61 intriguing psychology research topics to explore
Last updated
11 January 2024
Reviewed by
Brittany Ferri, PhD, OTR/L
Short on time? Get an AI generated summary of this article instead
Psychology is an incredibly diverse, critical, and ever-changing area of study in the medical and health industries. Because of this, it’s a common area of study for students and healthcare professionals.
We’re walking you through picking the perfect topic for your upcoming paper or study. Keep reading for plenty of example topics to pique your interest and curiosity.
- How to choose a psychology research topic
Exploring a psychology-based topic for your research project? You need to pick a specific area of interest to collect compelling data.
Use these tips to help you narrow down which psychology topics to research:

Focus on a particular area of psychology
The most effective psychological research focuses on a smaller, niche concept or disorder within the scope of a study.
Psychology is a broad and fascinating area of science, including everything from diagnosed mental health disorders to sports performance mindset assessments.
This gives you plenty of different avenues to explore. Having a hard time choosing? Check out our list of 61 ideas further down in this article to get started.
Read the latest clinical studies
Once you’ve picked a more niche topic to explore, you need to do your due diligence and explore other research projects on the same topic.
This practice will help you learn more about your chosen topic, ask more specific questions, and avoid covering existing projects.
For the best results, we recommend creating a research folder of associated published papers to reference throughout your project. This makes it much easier to cite direct references and find inspiration down the line.
Find a topic you enjoy and ask questions
Once you’ve spent time researching and collecting references for your study, you finally get to explore.
Whether this research project is for work, school, or just for fun, having a passion for your research will make the project much more enjoyable. (Trust us, there will be times when that is the only thing that keeps you going.)
Now you’ve decided on the topic, ask more nuanced questions you might want to explore.
If you can, pick the direction that interests you the most to make the research process much more enjoyable.
- 61 psychology topics to research in 2024
Need some extra help starting your psychology research project on the right foot? Explore our list of 61 cutting-edge, in-demand psychology research topics to use as a starting point for your research journey.
- Psychology research topics for university students
As a university student, it can be hard to pick a research topic that fits the scope of your classes and is still compelling and unique.
Here are a few exciting topics we recommend exploring for your next assigned research project:
Mental health in post-secondary students
Seeking post-secondary education is a stressful and overwhelming experience for most students, making this topic a great choice to explore for your in-class research paper.
Examples of post-secondary mental health research topics include:
Student mental health status during exam season
Mental health disorder prevalence based on study major
The impact of chronic school stress on overall quality of life
The impacts of cyberbullying
Cyberbullying can occur at all ages, starting as early as elementary school and carrying through into professional workplaces.
Examples of cyberbullying-based research topics you can study include:
The impact of cyberbullying on self-esteem
Common reasons people engage in cyberbullying
Cyberbullying themes and commonly used terms
Cyberbullying habits in children vs. adults
The long-term effects of cyberbullying
- Clinical psychology research topics
If you’re looking to take a more clinical approach to your next project, here are a few topics that involve direct patient assessment for you to consider:
Chronic pain and mental health
Living with chronic pain dramatically impacts every aspect of a person’s life, including their mental and emotional health.
Here are a few examples of in-demand pain-related psychology research topics:
The connection between diabetic neuropathy and depression
Neurological pain and its connection to mental health disorders
Efficacy of meditation and mindfulness for pain management
The long-term effects of insomnia
Insomnia is where you have difficulty falling or staying asleep. It’s a common health concern that impacts millions of people worldwide.
This is an excellent topic because insomnia can have a variety of causes, offering many research possibilities.
Here are a few compelling psychology research topics about insomnia you could investigate:
The prevalence of insomnia based on age, gender, and ethnicity
Insomnia and its impact on workplace productivity
The connection between insomnia and mental health disorders
Efficacy and use of melatonin supplements for insomnia
The risks and benefits of prescription insomnia medications
Lifestyle options for managing insomnia symptoms
The efficacy of mental health treatment options
Management and treatment of mental health conditions is an ever-changing area of study. If you can witness or participate in mental health therapies, this can make a great research project.
Examples of mental health treatment-related psychology research topics include:
The efficacy of cognitive behavioral therapy (CBT) for patients with severe anxiety
The benefits and drawbacks of group vs. individual therapy sessions
Music therapy for mental health disorders
Electroconvulsive therapy (ECT) for patients with depression
- Controversial psychology research paper topics
If you are looking to explore a more cutting-edge or modern psychology topic, you can delve into a variety of controversial and topical options:
The impact of social media and digital platforms
Ever since access to internet forums and video games became more commonplace, there’s been growing concern about the impact these digital platforms have on mental health.
Examples of social media and video game-related psychology research topics include:
The effect of edited images on self-confidence
How social media platforms impact social behavior
Video games and their impact on teenage anger and violence
Digital communication and the rapid spread of misinformation
The development of digital friendships
Psychotropic medications for mental health
In recent years, the interest in using psychoactive medications to treat and manage health conditions has increased despite their inherently controversial nature.
Examples of psychotropic medication-related research topics include:
The risks and benefits of using psilocybin mushrooms for managing anxiety
The impact of marijuana on early-onset psychosis
Childhood marijuana use and related prevalence of mental health conditions
Ketamine and its use for complex PTSD (C-PTSD) symptom management
The effect of long-term psychedelic use and mental health conditions
- Mental health disorder research topics
As one of the most popular subsections of psychology, studying mental health disorders and how they impact quality of life is an essential and impactful area of research.
While studies in these areas are common, there’s always room for additional exploration, including the following hot-button topics:
Anxiety and depression disorders
Anxiety and depression are well-known and heavily researched mental health disorders.
Despite this, we still don’t know many things about these conditions, making them great candidates for psychology research projects:
Social anxiety and its connection to chronic loneliness
C-PTSD symptoms and causes
The development of phobias
Obsessive-compulsive disorder (OCD) behaviors and symptoms
Depression triggers and causes
Self-care tools and resources for depression
The prevalence of anxiety and depression in particular age groups or geographic areas
Bipolar disorder
Bipolar disorder is a complex and multi-faceted area of psychology research.
Use your research skills to learn more about this condition and its impact by choosing any of the following topics:
Early signs of bipolar disorder
The incidence of bipolar disorder in young adults
The efficacy of existing bipolar treatment options
Bipolar medication side effects
Cognitive behavioral therapy for people with bipolar
Schizoaffective disorder
Schizoaffective disorder is often stigmatized, and less common mental health disorders are a hotbed for new and exciting research.
Here are a few examples of interesting research topics related to this mental health disorder:
The prevalence of schizoaffective disorder by certain age groups or geographic locations
Risk factors for developing schizoaffective disorder
The prevalence and content of auditory and visual hallucinations
Alternative therapies for schizoaffective disorder
- Societal and systematic psychology research topics
Modern society’s impact is deeply enmeshed in our mental and emotional health on a personal and community level.
Here are a few examples of societal and systemic psychology research topics to explore in more detail:
Access to mental health services
While mental health awareness has risen over the past few decades, access to quality mental health treatment and resources is still not equitable.
This can significantly impact the severity of a person’s mental health symptoms, which can result in worse health outcomes if left untreated.
Explore this crucial issue and provide information about the need for improved mental health resource access by studying any of the following topics:
Rural vs. urban access to mental health resources
Access to crisis lines by location
Wait times for emergency mental health services
Inequities in mental health access based on income and location
Insurance coverage for mental health services
Systemic racism and mental health
Societal systems and the prevalence of systemic racism heavily impact every aspect of a person’s overall health.
Researching these topics draws attention to existing problems and contributes valuable insights into ways to improve access to care moving forward.
Examples of systemic racism-related psychology research topics include:
Access to mental health resources based on race
The prevalence of BIPOC mental health therapists in a chosen area
The impact of systemic racism on mental health and self-worth
Racism training for mental health workers
The prevalence of mental health disorders in discriminated groups
LGBTQIA+ mental health concerns
Research about LGBTQIA+ people and their mental health needs is a unique area of study to explore for your next research project. It’s a commonly overlooked and underserved community.
Examples of LGBTQIA+ psychology research topics to consider include:
Mental health supports for queer teens and children
The impact of queer safe spaces on mental health
The prevalence of mental health disorders in the LGBTQIA+ community
The benefits of queer mentorship and found family
Substance misuse in LQBTQIA+ youth and adults
- Collect data and identify trends with Dovetail
Psychology research is an exciting and competitive study area, making it the perfect choice for projects or papers.
Take the headache out of analyzing your data and instantly access the insights you need to complete your next psychology research project by teaming up with Dovetail today.
Should you be using a customer insights hub?
Do you want to discover previous research faster?
Do you share your research findings with others?
Do you analyze research data?
Start for free today, add your research, and get to key insights faster
Editor’s picks
Last updated: 30 January 2024
Last updated: 11 January 2024
Last updated: 17 January 2024
Last updated: 12 December 2023
Last updated: 30 April 2024
Last updated: 4 July 2024
Last updated: 12 October 2023
Last updated: 5 March 2024
Last updated: 6 March 2024
Last updated: 31 January 2024
Last updated: 23 January 2024
Last updated: 13 May 2024
Last updated: 20 December 2023
Latest articles
Related topics, decide what to build next, log in or sign up.
Get started for free
Clinical Psychology Research Paper Topics

This page provides a comprehensive list of clinical psychology research paper topics , designed to support students navigating the complexities of mental health studies. Aimed at fostering a deeper understanding of psychological assessment, therapeutic methods, and the myriad issues faced by individuals with mental health disorders, these topics cover a broad spectrum of areas within clinical psychology. From exploring the efficacy of different therapeutic approaches to examining the impact of cultural and social factors on mental health, this list serves as a vital resource for students seeking to contribute meaningful research to the field. Whether you are interested in the latest trends in neuropsychology, the intricacies of forensic psychology, or the challenges of mental health in children and adolescents, these carefully selected topics offer a rich foundation for your academic inquiries and research endeavors.
100 Clinical Psychology Research Paper Topics
Clinical psychology plays a pivotal role in understanding, diagnosing, and treating mental health issues, standing at the forefront of efforts to improve psychological well-being and quality of life. This field combines rigorous academic research with practical therapeutic applications, making it essential for students to engage with a wide range of topics that reflect the diversity and complexity of human psychology. The topics listed here span foundational theories, cutting-edge therapeutic interventions, and the nuanced interplay between mental health and societal factors, offering students a comprehensive overview of the landscape of clinical psychology.
Academic Writing, Editing, Proofreading, And Problem Solving Services
Get 10% off with 24start discount code.
- The history and evolution of clinical psychology
- Major theoretical approaches in clinical psychology
- The role of clinical psychology in integrated healthcare
- Ethics in clinical practice and research
- The impact of technology on clinical psychology
- Psychoanalytic theories and techniques
- Cognitive-behavioral therapy: Foundations and evolutions
- The scientist-practitioner model
- Measurement and evaluation in clinical psychology
- Training and professional development in clinical psychology
- Psychological testing and assessment tools
- Neuropsychological testing for cognitive disorders
- Behavioral assessment strategies
- The DSM-5 and diagnostic criteria
- Cultural competence in psychological assessment
- The role of functional assessments in clinical settings
- Innovations in diagnostic methodologies
- Assessing risk and protective factors
- Personality assessment instruments
- Challenges in diagnosing complex cases
- Comparative effectiveness of psychotherapeutic techniques
- Mindfulness and acceptance-based interventions
- The efficacy of short-term psychodynamic therapies
- Innovations in cognitive-behavioral therapy
- Group therapy dynamics and outcomes
- Teletherapy and digital interventions
- Integrative and holistic therapeutic models
- The therapeutic alliance and outcome research
- Psychotherapy for chronic illness
- Ethical considerations in therapeutic practices
- Advances in understanding and treating depression
- Anxiety disorders: Phenomenology and treatment
- Schizophrenia and psychotic disorders
- Personality disorders: Challenges and therapeutic strategies
- Eating disorders: From etiology to recovery
- Bipolar disorder across the lifespan
- Substance use disorders and dual diagnoses
- Post-traumatic stress disorder and trauma-informed care
- Child and adolescent mental health disorders
- The psychology of chronic pain and its management
- Developmental psychopathology
- Behavioral interventions in schools
- Autism spectrum disorders: Diagnosis and intervention
- Adolescent mental health and identity formation
- Parent-child interactions and therapy outcomes
- The impact of technology on youth mental health
- Eating disorders in adolescents
- Childhood anxiety and depression
- ADHD: Contemporary approaches to assessment and treatment
- The role of family therapy in treating childhood disorders
- The brain-behavior relationship
- Cognitive rehabilitation strategies
- Neuroimaging techniques in clinical assessment
- Neuropsychological impacts of neurological disorders
- Aging and cognitive decline
- Pediatric neuropsychology
- Concussions and traumatic brain injury
- The neuropsychology of emotion
- Memory disorders and dementia
- Psychopharmacology for neuropsychological disorders
- The psychology of chronic illness management
- Behavioral interventions for physical health
- Psychoneuroimmunology: Stress and immunity
- Health behavior change models and strategies
- The role of psychology in pain management
- Psychological aspects of cancer care
- The impact of sleep on mental and physical health
- Eating behaviors and nutrition psychology
- The psychology of addiction and substance misuse
- Mind-body interventions in health care
- Psychological assessment in legal contexts
- Competency and insanity evaluations
- The psychology of criminal behavior
- Treatment of offenders and risk assessment
- Victimology and psychological impacts of crime
- Eyewitness testimony and memory reliability
- The role of psychology in law enforcement
- Ethical dilemmas in forensic psychology
- Child custody and family law
- Psychological interventions in correctional settings
- Cross-cultural psychology and mental health
- The impact of socioeconomic status on mental health
- Gender and sexuality issues in clinical psychology
- Racial and ethnic disparities in mental health care
- The psychology of immigration and acculturation
- Indigenous mental health and healing practices
- Stigma and mental illness
- Community psychology and social change
- The role of religion and spirituality in therapy
- Cultural competence in therapeutic settings
- The future of psychotherapy: Trends and predictions
- Virtual reality and augmented reality in therapy
- The use of artificial intelligence in mental health services
- Digital phenotyping and mobile health
- Genomics and personalized medicine in mental health
- Ethical considerations in the use of technology
- The impact of social media on mental health
- Neurofeedback and biofeedback
- E-mental health interventions and apps
- Integrating technology into traditional therapeutic models
The depth and breadth of clinical psychology research paper topics reflect the field’s dynamic nature and its critical role in addressing mental health issues. These topics not only offer students a wealth of areas to explore but also the opportunity to contribute meaningful insights and advancements to the discipline. By delving into these diverse areas of clinical psychology, students can play a part in shaping the future of mental health treatment and understanding, enriching their academic journey and the field at large.
What is Clinical Psychology
Introduction to the Field of Clinical Psychology
Clinical psychology merges the science of psychology with the treatment of complex human problems, making it one of the most critical areas within the realm of psychological study and application. It encompasses a wide range of practices, including assessment, diagnosis, treatment, and prevention of mental disorders. Clinical psychologists employ various therapeutic approaches to treat individuals across the lifespan, dealing with everything from minor stress and life transitions to severe psychopathology.
Importance of Research in Advancing Clinical Practice and Understanding
The bedrock of clinical psychology lies in rigorous research. Research in this field serves multiple purposes: it enhances our understanding of the etiology and progression of mental disorders, evaluates the efficacy of therapeutic interventions, and tests new treatment approaches. Without research, clinical practice would lack the empirical basis necessary for effectively treating patients. Research ensures that clinical interventions are both safe and effective, thereby safeguarding the well-being of clients and advancing the field.
Exploration of Diverse Research Topics in Clinical Psychology
Research in clinical psychology is as diverse as the field itself, covering a wide array of topics that reflect the complexity of human behavior and mental health. These topics range from understanding the neurological underpinnings of mental disorders to exploring the effectiveness of new psychotherapeutic techniques. Research in this field also investigates the social, cultural, and environmental factors that influence mental health, thereby contributing to more holistic approaches to treatment and prevention. This diversity not only broadens the scope of clinical psychology but also ensures that the field remains responsive to the changing needs of society.
Recent Advancements and Innovations in Clinical Psychology Research
The field of clinical psychology has witnessed significant advancements and innovations, thanks in part to technological progress and a deeper understanding of psychological processes. Recent research has explored the potential of teletherapy, digital interventions, and mobile health applications, providing access to mental health services for individuals who might otherwise face barriers to treatment. Additionally, advances in neuroimaging and psychopharmacology have offered new insights into the biological aspects of mental disorders, leading to more targeted and effective treatments. These advancements underscore the dynamic nature of clinical psychology and its continuous evolution in response to scientific discoveries and societal changes.
Ethical Considerations in Clinical Psychology Research
Ethical considerations hold paramount importance in clinical psychology research, given the vulnerability of the populations often involved. Ethical guidelines ensure that research is conducted in a manner that respects the dignity, rights, and welfare of participants. This includes obtaining informed consent, ensuring confidentiality, and minimizing potential harm. Ethical research practices are crucial for maintaining trust between researchers and participants and for upholding the integrity of the field.
Future Directions for Research in Clinical Psychology
Looking ahead, the field of clinical psychology is poised to explore new frontiers that promise to further enhance our understanding of mental health and improve treatment outcomes. One area of future research may focus on personalized medicine, tailoring interventions to the unique genetic, biological, and environmental factors of each individual. Another promising area involves integrating clinical psychology more closely with other disciplines, such as neuroscience and public health, to develop more comprehensive and effective approaches to mental health care. Additionally, as society continues to evolve, ongoing research will be necessary to address the psychological impacts of emerging societal challenges.
The Impact of Research on the Evolution of Clinical Psychology Practices
The trajectory of clinical psychology is indelibly shaped by research. It is through the diligent efforts of researchers that the field continues to advance, offering new insights into the human psyche and more effective treatments for mental disorders. Research in clinical psychology not only enriches our understanding of mental health but also plays a critical role in shaping policies, therapeutic practices, and public perceptions of mental health issues. As we move forward, the continued emphasis on research will ensure that clinical psychology remains a vital force for good in the lives of individuals and communities worldwide, epitomizing the profound impact that research has on the evolution of clinical practices.
iResearchNet’s Writing Services
At iResearchNet, we recognize the unique challenges and complexities involved in crafting research papers within the field of clinical psychology. That’s why we offer specialized writing services tailored specifically for clinical psychology students and professionals. Our mission is to support your academic and research endeavors by providing custom, high-quality papers that reflect the latest advancements and ethical considerations in clinical psychology. Whether you’re exploring novel therapeutic interventions, dissecting complex case studies, or examining the societal impact of mental health issues, iResearchNet is your partner in navigating the intricacies of clinical psychology research.
- Expert Writers with Advanced Degrees in Clinical Psychology : Our team consists of professionals who not only have advanced degrees in clinical psychology but also possess extensive research and writing experience in the field.
- Custom Papers Crafted to Meet Individual Academic Requirements : We understand that each research project has unique requirements, and we tailor our services to meet your specific academic needs.
- Comprehensive Research Incorporating the Latest Studies and Findings : Our writers stay abreast of current research trends and findings in clinical psychology to ensure your paper is informed by the latest insights.
- Adherence to All Academic Formatting Guidelines : Whether you need your paper formatted in APA, MLA, Chicago/Turabian, or Harvard style, our writers are experts in adhering to academic formatting guidelines.
- Unwavering Commitment to Producing Top-Quality Work : Quality is at the heart of what we do. We’re committed to delivering papers that meet the highest standards of academic excellence.
- Personalized Solutions for Each Research Topic : We offer customized writing solutions, ensuring that your paper is tailored to the specific requirements of your research topic.
- Competitive Pricing Designed with Students in Mind : Our pricing model is designed to be affordable for students, balancing high-quality services with competitive pricing.
- Capacity to Meet Even the Most Urgent Deadlines : We understand the pressures of academic deadlines and are equipped to handle urgent requests, ensuring timely completion of your project.
- Assurance of On-Time Delivery for All Projects : Timeliness is crucial, and we guarantee the on-time delivery of your research paper, allowing you to submit your work with confidence.
- Round-the-Clock Support for Queries and Updates : Our customer support team is available 24/7 to address any queries you may have and provide updates on your project’s progress.
- Strict Privacy Policies to Protect Client Information : We take your privacy seriously and adhere to strict policies to protect your personal and academic information.
- User-Friendly System for Tracking Order Progress : Our online platform makes it easy for you to track the progress of your order, offering transparency and peace of mind.
- Money-Back Guarantee if Expectations Are Not Met : We stand by the quality of our work. If your paper does not meet your expectations, we offer a money-back guarantee.
At iResearchNet, our dedication to supporting students and professionals in their clinical psychology research endeavors is unwavering. We understand the critical importance of your academic and professional contributions to the field of clinical psychology. By providing high-quality, customized research papers, we aim to help you advance your academic journey and make meaningful contributions to the field. Choose iResearchNet for your clinical psychology research paper needs and experience the difference that professional, tailored writing services can make in achieving academic excellence.
Advance Your Academic Journey with Custom Research Papers!
Embark on a path of academic distinction in the field of clinical psychology with iResearchNet at your side. Our expert writing services are meticulously designed to cater to your unique research paper needs, empowering you to delve deeper into the complexities of mental health and therapeutic practices. Whether you’re tackling the intricacies of psychological assessments, exploring innovative therapeutic approaches, or analyzing the societal implications of mental health policies, our custom research papers are your gateway to academic excellence.
We invite you to take full advantage of the unparalleled support and expertise offered by iResearchNet. Our process is streamlined for your convenience, ensuring that ordering your custom research paper is as straightforward as possible. From the moment you reach out to us, you’ll experience the comprehensive support that sets us apart. Our team is dedicated to your success, offering personalized assistance every step of the way, from initial consultation to the final delivery of your project.
Don’t let the opportunity to elevate your academic and professional prospects pass you by. Choose iResearchNet for your clinical psychology research paper needs and step confidently into your future, armed with insights and knowledge that will distinguish your work in the field. Your journey towards academic and professional excellence in clinical psychology begins here, with iResearchNet’s commitment to providing you with top-quality, customized research papers.
ORDER HIGH QUALITY CUSTOM PAPER

- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
Clinical Psychology Research Topics
Stumped for ideas? Start here
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Emily is a board-certified science editor who has worked with top digital publishing brands like Voices for Biodiversity, Study.com, GoodTherapy, Vox, and Verywell.
:max_bytes(150000):strip_icc():format(webp)/Emily-Swaim-1000-0f3197de18f74329aeffb690a177160c.jpg)
Clinical psychology research is one of the most popular subfields in psychology. With such a wide range of topics to cover, figuring out clinical psychology research topics for papers, presentations, and experiments can be tricky.
Clinical Psychology Research Topic Ideas
Topic choices are only as limited as your imagination and assignment, so try narrowing the possibilities down from general questions to the specifics that apply to your area of specialization.
Here are just a few ideas to start the process:
- How does social media influence how people interact and behave?
- Compare and contrast two different types of therapy . When is each type best used? What disorders are best treated with these forms of therapy? What are the possible limitations of each type?
- Compare two psychological disorders . What are the signs and symptoms of each? How are they diagnosed and treated?
- How does "pro ana," "pro mia," " thinspo ," and similar content contribute to eating disorders? What can people do to overcome the influence of these sites?
- Explore how aging influences mental illness. What particular challenges elderly people diagnosed with mental illness face?
- Explore factors that influence adolescent mental health. Self-esteem and peer pressure are just a couple of the topics you might explore in greater depth.
- Explore the use and effectiveness of online therapy . What are some of its advantages and disadvantages ? How do those without technical literacy navigate it?
- Investigate current research on the impact of media violence on children's behavior.
- Explore anxiety disorders and their impact on daily functioning. What new therapies are available?
- What are the risk factors for depression ? Explore the potential risks as well as any preventative strategies that can be used.
- How do political and social climates affect mental health?
- What are the long-term effects of childhood trauma? Do children continue to experience the effects later in adulthood? What treatments are available for PTSD (post-traumatic stress disorder) in childhood?
- What impact does substance use disorder have on the family? How can family members help with treatment?
- What types of therapy are most effective for childhood behavioral issues ?
Think of books you have read, research you have studied, and even experiences and interests from your own life. If you've ever wanted to dig further into something that interested you, this is a great opportunity. The more engaged you are with the topic, the more excited you will be to put the work in for a great research paper or presentation.
Consider Scope, Difficulty, and Suitability
Picking a good research topic is one of the most important steps of the research process. A too-general topic can feel overwhelming; likewise, one that's very specific might have limited supporting information. Spend time reading online or exploring your library to make sure that plenty of sources to support your paper, presentation, or experiment are available.
If you are doing an experiment , checking with your instructor is a must. In many cases, you might have to submit a proposal to your school's human subjects committee for approval. This committee will ensure that any potential research involving human subjects is done in a safe and ethical way.
Once you have chosen a topic that interests you, run the idea past your course instructor. (In some cases, this is required.) Even if you don't need permission from the instructor, getting feedback before you delve into the research process is helpful.
Your instructor can draw from a wealth of experience to offer good suggestions and ideas for your research, including the best available resources pertaining to the topic. Your school librarian may also be able to provide assistance regarding the resources available for use at the library, including online journal databases.
Kim WO. Institutional review board (IRB) and ethical issues in clinical research . Korean Journal of Anesthesiology . 2012;62(1):3-12. doi:10.4097/kjae.2012.62.1.3
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Mental Health and Clinical Psychological Science in the Time of COVID-19: Challenges, Opportunities, and a Call to Action
June gruber, lee anna clark, jonathan s abramowitz, amelia aldao, tammy chung, erika e forbes, gordon c nagayama hall, stephen p hinshaw, steven d hollon, daniel n klein, robert w levenson, jane mendle, enrique w neblett, bunmi o olatunji, mitchell j prinstein, jonathan rottenberg, anne marie albano, jessica l borelli, joanne davila, dylan g gee, lauren s hallion, stefan g hofmann, jutta joormann, alan e kazdin, annette m la greca, angus w macdonald iii, katie a mclaughlin, adam bryant miller, matthew nock, jacqueline b persons, david c rozek, george m slavich, jessica l schleider, bethany a teachman, lauren m weinstock.
- Author information
- Article notes
- Copyright and License information
All author names for the full article are listed alphabetically (by last name) after the four coordinating authors. Authorship contributions are as follows: June Gruber: Oversaw and organized overall article ideas and editing; contributed to writing the introduction, middle-aged adulthood, and concluding comments; approved final article; Mitchell J. Prinstein: Oversaw and organized overall article ideas and editing; contributed to writing the introduction, suicide, adolescence, social relationships, and concluding comments; approved final article; Lee Anna Clark: Edited the overall article, contributed to writing on assessment and treatment challenges, training models for mental health delivery; approved final article; Jonathan Rottenberg: Edited overall article, contributed to writing the introduction; approved final article; Jonathan S. Abramowitz: Contributed to writing on anxiety and depression; approved final article; Anne Marie Albano: Contributed to writing on adolescents and young adults; approved final article; Amelia Aldao: Contributed to writing on assessment and treatment challenges, training models for mental health delivery; approved final article; Jessica L. Borelli: Contributed to writing on older adults, family and interpersonal dynamics; approved final article; Tammy Chung: Contributed to writing on section pertaining to substance use disorders; approved final article; Joanne Davila: Contributed to writing on family and interpersonal dynamics; approved final article; Erika E. Forbes: Contributed to writing on anxiety and depression, adolescents and young adults, research agenda and priorities; approved final article; Dylan G. Gee: Contributed to writing on childhood; approved final article; Gordon C. Nagayama Hall: Contributed to writing on marginalized racial and ethnic groups and health disparities; approved final article; Lauren S. Hallion: Contributed to writing on anxiety and depression, assessment and treatment challenges; approved final article; Stephen P. Hinshaw: Contributed to writing on stigma; approved final article; Stefan G. Hofmann: Contributed to writing on anxiety and depression; reviewed and edited overall article; approved final article; Steven D. Hollon: Contributed to writing on anxiety and depression; approved final article; Jutta Joormann: Contributed to writing on anxiety and depression; approved final article; Alan E. Kazdin: Contributed to writing on clinical science psychology delivery; approved final article; Daniel N. Klein: Contributed to writing on anxiety and depression, adolescents and young adults; approved final article; Annette M. La Greca: Contributed to writing on PTSD; approved final article; Robert W. Levenson: Contributed to writing on older adults; approved final article; Angus W. MacDonald III: Contributed to writing the introduction, psychosis and other severe mental disorders; approved final article; Dean McKay: Contributed to writing on anxiety and depression, mental health care; approved final article; Katie A. McLaughlin: Contributed to writing on childhood, anxiety and depression, mental health disparities; approved final article; Jane Mendle: Contributed to writing on adolescents and young adults; approved final article; Adam Bryant Miller: Contributed to writing on suicide, childhood, adolescents and young adults; approved final article; Enrique W. Neblett: Contributed to writing on members of marginalized racial and ethnic groups and health disparities; approved final article; Matthew Nock: Contributed to writing on suicide; approved final article; Bunmi O. Olatunji: Contributed to writing on mental health care; approved final article; Jacqueline B. Persons: Contributed to writing on assessment and treatment challenges; approved final article; David C. Rozek: Contributed to writing on suicide, research agenda and priorities; approved final article; Jessica L. Schleider: Contributed to writing on training models for mental health delivery and interventions; approved final article; George M. Slavich: Contributed to writing on stress and loss of protective factors; anxiety and depression; approved final article; Bethany A. Teachman: Contributed to writing on training models for mental health delivery and care; approved final article; Vera J. Vine: Contributed to writing on research agenda and priorities; approved final article; Lauren M. Weinstock: Contributed to writing on training models for mental health delivery; approved final article.
June Gruber served as lead for conceptualization, writing – original draft, and writing – review and editing. Mitchell J. Prinstein served as lead for conceptualization, writing – original draft, and writing – review and editing. Lee Anna Clark served as lead for writing – review and editing. Jonathan Rottenberg served as lead for writing – review and editing. Lee Anna Clark, Jonathan Rottenberg, Jonathan S. Abramowitz, Anne Marie Albano, Amelia Aldao, Jessica L. Borelli, Tammy Chung, Joanne Davila, Erika E. Forbes, Dylan G. Gee, Gordon C. Nagayama Hall, Lauren S. Hallion, Stephen P. Hinshaw, Stefan G. Hofmann, Steven D. Hollon, Jutta Joormann, Alan E. Kazdin, Daniel N. Klein, Annette M. La Greca, Robert W. Levenson, Angus W. MacDonald III, Dean McKay, Katie A. McLaughlin, Jane Mendle, Adam Bryant Miller, Enrique W. Neblett, Matthew Nock, Bunmi O. Olatunji, Jacqueline B. Persons, David C. Rozek, Jessica L. Schleider, George M. Slavich, Bethany A. Teachman, Vera J. Vine, and Lauren M. Weinstock contributed to conceptualization equally. Lee Anna Clark, Jonathan Rottenberg, Jonathan S. Abramowitz, Anne Marie Albano, Amelia Aldao, Jessica L. Borelli, Tammy Chung, Joanne Davila, Erika E. Forbes, Dylan G. Gee, Gordon C. Nagayama Hall, Lauren S. Hallion, Stephen P. Hinshaw, Stefan G. Hofmann, Steven D. Hollon, Jutta Joormann, Alan E. Kazdin, Daniel N. Klein, Annette M. La Greca, Robert W. Levenson, Angus W. MacDonald III, Dean McKay, Katie A. McLaughlin, Jane Mendle, Adam Bryant Miller, Enrique W. Neblett, Matthew Nock, Bunmi O. Olatunji, Jacqueline B. Persons, David C. Rozek, Jessica L. Schleider, George M. Slavich, Bethany A. Teachman, Vera J. Vine, and Lauren M. Weinstock contributed to writing – original draft equally. Jonathan S. Abramowitz, Anne Marie Albano, Amelia Aldao, Jessica L. Borelli, Tammy Chung, Joanne Davila, Erika E. Forbes, Dylan G. Gee, Gordon C. Nagayama Hall, Lauren S. Hallion, Stephen P. Hinshaw, Stefan G. Hofmann, Steven D. Hollon, Jutta Joormann, Alan E. Kazdin, Daniel N. Klein, Annette M. La Greca, Robert W. Levenson, Angus W. MacDonald III, Dean McKay, Katie A. McLaughlin, Jane Mendle, Adam Bryant Miller, Enrique W. Neblett, Matthew Nock, Bunmi O. Olatunji, Jacqueline B. Persons, David C. Rozek, Jessica L. Schleider, George M. Slavich, Bethany A. Teachman, Vera J. Vine, and Lauren M. Weinstock contributed to writing – review and editing equally.
Correspondence concerning this article should be addressed to June Gruber, Department of Psychology and Neuroscience, University of Colorado Boulder, 345 UCB Muenzinger D321C, Boulder, CO 80309-0345, or to Mitchell J. Prinstein, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill, 240 Davie Hall, CB 3270, Chapel Hill, NC 27599-3270. [email protected] or [email protected]
Issue date 2021 Apr.
COVID-19 presents significant social, economic, and medical challenges. Because COVID-19 has already begun to precipitate huge increases in mental health problems, clinical psychological science must assert a leadership role in guiding a national response to this secondary crisis. In this article, COVID-19 is conceptualized as a unique, compounding, multidimensional stressor that will create a vast need for intervention and necessitate new paradigms for mental health service delivery and training. Urgent challenge areas across developmental periods are discussed, followed by a review of psychological symptoms that likely will increase in prevalence and require innovative solutions in both science and practice. Implications for new research directions, clinical approaches, and policy issues are discussed to highlight the opportunities for clinical psychological science to emerge as an updated, contemporary field capable of addressing the burden of mental illness and distress in the wake of COVID-19 and beyond.
Keywords: clinical psychological science, clinical psychology, mental health, treatment, COVID-19
COVID-19, the illness produced by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), has been associated with some of the greatest social, economic, and medical challenges of the 21st century. Between November 2019, when the outbreak began, and early May 2020, over 4.6 million people worldwide tested positive for infection with the virus, and more than 300,000 have died. Understandably, the first response phase focused on reducing infection rates, thereby preserving hospital resources (i.e., “flattening the curve”; Adhanom Ghebreyesus, 2020 ; Gruber & Rottenberg, 2020 ). As such, the initial contribution of clinical psychological science was attenuated relative to such fields as virology, epidemiology, and public health. Increasingly, however, it is becoming clear that the pandemic confers grave and potentially long-term mental health implications for the nation. The toxic psychosocial stressors that the pandemic has created (e.g., physical risks, daily disruptions, uncertainty, social isolation, financial loss, etc.) are well known to affect mental health (and thereby also physical health) adversely, and collectively encompass many characteristics that have been identified as having the greatest negative effects. Moreover, preliminary evidence suggests that the virus has direct behavioral-health sequelae and exacerbates existing psychopathology ( Adhanom Ghebreyesus, 2020 ). Accordingly, the field of clinical psychological science must play a leadership role in guiding a national response for the foreseeable future.
There are three ways in which the COVID-19 pandemic may be particularly, and perhaps uniquely, detrimental to mental health. First, it is long term and widespread, with an uncertain end date; the stakes are high, the disruption to daily routines is severe, and the loss of resources to meet both immediate (e.g., food, cleaning supplies) and future needs (e.g., due to unemployment) is significant.
Second, the COVID-19 pandemic is a multidimensional stressor, affecting individual, family, educational, occupational, and medical systems, with broader implications for the macrosystem, as it exacerbates political rifts, cultural and economic disparities, and prejudicial beliefs. Concerns regarding interpersonal disruption may be particularly relevant for understanding its psychological effects and both physical and psychological outcomes. Reduced social interaction is a notable risk factor for mental health difficulties and the negative impact of loneliness on mental and physical health is well-documented ( Cacioppo, Grippo, London, Goossens, & Cacioppo, 2015 ). Many individuals are facing serious illness—and thus, prolonged separation or even death—of loved ones, made even more difficult by interruptions in typical modes of grieving (e.g., funerals, spending time with family, sitting shiva, religious services), or by ongoing concerns regarding one’s own or one’s family members’ safety. Social disruptions during COVID-19 also include role confusion and conflict: Many parents are serving as both home-school teachers and care providers while also maintaining occupational responsibilities. These role changes thus increase parental stress and fatigue which, in turn, result in lower parenting satisfaction, self-efficacy, and distress tolerance (e.g., Kinnunen & Mauno, 1998 ). Strict stay-at-home guidelines also confer risk for sustained exposure to many interpersonal sources of adversity (e.g., marital discord, parent–child conflicts, interpersonal threat and deprivation, parental psychopathology, addictive behaviors, unemployment and economic instability, and lack of social support), many of which are known risk factors for child abuse ( Brown, Cohen, Johnson, & Salzinger, 1998 ; Stoltenborgh, Bakermans-Kranenburg, & Van Ijzendoorn, 2013 ) and the onset of psychopathology ( McLaughlin et al., 2012 ).
Third, the protections needed to safeguard against infection necessarily, but ironically, block access to protective factors that are known to reduce the effects of stress (e.g., enjoyable distractions, behavioral activation, social relationships) because they are difficult to employ while adhering to stay-at-home and social-distancing mandates. The lack of protective factors may be especially marked among socially isolated older adults who also are among the most vulnerable to the virus.
This article, therefore, aims to highlight the most urgent areas to address, and to suggest research directions, clinical approaches, and policy issues that need attention. Although numerous scientific fields and psychological subdisciplines, will need to be involved to address a myriad of interrelated relevant issues, this article focuses specifically on necessary contributions from “clinical psychological science,” a sub-field within mental health disciplines that reflects “a broad intellectual commitment to the importance of empirical research, its integration with clinical practice, and the central role that science must play in the training of clinical psychologists” ( Oltmanns & Krasner, 1993 ). 1 Extant findings are used to articulate briefly the unique mental health issues across developmental age levels that are likely to result from COVID-19. Next, acute challenge areas that are likely to emerge during the course of the pandemic are considered. A path forward is then discussed, highlighting new areas for discovery and potential paradigm shifts from traditional models of clinical psychological science implementation. It may be that the COVID-19 pandemic will prompt changes to mental health fields that have long been needed—only now, the changes are required to survive. In short, this article has two main goals: (a) to leverage what is known within clinical psychological science to address the enormous U.S. mental health needs exposed by COVID-19 and (b) to highlight what is unknown, perhaps prompting reforms to practices that are overdue for an update.
Psychological Impacts of COVID-19 Across the Life Span
Within the U. S., government officials and the popular media have begun to recognize the mental health crises that are likely to follow the immediate physical threat associated with the COVID-19 pandemic. Substantial research suggests that these needs can now be predicted from theoretical models regarding psychopathology risks and articulated with some clarity and detail. This section provides a brief review of this literature to highlight unique risks applicable to different developmental stages, including childhood, adolescence and young adulthood, middle adulthood, and older adulthood.
Children’s emotional/behavioral responses to COVID-19 are likely to result more from significant disruptions to typical roles and daily routines than an appraisal of the health and economic concomitants of the pandemic. Government-mandated school closures affected more than 45 million children in the U.S. as of this writing May 2020. Worldwide, this included school closures in 138 countries, affecting approximately 80% of school-age children ( Van Lancker & Parolin, 2020 ). In combination with changes in parents’ and caregivers’ schedules or availability, this process has been the most disruptive, prolonged shift to children’s daily lives in many decades, scrambling their familiar routines and reducing the number of adult and peer resources available to them. Indeed, schools are a major point of access to mental health resources for children ( Merikangas et al., 2011 ) and serve as gateways for identification and referral to specialty mental health providers ( Farmer, Burns, Phillips, Angold, & Costello, 2003 ). Importantly, developmental and mental health risks associated with the vast societal changes triggered by the COVID-19 pandemic are likely to be felt disproportionately by children living in families with lower economic resources and/or experiencing high levels of adversity prior to the pandemic.
Adolescence
Many forms of psychopathology increase in severity and/or prevalence during adolescence. COVID-19 pandemic-related disruptions are likely to exacerbate developmental vulnerabilities to a wide range of internalizing, externalizing, and health-risk behaviors. Numerous factors may explain the increased risk to adolescents, including an increased exposure to parents’ mental health problems, a loss of important “rite of passage” milestones (e.g., senior prom, graduation), uncertainty about the future, and a loss of autonomy. Yet perhaps the most important impact on adolescent lives will be the significant disruption to peer experiences that are critical for youths’ emotional, moral, behavioral, and identity development ( Prinstein & Giletta, 2016 ). During the COVID-19 crisis, many adolescents have increased their already remarkably frequent use of digital media to compensate for the loss of in-person social interactions, yet emerging research suggests that digitally mediated social interactions may be distinct in form and psychological function from face-to-face experiences ( Prinstein, Nesi, & Telzer, 2020 ). Separated from their peers, adolescents also will miss chances to engage in reward-seeking behaviors that characterize this developmental period, and that often enable opportunities for growth and exploration ( Forbes & Dahl, 2012 ; Tezler, 2016 ).
Young Adulthood
The combination of mental health, financial, and social changes during COVID-19 also poses unique challenges for young adults (e.g., Arnett, 2014 ). Although some young adults will experience many of the same challenges as adolescents with regard to missed rites of passage and disrupted social lives, others who return to living with parents may find a stalling or regression of key developmental milestones, including their independence in sexual relationships, expression of their sexual and gender identity, and ability to engage (or not) in religious, political, or other pursuits of their choice. This can result in unprecedented role confusion if forced into an unwelcome adolescent role (e.g., back living with family after a period of independence) or an adult role for which they feel unprepared (e.g., economic self-sufficiency). In addition to the immediate financial constraints of a tenuous economy and high unemployment, long-term vocational and social growth may be narrowed through curtailed education, limited ability to travel, difficulty obtaining vocational training or experience, and a slow ramp-up of the economy as restrictions begin to ease, with limited employment opportunities for entry-level workers.
Middle Adulthood
Adults in the middle-adulthood life span phase face unique and compounding economic and social stressors during the COVID-19 crisis that put them at heightened risk for mental health challenges. These include economic stressors tied to sudden unemployment or furloughs, and salary cuts that threaten their current and future economic stability. Middle-aged adults with children may also face abrupt role shifts as they transition to full-time homeschool teachers with little to no preparation, while also juggling work demands with little childcare support, which can quickly cause parental burnout and mental exhaustion ( Manjoo, 2020 ). In addition to the immediate financial and caregiving stressors during COVID-19, those middle-aged adults with living parents may additionally face increased anxiety and worry about the health and ability to care for (or even visit) their parents while physical-distancing guidelines are enforced.
Older Adulthood
Older adults are uniquely vulnerable during COVID-19, both physically and psychosocially. Older adults may have a heightened susceptibility to infection and its adverse consequences, and they may experience a loss of usual social support, such as family members visiting ( Garnier-Crussard, Forestier, Gilbert, & Krolak-Salmon, 2020 ). This abrupt physical threat and loss of social resources may increase risk for loneliness, isolation, and depression among older adults (e.g., Armitage & Nellums, in press ). Research during the 2002–2004 SARS outbreak documented that greater levels of stress, anxiety, and social isolation among older adults were associated with higher suicide rates ( Chan, Tang, & Hui, 2006 ; Yip, Cheung, Chau, & Law, 2010 ). Particularly vulnerable are older adults with dementia, which interferes with full cognitive understanding of the threat of the virus and hampers remembering to use safety behaviors (e.g., hand washing, wearing a mask when necessary). Family members providing care for people with dementia (over 16 million in the U.S. alone; Alzheimer’s Association, 2020 ) already are highly vulnerable to mental health problems ( Schulz, O’Brien, Bookwala, & Fleissner, 1995 ). For them, sheltering in place can add to social isolation, reduce access to external resources, and increase burden. Finally, for older adults living in congregated nursing-home facilities, risk of infection spread can be dramatically heightened ( Wang et al., 2020 ).
Psychological Sequelae of COVID-19
The COVID-19 pandemic introduced a complex worldwide stressor, and the strategies used to reduce physical health threats ironically may undercut critical protective factors known to buffer the negative effects of psychological stress. It is thus reasonable to assume that the pandemic will be associated with a substantial, sustained, and potentially severe “mental health curve” that, like the prevalence of the virus itself, will also need flattening given already-insufficient mental health resources in the U.S. Ideally, federal and state resources would be allocated to address mental health needs with the same vigor and attention that has been dedicated toward physical health threats. Yet this response seems unrealistic in light of a long history of inadequate attention to, or funding for mental health; thus, it is incumbent upon clinical psychological scientists and practitioners to conceive of innovative approaches to meet the increased burden of mental illness. This section discusses a model for understanding the psychological sequelae of COVID-19-related phenomena; briefly reviews preliminary, emerging research confirming an increased rate of mental health distress; and then discusses specific presentations of psychopathology that may deserve special attention.
Stress and Loss of Protective Factors
Increased psychological difficulties following the COVID-19 pandemic are likely to result from stress, defined as the physical and psychological responses that occur when situational demands outweigh one’s real or perceived resources to address them ( Brooks et al., 2020 ; Lazarus & Folkman, 1984 ; Monroe, 2008 ). As noted earlier, this complex stressor is characterized by great uncertainty, life-threatening conditions, prolonged exposure to anxiety-inducing information, and losses (e.g., of loved ones, financial security, daily routines, perceived control, and social roles), as well as actual physical threat. COVID-19 may represent a “perfect storm” of stress with high potential for adverse mental health consequences.
Psychobiological models have described clear associations between stress, the activation of brain systems (e.g., amygdala) that process fear and threat, and the release of cortisol, epinephrine, and norepinephrine into the blood-stream (e.g., O’Donovan, Slavich, Epel, & Neylan, 2013 ). These responses are adaptive in the short term, mobilizing needed resources to address acute threats. When prolonged, however, these responses can take a toll on the body known as allostatic load ( McEwen & Stellar, 1993 ), which negatively affects the brain (e.g., hippocampus), cardiovascular system (e.g., high blood pressure), and immune system (e.g., increased inflammation; McEwen & Wingfield, 2003 ). Inflammation, in turn, increases risk for psychopathology and related physical health problems ( Furman et al., 2019 ; Slavich, 2020 ). Populations experiencing increased stress due to COVID-19 are thus likely to suffer from a wide range of mental as well as physical health difficulties.
Several literatures support this supposition. For instance, work on highly disruptive or life-threatening natural and human-made disasters suggests markedly high risk for psychopathology following stress exposure, including increased internalizing and externalizing symptoms across age groups ( Bonanno, Brewin, Kaniasty, & La Greca, 2010 ; La Greca, Silverman, Vernberg, & Roberts, 2002 ). These adverse mental health impacts are most prevalent in vulnerable populations (e.g., those at socioeconomic disadvantage, minority groups; Tang, Liu, Liu, Xue, & Zhang, 2014 ), and various risk factors (e.g., temperamental fear, neural reactivity to emotional stimuli) are associated with more postdisaster symptoms ( Kujawa et al., 2016 ; Meyer et al., 2017 ). For some individuals, these effects persist long after the disaster has passed ( Bonanno et al., 2010 ).
Early, descriptive data examining mental health concomitants of COVID-19 also support this prediction. In an early 2020 sample of 1,200+ Wuhan-area nurses and physicians, relatively high prevalence estimates (i.e., 12% 15%, and 36%) of moderate-to-severe levels of anxiety, depression, and general distress, respectively, were reported ( Lai et al., 2020 ). The pandemic is also already affecting national mental health in countries that were hit early; for example, there have been sharp rises in anxiety and depression in China ( Gao et al., 2020 ). A similar pattern is likely to occur following COVID-19 more globally, especially among vulnerable populations, with the severity and duration of mental health difficulties being proportionally greater as a function of the severity and duration of the stressors. In this context, there are several areas of psychopathology that are most likely to result from COVID-19. Five of these areas are addressed in the sections that follow, although there is insufficient space to do full justice to them all.
Anxiety and Depression
Anxiety and depressive symptoms are likely to increase during the COVID-19 pandemic, resulting in greater vulnerability to psychological distress in the population at large and more individuals with diagnosable psychiatric disorders. This supposition is supported by data from the 2008 U.S. financial crisis, which suggested that chronic stress acutely increases risk for internalizing disorders (specifically, depressive, anxiety, and panic symptoms; Forbes & Krueger, 2019 ). This possibility is also supported by contemporary models that articulate how stress affects psychological and biological systems associated with anxiety and depression (e.g., Slavich, 2020 ). For instance, extant research reveals that psychological stressors increase emotional reactivity and reliance on maladaptive emotionregulation strategies that are known to exacerbate risk for internalizing symptoms (e.g., Nolen-Hoeksema, Wisco, & Lyubomirsky, 2008 ; Segerstrom, Tsao, Alden, & Craske, 2000 ). COVID-19 related stressors, such as social-distancing mandates, may also reduce access to regular social interactions that are recognized as an important process for promoting psychosocial resilience and overall well-being ( Cohen, 2004 ; Hofmann, 2014 ; Slavich, 2020 ).
The COVID-19 pandemic is also likely to precipitate substantial increases in depression. Depression is generally theorized as an abnormal response to loss, and the pandemic is likely to engender loss experiences in several life domains. Most notably, COVID-19 will lead to the death of loved ones for many individuals, with such deaths being relatively sudden and otherwise unexpected. In addition, the pandemic is leading to losses in social connectedness, daily routines, social roles, jobs, and financial stability. COVID-19 also directly affects other risk factors for depression, such as emotion regulation and coping ( Gross & Jazaieri, 2014 ) and may interfere with many protective forms of responding, such as seeking of social support and use of problem-focused coping strategies (e.g., thinking of various ways to solve a problem, selecting one, and taking action; Compas et al., 2017 ; Hofmann, Sawyer, Fang, & Asnaani, 2012 ). At the same time, social isolation and ongoing media coverage focusing on social-environmental threat may result in increased rumination and worry that drive biological processes such as inflammation that increase risk for depression ( Slavich & Irwin, 2014 ). Social isolation and stay-at-home orders also may interfere with the ability to experience positive affect, apply social strategies for regulating affect, and use rewarding experiences to offset negative emotions. Given the importance of social connection and belonging for regulating positive affect for resilience to depression and resilience in general, COVID-19 may be particularly likely to increase risk for depression.
Although anxiety and depression overlap both temporally and in terms of phenotypic presentation, anxiety is generally considered a primary response to threat or uncertainty, whereas depression is typically conceptualized as an abnormal response to loss. Notably, the COVID-19 pandemic is a complex, multifaceted stressor that includes elements of threat, uncertainty, and potential loss. It is well known that not all individuals who experience major life stress develop affective disorders, with cognitive and emotional responses playing a critical role in determining whether anxiety or depression follows such stress ( Aldao & Nolen-Hoeksema, 2010 ). Therefore, it will be important to pay attention to exaggerated perceptions of threat (which have been linked to anxiety) and loss (which have been linked to depression). It will also be important to ensure that the behaviors required to ensure physical safety, such as avoidance (e.g., of other people and public spaces) and vigilance (e.g., scanning the body for signs of disease), do not have the unintended consequence of increasing risk for the onset, exacerbation, or relapse of these two disorders.

Traumatic Stress Reactions
Acute stress disorder (ASD) and posttraumatic stress disorder (PTSD) are trauma- and stressor-related disorders that may occur at any age, and may result from direct exposure to a traumatic event involving actual or perceived life-threat, as well as from repeated or extreme exposure to aversive details of a traumatic event ( American Psychiatric Association, 2013 ). ASD symptoms are shorter in duration (3 days to 1 month) than for PTSD (at least 1 month) but, for both, symptoms include intrusion (e.g., nightmares), negative mood or cognitions, avoidance, and arousal (e.g., hypervigilance, insomnia).
Traumatic stress symptoms are likely to increase as a result of the COVID-19 pandemic because the multiple stressors that characterize it, including the threat to personal safety and security, significant life disruption, loss of loved ones and of financial resources, and disruption and erosion of interpersonal support systems, have been implicated in the development or maintenance of ASD and PTSD symptoms (e.g., Bonanno et al., 2010 ). In fact, the disaster mental health and medical-trauma literatures are pertinent to understanding the mental health impacts of COVID-19, which has exposed many individuals to medically related traumatic events associated with symptoms of ASD and PTSD, such as the sudden death of a loved one, near-death experiences, and life-threatening medical procedures (e.g., Hatch et al., 2018 ). Increased symptoms of traumatic stress (e.g., arousal, negative intrusive thoughts) are likely to occur in the general population, potentially fueled by media exposure to traumatic aspects of COVID-19 ( Gao et al., 2020 ). Although such symptoms may reflect a normative response to an unusually stressful situation, such symptoms are of substantial mental health concern when they are severe, persistent, and interfere with functioning.
Vulnerable populations in high-impact disasters, such as first responders and health care providers ( Bonanno et al., 2010 ; Norris et al., 2002 ), as well as other essential workers, are likely to be at risk for developing subclinical or clinical levels of ASD or PTSD in the COVID-19 pandemic. Health care providers and first responders may be exposed to extreme stressors, often referred to as secondary traumatic stress ( Greinacher, Derezza-Greeven, Herzog, & Nikendei, 2019 ), such as the sudden death of patients and moral decision-making regarding for whom to provide lifesaving intervention ( Griffin et al., 2019 ). First responders and essential workers also provide direct services to individuals with COVID-19 or have increased exposure to the general public, thereby increasing their own COVID-19 risk. Further, these vulnerable groups are advised to self-isolate away from family ( Ellis, 2020 ), thereby restricting social support, and further increasing their risk of traumatic stress reactions (e.g., Kaniasty & Norris, 2008 ; La Greca, Silverman, Lai, & Jaccard, 2010 ). Family members of first responders also may be at elevated risk for traumatic stress reactions, as they fear for loved ones’ safety (e.g., Duarte et al., 2006 ). Furthermore, elevated rates of PTSD have been observed among women and children and among disadvantaged minority groups in the aftermath of disasters ( Bonanno et al., 2010 ; Norris et al., 2002 ), and are likely to emerge for the current pandemic. PTSD symptoms also confer risk for alcohol and substance use, relationship difficulties, and suicidal thoughts and behaviors (e.g., Sareen, 2014 ). Elevated symptoms of PTSD also commonly co-occur with symptoms of depression, which bodes poorly for recovery (e.g., Lai, La Greca, Auslander, & Short, 2013 ), and complicates treatment (e.g., Cohen & the Workgroup on Quality Issues, 2010 ; La Greca & Danzi, 2019 ).
Overall, the “good news” is that most youth and adults exposed to traumatic events recover over time, although a significant minority (15% to 30%) continue to display elevated symptoms of PTSD a year or more postdisaster ( Alisic et al., 2014 ; Bonanno et al., 2010 ) and will benefit from psychological interventions ( APA, 2017 ; Cohen & the Workgroup on Quality Issues, 2010 ; La Greca & Danzi, 2019 ). Psychological first aid ( Brymer et al., 2006 ), widely used for short-term crisis and disaster intervention, may be important for use with people displaying traumatic stress symptoms during the COVID-19 pandemic. Increasing access to psychological treatments, such as via telehealth procedures, will be critical to address the anticipated widespread need for COVID-19-related mental health services for youth and adults.
Substance Use Disorders
Individuals with substance use disorders (SUDs), particularly those who smoke, vape, or use opioids, may be at increased risk for COVID-19 illness severity and even death ( Smith et al., 2020 ; Vardavas & Nikitara, 2020 ; Volkow, 2020 ). For some, pandemic-related stressors (e.g., job loss and financial strain), anxiety, and boredom due to extended stays at home could lead to an increase in smoking or other substance use as a way to cope with negative moods ( Nagelhout et al., 2017 ). In this regard, in March 2020, during the initial stay-at-home weeks in the United States, a survey of adults identified an association between more frequent alcohol and cannabis use in the past week and significantly higher mental distress ( Johns Hopkins COVID-19 Mental Health Measurement Working Group, 2020 ).
For individuals in recovery from SUD or seeking addiction treatment, the pandemic has presented unique challenges. Mandated stay-at-home orders have increased social isolation and concomitant risk for relapse for some individuals ( Volkow, 2020 ). Specifically, staying-at-home can involve domestic stressors (e.g., intimate partner violence), which can challenge recovery efforts. These stressors, in turn, can lead to or exacerbate co-occurring mental health conditions such as depression and anxiety among individuals with SUD ( Tripp, Jones, Back, & Norman, 2019 ). In addition, marginalized individuals, who are homeless or imprisoned, have high rates of SUD (e.g., up to 50% of prisoners have an SUD; Fazel, Yoon, & Hayes, 2017 ), and increased risk for COVID-19 infection ( Volkow, 2020 ) are less likely to receive care during the pandemic due to service provision cut-backs ( Alexander, Stoller, Haffajee, & Saloner, 2020 ). In-person social support, which can provide daily structure for individuals with SUD, especially during early recovery, has shifted to virtual or telehealth platforms ( Volkow, 2020 ). Federal guidelines have rapidly expanded to support access to and more flexible delivery of evidence-based eHealth ( APA, 2020 ), as well as to provide needed medications to support abstinence (e.g., medication-assisted treatment for opioid use disorder; Alexander et al., 2020 ) and other e-recovery support groups facilitated by psychologists in response to the pandemic ( Khatri & Perrone, 2020 ). Through evidence-based eHealth interventions, psychologists are using this opportunity in a time of crisis to create structured, safe, social, virtual spaces to facilitate recovery mindfully among individuals with SUD, and to reduce stigma and harms related to substance use disorder.
Before the onset of COVID-19, suicide already was a relatively neglected public health problem ( U. S. Department of Health and Human Services, Office of the Surgeon General, and National Action Alliance for Suicide, 2012 ). The current pandemic increases the risk for suicide in at least four ways that require a far greater investment in suicide science, along with new approaches to suicide screenings and imminent risk assessments across all types of clinical care. The risk is perhaps most obviously increased in psychologically vulnerable populations through introduction of a novel, pervasive, relatively uncontrollable stressor. Those with histories of depressive symptoms, selfinjury, prior suicidality, maltreatment, PTSD, substance use, and disruptive behavior disorders (particularly among youth) are especially at risk for increased suicidal thoughts and behaviors for all the stress-related reasons already discussed ( Nock & Kessler, 2006 ). In particular, maladaptive interpersonal patterns experienced with few opportunities to escape or distract (due to stay-at-home orders) may elevate individuals’ risk for suicide, and may intensify stressful experiences over time. Second, new at-risk populations may emerge from COVID-19, including trauma-exposed first responders, health care workers, particularly physicians ( Gold, Sen, & Schwenk, 2013 ) who have had to make unspeakably difficult medical-care decisions under high-pressure conditions, as well as other essential workers. Children who have experienced increased exposure to other kinds of trauma (e.g., child maltreatment; Gawęda et al., 2020 ) also may be at increased risk for suicidal behavior.
Third, it should be noted that suicide rates are associated closely with economic indices, with periods of recession associated with higher rates of suicide ideation, attempts, and deaths by suicide among all age and all racial/ethnic groups (e.g., Reeves et al., 2012 ). The worldwide economic changes associated with COVID-19 are likely to be associated with changes in a wide range of self-injurious thoughts and behaviors. Last, most theories offered to explain suicidal behavior have implicated interpersonal stress (e.g., conflict, loss) as a common factor that significantly enhances individuals’ risk ( Miller & Prinstein, 2019 ). Reports of increased isolation, loneliness, interpersonal loss, and limited interpersonal contact thus present a uniquely high-risk period for suicide within the general population as well, requiring ongoing monitoring in the years that follow COVID-19. Unfortunately, many of the existing resources designed to address imminent suicide risk may prove less effective during or after the COVID-19 crisis. Perhaps most importantly, there may be greater reluctance to call 911 or visit a local emergency room to ensure safety from suicidal urges during the pandemic for fear of infection or out of concern that one’s suicidality may overburden hospital staff who are needed to attend to COVID-19 patients.
Research on suicide rates following other extremely stressful events has yielded mixed findings. For many natural disasters, suicide rates often stay stable initially (for a review, see Kolves, Kolves, & De Leo, 2013 ). Following natural disasters, results are mixed for longer term outcomes, with some showing an increase and others showing a decrease in suicide rates. After other extreme stressors (e.g., terrorist attacks), suicide rates have been shown to be stable or even to decrease, which may be due to individuals in a population “coming together” ( Claassen et al., 2010 ) and receiving social support in doing so. As mentioned, however, an increase in social support—at least as long as social-distancing and stay-at-home orders are in effect—is not a viable option in the current disaster. Previous data-points on pandemics are scarce, although some suggest an increase in suicide rates following the 1918 pandemic ( Wasserman, 1992 ). Given the variation in data and extreme stressors, it is clear that clinical psychological scientists should continue to assess patients for suicidality, employ prevention strategies, and continue to collect data to inform how the COVID-19 pandemic is affecting suicide rates.
Psychosis and Other Severe Mental Disorders
Schizophrenia and bipolar affective disorder are also affected by stress-related pathways. Stress is a key factor in the emergence of psychotic illnesses ( Walker & Diforio, 1997 ), and repeated stress can alter the stress response itself, increasing risk for relapse and rehospitalization ( Belvederi Murri et al., 2016 ; Tessner, Mittal, & Walker, 2011 ). The mechanism for this alteration may be stress-related increases in cortisol release, via the HPA axis, altering related brain structures and increasing relapse ( Corcoran et al., 2003 ). Symptom exacerbations magnify the challenges of COVID-19 for people suffering from psychotic disorders, and, as noted below, create additional burdens for family members and other caregivers. Space precludes a more lengthy discussion of how COVID-19-related threats and disruptions potentiate new delusions, exacerbate kindling, or trigger mood symptoms, but there is an acute need to understand and propagate best practices to help the most vulnerable citizens with serious mental disorders and those in their care networks.
Challenges for Clinical Psychological Science Following COVID-19
COVID-19 will produce a series of mental health challenges, yet current practices in the field of clinical psychological science will require substantial adaptation to address them. These challenges relate not only to the expected high prevalence of mental health-related problems but also to the various unique populations that will require services, the critical need to address significant health disparities that have long been underaddressed in most mental health fields, and changes required that are related to the contexts of service delivery. This section describes these challenges and offers recommendations from the available science regarding intervention.
Who Will Need Mental Health Services?
Although the field has a rich literature on treating psychological symptoms and distress among individuals, COVID-19 will lead to an increased need for services among populations that have been understudied. Below, two populations that may need additional attention within research and practice efforts are discussed: health care workers and individuals in racial/ethnic minority groups. This section also addresses issues related to mental health stigma that may limit the number of people who receive psychological services.
Health-care workers.
Substantial research has been conducted to understand how to address trauma among those exposed to horrific, life-threatening events, especially veterans, yet this review suggests that far less research has addressed strategies to work with health care workers. This is a new and urgent need for the field. Such work will need to recognize that front-line health care responders have cared for COVID-19 patients while managing significant risks to their own and their colleagues’ personal health. Moreover, research on prior pandemics reveals that health care workers may face additional public stigma and isolation because of others’ perception that they may be at heightened risk for disease transmission ( Williams, Gonzalez-Medina, & Le, 2011 ). There are many open questions about the extent to which COVID-19 health care workers may develop a range of emotional disorders, from “simple” burnout to depression and PTSD.
A review of extant programs offered for health care workers indicates the content mainly focuses on basic self-care recommendations. Given strong evidence that the majority of people will be resilient after trauma exposure ( Galatzer-Levy, Huang, & Bonanno, 2018 ), along with evidence that overtreating can be harmful ( Bootzin & Bailey, 2005 ), for the majority of workers recommendations to bolster basic self-care (e.g., sleep hygiene, breaks from work, exercise), stress management (e.g., mindfulness), and emotional support may suffice. Further study is needed to determine how to apply the existing literature on risk for PTSD and resilience trajectories to the current circumstances. Importantly, the field needs to think broadly about the appropriate targets of interventions. For example, although it certainly makes sense to focus on deploying resources directly to health care workers who are struggling, another, more efficient approach may be to work with hospitals and other institutions to help them create supportive environments (e.g., allowing workers to voice concerns about virus exposure or working conditions; not stigmatizing workers who express mental health needs) and to create systems that allow for more consistent monitoring of mental health concerns.
Observed mental health patterns among health care workers during previous outbreaks may be informative ( Lai et al., 2020 ). For example, Lancee, Maunder, Goldbloom, and the Coauthors for the Impact of SARS Study (2008) found that new episodes of psychiatric disorders after the SARS outbreak were positively associated with a history of previously having a psychiatric disorder and inversely associated with years of health care experience and the perceived adequacy of training and support. This pattern suggests a need to target resources toward COVID-19 health care workers at higher risk, that is, those newer to the field and those with preexisting mental health issues. Another lesson from the SARS outbreak is that a major focus of intervention for high risk COVID-19 health care workers could include increasing access to resources for reducing daily life stress ( Lung, Lu, Chang, & Shu, 2009 ). In fact, health care workers who reported mental health problems following the SARS crisis were more likely to report symptoms that were related to daily life stress than to SARS itself ( Lung et al., 2009 ). Of course, COVID-19 adds additional daily stressors for health care workers, as many try to manage childcare, home schooling, and financial challenges on top of their extensive occupational demands. Given that those with limited training also represent a high-risk group ( Lancee, Maunder, Goldbloom, & the Coauthors for the Impact of SARS Study, 2008 ), assessing training needs of COVID-19 health care workers will be crucial. For example, the National Ebola Training and Education Center (NETEC) was established in response to the Ebola outbreak to increase health care workers’ competency to deliver effective care to infected patients ( Kratochvil et al., 2017 ). The NETEC also includes training in behavioral-health considerations for staff that may be relevant to the current pandemic.
In all cases, interventions for health care workers must consider cultural responsiveness, as there will be no unitary solution that works across contexts and populations. That is, different needs may arise as a function of race and ethnicity. For instance, given rising bias against Asians in the U. S., health care workers with Asian or Asian American identities may have to navigate increased discrimination from patients and/or coworkers that adversely affects their mental health. Further, subcultures exist within health care environments, and different professions may require distinct types of supports (e.g., physicians and nurses showed different post-SARS symptoms; Lung et al., 2009 ). Continuously and persistently monitoring mental health will be critical to optimizing care for health care workers.
Members of marginalized racial and ethnic groups.
The COVID-19 pandemic is disproportionately affecting members of marginalized racial and ethnic minority groups and those from lower socioeconomic backgrounds. Indeed, the pandemic has the potential to widen racial/ethnic and socioeconomic status (SES) disparities in health and life expectancy that have steadily grown in recent decades ( Singh & Siahpush, 2006 ). Emerging evidence indicates stark racial/ethnic disparities in the impact of COVID-19 in the U.S., with notably higher rates of illness and mortality among Black and Latinx people ( Zephyrin, Radley, Getachew, Baumgartner, & Schneider, 2020 ). Although similar data on infection and mortality rates as a function of SES are limited, the risks may be higher for people with low SES. Factors that contribute to a higher probability of contracting the illness include high population density, crowding, reliance on public transportation, and employment in low-wage jobs that are considered essential during even the most intense period of physical distancing and social isolation, such as transportation, production, and food and grocery services ( Soloman, Maxwell, & Castro, 2019 ). Black, Latinx, and people of low SES are also more likely to have preexisting conditions that exacerbate risk for serious COVID-19 illness and mortality once infected, including hypertension, obesity, diabetes, and cardiovascular disease ( Adler & Rehkopf, 2008 ). These groups are also less likely to have access to high-quality health care ( Schneider, Zaslavsky, & Epstein, 2002 ). Higher rates of COVID-19 infection and mortality among these groups present innumerable sources of stress, including high potential to lose family, friends, and neighbors to the disease, strong risk factors for depression, anxiety, and other mental health problems ( Kendler, Hettema, Butera, Gardner, & Prescott, 2003 ).
Scapegoating of immigrants and other outgroups is common when people seek reassurance while experiencing the threat of disease ( Kam, 2019 ). Thus, racist and xenophobic rhetoric around the origins of the novel coronavirus carries additional risks, particularly for people of Asian ancestry, who have been uniquely scapegoated as carriers of COVID-19. The Asian Pacific Policy and Planning Council ( Jeung & Nham, 2020 ) received nearly 1,500 reports of coronavirus discrimination (e.g., stigma, physical attack, suspicion) from Asian Americans across the United States in a 4-week period. Racial discrimination has general adverse physical and mental health effects for Asian Americans ( Gee, Ro, Shariff-Marco, & Chae, 2009 ), but they are the least likely ethnic group to use mental health services ( Smith & Trimble, 2016 ), and fear of COVID-19 discrimination may further interfere with help-seeking for physical or mental health problems. Thus, the effects of COVID-19 warrant a response that addresses racial/ethnic and socioeconomic disparities broadly, but also one that is specific to the needs of Asian Americans ( Hall et al., 2020 ).
Stigma in the COVID-19 era and beyond.
It is highly likely that only a small proportion of those in need of psychological services will receive them, often because they do not seek them. One factor limiting help seeking is ongoing stigmatization of mental health difficulties. Despite far greater public knowledge about mental illness over recent decades, public stigma related to mental and neuro-developmental disorders remains quite high ( Martinez & Hinshaw, 2016 ). In the COVID-19 era, with the distinct possibility of real increases in clinically significant anxiety, depression, posttraumatic responses to the pandemic and its sequelae (i.e., financial difficulties, family violence, etc.), how public attitudes and behavioral responses may change is unknown. That is, will the vast shared experience give rise to increased identification, compassion, and acceptance? Or will scapegoating and blaming rise, in terms of not only supposed ethnic origins of the virus, but also the perceived psychological threat that still accompanies perceptions of depressive, disorganized, or potentially violent behavior, during times of deprivation? Past research indicates that stigma rises against disenfranchised outgroups during economic downturns ( Hinshaw, 2007 ).
Optimistically, mental health may come to receive the attention it deserves in the wake of COVID-19. Also, as highlighted elsewhere herein, the necessity of providing mental health care remotely may promote greater access for many, if economic disparities regarding tele- and e-access are addressed. On the other hand, a core “module” believed to trigger stigmatizing responses is fear of contagion ( Goffman, 1963 ; Kurzban & Leary, 2001 ). In an era when literal contagion is on everyone’s mind—and when, for valid public health reasons, everyone must try to prevent viral spread—messaging is key. Indeed, “social distance” is a major target of antistigma interventions, countered largely through contact, disclosure, support, and humanization. The public-health term of “physical distancing” in the COVID era may be less inherently stigmatizing. How amazing it would be if this crisis actually plants seeds for reductions in stigma and enhances the push for prevention, self-care, and treatment.
How Will Treatment Be Conducted?
For nearly a century, the standard for treatment delivery of psychological services has been a single patient/single provider in a physical office. However, this system has not addressed the population-wide mental health need. In the years preceding COVID-19, up to 67% of adults and up to 80% of youths with mental health needs have gone without services each year ( Cummings, Wen, & Druss, 2013 ; Kessler et al., 2005 ). Even when services were accessed, many individuals dropped out due to financial and logistical barriers, and provision of evidence-based services remains the exception rather than the rule.
COVID-19 has necessitated a dramatic and immediate change to mental health care delivery that creates important and exciting opportunities to apply clinical psychological science more efficiently and effectively. Below, a variety of changes to this standard of care are discussed and opportunities for research and practice to evolve, perhaps well beyond the offset of COVID-19, are presented. Clinical psychological scientists are ideally positioned to lead the charge toward a transformation in mental health care delivery. As new treatment models are developed and deployed, their feasibility, acceptability, benefits, and potential harms will require careful, nuanced evaluation. Clinical psychological scientists possess expertise in many domains key to this goal: program design and evaluation, intervention and implementation science, and mental health care delivery. As such, a roadmap for realizing practical innovation in mental health care delivery is provided, with the goals of (a) ensuring that a greater proportion of vulnerable individuals, families, and groups gain access to the mental health care system; and (b) creating more accessible, inclusive avenues to mental health support than have ever existed.
Telehealth.
Seemingly overnight, clinical practice required delivery almost exclusively over telehealth platforms, requiring clinicians to learn and execute HIPAA-compliant video conference systems, identify confidential space to conduct clinical practice within their homes, teach technology to their patients, and examine rapid changes to reimbursement practices to ensure that insurance companies, including Medicare, would reimburse tele-health sessions, including across state lines. In many ways, this modality shift was overdue. Nevertheless, clinical psychological science is now needed to understand a wide array of new variables related to treatment efficacy and effectiveness. For instance, more research is needed on hybrid service provision models, integrating combinations of therapist-, digital/electronic, self-, and lay-provider-delivered service components to maximize efficiency of service delivery. Needed investigations include research to determine which telehealth services (i.e., using video, audio-only) are most helpful for individual patients, as well as which patients are most likely to benefit from telehealth relative to more intensive, in-person care. Ultimately, research on these and related questions will permit replacement of “expert consensus” clinical decision-making with empirically driven telemental health practice guidelines. In parallel, research is needed to determine the most effective procedures to conduct valid assessments remotely, including cognitive assessments, observational protocols, and child assessments that may require creative strategies to keep young children engaged without a mutual set of play materials available.
Telehealth also introduces questions regarding the ability to monitor and immediately intervene in high-risk situations. The assessment of imminent suicidality, for instance, or the ability to assist patients with calls to the department of social services in the event of maltreatment, will require modified procedures. Indeed, a formalized, field-wide set of standards for assessing and mitigating imminent risk and monitoring outcomes via telehealth platforms is a high priority. Guidance is needed to work remotely with patients who may develop COVID-19 during treatment, who may not be able to participate in techniques such as diaphragmatic breathing and progressive muscle relaxation. At least during periods of stay-at-home orders, exposure exercises will be limited as well, given restrictions on interaction outside the home.
The switch to telehealth also has implications for training. Specifically, training programs might consider a wider array of predoctoral internship clinical experiences, not limited to those within a close geographic community. Training to deliver services remotely will require a modification of current practices, and supervision skills similarly may need to be modified. Specifically, training may well require (a) integrating practicum and internship opportunities in telehealth, determining standards for evaluating competence in this domain; (b) prioritizing research on the effectiveness of diverse tele-mental health services; and (c) careful consideration of ethical issues that arise with remote provision of telemental health care (e.g., protecting private communication in a globally connected world). Relatedly, in place of the ad hoc telemental health technology systems that clinicians and training programs have implemented in a compressed time period, national technology-system standards for secure, private provision of telemental health services are needed. It also is important to increase understanding of—and account for—significant distress experienced by psychologists who provide treatment. Although psychologists are trained to recognize and account for personal issues that may interfere with their ability to meet their patients’ needs, the enormous disruptions experienced by all humans (including psychologists), coupled with providers’ ethical responsibility to meet the increasing needs of a distressed public, may well create an unusual situation in which typical strategies for self-care may be insufficient.
The switch to telehealth also offers exciting opportunities that may improve clinical psychological science. For instance, telehealth may prompt therapists to utilize technology to collect progress monitoring data and use it to inform treatment, which may lead to better outcomes (cf., Lewis et al., 2019 ). The expansion of telehealth also offers a solution to address significant disparities in access to mental health treatment, particularly in rural and other areas where few providers reside. Telehealth also creates opportunities to incorporate in-home observational assessments or perhaps even in vivo exercises into the therapeutic process. Research may further explore the utility of behavioral practice at home, observations of patient’s behavior as it occurs, and the provision of immediate feedback in situ.
Brief, mass-delivered interventions.
Brief and low-intensity interventions must become a research and clinical practice priority. This includes, as one well-studied example, single-session interventions (SSIs): structured, evidence-based interventions that require just one encounter with a provider or program ( Schleider, Dobias, Sung, & Mullarkey, 2020 ). Evidence suggests that SSIs can reduce or prevent psychopathology in youths and adults (e.g., Schleider et al., 2020 ; Schleider & Weisz, 2017 ), and are effective in treating self-harm ( Lamprecht et al., 2007 ), depressive symptoms ( Schleider et al., 2020 ), and conduct problems ( Mejia, Calam, & Sanders, 2015 ). Importantly, clinically significant, positive SSI effects emerge even for programs that are self-administered (e.g., web-based SSIs), without therapist guidance ( Schleider et al., 2020 ; Schleider & Weisz, 2017 ). SSIs’ overall effects are slightly smaller than those observed for multisession psychotherapy, but their brevity and accessibility magnify their potential public health impact, especially in the case of digital, self-administered SSIs, which are often accessible free-of-charge from any location (e.g., Schleider et al., 2020 ). Moving ahead, it will be critical to integrate SSIs and other low-intensity interventions into service delivery ecosystems. It will be most helpful to learn from other social and behavioral science fields as to how they have integrated brief interventions, from belongingness interventions that reduce the achievement gap among racial and ethnic minority students to governments using “nudges” to shift unhealthy behaviors ( Walton & Wilson, 2018 ). Evaluating these approaches will require a “flip” of standard research paradigms. Too often, research targets lengthy interventions that include only short-term follow-up assessments, rather than tracking durability of outcomes. Instead, research on short interventions, including SSIs, is needed, as is tracking outcomes for longer follow-up periods. This will provide information regarding which brief interventions have durable effects and which act simply as a prime or state manipulation that would require repetition as the effect fades—akin to an “aspirin” model, wherein taking aspirin helps when one has a headache, but one dose is not expected to prevent all future headaches.
Lay-provider service delivery.
An investment and stringent evaluation of scalable lay-provider-delivered supports also will be essential. Highly trained clinicians, including clinical psychological scientists, will remain key to flexible, next-generation service provision, but the need for care will continue to outpace demand. Given substantial evidence that nonprofessionals can deliver effective, sensitive, and acceptable care for a diversity of mental health challenges (e.g., Barnett, Lau, & Miranda, 2018 ), structures to broaden and formalize lay-provider training are needed. There are impressive non-specialist-provider models from the global mental health field that can help guide work domestically ( Singla et al., 2017 ).
Prevention and public health.
To address population-wide mental health needs, it will be important for clinical psychological science to look more broadly at strategies and practices to ameliorate or prevent significant psychological distress. In the short run, empirically supported interventions that are readily available and scalable are recommended, and where they do not exist, should be fostered. However, it will be important for the field also to examine interventions that have emerged from outside of clinical psychological science ( Kazdin, 2018 ); it is better to focus on solving problems than on “taking credit” for the solutions. For example, exercise exemplifies a broadly available intervention that benefits mental and physical health, and much more could be done to help ensure it is part of daily life (e.g., in workplaces or schools). Research also suggests that contact with nature, including interactions with living systems in the form of greenery, vegetation, and nonhuman animals in open spaces including parks, gardens, and forests, also has been well characterized and has surprisingly robust benefits in both lab studies and randomized controlled trials for depression, anxiety, and social isolation (e.g., Bratman et al., 2019 ). The field has an opportunity to be more innovative and vigorous in promoting such broadly available interventions, moving beyond usual “lobbying” and “task force reports” to develop concrete action plans, to partner with agencies and foundations to implement, and then to evaluate impact.
In the longer term, clinical psychological science should take a leadership role in preventing or treating clinical and subclinical mental disorders, as well as known risk factors, not by “merely” providing services but by coordinating cross-disciplinary efforts to offer preventive treatment for mental and physical problems. An exciting opportunity for research will be the identification of psychologically active interventions that can be delivered at scale (cf. fluoride in the water) to build resilience and reduce risks among large segments of the population that may never find their way to a traditional psychotherapy session. Fortunately, alternative models of good treatment delivery already exist in other fields (e.g., public health, law, social policy, business, entertainment) and may help to provide larger scale treatment. Similarly, many sectors of society (e.g., primary, secondary, and higher education systems, corporate human resource centers, justice and correctional systems) are increasingly interested in mental health wellness, and many new industries (e.g., technological tools, genetic/ancestry tracing) are willing partners to help advance clinical psychological science and its applications.
How Best to Evaluate These New Approaches?
Of course, new approaches to psychological service delivery will require careful empirical examination. For instance, research on resilience trajectories and stepped-care models will be critical to determining who can be served adequately with lower versus higher intensity treatments. Partnership with lay providers will require far greater community involvement, training programs to teach students how to partner with community leaders (e.g., faith leaders, social justice advocates), providers, and persons with lived experience so that interventions are ultimately acceptable to communities, fit their context, and address outcomes they value. Primary prevention approaches will require collaboration with new disciplines, including for-profit industries, that will utilize different methodological approaches and collect data with different priorities and values that may require methodological compromises. Yet, these adaptations may be necessary to change clinical psychological science in fundamental ways needed to meet the new demands of COVID-19 and its aftermath.
Already, scientists have begun to experience the challenge of research relying on the status quo. Obviously, human subjects research has been challenging during COVID-required physical distancing. Some methods—physiological measurement, experience sampling—have already lent themselves to ambulatory techniques. Additionally, interviews can often be conducted by video or phone. Questionnaires can be administered through online systems like Qualtrics. Psychosocial interventions can be conducted via telemedicine approaches, and behavior observation tasks can be carried in the home via video. Importantly, such remote methods may be compatible with the increasingly socially oriented research questions, which as noted further below, are particularly relevant in the COVID era. When lab-based methods are used (e.g., MRI scanning), there must be allowances for physical distancing with participants and among research staff (e.g., staggering work schedules). Further, COVID-19 must be met with increased cooperation and innovations in the process of scientific discourse. Collaborations will be critical to pooling resources to mine existing data and collect new data quickly. New findings will then need both rapid dissemination (e.g., at this writing, over 300 preprints of COVID-19 projects are circulating) and careful evaluation. There is a critical needle to thread: How can scientific peer-review be accelerated to accommodate the urgency of studying COVID-19, while maintaining the quality of the vetting process?
Conceptually, COVID-19 has laid bare the interconnectedness of so many aspects of human existence—of humans with one another; of social and economic systems and institutions; of structural inequities with adaptive functioning; of mental with physical health. In this way, the pandemic spotlights the need for a multidimensional understanding of human adaptation. Clinical psychological science must embrace this complexity and seek to understand the impact and inequities of COVID-19 within an interactional, intersectional, and interdisciplinary framework. Relatedly, it will be important to learn whether existing interventions—which may already be evidence-based in other contexts—can also reduce the burden of mental health related to the intersecting challenges of COVID-19. Existing interventions may require adaptations to help recipients build resilience in the COVID-19 context. Additionally, because COVID-19 affects functioning in many bodily systems, it will be valuable to delineate how the disease influences mental health via neurobiological, cardiovascular, respiratory, and other changes. Even more, clinical psychological science will need to reconcile the complementary strengths of psychiatric, disease-oriented perspectives on mental illness with perspectives locating causes of suffering within the social ecology. In sum, clinical psychological science research must rise to the occasion and learn from this moment to increase the versatility of both its methods and conceptual perspectives.
Concluding Comments
Clinical psychological science is needed more than ever in response to both the acute and enduring psychological effects of COVID-19 ( Adhanom Ghebreyesus, 2020 ). This article is intended to inspire dialogue surrounding the challenges the field faces and how it must adapt to meet the mental health demands of a rapidly evolving psychological landscape. Of course, sustained change will require strong advocacy to ensure that mental health research funding is available to understand and address mental health challenges following COVID-19. To secure a leadership role, clinical psychological scientists must be prepared to raise their voices not only within scientific outlets, but also in public discussions on the airwaves (radio, cable news), alongside colleagues in other scientific fields. Sustained effort, collaboration with other disciplines, and unity within psychology will be necessary to address the multifaceted impacts of COVID-19 on humanity.
Public Significance Statement.
Clinical psychological science must lead a national response to address mental health issues following COVID-19. This article highlights urgent challenges to confront, and timely opportunities to contemporize a field to better address mental health issues now and long after. The article concludes by discussing implications for new research directions, clinical approaches, and policy issues.
The term developed over a period of years (1964 to 1991) that saw an increasing belief among clinical psychologists that there was a “fundamental incompatibility of the roles of scientist and professional within one individual” ( Albee, 1970 , p. 1071). In contrast, a subgroup of clinical psychologists believed that “the scientist and the practitioner not only can be reunited but must be in order to continue the profession of clinical psychology as a viable, useful, and unique one in society” ( Oltmanns & Krasner, 1993 ).
The idea for this article came from an initial discussion between two of the corresponding authors (June Gruber and Mitchell J. Prinstein). The article was divided into several smaller working groups of authors covering specific topics of expertise or interest. Each of these smaller working groups continually updated a shared Google document for the article which all authors had access to. There was a smaller group of four coordinating authors (June Gruber, Mitchell J. Prinstein, Lee Anna Clark, and Jonathan Rottenberg) who coordinated the framework of the article and helped oversee organization of writing contributions among the broader authorship group and provided ongoing feedback and tracked article progress, and edited and organized the article as a whole throughout the preparation process.
Contributor Information
June Gruber, Department of Psychology and Neuroscience, University of Colorado Boulder;.
Lee Anna Clark, Department of Psychology, University of Notre Dame;.
Jonathan S. Abramowitz, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill; Ann
Amelia Aldao, Teachers’ College, Columbia University, and Department of Psychiatry, Mount Sinai Hospital, New York, New York;.
Tammy Chung, Institute for Health, Healthcare Policy and Aging Research and Department of Psychiatry, Rutgers, The State University of New Jersey;.
Erika E. Forbes, Department of Psychiatry, University of Pittsburgh;
Gordon C. Nagayama Hall, Department of Psychology, University of Oregon;
Stephen P. Hinshaw, Department of Psychology, University of California, Berkeley, and Department of Psychiatry, University of California, San Francisco;
Steven D. Hollon, Department of Psychology, Vanderbilt University;.
Daniel N. Klein, Department of Psychology, Stony Brook University;
Robert W. Levenson, Department of Psychology, University of California, Berkeley;.
Dean McKay, Department of Psychology, Fordham University;.
Jane Mendle, Department of Human Development, Cornell University;.
Enrique W. Neblett, School of Public Health, University of Michigan;
Bunmi O. Olatunji, Department of Psychology, Vanderbilt University;
Mitchell J. Prinstein, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill;.
Jonathan Rottenberg, Department of Psychology, University of South Florida;.
Anne Marie Albano, Columbia University Vagelos College of Physicians and Surgeons;.
Jessica L. Borelli, Department of Psychological Science, University of California, Irvine;
Joanne Davila, Department of Psychology, Stony Brook University;.
Dylan G. Gee, Department of Psychology, Yale University;
Lauren S. Hallion, Department of Psychology, University of Pittsburgh;.
Stefan G. Hofmann, Department of Psychological and Brain Sciences, Boston University;.
Jutta Joormann, Department of Psychology, Yale University;.
Alan E. Kazdin, Department of Psychology, Yale University;
Annette M. La Greca, Department of Psychology, University of Miami;.
Angus W. MacDonald, III, Department of Psychology, University of Minnesota;.
Katie A. McLaughlin, Department of Psychology, Harvard University;
Adam Bryant Miller, Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill;.
Matthew Nock, Department of Psychology, Harvard University;.
Jacqueline B. Persons, Oakland Cognitive Behavior Therapy Center, Oakland, California;
David C. Rozek, UCF RESTORES and Department of Psychology, University of Central Florida;.
George M. Slavich, Cousins Center for Psychoneuroimmunology and Department of Psychiatry and Biobehavioral Sciences, University of California, Los Angeles;.
Vera Vine, Department of Psychiatry, University of Pittsburgh;.
Jessica L. Schleider, Department of Psychology, Stony Brook University;.
Bethany A. Teachman, Department of Psychology, University of Virginia;
Lauren M. Weinstock, Department of Psychiatry, Brown University..
- Adhanom Ghebreyesus T (2020). Addressing mental health needs: An integral part of COVID-19 response. World Psychiatry, 19, 129–130. 10.1002/wps.20768 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Adler NE, & Rehkopf DH (2008). US disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health, 29, 235–252. [ DOI ] [ PubMed ] [ Google Scholar ]
- Albee GW (1970). The uncertain future of clinical psychology. American Psychologist, 25, 1071–1080. 10.1037/h0030393 [ DOI ] [ PubMed ] [ Google Scholar ]
- Aldao A, & Nolen-Hoeksema S (2010). Specificity of cognitive emotion regulation strategies: A transdiagnostic examination. Behaviour Research and Therapy, 48, 974–983. 10.1016/j.brat.2010.06.002Alexander, [ DOI ] [ PubMed ] [ Google Scholar ]
- G. C, Stoller KB, Haffajee RL, & Saloner B (2020). An epidemic in the midst of a pandemic: Opioid use disorder and COVID-19. Annals of Internal Medicine. Advance online publication. 10.7326/M20-1141 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alisic E, Zalta AK, van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, & Smid GE (2014). Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: Meta-analysis. The British Journal of Psychiatry, 204, 335–340. 10.1192/bjp.bp.113.131227 [ DOI ] [ PubMed ] [ Google Scholar ]
- Alzheimer’s Association. (2020). 2020 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association, 16, 391–460. [ DOI ] [ PubMed ] [ Google Scholar ]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [ Google Scholar ]
- American Psychological Association. (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Washington, DC: Author. [ Google Scholar ]
- American Psychological Association. (2020). Telehealth guidance by state during COVID-19: State emergency orders relevant to licensed psychologists during the COVID-19 public health crisis. Retrieved from https://www.apaservices.org/practice/clinic/covid-19-telehealth-state-summary?_ga=2.7791794.1068186990.1590015193-1603345642.1590015193
- Armitage R, & Nellums LB (in press). COVID-19 and the consequences of isolating the elderly. The Lancet Public Health. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Arnett JJ (2014). Emerging adulthood: The winding road from the late teens through the twenties. Oxford, UK: Oxford University Press. 10.1093/acprof:oso/9780199929382.001.0001 [ DOI ] [ Google Scholar ]
- Barnett ML, Lau AS, & Miranda J (2018). Lay health worker involvement in evidence-based treatment delivery: A conceptual model to address disparities in care. Annual Review of Clinical Psychology, 14, 185–208. 10.1146/annurev-clinpsy-050817-084825 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Belvederi Murri M, Prestia D, Mondelli V, Pariante C, Patti S, Olivieri B, … Amore M (2016). The HPA axis in bipolar disorder: Systematic review and meta-analysis. Psychoneuroendocrinology, 63, 327–342. 10.1016/j.psyneuen.2015.10.014 [ DOI ] [ PubMed ] [ Google Scholar ]
- Bonanno GA, Brewin CR, Kaniasty K, & La Greca AM (2010). Weighing the costs of disaster: Consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest, 11, 1–49. 10.1177/1529100610387086 [ DOI ] [ PubMed ] [ Google Scholar ]
- Bootzin RR, & Bailey ET (2005). Understanding placebo, nocebo, and iatrogenic treatment effects. Journal of Clinical Psychology, 61, 871–880. 10.1002/jclp.20131 [ DOI ] [ PubMed ] [ Google Scholar ]
- Bratman GN, Anderson CB, Berman MG, Cochran B, de Vries S, Flanders J, … Daily GC (2019). Nature and mental health: An ecosystem service perspective. Science Advances, 5, eaax0903. 10.1126/sciadv.aax0903 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brown J, Cohen P, Johnson JG, & Salzinger S (1998). A longitudinal analysis of risk factors for child maltreatment: Findings of a 17-year prospective study of officially recorded and self-reported child abuse and neglect. Child Abuse & Neglect, 22, 1065–1078. 10.1016/S0145-2134(98)00087-8 [ DOI ] [ PubMed ] [ Google Scholar ]
- Brymer M, Jacobs A, Layne C, Pynoos R, Ruzek J, Steinberg A, … Watson P (2006). Psychological first aid (PFA): Field operations guide (2nd ed.). National Child Traumatic Stress Network and National Center for PTSD. Retrieved from https://www.ptsd.va.gov/professional/treat/type/PFA/PFA_2ndEditionwithappendices.pdf [ Google Scholar ]
- Cacioppo S, Grippo AJ, London S, Goossens L, & Cacioppo JT (2015). Loneliness: Clinical import and interventions. Perspectives on Psychological Science, 10, 238–249. 10.1177/1745691615570616 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chan PKS, Tang JW, & Hui DSC (2006). SARS: Clinical presentation, transmission, pathogenesis and treatment options. Clinical Science, 110, 193–204. 10.1042/cs20050188 [ DOI ] [ PubMed ] [ Google Scholar ]
- Claassen CA, Carmody T, Stewart SM, Bossarte RM, Larkin GL, Woodward WA, & Trivedi MH (2010). Effect of 11 September 2001 terrorist attacks in the USA on suicide in areas surrounding the crash sites. The British Journal of Psychiatry, 196, 359–364. 10.1192/bjp.bp.109.071928 [ DOI ] [ PubMed ] [ Google Scholar ]
- Cohen JA, & the Workgroup on Quality Issues. (2010). Practice parameters for the assessment and treatment of children and adolescents with PTSD. Journal of the American Academy of Child & Adolescent Psychiatry, 49, 414–430. [ PubMed ] [ Google Scholar ]
- Cohen S (2004). Social relationships and health. American Psychologist, 59, 676–684. 10.1037/0003-066X.59.8.676 [ DOI ] [ PubMed ] [ Google Scholar ]
- Compas BE, Jaser SS, Bettis AH, Watson KH, Gruhn MA, Dunbar JP, … Thigpen JC (2017). Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychological Bulletin, 143, 939–991. 10.1037/bul0000110 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Corcoran C, Walker E, Huot R, Mittal V, Tessner K, Kestler L, & Malaspina D (2003). The stress cascade and schizophrenia: Etiology and onset. Schizophrenia Bulletin, 29, 671–692. 10.1093/oxfordjournals.schbul.a007038 [ DOI ] [ PubMed ] [ Google Scholar ]
- Cummings JR, Wen H, & Druss BG (2013). Improving access to mental health services for youth in the United States. Journal of the American Medical Association, 309, 553–554. 10.1001/jama.2013.437 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Duarte CS, Hoven CW, Wu P, Bin F, Cotel S, Mandell DJ, … Markenson D (2006). Posttraumatic stress in children with first responders in their families. Journal of Traumatic Stress, 19, 301–306. 10.1002/jts.20120 [ DOI ] [ PubMed ] [ Google Scholar ]
- Ellis EG (2020). How health care workers avoid bringing COVID-19 home. Retrieved May 21, 2020, from https://www.wired.com/story/coronavirus-covid-19-health-care-workers-families/
- Farmer EM, Burns BJ, Phillips SD, Angold A, & Costello EJ (2003). Pathways into and through mental health services for children and adolescents. Psychiatric Services, 54, 60–66. 10.1176/appi.ps.54.1.60 [ DOI ] [ PubMed ] [ Google Scholar ]
- Fazel S, Yoon IA, & Hayes AJ (2017). Substance use disorders in prisoners: An updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction, 112, 1725–1739. 10.1111/add.13877 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Forbes EE, & Dahl RE (2012). Research Review: Altered reward function in adolescent depression: What, when and how? Journal of Child Psychology and Psychiatry, 53, 3–15. 10.1111/j.1469-7610.2011.02477.x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Forbes MK, & Krueger RF (2019). The great recession and mental health in the United States. Clinical Psychological Science, 7, 900–913. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, … Slavich GM (2019). Chronic inflammation in the etiology of disease across the life span. Nature Medicine, 25, 1822–1832. 10.1038/s41591-019-0675-0 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Galatzer-Levy IR, Huang SH, & Bonanno GA (2018). Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clinical Psychology Review, 63, 41–55. 10.1016/j.cpr.2018.05.008 [ DOI ] [ PubMed ] [ Google Scholar ]
- Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, … Dai J (2020). Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE, 15, e0231924. 10.1371/journal.pone.0231924 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Garnier-Crussard A, Forestier E, Gilbert T, & Krolak-Salmon P (2020). Novel coronavirus (COVID-19) epidemic: What are the risks for older patients? Journal of the American Geriatrics Society, 68, 939–940. 10.1111/jgs.16407 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gawęda Ł, Pionke R, Krężołek M, Frydecka D, Nelson B, & Cechnicki A (2020). The interplay between childhood trauma, cognitive biases, psychotic-like experiences and depression and their additive impact on predicting lifetime suicidal behavior in young adults. Psychological Medicine, 50, 116–124. 10.1017/S0033291718004026 [ DOI ] [ PubMed ] [ Google Scholar ]
- Gee GC, Ro A, Shariff-Marco S, & Chae D (2009). Racial discrimination and health among Asian Americans: Evidence, assessment, and directions for future research. Epidemiologic Reviews, 31, 130–151. 10.1093/epirev/mxp009 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Goffman E (1963). Stigma: Notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice Hall. [ Google Scholar ]
- Gold KJ, Sen A, & Schwenk TL (2013). Details on suicide among U.S. physicians: Data from the National Violent Death Reporting System. General Hospital Psychiatry, 35, 45–49. 10.1016/j.genhosppsych.2012.08.005 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Greinacher A, Derezza-Greeven C, Herzog W, & Nikendei C (2019). Secondary traumatization in first responders: A systematic review. European Journal of Psychotraumatology, 10, 1562840. 10.1080/20008198.2018.1562840 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Griffin BJ, Purcell N, Burkman K, Litz BT, Bryan CJ, Schmitz M, … Maguen S (2019). Moral injury: An integrative review. Journal of Traumatic Stress, 32, 350–362. 10.1002/jts.22362 [ DOI ] [ PubMed ] [ Google Scholar ]
- Gross JJ, & Jazaieri H (2014). Emotion, emotion regulation, and psychopathology: An affective science perspective. Clinical Psychological Science, 2, 387–401. 10.1177/2167702614536164 [ DOI ] [ Google Scholar ]
- Gruber J, & Rottenberg J (2020). Flattening the mental health curve is the next big coronavirus challenge. Retrieved from https://theconversation.com/flattening-the-mental-health-curve-is-the-next-big-coronavirus-challenge-139066 [ Google Scholar ]
- Hall GCN, Berkman ET, Zane NW, Leong FTL, Hwang W-C, Nezu AM, … Huang ER (2020). Reducing mental health disparities by increasing the personal relevance of interventions. American Psychologist. Advance online publication. 10.1037/amp0000616 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hatch R, Young D, Barber V, Griffiths J, Harrison DA, & Watkinson P (2018). Anxiety, depression and post traumatic stress disorder after critical illness: A U. K.-wide prospective cohort study. Critical Care, 22, 310. 10.1186/s13054-018-2223-6 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hinshaw SP (2007). The mark of shame: Stigma of mental illness and an agenda for change. New York, NY: Oxford University Press. [ Google Scholar ]
- Hofmann SG (2014). Interpersonal emotion regulation model of mood and anxiety disorders. Cognitive Therapy and Research, 38, 483–492. 10.1007/s10608-014-9620-1 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hofmann SG, Sawyer AT, Fang A, & Asnaani A (2012). Emotion dysregulation model of mood and anxiety disorders. Depression and Anxiety, 29, 409–416. 10.1002/da.21888 [ DOI ] [ PubMed ] [ Google Scholar ]
- Jeung R, & Nham K (2020). Incidents of coronavirus-related discrimination. Los Angeles, CA: Asian Pacific Policy and Planning Councl. Retrieved from http://www.asianpacificpolicyandplanningcouncil.org/wp-content/uploads/STOP_AAPI_HATE_MONTHLY_REPORT_4_23_20.pdf [ Google Scholar ]
- Johns Hopkins COVID-19 Mental Health Measurement Working Group. (2020). Measuring mental distress amid a pandemic: Understanding COVID-19’s psychological effects over time. Retrieved from https://www.jhsph.edu/covid-19/articles/measuring-mental-distress-amid-a-pandemic.html
- Kam CD (2019). Infectious disease, disgust, and imagining the other. The Journal of Politics, 81, 1371–1387. 10.1086/704438 [ DOI ] [ Google Scholar ]
- Kaniasty K, & Norris FH (2008). Longitudinal linkages between perceived social support and posttraumatic stress symptoms: Sequential roles of social causation and social selection. Journal of Traumatic Stress, 21, 274–281. 10.1002/jts.20334 [ DOI ] [ PubMed ] [ Google Scholar ]
- Kazdin AE (2018). Innovations in psychosocial interventions and their delivery: Leveraging cutting-edge science to improve the world’s mental health. New York, NY: Oxford University Press. 10.1093/med-psych/9780190463281.001.0001 [ DOI ] [ Google Scholar ]
- Kendler KS, Hettema JM, Butera F, Gardner CO, & Prescott CA (2003). Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Archives of General Psychiatry, 60, 789–796. 10.1001/archpsyc.60.8.789 [ DOI ] [ PubMed ] [ Google Scholar ]
- Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, … Zaslavsky AM (2005). Prevalence and treatment of mental disorders, 1990 to 2003. The New England Journal of Medicine, 352, 2515–2523. 10.1056/NEJMsa043266 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Khatri UG, & Perrone J (2020). Opioid use disorder and COVID-19: Crashing of the crises. Journal of Addiction Medicine. Advance online publication. 10.1097/ADM.0000000000000684 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kinnunen U, & Mauno S (1998). Antecedents and outcomes of work-family conflict among employed women and men in Finland. Human Relations, 51, 157–177. 10.1177/001872679805100203 [ DOI ] [ Google Scholar ]
- Kolves K, Kolves KE, & De Leo D (2013). Natural disasters and suicidal behaviours: A systematic literature review. Journal of Affective Disorders, 146, 1–14. 10.1016/j.jad.2012.07.037 [ DOI ] [ PubMed ] [ Google Scholar ]
- Kratochvil CJ, Evans L, Ribner BS, Lowe JJ, Harvey MC, Hunt RC, … Smith PW (2017). The National Ebola Training and Education Center: Preparing the United States for Ebola and other special pathogens. Health Security, 15, 253–260. 10.1089/hs.2017.0005 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kujawa A, Hajcak G, Danzig AP, Black SR, Bromet EJ, Carlson GA, … Klein DN (2016). Neural reactivity to emotional stimuli prospectively predicts the impact of a natural disaster on psychiatric symptoms in children. Biological Psychiatry, 80, 381–389. 10.1016/j.biopsych.2015.09.008 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kurzban R, & Leary MR (2001). Evolutionary origins of stigmatization: The functions of social exclusion. Psychological Bulletin, 127, 187–208. 10.1037/0033-2909.127.2.187 [ DOI ] [ PubMed ] [ Google Scholar ]
- La Greca AM, & Danzi BA (2019). Posttraumatic stress disorder. In Prinstein MJ, Youngstrom EA, Mash EJ, and Buckley RA (Eds.), Treatment of childhood disorders (4th ed., pp. 493–538). New York, NY: Guilford Press. [ Google Scholar ]
- La Greca AM, Silverman WK, Lai B, & Jaccard J (2010). Hurricane-related exposure experiences and stressors, other life events, and social support: Concurrent and prospective impact on children’s persistent posttraumatic stress symptoms. Journal of Consulting and Clinical Psychology, 78, 794–805. [ DOI ] [ PubMed ] [ Google Scholar ]
- La Greca AM, Silverman WK, Vernberg EM, & Roberts MC (Eds.). (2002). Helping children cope with disasters and terrorism. Washington, DC: American Psychological Association. 10.1037/10454-000 [ DOI ] [ Google Scholar ]
- Lai BS, La Greca AM, Auslander BA, & Short MB (2013). Children’s symptoms of posttraumatic stress and depression after a natural disaster: Comorbidity and risk factors. Journal of Affective Disorders, 146, 71–78. 10.1016/j.jad.2012.08.041 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, … Hu S (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. Journal of the American Medical Association Network Open, 3, e203976. 10.1001/jamanetworkopen.2020.3976 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lamprecht H, Laydon C, McQuillan C, Wiseman S, Williams L, Gash A, & Reilly J (2007). Single-session solution-focused brief therapy and self-harm: A pilot study. Journal of Psychiatric and Mental Health Nursing, 14, 601–602. 10.1111/j.1365-2850.2007.01105.x [ DOI ] [ PubMed ] [ Google Scholar ]
- Lancee WJ, Maunder RG, Goldbloom DS, & the Coauthors for the Impact of SARS Study. (2008). Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatric Services, 59, 91–95. 10.1176/ps.2008.59.1.91 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lazarus R, & Folkman S (1984). Stress, appraisal and coping. New York, NY: Springer. [ Google Scholar ]
- Lewis CC, Boyd M, Puspitasari A, Navarro E, Howard J, Kassab H, … Kroenke K (2019). Implementing measurement-based care in behavioral health: A review. Journal of the American Medical Association Psychiatry, 76, 324–335. 10.1001/jamapsychiatry.2018.3329 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lung FW, Lu YC, Chang YY, & Shu BC (2009). Mental symptoms in different health professionals during the SARS attack: A follow-up study. Psychiatric Quarterly, 80, 107–116. 10.1007/s11126-009-9095-5 [ DOI ] [ PubMed ] [ Google Scholar ]
- Manjoo F (2020, April 22). Two parents. Two kids. Two jobs. No childcare. New York Times. Retrieved from https://www.nytimes.com/2020/04/22/opinion/coronavirus-parenting-burnout.html [ Google Scholar ]
- Martinez A, & Hinshaw SP (2016). Mental health stigma: Theory, developmental issues, and research priorities. In Cicchetti D (Ed.), Developmental psychopathology: Vol. 4. Risk, resilience, and intervention (3rd ed., pp. 997–1039). Hoboken, NJ: Wiley. 10.1002/9781119125556.devpsy420 [ DOI ] [ Google Scholar ]
- McEwen BS, & Stellar E (1993). Stress and the individual. Mechanisms leading to disease. Archives of Internal Medicine, 153, 2093–2101. 10.1001/archinte.1993.00410180039004 [ DOI ] [ PubMed ] [ Google Scholar ]
- McEwen BS, & Wingfield JC (2003). The concept of allostasis in biology and biomedicine. Hormones and Behavior, 43, 2–15. 10.1016/S0018-506X(02)00024-7 [ DOI ] [ PubMed ] [ Google Scholar ]
- McLaughlin KA, Green J, Gruber MJ, Sampson NA, Zaslavsky AM, & Kessler RC (2012). Childhood adversities and first onset of psychiatric disorders in a national sample of U.S. adolescents. Archives of General Psychiatry, 69, 1151–1160. 10.1001/archgenpsychiatry.2011.2277 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mejia A, Calam R, & Sanders MR (2015). A pilot randomized controlled trial of a brief parenting intervention in low-resource settings in Panama. Prevention Science, 16, 707–717. 10.1007/s11121-015-0551-1 [ DOI ] [ PubMed ] [ Google Scholar ]
- Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, Case B, … Olfson M (2011). Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey-Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 50, 32–45. 10.1016/j.jaac.2010.10.006 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meyer A, Danielson CK, Danzig AP, Bhatia V, Black SR, Bromet E, … Klein DN (2017). Neural biomarker and early temperament predict increased internalizing symptoms after a natural disaster. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 410–416. 10.1016/j.jaac.2017.02.005 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Miller AB, & Prinstein MJ (2019). Adolescent suicide as a failure of acute stress-response systems. Annual Review of Clinical Psychology, 15, 425–450. 10.1146/annurev-clinpsy-050718-095625 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Monroe SM (2008). Modern approaches to conceptualizing and measuring human life stress. Annual Review of Clinical Psychology, 4, 33–52. 10.1146/annurev.clinpsy.4.022007.141207 [ DOI ] [ PubMed ] [ Google Scholar ]
- Nagelhout GE, Hummel K, de Goeij MCM, de Vries H, Kaner E, & Lemmens P (2017). How economic recessions and unemployment affect illegal drug use: A systematic realist literature review. The International Journal on Drug Policy, 44, 69–83. 10.1016/j.drugpo.2017.03.013 [ DOI ] [ PubMed ] [ Google Scholar ]
- Nock MK, & Kessler RC (2006). Prevalence of and risk factors for suicide attempts versus suicide gestures: Analysis of the National Comorbidity Survey. Journal of Abnormal Psychology, 115, 616–623. 10.1037/0021-843X.115.3.616 [ DOI ] [ PubMed ] [ Google Scholar ]
- Nolen-Hoeksema S, Wisco BE, & Lyubomirsky S (2008). Rethinking Rumination. Perspectives on Psychological Science, 3, 400–424. 10.1111/j.1745-6924.2008.00088.x [ DOI ] [ PubMed ] [ Google Scholar ]
- Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, & Kaniasty K (2002). 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry, 65, 207–239. 10.1521/psyc.65.3.207.20173 [ DOI ] [ PubMed ] [ Google Scholar ]
- O’Donovan A, Slavich GM, Epel ES, & Neylan TC (2013). Exaggerated neurobiological sensitivity to threat as a mechanism linking anxiety with increased risk for diseases of aging. Neuroscience and Biobehavioral Reviews, 37, 96–108. 10.1016/j.neubiorev.2012.10.013 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Oltmanns TF, & Krasner L (1993). A voice for clinical science in clinical psychology: The history of section III of division 12. Clinical Psychologist, 46, 25–32. Retrieved from https://sites.google.com/site/sscpwebsite/Home/history-of-sscp#return3 [ Google Scholar ]
- Prinstein MJ, & Giletta M (2016). Peer relations and developmental psychopathology. In Cicchetti D (Ed.), Developmental psychopathology (3rd ed., Vol. 1, pp. 527–579). Hoboken, NJ: Wiley. [ Google Scholar ]
- Prinstein MJ, Nesi J, & Telzer EH (2020). Commentary: An updated agenda for the study of digital media use and adolescent development–future directions following Odgers & Jensen (2020). Journal of Child Psychology and Psychiatry, 61, 349–352. [ DOI ] [ PubMed ] [ Google Scholar ]
- Reeves A, Stuckler D, McKee M, Gunnell D, Chang SS, & Basu S (2012). Increase in state suicide rates in the USA during economic recession. Lancet, 380, 1813–1814. 10.1016/S0140-6736(12)61910-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- Sareen J (2014). Posttraumatic stress disorder in adults: Impact, comorbidity, risk factors, and treatment. Canadian Journal of Psychiatry, 59, 460–467. 10.1177/070674371405900902 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schleider JL, Dobias ML, Sung JY, & Mullarkey MC (2020). Future directions in single-session youth mental health interventions. Journal of Clinical Child and Adolescent Psychology, 49, 264–278. 10.1080/15374416.2019.1683852 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Schleider JL, & Weisz JR (2017). Little treatments, promising effects? Meta-analysis of single session interventions for youth psychiatric problems. Journal of the American Academy of Child & Adolescent Psychiatry, 56, 107–115. 10.1016/j.jaac.2016.11.007 [ DOI ] [ PubMed ] [ Google Scholar ]
- Schneider EC, Zaslavsky AM, & Epstein AM (2002). Racial disparities in the quality of care for enrollees in Medicare managed care. Jama, 287, 1288–1294. [ DOI ] [ PubMed ] [ Google Scholar ]
- Schulz R, O’Brien AT, Bookwala J, & Fleissner K (1995). Psychiatric and physical morbidity effects of dementia caregiving: Prevalence, correlates, and causes. The Gerontologist, 35, 771–791. [ DOI ] [ PubMed ] [ Google Scholar ]
- Segerstrom SC, Tsao JCI, Alden LE, & Craske MG (2000). Worry and rumination: Repetitive thought as a concomitant and predictor of negative mood. Cognitive Therapy and Research, 24, 671–688. 10.1023/A:1005587311498 [ DOI ] [ Google Scholar ]
- Singh GK, & Siahpush M (2006). Widening socioeconomic inequalities in U.S. life expectancy, 1980–2000. International Journal of Epidemiology, 35, 969–979. 10.1093/ije/dyl083 [ DOI ] [ PubMed ] [ Google Scholar ]
- Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, & Patel V (2017). Psychological treatments for the world: Lessons from low-and middle-income countries. Annual Review of Clinical Psychology, 13, 149–181. 10.1146/annurev-clinpsy-032816-045217 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Slavich GM (2020). Social safety theory: A biologically based evolutionary perspective on life stress, health, and behavior. Annual Review of Clinical Psychology, 16, 265–295. 10.1146/annurev-clinpsy-032816-045159 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Slavich GM, & Irwin MR (2014). From stress to inflammation and major depressive disorder: A social signal transduction theory of depression. Psychological Bulletin, 140, 774–815. 10.1037/a0035302 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith JC, Sausville EL, Girish V, Yuan ML, Vasudevan A, John KM, & Sheltzer JM (2020). Cigarette smoke exposure and inflammatory signaling increase the expression of the SARS-CoV-2 receptor ACE2 in the respiratory tract. Developmental Cell, 53, 514–529.e3. 10.1016/j.devcel.2020.05.012 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Smith TB, & Trimble JE (2016). Foundations of multicultural psychology: Research to inform effective practice. Washington, DC: American Psychological Association. 10.1037/14733-000 [ DOI ] [ Google Scholar ]
- Soloman D, Maxwell C, & Castro A (2019). Systematic inequality and economic opportunity. Washington, DC: Center for American Progress. Retrieved from https://www.americanprogress.org/issues/race/reports/2019/08/07/472910/systematic-inequality-economic-opportunity / [ Google Scholar ]
- Stoltenborgh M, Bakermans-Kranenburg MJ, & van Ijzendoorn MH (2013). The neglect of child neglect: A meta-analytic review of the prevalence of neglect. Social Psychiatry and Psychiatric Epidemiology, 48, 345–355. 10.1007/s00127-012-0549-y [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tang B, Liu X, Liu Y, Xue C, & Zhang L (2014). A meta-analysis of risk factors for depression in adults and children after natural disasters. BMC Public Health, 14, 623. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Telzer EH (2016). Dopaminergic reward sensitivity can promote adolescent health: A new perspective on the mechanism of ventral striatum activation. Developmental Cognitive Neuroscience, 17, 57–67. 10.1016/j.dcn.2015.10.010 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tessner KD, Mittal V, & Walker EF (2011). Longitudinal study of stressful life events and daily stressors among adolescents at high risk for psychotic disorders. Schizophrenia Bulletin, 37, 432–441. 10.1093/schbul/sbp087 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tripp JC, Jones JL, Back SE, & Norman SB (2019). Dealing With complexity and comorbidity: Comorbid PTSD and substance use disorders. Current Treatment Options in Psychiatry, 6, 188–197. 10.1007/s40501-019-00176-w [ DOI ] [ Google Scholar ]
- U. S. Department of Health and Human Services, Office of the Surgeon General, and National Action Alliance for Suicide. (2012). National strategy for suicide prevention: Goals and objectives for action. Washington, DC: HHS. [ PubMed ] [ Google Scholar ]
- Van Lancker W, & Parolin Z (2020). COVID-19, school closures, and child poverty: A social crisis in the making. The Lancet. Public Health, 5, e243–e244. 10.1016/S2468-2667(20)30084-0 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Vardavas CL, & Nikitara K (2020). COVID-19 and smoking: A systematic review of the evidence. Tobacco Induced Diseases, 18, 20. 10.18332/tid/119324 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Volkow ND (2020). Collision of the COVID-19 and addiction epidemics. Annals of Internal Medicine, 173, 61–62. 10.7326/m20-1212 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Walker EF, & Diforio D (1997). Schizophrenia: A neural diathesis-stress model. Psychological Review, 104, 667–685. 10.1037/0033-295X.104.4.667 [ DOI ] [ PubMed ] [ Google Scholar ]
- Walton GM, & Wilson TD (2018). Wise interventions: Psychological remedies for social and personal problems. Psychological Review, 125, 617–655. 10.1037/rev0000115 [ DOI ] [ PubMed ] [ Google Scholar ]
- Wang H, Li T, Barbarino P, Gauthier S, Brodaty H Molinuevo, … Yu X (2020). Dementia care during COVID-19. Lancet, 395, 1190–1191. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wasserman IM (1992). The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide & Life-Threatening Behavior, 22, 240–254. [ PubMed ] [ Google Scholar ]
- Williams J, Gonzalez-Medina D, & Le Q (2011). Infectious diseases and social stigma. Applied Technologies and Innovations, 4, 58–70. 10.15208/ati.2011.7 [ DOI ] [ Google Scholar ]
- Yip PS, Cheung YT, Chau PH, & Law YW (2010). The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 31, 86. [ DOI ] [ PubMed ] [ Google Scholar ]
- Zephyrin L, Radley DC, Getachew Y, Baumgartner JC, & Schneider EC (2020). COVID-19 more prevalent, deadlier in U.S. counties with higher Black populations. New York, NY: The Commonwealth Fund. Retrieved from https://www.commonwealthfund.org/blog/2020/covid-19-more-prevalent-deadlier-us-counties-higher-black-populations [ Google Scholar ]
- View on publisher site
- PDF (137.3 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

- University Safety and Response
- (866) 825-5426
10 Clinical Psychology Research Topics to Explore
Whether you’re working toward a PsyD or a PhD in Clinical Psychology , landing on a research paper that will sustain your interest throughout your doctoral program can be both thrilling and challenging.
Should you go with a niche you know well or branch out to another psychology specialization ? Should you choose a research topic you’re passionate about or opt for something more topical and needed in the broader realm of behavioral and mental health?
Only you can answer these questions—however, this blog may provide you with some inspiration and direction. Let’s walk through 10 of the most fascinating clinical psychology research topics and how they might bring you closer to your educational and professional objectives.
Explore Clinical Psychology Programs
10 Emerging Research Topics in Clinical Psychology
One of the benefits of clinical psychology is that it’s far from a static field.
With each passing year, we gain more and more insight into the brain and how it affects behavior. In the last few years alone, for example, we’ve obtained a clearer picture of the negative effects of digital media on mental health and behavior. But we’ve also seen how digital media (specifically, mobile apps) can enhance mental health when used correctly. 1
Put simply, clinical psychology is a dynamic, exhilarating realm with seemingly boundless possibilities for further research.
Nonetheless, it’s easy to feel overwhelmed when settling on a clinical psychology research paper topic, especially when it’s one that you may be intimate with for years. To that end, consider these top 10 psychology topics to get you started in your research area:
#1. Mental Health Technology and Digital Interventions
The pandemic dramatically altered how healthcare practitioners interact with their patients and clients. Whereas psychotherapy and other forms of counseling were once performed almost exclusively in person, COVID-19 turned mental telehealth into our new reality.
But what might the long-term effects of this be? And will it persist as we march into the future?
Exploring the impact of digital mental health interventions (such as apps, other digital tools, and teleconferences) on well-being may open up a world of possible clinical psychology research topics and questions. 2 For instance, it may compel you to ask and research thoughts like:
- How will AI alter mental health treatments, if at all?
- Will digital mental health interventions ultimately cause or worsen isolation?
- What are the downsides and perks of turning to social media for mental health information?
- What is the relevance and value of in-person counseling sessions, post-pandemic?
- Do clients feel safer in online sessions?
- How can technology be employed to monitor patients outside of sessions?
- How does mental telehealth affect the elderly?
Technology is rapidly and constantly changing. In other words, psychology and technology may be exciting subjects to explore as you work towards starting or completing your doctorate.
#2. Cross-Cultural and Global Mental Health
Globalization has its pros and cons. Studies indicate that while it may have its advantages, it can also heighten: 4
- Discrimination
Each of these may have lasting effects, including increasing the risk of mental disorders like addiction, depression, and anxiety. In other words, it needs to be examined by experts from multiple standpoints.
As a doctoral student, you’re in an ideal spot to investigate this complex issue. It also emphasizes the need to gain cultural competency and a global mindset as a mental health practitioner, which is another possible research topic in and of itself.
#3. Neuropsychology and Cognitive Processes
The field of neuropsychology and cognitive processes continues to grow, particularly with the advent of digital tools and their ability to monitor cognition. 5 Exploring our advancing knowledge of how the brain affects behavior may allow you to look at a wide range of mental health disorders and the newest clinical interventions that are being made available, such as treating:
- Alcohol use disorder (AUD)
- Eating disorders
- Post-traumatic stress disorder (PTSD)
#4. Trauma and Resilience Studies
Psychologists and psychiatrists ranging from Bessel Van der Kolk to Peter Levine forever altered our understanding of trauma. What was once thought of as a purely psychological issue is now understood as a bodily ailment. 6
But how might this look as we move forward in time and gain an enhanced understanding of neuroplasticity? Will somatics continue to play a role in treating trauma, or will technological advances send practitioners and their clients in a completely different direction?
You may be in a position to dig deeper and find out.
#5. Behavioral Health and Chronic Conditions
The unique relationship between chronic conditions and behavioral health is also up for exploration. Growing research indicates that chronic conditions (such as diabetes) can trigger mental health complications like depression, which can then perpetuate the cycle of the chronic condition.
This topic may be especially timely and relevant as it emphasizes the need to bridge the gap between a patient’s full healthcare team and points out flaws in treating chronic conditions solely from a pharmaceutical stance.
#6. Psychotherapy Process and Outcome Research
Cognitive behavioral therapy (CBT), acceptance and commitment therapy (ACT), and other forms of traditional “talk therapy” have been mainstays in the field of clinical psychology for decades. But this, too, isn’t static, especially as clients continue to look more toward body-based therapies and technology-fueled solutions, like: 8
- Transcranial magnetic stimulation (TMS)
- Neurofeedback therapy
- Brainspotting
- Somatic Experiencing (SE)
Is it too soon to know if these and other fresh forms of mental health treatments have the same staying power as, say, cognitive behavioral therapy? This might be optimal for exploration.
#7. Social Determinants of Mental Health
Social determinants of mental health (SDOMH) refer to the external circumstances that may impact an individual’s mental well-being and make them more vulnerable to conditions ranging from depression to addiction. SDOMH includes: 9
- Unemployment
- Social isolation
- Urban crowding
How will SDOMH change as we move forward? Will it? Additionally, what is a clinical psychologist’s role in addressing these issues? What are the most effective strategies for working with those who have been disadvantaged?
This is an important topic as we, as a society, continue to address long-buried issues of race and class.
#8. Addiction and Substance Use Disorders
Addiction remains a prevalent topic: Alcohol use disorder (AUD) affects roughly 10.5% of the population, while 46.8 million Americans wrestled with a substance abuse disorder in 2022 alone. 10
Analyzing the most recent treatments and the future of treatments might not only pave the way for your own work after completion of your PsyD or PhD but also do a tremendous service for those who suffer from addiction (and their loved ones and families).
#9. Child and Adolescent Mental Health
Numerous studies indicate that kids and teens now have unusually high rates of: 11
- Substance use
What plays into this? Is social media entirely to blame, or can social sites also be a resource for youngsters? And how can clinical psychologists tweak their methods to resonate with kids and teens?
These are just three of the many questions you might ask if you decide to adopt this topic for your clinical research.
#10. Ethics and Professional Issues in Clinical Psychology
Last but not least, consider the value of examining both the main and more subtle ethics and professional issues in clinical psychology at work today, such as:
- Privacy
- Informed consent
- Cultural sensitivity
- Termination of counseling
Shape the Future of Mental Health with Alliant International University
From making a substantial difference in the lives of others to eradicating the stigmas that surround certain mental health conditions, clinical psychologists are in a prime position to fuel lasting change. Selecting a clinical research topic that ignites your spirit and works toward solving larger social issues takes this notion to the next level.
Alliant International University may get you closer to becoming the type of clinical psychologist who can make an impact. Whether you’re exploring our PsyD in Clinical Psychology or have just started college, we’re proud to offer doctoral programs for psychology that can help you excel in your future profession. And with online and in-person classes and training, you might find the flexibility your life requires.
Learn more about our clinical psychology programs today.
Sources:
- “Exploring the Latest Frontiers in Clinical Psychology Research.” The Clinic, March 25, 2024. https://theclinicca.org/exploring-the-latest-frontiers-in-clinical-psyc… .
- Park, Susanna Y, Chloe Nicksic Sigmon, and Debra Boeldt. “A Framework for the Implementation of Digital Mental Health Interventions: The Importance of Feasibility and Acceptability Research.” Cureus, September 19, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9580609/.
- Bond, Raymond R., Maurice D. Mulvenna, Courtney Potts, Siobhan O’Neill, Edel Ennis, and John Torous. “Digital Transformation of Mental Health Services.” Nature News, August 22, 2023. https://www.nature.com/articles/s44184-023-00033-y.
- “Cross-Cultural Mental Health.” CMHA British Columbia, July 14, 2016. https://bc.cmha.ca/documents/cross-cultural-mental-health-and-substance-use-2/.
- “New Research Looks at the Promise of ‘Digital Neuropsychology.’” McLean News | New Research Looks at the Promise of “Digital Neuropsychology,” January 7, 2019. https://www.mcleanhospital.org/news/new-research-looks-promise-digital-neuropsychology.
- Kuhfuß, Marie, Tobias Maldei, Andreas Hetmanek, and Nicola Baumann. “Somatic Experiencing - Effectiveness and Key Factors of a Body-Oriented Trauma Therapy: A Scoping Literature Review.” European journal of psychotraumatology, July 12, 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8276649/.
- “The Intersection of Mental Health and Chronic Disease.” Johns Hopkins Bloomberg School of Public Health. Accessed April 17, 2024. https://publichealth.jhu.edu/2021/the-intersection-of-mental-health-and-chronic-disease.
- Theodora Blanchfield, AMFT. “What to Know about Brainspotting Therapy.” Verywell Mind, January 16, 2024. https://www.verywellmind.com/brainspotting-therapy-definition-techniques-and-efficacy-5213947.
- Social Determinants of Health and Mental Health. Accessed April 17, 2024. https://www.ncsc.org/__data/assets/pdf_file/0025/70864/Social-Determinants-of-Health.pdf.
- “Alcohol and Drug Abuse Statistics (Facts about Addiction).” American Addiction Centers, April 4, 2024. https://americanaddictioncenters.org/addiction-statistics#.
- “Data and Statistics on Children’s Mental Health.” Centers for Disease Control and Prevention, March 8, 2023. https://www.cdc.gov/childrensmentalhealth/data.html.

David Stewart
Dean, California School of Professional Psychology
David G. Stewart, PhD, ABPP, is a board-certified clinical child and adolescent psychologist and Dean of the California School of...
Other Categories
University announcements, featured news, nursing and health sciences, start on your path to succeed on purpose, request information.
- 1 Current Select Interests
- 2 Provide Information
You might also like
Student career spotlight: xiaowei lu.
Xiaowei Lu Doctoral Respecialization Program (DRP) in Clinical Psychology CSPP at Alliant International University, San Francisco...
Student Career Spotlight: Courtney Goodwin
Courtney Goodwin PhD in Clinical Psychology CSPP at Alliant International University, Fresno Q: What inspired you to get into...
Student Career Spotlight: Delaney Gilman
Delaney Gilman PhD in Clinical Psychology CSPP at Alliant International University, Fresno Q: What inspired you to pursue a...
New Ideas in: Psychology for Clinical Settings 2022
Loading... Editorial 13 March 2024 Editorial: New ideas in: psychology for clinical settings 2022 Giulia Landi , Burkhard Brosig and Eliana Tossani 857 views 0 citations
Brief Research Report 18 December 2023 How to reach people who do not want to be reached: psychosocial counseling for school-dropouts in vocational training Julian Valentin Möhring , 1 more and Burkhard Brosig 920 views 0 citations
Original Research 08 June 2023 Trauma-Informed Care on mental health wards: the impact of Power Threat Meaning Framework Team Formulation and Psychological Stabilisation on self-harm and restrictive interventions Faye Nikopaschos , 2 more and Ana Salgueiro 11,858 views 7 citations
Clinical Trial 06 June 2023 Evaluation of multidimensional pediatric-psychosomatic inpatient therapy: a pilot study comparing two treatment modalities Tim Botschek , 6 more and Burkhard Brosig 1,246 views 1 citations
Original Research 13 January 2023 An auditory processing advantage enables communication in less complex social settings: Signs of an extreme female brain in children and adolescents being assessed for Autism Spectrum Disorders Sofia Åkerlund , 1 more and Emma Claesdotter-Knutsson 2,005 views 2 citations
Original Research 09 January 2023 Inclusive leadership can improve nurses’ psychological ownership and reduce their turnover intention under the normalization of COVID-19 prevention Dongyu Zeng , 1 more and Weiju Chen 3,099 views 8 citations
Original Research 01 November 2022 Constant installation of present orientation and safety (CIPOS) - subjective and physiological effects of an ultrashort-term intervention combining both stabilizing and confrontational elements Markus Stingl , 4 more and Valeska Reichel Pape 1,829 views 2 citations
Loading... Conceptual Analysis 25 October 2022 A process-based approach to cognitive behavioral therapy: A theory-based case illustration Clarissa W. Ong , 1 more and Stefan G. Hofmann 34,708 views 28 citations
Original Research 02 September 2022 Are depression and suffering distinct? An empirical analysis Richard G. Cowden , 2 more and Tyler J. VanderWeele 3,890 views 7 citations
- How it works
"Christmas Offer"
Terms & conditions.
As the Christmas season is upon us, we find ourselves reflecting on the past year and those who we have helped to shape their future. It’s been quite a year for us all! The end of the year brings no greater joy than the opportunity to express to you Christmas greetings and good wishes.
At this special time of year, Research Prospect brings joyful discount of 10% on all its services. May your Christmas and New Year be filled with joy.
We are looking back with appreciation for your loyalty and looking forward to moving into the New Year together.
"Claim this offer"
In unfamiliar and hard times, we have stuck by you. This Christmas, Research Prospect brings you all the joy with exciting discount of 10% on all its services.
Offer valid till 5-1-2024
We love being your partner in success. We know you have been working hard lately, take a break this holiday season to spend time with your loved ones while we make sure you succeed in your academics
Discount code: RP0996Y

Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
Clinical Psychology Dissertation Topics
Published by Owen Ingram at January 3rd, 2023 , Revised On August 11, 2023
Clinical psychology is a highly popular area of research for Masters and PhD nursing students. A well-thought-out and appropriate clinical psychology dissertation topic will address trending issues in the field of clinical psychology. You can develop a clinical psychology dissertation topic or idea by addressing a certain clinical experience.
If you are a nursing student looking for an intriguing topic in clinical psychology, you will find all the necessary information on this page. So without further ado, here is our selection of clinical psychology dissertation topics that you can choose from.
Related Links:
- Cognitive psychology dissertationtopics
- Educational psychology dissertation topics
- Counselling psychology dissertation topics
- Forensic-psychology-dissertation-topics
- Social Psychology Dissertation Topics
- Criminal Psychology Dissertation Ideas
- Neuro Psychology Dissertation Ideas
- Consumer Psychology Dissertation Ideas
- How to Identify and Differentiate Treatment-Resistant Depression?
- Understanding the Reasons People Join the Military
- Comprehensive Treatment for Postpartum Mood Disorders
- Using a Meaning-Making Process to Cope with Death
- What Kind of Relationship Do Teenagers Have with Video Games?
- Depression vs ADHD in Young Children
- Severe and Chronic Mental Illness and Life Quality
- Analyze the views of cancer patients suffering from advanced stages and their partners
- What therapy is available to treat panic attacks and anxiety disorders?
- What treatments and medications work best to treat addiction?
- Describe the many medical approaches to treating insomnia
- Analyze the efficacy of antidepressant medications in therapeutic interventions
- Describe the most successful depression treatments
- How does post-traumatic stress disorder develop?
- Antidepressants: are they addictive? Describe their efficacy and any possible negative effects
- Is behavioural therapy the ideal kind of care for offenders?
- How could psychology be used to treat persistent pain?
- What clinical and demographic factors cause individuals with obsessions and compulsions to have poor insight?
- The educational process for clinical psychologists who sought out personal therapy: a narrative assessment
- Dialysis patients’ psycho-social adjustment to their cases of renal failure and the resulting treatment
- Within a bio-psycho-social paradigm of a psychosis episode, the experiences connected to the psycho-social formulation
- The experiences and how they relate to eating habits in maturity
- A cognitive paradigm for assessing major depressive disorder
- The difficulties in communicating sexual dysfunction symptoms after a heart injury
- What are the main causes of adult anorexia?
- Examine major depressive disorder (MDD) in the context of cognitive theory
- Describe the communication obstacles caused by sexual dysfunction after cardiac trauma
- What relationship exists between adult eating habits and experiences?
- Investigate the idea of body image and identity in people who have had a heart or lung transplant
- Describe the clinical and demographic characteristics that predict insight in people with compulsions and obsessions
- Define schizophrenia and list possible treatments
- What drugs and therapies can be used to treat phobias and paranoia?
Hire Dissertation Specialist
Orders completed by our expert writers are
- Formally drafted in an academic style
- Free Amendments and 100% Plagiarism Free – or your money back!
- 100% Confidential and Timely Delivery!
- Free anti-plagiarism report
- Appreciated by thousands of clients. Check client reviews
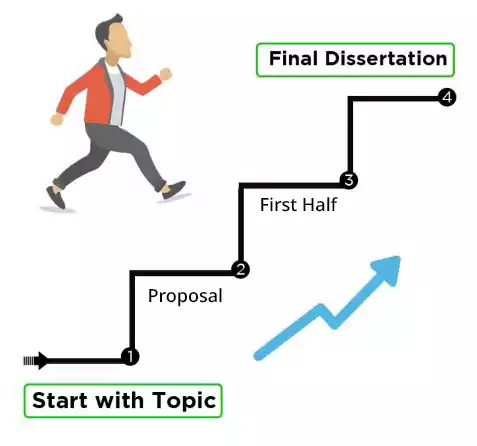
Something is mesmerising about the human mind. By writing clinical psychology-based dissertation papers, students can engage in formally conducting research on a variety of topics, including intellect, personality, addiction, relationship dynamics, and so on. Use these clinical psychology dissertation topics to start your academic research now!
If you are struggling with your dissertation and need a helping hand, you may want to read about our dissertation writing services.
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find clinical psychology dissertation topics.
To find Clinical Psychology dissertation topics:
- Study recent research in the field.
- Focus on emerging therapies or disorders.
- Address gaps in current literature.
- Consider ethical and practical aspects.
- Explore diverse populations or age groups.
- Seek topics aligning with your passion and expertise.
You May Also Like
Need interesting and manageable Economics dissertation topics? Here are the trending Economics dissertation titles so you can choose the most suitable one.
Need interesting and manageable international relations and geopolitics dissertation topics or thesis? Here are the trending international relations and geopolitics dissertation titles so you can choose the most suitable one.
As the field of forensic psychology is still relatively new, there are numerous research issues to address. Investigate how psychology has been used to support certain legal theories.
As Featured On

USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

Splash Sol LLC
- How It Works

COMMENTS
Explore interesting psychology research topics—ideal for students and professionals. Get ideas for your next research project here. Dovetail 3.0: Automated analysis, Channels, Ask ... Read the latest clinical studies. Once you've picked a more niche topic to explore, ...
from Psychology of Sexual Orientation and Sexual Diversity September 16, 2014; Easier to Stomach from Clinical Practice in Pediatric Psychology August 5, 2014; To Be Considered from Clinical Practice in Pediatric Psychology July 29, 2014; There's No Place Like Home from American Journal of Orthopsychiatry June 11, 2014
This page provides a comprehensive list of clinical psychology research paper topics, designed to support students navigating the complexities of mental health studies.Aimed at fostering a deeper understanding of psychological assessment, therapeutic methods, and the myriad issues faced by individuals with mental health disorders, these topics cover a broad spectrum of areas within clinical ...
Topics in Psychology. Explore how scientific research by psychologists can inform our professional lives, family and community relationships, emotional wellness, and more. ... Recent discoveries about the biological underpinnings of human behavior are helping psychologists find new ways to improve people's lives. ... Psychology Topics ...
With such a wide range of topics to cover, figuring out clinical psychology research topics for papers, presentations, and experiments can be tricky. Clinical Psychology Research Topic Ideas Topic choices are only as limited as your imagination and assignment, so try narrowing the possibilities down from general questions to the specifics that ...
Topics in Psychology. Explore how scientific research by psychologists can inform our professional lives, family and community relationships, emotional wellness, and more. ... Driven by a sense of purpose, psychologists are finding new ways to get research and clinical advice to those who need it.
The central role of lifelong learning and humility in clinical psychology. Clinical Psychological Science, 11(4), 744-756. Crossref. Web of Science. Google Scholar. Wood J. M., Nezworski M. T., Lilienfeld S. O., Garb H. N. (2003). ... Sage Research Methods Supercharging research opens in new tab; Sage Video Streaming knowledge opens in new ...
The article concludes by discussing implications for new research directions, clinical approaches, and policy issues. Footnotes 1 The term developed over a period of years (1964 to 1991) that saw an increasing belief among clinical psychologists that there was a "fundamental incompatibility of the roles of scientist and professional within ...
Read the latest articles of Clinical Psychology Review at ScienceDirect.com, Elsevier's leading platform of peer-reviewed scholarly literature. Skip to main content. ... (When and how) does basic research in clinical psychology lead to more effective psychological treatment for mental disorders? Thomas Ehring, Karina Limburg, Anna E. Kunze ...
This Research Topic is part of the Insights in Psychology series.<br/><br/>We are now entering the third decade of the 21st Century, and, especially in the last years, the achievements made by scientists have been exceptional, leading to major advancements in the fast-growing field of Psychology. Frontiers has organized a series of Research Topics to highlight the latest advancements in ...
Let's walk through 10 of the most fascinating clinical psychology research topics and how they might bring you closer to your educational and professional objectives. Explore Clinical Psychology Programs. 10 Emerging Research Topics in Clinical Psychology. One of the benefits of clinical psychology is that it's far from a static field.
Journal of Clinical Psychology: In Session is seeking for guest editors for an upcoming issue devoted to treatment of patients with comorbid eating disorders and personality disorders. The issue will include an introduction written by the guest editors, 6 papers each based on a clinical case coming from different orientations and possibly from different countries and continents, and then one ...
AIMS AND SCOPE OF JOURNAL: The Annual Review of Clinical Psychology provides comprehensive reviews of significant developments in the field of clinical psychology and psychiatry. The journal covers research, theory, and the application of psychological principles to address recognized disorders, including schizophrenia, mood, anxiety, childhood, substance use, cognitive, and personality disorders.
The journal also publishes invited commentaries that provide additional perspectives regarding the topics of such reviews. It is the official publication of APA Division 12, the Society of Clinical Psychology. The journal publishes papers from all theoretical perspectives in clinical psychology and considers all methods and approaches to research.
The achievements made by scientists over the last years have contributed to exceptional advancements in the fast-growing field of Psychology for Clinical Settings. We are organizing a series of Research Topics to build on the new and novel content within the section of Psychology for Clinical Settings. This editorial initiative is focused on new insights, novel developments, latest discoveries ...
New Research From Clinical Psychological Science. A sample of research on parent reinforcement and relationship behaviors, global well-being and mental health, predicting transdiagnostic symptom change across diverse demographic groups, and much more. New Content From Advances in Methods and Practices in Psychological Science
Clinical psychology is a highly popular area of research for Masters and PhD nursing students. A well-thought-out and appropriate clinical psychology dissertation topic will address trending issues in the field of clinical psychology. You can develop a clinical psychology dissertation topic or idea by addressing a certain clinical experience ...
Group for those interested in understanding and treating psychological disorders. | Explore the latest full-text research PDFs, articles, conference papers, preprints and more on CLINICAL PSYCHOLOGY.
I f you're starting out on the dissertation or thesis journey for your psychology degree, the very first challenge you'll face is finding a solid research topic.In this post, we'll help get the topic ideation process started by providing a meaty list of research ideas, spanning a range of psychology sub-disciplines.We'll also look at some examples from actual theses and dissertations ...
Clinical psychology has evolved and changed rapidly during its 125+-year history. This chapter examines the contemporary trends and issues in clinical psychology. One of the best examples of a current hot topic in clinical psychology is managed health care and health-care reform. The American family has changed a great deal in recent years.