

Root-Cause Analysis Comprehensive Solved Nursing Paper Example
Root cause analysis is a tool organizations, and institutions use to assess the operationality of various processes and functions. The same approach is used to investigate adverse events in health care and identify and address factors contributing to patient outcomes. Quality improvement is a critical aspect of the contemporary healthcare continuum, which seeks to deliver patient-centred care, improve access and enhance outcomes. Therefore, investigating how and why a patient incident has occurred is a foundational element for change and the development of recommendations. While medical administration is essential across health settings, this paper highlights a patient safety issue, root cause analysis, improvement plan with evidence-based and best-practice strategies, and existing organizational resources. (Root-Cause Analysis Comprehensive Solved Nursing Paper Example)

Root Cause Analysis
Over the past six months, Clarion Court Skilled Nursing Facility has recorded alarming figures of medication errors. This has concerned the facility’s management and the nursing staff as well as patients. The institution has a dedicated workforce comprised of Registered Nurses, Licensed Practical Nurses, and Certified Nursing Assistants (Cutler et al., 2018). Most recently, an incident occurred where a patient nearly experienced an overdose, and due to the increasing incidents of medication errors, Clarion Court Skilled Nursing Facility completed a root cause analysis to identify reasons for cause, strategies to mitigate them, and improvement plans for patient safety.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
Analysis of the Root Cause
The Clarion Court Skilled Nursing Facility has a well-established workforce whose precise roles and responsibilities should be accomplished accordingly. Registered Nurses, Licensed Practical Nurses, and Certified Nursing Assistants have different roles but are conjoined to pass medications to patients. Medication errors form a large percentage of all hospital cases, and in the last six months, at Clarion Court Skilled Nursing Facility, the cases have risen to 7%. A root cause analysis was necessary due to the many incidents, but the most recent one where a patient has received the wrong instructions for the medication administered.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
The patient was a regular and was on prescription medication. The medication incident occurred after the patient received a much stronger dosage than was actually prescribed on that day. The nurse on duty was not settled at work yet because she had just arrived for her morning shift. Although the patient was on a prescription, what changed was the strength of the medication, and she failed to take note of the change. Due to interruptions and miscommunication, the usual three pills were administered instead of the new dose of one pill, making the patient lethargic and unattended. Although the patient did not suffer any serious harm, a critical situation was in the offing, hence the need for a thorough root cause analysis.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
Most, if not all, health settings strive to attain acceptable health standards free of medication errors and related deficiencies. Therefore, RNs, LPNs, and CNAs should adhere to the five rights of medication: right route, right patient, right time, right dose, and the right medication (Ghorbanzadeh et al., 2019). In Clarion Court Skilled Nursing Facility’s case, the RN administering dose to a patient failed to check drug labels against electronic medical records contravening the right dose and medication. Her actions resulted in an oversight that may result in serious patient harm if unchecked in future scenarios. Such errors are often attributed to technological hitches, but this was one. Sometimes nurses want to complete a task quickly and proceed to another activity disregarding policies and procedures. The RN in charge of the round should have been keen on the medication dosage. Similarly, a flag indicating a change in the medication should have been highlighted to all staff, including RNs, LPNs, and CNAs attending to the patient.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
Lack of respect among personnel could have resulted in the medication error. Since CNAs work under the supervision of LPNs and RNs, their roles are mainly to assist and check on patients meaning. Therefore, some of their recommendations and observations can be ignored, leading to unpleasant outcomes. The RN was notified of the patient’s condition but seemingly was distracted and could not act on the CNA’s report observations of unusual behavior and lethargy. Health settings should establish better communication channels and collaboration between RNs, LPNs, and CNAs to improve patient safety outcomes. In addition, since CNAs interact with patients often, they observe the patients, their behavior patterns, and any other unusual activity; hence their input becomes vital. Health care settings should discourage staff from skipping essential procedures because of distractions and limited time to absolve themselves from unethical conduct and medication errors.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
Improvement Plan with Evidence-Based and Best-Practice Strategies
Medical and safety issues create an unhealthy environment for health care management, staff, and residents. The last six months have been a nightmare for Clarion Court Skilled Nursing Facility, given that it has had to undergo scrutiny due to the high medication errors. RNs and LPNs strive to perform optimally in their capacities and save time resulting in unnecessary pressure (Harrington et al., 2016). Activity-filled environments cause many distractions for nursing staff and, in the process, may not follow policies and procedures, negatively impacting patient care and outcomes (Walpola et al., 2017). The level of nurse staffing in a health facility is an excellent determinant of outcomes; therefore, there is a need for institutions to ascertain if increasing or increasing staff can lead to better outcomes.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
The rights of medication administration have significant impacts on patient safety and outcomes. Bypassing a right of medication indicates an intention to skip policies and procedures, presenting unpleasant outcomes on patient health and the medical field. Although medication administration processes may be complex, RNs, LPNs, and CNAs should adhere to procedures not unless stated otherwise by governing institutions.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
Some procedural errors can be mitigated by utilizing health resources effectively and being cautious. The HALT (hunger, angry, lonely, tired) model has proven effective in reducing human errors in the recent past. It employs an educative approach for staff through supportive frameworks that foster healthy relationships, guide emotional affliction on patient safety, and increase self and group awareness (“HALT: The dangers of hunger, anger, loneliness, and tiredness | Rehab,” 2021). Another approach that perhaps is the most advocated is fostering interprofessional collaboration and communication. Effective communication in the workplace means sharing ideas and educating others through open conversations. On the other hand, collaboration is based on learning essential skills and cultures, including accountability, autonomy, responsibility, respect, cooperation, and coordination. (Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
Existing Organizational Resources
A mission and vision guide every organization. Available resources at Clarion Court Skilled Nursing Facility foster collaborative environments that focus on in-service education and quality improvement programs. Due to a lack of synchrony between nursing staff, leadership becomes an essential component that health care management systems should address urgently. Some of the available resources for in-service education would include but are not limited to conference halls equipped with overhead projectors. Banners and other advertisement products will be placed around the facility, while management systems will recruit additional staff.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)
To sum up, Clarion Court Skilled Nursing Facility has in the past provided exceptional patient care; however, the past six months have presented a different picture altogether for the institution. Increasing incidents of medication errors necessitated a root cause analysis which identified several causal factors, including lack of communication and collaboration, distractive environments, and skipping procedures due to time constraints. Recommendations to address the errors are improved interprofessional collaboration and communication, adopting the HALT model and in-service programs, and hiring new staff. Research shows that these strategies are essential for medication administration to reduce errors and improve patient safety outcomes. (Root-Cause Analysis Comprehensive Solved Nursing Paper Example)

Cutler, S., Morecroft, C., Carey, P., & Kennedy, T. (2018). Are interprofessional healthcare teams meeting patient expectations? An exploration of the perceptions of patients and informal caregivers. Journal of Interprofessional Care , 33 (1), 66-75.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example) https://doi.org/10.1080/13561820.2018.1514373
Ghorbanzadeh, M., Gholami, S., Sarani, A., Badeli, F., & Nasimi, F. (2019). The prevalence, barriers to medication error reports, and nurses’ perceptions toward the causes of medication errors in the hospitals affiliated to north Khorasan University of medical sciences, Iran. Iran Journal of Nursing , 32 (117), 58-68(Root-Cause Analysis Comprehensive Solved Nursing Paper Example). https://doi.org/10.29252/ijn.32.117.58
HALT: The dangers of hunger, anger, loneliness, and tiredness | Rehab . (2021, August 19). Bradford Health Services – Drug and Alcohol Rehabilitation Center(Root-Cause Analysis Comprehensive Solved Nursing Paper Example). https://bradfordhealth.com/halt-hunger-anger-loneliness-tiredness/
Harrington, C., Schnelle, J. F., McGregor, M., & Simmons, S. F. (2016). Article Commentary: The need for higher minimum staffing standards in U.S. nursing homes. Health Services Insights , 9 , HSI.S38994(Root-Cause Analysis Comprehensive Solved Nursing Paper Example). https://doi.org/10.4137/hsi.s38994
Samaei, S., Amrollahi, M., Khanjani, N., Raadabadi, M., Hosseinabadi, M., & Mostafaee, M. (2017). Nurses’ perspectives on the reasons behind medication errors and the barriers to error reporting. Nursing and Midwifery Studies , 6 (3), 132.(Root-Cause Analysis Comprehensive Solved Nursing Paper Example) https://doi.org/10.4103/nms.nms_31_17
Walpola, R., Fois, R., McLachlan, A., & Chen, T. (2017). Evaluating the effectiveness of an educational intervention to improve the patient safety attitudes of intern pharmacists. American Journal of Pharmaceutical Education , 81 (1), 5. doi: 10.5688/ajpe8115(Root-Cause Analysis Comprehensive Solved Nursing Paper Example)

Working On an Assignment With Similar Concepts Or Instructions?
A Page will cost you $12, however, this varies with your deadline.
We have a team of expert nursing writers ready to help with your nursing assignments. They will save you time, and improve your grades.
Whatever your goals are, expect plagiarism-free works, on-time delivery, and 24/7 support from us.
Here is your 15% off to get started. Simply:
- Place your order ( Place Order )
- Click on Enter Promo Code after adding your instructions
- Insert your code – Get20
All the Best,
Post navigation
Previous post.
Root-Cause Analysis
For this assessment, you can use a supplied template to conduct a root-cause analysis. The completed assessment will be a scholarly paper focusing on a quality or safety issue in a health care setting of your choice as well as a safety improvement plan
Root-Cause Analysis and Safety Improvement Plan for Medication Errors in a Hospital Setting
Introduction.
Medication errors are a significant quality and safety issue in healthcare settings, leading to adverse patient outcomes, increased healthcare costs, and loss of trust in the healthcare system. This essay conducts a root-cause analysis of medication errors in a hospital setting and proposes a safety improvement plan aimed at reducing the incidence of these errors.
The root-cause analysis (RCA) is a systematic approach used to identify the underlying causes of a problem or adverse event. In the context of medication errors, the RCA focuses on understanding the contributing factors and processes that lead to these errors.
- Problem Identification : Medication errors can occur at various stages of the medication process, including prescribing, transcribing, dispensing, administering, and monitoring. Common types of errors include incorrect dosage, wrong medication, and errors in patient identification. These errors often result from a combination of human factors, system flaws, and environmental conditions.
- Data Collection : To conduct an RCA, data on medication errors were collected from incident reports, patient safety records, and interviews with healthcare staff. Key findings revealed that errors were frequently associated with high workload, inadequate communication among healthcare providers, interruptions during medication administration, and the complexity of the medication regimens.
- Human Factors : Fatigue, cognitive overload, and lack of proper training were significant contributors to errors.
- Systemic Issues : Inadequate electronic health records (EHR) systems, poor communication channels, and the absence of standardized procedures were critical systemic issues.
- Environmental Factors : Frequent interruptions and a chaotic work environment, especially in emergency and high-intensity settings, increased the likelihood of errors.
- Causal Chain Analysis : The RCA revealed a causal chain leading to medication errors. High workload and inadequate staffing led to cognitive overload among nurses and pharmacists, resulting in attention lapses and errors in medication administration. Additionally, the lack of a robust double-check system and poor communication between healthcare teams contributed to the errors.
Safety Improvement Plan
To address the identified root causes, a safety improvement plan is proposed, focusing on enhancing system reliability, improving communication, and reducing human error.
- Implementation of Electronic Medication Administration Records (eMAR) : Integrating eMAR with barcoding technology can help ensure that the correct medication is administered to the correct patient. The system can alert healthcare providers to potential errors, such as incorrect dosages or drug interactions.
- Standardization of Medication Processes : Developing standardized protocols for prescribing, transcribing, dispensing, and administering medications can reduce variability and prevent errors. This includes clear labeling of medications and standardized dosing units.
- Interdisciplinary Team Rounds : Implementing regular interdisciplinary team rounds can improve communication among healthcare providers. This allows for real-time discussions about patient care plans and potential medication concerns.
- SBAR (Situation-Background-Assessment-Recommendation) Communication : Training staff to use the SBAR framework for all communications regarding medication orders can ensure that critical information is conveyed accurately and efficiently.
- Workload Management : Adjusting nurse-to-patient ratios and implementing staggered shift changes can reduce cognitive overload and fatigue among healthcare providers.
- Simulation-Based Training : Providing simulation-based training on medication administration can enhance nurses’ skills and confidence, reducing the likelihood of errors.
- Regular Audits and Feedback : Conducting regular audits of medication administration processes and providing feedback to healthcare providers can help identify areas for improvement and reinforce adherence to safety protocols.
- Patient Involvement : Encouraging patients to actively participate in their care by verifying their medications and asking questions can serve as an additional safety check.
Medication errors are a critical patient safety issue in healthcare settings, but they can be mitigated through a comprehensive safety improvement plan. By addressing the root causes identified in the RCA, such as system reliability, communication, and human factors, healthcare organizations can significantly reduce the incidence of medication errors and enhance patient safety. Continuous monitoring, feedback, and a commitment to fostering a culture of safety are essential components of this improvement strategy.
WhatsApp us

Adverse event reporting and root cause analysis
Increasing nurses’ understanding can reduce errors..
- Maintaining patient safety is pivotal to nursing practice; the complexities of healthcare call for more in-depth attention to recognizing adverse events, utilizing incident reporting systems, and performing root cause analysis (RCA) to improve patient care.
- An organization that promotes just culture encourages nurses and other healthcare providers to speak up when faulty processes and safety hazards are identified, and report concerns in the incident reporting system.
- It is important that institutions prioritize the communication of the findings learned from the RCA process to promote transparency on what happened and the improvements made to prevent recurrence
Nurse leaders play a pivotal role in patient safety. By ensuring an effective incident reporting system is in place and engaging staff in root cause analysis (RCA), leaders can create a collaborative environment where nurses feel free to speak up about errors and participate in finding solutions. This article discusses reporting systems and uses a case study to illustrate RCA in action.
Incident reporting system
Nurses, who are among the highest reporters of adverse events, work most closely with patients and can identify errors that warrant further investigation. Incident reporting systems provide a secure mechanism to report safety concerns about vulnerabilities in the healthcare system and serve as a repository for tracking and trending adverse events. Leaders should reinforce with staff that these tools are meant to identify safety issues, not find blame. In fact, the reports are confidential and protected from discovery in legal proceedings. Some organizations even allow anonymous reporting for those who are afraid to speak up.
Most incident reporting systems are online and are routed directly to trained staff members (including nurses, physicians, and other leaders) who review each event as appropriate for their specialty areas. Unit leaders are responsible for interviewing staff to determine what, how, and why something happened. Lessons learned are shared with other patient care areas and immediate actions aim to mitigate an adverse event and prevent recurrence. When leaders close the loop with the staff member who reported the incident, they provide reassurance that the report won’t disappear into a black hole. This action builds trust with employees and highlights that the organization values staff safety concerns.
Safety reports also can serve as baseline data to identify care deficiencies as well as drive safety, performance, and quality improvement initiatives. The organization’s patient safety team selects adverse events on which to perform in-depth reviews and, depending on the severity of the patient harm, may escalate an event to various leaders within the organization. In many cases, an RCA is performed to gain a better understanding of the system issues underlying the adverse event.
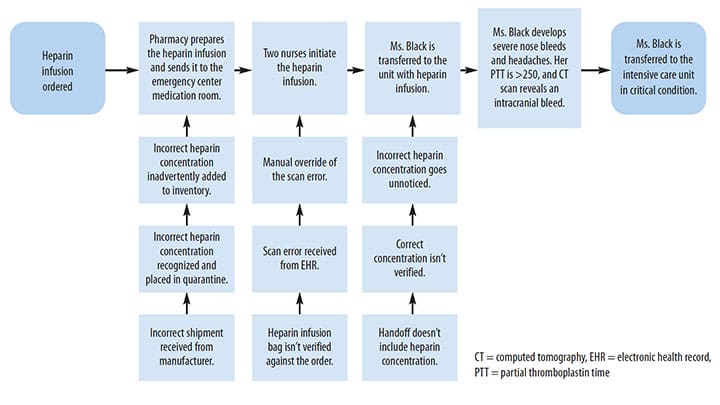
In the following case study, in which a patient receives the incorrect heparin concentration, RCA evaluates the process for system flaws that may have contributed to the event.
Mary Black*, a 75-year-old woman with a history of hypertension, is admitted for chest discomfort. She’s diagnosed with a pulmonary embolism. After the appropriate laboratory and diagnostic workups are completed, Ms. Black is started on a weight-based heparin protocol infusion. When she develops severe nose bleeds and headaches, the nurse re-assesses the patient and discovers that the incorrect concentration of heparin is infusing. The nurse stops the infusion and notifies the physician. Orders are received for lab work and to perform a brain computed tomography (CT) scan. The lab results reveal an abnormally high partial thromboplastin time (>250 seconds), and the CT scan indicates that the patient suffered a stroke . The nurse immediately transfers Ms. Black to the intensive care unit and later enters an adverse event report into the organization’s reporting system.
Root cause analysis process
An RCA provides a structured and systematic approach to evaluating errors. It’s usually led by an individual with training and experience in investigative and event analysis methodology. An RCA aims to improve patient safety, tighten system vulnerabilities, and facilitate organizational learning. Some organizations include individuals involved in the adverse event as part of the RCA process, whereas others limit participation to subject-matter experts. Critical actions to the process include interviewing the staff involved, gaining an understanding of what happened, determining what usually happens, and identifying interventions to prevent event recurrence.
Information acquired during the interviews, from observing the area’s workflow, and by mapping the sequence of events is essential to understanding what led to the adverse event. Comparing that information to the standard operating procedure or policy set by the organization uncovers the breakdown in the system or process, revealing the event’s causal and contributing factors. Causal factors have a direct cause and effect relationship and tell what caused the event to occur; contributing factors identify the issues that led to the adverse event.
Individuals closest to the work bring valuable information to recognizing safety issues and may be called to help develop solutions. When adverse events occur, rarely is there one individual or system issue contributing to the error. Organizational variables—such as staffing, environmental factors, and lack of organizational policies—signal system issues that should be addressed during the RCA process. Although each organization’s RCA process varies, the most common tools used include an event flow diagram, the 5-whys technique, and the fishbone diagram.
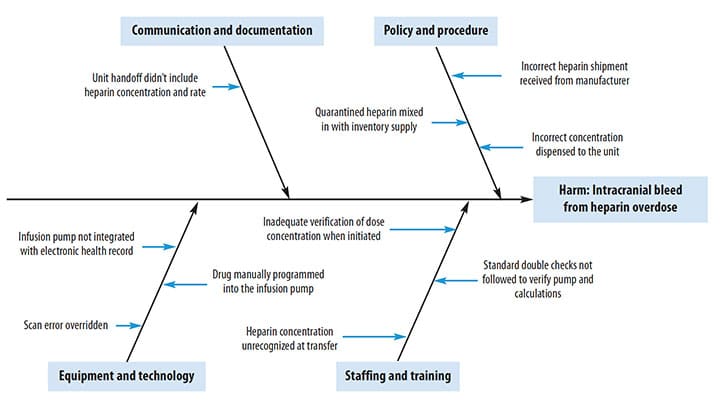
After reviewing Ms. Black’s chart and interviewing the staff involved, an individual skilled in RCA methodology (RCA analyst) creates a timeline and maps out the details of the event using a flow diagram (See Process mapping .) Using a fishbone diagram, the analyst identifies all the possible contributing factors (people, processes, equipment, materials, environmental) leading up to the error. (See Fishbone diagram .) The main headings can be adapted to reflect the process being analyzed. The analyst then uses the 5 whys to get to the root cause of the problem. Each question starts with a problem (Why did this problem occur?). The statement answering each why question is rephrased as a new question until no more “why” questions can be elicited. To get to the root of what caused the adverse event in this case, the analyst asks these questions:
- Why did Ms. Black develop an intracranial hemorrhage?
- Because the heparin dose was too high.
- Why was the heparin dose too high?
- Because the wrong concentration was infusing.
- Why was the wrong concentration infusing?
- Because the scan error was overridden.
- Why was the scan error overridden?
- Because the wrong concentration went unnoticed.
- Why did the wrong concentration go unnoticed?
- Because of the belief that the correct bag was dispensed from the pharmacy.
Process mapping
Use a flow chart to map a process and identify errors. This flow chart follows the process of ordering and administering heparin in the case study with Ms. Black.
Fishbone diagram
Use a fishbone diagram to identify all factors (people, processes, equipment, materials, and environmental) that may have contributed to an error. This diagram illustrates the factors that contributed to the heparin error in the case study with Ms. Black.
A team of key stakeholders (including nurses, pharmacists, managers, and providers) participates in the RCA to discuss the event and confirm the root causes associated with the heparin overdose. Action plans, which are selected based on the RCA outcomes, should address system issues and any gaps in training and education. Meaningful and sustainable changes start with implementing actions that improve the systems in which people work. For example, adding a force function or automating a system or process can eliminate user error and mitigate future events.
In Ms. Black’s case, the RCA finds six causes behind the adverse event. Corresponding steps are taken to prevent future events.
Cause: Standardized heparin concentrations are used, but the shipment received from the manufacturer was incorrect.
Solution: Report the error to the manufacturer.
Cause: The pharmacy process caught the error, but the quarantined shipment was accidently included with the inventory supply.
Solution: Designate an area or room for quarantined shipments with clear box labeling or area signage.
Cause: The medication was correctly labeled, but the incorrect concentration went unnoticed and was dispensed to the unit.
Solution: Implement independent double-checks before dispensing high-alert drugs to the unit.
Cause: When the heparin was initiated, the scan error from the electronic health record (EHR) was overridden.
Solution: Automate smart infusion pumps with the EHR to prevent manual data entry.
Cause: Standard double checks verifying the pump and calculations weren’t followed.
Solution: Drugs requiring double checks before administration should be programmed into the EHR using a best practice advisory popup alert (BPA) to improve adherence.
Cause: The incorrect concentration was manually entered.
Solution: Implement anticoagulation stewardship to improve monitoring and surveillance.
To help ensure adherence with the solutions, units will observe or audit the double-check process. They’ll also monitor BPA reports to determine the adherence rate with documentation of the double-check process, and the organization will monitor heparin infusion error rates.
If it appears that negligence or risky behavior contributed to the event, RCA investigations can result in referrals to peer review or risk management. Just culture, which is tied closely to the RCA process, is a fair and unbiased approach to addressing systems issues rather than blaming individuals. An organization that promotes just culture encourages nurses and other healthcare providers to speak up when faulty processes and safety hazards are identified and immediately report concerns in the incident reporting system.
Implications for nurse leaders
Nurses frequently share concerns about the lack of closed-loop feedback when an adverse event is reported. Although many organizations have mechanisms for sharing best practices or lessons learned, nurses may not make connections between the incident they reported and the actions taken. To promote transparency, organizations must prioritize communicating findings from the RCA process and the improvements made to prevent recurrence, increase safety issue understanding, and enhance staff buy-in and participation in improvements. In many cases, quality improvement initiatives and policies, algorithm development, and medical equipment and device changes are a direct result of mining an organization’s reporting system or implementing corrective actions from an RCA. Leaders should make that clear to staff so they understand the importance of their reports.
Nurses are vital to identifying safety issues in their work environments. When nurses are educated about the importance of adverse event reporting, leaders can aggregate data from those reports to detect and analyze events. As champions for patient safety, nurses and nurse leaders can use incident reporting and the RCA process to help narrow the knowledge gap, encourage learning from errors, and improve safe nursing practice. AN
*Name is fictitious.
Access references at myamericannurse.com/?p=112415.
Tamu Abreu is the program manager for patient safety at MD Anderson Cancer Center in Houston, Texas.
Aboumrad M, Fuld A, Soncrant C, Neily J, Paull D, Watts BV. Root cause analysis of oncology adverse events in the Veterans Health Administration. J Oncol Pract . 2018;14(9):e579-90. doi:10.1200/JOP.18.00159
Aboumrad M, Neily J, Watts BV. Teaching root cause analysis using simulation: Curriculum and outcomes. J Med Educ Curric Dev . 2019;6:2382120519894270. doi:10.1177/2382120519894270
Archer S, Hull L, Soukup T, et al. Development of a theoretical framework of factors affecting patient safety incident reporting: A theoretical review of the literature. BMJ Open. 2017;7(12):e017155. doi:10.1136/bmjopen-2017-017155
Charles R, Hood B, Derosier JM, et al. How to perform a root cause analysis for workup and future prevention of medical errors: A review . Patient Saf Surg 2016;10:20. doi:10.1186/s13037-016-0107-8
Hagley G, Mills PD, Watts BV, Wu AW. Review of alternatives to root cause analysis: Developing a robust system for incident report analysis. BMJ Open Qual . 2019;8(3):e000646. doi:10.1136/bmjoq-2019-000646
Hibbert PD, Thomas MJW, Deakin A, et al. Are root cause analyses recommendations effective and sustainable? An observational study. Int J Qual Health Care . 2018;30(2):124-31. doi:10.1093/intqhc/mzx181
The Joint Commission. Root Cause Analysis in Health Care: Tools and Techniques . 6th ed. Oakbrook Terrace, IL: The Joint Commission; 2017.
National Patient Safety Foundation. RCA 2 : Improving Root Cause Analyses and Actions to Prevent Harm . 2015. cdn.ymaws.com/www.npsf.org/resource/resmgr/PDF/RCA2_first-online-pub_061615.pdf
Peerally MF, Carr S, Waring J, Dixon-Woods M. The problem with root cause analysis. BMJ Qual Saf . 2017;26(5):417-22. doi:10.1136/bmjqs-2016-005511
Vacher A, El Mhamdi S, dʼHollander A, et al. Impact of an original methodological tool on the identification of corrective and preventive actions after root cause analysis of adverse events in health care facilities: Results of a randomized controlled trial. J Patient Saf . 2017. doi:10.1097/PTS.0000000000000437
1 Comment . Leave new
Excellent article!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.
Built to fit

ANA Enterprise News, October 2024

Responding to workplace violence

Creating an organization for future generations


Firearm safety: Nurses’ knowledge and comfort

The Secret Garden: A staff-only wellness and respite space
Healthy Nurse, Healthy Nation: 2024 Highlights Report
Nurses build coalitions at the Capitol

Stop fall prevention practices that aren’t working

Self-compassion in practice

Mitigating patient identification threats

Reflections: My first year as a Magnet® Program Director

Collective wisdom

The role of hospital-based nurse scientists

Professionalism and professional identity
- Cancer Nursing Practice
- Emergency Nurse
- Evidence-Based Nursing
- Learning Disability Practice
- Mental Health Practice
- Nurse Researcher
- Nursing Children and Young People
- Nursing Management
- Nursing Older People
- Nursing Standard
- Primary Health Care
- RCN Nursing Awards
- Nursing Live
- Nursing Careers and Job Fairs
- CPD webinars on-demand
- --> Advanced -->

- Clinical articles
- CPD articles
- CPD Quizzes
- Expert advice
- Clinical placements
- Study skills
- Clinical skills
- University life
- Person-centred care
- Career advice
- Revalidation
Evidence & Practice Previous Next
How to undertake a root cause analysis investigation to improve patient safety, elizabeth haxby lead clinician in clinical risk, royal brompton hospital, london, england, caroline shuldham independent consultant and chair, rcni editorial advisory board, surrey, england.
Rationale and key points
Root cause analysis is a tool that can be used when determining how and why a patient safety incident has occurred. Incidents that usually require a root cause analysis include the unexpected death of a patient, serious pressure ulcers, falls that result in injury, and some infections and medication errors. This article outlines the stages of the investigation process for undertaking a root cause analysis.
Root causes are the fundamental issues that led to the occurrence of an incident and can be identified using a systematic approach to investigation. Contributory factors related to the incident may also be identified.
Crucial questions in a root cause analysis are: what happened? How did it happen? And why did it happen?
Undertaking a root cause analysis can assist in identifying areas for change and developing recommendations, with the aim of providing safe patient care.
Reflective activity
‘How to’ articles can help update your practice and ensure it remains evidence-based. Apply this article to your practice. Reflect on and write a short account of:
A patient safety incident that has occurred in your clinical practice, such as the unexpected death of a patient, a fall that resulted in injury, a serious pressure ulcer, an infection or a medication error. What happened next? Was a root cause analysis undertaken and what was the outcome of this?
How you can support your colleagues to undertake a root cause analysis after a patient safety incident occurs.
Nursing Standard . 32, 20, 41-46. doi: 10.7748/ns.2018.e10859
@CMShuldham
This article has been subject to external double-blind peer review and checked for plagiarism using automated software
None declared
To suggest a ‘How to…’ article, please email [email protected] with a synopsis of your idea
Received: 02 March 2017
Accepted: 16 October 2017
clinical procedures - clinical skills - duty of candour - incident reporting - investigations - patient safety - root cause analysis - service improvement
User not found
Want to read more?
Already have access log in, 3-month trial offer for £5.25/month.
- Unlimited access to all 10 RCNi Journals
- RCNi Learning featuring over 175 modules to easily earn CPD time
- NMC-compliant RCNi Revalidation Portfolio to stay on track with your progress
- Personalised newsletters tailored to your interests
- A customisable dashboard with over 200 topics
Alternatively, you can purchase access to this article for the next seven days. Buy now
Are you a student? Our student subscription has content especially for you. Find out more

10 January 2018 / Vol 32 issue 20
TABLE OF CONTENTS
DIGITAL EDITION
- LATEST ISSUE
- SIGN UP FOR E-ALERT
- WRITE FOR US
- PERMISSIONS
Share article: How to undertake a root cause analysis investigation to improve patient safety
We use cookies on this site to enhance your user experience.
By clicking any link on this page you are giving your consent for us to set cookies.
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Key Performance Outcomes of Patient Safety Curricula: Root Cause Analysis, Failure Mode and Effects Analysis, and Structured Communications Skills
William e fassett , phd.
- Author information
- Article notes
- Copyright and License information
Corresponding Author: William E. Fassett, PhD, Professor, Department of Pharmacotherapy, College of Pharmacy, Washington State University, PO Box 1495, Spokane WA 99210-1495. Tel: 509-358-7666. Fax: 509-358-7745. E-mail: [email protected]
Corresponding author.
Received 2011 Apr 12; Accepted 2011 May 26.
As colleges and schools of pharmacy develop core courses related to patient safety, course-level outcomes will need to include both knowledge and performance measures. Three key performance outcomes for patient safety coursework, measured at the course level, are the ability to perform root cause analyses and healthcare failure mode effects analyses, and the ability to generate effective safety communications using structured formats such as the Situation-Background-Assessment-Recommendation (SBAR) situational briefing model. Each of these skills is widely used in patient safety work and competence in their use is essential for a pharmacist's ability to contribute as a member of a patient safety team.
Keywords: performance outcomes, patient safety, root cause analysis, failure mode and effects analysis, structured communication
The 1995 background papers of the Commission to Implement Change in Pharmaceutical Education set forth key elements to train pharmacists capable of participating in the healthcare system of the future. 1 Yanchick demonstrated that the broad competency categories identified in background paper 5 2 aligned well with the 2003 recommendations of the Health Professions Education Summit, which called for all health professionals to be able to demonstrate proficiency in delivering patient-centered care, working in interdisciplinary teams, employing evidence-based practice, applying quality improvement approaches, and using informatics. 3 As pharmacy programs establish coursework to prepare student pharmacists to participate in patient safety and quality improvement activities, both knowledge-based outcomes and performance outcomes must be developed. This paper discusses 3 performance outcomes that should be included and assessed at the course level to ensure that pharmacists on health care teams are able to effectively implement quality assurance programs and communicate patient safety concerns. Two of the competencies deal with widely-adopted formal approaches to assessing or predicting potential medical errors: root cause analysis (RCA) and failure mode and effects analysis (FMEA). The third competency is the ability to effectively use situational briefing formats; specifically, the Situation-Background-Assessment-Recommendation (SBAR) model, which is becoming the primary format for communication among nurses, physicians, and other health care providers regarding specific patient care situations.
RESIDENCY COMPETENCIES AS GUIDES FOR A PATIENT SAFETY CURRICULUM
In response to the growing awareness of morbidity and mortality arising from medical errors, and to the recommendations of the Health Professions Education Summit, health professions residency directors have increased their programs’ attention to patient safety skills and behaviors. The Accrediting Council on Graduate Medical Education (ACGME) has established 6 core competencies that should form the basis of medical residency training: patient care, medical knowledge, practice-based learning, communication, professionalism, and system-based practice. 4 Patient safety competencies are imbedded in each of these areas.
Two reports have examined specific performance outcomes that should be included in a medical residency. A needs assessment for a patient safety curriculum for residencies at the Mayo School of Graduate Medical Education surveyed the medical directors and key informants in 8 of the school's largest specialty programs. 5 Four content areas were identified as critical by all of the programs: training the resident to explicitly seek help when in doubt; achieving residents’ understanding of the role of fatigue in medical error; life support skills; and sentinel event reporting and management.
Faculty members from the schools of medicine, nursing, and pharmacy at the State University of New York - Buffalo developed the following patient safety performance objectives, which correspond to the 6 ACGME competencies, for their family medicine residency program 6 :
Patient care: (a) recognize and understand team behaviors that strengthen/weaken patient safety; (b) Incorporate effective team behaviors into their practices
Medical knowledge: (a) recognize and analyze inappropriate prescribing in elderly patients; (b) practice appropriate prescribing for elderly patients
Practice-based learning: (a) identify errors in their practices, analyze them, and learn from them; (b) develop system-based strategies to prevent recurrence of errors
Communication: (a) recognize and understand communication behaviors that strengthen/weaken patient safety; (b) incorporate effective communication behaviors into their practices
Professionalism: (a) understand ethical and legal issues surrounding error disclosure; (b) provide appropriate disclosure to patients when errors occur
System-based practice: (a) identify and prioritize vulnerabilities in their practice systems; (b) develop and implement system-based solutions to the identified vulnerabilities
The curriculum is divided into 3 modules taught across the 3 residency years. The curriculum in the first postgraduate year (PGY1) focuses on a behavioral skills cluster, including patient care, communications, and professionalism. The curriculum for PGY2 focuses on polypharmacy or the medication safety cluster, including medical knowledge and practice-based learning, with a pharmacist faculty member directly involved in the training. In the final, PGY3, year, the curriculum focuses on systems approaches in a systems safety cluster featuring practice-based learning and systems-based practice competencies. Two key objectives included in PGY3 are demonstration of ability to take part in RCA and FMEA processes.
Pharmacy practice residency accreditation guidelines also include standards that require residents to gain skills to ensure patient safety and improve quality of care in their practice settings. For example, the American Society of Health-System Pharmacists/American Pharmacists Association's required outcomes for PGY1 community pharmacy practice residents include that they be able to “Identify, design, and implement quality improvement changes to the organization's (eg, community pharmacy, corporation, health-system) medication-use system.” The objectives for this goal include an understanding of the role of RCA and FMEA as tools for analyzing medication use processes. 7
As pharmacy curricula better emphasize interdisciplinary training, patient safety, and quality improvement, pharmacy educators should be able to recognize how these performance outcomes in medical and pharmacy residencies also are skills needed by pharmacy graduates entering practice. Because the system-based practice outcomes depend on effective team activities, and because effective communication among team members is essential to patient safety and quality clinical outcomes, 8 doctor of pharmacy programs should teach approaches that are currently being taught to and used by other health professionals who will be participating with pharmacists on patient care teams.
THREE KEY PERFORMANCE OUTCOMES
Root cause analysis.
Root cause analysis is a retrospective assessment used “to identify the critical underlying reasons for the occurrence of an adverse event or close call (near miss).” 9 In an early description of RCA in 1991, Dew contrasted the importance of distinguishing between finding blame for a catastrophic event and determining the underlying, or root, cause of the disaster. 10 He summarized the search for the root cause as identifying the problem, finding the immediate cause, taking action to resolve immediate concerns, and then looking for root causes which, when found, will aid in system redesign to prevent future catastrophes. “In nature,” Dew wrote, “roots are found in the soil. In organizations, the soil is the systematic factors that deal with how management plans, organizes, controls, and provides assurance of quality and safety in 5 key areas …” Dew introduced 3 tools to aid in finding root causes: the event and causal factor diagram, safeguard analysis (safeguards that can be put in place to reduce hazards, enforce compliance, or make targets invulnerable to hazards), and change analysis (a comparison of the current state with the prior state of the organization or system). Dew's 5 key areas for system analysis include personnel, procedures, equipment, materials, and environment.
RCA and FMEA are required elements of patient safety programs in inpatient and acute care institutions, but they are applicable to all practice settings. The Department of Veterans Affairs adopted a system of RCA in 1998 as 1 of 3 major tools for its Patient Safety Initiative, along with a patient safety reporting system and a Veterans Affairs version of FMEA. 11 The initiative is applied in both inpatient and outpatient settings. The Joint Commission subsequently adopted a requirement for accredited institutions, centers, and clinics, to identify sentinel events and investigate each using RCA. 12 Jackson urged that continuous quality improvement (CQI) be undertaken in community pharmacies, as well; he further advocated that “the entire pharmacy staff should be invited” to participate in the CQI effort, and he discussed RCA and FMEA as 2 important tools for identifying CQI priority targets. 13 The Institute for Safe Medication Practices has announced a goal for 2011 to “develop a root cause analysis workbook for community pharmacies.” 14
Great Britain and other European countries have adopted RCA for assessing errors in community pharmacies as well as inpatient pharmacies. An interdisciplinary team in Denmark performed RCAs on transcription errors in 40 Danish community pharmacies. 15 In England, CQI is referred to as clinical governance and engaging in clinical governance is an essential requirement of the contract between primary care trusts (the 151 regional organizations in England that govern and administer primary, community, and secondary care under the National Health Service 16 ) and community pharmacies. 17 The South East Essex NHS Primary Care Trust includes basic information on RCA in a “clinical governance resource pack for community pharmacies,” and provides specific training to pharmacists in the Trust. 18
In the United States, California expects new pharmacy graduates, regardless of their eventual practice setting, to be trained in the concepts of RCA, and includes questions regarding RCA in the California Practice Standards and Jurisprudence Examination for Pharmacists. The examination's content outline provides a good example of an outcome measure related to patient safety, indicating that the candidate should be able to “Participate in a system for medication error prevention, assessment, and reporting (eg, root cause analysis, National Patient Safety Goals, medication error reduction program).” 19 The Massachusetts Board of Registration in Pharmacy adopted new rules in 2005 mandating CQI programs for community pharmacies, built on the experience in hospitals; its “best practices” suggested quarterly reviews of quality-related events and investigation of the root causes for quality-related events. The 23 best practice recommendations in its report provide a large variety of potential policy issues that could form the basis for student assignments or group case work. 20
One national safety consultant has identified 4 classes of personnel who participate on RCA training teams (program champion, super-users, facilitators [safety practitioners], and participants) and their training needs, which range from attendance at a 3-day class/seminar to completion of an online computer learning program. 21 Of the 4 personnel categories, doctor of pharmacy (PharmD) graduates entering practice fit best under the “participants” category, those who will be asked to serve on RCA teams and need to be able to perform basic RCA on individual problems and address the causes identified. Without more than institution-specific training by an employer, PharmD graduates should be prepared to participate effectively on RCA teams and identify and properly report sentinel events.
Failure Mode and Effects Analysis
While RCA is retrospective, FMEA is a forward-looking assessment of systems and processes designed to predict ways in which things can go wrong (failure modes), and the likely degree of injury or cost (effects) associated with each failure mode. FMEA thus provides a way to predesign systems and processes to improve their safety, and also serves as a tool to establish the highest priorities for investment of time and money to reduce harm. The Joint Commission sees FMEA as the logical follow up to RCA, providing the institution a means for “designing and implementing an action plan for improvement.” 22
Two major forms of FMEA are currently in use. The VA uses a system called healthcare failure mode effects analysis (HFMEA), 23 and many other institutions follow the guidelines for FMEA provided by the Institute for Healthcare Improvement (IHI). The principles of FMEA can be effectively taught by having students practice either approach; however, learning outcomes should assess students’ understanding of the differences in how each form implements these principles.
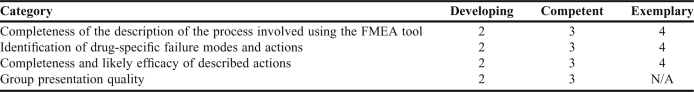
The IHI Web site features significant training materials and an interactive FMEA tool that can be used to provide teams of students with hands-on experience in developing an FMEA from an instructional case (personal memberships in IHI are available to faculty members and students without a fee.) 24 In a patient safety course at Washington State University, we have assigned students to work in teams to develop an FMEA (using the IHI tool) relating to newly-released drugs that have required risk evaluation and mitigation strategies (REMS) as a condition of marketing. The grading rubric for this assignment is shown in Table 1 . This project arose from Cohen's suggestion that FMEA is one approach to “proactively identify” ways in which high-risk drugs could lead to harm and allow for the design of safeguards for high-alert medications. 25
Example Rubric for a 15-Point FMEA Group Assignment Involving a Written FMEA and a Group Presentation
As they should for RCA, PharmD graduates entering practice should be able to participate on a team assigned to undertake FMEA or HFMEA. Because the scope of an FMEA can be limited to a specific process, entry-level pharmacists may be asked to lead a focused-FMEA and should be capable of using or adapting available FMEA tools.
Situational Briefing Model
Recognizing that the majority of sentinel events reported to the Joint Commission include communication difficulties as a contributing factor, the Joint Commission established a National Patient Safety Goal in 2006 to improve the effectiveness of communication among caregivers, and a requirement that facilities implement standardized approaches to hand-offs (ie, transfer of care of the patient from one practitioner to another) that include opportunities to ask questions and respond to them. 26 Perhaps the most widely adopted approach to communicating information about a patient's condition and immediate needs is a situational briefing model adapted from practices in the US Navy. SBAR stands for situation-background-assessment-recommendation, which are the 4 organizing elements around which a message is structured.
Prior to the phone call or face-to-face consultation, a practitioner seeking to communicate information about a patient's condition or needs uses a standardized template to organize his or her message. Relevant records or other patient information is kept at hand, and the important elements are placed into the appropriate SBAR sections of the template. The situation section of the SBAR message contains the reason for the contact, where the practitioner identifies him- or herself; the patient's name; location; and a brief statement of the problem; when it happened or started; and how severe the situation is. Pope and colleagues recommend that this should be done in no more than 10 seconds. 27 The background section contains the patient's essential and relevant medical history. The assessment section should state the practitioner's analysis of what might be going on or what drug-therapy-related problem is at issue. The assessment should include information on severity and urgency. The recommendation section should present an explanation to the other provider of what the practitioner believes must be done or what action he or she is requesting of the other provider.
In addition to its widespread adoption in the United States, SBAR also has become the standard structured communication model in the United Kingdom's National Health Service for all professionals, including pharmacists in hospitals and in community pharmacies. The University Hospitals of Coventry and Warwickshire have created a “community pharmacy escalation” training video on the use of SBAR between a community-based pharmacist and a physician's office. 28
Although the VA and many institutional pharmacies have adopted SBAR, there is little documentation that pharmacy educators teach SBAR as an integral part of the communications curriculum. Searches in PubMed Central using “SBAR” or “Situational Briefing” and “pharmacy,” or “ Am J Pharm Educ ,” yielded a single citation to a report by Brownlee and Bruce that described their use of SBAR presentations by student pharmacists as an element of pharmacy skills assessments conducted at 3 stages of the curriculum prior to student entry into advanced pharmacy practice experiences. 29
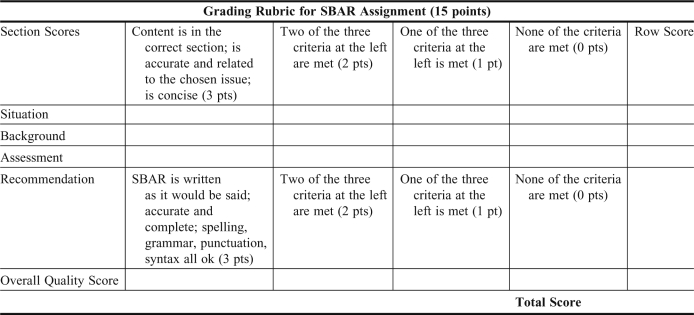
Using SOAP (subjective, objective, assessment, plan) notes to document patient encounters and treatment plans is firmly entrenched in PharmD curricula; a search on PubMed Central using “SOAP Am J Pharm Educ ” yielded 42 articles in the Journal mentioning SOAP notes since 2006. The use of SBAR should be taught routinely as well. In the patient safety course at Washington State University, which is taught in the third year, students are assigned to develop SBARs from cases analyzed in other courses, choosing one of the recommendations from their case work to be the subject of the SBAR. A grading rubric for such an SBAR assignment is shown in Appendix 1 .
RECOMMENDATIONS
The outcomes discussed here measure only a subset of the knowledge, skills, and attitudes necessary to promote a culture of patient safety and which must be acquired and assessed throughout the PharmD curriculum. Early instruction and practice in setting patient care goals, monitoring their achievement, and ensuring effective communication with others is essential to build the habits needed for safe professional practice. In-depth knowledge of risks and benefits of pharmacotherapy must be part of the pharmacist's expertise, especially as it is applied to geriatric and pediatric patients. Finally, PharmD graduates must have the informatics and systems skills to participate effectively in patient care and safety initiatives.
SBAR, RCA, and FMEA are well-established patient safety tools in inpatient and acute care settings. However, their use in community pharmacy practice is not the norm at present. This paper's emphasis on the need for community pharmacists to become greater participants on the health care team was not intended to deemphasize the need for these skills in inpatient practice, but to build the case for teaching SBAR, RCA, and FMEA in the PharmD curriculum as skills that graduates would need upon entry into practice rather than abilities used solely during or following postgraduate training.
Structured communication models, such as SBAR, should be taught early and practiced often, at least as early and often as the development of SOAP notes. In our experience, the SBAR format is best learned by requiring students in every skill laboratory or experiential practice setting to take time to develop an SBAR message for any brief communication intended to communicate a patient need to another practitioner. Students should not be expected to master SBAR messages in a single patient safety course.
RCA and FMEA approaches are probably best taught in the context of a specific patient safety curriculum component. Because RCA is retrospective, we have found it difficult for students to fully practice participating in an RCA team unless they can be provided with richly-detailed cases. Also, because an RCA in actual practice is performed in response to sentinel events, it is challenging to provide a student with a guaranteed opportunity to be involved on an RCA team while completing advance pharmacy practice experiences. Our current outcome objectives relating to RCA are primarily knowledge-based and focus on students’ ability to articulate on an examination the goals, purposes, and process of RCA.
FMEA, on the other hand, is used to anticipate possible ways in which a system can fail and does not depend on an adverse event to trigger its application. FMEA also may be used to improve existing systems, even in the absence of sentinel events. Group projects, ideally undertaken in an interdisciplinary setting with nursing, medical, dental, and other health professions students, provide the best approach to developing students’ skills as potential FMEA team members. Improvement stories at IHI include reports on successful redesign of processes in ambulatory pharmacy, medication dispensing and distribution, inpatient pharmacy services, oncology pharmacotherapy, and many other pharmacy-related areas. 30 These reports provide a wide range of subjects that are suitable for student teams to build upon in practicing development of an FMEA.
Though not the only skill sets needed by pharmacists to engage in protecting patient safety, these 3 performance outcomes – using SBAR regularly to communicate to other providers, participating effectively in RCA teams, and participating effectively in FMEA teams –are so widely taught and adopted by other health professions that they are essential to PharmD graduates’ ability to be members of interdisciplinary teams when they enter practice. Thus, these performance outcomes deserve special attention from curriculum developers in PharmD programs.
Appendix 1. Example of a rubric used to assess a 15-point SBAR assignment. A mark is placed in each column for the rows labeled S, B, A, R to indicate that the student met 3, 2, 1, or none of the criteria. A row score is placed in the far right column for each of the elements assessed. The overall quality score is similarly rated based on the student meeting 3, 2, 1 or none of the criteria listed, a check mark is placed in the appropriate column of the overall quality score row, and the score is entered in the right most column. The 5 row scores are added to determine the student's total score.
- 1. Commission to Implement Change in Pharmaceutical Education. Arlington, VA: American Association of Colleges of Pharmacy; 1995. Background Paper V: Maintaining our Commitment to Change. [ Google Scholar ]
- 2. Yanchick VA. Greater implementation of competency guidelines in the pharmacy curriculum needed. Am J Pharm Educ. 2005;59(2):Article 37. [ Google Scholar ]
- 3. Greiner AC, Knebel E, editors. Health Professions Education: A Bridge to Quality. Washington, DC: Institute of Medicine; 2003. [ PubMed ] [ Google Scholar ]
- 4. Accreditation Council for Graduate Medical Education. Common program requirements: general competencies. 2007. http://www.acgme.org/outcome/comp/GeneralCompetenciesStandards21307.pdf . Accessed August 27, 2011.
- 5. Varkey P, Karlapudi S, Rose S, Swensen S. A patient safety curriculum for graduate medical education: results from a needs assessment of educators and patient safety experts. Am J Med Qual. 2009;24(3):214–221. doi: 10.1177/1062860609332905. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Singh R, Naughton B, Taylor JS, et al. A comprehensive collaborative patient safety residency curriculum to address the ACGME core competencies. Med Educ. 2005;39(12):1195–1204. doi: 10.1111/j.1365-2929.2005.02333.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. American Society of Health-Systems Pharmacists and American Pharmacists Association. Required and Elective Educational Outcomes, Goals, Objectives and Instructional Objectives for Postgraduate Year One (PGY1) Community Pharmacy Residency Programs. http://www.ashp.org/DocLibrary/Accreditation/RTPCommunityCareGoalsObj2010.aspx . Accessed August 27, 2011.
- 8. Kohn LT, Corrigan JM, Donaldson MS, editors. To Err is Human: Building a Safer Health System. Washington, DC: National Academy Press; 2000. pp. 173–174. [ PubMed ] [ Google Scholar ]
- 9. Burkhardt M, Lee C, Taylor L, Williams R, Bagian J. Root cause analysis of medication errors. In: Cohen MR, editor. Medication Errors. 2nd ed. Washington, DC: American Pharmacists Association; 2007. p. 67. [ Google Scholar ]
- 10. Dew JR. In search of the root cause. Qual Progress. 1991;24(3):97–102. [ Google Scholar ]
- 11. Bagian JP, Gosbee J, Lee CZ, Williams L, McKnight SD, Mannos DM. The Veterans Affairs root cause analysis system in action. Jt Comm J Qual Improv. 1998;28(10):531–545. doi: 10.1016/s1070-3241(02)28057-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. McKee J, editor. Joint Commission Resources: Root Cause Analysis in Health Care. 3rd ed. Oakbrook Terrace, IL: Joint Commission Resources; 2005. p. 2. [ Google Scholar ]
- 13. Jackson TL. Ensuring quality in pharmacy operations. In: Deselle SP, Zgarrick DP, editors. Pharmacy Management: Essentials for All Practice Settings. New York: McGraw-Hill; 2005. pp. 132–133. [ Google Scholar ]
- 14. Institute for Safe Medication Practices. Key Plans for 2011. http://www.ismp.org/about/support.asp . Accessed August 27, 2011.
- 15. Knudsen P, Herborg H, Mortensen AR, Knudsen M, Hellebek A. Preventing medication errors in community pharmacy: root-cause analysis of transcription errors. Qual Saf Health Care. 2007;16(4):285–290. doi: 10.1136/qshc.2006.022053. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. NHS Choices. A-Z of NHS authorities and trusts; Primary care trusts. http://www.nhs.uk/NHSEngland/thenhs/about/Pages/authoritiesandtrusts.aspx#primary . Accessed August 27, 2011.
- 17. Pharmacy Services Negotiating Committee (United Kingdom) Essential Service: Clinical Governance. http://www.psnc.org.uk/pages/essential_service_clinical_governance.html . Accessed August 27, 2011.
- 18. Anon . Southend-on-Sea, Essex, United Kingdom: National Health Service, South East Essex Primary Care Trust; 2010. A clinical governance resource pack for community pharmacists. http://www.see-pct.nhs.uk/content/file/Clinical%20Governance%20resource%20pack%20for%20community%20pharmacists.pdf . Accessed August 27, 2011. [ Google Scholar ]
- 19. California State Board of Pharmacy. California Practice Standards and Jurisprudence Examination for Pharmacists: Candidate Information Bulletin. March 21, 2011. http://www.pharmacy.ca.gov/publications/phy_handbook_psi.pdf . Accessed August 27, 2011.
- 20. Massachusetts Board of Registration in Pharmacy. Report on analysis of quality related events (medication errors) 2005. http://www.mass.gov/Eeohhs2/docs/dph/quality/boards/report_med_errors.doc . Accessed August 27, 2011.
- 21. Apollo Associated Services, LLC. Apollo Root Cause Analysis Program Institutionalization. 2008. pp. 4–5. http://www.apollorca.com/_public/site/files/2008_Program_Institutionalization.pdf . Accessed August 27, 2011.
- 22. McKee J, editor. Joint Commission Resources: Root Cause Analysis in Health Care. 3rd ed. Oakbrook Terrace, IL: Joint Commission Resources; 2005. p. 105. [ Google Scholar ]
- 23. DeRosier J, Stalhandske E, Bagian JP, Nudell T. Using health care failure mode and effect analysis: the VA National Center for Patient Safety's prospective risk analysis system. Jt Comm Qual Improv. 2002;28(5):248–267. doi: 10.1016/s1070-3241(02)28025-6. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Institute for Healthcare Improvement. Failure Mode and Effects Analysis (FMEA) Tool. http://www.ihi.org/knowledge/Pages/Tools/FailureModesandEffectsAnalysisTool.aspx . Accessed September 7, 2011.
- 25. Cohen MR, Smetzer JL, Tuohy NR, Kilo CM. High-alert medications: safeguarding against errors. In: Cohen MR, editor. Medication Errors. 2nd ed. Washington, DC: American Pharmacists Association; 2007. pp. 317–328. [ Google Scholar ]
- 26. Haig KM, Sutton S, Whittington J. SBAR: a shared mental model for improving communication between clinicians. Jt Comm J Qual Pat Safety. 2006;32(3):167–175. doi: 10.1016/s1553-7250(06)32022-3. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Pope BB, Rodzen L, Spross G. Raising the SBAR: how better communication improves patient outcomes. Nursing. 2008;38(3):41–43. doi: 10.1097/01.NURSE.0000312625.74434.e8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. University Hospitals of Coventry and Warwickshire. SBAR – Community Pharmacy Escalation. http://www.mededcoventry.com/Guidelines/SBAR/Video/Escalation/CommunityPharmacy.aspx . Accessed August 27, 2011.
- 29. Brownlee SP, Bruce SP. Development of Pharmacy Skills Assessments (PSA) to evaluate clinical and communication skills of pharmacy students [abstract]. 111th annual meeting of the American Association of Colleges of Pharmacy, Seattle, Washington, July 10-14, 2010. Am J Pharm Educ. 2010;74(5):Article 96. [ Google Scholar ]
- 30. Institute for Healthcare Improvement. Improvement stories. http://www.ihi.org/knowledge/Pages/ImprovementStories/default.aspx . Accessed September 7, 2011.
- View on publisher site
- PDF (459.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Conducting root cause analysis with nursing students: best practice in nursing education
Affiliation.
- 1 University of San Francisco, CA 94117, USA. [email protected]
- PMID: 20438032
- DOI: 10.3928/01484834-20100430-03
This article describes a novel approach that allows students to actively participate in a root cause analysis, whether the error was committed in the clinical setting or in the simulation setting. This process can develop student awareness of the responsibility and professional duty to participate in creating a safer patient environment.
- Benchmarking
- Clinical Competence
- Data Collection
- Data Interpretation, Statistical*
- Education, Nursing, Baccalaureate / organization & administration*
- Faculty, Nursing / organization & administration
- Medical Errors / nursing
- Medical Errors / prevention & control*
- Medical Errors / statistics & numerical data*
- Role Playing
- Safety Management / organization & administration*
- Students, Nursing

IMAGES
VIDEO
COMMENTS
Root cause analysis with corrective measures: A root cause analysis was performed, and measures were taken to avoid this problem. The RCA team noted that the nurse caring for both patients had worked in the hospital for 5 years and was recently transitioned to the obstetric ward. This had never happened to her before.
Introduction. Root cause analysis (RCA) is a process which is implemented and used by health professionals to learn how and why errors occurred. Millions of patients are harmed in the United States (US) every year in the health care they provide (Agency for health care research and Quality (2014).This harm can result in death or injury to the ...
Root cause analysis analysis and safety improvement plan lisa bryant school of nursing and health sciences, capella university improving quality of care and ... Assignments. 100% (22) 10. NURS FPX 4020 Carmella Assessment 3 ... The root-cause analysis shows that interruptions during medication administration can cause the nurse to not adhere to ...
Identify the Root Cause •The process is the focus, not individual performance. •The event or combination of events that initiate a failure. •Consider WHY the individual committed the inappropriate act. •Determine HOW the system influenced the individual's thinking. •Root Cause -Event or events that initiate failure •Contributory ...
Your Name School of Nursing and Health Sciences, Capella University NURS4020: Improving Quality of Care and Patient Safety Instructor Name Month, Year. Root-Cause Analysis and Safety Improvement Plan Introduce a general summary of the issue or sentinel event that the root-cause analysis (RCA) will be exploring. Provide a brief context for the ...
rehensive systematic analysis is the Root Cause Analysis (RCA). The RCA is a process for identifying the basic causal factor(s) underlying system failures. and is a widely understood methodology used in many industries. Root cause analysis can be used to uncover factors that lead to pat.
A root cause analysis was necessary due to the many incidents, but the most recent one where a patient has received the wrong instructions for the medication administered. (Root-Cause Analysis Comprehensive Solved Nursing Paper Example) The patient was a regular and was on prescription medication. The medication incident occurred after the ...
By Tamu Abreu, RN-BC, CPHQ, CPPS. NURSE LEADERS play a pivotal role in patient safety. By ensuring an effective incident re-porting system is in place and engaging staff in root cause analysis (RCA), leaders can cre-ate a collaborative environment where nurses feel free to speak up about errors and partici-pate in finding solutions.
This essay conducts a root-cause analysis of medication errors in a hospital setting and proposes a safety improvement plan aimed at reducing the incidence of these errors. Root-Cause Analysis. The root-cause analysis (RCA) is a systematic approach used to identify the underlying causes of a problem or adverse event.
Root cause analysis process. An RCA provides a structured and systematic approach to evaluating errors. It's usually led by an individual with training and experience in investigative and event analysis methodology. An RCA aims to improve patient safety, tighten system vulnerabilities, and facilitate organizational learning.
RCA2 tools (e.g., interviewing techniques, Flow Diagramming, Cause and Effect Dia-gramming, Five Rules of Causation, Action Hierarchy, Process/Outcome Measures) should be used by teams to assist in the investigation process and the identification of strong and intermediate strength corrective actions.
paper example root cause analysis candace mabry college of nursing, grand canyon university nsg 436: leadership, ethics, and policy in healthcare sandra white ... D. & Joseph, M. L. (2021). Leadership and nursing care management (7th ed.). Elsevier- Saunders. ISBN-13: 9780323829694. Download. AI Quiz. ... Root Cause Analysis Assignment ...
Root cause analysis (RCA) provides an evidence-based structure for methodical investigation and comprehensive review of an event enabling appropriate identification of opportunities for improvement. Use of RCA is described in the home care setting. Adverse events, including sentinel events, require comprehensive review to improve patient safety ...
Root cause analysis is a tool that can be used when determining how and why a patient safety incident has occurred. Incidents that usually require a root cause analysis include the unexpected death of a patient, serious pressure ulcers, falls that result in injury, and some infections and medication errors. This article outlines the stages of ...
Assignment 1 Nurse Informatics. Module 03 Written Assignment Respiratory Disease 042318. NUR2571 Module 01 Comparison of Bowel Elimination Disorder v2. Module 7 Diabetes Practice Quiz. this assignment is about root-cause analysis analysis and safety improvement plan name of student institutional affiliation course code: course name name date.
Root Cause Analysis. Root cause analysis is a retrospective assessment used "to identify the critical underlying reasons for the occurrence of an adverse event or close call (near miss)." 9 In an early description of RCA in 1991, Dew contrasted the importance of distinguishing between finding blame for a catastrophic event and determining ...
The root cause analysis technique is a versatile and flexible learning resource for nursing students that can help them understand complex patient safety incidents while also fostering critical and problem-solving thinking, teamwork and systematic communication.
Conducting root cause analysis with nursing students: best practice in nursing education J Nurs Educ. 2010 Aug;49(8):444-8. doi: 10.3928/01484834-20100430-03. Authors Judith Lambton 1 , Laura Mahlmeister. Affiliation 1 University of San Francisco, CA ...
Root-Cause Analysis and Safety Improvement Plan Yaa Yaa School of Nursing and Health Sciences, Capella University NURS4020: Improving Quality of Care and Patient Safety Dr. ABC Sep, 2022 In today's fast-paced healthcare environment, it is crucial for organizations to effectively manage root causes of issues that can impact patient care and ...
Root cause analysis (RCA) is a typical strategy to reduce healthcare errors and adverse patient outcomes in all clinical scopes to establish and improve patient safety and quality improvement frameworks (Martin-Delgado et al., 2020). RCAs allow for a methodical or analytical implementation of systemic interventions (Lakbala et al., 2024).