- BOOK CONSULTATION
- The Surgical Journey
- Where do I start?
- Am I eligible for surgery?
- Preparing for Surgery
- General Recovery Info
- Risks & Safety
- Top Surgery
- Top Surgery Techniques
- Techniques Beyond the Binary
- Top Surgery Videos
- Breast Augmentation
- Facial Surgery
- Techniques & Incisions
- Body Contouring
- Body Feminization
- Body Masculinization
- Non-Binary Body Contouring
- Bottom Surgery
- “Feminizing” Techniques & Recovery
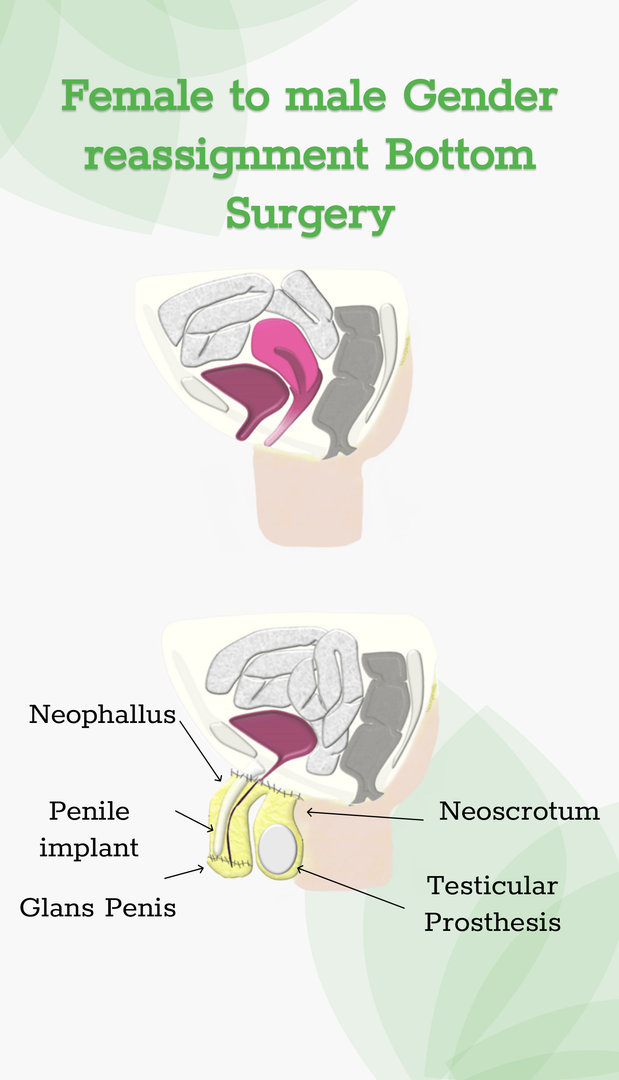
- “Masculinizing” Techniques & Recovery
Medical Tattooing & Scar Microneedling
- Medical Tattooing & Microneedling
- Outside Services
- Transition 101
- Introduction to Transitioning
- Support Services: Helpful Links
- Transitioning Later In Life
- Legal Name & Gender Change
- Transmasculine & Pregnancy
- Transgender Healthcare
- Mental Health
- Hormone Therapy
Trans Youth & Adolescents
- Mental Health Support
- Common Questions About Your Child’s Transition
- For Caregivers
- Explaining Your Child’s Identity
- Talking With Schools About Your Child
- Puberty Blockers
- Challenging Topics
- Detransition
- Adolescents
- Gatekeeping vs Empowerment
- Rapid Onset Gender Dysphoria
- Double Incision
- Periareolar
- Inverted T / Aggressive Breast Reduction
- Gynecomastia
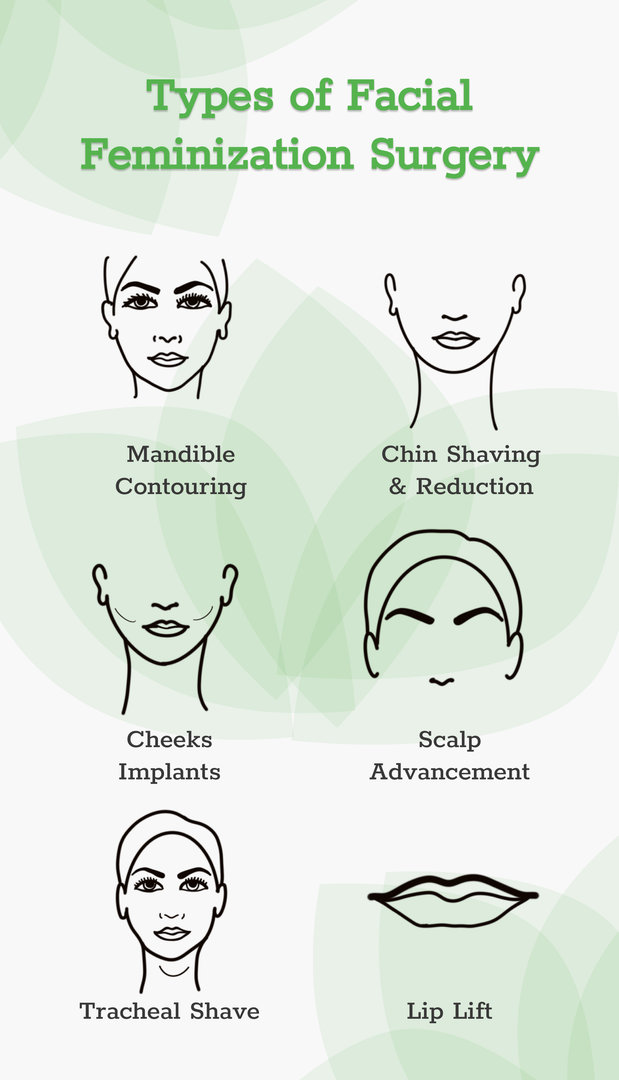
- Facial Feminization
- Facial Masculinization
- Labiaplasty
- Vaginoplasty
Costs and Financing
- Insurance Approval
- Insurance Denial
- Insurance Accepted
- Referral Letters
- Advocacy Team
- Make a Payment Now
- Our Philosophy
- Meet Our Team
Office & Facilities
- Testimonials
- Get in Touch
- For Current Patients
- For Providers
Consultation request
- Interpretation Services
- Privacy Policy

Do you have any questions? Check our F.A.Q. section or contact us directly!
- Gender Reassignment Surgery Cost Guide | Price Breakdown

How Much is Gender Reassignment Surgery?
Medically reviewed by Jennifer Richman on October 09, 2024.

Gender reassignment surgery (GRS) is now a less commonly used term in the field of gender-affirming care that refers to surgeries that help transgender patients experience greater gender congruence with their bodies. In this article, we discuss the costs of what some patients call “male to female (MTF)” and “female to male (MTF)” procedures like breast augmentation, chest reconstruction top surgery, facial surgery, body contouring and bottom surgery. We also go over insurance coverage, medical credit and financial assistance resources that help patients reduce the financial burdens of medically necessary gender reassignment surgery.
We recognize that terms like MTF and FTM do not resonate with the majority of the trans, non-binary and gender non-conforming communities we serve. After all, we believe that surgeries do not “reassign” anyone’s gender. Still, many patients that we serve identify with these terms or use them to search for resources and information to help them through transition.
Understanding the Cost of Gender Reassignment Surgery
Below you will find general cost estimates for different gender-affirming surgeries. Generally speaking, these price ranges do not include anesthesia fees, facility fees (staying overnight in the hospital) and/or pathology fees (sending removed organs or tissue for pathology testing). Prices vary depending on a number of factors we discuss below.
Please note that patients who are able to secure insurance coverage for their medically necessary, gender-affirming procedures will not have to pay the full price listed below.
Factors Affecting the Cost
The following factors can determine the price of the gender reassignment surgery or gender-affirming procedure in question.
For instance, surgeons with lots of experience may charge more than a surgeon who is just starting out.
- The surgical technique(s) used are a major determinant in the final cost of surgery. For example, metoidioplasty is a common GRS or masculinizing bottom surgery procedure that we perform. The cost of the metoidioplasty procedure will vary greatly depending on if a patient chooses to undergo a simultaneous primary urethral lengthening procedure, which facilitates urinating standing up.
- At the Gender Confirmation Center (GCC), sometimes chest liposuction is performed as a part of a chest reconstruction top surgery procedure to prevent dog ears and/or help flatten the chest contour. Cash pay patients are never charged extra for chest liposuction.
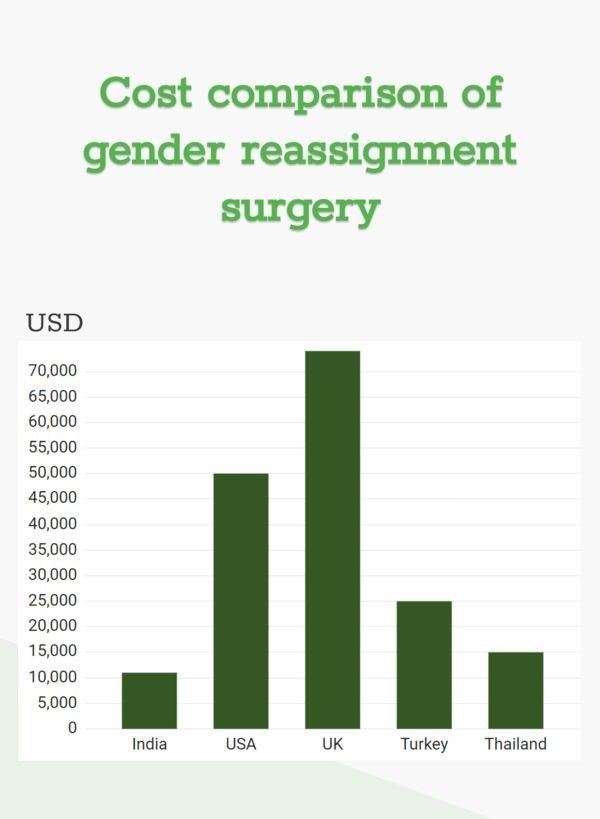
- Prices for surgery vary depending on the city and country you choose to undergo your operation.
- It is important to ensure that your surgeon is board-certified by the American Board of Plastic Surgery or a similarly reputable organization. This standard is indicative of their extensive training and expertise in plastic and reconstructive surgery.
- Some surgeons will charge a higher surgeon fee depending on their credentials, years of experience, and reputation.
- Facility-related costs include operating room fees, anesthesia fees, and hospital stay, which can vary by location and procedure. Generally speaking, most bottom surgery and facial surgery procedures involve a patient staying one or more nights in a hospital after surgery. Likewise, patients with certain medical conditions may need to stay the night in the hospital after their procedure.
- Prior to surgery, patients will be charged for all postoperative supplies that the surgeon will provide for recovery. This includes bandages, gauze, compression garments and any other materials such as medical-grade dilators for vaginoplasty patients.
- At the GCC, patients are not charged out-of-pocket for follow-up consultations or revision surgeries if they are scheduled within a year after your initial procedure. Not all gender-affirming surgical practices have this policy, so be sure to check with your surgeon.
- Many patients who undergo facial surgery and body contouring elect to undergo lymphatic massages to help facilitate their healing and recovery processes. We recommend that our patients go to licensed, experienced professionals for postoperative lymphatic massages. Since this is an outside service we do not offer, it will be an extra cost to the patient.
Additional Costs and Considerations
- Some patients will undergo revision procedures after their initial gender reassignment surgery or gender-affirming procedure. Occasionally, this is to treat medical complications. In other cases, patients request a revision surgery to correct aesthetic issues. Regardless, GCC patients who undergo a revision procedure one year after their initial surgery will not be charged.
- Most reputable, board-certified surgeons with extensive experience in gender care have a very low revision rate. This means that there is a low percentage of their patients that seek out revision surgeries. It is a good idea to ask your surgeon what percentage of their patients have requested a revision. That said, please note that certain procedures like a phalloplasty or metoidioplasty with primary urethral lengthening have a higher risk of complication than others.
- Individuals traveling to a different city or country for surgery, will incur additional expenses related to travel and accommodation. Many of our patients in the United States and internationally come to the GCC because they do not have access to high-quality gender-affirming surgical care near them. In the case of top surgery, we are one of the few providers in the US that will operate on patients with a body mass index (BMI) between 30-60. We have compiled a free travel guide with tips on how to save money traveling to the San Francisco Bay Area for surgery.
- Recovery from surgery may result in lost wages for those that are not able to get paid time off for the initial stages of healing. While procedures like top surgery and body contouring may only require that a patient take two weeks off work, more intensive surgeries may require more rest time. Likewise, if your job involves heavy lifting, you will not be able to take up that or other vigorous physical activities for at least six weeks post-op. Be sure to check with your surgeon’s office about how much time you will need off work.
- Most gender-affirming procedures do not involve long-term healthcare costs after the initial recovery. Patients who follow recovery instructions closely––for example, the top surgery arm mobility protocol––are unlikely to experience future complications that could result in greater costs.
Insurance Coverage and Financial Assistance
- Insurance Coverage
- Navigating insurance coverage for gender reassignment surgery can be complex, but many insurance providers now recognize these forms of healthcare for transgender individuals as medically necessary and thereby deserving of coverage. We encourage you to look into what your insurance plan covers––i.e., if they have gender benefits––by calling your insurance company and ask what medical policies on gender dysphoria treatment are applicable to your plan. You may also find this information in the Member Handbook provided by your insurance.
- Medical Credit or Financing Options
- The GCC and many other gender-affirming surgical practices do not offer payment plans for after surgery. For example, our patients must pay their full financial responsibility six weeks prior to surgery in order to keep their operation date. For patients that are not able to meet this requirement, we are pleased to partner with Care Credit to help our patients with or without insurance to finance the costs of their surgical procedure. The CareCredit card is North America’s leading patient payment program . The CareCredit card is easy to use, includes no hidden costs, and can be applied towards both surgical costs and follow-up appointments.
- Grants and Financial Assistance
- Through philanthropic partnerships the GCC collaborates with organizations such as Point of Pride , the Jim Collins Foundation and Genderbands because of their developed expertise in assessing need and selecting applicants with high levels of need. Patients still pass through the regular surgical consultation process after they are first selected by the organization. Our clinical team confirms their candidacy for surgery as a second step. Grants from these foundations and others can significantly reduce the costs of surgery for patients.
- Outside of the previously mentioned resource, many trans, non-binary and gender non-conforming communities use crowdfunding and other creative fundraising techniques to help them pay for gender-affirming surgery.
International Surgery Options
Many individuals in the United States choose to travel to other countries for gender-affirming surgery to save on costs. While medical tourism has been a popular option for gender reassignment surgery for decades, it is important to do your research on the credentials, experience and reputation of your provider. Some of the most popular destinations for surgeries abroad include Thailand, Mexico and Turkey. Especially because many countries do not have board-certification for surgeons, patients may need to do extra research to ensure the integrity of their provider. Not to mention, getting surgery outside of the US may involve less legal protections and greater difficulty with post-operative care like revision surgeries. For more information on comparing costs abroad, you can consult this guide .
More Articles
Gender surgeon of excellence, what is facial feminization surgery, your guide to top surgery in san francisco, request a free surgical consultation today..
All virtual and in-person consultations with our board-certified surgeons are free. Once you fill out this form, our patient care team will reach out and guide you through every step to get to surgery.
Suite 1010, 450 Sutter St San Francisco, CA 94108 Phone: (415) 780-1515 Fax: ( 628) 867-6510
Gender Journey Resources
- Our Services
- Trans Youth & Adolescents
Before & After
- Top surgery
- Pricing and Financing
- Office & Facilities
- Virtual Consultations
Board Certification & Memberships

- Terms of Use
Copyright © 2023 Gender Confirmation Center. All Rights Reserved.
- Credit cards
- View all credit cards
- Banking guide
- Loans guide
- Insurance guide
- Personal finance
- View all personal finance
- Small business
- Small business guide
- View all taxes
You’re our first priority. Every time.
We believe everyone should be able to make financial decisions with confidence. And while our site doesn’t feature every company or financial product available on the market, we’re proud that the guidance we offer, the information we provide and the tools we create are objective, independent, straightforward — and free.
So how do we make money? Our partners compensate us. This may influence which products we review and write about (and where those products appear on the site), but it in no way affects our recommendations or advice, which are grounded in thousands of hours of research. Our partners cannot pay us to guarantee favorable reviews of their products or services. Here is a list of our partners .
How Much Does Gender-Affirming Surgery Cost?

Many, or all, of the products featured on this page are from our advertising partners who compensate us when you take certain actions on our website or click to take an action on their website. However, this does not influence our evaluations. Our opinions are our own. Here is a list of our partners and here's how we make money .

Gender-affirming care encompasses a broad range of psychological, behavioral and medical treatments for transgender, nonbinary and gender-nonconforming people.
The care is designed to “support and affirm an individual’s gender identity” when it is at odds with the sex they were assigned at birth, as defined by the World Health Organization.
What is gender-affirming surgery?
Gender-affirming surgery refers to the surgical and cosmetic procedures that give transgender and nonbinary people “the physical appearance and functional abilities of the gender they know themselves to be,” according to the American Society of Plastic Surgeons. It is sometimes called gender reassignment surgery.
There are three main types of gender-affirming surgeries, per the Cleveland Clinic:
Top surgery , in which a surgeon either removes a person’s breast tissue for a more traditionally masculine appearance or shapes a person’s breast tissue for a more traditionally feminine appearance.
Bottom surgery , or the reconstruction of the genitals to better align with a person’s gender identity.
Facial feminization or masculinization surgery , in which the bones and soft tissue of a person’s face are transformed for either a more traditionally masculine or feminine appearance.
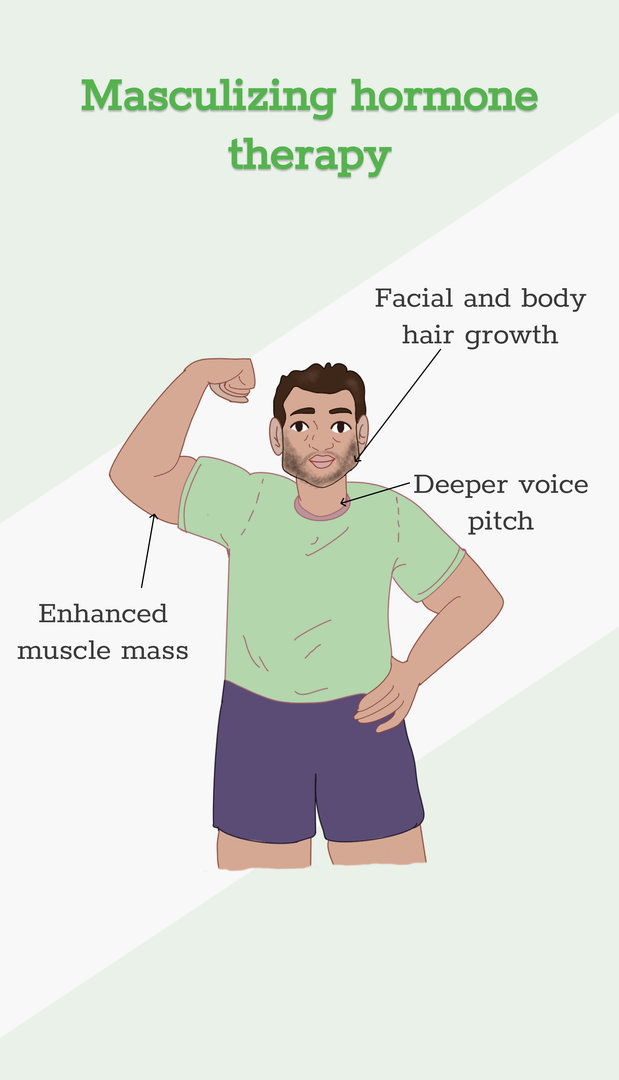
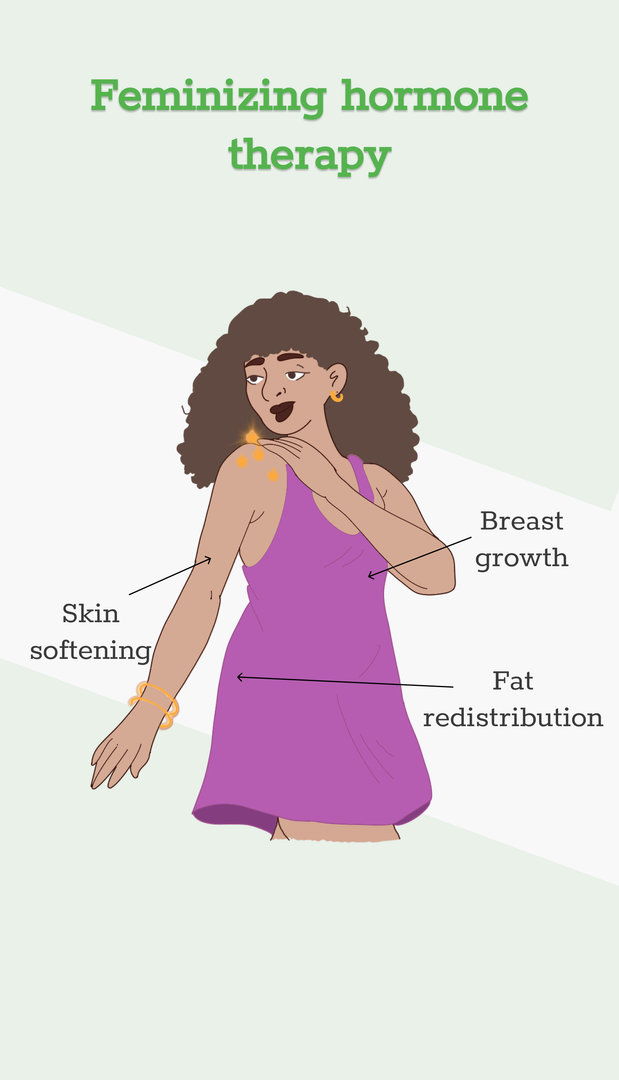
Some people who undergo gender-affirming surgeries also use specific hormone therapies. A trans woman or nonbinary person on feminizing hormone therapy, for example, takes estrogen that’s paired with a substance that blocks testosterone. And a trans man or nonbinary person on masculinizing hormone therapy takes testosterone.
Gender-affirming surgeries and treatments are the recommended course of treatment for gender dysphoria by the American Medical Association. Gender dysphoria is defined as “clinically significant distress or impairment related to gender incongruence, which may include desire to change primary and/or secondary sex characteristics,” according to the American Psychiatric Association.
Some LGBTQ+ advocates and medical professionals feel that gender dysphoria shouldn't be treated as a mental disorder, and worry that gender dysphoria’s inclusion in the DSM-5 — the authoritative source on recognized mental health disorders for the psychiatric industry — stigmatizes trans and nonbinary people.
How much does gender-affirming surgery cost?
Gender-affirming surgery can cost between $6,900 and $63,400 depending on the precise procedure, according to a 2022 study published in The Journal of Law, Medicine and Ethics.
Out-of-pocket costs can vary dramatically, though, depending on whether you have insurance and whether your insurance company covers gender-affirming surgeries.
There are also costs associated with the surgery that may not be represented in these estimates. Additional costs may include:
Surgeons fees
Hospital fees
Consultation fees
Insurance copays
The cost of psychiatric care or therapy, as most insurance companies and surgeons require at least one referral letter prior to the surgery. An hour of therapy can cost between $65 and $250, according to Good Therapy, an online platform for therapists and counselors.
Time off work. After bottom surgery, you can expect to miss six weeks of work while recovering. Most people miss around two weeks of work after top surgery.
Miscellaneous goods that’ll help you recover. For example, after bottom surgery, you might need to invest in a shower stool, waterproof bed sheets, cheap underwear and sanitary towels. Top surgery patients may need, depending on the procedure, a mastectomy pillow, chest binder and baggy clothes.
Is gender-affirming surgery covered by insurance?
It’s illegal for any federally funded health insurance program to deny coverage on the basis of gender identity, sexual orientation or sexual characteristics, per Section 1557, a section of the Affordable Care Act. Section 1557 doesn’t apply to private insurance companies, though, and several U.S. states have passed laws banning gender-affirming care.
The following states have banned gender-affirming surgery for people under 18 years old, according to the Human Rights Campaign: Alabama, Arkansas, Florida, Georgia, Idaho, Indiana, Iowa, Kentucky, Louisiana, Mississippi, Missouri, Montana, Nebraska, North Carolina, North Dakota, Oklahoma, South Dakota, Tennessee, Texas, Utah, West Virginia. In four of these states — Alabama, Arkansas, Florida and Indiana — court injunctions are currently ensuring access to care.
And these states have either passed laws — or have governors who issued executive orders — protecting access to gender-affirming surgery, according to the Movement Advancement Project, a public policy nonprofit: California, Colorado, Connecticut, Illinois, Maryland, Massachusetts, Minnesota, New Jersey, New Mexico, New York, Oregon, Vermont and Washington, D.C.
But even if your state has enshrined protections for gender-affirming care, some private insurance companies may consider surgeries “cosmetic” and therefore “not medically necessary,” according to the Transgender Legal Defense and Education Fund. If you have private insurance or are insured through your employer, contact your insurance company and see if they cover gender-affirming care. Also, ask about any documentation the insurance company requires for coverage.
The Williams Institute estimates that 14% of trans Americans currently enrolled in Medicaid live in states where such coverage is banned, while another 27% of trans Americans live in states where coverage is “uncertain,” because their state laws are “silent or unclear on coverage for gender-affirming care.”
Because of Section 1557, Medicaid is federally banned from denying coverage on the basis of sex or gender; among the roughly 1.3 million transgender Americans, around 276,000 have Medicaid coverage, according to a 2022 report from the Williams Institute.
How to pay for gender-affirming surgery
If your private insurance company won’t cover gender-affirming care, and you’re unable to obtain coverage through the federal marketplace, consider these sources:
Online personal loan.
Credit union personal loan.
Credit card.
CareCredit.
Home equity line of credit.
Family loan.
There are also several nonprofits that offer financial assistance for gender-affirmation surgeries. Those organizations include:
Point of Pride , which offers grants and scholarships to trans and nonbinary people seeking gender-affirming surgery and care.
The Jim Collins Foundation , which raises money to fund gender-affirming surgeries.
Genderbands , which offers grants for gender-affirming surgeries and care.
Black Transmen Inc. , which funds gender-affirming surgeries for Black trans men.
On a similar note...
Understanding the Cost and Criteria for Gender Reassignment Coverage

By Holly Hanson, CFP, CIMA, ADPA
There are certain steps that a transgender individual must go through before transition, one of which is receiving a diagnosis of gender identity disorder (GID). GID is characterized by a person’s strong and persistent desire to be, or belief that he or she is, the other sex, including:
- A preoccupation with getting rid of primary or secondary sex characteristics.
- An absence of any physical intersex condition.
- Clinically significant distress or impairment in social, occupational or other areas of functioning due to perceived incongruence between anatomical sex and perceived gender identity
GID Clearance
Clearance from a mental health professional/therapist is required for any type of body modification procedure except cosmetic surgery. The therapist should have familiarity with gender non-conformity and exhibit sensitivity in providing care.
The therapist will perform a psychological screening/assessment covering areas of emotional functioning, including peer and other social relationships. He or she will discuss possibilities and limitations of different treatments for GID.
Individuals with GID typically undergo treatment as prescribed by the World Professional Association for Transgender Health. This treatment follows a three-step approach to gender reassignment. It begins with the administration of cross-gender hormones to affect changes in physical appearance. The person being treated must then go through the “real-life” experience, which is a trial period of living as his or her true gender. The 12-month duration of the trial allows for the range of different life experiences and events that may occur throughout the year, including family events, holidays, vacations and season-specific work and/or school events.
Once this is complete, sex reassignment surgery — consisting of genital sex reassignment and/or nongenital sex reassignment — may be considered.
Preparing for GID Surgery
Here’s a snapshot of what is required before each surgery as well as the estimated costs.
Criteria for breast/chest surgery for transgender men
- Referral from ONE mental health professional
- Evidence of persistent, well-documented gender dysphoria
- Capacity to make a fully informed decision and consent to treatment
- Legal age (18+)*
- Reasonable control of any preexisting medical concerns. (Hormone therapy is not a prerequisite.)
Some younger individuals may be eligible.
( Read more about FTM top surgery .)
Criteria for breast/chest surgery for transgender females
- Persistent, well-documented gender dysphoria
- Capacity to make fully informed decision and consent to treatment
- Reasonable control of any preexisting medical concerns
Although not a criterion, it is recommended that male to female (MTF) patients receive hormonal therapy for a minimum of 12 months prior to breast implant surgery to maximize breast growth.
( Read more about breast augmentation for transgender women .)
Criteria for genital surgery
Hysterectomy (removal of uterus and ovaries) for transgender males and orchiectomy (removal of testicles) in transgender females.
- Referral from TWO mental health professionals
- Legal age (18+)
- One year of hormone therapy to meet gender goals (unless hormones are contraindicated for any medical reason).
Criteria for genital reconstructive surgery
Metoidioplasty/Phalloplasty in transgender males and vaginoplasty in transgender females.
- Capacity to make fully informed decision and consent for treatment
- One year of hormone therapy to meet gender goals
- One year spent living in a gender role that is congruent with their gender identity
Although not a criteria, it is recommended that these patients also have regular visits with a mental health or other medical professional.
Average Cost for Gender Reassignment
Electrolysis for unwanted hair removal can cost $100 to $200 per session. This is optional, but can be among the most costly of procedures for transgender females. Electrolysis is not covered by insurance in these cases.
The average total cost for transgender males is $50,000.
The average total cost for transgender females is $7,000 – $25,000.
The overall cost varies greatly. For starters, different doctors charge different amounts based on where their practice is based. In addition, some transgender individuals leave the country for the procedure(s). Some may not choose cosmetic surgery, and others may only undergo one or two procedures rather than committing to them all.
Insurance companies generally cover medically necessary procedures such as genital surgery and any surgery that alleviates severe gender dysphoria. Some insurance companies even partially cover hormone therapy since it could be considered hormone imbalance. Cosmetic surgery is not considered medically necessary and is not covered by most insurers.
Holly Hanson is the author of The LGBT and Modern Family Money Manual: Financial Strategies For You & Your Loved Ones. http://www.harmony-financial.com/
You Won't Believe How Much It Costs to Be Transgender in America

I decided to come out to my family and friends as transgender at 15. At the time I didn't really know what impact that decision would have on my life, but I knew I'd been in the wrong body for as long as I could remember. I didn't quite have the words to articulate my feelings until I found a YouTube of someone transitioning. I realized there was a medical term for the feelings, and that I too could transition to the gender I identified with — I was born a boy, but now I could become a girl.
Luckily, everyone I told was extremely understanding and supportive. My parents took the time to educate themselves on the issue and did everything in their power to make my transition as easy as possible. I was incredibly fortunate to have this foundation of support, as one of the greatest setbacks that transgender teens face is being shunned by families. Many in fact, end up homeless or attempting suicide .
Another frequent setback is the cost of transition. It's a very expensive process, and unfortunately, unlike in other Western countries, healthcare doesn't automatically cover most (or any) of these costs . (Some insurances and employers do, however, and the Human Rights Campaign website has an excellent resource that can walk you through the process.) This makes the prospect of transitioning seem unachievable to a lot of people struggling with gender identity. So how much does it all cost exactly? It depends of course on the desired transition, but here are some of the most popular treatments and procedures, and what they've cost me so far. It should also be noted, however, that no one has to undergo any of the below in order to identify as transgender. This is simply my journey.
Hormone Therapy: $1,500/Year
Deciding to transition into the opposite gender is not a decision that should be taken lightly. I underwent two years of therapy despite knowing in my heart that I was making the right choice. This process was one of the most rewarding stages of my transition. It felt liberating to have a healthcare professional validate my decision and help me understand my feelings on a deeper level. Unfortunately, professional therapy costs thousands of dollars a year, and most trans youth simply can’t afford it. Once my therapist and I decided that transitioning was the right decision for me, I began hormone replacement therapy, also known by its nickname: HRT. It's one of the most powerful tools a person transitioning can have at their disposal. I was initially put on anti-androgens to halt my body’s production of testosterone. This stopped my male puberty right in its tracks, and prevented the development of things like facial hair, excessive muscle, and a deeper voice. Three months later I was placed on estrogen, which was super exciting for me. Soon thereafter my body began to change—my skin became softer, my fat began redistributing itself to my breasts and hips, and my voice started changing. You can’t even begin to imagine how rewarding this process can be for a transgender teenager. Sadly, this incredibly crucial transformation also comes at a price. I had to visit my MD once a month to have my hormone levels checked, and to renew the prescription for my medication. It also costs a whopping $1,500 every year (at least). Once some people complete their gender reassignment surgery, they stop taking this medication, but I'm still on it. I started when I was 16 and am now 25, so that's about $13,500 so far, and I plan to be on HRT for the rest of my life.
Gender Reassignment Surgery: $30,000-Plus
Nearly two years after beginning my therapy and hormone replacement therapy, I was ready for my gender reassignment surgery at 18. In order to have this surgery, most doctors will require proof of at least two years of therapy, as this is not a reversible procedure. They also need to be certain that you're fully aware of the decision that you're making and all of its consequences. For me, it was one of the happiest moments in my life. There are really no words to describe the excitement and anticipation I felt leading up to surgery. I will say, however, that I cannot stress enough enough how important it is to do your research before choosing a GRS surgeon. Only a handful of doctors in the world are truly experts in this field, and choosing the wrong one can lead to catastrophic results. This step in the transition is very expensive, and the average cost is upwards of $30,000. In addition to the actual procedure, you also have to pay for travel costs and hotel accommodations if a good physician does not live in your neighborhood. But in my opinion, this is a small price to pay for a lifetime of completion. I feel incredibly blessed that I had the opportunity at such a young age, and the opportunity to live my life in a way that feels true to me, in part, because of this surgery.
Facial Feminization Surgery: $25,000-$60,000
A year after having gender reassignment surgery, I went back under the knife for facial feminization surgery — a set of reconstructive procedures that alter typically male facial features to bring them closer in shape and size to typical female facial features. In my personal experience, this is the most life changing surgery of them all. As a young transgender woman, nothing was more important to me than being able to "blend" into society seamlessly. It's not only crucial for vanity reasons (what girl wants to look like a boy?), but also for safety reasons. Being trans often subjects you to discrimination, bullying, and physical aggression .
It's so important to members of the trans community that our outward appearance and inner self are in complete harmony. Speaking from personal experience, although not often, I did occasionally come across some level of bullying prior to having FFS. It's simply a lot easier to be singled out and targeted when the aggressor can identify you as being trans. But again, there's a price to pay for the procedure. Board certified surgeons that are qualified to do these procedures will charge anywhere from $25,000 to $60,000 depending on the amount of work you get. Mine cost about $30,000 , as I only opted for the procedures that I thought would benefit me the most at the time, which were forehead and jawline contouring.

Breast Augmentation: $5,000-$10,000
Having a breast augmentation as a transgender woman is an entirely personal choice. I know many who have chosen not to, and instead let their hormones do all the work when it comes to breast development. I chose to have surgery because I wanted a fuller bosom, and my hormones didn't help completely on that front. This surgery will cost between $5,000 and $10,000, and it all depends on the surgeon you choose, where that person is located, and what type of implant you want. Breast augmentation was by far the most painful of all the surgeries. In fact, after all the other procedures, I usually only felt some level of discomfort. When I woke up from this one, it was like an elephant was sitting on my chest.
Looking back at those two years of my life, from about 16 to 19, in which most of my transition took place, I often tell friends that I didn’t feel any less "female" prior to having the surgeries. And I think this is very important. Transitioning simply brought all the puzzle pieces together. I never had a waking moment where I thought in order to feel or be female, I needed to undergo multiple surgeries. My brain, heart, and soul felt 100% female prior to transition. Oftentimes, after surgery, my relatives would ask if I felt any different. My answer was always the same: no. I've always been the same old Elle.
I chose to undergo these surgeries to better my life experience, not to "become" female because I already was. Nowadays, I really only think about the process of transition when I am filming a Youtube video related to it. My journey into the person I am today would not have been possible if that 15-year-old me hadn't stumbled upon someone else going through the same thing. I hope I can help others in the same way.
For more information on transgender individuals and some of the issues and hardships they frequently face, check out the LGBT organization, the Human Rights Campaign .
Related: Trans Teen Wins Right to Use Bathroom of His Choice
Check out Teen Vogue ’s December/January issue cover star, Fernanda Ly.

Get doctor listing on ClinicSpots.
Gynecologist
Cardiologist
Get answers for your health queries from top Doctors for FREE!
100% Privacy Protection
We maintain your privacy and data confidentiality.
Verified Doctors
All Doctors go through a stringent verification process.
Quick Response
Reduce Clinic Visits
Save your time and money from the hassle of visits.
Gender Reassignment Surgery Cost (MTF & FTM)
Explore the rising demand for gender reassignment surgery worldwide. Learn about the various procedures and their detailed costs in this comprehensive article.
- Transgender Surgery
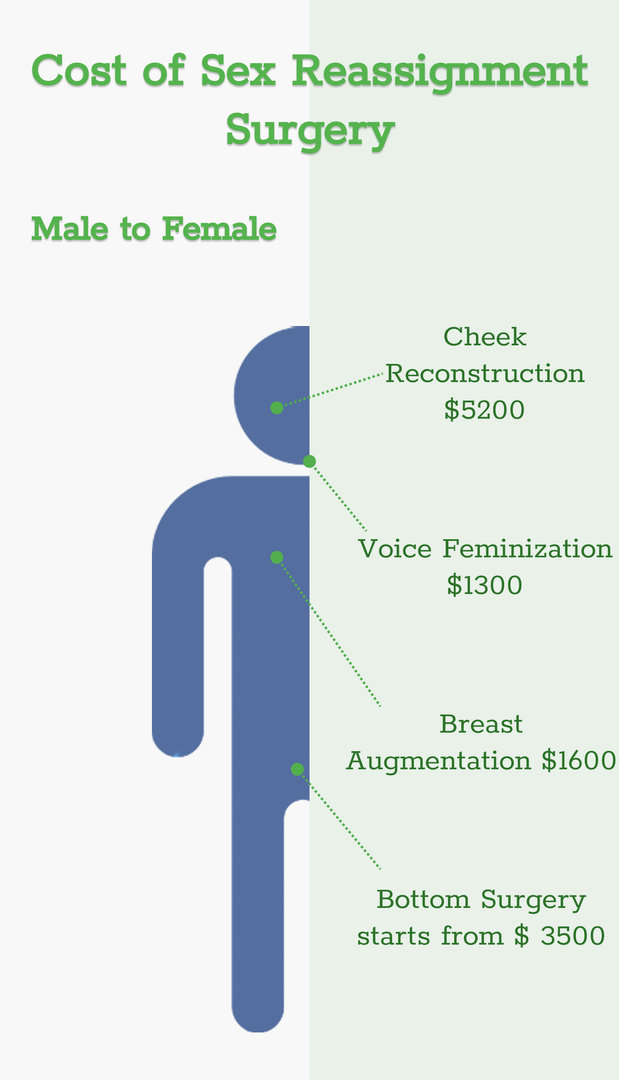
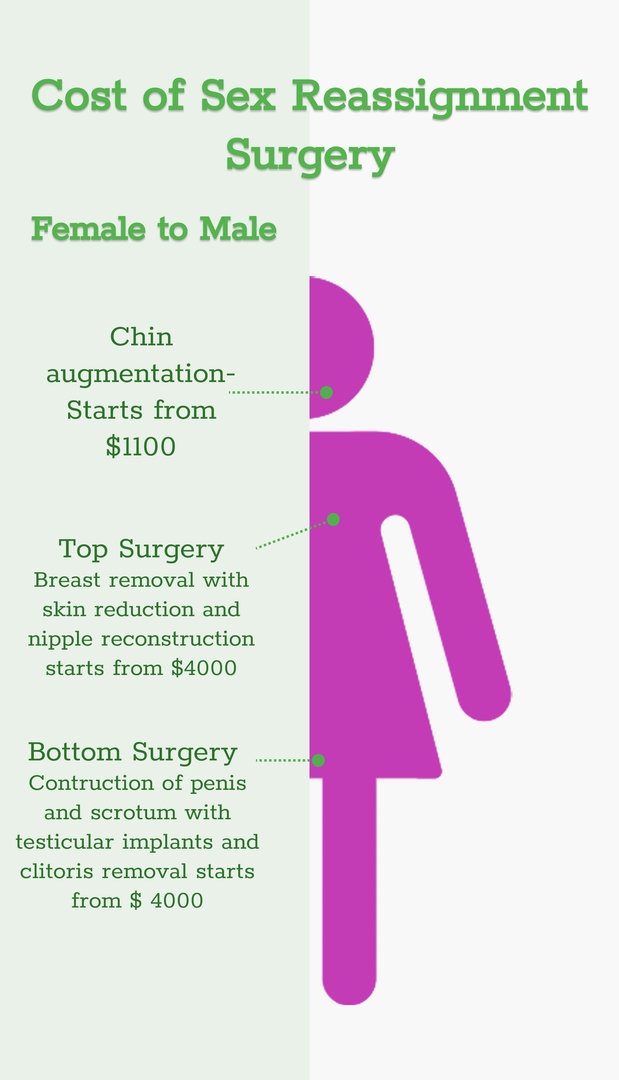
Gender reassignment surgery cost varies depending on the type of transition.
- For male to female (MTF) transition, the cost ranges from $2438 to $6095 and
- For female to male (FTM) transition, the cost falls between $4876 and $9752 .
When considering the cost of gender reassignment surgery, it's important to note that these figures encompass the surgical expenses alone. Additional costs, such as:
- pre-operative consultations
- post-operative care
- hospitalization may also be involved
For a precise cost estimate that aligns with your specific needs, it is highly recommended that you consult reliable healthcare providers or clinics.
Begin with clarity. Contact us for detailed cost insights now.
There are two broad types of gender reassignment surgery : top surgery and bottom surgery. The top surgery is performed for both people assigned female at birth (AFAB) and assigned male at birth (AMAB).
- Male to female or non-binary (MTF/N): This procedure entails using saline or silicone implants to boost chest size and form for a more feminine or female appearance. Male-to-female top surgery is done under general anesthesia.
- Female to male or non-binary (FTM/N): During FTM top surgery, breast tissue is removed and the chest is shaped to give the patient a flat, masculine, or male appearance. Following this, a nipple graft is planted to give a complete look .
Before we discuss each service's cost, let's take a quick look at overall transgender surgery costs in different countries.
You must be curious to know the gender change surgery cost of different surgical procedures. Let's read.
What is the Cost of Male-to-Female Top Surgery?
Breast augmentation or augmentation mammoplasty is another name for MTF and MTN top surgery.
The MTF/N top surgery or breast augmentation surgery cost in India is around USD 1290 to USD 1940 . The surgeon's expertise and experience are two of the most critical aspects that affect the cost.
For the duration of the surgery, you will be put under general anesthesia. Your surgeon may choose different breast augmentation methods depending on your desired chest size, implant kind, and incision site. The average time for MTF and MTN top surgery is 1 to 2 hours .
The insertion cost and the implant cost are the two components of the surgery cost.
Navigating your options? Contact us today for more information on cost!
What is the cost of female-to-male top surgery?
An FTM or FTN top surgery procedure takes from 1.5 to 4 hours . Various treatments are performed to get a more flat, masculine, or male-looking chest. Double incision, periareolar, and keyhole are the most popular procedures used by surgeons.
The FTM top surgery cost ranges around USD 3870 .
Now that we have already discussed top surgery costs, let's take a look at how much mtf bottom surgery costs.
AFAB and AMAB people can undergo bottom surgery as part of their gender confirmation process. Bottom surgery involves transforming or reconstructing the bottom or genitalia. This involves Vaginoplasty, penile transplant , phalloplasty, and metoidioplasty.
What is the cost of male-to-female bottom surgery?
Vaginoplasty surgery is the major procedure performed in bottom surgery . There are three main options under Vaginoplasty. Penile inversion, non-penile inversion Vaginoplasty, and recto-sigmoid or colon graft.
The clitoris is moulded from the head/tip of the penis in all three surgical approaches. The Vaginoplasty cost is around USD 3870 to USD 4520.
Now, let's look at female to male bottom surgery cost.
What is the Cost of Female-to-Male Bottom Surgery?
This procedure involves the removal of the female organs in the lower region and reassigning them to male sexual parts. It includes removing the uterus, vaginal remodeling, labia reconstruction, metoidioplasty, and phalloplasty.
The whole procedure may cost somewhere around USD 5160 to USD 10,335 .
To get a clearer picture of gender reassignment surgery cost, connect with us now .
What is the Cost of Facial Feminization Surgery?
Facial feminization surgery is a technique that involves changing your facial characteristics to make them appear more feminine. FFS is concerned with bone structure and nose shape. FFS is distinct for each person and can affect any part of the face or neck.
The facial feminization surgery cost is USD 1350 .
What is Hormonal Replacement Cost?
Hormonal replacement therapy is for both MTF/N and FTM/N transitioning.
MTF/N: The hormones for a male-to-female transition enhance the alignment of your gender identity. It helps induce physical changes in your body produced by female hormones during puberty (gender congruence). Male secondary sex traits can be avoided if feminizing hormone therapy like progesterone is initiated before male puberty. The hormonal replacement therapy cost for MTF/N is USD 12/month.
FTM/N: You'll be administered the male hormone testosterone during masculinizing hormone therapy. It suppresses your menstrual cycles and lowers oestrogen synthesis in your ovaries. The hormonal replacement therapy cost FTM/N is USD 7/month.
To make a more informed decision, talk to us today.
Factors affecting the cost of gender reassignment surgery:
- Hospital charges: It depends on the type of hospital you choose. Moreover, the cost also depends on whether you are admitted to a general ward or a private room.
- Psychiatrist : If you need a psychiatrist to deal with your physical changes, your cost will impact you. A psychiatrist is recommended to understand better the complex procedures and adjustments you will need before and after your surgery.
- Clinical Experts and Surgeons : You will discuss the specifics of your gender change surgery with your doctor. It includes an assessment of your medical health status, discussing your long-term gender confirmation goals, and evaluating which procedures may be most appropriate to assist you in your journey. You can ask for specific details such as risks, benefits, and what to expect from the surgery.
- Medical Insurance: Your medical insurance will play an essential role in the procedure, saving you a lot of money.
- Accommodation Charges: The accommodation charges are included for international patients.
- Medication charges : These charges include all the medication you will receive before and after the procedure ends.
- Pre- and Post-treatment charges: The pre-treatment charges include doctor consultation fees, diagnosis charges, etc. The post-treatment charges may include medicine costs, doctor's revisit charges, etc.
Your health is too important to ignore – schedule your appointment now.
Do Insurance Companies Cover Gender Reassignment Surgery?
Yes, insurance companies that cover gender reassignment surgery! There is no legal prohibition for that. Not all employers provide insurance coverage to unmarried or live-in partners of straight employees. But, several organizations nowadays provide medical insurance to their employees' same-sex partners, including coverage for gender-reassignment surgery.
Some independent companies have made it a goal to try and incorporate this coverage into their medical insurance for employees.
Note: This article is on the cost of gender reassignment surgery, and data about it is only for your informational purposes and is subject to change.
1. Side effects of gender reassignment surgery
- Infections.
- Side effects of anesthesia.
- Difficulty in urinating.
- Severe complications in intestines.
- Leakage of urine through openings.
- Closure of vaginal opening.
2. Who typically undergoes gender reassignment surgery?
Gender reassignment surgery is typically undergone by individuals who experience gender dysphoria, a condition where an individual's gender identity does not match their assigned sex at birth. It is usually recommended as a last resort after other treatments such as therapy, hormone therapy, and social transition have been tried.
3. What are the types of gender reassignment surgery?
The two main types of gender reassignment surgery are "top surgery," which refers to surgeries that alter the chest and breast area, and "bottom surgery," which refers to surgeries that alter the genital area. Top surgery may involve a mastectomy, breast augmentation, or breast reduction. Bottom surgery may involve genital reconstruction, orchiectomy, metoidioplasty, or phalloplasty. 4. Do the costs vary for different types of gender affirmation procedures? Yes, the cost can vary based on the specific surgeries involved, such as chest or breast augmentation, facial feminization, or genital reconstruction. References:
https://my.clevelandclinic.org/
Dr. Josef Hadeed Plastic Surgery | Beverly Hills & Los Angeles (josefhadeedmd.com)
The Economic Times: Business News, Personal Finance, Financial News, India Stock Market Investing, Economy News, SENSEX, NIFTY, NSE, BSE Live, IPO News (indiatimes.com)
Market research reports, consulting: Global Market Insights Inc. (gminsights.com)
Transgender surgery – Knowledge gap among physicians impacti... : Current Urology (lww.com)
https://jamanetwork.com/journals/jamasurgery/fullarticle/2779429
Related Blogs
How much does male to female (MTF) surgery cost in 2024?
Explore the interactive cost guide below for detailed pricing information on a range of MTF surgeries and compare costs in different countries.
Female to Male (FTM) Surgery Cost in 2024
Explore managing fibrocystic breast disease post-menopause. Gain insights and support for optimal health beyond this stage.

Transgender Surgery Gone Wrong, How To Reverse It?
Discover solutions for transgender surgery gone wrong. Learn how to reverse complications and regain confidence. Your guide to a corrective journey awaits.

MTF Top Surgery Scars, Are They Normal & How To Treat Them?
Understanding MTF top surgery scars: types, management, and scar reduction techniques. Empowering choices for a smooth transition.

Progesterone Transgender: Effects and Considerations
Explore the use of progesterone in transgender hormone therapy. Learn about its role in feminizing or masculinizing effects and its potential benefits and risks for individuals undergoing gender transition.

Gender Dysphoria in Adults: Understanding and Support
Explore gender dysphoria in adults. Gain insights, support, and resources for understanding and navigating this complex experience with compassion and dignity.
FTM Post Op: Expectations After Transgender Surgery
Explore the transformative journey of FTM post-op experiences. Discover insights, support, and resources for a fulfilling and affirming transition.

Post Op MTF: Expectations After Transgender Surgery
Find out post-operative care for MTF (Male-to-Female) gender confirmation surgery. Learn about recovery, potential complications, and ongoing support for a successful transition journey.
Question and Answers
I am 27 years i am trans female had a surgery from mtf and now want to have reversal surgery ftm now is it possible in india to have a surgery.
You want to know if there's an option for surgery to change from a trans female to a trans male in India. These surgeries are legal in India, but it is important to first talk to a plastic surgeon who is experienced in gender-affirming surgeries. They will look at your particular case, go over your reasons for reversal surgery with you, and help you with the process.
Answered on 22nd Oct '24
Dr. Vinod Vij
48! yaşında bir erkeğim trans birey olarak kadın olmak istiyorum Hormon tedavisi istiyorum. Hangi ilaçlardan başlamalıyım
For someone who is 48 years old and seeking to transition from male to female, it's important to consult with an endocrinologist before starting any hormone therapy. They will guide you on the appropriate medications and dosages based on your specific needs.
Answered on 2nd Aug '24
if I have top surgery without T can I develop pecs if I hit the gym a lot?
If you don't take testosterone or undergo top surgery, you can still build your pecs by lifting weights. Pecs, short for pectoral muscles, can grow with exercises like chest presses and push-ups, which target these muscles. Pace yourself, use the correct form, and be consistent with your workouts. Your pecs can still develop even without testosterone.
Answered on 29th July '24
I'm male and would like to know how to grow breasts without HRT?
Hormones and surgery are the only ways of growing breasts safely. The appearance of women's breasts in some regions is partly dependent on hormones during puberty and pregnancy. Trying to get a larger breast by force can cause some serious medical issues. If you are worried about your body, it's important to talk to a plastic surgeon for safe and honest guidance.
Answered on 19th Sept '24
I am a 32 years old male who has got into cross dressing some 8 years back, now my urge of being like this has grown, last two years I have been I’m eating dian35 prescribed by a doctor in Malaysia, but now I believe I shall be needing more strong dose since the transformation is already 2 years and can see few changes
It seems like you may be going through some changes about turning into the opposite sex. Understand that these changes are complicated and might need some medical interventions. You might require different amounts of hormones to help you through the process. Talk about what is bothering you and your symptoms with a doctor who can help you figure out the best way forward.
Answered on 18th July '24
Transgender Surgery Hospitals In Other Cities
Transgender surgery hospitals in delhi, transgender surgery hospitals in ahmedabad, transgender surgery hospitals in bangalore, transgender surgery hospitals in mumbai, transgender surgery hospitals in pune, transgender surgery hospitals in chennai, transgender surgery hospitals in hyderabad, transgender surgery hospitals in kolkata, top related speciality doctors in other cities, gynecologist/obstetrician in delhi, gynecologist/obstetrician in ahmedabad, gynecologist/obstetrician in bangalore, gynecologist/obstetrician in mumbai, gynecologist/obstetrician in pune, gynecologist/obstetrician in chennai, gynecologist/obstetrician in hyderabad, gynecologist/obstetrician in kolkata, plastic surgeon in delhi, plastic surgeon in ahmedabad.
How Gender Reassignment Surgery Works (Infographic)
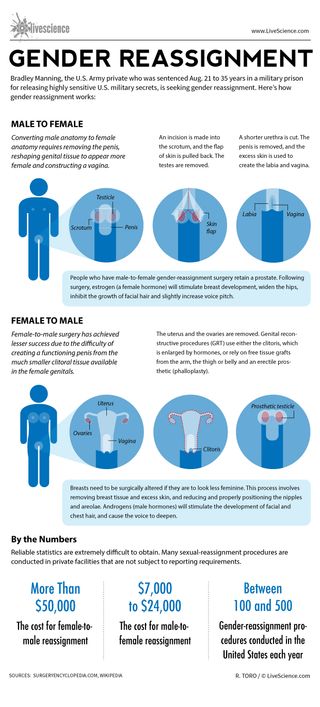
Bradley Manning, the U.S. Army private who was sentenced Aug. 21 to 35 years in a military prison for releasing highly sensitive U.S. military secrets, is seeking gender reassignment. Here’s how gender reassignment works:
Converting male anatomy to female anatomy requires removing the penis, reshaping genital tissue to appear more female and constructing a vagina.
An incision is made into the scrotum, and the flap of skin is pulled back. The testes are removed.
A shorter urethra is cut. The penis is removed, and the excess skin is used to create the labia and vagina.
People who have male-to-female gender-reassignment surgery retain a prostate. Following surgery, estrogen (a female hormone) will stimulate breast development, widen the hips, inhibit the growth of facial hair and slightly increase voice pitch.
Female-to-male surgery has achieved lesser success due to the difficulty of creating a functioning penis from the much smaller clitoral tissue available in the female genitals.
The uterus and the ovaries are removed. Genital reconstructive procedures (GRT) use either the clitoris, which is enlarged by hormones, or rely on free tissue grafts from the arm, the thigh or belly and an erectile prosthetic (phalloplasty).
Breasts need to be surgically altered if they are to look less feminine. This process involves removing breast tissue and excess skin, and reducing and properly positioning the nipples and areolae. Androgens (male hormones) will stimulate the development of facial and chest hair, and cause the voice to deepen.
Reliable statistics are extremely difficult to obtain. Many sexual-reassignment procedures are conducted in private facilities that are not subject to reporting requirements.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000.
Between 100 to 500 gender-reassignment procedures are conducted in the United States each year.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Scientists made mice with Y chromosomes female by deleting just 6 tiny molecules
Man's years of premature ejaculation had a rare cause
How old is planet Earth?
Most Popular
- 2 Euclid telescope reveals 1st section of largest-ever 3D map of the universe — and there's still 99% to go
- 3 1st wheel was invented 6,000 years ago in the Carpathian Mountains, modeling study suggests
- 4 Doctors no longer recommend 'self-checks' for breast cancer — here's what to know
- 5 Key Atlantic current could collapse soon, 'impacting the entire world for centuries to come,' leading climate scientists warn
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
Understanding Insurance Requirements for Gender Affirmation Surgery
- Type of Surgeries
- Barriers to Access
- WPATH Standards
Restrictions to Coverage
Getting started, what you can do.
Insurance coverage for orchiectomy, genitoplasty, and other types of gender-affirmation surgery is largely governed by standards issued by the World Professional Association for Transgender Health (WPATH). Many health insurance providers use these guidelines to direct which procedures are medically necessary. However, not every insurer—or state—does.
Because acceptance of WPATH guidelines can vary, it can sometimes be hard to determine which procedures are covered by your health plan and whether gender affirmation is even affordable.
This article describes the types of surgeries pursued by transgender or gender-nonconforming people as a part of gender affirmation and the barriers they face. It also explains the WPATH standards of care for each type of surgery, how insurance companies use them to determine eligibility, and what restrictions are imposed by providers or states.
Gender-affirmation surgery is the preferred term but gender-confirmation surgery and gender-alignment surgery can also be used. Outdated terms like "sex reassignment" or "sex change" should not be used.
Gender affirmation reflects the process a person goes through when they begin to live as their authentic gender rather than the gender assigned to them a birth.
Medical or surgical procedures are only one facet of gender affirmation.
Types of Gender-Affirmation Surgery
Not all transgender, non-binary , and genderqueer individuals want surgery to align their bodies to their gender identity. Some people are content with social or other medical transition options .
Others want one or more surgeries, including those referred to as " top surgery ” (occurring above the waist) and "bottom surgery" (occurring below the waist).
An extensive national survey of transgender people found that:
- 66% of transgender women either had or wanted vaginoplasty or labiaplasty .
- 51% of transgender women either had or wanted breast augmentation.
- 50% of transgender women either had or wanted facial feminization (surgery to make a face appear more feminine).
- 37% of transgender women either had or wanted a tracheal shave (removal of the Adam’s apple).
- 58% of transgender women either had or wanted orchiectomy (removal of the testicles).
- 22% of transgender men either had or wanted phalloplasty (the creation of a penis).
- 27% of transgender men either had or wanted metoidioplasty (surgery that uses existing genitalia to create a penis).
- 97% of transgender men either had or wanted chest reconstruction or mastectomy (removal of the breasts).
- 71% of transgender men either had or wanted a hysterectomy (removal of the uterus).
Common Barriers to Gender-Affirmation Surgery
Cost, surgeon availability, and a process referred to "gatekeeping" are three major hurdles commonly faced by people undergoing gender affirmation.
Cost is one of the primary reasons people have limited access to gender-affirmation surgeries. Historically, most public or private insurance companies have not covered these procedures. Fortunately, that is changing.
Some public and private insurance companies cover some or all gender-affirmation surgery options. But that coverage often comes with many hoops that people need to jump through. It is also not available to all people in all states.
Surgeon Availability
Another major factor limiting access to surgery is the small number of surgeons trained to perform them. These surgeons, particularly very experienced ones, are often booked months or years in advance.
In addition, many don’t take insurance. Fortunately, as insurance coverage for gender-affirmation surgeries has increased, so too has physician interest in training. Today, there are many hospitals across the country that routinely perform vaginoplasty and accept insurance to pay for them.
"Gatekeeping"
Another barrier is a process called “gatekeeping" currently endorsed by WPATH. Gatekeeping involves undergoing a significant therapy or psychiatric assessment before they are allowed to transition medically.
It is a process that attracted considerable debate given that this level of scrutiny is not required for other major surgeries. It ultimately places the decision in the hands of a psychiatrist who can determine if a person is mentally "fit" to pursue treatment.
Discrimination and Stigma
In addition to barriers like cost and surgeon availability/competency, there is also a long history of discrimination and stigma limiting transgender patients’ access to care.
Insurance and the WPATH Standards
When determining eligibility for gender-affirming surgery coverage, many insurers turn to the WPATH Standards of Care to inform their eligibility guidelines. These are also known as the WPATH criteria or WPATH requirements.
WPATH updates its guidelines every five to 10 years. These standards of care help define which treatments are medically necessary and under which conditions they should be authorized. The standards have become less restrictive over time, reflecting the growing recognition of gender diversity in society.
The standards of care are broadly described as follows:
Standards for Top Surgery
“Top surgery” refers to gender-affirmation surgery of the breast or chest. For transmasculine people, this surgery is called chest reconstruction. For transfeminine people, it is breast augmentation.
The WPATH criteria for top surgery include:
- Persistent, well-documented gender dysphoria (distress caused by the difference between a person’s gender and the gender they were assigned at birth)
- The ability to make an informed decision and consent to treatment
- Any significant medical or mental health conditions are “reasonably well controlled”
Standards for Hormone Therapy
It is important to note that hormone therapy is not required for these surgeries. However, a year of hormone therapy is recommended for transgender women because it allows them to get the maximum possible breast growth without surgery, which improves surgical outcomes.
For transgender men, there is no hormone requirement or recommendation. That’s because some transmasculine people are only dysphoric about their chests. Therefore, they do not want or need testosterone treatment.
There are also several physical and psychological reasons people choose to undergo top surgery without hormone use. That said, people who are taking testosterone and are very active may wish to wait a year for surgery because testosterone and exercise can significantly reshape the chest. Therefore, waiting a year may result in a more aesthetic outcome.
Standards for Orchiectomy, Hysterectomy, and Ovariectomy
These surgeries involve the removal of the testicles (orchiectomy), uterus (hysterectomy), or ovaries (ovariectomy).
WPATH criteria for these surgeries include:
- Persistent, well-documented gender dysphoria
- Any significant medical or mental health conditions are “well controlled”
- At least 12 continuous months of appropriate hormone therapy, unless there are reasons someone can’t or won’t take hormones. The purpose of this guideline is so that people can experience reversible hormone changes before they undergo irreversible ones.
Surgeries to remove the gonads (testes, ovaries) and the uterus may be performed independently. They may also be performed alongside other gender-affirmation surgeries.
Removing the gonads alone can lower the amount of cross-sex hormone therapy required to get results. In addition, removing the uterus or cervix eliminates the need to screen those organs. That’s important because those screening exams can cause dysphoria and discomfort in many transgender men.
Standards for Vaginoplasty, Phalloplasty, and Metoidioplasty
This group of surgeries constructs a vagina (vaginoplasty) or penis (phalloplasty, metoidioplasty). These procedures make a person’s genitalia more in line with their gender identity.
- Any significant medical or mental health conditions are “well controlled”
- Appropriate hormone therapy for 12 continuous months, unless there are reasons why someone can’t or won’t take hormones
- Living in a gender role that is consistent with their gender identity for 12 continuous months
The requirement for a year of living in a gender role is because it gives people time to adjust to their desired gender. In addition, doctors widely believe that a year is a sufficient time for that adjustment before undergoing a complicated, expensive, and irreversible surgery.
Aftercare for these surgeries can be emotionally intense and difficult. For example, following vaginoplasty , consistent vaginal dilation is required to maintain depth and girth and avoid complications. These requirements can sometimes be challenging for people with a history of sexual trauma.
Aftercare Recommendations
Due to these surgeries’ physical and emotional intensity, experts recommend that those considering them have regular visits with a mental or medical health professional.
Standards for Facial Feminization Surgery
There are no formal guidelines for facial feminization surgery. In addition, it has historically been tough to get this procedure covered by insurance due to a lack of research on the benefits.
However, some individuals have been able to have it successfully covered by arguing that it is as medically necessary as genital surgery and has equally positive effects on quality of life.

Standards for Children and Adolescents
WPATH guidelines for children and adolescents include criteria for fully reversible interventions ( puberty blockers that pause puberty, for example) or partially reversible ones (hormones, for example). However, they do not recommend irreversible (surgical) interventions until the age of majority in their given country.
One exception is chest surgery for transmasculine adolescents. WPATH criteria suggest this could be carried out before adulthood, after ample time of living in their gender role, and after being on testosterone treatment for one year.
Despite the increasing uptake of WPATH guidelines by insurers, not every organization embraces them or applies them in the same way. Even WPATH notes that “the criteria put forth in this document... are clinical guidelines. Individual health professionals and programs may modify them.” And many times, they do.
Generally speaking, private insurance companies are more likely to offer coverage for some or all procedures than government agencies like Medicaid and Medicare. Even so, eligibility requirements can vary as can copayment and coinsurance costs.
Medicaid is the U.S. government health coverage program for low-income people, jointly funded by the federal government and states. Of the estimated 1.4 million transgender adults living in the United States, approximately 152,000 have Medicaid coverage, according to the Kaiser Family Foundation.
Many state Medicaid programs cover aspects of gender-affirming health services. But only two states—Maine and Illinois—cover all five WPATH standards of care as of October 2022 (hormone therapy, surgery, fertility assistance, voice and communication therapy, primary care, and behavioral intervention).
Current Medicaid Coverage Status
In terms of gender-affirming surgery, 23 states provide coverage for adults, while nine states (Alabama, Arizona, Florida, Hawaii, Iowa, Kansas, Missouri, Texas, and Wyoming) currently deny coverage. The remaining states either have no policies in place or offer no reporting of coverage.
Medicare is federal health insurance for people 65 or older and some younger people with disabilities. Original Medicare (Part A and Part B) will cover gender-affirmation surgery when it is considered medically necessary. Prior to 2014, no coverage was offered.
The challenge with accessing surgery is that Medicare has no national precedent for approving or denying coverage. As such, approval or denial is based largely on precedents within your state and is conducted on a case-by-case basis.
This suggests that approval may be more difficult in states that deny coverage to Medicaid recipients given that Medicare is administered by a central agency called the Centers for Medicare & Medicaid Services (CMS).
As a general guideline, the CMS states that the following is needed for you to be an eligible candidate for gender-affirmation surgery:
- Have a diagnosis of gender dysphoria
- Provide proof of counseling
- Provide evidence of hormone therapy (for transgender women)
If coverage is denied, there is an appeal process you can undergo to overturn the denial.
Private Insurance
Most private insurance companies in the United States will offer coverage for some—but not necessarily all—gender-affirming surgeries.
According to the Transgender Legal Defense & Education Fund (TLDEF), many of the larger insurers offer coverage for a comprehensive array of surgeries, including providers like:
- Blue Cross/Blue Shield
- UnitedHealthcare
Others have different standards in different states (such as AmeriHealth) or only offer coverage for specific surgeries like facial feminization surgery (Prestige and AmeriHealth New Hampshire).
Though coverage of gender-affirmation surgery is increasing, many private insurers still require you to meet extensive criteria before approval is granted. By way of example, to get approval for breast augmentation, a transgender woman would need to provide a company like Aetna:
- A signed letter from a qualified mental health professional stating their readiness for physical treatment as well as their capacity to consent to a specific treatment
- Documentation of marked and sustained gender dysphoria
- Documentation that other possible causes of gender dysphoria have been excluded
- The completion of six to 12 months of hormone therapy
- A risk assessment of breast cancer screening by a qualified healthcare provider
Even if approval is granted, copayment, coinsurance, and out-of-pocket costs can vary, often considerably.
Out-of-Pocket Costs
According to a 2022 study from Oregon Health & Science University, a transgender person who underwent "bottom" surgery from 2007 to 2019 paid an average of $1,781 out of pocket.
With that said, 50% had to leave their state due to the restriction or unavailability of gender-affirmation surgery and ended up paying an average of $2,645 out of pocket, not including travel or living expenses.
Showing that a person has “persistent, well-documented gender dysphoria” usually requires a letter from a mental health provider. This letter usually states that the person meets the criteria for gender dysphoria, including the length of time that has been true.
This letter often also contains a narrative of the person’s gender history in detail. In addition, the letter should state how long the provider has been working with the person.
Well or Reasonably Controlled
It is important to note that some standards require that medical and mental health problems be well controlled, while others only require them to be reasonably well controlled. Documentation of this is also usually in a letter from the relevant healthcare provider.
This letter should contain information about the history of the condition, how it is controlled, and the length of the clinician’s relationship with the person. Ideally, the phrases “well controlled” or “reasonably well controlled” are used in the letter as appropriate.
Using terminology referenced in the WPTH criteria makes it easier for providers and insurance companies to determine that the conditions of the standards of care have been met.
Of note, mental health conditions are not a contraindication for gender affirmation surgeries. In fact, these procedures can help resolve symptoms in many transgender people and others with gender dysphoria. Symptom relief is true not just for anxiety and depression but for more severe conditions such as psychosis.
Getting insurance coverage for gender confirmation surgery can be a frustrating process. However, it can help to prepare a copy of the WPATH guidelines and any relevant research papers to support your goals. That’s particularly true if they include surgeries other than those listed above.
In addition, it may be a good idea to reach out to your local LGBT health center for assistance. Many health centers are now hiring transgender patient navigators who have extensive experience with the insurance process. They can be a great resource.
Local and national LGBTQ-focused legal organizations often have helplines or access hours where people can seek information.
Gender-affirmation surgery refers to various surgeries that allow people to align their bodies with their gender. WPATH guidelines offer criteria for determining whether someone is a good candidate for gender-affirmation surgery.
Not all insurance offers coverage for gender-affirmation surgery, but some do. First, however, you need to provide the proper documentation to show that you meet specific surgery criteria. This documentation is usually in a letter written by your physician or mental health clinician.
Morrison SD, Capitán-Cañadas F, Sánchez-García A, et al. Prospective quality-of-life outcomes after facial feminization surgery: an international multicenter study . Plast Reconstr Surg . 2020;145(6):1499-1509. doi:10.1097/PRS.0000000000006837
National Center for Transgender Equality. The report of the 2015 U.S. transgender survey .
World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people, 7th version .
Kaiser Family Foundation. Update on Medicaid coverage of gender-affirming health services .
CMS.gov. Gender dysphoria and gender reassignment surgery .
Transgender Legal Defense & Education Fund. Health insurance medical policies: gender dysphoria / gender reassignment .
Aetna. Gender-affirming surgery .
Downing J, Holt SK, Cunetta M, Gore JL, Dy GW. Spending and out-of-pocket costs for genital gender-affirming surgery in the US . JAMA Surg. 2022;157(9):799-806. doi:10.1001/jamasurg.2022.2606
Meijer JH, Eeckhout GM, van Vlerken RH, de Vries AL. Gender dysphoria and co-existing psychosis: review and four case examples of successful gender affirmative treatment . LGBT Health . 2017;4(2):106-114. doi:10.1089/lgbt.2016.0133
By Elizabeth Boskey, PhD Boskey has a doctorate in biophysics and master's degrees in public health and social work, with expertise in transgender and sexual health.
- Introduction
- Conclusions
- Article Information
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Digital Health
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Sexual Health
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Wright JD , Chen L , Suzuki Y , Matsuo K , Hershman DL. National Estimates of Gender-Affirming Surgery in the US. JAMA Netw Open. 2023;6(8):e2330348. doi:10.1001/jamanetworkopen.2023.30348
Manage citations:
© 2024
- Permissions
National Estimates of Gender-Affirming Surgery in the US
- 1 Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, New York, New York
- 2 Department of Obstetrics and Gynecology, University of Southern California, Los Angeles
Question What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Importance While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth. 1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS). 2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance. 2 - 4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery. 2 , 4 Prior studies 2 - 7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety. 8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications. 2 , 4
Given the benefits of GAS, the performance of GAS in the US has increased over time. 9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable. 10 , 11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking. 9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates. 12 , 13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline.
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision ( ICD-10 ) diagnosis codes for gender identity disorder or transsexualism ( ICD-10 F64) or a personal history of sex reassignment ( ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1 ). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures. 2 , 4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1 ). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified). 9
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score. 14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS. 8 Patients with missing data were classified as the unknown group and were included in the analysis.
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases. 15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ 2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
A total of 48 019 patients who underwent GAS were identified ( Table 1 ). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently ( Table 1 ).
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 ( Figure 1 and eFigure in Supplement 1 ). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) ( Table 2 ). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 ( Figure 1 ). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis ( Table 3 ).
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 ( Figure 2 ). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients ( Figure 2 ). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years ( P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years ( P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined ( P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time. 9 , 16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020. 9 , 17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic. 18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments. 19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states. 20 , 21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years. 16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS. 9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care. 22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence. 20 , 21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
Accepted for Publication: July 15, 2023.
Published: August 23, 2023. doi:10.1001/jamanetworkopen.2023.30348
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Wright JD et al. JAMA Network Open .
Corresponding Author: Jason D. Wright, MD, Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Columbia University College of Physicians and Surgeons, 161 Fort Washington Ave, 4th Floor, New York, NY 10032 ( [email protected] ).
Author Contributions: Dr Wright had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Wright, Chen.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Wright.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Wright, Chen.
Administrative, technical, or material support: Wright, Suzuki.
Conflict of Interest Disclosures: Dr Wright reported receiving grants from Merck and personal fees from UpToDate outside the submitted work. No other disclosures were reported.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- FIND A PROVIDER
I'm a Candidate
I'm a Provider
Log In / Sign Up
I'm a candidate
Provider login
I'm a provider
List your practice
MTF Gender Confirmation: Genital Construction
The specifics, the takeaway.
Download the app
As part of a transgender individual’s transition, genital reassignment surgery alters male genitalia into female genitalia.
Written By: Erin Storm, PA-C
Published: October 07, 2021
Last updated: February 18, 2022
- Procedure Overview
- Ideal Candidate
- Side Effects
- Average Cost
thumbs-up Pros
- Can Help Complete A Gender Affirmation Journey
thumbs-down Cons
- Potentially Cost Prohibitive
Invasiveness Score
Invasiveness is graded based on factors such as anesthesia practices, incisions, and recovery notes common to this procedure.
Average Recovery
Application.
Surgical Procedure
$ 7000 - $ 24000
What is a male to female (MTF) gender reassignment surgery?
Male to female (MTF) gender reassignment surgery is also known as sex reassignment surgery (SRS), genital construction, and generally as Gender Confirmation Surgery. These procedures are used to remove and alter male genitalia into traditional female genitalia. Plastic surgeons will remove the scrotum, perform a penile inversion to create the neovagina, remove and alter penile erectile tissue to form the clitoral tissue of the clitoris, and construct labia usually from scrotal tissue. The prostate gland is left intact. These procedures create fully functional female genitalia in transgender patients.
Typically gender reassignment surgery is performed as a last step in a transgender individuals transition journey. Guidelines from The World Professional Association for Transgender Health (WPATH) state candidates must have letters of recommendation from their mental health provider and physician, have been living full time as a woman for one year, and have completed one year of hormonal therapy to be eligible.
Information on facial feminization surgeries, top surgeries (like a breast construction), and other male to female gender affirming surgeries as part of a gender transition for transwomen can be found in our comprehensive guide to MTF gender affirmation solutions .
What concerns does a MTF gender reassignment surgery treat?
- Transfeminine Bottom Surgery & Genital Construction : Male to female gender reassignment surgery creates female genitalia that are aesthetically authentic and functional. A vaginoplasty, penectomy, orchiectomy (testicle removal), clitoroplasty, and labiaplasty are typically performed.
Who is the ideal candidate for a MTF gender reassignment surgery?
The ideal candidate for MTF gender reassignment surgery is a transgender women seeking to complete her physical embodiment of her gender identity. This reconstructive genital surgery creates functioning female genitalia.
MTF gender reassignment surgery is not recommended for those who have not been on hormone therapy for one year, have not been living full time as a woman for one year, do not have letters of recommendation from their mental health provider and physician, children under the age of 18, and those with certain chronic medical conditions.
What is the average recovery associated with a MTF gender reassignment surgery?
Most patients experience four to six weeks of recovery time following a MTF gender reassignment surgery. Patients can expect bruising, swelling, and tenderness following the procedure. A urinary catheter is placed for one week and vaginal packing as well which may cause a sensation of fullness. Vaginal dilation is a component of the procedure and the patient will be advised on how to complete this progressive dilation at home over the course of a few weeks.
What are the potential side effects of a MTF gender reassignment surgery?
Possible side effects following a MTF gender reassignment surgery include bleeding, swelling, bruising, site infection, altered sensation, difficulty urinating, difficulty with sexual function, prolonged edema, and complications from anesthesia or the procedure.
What can someone expect from the results of a MTF gender reassignment surgery?
The results of MTF gender reassignment surgery are permanent. This procedure creates functional female genitalia and removes all male genitalia. The prostate gland is left intact which is important for transgender individuals ongoing healthcare and preventative screenings.
What is the average cost of a MTF gender reassignment surgery?
What to expect.
A MTF Gender Reassignment Surgery creates female genitalia. Here is a quick guide for what to expect before, during, and after a MTF Gender Reassignment Surgery:
Before Surgery
- Prophylactic antibiotics or antivirals may be prescribed
- Stop taking blood thinning medications two weeks prior to surgery. Blood thinners may include, Advil, Tylenol, Aspirin, and prescription anticoagulants
- Stop smoking four weeks prior to the procedure and continue cessation for four weeks post op
- No alcohol two days prior to the procedure
- Do not eat or drink six hours before
During Surgery
- General anesthesia
- A penile inversion is performed to create the vaginal canal
- The scrotum is removed
- Skin grafts are used to create the labia and vulva
- Erectile tissue is removed from the new vaginal walls, and erectile tissue from the head of the penis is used to create the clitoris
- The urethra is shortened
Immediately After Treatment
- Swelling, bruising, and tenderness
1 - 30 After Treatment & Beyond
- Resume most activities after a few days
- Swelling typically resolves within a few weeks
- Avoid strenuous activity for two to four weeks
- Remove urinary catheter and vaginal packing after one week
- Continue progressive vaginal dilation
Result Notes
- Results are permanent
- Proper aftercare will ensure optimal results
Gender confirmation surgeries for transgender individuals are an important component of transgender health and in creating an embodied gender identity. Gender reassignment surgery allows transgender women who feel it is a part of their transition to more fully embrace their gender identity.
To learn more about our content creation practices, visit our Editorial Process page .
Source List
AEDIT uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- American Society of Plastic Surgeons Gender Confirmation Surgeries plasticsurgery.org
- Karel E Y Claes Chest Surgery for Transgender and Gender Nonconforming Individuals PubMed.gov ; 2018-07-02
Related Procedures

MTF Gender Confirmation Solutions

MTF Gender Confirmation: Facial Feminization

Adam’s Apple Reduction

MTF Gender Confirmation: Transfeminine Top & Bottom Surgeries
View all procedures
Learn More About MTF Gender Confirmation: Genital Construction in The AEDITION

Gender Transitioning And Skincare: Taking Care Of Your Changing Face
Side effects of hormone therapy often show up on the skin in the form of acne, pigmentation, and uneven skin texture. Here’s what you need to know about the most common skin concerns and treatment options.

A Guide To Non-Surgical Facial Feminization
Facial feminization procedures have been gaining popularity among men hoping to look more approachable or transition to female as well as among women hoping to have a more feminine appearance.

Finding The Right Plastic Surgeon, Dermatologist, Or Cosmetic Dentist
When considering a cosmetic procedure, it is so important to find the right doctor for you.
Discover more articles

‘Try on’ aesthetic procedures and instantly visualize possible results with AEDIT and our patented 3D aesthetic simulator.
Find Top Aesthetic Providers Near You
Providers by locations.
- Alpharetta, GA Providers
- Boston, MA Providers
- Cockeysville, MD Providers
- Fort Lauderdale, FL Providers
- Lone Tree, CO Providers
- Metairie, LA Providers
- More Locations
- New Haven, CT Providers
- Prairie Village, KS Providers
- Scottsdale, AZ Providers
- Skokie, IL Providers
- Southfield, MI Providers
- Springdale, AR Providers
- Washington, DC Providers
- West Hollywood, CA Providers
Providers by Specialties
- Cosmetic Dentistry Providers
- Cosmetic Dermatology Providers
- Cosmetic Surgery Providers
- Dermatologic Surgery Providers
- Dermatology Providers
- Esthetician Providers
- Facial Plastic and Reconstructive Surgery Providers
- General Surgery Providers
- Hair Restoration Surgery Providers
- Head and Neck Surgery Providers
- Medspa Providers
- More Procedures
- Oculoplastic Surgery Providers
- Other Providers
- Plastic and Reconstructive Surgery Providers
Providers by Procedures
- Acne Scar Treatment Providers
- Acne Treatment Providers
- Birthmark Removal Providers
- Blepharoplasty Providers
- Botox Providers
- Brow Lift Providers
- Buccal Fat Removal (Cheek Reduction) Providers
- Cheek Augmentation (Cheek Implants) Providers
- Cheek Surgery Providers
- Chemical Peels Providers
- Chin Surgery (Mentoplasty) Providers
- Dental Treatments Providers
- Dermabrasion Treatment Providers
- Dermal Fillers & Injectables Providers
- More Specialties
- Search Search Please fill out this field.
Does Insurance Cover Gender-Affirming Care?
Determining what your plan covers.
- Gender-Affirming Surgery Costs
- Gender-Affirming Medication Costs
Other Ways to Pay for Gender-Affirming Care and Surgery
Tips for financing gender-affirming care and surgery, the bottom line.
- Health Insurance
- Guide to Finance for LGBTQ+ People
- LGBTQ+ Marriage and Personal Finance
- The Costs of LGBTQ+ Family Planning
- Mortgage Lending for LGBTQ+ People
- Banks that Support the LGBTQ+ Community
- Overcoming LGBTQ+ Credit Barriers
- Top LGBTQ+ Financial Influencers
- Paying for College as an LGBTQ+ Student
- LGBTQ+ Representation in the Workforce
- LGBTQ+ Pay Gap and Unemployment
- Health Insurance for LGBTQ+ People
- How Being Nonbinary Affects Getting Life Insurance
- Qualifying for Life Insurance for Transgender People
- Paying for Transgender Surgeries CURRENT ARTICLE
- Investing in LGBTQ+ Friendly Investments
- Preparing for Retirement as an LGBTQ+ Person
- Social Security Benefit Equality for Same-Sex Couples
- LGBTQ+ Elder Care in Retirement
In many cases, health insurance in the U.S. covers gender-affirming care. However, whether or not your insurance plan will cover a specific gender-affirming treatment can depend on your state, your employer, and your plan's benefits.
Key Takeaways
- Health insurance generally covers gender-affirming care.
- Not all plans cover all procedures, however, and the process can be murky and require preauthorization.
- Gender-affirming care can cost tens of thousands of dollars without insurance coverage.
Major insurance companies today generally recognize transgender-related care as being medically necessary . However, at least 24 states have passed new laws or enacted new policies limiting coverage of gender-affirming care for people up to age 18. And some transgender people may still be denied coverage for certain procedures by their insurers.
1.6 million
The estimated number of Americans age 13 or older who identify as transgender, according to a 2022 study.
Health insurers generally cover an array of medically necessary services that affirm gender or treat gender dysphoria, according to the American Medical Association, which reaffirmed its advocacy for such care in 2023. Gender dysphoria is a condition that occurs when someone feels a conflict between the sex they were assigned at birth and the one they now identify with.
Gender-affirming care is the phrase used by most medical groups for dysphoria treatment. This care can include hormones, surgery, or counseling. The care aligns a person's gender identity with gender expression in appearance, anatomy, and voice.
In 2010, the federal Affordable Care Act (ACA) banned health insurance discrimination based on sexual orientation and gender identity. Before the law's passage, medically necessary gender-affirming surgeries and hormones often weren't covered by insurers.
A 2024 rule from the Department of Health and Human Services stated that covered entities (a term that includes both insurance plans and providers such as doctors) could not "deny or limit coverage, deny or limit coverage of a claim, or impose additional cost sharing or other limitations or restrictions on coverage, for specific health services related to gender transition or other gender-affirming care if such denial, limitation, or restriction results in discrimination on the basis of sex."
However, insurance is also regulated at the state level and rules can vary based on whether it is an ACA, public, or employer plan, so they don't apply evenly to all insurers.
Investopedia / Candra Huff
Policyholders and plan members can generally find out what's available to them in their member booklet. This should have been given to you when you got the policy or, if it's an employee plan, when you joined the company. It may be called a certificate of coverage, a benefit plan, a summary plan description, a certificate of insurance, or something similar.
This document should describe the insurer's clinical evidence criteria to qualify for claim coverage. For example, to begin hormone therapy, the requirements might include a diagnosis of gender dysphoria from a licensed mental health professional.
Some plans may list exclusions for certain procedures. Even if an exclusion exists in the documentation, it can still be worthwhile to apply for pre-authorization or pre-approval for the procedure to obtain an official decision. For one thing, as the Transgender Legal Defense & Education Fund, notes, "the plan booklet may simply be out of date."
Even if you're turned down, that is not necessarily the final word. If a preauthorization request or a claim is denied, an attorney, healthcare advocate, or your human resources department may be able to help with filing an appeal. Appeals should include individualized, extensive documentation of a service's medical necessity and appropriateness.
Here, we list four types of health insurance and how they might cover gender-affirming care.
Employer-Provided Insurance
Altogether, 24 states and the District of Columbia prohibit transgender exclusions in private health insurance coverage, according to the nonprofit LGBTQ+ advocacy organization Movement Advance Project, leaving half the states without such protections.
However, health coverage benefits that a private employer provides can vary based on whether the employer buys its coverage from an insurance company or is funding the plan itself. If the employer's plan is self-funded, it is governed by the federal law ERISA, the Employee Retirement Income Security Act , which overrides any state nondiscrimination law. The employer can decide what health care is or is not covered.
In the Human Rights Campaign's 2023-2024 Corporate Equality Index, a record 94% of the companies it evaluated offered at least one transgender-inclusive plan option.
Employer-based plans are governed in the state where the plan was issued, not where you live.
Affordable Care Act Plan Coverage
Individuals can buy their own health insurance policies, often with the help of federal subsidies, through the Healthcare.gov Marketplace. Most insurers have eliminated transgender-specific exclusions, which ACA regulations explicitly ban.
Still, policies vary by state and in what they cover. As the Healthcare.gov website notes, "Many health plans are still using exclusions such as 'services related to sex change' or 'sex reassignment surgery' to deny coverage to transgender people for certain health care services."
It suggests that before enrolling in a plan, consumers should carefully review its terms: "Plans might use different language to describe these kinds of exclusions. Look for language like 'All procedures related to being transgender are not covered.' Other terms to look for include 'gender change,' 'transsexualism,' 'gender identity disorder,' and 'gender identity dysphoria.'"
Fortunately, according to Out2Enroll, an organization connecting the LGBT+ community with healthcare coverage, when it recently reviewed silver Marketplace options in 32 states it found that "the vast majority of insurers did not use transgender-specific exclusions" and that "40% of plans had language indicating that all or some medically necessary gender-affirming care would be covered by the plan." (ACA coverage is broken down into bronze, silver, gold, and platinum plans, with silver being a moderately priced level.)
Out2Enroll also has state-specific Transgender Health Insurance Guides on its website for help in choosing a plan.
Medicare and Medicaid Coverage
About 6% of transgender adults receive their health coverage from Medicare, the federal insurance program primarily for Americans over age 65. Under these plans, medically necessary care—including some gender-affirming procedures—is covered. Private Medicare Advantage plans should abide by the same rules as traditional Medicare, but patients on such plans should try to get preauthorization before accessing transition-related services, the National Center for Transgender Equality advises.
Some 21% of transgender adults receive Medicaid, the joint federal and state health insurance plan for low-income Americans. On a state-by-state basis, Medicaid coverage is uneven. Medicaid programs explicitly cover transgender-related care in 26 states and the District of Columbia. Meanwhile, programs in 10 states bar coverage of transgender-related care for people of all ages, and programs in three states prohibit coverage of transgender-related care for minors.
Military and Veteran Coverage
Active military members can access some types of gender-affirming care. TRICARE, the health benefits provider for military members, says it "covers hormone therapy and psychological counseling for gender dysphoria. TRICARE generally doesn't cover surgery for the treatment of gender dysphoria. However, active duty service members may request a waiver for medically necessary, gender affirming surgery."
The Veterans Health Administration offers gender-affirming healthcare, including hormones and prosthetics, mental health care, and other healthcare. Coverage for gender-affirming surgery has traditionally been denied but is currently undergoing a review.
How Much Does Gender-Affirming Surgery Cost?
The cost of gender-affirming care might range from $25,000 to $75,000, according to an estimate from the Human Rights Campaign.
Gender-affirming surgeries may include top surgery (breast removal or augmentation), bottom surgery, vocal surgery, and face and body surgeries such as browlifts, jawline contouring, Adam's apple removal, and forehead reduction.
Bottom surgery may include:
- Phalloplasty : Creation of penis
- Metoidioplasty : Phallus created from existing genital region tissue.
- Hysterectomy : Uterus and cervix removal
- Nullification surgery : Creating a gender-neutral look in the groin
- Oophorectomy : Removal of one or both ovaries
- Vaginoplasty and vulvoplasty : Creation of vagina and vulva
- Orchiectomy : Testicle removal
Research published in 2022 by JAMA Surgery found that while gender-affirming surgery can be costly, insurance (for patients who have it) will often cover most of the cost. Looking at phalloplasty and vaginoplasty procedures specifically, it reported:
However, not all transgender people desire surgery. According to 2019 research statistics, only 28% of transgender women get any type of surgery, and only 4% to 13% receive genital surgery. Surgery is more common among transgender men, with 42% to 54% getting some type of surgery; up to 50% get genital surgery.
How Much Does Gender-Affirming Medication Cost?
Gender-affirming medication is far more common than surgery. As many as 65% of transgender people received gender-affirming hormone therapy in 2019, up from 17% in 2011, according to the Journal of Law, Medicine & Ethics .
The costs of gender-affirming medications can vary widely. While they are often at least partially covered by insurance, they also come with out-of-pocket costs, which may continue through the patient's lifetime.
For example, a study in the Journal of General Internal Medicine reported that, "in 2019, median prices for feminizing and masculinizing hormone therapy ranged from $6.76 to $91.15 and $31.82 to $398.99, respectively." At the same time, patients' "median out-of-pocket costs ranged from $5.00 to $10.71 and $10.00 to $12.86 for feminizing and masculinizing hormone therapy, respectively." Those prices refer to a 30-day supply.
Other costs can be involved as well. For example, patients who are taking hormones may need periodic blood tests to monitor their health.
A 2020 study in Annals of Family Medicine found that among insured respondents taking gender-affirming hormones, almost 21% reported that their claims were denied. This group (and those who are uninsured) were more likely to take nonprescription hormones from unlicensed sources, which may not be monitored for quality and potentially carry serious health risks.
Aside from health insurance, how can you pay for gender-affirming care or surgery? Here are some options.
Payment Plans
Some healthcare providers offer payment plans directly or through lenders that let you pay off medical bills over time.
You might take out a personal loan or even a type of personal loan called a medical loan to cover expenses related to gender-affirming care or surgery. A medical loan is just a personal loan used to pay for medical expenses.
Credit Cards
Credit cards cab be another avenue for covering the costs of gender-affirming care or surgery, although they tend to have very high interest rates if you run a balance.
Even with health insurance, hormone therapy may be less expensive if you comparison shop and use pharmacy programs, such as GoodRx.
Surgery Grants
Several organizations, such as the Jim Collins Foundation, offer grants for people seeking gender-affirming care or surgery.
Health Accounts
If you have a flexible spending account (FSA) or health savings account (HSA) , consider allocating some account money for gendering-affirming care or surgery if you are anticipating it.
Health Reimbursement Agreement
A health reimbursement agreement (HRA) is an employer-funded group health plan that reimburses employees for qualified medical expenses, which might include gender-affirming care or surgery.
Home Equity Loan or Line of Credit (HELOC)
You could take out a home equity loan or line of credit to cover the costs of gender-affirming care or surgery. With these types of loans, you can typically borrow up to a certain percentage of your home's equity. Interest rates are generally lower than those on a personal loan, because your home serves as collateral. Just realize that if you can't repay the loan, your could lose your home.
Friends and Family Loans
If you've got supportive friends or relatives, they might be willing to chip in money to pay for your gender-affirming care or surgery. To avoid misunderstandings, it's usually best to have a written agreement and repayment plan.
Crowdfunding
You might consider setting up a crowdfunding campaign on a platform like GoFundMe to raise money from friends, relatives, colleagues, or even strangers.
When you're financing gender-affirming care or surgery, you may be able to save some money if you follow these tips.
Shop Around
A number of online tools such as Hospital Cost Compare and Healthcare Bluebook allow you to compare costs for the same procedures and treatments offered by different healthcare providers. Doing this homework could save you a lot of money.
Check the Interest Rate Before You Borrow
Be sure to investigate how much you'll pay to borrow money if you decide to go the credit card or loan route.
Try Negotiating or Set up a Payment Plan
You can sometimes negotiate with a healthcare provider to lower the costs of gender-affirming care or surgery. For instance, a healthcare provider might discount your services if you agree to pay off your medical bills quickly. If a healthcare provider isn't willing to provide a discount, they might let you make interest-free payments as part of a payment plan.
Ask About Financial Assistance
Some nonprofit healthcare providers offer financial assistance programs that will cover all or some of your medical expenses.
What Are the Different Types of Gender-Affirming Care?
Various types of gender-affirming care include puberty-blocking medication, hormone therapy, top surgery, bottom surgery, nullification surgery, laser hair removal, facial feminization surgery, speech therapy, and mental health services.
How Much Does Gender-Affirming Care Cost in the U.S.?
The cost of gendering-affirming care varies widely, depending on the type of procedure or treatment involved. A common range is anywhere from $25,000 to $75,000, according to the Human Rights Campaign. Health insurance may cover these costs to varying degrees.
Does Insurance Cover Puberty Blockers?
According to one 2019 study, about 31% of the plans it looked at online claimed to cover puberty blockers. That makes it all the more important for patients and their families to shop around for insurance.
The campaign for transgender rights in the U.S. has experienced victories and setbacks in recent years—in some cases affecting coverage of gender-affirming care. Even amid progress, some people still encounter problems obtaining health insurance to cover such care or paying the out-of-pocket costs involved. People who expect to need gender-affirming care will want to read their insurance plan's coverage details carefully and ask questions if they're unsure about what's covered.
Human Rights Campaign. " Map: Attacks on Gender-Affirming Care by State ."
KFF. " Policy Tracker: Youth Access to Gender Affirming Care and State Policy Restrictions ."
The Williams Institute at UCLA. " How Many Adults and Youth Identify as Transgender in the United States? "
UCSF Transgender Care. " Initiating Hormone Therapy ."
American Medical Association. " Transgender Coverage Issue Brief ."
U.S. Department of Health and Human Services. " Section 1557 of the Patient Protection and Affordable Care Act ."
Transgender Legal Defense & Education Fund. " Health Insurance – Understanding Your Plan ."
Federal Register. " Vol. 89, No. 88 / Monday, May 6, 2024 / Rules and Regulations ," Page 37701.
Movement Advance Protect. " Healthcare Laws and Policies ."
Transgender Legal Defense & Education Fund. " Health Insurance – Understanding Your Plan: Differences Between Self-Funded and Insured Plans. "
Human Rights Campaign. " Corporate Equality Index 2023-2024 ."
HealthCare.gov. " Transgender Health Care ."
Out2Enroll. " Plan Information for 2024 ."
Healthcare.gov. " How to Pick a Health Insurance Plan ."
KFF. " Trans People in the U.S.: Identities, Demographics, Wellbeing. "
Movement Advancement Project. " Medicaid Coverage of Transgender-Related Health Care ."
TRICARE. " Gender Dysphoria Services ."
U.S. Department of Veterans Affairs. "VHA LGBTQ+ Health Program. "
Annals of Family Medicine, November 2020. " Insurance Coverage and Use of Hormones Among Transgender Respondents to a National Survey ," See Abstract: Results.
Translational Andrology and Urology. " Demographic and Temporal Trends in Transgender Identities and Gender Confirming Surgery ."
JAMA Surgery. " Spending and Out-of-Pocket Costs for Genital Gender-Affirming Surgery in the U.S. "
The Journal of Law, Medicine, and Ethics. " Utilization and Costs of Gender-Affirming Care in a Commercially Insured Transgender Population ."
Journal of General Internal Medicine. " Gender Affirming Hormone Therapy Spending and Use in the USA, 2013-2019 ."
Transgender Health. April 11, 2019. " Health Care Insurance of Recommended Gender-Affirming Health Care Services for Transgender Youth: Shopping Online for Coverage Information ," See Table 1.
:max_bytes(150000):strip_icc():format(webp)/DentalInsurance-Roundups-BestDentalInsuranceCompanies2-b2006ba5d079402bae6fe4d217ee1f43.png)
- Terms of Service
- Editorial Policy
- Privacy Policy
- Your Privacy Choices
We use cookies to personalize content and to analyze our traffic.
By clicking “Accept and continue” you agree with the use of analytical and tracking cookies. For more information, check the Cookie Policy
How Much Does Male-to-Female (MTF) Surgery Cost in 2024?

Medically reviewed by
Planning on conquering gender dysphoria through surgery but feeling worried about the cost? This comprehensive guide will clear up the financial fog and break down the costs of MTF gender-affirming surgery so you can focus on what truly matters— a journey to becoming your most authentic self.

Quick Overview:
- Average MTF top surgery cost: $5,000-$10,000.
- Average MTF bottom surgery cost: $10,000-$30,000.
- Average facial feminization surgery (FFS) costs: $20,000-$50,000.
- Average voice feminization surgery cost: $5,500-$9,000.
- 🗽 The US: $5,000-$30,000.
- 💂♂️ The UK: $3,700-$42,000.
- 🛕 Thailand : $3,200-$15,000.
- 🕌 Turkey : $2,500-$13,000.
Table of Contents
How much is male-to-female (mtf) gender reassignment surgery.
- How Much Does Male-to-Female Surgery Cost Worldwide?
How Much Does MTF Top Surgery Cost?
How much is mtf bottom surgery, how much does facial feminization surgery (ffs) cost, how much does voice feminization surgery cost, what factors affect mtf surgery cost, what is included in the male-to-female transgender surgery cost, does health insurance cover mtf surgery.
- Additional Costs of MTF Gender-Affirming Surgeries
Male-to-female (MTF) gender reassignment surgery involves various medical procedures that alter the physical characteristics of a person assigned male at birth to match their female gender identity. This can include breast augmentation, genital surgery, facial feminization surgery (FFS), and voice feminization surgery.
Because of the variety and complexity of procedures, the total cost of MTF gender-affirming surgery can reach up to $140,500. However, the average cost typically falls between $5,000 and $30,000 . It all depends on the specific surgeries and results you are aiming for.
Below, you can compare costs for some standard MTF gender reassignment procedures:

You might also like
- Technique: High intensity focused ultrasound ablation (HIFU)
- Dr. Baris Nuhoglu provides a wide range of operations.
- AquaHealth Clinic serves 50 patients annually, primarily from Europe and the Commonwealth.
- Included Services: 5* hotel, transfer airport-hotel-clinic-airport.
- Stay Info: 2 days stay in the patient room, 10 days stay in the hotel, included in the price.
- Technique: Premium MTF Vaginoplasty
- Dr. Pichet Rodchareon Md is a board-certified plastic surgeon specializing in a wide range of gender-affirming surgeries.
- Bangkok Plastic Surgery has performed over 3,000 procedures with remarkable patient satisfaction and functional results.
- Included Services: General anesthesia, medications, post-op medications, consultation with an anesthesiologist, consultation with a surgeon, hospitalization, transfer airport-hotel-clinic-airport.
- Stay Info: 4 days stay in the hospital, 14 days stay in the hotel, both included in the price.
- Method: Premium sex reassignment surgery
- Dr. Baris Nuhoglu has over 100 publications demonstrating his dedication to urooncology and endourology.
- Included Services: Consultation with a doctor, hospitalization, hotel stay, transfer airport-hotel-clinic-airport.
- Stay Info: 2 days in the hospital, 10 days in the hotel, included in the price.
- Dr. Tanongsak Panyayvirulroj is a renowned plastic surgeon specializing in sex reassignment surgery.
- Asia Cosmetic Hospital holds prestigious Joint Commission International (JCI) accreditation for maintaining high patient care standards.
- Included Services: Hotel, General anesthesia, Preoperative tests, Medications, Follow-up examination, Post-op medications, Neck pillow, Language assistance, Consultation with a surgeon, Follow-up visit, Consultation with a cardiologist, 4* Hotel, Transfer airport-hotel-clinic-airport.
- Stay Info: 7 Days stay in the hospital, 14 Days stay in the hotel, included in the price.
- Technique: Peritoneal Pull-Through Vaginoplasty (PPV)
- Saran Wannachamras is certified by the Medical Council of Thailand in medical practice expertise.
- Wansiri Hospital has a dedicated team specializing in advanced sex reassignment surgeries.
- Included Services: Language assistance, personalized beauty advice, multiple consultations, general anesthesia, post-op medications, preoperative tests, chest X-ray, hospitalization, hotel stay, airport transfers.
- Stay Info: 10 days in the hospital, 11 days in the hotel, included in the price.
How Much Does Male-to-Female Surgery Cost Worldwide?

Male-to-female surgery costs vary significantly around the world, influenced by factors such as local economic conditions, healthcare infrastructure, and the prevalence of medical tourism. In countries like Thailand and Turkey , the costs for MTF procedures are often lower than average, making these countries popular destinations for affordable gender-affirming care.
Here’s a comparative table of average male-to-female surgery costs in the most popular countries:
Get a Free Personalized Quote

Male-to-female (MTF) top surgery, or chest feminization, is a procedure that enhances breast volume and shape to have a more traditionally feminine appearance. A surgeon places breast implants either behind the natural breast tissue or beneath the pectoral muscle. Each implant is carefully centered beneath the nipples to ensure a natural and symmetric appearance.
MTF breast augmentation surgery cost ranges from $5,000 to $10,000 . The final price depends on the desired size, the type of implants, and the surgical technique.
Transgender people can choose between two types of implants:
- Saline implants are filled with sterile salt water. Due to the less expensive filling material, they can be up to 77% cheaper than their silicone counterparts. Saline implants also require smaller incisions because they are filled after being inserted.
- Silicone implants have a soft and natural feel. Although they are costlier, their texture feels more lifelike.
🤔 Learn more about what to expect from top surgery.

Male-to-female (MTF) bottom surgery encompasses a range of surgical procedures that align male genitalia with a transgender woman's gender identity. The average cost of MTF bottom surgery is around $25,000 .
- Orchiectomy: $2,000 to $8,000. This procedure involves the surgical removal of the testicles. This type of MTF bottom surgery is relatively simple and less invasive. It can be conducted alone or as part of a broader genital reconstruction.
- Vaginoplasty/ Vulvoplasty : $10,000-$30,000. Vaginoplasty constructs a functional vagina, which includes a vaginal canal capable of intercourse and a depth that supports penetration. Vulvoplasty, or zero-depth vaginoplasty, creates the external genitalia (vulva) without a vaginal canal.
Get a Cost Estimate
📸Click on the offers below to check out before-and-after photos from renowned surgeons in Thailand and Turkey:
📢Don’t miss out on our comprehensive guide to male-to-female bottom surgery !
Facial feminization surgery (FFS) is a subset of gender-affirming surgeries that soften facial features to reflect a more feminine appearance. FFS not only enhances aesthetic appeal but also offers profound psychological benefits. It can significantly alleviate gender dysphoria and boost self-confidence. Achieving a more traditionally feminine appearance and the ability to “pass” can also provide increased safety in a world where transphobia remains a genuine concern.
Out-of-pocket costs of FFS are quite variable and typically range from $20,000 to $50,000 , depending on which procedures you decide to have.
Below is a breakdown of common FFS procedures and their average costs:
☝️Tip: While it's usually more cost-effective to have multiple FFS procedures done in a single operation, it's crucial not to overdo it. Sometimes, a single change can significantly enhance femininity. If your budget is limited, discuss with your doctor which procedures would most effectively soften your features and give you the most value for your money.
🔎Read our in-depth guide to facial feminization surgery costs.
Voice feminization surgery is a specialized procedure that permanently raises the pitch of your voice, making it sound higher. Because certain voice qualities are traditionally associated with gender, trans women often seek this type of surgery as part of their medical male-to-female transition. The average cost for voice feminization surgery ranges from $5,500 to $9,000 .
🗣️How does it work? Your vocal cords determine the pitch of your voice based on their thickness and length. Typically, men and transgender individuals assigned male at birth (AMAB) have vocal cords that produce lower pitches compared to women and those assigned female at birth (AFAB). During this gender-affirming surgery, a laryngologist will permanently shorten, thin, or tighten your vocal cords to increase the pitch, helping your voice sound higher and more feminine.
Get a Free Consultation
🔎 Take a look at our comprehensive guide to voice feminization surgery costs.

Each male-to-female surgery is adapted to the patient’s needs, making each person’s experience and medical expenses unique. Here are some key elements that influence the overall cost:
- Type of gender-affirming surgery. Different MTF surgeries come with varying price tags depending on their complexity and the specific techniques used.
- Number of gender-affirming surgeries. Patients can combine surgeries. For example, facial feminization surgery often involves multiple procedures—such as rhinoplasty, jaw reshaping, and a brow lift—all performed in one surgical session to maximize results and minimize recovery time. Additionally, revision surgeries may be necessary to refine the outcomes.
- Surgeon's experience. Highly experienced surgeons charge more for their services, but they also often offer a higher level of skill and potentially better outcomes.
- Geographic location. MTF surgery cost can vary significantly depending on where it's performed. For example, surgery costs might be higher in major cities than in smaller towns. Likewise, some countries offer more advantageous options. Countries like Turkey and Thailand offer lower MTF surgery costs due to lower living expenses, favorable currency exchange rates, and competitive medical tourism markets.
- Clinic fees. The choice of facility also influences the total cost. Private clinics might have different pricing structures compared to public hospitals. Some offer package deals for multiple procedures.
- Additional medical treatments. Additional procedures or treatments may sometimes be necessary, either before or after surgery, which can add to the total cost.
Understanding what is typically included in the quoted MTF surgery cost helps ensure that there are no unexpected expenses during your journey.
The cost of male-to-female gender-affirming surgery usually covers:
- surgeon's fees;
- anesthesia fees;
- hospital costs (the use of the surgery room, hospital stay, and any necessary medical equipment);
- pre-operative consultations and necessary pre-surgery medical tests;
Additional costs of MTF gender-affirming surgeries

When planning for male-to-female (MTF) transgender surgery, it’s crucial to account for out-of-pocket costs. These extra expenses can significantly impact your overall budget. Here’s what to consider:
- Additional medications such as pain relief, antibiotics, and hormone therapy.
- Travel and accommodation for those traveling out of town or internationally for surgery.
- Secondary or revision surgeries if further procedures are needed for optimal results.
- Hair removal is often necessary as a preparatory step before certain gender-affirming surgeries like genital reconstruction. This process involves frequent sessions at $75-$100 per session.
- Hiring help at home if recovering alone, to assist with daily tasks during recovery.
- Therapy sessions , costing between $65 and $250, may be required to obtain referrals for surgery.
- Post-surgery items like compression garments, shower stools, waterproof bed sheets, cheap underwear, and sanitary towels.
- Factor in taking some time off work — about 6-8 weeks for bottom surgery recovery and 1-2 weeks for top surgery.
- Include a buffer for unexpected costs like extended hospital stays or emergency medical care.
Why choose all-inclusive MTF surgery packages?
It’s common for clinics, especially those in popular medical tourism destinations, to offer comprehensive sex reassignment surgery packages. These packages can provide a range of additional conveniences and necessities, simplifying the process for patients.
Here’s what you might find included:
- several compatible gender-affirming surgeries in one trip (based on your preferences);
- airport-hotel-hospital transfers;
- accommodation in hotels near the clinic;
- compression underwear for post-surgery recovery;
- post-operative care.
Always compare offers to ensure you get the necessary services and the best value.
Get a Personalized Treatment Program

Yes, health insurance often covers certain types of male-to-female (MTF) transgender surgeries, but coverage can vary depending on the specific policy and the provider. A typical insurance plan will cover surgeries considered essential for gender affirmation, such as top and bottom surgeries. Health insurance plans usually deny coverage for gender-affirming procedures deemed cosmetic, such as facial feminization surgery (FFS) and voice feminization.
To qualify for health insurance coverage, transgender people usually need to follow the guidelines set by the World Professional Association for Transgender Health (WPATH). Common requirements include:
- letters of readiness from mental health professionals;
- evidence of hormone replacement therapy for at least 1 year;
💰Struggling to fund your surgery with health insurance alone? Discover which organizations offer grants and other ways to fund gender-affirming surgeries here .
- Male-to-female (MTF) gender reassignment surgery includes procedures like breast augmentation, genital reconstruction, facial feminization, and voice feminization.
- Total costs for MTF surgery can reach up to $140,500; average costs generally range from $5,000 to $30,000 , depending on the procedure.
- MTF top surgery typically costs $5,000 to $10,000; bottom surgery ranges from $10,000 to $30,000; facial feminization surgery costs between $20,000 and $50,000; and voice feminization surgery ranges from $5,000 to $9,000.
- MTF surgery is especially expensive in the US and the UK , where costs can reach $42,000 and more . Thailand and Turkey offer options that are up to 3 times more affordable .
- Insurance covers procedures like top and bottom surgeries per WPATH guidelines but does not usually provide for cosmetic procedures.
- Expect to budget for extra expenses such as medications, travel, accommodation, hair removal, home assistance, therapy sessions, and time off work for recovery.
Related Articles
- How Much Does Facial Feminization Surgery Cost in 2024?
- How Much Does Voice Feminization Surgery Cost in 2024?
- How Much Does Top Surgery Cost in 2024?
- How Does Male-to-Female (MTF) Bottom Surgery Work?
- How Does Top Surgery Work?
- Forbes. (2022). How To Afford Transgender Surgery Expenses. https://www.forbes.com/advisor/personal-loans/transgender-surgery-cost/
- Business Insider. (2019). The staggering costs of being transgender in the US, where even patients with health insurance can face six-figure bills. https://www.businessinsider.com/transgender-medical-care-surgery-expensive-2019-6
- Healthline. (2023). Everything You Need to Know About Voice Feminization Surgery. https://www.healthline.com/health/voice-feminization-surgery

IMAGES
VIDEO
COMMENTS
Understanding the Cost of Gender Reassignment Surgery. Below you will find general cost estimates for different gender-affirming surgeries. Generally speaking, these price ranges do not include anesthesia fees, facility fees (staying overnight in the hospital) and/or pathology fees (sending removed organs or tissue for pathology testing). ...
For a female-to-male transition, masculinization chest surgery (also known as top surgery) might cost $3,000 to $10,000 while chest surgery for a male-to-female transition could cost $5,000 to ...
Gender Confirmation (GCS), formerly known as sex reassignment surgery, can be very complex. Find out more about these procedures.
It is sometimes called gender reassignment surgery. ... Gender-affirming surgery can cost between $6,900 and $63,400 depending on the precise procedure, according to a 2022 study published in The ...
They may also decide that bottom surgery — also known as genital surgery, sex reassignment surgery (SRS), or preferably, gender confirmation surgery (GCS) — is the right choice for them ...
Factors affecting the cost of male-to-female surgery. The number of surgical procedures performed for gender reassignment is on the rise. With the surge in cases, the male-to-female surgery cost is also becoming more affordable and nominal in Asian countries compared to other nations. However, a few factors still affect the total cost of surgery.
Many government healthcare plans, like Medicare, cover some form of gender affirming care, including surgery. You may still have to pay out of pocket costs.
Once this is complete, sex reassignment surgery — consisting of genital sex reassignment and/or nongenital sex reassignment — may be considered. ... Average Cost for Gender Reassignment. Counseling: $50 - $200 per session: Hormone Therapy: $300 - $2,500 yearly: Therapy + Letter of Referral:
The cost of medical treatments can add up to more than $100,000, and they're often not covered by health insurance. Plus, transgender people face discrimination in the workplace, which translates to unemployment rates that are as much as three times as high than they are for the general public.
Gender Reassignment Surgery: $30,000-Plus Nearly two years after beginning my therapy and hormone replacement therapy, I was ready for my gender reassignment surgery at 18.
Gender reassignment surgery cost varies depending on the type of transition. For male to female (MTF) transition, the cost ranges from $2438 to $6095 and ; For female to male (FTM) transition, the cost falls between $4876 and $9752.; When considering the cost of gender reassignment surgery, it's important to note that these figures encompass the surgical expenses alone.
The cost for female-to-male reassignment can be more than $50,000. The cost for male-to-female reassignment can be $7,000 to $24,000. Between 100 to 500 gender-reassignment procedures are ...
CMS.gov. Gender dysphoria and gender reassignment surgery. Transgender Legal Defense & Education Fund. Health insurance medical policies: gender dysphoria / gender reassignment. Aetna. Gender-affirming surgery. Downing J, Holt SK, Cunetta M, Gore JL, Dy GW. Spending and out-of-pocket costs for genital gender-affirming surgery in the US.
Papadopulos NA, Zavlin D, Lellé JD, et al. Male-to-female sex reassignment surgery using the combined technique leads to increased quality of life in a prospective study. Plast ... 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP ...
What is the average cost of a MTF gender reassignment surgery? MTF gender reassignment surgery cost generally ranges from $7,000 to $24,000. The actual cost of a surgical procedure will be dependent on location, surgeon, and length and involvement of the surgery.
Surgery is more common among transgender men, with 42% to 54% getting some type of surgery; up to 50% get genital surgery. How Much Does Gender-Affirming Medication Cost? Gender-affirming ...
Total costs for MTF surgery can reach up to $140,500; average costs generally range from $5,000 to $30,000, depending on the procedure. MTF top surgery typically costs $5,000 to $10,000; bottom surgery ranges from $10,000 to $30,000; facial feminization surgery costs between $20,000 and $50,000; and voice feminization surgery ranges from $5,000 ...