- Our Research
- Working with Business
- Our Partnerships

I’d like to learn more about Newcastle!
Professor roy taylor on discovering the cause of type 2 diabetes.
Once considered an irreversible condition that worsens with time, research at Newcastle University has shattered conventional beliefs about type 2 diabetes.
Professor Roy Taylor's pioneering discoveries have been accepted by the NHS - signifying more than just a scientific breakthrough, but marking a shift in how we perceive and treat type 2 diabetes (T2D). His findings - demonstrating the reversibility of T2D - have become a beacon of hope for thousands, empowering patients to transform their lives. Here, he shares with us what his research has involved.
What happens to food after you eat?
The role of the newcastle magnetic resonance centre, testing the hypothesis : counterpoint study, the personal fat threshold hypothesis, rolling out the weight loss method in primary care: direct, but how about t2d in people who are not overweight, the retune study: testing the second hypothesis, the retune study: a dditional findings, the nhs england path to remission programme.
Many scientific breakthroughs start with a simple question. What happens to food after you eat? When I moved to Newcastle as a junior doctor in 1979, we simply did not know.
Using newly developed advance magnetic resonance methods, we found that people destined to get type 2 diabetes (T2D) stored almost none of their meal carbohydrate as glycogen in muscle - we then showed that fat levels in the liver were high in such people. But all this research was done using MR scanners in other universities, and to take the research forwards, Newcastle University needed a dedicated MR Centre.

Pictured above, Newcastle Magnetic Resonance Centre opened in 2006 and is situated on the Health Innovation Neighbourhood.
Evoking enthusiasm for such a Magnetic Resonance Centre in Newcastle was the next task. It took from 2000 to 2004 to raise the necessary £5.2 million. A fine new building containing a 3 Tesla MR scanner opened in 2006 on what is now the Health Innovation Neighbourhood .
But by one of those quirks of fate, the final piece of the jigsaw of what causes T2D occurred to me just 3 months after the Newcastle MR Centre opened. When people with T2D were unable to eat after bariatric surgery, their blood sugar levels fell. This was widely thought to have other explanations, but to me it all fitted together: Over a period of years, people unable to store glucose normally after eating would steadily increase the level of fat in the liver with a knock-on increase in fat on the pancreas.
I called this my Twin Cycle Hypothesis , publishing this in 2008.
In this, I postulated that T2D might be caused in pre-disposed people taking in a little too much food daily, causing liver fat to build up with the release of too much glucose from the liver. The Newcastle MR Centre allowed me and my team of medics and scientists to test these ideas.
‘Counterpoint’ refers to COUNTERing the Pancreatic inhibition of Insulin secretion by Triglyceride (with a passing nod to my favourite Aldous Huxley novel, Point Counterpoint).
The design was simple: If the hypothesis was correct, I could test it to destruction by removing the driving factor of excess liver fat, so if glucose levels did not return to normal it was wrong. The charity, Diabetes UK , had the courage to fund this speculative idea.
The big challenge was devising a way to obtain what I calculated would have to be 15kg of weight loss. It had to be all within 8 weeks because the period of grant support was short. From listening to my patients describe the difficulties in losing weight over decades, I knew the two main problems had to be avoided: hunger, and the cumulative strain of deciding what and how much to eat every day.
That led to us using one 200-calorie liquid meal (the participants’ only choice being the flavour) at three mealtimes per day, plus salads or leafy vegetables. Somewhat to my surprise, it was highly effective and the participants actually liked it - so much so, that they lost an average of 15.3kg in 8 weeks. As can be seen in this diagram, their fasting blood glucose dropped to near-normal levels:
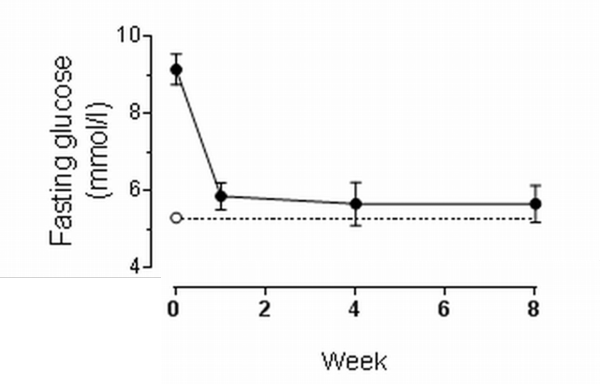
This graph shows the dramatic fall in blood glucose (sugar) levels before breakfast only one week after stopping glucose-lowering medications and starting the 800 calories per day diet. The dotted line shows glucose levels in a matched non-diabetic group.
The team - with special mention of Dr EeLin Lim, clinical research fellow, and Dr Kieren Hollingsworth, MR physicist - measured each of the mechanisms postulated in the Twin Cycle Hypothesis. To my astonishment, they were all as predicted. The amount of fat in the liver of these people with ordinary T2D was shocking – and disappeared remarkably with the weight loss , as shown in these MRI scans:
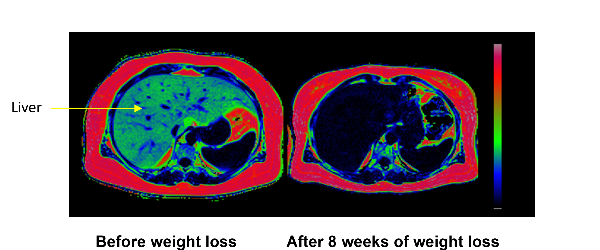
Every pixel in these images is colour-coded for the percentage of fat at that point in space. The fatty tissue under the skin is red, and black areas show very little fat. The arrow points to the liver which was 36% fat before weight loss and only 2% after weight loss.
Because of this decrease in liver fat, the liver stopped pouring out glucose and fat, and the cells making insulin in the pancreas were released from the inhibitory effect of the excess fat. Thus, the Twin Cycle Hypothesis was proven! The resulting paper in the main European diabetes journal, Diabetologia, became the journal’s most highly cited paper for the next two years. But this was just the beginning. Would the reversal of the underlying processes last once people returned to normal eating and keeping weight steady?
That was tested in the next study, Counterbalance (Counteracting BetA cell failure by Long term Action to Normalize Calorie intakE) which showed that all the underlying mechanisms remained normal for 6 months of normal eating .
In addition , this study addressed the question of whether people with a long duration of T2D could also return to normal. The sooner the better! After 10 years, the chance of achieving remission was very much lower.
Ingrained in medical thinking is the concept that T2D is caused by obesity. ‘Obesity’ is defined from population data as a BMI above 30kg/m 2 . It seemed that T2D only developed when a person became heavier than they personally could tolerate.
But throughout the Counterpoint and Counterbalance studies, the response to 15kg weight loss was the same at both ends of the spectrum of body mass index tested – from 27 to 45kg/m 2 . The reason appeared to be that fat is entirely safe when stored under the skin, but simple observation suggested that the capacity of this ‘subcutaneous’ compartment was genetically determined. So, each individual would have a Personal Fat Threshold which, if exceeded, may lead to fat being left inside the important organs – in particular, the liver and pancreas.
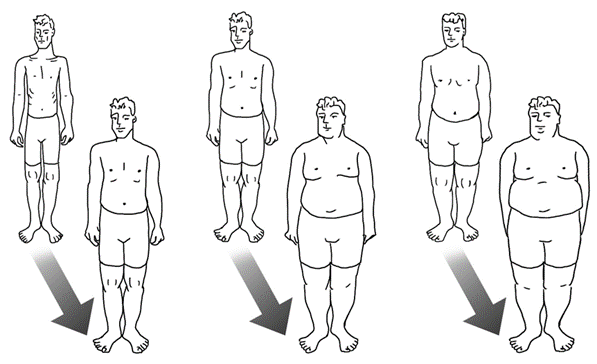
This image helps us understand the individual. The three 45-year-old men in the front row all have type 2 diabetes. How can this be if it is simply caused by excess fat? We must consider each individual separately, not compare between them. The back row shows the same men when they were 25 years old. Each has put on a similar percentage weight, and all weight gain in adult life is gain of fat. The man on the left simply has a lower threshold of tolerance for the absolute amount of fat in the body. A few years later, researchers at Oxford University showed that the capacity of safe storage of fat (under the skin) was genetically determined by 53 separate genes.
To publish a well-argued hypothesis, I sought the help of Prof Rury Holman of Oxford University, as he held the database of the most famous study in the history of T2D research.
Over one-third (36%) of the people in the UK Prospective Diabetes Study had a ‘normal’ BMI - that is difficult for modern-day doctors to comprehend - but at the time of recruitment (between 1977-1991), only 7% of people in the population of the UK were obese. And yet this was the study that told us most of what we know about T2D: a disease currently believed to be caused by obesity. Our rethink was overdue.
Rury and I published the Personal Fat Hypothesis in 2015 to draw attention to this matter. Conducting a formal study to test the hypothesis had to wait until more pressing research had been finished.
A very practical question had to be answered. Could the method of reversing the underlying processes of T2D be used in routine Primary Care, where most people with T2D are managed? Diabetes UK was willing to consider extending its grant support for this people-centred question.
My colleague, Prof Mike Lean of Glasgow University, had applied the method developed in Counterpoint to find out if it could be used in Primary Care to treat obesity, and had developed a routine of training primary care nurses or dietitians in how to use the diet. Diabetes UK suggested that Mike and I collaborated to run a large study, and the Diabetes Remission Clinical Trial (DiRECT) was born. It is the largest study funded by Diabetes UK.
DiRECT was a simple randomised study in Primary Care to compare the rapid weight loss method in T2D with another group, who were managed according to best practice guidelines. Each practice nurse (or dietitian in Scotland) was provided with a structured 8 hours of training. After one year, almost half of all the 149 people in the weight loss group were free of their diabetes and off all diabetes medications, having lost an average of 10kg. After two years some weight regain had occurred, but still over one-third of participants were free of diabetes.
However, we were able to confirm in the Newcastle cohort, that the underlying mechanisms causing the disease were reversed - exactly as already shown in our earlier studies - when supervised by nurses out in the real world. Even more excitingly, we showed that the insulin-secreting cells of the pancreas recovered very gradually over a one-year period. Therefore concluding that the previous belief that these cells had died, was wrong – they were merely inhibited by the excess of fat and sugar.
This question had come sharply into focus as soon as the Counterpoint results were published in 2011. Following this, I received an extraordinary influx of emails from people with diabetes, requesting how-to-do-it information which led to the hasty construction of information available on the Newcastle University website .
Then came a wave of emails either reporting the outcome of following the ‘Newcastle diet’ or reporting upon what happened when people discussed this with their diabetes nurse or GP. Together with Dr Sarah Steven - the brilliant doctor who conducted the Counterbalance study - I published an analysis of this real-world experience in 2014.
But by far the most anguished emails came from people reporting that they had been told they must not lose weight as their present body mass index was already in the normal range, and weight loss would be unhealthy.
Many of these ‘normal’ weight people decided to take matters into their own hands and discovered that they too could reverse their diabetes by weight loss. But we needed a formal study to test the Personal Fat Threshold Hypothesis - and so in 2018, Diabetes UK funded a research grant to carry this out.
The ReTUNE study - Reversal of Type 2 diabetes Upon Normalisation of Energy intake in non-obese people – was designed to test the Personal Fat Threshold Hypothesis. Would T2D return to normal with weight loss in a group of people with lower BMI? And how much weight loss was required to cross the threshold?
The answers were clear.
Yes, weight loss did normalise all the underlying mechanisms exactly as it did in heavier people. It was discovered that weight loss of 6.5% was required to cross the threshold on average for this group. This led us to decide that doctors need to change their practice: If a person has ordinary T2D , then they have become too heavy for their own body (or genetic makeup); weight loss has to be the first therapeutic move by whatever means suitable for the individual; only if this fails for whatever reason should there be a resort to drugs.
It will take a long time for this to be accepted into routine practice, but the hard evidence is available.
The results of the ReTUNE study were remarkable. At baseline, these apparently slim people had three times as much fat inside their livers compared to the weight-matched non-diabetic control group. As a result of the study, liver fat decreased rapidly and 70% of people returned to the non-diabetic state having stopped all diabetes medications. ‘Looking’ inside these research participants using MRI gives an idea of how clogged up with fat their bodies had become – without showing as readily visible fat under the skin.
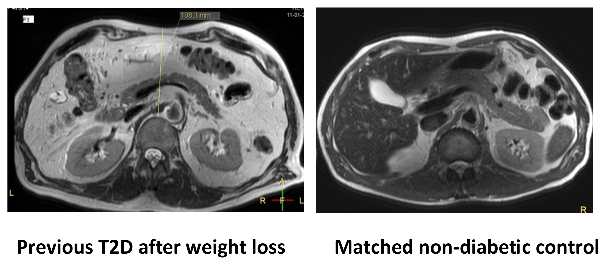
Compared to the group without T2D, those with T2D had excess fat inside the tummy cavity even after weight loss (although no longer any excess inside the liver and pancreas). Unlike most people of their weight, the ex-diabetic group had been unable to store the fat safely under the skin.
There was another important result from ReTUNE. Because we thought that some rare forms of diabetes may be more common in people of lower BMI, we carried out careful testing of all 24 people in this study. This was done at the national testing Centre in Exeter. We had to be sure that we were studying genuine T2D, not conditions caused by other factors.
Two people turned out to have monogenic diabetes, a rare genetic reason for glucose levels to be high. Two others had a slow onset form of type 1 diabetes. From this, we learnt that doctors need to bear in mind that some of the people who do not return to normal after weight loss may have a rarer type of diabetes than the vast majority.
The health benefits and economic advantages of helping large numbers of people escape from T2D resulted in a pilot scheme to establish whether the research findings could be reproduced on a large scale. They could, and the scheme transitioned to being a full national programme in 2022. It is still being rolled out across the country , but success in the pilot scheme saw several thousand people achieve 10kg weight loss - a level expected to bring about remission in 30-40% of participants in one year.
By establishing the underlying cause of type 2 diabetes it has been possible to improve the health of many people. Cutting-edge MR techniques, combined with good old-fashioned physiological research and clinical insight, have transformed the understanding and management of type 2 diabetes.
You might also like:
- Learn more about Professor Roy Taylor , his research, teaching, publications and more
- Discover the Newcastle Magnetic Resonance Centre and the diabetes research we do there
- Find out more information about reversing type 2 diabetes and ongoing remission
- Explore further insights into Professor Roy Taylor’s work on the FROM Blog
- Learn about Professor Roy Taylor's 2024 Rank Prize for Nutrition win
Tags: Research , Research Excellence , Ageing and Health , Research Culture
Related Articles
The impact of storms and saving the oak treescape.
Topics: Data , One Planet , Research Excellence , Sustainable Development , Biodiversity
Poverty Proofing schools: how to tackle the stigma
Topics: Cities and Place , Research Excellence
Big data need big ideas to predict species responses to climate change
Topics: One Planet , Research Excellence , Sustainable Development , Biodiversity
- Recent Posts
- Healthier Lives
- © 2019 Newcastle University All Rights Reserved

Newcastle University leads the way in Type 2 diabetes research
Research by professor roy taylor of newcastle university has proven that type 2 diabetes is reversible..
It is estimated that diabetes costs the NHS £10 billion a year, while almost one in 20 prescriptions written by GPs is for diabetes treatment. Once thought to be an incurable, lifelong condition, Professor Roy Taylor's findings have proven that it can be reversed, and have since been incorporated by the NHS who are currently running a pilot to help effectively treat patients with Type 2 diabetes and significantly reduce costs.
Professor Roy Taylor is Director of Newcastle Magnetic Resonance Centre and one of the world’s leading experts on Type 2 diabetes. His research has been pivotal in identifying the causes of Type 2 diabetes and showing how weight loss can reverse the condition. More recently, further research has been able to show that remission from Type 2 diabetes is also possible for those with lower BMIs. Below, we look back over the developments in Type 2 diabetes research.
Reversing Type 2 diabetes
Professor Roy Taylor discovered that Type 2 diabetes is caused by excess fat within the liver and pancreas. This happens when people reach their Personal Fat Threshold. Fat is normally stored under the skin but when the Personal Fat Threshold is reached, fat must find elsewhere in the body to go. Initially, this ends up being stored in the liver and then overspills to the rest of the body, including the pancreas. In the liver, this fat causes a poor response to insulin and it produces too much glucose. In the pancreas, the fat switches off the genes which direct how insulin should effectively be produced, and this causes Type 2 diabetes.
With this knowledge, it was found that Type 2 diabetes could be reversed by placing those diagnosed with the condition on a low-calorie diet. This decreases the fat levels in both the liver and pancreas, re-starts the normal production of insulin and reverses Type 2 diabetes. To achieve this, 15 kg of weight loss is required.
A research trial, DiRECT (Diabetes Remission Clinical Trial), was originally carried out to discover whether this knowledge could be used for routine treatment of the condition. A quarter of participants achieved a 15 kg or more weight loss, and of these, almost 9 out of 10 people put their Type 2 diabetes into remission. The study also found that almost half of those were still off all their Type 2 diabetes medication with normal blood glucose levels after one year. After two years, more than one third of the group had been free of diabetes and off all diabetes medication for at least two years.
A further study with a subset of DiRECT participants was able to show that if remission is achieved, the insulin-producing capacity of the pancreas can be restored to levels similar to those who had never been diagnosed with Type 2 diabetes. This disproved the assumption that insulin-producing cells are damaged forever in people diagnosed with Type 2 diabetes.
NHS pilot study
Following the success of the DiRECT trial, Professor Roy Taylor’s findings were incorporated into a three-year NHS England pilot in 2020. During the pilot up to 5,000 patients will be enrolled onto a life-changing weight-loss programme. Patients will be provided with low-calorie total diet replacement products for three months, alongside support to increase their exercise levels. This will result in the desired weight loss of over 15 kg if followed fully. After the 12-week weight loss period, patients are then offered managed plans for reintroducing ordinary, nutritious food, with ongoing support from clinicians and coaches after that.
Type 2 diabetes with a lower BMI
Obesity is known to increase the risk of developing Type 2 diabetes. However, 10% of people living with Type 2 diabetes have a BMI considered in the healthy range.
The latest findings by Professor Roy Taylor and his team have now shown that remission from Type 2 diabetes is possible even for people with lower BMIs.
20 people with Type 2 diabetes and a BMI at or just below the healthy range (BMI below 27) were enrolled onto the Diabetes UK-funded Reversal of Type 2 Diabetes upon Normalisation of Energy Intake in the Non-obese (ReTUNE). They were also placed on a low-calorie diet programme. However, the period of the low-calorie diet was for 2-4 weeks, rather than 3 months, and the period of weight loss maintenance for reintroducing normal foods was 4-6 weeks. This cycle of weight loss and maintenance was repeated up to three times, until participants lost between 10 and 15% of their bodyweight.
After each cycle, the research team measured the amount of fat in the participants’ pancreas and liver and looked to see who how remission was produced. 50% of participants went into Type 2 remission after the first weight loss cycle. Overall, 70% went into remission through diet-induced weight loss, despite not living with obesity or overweight.
The study confirms for the first time that people with Type 2 diabetes and lower BMIs can be supported to put their Type 2 into remission through a structured low-calorie diet programme, and that the key to this is losing harmful fat from the liver and pancreas.
‘Your Simple Guide to Reversing Type 2 Diabetes’
Professor Roy Taylor has published a book ‘Your Simple Guide to Reversing Type 2 Diabetes’ which provides a useful guide for those diagnosed with Type 2 diabetes to understand their condition and guidance on how to incorporate the weight loss programme. Proceeds from the book sales are donated by Professor Roy Taylor to Diabetes UK. The book has been endorsed by celebrities who have benefitted from the programme themselves. Hairy Biker Dave Myers said, “‘When I met Roy in 2012, I had Type 2 diabetes – and he showed me another way. Now my blood sugars are normal and my diabetes is a thing of the past.”
Find out more
If you would like to find out more about how you can help us continue our world-leading research to improve health and wellbeing, click the button below.

- You are here:
- research.ncl.ac.uk »
- Newcastle University »
- Skip to Content
Newcastle University
- Contact Information
Improving type 2 Diabetes management through Examining, Advising and prescribing (IDEA) trial
New clinical research findings may require clinicians to change their behaviour in order to provide high quality care to people with diabetes. The present study builds upon findings from our recently completed UK-wide study of theory-based behavioural and organisational factors associated with high quality diabetes care.
We have developed a workshop for primary care clinicians to help to support their provision of high quality type 2 diabetes care. We will conduct a two-armed cluster randomised controlled trial in 44 general practices in the North of England. We will focus on improvement in six clinical actions highlighted in NICE’s quality standards for type 2 diabetes which our previous work has shown have scope for improvement: prescribing for hypertension and glycaemic control, providing physical activity and nutrition advice, and on-going diabetes-related education, and examination of feet.
This website provides background information about the study, the research team and workshop facilitators
2013 - Institute of Health and Society, Newcastle University, Newcastle upon Tyne
NE2 4AX, United Kingdom
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
April 19, 2023
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Weight loss puts type 2 diabetes into remission for five years, finds research
by Newcastle University

New findings have revealed that nearly a quarter (23%) of participants who were in remission from type 2 diabetes at two years in a clinical trial remained in remission at five years.
The participants no longer needed to use diabetes medications to manage their blood sugar levels . Those who were still in remission had an average weight loss of 8.9kg at five years.
The research revealed that the proportion of participants in the extension of the landmark Diabetes Remission Clinical Trial (DiRECT) remission after five years was more than three times that of the DiRECT control group, who did not take part in the original low-calorie diet program or receive continued low-intensity weight management support in the extension trial.
The research, led by Professor Roy Taylor, at Newcastle University and Professor Mike Lean, at the University of Glasgow, and will be presented at the Diabetes UK Professional Conference 2023 in Liverpool on April 26.
Professor Roy Taylor at Newcastle University said, "The DiRECT five-year follow up shows that the rapid weight loss program brings about considerable weight loss at five years with low-intensity support. The most important question now is how the follow-up program can be even more successful at an affordable cost.
"We have found major overall benefits to people who were originally assigned to the weight loss group. They had around half the number of serious health issues causing admission to hospital. They also reported feeling much better as a result of the weight loss. For those who remain free of diabetes , the study has been life-changing. It is difficult for people who do not have type 2 diabetes to appreciate what it means to have escaped from the shadow of this serious condition."
The original DiRECT trial of a weight management program for people with a diagnosis of type 2 diabetes within the last six years, involved a 12-week low-calorie formula diet, followed by support to gradually reintroduce healthy food and maintain weight loss. The landmark trial carried out at Newcastle University was the first to show that remission from type 2 diabetes is possible through a dietary intervention in primary care , with almost half (46%) of people in remission at one year, and 36% at two years.
In the extension study, to understand the longer-term benefits of the program, 95 intervention group participants of the original two-year DiRECT study (48 of whom were in remission at the start of the extension) continued to receive support to help maintain weight loss over the next three years. They received nurse or dietitian appointments at their GP surgery every three months to review their weight, blood sugar levels and blood pressure, and were offered advice and support to maintain their weight loss.
Participants who regained over 2kg during years 3–5 were offered an additional package of support, available once each year, consisting of the low-calorie 'soups and shakes' diet for four weeks, followed by support while reintroducing normal meals.
During the three-year extension, 82 participants from the original DiRECT control group—who originally received best type 2 diabetes care according to guidelines—were advised to lose weight. Control participants did not receive the three-monthly appointments, or additional "soups and shakes" packages during the extension period.
- Data from 85 participants of the original DiRECT intervention group revealed an average five-year weight loss of 6.1kg.
- Of the 48/85 participants who were in remission at the start of the extension period, 11 (23%) were still in remission at five years, with an average five-year weight loss of 8.9kg.
- Data, available from 82 participants of the original DiRECT control group, showed an average five-year weight loss of 4.6kg, with 3.4% in remission.
- Overall, the intervention group saw greater improvements in blood pressure and blood sugar levels, and fewer needed medication, compared to the control group.
- The number of "serious adverse events" (events resulting in hospital admission) in the intervention group was less than half that in the control group. The findings also support growing evidence that weight loss, and remission from type 2 diabetes, can prevent or delay the complications of diabetes.
Dr. Elizabeth Robertson, Director of Research at Diabetes UK, said, "Diabetes UK is proud to be at the forefront of over a decade of pioneering research into type 2 diabetes remission. Our DiRECT study has been pivotal in transforming the lives of people with type 2 diabetes by showing that the condition can be put into remission through weight loss. The new findings from DiRECT confirm that for some people, it is possible to stay in remission for at least five years.
"For those who put type 2 diabetes into remission, it can be life-changing, offering a better chance of a healthier future. For those that aren't able to go into remission, losing weight can still lead to major health benefits, including improved blood sugar levels, and reduced risk of serious diabetes complications such as heart attack and stroke.
"DiRECT inspired the NHS low-calorie diet program, granting many more people with type 2 diabetes the opportunity to put the condition into remission. We now need to understand how best to support more people to maintain weight loss and stay in remission in the long term."
Explore further
Feedback to editors

Neuroscientists use AI to simulate how the brain makes sense of the visual world
4 hours ago

The light or the content? What we know about screens and sleep disruption
5 hours ago

For some endometriosis-related ovarian cancers, timing is everything

Researchers genetically modify E. coli bacteria with part of HIV virus in bid for successful vaccine

Researchers develop 3D model to better treat neurological disorders

Investigating hyperactivation of memory circuits and Alzheimer's disease risk

Targeting 'monster cancer cells' could reduce recurrence rates after cancer therapy
6 hours ago

What happens when auditory cues affect body representation and vice-versa?

Chatbots are poor multilingual health care consultants, study finds

Research identifies mechanisms for selective multiple sclerosis treatment strategy
7 hours ago
Related Stories

Intermittent fasting may reverse type 2 diabetes
Dec 14, 2022

South Asian people undergo type 2 diabetes remission with low calorie diets
Nov 25, 2022

Diabetes remission diet also lowers blood pressure and reduces need for medication
Jun 1, 2021

Type 2 diabetes remission is possible for people with lower BMIs
Apr 1, 2022

Seemingly healthy levels of liver fat can trigger type 2 diabetes, UK study suggests
Sep 28, 2021

Type 2 diabetes remission is possible even in people with lower body weight, supporting idea of 'personal fat threshold'
Sep 22, 2022
Recommended for you

Binge-eating disorder not as transient as previously thought
15 hours ago

Century-old vaccine found to protect type 1 diabetics from infectious diseases
May 22, 2024

Young people are increasingly using Wegovy and Ozempic, study finds

New biomarkers found to predict kidney failure in type 1 diabetes patients

Study finds ultraviolet radiation may affect subcutaneous fat regulation, could lead to new obesity treatments

Specialized weight navigation program shows higher use of evidence-based treatments, more weight lost than usual care
May 21, 2024
Let us know if there is a problem with our content
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy

Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Type 2 diabetes is a reversible condition
A body of research putting people with Type 2 diabetes on a low calorie diet has confirmed the underlying causes of the condition and established that it is reversible.
Professor Roy Taylor at Newcastle University, UK has spent almost four decades studying the condition and will present an overview of his findings at the European Association For The Study Of Diabetes (EASD 2017) in Lisbon.
In the talk he will be highlighting how his research has revealed that for people with Type 2 diabetes:
- Excess calories leads to excess fat in the liver
- As a result, the liver responds poorly to insulin and produces too much glucose
- Excess fat in the liver is passed on to the pancreas, causing the insulin producing cells to fail
- Losing less than 1 gram of fat from the pancreas through diet can re-start the normal production of insulin, reversing Type 2 diabetes
- This reversal of diabetes remains possible for at least 10 years after the onset of the condition
"I think the real importance of this work is for the patients themselves," Professor Taylor says. "Many have described to me how embarking on the low calorie diet has been the only option to prevent what they thought -- or had been told -- was an inevitable decline into further medication and further ill health because of their diabetes. By studying the underlying mechanisms we have been able to demonstrate the simplicity of type 2 diabetes."
Get rid of the fat and reverse Type 2 diabetes
The body of research by Professor Roy Taylor now confirms his Twin Cycle Hypothesis -- that Type 2 diabetes is caused by excess fat actually within both liver and pancreas.
This causes the liver to respond poorly to insulin. As insulin controls the normal process of making glucose, the liver then produces too much glucose. Simultaneously, excess fat in the liver increases the normal process of export of fat to all tissues. In the pancreas, this excess fat causes the insulin producing cells to fail.
The Counterpoint study which was published in 2011, confirmed that if excess food intake was sharply decreased through a very low calorie diet, all these abnormal factors would be reversed.
The study showed a profound fall in liver fat content resulting in normalisation of hepatic insulin sensitivity within 7 days of starting a very low calorie diet in people with type 2 diabetes. Fasting plasma glucose became normal in 7 days. Over 8 weeks, the raised pancreas fat content fell and normal first phase insulin secretion became re-established, with normal plasma glucose control.
Keep the weight off and keep the diabetes at bay
"The good news for people with Type 2 diabetes is that our work shows that even if you have had the condition for 10 years, you are likely to be able to reverse it by moving that all important tiny amount of fat out of the pancreas. At present, this can only be done through substantial weight loss," Professor Taylor adds.
The Counterbalance study published in 2016, demonstrated that Type 2 diabetes remains reversible for up to 10 years in most people, and also that the normal metabolism persists long term, as long as the person doesn't regain the weight.
Professor Taylor explained the science behind the mechanisms: "Work in the lab has shown that the excess fat in the insulin producing cell causes loss of specialised function. The cells go into a survival mode, merely existing and not contributing to whole body wellbeing. Removal of the excess fat allows resumption of the specialised function of producing insulin. The observations of the clinical studies can now be fully explained."
He added: "Surprisingly, it was observed that the diet devised as an experimental tool was actually liked by research participants. It was associated with no hunger and no tiredness in most people, but with rapidly increased wellbeing. The 'One, Two' approach used in the Counterbalance study was a defined two phase programme. The Phase 1 is the period of weight loss -- calorie restriction without additional exercise. A carefully planned transition period leads to Phase 2 -- long term supported weight maintenance by modest calorie restriction with increased daily physical activity."
This approach consistently brings about 15kg of weight loss on average.
After the details were posted on the Newcastle University, UK website, this has been applied clinically and people who were highly motivated have reported that they have reversed their type 2 diabetes and continued to have normal glucose levels (normoglycaemic) over years.
A further study in general practice, the Diabetes Remission Clinical Trial (DiRECT) funded by Diabetes UK is now underway to determine the applicability of this general approach to routine Primary Care practice with findings due before the end of the year.
Patients or GPs who would like more information about the diet that reverses Type 2 diabetes see the Magnetic Resonance Centre website.
- Diet and Weight Loss
- Hormone Disorders
- Liver Disease
- Chronic Illness
- Diabetes mellitus type 1
- Diabetic diet
- Diabetes mellitus type 2
- Hyperglycemia
Story Source:
Materials provided by Newcastle University . Note: Content may be edited for style and length.
Cite This Page :
Explore More
- Future Climate Impacts Put Whale Diet at Risk
- Charge Your Laptop in a Minute?
- Caterpillars Detect Predators by Electricity
- 'Electronic Spider Silk' Printed On Human Skin
- Engineered Surfaces Made to Shed Heat
- Innovative Material for Sustainable Building
- Human Brain: New Gene Transcripts
- Epstein-Barr Virus and Resulting Diseases
- Origins of the Proton's Spin
- Symbiotic Bacteria Communicate With Plants
Trending Topics
Strange & offbeat.
The New York Times
Well | hope for reversing type 2 diabetes.

Hope for Reversing Type 2 Diabetes

Many experts believe Type 2 diabetes is an incurable disease that gets worse with time. But new research raises the tantalizing possibility that drastic changes in diet may reverse the disease in some people.
Recently, a small clinical trial in England studied the effects of a strict liquid diet on 30 people who had lived with Type 2 diabetes for up to 23 years. Nearly half of those studied had a remission that lasted six months after the diet was over. While the study was small, the finding offers hope to millions who have been told they must live with the intractable disease.
“This is a radical change in our understanding of Type 2 diabetes,” said Dr. Roy Taylor, a professor at Newcastle University in England and the study’s senior author. “If we can get across the message that ‘yes, this is a reversible disease — that you will have no more diabetes medications, no more sitting in doctors’ rooms, no more excess health charges’ — that is enormously motivating.”
It is not the first time that people have reversed type 2 diabetes by losing a lot of weight shortly after a diagnosis. Studies have also shown that obese individuals who have bariatric surgery frequently see the condition vanish even before they lose very much weight.
But the new study, published in Diabetes Care , proved the reversal after diet can persist for at least half a year as long as patients keep weight off, and can occur in people who have had the disease for many years.
The researchers followed the participants after they had completed an eight-week low-calorie-milkshake diet and returned to normal eating. Six months later, those who had gone into remission immediately after the diet were still diabetes-free. Though most of those who reversed the disease had had it for less than four years, some had been diabetic for more than eight years.

When Allan Tutty, 57, learned five years ago that he had Type 2 diabetes, he asked health care providers if there was a cure. “It was a case of, look, you’ve got it, deal with it, there’s no cure,” said Mr. Tutty, who manages a home for people with brain injuries in Newcastle.
Later, Mr. Tutty spotted a notice recruiting volunteers for a diabetes study that asked, “Would you like the opportunity to reverse your condition?”
Mr. Tutty said he jumped at the chance, becoming one of 30 men and women ages 25 to 80 to sign up. Mr. Tutty was one of 13 participants whose fasting plasma glucose dropped, and during the six-month follow-up remained below the seven millimole per liter (or 126 milligrams per deciliter) that defines diabetes. Although Mr. Tutty completed the study nearly three years ago, his fasting blood sugars continue to range from 5.2 to 5.6 mmol/L, he said.
Type 2 diabetes develops when the body cannot use insulin properly or make enough insulin, so the body cannot properly use or store glucose (a form of sugar) and sugar backs up into the bloodstream, raising blood sugar levels. In the United States, some 8.9 percent of adults 20 and older have been found to have diabetes, and health officials estimate that another 3.5 percent have undiagnosed diabetes.
Although no one knows exactly why the diet appeared to reverse diabetes, Dr. Taylor said the explanation may be related to how the body stores fat. Excess fat in the liver can spill into the pancreas, inhibiting insulin secretion and the liver’s response to insulin, resulting in insulin resistance and diabetes.
Going on a very-low-calorie diet may allow the body to use up fat from the liver, causing fat levels to drop in the pancreas as well. That “wakes up” the insulin-producing cells in the pancreas, normalizing blood glucose levels.
While some previous studies have shown that blood sugars can normalize after significant weight loss, endocrinologists said they were impressed by the persistence of the lower blood sugar levels for months after the diet.
“Decreasing caloric intake for any reason brings with it a rapid improvement in glucose control,” said Dr. Robert Lash, the chairman of the Endocrine Society’s clinical affairs committee and a professor of internal medicine at the University of Michigan. “What’s exciting here is that the improvements in glucose control persisted when the participants went back to eating a diet with a normal number of calories.”
While the research suggests the potential for a cure, questions remain about how long the effect will last and whether it can work for the typical patient with diabetes.
“It’s definitely doable,” said Dr. George King, the chief scientific officer at Joslin Diabetes Center and a professor at Harvard Medical School. The question, he said, is: Can people maintain the weight loss and “continue to have this reversal for many, many years?”
“That is the difficult part,” he added.
Dr. King said that even short-term remission would reduce or put off some of the serious complications associated with diabetes, like nerve damage, kidney damage, loss of vision, heart attacks and strokes. Yet structured weight loss programs are expensive and often not covered by insurance, and physicians — who are often not well-versed in nutrition — may not take the time to counsel patients about diet, Dr. King said.
The participants in the Newcastle trial, who ranged from overweight to extremely obese, were told to stop their diabetes medications and start a 600- to 700-calorie-a-day diet, consisting of three diet milkshakes a day at mealtimes and half a pound of nonstarchy vegetables a day.
Mr. Tutty, who weighed about 213 pounds before the trial, lost a little more than 30 pounds, the average weight loss in the trial. The people in the study most likely to respond to the treatment were in their early 50s on average and younger than the nonresponders, and they had had diabetes for fewer years. The responders were also healthier before the trial: They had been taking fewer medications than nonresponders, had lower fasting glucose and hemoglobin A1c before the trial, and had higher baseline serum insulin levels. Three of those who went into remission had lived with diabetes for more than eight years.
Many of the responders are still in the prediabetes zone and at risk for developing diabetes, Dr. Taylor said. “It’s not fair to say they were completely normalized, but they’re at a level of blood sugar where we don’t expect to see the serious complications associated with diabetes,” he said. “That’s why it’s such good news.”
The big challenge for dieters was returning to normal eating, and trial participants received intensive counseling from a researcher on the team about how to eat after ending the liquid diet, Dr. Taylor said.
“They would describe going back to the kitchen and almost having a panic attack,” he said. “We used that as an opportunity to instill new habits, and were very directive about how much to cook and how much to eat.”
- Ask Well: Eating With Diabetes
- An Eating Disorder in People With Diabetes
- Wine May Help With Diabetes
For more fitness, food and wellness news, follow us on Facebook and Twitter , or sign up for our newsletter.
What's Next

Type 2 diabetes remission is possible for people with lower BMIs
A new ‘game-changing’ study by professor roy taylor and his team shows remission from type 2 diabetes is possible for people with lower bmis. .
The new study has shown that remission of type 2 diabetes is possible even for some people with lower body weights.
Results from the Diabetes UK-funded Reversal of Type 2 Diabetes upon Normalisation of Energy Intake in the Non-obese (ReTUNE) trial show a staggering 70% of participants with lower bodyweights went into type 2 remission through diet-induced weight loss, despite not living with obesity or overweight.
While obesity increases the risk of developing type 2 diabetes, 10% of people with type 2 diabetes have a BMI that is not in the obesity or overweight category.
Professor Roy Taylor, principal investigator on the ReTUNE trial, Newcastle University said:
“This is very good news for everyone with type 2 diabetes, not only pointing the way forward for effective return to health but also challenging the misconceptions clinging to the condition.”
Read the full article here: https://www.ncl.ac.uk/press/articles/latest/2022/04/diabetesremissionforlowbmi/
- Newcastle University
- News & Events
- Research output
- Our partnership
- Our strategy
- Who we work with
- Equality, Diversity and Inclusion
- Newcastle and the North East region
- Biomedical Research Building
- For collaborators
- Ageing, sarcopenia and multimorbidity
- Dementia, mental health and neurodegeneration
- Liver disease, multimorbidity and lifestyle
- Musculoskeletal disease and inflammation medicine
- Neuromuscular disease, rare diseases and mitochondrial dysfunction
- Skin disease, oral disease and immunogenomics
- Multiple long-term conditions
- Our training programme
- Meet our trainees
- NIHR Academy
- I want to learn about research
- Why get involved in research?
- I want to take part in research
- Multiverse Lab
NIHR Newcastle Biomedical Research Centre NIHR Newcastle Biomedical Research Centre Biomedical Research Building Campus for Ageing and Vitality Newcastle upon Tyne NE4 5PL United Kingdom Tel: +44(0)1912081148 Email: [email protected]
Privacy Overview
Diabetes Remission Clinical Trial
Direct 2024 update.
The much anticipated 5-year results, from the 2-year DiRECT trial and its 3-year DiRECT Extension Study, were published in The Lancet Diabetes & Endocrinology, on 23rd February 2024. (See Publications page)
In nutshell, NHS data on all the original DiRECT participants were collected for a total of 5 years, to see how well the remarkable one and two year results from a dietary weight management programme (remission of diabetes for 46% at 1 year, 36% at 2 years) would be maintained, and whether longer durations of weight loss, of freedom from diabetes medications and of remissions from type 2 diabetes might be associated with better clinical outcomes.
The original DiRECT Intervention group were offered and accepted low intensity dietary support from their practice nurse or a dietitian if one was available. However, follow up to 5 years was no longer a randomised trial: the original Control group participants were all provided with the one and two-year results, showing high rates of remission, and given advice to lose as much weight as they could. Many of them did exactly that, and some did achieve remissions through weight loss either on their own or with local help.
There was considerable weight regain in the first 3 years after starting the diet intervention, but the original DiRECT Intervention group still had an average weight loss of over 6kg (almost 1 stone) after 5 years, and about a quarter of those who had achieved remission of diabetes ate 2 years remained in remission at 5 years.
The diet intervention programme designed for in DiRECT was not perfect, or the last word, but it generated much better results with better sustained weight losses, than previous diets, and there were no unexpected hazards. Indeed, it appears safer to have the intervention than not to: there were half as many serious medical problems requiring hospital admission in the Intervention group over 5 years, compared to those who did not have the DiRECT intervention.
Excitingly, the 5-year results provided new support for making evidence-based weight management, to seek remission, an important early target for medical management of type 2 diabetes. In line with other studies of remission, the results suggested that maintaining substantial weight loss for longer, and maintaining lower HbA1c, off anti-diabetes medication and longer emissions, were all associated with suffering fewer clinical illnesses caused by diabetes.
The message for people diagnosed with type 2 diabetes is good. Based on all the results from DiRECT and other studies, we are now very confident that achieving and maintaining substantial weight loss (over 10 or 15 kg if possible) is the best start to control a very unpleasant progressive disease. Weight loss helps at any stage but remission of type 2 diabetes is most likely with weight loss soon after diagnosis. And other research has taught us that people with type 2 diabetes who are not overweight may still have abnormal body fat accumulations in vital organs, which can be removed to generate remission by relatively modest weight loss.
We all know that under the influence of modern foods and persuasive marketing it is very hard to overcome appetites and sustain substantial weight losses. The message for healthcare professionals from DiRECT is that many people can succeed, with consistent sensible advice and encouragement, and professional diet support programmes like the one used in DiRECT are now available. A bonus from the DiRECT intervention was that ‘quality of life’, or wellbeing, was significantly improved at every year up to 5 years in the participants who received the intervention within their routine primary care management of diabetes, including those who were less successful. Researchers must now seek even better diet programmes, particularly to help people maintain weight loss longer, but the DiRECT intervention is a good start.
DiRECT 2023 Update
The main task for 2023 has been to complete analyses on the DiRECT Extension Study, after all data collection finished in 2022.
For the DiRECT Extension study low-intensity support was provided to try to help maintain weight loss and remission for all the remaining DiRECT Intervention group participants, for 3 more years after the 2-year randomised trial ended. The preliminary 5-year results were presented at the annual UK Association of Physicians meeting, and also at the Diabetes UK Professional Meeting, both in Liverpool. A full paper has been written and submitted for publication.
Several secondary analyses from the original 2-year DiRECT trial have also been completed, and the DiRECT data have been shared with other research groups in collaborations to examine how genetic markers of coronary heart disease risk predict clinical events, and how metabolomic markers (small peptides, and parts of proteins which are associated with diabetes and cardiovascular disease) in the bloodstream improve with the DiRECT intervention. Links to the publications are in the Publications section of this website.
The impacts of the DiRECT trial continues to grow, both within Britain and internationally. New clinical guidelines in several countries, and from the European Association for the Study of Diabetes, now recommend weight loss and remission as a primary management target for people with type 2 diabetes. In both Scotland and England, the National Health Services have established strategies to divert resources and provide effective weight management in national-level Diabetes Remission programmes. People living with type 2 diabetes across the world are asking for treatment and support to achieve remission, and large numbers have been successful. Importantly, the STANDby trial, using the same Counterweight intervention as DiRECT, showed that people of South Asian ancestry, who have very high rates of type 2 diabetes at lower BMI and younger ages, can achieve remission, with loss of ectopic liver fat, just like people of European heritage. https://doi.org/10.1016/j.lansea.2022.100111
Further afield, Type 2 Diabetes Remission projects based on DiRECT have been conducted in many other countries, notably including Australia and New Zealand. Pilot food-based intervention projects based on DiRECT are also running in Lower and Middle Income Countries such as Nepal, where the personal risks and community burdens from Type 2 Diabetes are much greater, but modern drug treatments are unavailable or unaffordable.
DiRECT 2021 Update
In 2020 and 2021, we are continuing to collect data from participants in DiRECT, into their 4th and 5th years of support and follow-up. Covid 19 has made both weight-loss maintenance and data collection difficult, but the Glasgow and Newcastle University research teams have continued to analyse the 2-year results. Important new papers from DiRECT have been published, on the predictors of success for weight loss and remission, the cost-effectiveness of the treatment (it saves healthcare money!) and on the detailed mechanisms behind repairing the pancreas and restoring insulin production.
Link to our Publications page
Now that providing the DiRECT intervention has been shown to save NHS costs, it is now becoming widely available in UK. All Scottish Health Boards received the training to provide the DiRECT/Counterweight-Plus intervention for remission of type 2 diabetes in NHS Scotland by December 2019. In September 2020, a programme was launched to introduce the intervention for 5000 people with type 2 diabetes in selected areas of England.
Published results
On the 6th March 2019 the 2nd year results of the Diabetes Remission Clinical Trial (DiRECT) were presented at the DUK Professional Conference
Two-year results of the randomised Diabetes Remission Clinical Trial (DiRECT) (Final accepted draft, prior to editing and corrections.)
A PDF document containing the presentation slides can now be found on the Study Information page.
The results have been published at The Lancet - Diabetes & Endocrinology website and these results have also been reported in prominent UK media organisations including The Times and the Daily Mail
* A press release for this can opened by clicking this link

On the 5th December 2017 the 12 month primary outcome results of the Diabetes Remission Clinical Trial (DiRECT) were presented at the International Diabetes Federation Congress hosted in Abu Dhabi. Talks were delivered by both Professor Roy Taylor and Professor Mike Lean, with both pictured here with Professor Naveed Sattar enjoying some refreshments following the event.
Information and resources for weight loss and remission of type 2 diabetes are listed further down this page.

Trial description
DiRECT is a research study investigating whether offering an intensive programme for weight loss and weight loss maintenance would be advantageous for people with Type 2 diabetes. Specifically, this programme aims to increase the number of people who can become non-diabetic. Participants are recruited only via NHS General Practices which are taking part in the study, and individuals cannot be accepted in DiRECT. General Practices are randomly allocated to offer their patients one of two treatments. Each treatment has already been shown to be effective, and the question of DiRECT is whether one is better than the other. All participants will be followed for at least 2 years, to see how many remain diabetic under each treatment, and how that relates to their weight. Some participants will also undergo detailed tests concerning the amount of fat in their liver and pancreas.
DiRECT is the largest research study, to date, ever supported by the charity Diabetes UK . Additional support is provided by Cambridge Weight Plan pro bono but with no input into study design, execution or analysis. It is being conducted in NHS primary care practices in Scotland and in Tyneside, the intervention being delivered by NHS staff in routine practice. Defined training for these staff is being provided using the Counterweight Plus approach. The NHS “sponsor” is NHS Greater Glasgow and Clyde
Trial Status
Recruitment Status: Recruitment Closed
Funder: Diabetes UK
Primary Sponsor: NHS Greater Glasgow and Clyde(UK)
Recruitment countries: United Kingdom
Health condition studied: Type 2 Diabetes, Nutritional, Metabolic, Endocrine
Target Sample size: 280
URL: World Health Organization webpage
URL: NHS DiRECT webpage
Study Protocol DiRECT Protocol
What is diabetes?
There are several types of diabetes. All are metabolic disorders which can result in progressive damage to the main organs in the body. Diabetes especially damages the heart, brain, feet and legs, eyes, kidneys and nerves. There are two main types of diabetes: Type 1 (caused by an immune attack destroying the pancreas cells which make insulin), and Type 2 (caused by being overweight and resistant to the effect of insulin, with gradual loss of ability to make enough insulin). DiRECT is researching the treatment of Type 2 diabetes, which is the most common type, and the most expensive for health services.
Why is DiRECT important?
Some people with Type 2 diabetes can become non-diabetic again, at least for a period. That is called a remission of diabetes. A remission of diabetes will allow the patient to stop taking anti-diabetic drugs. This is important as the drugs are inconvenient and can cause side-effects. Also these drugs cost the NHS around £800million per year. If diabetes remission is long term this would prevent or delay the long-term damage which diabetes causes in different body-organs. The mechanisms underlying the return of normal glucose control will also be examined in the Tyneside cohort. Detailed tests using magnetic resonance scans and insulin secretion tests will be carried out. A new treatment programme which helps to produce remissions in type 2 diabetes could therefore be advantageous for people with diabetes, and also save treatment costs. For people who achieve a long term remission, the effect upon their future health and well being could be very great indeed.
Talk to us about diabetes
0345 123 2399
customer support
Weight loss can put type 2 diabetes into remission for at least 5 years, DiRECT study reveals

UPDATE, 26 FEBRUARY, 2024: This article has been updated following new findings into our landmark DiRECT study which have been published in the Lancet.
Results from a three-year extension of our landmark DIRECT study reveal that for some it’s possible to stay in remission of type 2 diabetes for at least five years. But the findings highlight that maintaining weight loss and staying in remission can be challenging.
New findings show that 13% of people who had received the weight management programme and continued to have support through the extension study were in remission of type 2 diabetes at five years.
Remission means blood sugar levels return to a non-diabetes range long term, without the need for diabetes medication.
The findings also show that the programme can have lasting benefits to health although in the extension period – three to five years on from receiving the ‘soups and shakes’ weight management programme – it was common for people to regain weight and fall out of remission.
The DiRECT extension was led by Professors Roy Taylor and Mike Lean (both pictured) and published in the Lancet.
Remission in the long term
The original DiRECT trial, which started in 2014, ran for two years. Previous results showed that almost half (46%) of people with type 2 diabetes who received the weight management programme were in remission one year later, and 36% at two years.
We funded the DiRECT extension study to help us understand more about the longer-term benefits of the programme.
In the extension study, the researchers followed participants from the original DiRECT intervention group – who had received the weight management programme – and the original control group – who hadn’t received the programme but did receive advice about managing their weight – for a further three years.
Some participants from the original intervention group opted to continue to receive support and advice from their GP surgery to help them maintain weight loss over the next three years. Anyone who regained more than 2kg during the three years was offered an additional package of support. This consisted of the low-calorie ‘soups and shakes’ diet for four weeks and support to reintroduce normal meals.
The latest remission results
At year five, remission data was available for 93 people from the original control group and 118 people from the original intervention group (including the 85 people who had continued to receive support from their GP during years 3-5).
12 out of 118 (10%) in the intervention group were still in remission at year five, compared to 5 out of 93 (5%) in the control group.
In the intervention group, of the 85 who had continued to receive support from their GP, 11 (13%) were still in remission.
At year five, the average weight loss in the intervention group was 5.6kg and in the control group this was 4.6kg.
For the 85 people in the intervention group who continued to receive GP support, the average weight loss was 6.1kg. The average weight loss of the 11 people in this group who stayed in remission was 8.9kg.
Over the whole five-year study period, people in the intervention group spent on average 27% of the time in remission. This compares to 4% for the control group who didn’t receive the weight management programme. The intervention group also spent more time with their bodyweight lower than baseline, off blood sugar lowering medications and with blood sugar levels in the non-diabetes range than the control group.
Benefits of remission and weight loss
While it's encouraging that the latest findings show that some people could stay in remission for five years, we also saw that this wasn’t possible for most. Many who regained the weight they had lost came out of remission. But it's important to remember that no matter how long you stay in remission for, spending any time in remission can have lasting benefits to health.
Another landmark remission study, called Look AHEAD, recently found that over a 12-year period going into remission at any point over the study was linked with a lower risk of heart and kidney complications, compared to never going into remission.
Staying in remission can be challenging. It is always possible that your blood sugar levels and weight can increase again, and you can go in and out of remission.
But even if you stay in remission for only a short time or don’t quite get there, by attempting it, a combination of lower blood sugar levels and lower body weight can bring significant health benefits. Putting weight back on and coming out of remission doesn’t mean that you’ve failed, you will have improved your health by trying and you might go back into remission again in the future.
People living with overweight or obesity on a weight management journey are fighting against their biology and the food environment. Over time, this complex interplay can make it difficult to avoid regaining weight. That’s why getting the right support to maintain weight loss and stay in remission is so important.
You can get more information on remission and its benefits.
Kieran Ball was diagnosed with type 2 diabetes in 2013 and started DiRECT the following year. Kieran lost 22kg and put his type 2 diabetes into remission in the first year of the study. Having taken part in the DiRECT extension, he is still in remission today. Kieran said:
“DiRECT has 100% been life changing. Those few months on the low-calorie diet were hard, but I’d do it again no question. DiRECT was an opportunity to reboot the way I was living and I’m so grateful for what being healthy has given me the opportunity to do. It’s amazing that what I went through all those years ago is still benefiting me today. I’m still in remission and not on any diabetes medication – I can’t quite believe how long it has been.”
Read Kieran’s story .
What's next?
Scientists have made significant strides in building our knowledge of dietary approaches to remission over the last decade, but it’s still a fairly new idea. There’s still much to learn so we can give more people the best chance to lose weight, maintain weight loss and stay in remission.
We’re proud that DiRECT’s findings have already influenced diabetes care, inspiring the NHS Type 2 Diabetes Path to Remission Programme . As this is rolled out across England we’ll get more valuable real-word data on weight loss, remission and its benefits for people newly diagnosed with type 2 diabetes.
We also need more research to understand how best to support people with type 2 diabetes to maintain weight loss and remission over time. And because a DiRECT style approach isn't suitable for everyone with type 2 diabetes, we need to find new or better routes to remission.
That’s why we’re investing in vital research like the NewDAWN study . Our researchers are developing a new nationwide NHS support service that will offer a range of weight loss diets for people with overweight or obesity and newly diagnosed with type 2 diabetes. We hope it will help everyone who could benefit find an approach that suits them, and have the opportunity of time free from type 2 diabetes.
Right now, we’re also calling on scientists to come up with research ideas and apply for our funding with proposals that will improve our understanding of, and support for people with type 2 who are seeking to go into or stay in remission.
Dr Elizabeth Robertson, our Director of Research, said:
“Diabetes UK is proud to have funded over a decade of research that has forged new frontiers for people with type 2 diabetes and put remission on the map. “Remission from type 2 diabetes lifts the burden of 24/7 diabetes management and can transform health and wellbeing. But we know that going into remission can be challenging and staying there even more so. That’s why we’ve just launched our new remission information and support hub and are continuing to fund research to understand how to help more people go into remission and stay there for longer.”
Professor Mike Lean, at the University of Glasgow, said:
“DiRECT has made a world-wide paradigm-shift in understanding and treating type 2 diabetes. The disease is not necessarily permanent, and the five-year results now suggest that diet treatment for weight loss to achieve a period of remission is accompanied by greater freedom from some diabetes complications, and fewer people being admitted to hospital with medical problems. “We must now call for much more effective, long-term funding for research to improve on these results – especially to prevent weight regain.”
Professor Roy Taylor, at Newcastle University, said:
“This five-year study demonstrates that long-term remission from type 2 diabetes is possible if sufficient weight loss is achieved and maintained. “Whether or not remission of diabetes was achieved, those who were assigned to the weight loss group had less than half of the serious health issues experienced by the conventionally treated group. These are dramatic outcomes which should change how this serious condition is managed.”
Share this Page
© The British Diabetic Association operating as Diabetes UK, a charity registered in England and Wales (no. 215199) and in Scotland (no. SC039136). A company limited by guarantee registered in England and Wales with (no.00339181) and registered office at Wells Lawrence House, 126 Back Church Lane London E1 1FH

Post-trial monitoring of a randomised controlled trial of intensive glycaemic control in type 2 diabetes extended from 10 years to 24 years (UKPDS 91)
Affiliations.
- 1 Diabetes Trials Unit, Radcliffe Department of Medicine, University of Oxford, Oxford, UK; NIHR Oxford Biomedical Research Centre, Oxford, UK.
- 2 NIHR Oxford Biomedical Research Centre, Oxford, UK; Health Economics Research Centre, University of Oxford, Oxford, UK.
- 3 Health Economics Research Centre, University of Oxford, Oxford, UK; Centre for Clinical Brain Sciences, University of Edinburgh, Edinburgh, UK; Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, Edinburgh, UK; British Heart Foundation Data Science Centre, Health Data Research UK, London, UK.
- 4 Diabetes Trials Unit, Radcliffe Department of Medicine, University of Oxford, Oxford, UK; Diabetes Trials Unit, OCDEM, Churchill Hospital, Oxford, UK. Electronic address: [email protected].
- PMID: 38772405
- DOI: 10.1016/S0140-6736(24)00537-3
Background: The 20-year UK Prospective Diabetes Study showed major clinical benefits for people with newly diagnosed type 2 diabetes randomly allocated to intensive glycaemic control with sulfonylurea or insulin therapy or metformin therapy, compared with conventional glycaemic control. 10-year post-trial follow-up identified enduring and emerging glycaemic and metformin legacy treatment effects. We aimed to determine whether these effects would wane by extending follow-up for another 14 years.
Methods: 5102 patients enrolled between 1977 and 1991, of whom 4209 (82·5%) participants were originally randomly allocated to receive either intensive glycaemic control (sulfonylurea or insulin, or if overweight, metformin) or conventional glycaemic control (primarily diet). At the end of the 20-year interventional trial, 3277 surviving participants entered a 10-year post-trial monitoring period, which ran until Sept 30, 2007. Eligible participants for this study were all surviving participants at the end of the 10-year post-trial monitoring period. An extended follow-up of these participants was done by linking them to their routinely collected National Health Service (NHS) data for another 14 years. Clinical outcomes were derived from records of deaths, hospital admissions, outpatient visits, and accident and emergency unit attendances. We examined seven prespecified aggregate clinical outcomes (ie, any diabetes-related endpoint, diabetes-related death, death from any cause, myocardial infarction, stroke, peripheral vascular disease, and microvascular disease) by the randomised glycaemic control strategy on an intention-to-treat basis using Kaplan-Meier time-to-event and log-rank analyses. This study is registered with the ISRCTN registry, number ISRCTN75451837.
Findings: Between Oct 1, 2007, and Sept 30, 2021, 1489 (97·6%) of 1525 participants could be linked to routinely collected NHS administrative data. Their mean age at baseline was 50·2 years (SD 8·0), and 41·3% were female. The mean age of those still alive as of Sept 30, 2021, was 79·9 years (SD 8·0). Individual follow-up from baseline ranged from 0 to 42 years, median 17·5 years (IQR 12·3-26·8). Overall follow-up increased by 21%, from 66 972 to 80 724 person-years. For up to 24 years after trial end, the glycaemic and metformin legacy effects showed no sign of waning. Early intensive glycaemic control with sulfonylurea or insulin therapy, compared with conventional glycaemic control, showed overall relative risk reductions of 10% (95% CI 2-17; p=0·015) for death from any cause, 17% (6-26; p=0·002) for myocardial infarction, and 26% (14-36; p<0·0001) for microvascular disease. Corresponding absolute risk reductions were 2·7%, 3·3%, and 3·5%, respectively. Early intensive glycaemic control with metformin therapy, compared with conventional glycaemic control, showed overall relative risk reductions of 20% (95% CI 5-32; p=0·010) for death from any cause and 31% (12-46; p=0·003) for myocardial infarction. Corresponding absolute risk reductions were 4·9% and 6·2%, respectively. No significant risk reductions during or after the trial for stroke or peripheral vascular disease were observed for both intensive glycaemic control groups, and no significant risk reduction for microvascular disease was observed for metformin therapy.
Interpretation: Early intensive glycaemic control with sulfonylurea or insulin, or with metformin, compared with conventional glycaemic control, appears to confer a near-lifelong reduced risk of death and myocardial infarction. Achieving near normoglycaemia immediately following diagnosis might be essential to minimise the lifetime risk of diabetes-related complications to the greatest extent possible.
Funding: University of Oxford Nuffield Department of Population Health Pump Priming.
Copyright © 2024 The Author(s). Published by Elsevier Ltd. This is an Open Access article under the CC-BY 4.0 license. Published by Elsevier Ltd.. All rights reserved.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Sign up for alerts
- RESEARCH HIGHLIGHT
- 27 May 2024
New tool to predict Type 2 diabetes
You can also search for this author in PubMed Google Scholar
A glucose test being carried out in a Harare, Zimbabwe clinic. Credit: Majority World CIC / Alamy Stock Photo
Lire en français
A new tool has been developed in Nigeria for early identification of patients at risk for Type 2 diabetes, which can be routinely administered by doctors in primary health settings.
The predictive model addresses a lack of accessibility to testing, especially in remote areas, and a lack of awareness that contributes to patients going undiagnosed until complications arise, raising the risk of long-term health complications. The authors of the study , published in Health Science Reports , call for its integration and use in Nigeria’s primary healthcare system as a primary screening tool.
The web-based application tested by the Nigerian scientists is one of the latest in a series of unique models that are collectively advancing diabetes prediction around the world. Using health check-up data from 444 patients in hospitals in Nigeria, they reported achieving highly accurate results, with training and test set accuracies of 95% and 91% respectively. This was “a notable advantage in terms of accuracy and reliability compared to similar studies in the field”, they said.
“Predictive modelling has become crucial for early detection, particularly in populations with low routine medical checkup profiles. The deployment of the proposed application has the potential to be transformative,” said Olubunmi Ayelagbe, from Nigeria’s Ladoke Akintola University of Technology, one of the authors.
Its capacity to deliver personalised risk scores has a dual benefit – empowering people with crucial information about their health, while guiding healthcare professionals to initiate timely and targeted interventions.
“It is imperative to raise awareness of diabetes risk factors, promote healthy lifestyles, and emphasise the importance of early diagnosis and treatment,” Ayelagbe said. “By promptly identifying high‐risk patients, clinicians can recommend specialised care or more frequent monitoring, directing resources to those who need them the most.”
World Health Organization estimates are that about 24 million people are living with diabetes in the African region, about 95% with Type 2 diabetes. The comparative figure for Nigeria, according to International Diabetes Federation (IDF) statistics, is 3.6 million total cases among adults.
Central to the challenge is that Africa is also home to the highest number of people worldwide who are unaware that they are living with the condition. A 2021 study suggested that the prevalence of prediabetes in Nigeria is about double the International Diabetes Federation’s 7.3% estimate.
doi: https://doi.org/10.1038/d44148-024-00162-2
Ojurongbe, T.A., Afolabi, H.A., Adegoke, N.A., et al Predictive model for early detection of type 2 diabetes using patients' clinical symptoms, demographic features, and knowledge of diabetes H. Sci. Rep 2024 https://doi.org/10.1002/hsr2.1834
Google Scholar
Bashir, M.A., Yahaya, A.I., et al Prediabetes Burden in Nigeria: A Systematic Review and Meta-Analysis (2021) Front. Pub Health https://doi.org/10.3389/fpubh.2021.762429
Download references
Assistant, Associate or Full Professor
The McLaughlin Research Institute and Touro University – Montana campus invite applications for open rank faculty positions.
McLaughlin Research Institute
Postdoctoral Associate- Neuroscience
Houston, Texas (US)
Baylor College of Medicine (BCM)
Call for applications- junior and senior scientists
The BORDEAUX INSTITUTE OF ONCOLOGY (BRIC U1312, https://www.bricbordeaux.com/) is seeking to recruit new junior and senior researchers
Bordeaux (Ville), Gironde (FR)
INSERM - U1312 BRIC
Postdoctoral Scholar - Organic Synthesis
Memphis, Tennessee
The University of Tennessee Health Science Center (UTHSC)
Postdoctoral Scholar - Chemical Biology
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Skip to main content
We use cookies
Necessary cookies.
Necessary cookies enable core functionality. The website cannot function properly without these cookies, and can only be disabled by changing your browser preferences.
Analytics cookies
Analytical cookies help us improve our website. We use Google Analytics. All data is anonymised.
Clarity helps us to understand our users’ behaviour by visually representing their clicks, taps and scrolling. All data is anonymised.
Privacy policy
- University news
- Archive of news
Diet intervention links longer remissions of type 2 diabetes and improved health over 5 years
Published: 23 February 2024
New findings from a three-year observational extension of the landmark Diabetes Remission Clinical Trial DiRECT reveal that, for those in remission from type 2 diabetes at the end of year two of the original study, 26% still remained in remission at year five. The overall remission rate was 13% of those with data at 5 years
New findings from a three-year observational extension of the landmark Diabetes Remission Clinical Trial DiRECT reveal that, for those in remission from type 2 diabetes at the end of year two of the original study, 26% still remained in remission at year five. The overall remission rate was 13% of those with data at 5 years.
The 5-year results break new ground, showing a halving of the number of serious medical events needing hospitalisation in those who received the diet intervention. Furthermore, the longer participants were able to maintain lower weight and remission of their type 2 diabetes, the less likely they were to suffer from some diabetes-related medical complications.

The important new findings, which are published in The Lancet Diabetes & Endocrinology, demonstrate how effective a weight management and diet programme can be for the control and remission of type 2 diabetes, highlighting the critical need for more clinical investment in diet-based therapies for the disease. Research is particularly needed to help people maintain the long-term weight losses required to achieve remission and other health benefits.
Designed and managed by researchers at the Universities of Glasgow and Newcastle and funded by Diabetes UK, the DiRECT trial proved highly effective at lowering blood pressure and reducing the need for anti-hypertensive medications, as well as bringing remissions of type 2 diabetes. DiRECT involved a 12-week 830-calorie formula diet to induce weight loss, followed by support to gradually reintroduce healthy meals from ordinary foods and maintain weight loss. The landmark trial was the first to show that remission from type 2 diabetes is possible through a dietary intervention programme in primary care, with almost half (46%) of people in remission at one year, and 36% at two years. With a weight loss of over 10 kg, 75% (three-quarters) of intervention group participants were in remission at both 1 and 2 years.
To investigate how much of the weight losses and remissions in the original two-year trial could be sustained – and whether there might be wider health benefits – the DiRECT-Extension study delivered a low-intensity weight-loss maintenance support programme to 95 participants who remained from the original DiRECT trial. Over the course of three years, participants received appointments at their GP surgery, or remotely during COVID-19 lockdowns, every three months to review their weight, blood sugar levels and blood pressure, and were offered advice and support to maintain their weight loss.
The DiRECT-Extension results demonstrated the continued effectiveness of prolonged weight management for the control and remission of type 2 diabetes. However, there was notable weight regain in some participants, especially up to year 3, underscoring the difficulty that maintaining weight loss poses – and also the need to find new ways to deliver this kind of support to patients. Importantly, however, those who maintained remission achieved an average weight loss of 8.9kg at five years.
Overall, at 5 years, those in the DiRECT-Extension group lost an average of 6.1kg. People in the original DiRECT control group who were receiving routine diabetes care, but with clear advice to lose weight, lost an average of 4.6kg. The original intervention group spent more of the 5 years than the original control group with weight over 5% below baseline (61% vs 29%), with HbA1c below the diabetes threshold of 48 mmol/mol (29% vs 15%), without needing anti-diabetes medication (51% vs 16%), and in remission (27% vs 4%). Of those in remission at year-2, over a quarter (26%) remained in remission at 5 years.
In keeping with results from other studies, the 5-year results also suggested wider health benefits from the diet intervention. Those in the original DiRECT intervention group had under half the number of illnesses needing hospital admission (4.8 events per 100 patient-years) than the original DiRECT control group (10.2 events per 100 patient-years), and participants had fewer diabetes-related clinical events if they maintained weight losses, lower HbA1c and remissions.
Professor Mike Lean, who co-designed the original DiRECT trial, and is the senior author of the latest DiRECT-Extension study, said: “Previously considered permanent, requiring life-long drug treatment, type 2 diabetes is now recognised to be a potentially reversible consequence of excessive or abnormal accumulation of body fat. When fat accumulates in vital organs, like liver, pancreas or heart, these organs stop functioning normally. Weight loss of 10-15kg (about 2 stones) is enough to remove that abnormal fat from vital organs, and the key to any type 2 remission.
“DiRECT has made a world-wide paradigm-shift in understanding and treating type 2 diabetes. The disease is not necessarily permanent, and the 5-year results now suggest that diet treatment for weight loss to achieve a period of remission is likely to be accompanied by greater freedom from some diabetes complications and fewer people being admitted to hospital with medical problems.
“We must now call for much more effective, long-term funding for research to improve on these results – especially to prevent weight regain. However the evidence means that we should no longer merely reduce high blood sugar with medication, but to try to check the underlying disease-process with effective weight management as a priority when type 2 diabetes is diagnosed. Previous research has shown that people who have type 2 diabetes but who are not overweight have excess or anormal body fat, and may be able to achieve remission with quite modest weight loss. New drugs being developed for type 2 diabetes and obesity are exciting, but they should not be prescribed without sound dietary weight-management.”
Professor Roy Taylor, from Newcastle University, who co-designed the original DiRECT trial, and is a senior author of the latest DiRECT-Extension study, said: “This five-year study demonstrates that long-term remission from type 2 diabetes is possible if sufficient weight loss is achieved and maintained.
“Whether or not remission of diabetes was achieved, those people who were assigned to the weight loss group had less than half of the serious health issues experienced by the conventionally treated group. These are encouraging outcomes which should help change how this serious condition is managed.”
Dr Elizabeth Robertson, Director of Research at Diabetes UK, said: “Diabetes UK is proud to have funded over a decade of research that has forged new frontiers for people with type 2 diabetes and put remission on the map. Remission from type 2 diabetes lifts the burden of 24/7 diabetes-management and can transform health and wellbeing. But we know that going into remission can be challenging and staying there even more so. That’s why we’ve just launched our new remission information and support hub and are continuing to fund research to understand how to help more people go into remission and stay there for longer.”
The study, ‘Five-year follow-up of the randomised Diabetes Remission Clinical Trial (DiRECT): Extension study of continued support for weight loss maintenance’ is published in The Lancet Diabetes & Endocrinology. The work was funded by Diabetes UK.
Enquiries: [email protected] or [email protected]
First published: 23 February 2024
<< February
<< previous story
in this issue
next story >>
Related Links
Professor Michael Lean, research profile
School of Medicine, Dentistry & Nursing
College of Medical, Veterinary & Life Sciences
The DiRECT Trial
Diabetes UK
Link to the paper

Credit: Shutterstock / Fahkamram
Early blood glucose control for people with type 2 diabetes is crucial for reducing complications and prolonging life
Research led by scientists from the Universities of Oxford and Edinburgh has found that early good blood glucose control can minimise the lifetime risk of diabetes-related complications, including heart attacks, kidney failure and vision loss.
These latest results from the UK Prospective Diabetes Study (UKPDS) , one of the longest ever clinical trials in type 2 diabetes, were made feasible by incorporating NHS data.
Professor Rury Holman of Oxford's Radcliffe Department of Medicine , the founding Director of the University of Oxford Diabetes Trials Unit and Chief Investigator of the UKPDS, said, ‘These remarkable findings emphasise the critical importance of detecting and treating type 2 diabetes intensively at the earliest possible opportunity.
‘People may have type 2 diabetes for several years before being diagnosed as they may have few symptoms until their blood sugars become substantially elevated.’
20-year trial led to worldwide guideline changes in blood glucose control
Starting in 1977, the UKPDS randomly allocated people with newly diagnosed type 2 diabetes to an intensive blood glucose control strategy with sulfonylureas, insulin, or metformin, or to a conventional blood glucose control strategy, primarily with diet.
The 20-year trial results, published in 1998, showed that good blood glucose control reduced the risk of diabetic complications. Worldwide, UKPDS changed guidelines to recommend intensive blood glucose control for everyone with type 2 diabetes.
‘This meant that the therapies and blood glucose levels in the two UKPDS groups rapidly became similar,’ explains Professor Holman.
‘Despite this, the 10-year post-trial monitoring study, published in 2008, showed those who had been allocated to early intensive blood glucose control continued to experience fewer diabetic complications compared with those allocated to conventional blood glucose control.’
Continuing benefits described as a ‘legacy’ effect
The new results show that the legacy effects of implementing intensive blood glucose control straight after diagnosis of diabetes continue to persist for up to 24 years after the trial ended.
Early intensive blood glucose control with insulin injections or sulfonylurea tablets led to 10% fewer deaths, 17% fewer heart attacks and 26% fewer diabetic complications such as kidney failure and vision loss. Early intensive blood glucose control with metformin led to 31% fewer heart attacks and 20% fewer deaths. The treatments used in the UKPDS remain in common use worldwide at low cost.
Professor Amanda Adler , Director of the Diabetes Trial Unit, said, ‘This shows that treating type 2 diabetes early and thoroughly is crucial. Playing catch-up with blood glucose control is not sufficient.’
Professor Philip Clarke , Director of the University of Oxford Health Economics Research Centre , said ‘A major life-time benefit is the increased life-expectancy in those allocated to intensive blood glucose control. The reduced rate of many diabetes-related complications will have a positive impact on overall quality of life’.
Dr Will Whiteley , Professor in Neurology and Epidemiology at the University of Edinburgh Centre for Clinical Brain Sciences , and Associate Director at BHF Data Science Centre, HDRUK , added: ‘Following up UKPDS participants for up to 42 years was possible only with the rich linked NHS data sources across UK nations. This meant we could study the effects of treatments given in midlife on diseases of ageing, such as dementia. This shows the value for clinical trials of accessing NHS data.’
The paper, ' Post-trial monitoring of a randomised controlled trial of intensive glycaemic control in type 2 diabetes extended from 10 years to 24 years (UKPDS 91) ', was presented at the 67th Japan Diabetes Society meeting, Tokyo, Japan, and is published in The Lancet .
DISCOVER MORE
- Support Oxford's research
- Partner with Oxford on research
- Study at Oxford
- Research jobs at Oxford
You can view all news or browse by category
You are using an outdated browser. Please upgrade your browser to improve your experience.
Newcastle Magnetic Resonance Centre
Diabetes Research
The Diabetes Research Group in Newcastle has applied magnetic resonance spectroscopy and imaging to explain the abnormal storage of fat and glycogen in pancreas, liver and muscle in Type 2 diabetes.
Type 2 diabetes is escalating as a national public health problem, and the rapidly rising incidence in younger people will certainly be followed by premature coronary and stroke disease.
Our work has shown that Type 2 diabetes is caused by abnormal fat storage accumulation in the pancreas. Research on how Type 2 may be reversed is available. Application of a newly developed magnetic resonance method has allowed the importance of the pancreas fat content to be evaluated.
Other current studies have allowed identification of the failure of muscle glycogen storage and abnormal storage of fat in muscle after eating in Type 2 diabetes. This work is revolutionising concepts of intra-organ energy storage after eating both in normal health and in diabetes. Additionally it has been demonstrated that DPP-4 inhibitors (specifically Vildagliptin) decrease liver fat stores.
We have shown that there is no intrinsic abnormality in mitochondrial ATP production in muscle of people with Type 2 diabetes.
We have developed methods to evaluate kidney disease in diabetes.
View Prof Roy Taylor 's staff profile.
Current and planned work
The DiRECT study will find out how well reversal of Type 2 diabetes works when done by Practice Nurses in General Practice. It is a cluster randomised controlled trial which will also define how durable is the return to normal glucose control, how people cope with the programme and what underlying changes in liver and pancreas determine outcome. Visit the DiRECT website .
Studies of the effect of exercise training on the previously defined abnormal muscle metabolism in Type 2 diabetes.
These studies have been supported by:
- Diabetes UK
- the Diabetes Research and Wellness Foundation
- the Wellcome Trust
- Novartis Pharma AG
- the European Foundation for the Study of Diabetes
Diabetes projects
- Remission of type 2 diabetes with Total Diet Replacement and long-term maintenance, within routine NHS care (DiRECT – Diabetes REmission Clinical Trial). Project Leader(s): Professor Roy Taylor Project Dates: From April 2014
Publications
- Sattar N, Taheri S, Astling DP, Chadwick J, Hinterberg MA, Holmes MV, Troth EV, Welsh P, Zaghloul H, Chagoury O, Lean M, Taylor R, Williams S. Prediction of cardiometabolic health through changes in plasma proteins with intentional weight loss in the DiRECT and DIADEM-I randomised clinical trials of type 2 diabetes remission. Diabetes Care 2023; Sep 26:dc230602. doi: 10.2337/dc23-0602. Online ahead of print.
- Corbin LJ, Hughes DA, Bull CJ, Vincent EE, SmithML, McConnachie A, Messow C, Welsh P, Taylor R, Lean MEJ, Sattar N, Timpson NJ. The metabolomic signature of weight loss and remission in the Diabetes Remission Clinical Trial (DiRECT). Diabetologia 2023 Online
- Taylor R, Barnes AC, Hollingsworth KG, Irvine KM, Solovyova A, Clark. L, Martin-Ruiz C, Romeres R, Koulman A, Meek,CM, Jenkins B, Cobelli C, Holman R. Aetiology of Type 2 diabetes in people with a ‘normal’ body mass index: testing the personal fat threshold hypothesis. Clin Sci (Lond) (2023)137: 1333–1346 doi.org/10.1042/CS20230586
- Jesuthasan, Aaron, Sviatlana Zhyzhneuskaya, Carl Peters, Alison C. Barnes, Kieren G. Hollingsworth, Naveed Sattar, Michael E. J. Lean, Roy Taylor, and Ahmad H. Al-Mrabeh. "Sex Differences in Intraorgan Fat Levels and Hepatic Lipid Metabolism: Implications for Cardiovascular Health and Remission of Type 2 Diabetes after Dietary Weight Loss." Diabetologia 65, no. 1 (2022/01/01 2022): 226-33. https://dx.doi.org/10.1007/s00125-021-05583-4 .
- Rehackova L, Rodrigues AM, Thom G, Brosnahan N, Barnes AC, McCombie L, Leslie WS, Zhyzhneuskaya S, Peters C, Adamson AJ, Lean MEJ, Taylor R, Sniehotta FF. Delivering the Diabetes Remission Clinical Trial (DiRECT) in primary care: A mixed-methods study of experiences of health care. Diabet Med 2022 39:e14952; DOI: 10.1111/dme.14752
- Williams SA, Rachel Ostroff, Michael A. Hinterberg, Josef Coresh, Christie M. Ballantyne, Matsushita K, Mueller CE, Walter J, Jonasson C, Holman RR, Shah SH, Sattar N, Taylor R, et al. A proteomic surrogate for cardiovascular outcomes that is sensitive to multiple mechanisms of change in risk. Science Translational Reports 2022, 14, eabj9625.
- Cassidy S, Trenell M, Stefanetti RJ, Charman SJ, Barnes AC, Brosnahan N, McCombie L, Thom G, Peters C, Zhyzhneuskaya S, Leslie WS, Catt C, Catt M, McConnachie A, Sattar N, Sniehotta FF, Lean MEJ, Taylor R. Physical activity, inactivity and sleep during the Diabetes Remission Clinical Trial (DiRECT). Diabetic Medicine 2022 40:e15010. doi: 10.1111/dme.15010
- Unwin D, Delon C, Unwin J, Tobin S, Taylor R. What predicts drug-free type 2 diabetes remission? Insights from an 8-year general practice service evaluation of a lower carbohydrate diet with weight loss BMJ Nutrition, Prevention and Health 2022 0:e000544. Doi:10.1136/bmjnph-2022-000544
- Taylor R. Type 2 Diabetes: The Problem and the Solution. Br J Diabetes 2022;22(Supp1):S55-S58 https://bjd-abcd.com/index.php/bjd/article/view/1055/1307
- Riddle MC, Cefalu WT, Evans PH, Gerstein HC, Nauck MA, Oh WK, Rothberg AE, le Roux CW, Rubino F, Schauer P, Taylor R, Twenefour D Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes Diabetes Care 2021;44(10):2438–2444 https://doi.org/10.2337/dci21-0034
- Leslie, Wilma S., Eman Ali, Leanne Harris, C. Martina Messow, Naomi T. Brosnahan, George Thom, E. Louise McCombie, Alison C. Barnes, Naveed Sattar, Roy Taylor, and Michael E. J. Lean. "Antihypertensive Medication Needs and Blood Pressure Control with Weight Loss in the Diabetes Remission Clinical Trial (Direct)." Diabetologia 64, no. 9 (2021/09/01 2021): 1927-38. https://dx.doi.org/10.1007/s00125-021-05471-x .
- Riddle, Matthew C., William T. Cefalu, Philip H. Evans, Hertzel C. Gerstein, Michael A. Nauck, William K. Oh, Amy E. Rothberg, Carel W. le Roux, Francesco Rubino, Philip Schauer, Roy Taylor, and Douglas Twenefour. "Consensus Report: Definition and Interpretation of Remission in Type 2 Diabetes." Diabetologia 64, no. 11 (2021/11/01 2021): 2359-66. https://dx.doi.org/10.1007/s00125-021-05542-z .
- Al-Mrabeh A, Peters C, Hollingsworth KG, Taylor R. Measurement of intraorgan fat and hepatic output of triglycerides in human type 2 diabetes by magnetic resonance and intralipid infusion techniques. Star Protocols 2021; 2:1 https://doi.org/10.1016/j.xpro.2021.100355
- Brosnahan N, Leslie W, McCombie L, Barnes A, Thom G, McConnachie A, Messow C M, Sattar N, Taylor R, Lean M E J. Brief formula low-energy-diet for relapse management during weight loss maintenance in the Diabetes Remission Clinical Trial (DiRECT). J Hum Nutr Diet. 2021;00:1-8 https://doi.org/10.1111/jhn.12839
- Rehackova L, Rodrigues AM, Thom G, Brosnahan N, Barnes AC, McCombie L, Leslie WS, Zhyzhneuskaya S, Peters C, Adamson AJ, Lean MEJ, Taylor R, Sniehotta FF. Participant experiences in the Diabetes REmission Clinical Trial (DiRECT). Diabet Med 2021;00:e14689 https://doi.org/10.1111/dme.14689
- Leslie WS, Ali E, Harris L, Martina Messow C, Brosnahan NT, Thom G, McCombie EL, Barnes AC, Sattar N, Taylor R, Lean MEJ. Antihypertensive medication needs and blood pressure control with weight loss in the Diabetes REmission Clinical Trial (DiRECT). Diabetologia (2021) 64:1927–1938 https//doi.org/10.1007/s00125-021-05471-x
- Taylor R. Type 2 diabetes and remission: practical management guided by pathophysiology. Journal of Internal Medicine 2021; 289: 754–770 http://dx.doi.org/10.1111/joim.13214
- Taylor R, Ramachandran A, Yancy Jr WS, Forouhi NG. Nutritional basis of type 2 diabetes remission. Brit Med J 2021; 373: n1449.
- Petrov M, Taylor R. Intra-pancreatic fat deposition: Piecing the exocrine and endocrine pancreas together. Nature Reviews Gastroenterology & Hepatology 2021 online https://doi.org/10.1038/s41575-021-00551-0 . [View only https://rdcu.be/cCQzO ]
- Al-Mrabeh A , Hollingsworth KG. Shaw JAM, McConnachie A, Sattar N; Lean MEJ, Taylor R. 2-year remission of type 2 diabetes and pancreas morphology: a post-hoc analysis of the DiRECT open-label, cluster-randomised trial. Lancet Diabetes Endocrinol 2020; 8: 939-948; doi: 10.1016/S2213-8587(20)30303-X
- Yiqiao X, Davies A, Briggs A, McCombie L, Martina Messow C, Grieve E, Leslie WM, Taylor R , Lean MEJ. Type 2 diabetes remission: 2 year within-trial and lifetime-horizon cost-effectiveness of the Diabetes Remission Clinical Trial (DiRECT)/Counterweight-Plus weight management programme. Diabetologia 2020; DOI: 10.1007/s00125-020-05220-6; In press.
- Kusinski LC, Murphy HR, De Lucia Rolfe E, Rennie KL, Oude Griep LM, Hughes D, Taylor R , Meek CL. Dietary Intervention in pregnant women with gestational diabetes; protocol for the DiGest randomised controlled trial. Nutrients 2020; April 22; doi: 10.3390/nu12041165.
- Preshaw PM, Taylor JJ, Jaedicke KM, De Jager M, Bikker JW, Selten W, Bissett SM, Whall KM, Van de Merwe R, Areibi A, Jitprasertwong P, Al-Shahwani R, Weaver J, Taylor R , Wassall RR. Treatment of periodontitis reduces systemic inflammation in type 2 diabetes. Journal of Clinical Periodontology 2020; February 27; doi: 10.111/jcpe.13274.
- Zhyzhneuskaya SV, Al-Mrabeh A , Peters C, Barnes AC, Aribasala B, Hollingsworth KG, McConnachie A, Sattar N, Lean MEJ, Taylor R. Time course of normalisation of functional beta cell capacity in DiRECT after weight loss in type 2 diabetes. Diabetes Care 2020; April; doi: 10.2337/dc19-0371.
- Al-Mrabeh A , Zhyzhneuskaya SV, Peters C, Barnes AC, Melhem S, Jesuthasan A, Aribisala B, Hollingsworth KG, Lietz G, Mather JC, Sattar N, Lean MEJ, Taylor R. Hepatic Lipoprotein Export and Remission of Human Type 2 Diabetes after Weight Loss. Cell Metabolism 2020 Feb 4;31(2):233-249.e4. doi: 10.1016/j.cmet.2019.11.018.
- Thom G, McIntosh A, Messow C-M, Leslie WS, Barnes A, Brosnahan N, McCombie L, Malkova D, Al-Mrabeh A, Zhyzhneuskaya S, Welsh P, Sattar N, Taylor R, Lean MEJ. Weight loss-induced increase in fasting ghrelin concentration is a predictor of weight regain: Evidence from the Diabetes Remission Clinical Trial (DiRECT). Diabetes Obes Metab 2020; Dec 2;DOI: 10.1111/dom.14274
- Thom G, Messow C‐M, Leslie WS, Barnes AC, Brosnahan N, McCombie EL, Al‐Mrabeh A, Zhyzhneuskaya S, Welsh P, Sattar N, Taylor R, Lean MEJ. Predictors of type 2 diabetes remission in the Diabetes Remission Clinical Trial (DiRECT). Diabetic Medicine 2020 https://doi.org/10.1111/dme.14395
- Shaden M, Steven S, Taylor R, Al-Mrabeh A . Effect of Weight Loss by Low-Calorie Diet on Cardiovascular Health in Type 2 Diabetes: An Interventional Cohort Study. Nutrients 2021, 13(5), 1465 doi: 10.3390/nu13051465
- Taylor R. Remission of type 2 diabetes – Latest Information for Health care Professionals. Practical Diabetes 2020 37:177-182
- Rehackova L, Araujo-Soares V, Steven S, Adamson AJ, Taylor R , Sniehotta FF. Behaviour change during dietary type 2 diabetes remission: A longitudinal qualitative evaluation of an intervention using a very low energy diet. Diabetic Med 2020 June;37(6):953-962. doi: 10.1111/dme.14066. Epub 2019 Aug 8.
- Xin Y, Davies A, McCombie L, Briggs A, Messow, C-M, Grieve E, Leslie WS, Taylor R , Lean MEJ. Type 2 diabetes remission: economic evaluation of the DiRECT/Counterweight-Plus weight management programme within a primary care randomized controlled trial. Diabetic Med 2019. April 26 doi:10.1111/dme.13981.
- Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, Peters C, Zhyzhneuskaya S, Al-Mrabeh A, Hollingsworth KG, Rodrigues AM, Rehackova L, Adamson AJ, Sniehotta FF, Mathers JM, Ross HM, McIlvenna Y, Welsh, P, Kean, S, Ford I, McConnachie A, Messow, C-M Sattar N, Taylor R. Durability of a primary care-led weight-management intervention for remission of type 2 diabetes: 2-year results of the DiRECT open-label, cluster-randomised trial. Lancet 2019; 7: 344–55; doi:10.1016/s2213-8587(19)30068-3.
- Taylor R, Al-Mrabeh A, Sattar N. Understanding the mechanisms of reversal of type 2 diabetes. Lancet Diabetes and Endocrinol. 2019; 7:726-736. doi: 10.1016/S2213-8587(19)30076-2
- Taylor R , Al-Mrabeh A, Zhyzhneuskaya S, Peters C, Barnes A, Aribisala B, Hollingsworth KG, Mathers JC, Sattar N, Lean MEJ. Remission of human type 2 diabetes requires decrease in liver and pancreas fat content but is dependent upon capacity for beta cell recovery. Cell Metab. 2018 Oct 2;28(4):547-556.e3. doi: 10.1016/j.cmet.2018.07.003.
- Taylor R , Barnes AC. Translating aetiological insight into sustainable management into type 2 diabetes. Diabetologia 2018: 61 273-283 doi: 10.1007/s00125-017-4504.
- Lean MEJ, Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, Peters C, Zhyzhneuskaya S, Al-Mrabeh A, Hollingsworth KG, Rodrigues AM, Rehackova L, Adamson AJ, Sniehotta FF, Mathers JM, Ross HM, McIlvenna Y, Stefanetti R, Trenell M, Welsh P, Kean S, Ford I, McConnachie A, Sattar N, Taylor R . Primary care weight-management for type 2 diabetes: the cluster-randomised Diabetes Remission Clinical Trial (DiRECT). Lancet 2017; 391:541-51 doi.org/10.1016/S0140-6736(17)33102-1 (IF 44)
- Taylor R , Leslie WS, Barnes AC, Brosnahan N, Thom G, McCombie L, Peters C, Zhyzhneuskaya S, Al-Mrabeh A, Hollingsworth KG, Rodrigues AM, Rehackova L, Adamson2 AJ, Sniehotta FF, Mathers JM, Ross HM, McIlvenna Y, Stefanetti R, Trenell M, Welsh P, Kean S, Ford I, McConnachie A, Sattar N, Lean MEJ. Clinical and metabolic features of the randomised controlled Diabetes Remission Clinical Trial (DiRECT) cohort. Diabetologia 2017; 61:589-98 https://doi.org/10.1007/s00125-017-4503-0 (IF 6.2)
- Rehackova L, Araujo-Soares V, Adamson AJ, Steven S, Taylor R , Sniehotta F. F. Acceptability of a very-low-energy diet in Type 2 diabetes: patient experiences and behaviour regulation Diabetic Med 2017; 34: 1554–1567
- Al-Mrabeh A, Hollingsworth KG, Steven S, Tiniakos D and Taylor R. Quantification of intrapancreatic fat in type 2 diabetes by MRI. PLOS One. April 3, 2017https://doi.org/10.1371/journal.pone.0174660.
- Hodson K , Dalla Man C, Smith FE, Barnes A, McParlin C, Cobelli C, Robson SC, Araujo-Soares V, Taylor R. Liver triacylglycerol content and gestational diabetes: Effects of moderate calorie restriction. Diabetologia. 2017 Feb;60(2):306-313. doi: 10.1007/s00125-016-4143-9. PMID: 27817155.
- Leslie WS, Taylor R , Harris L, Lean M. Weight losses with low energy formula diets in obese patients with and without type 2 diabetes: Systematic review and meta-analysis. Int J Obes (Lond). 2017; 41:96-101. doi: 10.1038/ijo.2016.175.
- White MG, Shaw JAM, Taylor R . Type 2 diabetes: The pathologic basis of reversible beta-cell dysfunction. Diabetes Care 2016; 39:2080-88. doi 10.2337/dc16-0619.
- Steven S , Hollingsworth KG, Small PK, Woodcock SA, Pucci A, Aribisala B, Al-Mrabeh A, Batterham RL, Taylor R. Calorie restriction and not glucagon-like peptide-1 explains the acute improvement in glucose control after gastric bypass in Type 2 diabetes. Diabet Med. 2016 Dec;33(12):1723-1731. doi: 10.1111/dme.13257. Epub 2016 Oct 8.
- Al-Mrabeh A , Hollingsworth KG, Steven S, Taylor R. Morphology of the pancreas in type 2 diabetes: effect of weight loss with or without normalisation of insulin secretory capacity. Diabetologia. 2016 Aug;59(8):1753-9. doi: 10.1007/s00125-016-3984-6. [Epub 2016 May 14].
- Avery L, Charman S, Taylor L, Flynn D, Mosely K, Speight J, Lievesley M, Taylor R , Sniehotta F, Trenell M. Systematic development of a theory-informed multifaceted behavioural intervention to increase physical activity of adults with type 2 diabetes in routine primary care: Movement as Medicine for Type 2 Diabetes. Implementation Science. 2016 Jul 19;11:99. doi: 10.1186/s13012-016-0459-6.
- Steven S , Hollingsworth KG, Al-Mrabeh A, Avery L, Aribisal B, Caslake M and Taylor R. Very-Low-Calorie Diet and 6 Months of Weight Stability in Type 2 Diabetes: Pathophysiologic Changes in Responders and Nonresponders. Diabetes Care. 2016 May;39(5):808-15. doi: 10.2337/dc15-1942. Epub 2016 Mar 21. PMID: 27002059.
- Steven S , Hollingsworth KG, Small PK, Woodcock SA, Pucci A, Aribisala B, Al-Mrabeh A, Daly AK, Batterham RL, Taylor R. Weight Loss Decreases Excess Pancreatic Triacylglycerol Specifically in Type 2 Diabetes. Diabetes Care. 2016 Jan;39(1):158-65. doi: 10.2337/dc15-0750. Epub 2015 Dec 1. PMID: 26628414.
- Steven S , Hollingsworth KG, Small PK, Woodcock SA, Pucci A, Aribasala A, Al-Mrabeh A, Batterham RL and Taylor R. Increased GLP-1 at 7 days following RYGB does not translate into improved insulin secretion rates or glucose control compared to 7 days of VLCD.
- Wilma Leslie; Ian Ford; Naveed Sattar; Kieren Hollingsworth; Ashley Adamson; Falko Sniehotta; Louise McCombie; Naomi Brosnahan; Hazel Ross; John Mathers; Carl Peters; George Thom; Alison Barnes; Sharon Kean; Yvonne McIlvenna; Angela Rodrigues; Lucia Rehackova; Sviatlana Zhyzhneuskaya; Roy Taylor ; Mike Lean. The Diabetes Remission Clinical Trial (DiRECT): protocol for a cluster randomised trial. BMC Family Practice. 2016 Feb 16;17:20. doi:10.1186/s12875-016-0406-2. PMID: 26879684.
- Cassidy S, Thoma C, Hallsworth K, Parikh J , Hollingsworth KG, Taylor R, Jakovljevic DG, Trenell MI. High intensity intermittent exercise improves cardiac structure and function and reduces liver fat in patients with type 2 diabetes: a randomised controlled trial. Diabetologia. 2016 Jan;59(1):56-66. doi: 10.1007/s00125-015-3741-2. Epub 2015 Sep 9.
- Steven S , Taylor R. Restoring normoglycaemia by use of a very low calorie diet in long- and short-duration Type 2 diabetes. Diabet Med. 2015 Feb 12. doi: 10.1111/dme.12722. [Epub ahead of print]. PMID: 25683066.
- Macauley M , Hollingsworth KG, Smith FE, Thelwall PE, Al-Mrabeh A, Schweizer A, Foley JE, Taylor R. Effect of Vildagliptin on Hepatic Steatosis. J Clin Endocrinol Metab. 2015 Feb 12. doi: 10.1111/dme.12722. PMID: 25683066.
- Macauley M , Percival K, Thelwall PE, Hollingsworth KG, Taylor R. Altered volume, morphology and composition of the pancreas in type 2 diabetes. PLOS ONE. 2015. In Press.
- Steven S , Carey PE, Small PK, Taylor R. Reversal of Type 2 diabetes after bariatric surgery is determined by the degree of achieved weight loss in both short- and long-duration diabetes. Diabetic Medicine. 2015 Jan; 32(1):47-53. doi: 10.1111/dme.12567. Epub 2014 Sep 12. PMID: 25132043.
- Macauley M , Smith FE, Thelwall P, Taylor R. Diurnal variation in skeletal muscle and liver glycogen in humans with normal health and type 2 diabetes. Clinical Science. 2015 Jan 13. PMID: 25583442. In Press.
- Talks J, Manjunath V, Steel DHW, Peto T, Taylor R . New vessels detected on wide field imaging compared to 2-field and 7-field imaging: implications for diabetic retinopathy screening image analysis. Br J Ophthalmol 2015 doi:10.1136/bjophthalmol-2015-306719.
- Cassidy S, Hallsworth K, Thoma C, MacGowan GA, Hollingsworth KG , Day CP, Taylor R, Jakovljevic DG, Trenell MI. Cardiac structure and function are altered in Type 2 diabetes and Non-alcoholic fatty liver disease and associate with glycemic control. Cardiovasc Diabetol. 2015 Feb 13;14:23. doi: 10.1186/s12933-015-0187-2.
- Hodson K , DellaMan C, Smith FE, Thelwall PE, Cobelli C, Robson SC, Taylor R. Mechanism of insulin resistance in normal pregnancy. Horm Metab Res. 2013 Aug;45(8):567-71. doi: 10.1055/s-0033-1337988. Epub 2013 Apr 2. PMID: 23549674.
- Avery L, Sniehotta FF, Denton SJ, Steen N, McColl E, Taylor R , Trenell MI. Movement as Medicine for Type 2 Diabetes: protocol for an open pilot study and external pilot clustered randomised controlled trial to assess acceptability, feasibility and fidelity of a multifaceted behavioural intervention targeting physical activity in primary care. Trials 2014 Feb 3; 15:46. doi: 10.1186/1745-6215-15-46. PubMed PMID: 24491134.
- Taylor R . Type 2 Diabetes: Etiology and Reversibility. Diabetes Care. 2013 Apr;36(4):1047-55. doi: 10.2337/dc12-1805. PubMed PMID: 23520370.
- Taylor R . Reversing the Twin Cycles of Type 2 Diabetes: The Banting Lecture 2012. Diabet Med. 2013 Mar;30(3):267-75. doi: 10.1111/dme.12039. PubMed PMID: 23075228.
- Steven S , Lim EL, Taylor R. Population response to information on reversibility of Type 2 diabetes. Diabet Med. 2013 Jan 15. doi: 10.1111/dme.12116. [Epub ahead of print].
- Knop F, Taylor R . Mechanism of metabolic advantage after bariatric surgery - it’s all gastrointestinal factors vs. it’s all food restriction. Diabetes Care. 2013 Aug;36 Suppl 2:S287-91. doi: 10.2337/dcS13-2032. PubMed PMID: 23882061.
- Taylor R . Insulin resistance and type 2 diabetes. Diabetes. 2012 Apr;61(4):778-9. doi: 10.2337/db12-0073. PubMed PMID: 22442298.
- Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R . Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011 Jun 9.
- Lim EL , Hollingsworth KG, Smith F, Thelwall PE, Taylor R. Inhibition of lipolysis in type 2 diabetes normalizes glucose disposal without change in muscle glycogen synthesis rates. Clin. Sci. 2011; 121: 169-177.
- Lim EL , Hollingsworth KG, Smith F, Thelwall PE, Taylor R. Effects of raising muscle glycogen synthesis on skeletal muscle ATP turnover rate in type 2 diabetes. American J Physiology 2011 PMID 21917633.
- Thelwall PE , Taylor R, Marshall SM. Non-invasive investigation of kidney disease in Type 1 diabetes by magnetic resonance imaging. Diabetologia 2011; 54(9):2421-9.
- Taylor R. Reversing Type 2 diabetes. Practical Diabetes 2011; 28: 377-378.
- Lim EL , Hollingsworth KG, Thelwall P, Taylor R. Measuring the acute effect of insulin infusion on ATP turnover rate in human skeletal muscle using phosphorus-31 magnetic resonance saturation transfer spectroscopy. NMR in Biomedicine 2010; 23:952-7.
- Chen MJ , Jovanovic A, Taylor R. Utilizing the Second-Meal Effect in Type 2 Diabetes: Practical Use of a Soya-Yogurt Snack. Diabetes Care 2010; 2552-54.
- Steven S , Lim EL, Taylor R. Reversal of type 2 diabetes. Diabetic Medicine 2010; 27: 724-725.
- Balasubramanian R, Gerrard J, Dalla Man C, Firbank MJ, Lane A, English PT, Cobelli C, Taylor R . Combination peroxisome proliferator-activated receptor gamma and alpha agonist treatment in type 2 diabetes prevents the beneficial pioglitazone effect on liver fat content. Diabetic Medicine 2010; 27:150-156.
- Hayes L, Pearce MS, Firbank MJ, Walker M, Taylor R , Unwin N. Do obese but metabolically normal women differ in intra-abdominal fat and physical activity levels from those with the expected metabolic abnormalities? A cross-sectional study. BMC Public Health. 2010; 10:723.
- Jovanovic A , Leverton E, Solanky B, Snaar JEM, Morris PEG, Taylor, R. The second meal phenomenon is associated with enhanced muscle glycogen storage. Clin. Sci. 2009 Jul 2;117(3):119-27.
- Jovanovic A , Gerrard, J., Taylor, R. The second meal phenomenon in type 2 diabetes. Diabetes Care 2009 Jul;32(7):1199-201.
- Taylor R . Pathogenesis of type 2 diabetes: tracing the reverse route from cure to cause. Diabetologia. 2008;51(10):1781-9.
- Trenell MI , Hollingsworth KG, Lim EL, Taylor R. Increased daily walking improves lipid oxidation without changes in mitochondrial function in type 2 diabetes. Diabetes Care. 2008 Aug;31(8):1644-9.
- Sorensen L, Siddall PJ, Trenell MI , Yue DK. Differences in Metabolites in Pain-Processing Brain Regions in Patients With Diabetes and Painful Neuropathy. Diabetes Care. 2008 May 1, 2008;31(5):980-1.
- Lim, E; Trenell, MI; Hollingsworth, KG; Smith, FE; Thelwell, PE; Taylor, R. Is the sub-normal insulin stimulation of muscle ATP synthesis in type 2 diabetes always a consequence of low rates of muscle glycogen synthesis? Diabetologia 51: 766 (2008).
- Trenell, MI; Thelwall, P; Thomas, K; Stevenson, E. Effect of high and low glycaemic index diets on skeletal muscle and liver substrate storage and utilisation during exercise. Diabetologia 51: 248 (2008).
- Ravikumar B , Gerrard J, Man CD, Firbank MJ, Lane A, English PT, et al. Poglitazone decreases fasting and postprandial endogenous glucose production in proportion to decrease in hepatic triglyceride content. Diabetes 2008; 57(9):2288-95.

IMAGES
COMMENTS
Newcastle research has established that type 2 diabetes is caused by excess fat in liver and pancreas. If this fat is removed in the first ~6 years of diabetes, functional beta cell mass gradually returns to a completely normal level over 12 months in most people. The immediate loss of fat from the pancreas following weight loss is from a ...
Type 2 diabetes has long been regarded as a chronic disease and one with a complex, obscure cause. However, research by Newcastle University's Professor Roy Taylor using innovative magnetic resonance methods has confirmed his Twin Cycle Hypothesis - that Type 2 diabetes is simply caused by excess fat within the liver and pancreas.
Weight loss puts type 2 diabetes into remission for five years. Published on: 19 April 2023. New findings have revealed that nearly a quarter (23%) of participants who were in remission from type 2 diabetes at two years in a clinical trial remained in remission at five years. Prof Roy Taylor in the lab. For those who remain free of diabetes ...
Once considered an irreversible condition that worsens with time, research at Newcastle University has shattered conventional beliefs about type 2 diabetes. Professor Roy Taylor's pioneering discoveries have been accepted by the NHS - signifying more than just a scientific breakthrough, but marking a shift in how we perceive and treat type 2 ...
University research into reversing diabetes has been turned into a concise book explaining what happens to us when we get type 2 and how we can escape it. ... With his team of researchers at Newcastle University he has demonstrated that type 2 is caused by just one factor - too much internal fat in the liver and pancreas - and that to ...
Research by Professor Roy Taylor of Newcastle University has proven that Type 2 Diabetes is reversible. It is estimated that diabetes costs the NHS £10 billion a year, while almost one in 20 prescriptions written by GPs is for diabetes treatment. Once thought to be an incurable, lifelong condition, Professor Roy Taylor's findings have proven ...
Improving type 2 Diabetes management through Examining, Advising and prescribing (IDEA) trial. ... the research team and workshop facilitators . 2013 - Institute of Health and Society, Newcastle University, Newcastle upon Tyne. NE2 4AX, United Kingdom ...
Blood Glucose. Clinical and pathophysiological studies have shown type 2 diabetes to be a condition mainly caused by excess, yet reversible, fat accumulation in the liver and pancreas. Within the liver, excess fat worsens hepatic responsiveness to insulin, leading to increased glucose production. Within the pancre ….
The landmark trial carried out at Newcastle University was the first to show that remission from type 2 diabetes is possible through a dietary intervention in primary care, with almost half (46% ...
Roy Taylor and colleagues explain how type 2 diabetes can be reversed by weight loss and avoidance of weight regain Nutritional basis of type 2 diabetes remission BMJ. 2021 Jul 7:374:n1449. doi: 10. ... Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, UK.
Type 2 diabetes is a reversible condition Date: September 13, 2017 Source: Newcastle University Summary: People with type 2 diabetes can reverse the condition through a low calorie diet.
April 18, 2016 1:33 pm. Allan Tutty, who reversed his Type 2 diabetes with a special diet, on the beach in his home town of Sunderland, Great Britain. Robert Ormerod for The New York Times. Many experts believe Type 2 diabetes is an incurable disease that gets worse with time. But new research raises the tantalizing possibility that drastic ...
The new study has shown that remission of type 2 diabetes is possible even for some people with lower body weights. Results from the Diabetes UK-funded Reversal of Type 2 Diabetes upon Normalisation of Energy Intake in the Non-obese (ReTUNE) trial show a staggering 70% of participants with lower bodyweights went into type 2 remission through ...
2023-01-06. Congratulations to Diabetes UK-funded researcher Professor Roy Taylor, who has been awarded an MBE in the New Year Honours list, recognising his world-leading work in diabetes research. Professor Taylor is Emeritus Professor of Medicine and Metabolism at Newcastle University and a Diabetes UK-funded researcher.
Prof Roy Taylor, Newcastle University. The new study has shown that remission of type 2 diabetes is possible even for some people with lower body weights, delegates at the 2022 Diabetes UK Professional Conference heard today (1 st April 2022). Results from the Diabetes UK-funded Reversal of Type 2 Diabetes upon Normalisation of Energy Intake in ...
28 Institute of Cellular Medicine, Newcastle University, Newcastle, UK. 29 Diabetes Research Network, Royal Victoria Infirmary, Newcastle, UK. 30 Centre for Health, Law and Emerging Technologies (HeLEX), Faculty of Law, University of Oxford, Oxford, UK. 31 Lund University Diabetes Centre, Department of Clinical Sciences, Lund University, Malmö ...
A calorie-restricted meal replacement diet dubbed the "Newcastle diet" has achieved type 2 diabetes remission in half of patients after one year of a groundbreaking UK research trial. ... co-led by researchers at the University of Newcastle and the University of Glasgow, followed around 300 patients from 49 primary care services in Scotland ...
Further afield, Type 2 Diabetes Remission projects based on DiRECT have been conducted in many other countries, notably including Australia and New Zealand. ... Covid 19 has made both weight-loss maintenance and data collection difficult, but the Glasgow and Newcastle University research teams have continued to analyse the 2-year results ...
Dr Elizabeth Robertson, our Director of Research, said: "Diabetes UK is proud to have funded over a decade of research that has forged new frontiers for people with type 2 diabetes and put remission on the map. "Remission from type 2 diabetes lifts the burden of 24/7 diabetes management and can transform health and wellbeing.
Type 2 diabetes mellitus, the most frequent subtype of diabetes, is a disease characterized by high levels of blood glucose (hyperglycaemia). ... Research Highlights 02 Apr 2024 Nature Reviews ...
The research, led by Professor Roy Taylor at Newcastle University, UK, is published today in the academic journal, Cell Metabolism. The study involved a group of people from Tyneside who previously had Type 2 diabetes but had lost weight and successfully reversed the condition as part of the DiRECT trial, which was funded by Diabetes UK and led ...
Background: The 20-year UK Prospective Diabetes Study showed major clinical benefits for people with newly diagnosed type 2 diabetes randomly allocated to intensive glycaemic control with sulfonylurea or insulin therapy or metformin therapy, compared with conventional glycaemic control. 10-year post-trial follow-up identified enduring and emerging glycaemic and metformin legacy treatment effects.
A new tool has been developed in Nigeria for early identification of patients at risk for Type 2 diabetes, which can be routinely administered by doctors in primary health settings. The predictive ...
New findings from a three-year observational extension of the landmark Diabetes Remission Clinical Trial DiRECT reveal that, for those in remission from type 2 diabetes at the end of year two of the original study, 26% still remained in remission at year five. The overall remission rate was 13% of those with data at 5 years
These latest results from the UK Prospective Diabetes Study (UKPDS), one of the longest ever clinical trials in type 2 diabetes, were made feasible by incorporating NHS data.. Professor Rury Holman of Oxford's Radcliffe Department of Medicine, the founding Director of the University of Oxford Diabetes Trials Unit and Chief Investigator of the UKPDS, said, 'These remarkable findings emphasise ...
A body of research putting people with Type 2 diabetes on a low calorie diet has confirmed the underlying causes of the condition and established that it is reversible. Professor Roy Taylor at Newcastle University, UK has spent almost four decades studying the condition and will present an overview of his findings at the European Association ...
The £1m award will help the University of Leeds look at how diabetes can lead to heart failure. ... A £1m grant has been given to a university to support research into type 2 diabetes.
Diabetes Research. The Diabetes Research Group in Newcastle has applied magnetic resonance spectroscopy and imaging to explain the abnormal storage of fat and glycogen in pancreas, liver and muscle in Type 2 diabetes. Type 2 diabetes is escalating as a national public health problem, and the rapidly rising incidence in younger people will ...