Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 21 January 2021
- Hepatocellular carcinoma
- Josep M. Llovet ORCID: orcid.org/0000-0003-0547-2667 1 , 2 , 3 ,
- Robin Kate Kelley 4 ,
- Augusto Villanueva ORCID: orcid.org/0000-0003-3585-3727 1 ,
- Amit G. Singal 5 ,
- Eli Pikarsky 6 ,
- Sasan Roayaie 7 ,
- Riccardo Lencioni 8 , 9 ,
- Kazuhiko Koike 10 ,
- Jessica Zucman-Rossi ORCID: orcid.org/0000-0002-5687-0334 11 , 12 &
- Richard S. Finn 13
Nature Reviews Disease Primers volume 7 , Article number: 6 ( 2021 ) Cite this article
239k Accesses
2676 Citations
1069 Altmetric
Metrics details
An Author Correction to this article was published on 12 February 2024
This article has been updated
Liver cancer remains a global health challenge, with an estimated incidence of >1 million cases by 2025. Hepatocellular carcinoma (HCC) is the most common form of liver cancer and accounts for ~90% of cases. Infection by hepatitis B virus and hepatitis C virus are the main risk factors for HCC development, although non-alcoholic steatohepatitis associated with metabolic syndrome or diabetes mellitus is becoming a more frequent risk factor in the West. Moreover, non-alcoholic steatohepatitis-associated HCC has a unique molecular pathogenesis. Approximately 25% of all HCCs present with potentially actionable mutations, which are yet to be translated into the clinical practice. Diagnosis based upon non-invasive criteria is currently challenged by the need for molecular information that requires tissue or liquid biopsies. The current major advancements have impacted the management of patients with advanced HCC. Six systemic therapies have been approved based on phase III trials (atezolizumab plus bevacizumab, sorafenib, lenvatinib, regorafenib, cabozantinib and ramucirumab) and three additional therapies have obtained accelerated FDA approval owing to evidence of efficacy. New trials are exploring combination therapies, including checkpoint inhibitors and tyrosine kinase inhibitors or anti-VEGF therapies, or even combinations of two immunotherapy regimens. The outcomes of these trials are expected to change the landscape of HCC management at all evolutionary stages.

Similar content being viewed by others

A global view of hepatocellular carcinoma: trends, risk, prevention and management

Molecular pathogenesis and systemic therapies for hepatocellular carcinoma
Insights into the success and failure of systemic therapy for hepatocellular carcinoma
Introduction.
Liver cancer remains a global health challenge and its incidence is growing worldwide 1 , 2 . It is estimated that, by 2025, >1 million individuals will be affected by liver cancer annually 3 . Hepatocellular carcinoma (HCC) is the most common form of liver cancer and accounts for ~90% of cases. Hepatitis B virus (HBV) infection is the most prominent risk factor for HCC development, accounting for ~50% of cases 4 . The risk attributed to hepatitis C virus (HCV) infection has substantially decreased owing to patients achieving sustained virological response (SVR) with antiviral drugs 5 . Nonetheless, patients with cirrhosis are still considered to be at high risk for HCC incidence even after HCV clearance. Non-alcoholic steatohepatitis (NASH), associated with metabolic syndrome or diabetes mellitus, is becoming the fastest growing aetiology of HCC, particularly in the West 6 . Additionally, reports on mutational signatures have established aristolochic acid and tobacco as potential pathogenetic cofactors in HCC 7 .
The molecular pathogenesis of HCC varies according to the distinct genotoxic insults and aetiologies. Although our understanding of the pathophysiology and drivers of the disease has improved, this knowledge is yet to be translated into clinical practice. Approximately 25% of HCC tumours present actionable mutations; however, the prevalence of most mutations is <10%, thereby complicating proof-of-concept studies 7 , 8 . Indeed, dominant mutational drivers in HCC, such as TERT , TP53 and CTNNB1 , remain undruggable 9 . In addition, the translation of molecular and immune classes into biomarkers that guide therapies is still under investigation. Currently, specific advancements in our understanding of the mechanisms underlying NASH-associated HCC have provided new insights into the contributions of the tumour microenvironment, particularly the immune system and platelet activation, in the pathophysiology of this disease 10 , 11 .
The diagnosis of HCC is usually based on non-invasive criteria, although there is a growing need for molecular characterization of the tumour using tissue biopsies in clinical practice 12 , 13 . In terms of prevention, beyond vaccines preventing HBV infection and anti-viral therapies for HBV and HCV infection, cumulative data support the preventive role of coffee and aspirin 14 . The management of HCC has markedly improved since the early 2010s 8 , 12 , 13 , 15 . Hepatic resection and liver transplantation have been the mainstay curative treatments in HCC cases. Refinements in patient selection have resulted in enhanced surgical resection outcomes and remarkable 10-year post-liver transplantation survival rates for tumours down-staged beyond Milan criteria 12 , 16 . Local ablation with radiofrequency remains the backbone of image-guided ablation for non-surgical early-stage HCC, despite progress in other techniques 15 . Adjuvant therapies to preclude relapse, following these potentially curative approaches, are an unmet medical need, as randomized controlled trials (RCTs) have so far yielded negative results. For intermediate-stage HCC, transarterial chemoembolization (TACE) has been the most widely used treatment and the standard of care over the past two decades 17 . Transarterial radioembolization (TARE) has shown efficacy in phase II investigations 18 but has not been established as a primary standard of care by guidelines. Other loco-regional devices or radiation oncology approaches are not expected to improve the intermediate treatment armamentarium in the short term.
Currently, systemic therapies, including immune-checkpoint inhibitors (ICIs), tyrosine kinase inhibitors (TKIs) and monoclonal antibodies, have challenged the use of conventional therapies for HCC. Approximately, 50–60% of patients with HCC are estimated to be exposed to systemic therapies in their lifespan, particularly in advanced stages of the disease 8 . The field has witnessed substantial progress in the development of systemic therapies in the past 5 years, with studies reporting a marked increase in overall survival and in the quality of life of patients 8 . For example, the natural history of advanced-stage HCC cases involves a median survival of ~8 months and the approved combination of atezolizumab (anti-PDL1 antibody) and bevacizumab (anti-VEGF antibody) has more than doubled this life expectancy and improved the patient-reported outcomes 19 . Sorafenib 20 and lenvatinib 21 remain as the most effective single-drug therapies. In case of progression to single-agent regimens, regorafenib 22 , cabozantinib 23 and ramucirumab 24 have also proven improved survival benefits. Single-agent ICIs provide substantial clinical benefits in 15–20% of responders but, so far, biomarkers have failed to identify this group 25 , 26 . Furthermore, phase III trials investigating the efficacy of combination therapy, that is, combining ICIs with TKIs or combining PD1/PDL1 axis inhibitors with CTLA4 inhibitors, are ongoing. The results of these trials are expected to change the landscape of HCC management at all evolutionary stages.
This Primer provides an update on the advancements in HCC pathogenetic mechanisms and its treatment since our first review 1 . We discuss the increasing contribution of non-alcoholic fatty liver disease (NAFLD) and NASH to the development of HCC as well as the specific key molecular mechanisms associated with this risk factor. Additionally, we summarize the current knowledge and trends in epidemiology, diagnosis, screening and management. In particular, we describe the evidence-based data generated with new therapies and the prospects of novel combination therapies in the adjuvant setting as well as in intermediate-stage and advanced-stage HCC. Finally, we discuss the role of biomarkers, liquid biopsy and patient-reported outcomes in the future management of this devastating disease.
Epidemiology
Liver cancer is the sixth most common cancer worldwide, with 841,080 new liver cancer cases in 2018, and the fourth leading cause of cancer-related death globally 3 (Fig. 1 ). The highest incidence and mortality of HCC are observed in East Asia and Africa, although HCC incidence and mortality are increasing in different parts of Europe and in the USA 27 . Indeed, Surveillance Epidemiology End Results (SEER) reported HCC as the fastest increasing cause of cancer-related death in the USA since the early 2000s and HCC is projected to become the third leading cause of cancer-related death by 2030 if these trends continue 28 .

The incidence and major aetiological factors involved in hepatocarcinogenesis are depicted in this figure. The highest incidence of hepatocellular carcinoma (HCC) is observed in East Asia, with Mongolia demonstrating the highest incidence of HCC worldwide. Hepatitis B virus (HBV) is the major aetiological factor in most parts of Asia (except Japan), South America and Africa; Hepatitis C virus (HCV) is the predominant causative factor in Western Europe, North America and Japan, and alcohol intake is the aetiological factor in Central and Eastern Europe. Non-alcoholic steatohepatitis (NASH), the main aetiology included in the category ‘Other’, is a rapidly increasing risk factor that is expected to become the predominant cause of HCC in high income regions in the near future. ASR, age-standardized incidence rate. Data from refs 3 , 129 . Reprinted from ref. 3 , Global Cancer Observatory, World Health Organization, Estimated age-standardized incidence rates (World) in 2020, liver, both sexes, all ages, Copyright (2020) ( https://gco.iarc.fr/today/online-analysis-map?v=2020&mode=population&mode_population=continents&population=900&populations=900&key=asr&sex=0&cancer=11&type=0&statistic=5&prevalence=0&population_group=earth&color_palette=default&map_scale=quantile&map_nb_colors=5&continent=0&rotate=%255B10%252C0%255D ).
Risk factors
Over 90% of HCC cases occur in the setting of chronic liver disease. Cirrhosis from any aetiology is the strongest risk factor for HCC 12 , 13 . HCC is the leading cause of death in patients with cirrhosis, with an annual HCC incidence of 1–6% 29 . The major risk factors for HCC include chronic alcohol consumption, diabetes or obesity-related NASH, and infection by HBV or HCV (Fig. 1 ). Other less prevalent risk factors for HCC include cirrhosis from primary biliary cholangitis, haemochromatosis and α1-antitrypsin deficiency. Indeed, patients developing cirrhosis from haemochromatosis are at a particularly high risk of HCC, with up to 45% developing HCC in their life span 30 .
Hepatitis B virus infection
HBV infection accounts for ~60% of HCC cases in Asia and Africa and 20% of cases in the West 4 (Fig. 1 ). HBV is a DNA virus that can integrate into the host genome inducing insertional mutagenesis, leading to oncogene activation 31 . HBV increases the risk of HCC even in the absence of cirrhosis, although most patients with HBV-induced HCC have cirrhosis at presentation. The high prevalence of endemic HBV infection in East Asia has resulted in a risk of HCC exceeding cost-effectiveness thresholds in men (40 years of age) and in women (50 years of age), thereby justifying surveillance programmes. In Africa, patients in their early 30s or 40s present with HCC, likely because of exposure to aflatoxin B1 , which acts synergistically with HBV to increase the risk of HCC 32 . HBV vaccination programmes have led to a decrease in HCC incidence in some parts of Asia, although many jurisdictions are yet to implement universal vaccination programmes 33 .
Hepatitis C virus infection
Chronic HCV infection is the most common underlying liver disease among patients with HCC in North America, Europe and Japan 4 (Fig. 1 ). Unlike HBV, HCV is an RNA virus that does not integrate into the host genome and, therefore, the risk of HCC is primarily limited to those who develop cirrhosis or chronic liver damage with bridging fibrosis . With the use of direct-acting antiviral (DAA) therapy, an increasing proportion of patients with HCV infection have been successfully treated to achieve an SVR, resulting in a 50–80% reduction in the risk of HCC 5 . However, several patients, particularly, racial minorities, ethnic minorities or people from low socioeconomic regions, are yet to be tested for HCV and remain unaware of their infection 34 . Additionally, patients with HCV-induced cirrhosis continue to have a persistent risk of developing HCC (>2% per year) even after SVR and should therefore remain under close surveillance 35 , 36 .
Hepatitis D virus infection
Hepatitis D virus (HDV) is an RNA virus that requires the presence of HBV surface antigens for its replication and, therefore, for infectivity. HDV is estimated to affect 20–40 million people globally and is associated with a more severe course of liver disease, including increased fibrosis and risk of cirrhosis, than patients with HBV infection alone. Similarly, several cohort studies suggest that HBV/HDV co-infection is associated with an increased risk of HCC compared with HBV infection alone. In one of the largest studies to date, the risk of HCC was significantly higher among those with acute HDV infection (RR 6.1, 95% CI 2.8–11.7) or chronic HDV infection (RR 3.9, 95% CI 1.6–7.2) than among those with HBV infection alone 37 .
Excessive alcohol intake causes alcoholic liver disease, cirrhosis and HCC. Currently, an increasing number of persons have cirrhosis from chronic alcohol consumption or NASH. Alcohol-related cirrhosis has an annual incidence ranging from 1% in population-based studies to 2–3% in tertiary care referral centres and accounts for ~15–30% of HCC cases depending on the geographical region 38 . Chronic alcohol intake can also increase the risk of HCC from other aetiologies; for example, several studies reveal an increased risk of HCC in HBV carriers who consume alcohol compared with those who do not consume alcohol 39 . Although alcohol consumption shares many pathophysiological processes with other forms of cirrhosis, in particular NASH, there is evidence supporting distinct alcohol-specific pro-tumorigenic mechanisms in patients.
Another common aetiological factor for cirrhosis in people is NASH, which is the precursor step in the development of HCC in patients with diabetes mellitus or obesity. Owing to the increasing prevalence of obesity, NASH has become the most common cause of cirrhosis in most regions of the world. Since 2010, the proportion of HCC attributed to NASH has rapidly increased, currently representing 15–20% of cases in the West 6 . Furthermore, the population attributable fraction of metabolic syndrome and NASH is likely to be >20% owing to its co-existence in patients with other liver diseases 40 . Although the annual incidence of HCC is lower in NASH-related cirrhosis (1–2% per year) than in viral-mediated cirrhosis (3–5% per year), the incidence is >1.1 per 100 person-years, indicating that surveillance is cost-effective and should therefore be implemented 41 . Several studies have demonstrated that 25–30% of NASH-associated HCC cases occur in the absence of cirrhosis, which hampers the applicability of surveillance programmes currently targeting only patients with cirrhosis. However, a cohort study from the national Veterans Affairs health system found that the annual incidence of HCC in individuals with non-cirrhotic NASH falls below the cost-effectiveness threshold, thus advising against surveillance 41 , 42 .
Age, sex and other factors
Several sociodemographic characteristics have been associated with HCC, particularly in patients with cirrhosis. Ageing is a strong risk factor, with the highest age-specific incidence reported in individuals >70 years of age 43 . Furthermore, HCC also has a strong male predominance (male to female ratio of 2–3:1), likely related to a clustering of risk factors among men as well as differences in sex hormones 44 . Studies have reported a higher incidence of HCC among racial or ethnic minorities, in particular Hispanics, than among white individuals. This discrepancy in incidence might partly be due to the high incidence of single-nucleotide variants in PNPLA3 , linked to NASH-associated HCC 45 . Epidemiological studies have also highlighted the increased risk of HCC associated with smoking 46 . However, the role of diet in moderating the risk of HCC remains unclear, with the exception of studies showing a preventive effect of coffee and aspirin 47 .
Mechanisms/pathophysiology
The pathophysiology of HCC is a complex multistep process. The interplay of various factors is at the origin of the early steps of hepatocyte malignant transformation and HCC development. These factors include a genetic predisposition, reciprocal interactions between viral and non-viral risk factors, the cellular microenvironment and various immune cells, and the severity of the underlying chronic liver disease. An altered microenvironment is a key enabling characteristic of cancer and is known to participate in all stages of malignant progression, from the initial transformation phases, through to invasion and, ultimately, to metastasis. In our previous Primer, we described the main oncogenic drivers and signalling pathways involved in the initiation, development and progression of HCC 1 . Herein, we explain in detail our current understanding of the mechanisms underlying NASH-associated HCC.
Cell of origin
The cell of origin of HCC is debated. Similar to any type of cancer, the cell of origin could be a liver stem cell, a transit amplifying population or mature hepatocytes. In general, the presence and role of stem cells in the liver is in itself debatable. Moreover, mature hepatocytes are long-lived cells and retain considerable proliferative potential in response to injury. Many mouse models support the possibility that HCC originates in transformed mature hepatocytes, although others posit that putative liver stem cells could be the source 48 . Paradoxically, intrahepatic cholangiocarcinomas and tumours showing mixed HCC or cholangiocarcinoma morphology often seem to arise from mature hepatocytes, emphasizing the concepts of metaplasia and cell plasticity (that is, transdifferentiation ). This finding confirms the notion that the morphology and epigenetic landscape of a tumour does not necessarily reflect its cell of origin 49 , 50 .
Cancer driver gene mutations in HCC
High throughput next-generation sequencing has enabled the identification of cancer driver genes with oncogenic functions or tumour suppressive functions that are recurrently altered in HCC. Telomerase activation via TERT promoter mutations, viral insertions, chromosome translocation or gene amplification are the most frequent driver gene alterations, observed in ~80% of HCC 7 , 51 . Studies have demonstrated the activation of the Wnt–β-catenin signalling pathway in 30–50% of the cases, caused by mutations in CTNNB1 (encoding β-catenin), AXIN1 or APC (inhibitors of Wnt pathway) inactivation 7 , 51 . Other frequent mutations or genetic alterations are found in TP53 , RB1 , CCNA2 , CCNE1 , PTEN , ARID1A , ARID2 , RPS6KA3 or NFE2L2 , all of which alter cell cycle control. Additionally, variants in genes involved in epigenetic regulation, oxidative stress, and the AKT–mTOR and MAPK pathways have been implicated in HCC (see previous Primer 1 ). Furthermore, recurrent focal chromosome amplifications in CCND1 , FGF19 , VEGFA , MYC or MET leading to over-expression result in the activation of various oncogenic signalling pathways, including of receptor tyrosine kinases 52 . Although cancer driver gene mutations accumulate randomly, specific genes are related to precise molecular HCC subclasses, defined by transcriptomic profiles and histological phenotypes 8 , 9 , 53 (Fig. 2 ). Overall, only ~20–25% of patients with HCC have at least one potential actionable mutation as per current standards 7 , 8 , 54 .
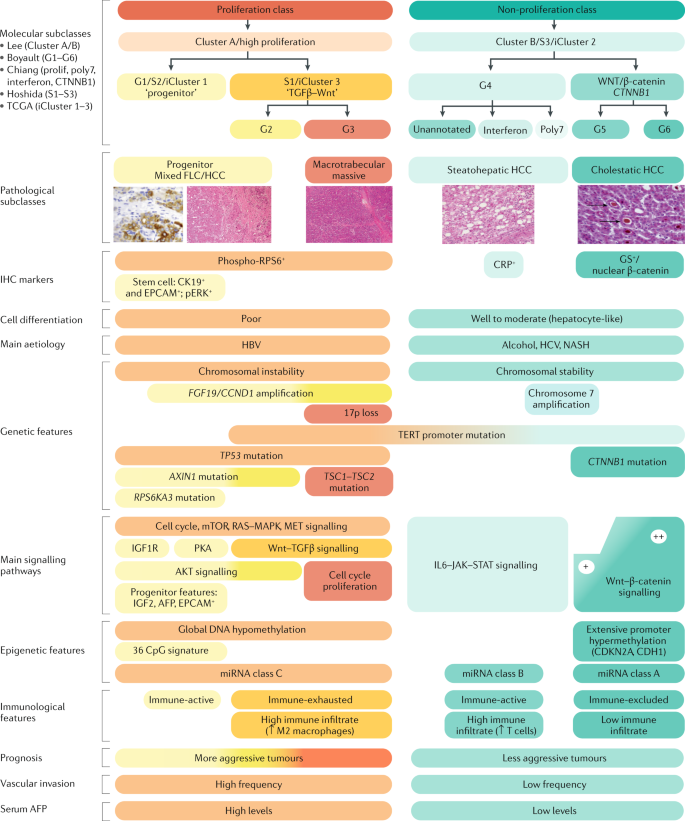
Hepatocellular carcinoma (HCC) can be classified into two major molecular groups based on transcriptomic-based phenotypic classes 52 , 67 , 68 , 69 , 70 . The proliferation class is characterized by more aggressive tumours with poor histological differentiation, high vascular invasion and increased levels of α-fetoprotein (AFP) 53 . This class can be further divided into two subclasses: S1 or iCluster 3 (refs 67 , 68 ), characterized by Wnt–TGFβ activation, which drives an immune-exhausted phenotype 71 , and S2 or iCluster 1 (refs 67 , 68 ), characterized by a progenitor-like phenotype, with the expression of stem cell markers (CK19, EPCAM) and activated IGF2 and EPCAM signalling pathways 53 . Hepatitis B virus (HBV)-associated tumours present frequent activation of classical cell proliferation pathways such as PI3K–AKT–mTOR, RAS–MAPK, MET and IGF cascades. In addition, frequent TP53 mutations, high chromosomal instability and global DNA hypomethylation represent additional hallmarks of this class. The non-proliferation class 52 , 67 , 68 , 69 , 70 is characterized by less aggressive tumours with well to moderate histological differentiation, low levels of AFP and less frequent vascular invasion 53 . These tumours are related to non-alcoholic steatohepatitis (NASH), alcoholic steatohepatitis and hepatitis C virus (HCV) infection. Distinct subgroups have been characterized within this class: the WNT–β-catenin CTNNB1 subclass presents frequent CTNNB1 mutations and activation of the WNT–β-catenin signalling pathway, which drives an immune-excluded phenotype with low immune infiltration 52 , 70 , 71 , and the interferon subclass presents a highly activated IL6–JAK–STAT signalling pathway, with a more inflamed tumour microenvironment. This class present chromosomal stability with frequent TERT promoter mutations. Data from refs 1 , 7 , 8 , 9 , 52 , 53 , 66 , 67 , 68 , 69 , 70 , 71 . FLC, fibrolamellar carcinoma; IHC, immunohistochemistry; miRNA, microRNA; TCGA, The Cancer Genome Atlas.
In addition to cancer driver mutations, the cooperation of risk factors is well described in the pathogenesis of HCC. For example, the toxic effect of aflatoxin B1 is potentiated by HBV infection, particularly in patients with a null polymorphism of GSTT1 (refs 55 , 56 ). In addition, polymorphisms in PNPLA3 , TM6SF2 and HSD17B13 have been identified to be associated with the severity of NASH and HCC incidence, specifically in patients with high chronic alcohol intake 57 , 58 .
Viral infection-associated molecular alterations
The most frequent site of HBV-mediated insertional mutagenesis is located within the TERT promoter, leading to an overexpression of telomerase, the enzyme responsible for the maintenance of telomere length 59 . The activation of telomerase prevents the erosion of the chromosomes that physiologically occur at each cell division during ageing. The ectopic activation of telomerase protects cells from senescence and promotes cell transformation 60 . Other recurrent insertions associated with HBV were identified to activate potent oncogenes, such as CCNA2 or CCNE1 , involved in cell cycle control. These oncogenic alterations induce replicative stress and complex rearrangements throughout the genome 61 . In a small set of patients with HCC, adeno-associated virus 2 demonstrated a similar insertional oncogenic mutagenesis, with a common hot spot of viral insertion within the TERT promoter, CCNA2 and CCNE1 (ref. 62 ). These observations illustrate that specific oncogenes, activated by viral infection, act as early facilitators of hepatocyte transformation. By contrast, HCV infection does not drive a strong, direct oncogenic effect and the induction of mutations results from the oxidative stress caused by chronic inflammation.
HCC-related mutational signatures
During the development of chronic liver disease and cirrhosis, which are the basis for the onset of HCC in most cases, hepatocytes progressively accumulate numerous genetic mutations and epigenetic changes. During this process, several risk factors inducing DNA mutations are associated with specific mutational signatures 7 , 63 . Exome sequencing analyses of HCC have identified mutational signature 22 and signature 24, especially in patients from Asia and Africa exposed to aristolochic acid (A>T mutations in CTG trinucleotide) and aflatoxin B1 (C>A mutations), respectively 7 , 64 . Signature 4 (C>A and dinucleotide mutations) and signature 16 (T>C mutation at TpA dinucleotide) were respectively associated with tobacco smoking and alcohol intake 65 . Whether this observation could be translated for preventive measures remains to be elucidated. These observations underline the role of the liver in detoxifying numerous metabolites, which can damage the hepatocyte genome by inducing passenger or driver mutations, leading to carcinogenesis.
Molecular classes of HCC
Several studies based on genomic, epigenomic, histopathological and immunological analyses have established a molecular and immune classification of HCC 1 , 9 , 66 (Fig. 2 ). Molecular classes of HCC have been defined based on the main molecular drivers and pathways involved 9 , 66 , 67 , 68 , 69 , 70 or depending on the immune status of the tumour 8 , 71 . These molecular classes correlate with specific genomic disturbances, histopathological fingerprints and clinical outcomes. The proliferation class accounts for ~50% of HCCs and is overall enriched in mutations in TP53 and in amplifications of FGF19 or CCND1 (ref. 52 ); additionally, it is more common in HBV-associated HCC and has the worst prognosis. The proliferation class includes two subclasses — the proliferation-progenitor cell group and the proliferation–Wnt–TGFβ group. The proliferation-progenitor cell group, which represents 25–30% of HCC 52 , 67 , is characterized by the activation of classic cell proliferation pathways (such as PI3K–AKT–mTOR signalling, RAS–MAPK pathway and MET and IGF signalling cascades 9 ) and by the expression of progenitor cell markers (such as EPCAM and α-fetoprotein), and corresponds to cluster 1 of The Cancer Genome Atlas (TCGA) 68 . The proliferation–WNT–TGFβ group, which represents 20% of HCC cases, is characterized by non-canonical activation of Wnt and correlates with cluster 3 of the TCGA. Conversely, the non-proliferation tumour class, which accounts for 50% of HCC, is more prevalent in alcohol-associated HCC and HCV-related HCC; these tumours present better outcomes and correlate with cluster 2 of the TCGA 68 . Within the non-proliferative class, at least two distinct subgroups have been delineated — one characterized by a dominant canonical Wnt signalling associated with mutations in CTNNB1 (ref. 72 ) and the second characterized by the activation of IFNα signaling 52 .
Reports on the classification of HCC according to the immune cell status have further expanded our understanding of the molecular traits of HCC 71 (Fig. 2 ). This classification provides complementary information based upon immune traits and divides HCC tumours into distinct subclasses — immune-active, immune-exhausted, immune-intermediate and immune-excluded. The immune class, which includes both the immune-active and immune-exhausted subclasses, is characterized by immune cell infiltrates of distinct nature. The immune-active HCC tumours (found in 20% of cases) are enriched with active helper T (CD4 + ) cell infiltrates and cytotoxic T (CD8 + ) cell infiltrates and respond to ICIs. Conversely, immune-exhausted tumours are dominated by TGFβ-driven CD8 + cell exhaustion status . Immune-excluded tumours, which represent the other end of the spectrum, are characterized by a paucity of T cell infiltrates and an increase of regulatory T (T reg ) cells and are dominated by canonical Wnt signalling and other immune-dissuasive cascades. Immune-excluded tumours are proposed to be primarily resistant to ICIs 73 .
NASH-associated HCC
Obesity is linked to an increased risk of cancer in multiple organs 74 . Obesity can induce systemic changes, including altered immune function and systemic endocrine changes, which are hallmarks of multiple types of cancer. Current evidence shows that fatty liver disease is rapidly becoming the leading cause of HCC in the West 6 . Studies have demonstrated that liver-specific mechanisms through which NAFLD or NASH promote HCC involve metabolic and oxidative stress, altered immune function, pathological inflammatory responses, and altered endocrine or adipokine signalling 10 , 75 .
Oxidative stress
Hepatocytes overloaded by fatty acids cause oxidative stress and endoplasmic reticulum (ER) stress, which induce pathological inflammation and cell damage 10 , 11 . One study proved the causative role for ER stress in NASH-induced HCC in mice; ER stress in mouse hepatocytes led to the activation of inflammatory signalling pathways, specifically NF-κB and TNF, leading to HCC induction 76 . However, these pathogenic mechanisms are yet to be proven in human HCC. The deranged fatty acid metabolism in hepatocytes can cause DNA damage owing to increased reactive oxygen species (ROS), produced as a result of mitochondrial dysfunction 77 . In addition, the altered expression of specific metabolic enzymes can affect hepatocytes by decreasing their ability to repair DNA damage 78 . The metabolic dysfunction also results in altered inflammatory signalling; for example, high expression levels of IL-17 (a tumour-promoting cytokine) have been observed in human NASH 79 . In NASH, lipid generation might not only be increased but possibly also altered to generate more pathogenic lipids that serve as oncometabolites 80 , 81 . For example, continuous activation of mTORC2 in mouse hepatocytes increased the generation of the sphingolipid glucosylceramide, causing increased ROS production, which can ultimately lead to HCC development 80 . Similarly, altered cholesterol metabolism may also contribute to HCC pathogenesis 81 , potentially through the production of pro-tumorigenic nuclear receptor ligands. Although autophagy can have anti-tumour functions, one study demonstrated an important role for lipophagy (that is, autophagic degradation of lipid droplets) in HCC pathogenesis. The overexpression of sequestosome 1 (also known as p62), which regulates lipophagy, in hepatocytes of patients with NASH and in a mouse model was linked to HCC development 82 .
Studies have shown a higher risk of HCC in patients with NASH than in those with NAFLD 6 . One experimental study revealed that fatty acid-induced oxidative stress in hepatocytes upregulated STAT1 and STAT3, both of which are pro-inflammatory transcription factors that usually act in parallel 83 . Remarkably, in this mouse model, high levels of STAT1 caused progression to NASH, while high levels of STAT3 promoted HCC, independently of each other 83 . This suggests that similar inflammatory signals can differentially promote the progression of NAFLD to NASH or to HCC. As NAFLD is more prevalent than NASH in the general population 6 , this finding underscores the need for a better understanding of how NAFLD per se, irrespective of NASH, can progress to HCC.
Taken together, ER stress, pathological lipophagy, increased ROS production and diminished reducing power (low NADH or NADPH levels) could cause oncogenic genetic alterations in fatty acid-overloaded hepatocytes and promote the expansion of malignant cells.
Immune infiltration of fatty liver
Immune cell infiltration of the fatty liver is a histopathological hallmark of NASH 10 . The development of animal models that accurately replicates human HCC is essential for basic studies exploring pathogenesis and for translational studies 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 (Fig. 3 ; Box 1 ). Several experimental models have shown that immune cells and cytokines play an important role in HCC pathogenesis. For example, prolonged NASH in mouse models induces CD8 + T cell activation, which results in hepatocyte damage, leading to HCC 99 . In addition, NAFLD causes a selective loss of intrahepatic CD4 + T cells, which are crucial for eliciting an effective anti-tumour adaptive immune response 100 . Other immune cell types, including B cells, T reg cells, natural killer cells and different types of myeloid cell, have been linked to NASH-induced HCC pathogenesis 10 , 75 . Interestingly, in line with clinical data 14 (see section on prevention), platelet recruitment and activation in the liver also contribute to HCC development in mice, specifically via platelet glycoprotein Ibα (GPIbα) signalling, suggesting a therapeutic potential of this pathway 101 . An altered cytokine milieu was also shown to underlie the causative role of NASH in HCC 11 . For example, NASH was shown to overexpress hepatic IL-6 and TNF, which are drivers of HCC in other aetiologies as in NASH 102 .
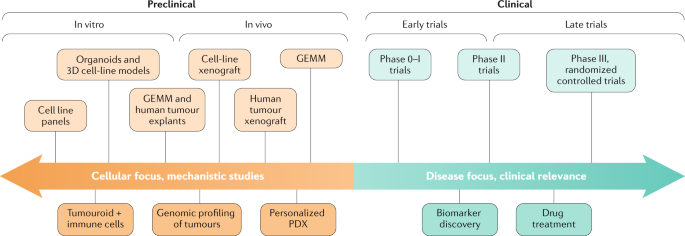
Translational research in hepatocellular carcinoma (HCC) represents a two-way road between preclinical and clinical models. At one end, preclinical models aim at understanding the pathogenesis and mechanisms involved in disease initiation and progression and build the groundwork for the development of clinical therapies. The selection of preclinical models represents a compromise between time, complexity and clinical relevance. For instance, cell lines provide fast, relatively simple but less clinically relevant information while patient-derived xenograft (PDX) models are slow, complex but more relevant. At the other end, clinical studies are focused on drug development and biomarker discovery and their outcomes, albeit negative, often lead to new hypotheses that require preclinical investigation. Phase I studies aim at understanding the pharmacokinetics and toxicity profiles of newly developed drugs, phase II studies are meant to explore preliminary efficacy and phase III randomized controlled trials represent the highest level of evidence necessary for regulatory approval. Biomarkers allow for the selection of enriched populations that are most likely to benefit from certain treatments based on their mechanism of action. GEMM, genetically engineered mouse model.
All of the above-described mechanisms could simultaneously promote HCC on a background of fatty liver disease. However, their relative contribution in human HCC is currently unknown. The analysis of mutational signatures in NASH-associated HCC versus HCC from other aetiologies could help to delineate the relative contributions of various factors.
Box 1 Experimental animal models of HCC
The establishment of experimental models that truly replicate the human disease is crucial for an improved understanding of the pathogenesis and to test novel therapeutic strategies. Animal models of hepatocellular carcinoma (HCC), consistent with the mouse tumour models proposed by The National Cancer Institute (see review 90 ) are categorized as explained below.
Chemically induced models 114 allow the detailed analysis of the progression of liver injury into HCC using well-established chemical carcinogens.
Genetically engineered (transgenic or knockout) models 91 allow analysis of the consequences of institution or retraction of specific gene expression. These models have been widely used to preclinically assess the therapeutic efficacy of drugs in HCC 73 and other types of cancer 89 . These models comprise immunocompetent animals with tumours driven by clear molecular aberrations. Nonetheless, the stroma, proteins and targets for therapies are non-human. New chimeric genetically engineered mouse models have been designed with novel techniques, such as CRISPR–Cas9 gene editing 88 , and have led to discoveries of oncogenes 87 or mechanisms of resistance of sorafenib in HCC 86 .
Engrafted models comprise three different categories.
Cell line xenograft, including 3D cell culture xenografts 92 . Although these models have been widely used in the preclinical development of targeted agents, they fail to recapitulate the complex microenvironment of the tumour 96 , 98 .
Mouse allograft models are used if there is a clear need to reproduce the microenvironment, including the immune system.
Patient-derived xenografts. These models allow studies using human tumour tissue, carrying human genetic material, to be performed in a natural or artificially modified microenvironment in animals. These models have been widely used in cancer 95 and in the development of drugs in HCC 94 .
The ideal animal model should reproduce the natural history, pathophysiology and biochemistry of human HCC according to distinct aetiologies. Several hepatitis C virus-related HCC 93 and non-alcoholic fatty liver disease-related HCC 85 models have been produced 97 to decipher the molecular pathogenesis of this disease, the advantages and disadvantages of which are reviewed elsewhere 90 .
Chronic inflammation
HCC is a prototypical inflammation-associated cancer, with ~90% of the HCC burden being associated with prolonged inflammation owing to viral hepatitis, excessive alcohol intake, NAFLD or NASH. The immune microenvironment plays a pivotal role in the pathogenesis of HCC 103 . In HCC, the presence of immune infiltrates is associated with a better prognosis, likely owing to more effective anti-tumour immunity 71 , 104 . Mouse models of HCC have revealed that immune signals, such as IL-6, lymphotoxin-α and TNF, can accelerate hepatocarcinogenesis and affect tumour aggressiveness 50 , 105 ; nevertheless, immune responses also limit liver cancer progression 103 . Importantly, the liver harbours the largest number of immune cells in the body and maintains a unique immune state, considerably more tolerant than other organs, allowing it to withstand the constant flow of inflammatory signals from the gut 103 . Understanding this unique hepatic immune system is likely important in the context of the complex interaction between malignant hepatocytes and the liver immune system 103 , 106 . Remarkably, studies in mice and humans suggest that VEGF secreted by malignant hepatocytes generates an immune-tolerant, pro-tumorigenic microenvironment 52 , 107 , suggesting that blocking the VEGF cascade could be effective by altering liver immune tolerance. Interestingly, combinations of an ICI with specific targeted therapies, such as VEGF inhibitors, showed more potent survival benefits than the use of single agents 19 , 108 .
In the chronically inflamed liver, multiple cell types, including macrophages, stellate cells, endothelial cells and different lymphocyte subtypes, interact with hepatocytes 103 , 106 . The role of innate immune cells and fibroblasts in HCC pathogenesis was described in detail in our previous Primer 1 . Understanding the role of the adaptive immune system is gaining increased attention in view of its importance in immuno-oncology therapies. Notably, insights from mouse models reveal that virtually every immune cell type can have both pro-tumour and anti-tumour roles 103 . The two major pro-tumorigenic mechanisms through which immune cells promote HCC include the secretion of cytokines and growth factors that favour proliferation or counteract apoptosis of tumour cells as well as, paradoxically, suppressing the anti-tumour function of neighbouring lymphocytes. Studies have demonstrated the NF-κB and JAK–STAT pathways as the key inflammatory signalling pathways involved in promoting HCC 109 ; this finding was further supported in a transcriptome analysis of human HCC 110 . The major anti-tumour function of the adaptive immune system is mediated via immune surveillance and by the elimination of pre-malignant or fully transformed malignant hepatocytes 104 .
Adaptive immune system in HCC
Cytotoxic T (CD8 + ) cells are considered the key effectors of anti-tumour immunity. Accordingly, one study showed that their depletion in mice could increase HCC burden 111 and another study showed that these T cells mediate the surveillance of premalignant hepatocytes 112 . Paradoxically, in several specific cases, CD8 + T cell depletion in mice resulted in a reduced tumour load, indicating that these cells can also have pro-tumorigenic functions 99 . Analyses of human HCC samples revealed the presence of functional CD8 + T cells expressing anti-tumour effector molecules, such as granzyme A, granzyme B and perforin, in some patients 113 . Nonetheless, single-cell RNA sequencing of T cells in human HCC suggests that, in many cases, these CD8 + T cells are dysfunctional 114 . The causes of CD8 + T cell dysfunction, evident by decreased proliferation and a decreased ability to produce cytotoxic effector molecules, are not sufficiently clarified to date. T reg cells are considered a major culprit in mediating T cell dysfunction in HCC and higher numbers of T reg cells within the tumour are associated with worse disease outcomes 115 . The immunosuppressive functions of T reg cells might be mediated via the secretion of CD10 and TGFβ 116 , suggesting that targeting these cytokines might sensitize HCC to ICIs. Interestingly, the hyaluronic acid receptor, layilin, was linked to the suppressive function of HCC-infiltrating T reg cells. Layilin induction caused CD8 + T cell dysfunction in human HCC and its overexpression in human lymphocytes was associated with a unique mRNA expression signature 114 .
Although B cells were thought to be innocent bystanders in cancer, the emerging evidence supports their active participation in the crosstalk between the adaptive immune system and cancer 117 . In mouse models of HCC, B cells both promoted and supressed tumour growth 118 . Furthermore, one study showed that IgA-expressing lymphocytes supported HCC growth by actively suppressing CD8 + T cell function 111 . Finally, human and mouse studies have shown that tertiary lymphoid structures , which have important roles in the adaptive immune response to cancer 119 , demonstrated pro-tumour and anti-tumour response capacities in HCC 120 , 121 . Thus, tertiary lymphoid structures, similar to macrophages and lymphocytes, could be either anti-tumorigenic or pro-tumorigenic in HCC.
Cirrhotic microenvironment and cancer field
Although some aetiologies are more likely to induce HCC than others (for example, HCV versus autoimmune hepatitis), once the patient reaches the cirrhotic stage, the risk of HCC is adequate to render surveillance cost effective 12 , 13 . The key cell involved in the liver response to chronic damage is the hepatic stellate cell 122 , which, upon activation, undergoes phenotypic changes and synthesizes extracellular matrix components, mostly collagen and growth factors, that promote the migration of endothelial cells, neoangiogenesis and fibrosis 123 . The subsequent distortion of the hepatic architecture and disorganized vasculature are the histological substrate for cirrhosis and portal hypertension. In response, premalignant senescent hepatocytes secrete chemokines that interfere with senescent surveillance and impair immune-mediated tumour suppression in vivo 112 . Furthermore, experimental models have documented the importance of CD4 + lymphocytes in NAFLD-related HCC 100 as well as the interplay between the innate immune system and the intestinal microbiota to favour HCC development 124 , 125 . Thus, besides fibrosis, the immune system contributes substantially to the cancer field effect in HCC.
The permissive microenvironment in cirrhosis that promotes tumour development is commonly referred to as the cancer field effect. Different genomic studies have characterized the dominant molecular elements deregulated in this microenvironment. Numerous gene signatures derived from cirrhotic tissue correlate with the risk of HCC development and can be used to risk-stratify patients 110 , 126 , 127 . These gene signatures correlate with cancer risk as well as with likelihood of patient hepatic decompensation and overall survival 126 , 127 . More studies have detailed the genomic traits of the inflammatory microenvironment in cirrhosis that contribute to HCC development 128 . An immune-mediated cancer field molecular subclass was detected in 50% of adjacent cirrhotic tissue from patients with HCC. This subclass can be further stratified based on lymphocyte infiltration and on the activation of either immunosuppressive or pro-inflammatory signals. The immunosuppressive subclass, which showed enrichment in TGFβ signalling, T cell exhaustion and overexpression of immune checkpoints (such as CTLA4, TIGIT, LAG3), represented 10% of patients and had a higher risk of HCC development (threefold increased risk at 5 and 10 years) 128 .
The crucial part played by the tumour microenvironment in the natural history of HCC is a strong rationale for modulating the dynamic cross-talk between hepatocytes and the liver immune system as a therapeutic strategy 103 .
Diagnosis, screening and prevention
Given that most cases of HCC occur in an identifiable patient population, that is, in those with chronic hepatitis B or cirrhosis, many patients are diagnosed through surveillance 129 , 130 . Nevertheless, given the under-implementation of screening in some clinical practices, a proportion of patients with HCC might present incidentally with a liver mass, identified on cross-sectional imaging performed for other reasons or owing to symptomatic advanced-stage HCC after developing abdominal pain, weight loss or worsening of liver dysfunction. Such incidental diagnosis has been estimated to occur in 50% of cases globally, particularly in developing jurisdictions.
Patients with an abnormal surveillance test, that is, detection of a liver nodule in abdominal ultrasonography or high serum α-fetoprotein levels (>20 ng/ml), belong to at-risk populations and require timely diagnostic evaluation. Most lesions <1 cm in diameter detected on ultrasonography are not HCC or are very difficult to diagnose. Hence, cross-sectional imaging is not required and short-term follow-up with a repeat ultrasonography after 3 months is sufficient. For lesions ≥1 cm in diameter, either quadruple-phase CT or dynamic contrast-enhanced MRI should be performed 13 , 14 . HCC lesions are brighter than the surrounding liver in the arterial phase in a CT scan or MRI and less bright than the surrounding parenchyma in the venous and delayed phases, related to the differential blood supply of the tumour compared with the background liver 131 . This phenomenon of ‘arterial enhancement and delayed washout’ has a sensitivity of 89% and a specificity of 96% for HCC and is regarded as the radiological hallmark of HCC , which is sufficient for a diagnosis without requiring histological confirmation 132 . The specificity of MRI using hepatobiliary contrast agents seems to be lower than that using extracellular agents; therefore, its role in the non-invasive diagnosis of HCC remains unclear 133 . Nonetheless, practice guidelines are increasingly recommending biopsies to molecularly characterize HCC 13 . Importantly, imaging criteria for HCC diagnosis only applies to at-risk patients, including those with cirrhosis or chronic HBV infection.
Histopathology
Although most HCCs have characteristic features in imaging, ~10% of the tumours (but up to 30% of tumours 1–2 cm in diameter) have an atypical presentation, lacking the imaging hallmarks of HCC. The International Consensus Group for Hepatocellular Neoplasia has proposed major histological features of HCC, which include stromal invasion, increased cell density, intratumoural portal tracts, unpaired arteries, pseudo-glandular pattern and diffuse fatty changes 134 . If there is a clinical suspicion for HCC but the appearance is atypical by imaging, a biopsy or second contrast-enhanced study should be performed 13 . The sensitivity of a biopsy is ~70% and is even lower in tumours <2 cm because of the potential for missed lesions as well as the difficulty in distinguishing well-differentiated HCC from dysplastic nodules. Some patients require multiple biopsies for a diagnosis, so patients with a negative biopsy should continue to be followed with serial contrast-enhanced imaging 135 . If the lesion enlarges but retains its atypical appearance for HCC, a repeat biopsy should be considered.
The prognosis for HCC is driven by the tumour stage, with curative options providing a 5-year survival exceeding 70% for early-stage HCC compared with a median survival of ~1–1.5 years for symptomatic advanced-stage cases treated with systemic therapies 1 , 2 . Thus, professional societies recommend HCC surveillance in high-risk individuals, including those with cirrhosis and subgroups of patients with chronic HBV infection (Table 1 ). The highest level of data supporting HCC surveillance comes from an RCT in China among 17,920 persons with HBV infection 136 . HCC-related mortality was decreased by 37% in patients randomized to surveillance compared with those who were not screened for HCC. Whether the survival benefit would have persisted if the analytic plan accounted for the use of block randomization (that is, using randomization of villages as opposed to individuals) is unclear 137 . A subsequent RCT among patients with cirrhosis was terminated given poor enrolment as patients did not accept the risk of being randomized to the no-surveillance arm 138 . Hence, surveillance recommendations in patients with cirrhosis are based on level II data, with cohort studies demonstrating an association between HCC surveillance and early tumour detection, curative treatment receipt and improved overall survival, which persists after adjusting for lead-time and length-time biases 139 . Decision analysis models have demonstrated that surveillance is cost effective in patients with compensated cirrhosis and, therefore, this strategy has been adopted by guidelines in this population 140 .
Guidelines across scientific societies concur that screening for HCC should be performed semi-annually as a 6-month interval yields improved survival compared with annual surveillance and non-inferior outcomes compared with a 3-month interval 141 . Nevertheless, optimal surveillance modalities are being debated. Increasing data have highlighted that abdominal ultrasonography, the most commonly recommended surveillance modality, is operator-dependent and has a poor performance in patient subgroups such as those with obesity and NASH 142 . These data have led to an increased interest in blood-based biomarkers and alternative imaging modalities for screening purposes. Although several biomarkers and biomarker panels (for example, GALAD score) have shown promising results in phase II (case–control) biomarker studies, most still require validation in large phase III (cohort) studies 143 , 144 . The only blood-based biomarker currently validated for HCC surveillance is α-fetoprotein 139 . A meta-analysis evaluating surveillance modalities found that the pooled sensitivity of ultrasonography for early HCC detection was significantly increased from 45% when used alone to 63% when combined with α-fetoprotein, albeit with a small decrease in specificity owing to false-positive results with α-fetoprotein 145 . Even though surveillance with CT or MRI likely has increased sensitivity for the early detection of HCC 145 , concerns about radiation, contrast exposure, radiologic capacity and cost limit their widespread implementation. As we await the evaluation of newer surveillance modalities, semi-annual ultrasonography with 13 or without α-fetoprotein 12 remains the recommended surveillance strategy. Given the higher burden of HCC in East Asia, surveillance is typically performed using more intensive protocols — with a combination of ultrasonography, cross-sectional imaging and serum biomarkers.
The ideal surveillance tool should be highly reproducible, not operator dependent (unlike abdominal ultrasonography), have a good accuracy, and easy to implement in different clinical settings. Liquid biopsy is one such tool that fulfils all these requirements. Mutation analysis of circulating tumour DNA (ctDNA) detects tissue mutations in patients at early-stage HCC after resection 146 . Similarly, aberrant ctDNA methylation patterns have been studied as surveillance tools in HCC 146 , 147 , 148 , 149 , 150 , 151 (Box 2 ). The accuracy of these approaches as surveillance tools is currently being investigated.
Box 2 Role of liquid biopsy in HCC
Liquid biopsy refers to the analysis of tumour components, mainly fragments of DNA (circulating tumour DNA; ctDNA), extracellular vesicles (exosomes) or actual tumour cells (circulating tumour cells). The clinical applications of liquid biopsy in oncology include cancer surveillance, early detection of minimal residual disease after curative therapies, prognosis prediction and molecular monitoring of therapeutic response.
Unlike tissue biopsies, liquid biopsy provides an easy access to the molecular information of the tumour. It also enables sequential sampling, which is crucial to implement molecular monitoring of hepatocellular carcinoma (HCC) and to streamline the real-time detection of mechanisms of resistance and tumour clonal composition. Indeed, the FDA has approved the use of ctDNA-based testing to detect mutations in EGFR in patients with lung cancer who are candidates for mutant EGFR therapies.
In HCC, liquid biopsy is being explored as a source to identify novel HCC surveillance tools and to predict the response to systemic therapies. Mutation analysis of ctDNA can detect tissue mutations in patients at early-stage HCC treated with resection 146 . A combined blood-based approach of α-fetoprotein and ctDNA mutation analysis had a 100% sensitivity and 95% specificity for the detection of HCC 149 . However, the positive predictive value of this approach was very low (17%), which could negatively impact the surveillance recall policy.
Methylation analysis of ctDNA has also been shown to detect early HCC in case–control studies across multiple aetiologies 147 , 148 . Evidence shows that VEGFA gene amplifications detected in ctDNA were associated with better outcomes in patients receiving sorafenib 150 .
The limitations of liquid biopsy include a lack of level 1 evidence supporting its role as a source of new biomarkers in HCC, for any clinical application. Furthermore, there is no harmonization on the analytical approaches and data interpretation for liquid biopsy, which has led to inconsistent results when calling DNA mutations in ctDNA using different commercially available methods in patients with prostate cancer 151 .
In our original Primer 1 , we discussed the primary prevention of HCC with vaccines, whereas here we focus on the different emerging prevention strategies. Besides treating the primary cause (for example, viral hepatitis), no intervention proven to prevent HCC development is currently available in patients at high risk. The effective suppression of HBV replication with antivirals and universal HBV vaccination have decreased HCC incidence 152 , 153 . Similarly, the high cure rate of HCV with the new DAA therapy has reduced the incidence of HCC in patients with chronic HCV infection 5 . However, evidence on the impact of alcohol cessation or reversion of NAFLD and the risk of HCC is lacking. Studies have tested different therapies, such as vitamin A, vitamin K and retinol analogues, for HCC chemoprevention. Currently, numerous uncontrolled, retrospective, population-based studies have suggested a role for metformin, statins, coffee and aspirin in HCC prevention 154 , regardless of the aetiology of liver disease. However, statins have been extensively studied for therapeutic repurposing in different indications, with disappointing results in controlled trials showing no evidence for a decreased incidence of HCC. Conversely, reports on aspirin are compelling in terms of HCC prevention, including data from nationwide Swedish registries 14 showing that, after a median follow-up of 8 years, aspirin use reduced the estimated cumulative incidence of HCC from 8% to 4%. Several cohort and case–control studies demonstrated a dose-dependent relationship between coffee consumption and reduced HCC incidence in the general population as well as in patients with chronic liver disease 155 . Based on available data, European Association for the Study of Liver (EASL) guidelines offer a strong recommendation for coffee consumption as a chemoprevention strategy in patients with chronic liver disease 12 . Nevertheless, controlled studies are needed to establish the role of these interventions.
HCC is a unique neoplasm as ~80–90% of cases develop in patients with cirrhosis and, therefore, the application of different therapeutic options might be limited because of the patient’s overall health status. The management of HCC has substantially improved over the past decade. The treatment is assigned according to tumour stages and the expected benefits of major interventions, following the Barcelona Clinic Liver Cancer (BCLC) staging system 12 , 156 , 157 (Fig. 4 ). In principle, patients with early-stage HCC tumours are the preferred candidates for resection, transplantation and local ablation (Fig. 4 ), whereas patients at intermediate stages are first candidates for TACE and those with advanced disease will first receive systemic therapies. These therapies have substantially improved the reported natural history of untreated cases at each of the stages, with median survival times for early, intermediate and advanced HCC of ~36, ~16 and ~6 months, respectively, in patients with well-preserved liver function defined as Child-Pugh A (according to the Child-Pugh score ) and compensated disease 158 , 159 . In order to prevent collateral liver dysfunction, certain therapies (such as resection and systemic therapies) are mostly applied in this patient population.
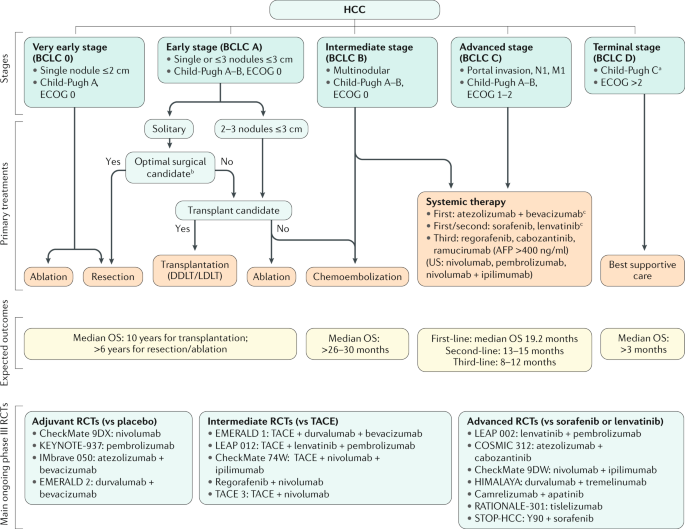
The Barcelona Clinic Liver Cancer (BCLC) staging system consists of five stages depending on disease extension, liver function and performance status. Asymptomatic patients with low tumour burden and good liver function (BCLC 0/A) should be treated with local curative treatments (resection, ablation or transplantation, depending on the presence of portal hypertension, number of nodules and liver function). Asymptomatic patients with multinodular disease and adequate liver function (BCLC B) should receive chemoembolization and patients with portal thrombosis or extrahepatic spread (BCLC C) should be treated with systemic therapies. Ongoing phase III trials in all disease stages are depicted. AFP, α-fetoprotein; DDLT, deceased-donor liver transplantation; ECOG, Eastern Cooperative Oncology Group; HCC, hepatocellular carcinoma; LDLT, living-donor liver transplantation; M1, distant metastasis; N1, lymph node metastasis; OS, overall survival; RCT, randomized controlled trial; TACE, transarterial chemoembolization. a Patients with end-stage liver disease Child-Pugh class C should first be considered for liver transplantation. b Patients with preserved hepatic function Child-Pugh class A with normal bilirubin and no portal hypertension are optimal candidates for hepatic resection. c Sorafenib and lenvatinib are also considered first-line treatment in case of contraindication for atezolizumab + bevacizumab. Adapted with permission from ref. 156 , Wiley.
Surgical interventions
Surgical treatment, which includes both hepatic resection and liver transplantation, has long been the backbone of curative therapies for HCC, yielding the best outcomes, with a 5-year survival of ~70–80% 12 , 13 (Table 2 ; Supplementary Table 1 ). The decision between resection and transplantation requires consideration of the patient’s liver function, the presence and extent of portal hypertension, performance status, and tumour characteristics such as size, number and involvement of the hepatic and portal veins. The local regulations governing the availability and allocation of organs must also be incorporated into the decision-making process. Western guidelines have advocated on the principal of selecting the ideal candidates leading to the best outcomes for surgical resection whilst relegating the non-ideal candidates to other therapies 12 , 13 . However, several studies now challenge this principal based on the fact that resection on suboptimal candidates for surgery might provide similar or even better outcomes than loco-regional therapies. Nonetheless, level 1 evidence supporting this approach of resection for non-ideal candidates is not yet available.
Hepatic resection is considered the treatment of choice in patients with HCC without cirrhosis in whom post-operative hepatic decompensation is not a major concern 12 , 13 , 160 . Of note, however, resection for HCC in non-cirrhotic NAFLD livers is associated with morbidity as high as 20%, similar to that observed in patients with cirrhosis 161 , 162 . In patients with cirrhosis, Western guidelines have restricted resection to those with a single tumour (regardless of size), with well-preserved liver function (Child-Pugh A with total bilirubin <1 mg/dl), the absence of clinically relevant portal hypertension (no varices or ascites) or a hepatic venous pressure gradient (<10 mmHg), as well as with a preserved performance status Eastern Cooperative Oncology Group score (( ECOG score ) 0). Adherence to these selection criteria have resulted in a 5-year survival of ~70% and perioperative mortality of <3% 163 . The Child-Pugh score, model for end-stage liver disease and indocyanine green clearance are the conventionally used tests to assess liver function prior to resection 12 . Currently, several studies have validated the albumin–bilirubin score (ALBI score) to be able to accurately stratify patients for resection with more granularity than the Child-Pugh score 164 , 165 .
Analysis of data from a large prospective registry found that the majority (>60%) of hepatic resections were performed in patients who did not meet the criteria of Western guidelines, either in terms of liver function, performance status or tumour characteristics 166 (Table 2 ). This study showed that the presence of one risk factor did not adversely affect overall survival, although resection in patients with both portal hypertension and elevated bilirubin resulted in a significantly lower survival than in candidates who met the criteria. Other studies have reported that resection in patients with portal hypertension or Child-Pugh B resulted in a 5-year survival of <50% with high morbidity and a perioperative mortality of 4% 167 , 168 . Overall, liver function, portal hypertension and the extent of liver resection directly impact outcome and, therefore, these variables should all be integrated into the selection process 169 . Whether outcomes can be improved with a minimally invasive approach still needs to be confirmed 170 .
Other potential indications for resection that require further study prior to being adopted in the management guidelines are the expansion of criteria to multinodular tumours or segmental vein invasion. One randomized trial and several retrospective studies suggest that expanding the criteria for resection to patients with multiple tumours and well-preserved liver function might lead to better outcomes for resection when compared with TACE 171 . Similarly, resection for HCC invading the segmental branches of the portal vein led to survival outcomes ranging from 29 to 49 months in Western and Japanese series 172 , 173 .
The recurrence of HCC after hepatic resection remains a major obstacle, with recurrence rates as high as 70% at 5 years, even in patients with a single tumour ≤2 cm (ref. 174 ). Recurrences can be divided into either early (<2 years), resulting from micrometastases following resection, or late (>2 years), resulting from de novo tumours arising in a microenvironment predisposed to carcinogenesis 175 . Modifications of surgical technique, such as the anatomical approach , as well as non-anatomical resection with a margin of 2 cm, have shown varying degrees of success in reducing recurrence 176 , 177 . Neoadjuvant treatment with embolization as well as adjuvant administration of retinoids, adoptive immunotherapy and 131 I-lipiodol embolization have all been tested unsuccessfully 178 , 179 . Additionally, the STORM trial randomizing patients to sorafenib versus placebo after resection or ablation showed no benefit in recurrence-free survival 180 . A decrease in late recurrence after resection has been reported with the use of antiviral agents for HBV in uncontrolled investigations 181 . Similarly, DAA therapy in patients with HCV cirrhosis and a history of treated HCC has been shown to be safe and likely beneficial, with improved overall survival in a meta-analyses 182 , 183 , thus not confirming preliminary discouraging results 184 . Current data suggest that treatment of HCC recurrence with resection, salvage transplantation , ablation, TACE and systemic therapies achieves outcomes close to those achieved in primary HCC 185 . Finally, pre-emptive liver transplantation has been proposed for patients with high risk of recurrence (that is, those with microvascular invasion) 186 .
Liver transplantation
Patients with cirrhosis and a limited tumour burden (the Milan Criteria — single tumour ≤5 cm or 2–3 tumours ≤3 cm without vascular invasion) are considered for liver transplantation 187 . The outcomes have been excellent, with a 5-year and a 10-year survival of 70% and 50%, respectively, and recurrence rates of 10–15% at 5 years 16 (Table 2 ; Supplementary Table 1 ). Long-term outcomes of liver transplantation are considered superior than resection, which has a 70% recurrence rate and a 10-year survival of 7–15% 188 . However, transplantation is plagued by organ shortage with prolonged waiting times, leading to patient dropout from the waiting list because of tumour progression. The probability of a cure via resection becomes similar to liver transplantation when drop-out rates exceed 20% 189 , 190 .
The use of extended criteria for liver transplantation has been an active area of investigation. Some proposed measures, such as the University of California San Francisco (UCSF) criteria, Up-to-Seven criteria, total tumour volume and α-fetoprotein criteria, and the Milan and α-fetoprotein model have been validated in studies 191 , 192 , 193 . Among these, only the UCSF criteria have been adopted as an upper limit of tumour burden for down-staging to Milan criteria for liver transplantation by the American Association for the Study of Liver Diseases (AASLD) guidelines 13 . Other retrospective and non-validated studies involving ~2,000 patients transplanted for a single tumour ≤6 cm or 2–3 tumours ≤5 cm demonstrated a 10-year survival rate similar to the Milan criteria 194 , 195 . Overall, the ‘Metroticket’ concept clarifies that an ideal cut-off value is difficult to establish owing to a continuous spectrum of outcomes that are incrementally correlated based on tumour size, number and α-fetoprotein levels 193 , 196 . Another approach to expand the transplantation criteria is based on the biological behaviour of a tumour, determined by a combination α-fetoprotein level and 18 F-fluorodeoxyglucose uptake on PET scans 197 . Nevertheless, transplantation of HCC beyond the Milan criteria remains experimental except in cases where the tumour has been successfully down-staged to within the criteria.
Studies have explored neoadjuvant therapies, such as TACE or ablation, to prevent tumour progression while on the waiting list (bridging therapy) or to reduce tumour burden to within the Milan criteria (down-staging). A response to neoadjuvant therapies reduces dropout from the waiting list as well as the risk of post-transplant recurrence 198 , 199 . A multicentre analysis involving ~2,500 patients demonstrated a 10-year survival of 52% in patients successfully down-staged to Milan criteria 16 . The response to neoadjuvant therapy assessed by the modified Response Evaluation Criteria In Solid Tumours (mRECIST) has been proposed as a criterion for selecting patients for transplantation and as predictor of death after liver transplantation 200 . Similarly, a response (evident by a decrease in α-fetoprotein levels) while on the waiting list has been shown to correlate with recurrence-free survival after transplantation 201 . However, these models need further validation before they can be incorporated into guidelines.
The scarcity of cadaveric organs has led to long waiting times for transplantation, resulting in dropout owing to tumour progression; the use of marginal donors (donors >60 years of age, those with diabetes, BMI >35 kg/m 2 or severe graft steatosis) and of living donors has been advocated to expand the access to transplantation. However, some notes of caution have been raised. Although the use of living donors yields similar survival rates as using deceased donors, some studies reported higher recurrence rates with the former despite adjustment for tumour characteristics (mostly size and number) 202 . This high recurrence may potentially be explained by the fact that a shorter waiting time with living donors prevents the identification of molecularly aggressive HCCs, which are prone to dropout with longer waiting times 203 . In this regard, genomic studies have identified the proliferative–progenitor subclass of HCC, characterized by an aggressive phenotype and high α-fetoprotein levels, to be associated with high recurrence rates after liver transplantation 203 . As patients with HCC listed for liver transplantation often have better liver function than those listed for hepatic decompensation, the preferential use of marginal organs has been proposed for patients with HCC. Nonetheless, studies have shown that the use of marginal donors is linked with a significantly higher risk of HCC recurrence 198 , 199 .
The 10-year recurrence rate after transplantation is 10–15% for HCC tumours within Milan criteria and 20% in those down-staged to the Milan criteria 16 . So far, no adjuvant treatment has been shown to prevent recurrence after liver transplantation. An RCT exploring sirolimus-based immunosuppression versus standard immunosuppression revealed no difference in overall survival or recurrence-free survival 204 . In summary, selection based on Milan criteria leads to low recurrence rates, which so far have not been able to further decrease with molecular therapies.
Image-guided ablation
Image-guided ablation is accepted as a potentially curative therapy for small, early-stage HCC tumours 12 , 205 . In principle, there are two indications for these therapies according to guidelines, either as first choice therapy for single, very early tumours <2 cm or as an alternative to surgery in early-stage single tumours, generally up to 4 cm, or 2–3 tumours ≤3 cm (refs 12 , 205 ) (Fig. 4 ). The latter patients are unsuitable for resection due to liver dysfunction or tumour multi-nodularity and additionally present with formal contraindications for liver transplantation. Ablation is used to direct injury to the tumour and is achieved via chemical, thermal or electrical methods 15 . Historically, percutaneous ethanol injection is the seminal technique for local ablation and is still recommended for tumours <2 cm, especially when located in the proximity of major vessels or bile ducts. Currently, radiofrequency ablation (RFA) is the established thermal technology along with microwave ablation (MWA), whereas other ablative techniques, such as cryoablation (CRA) and laser interstitial thermotherapy, are less used 15 . Irreversible electroporation (IRE) achieves tumour destruction by inducing electrical damage to the tumour cells without a significant thermal component.
Assessment of response
Identifying patients who respond to image-guided ablation as well as to loco-regional and systemic therapies is essential to guide appropriate management of these patients. RECIST is the standard imaging approach in oncology, but this approach has several limitations in the assessment of treatment response of HCC. Consequently, several groups have proposed the mRECIST for HCC, aimed at capturing differences in the viable tumour (that is, non-necrotic tissue) as opposed to differences in absolute tumour shrinkage 206 , 207 . These criteria have been recently refined and their performance reviewed elsewhere 208 . Overall, mRECIST identifies 2–3-fold more responders than standard RECIST in patients receiving loco-regional treatments as well as in those receiving systemic therapies 21 , 209 . Similarly, overall response rates (ORRs) assessed by mRECIST have been associated with better survival in patients receiving local therapies and systemic therapies 208 , 209 , 210 , 211 .
Radiofrequency ablation
RFA is the most used technique for local ablation and several RCTs have demonstrated the superiority of RFA to percutaneous ethanol injection in objective response rates and overall survival 212 , 213 , 214 as well as similar survival rates when compared with surgical resection in appropriately selected patients 215 , 216 , 217 , 218 (Table 2 ; Supplementary Table 1 ). Thus, AASLD and EASL guidelines have adopted RFA as the front-line primary treatment for single tumours <2 cm and as an alternative for surgery in early-stage single tumours 3–4 cm or 2–3 tumours <3 cm (refs 12 , 205 ). The main predictor of treatment failure is tumour size. When RFA is used as first-line therapy for early-stage HCC, complete response rates by mRECIST range from 70% to 90% 219 , 220 and is significantly associated with better overall survival 220 . In addition, studies have reported a median overall survival of ~60 months and a 5-year recurrence rate of 50–70% with RFA 12 , 205 , 221 .
Microwave ablation
MWA has the advantage of achieving a larger ablation zone than RFA as several needles can be used at simultaneously 15 . Several trials comparing RFA and MWA reported no differences in the primary endpoint or in local tumour progression at 2 years 222 . Similarly, three meta-analyses comparing percutaneous MWA and RFA showed a similar efficacy between the two percutaneous techniques 223 , 224 , with a trend towards greater efficacy but higher complication rates in tumours >3 cm treated with MWA compared with treatment with RFA 225 . The lack of phase III data led to the proposal of this treatment in early-stage HCC with only a low level of evidence 12 . Overall, MWA is easy to deliver and is widely used in clinical practice, although no evidence of superiority to RFA is available.
Other ablative techniques
Other ablative techniques have been the subject of limited research so far. Combining RFA with TACE or lyso-thermosensitive liposomal doxorubicin has not improved outcomes compared with RFA alone 226 , 227 . A multicentre randomized trial comparing RFA and CRA reported no differences in overall survival and tumour-free survival 228 , whereas a large retrospective study showed a significant advantage for CRA in liver cancer-specific survival compared with RFA 229 . IRE is a mostly non-thermal technology with the theoretical advantage that it avoids unnecessary thermal damage to critical structures; however, this advantage is counterbalanced by the complexity of multiprobe technology requiring general anaesthesia. Preliminary results from small series have shown early signals of efficacy with IRE 224 and laser ablation 230 . Nevertheless, these techniques are not yet ready for recommendation in conventional clinical practice 15 .
Radiotherapy
External beam radiation therapy can achieve radiological responses in HCC tumours across a range of sizes and stages within the liver as well as palliation of extrahepatic metastases. In HCC tumours confined to the liver, prospective studies of stereotactic body radiation therapy with photons or protons show high rates of radiological responses with acceptable safety in predominantly Child-Pugh A populations, although these findings are limited by uncontrolled study designs 231 , 232 . A pooled analysis examined the outcomes of 102 patients with unresectable HCC and Child-Pugh A liver function treated with photon stereotactic body radiation therapy from 24 to 54 Gy over six fractions and reported objective responses in 54% of patients and a median overall survival of 17 months 231 . Other smaller uncontrolled studies have reported better outcomes in this population 232 as well as in HCC lesions with tumour macrovascular invasion 233 , 234 .
Most studies comparing radiotherapy with other locoregional therapies in HCC are retrospective in nature and are limited due to selection bias and population heterogeneity 235 , 236 . The randomized phase III APROH trial comparing proton beam radiotherapy to RFA under a non-inferiority design, involving 144 patients with small HCC tumours (that is, up to 2 tumours <3 cm) and well-preserved liver function, met the pre-specified target for non-inferiority in the per-protocol population, with a hazard ratio of 0.52 (95% CI 0.26–1.05) for 2-year liver progression-free survival (PFS) 237 .
Collectively, these studies support a potential role for radiotherapy in selected patients, particularly those with small tumours not amenable to resection or transplantation. Additional randomized studies with longer follow-up and pooled analyses are required to confirm whether these approaches are similar to RFA and to define the optimal radiation modality. Studies combining palliative radiotherapy with immunotherapy in advanced HCC are under way.
Transarterial therapies
Two RCTs and a subsequent meta-analysis involving patients with intermediate-stage HCC have demonstrated survival benefits with TACE compared with suboptimal therapies, including tamoxifen or best supportive care (that is, management of pain and nutritional and psychological support) 17 , 238 , 239 . As a result of these studies, TACE has been globally adopted as standard of care for patients with intermediate-stage HCC 12 , 205 , 240 . Overall, the median survival ranges from 19.4 months in uncontrolled investigations 241 and up to 37 months in RCTs 242 , 243 , 244 , 245 , with an estimated average of median overall survival of ~30 months 15 (Table 3 ; Supplementary Table 1 ). Large case-series assessing the safety of conventional TACE reported a treatment-related mortality of 0.6% 241 . Over the past few years, the introduction of drug-eluting bead TACE has offered an alternative to conventional lipiodol TACE. Drug-eluting bead TACE has been associated with a reduction in systemic drug exposure and drug-related adverse events 246 , 247 , albeit with similar outcomes to conventional TACE, except for a median survival of >45 months in single-arm studies 248 . TACE is usually indicated by physicians on demand according to radiological response, generally assessed according to mRECIST 206 , 208 . Indeed, according to a large meta-analysis, response to mRECIST was associated with better survival (HR 0.39, 95% CI 0.26–0.61) 249 . However, combinations of TACE and TKIs have so far failed to provide beneficial clinical outcomes 243 , 250 , 251 , 252 , 253 , 254 .
TARE is a procedure involving the intra-arterial delivery of glass microspheres or resin microspheres embedded with yttrium. Uncontrolled studies and small RCTs in highly selected centres have reported results similar to TACE for the treatment of intermediate-stage HCC or even better outcomes in terms of time to progression 18 , 255 , 256 . The AASLD guidelines recommend TARE to patients with intermediate-stage HCC with a level 2 evidence 12 , 205 . TARE was explored owing to preliminary encouraging results in patients with portal vein thrombosis 255 , 257 but three consecutive RCTs comparing TARE with sorafenib in advanced-stage HCC failed to meet the primary endpoint of superior overall survival 258 , 259 , 260 . Consequently, guidelines have adopted a negative recommendation for this indication 12 , 205 , 240 .
Systemic therapies
The benchmark for clinical trial design in HCC is the SHARP study 20 , which established the selection criteria and stratification factors, such as the use of the BCLC staging system, Child-Pugh A liver function and performance status (ECOG 0 or 1), all of which form the basis for future phase III trials investigating advanced-stage HCC. Several studies over the past decade have established other prognostic factors that led to modifications in study designs. These modifications include the separation of extrahepatic spread and macrovascular invasion, the importance of elevated α-fetoprotein levels, and the incorporation of mRECIST assessments 156 .
First-line therapies
In patients with advanced-stage HCC, the SHARP trial demonstrated the superiority of sorafenib to placebo (overall survival, 10.7 months versus 7.9 months), which represented a breakthrough in HCC management (Table 4 ). Sorafenib was the only available standard of care for advanced HCC for a decade. A further meta-analysis established that sorafenib was more effective in patients with HCV-associated HCC and liver-only disease (that is, without metastases) than in those with HCC from non-HCV causes or in patients with extrahepatic disease 261 . Since the approval of sorafenib in 2007, several new effective drugs have been established as second-line treatment after progression on sorafenib as have more effective drugs in the first-line setting (Fig. 5 ).
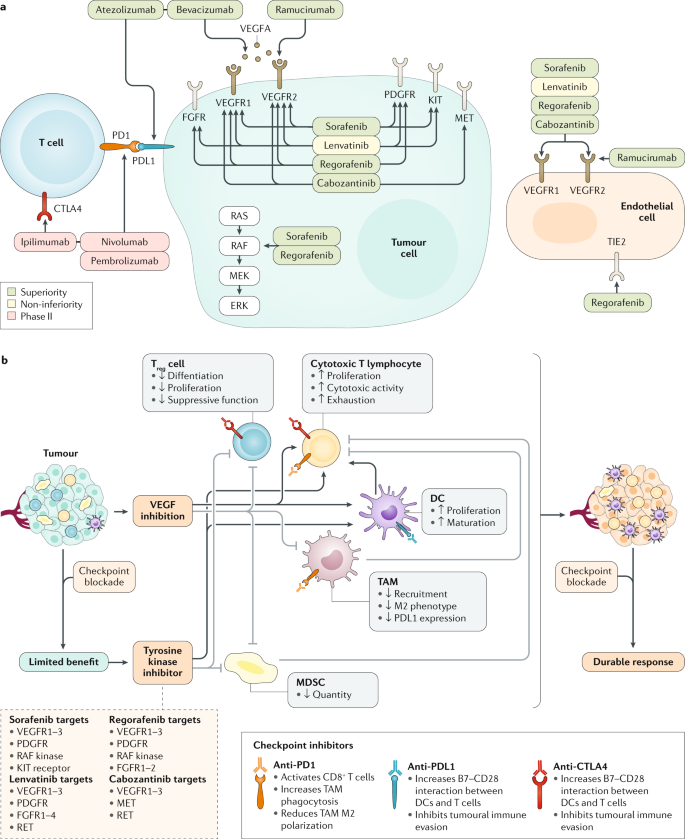
a | The mechanisms of action of targeted therapies approved based on phase III data. Green boxes indicate positive results based on phase III trials with a superiority design, in the first-line setting compared with placebo (versus sorafenib) or sorafenib (versus atezolizumab plus bevacizumab) or in the second-line setting compared with placebo (versus regorafenib, cabozantinib and ramucirumab). Yellow boxes indicate positive results based on phase III trials with a non-inferiority design (lenvatinib). Red boxes indicate other FDA-approved drugs based on non-randomized phase II trials (nivolumab, pembrolizumab and nivolumab plus ipilimumab). b | Mechanisms of action of the combination of molecular and immune targeted therapies. Checkpoint blockade monotherapies benefit a small subset of patients (~15–20%). Combining tyrosine kinase inhibitors or VEGF inhibitors with immune-checkpoint inhibitors can modulate the immune microenvironment by enhancing both dendritic cells (DCs) and cytotoxic T lymphocytes and inhibiting tumour-associated macrophages (TAMs), regulatory T (T reg ) cells and myeloid-derived suppressor cells (MDSCs), thereby creating a more inflamed microenvironment and favouring the development of more effective and durable responses to checkpoint inhibitors. Data from refs 1 , 8 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 263 , 264 . Part a adapted from ref. 8 , Springer Nature Limited. Part b adapted from ref. 15 , Springer Nature Limited.
A global open label randomized phase III study (REFLECT) demonstrated the efficacy of lenvatinib, which was the first new drug approved for advanced-stage HCC in the first-line setting in over 10 years 21 . The REFLECT study excluded patients with extrahepatic main portal vein invasion or in whom >50% of the liver was involved. The primary endpoint of the study was overall survival and was powered for superiority and non-inferiority, but the trial met only the latter endpoint. The final results established an improved median overall survival for lenvatinib (13.6 months) compared with sorafenib (12.3 months). In addition, lenvatinib also significantly improved PFS (7.4 months versus 3.7 months; HR 0.66, 95% CI 0.57–0.77; P < 0.001) and ORR (24.1% versus 9.2%; OR 3.13, 95% CI 2.15–4.56; P < 0.0001) compared with sorafenib according to mRECIST (Table 4 ). Unlike sorafenib, lenvatinib is a small molecular type V TKI, with more potent activity against VEGF receptors and the FGFR family. In this regard, the side effect profiles are different, with higher grade hypertension and proteinuria occurring with lenvatinib and increased hand–foot skin reaction occurring with sorafenib; both drugs are associated with asthenia, anorexia, diarrhoea and weight loss. Overall, both treatments are associated with grade 3–4 drug-related adverse events in ~50% of the treated patients, resulting in a ~15% withdrawal rate (Table 4 ).
The combination of atezolizumab (anti-PDL1 antibody) and bevacizumab (anti-VEGF antibody) was the first regimen to improve overall survival compared with sorafenib 19 , 262 . The IMbrave150 trial, an open-label study that randomized patients to sorafenib or to a combination of atezolizumab and bevacizumab as first-line therapy for advanced HCC, demonstrated an improvement in overall survival with the combination therapy. An updated analysis published as a conference abstract shows the median survival of patients receiving sorafenib was 13.4 months and the median survival of the combination arm was 19.2 months. PFS was improved from 4.3 months in the sorafenib arm to 6.8 months in the combination arm and RECIST ORR was increased from 11% in the sorafenib arm to 30% in the combination arm, and the median duration of response for the combination arm was 18.1 months by RECIST 1.1 and 16.3 months by mRECIST 19 , 262 (Table 4 ). Patient-reported outcomes were also favourable for the combination arm, with the median time to deterioration of quality of life being 11.2 months compared with 3.6 months for sorafenib. Tolerability was more favourable in the combination group compared with sorafenib, with the most common side effects being hypertension, proteinuria and low-grade diarrhoea. The autoimmune events that occurred with atezolizumab were reported as manageable. Upper-gastrointestinal endoscopies were required within 6 months prior to enrolment for the treatment of varices in all patients to mitigate the risk of bleeding associated with bevacizumab. This concept represents a change in practice, especially for the screening of patients in first-line therapy, as upper gastrointestinal endoscopies will have to be performed prior to treatment initiation. As a consequence of the positive findings, atezolizumab plus bevacizumab have become the standard of care in first-line therapies for advanced HCC, except in patients with untreated varices or in those with contraindications for VEGF inhibitors or immunotherapy 156 .
Second-line therapies
Currently, based on positive phase III data, three regimens (regorafenib, cabozantinib and ramucirumab) are approved for the treatment of advanced HCC after progression on sorafenib according to guidelines (Table 4 ). In addition, based upon promising phase Ib/II studies, three additional therapies, namely nivolumab, pembrolizumab and nivolumab plus ipilimumab, have been approved by the FDA 25 , 263 , 264 after first-line treatment with sorafenib.
Regorafenib, a multi-kinase inhibitor targeting VEGFR1–3 and other kinases, was the first agent to be approved in the second-line setting upon demonstrating a survival advantage over placebo (10.6 months versus 7.8 months) for patients who tolerated and had documented progression on sorafenib 22 (Table 4 ). The median survival with regorafenib was 10.6 months versus 7.8 months with placebo (HR 0.63, 95% CI 0.50–0.79; P < 0.0001). The median PFS was 3.1 months versus 1.5 months (HR 0.46, 95% CI 0.37–0.56; P < 0.0001) and ORR was 11% and 4% for regorafenib and placebo, respectively. The most common grade 3–4 events were hypertension, hand–foot skin reaction, fatigue and diarrhoea.
Cabozantinib is a multi-kinase inhibitor with unique activity against VEGFR2, AXL and MET. The CELESTIAL trial demonstrated an improvement in the median overall survival for cabozantinib (10.2 months) compared with placebo (8 months; HR 0.76, 95% CI 0.63–0.92; P = 0.0049) and an improvement in median PFS (5.2 months with cabozantinib versus 1.9 months with placebo; HR 0.44, 95% CI 0.36–0.52; P < 0.001) 23 . Both treatment arms had single digit objective response rates. The most common grade 3–4 events were palmar–plantar erythrodysesthesia , hypertension, increased aspartate aminotransferase levels, fatigue and diarrhoea.
Ramucirumab is the only biomarker-guided therapy for HCC. The REACH-2 trial that investigated ramucirumab was enriched for patients with baseline α-fetoprotein levels of ≥400 ng/dl. Ramucirumab demonstrated an improvement in overall survival (8.5 months versus 7.3 months in the placebo group; HR 0.710, 95% CI 0.531–0.949; P = 0.0199) 24 . PFS was increased with ramucirumab compared with placebo (2.8 months versus 1.6 months; HR 0.452, 95% CI 0.339–0.603; P < 0.0001) but the proportion of patients with objective response did not differ significantly between groups. The most common grade 3–4 treatment-related adverse events were hypertension, hyponatraemia and increased aspartate aminotransferase levels. All six regimens tested in phase III trials for advanced HCC with beneficial effects in survival showed an HR of ≤0.6 for PFS in contrast to ~15 randomized negative studies assessing systemic therapies. This observation led to the proposition of this restrictive threshold as a cut-off for assessing PFS-based benefits with molecular therapies highly likely to ultimately capture overall survival differences 156 , 265 . This PFS–HR threshold has been validated in five new RCTs and, as a result, it has been proposed as a primary endpoint for the trial design of studies in advanced HCC 156 .
Based on phase Ib/II data, nivolumab and pembrolizumab (anti-PD1 inhibitors) were approved as single agents and ipilimumab (CTLA4 monoclonal antibody) was approved in combination with nivolumab 263 , 266 . CheckMate 040 assessed nivolumab as monotherapy in 262 patients mostly as second line, demonstrating an ORR of 14% by RECIST with a median duration of response of 17 months (95% CI 6–24) 25 . The median overall survival was 15.6 months and the treatment was generally well tolerated. Similarly, the KEYNOTE-224 trial showed an ORR of 17% (RECIST v1.1) with pembrolizumab and these rates were durable with a median time to progression and progression-free survival of 4.9 months and a median overall survival of 12.9 months 264 . The pembrolizumab-associated adverse effects were tolerable. However, two phase III studies were unable to confirm the findings of these single-arm studies. CheckMate 459, exploring nivolumab versus sorafenib in the first-line setting, reported a median overall survival of 16.4 months for nivolumab and 14.7 months for sorafenib ( P = 0.07) 267 . Similarly, KEYNOTE-240 reported a median survival of 13.9 months for pembrolizumab compared with 10.6 months for placebo ( P = 0.02); however, the results did not hit the pre-specified P value required for statistical significance 26 . Both drugs achieved a durable ORR of 15–18% and remain approved in the USA. An expansion arm in the CheckMate 040 study evaluated the combination of nivolumab plus ipilimumab in patients who progressed on prior sorafenib in a three-arm randomized study involving 148 patients 263 . The combination of nivolumab plus ipilimumab achieved an objective response of 31% with a median duration of response of 17 months and a median overall survival of 23 months. Although the combination regimen induced immune-related toxicities requiring systemic corticoid administration in 51% of cases, the efficacy of outcomes resulted in an accelerated approval by the FDA for second-line therapy. As a result, phase III trials are currently exploring this combination therapy versus either sorafenib or lenvatinib 268 .
Emerging combination regimens
Across tumour types in oncology, new immunotherapy combination strategies are being developed to augment tumour responsiveness to immune-checkpoint inhibition 269 . In HCC, ICIs have shown promising activity when paired with anti-angiogenic agents, other molecularly targeted therapies and complementary ICIs (Fig. 5 ). The VEGF pathway promotes local immune suppression through the inhibition of antigen-presenting cells and effector cells as well as through the activation of suppressive elements, including T reg cells, myeloid-derived suppressor cells and tumour-associated macrophages, providing the rationale for combining ICIs with anti-angiogenic agents 270 . A phase Ib trial of the combination of lenvatinib and pembrolizumab as first-line therapy in 100 unresectable patients with HCC demonstrated durable, objective radiographic responses by mRECIST in 46%, with a median PFS of 9.5 months and a median overall survival of 22 months 108 . The efficacy of this combination has prompted an ongoing phase III trial investigating this combination therapy versus lenvatinib as monotherapy 271 . Based upon the unique immunomodulatory and antiangiogenic profile of cabozantinib, another phase III trial to determine the efficacy of the combination of cabozantinib with atezolizumab compared with sorafenib or cabozantinib alone 272 , is ongoing 273 . A number of trials testing the combinations of a variety of other multi-kinase inhibitors plus ICIs are under way (Fig. 5 ).
The inhibition of complementary, non-redundant immune-checkpoint pathways may augment the proportion of patients achieving anti-tumour immune responses 274 (Fig. 5 ). The addition of a CTLA4 inhibitor to the inhibition of PD1 or PDL1 has shown higher rates of durable responses in multiple tumour types, albeit with higher rates of immune-related toxicity 275 . Phase III trials testing the combination of nivolumab and ipilimumab as front-line therapy 268 are ongoing. A trial tested the combination of durvalumab with tremelimumab in 75 patients with advanced HCC after failure of prior sorafenib 276 . Radiographic responses by RECISTv1.1 occurred in 24% of patients, with a median PFS and overall survival of 2.7 and 18.7 months, respectively. This regimen was tolerable, with a requirement of systemic corticosteroid in 24% of patients. A confirmatory phase III trial of this combination regimen compared with durvalumab or sorafenib as monotherapy 277 has been completed and results are awaited.
An important question in the evaluation of the efficacy of the combination regimen is to understand whether improvements in time-to-event medians and objective response rates are due to synergy and not because of the independent additive effects of two active agents, which can also be achieved by a sequential approach. The depth and the durability of objective radiographic responses may inform this inference 278 . In the absence of head-to-head trials or established biomarkers to guide the choice of therapy, treatment decisions must rely upon the magnitude of benefits, the toxicity profile and drug availability.
Biomarkers of response to systemic therapy
To date, biomarker data to help decision-making and to guide treatment for advanced stages of HCC are limited. An elevated level of serum α-fetoprotein is an established biomarker of poor prognosis across all stages of HCC and is associated with tumour VEGF pathway activation 279 , 280 . Pre-treatment serum levels of α-fetoprotein became the first biomarker predictive of response, with the finding of a survival benefit of ramucirumab over placebo only in patients with α-fetoprotein levels ≥400 ng/ml (ref. 24 ). Thus, ramucirumab is only indicated when α-fetoprotein levels are beyond this cut-off value. However, unlike ramucirumab, the treatment benefits from multi-kinase inhibitors, including sorafenib, lenvatinib, regorafenib and cabozantinib, occur across a range of baseline α-fetoprotein values, likely owing to a broader spectrum of target inhibition 22 , 23 , 245 , 261 . In patients with elevated α-fetoprotein levels at baseline, changes in α-fetoprotein levels on treatment were shown to correlate with clinical outcomes on systemic therapy, with declining α-fetoprotein levels linked to prolonged PFS and overall survival and increasing α-fetoprotein levels associated with tumour progression 245 , 280 . Nevertheless, additional studies of α-fetoprotein kinetics are required.
Few studies evaluating TKIs in HCC have reported on the biomarkers associated to response 281 , 282 . A variety of candidate biomarkers of benefit from immune-checkpoint inhibition are under investigation across different solid tumours, including HCC. A meta-analysis of outcomes from >3,500 patients showed that tumour PDL1 expression is associated with a worse prognosis in HCC, including a poorly differentiated histology, high levels of α-fetoprotein and shorter overall survival 283 . Non-randomized studies of nivolumab and pembrolizumab suggest higher rates of radiographic response 25 , 264 and prolonged PFS 264 in patients with positive tumour or combined tumour and non-tumour PDL1 expression scores, although interpretation is limited owing to assay heterogeneity and small sample sizes. Analyses of PDL1 expression and its association with survival endpoints are awaited from RCTs of ICIs in monotherapy as well as in combination regimens. Tumour lymphocytic infiltration 53 , immune class gene signature 71 and CTNNB1 mutation status 73 in subsets of HCC tumours also warrant examination for predictive value in patients treated with ICIs.
Proof-of-concept studies in HCC based on trial enrichment for biomarkers have shown distinct results. Early clinical trials demonstrated that enriching patients with advanced HCC with immunopositivity for FGF19 (a known oncogene in HCC) led to a significant ORR of 16% (versus 0% in patients with no immunoreactivity) when treated with FGFR4 inhibitors 284 . Conversely, other trials enriching patients for RAS mutations 285 or MET 286 immunoreactivity have resulted in negative outcomes.
COVID-19 infection and HCC
There is no definitive data on the impact of COVID-19 (a disease caused by the SARS-CoV-2 coronavirus that causes fever, shortness of breath and, in rare cases, acute respiratory distress) in patients with HCC. The known indirect impacts relate to the large numbers of patients with COVID-19 requiring hospitalization and critical care, which has diverted the resources away from patients with HCC. This diversion will likely result in a second wave of patients with other ailments requiring health-care services at an increased rate once the pandemic wave settles and social restrictions are de-escalated 287 . A survey from the American Cancer Society found that 50% of patients with cancer reported an impact to their cancer care, including delays in therapy. Further, over one-third of patients expressed concern about their ability to afford cancer-related care given the repercussions of the COVID-19 pandemic on the job market 288 . In 15–54% of patients with COVID-19, an elevation of transaminases has been observed 289 ; however, the long-term impact of elevated transaminases in HCC outcomes is currently unknown. In addition, considering the potential role of immune derangement in the pathophysiology of COVID-19, the effect of immune-based therapies in the course or outcomes of patients with HCC with COVID-19 is unclear. To address these issues, the International Liver Cancer Association has developed a guidance document to help adapt the clinical management of patients with HCC during this unprecedented time 290 .
Quality of life
Quality of life is becoming a major endpoint in oncology research. Improvements in quality of life are captured by changes in patient-reported outcomes, which result from clinical benefits from treatments and from the impact of adverse events and tolerability of potentially toxic drugs. A longstanding challenge to systemic therapy in advanced HCC has been the limited tolerability to treatment, owing in part to adverse events from the treatments themselves and in part to symptomatic comorbidity from the underlying liver disease, which, in turn, is confounded by the increasing tumour burden. In the pivotal clinical trials investigating multi-kinase inhibitors such as sorafenib, lenvatinib or regorafenib, the rate of treatment-related adverse events of grade ≥3 generally exceeded 50% 20 , 21 , 22 , 291 . However, dose reductions to delay treatment-related adverse events are prevalent but may interfere with efficacy.
Treatment-related adverse events
The advent of immune-checkpoint inhibition for advanced HCC has expanded the treatment landscape to include ICIs as monotherapy as well as in combination 19 , 25 , 26 . Beyond the potential for deep and durable immune responses with immune-targeted therapies in subsets of patients, ICIs have also shown favourable adverse event profiles in comparison to standard therapies such as sorafenib. In phase III RCTs of ICIs as monotherapy in HCC, the rates of grade 3–4 treatment-related adverse events ranged from 18.2% to 22% 26 , 267 for single agents and 37% for combination regimens 19 . Although the adverse event profiles are favourable overall, immune-related toxicity can occur in any organ system, ranging from mild and manageable events such as rash, joint aches or hypothyroidism, to severe and potentially life-threatening events such as pneumonitis, enterocolitis or myocarditis 292 . Immune-related adverse events of any grade occur in ~27% of patients treated with drugs targeting PD1 or PDL1, with adverse events of grade ≥3 occurring in 6% of cases 292 . Systemic corticosteroids for the management of immune-related toxicity were required in 8.2% of patients treated with pembrolizumab as monotherapy in an RCT but in up to 50% of patients receiving nivolumab plus ipilimumab 263 . The generally favourable safety profile of ICIs has enabled their combination with other agents, as discussed in prior sections, with varying degrees and types of additive toxicity 19 , 263 . The toxicity associated with various new ICI combinations may impact the choice of therapy for individual patients.
Health-related quality of life
Beyond treatment-related adverse events, comorbidity from the underlying liver disease also impacts the quality of life in patients with advanced HCC. Owing to the complex relationship between tumour burden and underlying liver function, HCC-specific health-related quality of life (HRQOL) assessments are necessary in clinical management as well as in assessing the safety and efficacy of new therapies 19 , 20 , 22 , 293 (Table 5 ; Supplementary Table 2 ). The most common instruments used to assess HRQOL in patients with HCC are the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire Core-30 (EORTC QLQ-C30 and its HCC-specific module, the EORTC QLQ-HCC18 (ref. 294 )), the Functional Assessment of Cancer Therapy-Hepatobiliary (FACT-Hep) survey and its derivative the FACT Hepatobiliary Symptom Index (FHSI8) 295 . Patients with HCC report significantly lower physical well-being and lower overall HRQOL than the general population, patients with chronic liver disease and patients with other cancers 296 . The most commonly reported symptoms driving HRQOL were fatigue, pain, insomnia, anorexia and weight loss, and sexual dysfunction. Poor HRQOL seems to be driven by a combination of liver-related and tumour-related factors, with worse Child-Pugh class and increased tumour burden being independently associated with lower HRQOL scores. Emerging data suggest that HRQOL, particularly role functioning (involvement in life situations involving family, partner relationship, work or household chores), may be independently associated with survival in patients with advanced HCC 297 .
HRQOL assessments are now incorporated into most HCC RCTs as a secondary endpoint. In the phase III trial of nivolumab versus sorafenib, HRQOL assessments using the FACT-Hep survey showed substantially higher scores for HRQOL in the nivolumab arm than in the sorafenib arm, extending for >100 weeks on treatment and with at least 70% instrument completion rate at all time points 267 . Similarly, the RCT of atezolizumab plus bevacizumab in advanced HCC also showed substantial prolongation in time to deterioration in quality of life, physical functioning and role functioning using the EORTC QLQ-C30 instrument for the combination regimen compared with sorafenib 19 (Supplementary Table 2 ). The HRQOL outcomes from these trials reinforce the favourable benefit-to-risk ratio for immune-checkpoint inhibition in advanced HCC and establish the utility of patient-reported outcomes in HCC clinical trials.
HCC is one of the few malignancies where the major risk factors have been delineated. Although vaccinations and anti-viral therapies have dramatically reduced HCC occurrence, its incidence is steadily growing as a result of other aetiological factors, such as alcohol abuse and NASH, especially in the West 41 . Strategies aimed at decreasing the risk factors of NASH might also decrease HCC incidence in the future. Enhanced surveillance methods for patients at risk might facilitate the identification of more patients with curative stage disease. New serum biomarkers or ctDNA have the potential to replace imaging as a screening modality or even as a diagnostic modality in the future 143 , 149 . With these advancements, in the future, more patients are likely to present with early-stage disease that is more amenable to curative approaches. In addition, even those that present beyond resection or transplant criteria may have better preserved liver function, which will allow the sequential use of numerous lines of systemic anti-cancer therapies leading to improvements in survival.
The marked survival benefit of atezolizumab plus bevacizumab has validated the use of combination therapies as an approach to improving outcomes in patients. More specifically, targeting angiogenesis has proven to be a specifically important part of HCC management. The importance of targeting angiogenesis was emphasized with ramucirumab, which demonstrated survival advantages in second-line treatment for advanced HCC. Nonetheless, the effect of bevacizumab plus atezolizumab goes beyond the expected anti-VEGF effect, particularly to expand the target population to anti-PDL1 responders. The effects of such combination have been reviewed elsewere 298 , 299 . In summary, besides normalizing angiogenesis, VEGF inhibitors have been shown to suppress T reg cells, myeloid-derived suppressor cells, and tumour-associated macrophages and to increase cytotoxic T cell activity as well as the maturation of dendritic cells. Overall, these effects might enable the switching of cold tumours into hot tumours, thereby allowing an additional effect of ICIs. A similar mechanism has been identified with TKIs 300 , where oncogene-mediated T cell exclusion can be reverted by blocking, for instance, CDK4 or CDK6 or MAPK signalling, resulting in dendritic cell activation, T cell infiltration, increased tumour antigen presentation and increased IFNγ sensitivity.
Numerous ongoing phase III trials exploring combinations of TKIs (lenvatinib, cabozantinib and apatinib) and ICIs and combinations of CTLA4 inhibitors (ipilimumab and tremelimumab) and other ICIs are currently ongoing. In the latter of the two combination regimens, a major role in priming and peripheral activation of the immune system is expected 301 . The next big challenge in the field is to identify the novel combination regimens for a continued improvement in overall survival in the front-line setting. With a high bar now set with a HR 0.66 (for overall survival with bevacizumab plus atezolizumab versus sorafenib) and a median overall survival of 19.2 months 19 , 262 , there is no obvious combination partner. The next several years will incorporate the testing of new agents in clinical trials, which will be rationally designed based on basic science and will simultaneously drive future research.
Our understanding of the molecular pathogenesis and heterogeneity of the disease has also advanced, although this knowledge is yet to influence clinical practice or trial design. Developing data linking molecular subtypes with therapeutic interventions will bridge this gap. As technology evolves, the increasing ability to classify tumours using liquid biopsies or other techniques will serve as a platform for incorporating our molecular understanding of the disease into treatment decisions. These data will also help delineate the mechanisms of resistance to current therapies and lead to personalized medicine tailored to individual patient needs. Ultimately, translating tumour biology into the clinic will continue to improve patient outcomes.
Currently, image-based diagnoses are being challenged because of the need for a more profound molecular understanding of the disease. In this regard, a standardized routine for collecting tumour biopsies in clinical practice is emerging and recommended 8 , 15 . The therapeutic armamentarium of HCC has been growing, including improvements in ablation techniques, loco-regional therapies and systemic therapies 8 , 15 . As is typical in cancer medicine, once agents have shown efficacy in the advanced setting, they are shifted into earlier stages of the disease, where survival benefits can be amplified. Unfortunately, sorafenib failed to improve outcomes in the adjuvant 180 and intermediate-stage settings 250 . Now, phase III trials with newer immunotherapy agents (alone or in combination) in the adjuvant setting after curative resection or ablation and in combination with locoregional therapies are ongoing (Fig. 4 ). Shifting these agents into earlier lines of therapy and for patients with earlier disease stages holds the promise of curative treatment for more patients. In addition, the pursuit of biomarkers for assessing response to therapy is ongoing. Although single agent PD1 inhibitors are very active in ~15–20% of patients, this activity was not sufficient to improve survival in randomized studies. The ability to select patients most likely to benefit from a given regimen providing long-lasting responses would be of great value and ongoing translational studies will hopefully offer answers, including an elucidation of the mechanisms of resistance 71 , 73 . The capacity of combinations of ICIs with TKIs or VEGF inhibitors to switch cold tumours into hot tumours 299 , 300 (Fig. 5 ) has already resulted in nearly doubled response rates and survival benefits compared with single agents 108 (Fig. 4 ). With the advent of atezolizumab plus bevacizumab demonstrating significant survival benefits over sorafenib, two major questions emerge: whether other combination regimens will be equally efficacious or improve the survival mark currently established in advanced HCC, and whether the current combination regimen and other regimens reaching ≥30% objective responses can improve outcomes at earlier disease stages. Although vaccine-related therapeutic strategies have not yet yielded significant clinical activity, there is growing interest in cell-based strategies such as chimeric antigen receptor T cell therapy, which is now being studied in early-stage HCC based on its approval in haematologic cancers 302 . Novel antibody targets are being pursued with both naked antibodies and antibody–drug conjugates to novel epitopes unique to HCC. Overall, we envision major advancements in the management of all stages of the disease based on current investigations in the next 5 years.
Change history
12 february 2024.
A Correction to this paper has been published: https://doi.org/10.1038/s41572-024-00500-6
Llovet, J. M. et al. Hepatocellular carcinoma. Nat. Rev. Dis. Prim. 2 , 16018 (2016).
PubMed Google Scholar
Villanueva, A. Hepatocellular carcinoma. N. Engl. J. Med. 380 , 1450–1462 (2019).
CAS PubMed Google Scholar
International Agency for Research on Cancer. GLOBOCAN 2018. IARC https://gco.iarc.fr/today/online-analysis-map?v=2020&mode=population&mode_population=continents&population=900&populations=900&key=asr&sex=0&cancer=11&type=0&statistic=5&prevalence=0&population_groupearth&color_palette=default&map_scale=quantile&map_nb_colors=5&continent=0&rotate=%255B10%252C0%255D (2020).
Akinyemiju, T. et al. The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level. JAMA Oncol. 3 , 1683 (2017).
PubMed PubMed Central Google Scholar
Kanwal, F. et al. Risk of hepatocellular cancer in HCV patients treated with direct-acting antiviral agents. Gastroenterology 153 , 996–1005.e1 (2017).
Estes, C., Razavi, H., Loomba, R., Younossi, Z. & Sanyal, A. J. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology 67 , 123–133 (2018).
Schulze, K. et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 47 , 505–511 (2015). A comprehensive genomic study conducted in HCC describing the landscape of mutations and mutational signatures .
CAS PubMed PubMed Central Google Scholar
Llovet, J. M., Montal, R., Sia, D. & Finn, R. S. Molecular therapies and precision medicine for hepatocellular carcinoma. Nat. Rev. Clin. Oncol. 15 , 599–616 (2018).
Zucman-Rossi, J., Villanueva, A., Nault, J.-C. & Llovet, J. M. Genetic landscape and biomarkers of hepatocellular carcinoma. Gastroenterology 149 , 1226–1239.e4 (2015).
Anstee, Q. M., Reeves, H. L., Kotsiliti, E., Govaere, O. & Heikenwalder, M. From NASH to HCC: current concepts and future challenges. Nat. Rev. Gastroenterol. Hepatol. 16 , 411–428 (2019).
Friedman, S. L., Neuschwander-Tetri, B. A., Rinella, M. & Sanyal, A. J. Mechanisms of NAFLD development and therapeutic strategies. Nat. Med. 24 , 908–922 (2018).
European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J. Hepatol. 69 , 182–236 (2018).
Google Scholar
Marrero, J. A. et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology 68 , 723–750 (2018).
Simon, T. G. et al. Association of aspirin with hepatocellular carcinoma and liver-related mortality. N. Engl. J. Med. 382 , 1018–1028 (2020).
Llovet, J. M. et al. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma. Nat. Rev. Gastroenterol. Hepatol. https://doi.org/10.1038/s41575-020-00395-0 (2020).
Tabrizian, P. et al. A US multicenter analysis of 2529 HCC patients undergoing liver transplantation: 10-year outcome assessing the role of down-staging to within Milan criteria [abstract 15]. Hepatology 70 , 10–11 (2019).
Llovet, J. & Bruix, J. Systematic review of randomized trials for unresectable hepatocellular carcinoma: chemoembolization improves survival. Hepatology 37 , 429–442 (2003). This paper is a meta-analysis of randomized studies providing the rationale to use transarterial chemoembolization in intermediate HCC as standard of care .
Salem, R. et al. Y90 radioembolization significantly prolongs time to progression compared with chemoembolization in patients with hepatocellular carcinoma. Gastroenterology 151 , 1155–1163.e2 (2016).
Finn, R. S. et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N. Engl. J. Med. 382 , 1894–1905 (2020). This paper is the first study demonstrating survival benefit for any systemic therapies compared with the standard of care sorafenib in advanced HCC .
Llovet, J. M. et al. Sorafenib in advanced hepatocellular carcinoma. N. Engl. J. Med. 359 , 378–390 (2008). The first study demonstrating survival benefit for systemic therapies (sorafenib) in advanced HCC compared with placebo .
Kudo, M. et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet 391 , 1163–1173 (2018). This is the first study demonstrating a survival benefit similar to the standard of care sorafenib in advanced HCC compared with placebo .
Bruix, J. et al. Regorafenib for patients with hepatocellular carcinoma who progressed on sorafenib treatment (RESORCE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 389 , 56–66 (2017). The first study demonstrating survival benefit in second-line treatment for patients with advanced HCC progressing to sorafenib therapy .
Abou-Alfa, G. K. et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N. Engl. J. Med. 379 , 54–63 (2018).
Zhu, A. X. et al. Ramucirumab after sorafenib in patients with advanced hepatocellular carcinoma and increased α-fetoprotein concentrations (REACH-2): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 20 , 282–296 (2019).
El-Khoueiry, A. B. et al. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet 389 , 2492–2502 (2017).
Finn, R. S. et al. Pembrolizumab as second-line therapy in patients with advanced hepatocellular carcinoma in KEYNOTE-240: a randomized, double-blind, phase III trial. J. Clin. Oncol. 38 , 193–202 (2020).
McGlynn, K. A., Petrick, J. L. & London, W. T. Global epidemiology of hepatocellular carcinoma: an emphasis on demographic and regional variability. Clin. Liver Dis. 19 , 223–238 (2015).
Rahib, L. et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 74 , 2913–2921 (2014).
Trinchet, J.-C. et al. Complications and competing risks of death in compensated viral cirrhosis (ANRS CO12 CirVir prospective cohort). Hepatology 62 , 737–750 (2015).
Fracanzani, A. Increased cancer risk in a cohort of 230 patients with hereditary hemochromatosis in comparison to matched control patients with non–iron-related chronic liver disease. Hepatology 33 , 647–651 (2001).
Wang, J., Chenivesse, X., Henglein, B. & Bréchot, C. Hepatitis B virus integration in a cyclin A gene in a hepatocellular carcinoma. Nature 343 , 555–557 (1990).
Kew, M. C. Synergistic interaction between aflatoxin B1 and hepatitis B virus in hepatocarcinogenesis. Liver Int. 23 , 405–409 (2003).
Chang, M. H. et al. Long-term effects of hepatitis B immunization of infants in preventing liver cancer. Gastroenterology 151 , 472–480.e1 (2016).
Jain, M. K. et al. Evaluation of a multifaceted intervention to reduce health disparities in hepatitis C screening: a pre-post analysis. Hepatology 70 , 40–50 (2019).
Ioannou, G. N. et al. Increased risk for hepatocellular carcinoma persists up to 10 years after HCV eradication in patients with baseline cirrhosis or high FIB-4 scores. Gastroenterology 157 , 1264–1278.e4 (2019).
Llovet, J. M. & Villanueva, A. Effect of HCV clearance with direct-acting antiviral agents on HCC. Nat. Rev. Gastroenterol. Hepatol. 13 , 561–562 (2016).
Puigvehí, M., Moctezuma-Velázquez, C., Villanueva, A. & Llovet, J. M. The oncogenic role of hepatitis delta virus in hepatocellular carcinoma. JHEP Rep. 1 , 120–130 (2019).
Jepsen, P., Ott, P., Andersen, P. K., Sørensen, H. T. & Vilstrup, H. Risk for hepatocellular carcinoma in patients with alcoholic cirrhosis. Ann. Intern. Med. 156 , 841 (2012).
Lin, C. W. et al. Heavy alcohol consumption increases the incidence of hepatocellular carcinoma in hepatitis B virus-related cirrhosis. J. Hepatol. 58 , 730–735 (2013).
Welzel, T. M. et al. Population-attributable fractions of risk factors for hepatocellular carcinoma in the United States. Am. J. Gastroenterol. 108 , 1314–1321 (2013).
Kanwal, F. et al. Risk of hepatocellular cancer in patients with non-alcoholic fatty liver disease. Gastroenterology 155 , 1828–1837.e2 (2018).
Mittal, S. et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin. Gastroenterol. Hepatol. 14 , 124–131.e1 (2016).
Rich, N. E., Yopp, A. C., Singal, A. G. & Murphy, C. C. Hepatocellular carcinoma incidence is decreasing among younger adults in the United States. Clin. Gastroenterol. Hepatol. 18 , 242–248.e5 (2020).
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. Cancer J. Clin. 68 , 394–424 (2018).
Rich, N. E. et al. Racial and ethnic differences in presentation and outcomes of hepatocellular carcinoma. Clin. Gastroenterol. Hepatol. 17 , 551–559.e1 (2019).
Lee, Y.-C. A. et al. Meta-analysis of epidemiologic studies on cigarette smoking and liver cancer. Int. J. Epidemiol. 38 , 1497–1511 (2009).
Bravi, F., Bosetti, C., Tavani, A., Gallus, S. & La Vecchia, C. Coffee reduces risk for hepatocellular carcinoma: an updated meta-analysis. Clin. Gastroenterol. Hepatol. 11 , 1413–1421.e1 (2013).
Sia, D., Villanueva, A., Friedman, S. L. & Llovet, J. M. Liver cancer cell of origin, molecular class, and effects on patient prognosis. Gastroenterology 152 , 745–761 (2017).
Pikarsky, E. Neighbourhood deaths cause a switch in cancer subtype. Nature 562 , 45–46 (2018).
Seehawer, M. et al. Necroptosis microenvironment directs lineage commitment in liver cancer. Nature 562 , 69–75 (2018).
Guichard, C. et al. Integrated analysis of somatic mutations and focal copy-number changes identifies key genes and pathways in hepatocellular carcinoma. Nat. Genet. 44 , 694–698 (2012).
Chiang, D. Y. et al. Focal gains of VEGFA and molecular classification of hepatocellular carcinoma. Cancer Res. 68 , 6779–6788 (2008).
Calderaro, J., Ziol, M., Paradis, V. & Zucman-Rossi, J. Molecular and histological correlations in liver cancer. J. Hepatol. 71 , 616–630 (2019).
Hyman, D. M., Taylor, B. S. & Baselga, J. Implementing genome-driven oncology. Cell 168 , 584–599 (2017).
Bressac, B., Kew, M., Wands, J. & Ozturk, M. Selective G to T mutations of p53 gene in hepatocellular carcinoma from southern Africa. Nature 350 , 429–431 (1991).
Wang, B. et al. Null genotypes of GSTM1 and GSTT1 contribute to hepatocellular carcinoma risk: Evidence from an updated meta-analysis. J. Hepatol. 53 , 508–518 (2010).
Romeo, S. et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat. Genet. 40 , 1461–1465 (2008).
Buch, S. et al. A genome-wide association study confirms PNPLA3 and identifies TM6SF2 and MBOAT7 as risk loci for alcohol-related cirrhosis. Nat. Genet. 47 , 1443–1448 (2015).
Paterlini-Bréchot, P. et al. Hepatitis B virus-related insertional mutagenesis occurs frequently in human liver cancers and recurrently targets human telomerase gene. Oncogene 22 , 3911–3916 (2003).
Nault, J.-C., Ningarhari, M., Rebouissou, S. & Zucman-Rossi, J. The role of telomeres and telomerase in cirrhosis and liver cancer. Nat. Rev. Gastroenterol. Hepatol. 16 , 544–558 (2019).
Bayard, Q. et al. Cyclin A2/E1 activation defines a hepatocellular carcinoma subclass with a rearrangement signature of replication stress. Nat. Commun. 9 , 5235 (2018).
Nault, J.-C. et al. Recurrent AAV2-related insertional mutagenesis in human hepatocellular carcinomas. Nat. Genet. 47 , 1187–1193 (2015).
Letouzé, E. et al. Mutational signatures reveal the dynamic interplay of risk factors and cellular processes during liver tumorigenesis. Nat. Commun. 8 , 1315 (2017).
Ng, A. W. T. et al. Aristolochic acids and their derivatives are widely implicated in liver cancers in Taiwan and throughout Asia. Sci. Transl. Med. 9 , eaan6446 (2017).
Alexandrov, L. B. et al. Signatures of mutational processes in human cancer. Nature 500 , 415–421 (2013).
Rebouissou, S. & Nault, J.-C. Advances in molecular classification and precision oncology in hepatocellular carcinoma. J. Hepatol. 72 , 215–229 (2020).
Hoshida, Y. et al. Integrative transcriptome analysis reveals common molecular subclasses of human hepatocellular carcinoma. Cancer Res. 69 , 7385–7392 (2009).
Cancer Genome Atlas Research Network. Comprehensive and integrative genomic characterization of hepatocellular carcinoma. Cell 169 , 1327–1341.e23 (2017).
Lee, J.-S. et al. A novel prognostic subtype of human hepatocellular carcinoma derived from hepatic progenitor cells. Nat. Med. 12 , 410–416 (2006).
Boyault, S. et al. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology 45 , 42–52 (2007).
Sia, D. et al. Identification of an immune-specific class of hepatocellular carcinoma, based on molecular features. Gastroenterology 153 , 812–826 (2017).
Lachenmayer, A. et al. Wnt-pathway activation in two molecular classes of hepatocellular carcinoma and experimental modulation by sorafenib. Clin. Cancer Res. 18 , 4997–5007 (2012).
Ruiz de Galarreta, M. et al. β-Catenin activation promotes immune escape and resistance to anti-PD-1 therapy in hepatocellular carcinoma. Cancer Discov. 9 , 1124–1141 (2019).
Renehan, A. G., Tyson, M., Egger, M., Heller, R. F. & Zwahlen, M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 371 , 569–578 (2008).
Sutti, S. & Albano, E. Adaptive immunity: an emerging player in the progression of NAFLD. Nat. Rev. Gastroenterol. Hepatol. 17 , 81–92 (2020).
Nakagawa, H. et al. ER stress cooperates with hypernutrition to trigger TNF-dependent spontaneous HCC development. Cancer Cell 26 , 331–343 (2014).
Nishida, N. et al. Unique features associated with hepatic oxidative DNA damage and DNA methylation in non-alcoholic fatty liver disease. J. Gastroenterol. Hepatol. 31 , 1646–1653 (2016).
Tummala, K. S. et al. Inhibition of de novo NAD + synthesis by oncogenic URI causes liver tumorigenesis through DNA damage. Cancer Cell 26 , 826–839 (2014).
Gomes, A. L. et al. Metabolic inflammation-associated IL-17A causes non-alcoholic steatohepatitis and hepatocellular carcinoma. Cancer Cell 30 , 161–175 (2016).
Guri, Y. et al. mTORC2 promotes tumorigenesis via lipid synthesis. Cancer Cell 32 , 807–823.e12 (2017).
Liu, D. et al. Squalene epoxidase drives NAFLD-induced hepatocellular carcinoma and is a pharmaceutical target. Sci. Transl. Med. 10 , eaap9840 (2018).
Umemura, A. et al. p62, upregulated during preneoplasia, induces hepatocellular carcinogenesis by maintaining survival of stressed HCC-initiating cells. Cancer Cell 29 , 935–948 (2016).
Grohmann, M. et al. Obesity drives STAT-1-dependent NASH and STAT-3-dependent HCC. Cell 175 , 1289–1306.e20 (2018).
Henderson, J. M., Zhang, H. E., Polak, N. & Gorrell, M. D. Hepatocellular carcinoma: mouse models and the potential roles of proteases. Cancer Lett. 387 , 106–113 (2017).
Negro, F. Natural history of NASH and HCC. Liver Int. 40 , 72–76 (2020).
Rudalska, R. et al. In vivo RNAi screening identifies a mechanism of sorafenib resistance in liver cancer. Nat. Med. 20 , 1138–1146 (2014).
Martinez-Quetglas, I. et al. IGF2 is up-regulated by epigenetic mechanisms in hepatocellular carcinomas and is an actionable oncogene product in experimental models. Gastroenterology 151 , 1192–1205 (2016).
Doudna, J. A. & Charpentier, E. The new frontier of genome engineering with CRISPR-Cas9. Science 346 , 1258096 (2014).
Cook, N., Jodrell, D. I. & Tuveson, D. A. Predictive in vivo animal models and translation to clinical trials. Drug Discov. Today 17 , 253–260 (2012).
Singh, M. & Ferrara, N. Modeling and predicting clinical efficacy for drugs targeting the tumor milieu. Nat. Biotechnol. 30 , 648–657 (2012).
Newell, P., Villanueva, A., Friedman, S. L., Koike, K. & Llovet, J. M. Experimental models of hepatocellular carcinoma. J. Hepatol. 48 , 858–879 (2008).
Bresnahan, E., Ramadori, P., Heikenwalder, M., Zender, L. & Lujambio, A. Novel patient-derived preclinical models of liver cancer. J. Hepatol. 72 , 239–249 (2020).
Moriya, K. et al. The core protein of hepatitis C virus induces hepatocellular carcinoma in transgenic mice. Nat. Med. 4 , 1065–1067 (1998).
Hagel, M. et al. First selective small molecule inhibitor of FGFR4 for the treatment of hepatocellular carcinomas with an activated FGFR4 signaling pathway. Cancer Discov. 5 , 424–437 (2015).
Day, C.-P., Merlino, G. & Van Dyke, T. Preclinical mouse cancer models: a maze of opportunities and challenges. Cell 163 , 39–53 (2015).
Jayson, G. & Harris, J. How participants in cancer trials are chosen: ethics and conflicting interests. Nat. Rev. Cancer 6 , 330–336 (2006).
Febbraio, M. A. et al. Preclinical models for studying NASH-driven HCC: how useful are they? Cell Metab. 29 , 18–26 (2019).
Sharpless, N. E. & DePinho, R. A. The mighty mouse: genetically engineered mouse models in cancer drug development. Nat. Rev. Drug Discov. 5 , 741–754 (2006).
Wolf, M. J. et al. Metabolic activation of intrahepatic CD8 + T cells and NKT cells causes nonalcoholic steatohepatitis and liver cancer via cross-talk with hepatocytes. Cancer Cell 26 , 549–564 (2014).
Ma, C. et al. NAFLD causes selective CD4 + T lymphocyte loss and promotes hepatocarcinogenesis. Nature 531 , 253–257 (2016).
Malehmir, M. et al. Platelet GPIbα is a mediator and potential interventional target for NASH and subsequent liver cancer. Nat. Med. 25 , 641–655 (2019).
Park, E. J. et al. Dietary and genetic obesity promote liver inflammation and tumorigenesis by enhancing IL-6 and TNF expression. Cell 140 , 197–208 (2010).
Ringelhan, M., Pfister, D., O’Connor, T., Pikarsky, E. & Heikenwalder, M. The immunology of hepatocellular carcinoma. Nat. Immunol. 19 , 222–232 (2018).
Wada, Y., Nakashima, O., Kutami, R., Yamamoto, O. & Kojiro, M. Clinicopathological study on hepatocellular carcinoma with lymphocytic infiltration. Hepatology 27 , 407–414 (1998).
Yuan, D. et al. Kupffer cell-derived TNF triggers cholangiocellular tumorigenesis through JNK due to chronic mitochondrial dysfunction and ROS. Cancer Cell 31 , 771–789.e6 (2017).
Crispe, I. N. The liver as a lymphoid organ. Annu. Rev. Immunol. 27 , 147–163 (2009).
Horwitz, E. et al. Human and mouse VEGFA-amplified hepatocellular carcinomas are highly sensitive to Sorafenib treatment. Cancer Discov. 4 , 730–743 (2014).
Finn, R. S. et al. Phase Ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J. Clin. Oncol. 38 , 2960–2970 (2020).
Hou, J., Zhang, H., Sun, B. & Karin, M. The immunobiology of hepatocellular carcinoma in humans and mice: basic concepts and therapeutic implications. J. Hepatol. 72 , 167–182 (2020).
Hoshida, Y. et al. Gene expression in fixed tissues and outcome in hepatocellular carcinoma. N. Engl. J. Med. 359 , 1995–2004 (2008). This study is the first molecular indication of the importance of the cancer field effect in the outcome of patients with HCC .
Shalapour, S. et al. Inflammation-induced IgA + cells dismantle anti-liver cancer immunity. Nature 551 , 340–345 (2017).
Kang, T. W. et al. Senescence surveillance of pre-malignant hepatocytes limits liver cancer development. Nature 479 , 547–551 (2011).
Flecken, T. et al. Immunodominance and functional alterations of tumor-associated antigen-specific CD8 + T-cell responses in hepatocellular carcinoma. Hepatology 59 , 1415–1426 (2014).
Zheng, C. et al. Landscape of infiltrating T cells in liver cancer revealed by single-cell sequencing. Cell 169 , 1342–1356.e16 (2017).
Langhans, B. et al. Role of regulatory T cells and checkpoint inhibition in hepatocellular carcinoma. Cancer Immunol. Immunother. 68 , 2055–2066 (2019).
Garnelo, M. et al. Interaction between tumour-infiltrating B cells and T cells controls the progression of hepatocellular carcinoma. Gut 66 , 342–351 (2017).
Bruno, T. C. New predictors for immunotherapy responses sharpen our view of the tumour microenvironment. Nature 577 , 474–476 (2020).
Schneider, C. et al. Adaptive immunity suppresses formation and progression of diethylnitrosamine-induced liver cancer. Gut 61 , 1733–1743 (2012).
Sautès-Fridman, C., Petitprez, F., Calderaro, J. & Fridman, W. H. Tertiary lymphoid structures in the era of cancer immunotherapy. Nat. Rev. Cancer 19 , 307–325 (2019).
Calderaro, J. et al. Intra-tumoral tertiary lymphoid structures are associated with a low risk of early recurrence of hepatocellular carcinoma. J. Hepatol. 70 , 58–65 (2019).
Finkin, S. et al. Ectopic lymphoid structures function as microniches for tumor progenitor cells in hepatocellular carcinoma. Nat. Immunol. 16 , 1235–1244 (2015).
Tsuchida, T. & Friedman, S. L. Mechanisms of hepatic stellate cell activation. Nat. Rev. Gastroenterol. Hepatol. 14 , 397–411 (2017).
Higashi, T., Friedman, S. L. & Hoshida, Y. Hepatic stellate cells as key target in liver fibrosis. Adv. Drug Deliv. Rev. 121 , 27–42 (2017).
Dapito, D. H. et al. Promotion of hepatocellular carcinoma by the intestinal microbiota and TLR4. Cancer Cell 21 , 504–516 (2012).
Ma, C. et al. Gut microbiome-mediated bile acid metabolism regulates liver cancer via NKT cells. Science 360 , eaan5931 (2018).
Hoshida, Y. et al. Prognostic gene expression signature for patients with hepatitis C–related early-stage cirrhosis. Gastroenterology 144 , 1024–1030 (2013).
Budhu, A. et al. Prediction of venous metastases, recurrence, and prognosis in hepatocellular carcinoma based on a unique immune response signature of the liver microenvironment. Cancer Cell 10 , 99–111 (2006).
Moeini, A. et al. An immune gene expression signature associated with development of human hepatocellular carcinoma identifies mice that respond to chemopreventive agents. Gastroenterology 157 , 1383–1397.e11 (2019).
Singal, A. G., Lampertico, P. & Nahon, P. Epidemiology and surveillance for hepatocellular carcinoma: new trends. J. Hepatol. 72 , 250–261 (2020).
Papatheodoridis, G. et al. PAGE-B predicts the risk of developing hepatocellular carcinoma in Caucasians with chronic hepatitis B on 5-year antiviral therapy. J. Hepatol. 64 , 800–806 (2016).
Shinmura, R. et al. Cirrhotic nodules: association between MR imaging signal intensity and intranodular blood supply. Radiology 237 , 512–519 (2005).
van der Pol, C. B. et al. Accuracy of the liver imaging reporting and data system in computed tomography and magnetic resonance image analysis of hepatocellular carcinoma or overall malignancy — a systematic review. Gastroenterology 156 , 976–986 (2019).
Paisant, A. et al. Comparison of extracellular and hepatobiliary MR contrast agents for the diagnosis of small HCCs. J. Hepatol. 72 , 937–945 (2020).
Kojiro, M. et al. Pathologic diagnosis of early hepatocellular carcinoma: a report of the international consensus group for hepatocellular neoplasia. Hepatology 49 , 658–664 (2009).
Forner, A. et al. Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: Prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology 47 , 97–104 (2007).
Zhang, B.-H., Yang, B.-H. & Tang, Z.-Y. Randomized controlled trial of screening for hepatocellular carcinoma. J. Cancer Res. Clin. Oncol. 130 , 417–422 (2004).
Lederle, F. A. Screening for liver cancer: the rush to judgment. Ann. Intern. Med. 156 , 387 (2012).
Poustchi, H. et al. Feasibility of conducting a randomized control trial for liver cancer screening: is a randomized controlled trial for liver cancer screening feasible or still needed? Hepatology 54 , 1998–2004 (2011).
Singal, A. G., Pillai, A. & Tiro, J. Early detection, curative treatment, and survival rates for hepatocellular carcinoma surveillance in patients with cirrhosis: a meta-analysis. PLoS Med. 11 , e1001624 (2014). This paper is a meta-analysis defining the accuracy of distinct surveillance strategies for the early detection of HCC .
Andersson, K. L., Salomon, J. A., Goldie, S. J. & Chung, R. T. Cost effectiveness of alternative surveillance strategies for hepatocellular carcinoma in patients with cirrhosis. Clin. Gastroenterol. Hepatol. 6 , 1418–1424 (2008).
Trinchet, J.-C. et al. Ultrasonographic surveillance of hepatocellular carcinoma in cirrhosis: a randomized trial comparing 3- and 6-month periodicities. Hepatology 54 , 1987–1997 (2011).
Atiq, O. et al. An assessment of benefits and harms of hepatocellular carcinoma surveillance in patients with cirrhosis. Hepatology 65 , 1196–1205 (2017).
Marrero, J. A. et al. α-Fetoprotein, DES-γ carboxyprothrombin, and lectin-bound α-fetoprotein in early hepatocellular carcinoma. Gastroenterology 137 , 110–118 (2009).
Pepe, M. S. et al. Phases of biomarker development for early detection of cancer. J. Natl. Cancer Inst. 93 , 1054–1061 (2001).
Tzartzeva, K. et al. Surveillance imaging and alpha fetoprotein for early detection of hepatocellular carcinoma in patients with cirrhosis: a meta-analysis. Gastroenterology 154 , 1706–1718.e1 (2018).
Labgaa, I. et al. A pilot study of ultra-deep targeted sequencing of plasma DNA identifies driver mutations in hepatocellular carcinoma. Oncogene 37 , 3740–3752 (2018).
Kisiel, J. B. et al. Hepatocellular carcinoma detection by plasma methylated DNA: discovery, phase I pilot, and phase II clinical validation. Hepatology 69 , 1180–1192 (2019).
Xu, R. et al. Circulating tumour DNA methylation markers for diagnosis and prognosis of hepatocellular carcinoma. Nat. Mater. 16 , 1155–1161 (2017).
Qu, C. et al. Detection of early-stage hepatocellular carcinoma in asymptomatic HBsAg-seropositive individuals by liquid biopsy. Proc. Natl Acad. Sci. USA 116 , 6308–6312 (2019).
Oh, C. R. et al. Genome-wide copy number alteration and VEGFA amplification of circulating cell-free DNA as a biomarker in advanced hepatocellular carcinoma patients treated with Sorafenib. BMC Cancer 19 , 292 (2019).
Torga, G. & Pienta, K. J. Patient-paired sample congruence between 2 commercial liquid biopsy tests. JAMA Oncol. 4 , 868 (2018).
Papatheodoridis, G. V., Chan, H. L.-Y., Hansen, B. E., Janssen, H. L. A. & Lampertico, P. Risk of hepatocellular carcinoma in chronic hepatitis B: assessment and modification with current antiviral therapy. J. Hepatol. 62 , 956–967 (2015).
Chang, M.-H. et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. N. Engl. J. Med. 336 , 1855–1859 (1997).
Singh, S., Singh, P. P., Singh, A. G., Murad, M. H. & Sanchez, W. Statins are associated with a reduced risk of hepatocellular cancer: a systematic review and meta-analysis. Gastroenterology 144 , 323–332 (2013).
Kennedy, O. J. et al. Coffee, including caffeinated and decaffeinated coffee, and the risk of hepatocellular carcinoma: a systematic review and dose–response meta-analysis. BMJ Open 7 , e013739 (2017).
Llovet, J. M. et al. Trial design and endpoints in hepatocellular carcinoma: AASLD consensus conference. Hepatology https://doi.org/10.1002/hep.31327 (2020).
Article PubMed Google Scholar
Llovet, J., Brú, C. & Bruix, J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin. Liver Dis. 19 , 329–338 (1999). The first description of the BCLC classification widely used in guidelines of management of HCC .
D’Amico, G. et al. Clinical states of cirrhosis and competing risks. J. Hepatol. 68 , 563–576 (2018).
Llovet, J. M. et al. Natural history of untreated nonsurgical hepatocellular carcinoma: rationale for the design and evaluation of therapeutic trials. Hepatology 29 , 62–67 (1999).
Shrager, B., Jibara, G., Schwartz, M. & Roayaie, S. Resection of hepatocellular carcinoma without cirrhosis. Ann. Surg. 255 , 1135–1143 (2012).
Viganò, L. et al. Liver resection for hepatocellular carcinoma in patients with metabolic syndrome: a multicenter matched analysis with HCV-related HCC. J. Hepatol. 63 , 93–101 (2015).
Piscaglia, F. et al. Clinical patterns of hepatocellular carcinoma in nonalcoholic fatty liver disease: a multicenter prospective study. Hepatology 63 , 827–838 (2016).
Zhou, X.-D. et al. Experience of 1000 patients who underwent hepatectomy for small hepatocellular carcinoma. Cancer 91 , 1479–1486 (2001).
Johnson, P. J. et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach — the ALBI grade. J. Clin. Oncol. 33 , 550–558 (2015).
Pinato, D. J. et al. The ALBI grade provides objective hepatic reserve estimation across each BCLC stage of hepatocellular carcinoma. J. Hepatol. 66 , 338–346 (2017).
Roayaie, S. et al. The role of hepatic resection in the treatment of hepatocellular cancer. Hepatology 62 , 440–451 (2015).
Berardi, G. et al. Development of a nomogram to predict outcome after liver resection for hepatocellular carcinoma in Child-Pugh B cirrhosis. J. Hepatol. 72 , 75–84 (2020).
Ishizawa, T. et al. Neither multiple tumors nor portal hypertension are surgical contraindications for hepatocellular carcinoma. Gastroenterology 134 , 1908–1916 (2008).
Citterio, D. et al. Hierarchic interaction of factors associated with liver decompensation after resection for hepatocellular carcinoma. JAMA Surg. 151 , 846–853 (2016).
Vitale, A. et al. Survival benefit of liver resection for patients with hepatocellular carcinoma across different Barcelona clinic liver cancer stages: a multicentre study. J. Hepatol. 62 , 617–624 (2015).
Yin, L. et al. Partial hepatectomy vs. transcatheter arterial chemoembolization for resectable multiple hepatocellular carcinoma beyond Milan criteria: a RCT. J. Hepatol. 61 , 82–88 (2014).
Kokudo, T. et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J. Hepatol. 65 , 938–943 (2016).
Roayaie, S., Jibara, G., Taouli, B. & Schwartz, M. Resection of hepatocellular carcinoma with macroscopic vascular invasion. Ann. Surg. Oncol. 20 , 3754–3760 (2013).
Roayaie, S. et al. Resection of hepatocellular cancer ≤2 cm: results from two Western centers. Hepatology 57 , 1426–1435 (2013).
Imamura, H. et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J. Hepatol. 38 , 200–207 (2003).
Shi, M. et al. Partial hepatectomy with wide versus narrow resection margin for solitary hepatocellular carcinoma: a prospective randomized trial. Ann. Surg. 245 , 36–43 (2007).
Hidaka, M. et al. Impact of anatomical resection for hepatocellular carcinoma with microportal invasion (vp1): a multi-institutional study by the Kyushu study group of liver surgery. Ann. Surg. 271 , 339–346 (2020).
Samuel, M., Chow, P. K. H., Shih-Yen, E. C., Machin, D. & Soo, K. C. Neoadjuvant and adjuvant therapy for surgical resection of hepatocellular carcinoma. Cochrane Database Syst. Rev. 2009 , CD001199 (2009).
Lee, J. H. et al. Adjuvant immunotherapy with autologous cytokine-induced killer cells for hepatocellular carcinoma. Gastroenterology 148 , 1383–1391.e6 (2015).
Bruix, J. et al. Adjuvant sorafenib for hepatocellular carcinoma after resection or ablation (STORM): a phase 3, randomised, double-blind, placebo-controlled trial. Lancet Oncol. 16 , 1344–1354 (2015).
Yin, J. et al. Effect of antiviral treatment with nucleotide/nucleoside analogs on postoperative prognosis of hepatitis B virus-related hepatocellular carcinoma: a two-stage longitudinal clinical study. J. Clin. Oncol. 31 , 3647–3655 (2013).
Singal, A. G. et al. Direct-acting antiviral therapy for hepatitis C virus infection is associated with increased survival in patients with a history of hepatocellular carcinoma. Gastroenterology 157 , 1253–1263.e2 (2019).
Waziry, R. et al. Hepatocellular carcinoma risk following direct-acting antiviral HCV therapy: a systematic review, meta-analyses, and meta-regression. J. Hepatol. 67 , 1204–1212 (2017).
Reig, M. et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J. Hepatol. 65 , 719–726 (2016).
Tabrizian, P., Jibara, G., Shrager, B., Schwartz, M. & Roayaie, S. Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann. Surg. 261 , 947–955 (2015).
Ferrer-Fàbrega, J. et al. Prospective validation of ab initio liver transplantation in hepatocellular carcinoma upon detection of risk factors for recurrence after resection. Hepatology 63 , 839–849 (2016).
Mazzaferro, V. et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N. Engl. J. Med. 334 , 693–700 (1996). This is a landmark study establishing the criteria for liver transplantation in HCC .
Franssen, B., Jibara, G., Tabrizian, P., Schwartz, M. E. & Roayaie, S. Actual 10-year survival following hepatectomy for hepatocellular carcinoma. HPB 16 , 830–835 (2014).
Cucchetti, A. et al. The chances of hepatic resection curing hepatocellular carcinoma. J. Hepatol. 72 , 711–717 (2020).
Llovet, J. M., Fuster, J. & Bruix, J. Intention-to-treat analysis of surgical treatment for early hepatocellular carcinoma: resection versus transplantation. Hepatology 30 , 1434–1440 (1999).
Yao, F. Y. et al. Liver transplantation for hepatocellular carcinoma: Expansion of the tumor size limits does not adversely impact survival. Hepatology 33 , 1394–1403 (2001).
Yao, F. Y. et al. Liver transplantation for hepatocellular carcinoma: validation of the UCSF-expanded criteria based on preoperative imaging. Am. J. Transplant. 7 , 2587–2596 (2007).
Mazzaferro, V. et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 10 , 35–43 (2009).
Commander, S. J. et al. A long-term experience with expansion of Milan criteria for liver transplant recipients. Clin. Transplant. 32 , e13254 (2018).
Ravaioli, M. et al. Liver transplantation for hepatocellular carcinoma: results of down-staging in patients initially outside the Milan selection criteria. Am. J. Transpl. 8 , 2547–2557 (2008).
CAS Google Scholar
Mazzaferro, V. et al. Metroticket 2.0 model for analysis of competing risks of death after liver transplantation for hepatocellular carcinoma. Gastroenterology 154 , 128–139 (2018).
Hong, G. et al. Alpha-fetoprotein and 18F-FDG positron emission tomography predict tumor recurrence better than Milan criteria in living donor liver transplantation. J. Hepatol. 64 , 852–859 (2016).
Kulik, L. et al. Therapies for patients with hepatocellular carcinoma awaiting liver transplantation: a systematic review and meta-analysis. Hepatology 67 , 381–400 (2018).
Yao, F. Y. et al. Downstaging of hepatocellular cancer before liver transplant: long-term outcome compared to tumors within Milan criteria. Hepatology 61 , 1968–1977 (2015).
Cucchetti, A. et al. Including mRECIST in the Metroticket 2.0 criteria improves prediction of hepatocellular carcinoma-related death after liver transplant. J. Hepatol. 73 , 342–348 (2020).
Halazun, K. J. et al. Is it time to abandon the Milan criteria? Results of a bicoastal US collaboration to redefine hepatocellular carcinoma liver transplantation selection policies. Ann. Surg. 268 , 690–699 (2018).
Kulik, L. M. et al. Outcomes of living and deceased donor liver transplant recipients with hepatocellular carcinoma: results of the A2ALL cohort. Am. J. Transpl. 12 , 2997–3007 (2012).
Miltiadous, O. et al. Progenitor cell markers predict outcome of patients with hepatocellular carcinoma beyond Milan criteria undergoing liver transplantation. J. Hepatol. 63 , 1368–1377 (2015).
Geissler, E. K. et al. Sirolimus use in liver transplant recipients with hepatocellular carcinoma. Transplantation 100 , 116–125 (2016).
Heimbach, J. K. et al. AASLD guidelines for the treatment of hepatocellular carcinoma. Hepatology 67 , 358–380 (2018).
Lencioni, R. & Llovet, J. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin. Liver Dis. 30 , 52–60 (2010).
Lencioni, R. New data supporting modified RECIST (mRECIST) for hepatocellular carcinoma. Clin. Cancer Res. 19 , 1312–1314 (2013).
Llovet, J. M. & Lencioni, R. mRECIST for HCC: performance and novel refinements. J. Hepatol. 72 , 288–306 (2020).
Meyer, T. et al. mRECIST to predict survival in advanced hepatocellular carcinoma: analysis of two randomised phase II trials comparing nintedanib vs sorafenib. Liver Int. 37 , 1047–1055 (2017).
Lencioni, R. et al. Objective response by mRECIST as a predictor and potential surrogate end-point of overall survival in advanced HCC. J. Hepatol. 66 , 1166–1172 (2017).
Kudo, M. et al. Analysis of survival and objective response (OR) in patients with hepatocellular carcinoma in a phase III study of lenvatinib (REFLECT). J. Clin. Oncol. 37 , 186–186 (2019).
Lencioni, R. A. et al. Small hepatocellular carcinoma in cirrhosis: randomized comparison of radio-frequency thermal ablation versus percutaneous ethanol injection. Radiology 228 , 235–240 (2003).
Lin, S.-M., Lin, C.-J., Lin, C.-C., Hsu, C.-W. & Chen, Y.-C. Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma ≤4 cm. Gastroenterology 127 , 1714–1723 (2004).
Shiina, S. et al. A randomized controlled trial of radiofrequency ablation with ethanol injection for small hepatocellular carcinoma. Gastroenterology 129 , 122–130 (2005).
Ng, K. K. C. et al. Randomized clinical trial of hepatic resection versus radiofrequency ablation for early-stage hepatocellular carcinoma. Br. J. Surg. 104 , 1775–1784 (2017).
Xu, X.-L., Liu, X.-D., Liang, M. & Luo, B.-M. Radiofrequency ablation versus hepatic resection for small hepatocellular carcinoma: systematic review of randomized controlled trials with meta-analysis and trial sequential analysis. Radiology 287 , 461–472 (2018).
Izumi, N. et al. A multicenter randomized controlled trial to evaluate the efficacy of surgery vs. radiofrequency ablation for small hepatocellular carcinoma (SURF trial). J. Clin. Oncol. 37 , 4002–4002 (2019).
Xia, Y. et al. Long-term effects of repeat hepatectomy vs percutaneous radiofrequency ablation among patients with recurrent hepatocellular carcinoma. JAMA Oncol. 6 , 255–263 (2020).
Lencioni, R. et al. Early-stage hepatocellular carcinoma in patients with cirrhosis: long-term results of percutaneous image-guided radiofrequency ablation. Radiology 234 , 961–967 (2005).
Sala, M. et al. Initial response to percutaneous ablation predicts survival in patients with hepatocellular carcinoma. Hepatology 40 , 1352–1360 (2004).
Breen, D. J. & Lencioni, R. Image-guided ablation of primary liver and renal tumours. Nat. Rev. Clin. Oncol. 12 , 175–186 (2015).
Yu, J. et al. Percutaneous cooled-probe microwave versus radiofrequency ablation in early-stage hepatocellular carcinoma: a phase III randomised controlled trial. Gut 66 , 1172–1173 (2017).
Hu, J. et al. Image-guided percutaneous microwave ablation versus cryoablation for hepatocellular carcinoma in high-risk locations: intermediate-term results. Cancer Manag. Res. 11 , 9801–9811 (2019).
Cheng, R. G., Bhattacharya, R., Yeh, M. M. & Padia, S. A. Irreversible electroporation can effectively ablate hepatocellular carcinoma to complete pathologic necrosis. J. Vasc. Interv. Radiol. 26 , 1184–1188 (2015).
Sutter, O. et al. Safety and efficacy of irreversible electroporation for the treatment of hepatocellular carcinoma not amenable to thermal ablation techniques: a retrospective single-center case series. Radiology 284 , 877–886 (2017).
Peng, Z.-W. et al. Radiofrequency ablation with or without transcatheter arterial chemoembolization in the treatment of hepatocellular carcinoma: a prospective randomized trial. J. Clin. Oncol. 31 , 426–432 (2013).
Tak, W. Y. et al. Phase III HEAT study adding lyso-thermosensitive liposomal doxorubicin to radiofrequency ablation in patients with unresectable hepatocellular carcinoma lesions. Clin. Cancer Res. 24 , 73–83 (2018).
Wang, C. et al. Multicenter randomized controlled trial of percutaneous cryoablation versus radiofrequency ablation in hepatocellular carcinoma. Hepatology 61 , 1579–1590 (2015).
Xu, J. et al. Radiofrequency ablation vs. cryoablation for localized hepatocellular carcinoma: a propensity-matched population study. Anticancer. Res. 38 , 6381–6386 (2018).
Di Costanzo, G. G. et al. Radiofrequency ablation versus laser ablation for the treatment of small hepatocellular carcinoma in cirrhosis: a randomized trial. J. Gastroenterol. Hepatol. 30 , 559–565 (2015).
Bujold, A. et al. Sequential phase I and II trials of stereotactic body radiotherapy for locally advanced hepatocellular carcinoma. J. Clin. Oncol. 31 , 1631–1639 (2013).
Hong, T. S. et al. Multi-institutional phase II study of high-dose hypofractionated proton beam therapy in patients with localized, unresectable hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J. Clin. Oncol. 34 , 460–468 (2016).
Tse, R. V. et al. Phase I study of individualized stereotactic body radiotherapy for hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J. Clin. Oncol. 26 , 657–664 (2008).
Yang, J.-F. et al. Stereotactic ablative radiotherapy versus conventionally fractionated radiotherapy in the treatment of hepatocellular carcinoma with portal vein invasion: a retrospective analysis. Radiat. Oncol. 14 , 180 (2019).
Wahl, D. R. et al. Outcomes after stereotactic body radiotherapy or radiofrequency ablation for hepatocellular carcinoma. J. Clin. Oncol. 34 , 452–459 (2016).
Shen, P. C. et al. Comparison of stereotactic body radiation therapy and transarterial chemoembolization for unresectable medium-sized hepatocellular carcinoma. Int. J. Radiat. Oncol. Biol. Phys. 105 , 307–318 (2019).
Kim, T. H. et al. Proton beam radiotherapy vs. radiofrequency ablation for recurrent hepatocellular carcinoma: a randomized phase III trial. J. Hepatol . https://doi.org/10.1016/j.jhep.2020.09.026 (2020)
Llovet, J. M. et al. Arterial embolisation or chemoembolisation versus symptomatic treatment in patients with unresectable hepatocellular carcinoma: a randomised controlled trial. Lancet 359 , 1734–1739 (2002).
Lo, C. et al. Randomized controlled trial of transarterial lipiodol chemoembolization for unresectable hepatocellular carcinoma. Hepatology 35 , 1164–1171 (2002).
Vogel, A. et al. Hepatocellular carcinoma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 29 (Suppl. 4), iv238–iv255 (2018).
Lencioni, R., de Baere, T., Soulen, M. C., Rilling, W. S. & Geschwind, J.-F. H. Lipiodol transarterial chemoembolization for hepatocellular carcinoma: a systematic review of efficacy and safety data. Hepatology 64 , 106–116 (2016).
Meyer, T. et al. Sorafenib in combination with transarterial chemoembolisation in patients with unresectable hepatocellular carcinoma (TACE 2): a randomised placebo-controlled, double-blind, phase 3 trial. Lancet Gastroenterol. Hepatol. 2 , 565–575 (2017).
Kudo, M. et al. Brivanib as adjuvant therapy to transarterial chemoembolization in patients with hepatocellular carcinoma: a randomized phase III trial. Hepatology 60 , 1697–1707 (2014).
Okusaka, T. et al. Transarterial chemotherapy alone versus transarterial chemoembolization for hepatocellular carcinoma: a randomized phase III trial. J. Hepatol. 51 , 1030–1036 (2009).
Chau, I. et al. Alpha-fetoprotein kinetics in patients with hepatocellular carcinoma receiving ramucirumab or placebo: an analysis of the phase 3 REACH study. Br. J. Cancer 119 , 19–26 (2018).
Lammer, J. et al. Prospective randomized study of doxorubicin-eluting-bead embolization in the treatment of hepatocellular carcinoma: results of the PRECISION V study. Cardiovasc. Intervent. Radiol. 33 , 41–52 (2010).
Varela, M. et al. Chemoembolization of hepatocellular carcinoma with drug eluting beads: efficacy and doxorubicin pharmacokinetics. J. Hepatol. 46 , 474–481 (2007).
Burrel, M. et al. Survival of patients with hepatocellular carcinoma treated by transarterial chemoembolisation (TACE) using drug eluting beads. Implications for clinical practice and trial design. J. Hepatol. 56 , 1330–1335 (2012).
Vincenzi, B. et al. Prognostic relevance of objective response according to EASL criteria and mRECIST criteria in hepatocellular carcinoma patients treated with loco-regional therapies: a literature-based meta-analysis. PLoS ONE 10 , e0133488 (2015).
Lencioni, R. et al. Sorafenib or placebo plus TACE with doxorubicin-eluting beads for intermediate stage HCC: the SPACE trial. J. Hepatol. 64 , 1090–1098 (2016).
Kudo, M. et al. Orantinib versus placebo combined with transcatheter arterial chemoembolisation in patients with unresectable hepatocellular carcinoma (ORIENTAL): a randomised, double-blind, placebo-controlled, multicentre, phase 3 study. Lancet Gastroenterol. Hepatol. 3 , 37–46 (2018).
Kudo, M. et al. Sorafenib plus low-dose cisplatin and fluorouracil hepatic arterial infusion chemotherapy versus sorafenib alone in patients with advanced hepatocellular carcinoma (SILIUS): a randomised, open label, phase 3 trial. Lancet Gastroenterol. Hepatol. 3 , 424–432 (2018).
Park, J. W. et al. Sorafenib with or without concurrent transarterial chemoembolization in patients with advanced hepatocellular carcinoma: the phase III STAH trial. J. Hepatol. 70 , 684–691 (2019).
Kudo, M. et al. Phase III study of sorafenib after transarterial chemoembolisation in Japanese and Korean patients with unresectable hepatocellular carcinoma. Eur. J. Cancer 47 , 2117–2127 (2011).
Hilgard, P. et al. Radioembolization with yttrium-90 glass microspheres in hepatocellular carcinoma: European experience on safety and long-term survival. Hepatology 52 , 1741–1749 (2010).
Salem, R. et al. Radioembolization for hepatocellular carcinoma using Yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology 138 , 52–64 (2010).
Mazzaferro, V. et al. Yttrium-90 radioembolization for intermediate-advanced hepatocellular carcinoma: a phase 2 study. Hepatology 57 , 1826–1837 (2013).
Vilgrain, V. et al. Efficacy and safety of selective internal radiotherapy with yttrium-90 resin microspheres compared with sorafenib in locally advanced and inoperable hepatocellular carcinoma (SARAH): an open-label randomised controlled phase 3 trial. Lancet Oncol. 18 , 1624–1636 (2017).
Chow, P. K. H. et al. SIRveNIB: selective internal radiation therapy versus sorafenib in Asia-Pacific patients with hepatocellular carcinoma. J. Clin. Oncol. 36 , 1913–1921 (2018).
Ricke, J. et al. Impact of combined selective internal radiation therapy and sorafenib on survival in advanced hepatocellular carcinoma. J. Hepatol. 71 , 1164–1174 (2019).
Bruix, J. et al. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: analysis of two phase III studies. J. Hepatol. 67 , 999–1008 (2017).
Finn R. S. et al. IMbrave150: Updated overall survival (OS) data from a global, randomized, open-label phase III study of atezolizumab (atezo) + bevacizumab (bev) versus sorafenib(sor) in patients (pts) with unresectable hepatocellular carcinoma (HCC). J. Clin. Oncol. 39 , (suppl 3; abstr 267) (2021).
Yau, T. et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the CheckMate 040 randomized clinical trial. JAMA Oncol. 6 , e204564 (2020).
Zhu, A. X. et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 19 , 940–952 (2018).
Llovet, J. M., Montal, R. & Villanueva, A. Randomized trials and endpoints in advanced HCC: role of PFS as a surrogate of survival. J. Hepatol. 70 , 1262–1277 (2019).
Office of the Commissioner. FDA grants accelerated approval to nivolumab and ipilimumab combination for hepatocellular carcinoma. FDA https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-nivolumab-and-ipilimumab-combination-hepatocellular-carcinoma (2020).
Yau, T. et al. CheckMate 459: a randomized, multi-center phase III study of nivolumab (NIVO) vs sorafenib (SOR) as first-line (1L) treatment in patients (pts) with advanced hepatocellular carcinoma (aHCC). Ann. Oncol. 30 , v874–v875 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT04039607 (2019).
Zappasodi, R., Merghoub, T. & Wolchok, J. D. Emerging concepts for immune checkpoint blockade-based combination therapies. Cancer Cell 33 , 581–598 (2018).
Rahma, O. E. & Hodi, F. S. The intersection between tumor angiogenesis and immune suppression. Clin. Cancer Res. 25 , 5449–5457 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03713593 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03755791 (2018).
Bergerot, P., Lamb, P., Wang, E. & Pal, S. K. Cabozantinib in combination with immunotherapy for advanced renal cell carcinoma and urothelial carcinoma: rationale and clinical evidence. Mol. Cancer Ther. 18 , 2185–2193 (2019).
Ott, P. A., Hodi, F. S., Kaufman, H. L., Wigginton, J. M. & Wolchok, J. D. Combination immunotherapy: a road map. J. Immunother. Cancer 5 , 16 (2017).
Hellmann, M. D. et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N. Engl. J. Med. 378 , 2093–2104 (2018).
Kelley, R. K. et al. Efficacy, tolerability, and biologic activity of a novel regimen of tremelimumab (T) in combination with durvalumab (D) for patients (pts) with advanced hepatocellular carcinoma (aHCC). J. Clin. Oncol. 38 , 4508–4508 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03298451 (2017).
Schmidt, E. V. et al. Assessment of clinical activity of PD-1 checkpoint inhibitor combination therapies reported in clinical trials. JAMA Netw. Open 3 , e1920833 (2020).
Montal, R. et al. Molecular portrait of high alpha-fetoprotein in hepatocellular carcinoma: implications for biomarker-driven clinical trials. Br. J. Cancer 121 , 340–343 (2019).
Galle, P. R. et al. Biology and significance of alpha-fetoprotein in hepatocellular carcinoma. Liver Int. 39 , 2214–2229 (2019).
Teufel, M. et al. Biomarkers associated with response to regorafenib in patients with hepatocellular carcinoma. Gastroenterology 156 , 1731–1741 (2019).
Pinyol, R. et al. Molecular predictors of prevention of recurrence in HCC with sorafenib as adjuvant treatment and prognostic factors in the phase 3 STORM trial. Gut 68 , 1065–1075 (2019).
Li, X.-S., Li, J.-W., Li, H. & Jiang, T. Prognostic value of programmed cell death ligand 1 (PD-L1) for hepatocellular carcinoma: a meta-analysis. Biosci. Rep. 40 , BSR20200459 (2020).
Kim, R. D. et al. First-in-human phase I study of Fisogatinib (BLU-554) validates aberrant fibroblast growth factor 19 signaling as a driver event in hepatocellular carcinoma. Cancer Discov. 9 , 1696–1707 (2019).
Lim, H. Y. et al. Phase II studies with refametinib or refametinib plus sorafenib in patients with RAS-mutated hepatocellular carcinoma. Clin. Cancer Res. 24 , 4650–4661 (2018).
Rimassa, L. et al. Tivantinib for second-line treatment of MET-high, advanced hepatocellular carcinoma (METIV-HCC): a final analysis of a phase 3, randomised, placebo-controlled study. Lancet Oncol. 19 , 682–693 (2018).
Tapper, E. B. & Asrani, S. K. The COVID-19 pandemic will have a long-lasting impact on the quality of cirrhosis care. J. Hepatol. https://doi.org/10.1016/j.jhep.2020.04.005 (2020).
Article PubMed PubMed Central Google Scholar
US Census Bureau. Coronavirus (COVID-19) pandemic. US Census Bureau https://www.census.gov/coronavirus (2020).
Huang, C. et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395 , 497–506 (2020).
International Liver Cancer Association. Management of HCC during COVID-19: ILCA guidance. ILCA https://ilca-online.org/news/management-of-hcc-during-covid-19-ilca-guidance/ (2020).
Cheng, A. L. et al. Efficacy and safety of sorafenib in patients in the Asia-Pacific region with advanced hepatocellular carcinoma: a phase III randomised, double-blind, placebo-controlled trial. Lancet Oncol. 10 , 25–34 (2009).
Sangro, B. et al. Diagnosis and management of toxicities of immune checkpoint inhibitors in hepatocellular carcinoma. J. Hepatol. 72 , 320–341 (2020).
Zhu, A. X. et al. Effect of everolimus on survival in advanced hepatocellular carcinoma after failure of sorafenib: the EVOLVE-1 randomized clinical trial. JAMA 312 , 57–67 (2014).
Blazeby, J. M. et al. Development of a questionnaire module to supplement the EORTC QLQ-C30 to assess quality of life in patients with hepatocellular carcinoma, the EORTC QLQ-HCC18. Eur. J. Cancer 40 , 2439–2444 (2004).
Heffernan, N. et al. Measuring health-related quality of life in patients with hepatobiliary cancers: the functional assessment of Cancer Therapy-Hepatobiliary Questionnaire. J. Clin. Oncol. 20 , 2229–2239 (2002).
Fan, S. Y., Eiser, C. & Ho, M. C. Health-related quality of life in patients with hepatocellular carcinoma: a systematic review. Clin. Gastroenterol. Hepatol. 8 , 559–564 (2010).
Diouf, M. et al. The added value of quality of life (QoL) for prognosis of overall survival in patients with palliative hepatocellular carcinoma. J. Hepatol. 58 , 509–521 (2013).
Fukumura, D., Kloepper, J., Amoozgar, Z., Duda, D. G. & Jain, R. K. Enhancing cancer immunotherapy using antiangiogenics: opportunities and challenges. Nat. Rev. Clin. Oncol. 15 , 325–340 (2018).
Sharma, P. & Allison, J. P. The future of immune checkpoint therapy. Science 348 , 56–61 (2015).
Kalbasi, A. & Ribas, A. Tumour-intrinsic resistance to immune checkpoint blockade. Nat. Rev. Immunol. 20 , 25–39 (2020).
Rotte, A. Combination of CTLA-4 and PD-1 blockers for treatment of cancer. J. Exp. Clin. Cancer Res. 38 , 255 (2019).
Rafiq, S., Hackett, C. S. & Brentjens, R. J. Engineering strategies to overcome the current roadblocks in CAR T cell therapy. Nat. Rev. Clin. Oncol. 17 , 147–167 (2020).
Download references
Acknowledgements
The authors thank Florian Castet for his invaluable support in the production of this manuscript. J.M.L. acknowledges his research funding from the Accelerator Award (HUNTER, Ref. C9380/A26813, partnership between the CRUK, AECC and AIRC), National Cancer Institute (P30-CA196521), U.S. Department of Defense (CA150272P3), Samuel Waxman Cancer Research Foundation, Spanish National Health Institute (PID2019-105378RB-100) and the Generalitat de Catalunya/AGAUR (SGR-1358). E.P. acknowledges his grants from the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation and the Israel Science Foundation.
Author information
Authors and affiliations.
Mount Sinai Liver Cancer Program, Division of Liver Diseases, Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Josep M. Llovet & Augusto Villanueva
Translational Research in Hepatic Oncology, Liver Unit, IDIBAPS, Hospital Clinic, University of Barcelona, Catalonia, Spain
Josep M. Llovet
Institució Catalana d’Estudis Avançats (ICREA), Barcelona, Catalonia, Spain
Helen Diller Family Comprehensive Cancer Center, University of California, San Francisco (UCSF), San Francisco, CA, USA
Robin Kate Kelley
Department of Internal Medicine, University of Texas Southwestern Medical Center, Dallas, Texas, USA
Amit G. Singal
The Lautenberg Center for Immunology and Cancer Research, IMRIC, The Hebrew University of Jerusalem, Jerusalem, Israel
Eli Pikarsky
White Plains Hospital Center for Cancer Care, Montefiore Health, White Plains, NY, USA
Sasan Roayaie
Department of Radiology, Pisa University School of Medicine, Pisa, Italy
Riccardo Lencioni
Department of Radiology, Miami Cancer Insitute, Miami, FL, USA
The University of Tokyo, Department of Gastroenterology, Tokyo, Japan
Kazuhiko Koike
Centre de Recherche des Cordeliers, Sorbonne Université, Inserm, USPC, Université Paris Descartes, Université Paris Diderot, Paris, France
Jessica Zucman-Rossi
Hôpital Européen Georges Pompidou, Assistance Publique-Hôpitaux de Paris, Paris, France
Department of Oncology, Geffen School of Medicine at UCLA, Los Angeles, CA, USA
Richard S. Finn
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (J.M.L.); Epidemiology (A.G.S.); Mechanisms/pathophysiology (J.Z-R., E.P., K.K. and A.V.); Diagnosis, screening and prevention (A.G.S. and A.V.); Management (J.M.L., R.K.K., S.R., R.S.F., A.V. and R.L.); Quality of life (R.K.K., A.G.S. and A.V.); Outlook (J.M.L. and R.S.F.); Overview of Primer (J.M.L.).

Corresponding author
Correspondence to Josep M. Llovet .
Ethics declarations
Competing interests.
J.M.L. receives research support from Bayer HealthCare Pharmaceuticals, Bristol-Myers Squibb, Boehringer-Ingelheim, Eisai Inc., and Ipsen and received consulting fees from AstraZeneca, Bayer HealthCare Pharmaceuticals, Bristol-Myers Squibb, Can-Fite Biopharma, Celsion Corporation, Eli Lilly, Eisai Inc., Exelixis, Genentech, Glycotest, Merck, Nucleix and Roche. R.K.K. receives research support to the institution from Adaptimmune, Agios Inc., AstraZeneca, Bayer, Bristol-Myers Squibb, Eli Lilly, EMD Serono, Exelixis, Merck, Novartis, Partner Therapeutics, QED and Taiho; R.K.K. has received consulting for Independent Data Monitoring Committee fees from Genentech or Roche and Gilead, and travel support from Ipsen. A.V. has received consulting fees from Guidepoint and Fujifilm and advisory board fees from Exact Sciences, Gilead, Nucleix and NGM Pharmaceuticals. A.G.S. has received consulting fees from AstraZeneca, Bayer, Bristol-Myers Squibb, Eisai, Exact Sciences, Exelixis, Fujifilm, Genentech, Glycotest, GRAIL and Roche. S.R. is a consulting director and a course director for Medtronic. R.L. reports advisory fees from AstraZeneca, Celsion and Guerbet. K.K. is receiving support from AbbVie GK, Asuka Pharmaceutical, Astellas, Bristol-Myers Squibb, Dainippon-Sumitomo Pharma, EA Pharma, Eisai Inc., Gilead Sciences, Merck, Otsuka Pharmaceuticals, Shionogi and Takeda Pharmaceuticals. R.S.F. reports consulting fees from AstraZeneca, Bayer, Bristol-Myers Squibb, CStone, Eisai, Eli Lilly, Merck, Novartis, Pfizer and Roche/Genentech. All other authors declare no competing interests.
Additional information
Peer review information.
Nature Reviews Disease Primers thanks Hellmut Augustin, Massimo Colombo, Chih-Che Lin, Michael Peter Manns, Timothy Pawlik and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information.
(SVR). An undetectable hepatitis C virus RNA in the serum with the use of a sensitive polymerase chain assay at 6 months after completion of antiviral therapy.
(NASH). Inflammation of the liver caused by excess accumulation of fat in hepatocytes.
A multifactorial metabolic disorder, characterized by a cluster of risk factors, including abdominal obesity, insulin resistance, dyslipidaemia and elevated blood pressure, that promote the development of type 2 diabetes mellitus and cardiovascular disease.
Mutational fingerprints of specific genotoxins.
(ICIs). Drugs that stimulate anti-tumour immune response by blocking checkpoint proteins and promoting immune-mediated elimination of tumour cells.
A measurement of any aspect of a patient’s health status that comes directly from the patient, without interpretation of the patient’s responses by a health-care professional or anyone else.
A mycotoxin produced by Aspergillus species in a variety of food commodities; consumption of the toxin can cause adverse health effects, including liver cancer.
A histological finding in the advanced stage of liver fibrosis characterized by thin and long fibrous septa that extend across lobules and connect portal spaces and central veins.
The proportion of hepatocellular carcinoma cases that would be prevented if a risk factor were eliminated.
The process by which one somatic cell is transformed into another mature somatic cell without undergoing a pluripotent state.
A progressive loss of effector function due to prolonged exposition to inflammatory signals and antigen stimulation, characteristic of chronic infections and cancer.
Lymphoid micro-organs that develop at sites of chronic inflammation, including the liver.
Liver-specific mesenchymal cells that play a vital role in liver physiology and in wound healing, in particular fibrogenesis.
A hepatocyte that is metabolically active but with permanently arrested growth and resistant to apoptosis.
A pathognomonic radiological finding of hepatocellular carcinoma (HCC) characterized by hyperenhancement in the arterial phase (wash-in) and hypoenhancement in the portal venous and/or delayed phases of acquisition (wash-out) in the setting of liver cirrhosis.
A scoring system that assesses the prognosis of chronic liver disease by integrating three analytical and two clinical items, including blood levels of bilirubin, albumin, prothrombin time, presence of encephalopathy and ascites.
Abnormal and enlarged veins that develop as a result of portal hypertension and may leak or rupture, causing potentially life-threatening upper gastrointestinal bleeding.
A standardized scale for measuring a patient’s performance status and the impact of disease on their daily living abilities and level of daily functioning.
A small collection of tumour cells (<2 mm in size) shed from the primary tumour that spread to another organ through blood or lymph nodes.
The removal of the entire neoplasm together with the segment of the liver where the tumour is located.
Therapies that transfer immune cells with anti-tumour activity into a patient to mediate tumour regression.
Transplantation of liver specimens in patients with hepatocellular carcinoma recurrence after initial tumour resection.
A mathematical model estimating the exact outcomes after transplantation based upon size and number of nodules at pathological explant.
Organs recovered from elderly donors or with comorbidities that convey a higher risk of technical complications and/or post-transplantation dysfunction.
A measure of treatment efficacy used in clinical trials and defined as a reduction in tumour size on radiological evaluation.
A dermatological adverse reaction to certain drugs, mainly tyrosine kinase inhibitors, causing a painful erythematous rash localized in palms, fingers and feet.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Llovet, J.M., Kelley, R.K., Villanueva, A. et al. Hepatocellular carcinoma. Nat Rev Dis Primers 7 , 6 (2021). https://doi.org/10.1038/s41572-020-00240-3
Download citation
Accepted : 08 December 2020
Published : 21 January 2021
DOI : https://doi.org/10.1038/s41572-020-00240-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Open access
- Published: 14 March 2022
Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss
- Sjaak Pouwels ORCID: orcid.org/0000-0002-6390-7692 1 ,
- Nasser Sakran 2 ,
- Yitka Graham 3 , 4 ,
- Angela Leal 5 ,
- Tadeja Pintar 6 ,
- Wah Yang 7 ,
- Radwan Kassir 8 ,
- Rishi Singhal 9 ,
- Kamal Mahawar 3 , 10 &
- Dharmanand Ramnarain 1 , 11
BMC Endocrine Disorders volume 22 , Article number: 63 ( 2022 ) Cite this article
41k Accesses
211 Citations
21 Altmetric
Metrics details
Given the increasing prevalence of diabetes and obesity worldwide, the deleterious effects of non-alcoholic fatty liver disease (NAFLD) are becoming a growing challenge for public health. NAFLD is the most common chronic liver disease in the Western world. NAFLD is closely associated with metabolic disorders, including central obesity, dyslipidaemia, hypertension, hyperglycaemia and persistent abnormalities of liver function tests.
In general NAFLD is a common denominer for a broad spectrum of damage to the liver, which can be due to hepatocyte injury, inflammatory processes and fibrosis. This is normally seen on liver biopsy and can range from milder forms (steatosis) to the more severe forms (non-alcoholic steatohepatitis (NASH), advanced fibrosis, cirrhosis and liver failure). In these patients, advanced fibrosis is the major predictor of morbidity and liver-related mortality, and an accurate diagnosis of NASH and NAFLD is mandatory. Histologic evaluation with liver biopsy remains the gold standard to diagnose NAFLD. Diagnosis of NAFLD is defined as presence of hepatic steatosis, ballooning and lobular inflammation with or without fibrosis. Weight loss, dietary modification, and the treatment of underlying metabolic syndrome remain the mainstays of therapy once the diagnosis is established. Dietary recommendations and lifestyle interventions, weight loss, and the treatment of underlying metabolic syndrome remain the mainstays of therapy once the diagnosis is established with promising results but are difficult to maintain. Pioglitazone and vitamin E are recommended by guidelines in selected patients. This review gives an overview of NAFLD and its treatment options.
Peer Review reports
Non-alcoholic fatty liver disease (NAFLD) is a common cause of chronic liver disease worldwide. NAFLD is a spectrum of the disease characterized by hepatic steatosis when no other causes for secondary hepatic fat accumulation (e.g., excessive alcohol consumption) can be identified. NAFLD ranges from the more benign condition of non-alcoholic fatty liver (NAFL) to non-alcoholic steatohepatitis (NASH), which is at the more severe end of the spectrum. NAFLD may progress to fibrosis and cirrhosis [ 1 , 2 ]. In NAFLD, hepatic steatosis is present without evidence of inflammation, whereas in NASH, hepatic steatosis is associated with lobular inflammation and apoptosis that can lead to fibrosis and cirrhosis [ 1 , 2 , 3 , 4 ].
Before the middle of the last decade, NASH was widely considered a serious condition, occurring almost exclusively in females with obesity, often associated with Type 2 Diabetes Mellitus (T2DM), and relatively benign prognosis, that are predictive risk factors of cardiovascular disease, stroke, and diabetes [ 1 , 2 , 3 , 4 ]. The prevalence of liver disease (NAFLD) has risen rapidly in Western countries, with a worldwide prevalence of 25%. NAFLD is becoming more common chronic liver disease in Western industrialized countries, particularly in patients with central obesity, T2DM, dyslipidaemia, and metabolic syndrome [ 5 ].
In terms of diagnostic tests, the gold standard to investigate any form of liver inflammation e.g. damage is a liver biopsy. In the diagnosis of NAFLD and related disorders, liver biopsies can be extremely helpful and its findings can range from triglyceride deposition as droplets in the hepatocyte to more extensive forms of non-alcoholic steatohepatitis (NASH). NASH is normally characterised by the earlier mentioned lipid droplets in hepatocytes, with concomitant inflammation and a variable degree of hepatic fibrosis. In the majority of the liver steatosis patients, the disease is ‘non-progressive’, however a small portion of these patients develop the earlier mentioned NASH, which can lead to liver failure and even hepatocellular carcinoma [ 5 , 6 ].
NAFLD management’s US guidelines define NAFLD as steatosis with ≥5% fat infiltration in imaging or histology and b) no alcohol, drug, or viral-induced steatosis. NAFLD patients may present with elevated liver enzymes [ 6 ].
Patients with NAFLD often have one or more components of the metabolic syndrome (MS) like systemic hypertension, dyslipidaemia, Insulin resistance, or overt diabetes [ 7 ]. There is increasing evidence that visceral obesity is a risk factor for NAFLD and it also has to be taken into account that MS is a known risk factor in cardiovascular disease development [ 5 , 7 ]. Based on current literature cardiac and vascular diseases seem to be the most important cause of death in these patients, however the pathophysiological mechanisms connecting cardiovascular disease and NAFLD are not fully understood [ 5 , 7 ]. It is thought that insulin resistance is a common factor in the pathogenesis linking both entities [ 5 , 7 ].
Evaluation of abnormal liver enzyme levels in an otherwise healthy patient can pose a challenge to even an experienced clinician. NAFLD is a common explanation for abnormal liver test results in blood donors. It determines asymptomatic elevation of alanine aminotransferase (ALT) and asparate aminotransverase (AST) levels in up to 90% of cases, once other liver disease causes are excluded [ 8 , 9 ]. The World Health Organization Global Health Observatory data in 2014 indicates that globally obesity occurs in 15% of women and 11% of men aged 18 and over [ 8 , 9 ]. A study evaluating the prevalence of NASH estimated that 5.7–17% of the US population is affected [ 8 , 9 ].
The spectrum of NAFLD and related disease, including its complex relationship with MS poses challenges for clinicians. This review aims to summarise the pathophysiology of NAFLD, risk factors, diagnostic measures and conservative and surgical treatment options.
Pathophysiology of NAFLD/NASH
The development of NASH is a complex process and is not completely understood. In the recent years a lot of animal research has been conducted investigating the pathophysiology of NAFLD and NASH, mainly difference in dietary models (high fructose, high fat or methionine/choline deficient diet (MCD) [ 10 , 11 ]. Based on this body of evidence, it has been suggested that the development of NASH is a two-step process. The first step of this process is fat deposition in the liver that will increase insulin resistance. The second part of this process is cellular and molecular changes involving oxidative stress, and oxidation of fatty acids in the liver due to a variety of factors (cytokine injury, hyperinsulinemia, hepatic iron and/or lipid peroxidation, variation of the extracelular matrix, energy homeostasis, and change in the immune system function) [ 9 , 12 ]. The development of insulin resistance is an intricate process. In the setting of the MS, as is the case for many patients with NASH, the increase in fat mass and adipocyte differentiation plays a key role in developing insulin resistance.
NAFLD can be divided into two distinct types. The first type of NAFLD has a narrow relationship with metabolic syndrome and the current beliefs are that insulin resistance is the primary pathophysiological mechanism. The second type of NAFLD has a relationship with infectious pathologies that can lead to the occurrence of liver steatosis. In this case infections like hepatitis C and HIV can be a cause, but it is also associated with medication (total parenteral nutrition, glucocorticoids, tamoxifen, tetracycline, amiodaron, methotrexate, valproic acid, vinyl chloride) and specific toxins or inherited/acquired metabolic diseases (e.g. lipodystrophy or cachexia or intestinal bypass surgery) [ 13 , 14 ].
Risk factors
People with NAFLD generally have characteristics of MS, with the associated cardiovascular disease risk factors [ 15 , 16 ]. As stated earlier NAFLD is closely related to metabolic syndrome and obesity, type 2 diabetes mellitus (T2DM), and dyslipidaemia are considered to be important risk factors for NAFLD [ 17 ]. Studies have shown the increased prevalence of cardiovascular disease (CVD) in patients with NAFLD, without and without diabetes [ 18 , 19 ]. Thus, NAFLD is generally associated with an unhealthy lifestyle, with evidence, to suggest that changes in unhealthy lifestyles can reduce the transaminase levels and improve NAFLD [ 20 ]. A study of patients with T2DM found a higher prevalence of peripheral vascular, coronary and cerebrovascular diseases in subjects with NAFLD than without, with coronary, cerebrovascular and peripheral vascular disease was greater among those with NAFLD than among those without this disease, aside from normal CVD risk factors, medication use and diabetes-related variables [ 21 ]. Byrne et al. stated there are over 20 published studies, both prospective and retrospective, that have studied the relationship between NAFLD and cardiovascular disease and concluded that CVD is a clear and present threat [ 15 ], which continues to be confirmed in on-going studies [ 22 ].
The relationship between NAFLD and smoking is controversial [ 23 , 24 ]. Overall, smoking is a major risk factor for the development of chronic, non-communicable diseases (NCD) such as cancer, T2DM, respiratory and cardiovascular conditions globally [ 25 ]. A study of obese rats found that cigarette smoke increased the histological severity of NAFLD [ 26 ]. A cross-sectional study of NAFLD patients (smokers and non-smokers) found the proportions of patients with liver significant fibrosis and advanced liver fibrosis among the smokers were significantly higher than those among the non-smokers [ 20 ]. A systematic review and meta-analysis of 20 published studies found smoking is greatly associated with NAFLD, and recommended further studies to understand the underlying mechanisms of the association [ 27 ]. Smoking was considered an independent risk factor for the development of NAFLD [ 23 ], however, a cross-sectional study of 933 patients (368 smokers and 565 non-smokers as controls) found no difference in the prevalence of NAFLD in the two groups (22.2% versus 29%), nor with heavy smokers (> 20 packs of cigarettes per year) [ 28 ].
Symptoms and signs
The majority of the patients with NAFLD do not experience any symptoms, however some of them may complain of fatigue, right upper quadrant discomfort, hepatomegaly, acanthosis nigricans, and lipomatosis [ 29 ]. A significant amount of patients with cirrhosis can be present themselves with end-stage liver disease. In approximately 48-100% NASH can be asymptomatic and very often it is discovered during medical evaluations for other reasons. Although clinical stigmata of chronic liver failure are rarely seen in this population, one study showed that at the time of diagnosis splenomegaly was present in 25% of the patients [ 29 ].
Very often a diagnosis like NASH or NAFLD is discovered due to abnormal liver function tests such as aminotransferases (ALT and AST) or incidental finding of hepatic steatosis on radiologic abdominal finding. Hepatomegaly can present during physical examination and this is caused by the liver’s fatty infiltration [ 29 ].
Laboratory findings
When performing laboratory tests, serum markers like aminotransferases (AST, ALT), are mild to moderately elevated [ 30 ]. However, the AST and ALT levels can be aspecific in patients with NAFLD or related conditions. In other words, AST and ALT levels can either be elevated or normal, but both do exclude the presence of NAFLD [ 30 , 31 , 32 ]. In patients with NAFLD, ALT elevations are more common than elevations of AST. The ALT levels tend to be higher in NASH than in simple steatosis. Elevated serum ferritin levels are commonly elevated in patients with NAFLD, and increased transferrin saturation is found in 6–11% of patients [ 30 , 31 , 32 ].
Other markers of interest are alkaline phosphatase (ALP) and clotting factors. In patients with NAFLD ALP can be abnormal and even be elevated 2-3 times the upper limit of its normal value.
In addition, other laboratory values can be helpful in diagnosing NAFLD. Both albumin and bilirubin levels may be high in patients who have developed chronic progressive disease. In cirrhotic patients laboratory measurements of clotting times can be abnormal. Most of the time patients who have developed cirrhosis have a prolonged prothrombin time, thrombocytopenia, and a concomitant neutropenia [ 30 , 31 , 32 ].
Imaging in NAFLD
In liver diseases such as NAFLD and NASH, various imaging modalities can be used to substantiate the diagnosis, however none of them are routinely used for differentiating between (histological) subtypes of NAFLD or NASH [ 33 ]. Computed tomography (CT) scans, abdominal ultrasound (US), or Magnetic Resonance Imaging (MRI) can detect these liver diseases. Imaging findings in patients with NAFLD include increased echogenicity on ultrasound, decreased hepatic attenuation on CT, and an increased fat signal on MRI [ 33 ].
US often reveals a hyperechoic texture or a bright liver because of diffuse fatty infiltration [ 34 ]. The sensitivity and the specificity of US are respectively 89 and 93% in detecting increased fibrosis and steatosis [ 35 ]. However, the US is the cheapest method and has been the most common modality used in clinical practice. The sensitivity of US is decreased in patients with obesity [ 36 , 37 ]. The US showing hyperechogenic liver tissue in contrast to the spleen or kidney echogenicity is suggestive of steatosis. However, the sensitivity of the US is only 60–94% in these instances [ 38 ].
Vibration-controlled transient Elastography (VCTE)
VCTE is a non-invasive method for excluding advanced fibrosis in measuring liver stiffness with VCTE [ 39 , 40 , 41 ]. A meta-analysis of 19 biopsy-controlled studies including over 2700 patients, the optimal cut-off value for steatosis grade > S0 was 248 dB/m (95% Confidence Interval (CI) 237-261) and for steatosis grade > S1 was 268 dB/m (95% CI 257-284) [ 40 ].
CT, MRI, and magnetic resonance spectroscopy (MRS)
Both imaging modalities are able to detect steatosis, but lack sensitivity to detect inflammatory or fibrotic process of the liver [ 42 ].
Unfortunately MRS has a higher sensitivity to detect the earlier mentioned pathological processes it is (not yet) widely available [ 43 ]. In general the sensitivity of CT, MRI and MRS to detect steatosis of the liver was 33, 50, and 88%, respectively. Specificity of all three for detection of hepatic steatosis was 100, 83, and 63%, respectively [ 44 ].
Histological findings in NAFLD
The liver biopsy is the Gold standard for diagnosis of NASH or NAFLD. Performing a liver biopsy on every patient with suspected NAFLD remains controversial. The general indications for performing a liver biopsy in patients with NAFLD confirm or exclude the diagnosis. To many, the liver biopsy is considered to be the golden standard in diagnosing NAFLD, but a pre-emptive diagnosis is mostly made up using the medical history, laboratory work and imaging of the patient. A liver biopsy can be very helpful in assessing the amount of hepatic damage in general, but also in patients that remain to have an unclear diagnosis after non-invasive assessments [ 45 , 46 , 47 ].
Limitations of liver biopsy are sampling error variability, inter and intra-observer variability, and risk and complications—problems with a pathological diagnosis that may lead to misdiagnosis and staging inaccuracies. Many studies have shown sampling variability and uneven distribution of NASH histologic lesions during the evaluation of paired biopsies [ 45 , 46 , 47 ].
The NAFLD Activity Score (NAS) is a validated score that is used to grade disease activity in patients with NAFLD [ 48 ]. The NAS has several components and each of them has a minimum and maximum score; steatosis (0 to 3), lobular inflammation (0 to 3), hepatocellular ballooning (0 to 2) [ 48 ]. Fibrosis is not included in the NAS. In the original study that derived the NAS, scores of 0 to 2 occurred in cases mainly considered not diagnostic of NASH; scores of 3 to 4 were evenly divided among those considered not diagnostic, borderline, or positive for NASH; and scores of 5 to 8 occurred in cases that were considered mainly diagnostic of NASH [ 48 ].
The treatment of NAFLD and related diseases (including but not limited to components of MS) consists of several tiers of which conservative and surgical therapies are known treatments. Very often the treatment of patients with NAFLD consists of a multimodal intervention targeting multiple aspects like weight loss, lifestyle modifications and possible medication optimisation.
Conservative treatment - lifestyle modifications and weight loss
To date, there is no specific drug treatment for NAFLD, however it is believed that a combination of treatment goals (lifestyle adjustments, increasing physical activity and smoking/ alcohol cessation) can be beneficial [ 49 , 50 ].
NAFLD patients, whether living with obesity are not, should be encouraged and educated to partake in a healthy lifestyle approach, which exists irrespective of weight-loss [ 49 ]. A healthy diet i.e. reduction of caloric intake and high-glycaemic index (GI) foods, increased consumption of monounsaturated fatty acids, omega-3 fatty acids, fibers, and specific protein sources such as fish and poultry are suggested to have beneficial effects [ 51 ]. Studies suggest that a Mediterranean diet, defined as reduced carbohydrate intake (especially sugars and refined carbohydrates) and increased monosaturated and omega-3 fatty acid intake, can reduce liver fat and thus positively contribute to the management of NAFLD [ 50 , 52 ]. Research into the effect of diet on risk and management of NAFLD found that prolonged consumption of sugary drinks had a positive correlation to NAFLD [ 53 ] and many people with NAFLD tended to consume high levels of sugary drinks and red meat compared to others [ 54 ]. Whilst the reduction of and type of carbohydrates on prevention and management of NAFLD has been widely studied, the effects of protein consumption are not as widely known [ 55 , 56 ]. A high protein diet is suggested to be beneficial for NAFLD management, but the source of protein needs to be considered given the evidence on consumption of red meat on cardiovascular disease, and consideration of proteins in a vegetarian diet [ 57 ].
Other dietary components can also be beneficial in the treatment of NAFLD, like changes in Vitamin E, caffeine and polyphenol intake. Vitamin E is a fat-soluble vitamin that works as an antioxidant [ 58 ]. Current data support the use of Vitamin E in non-diabetic patients with nonalcoholic fatty liver disease. However, it should not be considered as the first option for treatment [ 58 ]. Vitamin E therapy should be considered as treatment if lifestyle modifications do not produce the expected results due to non-compliance or ineffectiveness [ 59 ].
The PIVENS study showed that a 2-year period of treatment with Vitamin E at 800 IU / day in adult patients significantly reverses steatohepatitis and significantly reduced hepatic steatosis and alanine aminotransferase (ALT), but did not had significant changes in fibrosis compared to placebo [ 58 , 60 ]. Long-term safety is of concern, several meta-analyses suggest increased mortality in patients taking Vitamin E supplements. Some of them showed a 20% increased risk of haemorrhagic stroke; and another test suggested an increased risk of prostate cancer in men over the age of 50 [ 60 ].
Caffeine is a strong antioxidant that could help reduce the burden of oxidative stress and inflammation in the liver and may provide hepatoprotective effect [ 61 ]. Many studies have linked coffee consumption to improvement in liver enzymes in a dose-dependent manner in individuals who are at risk of liver diseases [ 61 ]. There is an evident protective role of more than 3 cups of coffee consumption per day but not less than 2 cups according a meta-analysis study [ 62 ].
Finally, polyphenols are a heterogeneous class of plant-derived compounds that include several hydro soluble antioxidants reported as health promoting agents and proposed in the treatment of different metabolic disorders [ 63 ]. Natural polyphenols are present in nature and particularly have been found in high quantities in many foods and plants, such as vegetables, fruits, cereals, spices, mushrooms, tea, microalgae, medical plants, wild fruits, and flowers [ 64 ].
There exists a considerable amount of evidence indicating the hepatoprotective effects of these biomolecules, unless they are in cultured cells and animal models. Their optimal dose and the concomitant length of the treatment period are not known [ 60 ].
Weight loss – conservative and surgical
Weight loss is the primary therapy for most patients with NAFLD. Weight loss can improve liver biochemical tests, liver histology, serum insulin levels, and quality of life in patients with NAFLD [ 65 , 66 , 67 , 68 , 69 ].
A significant body of literature has shown that weight loss induces a clinical improvement in patients with NAFLD or NASH. Several studies showed improvement of liver biochemistry after significant weight loss [ 65 , 66 , 67 , 68 , 69 , 70 ]. In a study of 25 Japanese individuals aminotransferases, cholesterol and fasting glucose improved significantly after a 3-months of combined exercise and dieting [ 69 ]. In a study done by Knobler et al. in 48 patients these results were substantiated by the fact that the majority of the patients had improved liver biochemistry and half of them had a complete normalisation of their transaminase profiles [ 68 ].
In the last few years there have been promising outcomes using pioglitazone (and related medication) [ 71 , 72 ], but also the use of Glucagon-like peptide-1 (GLP-1) receptor agonists has shown significant improvement in hepatic outcomes in patients with NAFLD [ 73 , 74 ].
In the last years, bariatric and metabolic surgery has made enormous developments. Its benefits regarding weight loss and improvement of several metabolic diseases, like T2DM has been well established [ 75 , 76 ]. It even has lead to a significantly better long-term overall survival compared to patients treated conservatively [ 75 , 76 , 77 ].
Specifically looking at NAFLD related outcomes, bariatric and metabolic surgery has not been taken into account as treatment option in many meta-analyses to date, despite the increasing body of evidence and properly designed studies on this subject. Lassailly et al. [ 78 ] found that bariatric and metabolic surgery results in resolution of NAFLD/NASH in the majority of the patients (64.2% in patients that underwent Roux-Y Gastric Bypass (RYGB) and 5.5% in Sleeve Gastrectomy (SG)). Secondly they found regression of the present liver fibrosis [ 78 ].
A meta-analysis on 48 studies showed that the combination of pioglitazone and Roux-en Y Gastric Bypass surgery had the best effects on the NAFLD Activity Score. This suggests a possible causal connection between glucose metabolism and NAFLD development [ 79 ]. It needs to be said that bariatric and metabolic surgery solely can impact the amelioration of NAFLD and related disorders, but also its impact on postoperative outcomes after surgery needs to be taken into account [ 80 ].
It has to be said that a small proportion of the patients undergoing bariatric and metabolic surgery develop NASH or suffer from aggravation of the disease (NAFLD/NASH/ live fibrosis) after bariatric surgery [ 81 ]. Also the patients on the ‘end of the spectrum’, with liver cirrhosis are in need of special preparation before and after bariatric and metabolic surgery, as highlighted in the systematic reviews done by Jan et al. [ 82 ] and Ahmed et al. [ 83 ] We need to consider that different surgical procedures have different effects on postoperative physiological remodelling and also can lead to (liver-related) complications. (See Fig. 1 ).
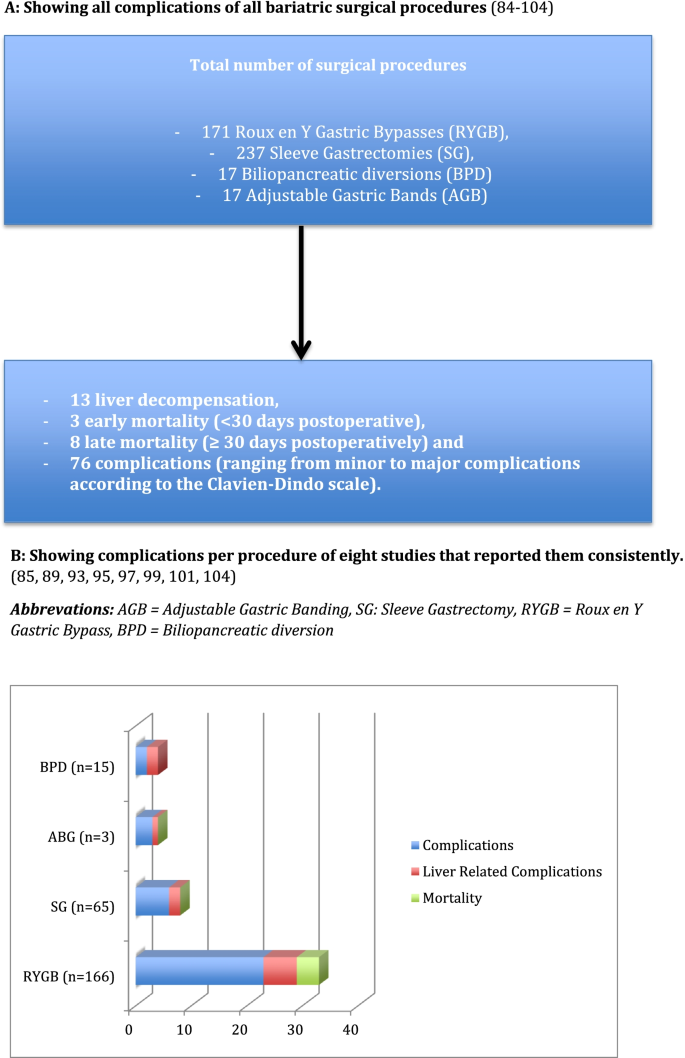
Complications in patients with liver cirrhosis undergoing bariatric and metabolic surgery. * Studies used in both the reviews by Jan et al. [ 82 ] en Ahmed et al. [ 83 ] (References [ 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 ]). A Showing all complications of all bariatric surgical procedures [ 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 ]. B Showing complications per procedure of eight studies that reported them consistently [ 85 , 89 , 93 , 95 , 97 , 99 , 101 , 104 ]. .Abbrevations: AGB = Adjustable Gastric Banding, SG: Sleeve Gastrectomy, RYGB = Roux en Y Gastric Bypass, BPD = Biliopancreatic diversion
Conclusions
With the growing obesity pandemic and the rising prevalence of comorbid conditions like T2DM and NAFLD, the management of these patients has become even more complex. There are some treatment methods, however there is lack of high-quality studies that compared different treatment methods with each other. Considering that bariatric surgery is increasingly utilized, prospective studies answering the remaining questions on the connection of insulin resistance, fatty liver, and fibrosis progression should become available in the near future.
Availability of data and materials
Not applicable.
Ahmed A, Wong RJ, Harrison SA. Nonalcoholic fatty liver disease review: diagnosis, treatment, and outcomes. Clin Gastroenterol Hepatol. 2015;13(12):2062–70.
Article PubMed Google Scholar
Machado MV, Diehl AM. Pathogenesis of nonalcoholic Steatohepatitis. Gastroenterology. 2016;150(8):1769–77.
Article CAS PubMed Google Scholar
Nasr P, Ignatova S, Kechagias S, Ekstedt M. Natural history of nonalcoholic fatty liver disease: a prospective follow-up study with serial biopsies. Hepatol Commun. 2018;2(2):199–210.
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018;15(1):11–20.
Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology (Baltimore, Md). 2004;40(6):1387–95.
Article Google Scholar
Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Gastroenterological Association, American Association for the Study of Liver Diseases, and American College of Gastroenterology. Gastroenterology. 2012;142(7):1592–609.
Dixon JB, Bhathal PS, O'Brien PE. Nonalcoholic fatty liver disease: predictors of nonalcoholic steatohepatitis and liver fibrosis in the severely obese. Gastroenterology. 2001;121(1):91–100.
Clark JM, Brancati FL, Diehl AM. The prevalence and etiology of elevated aminotransferase levels in the United States. Am J Gastroenterol. 2003;98(5):960–7.
Edmison J, McCullough AJ. Pathogenesis of non-alcoholic steatohepatitis: human data. Clin Liver Dis. 2007;11(1):75–104, ix.
Erbas O, Erdogan MA, Khalilnezhad A, Gürkan FT, Yiğittürk G, Meral A, et al. Neurobehavioral effects of long-term maternal fructose intake in rat offspring. Int J Dev Neurosci. 2018;69:68–79.
Lau JK, Zhang X, Yu J. Animal models of non-alcoholic fatty liver disease: current perspectives and recent advances. J Pathol. 2017;241(1):36–44.
Day CP, Saksena S. Non-alcoholic steatohepatitis: definitions and pathogenesis. J Gastroenterol Hepatol. 2002;17(Suppl 3):S377–84.
Chitturi S, Farrell GC. Etiopathogenesis of nonalcoholic steatohepatitis. Semin Liver Dis. 2001;21(1):27–41.
Fromenty B, Pessayre D. Impaired mitochondrial function in microvesicular steatosis. Effects of drugs, ethanol, hormones and cytokines. J Hepatol. 1997;26(Suppl 2):43–53.
Byrne CD, Targher G. NAFLD: a multisystem disease. J Hepatol. 2015;62(1):S47–64.
Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10(6):330–44.
EASL. EASD&EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388–402.
Bhatia LS, Curzen NP, Calder PC, Byrne CD. Non-alcoholic fatty liver disease: a new and important cardiovascular risk factor? Eur Heart J. 2012;33(10):1190–200.
Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363(14):1341–50.
Ou H, Fu Y, Liao W, Zheng C, Wu X. Association between smoking and liver fibrosis among patients with nonalcoholic fatty liver disease. Can J Gastroenterol Hepatol. 2019;2019:6028952.
Article PubMed PubMed Central Google Scholar
Targher G, Bertolini L, Padovani R, Rodella S, Tessari R, Zenari L, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30(5):1212–8.
Lonardo A, Sookoian S, Pirola CJ, Targher G. Non-alcoholic fatty liver disease and risk of cardiovascular disease. Metabolism. 2016;65(8):1136–50.
Hamabe A, Uto H, Imamura Y, Kusano K, Mawatari S, Kumagai K, et al. Impact of cigarette smoking on onset of nonalcoholic fatty liver disease over a 10-year period. J Gastroenterol. 2011;46(6):769–78.
Akhavan Rezayat A, Dadgar Moghadam M, Ghasemi Nour M, Shirazinia M, Ghodsi H, Rouhbakhsh Zahmatkesh MR, et al. Association between smoking and non-alcoholic fatty liver disease: a systematic review and meta-analysis. SAGE Open Med. 2018;6:2050312117745223.
Control CfD. Current cigarette smoking among adults - United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(44):889–94.
Google Scholar
Azzalini L, Ferrer E, Ramalho LN, Moreno M, Domínguez M, Colmenero J, et al. Cigarette smoking exacerbates nonalcoholic fatty liver disease in obese rats. Hepatology. 2010;51(5):1567–76.
Al-Dayyat HM, Rayyan YM, Tayyem RF. Non-alcoholic fatty liver disease and associated dietary and lifestyle risk factors. Diabetes Metab Syndr. 2018;12(4):569–75.
Chavez-Tapia NC, Lizardi-Cervera J, Perez-Bautista O, Ramos-Ostos MH, Uribe M. Smoking is not associated with nonalcoholic fatty liver disease. World J Gastroenterol. 2006;12(32):5196–200.
CAS PubMed PubMed Central Google Scholar
Bacon BR, Farahvash MJ, Janney CG, Neuschwander-Tetri BA. Nonalcoholic steatohepatitis: an expanded clinical entity. Gastroenterology. 1994;107(4):1103–9.
Mofrad P, Contos MJ, Haque M, Sargeant C, Fisher RA, Luketic VA, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology (Baltimore, Md). 2003;37(6):1286–92.
Noguchi H, Tazawa Y, Nishinomiya F, Takada G. The relationship between serum transaminase activities and fatty liver in children with simple obesity. Acta Paediatr Jpn Overseas Edition. 1995;37(5):621–5.
Charatcharoenwitthaya P, Lindor KD, Angulo P. The spontaneous course of liver enzymes and its correlation in nonalcoholic fatty liver disease. Dig Dis Sci. 2012;57(7):1925–31.
Schwenzer NF, Springer F, Schraml C, Stefan N, Machann J, Schick F. Non-invasive assessment and quantification of liver steatosis by ultrasound, computed tomography and magnetic resonance. J Hepatol. 2009;51(3):433–45.
Lonardo A, Bellini M, Tondelli E, Frazzoni M, Grisendi A, Pulvirenti M, et al. Nonalcoholic steatohepatitis and the "bright liver syndrome": should a recently expanded clinical entity be further expanded? Am J Gastroenterol. 1995;90(11):2072–4.
CAS PubMed Google Scholar
Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology (Baltimore, Md). 2011;54(3):1082–90.
Mottin CC, Moretto M, Padoin AV, Swarowsky AM, Toneto MG, Glock L, et al. The role of ultrasound in the diagnosis of hepatic steatosis in morbidly obese patients. Obes Surg. 2004;14(5):635–7.
de Moura AA, Cotrim HP, Barbosa DB, de Athayde LG, Santos AS, Bitencourt AG, et al. Fatty liver disease in severe obese patients: diagnostic value of abdominal ultrasound. World J Gastroenterol. 2008;14(9):1415–8.
Adams LA, Talwalkar JA. Diagnostic evaluation of nonalcoholic fatty liver disease. J Clin Gastroenterol. 2006;40(Suppl 1):S34–8.
Wong GL, Wong VW. Fat and fiber: how the controlled attenuation parameter complements noninvasive assessment of liver fibrosis. Dig Dis Sci. 2015;60(1):9–12.
Karlas T, Petroff D, Sasso M, Fan JG, Mi YQ, de Lédinghen V, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66(5):1022–30.
Shi KQ, Tang JZ, Zhu XL, Ying L, Li DW, Gao J, et al. Controlled attenuation parameter for the detection of steatosis severity in chronic liver disease: a meta-analysis of diagnostic accuracy. J Gastroenterol Hepatol. 2014;29(6):1149–58.
Rofsky NM, Fleishaker H. CT and MRI of diffuse liver disease. Semin Ultrasound CT MR. 1995;16(1):16–33.
Szczepaniak LS, Nurenberg P, Leonard D, Browning JD, Reingold JS, Grundy S, et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am J Physiol Endocrinol Metab. 2005;288(2):E462–8.
Borra RJ, Salo S, Dean K, Lautamäki R, Nuutila P, Komu M, et al. Nonalcoholic fatty liver disease: rapid evaluation of liver fat content with in-phase and out-of-phase MR imaging. Radiology. 2009;250(1):130–6.
Merriman RB, Ferrell LD, Patti MG, Weston SR, Pabst MS, Aouizerat BE, et al. Correlation of paired liver biopsies in morbidly obese patients with suspected nonalcoholic fatty liver disease. Hepatology (Baltimore, Md). 2006;44(4):874–80.
Arun J, Jhala N, Lazenby AJ, Clements R, Abrams GA. Influence of liver biopsy heterogeneity and diagnosis of nonalcoholic steatohepatitis in subjects undergoing gastric bypass. Obes Surg. 2007;17(2):155–61.
Ratziu V, Charlotte F, Heurtier A, Gombert S, Giral P, Bruckert E, et al. Sampling variability of liver biopsy in nonalcoholic fatty liver disease. Gastroenterology. 2005;128(7):1898–906.
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology (Baltimore, Md). 2005;41(6):1313–21.
Nseir W, Hellou E, Assy N. Role of diet and lifestyle changes in nonalcoholic fatty liver disease. World J Gastroenterol. 2014;20(28):9338–44.
Romero-Gómez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67(4):829–46.
Freidoony L, Kong ID. Practical approaches to the nutritional management of nonalcoholic fatty liver disease. Integr Med Res. 2014;3(4):192–7.
Pintó X, Fanlo-Maresma M, Corbella E, Corbella X, Mitjavila MT, Moreno JJ, et al. A Mediterranean diet rich in extra-virgin olive oil is associated with a reduced prevalence of nonalcoholic fatty liver disease in older individuals at high cardiovascular risk. J Nutr. 2019;149(11):1920–9.
Siddiqi Z, Karoli R, Fatima J, Khanduri S, Varshneya S, Ahmad SS. Soft drinks consumption and the risk of nonalcoholic fatty liver disease. J Assoc Physicians India. 2017;65(5):28–32.
PubMed Google Scholar
Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, Webb M, Blendis L, Halpern Z, et al. Long term nutritional intake and the risk for non-alcoholic fatty liver disease (NAFLD): a population based study. J Hepatol. 2007;47(5):711–7.
Hallsworth K, Adams LA. Lifestyle modification in NAFLD/NASH: facts and figures. JHEP Rep. 2019;1(6):468–79.
Ampong I, Watkins A, Gutierrez-Merino J, Ikwuobe J, Griffiths HR. Dietary protein insufficiency: an important consideration in fatty liver disease? Br J Nutr. 2020;123(6):601–9.
De Chiara F, Ureta Checcllo C, Ramón AJ. High protein diet and metabolic plasticity in non-alcoholic fatty liver disease: myths and truths. Nutrients. 2019;11(12):2985. https://doi.org/10.3390/nu11122985 .
Miller EF. Nutrition management strategies for nonalcoholic fatty liver disease: treatment and prevention. Clin Liver Dis. 2020;15(4):144–8.
Perumpail BJ, Li AA, John N, Sallam S, Shah ND, Kwong W, et al. The role of vitamin E in the treatment of NAFLD. Diseases (Basel, Switzerland). 2018;6(4):86. https://doi.org/10.3390/diseases6040086 .
Bugianesi E. Non-alcoholic fatty liver disease: a 360-degree overview. Switzerland: Springer Nature; 2020. https://doi.org/10.1007/978-3-319-95828-6 .
Wijarnpreecha K, Thongprayoon C, Ungprasert P. Coffee consumption and risk of nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2017;29(2):e8–e12.
Chen YP, Lu FB, Hu YB, Xu LM, Zheng MH, Hu ED. A systematic review and a dose-response meta-analysis of coffee dose and nonalcoholic fatty liver disease. Clin Nutr (Edinburgh, Scotland). 2019;38(6):2552–7.
Article CAS Google Scholar
Abenavoli L, Milic N, Luzza F, Boccuto L, De Lorenzo A. Polyphenols treatment in patients with nonalcoholic fatty liver disease. J Transl Intern Med. 2017;5(3):144–7.
Li S, Tan HY, Wang N, Cheung F, Hong M, Feng Y. The potential and action mechanism of polyphenols in the treatment of liver diseases. Oxidative Med Cell Longev. 2018;2018:8394818.
Petersen KF, Dufour S, Befroy D, Lehrke M, Hendler RE, Shulman GI. Reversal of nonalcoholic hepatic steatosis, hepatic insulin resistance, and hyperglycemia by moderate weight reduction in patients with type 2 diabetes. Diabetes. 2005;54(3):603–8.
Promrat K, Kleiner DE, Niemeier HM, Jackvony E, Kearns M, Wands JR, et al. Randomized controlled trial testing the effects of weight loss on nonalcoholic steatohepatitis. Hepatology (Baltimore, Md). 2010;51(1):121–9.
Article CAS PubMed Central Google Scholar
Keating SE, Hackett DA, George J, Johnson NA. Exercise and non-alcoholic fatty liver disease: a systematic review and meta-analysis. J Hepatol. 2012;57(1):157–66.
Knobler H, Schattner A, Zhornicki T, Malnick SD, Keter D, Sokolovskaya N, et al. Fatty liver--an additional and treatable feature of the insulin resistance syndrome. QJM. 1999;92(2):73–9.
Ueno T, Sugawara H, Sujaku K, Hashimoto O, Tsuji R, Tamaki S, et al. Therapeutic effects of restricted diet and exercise in obese patients with fatty liver. J Hepatol. 1997;27(1):103–7.
Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, Torres-Gonzalez A, Gra-Oramas B, Gonzalez-Fabian L, et al. Weight Loss Through Lifestyle Modification Significantly Reduces Features of Nonalcoholic Steatohepatitis. Gastroenterology. 2015;149(2):367–78 e5 quiz e14-5.
Colca JR, Scherer PE. The metabolic syndrome, Thiazolidinediones, and implications for intersection of chronic and inflammatory disease. Mol Metab. 2021;101409. https://doi.org/10.1016/j.molmet.2021.101409 .
Takahashi H, Kessoku T, Kawanaka M, Nonaka M, Hyogo H, Fujii H, et al. Ipragliflozin improves the hepatic outcomes of patients with diabetes with NAFLD. Hepatol Commun. 2022;6(1):120–32. https://doi.org/10.1002/hep4.1696 .
Ghosal S, Datta D, Sinha B. A meta-analysis of the effects of glucagon-like-peptide 1 receptor agonist (GLP1-RA) in nonalcoholic fatty liver disease (NAFLD) with type 2 diabetes (T2D). Sci Rep. 2021;11(1):22063.
Rezaei S, Tabrizi R, Nowrouzi-Sohrabi P, Jalali M, Atkin SL, Al-Rasadi K, et al. GLP-1 receptor agonist effects on lipid and liver profiles in patients with nonalcoholic fatty liver disease: systematic review and Meta-analysis. Can J Gastroenterol Hepatol. 2021;2021:8936865.
Sjöström L, Narbro K, Sjöström CD, Karason K, Larsson B, Wedel H, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357(8):741–52.
Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Carlsson LMS, Sjöholm K, Jacobson P, Andersson-Assarsson JC, Svensson PA, Taube M, et al. Life expectancy after bariatric surgery in the Swedish obese subjects study. N Engl J Med. 2020;383(16):1535–43.
Lassailly G, Caiazzo R, Buob D, Pigeyre M, Verkindt H, Labreuche J, et al. Bariatric surgery reduces features of nonalcoholic Steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149(2):379–88 quiz e15-6.
Panunzi S, Maltese S, Verrastro O, Labbate L, De Gaetano A, Pompili M, et al. Pioglitazone and bariatric surgery are the most effective treatments for non-alcoholic steatohepatitis: a hierarchical network meta-analysis. Diabetes Obes Metab. 2021;23(4):980–90.
Goossens N, Hoshida Y, Song WM, Jung M, Morel P, Nakagawa S, et al. Nonalcoholic Steatohepatitis is associated with increased mortality in obese patients undergoing bariatric surgery. Clin Gastroenterol Hepatol. 2016;14(11):1619–28.
Eilenberg M, Langer FB, Beer A, Trauner M, Prager G, Staufer K. Significant liver-related morbidity after bariatric surgery and its reversal-a case series. Obes Surg. 2018;28(3):812–9.
Jan A, Narwaria M, Mahawar KK. A systematic review of bariatric surgery in patients with liver cirrhosis. Obes Surg. 2015;25(8):1518–26.
Ahmed S, Pouwels S, Parmar C, Kassir R, de Luca M, Graham Y, et al. Outcomes of bariatric surgery in patients with liver cirrhosis: a systematic review. Obes Surg. 2021;31(5):2255–67.
Brolin RE, Bradley LJ, Taliwal RV. Unsuspected cirrhosis discovered during elective obesity operations. Arch Surg (Chicago, Ill : 1960). 1998;133(1):84–8.
Dallal RM, Mattar SG, Lord JL, Watson AR, Cottam DR, Eid GM, et al. Results of laparoscopic gastric bypass in patients with cirrhosis. Obes Surg. 2004;14(1):47–53.
Kral JG, Thung SN, Biron S, Hould FS, Lebel S, Marceau S, et al. Effects of surgical treatment of the metabolic syndrome on liver fibrosis and cirrhosis. Surgery. 2004;135(1):48–58.
Sarr MG. Is a bariatric procedure appropriate in patients with portal hypertension secondary to cirrhosis? Surgery for obesity and related diseases : official journal of the American Society for Bariatric. Surgery. 2006;2(3):405–6 discussion 6-7.
Takata MC, Campos GM, Ciovica R, Rabl C, Rogers SJ, Cello JP, et al. Laparoscopic bariatric surgery improves candidacy in morbidly obese patients awaiting transplantation. Surg Obes Relat Dis. 2008;4(2):159–64 discussion 64-5.
Shimizu H, Phuong V, Maia M, Kroh M, Chand B, Schauer PR, et al. Bariatric surgery in patients with liver cirrhosis. Surg Obes Relat Dis. 2013;9(1):1–6.
Rebibo L, Gerin O, Verhaeghe P, Dhahri A, Cosse C, Regimbeau JM. Laparoscopic sleeve gastrectomy in patients with NASH-related cirrhosis: a case-matched study. Surg Obes Relat Dis. 2014;10(3):405–10 quiz 565.
Woodford RM, Burton PR, O'Brien PE, Laurie C, Brown WA. Laparoscopic adjustable gastric banding in patients with unexpected cirrhosis: safety and outcomes. Obes Surg. 2015;25(10):1858–62.
Lin MY, Tavakol MM, Sarin A, Amirkiai SM, Rogers SJ, Carter JT, et al. Safety and feasibility of sleeve gastrectomy in morbidly obese patients following liver transplantation. Surg Endosc. 2013;27(1):81–5.
Pestana L, Swain J, Dierkhising R, Kendrick ML, Kamath PS, Watt KD. Bariatric surgery in patients with cirrhosis with and without portal hypertension: a single-center experience. Mayo Clin Proc. 2015;90(2):209–15.
Wolter S, Duprée A, Coelius C, El Gammal A, Kluwe J, Sauer N, et al. Influence of liver disease on perioperative outcome after bariatric surgery in a northern German cohort. Obes Surg. 2017;27(1):90–5.
Hanipah ZN, Punchai S, McCullough A, Dasarathy S, Brethauer SA, Aminian A, et al. Bariatric surgery in patients with cirrhosis and portal hypertension. Obes Surg. 2018;28(11):3431–8.
García-Sesma A, Calvo J, Manrique A, Cambra F, Justo I, Caso O, et al. Morbidly obese patients awaiting liver transplantation-sleeve Gastrectomy: safety and efficacy from a liver transplant unit experience. Transplant Proc. 2019;51(1):33–7.
Moulla Y, Lyros O, Blüher M, Simon P, Dietrich A. Feasibility and safety of bariatric surgery in high-risk patients: a single-center experience. J Obes. 2018;2018:7498258.
Miñambres I, Rubio MA, de Hollanda A, Breton I, Vilarrasa N, Pellitero S, et al. Outcomes of bariatric surgery in patients with cirrhosis. Obes Surg. 2019;29(2):585–92.
Younus H, Sharma A, Miquel R, Quaglia A, Kanchustambam SR, Carswell KA, et al. Bariatric surgery in cirrhotic patients: is it safe? Obes Surg. 2020;30(4):1241–8.
Frey S, Petrucciani N, Iannelli A. Bariatric surgery in the setting of liver cirrhosis with portal hypertension: the confection and particularities of roux-en-Y gastric bypass in a high-risk patient. Obes Surg. 2020;30(10):4165–6.
Quezada N, Maturana G, Irarrázaval MJ, Muñoz R, Morales S, Achurra P, et al. Bariatric surgery in cirrhotic patients: a matched case-control study. Obes Surg. 2020;30(12):4724–31. https://doi.org/10.1007/s11695-020-04929-y .
Kaul A, Singla V, Baksi A, Aggarwal S, Bhambri A, Shalimar A, et al. Safety and efficacy of bariatric surgery in advanced liver fibrosis. Obes Surg. 2020;30:4359–65.
Salman MA, Mikhail HMS, Nafea MA, Sultan A, Elshafey HE, Tourky M, et al. Impact of laparoscopic sleeve gastrectomy on fibrosis stage in patients with child-a NASH-related cirrhosis. Surg Endosc. 2021;35(3):1269–77. https://doi.org/10.1007/s00464-020-07498-4 .
Vuppalanchi R, McCabe MET, Tandra SR, Parcha SP, Ghafoor A, Schuh L, et al. Safety and efficacy of bariatric surgery in cirrhosis patients with extreme obesity. Ann Surg. 2022;275(1):e174–80. https://doi.org/10.1097/SLA.0000000000003891 .
Download references
Acknowledgements
Author information, authors and affiliations.
Department of Intensive Care Medicine, Elisabeth-Tweesteden Hospital, Hilvarenbeekseweg 60, P.O. Box 90151, 5000 LC, Tilburg, The Netherlands
Sjaak Pouwels & Dharmanand Ramnarain
Department of Surgery, Holy Family Hospital, Nazareth, Israel, and the Azrieli Faculty of Medicine, Bar-Ilan University, Safed, Israel
Nasser Sakran
Faculty of Health Sciences and Wellbeing, University of Sunderland, Sunderland, UK
Yitka Graham & Kamal Mahawar
Facultad de Psycologia, Universidad Anahuac Mexico, Mexico City, Mexico
Yitka Graham
Department of Bariatric Surgery, Christus Muguerza Conchita Hospital, Monterrey, Mexico
Angela Leal
Department of Abdominal Surgery, University Medical Center Ljubljana, Zaloška cesta, Ljubljana, Slovenia
Tadeja Pintar
Department of Metabolic and Bariatric Surgery, The First Affiliated Hospital of Jinan University, Guangzhou, China
CHU Félix Guyon, Allée des Topazes, Saint-Denis, France
Radwan Kassir
Bariatric and Upper GI Unit, Birmingham Heartlands Hospital, University Hospital Birmingham NHS Foundation Trust, Birmingham, UK
Rishi Singhal
Bariatric Unit, South Tyneside and Sunderland NHS Foundation Trust, Sunderland, UK
Kamal Mahawar
Department of Intensive Care Medicine, Saxenburg Medical Centre, Hardenberg, The Netherlands
Dharmanand Ramnarain
You can also search for this author in PubMed Google Scholar
Contributions
Collecting data and articles for the review: SP, NS, YG, AL, TP, WY, RK, RS, KM, and DR. Writing the manuscript: SP, NS, YG, AL, TP, WY, RK, RS, KM, and DR. Final approval: SP, NS, YG, AL, TP, WY, RK, RS, KM, and DR.
Corresponding author
Correspondence to Sjaak Pouwels .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Pouwels, S., Sakran, N., Graham, Y. et al. Non-alcoholic fatty liver disease (NAFLD): a review of pathophysiology, clinical management and effects of weight loss. BMC Endocr Disord 22 , 63 (2022). https://doi.org/10.1186/s12902-022-00980-1
Download citation
Received : 12 July 2021
Accepted : 02 March 2022
Published : 14 March 2022
DOI : https://doi.org/10.1186/s12902-022-00980-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Non-alcoholic fatty liver disease
- Weight management
- Bariatric surgery
- Metabolic surgery
- Conservative therapy
BMC Endocrine Disorders
ISSN: 1472-6823
- General enquiries: [email protected]
The regional disparities in liver disease comorbidity among elderly Chinese based on a health ecological model: the China Health and Retirement Longitudinal Study
Affiliations.
- 1 Public Health School, Ningxia Medical University, Yinchuan, 750004, China.
- 2 Key Laboratory of Environmental Factors and Chronic Disease Control, Yinchuan, 750004, China.
- 3 School of Medical Information and Engineering, Ningxia Medical University, Yinchuan, 750004, China.
- 4 School of Clinical Medicine, Ningxia Medical University, Yinchuan, 750004, China.
- 5 Public Health School, Ningxia Medical University, Yinchuan, 750004, China. [email protected].
- 6 Key Laboratory of Environmental Factors and Chronic Disease Control, Yinchuan, 750004, China. [email protected].
- 7 Research Center for Medical Science and Technology, Ningxia Medical University, Yinchuan, 750004, China. [email protected].
- 8 Ningxia Institute of Medical Science, Yinchuan, 750004, China. [email protected].
- 9 Public Health School, Ningxia Medical University, Yinchuan, 750004, China. [email protected].
- 10 Key Laboratory of Environmental Factors and Chronic Disease Control, Yinchuan, 750004, China. [email protected].
- PMID: 38654168
- PMCID: PMC11040959
- DOI: 10.1186/s12889-024-18494-x
Purpose: This study aimed to investigate the risk factors for liver disease comorbidity among older adults in eastern, central, and western China, and explored binary, ternary and quaternary co-morbid co-causal patterns of liver disease within a health ecological model.
Method: Basic information from 9,763 older adults was analyzed using data from the China Health and Retirement Longitudinal Study (CHARLS). LASSO regression was employed to identify significant predictors in eastern, central, and western China. Patterns of liver disease comorbidity were studied using association rules, and spatial distribution was analyzed using a geographic information system. Furthermore, binary, ternary, and quaternary network diagrams were constructed to illustrate the relationships between liver disease comorbidity and co-causes.
Results: Among the 9,763 elderly adults studied, 536 were found to have liver disease comorbidity, with binary or ternary comorbidity being the most prevalent. Provinces with a high prevalence of liver disease comorbidity were primarily concentrated in Inner Mongolia, Sichuan, and Henan. The most common comorbidity patterns identified were "liver-heart-metabolic", "liver-kidney", "liver-lung", and "liver-stomach-arthritic". In the eastern region, important combination patterns included "liver disease-metabolic disease", "liver disease-stomach disease", and "liver disease-arthritis", with the main influencing factors being sleep duration of less than 6 h, frequent drinking, female, and daily activity capability. In the central region, common combination patterns included "liver disease-heart disease", "liver disease-metabolic disease", and "liver disease-kidney disease", with the main influencing factors being an education level of primary school or below, marriage, having medical insurance, exercise, and no disabilities. In the western region, the main comorbidity patterns were "liver disease-chronic lung disease", "liver disease-stomach disease", "liver disease-heart disease", and "liver disease-arthritis", with the main influencing factors being general or poor health satisfaction, general or poor health condition, severe pain, and no disabilities.
Conclusion: The comorbidities associated with liver disease exhibit specific clustering patterns at both the overall and local levels. By analyzing the comorbidity patterns of liver diseases in different regions and establishing co-morbid co-causal patterns, this study offers a new perspective and scientific basis for the prevention and treatment of liver diseases.
Keywords: Association rules; Co-morbid co-causal pattern; Elderly people; Geographic information system; Liver disease comorbidity.
© 2024. The Author(s).
Publication types
- Research Support, Non-U.S. Gov't
- Aged, 80 and over
- China / epidemiology
- Comorbidity*
- East Asian People
- Health Status Disparities
- Liver Diseases* / epidemiology
- Longitudinal Studies
- Middle Aged
- Risk Factors
Grants and funding
- No. XT2020024/Scientific research project of Ningxia Medical University in 2020
- No. 82060597/This work was supported by the National Natural Science Foundation of China
- 2021BEG03031/Key research and development project in Ningxia
Scientists Discover a New Signaling Pathway and Design a Novel Drug for Liver Fibrosis
Their research could lead to treatment for a variety of liver diseases and conditions..
- Judith Myers - [email protected]
Media contact:
- Miles Martin - [email protected]
Published Date
Topics covered:.
- Liver fibrosis
- Fatty liver disease
Share This:
Article content.
A healthy liver filters all the blood in your body, breaks down toxins and digests fats. It produces collagen to repair damaged cells when the liver is injured. However, a liver can produce too much collagen when an excess accumulation of fat causes chronic inflammation, a condition called metabolic dysfunction-associated steatohepatitis (MASH). In an advanced state, MASH can lead to cirrhosis, liver cancer and liver-related death.
The cells that produce collagen in livers are called hepatic stellate cells (HSC). In a new paper published in Cell Metabolism , scientists from the University of California San Diego investigated how these cells are activated. They found a three-component signaling pathway in the nucleus that functions according to a sort of police-controlling-the-police model.
In healthy livers, the first molecule in the pathway inhibits a second molecule, which inhibits the molecule that stimulates collagen-producing genes. MASH scales down the first molecule, so that inhibition is lifted on the second and third molecules, leading to stimulation of collagen production.
After discovering the signaling pathway, the scientists designed a short piece of RNA to prove the pathway behaved the way they thought it did. This RNA, called an antisense oligonucleotide (ASO), was so effective that it not only proved the viability of the pathway but also prevented liver fibrosis — too much collagen in the liver — without causing any side effects. The scientists are currently discussing licensing the ASO as a therapeutic with various pharmaceutical and biotech companies.
“All the molecules in the pathway were known, but no one knew if or how they interacted. We put the pathway together, showing each step in this intracellular signaling module. That was the science of the research. The clinical message is this ASO, which can actually block liver fibrosis,” said Jerrold Olefsky, a professor of medicine and assistant vice chancellor for integrative research at UC San Diego Health Sciences, and senior author on the paper.
The scientists carried out their investigations in organoids — tiny little livers in a dish made from three types of liver cells fed a MASH cocktail of fatty acids, fructose and sugars. They found that in normal livers, the first component of the pathway, a nuclear seven-transmembrane protein called TM7SF3, inhibits a splicing factor called hnRNPU. hnRNPU refrains from splicing out an inhibitory exon in the messenger RNA (mRNA) of TEAD1, a transcription factor that controls the genes that produce collagen. The inhibitory exon, exon 5, keeps TEAD1 from turning on the collagen-producing genes.
{/exp:typographee}
Schematic of the TEAD 1 signaliing module that drives liver fibrosis. Photo by UC San Diego Health Sciences
In the MASH-fed organoids, TM7SF3 is reduced and does not inhibit the splicing factor. The active splicing factor splices out the inhibitory exon in the transcription factor, which turns on the genes that produce collagen. This is called alternative splicing.
Furthering their investigations, they designed an ASO to keep hnRNPU from splicing out exon 5. “It had the sequence that would put it just upstream of exon 5 where hnRPU binds. The ASO prevented the splicing factor from binding to the TEAD mRNA, so it couldn’t ultimately splice it out. We got pretty much only inactive TEAD when we treated MASH mice with the ASO,” said Olefsky. With TEAD inactivated, collagen wasn’t produced. Neither was fibrosis.
“These findings show the key role of alternative splicing in shaping progression of fibrotic liver disease,” said Roi Isaac, Ph.D., assistant project scientist, Medicine, and first author on the paper.
When ASOs are administered intravenously, they enter every cell in the body, not just the target cells. Serendipitously, the scientists found that within the liver, this hnRNPU mechanism only operated in stellate cells. That made their ASO both highly effective and highly specific — the epitome of good drug design.
According to Olefsky, a quarter of the U.S. population has MASH. While the scientists’ ASO may well be an effective treatment, getting FDA approval for it would necessitate enormous clinical studies and could cost up to a billion dollars.
Olefsky and his team identified a much less common disease called primary sclerosing cholangitis, or PSC. It's relatively rare, often fatal, and until now there were no good treatments. When the scientists tested their ASO on a mouse model of PSC, they found that their ASO almost completely blocked the development of the disease. “Getting FDA approval for PSC would be easier than getting it for MASH,” said Olefsky, “so we’re currently talking to biotech and pharma partners about licensing the ASO for PSC.”
Additional authors are: Gautam Bandyopadhyay, Theresa V. Rohm, Sion Kang, Jinyue Wang, Narayan Pokhre, Sadatsugu Sakane, Rizaldy Zapata, Avraham M. Libster, Asres Berhan,Tatiana Kisseleva, Zea Borok, Francesca Telese, Nicholas JG Webster of the University of California San Diego, and Varon Vinik and Yehiel Zick of the Weizmann Institute of Science, Israel.
This study was funded by the National Institutes of Health, the Swiss National Science Foundation, the Larry L. Hillblom Foundation, and Janssen Pharmaceuticals.
Disclosures: Roi Isaac and Jerrold Olefsky are co-inventors on a provisional patent for the use of ASO 56 as an inhibitor of liver fibrosis.
“All the molecules in the pathway were known, but no one knew if or how they interacted. We put the pathway together. That was the science of the research. The clinical message is this ASO, which can actually block liver fibrosis.”
You May Also Like
Soft robots, tough problems, a message from chancellor pradeep k. khosla, closing the u.s./mexico border during covid-19 increased hiv transmission, scientists show ancient village adapted to drought, rising seas, stay in the know.
Keep up with all the latest from UC San Diego. Subscribe to the newsletter today.
You have been successfully subscribed to the UC San Diego Today Newsletter.
Campus & Community
Arts & culture, visual storytelling.
- Media Resources & Contacts
Signup to get the latest UC San Diego newsletters delivered to your inbox.
Award-winning publication highlighting the distinction, prestige and global impact of UC San Diego.
Popular Searches: Covid-19 Ukraine Campus & Community Arts & Culture Voices
- Un common compassion
- Un wavering dedication
- Un breakable resolve
- Find a Provider
Featured Services
Specialty services.
- < Back Locations
- VCU Medical Center (Downtown Richmond)
- Children's Hospital of Richmond at VCU
- Community Memorial
- VCU Massey Comprehensive Cancer Center
- Pauley Heart Center
- Search VCU Health
- VCU Health Home
- Medical Services
Find a Location
Request an Appointment
- Refer your Patient
Patients & Visitors
VCU Health MyChart
Pay My Bill
For Your Health
Hospitals & care centers.
- VCU Health Community Memorial Hospital
- VCU Health Tappahannock Hospital
Comprehensive Care Centers
- Hume-Lee Transplant Center
- Neurosciences
Research & Clinical Trials
Health professionals, vcu health sciences: education.
How can we help you today?
General Information
1-800-762-6161
Get Directions with VCU Health Way Finder
COVID-19 Information
EpicCare Link
Traffic Updates
Traffic updates at our MCV Campus
What can we help you find?
Popular search terms.
- Medical Records
- Our Services
Related Search Terms
Related search results, providers ( 0 ), locations ( 0 ), classes & events ( 0 ), providers by specialty ( 0 ), suggested terms, news center.
- COVID-19 Vaccine
- Sign up for COVID-19 and Vaccine Updates
- COVID-19 Symptom Checker
- Latest News
- In The Media
- Inspiring Stories
- News Releases
- Health and Wellness
- Removing obstacles facing our community
- Helping our communities during COVID-19
- Creating opportunities in our workforce
- Research on health disparities
- For Journalists
- Search Our News

New study shows liver patients see benefits after going meatless for one meal
Vcu school of medicine, richmond va medical center researchers discover that replacing meat with plant-based proteins for one meal lowers harmful ammonia levels..
5/2/2024 12:00:00 AM

By A.J. Hostetler Just one meal without meat can lower levels of harmful ammonia in people with advanced liver disease, researchers from Virginia Commonwealth University’s School of Medicine and Richmond VA Medical Center report. The study, a small clinical trial conducted on adults whose livers are permanently damaged by cirrhosis who eat a Western non-vegetarian diet, explored the effects of substituting one meal with a meatless option, vegan or vegetarian. High levels of ammonia in the blood are linked to cirrhosis and a type of cognitive decline called hepatic encephalopathy. Ammonia levels are also known to be influenced by factors such as gut bacteria and diet. While earlier studies hinted at the benefits of a vegetarian diet for those with cognitive problems caused by cirrhosis, implementing long-term dietary changes can be challenging for patients to make and sustain. Further research is still needed to investigate the impact of vegan diets on cirrhosis and ammonia. These factors prompted VCU gastroenterologist Jasmohan Bajaj , M.D., and a team of international colleagues to wonder whether a temporary dietary switch could make a significant impact on the interplay among ammonia levels, diet, and cirrhosis. Among the paper’s authors include Bryan Badal, M.D., a fellow in the VCU Department of Internal Medicine’s Division of Gastroenterology, Hepatology and Nutrition , and associate professor Leroy Thacker , Ph.D., of the VCU School of Population Health’s Department of Biostatistics . According to the preliminary results published today, May 2, in the journal Clinical and Translational Gastroenterology , even a single meatless meal eaten by patients with cirrhosis generates less harmful ammonia. “It was exciting to see that even small changes in your diet, like having one meal without meat once in a while, could benefit your liver by lowering harmful ammonia levels in patients with cirrhosis,” said Bajaj, a world-renowned expert in hepatic encephalopathy with the Richmond VA Medical Center, where the study was conducted, and the VCU Stravitz-Sanyal Institute for Liver Disease and Metabolic Health . “We now need more research to learn if consuming meals without meat goes beyond reducing ammonia to preventing problems in brain function and liver disease progression.” Ammonia is a waste product that bacteria in the intestines make when digesting food. It is normally processed in the liver, sent to the kidneys and then eliminated through urine. Livers severely damaged by cirrhosis, however, can’t process the ammonia, allowing dangerous levels of the toxin to rise and travel to the brain. Once there, the ammonia can impair cognitive function, causing confusion or delirium. This hepatic encephalopathy can lead to coma and can sometimes be fatal without treatment. Western-style meals, which are high in carbohydrates and red meat while low in fiber, can increase levels of ammonia. Could even a simple, infrequent adjustment in the diet, such as switching to non-meat options for a single meal, reduce ammonia levels and benefit liver patients? “It can be so hard to make long-term dietary and behavioral changes. We wondered if making an occasional change could be an option for these patients. Liver patients with cirrhosis should know that making positive changes in their diet doesn't have to be overwhelming or difficult,” Bajaj said. They studied 30 adults (including non-veterans) with cirrhosis who were treated at the Richmond VA Medical Center and who usually ate meat. They split them into three groups of 10 to eat three kinds of burgers: one made of pork/beef, one with a vegan meat substitute, and a vegetarian bean burger. Each burger contained 20 grams of protein, reflecting the amount in a typical Western meal. In addition to the burgers, participants ate low-fat potato chips and a whole-grain bun, along with water. No condiments or toppings were allowed. Although the patients had similar gut bacteria profiles initially, the type of meal seemed to affect ammonia levels differently. Blood and urine samples taken before and after meals revealed noteworthy differences. Just a few hours after eating, the samples revealed that those who ate a meat burger had higher amino acids associated with ammonia production and hepatic encephalopathy than those who ate the non-meat burgers. “The main take-home message was that occasionally skipping meat from just a single meal can have benefits for patients with cirrhosis. A simple change to a patient’s diet or substituting some parts of it could be a simple and accessible method to reduce ammonia generation,” Bajaj said. Although the results are preliminary, the study’s authors suggested that physicians should encourage liver patients who regularly eat meat to try and substitute meat with sources of protein from plant or dairy sources. A nutrition expert could provide valuable insights into the best foods for liver patients with cirrhosis, who still need to eat protein as part of a healthy diet. The researchers noted that the findings should be confirmed by exploring how changes in diet over time could have an even greater impact on patients with cirrhosis, the ninth-leading cause of death in the United States. The study was partly funded by grants from the American College of Gastroenterology Clinical Research Award, the Veterans Affairs Merit Review, the Richmond Institute for Veterans Research and the National Institute on Alcohol Abuse and Alcoholism.
Learn more about the VCU Stravitz-Sanyal Institute for Liver Disease and Metabolic Health.
Read more stories about the innovative researchers at VCU and VCU Health.

VCU community unites to promote organ donation awareness
Delving into the intricacies of drug development

With quick thinking and CPR skills, aspiring doctor helped save a restaurant customer’s life

IMAGES
VIDEO
COMMENTS
The first edition of the clinical practice guidelines for liver cirrhosis was published in 2010, and the second edition was published in 2015 by the Japanese Society of Gastroenterology (JSGE). The revised third edition was recently published in 2020. This version has become a joint guideline by the JSGE and the Japan Society of Hepatology (JSH).
Cirrhosis is widely prevalent worldwide and can be a consequence of different causes, such as obesity, non-alcoholic fatty liver disease, high alcohol consumption, hepatitis B or C infection, autoimmune diseases, cholestatic diseases, and iron or copper overload. Cirrhosis develops after a long period of inflammation that results in replacement of the healthy liver parenchyma with fibrotic ...
The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 2018;67:328-357. Crossref
Abstract. Liver disease is the major cause of death every year. Approximately 29 million people suffer from a chronic liver condition (Blachier M, et al, 2013 [1]) and more than 30 million ...
Steatotic liver disease is part of a revised nomenclature to replace the term fatty liver disease, but this should also drive forward innovation in research, diagnostics and treatments. Aleksander ...
Explore Liver Disease articles from The New England Journal of Medicine ... Research 625; Clinical Cases 408; Other 279; Review 256; Commentary 215; Media 69; Perspective 33; By Date. Past 6 months;
Liver inflammation is a key process that orchestrates intrahepatic injury. This Review offers a comprehensive overview of the inflammatory mechanisms of hepatic fibrosis and discusses current ...
Introduction. Liver disease accounts for over two million deaths annually (cirrhosis, viral hepatitis, and liver cancer) and accounts for 4% of all deaths worldwide (1 out of every 25 deaths); 1 out of 3 liver-related deaths occur among females ( Box 1 ). Within this estimate, liver cancer accounts for 600,000 to 900,000 deaths.
Liver Research is an international, open-access, peer-reviewed English journal that publishes reviews, editorials, and original articles describing novel developments covering all aspects of liver and biliary science on a quarterly basis. Liver Research delivers original research on the biology and diseases of the liver and biliary tree in both human and experimental models.
It is estimated that, by 2025, >1 million individuals will be affected by liver cancer annually 3. Hepatocellular carcinoma (HCC) is the most common form of liver cancer and accounts for ~90% of ...
Given the increasing prevalence of diabetes and obesity worldwide, the deleterious effects of non-alcoholic fatty liver disease (NAFLD) are becoming a growing challenge for public health. NAFLD is the most common chronic liver disease in the Western world. NAFLD is closely associated with metabolic disorders, including central obesity, dyslipidaemia, hypertension, hyperglycaemia and persistent ...
Among them, non-alcoholic fatty liver disease (NAFLD) is the primary cause, representing more than 50% of cases. NAFLD is characterized by the intracellular deposition of lipids in hepatocytes, often associated with a wide spectrum of metabolic abnormalities, such as obesity, diabetes, dyslipidemia, hypertension, and insulin resistance [].NAFLD represents a different range of liver disease ...
The computer-based approach is required for the non-invasive detection of chronic liver diseases that are asymptomatic, progressive, and potentially fatal in nature. In this study, we review the computer-aided diagnosis of hepatic lesions in view of diffuse- and focal liver disorders. This survey mainly focuses on three image acquisition ...
Thus, this suggests that ML methods predict liver disease by incorporating the risk factors, which may improve the inference-based diagnosis of patients. ... Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several ...
Chronic liver disease (CLD) is a major health concern for millions of people all over the globe. ... In this paper, research is applied on Resnet50 model for classification of DR and DME based on ...
This Special Issue welcomes contributions covering the current aspects of diagnosis and management of liver diseases. Submissions may include articles of current original research, new experimental methodology, and/or review articles summarizing the current state of the art for clinical diagnosis, state-of-the-art treatment, and management of ...
Purpose: This study aimed to investigate the risk factors for liver disease comorbidity among older adults in eastern, central, and western China, and explored binary, ternary and quaternary co-morbid co-causal patterns of liver disease within a health ecological model. Method: Basic information from 9,763 older adults was analyzed using data from the China Health and Retirement Longitudinal ...
Conversely, some xenobiotics and micronutrients have been recognized to have a protective effect in several liver diseases. This paper offers an overview of the current knowledge on the role of xenobiotics and micronutrients in liver damage. Keywords: xenobiotics, micronutrients, P450 enzymes, vitamins, herbs, red vine, spices.
In an advanced state, MASH can lead to cirrhosis, liver cancer and liver-related death. The cells that produce collagen in livers are called hepatic stellate cells (HSC). In a new paper published in Cell Metabolism, scientists from the University of California San Diego investigated how these cells are activated. They found a three-component ...
By A.J. Hostetler Just one meal without meat can lower levels of harmful ammonia in people with advanced liver disease, researchers from Virginia Commonwealth University's School of Medicine and Richmond VA Medical Center report. The study, a small clinical trial conducted on adults whose livers are permanently damaged by cirrhosis who eat a Western non-vegetarian diet, explored the ...
Liver diseases are diagnosed based on the liver functional test[1]. Several diseases states can disturb the liver. Some of the diseases are Wilson's disease, hepatitis (an inflammation of ... it was depicted that the past research studies have implemented different data mining techniques for classification of liver dataset. A hybrid model can ...