- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs


Chapter 7: 10 Real Cases on Transient Ischemic Attack and Stroke: Diagnosis, Management, and Follow-Up
Jeirym Miranda; Fareeha S. Alavi; Muhammad Saad
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Case review, case discussion, clinical symptoms.
- Radiologic Findings
- Full Chapter
- Supplementary Content
Case 1: Management of Acute Thrombotic Cerebrovascular Accident Post Recombinant Tissue Plasminogen Activator Therapy
A 59-year-old Hispanic man presented with right upper and lower extremity weakness, associated with facial drop and slurred speech starting 2 hours before the presentation. He denied visual disturbance, headache, chest pain, palpitations, dyspnea, dysphagia, fever, dizziness, loss of consciousness, bowel or urinary incontinence, or trauma. His medical history was significant for uncontrolled type 2 diabetes mellitus, hypertension, hyperlipidemia, and benign prostatic hypertrophy. Social history included cigarette smoking (1 pack per day for 20 years) and alcohol intake of 3 to 4 beers daily. Family history was not significant, and he did not remember his medications. In the emergency department, his vital signs were stable. His physical examination was remarkable for right-sided facial droop, dysarthria, and right-sided hemiplegia. The rest of the examination findings were insignificant. His National Institutes of Health Stroke Scale (NIHSS) score was calculated as 7. Initial CT angiogram of head and neck reported no acute intracranial findings. The neurology team was consulted, and intravenous recombinant tissue plasminogen activator (t-PA) was administered along with high-intensity statin therapy. The patient was admitted to the intensive care unit where his hemodynamics were monitored for 24 hours and later transferred to the telemetry unit. MRI of the head revealed an acute 1.7-cm infarct of the left periventricular white matter and posterior left basal ganglia. How would you manage this case?
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging. He had multiple comorbidities, including hypertension, diabetes, dyslipidemia, and smoking history, which put him at a higher risk for developing cardiovascular disease. Because his symptoms started within 4.5 hours of presentation, he was deemed to be a candidate for thrombolytics. The eligibility time line is estimated either by self-report or last witness of baseline status.
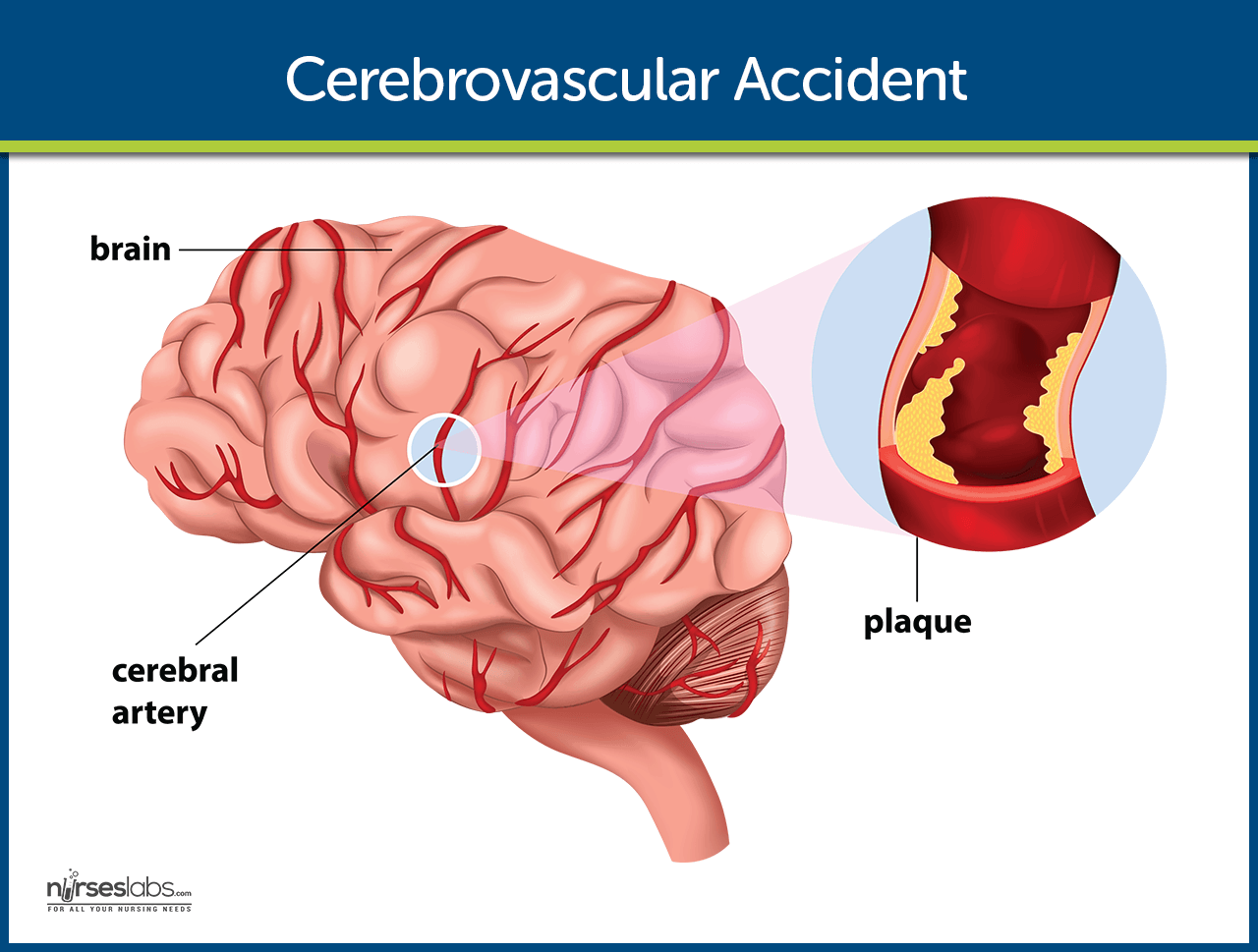
Ischemic strokes are caused by an obstruction of a blood vessel, which irrigates the brain mainly secondary to the development of atherosclerotic changes, leading to cerebral thrombosis and embolism. Diagnosis is made based on presenting symptoms and CT/MRI of the head, and the treatment is focused on cerebral reperfusion based on eligibility criteria and timing of presentation.
Symptoms include alteration of sensorium, numbness, decreased motor strength, facial drop, dysarthria, ataxia, visual disturbance, dizziness, and headache.
Get Free Access Through Your Institution
Download the Access App: iOS | Android
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait

- < Previous
Home > Symposia and Research Days > Campus Research Day > San Marcos Campus > Fall 2019 > 13
San Marcos, Fall 2019

Case Study: Efficacy of Physical Therapy on a Patient with CVA in Normalizing Gait and Shoulder Mechanics
Jane Mongkolvipakul , University of St. Augustine for Health Sciences Follow Amanda Orr , University of St. Augustine for Health Sciences Follow Queenie Lim , University of St. Augustine for Health Sciences Follow Rajbir Basati , University of St. Augustine for Health Sciences Follow Faris Alshammari , University of St. Augustine for Health Sciences Follow
Download Poster (514 KB)
Description
Background & Purpose : Cerebrovascular Accident (CVA) is known as Stroke. It is a damage to the brain due to an interruption of blood supply. Two main types of stroke are ischemic stroke and hemorrhagic stroke. Ischemic stroke, the most common type of stroke, is due to a blocked artery and a hemorrhagic stroke is due to a leak or burst of a blood vessel. Signs and symptoms of stroke are presented contralaterally. The purpose of this case report is to demonstrate the use of PT interventions to improve shoulder function and gait mechanics in a post CVA patient.
Case Description : Patient is a retired 75-yo male who sustained a left ischemic CVA in 2017 with an insidious onset. Comorbidities include Central and Obstructive Sleep Apnea, HTN, and Benign Prostatic Hyperplasia. He has been receiving PT, OT, and SLP intermittently for the past 2 years. The patient’s body structure and function impairments include balance and coordination deficits, R hemiparesis, impaired sensation RUE, decreased ROM of RUE, RUE partial flexor synergy, difficulty speaking, right homonymous hemianopsia, and decreased endurance. Activity limitations include difficulty walking greater than 1 mile and inability to reach overhead with the RUE. Participation restrictions include difficulty cooking independently (I) and socializing in groups due to his speech impairment. Specific interventions included balance and gait training, therapeutic exercise and neuromuscular re-education for RUE and RLE, and patient education. PT services were provided 1 time per week for 4 weeks.
Outcomes : Patient had significant improvement in functional gait as well as awareness of ankle motion. Dynamic Gait Index (DGI) increased from 18/24 to 20/24 with improvements in alternating gait speed, ambulation with head turns, and pivoting on command compared to pre-test. Although his time for Timed Up and Go (TUG) went from 7 sec to 7.3 sec, he did not stumble as compared to the pre-test. Patient also demonstrated decreased RUE partial synergy during TUG and DGI. He was d/c from PT services with a plan to continue progressing shoulder flexion ROM, increasing endurance of R ankle dorsiflexors, and continuation of LE stretches to improve gait.
Discussion: For a patient who has experienced a CVA, scapulohumeral rehabilitation and gait training are effective PT management options to increase functional mobility and (I). This study supports previous research for the effectiveness of scapulohumeral rhythm in increasing shoulder ROM and gait training in implementing proper gait mechanics, efficiency, and endurance. Although the patient’s stroke had occurred two years ago, the patient was able to make significant functional improvement with shoulder ROM and improved quality in gait mechanics. The outcome of this study may help guide future clinicians in decision making with stroke patients who need improvement with shoulder ROM and gait mechanics.
Publication Date
San Marcos, CA
Stroke, Walking, Gait, Shoulder, Range of Motion, Articular, Exercise Therapy, Physical Therapy Modalities, Male, Humans
- Disciplines
Occupational Therapy | Rehabilitation and Therapy
Poster presented at the Fall 2019 Research Day on the San Marcos, CA, campus of the University of St. Augustine for Health Sciences, December 13, 2019.
- Abdul Rahman K, Azaman A, Mohd Latip HF, Mat Dzahir MA, Balakrishnan M. Comparison of tibialis anterior and gastrocnemius muscles activation on balance training devices and hoverboard. Malaysian Journal of Fundamental and Applied Sciences . 2017;13(4-2):495-500. doi:10.11113/mjfas.v13n4-2.820.
- Ratanapinunchai J, Mathiyakom W, Sungkarat S. Scapular upward rotation during passive humeral abduction in individuals with hemiplegia post-stroke. Annals of Rehabilitation Medicine . 2019;43(2):178-186. doi:10.5535/arm.2019.43.2.178.
- Burpee JL, Lewek MD. Biomechanical gait characteristics of naturally occurring unsuccessful foot clearance during swing in individuals with chronic stroke. Clin Biomech . 2015;30(10):1102-1107. doi:10.1016/j.clinbiomech.2015.08.018
Recommended Citation
Mongkolvipakul, J., Orr, A., Lim, Q., Basati, R., & Alshammari, F. (2019, December 13). Case Study: Efficacy of Physical Therapy on a Patient with CVA in Normalizing Gait and Shoulder Mechanics. Poster presented at the Campus Research Day Symposium, University of St Augustine for Health Sciences. Retrieved from https://soar.usa.edu/casmfall2019/13 Mongkolvipakul, Jane; Orr, Amanda; Lim, Queenie; Basati, Rajbir; and Alshammari, Faris, "Case Study: Efficacy of Physical Therapy on a Patient with CVA in Normalizing Gait and Shoulder Mechanics" (2019). San Marcos, Fall 2019 . 13. Retrieved from https://soar.usa.edu/casmfall2019/13
Since March 11, 2020
Included in
Occupational Therapy Commons
- Collections
Advanced Search
- Notify me via email or RSS
Author Corner
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Cerebrovascular Accident (Stroke)
Learn about the nursing care management of patients with cerebrovascular accident in this nursing study guide .
Table of Contents
- What is Cerebrovascular Accident?

Classification
Risk factors, pathophysiology, statistics and epidemiology, clinical manifestations, complications, assessment and diagnostic findings, medical management, surgical management, nursing assessment, nursing diagnosis, nursing care planning & goals, nursing interventions, discharge and home care guidelines, documentation guidelines, what is cerebrovascular accident.
A cerebrovascular accident (CVA), an ischemic stroke or “ brain attack,” is a sudden loss of brain function resulting from a disruption of the blood supply to a part of the brain.
- Cerebrovascular accident or stroke is the primary cerebrovascular disorder in the United States.
- A cerebrovascular accident is a sudden loss of brain functioning resulting from a disruption of the blood supply to a part of the brain.
- It is a functional abnormality of the central nervous system .
- Cryptogenic strokes have no known cause, and other strokes result from causes such as illicit drug use, coagulopathies, migraine, and spontaneous dissection of the carotid or vertebral arteries.
- The result is an interruption in the blood supply to the brain, causing temporary or permanent loss of movement, thought, memory , speech, or sensation.
Strokes can be divided into two classifications.
- Ischemic stroke. This is the loss of function in the brain as a result of a disrupted blood supply.
- Hemorrhagic stroke. Hemorrhagic strokes are caused by bleeding into the brain tissue, the ventricles, or the subarachnoid space.
The following are the nonmodifiable and modifiable risk factors of Cerebrovascular accident:
Nonmodifiable
- Advanced age (older than 55 years)
- Gender (Male)
- Race (African American)
- Hypertension
- Atrial fibrillation
- Hyperlipidemia
- Asymptomatic carotid stenosis and valvular heart disease (eg, endocarditis, prosthetic heart valves)
- Periodontal disease
The disruption in the blood flow initiates a complex series of cellular metabolic events.
- Decreased cerebral blood flow. The ischemic cascade begins when cerebral blood flow decreases to less than 25 mL per 100g of blood per minute.
- Aerobic respiration. At this point, neurons are unable to maintain aerobic respiration.
- Anaerobic respiration. The mitochondria would need to switch to anaerobic respiration, which generates large amounts of lactic acid , causing a change in pH and rendering the neurons incapable of producing sufficient quantities of ATP.
- Loss of function. The membrane pumps that maintain electrolyte balances fail and the cells cease to function.
Stroke is a worldwide phenomenon suffered through all walks of life.
- Morbidity: In 2005, prevalence of stroke was estimated at 2.3 million males and 3.4 million females; many of the approximately 5.7 million U.S. stroke survivors have permanent stroke-related disabilities.
- Mortality: In 2004, stroke ranked fifth as the cause of death for those aged 45 to 64 years and third for those aged 65 years or older (National Heart, Lung and Blood Institute [NHLBI], 2007), with 150,000 deaths (American Heart Association and American Stroke Association, 2008); hemorrhagic strokes are more severe, and mortality rates are higher than ischemic strokes, with a 30-day mortality rate of 40% to 80%.
- Cost: Estimated direct and indirect cost for 2008 was $65.5 billion (American Heart Association and American Stroke Association, 2008).
- Stroke is the third leading cause of death after heart disease and cancer .
- Approximately 780, 000 people experience a stroke each year in the United States.
- Approximately 600, 000 of these are new strokes, and 180, 000 are recurrent strokes.
- About 5.6 million noninstitutionalized stroke survivors are alive today.
- Stroke is the leading cause of serious, long-term disability in the United States.
- Direct and indirect costs for stroke cost $65.5 billion in 2008.
- Strokes are usually hemorrhagic (15%) or ischemic/nonhemorrhagic (85%).
- Ischemic strokes are categorized according to their cause: large artery thrombotic strokes (20%), small penetrating artery thrombotic strokes (25%), cardiogenic embolic strokes (20%), cryptogenic strokes (30%), and other (5%).
Strokes are caused by the following:
- Large artery thrombosis . Large artery thromboses are caused by atherosclerotic plaques in the large blood vessels of the brain.
- Small penetrating artery thrombosis. Small penetrating artery thrombosis affects one or more vessels and is the most common type of ischemic stroke.
- Cardiogenic emboli. Cardiogenic emboli are associated with cardiac dysrhythmias, usually atrial fibrillation .
Stroke can cause a wide variety of neurologic deficits, depending on the location of the lesion, the size of the area of inadequate perfusion, and the amount of the collateral blood flow. General signs and symptoms include numbness or weakness of face, arm, or leg (especially on one side of the body); confusion or change in mental status; trouble speaking or understanding speech; visual disturbances; loss of balance, dizziness, difficulty walking ; or sudden severe headache.
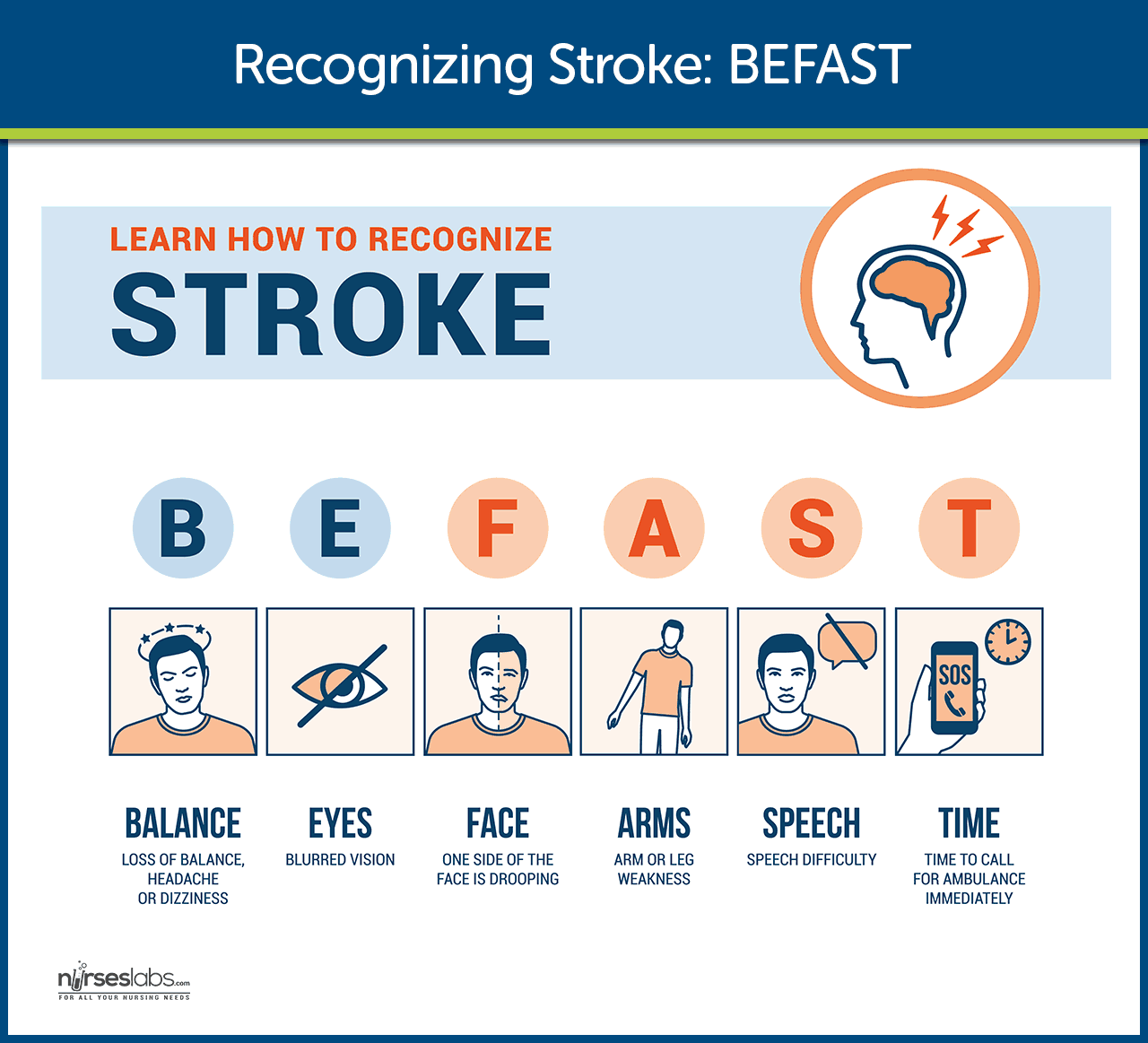
General signs and symptoms include numbness or weakness of face, arm, or leg (especially on one side of the body); confusion or change in mental status; trouble speaking or understanding speech; visual disturbances; loss of balance, dizziness, difficulty walking ; or sudden severe headache.
- Numbness or weakness of the face. Without adequate perfusion, oxygen is also low, and facial tissues could not function properly without them.
- Change in mental status. Due to decreased oxygen, the patient experiences confusion .
- Trouble speaking or understanding speech. Cells cease to function as a result of inadequate perfusion.
- Visual disturbances. The eyes also need enough oxygen for optimal functioning.
- Homonymous hemianopsia. There is loss of half of the visual field.
- Loss of peripheral vision . The patient experiences difficulty seeing at night and is unaware of objects or the borders of objects.
- Hemiparesis. There is a weakness of the face, arm, and leg on the same side due to a lesion in the opposite hemisphere.
- Hemiplegia. Paralysis of the face, arm, and leg on the same side due to a lesion in the opposite hemisphere.
- Ataxia. Staggering, unsteady gait and inability to keep feet together.
- Dysarthria. This is the difficulty in forming words.
- Dysphagia . There is difficulty in swallowing.
- Paresthesia. There is numbness and tingling of extremities and difficulty with proprioception.
- Expressive aphasia . The patient is unable to form words that is understandable yet can speak in single-word responses.
- Receptive aphasia . The patient is unable to comprehend the spoken word and can speak but may not make any sense.
- Global aphasia. This is a combination of both expressive and receptive aphasia.
- Hemiplegia, hemiparesis
- Flaccid paralysis and loss of or decrease in the deep tendon reflexes (initial clinical feature) followed by (after 48 hours) reappearance of deep reflexes and abnormally increased muscle tone (spasticity)
Communication Loss
- Dysarthria (difficulty speaking)
- Dysphasia (impaired speech) or aphasia (loss of speech)
- Apraxia (inability to perform a previously learned action)
Perceptual Disturbances and Sensory Loss
- Visual-perceptual dysfunctions (homonymous hemianopia [loss of half of the visual field])
- Disturbances in visual-spatial relations (perceiving the relation of two or more objects in spatial areas), frequently seen in patients with right hemispheric damage
- Sensory losses: slight impairment of touch or more severe with loss of proprioception; difficulty in interrupting visual, tactile, and auditory stimuli
Impaired Cognitive and Psychological Effects
- Frontal lobe damage: Learning capacity, memory, or other higher cortical intellectual functions may be impaired. Such dysfunction may be reflected in a limited attention span, difficulties in comprehension, forgetfulness, and lack of motivation.
- Depression , other psychological problems: emotional lability, hostility, frustration, resentment, and lack of cooperation.
Primary prevention of stroke remains the best approach.
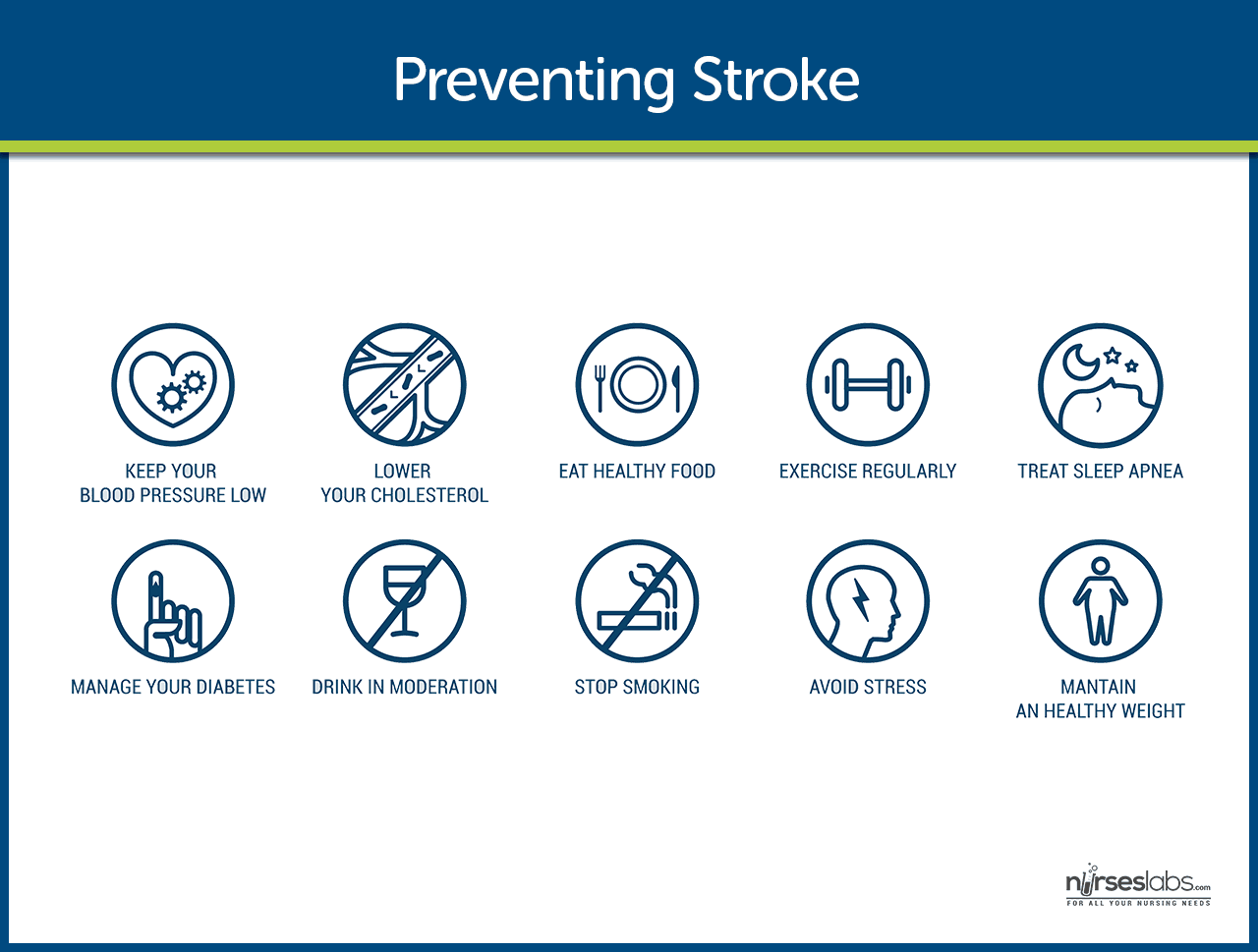
- Healthy lifestyle. Leading a healthy lifestyle which includes not smoking, maintaining a healthy weight, following a healthy diet, and daily exercise can reduce the risk of having a stroke by about one half.
- DASH diet. The DASH ( Dietary Approaches to Stop Hypertension ) diet is high in fruits and vegetables, moderate in low-fat dairy products, and low in animal protein and can lower the risk of stroke.
- Stroke risk screenings. Stroke risk screenings are an ideal opportunity to lower stroke risk by identifying people or groups of people who are at high risk for stroke.
- Education. Patients and the community must be educated about recognition and prevention of stroke.
- Low-dose aspirin . Research findings suggest that low-dose aspirin may lower the risk of stroke in women who are at risk.
If cerebral oxygenation is still inadequate; complications may occur.
- Tissue ischemia . If cerebral blood flow is inadequate, the amount of oxygen supplied to the brain is decreased, and tissue ischemia will result.
- Cardiac dysrhythmias. The heart compensates for the decreased cerebral blood flow, and with too much pumping, dysrhythmias may occur.
Any patient with neurologic deficits needs a careful history and complete physical and neurologic examination.
- CT scan . Demonstrates structural abnormalities, edema , hematomas, ischemia , and infarctions. Demonstrates structural abnormalities, edema , hematomas, ischemia, and infarctions. Note: May not immediately reveal all changes, e.g., ischemic infarcts are not evident on CT for 8–12 hr; however, intracerebral hemorrhage is immediately apparent; therefore, emergency CT is always done before administering tissue plasminogen activator (t-PA). In addition, patients with TIA commonly have a normal CT scan
- PET scan. Provides data on cerebral metabolism and blood flow changes.
- MRI. Shows areas of infarction, hemorrhage , AV malformations, and areas of ischemia.
- Cerebral angiography. Helps determine specific cause of stroke, e.g., hemorrhage or obstructed artery, pinpoints site of occlusion or rupture. Digital subtraction angiography evaluates patency of cerebral vessels, identifies their position in head and neck, and detects/evaluates lesions and vascular abnormalities.
- Lumbar puncture . Pressure is usually normal and CSF is clear in cerebral thrombosis, embolism, and TIA. Pressure elevation and grossly bloody fluid suggest subarachnoid and intracerebral hemorrhage. CSF total protein level may be elevated in cases of thrombosis because of inflammatory process. LP should be performed if septic embolism from bacterial endocarditis is suspected.
- Transcranial Doppler ultrasonography. Evaluates the velocity of blood flow through major intracranial vessels; identifies AV disease, e.g., problems with carotid system (blood flow/presence of atherosclerotic plaques).
- EEG. Identifies problems based on reduced electrical activity in specific areas of infarction; and can differentiate seizure activity from CVA damage.
- Skull x-ray. May show a shift of pineal gland to the opposite side from an expanding mass; calcifications of the internal carotid may be visible in cerebral thrombosis; partial calcification of walls of an aneurysm may be noted in subarachnoid hemorrhage.
- ECG and echocardiography . To rule out cardiac origin as source of embolus (20% of strokes are the result of blood or vegetative emboli associated with valvular disease, dysrhythmias, or endocarditis).
- Laboratory studies to rule out systemic causes: CBC, platelet and clotting studies, VDRL/RPR, erythrocyte sedimentation rate (ESR), chemistries ( glucose , sodium ).
Patients who have experienced TIA or stroke should have medical management for secondary prevention.
- Recombinant tissue plasminogen activator would be prescribed unless contraindicated, and there should be monitoring for bleeding .
- Increased ICP. Management of increased ICP includes osmotic diuretics , maintenance of PaCO2 at 30-35 mmHg, and positioning to avoid hypoxia through elevation of the head of the bed.
- Endotracheal Tube. There is a possibility of intubation to establish patent airway if necessary.
- Hemodynamic monitoring. Continuous hemodynamic monitoring should be implemented to avoid an increase in blood pressure .
- Neurologic assessment to determine if the stroke is evolving and if other acute complications are developing
Surgical management may include prevention and relief from increased ICP.
- Carotid endarterectomy. This is the removal of atherosclerotic plaque or thrombus from the carotid artery to prevent stroke in patients with occlusive disease of the extracranial cerebral arteries.
- Hemicraniectomy. Hemicraniectomy may be performed for increased ICP from brain edema in severe cases of stroke.
Nursing Management
After the stroke is complete, management focuses on the prompt initiation of rehabilitation for any deficits.
During the acute phase , a neurologic flow sheet is maintained to provide data about the following important measures of the patient’s clinical status:
- Change in level of consciousness or responsiveness.
- Presence or absence of voluntary or involuntary movements of extremities.
- Stiffness or flaccidity of the neck.
- Eye opening, comparative size of pupils, and pupillary reaction to light.
- Color of the face and extremities; temperature and moisture of the skin.
- Ability to speak.
- Presence of bleeding.
- Maintenance of blood pressure .
During the postacute phase , assess the following functions:
- Mental status (memory, attention span, perception, orientation, affect, speech/language).
- Sensation and perception (usually the patient has decreased awareness of pain and temperature).
- Motor control (upper and lower extremity movement); swallowing ability, nutritional and hydration status, skin integrity, activity tolerance , and bowel and bladder function.
- Continue focusing nursing assessment on impairment of function in patient’s daily activities.
Based on the assessment data, the major nursing diagnoses for a patient with stroke may include the following:
- Impaired physical mobility related to hemiparesis, loss of balance and coordination , spasticity, and brain injury .
- Acute pain related to hemiplegia and disuse.
- Deficient self-care related to stroke sequelae.
- Disturbed sensory perception related to altered sensory reception, transmission, and/or integration.
- Impaired urinary elimination related to flaccid bladder , detrusor instability, confusion , or difficulty in communicating.
- Disturbed thought processes related to brain damage.
- Impaired verbal communication related to brain damage.
- Risk for impaired skin integrity related to hemiparesis or hemiplegia and decreased mobility .
- Interrupted family processes related to catastrophic illness and caregiving burdens.
- Sexual dysfunction related to neurologic deficits or fear of failure.
Main article: Cerebrovascular Accident (Stroke) Nursing Care Plans
The major nursing care planning goals for the patient and family may include:
- Improve mobility.
- Avoidance of shoulder pain .
- Achievement of self-care .
- Relief of sensory and perceptual deprivation.
- Prevention of aspiration .
- Continence of bowel and bladder.
- Improved thought processes.
- Achieving a form of communication .
- Maintaining skin integrity .
- Restore family functioning.
- Improve sexual function.
- Absence of complications.
Nursing care has a significant impact on the patient’s recovery. In summary, here are some nursing interventions for patients with stroke:
- Positioning. Position to prevent contractures, relieve pressure, attain good body alignment, and prevent compressive neuropathies.
- Prevent flexion . Apply splint at night to prevent flexion of the affected extremity.
- Prevent adduction. Prevent adduction of the affected shoulder with a pillow placed in the axilla.
- Prevent edema. Elevate affected arm to prevent edema and fibrosis.
- Full range of motion. Provide full range of motion four or five times a day to maintain joint mobility.
- Prevent venous stasis. Exercise is helpful in preventing venous stasis, which may predispose the patient to thrombosis and pulmonary embolus .
- Regain balance. Teach patient to maintain balance in a sitting position, then to balance while standing and begin walking as soon as standing balance is achieved.
- Personal hygiene . Encourage personal hygiene activities as soon as the patient can sit up.
- Manage sensory difficulties. Approach patient with a decreased field of vision on the side where visual perception is intact.
- Visit a speech therapist. Consult with a speech therapist to evaluate gag reflexes and assist in teaching alternate swallowing techniques.
- Voiding pattern. Analyze voiding pattern and offer urinal or bedpan on patient’s voiding schedule.
- Be consistent in patient’s activities. Be consistent in the schedule, routines, and repetitions; a written schedule, checklists, and audiotapes may help with memory and concentration, and a communication board may be used.
- Assess skin. Frequently assess skin for signs of breakdown, with emphasis on bony areas and dependent body parts.
Improving Mobility and Preventing Deformities
- Position to prevent contractures; use measures to relieve pressure, assist in maintaining good body alignment, and prevent compressive neuropathies.
- Apply a splint at night to prevent flexion of affected extremity.
- Prevent adduction of the affected shoulder with a pillow placed in the axilla.
- Elevate affected arm to prevent edema and fibrosis.
- Position fingers so that they are barely flexed; place hand in slight supination. If upper extremity spasticity is noted, do not use a hand roll; dorsal wrist splint may be used.
- Change position every 2 hours; place patient in a prone position for 15 to 30 minutes several times a day.
Establishing an Exercise Program
- Provide full range of motion four or five times a day to maintain joint mobility, regain motor control, prevent contractures in the paralyzed extremity, prevent further deterioration of the neuromuscular system, and enhance circulation. If tightness occurs in any area, perform a range of motion exercises more frequently.
- Exercise is helpful in preventing venous stasis, which may predispose the patient to thrombosis and pulmonary embolus.
- Observe for signs of pulmonary embolus or excessive cardiac workload during exercise period (e.g., shortness of breath, chest pain , cyanosis , and increasing pulse rate ).
- Supervise and support the patient during exercises; plan frequent short periods of exercise, not longer periods; encourage the patient to exercise unaffected side at intervals throughout the day.
Preparing for Ambulation
- Start an active rehabilitation program when consciousness returns (and all evidence of bleeding is gone, when indicated).
- Teach patient to maintain balance in a sitting position, then to balance while standing (use a tilt table if needed).
- Begin walking as soon as standing balance is achieved (use parallel bars and have a wheelchair available in anticipation of possible dizziness).
- Keep training periods for ambulation short and frequent.
Preventing Shoulder Pain
- Never lift patient by the flaccid shoulder or pull on the affected arm or shoulder.
- Use proper patient movement and positioning (e.g., flaccid arm on a table or pillows when patient is seated, use of sling when ambulating).
- Range of motion exercises are beneficial, but avoid over strenuous arm movements.
- Elevate arm and hand to prevent dependent edema of the hand; administer analgesic agents as indicated.
Enhancing Self Care
- Encourage personal hygiene activities as soon as the patient can sit up; select suitable self-care activities that can be carried out with one hand.
- Help patient to set realistic goals; add a new task daily.
- As a first step, encourage patient to carry out all self-care activities on the unaffected side.
- Make sure patient does not neglect affected side; provide assistive devices as indicated.
- Improve morale by making sure patient is fully dressed during ambulatory activities.
- Assist with dressing activities (e.g., clothing with Velcro closures; put garment on the affected side first); keep environment uncluttered and organized.
- Provide emotional support and encouragement to prevent fatigue and discouragement.
Managing Sensory-Perceptual Difficulties
- Approach patient with a decreased field of vision on the side where visual perception is intact; place all visual stimuli on this side.
- Teach patient to turn and look in the direction of the defective visual field to compensate for the loss; make eye contact with patient, and draw attention to affected side.
- Increase natural or artificial lighting in the room; provide eyeglasses to improve vision.
- Remind patient with hemianopsia of the other side of the body; place extremities so that patient can see them.
Assisting with Nutrition
- Observe patient for paroxysms of coughing , food dribbling out or pooling in one side of the mouth , food retained for long periods in the mouth, or nasal regurgitation when swallowing liquids.
- Consult with speech therapist to evaluate gag reflexes; assist in teaching alternate swallowing techniques, advise patient to take smaller boluses of food, and inform patient of foods that are easier to swallow; provide thicker liquids or pureed diet as indicated.
- Have patient sit upright, preferably on chair, when eating and drinking; advance diet as tolerated.
- Prepare for GI feedings through a tube if indicated; elevate the head of bed during feedings, check tube position before feeding , administer feeding slowly, and ensure that cuff of tracheostomy tube is inflated (if applicable); monitor and report excessive retained or residual feeding .
Attaining Bowel and Bladder Control
- Perform intermittent sterile catheterization during the period of loss of sphincter control.
- Analyze voiding pattern and offer urinal or bedpan on patient’s voiding schedule.
- Assist the male patient to an upright posture for voiding.
- Provide highfiber diet and adequate fluid intake (2 to 3 L/day), unless contraindicated.
- Establish a regular time (after breakfast) for toileting.
Improving Thought Processes
- Reinforce structured training program using cognitive, perceptual retraining, visual imagery, reality orientation, and cueing procedures to compensate for losses.
- Support patient: Observe performance and progress, give positive feedback, convey an attitude of confidence and hopefulness; provide other interventions as used for improving cognitive function after a head injury.
Improving Communication
- Reinforce the individually tailored program.
- Jointly establish goals, with the patient taking an active part.
- Make the atmosphere conducive to communication , remaining sensitive to patient’s reactions and needs and responding to them in an appropriate manner; treat the patient as an adult.
- Provide strong emotional support and understanding to allay anxiety ; avoid completing patient’s sentences.
- Be consistent in schedule, routines, and repetitions. A written schedule, checklists, and audiotapes may help with memory and concentration; a communication board may be used.
- Maintain patient’s attention when talking with the patient, speak slowly, and give one instruction at a time; allow the patient time to process.
- Talk to aphasic patients when providing care activities to provide social contact.
Maintaining Skin Integrity
- Frequently assess skin for signs of breakdown, with emphasis on bony areas and dependent body parts.
- Employ pressure relieving devices; continue regular turning and positioning (every 2 hours minimally); minimize shear and friction when positioning.
- Keep skin clean and dry, gently massage the healthy dry skin and maintain adequate nutrition .
Improving Family Coping
- Provide counseling and support to the family.
- Involve others in patient’s care; teach stress management techniques and maintenance of personal health for family coping.
- Give family information about the expected outcome of the stroke, and counsel them to avoid doing things for the patient that he or she can do.
- Develop attainable goals for the patient at home by involving the total health care team, patient, and family.
- Encourage everyone to approach the patient with a supportive and optimistic attitude, focusing on abilities that remain; explain to the family that emotional lability usually improves with time.
Helping the Patient Cope with Sexual Dysfunction
- Perform indepth assessment to determine sexual history before and after the stroke.
- Interventions for patient and partner focus on providing relevant information, education, reassurance, adjustment
- of medications, counseling regarding coping skills, suggestions for alternative sexual positions, and a means of sexual expression and satisfaction.
Teaching points
- Teach patient to resume as much self care as possible; provide assistive devices as indicated.
- Have occupational therapist make a home assessment and recommendations to help the patient become more independent.
- Coordinate care provided by numerous health care professionals; help family plan aspects of care.
- Advise family that patient may tire easily, become irritable and upset by small events, and show less interest in daily events.
- Make a referral for home speech therapy. Encourage family involvement. Provide family with practical instructions to help patient between speech therapy sessions.
- Discuss patient’s depression with the physician for possible antidepressant therapy.
- Encourage patient to attend community-based stroke clubs to give a feeling of belonging and fellowship to others.
- Encourage patient to continue with hobbies, recreational and leisure interests, and contact with friends to prevent social isolation .
- Encourage family to support patient and give positive reinforcement.
- Remind spouse and family to attend to personal health and wellbeing.
Expected patient outcomes may include the following:
- Improved mobility.
- Absence of shoulder pain .
- Self-care achieved.
- Achieved a form of communication.
- Maintained skin integrity .
- Restored family functioning.
- Improved sexual function.
Patient and family education is a fundamental component of rehabilitation.
- Consult an occupational therapist. An occupational therapist may be helpful in assessing the home environment and recommending modifications to help the patient become more independent.
- Physical therapy. A program of physical therapy may be beneficial, whether it takes place in the home or in an outpatient program.
- Antidepressant therapy. Depression is a common and serious problem in the patient who has had a stroke.
- Support groups . Community-based stroke support groups may allow the patient and the family to learn from others with si milar problems and to share their experiences.
- Assess caregivers . Nurses should assess caregivers for signs of depression, as depression is also common among caregivers of stroke survivors.
The focus of documentation should involve:
- Individual findings including level of function and ability to participate in specific or desired activities.
- Needed resources and adaptive devices.
- Results of laboratory tests, diagnostic studies, and mental status or cognitive evaluation .
- SO/family support and participation.
- Plan of care and those involved in planning .
- Teaching plan.
- Response to interventions, teaching, and actions performed.
- Attainment or progress toward desired outcomes .
- Modifications to plan of care.
Posts related to Cerebrovascular Accident (Stroke):
- 8+ Cerebrovascular Accident (Stroke) Nursing Care Plans
- Drugs Affecting Coagulation
12 thoughts on “Cerebrovascular Accident (Stroke)”
I’m impressed, I have been challenged to read more.
The article was helpful
Am so impressed with the write up am student will wish to develop a research topic in CVA
As a nursing student, I want to thank this article for the valuable information on cerebrovascular accident nursing management. Understanding the importance of proper care and management for stroke patients is a crucial aspect of my education and future practice as a nurse. This article has provided me with a deeper insight into the role of the nurse in promoting positive outcomes for stroke patients, and I am grateful for the opportunity to learn more about this important topic. Thank you!
very presented alihamudulillah i got something
Hi Mugoya, Wonderful to hear you gained something valuable from the study guide! If you’re curious about more or have any questions, feel free to reach out. Always here to help!
well explained great article for students ……… Kindly increase the number of mcqs
Hi Abdur, Thanks for the positive feedback on the article! I’m glad to hear it’s helpful for students. All of our practice questions are available at our Nursing Test Bank page . If there are specific topics you’d like to see more questions on, just drop a suggestion. Your input helps us create better resources!
So interesting, very very good notes.
So interesting topic to learn
Excelente y completo artículo .muchas felicidades y gracias por la información
Very insightful. ⭐⭐⭐⭐
Can you add reference to the work.
Leave a Comment Cancel reply
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.10(7); 2018 Jul

A Case Report in Hemorrhagic Stroke: A Complex Disease Process and Requirement for a Multimodal Treatment Approach
Brain d sindelar.
1 Neurosurgery, University of Florida, Gainesville, USA
Vimal Patel
2 NorthShore Neurological Institute, NorthShore University Health System/University of Chicago Pritzker School of Medicine, Chicago, USA
Shakeel Chowdhry
3 Neurosurgery, NorthShore University Health System/University of Chicago Pritzker School of Medicine, Chicago, USA
Julian E Bailes
Intracerebral hemorrhage (ICH) with or without intraventricular hemorrhage (IVH) is a highly morbid disease process due to the mass effect and secondary injury that occurs upon the surrounding brain. Historically, surgical evacuation has failed to demonstrate improved outcomes in comparison to standard medical therapy likely due to the significant brain trauma when accessing the clot. Recent minimally invasive techniques have proposed a way to improve outcomes by reducing this injury. We report here a 62-year-old male with ICH and IVH with acute neurological deterioration due to hydrocephalus was found to have no improvement following external ventricular drainage. A repeat non-contrasted computed tomography (CT) head was obtained which demonstrated the worsening mass effect from peri-hematoma edema. Surgical intervention was employed that uses a variety of techniques (endoscopic and exoscopic visualization, stereotactic trans-sulcal approach and side cutting aspiration, and intraventricular thrombolytic therapy) to reduce cerebral trauma while effectively removing both ICH and IVH. The surgical intervention reduces the mass effect and associated secondary injury, lessens the likelihood of shunt placement and length of stay, and improves long-term morbidity. We conclude that the effectiveness of surgical management of ICH could potentially be improved by employing a multifaceted approach to address the different characteristics of the hemorrhagic stroke.
Introduction
Minimally invasive surgical interventions for evacuation of intracerebral hemorrhage (ICH) and/or intraventricular hemorrhage (IVH) (in order to remove mass effect, prevent secondary injury, and potentially reduce morbidity/mortality) have demonstrated a range of published clinical outcomes, and therefore the use of one specific or any surgical modality is greatly contested. Here, we will present our management of a particular case of significant ICH with IVH with the purpose of transitioning the dialogue away from choosing a single medical or specific surgical approach to suggesting a multifaceted treatment tactic of ICH in order to reduce this devastating affliction.
Case presentation
A 62-year-old male with a history of gastroesophageal reflux and deep vein thrombosis/pulmonary embolism, developed sudden onset headache prior to his scheduled Nissen fundoplication. The patient presented to an outside hospital neurologically intact, but due to intractable symptoms, a non-contrasted head computed tomography (CT) was ordered which was significant for a right-sided caudate ICH with ventricular extension but without hydrocephalus (Figure (Figure1A) 1A ) (ICH score 1). Of note, the patient’s coagulation labs were within normal range.

A) Right caudate intracerebral hemorrhage (ICH) (17 cm 3 ) (black arrow) with ventricular extension (red arrow) but without hydrocephalus. B) Repeat CT head significant for slight increased size of ICH (21 cm 3 ) (black arrow) with greater intraventricular hemorrhage (red arrow), casting of the right lateral and third ventricles, and hydrocephalus (blue arrow).
En route to our hospital, the patient declined dramatically requiring intubation upon arrival. Repeat imaging was significant for expansion of the ICH with worsening of the IVH and associated hydrocephalus (Figure (Figure1B). The 1B ). The patient was localizing on the right upper extremity and withdrawing in the left upper extremity and bilateral lower extremities to noxious stimuli (GCS 7t, ICH score 2). An external ventricular drain (EVD) was placed and the patient was admitted to the intensive care unit (ICU). Vascular imaging was negative for underlying malformations. A repeat CT head six hours post EVD placement demonstrated a collapsed ventricle secondary to cerebrospinal fluid (CSF) drainage, but the progression of perihematoma edema and midline shift (Figure (Figure2). With 2 ). With increasing mass effect and failure of neurological improvement with CSF drainage, it was decided to take the patient to the operating room for ICH evacuation.

Increased size of the intracerebral hemorrhage (23 cm 3 ), a collapsed left lateral ventricle (red arrow) secondary to cerebrospinal fluid drainage, entrapment of the left temporal horn, and peri-hematoma edema with 6.5 mm of midline shift.
Following anesthetization, a 5 cm curvilinear right frontal incision was made behind the hairline. A 4 cm craniotomy was performed followed by identification of the posterior aspect of the right frontal superior sulcus, and then stereotactic trans-sulcal introduction of a 75 mm sheath and obturator (BrainPath, NICO Corp, Indianapolis, Indiana). Under exoscope magnification, the inferior depth of the hematoma was evacuated with gentle irrigation and suction. A small opening into the right lateral ventricle was identified, and a straight rigid endoscope was used to atraumatically enter the ventricle for further ventricular clot evacuation and irrigation. The endoscope was removed and the trans-sulcal port was slightly retracted in successive fashion to deliver more of the frontal ICH into view. With the use of suction, irrigation, and a side cutting resection device (Myriad, NICO Corp, Indianapolis, Indiana), the remainder of parenchymal hematoma was extracted. A post-operative head CT showed near complete removal of the ICH and IVH from the right lateral ventricle but with residual hematoma predominantly within the left lateral and third ventricles (Figure (Figure3 3 ).

Almost complete removal of the intracerebral hemorrhage and intraventricular hemorrhage from the right lateral ventricle but with persistent clot within the left lateral and third ventricles.
Due to the persistence of third ventricle IVH, the patient received intrathecal tPA post-operative day two (two doses, 1 mg each, nine hours apart) followed by successful weaning and removal of the ventricular drain. After three days, the patient was discharged to a long-term acute care hospital. At the three-month follow-up visit, the patient had transitioned to a skilled nursing facility. At the five-month follow-up visit, the patient was living at home, neurologically intact except for a slight facial droop and mild gait imbalance with a goal to return to work in the coming month. At each follow-up, head CT at each outpatient visit was negative for hydrocephalus.
It has been long hypothesized and studied in pre-clinical models that surgical evacuation of an intracerebral hemorrhage aids in removing both the mass effect of the primary injury along with the reduction in the secondary injury associated with clot-induced blood-brain barrier breakdown, the release of inflammatory cytokines, and the development of perihematomal edema. But, two randomized clinical trials, STITCH and STITCH 2, failed to prove this theory due to their inability to strongly demonstrate a statistically significant difference in those offered surgical evacuation through a standard craniotomy compared with medical management, even in those with superficially located lesions [ 1 ]. Lack of clinical efficacy has been suggested to be due to the overall morbidity associated with large craniotomies and the cerebral trauma required to access deep-seeded lesions.
For this reason, minimally invasive techniques have been suggested in order to reduce the morbidity associated with a craniotomy, specifically the cerebral injury when retrieving the hematoma. These approaches can be subdivided into those that use thrombolytic agents or those that use mechanical methods for ICH/IVH evacuation. The most popularized approach to targeting intracerebral hemorrhage through thrombolytic means is by stereotactically aspirating the hematoma followed by infusion of either alteplase or urokinase. A phase two clinical trial for this method called “Minimally invasive surgery plus alteplase in intracerebral hemorrhage evacuation”, MISTIE, demonstrated efficacy in reducing clot burden and perihematomal edema and a correlation between outcomes and volume of clot removed [ 2 ]. The phase three trial has completed subject enrollment but study results are pending collection of final patient follow-up assessments. A thrombolytic therapy to address IVH has been studied in the “Clot lysis evaluating accelerated resolution,” or CLEAR. This study administered 1 mg of tPA through a ventricular drain every eight hours. This technique reduced overall clot burden but showed no difference in overall outcomes in comparison to control (saline ventricular injection) [ 3 ].
Variations in mechanical means to remove deep-seeded clots vary by the type of optics used (endoscope vs exoscope), ways to gain access to the clot, and also various devices to mechanically remove the clot. Case series and retrospective reviews have demonstrated efficacy in clot removal through endoscopic means, but there is only limited evidence demonstrating superior means to standard therapy (medical management). A newer technology published, “minimally invasive subcortical parafascicular access for clot evacuation” or MISPACE, uses an imaged guided placement of a trans-sulcal port with the use of a side cutting aspirator [ 4 ]. This approach allows a small craniotomy, practically atraumatic trans-sulcal access to the clot, minimal retraction to surrounding brain, and elimination of pulling that occurs with standard suction. There is currently a randomized multicenter trial (ENRICH: Early Minimally-Invasive Removal of ICH) evaluating the effectiveness of this method but results are still pending [ 5 ].
These techniques all bring great promise to possibly improving the standard of care, but due to limited trials directly comparing each to the other and medical management, there is great controversy to their role in ICH management. Due to the multidimensional presentations (size/location of ICH, presence or absence of IVH, etc.) of those with hemorrhagic stroke, we presented this case study in order to pose that a single surgical approach may not be the answer to improving outcomes in comparison to medical management but actually a transition to a multimodal manner that combines the various mechanical and thrombolytic methods to improve visualization, intracerebral and intraventricular clot retrieval, and weaning from ventricular drainage. It appears disadvantageous to not use our arsenal of techniques to provide individualized care to the heterogeneous nature of hemorrhagic stroke. Also, as this case report emphasizes, the standard heterogeneous clinical presentation and management is far different than the homogenous subject pool with two-arm treatment approach standard in clinical trials potentially influencing and explaining the limited benefit demonstrated in previous trials.
Conclusions
The presentation of a hemorrhagic stroke is multidimensional due to the size, location, and extent of secondary pathological processes (peri-hematomal edema, ventricular hemorrhage, hydrocephalus, etc.). This case report demonstrates the typical clinical presentation of an ICH and demonstrates a multimodal approach that involves not only the standard medical therapy of intracerebral hemorrhage, but also a combination of the various minimally invasive surgical, mechanical and thrombolytic methods in order to safely access and visualize both intracerebral and intraventricular clot to improve removal with the ultimate goal to potentially improve long-term functional outcomes and reduce the requirement of shunting. Though we understand the inherent limitations to an anecdotal case report, we hope that this brings contemplation and consideration in future clinical trials.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
- Careers in Physical Therapy
- Career Advancement
- APTA Learning Center
- APTA Combined Sections Meeting
- APTA Event Commitments
- Find PT and PTA Jobs
- Practice Models and Settings
- Scope of Practice
- APTA Fit for Practice
- Supervision and Teamwork
- Documentation
- National Provider Identifier
- Ethics and Professionalism
- APTA Article Search
- Clinical Summaries
- Clinical Practice Guidelines
- Tests and Measures
- Symptoms and Conditions
- Interventions
- Public Health and Population Care
- APTA Legislative Update Bill Status
- Take Action
- APTA Advocacy Network
- Explore Membership
- News and Publications
- Diversity, Equity, and Inclusion
- Chapters and Sections
- Leadership and Governance
- APTA Community (Online Communities)
- Volunteer Opportunities
- Honors & Awards Program
- Strategic Alliances
- Join / Renew
- Pursue Specialist Certification
- Buy APTA Gear
- For Students
- For Early-Career PTs and PTAs
- For Educators
Apply for APTA Specialist Certification by the final deadline on Sept. 30.
By using this site, you are consenting to our use of cookies. To find out more visit our privacy policy .
ICD-10 Case Study: Outpatient PT-First Visit for CVA
Case study details.
Chief Complaint: Difficulty walking short distance and weakness in right arm
Log in or create a free account to keep reading.
Join APTA to get unlimited access to content.
Date: February 28, 2020 Contact: [email protected] Content Type: Resource
Coding & Billing
You Might Also Like...
Open Access
Sep 11, 2024
Access answers to the most frequently asked questions on ICD-10.
Access guidelines and information on how to identify the correct codes for ICD-10.
Apr 2, 2024
After helping create the CPT codes and advocate for their adoption, APTA launched an education campaign featuring a practice advisory.

COMMENTS
NIHSS 23 on presentation, consistent with large left MCA syndrome. Non-contrast head CT showed a dense L MCA (figure 1A) without early infarct changes, ASPECTS 10 (figure 1B). He received Alteplase IV r-tPA with a door-to-needle time of 27 minutes, 54 minutes from symptom onset.
C. Diff Sepsis - Case Study - C. difficile Sepsis Unfolding Reasoning Minnie Taylor, 62 years old - Studocu; Ncsbn Clinical Judgment Tool Blank; ... CVA case study - LPN Program. Course: Foundations of Clinical Nursing (KSPN-0104) 46 Documents. Students shared 46 documents in this course.
This case scenario presents a patient with acute ischemic cerebrovascular accident (CVA) requiring intravenous t-PA. Diagnosis was based on clinical neurologic symptoms and an NIHSS score of 7 and was later confirmed by neuroimaging.
Some case studies in Wuhan described immense inflammatory responses to COVID-19, including elevated acute phase reactants, such as CRP and D-dimer. Raised D-dimers are a non-specific marker of a prothrombotic state and have been associated with greater morbidity and mortality relating to stroke and other neurological features. 14.
SCENARIO 1: Suspected Ischemic Stroke without Large Vessel Occlusion. PREHOSPITAL. ACTORS: Patient: 68 y/o female. Husband: approximately same age. 911 Call Taker. Engine Company (3): Firefighter/EMT, Driver Engineer, Lieutenant. ALS Ambulance crew (2): paramedics. A sixty-eight year-old female patient has a sudden onset of left-sided weakness ...
CVA is a significant global health problem and a major cause of mortality and morbidity in developed countries. ... This case study shows improvement in tongue strength and swallowing function in ...
A stroke or cerebrovascular accident (CVA) is an acute compromise of the cerebral perfusion or vasculature. Approximately 85% of strokes are ischemic and rest are hemorrhagic.[1] In this discussion, we mainly confine to ischemic strokes. Over the past several decades, the incidence of stroke and mortality is decreasing.[2] Stroke is the leading cause of adult disability worldwide.
Current status and quality of radiomics studies for predicting outcome in acute ischemic stroke patients: a systematic review and meta-analysis, Frontiers in Neurology, 14, (2024). https://doi.org ...
Background & Purpose: Cerebrovascular Accident (CVA) is known as Stroke. It is a damage to the brain due to an interruption of blood supply. Two main types of stroke are ischemic stroke and hemorrhagic stroke. Ischemic stroke, the most common type of stroke, is due to a blocked artery and a hemorrhagic stroke is due to a leak or burst of a blood vessel. Signs and symptoms of stroke are ...
Rupture of the arteries leading to the brain during stroke results in the sudden death of brain cells owing to a lack of oxygen. Stroke can also lead to depression and dementia. Until the International Classification of Disease 11 (ICD-11) was released in 2018, stroke was classified as a disease of the blood vessels.
(CVA) , commonly known as a stroke, leaving 40% of stroke patients with moderate impairments and up to 30% with severe disabilities. 1 . ... This case study pertains to an individual in the sub-acute phase, 5 months post ischemic stroke. As most intensive therapies are started in the acute phase,
A cerebrovascular accident (CVA), an ischemic stroke or " brain attack," is a sudden loss of brain function resulting from a disruption of the blood supply to a part of the brain. Cerebrovascular accident or stroke is the primary cerebrovascular disorder in the United States. A cerebrovascular accident is a sudden loss of brain functioning ...
Abstract. Despite advances in acute management and prevention of cerebrovascular disease, stroke and vascular cognitive impairment together remain the world's leading cause of death and neurological disability. Hypertension and its consequences are associated with over 50% of ischemic and 70% of hemorrhagic strokes but despite good control of ...
The goal of the case is to have the learners appropriately assess the patient with an acute CVA in a timely manner, obtain the appropriate imaging studies, evaluate indications and contraindications for a patient who is a potential candidate for iv-TPA, manage significant hypertension, and discuss with the patient the risks and benefits of iv-TPA.
General Submissions: Presentations (Oral and Poster) Ischemic stroke: A case study. Rudolf Cymorr Kirby P. Martinez, PhD, MA, RN, CAA, LMT, CSTP, FRIN. Item Link - Use this link for citations and online mentions. This presents an analysis of a case of Ischemic stroke in terms of possible etiology, pathophysiology, drug analysis and nursing care.
Cerebral Vascular Accident (CVA) John Gates, 59 years old Primary Concept Perfusion Interrelated Concepts (In order of emphasis) 1. Stress 2. Coping 3. Clinical Judgment 4. Patient Education RAPID Reasoning Case Study: STUDENT Cerebral Vascular Accident (CVA) History of Present Problem:
Due to the multidimensional presentations (size/location of ICH, presence or absence of IVH, etc.) of those with hemorrhagic stroke, we presented this case study in order to pose that a single surgical approach may not be the answer to improving outcomes in comparison to medical management but actually a transition to a multimodal manner that ...
Case Study 64 Acute Cerebrovascular Accident (CVA) N., a 79-year-old woman, arrives at the emergency room with expressive aphasia, left facial droop, left- sided hemiparesis, and mild dysphagia. Her husband states that when she awoke that morning at 0600, she stayed in bed, complaining of a mild headache over the right temple and feeling ...
have selected a patient with CVA for my medical case study in critical care nursing [11]. The material is presented here to provide an overall frame work of nursing care for patient with cerebro vascular accident [12]. OBJECTIVES To perform a health assessment of the client with cerebro vascular accident.
CVA case study. cva case study. Course. Nursing Care of Adult I (NUR 390) 127 Documents. Students shared 127 documents in this course. University Concordia University Saint Paul. Academic year: 2023/2024. Uploaded by: Anonymous Student. This document has been uploaded by a student, just like you, who decided to remain anonymous.
Case Study: Outpatient CVA; ICD-10 Case Study: Outpatient PT-First Visit for CVA. Resource. Date: Friday, February 28, 2020 Case Study Details. Chief Complaint: Difficulty walking short distance and weakness in right arm. Log in or create a free account to keep reading. Join APTA ...