Loading metrics
Open Access
Peer-reviewed
Research Article

Digital transformation of an academic hospital department: A case study on strategic planning using the balanced scorecard
Roles Conceptualization, Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Rheumatology, Departement Appareil Locomoteur (DAL), University Hospital Lausanne (CHUV) and University of Lausanne, Switzerland
Roles Conceptualization, Data curation, Formal analysis, Methodology, Software, Writing – review & editing
Affiliations Department of Rheumatology, Departement Appareil Locomoteur (DAL), University Hospital Lausanne (CHUV) and University of Lausanne, Switzerland, Department of Urology,Inselspital and University of Bern,Bern, Switzerland
- Thomas Hügle,
- Vincent Grek

- Published: November 17, 2023
- https://doi.org/10.1371/journal.pdig.0000385
- Peer Review
- Reader Comments
Digital transformation has a significant impact on efficiency and quality in hospitals. New solutions can support the management of data overload and the shortage of qualified staff. However, the timely and effective integration of these new digital tools in the healthcare setting poses challenges and requires guidance. The balanced scorecard (BSC) is a managerial method used to translate new strategies into action and measure their impact in an institution, going beyond financial values. This framework enables quicker operational adjustments and enhances awareness of real-time performance from multiple perspectives, including customers, internal procedures, and the learning organization. The aim of this study was to adapt the BSC to the evolving digital healthcare environment, encompassing factors like the recent pandemic, new technologies such as artificial intelligence, legislation, and user preferences. A strategic mapping with identification of corresponding key performance indicators was performed. To achieve this, we employed a qualitative research approach involving retreats, interdisciplinary working groups, and semi-structured interviews with different stakeholders (administrative, clinical, computer scientists) in a rheumatology department. These inputs served as the basis for customizing the BSC according to upcoming or already implemented solutions and to define actionable, cross-level performance indicators for all perspectives. Our defined values include quality of care, patient empowerment, employee satisfaction, sustainability and innovation. We also identified substantial changes in our internal processes, with the electronic medical record (EMR) emerging as a central element for vertical and horizontal digitalization. This includes integrating patient-reported outcomes, disease-specific digital biomarker, prediction algorithms to increase the quality of care as well as advanced language models in order save resources. Gaps in communication and collaboration between medical departments have been identified as a main target for new digital solutions, especially in patients with more than one disorder. From a learning institution’s perspective, digital literacy among patients and healthcare professionals emerges as a crucial lever for successful implementation of internal processes. In conclusion, the BSC is a helpful tool for guiding digitalization in hospitals as a horizontally and vertically connected process that affects all stakeholders. Future studies should include empirical analyses and explore correlations between variables and above all input and user experience from patients.
Author summary
Digital transformation enhances hospital efficiency and quality, yet the integration of these technologies poses challenges that require clear direction. The Balanced Scorecard (BSC) is a tool that helps institutions gauge and action new strategies, not limited to financial metrics. It promotes rapid adjustments and offers clarity on performance on different perspectives. The university hospital sector is suitable for the application of the BSC, as the financial perspective is important, but other perspectives such as patient care and safety or research and innovation are equally important. This study adapted the BSC for current and future digital health solutions such as digital therapeutics or biomarker, AI or automation. Key performance indicators span across education, employee satisfaction and patient empowerment. By collecting insights from diverse stakeholders at a Swiss University Hospital, we developed a custom BSC. This updated BSC accentuates the role of electronic medical records in digitalization and underscores communication challenges between departments. A crucial insight is the importance of digital health literacy for both patients and staff. In essence, the BSC adeptly steers hospitals through digital transitions. Future studies should emphasize real-world testing and patient feedback.
Citation: Hügle T, Grek V (2023) Digital transformation of an academic hospital department: A case study on strategic planning using the balanced scorecard. PLOS Digit Health 2(11): e0000385. https://doi.org/10.1371/journal.pdig.0000385
Editor: Benjamin P. Geisler, Massachusetts General Hospital, UNITED STATES
Received: February 3, 2023; Accepted: October 10, 2023; Published: November 17, 2023
Copyright: © 2023 Hügle, Grek. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are included in the manuscript.
Funding: The authors received no specific funding for this work.
Competing interests: I have read the journal’s policy and the authors of this manuscript have the following competing interests: TH has received speaker fees or research grants from Fresenius Kabi, Abbvie, BMS, Lilly, Janssen and GSK. He is a scientific board member of Atreon and Vtuls and patent holder of a digital biomarker for joint swelling. VG has no competing interest.
Introduction
Digital transformation is an ongoing process in hospitals that has enormous potential to improve patient care, optimize costs, and streamline resources [ 1 ]. The advancements in computing power, data storage, and interoperability, such as the electronic medical records (EMR) with mobile devices, and the growing availability of artificial intelligence (AI) to harness this data flood, are reshaping healthcare [ 2 ]. These changes are occurring against the backdrop of an aging society with more comorbidities, increasing the need for interdisciplinary collaboration. However, healthcare systems are also encountering rising costs due to advanced diagnostic and therapeutic interventions and a critical shortage of healthcare professionals. Therefore, it is essential to reorganize healthcare at the point of care as well as on institutional and systemic levels using new digital tools, including AI and automation [ 3 ].
Integrating new digital solutions in hospitals is challenging and requires breaking down data and knowledge silos. On a vertical level, healthcare professionals, administrative staff, and patients use different indicators to measure quality and satisfaction and often do not speak the same language. The same is true horizontally, with a considerable lack of communication and data usage both between medical specialties and patients. This notably applies for overlapping pathologies such as immune-mediated disorders or chronic pain requiring parallel care. Hospitals hardly use digital devices to overcome these silos, apart from using the same EMR. Interdisciplinary case discussions in person, by email, or phone are rare occasions to interact with colleagues from other disciplines to take decisions and learn from each other. However, due to the lack of time and staff, such meta-networks are hardly scalable.
A range of new digital solutions addresses these issues. Many are already certified, such as >500 FDA-cleared AI algorithms, certified mobile health applications, and digital therapeutics such as the German DIGAs (Digitale Gesundheitsanwendung). Other solutions with a potentially large impact are upcoming, such as large language models (LLM) and transfer learning models that exploit and harmonize unstructured clinical data and biomarkers across disciplines. New applications are also available for the EMR as a central digital element in patient care, expanding and leveraging it horizontally and vertically, such as AI or mobile patient applications.
Responsible persons in hospitals are aware of this development, but the implementation of digital tools in clinical practice is anything but easy. Digital transformation requires a high investment in technology and stakeholder training to create gains in operational efficiency, medical care, and cost-reduction. Different expectations from the economic, clinical, and patient perspective make it difficult to prioritize and approach digitalization implementation.
This study analyzes existing and emerging needs of our hospital department and projects existing and new digital solutions across the value chain. The article presents a systematic methodology that takes into account the mission and vision of the institution, current healthcare trends, and shows the impact of digital tools on key processes and their indicators. A central element of this study is the Balanced Scorecard (BSC) as a strategic management and planning system to improve internal operations and project external outcomes [ 4 ]. It has been developed to monitor and improve real-time performances, for operational adjustments and for implementation of new strategies [ 5 ]. The BSC is adapted to the hospital perspective with a focus on clinical, patient, quality of care, and innovation outcomes and their key performance indicators (KPIs) [ 6 ]. The possible impact of existing and upcoming digital solutions on these outcomes is analyzed, and internal processes and knowledge are discussed to implement them in clinical practice.
This monocentric, observational study on strategic planning was conducted in the rheumatology department of the University Hospital in Lausanne (CHUV), Switzerland from 2017–2023. It included restrictions and subsequent new digital developments during the SARS-Cov2 pandemic. Data were used from a general retreat, working and focus groups as well as semi-structured interviews with different stakeholders and a literature and social media review. The methodological process is illustrated in Fig 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pdig.0000385.g001
Retreat and working groups
An initital retreat with all institutional stakeholders on a cadre level (doctors, nurses, adminsitrative) was performed 2017 to define visions, missions and clinical priorities. A SOAR analysis (Strengths, Opportunities, Aspirations, and Results) has been performed [ 7 ]. Clinical needs and potential digital solutions were further elaborated in monthly working groups over six months. Subsequently, existing key processes were analyzed in four working groups (patient care, organisation, research and education).
Semi-structured interviews, focus groups and conferences on an institutional level
We performed interviews with all stakeholders, including the informatic department, administration, clinicians, nurses and researchers. The status quo of implemented digital solutions and ongoing projects in terms of digital transformation were investigated. Data access and interfaces on an institutional level were discussed. From a clinical side, we organised a yearly interdisciplinary conference between rheumatology, gastro-enterology and dermatology on immune-mediated diseases to understand the clinical needs and developments of each speciality ( www.common-ground-meeting.org ).
Technological review
Information on existing digital solutions for health care insititutions was obtained by literature review on Pubmed, Google, social media (mainly LinkedIn) and podcasts (e.g. Medical AI Podcast, DTx Podcast, Faces of Digital Health, Deep Minds). We created the « Digital Rheumatology Network » ( www.digitalrheumatology.org ) as international platform to educate digitalization in rheumatology along with a conference series called Digital Rheumatology Day was started 2019. This platform served inform and connect clinicians and researcher with digital companies and start-ups in the field.
Adapted Balanced Scorecard and Strategy Mapping
The Balanced Scorecard was adapted to measure or project performances of digital solutions according four perspectives: financial, customer, internal processes and learning and growth. Vision, mission and have been elaborated in the working groups. Internal and external customers have been defined as patients, clinicians, health care professionals and administration. Financial performance has been shifted to « values », which were defined as: patient empowerment, clinical-decision support, time-saving, cost-effectiveness and quality.
Variables and KPI
KPI have been identified and assessed for measurability and feasibility in the working groups based on a clinical, internal, learning, quality of care or innovation perspective. According the clinical focus of this work KPIs shown in Fig 1 concern efficiency and effectiveness, qualiy of care, time management, scientific development of health care professionals, patient-centeredness, technology and information systems and interdisciplinary communication.
Strategic mapping
The primary result of this work is a strategic map based on an adapted Balanced Scorecard according key procedures for digitalization ( Fig 2 ). Previously, missions, visions and values facing new medical trends have been elaborated in a retreate and subsequent working groups. Internal processes and knowledge in terms of digitalisation have been worked out in semi-structured interviews, literature and social media search. Each chosen subset of the BSC was aligned with current developments in healthcare and digital technology.
From bottom-up the figure shows people & organisation, internal processes, customers, values and missions. Values have been adapted to current healthcare trends. Exemplary indicators are listed on the right. Artificial intelligence based models are indicated in orange. DTX: Digital therapeutics. PRO: Patient reported outcomes. EMR: Electronic medical record.
https://doi.org/10.1371/journal.pdig.0000385.g002
Mission and vision
We defined the mission of our academic department as cost-effective and state-of-the-art patient care, combined with a high level education and research. The vision was to overcome the challenges that come along with demographic changes of our society and staff shortage by becoming a smart hospital. We envision a countinously fluctuating healthcare system, e.g. due to the occurrence of infection waves, accidents or natural phenomena (heat or cold waves etc.). We aim to foster digital transformation but also to celebrate human interaction and contact with patients that are in control of their decisions and data.
Apart from a financial aspect, we defined four health care developments as the key values in our department:
- 1 . Patient empowerment and convenience
Healthcare is developing towards a consumer-driven service. Patients want to actively chose their site of patient care and doctors. Less wating times, accessiblity via email ect. appointments online ect. This also applies at least for a portion of the patients that prefer a more active role in managing their chronic disease by monitoring their symptoms, providing patient reported outcomes (PROs) or even taking over clinical decisions after appropriate training [ 8 ]. Patient convenience from the medical and digital side (not in terms of hospitality) has so far remained largely unexamined in hospitals, although it has a significant impact on the quality of life as a measurable indicator. Of note, convencience can be more important to patients than quality of care [ 9 ].
- 2. Personalized medicine
Personalized medicine approaches aim to streamline individualized diagnostic and therapeutic procedures for high efficacy and safety of care. This means a higher diagnostic effort (e.g. by -omics) and the integration of digital biomarkers and real world data in our workflow [ 10 ]. The exploitation of biomedical and clinical data by machine learning algorithms allows the prediction of individual disease courses, treatment response or phenotyping (clustering) as clinical decision support systems [ 11 ]. Thus, higher costs in diagnostics and data analysis might be compensated by better efficiency, lower complications and secondary healthcare costs.
- 3. Interdisciplinary care
In many chronic diseases, notably immune-mediated diseases or cancer, symptoms of different body systems often are compulsorily connected e.g. skin and joint inflammation in psoriasis arthritis, immune dysregulation due to immunotherapy in cancer or chronic pain and depression [ 12 ]. Quality of care depends on an optimal exchange of data and clinical decision between medical and paramedical information which bears a substantial number of barriers in terms of data interoperability. The individual ’point of care’ which is not always clear to the patient (private practice, hospital, pharmacy, online), needs to be redefined. Digital platforms or EMR with interdisciplinary dashboards may support an efficient and time saving exchange [ 13 ].
- 4. Sustainability and automatisation
The shortage of healthcare professionals, notably nurses, doctors or administrative staff is an emerging problem which leads to employee dissatisfaction and sick leave. Automatisation of simple procedures such as voice, image or text recognition has largely been implemented e.g. for medical documentation. There are several FDA-approved algorithms for automated evaluation of radiographs e.g. for fracture detection on the market. So far, those solutions are not an active clinical decision support but they likely increase quality as ‘double check’ or if no radiologist is available. Finally, advanced technology in chatbots such as ChatGPT from OpenAI could potentially support administrative tasks such as writing and correcting medical reports. Care robots are slowly touching ground in hospitals and care homes in order for transport but also for vital signs and PRO assessment [ 14 ].
Customers of our structure are patients (whether face-to-face or remote), clinicians, healthcare professionals, administrative staff and scientists. Accordingly, the needs of those internal and external customers on the BSC are anchored as clinical decision support, patient support, administrative support and research infrastructure. New types of customers are entering healthcare systems such as remote healthcare professionals (e.g. telenurse or online coaches), DIGA (Digital health application) providers ect. [ 15 ].
Internal processes (Digital Care Pathways)
Internal processes in hospitals are responsible to maintain and improve quality, efficiency and safety. Fig 2 (left) shows various forms of digital data collection (telemonitoring, digital biomarkers, biosensors ect.) as the basis for a personalized medicine. AI-models likely integrated in the EMR permit to define phenotypes, disease predictions and to perform transfer learning from concomitant (autoimmune) diseases. This supports the creation of digital care pathways that organise individual patient monitoring and treatment and orchestrate ressouces optimally. Data accessibility and connectibility is a main process for horizontal digitalization, both in terms of providing user interfaces, data privacy and legal certainty. Usability and intepretability of data is considered as a key process to avoid data and knowledge silos. This concerns structured data at the moment, but can be enlarged unstructured data e.g. by large language models. Clearly, external registries or other data sources should be interoperable with hospital systems, especially the EMR.
Generally, the EMR can be considered as the main tool to integrate new digital solutions horizontally and vertically ( Fig 3 ). For example. EMR can be extended vertically by integrating PROs, Patient reported experiences (PREs), digital biomarker or apps [ 16 ]. According to the ‘Internet of Things’ (IoT), the concept ‘Internet of Medical Devices’ (IoMD) should be promoted. Horizontally, dashboards increase usability of EMR between specialities and AI-generated predictions (including transfer learning algorithms) can be included in those interdisciplinary dashboards. New generation clinical dashboards also should show a holistic patient journey including predictions and outlier analysis etc. In the sense of horizontal integration along the value chain, the prediction should be connected to data on the availability of follow-up care facilities. The first step of AI-guided clinical pathway / decision support will likely be auto-care loops in stable disease courses. A maximal amount of collected data will be analyzed by clustering and prediction models, a digital treatment plan will be established and automatically monitored and reported to health care professionals including remote nurses. Smart agenda planning allows to identify and planify patients with a high flare risk for a conventional visit.
Elements around the EMR have been taken from the Balanced Scorecard (internal procedure perspective) and regrouped for a better demonstration.
https://doi.org/10.1371/journal.pdig.0000385.g003
Finally, automatisation is a sine qua non to encounter the shortage of rheumatologists and health care professionals. Large language models (LLM) such as GPT4 can be used to screen EMR and hospital databases for data or for the generation of discharge letters [ 17 ]. Voice recognition systems have widely been introduced in the clinic. New generation chatbots are able to extract the necessary information to create discharge reports and thus save time for the clinician to spend more time with patients or in interdisciplinary discussion. It seems primordial that all staff are equipped with smartphones and apps for those dashboards. Communication between colleagues in- and outside the hospital is via Email, which seems not adequate for several reasons (high number of unreplied messages, spam, security ect). It is obvious to connect case-based communication to dashboards in order to save time and to get relevant Information in a few clicks. All those digital processes together with their KPIs illustrate digital care pathways.
People and organisation (learning organisation)
In order to implement (digital or other) innovations, the human factor remains indispensable. This is especially true in medicine, where human interaction and ethical concerns are or paramount importance. Therefore, change management is the basis for creating readiness and acceptance for new technologies. In chronic diseases, a holistic view on patient journeys (or digital clinical pathways) with patient-centered endpoints and indicators are of increasing importance. Both patients and healthcare professionals need to understand how to access and inteprete this data and how to guarantee data privacy. To this end, knowledge about the inhouse databases (data warehouse etc.) and external data sources (registries or apps) as well as basic knowledge on data science is required and should be educated as a first step. The national or federal strategy for education of digital health is currently being actively discussed, but is only interoperable to a limited extent due to the different health systems [ 18 ]. Thus, a regular exchange between institutional, pan-departmental data scientists and collaborators within clinical departments ‘closer to clinical action’, shoud be established. Clinical-informaticians within medical departments are key elements for horizontal digitalization. For exemple they can educate clinicians use EMR more efficiently, including processes such as billing or implementing new processes such as prescribing DIGAs (Digitale Gesundheitsanwendung, digital health application) [ 15 ].
Human clinical know-how is also required to build and to control machine learning algorithms. As for input variables for algorithms (e.g. for clinical predictions), it is obviously not just about the availability but also the quality of the clinical data (e.g. what, when and how was measured). Clinicians need to specify the relevance of the data. As an exemple in image recognition, clinically defined pre-processing increases the prediction performance. As an example focusing on the hip shape to predict radiographic progression of hip ostearthritis [ 19 ].
No-coding platforms for image recognition or natural language processing can support clinicians in creating on predictions based on the insitutional data. For natural language processing, chatbots such as the openAI chatbot can leverage the work of doctors and scientists by support of writing articles or create automated reports and save precious time. Those tools are typically explored in defined research projects or audits before integrating them in the clinical workflow. Clearly, data safety issues have to be addressed rigourously and with new technological tools, its strengths and weaknesses are yet to be fully understood–and there appears early indication that such chatbots can be prone to confabulating information. An example of a medical report generated by the chatGPT3 chatbot can be found in S1 Table .
Patient education in the use of wearables, apps, digital therapeutics or biomarkers is pivotal. However low adherence to digital tools such as DIGAs is a widely undadressed problem [ 20 ]. Beside gamification, avatars or better human companion (e.g. health coaches) are necesary to assure adherence and quality of care. For mental health care, which also affects a substantial part of patients with immune-mediated diseases in form of secondary fibromyalgia, the human companionship seems even more important. Therefore, the need for trained remote health care professionals, e.g. as health coaches, will increase strongly in the future. A new profession of online nurses is also emerging among nurses, who work for hospitals or insurance companies and are connected to patients via a wide range of digital tools [ 21 ].
On a national and internationa level, both societies such as EULAR and patient organisations foster education and exchange of digital solutions [ 22 ]. To support this endavour, we created the digital rheumatology network ( www.digitalrheumatology.org ) organising yearly conferences (Digital Rheumatology Days) and regular pod-and webcasts.
The BSC has been developed around key indicators so they can and should be obtained at all levels. In other words, what is measurable within a digital care pathway should be measured. In our opinion, extra hours, sick leave and employer satisfaction are among the most urgent KPI, given the shortness of health care professionals and the wish for part-time positions. Patient empowerment and convenience measured by patient satifaction is also notably important to create and maintain trust as the basis of successful care.
For skills, education levels both of patients and clinicians can be measured by the number of attended courses, podcasts ect. Prescribed DIGAs and telemonitoring reports and patient adherence to those can be measured and discussed during face-to-face consultatons. PREs can be used to reflect the mix of human and digital therapeutic services offered by the department. Internal processes, including automatisation procedures, can be monitored by reduced extra-hours. Measuring ’connected care’ is more subtle but could be measurable by reduced length of hospital stay or readmission rates and patient satisfaction. Of note, many aspects of patient care such as empathy, time for listening can not be measured.
Implementation in our department and first results
In our and many other hospitals, the key aspects of digital transformation are initiated top-down from an institutional level. For example, the online assignment of patients for consultations or hospitalisation or telemonitoring via an app for post-operative patients that is supervised by a central nurse team. The access to the data warehouse for scientific purposes has been facilitated and a machine learning team for clinical predictions or biomedical (big) data analysis collaborates closely with medical departments on a project level. To leverage these and other opportunities, we initiated a bottom-up strategy according to the above mentioned factors. On a departimental level, we have introduced regularly scheduled meetings between clinicians and institutional IT specialists. A clinician-informatician consultant provides regular training in basic machine learning coding and institutional data access to our clinical and research team. Clinical data science training using data from registries and our datawarehouse has been added to the curriculum for new assistant doctors. A specialized nurse consultation for rheumatic patients has been implemented to instruct patients in the use of apps with PROs, here within our national registry SCQM (Swiss Cohort for Quality Management), wearable data and the use of digital therapeutics. As our current EMR is lacking clinical scores and indicators such as the DAS28 score, we included the mannequin for tender and swolen joints and were thus able to synchonize EMR with the registry. Patients can send pictures or videos of their hands into our system via apps. We have developed an algorithms that automatically measure the finger folds, joint diameter etc. on hand images to monitor joint swelling [ 23 ]. The range of motion can be estimated on self-recorded videos of patients by automatically measuring the angles of the different joints and comparing them with the previous values. In the future, hopefully such disease-specific biomarker will earlier detect of arthritis flares.
A telemonitoring & communication office is currently being set up where medical medical assistants are trained to become ‘clinical workflow & communication manager’ with access to PROs, wearables, photos, videos etc. on specific dashboards and obviously the agenda of our consultation. In parallel to telephone calls and emails from patients they forward information (or not) to specialized nurses or our rheumatologist and to refer patients to the consultation.
Five years ago we started an international conference series called the ’Digital Rheumatology Days’ ( www.digitalrheumatology.org ) for healthcare professionals to educate them on telemonitoring, digital therapeutics/DIGAs, digital biomarkers, social media usage, machine learning ect. The annual conference was complemented by the Digital Rheumatology Network as an educational platform where information, podcasts, webcasts, etc. are permanently published and distributed via social media. To foster interdisciplinarity as part of the connected care model, the Common Ground Meeting for Immune-mediated Diseases has been created (common-ground-meeting.org), assembling different specialties for disease updates, the use of data (e.g. presentation of digital biomarkers) and case discussions by rheumatologists, dermatologists, gastro-enterologists, immunologists, nephrologists and pneumologists.
So far, the internal processes mentioned above have been partially implemented. Digital tools and data science have mainly been introduced on a project basis, with ongoing studies ( S1 Table ).
We present a comprehensive mapping of digital transformation in a rheumatology hospital department, focusing on current digital developments and the evolving values in healthcare. By utilizing the BSC framework, we effectively illustrate how the implementation of digital solutions, both existing and upcoming, can enhance our performance on different levels towards achieving a ’connected care model’ that aligns with the institution’s mission and vision.
First of all, this strategic mapping emphasizes the significance of bottom-up education for all stakeholders, including patients, to promote the adoption of new digital tools. We propose that knowledge on data science, app technology, cloud computing, and the fundamentals of AI, such as large language models, is a vital process in transforming healthcare organizations into learning environments that better support patients, administration, and healthcare professionals. In this context, the BSC may improve organizational performance by facilitating double-loop learning and disseminating the hospital’s vision as a learning organization [ 24 ].
During our research, we identified a knowledge gap concerning institutional digital solutions or collaborative projects developed within the hospital. For instance, a platform designed for accessing clinical data for research purposes faced low adoption rates primarily due to a lack of awareness among clinical departments. Regular meetings between the institution and clinicians or the appointment of a clinician-informatician emerged as crucial strategies to leverage digitalization and foster adoption.
Furthermore, we demonstrate that the electronic EMR plays a pivotal role in the digital transformation of healthcare. As illustrated in Fig 3 , The EMR can be expanded both horizontally and vertically e.g. through the integration of AI algorithms, apps, interdisciplinary dashboards, wearable data, patient-reported outcomes (PROs), ultimately serving as the central point of care within a hospital.
Initially, the BSC was developed to establish relationships between actions and process performance in business institutions at levels beyond financial values. The hospital as ‘institution’ has evolving values and a very short half-life of knowledge and technology.
In a first step, we established a BSC framework that corresponds to the current state of knowledge and digitalization. Over time, key success factors in hospitals have undergone changes, particularly in terms of employee satisfaction and patient empowerment. Interdependencies with other sub-units (= interdisciplinarity) have also become increasingly important and should be taken into account when selecting KPI.
It is important to note that this strategic mapping does not serve as a manual for digitalization but rather aims to inspire others to conduct similar exercises in order to create a ’compass’ for responsible healthcare professionals.
We must acknowledge several limitations of this work. KPI implementation was only partial, and processes at different levels have not yet been fully connected or supported by empirical data. Thus, we cannot demonstrate causal relationships among key indicators within or across the four perspectives, as previously shown in hospital settings [ 25 ]. Therefore, the full potential of the BSC remains untapped. Adoption of the BSC healthcare professionals may prove challenging [ 5 ]. Another limitation lies in the fact that the BSC has shown limitations in measuring human relations, which are crucial components of learning organizations in the healthcare sector [ 26 ].
In conclusion, digital transformation is a complex and ongoing process that requires meticulous planning on various levels. The BSC proves to be a suitable tool for both planning and monitoring this significant endeavor. Digital tools should enable better care and save time, allowing healthcare professionals to focus on valuable human interaction that algorithms can never replace.
Supporting information
S1 table. implemented digital aspects in our rheumatology department..
https://doi.org/10.1371/journal.pdig.0000385.s001
Acknowledgments
We thank Dr. Chris Lovejoy for his valuable review of the manuscript.
- View Article
- PubMed/NCBI
- Google Scholar
Europe PMC requires Javascript to function effectively.
Either your web browser doesn't support Javascript or it is currently turned off. In the latter case, please turn on Javascript support in your web browser and reload this page.
Search life-sciences literature (44,031,989 articles, preprints and more)
- Available from publisher site using DOI. A subscription may be required. Full text
- Citations & impact
- Similar Articles
Priority-setting and hospital strategic planning: a qualitative case study.
Author information, affiliations.
Journal of Health Services Research & Policy , 01 Oct 2003 , 8(4): 197-201 https://doi.org/10.1258/135581903322403254 PMID: 14596753
Abstract
Full text links .
Read article at publisher's site: https://doi.org/10.1258/135581903322403254
Citations & impact
Impact metrics, citations of article over time, alternative metrics.

Article citations
Ethics education and moral decision-making in clinical commissioning: an interview study..
Knight S , Hayhoe BW , Frith L , Ashworth M , Sajid I , Papanikitas A
Br J Gen Pract , 70(690):e45-e54, 26 Dec 2019
Cited by: 1 article | PMID: 31848203 | PMCID: PMC6917357
Free full text in Europe PMC
'You can give them wings to fly': a qualitative study on values-based leadership in health care.
Denier Y , Dhaene L , Gastmans C
BMC Med Ethics , 20(1):35, 27 May 2019
Cited by: 3 articles | PMID: 31133017 | PMCID: PMC6537214
Leadership styles in two Ghanaian hospitals in a challenging environment.
Aberese-Ako M , Agyepong IA , van Dijk H
Health Policy Plan , 33(suppl_2):ii16-ii26, 01 Jul 2018
Cited by: 6 articles | PMID: 30053032 | PMCID: PMC6037062
Setting healthcare priorities: a description and evaluation of the budgeting and planning process in county hospitals in Kenya.
Barasa EW , Cleary S , Molyneux S , English M
Health Policy Plan , 32(3):329-337, 01 Apr 2017
Cited by: 23 articles | PMID: 27679522 | PMCID: PMC5362066
Setting Healthcare Priorities at the Macro and Meso Levels: A Framework for Evaluation.
Barasa EW , Molyneux S , English M , Cleary S
Int J Health Policy Manag , 4(11):719-732, 16 Sep 2015
Cited by: 31 articles | PMID: 26673332 | PMCID: PMC4629697
Review Free full text in Europe PMC
Similar Articles
To arrive at the top five similar articles we use a word-weighted algorithm to compare words from the Title and Abstract of each citation.
Hospital priority setting with an appeals process: a qualitative case study and evaluation.
Madden S , Martin DK , Downey S , Singer PA
Health Policy , 73(1):10-20, 10 Dec 2004
Cited by: 22 articles | PMID: 15911053
Priority setting in a hospital critical care unit: qualitative case study.
Mielke J , Martin DK , Singer PA
Crit Care Med , 31(12):2764-2768, 01 Dec 2003
Cited by: 37 articles | PMID: 14668612
SARS and hospital priority setting: a qualitative case study and evaluation.
Bell JA , Hyland S , DePellegrin T , Upshur RE , Bernstein M , Martin DK
BMC Health Serv Res , 4(1):36, 19 Dec 2004
Cited by: 26 articles | PMID: 15606924 | PMCID: PMC544195
A strategic approach for negotiating with hospital stakeholders.
Blair JD , Savage GT , Whitehead CJ
Health Care Manage Rev , 14(1):13-23, 01 Jan 1989
Cited by: 2 articles | PMID: 2647668
The use of cost-effectiveness by the National Institute for Health and Clinical Excellence (NICE): no(t yet an) exemplar of a deliberative process.
Schlander M
J Med Ethics , 34(7):534-539, 01 Jul 2008
Cited by: 30 articles | PMID: 18591289
Europe PMC is part of the ELIXIR infrastructure
Essentials of Strategic Planning in Healthcare, Third Edition
Jeffrey p. harrison, phd, fache.
- Member Price: $68.60
- Non Member Price: $98.00
- Strategic Planning
Book Description
- Current data on healthcare spending, hospital statistics, healthcare employment, and the use of healthcare technology
- New content on the use of artificial intelligence and big data in healthcare, as well as the benefits of block chain technology
- Coverage of future advances in healthcare, including genomics and Medicare for All
- Expanded marketing content, including the latest trends in websites, digital outlets, and social media
- Table of Contents (PDF)
- Preface (PDF)
- Book Excerpt (PDF)
- Transition Guide
- Instructor Resource Sample
- Corrections
- PURCHASE EBOOK FROM AMAZON KINDLE SALES
- PURCHASE EBOOK FROM CHEGG
- PURCHASE EBOOK FROM VITALSOURCE (INGRAM)

Futurescan 2017: Healthcare Trends and Implications 2017-2022

Futurescan 2018: Healthcare Trends and Implications 2018-2023
Looking Back to Look Forward: AUPHA at 70

Futurescan 2016: Healthcare Trends and Implications 2016-2021
-b084e1dd.jpg?w=160)
Management of Healthcare Organizations: An Introduction, Third Edition

Evidence-Based Management in Healthcare: Principles, Cases, and Perspectives, Second Edition
Strategic Healthcare Management: Planning and Execution, Second Edition

Futurescan 2019–2024: Healthcare Trends and Implications
Exceptional Leadership: 16 Critical Competencies for Healthcare Executives, Second Edition

Futurescan 2022–2027: Health Care Trends and Implications
Marketing Health Services, Fourth Edition

Getting It Done: Experienced Healthcare Leaders Reveal Field-Tested Strategies for Clinical and Financial Success

Why Hospitals Should Fly: The Ultimate Flight Plan to Patient Safety and Quality Care
Transformative Planning: How Your Healthcare Organization Can Strategize for an Uncertain Future
Leadership for Public Health: Theory and Practice
An Insider’s Guide to Working with Healthcare Consultants

Healthcare Strategic Planning, Fourth Edition
Strategic Analysis for Healthcare: Concepts and Practical Applications, Second Edition

Make It Happen: Effective Execution in Healthcare Leadership

The Future of Healthcare: Global Trends Worth Watching
Use of Q methodology for hospital strategic planning: a case study
Affiliation.
- 1 Cardinal Health Alliance, Muncie, Indiana, USA. [email protected]
- PMID: 11187361
This study was designed to illustrate how Q Methodology can be used as a tool for strategic planning. Potential plans for the future of a small Indiana hospital were formulated and Q sorted to determine support or resistance by key leaders from within hospital management, the board, and the medical staff. The hospital was able to identify stakeholder perceptions that resulted in strong consensus that integration should be a priority for the hospital. This exercise provided a list of objectives for hospital leadership and the results were also used to justify the cessation of several programs that the hospital leadership had been pursuing.
- Attitude of Health Personnel
- Decision Making, Organizational
- Governing Board
- Group Processes
- Hospital Administrators
- Hospital Bed Capacity, 100 to 299
- Hospital Planning / methods*
- Hospital Planning / statistics & numerical data
- Hospitals, Community / organization & administration*
- Leadership*
- Medical Staff, Hospital
- Organizational Case Studies
- Planning Techniques*
- Open access
- Published: 18 September 2020
An analysis of the strategic plan development processes of major public organisations funding health research in nine high-income countries worldwide
- Cristina Morciano 1 ,
- Maria Cristina Errico 1 ,
- Carla Faralli 2 &
- Luisa Minghetti 1
Health Research Policy and Systems volume 18 , Article number: 106 ( 2020 ) Cite this article
11k Accesses
9 Citations
3 Altmetric
Metrics details
There have been claims that health research is not satisfactorily addressing healthcare challenges. A specific area of concern is the adequacy of the mechanisms used to plan investments in health research. However, the way organisations within countries devise research agendas has not been systematically reviewed. This study seeks to understand the legal basis, the actors and the processes involved in setting research agendas in major public health research funding organisations.
We reviewed information relating to the formulation of strategic plans by 11 public funders in nine high-income countries worldwide. Information was collected from official websites and strategic plan documents in English, French, Italian and Spanish between January 2019 and December 2019, by means of a conceptual framework and information abstraction form.
We found that the formulation of a strategic plan is a common and well-established practice in shaping research agendas across international settings. Most of the organisations studied are legally required to present a multi-year strategic plan. In some cases, legal provisions may set rules for actors and processes and may establish areas of research and/or types of research to be funded. Commonly, the decision-making process involves both internal and external stakeholders, with the latter being generally government officials and experts, and few examples of the participation of civil society. The process also varies across organisations depending on whether there is a formal requirement to align to strategic priorities developed by an overarching entity at national level. We also found that, while actors and their interactions were traceable, information, sources of information, criteria and the mechanisms/tools used to shape decisions were made less explicit.
Conclusions
A complex picture emerges in which multiple interactive entities appear to shape research plans. Given the complexity of the influences of different parties and factors, the governance of the health research sector would benefit from a traceable and standardised knowledge-based process of health research strategic planning. This would provide an opportunity to demonstrate responsible budget stewardship and, more importantly, to make efforts to remain responsive to healthcare challenges, research gaps and opportunities.
Peer Review reports
Advances in scientific knowledge have contributed greatly to improvements in healthcare, but there have been claims that health research is not adequately addressing healthcare challenges. These concerns are reflected in the increasing debate over the adequacy of the mechanisms used to plan investment in health research and ensure its optimal distribution [ 1 , 2 , 3 , 4 , 5 ].
Over recent decades, methods and tools have been produced in order to guide the process of setting the health research agenda and facilitate more explicit and transparent judgment regarding research priorities. There is no single method that is considered appropriate for all settings and purposes, yet it is recognised that their optimal application requires a knowledge of health needs, research gaps and the perspectives of key stakeholders [ 6 , 7 , 8 , 9 , 10 ].
A number of studies have described initiatives to set health research agendas. Several articles refer to experiences focusing on specific health conditions, for example, those undertaken under the framework of the James Lind Alliance [ 11 ]. There are also reviews of disparate examples of research agenda-setting in low- and middle-income countries [ 12 , 13 ] as well as in high-income countries (HICs) [ 14 ]. These initiatives were highly heterogeneous with regard to their promotor (public organisations, academics, advocacy groups, etc.), the level of the research system (global, regional, national, sub-national, organisational or sub-organisational) and the scope of the prioritisation process (broad themes or specific research questions).
However, there are no studies that have specifically investigated the way large public organisations in HICs devise their research agendas and to what extent this is linked to regulations and organisational setup. In 2016, Moher et al. reported on how research funders had addressed recommendations to increase value and reduce waste in biomedical research [ 15 ]. Within this framework, they provided a general overview of setting the overall agenda in a convenient sample of six public funders of health research. They also affirmed the need for a “ periodic survey of information on research funders’ websites about their principle and methods used to decide what research to support ” [ 15 ]. At the same time, Viergever et al. identified the 10 largest funders of health research in the world and recommended further study of their priority-setting processes [ 16 ].
Given this context, we wished to provide an updated and thorough description of the way public funders of research in HICs devise their research agenda. We therefore analysed the regulatory framework for the actors and processes involved in developing the strategic plan in 11 major English and non-English speaking public research funders across 9 HICs worldwide.
Strategic planning
Our analysis focused on the development of the strategic plan, or strategic planning, at organisational level as a crucial step in the setting of the research agenda by the organisation. By the term ‘setting the research agenda’, we meant the whole-organisation research management planning cycle, which may encompass multiple decision-making level (organisational, sub-organisational, research programme level, etc.) actors and funding flows.
Strategic planning has been defined in social science as a “ deliberative, disciplined effort to produce fundamental decisions and actions that shape and guide what an organization (or other entity) is, what it does, and why ” [ 17 ].
The strategic plan is assumed to be the final outcome of the strategic planning process, in which priority-setting is the key milestone. It is therefore expected that the research priorities of the organisation will be included. Depending on mandate, priorities could be related to research topics (e.g. health conditions or diseases), types of research (e.g. basic or clinical) and/or other planned initiatives (e.g. workforce or research integrity).
The choice to focus on strategic planning was also guided by the fact that it is known from social science that strategic planning is a well-established practice within public organisations worldwide [ 17 , 18 ]. This would enable us to ensure comparability of information on modalities of decision-making in research planning across organisations from different countries.
Selection of public organisations
We created a list of public funders of health research, drawing from a previous study in which the authors identified 55 public and philanthropic organisations and listed them according to their annual expenditure on health research [ 16 ]. In order to strike a balance between learning about the practices of health research funders, and keeping data collection feasible and manageable, we restricted our sample to two organisations per country, with health research budgets of more than 200 million USD annually. In doing so, we identified a manageable subsample of 35 organisations having the greatest potential influence on research agendas, both locally and globally, and representing different health research systems in different countries.
We based our overview on publicly available information and restricted our sample to those organisations with published strategic research plans in English, French, Italian or Spanish (Additional file 1 ).
Information search and abstraction
Since we expected processes to vary across organisations, we did not use guidelines or best practices for strategic planning, which allowed us to document a wide range of experiences. As mentioned earlier, we based this overview on the collection of publicly available information by means of a conceptual framework and an information abstraction form (Box 1 , Additional file 1 ).
We based the conceptual framework on Walt and Gilson’s policy analysis model [ 19 ] and the information that could actually be retrieved after an initial assessment of the available information. The conceptual framework and the data abstraction form were conceived in an effort to (1) standardise the search for and collection of information across organisations, (2) render the collection process more transparent, and (3) make the retrieved information more understandable to readers.
Three authors (CM, CF and MCE) performed the review of information and the compilation of the form independently, with differences of opinion resolved by discussion. Information was collected in duplicate from 1 January 2019 to 31 July 2019. Before submitting the article, we updated the information by accessing and reviewing the official websites of the included organisations until 10 December 2019.
We searched for information that answered our questions by (1) browsing the funding organisations’ official websites and following links providing information about the organisations, e.g. Who we are, About us, Mission, Laws and statutes, Funding opportunities and other similar web pages, and by (2) identifying and reviewing strategic plans. When an organisation was composed of multiple sub-organisations, we limited our analysis to the strategic planning of the overarching organisation.
A second phase of research consisted of producing a profile for each organisation according to the data extraction form (Additional file 1 ). Bearing in mind that the results of this analysis could have been very general, we also used two organisations as case studies to provide more detailed examples of planning and implementing research priorities at the organisational level. We accessed and reviewed the official websites of the case study organisations until 14 April 2020. We did not contact organisations directly to obtain additional information. After collecting and analysing the information, we produced a narrative overview of our findings.
Box 1 Conceptual framework
Organisation profile
This section describes the funding organisation and its role and relationship with other overarching governmental bodies.
What are the contents of the strategic plan?
This section examines the publicly available strategic plan of the funding organisation. The strategic plan is assumed to be the final outcome of the strategic planning process and includes the research priorities of the organisation. Depending on the mandate of the organisation, the research priorities are those related to research topics (for example, health conditions/diseases), types of research (for example, basic research, clinical research) and/or other planned initiatives within the mandate of the organisation (e.g. workforce, research integrity).
Regulatory basis
This part seeks to understand if there is an official basis for strategic planning, for example, a law or a government document that establishes processes and actors for setting priorities.
What are the process and tools of strategic planning?
This section seeks to describe the processes and tools for identifying the research priorities included in the strategic plan, including whether or not there are explicit mechanisms, criteria, instruments and information to guide and inform the process of strategic planning such as a research landscape analysis or a more structured experience of priority-setting.
Who are the actors involved?
This section examines who the involved actors are in preparing the strategic plan; for example, who coordinates the process and who is involved in the process (e.g. clinicians, patients, citizens, researchers) and how the organisation relates with other entities in preparing the strategic plan.
Included organisations
We included 11 public organisations with a publicly available strategic plan in English, Spanish, French or Italian (Additional file 1 ). There were two from the United States, two from France, and one each from the United Kingdom, Canada, Australia, Japan, Italy, Spain and Singapore. The mandates of the organisations were diverse – some had the task of funding research and other activities in support of health research, while others were involved in both funding and conducting health research (Table 1 ).
The strategic plan: format and content
The strategic plans varied in format (Additional file 1 ). While some organisations indicated broad lines of research, others structured their strategic plan in a complex hierarchy with high-level priorities connected to goals and sub-goals. In some cases, indicators, or menus of indicators, were added to monitor progress of the planned work and/or assess the impact of the research. In some research plans, the type of research funding (e.g. responsive, commissioned, research training) and budget were explicitly linked to research priorities.
With regard to content, some organisations focused their strategy on supporting the production of new knowledge of specific diseases or conditions. Others prepared a comprehensive strategy to support different functions of the health research system, such as producing knowledge, sustaining the workforce and infrastructure, developing policies for research integrity and conceiving processes for making more informed decisions. Some strategic plans briefly described the research environment at the national, organisational or programme level. One organisation described the process used to develop health research priorities.
Most of the organisations are legally required to present a multi-year strategic plan or at least annual research priorities. In addition, legislation sets rules and procedures by covering subjects such as the actors to be involved, the documents to be consulted and the format of the strategic plan document to be adopted. In some cases, legal provisions indicate areas and/or types of research to be funded (Table 1 ).
Commonly, the main actors are the top-level policy-makers of the organisations. A spectrum of external stakeholders from multiple sectors may be involved and their participation varies across organisations. External stakeholders can be members of academia or government research agencies, or industry professionals and policy-makers. Most frequently, they have a membership role in organisational governing bodies (boards and committees) (Table 1 ).
The government maintains a role in shaping the strategic plan to various extents in different organisations. This may involve producing nationwide strategic plans for research that the organisations have to adopt or align to, directing attention to specific research priorities or types of research, having representatives in the governing bodies of the organisations and retaining the power of final approval of the organisations’ strategic plans (Table 1 ). Other actors involved are overarching government agencies, which play a role in managing or coordinating the research plan at the national level. Examples of this are the Spanish National Research Agency and United Kingdom Research and Innovation (UKRI). When this study was being conducted, the latter had just been established and been given the role of developing a coherent national research strategy.
The participation of civil society in governing bodies, temporary committees or consultation exercises was far less common. There are representatives of the public in the advisory bodies of the National Institutes of Health (NIH; e.g. the Advisory Committee to the Director).
The Chief Executive Officer of the National Health and Medical Research Council (NHMRC), acting under the terms of the NHMRC Act, established the Community and Consumer Advisory Group. This is a working committee whose function is to provide advice on health questions and health and medical research matters, from consumer and community perspectives. Most notably, the United States Department of Defense – Congressionally Directed Medical Research Programs (DoD-CDMRP) involve consumers (patients, their representatives and caregivers) at all levels of the funding process, from strategic planning to the peer-review process of research proposals. Organisations also have external consultation exercises, in which the target audiences and mechanisms implemented vary (Table 1 ).
In order to illustrate the interactions between different actors, we identified two broad categories of organisation. The first comprises those organisations that develop their own plans with a certain degree of independence. Government and legal provisions might provide some direction. In this group are the NIH, the Institut national de la santé et de la recherche médicale (Inserm), the Italian Ministry of Health (MoH), the NHMRC, the Canadian Institutes of Health Research (CIHR), the Medical Research Council (MRC), the DoD-CDMRP, the Centre National de la Recherche Scientifique (CNRS) and the Japan Society for the Promotion of Science (JSPS) (Table 1 ).
The second category is made up of those organisations whose research planning derives from the strategic plan of an overarching entity. In this group are the Instituto de Salud Carlos III (ISCIII), the National Medical Research Council (NMRC) and the MRC. Both categories are represented in the case studies below.
An example of the first category from the United States is the 5-year strategic plan, NIH-Wide Strategic Plan, Fiscal Years 2016–2020: Turning Discovery Into Health, developed by the NIH at the request of Congress. Legislation provides direction on some criteria for setting priorities in the plan, but it is the NIH Director who develops it in consultation with internal (Centres, Institutes and Offices) and external stakeholders (see the NIH case study).
In Australia, the Chief Executive Officer of the NHMRC identifies major national health issues likely to arise during the 4-year period covered by the plan and devises the strategy in consultation with the Minister for Health and the NHMRC governing bodies. The Minister provides guidance on the NHMRC’s strategic priorities and approves or revises the plan. In Canada, the governing bodies of the CIHR are responsible for devising the strategic plan. The Deputy Minister of the Department of Health participates as a non-voting member of one of the governing bodies.
The common characteristic of the second category is that the process of strategic planning derives from one or more overarching entities. This means that the strategic plans of the organisations are informed to various extents by the research programmes of such an entity or entities. In some cases, there is a main institution with research coordination and/or management roles at the national level. For example, in Spain, in order to inform funding grants, the ISCIII adopted the research priorities set out in the Strategic Action for Health included in the State Plan for Science, Innovation and Technology 2017–2020 . This plan, elaborated by the Government Delegated Committee for the Policies for Research, Technology and Innovation ( la Comisión Delegada del Gobierno para Política Scientífica, Tecnológica y de Innovación ), in cooperation with the Ministry of Fianance, is aligned with the four strategic objectives of the Spanish Strategy for Science, Technology and Innovation 2013–2020. The newly established Spanish State Research Agency ( Agencia Estatal de Investigacion ) also participated in the development of the State Plan. However, its role is mainly in monitoring the plan’s funding, including ISCIII funding for the Strategic Action for Health.
UKRI, sponsored by the Department for Business, Energy and Industrial Strategy, is the body responsible for the development of a coherent national research strategy that balances the allocation of funding across different disciplines. In 2018, the MRC became a committee body of UKRI, alongside eight other committees, called ‘Councils’, which represent various research sectors. The MRC is required to develop a strategic plan that is coherent with the strategic objectives set by UKRI. This plan must be approved by the UKRI Board, the governing body responsible for ensuring that Council plans are consistent with the UKRI strategy.
In Singapore, the NMRC refers to the strategic plan developed by the National Research Foundation, a department within the Prime Minister’s Office. The NMRC has a well-described system for incorporating national priorities into the organisation’s research plan (see the NMRC case study).
With regard to the information, sources of information, criteria and mechanisms used to shape decisions, the included organisations were less explicit. Most commonly, organisations introduced health research priorities with an overview of major general advancements in biomedical research or a catalogue of organisational activities and a research portfolio.
A small number of organisations presented a brief situational analysis of the health and health research sectors. In these cases, the scope and nature of the presented information varied from one organisation to another (Additional file 1 ).
For example, the NIH-Wide Strategic Plan contains a brief summary of the state of research at the organisational level. The plans of each DoD-CDMRP health research programme present a summary of both the current health and health research landscapes at the national level.
Other organisations stated that the plan had been supported by information analysis of the research field, but they did not report explicitly on this work.
Case studies
The national institutes of health (nih).
The NIH is an operating division of the United States Department of Health and Human Services whose mission is to improve public health by conducting and funding basic and translational biomedical research. It is made up of 27 theme-based Institutes, Centers and Offices, each of which develops an individual strategic plan [ 20 ].
The first 5-year strategic plan, NIH-Wide Strategic Plan, Fiscal Years 2016–2020: Turning Discovery into Health, was prepared at the request of Congress and published in 2016 [ 21 ]. The legal framework stipulates that the NIH-coordinated strategy will inform the individual strategic plans of the Institutes and Centers. In addition, it provides some direction regarding content and the process to be adopted for generating the overall NIH strategy [ 22 , 23 ]. For example, it sets out specific requirements for the identification of research priorities. These include “ an assessment of the state of biomedical and behavioural research ” and the consideration of “ (i) disease burden in the United States and the potential for return on investment to the United States; (ii) rare diseases and conditions; (iii) biological, social, and other determinants of health that contributes to health disparities; and (iv) other factors the Director of National Institutes of Health determines appropriate ” [ 23 ]. The NIH Director is also required to consult “ with the directors of the national research institutes and national centers, researchers, patient advocacy groups and industry leaders ” [ 23 ]. To fulfil the request of Congress, the NIH Director and the Principal Deputy Director initiated the process by creating a draft ‘framework’ for the strategic plan. This framework was designed with the purposes of identifying major areas of research that cut across NIH priorities and of setting out principles to guide the NIH research effort (‘unifying principles’).
The development of the NIH-Wide Strategic Plan involved extensive internal and external consultations throughout the process. Consultees included the ad hoc NIH-Wide Strategic Plan Working Group, composed of representatives of all 27 Institutes, Centers and Offices, the Advisory Committee to the Director, which is an NIH standing committee of experts in research fields relevant to the NIH mission, and representatives of the research community (from academia and the private sector) and the general public. The framework was also presented at meetings with the National Advisory Councils of the Institutes and Centers.
In addition, the framework was disseminated to external stakeholders for comments and suggestions, which were solicited via a series of public webinars and through the initiative Request for Information: Inviting Comments and Suggestions on a Framework for the NIH-Wide Strategic Plan. In this case, a web-based form collected comments and suggestions on a predefined list of topic areas from a wide array of stakeholders representative of patient advocacy organisations, professional associations, private hospitals and companies, academic institutions, government and private citizens [ 24 , 25 , 26 , 27 ]. A report on the analysis of the public comments is publicly available [ 27 ].
The National Medical Research Council (NMRC)
The NMRC is the organisation that has the role of promoting, coordinating and funding biomedical research in Singapore [ 28 ]. It has developed its own research strategy by adopting the research priorities indicated by the national research strategy in the domain of health and biomedical sciences [ 29 ].
The national research strategy is the responsibility of the National Research Foundation, a department of the Prime Minister’s Office. It defines broad research priorities relating to various areas of research identified as ‘domains’. Within the health and biomedical sciences domain, five areas of research have been proposed with input from the Ministry of Health and the Health and Biomedical Sciences International Advisory Council. These are cancer, cardiovascular diseases, infectious diseases, neurological and sense disorders, diabetes mellitus and other metabolic/endocrine conditions. Criteria for selection of the areas of focus were “ disease impact, scientific excellence in Singapore and national needs ” [ 29 ].
The approach of NMRC to implementing the national research strategy at organisational level involves the establishment of ‘task forces’, i.e. groups of experts, with the role of defining the specific research strategy for each of the five areas of focus. Each task force provides documentation of research recommendations and methods used to prioritise research topics [ 30 ].
For example, the Neurological and Sense Disorders Task Force identified sub-areas of research Footnote 1 after analysing the local burden of neurological and sense disorders as well as considering factors such as local scientific expertise and research talent, ongoing efforts in neurological and sense disorders, industry interest, and opportunities for Singapore. As part of the effort, input was also solicited from the research community and policy-makers. This research prioritisation exercise served for both the NMRC grant scheme and a 10-year research roadmap [ 31 ].
Our study is the first to report on the processes used by a set of large national public funders to develop health research strategic plans. In line with findings from public management literature [ 16 , 17 ], we found that the formulation of a strategic plan is a well-established practice in shaping research agendas across international settings and it is a legal requirement for the majority of the organisations we studied.
We were able to reconstruct the process for developing the strategic plan by identifying the main actors involved and how they are connected. A complex picture emerges, in which multiple interactive entities and forces, often organised in a non-linear dynamic, appear to shape the research plans. In general, an organisation has to take into account legislative provisions, government directives, national overall research plans, national health plans and specific disease area plans. In some cases, it has to consider ‘institutionalised’ allocation of resources across organisations’ sub-entities (institutes, centres and units), which are historically associated with a particular disease or type of research.
On the other hand, we found little documentation of the decision-making mechanisms and information used to inform decision-making. There were, for example, few references to health research needs, research capabilities, the sources of information consulted, and the principles and criteria applied. This despite the increasing attention being paid nationally and internationally to the need for an explicit evidence-based or rational approach to setting health research priorities, particularly in the light of current economic constraints [ 3 , 32 , 33 ]. Given the complexity of the influences of different parties and factors, the governance of the health research sector would benefit from a traceable knowledge-based process of strategic planning, similar to that advocated for the health sector [ 34 ].
We found, however, evidence of an increasing interest in improving ways to establish research priorities at the organisational level. For example, NIH has brought forward the Senate request to develop a coordinated research strategy by including, in the strategic plan, the intention to further improve the processes for setting NIH research priorities and to optimise approaches to making informed funding decisions [ 21 ].
Recently, the DoD-CDMRP, the second largest funder of health research in the United States, reviewed its research management practices upon the recommendations of an ad hoc committee of the National Academies of Sciences, Engineering and Medicine. In the area of strategic planning, the committee recommended an analysis of the funding landscape across different agencies and organisations, the identification of short- and long-term research needs, and harmonisation with the research priorities of other organisations [ 35 ].
In its strategic plan, the JSPS has placed particular emphasis on the development of research-on-research capacity and infrastructures to analyse the research landscape at organisational, national and international levels in order to ensure that funding decisions are evidence based [ 36 ].
The allocation of sufficient resources to develop the infrastructure and technical expertise required for collection, analysis and dissemination of a portfolio of relevant data should be considered a necessary step when a funding organisation or country decides to implement standardised approaches for strategic planning and priority-setting.
Additionally, from the perspective of health research as a system, data collection and analyses should not be limited to ‘what is funded’, but should also include ‘who is funded and where’, and be linked to research policies and their long-term outcomes. The benefit of such an approach is not limited to the prevention of unnecessary duplication of research. Support would also be provided for producing formal mechanisms to coordinate research effort across research entities, within and among countries. Collaborations with other non-profit as well as for-profit organisations would be promoted and the capacity for research would be created and strengthened where necessary.
A number of resources and initiatives in this field already exist at organisational and national level. For example, the NIH has the Research Portfolio Online Reporting Tools, a public repository of data and other tools from NIH research activities [ 37 ]. This repository is linked to Federal RePORTER, an infrastructure that makes data on federal investments in science available. In the United Kingdom, the Health Research Classification System performs regular analysis of the funding landscape of United Kingdom health research to support monitoring, strategy development and coordination [ 38 ].
At the international level, there is ongoing global work to shape evidence-based health research decisions and coordination. In 2013, the WHO Global Observatory on Health R&D was established “ in order to monitor and analyze relevant information on health research and development, […] with a view to contributing to the identification of gaps and opportunities for health research and development and defining priorities […] and to facilitate the development of a global shared research agenda ” [ 33 ]. This effort has been coupled with a global call to action, which asks governments to create or strengthen national health research observatories and contribute to the WHO Observatory. Furthermore, the Clinical Research Initiative for Global Health, a consortium of research organisations across the world, has ongoing projects that will map clinical research networks and funding capacity and conduct clinical research at a global level [ 39 ].
A further key area that deserves comment is the engagement of stakeholders. In general, a spectrum of external stakeholders from multiple sectors is involved and the extent of this involvement varies across organisations. Decision-making processes commonly include people from government bodies, academia, research agencies and industry. However, we found that the participation of civil society, here represented by the intended beneficiaries of research such as health professionals, patients and their carers, remains limited. The fact that decision-making is still the domain of government officials and experts is an unexpected finding. There is a widespread consensus that the participation of a mix of stakeholders can improve the process of strategic planning. The logic behind this is that representatives of those who are affected by decisions can bring new information and perspectives and improve the effectiveness of the process [ 17 , 32 , 40 ]. Broader inclusion is desirable, both for granting legitimacy to strategic planning and for advancing equity in healthcare. Decisions on research priorities shape knowledge and, ultimately, they determine whether patients and their carers will have access to healthcare options that meet their needs [ 41 ].
Additionally, our study shows that the involvement of civil society is not only desirable but is also feasible. Organisations that support the participation of civil society have this practice firmly embedded in their governance, although it may be implemented in different ways.
Strengths and limitations
A particular strength of our study is the innovative way in which we approached the disorienting complexity of whole-organisation planning cycle management. This allowed us to contribute to an understanding of the processes used by large public funders not only in English-speaking countries but also in France, Italy and Spain.
However, one potential limitation concerns the accuracy and completeness of the information. This drawback was imposed by both the unstructured nature of the information and its fragmentation across multiple webpages and legal and/or administrative documents. Nevertheless, we strove to ensure accuracy, consistency and a clear presentation of the relevant information by means of a conceptual framework and a data abstraction form. In addition, to guarantee the reliability of the data, two reviewers abstracted the information independently, before discussing it and reaching a consensus. The use of more accessible information, e.g. through single documents, would therefore be advisable to improve accountability and transparency. This would also be of particular importance for exchanging knowledge and promoting research in the specific field of research governance.
In addition to the limitations imposed by the available data, there is a potential limitation in the methodology of the study. In conducting our research, we decided to rely only on publicly available information and we did not ask organisations for further details. Consequently, we may have missed some actions and drawn an incomplete picture of the organisations presented. Our strategy was based on the assumption that, if a strategic plan existed, both it and a description of its associated decision-making process would be present in the public domain, given that transparency in decision-making is an acknowledged element of good public organisation governance [ 42 ]. We would therefore counter that the process should be more transparent and should address, in particular, the criteria and information used to support decision-making.
In addition, it was not possible to ascertain in detail how processes actually took place. For example, engaging external stakeholders, such as representatives of civil society, is a key feature of the organisations included in the study but we do not know whether this engagement was meaningful or simply granted legitimacy to leadership decisions.
Furthermore, by limiting our inclusion criteria to organisations with strategic plans publicly available in English, French, Spanish and Italian, we excluded two German organisations (the German Research Foundation and the Bundesministerium für Bildung und Forschung – the Federal Ministry of Education and Research) and two Chinese bodies (the National Natural Science Foundation of China and the Ministry of Health). These organisations could have been included on the basis of their health research budgets. While it is unlikely that these bodies from two countries with similar health research systems have practices that would have changed our conclusions, it would nevertheless be useful in the future to acquire information regarding their experiences in this area.
Future research
Having considered the abovementioned limitations, we recommend that qualitative research be conducted to further validate our findings by complementing the information presented here with data gathered from key informants within each organisation. We also suggest that the study be extended to include other organisations and countries. Additional research should also expand on our study by more deeply exploring the perspectives of the members of external stakeholder bodies regarding their involvement in strategic planning within each organisation. Making this information accessible would benefit those funder organisations who wish to both increase public engagement in health research decision-making and make it more meaningful.
It would also be interesting to explore whether and why funder organisations are influenced by the research plans of other organisations (including academic, advocacy and international bodies) within and among countries, and whether they have formal mechanisms in place to coordinate with other such organisations. This information would be of use in guiding research coordination policies, with the aim of avoiding duplication of effort and identifying not only gaps in research but also overlapping interests and opportunities for partnerships.
Our study illustrates the variety of the processes adopted in developing strategic plans for health research in the international setting. A complex picture emerges in which multiple interactive entities appear to shape research plans. Although we found documentation of the actors involved in the processes, much less was available on the mechanisms, information, criteria and tools used to inform decision-making.
Given the complexity of the influences of different parties and factors, both funding organisations and health sector governance would benefit from a traceable knowledge-based process of strategic planning. The benefits of such an approach are not limited to demonstrating responsible budget stewardship as it would also provide opportunities to respond to research gaps and healthcare needs and to move more effectively from basic to translational research.

Availability of data and materials
All data generated or analysed during this study are included in this published article in Additional file 1 .
Neurodegenerative diseases (vascular dementia and Parkinson’s diseases), neurodegenerative eye diseases (age-related macular degeneration and glaucoma), mental health disorders (depression) and neurotechnology.
Abbreviations
High-income countries
United Kingdom Research and Innovation
National Institutes of Health
National Health and Medical Research Council
U.S. Department of Defense - Congressionally Directed Medical Research Programs
Institut national de la santé et de la recherche médicale
The Italian Ministry of Health
Canadian Institutes of Health Research
Medical Research Council
Centre National de la Recherche Scientifique
Japan Society for Promotion of Science
Instituto de Salud Carlos III
Singapore National Medical Research Council
Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. 2009;374:86–9. https://doi.org/10.1016/S0140-6736(09)60329-9 .
Article PubMed Google Scholar
World Health Organization. The WHO strategy on research for health. Geneva: WHO; 2012.
Google Scholar
Viergever RF. The mismatch between the health research and development (R&D) that is needed and the R&D that is undertaken: an overview of the problem, the causes, and solutions. Glob Health Action. 2013;6:22450. https://doi.org/10.3402/gha.v6i0.22450 .
Chalmers I, Bracken MB, Djulbegovic B, Garattini S, Grant J, Gülmezoglu AM, et al. How to increase value and reduce waste when research priorities are set. Lancet. 2014;383:156–65. https://doi.org/10.1016/S0140-6736(13)62229-1 .
UCL Institute for Innovation and Public Purpose. The people’s prescription: re-imagining health innovation to deliver public value. IIPP policy report, 2018–10. London: IIPP, Global Justice Now, Just Treatment, STOPAIDS; 2018.
Global Forum for Health Research. The 3D combined approach matrix: an improved tool for setting priorities in research for health. Geneva: Global Forum for Health Research; 2009.
Montorzi G, de Haan S, IJIsselmuiden C. Priority setting for research for health: a management process for countries. Geneva: Council on Health Research for Development (COHRED); 2010.
Viergever RF, Olifson S, Ghaffar A, Terry RF. A checklist for health research priority setting: nine common themes of good practice. Health Res Policy Syst. 2010;8:36. https://doi.org/10.1186/1478-4505-8-36 .
Article PubMed PubMed Central Google Scholar
Nasser M, Ueffing E, Welch V, Tugwell P. An equity lens can ensure an equity-oriented approach to agenda setting and priority setting of Cochrane reviews. J Clin Epidemiol. 2013;66(5):511–21. https://doi.org/10.1016/j.jclinepi.2012.11.013 .
Sharma T, Choudhury M, Rejón-Parrilla JC, Jonsson P, Garner S. Using HTA and guideline development as a tool for research priority setting the NICE way: reducing research waste by identifying the right research to fund. BMJ Open. 2018;8(3):e019777. https://doi.org/10.1136/bmjopen-2017-019777 .
James Lind Alliance. About the James Lind Alliance. http://www.jla.nihr.ac.uk/about-the-james-lind-alliance Accessed 14 Apr 2020.
Tomlinson M, Chopra M, Hoosain N, Rudan I. A review of selected research priority setting processes at national level in low and middle income countries: towards fair and legitimate priority setting. Health Res Policy Syst. 2011;9:19. https://doi.org/10.1186/1478-4505-9-19 .
McGregor S, Henderson KJ, Kaldor JM. How are health research priorities set in low and middle income countries? A systematic review of published reports. PLoS One. 2014;9(9):e108787. https://doi.org/10.1371/journal.pone.0108787 .
Article CAS PubMed PubMed Central Google Scholar
Bryant J, Sanson-Fisher R, Walsh J, Stewart J. Health research priority setting in selected high income countries: a narrative review of methods used and recommendations for future practice. Cost Eff Resour Alloc. 2014;12:23. https://doi.org/10.1186/1478-7547-12-23 .
Moher D, Glasziou P, Chalmers I, Nasser M, Bossuyt PM, Korevaar DA, et al. Increasing value and reducing waste in biomedical research: who’s listening? Lancet. 2016;387(10027):1573–86. https://doi.org/10.1016/S0140-6736(15)00307-4 .
Viergever RF, Hendriks TC. The 10 largest public and philanthropic funders of health research in the world: what they fund and how they distribute their funds. Health Res Policy Syst. 2016;14:12. https://doi.org/10.1186/s12961-015-0074-z .
Bryson JM, Hamilton Edwards L. Strategic planning in the public sector. In: Oxford research encyclopedia of business and management. https://doi.org/10.1093/acrefore/9780190224851.013.128 . Accessed date 2 Sep 2020.
Bryson JM, Hamilton Edwards L, Van Slyke DM. Getting strategic about strategic planning research. Public Manage Rev. 2018;20(3):317–39. https://doi.org/10.1080/14719037.2017.1285111 .
Article Google Scholar
Walt G, Gilson L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan. 1994;9(4):353–70. https://doi.org/10.1093/heapol/9.4.353 .
Article CAS PubMed Google Scholar
National Institutes of Health. Who we are. https://www.nih.gov/about-nih/who-we-are Accessed 14 Apr 2020.
National Institutes of Health. Department of Health & Human Services. NIH-Wide strategic plan. Fiscal year 2016–2020. https://www.nih.gov/sites/default/files/about-nih/strategic-plan-fy2016-2020-508.pdf Accessed 14 Apr 2020.
National Institute of Standards and Technology, U.S. Department of Commerce. Consolidated and further Continuing Appropriation Act 2015 (P.L.113–235). https://www.nist.gov/system/files/documents/director/legislation/fy2015/MAIN_NIST_APPN_LANG_PL-113-235.pdf . Accessed 14 Apr 2020.
21st Century Cures Act. H.R. 34, 114th Congress. 2016. https://www.congress.gov/bill/114th-congress/house-bill/34 . Accessed 14 Apr 2020.
National Institutes of Health. NIH Wide Strategic Plan. https://www.nih.gov/about-nih/nih-strategic-plan . Accessed 14 Apr 2020.
National Institutes of Health. Advisory Committee to the Director. https://acd.od.nih.gov . Accessed 14 Apr 2020.
National Institutes of Health. Council of Councils. https://dpcpsi.nih.gov/council . Accessed 14 Apr 2020.
National Institutes of Health. NIH Request for Information: Inviting Comments and Suggestions on a Framework for the NIH-wide Strategic Plan. Analysis of Public Comments. October 2015. https://www.nih.gov/sites/default/files/about-nih/nih-strategic-plan-rfi-comments-suggestions-framework.pdf Accessed 14 Apr 2020.
National Medical Research Council Singapore. Who we are. http://www.nmrc.gov.sg/about-us . Accessed 14 Apr 2020.
Singapore Government, National Research Foundation. Research, Innovation Enterprise 2020 Plan. https://www.nrf.gov.sg/docs/default-source/default-document-library/rie2020-publication-(final-web).pdf . Accessed 14 Apr 2020.
National Medical Research Council Singapore. Who we are. HBMS Disease Taskforces’ Reports. https://www.nmrc.gov.sg/who-we-are/hbms-disease-taskforces-reports . Accessed 14 Apr 2020.
National Medical Research Council Singapore. Neurological and Sense Disorders Taskforce Report. http://www.nmrc.gov.sg/docs/default-source/about-us-library/nstf-summary-report.pdf . Accessed 14 Apr 2020.
Nuyens Y. Setting priorities for health research: lessons from low- and middle-income countries. Bull World Health Organ. 2007;85(4):319–21. https://doi.org/10.2471/blt.06.032375 .
World Health Organization. Follow up of the report of the Consultative Expert Working Group on Research and Development: Financing and Coordination. Resolution WHA66.22, 27 May 2013. https://www.who.int/phi/resolution_WHA-66.22.pdf . Accessed 27 Mar 2020.
World Health Organization. WHO strategizing national health in the 21 century: a handbook. Geneva: WHO; 2016. https://apps.who.int/iris/handle/10665/250221 . Accessed 14 Apr 2020.
National Academies of Sciences, Engineering, and Medicine. Evaluation of the congressionally directed medical research programs review process. Washington, DC: The National Academies Press; 2016.
Japan Society for the Promotion of Science. About us, Brochure JSPS 2017–2018. http://www.jsps.go.jp/english/aboutus/data/brochure17-18_e.pdf . Accessed 10 Dec 2019.
National Institutes for Health. Research Portfolio Online Reporting Tools (RePORT). https://report.nih.gov/index.aspx . Accessed 14 Apr 2020.
Carter JG, Sherbon BJ, Viney IS. United Kingdom health research analyses and the benefits of shared data. Health Res Policy Syst. 2016;14:48. https://doi.org/10.1186/s12961-016-0116-1 .
Clinical Research Initiative for Global Health. About Crigh. https://crigh.org/about-crigh . Accessed 14 Apr 2020.
Fung A. Varieties of participation in complex governance. Public Adm Rev. 2006;66:66–75.
Pratt B, Merritt MM, Hyder AA. Towards deep inclusion for equity-oriented health research priority-setting: a working model. Soc Sci Med. 2016;151:215–24. https://doi.org/10.1016/j.socscimed.2016.01.018 .
Greer SL, Vasev N, Jarman H, Wismar M, Figueras J. It’s the governance, stupid! TAPIC: a governance framework to strengthen decision making and implementation (Policy Brief 33). Geneva: WHO; 2019. http://www.euro.who.int/__data/assets/pdf_file/0012/416100/PolicyBrief_PB33_TAPIC.pdf?ua=1 . Accessed 14 Apr 2020.
Download references
Acknowledgements
The authors thank Letizia Sampaolo, Istituto Superiore di Sanità, the information specialist who made an initial search of relevant scientific articles, and Stephen James for English language review of the manuscript.
This research was partly supported by funding for 'Ricerca Corrente' of the Istituto Superiore di Sanità.
Author information
Authors and affiliations.
Research Coordination and Support Service, Istituto Superiore di Sanità, Viale Regina Elena, 299, 00161, Rome, Italy
Cristina Morciano, Maria Cristina Errico & Luisa Minghetti
National Centre for Disease Prevention and Health Promotion, Istituto Superiore di Sanità, Rome, Italy
Carla Faralli
You can also search for this author in PubMed Google Scholar
Contributions
CM conceived of the study and made a first drafted the work. CM, MCE and CF abstracted the data and compiled the organisations’ profiles. LM contributed to the draft and substantively revised the work. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Cristina Morciano .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1..
Data abstraction form. (a) Table of the included and excluded organisations with reasons; (b) table of the included organisations with budget; (c) the organisations’ profiles according to the fields of the conceptual framework; and (d) full list of the consulted references and web pages for each organisation’s profile.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Morciano, C., Errico, M.C., Faralli, C. et al. An analysis of the strategic plan development processes of major public organisations funding health research in nine high-income countries worldwide. Health Res Policy Sys 18 , 106 (2020). https://doi.org/10.1186/s12961-020-00620-x
Download citation
Received : 18 April 2020
Accepted : 09 August 2020
Published : 18 September 2020
DOI : https://doi.org/10.1186/s12961-020-00620-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health research
- Research plan
- Health research system
- Research priority-setting
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

How To Implement Effective Strategic Planning In Healthcare

Are you feeling overwhelmed and uncertain about the future?
According to Deloitte , “The global healthcare sector stands at a crossroads in 2024, poised for profound changes. The future of global healthcare is likely to be shaped by innovation, sustainability, social care integration, cost management, and workforce adaptation.”
If you work in the healthcare industry, you know firsthand how quickly things can change. As technology advances, regulations change, the population ages, and new diseases evolve at lightning speed, it can be tough to keep up.
That's why implementing an effective strategic planning process that is execution-ready is so important. It's a tool that helps healthcare organizations prioritize their goals, anticipate potential roadblocks, and quickly adapt to seize new opportunities.
Whether you’re a manager or a top-level executive, this article will provide valuable insights and guidance to help you develop and execute a successful strategic plan.
We'll also show you how Cascade can help you successfully plan, execute, and track your healthcare strategy in one centralized location. Plus, as a bonus, we'll provide a free strategic planning template prefilled with healthcare examples to help you get started.
So, let's dive in and discover how strategic planning can help you navigate the changing landscape of the healthcare environment and achieve your organization’s goals.

Strategic Planning In Healthcare: What Is It?
Strategic planning in healthcare helps you set business goals and decide how to allocate resources to achieve these goals. It involves looking at your organization’s internal and external environments using established strategic tools .
Doing so lets you develop a strategic plan outlining what you want to achieve and an action plan to get there. Think of it like building a roadmap that helps you get to where you want to go.
With a healthcare strategy, you’ll have a framework for improved decision-making that is aligned with your overarching business objectives . This ensures you’re moving towards your long-term goals and objectives, even when making short-term decisions.
Examples Of Strategic Planning In Healthcare
Strategic planning can significantly enhance the operational efficiency and service quality of healthcare organizations. Here are some specific examples of how you can use strategic planning:
- Boosting Patient Care Quality : Tackle specific challenges like lowering the rates of hospital-acquired infections or enhancing the coordination of patient care. By pinpointing these areas, you can implement targeted improvements that directly benefit patient outcomes.
- Optimizing Staff and Resource Management : Utilize data analytics to make evidence-based decisions regarding staffing and resource distribution. This approach ensures that your workforce is optimally aligned with patient needs, and your resource allocation is efficient, contributing to a more effective healthcare system.
- Exploring New Avenues for Growth : Seize opportunities to expand your services and reach by integrating telehealth, offering home healthcare solutions, or developing specialized programs tailored to unique patient demographics. Such strategic initiatives can open new revenue streams and meet the evolving needs of your community.
- Improving Financial Health : Identify strategies for cost reduction and revenue enhancement, such as streamlining supply chain operations or venturing into untapped markets. These measures can bolster your organization's financial stability, allowing for reinvestment in key areas.
- Fostering Partnerships for Comprehensive Care : Establish collaborations with community organizations, other healthcare providers and facilities, or specialists to broaden your service offerings and improve patient care. Partnerships can lead to a more integrated care model that addresses a wide range of patient needs.
📚 Recommended read: Strategy study: The Ramsay Health Care Growth Study
Healthcare Strategic Planning: Why Is It Important?
Strategic planning in healthcare is more than just setting goals; it's about ensuring your organization is on the right track for success.
These are some of the countless benefits of strategic planning in healthcare:
Boost profitability
Strategic planning helps healthcare leaders improve their organization’s financial performance and achieve long-term sustainability. It's about using resources wisely, cutting costs where possible, and smoothing out inefficiencies by streamlining processes and creating better strategic initiatives to increase patient volume and improve experience.
Additionally, strategic planning plays a crucial role in uncovering new opportunities for revenue, enabling healthcare organizations to diversify their sources of income.
Enhance collaboration and engagement
Strategic planning in healthcare goes beyond identifying operational challenges; it's about bringing to light the issues that affect our teams daily, such as the strain of long work hours. When staff feel overburdened, their motivation dips, leading to decreased engagement and higher turnover rates.
By articulating a clear vision for the organization and actively involving employees in the strategic planning process, we can significantly boost morale. It's about making sure everyone feels seen and heard, understanding that their contributions are valued. This inclusive approach not only enhances team engagement but also encourages stronger retention.
Strategic planning also fosters collaboration across different teams and business units within the healthcare organization. By working together towards common goals, departments can better align their efforts, share insights, and support each other in achieving the organization's objectives. This synergy not only improves efficiency but also builds a more cohesive and motivated workforce.
💡Pro Tip : Ensure your vision statement is crystal clear organization-wide for unified strategic alignment.
Increase efficiency
Strategic planning helps you align your operational activities with the organization’s goals. This ensures that every action contributes toward achieving your business objectives. Strategic planning also empowers healthcare leaders, providing them with the insights needed to make resource allocation decisions wisely in the dynamic healthcare landscape.
Improve communication
A good strategic plan should be shared with all stakeholders so they can form a clear picture of how their actions affect a future outcome. This transparency promotes better communication within the organization, as employees align their efforts towards achieving a common goal. The end result is a more collaborative environment where the collective focus is on attaining shared objectives.
Drive alignment and strategy execution
Involving key stakeholders in the strategic planning process is crucial for aligning your healthcare organization's goals with its overarching strategy. This ensures that everyone, from top management to frontline staff, is aligned and moving in the same direction. Achieving this level of strategic harmony across the organization reduces confusion and clarifies the collective mission, paving the way for successful strategy implementation. This collaborative approach not only fosters a unified effort towards common objectives but also enhances the overall effectiveness of the organization's strategic initiatives.
💡Pro Tip : Ensure you balance a top-down and bottom-up for enhanced vertical and horizontal strategic alignment .
5 Strategic Planning Tools For Your Healthcare Strategy
Here’s a list of strategy tools and frameworks that can help you identify gaps in your healthcare strategy, prioritize strategic initiatives, and develop business goals:
1. Balanced Scorecard (BSC)
The Balanced Scorecard translates strategic goals into measurable indicators or metrics to help you balance four critical organizational perspectives: financial, customer, internal processes, and organizational capacity.
Using this tool ensures that your organization aligns with your strategic objectives and that you’re measuring the right KPIs to track progress toward those objectives.
2. Objectives and key results (OKR)
The OKR framework sets specific and measurable objectives and tracks progress toward them using key results. Objectives should be ambitious and challenging but achievable. Meanwhile, key results should be specific and measurable and have defined target values.
This framework promotes accountability and transparency since everyone works toward the same goals.
3. Political, economic, sociocultural, and technological (PEST) analysis
PEST analysis helps you understand the external factors that may impact your operations. By using this tool, you can identify potential opportunities and threats so you can anticipate and respond to changes in the external environment.
For example, PEST can help you identify a shift toward consumer-driven healthcare. Consequently, this enables you to invest in telemedicine and other digital healthcare technologies to meet patients’ changing needs.
4. Strengths, weaknesses, opportunities, threats (SWOT) analysis
SWOT analysis is a simple yet powerful way to identify the internal and external factors that can impact your organization’s success.
For example, if you discover that staffing levels are a weakness, you may decide to invest in staff training or recruitment programs. Or, if you identify an opportunity to expand into a new service area, you may choose to allocate resources for the expansion.
By leveraging your organization's strengths through this analysis, you can craft targeted strategies that address challenges and capitalize on opportunities for sustained success.
5. Theory of change (TOC)
The theory of change is a framework that helps your organization articulate the desired outcomes and specific steps you need to take to achieve them. This model provides a more structured approach to achieving goals by identifying the inputs required for success.
For example, if you want to reduce hospital readmissions, you may use the theory of change to identify the inputs needed (staff training on patient education), activities needed (discharge planning), and desired outcomes (reduction in hospital readmissions). By mapping out this logic model and continuously evaluating the initiative, your organization can adjust its activities to achieve your desired outcomes and improve the quality of care for your patients.
📚 Recommended read: 26 Best Strategy Tools For Your Organization in 2024
How To Implement A Strategic Plan In Healthcare
Implementing a strategic healthcare plan can be challenging. Follow this step-by-step framework to help you get started.
💡Pro Tip : Streamline your healthcare strategy planning, execution, and tracking with Cascade Strategy Execution Platform . It serves as a centralized hub for enhanced decision-making and accelerated results. Unsure of where to begin? Kickstart your strategic planning process with our complimentary pre-filled healthcare strategy template .
1. Establish goals
The first step is to establish clear and measurable goals. These goals should align with your organization’s mission and vision , and be SMART (specific, measurable, achievable, relevant, and time-bound).
Examples of goals in healthcare include reducing hospital readmission rates, improving patient satisfaction scores, or increasing revenue.
👉🏻How Cascade can help? With Cascade's Planner feature , you can simplify the process of constructing your strategies. It provides a structured approach, making it effortless to break down complex high-level initiatives into actionable outcomes.
2. Set milestones and measure progress
Once you establish goals, it’s important to set milestones and measure progress regularly. This allows your organization to track its progress toward achieving its goals, identify areas for improvement, and make necessary adjustments.
Make sure to establish a timeframe for your milestones, whether it's monthly, quarterly, or yearly, depending on the nature of your goal.
👉🏻How Cascade can help? Cascade's Metrics Library offers a centralized repository for your business metrics, allowing you to seamlessly link these metrics to your plan's Key Performance Indicators (KPIs). Integrating core metrics becomes a breeze, whether they originate from your business systems, data lakes, Business Intelligence (BI) tools, or spreadsheets.
3. Develop an execution plan
To successfully achieve your goals, it is essential to have a comprehensive execution plan . This plan should detail all the necessary activities and strategies that will guide you toward success.
An effective execution plan must include a well-structured timeline, a checklist of required resources, and clearly defined responsibilities for each action or project.
👉🏻How Cascade can help? Cascade's Alignment Maps feature empowers you to monitor the interactions between activities by documenting and examining dependencies, blockers, and risks that might arise during your strategic journey. This ensures a smooth path to successful strategy execution.
4. Monitor performance and adapt as needed
Once the plan is in motion, you should monitor its performance regularly and make necessary adjustments when you notice deviations. You must be flexible and willing to change your execution plan as needed.
For example, if the original plan doesn't turn out to be effective, it's important to quickly reevaluate and come up with an alternative strategy.
👉🏻How Cascade can help? Cascade's Dashboards & Reports allow you to gain accurate, real-time insights into your strategic performance, enabling you to easily share this information with your stakeholders.
5. Communicate regularly
Communication is key in implementing a strategic plan . Each stakeholder should understand their role and how their work fits into the big picture. You must inform them of progress toward the established goals, any changes to the execution plan, and other relevant information. This will help you build trust and get buy-in, which are essential for successful strategy execution.
6. Celebrate successes
Celebrating successes helps maintain motivation and momentum. It shows staff and stakeholders that their hard work is paying off. This can be done in various ways, such as recognizing staff members who have contributed significantly to the plan or sharing positive feedback from patients.
Positive reinforcement will motivate employees to keep striving to achieve your organization’s objectives.
📚 Recommended read: How Parker University uses Cascade to help them hold a position as a leader in Patient-Centric Healthcare
Case Study: Perley Health’s Strategic Ambition
Perley Health, a healthcare organization dedicated to improving care for veterans and seniors, faced some significant challenges in their strategic planning and execution processes. These challenges included making assumptions about the stability of the external environment in their long-term planning, inconsistency in how different departments planned and reported, a lack of clarity in how they measured success, and a somewhat fragmented approach to strategic and departmental plans.
Perley Health's journey toward strategic improvement began with the adoption of Cascade, a pivotal decision for them. Initially, they used Cascade to bring together all their strategic plans and initiatives, which brought about greater transparency and alignment with their organizational priorities. This not only made resource allocation more efficient but also provided a standardized way to measure results, making it easier to discuss return on investment (ROI) and track progress systematically.
Empowered by Cascade's capabilities, the management and various teams could now propose forward-thinking initiatives with a clear view of how they aligned with strategic priorities. This sped up decision-making and made funding allocation more precise.
With the right tools in place, Perley Health is now confidently working towards their goal of doubling senior care and establishing themselves as a center of excellence in frailty-informed care. They keep a close eye on their progress using the Cascade platform.
This case underscores the critical importance of strategic planning in navigating the complexities of healthcare, demonstrating a clear path to achieving and surpassing organizational objectives.
📚 Read the complete Perley Health Case Study!
Execute Your Healthcare Strategy With Cascade 🚀
Take the guesswork out of strategic planning in healthcare. With Cascade , you can easily create an execution plan customized to your goals and objectives, including assigning initiatives and setting deadlines for each team member involved.
Take a look at this example of a healthcare strategic plan in Cascade:

You can also leverage easy-to-use dashboards and visualizations that provide real-time data on your progress toward your goals.
Here’s an example of a real-time dashboard:

Cascade lets you collaborate with your team, assign responsibilities, and communicate progress, ensuring everyone is aligned and working toward the same objectives.
Whether you run a small clinic or a large healthcare organization, Cascade will help you make strategic planning in healthcare a breeze. Learn more about Cascade for healthcare !
Looking for a tailored tour of our platform? Book a demo with one of our Strategy Execution experts.
Popular articles

Viva Goals Vs. Cascade: Goal Management Vs. Strategy Execution

What Is A Maturity Model? Overview, Examples + Free Assessment
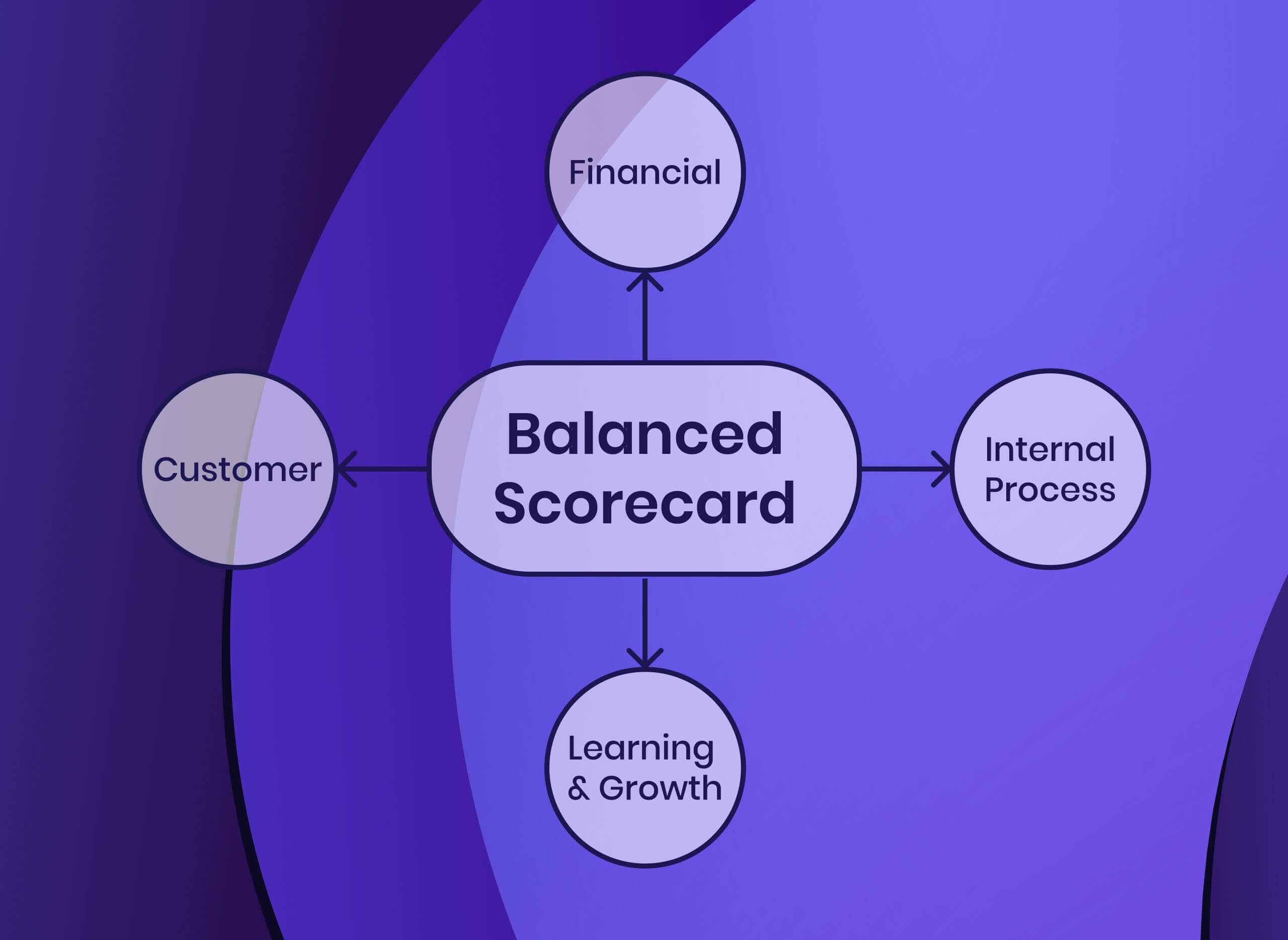
How To Implement The Balanced Scorecard Framework (With Examples)

The Best Management Reporting Software For Strategy Officers (2024 Guide)
Your toolkit for strategy success.

- Research article
- Open access
- Published: 26 February 2015
Training hospital managers for strategic planning and management: a prospective study
- Zorica Terzic-Supic 1 ,
- Vesna Bjegovic-Mikanovic 2 ,
- Dejana Vukovic 1 ,
- Milena Santric-Milicevic 1 ,
- Jelena Marinkovic 3 ,
- Vladimir Vasic 4 &
- Ulrich Laaser 5
BMC Medical Education volume 15 , Article number: 25 ( 2015 ) Cite this article
24k Accesses
17 Citations
4 Altmetric
Metrics details
Training is the systematic acquisition of skills, rules, concepts, or attitudes and is one of the most important components in any organization’s strategy. There is increasing demand for formal and informal training programs especially for physicians in leadership positions. This study determined the learning outcomes after a specific training program for hospital management teams.
The study was conducted during 2006 and 2007 at the Centre School of Public Health and Management, Faculty of Medicine, University of Belgrade and included 107 participants involved in the management in 20 Serbian general hospitals. The management teams were multidisciplinary, consisting of five members on average: the director of the general hospital, the deputy directors, the head nurse, and the chiefs of support services. The managers attended a training program, which comprised four modules addressing specific topics. Three reviewers independently evaluated the level of management skills at the beginning and 12 months after the training program. Principal component analysis and subsequent stepwise multiple linear regression analysis were performed to determine predictors of learning outcomes.
The quality of the SWOT (strengths, weaknesses, opportunities and threats) analyses performed by the trainees improved with differences between 0.35 and 0.49 on a Likert scale ( p < 0.001). Principal component analysis explained 81% of the variance affecting their quality of strategic planning. Following the training program, the external environment, strategic positioning, and quality of care were predictors of learning outcomes. The four regression models used showed that the training program had positive effects ( p < 0.001) on the ability to formulate a Strategic Plan comprising the hospital mission, vision, strategic objectives, and action plan.
This study provided evidence that training for strategic planning and management enhanced the strategic decision-making of hospital management teams, which is a requirement for hospitals in an increasingly competitive, complex and challenging context. For the first time, half of state general hospitals involved in team training have formulated the development of an official strategic plan. The positive effects of the formal training program justify additional investment in future education and training.
Peer Review reports
Strategic management comprises drafting, implementing, and evaluating cross-functional decisions that enable an organization to achieve its long-term strategic objectives [ 1 ]. Changes in the external environment (i.e., demographic and epidemiological transitions, economic fluctuations, public and political expectations), and within the health care system (i.e., health market, demands, costs, new technologies, regulations) have put pressure on hospital managers to implement strategic management programs to respond to environmental challenges [ 2 - 5 ]. Leadership development [ 6 ] implies that a Strategic Plan should be in place, with the organization’s mission, vision, strategic objectives, and action plans aimed at achieving these objectives [ 7 ]. A hospital develops strategies, which must be derived from a situational or strategic analysis, which most often is performed by a SWOT analysis (strengths, weaknesses, opportunities and threats).
Continuing education and training have become part of the ongoing processes of organizational learning and permanent change, employee evaluation, and career development [ 8 ]. In addition, they are essential tools for managers to improve their management skills and to learn new skills [ 9 - 11 ]. Training can be defined as the systematic acquisition of skills, rules, concepts, or attitudes, which result in improved performance [ 12 ]. There is an increasing demand for formal and informal training programs in health organizations, especially for physicians in leadership positions who need to acquire managerial and leadership skills. In some hospitals, significant resources are devoted to educate the institution’s managers [ 13 ]. Training is one of the most important components in any organization’s strategy, and evaluation is an essential part of the training system [ 14 ].
However, organizations, including hospitals, spend little time on evaluating their training programs [ 15 - 20 ]. Numerous reasons have been identified: disbelief in the benefits of evaluation, lack of confidence in whether training has an impact on the organization, as well as lack of resources, expertise, and organizational support [ 21 ]. The expansion of Kirkpatrick’s four-level evaluation model has emphasized the importance of training evaluation [ 15 ]. This model includes measurement of reactions to training, learning attainment, transfer and subsequent individual behavior, and organizational results [ 16 ]. Most evaluations of this model have focused on its first two levels. Several authors have also researched the effect of training on individual job performance or the results achieved within their own organization [ 17 - 19 ]. The benefits of training evaluation are widely recognized as a diagnostic tool for training revisions, and for evidence of training effectiveness, such as successful learning, improved on-the-job performance, changes in key business measures, and return on investment. In addition, training evaluation should influence decision making [ 22 - 24 ]. Furthermore, training evaluation may have ethical implications for professional development [ 25 ].
In Serbia, the health care system has declined during the past two decades due to the country’s unstable political situation and long-term, weak economic development [ 25 ]. Consequently, in many cases the performance of Serbian hospitals has yet to reach a satisfactory level [ 25 ]. Therefore, there is a demand for systematic interventions, including multidisciplinary management training for stronger management of the health care system in Serbia. This was recognized by different international organizations and supporting management capacity building programs [ 26 , 27 ]. Formal training of health managers was not common in Serbia before the democratic transition that took place in the year 2000 [ 28 ]. In the mid - 2000, the Serbian government adopted laws which supported formal education and the necessity to improve the specific skills and knowledge of health professionals in the field of health care management (continuing education, postgraduate academic programs) [ 29 - 31 ]. The recognition and application of advanced managerial skills became basic requirements for managing hospitals as well as other health care institutions in Serbia. This has influenced the quality of services, accountability and effectiveness in the hospitals [ 32 , 33 ].
An earlier study focused on the skills improvement of individual hospital managers [ 34 ]. The aim of this study was to determine the learning outcomes after a specific training program for hospital management teams.
Study design
The study was conducted during 2006 and 2007 at the Centre School of Public Health and Management, Faculty of Medicine, University of Belgrade. Twenty management teams from 40 general hospitals in Serbia took part. Hospitals eligible for training were selected by the Ministry of Health of Serbia and participated in the capacity-building project sponsored by the Ministry and the European Agency for Reconstruction [ 35 ]. The participating hospitals had an average number of approximately 300 beds.
The management teams were multidisciplinary, consisting of five members on average: the director of the general hospital, the deputy directors, the head nurse, and the chiefs of support services. The total number of managers was 107. Managerial teams comprised clinical physicians (27.1%), economists (21.5%), lawyers (18.7%), engineers (16.8%), and nurses (14.0%). The specialists among the physicians were mostly from surgery (24.3%) and internal medicine (12.6%). The average age of the managers was 47.7 ± 7.0 years. The average number of years of service was 21.9 ± 7.8 and for managerial experience 11.1 ± 8.0 years. The share of female managers who held the position of director or deputy director was 30.6%. Almost two-thirds (63.6%) of the participating managers had previously attended some form of managerial training (seminars, workshops), but without obtaining a formal management degree or certificate.
Description of training program
During a six-month period, the hospital management teams attended training for health management that comprised four sessions of 48-hour modules addressing specific topics: Basic Health Management, Hospital Management, Health Information Management, and Total Quality Management. Twenty hours were contact hours in the classroom and 40 included individual work, which involved 60 learning hours per module.
The module of Basic Health Management included basic functions of management, the specifics of management in health care organizations, and the application of strategic management tools, such as SWOT and Strategic Plan development (the mission, vision, objectives, and action plan) [ 36 , 37 ] (Table 1 ).
During the module of Basic Health Management, each participating management team performed the first SWOT analysis of their hospital. Throughout the entire six-month training period, the management teams were able to consult with trainers, either by e-mail or directly, regarding their work in the context of preparing the second SWOT analysis and developing a Strategic Plan for the hospital.
Based on identification of the strengths, weaknesses (Table 2 ), opportunities, and threats (Table 3 ), the teams attempted to agree on the best of the four SWOT strategies [ 36 - 39 ] for their own hospital, listed below (Table 4 ).
Comparative Advantage Strategy or Maxi-Maxi means the ability of hospitals to maximize strengths and opportunities and take advantage of the market. Investment/Divestment Strategy or Mini-Maxi means to minimize the weaknesses and to maximize the opportunities. The question is, should a hospital invest its scarce resources in weak programs in order to make them more competitive vis-à-vis a perceived opportunity? Mobilization Strategy or Maxi-Mini is based on the strengths of the hospital that can deal with the threats of the environment and the possibility of mobilizing its strengths to avert a perceived threat or even transform this threat into an opportunity. Damage Control Strategy or Mini-Mini is a survival strategy, which includes temporary measures to minimize weaknesses of, and threats to, a hospital (Table 4 ).
The Hospital Management module aimed to develop management and leadership capacity for hospital management, using the basic principles of social marketing and also to assess hospital performance, payment, and organizational modalities. The third module, Health Information Management, explored information flow in the health care system, computer-assisted learning, and document-management systems. Finally, within the fourth module, Total Quality Management (TQM), managers learned about quality in health care, analysis of quality indicators, and the application of the TQM method.
Twelve months after the beginning of the training program, within the Change Management module, the hospital management teams presented a Strategic Plan for their hospital based on the second SWOT analysis. The managers had been prepared for this task throughout the four modules by a combination of lectures, case studies, task-orientated activities, and directed learning.
Evaluation procedure
Three independent reviewers of the training program, from the university environment (Faculty of Organizational Sciences and Faculty of Medicine, Departments of Epidemiology and of Social Medicine) performed a review after the end of the training program. Two reviewers had a PhD degree in Management, while the third one had certificates from several relevant international training centres in the field of Health Management. All three reviewers had experience and were involved in health care system work. The average length of managerial experience was 18 ± 1.63 years. They assessed the quality of the two anonymous SWOT analyses carried out by the 20 management teams: the first SWOT was delivered at the beginning of training during the first module (20 analyses of SWOT-I), and the second SWOT, 12 months later (20 analyses of SWOT-II). They also assessed the quality of the Strategic Plans (20 hospital plans) developed by the teams after the second SWOT analysis. The reviewers did not know in advance which hospital SWOT analyses or Strategic Plans they would evaluate. Each reviewer assessed 40 SWOT analyses (SWOT-I and SWOT-II) and 20 hospital strategic plans.
The reviewers used a specific questionnaire comprising 37 questions, organized in four parts following the hospital’s mission and vision and its objectives and action plan [ 36 , 39 ]. The answers to the questionnaire were ranked on a Likert scale from 1 (very poor) to 5 (excellent). Questions relating to the quality of SWOT analysis were directed at the analysis of the external and internal environment and how technical rules were applied in the SWOT analyses. For example, the number of items pertaining to the external and internal environment, whether the items were arranged from most to least important and according to the external and internal environment, and identification and clarification of hospital strategies.
Next, questions regarding the managers’ vision statements focused on the hospital’s state and function and whether the vision was culture-specific, brief, verifiable, focused, flexible, understandable to all employees, and inspirational. Questions relating to the mission statement addressed the organization’s purpose, its business values, client orientation, and use of proactive verbs to describe what hospitals do. The evaluation of strategic objectives considered the number of objectives and whether they were SMART (i.e. specific, measurable, achievable, relevant, and time frame) [ 39 ]. Finally, the action plan was evaluated in relation to activities, results, staff responsibility, realistic budgeting, and the existence of a time frame for each objective.
Statistical analysis
The continuous variables, according to the Likert scale, were expressed as means and their standard deviation. If the group variances were not homogenous, as evidenced by Levene’s test , the p -values were adjusted. The internal consistency and reliability of each reviewer were determined using intra-class correlation coefficients (ICC) related to the means. The significance of the ICCs was tested by a two - way ANOVA random effects model. Cronbach's alpha was used to estimate the internal consistency of questions that comprised several items, such as those regarding technical skills in the SWOT analysis, SMART objectives, and action plan. The internal consistency was considered acceptable when Cronbach’s alpha coefficient ≥0.7 [ 40 ]. Paired sample tests were used to compare means and thus identify differences indicative of improvement for items of the SWOT analyses conducted at the beginning of the program and again 12 months later. Principal component (PC) analysis with varimax rotation and the Kaiser criterion was applied with 13 variables in the SWOT analyses, before and after training, to detect common dimensions. Principal components were described by variables with a loading > 0.7. A stepwise multiple linear regression analysis was applied to determine predictors of quality of the Strategic Plans developed by the managerial teams (hospital mission, vision, strategic SMART objectives, and action plan).
Ethical approval
The study was reviewed and given ethical approval by the Ethics Committees at the School of Medicine in Belgrade. All participants received cover letters which contained detailed information on objectives and methodology of the research and consent forms. All participants gave written, informed consent.
The consistency of judgments given by each reviewer for the SWOT analyses ranged between 0.50 and 1.00 (Table 5 ) and for the Strategic Plans between 0.92 and 0.97 (Table 6 ). There was a high degree of matching among the reviewers, especially in the evaluation of the Strategic Plan ( p < 0.001 for the intra-class correlation coefficient), assessed twelve months after the end of the training program (Table 6 ).
In the first SWOT analysis, the reviewers gave the lowest grades for the analysis of several external factors (evidence-based analysis of the environment, analysis of competitors and stakeholders). However, all grades improved significantly in the second SWOT analysis after the training program ( p < 0.001). With regard to the Strategic Plan, the three reviewers assessed the learning outcomes with grades ranging from 3.30 (realistic budgeting) to 4.19 (hospital vision).
In a PC analysis of the 13 SWOT variables, two components (PC I) before training and three components (PC II) after training together explained 70.2% and 80.9%, respectively, of the variance affecting strategic planning. Prior to training, the first principal component was strategic planning ability (PC I-1); the second was internal environment (PC I-2). After training, the principal components were: external environment (PC II-1), strategic positioning (PC II-2), and quality of care (PC II-3) (Table 7 ). These new variables, i.e., the principal components, were used as independent variables in the subsequent regression analysis to determine predictors of learning outcomes (Table 8 ).
The four regression models, hospital mission, vision, SMART objectives, and action plan, as outcome dimensions were significant. At the start of the training program, strategic planning ability (PC I-1) and internal environment (PC I-2) had a positive significant influence on the quality of the description of the hospital’s mission, vision, and action plan, while only strategic planning ability (PC I-1) had a positive significant influence on SMART objectives. Twelve months after the end of the training program, the external environment (PC II-1), strategic positioning (PC II-2), and quality of care (PC II-3) had a positive significant influence on the quality of the description of the hospital’s mission and vision. External environment (PC II-1) and strategic positioning (PC II-2) had a positive significant influence on SMART objectives and the action plan (Table 8 ).
The aim of this study was to determine learning outcomes after a specific training program for hospital management teams. The results of our training program for hospital management teams, offered by the Centre School of Public Health and Management in Belgrade, for the first time in Serbia, provide evidence which support training hospital managerial teams in strategic planning and management. The framing of strategic issues is a critical component of hospital management as it can provide health policy makers with the opportunity to take the initiative.
Тhis study analysed the possibility of transferring management principles to healthcare management, throughout assessment of the learning outcomes in management teams, regarding the quality of SWOT analysis and the development of a Strategic Plan. Multiple linear regression analysis identified four significant models: hospital mission, vision, SMART objectives, and the action plan.
Following the training program, external environment, strategic positioning, and the quality of care were predictors of learning outcomes. The quality of the second SWOT analyses was improved mainly because hospital managers recognized the relevance of the external environment exploration and their position in it, based on evidence (patterns of disease, quality of care, costs), stakeholder analysis (i.e., the private sector and other public hospital services and customers) and financial resources. As a result, the teams were able to better describe market dynamics and to propose specific strategies for hospitals, SMART objectives and the action plan. In relation to the open market, hospitals managerial teams tried to improve their position through delivery of new services and resources.
Quality of care was the most important independent component in the definition of hospital mission and vision. The managerial teams recognized the relevance of customers’ and employees’ perspectives for the improvement of mission and vision statements, capacity to deliver better quality of care, and patient satisfaction enhancement.
SWOT analysis is one of the most common tools in strategic management, e.g. in the Netherlands more than 80% of health managers in hospitals, home care organizations and nursing homes are reported to use the SWOT analysis as part of their strategic process [ 38 ]. SWOT, when used properly, can provide a good basis for the formulation of strategy [ 41 ]. In our study, terms in the questionnaire, used by reviewers for evaluation of SWOT analysis, could be queried in many ways, but together were able to demonstrate improvement after completion of the training program. Furthermore, external evaluation and review were designed to provide support to hospitals by improving systematic determination of quality, “valued outcomes”, and “key contributing processes” [ 42 ]. The reviewer-based evaluation was characterized by a high level of internal consistency.
In Serbia, a transitional country with a socialist heritage and little modern management experience, defining a hospital’s mission, vision, action plan, and especially its SMART objectives, seems to be dependent on the political environment and existing legislation. The measurement and evaluation of hospital performance were recognized as essential, partly because of the recently established reporting system of quality indicators [ 43 ] and partly due to recognition of the usefulness for benchmarking. Only a few stakeholders, i.e., the Ministry of Health, the Republic Health Insurance Fund and project agencies were considered relevant for the hospitals services and financial flow. This demonstrated that the managerial teams were predominantly oriented toward the fulfillment of legal obligations and contracts. The hospital’s internal environment (staff, their training and development, management, information system, equipment, customers and their satisfaction, and type and quality of health services) was included in the government’s health reform initiatives [ 25 ].
Positive effects of the independent components on learning outcomes, i.e., mission and vision, SMART objectives, and action plan, indicated that the extensive discussions initiated between the members of the managerial teams led to improved operation, even though their approach has not yet been formalized optimally. The teams understood the critical elements of the strategic planning process, but had difficulties in making maximum use of them in concretely planning their activities, e.g. balancing appropriate efficiency and quality [ 44 ]. This is obviously a desideratum in the improvement and better focusing of the didactic elements in training programs and their operational transfer.
However, the weakness of our study is the lack of control group, so our results cannot be fully attributed to the training programme. An alternative explanation is that some managers might have had some individual training or previous experience or some of them were interested in deeper research in specific fields. A potential weakness was the composite judgment of “teams”, without singling out individual members of the management teams. This is especially relevant as the composition of the multidisciplinary teams varied to some degree with respect to their professional background, reflecting the specific circumstances of the 20 participating hospitals. However, the chosen team approach is an asset in terms of sustainability of the training effects in transferring advanced managerial competence to several lead persons within a certain hospital. Accordingly, mutual understanding as well as a stronger impact in pursuing the necessary organizational changes in the hospital can be expected.
Research evidence demonstrates that improving hospitals’ strategic planning practices can be effective, but many health care organizations have difficulties in implementing their Strategic Plan to result in successful performance [ 45 , 46 ]. Also, both the hospital’s mission and vision statement and its clearly defined objectives are related to improved performance, staff behavior, and staff motivation [ 47 , 48 ]. This is evidenced by the formal training programs that have been ongoing in some countries, in which it was concluded that the positive effects of those programs justified additional investment in future education and training [ 49 ]. In Serbia, this was the first time that communities had the possibility of learning about their hospitals. When the managerial teams presented their strategies and action plans at a public event, this had a positive impact on the recognition of hospitals in their local environment.
The need for stronger management in Serbian health care is well recognized and the European Union, in particular, is supporting management capacity building programs [ 25 - 28 ]. Continuing education in health care management is being offered in Serbia at an increasing scale, in response to the health care system’s well-known deficits. A Masters program in health policy and management was recently established at the Belgrade Faculty of Medicine. Furthermore, a separate Masters in health management was also initiated. However, those programs have not been evaluated.
Through its policy and organization of the health care system, Serbia allows directors of the healthcare institutions to be physicians without formal managerial education. In such cases, introduction of training for the complete managerial team creates the conditions to maximize knowledge transfer in the workplace and encourage action oriented leadership. This is the value of our study for the international audience, since multidisciplinary managerial teamwork leads to success with a strong focus on organizational values, culture and interpersonal relationship.
In Serbia, for the first time, hospital managers were trained as a team by the Centre School of Public Health and Management in Belgrade to develop an official Strategic Plan for their hospitals and to implement monitoring and adjustment of their strategies. The training program had positive effects on the teams’ abilities to develop their hospital’s mission and vision, strategic objectives, and action plan as learning outcomes.
David F. Strategic Management. Columbus: Merrill Publishing Company; 1989.
Google Scholar
Liu CF, Rubenstein LV, Kirchner JE, Rortney JC, Parkins MW, Ober SK, et al. Organizational Cost of Quality Improvement for Depression Care. Health Serv Res. 2009;44:225–44.
Article Google Scholar
Pettersen IJ, Nyland K. Management and control of public hospitals-the use of performance measures in Norwegian hospitals, a case-study. Int J Health Plann Manage. 2006;21:133–49.
Garcia CM, de Val PI. Strategies and performance in hospitals. Health Policy. 2004;67:1–13.
McKee M, Helay J. Hospitals in a changing Europe. Buckingham: Open University Press; 2002.
Kim TH, Thompson JM. Organizational and market factors associated with leadership development programs in hospitals, a national study. J Healthc Manag. 2012;57:113–31.
Byars LL, Rue LW, Zahra SA. Strategic Management: Formulation and Implementation. Chicago: Irwin; 1996.
Lingham T, Richley B, Rezania D. An evaluation system for training programs, a case study using a four-phase approach. Career Dev Int. 2006;11:334–51.
Davies S. Health services management education: why and what? J Health Organ Manag. 2006;20:325–34.
Gregory D, Baigelman W, Wilson IB. Hospital economics of the hospitalist. Health Serv Res. 2003;38:905–18.
Hanlon NT. Sense of place, organizational context and the strategic management of publicly funded hospitals. Health Policy. 2001;58:151–73.
Goldstein IL, Ford JK. Training in organizations. Belmont CA: Wadsworth; 2002.
Pappas JM, Flaherty KE, Wooldridge B. Tapping into hospital champions – strategic middle managers. Health Care Manage Rev. 2004;29:8–6.
Geertshuis S, Holmes M, Geertshuis H, Clancy D, Bristol A. Evaluation of workplace learning. J Workplace Learn. 2002;14:11–8.
Collins BD. Performance-level evaluation methods used in management development studies from 1986 to 2000. Hum Resource Dev Rev. 2002;1:91–110.
Kirkpatrick D. Revisiting Kirkpatrick’s four – level model. Alexandria VA: American Society for Training and Development; 1996.
Mann S, Robertson IT. What should training evaluations evaluate? JEIT. 1996;20:14–20.
Rummler GA, Branche A. Improving Performance: How to Manage the White Space on the Organization Chart. San Francisco: Jossey Bass; 1995.
Wang GG, Wilcox D. Training evaluation, knowing more than is practiced. ADHR. 2006;8:528–39.
Kim CY, Cho SH. Institutionalization of quality improvement programs in Korean hospitals. Int J Qual Health Care. 2000;12:419–23.
Moller L, Mallin P. Evaluation Practices of instructional designers and organizational supports and barriers. PIQ. 1996;9:82–92.
Collins BD. Organizational performance: the future focuses of leadership development. J Leader Stud. 2000;7:43–54.
Philips PP, Philips JJ. Symposium on the evaluation of training. Int J Train Dev. 2001;5:240–7.
Unger JP, Marchal B, Green A. Quality standards for health care delivery and management in publicly oriented health services. Int J Health Plann Manage. 2003;18:s79–S88.
McCarthy M. Serbia rebuilds and reforms its health-care system. Lancet. 2007;369:360.
Markovic R, Vasic M, Segar C, Deljanin Z, Rancic N, Marjanovic S. Need for systematic education and training in health care management in the Republic of Serbia. Ata Fac Med Naiss. 2009;26:143–9.
O’Rourke M, Lukic N, Jones M, McCarley N. Management training and education to strengthen the nursing profession in Serbia. Manag Health. 2011;15:20–4.
Matovic Miljanovic S, Jankovic S. The international community and the reconstruction of health care in South Eastern Europe. J Public Health. 2006;14:246–56.
Nelson BD, Dierberg K, Scepanovic M, Mitrovic M, Vuksanovic M, Milic L, et al. Integrating quantitative and qualitative methodologies for the assessment of health care systems, emergency medicine in post-conflict Serbia. Health Serv Res. 2005;5:1–11.
Zakon o komorama zdravstvenih radnika. Sluzbeni glasnik RS” br. 107/2005 i 99/2010. [ http://www.paragraf.rs/propisi/zakon_o_komorama_zdravstvenih_radnika.html ]
Zakon o zdravstvrnoj zastiti. Sluzbeni glasnik RS” br. 107/05, 72/09 – dr. zakon, 88/10, 99/10, 57/11, 119/12, 45/13 – dr. zakon i 93/2014. [ http://www.paragraf.rs/propisi/zakon_o_zdravstvenoj_zastiti.html ]
Lammintakanen J, Kivinen T, Kinnunen J. Managers’ perspectives on recruitment and human resource development practices in primary health care. Int J Circumpolar Health. 2010;69:462–9.
McHugh M, Johnston K, McClelland D. HRM and the management of clinicians within the NHS. Int J Public Sector Man. 2007;20:314–24.
Terzic Supic Z, Bjegovic V, Marinkovic J, Santric Milicevic M, Vasic V. Hospital management training and improvement in managerial skills, Serbian experience. Health Policy. 2010;96:80–9.
Ministry of Health of the Republic of Serbia. Finalized projects. International projects; 2007 [ http://www.zdravlje.gov.rs/showpage.php?id=79 ]
Weihrich H. The TOWS matrix–a tool for situation analysis. Long Range Plann. 1982;15:54–66.
Vankova D, de Leeuw E. Public health human capacity building in Bulgaria – theory and application of SWOT analysis. I-JPHE. 2001;3:B 18–48.
van Wijngaarden JDH, Scholten GRM, van Wijk KP. Strategic analysis for health care organizations, the suitability of the SWOT-analysis. Int J Health Plann Manage. 2012;27:34–49.
Bernroider E. Factors in SWOT analysis applied to micro, small–to–medium, and large software enterprise: an Austrian study. Emerg Med J. 2002;20:562–73.
Klijn PH, van Stel HF, Quittner AL, van der Net HJ, Doeleman W, van der Schans CP, et al. Validation of the Dutch cystic fibrosis questionnaire (CFQ) in adolescents and adults. J Cyst Fibros. 2004;3:29–36.
Yuksel I, Dagdeviren M. Using the analytic network process (ANP) in a SWOT analysis – a case study for a textile firm. Inform Sci. 2007;177:3364–82.
Expert Advisory Group. Principles of an evaluative approach to quality assurance. Auckland: New Zealand Qualifications Authority; 2007.
Pravilnik o pokazateljima kvaliteta zdravstvene zastite. Sluzbeni glasnik RS” br. 107/05. Clan 19. Zakon o zdravstvrnoj zastiti. „Sluzbeni glasnik RS” br. 107/05. [ http://www.zdravlje.gov.rs/tmpmz-admin/downloads/zakoni1/Pravilnik_pracenje_kvaliteta.pdf ]
Mennicken R, Kuntz L, Schwierz C. The trade-off between efficiency and quality in hospital departments. J Health Organ Manag. 2011;25:564–77.
Zuckerman AM. Advancing the state of the art in healthcare strategic planning. Front Health Serv Manage. 2006;23:3–1.
Adams J. Successful strategic planning: creating clarity. J Healthc Inf Manag. 2005;19:24–31.
Bart CK, Hupfer M. Mission statements in Canadian hospitals. J Health Organ Manag. 2004;18:92–110.
Forbes DJ, Seena S. The value of a mission statement in an association of not-for-profit hospitals. Int J Health Care Qual Assur Inc Leadership Health Serv. 2006;19:409–19.
Flessa S. Hospitals development plans: a new tool to break ground for strategic thinking in Tanzanian hospitals. Eur J Health Econ. 2005;6:s322–33.
Download references
Acknowledgements
This work was supported by Ministry of Education, Science and Technological Development, Republic of Serbia (Grant No. 41004, Contract No. 175042 (2011-2014) and Grant No.175087). Special thanks for English review to Mr. Jonathan Erskine, Research Fellow at the Centre for Public Policy and Health, School of Medicine, Pharmacy and Health, Durham University, UK.
Author information
Authors and affiliations.
Institute of Social Medicine, University of Belgrade, School of Medicine, Belgrade, Serbia
Zorica Terzic-Supic, Dejana Vukovic & Milena Santric-Milicevic
Centre-School of Public Health and Management, University of Belgrade, School of Medicine, Belgrade, Serbia
Vesna Bjegovic-Mikanovic
Institute of Medical Statistics and Informatics, University of Belgrade, School of Medicine, Belgrade, Serbia
Jelena Marinkovic
Department of Statistics and Mathematics, Faculty of Economics, University of Belgrade, Belgrade, Serbia
Vladimir Vasic
Section of International Public Health (S-IPH), Faculty of Health Sciences, University of Bielefeld, Bielefeld, Germany
Ulrich Laaser
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Zorica Terzic-Supic .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
ZTS, VBM created the study concept and design and completed the interpretation of data. DV and MSM analyzed and presented the data. JM and VV were responsible for statistical analysis and data presented. ZTS, VBM and UL wrote the manuscript. UL carried out a critical revision of the manuscript for important intellectual content. All authors had full access to all data, read the manuscript and approved the final version.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License ( http://creativecommons.org/licenses/by/4.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Terzic-Supic, Z., Bjegovic-Mikanovic, V., Vukovic, D. et al. Training hospital managers for strategic planning and management: a prospective study. BMC Med Educ 15 , 25 (2015). https://doi.org/10.1186/s12909-015-0310-9
Download citation
Received : 11 June 2014
Accepted : 17 February 2015
Published : 26 February 2015
DOI : https://doi.org/10.1186/s12909-015-0310-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Learning outcome
- Hospital management
- Strategic planning
- Professional development
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Skip to Content
- Skip to Menu
- Increase Text Size

Case Studies
Helping healthcare organizations succeed.
The Program Success Snapshots and Case Studies show how Tiller-Hewitt helps organizations succeed in physician engagement, alignment and growth strategies. Please take a look at some of the results achieved and contact us for additional information.
Program Success Snapshots
Fast-facts and at-a-glance results demonstrate the scope and effectiveness of Tiller-Hewitt HealthCare Strategies’ laser-focused programs.

Tiller-Hewitt’s Physician-Hospital Relations Program in action drives measurable results. Our case studies illustrate how our strategic operational and marketing solutions overcome barriers and lead to increased referrals, volume and revenue for hospitals and health systems.
Partnership Rapidly Generates $24.3 Million in Strategic Growth
LCMH engaged Tiller-Hewitt HealthCare Strategies’ Rapid Impact Strategic Growth solution and:
- Identified the opportunity to mitigate an estimated $100 million annual leakage
- Delivered 2.24% outpatient and 3.33% inpatient market share growth
View Case Study

Rapid Impact Strategic Growth Solution Drives $34 Million Incremental Net Revenue
The Tiller-Hewitt engagement with Archbold produced off-the-charts results and return on investment in year one:
- $122 million incremental top line revenue
- $34 million incremental net revenue
- 22% increase - outpatient CTs
- 19% increase - outpatient MRIs
Best-In-Class Physician Integration Sparks Improved Retention and Performance
Tiller-Hewitt’s assessment resulted in a comprehensive physician integration program which sparked a dramatic turnaround and improvement in in recruitment, retention and value-based operational performance. Working with leadership, the hospitalists became a unified force, gaining engagement and respect from specialist physicians. ‘Slam dunk’ results followed close behind.
PHR Accelerates Multi-Hospital Network Integration and Growth
The PHR program delivered double digit incremental increases in the first year by significantly improving network communication and collaboration with physicians and their staffs. With committed and collaborative senior leaders, the largest hospital’s results exceeded Tiller-Hewitt’s already strong average growth benchmarks, and the PHR program continues to show measurable results.
onboardPLUS Improves Engagement, Productivity And Retention
Dayton Children’s implemented onboardPLUS and achieved measurable improvements within the first two years. Their astounding results, include: a reduction in credentialing time from 322 to 84 days, acceleration in getting physicians working at full productivity from 14 months to 5 months; and reduction in turnover from 11.6% to 2.7%.
Transforming an In-House Liaison Program into a Growth Engine
Tiller-Hewitt’s program tripled the hospital’s physician referral base and generated measurable increases in referral activity. In conjunction with the Service Line Blitz, the PHR program included double-digit growth in imaging services. The PHR program team continues to exceed program goals for physician sales calls and new referrals from targeted physicians.
Physician-Hospital Relations Program Produces Rapid Improvement and Sustainable Growth
Tiller-Hewitt’s Physician-Hospital Relations program increased the hospital’s incremental revenue by $1.9 million in the first year, a 39% increase. Over two years, market share grew from 31% to 44% (a 42% increase). This trajectory for growth positioned the hospital to develop new funding sources, recruit and retain quality providers, pursue profitable care delivery and diversify reimbursement sources.
Check out our Resource Page often for updates, videos, webinars, articles and other strategic growth planning tools.
"Tiller-Hewitt gave us a jump start for early success. By focusing our program on the right initiatives and tracking the right data, we got our outreach ..."
Get started with a complimentary strategy call to pinpoint your most pressing challenges and areas of greatest opportunity.

IMAGES
VIDEO
COMMENTS
Methods: Qualitative case study and evaluation against the conditions of 'accountability for reasonableness' of a strategic planning process at a large urban university-affiliated hospital. Results : The hospital's strategic planning process met the conditions of 'accountability for reasonableness' in large part.
this hospital's strategic planning initiative comply with the conditions of AFR? Methods Design To describe priority-setting, we undertook a qualitative case study. A case study is 'an empirical inquiry that investigates a contemporary phenomenon within its real life context'.13 The case study method is appropriate because priority-setting in ...
inaapropriate strategic planning model, lack of team work morale, poor communication and coordination, inadequate educatio n. and training, lack of manag ers', employees' and physicians ...
A case study approach [ 47, 48] was adopted here to understand the deployment of a whole system change in the acute hospital along the four dimensions of STS outlined above. A case study is an approach that is used to generate an in-depth, multi-faceted understanding of a complex issue in its real-life context [ 49 ].
Results: The hospital's strategic planning process met the conditions of 'accountability for reasonableness' in large part.Specifically: the hospital based its decisions on reasons (both information and criteria) that the participants felt were relevant to the hospital; the number and type of participants were very extensive; the process, decisions and reasons were well communicated throughout ...
This monocentric, observational study on strategic planning was conducted in the rheumatology department of the University Hospital in Lausanne (CHUV), Switzerland from 2017-2023. It included restrictions and subsequent new digital developments during the SARS-Cov2 pandemic.
A case study linked to an evaluation using 'accountability for reasonableness' can serve to improve priority-setting in the context of hospital strategic planning. Objectives: To describe and evaluate the priority-setting element of a hospital's strategic planning process. Methods: Qualitative case study and evaluation against the conditions of 'accountability for reasonableness' of a ...
A case study linked to an evaluation using 'accountability for reasonableness' can serve to improve priority-setting in the context of hospital strategic planning. Discover the world's research 25 ...
A case study linked to an evaluation using 'accountability for reasonableness' can serve to improve priority-setting in the context of hospital strategic planning. Full text links Read article at publisher's site (DOI): 10.1258/135581903322403254
A comprehensive case study woven throughout the book allows readers to assume the role of strategic planners and apply what they are learning to the entire strategic planning process. This revised edition includes insight into the modern healthcare system and an exploration of trends in mergers and acquisitions, system growth, and value-based care.
Abstract. Background & Objectives: It is necessary to utilize hospital scare resources to meet patients' unlimited needs. Hospital managers should pay more attention to efficiency. This study ...
Methods: Qualitative case study and evaluation against the conditions of 'accountability for reasonableness' of a strategic planning process at a large urban university-affiliated hospital. Results: The hospital's strategic planning process met the conditions of 'accountability for reasonableness' in large part. Specifically: the hospital based ...
This study was designed to illustrate how Q Methodology can be used as a tool for strategic planning. Potential plans for the future of a small Indiana hospital were formulated and Q sorted to determine support or resistance by key leaders from within hospital management, the board, and the medical staff.
In Singapore, the NMRC refers to the strategic plan developed by the National Research Foundation, a department within the Prime Minister's Office. The NMRC has a well-described system for incorporating national priorities into the organisation's research plan (see the NMRC case study).
Strategic planning in healthcare helps you set business goals and decide how to allocate resources to achieve these goals. It involves looking at your organization's internal and external environments using established strategic tools. Doing so lets you develop a strategic plan outlining what you want to achieve and an action plan to get there.
Strategic planning for health in Turkey has been successful for a number of reasons. Conceptually speaking, there are two sets of reasons. The first has to do with the characteristics of the strategic plans and the way in which they were prepared, and the second with the way in which they were operationalized.
This study aimed to examine the impact of strategic planning on patient satisfaction in a hospital in 2012-2014. Methods: A participatory action research was used in this study. Hospital strategic ...
The four regression models used showed that the training program had positive effects (p < 0.001) on the ability to formulate a Strategic Plan comprising the hospital mission, vision, strategic objectives, and action plan. This study provided evidence that training for strategic planning and management enhanced the strategic decision-making of ...
Instead of having a one-product enterprise, we have a complex multi-product enterprise. There is no doubt that German hospital financing is in zone III and uncertainty with unexpected frequent substantial changes is a constant threat for hospital planning. The introduction of G-DRGs was a major call for strategic management in German hospitals.
Partnership Rapidly Generates $24.3 Million in Strategic Growth. LCMH engaged Tiller-Hewitt HealthCare Strategies' Rapid Impact Strategic Growth solution and: Identified the opportunity to mitigate an estimated $100 million annual leakage. Delivered 2.24% outpatient and 3.33% inpatient market share growth. View Case Study.
In another study, the researcher shows that adopting BSC in the integration of big data and strategic management, not only will help to overcome complexities in the organizations, but also will help to improve the effectiveness of the strategic plan performance, and new insight will be available for managers decisions. 7
This study aimed to identify the critical success factors (CSFs) of the strategic planning process in Iranian hospitals. Materials and Methods: This qualitative study was performed using semi ...
The study compares two hospital buildings with a very similar configuration and medical program but with significantly different architectural design strategies: One was designed for an unknown future medical function, and the second was designed for a specific medical function. ... Cole explained that strategic planning of new healthcare ...