology has been connected with a negative impact on the emotional and social wellbeing of adolescents involved. An earlier sexual debut such as the use of drugs and promiscuity have been all associated to the excessive use of sexting. It can also cause spreading of sexual content material without consent, to a third party as a method of bullying or revenge [ 21 , 26 , 51 , 74 ].
4.11. Social Media and Behavioral Problems
Out of the reports, seven explored the influence of social media and behavioral problems [ 22 , 49 , 64 , 75 , 76 , 77 , 78 ]. Table 10 outlines the highlighted findings ( Table 10 ). Behavioral outcomes usually cover five areas, including hyperactivity/inattention, emotional symptoms, conduct problems, peer relationship, and pro-social behavior.
Social media and behavioral problems.
For children aged 10–15 years old, limited time on social media has no effect on most emotional and behavioral outcomes (and can even positively impact social relationships), while there are strong negative associations between very long hours on social media and increased emotional distress and worse behavioral outcomes, which continue for several years [ 75 ].
In accordance to McNamee, the study by Okada conducted in Japan [ 76 ] among children aged 9–10 years old highlighted that mobile devices usage time of less than 1 h was a protective factor for behavior problems in boys. Instead, the usage time of 1 h or more was a risk factor in girls. Among girls, a dose–response positive association was found between duration of mobile devices usage and total difficulty score. A U-shaped association was found between duration of mobile devices usage and behavioral problems in boys: moderate use of mobile devices might be a tool for relaxation or alleviating distress through interactions with peers. However, in the subscale analysis, boys who use two or more hours of mobile devices showed higher risk of emotional problems and peer problems [ 76 ].
Moreover, the social media violent content exposure may be a risk factor for violent and aggressive behaviors. In this context, levels of aggression are directly proportional to exposure of types of violent media content. Electronic and social media showing contents with fights, stealing, dead bodies, and people’s belongings being destroyed influence young viewers, as per observational-learning theory, making them believe that reacting aggressively in response to perception of any offense is acceptable [ 77 ].
In line with Tahir’s report, Maurer underlined a significant association between exposure to media violence and aggressive behavior, aggressive thoughts, angry feelings, and physiologic arousal. Media exposure is also negatively related to personal adjustment and school performance and positively related to risk-taking behaviors [ 22 ].
Another study confirmed that longer the time spent on screens, higher the risk for behavioral problems among children 9–10 years old, and depending on the content type visualization, the risk for an aggressive and rule-breaking behavior. This association was mediated by sleep duration: longer sleep duration was associated with fewer problem behaviors [ 64 ].
Challenges and risk-taking attitudes are frequent in child and youth culture. However, online challenges take on new meanings when mediated by digital sociability; they appear as a powerful communicative resource to reaffirm belonging, recognition, and audience adherence. They are a media strategy adopted by youth in the construction of an internet-mediated identity in which risk and violence are crucial devices in building a self-image capable of maintaining an audience. Nevertheless, they can involve potential self-inflicted injuries to participants, with risks ranging from minor to even lethal [ 78 ].
Finally, an emerging problem is the social phenomenon called Shakaiteki Hikikomori (social withdrawal). Most of them are males and they usually experience a social reclusion range from 1 to 4 years. They refuse to communicate even with their own family and spend even more than 12 h a day in front of a screen [ 49 ].
4.12. Social Media and Body Image
On social media platforms such as Facebook, Snapchat, and Instagram, body image has become an important topic [ 17 , 25 , 45 , 46 , 50 , 73 ]. Table 11 summarized the evidence. ( Table 11 ). People post their most flattering photos and view those of others, creating an online environment that could be damaging to body image acceptance. Spending time on social media puts adolescents under a higher risk of comparing themselves to models that are more attractive. As a result, these unfavorable social comparisons of physical appearance may exacerbate body image apprehension [ 17 , 45 ].
Social media and body image.
Moreover, beauty trends are constantly reinforced through social media networks and image-editing tools are often used to alter images to fit beauty standards. Teenagers who, perhaps, are not aware of these digital changing made in commercial photos may become insecure of their image. This may reduce self-esteem and body satisfaction, mainly among adolescent girls, developing body image concerns, engaging in weight-modification behavior, and potentially developing eating disorders. Nowadays, adolescents, and, in particular, girls, need to fit “social media” standard for photo posting; they use to modify photos with specific programs in order to respect society beauty standard. In fact, 28% of girls aged 8–18 years admit to editing their photos to make themselves look more attractive prior to posting online [ 50 ].
In addition to social media causing body image problems, adolescents with body image misperception may look on the internet for advice on how to lose weight quickly. However, the suboptimal quality of online information contributes to the development of unhealthy eating attitudes and behaviors in young adolescents. It may be that the content of these sites promotes eating disorders by providing unhealthy weight loss advice [ 46 ].
Furthermore, the desire of perfection and selfie mania with repeated selfie can cause depression and self-harm. This is a typical symptom of body dysmorphic disorder [ 73 ].
Finally, this association between the use of social media, self-esteem and body image can be a correlation and not a cause-effect relation: girls with lower self-esteem and sensitive to body image complains may use social media more frequently than girls with a higher level of self-esteem. For example, users can make a “selective self-presentation” where they show themselves only in a positive way on their social media profiles [ 25 ].
4.13. Social Media and Physical Activity
Evidence supports a correlation between social media and physical activity [ 45 , 49 , 57 , 73 , 79 ]. Excessive use of smartphones and other digital devices can also cause physical problems, such as a more sedentary lifestyle [ 45 ], which is positively associated with childhood obesity. In addition, non-physiological postures assumed while using smartphones may lead to cervical rigidity and muscle pain resulting in neck strain or “Tech Neck”. Moreover, “texting thumb” is a form of tendinitis that comes from overusing the thumb from excessive texting, video gaming, and web browsing using a smartphone [ 49 , 73 ].
An Australian study found that non-organized physical activity declines between 11 and 13 years, especially in children with a large increase in activities of texting, emailing, social media, and other internet use [ 79 ].
Another study showed that problematic social media use is related to lower levels of vigorous physical activity, especially in girls [ 57 ].
In Table 12 are listed the reports related to this topic and their major content ( Table 12 ).
Social media and physical activity.
4.14. Online Grooming
Online grooming may be defined as a situation in which an adult builds a relationship with a minor finalized to a sexual abuse using social media. [ 47 , 80 ]. The risk of developing post-traumatic stress disorder in the victims is of note and may affect mental and well-being of children and adolescents [ 80 ].
Children are more vulnerable online as they often escape their parents’ control and may be more willing to share information or pictures about themselves than in real life.
Online grooming, differently to offline sexual abuse, is simpler to perpetrate, due to internet’s technology and accessibility. Furthermore, often the perpetrator misrepresents himself as another child or teenager, in order to establish a trusting relationship [ 21 ].
Teenage girls appear to be more at risk, even if the proportion of male victims is considerable too. In general, minors with problematic internet use are at greater risk of being groomed.
Sexual solicitation has been found to be more common in children spending longer time on internet on weekdays, being involved in sexting, having strangers in social networks friends list, playing online games, and chats. The risk is high even for adolescents whose curiosity and unconsciousness set them at risk of being deceived [ 80 ].
Table 13 presents the reports related to this topic and their major content ( Table 13 ).
Social media and online grooming.
4.15. Social Media and Sight
Studies have investigated the risk of social media on sight, in terms of visual imbalance [ 22 , 49 , 73 ]. Evidence underlines that children can develop ocular disorders from excessive screen time, including myopia, eye fatigue, dryness, blurry vision, irritation, burning sensation, conjunctival injection, ocular redness, dry eye disease, decreased visual acuity, strain, fatigue acute acquired concomitant esotropia, and macular degeneration. During smartphone use, there is a reduction of the blink rate to 5–6/min that promotes tear evaporation and accommodation, leading to dry eye disease [ 49 , 73 ].
In addition, excessive screen time and less time spent outdoors may lead to early development of myopia, particularly with smartphone and tablet use [ 22 ].
Table 14 presents the reports related to this topic and their major content ( Table 14 ).
Social media and sight.
4.16. Social Media and Headache
There are increased complaints of headaches related to staring at a screen for too long [ 62 , 73 , 81 ]. Reports dealing with social media and headache are listed in Table 15 ( Table 15 ).
Social Media and headache.
Headache is actually the most common neurologic disorder in the population, children and adolescents included [ 81 ]. It may negatively impact on children and adolescents’ well-being, leading to stress, tiredness, anxiety, and bad mood. Time of usage of media device has been directly connected to headache: in particular, adolescents using more than 3 h a screen have a significantly higher risk of headache compared with those using a device for less than 2 h ( p < 0.001). Spending even 2–3 h with a computer significantly increases the chance of suffering a headache in comparison with those using a computer for less than 2 h ( p < 0.01). Excessive use of electronic devices is considered a risk factor, especially for the development of migraine-type headache ( p < 0.05) [ 81 ].
According to recent studies, headache and somatic symptoms have been found mostly in patients with problematic social media usage, compared with non-problematic peers. There is a consistent association between the problematic use of social media and adolescent psychosomatic health [ 62 , 73 ].
4.17. Social Media and Dental Caries
The association between use of internet and social media has been studied in literature [ 35 , 82 ]. Table 16 summarizes the main findings ( Table 16 ).
Social media and dental caries.
The association between use of internet social media to obtain oral health information and dental caries has been highlighted in Almoddahi’s report [ 82 ]. In detail, problematic internet use has been associated with unhealthy lifestyles, poor oral health behaviors, and more oral symptoms such as toothache, bleeding gums, and poor self-perceived oral health. Caries and junk food have been both connected to excessive internet use and ads [ 82 ]. Therefore, social media may be a risk factor for caries, poor oral health, and dental outcomes.
In line with Almoddahi, Radesky underlines that advertisements on social media promote intake of foods that contribute to dental caries, such as fast food and sugar beverages [ 35 ]. Nevertheless, evidence suggests that smartphone applications may improve health and oral health when internet-based health interventions are in place. Delivering oral health information via social media may increase tooth brushing and dental outcome [ 82 ].
5. Limitations
From the literature, it is not possible to decide whether social media use causes internalizing symptoms and problematic behaviors examined in this manuscript or whether children and adolescents suffering from depression, anxiety, or other psychological distress are more likely to spend time on social media. We can just state that there is an association between social media use and health problems, but that is not necessarily cause-effect. Moreover, the articles included are different, ranging from reviewers to clinical studies to letters and to editors, so that it may be difficult to accurately compare them. Third, as specified in the materials and methods, we excluded reports not in English letter and not published in PubMed.
Nevertheless, through our manuscript we contribute to the existing literature to highlighting the impact of social media use on adolescents, providing advices to pediatricians in everyday practice.
6. Conclusions
Social media is increasingly being used by children and adolescents, especially during COVID-19 pandemic and the health emergency. Although social media use demonstrated to be of utility, an excessive or non-correct use may be a risk factor for mental health, including depression, anxiety, and addiction.
Social media use may also correlate to a non-adequate nutrition with consumption of junk food marketing leading to weight gain, obesity, dental caries, and unhealthy eating behaviors. Associations have been found also with increasing physical problems due to sedentary lifestyle, obesity, and non-physiological postures. On the other hand, social media can cause problems with body image visualization and acceptance, especially in young adolescent girls with lower self-esteem, who may look for contents for losing weight rapidly, and this can help the extension of anorexia disorders.
Children and adolescents who use social media for many hours a day, are also at higher risk for behavioral problems, cyberbullying, online grooming, sleep difficulties, eye problems, (such as myopia, eye fatigue, dryness, blurry vision, irritation, burning sensation, conjunctival injection, ocular redness, and dry eye disease), and headache. Moreover, uncontrolled social media use, can lead to sexting, exposure to pornography, exposed to unwanted sexual material online, and early sexual activity. Social media users meet more online risks than their peers do, with an increased risk for those who are more digitally competence.
Public and medical awareness must rise over this topic and new prevention measures must be found, starting with health practitioners, caregivers, and websites/application developers. Families should be educating on the dangers and concerns of having children and adolescence online. Prerequisite to inform families how to handle social media is to educate those responsible for training, including health practitioners. In detail, pediatricians should be reminded to screen for media exposure (amount and content) during periodic check-up visits. They need to keep in mind a potential correlation of problematic social media use with depression, obesity and unhealthy eating behavior, psychological problems, sleep disorder, addiction, anxiety, sex related problem, behavioral problem, body image, physical inactivity, online grooming, sight compromising, headache, and dental caries. Pediatricians can also counsel parents to guide children to appropriate content by consulting ratings, reviews, plot descriptions, and by a previous screening of the material. They should inform parents about the potential risk of digital commerce to facilitate junk food, poor nutrition and sweetened aliments, facilitating overweight and obesity. On the contrary, a healthy diet, adequate physical activity and sleep need to be recommended. Pediatricians may also play a role in preventing cyberbullying by educating both adolescent and families on appropriate online behaviors and on privacy respect. They should also promote a face-to-face communication and to limit online communication by social media. Pediatricians may encourage parents to develop rules and strategies about media device and social media use at home as well as in every day’s life.
Funding Statement
This research received no external funding.
Author Contributions
Conceptualization: E.B.; methodology: S.B.; formal analysis G.S. and A.D.M.; Resources R.A. and R.R.; writing E.S. and A.V.D.S.; visualization: C.C.; editing: A.S.; supervision G.C. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Data availability statement, conflicts of interest.
The authors declare no conflict of interest.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.

IMAGES
VIDEO
COMMENTS
Parental attitudes and practices influence child behavior and development, both in the. acquisition of prosocial skills and in the emergence of psychosocial adjustment difficulties (Ko tchick &. F ...
Parenting behavior may be one mediator of stress as a predictor of child behavior problems. Some research conducted with typically developing children has suggested that stress in the family context may lead to less competent and less responsive parenting (Belsky, Woodworth, & Crnic, 1996; Crnic & Low, 2002; Patterson, 1983), which has been ...
Research on CBCL scales (33, 34) found that comorbid clinical elevations on specific pairs of scales may have prognostic implications, ... The Child Behavior Checklist (CBCL) is a 113-item parent-rated assessment of a child's behavior problems and social competence . Raw scores are calculated and used to generate T-scores for eight clinical ...
The behavior of school-aged children is an important indicator of adaptation in this stage of development; however, not all children are successful and may present externalizing or internalizing behavioral problems, expressed within the family and/or school contexts (Achenbach, Ivanova, Rescorla, Turner, & Althoff, 2016; Linhares & Martins, 2015; Marturano, 2013).
Behavioral management programs have become an important tool in encouraging prosocial behavior among children who are considered disruptive or aggressive. Since 1995, a number of well-designed randomized controlled trials have found evidence for the effectiveness of these programs across settings. This comprehensive literature review describes the results of this research, concluding that the ...
Children's gender has been found to be important in the emergence of child behavior problems and how children respond to parenting styles, and several studies have suggested the role of gender differences in internalizing versus externalizing problems [50,51,52,53,54,55,56]. Early childhood is a critical period for child development related ...
Emotional, behavioral, and relationship problems can develop in very young children, especially those living in high-risk families or communities. These early problems interfere with the normative activities of young children and their families and predict long-lasting problems across multiple domains. A growing evidence base demonstrates the efficacy of specific family-focused therapies in ...
The severity of child psychopathology (i.e., child aggressive behavior, child attention problems, and child rule-breaking behavior from CBCL, and the mania score). was slightly lower in the sample ...
Challenging behavior exhibited by young children is becoming recognized as a serious impediment to social ... A review and recommendations for future research. Working Paper No. 97-36. ... National estimates of mental health utilization and expenditures for children in 1998. In Blueprint for change: Research on child and adolescent mental ...
Discrepancies between raters can be used to reveal key information regarding a child's behavior in ... Quality of life and childhood mental and behavioural disorders - A critical review of the research. Journal of Child ... WHOQOL Group. (1995). The World Health Organization quality of life assessment (WHOQOL): Position paper from the World ...
Consequences of childhood trauma. 1.1.1. Depression and anxiety. Childhood trauma has been linked to the development of anxiety and depression in later life ( Hovens et al., 2010) and a history of abuse may be more identifiable by adulthood as emotional and behavioral patterns have evolved by this period.
A large body of evidence has demonstrated that exposure to childhood maltreatment at any stage of development can have long-lasting consequences. It is associated with a marked increase in risk for psychiatric and medical disorders. This review summarizes the literature investigating the effects of childhood maltreatment on disease vulnerability for mood disorders, specifically summarizing ...
Abstract. Examined the hypothesis that distinct parenting practices may be associated with type and profile of a child's disruptive behavior problems (e.g., oppositional, aggressive, hyperactive). Parents of 631 behaviorally disruptive children described the extent to which they experienced warm and involved interactions with their children ...
Previous research suggests that adopted children are at a greater risk of experiencing ... Groza V, Ryan SD (2002) Pre-adoption stress and its association with child behavior in domestic special needs and international adoptions. ... Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta ...
behavior may impact their learning, which seems to be just a loop of the behaviors stemming. from the student work load. A child's behavior can be completely different than the next child's, so the researcher. was wondering how the screener and assessment scores look. The researcher has had a different.
Family-Based Factors and Child Behavior Problems Family structure and child behavioral problems. The increase in the prevalence of children being raised in a "nontraditional" family (Carlson & Corcoran, 2001) has led to more research exploring this relationship between family structure and child development (Wen, 2008).
However, this relationship seems to be more complicated. The Children's Ecological Behavior (CEB) Scale has been proposed as an alternative. Based on the Rasch model, it considers the different efforts needed to conduct a series of behaviors. This paper presents an improved adaptation of the CEB to Spanish population.
The behavior of a child is variable and depends on ... The present study revealed a significant association between loss of parents and prevalence rate of behavior problems. Most of the research studies related to mental illness and psychological disturbances have shown a significant correlation between loss of parent and psychopathology in ...
They said the therapy teaches children to manage their behavior and often results in significant reductions in behavior problems. It has also been shown to prevent future abuse because caregivers learn new behaviors and strategies for promoting family relationships and addressing externalizing behaviors without resorting to violent words or ...
Child maltreatment leads to behavior problems, but behavior problems seldom lead to child maltreatment, according to a new study by researchers in the Penn State Department of Human Development and Family Studies. Previous research had shown that maltreatment and behavior problems were linked but not whether one led to the other.
In both primary school and high school models, children's social media use has the highest impact on child's BMI [ 42 ]. In addition, heavy media use during preschool years is associated with small but significant increases in BMI, especially if used ≥ 2 h of media per day [ 21 ]. 4.2.4.