

Patient Case #1: 19-Year-Old Male With ADHD
Stephen Faraone, PhD, presents the case of a 19-year-old male with ADHD.

EP: 1 . Prevalence of Adult ADHD
Ep: 2 . diagnosis and management of adults adhd compared to children.
EP: 3 . Diagnosing Adults With ADHD Based on Patient Presentation

EP: 4 . Unmet Needs in the Treatment of Adult ADHD

EP: 5 . Efficacy and Safety of Treatment Options Utilized in Adult ADHD
Ep: 6 . future of adult adhd, ep: 7 . patient case #1: 19-year-old male with adhd.

EP: 8 . Patient Case #1: Prompting an ADHD Consultation
Ep: 9 . patient case #1: differentiating between adhd and other psychiatric comorbidities, ep: 10 . patient case #1: co-managing adhd, ep: 11 . patient case #1: dealing with treatment delay in adult adhd, ep: 12 . patient case #2: a 23-year-old patient with adhd, ep: 13 . patient case #2: impressions and challenges in adult adhd, ep: 14 . patient case #2: dealing with comorbidities in adult adhd, ep: 15 . patient case #2: addressing non-adherence and stigma of adult adhd, ep: 16 . patient case #2: importance of an integrative approach in adult adhd, ep: 17 . case 3: 24-year-old patient with adhd, ep: 18 . case 3: treatment goals in adult adhd, ep: 19 . case 3: factors driving treatment selection in adult adhd, ep: 20 . implications of pharmacogenetic testing in adhd, ep: 21 . novel drug delivery systems in adhd and take-home messages.
Stephen Faraone, PhD: That's a good one, yes, I'd like that, it's a very creative one, thank you, thank you. OK, let's move on to the case presentation. This first patient is a 19-year-old male, who presented to his psychiatrist after being referred by his primary care provider, PCP for ADHD consultation, during the interview, he noted he was a sophomore in college and is taking 17 credits. This semester chief complaint includes a lack of ability to focus in class as well as struggling with time management. He complained that every time he's in class, he finds himself thinking about many other responsibilities he must complete at home and feels that he cannot control it. He has had this complaint for the past 6 years, but refused to seek help, because he feared being put on medication. In high school, he was assigned a counselor who taught him behavior techniques such as making a schedule, and going on walks, which he found to be very effective. However, these techniques were less effective once he started college. His symptoms tend to get worse before exams, he often feels very anxious, leading to horrible performance on exams, he claimed that he has been this anxious since he took his LSAT tests. Currently, he is on academic probation, and is not allowed to be part of the Student Work Program, which was his only source of income. The patient has no history of substance abuse, no history of taking any medications for his symptoms, and no history of suicidal thoughts.
Transcript edited for clarity
The Cumulative Risks of ADHD

Treating ADHD in Children: Concerns, Controversies, Safety Measures

ADHD: Overlooked Cause of Persistent Anxiety and Depression in Adults

ADHD in Older Adults

Insights Into the New CDC Data on Adult ADHD
New CDC Data Highlights the Need for Guidelines on Adult ADHD
2 Commerce Drive Cranbury, NJ 08512
609-716-7777


- General Categories
- Mental Health
- IQ and Intelligence
- Bipolar Disorder

ADHD Case Study: Unveiling Real-Life Experiences and Treatment Approaches
Brace yourself for a journey through the kaleidoscopic world of ADHD, where case studies illuminate the vibrant, chaotic, and often misunderstood experiences of those living with this complex condition. Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder that affects millions of individuals worldwide, impacting their daily lives in profound and diverse ways. As we delve into the realm of ADHD case studies, we’ll uncover the intricate tapestry of symptoms, challenges, and triumphs that define the ADHD experience.
ADHD is characterized by persistent patterns of inattention, hyperactivity, and impulsivity that interfere with functioning and development. According to the Centers for Disease Control and Prevention (CDC), approximately 9.4% of children aged 2-17 years in the United States have been diagnosed with ADHD, with the prevalence in adults estimated to be around 4.4%. These statistics underscore the significant impact of ADHD on individuals, families, and society as a whole.
The value of case studies in understanding ADHD cannot be overstated. While statistical data and clinical definitions provide a framework for comprehending the disorder, it is through the lens of individual experiences that we truly grasp the nuanced reality of living with ADHD. Case studies offer a window into the personal struggles, adaptive strategies, and unique strengths of those navigating life with this condition. By examining these real-life narratives, we gain invaluable insights that inform treatment approaches, support systems, and ADHD research .
Understanding ADHD Through Case Studies
Case studies in ADHD research come in various forms, each offering a distinct perspective on the disorder. Some focus on longitudinal observations, tracking an individual’s journey from childhood through adulthood. Others provide snapshots of specific challenges or interventions at particular life stages. There are also comparative case studies that examine ADHD presentations across different demographics or in conjunction with comorbid conditions.
The benefits of analyzing real-life ADHD cases are manifold. Firstly, they humanize the disorder, moving beyond clinical descriptions to reveal the day-to-day realities of living with ADHD. This personal touch fosters empathy and understanding among healthcare providers, educators, and the general public. Secondly, case studies often uncover unique coping mechanisms and strategies developed by individuals with ADHD, which can inform and inspire others facing similar challenges.
Moreover, case studies contribute significantly to ADHD research and treatment by highlighting patterns, raising new questions, and sometimes challenging existing assumptions. They provide a rich source of qualitative data that complements quantitative research, offering a more holistic understanding of the disorder. This comprehensive approach is crucial in developing effective, personalized treatment plans and support systems for individuals with ADHD.
Case Study on ADHD: The Story of Sarah
To illustrate the power of case studies, let’s delve into the story of Sarah, a 28-year-old marketing professional whose journey with ADHD spans from childhood to her current career.
Background and Early Signs: Sarah’s parents first noticed her restlessness and difficulty focusing during preschool. She was constantly in motion, struggled to complete tasks, and often seemed to be “in her own world.” Despite being bright and creative, Sarah’s academic performance was inconsistent, and she frequently lost or forgot important items.
Challenges in School and Social Settings: As Sarah progressed through elementary and middle school, her ADHD symptoms became more pronounced. She struggled to organize her thoughts and materials, often turning in assignments late or incomplete. Socially, Sarah’s impulsivity and tendency to interrupt others made it difficult for her to maintain friendships. Her self-esteem suffered as she internalized the frustration of teachers and peers who misinterpreted her behavior as laziness or disrespect.
Diagnosis Process and Initial Treatment: At age 12, Sarah’s parents sought professional help. After a comprehensive evaluation involving interviews, behavioral assessments, and cognitive tests, Sarah was diagnosed with ADHD, predominantly inattentive type. The diagnosis was both a relief and a challenge for Sarah and her family. They embarked on a journey to understand the disorder and explore treatment options.
Initially, Sarah’s treatment plan included a combination of stimulant medication and behavioral therapy. The medication helped improve her focus and impulse control, while therapy sessions taught her strategies for organization, time management, and social skills. Sarah’s parents and teachers also received education on ADHD, enabling them to create a more supportive environment.
Long-term Management and Outcomes: As Sarah entered adulthood, she continued to refine her ADHD management strategies. She learned to leverage her creative strengths in her marketing career while implementing systems to compensate for her organizational challenges. Sarah’s journey exemplifies the ongoing nature of ADHD management and the potential for individuals with ADHD to lead fulfilling, successful lives.
ADHD Case Study Examples: Diverse Presentations
Sarah’s story is just one example of the myriad ways ADHD can manifest. Let’s explore three more case studies that highlight the diversity of ADHD presentations and the importance of tailored interventions.
Case 1: Adult ADHD in the Workplace John, a 35-year-old software engineer, was diagnosed with ADHD in his late twenties. Despite his technical brilliance, John struggled with project deadlines, time management, and interpersonal communication at work. His case study reveals the unique challenges of adult ADHD in professional settings and the effectiveness of workplace accommodations, such as flexible schedules and task management tools. John’s experience underscores the importance of mastering life with ADHD in professional contexts.
Case 2: ADHD in a Gifted Child Emma, a 9-year-old identified as intellectually gifted, exhibited classic ADHD symptoms that were initially masked by her high academic achievement. Her case study highlights the complexities of diagnosing and supporting twice-exceptional children. Emma’s journey emphasizes the need for nuanced approaches to ADHD and learning , balancing intellectual stimulation with strategies to address executive function deficits.
Case 3: ADHD with Comorbid Anxiety Disorder Michael, a 19-year-old college student, grapples with both ADHD and generalized anxiety disorder. His case study illustrates the challenges of managing co-occurring conditions and the importance of integrated treatment approaches. Michael’s experience sheds light on the interplay between ADHD symptoms and anxiety, informing strategies for addressing complex presentations of the disorder.
Comparing and contrasting these diverse ADHD presentations reveals the heterogeneity of the disorder and the necessity for individualized assessment and treatment plans. Each case offers unique insights into the varied manifestations of ADHD across different life stages, cognitive profiles, and comorbid conditions.
Analyzing Treatment Approaches in ADHD Case Studies
The case studies we’ve explored demonstrate the range of treatment approaches used in managing ADHD. Let’s examine these interventions in more detail:
Medication-based Interventions: Pharmacological treatments, particularly stimulant medications like methylphenidate and amphetamines, play a significant role in many ADHD management plans. Sarah’s case illustrates how medication can improve core symptoms of inattention and hyperactivity. However, as seen in Michael’s situation with comorbid anxiety, medication selection and dosing require careful consideration of individual factors and potential side effects.
Behavioral Therapy and Cognitive Strategies: Cognitive-behavioral therapy (CBT) and other psychosocial interventions are crucial components of comprehensive ADHD treatment. These approaches help individuals develop coping strategies, improve executive functioning, and address emotional regulation. In Emma’s case, cognitive strategies were particularly important in helping her harness her intellectual strengths while managing ADHD symptoms.
Educational Accommodations and Support: For children and adolescents with ADHD, school-based interventions are often essential. These may include individualized education plans (IEPs), classroom accommodations, and specialized tutoring. Emma’s case highlights the importance of tailoring educational approaches to meet the unique needs of gifted children with ADHD.
Holistic Approaches: Diet, Exercise, and Lifestyle Changes: Many case studies, including John’s, emphasize the role of lifestyle factors in ADHD management. Regular exercise, balanced nutrition, adequate sleep, and mindfulness practices can significantly impact ADHD symptoms and overall well-being. These holistic approaches often complement traditional treatments and empower individuals to take an active role in managing their condition.
The effectiveness of these treatment approaches varies among individuals, underscoring the importance of personalized care plans. ADHD clinical trials continue to explore new interventions and refine existing ones, contributing to the evolving landscape of ADHD treatment options.
Lessons Learned from ADHD Case Studies
The wealth of information gleaned from ADHD case studies offers valuable insights for healthcare professionals, educators, and individuals affected by the disorder:
Key Insights for Healthcare Professionals: Case studies underscore the importance of comprehensive assessment and individualized treatment planning. They highlight the need for ongoing monitoring and adjustment of interventions, as ADHD presentations can evolve over time. Healthcare providers are reminded of the significance of considering comorbid conditions and life circumstances when developing treatment strategies.
Implications for Educators and Parents: The diverse presentations of ADHD illustrated in case studies emphasize the need for flexible and supportive educational environments. Educators and parents can learn from these narratives to better understand the challenges faced by individuals with ADHD and implement effective support strategies. The success stories within these case studies also serve as powerful motivators, showcasing the potential for individuals with ADHD to thrive with appropriate support.
Importance of Personalized Treatment Plans: Perhaps the most crucial lesson from ADHD case studies is the necessity of tailored interventions. What works for one individual may not be effective for another, highlighting the need for a patient-centered approach to ADHD management. This personalization extends beyond medication to encompass behavioral strategies, environmental modifications, and lifestyle adjustments.
Future Directions in ADHD Research: Case studies often uncover areas requiring further investigation, driving new research questions and methodologies. They can reveal emerging trends, such as the increasing recognition of adult ADHD, and inform the development of novel treatment approaches. The rich, qualitative data provided by case studies complement quantitative research, offering a more nuanced understanding of ADHD’s impact on daily life.
As we conclude our exploration of ADHD case studies, we’re reminded of the profound value these narratives bring to our understanding of the disorder. They offer a vivid portrayal of the challenges, triumphs, and everyday realities of living with ADHD, moving beyond clinical definitions to capture the human experience of the condition.
The case studies we’ve examined underscore the critical importance of individualized approaches to ADHD management. From Sarah’s journey through childhood and into a successful career, to John’s workplace adaptations, Emma’s twice-exceptional experience, and Michael’s complex presentation with comorbid anxiety, each story highlights the unique constellation of symptoms, strengths, and needs that characterize ADHD.
These personal accounts serve as powerful tools for raising awareness and fostering empathy. They challenge stereotypes and misconceptions about ADHD, revealing the diverse ways in which the disorder manifests across different individuals and life stages. Moreover, they offer hope and inspiration, showcasing the potential for individuals with ADHD to lead fulfilling, successful lives with appropriate support and interventions.
As we move forward, it’s crucial to continue sharing and learning from ADHD stories . These narratives not only inform clinical practice and research but also empower individuals with ADHD and their support networks. They remind us that behind every diagnosis is a unique individual with their own story, challenges, and potential.
Let us carry forward the insights gained from these case studies to create more inclusive, understanding, and supportive environments for individuals with ADHD. By doing so, we can contribute to a world where ADHD is not seen as a limitation, but as a different way of experiencing and interacting with the world—one that comes with its own set of challenges and remarkable strengths.
As we continue to unravel the complexities of ADHD through research, clinical practice, and personal narratives, let us remain committed to supporting, empowering, and celebrating the diverse experiences of individuals living with this fascinating and challenging condition. After all, it is through understanding and embracing these differences that we can truly appreciate the rich tapestry of human neurodiversity.
References:
1. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
2. Barkley, R. A. (2015). Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment (4th ed.). New York: Guilford Press.
3. Faraone, S. V., Biederman, J., & Mick, E. (2006). The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychological Medicine, 36(2), 159-165.
4. Kessler, R. C., Adler, L., Barkley, R., Biederman, J., Conners, C. K., Demler, O., … & Zaslavsky, A. M. (2006). The prevalence and correlates of adult ADHD in the United States: results from the National Comorbidity Survey Replication. American Journal of Psychiatry, 163(4), 716-723.
5. National Institute for Health and Care Excellence. (2018). Attention deficit hyperactivity disorder: diagnosis and management. NICE guideline [NG87]. https://www.nice.org.uk/guidance/ng87
6. Sibley, M. H., Swanson, J. M., Arnold, L. E., Hechtman, L. T., Owens, E. B., Stehli, A., … & Jensen, P. S. (2017). Defining ADHD symptom persistence in adulthood: optimizing sensitivity and specificity. Journal of Child Psychology and Psychiatry, 58(6), 655-662.
7. Thapar, A., Cooper, M., & Rutter, M. (2017). Neurodevelopmental disorders. The Lancet Psychiatry, 4(4), 339-346.
8. Wilens, T. E., & Spencer, T. J. (2010). Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgraduate Medicine, 122(5), 97-109.
Was this article helpful?
Would you like to add any comments (optional), leave a reply cancel reply.
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Post Comment
Related Resources

Understanding ADHD Screening: ICD-10 Code Z13.30 and Its Implications

The High Cost of ADHD Testing: Understanding Why It’s So…

The Rise of ADHD: Understanding the Surge in Diagnoses and…

Why Do I Need a Blood Test for ADHD? Understanding…

Who Diagnoses ADHD: A Comprehensive Guide to Seeking Professional Help

Who Can Diagnose ADHD: A Comprehensive Guide to Getting the…

Understanding ADHD Diagnosis: Separating Fact from Fiction

Where is ADHD in the DSM-5? A Comprehensive Guide to…

When Can ADHD Be Diagnosed? A Comprehensive Guide for Parents

What Does an ADHD Test Look Like for Adults? A…
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Case Report: Treatment of a Comorbid Attention Deficit Hyperactivity Disorder and Obsessive–Compulsive Disorder With Psychostimulants
Ezgi dogan-sander, maria strauß.
- Author information
- Article notes
- Copyright and License information
Edited by: Mirko Manchia, University of Cagliari, Italy
Reviewed by: Pavel Golubchik, Geha Mental Health Center, Israel; Stefania Schiavone, University of Foggia, Italy
*Correspondence: Ezgi Dogan-Sander [email protected]
This article was submitted to Psychopharmacology, a section of the journal Frontiers in Psychiatry
Received 2021 Jan 5; Accepted 2021 Mar 29; Collection date 2021.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Introduction: Attention deficit hyperactivity disorder (ADHD) is a common disease in childhood and adolescence. In about 60% of pediatric patients, the symptoms persist into adulthood. Treatment guidelines for adult ADHD patients suggest multimodal therapy consisting of psychostimulants and psychotherapy. Many adult ADHD patients also suffer from psychiatric comorbidities, among others obsessive–compulsive disorder (OCD). The treatment of the comorbidity of ADHD and OCD remains challenging as the literature is sparse. Moreover, the impact of psychostimulants on obsessive–compulsive symptoms is still unclear.
Case Presentation: Here, we report on a 33-year-old patient with an OCD who was unable to achieve sufficient remission under long-term guideline-based treatment for OCD. The re-examination of the psychological symptoms revealed the presence of adult ADHD as a comorbid disorder. The patient has already been treated with paroxetine and quetiapine for the OCD. Due to the newly established diagnosis of ADHD, extended-release methylphenidate (ER MPH) was administered in addition to a serotonin reuptake inhibitor. After a dose of 30 mg ER MPH, the patient reported an improvement in both the ADHD and the obsessive–compulsive symptoms. After discharge, the patient reduced ER MPH without consultation with a physician due to subjectively described side effects. The discontinuation of medication led to a renewed increase in ADHD and obsessive–compulsive symptoms. The readjustment to ER MPH in combination with sertraline and quetiapine thereafter led to a significant improvement in the compulsive symptoms again.
Conclusion: The present case shows that in ADHD and comorbid obsessive–compulsive disorder, treatment with psychostimulants can improve the obsessive–compulsive symptoms in addition to the ADHD-specific symptoms. To our knowledge, this is only the second case report describing a treatment with ER MPH for an adult patient with OCD and ADHD comorbidity in the literature. Further research, especially randomized controlled trials, is needed to standardize treatment options.
Keywords: ADHD, OCD, comorbidity, psychostimulant, methylphenidate, case report
Introduction
Attention deficit hyperactivity disorder (ADHD) is a frequent mental disorder with childhood onset and a worldwide prevalence of at least 2.8% ( 1 ). It is characterized by the three core symptoms of attention deficit, hyperactivity, and impulsivity manifesting since childhood ( 2 ). Adult ADHD is also commonly associated with different comorbidities ( 3 , 4 ), particularly obsessive–compulsive disorder (OCD). The prevalence of OCD comorbidity in patients with ADHD varies widely in the literature, ranging from 1 to 13% ( 5 ). On the other hand, ADHD prevalence in patients with OCD has been reported as ranging from 0 to 23% ( 5 ). The high co-occurrence of these disorders has raised questions about their diagnoses, neurobiology, and treatment.
It has been discussed that the ADHD-like symptoms in OCD, for example inattention, may have contributed to the inconsistency of the reported co-occurrence rates. Furthermore, familial link between OCD and ADHD, disturbances in attention, and executive function and the high comorbidity of tic disorders are common features of these two disorders ( 6 – 9 ).
On the other hand, these disorders have reverse fronto-striatal abnormalities ( 5 ). OCD patients exhibit increased fronto-striatal activity and functional connectivity ( 5 ). In contrast, ADHD is found to be associated with hypoactivity in the prefrontal and striatal brain regions and a reduced fronto-striatal activity ( 5 ). Despite these differences, a shared dysfunction in the medio-fronto-striato-limbic brain region was reported in addition to disorder-specific dysfunctions ( 10 ).
Psychostimulants such as methylphenidate are regarded as the first-line treatment for ADHD. They increase prefrontal activation and improve both clinical symptomology and neurocognitive functioning in ADHD by modulating dopamine reuptake. Guidelines for the treatment of OCD recommend serotonin reuptake inhibitors as first-line pharmacotherapy, which are thought to modulate fronto-striatal hyperactivity. In the case of partial response to serotonin reuptake inhibitors, an augmentation therapy with antipsychotics has also been shown to have a useful effect ( 11 ).
Although the pharmacotherapy of each of these disorders has been well-established, the effective treatment and management of patients with comorbid ADHD and OCD remains challenging. While stimulant medication is recommended as the first-line treatment for ADHD, findings suggest that its use in OCD may exacerbate the OCD symptoms. To our knowledge, there have been only a few studies, mostly case reports and case studies, reporting on the pharmacotherapy of this comorbidity. Some of these reports have shown that the use of stimulants may cause obsessive–compulsive symptoms as side effects ( 12 – 14 ), while others have reported a decline of OCD symptoms under stimulant therapy ( 15 , 16 ).
In this report, we present a case of an adult patient with comorbid ADHD and OCD treated successfully with stimulants and serotonin reuptake inhibitors.

Case Presentation
In November 2017, a 33-year-old patient presented at our ADHD outpatient clinic in the Department of Psychiatry and Psychotherapy at the University Hospital of Leipzig for diagnostic clarification. During a previous psychiatric examination organized by the federal employment agency, a tentative ADHD diagnosis was made for the first time. The patient reported impulsiveness and physical restlessness that had persisted since childhood. He stated that he could hardly sit still or stay in one place for a longer period of time. He also described a lack of concentration and problems sustaining attention in given tasks (see Table 1 for the summary of clinical manifestations). In order to relax physically, he started practicing martial arts and has been doing a lot of gardening lately.
Summary of the clinical manifestations of ADHD and OCD.
ADHD, attention deficit hyperactivity disorder; OCD, obsessive–compulsive disorder .
A mental status examination was conducted according to the AMDP System ( 17 ). The patient was oriented with regard to time, place, person, and situation. He was friendly and cooperative in personal contact. In motor activity, he demonstrated restlessness (fidgeting with the legs, playing with the fingers, and partly increased body tension). He described his mood as slightly dysphoric; his affect was broad. He showed no evidence of delusions, hallucinations, or ideas of reference, but he had poor impulse control, attention deficits with quick distractibility, as well as concentration and short-term memory problems. The thought process was lightly circumstantial, but apart from that without a pathological finding. He did not display any sleep or eating disorders. Any kind of suicidal ideations were denied. The patient demonstrated insight into his mental disorder and was motivated for therapy. These aspects were also confirmed by a senior psychiatrist.
In further exploration, the patient stated that he had been suffering from an OCD since about the age of 10. At that time, a classmate had had an eye tumor, and in this context, he had first developed a washing compulsion for which a first presentation to a psychiatrist had taken place. Later on, he showed compulsive behavior in the form of compulsive counting and ritualized touching things and obsessive thoughts (fear of aliens and the special meaning of the color “blue”). These obsessions began after he watched a film about aliens as a teenager, which frightened him enormously although he does not believe in aliens. Overall, obsessive and compulsive symptoms have been affecting his life in many ways, but especially his work life, disrupting his functionality. He had been treated as an inpatient and outpatient several times, yet the OCD symptoms would still occupy 3–4 h per day (see Table 1 ). In addition, ambulatory psychotherapy (anamnestically cognitive behavioral therapy) had only helped him to a limited extent. However, the existing concentration problems were described as independent of obsessive–compulsive disorder. The current medication at the first visit consisted of paroxetine 30 mg/day and quetiapine 100 mg/day.
The patient also reported that, in the past, he had been drinking a lot of alcohol to compensate for his compulsions and impulsiveness. However, alcohol had disinhibited him in parts even more, and it had come to physical confrontations several times. He had lost control in situations in which he felt provoked. In the past, criminal proceedings had also been brought against him in this context. In the course of time, he developed an alcohol addiction. At the time of the first visit to our outpatient clinic, he had been completely abstinent from alcohol for 6 years. Drug consumption was also negated, which could also be confirmed by a toxicological screen at the inpatient admission.
The following information was gathered on the past psychiatric history: a first inpatient treatment because of the OCD (ICD-10: F42.2) took place in 2006. During that time, a suspected diagnosis of paranoid schizophrenia (ICD-10: F20.0) was made and treatment with risperidone 1.5 mg/day, olanzapine 10 mg/day, and lorazepam 1 mg/day was started. Risperidone was discontinued due to akathisia, and the patient was then treated with olanzapine 10 mg/day and paroxetine 20 mg/day. In 2008, the patient was treated in a day clinic for 1.5 months, where an OCD (ICD-10: F42.2) and an immature personality accentuation were diagnosed. During this treatment, the dose of sulpride was increased from 200 to 400 mg/day, which was prescribed during the outpatient treatment. Subsequently, sulpride was switched to paroxetine 60 mg/day. In 2009, the patient was hospitalized again due to worsening of the OCD symptoms. In 2012, an alcohol withdrawal treatment was completed. The discharge medication consisted of paroxetine 60 mg/day and olanzapine 10 mg/day. The diagnoses then consisted of alcohol dependence (ICD-10: F10.2), alcohol withdrawal syndrome (ICD-10: F10.3), OCD (ICD-10: F42.2), personality accentuation (ICD-10: F60.9), and an unspecified form of schizophrenia (ICD-10: F20.8). In 2013, another alcohol withdrawal treatment due to a relapse followed. Since then, he has been abstinent of alcohol according to his own statement. Discharge medication consisted of paroxetine 60 mg/day and promethazine 25 mg as needed. Since 2015, the patient has been undergoing an outpatient behavioral therapy treatment, without achieving complete remission of the OCD so far.
While there were no relevant diseases in the medical anamnesis, the family history revealed that his mother had been diagnosed with schizophrenia and his father had a history of alcohol addiction.
After the initial presentation in our outpatient clinic (December 2017), detailed diagnostic tests were performed, including the Diagnostic Interview for ADHD in adults (DIVA) and ADHD-specific questionnaires [Conners Adult ADHD Rating Scales (CAARS)—Self-Report: Long Version ( 18 ), Wender Utah Rating Scale (WURS), and Adult ADHD—Self-Report Scale (ADHD-SB)] as well as other questionnaires (e.g., Personality Styles and Disorder Inventory). The subjective assessment of ADHD-relevant symptoms was clearly significant in terms of inattention and hyperactivity, as well as temperament, affective instability, emotional overreaction, and impulsiveness. The CAARS revealed an ADHD index in percentile rank of 88, a DSM-IV Inattentive symptom scale in percentile rank of 98, a DSM-IV Hyperactive–Impulsive scale in percentile rank of 86, and a DSM-IV ADHD Symptoms Total in percentile rank of 96 (see Table 2 ). Available school reports were also reviewed: in primary school reports, the patient was described as an eager and endeavored student, who was partly distracted and showed fluctuations in cooperation with other students. A somewhat unfriendly behavior toward classmates was also reported. These descriptions were in accordance with the self-report of the patient and indicate the presence of ADHD in childhood. The available findings as well as the biographical and current anamnesis strongly suggested the diagnosis of ADHD in adulthood.
The patient's scores on CAARS (in percentile rank) and Y-BOCS.
ADHD, attention deficit hyperactivity disorder; ER MPH, extended-release methylphenidate; CAARS, Conners adult ADHD rating scales; DSM-I, DSM-IV inattentive symptoms; DSM-Hy/I, DSM-IV hyperactive–impulsive symptoms; DSM-Total, DSM-IV ADHD symptoms total; Y-BOCS, yale–brown obsessive compulsive scale .
Due to the complex comorbidity of psychiatric illnesses, the patient was admitted to our inpatient unit in January 2018 for medication adjustment. At that time, the Yale–Brown Obsessive Compulsive Scale (Y-BOCS) ( 19 ) was performed to assess the severity of the OCD symptoms. Concerning the last 7 days, the patient affirmed seven out of 37 typical obsessive thoughts and seven of 21 typical compulsive behaviors. In the severity rating, the patient reached a total score of 18 points, of which eight points were scored in the obsessive thoughts scale and 10 points were on the compulsive behavior scale. The laboratory tests showed a mild folic acid deficiency, which was substituted accordingly. Electrocardiography, electroencephalography, as well as magnetic resonance imaging of the brain showed no abnormal findings.
In accordance with existing literature, we switched the medication from paroxetine 30 mg to sertraline 50 mg/day because of the lack of therapy response to paroxetine treatment for many years ( 20 , 21 ). A psychostimulant treatment with extended-release methylphenidate (ER MPH) was initiated. ER MPH was gradually dosed up to 30 mg/day. Under this medication, not only the ADHD symptoms but also his OCD symptoms improved, so that sertraline could subsequently be reduced to 25 mg/day. At this time, the patient stated that his OCD had almost completely disappeared and that the time he spent with obsessive thoughts and compulsive actions had decreased severely. Furthermore, he felt more balanced and reported that he did not get into conflicts so quickly anymore. As the restlessness decreased, quetiapine could also be reduced and eventually stopped.
One day before discharge (after 42 days on board), Y-BOCS and CAARS were applied again. The patient reported observing one out of 37 typical obsessive thoughts and one of 21 typical compulsive behaviors in the last 7 days. In the severity rating, the patient reached a total score of seven points (five points for obsessive thoughts and two points for compulsive behavior). The CAARS resulted in an ADHD index in percentile rank of 5, a DSM-IV Inattentive symptom scale in percentile rank of 10, a DSM-IV Hyperactive–Impulsive symptom scale in percentile rank of 14, and a DSM-IV ADHD Symptoms Total in percentile rank of 10 (see Table 2 ). The medication at discharge consisted of ER MPH 30 mg/day and sertraline 25 mg/day.
After discharge, the patient attended our ADHD outpatient clinic for regular follow-ups. On his first visit (1 day after the discharge), he reported a good response to the medical therapy with ER MPH and assured that he did not notice any side effects. He expressed the wish to increase the sertraline dose from 25 to 37.5 mg/day. In the following visit after 26 days, the patient reported unspecific anxiety and panic attacks and claimed to have reduced ER MPH to 10 mg on his own responsibility after having read the package leaflet and worrying about potential side effects. Thus, the remaining medication consisted of sertraline 50 mg/day and quetiapine 25 mg/day, which he started again without a consultation with our outpatient clinic.
In March 2018, a month later after the discharge, a second inpatient admission was initiated after an emergency contact of the patient with the ward. He described an increase in obsessive–compulsive symptoms and restlessness and reported that he suffered from panic attacks and sleep disorders and that he lost his appetite. The patient observed severe mood swings and distrust toward other people. The medication at administration consisted of ER MPH 10 mg/day, sertraline 37.5 mg/day, and quetiapine 25 mg as needed. However, he reported that he did not want to continue to take ER MPH. Therefore, therapy with atomoxetine was started as ER MPH was discontinued. Due to the worsened symptomatology, the sertraline dose was increased to 150 mg/day and quetiapine was dosed up to 125 mg/day. However, the OCD symptoms worsened further after the discontinuation of ER MPH despite increasing the doses of sertraline and quetiapine. After weighing up the symptoms before and after treatment with ER MPH, we decided together with the patient to restart the treatment with ER MPH. Physical well-being and a reduction of the OCD and ADHD symptoms were described after switching the medication from atomoxetine to ER MPH. On the first day of the switch, we performed Y-BOCS and CAARS again. For the last 7 days, the patient reported observing four of 37 typical obsessive thoughts and four of 21 typical compulsive behaviors. In the severity rating, the patient reached a total score of 20 points, of which 11 points were on the scale of obsessive thoughts and nine points were on the scale of compulsive behavior. The CAARS showed an ADHD Index in percentile rank of 76, a DSM-IV Inattentive symptom scale in percentile rank of 54, a DSM-IV Hyperactive–Impulsive scale in percentile rank of 82, and a DSM-IV ADHD Symptoms Total in percentile rank of 69 (see Table 2 ).
An improvement of compulsive thoughts and joyfulness was observed when sertraline was added. The patient was discharged in April 2018 (after 27 days on board) into outpatient care at the ADHS outpatient clinic. Five days after discharge, CAARS and Y-BOCS were performed again: the patient reported observing two of 37 typical obsessive thoughts and four of 21 typical compulsive behaviors within the last 7 days. In the severity rating, the patient reached a total score of 18 points, of which 10 points were on the scale of obsessive thoughts and 8 points were on the scale of compulsive behavior. The CAARS revealed an ADHD Index in percentile rank of 42, a DSM-IV Inattentive symptom scale in percentile rank of 38, a DSM-IV Hyperactive–Impulsive scale in percentile rank of 35, and a DSM-IV ADHD Symptoms Total in percentile rank of 35 (see Table 2 ). Discharge medication consisted of ER MPH 10 mg/day, quetiapine 125 mg/day, and sertraline 200 mg per/day. A timeline of this case presentation is shown in Figure 1 .
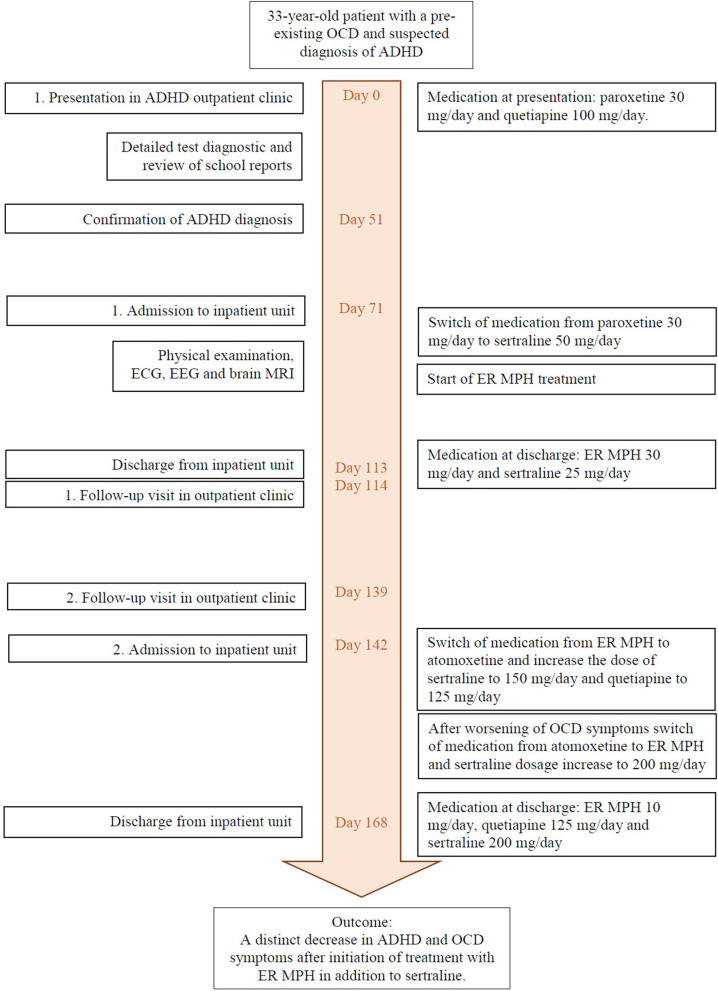
Timeline of events and medication.
Discussion and Conclusions
In this case report, we present a case of successful treatment with psychostimulants in an adult patient with ADHD and comorbid OCD. Due to the late diagnosis of ADHD (in addition to an apparent misdiagnosis of schizophrenia and personality disorder), no effective treatment was initiated in his early life, resulting in an impacted quality of life up to now. After diagnosing ADHD, we treated the patient with ER MPH in addition to antidepressants for OCD treatment and observed that the adjunctive use of ER MPH resulted in enhanced treatment response. Contrary to reports in the literature, treatment with a stimulant did not cause a worsening of the OCD symptoms. Rather, the patient reported a severe decrease in OCD symptoms, which was also observable by the treatment team. A second administration was necessary due to a worsening of the OCD and ADHD symptoms occurring after the patient had reduced the dose of ER MPH on his own, because he was worried about side effects, which he had never actually experienced during the inpatient treatment. This case highlights the importance of frequent reassessment of comorbid conditions in the case of low treatment response to serotonin reuptake inhibitors and psychotherapy in patients with OCD. Untreated ADHD as a comorbid condition to OCD may reduce the treatment response on the OCD, as shown in previous studies ( 22 ).
Recognizing ADHD and OCD comorbidity is important for the clinical course of these disorders considering that the onset of OCD is significantly higher in adults with childhood ADHD symptoms and that the comorbidity is associated with more severe OCD symptoms and their persistence ( 23 , 24 ). Despite the increasing awareness and interest in ADHD, many affected adults are still underdiagnosed and untreated ( 25 ). The overlap of ADHD symptoms with several other psychiatric disorders, including mood disorders, substance abuse, and anxiety, and the high incidence of comorbid psychiatric conditions are probable reasons for the high number of missed ADHD diagnoses in adults ( 1 , 4 ).
On the basis of neuroimaging findings, structural and functional abnormalities in ADHD and OCD have been reported ( 26 ). A shared dysfunction in the mesial frontal cortex has been shown in patients with ADHD and OCD. On the other hand, disorder-specific dysfunctions were found in the caudate, cingulate, and parietal brain regions in patients with ADHD and in the lateral prefrontal cortex in OCD patients ( 27 ). Furthermore, fronto-striatal hypoactivity was observed in ADHD, whereas OCD shows fronto-striatal hyperactivity, which is also associated positively with symptom severity ( 10 ). Regarding structural abnormalities, a recent meta-analysis reported that patients with OCD have larger insular–striatal regions, whereas patients with ADHS have smaller ventrolateral prefrontal/insular–striatal regions ( 28 ). Nonetheless, apart from these disorder-specific abnormalities, both disorders show a similar neuropsychological impairment in executive functions.
Despite the high prevalence of OCD and ADHD comorbidity, only a few reports on the treatment of this comorbidity exist. Most of these studies were performed in child and adolescent populations, and as far as we know, only one was conducted in an adult population ( 14 ). Some of the case reports described obsessive–compulsive symptoms as a side effect of MPH treatment in patients with ADHD ( 12 – 14 , 29 – 32 ). However, a few studies also described a decrease of the obsessive–compulsive symptoms with MPH treatment ( 15 , 16 ). The latter results are in line with our findings. Still, there are no longitudinal and clinical controlled trials investigating the effect of MPH on the treatment of ADHD and OCD comorbidity. Although this case presentation is the first published report of a positive effect of ER MPH for the treatment of ADHD and OCD comorbidity in an adult patient, it also has certain limitations. This case report describes only one patient and a psychostimulant treatment with ER MPH in addition to the therapy with sertraline and quetiapine instead of a monotherapy. Also, it cannot be determined whether the patient took his medication regularly as prescribed after the first discharge.
The present case report highlights that treatment with psychostimulants in addition to a serotonin reuptake inhibitor can improve the obsessive–compulsive symptoms as well as the ADHD-specific symptoms in patients with ADHD and OCD comorbidity. Still, the treatment of this comorbidity remains challenging. Underdetection, misdiagnosis, as well as delay in the diagnosis of this comorbidity may cause a reduction in quality of life and low treatment response. Treating both disorders concurrently may help to decrease the symptom severity of both conditions. Monitoring the progress may also support the treatment process, allowing improvement of the treatment compliance as well as observing side effects. Yet, longitudinal and clinical controlled trials are needed to gain more information about the treatment of this comorbidity and to observe the treatment response longitudinally.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: identifying/confidential patient data cannot be shared. Requests to access the data should be directed to the corresponding author.
Ethics Statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
ED-S and MS were the main authors of the manuscript. ED-S performed the literature research on the comorbidity of ADHD and OCD. Both authors participated substantially in the writing and editing of the final manuscript.
Conflict of Interest
MS has received speaker fees from Lilly, Medice Arzneimitte Pütter GmbH & Co. KG and Servier and was an advisory board member for Shire/Takeda. The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We acknowledge support from the German Research Foundation (DFG) and Leipzig University within the program of Open Access Publishing. We thank Tina Stibbe for her English editing.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.649833/full#supplementary-material
- 1. Fayyad J, Sampson NA, Hwang I, Adamowski T, Aguilar-Gaxiola S, Al-Hamzawi A, et al. The descriptive epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. Atten Defic Hyperact Disord. (2017) 9:47–65. 10.1007/s12402-016-0208-3 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association: Arlington, VA: (2013). [ Google Scholar ]
- 3. Katzman MA, Bilkey TS, Chokka PR, Fallu A, Klassen LJ. Adult ADHD and comorbid disorders: clinical implications of a dimensional approach. BMC Psychiatry. (2017) 17:302. 10.1186/s12888-017-1463-3 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Sobanski E. Psychiatric comorbidity in adults with attention-deficit/hyperactivity disorder (ADHD). Eur Arch Psychiatry Clin Neurosci. (2006) 256(Suppl 1):i26–31. 10.1007/s00406-006-1004-4 [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Abramovitch A, Dar R, Mittelman A, Wilhelm S. Comorbidity between attention deficit/hyperactivity disorder and obsessive-compulsive disorder across the lifespan: a systematic and critical review. Harv Rev Psychiatry. (2015) 23:245–62. 10.1097/HRP.0000000000000050 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J. Further evidence for co-segregation between pediatric obsessive compulsive disorder and attention deficit hyperactivity disorder: a familial risk analysis. Biol Psychiatry. (2007) 61:1388–94. 10.1016/j.biopsych.2006.09.026 [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J. Examining the relationship between obsessive-compulsive disorder and attention-deficit/hyperactivity disorder in children and adolescents: a familial risk analysis. Biol Psychiatry. (2007) 61:316–21. 10.1016/j.biopsych.2006.03.083 [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. de Geus F, Denys DA, Sitskoorn MM, Westenberg HG. Attention and cognition in patients with obsessive-compulsive disorder. Psychiatry Clin Neurosci. (2007) 61:45–53. 10.1111/j.1440-1819.2007.01609.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Çelebi F, Koyuncu A, Ertekin E, Alyanak B, Tükel R. The features of comorbidity of childhood ADHD in patients with obsessive compulsive disorder. J Atten Disord. (2020) 24:973–80. 10.1177/1087054716669228 [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Cabarkapa S, King JA, Dowling N, Ng CH. Co-morbid obsessive-compulsive disorder and attention deficit hyperactivity disorder: neurobiological commonalities and treatment implications. Front Psychiatry. (2019) 10:557. 10.3389/fpsyt.2019.00557 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Keuneman RJ, Pokos V, Weerasundera R, Castle DJ. Antipsychotic treatment in obsessive-compulsive disorder: a literature review. Aust N Z J Psychiatry. (2005) 39:336–43. 10.1080/j.1440-1614.2005.01591.x [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Jhanda S, Singla N, Grover S. Methylphenidate-induced obsessive-compulsive symptoms: a case report and review of literature. J Pediatr Neurosci. (2016) 11:316–8. 10.4103/1817-1745.199461 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 13. Kouris S. Methylphenidate-induced obsessive-compulsiveness. J Am Acad Child Adolesc Psychiatry. (1998) 37:135. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Serby M. Methylphenidate-induced obsessive-compulsive symptoms in an elderly man. CNS Spectr. (2003) 8:612–3. 10.1017/s1092852900018885 [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. King J, Dowling N, Leow F. Methylphenidate in the treatment of an adolescent female with obsessive-compulsive disorder and attention deficit hyperactivity disorder: a case report. Aust Psychiatry. (2017) 25:178–80. 10.1177/1039856216671664 [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Gürkan K, Bilgiç A, Türkoglu S, Kiliç BG, Aysev A, Uslu R. Depression, anxiety and obsessive-compulsive symptoms and quality of life in children with attention-deficit hyperactivity disorder (ADHD) during three-month methylphenidate treatment. J Psychopharmacol. (2010) 24:1810–8. 10.1177/0269881109348172 [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Broome MR, Bottlender R, Rösler M, Stieglitz R. editors. The AMDP System: Manual for Assesment and Documentation of Psychopathology in Psychiatry. Göttingen: Hogrefe Publishing; (2017). [ Google Scholar ]
- 18. Conners CK, Erhardt D, Sparrow EP. Conners' Adult ADHD Rating Scales (CAARS): Technical Manual. North Tonawanda, NY: Multi-Health Systems; (1999). [ Google Scholar ]
- 19. Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RN, Hill CL, et al. The Yale-brown obsessive compulsive scale: I. Development, use, and reliability. Arch Gen Psychiatry. (1989) 46:1006–11. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Koran LM, Hanna GL, Hollander E, Nestadt G, Simpson HB. Practice guideline for the treatment of patients with obsessive-compulsive disorder. Am J Psychiatry. (2007) 164:5–53. [ PubMed ] [ Google Scholar ]
- 21. Abudy A, Juven-Wetzler A, Zohar J. Pharmacological management of treatment-resistant obsessive-compulsive disorder. CNS Drugs. (2011) 25:585–96. 10.2165/11587860-000000000-00000 [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Geller DA, Biederman J, Faraone SV, Cradock K, Hagermoser L, Zaman N, et al. Attention-deficit/hyperactivity disorder in children and adolescents with obsessive-compulsive disorder: fact or artifact? J Am Acad Child Adolesc Psychiatry. (2002) 41:52–8. 10.1097/00004583-200201000-00011 [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Tan O, Metin B, Metin S. Obsessive-compulsive adults with and without childhood ADHD symptoms. Atten Defic Hyperact Disord. (2016) 8:131–8. 10.1007/s12402-016-0196-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Walitza S, Zellmann H, Irblich B, Lange KW, Tucha O, Hemminger U, et al. Children and adolescents with obsessive-compulsive disorder and comorbid attention-deficit/hyperactivity disorder: preliminary results of a prospective follow-up study. J Neural Transm. (2008) 115:187–90. 10.1007/s00702-007-0841-2 [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Asherson P, Buitelaar J, Faraone SV, Rohde LA. Adult attention-deficit hyperactivity disorder: key conceptual issues. Lancet Psychiatry. (2016) 3:568–78. 10.1016/S2215-0366(16)30032-3 [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Brem S, Grünblatt E, Drechsler R, Riederer P, Walitza S. The neurobiological link between OCD and ADHD. ADHD Atten Def Hyp Disord. (2014) 6:175–202. 10.1007/s12402-014-0146-x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 27. Rubia K, Cubillo A, Woolley J, Brammer MJ, Smith A. Disorder-specific dysfunctions in patients with attention-deficit/hyperactivity disorder compared to patients with obsessive-compulsive disorder during interference inhibition and attention allocation. Hum Brain Mapp. (2011) 32:601–11. 10.1002/hbm.21048 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Norman LJ, Carlisi C, Lukito S, Hart H, Mataix-Cols D, Radua J, et al. Structural and functional brain abnormalities in attention-deficit/hyperactivity disorder and obsessive–compulsive disorder: a comparative meta-analysis. JAMA Psychiatry. (2016) 73:815–25. 10.1001/jamapsychiatry.2016.0700 [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Kotsopoulos S, Spivak M. Obsessive-compulsive symptoms secondary to methylphenidate treatment. Can J Psychiatry. (2001) 46:89. [ PubMed ] [ Google Scholar ]
- 30. Guegant G, Crochette A. Méthylphénidate, tics et compulsions. Encephale. (2000) 26:45–7. [ PubMed ] [ Google Scholar ]
- 31. Vishwaraj S. Methylphenidate-induced obsessive compulsive disorder in attention deficit hyperactivity disorder. J Med Sci. (2016) 2:21–2. 10.5005/jp-journals-10045-0028 [ DOI ] [ Google Scholar ]
- 32. Coskun M. Methylphenidate induced obsessive-compulsive symptoms treated with sertraline. Klinik Psikofarmakoloji Bulteni. (2011) 21:275. 10.5455/bcp.20110904061403 [ DOI ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
- View on publisher site
- PDF (860.0 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions
- First Online: 02 March 2019
Cite this chapter

- Bijal Chheda-Varma 5
3555 Accesses
The male to female ratio of ADHD is 4:1. This chapter on ADHD provides a wide perspective on understanding, diagnosis and treatment for ADHD. It relies on a neurodevelopmental perspective of ADHD. Signs and symptoms of ADHD are described through the DSM-V criteria. A case example (K, a patient of mine) is illustrated throughout the chapter to provide context and illustrations, and demonstrates the relative merits of “doing” (i.e. behavioural interventions) compared to cognitive insight, or medication alone. Finally, a discussion of the Cognitive Behavioral Modification Model (CBM) for the treatment of ADHD provides a snapshot of interventions used by clinicians providing psychological help.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Durable hardcover edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others
Psychological Treatments in Adult ADHD: A Systematic Review
Attention-Deficit Hyperactivity Disorder

ADHD and Its Therapeutics
Alderson, R. M., Hudec, K. L., Patros, C. H. G., & Kasper, L. J. (2013). Working memory deficits in adults with attention-deficit/hyperactivity disorder (ADHD): An examination of central executive and storage/rehearsal processes. Journal of Abnormal Psychology, 122 (2), 532–541. http://dx.doi.org/10.1037/a0031742 .
Arcia, E., & Conners, C. K. (1998). Gender differences in ADHD? Journal of Developmental and Behavioral Pediatrics, 19 (2), 77–83. http://dx.doi.org/10.1097/00004703-199804000-00002 .
Barkley, R. A. (1990). Attention deficit hyperactivity disorder: A handbook for diagnosis and treatment . New York: Guildford.
Google Scholar
Barkley, R. A. (1997). ADHD and the nature of self-control . New York: Guilford Press.
Barkley, R. A. (2000). Commentary on the multimodal treatment study of children with ADHD. Journal of Abnormal Child Psychology, 28 (6), 595–599. https://doi.org/10.1023/A:1005139300209 .
Article Google Scholar
Barkley, R., Knouse, L., & Murphy, K. Correction to Barkley et al. (2011). Psychological Assessment [serial online]. June 2011; 23 (2), 446. Available from: PsycINFO, Ipswich, MA. Accessed December 11, 2014.
Beck, A. T. (1976). Cognitive therapy and the emotional disorders . New York, NY: International Universities Press.
Brown, T. E. (2005). Attention deficit disorder: The unfocused mind in children and adults . New Haven, CT: Yale University Press.
Brown, T. (2013). A new understanding of ADHD in children and adults . New York: Routledge.
Chacko, A., Kofler, M., & Jarrett, M. (2014). Improving outcomes for youth with ADHD: A conceptual framework for combined neurocognitive and skill-based treatment approaches. Clinical Child and Family Psychology Review . https://doi.org/10.1007/s10567-014-0171-5 .
Chronis, A., Jones, H. A., Raggi, V. L. (2006, August). Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Clinical Psychology Review, 26 (4), 486–502. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2006.01.002 .
Curatolo, P., D’Agati, E., & Moavero, R. (2010). The neurobiological basis of ADHD. Italian Journal of Pediatrics, 36 , 79. http://doi.org/10.1186/1824-7288-36-79 . http://www.sciencedirect.com/science/article/pii/S0272735806000031 .
Curtis, D. (2010). ADHD symptom severity following participation in a pilot, 10-week, manualized, family-based behavioral intervention. Child & Family Behavior Therapy, 32 , 231–241. https://doi.org/10.1080/07317107.2010.500526 .
De Young, R. (2014). Using the Stroop effect to test our capacity to direct attention: A tool for navigating urgent transitions. http://www.snre.umich.edu/eplab/demos/st0/stroopdesc.html .
Depue, B. E., Orr, J. M., Smolker, H. R., Naaz, F., & Banich, M. T. (2015). The organization of right prefrontal networks reveals common mechanisms of inhibitory regulation across cognitive, emotional, and motor processes. Cerebral Cortex (New York, NY: 1991), 26 (4), 1634–1646.
D’Onofrio, B. M., Van Hulle, C. A., Waldman, I. D., Rodgers, J. L., Rathouz, P. J., & Lahey, B. B. (2007). Causal inferences regarding prenatal alcohol exposure and childhood externalizing problems. Archives of General Psychiatry, 64, 1296–1304 [PubMed].
DSM-V. (2013). Diagnostic and statistical manual of mental disorders . American Psychological Association.
Eisenberg, D., & Campbell, B. (2009). Social context matters. The evolution of ADHD . http://evolution.binghamton.edu/evos/wp-content/uploads/2012/02/eisenberg-and-campbell-2011-the-evolution-of-ADHD-artice-in-SF-Medicine.pdf .
Gizer, I. R., Ficks, C., & Waldman, I. D. (2009). Hum Genet, 126 , 51. https://doi.org/10.1007/s00439-009-0694-x .
Hinshaw, S. P., & Scheffler, R. M. (2014). The ADHD explosion: Myths, medication, money, and today’s push for performance . New York: Oxford University Press.
Kapalka, G. M. (2008). Efficacy of behavioral contracting with students with ADHD . Boston: American Psychological Association.
Kapalka, G. (2010). Counselling boys and men with ADHD . New York: Routledge, Taylor & Francis Group.
Book Google Scholar
Knouse, L. E., et al. (2008, October). Recent developments in psychosocial treatments for adult ADHD. National Institute of Health, 8 (10), 1537–1548. https://doi.org/10.1586/14737175.8.10.1537 .
Laufer, M., Denhoff, E., & Solomons, G. (1957). Hyperkinetic impulse disorder in children’s behaviour problem. Psychosomatic Medicine, 19, 38–49.
Raggi, V. L., & Chronis, A. M. (2006). Interventions to address the academic impairment of children and adolescents with ADHD. Clinical Child and Family Psychology Review, 9 (2), 85–111. https://doi.org/10.1007/s10567-006-0006-0 .
Ramsay, J. R. (2011). Cognitive behavioural therapy for adult ADHD. Journal of Clinical Outcomes Management, 18 (11), 526–536.
Retz, W., & Retz-Junginger, P. (2014). Prediction of methylphenidate treatment outcome in adults with attention deficit/hyperactivity disorder (ADHD). European Archives of Psychiatry and Clinical Neuroscience . https://doi.org/10.1007/s00406-014-0542-4 .
Safren, S. A., Otto, M. W., Sprich, S., Winett, C. L., Wilens, T. E., & Biederman, J. (2005, July). Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms. Behaviour Research and Therapy, 43 (7), 831–842. ISSN 0005-7967. http://dx.doi.org/10.1016/j.brat.2004.07.001 . http://www.sciencedirect.com/science/article/pii/S0005796704001366 .
Sibley, M. H., Kuriyan, A. B., Evans, S. W., Waxmonsky, J. G., & Smith, B. H. (2014). Pharmacological and psychosocial treatments for adolescents with ADHD: An updated systematic review of the literature. Clinical Psychology Review, 34 (3), 218–232. https://doi.org/10.1016/j.cpr.2014.02.001 .
Simchon, Y., Weizman, A., & Rehavi, M. (2010). The effect of chronic methylphenidate administration on presynaptic dopaminergic parameters in a rat model for ADHD. European Neuropsychopharmacology, 20 (10), 714–720. ISSN 0924-977X. https://doi.org/10.1016/j.euroneuro.2010.04.007 . http://www.sciencedirect.com/science/article/pii/S0924977X10000891 .
Swanson, J. M., & Castellanos, F. X. (2002). Biological bases of ADHD: Neuroanatomy, genetics, and pathophysiology. In P. S. Jensen & J. R. Cooper (Eds.), Attention deficit hyperactivity disorder: State if the science, best practices (pp. 7-1–7-20). Kingston, NJ: Civic Research Institute.
Toplak, M. E., Connors, L., Shuster, J., Knezevic, B., & Parks, S. (2008, June). Review of cognitive, cognitive-behavioral, and neural-based interventions for attention-deficit/hyperactivity disorder (ADHD). Clinical Psychology Review, 28 (5), 801–823. ISSN 0272-7358. http://dx.doi.org/10.1016/j.cpr.2007.10.008 . http://www.sciencedirect.com/science/article/pii/S0272735807001870 .
Wu, J., Xiao, H., Sun, H., Zou, L., & Zhu, L.-Q. (2012). Role of dopamine receptors in ADHD: A systematic meta-analysis. Molecular Neurobiology, 45 , 605–620. https://doi.org/10.1007/s12035-012-8278-5 .
Download references
Author information
Authors and affiliations.
Foundation for Clinical Interventions, London, UK
Bijal Chheda-Varma
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
UCL, London, UK
John A. Barry
Norfolk and Suffolk NHS Foundation Trust, Wymondham, UK
Roger Kingerlee
Change, Grow, Live, Dagenham/Southend, Essex, UK
Martin Seager
Community Interest Company, Men’s Minds Matter, London, UK
Luke Sullivan
Rights and permissions
Reprints and permissions
Copyright information
© 2019 The Author(s)
About this chapter
Chheda-Varma, B. (2019). Attention Deficit Hyperactivity Disorder (ADHD): A Case Study and Exploration of Causes and Interventions. In: Barry, J.A., Kingerlee, R., Seager, M., Sullivan, L. (eds) The Palgrave Handbook of Male Psychology and Mental Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-04384-1_15
Download citation
DOI : https://doi.org/10.1007/978-3-030-04384-1_15
Published : 02 March 2019
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-04383-4
Online ISBN : 978-3-030-04384-1
eBook Packages : Behavioral Science and Psychology Behavioral Science and Psychology (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research

IMAGES
VIDEO
COMMENTS
Read four case studies of individuals with ADHD, ranging from 7 to 36 years old, who present with different symptoms and challenges. Learn about their family history, academic performance, behavioural issues, and coping strategies.
A video presentation of a case study of a 19-year-old male with ADHD, who presented to his psychiatrist for consultation. The video covers the patient's history, symptoms, diagnosis, and treatment options.
This was a case study using monopolar electroencephalogram recording (brain mapping known as MiniQ) for subsequent use in an intervention with neurofeedback for a 10-year-old girl presenting predominantly inattentive ADHD.
Jen is a 29 year-old woman who struggles with time management, disorganization, and anxiety. She is diagnosed with adult ADHD and receives treatment recommendations based on empirical evidence.
His case study reveals the unique challenges of adult ADHD in professional settings and the effectiveness of workplace accommodations, such as flexible schedules and task management tools. John’s experience underscores the importance of mastering life with ADHD in professional contexts. Case 2: ADHD in a Gifted Child.
In a 2020 study, researchers compared 444 adults with diagnosed ADHD with 1,055 adults who exhibited symptoms but had no formal diagnosis. After matching for age and gender, those with a diagnosis reported a higher quality of life, which included metrics for work productivity, self-esteem, and functional performance ( Pawaskar, M., et al ...
Untreated ADHD as a comorbid condition to OCD may reduce the treatment response on the OCD, as shown in previous studies . Recognizing ADHD and OCD comorbidity is important for the clinical course of these disorders considering that the onset of OCD is significantly higher in adults with childhood ADHD symptoms and that the comorbidity is ...
ADHD was initially considered to be solely a childhood disorder, and the diagnosis of adult ADHD 2 was controversial. 3 However, long-term follow-up studies revealed that in 40 to 60% of children ...
This chapter provides a wide perspective on understanding, diagnosis and treatment for ADHD, a neurodevelopmental disorder with genetic and environmental factors. It relies on a case example of a male patient with ADHD Combined type and illustrates the relative merits of behavioural interventions, medication and cognitive behavioural modification.
Characteristics of ADHD seen in children tend to persist into adulthood, but they are often overlooked. This means the prevalence might be higher in adults than reported (Katzman, Bilkey, Chokka, Fallu, & Klassen, 2017). Studies have shown that characteristics seen in children change when individuals enter their late teens or early adulthood.