- Introduction
- Conclusions
- Article Information
Flowchart describing the derivation of the study sample of patients with major depressive disorder (MDD) episodes (as defined in the eAppendix in Supplement 1 ), including the matched study sample of patients with MDD with and without suicidal behavior (SB). Suicidal behavior was defined using International Classification of Diseases, Tenth Revision codes X60 to X84 (intentional self-harm) recorded in any diagnosis position and in both outpatient and inpatient health care settings. The Methods section provides more information. For MDD with SB, the index is the date of first SB within the MDD episode. The matched controls (patients with MDD without SB) are given the same index date as their matched case. The matching procedure is explained in eFigure 1 in Supplement 1 .
Definition of an MDD episode is provided in the eAppendix in Supplement 1 . Suicidal behavior was defined using International Classification of Diseases, Tenth Revision codes X60 to X84 (intentional self-harm) recorded in any diagnosis position and in both outpatient and inpatient health care settings. The Methods section provides more information. For MDD with SB, index is the date of first SB within the MDD episode. The matched controls (MDD without SB) are given the same index date as their matched case. The matching procedure is explained in eFigure 1 in Supplement 1 .
Ongoing treatment with antidepressant therapy at 12 months before and 12 months after index.
eAppendix. Definition of Major Depressive Disorder (MDD) Episode
eFigure 1. Matching Procedure for Patients With Major Depressive Disorder (MDD) With and Without Suicidal Behavior (SB)
eTable 1. Definitions of Inclusion and Exclusion Criteria, Treatments, and Comorbid Conditions
eTable 2. Definition of Variables Included in the Development of the Cox Proportional Hazards Model on Determinants for Suicidal Behavior (SB) Within 1 Year After Start of a Major Depressive Disorder (MDD) Episode
eFigure 2. Cumulative Proportion of Major Depressive Disorder (MDD) Episodes With Records of Suicidal Behavior (SB) After Start of an MDD Episode, by Age Strata
eTable 3. Specification of Type of Suicidal Behavior (SB) Events in Descending Order Among the 2,240 Patients With Major Depressive Disorder (MDD) and SB
eFigure 3. Cumulative Probability of All-Cause Mortality in Patients With Major Depressive Disorder (MDD) With and Without Suicidal Behavior (MDD-SB) Compared With MDD-Non-SB, Sensitivity Analysis
eTable 4. Characteristics at Start of the Major Depressive Disorder (MDD) Episodes (MDD-Baseline) Among Patients With Records of Suicidal Behavior (SB) Within the Current MDD Episode Compared With All MDD Episodes (With and Without Records of SB)
eFigure 4. Prevalence of Psychiatric Comorbid Conditions 12 Months Before and 12 Months After Index (Time of First Suicidal Behavior [SB] Within the Major Depressive Disorder [MDD] Episode)
eFigure 5. Mean Monthly Health Care Resource Utilization (HCRU) and Work Loss 12 Months Before and 12 Months After Index (Time of First Suicidal Behavior [SB] Within the Major Depressive Disorder [MDD] Episode)
eFigure 6. Nonogram for the Cox Proportional Hazards Model on Determinants for Suicidal Behavior Within 1 Year After Start of a Major Depressive Disorder (MDD) Episode, Based on Patients With MDD Episodes Between 2015 and 2017 Residing in Stockholm for at Least 3 Year Prior to Start of MDD
eFigure 7. Calibration of the Cox Proportional Hazards Model on Determinants for Suicidal Behavior (SB) Within 1 Year After Start of a Major Depressive Disorder (MDD) Episode
Data Sharing Statement

See More About
Select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Lundberg J , Cars T , Lampa E, et al. Determinants and Outcomes of Suicidal Behavior Among Patients With Major Depressive Disorder. JAMA Psychiatry. 2023;80(12):1218–1225. doi:10.1001/jamapsychiatry.2023.2833
Manage citations:
© 2024
- Permissions
Determinants and Outcomes of Suicidal Behavior Among Patients With Major Depressive Disorder
- 1 Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institutet, and Stockholm Health Care Services, Stockholm, Sweden
- 2 Sence Research AB, Uppsala, Sweden
- 3 Department of Medical Sciences, Uppsala University, Uppsala, Sweden
- 4 Department of Women’s and Children’s Health, Uppsala University, Uppsala, Sweden
- 5 Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
- 6 Janssen-Cilag AB, Solna, Sweden
Question What are the clinical and societal outcomes, including all-cause mortality, associated with suicidal behavior in patients with major depressive disorder (MDD)?
Findings In this cohort study of 158 169 unipolar MDD episodes, 1.4% involved records of suicidal behavior. The all-cause mortality among patients with suicidal behavior was 2.6 times higher than among matched patients with MDD without records of suicidal behavior.
Meaning These findings show an association between suicidal behavior and all-cause mortality in patients with MDD and warrant additional interventional studies in health care practice.
Importance Major depressive disorder (MDD) is an important risk factor of suicidal behavior, but the added burden of suicidal behavior and MDD on the patient and societal level, including all-cause mortality, is not well studied. Also, the contribution of various prognostic factors for suicidal behavior has not been quantified in larger samples.
Objective To describe the clinical and societal outcomes, including all-cause mortality, of suicidal behavior in patients with MDD and to explore associated risk factors and clinical management to inform future research and guidelines.
Design, Setting, and Participants This population-based cohort study used health care data from the Stockholm MDD Cohort. Patients aged 18 years or older with episodes of MDD diagnosed between January 1, 2012, and December 31, 2017, in any health care setting were included. The dates of the data analysis were February 1 to November 1, 2022.
Exposures Patients with MDD with and without records of suicidal behavior.
Main Outcomes and Measures The main outcome was all-cause mortality. Secondary outcomes were comorbid conditions, medications, health care resource utilization (HCRU), and work loss. Using Region Stockholm registry variables, a risk score for factors associated with suicidal behavior within 1 year after the start of an MDD episode was calculated.
Results A total of 158 169 unipolar MDD episodes were identified in 145 577 patients; 2240 (1.4%) of these episodes, in 2219 patients, included records of suicidal behavior (mean [SD] patient age, 40.9 [18.6] years; 1415 episodes [63.2%] in women and 825 [36.8%] in men). A total of 11 109 MDD episodes in 9574 matched patients with MDD without records of suicidal behavior were included as controls (mean [SD] patient age, 40.8 [18.5] years; 7046 episodes [63.4%] in women and 4063 [36.6%] in men). The all-cause mortality rate was 2.5 per 100 person-years at risk for the MDD-SB group and 1.0 per 100 person-years at risk for the MDD-non-SB group, based on 466 deaths. Suicidal behavior was associated with higher all-cause mortality (hazard ratio, 2.62 [95% CI, 2.15-3.20]), as well as with HCRU and work loss, compared with the matched controls. Patients with MDD and suicidal behavior were younger and more prone to have psychiatric comorbid conditions, such as personality disorders, substance use, and anxiety, at the start of their episode. The most important factors associated with suicidal behavior within 1 year after the start of an MDD episode were history of suicidal behavior and age, history of substance use and sleep disorders, and care setting in which MDD was diagnosed.
Conclusions and Relevance This cohort study’s findings suggest that high mortality, morbidity, HCRU, and work loss associated with MDD may be substantially accentuated in patients with MDD and suicidal behavior. Use of medication aimed at decreasing the risk of all-cause mortality during MDD episodes should be systematically evaluated to improve long-term outcomes.
According to the World Health Organization, approximately 5% of the adult population worldwide experienced depression in 2021. 1 Depression is associated with increased all-cause mortality. 2 A recent populationwide study showed that all-cause mortality was more than doubled in patients with major depressive disorder (MDD) compared with population controls and that mortality is further increased in patients with treatment-resistant MDD. 3 , 4 Suicidal thoughts or behaviors are recognized as diagnostic criteria for MDD in the DSM-5 , and suicidal behavior, defined as self-inflicted harm with or without concurrent suicidal ideation, has been reported in up to 50% of patients with MDD; the longer the episodes, the higher the occurrence. 5 , 6 Furthermore, suicidal behavior and previous suicide attempts have been shown to increase the risk of death from suicide. Approximately 7% to 13% of patients with nonfatal suicide attempts have been reported to die from suicide at a later time, 7 , 8 and up to 7% of patients with MDD who are in contact with specialized psychiatric care have been reported to die from suicide. 6
However, most patients with MDD are not treated in specialized care, 9 , 10 and studies to date have been limited by nonrandom sampling due to nonuniversal access to health care and/or exclusion of primary care data. Thus, it is not established to what extent the aforementioned estimates are representative of patients with MDD as a whole or to what extent suicidal behavior is a risk factor for all-cause mortality. The focus on a specific cause of death (ie, suicide) may underestimate the overall risk of death in the population of patients with MDD and suicidal behavior. Thus, focusing on suicidal behavior and all-cause mortality in a population-wide observational study may result in more clinically relevant and replicable data. In Sweden, all residents have universal access to health care, 11 with a nominal copayment for health care visits, hospitalizations, and drugs. The opportunities for individual record linkage, together with near-complete information on population health care coverage, including mortality, help to overcome some of the limitations in data that may exist in other countries and from clinical cohorts.
In this study, we investigated the all-cause mortality associated with MDD episodes with suicidal behavior (MDD-SB) compared with MDD episodes without records of suicidal behavior (MDD-non-SB). We also aimed to describe patient clinical characteristics, such as comorbid conditions, treatment patterns, health care resource utilization (HCRU), and work loss. Furthermore, in a separate analysis, we identified risk factors of suicidal behavior in patients with MDD based on information available at the start of an MDD episode.
In this population-based cohort study, we used data from the Stockholm MDD Cohort (SMC), 3 , 4 which comprises all patients diagnosed with MDD according to International Classification of Diseases, Tenth Revision ( ICD-10 ) codes F32 to F33 in any health care setting in the region of Stockholm (approximate population, 2.4 million) between 2010 and 2018. 12 The data in SMC are based on the Regional Healthcare Data Warehouse of Region Stockholm, including information on all individual contacts with health care in Region Stockholm. The information in the data warehouse includes date of death but not cause of death. This project is a part of a framework to facilitate research collaboration between research-based companies and Region Stockholm and registered at the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (European Union Electronic Register of Post-Authorisation Studies No. 256646). The study was approved by the regional ethics committee, Stockholm, Sweden (No. 2018/546-31), with a waiver for informed consent because all analyses were performed using pseudonymized data. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We identified all recorded MDD episodes between January 1, 2012, and December 31, 2017, when patients were aged 18 years or older at the start of the episode (MDD baseline) (eAppendix in Supplement 1 ). Each patient could contribute more than 1 episode. To allow for analyses of MDD baseline conditions, patients residing in Stockholm for 12 months or less before the start of the MDD episode were excluded. We also excluded patients with a history of psychosis, bipolar disorder, manic episode, or dementia. Diagnostic criteria for MDD include suicidal thoughts or attempts (suicidal behavior); therefore, suicidal behavior was defined as ICD-10 codes for intentional self-harm (X60-X84). Diagnoses of harm of undetermined intent ( ICD-10 codes Y10-Y34) were not included in this study. Records in outpatient or inpatient health care settings were collected, and the date of the first recorded diagnosis of suicidal behavior within an MDD episode was set as the index. At the start of an MDD episode (MDD baseline), patients with MDD and suicidal behavior (MDD-SB group) were compared with all patients with MDD. At index, patients in the MDD-SB group were compared with patient with MDD but without records of suicidal behavior (MDD-non-SB group) by matching each patient in the MDD-SB group (ie, cases) on age (within 2 years), sex, year of MDD diagnosis, and sociodemographic status with up to 5 patients in the MDD-non-SB group (ie, controls). To be eligible for matching, controls were required to have an MDD episode duration at least as long as their matched case’s time from the start of MDD until record of first suicidal behavior. Controls were given the same index date as their matched case (eFigure 1 in Supplement 1 ). Definitions of inclusion and exclusion criteria are presented in eTable 1 in Supplement 1 .
The data analysis for this study was performed between February 1 and November 1, 2022. All data management and analyses were performed using R, version 3.6.0 software (R Foundation for Statistical Computing). Patient characteristics were described at MDD baseline and index (date of suicidal behavior). In the time-to-event analyses, patients were censored at first instance of emigration from Stockholm, death, a record of an exclusion criterion, or end of follow-up, whichever came first. The time to first suicidal behavior was calculated as the time from MDD baseline until index, and in this analysis, end dates of MDD episodes also qualified as censoring events. To evaluate the association of suicidal behavior with all-cause mortality, we used the Kaplan-Meier method and Cox proportional hazards regression models. Robust SEs were used to account for nonindependence (ie, that 1 patient could have had >1 case of suicidal behavior per MDD episode). Episodes of MDD-SB and MDD-non-SB were followed up from index until the outcome. In a sensitivity analysis, end dates of MDD episodes were also included as censoring events. Departures from the proportional hazards assumption were evaluated using Schoenfeld residuals.
We analyzed psychiatric comorbid conditions, ongoing antidepressant therapy, HCRU, and work loss from 12 months before to 12 months after the index date. Psychiatric comorbid conditions were expressed as cumulative proportions per month; ie, patients were included the first month they were diagnosed with a psychiatric comorbid condition, and this information was carried forward to all later time points. Ongoing treatment with antidepressant therapy (antidepressants, add-on medication, electroconvulsive therapy [ECT], repetitive transcranial magnetic stimulation, and psychotherapy) (eTable 1 in Supplement 1 ) was calculated as the proportion of patients treated per month. To be defined as receiving ongoing treatment with antidepressant and add-on medication, each patient had to have at least 1 pharmacy dispensation of medication that month or be covered with a medical supply from a previous dispensation. For electroconvulsive therapy, repetitive transcranial magnetic stimulation, or psychotherapy, patients were required to have at least 1 record of a clinical procedure code for that procedure that month. Health care resource utilization was defined as the mean number of outpatient physician visits and inpatient bed days per month, and work loss was defined as the mean number of days not worked per month. Analyses of work loss were performed for patients aged between 20 years and 64 years. Sick leave episodes lasting 14 days or less were not included, as they are not recorded in patient records.
Risk factors for suicidal behavior among patients with MDD were assessed using a study sample restricted to MDD episodes between 2015 and 2017. Only patients residing in Stockholm for 3 years or more prior to the start of the MDD episode were included to ensure a sufficient period of baseline data. Episodes where the start date of the MDD and date of suicidal behavior coincided were excluded. In the model, the outcome of interest was a record of suicidal behavior within 1 year after the start of an MDD episode. Potential risk factors (eTable 2 in Supplement 1 ) were selected based on previous reports and data availability, 13 - 16 and a Cox proportional hazards regression model was fitted following the steps by Harrell 17 (details provided in eFigure 6 in Supplement 1 ). The final prediction model was presented as a nomogram. The importance of each risk factor was measured by partial Wald χ 2 minus the predictor df . We adhered to the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis ( TRIPOD ) statement 18 in reporting of the results of the prediction model.
A total of 158 169 unipolar MDD episodes were identified between January 1, 2012, and December 31, 2017 ( Figure 1 ). Among these episodes, 2240 (1.4%) in 2219 patients had at least 1 record of suicidal behavior (MDD-SB group; mean [SD] patient age, 40.9 [18.6] years; 1415 episodes [63.2%] in women and 825 [36.8%] in men), and 552 (24.6%) of these contained 2 or more records of suicidal behavior. In MDD episodes lasting 5 years or more, 430 of 14 170 (3.0%) had at least 1 suicidal behavior (eFigure 2 in Supplement 1 ). The most common form of suicidal behavior was intentional self-poisoning (eTable 3 in Supplement 1 ). The median time from MDD baseline (ie, from start of episode until first suicidal behavior) was 165 days (IQR, 12-510 days). The matched MDD-non-SB control group included 11 109 MDD episodes in 9574 patients (mean [SD] patient age, 40.8 [18.5] years; 7046 episodes [63.4%] in women and 4063 [36.6%] in men) ( Figure 1 ). Patient characteristics at the time of the first suicidal behavior within an MDD episode (index) for the matched study sample are presented in the Table .
The all-cause mortality rate was 2.5 per 100 person-years at risk for the MDD-SB group and 1.0 per 100 person-years at risk for the MDD-non-SB group, based on 466 deaths. This rate corresponds to a hazard ratio of 2.62 (95% CI, 2.15-3.20) ( Figure 2 ). In a sensitivity analysis, MDD episodes were censored at the end of the MDD episode (eFigure 3 in Supplement 1 ).
Already at the start of the MDD episode, patients in the MDD-SB group appeared different compared with all patients with MDD. For example, they were younger, more often diagnosed while in specialized care, and had higher work loss (eTable 4 in Supplement 1 ). Patients in the MDD-SB group also had a gradual increase in the prevalence of comorbid conditions from approximately 12 months before index (eFigure 4 in Supplement 1 ). This increase was most pronounced for anxiety, stress, substance use, and personality disorders. These differences persisted at index between the MDD-SB and MDD-non-SB groups ( Table ). eFigure 5 in Supplement 1 displays the temporal distribution of monthly HCRU and work loss, with a clear peak at index for the MDD-SB group.
Up until index, 1880 patients (83.9%) in the MDD-SB group and 9012 patients (81.1%) in the MDD-non-SB group were treated with antidepressants ( Table ). The proportion of patients treated with add-on medication (including lithium in 21 patients [0.9%] and 25 patients [0.2%] in the MDD-SB and MDD-non-SB groups, respectively) and ECT was higher among those in the MDD-SB group both at index and 12 months after compared with the MDD-non-SB group. A total of 82 patients (3.8%) in the MDD-SB group received ECT during the index month, and the provision of psychotherapy ranged between 248 (11.5%) and 275 (14.2%) patients starting at the index month and through the 12 months after the index month ( Figure 3 ).
A risk score for factors associated with suicidal behavior within 1 year after the start of an MDD episode (outcome) was calculated using available variables. The 2 most important risk factors for suicidal behavior were a history of suicidal behavior together with age, which had a U-shaped association with the outcome, with individuals younger than 20 years or 70 years or older having the highest risks. The final risk score also included the following factors (in descending order), the presence of which increased the risk for the outcome: history of substance use, history of sleep disorders, health care level in which MDD was diagnosed, history of antidepressant use, and history of anxiety disorders. eFigure 6 in Supplement 1 displays the final prediction model, presented as a nomogram; all variables evaluated for entry are defined in eTable 2 in Supplement 1 . The risk score yielded a C index of 0.78, and the internal bootstrap validation indicated only minimal overfitting. The risk score was well calibrated (eFigure 7 in Supplement 1 ).
In this cohort study, we analyzed more than 158 000 MDD episodes during 6 years, of which 2240 (1.4%) also included suicidal behavior, with an average time from MDD diagnosis to first record of suicidal behavior of less than 6 months. We found that all-cause mortality was more than doubled in adults with MDD who had a diagnosis of suicidal behavior compared with those with MDD without suicidal behavior, which in and of itself is associated with a doubled risk compared with control patients without MDD. 2 , 3 We found an immediate increase in mortality after the first suicidal behavior event, which appeared to be elevated throughout the whole observation period. This suggests that suicidal behavior may be a marker for MDD episodes with an increased risk of mortality; although the SMC data were not linked to information regarding cause of death, and any inference regarding causality remains speculative. However, the incidence of somatic disorders was not increased in the MDD-SB group, indicating that unnatural causes, such as accidents and suicides, may have been the main contributors to the increased mortality.
The proportion of patients with suicidal behavior in our study appears to be lower than in other registry-based studies of patients with MDD 19 and compared with self-reports from a general population. 5 A possible explanation could be the virtually full coverage of the patient population with MDD with data from all health care settings in our study, thus not limiting the sample to populations that could be considered to have a higher risk of suicidal behavior, such as patients treated in hospitals or other specialized settings. To reduce the risk of misclassifications, we also chose a stricter definition of suicidal behavior by only including self-harm with intent diagnosed during an ongoing MDD episode. Although previous studies have shown that suicidal behavior is underdiagnosed, 5 our findings suggest that suicidal behavior in all patients with MDD may not be as common as previously described, although any estimate of suicidal behavior and/or suicide attempt could be subject to uncertainty and methodological considerations. However, in our data, suicidal behavior might be seen as a marker for a subgroup of MDD episodes with more psychiatric comorbidity, higher work loss, and substantially higher all-cause mortality. Thus, developing an evidence-based clinical guideline for both acute and long-term interventions for patients with MDD and suicidal behavior may be warranted.
In our study, the majority of patients were treated with antidepressants at the time of their suicidal behavior, indicating that the treatment may not have been sufficiently effective in ameliorating depressive symptoms and associated suicidal behavior. Although the proportion of patients in the MDD-SB group treated with add-on medications, ECT, and/or psychotherapy increased after the first record of suicidal behavior, the proportions were still low. This finding suggests that treatments for a majority of patients with MDD and suicidal behavior could be improved both before and especially after an suicidal behavior event. Specifically, long-term lithium treatment could be indicated given its suggested association with decreased all-cause mortality in affective disorders. 20 Still, our findings showed that less than 1% of patients with MDD and suicidal behavior had initiated treatment with lithium at the time of their first recorded suicidal behavior.
The baseline prevalence of nonpsychiatric comorbid conditions was lower in patients with MDD and suicidal behavior compared with all patients with MDD. This finding could be explained by the lower age at baseline, as the differences disappeared after matching. At baseline, patients in the MDD-SB group also had greater proportions of anxiety disorders and substance use than the MDD-non-SB group, which have previously been shown to be factors linked to suicide, suicide attempts, and deliberate self-harm. 13 , 15 , 21 - 25 Sleep disorders and substance use disorders have previously been reported to be associated with increased all-cause mortality, 26 , 27 whereas anxiety has not. 28 These specific comorbidities were all found to be associated with suicidal behavior in our data. Personality disorders have been linked to suicidal behavior, 13 and they constituted the highest relative difference in proportions between the MDD-SB group and MDD-non-SB group in our study. In addition, the number of patients with personality disorders almost doubled during the follow-up period, suggesting that they were previously underdiagnosed. In absolute numbers, however, the majority of suicidal behavior events were not linked to personality disorders.
The frequency of health care contacts and high rates of psychiatric comorbidity among patients with MDD who later develop suicidal behavior presents important opportunities for health care to identify and treat these patients at an early stage. A comprehensive approach that also includes diagnosing and addressing these comorbidities, in addition to treating depressive symptoms, would be beneficial. Should evidence-based guidelines be developed on how to best optimize treatments to avoid suicidal behavior, they should include early detection of potential patients with MDD and suicidal behavior. With future evidence-based guidelines in mind, we calculated a risk score based on variables present in our data. The risk score could be explored as a tool to help identify the risk of suicidal behavior among patients with MDD in clinical practice. In the risk score, the most important factors associated with suicidal behavior within 1 year after the start of an MDD episode were history of suicidal behavior and age, followed by history of substance use and sleep disorders. However, it is important to emphasize that the predictive ability of this tool needs to be evaluated in other patient populations and to acknowledge that some important variables, such as family history of psychiatric conditions, were not included. 23 Thus, this tool should be used as a complement and should not supersede a thorough clinical evaluation. It is important to acknowledge that not all patients with suicidal behavior present for treatment, 29 even in a universal health care system, which limits the assessment of risk factors and possibilities for prevention.
This study had several limitations. We defined suicidal behavior as any diagnosis of intentional self-harm ( ICD-10 codes X60-X84) and did not include diagnoses of harm of undetermined intent ( ICD-10 codes Y10-Y34). Even so, this broad definition probably gives a comprehensive picture of suicidal behavior among patients with MDD. An suicidal behavior episode was defined by records of consecutive events, and any additional records of suicidal behavior at later time points were attributed to a new episode. This strict definition might have slightly overestimated the number of suicidal behavior episodes, which should be contrasted to previous reports that suicidal behavior is underdiagnosed. 5 The study population consisted of unipolar MDD episodes and excluded patients with records of bipolar disorder, dementia, or psychosis before or at baseline, and patients who developed any of these conditions later were censored in time-to-event analyses, limiting our ability to draw conclusions on MDD-SB in these patient groups. However, suicidal behavior may also be associated with an increased risk of mortality in other psychiatric disorders. Other comorbid conditions, such as anxiety, substance use, and personality disorders, were included, which is important since they are common among patients with MDD in general, as well as among patients with MDD and suicidal behavior in particular.
In this cohort study, we found that 1.4% of MDD episodes in Stockholm, Sweden, involved records of suicidal behavior, which is lower than previously reported. 6 - 8 Among these patients, the all-cause mortality was more than doubled compared with MDD episodes without records of suicidal behavior. Our results also indicate that patients at risk for suicidal behavior can be identified at an early stage to allow for enhanced monitoring and optimized treatment with the goal of preventing suicidal behavior and reducing mortality.
Accepted for Publication: June 9, 2023.
Published Online: August 16, 2023. doi:10.1001/jamapsychiatry.2023.2833
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Lundberg J et al. JAMA Psychiatry .
Corresponding Author: Johan Lundberg, MD, PhD, Centre for Psychiatry Research, Department of Clinical Neuroscience, Karolinska Institutet, and Stockholm Health Care Services, Region Stockholm, Norra Stockholms Psykiatri, Vårdvägen 3, SE-112 81 Stockholm, Sweden ( [email protected] ).
Author Contributions: Drs Lundberg and Cars had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Lundberg, Cars, Leval, Gannedahl, Själin, Björkholm, Hellner.
Acquisition, analysis, or interpretation of data: Lundberg, Cars, Lampa, Ekholm Selling, Leval, Själin, Björkholm, Hellner.
Drafting of the manuscript: Lundberg, Cars, Lampa, Ekholm Selling, Gannedahl, Björkholm, Hellner.
Critical review of the manuscript for important intellectual content: Lundberg, Cars, Lampa, Ekholm Selling, Leval, Själin, Björkholm, Hellner.
Statistical analysis: Lundberg, Cars, Lampa, Ekholm Selling.
Obtained funding: Leval.
Administrative, technical, or material support: Lundberg, Ekholm Selling, Leval, Björkholm, Hellner.
Supervision: Själin, Hellner.
Conflict of Interest Disclosures: Dr Car reported being a co-owner of Sence Research, which is an independent company in epidemiology and biostatistics; Janssen-Cilag AB has funded Sence Research for statistical analyses within this research project. Dr Lampa reported receiving consulting fees from Biogen outside of the submitted work. Dr Leval reported holding shares from Johnson and Johnson outside the submitted work. No other disclosures were reported.
Funding/Support: This study was funded by Region Stockholm and Janssen-Cilag AB. This research project is part of a framework aimed to facilitate research collaborations between the public health care authorities in Stockholm County, Sweden, and research-based companies. All pharmaceutical companies in Sweden were invited to participate in this depression research program via the pharmaceutical industry trade association. Region Stockholm was the initiator of this research project and governed all research data. Region Stockholm further supported this project with scientific and clinical expertise.
Role of the Funder/Sponsor: The sponsor (research authority) Region Stockholm was responsible for the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Janssen-Cilag participated, provided scientific expertise, and supported the analytic work for this project via an external company in biostatistics (Sence Research). No financial transfers were made between Janssen-Cilag AB and Region Stockholm.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: The authors thank Karolinska University Hospital, Danderyds sjukhus AB, Södersjukhudet AB, TioHundra AB, Södertälje sjukhus, Stockholms läns sjukvårdsområde, and the public Health Care Services Administration for providing data for this study.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Global health
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 13, Issue 10
- Severe psychiatric disturbance and attempted suicide in a patient with COVID-19 and no psychiatric history
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-0270-9369 George Gillett 1 and
- Iain Jordan 2
- 1 Oxford University Clinical Academic Graduate School , University of Oxford , Oxford , UK
- 2 Oxford Psychological Medicine Centre , Oxford University Hospitals NHS Trust , Oxford , UK
- Correspondence to Dr George Gillett; george.gillett{at}live.co.uk
A previously fit and well 37-year-old male healthcare worker presented with confusion, psychotic symptoms and a suicide attempt in the context of a new COVID-19 diagnosis. Following surgical interventions and an extended admission to the intensive care unit, he made a good recovery in terms of both his physical and mental health. A number of factors likely contributed to his presentation, including SARS-CoV-2 infection, severe insomnia, worry, healthcare worker-related stress, and the unique social and psychological stressors associated with the COVID-19 pandemic. This case highlights the need to further characterise the specific psychiatric sequelae of COVID-19 in community settings, and should remind general medical clinicians to be mindful of comorbid psychiatric symptoms when assessing patients with newly diagnosed COVID-19.
- psychotic disorders (incl schizophrenia)
- public health
- infectious diseases
- suicide (psychiatry)
This article is made freely available for use in accordance with BMJ’s website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
https://doi.org/10.1136/bcr-2020-239191
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
COVID-19, caused by SARS-CoV-2 infection, remains an emerging disease with poorly defined psychological sequelae. Previous reports have identified that confusion, low mood, anxiety and insomnia are associated with severe coronavirus infection, 1 although the precise risk factors and mechanisms by which these symptoms develop are unclear.
It has been speculated that healthcare workers may be especially vulnerable to the neuropsychiatric manifestations of COVID-19 due to work-related stress, bereavement and their increased risk of infection. 2 3 Emerging evidence suggests healthcare workers may be at greater risk of depression, anxiety and insomnia during the COVID-19 pandemic, 3 although the prevalence of severe psychiatric symptoms among healthcare workers has not been thoroughly investigated.
We present the case of a 37-year-old healthcare worker presenting with severe psychiatric disturbance and attempted suicide following SARS-CoV-2 infection. We explore a number of potential contributing factors including encephalopathy, severe worry, ethnicity and work-related stress. The case highlights the importance of vigilance towards psychiatric symptoms in patients with SARS-CoV-2 infection in both inpatient and community settings.
Case presentation
The patient is a 37-year-old married man with two young children. Prior to this admission, he had no notable medical or psychiatric history, took no regular medications and had no allergies. He is a mental health nurse and works in the UK, where he has raised a family and lived for a number of years. He is of Black ethnicity. Regarding family history, his sister, aunt and grandfather were described as having experienced psychotic episodes, although the circumstances surrounding these and any subsequent diagnoses are not known.
During the COVID-19 pandemic, the patient experienced a 5-day history of fever, cough, breathlessness and myalgia. He experienced severe insomnia during this period, and reported feeling worried that he may infect his family. He had recently lost a number of patients to COVID-19 in the facility he worked at, which had been severely affected by the pandemic. Later, the patient would recall that he became preoccupied with biblical passages during this period, believing they were connected to the events happening in his life.
After self-isolating at home in line with current guidance, an ambulance was eventually called in relation to his worsening breathlessness. He was assessed by paramedics at home. It was agreed that he did not require hospital review, and he was advised to self-isolate at home.
That night, the patient’s family noted that he became increasingly confused and began acting bizarrely. He reported that he had both seen and heard the devil, and was also observed responding to auditory hallucinations. During the night he became increasingly anxious and was specifically preoccupied about dying and concerned he would infect his family. At approximately 04:00, he began to clean out the garden shed to sleep in, in order to be safely distanced from his children. In a phone-call with a family member, he was reported as being ‘confused’ and ‘paranoid’. He was also incontinent of urine.
Later that morning, the patient presented to the emergency department of a local hospital with ongoing concerns about his breathlessness. Clinical assessment, bloodwork and imaging (chest radiograph and CT of the head) did not indicate a need for admission. A swab test for SARS-CoV-2 was taken, and the patient was advised to return home and continue self-isolating. His family raised concerns about his mental state, but recall that no formal psychiatric assessment was performed.
The patient was driven home by a family member. On return, he went to the bathroom, stating he would wash to avoid infecting his family. Within approximately 20 minutes, his wife heard loud noises. On investigating, she found that the patient had lacerated his neck and jumped from an upstairs window. Emergency service attended the scene; the patient was heard telling clinicians “this is not me”. He was sedated, intubated, fluid resuscitated and transferred to a local trauma centre. On arrival, he was noted to have a deep anterior neck laceration (12 cm by 4 cm) and an open wound of his right knee.
Investigations
CT imaging of the patient’s neck and chest revealed pneumomediastinum and surgical emphysema of the neck secondary to tracheal injury, and ground glass opacification and consolidation in keeping with moderate COVID-19. A CT of the head revealed no intracranial pathology. Fractures of the left radius, left ulna, left and right ankles were noted on imaging, alongside a vertebral compression fracture of L1. Bloodwork revealed an elevated white cell count (24.18×10 9 /L) with lymphopenia (0.51×10 9 /L), normal C reactive protein (1.5 mg/L) and electrolytes within normal range. Toxicology tests (ethanol, paracetamol, salicylate) were all negative. A SARS-CoV-2 PCR test was positive.
During his subsequent intensive care admission, a repeat CT of the head, cerebrospinal fluid (CSF) studies (lactate, glucose, protein, microscopy, cytology, flow cytology and NMDA receptor antibodies) and serology tests (CASPPR2, LGI1, voltage-gated potassium channel and NMDA receptor antibodies, HIV and syphilis) were performed; all were negative.
Differential diagnosis
This patient’s case likely represents either a manifestation of either delirium, a single acute psychotic episode or a manic episode in keeping with bipolar affective disorder. Factors supporting a diagnosis of delirium include the lack of any personal psychiatric history, the rapid onset of symptoms, quick recovery, amnesia and predominance of confusion throughout the event. Meanwhile, the patient’s family history of psychotic episodes may support the diagnosis of a single acute psychotic episode. A manifestation of bipolar-spectrum illness is also possible, given the patient’s apparent decreased need for sleep, increased energy and psychotic symptoms. Regardless, the underlying causes are similar; SARS-CoV-2 infection, severe insomnia, stress, preoccupation and worry are likely to have contributed to the patient’s mental deterioration.
The patient was taken to operating theatres for an anterior tracheal repair and tracheostomy. The injury was noted to involve very deep lacerations of his larynx and neck resulting in severed cricothyroid joints, an open hole in the airway and bilateral external jugular venous haemorrhage. After surgery, he was kept sedated and admitted to the intensive care unit for ongoing support. Orthopaedic open reduction internal fixation and manipulation under anaesthesia were performed for his left radius and ankle fractures 2 days later.
The patient’s intensive care admission was complicated by haemodynamic instability, line sepsis, renal failure, refeeding syndrome and agitation. When sedative agents were reduced, he was noted to be agitated on a number of occasions, resulting in him pulling out his tracheostomy tube. Difficulty weaning sedative agents (propofol and fentanyl) contributed to a prolonged 32-day admission.
Regular olanzapine was commenced alongside PRN diazepam. The latter of these was introduced to facilitate weaning from intravenous sedatives rather than for primary treatment of psychiatric symptoms. Intravenous sedation was gradually weaned and the patient eventually began to wake safely. Communication was difficult due to the patient’s tracheostomy and oxygen requirements, however he smiled when family members visited and video-called, and he engaged with staff appropriately. At a bedside assessment, using a whiteboard to communicate, he calmly introduced himself to the consultant psychiatrist. He was orientated to being in hospital and the current year, and retained information about the exact date. The patient had no recollection of events leading to admission and was surprised to discover that he had jumped from a window. Although appearing tearful at times, he showed no signs of overt distress. He denied any current suicidal thoughts and expressed eagerness to recover and see his family.
The patient was weaned off oxygen support and stepped down to ward-level care. He remained settled, and worked cooperatively with physiotherapists both on and off the ward. His speech improved, and the psychiatry team assessed him on a number of occasions during this period. The patient recalled experiencing frightening disorientation, paranoia and hallucinations on the intensive care unit. It was explained that these are common features of delirium.
Outcome and follow-up
The patient continued to have limited recollection of the events leading up to admission, other than recalling severe worry about SARS-CoV-2 infection, insomnia and some religious preoccupation. He discussed the possibility of psychiatric illness openly and was curious towards a diagnosis to explain the events leading to admission. On the ward, he showed no signs of psychosis or suicidality, although did feel inexplicably tearful on occasion, struggled to concentrate while reading and had fragmented memories of the past week. These symptoms improved within days. At further assessments, he remained fully orientated, remembered previous conversations at each assessment and showed no signs of psychiatric illness. The patient’s tracheostomy was decannulated, and he was discharged on olanzapine, with appropriate medical and community mental health follow-up.
Since his discharge, the patient has remained well. On returning home, he initially experienced flashbacks of the events of deliberate self-harm, although these intrusions have now ceased. He is sleeping well, spending time with his family and showing no signs of agitation. He has been counselled on the importance of sleep and vigilance for signs of recurrence, and continues to take olanzapine while awaiting further community mental health review.
COVID-19 remains an emerging disease, with unknown psychological sequelae. A meta-analysis of severe coronavirus infection identified both delirium and insomnia to be common among such patients. 1 Delirium was especially prevalent despite the relatively young age of the sample. 1 Likewise, a separate analysis of 40 469 patients’ electronic medical records identified insomnia and delirium to be prevalent manifestations of COVID-19. 4
Neuroinflammation, neurotropic SARS-CoV-2 infection, hypoxia, cerebrovascular events and the effect of steroid treatment have all been speculated to act as biological mediators of psychiatric disturbance in COVID-19, although the quality of evidence is poor. 1 5 Previous reports have observed new-onset psychotic symptoms in patients with coronavirus infection, 6–9 although the difficulty of differentiating delirium and psychosis has been noted. 10 The vast majority of evidence focuses on psychiatric presentations in hospitalised patients and may be less generalisable to those with mild or moderate physical symptoms in community settings. 1 In this case, both neuroimaging and CSF studies were normal, although these findings cannot exclude the role of neuroinflammation, neurotropic infection or hypoxia as potential biological mediators of the patient’s psychiatric disturbance.
Evidence supporting an aetiological role for neuroinflammation triggered by COVID-19 includes the finding that patients with psychiatric disorders have elevated serum levels of IgG to human coronaviruses compared with controls, and that this association may be partially specific to psychotic, compared with mood, disorders. 11 Coronavirus strains tested include 229E, HKU1, NL63 and OC43, although to our knowledge, similar studies focused on immunoglobulins against SARS-CoV-2 are yet to be performed.
Neurotropic SARS-CoV-2 infection is also a plausible explanation of the patient’s psychiatric presentation in the above case. The functional receptor by which SARS-CoV-2 enters host cells is the ACE2 receptor, which is expressed in brain endothelium, allowing a plausible mechanism for neurotropic SARS-CoV-2 infection. 12 Peripheral nerve invasion has also been hypothesised as a potential route for neurotropic infection, while neuronal degeneration has been identified in the brains of patients with SARS-CoV infection, suggesting that neurotropism may plausibly mediate the psychiatric manifestations of COVID-19. 13 14
The coagulopathy associated with COVID-19 may also represent a potential aetiological factor in this case. Of particular interest are studies which have identified abnormalities consistent with hypercoagulability in patients with psychosis, and proteomic evidence which suggests complement activation and hypercoagulation may precede psychosis in the general population. 15 Although such evidence is limited, if associations between coagulation abnormalities and psychosis are rigorously established, hypercoagulability may represent a plausible mechanism by which COVID-19 mediates its neuropsychiatric sequelae.
A range of unique psychological and social factors associated with the COVID-19 pandemic may also have contributed to the patient’s presentation. Policy measures may detrimentally affect general population’s mental health regardless of infection through social distancing, decreased physical exercise, unemployment, domestic violence, loss of routine and health anxiety. 16 17 Social stress associated with the pandemic has been implicated in a number of reports of psychotic symptoms in patients without SARS-CoV-2 infection 18 19 and preliminary evidence suggests increased rates of new schizophrenia diagnoses in a region affected by the COVID-19 pandemic. 16
Similarly, social factors may specifically exacerbate the psychiatric consequences of COVID-19 compared with other physical illnesses. Quarantine measures may lead to psychiatric distress and insomnia, 20 while SARS-CoV-2 infection may be associated with greater anxiety symptoms compared with other non-COVID-19 pneumonias. 1 Specific anxieties commonly relate to transmission of the virus to family members and to death. 1
The patient’s occupation as a healthcare worker may have contributed to his presentation. Healthcare workers are thought to be at increased risk of mental ill-health during pandemic situations due to overwork, exhaustion, frustration, bereavement, risk of infection and discrimination. 2 3 Data from the COVID-19 pandemic suggests frontline healthcare workers, especially nursing staff, appear to be especially at risk of experiencing psychological symptoms and insomnia. 3 Specific to this case, the patient had lost a number of patients to COVID-19 at the facility he worked at, which may have contributed to his psychological distress and influenced the nature of his preoccupation and anxiety relating to the transmission of the virus to family members.
Another potentially relevant factor in the patient’s case is his ethnicity. The emerging literature suggests that COVID-19 disproportionately affects BAME (Black, Asian and minority ethnic) communities in terms of prevalence and mortality, 21 and more recently concerns have been expressed about a potentially disproportionate impact on the mental health of such communities. 22 Posited reasons for a racial disparity in mental ill-health include fear of contracting the virus, bereavement of social contacts and the disproportionate impact of social distancing measures on BAME communities. 23 Although the patient did not report any direct discrimination by healthcare workers during the admission, his ethnicity may have contributed to his presentation through the indirect risk factors previously described in the literature. 22 23
Regardless of whether any potential association between COVID-19 and mental illness is mediated through biological, psychological or social factors, this case should make general medical clinicians alert to psychiatric presentations and their associated risk when assessing patients with COVID-19. Of particular concern is a similar case of a man who jumped from a third-floor window during self-isolation with SARS-CoV-2 24 and a number of reports of nurses attempting suicide during the COVID-19 pandemic. 25 Likewise, psychiatrists should be mindful of the contribution of biological, psychological and social factors associated with the COVID-19 pandemic when assessing patients with primarily psychiatric presentations. Such associations are likely to be multifactorial, may require careful assessment and will likely go beyond the projected rise in post-traumatic symptoms associated with critical illness.
As well as aetiology, the treatment detailed in this case is also relevant to the association between SARS-CoV-2 and its psychiatric sequelae. This case adds to two previous reports of manic or psychotic episodes which have responded well to conventional antipsychotic treatments. 14 26 This preliminary evidence may reassure clinicians that COVID-19-associated psychiatric presentations are treatable with established pharmacotherapies. However, as aetiological factors are elucidated, it is possible that more specific therapies are identified for presentations involving psychiatric symptoms. For instance, the hypercoagulable state associated with SARS-CoV-2 infection may represent a potential area of future therapeutic interest.
In conclusion, we report on the case of a 37-year-old man with no psychiatric history, who presented with confusion, psychotic symptoms and a suicide attempt in the context of a new COVID-19 diagnosis. We suggest this case may represent delirium, psychosis or a manic episode, and discuss a number of potential precipitating factors including SARS-CoV-2 infection, severe insomnia, worry and healthcare worker-related stress. The array of psychiatric manifestations associated with COVID-19 remains unclear and the majority of literature focuses on secondary psychiatric symptoms among patients hospitalised for severe infection. This case may therefore highlight the need to further characterise the specific psychiatric sequelae of COVID-19 in community settings, which may be in part achieved by performing case–control serological studies as in previous epidemics. 1
Learning points
General medical clinicians should be alert to psychiatric symptoms in patients recently diagnosed with COVID-19 and their associated risks.
Psychiatrists should be mindful of the wide contribution of biological, psychological and social factors associated with the COVID-19 pandemic which may precipitate or perpetuate primarily psychiatric presentations.
The majority of research literature investigating comorbid psychiatric symptoms in COVID-19 has focused on patients hospitalised for severe infection. There may be an unmet need to characterise the specific psychiatric sequelae of COVID-19 in community settings.
- Rogers JP ,
- Chesney E ,
- Oliver D , et al
- McMahon L , et al
- Spoorthy MS ,
- Pratapa SK ,
- Nalleballe K ,
- Reddy Onteddu S ,
- Sharma R , et al
- Troyer EA ,
- Varatharaj A ,
- Ellul MA , et al
- Leung HCM , et al
- Losada CP , et al
- Ferrando SJ ,
- Klepacz L ,
- Lynch S , et al
- Rentero D ,
- Severance EG ,
- Dickerson FB ,
- Viscidi RP , et al
- Hamming I ,
- Bulthuis MLC , et al
- Li S , et al
- Mawhinney JA ,
- Wilcock C ,
- Haboubi H , et al
- Lo Monaco S , et al
- Zhao M , et al
- Valdés-Florido MJ ,
- López-Díaz Álvaro ,
- Palermo-Zeballos FJ , et al
- Huarcaya-Victoria J ,
- Herrera D ,
- Brooks SK ,
- Webster RK ,
- Smith LE , et al
- Webb Hooper M ,
- Nápoles AM ,
- Pérez-Stable EJ
- Kapilashrami A ,
- Bailey S , et al
- Epstein D ,
- Andrawis W ,
- Lipsky AM , et al
- Komisar JR ,
- Mourad A , et al
Twitter @george_gillett
Contributors Both authors made a substantial contribution to the conception, design, drafting and revising of the article. GG wrote the first draft of the manuscript and IJ supervised the project.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Obtained.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Change Password
Your password must have 6 characters or more:.
- a lower case character,
- an upper case character,
- a special character
Password Changed Successfully
Your password has been changed
Create your account
Forget yout password.
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password
Forgot your Username?
Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username

- Spring 2024 | VOL. 22, NO. 2 Autism Across the Lifespan CURRENT ISSUE pp.147-262
- Winter 2024 | VOL. 22, NO. 1 Reproductive Psychiatry: Postpartum Depression is Only the Tip of the Iceberg pp.1-142
The American Psychiatric Association (APA) has updated its Privacy Policy and Terms of Use , including with new information specifically addressed to individuals in the European Economic Area. As described in the Privacy Policy and Terms of Use, this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences.
Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
Ethics Commentary: Suicide Risk: Ethical Considerations in the Assessment and Management of Suicide Risk
- Rebecca A. Bernert , Ph.D , and
- Laura Weiss Roberts , M.D., M.A.
Search for more papers by this author
Suicide is the tragic outcome of a diverse interplay of biological, psychological, and social factors. Suicide affects all people and has long been considered a complex, but preventable, cause of disease burden throughout the world. Despite improvements in awareness and treatment, suicide continues to account for 1 million deaths annually—one life lost every 40 seconds. Suicide occurs in the general population at a rate of 11.3/100,000 in the United States. Suicide attempts occur even more frequently. For every death by suicide, the Institute of Medicine (IOM) reports that an additional 25 nonfatal suicide attempts (100-200 for youth) are estimated to occur. Suicide attempts are associated with approximately 500,000 emergency room visits every year in the United States alone ( 1 ). Risk for suicide cuts across mental disorders, socioeconomic status, age, and gender, and “psychological autopsy” studies indicate that nearly all suicide decedents have at least one psychiatric disorder at the time of death ( 2 ).
The detection, prediction, and management of suicidality present a diverse array of ethical challenges. Suicidal behaviors, now defined in a standardized nomenclature ( 3 ), exist on a spectrum, ranging in severity from suicidal ideation to suicide attempts to death by suicide. In seeking to prevent self-harm, clinicians ideally will use what have emerged as “best practice” techniques to assess suicide risk and intervene if necessary, yet fear of losing a patient to suicide, and worry surrounding malpractice claims, are significant concerns reported by clinicians ( 4 ). This may result in two kinds of responses: 1) a “better safe than sorry” approach, where suicidal risk is overestimated, and 2) an avoidant or dismissive approach, where risk is inadequately assessed, and thereby underestimated ( 5 ). An overestimation of suicide risk may deprive a patient of their rights and may misuse clinical resources. On the other hand, an underestimation of suicide risk may jeopardize the safety of the patient and increase the liability of the provider ( 6 ). Inaccurate assumptions about best practice treatment of suicidal behaviors may also heighten the fear and worry of clinicians. For example, despite advances in evidence-based suicide risk assessment and treatment, an inaccurate belief may persist that hospitalization is the optimal clinical response to a distressed patient. This is a problem, given the absence of evidence supporting the enduring efficacy of acute hospitalization, particularly compared to randomized controlled behavioral treatment trials reporting reduction of risk using psychosocial outpatient interventions for suicidal behaviors ( 7 , 8 ). Dispelling myths, or inaccurate beliefs that may result in harmful consequences to the patient or clinician, is thus critical within a discussion of ethical considerations on this topic. Ethically and legally, best practice and reasonable care should likewise be distinguished from the prediction of suicide, or the legal construct of foreseeability ( 9 ). Given its low rate of occurrence, suicide is not an outcome that clinicians can reliably predict. Rather, evidence-driven approaches and established guidelines in the assessment and management of suicide risk represent the optimal ethical approach in caring for patients at risk for suicide.
Several cardinal medical ethical principles in psychiatry shape ethical approaches to the care of patients at risk for suicide and inform “best practices” in this aspect of clinical care ( 10 ):
Respect for Persons —a deep regard for an individual’s worth and dignity;
Autonomy —self-governance;
Beneficence —the responsibility to act in a way that seeks to provide the greatest benefit and, for this reason, the notion of clinical excellence is an imperative in fulfilling this principle.
Other key principles include:
Fidelity —faithfulness to the interests of the patient;
Nonmaleficence —primum non nocere (“first, do no harm”);
Veracity —the duty of truth and honesty;
Justice —the act of fair treatment, without prejudice;
Privacy —protection of patients’ personal information; and
Integrity —honorable conduct within the profession.
Best practices in suicide risk assessment and management
Approaching the patient—informed consent.
Informed consent to treatment and risk management may be defined as informing the patient of all procedures that will be used in the evaluation and management of suicide risk, clinical decision-making, and emergency assessment and referral practices ( 9 ). Like evidence-based psychosocial interventions for suicidal behaviors, this process should be highly transparent, collaborative, and initiated at the onset of treatment to disclose ethical and legal responsibilities of the provider, limits to confidentiality, and to enhance understanding of treatment ground rules ( 11 , 12 ). In deeply respecting the rights and dignity of the individual, this process strongly supports the Autonomy of the patient, as well as Respect for Persons .
Informed consent to suicide risk management can be collaboratively described as working together to keep the patient safe. Such language compassionately stresses the equal importance of both the patient and clinician in safety planning. Assessment procedures, routinized clinical-decision making, and specific circumstances prompting an emergency referral should be made unambiguous as part of the informed consent process. Adequate time and effort should be devoted to answering questions and confirming understanding of such procedures. For example, a clinician can inform the patient about questions he or she may expect in a suicide risk assessment, under what circumstances they will be asked, how this information will be used, and any limits to confidentiality. The collaborative, transparent aspect of this approach embraces principles of Privacy and Veracity , as well as the dignity and the self-governing rights of the patient. Beneficence is also represented in informed consent, given that explanation of best-practice assessment both standardizes assessment and routinizes clinical decision-making ( 13 ). In this way, informed consent maximizes benefits, while minimizing risks to the fullest extent possible.
An opportunity to strengthen the therapeutic relationship is inherent to this process. Suicidal ideation is associated with significant distress, yet patients may be reluctant to disclose symptoms because of fear of stigma or judgment. This may promote shame, isolation, and secrecy in treatment. Informed consent of risk assessment and management has the potential to directly address these fears and compassionately correct harmful misperceptions, if present. Providing diagnostic feedback about risk (i.e., education that suicidal ideation is a symptom of depression, among a constellation of other diagnostic criteria) may empower the patient with accurate information about his or her symptoms, diagnosis, and treatment plan, whereas education about suicidal symptom severity and risk categorizations may address fears of involuntary hospitalization. The collaborative and transparent nature of assessments may here again be emphasized, with risk categorizations delineated (e.g., minimal, mild, moderate, serious, imminent risk) ( 14 ). The way in which risk categorizations guide decision-making may also be made explicit to clarify questions about circumstances that would prompt emergency referrals (e.g., informing the patient that referral for involuntary services will only be pursued when risk is judged to be serious/imminent, the patient is offered emergency services on a voluntary basis, and he or she refuses voluntary services).
Undertaking the next steps—assessing and managing patients at-risk
The ability to perform an adequate assessment of suicidality and to manage patients who are at risk for suicide is an essential clinical skill for psychiatrists. Because clinical excellence is vital to fulfilling one’s professional obligations, the ability to assess and manage high-risk patients is also an ethical commitment for psychiatrists. Psychiatric practitioners, acting on knowledge from training years ago, may rely on inadequate interventions, such as the “no-harm contract,” and may not be as knowledgeable about empirically supported behavioral treatments for suicidal behaviors ( 9 , 15 ). Best practice techniques in standardized suicide risk assessment and evidence-based clinical decision-making are strongly rooted in clinical science, and emerging standards that derive from the field of suicidology. Modern clinical practice requires knowledge and use of 1) suicide risk factors and warning signs; 2) standardized suicide risk assessment frameworks, risk categorizations, and decision-tree rules for outpatient management; and 3) suicidal symptom severity scales. For a list of evidence-based guidelines and materials, we refer clinicians to those listed in Figure 1 .
Evidence-based suicide risk assessment frameworks structure the assessment process in an alliance-based and nondefensive manner. Symptom measures (clinician administered or self-reported) are straightforward to use, and they aid the clinician in assessing the severity of suicidal symptoms across empirically derived domains (i.e., onset, duration, frequency, and intensity of suicidal ideation; suicidal intent and planning; history of suicidal behaviors; access to means for a suicide attempt). The structure, severity, and intensity of symptoms translate into quantifiably different risk categorizations, and may be reliably addressed using established measures. For example, the Columbia-Suicide Severity Rating Scale (C-SSRS) is a brief measure of suicidal ideation and behaviors that may be used in clinical practice to assess and regularly monitor suicide risk. It has excellent psychometric properties and is accessible and available in 103 languages; administration training is also offered in its use for research and clinical practice ( Figure 1 ). Among those at high risk for suicide, the use of evidence-based interventions, particularly those informed by cognitive-behavioral frameworks, is associated with a significantly decreased risk for suicide attempts, in some cases, reducing risk by half ( 8 , 16 ). In outpatient management of suicide risk, safety planning may be used to identify emergency resources, as well as cognitive and behavioral coping strategies, for the patient to elicit during a suicidal crisis.
Safety planning is highly tailored to the individual and is patient-driven, preferably with the patient identifying and recording his or her own internal coping strategies, in addition to mental health resources (e.g., contact information for local hospitals and emergency clinics, 24-hour crisis hotlines). Safety planning should be comprehensive, concise, and easily accessible and available to the patient. As with evidence-based psychosocial psychotherapies, safety planning is collaborative, transparent, and stresses agency on the part of the patient during the crisis. This honors the Autonomy of the patient, Respect for Persons , as well as Nonmaleficence, in protecting a patient from harm.
Throughout the processes of suicide risk assessment and the management of patient safety, wise and thoughtful clinicians use additional strategies to uphold the highest standards of care: 1) consultation with colleagues, and possible use of decisions by consensus, for difficult or complex cases; 2) regular documentation (i.e., risk level, action taken, safety planning); 3) diligence surrounding continuity of care, given that attrition in treatment is common, yet dangerous, for this high-risk group; and 4) continued education in suicidology. Beyond these strategies, mental health professionals carry an implicit ethical obligation to work to dispel myths about suicide, raise awareness about suicide prevention, and remove language that may be inaccurate, misleading, and potentially harmful to patients ( 9 ). Removal of harmful language related to suicidal behaviors, and dissemination that promotes suicide prevention, values the principles of Autonomy , Respect for Persons , Beneficence , and Nonmaleficence . Deconstructing misunderstandings about suicide is a clear expression of these ethical ideals. For instance, the myth that suicidal “gestures” should be “ignored” rather than “gratified” with a clinical response should be challenged—a dismissive approach to risk assessment is always inappropriate. When a patient endorses or behaves in a manner that suggests suicidality, it must be taken seriously and should be recognized as an opportunity for intervention that may prevent loss of life. Another harmful myth includes the belief that asking about suicidal thoughts and plans may produce suicidality—that questions regarding suicide create “iatrogenic” conditions. This is not grounded in clinical science. Research suggests that assessing suicidal thoughts and risk regularly and frequently does not exacerbate symptoms ( 17 ). Myths like these may discourage questioning about suicidal ideation and increase stigma and, in this way, thwart intervention and suicide prevention efforts. To help clarify optimal ways of addressing these difficult issues with patients, particularly with subgroups that may have heightened risk, several professional and advocacy organizations have worked together to propose guidelines for reporting on suicide to prevent language or nomenclature that may sensationalize or stigmatize suicide or result in suicide contagion. These guidelines, available online by the Suicide Prevention Resource Center, are an excellent resource for clinicians. One recommendation from such guidelines, which may be easily adopted into our daily nomenclature, is removal of the term “committed suicide” and replacement with “death by suicide.” Rationale is based on the stigma often tied to descriptions of suicide, in this case nuanced by negative connotations of the verb “committed,” as it is typically only used to describe sins or crimes. Dissemination of accurate, nonjudgmental information regarding suicide and its prevention is thus an expression of professional Integrity as well as fulfillment of the obligations of Beneficence and Nonmaleficence . These foundational principles are embraced both in continuing education (e.g., CE credits, curriculum development of residency training) and promotion of suicide prevention awareness.
Case vignette
Jane is a 46-year-old physician employed full-time at an emergency room, where she has worked for 2 years. She very recently ended her marriage of 8 years and has no children. She began feeling depressed around the time of her divorce 6 months ago and sought treatment from a psychiatrist. Jane reports having only a few friends in the area and becoming more isolative following the separation. She states that she felt depressed only one other time in her life—in college, for approximately 1 year.
Diagnosis and treatment
Jane was diagnosed with major depressive disorder—recurrent type with moderate severity—and initiated weekly psychotherapy with a psychiatrist. Jane was prescribed an SSRI, as well as a hypnotic for insomnia. Difficulty falling asleep began during her marital separation. She reports significant distress about the insomnia, which appears worsened by her rotating, extended shift work schedule. Jane recently reported thoughts of suicide—although she quickly stated that she would never act on such thoughts. This prompted questions from her psychiatrist about the frequency and quality of such thoughts, as well as her history of hospitalizations and past suicidal behaviors. She reported that she had been hospitalized once, when she was 20 years old, following a suicide attempt, but noted that she was “all screwed up back then.” The method of the attempt was by overdose, which required medical treatment. Regarding her current symptoms, Jane stated that on several occasions in the past week she thought about driving off the road and “ending it all.” Her psychiatrist asked when the symptoms began, and whether she had made plans for a suicide attempt. Jane denied any plans or preparation for an attempt, and said the thoughts began after signing her divorce papers several weeks ago.
During a session with the psychiatrist, Jane was asked to identify factors that appeared to prompt the suicidal thinking and to identify reasons for living. Jane reported that her divorce papers were a clear trigger, that she felt like a failure in her marriage. She said she felt hopeless about the future. In the remainder of this session, distorted thoughts were challenged and restructured using cognitive behavioral therapy, and the psychiatrist felt that Jane handled this intervention well. When she was asked to identify reasons for living, however, she had greater difficulty. After some time, she identified minimal enjoyment of work and love for her parents as reasons. The session ended with assessment and treatment planning. The psychiatrist asked Jane to rate the severity of her suicidal thoughts, which she described as “mild.” He asked her to agree to call him directly if her symptoms worsened and confirmed their appointment for next week. Jane agreed and appeared amenable to this plan.
Case discussion
In this difficult case, the psychiatrist appears to have had some success in establishing a therapeutic dialogue with the patient. Given the nature of the concerns, the psychiatrist could have taken additional time, however, to talk with the patient about the process of evaluating suicide risk and how they, together, would approach the next steps in understanding her concerns. Informing the patient of this process at the start of treatment presents the opportunity to assess and categorize risk level from the outset of therapy and lay the foundation for ongoing monitoring of symptoms. This conversation, which may be understood as fostering the therapeutic relationship as well as fulfilling informed consent, may promote earlier risk assessment and detection, as well as opportunity to reduce distress and suffering. Jane volunteered information of a deeply personal nature regarding her suicidal thoughts —which she had already been experiencing for 1 week and had contemplated acting on them. Explicit description of risk assessment and management procedures helps both the patient and the clinician, and if introduced at the beginning of treatment, may improve communication and provide structure to assessment and treatment. This “informed consent” conversation may be presented as a standard part of the diagnostic assessment process, even if the patient does not endorse suicidal thoughts initially.
In response to Jane’s endorsement of suicidal thinking, the psychiatrist expressed compassion and inquired directly about the quality and duration of symptoms. The psychiatrist intervened by addressing hopelessness and reasons for living. This intervention was valuable. Suggested additional next steps are noted below.
A formal and comprehensive evaluation of risk factors and suicide warning signs is recommended in this situation. Numerous suicide risk factors are present: divorced marital status; occupation (physician); a recent stressful event or loss (divorce); no children; and a past suicide attempt history. Jane also reported a number of suicide warning signs that should prompt a standardized suicide risk assessment: intense and pervasive suicidal ideation; social isolation; hopelessness; and disturbances in sleep. Addressing these factors would best inform assessment, Jane’s risk level, and the intervention process. For example, Jane’s risk level is raised by the severity of her depression, as well as the presence and severity of past suicidal behaviors, in this case, a suicide attempt that was more lethal in nature (i.e., resulting in physical injury requiring medical attention). Assessing the severity of current suicidal symptoms would have been helpful and important for these reasons. These steps can be readily accomplished using a brief, standardized scale (such as the C-SSRS). This would allow the psychiatrist to easily quantify the severity of symptoms and risk level to guide clinical decision-making and documentation of action taken.
Given Jane’s combination of risk factors and warning signs, the recommended best practice intervention would include construction of a safety plan in session. Although the psychiatrist’s response was in many ways consistent with, and adaptable to, a safety plan (i.e., explicitly addressing hopelessness and reasons for living; asking Jane to call if symptoms worsen and providing his number as a resource), a more formalized intervention is recommended. As a collaborative process, this involves construction of a safety plan tailored to the patient’s individual risk level and coping strategies. A small index card may be used to list emergency resources in the local area, which would include the clinician’s contact information, as well as free 24-hour crisis hotlines (e.g., National Suicide Prevention Lifeline, 1-800-273-TALK), nonemergency support resources (e.g., parents and close confidants whom the patient may call if in need of social support), as well as internal coping strategies (e.g., pleasurable activities, adaptive cognitions, and behavioral strategies that promote coping). Safety planning may also include a listing of protective factors that the patient may draw on as a source of additional support. Because Jane identified closeness to her family as a reason for living and a source of hope, the clinician might consider encouraging Jane to reach out, as part of her safety plan, about how she has been feeling. Documentation of all of the above assessment, risk level, and action taken is recommended.
As a safety precaution, limiting access to means for a suicide attempt would also be recommended in the case of Jane. She has a history of overdose, yet was prescribed a hypnotic for treatment of her insomnia. This is contraindicated. Avoidance of medications with overdose potential is recommended whenever risk is judged to be elevated. Assessing access to medications with potential for overdose, and limiting them wherever possible, is also suggested.
Last, when describing her suicide attempt, Jane used language that may be viewed as derogatory or shameful. In addressing suicide risk assessment, the nature and prevalence of suicidal behaviors, and evidence-based treatments, there may be opportunity to correct misconceptions about suicide and improve treatment. As a collaboration between the patient and the physician, this process facilitates transparency and communication that support the highest level of care.
Author Information and CME Disclosure
Rebecca A. Bernert, Ph.D., Instructor, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, CA.
Dr. Bernert reports no competing interests.
Laura Weiss Roberts, M.D., M.A., Professor, Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, CA.
Dr. Roberts reports: Owner, Investigator: Terra Nova Learning Systems.
1 Centers for Disease Control and Prevention, National Center for Injury Prevention and Control : Web-based Injury Statistics Query and Reporting System (WISQARS): www.cdc.gov/ncipc/wisqars ; August 6, 2012 Google Scholar
2 Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM : Psychological autopsy studies of suicide: a systematic review . Psychol Med 2003 ; 33:395–405 Crossref , Google Scholar
3 Crosby AE, Ortega L, Melanson C : Self-Directed Violence Surveillance: Uniform Definitions and Recommended Data Elements, Version 1.0 . Atlanta, GA, Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2011 Google Scholar
4 Jobes DA, Berman AL : Suicide and malpractice liability: assessing and revising policies, procedures, and practice in outpatient settings . Prof Psychol Res Pr 1993 ; 24:91–99 Crossref , Google Scholar
5 Wingate LR, Joiner TE, Walker RL, Rudd MD, Jobes DA : Empirically informed approaches to topics in suicide risk assessment . Behav Sci Law 2004 ; 22:651–665 Crossref , Google Scholar
6 Bryan CJ, Rudd MD : Advances in the assessment of suicide risk . J Clin Psychol 2006 ; 62:185–200 Crossref , Google Scholar
7 Bryan CG : Empirically-based outpatient treatment for a patient at risk for suicide: the case of “John” . Pragmatic Case Stud Psychother 2007 ; 3:1–40 Google Scholar
8 Comtois KA, Linehan MM : Psychosocial treatments of suicidal behaviors: a practice-friendly review . J Clin Psychol 2006 ; 62:161–170 Crossref , Google Scholar
9 Jobes DA, Rudd DM, Overholser JC, Joiner TE : Ethical and competent care of suicidal patients: contemporary challenges, new developments, and considerations for clinical practice . Prof Psychol Res Pr 2008 ; 39:405–413 Crossref , Google Scholar
10 Roberts LW, Hoop JG, Dunn LB : Ethical aspects of psychiatry , in The American Psychiatric Publishing Textbook of Psychiatry , 5th ed. Edited by Hales REYudofsky SCGabbard GO . Washington, DC, American Psychiatric Publishing, 2008 , pp 1601–1636 Google Scholar
11 Jobes DA : Managing Suicidal Risk: A Collaborative Approach . New York, Guilford Press, 2006 Google Scholar
12 Rudd MD, Joiner T, Brown GK, Cukrowicz K, Jobes DA, Silverman M, Cordero L : Informed consent with suicidal patients: rethinking risks in (and out of) treatment . Psychotherapy (Chic) 2009 ; 46:459–468 Crossref , Google Scholar
13 Joiner TE, Walker RL, Rudd MD, Jobes DA : Scientizing and routinizing the assessment of suicidality in outpatient practice . Prof Psychol Res Pr 1999 ; 30:447–453 Crossref , Google Scholar
14 Rudd MD, Joiner TE, Rajab H : Treating Suicidal Behavior: An Effective Time-Limited Approach . New York, Guilford Press, 2001 Google Scholar
15 Rudd MD, Mandrusiak M, Joiner TE : The case against no-suicide contracts: the commitment to treatment statement as a practice alternative . J Clin Psychol 2006 ; 62:243–251 Crossref , Google Scholar
16 Brown GK, Ten Have T, Henriques GR, Xie SX, Hollander JE, Beck AT : Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial . JAMA 2005 ; 294:563–570 Crossref , Google Scholar
17 Stanley B, Brown G, Brent DA, Wells K, Poling K, Curry J, Kennard BD, Wagner A, Cwik MF, Klomek AB, Goldstein T, Vitiello B, Barnett S, Daniel S, Hughes J : Cognitive-behavioral therapy for suicide prevention (CBT-SP): treatment model, feasibility, and acceptability . J Am Acad Child Adolesc Psychiatry 2009 ; 48:1005–1013 Crossref , Google Scholar
- Sutanaya Pal , M.D. , and
- Seetha Ramanathan , M.D., M.P.A.
- Nataly S. Beck , M.D. , and
- Jacob S. Ballon , M.D. , M.P.H.

Managing Suicidal Thoughts, Behaviors, and Risk in Treatment-Resistant Depression
A range of therapeutic targets are likely to be relevant for reducing risk of suicide in TRD. Here's what you need to know.

Tryfonov_AdobeStock

Suicidal thoughts and behaviors (STBs) are among the most dreaded complications of treatment-resistant depression (TRD), which is associated with elevated risk of death from suicide as well as from other conditions, even when compared with nonresistant depression. 1
According to 1 meta-analysis, the overall incidence of suicide and suicide attempts among adults with TRD is between 2 and 10 times that of individuals with nonresistant depression. 2 Approximately 30% of individuals with TRD attempt suicide at least once in their lifetime, compared with about 15% of those with nonresistant depression. 3 Even when compared with individuals with unipolar depression, patients with a history of TRD should be considered at high risk for STBs.
Risk Factors
Although many years of suicide research has generated a large body of knowledge about risk factors, we still know relatively little about the causal associations among risk factors and STBs, and the mechanisms through which risk factors translate into thoughts, behaviors, and fatal outcomes. As in other areas of clinical medicine, prediction models of suicide that work reasonably well in the general population may not generalize to diverse subpopulations, creating a risk of exacerbating rather than addressing health disparities. 4
While we know a lot about suicide risk factors, we know far less about how to predict imminent risk of suicide, which—given the tragic intractability of suicide death across the past century 5 —remains the holy grail of suicide research.
It remains unclear whether TRD is associated with any unique suicide risk profiles; still-growing knowledge indicates that risk factors for STBs among individuals with TRD closely resemble those for other individuals. For example, prior suicide attempts are the strongest risk factor for suicide death in TRD and in the general population. 6
Moreover, factors often associated with TRD are also independent risk factors for STBs. These factors include early life adversity, personality disorders, anxiety, insomnia, chronic pain, substance use disorders, other co-occurring medical conditions, hopelessness, diminished problem-solving ability, low socioeconomic status, a paucity of social supports, and recent psychiatric hospitalization. 7
While depression is associated with the presence of suicidal thoughts, other factors such as psychiatric comorbidity and impulsivity may be better predictors of STBs and suicide. 8
In terms of psychological components of suicide risk, the influential Interpersonal Theory of Suicide proposed by Joiner et al focuses on 3 interconnected risk factors for suicidal thoughts: “thwarted belongingness,” “perceived burdensomeness,” and “hopelessness.” 9 Although this theory is transdiagnostic, its relevance to the experience of many patients with TRD is clinically compelling.
The growing literature on suicide risk factors suggests that TRD may be associated with increased risk of STBs largely because of its close association with other risk factors for STBs; these factors are often connected with TRD as contributing factors to treatment resistance or as consequences.
The bad news is that managing depression itself may influence only part of the complex risk equation, potentially affecting suicidal thoughts more than acts. The good news is that there may be multiple levers that influence the transition from ideas to behavior. Many of these levers are directly relevant to the comprehensive, multimodal evaluation and care of patients with TRD.
A range of pharmacological, psychological, and neurostimulation therapies have shown promise for reducing STBs including among individuals with TRD. In some studies, the antisuicide effects of treatment have appeared to be somewhat dissociable from the antidepressant effects, though this remains an area of continued inquiry. In addition, the impacts of treatments on suicidal ideation and attempts have been better studied than their impact on suicide deaths.
Finally, in many treatment studies relevant to TRD and STBs, STBs have been assessed primarily as secondary outcome measures in studies not adequately powered to test these outcomes; there remains much need for well-designed studies in TRD cohorts in which STBs are the primary outcomes of interest.
Clozapine: Based largely on the International Suicide Prevention Trial, 10 clozapine was the first medication approved by the US Food and Drug Administration (FDA) to prevent suicidal behavior, specifically in individuals with schizophrenia or schizoaffective disorder.
Because of its substantial adverse effect burden and monitoring requirements, clozapine has not been widely used or studied as an antidepressant adjunct among TRD cohorts. Its superiority in reducing suicide risk compared with newer second-generation antipsychotics approved for antidepressant augmentation in TRD has not been established.
Ketamine and esketamine: Esketamine also carries a specific FDA indication for suicidality (since August 2020), particularly in the context of MDD, following its initial approval for TRD. Although data on the efficacy of intranasal esketamine or intravenous racemic ketamine for suicidality in TRD have been mixed, 11 some studies have shown rapid reduction in suicidal ideation after single or repeated doses, sometimes independent of reduction in other core depressive symptoms.
A topic of further research is whether effects on ideation persist beyond the period of active treatment and whether they translate into fewer suicide attempts and deaths.
Lithium: The potential antisuicide effects of lithium have been reported for several decades. These effects have had some support from large pharmaco-epidemiological studies, particularly among individuals with bipolar disorder. 12
A meta-analysis by Cipriani and colleagues 13 demonstrated reduction in STBs among individuals with unipolar as well as bipolar illness; the authors hypothesized that lithium’s apparent antisuicide benefits may be related to prevention of relapse and/or reduced aggression and impulsivity. No adequate studies to date have compared lithium against other combinations or adjunctive antidepressant strategies in TRD with suicide as a primary outcome.
Buprenorphine: Recent years have seen a resurgence of interest in opioid mechanisms in depression treatment, particularly κ receptor antagonists, which appear to be associated with little or no abuse liability compared with mu agonists.
Although no opioid agents have been approved for major depressive disorder (MDD) or TRD, a small proof-of-concept, placebo-controlled trial of ultralow-dose buprenorphine (mean dose 0.44 mg), a partial μ agonist and κ antagonist, showed rapid onset reduction of suicidal ideation among individuals with depression when added to ongoing pharmacotherapy. 14 This benefit persisted for the 4-week trial, suggesting potential promise in opioid mechanisms to reduce STBs in TRD.
Neurostimulation: Studies on most forms of neurostimulation treatments used in TRD have shown reductions in STBs. These include studies on electroconvulsive therapy, 15-17 repetitive transcranial magnetic stimulation, 18-20 and vagus nerve stimulation. 21
Among investigational neurostimulation treatments, similar preliminary promising results for STBs have been reported with magnetic seizure therapy 22 and transcranial direct current stimulation. 23 Anecdotal reports suggested increased suicide risk among depressed individuals receiving deep brain stimulation 24,25 though this has not been observed in other studies. 26
Psychotherapies: A large body of data suggests that psychological therapies have a role in treating TRD and are often critical in the approach to TRD. 27 Similarly, numerous studies suggest that first-line, evidence-based psychotherapies have a role in reducing risk of STBs.
These include cognitive behavior therapy 28 ; dialectical behavior therapy 29 ; interpersonal psychotherapy 30 ; acceptance and commitment therapy 31 ; and collaborative assessment and management of suicidality, 32 a therapeutic framework specifically designed for patients with suicidality.
Brief and ultrabrief therapy interventions have also been found to be effective. 33 Though promising, most studies have focused on suicidal ideation rather than suicide attempts or deaths, and no controlled trials to our knowledge have focused on STBs specifically in TRD populations.
Managing Risk
Core components in the management of suicide risk among patients with TRD include regular assessment, safety planning, and supporting a hopeful and realistic therapeutic stance.
Assessment of suicide risk: Comprehensive assessment of suicide risk includes appreciation of longer-term demographic and clinical risk factors, identification of current and past suicidal thoughts, and evaluation of potentially impulsive emotional and behavioral responses to stressful circumstances.
Psychiatric practice over the next decade will likely increasingly integrate a range of novel risk assessment and mitigation approaches, including machine learning techniques that scour electronic health records, behavioral tasks to evaluate implicit cognitions, and the use of ecological momentary assessment from digital devices coupled with patient prompts to support coping and help-seeking behaviors and messaging to clinical teams in the context of imminent risk.
Many health systems have adopted standardized suicide risk screens, such as the Columbia-Suicide Severity Rating Scale ( Figure 1 ), which includes questions clinicians use in routine assessments for patients with TRD.
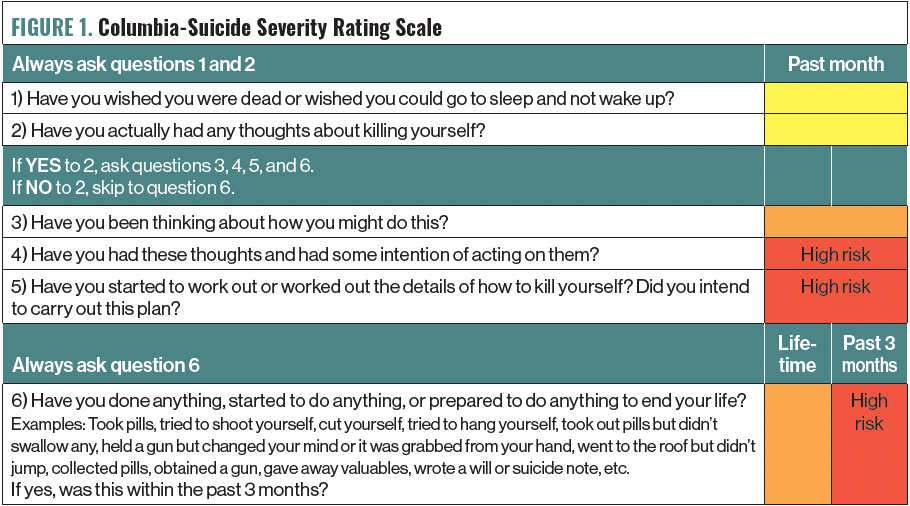
Figure 1. Columbia-Suicide Severity Rating Scale
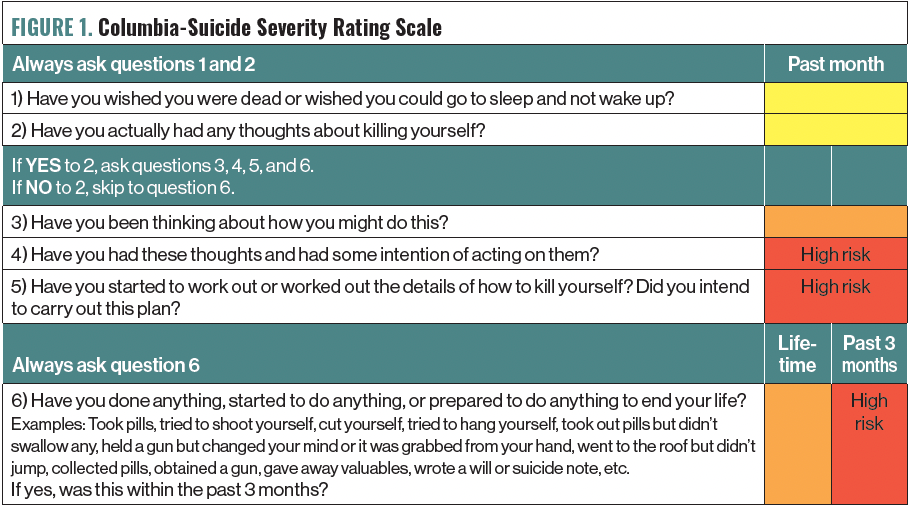
Using a standardized scale, routine assessment, and documentation of suicide risk among patients at elevated risk is integral to good clinical practice.
Safety planning: For the many patients with TRD who are at high risk for suicide, clinicians and patients should collaboratively agree upon a safety plan 34 that typically includes (1) identifying warning signs for suicidal behavior; (2) using coping activities, including relaxation and distraction; (3) reminding of individuals and social situations that can provide distraction; (4) listing contact information for personal supports in a crisis; (5) recording phone numbers for professional and emergency resources and the 988 suicide prevention lifelines; and (6) describing steps to make the environment safer (eg, reducing access to firearms or stockpiled medications).
We also include a section for reasons to live ( Figure 2 ). 35
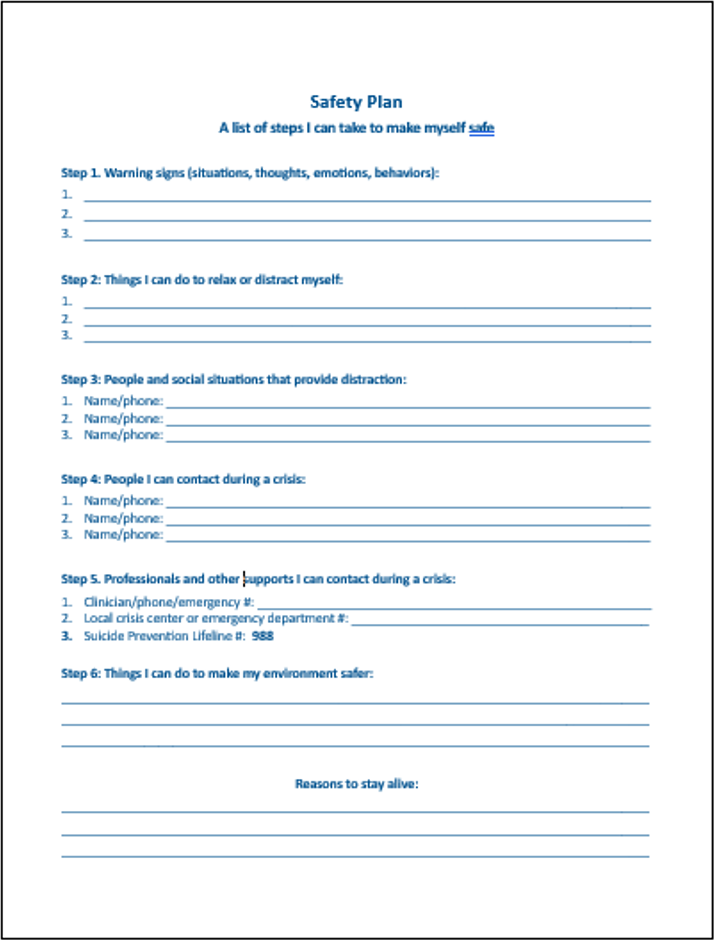
Figure 2. Suicide Safety Plan Template 35
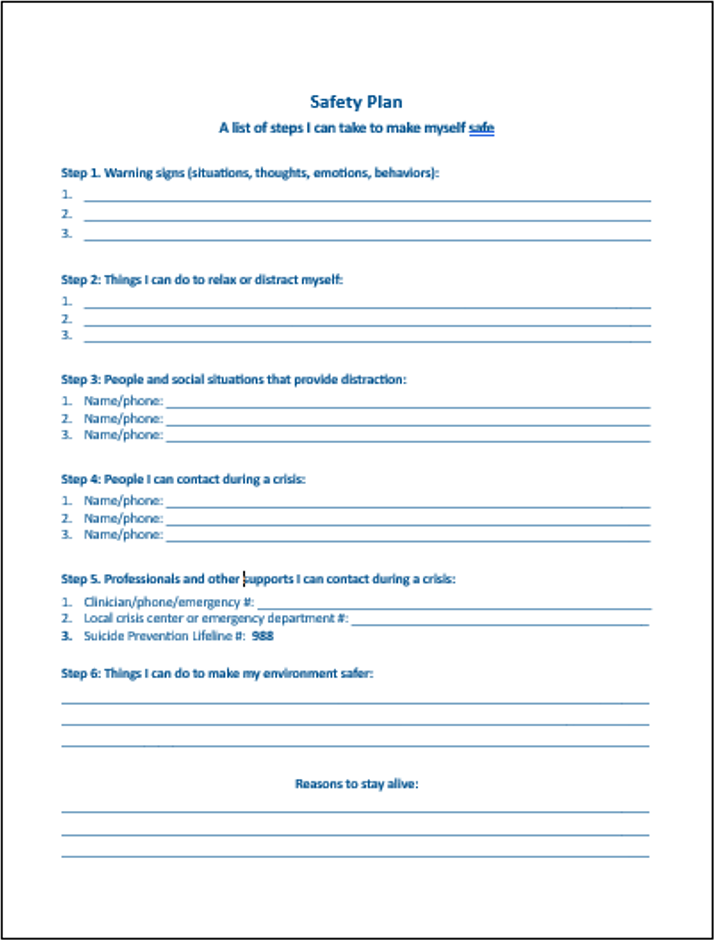
The safety plan should be maintained by the patient and clinician and updated regularly, particularly at key transitions such as hospital discharge.
Therapeutic stance: Recurrently dashed hopes, growing pessimism, self-blame, persistent suffering, and social isolation are often core experiences of individuals with TRD. Joiner’s triad of thwarted belongingness, perceived burdensomeness, and hopelessness are evocative of this experience and the enhanced risk of suicide they entail. Clinicians working with patients with TRD and suicidality are not immune to absorbing the nihilism of the individuals they work with. Aspects of a positive therapeutic approach can be found in the Table .

Table. Aspects of a Therapeutic Approach
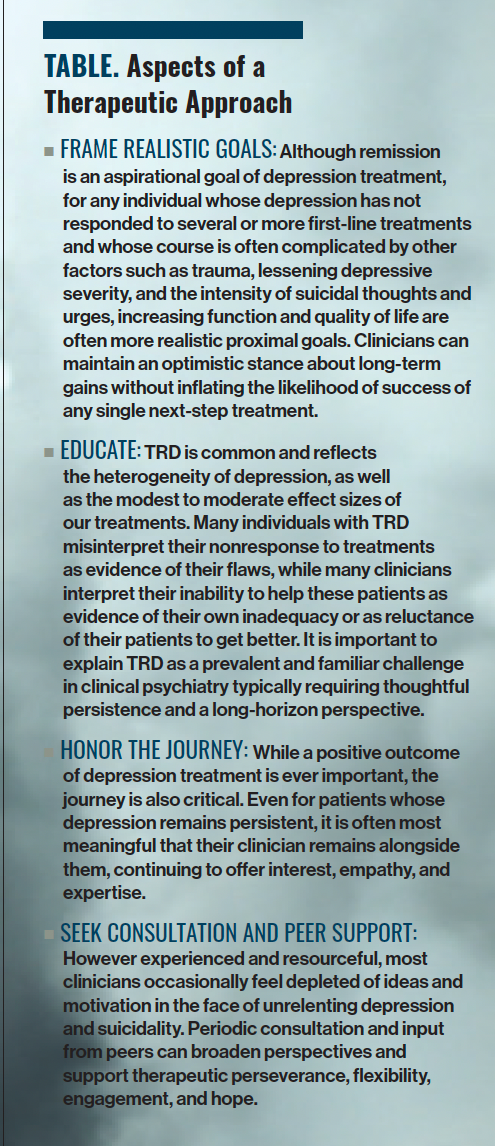
Concluding Thoughts
TRD is associated with elevated risk for STBs and suicide death even when compared with depression without documented resistance. Risk factors for suicide in TRD appear to be largely similar to those in the general population and are often themselves risk factors for and/or consequences of TRD.
A range of therapeutic targets are likely to be relevant for reducing risk of suicide in TRD. Several pharmacotherapies have shown potential antisuicide benefits, including clozapine, ketamine/esketamine, lithium, and buprenorphine. However, research in this area is still evolving with few studies involving active comparators or long-term follow-up and not all focused on TRD.
Most forms of neurostimulation have been associated with reduction in suicidal ideation though this remains a nascent area of research. Several psychotherapies show substantial promise for reducing STBs, though most have focused on suicidal thoughts rather than suicide and none have been adequately studied in TRD.
An optimal therapeutic approach to suicide in TRD involves screening and ongoing assessment, suicide planning, a hopeful but realistic therapeutic stance that emphasizes attainable goals and consistency in the treatment relationship, and recruitment of consultation and peer supports to address therapeutic blind spots and burnout. While TRD is associated with elevated risk of suicide, most individuals with TRD do not attempt suicide and many achieve reduction in suffering and a meaningful quality of life.
Dr Franz is an assistant professor of psychology at the Ferkauf Graduate School of Psychology, Yeshiva University. He is also an assistant professor in the Department of Psychiatry and Behavioral Sciences at Albert Einstein College of Medicine in Bronx, New York. Dr Alpert is chair of the Department of Psychiatry and Behavioral Sciences and professor of psychiatry and behavioral sciences, neuroscience, and pediatrics at the Montefiore Medical Center and Albert Einstein College of Medicine in Bronx, New York.
1. Brenner P, Reutfors J, Nijs M, Andersson TM. Excess deaths in treatment-resistant depression. Ther Adv Psychopharmacol . 2021;11:20451253211006508.
2. Bergfeld IO, Mantione M, Figee M, et al. Treatment-resistant depression and suicidality. J Affect Disord . 2018;235:362-367.
3. Kern DM, Canuso CM, Daly E, et al. Suicide-specific mortality among patients with treatment-resistant major depressive disorder, major depressive disorder with prior suicidal ideation or suicide attempts, or major depressive disorder alone. Brain Behav . 2023;13(8):e3171.
4. Coley RY, Johnson E, Simon GE, et al. Racial/ethnic disparities in the performance of prediction models for death by suicide after mental health visits. JAMA Psychiatry . 2021;78(7):726-734.
5. Suicide. Centers for Disease Control and Prevention National Center for Health Statistics. Reviewed June 26, 2023. Accessed October 19, 2023. https://www.cdc.gov/nchs/hus/topics/suicide.htm#featured-charts
6. Reutfors J, Andersson TM, Tanskanen A, et al. Risk factors for suicide and suicide attempts among patients with treatment-resistant depression: nested case-control study. Arch Suicide Res . 2021;25(3):424-438.
7. Turecki G, Brent DA, Gunnell D, et al. Suicide and suicide risk. Nat Rev Dis Primers . 2019;5(1):74.
8. Franklin JC, Ribeiro JD, Fox KR, et al. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol Bull . 2017;143(2):187-232.
9. Van Orden KA, Witte TK, Cukrowicz KC, et al. The interpersonal theory of suicide. Psychol Rev . 2010;117(2):575-600.
10. Meltzer HY, Alphs L, Green AI, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry. 2003;60(1):82-91.
11. McIntyre RS, Rosenblat JD, Nemeroff CB, et al. Synthesizing the evidence for ketamine and esketamine in treatment-resistant depression: an international expert opinion on the available evidence and implementation. Am J Psychiatry . 2021;178(5):383-399.
12. Hayes JF, Pitman A, Marston L, et al. Self-harm, unintentional injury, and suicide in bipolar disorder during maintenance mood stabilizer treatment: a UK population-based electronic health records study. JAMA Psychiatry . 2016;73(6):630-637.
13. Cipriani A, Hawton K, Stockton S, Geddes JR. Lithium in the prevention of suicide in mood disorders: updated systematic review and meta-analysis. BMJ . 2013;346:f3646.
14. Yovell Y, Bar G, Mashiah M, et al. Ultra-low-dose buprenorphine as a time-limited treatment for severe suicidal ideation: a randomized controlled trial. Am J Psychiatry . 2016;173(5):491-498.
15. Ahmadi N, Moss L, Simon E, et al. Efficacy and long-term clinical outcome of comorbid posttraumatic stress disorder and major depressive disorder after electroconvulsive therapy. Depress Anxiety . 2016;33(7):640-647.
16. Kellner CH, Fink M, Knapp R, et al. Relief of expressed suicidal intent by ECT: a consortium for research in ECT study. Am J Psychiatry . 2005;162(5):977-982.
17. Liang CS, Chung CH, Ho PS, et al. Superior anti-suicidal effects of electroconvulsive therapy in unipolar disorder and bipolar depression. Bipolar Disord . 2018;20(6):539-546.
18. Abdelnaim MA, Langguth B, Deppe M, et al. Anti-suicidal efficacy of repetitive transcranial magnetic stimulation in depressive patients: a retrospective analysis of a large sample. Front Psychiatry . 2020;10:929.
19. Weissman CR, Blumberger DM, Brown PE, et al. Bilateral repetitive transcranial magnetic stimulation decreases suicidal ideation in depression. J Clin Psychiatry . 2018;79(3):17m11692.
20. George MS, Raman R, Benedek DM, et al. A two-site pilot randomized 3 day trial of high dose left prefrontal repetitive transcranial magnetic stimulation (rTMS) for suicidal inpatients. Brain Stimul . 2014;7(3):421-431.
21. Aaronson ST, Sears P, Ruvuna F, et al. A 5-year observational study of patients with treatment resistant depression treated with vagus nerve stimulation or treatment as usual: comparison of response, remission, and suicidality. Am J Psychiatry . 2017;174(7):640-648.
22. Weissman CR, Blumberger DM, Dimitrova J, et al. Magnetic seizure therapy for suicidality in treatment-resistant depression. JAMA Netw Open . 2020;3(8):e207434.
23. Brunoni AR, Junior RF, Kemp AH, et al. Differential improvement in depressive symptoms for tDCS alone and combined with pharmacotherapy: an exploratory analysis from the sertraline vs. electrical current therapy for treating depression clinical study. Int J Neuropsychopharmacol . 2014;17(1):53-61.
24. Foncke EMJ, Schuurman PR, Speelman JD. Suicide after deep brain stimulation of the internal globus pallidus for dystonia. Neurology . 2006;66(1):142-143.
25. Mahgoub NA, Kotbi N. Acute depression and suicidal attempt following lowering the frequency of deep brain stimulation. J Neuropsychiatry Clin Neurosci . 2009;21(4):468.
26. Bergfeld IO, Mantione M, Hoogendoorn ML, et al. Deep brain stimulation of the ventral anterior limb of the internal capsule for treatment-resistant depression: a randomized clinical trial. JAMA Psychiatry . 2016;73(5):456-464.
27. Ijaz S, Davies P, Williams CJ, et al. Psychological therapies for treatment-resistant depression in adults. Cochrane Database Syst Rev . 2018;5(5):CD010558.
28. Gøtzsche P C, Gøtzsche PK. Cognitive behavioural therapy halves the risk of repeated suicide attempts: systematic review. J R Soc Med . 2017;110(10):404-410.
29. Linehan MM, Comtois KA, Murray AM, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Arch Gen Psychiatry . 2006;63(7):757-766.
30. Heisel MJ, Talbot NL, King DA, et al. Adapting interpersonal psychotherapy for older adults at risk for suicide. Am J Geriatr Psychiatry . 2015;23(1):87-98.
31. Tighe J, Nicholas J, Shand F, Christensen H. Efficacy of acceptance and commitment therapy in reducing suicidal ideation and deliberate self-harm: systematic review. JMIR Ment Health . 2018;5(2):e10732.
32. Swift JK, Trusty WT, Penix EA. The effectiveness of the collaborative assessment and management of suicidality (CAMS) compared to alternative treatment conditions: a meta-analysis. Suicide Life Threat Behav . 2021;51(5):882-896.
33. Stanley B, Brodsky B, Monahan M. Brief and ultra-brief suicide-specific interventions. Focus (Am Psychiatr Publ) . 2023;21(2):129-136.
34. Stanley B, Brown GK, Brenner LA, et al. Comparison of the safety planning intervention with follow-up vs usual care of suicidal patients treated in the emergency department. JAMA Psychiatry . 2018;75(9):894-900.
35. Stanley-Brown Safety Planning Intervention. Accessed November 6, 2023. https://suicidesafetyplan.com
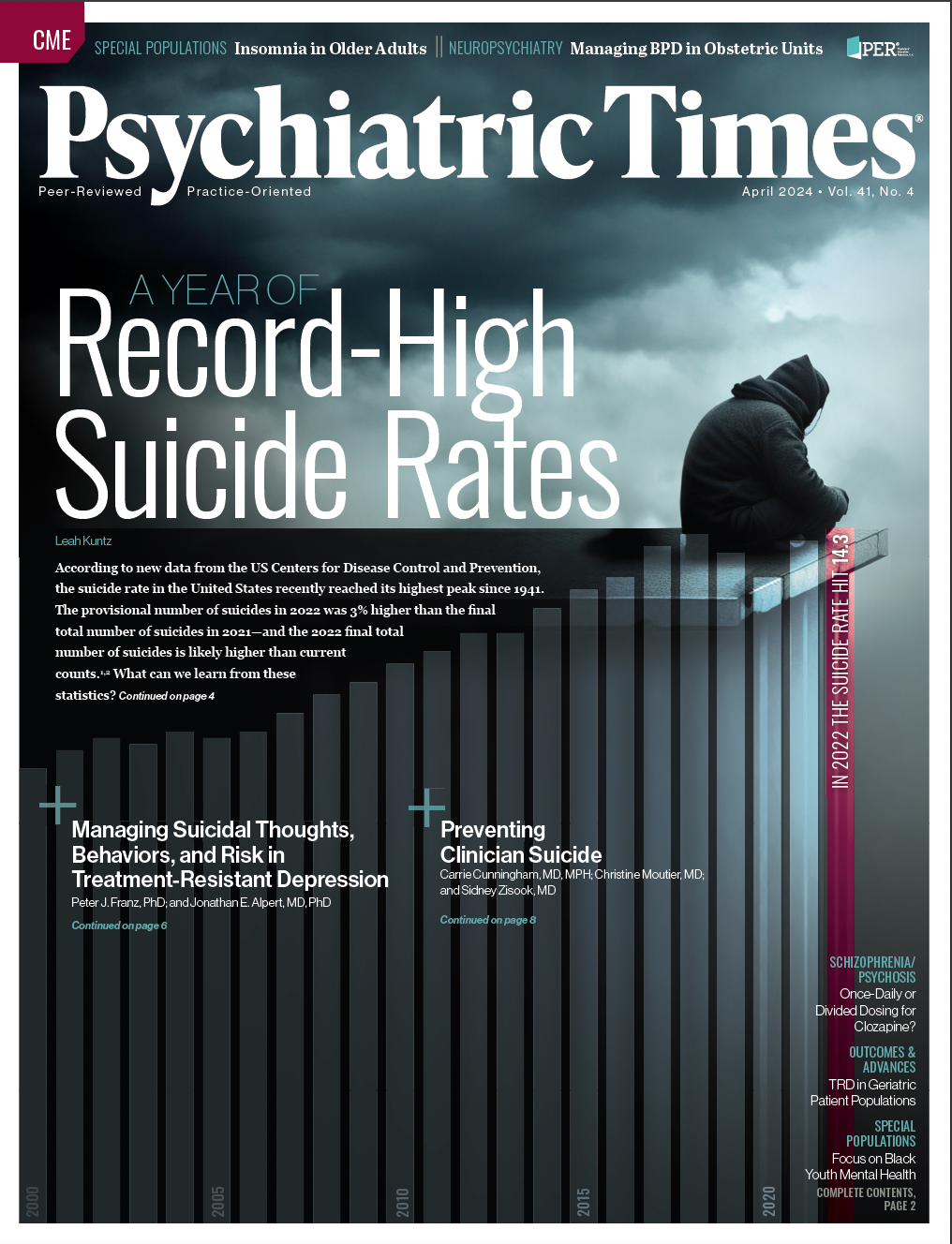
Blue Light Blockers: A Behavior Therapy for Mania
Preventing Clinician Suicide

Treating ‘Morally Objectionable’ Patients

The Week in Review: April 1-5
First Patient Dosed in Phase 2 Clinical Trial of NBI-1070770 for MDD
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

ORIGINAL RESEARCH article
Suicide in psychiatric inpatients— a case–control study.

- 1 Department of Psychiatry, Psychotherapy and Psychosomatics, Medical University of Innsbruck, Innsbruck, Austria
- 2 Department of Psychiatry and Psychotherapy, Center for Health Services Research in Medicine, Erlangen, Germany
- 3 Department of Psychiatry and Psychotherapy B, State Hospital Hall in Tirol, Hall in Tirol, Austria
- 4 Department of Psychiatry, County Hospital Kufstein, Kufstein, Austria
Objective: Psychiatric inpatients constitute a population at considerably increased risk for suicide. Identifying those at imminent risk is still a challenging task for hospital staff. This retrospective case–control study focused on clinical risk factors related to the course of the hospital stay.
Method: Inpatient suicide cases were identified by linking the Tyrol Suicide Register with the registers of three psychiatric hospitals in the state. Control subjects were patients who had also been hospitalized in the respective psychiatric unit but had not died by suicide. Matching variables included sex, age, hospital, diagnosis, and admission date. The study period comprised 7 years. Data were analyzed by the appropriate two-sample tests and by logistic regression.
Results: A total of 30 inpatient suicide cases and 54 control patients were included. A number of factors differentiated cases from controls; after correction for multiple testing, the following retained significance: history of aborted suicide, history of attempted suicide, history of any suicidal behavior/threats, suicidal ideation continuing during hospitalization, no development of prospective plans, no improvement of mood during the hospital stay, and leaving ward without giving notice. Logistic regression identified the latter three variables and history of attempted suicide as highly significant predictors of inpatient suicide.
Conclusions: Preventive measures during hospitalization include thorough assessment of suicidal features, an emphasis on the development of future perspectives, and a review of hospital regulations for patients who want to leave the ward.
Introduction
Mental illness is associated with an increased risk for suicide ( 1 – 4 ). Psychiatric patients requiring admission to hospital treatment constitute a particularly vulnerable population given that they suffer the most severe subjective burden of disease. On the other side, psychiatric inpatients are placed in an environment which provides the most intensive professional therapeutic and caring setting and therefore should constitute the relatively safest one. In recent years, however, a debate as to whether hospitalization is actually protective against suicides or may even have risk-increasing effects on patient suicides has emerged ( 5 , 6 ).
Inpatient suicide is defined as the suicide of a patient while hospitalized and also includes self-inflicted deaths occurring during a granted overnight or weekend leave if the continuation of the inpatient treatment was intended. A suicide occurring on the very same day of but after the patient's planned discharge is commonly (as far as the respective information is assessable) categorized as a post-discharge suicide.
Fortunately, inpatient suicides are relatively rare incidents. In a meta-analysis published a few years ago, the pooled estimate of suicide rates was 147 per 100,000 inpatient years ( 7 ). Related to admissions, rates range between 6 and 566 per 100,000 admissions ( 8 ). Recently, several studies suggested further decreasing rates, although some of these decreases may at least partially just be paralleling nationwide suicide rate declines ( 9 – 11 ). In contrast, Madsen et al. ( 12 ) found increases in inpatient suicide rates of 7.5% annually between 2009 and 2016 for Denmark. Still, the suicide of a hospitalized patient carries a significant emotional, sometimes even traumatic, load not only for the family, relatives, and friends but also for the hospital staff and fellow patients ( 13 – 15 ).
The prediction of a suicidal act, even during the period of inpatient treatment, where trained and experienced mental health staff is available day and night, still remains difficult ( 16 ). This is on one side due to the fluctuating nature of suicidal impulses and the reduced ability to communicate one's feelings inherent to suicidal individuals. On the other side, risk factors identified in studies oftentimes are distal ones, of limited specificity, or otherwise not utilizable for prevention (e.g., male gender, multiple hospitalizations, educational degree, and short duration of illness).
Case–control studies on inpatient suicides are scarce and had investigated varying aspects of suicide risk ( 17 – 20 ). In this study, we investigated risk factors for suicide during psychiatric hospitalization with a focus on variables assessed during the entire course of the hospital stay (i.e., clinical history, mode of and symptomatology at admission, and phase of hospitalization), i.e., predominantly proximal risk factors, comparing inpatient suicides with closely matched control patients.
For this case–control study which was part of a larger project focusing on hospital suicides, data of all suicides which occurred in the Austrian state of Tyrol between 01-Feb-2004 and 31-Jan-2011 were obtained from the Tyrol Suicide Register (TSR). The study period thus comprised 7 years during which a total of 775 suicides were documented in the TSR. The TSR was linked with the hospital registers of the, at that time, three psychiatric units in Tyrol [the respective departments of a university hospital in Innsbruck (UHI), a state hospital in Hall in Tirol (SHH), and a county hospital in Kufstein (CHK)]. Through this procedure, 30 inpatient suicide cases (3.9% of the total number) were identified.
Controls were defined as psychiatric hospital inpatients during the same period who had not died by suicide. Based on the decision to focus on clinical factors related to the hospital stay, a close matching strategy was chosen. Matching variables included sex, age (±max. 9 years), hospital, diagnosis (according to ICD-10 chapters: F1, F2, F3, etc.), and admission date (±max. 1 week). For each case, the respective closest potential controls were chosen. It was aimed to identify two controls for each case. Due to the thorough matching strategy, however, it was not possible to attain the targeted 60 controls, but only 54.
Patient and admission-related data were extracted from available hospital records (e.g., admission record, assessment for restraint measures, and documentation during stay) and included demographic and clinical history variables, symptoms at admission, mode of admission, treatment variables, and symptoms in the last record. Data were extracted by one of the authors only (E-MB-B), a psychologist clinically trained to assess psychopathological alterations.
The study procedure was approved by the Ethics Committee of the Medical University of Innsbruck.
Statistical Analysis
The two groups (inpatient suicides and controls) were compared with regard to the relevant demographic, clinical, and admission-related variables by means of the appropriate two-sample tests. The chi-square test was used for categorical variables, and Student's t -test or Mann–Whitney U -test for continuous variables depending on their distribution (approximately normal or non-normal, respectively). To quantify group differences, effect sizes and corresponding 95% confidence intervals (CI) were calculated, Cohen's d for metric variables and odds ratios (ORs) for dichotomous variables. Statistical testing was performed at a significance level of 0.05 and also at an adjusted α-level to correct for multiple testing by means of the Bonferroni method (α adj. = 0.05/number of tests performed). Both uncorrected and Bonferroni-corrected test results are reported.
To investigate the combined effects of the above variables, we performed a logistic regression analysis with group (inpatient suicide vs. control) as the dependent variable. To avoid problems with multiple testing, only those variables that had attained significance in the univariate analysis with Bonferroni correction were entered as independent variables. Significant predictors were determined by forward stepwise variable selection using the likelihood ratio test. As most of the ORs obtained in the analysis were undetermined due to almost complete separation [some combinations of predictors gave rise to estimated suicide risks of 0% or 100%, see ( 21 )], we summarized our findings in a way that is different than usual. We formed a sum score, S , based on the four significant risk factors, by counting how many of these risk factors were present in the individual patient. Confidence intervals (CIs) for the suicide risk in dependence of S were determined by means of the adjusted Wald method.
Demographic and clinical data of inpatient suicides and controls are displayed in Table 1 . The proportion of females was 60 and 57.4%, respectively. Two thirds of the suicides had occurred in the largest of the three units, the state hospital (SHH). The most frequent diagnosis in both groups was a mood disorder (ICD-10: F3; 70%). Jumping from a height accounted for 40% of the suicide methods applied, followed by hanging and jumping in front of a train (both 23.3%).
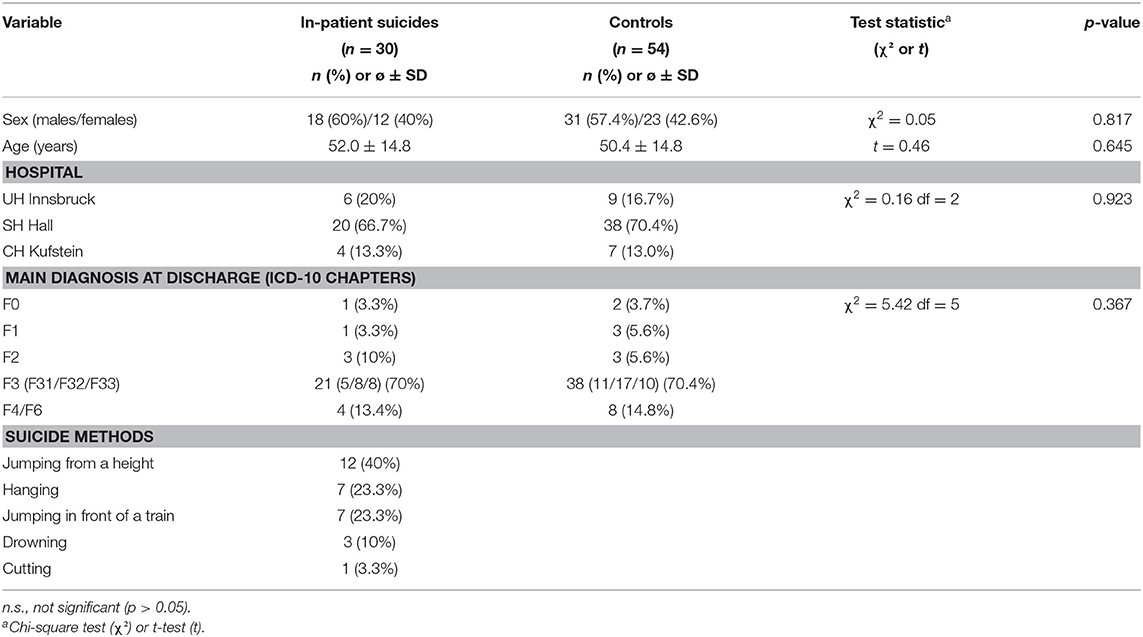
Table 1 . Demographic and clinical data of suicide and control patients.
Nine suicides (30%) occurred inside the hospital itself and only three (10% of the total) in a closed ward. Ten suicides (33.3%) occurred within 1 week after admission, six of these within 3 days and two on the day after admission. Sixteen suicides (53.3%) occurred after the patients had left the ward without informing the staff.
The total inpatient suicide rate was 45.7 per 100,000 admissions. The rates differed considerably between the three units [UHI, 21.8; SHH, 62.8; CHK, 63.1; significant for UHI vs. SHH only ( p = 0.018)].
Variables grouped according to phase of hospital stay (i.e., clinical history, admission, course of hospital stay, and day of discharge) are displayed in Tables 2 , 3 . In short, patients who died by suicide had significantly more often a history of aborted suicide attempts and of any suicidal behavior. They further reported more often suicidal ideation, depressive symptoms, and a current stressor at admission but showed less often aggressive behavior. Suicide patients were significantly more often referred from a nonpsychiatric unit and had less often made contact with the hospital by themselves. They were less often able to develop prospective plans for the time after discharge. In the respective last documentation, we found less often mood improvement and more often suicidal ideation. Only one of the control patients had left the ward without giving notice during the hospital stay while more than half of the inpatient suicide subjects had left the ward without notification at least once.
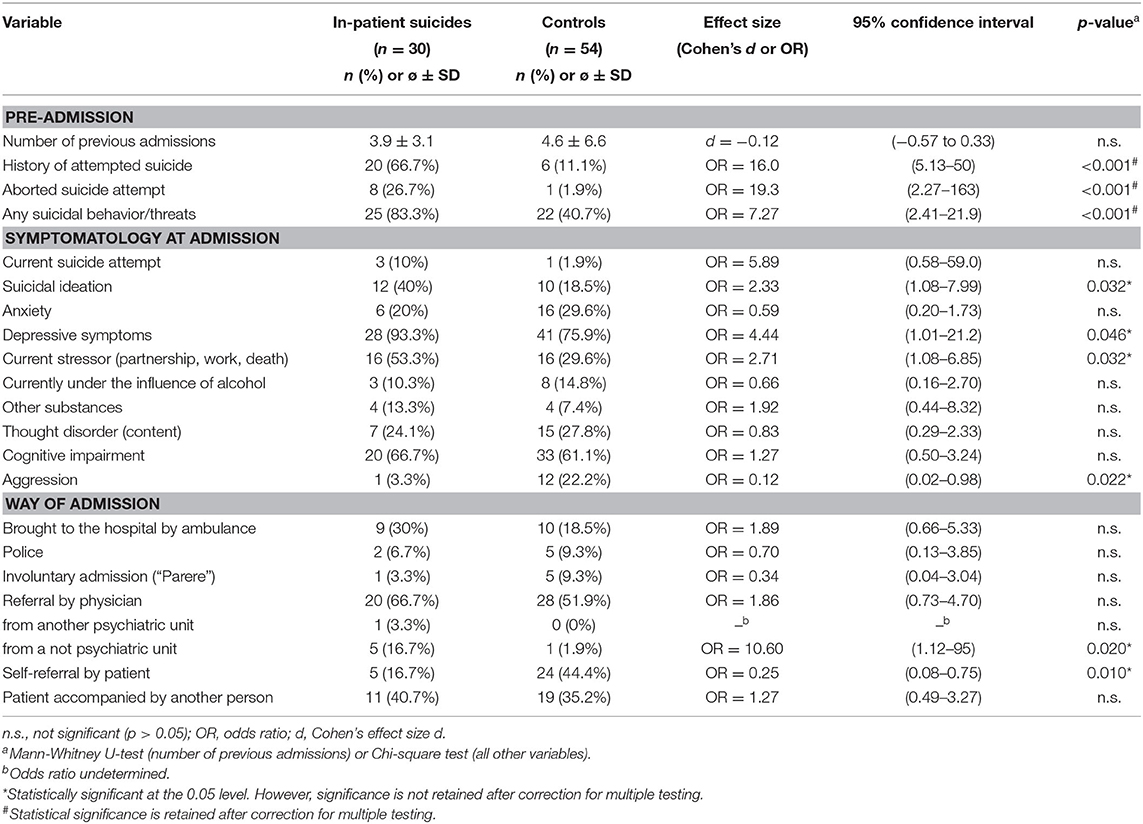
Table 2 . Pre-admission clinical history, symptoms at admission and mode of admission.
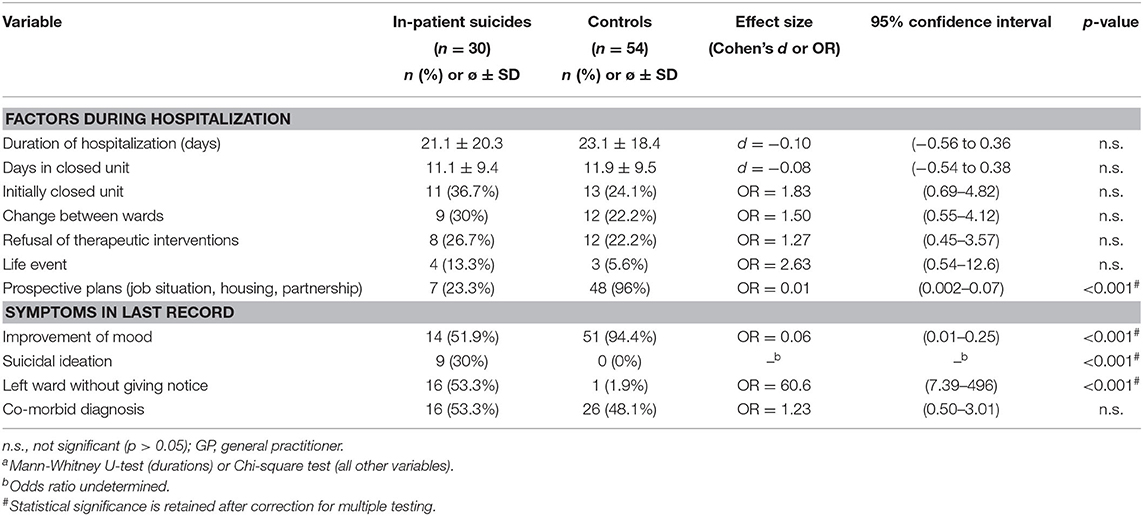
Table 3 . Factors during hospitalization and symptoms in last record.
After correction for multiple testing, the following variables retained significance: history of aborted suicide, history of any suicidal behavior or threats, no prospective plans, no improvement of mood, suicidal ideation continued during hospitalization, and leaving ward without giving notice.
The combined effects of the above variables on the risk of inpatient suicide were investigated by logistic regression. Of the independent variables taken into account (see Statistical Analysis), the following four emerged as significant predictors of an increased suicide risk: history of attempted suicide, leaving ward without notice, no prospective plans (always χ 2 > 14, p <0.001), and no improvement of mood at discharge (χ 2 = 7.36, p = 0.007). Table 4 shows how the risk of suicide increases with the number of risk factors. Among the patients without any of these risk factors, there were no suicides. The corresponding CI indicates a rather small risk of suicide (95% CI: 0–7.6%). Patients with one risk factor had a higher suicide risk (estimate of 28.6%). In the subgroup with two or more risk factors, all patients belonged to the inpatient suicide group. The corresponding 95% CIs indicate that the suicide risk in this group was very high: 75–100% for patients with two and 79–100% for those with three to four risk factors.
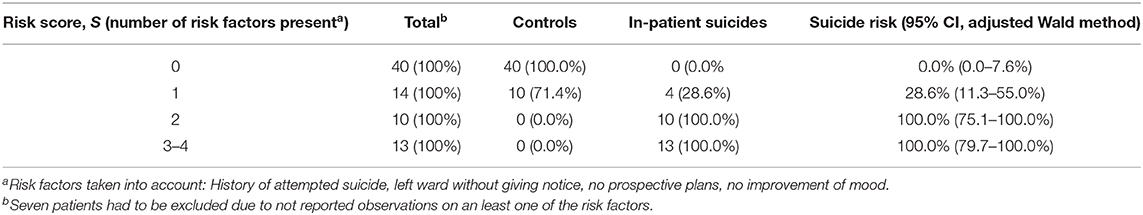
Table 4 . Risk of inpatient suicide in dependence of the number of risk factors.
The data presented here are part of a larger project investigating hospital-associated suicides in the state of Tyrol. A similar case–control procedure was used for a study in post-discharge suicides (i.e., suicides occurring within 12 weeks after discharge from a psychiatric hospital), which identified, among others, a history of suicidal behavior or threats, depression and thought disorder at admission, a change between wards during hospitalization, depression at discharge, and lack of a fixed appointment with a general practitioner for post-discharge care as suicide risk factors ( 22 ). In another study using data from this project, inpatient suicides were compared with post-discharge cases and suicides not recently hospitalized with the result of between-group differences in several variables including gender ratio and suicide method distribution ( 23 ).
In the present study in psychiatric inpatients focusing on clinical factors assessed during the entire hospitalization period, we found a number of significant differences between inpatient suicides and control subjects from which clinical recommendations for suicide prevention measures can be derived.
Of the factors retaining statistical significance after correction for multiple testing, a history of previous suicidal behavior (including aborted suicide attempts) or suicidal threats is one that has previously been reported in a number of studies. This risk factor is true not only for inpatient suicides ( 18 , 24 – 27 ) but also for post-discharge suicides ( 22 , 28 , 29 ). To address this issue, including a thorough assessment of previous suicidal ideation and behavior into the admission interview remains an important measure for the identification of potentially suicidal patients ( 30 ). In addition, this information should be kept in mind throughout the entire therapeutic process during the hospital stay and even beyond.
Several factors relating to symptoms at admission and the mode of admission lost statistical significance when applying a Bonferroni correction for multiple testing, possibly due to limited statistical power. However, most of these still appear to be plausible puzzle pieces in the risk profile of suicidal inpatients. These include suicidal ideation, depressive symptoms, a current stressor (in relation to partnership, work, or loss of a significant other), and less aggressive features at admission as well as being transferred from a nonpsychiatric unit more often and having contacted the hospital by oneself less often. While suicidal and depressive symptoms assessed at admission have been reported in previous studies ( 19 , 20 , 27 ) and are well comprehensible, less aggression noted in the admission record appears to be less obvious. However, although aggression has been related to suicidal behavior ( 31 , 32 ), this association is not unequivocal ( 33 ). From a psychodynamic point of view, the defense (or—in Adlerian terminology—safety) mechanism of turning inhibited aggression toward the self ( 34 ) may obscure aggressive impulses and thus result in a seemingly low-aggression appearance.
For patients who later died by suicide, treating physicians had less often stated in the records that they had generated prospective plans concerning their job situation, housing conditions, or partnership during the hospital stay. In recent years, research has emphasized the importance of such socioeconomic (in addition to clinical and psychological) factors for the occurrence of suicidal ideation and behavior ( 35 – 38 ). In the therapeutic setting in hospitals, it appears of utmost importance to include the interaction of depressive symptoms and other clinical features with the circumstances of the patient's life into treatment planning. Further, a focus should be laid on the development of perspectives to help the patient to free oneself from the suicidal entrapment.
The poorer course of inpatient suicide cases during the hospital stay compared with controls is also reflected by the psychopathological load described in the respective last patient records. Improvement of mood was less often documented and suicidal ideation was more often documented for patients who died by suicide shortly after.
We also found more often a record of a nonarranged leaving of the ward while hospitalized. Such a behavior during the hospital stay has been reported in previous studies to be associated with an increased suicide risk in inpatients ( 18 , 39 – 41 ). As a clinical preventive measure, it might be worth considering to review the respective hospital regulations for patients who want to leave the ward, e.g., for a walk or for smoking. For example, an obligatory presentation to a nurse before leaving the ward may reveal short-term behavioral alterations and lead to at least some form of communication (which is probably the most effective suicide preventive measure in an acute situation). As a further recommendation, establishing standard operating procedures in case a patient absconds from the ward (e.g., having a list of all phone numbers of the patient and significant others at hand, informing the hospital security service, or prompting a search by police) can be derived from these findings.
More than two thirds of the suicides happened outside the hospital. This is in line with the results of previous research ( 17 , 41 , 42 ) and supports the view of a general protective effect of being under professional observation. The hospital setting also, and probably even more importantly, facilitates the possibility to get into contact and communication with other people. This is provided on a ward by trained hospital staff more or less at any time, when suicidal urges acutely emerge.
The inpatient suicide rate of 45.7 per 100,000 admissions found in this study is a considerable reduction of about two thirds compared to the rate of 132 reported in a study we had conducted about 20 years ago in two of the hospitals included here ( 43 ). In contrast, the general suicide rate of Tyrol during the past decades decreased to a much lesser extent, from 21.9/100.000 inhabitants in 1995 to 16.4 in 2019. There was also no significant change in the number of psychiatric hospital beds in the region. The inpatient suicide rate decrease, which was also found in other European countries ( 44 , 45 ), may thus be an actual consequence of suicide preventive measures in psychiatric hospitals.
There were considerable and in part significant differences in inpatient suicide rates between the three hospitals (UHI, 21.8 per 100,000 admissions; SHH, 62.8; CHK, 63.1). Differences between categories of hospitals have so far been reported for post-discharge suicides only ( 22 , 46 ). Potential explanations for the variability in inpatient suicide rates include different patient populations, differences in hospital safety measures, varying patient-to-physician/psychotherapist/nurse ratios, differing regulations concerning overnight and weekend leaves, and many more. It should be noted, however, that case numbers in two of the hospitals were low.
In general, the relatively low number of suicide cases is one of the limitations of this study. Further, clinical information was not assessed with standardized instruments or scales but was extracted retrospectively from routine records, thus, on the other side, reflecting real-world availability of clinical data. Related to this, the required information may not have been documented for all patients, thus potentially leading to some degree of underassessment. The main strength of this study is the thorough matching strategy making it possible to focus on factors associated with the hospital stay, the time immediately preceding suicide.
In conclusion, in this study on psychiatric inpatient suicides, we found a number of factors associated with the risk of suicide. Preventive measures that can be derived from these results include a thorough and periodical assessment of suicidal features during the entire phase of hospitalization (and beyond), an emphasis on the development of future perspectives in the therapeutic working with the patient, and a review of hospital regulations for patients who want to leave or have absconded from the ward.
Data Availability Statement
The datasets presented in this article are not readily available because Personal data. Requests to access the datasets should be directed to Eberhard A. Deisenhammer, eberhard.deisenhammer@i-med.ac.at .
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Medical University of Innsbruck. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
EAD: design of the study writing. E-MB-B: extracting of data. CH: extracting of data. CM: extracting of data. GK: statistics. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Hawton K, Van Heeringen K. Suicide. Lancet . (2009) 373:1372–81. doi: 10.1016/S0140-6736(09)60372-X
CrossRef Full Text | Google Scholar
2. Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. (2014) 13:153–60. doi: 10.1002/wps.20128
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Holmstrand C, Bogren M, Mattisson C, Brådvik L. Long-term suicide risk in no, one or more mental disorders: the Lundby Study 1947-1997. Acta Psychiatr Scand . (2015) 132:459–69. doi: 10.1111/acps.12506
4. Too LS, Spittal MJ, Bugeja L, Reifels L, Butterworth P, Pirkis J. The association between mental disorders and suicide: a systematic review and meta-analysis of record linkage studies. J Affect Disord . (2019) 259:302–13. doi: 10.1016/j.jad.2019.08.054
5. Large MM, Chung DT, Davidson M, Weiser M, Ryan CJ. In-patient suicide: selection of people at risk, failure of protection and the possibility of causation. BJPsych Open . (2017) 3:102–5. doi: 10.1192/bjpo.bp.116.004309
6. Large MM, Kapur N. Psychiatric hospitalization and the risk of suicide. Br J Psychiatry . (2018) 212:269–73. doi: 10.1192/bjp.2018.22
7. Walsh G, Sara G, Ryan CJ, Large M. Meta-analysis of suicide rates among psychiatric in-patients. Acta Psychiatr Scand . (2015) 131:174–84. doi: 10.1111/acps.12383
8. Bowers L, Banda T, Nijman H. Suicide inside. A systematic review of inpatient suicides. J Nerv Ment Dis . (2010) 198:315–28. doi: 10.1097/NMD.0b013e3181da47e2
9. Kapur N, Hunt IM, Windfuhr K, Rodway C, Webb R, Rahman MS, et al. Psychiatric in-patient care and suicide in England, 1997 to 2008: a longitudinal study. Psychol Med . (2013) 43:61–71. doi: 10.1017/S0033291712000864
10. Levi L, Werbeloff N, Pugachova I, Yoffe R, Large M, Davidson M, et al. Has deinstitutionalization affected inpatient suicide? Psychiatric inpatient suicide rates between 1990 and 2013 in Israel. Schizophr Res . (2016) 173:75–8. doi: 10.1016/j.schres.2016.03.007
11. Tseng M-CM, Chang C-H, Liao S-C, Yeh Y-C. Rates and trends of psychiatric inpatient and postdischarge suicides in Taiwan, 2002-2013: a national register-based study. Soc Psychiatry Psychiatr Epidemiol . (2019) 54:591–8. doi: 10.1007/s00127-019-01656-3
12. Madsen T, Erlangsen A, Hjorthøj C, Nordentoft M. High suicide rates during psychiatric inpatient stay and shortly after discharge. Acta Psychiatr Scand. (2020) 142:355–65. doi: 10.1111/acps.13221
13. Walmsley P. Patient suicide and its effect on staff. J Nurs Manage . (2003) 10:24–6. doi: 10.7748/nm2003.10.10.6.24.c1947
14. Fairman N, Thomas LP, Whitmore S, Meier EA, Irwin SA. What did I miss? A qualitative assessment of the impact of patient suicide on hospice clinical staff. J Palliat Med . (2014) 17:832–6. doi: 10.1089/jpm.2013.0391
15. Miller D. When a patient dies by suicide - the physician's silent sorrow. N Engl J Med . (2019) 380:311–3. doi: 10.1056/NEJMp1808910
16. Large M, Myles N, Myles H, Corderoy A, Weiser M, Davidson M, et al. Suicide risk assessment among psychiatric inpatients: a systematic review and meta-analysis of high-risk categories. Psychol Med . (2018) 48:1119–27. doi: 10.1017/S0033291717002537
17. Hunt IM, Kapur N, Webb R, Robinson J, Burns J, Turnbull P, et al. Suicide in current psychiatric in-patients: a case-control study. Psychol Med . (2007) 37:831–7. doi: 10.1017/S0033291707000104
18. Hunt IM, Bickley H, Windfuhr K, Shaw J, Appleby L, Kapur N. Suicide in recently admitted psychiatric in-patients: a case-control study. J Affect Disord . (2013) 144:123–8. doi: 10.1016/j.jad.2012.06.019
19. Lin S-K, Hung T-M, Liao Y-T, Lee W-C, Tsai S-Y, Chen C-C, et al. Protective and risk factors for inpatient suicides: a nested case-control study. Psychiatry Res . (2014) 217:54–9. doi: 10.1016/j.psychres.2014.03.008
20. Lukaschek K, Baumert J, Krawitz M, Erazo N, Förstl H, Ladwig K-H. Determinants of completed railway suicides by psychiatric in-patients: case-control study. Br J Psychiatry . (2014) 205:398–406. doi: 10.1192/bjp.bp.113.139352
21. Heinze G. A comparative investigation of methods for logistic regression with separated or nearly separated data. Stat Med . (2006) 25:4216–26. doi: 10.1002/sim.2687
22. Deisenhammer EA, Behrndt EM, Kemmler G, Haring C, Miller C. Suicide risk factors in patients recently discharged from psychiatric hospital - a case control study. J Clin Psychiatry . (2019) 80:18m12702. doi: 10.4088/JCP.18m12702
23. Deisenhammer EA, Behrndt E-M, Kemmler G, Haring C, Miller C. A comparison of suicides in psychiatric in-patients, after discharge and in not recently hospitalized individuals. Compr Psychiatry . (2016) 69:100–5. doi: 10.1016/j.comppsych.2016.05.003
24. Høyer EH, Licht RW, Mortensen PB. Risk factors of suicide in inpatients and recently discharged patients with affective disorders. A case-control study. Eur Psychiatry . (2009) 24:317–21. doi: 10.1016/j.eurpsy.2008.03.011
25. Madsen T, Agerbo E, Mortensen PB, Nordentoft M. Predictors of psychiatric inpatient suicide: a national prospective register-based study. J Clin Psychiatry . (2012) 73:144–51. doi: 10.4088/JCP.10m06473
26. Lieb M, Palm U, Meyer S, Sarubin N, Mokhtari-Nejad R, Riedel M, et al. Risk factors for inpatient suicide. Psychiatr Praxis . (2014) 41:195–9. doi: 10.1055/s-0033-1343267
27. Large M, Smith G, Sharma S, Nielssen O, Singh SP. Systematic review and meta-analysis of the clinical factors associated with the suicide of psychiatric in-patients. Acta Psychiatr Scand . (2011) 124:18–29. doi: 10.1111/j.1600-0447.2010.01672.x
28. Large M, Sharma S, Cannon E, Ryan C, Nielssen O. Risk factors for suicide within a year of discharge from psychiatric hospital: a systematic meta-analysis. Aust N Z J Psychiatry . (2011) 45:619–28. doi: 10.3109/00048674.2011.590465
29. Haglund A, Lysell H, Larsson H, Lichtenstein P, Runeson B. Suicide immediately after discharge from psychiatric inpatient care: a cohort study of nearly 2.9 million discharges. J Clin Psychiatry . (2019) 80:18m12172. doi: 10.4088/JCP.18m12172
30. Tishler CL, Reiss NS. Inpatient suicide: preventing a common sentinel event. Gen Hosp Psychiatry . (2009) 31:103–9. doi: 10.1016/j.genhosppsych.2008.09.007
31. Gvion Y. Aggression, impulsivity, and their predictive value on medical lethality of suicide attempts: a follow-up study on hospitalized patients. J Affect Disord . (2018) 227:840–6. doi: 10.1016/j.jad.2017.11.033
32. Reich R, Gilbert A, Clari R, Burdick KE, Szeszko PR. A preliminary investigation of impulsivity, aggression and white matter in patients with bipolar disorder and a suicide attempt history. J Affect Disord . (2019) 247:88–96. doi: 10.1016/j.jad.2019.01.001
33. Buitron V, Hartley CM, Pettit JW, Hatkevich C, Sharp C. Aggressive behaviors and suicide ideation in inpatient adolescents: the moderating roles of internalizing symptoms and stress. Suicide Life Threat Behav . (2018) 48:580–8. doi: 10.1111/sltb.12375
34. Ringel E. The presuicidal syndrome. Suicide Life Threat Behav . (1976) 6:131–49. doi: 10.1111/j.1943-278X.1976.tb00328.x
35. Nordt C, Warnke I, Seifritz E, Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000-11. Lancet Psychiatry . (2015) 2:239–45. doi: 10.1016/S2215-0366(14)00118-7
36. Stickley A, Koyanagi A. Loneliness, common mental disorders and suicidal behavior: findings from a general population survey. J Affect Disord . (2016) 197:81–7. doi: 10.1016/j.jad.2016.02.054
37. Roelands M, Vanoverloop J, Maron L, Bilsen J. Socioeconomic risk factors for hospital admittance due to a suicide attempt in Belgium: a population-based study using administrative data. Soc Psychiatry Psychiatr Epidemiol . (2018) 53:53–61. doi: 10.1007/s00127-017-1458-x
38. Zhou L-B, Yao W, Yan Z, Giron MST, Pei J-J, Wang H-X. Impact of effort reward imbalance at work on suicidal ideation in ten European countries: the role of depressive symptoms. J Affect Disord . (2020) 260:214–21. doi: 10.1016/j.jad.2019.09.007
39. Dong JYS, Ho TP, Kan CK. A case-control study of 92 cases of in-patient suicides. J Affect Disord . (2005) 87:91–9. doi: 10.1016/j.jad.2005.03.015
40. Hunt IM, Windfuhr K, Swinson N, Shaw J, Appleby L, Kapur N. Suicide amongst psychiatric in-patients who abscond from the ward: a national clinical survey. BMC Psychiatry . (2010) 10:14. doi: 10.1186/1471-244X-10-14
41. Sakinofsky I. Preventing suicide among inpatients. Can J Psychiatry . (2014) 59:131–40. doi: 10.1177/070674371405900304
42. Ajdacic-Gross V, Lauber C, Baumgartner M, Malti T, Rössler W. In-patient suicide - a 13-year assessment. Acta Psychiatr Scand . (2009) 120:71–5. doi: 10.1111/j.1600-0447.2009.01380.x
43. Deisenhammer EA, DeCol C, Honeder M, Hinterhuber H, Fleischhacker WW. In-patient suicide in psychiatric hospitals. Acta Psychiatr Scand . (2000) 102:290–4. doi: 10.1034/j.1600-0447.2000.102004290.x
44. Madsen T, Nordentoft M. Changes in inpatient and postdischarge suicide rates in a nationwide cohort of Danish psychiatric inpatients, 1998-2005. J Clin Psychiatry . (2013) 74:e1190–e1194. doi: 10.4088/JCP.13m08656
45. Wolfersdorf M, Vogel R, Vogl R, Grebner M, Keller F, Purucker M, et al. Suicide in psychiatric hospitals. Results, risk factors and therapeutic measures [in German]. Nervenarzt . (2016) 87:474–82. doi: 10.1007/s00115-016-0111-3
46. Lin H-C, Lee H-C, Kuo N-W, Chu C-H. Hospital characteristics associated with post-discharge suicide of severely depressed patients. J Affect Disord . (2008) 110:215–21. doi: 10.1016/j.jad.2008.01.030
Keywords: suicide risk, in-patients, psychiatric hospital, hospitalization, admission
Citation: Deisenhammer EA, Behrndt-Bauer E-M, Kemmler G, Haring C and Miller C (2020) Suicide in Psychiatric Inpatients— A Case–Control Study. Front. Psychiatry 11:591460. doi: 10.3389/fpsyt.2020.591460
Received: 04 August 2020; Accepted: 23 November 2020; Published: 21 December 2020.
Reviewed by:
Copyright © 2020 Deisenhammer, Behrndt-Bauer, Kemmler, Haring and Miller. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eberhard A. Deisenhammer, eberhard.deisenhammer@i-med.ac.at
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- Undergraduate Admissions
- Graduate Admissions
- Teacher Certification Options
- International Admissions Information
- Financial Aid & Scholarships
- Undergraduate Majors and Minors
- Master’s Programs
- Certificates of Advanced Study
- Doctoral Programs
- Online, Hybrid, and Flexible Programs
- Faculty and Academic Advising
- Career Services and Certification
- Undergraduate Peer Advisors
- Student Organizations
- Learning Communities
- For Families
- Study Abroad
- Field Placements & Internships
- Bridge to the City
- Spector/Warren Fellowship
- Orange Holmes Scholars
- Engaged BIPOC Scholar-Practitioner Program
- Research News
- Faculty Bookshelf
- Faculty Publications
- Grants & Awards
- Doctoral Dissertations
- Research Resources and Support
- Office of Professional Research and Development
- Atrocity Studies Annual Lecture
- Antiracist Algebra Coalition
- Ganders Lecture Series
- InquiryU@Solvay
- Intergroup Dialogue Program
- Otto’s Fall Reading Kickoff
- Psycho-Educational Teaching Laboratory
- The Study Council
- Writing Our Lives
- Center for Academic Achievement and Student Development
- Center on Disability and Inclusion
- Center for Experiential Pedagogy and Practice
- Latest News
- Upcoming Events
- Education Exchange
- Get Involved
- Advisory Board
- Tolley Medal
- Administration
- From the Dean
- Convocation
- Accreditation
- Request Info
- Grants & Awards
Suicide Risk: Case Studies and Vignettes
Identifying warning signs case study.
Taken from Patterson, C. W. (1981). Suicide. In Basic Psychopathology: A Programmed Text.
Instructions: Underline all words and phrases in the following case history that are related to INCREASED suicidal risk. Then answer the questions at the end of the exercise.
History of Present Illness
The client is a 65-year-old white male, divorced, living alone, admitted to the hospital in a near comatose condition yesterday because of an overdose of approximately thirty tablets of Valium, 5 mgm, combined with alcoholic intoxication. The client was given supportive care and is alert at the present time.
A heavy drinker, he has been unemployed from his janitorial job for the past three months because of his drinking. He acknowledges feeling increasingly depressed since being fired, and for the past two weeks has had insomnia, anorexia, and a ten pound weight loss. He indicates he wanted to die, had been thinking of suicide for the past week, planned the overdose, but had to “get drunk” because “I didn’t have the guts” [to kill myself]. He is unhappy that the attempt failed, states that, “nobody can help me” and he sees no way to help himself. He denies having any close relationships or caring how others would feel if he committed suicide (“who is there who cares?”). He views death as a “relief.” His use of alcohol has increased considerably in the past month. He denies having any hobbies or activities, “just drinking.”
Past Psychiatric History
Hospitalized in 1985 at Pleasantview Psychiatric Hospital for three months following a suicide attempt after his fourth wife left him. Treated with ECT, he did “pretty good, but only for about two years” thereafter.
Social History
An only child, his parents are deceased (father died by suicide when client was eight years old; mother died of “old age” two years ago). Raised in Boston, he moved to Los Angeles at twenty-one and has lived here since. Completed eighth grade (without any repeat) but quit to go to work (family needed money). Has never held a job longer than two years, usually quitting or being fired because of “my temper.” Usually worked as a laborer. Denies any physical problems other than feeling “tired all the time.” Currently living on Social Security income, he has no other financial resources. He received a bad conduct discharge from the army after three months for “disobeying an order and punching the officer.” He has had no legal problems other than several arrests in the past two years for public intoxication. Married and divorced four times, he has no children or close friends.
Mental Status Examination
65 y.o. W/M, short, thin, grey-haired, unkempt, with 2-3 day-old beard, lying passively in bed and avoiding eye contact. His speech was slow and he did not spontaneously offer information. Passively cooperative. Little movement of his extremities. His facial expression was sad and immobile.
Thought processes were logical and coherent, and no delusions or hallucinations were noted. Theme of talk centered around how hopeless the future was and his wishes to be dead. There were no thoughts about wishing to harm others.
Mood was one of depression. He was oriented to person, place, and time, and recent and remote memory was intact. He could perform simple calculations and his general fund of knowledge was fair. His intelligence was judged average.
Diagnostic Impression
- drug overdose (Valium and alcohol)
- Dysthymic Disorder (depression)
- Substance Use Disorder (alcohol)
Questions for Exercise
You have interviewed the client, obtained the above history, and now have to make some decisions about the client. He wants to leave the hospital.
- Is he a significant risk for suicide?
- discharging him as he wishes and with your concurrence?
- discharging him against medical advice (A.M.A.)?
- discharging him if he promises to see a therapist at a nearby mental health center within the next few days?
- holding him for purposes of getting his psychiatric in-client care even though he objects?
- Discuss briefly why you would not have chosen the other alternatives in question #2.
Identifying Warning Signs Case Study: Feedback/Answers
The client is a 65-year-old white male , divorced , living alone , admitted to the hospital in a near comatose condition yesterday because of an overdose of approximately thirty tablets of Valium, 5 mgm, combined with alcoholic intoxication. The client was given supportive care and is alert at the present time. A heavy drinker , he has been unemployed from his janitorial job for the past three months because of his drinking. He acknowledges feeling increasingly depressed since being fired, and for the past two weeks has had insomnia and a ten pound weight loss . He indicates he wanted to die, had been thinking of suicide for the past week, planned the overdose, but had to “get drunk” because “I didn’t have the guts” [to kill myself]. He is unhappy that the attempt failed , states that, “ nobody can help me ” and he sees no way to help himself. He denies having any close relationships or caring how others would feel if he committed suicide (“who is there who cares?”). He views death as a “relief.” His use of alcohol has increased considerably in the past month. He denies having any hobbies or activities , “just drinking.”
Hospitalized in 1985 at Pleasantview Psychiatric Hospital for three months following a suicide attempt after his fourth wife left him . Treated with ECT, he did “pretty good, but only for about two years” thereafter.
An only child, his parents are deceased ( father died by suicide when client was eight years old; mother died of “old age” two years ago). Raised in Boston, he moved to Los Angeles at twenty-one and has lived here since. Completed eighth grade (without any repeat) but quit to go to work (family needed money). Has never held a job longer than two years , usually quitting or being fired because of “ my temper .” Usually worked as a laborer. Denies any physical problems other than feeling “tired all the time.” Currently living on Social Security income, he has no other financial resources . He received a bad conduct discharge from the army after three months for “disobeying an order and punching the officer.” He has had no legal problems other than several arrests in the past two years for public intoxication. Married and divorced four times , he has no children or close friends .
65 y.o. W/M, short, thin, grey-haired, unkempt, with 2-3 day-old beard, lying passively in bed and avoiding eye contact. His speech was slow and he did not spontaneously offer information . Passively cooperative. Little movement of his extremities. His facial expression was sad and immobile. Thought processes were logical and coherent, and no delusions or hallucinations were noted. Theme of talk centered around how hopeless the future was and his wishes to be dead . There were no thoughts about wishing to harm others. Mood was one of depression . He was oriented to person, place, and time, and recent and remote memory was intact. He could perform simple calculations and his general fund of knowledge was fair. His intelligence was judged average.
- Is he a significant risk for suicide? Yes. The client presents a considerable suicidal risk, with respect to demographic characteristics, psychiatric diagnosis and mental status findings.
- Discuss briefly why you would not have chosen the other alternatives in question #2. The client appears to be actively suicidal at the present time,and may act upon his feelings. Nothing about his life has changed because of his attempt. He still is lonely, with limited social resources. He feels no remorse for his suicidal behavior and his future remains unaltered. He must be hospitalized until some therapeutic progress can be made.
Short-Term Suicide Risk Vignettes
*Case study vignettes taken from Maris, R. W., Berman, A. L., Maltsberger, J. T., & Yufit, R. I. (Eds), (1992). Assessment and prediction of suicide. New York: Guilford. And originally cited in Stelmachers, Z. T., & Sherman, R. E. (1990). Use of case vignettes in suicide risk assessment. Suicide and Life-Threatening Behavior, 20, 65-84.
The assessment of suicide risk is a complicated process. The following vignettes are provided to promote discussion of suicide risk factors, assessment procedures, and intervention strategies. The “answers” are not provided, rather students are encouraged to discuss cases with each other and faculty. Two examples of how discussions may be facilitated are provided.
37-year-old white female, self-referred. Stated plan is to drive her car off a bridge. Precipitant seems to be verbal abuse by her boss; after talking to her nightly for hours, he suddenly refused to talk to her. As a result, patient feels angry and hurt, threatened to kill herself. She is also angry at her mother, who will not let patient smoke or bring men to their home. Current alcohol level is .15; patient is confused, repetitive, and ataxic. History reveals a previous suicide attempt (overdose) 7 years ago, which resulted in hospitalization. After spending the night at CIC and sobering, patient denies further suicidal intent.
16-year-old Native American female, self-referred following an overdose of 12 aspirins. Precipitant: could not tolerate rumors at school that she and another girl are sharing the same boyfriend. Denies being suicidal at this time (“I won’t do it again; I learned my lesson”). Reports that she has always had difficulty expressing her feelings. In the interview, is quiet, guarded, and initially quite reluctant to talk. Diagnostic impression: adjustment disorder.
49-year-old white female brought by police on a transportation hold following threats to overdose on aspirin (initially telephoned CIC and was willing to give her address). Patient feels trapped and abused, can’t cope at home with her schizophrenic sister. Wants to be in the hospital and continues to feel like killing herself. Husband indicates that the patient has been threatening to shoot him and her daughter but probably has no gun. Recent arrest for disorderly conduct (threatened police with a butcher knife). History of aspirin overdose 3 years ago. In the interview, patient is cooperative; appears depressed, anxious, helpless, and hopeless. Appetite and sleep are down, and so is her self-esteem. Is described as “anhedonic.” Alcohol level: .12.
23-year-od white male, self-referred. Patient bought a gun 2 months ago to kill himself and claims to have the gun and four shells in his car (police found the gun but no shells). Patient reports having planned time and place for suicide several times in the past. States that he cannot live any more with his “emotional pain” since his wife left him3 years ago. This pain has increased during the last week, but the patient cannot pinpoint any precipitant. Patient has a history of chemical dependency, but has been sober for 20 months and currently goes to AA.
22-year-old black male referred to CIC from the Emergency Room on a transportation hold. He referred himself to the Emergency Room after making fairly deep cuts on his wrists requiring nine stitches. Current stress is recent breakup with his girlfriend and loss of job. Has developed depressive symptoms for the last 2 months, including social withdrawal, insomnia, anhedonia, and decreased appetite. Blames his sister for the breakup with girlfriend. Makes threats to sister (“I will slice up that bitch, she is dead when I get out”). Patient is an alcoholic who just completed court-ordered chemical dependency treatment lasting 3 weeks. He is also on parole for attempted rape. There is a history of previous suicide attempts and assaultive behavior, which led to the patient being jailed. In the interview, patient is vague regarding recent events and history. He denies intent to kill himself but admits to still being quite ambivalent about it. Diagnostic impression: antisocial personality.
19-year-old white male found by roommate in a “sluggish” state following the ingestion of 10 sleeping pills (Sominex) and one bottle of whiskey. Recently has been giving away his possessions and has written a suicide note. After being brought to the Emergency Room, declares that he will do it again. Blood alcohol level: .23. For the last 3 or 4 weeks there has been sleep and appetite disturbance, with a 15-pound weight loss and subjective feelings of depression. Diagnostic impression: adjustment disorder with depressed mood versus major depressive episode. Patient refused hospitalization.
30-year-old white male brought from his place of employment by a personnel representative. Patient has been thinking of suicide “all the time” because he “can’t cope.” Has a knot in his stomach; sleep and appetite are down (sleeps only 3 hours per night); and plans either to shoot himself, jump off a bridge, or drive recklessly. Precipitant: constant fighting with his wife leading to a recent breakup (there is a long history of mutual verbal/physical abuse). There is a history of a serious suicide attempt: patient jumped off a ledge and fractured both legs; the precipitant for that attempt was a previous divorce. There is a history of chemical dependency with two courses of treatment. There is no current problem with alcohol or drugs. Patient is tearful, shaking, frightened, feeling hopeless, and at high risk for impulsive acting out. He states that life isn’t worthwhile.
Vignette Discussion Examples
Vignette example 1.
Twenty-six year old white female phoned her counselor, stated that she might take pills, and then hung up and kept the phone off the hook. The counselor called the police and the patient was brought to the crisis intervention center on a transportation hold. Patient was angry, denied suicidal attempt, and refused evaluation; described as selectively mute, which means she wouldn’t answer any of the questions she didn’t like.
Facilitator: How high a risk is this person for committing suicide? Low, moderate or high? Student Answer 1: Maybe moderate because the person is warning somebody, basically a plea for help. Facilitator: Okay, so we have suicidal talk. That’s one of our red flags. What else? She said she might take pills, so we didn’t know if she does have the pills. So she has a plan. The plan would be to take pills, but we don’t know if we have means. Student Answer 2: High. She’s also angry. I don’t know if she’s angry often. Facilitator: A person in this situation who is really thinking about killing themselves tends not to deny it. They tend not to deny it. There are exceptions to everything, but most of the time, for some reason, this is one of the things where people tend to mostly tell you the truth. If you ask people, they tend to tell you the truth. It’s a very funny thing about suicide that way. That’s certainly not true about most things. If you ask people how much they drink…But, “Are you thinking about killing yourself?” “Well, yes.” If you ask a question, you tend to get a more or less accurate, straight answer. Student question: Is that because it doesn’t matter anymore? If they’re going to die anyway, who’s going to care about what anybody thinks or what happens? Facilitator: My hypothesis would be, when someone is at that point, they’re talking about real, true things. They’re not into play. This is where they are. If they’re really looking at it, then they’re just at that place. What’s to hide at that point? You don’t have anything to lose. It’s a state of mind. And then if you’re not in that place—it’s like, how close are you to the edge of that cliff? “I’m not there. I know where that is, and I’m not there.” “If you get there, will you tell me?” “Yeah, I’m not there.” So, people have a sense—if they’ve gotten that close, they know where that line is, and they know about where they stand in regard to it, because it’s a very hard-edged, true thing.
Twenty-three year old white male, self-referred. Patient bought a gun two months ago to kill himself and claims to have the gun and four shells in his car. Police found the gun but no shells. Patient reports having planned time and place for suicide several times in the past. States that he cannot live anymore with his emotional pain since his wife left him three years ago. This pain has increased during the last week, but the patient cannot pinpoint any precipitant. Patient has a history of chemical dependency but has been sober for 20 months and currently goes to AA.
Facilitator: How high a risk is this person for committing suicide? Low, moderate or high? On a scale from 0 to 7 (7 being very high). Student Answer 1: High. On a scale of 0 to 7? Student Answer: Six. Student Answer 2: I would say three. I think it would be lower because if he’s already bought the gun two months ago and he’s self-referring himself to get help, he wants to live. He has not made peace with whatever, and he’s more likely not give away his things, and he’s going to AA meetings. I think it’s lower than really an extreme…I would say a three or four. Student Answer 3: I would say a four or five, moderate. Student Answer 4: About a five..several times and hasn’t followed through, tells me he doesn’t really want to follow through with it. Facilitator: And there are no shells, right? So we can see some of the red flags are there, but some of them aren’t. He’s still sober… Student: He has a support group. Student: He’s not using, though he bought a gun—so that’s a concern. There is a lot there. Student: He may not have the shells so he doesn’t have the opportunity to. So does that make him more…? Student 2: Think I’ll change mine to a five. Facilitator: So the mean was 4.68, so 5 was the mode. If we’re saying this is a moderate risk, what things would we look for that would make this a high risk? Student: Take away AA. Student: If he falls off the wagon, he goes right to the top. Student: And if he finds the shells. Facilitator: Because it probably is not that hard to find shells. All these stores around here, you can get shells quicker than you can get a gun, so he’s only a five-minute purchase away from having lethal—in contrast to not having the gun. Student: Could there be a difference in the time? Let’s say his wife left him just four to six months ago rather than three years. Would that be something that would be more serious? Facilitator: Yes, or if his wife just left him. So, say his wife left him a month ago that would bump it up. So that’s unresolved. That’s taking a person that was worried and that’s pushing him higher. Student: It also raises the homicide rate. Facilitator: Yes, because these tend to be murder-suicides. How often have we seen that? Murder-suicide is a big deal. If she won’t be with me, she won’t be with anybody.
- Case report
- Open access
- Published: 31 May 2019
Critical appraisal of major depression with suicidal ideation
- Maurizio Pompili ORCID: orcid.org/0000-0003-1886-4977 1
Annals of General Psychiatry volume 18 , Article number: 7 ( 2019 ) Cite this article
6646 Accesses
60 Citations
7 Altmetric
Metrics details
Regardless of its nature, suicidal ideation, in the absence of another diagnosis, is quintessentially associated with major clinical depression. Although for the characteristics of being depressed it is reasonable to have some wish to die, there is no real attempt to understanding the suicidal mind. Clinicians are therefore often inclined to consider suicidal ideation a symptom of major depression. Yet, most depressed patients do not die by suicide, and many of them never experience suicidal ideation even in the most severe depressing scenario. At a closer look, when one works with suicidal individual, suicide appears complex and not line with the obsolete medical model. There are often warning signs for suicide, and suicidal individuals experience mental pain as a common denominator of many adverse events.
Case presentation
A case report of an entrepreneur with no previous psychiatric history describes the process of meditating suicide as a dimension overlapping the depressive disorder. Details of how this 63-year-old male developed high suicide risk are reported, and clinicians are guided into the understanding of suicide risk.
Conclusions
Nowadays, clinicians are requested to provide an in-depth investigation into the suicidal mind, an assessment adjunctive to the psychiatric evaluation. A phenomenological approach may be the key to unlock the suicidal mind. Clinicians may use such tool in light of the need for the empathic understanding of human suffering as well as a paradigm shift in the care of suicidal individuals.
Notwithstanding the strong association between suicidal ideation and depression, it is time to re-consider both major depression and suicide risk. For both scholars and laypeople, depression does result in the wish to die, and clinicians are often inclined to include suicidal ideation as well as a suicidal crisis into the clinical manifestations of major depression. This assumption is reasonable for any patient. An individual who is depressed, with insomnia, anhedonia, and facing dysphoria and overall hopelessness about the future could easily conclude that life is not worth living, especially if a rapid reduction of such misery is not readily available or not possible. Moreover, lack of joy and pleasure, impaired ability to concentrate and unpleasant future expectations, as well as feeling of worthlessness and guilt, are all symptoms that can result in the wish to die. As Esquirol [ 1 ] noted, “Suicide presents all the characteristics of insanity of which it is but a symptom.”
Only a minority of depressed patients die by suicide, and a large percentage of severely depressed patients never think about suicide [ 2 ]. Although some researchers count the lives of those who die by suicide as part of the burden of depression, recent statistics challenge this view, indicating that more than the half of suicides do not merit a psychiatric diagnosis [ 3 ]. Furthermore, The US Centers for Disease Control and Prevention has launched an information campaign to shed light on suicide pointing to contributing factors other than mental illness [ 4 ].
Contrary to the obsolete medical model of suicide, pharmacological treatment results in the reduction of suicide risk, and this implies that these agents target the components of the suicidal scenario rather than the psychopathological symptoms of major depression. The evidence supporting this hypothesis suggests that there are two separate dimensions, one involving features of a psychiatric disorder and the other one presenting the characteristics of a suicidal crisis, often overlapping but still distinct. Such a conclusion emerges from various studies, among which, those involving lithium [ 5 ], ketamine [ 6 , 7 , 8 ] and clozapine [ 9 , 10 , 11 , 12 ]. Furthermore, some evidence supports the notion that being suicidal may limit response to antidepressant treatment in depressed major affective disorder patients, independent of overall symptomatic severity [ 13 , 14 ]. Such evidence seems to suggest that depressed, suicidal individual represent a peculiar subgroup of patients that request in-depth clinical observation.
Modern psychiatry now needs a new medical model with clinicians being able to appraise depressed individuals with suicidal ideation critically. Depression per se is not a useful tool for a proper understanding of the complexity of suicide, and suicidal ideation is not a proxy for the diagnosis of major depression. The uniqueness of each patient determines the variability of the threshold for sustaining mental pain, a condition dependent on personal experiences starting from childhood. This mental suffering, which has been shown to share the same neuroanatomical circuits of somatic pain [ 15 ], is referred to the hurt, anguish, or psychache that takes hold in the mind. Such negative emotions are tied to thoughts that erode the perspective of future expectations, making the future seem ominous. Efforts to manage psychological pain can last weeks, months and sometimes years and, at times, the suffering overcomes the threshold very rapidly, and suicide occurs.
It is possible that human sadness (such as in response to loss, grief, etc.) shares feature with major depression even in the absence of a validated psychiatric diagnosis. Clinical judgment is required to distinguish between the two entities [ 16 , 17 ].
In line with this, the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) states, “Diagnosis of a mental disorder should have clinical utility” but “the diagnosis of a mental disorder is not equivalent to a need for treatment. Need for treatment is a complex clinical decision that takes into consideration symptom severity, symptom salience (e.g., the presence of suicidal ideation), the patient’s distress (mental pain)” and “Clinicians may thus encounter individuals whose symptoms do not meet full criteria for a mental disorder but who demonstrate a clear need for treatment or care. The fact that some individuals do not show all symptoms indicative of a diagnosis should not be used to justify limiting their access to appropriate care” ([ 18 ], p. 20).
Mr. SL is a 63-year-old entrepreneur who has been running his own business for about 30 years, achieving success and admiration from his peers. However, due to the economic crisis, he started facing financial difficulties and had problems in carrying out his business, paying salaries to his long-lasting employees, and supporting his family. After trying many options to get support from banks, he realized that his company was in danger. Because of this situation, he started experiencing sadness, insomnia, loss of appetite, hopelessness, and irritability. He described how he saw no way out, and he described himself as in a tunnel with no real solution to his economic problems. Things got worse as the crisis eroded the money he had saved for emergencies.
He also experienced unimaginable physical suffering with unpleasant sensations at the hypochondrium (the upper part of the abdomen) related to anxiety, and he sometimes had dyspnea. Despite these symptoms, he tried his very best to continue and attend to his work activities. After almost 3 months of feeling depressed, he started thinking about suicide. He reported that suicidal ideation gradually became the companion that could provide help and relief from the pain he was experiencing. Having realized that he could rely on suicide as a way out from his problems, he experienced both the pressure of the precarious economic state and a state of relief when lousy news regarding his debts continued to arrive. He thought that he would not be alive anymore in a week or two. A peculiar aspect of his psychopathological state was an “ossimoric” feature, that is, while he was experiencing the sadness and despair for what has happened to his life, he was still able to enjoy some activities such as maintaining his status and playing at his tennis club, as well as going out for dinner and other leisure activities.
After experiencing depression with suicidal ideation for a while, he then concluded that suicide was the only option left. Although he had spent a pleasant bank holiday, early in the morning on returning to work, he thought that he had to put an end to his life. He went to his office, got his gun and started driving at random for hours. He had left two letters for his children explaining what was behind his choice. He had switched off his cellular phone, and his family lost his track oh him for hours. Just before the moment when he decided to use the gun for killing himself, he thought he wanted to speak to a friend to ask him to support his family. This friend proved to be skilled in maintaining a conversation and supporting the patients’ wish to live. The conversation on the cellular phone helped police to trace the patient. Police officers stopped him and brought to a psychiatrist who diagnosed major depression and the need for psychiatric hospitalization.
However, after a few days, he was able to decide whether to remain or discharge himself. After returning home, his children noticed the poor mental state of their father and sought a consultation with the author. The patient underwent a full psychiatric evaluation, as well as an in-depth assessment of suicide risk, with an analysis of his reasons for living versus his reasons for dying. Although the patient was depressed, an intervention for the treatment of depression would not have provided relief for this man. Lithium was prescribed, in association with small doses of an atypical antipsychotic at night, and regular sessions of psychiatric evaluation combined with sessions of psychotherapy were scheduled. This treatment proved to be of great relief for the patient, and he reported a feeling of being understood by my collaborators and by me. He improved dramatically over 2 months and, despite having the same economic problems that had led him to contemplate suicide; he never reported suicidal ideation again.
Discussion and conclusions
Suicidal individuals have many unmet needs, and they may not fit into diagnostic categories and may lack a full clinical picture. They should not be left alone with no treatment as if therapeutic options would prove to be of no use.
Psychological pain, as a main ingredient of suicide, is the pain of excessively felt shame, guilt, fear, anxiety, loneliness, and angst. This very human condition points to the fact that the nature of suicide is first mental, meaning that each suicidal drama occurs in the mind of a unique individual [ 19 ]. Depressed individuals are suicidal only when negative emotions are so painful that suicide is the only option left and when the suicidal mind is hosted in an individual’s depressed brain. Such individuals conclude that life cannot be accepted with unbearable suffering. Suicide is not, therefore, a specific and narrow symptom of depression. Instead, it is a behavior “combining features of a declaration of war with a petition for bankruptcy” [ 20 ].
What emerged from the case reported above is the fact this man was experiencing a narcissistic failure from having his business closed down, and his employees fired. He was between life and death, hoping somebody would rescue him and reduce his suffering. From the clinical picture, there also emerged a feature always traceable in suicidal individuals, that is, ambivalence. He was contemplating suicide, but he also was attached to life’s activities, such as his duties and his family, and he ultimately phoned a friend. This feature can be a crucial element in suicide prevention, providing a period available for rescuing the individual in crisis. During this phase, suicidal individuals often communicate, either covertly or explicitly, their intention to die [ 21 ]. The suicidal crisis is also often anticipated or accompanied by three symptoms: anxiety (inner turmoil), agitation and irritability [ 22 ], key features also found patients with depressive symptoms during mania [ 23 ]. Sleep symptoms are often reported occurring well before the emergence of the suicidal ideation. People contemplating suicide, but experiencing ambivalence, often consider what has been crucial in their lives. They may give away books, jewelers, and symbolic objects to someone who will take care of such things after their death.
From the case report above, we learn that two other essential items were at work in the suicidal mind: hopelessness (such as not having positive future expectations) and dramatic mood changes. Hopelessness has been reported as more indicative than depression in the prediction of suicide [ 24 , 25 ]. The patient, although continuing to work, saw no future in his activity, dismissing claims for payment as something, which he would not deal with anymore. He also alternated pessimistic thoughts with some recreational activities. Of note is that, before the final decision to die and collecting the gun, he had experienced a good mood and a state of enjoyment (playing golf with friends). Suicidal individuals often switch from sadness to positive and enthusiastic thinking, a feature that has been interpreted with having decided to die by suicide and eliminating the ambivalence. What causes suffering is the ruminations and thoughts that reiterate the failures, the shame, the loss and the rejections (to name just a few) so that imagining the abolition of the flow of thoughts in the conscious mind is seen as the ultimate relief. Clinicians must explore death fantasies in suicidal individuals. When suicide risk is deemed to be high, I always ask if the patients have ever thought about his or her afterlife, that is, the funeral, who will attend, or the reaction of the people who will discover the body. In highly suicidal individuals, such fantasies are reported, whereas they often (although not always) evoke horror if the risk of suicide is low.
Clinicians who consider suicidal ideation to be merely a symptom of depression may miss the rare opportunity to get to know a very private aspect of patients and reduce their suffering. They may even uncover the fact that what they are treating is not necessarily major depression with suicidal ideation but rather severe human sadness emerging with suicidal wishes. This critical distinction may dramatically change the outcome for patients. Treatments and therapeutic options depend on the clinical manifestations. Clinicians may use available treatments for targeting symptoms such as insomnia, agitation, and dysphoria. At the same time, major depression with suicidal ideation may benefit from both pharmacological and non-pharmacological interventions, while not ignoring the motives for wishing to be dead which should be at the center of the psychiatric intervention.
Modern psychiatry needs a better interpretation of suicide risk as compared with old models and reductionist explanations of a complex phenomenon. Rather than confining suicidal ideation to the realm of a symptom, clinicians should relocate such event in the complexity of each human being. Defining it as a symptom inevitably suggests that it is a manifestation of a given disease. We are however dealing with disorders rather than diseases, and suicidal ideation may emerge from the unfortunate combinations of various factors that threaten the stability of an individual. The result of such a state may belong to a different domain than the criteria of major depression. Despite the centrality of perspectives derived from genetics and epigenetics, neurobiology, psychobiology, far from being a manifestation of “normality,” suicide risk is ultimately a manifestation of overwhelming mental pain for which clinicians should be able to provide relief. Such clinical task reveals that suicidal impulses (thoughts and actions) are better understood as a pervasive condition whose roots originate from the internalization of pain-producing inner patterns derived from unsolved past experiences. Such vicissitudes influence proximal risk factors for suicide and exacerbate reactions to present adverse events.
Notions presented in this paper are in line with significant campaigns for preventing suicide, which point to the fact that any single factor rarely causes suicide. Factors can include relationship problems, substance misuse, a recent crisis as well as job, financial or legal stress [ 4 ]. Furthermore, recent results highlight the role of childhood traumatic experiences in determining vulnerability to both depression [ 26 ] and suicide [ 27 ]. Recent findings demonstrated that childhood traumatic experiences negatively influence the outcome of major depression in adulthood [ 28 ]. Besides, depressed patients who experienced trauma in childhood may be less likely to respond to treatment and achieve remission [ 29 ]. Such evidence goes to show that the focus is the person rather than the disorder and that a comprehensive analysis of both clinical assessments of major depression according to psychiatric criteria as well as an empathic understanding of what energizes mental pain is the key role of anyone who is professionally involved in helping such suicidal individuals.
Clinicians should put themselves into the shoes of the individual with whom they are dealing with. They should discern whether it is major depression or sadness and misery derived from accumulating adverse events. A more phenomenological approach would be of help in assessing the suicidal risk formulation in patients with major depression.
Availability of data and materials
Not applicable.
Abbreviations
Diagnostic and Statistical Manual of Mental Disorders, fifth edition
Esquirol JE. Des maladies mentales considérées sous les rapports médicals, hygiéniques et médico-légal (Vol. 1), Paris, J.B. Baillière. 1838, p. 639 [English translation by Hunt KE, entitled Mental Maladies: treatise on insanity [Philadelphia, 1845].
Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. Am J Psychiatry. 2000;157:1925–32.
Article CAS Google Scholar
Stone DM, Simon TR, Fowler KA, et al. Vital signs: trends in state suicide rates—United States, 1999–2016 and circumstances contributing to suicide—27 states, 2015. MMWR Morb Mortal Wkly Rep. 2018;67:617–24.
Article Google Scholar
Centers for Disease Control and Prevention. Suicide rising across the US More than a mental health concern. https://www.cdc.gov/vitalsigns/suicide/index.html . Accessed 28 May 2019.
Ahrens B, Müller-Oerlinghausen B. Does lithium exert an independent antisuicidal effect? Pharmacopsychiatry. 2001;34:132–6.
Grunebaum MF, Galfalvy HC, Choo TH, Keilp JG, Moitra VK, Parris MS, Marver JE, Burke AK, Milak MS, Sublette ME, Oquendo MA, Mann JJ. Ketamine for rapid reduction of suicidal thoughts in major depression: a midazolam-controlled randomized clinical trial. Am J Psychiatry. 2018;175:327–35.
Ionescu DF, Swee MB, Pavone KJ, Taylor N, Akeju O, Baer L, Nyer M, Cassano P, Mischoulon D, Alpert JE, Brown EN, Nock MK, Fava M, Cusin C. Rapid and sustained reductions in current suicidal ideation following repeated doses of intravenous ketamine: secondary analysis of an open-label study. J Clin Psychiatry. 2016;77:719–25.
Wilkinson ST, Ballard ED, Bloch MH, Mathew SJ, Murrough JW, Feder A, Sos P, Wang G, Zarate CA Jr, Sanacora G. The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. Am J Psychiatry. 2018;175:150–8.
Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, Bourgeois M, Chouinard G, Islam MZ, Kane J, Krishnan R, Lindenmayer JP, Potkin S, International Suicide Prevention Trial Study Group. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial [InterSePT]. Arch Gen Psychiatry. 2003;60:82–91.
Meltzer HY, Okayli G. Reduction of suicidality during clozapine treatment of neuroleptic-resistant schizophrenia: impact on risk-benefit assessment. Am J Psychiatry. 1995;152:183–90.
Reid WH, Mason M, Hogan T. Suicide prevention effects associated with clozapine therapy in schizophrenia and schizoaffective disorder. Psychiatr Serv. 1998;49:1029–33.
Walker AM, Lanza LL, Arellano F, Rothman KJ. Mortality in current and former users of clozapine. Epidemiology. 1997;8:671–7.
Pompili M, Baldessarini RJ, Tondo L, Innamorati M, Tatarelli R, Girardi P, De Pisa E. Response to intravenous antidepressant treatment by suicidal vs. nonsuicidal depressed patients. J Affect Disord. 2010;122:154–8.
Courtet P, Jaussent I, Lopez-Castroman J, Gorwood P. Poor response to antidepressants predicts new suicidal ideas and behavior in depressed outpatients. Eur Neuropsychopharmacol. 2014;24:1650–815.
Eisenberger NI, Lieberman MD, Williams KD. Does rejection hurt? An FMRI study of social exclusion. Science. 2003;302(5643):290–2.
Maj M. When does depression become a mental disorder? Br J Psychiatry. 2011;199:85–6.
Maj M. “Clinical judgment” and the DSM-5 diagnosis of major depression. World Psychiatry. 2013;12:89–91.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Arlington: American Psychiatric Publishing; 2013.
Book Google Scholar
Shneidman ES. Suicide as psychache. J Nerv Ment Dis. 1993;181:145–7.
Weisman AD. Is suicide a disease? Life Threat Behav. 1971;1:219–31.
Google Scholar
Pompili M, Belvederi Murri M, Patti S, Innamorati M, Lester D, Girardi P, Amore M. The communication of suicidal intentions: a meta-analysis. Psychol Med. 2016;46:2239–53.
Jobes DA. Collaborating to prevent suicide: a clinical-research perspective. Suicide Life Threat Behav. 2000;30(1):8–17.
CAS PubMed Google Scholar
Vieta E, Grunze H, Azorin JM, Fagiolini A. Phenomenology of manic episodes according to the presence or absence of depressive features as defined in DSM-5: results from the IMPACT self-reported online survey. J Affect Disord. 2014;156:206–13.
Maris RW. Suicide. Lancet. 2002;360:319–26.
Beck AT, Steer RA, Kovacs M, Garrison B. Hopelessness and eventual suicide: a 10-year prospective study of patients hospitalized with suicidal ideation. Am J Psychiatry. 1985;142:559–63.
Booij L, Wang D, Lévesque ML, Tremblay RE, Szyf M. Looking beyond the DNA sequence: the relevance of DNA methylation processes for the stress-diathesis model of depression. Philos Trans R Soc Lond B Biol Sci. 2013;368:20120251.
Turecki G, Ernst C, Jollant F, Labonté B, Mechawar N. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 2012;35(1):14–23.
Opel N, Redlich R, Dohm K, Zaremba D, Goltermann J, Repple J, Kaehler C, Grotegerd D, Leehr EJ, Böhnlein J, Förster K, Meinert S, Enneking V, Sindermann L, Dzvonyar F, Emden D, Leenings R, Winter N, Hahn T, Kugel H, Heindel W, Buhlmann U, Baune BT, Arolt V, Dannlowski U. Mediation of the influence of childhood maltreatment on depression relapse by cortical structure: a 2-year longitudinal observational study. Lancet Psychiatry. 2019;6:318–26.
Williams LM, Debattista C, Duchemin AM, Schatzberg AF, Nemeroff CB. Childhood trauma predicts antidepressant response in adults with major depression: data from the randomized international study to predict optimized treatment for depression. Transl Psychiatry. 2016;6:e799.
Download references

Acknowledgements
Disclosures.
Nor the author or immediate family member has financial relationships with commercial entities that might represent the appearance of a potential conflict of interest. No competing interests as related to this manuscript. The Ethics approval and consent to participate does not apply to this submission.
Author information
Authors and affiliations.
Department of Neurosciences, Mental Health and Sensory Organs, Suicide Prevention Center, Sant’Andrea Hospital, Sapienza University of Rome, Rome, Italy
Maurizio Pompili
You can also search for this author in PubMed Google Scholar
Contributions
The author read and approved the final manuscript.
Corresponding author
Correspondence to Maurizio Pompili .
Ethics declarations
Ethics approval and consent to participate.
Not applicable—material presented in the case report has been disguised to preserve patient confidentiality according to Clifft, M.A. (1986). Writing about psychiatric patients. Guidelines for disguising case material. Bulletin of The Menninger Clinic, 50, 511–524.; also, the patient released the original story through mass-media and gave it to the public domain;
Consent for publication
Competing interests.
The author declares no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Pompili, M. Critical appraisal of major depression with suicidal ideation. Ann Gen Psychiatry 18 , 7 (2019). https://doi.org/10.1186/s12991-019-0232-8
Download citation
Received : 13 March 2019
Accepted : 23 May 2019
Published : 31 May 2019
DOI : https://doi.org/10.1186/s12991-019-0232-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Annals of General Psychiatry
ISSN: 1744-859X
- Submission enquiries: [email protected]
- Patient Care & Health Information
- Diseases & Conditions
- Suicide and suicidal thoughts
Your doctor may do a physical exam, tests and in-depth questioning about your mental and physical health to help determine what may be causing your suicidal thinking and to determine the best treatment.
Assessments may include:
- Mental health conditions. In most cases, suicidal thoughts are linked to an underlying mental health issue that can be treated. If this is the case, you may need to see a doctor who specializes in diagnosing and treating mental illness (psychiatrist) or other mental health provider.
- Physical health conditions. In some cases, suicidal thinking may be linked to an underlying physical health problem. You may need blood tests and other tests to determine whether this is the case.
- Alcohol and drug misuse. For many people, alcohol or drugs play a role in suicidal thinking and completed suicide. Your doctor will want to know whether you have any problems with alcohol or drug use — such as bingeing or being unable to cut back or quit using alcohol or drugs on your own. Many people who feel suicidal need treatment to help them stop using alcohol or drugs, to reduce their suicidal feelings.
- Medications. In some people, certain prescription or over-the-counter drugs can cause suicidal feelings. Tell your doctor about any medications you take to see whether they could be linked to your suicidal thinking.
Children and teenagers
Children who are feeling suicidal usually need to see a psychiatrist or psychologist experienced in diagnosing and treating children with mental health problems. In addition to patient discussion, the doctor will want to get an accurate picture of what's going on from a variety of sources, such as the parents or guardians, others close to the child or teen, school reports, and previous medical or psychiatric evaluations.
- Schreiber J, et al. Suicidal ideation and behavior in adults. https://www.uptodate.com/contents/search. Accessed Feb. 20, 2018.
- Kennebeck S, et al. Suicidal ideation and behavior in children and adolescents: Evaluation and management. https://www.uptodate.com/contents/search. Accessed Feb. 20, 2018.
- Moreland CS, et al. Effect of antidepressants on suicide risk in children and adolescents. https://www.uptodate.com/contents/search. Accessed Feb. 20, 2018.
- Kennebeck S, et al. Suicidal behavior in children and adolescents: Epidemiology and risk factors. https://www.uptodate.com/contents/search. Accessed Feb. 20, 2018.
- AskMayoExpert. Suicide. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2017. Accessed Feb. 20, 2018.
- Risk factors and warning signs. American Foundation for Suicide Prevention. https://afsp.org/about-suicide/risk-factors-and-warning-signs/. Accessed Feb. 20, 2018.
- Understanding suicide: Fact sheet 2015. Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/suicide/index.html. Accessed Feb. 20, 2018.
- The relationship between bullying and suicide: What we know and what it means for schools. Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/suicide/index.html. Accessed Feb. 20, 2018.
- Suicide in America: Frequently asked questions. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/suicide-faq/index.shtml. Accessed Feb. 20, 2018.
- After an attempt. American Foundation for Suicide Prevention. https://afsp.org/find-support/ive-made-attempt/after-an-attempt/. Accessed Feb. 20, 2018.
- When a loved one has made an attempt. American Foundation for Suicide Prevention. https://afsp.org/find-support/my-loved-one-made-attempt/loved-one-made-attempt/. Accessed Feb. 20, 2018.
- Connecting the dots: An overview of the links among multiple forms of violence. Centers for Disease Control and Prevention. https://www.cdc.gov/violenceprevention/suicide/index.html. Accessed Feb. 20, 2018.
- Flynn S, et al. Homicide-suicide and the role of mental disorder: A national consecutive case series. Social Psychiatry and Psychiatric Epidemiology. 2016;51:877.
- Depression: FDA-approved medications may help. U.S. Food and Drug Administration. https://www.fda.gov/forconsumers/consumerupdates/ucm095980.htm. Accessed Feb. 20, 2018.
- Greer TL, et al. Improvements in psychosocial functioning and health-related quality of life following exercise augmentation in patients with treatment response but non-remitted major depressive disorder: Results from the TREAD study. Depression and Anxiety. 2016;33:870.
- Veterans Crisis Line. U.S. Department of Veteran Affairs. https://www.veteranscrisisline.net/. Accessed Feb. 24, 2018.
- Hall-Flavin DK (expert opinion). Mayo Clinic, Rochester, Minn. March 15, 2018.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 11
- Safe clinical practice for patients hospitalised in mental health wards during a suicidal crisis: qualitative study of patient experiences
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-0624-3727 Siv Hilde Berg 1 ,
- http://orcid.org/0000-0002-6657-1012 Kristine Rørtveit 2 , 3 ,
- http://orcid.org/0000-0001-5154-7397 Fredrik A. Walby 4 ,
- http://orcid.org/0000-0002-5363-5152 Karina Aase 5
- 1 Division of Adult Mental Health , Stavanger University Hospital , Stavanger , Norway
- 2 Health and Nursing Research Group, Department of Research , Stavanger University Hospital , Stavanger , Norway
- 3 Department of Caring and Ethics, Faculty of Health Sciences , University of Stavanger , Stavanger , Norway
- 4 National Centre for Suicide Research and Prevention, Faculty of Medicine , University of Oslo , Oslo , Norway
- 5 Centre for Resilience in Healthcare, Faculty of Health Sciences , University of Stavanger , Stavanger , Norway
- Correspondence to Dr Siv Hilde Berg; siv.h.berg{at}uis.no
Aim The aim of this study was to explore suicidal patients’ experiences of safe clinical practice during hospitalisation in mental health wards. The study was guided by the following research question: How do suicidal patients experience safe clinical practice during hospitalisation in mental health wards?
Design, setting and participants A qualitative design with semistructured individual interviews was applied. Eighteen patients hospitalised with suicidal behaviour in specialised mental health wards for adults at a Norwegian hospital participated in the study. Data were analysed thematically and inductively using qualitative content analysis.
Results Patients in a suicidal crisis experienced safe clinical care in mental health wards characterised by the following three themes: (1) being recognised as suicidal, (2) receiving tailor-made treatment and (3) being protected by adaptive practice.
Conclusion This study illuminates the experiences of safe clinical practice for patients in a suicidal crisis. The patient group was multifaceted, with variable experiences of how safe clinical practice affected their subjective experience of safety and suicidal behaviour. The finding highlights the importance of embracing personalised activities in all parts of safe clinical practice and to recognise rather than efface patients’ variability in patient safety efforts.
- adult psychiatry
- suicide & self-harm
- qualitative research
- health & safety
- quality in health care
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-040088
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This study used qualitative interviews to provide rich and variable in-depth data of inpatients with suicidal behaviour, which is an under-researched group.
The study results are suitable for analytical generalisations regarding suicidal patients’ perspectives on safe clinical practice.
The patient sample provided rich variability regarding diagnoses, symptom/function level, sex, number of previous hospital admissions and compulsory/voluntary admissions.
The qualitative methodological approach is not suited for assessing the effects of interventions.
Patients in mental health wards are a population at particular risk of suicide. 1 2 Inpatient suicide constitutes a proportionately small but clinically important fraction of suicides, and it is a major issue for patient safety in mental inpatient care. 3 How to define and understand patient safety in mental inpatient care has been rarely explored. 4 5 Patient safety in mental healthcare is commonly described in physical terms. 5 However, other topics emerge when suicidal patients’ experiences are considered. In a systematic review, 6 we found that suicidal inpatients felt safe due to their connection with healthcare professionals (HCPs), being protected against their suicidal impulses and through having a sense of control over their lives. Therapeutic alliance, 7 decreased access to lethal means 8 and locus of control 9 10 also have strong associations with suicidal behaviour, indicating that the processes patients emphasise are relevant to clinical outcomes. Patient experiences are positively associated with clinical effectiveness and patient safety across a range of disease areas and settings, and understanding them will thus increase the likelihood of improving the two other domains. 11
No studies have specifically explored what suicidal patients emphasise as vital for their perception of safety during inpatient care, and the literature on suicidal patients’ experiences of safe clinical practice is limited. Although asking patients at high risk of suicide about suicidal ideations is not associated with increased suicidal ideation, 12 knowledge of how suicidal patients experience suicide risk assessments is limited. Suicidal patients’ experiences of being behind locked doors 13 and under constant observation 14 15 have been sparsely documented in the literature. Although robust evidence supports restricting access to lethal means, 8 no studies have explored patients’ experiences of lethal means restriction in hospital wards.
Preventing suicides in wards is a challenging task. Like most healthcare activities, safe clinical practice for patients with suicidal behaviour is complex and unpredictable, as knowledge of its underlying principles is incomplete, which often leads to a high degree of uncertainty. 16 Even expert clinicians cannot predict which patients will commit suicide, 17–19 and some patients do not communicate their suicidal ideations to their HCPs. 13 20–22 The aetiological heterogeneity of suicidal behaviour further complicates the creation of an all-encompassing model of best treatment practices. Consequently, each patient is understood and approached differently. 23 More knowledge on the variability of safe clinical practice from suicidal patients’ perspectives is needed. Thus, this article aims to explore suicidal patients’ experiences of safe clinical practice during hospitalisation in mental health wards. The study was guided by the following question: How do suicidal patients experience safe clinical practice during hospitalisation in mental health wards?
A qualitative design with a phenomenological-hermeneutic approach 24 based on semistructured individual interviews 25 was applied.
The study was conducted at a university hospital in Norway that provides specialised mental health services for patients with mental illness. The hospital treats approximately 10 000 patients per year. Patients were recruited from seven mental health wards for adults: one locked acute ward, one locked specialised ward for affective disorders, four open general mental health wards and one short-term open crisis ward. A national patient safety programme for suicide prevention was taking place at the hospital wards during the data collection. The national programme included a checklist to document whether a patient had been assessed for suicide risk, had received an assessment by a specialist on the first day of admittance and had received a safety plan and follow-up appointment at discharge, as well as whether the next-of-kin had been contacted. 26 The hospital had developed specific forms for the documentation of risk factors and warning signs for suicide.
Participants
The study used a purposeful sampling strategy that aimed to recruit patients with serious suicidal behaviour and/or active suicide ideations and who were admitted to open or locked wards in specialised mental health settings for adults. Patients admitted with non-suicidal self-injury were not included in the study. 23 The participants were recruited by their therapists at the study sites and self-identified as ‘being in a suicidal crisis’. The sample consisted of 7 men and 11 women (n=18) aged 18–57 years (mean age 40 years). All but one of the participants were of Western origin. See table 1 for details regarding the participant characteristics. A sample size of 18 participants was considered an adequate size to offer sufficient information to respond to the study aim and ensure participant variability. 27
- View inline
Participants’ characteristics
Ethical considerations
A safety plan was established that outlined the procedures for the interviewer, the patient and the therapist in case participants required increased support or mental healthcare. All participants provided voluntary and informed consent to participate in the study. They were guaranteed that the information they provided would not be passed on to HCPs in the ward, and their therapist was informed that they were participating in the study for safety reasons. To participate, the patients had to have access to a therapist in specialised mental healthcare during the study. One patient needed additional support because he was worried that he would have no support system after his discharge. The interviewer obtained permission from this participant to inform his therapist about this issue. None of the patients reported increased distress or suicidal behaviour after taking part in the research study. The interviews were performed before discharge. The timing of the interviews was determined in collaboration with the participants and their therapists to ensure that the participants were sufficiently stable to engage in the interview and without acute suicidal ideation. The study protocol is provided in online supplemental file 1 . 28 The participants have been given fictitious names here.
Supplemental material
Data collection.
The interviews were conducted by the first author (SHB) between September 2016 and January 2017. The interviews were semi-structured and followed an interview guide ( online supplemental file 2 ) designed to explore safe clinical practice from different angles. The interview guide was developed in collaboration with an advisory panel and was tested in a pilot interview. The pilot interview was included in the study. The interviews focused on the patients’ experiences in the context of daily practices in mental health wards. Of interest were their interactions with HCPs and experiences of safe clinical practice. A phenomenological-hermeneutic approach was applied during the interviews, 24 which implied being sensitive to openness during the interviews by following up with the participants’ responses to the guided questions. 24 The median interview length was 70 min. The first author (SHB) transcribed the interviews verbatim.
The data were analysed using a phenomenological-hermeneutic approach to content analysis, which guided a systematic move from the manifest content towards a higher level of abstraction and interpretation. 29 30 Each interview transcript was read several times by SHB to gain an overall understanding of what the participant expressed. Collaborative discussions of first impressions were conducted with all authors. The unit of analysis was related to experiences of safe clinical practice across the entire dataset. These units were marked and condensed by SHB. In an attempt to understand the life world of each individual, the meaning units pertaining to each participant were condensed and coded separately before moving to more general codes across the dataset. 24 At this stage of analysis, the manifest content was coded. 30 The codes were sorted into five content areas that shed light on specific aspects (talking about suicide, recognising acute suicidality, relational interactions and therapeutic milieu, protection and treatment). Categories representing a thread through the codes were created using tables and abstracted into three themes and seven subthemes. The analytical process constantly moved between the whole and the parts. 24 The authors read and reread the text to grasp the meaning in relation to the study’s aim and to determine the meaning of the data for the participants. The interpretations and findings were continuously discussed by the authors, and feedback on the themes was provided by the advisory panel, which increased the study’s reflexivity and allowed interpretations to be contested and nuanced. 31
Patient and public involvement
Two patient experience consultants were involved in the design of the study and offered feedback on the recruitment strategy, the information material to patients, the consent form, the interview guides and early drafts of the manuscript. No patients were involved in the study recruitment. The participants were notified about the study results.
All participants had active suicidal ideations during their inpatient care, and nine had attempted suicide shortly before their admission to the mental health ward. Most of the patients attributed aggravations in their suicidal behaviour to deteriorations in their mental illness, unrelated to their experiences of harm during clinical practice. Safe clinical practice for suicidal inpatients was described by three themes and nine subthemes, as displayed in table 2 .
Themes and subthemes
Being recognised as suicidal
Patients experienced safe clinical practice when being recognised as suicidal during acute suicidal deteriorations. As they struggled to communicate their suicidal ideations, they were recognised by HCPs, who showed sensitivity to their deterioration. Their suicidal behaviours were better understood in trusted and familiar relationships.
Struggle to communicate suicidal ideations
Several participants found it difficult to verbalise their suicidal ideations, which they experienced as more profound during episodes of severe mental illness. This experience was related to losing the ability to articulate their inner thoughts when mentally ill, a fear of being locked inside a mental ward, being fixated on death or having suicidal impulses with sudden deteriorations and acting on impulse without telling anyone. They depended on others to recognise and express their psychological needs when they deteriorated. Family members fulfilled this function before admission, and HCPs did so in the ward:
I did not say so much (about my suicidal ideation) at the beginning. It was them (parents and girlfriend) who explained most of it because I did not manage to talk. I was completely broken down.(Nathan)
Because they were limited by fear, mental illness and difficulty with verbal expression, many of the participants stated that the severity of their suicidal ideations was never detected during formal risk assessments.
Many participants felt unsafe when they were hospitalised through the emergency room and the centralised acute ward because of reduced predictability in terms of whom they would meet and where they would be transferred next. For some of the participants, in particular those admitted for the first time, this insecurity prevented them from verbally communicating their suicidal ideations and reaching out to HCPs for help, as they feared being misunderstood, misinterpreted or mistreated in the form of punishment or seclusion.
Sensitivity to deterioration
Participants experienced that HCPs showed sensitivity to their acute suicidal state, which saved them from an impending suicide attempt. The HCP who responded was not always the participant’s contact person. The situations were described as ‘being picked up’ or ‘being read’ by someone who was aware of their needs, who cared about them as an individual, who was vigilant and who was able to immediately make sense of changes in their mental state by reading their body language, signs of instability or signs of withdrawal. Patients experienced being seen beyond spoken words by HCPs who acted as lifeguards; they noticed and heard everything:
There is one nurse who reads me like an open book. She picked me up and managed to read me so clearly and get hold of me. Her presence prevented suicide…She says that she can see it in my face, my eyes and my body posture and that I start tightening my fists . (Aina)
The participants experienced that the HCPs immediately understood how to change their suicidal mindset through, among other strategies, talking about casual everyday topics, addressing their sleep problems, connecting with them and showing genuine interest in them, thus helping them to regulate their emotions.
Some participants also described that they required HCPs to interpret their spoken words, as they struggled to use the term ‘suicidal’ when communicating their suicidal ideations; for example, “I am in pain; I need to go out for a walk” (Aina) and “My life is truly hard to live” (Ester). In another example, when Patricia said, “Just send me home; there is nothing here that works for me”, she planned to go home and take pills to commit suicide, but a nurse understood what she was communicating and told her that she had been neglected in the ward and that she should now be taken more seriously. Patricia expressed that this understanding stopped her from making a suicide attempt.
Understood in trusted and familiar relationships
The participants sought trusted and familiar relationships in the healthcare system because such relationships gave them predictability in terms of how their suicidal behaviour would be understood and treated. Participants who had been hospitalised previously described active strategies for being admitted to a familiar ward milieu. The safety plan helped them to be hospitalised in a familiar place. Being in a familiar place was emphasised as vital for the detection of acute deterioration because it meant that the participants would be close to HCPs who knew from experience how they deteriorated and how to intervene:
They know me, and that is why I think it is important to be admitted to the same ward. They have seen it in the change in my mental state, the things I say and do not say, my facial expressions. They have read me when I get truly, truly silent; then I am ill, and they watch me extra carefully… I have survived because they have watched me like hawks. They have given me my personal freedom, but not too much. (Gunn)
When patients did not have access to HCPs who they perceived as being able to read the fluctuations in their suicidal behaviour, their sense of trust in HCPs’ response to their suicidal crises was diminished. Lack of trust caused patients to withdraw from seeking help from HCPs and to cope with their suicidal deteriorations by themselves or by being recognised by their co-patients. These strategies were unfortunate and made the participants feel unsafe. Turid described how she was saved from suicide attempts by fellow patients who detected her behaviour and called ward personnel at times when she deteriorated and by ensuring that she used medications to fall asleep in order to keep her safe from her suicidal impulses at night.
Receiving tailor-made treatment
Safe clinical practice was experienced when receiving tailor-made treatment , which relieved emotional pressure by targeting underlying stressors and mental health issues. A collaborative dialogue was preferred during suicide risk assessments.
Relieved emotional pressure
The participants presented diverse reasons for their suicidal behaviours, which were approached with equally diverse interventions. When treated as an individual, their underlying issues and stressors could be addressed, enabling them to re-establish a feeling of internal emotional control that allowed them to cope with their lives without committing suicide, at least in the short term. Experiences of safe clinical practice were highly related to whether the treatment efficiently relieved emotional pressure. For some, the emotional pressure was due to chaos in their inner worlds (eg, difficult feelings, delusions, existential issues and sleep deprivation) and/or outer worlds (eg, relational or economic issues and lack of a place to live). For Eva, her emotional pressure was relieved when she was eventually medicated with a mood stabiliser, and her delusions telling her to die faded. For Hannah, her emotional pressure was relieved when she received practical support that helped her cope economically with her new life after surviving a suicide attempt:
I was very miserable in my job. You are in a prison and they have thrown away the key. The key was the assurance that I would never go back to that job. It gave me hope to live and took away my suicidal thoughts… I felt safe when the social worker guided me in the outer world, because I knew how to take hold of my new life. (Hannah)
The patients’ underlying issues were targeted by unique combinations of helpful and life-saving care at the wards that was tailored to the individual (eg, psychotherapy, medications, rest, isolation, having a strict daily structure, group therapy and activities) by diverse professionals (eg, social workers, psychologists, nurses and psychiatrists). When these issues were not addressed, the participants experienced being a great risk to themselves after discharge.
Tailor-made treatment was important to ensuring safe clinical practice for patients with complicated mental health issues, as exemplified by Janet. Janet had a history of trauma due to abuse and felt out of control of her suicidal impulses and flashbacks. She managed to find hope and to cope with her flashbacks by talking about her trapped emotions with a psychologist. However, during acute phases, she exhibited a severe lack of self-control, and any attempt to restrain her worsened her flashbacks and suicidality. She managed to gradually improve through treatment with sedatives during acute phases and the presence of HCPs who stayed with her in the bathroom in the dark, as this made her feel safe because no one could find her.
Feeling that the conversation relieved emotional pressure was important when talking about suicide. The participants longed for confirmation that their suffering and suicidal ideations were understandable. Many participants experienced HCPs asking them about their suicidal ideations, but their pain was not alleviated when they opened up.
They do not have the time; they are looking at their watch, as if they would rather be somewhere else. When they do not take my suicidal ideation seriously, I think I am worthless and should instead keep these thoughts to myself. (Aina)
Describing the difficult emotions and suicidal ideations involved with being in a vulnerable position, Gunn stated, “Elaborating on my suicidal thoughts is extremely personal for me. It is worse than undressing and being naked. It is like going to the gynaecologist.” A lack of emotional confirmation elicited feelings of hopelessness, shame and refusal to disclose suicidal thoughts.
Collaborative dialogue
The participants had positive experiences of being assessed for suicide risk when the questions appeared to occur naturally as part of a collaborative dialogue in which they were perceived as individuals and the HCPs validated their feelings. Merely asking questions about suicidal ideations was described as ‘ticking off boxes’, ‘being a part of a machine’, and ‘being interrogated’, leading to the impression that their personal experiences, stories and feelings were not important:
They should ask other questions than just about suicidality, such as what your life situation is like… It is meaningless to be asked about suicidal thoughts and plans when they do not understand the context of why I do not want to live. (Kate)
The participants said that when addressing suicidal ideation, the HCPs should tailor their responses and adjust the conversation about suicide towards topics that matter instead of only giving general advice. One example of what was perceived as generic advice was reminding patients to think of their children. However, having children was not necessarily a protective factor for keeping the patients alive at different stages of their suicidal crises. The participants said that they had periods when they struggled with guilt, felt like a burden and thought that their children would manage better without them. Whether the participants experienced a need to elaborate on their suicidal ideations also varied. While some experienced fewer suicidal ideation episodes when they shared their inner suicidal thoughts and feelings, others improved by focusing on different topics (eg, finding hope through coping with economic issues and delusions).
Being protected by adaptive practice
Safe clinical practice was experienced when being protected by adaptive practice as the participants’ suicidal behaviours fluctuated, and the need for protection varied between the participants. Safe clinical practice was experienced as a balance between withdrawing from and mastering the outside world, internal and external control, and closeness and distance during observation.
Withdrawing from and mastering the outside world
The participants experienced being protected from suicidal impulses during inpatient care by being removed from the overwhelming stressors and demands of the outside world that triggered their suicidal ideations. However, withdrawal was described as a short-term strategy, and they clearly stated they needed to cope with the outside world:
I struggle with guilt about not coping with things at home. When I am hospitalised, I do not get these reminders all the time, and I have fewer episodes of suicidal ideation. At home, I have so much to cope with that the suicidal thoughts are triggered. However, the experience is two-sided: I feel guilty about the fact that I am not with my family, and I feel defeated when I do not deal with my home situation because my life should not be here . (Ida)
The participants felt safe during discharge when HCPs balanced their need to withdraw from and master the outside world. They needed to feel able to cope with both their symptoms and their life situations to be ready to leave the ward. Safety was also experienced when the participants were involved in the discharge process of finding the right balance between activity and peace, testing this balance when leaving the ward and receiving support when the balance failed. The patients emphasised the need for predictability regarding follow-up after discharge for their own safety. They experienced severe anxiety about being discharged without feeling prepared. Gunn described how being discharged without being involved and feeling prepared diminished her trust in healthcare and triggered a suicide attempt:
To be notified about discharge on the same day is like hitting the pavement at 100 km per hour. I was discharged without being prepared, and I became very confused and even more of a danger to myself. If I am not worthy enough of getting help from mental health care, then there is nothing more to do for me; my suicidal thoughts turn active, and I have tried committing suicide. (Gunn)
Internal and external control
The participants described experiencing safety from their suicidal impulses through internal or external control, which are related to different needs for emotional regulation and trust in HCPs and the healthcare system. Feeling safe through internal or external control changed during their suicidal crises, as described in the following statement made by Magnus:
To feel safe from myself, I needed to get out of that psychosis where I believed that I was completely bound to kill myself because I had let everything and everyone down. Because I did not truly want to kill myself… I lost my sense of self, my motor control, my sight and my concentration during the psychosis. I thought this was the way my life had become… I needed rest, isolation and medication, and with time I understood that I would get better, and then I needed to experience that I could function normally again and trust that I would not kill myself. (Magnus)
When experiencing safety through external control, the participants felt safe by being physically held back from the impulses, delusions or hallucinations commanding them to commit suicide and moments of overwhelming agitation and despair. Locked doors or restraints replaced their sense of no control, and the lack of such protection placed greater demands on their emotional regulation to maintain their self-control. The participants emphasised the importance of not having access to any potentially lethal items, such as belts or medications, in both open and closed wards to prevent suicide during episodes of deterioration. In the aftermath, they perceived that they were being saved from death when they received proper protection:
Being restrained has a calming effect on me. I can hand control over to others and relax because I know that I cannot do any harm. My suicidal thoughts fade because I know that I am totally without control… When you are so intensely agitated, nothing stops you… Being hospitalised by force has been crucial for not committing suicide. (Klaus)
When experiencing safety through internal control, participants had the freedom to experience that nothing happened as a result of their ideations, which strengthened their perceptions of being in emotional control, making them feel safe from suicide. Barred windows, locked doors and having to walk through metal detectors increased their anxiety regarding losing this freedom and provoked thoughts such as being a prisoner , a child , or having passed the point of no return .
Feeling safe or unsafe through external control was highly dependent on the patients’ trust that the healthcare system would act in their best interests when they handed over some of their own power in a vulnerable situation. Patients who were admitted for the first time were sensitive to cues of trust, and locked wards could result in feelings of claustrophobia, panic attacks and more episodes of suicidal ideation. Patients’ anxiety was reduced when they intuitively understood or were told that the physical barriers and procedures were intended to help them. They felt safe because they began trusting in the healthcare system. Consequently, being deprived of their personal belongings was easily accepted and intuitively understood as necessary for their own safety, because it was experienced as a necessary protection for all participants during an acute suicidal crisis.
Closeness and distance during observation
Due to the invasiveness of the observations, the participants emphasised the need to balance closeness and physical distance. They needed a balance between being acknowledged and seen and being left in peace, having their privacy respected without being given too much freedom: ‘Firm but soft, but not too much freedom’.
The participants’ ability to establish relational contact during constant observation varied. Their needs and their ability to connect altered as their mental state fluctuated. Some participants needed active support and dialogue with the HCPs, while others wanted to be left in peace but needed confirmation that the HCPs were present (ie, outside the room with the door open) if required. Participants experiencing a psychotic episode reported being in a mental state that left them unable to communicate and establish relationships with the HCPs. In this state, they indicated that they simply needed the HCPs to show that they genuinely cared for them, keeping them within sight and recognising their fluctuations. They described being fixated on death and constantly thinking about suicide and thus experienced the constant presence of HCPs’ life-saving. Although constant observation was perceived as invasive, in the aftermath of their crises the participants perceived this practice as safe and necessary to preventing suicide:
I still hate being followed everywhere when I have a suicide plan, but they watch all the time because they care; it is a sign of humanity. They have saved me many times. (Janet)
However, observation was experienced as unsafe when the patients’ need for connection and acknowledgement was neglected and they felt left on their own and ignored. It was important that the HCPs established relationships with the patients and asked them how they were doing rather than just ‘checking whether they were alive’ and acting as though they were ‘guardians of a prison’. Such practices increased the participants’ suicidality, and for some, this had a devastating effect on trust.
While under intermittent observation, patients felt safe when they had relationships with HCPs based on trust rather than control. Trusting relationships were established when the participants felt they were treated as valuable and equal human beings. Such encounters could be in the form of simple informal contact, which made the participants feel that the HCPs were available and genuinely cared about them as individuals and were not just doing their jobs. It made them feel safe knowing that the HCPs would intervene during a suicidal crisis if they were unable to call for help themselves.
This article aimed to explore the experiences of safe clinical practice among patients hospitalised during suicidal crises. There was rich variation in the participants’ experiences of safe clinical practice expressed in the following themes: ‘being recognised as suicidal’, ‘receiving tailor-made treatment’ and ‘being protected by adaptive practice’.
Risk detection
‘Being recognised as suicidal’ highlights the experiences of patients who struggle to verbally communicate their suicidal ideations, which are more profound during severe mental illness. The connection between the severity of mental illness and the lack of verbal communication of suicidal ideations has been described among patients with depressive disorder. 21 Levi-Belz et al 32 found that suicide attempters who did not verbally communicate their suicidal ideations were characterised by higher levels of suicide ideation, distress and victimisation than those who did communicate their ideations. An inability to identify and communicate suicidal ideations has also been documented in a sample of patients with psychotic depression. 13 The findings of the present study are also in line with other findings in the literature that shame and trust issues inhibit honest communication during suicide risk assessment. 22 33 Nevertheless, knowledge regarding how patients who do not communicate their suicidal ideations are saved by others is limited. In the present study, HCPs’ awareness and engagement enabled the detection of suicidal behaviour in the participants. This study emphasises the importance of understanding warning signs among inpatients, 34 particularly those who struggle to participate in a collaborative dialogue about their suicidal ideations. As warning signs vary among the participants in the present study and vary over time, the success of such an understanding seems to be dependent on HCPs who are familiar with and vigilant about changes in a patient’s mental status, irrespective of whether they are that participant’s contact person in the ward. These findings emphasise the importance of a high level of expertise among all HCPs who interact with patients, enabling them to connect with each patient and make sense of her/his situation.
The findings also highlight the importance of being informed about a clear pathway on admission to hospital. The importance of suicidal patients having trust in their HCPs 35–39 has been well documented in the literature. Familiar and trusted relationships are important for enabling suicidal patients to feel safe because they provide predictability in how their suicidal behaviour is understood and approached. Considering that the suicide risk is highest in the first week after psychiatric hospitalisation, 40 immediate admission to familiar places that patients trust may be one strategy to employ during readmissions, as highlighted in the current study.
‘Receiving tailor-made treatment’ highlights the rich variation in underlying issues and associated treatment paths for patients displaying suicidal behaviours, emphasising that practice is characterised by differing treatment strategies across participants as opposed to practices with high similarity 41 and that suicidal behaviour is characterised by aetiological heterogeneity. 23 The findings indicated that tailor-made treatment efficiently relieved the patients’ emotional pressure by addressing the individual’s need to re-establish a feeling of control regarding their suicidal impulses. Individualised care and tailored services are central topics of patient experiences in healthcare 42 ; however, their relevance to suicidal patients’ experiences of safety has been less explored. The findings support the assumption that a sense of safety for the individual patient can be achieved by addressing her/his manifestations of suffering, as discussed by Undrill. 43 Furthermore, for the suicidal patient, experiences of safety are related to re-establishing a feeling of control, as found by Berg et al . 6
This study also addressed the processes that patients perceive as important to feel safe during suicide risk assessments. Through collaborative dialogue and by relieving emotional pressure during suicide risk assessments, harm may be avoided, and HCPs may help patients to re-establish feelings of control. The emphasis on the role of a collaborative assessment of suicide risk that accounts for the suicidal patients’ individual drivers has been described elsewhere. 44 45 Patients have stressed the importance of trust and support to verbally communicate their suicidal thoughts. 33 46 Consequently, this study supports the recommendations provided by the British National Institute for Health and Care Excellence guidelines 47 to avoid using tools and scales to predict suicide; to manage risk and not merely assess it; and to identify and agree with patients regarding their specific risks. 47 Experiencing safety during suicide risk assessments involves a collaborative dialogue that establishes a therapeutic alliance that includes trust, confirmation of feelings and tuning into the patient’s issues to manage their emotional pressure. The findings also reflect that some patients have difficulties participating in collaborative dialogue, which is emphasised under the theme ‘being recognised as suicidal’.
The theme ‘being protected by adapted practice’ adds knowledge regarding the dynamic, fluctuating and interactive nature of experiencing protection as a means of safe clinical practice. The experience of safe clinical practice as a balance between withdrawing from and mastering the outside world offers insights into a well-known aspect of suicide research: that suicidal risk appears to be especially high soon after hospitalisation. 48 The study findings imply that a lack of predictability regarding discharge induces anxiety and may aggravate suicidal behaviour. This corresponds with previous research stating that suicidal patients experience anxiety when leaving a place of safety 49 50 and require discharge preparedness to feel safe from themselves. 6 The study described how a lack of discharge preparedness triggered a suicide attempt among one of the participants, highlighting its importance. This study adds to the knowledge that discharge preparedness is created in the trusted collaborative relationships between the HCPs and the patients.
The ‘internal and external control’ subtheme demonstrates that patients have different experiences of safety in relation to locked doors, barred windows, restraints and involuntary commitment. This finding is in accordance with other descriptions in the literature; for example, locked doors have been experienced as both ‘being admitted to prison’ and ‘having access to shelter’, 51 while involuntary commitment has been experienced as both ‘necessary’ and ‘being cared for’ and as ‘unjust’ or a ‘restriction of autonomy’. 52 53 This does not imply that protective interventions are entirely good or bad; it depends on what works for whom. 54 It is not a matter of whether doors should be locked, but rather which patients need to be behind locked or open doors, along with when and how. Locking all wards as a means of safety may have consequences for help-seeking behaviour, compliance and recovery for patients experiencing being safe with internal control. To ensure that healthcare can adjust to a patient’s need for control, it is necessary to have both open and locked wards.
Furthermore, the study indicates that some patients experience emotional regulation of their suicidal impulses through internal and external locus of control, which may interchange during the crisis. Internal locus of control strengthens the perception that one’s environment, emotions and actions are under control, while external locus of control is the perception that one’s behaviour is under the control of external factors. 55 External locus of control has clear associations with higher levels of suicide risk 9 10 and is related to the emotional regulation of suicidal impulses in patients with borderline personality disorder. 56 For some patients, external locus of control may nevertheless be necessary in the acute phases of a suicidal crisis. This has also been described in a sample of psychotic and suicidal patients. 57 In our study, emotional regulation was achieved through physical protection where some patients found that they could not harm themselves.
Being under physical containment means giving power to the HCPs and trusting that they will act in accordance with the patient’s best interests. This is a highly vulnerable situation for the patient that depends on interpersonal trust. 58 The study implies that identifying patients who suffer emotionally when they are physically protected is crucial to minimising their catastrophic thoughts and emotional reactions. Explaining the rationale of such interventions may help patients reduce their uncertainty through interpersonal trust and predictability that they are in a safe place. To our knowledge, this is the first study of patients’ experiences of being deprived of lethal means in hospital wards. There is robust evidence for the preventive effect of not having access to any lethal means in hospital wards, 8 and this study provides evidence that patients do not perceive this procedure as invasive when they understand its purpose.
Safe clinical practice was also a matter of maintaining a balance between closeness and distance during observation. The importance of supportive HCPs who acknowledge patients during constant observation 15 59 60 and who consider the patient’s sense of control while building the therapeutic relationship 61 has been described in previous research. This study adds to the importance of understanding such dynamic relationships during observation. Patients’ needs change throughout a suicidal crisis, as does their capacity to connect to others. Safe clinical practice involves a flexible relationship during observations, where HCPs tune into patients’ need for closeness and distance. During this complex endeavour, HCPs can make a difference between life and death. Both experiencing inattentive HCPs and feeling ignored can potentially increase suicidal behaviours and cause patients to feel unsafe. Accordingly, this study supports the perspective of Cutcliffe and Barker 62 that observations should be regarded as a dynamic relational practice, without neglecting the importance of being watchful and physically present.
Strengths and weaknesses of the study
A phenomenological-hermeneutic approach was employed with a sample of 18 participants. While the methodological approach cannot study the effects of interventions, it can provide a deeper understanding of how safe clinical practice is experienced and how it varies among patients. Credibility is strengthened by including a sample that covers significant variations and participants with relevant experiences with the phenomenon under study, 29 as well as through providing a sample size with sufficient information power. 27 The findings of this study cannot be generalised to the entire population of patients hospitalised in mental health wards during a suicidal crisis and are not applicable to patients dying from suicide or patients who are not admitted to hospital wards during a suicidal crisis. Nevertheless, analytical generalisations can be made regarding suicidal patients’ perspectives on safe clinical practice. 63
This study contributes to the understanding of how suicidal patients experience safe clinical practice. Safe clinical practice is experienced by patients hospitalised during a suicidal crisis when they are recognised as suicidal, receive tailor-made treatment and are protected by adaptive practice. The patient group was multifaceted with fluctuating suicidal behaviours, which highlights the importance of embracing personalised activities in safe clinical practice. Safe clinical practice needs to recognise rather than efface patients’ variability. This requires patient safety efforts directed toward strengthening the expert knowledge of HCPs in terms of interpersonal skills to establish trusted relationships, competence and experience with understanding and recognising deteriorations in mental illness, and how to adapt practices such as observation and suicide risk assessment to individual patients.
Acknowledgments
We would like to thank the following advisory panel members for this study who offered feedback on the recruitment strategies, the interview guides and the manuscript draft: Dag Lieungh (patient experience consultant), Målfrid J. Frahm Jensen (patient experience consultant), Gudrun Austad (inpatient and community suicide prevention; mental health nurse), Kristin Jørstad Fredriksen (consultant psychiatrist), Liv Sand (consultant clinical psychologist) and Sigve Dagsland (consultant clinical psychologist).
- Sharma S , et al
- Kanerva A ,
- Lammintakanen J ,
- Brickell TA ,
- Nicholls TL ,
- Procyshyn RM
- Rørtveit K ,
- Dunster-Page C ,
- Haddock G ,
- Wainwright L , et al
- Zalsman G ,
- Wasserman D , et al
- Pearce CM ,
- Mathias CW ,
- Michael Furr R ,
- Sheftall AH , et al
- Fredriksen KJ ,
- Schoeyen HK ,
- Johannessen JO , et al
- Cardell R ,
- Pitula CR ,
- Braithwaite J ,
- Clay-Williams R ,
- Nugus P , et al
- Cannon E , et al
- Franklin JC ,
- Ribeiro JD ,
- Fox KR , et al
- Öncü B , et al
- Gothelf D , et al
- Richards JE ,
- Whiteside U ,
- Ludman EJ , et al
- Turecki G ,
- Dahlberg K ,
- Dahlberg H ,
- Johnson JM ,
- Directorate of Health
- Malterud K ,
- Siersma VD ,
- Guassora AD
- Walby FA , et al
- Graneheim UH ,
- Lindgren B-M ,
- Levi-Belz Y ,
- Gavish-Marom T ,
- Barzilay S , et al
- Ganzini L ,
- Denneson LM ,
- Press N , et al
- Knizek BL ,
- Hjelmeland H
- Talseth A-G ,
- Severinsson E
- Wiklander M ,
- Samuelsson M ,
- Åsberg M , et al
- Nordentoft M ,
- Nordentoft M
- Hoffman RR ,
- Militello LG
- Niederhauser V ,
- Marshburn D , et al
- Stänicke E ,
- Stanley IH ,
- Podlogar MC , et al
- National Institute for Health & Excellence
- Buscajoni A ,
- Fiorillo A , et al
- Cutcliffe J ,
- Harder H , et al
- Cutcliffe JR ,
- Harder HG , et al
- Ringnér A ,
- Molin J , et al
- Katsakou C ,
- Amos T , et al
- Wakefield MA ,
- Northey L , et al
- Schaufel MA ,
- Scrivener A , et al
- Stevenson C ,
- Jackson S , et al
- Procter N ,
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
Twitter @walby_a
Contributors All authors provided substantial contributions in the conception of the work and the analysis of the data. SHB was responsible for the design of the study, the data collection and the organisation of the data. Additionally, SHB read and coded all transcripts and developed summaries. KR and KA read half of the transcripts and drafted summaries of early impressions of the material. FW read the summaries and participated in collaborative discussions regarding first impressions of the material with all authors. All authors participated in analytical reflections and validation of the analysis. SHB drafted the manuscript, and all authors made critical revisions to the intellectual content.
Funding This study received financial support from the Western Norway Regional Health Authority, grant number 911846.
Competing interests None declared.
Patient consent for publication Not required.
Ethics approval This study was approved by the Regional Committees for Medical and Health Research Ethics (2016/34; Norway).
Provenance and peer review Not commissioned; externally peer reviewed.
Data availability statement The datasets generated and/or analysed during the present study are not publicly available due to restrictions regarding individual privacy; however, anonymised data are available from the corresponding author upon reasonable request.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Hopelessness predicts suicidal ideation but not attempts: A 10-year longitudinal study
Tianyou qiu.
University of British Columbia
E David Klonsky
Daniel n. klein.
Stony Brook University
Hopelessness is one of the most commonly cited risk factors for suicidal behaviors. However, several retrospective studies suggest that hopelessness, while strongly correlated with suicidal ideation, does not distinguish attempters from ideators without attempts. The present study is the first to utilize a prospective design to disambiguate the relationship of hopelessness to ideation vs. attempts. Participants were 142 depressed patients followed-up over 10-years. Hopelessness and suicidality (ideation and attempts) were assessed using validated questionnaires and structured interviews. Both retrospective and prospective analyses revealed that hopelessness was higher among those reporting any suicidality (ideation or attempts) compared to nonsuicidal individuals. However, hopelessness failed to meaningfully distinguish attempters from ideators in both retrospective and prospective analyses. Taken together with results from previous studies, our findings suggest hopelessness is best conceptualized as a risk factor for suicidal ideation but not progression from ideation to attempts.
Suicide is a leading cause of death worldwide. According to the latest estimates by the World Health Organisation (2014) , suicides account for 50% of all violent deaths in men and 71% in women. Beyond suicide death, research indicates that a much larger number of people attempt or consider suicide ( Goldsmith et al., 2002 ; Nock et al., 2008 ). However, despite considerable scientific and policy efforts at suicide intervention, the rates of suicide attempts have remained largely unchanged ( WHO, 2014 ). A critical task for suicide researchers is to identify robust risk factors for suicidal thoughts and behaviors.
One of the most oft-cited risk factors for suicidal behavior is hopelessness. First formulated by Beck (1967) , the hopelessness theory of suicide states that hopelessness – a negative attributional style about prospects for the future – leads depressed individuals to view suicide as the only way out of insoluble problems. Hopelessness is thus conceptualized as an important cognitive vulnerability for suicide. Consistent with this perspective, several studies have shown that individuals at elevated risks for suicide tended to experience greater level of hopelessness. In a large-scale community sample, for example, hopelessness predicted suicidal thoughts, suicide attempts, and suicide death over a 13-year interval ( Kuo, Gallo & Eaton, 2004 ). Similarly, in patients with psychosis, hopelessness reliably predicted attempted suicide up to 4 to 6 years later( Klonsky et al., 2012 ).
Despite these findings, a critical limitation of this research is a lack of clarity regarding the role of hopelessness in suicide. Studies that examine predictors of suicide attempts tend to compare individuals with suicidal attempts to individuals without attempts ( Klonsky & May, 2014 ). However, because all (or virtually all) attempters experience ideation, these research designs allow correlates of ideation to appear as correlates of attempts. Indeed, emerging evidence suggests that oft-cited risk factors for suicide such as depression and hopelessness are strong predictors of ideation, but fail to distinguish attempters from ideators without attempts ( Klonsky & May, 2014 ; May & Klonsky, 2016 ). Consequently, it is possible that hopelessness predicts outcomes such as suicide attempts and deaths solely through its relationship to suicidal ideation, but offers no prediction of these outcomes beyond its association with ideation. Correlational studies suggest this is indeed the case. For example, Apter et al (2001) found that hopelessness was elevated in depressed patients with histories of any form of suicidality compared to depressed patients without suicidality; however, Apter et al. also found that hopelessness was no higher in attempters than ideators, and this pattern held even when analyses compared patients with severe attempts to patients with only ideation. Similarly, in a sample of 102 bipolar outpatients, Acosta et al (2012) found that hopelessness was independently associated with suicidal thoughts but not suicide attempts.
While the above studies are useful for clarifying the role of hopelessness in suicide, they are limited by their retrospective design. Prospective research is necessary to further disambiguate the relationship of hopelessness to ideation vs. attempts. Thus, the present study seeks to extend the literature by examining the prospective ability of hopelessness to predict suicide ideation vs. attempts in depressed patients over a 10-year follow-up period.
Participants
Participants ( n = 142) were outpatients with DSM-IV major depressive disorder and/or dysthymic disorder recruited from the State University of New York at Stony Brook (SUSB) Hospital Outpatient Psychiatric Clinic and the SUSB Psychological Services Center, as part of a larger project investigating the naturalistic course of depressive disorders over 10 years ( Klein et al., 2006 ). These participants were then followed up at 30, 60, 90, and 120 months by in-person visits whenever possible and over the phone. Interviewers for this project were formally trained and regularly supervised, including a doctoral-level clinical psychologist, a master's-level psychiatric social worker, and graduate students in clinical psychology. This study was approved by the Stony Brook University Institutional Review Board. Written informed consent was obtained from all study participants.
Suicidality
Baseline suicide ideation was coded as present if it was either endorsed during the Structured Clinical Interview for DSM-III-R (SCID; Spitzer et al., 1990 ) or on the Inventory to Diagnose Depression (IDD; Zimmerman & Coryell, 1987 ) at baseline. Lifetime suicide attempts were assessed using the SCID. Suicidal ideation and attempts during follow-up intervals were assessed using a semi-structured interview, the Longitudinal Interval Follow-Up Evaluation (LIFE; Keller et al., 1987 ).
Hopelessness
Hopelessness was measured using the Beck Hopelessness Scale (BHS), a 20-item, true–false scale designed to index the extent to which one's cognition is organised around negative future expectancies ( Beck, 1988 ). The BHS has been shown to have high internal consistency reliability and concurrent and construct validity.
Retrospective analyses
First, participants were classified as individuals with either lifetime histories of suicidality (i.e., attempts or ideation) ( n = 78) or no history of suicidality (i.e., no previous attempts or ideation) ( n = 62). Hopelessness was significantly higher in lifetime suicidal individuals ( M = 10.68, SD = 5.74) compared to non-suicidal controls ( M = 8.63, SD = 5.15; p = .029, d = .38). Second, the individuals with lifetime histories of suicidality were further classified into participants with attempts ( n = 36, M = 11.68 SD = 5.70) vs. participants who denied attempts but reported ideation at baseline ( n = 42, M = 9.83 SD = 5.71). There was no significant difference in hopelessness between these two groups ( p = .158, d = .32).
Prospective analyses
Participants were first classified as individuals who reported suicidality (i.e., attempts or ideation) during the 10-year follow-up period ( n = 28) or who reported no suicidality during follow-up (i.e., no attempts or ideation) ( n = 85). Hopelessness was significantly higher in the prospective suicidal individuals ( M = 12.53, SD = 5.87) than non-suicidal controls ( M = 9.06, SD = 4.96),( p = .003; d = .64). Second, the suicidal individuals were further classified into those who made attempts during follow-up ( n = 11) vs. those who reported ideation during follow-up but no attempts ( n = 17). No significant difference in hopelessness was observed between attempters ( M = 11.94, SD = 6.63) and ideators ( M = 13.45, SD = 4.6), ( p = .51, d = .26).
The goal of this study is to elucidate the role of hopelessness in the prospective prediction of suicidal thoughts and behaviors. We thus examined hopelessness and suicide ideation and attempts in a 10-year follow-up study of depressed patients. Results indicated that baseline hopelessness robustly predicted future ideation but negligibly distinguished individuals who went on to make attempts from those who went on to experience ideation without attempts. These findings are consistent with those from retrospective studies ( Apter et al., 2001 ; Acosta et al., 2012 ), and suggest that hopelessness is a risk factor for suicide ideation but not for the progression from ideation to attempts.
There are indeed past studies reporting prospective relationships between hopelessness and suicide attempts (e.g. Beck, Brown & Steer, 1989 ). However, one implication of our findings is that hopelessness relates to suicide attempts to the extent it relates to suicide ideation, but does not predict suicidal outcomes beyond ideation. This finding is in partial contradiction with theories of suicide that implicate hopelessness as the primary factor in suicide ( Beck, 1967 ; Abramson et al., 2002 ). Instead, findings are consistent with the more recent perspective that hopelessness plays a key role in ideation, whereas other factors explain the progression from ideation to attempts ( Klonsky & May, 2015 ).
More broadly, findings from this study highlight the need to distinguish factors that predict suicidal ideation from those that predict suicide attempts among ideators. Notably, just as hopelessness is shown to predict suicidal ideation but not attempts, this same pattern has been found for many other commonly cited risk factors for suicide, including depression, most mental disorders, and even impulsivity – each predicts ideation, but fails to meaningfully differentiate attempters from ideators ( Klonsky & May, 2014 ; May & Klonsky, 2016 ). Unfortunately, relatively little is known about factors specifically contributing to the transition from suicidal thoughts to acts ( Klonsky & May, 2014 ). A critical task for future research is to elucidate distinct risk factors associated with suicidal ideation and its progression to attempts ( Glenn & Nock, 2014 ).
Findings from this study have important practical implications. Hopelessness is consistently highlighted in guidelines for suicide risk assessments and interventions ( Joiner et al., 1999 ; Chu et al., 2015 ). Our findings suggest that the relevance of hopelessness for suicide risk is relatively specific: hopelessness confers risk for suicidal ideation. It is important that risk guidelines start to distinguish factors that predict ideation versus progression from ideation to attempts ( Klonsky, May, & Saffer, 2016 ).
It was more difficult to place our retrospective findings in the context of previous literature. As expected, we found that the difference in hopelessness between individuals with histories of attempts vs. individuals reporting baseline ideation but no attempts was not statistically significant; however, the effect size indicated a modest elevation in hopelessness among attempters compared to ideators. Given the relatively small sizes of these subgroups, it is difficult to know whether the modest elevation is meaningful.
This study has limitations. First, this study included only small subsamples of individuals with ideation or attempts during the 10-year follow-up period, thus limiting the reliability and generalizability of findings. Second, this study was not able to distinguish the ability of hopelessness to predict suicidality over short-term (e.g., days or weeks) vs. long-term (e.g., months or years) periods. In light of recent evidence indicating distinct correlates associated with acute vs. long-term suicide risks ( Glenn & Nock, 2014 ), the role of hopelessness in suicidal ideation and attempt may change across time. Future studies, therefore, should not only replicate our prospective findings, but examine hopelessness as a predictor of suicidal thoughts and behaviors over both shorter and longer intervals.
Acknowledgement
Collected of data analysed for this study was supported by NIMH Grant RO1 MH45757 awarded to Dan Klein (PI).
Contributor Information
Tianyou Qiu, University of British Columbia.
E David Klonsky, University of British Columbia.
Daniel N. Klein, Stony Brook University.
- Abramson LY, Alloy LB, Hogan ME, Whitehouse WG, Gibb BE, Hankin BL, Cornette MM. Suicide Science. Springer; US: 2002. The hopelessness theory of suicidality. pp. 17–32. [ Google Scholar ]
- Acosta FJ, Vega D, Torralba L, Navarro S, Ramallo-Farina Y, Fiuza D, Siris SG. Hopelessness and suicidal risk in bipolar disorder. A study in clinically nonsyndromal patients. Comprehensive Psychiatry. 2012; 53 :1103–1109. doi: 10.1016/j.comppsych.2012.03.013; 10.1016/j.comppsych.2012.03.013. [ PubMed ] [ Google Scholar ]
- Apter A, Horesh N, Gothelf D, Graffi H, Lepkifker E. Relationship between self-disclosure and serious suicidal behavior. Comprehensive Psychiatry. 2001; 42 :70–75. doi: 10.1053/comp.2001.19748. [ PubMed ] [ Google Scholar ]
- Beck AT. Depression: Clinical, experimental, and theoretical aspects. University of Pennsylvania Press; 1967. [ Google Scholar ]
- Beck AT. Beck hopelessness scale. The Psychological Corporation; San Antonio, TX: 1988. [ Google Scholar ]
- Beck AT, Brown G, Steer RA. Prediction of eventual suicide in psychiatric inpatients by clinical ratings of hopelessness. Journal of consulting and clinical psychology. 1989; 57 (2):309. [ PubMed ] [ Google Scholar ]
- Chu C, Klein KM, Buchman-Schmitt JM, Hom MA, Hagan CR, Joiner TE. Routinized assessment of suicide risk in clinical practice: An empirically informed update. Journal of clinical psychology. 2015; 71 (12):1186–1200. [ PubMed ] [ Google Scholar ]
- Glenn CR, Nock MK. Improving the short-term prediction of suicidal behavior. American journal of preventive medicine. 2014; 47 (3):S176–S180. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE. Reducing suicide: a national imperative. National Academies Press; 2002. [ PubMed ] [ Google Scholar ]
- Joiner TE, Jr., Walker RL, Rudd DM, Jobes DA. Scientizing and routinizing the assessment of suicidality in outpatient practice. Professional Psychology: Research and Practice. 1999; 30 (5):447–453. [ Google Scholar ]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, Andreasen NC. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Archives of general psychiatry. 1987; 44 (6):540–548. [ PubMed ] [ Google Scholar ]
- Klein DN, Shankman SA, Rose S. Ten-year prospective follow-up study of the naturalistic course of dysthymic disorder and double depression. American Journal of Psychiatry. 2006 [ PubMed ] [ Google Scholar ]
- Klonsky ED, May AM. Differentiating suicide attempters from suicide ideators: A critical frontier for suicidology research. Suicide and Life-Threatening Behavior. 2014; 44 :1–5. [ PubMed ] [ Google Scholar ]
- Klonsky ED, May AM. The Three-Step Theory (3ST): A new theory of suicide rooted in the “Ideation-to-Action” framework. International Journal of Cognitive Therapy. 2015; 8 :114–129. [ Google Scholar ]
- Klonsky ED, May AM, Saffer BY. Suicide, suicide attempts, and suicidal ideation. Annual Review of Clinical Psychology. 2016; 12 :307–330. [ PubMed ] [ Google Scholar ]
- Klonsky ED, Kotov R, Bakst S, Rabinowitz J, Bromet EJ. Hopelessness as a predictor of attempted suicide among first admission patients with psychosis: A 10-year cohort study. Suicide and Life-Threatening Behavior. 2012; 41 :1–10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kuo WH, Gallo JJ, Eaton WW. Hopelessness, depression, substance disorder, and suicidality. Social psychiatry and psychiatric epidemiology. 2004; 39 (6):497–501. [ PubMed ] [ Google Scholar ]
- May AM, Klonsky ED. What distinguishes suicide attempters from suicide ideators? A meta-analysis of potential factors. Clinical Psychology: Science & Practice. 2016; 23 :5–20. [ Google Scholar ]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, De Graaf R. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. The British Journal of Psychiatry. 2008; 192 (2):98–105. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Spitzer RL, Williams JB, Gibbon M, First MB. User's guide for the structured clinical interview for DSM-III-R: SCID. American Psychiatric Association; 1990. [ Google Scholar ]
- World Health Organisation (WHO) Preventing suicide: A global imperative. 2014 Retrieved from http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/
- Zimmerman M, Coryell W. The Inventory to Diagnose Depression (IDD): a self- report scale to diagnose major depressive disorder. Journal of Consulting and Clinical Psychology. 1987; 55 :55e9. [ PubMed ] [ Google Scholar ]

IMAGES
VIDEO
COMMENTS
Case Study 142 Depressed Patient with ... Case Study 142 Depressed Patient with Suicidal Thoughts. you are working the day shift on a medical inpatient unit. you are discussing discharge instructions with J., an 86-year-old man who was admitted for mitral valve repair. His serum blood glucose had been averaging 250 mg/dL or higher for the past ...
jlm764. Preview. Case Studies for Midterm. 17 terms. celeste122567. Preview. Study with Quizlet and memorize flashcards containing terms like Characteristics that make patient at high risk for suicide, Psychiatric disorders that can result in suicidal ideation or gestures:, Depression vs Illness: depression and more.
A 37-year-old woman was admitted to the hospital because of suicidal ideation during the Covid-19 pandemic. She had presented with symptoms consistent with Covid-19 on two previous occasions and ha...
Flowchart describing the derivation of the study sample of patients with major depressive disorder (MDD) episodes (as defined in the eAppendix in Supplement 1), including the matched study sample of patients with MDD with and without suicidal behavior (SB).Suicidal behavior was defined using International Classification of Diseases, Tenth Revision codes X60 to X84 (intentional self-harm ...
There are other ways to approach the task of exploring the region of recent events. In another method (Figure 3), the clinician first generates the entire list of suicide methods contemplated by the patient and then explores each one in detail.Both strategies are easy to remember. The clinician can try both strategies or develop entirely new ones.
For both scholars and laypeople, depression does result in the wish to die, and clinicians are often inclined to include suicidal ideation as well as a suicidal crisis into the clinical manifestations of major depression. This assumption is reasonable for any patient. An individual who is depressed, with insomnia, anhedonia, and facing ...
How to Screen. The Patient Health Questionaire-9 (PHQ-9) is a quick, subjective reporting scale that can be incorporated into the medical record. Affirmative responses to item 9 regarding thoughts of death or self-harm have a hazard ratios of 10 and 8.5 for attempts and deaths in a community setting, respectively. 17 It is in the public domain and available with instructions through the ...
A 2000 meta ‐analysis of the FDA database of studies of seven antidepressant drugs involving 16,639 patients [ 18] revealed annual rates of suicide and attempted suicide of 0.4% and 2.7% with placebo, 0.7% and 3.4% with active comparitors, and 0.8% and 2.8% with investigational antidepressants, respectively.
6 APA Practice Guidelines GUIDE TO USING THIS PRACTICE GUIDELINE Practice Guideline for the Assessment and Treatment of Patients With Suicidal Behaviors consists of three parts (Parts A, B, and C) and many sections, not all of which will be equally useful for
A previously fit and well 37-year-old male healthcare worker presented with confusion, psychotic symptoms and a suicide attempt in the context of a new COVID-19 diagnosis. Following surgical interventions and an extended admission to the intensive care unit, he made a good recovery in terms of both his physical and mental health. A number of factors likely contributed to his presentation ...
Approaching the patient—informed consent. Informed consent to treatment and risk management may be defined as informing the patient of all procedures that will be used in the evaluation and management of suicide risk, clinical decision-making, and emergency assessment and referral practices ().Like evidence-based psychosocial interventions for suicidal behaviors, this process should be ...
Suicide assessment in emergency care settings is one of the most challenging tasks for front-line clinicians. Working in a busy ED without the benefit of more extensive training, clinicians may reflexively categorize patients being assessed for suicide, using their own experience and hunches as guides.
Suicidal thoughts and behaviors (STBs) are among the most dreaded complications of treatment-resistant depression (TRD), which is associated with elevated risk of death from suicide as well as from other conditions, even when compared with nonresistant depression. 1. According to 1 meta-analysis, the overall incidence of suicide and suicide attempts among adults with TRD is between 2 and 10 ...
Depression is the most common psychiatric illness in the general community, with 3% to 4% of depressives dying by suicide today. Studies have shown that depression has considerable morbidity and mortality. This article focuses on depressed patients and their management within the emergency department. Understanding the intricacies of the interview process and identifying which patients need ...
Discussion. The data presented here are part of a larger project investigating hospital-associated suicides in the state of Tyrol. A similar case-control procedure was used for a study in post-discharge suicides (i.e., suicides occurring within 12 weeks after discharge from a psychiatric hospital), which identified, among others, a history of suicidal behavior or threats, depression and ...
Identifying Warning Signs Case Study Taken from Patterson, C. W. (1981). Suicide. In Basic Psychopathology: A Programmed Text. Instructions: Underline all words and phrases in the following case history that are related to INCREASED suicidal risk. Then answer the questions at the end of the exercise. History of Present Illness The client is a 65-year-old white
Some of selective serotonin reuptake inhibitors (SSRI) may increase suicidal behaviour by stimulating depressed patients to act with preexisting suicidal thoughts . In 2004, the FDA issued a black box warning that using antidepressants was associated with an increased risk of suicidal ideation and behaviour in people under 18.
? o What are some coping mechanisms you have tried using? 2. What characteristics of J.B. put him at a high risk for suicide? o Characteristics of J.B. that put him at a high risk for suicide are the occurrence of his wife dying recently, feelings of loss and loneliness, feelings of sadness most of the time, interruption in his normal activities, loss of interaction with friends and family ...
Background Regardless of its nature, suicidal ideation, in the absence of another diagnosis, is quintessentially associated with major clinical depression. Although for the characteristics of being depressed it is reasonable to have some wish to die, there is no real attempt to understanding the suicidal mind. Clinicians are therefore often inclined to consider suicidal ideation a symptom of ...
Diagnosis. Your doctor may do a physical exam, tests and in-depth questioning about your mental and physical health to help determine what may be causing your suicidal thinking and to determine the best treatment. Assessments may include: Mental health conditions. In most cases, suicidal thoughts are linked to an underlying mental health issue ...
The emphasis on the role of a collaborative assessment of suicide risk that accounts for the suicidal patients' individual drivers has been described elsewhere.44 45 Patients have stressed the importance of trust and support to verbally communicate their suicidal thoughts.33 46 Consequently, this study supports the recommendations provided by ...
The present study is the first to utilize a prospective design to disambiguate the relationship of hopelessness to ideation vs. attempts. Participants were 142 depressed patients followed-up over 10-years. Hopelessness and suicidality (ideation and attempts) were assessed using validated questionnaires and structured interviews.