

Clinical Research Project Plan

Needless to say, medicine today is quite different from the past. It has also come from a long history. When we say ancient medicine, the first things that would come to our minds are the times where people still believed that illnesses served as punishments by the Gods due to the bad things that people did. Our ancestors from a particular era also thought that sicknesses such as diarrhea were perfectly normal and are just natural occurence. Thus, such occurrences didn’t require medicine or other medical interference to solve. However, that is just part of a long history of medicine. Along with the advancement of technology, smart people have come up with a better approach to deal with these illnesses, and clinical research is just one of the healthcare studies that we are practicing to better our health.
Clinical research, just like medical research , is a broad category to discuss in just one article, but today we are going to tackle one of the sections that make this type of research – Clinical Research Project Plan.
What is Clinical Research?
Generally speaking, clinical research is the study of human health. It aims to secure the safety and effectiveness of health-related tools and methods such as medications, medical devices, and treatment regimens. Through these studies, medical professionals can ensure the efficacy of the products that they use for diagnosis, treatment, and prevention of deceases that people may endure. This science healthcare branch includes the studies or clinical trials conducted under the following categories: mental health, social health, physical health.
Clinical researchers from university medical centers and affiliated research study sites are usually the ones who are executing this type of researches as part of their Ph.D. application or typical undergraduate research. These areas have access to more resources for medical participants. They have high standards in terms of following the proper ethical conduct of medical research, thus, making these grounds for effective clinical studies.
Simply put, the clinical research plan contains an overview of the clinical research that you are proposing. You will have to submit this document along with the other sections of your research proposal . This document is one of the things that your research stakeholders will look at when considering the approval of your proposed plan. To create a good research plan, make sure that your project answers the following questions.
What are the goals of the research? Why are these goals important?
Providing research goals is an essential part of conducting a study. In this part, you should state the specific objectives of your research. We recommend you to include a whole page document for this section.
What are the things that people, such as the researchers, concerning this project have done so far?
Is there existing research that needs a follow-up study? Is there a system that the hospital is following? You will have to specify all the current activities that the field is currently practicing and other existing factors in connection to your proposed research.
How are you going to achieve the goals of your research?
Aside from the goals, your research plan should include the steps that you are going to take to achieve these goals. To do that, you will have to include elements such as strategy. In this part, you will assure the research stakeholders that you will attain the goals of your study.
11+ Clinical Research Project Plan Examples & Templates
Now that you have a better understanding of the clinical research project plan take a look at these examples and templates. You can use these downloadable documents as a reference or guide to create a layout for your student research.
1. Research Plan Template for Pragmatic Clinical Studies
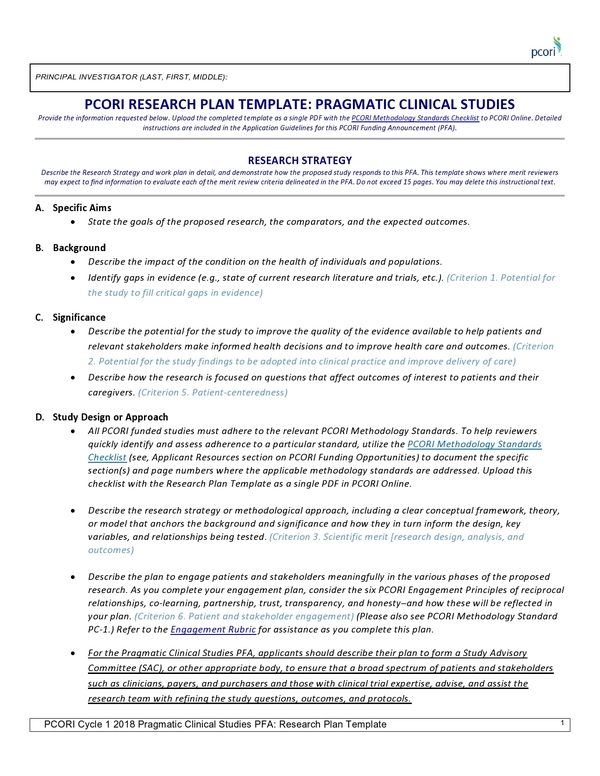
Size: 31 KB
2. Sample Research Plan Proposal
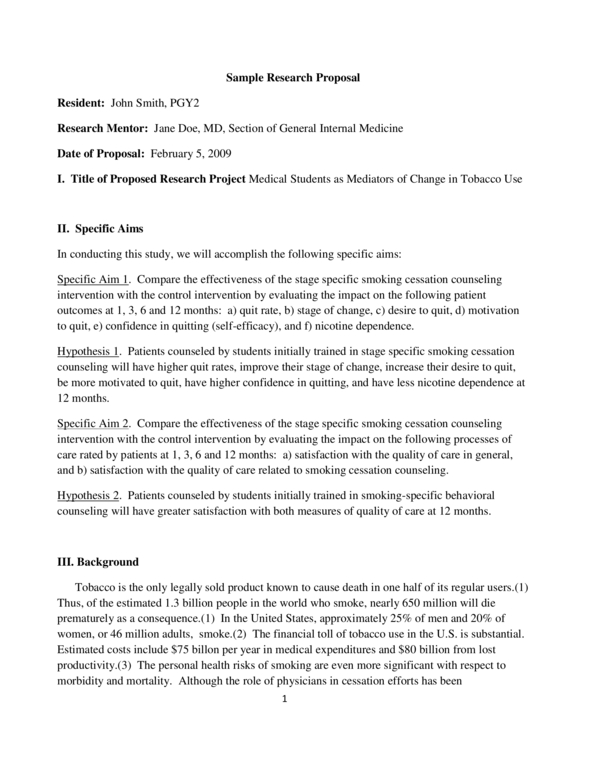
Size: 191 KB
3. Example of a Well-Written Clinical Research Plan Proposal
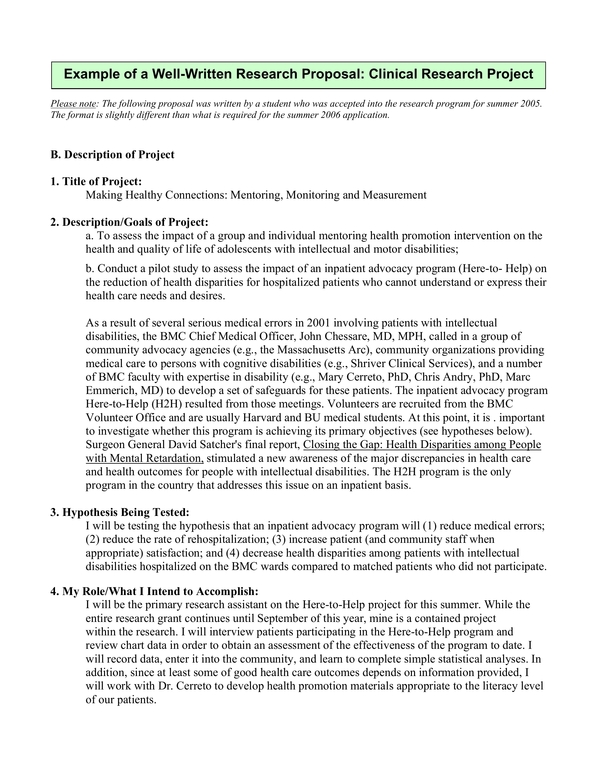
Size: 102 KB
4. Research Plan Proposal Sample
Size: 106 KB
5. Medical Student Resesarch Plan Proposal
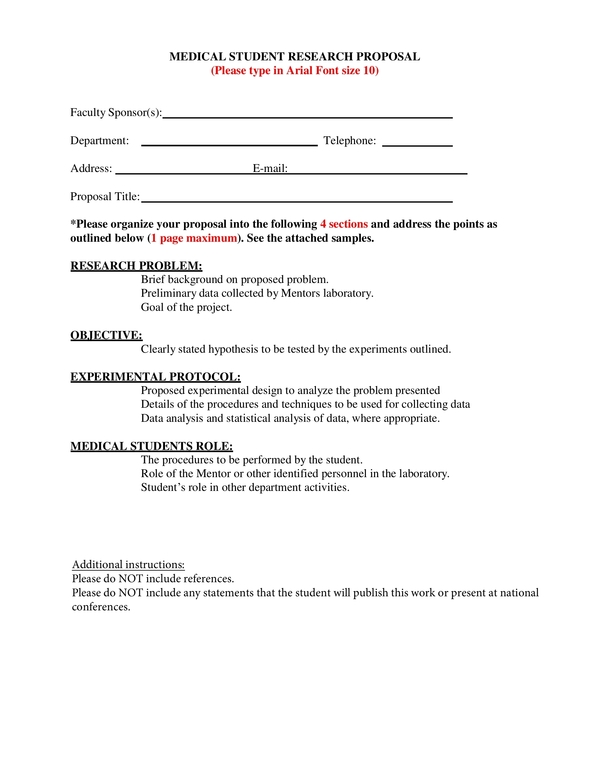
Size: 232 KB

6. Template for essential information to be provided for proposals including clinical trials / studies / investigations
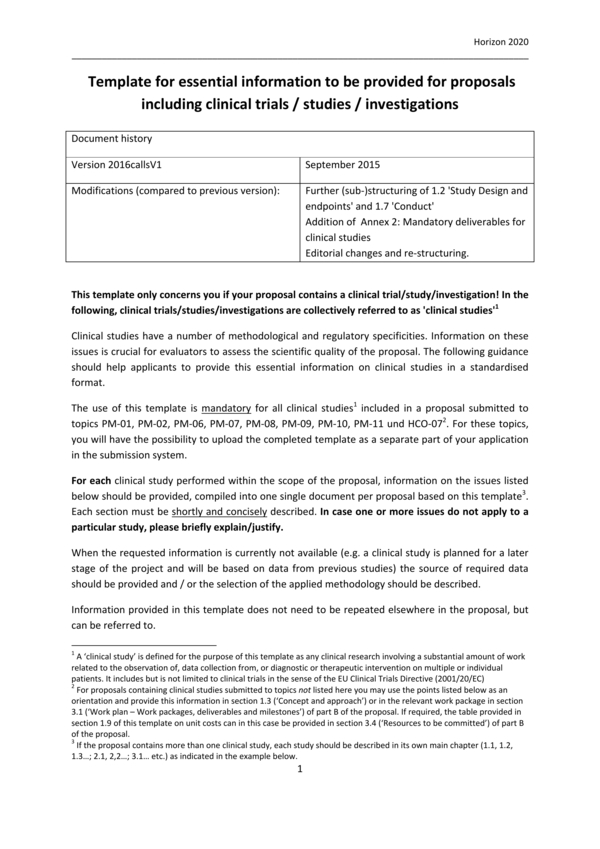
Size: 134 KB
7. Research Plan for Clinical Research Study With No External Sponsor
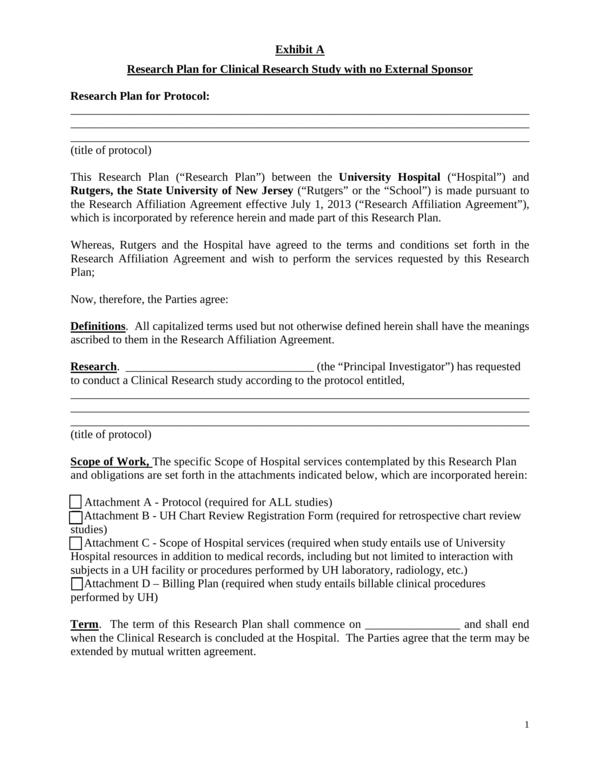
Size: 26 KB
8. Writing a Research Plan
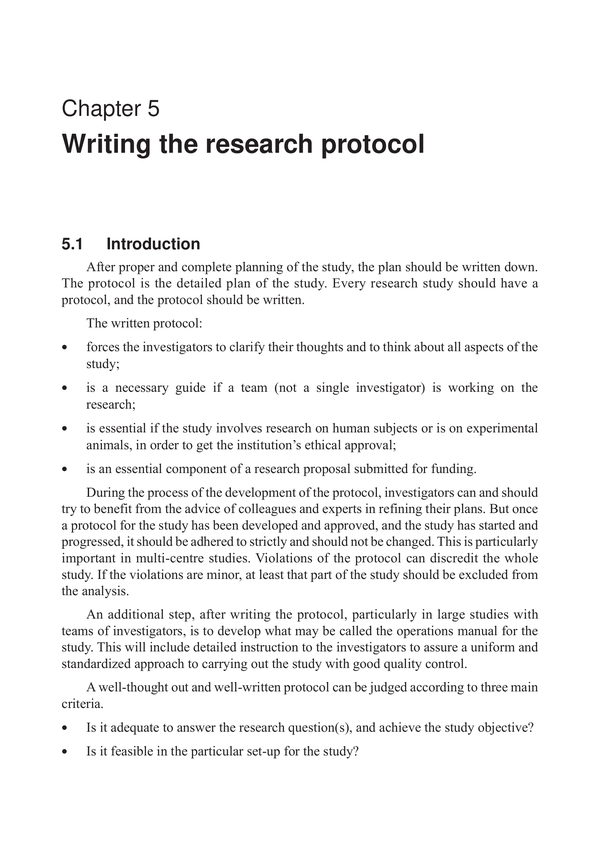
Size: 131 KB
9. Biomedical Research Protocol
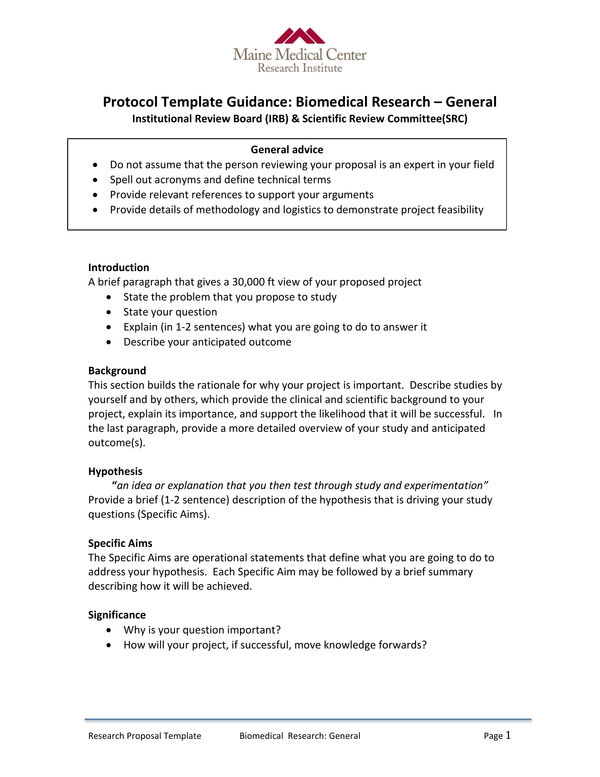
Size: 154 KB
10. Research Plan Proposal Form
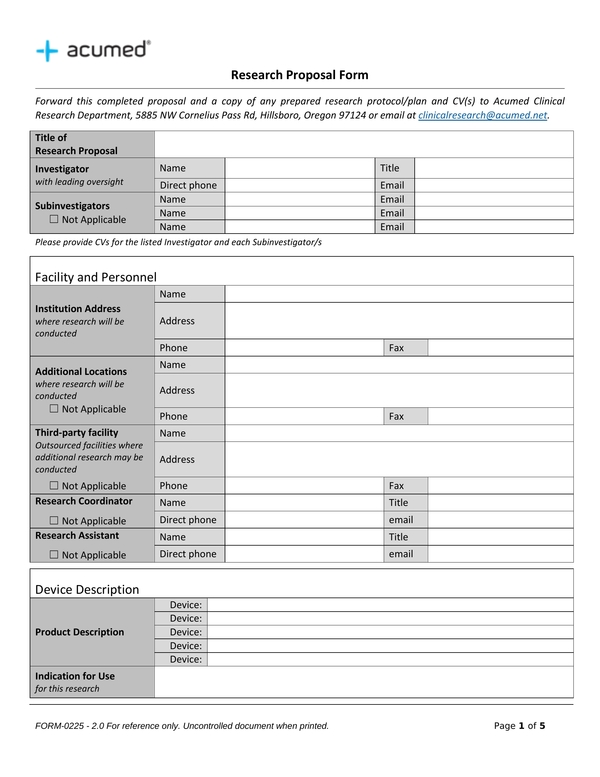
11. Research Plan Proposal Template
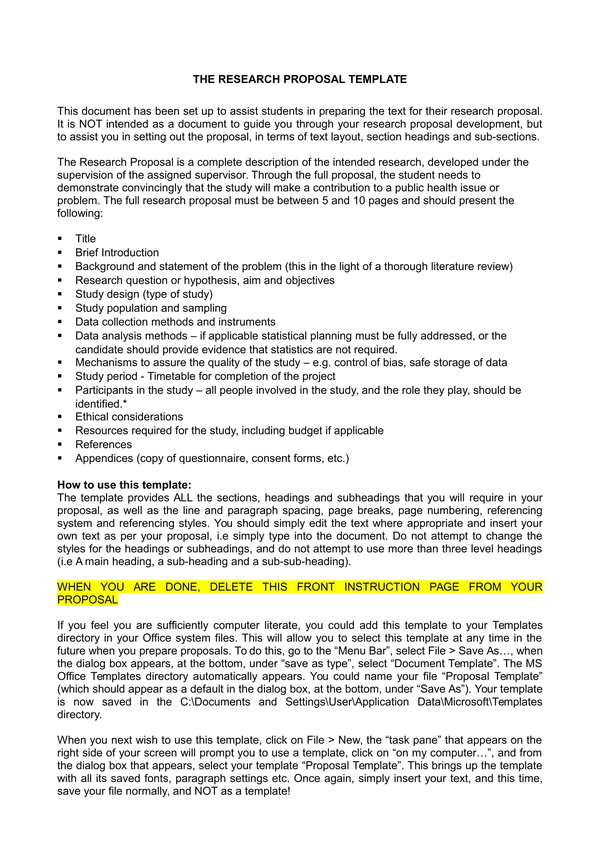
Size: 14 KB
12. Health Sector Workpace Violence Research Plan
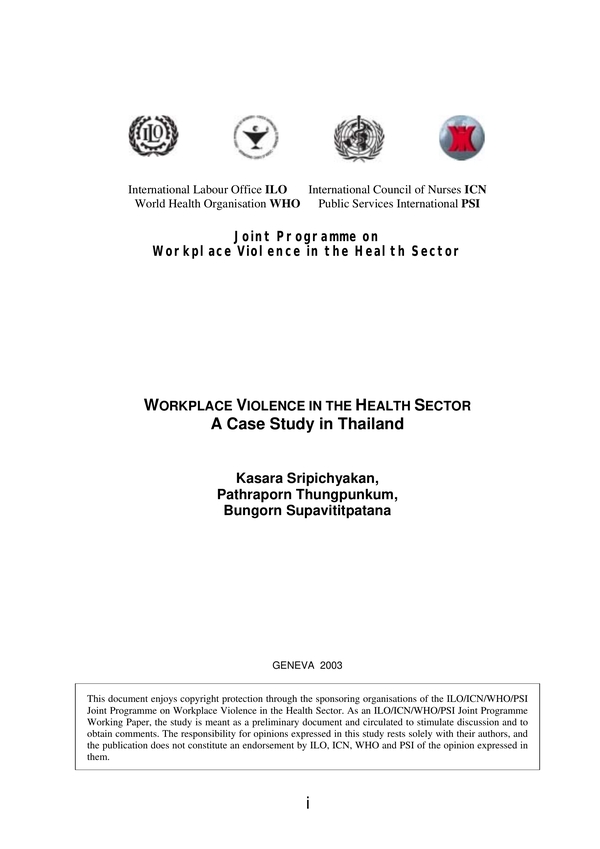
Size: 233 KB
Tips on Writing a Research Plan
Come up with a useful subject.
When writing a research plan, you should remember that your goal is for the stakeholders to approve your project, and selecting your research subject will play a significant role in the approval that you want. Choose a topic that will compel and impress your leaders. You can do some research and list the latest trends that you think are worth it to tackle. However, the best way to convince your leaders is to come up with a topic that you feel is important. In that way, it will be easier for you to persuade the importance of your work.
Make Your Plan Brief
Choosing a compelling topic is just the beginning. Think of a TV drama with a promising trailer or hit pilot episode but had to cancel after the first season due to the gradually declining ratings. What could have possibly happened? Aside from the story is not clicking, most of the time, this scenario occurs when the maker is stretching the storyline to the point that it becomes dragging and boring. You don’t want that to happen on your project plan. Make your research plan brief and concise. To do it, you have to refine your research plan in a way that you only include essential items.
Be Realistic
We know that coming up with an interesting topic is a great idea in creating a research plan. However, you should also remember that you are proposing a research plan to create a solution. Therefore, you have to ensure that your plan’s objective is realistic. In this way, you can ensure that there will be no holes in your plan, and it will also be easy for you to defend and answer the questions of the stakeholders, especially during the research project proposal period.
Include a Preliminary Data
Do your research! When proposing a research plan, you have to make specific preparations. One of them is researching the existing research made for the topic that you choose. As mentioned earlier, to create a good research plan, you have to ask yourself for things concerning your project that has done so far. Look for the data and results generated by prior research, demonstration, development such as structured and literature interviews. You will, then, include this data to your research plan.
Science has indeed enlightened us in so many ways. One of the best contributions that it has given to humanity is the advancement of clinical matters. Our great thinkers uncover better methods to deal with humans’ health. Through clinical research, we benefit from inventions that we have today with lesser adversaries. Better approaches to diagnose, treat, and prevent diseases are within reach. In this article, we have discussed one of the essential components of clinical research, which is the clinical research plan.
Text prompt
- Instructive
- Professional
Create a study plan for final exams in high school
Develop a project timeline for a middle school science fair.

IMAGES
VIDEO