What is Critical Thinking in Nursing? (With Examples, Importance, & How to Improve)

Successful nursing requires learning several skills used to communicate with patients, families, and healthcare teams. One of the most essential skills nurses must develop is the ability to demonstrate critical thinking. If you are a nurse, perhaps you have asked if there is a way to know how to improve critical thinking in nursing? As you read this article, you will learn what critical thinking in nursing is and why it is important. You will also find 18 simple tips to improve critical thinking in nursing and sample scenarios about how to apply critical thinking in your nursing career.

What is Critical Thinking in Nursing?
4 reasons why critical thinking is so important in nursing, 1. critical thinking skills will help you anticipate and understand changes in your patient’s condition., 2. with strong critical thinking skills, you can make decisions about patient care that is most favorable for the patient and intended outcomes., 3. strong critical thinking skills in nursing can contribute to innovative improvements and professional development., 4. critical thinking skills in nursing contribute to rational decision-making, which improves patient outcomes., what are the 8 important attributes of excellent critical thinking in nursing, 1. the ability to interpret information:, 2. independent thought:, 3. impartiality:, 4. intuition:, 5. problem solving:, 6. flexibility:, 7. perseverance:, 8. integrity:, examples of poor critical thinking vs excellent critical thinking in nursing, 1. scenario: patient/caregiver interactions, poor critical thinking:, excellent critical thinking:, 2. scenario: improving patient care quality, 3. scenario: interdisciplinary collaboration, 4. scenario: precepting nursing students and other nurses, how to improve critical thinking in nursing, 1. demonstrate open-mindedness., 2. practice self-awareness., 3. avoid judgment., 4. eliminate personal biases., 5. do not be afraid to ask questions., 6. find an experienced mentor., 7. join professional nursing organizations., 8. establish a routine of self-reflection., 9. utilize the chain of command., 10. determine the significance of data and decide if it is sufficient for decision-making., 11. volunteer for leadership positions or opportunities., 12. use previous facts and experiences to help develop stronger critical thinking skills in nursing., 13. establish priorities., 14. trust your knowledge and be confident in your abilities., 15. be curious about everything., 16. practice fair-mindedness., 17. learn the value of intellectual humility., 18. never stop learning., 4 consequences of poor critical thinking in nursing, 1. the most significant risk associated with poor critical thinking in nursing is inadequate patient care., 2. failure to recognize changes in patient status:, 3. lack of effective critical thinking in nursing can impact the cost of healthcare., 4. lack of critical thinking skills in nursing can cause a breakdown in communication within the interdisciplinary team., useful resources to improve critical thinking in nursing, youtube videos, my final thoughts, frequently asked questions answered by our expert, 1. will lack of critical thinking impact my nursing career, 2. usually, how long does it take for a nurse to improve their critical thinking skills, 3. do all types of nurses require excellent critical thinking skills, 4. how can i assess my critical thinking skills in nursing.
• Ask relevant questions • Justify opinions • Address and evaluate multiple points of view • Explain assumptions and reasons related to your choice of patient care options
5. Can I Be a Nurse If I Cannot Think Critically?

The Value of Critical Thinking in Nursing
- How Nurses Use Critical Thinking
- How to Improve Critical Thinking
- Common Mistakes

Some experts describe a person’s ability to question belief systems, test previously held assumptions, and recognize ambiguity as evidence of critical thinking. Others identify specific skills that demonstrate critical thinking, such as the ability to identify problems and biases, infer and draw conclusions, and determine the relevance of information to a situation.
Nicholas McGowan, BSN, RN, CCRN, has been a critical care nurse for 10 years in neurological trauma nursing and cardiovascular and surgical intensive care. He defines critical thinking as “necessary for problem-solving and decision-making by healthcare providers. It is a process where people use a logical process to gather information and take purposeful action based on their evaluation.”
“This cognitive process is vital for excellent patient outcomes because it requires that nurses make clinical decisions utilizing a variety of different lenses, such as fairness, ethics, and evidence-based practice,” he says.
How Do Nurses Use Critical Thinking?
Successful nurses think beyond their assigned tasks to deliver excellent care for their patients. For example, a nurse might be tasked with changing a wound dressing, delivering medications, and monitoring vital signs during a shift. However, it requires critical thinking skills to understand how a difference in the wound may affect blood pressure and temperature and when those changes may require immediate medical intervention.
Nurses care for many patients during their shifts. Strong critical thinking skills are crucial when juggling various tasks so patient safety and care are not compromised.
Jenna Liphart Rhoads, Ph.D., RN, is a nurse educator with a clinical background in surgical-trauma adult critical care, where critical thinking and action were essential to the safety of her patients. She talks about examples of critical thinking in a healthcare environment, saying:
“Nurses must also critically think to determine which patient to see first, which medications to pass first, and the order in which to organize their day caring for patients. Patient conditions and environments are continually in flux, therefore nurses must constantly be evaluating and re-evaluating information they gather (assess) to keep their patients safe.”
The COVID-19 pandemic created hospital care situations where critical thinking was essential. It was expected of the nurses on the general floor and in intensive care units. Crystal Slaughter is an advanced practice nurse in the intensive care unit (ICU) and a nurse educator. She observed critical thinking throughout the pandemic as she watched intensive care nurses test the boundaries of previously held beliefs and master providing excellent care while preserving resources.
“Nurses are at the patient’s bedside and are often the first ones to detect issues. Then, the nurse needs to gather the appropriate subjective and objective data from the patient in order to frame a concise problem statement or question for the physician or advanced practice provider,” she explains.
Top 5 Ways Nurses Can Improve Critical Thinking Skills
We asked our experts for the top five strategies nurses can use to purposefully improve their critical thinking skills.
Case-Based Approach
Slaughter is a fan of the case-based approach to learning critical thinking skills.
In much the same way a detective would approach a mystery, she mentors her students to ask questions about the situation that help determine the information they have and the information they need. “What is going on? What information am I missing? Can I get that information? What does that information mean for the patient? How quickly do I need to act?”
Consider forming a group and working with a mentor who can guide you through case studies. This provides you with a learner-centered environment in which you can analyze data to reach conclusions and develop communication, analytical, and collaborative skills with your colleagues.
Practice Self-Reflection
Rhoads is an advocate for self-reflection. “Nurses should reflect upon what went well or did not go well in their workday and identify areas of improvement or situations in which they should have reached out for help.” Self-reflection is a form of personal analysis to observe and evaluate situations and how you responded.
This gives you the opportunity to discover mistakes you may have made and to establish new behavior patterns that may help you make better decisions. You likely already do this. For example, after a disagreement or contentious meeting, you may go over the conversation in your head and think about ways you could have responded.
It’s important to go through the decisions you made during your day and determine if you should have gotten more information before acting or if you could have asked better questions.
During self-reflection, you may try thinking about the problem in reverse. This may not give you an immediate answer, but can help you see the situation with fresh eyes and a new perspective. How would the outcome of the day be different if you planned the dressing change in reverse with the assumption you would find a wound infection? How does this information change your plan for the next dressing change?
Develop a Questioning Mind
McGowan has learned that “critical thinking is a self-driven process. It isn’t something that can simply be taught. Rather, it is something that you practice and cultivate with experience. To develop critical thinking skills, you have to be curious and inquisitive.”
To gain critical thinking skills, you must undergo a purposeful process of learning strategies and using them consistently so they become a habit. One of those strategies is developing a questioning mind. Meaningful questions lead to useful answers and are at the core of critical thinking .
However, learning to ask insightful questions is a skill you must develop. Faced with staff and nursing shortages , declining patient conditions, and a rising number of tasks to be completed, it may be difficult to do more than finish the task in front of you. Yet, questions drive active learning and train your brain to see the world differently and take nothing for granted.
It is easier to practice questioning in a non-stressful, quiet environment until it becomes a habit. Then, in the moment when your patient’s care depends on your ability to ask the right questions, you can be ready to rise to the occasion.
Practice Self-Awareness in the Moment
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. Passing medication, changing dressings, and hanging intravenous lines all while trying to assess your patient’s mental and emotional status can affect your focus and how you manage stress as a nurse .
Staying present helps you to be proactive in your thinking and anticipate what might happen, such as bringing extra lubricant for a catheterization or extra gloves for a dressing change.
By staying present, you are also better able to practice active listening. This raises your assessment skills and gives you more information as a basis for your interventions and decisions.
Use a Process
As you are developing critical thinking skills, it can be helpful to use a process. For example:
- Ask questions.
- Gather information.
- Implement a strategy.
- Evaluate the results.
- Consider another point of view.
These are the fundamental steps of the nursing process (assess, diagnose, plan, implement, evaluate). The last step will help you overcome one of the common problems of critical thinking in nursing — personal bias.
Common Critical Thinking Pitfalls in Nursing
Your brain uses a set of processes to make inferences about what’s happening around you. In some cases, your unreliable biases can lead you down the wrong path. McGowan places personal biases at the top of his list of common pitfalls to critical thinking in nursing.
“We all form biases based on our own experiences. However, nurses have to learn to separate their own biases from each patient encounter to avoid making false assumptions that may interfere with their care,” he says. Successful critical thinkers accept they have personal biases and learn to look out for them. Awareness of your biases is the first step to understanding if your personal bias is contributing to the wrong decision.
New nurses may be overwhelmed by the transition from academics to clinical practice, leading to a task-oriented mindset and a common new nurse mistake ; this conflicts with critical thinking skills.
“Consider a patient whose blood pressure is low but who also needs to take a blood pressure medication at a scheduled time. A task-oriented nurse may provide the medication without regard for the patient’s blood pressure because medication administration is a task that must be completed,” Slaughter says. “A nurse employing critical thinking skills would address the low blood pressure, review the patient’s blood pressure history and trends, and potentially call the physician to discuss whether medication should be withheld.”
Fear and pride may also stand in the way of developing critical thinking skills. Your belief system and worldview provide comfort and guidance, but this can impede your judgment when you are faced with an individual whose belief system or cultural practices are not the same as yours. Fear or pride may prevent you from pursuing a line of questioning that would benefit the patient. Nurses with strong critical thinking skills exhibit:
- Learn from their mistakes and the mistakes of other nurses
- Look forward to integrating changes that improve patient care
- Treat each patient interaction as a part of a whole
- Evaluate new events based on past knowledge and adjust decision-making as needed
- Solve problems with their colleagues
- Are self-confident
- Acknowledge biases and seek to ensure these do not impact patient care
An Essential Skill for All Nurses
Critical thinking in nursing protects patient health and contributes to professional development and career advancement. Administrative and clinical nursing leaders are required to have strong critical thinking skills to be successful in their positions.
By using the strategies in this guide during your daily life and in your nursing role, you can intentionally improve your critical thinking abilities and be rewarded with better patient outcomes and potential career advancement.
Frequently Asked Questions About Critical Thinking in Nursing
How are critical thinking skills utilized in nursing practice.
Nursing practice utilizes critical thinking skills to provide the best care for patients. Often, the patient’s cause of pain or health issue is not immediately clear. Nursing professionals need to use their knowledge to determine what might be causing distress, collect vital information, and make quick decisions on how best to handle the situation.
How does nursing school develop critical thinking skills?
Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn about diseases, anatomy, and physiology, and how to improve the patient’s overall well-being. Learners also participate in supervised clinical experiences, where they practice using their critical thinking skills to make decisions in professional settings.
Do only nurse managers use critical thinking?
Nurse managers certainly use critical thinking skills in their daily duties. But when working in a health setting, anyone giving care to patients uses their critical thinking skills. Everyone — including licensed practical nurses, registered nurses, and advanced nurse practitioners —needs to flex their critical thinking skills to make potentially life-saving decisions.
Meet Our Contributors

Crystal Slaughter is a core faculty member in Walden University’s RN-to-BSN program. She has worked as an advanced practice registered nurse with an intensivist/pulmonary service to provide care to hospitalized ICU patients and in inpatient palliative care. Slaughter’s clinical interests lie in nursing education and evidence-based practice initiatives to promote improving patient care.

Jenna Liphart Rhoads is a nurse educator and freelance author and editor. She earned a BSN from Saint Francis Medical Center College of Nursing and an MS in nursing education from Northern Illinois University. Rhoads earned a Ph.D. in education with a concentration in nursing education from Capella University where she researched the moderation effects of emotional intelligence on the relationship of stress and GPA in military veteran nursing students. Her clinical background includes surgical-trauma adult critical care, interventional radiology procedures, and conscious sedation in adult and pediatric populations.

Nicholas McGowan is a critical care nurse with 10 years of experience in cardiovascular, surgical intensive care, and neurological trauma nursing. McGowan also has a background in education, leadership, and public speaking. He is an online learner who builds on his foundation of critical care nursing, which he uses directly at the bedside where he still practices. In addition, McGowan hosts an online course at Critical Care Academy where he helps nurses achieve critical care (CCRN) certification.

Effective clinical learning for nursing students
Approaches that meet student and nurse needs..
- Direct care nurses serve as significant teachers and role models for nursing students in the clinical setting.
- Building critical thinking skills is one of the most important outcomes in the clinical setting for nursing students.
- Collaboration with nursing faculty during the clinical rotation can ease the burden on direct care nurses and facilitate a positive learning experience for the student.
The nursing profession continues to experience several challenges—some longstanding and exacerbated by the COVID-19 pandemic. The shortage of nurses at the bedside and reports of nurses planning to leave the profession soon place stress on the workforce and the healthcare system. The situation has put even more pressure on nursing schools to recruit and retain students who enter the workforce well-prepared for practice and capable of filling these vacancies. However, concerns exist surrounding students’ critical thinking skills and their readiness for a demanding career.
The challenge
A longstanding shortage of nursing school faculty and a reliance on new graduate nurses to serve as preceptors create challenges to properly preparing nursing students for a demanding role that requires excellent critical thinking skills.
What-Why-How? Improving Clinical Judgement
New nurses and clinical judgment
Nurse faculty shortage
Lack of interest and incentives lead to difficulty recruiting nurses from the bedside or practice to education. Many 4-year schools require a terminal degree to teach full-time in their undergraduate programs, but only 1% of nurses hold a PhD. In addition, according to the National Advisory Council on Nurse Education and Practice (NACNEP), the average doctorally prepared nurse faculty member is in their 50s, which means they may soon retire. The surge in doctor of nursing practice programs has helped to bridge this gap, but attracting advanced practice nurses to academia from their more lucrative practice roles continues to prove difficult.
Concerns about the practice readiness of new graduate nurses have existed for several years. Missed clinical experiences and virtual learning during the COVID-19 pandemic heightened those concerns. The National Council of State Boards of Nursing (NCSBN) addressed the calls from nurse employers to make progress in this area by revamping the NCLEX-RN and NCLEX-PN exams to create Next Generation NCLEX (NGN), which includes more clinical judgment and critical thinking items. Nurse educators are working hard to prepare students for both practice and the new exam items by incorporating more active learning into classroom, clinical, and lab activities and emphasizing the importance of clinical judgment skills.
In most areas of the country, clinical student experiences have returned to pre-pandemic arrangements. State boards of nursing mandate maximum faculty-to-student ratios for clinical experiences. Schools can choose to have faculty supervise fewer students than the maximum, but faculty and clinical site shortages may eliminate that option. In many cases, preceptor-style experiences (such as capstone or practicum courses) have higher faculty-to-student ratios, and preceptors may have to meet specific criteria, such as a certain amount of experience.
Nursing faculty who facilitate on-site learning and supervise and teach students during their clinical experiences face several challenges. Some faculty supervise students across multiple units because unit size can’t accommodate 8 to 10 students at one time. Faculty may or may not have access to the organization’s electronic health records or other healthcare information technology, such as medication dispensing cabinets or glucometers.
In such instances, direct care nurses play an important role in the student’s experience at the clinical site. Their familiarity with the unit, the patient population, and the organization’s technology facilitates learning.
Direct care nurses
Allowing nursing students into the hospital can improve the patient care experience and potentially recruit students to work at the organization in the future. However, precepting a student or new employee creates an extra burden on an already overextended bedside nurse. NACNEP identifies several challenges for obtaining qualified preceptors, including lack of incentives and limited preparation in clinical teaching and learning strategies. Many hospitals have nursing students on the same unit several days a week to accommodate multiple area schools. This means that staff nurses are expected to teach students on most of their workdays during a typical school semester.
Unit nurse experience creates another barrier to effective precepting of nursing students. A study by Thayer and colleagues reported that the median length of experience for inpatient nurses working a 12-hour shift was less than 3 years at an organization. Without a better alternative, new graduate nurses frequently teach nursing students, although they may still be in what Benner describes as the advanced beginner stage of their career (still learning how to organize care, prioritize, and make clinical judgments). It’s difficult for someone who’s still learning and experiencing situations for the first time to teach complex concepts.
A guide to effective clinical site teaching
The following strategies promote critical thinking in students and collaboration with nurse faculty to ease direct care nurses’ teaching workload. Not every strategy is appropriate for all student clinical experiences. Consider them as multiple potential approaches to help facilitate meaningful learning opportunities.
Set the tone
Nursing students frequently feel anxious about clinical experiences, especially if they’ve been told or perceive that they’re a burden or unwanted on the unit. When meeting the student for the first time, welcome them and communicate willingness to have them on the unit.
If you feel that you can’t take on a student for the day, speak to the nurse faculty member and charge nurse to explore other arrangements. Nurse faculty recognize that work or personal concerns may require you to decline precepting a student. Faculty members want to find the best situation for everyone. If the charge nurse or supervisor determines that the student still needs to work with you, talk to the nurse faculty about how they can help ease the burden and facilitate the student’s learning experience for the day.
Begin your time with the student by asking about their experience level and any objectives for the day. Understanding what the student can or can’t do will help you make the most out of the clinical experience. You’ll want to know the content they’re learning in class and connect them with a patient who brings those concepts to life. A student may have assignments to complete, but their focus should be on patient care. Help the student identify the busiest parts of the day and the best time to review the electronic health record and complete assignments.
If a situation requires your full attention and limits training opportunities, briefly explain to the student what will happen. If you have time, provide the student with tasks or specific objectives to note during the observation. Involve the nursing faculty member to help facilitate the learning experience and make it meaningful.
Be a professional role model
Students like to hear about the benefits and rewards of being a nurse, and about each nurse’s unique path. Students also enjoy learning about the “real world” from nurses, but keep in mind that they’re impressionable. Speaking negatively about the unit, patients, organization, or profession may discourage the student. If you must deviate from standard care, such as performing a skill differently than it’s traditionally taught in school, provide the rationale or hospital policy behind the decision.
Feel free to discuss the student’s nursing school experience but don’t diminish the value of their education or assigned work. Keep in mind that school assignments, such as nursing care plans or concept maps, aren’t taught for job training but to deliberately and systematically promote critical thinking. These assignments allow a student to reflect on how a patient’s pathophysiology and nursing assessment and interventions relate to one another.
Reinforce how concepts students learn in school provide valuable knowledge in various settings. For example, if the student is on a medical-surgical unit but says that they want to work in obstetrics, engage the student by pointing out links between the two areas, such as managing diabetes and coagulation disorders. Provide encouragement and excitement about the student’s interest in joining the profession at a time of great need.
Build assessment skills
Explain to students your approach to performing assessments and organizing patient care. Most students learn comprehensive head-to-toe assessments but, in the clinical setting, need to focus on the most relevant assessments. To promote critical thinking, ask the student what data they should focus on gathering based on the patient’s condition. Many students focus on the psychomotor aspect of assessment (performing the assessment correctly); ask them about the subjective data they should gather.
Allow the student to perform an assessment and then compare findings. For example, a student may know that a patient’s lung sounds are abnormal but not remember what the sound is called or what it means. Provide them with the correct terminology to help connect the dots. Discuss with the student when reassessments are warranted. If appropriate, allow a student to reassess the patient (vital signs, output, pain, other physical findings) and then confirm their findings and discuss what any changes mean for the clinical situation. If you don’t have time for these types of discussions following a student’s patient assessment, ask nursing faculty to observe and discuss findings with the student.
Discuss care management
Take advantage of opportunities to discuss concepts such as prioritization, advocacy, delegation, collaboration, discharge planning, and other ways in which the nurse acts as a care manager. Pointing out what’s appropriate to delegate to unlicensed assistive personnel or a licensed practical nurse will prove valuable and help reinforce concepts frequently covered on the NGN exam.
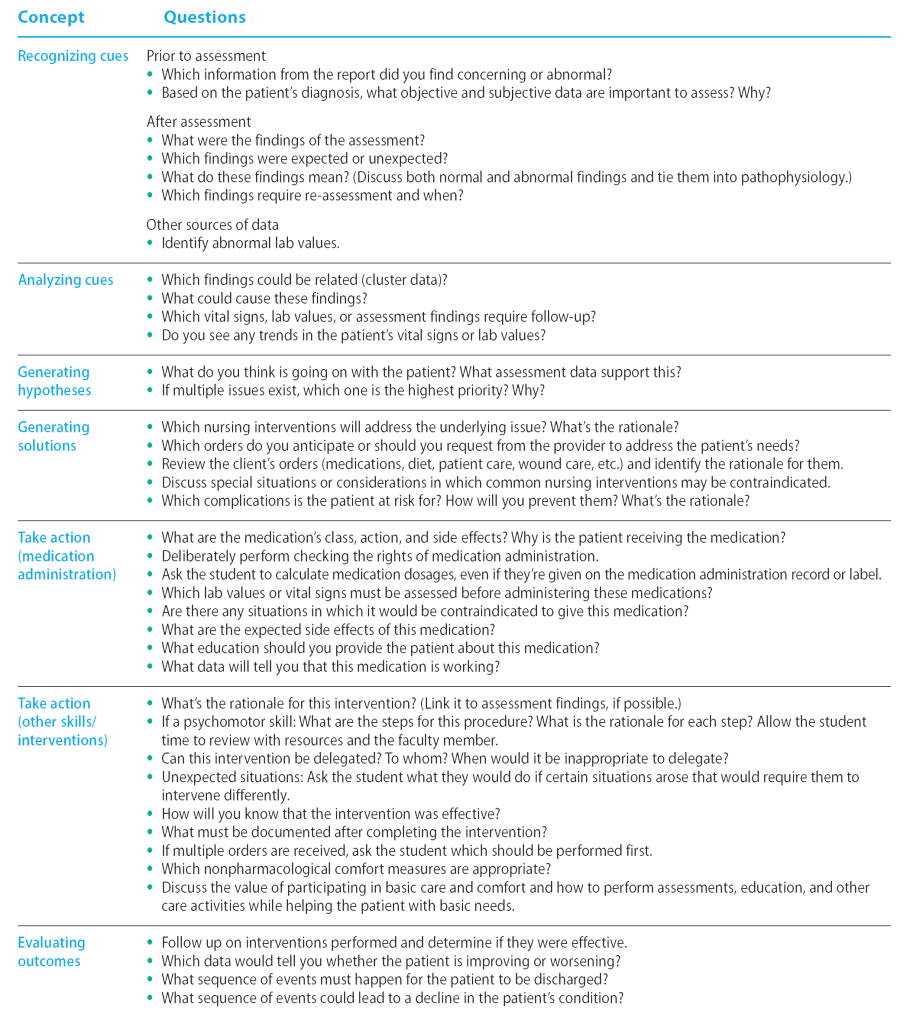
Promote critical thinking
The NCBSN has introduced the Clinical Judgment Measurement Model (CJMM) as a framework for evaluating the NGN exam, which incorporates unfolding case studies that systematically address six steps: recognize cues, analyze cues, generate hypotheses, generate solutions, take action, and evaluate outcomes. Each candidate encounters three case studies, with six questions, one for each step of the CJMM. Nursing faculty incorporate this framework and language into the nursing curriculum to help students think systematically and critically and prepare them for the exam.
Nurses with practice experience use this type of framework to gather information, make judgments, and take action. As a nurse approaches Benner’s competent stage of nursing practice, this type of thinking becomes intuitive, and nurses may not even be aware of the conclusions they draw and decisions they make based on their clinical judgment skills. To help students understand why something is happening, they should continue to work through a process like this deliberately. For example, many students view medication administration as a simple task and may say in post-conference discussion, “All I did was give meds.” You perform many assessments and make various judgments while administering medications, but you may not think to discuss them with students. Asking questions of students while they’re performing what may seem like repetitive tasks can help prompt critical thinking. (See Critical questions .)
Critical questions
Enhance self-efficacy
Many nurses believe that the student must follow them to every patient. This can be overwhelming for the direct care nurse and a barrier to agreeing to work with students. Other approaches can better facilitate learning. Most students will complete an assignment focused on one or two patients. Encourage the student to spend time alone with those patients to perform a more comprehensive history and assessment, help patients with basic care, and provide education. Select a patient who might enjoy the extra attention to ensure a mutually beneficial experience.
Also, consider asking the student to find information using available resources. Such inquiry can benefit you and the student. For example, prompt a student to answer one or more critical thinking questions using their textbooks or resources available on the hospital’s intranet. If time prevents you from explaining complex topics or helping the student problem-solve, ask the student to take the information they find to their faculty member to review. Nurse faculty won’t be familiar with the specific details of all patients on the unit, so identify the most appropriate questions for the student to consider to help the nurse faculty facilitate learning.
Allowing the student time to find answers themselves builds self-efficacy and confidence and also relieves some of the stress and anxiety associated with being asked questions on the spot. This strategy also models the professional approach of using evidence-based resources to find information as needed in the clinical setting.
To ensure a positive learning experience and reduce anxiety, provide the student with ample time to prepare for performance-based skills. For example, identify an approximate time that medications will be administered to one patient and ask the student to independently look up the medication information by that time. This is more beneficial for the student than observing every patient’s medication administration or participating only in psychomotor tasks, such as scanning and giving injections. This also can free up your time by setting the expectation that the student will have the chance to prepare for and be directly involved in one medication pass.
Similarly, if an opportunity exists for practicing a psychomotor skill, such as inserting a urinary catheter or suctioning a tracheostomy, ask the student to review the procedure with their instructor using hospital policy and resources. If time doesn’t allow for a review, have the student observe to ensure provision of the best care and efficient use of time and resources.
Opportunities in education
Nurses who enjoy working with students or new staff members may want to consider academic roles. Many advanced nursing degrees, available in various formats, focus on education. For those who want to try teaching or have an interest in teaching only in the clinical setting, opportunities exist to work as adjunct faculty or to participate in hospital-based professional development activities. Adjunct faculty (part-time instructors) teach a variety of assignments and workloads, including in clinical, lab, or classroom settings. Many clinical adjunct faculty are nurses who also work in the organization with patients and may teach one group of students one day a week. Clinical and lab assignments vary from 4- or 6-hour experiences to 12-hour shifts.
According to NACNEP, most nursing programs require that adjunct faculty and clinical preceptors have the same or higher level of educational preparation as the program; for example, a nurse with a bachelor of science in nursing (BSN) may be able to teach clinicals for associate degree in nursing or BSN programs, depending on the state’s requirements and the school’s needs. Educational requirements to work in nursing programs vary by school. In some cases, adjunct faculty who don’t have a master’s degree may be supervised by full-time faculty with advanced degrees.
Benefits for adjunct faculty can include extra income, professional development, personal reward, tuition discounts or remissions, and giving back to the profession. Locate opportunities on nursing school websites or by talking to the nursing instructors or administrators in the local area.
Everyone benefits
Applying teaching approaches that benefit students and nurses can help ensure a positive clinical learning experience for everyone. When you graciously accept and teach students you help create positive encounters that enhance student critical thinking skill development, aid program retention, and support organizational recruitment.
Jennifer Miller is an assistant professor of nursing at the University of Louisville School of Nursing in Louisville, Kentucky .
American Nurse Journal. 2024; 19(4). Doi: 10.51256/ANJ042432
American Association of Colleges of Nursing. Nursing faculty shortage fact sheet. October 2022. aacnnursing.org/news-information/fact-sheets/nursing-faculty-shortage
Benner P. From Novice to Expert: Excellence and Power in Clinical Nursing Practice . Menlo Park, CA: Addison-Wesley; 1984.
National Advisory Council on Nurse Education and Practice. Preparing nurse faculty, and addressing the shortage of nurse faculty and clinical preceptors. January 2021. hrsa.gov/sites/default/files/hrsa/advisory-committees/nursing/reports/nacnep-17report-2021.pdf
National Council of State Boards of Nursing. Clinical Judgment Measurement Model. 2023. nclex.com/clinical-judgment-measurement-model.page
Thayer J, Zillmer J, Sandberg N, Miller AR, Nagel P, MacGibbon A. ‘The new nurse’ is the new normal. June 2, 2022. Epic Research. epicresearch.org/articles/the-new-nurse-is-the-new-normal
Key words: nursing students, nursing education, critical thinking, precepting
Let Us Know What You Think
1 comment . leave new.
All nursing programs need to put in more clinical time. Students do not get the time in clinicals so they do not have the opportunities to develop their clinical judgement and thinking skills. Clinical time is what glues concept and theory together if they don’t get the clinical time they are less likely to develop these skills which contributes to errors, burnout and nurses leaving the field.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *

NurseLine Newsletter
- First Name *
- Last Name *
- Hidden Referrer
*By submitting your e-mail, you are opting in to receiving information from Healthcom Media and Affiliates. The details, including your email address/mobile number, may be used to keep you informed about future products and services.
Test Your Knowledge
Recent posts.
Built to fit

ANA Enterprise News, October 2024

Responding to workplace violence

Answering the call

Creating an organization for future generations

Firearm safety: Nurses’ knowledge and comfort

The Secret Garden: A staff-only wellness and respite space
Healthy Nurse, Healthy Nation: 2024 Highlights Report
Nurses build coalitions at the Capitol

Stop fall prevention practices that aren’t working

Self-compassion in practice

Mitigating patient identification threats

Reflections: My first year as a Magnet® Program Director

Collective wisdom

The role of hospital-based nurse scientists
Miller J. Effective clinical learning for nursing students. American Nurse Journal. 2024;19(4):32-37. doi:10.51256/anj042432 https://www.myamericannurse.com/effective-clinical-learning-for-nursing-students/
#1 Duquesne University Graduate School of Nursing is Ranked #1 for Veterans by Militaryfriendly.com for 7 years running

- Adult-Gerontology Acute Care Nurse Practitioner
- Executive Nurse Leadership and Health Care Management
- Family Nurse Practitioner
- Forensic Nursing
- Nursing Education and Faculty Role
- Psychiatric-Mental Health Nurse Practitioner
- Clinical Leadership
- Admissions & Aid
- About Duquesne
- Why Duquesne Online?

Developing Critical-Thinking Skills in Student Nurses
April 8, 2020
View all blog posts under Articles | View all blog posts under Master of Science in Nursing

Critical thinking skills for nurses include problem-solving and the ability to evaluate situations and make recommendations. Done correctly, critical thinking results in positive patient outcomes, Srinidhi Lakhanigam, an RN-BSN, said in a Minority Nurse article.
“Critical thinking is the result of a combination of innate curiosity; a strong foundation of theoretical knowledge of human anatomy and physiology, disease processes, and normal and abnormal lab values; and an orientation for thinking on your feet,” Lakhanigam said in “Critical Thinking: A Vital Trait for Nurses.” “Combining this with a strong passion for patient care will produce positive patient outcomes. The critical thinking nurse has an open mind and draws heavily upon evidence-based research and past clinical experiences to solve patient problems.”
Since the 1980s, critical thinking has become a widely discussed component of nurse education, and a significant factor for National League for Nursing (NLN) nursing school accreditation. Nursing school curriculum is expected to teach students how to analyze situations and develop solutions based on high-order thinking skills. For nurse educators who are responsible for undergraduate and graduate learners , teaching critical thinking skills is crucial to the future of healthcare.
Characteristics of Critical Thinkers
A landmark 1990 study found critical thinkers demonstrate similar characteristics. The Delphi Report by the American Philosophical Association (APA) identified these cognitive skills common to critical thinkers:
Interpretation
Critical thinkers are able to categorize and decode the significance and meaning of experiences, situations, data, events, and rules, among others.
Critical thinkers can examine varying ideas, statements, questions, descriptions and concepts and analyze the reasoning.
Critical thinkers consider relevant information from evidence to draw conclusions.
Explanation
Critical thinkers state the results of their reasoning through sound arguments.
Self-regulation
Critical thinkers monitor their cognitive abilities to reflect on their motivations and correct their mistakes.
In addition, critical thinkers are well-informed and concerned about a wide variety of topics. They are flexible to alternative ideas and opinions and are honest when facing personal biases. They have a willingness to reconsider their views when change is warranted.
In nursing, critical thinking and clinical reasoning are inextricably linked, columnist Margaret McCartney said in the BMJ . While experienced nurses are able to make sound clinical judgements quickly and accurately, novice nurses find the process more difficult, McCartney said in “Nurses must be allowed to exercise professional judgment.”
“Therefore, education must begin at the undergraduate level to develop students’ critical thinking and clinical reasoning skills,” McCartney said. “Clinical reasoning is a learnt skill requiring determination and active engagement in deliberate practice design to improve performance. In order to acquire such skills, students need to develop critical thinking ability, as well as an understanding of how judgments and decisions are reached in complex healthcare environments.”
Teaching Critical Thinking to Nurses
In 2015, a study in the Journal of College Teaching & Learning found a positive correlation between critical thinking skills and success in nursing school. The study said, “It is the responsibility of nurse educators to ensure that nursing graduates have developed the critical thinking abilities necessary to practice the profession of nursing.”
To help new nurses develop critical-thinking skills, the professional development resources provider Lippincott Solutions recommended nurse educators focus on the following in the classroom:
Promoting interactions
Collaboration and learning in group settings help nursing students achieve a greater understanding of the content.
Asking open-ended questions
Open-ended questions encourage students to think about possible answers and respond without fear of giving a “wrong” answer.
Providing time for students to reflect on questions
Student nurses should be encouraged to deliberate and ponder questions and possible responses and understand that perhaps the immediate answer is not always the best answer.
Teaching for skills to transfer
Educators should provide opportunities for student nurses to see how their skills can apply to various situations and experiences.
In the Minority Nurse article, Lakhanigam also said students who thirst for knowledge and understanding make the best critical thinkers. The author said novice nurses who are open to constructive criticism can learn valuable lessons that will translate into successful practice.
At the same time, however, critical thinking skills alone will not ensure success in the profession , Lakhanigam said in the article. Other factors count as well.
“A combination of open-mindedness, a solid foundational knowledge of disease processes, and continuous learning, coupled with a compassionate heart and great clinical preceptors, can ensure that every new nurse will be a critical thinker positively affecting outcomes at the bedside,” Lakhanigam said.
Another element that ensures success as both an educator and student is earning a nursing degree from a school that focuses on student accomplishments. At Duquesne University’s School of Nursing, students learn best practices in healthcare. The online master’s in nursing program prepares educators to train the next generation of nurses.
About Duquesne University’s online Master of Science in Nursing (MSN) Program
Duquesne University’s MSN curriculum for the Nursing Education and Faculty Role program focuses on preparing registered nurses (RNs) for careers as nurse educators. Students enrolled in the online master’s in nursing program learn the skills needed in the classroom and for clinical training. RNs learn how to empower student nurses to work to their fullest potential.
The MSN program is presented entirely online, so RNs can pursue their career goals and continue personal responsibilities simultaneously. Duquesne University has been recognized for excellence in education as a U.S. News & World Report Best Online Graduate Nursing Program and best among Roman Catholic universities in the nation.
For more information, contact Duquesne University today.
Critical Thinking: A Vital Trait for Nurses: Minority Nurse
Consensus Descriptions of Core CT Skills And Sub-Skills: Delphi
Margaret McCartney: Nurses must be allowed to exercise professional judgment: BMJ
Predicting Success in Nursing Programs: Journal of College Teaching & Learning
Turning New Nurses Into Critical Thinkers: Wolters Kluwer
- Study Protocol
- Open access
- Published: 14 October 2024
Exploring a learning model for knowledge integration and the development of critical thinking among nursing students with previous learning: a qualitative study protocol
- Chun-Chih Lin ORCID: orcid.org/0000-0001-7548-7720 1 , 2 ,
- Chin-Yen Han ORCID: orcid.org/0000-0002-7464-7507 2 , 3 ,
- Ya-Ling Huang ORCID: orcid.org/0000-0001-6156-4721 4 , 5 ,
- Han-Chang Ku ORCID: orcid.org/0000-0001-9371-0607 1 &
- Li-Chin Chen ORCID: orcid.org/0000-0002-5724-2946 2
BMC Medical Education volume 24 , Article number: 1140 ( 2024 ) Cite this article
291 Accesses
Metrics details
Students often struggle to apply their knowledge of bioscience to their care practice. Such knowledge is generally learned through remembering and understanding, but retention quickly fades. They also experience difficulty progressing to higher-order cognitive skills such as applying, analyzing, evaluating, and even creating, which are necessary to develop soft skills, such as critical thinking, in the care profession. In order to improve existing programs, there is a need to better understand students' prior learning experiences and processes. The proposed study will explore the previous learning experiences of nurses enrolled in a two-year nursing program at a Taiwan university and identify the challenges they face in integrating multidisciplinary knowledge and developing critical thinking competency. The study will adopt a constructivist grounded theory methodology to collect interview data. The findings are expected to improve higher cognitive learning performance and inform the revision of the two-year nursing curriculum.
Peer Review reports
Introduction
In nursing education, theoretical knowledge focuses on human body systems and is primarily or often imparted through lectures. This mode of teaching–learning results in a separation between theoretical knowledge and clinical practice. As a result, it is difficult for students to connect these two domains, and they often struggle to integrate these two types of knowledge in a care scenario. Nursing curricula aimed at basic medicine and applying it to nursing care learning. For instance, knowledge of biosciences such as physiology or pharmacology is not repeated in courses like Adult Nursing. In Bloom’s cognition hierarchy of learning [ 1 ], learning outcomes are primarily set in relation to remembering and understanding rather than higher-order outcomes such as applying or analyzing. Since knowledge retention fades over time [ 2 ], students may be unable to adequately apply academic knowledge when faced with complex health issues in individual cases.
In technical and vocational education in nursing, the curricula’s learning outcomes are based on three types of objectives—cognitive, affective, and skills-based—equivalent to remembering, learning attitude, and techniques in Bloom’s taxonomy [ 3 ]. If learning continues with constant practice, it is possible to achieve learning outcomes at a proficiency level. However, the acquired knowledge may gradually fade if learning is not continued. This could result in missed opportunities to achieve higher-order cognitive learning, such as the ability to analyze or create [ 2 ]. Additionally, prior knowledge may be difficult to internalize, and unfamiliar skills may become challenging to acquire.
The educational goals of the technical and vocational systems are likely to play a role in determining whether learning continues after graduation. Nursing students in junior college are expected to pass a national qualification examination and enter the workplace immediately afterward, meaning their cognitive, affective, and skills learning will continue to develop. They will advance to a higher level of learning performance. However, students who pursue a higher degree may lack extrinsic learning motivation, and these abilities may stagnate or regress. Continuing nursing education programs such as 2-year programs can improve students’ extrinsic learning motivation and transform it into intrinsic learning motivation, which leads to improved internalization and integration of knowledge and enhanced critical thinking skills [ 4 , 5 ]. A better understanding of students' prior learning experiences and processes is necessary to make appropriate revisions to the curriculum.
Memorization and understanding of learning concepts are essential for accumulating knowledge. However, merely holding onto this knowledge can weaken nursing graduates' critical thinking and problem-solving abilities [ 6 ]. While nursing graduates with associate degrees possess strong theoretical understanding, they are often unable to apply this knowledge to a holistic consideration of the circumstances of individual patients, relying instead on managing their patients' symptoms and practitioners' prescriptions. The consequences are less effective patient care and a devaluation of nursing professionalism.
In summary, nursing students are limited in their theoretical knowledge and critical thinking development, which hinders their ability to perform comprehensive evaluations of patients and make effective clinical care decisions. This gap between learning and practice could be addressed through further education that equips students to integrate and apply multidisciplinary knowledge to the practical care domain. To this end, the proposed study seeks to identify the factors that affect how students integrate academic knowledge to improve critical thinking and overall learning satisfaction, as Chang et al. [ 7 ] recommended. Such information is needed to inform the revision of the two-year nursing program curriculum.
Literature review
Learning models and knowledge integration.
The ability to synthesize knowledge is fundamental in all health professions, including nursing [ 8 ]. Competent nurses require theoretical knowledge of biosciences and care practice to make complex patient management decisions. Quality care depends on nurses’ ability to combine clinical reasoning (critical thinking) with accurate health information in real-time situations. Nursing education should aim to bridge the gap between theoretical concepts learned in classrooms and their practical application in clinical settings [ 9 ].
Nursing education fosters the development of complex knowledge and soft skills, known as core nursing values or competencies [ 10 ]. A scoping review conducted by Widad and Abdellah [ 11 ] identified various soft skills that should be included in the nursing curriculum and concluded that different teaching and learning strategies were required to enhance these skills. Other researchers have emphasized the centrality of effective learning with a learner-centered approach that encourages active participation in learning and an interdisciplinary model for integrative learning [ 12 ].
To date, a number of innovative teaching methods have been found to improve learning effectiveness. Kou [ 13 ] proposed a reward-learning model that focuses on how extrinsic rewards motivate individuals to engage in knowledge-acquisition behavior, noting that learning involves explaining and strengthening one's information-seeking behavior. Collaborative learning has improved cognitive integration or combining knowledge from multiple disciplines [ 8 ]. Challenge-based learning is a collaborative approach that encourages students to engage in multidisciplinary learning and take action to solve challenges [ 14 ]. Problem-based learning (PBL) has been shown to enhance students' critical thinking and self-directed learning for long-term knowledge retention [ 15 ]. For instance, Gao et al. [ 16 ] reported that an approach that combined mind mapping with PBL improved undergraduate nursing students' theoretical knowledge, practical abilities, and self-learning skills. In contrast, Manuaba et al. [ 17 ] concluded from their study that the PBL approach did not appear to improve critical thinking and problem-solving skills compared to the conventional teaching method. Another model, inquiry-based learning (IBL), has been identified as equipping students with the ability to investigate and solve problems [ 18 ]. Finally, a flipped classroom teaching model has been proposed as an effective way of supporting students to develop high-level cognitive skills [ 19 ], develop their critical thinking [ 20 ], and improve their motivation and interactions. The flipped classroom teaching model is a form of blended learning that centers around students and reverses their learning activities in groups while in class.
Critical thinking in nursing
According to Benner [ 21 ], the traditional classroom approach to teaching and learning theoretical knowledge needs to be transformed into one that focuses on cultivating learners' critical thinking and clinical judgment abilities to bridge the gap between theoretical knowledge and clinical practice. Similarly, Gonzalez et al. [ 22 ] argue that understanding the connection between learned knowledge and the clinical situation is crucial for developing critical thinking skills. Such understanding allows the learner to apply clinical decision-making abilities to the care situation. In other words, learners must integrate their knowledge, critical thinking, clinical reasoning, and clinical judgment skills into clinical practice. This learning method draws on various disciplines to help learners develop logical and critical thinking skills while eliminating the monotony of academic learning.
Critical thinking refers to the cognitive process of exploring existing information and analyzing available information to assist in judgment and decision-making. In simpler terms, critical thinking involves an individual's use of logical thinking to regulate their thoughts. As such critical thinking involves several skills, such as interpretation, reasoning, evaluation, self-regulation, analysis, and inductive and deductive logical reasoning [ 23 ]. The process enables individuals to thoughtfully consider information from the real world, construct questions, and bridge the gap between theory and practice. Demonstrating critical thinking skills is a significant component of professional practice in nursing [ 24 ]. Nursing can be regarded as a cognitive process in which critical thinking is necessary to gather information, make clinical decisions, and solve complex and diverse clinical health problems in individual cases. Accordingly, critical thinking is essential to developing care competencies at every stage of the nursing process. Consequently, reasoning or critical thinking has become a central component of nursing education [ 25 ].
There is a close relationship between critical thinking and deductive and inductive logic. Deductive and inductive reasoning are two distinct forms of logical thinking. Deductive reasoning starts from general concepts and reasons toward specific conclusions, whereas inductive reasoning draws conclusions from specific observations and infers general principles. Both types of reasoning play a crucial role in critical thinking [ 26 ], but their processes and outcomes differ. In the classroom, deductive logic learning explains the theoretical principles of the course content and demonstrates their application to situations. This kind of learning helps students acquire theoretical knowledge and connects various concepts to form a series of logical theoretical understandings. Concept mapping is an example of this approach. Inductive logic learning, on the other hand, can help students develop a deeper understanding of the concepts, which enables them to think more critically about what they have learned. This results in more comprehensive and long-lasting knowledge that is not based merely on memorization, which can have a negative effect on problem-solving skills. Therefore, incorporating deductive and inductive logic strategies in teaching can enhance learners' conceptual understanding and problem-solving abilities [ 27 ].
Critical thinking is usually associated with logical thinking, problem-solving, and critical reflection [ 28 ].Although these abilities are all related to building convincing arguments and enhancing thinking skills, they have important differences. Critical thinking focuses on uncovering the essence of things, with an emphasis on achieving a comprehensive understanding at the cognitive level. It is characterized by carefully collecting relevant information and objectively evaluating a phenomenon or state. It involves exploring and reconsidering the problem to avoid subjective biases and seek the most accurate factual situation. It seeks to present diverse views and positions on events, emphasizing logical and rational judgment. In contrast, critical reflection involves introspection and self-reflection. It emphasizes self-criticism and aims to identify right and wrong courses of action [ 29 ]. As a result, critical thinking is often considered an essential thinking skill for practice. Both reflection and critical thinking have been identified as essential nursing skills for appropriate patient care. Despite these conceptual and operational differences, critical thinking and reflection share many commonalities and can impact each other's development [ 30 ]. These include analysis, interpretation, evaluation, reasoning, information searching, logic, cognitive processes of reasoning, and knowledge translation, all of which are necessary for making well-considered clinical professional decisions. Clinical decision-making plays a crucial role in ensuring safe patient care, and critical thinking is a vital cognitive process for clinical decision-making. Accordingly, critical thinking is vital in clinical nursing practice. However, there is a lack of clarity around the most effective teaching–learning methods to foster problem-solving and critical-thinking abilities in students [ 31 ].
In summary, continuous improvement in students’ inductive and deductive logical reasoning skills is necessary to cultivate higher-order cognitive skills, such as critical thinking. The application of critical thinking in professional disciplines involves the cognitive processes of academic application, analysis, evaluation, and creation. This conceptual process is vital for clinical decision-making and safe patient care. Among the various learning strategies that have been proposed to cultivate students' problem-solving and critical thinking, there is broad agreement that critical thinking awareness (awareness) and reflection ability (reflection) are important components [ 32 , 33 ].
Academic self-efficacy and knowledge integration
The proposed study employs the concept of learning self-efficacy, which has been used to indicate the effectiveness of learners’ ability to integrate theoretical knowledge. According to Bandura [ 34 ], self-efficacy refers to an individual’s belief in their ability to perform a task and achieve a goal. Four factors influence self-efficacy: mastery experience, vicarious experience, verbal persuasion, and psychological and affective states. Individuals confident in their abilities are more likely to persevere and work hard until they succeed, regardless of the task’s difficulty. As a result, self-efficacy beliefs are considered predictors, mediators, or moderators of task completion [ 35 , 36 ].
Learning self-efficacy refers to students’ belief in their ability to achieve their learning goals and demonstrate their effectiveness in learning. Those who possess high learning self-efficacy show positive motivation towards learning even when faced with difficulties, and they persist in their efforts to solve problems. On the other hand, when students with low learning self-efficacy encounter learning difficulties, they hesitate and lack the motivation to resolve the issues. Bulfone et al. [ 35 ] reported that most students’ learning self-efficacy remained relatively stable. However, those with increased learning self-efficacy demonstrated improved learning motivation and problem-solving skills. Previous research has used learning self-efficacy to predict learning motivation [ 37 ] and learning effectiveness [ 36 ]. The results indicated that higher learning self-efficacy was associated with stronger self-directed learning ability, more psychologically safe learning, and more positive learning results, demonstrating learning resilience. Basith et al. [ 36 ] found that academic achievement was positively related to learning self-efficacy; students with strong beliefs in their learning abilities were more likely to act to achieve their learning goals. As a result, they were more likely to pass examinations, improve their academic performance, and achieve their learning objectives. The findings also found that individuals with lower learning self-efficacy were more likely to experience emotional breakdown when faced with learning pressure. Gulley et al. [ 38 ] found a positive correlation between learning self-efficacy and performance on national licensure exams, indicating that students with high self-efficacy are more likely to learn effectively and successfully.
Overall. The research findings indicate that motivation, learning self-efficacy, and effectiveness are interdependent. Enhancing learners’ intrinsic motivation can increase learning achievement [ 39 ]. At the same time, learning self-efficacy has the potential to predict both learning motivation [ 37 ] and learning effectiveness [ 36 ]. The relationship between intrinsic motivation, learning self-efficacy, involvement, and effectiveness is mutually reinforcing. Each factor has an impact on the others. According to Dunn and Kennedy [ 37 ], there is a positive correlation between intrinsic motivation and self-efficacy, which, in turn, predicts students’ learning involvement. Moreover, learning involvement is an indicator of students’ learning achievement. Therefore, enhancing learning self-efficacy can foster learning motivation and effectiveness [ 36 ].
Aim and objectives
The proposed study aims to identify the factors that influence the integration of multidisciplinary knowledge and the development of critical thinking among undergraduate nursing students in two-year programs. The specific objectives are to (1) document the learning experience of undergraduate nursing students in their previous Junior Nursing College, (2) develop learning opportunities that effectively incorporate knowledge integration, and (3) identify learning needs for the development of critical thinking skills.
Study design
Charmaz’s constructivist grounded theory (CGT) [ 40 ] will underpin the study design. CGT is a method derived from traditional grounded theory that focuses on group experiences rather than individual experiences by focusing on understanding interactions, processes, and events. It aims to generate concepts and ideas based on a distinction between reality and truth. This means that researchers manage their constructions and interpretations of the participants’ constructions and interpretations, and the results are contextualized. The theoretical concepts of a constructivist approach serve as interpretive frameworks and offer an abstract understanding rather than a theory for explanation and prediction. Knowledge is, therefore, created and constructed during the research process. In the proposed study, therefore, CGT is considered an appropriate method for an inductive exploration and analysis of the complex learning process in the context of undergraduate nursing education.
CGT will explore nursing students’ previous learning experiences and the challenges affecting their ability to integrate multidisciplinary knowledge and critical thinking competency. The study design will be based on the five key elements in this methodology for developing lesson plans: (1) The theoretical framework will inform the sampling strategy. (2) Study participants will be able to provide rich information on the phenomenon under investigation. (3) Data collection and analysis will proceed simultaneously until saturation as a sufficient sample size is achieved [ 41 ]. (4) Data collection may be modified as theoretical insights emerge. (5) continuous data collection, analysis, and integration will occur. These five elements will be deployed to explore the nursing learning process and identify the factors influencing integrating multidisciplinary knowledge and critical thinking development.
Chang Gung University of Science and Technology has two northern and southern Taiwan campuses. The study will be conducted at both campuses, with a total student population 6,100. This includes 4,300 students undertaking four- and two-year nursing programs at the baccalaureate level. Both campuses have an annual enrolment of nearly 1,000 students in the two-year nursing program. This study will recruit participants from two-year nursing programs who completed their five-year study in nursing with a diploma degree obtained, already have a nursing license, and could practice in clinical settings. However, they all wish to study further to get a bachelor's degree.
A theoretical and purposive sampling strategy will be used to recruit participants for the study. To be eligible for the study, potential participants must meet the following criteria: (1) aged 18 years or older, (2) currently enrolled in the Evaluation and Analysis of Adult Nursing Cases course, and (3) be willing to participate in face-to-face interviews that will be audio-recorded. Potential participants will be excluded if they (1) withdraw from the Evaluation and Analysis of Adult Nursing Cases course, (2) have prior clinical nursing experience, and/or (3) have a non-nursing academic background in Junior Nursing College.
Data collection
The primary investigator (PI) will conduct all interviews. A semi-structured interview guide format will be used to ensure both consistency and flexibility in data collection. The interview guide will also maintain focus and avoid bias toward the researcher’s specific areas of interest. Interviewing in the participants’ and interviewers’ common language will maximize data quality. Sharing the same nursing background and language will facilitate an in-depth understanding and interpretation of verbal and non-verbal cues and maximize data quality. With participants’ permission, interviews will be audio-recorded to ensure accuracy. Participants will be encouraged to share their perspectives and experiences of previous academic studies.
Data management and analysis
The interviews will be transcribed verbatim. The transcripts and audio recordings will be coded under the same filename. The audio recordings will be listened to repeatedly to gain a deeper insight into the data, and the transcripts will be read line-by-line to obtain a sense of the text’s whole meaning. Constant comparative data analysis will be performed to focus interviews on the subsequent process of theoretical sampling to develop the properties of categories until theoretical satisfaction. All transcripts will be carefully read several times and systematically coded using open coding. They will then be read again, and any keywords or phrases relating to the issues under investigation will be captured in the participants’ own words. The PI will undertake preliminary data analysis, and the results will be discussed with the study team to obtain consensus on the emerging interpretation.
Study rigor
The quality of the study will be evaluated based on its credibility, originality, resonance, and usefulness [ 42 ]. Credibility is ensured by having the primary author conduct all interviews to maintain consistency and quality. Credibility will be enhanced through purposive and theoretical sampling, audit trail techniques, member checking, and thick and rich descriptions. The research team will meet frequently to reach a consensus on identifying codes and categories and the process of theoretical sampling. The originality of the findings will be demonstrated in the use of verbatim quotes in the report and continuous searching of the literature. Resonance will be achieved by identifying categories that provide in-depth insights, and interviews will be recorded and transcribed accurately to provide thick and rich data. Furthermore, a nursing educator will read data from the coding process and report on the study. The study’s usefulness will be evaluated as follows: sole interviewer, audit trail, and a better understanding of nursing students’ learning difficulties in integrating knowledge and developing critical thinking skills .
Ethical considerations
Once organizational permission to conduct the study has been obtained from the university, participants will be recruited via an invitation to the school email system. The email will explain the importance of the study and invite students to participate in face-to-face semi-structured individual interviews. Only the PI will conduct an open-ended and in-depth interview with individuals.
Potential participants will receive an invitation via the university's email system. Potential participants who demonstrate interest in participating will receive an information sheet and consent form and be given time to read and consider the information. The participants will be fully informed about the study, including its purpose, the procedures for data collection, potential risks and benefits, time commitment, and how their rights to privacy and anonymity will be protected. An opportunity to ask questions will be given before signing the consent form. Participants will be advised that participation is voluntary and have the right to withdraw from the study without penalty. The decision to participate or not will in no way impact their involvement in the course. No coercive or deceptive tactics will be used to encourage participation. The interviews will be conducted at a time and place of the participant’s choosing, but preferably in an independent, safe, and quiet location in the workplace. Before the interview commences, the interviewer will explain the interviewee’s rights in relation to their participation, answer any questions, and obtain written consent.
Participants will be assigned a number code. No names or other identifying information will be recorded on the audio records, transcripts, or field notes. No physical risk to the participants is anticipated. Some participants may experience psychological discomfort in reflecting on their experiences during interviews. The risk management plan includes continuous assessment of a participant’s level of comfort or anxiety through the interview, and interviews will be terminated and rescheduled if any discomfort or anxiety occurs. Participants will be referred to a free counseling service if this meets their needs. Participants will be informed that they can refuse to answer questions during the interview.
Interpretation
This study employs constructivist grounded theory to investigate how previous learning experiences and perspectives affect nursing students' knowledge integration and critical thinking development.
Limitations
Different universities in Taiwan may have varying criteria for selecting students for enrollment based on their academic achievements in the two-year nursing program entrance system. This study will only be conducted in a single university, based on the institution's goals of nursing student cultivation. Therefore, the findings may not apply to other institutions. Furthermore, the study saturation or theoretical saturation in qualitative studies may not be suitable for this study. Therefore, a sufficient sample size [ 41 ] will be used in the current study's data collection and analysis process.
The proposed study will investigate how students' learning experiences during their associate degree in nursing affect their ability to integrate knowledge and develop critical thinking skills. The two-year nursing degree serves as a lead for a bachelor's degree for students with a five-year nursing associate degree. Also, a bachelor's degree in nursing is becoming a standard educational qualification for clinical practice. Accordingly, it is important to ensure that the curriculum design in the two-year program is effective in cultivating students' development of these 'soft' skills to bridge the gap between nursing education systems.
Availability of data and materials
No datasets were generated or analysed during the current study.
Bloom BS, Engelhart MD, Furst E J, Krathwohl DR. Taxonomy of educational objectives: The classification of educational goals. 1956; David McKay
Molina-Torres G, Rodriguez-Arrasti M, Alarcón R, Sánchez-Labraca N, Sánchez-Joya M, Roman P, Requena M. Game-based learning outcomes among physiotherapy students: comparative study. JMIR Serious Games. 2021;9(1):e26007.
Article Google Scholar
Bloom BS. In: Anderson LW, Krathwohl DR, editors. A Taxonomy for Learning, Teaching, and Assessing: a revision of Bloom’s taxonomy of educational objectives, complete ed. New York: Longman; 2001.
Google Scholar
Vu T, Magis-Weinberg L, Jansen BRJ, Atteveldt NV, Janssen TWT, Lee NC, Maask HLJ, Raijmakers MEJ, Sachisthal MSM, Meeter M. Motivation-Achievement Cycles in Learning: A Literature Review and Research Agenda. Educ Psychol Rev. 2022;34:39–71.
Walsh P, Owen PA, Mustaf N, Beech R. Learning and teaching approaches promoting resilience in student nurses: an integrated review of the literature. Nurse Educ Prac. 2020;45:102748.
Yeung MM, Yuen JW, Chen JM, Lam KK. The efficacy of team-based learning in developing the generic capability of problem-solving ability and critical thinking skills in nursing education: A systematic review. Nurse Educ Today. 2023;122:105704.
Chang CY, Kuo SY, Hwang GH. Chatbot-facilitated nursing education. Educ Technol Soc. 2022;25(1):15–27.
Ignacio J, Chen H-C. Cognitive integration in health professions education: Development and implementation of a collaborative learning workshop in an undergraduate nursing program. Nurse Educ Today. 2020;90:104436.
Culyer LM, Jatulis LL, Cannistraci P. Brownel CAEvidence-based teaching strategies that facilitate transfer of knowledge between theory and practice: what are nursing faculty using? Teach Learn Nurs. 2018;13(3):174–9.
Sancho-Cantus D, Cubero-Plazas L, BotellaNavas M, Castellano-Rioja E, Cañabate Ros M. Importance of Soft Skills in Health Sciences Students and Their Repercussion after the COVID-19 Epidemic: Scoping Review. Int J Environ Res Public Health. 2023;20:4901.
Widad A, Abdellah G. Strategies used to teach soft skills in undergraduate nursing education: a scoping review. J Prof Nurs. 2022;42:209–18.
Berg C, Philipp R, Taff SD. Scoping review of critical thinking literature in healthcare education. Occup Ther Health Care. 2023;37(1):18–39. https://doi.org/10.1080/07380577.2021.1879411 .
Kou M. A reward-learning framework of knowledge acquisition: an integrated account of curiosity, interest, and intrinsic-extrinsic rewards. Psychol Rev. 2022;129(1):175–98.
Nichols M, Cator K, Torres M. Challenge-based learner user guide. Digital Promise. Redwood City: ENGAGE; 2016.
Lund B, Jensen AA. In: Peters MA, editor. PBL Teachers in Higher Education: Challenges and Possibilities. Encyclopedia of Teacher Education Springer; 2020.
Gao X, Wang L, Deng J, Wan C, Mu D. The effect of the problem-based learning teaching model combined with mind mapping on nursing teaching: A meta-analysis. Nurse Educ Today. 2022;111:105306. https://doi.org/10.1016/j.nedt.2022 .
Manuaba IBAP, No Y, Wu CC. The effectiveness of problem-based learning in improving critical thinking, problem-solving and self-directed learning in first-year medical students: a meta-analysis. PLoS One. 2022;17(11):e0277339.
Archer-Kuhn B, MacKinnon S. Inquiry-based learning in higher education: A pedagogy of trust. J Educ Train Stud. 2020;8(9):1–14.
Betihavas V, Bridgman H, Kornhaber R, Cross M. The evidence for ‘flipping out’: a systematic review of the flipped classroom in nursing education. Nurse Educ Today. 2016;38:15–21.
Nugraheni BI, Surjono HD, Aji GP. How can flipped classroom develop critical thinking skills? A literature review. Int J Inform Educ Technol. 2022;12(1):82–9.
Benner P, Sutphen M, Leonard V, Day L. Educating nurses: A call for radical transformation. Jossey-Bass; 2010.
Gonzalez L, Nielsen A, Lasater K. Developing students’ clinical reasoning skills: a faculty guide. J Nurs Educ. 2021;60(9):485–93.
Altun E, Yildirim N. What does critical thinking mean? Examination of pre-service teachers’ cognitive structures and definitions for critical thinking. Thinking Skills Creativity. 2023;49:101367.
Ilaslan E, Adibelli D, Tesjerecu G, Cura SU. Development of nursing students’ critical thinking and clinical decision-making skills. Teach Learn Nurs. 2023;18(1):152–9.
Lee DS, Abdullah KL, Chinna K, Subramanian P, Bachmann RT. Critical thinking skills of RNs: exploring demographic determinants. J Contin Educ Nurs. 2020;51(3):109–17.
Karlse B, Hillestad TM, Dysvik E. Abductive reasoning in nursing: Challenges and possibilities. Nurs Inq. 2021;28(1):e12374.
Wardaini S, Kusuma IW. Comparison of learning in inductive and deductive approach to increase student’s conceptual understanding based on international standard curriculum. J Pendidikan IPA Indonesia. 2020;9(1):70–8.
Ng SL, Mylopoulos M, Kangasjarvi E, Boyd VA, Teles S, Orsino A, Lingard L, Phelan S. Critically reflective practice and its sources: A qualitative exploration. Med Educ. 2020;54:312–9.
Rolfe G, Jasper M, Freshwater D. Critical reflection in practice: Generating knowledge for care. 2nd ed. London: Red Globe Press; 2011.
Berg E, Lepp M. The meaning and application of student-centered learning in nursing education: an integrative review of the literature. Nurs Educ Pract. 2023;69:103622.
Carter AG, Creedy DK, Sidebotham M. Efficacy of teaching methods used to develop critical thinking in nursing and midwifery undergraduate students: a systematic review of the literature. Nurs Educ Today. 2016;40:209–18.
Lin CC, Chen LC, Han CY, Su CC, Huang YL. Exploring the experience of reflective writing among Taiwanese undergraduate nursing students: a qualitative study. J Prof Nurs. 2022;40:105–10.
Lin CC, Han CY, Wu ML, Hsiao R, Wang LH, Chen LC. Enhancing reflection on medical and surgical nursing among nursing students: a participatory action research study. Nurs Educ Today. 2021;102:104935.
Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44(9):1175–84.
Bulfone G, Badolamenti S, Biagioli V, Maurici M, Macale L, Sili A, Vellone E, Alvaro R. Nursing students’ academic self-efficacy: a longitudinal analysis of academic self-efficacy changes and predictive variables over time. J Adv Nurs. 2021;77(5):2353–62.
Basith A, Syahputra A, Ichwanto MA. Academic self-efficacy as predictor of academic achievement. JPI (Jurnal Pendidikan Indonesia). 2020;9(1):163–70.
Dunn TJ, Kennedy M. Technology enhanced learning in higher education; motivations, engagement and academic achievement. Comput Educ. 2019;137:104–13.
Gulley T, Hall T, Newsome A, Sidle MW, Simpson MR. Perceived self-efficacy among nursing students during a pandemic: A pilot study. Teach Learn Nurs. 2021;16:215–9.
Lisa U, Andriani F, Ahzaliza D. The effectiveness of online learning on student practicum skills. Adv Soc Sci Educ Humanit Re. 2020;506:204–43.
Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. SAGE Publication Ltd; 2006.
Johnson JL, Adkins D, Chauvin S. Qualitative research in pharmacy education: A review of the quality indicators of rigor in qualitative research. Am J Pharmaceut Educ. 2020;84(1):138–46.
Charmaz K. Constructing Grounded Theory (2nd ed). SAGE Publications Ltd; 2014.
Download references
Acknowledgements
CC-L, the primary researcher and project leader, acknowledges the study's co-investors, who generously shared their time, experience, and opinions for this research protocol.
This study was supported by the Ministry of Science and Technology (NSTC 112-2410-H-255-005 -). The organization was not involved in any stages of this manuscript.
Author information
Authors and affiliations.
Department of Nursing, Chang Gung University of Science and Technology, 2, Jiapu Rd, West Sec. Putz, Chiayi, 61363, Taiwan
Chun-Chih Lin & Han-Chang Ku
New Taipei Municipal TuCheng Hospital, Built and Operated By Chang Gung Medical Foundation, No.6, Sec.2, Jincheng Rd., Tucheng Dist., New Taipei City, 236, Taiwan
Chun-Chih Lin, Chin-Yen Han & Li-Chin Chen
Department of Nursing, Chang Gung University of Science and Technology, No.261, Wenhua 1st Rd., Guishan Dist., Taoyuan City, 33303, Taiwan
Chin-Yen Han
School of Nursing and Midwifery, University of Southern Queensland, UniSQ Ipswich Campus, 11 Salisbury Road, Ipswich, QLD, 4305, Australia
Ya-Ling Huang
Department of Emergency Medicine, Gold Coast Hospital and Health Service, 1 Hospital Boulevard Southport, Southport, QLD, 4215, Australia
You can also search for this author in PubMed Google Scholar
Contributions
CC-L is the primary researcher and project lead. She is also applying for this study's grant. CC-L, CY-H, LC-C, HC-Ku, and YL-H contributed to the study's conception and design and have reviewed and approved the protocol. All authors listed will be involved in the research project, from this protocol paper to a completed manuscript. The research assistant, YY-Tseng, will be responsible for recruiting participants. All authors have read and approved the final manuscript of the research protocol.
Corresponding author
Correspondence to Chun-Chih Lin .
Ethics declarations
Ethics approval and consent to participate.
The Chang Gung Medical Foundation Institutional Review Board (202301954B0) has approved full ethics.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Lin, CC., Han, CY., Huang, YL. et al. Exploring a learning model for knowledge integration and the development of critical thinking among nursing students with previous learning: a qualitative study protocol. BMC Med Educ 24 , 1140 (2024). https://doi.org/10.1186/s12909-024-06118-2
Download citation
Received : 05 August 2024
Accepted : 01 October 2024
Published : 14 October 2024
DOI : https://doi.org/10.1186/s12909-024-06118-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Knowledge integration
- Critical thinking
- Constructivist grounded theory
- Undergraduate nursing students
- Learning model
BMC Medical Education
ISSN: 1472-6920
- General enquiries: [email protected]
Unlock Critical Thinking: Fun Activities To Enhance Nursing Skills
- by Carlos Manuel Alcocer
- September 7, 2024 June 18, 2024
Interactive activities foster critical thinking in nursing students. Case studies, simulations, and creative writing stimulate analysis and imagination. Games, discussions, and group projects enhance problem-solving and communication skills. Role-playing, scenarios, and think-pair-share exercises promote immersive learning and idea generation, preparing students for real-world challenges in nursing.
Table of Contents
Active Learning: A Path to Excellence in Nursing Education
In the dynamic and ever-evolving field of nursing, critical thinking and problem-solving are essential skills that empower healthcare professionals to make sound decisions and deliver exceptional patient care. Embracing active learning methods in nursing education is a game-changer, fostering a deep understanding and critical思考 that prepares students for the challenges they will encounter on the front lines.
Unleashing the Power of Active Learning
Active learning ignites a spark in nursing students, transforming them from passive recipients of information into active participants in their learning journey. By engaging in interactive and hands-on activities, students delve deeply into concepts, develop their analytical skills, and hone their problem-solving abilities.
The benefits of active learning extend beyond the classroom, extending into the clinical setting. Students who have experienced active learning methods demonstrate increased confidence in their decision-making, enhanced communication skills, and a profound understanding of the nursing process. These qualities pave the way for safe and effective patient care, ensuring the well-being of those in their hands.
Why Active Learning is Vital in Nursing Education
Nursing students require a solid foundation in critical thinking and problem-solving to navigate the complexities of healthcare. Active learning, a pedagogical approach that emphasizes student engagement and interaction, plays a pivotal role in fostering these essential skills.
Benefits of Active Learning:
Active learning techniques engage students intellectually and emotionally, making learning more meaningful and enjoyable. Unlike passive lectures, active learning promotes student involvement , encouraging them to participate in discussions, solve problems, and share their perspectives.
This student-centered approach fosters higher levels of understanding. By actively participating in their learning, students develop a deeper comprehension of concepts and make stronger connections to real-world applications. Active learning prepares students to think critically, analyze information, and make informed decisions.
Examples of Active Learning Activities:
Case Studies: Present real-life scenarios for students to analyze and discuss. This immerses students in complex situations , enabling them to apply their knowledge and develop critical thinking skills.
Clinical Simulations: Provide a safe and controlled environment for students to practice patient care. Simulations enhance collaboration and problem-solving through group work and immersive scenarios.
Creative Writing Activities: Stimulate imagination and encourage out-of-the-box thinking. These activities integrate personal experiences and perspectives , fostering empathy and understanding of diverse patient experiences.
Active learning methods are essential in nursing education as they transform students from passive learners to active participants. By engaging students in meaningful activities, active learning promotes critical thinking, problem-solving, and a deeper understanding of nursing concepts. These skills are crucial for successful nursing practice , equipping students to provide high-quality care and make informed decisions in the ever-evolving healthcare landscape.
Case Studies: Empowering Critical Thinking in Nursing Education
Case studies present nursing students with real-life scenarios that mirror the complexities and dilemmas they’ll encounter in their profession. These scenarios immerse students in authentic clinical experiences, allowing them to apply their knowledge, analyze data, and make informed decisions.
In a case study, students are presented with a detailed patient case history, including symptoms, assessments, and medical interventions. They then work in groups or individually to critically examine the case, identify key issues, and develop evidence-based care plans.
The beauty of case studies lies in their flexibility , allowing instructors to tailor them to specific learning objectives and student needs. They can be combined with discussions, role-playing, and problem-solving exercises to further deepen students’ understanding and enhance their problem-solving abilities.
For example, a case study may present a patient with a complex medical condition that requires a multidisciplinary approach. Students would work together to analyze the patient’s symptoms, consult with different healthcare professionals, and formulate a comprehensive care plan. This type of active learning exercise would not only hone their critical thinking skills but also foster collaboration and teamwork.
In another instance, a case study could focus on an ethical dilemma faced by a nurse. Students would engage in discussions and role-playing exercises to explore the ethical considerations, weigh the potential consequences, and develop defensible rationales for their decisions. Such activities prepare students to face the moral and ethical challenges they’ll encounter in their nursing practice.
By integrating case studies into nursing education, instructors can create engaging and transformative learning experiences that empower students to develop the critical thinking abilities essential for thriving in the dynamic and demanding field of nursing.
Clinical Simulations: Nurturing Critical Thinking in Nursing Education
Immersive Learning for Future Healthcare Heroes
In the realm of nursing education, clinical simulations have emerged as a beacon of innovation, offering students a safe and captivating environment to hone their skills and develop critical thinking abilities. These simulations, meticulously designed to mirror real-life healthcare scenarios, provide an unparalleled opportunity for students to navigate complex patient cases, test their knowledge, and refine their decision-making processes.
Collaborative Excellence
Clinical simulations foster a spirit of collaboration, encouraging students to work together as a team, just as they would in an actual clinical setting. Through engaging games and interactive group projects, they learn the importance of communication, problem-solving, and mutual support. This fosters a sense of unity and prepares them for the collaborative nature of the nursing profession.
Interactive Immersion for Enhanced Learning
By immersing students in a virtual reality that mimics the clinical environment, simulations provide a realistic playground for practicing patient care. Students are presented with various scenarios that challenge their critical thinking, enabling them to apply their knowledge in a simulated setting, free from the potential consequences of real-life situations. This allows them to make mistakes, learn from them, and develop their confidence without compromising patient safety.
Clinical simulations are indispensable tools in the arsenal of nursing education. They provide an immersive and engaging learning experience, empowering students with the critical thinking skills, collaborative spirit, and practical knowledge necessary to thrive as compassionate and competent nurses. By embracing these simulations, educators create a bridge between theoretical concepts and real-world applications, preparing students for the challenges and rewards that lie ahead in the healthcare field.
Creative Writing Activities: Fostering Imagination and Empathy in Nursing Education
Engage in Storytelling to Enhance Learning
Creative writing activities are an innovative way to stimulate imagination and encourage out-of-the-box thinking in nursing students. By embracing storytelling techniques, educators can create immersive and engaging experiences that promote critical thinking , perspective-taking , and empathy among learners.
Integrate Creative Writing with Discussions and Role-Playing
Integrating creative writing with discussions and role-playing allows students to explore complex nursing scenarios from multiple perspectives. Writing reflective essays, short stories, or narratives encourages them to analyze situations, develop empathy for patients and families , and appreciate the multifaceted nature of healthcare. Role-playing activities, coupled with creative writing assignments, provide a safe space for students to practice communication skills, ethical decision-making , and interpersonal dynamics .
Example: As part of a discussion on patient advocacy, students are tasked with writing a short story from the perspective of a patient navigating the challenges of a healthcare system. This activity fosters empathy, critical thinking , and communication skills , preparing students for the complexities of real-world nursing practice.
Creative Thinking in Nursing Education: Unleashing the Imagination
In the realm of nursing education, fostering critical thinking is paramount. Embracing active learning methodologies empowers students to engage deeply with course material, enhancing their understanding and preparing them for the challenges of the nursing profession.
Among the myriad active learning strategies, creative thinking activities play a pivotal role in nurturing critical analysis, argumentation, and idea generation . By immersing students in debates, discussion boards, and engaging games, educators ignite their imagination and cultivate out-of-the-box perspectives .
Debates ignite intellectual discourse, encouraging students to articulate their views and defend their positions with logical reasoning. They learn to evaluate evidence, support their claims, and engage in respectful dialogue, fostering critical thinking and problem-solving abilities.
Discussion boards provide a platform for asynchronous exchange of ideas. Students can post their thoughts, respond to others, and participate in thought-provoking discussions. This format encourages collaboration , promotes critical evaluation , and enhances their ability to synthesize information .
Games can transform learning into an enjoyable and interactive experience. Nursing educators can leverage games to present complex scenarios, challenge students’ assumptions, and encourage creative problem-solving . By engaging in games that simulate real-world situations, students develop critical thinking , decision-making , and teamwork skills.
By incorporating creative thinking activities into their teaching repertoire, nursing educators empower students to become dynamic thinkers and effective decision-makers . These activities cultivate essential cognitive abilities, preparing students to navigate the complexities of the nursing profession with confidence and competence.
Group Projects: Collaborative Learning for Budding Nurses
Group projects serve as an exceptional platform for nursing students to hone their collaboration, communication, and team-building prowess. These initiatives foster an environment where critical thinking , idea generation , and problem-solving thrive.
Collaboration at its Finest:
As nurses, collaboration is paramount. Group projects provide a safe space for students to develop these vital skills. By working together, they learn to value diverse perspectives , share ideas respectfully , and achieve a common goal .
Communication Skills Sharpened:
Effective communication is essential in nursing. Group projects provide ample opportunities for students to practice active listening , articulate their thoughts clearly , and resolve conflicts constructively .
Teamwork and Unity:
Nurses often work in teams. Group projects mirror this reality, allowing students to build strong relationships , assign roles effectively , and overcome challenges collectively .
Research, Case Studies, and Presentations:
Group projects can take various forms. Some may focus on research , enabling students to delve into specific nursing topics and develop evidence-based solutions . Others may involve case studies , presenting students with real-world scenarios to analyze and offer recommendations . Finally, presentations provide students with a chance to showcase their findings and engage in thought-provoking discussions .
By embracing group projects, nursing students not only enhance their critical thinking and problem-solving abilities but also develop the essential teamwork and communication skills that will serve them well throughout their careers.
Problem-Solving Exercises: Equipping Nursing Students for Real-World Challenges
In the dynamic and demanding field of nursing, critical thinking and problem-solving are essential qualities for delivering optimal patient care. Active learning methods, including problem-solving exercises, provide an effective means of developing these crucial skills in nursing students.
These exercises present students with intricate healthcare scenarios that require analytical thinking, evaluation, and the development of effective solutions. They challenge students to apply their knowledge, assess the situation from different perspectives, and make well-informed decisions to achieve the best possible outcomes.
Through these exercises, students engage in systematic analysis of complex scenarios, considering the various factors involved, such as patient health history, clinical manifestations, and potential treatment options. They learn to prioritize needs, identify potential risks and complications, and formulate comprehensive care plans that address the multidimensional aspects of patient care.
Problem-solving exercises foster critical thinking by encouraging students to question assumptions, challenge existing knowledge, and seek evidence-based solutions. It enables them to develop a deeper understanding of nursing concepts and their practical application, equipping them with the ability to think beyond rote memorization and apply their knowledge in real-world settings.
Moreover, these exercises promote collaboration and teamwork, as students often work together in groups to analyze scenarios and brainstorm solutions. They learn the importance of communication, consensus-building, and leveraging diverse perspectives to reach the best possible outcomes. By actively engaging in problem-solving exercises, nursing students develop a solid foundation for facing the challenges of the nursing profession and providing exceptional care to patients.
Role-Playing: Immersive Learning for Nursing Students
Role-playing is an active learning technique that transports nursing students into real-world scenarios, enabling them to experience the complexities of patient care firsthand. This immersive approach provides a safe and engaging environment for students to practice their skills, navigate ethical dilemmas, and develop interpersonal dynamics.
During role-playing exercises, students assume the roles of patients, nurses, and other healthcare professionals. They interact with each other, simulating real-life situations such as patient assessments, medication administration, and crisis management. This hands-on experience allows students to feel the challenges and respond appropriately.
One of the most valuable aspects of role-playing is the opportunity it provides for students to practice patient interactions . By embodying the perspectives of patients, students can develop empathy and understanding for the experiences of those they care for. They learn to communicate effectively, build rapport, and address patient concerns with compassion.
Role-playing also equips students to navigate ethical dilemmas . Nursing practice often presents complex ethical challenges. Through role-playing, students can explore these issues in a safe space, consider different perspectives, and develop a nuanced understanding of ethical principles. By grappling with real-world scenarios, they develop the ability to think critically and make informed decisions.
Furthermore, role-playing enhances interpersonal dynamics among students. By working together in different roles, they learn to collaborate effectively, manage conflicts, and support each other as a team. These interpersonal skills are crucial for successful nursing practice, where teamwork and communication are essential.
In conclusion, role-playing is an invaluable active learning technique that fosters critical thinking, empathy, and interpersonal dynamics in nursing students. By simulating real-life scenarios, it prepares students for the challenges of the nursing profession and empowers them to provide the highest quality of patient care.
Scenarios: Engaging Students in Real-World Nursing Challenges
Scenarios present students with compelling real-world situations or patient cases, immersing them in the complexities of the nursing profession. These immersive learning experiences challenge students to critically think , apply their knowledge , and develop problem-solving skills essential in the clinical setting.
Scenarios can be tailored to specific nursing disciplines, such as medical-surgical nursing, critical care nursing, or pediatric nursing. By simulating real-world challenges, scenarios provide a safe and controlled environment for students to practice their skills and make informed decisions .
For instance, a medical-surgical nursing scenario might present students with a patient who exhibits signs of a pulmonary embolism. Students are required to assess the patient’s condition , formulate a differential diagnosis , and develop a plan of care . This scenario challenges students to think critically and apply their knowledge of pulmonary embolism, while providing a safe space to practice their decision-making skills.
Scenarios can also be used to teach interpersonal skills and ethical decision-making . In a pediatric nursing scenario, students might encounter a family who is struggling to cope with the diagnosis of their child. Students are tasked with providing emotional support , answering questions , and advocating for the family’s needs . This type of scenario helps students develop empathy and communication skills, while also challenging them to navigate ethical considerations.
By incorporating scenarios into nursing education, educators can create immersive learning experiences that prepare students for the challenges they will face in the clinical setting. Scenarios encourage critical thinking , promote problem-solving , and foster interpersonal skills , ultimately equipping students with the knowledge and confidence they need to succeed as professional nurses.
Think-Pair-Share: Fostering Collaboration and Critical Thinking
Think-Pair-Share is an active learning technique that enhances critical thinking and collaboration among nursing students. By engaging in structured discussions, students are encouraged to generate ideas, communicate their perspectives, and solve problems collectively.
In the “Think” phase, students are given a topic or question to consider individually. This allows them to formulate their own thoughts and ideas. Subsequently, in the “Pair” phase, students pair up with a classmate to discuss their insights and perspectives. This exchange of ideas fosters collaboration and allows students to learn from each other.
The “Share” phase involves sharing their combined ideas and solutions with the class. This stage encourages students to present their findings, engage in respectful debate, and synthesize different viewpoints. Through this process, students not only develop their critical thinking skills but also improve their communication and presentation abilities.
Think-Pair-Share promotes a collaborative learning environment where students feel comfortable sharing their thoughts and actively contributing to class discussions. It creates a supportive atmosphere that encourages idea generation, problem-solving, and teamwork – essential skills for nurses in the real world.
Carlos Manuel Alcocer is a seasoned science writer with a passion for unraveling the mysteries of the universe. With a keen eye for detail and a knack for making complex concepts accessible, Carlos has established himself as a trusted voice in the scientific community. His expertise spans various disciplines, from physics to biology, and his insightful articles captivate readers with their depth and clarity. Whether delving into the cosmos or exploring the intricacies of the microscopic world, Carlos’s work inspires curiosity and fosters a deeper understanding of the natural world.
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
Critical thinking in nursing clinical practice, education and research: From attitudes to virtue
Affiliations.
- 1 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group Quantitative Psychology (2017-SGR-269), University of Barcelona, Barcelona, Spain.
- 2 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, Consolidated Research Group on Gender, Identity and Diversity (2017-SGR-1091), University of Barcelona, Barcelona, Spain.
- 3 Department of Fundamental Care and Medical Surgital Nursing, Faculty of Medicine and Health Sciences, School of Nursing, University of Barcelona, Barcelona, Spain.
- 4 Multidisciplinary Nursing Research Group, Vall d'Hebron Research Institute (VHIR), Vall d'Hebron Hospital, Barcelona, Spain.
- PMID: 33029860
- DOI: 10.1111/nup.12332
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing profession. In this context, the ethics of virtue is a theoretical framework that becomes essential for analyse the critical thinking concept in nursing care and nursing science. Because the ethics of virtue consider how cultivating virtues are necessary to understand and justify the decisions and guide the actions. Based on selective analysis of the descriptive and empirical literature that addresses conceptual review of critical thinking, we conducted an analysis of this topic in the settings of clinical practice, training and research from the virtue ethical framework. Following JBI critical appraisal checklist for text and opinion papers, we argue the need for critical thinking as an essential element for true excellence in care and that it should be encouraged among professionals. The importance of developing critical thinking skills in education is well substantiated; however, greater efforts are required to implement educational strategies directed at developing critical thinking in students and professionals undergoing training, along with measures that demonstrate their success. Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student education and the growth of nursing science.
Keywords: critical thinking; critical thinking attitudes; nurse education; nursing care; nursing research.
© 2020 John Wiley & Sons Ltd.
- Attitude of Health Personnel*
- Education, Nursing / methods
- Nursing Process
- Nursing Research / methods
Grants and funding
- PREI-19-007-B/School of Nursing. Faculty of Medicine and Health Sciences. University of Barcelona
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Clinical supervision strategies, learning, and critical thinking of nursing students
Estrategias de supervisión clínica, aprendizaje y pensamiento crítico de los estudiantes de enfermería, estratégias de supervisão clínica, aprendizagem e pensamento crítico dos estudantes de enfermagem, angélica oliveira veríssimo da silva, antónio luís rodrigues faria de carvalho, rui marques vieira, cristina maria correia barroso pinto.
- Author information
- Article notes
- Copyright and License information
Corresponding author: Angélica Oliveira Veríssimo da Silva, E-mail: [email protected]
EDITOR IN CHIEF: Álvaro Sousa
ASSOCIATE EDITOR: Rafael Silva
Received 2022 Nov 23; Accepted 2023 Mar 10; Collection date 2023.
This is an Open Access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
To identify the supervisory strategies that Nursing students consider facilitators of the development of critical thinking skills in clinical teaching.
This is a qualitative study, within the interpretative paradigm, using the focus group methodology. Eight undergraduate nursing students participated in the study.
Participants recognized the indispensability of critical thinking for professional responsibility and quality of care and highlighted the importance of using supervisory strategies adapted to their needs, learning objectives, and the context of clinical practice.
Final considerations:
This study highlights the urgent need to establish, within the Nursing curricula, clinical supervision strategies that promote critical thinking and favor the development of skills for good clinical judgment, problem solving, and safe, effective, and ethical decision-making.
Descriptors: Thinking, Clinical Decision Making, Nursing Students, Learning, Nursing Education.
Identificar as estratégias supervisivas que os estudantes de Enfermagem consideram facilitadoras do desenvolvimento das capacidades de pensamento crítico no contexto de ensino clínico.
Estudo de natureza qualitativa, inserido no paradigma interpretativo, com recurso à metodologia focus group . Participaram do estudo oito estudantes do curso de licenciatura em Enfermagem.

Resultados:
Os participantes reconheceram a imprescindibilidade do pensamento crítico para a responsabilidade profissional e qualidade na assistência; e destacaram a importância da utilização de estratégias supervisivas adequadas às suas necessidades, aos objetivos de aprendizagem e ao contexto da prática clínica.
Considerações finais:
Este estudo sobreleva a premência em se estabelecer, dentro dos currículos do curso de Enfermagem, estratégias de supervisão clínica promotoras do pensamento crítico, que favoreçam o desenvolvimento de capacidades para o bom julgamento clínico, resolução de problemas e tomada de decisão segura, eficaz e ética.
Descritores: Pensamento, Tomada de Decisão Clínica, Estudantes de Enfermagem, Aprendizagem, Educação em Enfermagem.
Identificar las estrategias de supervisión que los estudiantes de Enfermería consideran facilitadoras del desarrollo de las capacidades de pensamiento crítico en el contexto de enseñanza clínica.
Estudio de naturaleza cualitativa, inserido en el paradigma interpretativo, con recurso a la metodología focus group . Participaron del estudio ocho estudiantes del curso de licenciatura en Enfermería.
Los participantes reconocieron la imprescindibilidad del pensamiento crítico para la responsabilidad profesional y calidad en la asistencia; y destacaron la importancia de la utilización de estrategias de supervisión adecuadas a sus necesidades, a los objetivos de aprendizaje y al contexto de la práctica clínica.
Consideraciones finales:
Este estudio sobrepasa la urgencia en establecerse, dentro de los currículos del curso de Enfermería, estrategias de supervisión clínica promotoras del pensamiento crítico, que favorezcan el desarrollo de capacidades para el bueno juicio clínico, resolución de problemas y toma de decisión segura, eficaz y ética.
Descriptores: Pensamiento, Toma de Decisiones Clínicas, Estudiantes de Enfermería, Aprendizaje, Educación en Enfermería.
INTRODUCTION
The complex challenges that globalization imposes incorporate the need to establish critical thinking (CT) as a pillar today. It is the duty of educational institutions to prepare their students adequately so that they can provide timely and appropriate answers to the diverse and emerging problems that society and patients impose on them ( 1 ) . Critical thinking, as a set of skills and dispositions, has sparked the interest of the scientific community and of national and international organizations ( 2 - 3 ) . In recent years, efforts have been made to incorporate it into the curricula in different educational institutions.
Widely studied in the last decades, CT can be defined as intentional, rational, and reflective thinking, focused on what one should believe and do ( 4 ) , which results in interpretation, analysis, evaluation, inference, explanation, and self-regulation ( 5 ) . It is considered essential for the development of the ability to process information and evaluate its plausibility, to clearly argue and defend one’s position, to foresee consequences, to examine the pros and cons in the decision-making process ( 6 - 7 ) . Being able to think critically is evidenced as an important predictor of good academic performance ( 8 ) . Students with high CT skills are capable of organizing their learning, monitor and evaluate their performance ( 9 ) , and such skills favor successful decision making ( 8 ) .
Like globalization, health care has also become complex and demanding; nursing has evolved as a profession, a fact that has generated the need for professionals to demonstrate critical-reflexive characteristics in their daily practice ( 10 ) . Nursing as a profession is configured as the largest workforce in health care, both by the number of professionals and by its proximity to patients and their families, because it is the nursing professionals who ensure 24 hours of patient care. This proximity and all the complexity involved in nursing care, along with technological advances, require skills that allow nurses to provide safe and quality care ( 11 - 15 ) .
In the context of health care, CT can be defined as the rigorous, intentional, and result-focused reasoning based on the patient’s needs ( 16 ) . For the promotion of safe and quality care, nursing students should be trained in a reflective manner to be able to act and respond assertively to the complex tangle of issues that emerge from the clinical context in the face of dynamic, uncertain, unpredictable, and inconstant situations ( 15 , 17 ) . Thus, CT skills are considered essential components for professional responsibility and quality in nursing care ( 11 - 12 , 14 , 16 , 18 - 19 ) .
Thinking critically is not innate, so it requires effort and integration of contexts and teaching and learning proposals that favor its evolution ( 20 ) . For the development of CT skills, it is important to ensure learning environments that enable the active involvement of students ( 21 ) , since active learning methodologies can stimulate the development of higher order cognitive processes ( 12 , 15 , 22 - 23 ) . Active learning methodologies are considered the key to success that guarantees students the ability to analyze evidence and proposals, make fair judgments, propose solutions ( 22 , 24 - 25 ) , evaluate their decisions and, if necessary, go back to the start and reconstruct the whole process ( 26 ) .
Thus, the clinical teaching context constitutes the space of choice for the development of CT skills due to its dynamic, interactive, unpredictable, mediating, facilitating, and enhancing nature of practical learning ( 27 - 28 ) . Clinical teaching, performed in health institutions, is characterized by learning in real context, where the student applies theoretical knowledge in practice, that is, it integrates knowing with doing, resulting in a reflective and critical process and in the improvement of clinical skills and competencies that, when properly conducted, culminates in a conscious, critical, and creative student action ( 11 , 29 - 30 ) . Clinical teaching, through the supervisory process, aims to guarantee the student the acquisition of knowledge and the development of skills and attitudes for the performance of autonomous, conscious, and grounded interventions ( 29 - 31 ) .
It is possible to state that CT, as a set of skills, can be taught, and the more these skills are trained, the greater the probability of favorable results, which contributes to the training of students capable of providing assertive answers to the complex problems presented ( 5 , 22 , 32 ) . Critical teaching, due to its real-world nature, favors the development of these abilities (professional competencies), since it enables the articulation between theory and practice, enhanced by the adoption of a proactive learning attitude ( 29 ) . Clinical supervision strategies (CSS) can influence the development of nursing students’ CT skills, which are essential for their performance in care practice.
Currently, there are several studies that address CT issues ( 1 - 6 , 8 , 19 , 32 ) in a general manner and others more directed to nursing ( 18 , 21 - 22 , 26 ) ; however, there are still no studies relating supervision strategies to the development of CT in nursing students. Based on the premise that CT is a fundamental aspect during the critical teaching of these students, the adoption of constructivist teaching strategies that allow them to improve CT learning should be encouraged. In this sense, it is essential to identify the students’ CT skills and the CSSs that most promote their development.
To identify the supervisory strategies that Nursing students consider facilitators of the development of CT skills in clinical teaching.
Ethical aspects
This study was submitted to the opinion of the Ethics Committee of a Nursing School in Northern Portugal, and its ethical and methodological aspects were approved. All study participants signed the Informed Consent Form, which guarantees the right to data privacy, anonymity, and confidentiality.
Theoretical and methodological framework
The theoretical and methodological framework is based on the qualitative approach. This seeks to interpret and understand a reality from the perspective of the actors involved in the process ( 33 ) .
The qualitative nature, as a theoretical and methodological foundation, enables the unveiling of the undergraduate nursing students’ thought referential about their experience in the critical teaching context, namely to identify the clinical supervision strategies considered by them as facilitators of the development of their CT skills.
This is a qualitative study, inserted in the interpretative paradigm, since it seeks to interpret and understand the meanings of human action from the perspective of those who live it ( 33 ) , namely undergraduate nursing students in the context of critical teaching. It is an exploratory and cross-sectional study, using the focus group methodology. For the preparation of the manuscript, to ensure rigor and transparency in the writing of the summary of results, this work was conducted and structured based on the Standards for Reporting Qualitative Research (SRQR), whose objective is to establish standards for reporting qualitative research.
The qualitative nature of focus group data collection provides a rich environment for discussion among several participants, as it allows the researcher to gain an in-depth view of different opinions, knowledge, perceptions, feelings, and experiences on a given topic, which may be analyzed later ( 34 ) . Its objective is to understand the human being and his/her relations with the theme under investigation, by observing the participants’ discourses, behaviors, and reactions ( 33 ) . Among the benefits of this methodology, we can highlight its quick execution, the ease of being performed nowadays by videoconference, its dynamic character due to flexibility in its conduction, and contact between the participants and moderator ( 34 ) .
Study setting
Study carried out in a Nursing School in Northern Portugal, during the months of May to July 2021. The research was carried out with students enrolled in the 2020/2021 academic year of the Bachelor of Science in Nursing (BSN) course.
Data source
Bachelor of science in nursing students were part of the sample for this study. The eligibility criteria were: active enrollment in the year 2020/2021 and having at least one critical teaching experience, due to familiarity with the critical teaching context and the CSSs. Eight fourth-year BSN students participated in the focus group session.
During the planning phase of data collection, there was concern about how to recruit the students. Thus, the main researcher was allowed to contact the coordinators of the Clinical Practice curricular units (CU), and they, in turn, contacted the students and explained the nature and objectives of the research. To those who expressed interest in participating, the coordinator requested authorization to give their electronic address, and, by this means, a formal invitation was sent to each student. After accepting the invitation, the students received, also by e-mail, the Free and Informed Consent Form to sign and return to the main researcher. A date and time was then scheduled for the focus group session, and the respective link to access the session was sent to all participants.
Data collection and organization
Due to the pandemic context caused by covid-19 and the restrictions it imposed on educational establishments and health services, data collection was conducted via videoconference, through the Zoom platform, adopting a focus group session format.
To conduct the focus group, a script consisting of a set of open questions was constructed. In its elaboration, fidelity and validity - essential characteristics that determine the quality of any measurement instrument - were considered. Fidelity is a condition that shows if the measurement instrument provides constant values from one use to the next; in this sense, a pre-test of the script was carried out with a focus group composed of four students who met the eligibility criteria for the research and who were not part of the group of participants. After analysis, there was no need for reformulation. Validity was checked through the evaluation of the script by an expert external to the study: a professor and researcher in nursing with 20 years of experience in clinical supervision, who gave a favorable opinion about the instrument.
The execution or moderation of the focus group was carried out by the main researcher, assisted by another researcher of the team, experienced in using the methodology. The session lasted about two hours. The session was recorded in image and audio and was destroyed after being transcribed.
Analysis of results
Content analysis was used globally, according to the methodology proposed by Bardin. Such analysis allows us to verify the order, intensity, and frequency of a discourse ( 33 ) , with the aim of improving the results, expanding its validity and, consequently, enabling a reliable final interpretation ( 35 ) .
Data analysis was performed by two independent researchers, with a backup researcher who was involved in case of disagreement, and followed three phases: organization, coding, and categorization. The first phase comprised the full transcription of the focus group participants’ speeches according to their sequence. To guarantee focus group anonymity, each participant was classified with the letter P (Participant) plus a number corresponding to the order of his or her speech (P1, P2, ...P8). Next, a skimming of the entire document that composed the corpus of analysis was performed, followed by an exhaustive reading. In the second phase, we performed the codification based on the theme and listed according to the frequency and intensity in the speeches. Finally, the semantic and lexical categorization was performed considering the meanings and reasoning of the speeches, based on which the categories and respective subcategories emerged ( 35 ) .
Eight BSN students participated in the focus group session, six female and two male. All of them were attending the 4th year of the Clinical Practices CUs course; and their ages ranged from 21 to 24 years, with an average age of 22.
The content analysis of the participants’ discourse allowed us to organize the information into categories and subcategories as shown in Chart 1 . The categories found were “Critical thinking skills”, “Factors that facilitate the development of critical thinking”, “Factors that hinder the development of critical thinking”, and “Clinical supervision strategies”.
Chart 1. Categories and subcategories of the content analysis of the focus group participants’ discourse.
Critical thinking skills.
The participants recognized the importance of CT in the initial training of nurses, listing it as a factor that favors professional responsibility and quality in nursing care, since it promotes reflective thinking, meaningful and autonomous involvement in the complex context of health care, clinical judgment, and the development of decision-making skills.
I think it’s quite important that we develop our critical thinking because I think that’s one of the foundations of nursing practice; and I think that we as students, the earlier we develop it, the easier it will be for us when we are nurses. (P1) [...] I think it’s a fundamental part of being a good nurse [...]. (P5)
However, despite the extensive dissemination of the need for CT in nursing education, it is perceived that students are often not stimulated or are even prevented from putting their competencies into practice. Such difficulty is evidenced in their speech:
[...] it is true, sometimes we enact our critical thinking and we even manage to sustain it, but it is not always used, because many times we are even told “This is the protocol here”, and we actually end up performing the intervention according to the protocol, and not according to what we think, which is even more based on the most current evidence [...]. (P7)
In addition to recognizing its importance, participants also highlighted that the CT skills (evaluation, interpretation, analysis, inference, explanation, and self-regulation) are essential for their good performance in critical teaching, namely for clinical judgment, decision-making, and problem solving.
It is basically having the tendency not to say, oh, this is like this, it’s like that, because that person is telling me it’s like that; it’s having the ability to make the decision ourselves, taking into account the data that we have and the information that we can collect from that problem. (P7) Even if there are protocols at the service level, whatever they are, we shouldn’t look at them as a norm or a rule. We should respect them, but take into consideration what principles or what kind of bibliography they are based on... we should always look for evidence that justifies and supports the practices [...]. (P8)
Factors that facilitate the development of critical thinking
In the critical teaching context, the relationship between supervisors, students, and multiprofessional team is key to facilitate student learning. The spirit of cooperation favors autonomy, good clinical judgment, and the decision-making process. Regarding facilitating factors for the development of CT, participants highlight the importance of having a supervisor, having multiple supervisors, the supervisory relationship, experience in clinical supervision, student characteristics, the role of the supervisor, and integration into the team.
The establishment of a good supervisory relationship I think is the key, because from a good supervisory relationship comes all the rest, comes questioning, autonomy, trust, and also availability, which then will encourage us to seek more information, to question more, and learn more about the service we are in. (P4) [...] much more important than the strategies used, is also knowing the role that the supervisor has [...] knowing for a fact where he can really contribute to our critical thinking. (P6)
Factors that hinder the development of critical thinking
As supervisors move away from the characteristics previously described, they establish an authoritarian, oppressive, hostile, apathetic environment with little communication and make it impossible to create a good supervisory relationship, besides causing negative experiences in students. The absence of a good relationship between supervisor and supervised shows itself as a hindrance to the development of CT.
The analysis of the participants’ discourse allowed us to identify the following aspects as hindering the development of CT: nurse’s attitude, lack of feedback, communication problems, not wanting to be a supervisor, not having a supervisor, lack of support, and negative experience.
[...] I did many shifts with this supervisor, and she had a very authoritarian and very hostile attitude [...] I think I could have learned a lot more, and I didn’t learn exactly because of this attitude of hostility and neglect. (P3) [...] there was a little bit of a mocking attitude towards me for not knowing, and “how is it possible that you don’t know this? ” (P3) [...] my family was worked up, everything was going wrong, and the supervisor [...] never showed any concern, not even on a knowledge level, not on a personal level, nothing. It was the same thing being with her, I did things with her, and if I wasn’t with her it was the same, that was it. (P4) Having been placed with a supervisor who didn’t want to have students, I know it’s a little contradictory, but she told me, in this case directly, that she didn’t want to have students; and I think that makes clinical teaching a little difficult, because the person in particular didn’t ask me questions, when I asked questions she answered me in a less than friendly way, or sometimes she didn’t answer me at all. And then, throughout the clinical teaching, it felt a little bit as if the person was doing me a favor, and I didn’t feel secure and confident to be able to develop what I wanted, and I think it hindered my learning a little bit. (P1)
Clinical supervision strategies
The strategy adopted by the supervisor is established as the structuring axis of the teaching and learning process within critical teaching, since it allows students to develop essential clinical skills aiming at success in their performance. Regarding the CSSs, the participants highlight the pedagogical questions, reflection, individualized study, guidance, support, encouragement, feedback, discussion of clinical cases, definition of individual goals, observation and stimulation, and communication with the team.
[...] the fact that the supervisors ask us questions helps us to reflect on certain issues that are important and that, perhaps, we would not pay much attention to. (P2) [...] the fact that those questions, which are questions of another level, that ultimately take us further, are those questions that are not basic, but that we have to study in depth and understand different relationships to answer those questions [...]. (P8) [...] the questions, I think are important, but I think the moment, that is, when they ask us the questions is fundamental; I just don’t think it should be a stressful moment [...]. (P5) It really made me reflect and think [...]. (P1) [...] that is, with one question, I think I could encompass great knowledge, which would then have repercussions on my critical thinking in the short or long term. (P7) [...] but also, at the same time, it would guide my study at the initial moment; it would help, for example, “Look, right now, I think it makes sense for you to study this.” (P3) [...] she was a supervisor who cared about me as a person. For example, if there was any change, she was the first to say: “If you can’t make it, you can come and do it on another day; there’s no problem. (P3) [...] in more stressful situations, she was the first one to say: “Calm down, I’ll help you, I’m here and you can do it”. (P3) I consider feedback as something central, that is, to understand how well we are doing in clinical teaching, because we often have a wrong perception [...]. I think we should always understand how we are doing and what we can improve on. (P8) [...] and I think that, in the third year, in some of the initial clinical teaching, it was essential to establish objectives [...], also because when we start clinical teaching, we somehow feel lost, because there are a lot of things that we must know, so the definition of objectives ends up guiding us in some way. (P8)
The participants recognized the indispensability of CT for clinical practice, describing it as essential for professional responsibility and quality in nursing care, by virtue of being an enabling factor for reflective thinking, autonomy, good clinical judgment, acquisition of problem-solving skills, and safe, effective, and ethical decision-making. In addition, they highlighted the importance of establishing a good supervisory relationship, i.e., the need for the supervisor to get to know the student within his or her personal and academic journey. This close relationship was considered essential in determining the supervisory strategy best suited to the students’ needs, learning objectives, and clinical teaching context.
Peter Facione, through the memorable The Delphi Report, emphasizes the indispensability of the development of CT capabilities for the execution of sensible judgments and correct decisions. The abilities, also recognized as cognitive competencies or skills, are classified into six spheres: interpretation, analysis, evaluation, inference, explanation, and self-regulation ( 5 - 6 , 36 ) . These competencies are considered primordial for the student’s good academic, personal, and professional performance ( 36 ) since they allow them to improve problem-solving skills and, in turn, make assertive decisions ( 9 ) .
The participants’ discourse makes it possible to identify the critical thinker as one updated in knowledge, diligent in the search for a valid reason, thoughtful, flexible in his judgments, able to judge the credibility of information. However, it can be inferred that the absence of a cordial relationship between supervisor and supervised as well as the impossibility of putting current scientific knowledge into practice constitute major hindrances to the development of the students’ CT. Similarly, the critical thinker is described as curious, well-informed, creative, open to different possibilities, possessing reflective thinking, and therefore capable of judging the credibility of information ( 17 ) . Because the context of health care demands prudence from the nursing student in the search for and selection of information ( 10 ) , it becomes urgent to develop the habit of questioning and searching for scientific evidence to support safe and quality care.
Critical teaching allows the student to experience valuable moments of observation and interaction, as it favors the development of essential knowledge, skills, and attitudes for professional practice, provides self-regulation resources, besides facilitating the appropriation, mobilization, and materialization of knowledge ( 29 ) . In this environment, the supervisory process is configured as dynamic, interactive, facilitator, and which empowers learning, since it is based on a relationship of trust and mutual help, in which the supervisor adopts strategies for the personal and professional development of those supervised ( 37 ) .
The clinical supervisor, as the mediator of the students’ learning and professional development, ensures the transition from being a student to being a professional ( 29 ) . In this framework, the supervisory strategy constitutes an important phase in the training process since it provides the planning of actions and the organization of activities that favors students’ personal and professional development ( 37 ) .
Anchored in the principle of equity, supervisors should not treat students in an exactly equal manner regarding learning, a fact that is justified by the individual needs inherent to each supervisee ( 38 ) . There is no single, incontestable strategy that fits all contexts and all students; rather, there are different strategies that can be used in different combinations. For the strategy selection to be successful, it is important to consider the clinical context, the students, the learning objectives, and the available resources, which is why individualization of teaching is indispensable ( 37 ) .
Reflection allows students to construct and appropriate knowledge through their professional practice. In this process, the supervisor has a fundamental role in leading the student in the reflective process, either by creating real learning opportunities, or by provoking him/her in the search for more knowledge. Upon a doubt or difficulty, reflective thinking is initiated, followed by a mental process of questioning, which motivates the student to research so that he can then resolve that doubt or difficulty ( 39 ) . Reflection improves the capacity to solve problems and makes it possible to revisit and reformulate the experience lived, with the objective of establishing alternatives and constructing new learning ( 37 ) . The reflective process is enunciated as an effective strategy for the promotion of CT ( 17 ) , since reflecting on priorities in care promotes the development of confidence, autonomy, and communication skills ( 28 ) .
To formulate questions that instigate students’ restlessness and motivate them in the search for answers is pointed out as a propulsive strategy for reflective and creative thinking ( 37 ) . As the questions increase the students’ interest and curiosity, they contribute to experiential learning, enabling the connection between knowledge and practice ( 17 ) . At the same time, the supervisor, at opportune moments, in a friendly manner and withholding his/her evaluative character, asks questions. Besides facilitating the construction of a competent professional, it also instills in the student the habit of asking questions, allowing progress toward the potential development of CT skills.
Providing feedback allows students to become active subjects in the teaching and learning process, since it facilitates the self-evaluation process, and reflective, creative, and critical thinking ( 40 ) , and autonomy ( 17 ) , characteristics that are indispensable to nurses. Thus, the supervisor should find the most opportune moment to provide effective, clear, and constructive feedback ( 40 ) .
Study limitations
There are two limitations. First, the participants are only 4th year BSN students, i.e., graduates; this made it impossible to determine the strategies that promote CT for all BSN students in a critical teaching context. The second limitation relates to the fact that the study was conducted in a pandemic context, so online data collection did not allow establishing a physical meeting place with the participants, a fact that may have conditioned the responses due to the lack of familiarity with this format. In this sense, it is suggested to carry out studies in post-pandemic contexts, with students at different stages of critical teaching, in the early and final academic years, which will make it possible to demonstrate the causal relationship between the CSSs and the CT skills in students throughout the Nursing course.
Contributions to the field
The study highlights the need for the use of CSSs that favor the reflective process. It also reiterates the urgency to establish within the curricula of undergraduate nursing courses constructivist teaching strategies that allow students to develop CT, essential skills for good clinical judgment, problem solving, and safe, effective, and ethical clinical decision-making.
FINAL CONSIDERATIONS
Students recognized the importance of CT skills in the critical teaching context, considering them fundamental for clinical judgment, decision making, and problem solving. Since critical thinking demands effort and association of contexts and strategies that enable its development, this study highlights the importance of using different CSSs. Thus, the perspective of strategies acting in interchangeable and complementary ways is emphasized. Pedagogical questions, reflection, individualized study, orientation, support, encouragement, feedback, discussion of clinical cases, definition of individual goals, observation, and stimulation of communication with the team are the strategies identified as the most favorable for CT. At certain times, it is appropriate to use several strategies at the same time; at other times, only one is sufficient to achieve the learning objectives. To establish the most appropriate supervisory strategy for the student and the learning context, it is essential that the supervisor, in addition to knowing the academic path of his supervisee, recognize his individuality and needs.
AVAILABILITY DATA AND MATERIAL
https://doi.org/10.48331/scielodata.PC3XOX
- 1. Lopes J, Silva H, Morais T. In: Educar para o pensamento crítico na sala de aula. Lopes J, Silva H, Dominguez C, Nascimento M., editors. Lisboa: Pactor;; 2020. A aprendizagem cooperativa na promoção do pensamento crítico; pp. 125–142. [ Google Scholar ]
- 2. Cruz G, Dominguez C, Payan-Carreira R. In: Educar para o pensamento crítico na sala de aula. Lopes J, Silva H, Dominguez C, Nascimento M., editors. Lisboa: Pactor;; 2020. A importância e o desafio de educar para o pensamento crítico no séc. XXi; pp. 1–22. [ Google Scholar ]
- 3. Tenreiro-Vieira C, Vieira RM. Promover o pensamento crítico e criativo no ensino das ciências: propostas didáticas e seus contributos em alunos Portugueses. IENCI. 2021;26(1):70–84. doi: 10.22600/1518-8795.ienci2021v26n1p70. [ DOI ] [ Google Scholar ]
- 4. Ennis RH. The nature of critical thinking: an outline of critical thinking dispositions and abilities. 2011. [cited 2021 May 20]. [Internet] Available from: https://education.illinois.edu/docs/default-source/faculty-documents/robert-ennis/thenatureofcriticalthinking_51711_000.pdf .
- 5. Facione P. Critical thinking: a statement of expert consensus for purposes of educational assessment and instruction [Internet] California; 1990. [cited 2021 May 20]. Available from: https://www.qcc.cuny.edu/socialsciences/ppecorino/CT-Expert-Report.pdf .
- 6. Facione P. Critical thinking: what it is and why it counts leadership thinking resources view project Critical Thinking, Decision Making, and Problem Solving View project. 2015. [cited 2021 May 20]. [Internet] Available from: https://www.researchgate.net/publication/251303244 .
- 7. Pastén LE. Metacognitive, critical and creative thinking in educative contexts: conceptualization and didactic suggestions. Psicol Esc Educ. 2021;25:1–8. doi: 10.1590/2175-35392021220278. [ DOI ] [ Google Scholar ]
- 8. Bellaera L, Weinstein-Jones Y, Ilie S, Baker ST. Critical thinking in practice: the priorities and practices of instructors teaching in higher education. Think Skills Creat. 2021 Sep;:41. doi: 10.1016/j.tsc.2021.100856. [ DOI ] [ Google Scholar ]
- 9. Ayçiçek B. Integration of critical thinking into curriculum: perspectives of prospective teachers. Think Skills Creat. 2021:41. doi: 10.1016/j.tsc.2021.100895. [ DOI ] [ Google Scholar ]
- 10. Jiménez-Gómez MA, Cárdenas-Becerril L, Velásquez-Oyola MB, Carrillo-Pineda M, Barón-Díaz LY. Reflective and critical thinking in nursing curriculum. Rev Latino-Am Enferm. 2019:27. doi: 10.1590/1518-8345.2861.3173. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Baixinho CL, Ferreira ÓR. Ser estudante de enfermagem em tempos de COVID-19. Esc Anna Nery. 2021;25(spe) doi: 10.1590/2177-9465-ean-2020-0541. [ DOI ] [ Google Scholar ]
- 12. Nunes JGP, Amendoeira JJP, Cruz DALM, Lasater K, Morais SCRV, Carvalho EC. Clinical judgment and diagnostic reasoning of nursing students in clinical simulation. Rev Bras Enferm. 2020;73(6):1–7. doi: 10.1590/0034-7167-2018-0878. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Cantante APSR, Fernandes HIVM, Teixeira MJ, Frota MA, Rolim KMC, Albuquerque FHS. Health systems and nursing skills in Portugal. Cienc Saude Coletiva. 2020;25(1):261–272. doi: 10.1590/1413-81232020251.27682019. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Oliveira JF, Perez EZ, Ferreira MBG, Pires PS, Barichello E, Barbosa MH. Cultural adaptation and validation of an instrument about nursing critical thinking skills. Rev Bras Enferm. 2021;74(2):e20200720. doi: 10.1590/0034-7167-2020-0720. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Carvalho DP de SRP, Vitor AF, Cogo ALP, Bittencourt GKGD, Santos VEP, Ferreira MA., Júnior Critical thinking in nursing students from two Brazilian regions. Rev Bras Enferm. 2020;73(1):e20170742. doi: 10.1590/0034-7167-2017-0742. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Alfaro-LeFevre R. Fundamentos para o raciocínio clinico. 8a. Porto Alegre: Artmed;; 2014. Aplicação do processo de enfermagem. [ Google Scholar ]
- 17. Willers S, Jowsey T, Chen Y. How do nurses promote critical thinking in acute care? a scoping literature review. Nurs Educ Pract. 2021;53:103074. doi: 10.1016/j.nepr.2021.103074. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Carvalho DPSRP, Azevedo IC, Cruz GKP, Mafra GAC, Rego ALC, Vitor AF, et al. Strategies used for the promotion of critical thinking in nursing undergraduate education: a systematic review. Nurs Educ Today. 2017;57:103–107. doi: 10.1016/j.nedt.2017.07.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 19. Riegel F, Crossetti MGO. Referenciais teóricos e instrumentos para avaliação do pensamento crítico na enfermagem e na educação. Rev Gaúcha Enferm. 2018;39:1–9. doi: 10.1590/1983-1447.2018.2017-0097. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Tenreiro-Vieira C, Vieira RM. Promover o Pensamento Crítico em Contextos CTS: desenvolvimento de propostas didáticas para o ensino básico. Indagatio Didactica. 2020;12(4):2020. doi: 10.34624/id.v12i4.21823. [ DOI ] [ Google Scholar ]
- 21. Carvalho DPSRP, Vitor AF, Cogo ALP, Bittencourt GKGD, Santos VEP, Ferreira MA., Júnior Measurement of general critical thinking in undergraduate nursing students: experimental study. Texto Contexto Enferm. 2020:29. doi: 10.1590/1980-265x-tce-2018-0229. [ DOI ] [ Google Scholar ]
- 22. Riegel F, Martini JG, Bresolin P, Mohallem AGC, Nes AAG. Desenvolvendo o pensamento crítico no ensino de Enfermagem: um desafio em tempos de pandemia de Covid-19. Esc Anna Nery. 2021;25(spe) doi: 10.1590/2177-9465-ean-2020-0476. [ DOI ] [ Google Scholar ]
- 23. Carbogim F, Luiz F, Oliveira L, Braz P, Santos K, Püschel V. Effectiveness of a teaching model in a first aid course: a randomized clinical trial. Texto Contexto Enferm. 2020:29. doi: 10.1590/1980-265x-tce-2018-0362. [ DOI ] [ Google Scholar ]
- 24. Dominguez C, Payan-Carreira R, Morais F, Nascimento M, Maia A, Pedrosa D, et al. In: Pensamento crítico na educação: perspectivas atuais no panorama internacional. Vieira RM, Tenreiro-Vieira C, Chaves IS, Machado C., editors. Aveiro: UA Editora;; 2014. [cited 2021 Jun 11]. Revisão entre pares e pensamento críticopercurso para uma metodologia transversal. Available from: https://www.researchgate.net/publication/269334637_Revisao_entre_pares_e_pensamento_critico_percurso_para_uma_metodologia_transversal . [ Google Scholar ]
- 25. Ghezzi JFSA, Higa EFR, Lemes MA, Marin MJS. Strategies of active learning methodologies in nursing education: an integrative literature review. Rev Bras Enferm. 2021;74(1):e20200130. doi: 10.1590/0034-7167-2020-0130. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Facione PA, Facione NC, Riegel F, Martini JG, Crossetti MGO. Holistic critical thinking in times of covid-19 pandemic: unveiling fundamental skills to clinical nursing practice. Rev Gaucha Enferm. 2021;42:e20210235. doi: 10.1590/1983-1447.2021.20210235. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Abreu WC. Formação e Aprendizagem em Contexto Clínico. Coimbra: Formasau;; 2007. [ Google Scholar ]
- 28. Peixoto T, Peixoto N. Critical thinking of nursing students in clinical teaching: an integrative review. Rev Enferm Ref. 2017;IV(13):125–138. doi: 10.12707/riv16029. [ DOI ] [ Google Scholar ]
- 29. Esteves LSF, Cunha ICKO, Bohomol E, Santos MR. Clinical supervision and preceptorship/tutorship: contributions to the Supervised Curricular Internship in Nursing Education. Rev Bras Enferm. 2019;72(6):1730–1735. doi: 10.1590/0034-7167-2018-0785. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Karaduman GS, Bakir GK, Sim-Sim MMSF, Basak T, Goktas S, Skarbalienė A, et al. Percepções de estudantes de enfermagem sobre o ambiente de aprendizagem clínica e saúde mental: um estudo multicêntrico. Rev Latino-Am Enferm. 2022:30. doi: 10.1590/1518-8345.5577.3581. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Rocha IARES, Pinto CMCB, Carvalho ALRF. Impact of clinical supervision on job satisfaction and emotional competence of nurses. Rev Bras Enferm. 2021;74(6):e20210125. doi: 10.1590/0034-7167-2021-0125. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Halpern DF. Teaching for critical thinking: helping college students develop the skills and dispositions of a critical thinker. 1999. [cited 2021 May 20]. [Internet] Available from: www.psychplace.com .
- 33. Coutinho C. Metodologias de Investigação em Ciências Sociais e Humanas: teoria e prática. Coimbra: Edições Almedina;; 2019. [ Google Scholar ]
- 34. Halliday M, Mill D, Johnson J, Lee K. Let’s talk virtual! online focus group facilitation for the modern researcher. Res Soc Admin Pharm. 2021 doi: 10.1016/j.sapharm.2021.02.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Bardin L. Análise de Conteúdo. Lisboa: Edições 70;; 2021. [ Google Scholar ]
- 36. Hart C, Costa C, D’Souza D, Kimpton A, Ljbusic J. Exploring higher education students’ critical thinking skills through content analysis. Think Skills Creat. 2021:41. doi: 10.1016/j.tsc.2021.100877. [ DOI ] [ Google Scholar ]
- 37. Fonseca MJL. Supervisão em ensinos clínicos de enfermagem: perspectiva do docente. Coimbra: Formasau;; 2006. [ Google Scholar ]
- 38. Alarcão I, Tavares J. Supervisão da prática pedagógica: uma perspectiva de desenvolvimento e aprendizagem. 2a. Coimbra: Livraria Almedina;; 2003. [ Google Scholar ]
- 39. Peixoto N, Peixoto T. Reflective practice among nursing students in clinical teaching. Rev Enferm Ref. 2016 Dec;IV(11):121–132. doi: 10.12707/riv16030. [ DOI ] [ Google Scholar ]
- 40. Jackson D, Power T, Usher K. Feedback as a balancing act: qualitative insights from an experienced multi-cultural sample of doctoral supervisors in nursing. Nurs Educ Pract. 2021:54. doi: 10.1016/j.nepr.2021.103125. [ DOI ] [ PubMed ] [ Google Scholar ]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
- View on publisher site
- PDF (178.4 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 1
- Teaching strategies and outcome assessments targeting critical thinking in bachelor nursing students: a scoping review protocol
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-4086-0086 Frida Westerdahl 1 ,
- Elisabeth Carlson 1 ,
- Anne Wennick 1 ,
- Gunilla Borglin 1 , 2
- 1 Department of Care Science , Malmö University , Malmö , Sweden
- 2 Nursing Education , Lovisenberg Diaconal University College , Oslo , Norway
- Correspondence to Frida Westerdahl; frida.nygren{at}mau.se
Introduction Applying critical thinking is essential for nursing students both in an academic and clinical context. Particularly, as critical thinking is a vital part of nurses’ everyday problem-solving and decision-making processes. Therefore, regardless of the topic taught or the setting in which it is taught, it requires teaching strategies especially targeting students’ critical thinking skills and abilities. One challenge with the latter is the difficulties to assess and evaluate the impact of such teaching strategies on the students’ critical thinking disposition. Hence, our objective will be to review published literature on; existing teaching strategies and outcomes assessments targeting nursing students’ critical thinking skills and abilities.
Methods and analysis Our scoping review will be conducted in accordance with Arksey and O’Malley’s framework for scoping studies. Search strategies will be developed in cooperation with an experienced librarian, and adjusted to each individual database for example, CINAHL, PubMed, PsycINFO, ERIC and ERC. A preliminary search in CINAHL was conducted on the 17 th of July 2019. Peer-reviewed published studies conducted with a qualitative, quantitative or mixed method design and focussing our objectives, will be eligible for inclusion. Included studies will be quality assessed in accordance with their study design. Data will be charted using a standardised extraction form. The qualitative data will be presented through a thematic analyses, and the quantitative data by descriptive numerical analysis. Lastly, nurse educators and nursing students will be consulted for validation of the findings from the scoping review.
Ethics and dissemination Under the Swedish Ethical Review Act (2003:460) this study does not need ethical clearance by a Regional Ethical Review Authority as it not includes any primary empirical data on biological material or sensitive information. The findings will be used to inform the design of a future study aiming to develop an, and subsequently evaluate it, educational intervention targeting teaching strategies focussing on nursing students’ critical thinking skills and abilities.
- critical thinking abilities
- critical thinking skills
- descriptive numerical analysis
- nurse educators
- thematic analysis
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2019-033214
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
To ensure rigour and transparency the upcoming scoping review will be based on (1) a solid methodological framework for scoping studies and (2) the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews checklist.
A minimum of two members of the review team will independently assess study eligibility.
Eligible studies will be quality assessed in accordance with their study design.
To achieve a comprehensive picture of the existing research qualitative, quantitative and mixed methods designs will be included in this scoping review.
One limitation might be the potential risk for publication bias since grey literature will not be included, as this will facilitate charting of teaching strategies and outcome assessments targeting critical thinking skills and abilities as described solely in published research.
Introduction
Applying critical thinking is essential for bachelor nursing students (hereafter nursing students); particularly, considering the complex care situations they regularly will find themselves in after graduation. 1 Care situations that among others require them to work in accordance with established standards 2 to be able to contribute to a safe, evidence based and optimal clinical practice. Given that nursing is based on scientific knowledge, critical thinking is the reasonable reflection to justify nursing actions based on evidence. Skills and abilities in critical thinking have consequently been found to predict nursing competence together with working years, position, title and educational level, that is, Bachelor or Master in Nursing. 3 Critical thinking is, therefore, a crucial component of every registered nurse’s daily activities, aiding problem-solving and decision-making processes. 4
According to Scheffer and Rubenfeld the ability to execute critical thinking in nursing could be seen from two perspectives; habits of the mind (cognition), and skills employed by the critical thinker. 5 Critical thinking can also be seen as a consecutive process including (i) gathering information, (ii) questioning, (iii) analysis and evaluation and (iv) problem-solving and application of theory, that is, the nursing process. 6 This consecutive process of critical thinking needs to be applied both in the clinical area and in the classroom. 7 However, to develop this ability among nursing students is a complex process. To apply critical thinking, the necessary skills and abilities need to be taught and developed during both the students’ clinical placements as well as during their theory courses throughout the nursing education. 4
One challenge with the concept of critical thinking, often highlighted in the literature, and despite its priority within the nursing education, is the interchangeable use of the concepts of critical thinking, clinical reasoning and clinical judgement. 7–9 Concepts that Victor-Chmil describe as; ‘they are not one and the same’ (p 34). It needs to be acknowledged, as the authors of this current protocol do, that critical thinking often is used as a broader term which includes the concepts of clinical reasoning and clinical judgement. 8 According to Alfaro-LeFevre clinical reasoning refers to the process used to solve clinical issues and clinical judgement refers to the outcome or conclusion of this process. 7 Therefore, regardless of the topic taught or the setting in which it is taught, requires teaching strategies especially targeting nursing students’ critical thinking skills and abilities. For these strategies to be favourable, it requires implementation throughout the nursing education, and thereby reflected in all parts of the nursing programmes’ learning objectives and curricula. 10 It has been outlined that teaching strategies such as, problem-based learning, concept-mapping, case-based learning interventions and reflective writing are often used in nursing programmes to support critical thinking. 6 10 11 However, another challenge with critical thinking, besides the interchangeable use of concepts, is the difficulty to assess and evaluate the impact of different teaching strategies on the students’ critical thinking disposition (ie, skills and abilities) as well as the assessment of the different components in the critical thinking process. 8 Previous reviews in the current research area have only included either experimental studies 12 or randomised clinical trials 13 measuring the effectiveness of teaching strategies. Further, other reviews have involved mixed populations including not only nursing students, but also working nurses and nursing managers 14 and midwifery students. 15 Since critical thinking is a vital part of registered nurses’ problem-solving and decision-making, this ability needs to be taught already during the nursing education. It is therefore necessary to focus the educational context of undergraduate nursing taking an extended approach on how teaching strategies targeting critical thinking are described, experienced and assessed. Hence, our overarching objective will be to review published literature on; existing teaching strategies and outcomes assessments targeting nursing students’ critical thinking skills and abilities.
Methods and analysis
The upcoming scoping review will address a broad topic (ie, teaching strategies targeting nursing students’ critical thinking skills and abilities, as well as outcome assessments of such skills and abilities), where a diverse range of study designs can be considered relevant in answering our additionally wide review questions. Our scoping review will therefore be designed in accordance with Arksey and O’Malley’s methodological framework for scoping studies. 16 However, our design will also be informed by other more recent methodological accounts. 17 18 The framework will enable us to identify existing gaps in the literature as well as to summarise, evaluate and disseminate the overall state of research activities within the field. 16 The Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews checklist (PRISMA-ScR) was used to prepare this protocol. 19 PRISMA-ScR will also form the base for the upcoming scoping review as standardised reporting guidelines can according to Colquhoun et al support the critical appraisals of published reviews by expanding on their transparency and reproducibility. 20
Stage 1: identifying the research question
The research questions for the upcoming scoping review aims for comprehensiveness, that is, they will be broad to cover the breadth of research evidence in our field of focus. As scoping is an iterative methodological process, 16 it is possible for us to decide to add supplementary questions based on the findings emerging during the review process. A modified 21 PICOS (Population, Intervention, Comparison, Outcome and Study Setting) framework will aid us in determining the appropriateness of the research questions, as well as guide us in our database searches ( table 1 ).
- View inline
Framework (PICOS) for determination of eligibility of review questions
Since the subsequent goal of the upcoming scoping review is to further the knowledge and understanding about how nurse educators via teaching strategies can target the development of nursing students’ critical thinking skills and abilities we will additionally engage in findings of relevance to this. The following tentative research questions were developed to capture the objectives of the upcoming study:
Which are the teaching strategies described in the literature as targeting critical thinking skills and abilities among nursing students?
How are these teaching strategies conceptualised, described and experienced by students and/or nurse educators for example, pros and cons?
Which outcomes are described in the literature as used to assess critical thinking skills and abilities?
Stage 2: identifying relevant studies
The upcoming scoping review will include primary studies utilising qualitative, quantitative and mixed methods, published in peer-reviewed journals. This strategy will support us to achieve a comprehensive picture of the existing research focussing peer-reviewed studies on teaching strategies targeting critical thinking skills and abilities among nursing students, as well as on existing research focussing on outcome assessments of such skills and abilities. No limits will be applied concerning publication year, since we aim at conducting a comprehensive overview of published studies. Studies will be excluded if the population is not identifiable, qualitative and quantitative data is not possible to extract in case of mixed method design or published in other languages than English. All reasons for exclusion will be documented.
In our upcoming scoping review the term ‘teaching strategies’ will be used. Thus, our focus is not the overall educational organisation of teaching (ie, educational strategies) or the students’ individual general learning process (ie, learning strategies). However, as we are aware of the commonly interchangeable use in the literature of the terms; teaching strategies, educational strategies and learning strategies, they will all be included in our searches. Here the term teaching strategies are operationalised in accordance with Banning, and as encompassing three different perspectives; (i) the didactic perspective, which is teacher centred and mainly involves lectures; (ii) the facilitative perspective, focussing on self-directed learning making the students articulate their knowledge and lastly (iii) the Socratic perspective which is emphasising student-centredness and use objective questioning from the teacher. 22
The following databases; CINAHL, PubMed, PsycInfo, ERIC and ERC will be used to search for eligible studies. These databases are chosen to cover a comprehensive sample of literature from healthcare science and education. A search strategy for each database will be developed by the review team with assistance from an experienced librarian. Our strategies will include both database specific heading that is, Medical Subject Headings, keywords and synonyms. All specific headings and key words will be combined using the Boolean operators OR as well as AND. To ensure comprehensiveness, included studies reference lists will be manually searched. As outlined by Arksey and O’Malley the search strategy should be an iterative process and the search terms could be adjusted while an increased familiarity with the literature is achieved. For this reason, a preliminary pilot search strategy will be applied to the databases and the first 100 search results will be reviewed by the review team to assess validity. 16 During the review team meetings, adjustments will be applied to the search strategy and search terms until full agreement is reached. Grey literature (ie, literature that is not formally published in sources such as journal articles or books) will not, as described elsewhere, be included in our upcoming scoping study. 23 This will support us to focus on and to chart how teaching strategies targeting skills and abilities such as critical thinking is described in published peer-reviewed research. A draft of a preliminary search in CINAHL conducted on the 17 th of July 2019 is attached in online supplementary file 1 .
Supplemental material
Stage 3: study selection.
The study selection will first consist of a title and abstract scan. If the title and abstract are in line with the scoping review’s objectives and questions to the literature or if the relevance of the study is unclear a full-text review will follow. Retrieved studies from each database are going to be divided equally among a minimum of two reviewers, who independently will conduct the selection process. 17 To facilitate the process, we are going to use the data programme Rayyan. The programme is a mobile and web application developed to facilitate the screening of title and/or abstract as well as the collaboration between the reviewers. 24 During the study selection process, the first reviewer (FW) will be responsible for regularly convoking the review team for discussions concerning uncertainties and to refine the study selection process. 17 Criteria for inclusion can also be applied ad hoc during the process when acquaintance with the field of research is increased. 16 If any disagreements on study inclusion occur, an additional reviewer will be consulted to determine the final inclusion. 17 The study selection process ( figure 1 ) will be accounted for by the PRISMA flow diagram. 25
- Download figure
- Open in new tab
- Download powerpoint
Overview study selection process.
Contrary to Arksey and O’Malley’s methodological framework, 16 studies eligible for inclusion in our scoping review are going to be quality assessed. The assessment of the included studies’ quality will allow us to identify where the research itself is of poor quality, that is, identifying gaps in the existing literature review. According to Grant and Booth the lack of quality assessments in scoping reviews are likely to limit the uptake of the findings. 26 Their sentiment is supported by both Levac, Colquhoun and O’Brien 17 and Daudt, van Mossel and Scott 18 who state that a quality assessment of included studies will likely result in findings more useful for practice. The quality assessment will be conducted by a minimum of two reviewers, who will use the relevant study design checklists from the Critical Appraisal Skills Programme (CASP). 27 As, CASP lack a checklist for mixed methods studies, the mixed method appraisal tool will be applied. 28 In the case of any ambiguity concerning a study’s quality assessment, an additional reviewer is going to be consulted. No exclusion of eligible studies will be made on behalf of the quality assessment as studies with limited quality nevertheless can provide a valid rationale as guidance as to where more research is required.
Stage 4: charting data
A data charting form would be developed, and piloted on the first 5 to 10 included studies in this review. The piloting will support the team to reach an agreement on extraction consistency. The latter is especially important, as the extraction will be conducted individually and independently by a minimum of two reviewers. 17 A systematic and analytical approach will be utilised to extract the relevant information of each included study. The variables and themes to be included in order to answer the review’s objective and questions to the literature will be established iteratively ( box 1 ). Thus, the data charting form will be updated throughout the review by one of the reviewers (FW) who will also hold regular discussion with the others in the review team. 17
Tentative data charting form
Author and date.
Study title.
Journal full reference.
Aim, objective and/or research questions.
Study and recruitment context (eg, in what country and where people were recruited).
Participant characteristics (eg, age, gender, education year/semester of study, course (ie, theoretical or clinical placement)).
Sampling method.
Number of study participants.
Study design.
Data collection (eg, what data collection methods were used?).
Data analysis (eg, how was the data analysed?).
Described ethical approval and/or considerations. 29
Described teaching strategies and/or interventions targeting review focus.
Described outcomes and assessments.
Most relevant findings.
Study quality appraisal. 27 28
Tentative ethical requirements influenced by Weingarten, Paul and Leibovici.
Was the study approved by a research ethical committee? (Yes/No)
Was informed consent obtained? (Yes/No)
Were adequate measurements taken to protect personal data? (Yes/No)
Is there a declaration on financial support? (Yes/No)
Is there a declaration on potential conflict of interest? (Yes/No)
Influenced by Weingarten, Paul and Leibovici’s substantial contribution to raise the ethical awareness in reviews, an ethical assess form ( box 2 ) was developed for the upcoming scoping review including five requirements. 29 Included studies valued by the review team as not adhering to the ethical requirements will be excluded at this stage of the scoping review process.
Stage 5: collating, summarising and reporting the results
In the fifth stage, an overview and narrative account of variables and information extracted in stage 4 will be presented, and as highlighted by Arksey and O’Malley no evidence grading will be executed. 16 Levac, Colquhoun and O’Brien 17 and Daudt, Van Mossel and Scott 18 suggest that the extracted qualitative data should be presented through thematic analysis, since no synthesis of data is required. 16 For this purpose, the thematic analysis by Braun and Clarke will be applied which is a flexible method suitable when the data is broad and allowing for a wide range of analytical options. 30 This cohere with the upcoming scoping review, which will include studies with a wide range of research questions and methods. Quantitative data will be reviewed through basic descriptive numerical analysis and presented in tables and charts to highlight the range of data. 16 If studies with a mixed method design are included in stage 3, the qualitative and quantitative data will be extracted and analysed separately. A minimum of two reviewers will be responsible for this stage of the scoping review process. During the process, meetings with the entire review team will be scheduled by the first reviewer (FW) to discuss and come to agreement concerning analysis and presentation of extracted data.
Stage 6: consultation stage
To validate the findings of this scoping study and make it more useful for practice the optional stage consultation will be applied. For this purpose, the findings from the scoping review will be presented to a group of educators and students connected to a nursing programme as a means to contribute with valuable insights on issues connected to the application and implementation of the findings.
Patient and public involvement
No patients have been involved in the design of this study. However, to conduct a study targeting teaching strategies for critical thinking in nursing education will eventually benefit patients since education is the foundation for raising future nurses and improve patient care.
Ethics and dissemination
Under the Swedish Ethical Review Act (2003:460) 31 this study does not need ethical clearance by a Regional Ethical Review Authority as it does not include any primary empirical data on biological material or sensitive information (eg, ethnicity, political or sexual orientation). However, the issue of ethical consideration in the execution of reviews is raised by Vergnes et al 32 as well as by Weingarten, Paul and Leibovici. 29 They state that without an ethical judgement of the included studies it could result in establishing clinical practise and guidelines based on studies with poor ethical quality and even unethical studies. It could further be seen as a way of increasing the awareness and necessity of high ethical standards in research. To meet these requirements one variable in the charting form will be ethical consideration and for that purpose a tentative checklist for ethical requirements was developed ( box 2 ). The checklist will be tested on a minimum of 10 publications, and revised accordingly if necessary.
The upcoming scoping review will contribute to the advancement of research concerning teaching strategies targeting nursing students’ skills and abilities in critical thinking and the outcome assessment of it. It will also provide an indication of the maturity of the literature by identifying research gaps. Gaining more knowledge of the targeted research area can act as a benchmark to implement new teaching strategies facilitating students’ critical thinking disposition within the nursing education. This will better prepare future nurses for the complex care situations they will approach. Our findings will be used to inform the design of a future study aiming to develop and evaluate an educational intervention targeting teaching strategies focussing on nursing students’ critical thinking skills and abilities. The upcoming scoping review will be published in a peer-reviewed journal. We expect to report in late spring 2020.
- Von Colln-Appling C ,
- Cronenwett L ,
- Sherwood G ,
- Barnsteiner J , et al
- Chang Y-J ,
- Kuo S-H , et al
- Andrea Sullivan E ,
- Sullivan EA
- Scheffer BK ,
- Rubenfeld MG
- Alfaro-LeFevre R
- Victor-Chmil J
- Simpson E ,
- Carvalho DPSRP ,
- Azevedo IC ,
- Cruz GKP , et al
- De Oliviera LB ,
- Carbogim FDC , et al
- Zuriguel Pérez E ,
- Lluch Canut MT ,
- Falcó Pegueroles A , et al
- Carter AG ,
- Creedy DK ,
- Sidebotham M
- Colquhoun H ,
- Daudt HML ,
- van Mossel C ,
- Tricco AC ,
- Zarin W , et al
- Colquhoun HL ,
- O'Brien KK , et al
- Mashamba-Thompson TP
- Stoffels M ,
- Peerdeman SM ,
- Daelmans HEM , et al
- Ouzzani M ,
- Hammady H ,
- Fedorowicz Z , et al
- Liberati A ,
- Tetzlaff J , et al
- Fbregues S , et al
- Weingarten MA ,
- Leibovici L
- ↵ Act concerning the ethical review of research involving humans (SFS 2003:460) .
- Vergnes J-N ,
- Marchal-Sixou C ,
- Nabet C , et al
Contributors FW, EC, AW and GB were responsible for the initial design of this study. FW conceptualised the review approach and led the writing of the manuscript. FW, EC, AW and GB contributed to the protocol’s development and approved the final version of this protocol. GB, EC and AW led the supervision of the manuscript preparation.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests None declared.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:

What is Critical Thinking in Nursing? (Explained W/ Examples)
Last updated on August 23rd, 2023
Critical thinking is a foundational skill applicable across various domains, including education, problem-solving, decision-making, and professional fields such as science, business, healthcare, and more.
It plays a crucial role in promoting logical and rational thinking, fostering informed decision-making, and enabling individuals to navigate complex and rapidly changing environments.
In this article, we will look at what is critical thinking in nursing practice, its importance, and how it enables nurses to excel in their roles while also positively impacting patient outcomes.
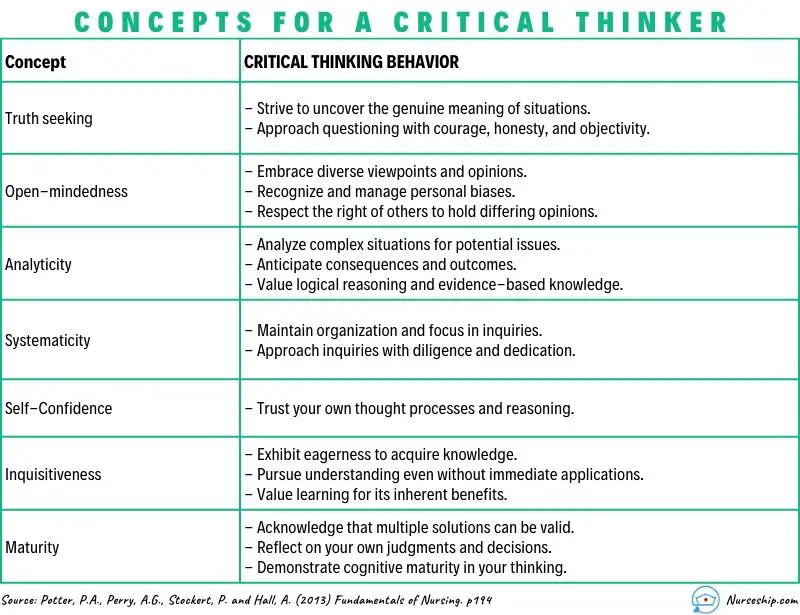
What is Critical Thinking?
Critical thinking is a cognitive process that involves analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
It’s a mental activity that goes beyond simple memorization or acceptance of information at face value.
Critical thinking involves careful, reflective, and logical thinking to understand complex problems, consider various perspectives, and arrive at well-reasoned conclusions or solutions.
Key aspects of critical thinking include:
- Analysis: Critical thinking begins with the thorough examination of information, ideas, or situations. It involves breaking down complex concepts into smaller parts to better understand their components and relationships.
- Evaluation: Critical thinkers assess the quality and reliability of information or arguments. They weigh evidence, identify strengths and weaknesses, and determine the credibility of sources.
- Synthesis: Critical thinking involves combining different pieces of information or ideas to create a new understanding or perspective. This involves connecting the dots between various sources and integrating them into a coherent whole.
- Inference: Critical thinkers draw logical and well-supported conclusions based on the information and evidence available. They use reasoning to make educated guesses about situations where complete information might be lacking.
- Problem-Solving: Critical thinking is essential in solving complex problems. It allows individuals to identify and define problems, generate potential solutions, evaluate the pros and cons of each solution, and choose the most appropriate course of action.
- Creativity: Critical thinking involves thinking outside the box and considering alternative viewpoints or approaches. It encourages the exploration of new ideas and solutions beyond conventional thinking.
- Reflection: Critical thinkers engage in self-assessment and reflection on their thought processes. They consider their own biases, assumptions, and potential errors in reasoning, aiming to improve their thinking skills over time.
- Open-Mindedness: Critical thinkers approach ideas and information with an open mind, willing to consider different viewpoints and perspectives even if they challenge their own beliefs.
- Effective Communication: Critical thinkers can articulate their thoughts and reasoning clearly and persuasively to others. They can express complex ideas in a coherent and understandable manner.
- Continuous Learning: Critical thinking encourages a commitment to ongoing learning and intellectual growth. It involves seeking out new knowledge, refining thinking skills, and staying receptive to new information.
Definition of Critical Thinking
Critical thinking is an intellectual process of analyzing, evaluating, and synthesizing information to make reasoned and informed decisions.
What is Critical Thinking in Nursing?
Critical thinking in nursing is a vital cognitive skill that involves analyzing, evaluating, and making reasoned decisions about patient care.
It’s an essential aspect of a nurse’s professional practice as it enables them to provide safe and effective care to patients.
Critical thinking involves a careful and deliberate thought process to gather and assess information, consider alternative solutions, and make informed decisions based on evidence and sound judgment.
This skill helps nurses to:
- Assess Information: Critical thinking allows nurses to thoroughly assess patient information, including medical history, symptoms, and test results. By analyzing this data, nurses can identify patterns, discrepancies, and potential issues that may require further investigation.
- Diagnose: Nurses use critical thinking to analyze patient data and collaboratively work with other healthcare professionals to formulate accurate nursing diagnoses. This is crucial for developing appropriate care plans that address the unique needs of each patient.
- Plan and Implement Care: Once a nursing diagnosis is established, critical thinking helps nurses develop effective care plans. They consider various interventions and treatment options, considering the patient’s preferences, medical history, and evidence-based practices.
- Evaluate Outcomes: After implementing interventions, critical thinking enables nurses to evaluate the outcomes of their actions. If the desired outcomes are not achieved, nurses can adapt their approach and make necessary changes to the care plan.
- Prioritize Care: In busy healthcare environments, nurses often face situations where they must prioritize patient care. Critical thinking helps them determine which patients require immediate attention and which interventions are most essential.
- Communicate Effectively: Critical thinking skills allow nurses to communicate clearly and confidently with patients, their families, and other members of the healthcare team. They can explain complex medical information and treatment plans in a way that is easily understood by all parties involved.
- Identify Problems: Nurses use critical thinking to identify potential complications or problems in a patient’s condition. This early recognition can lead to timely interventions and prevent further deterioration.
- Collaborate: Healthcare is a collaborative effort involving various professionals. Critical thinking enables nurses to actively participate in interdisciplinary discussions, share their insights, and contribute to holistic patient care.
- Ethical Decision-Making: Critical thinking helps nurses navigate ethical dilemmas that can arise in patient care. They can analyze different perspectives, consider ethical principles, and make morally sound decisions.
- Continual Learning: Critical thinking encourages nurses to seek out new knowledge, stay up-to-date with the latest research and medical advancements, and incorporate evidence-based practices into their care.
In summary, critical thinking is an integral skill for nurses, allowing them to provide high-quality, patient-centered care by analyzing information, making informed decisions, and adapting their approaches as needed.
It’s a dynamic process that enhances clinical reasoning , problem-solving, and overall patient outcomes.
What are the Levels of Critical Thinking in Nursing?
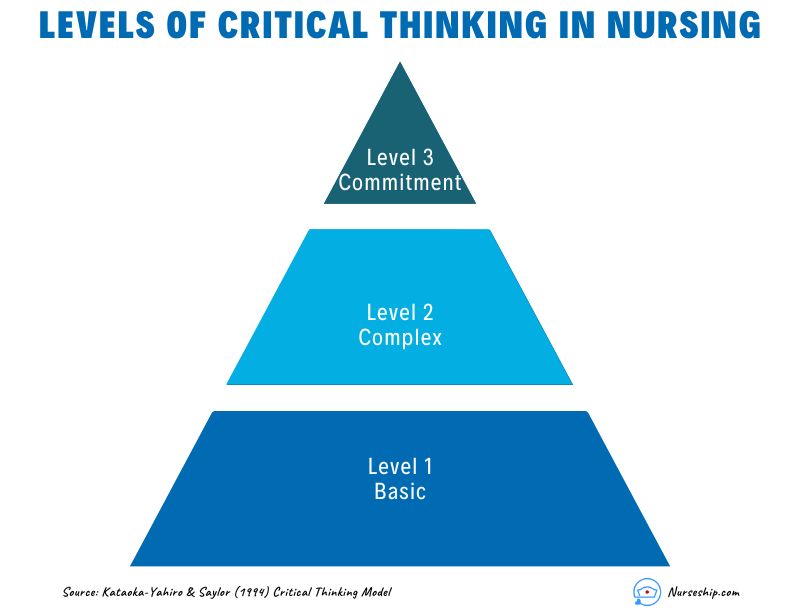
The development of critical thinking in nursing practice involves progressing through three levels: basic, complex, and commitment.
The Kataoka-Yahiro and Saylor model outlines this progression.
1. Basic Critical Thinking:
At this level, learners trust experts for solutions. Thinking is based on rules and principles. For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted.
2. Complex Critical Thinking:
Learners start to analyze choices independently and think creatively. They recognize conflicting solutions and weigh benefits and risks. Thinking becomes innovative, with a willingness to consider various approaches in complex situations.
3. Commitment:
At this level, individuals anticipate decision points without external help and take responsibility for their choices. They choose actions or beliefs based on available alternatives, considering consequences and accountability.
As nurses gain knowledge and experience, their critical thinking evolves from relying on experts to independent analysis and decision-making, ultimately leading to committed and accountable choices in patient care.
Why Critical Thinking is Important in Nursing?
Critical thinking is important in nursing for several crucial reasons:
Patient Safety:
Nursing decisions directly impact patient well-being. Critical thinking helps nurses identify potential risks, make informed choices, and prevent errors.
Clinical Judgment:
Nursing decisions often involve evaluating information from various sources, such as patient history, lab results, and medical literature.
Critical thinking assists nurses in critically appraising this information, distinguishing credible sources, and making rational judgments that align with evidence-based practices.
Enhances Decision-Making:
In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and weigh different options based on evidence and analysis.
This process empowers them to make informed decisions about patient care, treatment plans, and interventions, ultimately leading to better outcomes.
Promotes Problem-Solving:
Nurses encounter complex patient issues that require effective problem-solving.
Critical thinking equips them to break down problems into manageable parts, analyze root causes, and explore creative solutions that consider the unique needs of each patient.
Drives Creativity:
Nursing care is not always straightforward. Critical thinking encourages nurses to think creatively and explore innovative approaches to challenges, especially when standard protocols might not suffice for unique patient situations.
Fosters Effective Communication:
Communication is central to nursing. Critical thinking enables nurses to clearly express their thoughts, provide logical explanations for their decisions, and engage in meaningful dialogues with patients, families, and other healthcare professionals.
Aids Learning:
Nursing is a field of continuous learning. Critical thinking encourages nurses to engage in ongoing self-directed education, seeking out new knowledge, embracing new techniques, and staying current with the latest research and developments.
Improves Relationships:
Open-mindedness and empathy are essential in nursing relationships.
Critical thinking encourages nurses to consider diverse viewpoints, understand patients’ perspectives, and communicate compassionately, leading to stronger therapeutic relationships.
Empowers Independence:
Nursing often requires autonomous decision-making. Critical thinking empowers nurses to analyze situations independently, make judgments without undue influence, and take responsibility for their actions.
Facilitates Adaptability:
Healthcare environments are ever-changing. Critical thinking equips nurses with the ability to quickly assess new information, adjust care plans, and navigate unexpected situations while maintaining patient safety and well-being.
Strengthens Critical Analysis:
In the era of vast information, nurses must discern reliable data from misinformation.
Critical thinking helps them scrutinize sources, question assumptions, and make well-founded choices based on credible information.
How to Apply Critical Thinking in Nursing? (With Examples)
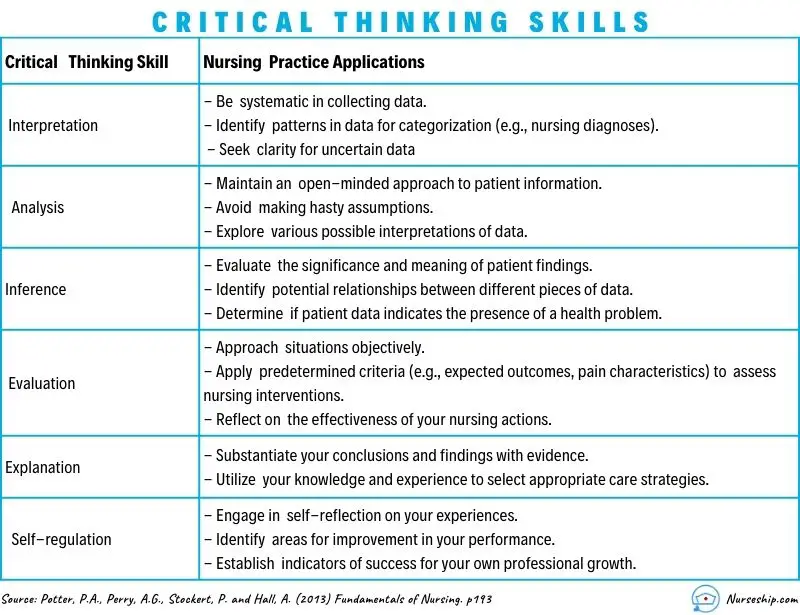
Here are some examples of how nurses can apply critical thinking.
Assess Patient Data:
Critical Thinking Action: Carefully review patient history, symptoms, and test results.
Example: A nurse notices a change in a diabetic patient’s blood sugar levels. Instead of just administering insulin, the nurse considers recent dietary changes, activity levels, and possible medication interactions before adjusting the treatment plan.
Diagnose Patient Needs:
Critical Thinking Action: Analyze patient data to identify potential nursing diagnoses.
Example: After reviewing a patient’s lab results, vital signs, and observations, a nurse identifies “ Risk for Impaired Skin Integrity ” due to the patient’s limited mobility.
Plan and Implement Care:
Critical Thinking Action: Develop a care plan based on patient needs and evidence-based practices.
Example: For a patient at risk of falls, the nurse plans interventions such as hourly rounding, non-slip footwear, and bed alarms to ensure patient safety.
Evaluate Interventions:
Critical Thinking Action: Assess the effectiveness of interventions and modify the care plan as needed.
Example: After administering pain medication, the nurse evaluates its impact on the patient’s comfort level and considers adjusting the dosage or trying an alternative pain management approach.
Prioritize Care:
Critical Thinking Action: Determine the order of interventions based on patient acuity and needs.
Example: In a busy emergency department, the nurse triages patients by considering the severity of their conditions, ensuring that critical cases receive immediate attention.
Collaborate with the Healthcare Team:
Critical Thinking Action: Participate in interdisciplinary discussions and share insights.
Example: During rounds, a nurse provides input on a patient’s response to treatment, which prompts the team to adjust the care plan for better outcomes.
Ethical Decision-Making:
Critical Thinking Action: Analyze ethical dilemmas and make morally sound choices.
Example: When a terminally ill patient expresses a desire to stop treatment, the nurse engages in ethical discussions, respecting the patient’s autonomy and ensuring proper end-of-life care.
Patient Education:
Critical Thinking Action: Tailor patient education to individual needs and comprehension levels.
Example: A nurse uses visual aids and simplified language to explain medication administration to a patient with limited literacy skills.
Adapt to Changes:
Critical Thinking Action: Quickly adjust care plans when patient conditions change.
Example: During post-operative recovery, a nurse notices signs of infection and promptly informs the healthcare team to initiate appropriate treatment adjustments.
Critical Analysis of Information:
Critical Thinking Action: Evaluate information sources for reliability and relevance.
Example: When presented with conflicting research studies, a nurse critically examines the methodologies and sample sizes to determine which study is more credible.
Making Sense of Critical Thinking Skills
What is the purpose of critical thinking in nursing.
The purpose of critical thinking in nursing is to enable nurses to effectively analyze, interpret, and evaluate patient information, make informed clinical judgments, develop appropriate care plans, prioritize interventions, and adapt their approaches as needed, thereby ensuring safe, evidence-based, and patient-centered care.
Why critical thinking is important in nursing?
Critical thinking is important in nursing because it promotes safe decision-making, accurate clinical judgment, problem-solving, evidence-based practice, holistic patient care, ethical reasoning, collaboration, and adapting to dynamic healthcare environments.
Critical thinking skill also enhances patient safety, improves outcomes, and supports nurses’ professional growth.
How is critical thinking used in the nursing process?
Critical thinking is integral to the nursing process as it guides nurses through the systematic approach of assessing, diagnosing, planning, implementing, and evaluating patient care. It involves:
- Assessment: Critical thinking enables nurses to gather and interpret patient data accurately, recognizing relevant patterns and cues.
- Diagnosis: Nurses use critical thinking to analyze patient data, identify nursing diagnoses, and differentiate actual issues from potential complications.
- Planning: Critical thinking helps nurses develop tailored care plans, selecting appropriate interventions based on patient needs and evidence.
- Implementation: Nurses make informed decisions during interventions, considering patient responses and adjusting plans as needed.
- Evaluation: Critical thinking supports the assessment of patient outcomes, determining the effectiveness of intervention, and adapting care accordingly.
Throughout the nursing process , critical thinking ensures comprehensive, patient-centered care and fosters continuous improvement in clinical judgment and decision-making.
What is an example of the critical thinking attitude of independent thinking in nursing practice?
An example of the critical thinking attitude of independent thinking in nursing practice could be:
A nurse is caring for a patient with a complex medical history who is experiencing a new set of symptoms. The nurse carefully reviews the patient’s history, recent test results, and medication list.
While discussing the case with the healthcare team, the nurse realizes that the current treatment plan might not be addressing all aspects of the patient’s condition.
Instead of simply following the established protocol, the nurse independently considers alternative approaches based on their assessment.
The nurse proposes a modification to the treatment plan, citing the rationale and evidence supporting the change.
This demonstrates independent thinking by critically evaluating the situation, challenging assumptions, and advocating for a more personalized and effective patient care approach.
How to use Costa’s level of questioning for critical thinking in nursing?
Costa’s levels of questioning can be applied in nursing to facilitate critical thinking and stimulate a deeper understanding of patient situations. The levels of questioning are as follows:
- 15 Attitudes of Critical Thinking in Nursing (Explained W/ Examples)
- Nursing Concept Map (FREE Template)
- Clinical Reasoning In Nursing (Explained W/ Example)
- 8 Stages Of The Clinical Reasoning Cycle
- How To Improve Critical Thinking Skills In Nursing? 24 Strategies With Examples
- What is the “5 Whys” Technique?
- What Are Socratic Questions?
Critical thinking in nursing is the foundation that underpins safe, effective, and patient-centered care.
Critical thinking skills empower nurses to navigate the complexities of their profession while consistently providing high-quality care to diverse patient populations.
Reading Recommendation
Potter, P.A., Perry, A.G., Stockert, P. and Hall, A. (2013) Fundamentals of Nursing
Comments are closed.
Medical & Legal Disclaimer
All the contents on this site are for entertainment, informational, educational, and example purposes ONLY. These contents are not intended to be used as a substitute for professional medical advice or practice guidelines. However, we aim to publish precise and current information. By using any content on this website, you agree never to hold us legally liable for damages, harm, loss, or misinformation. Read the privacy policy and terms and conditions.
Privacy Policy
Terms & Conditions
© 2024 nurseship.com. All rights reserved.
- Open access
- Published: 17 June 2024
The effects of simulation-based education on undergraduate nursing students' competences: a multicenter randomized controlled trial
- Lai Kun Tong 1 ,
- Yue Yi Li 1 ,
- Mio Leng Au 1 ,
- Wai I. Ng 1 ,
- Si Chen Wang 1 ,
- Yongbing Liu 2 ,
- Yi Shen 3 ,
- Liqiang Zhong 4 &
- Xichenhui Qiu 5
BMC Nursing volume 23 , Article number: 400 ( 2024 ) Cite this article
2390 Accesses
Metrics details
Education in nursing has noticed a positive effect of simulation-based education. There are many studies available on the effects of simulation-based education, but most of those involve a single institution, nonrandomized controlled trials, small sample sizes and subjective evaluations of the effects. The purpose of this multicenter randomized controlled trial was to evaluate the effects of high-fidelity simulation, computer-based simulation, high-fidelity simulation combined with computer-based simulation, and case study on undergraduate nursing students.
A total of 270 nursing students were recruited from five universities in China. Participants were randomly divided into four groups at each institution: the high-fidelity simulation group, the computer-based simulation group, the high-fidelity simulation combined with computer-based simulation group, and the case study group. Finally, 239 participants completed the intervention and evaluation, with 58, 67, 57, and 57 participants in each group. The data were collected at three stages: before the intervention, immediately after the intervention, and three months after the intervention.
The demographic data and baseline evaluation indices did not significantly differ among the four groups. A statistically significant difference was not observed between the four methods for improving knowledge, interprofessional collaboration, critical thinking, caring, or interest in learning. While skill improvement differed significantly among the different groups after the intervention ( p = 0.020), after three months, no difference was observed ( p = 0.139). The improvement in skill in the computer-based simulation group was significantly lower at the end of the intervention than that in the high-fidelity simulation group ( p = 0.048) or the high-fidelity simulation combined with computer-based simulation group ( p = 0.020).
Conclusions
Nursing students benefit equally from four methods in cultivating their knowledge, interprofessional collaboration, critical thinking, caring, and interest in learning both immediately and over time. High-fidelity simulation and high-fidelity simulation combined with computer-based simulation improve skill more effectively than computer-based simulation in the short term. Nursing educators can select the most suitable teaching method to achieve the intended learning outcomes depending on the specific circumstances.
Trial registration
This clinical trial was registered at the Chinese Clinical Trial Registry (clinical trial number: ChiCTR2400084880, date of the registration: 27/05/2024).
Peer Review reports
Introduction
There are many challenges nursing students face in the clinical setting because of the gap between theory and practice, the lack of resources, and unfamiliarity with the medical environment [ 1 ]. Nursing education needs an innovative teaching method that is more closely related to the clinical environment. Simulation-based education is an effective teaching method for nursing students [ 2 ]. It provides students with an immersive clinical environment for practicing skills and gaining experience in a safe, controlled setting [ 3 ]. This educational approach not only supports the development of various competencies [ 2 , 4 ], including knowledge, skill, interprofessional collaboration, critical thinking, caring, and interest in learning, but also enables students to apply learned concepts to complex and challenging situations [ 5 ].
Manikin-based and computer-based simulations are commonly employed simulators in nursing education. Manikin-based simulation involves the use of a manikin to mimic a patient’s characteristics, such as heart and lung sounds [ 6 ]. Computer-based simulation involves the modeling of real-life processes solely using computers, usually with a keyboard and monitor as inputs and outputs [ 6 ]. According to a recent meta-analysis, manikin-based simulation improves nursing students' knowledge acquisition more than computer-based simulation does, but there are no significant differences in confidence or satisfaction with learning [ 4 ].
Based on the level of fidelity, manikin-based simulation can be categorized as low, medium, or high fidelity [ 7 ]. High-fidelity simulation has become increasingly popular since it replaces part of clinical placement without compromising nursing student quality [ 8 ]. Compared to other teaching methods, high-fidelity simulation is associated with elevated equipment and labor costs [ 9 ]. To enhance cost-effectiveness, it is imperative to maximize the impact of high-fidelity simulation. To improve learning outcomes, mixed learning has gained popularity across higher education in recent years [ 10 ]. The most widely used mixed learning method for simulation education in the nursing field is high-fidelity simulation combined with computer-based simulation. There have been only a few studies on the effect of high-fidelity simulation combined with computer-based simulation on nursing students, and these are either pre-post comparison studies without control groups [ 11 ] or quasi-experimental studies without randomization [ 12 ]. To obtain a better grasp of the effects of combining high-fidelity simulation and computer-based simulation, a randomized controlled trial is needed.
In addition to enhancing effectiveness, optimizing cost-effectiveness can be achieved by implementing cost reduction measures. Case study, which eliminates the need for additional equipment, offers a relatively low-cost alternative. A traditional case study provides all pertinent information, whereas an unfolding case study purposefully leaves out information [ 13 ]. It has been shown that unfolding case study fosters critical thinking in students more effectively than traditional case studies [ 14 ]. Despite being regarded as an innovative and inexpensive teaching method, there is little research comparing unfolding case study with other simulation-based teaching methods. To address this knowledge gap, further study is necessary.
An umbrella review highlights that the existing literature on the learning outcomes of simulation-based education predominantly emphasizes knowledge and skills, while conferring limited focus on other core competencies, such as interprofessional collaboration and caring [ 15 ]. Therefore, future research should evaluate various learning outcome indicators.
This multicenter randomized controlled trial aimed to assess the effectiveness of high-fidelity simulation, computer-based simulation, high-fidelity simulation combined with computer-based simulation, and case study on nursing students’ knowledge, skill, interprofessional collaboration, critical thinking, caring, and interest in learning.
Study design
A multicenter randomized controlled trial was conducted between March 2022 and May 2023 in China. The study conforms to the CONSORT guidelines. This clinical trial was registered at the Chinese Clinical Trial Registry (clinical trial number: ChiCTR2400084880, date of the registration: 27/05/2024).
Participants and setting
Participants were recruited from five universities in China, two of which were private and three of which were public. Among the five universities, four were equipped with two high-fidelity simulation laboratories. Specifically, three universities had laboratories simulating intensive care unit wards and delivery rooms, while the remaining university had two laboratories simulating general wards. Additionally, one university possessed a high-fidelity simulation laboratory specifically designed to simulate a general ward setting. Three universities utilized Laerdal patient simulators in their laboratories, while the other two universities employed Gaumard patient simulators.
A recruitment poster with the time and location of the project promotion was posted on the school bulletin board. The research team provided a briefing to students at the designated time and location indicated on the poster, affording them the opportunity to inquire about and enhance their understanding of the project.
The study mandated that participants fulfill the following criteria: 1) enroll in a nursing undergraduate program; 2) have full-time student status; 3) complete courses in Anatomy and Physiology, Pathophysiology, Pharmacology, Health Assessment, Basic Nursing, and Medical and Surgical Nursing (Respiratory System); 4) have proficiency in reading and writing Chinese; and 5) participate voluntarily. Those who met the following criteria were excluded: 1) had a degree or diploma and 2) took the course again.
The sample size was calculated through the use of G*Power 3.1, which was based on F tests (ANOVA: Repeated measures, between factors). Several assumptions were taken into consideration, including a 5% level of significance, 80% power, four groups, three measurements, and a 0.50 correlation between pre- and postintervention time points. Compared to other teaching methods, high-fidelity simulation exhibited a medium effect size (d = 0.49 for knowledge, d = 0.50 for performance) [ 16 ]. The calculation employed a conservative approach, accommodating a small yet clinically significant effect size (0.25), thereby bolstering the reliability and validity of the findings. Based on these assumptions, the total sample size required was determined to be 124, with each group requiring 31 participants.
Randomization and blinding
Due to inconsistent teaching schedules at the five universities involved in the study, the participants were divided into four groups at each institution: the high-fidelity simulation group, the computer-based simulation group, the high-fidelity simulation combined with computer-based simulation group, and the case study group. Participant grouping was carried out by study team members who were not involved in the intervention or evaluation. The participants were each assigned a random nonduplicate number between zero and 100 using Microsoft Excel. The random numbers/participants were divided into four groups based on quartiles: the lower quarter, the lower quarter to a half, the half to three-fourths, and the upper quarter were assigned to the high-fidelity simulation group, the computer-based simulation group, the high-fidelity simulation combined with computer-based simulation group, and the case study group, respectively. It was not possible to implement participant blinding because the four teaching methods differed significantly, while effect evaluation and data analysis were conducted in a blinded manner. Each participant was assigned a unique identifier to maintain anonymity throughout the study.
Baseline test
Baseline testing started after participant recruitment had ended, so the timing of the study varied between universities. The baseline test items were the same for all participants and included general characteristics, knowledge, skills, interprofessional collaboration, critical thinking, caring, and interest in learning. The evaluation of skills was conducted by trained assessors, whereas a non-face-to-face online survey was utilized for the assessment of others.
Intervention
The four groups were taught with three scenarios covering the three different cases, in the following order: asthma worsening, drug allergy, and ventricular fibrillation. These three cases represent commonly encountered scenarios necessitating emergency treatment. It is anticipated that by means of training, students can enhance their aptitude to effectively handle emergency situations within clinical settings. It is vital that the case used in simulation-based education is valid so that its effectiveness can be enhanced [ 17 ]. The cases used in this study were from vSim® for Nursing | Lippincott Nursing Education, which was developed by Wolters Kluwer Health (Lippincott), Laerdal Medical, and the National League for Nursing. Hence, the validity of the cases can be assured. Participants received all the materials, including learning outcomes, theoretical learning materials, and case materials (medical history and nursing document), at least one day before teaching. All the teachers in charge of teaching participated in the meeting to discuss the lesson plans to reach a consensus on the lesson plans. The lesson plans were written by three members of the research team and revised according to the feedback. Table 1 shows the teaching experience of each case in the different intervention groups. The instructors involved had at least five years of teaching experience and a master's degree or higher.
Posttest and follow-up test
The posttest was conducted within one week of the intervention using the same items as those used in the baseline test. The follow-up test was administered after three months of the intervention.
General characteristics
The general characteristics of the participants included gender, age, and previous semester grade.
This was measured by five multiple-choice items developed for this study. The items were derived from the National Nurse Licensing Examination [ 18 ]. The maximum score was five, with one awarded for each correct answer. The questionnaire exhibited high content validity (CVI = 1.00) and good reliability (Kuder-Richardson 20 = 0.746).
The Creighton Competency Evaluation Instrument (CCEI) is designed to assess clinical skills in a simulated environment by measuring 23 general nursing behaviors. This tool was originally developed by Todd et al. [ 19 ] and subsequently modified by Hayden et al. [ 20 ]. The Chinese version of the CCEI has good reliability (Cronbach’s α = 0.94) and validity (CVI = 0.98) [ 21 ]. The CCEI was scored by nurses with master’s degrees who were trained by the research team and blinded to the intervention information. A dedicated person was assigned to handle the rating for each university, and the raters did not rotate among the participants. The Kendall's W coefficient for the raters' measures was calculated to be 0.832, indicating a high level of interrater agreement and reliability. All participants were tested using a high-fidelity simulator, with each test lasting ten minutes. The skills test without debriefing employed a single-person format, and the nursing procedures did not rely on laboratory results, so the items "Delegates Appropriately," "Reflects on Clinical Experience," "Interprets Lab Results," and "Reflects on Potential Hazards and Errors" were excluded from the assessment. The total score ranged from 0–19 and a higher score indicated a higher level of skill.
- Interprofessional collaboration
The Assessment of the Interprofessional Team Collaboration Scale for Students (AITCS-II Student) was used to assess interprofessional collaboration. It consists of 17 items rated on a 5-point Likert scale (1 = never, 5 = always), for a total score ranging from 17 to 85 [ 22 ]. The Chinese version of the AITCS-II has good reliability (Cronbach’s α = 0.961) and validity [ 23 ].
- Critical thinking
Critical thinking was measured by Yoon's Critical Thinking Disposition Scale (YCTD). It is a five-point Likert scale with values ranging from 1 to 5, resulting in a total score ranging from 27 to 135 [ 24 ]. Higher scores on this scale indicate greater critical thinking ability. The YCTD has good reliability (Cronbach’s α = 0.948) and validity when applied to Chinese nursing students [ 25 ].
Caring was assessed using the Caring Dimensions Inventory (CDI), which employs a five-point Likert scale ranging from 25 to 125 [ 26 ]. Higher scores on the CDI indicate a greater level of caring. The Chinese version of the CDI exhibited good reliability (Cronbach’s α = 0.97) and validity [ 27 ].
- Interest in learning
The Study Interest Questionnaire (SIQ) was used to assess interest in learning. The SIQ is a four-point Likert scale ranging from 18 to 72, where a higher total score indicates a greater degree of interest in the field of study [ 28 ]. The SIQ has good reliability (Cronbach’s α = 0.90) and validity when applied to Chinese nursing students [ 29 ].
Ethical considerations
The institution of the first author granted ethical approval (ethical approval number: REC-2021.801). Written informed consent was obtained from all participants. Participants were permitted to withdraw for any reason at any time without penalty. Guidelines emphasizing safety measures and precautions during the intervention were provided to participants, and study coordinators closely monitored laboratory and simulation sessions to address concerns or potential harm promptly.
Data analysis
Descriptive statistics were used to describe the participant characteristics and baseline characteristics. Continuous variables are presented as the mean and standard deviation, while categorical variables are presented as frequencies and percentages. According to the Quantile–Quantile Plot, the data exhibited an approximately normal distribution. Furthermore, Levene's test indicated equal variances for the variables of knowledge, skill, interprofessional collaboration, critical thinking, caring, and interest in learning, with p-values of 0.171, 0.249, 0.986, 0.634, 0.992, and 0.407, respectively. The baseline characteristics of the four groups were compared using one-way analysis of variance. The indicators of knowledge, skill, interprofessional collaboration, critical thinking, caring, and interest in learning were assessed at baseline, immediately after the intervention, and three months postintervention. Changes in these indicators from baseline were calculated for both the postintervention and three-month follow-up periods. The changes among the four groups were compared using one-way analysis of variance. Cohen's d effect sizes were computed for the between-group comparisons (small effect size = 0.2; medium effect size = 0.5; large effect size = 0.8). Missing data were treated as missing without imputation. The data analysis was conducted using jamovi 2.3.28 ( https://www.jamovi.org/ ). Jamovi was developed on the foundation of the R programming language, and is recognized for its user-friendly interface. The threshold for statistical significance was established at a two-sided p < 0.05.
Participants
A total of 270 participants were initially recruited from five universities for this study. However, an attrition rate of 11.5% was observed, resulting in 31 participants discontinuing their involvement. Consequently, the final analysis included data from 239 participants who successfully completed the intervention and remained in the study. Specifically, there were 58 participants in the high-fidelity simulation group, 67 in the computer-based simulation group, 57 in the high-fidelity simulation combined with computer-based simulation group, and 57 in the case study group (Fig. 1 ). The participant demographics and baseline characteristics are displayed in Table 2 , and no significant differences were observed in these variables.
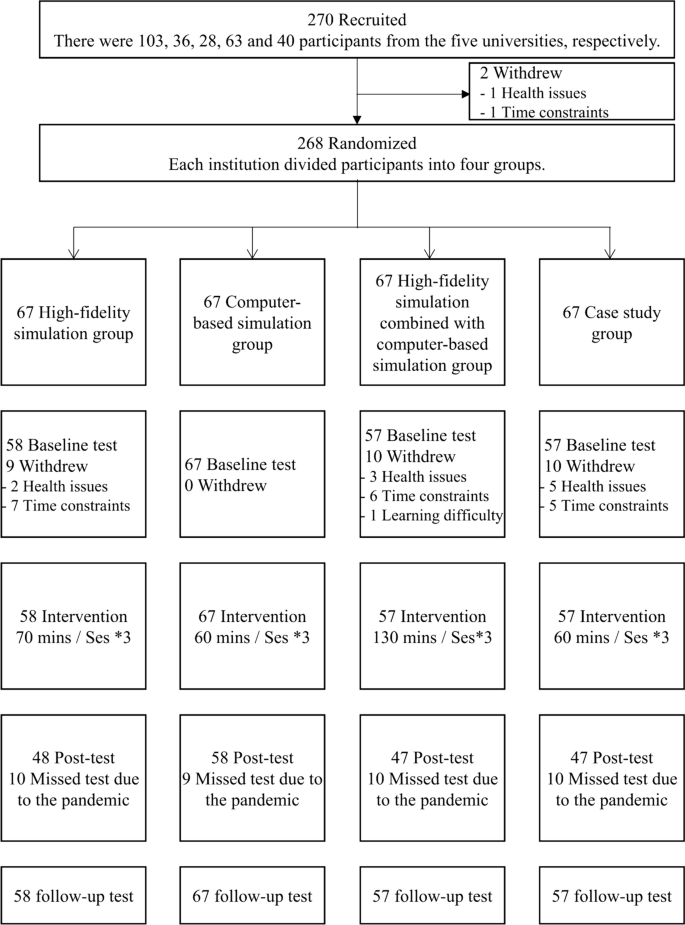
Study subject disposition flow chart
Efficacy outcomes
All the intervention groups showed improvements in knowledge after the intervention, with the high-fidelity simulation group showing the greatest improvement (Fig. 2 ). However, there were no significant differences in knowledge improvement among the groups (p = 0.856). The computer-based simulation group and case study group experienced a decrease in knowledge compared to baseline three months after the intervention, while the other groups showed an increase in knowledge. The high-fidelity simulation combined with computer-based simulation group performed best (Fig. 3 ), but no significant differences were observed (p = 0.872). The effect sizes between groups were found to be small, both immediately after the intervention and at the three-month follow-up (Table 3 ).
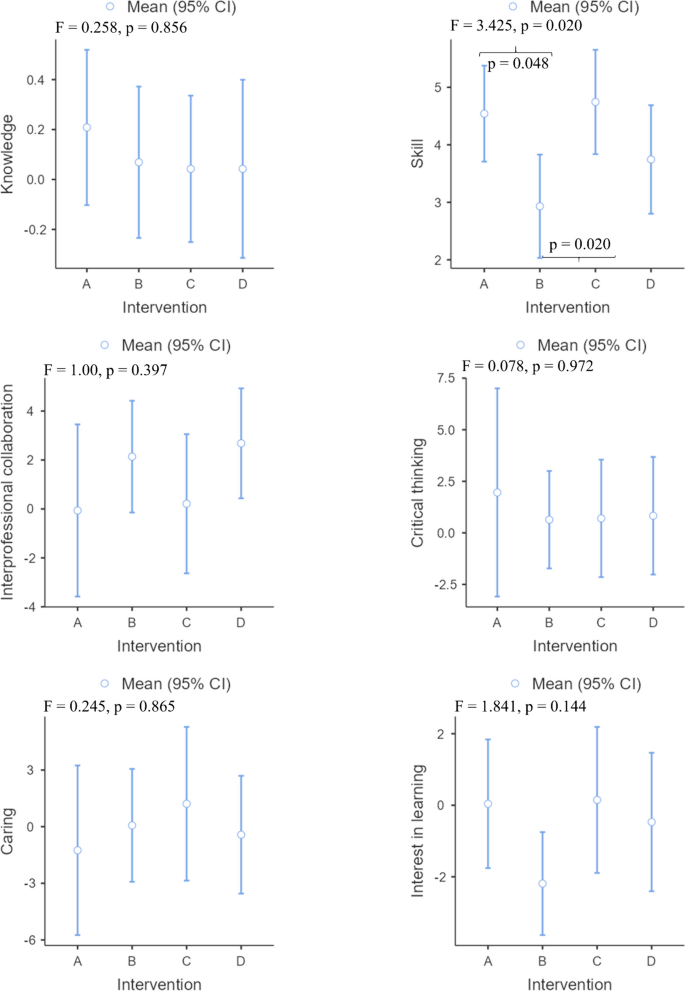
Changes in all effectiveness outcomes at post intervention. Note: A High-fidelity simulation group; B Computer-based simulation group; C High-fidelity simulation combined with computer-based simulation group; D Case study group
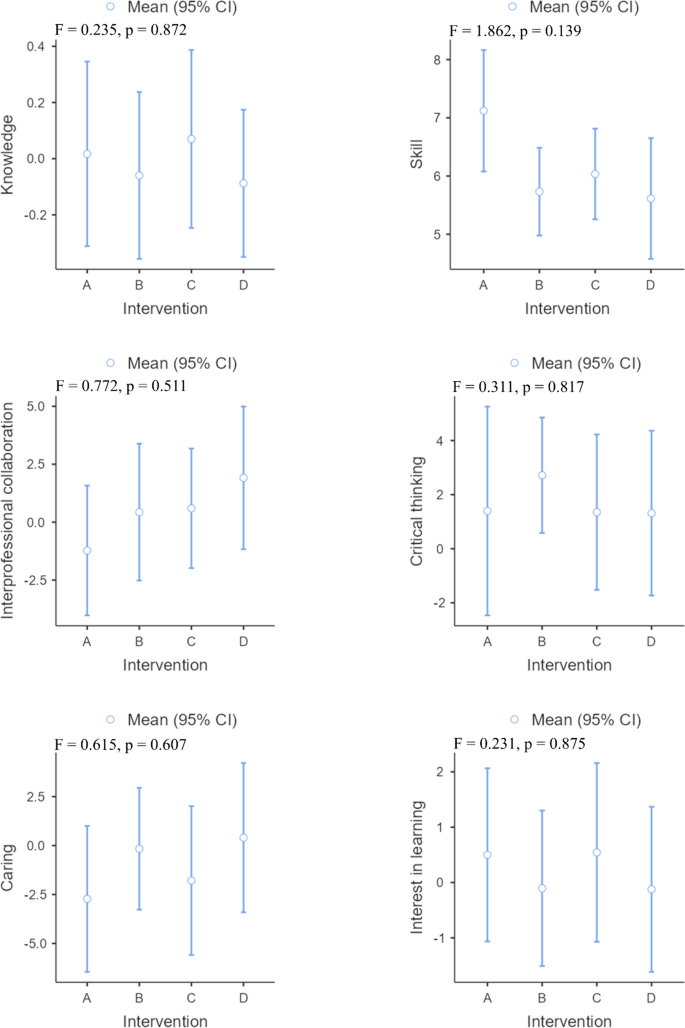
Changes in all effectiveness outcomes at three months of intervention. Note: A High-fidelity simulation group; B Computer-based simulation group; C High-fidelity simulation combined with computer-based simulation group; D Case study group
The different intervention groups showed improvements in skills after the intervention and three months after the intervention. The high-fidelity simulation combined with computer-based simulation group showed the greatest improvement after the intervention (Fig. 2 ), while the greatest improvement was observed in the high-fidelity simulation group three months after the intervention (Fig. 3 ). There was a significant difference in the improvement in skills among the different groups after the intervention ( p = 0.020). Specifically, the improvement observed in the computer-based simulation group was significantly lower than that in both the high-fidelity simulation group ( p = 0.048) and the high-fidelity simulation combined with computer-based simulation group ( p = 0.020). However, three months after the intervention, there was no statistically significant difference in skill improvement among the groups ( p = 0.139). Except for the between-group effect sizes of the high-fidelity simulation group compared to the computer-based simulation group (Cohen d = 0.51) and the computer-based simulation group compared to the high-fidelity simulation combined with computer-based simulation group (Cohen d = 0.56), the effects were found to be medium after the intervention, while the other between-group effect sizes were small both after the intervention and three months after the intervention (Table 3 ).
In all intervention groups except for the high-fidelity simulation group, interprofessional collaboration improved after the intervention and three months after the intervention, with the case study group (Figs. 2 and 3 ) demonstrating the greatest improvement. No significant difference was found between the intervention groups after or three months after the intervention in terms of changes in interprofessional collaboration. Both immediately following the intervention and three months later, the effect sizes between groups were small (Table 3 ).
After the intervention and three months after the intervention, the critical thinking of all the intervention groups improved. Among them, the high-fidelity simulation group improved the most after the intervention (Fig. 2 ), while the computer-based simulation group improved the most three months after the intervention (Fig. 3 ). However, no statistically significant differences were observed in the improvement of critical thinking across the different groups. The between-group effect sizes of each group were small both after the intervention and three months after the intervention (Table 3 ).
Caring improved following the intervention in all intervention groups, with the exception of the high-fidelity simulation group and case study group (Fig. 2 ). However, no significant difference was observed between the intervention groups in terms of changes ( p = 0.865). A decrease in caring was observed three months after the intervention in all intervention groups, except for the case study group (Fig. 3 ). Nevertheless, no statistically significant difference was detected between the intervention groups in terms of changes (p = 0.607). Both immediately following the intervention and three months later, the effect sizes between groups were small (Table 3 ).
In terms of interest in learning, both the high-fidelity simulation group and the high-fidelity simulation combined with computer-based simulation group improved after the intervention or three months later. Among the groups, the high-fidelity simulation combined with computer-based simulation group improved the most after both the intervention and three months after the intervention (Figs. 2 and 3 ). However, no statistically significant difference was detected between the intervention groups in terms of changes either after the intervention (p = 0.144) or three months after the intervention (p = 0.875). Both immediately following the intervention and three months later, the effect sizes between groups were small (Table 3 ).
To our knowledge, this study is the first multicenter randomized controlled trial to explore the effects of different simulation teaching methods on nursing students' competence and the first study in which multiple different indicators were evaluated simultaneously. The indicators included both objectively assessed indicators of knowledge and skills and subjectively assessed indicators of interprofessional collaboration, critical thinking, caring, and interest in learning. This study assessed the immediate and long-term effects of the intervention by examining its immediate impact as well as its effects three months postintervention.
The results obtained from this study indicate that high-fidelity simulation, computer-based simulation, high-fidelity simulation combined with computer-based simulation, and case study could improve nursing students’ knowledge immediately after intervention. Furthermore, these four teaching methods exhibited comparable effectiveness in improving knowledge. The findings of this study contradict previous meta-analyses that showed that high-fidelity simulation improved nursing students' knowledge over other teaching techniques [ 2 ]. This discrepancy may be attributed to the inclusion of simulation teaching in the previous study alongside theoretical teaching [ 12 ], whereas the current study solely employed simulation teaching without incorporating theoretical instruction. Notably, three months following the intervention, computer-based simulation and case study did not result in knowledge retention. Conversely, high-fidelity simulation, particularly when combined with computer-based simulation, demonstrated knowledge retention, with the latter exhibiting superior performance in this regard. The realistic nature of the simulation provided students with a context in which to apply their knowledge, enhancing their understanding of key concepts [ 30 ]. High-fidelity simulation surpasses computer-based simulation and case study in terms of realism. When combined with computer-based simulation, this approach affords students the opportunity to practice their knowledge in a safe environment while also providing them with access to additional resources and learning opportunities [ 31 ]. Therefore, in this study, high-fidelity simulation combined with computer-based simulation proved to be the most effective at retaining knowledge.
Four simulation-based education strategies were found to be effective at acquiring and retaining skills by the students in this study. High-fidelity simulation combined with computer-based simulation was found to be more effective at acquiring skill than was using either method alone. This method combines the benefits of both teaching methods, providing students with a comprehensive learning experience that combines physical realism and virtual interactivity [ 32 ]. Hybrid simulation creates a seamless learning experience in which individuals can practice their skills in a simulated environment, receive immediate feedback, and then transfer those skills to real-world situations. This integration provides a seamless transition from theoretical knowledge to practical skills, making it easier for individuals to apply what they have learned and enhance their overall performance [ 33 ]. Hybrid simulation may seem to be an attractive option [ 34 ]; however, this study found that hybrid simulation had no advantage in terms of skill retention; rather, high-fidelity simulation performed best. More research is needed in the future to confirm the results of this study and the underlying reasons since previous studies have not compared hybrid simulation with high-fidelity simulation on skill retention.
The findings of this study reveal a noteworthy observation: interprofessional collaboration improved across all interventions, except for high-fidelity simulation. This finding diverges from prior studies that indicated high-fidelity simulation as a more effective method for enhancing students' interprofessional collaboration compared to traditional case study [ 35 ]. This discrepancy may be attributed to the use of an unfolding case study in the current study, wherein patient scenarios evolve unpredictably, thereby prompting students and team members to engage in heightened collaborative efforts to address evolving patient care challenges [ 36 ]. Interprofessional collaboration plays a crucial role in improving healthcare outcomes. Studies have shown that when healthcare professionals collaborate effectively, patients experience better outcomes, fewer errors, and shorter hospital stays [ 37 ]. While high-fidelity simulation has gained popularity as a training tool, according to the results of this study, its impact on interprofessional collaboration remains limited. There may be two reasons for this. First, high-fidelity simulation scenarios are often time constrained [ 38 ], which can hinder effective interprofessional collaboration. Each team member may prioritize their individual goals or tasks, making it difficult to achieve optimal teamwork and coordination. Second, interprofessional team members may not have worked together extensively, which can hinder their ability to collaborate effectively in a high-fidelity simulation setting. It takes time to build trust and rapport, which may not be readily available in a simulated environment [ 39 ]. Despite being assigned the roles of senior nurse or junior nurse, participants in the high-fidelity simulation group were provided with the opportunity to engage with peers at various levels and individuals from different professions, such as instructors assuming the role of doctors. However, the duration of the simulation section for this group was limited to only 10 min. In contrast, participants in the computer-based simulation group and case study group were allocated 30 min and 35 min, respectively. It is crucial for healthcare institutions and educators to critically evaluate their simulation-based training programs and incorporate key components that promote interprofessional collaboration [ 40 ].
This study revealed that four interventions effectively promoted students' critical thinking, and these effects lasted for three months after the interventions. Furthermore, high-fidelity simulation was most effective at improving critical thinking in the short term, whereas computer-based simulation was most effective at fostering long-term improvements. High-fidelity simulation involves creating a realistic and immersive environment that closely resembles a real-world scenario [ 41 ]. This approach affords individuals the opportunity to actively participate and immerse themselves in the simulated scenario, thereby enhancing their experiential understanding [ 3 ]. Computer-based simulation does not provide the same immediate and tangible experience as high-fidelity simulation. High-fidelity simulation commonly incorporates the utilization of medical devices and mannequins that closely resemble clinical scenarios, thereby affording students a more authentic and immersive learning encounter. Only 5% of students perceive computer-based simulation as a viable substitute for mannequin-based simulation within the curriculum [ 42 ]. As a result, high-fidelity simulation is highly effective in the short term, and a previous meta-analysis reported similar results [ 43 ]. However, computer-based simulation provides advantages for data collection and analysis that contribute to the long-term development of critical thinking skills. In the simulation, participants can record their actions, decisions, and results [ 3 ]. These data can be used to compare different strategies and approaches, allowing participants to reflect on their own critical thinking skills and identify areas for improvement. Furthermore, it is noteworthy that the four simulation teaching methods demonstrated the ability to enhance students' critical thinking. However, it is important to consider the substantial disparity in costs among these methods. Therefore, educators should carefully evaluate their available resources and opt for the most cost-effective approach to foster students' critical thinking.
This study found limited evidence that all four simulation teaching methods contribute to improve caring among students. High-fidelity simulation often focuses on technical skills rather than patient interaction or emotional sensitivity [ 44 , 45 ]. Moreover, research has demonstrated that using mannequins in high-fidelity simulation leads some students to perceive them as separate from real-life patients [ 45 ]. This perception reduces students' concern for the consequences of their actions during the simulation [ 45 ], hindering empathy development and limiting the cultivation of their caring abilities [ 46 ]. Unlike high-fidelity simulation, which provides tactile experiences and simulates real-life interactions, computer-based simulation is characterized by the absence of human connections. This lack of physical proximity can hinder the development of caring behaviors such as nonverbal communication, empathy, and sympathy [ 47 , 48 ]. Similarly, the absence of direct patient interaction is a notable drawback of case study. Although case study simulates complex patient care scenarios, they do not allow students to practice hands-on or experience caregiving emotions. Similarly, the absence of direct patient interactions in case study is a notable limitation. This lack of personal connection and guided practice may hinder the development of caring behaviors. By recognizing these limitations and seeking alternative instructional methods, educational institutions can strive to enhance students' caring skills and equip them with the qualities and behaviors necessary for providing compassionate and patient-centered care.
The findings of this study revealed that neither computer-based simulation nor case study improved students' interest in learning, whereas high-fidelity simulation combined with computer-based simulation was most effective. One possible explanation for the ineffectiveness of computer-based simulation and case study in promoting students' interest is that they may lack the authenticity and immersive nature of real-world experiences [ 47 , 48 ]. High-fidelity simulation, on the other hand, provides a more lifelike and interactive learning environment, which may enhance students' engagement, interest, and retention [ 49 ]. High-fidelity simulation combined with computer-based simulation allows students to interact with the simulation in a hands-on manner while also having access to additional resources and information through computer-based simulation [ 50 ]. This combination provides a well-rounded learning experience that can captivate students' attention and keep them engaged. Notably, these findings are exploratory and should be further explored and validated in future studies. Further research should aim to identify the reasons behind the lack of improvement in students' interest in learning when using computer-based simulation and case study alone. Additionally, the impact of different combinations of simulation techniques on students' interest in learning should be investigated to further refine instructional practices.
Limitations
This study provides valuable insights into the effectiveness of simulation-based education in improving nursing students' competences. However, it is essential to acknowledge and address the study's limitations. One of the limitations is the possible selection bias introduced by the recruiting process. It is possible that students who were more motivated or had a greater interest in simulation-based education may have been more likely to participate in the study. This bias may have influenced the outcomes and interpretation of the results. Additionally, the participants were primarily from one cultural background, which may limit the generalizability of the findings. Future studies should include participants from diverse backgrounds to enhance generalizability. Third, participants assigned to different intervention groups may engage in communication and information sharing, potentially leading to contamination effects. To mitigate this issue, future studies could employ cluster randomized controlled trials, which can effectively minimize the risk of contamination among participants. Finally, the follow-up period was relatively short, which limits the understanding of the long-term impact of simulation-based education on competence. Long-term follow-up studies are needed to evaluate the sustained effect of simulation-based education on competence. Future research should aim to address these limitations to further our understanding of the effects of simulation-based education on undergraduate nursing students' competences.
The four methods are effective at improving skills and critical thinking both immediately and over time. In addition to high-fidelity simulation, the other three methods promote interprofessional collaboration both immediately and long term. High-fidelity simulation combined with computer-based simulation is the most effective approach for enhancing interest in learning both immediately and long term. Undergraduate nursing students benefit equally from four methods in cultivating their knowledge, interprofessional collaboration, critical thinking, caring, and interest in learning both immediately and over time. High-fidelity simulation and high-fidelity simulation combined with computer-based simulation improve skill more effectively than computer-based simulation in the short term. Nursing educators can select the most suitable teaching method to achieve the intended learning outcomes depending on the specific circumstances.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
Panda S, Dash M, John J, Rath K, Debata A, Swain D, et al. Challenges faced by student nurses and midwives in clinical learning environment – A systematic review and meta-synthesis. Nurse Educ Today. 2021;101: 104875. https://doi.org/10.1016/j.nedt.2021.104875 .
Article PubMed Google Scholar
Li YY, Au ML, Tong LK, Ng WI, Wang SC. High-fidelity simulation in undergraduate nursing education: A meta-analysis. Nurse Educ Today. 2022;111: 105291. https://doi.org/10.1016/j.nedt.2022.105291 .
Tamilselvan C, Chua SM, Chew HSJ, Devi MK. Experiences of simulation-based learning among undergraduate nursing students: A systematic review and meta-synthesis. Nurse Educ Today. 2023;121: 105711. https://doi.org/10.1016/j.nedt.2023.105711 .
Mulyadi M, Tonapa SI, Rompas SSJ, Wang R-H, Lee B-O. Effects of simulation technology-based learning on nursing students’ learning outcomes: A systematic review and meta-analysis of experimental studies. Nurse Educ Today. 2021;107: 105127. https://doi.org/10.1016/j.nedt.2021.105127 .
Chernikova O, Heitzmann N, Stadler M, Holzberger D, Seidel T, Fischer F. Simulation-Based Learning in Higher Education: A Meta-Analysis. Rev Educ Res. 2020;90(4):499–541. https://doi.org/10.3102/0034654320933544 .
Article Google Scholar
Lioce L. Healthcare Simulation Dictionary. 2nd ed. Rockville: Agency for Healthcare Research and Quality; 2020.
Book Google Scholar
Kim J, Park J-H, Shin S. Effectiveness of simulation-based nursing education depending on fidelity: a meta-analysis. BMC Med Educ. 2016;16(1):152. https://doi.org/10.1186/s12909-016-0672-7 .
Article PubMed PubMed Central Google Scholar
Roberts E, Kaak V, Rolley J. Simulation to Replace Clinical Hours in Nursing: A Meta-narrative Review. Clin Simul Nurs. 2019;37:5–13. https://doi.org/10.1016/j.ecns.2019.07.003 .
Lapkin S, Levett-Jones T. A cost–utility analysis of medium vs. high-fidelity human patient simulation manikins in nursing education. J Clin Nurs. 2011;20(23–24):3543–52. https://doi.org/10.1111/j.1365-2702.2011.03843.x .
Dziuban C, Graham CR, Moskal PD, Norberg A, Sicilia N. Blended learning: the new normal and emerging technologies. Int J Educ Technol High Educ. 2018;15(1):3. https://doi.org/10.1186/s41239-017-0087-5 .
Goldsworthy S, Ferreira C, Shajani Z, Snell D, Perez G. Combining Virtual and High-fidelity Simulation to Foster Confidence and Competency in Postpartum Assessment Complications among Undergraduate Nursing Students. Clin Simul Nurs. 2022;66:18–24. https://doi.org/10.1016/j.ecns.2022.02.001 .
Kang KA, Kim SJ, Lee MN, Kim M, Kim S. Comparison of Learning Effects of Virtual Reality Simulation on Nursing Students Caring for Children with Asthma. Int J Enviro Res Public Health. 2020;17(22):8417. https://doi.org/10.3390/ijerph17228417 .
Ellis M, Hampton D, Makowski A, Falls C, Tovar E, Scott L, et al. Using unfolding case scenarios to promote clinical reasoning for nurse practitioner students. J Am Assoc Nurse Pract. 2023;35(1):55–62. https://doi.org/10.1097/jxx.0000000000000806 .
Englund H. Using unfolding case studies to develop critical thinking skills in baccalaureate nursing students: A pilot study. Nurse Educ Today. 2020;93: 104542. https://doi.org/10.1016/j.nedt.2020.104542 .
Wang X, Yang L, Hu S. Teaching nursing students: As an umbrella review of the effectiveness of using high-fidelity simulation. Nurse Educ Pract. 2024;77: 103969. https://doi.org/10.1016/j.nepr.2024.103969 .
La Carmen C, Angelo D, Valeria C, Ilaria F, Elona G, Cristina P, et al. Effects of high-fidelity simulation based on life-threatening clinical condition scenarios on learning outcomes of undergraduate and postgraduate nursing students: a systematic review and meta-analysis. BMJ Open. 2019;9(2): e025306. https://doi.org/10.1136/bmjopen-2018-025306 .
Au ML, Tong LK, Li YY, Ng WI, Wang SC. Impact of scenario validity and group size on learning outcomes in high-fidelity simulation: A systematics review and meta-analysis. Nurse Educ Today. 2023;121: 105705. https://doi.org/10.1016/j.nedt.2022.105705 .
Book ECfAtNNLE. 2022 National Nurse Licensing Examination Guided Simultaneous Practice Question Set. Beijing: People's Medical Publishing House Co. LTD; 2022.
Todd M, Manz JA, Hawkins KS, Parsons ME, Hercinger M. The Development of a Quantitative Evaluation Tool for Simulations in Nursing Education. Int J Nurs Educ Scholarsh. 2008;5(1). https://doi.org/10.2202/1548-923X.1705
Hayden J, Keegan M, Kardong-Edgren S, Smiley RA. Reliability and Validity Testing of the Creighton Competency Evaluation Instrument for Use in the NCSBN National Simulation Study. Nurs Educ Perspect. 2014;35(4):244–52. https://doi.org/10.5480/13-1130.1 .
Song X, Jin R. Chinese revised CCEI cross-cultural debugging and measurement features evaluation. Int J Nurs. 2018;37(19):2622–7. https://doi.org/10.3760/cma.j.issn.1637-4351.2019.19.009 .
Orchard C, Mahler C, Khalili H. Assessment of the Interprofessional Team Collaboration Scale for Students-AITCS-II (Student): Development and Testing. J Allied Health. 2021;50(1):E1–7.
PubMed Google Scholar
Shi Y, Zhu Z, Hu Y. The reliability and validity of the Chinese version of the Assessment of Interprofessional Team Collaboration in Student Learning Scale. Chinese J Nurs Educ. 2020;17(5):435–8. https://doi.org/10.3761/j.issn.1672-9234.2020.05.011 .
Shin H, Park CG, Kim H. Validation of Yoon’s Critical Thinking Disposition Instrument. Asian Nurs Res. 2015;9(4):342–8. https://doi.org/10.1016/j.anr.2015.10.004 .
Au ML, Li YY, Tong LK, Wang SC, Ng WI. Chinese version of Yoon Critical Thinking Disposition Instrument: validation using classical test theory and Rasch analysis. BMC Nurs. 2023;22(1):362. https://doi.org/10.1186/s12912-023-01519-y .
Watson R, Lea A. The caring dimensions inventory (CDI): content validity, reliability and scaling. J Adv Nurs. 1997;25(1):87–94. https://doi.org/10.1046/j.1365-2648.1997.1997025087.x .
Article CAS PubMed Google Scholar
Tong LK, Zhu MX, Wang SC, Cheong PL, Van IK. A Chinese Version of the Caring Dimensions Inventory: Reliability and Validity Assessment. Int J Environ Res Public Health. 2021;18(13):6834. https://doi.org/10.3390/ijerph18136834 .
Schiefele U, Krapp A, Wild KP, Winteler A. Der Fragebogen zum Studieninteresse (FSI). [The Study Interest Questionnaire (SIQ)]. Diagnostica. 1993;39(4):335–51.
Google Scholar
Tong LK, Au ML, Li YY, Ng WI, Wang SC. The mediating effect of critical thinking between interest in learning and caring among nursing students: a cross-sectional study. BMC Nurs. 2023;22(1):30. https://doi.org/10.1186/s12912-023-01181-4 .
Graham AC, McAleer S. An overview of realist evaluation for simulation-based education. Adv Simul. 2018;3(1):13. https://doi.org/10.1186/s41077-018-0073-6 .
Sharoff L. Faculty’s Perception on Student Performance using vSim for Nursing® as a Teaching Strategy. Clin Simul Nurs. 2022;65:1–6. https://doi.org/10.1016/j.ecns.2021.12.007 .
Cole R, Flenady T, Heaton L. High Fidelity Simulation Modalities in Preregistration Nurse Education Programs: A Scoping Review. Clin Simul Nurs. 2023;80:64–86. https://doi.org/10.1016/j.ecns.2023.04.007 .
Park S, Hur HK, Chung C. Learning effects of virtual versus high-fidelity simulations in nursing students: a crossover comparison. BMC Nurs. 2022;21(1):100. https://doi.org/10.1186/s12912-022-00878-2 .
Goldsworthy S, Patterson JD, Dobbs M, Afzal A, Deboer S. How Does Simulation Impact Building Competency and Confidence in Recognition and Response to the Adult and Paediatric Deteriorating Patient Among Undergraduate Nursing Students? Clin Simul Nurs. 2019;28:25–32. https://doi.org/10.1016/j.ecns.2018.12.001 .
Tosterud R, Hedelin B, Hall-Lord ML. Nursing students’ perceptions of high- and low-fidelity simulation used as learning methods. Nurse Educ Pract. 2013;13(4):262–70. https://doi.org/10.1016/j.nepr.2013.02.002 .
Cheng C-Y, Hung C-C, Chen Y-J, Liou S-R, Chu T-P. Effects of an unfolding case study on clinical reasoning, self-directed learning, and team collaboration of undergraduate nursing students: A mixed methods study. Nurse Educ Today. 2024;137: 106168. https://doi.org/10.1016/j.nedt.2024.106168 .
Kaiser L, Conrad S, Neugebauer EAM, Pietsch B, Pieper D. Interprofessional collaboration and patient-reported outcomes in inpatient care: a systematic review. Syst Rev. 2022;11(1):169. https://doi.org/10.1186/s13643-022-02027-x .
Tong LK, Li YY, Au ML, Wang SC, Ng WI. High-fidelity simulation duration and learning outcomes among undergraduate nursing students: A systematic review and meta-analysis. Nurse Educ Today. 2022;116: 105435. https://doi.org/10.1016/j.nedt.2022.105435 .
Livne N. High-fidelity simulations offer a paradigm to develop personal and interprofessional competencies of health students: A review article. Int J Allied Health Sci Pract. 2019;17(2). https://doi.org/10.46743/1540-580X/2019.1835
Marion-Martins AD, Pinho DLM. Interprofessional simulation effects for healthcare students: A systematic review and meta-analysis. Nurse Educ Today. 2020;94: 104568. https://doi.org/10.1016/j.nedt.2020.104568 .
Macnamara AF, Bird K, Rigby A, Sathyapalan T, Hepburn D. High-fidelity simulation and virtual reality: an evaluation of medical students’ experiences. BMJ simulation & technology enhanced learning. 2021;7(6):528–35. https://doi.org/10.1136/bmjstel-2020-000625 .
Foronda CL, Swoboda SM, Henry MN, Kamau E, Sullivan N, Hudson KW. Student preferences and perceptions of learning from vSIM for Nursing™. Nurse Educ Pract. 2018;33:27–32. https://doi.org/10.1016/j.nepr.2018.08.003 .
Lei Y-Y, Zhu L, Sa YTR, Cui X-S. Effects of high-fidelity simulation teaching on nursing students’ knowledge, professional skills and clinical ability: A meta-analysis and systematic review. Nurse Educ Pract. 2022;60: 103306. https://doi.org/10.1016/j.nepr.2022.103306 .
Najjar RH, Lyman B, Miehl N. Nursing Students’ Experiences with High-Fidelity Simulation. Int J Nurs Educ Scholarsh. 2015;12(1):27–35. https://doi.org/10.1515/ijnes-2015-0010 .
Au ML, Lo MS, Cheong W, Wang SC, Van IK. Nursing students’ perception of high-fidelity simulation activity instead of clinical placement: A qualitative study. Nurse Educ Today. 2016;39:16–21. https://doi.org/10.1016/j.nedt.2016.01.015 .
Dean S, Williams C, Balnaves M. Practising on plastic people: Can I really care? Contemp Nurse. 2015;51(2–3):257–71. https://doi.org/10.1080/10376178.2016.1163231 .
Chang YM, Lai CL. Exploring the experiences of nursing students in using immersive virtual reality to learn nursing skills. Nurse Educ Today. 2021;97: 104670. https://doi.org/10.1016/j.nedt.2020.104670 .
Jeon J, Kim JH, Choi EH. Needs Assessment for a VR-Based Adult Nursing Simulation Training Program for Korean Nursing Students: A Qualitative Study Using Focus Group Interviews. Int J Environ Res Public Health. 2020;17(23):8880. https://doi.org/10.3390/ijerph17238880 .
Davis R. Nursing Student Experiences with High-Fidelity Simulation Education [Ed.D.]. Arizona: Grand Canyon University; 2021.
Saab MM, Landers M, Murphy D, O’Mahony B, Cooke E, O’Driscoll M, et al. Nursing students’ views of using virtual reality in healthcare: A qualitative study. J Clin Nurs. 2022;31(9–10):1228–42. https://doi.org/10.1111/jocn.15978 .
Download references
Acknowledgements
Not applicable.
This work was supported by a research grant from Higher Education Fund of Macao SAR Government (project number: HSS-KWNC-2021–01). This funding source had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and affiliations.
Kiang Wu Nursing College of Macau, Edifício do Instituto de Enfermagem Kiang Wu de Macau, Avenida do Hospital das Ilhas no.447, Coloane, RAEM, Macau SAR, China
Lai Kun Tong, Yue Yi Li, Mio Leng Au, Wai I. Ng & Si Chen Wang
School of Nursing, Yangzhou University, No.136, Jiangyang Middle Road, Hanjiang District, Yangzhou, Jiangsu Province, China
Yongbing Liu
School of Nursing, Guangzhou Xinhua University, 19 Huamei Road, Tianhe District, Guangzhou, Guangdong Province, China
School of Nursing, Guangzhou Medical University, Dongfeng West Road, Yuexiu District, Guangzhou, Guangdong Province, China
Liqiang Zhong
School of Nursing, Shenzhen University, No. 3688, Nanhai Road, Nanshan District, Shenzhen, Guangdong Province, China
Xichenhui Qiu
You can also search for this author in PubMed Google Scholar
Contributions
Study conceptualization and planning were organized and performed by LKT, YYL, MLA, WIN, SCW, YBL, YS, LQZ, and XCHQ. Data collection, data analysis and data interpretation were performed by LKT, YYL, MLA, WIN, SCW, YBL, YS, LQZ, and XCHQ. LKT drafted the initial version of the manuscript. YYL, MLA, WIN, SCW, YBL, YS, LQZ, and XCHQ revised the manuscript for important intellectual content. All authors had full access to the data and have reviewed and approved the submitted version of the manuscript. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Correspondence to Mio Leng Au .
Ethics declarations
Ethics approval and consent to participate.
This research was approved by the Research Management and Development Department of Kiang Wu Nursing College of Macau (No. REC-2021.801) and conducted according to the Declaration of Helsinki. It was a completely voluntary, anonymous, and unrewarded study. Written consent was obtained from all participants.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tong, L.K., Li, Y.Y., Au, M.L. et al. The effects of simulation-based education on undergraduate nursing students' competences: a multicenter randomized controlled trial. BMC Nurs 23 , 400 (2024). https://doi.org/10.1186/s12912-024-02069-7
Download citation
Received : 21 March 2024
Accepted : 05 June 2024
Published : 17 June 2024
DOI : https://doi.org/10.1186/s12912-024-02069-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- High-fidelity simulation
- Computer-based simulation
- High-fidelity simulation combined with computer-based simulation
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The following are examples of attributes of excellent critical thinking skills in nursing. 1. The ability to interpret information: In nursing, the interpretation of patient data is an essential part of critical thinking. Nurses must determine the significance of vital signs, lab values, and data associated with physical assessment.
Critical thinking in nursing is invaluable for safe, effective, patient-centered care. You can successfully navigate challenges in the ever-changing health care environment by continually developing and applying these skills. Images sourced from Getty Images. Critical thinking in nursing is essential to providing high-quality patient care.
Critical thinking in nursing requires self-awareness and being present in the moment. During a hectic shift, it is easy to lose focus as you struggle to finish every task needed for your patients. ... Nursing school gives students the knowledge professional nurses use to make important healthcare decisions for their patients. Students learn ...
Building critical thinking skills is one of the most important outcomes in the clinical setting for nursing students. Collaboration with nursing faculty during the clinical rotation can ease the burden on direct care nurses and facilitate a positive learning experience for the student. The nursing profession continues to experience several ...
As such, nurse educators must also ensure that students can incorporate critical thinking skills into everyday practice. Critical thinking skills for nurses include problem-solving and the ability to evaluate situations and make recommendations. Done correctly, critical thinking results in positive patient outcomes, Srinidhi Lakhanigam, an RN ...
Continuing nursing education programs such as 2-year programs can improve students' extrinsic learning motivation and transform it into intrinsic learning motivation, which leads to improved internalization and integration of knowledge and enhanced critical thinking skills [4, 5]. A better understanding of students' prior learning experiences ...
Interactive activities foster critical thinking in nursing students. Case studies, simulations, and creative writing stimulate analysis and imagination. Games, discussions, and group projects enhance problem-solving and communication skills. Role-playing, scenarios, and think-pair-share exercises promote immersive learning and idea generation, preparing students for real-world challenges in ...
Critical thinking is a complex, dynamic process formed by attitudes and strategic skills, with the aim of achieving a specific goal or objective. The attitudes, including the critical thinking attitudes, constitute an important part of the idea of good care, of the good professional. It could be said that they become a virtue of the nursing ...
In Brief. After a brief interaction with a nursing student, this nurse educator saw the wisdom of using critical thinking when teaching critical thinking. IN NURSING SCHOOL, I learned about two types of thinking: There is the regular kind, and then there is critical thinking. Although it sounds like it means thinking about important things ...
develop and practice the critical thinking skills needed by successful students and competent nurses (Ward & Morris, 2016; Boso et al., 2020). Nursing students must begin learning critical thinking skills early in a nursing program, and the process of enhancing these skills should be reinforced and threaded throughout the
The main critical thinking skills in which nursing students should be exercised during their studies are critical analysis, introductory and concluding justification, valid conclusion, distinguish of facts and ... Key Words: critical thinking, nursing education, clinical nurse education, clinical nursing practice doi: 10.5455/aim.2014.22.283-286
76 nursing programs participated in the study. The Reflective and Critical Thinking was found as a subject, subject content and didactic strategies. Of the 562 subjects reviewed, this type of thinking is found in 46% of the humanities area and 42% in the area of research and professional discipline. It is important to train teachers to achieve ...
This study supports the need for different learning methods to develop nursing students' critical thinking and clinical decision-making levels. It is seen that there is a need for revision in the delivery of education and training in nursing schools, taking into account extraordinary situations (distance education, etc.) as in the COVID-19 ...
Lastly, we show that critical thinking constitutes a fundamental component in the research process, and can improve research competencies in nursing. We conclude that future research and actions must go further in the search for new evidence and open new horizons, to ensure a positive effect on clinical practice, patient health, student ...
Bachelor nursing students´ and their educators´ experiences of teaching strategies targeting critical thinking: A scoping review. Frida Westerdahl, ... Gunilla Borglin, in Nurse Education in Practice, 2022. 1 Introduction. Critical thinking in nursing is considered essential for delivering quality care and reflects the professional accountability of registered nurses (Chang et al., 2011).
This study highlights the urgent need to establish, within the Nursing curricula, clinical supervision strategies that promote critical thinking and favor the development of skills for good clinical judgment, problem solving, and safe, effective, and ethical decision-making. Descriptors: Thinking, Clinical Decision Making, Nursing Students ...
The process includes five steps: assessment, diagnosis, outcomes/planning, implementation and evaluation. "One of the fundamental principles for developing critical thinking is the nursing process," Vest says. "It needs to be a lived experience in the learning environment.". Nursing students often find that there are multiple correct ...
2. Meeting with Colleagues: Collaborative Learning for Critical Thinking. Regular interactions with colleagues foster a collaborative learning environment. Sharing experiences, discussing diverse viewpoints, and providing constructive feedback enhance critical thinking skills. Colleagues' insights can challenge assumptions and broaden ...
Clinical reasoning and critical thinking have been identified as competency deficient in many new graduate nurses (Herron, 2018; Theisen & Sandau, 2013). As a result enhancing critical thinking in undergraduate nursing education is a significant focus of contemporary nursing education research internationally (Alfaro-LeFevre, 2019; Carvalho et al., 2017; Levett-Jones, 2017). Developing ...
Introduction Applying critical thinking is essential for nursing students both in an academic and clinical context. Particularly, as critical thinking is a vital part of nurses' everyday problem-solving and decision-making processes. Therefore, regardless of the topic taught or the setting in which it is taught, it requires teaching strategies especially targeting students' critical ...
For instance, nursing students may strictly follow a procedure manual without personalization, as they lack experience. Answers are seen as right or wrong, and the opinions of experts are accepted. 2. Complex Critical Thinking: ... In nursing, critical thinking allows nurses to gather relevant patient information, assess it objectively, and ...
is aimed to investigate the impact of PBL interventions on critical thinking skills of nursing students. Methods: PubMed, Embase, Cochrane, and CINAHL databases were electronically searched. Methodological quality was examined using the Newcastle-Ottawa Scale and version 2 of the Cochrane risk-of-bias tool. Data were analyzed with 95% confidence intervals based on random-effect models. Results ...
l master's programs. The purpose of this study was to evaluate the impact of TBL on the critical thinking disposition of entry-level master's nursing students. Critical thinking disposition scores did not significantly improve, but students' confidence in reasoning skills and intellectual curiosity were strengthened, suggesting that TBL is an instructional strategy worth pursuing in ...
Nursing students benefit equally from four methods in cultivating their knowledge, interprofessional collaboration, critical thinking, caring, and interest in learning both immediately and over time. High-fidelity simulation and high-fidelity simulation combined with computer-based simulation improve skill more effectively than computer-based ...