Tobacco, Nicotine, and E-Cigarettes Research Report What are the physical health consequences of tobacco use?
Cigarette smoking harms nearly every organ in the body, 1,44 and smoking is the leading preventable cause of premature death in the United States. Although rates of smoking have declined, it is estimated that it leads to about 480,000 deaths yearly. 1 Smokers aged 60 and older have a twofold increase in mortality compared with those who have never smoked, dying an estimated 6 years earlier. 45 Quitting smoking results in immediate health benefits, and some or all of the reduced life expectancy can be recovered depending on the age a person quits. 46
Although nicotine itself does not cause cancer, at least 69 chemicals in tobacco smoke are carcinogenic, 1 and cigarette smoking accounts for at least 30 percent of all cancer deaths. 22 The overall rates of death from cancer are twice as high among smokers as nonsmokers, with heavy smokers having a four times greater risk of death from cancer than nonsmokers. 1
Foremost among the cancers caused by tobacco use is lung cancer. Cigarette smoking has been linked to about 80 to 90 percent of all cases of lung cancer, the leading cause of cancer death for both men and women, and it is responsible for roughly 80 percent of deaths from this disease. 22,47 Smoking increases lung cancer risk five to tenfold, with greater risk among heavy smokers. 48 Smoking is also associated with cancers of the mouth, pharynx, larynx, esophagus, stomach, pancreas, cervix, kidney, and bladder, as well as acute myeloid. 1 Cigarette smoking is not the only form of tobacco use associated with cancers. Smokeless tobacco (see " Other Tobacco Products ") has been linked to cancer of the pharynx, esophagus, stomach, and lung, as well as to colorectal cancer. 49
In addition to cancer, smoking causes lung diseases such as chronic bronchitis and emphysema, and it has been found to exacerbate asthma symptoms in adults and children. Cigarette smoking is the most significant risk factor for chronic obstructive pulmonary disease (COPD). 50 Survival statistics indicate that quitting smoking results in repair to much of the smoking-induced lung damage over time. However, once COPD develops, it is irreversible; COPD-related lung damage is not repaired with time.
Smoking also substantially increases the risk of heart disease, including stroke, heart attack, vascular disease, and aneurysm. 51,52 Cardiovascular disease is responsible for 40 percent of all smoking-related deaths. 53 Smoking causes coronary heart disease, the leading cause of death in the United States. Smoking is also linked to many other major health conditions—including rheumatoid arthritis, inflammation, and impaired immune function. 1 Even young smokers aged 26 to 41 report reduced health-related quality of life compared with nonsmoking peers, according to a cross-sectional population study. 54 Recent animal research also identified a pathway between the pancreas and a part of the brain active in nicotine intake, potentially linking cigarette smoking to the risk of developing Type 2 Diabetes.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 24 March 2022

Tobacco and nicotine use
- Bernard Le Foll 1 , 2 ,
- Megan E. Piper 3 , 4 ,
- Christie D. Fowler 5 ,
- Serena Tonstad 6 ,
- Laura Bierut 7 ,
- Lin Lu ORCID: orcid.org/0000-0003-0742-9072 8 , 9 ,
- Prabhat Jha 10 &
- Wayne D. Hall 11 , 12
Nature Reviews Disease Primers volume 8 , Article number: 19 ( 2022 ) Cite this article
70 Citations
96 Altmetric
Metrics details
- Disease genetics
- Experimental models of disease
- Preventive medicine
Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will die prematurely from tobacco-related complications. In addition, people who smoke have a significant reduction in their quality of life. Neurobiological findings have identified the mechanisms by which nicotine in tobacco affects the brain reward system and causes addiction. These brain changes contribute to the maintenance of nicotine or tobacco use despite knowledge of its negative consequences, a hallmark of addiction. Effective approaches to screen, prevent and treat tobacco use can be widely implemented to limit tobacco’s effect on individuals and society. The effectiveness of psychosocial and pharmacological interventions in helping people quit smoking has been demonstrated. As the majority of people who smoke ultimately relapse, it is important to enhance the reach of available interventions and to continue to develop novel interventions. These efforts associated with innovative policy regulations (aimed at reducing nicotine content or eliminating tobacco products) have the potential to reduce the prevalence of tobacco and nicotine use and their enormous adverse impact on population health.
Similar content being viewed by others

Associations of dietary patterns with brain health from behavioral, neuroimaging, biochemical and genetic analyses

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Distinct µ-opioid ensembles trigger positive and negative fentanyl reinforcement
Introduction.
Tobacco is the second most commonly used psychoactive substance worldwide, with more than one billion smokers globally 1 . Although smoking prevalence has reduced in many high-income countries (HICs), tobacco use is still very prevalent in low-income and middle-income countries (LMICs). The majority of smokers are addicted to nicotine delivered by cigarettes (defined as tobacco dependence in the International Classification of Diseases, Tenth Revision (ICD-10) or tobacco use disorder in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5)). As a result of the neuro-adaptations and psychological mechanisms caused by repeated exposure to nicotine delivered rapidly by cigarettes, cessation can also lead to a well-characterized withdrawal syndrome, typically manifesting as irritability, anxiety, low mood, difficulty concentrating, increased appetite, insomnia and restlessness, that contributes to the difficulty in quitting tobacco use 2 , 3 , 4 .
Historically, tobacco was used in some cultures as part of traditional ceremonies, but its use was infrequent and not widely disseminated in the population. However, since the early twentieth century, the use of commercial cigarettes has increased dramatically 5 because of automated manufacturing practices that enable large-scale production of inexpensive products that are heavily promoted by media and advertising. Tobacco use became highly prevalent in the past century and was followed by substantial increases in the prevalence of tobacco-induced diseases decades later 5 . It took decades to establish the relationship between tobacco use and associated health effects 6 , 7 and to discover the addictive role of nicotine in maintaining tobacco smoking 8 , 9 , and also to educate people about these effects. It should be noted that the tobacco industry disputed this evidence to allow continuing tobacco sales 10 . The expansion of public health campaigns to reduce smoking has gradually decreased the use of tobacco in HICs, with marked increases in adult cessation, but less progress has been achieved in LMICs 1 .
Nicotine is the addictive compound in tobacco and is responsible for continued use of tobacco despite harms and a desire to quit, but nicotine is not directly responsible for the harmful effects of using tobacco products (Box 1 ). Other components in tobacco may modulate the addictive potential of tobacco (for example, flavours and non-nicotine compounds) 11 . The major harms related to tobacco use, which are well covered elsewhere 5 , are linked to a multitude of compounds present in tobacco smoke (such as carcinogens, toxicants, particulate matter and carbon monoxide). In adults, adverse health outcomes of tobacco use include cancer in virtually all peripheral organs exposed to tobacco smoke and chronic diseases such as eye disease, periodontal disease, cardiovascular diseases, chronic obstructive pulmonary disease, stroke, diabetes mellitus, rheumatoid arthritis and disorders affecting immune function 5 . Moreover, smoking during pregnancy can increase the risk of adverse reproductive effects, such as ectopic pregnancy, low birthweight and preterm birth 5 . Exposure to secondhand cigarette smoke in children has been linked to sudden infant death syndrome, impaired lung function and respiratory illnesses, in addition to cognitive and behavioural impairments 5 . The long-term developmental effects of nicotine are probably due to structural and functional changes in the brain during this early developmental period 12 , 13 .
Nicotine administered alone in various nicotine replacement formulations (such as patches, gum and lozenges) is safe and effective as an evidence-based smoking cessation aid. Novel forms of nicotine delivery systems have also emerged (called electronic nicotine delivery systems (ENDS) or e-cigarettes), which can potentially reduce the harmful effects of tobacco smoking for those who switch completely from combustible to e-cigarettes 14 , 15 .
This Primer focuses on the determinants of nicotine and tobacco use, and reviews the neurobiology of nicotine effects on the brain reward circuitry and the functioning of brain networks in ways that contribute to the difficulty in stopping smoking. This Primer also discusses how to prevent tobacco use, screen for smoking, and offer people who smoke tobacco psychosocial and pharmacological interventions to assist in quitting. Moreover, this Primer presents emerging pharmacological and novel brain interventions that could improve rates of successful smoking cessation, in addition to public health approaches that could be beneficial.
Box 1 Tobacco products
Conventional tobacco products include combustible products that produce inhaled smoke (most commonly cigarettes, bidis (small domestically manufactured cigarettes used in South Asia) or cigars) and those that deliver nicotine without using combustion (chewing or dipping tobacco and snuff). Newer alternative products that do not involve combustion include nicotine-containing e-cigarettes and heat-not-burn tobacco devices. Although non-combustion and alternative products may constitute a lesser risk than burned ones 14 , 15 , 194 , no form of tobacco is entirely risk-free.
Epidemiology
Prevalence and burden of disease.
The Global Burden of Disease Project (GBDP) estimated that around 1.14 billion people smoked in 2019, worldwide, increasing from just under a billion in 1990 (ref. 1 ). Of note, the prevalence of smoking decreased significantly between 1990 and 2019, but increases in the adult population meant that the total number of global smokers increased. One smoking-associated death occurs for approximately every 0.8–1.1 million cigarettes smoked 16 , suggesting that the estimated worldwide consumption of about 7.4 trillion cigarettes in 2019 has led to around 7 million deaths 1 .
In most populations, smoking prevalence is much higher among groups with lower levels of education or income 17 and among those with mental health disorders and other co-addictions 18 , 19 . Smoking is also more frequent among men than women (Figs 1 – 3 ). Sexual and/or gender minority individuals have disproportionately high rates of smoking and other addictions 17 , 20 . In addition, the prevalence of smoking varies substantially between regions and ethnicities; smoking rates are high in some regions of Asia, such as China and India, but are lower in North America and Australia. Of note, the prevalence of mental health disorders and other co-addictions is higher in individuals who smoke compared with non-smokers 18 , 19 , 21 . For example, the odds of smoking in people with any substance use disorder is more than five times higher than the odds in people without a substance use disorder 19 . Similarly, the odds of smoking in people with any psychiatric disorder is more than three times higher than the odds of smoking in those without a psychiatric diagnosis 22 . In a study in the USA, compared with a population of smokers with no psychiatric diagnosis, subjects with anxiety, depression and phobia showed an approximately twofold higher prevalence of smoking, and subjects with agoraphobia, mania or hypomania, psychosis and antisocial personality or conduct disorders showed at least a threefold higher prevalence of smoking 22 . Comorbid disorders are also associated with higher rates of smoking 22 , 23 .
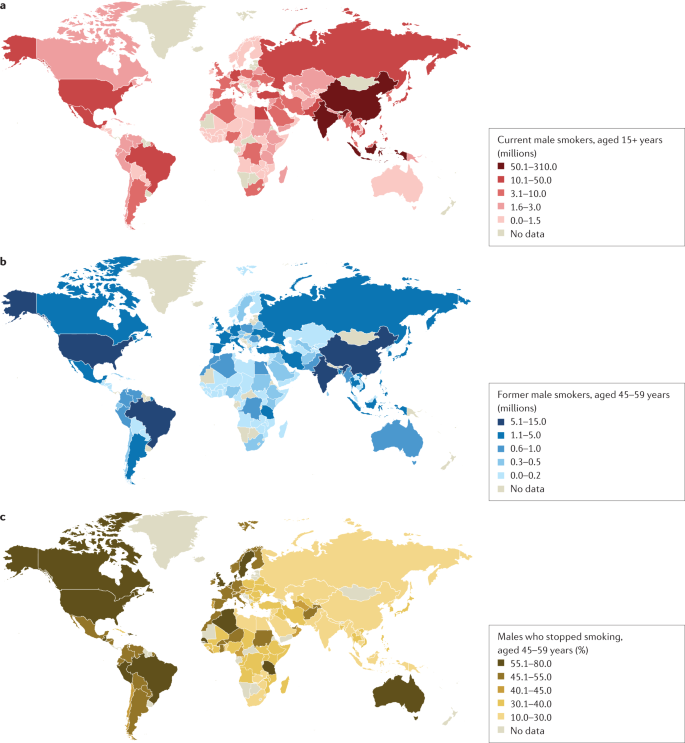
a | Number of current male smokers aged 15 years or older per country expressed in millions. b | Former male smokers aged 45–59 years per country expressed in millions. c | Former male smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for male smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among males is less variable than among females. Data from ref. 1 .
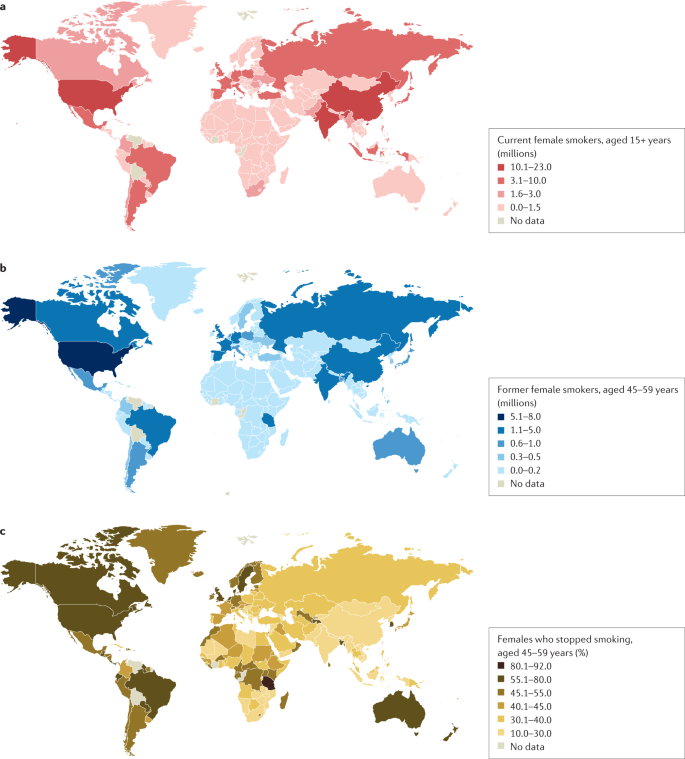
a | Number of current female smokers aged 15 years or older per country expressed in millions. b | Former female smokers aged 45–59 years per country expressed in millions. c | Former female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for female smokers for the period 2015–2019 from countries with direct smoking surveys. The prevalence of smoking among females is much lower in East and South Asia than in Latin America or Eastern Europe. Data from ref. 1 .
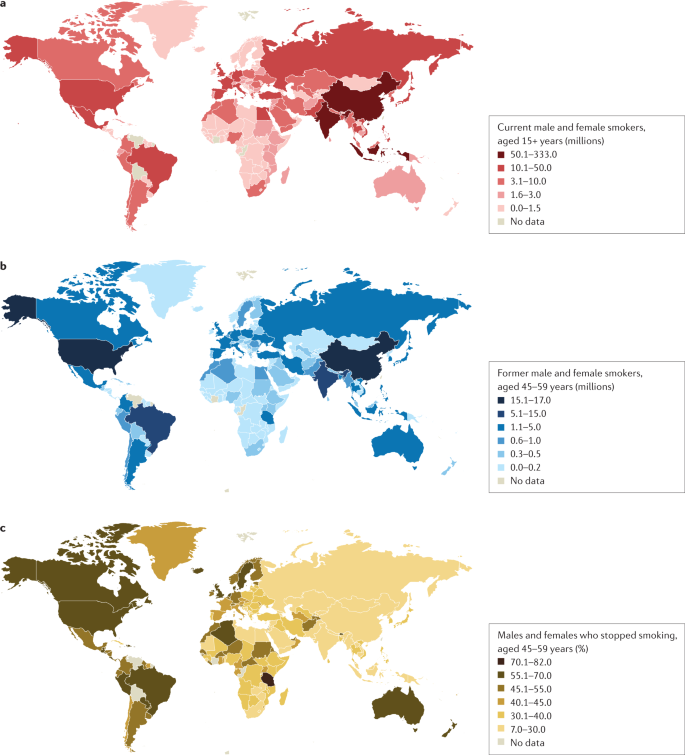
a | Number of current male and female smokers aged 15 years or older per country expressed in millions. b | Former male and female smokers aged 45–59 years per country expressed in millions. c | Former male and female smokers aged 45–59 years per country expressed as the percentage of smokers who stopped. The data shown are for the period 2015–2019 from countries with direct smoking surveys. Cessation rates are higher in high-income countries, but also notably high in Brazil. Cessation is far less common in South and East Asia and Russia and other Eastern European countries, and also low in South Africa. Data from ref. 1 .
Age at onset
Most smokers start smoking during adolescence, with almost 90% of smokers beginning between 15 and 25 years of age 24 . The prevalence of tobacco smoking among youths substantially declined in multiple HICs between 1990 and 2019 (ref. 25 ). More recently, the widespread uptake of ENDS in some regions such as Canada and the USA has raised concerns about the long-term effects of prolonged nicotine use among adolescents, including the possible notion that ENDS will increase the use of combustible smoking products 25 , 26 (although some studies have not found much aggregate effect at the population level) 27 .
Smoking that commences in early adolescence or young adulthood and persists throughout life has a more severe effect on health than smoking that starts later in life and/or that is not persistent 16 , 28 , 29 . Over 640 million adults under 30 years of age smoke in 22 jurisdictions alone (including 27 countries in the European Union where central efforts to reduce tobacco dependence might be possible) 30 . In those younger than 30 years of age, at least 320 million smoking-related deaths will occur unless they quit smoking 31 . The actual number of smoking-related deaths might be greater than one in two, and perhaps as high as two in three, long-term smokers 5 , 16 , 29 , 32 , 33 . At least half of these deaths are likely to occur in middle age (30–69 years) 16 , 29 , leading to a loss of two or more decades of life. People who smoke can expect to lose an average of at least a decade of life versus otherwise similar non-smokers 16 , 28 , 29 .
Direct epidemiological studies in several countries paired with model-based estimates have estimated that smoking tobacco accounted for 7.7 million deaths globally in 2020, of which 80% were in men and 87% were current smokers 1 . In HICs, the major causes of tobacco deaths are lung cancer, emphysema, heart attack, stroke, cancer of the upper aerodigestive areas and bladder cancer 28 , 29 . In some lower income countries, tuberculosis is an additional important cause of tobacco-related death 29 , 34 , which could be related to, for example, increased prevalence of infection, more severe tuberculosis/mortality and higher prevalence of treatment-resistant tuberculosis in smokers than in non-smokers in low-income countries 35 , 36 .
Despite substantial reductions in the prevalence of smoking, there were 34 million smokers in the USA, 7 million in the UK and 5 million in Canada in 2017 (ref. 16 ), and cigarette smoking remains the largest cause of premature death before 70 years of age in much of Europe and North America 1 , 16 , 28 , 29 . Smoking-associated diseases accounted for around 41 million deaths in the USA, UK and Canada from 1960 to 2020 (ref. 16 ). Moreover, as smoking-associated diseases are more prevalent among groups with lower levels of education and income, smoking accounts for at least half of the difference in overall mortality between these social groups 37 . Any reduction in smoking prevalence reduces the absolute mortality gap between these groups 38 .
Smoking cessation has become common in HICs with good tobacco control interventions. For example, in France, the number of ex-smokers is four times the number of current smokers among those aged 50 years or more 30 . By contrast, smoking cessation in LMICs remains uncommon before smokers develop tobacco-related diseases 39 . Smoking cessation greatly reduces the risks of smoking-related diseases. Indeed, smokers who quit smoking before 40 years of age avoid nearly all the increased mortality risks 31 , 33 . Moreover, individuals who quit smoking by 50 years of age reduce the risk of death from lung cancer by about two-thirds 40 . More modest hazards persist for deaths from lung cancer and emphysema 16 , 28 ; however, the risks among former smokers are an order of magnitude lower than among those who continue to smoke 33 .
Mechanisms/pathophysiology
Nicotine is the main psychoactive agent in tobacco and e-cigarettes. Nicotine acts as an agonist at nicotinic acetylcholine receptors (nAChRs), which are localized throughout the brain and peripheral nervous system 41 . nAChRs are pentameric ion channels that consist of varying combinations of α 2 –α 7 and β 2 –β 4 subunits, and for which acetylcholine (ACh) is the endogenous ligand 42 , 43 , 44 . When activated by nicotine binding, nAChR undergoes a conformational change that opens the internal pore, allowing an influx of sodium and calcium ions 45 . At postsynaptic membranes, nAChR activation can lead to action potential firing and downstream modulation of gene expression through calcium-mediated second messenger systems 46 . nAChRs are also localized to presynaptic membranes, where they modulate neurotransmitter release 47 . nAChRs become desensitized after activation, during which ligand binding will not open the channel 45 .
nAChRs with varying combinations of α-subunits and β-subunits have differences in nicotine binding affinity, efficacy and desensitization rate, and have differential expression depending on the brain region and cell type 48 , 49 , 50 . For instance, at nicotine concentrations found in human smokers, β 2 -containing nAChRs desensitize relatively quickly after activation, whereas α 7 -containing nAChRs have a slower desensitization profile 48 . Chronic nicotine exposure in experimental animal models or in humans induces an increase in cortical expression of α 4 β 2 -containing nAChRs 51 , 52 , 53 , 54 , 55 , but also increases the expression of β 3 and β 4 nAChR subunits in the medial habenula (MHb)–interpeduncular nucleus (IPN) pathway 56 , 57 . It is clear that both the brain localization and the type of nAChR are critical elements in mediating the various effects of nicotine, but other factors such as rate of nicotine delivery may also modulate addictive effects of nicotine 58 .
Neurocircuitry of nicotine addiction
Nicotine has both rewarding effects (such as a ‘buzz’ or ‘high’) and aversive effects (such as nausea and dizziness), with the net outcome dependent on dose and others factors such as interindividual sensitivity and presence of tolerance 59 . Thus, the addictive properties of nicotine involve integration of contrasting signals from multiple brain regions that process reward and aversion (Fig. 4 ).
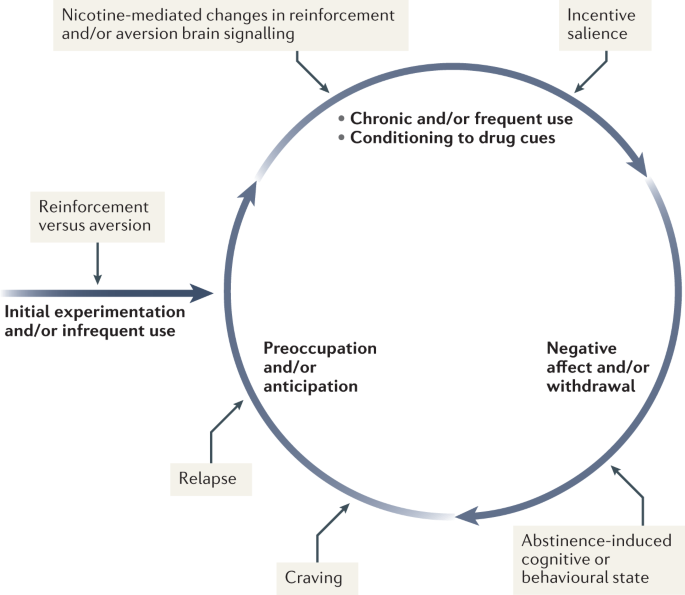
During initial use, nicotine exerts both reinforcing and aversive effects, which together determine the likelihood of continued use. As the individual transitions to more frequent patterns of chronic use, nicotine induces pharmacodynamic changes in brain circuits, which is thought to lead to a reduction in sensitivity to the aversive properties of the drug. Nicotine is also a powerful reinforcer that leads to the conditioning of secondary cues associated with the drug-taking experience (such as cigarette pack, sensory properties of cigarette smoke and feel of the cigarette in the hand or mouth), which serves to enhance the incentive salience of these environmental factors and drive further drug intake. When the individual enters into states of abstinence (such as daily during sleep at night or during quit attempts), withdrawal symptomology is experienced, which may include irritability, restlessness, learning or memory deficits, difficulty concentrating, anxiety and hunger. These negative affective and cognitive symptoms lead to an intensification of the individual’s preoccupation to obtain and use the tobacco/nicotine product, and subsequently such intense craving can lead to relapse.
The rewarding actions of nicotine have largely been attributed to the mesolimbic pathway, which consists of dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens and prefrontal cortex 60 , 61 , 62 (Fig. 5 ). VTA integrating circuits and projection regions express several nAChR subtypes on dopaminergic, GABAergic, and glutamatergic neurons 63 , 64 . Ultimately, administration of nicotine increases dopamine levels through increased dopaminergic neuron firing in striatal and extrastriatal areas (such as the ventral pallidum) 65 (Fig. 6 ). This effect is involved in reward and is believed to be primarily mediated by the action of nicotine on α 4 -containing and β 2 -containing nAChRs in the VTA 66 , 67 .
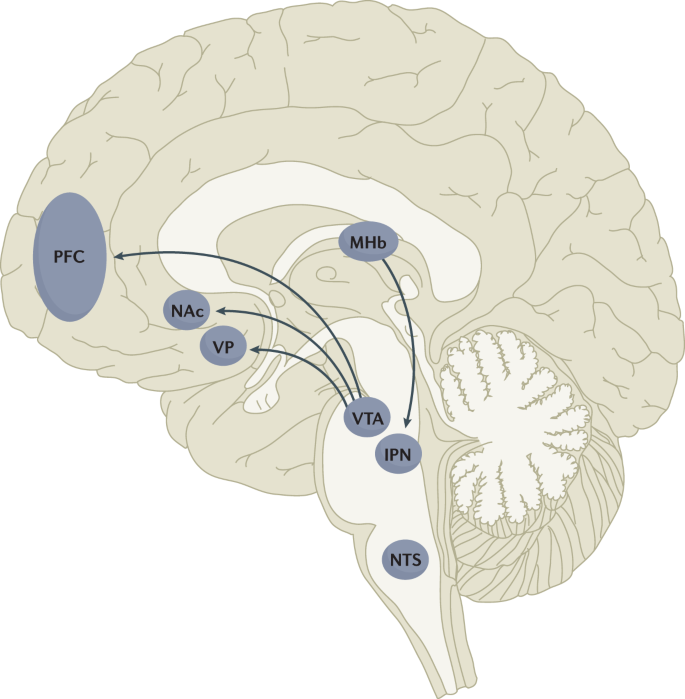
Multiple lines of research have demonstrated that nicotine reinforcement is mainly controlled by two brain pathways, which relay predominantly reward-related or aversion-related signals. The rewarding properties of nicotine that promote drug intake involve the mesolimbic dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens (NAc). By contrast, the aversive properties of nicotine that limit drug intake and mitigate withdrawal symptoms involve the fasciculus retroflexus projection from the medial habenula (MHb) to the interpeduncular nucleus (IPN). Additional brain regions have also been implicated in various aspects of nicotine dependence, such as the prefrontal cortex (PFC), ventral pallidum (VP), nucleus tractus solitarius (NTS) and insula (not shown here for clarity). All of these brain regions are directly or indirectly interconnected as integrative circuits to drive drug-seeking and drug-taking behaviours.
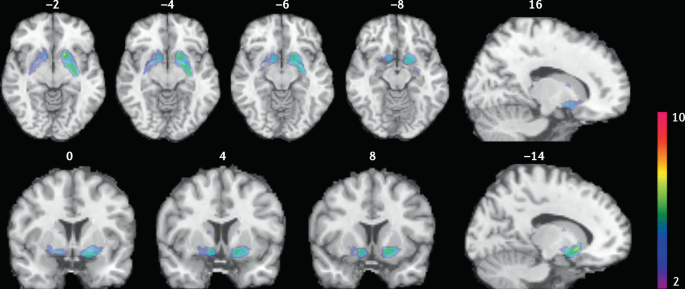
Smokers received brain PET scans with [ 11 C]PHNO, a dopamine D 2/3 PET tracer that has high sensitivity in detecting fluctuations of dopamine. PET scans were performed during abstinence or after smoking a cigarette. Reduced binding potential (BP ND ) was observed after smoking, indicating increased dopamine levels in the ventral striatum and in the area that corresponds to the ventral pallidum. The images show clusters with statistically significant decreases of [ 11 C]PHNO BP ND after smoking a cigarette versus abstinence condition. Those clusters have been superimposed on structural T1 MRI images of the brain. Reprinted from ref. 65 , Springer Nature Limited.
The aversive properties of nicotine are mediated by neurons in the MHb, which project to the IPN. Studies in rodents using genetic knockdown and knockout strategies demonstrated that the α 5 -containing, α 3 -containing and β 4 -containing nAChRs in the MHb–IPN pathway mediate the aversive properties of nicotine that limit drug intake, especially when animals are given the opportunity to consume higher nicotine doses 68 , 69 , 70 , 71 , 72 . In addition to nAChRs, other signalling factors acting on the MHb terminals in the IPN also regulate the actions of nicotine. For instance, under conditions of chronic nicotine exposure or with optogenetic activation of IPN neurons, a subtype of IPN neurons co-expressing Chrna5 (encoding the α 5 nAChR subunit) and Amigo1 (encoding adhesion molecule with immunoglobulin-like domain 1) release nitric oxide from the cell body that retrogradely inhibits MHb axon terminals 70 . In addition, nicotine activates α 5 -containing nAChR-expressing neurons that project from the nucleus tractus solitarius to the IPN, leading to release of glucagon-like peptide-1 that binds to GLP receptors on habenular axon terminals, which subsequently increases IPN neuron activation and decreases nicotine self-administration 73 . Taken together, these findings suggest a dynamic signalling process at MHb axonal terminals in the IPN, which regulates the addictive properties of nicotine and determines the amount of nicotine that is self-administered.
Nicotine withdrawal in animal models can be assessed by examining somatic signs (such as shaking, scratching, head nods and chewing) and affective signs (such as increased anxiety-related behaviours and conditioned place aversion). Interestingly, few nicotine withdrawal somatic signs are found in mice with genetic knockout of the α 2 , α 5 or β 4 nAChR subunits 74 , 75 . By contrast, β 2 nAChR-knockout mice have fewer anxiety-related behaviours during nicotine withdrawal, with no differences in somatic symptoms compared with wild-type mice 74 , 76 .
In addition to the VTA (mediating reward) and the MHb–IPN pathway (mediating aversion), other brain areas are involved in nicotine addiction (Fig. 5 ). In animals, the insular cortex controls nicotine taking and nicotine seeking 77 . Moreover, humans with lesions of the insular cortex can quit smoking easily without relapse 78 . This finding led to the development of a novel therapeutic intervention modulating insula function (see Management, below) 79 , 80 . Various brain areas (shell of nucleus accumbens, basolateral amygdala and prelimbic cortex) expressing cannabinoid CB 1 receptors are also critical in controlling rewarding effects and relapse 81 , 82 . The α 1 -adrenergic receptor expressed in the cortex also control these effects, probably through glutamatergic afferents to the nucleus accumbens 83 .
Individual differences in nicotine addiction risk
Vulnerability to nicotine dependence varies between individuals, and the reasons for these differences are multidimensional. Many social factors (such as education level and income) play a role 84 . Broad psychological and social factors also modulate this risk. For example, peer smoking status, knowledge on effect of tobacco, expectation on social acceptance, exposure to passive smoking modulate the risk of initiating tobacco use 85 , 86 .
Genetic factors have a role in smoking initiation, the development of nicotine addiction and the likelihood of smoking cessation. Indeed, heritability has been estimated to contribute to approximatively half of the variability in nicotine dependence 87 , 88 , 89 , 90 . Important advances in our understanding of such genetic contributions have evolved with large-scale genome-wide association studies of smokers and non-smokers. One of the most striking findings has been that allelic variation in the CHRNA5 – CHRNA3 – CHRNB4 gene cluster, which encodes α 5 , α 3 and β 4 nAChR subunits, correlates with an increased vulnerability for nicotine addiction, indicated by a higher likelihood of becoming dependent on nicotine and smoking a greater number of cigarettes per day 91 , 92 , 93 , 94 , 95 . The most significant effect has been found for a single-nucleotide polymorphism in CHRNA5 (rs16969968), which results in an amino acid change and reduced function of α 5 -containing nAChRs 92 .
Allelic variation in CYP2A6 (encoding the CYP2A6 enzyme, which metabolizes nicotine) has also been associated with differential vulnerability to nicotine dependence 96 , 97 , 98 . CYP2A6 is highly polymorphic, resulting in variable enzymatic activity 96 , 99 , 100 . Individuals with allelic variation that results in slow nicotine metabolism consume less nicotine per day, experience less-severe withdrawal symptoms and are more successful at quitting smoking than individuals with normal or fast metabolism 101 , 102 , 103 , 104 . Moreover, individuals with slow nicotine metabolism have lower dopaminergic receptor expression in the dopamine D2 regions of the associative striatum and sensorimotor striatum in PET studies 105 and take fewer puffs of nicotine-containing cigarettes (compared with de-nicotinized cigarettes) in a forced choice task 106 . Slower nicotine metabolism is thought to increase the duration of action of nicotine, allowing nicotine levels to accumulate over time, therefore enabling lower levels of intake to sustain activation of nAChRs 107 .
Large-scale genetic studies have identified hundreds of other genetic loci that influence smoking initiation, age of smoking initiation, cigarettes smoked per day and successful smoking cessation 108 . The strongest genetic contributions to smoking through the nicotinic receptors and nicotine metabolism are among the strongest genetic contributors to lung cancer 109 . Other genetic variations (such as those related to cannabinoid, dopamine receptors or other neurotransmitters) may affect certain phenotypes related to smoking (such as nicotine preference and cue-reactivity) 110 , 111 , 112 , 113 , 114 , 115 .
Diagnosis, screening and prevention
Screening for cigarette smoking.
Screening for cigarette smoking should happen at every doctor’s visit 116 . In this regard, a simple and direct question about a person’s tobacco use can provide an opportunity to offer information about its potential risks and treatments to assist in quitting. All smokers should be offered assistance in quitting because even low levels of smoking present a significant health risk 33 , 117 , 118 . Smoking status can be assessed by self-categorization or self-reported assessment of smoking behaviour (Table 1 ). In people who smoke, smoking frequency can be assessed 119 and a combined quantity frequency measure such as pack-year history (that is, average number of cigarettes smoked per day multiplied by the number of years, divided by 20), can be used to estimate cumulative risk of adverse health outcomes. The Association for the Treatment of Tobacco Use and Dependence recommends that all electronic health records should document smoking status using the self-report categories listed in Table 1 .
Owing to the advent of e-cigarettes and heat-not-burn products, and the popularity of little cigars in the US that mimic combustible cigarettes, people who use tobacco may use multiple products concurrently 120 , 121 . Thus, screening for other nicotine and tobacco product use is important in clinical practice. The self-categorization approach can also be used to describe the use of these other products.
Traditionally tobacco use has been classified according to whether the smoker meets criteria for nicotine dependence in one of the two main diagnostic classifications: the DSM 122 (tobacco use disorder) and the ICD (tobacco dependence) 123 . The diagnosis of tobacco use disorder according to DSM-5 criteria requires the presence of at least 2 of 11 symptoms that have produced marked clinical impairment or distress within a 12-month period (Box 2 ). Of note, these symptoms are similar for all substance use disorder diagnoses and may not all be relevant to tobacco use disorder (such as failure to complete life roles). In the ICD-10, codes allow the identification of specific tobacco products used (cigarettes, chewing tobacco and other tobacco products).
Dependence can also be assessed as a continuous construct associated with higher levels of use, greater withdrawal and reduced likelihood of quitting. The level of dependence can be assessed with the Fagerström Test for Nicotine Dependence, a short questionnaire comprising six questions 124 (Box 2 ). A score of ≥4 indicates moderate to high dependence. As very limited time may be available in clinical consultations, the Heaviness of Smoking Index (HSI) was developed, which comprises two questions on the number of cigarettes smoked per day and how soon after waking the first cigarette is smoked 125 . The HSI can guide dosing for nicotine replacement therapy (NRT).
Other measures of cigarette dependence have been developed but are not used in the clinical setting, such as the Cigarette Dependence Scale 126 , Hooked on Nicotine Checklist 127 , Nicotine Dependence Syndrome Scale 128 , the Wisconsin Inventory of Smoking Dependence Motives (Brief) 129 and the Penn State Cigarette Dependence Index 130 . However, in practice, these are not often used, as the most important aspect is to screen for smoking and encourage all smokers to quit smoking regardless of their dependence status.
Box 2 DSM-5 criteria for tobacco use disorder and items of the Fagerström Test for nicotine dependence
DSM-5 (ref. 122 )
Taxonomic and diagnostic tool for tobacco use disorder published by the American Psychiatric Association.
A problematic pattern of tobacco use leading to clinically significant impairment or distress as manifested by at least two of the following, occurring within a 12-month period.
Tobacco often used in larger amounts or over a longer period of time than intended
A persistent desire or unsuccessful efforts to reduce or control tobacco use
A great deal of time spent in activities necessary to obtain or use tobacco
Craving, or a strong desire or urge to use tobacco
Recurrent tobacco use resulting in a failure to fulfil major role obligations at work, school or home
Continued tobacco use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of tobacco (for example, arguments with others about tobacco use)
Important social, occupational or recreational activities given up or reduced because of tobacco use
Recurrent tobacco use in hazardous situations (such as smoking in bed)
Tobacco use continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco use
Tolerance, defined by either of the following.
A need for markedly increased amounts of tobacco to achieve the desired effect
A markedly diminished effect with continued use of the same amount of tobacco
Withdrawal, manifesting as either of the following.
Withdrawal syndrome for tobacco
Tobacco (or a closely related substance, such as nicotine) taken to relieve or avoid withdrawal symptoms
Fagerström Test for Nicotine Dependence 124
A standard instrument for assessing the intensity of physical addiction to nicotine.
How soon after you wake up do you smoke your first cigarette?
Within 5 min (scores 3 points)
5 to 30 min (scores 2 points)
31 to 60 min (scores 1 point)
After 60 min (scores 0 points)
Do you find it difficult not to smoke in places where you should not, such as in church or school, in a movie, at the library, on a bus, in court or in a hospital?
Yes (scores 1 point)
No (scores 0 points)
Which cigarette would you most hate to give up; which cigarette do you treasure the most?
The first one in the morning (scores 1 point)
Any other one (scores 0 points)
How many cigarettes do you smoke each day?
10 or fewer (scores 0 points)
11 to 20 (scores 1 point)
21 to 30 (scores 2 points)
31 or more (scores 3 points)
Do you smoke more during the first few hours after waking up than during the rest of the day?
Do you still smoke if you are so sick that you are in bed most of the day or if you have a cold or the flu and have trouble breathing?
A score of 7–10 points is classified as highly dependent; 4–6 points is classified as moderately dependent; <4 points is classified as minimally dependent.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Young people who do not start smoking cigarettes between 15 and 25 years of age have a very low risk of ever smoking 24 , 131 , 132 . This age group provides a critical opportunity to prevent cigarette smoking using effective, evidence-based strategies to prevent smoking initiation and reduce escalation from experimentation to regular use 131 , 132 , 133 , 134 , 135 .
Effective prevention of cigarette uptake requires a comprehensive package of cost-effective policies 134 , 136 , 137 to synergistically reduce the population prevalence of cigarette smoking 131 , 135 . These policies include high rates of tobacco taxation 30 , 134 , 137 , 138 , widespread and rigorously enforced smoke-free policies 139 , bans on tobacco advertising and promotions 140 , use of plain packaging and graphic warnings about the health risks of smoking 135 , 141 , mass media and peer-based education programmes to discourage smoking, and enforcement of laws against the sale of cigarettes to young people below the minimum legal purchase age 131 , 135 . These policies make cigarettes less available and affordable to young people. Moreover, these policies make it more difficult for young people to purchase cigarettes and make smoking a much less socially acceptable practice. Of note, these policies are typically mostly enacted in HICs, which may be related to the declining prevalence of smoking in these countries, compared with the prevalence in LMICs.
Pharmacotherapy
Three evidence-based classes of pharmacotherapy are available for smoking cessation: NRT (using nicotine-based patches, gum, lozenges, mini-lozenges, nasal sprays and inhalers), varenicline (a nAChR partial agonist), and bupropion (a noradrenaline/dopamine reuptake inhibitor that also inhibits nAChR function and is also used as an antidepressant). These FDA-approved and EMA-approved pharmacotherapies are cost-effective smoking cessation treatments that double or triple successful abstinence rates compared with no treatment or placebo controls 116 , 142 .
Combinations of pharmacotherapies are also effective for smoking cessation 116 , 142 . For example, combining NRTs (such as the steady-state nicotine patch and as-needed NRT such as gum or mini-lozenge) is more effective than a single form of NRT 116 , 142 , 143 . Combining NRT and varenicline is the most effective smoking cessation pharmacotherapy 116 , 142 , 143 . Combining FDA-approved pharmacotherapy with behavioural counselling further increases the likelihood of successful cessation 142 . Second-line pharmacotherapies (for example, nortriptyline) have some potential for smoking cessation, but their use is limited due to their tolerability profile.
All smokers should receive pharmacotherapy to help them quit smoking, except those in whom pharmacotherapy has insufficient evidence of effectiveness (among adolescents, smokeless tobacco users, pregnant women or light smokers) or those in whom pharmacotherapy is medically contraindicated 144 . Table 2 provides specific information regarding dosing and duration for each FDA-approved pharmacotherapy. Extended use of pharmacotherapy beyond the standard 12-week regimen after cessation is effective and should be considered 116 . Moreover, preloading pharmacotherapy (that is, initiating cessation medication in advance of a quit attempt), especially with the nicotine patch, is a promising treatment, although further studies are required to confirm efficacy.
Cytisine has been used for smoking cessation in Eastern Europe for a long time and is available in some countries (such as Canada) without prescription 145 . Cytisine is a partial agonist of nAChRs and its structure was the precursor for the development of varenicline 145 . Cytisine is at least as effective as some approved pharmacotherapies for smoking cessation, such as NRT 146 , 147 , 148 , and the role of cytisine in smoking cessation is likely to expand in the future, notably owing to its much lower cost than traditional pharmacotherapies. E-cigarettes also have the potential to be useful as smoking cessation devices 149 , 150 . The 2020 US Surgeon General’s Report concluded that there was insufficient evidence to promote cytisine or e-cigarettes as effective smoking cessation treatments, but in the UK its use is recommended for smoking cessation (see ref. 15 for regularly updated review).
Counselling and behavioural treatments
Psychosocial counselling significantly increases the likelihood of successful cessation, especially when combined with pharmacotherapy. Even a counselling session lasting only 3 minutes can help smokers quit 116 , although the 2008 US Public Health Service guidelines and the Preventive Services Task Force 151 each concluded that more intensive counselling (≥20 min per session) is more effective than less intensive counselling (<20 min per session). Higher smoking cessation rates are obtained by using behavioural change techniques that target associative and self-regulatory processes 152 . In addition, behavioural change techniques that will favour commitment, social reward and identity associated with changed behaviour seems associated with higher success rates 152 . Evidence-based counselling focuses on providing social support during treatment, building skills to cope with withdrawal and cessation, and problem-solving in challenging situations 116 , 153 . Effective counselling can be delivered by diverse providers (such as physicians, nurses, pharmacists, social workers, psychologists and certified tobacco treatment specialists) 116 .
Counselling can be delivered in a variety of modalities. In-person individual and group counselling are effective, as is telephone counselling (quit lines) 142 . Internet and text-based intervention seem to be effective in smoking cessation, especially when they are interactive and tailored to a smoker’s specific circumstances 142 . Over the past several years, the number of smoking cessation smartphone apps has increased, but there the evidence that the use of these apps significantly increases smoking cessation rates is not sufficient.
Contingency management (providing financial incentives for abstinence or engagement in treatment) has shown promising results 154 , 155 but its effects are not sustained once the contingencies are removed 155 , 156 . Other treatments such as hypnosis, acupuncture and laser treatment have not been shown to improve smoking cessation rates compared with placebo treatments 116 . Moreover, no solid evidence supports the use of conventional transcranial magnetic stimulation (TMS) for long-term smoking cessation 157 , 158 .
Although a variety of empirically supported smoking cessation interventions are available, more than two-thirds of adult smokers who made quit attempts in the USA during the past year did not use an evidence-based treatment and the rate is likely to be lower in many other countries 142 . This speaks to the need to increase awareness of, and access to, effective cessation aids among all smokers.
Brain stimulation
The insula (part of the frontal cortex) is a critical brain structure involved in cigarette craving and relapse 78 , 79 . The activity of the insula can be modulated using an innovative approach called deep insula/prefrontal cortex TMS (deep TMS), which is effective in helping people quit smoking 80 , 159 . This approach has now been approved by the FDA as an effective smoking cessation intervention 80 . However, although this intervention was developed and is effective for smoking cessation, the number of people with access to it is limited owing to the limited number of sites equipped and with trained personnel, and the cost of this intervention.
Quality of life
Generic instruments (such as the Short-Form (SF-36) Health Survey) can be used to evaluate quality of life (QOL) in smokers. People who smoke rate their QOL lower than people who do not smoke both before and after they become smokers 160 , 161 . QOL improves when smokers quit 162 . Mental health may also improve on quitting smoking 163 . Moreover, QOL is much poorer in smokers with tobacco-related diseases, such as chronic respiratory diseases and cancers, than in individuals without tobacco-related diseases 161 , 164 . The dimensions of QOL that show the largest decrements in people who smoke are those related to physical health, day-to-day activities and mental health such as depression 160 . Smoking also increases the risk of diabetes mellitus 165 , 166 , which is a major determinant of poor QOL for a wide range of conditions.
The high toll of premature death from cigarette smoking can obscure the fact that many of the diseases that cause these deaths also produce substantial disability in the years before death 1 . Indeed, death in smokers is typically preceded by several years of living with the serious disability and impairment of everyday activities caused by chronic respiratory disease, heart disease and cancer 2 . Smokers’ QOL in these years may also be adversely affected by the adverse effects of the medical treatments that they receive for these smoking-related diseases (such as major surgery and radiotherapy).
Expanding cessation worldwide
The major global challenge is to consider individual and population-based strategies that could increase the substantially low rates of adult cessation in most LMICs and indeed strategies to ensure that even in HICs, cessation continues to increase. In general, the most effective tools recommended by WHO to expand cessation are the same tools that can prevent smoking initiation, notably higher tobacco taxes, bans on advertising and promotion, prominent warning labels or plain packaging, bans on public smoking, and mass media and educational efforts 29 , 167 . The effective use of these policies, particularly taxation, lags behind in most LMICs compared with most HICs, with important exceptions such as Brazil 167 . Access to effective pharmacotherapies and counselling as well as support for co-existing mental health conditions would also be required to accelerate cessation in LMICs. This is particularly important as smokers living in LMICs often have no access to the full range of effective treatment options.
Regulating access to e-cigarettes
How e-cigarettes should be used is debated within the tobacco control field. In some countries (for example, the UK), the use of e-cigarettes as a cigarette smoking cessation aid and as a harm reduction strategy is supported, based on the idea that e-cigarette use will lead to much less exposure to toxic compounds than tobacco use, therefore reducing global harm. In other countries (for example, the USA), there is more concern with preventing the increased use of e-cigarettes by youths that may subsequently lead to smoking 25 , 26 . Regulating e-cigarettes in nuanced ways that enable smokers to access those products whilst preventing their uptake among youths is critical.
Regulating nicotine content in tobacco products
Reducing the nicotine content of cigarettes could potentially produce less addictive products that would allow a gradual reduction in the population prevalence of smoking. Some clinical studies have found no compensatory increase in smoking whilst providing access to low nicotine tobacco 168 . Future regulation may be implemented to gradually decrease the nicotine content of combustible tobacco and other nicotine products 169 , 170 , 171 .
Tobacco end games
Some individuals have proposed getting rid of commercial tobacco products this century or using the major economic disruption arising from the COVID-19 pandemic to accelerate the demise of the tobacco industry 172 , 173 . Some tobacco producers have even proposed this strategy as an internal goal, with the idea of switching to nicotine delivery systems that are less harmful ( Philip Morris International ). Some countries are moving towards such an objective; for example, in New Zealand, the goal that fewer than 5% of New Zealanders will be smokers in 2025 has been set (ref. 174 ). The tobacco end-game approach would overall be the best approach to reduce the burden of tobacco use on society, but it would require coordination of multiple countries and strong public and private consensus on the strategy to avoid a major expansion of the existing illicit market in tobacco products in some countries.
Innovative interventions
The COVID-19 pandemic has shown that large-scale investment in research can lead to rapid development of successful therapeutic interventions. By contrast, smoking cessation has been underfunded compared with the contribution that it makes to the global burden of disease. In addition, there is limited coordination between research teams and most studies are small-scale and often underpowered 79 . It is time to fund an ambitious, coordinated programme of research to test the most promising therapies based on an increased understanding of the neurobiological basis of smoking and nicotine addiction (Table 3 ). Many of those ideas have not yet been tested properly and this could be carried out by a coordinated programme of research at the international level.
GBD 2019 Tobacco Collaborators. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and attributable disease burden in 204 countries and territories, 1990-2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet 397 , 2337–2360 (2021). This study summarizes the burden of disease induced by tobacco worldwide .
Google Scholar
West, R. Tobacco smoking: health impact, prevalence, correlates and interventions. Psychol. Health 32 , 1018–1036 (2017).
PubMed PubMed Central Google Scholar
West, R. The multiple facets of cigarette addiction and what they mean for encouraging and helping smokers to stop. COPD 6 , 277–283 (2009).
PubMed Google Scholar
Fagerström, K. Determinants of tobacco use and renaming the FTND to the Fagerström test for cigarette dependence. Nicotine Tob. Res. 14 , 75–78 (2012).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Doll, R. & Hill, A. B. Smoking and carcinoma of the lung; preliminary report. Br. Med. J. 2 , 739–748 (1950).
CAS PubMed PubMed Central Google Scholar
Royal College of Physicians. Smoking and health. Summary of a report of the Royal College of Physicians of London on smoking in relation to cancer of the lung and other diseases (Pitman Medical Publishing, 1962).
Henningfield, J. E., Smith, T. T., Kleykamp, B. A., Fant, R. V. & Donny, E. C. Nicotine self-administration research: the legacy of Steven R. Goldberg and implications for regulation, health policy, and research. Psychopharmacology 233 , 3829–3848 (2016).
Le Foll, B. & Goldberg, S. R. Effects of nicotine in experimental animals and humans: an update on addictive properties. Hand. Exp. Pharmacol. https://doi.org/10.1007/978-3-540-69248-5_12 (2009).
Article Google Scholar
Proctor, R. N. The history of the discovery of the cigarette–lung cancer link: evidentiary traditions, corporate denial, global toll. Tob. Control. 21 , 87–91 (2012).
Hall, B. J. et al. Differential effects of non-nicotine tobacco constituent compounds on nicotine self-administration in rats. Pharmacol. Biochem. Behav. 120 , 103–108 (2014).
Musso, F. et al. Smoking impacts on prefrontal attentional network function in young adult brains. Psychopharmacology 191 , 159–169 (2007).
CAS PubMed Google Scholar
Goriounova, N. A. & Mansvelder, H. D. Short- and long-term consequences of nicotine exposure during adolescence for prefrontal cortex neuronal network function. Cold Spring Harb. Perspect. Med. 2 , a012120 (2012).
Fagerström, K. O. & Bridgman, K. Tobacco harm reduction: the need for new products that can compete with cigarettes. Addictive Behav. 39 , 507–511 (2014).
Hartmann-Boyce, J. et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9 , CD010216 (2021).
Jha, P. The hazards of smoking and the benefits of cessation: a critical summation of the epidemiological evidence in high-income countries. eLife https://doi.org/10.7554/eLife.49979 (2020).
Article PubMed PubMed Central Google Scholar
Palipudi, K. M. et al. Social determinants of health and tobacco use in thirteen low and middle income countries: evidence from Global Adult Tobacco Survey. PLoS ONE 7 , e33466 (2012).
Goodwin, R. D., Pagura, J., Spiwak, R., Lemeshow, A. R. & Sareen, J. Predictors of persistent nicotine dependence among adults in the United States. Drug Alcohol. Depend. 118 , 127–133 (2011).
Weinberger, A. H. et al. Cigarette use is increasing among people with illicit substance use disorders in the United States, 2002-14: emerging disparities in vulnerable populations. Addiction 113 , 719–728 (2018).
Evans-Polce, R. J., Kcomt, L., Veliz, P. T., Boyd, C. J. & McCabe, S. E. Alcohol, tobacco, and comorbid psychiatric disorders and associations with sexual identity and stress-related correlates. Am. J. Psychiatry 177 , 1073–1081 (2020).
Hassan, A. N. & Le Foll, B. Survival probabilities and predictors of major depressive episode incidence among individuals with various types of substance use disorders. J. Clin. Psychiatry https://doi.org/10.4088/JCP.20m13637 (2021).
Article PubMed Google Scholar
Smith, P. H., Mazure, C. M. & McKee, S. A. Smoking and mental illness in the U.S. population. Tob. Control. 23 , e147–e153 (2014).
Bourgault, Z., Rubin-Kahana, D. S., Hassan, A. N., Sanches, M. & Le Foll, B. Multiple substance use disorders and self-reported cognitive function in U.S. adults: associations and sex-differences in a nationally representative sample. Front. Psychiatry https://doi.org/10.3389/fpsyt.2021.797578 (2022).
Reitsma, M. B. et al. Spatial, temporal, and demographic patterns in prevalence of smoking tobacco use and initiation among young people in 204 countries and territories, 1990-2019. Lancet Public Health 6 , e472–e481 (2021).
Warner, K. E. How to think–not feel–about tobacco harm reduction. Nicotine Tob. Res. 21 , 1299–1309 (2019).
Soneji, S. et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 171 , 788–797 (2017).
Levy, D. T. et al. Examining the relationship of vaping to smoking initiation among US youth and young adults: a reality check. Tob. Control. 28 , 629–635 (2019).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The health consequences of smoking — 50 years of progress: a report of the Surgeon General (Centers for Disease Control and Prevention, 2014).
Jha, P. & Peto, R. Global effects of smoking, of quitting, and of taxing tobacco. N. Engl. J. Med. 370 , 60–68 (2014). This review covers the impact of tobacco, of quitting smoking and the importance of taxation to impact prevalence of smoking .
Jha, P. & Peto., R. in Tobacco Tax Reform: At the Crossroads of Health and Development . (eds Marquez, P. V. & Moreno-Dodson, B.) 55–72 (World Bank Group, 2017).
Jha, P. et al. 21st-century hazards of smoking and benefits of cessation in the United States. N. Engl. J. Med. 368 , 341–350 (2013).
Banks, E. et al. Tobacco smoking and all-cause mortality in a large Australian cohort study: findings from a mature epidemic with current low smoking prevalence. BMC Med. 13 , 38 (2015).
Pirie, K. et al. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet 381 , 133–141 (2013).
Jha, P. et al. A nationally representative case-control study of smoking and death in India. N. Engl. J. Med. 358 , 1137–1147 (2008).
Chan, E. D. et al. Tobacco exposure and susceptibility to tuberculosis: is there a smoking gun? Tuberculosis 94 , 544–550 (2014).
Wang, M. G. et al. Association between tobacco smoking and drug-resistant tuberculosis. Infect. Drug Resist. 11 , 873–887 (2018).
Jha, P. et al. Social inequalities in male mortality, and in male mortality from smoking: indirect estimation from national death rates in England and Wales, Poland, and North America. Lancet 368 , 367–370 (2006).
Jha, P., Gelband, H, Irving, H. & Mishra, S. in Reducing Social Inequalities in Cancer: Evidence and Priorities for Research (eds Vaccarella, S et al.) 161–166 (IARC, 2018).
Jha, P. Expanding smoking cessation world-wide. Addiction 113 , 1392–1393 (2018).
Jha, P. Avoidable global cancer deaths and total deaths from smoking. Nat. Rev. Cancer 9 , 655–664 (2009).
Wittenberg, R. E., Wolfman, S. L., De Biasi, M. & Dani, J. A. Nicotinic acetylcholine receptors and nicotine addiction: a brief introduction. Neuropharmacology 177 , 108256 (2020).
Boulter, J. et al. Functional expression of two neuronal nicotinic acetylcholine receptors from cDNA clones identifies a gene family. Proc. Natl Acad. Sci. USA 84 , 7763–7767 (1987).
Couturier, S. et al. A neuronal nicotinic acetylcholine receptor subunit (α7) is developmentally regulated and forms a homo-oligomeric channel blocked by α-BTX. Neuron 5 , 847–856 (1990).
Picciotto, M. R., Addy, N. A., Mineur, Y. S. & Brunzell, D. H. It is not “either/or”: activation and desensitization of nicotinic acetylcholine receptors both contribute to behaviors related to nicotine addiction and mood. Prog. Neurobiol. 84 , 329–342 (2008).
Changeux, J. P. Structural identification of the nicotinic receptor ion channel. Trends Neurosci. 41 , 67–70 (2018).
McKay, B. E., Placzek, A. N. & Dani, J. A. Regulation of synaptic transmission and plasticity by neuronal nicotinic acetylcholine receptors. Biochem. Pharmacol. 74 , 1120–1133 (2007).
Wonnacott, S. Presynaptic nicotinic ACh receptors. Trends Neurosci. 20 , 92–98 (1997).
Wooltorton, J. R., Pidoplichko, V. I., Broide, R. S. & Dani, J. A. Differential desensitization and distribution of nicotinic acetylcholine receptor subtypes in midbrain dopamine areas. J. Neurosci. 23 , 3176–3185 (2003).
Gipson, C. D. & Fowler, C. D. Nicotinic receptors underlying nicotine dependence: evidence from transgenic mouse models. Curr. Top. Behav. Neurosci. 45 , 101–121 (2020).
Hamouda, A. K. et al. Potentiation of (α4)2(β2)3, but not (α4)3(β2)2, nicotinic acetylcholine receptors reduces nicotine self-administration and withdrawal symptoms. Neuropharmacology 190 , 108568 (2021).
Lallai, V. et al. Nicotine acts on cholinergic signaling mechanisms to directly modulate choroid plexus function. eNeuro https://doi.org/10.1523/ENEURO.0051-19.2019 (2019).
Benwell, M. E., Balfour, D. J. & Anderson, J. M. Evidence that tobacco smoking increases the density of (-)-[3H]nicotine binding sites in human brain. J. Neurochem. 50 , 1243–1247 (1988).
Perry, D. C., Davila-Garcia, M. I., Stockmeier, C. A. & Kellar, K. J. Increased nicotinic receptors in brains from smokers: membrane binding and autoradiography studies. J. Pharmacol. Exp. Ther. 289 , 1545–1552 (1999).
Marks, M. J. et al. Nicotine binding and nicotinic receptor subunit RNA after chronic nicotine treatment. J. Neurosci. 12 , 2765–2784 (1992).
Le Foll, B. et al. Impact of short access nicotine self-administration on expression of α4β2* nicotinic acetylcholine receptors in non-human primates. Psychopharmacology 233 , 1829–1835 (2016).
Meyers, E. E., Loetz, E. C. & Marks, M. J. Differential expression of the beta4 neuronal nicotinic receptor subunit affects tolerance development and nicotinic binding sites following chronic nicotine treatment. Pharmacol. Biochem. Behav. 130 , 1–8 (2015).
Zhao-Shea, R., Liu, L., Pang, X., Gardner, P. D. & Tapper, A. R. Activation of GABAergic neurons in the interpeduncular nucleus triggers physical nicotine withdrawal symptoms. Curr. Biol. 23 , 2327–2335 (2013).
Jensen, K. P., Valentine, G., Gueorguieva, R. & Sofuoglu, M. Differential effects of nicotine delivery rate on subjective drug effects, urges to smoke, heart rate and blood pressure in tobacco smokers. Psychopharmacology 237 , 1359–1369 (2020).
Villanueva, H. F., James, J. R. & Rosecrans, J. A. Evidence of pharmacological tolerance to nicotine. NIDA Res. Monogr. 95 , 349–350 (1989).
Corrigall, W. A., Coen, K. M. & Adamson, K. L. Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res. 653 , 278–284 (1994).
Nisell, M., Nomikos, G. G., Hertel, P., Panagis, G. & Svensson, T. H. Condition-independent sensitization of locomotor stimulation and mesocortical dopamine release following chronic nicotine treatment in the rat. Synapse 22 , 369–381 (1996).
Rice, M. E. & Cragg, S. J. Nicotine amplifies reward-related dopamine signals in striatum. Nat. Neurosci. 7 , 583–584 (2004).
Mameli-Engvall, M. et al. Hierarchical control of dopamine neuron-firing patterns by nicotinic receptors. Neuron 50 , 911–921 (2006).
Picciotto, M. R., Higley, M. J. & Mineur, Y. S. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron 76 , 116–129 (2012).
Le Foll, B. et al. Elevation of dopamine induced by cigarette smoking: novel insights from a [11C]-+-PHNO PET study in humans. Neuropsychopharmacology 39 , 415–424 (2014). This brain imaging study identified the brain areas in which smoking elevates dopamine levels .
Maskos, U. et al. Nicotine reinforcement and cognition restored by targeted expression of nicotinic receptors. Nature 436 , 103–107 (2005). This article discusses the implication of the β 2 - containing nAChRs in the VTA in mammalian cognitive function .
Picciotto, M. R. et al. Acetylcholine receptors containing the beta2 subunit are involved in the reinforcing properties of nicotine. Nature 391 , 173–177 (1998). This article discusses the implication of the β 2 - containing nAChRs in addictive effects of nicotine .
Fowler, C. D., Lu, Q., Johnson, P. M., Marks, M. J. & Kenny, P. J. Habenular alpha5 nicotinic receptor subunit signalling controls nicotine intake. Nature 471 , 597–601 (2011). This article discusses the implication of the α5 nicotinic receptor located in the MHb in a mechanism mediating the aversive effects of nicotine .
Elayouby, K. S. et al. α3* Nicotinic acetylcholine receptors in the habenula-interpeduncular nucleus circuit regulate nicotine intake. J. Neurosci. https://doi.org/10.1523/JNEUROSCI.0127-19.2020 (2020).
Ables, J. L. et al. Retrograde inhibition by a specific subset of interpeduncular α5 nicotinic neurons regulates nicotine preference. Proc. Natl Acad. Sci. USA 114 , 13012–13017 (2017).
Frahm, S. et al. Aversion to nicotine is regulated by the balanced activity of β4 and α5 nicotinic receptor subunits in the medial habenula. Neuron 70 , 522–535 (2011).
Jackson, K. J. et al. Role of α5 nicotinic acetylcholine receptors in pharmacological and behavioral effects of nicotine in mice. J. Pharmacol. Exp. Ther. 334 , 137–146 (2010).
Tuesta, L. M. et al. GLP-1 acts on habenular avoidance circuits to control nicotine intake. Nat. Neurosci. 20 , 708–716 (2017).
Salas, R., Pieri, F. & De Biasi, M. Decreased signs of nicotine withdrawal in mice null for the β4 nicotinic acetylcholine receptor subunit. J. Neurosci. 24 , 10035–10039 (2004).
Salas, R., Sturm, R., Boulter, J. & De Biasi, M. Nicotinic receptors in the habenulo-interpeduncular system are necessary for nicotine withdrawal in mice. J. Neurosci. 29 , 3014–3018 (2009).
Jackson, K. J., Martin, B. R., Changeux, J. P. & Damaj, M. I. Differential role of nicotinic acetylcholine receptor subunits in physical and affective nicotine withdrawal signs. J. Pharmacol. Exp. Ther. 325 , 302–312 (2008).
Le Foll, B. et al. Translational strategies for therapeutic development in nicotine addiction: rethinking the conventional bench to bedside approach. Prog. Neuropsychopharmacol. Biol. Psychiatry 52 , 86–93 (2014).
Naqvi, N. H., Rudrauf, D., Damasio, H. & Bechara, A. Damage to the insula disrupts addiction to cigarette smoking. Science 315 , 531–534 (2007). This article discusses the implication of the insular cortex in tobacco addiction .
Ibrahim, C. et al. The insula: a brain stimulation target for the treatment of addiction. Front. Pharmacol. 10 , 720 (2019).
Zangen, A. et al. Repetitive transcranial magnetic stimulation for smoking cessation: a pivotal multicenter double-blind randomized controlled trial. World Psychiatry 20 , 397–404 (2021). This study validated the utility of deep insula/prefrontal cortex rTMS for smoking cessation .
Le Foll, B., Forget, B., Aubin, H. J. & Goldberg, S. R. Blocking cannabinoid CB1 receptors for the treatment of nicotine dependence: insights from pre-clinical and clinical studies. Addict. Biol. 13 , 239–252 (2008).
Kodas, E., Cohen, C., Louis, C. & Griebel, G. Cortico-limbic circuitry for conditioned nicotine-seeking behavior in rats involves endocannabinoid signaling. Psychopharmacology 194 , 161–171 (2007).
Forget, B. et al. Noradrenergic α1 receptors as a novel target for the treatment of nicotine addiction. Neuropsychopharmacology 35 , 1751–1760 (2010).
Garrett, B. E., Dube, S. R., Babb, S. & McAfee, T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob. Res. 17 , 892–897 (2015).
Polanska, K., Znyk, M. & Kaleta, D. Susceptibility to tobacco use and associated factors among youth in five central and eastern European countries. BMC Public Health 22 , 72 (2022).
Volkow, N. D. Personalizing the treatment of substance use disorders. Am. J. Psychiatry 177 , 113–116 (2020).
Li, M. D., Cheng, R., Ma, J. Z. & Swan, G. E. A meta-analysis of estimated genetic and environmental effects on smoking behavior in male and female adult twins. Addiction 98 , 23–31 (2003).
Carmelli, D., Swan, G. E., Robinette, D. & Fabsitz, R. Genetic influence on smoking–a study of male twins. N. Engl. J. Med. 327 , 829–833 (1992).
Broms, U., Silventoinen, K., Madden, P. A. F., Heath, A. C. & Kaprio, J. Genetic architecture of smoking behavior: a study of Finnish adult twins. Twin Res. Hum. Genet. 9 , 64–72 (2006).
Kendler, K. S., Thornton, L. M. & Pedersen, N. L. Tobacco consumption in Swedish twins reared apart and reared together. Arch. Gen. Psychiat 57 , 886–892 (2000).
Saccone, N. L. et al. The CHRNA5-CHRNA3-CHRNB4 nicotinic receptor subunit gene cluster affects risk for nicotine dependence in African-Americans and in European-Americans. Cancer Res. 69 , 6848–6856 (2009).
Bierut, L. J. et al. Variants in nicotinic receptors and risk for nicotine dependence. Am. J. Psychiatry 165 , 1163–1171 (2008). This study demonstrates that nAChR gene variants are important in nicotine addiction .
Bierut, L. J. et al. Novel genes identified in a high-density genome wide association study for nicotine dependence. Hum. Mol. Genet. 16 , 24–35 (2007).
Berrettini, W. et al. α-5/α-3 nicotinic receptor subunit alleles increase risk for heavy smoking. Mol. Psychiatry 13 , 368–373 (2008).
Sherva, R. et al. Association of a single nucleotide polymorphism in neuronal acetylcholine receptor subunit alpha 5 (CHRNA5) with smoking status and with ‘pleasurable buzz’ during early experimentation with smoking. Addiction 103 , 1544–1552 (2008).
Thorgeirsson, T. E. et al. Sequence variants at CHRNB3-CHRNA6 and CYP2A6 affect smoking behavior. Nat. Genet. 42 , 448–453 (2010).
Ray, R., Tyndale, R. F. & Lerman, C. Nicotine dependence pharmacogenetics: role of genetic variation in nicotine-metabolizing enzymes. J. Neurogenet. 23 , 252–261 (2009).
Bergen, A. W. et al. Drug metabolizing enzyme and transporter gene variation, nicotine metabolism, prospective abstinence, and cigarette consumption. PLoS ONE 10 , e0126113 (2015).
Mwenifumbo, J. C. et al. Identification of novel CYP2A6*1B variants: the CYP2A6*1B allele is associated with faster in vivo nicotine metabolism. Clin. Pharmacol. Ther. 83 , 115–121 (2008).
Raunio, H. & Rahnasto-Rilla, M. CYP2A6: genetics, structure, regulation, and function. Drug Metab. Drug Interact. 27 , 73–88 (2012).
CAS Google Scholar
Patterson, F. et al. Toward personalized therapy for smoking cessation: a randomized placebo-controlled trial of bupropion. Clin. Pharmacol. Ther. 84 , 320–325 (2008).
Rodriguez, S. et al. Combined analysis of CHRNA5, CHRNA3 and CYP2A6 in relation to adolescent smoking behaviour. J. Psychopharmacol. 25 , 915–923 (2011).
Strasser, A. A., Malaiyandi, V., Hoffmann, E., Tyndale, R. F. & Lerman, C. An association of CYP2A6 genotype and smoking topography. Nicotine Tob. Res. 9 , 511–518 (2007).
Liakoni, E. et al. Effects of nicotine metabolic rate on withdrawal symptoms and response to cigarette smoking after abstinence. Clin. Pharmacol. Ther. 105 , 641–651 (2019).
Di Ciano, P. et al. Influence of nicotine metabolism ratio on [11C]-(+)-PHNO PET binding in tobacco smokers. Int. J. Neuropsychopharmacol. 21 , 503–512 (2018).
Butler, K. et al. Impact of Cyp2a6 activity on nicotine reinforcement and cue-reactivity in daily smokers. Nicotine Tob. Res. https://doi.org/10.1093/ntr/ntab064 (2021).
Benowitz, N. L., Swan, G. E., Jacob, P. 3rd, Lessov-Schlaggar, C. N. & Tyndale, R. F. CYP2A6 genotype and the metabolism and disposition kinetics of nicotine. Clin. Pharmacol. Ther. 80 , 457–467 (2006).
Liu, M. et al. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat. Genet. 51 , 237–244 (2019).
McKay, J. D. et al. Large-scale association analysis identifies new lung cancer susceptibility loci and heterogeneity in genetic susceptibility across histological subtypes. Nat. Genet. 49 , 1126–1132 (2017).
Chukwueke, C. C. et al. The CB1R rs2023239 receptor gene variant significantly affects the reinforcing effects of nicotine, but not cue reactivity, in human smokers. Brain Behav. 11 , e01982 (2021).
Ahrens, S. et al. Modulation of nicotine effects on selective attention by DRD2 and CHRNA4 gene polymorphisms. Psychopharmacology 232 , 2323–2331 (2015).
Harrell, P. T. et al. Dopaminergic genetic variation moderates the effect of nicotine on cigarette reward. Psychopharmacology 233 , 351–360 (2016).
Lerman, C. et al. Role of functional genetic variation in the dopamine D2 receptor (DRD2) in response to bupropion and nicotine replacement therapy for tobacco dependence: results of two randomized clinical trials. Neuropsychopharmacology 31 , 231–242 (2006).
Le Foll, B., Gallo, A., Le Strat, Y., Lu, L. & Gorwood, P. Genetics of dopamine receptors and drug addiction: a comprehensive review. Behav. Pharmacol. 20 , 1–17 (2009).
Chukwueke, C. C. et al. Exploring the role of the Ser9Gly (rs6280) dopamine D3 receptor polymorphism in nicotine reinforcement and cue-elicited craving. Sci. Rep. 10 , 4085 (2020).
The Clinical Practice Guideline Treating Tobacco Use and Dependence 2008 Update Panel, Liaisons, and Staff A clinical practice guideline for treating tobacco use and dependence: 2008 update: a U.S. Public Health Service report. Am. J. Prev. Med. 35 , 158–176 (2008).
Hackshaw, A., Morris, J. K., Boniface, S., Tang, J. L. & Milenković, D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 360 , j5855 (2018).
Qin, W. et al. Light cigarette smoking increases risk of all-cause and cause-specific mortality: findings from the NHIS cohort study. Int. J. Env. Res. Public Health https://doi.org/10.3390/ijerph17145122 (2020).
Rodu, B. & Plurphanswat, N. Mortality among male smokers and smokeless tobacco users in the USA. Harm Reduct. J. 16 , 50 (2019).
Kasza, K. A. et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 376 , 342–353 (2017).
Richardson, A., Xiao, H. & Vallone, D. M. Primary and dual users of cigars and cigarettes: profiles, tobacco use patterns and relevance to policy. Nicotine Tob. Res. 14 , 927–932 (2012).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental disorders 5th edn (American Psychiatric Association, 2013).
World Health Organization. Tobacco fact sheet. WHO https://www.who.int/news-room/fact-sheets/detail/tobacco (2021).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C. & Fagerström, K. O. The Fagerström test for nicotine dependence: a revision of the Fagerström tolerance questionnaire. Br. J. Addict. 86 , 1119–1127 (1991).
Heatherton, T. F., Kozlowski, L. T., Frecker, R. C., Rickert, W. & Robinson, J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 84 , 791–799 (1989).
Etter, J. F., Le Houezec, J. & Perneger, T. V. A self-administered questionnaire to measure dependence on cigarettes: the cigarette dependence scale. Neuropsychopharmacology 28 , 359–370 (2003).
DiFranza, J. R. et al. Measuring the loss of autonomy over nicotine use in adolescents: the DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Arch. Pediatr. Adolesc. Med. 156 , 397–403 (2002).
Shiffman, S., Waters, A. & Hickcox, M. The Nicotine Dependence Syndrome Scale: a multidimensional measure of nicotine dependence. Nicotine Tob. Res. 6 , 327–348 (2004).
Smith, S. S. et al. Development of the Brief Wisconsin Inventory of Smoking Dependence Motives. Nicotine Tob. Res. 12 , 489–499 (2010).
Foulds, J. et al. Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking E-cigarette users. Nicotine Tob. Res. 17 , 186–192 (2015).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Preventing tobacco use among youth and young adults: a report of the Surgeon General (Centers for Disease Control and Prevention, 2012).
World Health Organization. Tobacco control to improve child health and development. Thematic brief (WHO, 2021).
Lantz, P. M. et al. Investing in youth tobacco control: a review of smoking prevention and control strategies. Tob. Control. 9 , 47–63 (2000).
Leão, T., Kunst, A. E. & Perelman, J. Cost-effectiveness of tobacco control policies and programmes targeting adolescents: a systematic review. Eur. J. Public Health 28 , 39–43 (2018).
Royal College of Physicians. Smoking and health 2021: a coming of age for tobacco control? (RCP, 2021).
Higashi, H. et al. Cost effectiveness of tobacco control policies in Vietnam: the case of population-level interventions. Appl. Health Econ. Health Policy 9 , 183–196 (2011).
Ranson, M. K., Jha, P., Chaloupka, F. J. & Nguyen, S. N. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tob. Res. 4 , 311–319 (2002).
International Agency for Research on Cancer. I ARC Handbooks of Cancer Prevention: Tobacco control Vol. 14 (IARC, 2011).
Frazer, K. et al. Legislative smoking bans for reducing harms from secondhand smoke exposure, smoking prevalence and tobacco consumption. Cochrane Database Syst. Rev. 2 , CD005992 (2016).
Hoffman, S. J. & Tan, C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health 15 , 744 (2015).
McNeill, A. et al. Tobacco packaging design for reducing tobacco use. Cochrane Database Syst. Rev. 4 , CD011244 (2017).
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking cessation: a report of the Surgeon General (Department of Health and Human Services, 2020).
Lindson, N. et al. Different doses, durations and modes of delivery of nicotine replacement therapy for smoking cessation. Cochrane Database Syst. Rev. 4 , CD013308 (2019).
Krist, A. H. et al. Interventions for tobacco smoking cessation in adults, including pregnant persons: US Preventive Services Task Force recommendation statement. JAMA 325 , 265–279 (2021).
Tutka, P. & Zatonski, W. Cytisine for the treatment of nicotine addiction: from a molecule to therapeutic efficacy. Pharmacol. Rep. 58 , 777–798 (2006).
Courtney, R. J. et al. Effect of cytisine vs varenicline on smoking cessation: a randomized clinical trial. JAMA 326 , 56–64 (2021).
Walker, N. et al. Cytisine versus nicotine for smoking cessation. N. Engl. J. Med. 371 , 2353–2362 (2014). This study validated the utility of cytisine for smoking cessation .
West, R. et al. Placebo-controlled trial of cytisine for smoking cessation. N. Engl. J. Med. 365 , 1193–1200 (2011).
Hajek, P. et al. E-cigarettes compared with nicotine replacement therapy within the UK Stop Smoking Services: the TEC RCT. Health Technol. Assess. 23 , 1–82 (2019).
Walker, N. et al. Nicotine patches used in combination with e-cigarettes (with and without nicotine) for smoking cessation: a pragmatic, randomised trial. Lancet Respir. Med. 8 , 54–64 (2020).
Siu, A. L., U.S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force recommendation statement. Ann. Intern. Med. 163 , 622–634 (2015).
Black, N. et al. Behaviour change techniques associated with smoking cessation in intervention and comparator groups of randomized controlled trials: a systematic review and meta-regression. Addiction 115 , 2008–2020 (2020).
Center for Substance Abuse and Treatment. Detoxification and Substance Abuse Treatment (Center for Substance Abuse and Treatment, 2006).
Cahill, K., Hartmann-Boyce, J. & Perera, R. Incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub5 (2015).
Secades-Villa, R., Aonso-Diego, G., García-Pérez, Á. & González-Roz, A. Effectiveness of contingency management for smoking cessation in substance users: a systematic review and meta-analysis. J. Consult. Clin. Psychol. 88 , 951–964 (2020).
Cahill, K. & Perera, R. Competitions and incentives for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD004307.pub4 (2011).
Trojak, B. et al. Transcranial magnetic stimulation combined with nicotine replacement therapy for smoking cessation: a randomized controlled trial. Brain Stimul. 8 , 1168–1174 (2015).
Wing, V. C. et al. Brain stimulation methods to treat tobacco addiction. Brain Stimul. 6 , 221–230 (2013).
Dinur-Klein, L. et al. Smoking cessation induced by deep repetitive transcranial magnetic stimulation of the prefrontal and insular cortices: a prospective, randomized controlled trial. Biol. Psychiatry 76 , 742–749 (2014).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23 , 540–562 (2014).
Heikkinen, H., Jallinoja, P., Saarni, S. I. & Patja, K. The impact of smoking on health-related and overall quality of life: a general population survey in Finland. Nicotine Tob. Res. 10 , 1199–1207 (2008).
Moayeri, F., Hsueh, Y. A., Dunt, D. & Clarke, P. Smoking cessation and quality of life: insights from analysis of longitudinal Australian data, an application for economic evaluations. Value Health 24 , 724–732 (2021).
Taylor, G. M. et al. Smoking cessation for improving mental health. Cochrane Database Syst. Rev. 3 , CD013522 (2021).
López-Nicolás, Á., Trapero-Bertran, M. & Muñoz, C. Smoking, health-related quality of life and economic evaluation. Eur. J. Health Econ. 19 , 747–756 (2018).
Morris, A. Linking nicotine addiction and T2DM. Nat. Rev. Endocrinol. 16 , 6 (2020).
Willi, C., Bodenmann, P., Ghali, W. A., Faris, P. D. & Cornuz, J. Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis. Jama 298 , 2654–2664 (2007).
World Health Organization. WHO report on the global tobacco epidemic (WHO, 2019).
Donny, E. C. et al. Randomized trial of reduced-nicotine standards for cigarettes. N. Engl. J. Med. 373 , 1340–1349 (2015). This study tested the impact of reducing the quantity of nicotine present in cigarettes on smoking .
Benowitz, N. L. & Henningfield, J. E. Establishing a nicotine threshold for addiction. The implications for tobacco regulation. N. Engl. J. Med. 331 , 123–125 (1994).
Benowitz, N. L. & Henningfield, J. E. Reducing the nicotine content to make cigarettes less addictive. Tob. Control. 22 , i14–i17 (2013).
Gottlieb, S. & Zeller, M. A nicotine-focused framework for public health. N. Engl. J. Med. 377 , 1111–1114 (2017).
Hall, W. & West, R. Thinking about the unthinkable: a de facto prohibition on smoked tobacco products. Addiction 103 , 873–874 (2008).
Ioannidis, J. P. A. & Jha, P. Does the COVID-19 pandemic provide an opportunity to eliminate the tobacco industry? Lancet Glob. Health 9 , e12–e13 (2021).
Smokefree. Smokefree 2025. Smokefree https://www.smokefree.org.nz/smokefree-in-action/smokefree-aotearoa-2025 (2021).
Morgan, C. J., Das, R. K., Joye, A., Curran, H. V. & Kamboj, S. K. Cannabidiol reduces cigarette consumption in tobacco smokers: preliminary findings. Addict. Behav. 38 , 2433–2436 (2013).
Elsaid, S., Kloiber, S. & Le Foll, B. Effects of cannabidiol (CBD) in neuropsychiatric disorders: a review of pre-clinical and clinical findings. Prog. Mol. Biol. Transl. Sci. 167 , 25–75 (2019).
Butler, K. & Le Foll, B. Novel therapeutic and drug development strategies for tobacco use disorder: endocannabinoid modulation. Expert Opin. Drug Discov. 15 , 1065–1080 (2020).
D’Souza, D. C. et al. Efficacy and safety of a fatty acid amide hydrolase inhibitor (PF-04457845) in the treatment of cannabis withdrawal and dependence in men: a double-blind, placebo-controlled, parallel group, phase 2a single-site randomised controlled trial. Lancet Psychiatry 6 , 35–45 (2019).
Robinson, J. D. et al. Pooled analysis of three randomized, double-blind, placebo controlled trials with rimonabant for smoking cessation. Addict. Biol. 23 , 291–303 (2018).
Gueye, A. B. et al. The CB1 neutral antagonist AM4113 retains the therapeutic efficacy of the inverse agonist rimonabant for nicotine dependence and weight loss with better psychiatric tolerability. Int. J. Neuropsychopharmacol. https://doi.org/10.1093/ijnp/pyw068 (2016).
Yammine, L. et al. Exenatide adjunct to nicotine patch facilitates smoking cessation and may reduce post-cessation weight gain: a pilot randomized controlled trial. Nicotine Tob. Res. 23 , 1682–1690 (2021).
Eren-Yazicioglu, C. Y., Yigit, A., Dogruoz, R. E. & Yapici-Eser, H. Can GLP-1 be a target for reward system related disorders? A qualitative synthesis and systematic review analysis of studies on palatable food, drugs of abuse, and alcohol. Front. Behav. Neurosci. 14 , 614884 (2020).
Vanderkam, P. et al. Effectiveness of drugs acting on adrenergic receptors in the treatment for tobacco or alcohol use disorders: systematic review and meta-analysis. Addiction 116 , 1011–1020 (2021).
Sokoloff, P. & Le Foll, B. The dopamine D3 receptor, a quarter century later. Eur. J. Neurosci. 45 , 2–19 (2017).
David, S. P., Lancaster, T., Stead, L. F., Evins, A. E. & Prochaska, J. J. Opioid antagonists for smoking cessation. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003086.pub3 (2013).
Ray, L. A. et al. Efficacy of combining varenicline and naltrexone for smoking cessation and drinking reduction: a randomized clinical trial. Am. J. Psychiatry 178 , 818–828 (2021).
Mooney, M. E. et al. Bupropion and naltrexone for smoking cessation: a double-blind randomized placebo-controlled clinical trial. Clin. Pharmacol. Ther. 100 , 344–352 (2016).
Justinova, Z., Le Foll, B., Redhi, G. H., Markou, A. & Goldberg, S. R. Differential effects of the metabotropic glutamate 2/3 receptor agonist LY379268 on nicotine versus cocaine self-administration and relapse in squirrel monkeys. Psychopharmacology 233 , 1791–1800 (2016).
Le Foll, B., Wertheim, C. E. & Goldberg, S. R. Effects of baclofen on conditioned rewarding and discriminative stimulus effects of nicotine in rats. Neurosci. Lett. 443 , 236–240 (2008).
Franklin, T. R. et al. The GABA B agonist baclofen reduces cigarette consumption in a preliminary double-blind placebo-controlled smoking reduction study. Drug Alcohol. Depend. 103 , 30–36 (2009).
Lotfy, N., Elsawah, H. & Hassan, M. Topiramate for smoking cessation: systematic review and meta-analysis. Tob. Prev. Cessat. 6 , 14 (2020).
Shanahan, W. R., Rose, J. E., Glicklich, A., Stubbe, S. & Sanchez-Kam, M. Lorcaserin for smoking cessation and associated weight gain: a randomized 12-week clinical trial. Nicotine Tob. Res. 19 , 944–951 (2017).
Higgins, G. A., Fletcher, P. J. & Shanahan, W. R. Lorcaserin: a review of its preclinical and clinical pharmacology and therapeutic potential. Pharmacol. Ther. 205 , 107417 (2020).
Stead, L. F. & Lancaster, T. Interventions to reduce harm from continued tobacco use. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD005231.pub2 (2007).
Download references
Acknowledgements
B.Le F. is supported by a clinician-scientist award from the Department of Family and Community Medicine at the University of Toronto and the Addiction Psychiatry Chair from the University of Toronto. The funding bodies had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication. The authors thank H. Fu (University of Toronto) for assistance with Figs 1–3.
Author information
Authors and affiliations.
Translational Addiction Research Laboratory, Campbell Family Mental Health Research Institute, Centre for Addiction and Mental Health, University of Toronto, Toronto, Ontario, Canada
Bernard Le Foll
Departments of Family and Community Medicine, Psychiatry, Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada
Department of Medicine, University of Wisconsin, Madison, WI, USA
Megan E. Piper
University of Wisconsin Center for Tobacco Research and Intervention, Madison, WI, USA
Department of Neurobiology and Behaviour, University of California Irvine, Irvine, CA, USA
Christie D. Fowler
Section for Preventive Cardiology, Department of Endocrinology, Morbid Obesity and Preventive Medicine, Oslo University Hospital, Oslo, Norway
Serena Tonstad
Department of Psychiatry, Washington University School of Medicine, St. Louis, MO, USA
Laura Bierut
Institute of Mental Health, Peking University Sixth Hospital, Peking University, Beijing, China
National Institute on Drug Dependence, Peking University Health Science Center, Beijing, China
Centre for Global Health Research, Unity Health Toronto, University of Toronto, Toronto, Ontario, Canada
- Prabhat Jha
National Centre for Youth Substance Use Research, The University of Queensland, St Lucia, Queensland, Australia
Wayne D. Hall
Queensland Alliance for Environmental Health Sciences, The University of Queensland, Woolloongabba, Queensland, Australia
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (B.Le F.); Epidemiology (P.J. and W.D.H.); Mechanisms/pathophysiology (C.D.F., L.B., L.L. and B.Le F.); Diagnosis, screening and prevention (P.J., M.E.P., S.T. and B.Le F.); Management (M.E.P., S.T., W.D.H., L.L. and B.Le F.); Quality of life (P.J. and W.D.H.); Outlook (all); Conclusions (all). All authors contributed substantially to the review and editing of the manuscript.
Corresponding author
Correspondence to Bernard Le Foll .
Ethics declarations
Competing interests.
B.Le F. has obtained funding from Pfizer (GRAND Awards, including salary support) for investigator-initiated projects. B.Le F. has received some in-kind donations of cannabis product from Aurora and medication donation from Pfizer and Bioprojet and was provided a coil for TMS study from Brainsway. B.Le F. has obtained industry funding from Canopy (through research grants handled by CAMH or the University of Toronto), Bioprojet, ACS, Indivior and Alkermes. B.Le F. has received in-kind donations of nabiximols from GW Pharma for past studies funded by CIHR and NIH. B.Le F. has been an advisor to Shinoghi. S.T. has received honoraria from Pfizer the manufacturer of varenicline for lectures and advice. All other authors declare no competing interests.
Peer review
Peer reviewer information.
Nature Reviews Disease Primers thanks Jamie Brown, Elisardo Iglesias and Ming Li for their contribution to the peer review of this work.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
CTRI website: https://d3futrf33lk36a.cloudfront.net/wp-content/uploads/sites/240/2019/04/Meds-Chart.pdf
Philip Morris International: https://www.pmi.com/
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Le Foll, B., Piper, M.E., Fowler, C.D. et al. Tobacco and nicotine use. Nat Rev Dis Primers 8 , 19 (2022). https://doi.org/10.1038/s41572-022-00346-w
Download citation
Accepted : 07 February 2022
Published : 24 March 2022
DOI : https://doi.org/10.1038/s41572-022-00346-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Integrated mrna- and mirna-sequencing analyses unveil the underlying mechanism of tobacco pollutant-induced developmental toxicity in zebrafish embryos.
- Jiasheng Chen
- Xiaoping Zhong
Journal of Translational Medicine (2024)
Influence of substance use on male reproductive health and offspring outcomes
- Jamie O. Lo
- Jason C. Hedges
- Charles A. Easley
Nature Reviews Urology (2024)
Reductions in smoking due to ratification of the Framework Convention for Tobacco Control in 171 countries
- Guillermo Paraje
- Mauricio Flores Muñoz
Nature Medicine (2024)
Impact of benzoic acid and 2,2’-methylenebis (6-tert-butyl-4-methylphenol) on the metabolome of flue-cured tobacco and rhizosphere microbial communities: implications for continuous cropping obstacles
- Qiulian Peng
- Jiayan Zhang
Plant and Soil (2024)
Nicotinic regulation of microglia: potential contributions to addiction
- Alexa R. Soares
- Marina R. Picciotto
Journal of Neural Transmission (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Essay on Smoking
500 words essay on smoking.
One of the most common problems we are facing in today’s world which is killing people is smoking. A lot of people pick up this habit because of stress , personal issues and more. In fact, some even begin showing it off. When someone smokes a cigarette, they not only hurt themselves but everyone around them. It has many ill-effects on the human body which we will go through in the essay on smoking.

Ill-Effects of Smoking
Tobacco can have a disastrous impact on our health. Nonetheless, people consume it daily for a long period of time till it’s too late. Nearly one billion people in the whole world smoke. It is a shocking figure as that 1 billion puts millions of people at risk along with themselves.
Cigarettes have a major impact on the lungs. Around a third of all cancer cases happen due to smoking. For instance, it can affect breathing and causes shortness of breath and coughing. Further, it also increases the risk of respiratory tract infection which ultimately reduces the quality of life.
In addition to these serious health consequences, smoking impacts the well-being of a person as well. It alters the sense of smell and taste. Further, it also reduces the ability to perform physical exercises.
It also hampers your physical appearances like giving yellow teeth and aged skin. You also get a greater risk of depression or anxiety . Smoking also affects our relationship with our family, friends and colleagues.
Most importantly, it is also an expensive habit. In other words, it entails heavy financial costs. Even though some people don’t have money to get by, they waste it on cigarettes because of their addiction.
How to Quit Smoking?
There are many ways through which one can quit smoking. The first one is preparing for the day when you will quit. It is not easy to quit a habit abruptly, so set a date to give yourself time to prepare mentally.
Further, you can also use NRTs for your nicotine dependence. They can reduce your craving and withdrawal symptoms. NRTs like skin patches, chewing gums, lozenges, nasal spray and inhalers can help greatly.
Moreover, you can also consider non-nicotine medications. They require a prescription so it is essential to talk to your doctor to get access to it. Most importantly, seek behavioural support. To tackle your dependence on nicotine, it is essential to get counselling services, self-materials or more to get through this phase.
One can also try alternative therapies if they want to try them. There is no harm in trying as long as you are determined to quit smoking. For instance, filters, smoking deterrents, e-cigarettes, acupuncture, cold laser therapy, yoga and more can work for some people.
Always remember that you cannot quit smoking instantly as it will be bad for you as well. Try cutting down on it and then slowly and steadily give it up altogether.
Get the huge list of more than 500 Essay Topics and Ideas
Conclusion of the Essay on Smoking
Thus, if anyone is a slave to cigarettes, it is essential for them to understand that it is never too late to stop smoking. With the help and a good action plan, anyone can quit it for good. Moreover, the benefits will be evident within a few days of quitting.
FAQ of Essay on Smoking
Question 1: What are the effects of smoking?
Answer 1: Smoking has major effects like cancer, heart disease, stroke, lung diseases, diabetes, and more. It also increases the risk for tuberculosis, certain eye diseases, and problems with the immune system .
Question 2: Why should we avoid smoking?
Answer 2: We must avoid smoking as it can lengthen your life expectancy. Moreover, by not smoking, you decrease your risk of disease which includes lung cancer, throat cancer, heart disease, high blood pressure, and more.
Customize your course in 30 seconds
Which class are you in.

- Travelling Essay
- Picnic Essay
- Our Country Essay
- My Parents Essay
- Essay on Favourite Personality
- Essay on Memorable Day of My Life
- Essay on Knowledge is Power
- Essay on Gurpurab
- Essay on My Favourite Season
- Essay on Types of Sports
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Download the App

Smoking and Its Effects on Human Body Essay
Introduction, works cited.
Smoking is one of the oldest traditions followed by millions of people in the world. Despite pleasure and positive feelings, smoking is dangerous as it harms the human body and tissues. Smoking is dangerous as it leads to health-related problems including cardiovascular disease. According to Carr (22), one-third of all deaths in America are caused by coronary heart disease, and at least 30 percent of these deaths are related to smoking. Smoking affects the lungs and respiratory organs causing such terrible diseases as cancer. Among the most wider spread diseases are peptic ulcers, cancer of the larynx, kidney, pancreas, and other major organs. The resins from the smoke enter the blood and ruin cells. This process is inevitable if a person smokes for years. Also, smoking harms the fetus, increasing the risk of spontaneous abortion and low birth weight.
The investigators explain the effects of smoking on the breath as follows: the rapid pulse rate of smokers decreases the stroke volume during rest since the venous return is not affected and the ventricles lose the habit and ability to make large strokes. Similar conditions arise during strenuous exercise, that is, with the rapid heart rate, the diastolic filling is incomplete and the stroke output remains small. This results in a relatively small unit circulation and oxygen supply to the tissues with the result that an oxygen debt must be incurred. This ends in breathlessness and dyspnœa. Just giving the facts is not enough. Attitudes and behaviors need to be addressed (Rabin and Sugarman, p. 43).
Students want behavioral tips on how to maintain peer acceptability while avoiding the pressure to show how cool they are b smoking. While cigarette ads on television and radio are forbidden, “gifts” of cigarettes to minors (particularly in minority communities) are not discouraged as an advertisement ploy. Moreover, the interlacing of beer ads with sports events and wine cooler ads with upscale women’s television programming sends strong messages to young people about how society views substance use. Role-plays, debates, “raps,” and antismoking jingles allow students an active exploration of their motivation for wanting or not wanting to smoke. These techniques encourage youngsters to think for themselves, to develop their judgments and attitudes (Carr, p. 87). Recently, studies by Rabin and Sugarman (2003) have demonstrated an increased cancer risk in adulthood among children who were exposed to parental smoking in their early years. An overview of the health effects of passive smoking on children and adults is the same as on active smokers. Smoking has direct physiological effects on the body, and the cumulative wear and tear on the system caused by recurring stress can eventually cause damage to the system. Indeed, there is abundant evidence that stress can cause several physiological and biochemical changes (Cnossen, p. 31).
In sum, smoking harms the human body ruining healthy cells and tissues. Smoking is dangerous as it leads to inevitable changes in blood and tissues of the heart and lungs. Smoking can cause neural and endocrine change that alters the normal functioning of the organism (e.g., change in cardiovascular activity or immune system functioning). This physiological stress response is accompanied by behavioral responses as well. Smoking and the subsequent behavioral response to it can affect health and facilitate, if not cause, some illnesses.
- Carr, A. The Easy Way to Stop Smoking: Join the Millions Who Have Become Non-Smokers Using Allen Carr’s Easyway Method. Sterling; 1 edition, 2005.
- Cnossen, S. Theory and Practice of Excise Taxation: Smoking, Drinking, Gambling, Polluting, and Driving. Oxford University Press, 2005.
- Rabin, R. L., Sugarman, S.D. Regulating Tobacco. Oxford University Press, 2001.
- You Can’t Smoke Before 18
- Stroke as a Prevalent Chronic Condition
- Clinical Effects of Cigarette Smoking
- Cultural Perceptions of Health and Related Issues
- Community Health Assessment in Crown Heights District
- Community Health Promotion for Aged People in Warren
- Analyzing the Truth of "Sicko" for Canadian Health Care
- Public Health Model and Its Application
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, October 19). Smoking and Its Effects on Human Body. https://ivypanda.com/essays/smoking-and-its-effects-on-human-body/
"Smoking and Its Effects on Human Body." IvyPanda , 19 Oct. 2021, ivypanda.com/essays/smoking-and-its-effects-on-human-body/.
IvyPanda . (2021) 'Smoking and Its Effects on Human Body'. 19 October.
IvyPanda . 2021. "Smoking and Its Effects on Human Body." October 19, 2021. https://ivypanda.com/essays/smoking-and-its-effects-on-human-body/.
1. IvyPanda . "Smoking and Its Effects on Human Body." October 19, 2021. https://ivypanda.com/essays/smoking-and-its-effects-on-human-body/.
Bibliography
IvyPanda . "Smoking and Its Effects on Human Body." October 19, 2021. https://ivypanda.com/essays/smoking-and-its-effects-on-human-body/.

Essay on Harmful Effects of Smoking
Students are often asked to write an essay on Harmful Effects of Smoking in their schools and colleges. And if you’re also looking for the same, we have created 100-word, 250-word, and 500-word essays on the topic.
Let’s take a look…
100 Words Essay on Harmful Effects of Smoking
Introduction.
Smoking is a dangerous habit that poses significant health risks. It’s not only harmful to smokers, but also to those around them.
Health Risks
Smoking can cause lung cancer, heart disease, and stroke. It damages nearly every organ in the body, leading to premature death.
Secondhand Smoke
Non-smokers exposed to secondhand smoke face similar health risks. They can develop respiratory problems and increased risk of heart disease.
Impact on Environment
Cigarette butts litter the environment and release toxic chemicals into the soil and water, harming wildlife.
Smoking is harmful for everyone. It’s important to stay away from this deadly habit.
250 Words Essay on Harmful Effects of Smoking
Smoking is a widespread habit, yet it is one of the most detrimental practices to human health. Despite the awareness campaigns and statutory warnings, many continue to smoke, oblivious of the damaging effects it has on their health and wellbeing.
Physical Health Risks
Primarily, smoking causes numerous fatal diseases. It is the leading cause of lung cancer, accounting for about 85% of all cases. It also significantly increases the risk of heart diseases and stroke. The harmful chemicals in cigarettes damage blood vessels, leading to atherosclerosis, which can result in heart attack or stroke.
Impact on Respiratory System
Moreover, smoking adversely affects the respiratory system. It leads to chronic bronchitis, emphysema, and other lung diseases. The smoke and toxins inhaled damage the airways and alveoli, the tiny air sacs in the lungs, causing chronic obstructive pulmonary disease (COPD).
Effect on Mental Health
Smoking also influences mental health. Nicotine addiction can lead to increased stress, anxiety, and depression. The temporary relief from stress that smoking provides is often mistaken for a stress reliever, while it is actually exacerbating the problem.
In conclusion, smoking is a harmful habit that poses significant threats to physical and mental health. The myriad diseases it causes, coupled with its addictive nature, make it a dangerous lifestyle choice. It is imperative to raise awareness about these harmful effects and encourage cessation to safeguard public health.
500 Words Essay on Harmful Effects of Smoking
Smoking is a prevalent habit, often started out of curiosity, peer pressure, or stress management. However, its harmful effects are well-documented, impacting nearly every organ in the human body. Despite the widespread knowledge of its adverse effects, smoking continues to be a significant public health concern.
The Impact on Physical Health
One of the most severe consequences of smoking is its impact on physical health. Smokers are at a higher risk of developing a plethora of diseases, including lung cancer, heart disease, stroke, and chronic obstructive pulmonary disease (COPD). These conditions are often fatal, leading to premature death. The toxins in cigarette smoke damage the lining of the lungs, making smokers more susceptible to infections like pneumonia.
Detrimental Effects on Mental Health
Smoking doesn’t just harm the physical body; it also has a profound effect on mental health. Nicotine, the addictive substance in tobacco, alters the brain chemistry, leading to dependence. This dependence can exacerbate mental health conditions such as anxiety and depression. Furthermore, the stress of addiction and the struggle to quit smoking can also take a toll on mental well-being.

Smoking and Second-hand Smoke
The harmful effects of smoking are not confined to the smoker alone. Second-hand smoke, also known as passive smoking, is a significant concern. Non-smokers exposed to second-hand smoke inhale the same dangerous chemicals as smokers. This exposure increases their risk of developing heart disease, lung cancer, and other respiratory conditions.
Societal Impact
Smoking also has societal implications. The economic burden of smoking is substantial, with healthcare costs for smoking-related illnesses reaching astronomical levels. Additionally, the loss of productivity due to illness or premature death contributes to economic strain.
In conclusion, the harmful effects of smoking are far-reaching, affecting not only the smoker but also those around them and society at large. The physical and mental health implications, coupled with the economic burden, make it a significant public health issue. Despite the addictive nature of smoking, quitting is possible with the right support and resources, leading to improved health outcomes and quality of life. Understanding the full scope of smoking’s harmful effects is crucial in motivating smokers to quit and preventing non-smokers from starting.
That’s it! I hope the essay helped you.
If you’re looking for more, here are essays on other interesting topics:
- Essay on Effects of Smoking
- Essay on Dangers of Smoking
- Essay on Cyclone
Apart from these, you can look at all the essays by clicking here .
Happy studying!
Leave a Reply Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

Australian Government Department of Health and Aged Care
Effects of smoking and tobacco
Within 10 seconds of your first puff, the toxic chemicals in tobacco smoke reach your brain, heart and other organs. Smoking harms almost every part of your body and increases your risk of many diseases. Smoking also affects how you look and feel, your finances and the people close to you.
What happens in your body
When you smoke, harmful chemicals enter your lungs, move into your blood stream and spread through your body. They can:
- reach your brain, heart and other organs within 10 seconds of your first puff
- go everywhere your blood flows, causing damage anywhere they go.
Did you know?
Even if you don’t inhale tobacco smoke, you still absorb harmful chemicals through the lining of your mouth.
How you become addicted
The nicotine in tobacco is highly addictive. It makes your brain release a chemical called dopamine. Dopamine is a ‘feel good’ chemical that:
- makes you feel happy
- helps you to concentrate
- gives you more energy.
But this effect doesn’t last long.
As the nicotine levels in your body fade, your brain craves more dopamine. The longer you have been smoking, the more dopamine you need to feel good. You become dependent on nicotine to create this feeling.
Once you are dependent on nicotine, without it you will have withdrawal symptoms. You may find it difficult to concentrate or feel nervous, restless, irritable or anxious.
These 2 things – nicotine dependence and nicotine withdrawal – make you want to smoke more. You have become addicted to tobacco.
How tobacco damages your body
Tobacco contains over 100 dangerous chemicals. These chemicals can damage your body in many ways. For example:
- damage your heart by forcing it to work faster and harder
- slow your blood and reduce oxygen to your feet and hands.
- Carbon monoxide deprives your heart of the oxygen it needs to pump blood around your body. Over time, your airways swell up and let less air into your lungs.
- Tar is a sticky substance that coats your lungs like soot in a chimney. This damages your lungs and is known to cause lung disease, which can make it harder to breathe.
- Phenols paralyse and kill the hair-like cells in your airways. These means the cells cannot sweep clean the lining of your airways and protect you against infections.
- Tiny particles in tobacco smoke irritate your throat and lungs and cause ‘smoker’s cough’. This makes you produce more mucus and damages lung tissue.
- Ammonia and formaldehyde irritate your eyes, nose and throat.
- Cancer-causing chemicals make your cells grow too fast or abnormally- which can result in cancer cells. Smoking is known to cause at least 16 types of cancer.
How tobacco affects the way you look
Smoking tobacco can:
- cause yellow-brown stains on your fingers, tongue and teeth
- increase your risk of tooth loss, damaged gums and bad breath
- make your skin saggy and give you early wrinkles
- make your hair lose its natural shine.
Health effects
Smoking is the leading cause of preventable disease and death in Australia.
If you smoke, you:
- reduce your life expectancy and your quality of life
- increase your risk of many conditions and diseases as well as of dying prematurely.
It can be a long time before smokers get a smoking-related condition or disease. Because of this, some people believe it won’t happen to them.
In fact, up to ⅔ of long-term smokers will:
- die of a smoking-related disease
- have their life cut short by about 10 years on average, compared to non-smokers.
There is also growing evidence to suggest that smoking has a negative impact on mental health. For example, some studies show that smoking is associated with increased rates of anxiety, panic attacks, depression, suicide attempts and schizophrenia.
Increased risk of conditions and diseases
Tobacco use is the only risk factor that contributes to 4 of the main types of non-communicable diseases: cardiovascular disease, cancer, chronic lung disease and diabetes.
Smoking causes most lung cancers and can cause cancer almost anywhere on the body. This includes the mouth and nose, throat and voice box, oesophagus, blood cells, liver, stomach, kidney, pancreas, mucinous ovary, ureter, cervix, colon and bladder.
Breathing problems and chronic respiratory conditions
Smoking is the main cause of chronic obstructive pulmonary disease (COPD), a serious, progressive and disabling condition that limits airflow in the lungs. Active smoking also worsens asthma in active smokers and is associated with an increased risk for asthma in adolescents and adults.
Heart disease, stroke and blood circulation problems
Smoking is major cause of cardiovascular disease, such as heart disease and stroke, and cardiovascular disease is one of the major causes of death for both men and women. Smoking increases the risk of blood clots, which block blood flow to the heart, brain or legs. Some smokers end up having their limbs amputated due to blood circulation problems caused by smoking.
People who smoke have more heart attacks than people who don’t smoke. They are also more likely to die from a heart attack at a younger age, even in their 40s.
Smoking causes type 2 diabetes . The risk of developing diabetes is 30 to 40% higher for active smokers compared to non-smokers. Smoking can also worsen some of the health conditions related to type 1 diabetes , such as kidney disease, eye disease and poor circulation which can lead to gangrene.
Smoking weakens your immune system so you’re more likely to get bacterial and viral infections .
Smoking reduces blood flow in your body, so wounds can take longer to heal.
Dental problems
Smoking increases the risk of gum diseases , tooth loss and tooth sensitivity. Once a person has gum damage, smoking also makes it harder for their gums to heal.
People with dental problems can find it harder to chew and swallow, which can lead to poor nutrition and further health issues.
Hearing loss
Smoking reduces blood flow to the inner ear. It can also cause irritation and swelling to the Eustachian tubes (the tubes which connect the back of the nose with the middle ear) resulting in pain and infection.
Smokers may lose their hearing earlier than a non-smoker.
Vision loss
Smoking damages the eye and can lead to macular degeneration – the main cause of blindness in Australia.
Fertility problems
Smoking can make it more difficult to fall pregnant and affect sperm quality. Find out more about smoking, vaping and tobacco and pregnancy .
Osteoporosis and menopause
Smoking is a risk factor for osteoporosis – a condition that weakens your bones and makes them more likely to break – and in women, may result in early menopause compared to a non-smoker.
What the numbers say
- The most recent available estimates show that almost 20,500 Australians died from tobacco use in 2018. This equates to one tobacco-related death every 26 minutes.
- Up to ⅔ of deaths in current smokers can be attributed to smoking and current smokers are estimated to die an average of 10 years earlier than non-smokers.
Effects on those around you
As a smoker, you can affect the health of other people when they breathe in your second-hand smoke. This means they’re breathing in the same toxic and cancer-causing chemicals that you are.
Find out about:
- the health risks of passive smoking
- pregnancy and smoking, vaping and tobacco
- children and smoking, vaping and tobacco
- young people and smoking and tobacco
- First Nations people and smoking, vaping and tobacco .
Financial effects
Smoking is expensive. To work out how much you could save if you stopped smoking, try the I Can Quit calculator . The numbers add up over a year.
If you smoke a pack of cigarettes a day, you could be spending more than $15,000 a year on cigarettes.
Reducing the effects
There is no safe level of smoking.
To reduce your risk, the best option is to quit smoking . You’ll feel the health benefits almost straight away.
- Smoking, vaping and tobacco
Is there anything wrong with this page?
Help us improve health.gov.au
If you would like a response please use the enquiries form instead.

8 Strategies to Use if You Want to Quit Smoking in 2024
E very year, we write our lists of things we want to accomplish to become a better version of ourselves in the new year. For many people, quitting smoking is at the top of the list. Unfortunately, not everyone is successful because they haven't adequately prepared to quit.
Making a plan that works for you is essential. Whether you want to know how to quit smoking cold turkey or how to stop smoking with a more gradual method, we're here to help. With these practical tips, you can start 2024 on the right foot and achieve your goals.
For more health tips, check out this supplement that will help you sleep and five tips to cope with sleep anxiety .
How to make a plan to quit smoking that works for you
Setting up a plan is a great way to start the process of giving up nicotine. That plan begins with examining your habits and considering what will work best for you.
Examine your current smoking habits
Once you've decided you want to stop smoking, it's a good practice to come up with a plan you will follow through with. That starts with looking at your smoking habits and figuring out how to change them
- Become aware of how much you smoke: Before you cut back, it's important to understand how much you're smoking to begin with. It might be more than you think. Count how many cigarettes you're smoking each day and write it down so you can look at that number.
- Identify the reasons you smoke: There are certainly reasons that you smoke or use tobacco and the next step in your journey is understanding them. There's a good possibility that it's a years-old habit that doesn't feel like it has its reasons anymore -- but think about why you started in the first place and why you turn to it throughout the day now. Every time you want to smoke, write down why you're doing it.
- Think about why you want to quit smoking: Having a reason in place will help you stick to your guns when it comes to giving up tobacco. Whether it's for your health, the sake of your children or another reason, figure out why you really want to quit smoking -- beyond just quitting for the sake of quitting. While that is a great way to start, having something you can visualize in the tough parts of this journey can help you push through when you feel like giving up.
Learn how smoking affects your body
Smoking and general tobacco use can have a very negative effect on your body. According to the Centers for Disease Control and Prevention , "smoking can cause cancer, heart disease, stroke, lung diseases, diabetes and chronic obstructive pulmonary disease, which includes emphysema and chronic bronchitis. Smoking also increases risk for tuberculosis, certain eye diseases and problems of the immune system, including rheumatoid arthritis." All of these physical concerns can also lead to issues with your mental health with the added stress of a medical condition.
Studies have also proven that smoking at night may be a direct cause of insomnia , and poor sleep health can lead to other health issues like obesity and heart problems. The CDC also points out how harmful secondhand smoke is, especially around children: Secondhand smoke causes around 400 infant deaths each year.
Set a goal
Goals can help keep you motivated, but beyond one big goal of "quit smoking," set smaller goals that you can achieve along the way. Maybe you start with giving up smoking one day at a time. For a month, commit to not smoking on weekends. When you make it through the month, treat yourself and move on to the next goal. This feels more manageable than quitting cold turkey (although that method certainly works for some people).
Try nicotine replacement therapy
Nicotine replacement therapy -- like a nicotine patch or gum -- can help curb cravings for nicotine. These low doses of nicotine have been proven in numerous studies as a positive resource in giving up smoking. If you're considering nicotine replacement therapy, it's not a bad idea to speak to your healthcare provider to decide which product may work best for you.
Consider prescription pills
You can also speak to your doctor about a prescription medication to help you quit smoking. Chantix and Zyban are two popular prescription medications for smoking cessation that you can discuss with your doctor. Pfizer shared research on the effectiveness of Chantix , with various studies demonstrating upwards of 40% of participants successfully abstaining from smoking while using the drug.
Create a support system
Surrounding yourself with people to lean on while you're going through what will certainly be a difficult time can help you not only be successful but also stay motivated. When you're feeling like you want to give up, these people can help you keep going.
- Let your friends and family know your goals: Share your goals with your trusted circle who will support you -- but leave out anyone who won't. Let them know what your goals are and let them know how they can help you. If you want them to not smoke around you, mention it. If you want them to cheer you on, tell them that. If you want them to be a silent supporter, express just that.
- Create your community: It's also important to find people who are either currently going through the same journey as you or have at some point because they'll understand you better than anyone. Online communities and in-person communities like Nicotine Anonymous and Smokers Anonymous can be helpful.
- Seek professional help: You can also turn to your doctor or therapist for guidance and support while you give up smoking. They can provide you with further resources or medically backed reasons for quitting. They can also help you see the positive effects your physical and mental health are going through as you smoke less and less, which can help keep you motivated.
Plan for the side effects
Most people who give up smoking experience withdrawal symptoms. When weaning yourself off tobacco, the CDC says you can expect to feel irritable, restless, hungry, depressed, and sad. You may also have trouble sleeping and see some weight gain. All of these are common but speak to your doctor about anything that doesn't feel right to you.
The CDC also recommends exercise to deal with restless, anxious feelings. Exercise will raise your heart rate and get your endorphins going, which can improve your mood. Plus, it's a way to channel those negative side effects into something positive.
Celebrate your wins
While it's great to celebrate reaching your big goal, it's just as important to celebrate smaller goals along the way. The first day you fully go without smoking, treat yourself. Once you hit a week, treat yourself again. Buy yourself a nice meal out or go get ice cream. Go have a spa day or buy yourself some shoes you've been eyeing. When you start, set up a bank of rewards you'll give yourself so you know exactly what you're working toward.

A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Cannabis
- Health Effects
- Cannabis FAQs
- Facts and Stats
- Journal Articles
- MMWR Articles
- Related Websites
Cannabis Health Effects
- Cannabis use may have a wide range of health effects on the body and brain.
- There are several risk factors and negative health outcomes associated with cannabis use.

How cannabis can affect your health
Cannabis is the most commonly used federally illegal drug in the United States, with an estimated 61.9 million people using it in 2022. 1 Cannabis use may have a wide range of health effects on the body and brain. 2 Click on the sections below to learn more about how cannabis use can affect your health.
Cannabis health effects
There are health risks associated with using cannabis regardless of how it is used. These include:
Cannabis Use Disorder
People who use cannabis can struggle with physical dependency and controlling their use. This is concerning as there is evidence suggesting the use of highly concentrated THC products is associated with more severe cannabis use disorder symptoms. 3 While approximately 3 in 10 persons who report cannabis have a cannabis use disorder, this figure is rising. 1 4 Some signs and symptoms of cannabis use disorder include trying but failing to quit using cannabis or giving up important activities with friends and family in favor of using cannabis. 5 The risk of developing cannabis use disorder is stronger in people who start using cannabis during youth or adolescence and who use cannabis more frequently. 6
Brain Health
Cannabis use directly affects brain function—specifically the parts of the brain responsible for memory, learning, attention, decision making, coordination, emotions, and reaction time. 7 8
Heart Health
Cannabis can make the heart beat faster and raise blood pressure immediately after use. 9 10 It could also lead to increased risk of stroke, heart disease, and other vascular diseases. 11 12 13 14 15
Cannabis, like alcohol, negatively affects several skills required for safe driving. You can choose not to drive—and remind your friends and family to do the same—after using cannabis.
- It can slow reaction time and ability to make decisions. 7 16
- Cannabis can impair coordination and distort perception. 7 16
- The use of multiple substances (such as cannabis and alcohol) at the same time can increase impairment. 17
- Some studies have shown an association between cannabis use and car crashes; however, more research is needed. 7 17
Lung Health
Smoked cannabis, regardless of how it is smoked, can harm lung tissues and cause scarring and damage to small blood vessels. 18 19
Mental Health
Cannabis use has been linked to social anxiety, depression, and schizophrenia (a type of mental illness where people might see or hear things that aren't really there), but scientists don't yet fully understand the relationships between these mental health disorders and cannabis use. 20 21
Unintentional Poisoning
Edibles, or food and drink products infused with cannabis, have some different risks than smoked cannabis, including a greater risk of poisoning. 7 Some cannabis edibles have packaging designed to mimic the appearance of well-known branded snacks and candy that appeal to children, which increases the risk for unintentional ingestion. Children who consume THC-containing products can become very sick. 22
If You Use Cannabis Products
If you use cannabis products, keep them in a locked childproof container and out of the sight and reach of children. For additional questions, you can contact your healthcare provider, your health department, your local or regional poison control center at 1-800-222-1222 , or 911 if it's an emergency.
FDA Warns About Children Accidentally Ingesting Food Products Containing THC
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2022 National Survey on Drug Use and Health (HHS Publication No. PEP23-07-01-006, NSDUH Series H-58). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. 2023. https://www.samhsa.gov/data/sites/default/files/reports/rpt42731/2022-nsduh-nnr.pdf . Accessed on February 9, 2024.
- Rosenberg EC, Tsien RW, Whalley BJ, et al. Cannabinoids and Epilepsy. Neurotherapeutics . 2015;12(4):747-768. doi: 10.1007/s13311-015-0375-5.
- Freeman TP, Winstock AR. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med. 2015;45(15):3181-3189. doi: 10.1017/S0033291715001178
- Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2021 National Survey on Drug Use and Health (HHS Publication No. PEP22-07-01-005, NSDUH Series H-57). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/report/2021-nsduh-annual-national-report . Accessed on February 9, 2024.
- American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA, 2013.
- Winters KC, Lee C-YS. Likelihood of developing an alcohol and cannabis use disorder during youth: Association with recent use and age. Drug Alcohol Depend . 2008;92(1-3):239-247. doi: 10.1016/j.drugalcdep.2007.08.005.
- National Academies of Sciences, Engineering, and Medicine. The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, DC: The National Academies Press; 2017. https://nap.nationalacademies.org/catalog/24625/the-health-effects-of-cannabis-and-cannabinoids-the-current-state . Accessed February 8, 2024.
- Batalla A, Bhattacharyya S, Yücel M, et al. Structural and functional imaging studies in chronic cannabis users: A systematic review of adolescent and adult findings. PLoS One . 2013;8(2):e55821. doi: 10.1371/journal.pone.0055821.
- Sidney S. Cardiovascular consequences of marijuana use. J Clin Pharmacol . 2002;42(S1):64S-70S. https://doi.org/10.1002/j.1552-4604.2002.tb06005.x
- Subramaniam VN, Menezes AR, DeSchutter A, et al. The cardiovascular effects of marijuana: Are the potential adverse effects worth the high? Mo Med . 2019;116(2):146-153.
- Wolff V, Armspach JP, Lauer V, et al. Cannabis-related stroke: Myth or reality? Stroke . 2013;44(2):558-563. doi: 10.1161/STROKEAHA.112.671347.
- Wolff V, Zinchenko I, Quenardelle V, et al. Characteristics and prognosis of ischemic stroke in young cannabis users compared with non-cannabis users. J Am Coll Cardiol . 2015;66(18):2052-2053. doi: 10.1016/j.jacc.2015.08.867.
- Franz CA, Frishman WH. Marijuana use and cardiovascular disease. Cardiol Rev . 2016;24(4):158-162. doi: 10.1097/CRD.0000000000000103.
- Rumalla K, Reddy AY, Mittal MK. Association of recreational marijuana use with aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis . 2016;25(2):452-460. doi: 10.1016/j.jstrokecerebrovasdis.2015.10.019.
- Rumalla K, Reddy AY, Mittal MK. Recreational marijuana use and acute ischemic stroke: A population-based analysis of hospitalized patients in the United States. J Neurol Sci . 2016;364:191-196. doi: 10.1016/j.jns.2016.01.066.
- Compton R. Marijuana-impaired driving. A report to Congress. Washington, DC: National Highway Traffics Safety Administration, 2017. https://www.nhtsa.gov/sites/nhtsa.dot.gov/files/documents/812440-marijuana-impaired-driving-report-tocongress.pdf . Accessed February 9, 2024.
- Lacey JH, Kelley-Baker T, Berning A, et al. Drug and alcohol crash risk: A case-control study (Report No. DOT HS 812 355). Washington, DC: National Highway Traffic Safety Administration; 2016.
- Tashkin DP, Simmons MS, Tseng CH. Impact of changes in regular use of marijuana and/or tobacco on chronic bronchitis. COPD . 2012;9(4):367-374. doi: 10.3109/15412555.2012.671868.
- Wang X, Derakhshandeh R, Liu J, et al. One minute of marijuana secondhand smoke exposure substantially impairs vascular endothelial function. J Am Heart Assoc . 2016;5(8):e003858. doi: 10.1161/JAHA.116.003858.
- Fattore L, Fratta W. How important are sex differences in cannabinoid action? Br J Pharmacol . 2010;160(3):544-548. doi: 10.1111/j.1476-5381.2010.00776.x.
- Volkow ND, Swanson JM, Evins AE, et al. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: A review. JAMA Psychiatry . 2016;73(3):292-297. doi: 10.1001/jamapsychiatry.2015.3278.
- Richards JR, Smith NE, Moulin AK. Unintentional cannabis ingestion in children: A systematic review. J Pediatr . 2017;190:142-152. doi: 10.1016/j.jpeds.2017.07.005.
Cannabis and Public Health
Cannabis—which can also be called marijuana —is the most commonly used federally illegal drug in the United States.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Office of the Surgeon General (US); Office on Smoking and Health (US). The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2004.

The Health Consequences of Smoking: A Report of the Surgeon General.
4 respiratory diseases.
- Introduction
Smoking has adverse health effects on the entire lung—affecting every aspect of lung structure and function—including impairing lung defenses against infection and causing the sustained lung injury that leads to chronic obstructive pulmonary disease ( COPD ). In fact, among the postulated causes of COPD are acute respiratory infections, for which smokers are at an increased risk. This chapter addresses smoking and acute and chronic respiratory diseases other than lung cancer (see Chapter 2 , “Cancer”), and discusses the relevant evidence of the underlying mechanisms. COPD was the focus of the 1984 Surgeon General’s report ( U.S. Department of Health and Human Services [USDHHS] 1984 ), and a number of previous reports have addressed acute respiratory infections, which can range in severity from minor to fatal. This chapter emphasizes acute respiratory illnesses and COPD, which are leading causes of morbidity and mortality in the United States and worldwide.
- Acute Respiratory Illnesses
Acute respiratory illnesses are presumed to have an infection as the predominant underlying cause. Smoking might act to increase the frequency or severity of infections. In this section, acute respiratory infections are examined separately for persons with and without smoking-related chronic obstructive lung diseases (COLDs), because patients with smoking-related diseases have frequent exacerbations of their underlying diseases. Whenever possible, effects of smoking that increase the incidence of disease are distinguished from effects that relate to the severity of the disease.
A MEDLINE search was conducted to identify relevant studies published between 1966 and 2000. To identify studies focusing on the biologic basis of and the evidence linking smoking and acute respiratory infections in persons without COPD , the following Medical Subject Headings ( MeSH ) terms were searched: “respiratory tract infections” and “smoking,” “respiratory tract infections” and “immunology,” “smoking” and “immunology,” “nicotine” and “immunology,” and “smoking” and “respiratory tract infections” and “epidemiology.” To identify studies focusing on smoking and acute respiratory infections accompanied by COPD and asthma, the MeSH term “lung diseases, obstructive” was searched in combination with multiple key words: “antibiotic(s),” “respiratory infection(s),” “respiratory tract infection(s),” “infection(s),” “Tecumseh,” “immunization,” and “immunotherapy.” The MeSH terms “bronchitis” and “asthma” were also searched in conjunction with the above key words. The searches were then repeated substituting the key words “COPD,” “chronic obstructive pulmonary disease,” “asthma,” “chronic bronchitis,” and “acute bronchitis.” The Cochrane database was also searched. All searches included a hand search of bibliographies and authors’ files.
Acute respiratory illnesses are usually divided into those that include the upper respiratory tract (nose and pharynx) and larynx, and those that include the lower respiratory tract (below the larynx). In people with normal immune systems, viruses account for most cases of upper respiratory syndromes ( Gwaltney 1995c ): acute bronchitis ( Gwaltney 1995a ), bronchiolitis ( Hall and Hall 1995 ), and a majority of pneumonia cases ( Marrie et al. 1989 ). Bacteria can cause pharyngitis ( Gwaltney 1995b ) and some pneumonias ( Marrie et al. 1989 ). Cigarette smoke combustion products reportedly increase morbidity and mortality in acute respiratory infections by impairing physical defenses in the respiratory tract, and by impairing cellular and humoral immune responses to microbes ( Donowitz and Mandell 1995 ). Moreover, the effects of smoking can be expected to differ in respiratory infections caused by viruses and in infections caused by bacteria, because each class of microbes stimulates different immune responses specific to the infection ( Mandell et al. 1995 ).
Conclusions of Previous Surgeon General’s Reports
Previous Surgeon General’s reports on smoking and health have noted possible adverse effects of cigarette smoking on acute respiratory infections. The 1979 report ( U.S. Department of Health, Education, and Welfare [USDHEW] 1979 ) cited data from the 1964–1965 Health Interview Survey, which found a higher age-adjusted incidence of self-reported influenza in male and female smokers when compared with non-smokers, and more upper respiratory illnesses (URIs) in female smokers than in female nonsmokers. The 1989 report ( USDHHS 1989a ) identified a number of studies that reported higher mortality ratios for smokers than for nonsmokers suffering from respiratory tuberculosis (the range of ratios was 1.27–5.0 in three studies), and from influenza and pneumonia as one combined category (the range of ratios was 1.4–2.6 in seven studies). The 1990 report focused on the health benefits of smoking cessation, and it comprehensively reviewed evidence suggesting that smoking increased the risk of acute respiratory illnesses ( USDHHS 1990 ).
Providing a more detailed analysis of the smoking-related mortality data presented in the 1989 report, the 1990 report identified exposure-response relationships between mortality from pneumonia and influenza and the number of cigarettes currently smoked, and identified reductions in mortality rates of former smokers in relation to years of not smoking ( USDHHS 1990 ). A review of possible mechanisms related to acute respiratory illnesses documented a variety of effects on host defenses: increases in peripheral blood total leukocyte counts, increases in poly-morphonuclear leukocyte and monocyte counts, decreases in monocyte intracellular killing, decreases in the CD4/CD8 ratio in heavy smokers, decreases in concentrations of serum immunoglobulins (other than IgE), an increase in alveolar macrophage release of superoxide anions, a decrease in microbicidal activity of the macrophages, and a blunted immune response to an influenza vaccination. Although the 1990 report noted that smoking cessation restored many of these impaired defenses, it also found that few epidemiologic studies directly addressed the effects of smoking on acute respiratory morbidity. Conflicting data were observed for nonspecific acute lower respiratory illnesses (LRIs), but findings for increased morbidity from influenza virus infections in smokers were more consistent. The 1994 report ( USDHHS 1994 ), which focused on young people, added little new information.
Biologic Basis
Animal studies.
More than 25 years ago, in vitro exposure of rabbit alveolar macrophages to a water soluble fraction of tobacco smoke was shown to impair the ability of macrophages to kill bacteria ( Green and Carolin 1967 ). An extensive body of data has since accumulated on the effects of exposure to tobacco smoke on immune and cellular function in animal models. However, differences in responses among species to different experimental exposures of tobacco smoke and its products make it difficult to provide a simple, unifying summary of the animal data. Impaired immunoglobulin responses to immunization ( Roszman and Rogers 1973 ) and dose-dependent decreases in responses to T cell and B cell mitogens have been reported for both short-term in vitro ( Roszman et al. 1975 ) and in vivo ( Johnson et al. 1990 ) exposures to tobacco smoke. Johnson and colleagues (1990) provide a comprehensive review of in vivo subchronic exposures in animals ( Table 4.1 ) and of the voluminous relevant animal toxicology literature through 1990. In addition to the general immunologic effects summarized in Table 4.1 , direct effects of tobacco smoke exposure on lung defenses include suppressed functioning of bronchial-associated lymphoid tissue, increased numbers of alveolar macrophages that have a higher than normal metabolic rate, and increased generation of reactive oxygen species precursors during phagocytosis, but without changes in bactericidal capacity (rat alveolar macrophages [summarized in Johnson et al. 1990 ]).
Summary of subchronic exposure to cigarette smoke on immune function in animals.
Studies of the effects of nicotine on the immune function of rodents provide some relevant insights into the effects of tobacco smoke on host responses. Exposing rats to a four-week continuous infusion of nicotine inhibited the increase of intracellular calcium that usually happens when the T cell antigen receptor is blocked ( Sopori et al. 1998 ). The calcium ion plays a role in the early receptor-mediated activation of cells in general ( Sopori and Kozak 1998 ), and this effect of nicotine on calcium fluxes could explain a number of observed nicotine effects on host defenses: (1) suppressed febrile response to turpentine-induced abscesses in mice ( Sopori and Kozak 1998 ), (2) decreased inflammatory response to influenza infections with an increased proliferation of virus in mice ( Sopori and Kozak 1998 ), (3) decreased responses to T cell mitogens in mice ( McAllister-Sistilli et al. 1998 ) (T cell anergy [ Sopori and Kozak 1998 ]), and (4) decreased induction of antibody-forming cells and proliferative response to anti-CD3 antibody in rats ( McAllister-Sistilli et al. 1998 ).
Human Studies
Studies of the effects of tobacco smoke on immune function and host defenses can be broadly grouped as those focusing on markers in peripheral blood, serologic responses to specific antigens, and markers in specimens obtained by bronchoalveolar lavage.
Studies of immune response markers in peripheral blood to acute respiratory infections are summarized in Table 4.2 . However, the interpretive value of many of these studies is limited by insufficient information on the sources and health status of the participants. Of the studies noted in Table 4.2 , only those by Gulsvik and Fagerhol (1979) , Tollerud and colleagues (1989a , b ), Mili and colleagues (1991) , Kurtti and colleagues (1997) , and Sankilampi and colleagues (1997) are based on population samples with clearly defined criteria for classifying the health status of smokers and nonsmokers. Torres and colleagues (1996) also examined population samples in an effort to assess clinical characteristics of COPD patients with community-acquired pneumonia. The remaining studies have small samples, and the sources of the participants are not always clear. Although innumerable studies have observed increased peripheral white blood cell counts in smokers when compared with nonsmokers, the consequences of this increase remain unclear, especially because few data exist on the effects of smoking on peripheral phagocytic and immune-competent cells. Inconsistent findings in studies observing exposure-response relationships based on the amount of smoking may reflect varying definitions of smoking and the small numbers of persons in some of the studies. Even among those studies that were population-based or those that were larger, exposure-response relationships have not been consistently demonstrated ( Gulsvik and Fagerhol 1979 ; Petitti and Kipp 1986 ; Tollerud et al. 1989b ).
Studies on the effects of smoking on markers of human immune function and host defenses, derived from analyses of peripheral blood.
Nasal mucociliary clearance is probably important in the clearing of microorganisms from the nasopharynx. A study of the rate of nasociliary clearance found the rate of clearance to be delayed in smokers (20.8 [standard deviation = 9.3] minutes versus 11.1 [standard deviation = 3.8] minutes in nonsmokers). In this study the beat frequency of the cilia was not affected in smokers, and this finding suggests that the slower clearance is due either to a loss of cilia and/or changes in the viscoelastic properties of nasal mucus caused by cigarette smoke ( Stanley et al. 1986 ). A study of bacterial adherence to buccal cells found that Streptococcus pneumoniae ( S. pneumoniae ) but not Hemophilus influenzae ( H. influenzae ) had an increased adherence in cigarette smokers. Since bacterial adherence to the cell is the first step in the colonization of bacteria, this finding may indicate an important mechanism for enhancing bacterial colonization and infection in smokers ( Piatti et al. 1997 ).
Although smoking generally seems to suppress immune function, the evidence does not suggest particular mechanisms by which smoking might act to increase the risk of an acute infection ( Table 4.2 ). One possible mechanism relates to the effect of cigarette smoke on the enhancement of IgE immunoglobulin responses through effects on interleukin-4 ( IL -4) production by CD4 lymphocytes ( Byron et al. 1994 ). IgE levels tend to be higher in smokers than in nonsmokers, and the age-related decline in serum IgE levels is not seen in smokers ( Burrows et al. 1981 ). Exposure to cigarette smoke also skews immune responses away from a T-helper ( Th ) 1 type response, characterized by the production of interferon γ, IL-2, tumor necrosis factor alpha, and IL-12 that lead to phagocytosis and the destruction of microbial pathogens ( Fearon and Locksley 1996 ; Locksley et al. 1998 ). As a result, smoking may enhance the ability of common respiratory microbial pathogens (e. g ., viruses) both to infect the host and decrease the host’s ability to control the infection.
Studies of markers in bronchoalveolar lavage specimens provide additional insights into how exposure to tobacco smoke could alter host defenses and increase morbidity from acute infections ( Table 4.3 ). Moreover, the differences in marker profiles (e. g ., distribution of CD4 and CD8 T lymphocytes) between peripheral blood and bronchoalveolar lavage data suggest that both systemic and pulmonary responses need to be evaluated to assess the effects of smoking on host defenses against respiratory pathogens. New data from bronchoalveolar lavage studies also suggest that smoking can alter regulation of the cytokine network. The lower production in smokers of the cytokine IL -1 by alveolar macrophages may be responsible for decreased levels of serum immunoglobulins and decreased antibody responses to vaccines because of IL-1’s role in the production of κ light chains in B cells ( Yamaguchi et al. 1989 ). The suppression of regulatory cytokines IL-1 receptor antagonist and IL-6 ( Mikuniya et al. 1999 ), the inhibition of the chemotactic factor inactivator by tobacco smoke, and the increase in numbers of neutrophils in the lung ( Robbins et al. 1990 ; Costabel et al. 1992 ; Repine et al. 1997 ) could contribute to a heightened inflammatory response that increases morbidity and/or mortality from a respiratory infection.
Studies on the effects of smoking on markers of human immune function and host defenses, derived from analyses of bronchoalveolar lavage fluid.
In summary, since the last Surgeon General’s reports to address the topic ( USDHHS 1989a , 1990 ), new evidence has emerged buttressing the biologic basis of how cigarette smoking could increase the risk of and morbidity from acute respiratory infections: (1) animal data on the inhibitory effects of nicotine on T cell receptor stimulation indicate a plausible basis for the decreased mitogenic responses observed in smokers; (2) bronchoalveolar lavage fluid in smokers shows a more pro-inflammatory cytokine profile than in nonsmokers, suggesting that dysregulation of the cytokine network and inhibition of inflammation regulators provide a basis for more severe inflammation in smokers with respiratory infections; and (3) the emergent understanding of the role of Th -1 and Th-2 lymphocyte phenotypes on immune responses to foreign antigens indicates that the capacity of cigarette smoke to skew immune responses to a Th-2 phenotype could play a role in host responses to an infection. These immunologic alterations can be expected to increase the risk of acute infections through various effects on pulmonary airways, including decreased ciliary function and impaired mucociliary clearance ( Janoff et al. 1987 ), and metaplasic changes in the airway epithelium ( Sherman 1992 ) that diminish the capacity of physical clearance mechanisms.
Acute Respiratory Infections in Persons Without Chronic Obstructive Pulmonary Disease
Epidemiologic evidence, influenza infections.
Some of the earliest studies of the effects of cigarette smoking on acute respiratory infections focused on the influenza virus ( Table 4.4 ). Studies have shown an increased incidence of clinical influenza illness and infection in young, healthy smokers when compared with young, healthy nonsmokers ( Finklea et al. 1969 , 1971a ; Kark and Lebiush 1981 ; Kark et al. 1982 ). An attributable risk of 31.2 percent (95 percent confidence interval [ CI ], 16.5–43.1) was reported for clinical influenza in U.S. male military recruits in a closed outbreak environment ( Kark et al. 1982 ). The data for the severity of an illness are less clear, with studies of young, healthy persons providing conflicting results ( Table 4.4 ) ( Finklea et al. 1969 ; Kark et al. 1982 ). The evidence on smoking and influenza-like illnesses in older populations is even more limited. A randomized, placebo-controlled Dutch trial of influenza vaccines in persons aged 60 years and older ( Cruijff et al. 1999 ) did not show an increase in clinical disease among smokers, but did show an increase in asymptomatic (by serology) infections in smokers in the placebo arm of the trial (the odds ratio [ OR ] adjusted for age, gender, and an underlying risk group = 1.61 [95 percent CI, 0.91–2.83]). A study of adults (age distribution not given) from a health maintenance organization in the United States found an increased OR for a physician/nurse practitioner visit for pneumonia/influenza (no distinction made) among smokers of high-tar cigarettes compared with low-tar cigarette smokers ( Table 4.4 ) ( Petitti and Friedman 1985b ). Unfortunately, the study depended on a medical record review of practitioner diagnoses, with no criteria in the report as to how the “pneumonia/influenza” diagnosis was assigned. Without these criteria, it is difficult to interpret the OR of 1.7 (95 percent CI, 1.0–3.0) for the occurrence of illness in smokers of low-tar cigarettes compared with non-smokers, since this analysis was not adjusted for the presence of COPD in the smokers.
Studies on the association between smoking and the occurrence of influenza virus illness and infection.
Whether smokers have an increased risk of infection with influenza viruses in contrast to more often having a clinically recognizable illness remains clouded. A study of healthy U.S. military cadets found evidence of increased asymptomatic infections among smokers in addition to a larger percentage of smokers with high hemagglutination inhibition ( HI ) titers (>1:40) to influenza A ( Finklea et al. 1969 , 1971a ). As a group, however, ill smokers tended to have lower HI titers to influenza A 2 than ill lifetime nonsmokers, after adjusting for the effects of illness and vaccination status. Ill smokers also had higher titers to influenza B but poorer responses to vaccination with influenza B antigen. Overall responses to vaccination with influenza A and B antigens did not differ among various smoking groups and lifetime nonsmokers. However, smokers had a decreased persistence of antibody at a one-year follow-up evaluation. In the Dutch study of persons aged 60 years or older ( Cruijff et al. 1999 ), smoking status was inversely related to the likelihood of a serologic infection among those who were vaccinated—possibly because smokers develop a better immunologic protection after vaccination than nonsmokers—but showed a direct relationship in those who received a placebo ( Table 4.4 ). These findings do not suggest that smokers are less responsive to the beneficial effects of influenza vaccination, at least in the elderly.
Pneumonia and Infections with Pathogens that Infect the Lower Respiratory Tract
Several well-designed and well-executed U.S. population-based studies have provided evidence of a link between cigarette smoking and acute lower respiratory tract infections ( Table 4.5 ). A population-based, case-control study of 205 cases of community-acquired pneumonia ( Almirall et al. 1999a , b ) reported an attributable risk of 23.0 percent (95 percent CI , 3.3–42.7) for a history of ever smoking. An exposure-response relationship based on the number of cigarettes smoked per day was observed in former smokers, who had an adjusted OR close to that of current smokers of 10 to 20 cigarettes per day ( Table 4.5 ). The Centers for Disease Control and Prevention sponsored a case-control study of invasive pneumococcal disease based on a population surveillance system ( Nuorti et al. 2000 ). Although the number of cases for which pneumonia was the underlying source of the invasive disease was not given, pneumonia is likely to have been the main diagnosis in the 216 (out of a total sample of 228) cases in patients with bacteremia. The population attributable risk estimate for smoking was 51 percent (no CIs were given), compared with 14 percent for chronic illnesses. The authors estimated that reducing the prevalence of smoking to 15 percent among persons aged 18 through 64 years would prevent 4,000 cases per year of invasive pneumococcal disease in the United States. Of particular interest in this study was the observation that after 10 years of smoking cessation, the risk of invasive pneumococcal disease reached that of nonsmokers.
Studies on the association between smoking and the occurrence of pneumonia and infection with pathogens that infect the lower respiratory tract.
Serologic evidence of infection with Chlamydia pneumoniae ( C. pneumoniae ) was evaluated in a sample from the European Respiratory Health Survey ( Table 4.5 ) ( Ferrari et al. 2000 ). The adjusted OR as evidence of recent infection (IgG titer >512 or IgM titer >16) with C. pneumoniae in smokers compared with non-smokers was 3.51 (95 percent CI , 1.26–9.67). Finally, a matched, case-control study of community-acquired infections with Legionella pneumophila was carried out with cases derived from a prospective pneumonia surveillance system in the United States ( Table 4.5 ) ( Straus et al. 1996 ). The univariate OR for infection in current smokers compared with nonsmokers was 3.75 (95 percent CI, 2.27–6.17). However, in a multivariable logistic regression model, an effect from current smoking was observed only in those patients with no evidence of an underlying disease (OR = 7.49 [95 percent CI, 3.27–17.17]).
A study of Finnish twins (all zygosities) discordant for smoking reported that male current and former smokers were more likely to have evidence of ongoing infections with C. pneumoniae (IgA titer >40) than their male twins who had never smoked ( Table 4.5 ) ( von Hertzen et al. 1998a , b ). Antigen-specific lymphocyte responses to C. pneumoniae , but not to other Chlamydia antigens, also were decreased in the male smokers ( von Hertzen et al. 1998b ). No effects were observed in female twins. The authors interpreted the lymphocyte data as being consistent with Th -2 skewing of the immune response in males. The gender differences in these responses are not explained.
Data from several different types of studies have suggested a link between smoking and infection with Mycobacterium tuberculosis ( Table 4.5 ). A study of one million deaths from 1988–1990 in 98 urban and rural areas of China estimated that 11.3 percent of deaths from tuberculosis could be attributed to smoking ( Table 4.5 ) ( Liu et al. 1998 ). Exposure-response relationships with the number of cigarettes smoked per day and time since onset of smoking were observed in both urban and rural environments. However, a survey of the occurrence of positive tuberculin skin tests in a large nursing home population in Hong Kong ( Woo et al. 1996 ) failed to find an association with smoking ( Table 4.5 ). In contrast, three case-control studies provided evidence of an association. A nonpopulation-based, case-control study in Spain evaluated smoking as a risk factor for newly diagnosed tuberculosis ( Table 4.5 ) ( Alcaide et al. 1996 ), and found an estimated attributable risk of 48 percent (95 percent CI , 13–69). Moreover, the authors observed a strong exposure-response relationship with the number of cigarettes smoked per day and an additive effect from passive exposure to tobacco smoke. Two other case-control studies in the United States (both in Washington state) demonstrated associations between the duration of smoking and risk for newly diagnosed tuberculosis ( Buskin et al. 1994 ) and skin test conversion ( Anderson et al. 1997 ), but no association with the current number of cigarettes smoked per day ( Table 4.5 ).
Acute Upper and Lower Respiratory Illnesses with and Without Identification of Specific Pathogens
A large number of studies on the incidence of URI and LRI in relation to cigarette smoking were reviewed in the 1990 Surgeon General’s report on smoking and health ( USDHHS 1990 ), some of which are summarized in Table 4.6 . Although not provided in the text of the papers, attributable risk estimates for the effects of smoking ( Rockhill et al. 1998 ) can be calculated for several of the previously reviewed studies ( Table 4.6 ) ( Parnell et al. 1966 ; Finklea et al. 1971b ; Monto et al. 1975 ; Blake et al. 1988 ). Attributable risk estimates of URI for smokers were similar in studies from divergent populations: 31 percent (95 percent CI , 23–39) in student nurses ( Parnell et al. 1966 ) and 22 percent (95 percent CI, 12–30) and 29 percent (95 percent CI, 10–44) in two military trainee populations ( Finklea et al. 1971b ; Blake et al. 1988 ). A similar coherence was found for LRI ( Table 4.6 ) ( Parnell et al. 1966 ; Finklea et al. 1971b ). In the Tecumseh, Michigan, population-based cohort study ( Monto et al. 1975 ), smokers tended to have a higher incidence of serologically determined infections ( Table 4.6 ).
Studies on the association between smoking and the occurrence of acute upper respiratory illness (URI) and lower respiratory illness (LRI), with and without identification of specific pathogens.
Of three studies published since the 1990 report, two supported an association between smoking and acute respiratory illnesses ( Table 4.6 ) ( Cohen et al. 1993 ; Nicholson et al. 1996 ). The third study, which did not support this association ( Jaakkola and Heinonen 1995 ), was based entirely on self-reported illnesses. A study of volunteers who received an intranasal challenge with rhinovirus and coronavirus ( Table 4.6 ) ( Cohen et al. 1993 ) found an adjusted OR for infection in smokers compared with nonsmokers (virus isolation or serologic response at 28 days) of 2.03 (95 percent CI , 1.18–3.70). A prospective study of a community sample of people aged 60 through 90 years ( Nicholson et al. 1996 ) reported an adjusted OR associated with current smoking for complicated LRI of 1.47 (95 percent CI, 1.14–1.90).
Acute Respiratory Infections in Persons with Human Immunodeficiency Virus Infection
Respiratory infections are a main source of morbidity in persons with human immunodeficiency virus ( HIV ) infection. Several studies have evaluated cigarette smoking and risk for incident lower respiratory infections in persons infected with HIV ( Table 4.7 ).
Studies on the association between smoking and the occurrence of acute respiratory infections in persons with human immunodeficiency virus (HIV) infection.
A large observational cohort study with up to four years of follow-up found a CD4-adjusted relative hazard ( RH ) for bacterial pneumonia in HIV -infected current smokers of 1.57 (95 percent CI , 1.14–2.15) ( Table 4.7 ) ( Burns et al. 1996 ). No excess risk from tuberculosis or infection with Pneumocystis carinii ( P. carinii ) was observed. A second cohort study did not find an excess risk of bacterial pneumonia in HIV-infected patients who smoked when compared with infected patients who did not smoke ( Hirschtick et al. 1995 ). However, among HIV-infected patients with a CD4 count below 200/ mm 3 , smokers had an incidence of pneumonia more than three times higher (13.8/100 person-years compared with 4.0 in nonsmokers) ( Table 4.7 ). A cross-sectional study of a variety of infections within the past six months in HIV-positive and HIV-negative women with similar characteristics based on self-reporting documented an OR for pneumonia in smokers of 2.7 (95 percent CI, 1.2–5.9) ( Table 4.7 ) ( Flanigan et al. 1999 ). No other infections were associated with smoking. A study based on a retrospective evaluation of medical records found that the median time from the onset of HIV infection to a clinical infection with P. carinii was significantly shorter in smokers (9 months) than in nonsmokers (16 months) ( Nieman et al. 1993 ). Smoking did not appear to affect the time of onset of acquired immunodeficiency syndrome ( AIDS ) for non- Pneumocystis AIDS-defining conditions.
Evidence Synthesis
Since the publication of the 1990 Surgeon General’s report ( USDHHS 1990 ), the biologic basis for evaluating associations between cigarette smoking and acute respiratory infections has been strengthened, adding to the plausibility of an association of smoking with respiratory infection. Animal studies on the effects of nicotine demonstrate a mechanism for immune suppression. The effects of cigarette smoke on the regulation of the cytokine network and in producing a Th -2 bias in lymphocyte responses to antigens imply that smokers will have an increase in inflammation and a decrease in protective host responses to infections with respiratory pathogens.
A review of the evidence across all of the studies indicates that cigarette smokers, particularly current smokers, have an increased risk for an acute URI or LRI . The findings are generally consistent among studies and some provide evidence for dose-response with amount of smoking. When persons are classified as current or former smokers or lifetime nonsmokers, ORs generally have been above 1.5 for acute respiratory infections in smokers without an underlying illness compared with nonsmokers ( Tables 4.4 through 4.6 ). However, ORs as high as seven have been reported in at least one well-conducted study of Legionella infection ( Straus et al. 1996 ). The few studies that focused on persons with HIV infection documented a similar range of excess infection rates ( Table 4.7 ). When current smokers are classified by the number of cigarettes smoked per day, exposure-response relationships have been found in some studies. The lack of a standardized measure for current smoking makes the comparison of estimates from various studies difficult. Lower tar content of cigarettes is associated with a decrease in the incidence of acute respiratory illnesses ( Petitti and Friedman 1985b ), consistent with the exposure-response relationship observed with the amount smoked each day and with population-based studies showing a decreased incidence in former smokers when compared with current smokers ( Almirall et al. 1999a , b ; Nuorti et al. 2000 ). A range of potential confounding factors has been considered across the studies.
The evidence is less clear as to whether the risk associated with smoking varies for lower versus upper respiratory infections. In studies reporting an excess incidence of lower respiratory infections, infections tended to be in the heaviest smokers. Studies of military populations have produced conflicting results. A single study of persons aged 60 years or older ( Nicholson et al. 1996 ) indicated that smokers were more likely than nonsmokers to have a complicated LRI .
Finally, the available data do not provide a basis for identifying subgroups particularly susceptible to the smoking-induced risks of acute respiratory illnesses. Studies of HIV -infected persons suggest that the incremental incidence of disease is similar to that in non-HIV-infected people. One study did provide evidence that the effects of smoking on acute respiratory illnesses might be greatest in those most severely immunocompromised ( Hirschtick et al. 1995 ).
- The evidence is sufficient to infer a causal relationship between smoking and acute respiratory illnesses, including pneumonia, in persons without underlying smoking-related chronic obstructive lung disease.
Implications
There are numerous studies providing population attributable risk estimates of the effects of smoking on respiratory illness outcomes ( Table 4.8 ). Two of these estimates have limited generalizability because they were based on selected military populations ( Kark and Lebiush 1981 ; Kark et al. 1982 ). The estimate based on a surveillance system of invasive pneumococcal disease ( Nuorti et al. 2000 ) is indirectly useful, because it has to be assumed that in most of the cases studied the disease originated in the respiratory tract. Although this assumption is reasonable given the particular bacterium, no data on this point were given. Nonetheless, the 51 percent estimate indicates a large contribution to disease burden in the populations studied. The remaining estimates in Table 4.8 are the attributable fractions for smokers. Excluding the estimate with CIs including 1, estimates ranged from 19 to 63 percent. Because the various estimates are based on incidence density data as well as on cumulative incidence data, it is not possible to give a unifying interpretation (etiologic or excess fraction) for all of the estimates ( Greenland and Robins 1988 ). However, considering all of these estimates as “excess” cases ( Greenland 1999 ) of acute respiratory illness provides a maximum estimate of the excess burden that smoking imposes on the occurrence of these illnesses. In most cases, the estimated amount of excess cases is greater than 20 percent.
Estimates of attributable risk fractions for smoking and acute respiratory illness (ARI) in persons without chronic obstructive pulmonary disease.
From a public health standpoint, an argument could be made that additional studies on the broad question of smoking and acute respiratory illnesses are not needed. However, studies to assess the economic and social impacts of this association may still be useful, particularly if they establish common definitions of and criteria for acute respiratory conditions and smoking status. Ideally, these studies should provide data detailing current smoking patterns and smoking patterns for the five years before the study. Using open populations in these studies should make estimates of both population and smoking attributable fractions possible. Such studies must be large enough to provide precise estimates of these fractions and to take into account whatever confounders may be relevant. Small studies are not likely to be useful. National studies, such as the National Health and Nutrition Examination Survey, would be an ideal venue for addressing these components.
Finally, in the context of health care services, health care providers need to make all smokers aware of the implications of these data for their health. The effects of smoking on the incidence of acute respiratory diseases should be included in all health care messages to smokers.
Acute Respiratory Infections in Persons with Chronic Obstructive Pulmonary Disease and Asthma
The population-based Tecumseh study was one of the most extensive epidemiologic investigations examining the effects of cigarette smoking on acute respiratory infections in persons with and without chronic lung disease in the United States ( Monto et al. 1975 ; Monto and Ross 1977 , 1978 ). This multiyear study recruited several stratified random samples of families. During a one-year period, people participated in weekly telephone interviews to identify prospectively the occurrence of an acute respiratory illness. Each participant also underwent serial clinical, spirometric, and serologic examinations. Two definitions of an acute respiratory infection were used: self-reported acute respiratory symptoms and serology (a fourfold rise in serum antibody titer to selected respiratory pathogens).
The observed association between current smoking and self-reported acute respiratory infections was addressed in a series of study reports ( Table 4.9 ). The small sample sizes in subgroups resulted in wide CIs, complicating the interpretation of results. However, smoking has been associated with an increased risk for several indexes of illness: acute respiratory infections in healthy men, based on both self-reported and serologic evidence of infection ( Monto et al. 1975 ); serologic evidence of respiratory infections in women with or without chronic bronchitis ( Monto and Ross 1978 ); and acute, self-reported lower respiratory tract infections in men, especially in those with chronic bronchitis ( Monto and Ross 1977 ). However, not all of the analyses found smoking to be associated with a higher risk of acute respiratory infections in persons with chronic bronchitis ( Table 4.9 ).
Studies on the association between smoking and the risk of acute respiratory illness (ARI)— Results from the Tecumseh Study.
In the Tecumseh study, COPD , as indicated by chronic bronchitis or pulmonary function impairment, was itself associated with a greater risk of developing an acute respiratory infection ( Table 4.10 ), although the effects of smoking were stronger and more consistent among men. In men, the risk varied with the number of cigarettes smoked and the presence of chronic bronchitis, with the risk of an acute respiratory illness highest in heavy smokers of more than one pack per day with chronic bronchitis (relative risk [ RR ] = 1.63), followed by moderate smokers of approximately one and one-half packs per day (RR = 1.45), and nonsmokers (RR = 1.16). (The smoking categories were based on the sum of three reports measuring the number of cigarettes smoked per day: none equals zero packs, category 1 equals less than one pack, category 2 equals one to one and one-half packs, and category 3 equals one and one-half packs or more per day; moderate smokers were in the four to six packs category and heavy smokers were in the seven to nine packs category.) This pattern was not apparent in women.
Studies on the association between smoking, chronic obstructive pulmonary disease, and the risk of acute respiratory illness (ARI)—Results from the Tecumseh Study.
Many studies have documented a high prevalence of potentially pathogenic bacteria isolated from the sputum of persons with an exacerbation of COPD ( Tager and Speizer 1975 ; Fagon et al. 1990 ; Murphy and Sethi 1992 ; Monsó et al. 1995 ; Murphy et al. 2000 ; Voelkel and Tuder 2000 ). In most studies, the specific role of current cigarette smoking in acute infections was not examined. Soler and colleagues (1998) used bronchoscopy with a protected specimen brush to examine bacterial infections in 50 patients with severe COPD exacerbations requiring mechanical ventilation. The prevalence of a positive culture for gram-negative bacilli, including Pseudomonas species, was similar in former and current smokers (23 percent versus 32 percent). In contrast, a study of 91 ambulatory patients with an acute exacerbation of COPD demonstrated an association between current smoking and a greater risk for a quantitative sputum culture yielding H. influenzae ( OR = 8.16 [95 percent CI , 1.9–43]) ( Miravitlles et al. 1999 ).
A population-based, cross-sectional study from Norway examined the association between a clinical diagnosis of obstructive lung disease ( COPD or asthma) and serologic evidence of a respiratory viral infection (influenza A and influenza B viruses, para-influenza virus types 1–3, adenovirus, and respiratory syncytial virus [ RSV ]) ( Omenaas et al. 1996 ). The prevalence of a positive serology, indicating recent or past infections, was higher among persons with obstructive lung disease (74 percent) than among those with chronic respiratory symptoms (60 percent) or persons who were asymptomatic (48 percent). Compared with persons without evidence of infections, those with positive serology for RSV and influenza B virus had lower standardized forced expiratory volume in one second ( FEV 1 ) residuals (−0.61 and −0.54, respectively). For these viruses, an exposure-response relationship was observed between viral titers and FEV 1 residuals. The association between a positive RSV serology and FEV 1 residuals was of a greater magnitude in smokers (−0.93) than in former smokers (−0.65) or nonsmokers (−0.48), although the interaction between smoking and RSV infections was not significant. The investigators observed a similar pattern of results for influenza B virus serology (−1.02 among smokers, −0.46 among former smokers, and −0.30 among nonsmokers). Analyses were not carried out to assess the interaction between the joint effect of having obstructive lung disease and smoking, which would directly address the risk posed by smoking for viral infections among persons with COPD. The cross-sectional design precludes determining whether a viral infection reduces lung function or whether decreased lung function increases susceptibility to viral infections.
The impact of smoking on the risk of death from pulmonary infections among persons with COPD was examined in the population-based Copenhagen City Heart Study ( Prescott et al. 1995 ). In the cohort of 13,888 persons followed for 10 to 12 years, 214 persons died from COPD (8 percent of deaths). Of these deaths, 133 occurred in the hospital. Medical records were reviewed for 101 patients to determine whether death was due to a pulmonary infection. Compared with persons who died without pulmonary infections ( n = 51), those who died from a pulmonary infection (n = 38) had similar smoking statuses. Both groups also had similar prevalence rates of current smoking (75 percent of those without pulmonary infection versus 82 percent of those with infection) and current heavy smoking (53 percent for both), and a similar mean duration of smoking (36 years versus 40 years). In a Cox proportional hazard model that controlled for age, gender, and FEV 1 , daily tobacco use was related to the risk of death from a pulmonary infection ( RH = 1.4 per 10 grams of tobacco used; 95 percent CI , 1.04–1.80). When current smokers and lifetime nonsmokers were compared, smoking was not associated with an increased risk. Although a selection bias from examining a subset of COPD deaths cannot be excluded, the data strongly suggest a relationship between current smoking intensity and the risk of death from a pulmonary infection.
A population-based, case-control study demonstrated that cigarette smoking was a strong risk factor for invasive pneumococcal disease ( Nuorti et al. 2000 ). Moreover, both COPD and asthma were associated with a greater risk of pneumococcal infection ( OR = 3.4 [95 percent CI , 1.6–7.0] and OR = 2.5 [95 percent CI, 1.4–4.7]), respectively. In a multivariate analysis that included smoking variables and demographic characteristics, neither disease was associated with a greater risk of pneumococcal infection. Other investigators also found that COPD was associated with a greater risk of pneumococcal pneumonia and bronchitis ( RR = 1.96 [95 percent CI, 1.51–2.56]) ( Simberkoff et al. 1986 ).
A recent report from the Lung Health Study evaluated the effects of the frequency of self-reported nonspecific LRI that resulted in a visit to a physician on the annual rate of change in FEV 1 levels in participants with mild COPD ( Kanner et al. 2001 ). The number of illness episodes was few in this population, averaging about 0.24 per year for the study population as a whole. Illnesses in the year before the study and female gender were the best predictors of subsequent illnesses, but these two variables explained only 8.4 percent of the total variation. However, during the five-year observation period, participants who were continuous smokers had significantly more illnesses than those who had quit smoking for the entire five-year period ( p = 0.0003). Intermittent smokers had illness rates that fell between the continuing smoker and sustained quitter groups. In this study, nonspecific lower respiratory tract illnesses that resulted in a physician visit had an adverse effect on the annual rate of change in lung function only in those who continued to smoke. The illness effect on changes in the FEV 1 was not seen in sustained quitters ( Kanner et al. 2001 ).
Evidence from Antibiotic Trials
The potential etiologic role of smoking in acute respiratory infections among persons with COPD can be assessed indirectly by examining data from clinical trials of the efficacy of antibiotic treatments for acute exacerbations of COPD. If a bacterial infection plays an important causal role in the acute exacerbation of COPD, characterized by increases in coughing, sputum production, wheezing, dyspnea (difficulty breathing and shortness of breath), and/or airflow obstruction, then treatment with appropriate antibiotics should accelerate symptomatic resolution. Current smoking might decrease the efficacy of antibiotic therapy, and past smoking might influence the risk for infections by determining the level of lung function. This section considers the evidence from trials of antibiotics in exacerbations of COPD. These trials are potentially informative as to the role of bacteria in causing these exacerbations and whether current smoking modifies the effects of antibiotics. Furthermore, they offer evidence on the role of bacteria in causing the exacerbations and provide insights into a causal pathway that begins with smoking, is followed by the onset of COPD, and finally leads to an increased risk for a bacterial infection. However, these studies do not address the role of viruses, which cause the majority of acute upper respiratory infections in the general population.
Beginning in 1957, randomized placebo-controlled clinical trials have examined the efficacy of antibiotics in acute exacerbations of chronic bronchitis characterized by coughing, sputum production, wheezing, or dyspnea ( Table 4.11 ). Studies have examined patients hospitalized for acute exacerbations of chronic bronchitis ( Elmes et al. 1965 ; Petersen et al. 1967 ; Pines et al. 1968 , 1972 ; Nicotra et al. 1982 ) and persons treated as outpatients ( Elmes et al. 1957 ; Berry et al. 1960 ; Fear and Edwards 1962 ; Anthonisen et al. 1987 ; Jørgensen et al. 1992 ; Sachs et al. 1995 ). Except for one single-blind study ( Petersen et al. 1967 ), all trials were double-blind. Several trials demonstrated that antibiotic treatments reduced respiratory symptoms ( Elmes et al. 1957 ; Anthonisen et al. 1987 ), physician-assessed clinical severity ( Berry et al. 1960 ; Pines et al. 1968 , 1972 ), work loss ( Elmes et al. 1957 ), and sputum purulence ( Pines et al. 1972 ). Other trials found that antibiotic treatment improved peak expiratory flow rates ( Elmes et al. 1965 ; Anthonisen et al. 1987 ). Conversely, other clinical trials showed no effects of antibiotics on respiratory symptoms ( Fear and Edwards 1962 ; Sachs et al. 1995 ), clinical severity ( Elmes et al. 1965 ; Jørgensen et al. 1992 ), sputum volume or purulence ( Elmes et al. 1965 ; Petersen et al. 1967 ; Nicotra et al. 1982 ), or peak expiratory flow or other pulmonary function testing ( Petersen et al. 1967 ; Pines et al. 1972 ; Nicotra et al. 1982 ; Jørgensen et al. 1992 ; Sachs et al. 1995 ).
Studies on the efficacy of antibiotic treatment in acute exacerbations of chronic obstructive pulmonary disease.
In a randomized controlled trial that has been widely cited, Anthonisen and colleagues (1987) tested three different antibiotic treatments (trimethoprim-sulfamethoxazole, ampicillin, or doxycycline) against a placebo. In contrast to earlier studies, all patients had a clinical diagnosis of COPD and a FEV 1 /forced vital capacity ( FVC ) ratio of less than 70 percent. Nearly all patients had a history of smoking cigarettes (95 percent), with 21 percent indicating current smoking. After two weeks of standard treatments for COPD, patients received an antibiotic or placebo for acute exacerbations characterized by increased dyspnea, sputum volume, and sputum purulence. In the trial, 173 patients had 362 exacerbations. Treatment success, defined as symptom resolution within 21 days, was significantly more apparent in the antibiotic group than in the placebo group (68 percent versus 55 percent of exacerbations). The duration of antibiotic-treated exacerbations was also shorter (averaging 2.2 days less). When the analysis was restricted to first exacerbations, the results were similar. Increases in peak expiratory flow rates were also greater in patients treated with antibiotics.
In the largest clinical trial, Jørgensen and colleagues (1992) randomly assigned 278 general practice patients with acute exacerbations of chronic bronchitis to amoxicillin or a placebo. Smoking history was not reported. Based on blinded physician assessments, there were no differences in clinical outcomes between the amoxicillin (63 percent) or placebo (64 percent) groups after eight days. Although peak expiratory flows improved in all patients, there were no differences between the groups.
These studies are limited by a small sample size and low statistical power, which likely reduced the ability to detect antibiotic efficacy. One study of hospitalized patients included patients with radiographic infiltrates, suggesting pneumonia ( Elmes et al. 1965 ); other studies of inpatients did not explicitly exclude persons with pneumonia ( Petersen et al. 1967 ; Pines et al. 1968 ). Inclusion of patients with pneumonia would likely inflate the apparent efficacy of antibiotics in acute COPD exacerbations. Although most patients with chronic bronchitis have smoked cigarettes, most studies did not report smoking histories ( Elmes et al. 1957 , 1965 ; Berry et al. 1960 ; Fear and Edwards 1962 ; Petersen et al. 1967 ; Pines et al. 1972 ; Nicotra et al. 1982 ; Anthonisen et al. 1987 ; Jørgensen et al. 1992 ). Even if the efficacy of antibiotics were to suggest that smoking plays a causal role in acute bacterial infections, none of the studies separated remote effects from immediate effects of cigarette smoking on the risk of infection. Remote effects of smoking on acute respiratory infections are those mediated through chronic airway obstruction, mucous hyper-secretion, and impaired mucociliary clearance; immediate effects are the alteration of immune and inflammatory functions ( USDHHS 1990 ).
The limitations of low study power were addressed by a meta-analysis that combined 11 of the randomized controlled trials ( Elmes et al. 1957 , 1965 ; Berry et al. 1960 ; Fear and Edwards 1962 ; Petersen et al. 1967 ; Pines et al. 1968 , 1972 ; Nicotra et al. 1982 ; Anthonisen et al. 1987 ; Jørgensen et al. 1992 ; Sachs et al. 1995 ). Because the studies used many different outcome measures, Saint and colleagues (1995) calculated a standardized effect size. The overall summary effect size, which was the difference between mean outcomes in the antibiotic and placebo groups divided by the pooled standard deviation, was 0.22 (95 percent CI , 0.10–0.34), indicating a small benefit from antibiotics. Combining the six trials that measured peak expiratory flow rates yielded a summary improvement of 10.75 liters per minute with antibiotic treatments (95 percent CI, 4.96–16.54 liters per minute).
Observational data also support the efficacy of antibiotics in treating acute exacerbations of COPD . A nonrandomized clinical trial examined the efficacy of cefaclor in 106 outpatients with acute exacerbations of chronic bronchitis ( Cazzola et al. 1991 ). In this trial all patients were current cigarette smokers, and potentially pathogenic bacteria were isolated from the sputum of most participants. On the basis of clinical examinations, the majority of patients were considered to be cured (75.5 percent) or improved (17 percent). There was no significant change in pulmonary function. A major limitation of this trial is the absence of a placebo control group. Taken together with randomized trials, this trial suggests the efficacy of antibiotics for current smokers with acute exacerbations of chronic bronchitis.
A cohort study examined 173 patients who had 362 emergency department visits for acute exacerbations of COPD during an 18-month period ( Adams et al. 2000 ). For patients to be included, the investigators required evidence of airway obstruction verified by pulmonary function testing during the previous three years. Of 1,754 patient visits to the emergency department for an acute COPD exacerbation, 1,392 were excluded. The most common reason for exclusion was no record of recent pulmonary function testing (1,122 visits). Although antibiotics were prescribed preferentially to patients with more severe exacerbations, antibiotic administration was associated with a lower proportion of recurrent emergency department visits during the ensuing 14 days (19 percent versus 32 percent, p <0.001). Active cigarette smoking was associated with a greater risk of relapse ( OR = 4.45 [95 percent CI , 2.09–10.13]), which suggests that smoking may increase the severity of an acute exacerbation. Selection bias, introduced by excluding many emergency department visits by patients without recent pulmonary function testing, limits any conclusions based on this study.
Prevention of COPD Exacerbation. Randomized trials of antibiotic prophylaxis in patients with COPD, conducted mostly in the 1950s and 1960s, provide evidence on cigarette smoking and the risk of respiratory infections in persons with chronic lung disease. If data indicate that antibiotics could prevent exacerbations of COPD, the indication would be that bacterial infection plays a role in COPD exacerbation. Because smoking is the principal cause of COPD, smoking would then have been shown to act on the causal pathway to acute bacterial respiratory infections in this patient group.
Placebo-controlled, randomized clinical trials have tested a variety of antibiotics, including tetracycline, penicillin, sulfonamides, and combination agents ( Table 4.12 ). Preventive treatment with antibiotics was administered for 2 weeks to 20 months, with treatment in most trials lasting 4 to 6 months during the winter months ( McVay and Sprunt 1953 ; Buchanan et al. 1958 ; Cherniack et al. 1959 ; Francis and Spicer 1960 ; Pirdie et al. 1960 ; Davis et al. 1961 , 1965 ; Francis et al. 1961 ; Johnston et al. 1961 , 1969 ; Fear and Edwards 1962 ; Medical Research Council 1966 ; Pines 1967 ; Liippo et al. 1987 ). Only three trials reported smoking status: 79 to 95 percent ever smoked, and 29 to 79 percent were current smokers ( Medical Research Council 1966 ; Johnston et al. 1969 ; Liippo et al. 1987 ).
Studies on the efficacy of antibiotic preventive treatment of persons with chronic obstructive pulmonary disease.
Of the various study outcomes examined, preventive antibiotics have demonstrated the most consistent efficacy in reducing missed workdays among persons with chronic bronchitis ( Table 4.12 ). In two early large-scale, well-conducted clinical trials, Francis and Spicer (1960) and Francis and colleagues (1961) demonstrated that the prophylactic administration of tetracycline decreased the number of lost workdays by about 50 percent. The benefits of penicillin were less clear. A later clinical trial conducted by the Medical Research Council (1966) of Great Britain also suggested that oxytetracycline reduced the duration of missed workdays (22 percent reduction, 95 percent CI , 55 percent reduction to 4 percent increase, but the CI did not exclude a lack of benefit). Smaller or less well-controlled trials suggested that antibiotic prophylaxis reduced lost workdays ( Pirdie et al. 1960 ; Johnston et al. 1961 , 1969 ).
The salutary impact of prophylactic antibiotics on other clinical outcomes has been less consistent. Some clinical trials demonstrated that preventive antibiotics reduced acute exacerbations of chronic bronchitis ( McVay and Sprunt 1953 ; Buchanan et al. 1958 ; Cherniack et al. 1959 ; Davis et al. 1961 ; Pines 1967 ), whereas others showed no benefit ( Francis and Spicer 1960 ; Francis et al. 1961 ; Davis et al. 1965 ; Medical Research Council 1966 ; Johnston et al. 1969 ; Liippo et al. 1987 ). Despite reducing lost workdays, the two early British trials found that antibiotics did not reduce the incidence of symptomatic exacerbation, suggesting an effect mostly on symptom severity or duration ( Francis and Spicer 1960 ; Francis et al. 1961 ). Although patients receiving prophylactic antibiotics may experience subjective ( McVay and Sprunt 1953 ) or clinical improvements as determined by physicians ( Fear and Edwards 1962 ), these benefits were not always observed ( Davis et al. 1961 , 1965 ; Johnston et al. 1961 ). In all trials that examined pulmonary function, antibiotics were not associated with any benefit ( Francis and Spicer 1960 ; Pirdie et al. 1960 ; Davis et al. 1961 , 1965 ; Medical Research Council 1966 ; Johnston et al. 1969 ; Liippo et al. 1987 ). Taken together, the conflicting evidence does not allow for a clear conclusion regarding the efficacy of prophylactic antibiotics in persons with COPD .
Randomized, placebo-controlled clinical trials tested the efficacy of an oral vaccination against formalin-killed H. influenzae bacteria in patients with COPD ( Clancy et al. 1985 , 1990 ; Lehmann et al. 1991 ; Tandon and Gebski 1991 ). The efficacy of vaccinations would support a role for bacterial infections in acute exacerbations of COPD, with smoking acting on the causal pathway. Most persons in these trials reported having ever smoked cigarettes (78 to 91 percent), and fewer indicated current smoking (10 to 73 percent). In an early trial of 50 patients, Clancy and colleagues (1985) reported a tenfold reduction in the cumulative incidence of acute episodes of bronchitis after oral immunizations (6 percent in the placebo group versus 63 percent in the immunized group, RR = 0.10 [95 percent CI , 0.014–0.64]). The same investigators demonstrated in a subsequent controlled trial ( n = 40) a reduction in episodes of acute wheezy bronchitis (30 percent versus 80 percent, RR = 0.38 [95 percent CI, 0.19–0.76]) and a decreased use of antibiotics (25 percent versus 60 percent, RR = 0.42 [95 percent CI, 0.18–0.96]) ( Clancy et al. 1990 ). The study also suggested a reduction in the cumulative incidence of acute bronchitis exacerbations (50 percent versus 80 percent, RR = 0.63 [95 percent CI, 0.38–1.02]). Compared with the placebo group, the group that received oral vaccinations had no reductions in symptom duration or reports of dyspnea, and no improvement in FEV 1 . The RRs and CIs for both studies by Clancy and colleagues (1985 , 1990) were not published; the calculations were based on data available in the papers. A similar trial conducted in the highlands of Papua, New Guinea, enrolled 62 adults with chronic bronchitis ( Lehmann et al. 1991 ). Oral vaccinations were associated with a reduced risk of acute bronchitis (RR for placebo group = 1.92 [95 percent CI, 1.58–2.26]). There was no impact on the risk of pneumonia (RR = 0.66 [95 percent CI, 0.23–1.09]). In a similar study of 64 persons with chronic bronchitis, an oral vaccination was associated with a reduced risk of acute lower respiratory tract infections ( OR = 0.4 [95 percent CI, 0.2–0.9]) and improved general well-being assessed by a visual analog scale (median score 5.0 versus 2.5) ( Tandon and Gebski 1991 ).
Large-scale randomized controlled trials also have examined the efficacy of an oral vaccination with OM-85 BV, an antigenic extract of eight microorganisms commonly found in the respiratory tract that has been subjected to alkaline lysis. These agents are thought to activate lung macrophages and enhance antigen presentation to T lymphocytes ( Collet et al. 1997 ). For the following studies, the RRs and CIs were calculated based on data available in the papers. In a study by Orcel and colleagues (1994) , 354 adults aged 65 years or older with chronic bronchitis were randomly selected to receive OM-85 BV or a placebo. Of these patients, 51 percent had ever smoked and 25 percent were current smokers. Among the 290 patients analyzed, the cumulative incidence of acute lower respiratory tract infections was lower in the active treatment group (35 percent versus 52 percent, RR = 0.67 [95 percent CI , 0.51–0.88]). More recently, Collet and colleagues (1997) conducted a multicenter trial that enrolled patients with COPD , a history of heavy smoking (20 or more pack-years 1 ), and airway obstruction ( FEV 1 less than 70 percent predicted). There was no difference in the cumulative incidence of acute symptomatic exacerbation between the placebo group and the treatment group (44.5 percent versus 43.7 percent, RR = 1.02 [95 percent CI, 0.81–1.28]). The risk of hospitalization for a respiratory problem was lower in the treatment group (16.2 percent versus 23.2 percent, RR = 0.70 [95 percent CI, 0.46–1.06]). Moreover, the average duration of hospitalization for a respiratory problem was lower in the oral vaccination group (1.5 versus 3.4 days per person). The treatment had no impact on FEV 1 levels, which declined 5.5 mL in the treatment group and 7.5 mL in the placebo group, or on a health-related quality-of-life index (health status questionnaire SF-36 physical and mental component summary scores and eight subscales). Although the evidence is mixed, the oral vaccination trials suggest that bacterial infections play a role in COPD exacerbations and that smoking, as the major cause of COPD, acts on the causal pathway to acute infections.
Antibiotics and Acute Bronchitis. Clinical trials assessing the efficacy of antibiotic treatments for acute bronchitis also indirectly addressed the role of smoking in acute respiratory infections among persons with chronic lung disease ( Howie and Clark 1970 ; Stott and West 1976 ; Franks and Gleiner 1984 ; Williamson 1984 ; Brickfield et al. 1986 ; Dunlay et al. 1987 ; Scherl et al. 1987 ; Hueston 1994 ; Verheij et al. 1994 ; King et al. 1996 ). Although these clinical trials excluded persons with overt COPD , the prevalence of current smoking among patients was substantial (32 to 55 percent). In three trials, at least 50 percent of patients indicated current smoking ( Howie and Clark 1970 ; Franks and Gleiner 1984 ; Hueston 1994 ). Other reviews have established the strong association between current smoking and a decrement in pulmonary function ( USDHHS 1990 ; see “Chronic Respiratory Diseases” later in this chapter). Epidemiologic studies also indicate a higher risk of acute bronchitis in persons with COPD ( Monto and Ross 1977 , 1978 ). As a consequence, these clinical trials of acute bronchitis likely included persons with smoking-related airway obstruction.
Taken together, these randomized, double-blind, controlled clinical trials suggest that antibiotic treatments provide a small clinical benefit compared with a placebo ( Howie and Clark 1970 ; Stott and West 1976 ; Franks and Gleiner 1984 ; Williamson 1984 ; Brickfield et al. 1986 ; Dunlay et al. 1987 ; Scherl et al. 1987 ; Hueston 1994 ; Verheij et al. 1994 ; King et al. 1996 ). A meta-analysis of these clinical trials indicated that antibiotic treatments were associated with a duration of cough and sputum production that was one-half day shorter ( Bent et al. 1999 ). The efficacy of antibiotics supports a causal role of bacterial infections in acute bronchitis.
Of the five clinical trials that used current smoking status to stratify analyses of clinical outcomes ( Franks and Gleiner 1984 ; Brickfield et al. 1986 ; Dunlay et al. 1987 ; Verheij et al. 1994 ; King et al. 1996 ), all but one found no evidence of an effect modification from smoking ( Brickfield et al. 1986 ). All of the studies found a similar salutary effect from antibiotics on the duration of respiratory symptoms in both smokers and nonsmokers ( Franks and Gleiner 1984 ; Brickfield et al. 1986 ; Dunlay et al. 1987 ; Verheij et al. 1994 ; King et al. 1996 ). In a randomized, placebo-controlled trial of erythromycin for acute bronchitis involving 50 patients from a family practice clinic, antibiotics appeared to attenuate the duration of coughing and sputum production only among non-smokers ( Brickfield et al. 1986 ). Although these studies are limited by low power for stratified analysis, the overall evidence suggests no difference in antibiotic efficacy between smokers or nonsmokers.
These findings suggest that the incidence of bacterial infection as a cause of acute bronchitis is similar in smokers and nonsmokers. As a consequence, these studies provide indirect evidence that current smoking does not cause acute bacterial bronchitis in persons who, on average, are likely to have decreased pulmonary function. A major limitation of these studies is the absence of any evaluation of viral respiratory infections.
Although previous Surgeon General’s reports have examined the effects of smoking on acute respiratory infections ( USDHHS 1990 , 1994 ), the impact of smoking on persons with a preexisting chronic lung disease was not previously reviewed. The preponderance of evidence presented in this section implicates smoking as a cause of acute respiratory infections among persons with COPD . The Tecumseh study indicated that COPD predisposes smokers to a greater risk of acute respiratory infections, and more recent data confirm that COPD is strongly associated with the development of invasive pneumococcal disease ( Nuorti et al. 2000 ). Although the epidemiologic data are not consistent across studies and study outcomes (i.e., self-reported acute respiratory infection, serologic evidence, pulmonary function decrement, and death from respiratory infection), controlled clinical trials have established the efficacy of antibiotics in treating acute COPD exacerbations. Clinical trials of antibiotics as a prophylaxis against acute infections yielded conflicting results and did not clearly establish efficacy in persons with COPD. The evidence did not clearly establish efficacy in persons with COPD, or whether smoking increases the frequency of acute bacterial bronchitis or modifies the effects of antibiotics in persons with reduced lung function. The oral vaccination trials indicated a reduction in the risk of acute infections. However, none of these studies explicitly evaluated the interaction between COPD and smoking, which would directly address the specific effects of smoking on acute respiratory infections in persons with chronic lung diseases.
Taken together, the epidemiologic and clinical trial evidence indicates that smoking probably acts on the causal pathway to an acute respiratory infection in persons with COPD . However, studies did not clearly separate the risk from remote effects of cigarette smoking (mediated by chronic airway obstruction and its attendant complications) from the immediate effects (through the alteration of immune or inflammatory functions). In vitro and in vivo studies support a biologic basis for the immediate adverse impact of smoking on acute respiratory infections.
The data also support an exposure-response relationship between smoking intensity and the risk of chronic bronchitis ( Monto and Ross 1978 ) and the risk of self-reported acute lower respiratory tract infections among persons with chronic bronchitis ( Monto and Ross 1978 ). For other outcome measures, exposure-response relationships have not been clearly demonstrated ( Monto and Ross 1977 ). One investigation demonstrated an association between smoking intensity and the risk of death from an infection among persons with COPD ( Prescott et al. 1995 ).
The evidence supports the causal role of cigarette smoking in acute asthma exacerbations, and acute respiratory viral infections are an important cause of asthma exacerbations. As a consequence, smoking may precipitate an exacerbation by promoting a viral infection. However, evidence does not directly address this possible mechanism, and further research is needed to clarify the precise impact of smoking on acute asthma.
- Conclusions
- The evidence is suggestive but not sufficient to infer a causal relationship between smoking and acute respiratory infections among persons with preexisting chronic obstructive pulmonary disease.
- In persons with asthma, the evidence is inadequate to infer the presence or absence of a causal relationship between smoking and acute asthma exacerbation.
Both COPD and asthma are chronic respiratory conditions associated with substantial morbidity, activity limitation, and economic costs. Although sufficient data exist to infer a causal relationship between smoking and an increased risk for acute respiratory infections in persons without chronic respiratory diseases, effects in persons with chronic lung diseases are less clearly established. Further research should specifically evaluate the impact of current smoking status on acute respiratory infections among persons with COPD and asthma. Particularly in persons with COPD, the effects of past and current smoking should be evaluated both separately and together. The effects of current and past smoking intensity also should be examined.
Conclusive data confirming the health care costs of smoking-related respiratory infections would place the problem in a larger public health context. Clinical practice guidelines could then incorporate more precise information about the potential benefits of smoking cessation.
- Chronic Respiratory Diseases
Chronic respiratory diseases are a heterogeneous group of disorders that affect mainly the conducting airways and alveoli, two main components of the respiratory system. A major function of the airways is to conduct air to the alveoli, also known as the lung parenchyma, where gas exchange occurs. There, oxygen is taken up by red blood cells, and carbon dioxide is removed from the bloodstream. In addition, the airways provide defenses against inhaled particles and other agents that impact the airway walls.
Past reports of the Surgeon General on active cigarette smoking and chronic respiratory diseases have emphasized respiratory symptoms, lung function, and COPD . Key conclusions of those reports relevant to these topics are summarized in Table 4.13 . Although these topics continue to be important public health concerns and are updated in this review, this report also addresses other chronic respiratory diseases including diseases of the airways, such as asthma, and diffuse parenchymal lung diseases, such as pulmonary fibrosis. The rationale for broadening the scope of diseases discussed in this report is based on a growing body of research on associations of cigarette smoking with other chronic respiratory diseases. The potential for synergism between cigarette smoking and specific occupational exposures, which was reviewed in the 1985 Surgeon General’s report ( USDHHS 1985 ), is not considered in this report.
Conclusions from previous Surgeon General’s reports concerning smoking as a cause of chronic respiratory diseases.
Because of the extensive literature reviews in previous Surgeon General’s reports on chronic respiratory diseases, this section is limited largely to research published between 1989 and January 2000. The search strategy used to identify references in the MEDLINE database included smoking as a major MEDLINE term, or smoking as a descriptor with tobacco or smoking in the title field. These terms were then linked to lung growth and development, lung function, respiratory symptoms, obstructive lung diseases, asthma, and pulmonary fibrosis. In addition, tables of contents were reviewed from two publications, American Journal of Respiratory and Critical Care Medicine and Thorax , for issues published through April 2000.
The organization of this review follows lung growth and development through developmental periods (i.e., childhood versus adulthood) during which time the various respiratory diseases become clinically apparent. The available evidence suggests that the development of chronic respiratory diseases, particularly chronic airflow obstruction, may result from impaired lung development and growth, a premature onset of declining lung function, an accelerated decline in lung function, or any combination of these conditions ( Figure 4.1 ).
Theoretical curves depicting varying rates of decline of forced expiratory volume in one second (FEV 1 ). Note: Curves A and B represent never smokers and smokers, respectively, declining at normal rates. Curve C shows increased declines without the development (more...)
Airway development in utero, alveolar proliferation during the first 12 through 24 months of life ( Burri 1997 ), and lung growth to adulthood are critical to the level of mechanical functioning of the lungs. Impaired growth in utero from exposure to maternal smoking may begin a process that predisposes the infant to chronic respiratory diseases in childhood or adulthood. Exposure to secondhand smoke in infancy and childhood, and active smoking during childhood and adolescence, further contribute to impaired lung growth and the risk of developing respiratory diseases ( Fletcher et al. 1976 ; Samet et al. 1983 ; USDHHS 1984 ; Tager et al. 1988 ; Sherrill et al. 1991 ; Helms 1994 ; Samet and Lange 1996 ). Active smoking in adulthood leads to an accelerated decline of FEV 1 in some smokers and ultimately to the development of clinically apparent COPD ( USDHHS 1984 ).
Lung Development In Utero
Although measuring lung function during infancy to detect in utero effects presents many challenges and is an evolving technique, during the past decade our knowledge about the effects of maternal smoking during pregnancy has grown ( Dezateux and Stocks 1997 ; Morgan and Martinez 1998 ). Studies have consistently documented evidence of impaired lung function in early infancy following in utero exposure to maternal smoking ( Table 4.14 ) ( Young et al. 1991 ; Hanrahan et al. 1992 ; Tager et al. 1995 ; Stick et al. 1996 ; Lødrup Carlsen et al. 1997 ; Hoo et al. 1998 ; Dezateux et al. 1999 ; Milner et al. 1999 ). A number of measures of ventilatory function have been used, including (1) measures of expiratory flow: maximal flow at functional residual capacity ( V max FRC ) and the ratio of time to peak tidal expiratory flow to expiratory time ( tPTEF/tE ); (2) airway resistance and respiratory system conductance; and (3) respiratory system compliance. In addition, bronchial responsiveness to pharmacologic agents has been measured in a smaller number of studies ( Young et al. 1991 ; Clarke et al. 1995 ).
Studies on the association between maternal smoking during pregnancy and infant lung function.
To determine the effects of in utero exposures to maternal smoking, separate from later exposures to secondhand smoke and lower respiratory tract infections, pulmonary function tests have been performed in healthy infants soon after birth and even before hospital discharge ( Stick et al. 1996 ; Lødrup Carlsen et al. 1997 ; Hoo et al. 1998 ; Milner et al. 1999 ). Three studies that looked at examinations conducted before hospital discharge identified decrements in tPTEF/tE in relation to maternal smoking during pregnancy ( Stick et al. 1996 ; Lødrup Carlsen et al. 1997 ; Hoo et al. 1998 ). Instead of using a measure of airflow, Milner and colleagues (1999) measured respiratory system conductance and respiratory system compliance and found decrements in these parameters that differed between male and female infants ( Table 4.14 ). An inverse dose-response relationship between the number of cigarettes smoked per day during pregnancy and the level of pulmonary function was found in two of the investigations ( Stick et al. 1996 ; Lødrup Carlsen et al. 1997 ).
Further evidence for an adverse effect from maternal smoking during pregnancy has been found in infants who had pulmonary function measurements later in infancy but before having any LRI ( Young et al. 1991 ; Hanrahan et al. 1992 ; Tager et al. 1995 ; Dezateux et al. 1999 ). Young and colleagues (1991) measured pulmonary function and airway hyper-responsiveness to histamine in 63 healthy infants from a prenatal clinic in Perth, Australia. The infants were categorized into four groups on the basis of a family history of asthma and parental cigarette smoking during pregnancy, but prenatal and postnatal exposures to cigarette smoke could not be separated. At a mean age of 4.5 weeks, rates of forced expiratory flow ( FEF ) did not differ among the four groups. However, airway responsiveness was greater in infants whose parents had smoked during pregnancy.
An increased risk of lower respiratory tract illnesses, including wheezing, and subsequent reductions in expiratory airflow and airway hyperresponsiveness during infancy may be consequences of maternal smoking during pregnancy ( Martinez et al. 1988 ; Stick et al. 1991 ; Tager et al. 1993 ; Clarke et al. 1995 ; Dezateux et al. 1999 ). Martinez and colleagues (1988) measured pulmonary function in 124 infants from Tucson, Arizona, before any lower respiratory tract illness had occurred, and found that infants whose total respiratory conductance was in the lowest third of the group had an increased risk of a subsequent wheezing illness ( OR = 3.7 [95 percent CI , 0.9–15.5]). In a sample of 97 infants from the East Boston, Massachusetts, Neighborhood Health Center, Tager and colleagues (1993) found an association between maternal smoking during pregnancy and an elevated risk for lower respiratory tract illnesses (OR = 1.47 [95 percent CI, 1.08–1.99]). Clarke and colleagues (1995) conducted pulmonary function studies on 79 healthy infants approximately one month of age and followed them during their first year of life. Lower expiratory airflow was associated with a wheezing illness in boys but not in girls, and bronchial hyperreactivity was associated with a wheezing illness in girls but not boys. Dezateux and colleagues (1999) found a significantly higher expiratory airway resistance before there was any evidence of a lower respiratory tract illness in 28 infants who had developed at least one subsequent wheezing illness by one year of age or less, compared with 73 infants who did not have a wheezing illness.
The decrement in pulmonary function associated with in utero exposure to tobacco smoke that is detectable at birth and throughout infancy may persist across childhood and into adulthood. In a cross-sectional survey, Cunningham and colleagues (1994) measured pulmonary function in 8,863 children aged 8 through 12 years from 22 North American communities. In multivariate analyses the children whose mothers reported smoking during pregnancy had significantly lower FEFs and reductions in FEV 0.75 and FEV 1 / FVC , compared with the children of mothers who did not smoke during pregnancy. After adjusting for maternal smoking during pregnancy, current maternal smoking was not associated with a significant decrement in lung function. Gilliland and colleagues (2000) examined the relationship between maternal smoking and pulmonary function among 3,357 school children (grades 4, 7, and 10) living in 12 southern California communities. After adjusting for secondhand smoke exposure and other potential confounders, maternal smoking during pregnancy was associated with significant decrements in peak expiratory flows, maximum midexpiratory flows, and FEFs at 75 percent of FVC, but not in FEV 1 levels.
These findings consistently show the effects of maternal smoking during pregnancy, including impaired pulmonary function and lower respiratory tract illnesses during infancy and childhood. Evidence for a causal role of maternal smoking is further strengthened by the dose-response relationship between maternal smoking during pregnancy and the magnitude of decrements in pulmonary function ( Stick et al. 1996 ; Lødrup Carlsen et al. 1997 ). Because these studies have been restricted to healthy full-term infants, it is unlikely that the findings are a result of other factors that may adversely affect in utero development including poor maternal nutrition, alcohol use, or the intake of other potentially toxic agents.
In utero exposure to maternal smoking may be associated with lower respiratory tract illnesses in childhood, and the subsequent risk for chronic respiratory diseases in adulthood through its effect on birth weights. Lower birth weight has been associated with reduced lung function in childhood. Data on the relationship between birth weight and adult lung function also provide similar indirect evidence ( Chan et al. 1989 ; Barker et al. 1991 ; Rona et al. 1993 ). Maternal smoking during pregnancy has been associated with decreased birth weights (see Chapter 5 , “Reproductive Effects”), and several studies indicate that birth weight is directly related to the level of expiratory airflow during childhood ( Chan et al. 1989 ; Rona et al. 1993 ) and adulthood ( Barker et al. 1991 ). Furthermore, self-reports of childhood lower respiratory tract illnesses are associated with chronic airflow obstruction in adulthood ( Berglund et al. 1999 ).
- The evidence is sufficient to infer a causal relationship between maternal smoking during pregnancy and a reduction of lung function in infants.
- The evidence is suggestive but not sufficient to infer a causal relationship between maternal smoking during pregnancy and an increase in the frequency of lower respiratory tract illnesses during infancy.
- The evidence is suggestive but not sufficient to infer a causal relationship between maternal smoking during pregnancy and an increased risk for impaired lung function in childhood and adulthood.
Implication
Although the biologic basis for impaired infant lung function from maternal smoking during pregnancy is not yet fully understood, the causal link provides yet another strong rationale for smoking cessation during pregnancy.
Pathogenesis of Smoking-Induced Lung Injury
The rate of expiratory airflow depends on elastic recoil forces of the alveoli and on the diameter of the small airways. Complex interactions between smoking-caused changes in the structure and function of small airways and lung parenchyma result in the physiologic finding of chronic airflow limitation ( Wright 1992 ; Thurlbeck 1994 ). The literature relevant to understanding the mechanisms of smoking-induced COPD has grown substantially in recent years, and points to a complex interplay among a number of biologic processes including oxidative stress, inflammation, protease-antiprotease imbalances, repair processes, and the genetic variations that control these processes ( Figure 4.2 ) ( Sandford et al. 1997 ; Barnes 1999 ; MacNee and Rahman 1999 ). The inhalation of cigarette smoke exposes the lungs to high concentrations of oxidant agents and free radicals, which decrease the antioxidant capacity that normally protects epithelial cells from oxidant injury ( Repine et al. 1997 ; Rahman and MacNee 1999 ). Moreover, several enzymes found in the lungs generate reactive oxygen molecules that may contribute further to the oxidative stress in the lungs. Genetic variations that alter the function of enzymes that generate reactive oxygen molecules, or that affect the activity of antioxidant enzymes, may determine individual susceptibility to COPD from cigarette smoking ( Barnes 1999 ).
Summary diagram of cigarette-related mechanisms of lung injury. Source: MacNee and Rahman 1999, p. S63. Reprinted with permission.
Epithelial injury results in the release of proinflammatory mediators (i.e., cytokines) from epithelial cells and inflammatory cells in the airway walls (i.e., lymphocytes and macrophages). These mediators lead to an influx of neutrophils, which also release mediators that perpetuate the cycle of injury and inflammation ( Figure 4.2 ) ( MacNee and Rahman 1999 ; Mills et al. 1999 ). The inflammatory process is found in the central airways, peripheral airways, and lung parenchyma, even in smokers with normal lung function ( Saetta 1999 ; Saetta et al. 2001 ). Although an inflammatory process in the small airways (respiratory bronchiolitis) appears to develop in all cigarette smokers, in susceptible smokers the injury progresses and leads to a narrowing of these airways ( Bosken et al. 1990 ; USDHHS 1990 ; Aguayo 1994 ). Available evidence suggests that changes in the structure and function of small airways (bronchioles) are fundamental to the development of smoking-induced COPD ( Wright 1992 ; Thurlbeck 1994 ). Genetic variations that alter the function of several inflammatory mediators, and thus the type of inflammatory response, probably contribute in part to susceptibility to COPD ( Barnes 1999 ). For example, smokers with COPD have a predominance of CD8-positive T lymphocytes in the central and peripheral airways compared with smokers without COPD ( O’Shaughnessy et al. 1997 ; Saetta et al. 1998 , 2001 ).
The inflammatory process may extend into the peribronchiolar alveoli and destroy the alveolar walls—the hallmark of emphysema—when there is an imbalance between proteases and antiproteases. Proteases are enzymes released from neutrophils and macrophages that degrade structural proteins (e. g ., elastin and collagen) of the airways and lung parenchyma. Evidence for increased elastin degradation was reported by Gottlieb and colleagues (1996) , who found increased urine desmosine (a by-product of elastin degradation) in smokers who had rapid declines in lung function. Antiproteases released from macrophages and the liver provide a natural defense against proteases. A deficiency in alpha 1 -antitrypsin, an antiprotease, is a rare genetic variation that causes emphysema, but it is found only in 1 to 2 percent of patients with COPD .
To date, except for an alpha 1 -antitrypsin deficiency, the role of genetic variations in the development of COPD has received limited attention ( Sandford et al. 1997 ; Barnes 1999 ; Takizawa et al. 2001 ). Family studies have demonstrated a genetic influence on the level of FEV 1 , and segregation analysis has provided evidence that the effect is polygenic. Moreover, in case-control studies of COPD patients, a family history of COPD has proven to be a risk factor for COPD. Candidate genes for susceptibility to cigarette smoke and COPD that are under active investigation include the numerous genes that control peripheral airway inflammation, oxidant levels, and the protease-antiprotease balance ( Higham et al. 2000 ; Sakao et al. 2001 ; Sandford et al. 2001 ).
- Active smoking causes injurious biologic processes (i.e., oxidant stress, inflammation, and a protease-antiprotease imbalance) that result in airway and alveolar injury. This injury, if sustained, ultimately leads to the development of chronic obstructive pulmonary disease.
Although smoking prevention and cessation remain the cornerstones for preventing smoking-induced chronic respiratory diseases ( USDHHS 1990 ), further research on the biologic mechanisms of airway and alveolar injury caused by smoking may provide new approaches for preventing smoking-induced lung diseases among smokers unable to quit.
Growth of Lung Function in Infancy and Childhood
In addition to the adverse effects on pulmonary function of in utero exposure to maternal smoking and postnatal exposure to parental smoking ( National Research Council 1986 ; USDHHS 1986 ; U.S. Environmental Protection Agency 1992 ), active cigarette smoking during childhood and adolescence has the potential for retarding the rate of lung growth and the level of maximum lung function ( Table 4.13 ) ( USDHHS 1994 ), thus increasing the risk for COPD in adulthood ( Figure 4.1 ). Results from six cohort studies of lung function in children and adolescents published from 1982–1992 were reviewed in the 1994 Surgeon General’s report ( USDHHS 1994 ). Two representative publications from that report ( Tager et al. 1985 , 1988 ) are summarized here along with two investigations that were not reviewed in the 1994 report ( Sherrill et al. 1991 ; Gold et al. 1996 ).
In a longitudinal study of 669 children and adolescents aged 5 through 19 years in East Boston, Massachusetts, Tager and colleagues (1985) found that among adolescents who started to smoke at 15 years of age and continued to smoke, the percent predicted FEV 1 level at 20 years of age was only 92 percent of the expected FEV 1 level for nonsmokers. Subsequently, Tager and colleagues (1988) analyzed spirometric measurements from at least one FVC test performed during 1975–1985 in each of 974 females and 913 males aged 5 years and older. For girls, a linear increase in FEV 1 levels ended approximately one year earlier for current smokers (at 17 years of age) than for nonsmokers without respiratory symptoms (at 18 years of age); the average maximal FEV 1 values were 2.9 L and 3.1 L, respectively. For nonsmokers with respiratory symptoms, the estimated maximal FEV 1 level was identical to that for current smokers (2.9 L). For boys, the estimated maximal FEV 1 level was identical for asymptomatic nonsmokers (those who do not have a diagnosis of chronic bronchitis or emphysema, or evidence of chronic respiratory symptoms), symptomatic non-smokers, and current smokers (4.9 L), but was attained at a much earlier age for current smokers (at 18 through 19 years of age) compared with asymptomatic non-smokers (aged 20 through 34 years) and symptomatic nonsmokers (21 years). Sherrill and colleagues (1991) assessed growth curves in smokers classified as asymptomatic. They found that among women, cessation of lung function growth occurred at 22 years of age in asymptomatic smokers and at 23 years of age in asymptomatic women who had never smoked. Among female smokers with respiratory symptoms, lung function growth ended at 21 years of age, three years earlier than for those who had never smoked. Among asymptomatic men, the authors found no differences in the age of lung growth cessation between nonsmokers and smokers (23 years of age). Among symptomatic male smokers, however, lung growth cessation occurred at a younger age (25 years of age) compared with symptomatic nonsmokers (27 years of age).
In a cohort of 4,902 girls and 5,158 boys from 10 to 18 years of age tested annually with spirometry, Gold and colleagues (1996) examined the effects of cigarette smoking on the rate of lung function growth and the level of lung function attained. Among girls smoking five or more cigarettes per day, the rate of increase in FEV 1 levels was slower by 31 mL /year (95 percent CI , 16.0–46.0 mL/year) than among girls who had never smoked. At 17 to 18 years of age, FEV 1 levels began to decline among girls who smoked while staying at a plateau among girls who did not smoke. Although smoking five or more cigarettes per day slowed the rate of increase in FEV 1 levels in boys, the magnitude of the effect (slower by 9 mL/year; 95 percent CI, −6.0 to 24.0 mL/year) was less than that in girls. There was an inverse association between the amount smoked and the level of FEV 1 / FVC and FEF between 25 and 75 percent of the FVC (FEF 25–75% ). The number of cigarettes smoked was not associated with FVC or FEV 1 levels.
There have been only a limited number of longitudinal investigations of active smoking during childhood and adolescence because of the complex logistics of such studies. However, the findings are consistent for various populations. In smokers, lung function growth is slower during childhood and adolescence, prematurely ceases, and begins to decline in late adolescence and early adulthood. The evidence suggests a causal role for active smoking. This causal link is strengthened by the finding of a dose-response relationship between smoking and the level of FEV 1 / FVC and between smoking and FEF 25–75% . Additionally, the inflammatory process caused by smoking would be initiated at any age, and the lungs of young smokers show evidence of airways inflammation and injury.
- The evidence is sufficient to infer a causal relationship between active smoking and impaired lung growth during childhood and adolescence.
- The evidence is sufficient to infer a causal relationship between active smoking and the early onset of lung function decline during late adolescence and early adulthood.
These conclusions provide a strong rationale for interventions to prevent children and adolescents from starting to smoke and for helping young smokers to quit. Future studies should determine the effects of smoking cessation on the rate of lung growth, and they should follow smokers from adolescence into their fourth and fifth decades of life when COPD is first diagnosed. Addressing these gaps in knowledge could provide further evidence of a causal link between active smoking during childhood and the risk for later development of COPD.
Decline of Lung Function
Results from longitudinal investigations of adults between their second and third decades—the period of transition from lung growth to a plateau of variable length and then to decline—suggest that cigarette smoking causes a premature onset of lung function decline and, to a lesser extent, a more rapid decline ( Tager et al. 1988 ; Sherrill et al. 1991 ). In the East Boston study, estimates of the age range when lung function begins to decline were wide but tended to be earlier for current smokers compared with asymptomatic or symptomatic nonsmokers ( Tager et al. 1988 ). After the period of maximal lung growth, there is a prolonged plateau period for the FEV 1 level in nonsmoking men before the FEV 1 declines (late in the fourth decade of life). This decline is estimated to begin 10 years earlier (i.e., late in the third decade of life) in asymptomatic nonsmokers and 15 years earlier in current smokers (i.e., in the middle of the third decade). Among all women, the onset of decline begins at an earlier age compared with that of men, and female current smokers had a more rapid earlier decline (−20 mL /year) and an earlier age of onset of a more rapid decline compared with nonsmoking women. In the population-based study of respiratory diseases in Tucson, Arizona, Sherrill and colleagues (1991) also found that symptom status modified the rate of decline. The rate of decline was similar for asymptomatic male smokers and nonsmokers until approximately 48 years of age, when the average rate of decline for smokers increased from −29 mL/year to −46 mL/year. Among symptomatic smokers, the increased rate of decline occurred at a younger age (34 years of age). The FEV 1 level was lower for symptomatic female smokers beginning in the late teenage years, but there was little difference in the subsequent rate of FEV 1 decline between smokers and nonsmokers.
In cross-sectional and cohort studies of ventilatory function, a higher average rate of FEV 1 decline has been consistently found in current cigarette smokers compared with former smokers and nonsmokers ( Table 4.15 ) ( USDHHS 1984 , 1990 ). In cohort studies the average rate of FEV 1 decline among nonsmokers ranged from 17 to 61 mL /year, and the decline among smokers exceeded the decline among nonsmokers by 7 to 27 mL/year ( USDHHS 1990 ). Furthermore, while the rate of FEV 1 decline for smokers and nonsmokers is highly variable, the distribution of FEV 1 decline rates is shifted toward a higher proportion of sustained smokers with rapid rates of decline. As the amount of cigarette smoking increases, the rate of decline increases ( Xu et al. 1992 , 1994 ; Burchfiel et al. 1996 ; Vestbo et al. 1996 ; Belousova et al. 1997 ; Scanlon et al. 2000 ; Vollmer et al. 2000 ). For some smokers, the increased rate of decline eventually results in a FEV 1 level associated with dyspnea and a limitation of activities; at this level, the clinical diagnosis of COPD is usually made ( Figure 4.1 ).
Studies on the association between smoking and rates of forced expiratory volume in one second (FEV 1 ) decline.
Because not all smokers develop COPD , research is increasingly directed at identifying factors that may heighten susceptibility to rapid rates of FEV 1 decline. Factors that have been examined include gender ( Xu et al. 1994 ; Scanlon et al. 2000 ; Vollmer et al. 2000 ), race and ethnicity ( Scanlon et al. 2000 ; Vollmer et al. 2000 ), alcohol use ( Burchfiel et al. 1996 ), diet and use of nutritional supplements ( Carey et al. 1998 ), anthropometric characteristics ( Burchfiel et al. 1996 ), respiratory symptoms ( Jaakkola et al. 1991a , b ; Sherman et al. 1992 ; Burchfiel et al. 1996 ; Scanlon et al. 2000 ), FEV 1 levels ( Burrows et al. 1987 ; Scanlon et al. 2000 ), airways hyperresponsiveness ( Frew et al. 1992 ; Tashkin et al. 1996 ), comorbid conditions such as asthma and coronary heart disease ( Burchfiel et al. 1996 ; Lange et al. 1998 ), and occupational and environmental exposures ( Xu and Wang 1998 ). Investigations of these factors are ongoing and firm conclusions cannot yet be reached on their roles in modifying the risk for COPD in smokers.
Available investigations provide conflicting results about the relative rates of FEV 1 decline among women who smoke compared with men who smoke ( Xu et al. 1994 ; Scanlon et al. 2000 ; Vollmer et al. 2000 ). Xu and colleagues (1994) suggested that women may have a higher rate of FEV 1 decline. They hypothesized that different distributions of unhealthy participants by gender in nonsmoking reference groups may explain conflicting results in studies that compared rates of FEV 1 decline in women and men. Other factors that may modify the effects of smoking and contribute to gender differences in study findings include the year of birth of study participants (birth cohort) and the time period of a study ( Samet and Lange 1996 ). In a study from the Netherlands, Xu and colleagues (1995) reported a significant interaction between age and birth cohorts in relation to declines in FEV 1 levels in women but not in men. The modifying effects of a birth cohort may partially reflect changes in smoking behavior and perhaps in the products smoked.
Several studies have shown that women have a higher prevalence and degree of bronchial hyperreactivity ( Leynaert et al. 1997 ), associated with an accelerated rate of decline in FEV 1 levels, compared with men ( Tashkin et al. 1996 ; Scanlon et al. 2000 ). This gender difference in bronchial hyperreactivity may contribute to a higher risk in women for developing COPD . Scanlon and colleagues (2000) found in the Lung Health Study that women who continued to smoke over a five-year period had a greater annual decline in FEV 1 levels than did men with comparable levels of smoking (−1.08 percent predicted and −0.77 percent predicted, respectively), but the statistical significance of the difference was not reported. The increased rate of decline among women was associated with a greater degree of bronchial hyperreactivity.
Biologic differences between women and men, including differences in lung mechanics and hormonal factors, may affect susceptibility to the adverse effects of cigarette smoke, but limited data are available to test these hypotheses. Whether there are gender differences from the effects of smoking on changes in lung function remains unclear.
Scant data are available on racial and ethnic differences in the rates of FEV 1 decline ( Scanlon et al. 2000 ; Vollmer et al. 2000 ). In the Lung Health Study, Vollmer and colleagues (2000) combined spirometric data from eight population-based observational studies or clinical trials conducted in North America to examine the relationship between smoking, lung function, race, and ethnicity. Overall, this cross-sectional analysis included 23,812 men (66 percent white, 14 percent black, 4 percent Hispanic, 12 percent Asian/Pacific Islander, and 3 percent American Indian) and 16,921 women (62 percent white, 25 percent black, 6 percent Hispanic, and 7 percent American Indian). The estimated average excess FEV 1 decline attributed to smoking was highest among whites (−6 mL /pack-year) and similar in the other racial and ethnic groups (−3 to −4 mL/pack-year). However, the greatest differences among racial and ethnic groups were limited to the heaviest smokers (more than 10 cigarettes per day). Overall, during the five-year period of the Lung Health Study, there were no differences in the rates of change in FEV 1 declines among these participants ( Scanlon et al. 2000 ).
The presence of respiratory symptoms, particularly coughing, phlegm, and wheezing, has been associated with an accelerated decline in FEV 1 levels in cigarette smokers and nonsmokers in a number of studies ( Jaakkola et al. 1991a , b ; Sherman et al. 1992 ; Burchfiel et al. 1996 ; Vestbo et al. 1996 ). Among Japanese American men in the Honolulu Heart Program who were continuous smokers, Burchfiel and colleagues (1996) found an increased risk of rapid FEV 1 declines (−60 mL /year or greater) associated with wheezing ( OR = 3.9 [95 percent CI , 1.8–8.3]). However, respiratory symptoms have not been predictive of FEV 1 declines in all studies. Although Scanlon and colleagues (2000) did not find an association between respiratory symptoms and the rate of FEV 1 declines in the Lung Health Study, their ability to detect an association may have been limited because participants in this study were restricted to smokers with mild to moderate chronic airflow obstruction.
The presence of other diseases including asthma ( Lange et al. 1998 ) and coronary heart disease ( Burchfiel et al. 1996 ) has been associated with an accelerated FEV 1 decline among smokers. In the Copenhagen City Heart Study, Lange and colleagues (1998) followed 9,370 women and 8,136 men, 20 to 79 years of age, over a 15-year period. Except for the youngest women (20 to 39 years of age) and the oldest men (60 to 79 years of age), smokers with asthma averaged greater FEV 1 reductions than smokers without asthma. In the Honolulu Heart Program, Japanese American men with coronary heart disease who continued to smoke had an increased risk for a rapid FEV 1 decline (−60 mL /year or greater) ( OR = 1.99 [95 percent CI , 0.96–4.14]).
Nutritional factors such as dietary intake ( Carey et al. 1998 ) and anthropometric characteristics ( Burchfiel et al. 1996 ) have been associated with rates of FEV 1 decline. In a national sample of 2,171 British adults aged 18 through 73 years, Carey and colleagues (1998) found that current smokers who consumed the smallest quantities of fresh fruits (sources of antioxidant vitamins) over a seven-year period had a higher rate of FEV 1 decline than lifetime nonsmokers, with adjustments for social class, region, pack-years, and average fresh fruit scores (by rating consumption as more than one per day, one per day most days, once or twice per week, less than one per week, or never).
Anthropometric characteristics have been associated with a rapid FEV 1 decline among cigarette smokers ( Burchfiel et al. 1996 ). Burchfiel and colleagues (1996) found that increasing body mass, measured by subscapular skinfold thickness, was associated with a lower risk for rapid FEV 1 declines (−60 mL /year or greater). A 10- mm increase in subscapular skinfold thickness was associated with a 30 percent decrease in the risk for a rapid FEV 1 decline ( OR = 0.70 [95 percent CI , 0.55–0.88]).
The relationship between a single measure of and a subsequent rate of change in the FEV 1 level has been termed the “horse-racing effect”; a low FEV 1 level is a predictor of a rapid decline in the FEV 1 ( Fletcher et al. 1976 ; Burrows et al. 1987 ). The term “horse-racing” was proposed because a low FEV 1 level at any point reflects a high rate of prior loss and hence is predictive of a future decline. As an integrated consequence of a prior decline, the FEV 1 level is also a potential marker for susceptibility to the factors driving the decline.
Burrows and colleagues (1987) proposed that a low FEV 1 level may be an early marker for identifying smokers who are susceptible to COPD . The investigators examined relationships between FEV 1 levels and other spirometric parameters and the rates of FEV 1 decline in 620 women and 475 men from Tucson, Arizona. For both men and women, a low initial FEV 1 decline. In level was not associated with a rapid FEV 1 men, however, an initially low ratio of FEV 1 / FVC (less than 70 percent) was associated with a rapid FEV 1 decline; trends in women were reported to be similar but less marked, although the data were not provided. Similarly, in the Lung Health Study, Scanlon and colleagues (2000) found no differences in the rates of FEV 1 decline over four years of follow-up when comparing continuing smokers with a baseline FEV 1 in the lowest quintile (−63 mL /year) with those in the highest quintile (−61 mL/year). However, the investigators did find a significant association between the baseline FEV 1 percent predicted and the rate of decline. These findings need to be interpreted with attention to the characteristics of the study participants: middle-aged smokers with mild-to-moderate airflow obstruction. Overall, the available results suggest that various indicators of impaired ventilatory function predict subsequent FEV 1 declines.
Among cigarette smokers, bronchial hyper-responsiveness to a variety of stimuli (e. g ., histamine and methacholine) has been associated with an accelerated rate of decline in FEV 1 levels ( Frew et al. 1992 ; Rijcken et al. 1995 ; Villar et al. 1995 ; Tashkin et al. 1996 ). In the Lung Health Study, Tashkin and colleagues (1996) examined the relationship between bronchial hyperreactivity to methacholine and FEV 1 declines among 5,733 smokers aged 35 through 60 years with mild COPD (mean FEV 1 / FVC , 65 percent; FEV 1 , 78 percent predicted). After adjusting for age, gender, baseline smoking history, changes in smoking status, and baseline lung function levels, the investigators found that airway hyperreactivity during the five-year follow-up was a strong predictor of changes in FEV 1 levels percent predicted. The greatest decline of 2.2 percent predicted was in women who had the highest degree of hyperreactivity and who continued to smoke. The corresponding value in men was 1.7 percent predicted.
In addition to cigarette smoking, exposures to ambient air pollutants or workplace exposures may accelerate FEV 1 declines and increase future risks for COPD ( Garshick et al. 1996 ; Xu and Wang 1998 ). For example, Xu and Wang (1998) examined the effects of smoking, urban air pollution, and workplace exposures on lung function levels in a 1986 cross-sectional survey of 3,287 randomly selected adults 40 to 69 years of age residing in Beijing, China. The investigators found that smokers had an increased reduction in FEV 1 levels of 6.5 mL for each year of smoking compared with adults who had never smoked; smokers living in residential and industrial areas with high levels of ambient pollutants had further decrements in pulmonary function.
Effects of Smoking Cessation
The beneficial effects of smoking cessation on the decline were extensively reviewed in the rates of FEV 1 1990 Surgeon General’s report. A major conclusion of that report relevant to FEV 1 declines and smoking cessation was that “cigarette smoking accelerates the age-related decline in lung function that occurs among never smokers. With sustained abstinence from smoking, the rate of decline in pulmonary function among former smokers returns to that of never smokers” ( Table 4.13 ) ( USDHHS 1990 , p . 11). Since that report, there have been additional studies supporting these conclusions ( Townsend et al. 1991 ; Anthonisen et al. 1994 ; Sherrill et al. 1994 ; Xu et al. 1994 ; Burchfiel et al. 1995 ; Frette et al. 1996 ; Murray et al. 1998 ; Berglund et al. 1999 ; Scanlon et al. 2000 ). These studies also have advanced an understanding of factors that modify the effects of smoking cessation on rates of FEV 1 decline.
The Lung Health Study provides powerful clinical trial data on the effects of smoking cessation on the rates of FEV 1 decline and lung function levels ( Anthonisen et al. 1994 ; Scanlon et al. 2000 ). This five-year, multicenter clinical trial of smoking cessation interventions was conducted in 10 North American centers. Between 1986 and 1989, 5,887 women (37 percent) and men (63 percent) aged 35 through 60 years who were current smokers with mild to moderate air-flow obstruction (FEV 1 / FVC of 70 percent or less and FEV 1 between 55 percent and 90 percent of predicted normal) were randomized into three groups: usual care, smoking cessation intervention with a placebo inhaler, and smoking cessation intervention with an inhaled bronchodilator (ipratropium bromide). Participants in the smoking cessation intervention placebo group and the usual care group who stopped smoking in the first year of the trial had an average increase in FEV 1 levels of 47 mL compared with a 49 mL decrease among persons who continued to smoke ( Scanlon et al. 2000 ). Between year one and year five of the trial, the average rate of FEV 1 reduction among continuous smokers was −62 mL/year, twice that of sustained quitters (−31 mL/year) during the same time period. Quitting intermittently during the follow-up period was associated with an intermediate rate of decline (−43 mL/year). The degree of improvement during the first year of cessation and the rates of FEV 1 decline after cessation varied with age at cessation, gender, amount of smoking, level of baseline lung function, and airways hyperreactivity.
Results from several investigations suggest that the benefits of smoking cessation are greatest for persons who stop smoking at younger ages ( Camilli et al. 1987 ; Sherrill et al. 1994 ; Xu et al. 1994 ; Frette et al. 1996 ; Scanlon et al. 2000 ). In the Lung Health Study, Scanlon and colleagues (2000) found that sustained quitters younger than 50 years of age had the slowest rates of FEV 1 decline during the five-year follow-up period compared with sustained quitters 50 years of age and older ( Figure 4.3 ). Among 147 women and 141 men who were new quitters in the prospective Tucson Epidemiological Study of Airways Obstructive Disease, Sherrill and colleagues (1994) estimated that smoking cessation among women improved FEV 1 levels by 4.3 percent at 20 years of age and by 2.5 percent at 80 years of age. For men, FEV 1 improvements were less at both ages: 1.2 percent at 20 years of age and zero at 80 years of age. During the 24 years of follow-up in the Dutch Vlagtwedde-Vlaardingen Study ( Xu et al. 1994 ), the mean FEV 1 loss in former compared with current smokers was 20 mL /year less for women who stopped smoking before 45 years of age, but only 5.4 mL/year less for women who stopped smoking at 45 years of age or older. The corresponding values for men were 28.2 mL/year less for men younger than 45 years of age, and 10.4 mL/year less for men 45 years of age and older. In the Rancho Bernardo (California) Heart and Chronic Disease Study, 826 women and 571 men aged 51 through 95 years had spirometry testing from 1988–1991 ( Frette et al. 1996 ). Women who were former smokers who stopped smoking before 40 years of age had FEV 1 levels similar to those for women who had never smoked (2.09 L and 2.13 L, respectively). The average FEV 1 level for women who stopped smoking at 40 through 60 years of age was 2.02 L, which was between that for female nonsmokers (2.13 L) and female current smokers (1.71 L). Women who stopped smoking at 60 years of age or older had a FEV 1 level similar to that of current smokers (1.72 L and 1.71 L, respectively); the same pattern in relation to age at smoking cessation was found for men.
Mean change and 95 percent confidence interval in forced expiratory volume in one second (FEV 1 ) percent predicted from years 1–5 of the Lung Health Study for sustained quitters, intermittent quitters, and continuous smokers, by quintile of age. (more...)
Limited data suggest that smoking cessation more significantly benefits lung function and the rate of FEV 1 decline in women than in men ( Sherrill et al. 1994 ; Scanlon et al. 2000 ). The Tucson Epidemiological Study of Airways Obstructive Disease ( Sherrill et al. 1994 ) estimated that the average improvement in FEV 1 levels at 80 years of age was higher among women who had quit smoking (2.5 percent) than among men who had stopped smoking (0.0 percent). Women who were sustained quitters in the Lung Health Study had improvements in FEV 1 levels in the first year of cessation 2.5 times greater than did men ( Scanlon et al. 2000 ). The report from Scanlon and colleagues (2000) did not provide gender-specific effects on subsequent FEV 1 rates of decline.
The amount of exposure to cigarette smoke, which may be measured in several ways, may also influence the effects of smoking cessation ( Burchfiel et al. 1995 ; Scanlon et al. 2000 ). Burchfiel and colleagues (1995) found slower FEV 1 declines after quitting in Japanese American men with the highest level of baseline smoking (−9.1 mL /year) compared with men with the lowest level (−24.1 mL/year). In the Lung Health Study, Scanlon and colleagues (2000) found no differences in the rates of FEV 1 decline among sustained quitters from year one through year five of follow-up in relation to the number of cigarettes smoked at baseline. However, they did find that the largest improvements in FEV 1 levels after smoking cessation for the first year were among persons who smoked the most cigarettes per day before quitting ( Figure 4.4 ) ( Scanlon et al. 2000 ). Among sustained quitters in the Lung Health Study, for the subgroup with the highest quintile of cigarettes smoked per day before quitting, improvement in FEV 1 levels was 3.33 percent predicted in the first year of cessation compared with only 0.51 percent predicted for the lowest smoking quintile.
Mean change and 95 percent confidence interval in forced expiratory volume in one second (FEV 1 ) percent predicted during year 1 of the Lung Health Study, for persons who quit smoking and for persons who continued to smoke during year 1, by quintile of (more...)
Limited data are available on the relationship between the FEV 1 level at quitting and the consequences of smoking cessation ( Burchfiel et al. 1995 ; Scanlon et al. 2000 ). In the Honolulu Heart Program, Burchfiel and colleagues (1995) found that after adjusting for age, height, and amount smoked, the benefits of quitting were more evident in persons with lower baseline FEV 1 levels. In contrast, Scanlon and level was colleagues (2000) found that a baseline FEV 1 not predictive of subsequent rates of decline in the FEV 1 level and baseline level was not associated with greater improvements after the first year of cessation. The conflicting results between these two studies may reflect differing study populations. The Honolulu Heart Program was population-based and began with middle-aged Japanese American men, whereas the Lung Health Study used volunteer smokers with evidence of mild-to-moderate airflow obstruction.
The degree of bronchial reactivity has been strongly associated with the magnitude of improvements in FEV 1 levels in the first year of cessation, and with the subsequent rates of FEV 1 decline. In the Lung Health Study, Tashkin and colleagues (1996) found that persons with higher airway reactivity had the greatest improvements in FEV 1 levels within the first year after quitting, whereas the slowest rates of FEV 1 decline occurred among sustained quitters with the lowest airway reactivity.
Although the benefits of smoking cessation on rates of decline and lung function levels are well established, weight gain associated with quitting may reduce lung function levels and increase FEV 1 declines, thus counterbalancing the benefits of quitting. In the Lung Health Study, Wise and colleagues (1998) found that the FVC was affected more than the FEV 1 by the weight gain. The estimated loss of FEV 1 was 11.1 mL / kg of weight gain for men and 10.6 mL/kg for women, and the mean weight gains over five years among sustained quitters were 7.6 kg and 8.8 kg, respectively. Furthermore, the average FEV 1 decline was greater in those who gained the most weight during the five years of follow-up ( Figure 4.5 ). However, the effect of weight gain on the rates of FEV 1 decline was relatively small compared with the effects of continued smoking, and the FVC and FEV 1 would be expected to increase with weight loss.
The relationship between mean changes in forced expiratory volume in one second (FEV 1 ) percent predicted to quintiles of mean changes in weight for each smoking category. Note: Corrected data presentation shown here. The interval for changes in FEV 1 percent (more...)
The adverse effects of active smoking and the benefits of smoking cessation on lung function decline have been firmly established ( USDHHS 1984 , 1990 ). Research emphasis has shifted to finding determinants of susceptibility to rapid lung function decline in active smokers and determinants of improvements after smoking cessation. Factors that predict the greatest susceptibility to rapid lung function decline while actively smoking include a greater number of cigarettes smoked, wheezing, asthma, bronchial hyperreactivity, low body mass, low lung-function level ( FEV 1 percent predicted or low FEV 1 / FVC ), occupational exposures, and ambient air pollution. However, there is limited evidence available on how modifying active smoking affects the rate of lung function decline by gender, ethnicity, and antioxidant dietary intake.
- The evidence is sufficient to infer a causal relationship between active smoking in adulthood and a premature onset of and an accelerated age-related decline in lung function.
- The evidence is sufficient to infer a causal relationship between sustained cessation from smoking and a return of the rate of decline in pulmonary function to that of persons who had never smoked.
These conclusions provide a strong rationale for smoking cessation interventions for active smokers. The greatest benefits from smoking cessation will occur at younger ages, but all smokers benefit from cessation regardless of age. Identifying smokers with the greatest susceptibility for a rapid decline in lung function may lead to more targeted interventions, but cessation for all smokers is central to preventing COPD .
Chronic Respiratory Symptoms and Diseases
Substantial observational evidence has long shown that respiratory symptoms and diagnoses, the most relevant health outcomes to patients, are causally associated with smoking. Respiratory symptoms— coughing, productive coughing, wheezing, and dyspnea (difficulty breathing and shortness of breath)—are nonspecific and are associated with a number of acute and chronic respiratory diseases and even nonrespiratory diseases. Despite the nonspecificity of respiratory symptoms, their presence is a sensitive indicator of underlying lung injury and disease ( Torén et al. 1993 ), and they have clinical relevance because they may impair functioning and reduce the quality of life. Selected diseases, particularly asthma and respiratory symptoms such as wheezing, may be sufficiently specific in children to be used to define the disease. However, the specificity of wheezing for asthma declines with age because of the increasing prevalence of COPD .
Respiratory Symptoms: Childhood and Adolescence
Overall, the frequency of respiratory symptoms in children and adolescents is greater in current smokers compared with nonsmokers or former smokers, and the duration and amount of smoking further increase the frequency of symptoms ( USDHHS 1994 ; Arday et al. 1995 ; Larsson 1995 ; Lam et al. 1998 ; Withers et al. 1998 ). A major conclusion of the 1994 Surgeon General’s report was that “Cigarette smoking during childhood and adolescence produces significant health problems among young people, including cough and phlegm production, an increased number and severity of respiratory illnesses” and “decreased physical fitness” ( USDHHS 1994 , p . 41). Since the 1994 report, several investigations have confirmed and extended the conclusions relevant to respiratory symptoms in childhood and adolescence ( Arday et al. 1995 ; Lam et al. 1998 ; Withers et al. 1998 ).
To examine the relationship between smoking status and respiratory symptoms, Arday and colleagues (1995) used self-reported questionnaire data obtained from a random sample of 26,504 high school seniors in the 48 contiguous United States from 1982– 1989. Compared with students who had never smoked or who had smoked only once or twice in the past, current regular smokers (i.e., reported smoking at least one cigarette within the past 30 days) who began to smoke daily by ninth grade were more likely to report at least one episode in the past 30 days of coughing spells ( OR = 2.1 [95 percent CI , 1.90–2.33]), shortness of breath when not exercising (OR = 2.67 [95 percent CI, 2.38–2.99]), and wheezing or gasping (OR = 2.58 [95 percent CI, 2.29–2.90]). These risk estimates were adjusted for gender, marijuana and cocaine use, parental education, and the year of the survey. The prevalence of respiratory symptoms increased with the amount and duration of smoking.
Lam and colleagues (1998) conducted a cross-sectional survey of 6,304 students 12 to 15 years of age who were attending school in Hong Kong. Students who reported smoking more than six cigarettes per week had a higher prevalence of coughing for three months compared with students who had never smoked ( OR = 3.02 [95 percent CI , 1.95–4.69]), and a higher prevalence of wheezing in the past three months (OR = 2.91 [95 percent CI, 1.99–4.26]). These risk estimates were adjusted for gender, age, area of residence, and type of housing. Statistically significant increases in the prevalence of respiratory symptoms were associated with an increased frequency of smoking.
Withers and colleagues (1998) reported results from following a cohort of 2,289 children from the ages of 6 to 8 years to 14 to 16 years of age; all were registered with 1 of 86 family practitioners in Southampton, United Kingdom. Regular smoking (i.e., smoking at least one cigarette per week during the 12 months before completing the questionnaire) was associated with a current cough ( OR = 1.71 [95 percent CI , 1.21–2.43]), the onset of a cough between the surveys (OR = 1.91 [95 percent CI, 1.12–3.25]), a persistent wheeze in boys (OR = 4.35 [95 percent CI, 1.20–14.3]), and a new report of wheezing (OR = 1.65 [95 percent CI, 1.14–2.39]).
In the three investigations published since the 1994 Surgeon General’s report, the prevalence of respiratory symptoms was consistently higher among cigarette smokers than among nonsmokers ( Arday et al. 1995 ; Lam et al. 1998 ; Withers et al. 1998 ). Furthermore, limited evidence suggests that the prevalence of symptoms increases with the duration and amount of smoking ( Arday et al. 1995 ; Lam et al. 1998 ). Although the results from these investigations are not directly comparable because the survey questions on smoking status and respiratory symptoms vary across studies, in three distinct settings each study shows an increase in symptom rates for children who smoke.
Other factors that may also contribute to respiratory symptoms include gender, associated diseases (e. g ., atopy or asthma), passive exposure to smoking if parents or other household members smoke, marijuana and cocaine use, ambient air pollution, workplace exposures, and socioeconomic factors. These factors have been considered to an extent in some studies. Arday and colleagues (1995) adjusted for gender, marijuana and cocaine use, and parental education. Lam and colleagues (1998) considered gender, age, area of residence, and housing type. Withers and colleagues (1998) included gender, personal and family history of atopy, passive smoking, other household exposures, and social factors. However, despite inconsistent controls for other factors that may contribute to the occurrence of respiratory symptoms, none is likely to substantially confound the strong association between smoking and respiratory symptoms.
Limited data are available on the relationship between smoking cessation and the occurrence of respiratory symptoms in children and adolescents ( Arday et al. 1995 ; Lam et al. 1998 ). Compared with nonsmokers, former smokers report more frequent respiratory symptoms, but they generally have fewer occurrences of symptoms than regular smokers. Several factors may partially explain this higher occurrence in former smokers compared with nonsmokers, including a relatively short duration of cessation, false reporting of their smoking status, and the “healthy smoker” effect. This effect refers to the observation that persons who continue to smoke are less likely to have respiratory symptoms, in contrast to former smokers who quit smoking because of frequent respiratory symptoms ( Weiss et al. 1989 ).
Since the 1994 Surgeon General’s report on smoking and health, several investigations have been published that confirm and extend conclusions of that report that are relevant to respiratory symptoms in childhood and adolescence ( Table 4.13 ). These studies establish that respiratory symptoms increase with the amount and duration of smoking. Further, these studies also show that the effects of active smoking on respiratory symptoms are not due to other factors that increase respiratory symptoms. Limited data are available on the effects of smoking cessation on respiratory symptoms among youth.
- The evidence is sufficient to infer a causal relationship between active smoking and respiratory symptoms in children and adolescents, including coughing, phlegm, wheezing, and dyspnea.
This conclusion provides yet another strong rationale for smoking cessation interventions among youth.
Asthma. In the Guidelines for the Diagnosis and Management of Asthma of the National Heart, Lung, and Blood Institute ( NHLBI 1997 ), asthma is defined as “a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role . . . . In susceptible individuals, this inflammation causes recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread but variable airflow obstruction that is often reversible either spontaneously or with treatment. The inflammation also causes an associated increase in the existing bronchial hyperresponsiveness to a variety of stimuli” ( p . 3).
Asthma is the most common chronic respiratory childhood disease, and it has been increasing in frequency in the United States and worldwide for several decades ( NHLBI 1997 ; Warner 1999 ). This complex disease is associated with a number of environmental exposures, particularly aeroallergens, and with genetic susceptibility. Although the literature documenting the association between secondhand smoke exposure and childhood asthma is extensive ( Cook and Strachan 1999 ), only a limited number of studies on active smoking and childhood asthma have been conducted ( Larsson 1995 ; Kaplan and Mascie-Taylor 1997 ; Lam et al. 1998 ; Norrman et al. 1998 ; Withers et al. 1998 ; Chen et al. 1999 ).
Epidemiologic Evidence. Establishing the presence of asthma in epidemiologic studies is one of the greatest challenges in investigating cigarette smoking and asthma, primarily because of the lack of an agreed-upon operational definition of asthma ( Torén et al. 1993 ). However, during childhood and adolescence physician-diagnosed asthma and standardized questions about asthma-related symptoms (i.e., wheezing or wheezing with dyspnea) provide sufficient specificity. Asking such questions has been the main method used to examine active smoking and asthma among youth ( Larsson 1995 ; Kaplan and Mascie-Taylor 1997 ; Lam et al. 1998 ; Withers et al. 1998 ; Chen et al. 1999 ).
Larsson (1995) examined the association between smoking and self-reported asthma incidence among 2,308 persons aged 16 through 19 years living in Sweden. Between 1990 and 1993, the overall incidence of physician-diagnosed asthma was 1.3 percent per year, and the incidence among females was higher (1.8 percent per year) than that among males (0.9 percent per year). The risk for physician-diagnosed asthma was also higher among female smokers ( OR = 2.0 [95 percent CI , 1.0–4.0]) than among male smokers (OR = 1.7 [95 percent CI, 0.6–4.8]). The risks for asthma-related symptoms and the use of asthma medications also were higher among females than among males. This analysis was limited by the lack of information on other factors associated with asthma, including personal atopy, family history of atopy and asthma, parental smoking, and other potential confounding variables.
Kaplan and Mascie-Taylor (1997) examined smoking and asthma in a cohort of 8,860 participants from England, Wales, and Scotland participating in the National Child Development Study. The analysis was based on self-reports at 16 and 23 years of age. In a univariate analysis that included males and females, regular smoking since 16 years of age was associated with reports of asthma or wheezy bronchitis between 16 and 23 years of age ( OR = 1.55). Stratified or multivariate analyses, adjusting for other factors, were not performed.
In a 1994 cross-sectional survey of Hong Kong schoolchildren aged 12 through 15 years, Lam and colleagues (1998) did not find an association between active smoking and physician-diagnosed asthma. The prevalence of asthma was 8.6 percent among children who reported smoking six or more cigarettes per week compared with 8.1 percent among children who had never smoked ( OR = 1.18 [95 percent CI , 0.76–1.83]).
In a cohort of persons from 2,150 households in the United Kingdom, Withers and colleagues (1998) obtained questionnaire responses on smoking behaviors and asthma from participants aged 14 through 16 years. Smoking at least one cigarette per week in the 12 months preceding the survey was not associated with physician-diagnosed asthma (26.3 percent) compared with children who did not report smoking (21.9 percent). However, the prevalence of asthma was not examined separately with greater amounts of smoking.
Norrman and colleagues (1998) surveyed 1,112 Swedish eighth graders 13 to 16 years of age in 1987 and again in 1991. Overall, the incidence of self-reported asthma was 1.1 percent per year. The onset of asthma was significantly associated with current smoking ( OR = 3.4 [95 percent CI , 1.2–9.3]) but not with former smoking (OR = 2.8 [95 percent CI, 0.4–23.0]).
Among 3,240 persons aged 12 through 24 years who participated in the 1994–1995 Canadian National Population Health Study, Chen and colleagues (1999) found a significant association between asthma diagnosed by a health professional and smoking, but only among females. The OR for asthma among female smokers compared with female nonsmokers, adjusted for age, was 2.18 (95 percent CI , 1.41–3.44). Among males, the OR for smokers was 0.98 (95 percent CI, 0.56–1.70) compared with nonsmokers.
In addition to the potential etiologic role of active smoking in asthma, there is strong evidence that smoking adversely affects the course of the disease in children with asthma ( Godden et al. 1994 ; Lam et al. 1998 ). Godden and colleagues (1994) examined the levels prevalence of respiratory symptoms and FEV 1 among 360 persons from Scotland aged 34 through 40 years, who were participants in a population-based survey as children and who had been diagnosed with childhood asthma ( n = 97), wheezing with an upper respiratory infection (n = 132), or no respiratory symptoms (n = 131). In the entire group, current smoking was associated with an increased risk of a current wheeze ( OR = 2.02 [95 percent CI , 1.15–3.52]), cough (OR = 7.24 [95 percent CI, 3.39–15.49]), and phlegm (OR = 3.08 [95 percent CI, 1.27–7.39]). The risk associated with all three respiratory symptoms was substantially lower for former smokers, and only phlegm (OR = 1.68 [95 percent CI, 1.30–10.38]) was significantly associated with past smoking. In addition, current smoking was associated with a lower mean FEV 1 percent predicted level (−5.64 percent [95 percent CI, -19.4 to 1.09]). In the 1994 cross-sectional survey of Hong Kong schoolchildren reported by Lam and colleagues (1998) , children with asthma who smoked more than six cigarettes per week were more likely to report using asthma medications during the previous two days compared with children who had never smoked (OR = 3.07 [95 percent CI, 1.58–5.97]).
Evidence Synthesis. Although the prevalence of wheezing, an asthma-related symptom, is consistently higher in current smokers than in former smokers and nonsmokers, available investigations provide inconsistent findings on the relationship between smoking and reports of physician-diagnosed asthma. Moreover, none of the investigations have fully controlled for known risk factors for asthma. There is limited but consistent evidence that active smoking worsens the prognosis of asthma in children.
- The evidence is sufficient to infer a causal relationship between active smoking and asthma-related symptoms (i.e., wheezing) in childhood and adolescence.
- The evidence is inadequate to infer the presence or absence of a causal relationship between active smoking and physician-diagnosed asthma in childhood and adolescence.
- The evidence is suggestive but not sufficient to infer a causal relationship between active smoking and a poorer prognosis for children and adolescents with asthma.
Implications. These conclusions provide a strong rationale for preventing active smoking among children and adolescents to preclude the occurrence of asthma-related symptoms. The promotion of smoking cessation should improve the prognosis for children and adolescents with asthma who smoke. Future studies of causes of childhood asthma should include active smoking as a potential etiologic agent.
Respiratory Symptoms: Adulthood
Evidence continues to accumulate confirming the long-established causal association between active smoking and respiratory symptoms in adults. Among adults, all respiratory symptoms are strongly and consistently associated with cigarette smoking ( Freund et al. 1993 ; David et al. 1996 ; Bodner et al. 1998 ; Forastiere et al. 1998 ; Butland et al. 1999 ), and smoking cessation reduces their frequency ( Kanner et al. 1999 ). In the Framingham Study, Freund and colleagues (1993) found that among persons aged 45 years and older, the prevalence of a cough was higher among cigarette smokers than among nonsmokers, and the prevalence increased as the amount smoked increased. Persons who smoked more than 30 cigarettes per day were seven times more likely than nonsmokers to report a chronic cough.
Among 677 women 18 to 43 years of age who were seen for prenatal care at an East Boston clinic, David and colleagues (1996) examined the relationship between cigarette smoking and a persistent wheeze without asthma. In a multiple logistic regression model adjusting for ethnicity, parental history of asthma, educational level, and the presence of a cat or dog at home, current smokers had a fivefold increased risk ( OR = 4.97 [95 percent CI , 2.46–10.1]) of a persistent wheeze compared with lifetime nonsmokers. There was no increase in this risk among former smokers (OR = 1.13 [95 percent CI, 0.50–2.55]).
Bodner and colleagues (1998) conducted a nested case-control study of 117 adults aged 39 through 45 years with adult onset of wheezing and 277 randomly selected persons without wheezing who were participants in a population-based cohort study in Scotland. After adjusting for family history, atopy, and social class, the investigators found that current smoking was associated with adult onset of wheezing ( OR = 2.01 [95 percent CI , 1.08–3.74]) and with chronic cough and phlegm (OR = 11.48 [95 percent CI, 2.49–52.89]). Former smokers were at a lower risk for adult onset of wheezing (OR = 1.48 [95 percent CI, 0.74–2.95]), but the risk remained significant for chronic cough and phlegm (OR = 5.24 [95 percent CI, 1.00–27.53]).
In a population-based study of 1,226 women aged 55 years and older living in Sonoma, California, Forastiere and colleagues (1998) examined relationships of chronic respiratory symptoms with a number of risk factors. Among women who reported shortness of breath with a wheeze or chronic wheeze during the past 12 months without a physician’s diagnosis of asthma or chronic bronchitis/emphysema, the investigators found that the risk for these symptoms was highest in current smokers ( OR = 3.8 [95 percent CI , 2.2–6.5]) and that the risk declined but remained statistically significant for former smokers who had quit for 10 or fewer years (OR = 1.8 [95 percent CI, 1.1–3.2]) or for more than 10 years (OR = 1.8 [95 percent CI, 1.2–2.5]). Overall, the population attributable risk for these symptoms in this population of women who had ever smoked was 35 percent.
In a longitudinal study in the Netherlands that included 792 women and 995 men, Jansen and colleagues (1999) found a dose-response relationship between the number of cigarettes smoked and any occurrence of chronic respiratory symptoms. When smokers were compared with nonsmokers, the risk ( OR ) of any chronic respiratory symptom was 1.89 (95 percent CI , 1.37–2.60) for those who smoked 1 to 14 cigarettes per day, 2.98 (95 percent CI, 2.14–4.29) for those who smoked 15 to 24 cigarettes per day, and 3.57 (95 percent CI, 2.32–5.48) for those who smoked 25 or more cigarettes per day. Among former smokers, the risk was lower but not statistically significant (OR = 1.21 [95 percent CI, 0.85–1.74]).
Butland and colleagues (1999) conducted a cross-sectional survey of 5,770 women and 5,582 men aged 33 years living in the United Kingdom. The prevalence of any wheezing or wheezing five or more times in the past 12 months increased with the amount smoked and was lower for former smokers. The prevalence of these symptoms was similar when comparing non-smokers with former smokers who had quit for more than five years.
In the Lung Health Study ( Kanner et al. 1999 ), the prevalence of all respiratory symptoms significantly decreased during the five-year sustained cessation follow-up period. Compared with current smokers, intermittent quitters had a lower prevalence of respiratory symptoms. When compared with those in the sustained cessation category, intermittent quitters had a greater prevalence of respiratory symptoms ( Figure 4.6 ) ( Kanner et al. 1999 ).
Proportion (95 percent confidence interval) of participants reporting chronic cough at each annual follow-up visit, stratified by final smoking status. Note: (A) Restricted to participants who did not report the symptom of cough at entry into the study. (more...)
Active cigarette smoking is consistently associated with an increased risk for respiratory symptoms, including coughing, phlegm, wheezing, and dyspnea. Moreover, the occurrence of respiratory symptoms increases with the number of cigarettes smoked and decreases with smoking cessation. These symptoms reflect the consequences of the smoking-caused changes throughout the respiratory tract.
- The evidence is sufficient to infer a causal relationship between active smoking and all major respiratory symptoms among adults, including coughing, phlegm, wheezing, and dyspnea.
Respiratory symptoms are common among cigarette smokers and probably contribute substantially to an impaired quality of life and a higher utilization of health care resources. Thus, a decrease in the occurrence of these symptoms with smoking cessation will provide important benefits to public health and to the well-being of successful quitters.
Asthma. Epidemiologic Evidence. Asthma in adults is a complex and heterogeneous disorder, likely caused by a number of occupational and environmental exposures as well as by genetic or other intrinsic predispositions. The majority of asthma begins in childhood and may remit for a number of years before manifesting again in adulthood. This phenomenon may complicate the interpretation of epidemiologic investigations of risk factors for adult-onset asthma, because this condition most likely comprises both childhood asthma and true adult-onset asthma. The role of smoking as an etiologic agent in adults with asthma has been investigated in a number of studies using both longitudinal and cross-sectional designs ( Tables 4.16 and 4.17 ). The results indicate a complicated relationship between cigarette smoking and asthma that may be modified by smoking status (i.e., current, former, or never smoker), gender, age, other established risk factors for asthma (e. g ., family history of asthma or personal atopy), and the bias arising from the “healthy smoker effect” ( Weiss et al. 1989 ).
Longitudinal studies on the association between smoking and adult asthma.
Cross-sectional studies on the association between smoking and adult asthma.
The interpretation of the evidence for cigarette smoking and asthma is constrained by a number of methodologic considerations including varying study designs, different definitions of asthma, and different indexes for defining smoking status. Although the longitudinal design is the strongest for investigating the relationship between smoking and adult-onset asthma, the studies that have been conducted arrived at conflicting results ( Table 4.16 ). In those studies, current smoking was associated with an increased risk of asthma among men ( Vesterinen et al. 1988 ) and among men and women aged 40 years or older ( Krzyzanowski and Lebowitz 1992 ). However, neither Vesterinen and colleagues (1988) nor Troisi and colleagues (1995) found an association between current smoking and asthma in women. Furthermore, Troisi and colleagues (1995) did not find a dose-response relationship between the amount smoked and asthma. The strongest associations between smoking and asthma were reported by Strachan and colleagues (1996) and Plaschke and colleagues (2000) . However, their results are difficult to interpret. For example, Strachan and colleagues (1996) combined asthma with wheezy bronchitis, and Plaschke and colleagues (2000) did not define “smokers,” which may have included former smokers. Finally, McWhorter and colleagues (1989) only examined ever smoking in their longitudinal investigation and did not find an association with asthma.
A number of cross-sectional studies have examined the association between asthma and smoking, with inconsistent results for both current and former smokers ( Table 4.17 ). Of the 10 publications that provided quantitative results, 3 found an association between current smoking and asthma in men and women ( Ben-Noun 1999 ; Chen et al. 1999 ; Torén and Hermansson 1999 ), and 1 found an association only in women ( Chen et al. 1999 ). No association was reported in seven cross-sectional studies ( Flodin et al. 1995 ; David et al. 1996 ; Bodner et al. 1998 ; Forastiere et al. 1998 ; Zhang et al. 1999 ; de Marco et al. 2000 ; Kotaniemi et al. 2001 ). Moreover, two investigations provided indirect evidence that current smoking was not associated with asthma ( Hansen et al. 2000 ; Kilpelainen et al. 2001 ), and limited data suggest that the risk of asthma may be greater because of a family history of asthma or the presence of other atopic conditions (i.e., hay fever, atopic dermatitis) ( Melbostad et al. 1998 ; Torén and Hermansson 1999 ). However, this finding was contradicted by the results reported by Plaschke and colleagues (2000) .
Among former smokers, an association with asthma has been inconsistent ( Table 4.17 ). Out of nine studies, five found an increased risk for asthma among former smokers compared with current smokers ( Flodin et al. 1995 ; Troisi et al. 1995 ; Bodner et al. 1998 ; Forastiere et al. 1998 ; Siroux et al. 2000 ), with ORs ranging from 1.4 to 5.24. In contrast, four studies found no association ( David et al. 1996 ; Chen et al. 1999 ; de Marco et al. 2000 ; Kotaniemi et al. 2001 ).
In four cross-sectional studies that examined ever smokers defined as current and former smokers ( Table 4.17 ) ( Flodin et al. 1995 ; Melbostad et al. 1998 ; Ben-Noun 1999 ; Siroux et al. 2000 ), three of the studies associated asthma with ever smoking ( Flodin et al. 1995 ; Melbostad et al. 1998 ; Ben-Noun 1999 ) with ORs ranging from 1.3 to 1.9.
Investigating the relationship between smoking and asthma offers a number of challenges, including diagnostic misclassifications and changes in smoking behaviors because of asthma. Dodge and colleagues (1986) found that among persons aged 40 years or older with newly diagnosed asthma, emphysema, or chronic bronchitis based on self-reports, women were more likely than men to receive a physician’s diagnosis of asthma or chronic bronchitis, and men were more likely to receive a diagnosis of emphysema. In the Nurses Health Study, Troisi and colleagues (1995) found that among women diagnosed with chronic bronchitis, smokers were more likely to receive a subsequent diagnosis of asthma than were nonsmokers ( RR = 2.02 [95 percent CI , 1.01–4.02]). This labeling pattern in women may tend to bias toward an association of asthma with smoking.
Because the bronchial hyperresponsiveness of asthma may cause an intolerance to tobacco smoke, and because smoking worsens respiratory symptoms in persons with asthma ( Althuis et al. 1999 ; Sippel et al. 1999 ), some persons alter their smoking habits and thereby obscure a possible causal association ( Weiss et al. 1989 ). The result is that persons with asthma may not start smoking or may be more likely to quit, a phenomenon referred to as the “healthy smoker effect” ( Weiss et al. 1989 ); however, few data support these suggested biases. In a population-based survey of 3,019 persons from Australia, Wakefield and colleagues (1995) found no differences in the prevalence of smoking between persons with asthma (28.5 percent) and persons without asthma (26.9 percent), or in the amount smoked. Moreover, there were no differences between those two groups in reports of ever trying to quit or trying to quit in the past year.
Siroux and colleagues (2000) examined smoking behaviors among 200 adult patients with asthma and 265 controls without asthma, and found that childhood asthma was not associated with a reduced initiation of smoking. However, patients with asthma were more likely than those without asthma to quit smoking ( OR = 2.76 [95 percent CI , 1.19–6.42] for men; OR = 2.20 [95 percent CI, 1.11–4.34] for women).
Surrogate evidence for a link between cigarette smoking and asthma may be obtained from investigations of the relationship between smoking and non-specific bronchial hyperresponsiveness ( Weiss et al. 1989 ). Although the results are not entirely consistent, available evidence suggests that current smokers have greater bronchial hyperresponsiveness compared with nonsmokers, thus establishing a biologically plausible link for a causal role for smoking in the development of asthma ( Weiss et al. 1989 ; Kennedy et al. 1990 ; Rijcken et al. 1993 ; Sunyer et al. 1997 ).
A possible biologic link between smoking and asthma was also described by Wang and colleagues (2001) in their case-control study of 128 patients with asthma and 136 controls, identified through a community-based survey of 10,014 patients in China. Patients and controls were all examined for the prevalence of two genetic variations of the β 2 -adrenergic receptor gene, which controls airway dilatation. Compared with lifetime nonsmokers, ever smokers who were homozygotes for a specific genetic variation of the β 2 -adrenergic receptor gene on chromosome 16 (arginine/arginine-16) had a markedly increased risk for asthma ( OR = 7.81 [95 percent CI , 2.07–29.5]). In addition, there was a strong dose-response relationship with the amount smoked.
Although the relationship between active smoking and adult-onset asthma is inconsistent, there is consistent evidence that smoking adversely affects the control and severity of asthma ( Prescott et al. 1997 ; Cassino et al. 1999 ; Siroux et al. 2000 ; Beeh et al. 2001 ). As part of the Copenhagen City Heart Study, Prescott and colleagues (1997) examined 13,540 patients for factors associated with hospital admissions for asthma between 1977 and 1993. Overall, the risk of hospitalization for asthma was 20 percent greater in current and former smokers compared with lifetime nonsmokers (95 percent CI , 1.1–1.4) for each 10-year period of smoking. Cassino and colleagues (1999) examined determinants of emergency department visits for asthma among 1,216 adults with asthma living in New York City. Compared with nonsmokers, the RRs for emergency department visits were 1.07 (95 percent CI, 0.97– 1.18) for 1 to 5 pack-years of smoking, 1.69 (95 percent CI, 1.56–1.84) for 6 to 13 pack-years, 0.93 (95 percent CI, 0.84–1.04) for 14 to 30 pack-years, and 1.11 (95 percent CI, 1.00–1.22) for 31 or more pack-years. They also identified heavy cigarette use (13 or more pack-years) as a predictor of emergency department visits following days that had high outdoor ozone levels. In a case-control study of 200 adults with asthma from six specialty clinics in France and 265 controls without asthma, Siroux and colleagues (2000) found that active smoking was associated with an increase in asthma severity. For example, compared with nonsmokers, current smokers more often reported one or more asthma attacks per day ( OR = 2.39 [95 percent CI, 1.06– 5.36]) and abnormal breathing between attacks (OR = 2.06 [95 percent CI, 0.97–4.36]) than nonsmokers. Among 112 persons with asthma seen at a pulmonary specialist practice in Germany, Beeh and colleagues (2001) found that severe asthma, defined as a FEV 1 less than 60 percent predicted, was strongly associated with current smoking (OR = 4.8 [95 percent CI, 1.3–18.3]).
Evidence Synthesis. Although limited evidence suggests that smoking is a biologically plausible cause of asthma, the available epidemiologic evidence of an association between smoking and adult-onset asthma is inconsistent ( Tables 4.16 and 4.17 ). A number of methodologic limitations, including different definitions of asthma, different study designs, and biases such as recall bias and healthy smoker bias, probably contribute to the inconsistent results. In contrast to studies on the causation of asthma, smoking is consistently associated with a greater severity of asthma and increased uses of emergency and hospital services. By increasing the degree of airways inflammation, smoking may worsen the inflammatory process that is considered central in the pathogenesis of asthma. The impairment of airways function caused by smoking may also increase the likelihood of more severe asthma on a clinical basis.
- The evidence is inadequate to infer the presence or absence of a causal relationship between active smoking and asthma in adults.
- The evidence is suggestive but not sufficient to infer a causal relationship between active smoking and increased nonspecific bronchial hyper-responsiveness.
- The evidence is sufficient to infer a causal relationship between active smoking and poor asthma control.
Implications. Because of the large numbers of persons with asthma and an increasing prevalence of asthma worldwide, the potential role of active smoking in the causation of asthma has major public health implications. Therefore, this problem is highly relevant for further research despite methodologic challenges. Patients with asthma need to be strongly encouraged to quit smoking.
COPD . COPD is defined differently by clinicians, pathologists, and epidemiologists; each discipline uses different criteria based on physiologic impairments, pathologic abnormalities, and symptoms ( Samet 1989 ). The hallmark of COPD is airflow obstruction based on spirometric testing, with a persistently low FEV 1 and a low ratio of FEV 1 / FVC despite treatment. Clinicians often diagnose COPD when an adult cigarette smoker presents with chronic dyspnea, coughing, and consistent spirometric abnormalities.
Chronic bronchitis and emphysema with airflow obstruction are both included in the clinical syndrome of COPD . Other specific diseases associated with airflow obstruction, such as asthma, bronchiectasis, and cystic fibrosis, are specifically excluded from the clinical definition of COPD, although there may be overlapping clinical features. Chronic bronchitis and emphysema have specific definitions, although the terms are used more loosely in clinical practice. Chronic bronchitis is characterized by a chronic cough productive of sputum with airflow obstruction. Emphysema is defined as “a condition of the lung characterized by abnormal permanent enlargement of the airspaces distal to the terminal bronchiole, accompanied by destruction of their walls, and without obvious fibrosis” ( American Thoracic Society 1987 , p . 225). On the basis of this definition, the diagnosis of emphysema requires an examination of gross or microscopic lung specimens or an assessment of the lungs based on computed tomography, a recently developed tool ( Thurlbeck 1994 ).
Epidemiologic Evidence. In epidemiologic studies, the diagnosis of COPD may be derived from surveys or clinical databases. Questionnaire responses that may be used to diagnose COPD include reports of symptoms (e. g ., dyspnea, coughing, or phlegm), reports of physician diagnoses (e.g., emphysema, chronic bronchitis, or COPD), or both. Spirometry is often performed in epidemiologic studies to provide objective evidence of airflow obstruction in persons with or without symptoms. Sources of data for descriptive or analytic studies of COPD include databases containing hospital discharge information or vital statistics (e.g., from death certificates). However, the quality of these data sources may vary greatly. The standard terms used for COPD in the databases include terms from the International Classification of Diseases, 9th Revision, such as “chronic bronchitis” (code 491), “emphysema” (code 492), and “chronic airway obstruction not elsewhere classified” (code 496) ( USDHHS 1989b ).
Cigarette smoking as a cause of COPD has been reviewed extensively in earlier reports of the Surgeon General ( Table 4.13 ) ( USDHHS 1984 , 1989a , 1990 ). A considerable amount of more recent research on the relationship between COPD and cigarette smoking has focused on determining predictors of susceptibility, as discussed previously, and on early detection. The following discussion summarizes more current key research on the epidemiology of COPD.
COPD Morbidity. COPD is a common chronic disease in the United States and a major cause of morbidity associated with limitations on physical functioning and a high utilization of medical care services ( Verbrugge and Patrick 1995 ; Mapel et al. 2000 ). Approximately 10 million people in the United States have been diagnosed with COPD ( Wise 1997 ). Verbrugge and Patrick (1995) used data collected from the National Health Interview Survey conducted from 1983–1985 to calculate the prevalence of chronic conditions in the United States and to determine their relative impact on functioning. Among adults aged 18 years and older the prevalence of COPD, which included chronic bronchitis, emphysema, and asthma, was consistently among the top 10 chronic conditions. The prevalence was highest in men and women aged 65 years and older (16.7 percent among men and 12.6 percent among women), intermediate for men and women aged 45 through 64 years (8.8 percent and 11.4 percent, respectively), and lowest for men and women aged 18 through 44 years (5.5 percent and 9.3 percent, respectively). In addition, COPD consistently ranked among the top 10 conditions in all age groups that resulted in limitations on job-related responsibilities and other activities of daily living.
More recent national data are available from the Third National Health and Nutrition Examination Survey ( Mannino et al. 2000 ). This survey included 20,050 U.S. adults who participated from 1988–1994 and who completed an examination that included spirometry and respiratory health questions. The findings suggest that COPD occurs frequently in the United States. The authors categorized current obstructive lung disease as a report of current asthma, bronchitis, or ever having a diagnosis of emphysema. A prior but not current diagnosis of either chronic bronchitis or asthma was categorized as past obstructive lung disease. With these definitions, obstructive lung disease was found to affect 12.5 percent of current smokers, 9.4 percent of former smokers, and 5.8 percent of lifetime nonsmokers.
COPD is associated with high medical care utilization rates, including office-based physician visits and hospitalizations ( Verbrugge and Patrick 1995 ; Sullivan et al. 2000 ). In the 1985 National Ambulatory Medical Care Survey, COPD was consistently among the top 10 conditions leading to a physician visit. Verbrugge and Patrick (1995) found that the largest percentage of physician visits for COPD were among men and women aged 65 years and older (10.8 percent among men and 9.4 percent among women), intermediate for men and women aged 45 through 64 years (6.1 percent and 8.2 percent, respectively), and lowest for men and women aged 18 through 44 years (3.4 percent and 4.8 percent, respectively). In 1995, more than 16 million visits were made to physicians’ offices for COPD, a 72 percent increase from 1985 ( Sullivan et al. 2000 ). In contrast to other chronic conditions (e. g ., cancer or cardiovascular disease), COPD was a less common primary cause of hospitalization in the 1984 National Hospital Discharge Survey ( Verbrugge and Patrick 1995 ), but in 1995 it accounted for more than 500,000 hospitalizations in the United States ( Sullivan et al. 2000 ). However, COPD often is a comorbid condition associated with other chronic conditions, including cancer and cardiovascular diseases ( Ferrer et al. 1997 ; Mapel et al. 2000 ). Total estimated costs associated with COPD in 1993 were $23.9 billion, or about $1,522 per person per year, three times the per capita cost of asthma ( Sullivan et al. 2000 ).
More recent epidemiologic investigations continue to provide strong evidence for the causal link between active smoking and COPD ( Troisi et al. 1995 ; Forastiere et al. 1998 ). In the Nurses Health Study, a prospective cohort study of 74,072 women aged 34 through 68 years, the RR for self-reported, physician-diagnosed chronic bronchitis among current smokers compared with women who had never smoked was 2.85 (95 percent CI , 2.45–3.32) ( Troisi et al. 1995 ). Forastiere and colleagues (1998) , in a population-based cross-sectional survey of 1,226 women aged 55 years and older, found a marked increase in risk for self-reported, physician-diagnosed chronic bronchitis/emphysema among current smokers compared with former and lifetime nonsmokers ( OR = 6.4 [95 percent CI, 3.2–12.6]).
Smoking Cessation and COPD Morbidity. Although smoking cessation slows the rate of FEV 1 decline, thus decreasing the risk for developing chronic airflow obstruction ( Figure 4.1 ), the risk may not return to that for nonsmokers. In a population-based study of 1,391 Seventh-Day Adventists from California, which included nonsmokers and former smokers (aged 16 years or older), Berglund and colleagues (1999) found that, compared with never smoking, past smoking for 10 years was associated with a small but significant risk ( OR = 1.29 [95 percent CI , 1.00–1.66]) of airflow obstruction (FEV 1 / FVC less than 65 percent or FEV 1 percent predicted less than 75 percent).
The risk of self-reported physician-diagnosed chronic bronchitis returns close to that of nonsmokers, but only after 5 to 10 years of cessation ( Troisi et al. 1995 ; Forastiere et al. 1998 ). In the Nurses Health Study, Troisi and colleagues (1995) found that among former smokers the incidence of chronic bronchitis among women was equal to the incidence in those who had completely abstained from smoking for five or more years. Among women aged 55 years and older from Sonoma, California, Forastiere and colleagues (1998) found that the occurrence of physician-diagnosed chronic bronchitis/emphysema was higher in former smokers who had stopped smoking for 10 years or less ( OR = 4.7 [95 percent CI , 2.5–8.7]) compared with nonsmokers, but the risk returned close to that of nonsmokers after more than 10 years of cessation (OR = 1.6 [95 percent CI, 0.9–2.8]).
COPD Mortality. In 2001, COPD (excluding asthma) was the fourth leading cause of death in the United States with more than 118,000 deaths (4.9 percent of all deaths) and an overall mortality rate of 41.7 per 100,000 ( Arias et al. 2003 ). Over the past 30 years, the age-adjusted mortality rate from COPD has been increasing. Of the 10 leading causes of death in the United States, only COPD has increased during this period ( Wise 1997 ). Factors that contribute to the rising COPD mortality rates include decreasing mortality from other causes of death (e. g ., cardiovascular diseases) and increasing mortality among women and nonwhite males ( Mannino et al. 1997 ).
Although COPD prevalence and mortality rates since the late 1970s have been substantially higher in men than in women, the estimated percentage increases have been higher for women ( Thun et al. 1995 , 1997a ; Mannino et al. 1997 ). In fact, from 1979–1988 mortality rates for men worldwide either remained stable or decreased ( Brown et al. 1994 ). These patterns may be partially explained by differences between the prevalence of smoking and smoking behaviors in women and men that have occurred over time. During the past 20 to 30 years, the prevalence and amount of smoking among women have become increasingly similar to those of men ( USDHHS 2001 ).
The prospective studies of the American Cancer Society (Cancer Prevention Study I [ CPS-I ] and Cancer Prevention Study II [ CPS-II ]), which were conducted in the early- to mid-1960s and in the 1980s, provide evidence for a marked increase in the risk of mortality from COPD among women ( Thun et al. 1995 , 1997a ). In CPS-II the death rate for female current smokers (61.6 per 100,000 person-years) was three times higher than in CPS-I. The mortality RR was 12.8 for female current smokers compared with women who had never smoked. For male current smokers in CPS-II, the death rate (103.9 per 100,000 person-years) was 41 percent higher than for male current smokers in CPS-I. The mortality RR was 11.7 for male current smokers compared with men who had never smoked.
Thun and colleagues (1997b) examined mortality rates for COPD in CPS-II in relation to the number of cigarettes currently smoked at baseline. The RR for death from COPD increased with the number of cigarettes smoked per day. For female current smokers compared with women who had never smoked, the RR was 5.6 for 1 to 9 cigarettes per day, 7.9 for 10 to 19 cigarettes per day, 23.3 for 20 cigarettes per day, 22.9 for 21 to 39 cigarettes per day, and 25.2 for 40 or more cigarettes per day. The corresponding RRs for current male smokers compared with men who had never smoked were 8.8 for 1 to 9 cigarettes per day, 8.9 for 10 to 19 cigarettes per day, 10.4 for 20 cigarettes per day, 16.5 for 21 to 39 cigarettes per day, and 9.3 for 40 or more cigarettes per day.
Using CPS-I and CPS-II data on the RR of COPD mortality, Thun and colleagues (1997a , b ) calculated the percentage of COPD deaths attributable to cigarette smoking. Among women in CPS-I, 85 percent of COPD deaths were attributable to smoking; this percentage increased to 92.2 percent in CPS-II. The corresponding values among men were 89.2 percent and 91.4 percent, respectively.
Mannino and colleagues (1997) analyzed mortality trends for obstructive lung disease (including asthma) among people who died in the United States from 1979–1993. Of all the deaths during this time period, 8.2 percent had obstructive lung disease listed on the death certificate, but in only 43.3 percent was the death attributed to obstructive lung disease. Over the time of the study, the age-adjusted mortality rates for obstructive lung disease were highest in white men (ranging from 98.8 to 115.5 per 100,000 per year), followed by black men (77.5 to 100.2 per 100,000), men of other races (38.1 to 58.6 per 100,000), white women (25.5 to 57.7 per 100,000), black women (14.9 to 38.5 per 100,000), and women of other races (10.9 to 20.9 per 100,000). The percentage increases in mortality rates were highest for black women (158.3 percent), followed by white women (126.3 percent), other women (91.7 percent), other men (57.8 percent), black men (29.3 percent), and lowest among white men (16.9 percent).
Smoking Cessation and COPD Mortality. The literature on the effects of smoking cessation on mortality from COPD was extensively reviewed in the 1990 Surgeon General’s report, and the major conclusion relevant to mortality from that report was “With sustained abstinence, the COPD mortality rates among former smokers decline in comparison with continuing smokers” ( Table 4.13 ) ( USDHHS 1990 , p . 11). However, the risk of COPD mortality among former smokers, even after 20 years or more of abstinence, remains elevated compared with the risk among people who have never smoked. Moreover, within approximately the first five years of cessation, mortality rates from COPD initially increase above the rates for continuing smokers and then gradually decline with an increase in the duration of abstinence.
Evidence Synthesis. The recent literature on smoking and COPD provides further support for the conclusion of the 1984 Surgeon General’s report that “cigarette smoking is the major cause of COLD in the United States for both men and women. The contribution of cigarette smoking to COLD morbidity and mortality far outweighs all other factors” ( USDHHS 1984 , p . 8). Whereas the risks for COPD morbidity and mortality decline with smoking cessation, they may not return to the levels of nonsmokers, probably because smoking has resulted in irreversible injury to the airways and parenchyma. A growing body of literature in recent years is providing evidence for major socioeconomic consequences of COPD associated with a marked increase in the utilization of medical care resources.
- The evidence is sufficient to infer a causal relationship between active smoking and chronic obstructive pulmonary disease morbidity and mortality.
Implication. COPD represents a major public health problem that is increasing but could be almost completely prevented with the elimination of smoking.
Cigarette Type and Risk for Chronic Respiratory Diseases. The effect of cigarette type on respiratory symptoms and COLD was reviewed in the 1984 Surgeon General’s report, by Samet (1996) , and by the National Cancer Institute ( NCI ) Tobacco Control Monograph 13 ( NCI 2001 ). A conclusion from the 1984 report was as follows:
Although a reduction in cigarette tar content appears to reduce the risk of cough and mucus hypersecretion, the risk of shortness of breath and airflow obstruction may not be reduced. Evidence is unavailable on the relative risks of developing COLD consequent to smoking cigarettes with the very low tar and nicotine yields of current and recently marketed brands ( USDHHS 1984 , p . 12).
Since the publication of that report, few new data are available on the relationship between cigarette type and chronic respiratory diseases ( Lange et al. 1990 , 1992 ).
Epidemiologic Evidence. Using longitudinal spirometric data obtained during five years (1976–1978 and 1981–1983) from 4,372 smokers and 3,753 non-smokers who participated in the Copenhagen City Heart Study, Lange and colleagues (1990) examined the relationship between cigarette type (filter-tipped versus unfiltered) and lung function deterioration. Overall, there was no significant difference in FEV 1 reductions among filter-tipped cigarette smokers compared with unfiltered cigarette smokers. On average, during the time of the study the tar content of Danish unfiltered cigarettes was 35 mg per cigarette compared with 23 mg per cigarette for filter-tipped cigarettes.
Lange and colleagues (1992) also examined risks of COPD mortality associated with the type of cigarette smoked (filter-tipped versus unfiltered) and inhalation patterns in 7,703 women and 6,511 men who participated in the Copenhagen City Heart Study. The RRs for COPD-related mortality differed little between women and men based on the type of cigarette smoked. Compared with women who were nonsmokers, women who smoked unfiltered cigarettes had a RR for COPD-related mortality of 15 (95 percent CI , 3.1–65.0), and women who smoked filter-tipped cigarettes had a RR of 16 (95 percent CI, 3.6–70.0). The corresponding RRs for men were 6.4 (95 percent CI, 2.0– 20.0) and 7.9 (95 percent CI, 2.3–27.0), respectively.
In four prospective cohort studies in the United Kingdom, Tang and colleagues (1995) assessed mortality in 56,225 men for smoking-induced diseases, comparing filter-tipped and unfiltered cigarettes and estimated tar yields. The mortality risk for COPD was somewhat lower for smokers of filter-tipped cigarettes, but not significantly in comparison with smokers of unfiltered cigarettes. For a tar reduction of 15 mg per cigarette, Tang and colleagues (1995) estimated that COPD mortality would drop by about 20 percent, but this estimate was quite imprecise.
Histopathologic findings have also been reported that provide insights concerning tar and nicotine yields, respiratory symptoms, and lung function levels. Auerbach and colleagues (1979) quantitated smoking-related changes in the autopsied lungs of men from a Veterans Administration hospital in New Jersey. In a rigorously studied series of autopsied lungs, these investigators showed that smokers from a period when cigarettes had comparatively high tar and nicotine yields (1955–1960) had more changes in the airways at various smoking levels compared with smokers from a later period (1970–1977). They interpreted this temporal pattern as an indication that cigarettes with lower tar and nicotine yields had fewer effects on the lungs than did higher-yield cigarettes.
A number of studies have shown that smokers of lower-yield cigarettes have comparatively lower rates of respiratory symptoms ( Table 4.18 ). Respiratory questionnaire data collected in the late 1970s from approximately 6,000 Pennsylvania women are illustrative ( Schenker et al. 1982 ). The brand of cigarettes currently smoked was identified and used with Federal Trade Commission tar yield information to classify the smokers according to tar exposure. A higher-tar yield was positively associated with coughing and phlegm but not with wheezing or shortness of breath. For coughing and phlegm, there were consistent exposure-response relationships with an approximate doubling of symptom frequency from the lowest to the highest exposure category. The findings of other studies are similar. For example, a large study of civil servants in the United Kingdom, the Whitehall Study, showed that the percentage of smokers reporting phlegm increased with tar yield within each stratum of cigarettes smoked per day, even the lowest ( Higenbottam et al. 1980 ).
Studies on the association between cigarette tar yields and chronic respiratory diseases.
Not all studies show less disease associated with lower-yield cigarettes ( Table 4.18 ). One study from Finland found that symptom levels in young smokers who were just initiating smoking did not depend greatly on tar yield ( Rimpela and Teperi 1989 ). In this six-year follow-up study, the youth were surveyed on several occasions to determine the relationship between tar yield and symptom onset. There was little evidence of less symptom occurrence in the new smokers using low-tar cigarettes in comparison with those smoking higher-tar cigarettes. Moreover, symptoms were far more frequent in the low-tar smokers than in nonsmokers. In a randomized trial in the United Kingdom, lower-tar cigarettes were not associated with either lower symptom frequency or a higher level of ventilatory function, which was assessed by measuring the peak expository flow rate ( Withey et al. 1992a , b ). The investigators monitored urinary nicotine metabolites and concluded that compensation led to comparable levels across the trial period.
Respiratory morbidity also has been investigated. Follow-ups of outpatient visits by enrollees in a Kaiser Permanente group over one year showed that there was a reduced risk for pneumonia and influenza, but not for other respiratory conditions, associated with the use of low-tar and low-nicotine products compared with the use of products higher in tar and nicotine ( Petitti and Friedman 1985a ). However, in comparison with nonsmokers, smokers using low-tar and low-nicotine cigarettes had an increased risk for pneumonia, influenza, and COPD .
The evidence does not suggest a relationship between tar yield and lung function level. For example, in the Whitehall Study there was no cross-sectional relationship between tar yield and the FEV 1 level ( Higenbottam et al. 1980 ). In the Normative Aging Study, a longitudinal study of U.S. veterans, tar yields of the usual brands of cigarettes smoked were not associated with a decline of FEV 1 levels ( Sparrow et al. 1983 ), and the Tucson Study found a weak association between lung function decline and higher tar yields ( Krzyzanowski et al. 1991 ).
In general, cohort studies assessing cigarette type and yield with COPD risks show little evidence for an association. In the CPS-I study comparing “low-” or “medium-” tar and nicotine smokers with “high-” tar and nicotine smokers, mortality from emphysema was reduced somewhat, although not significantly ( Table 4.18 ) ( Lee and Garfinkel 1981 ).
Evidence Synthesis. Little new evidence is available, and it does not conflict with the conclusion of the 1984 Surgeon General’s report ( USDHHS 1984 ) that “reduction in cigarette tar content appears to reduce the risk of cough and mucus hypersecretion” ( p . 12). Limited evidence published since that report suggests that cigarette type does not influence the rate of FEV 1 decline or COPD -related mortality.
- The evidence is suggestive but not sufficient to infer a causal relationship between lower machine-measured cigarette tar and a lower risk for cough and mucus hypersecretion.
- The evidence is inadequate to infer the presence or absence of a causal relationship between a lower cigarette tar content and reductions in forced expiratory volume in one second decline rates.
- The evidence is inadequate to infer the presence or absence of a causal relationship between a lower cigarette tar content and reductions in chronic obstructive pulmonary disease-related mortality.
Implications. Although there are limited data on the relationship between cigarette type and the risk for chronic respiratory diseases, the strong benefits from smoking cessation combined with the availability of effective methods for controlling tobacco use suggest that little public health benefit will be gained by further research on the relationship between cigarette type and chronic respiratory diseases.
Diffuse Parenchymal Lung Diseases. Diffuse parenchymal lung diseases, also known as interstitial lung diseases, are a heterogeneous group of disorders associated with different types of inflammation primarily in the walls and airspaces of alveoli. Although there are more than 100 different diffuse parenchymal lung diseases, only small numbers of patients with these diseases are seen regularly by clinicians ( Coultas et al. 1994 ), and the role of cigarette smoking has been investigated only for a few of these diseases.
Although the pathogenesis of these diseases is varied, conceptually they result from an inflammatory response in the lungs that follows the inhalation of a wide variety of particles (e. g ., inorganic and organic). For some of the diseases (i.e., idiopathic pulmonary fibrosis [ IPF ] or sarcoidosis), emerging evidence suggests a causal role for a number of inhaled agents, but causality remains to be established. The role of cigarette smoking in the pathogenesis of diffuse parenchymal lung diseases, although not fully defined, is potentially complex and may involve altered clearance, deposition of particles, and modification of the inflammatory response. Evidence for a complex interaction between cigarette smoking and the pathogenesis of diffuse parenchymal lung diseases is based on observations that cigarette smoking is associated with an increased disease risk for some (e.g., IPF or pneumoconiosis), and a decreased risk for others (e.g., hypersensitivity pneumonitis or sarcoidosis). Available evidence suggests that modification of the inflammatory/immune response may be the mechanism for lowering the risks for hypersensitivity pneumonitis ( Baron 1996 ) and sarcoidosis ( Soliman and Twigg 1992 ; Baron 1996 ).
Idiopathic Pulmonary Fibrosis. Epidemiologic Evidence. Scant epidemiologic data are available on the occurrence of IPF ( Coultas et al. 1994 ), but the available information suggests that IPF may be the most common diffuse parenchymal lung disease in the general population ( Coultas et al. 1994 ). Until recently, etiologic investigations of this disorder had not been conducted. It is relatively uncommon, and without a lung biopsy misclassification of the diagnosis may result, making investigation of this disorder difficult. Although the term “idiopathic” means of unknown cause, during the past decade four case-control studies have been conducted to examine potential etiologic agents, including cigarette smoking ( Scott et al. 1990 ; Iwai et al. 1994 ; Hubbard et al. 1996 ; Baumgartner et al. 1997 ). One case-control study of environmental exposures was conducted with 17 patients, but cigarette smoking was not examined ( Mullen et al. 1998 ).
Overall, significant associations were found in three of the four studies. Scott and colleagues (1990) identified 40 cases of IPF seen by pulmonary physicians or tested at pulmonary function laboratories in Nottingham, England, and 106 age- and gender-matched controls were identified from patients registered with the index patient’s general practitioner. In this case-control study, cigarette smoking was not significantly associated with IPF ( OR = 1.11 [95 percent CI , 0.13–1.40]).
Cases of IPF seen between 1992 and 1994 at four teaching hospitals in the Trent Region, United Kingdom, were identified by Hubbard and colleagues (1996) . Controls matched by age, gender, and community were identified from patients registered with the same general practitioner. Information on smoking and other exposures was obtained from 218 patients and 569 controls who returned a mailed questionnaire; 165 cases and 408 controls completed telephone interviews for verification. Having ever smoked was significantly associated with IPF ( OR = 1.57 [95 percent CI , 1.01– 2.43]).
Iwai and colleagues (1994) identified 86 patients with IPF evaluated by two research committees in Japan. Two controls for each patient were matched for age, gender, and residential area: a person selected from voters’ lists and a hospital patient with a non-IPF respiratory disease. Compared with healthy controls, IPF patients were significantly more likely to smoke ( OR = 2.94 [95 percent CI , 1.37–6.30]).
Baumgartner and colleagues (1997) conducted a multicenter case-control study in the United States that included 16 institutions in 15 states. A total of 248 patients had been diagnosed with IPF between 1989 and 1993; and 491 community controls matched for age, gender, and geographic location were identified using random-digit telephone dialing. Standardized telephone interviews were used to obtain risk factor information from cases and controls. Ever smoking was significantly associated with IPF ( OR = 1.6 [95 percent CI , 1.1–2.4]), but there was no dose-response relationship with pack-years of smoking. Moreover, there was no increased risk in current smokers (OR = 1.06 [95 percent CI, 0.6–1.8]). However, among former smokers there was an inverse trend in risk with time since cessation (OR = 3.5 [95 percent CI, 1.1–11.9] for cessation of less than 2.5 years, OR = 2.3 [95 percent CI, 1.3–4.2] for cessation of 2.5 to 10 years, OR = 1.9 [95 percent CI, 1.1–3.2] for cessation of 10 to 25 years, and OR = 1.3 [95 percent CI, 0.7–2.3] for cessation of 25 or more years).
Evidence Synthesis. Inflammation is thought to have a central role in the pathogenesis of IPF . Smoking, which increases lung inflammation, could plausibly increase the risk for IPF. Several studies show an association between ever smoking and IPF; however, the data are limited and further studies are needed.
- The evidence is inadequate to infer the presence or absence of a causal relationship between active smoking and idiopathic pulmonary fibrosis.
Implication. Further research will be needed to determine whether there is a causal relationship between active smoking and pulmonary fibrosis.
1. The evidence is sufficient to infer a causal relationship between smoking and acute respiratory illnesses, including pneumonia, in persons without underlying smoking-related chronic obstructive lung disease.
2. The evidence is suggestive but not sufficient to infer a causal relationship between smoking and acute respiratory infections among persons with preexisting chronic obstructive pulmonary disease.
3. In persons with asthma, the evidence is inadequate to infer the presence or absence of a causal relationship between smoking and acute asthma exacerbation.
4. The evidence is sufficient to infer a causal relationship between maternal smoking during pregnancy and a reduction of lung function in infants.
5. The evidence is suggestive but not sufficient to infer a causal relationship between maternal smoking during pregnancy and an increase in the frequency of lower respiratory tract illnesses during infancy.
6. The evidence is suggestive but not sufficient to infer a causal relationship between maternal smoking during pregnancy and an increased risk for impaired lung function in childhood and adulthood.
7. Active smoking causes injurious biologic processes (i.e., oxidant stress, inflammation, and a protease-antiprotease imbalance) that result in airway and alveolar injury. This injury, if sustained, ultimately leads to the development of chronic obstructive pulmonary disease.
8. The evidence is sufficient to infer a causal relationship between active smoking and impaired lung growth during childhood and adolescence.
9. The evidence is sufficient to infer a causal relationship between active smoking and the early onset of lung function decline during late adolescence and early adulthood.
10. The evidence is sufficient to infer a causal relationship between active smoking in adulthood and a premature onset of and an accelerated age-related decline in lung function.
11. The evidence is sufficient to infer a causal relationship between sustained cessation from smoking and a return of the rate of decline in pulmonary function to that of persons who had never smoked.
12. The evidence is sufficient to infer a causal relationship between active smoking and respiratory symptoms in children and adolescents, including coughing, phlegm, wheezing, and dyspnea.
13. The evidence is sufficient to infer a causal relationship between active smoking and asthma-related symptoms (i.e., wheezing) in childhood and adolescence.
14. The evidence is inadequate to infer the presence or absence of a causal relationship between active smoking and physician-diagnosed asthma in childhood and adolescence.
15. The evidence is suggestive but not sufficient to infer a causal relationship between active smoking and a poorer prognosis for children and adolescents with asthma.
16. The evidence is sufficient to infer a causal relationship between active smoking and all major respiratory symptoms among adults, including coughing, phlegm, wheezing, and dyspnea.
17. The evidence is inadequate to infer the presence or absence of a causal relationship between active smoking and asthma in adults.
18. The evidence is suggestive but not sufficient to infer a causal relationship between active smoking and increased nonspecific bronchial hyper-responsiveness.
19. The evidence is sufficient to infer a causal relationship between active smoking and poor asthma control.
20. The evidence is sufficient to infer a causal relationship between active smoking and chronic obstructive pulmonary disease morbidity and mortality.
21. The evidence is suggestive but not sufficient to infer a causal relationship between lower machine-measured cigarette tar and a lower risk for cough and mucus hypersecretion.
22. The evidence is inadequate to infer the presence or absence of a causal relationship between a lower cigarette tar content and reductions in forced expiratory volume in one second decline rates.
23. The evidence is inadequate to infer the presence or absence of a causal relationship between a lower cigarette tar content and reductions in chronic obstructive pulmonary disease-related mortality.
24. The evidence is inadequate to infer the presence or absence of a causal relationship between active smoking and idiopathic pulmonary fibrosis.
- Adams SG, Melo J, Luther M, Anzueto A. Antibiotics are associated with lower relapse rates in outpatients with acute exacerbations of COPD. Chest. 2000; 117 (5):1345–52. [ PubMed : 10807821 ]
- Aguayo SM. Determinants of susceptibility to cigarette smoke: potential roles for neuroendocrine cells and neuropeptides in airway inflammation, airway wall remodeling, and chronic airflow obstruction. American Journal of Respiratory and Critical Care Medicine. 1994; 149 (6):1692–8. [ PubMed : 7911710 ]
- Alcaide J, Altet MN, Plans P, Parrón I, Folguera L, Saltó E, Domínquez A, Pardell H, Salleras L. Cigarette smoking as a risk factor for tuberculosis in young adults: a case-control study. Tubercle and Lung Disease. 1996; 77 (2):112–6. [ PubMed : 8762844 ]
- Alderson MR, Lee PN, Wang R. Risks of lung cancer, chronic bronchitis, ischaemic heart disease, and stroke in relation to type of cigarette smoked. Journal of Epidemiology and Community Health. 1985; 39 (4):286–93. [ PMC free article : PMC1052459 ] [ PubMed : 4086957 ]
- Almirall J, Bolíbar I, Balanzó X, González CA. Risk factors for community-acquired pneumonia in adults: a population-based case-control study. European Respiratory Journal. 1999a; 13 (2):349–55. [ PubMed : 10065680 ]
- Almirall J, González CA, Balanzó X, Bolíbar I. Proportion of community-acquired pneumonia cases attributable to tobacco smoking. Chest. 1999b; 116 (2):375–9. [ PubMed : 10453865 ]
- Althuis MD, Sexton M, Prybylski D. Cigarette smoking and asthma symptom severity among adult asthmatics. Journal of Asthma. 1999; 36 (3):257–64. [ PubMed : 10350222 ]
- American Thoracic Society. Standards for the diagnosis and care of patients with chronic obstructive pulmonary disease (COPD) and asthma. American Review of Respiratory Disease. 1987; 136 (1):225–44. [ PubMed : 3605835 ]
- Anderson RH, Sy FS, Thompson S, Addy C. Cigarette smoking and tuberculin skin test conversion among incarcerated adults. American Journal of Preventive Medicine. 1997; 13 (3):175–81. [ PubMed : 9181204 ]
- Anthonisen NR, Connett JE, Kiley JP, Altose MD, Bailey WC, Buist AS, Conway WA Jr, Enright PL, Kanner RE, O’Hara P, Owens GR, Scanlon PD, Tashkin DP, Wise RA. Effects of smoking intervention and the use of inhaled anticholinergic bronchodilator on the rate of decline of FEV 1 : the Lung Health Study. Journal of the American Medical Association. 1994; 272 (19):1497–505. [ PubMed : 7966841 ]
- Anthonisen NR, Manfreda J, Warren CPW, Hershfield ES, Harding GKM, Nelson NA. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Annals of Internal Medicine. 1987; 106 (2):196–204. [ PubMed : 3492164 ]
- Arday DR, Giovino GA, Schulman J, Nelson DE, Mowery P, Samet JM. Cigarette smoking and self-reported health problems among U.S. high school seniors, 1982–1989. American Journal of Health Promotion. 1995; 10 (2):111–6. [ PubMed : 10160044 ]
- Arias E, Anderson RN, Kung H-C, Murphy SL, Kochanek KD. Deaths: final data for 2001. National Vital Statistics Reports. 2003; 52 (3):1–116. [ PubMed : 14570230 ]
- Aronson MD, Weiss ST, Ben RL, Komaroff AL. Association between cigarette smoking and acute respiratory tract illness in young adults. Journal of the American Medical Association. 1982; 248 (2):181–3. [ PubMed : 7087108 ]
- Auerbach O, Garfinkel L, Parks VR. Scar cancer of the lung: increase over a 21 year period. Cancer. 1979; 43 (2):636–42. [ PubMed : 217523 ]
- Barker DJP, Godfrey KM, Fall C, Osmond C, Winter PD, Shaheen SO. Relation of birth weight and childhood respiratory infection to adult lung function and death from chronic obstructive airways disease. British Medical Journal. 1991; 303 (6804):671–5. [ PMC free article : PMC1670943 ] [ PubMed : 1912913 ]
- Barnes PJ. Molecular genetics of chronic obstructive pulmonary disease. Thorax. 1999; 54 (3):245–52. [ PMC free article : PMC1745439 ] [ PubMed : 10325902 ]
- Baron JA. Beneficial effects of nicotine and cigarette smoking: the real, the possible and the spurious. British Medical Bulletin. 1996; 52 (1):58–73. [ PubMed : 8746297 ]
- Baumgartner KB, Samet JM, Stidley CA, Colby TV, Waldron JA. Cigarette smoking: a risk factor for idiopathic pulmonary fibrosis. American Journal of Respiratory and Critical Care Medicine. 1997; 155 (1):242–8. [ PubMed : 9001319 ]
- Beeh KM, Micke P, Ksoll M, Buhl R. Cigarette smoking, but not sensitization to Alternaria, is associated with severe asthma in urban patients. Journal of Asthma. 2001; 38 (1):41–9. [ PubMed : 11256553 ]
- Belousova EG, Haby MM, Xuan W, Peat JK. Factors that affect normal lung function in white Australian adults. Chest. 1997; 112 (6):1539–46. [ PubMed : 9404751 ]
- Ben-Noun L. Is there a relationship between smoking and asthma in adults? Journal of International Medical Research. 1999; 27 (1):15–21. [ PubMed : 10417957 ]
- Bent S, Saint S, Vittinghoff E, Grady D. Antibiotics in acute bronchitis: a meta-analysis. American Journal of Medicine. 1999; 107 (1):62–7. [ PMC free article : PMC7124195 ] [ PubMed : 10403354 ]
- Berglund DJ, Abbey DE, Lebowitz MD, Knutsen SF, McDonnell WF. Respiratory symptoms and pulmonary function in an elderly nonsmoking population. Chest. 1999; 115 (1):49–59. [ PubMed : 9925062 ]
- Berry DG, Fry J, Hindley CP, Hodson JM, Horder EJ, Horder JP, Marien EAW, Rea JN, Ryle A, Curwen MP, Tomlinson AJH. Exacerbations of chronic bronchitis: treatment with oxytetracycline. Lancet. 1960; 1 :137–9. [ PubMed : 13799872 ]
- Blake GH, Abell TD, Stanley WG. Cigarette smoking and upper respiratory infection among recruits in basic combat training. Annals of Internal Medicine. 1988; 109 (3):198–202. [ PubMed : 3389603 ]
- Boake WC. A study of illness in a group of Cleveland families. XVIII: tobacco smoking and respiratory infections. New England Journal of Medicine. 1958; 259 (26):1245–9. [ PubMed : 13622921 ]
- Bodner CH, Ross S, Little J, Douglas JG, Legge JS, Friend JAR, Godden DJ. Risk factors for adult onset wheeze: a case control study. American Journal of Respiratory and Critical Care Medicine. 1998; 157 (1):35–42. [ PubMed : 9445276 ]
- Bosken CH, Wiggs BR, Pare PD, Hogg JC. Small airway dimensions in smokers with obstruction to airflow. American Review of Respiratory Disease. 1990; 142 (3):563–70. [ PubMed : 2389908 ]
- Brickfield FX, Carter WH, Johnson RE. Erythromycin in the treatment of acute bronchitis in a community practice. Journal of Family Practice. 1986; 23 (2):119–22. [ PubMed : 3525736 ]
- Brown CA, Crombie IK, Smith WC, Tunstall-Pedoe H. Cigarette tar content and symptoms of chronic bronchitis: results of the Scottish Heart Health Study. Journal of Epidemiology and Community Health. 1991; 45 (4):287–90. [ PMC free article : PMC1059462 ] [ PubMed : 1795148 ]
- Brown CA, Crombie IK, Tunstall-Pedoe H. Failure of cigarette smoking to explain international differences in mortality from chronic obstructive pulmonary disease. Journal of Epidemiology and Community Health. 1994; 48 (2):134–9. [ PMC free article : PMC1059921 ] [ PubMed : 8189166 ]
- Buchanan J, Buchanan WW, Melrose AG, McGuinness JB, Price AU. Long-term prophylactic administration of tetracycline to chronic bronchitics. Lancet. 1958; 2 :719–22. [ PubMed : 13588985 ]
- Buist AS, Vollmer WM, Wu Y, Tsai R, Johnson LR, Hurd S, Davis CE, Williams OD, Li Y, Chen B, Ma L. Effects of cigarette smoking on lung function in four population samples in the People’s Republic of China: the PRC-US Cardiovascular and Cardiopulmonary Epidemiology Research Group. American Journal of Respiratory and Critical Care Medicine. 1995; 151 (5):1393–400. [ PubMed : 7735591 ]
- Burchfiel CM, Marcus EB, Curb JD, MacLean CJ, Vollmer WM, Johnson LR, Fong K-O, Rodriguez BL, Masaki KH, Buist AS. Effects of smoking and smoking cessation on longitudinal decline in pulmonary function. American Journal of Respiratory and Critical Care Medicine. 1995; 151 (6):1778–85. [ PubMed : 7767520 ]
- Burchfiel CM, Marcus EB, Sharp DS, Enright PL, Rodriguez BL, Masaki KH, Hwang L-J, Curb JD. Characteristics associated with rapid decline in forced expiratory volume. Annals of Epidemiology. 1996; 6 (3):217–27. [ PubMed : 8827157 ]
- Burns DN, Hillman D, Neaton JD, Sherer R, Mitchell T, Capps L, Vallier WG, Thurnherr MD, Gordin FM. Cigarette smoking, bacterial pneumonia, and other clinical outcomes in HIV-1 infection. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1996; 13 (4):374–83. [ PubMed : 8948377 ]
- Burri PH. Postnatal development and growth. In: Crystal RG, West JB, Barnes PJ, Weibel ER, editors. The Lung: Scientific Foundations. 2nd ed. Philadelphia (PA): Lippincott-Raven; 1997. pp. 1013–7.
- Burrows B, Halonen M, Barbee RA, Lebowitz MD. The relationship of serum immunoglobulin E to cigarette smoking. American Review of Respiratory Disease. 1981; 124 (5):523–5. [ PubMed : 7305105 ]
- Burrows B, Knudson RJ, Camilli AE, Lyle SK, Lebowitz MD. The “horse-racing effect” and predicting decline in forced expiratory volume in one second from screening spirometry. American Review of Respiratory Disease. 1987; 135 (4):788–93. [ PubMed : 3565926 ]
- Buskin SE, Gale JL, Weiss NS, Nolan CM. Tuberculosis risk factors in adults in King County, Washington, 1988 through 1990. American Journal of Public Health. 1994; 84 (11):1750–6. [ PMC free article : PMC1615189 ] [ PubMed : 7977912 ]
- Butland BK, Strachan DP, Anderson HR. Fresh fruit intake and asthma symptoms in young British adults: confounding or effect modification by smoking? European Respiratory Journal. 1999; 13 (4):744–50. [ PubMed : 10362034 ]
- Byron KA, Varigos GA, Wootton AM. IL-4 production is increased in cigarette smokers. Clinical and Experimental Immunology. 1994; 95 (2):333–6. [ PMC free article : PMC1534911 ] [ PubMed : 8306509 ]
- Camilli AE, Burrows B, Knudson RJ, Lyle SK, Lebowitz MD. Longitudinal changes in forced expiratory volume in one second in adults: effects of smoking and smoking cessation. American Review of Respiratory Disease. 1987; 135 (4):794–9. [ PubMed : 3565927 ]
- Carey IM, Strachan DP, Cook DG. Effects of changes in fresh fruit consumption on ventilatory function in healthy British adults. American Journal of Respiratory and Critical Care Medicine. 1998; 158 (3):728–33. [ PubMed : 9730997 ]
- Cassino C, Ito K, Bader I, Ciotoli C, Thurston G, Reibman J. Cigarette smoking and ozone-associated emergency department use for asthma by adults in New York City. American Journal of Respiratory and Critical Care Medicine. 1999; 159 (6):1773–9. [ PubMed : 10351917 ]
- Cazzola M, Franco C, Gioia V, Legnani D, Mancini V, Polverino M, Sevieri G. Cefaclor in the treatment of infective exacerbations of chronic bronchitis in cigarette smokers. Journal of Chemotherapy. 1991; 3 (4):245–9. [ PubMed : 1779259 ]
- Chan KN, Noble-Jamieson CM, Elliman A, Bryan EM, Silverman M. Lung function in children of low birth weight. Archives of Disease in Childhood. 1989; 64 (9):1284–93. [ PMC free article : PMC1792739 ] [ PubMed : 2817949 ]
- Chen Y, Dales R, Krewski D, Breithaupt K. Increased effects of smoking and obesity on asthma among female Canadians: the National Population Health Survey, 1994–1995. American Journal of Epidemiology. 1999; 150 (3):255–62. [ PubMed : 10430229 ]
- Cherniack NS, Vosti KL, Dowling HF, Lepper MH, Jackson GG. Long-term treatment of bronchiectasis and chronic bronchitis. Archives of Internal Medicine. 1959; 103 :345–53. [ PubMed : 13626263 ]
- Clancy R, Cripps A, Murree-Allen K, Yeung S, Engel M. Oral immunisation with killed Haemophilus influenzae for protection against acute bronchitis in chronic obstructive lung disease. Lancet. 1985; 2 (8469–70):1395–7. [ PubMed : 2867396 ]
- Clancy RL, Cripps AW, Gebski V. Protection against recurrent acute bronchitis after oral immunization with killed Haemophilus influenzae . Medical Journal of Australia. 1990; 152 (8):413–6. [ PubMed : 2184330 ]
- Clarke JR, Salmon B, Silverman M. Bronchial responsiveness in the neonatal period as a risk factor for wheezing in infancy. American Journal of Respiratory and Critical Care Medicine. 1995; 151 (5):1434–40. [ PubMed : 7735597 ]
- Clerici N, Reboiras S, Fierro C, Leyva-Cobian F. Expression of Ia like (HLA-DR) antigens on human alveolar macrophages. Clinical and Experimental Immunology. 1984; 58 (2):388–94. [ PMC free article : PMC1577058 ] [ PubMed : 6209043 ]
- Cohen S, Tyrrell DAJ, Russell MAH, Jarvis MJ, Smith AP. Smoking, alcohol consumption, and susceptibility to the common cold. American Journal of Public Health. 1993; 83 (9):1277–83. [ PMC free article : PMC1694990 ] [ PubMed : 8363004 ]
- Collet JP, Shapiro P, Ernst P, Renzi T, Ducruet T, Robinson A. Effects of an immunostimulating agent on acute exacerbations and hospitalizations in patients with chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1997; 156 (6):1719–24. [See also comments in American Journal of Respiratory and Critical Care Medicine 1997;156(6):1713–4] [ PubMed : 9412546 ]
- Cook DG, Strachan DP. Health effects of passive smoking-10: summary of effects of parental smoking on the respiratory health of children and implications for research. Thorax. 1999; 54 (4):357–66. [ PMC free article : PMC1745458 ] [ PubMed : 10092699 ]
- Corberand J, Nguyen F, Do AH, Dutau G, Laharrague P, Fontanilles AM, Gleizes B. Effect of tobacco smoking on the functions of polymorphonuclear leukocytes. Infection and Immunity. 1979; 23 (3):577–81. [ PMC free article : PMC414204 ] [ PubMed : 222675 ]
- Costabel U, Bross KJ, Reuter C, Rühle K-H, Matthys H. Alterations in immunoregulatory T-cell subsets in cigarette smokers: a phenotypic analysis of bronchoalveolar and blood lymphocytes. Chest. 1986; 90 (1):39–44. [See also erratum in Chest 1987; 92(6):1124.] [ PubMed : 2941248 ]
- Costabel U, Maier K, Teschler H, Wang YM. Local immune components in chronic obstructive pulmonary disease. Respiration. 1992; 59 (Suppl 1):17–9. [ PubMed : 1579726 ]
- Coultas DB, Zumwalt RE, Black WC, Sobonya RE. The epidemiology of interstitial lung diseases. American Journal of Respiratory and Critical Care Medicine. 1994; 150 (4):967–72. [ PubMed : 7921471 ]
- Cruijff M, Thijs C, Govaert T, Aretz K, Dinant GJ, Knottnerus A. The effect of smoking on influenza, influenza vaccination efficacy and on the antibody response to influenza vaccination. Vaccine. 1999; 17 (5):426–32. [ PMC free article : PMC7130566 ] [ PubMed : 10073719 ]
- Cunningham J, Dockery DW, Speizer FE. Maternal smoking during pregnancy as a predictor of lung function in children. American Journal of Epidemiology. 1994; 139 (12):1139–52. [ PubMed : 8209873 ]
- Daniele RP, Dauber JH, Altose MD, Rowlands DT Jr, Gorenberg DJ. Lymphocyte studies in asymptomatic cigarette smokers: a comparison between lung and peripheral blood. American Review of Respiratory Disease. 1977; 116 (6):997–1005. [ PubMed : 303879 ]
- David MM, Hanrahan JP, Carey V, Speizer FE, Tager IB. Respiratory symptoms in urban Hispanic and non-Hispanic white women. American Journal of Respiratory and Critical Care Medicine. 1996; 153 (4 Pt 1):1285–91. [ PubMed : 8616555 ]
- Davis AL, Grobow EJ, Kaminski T, Tompsett R, McClement JH. Bacterial infection and some effects of chemoprophylaxis in chronic pulmonary emphysema. American Review of Respiratory Disease. 1965; 92 (6):900–13. [ PubMed : 4378906 ]
- Davis AL, Grobow EJ, Tompsett R, McClement JH. Bacterial infection and some effects of chemoprophylaxis in chronic pulmonary emphysema. American Journal of Medicine. 1961; 31 :619–37. [ PubMed : 13720140 ]
- de Marco R, Locatelli F, Sunyer J, Burney P. Differences in incidence of reported asthma related to age in men and women: a retrospective analysis of the data of the European Respiratory Health Survey. American Journal of Respiratory and Critical Care Medicine. 2000; 162 (1):68–74. [ PubMed : 10903222 ]
- Dean G, Lee PN, Todd GF, Wicken AJ, Sparks DN. Factors related to respiratory and cardiovascular symptoms in the United Kingdom. Journal of Epidemiology and Community Health. 1978; 32 (2):86–96. [ PMC free article : PMC1060924 ] [ PubMed : 681591 ]
- Dezateux C, Stocks J. Lung development and early origins of childhood respiratory illness. British Medical Bulletin. 1997; 53 (1):40–57. [ PubMed : 9158283 ]
- Dezateux C, Stocks J, Dundas I, Fletcher ME. Impaired airway function and wheezing in infancy: the influence of maternal smoking and a genetic predisposition to asthma. American Journal of Respiratory and Critical Care Medicine. 1999; 159 (2):403–10. [ PubMed : 9927350 ]
- Dodge R, Cline MG, Burrows B. Comparisons of asthma, emphysema, and chronic bronchitis diagnoses in a general population sample. American Review of Respiratory Disease. 1986; 133 (6):981–6. [ PubMed : 3717770 ]
- Donowitz GR, Mandell GL. Acute pneumonia. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 4th ed. New York: Churchill Livingston; 1995. pp. 619–37.
- Dunlay J, Reinhardt R, Roi LD. A placebo-controlled, double-blind trial of erythromycin in adults with acute bronchitis. Journal of Family Practice. 1987; 25 (2):137–41. [ PubMed : 3302093 ]
- Elmes PC, Fletcher CM, Dutton AAC. Prophylactic use of oxytetracycline for exacerbations of chronic bronchitis. British Medical Journal. 1957; 2 :1272–5. [ PMC free article : PMC1963159 ] [ PubMed : 13479695 ]
- Elmes PC, King TKC, Langlands JHM, Mackay JA, Wallace WFM, Wade OL, Wilson TS. Value of ampicillin in the hospital treatment of exacerbations of chronic bronchitis. British Medical Journal. 1965; 2 (5467):904–8. [ PMC free article : PMC1846431 ] [ PubMed : 5318963 ]
- Fagon J-Y, Chastre J, Trouillet J-L, Domart Y, Dombret M-C, Bornet M, Gibert C. Characterization of distal bronchial microflora during acute exacerbation of chronic bronchitis: use of the protected specimen brush technique in 54 mechanically ventilated patients. American Review of Respiratory Disease. 1990; 142 (5):1004–8. [ PubMed : 2240819 ]
- Fear EC, Edwards G. Antibiotic regimes in chronic bronchitis. British Journal of Diseases of the Chest. 1962; 56 (4):153–62. [ PubMed : 13944632 ]
- Fearon DT, Locksley RM. Instructive role of innate immunity in the acquired immune response. Science. 1996; 272 (5258):50–3. [ PubMed : 8600536 ]
- Ferrari M, Poli A, Olivieri M, Tardivo S, Biasin C, Balestreri F, Dal Molin G, Lo Cascio V, Campello C. Seroprevalence of Chlamydia pneumoniae antibodies in a young adult population sample living in Verona. Infection. 2000; 28 (1):38–41. [ PubMed : 10697790 ]
- Ferrer M, Alonso J, Morera J, Marrades RM, Khalaf A, Aguar MC, Plaza V, Prieto L, Antó JM. Chronic obstructive pulmonary disease stage and health-related quality of life. Annals of Internal Medicine. 1997; 127 (12):1072–9. [ PubMed : 9412309 ]
- Finklea JF, Hasselblad V, Riggan WB, Nelson WC, Hammer DI, Newill VA. Cigarette smoking and hemagglutination inhibition response to influenza after natural disease and immunization. American Review of Respiratory Disease. 1971a; 104 (3):368–76. [ PubMed : 5098670 ]
- Finklea JF, Hasselblad V, Sandifer SH, Hammer DI, Lowrimore GR. Cigarette smoking and acute non-influenzal respiratory disease in military cadets. American Journal of Epidemiology. 1971b; 93 (6):457–62. [ PubMed : 5562718 ]
- Finklea JF, Sandifer SH, Smith DD. Cigarette smoking and epidemic influenza. American Journal of Epidemiology. 1969; 90 (5):390–9. [ PubMed : 5356947 ]
- Flanigan TP, Hogan JW, Smith D, Schoenbaum E, Vlahov D, Schuman P, Mayer K. Self-reported bacterial infections among women with or at risk for human immunodeficiency virus infection. Clinical Infectious Diseases. 1999; 29 (3):608–12. [ PubMed : 10530455 ]
- Fletcher CM, Peto R, Tinker C, Speizer FE. The Natural History of Chronic Bronchitis and Emphysema An Eight-Year Study of Early Chronic Obstructive Lung Disease in Working Men in London. New York: Oxford University Press; 1976.
- Flodin U, Jönsson P, Ziegler J, Axelson O. An epidemiologic study of bronchial asthma and smoking. Epidemiology. 1995; 6 (5):503–5. [ PubMed : 8562626 ]
- Forastiere F, Balmes J, Scarinci M, Tager IB. Occupation, asthma, and chronic respiratory symptoms in a community sample of older women. American Journal of Respiratory and Critical Care Medicine. 1998; 157 (6 Pt 1):1864–70. [ PubMed : 9620919 ]
- Francis RS, May JR, Spicer CC. Chemotherapy of bronchitis. British Medical Journal. 1961; 2 :979–84. [ PMC free article : PMC1970155 ] [ PubMed : 13894512 ]
- Francis RS, Spicer CC. Chemotherapy in chronic bronchitis. British Medical Journal. 1960; 1 :297–303. [ PMC free article : PMC1966487 ] [ PubMed : 13824401 ]
- Franks P, Gleiner JA. The treatment of acute bronchitis with trimethoprim and sulfamethoxazole. Journal of Family Practice. 1984; 19 (2):185–90. [ PubMed : 6611385 ]
- Frette C, Barrett-Connor E, Clausen JL. Effect of active and passive smoking on ventilatory function in elderly men and women. American Journal of Epidemiology. 1996; 143 (8):757–65. [ PubMed : 8610685 ]
- Freund KM, Belanger AJ, D’Agostino RB, Kannel WB. The health risks of smoking. The Framingham study: 34 years of follow-up. Annals of Epidemiology. 1993; 3 (4):417–24. [ PubMed : 8275219 ]
- Frew AJ, Kennedy SM, Chan-Yeung M. Methacholine responsiveness, smoking, and atopy as risk factors for accelerated FEV 1 decline in male working populations. American Review of Respiratory Disease. 1992; 146 (4):878–83. [ PubMed : 1416413 ]
- Garshick E, Schenker MB, Dosman JA. Occupationally induced airways obstruction. Medical Clinics of North America. 1996; 80 (4):851–78. [ PubMed : 8676617 ]
- Gilliland FD, Berhane K, McConnell R, Gauderman WJ, Vora H, Rappaport EB, Avol E, Peters JM. Maternal smoking during pregnancy, environmental tobacco smoke exposure and childhood lung function. Thorax. 2000; 55 (4):271–6. [ PMC free article : PMC1745733 ] [ PubMed : 10722765 ]
- Ginns LC, Ryu JH, Rogol PR, Sprince NL, Oliver LC, Larsson CJ. Natural killer cell activity in cigarette smokers and asbestos workers. American Review of Respiratory Disease. 1985; 131 (6):831–4. [ PubMed : 4003932 ]
- Godden DJ, Ross S, Abdalla M, McMurray D, Douglas A, Oldman D, Friend JAR, Legge JS, Douglas JG. Outcome of wheeze in childhood: symptoms and pulmonary function 25 years later. American Journal of Respiratory and Critical Care Medicine. 1994; 149 (1):106–12. [ PubMed : 8111567 ]
- Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW. Effects of cigarette smoking on lung function in adolescent boys and girls. New England Journal of Medicine. 1996; 335 (13):931–7. [ PubMed : 8782500 ]
- Gottlieb DJ, Stone PJ, Sparrow D, Gale ME, Weiss ST, Snider GL, O’Connor GT. Urinary desmosine excretion in smokers with and without rapid decline of lung function: the Normative Aging Study. American Journal of Respiratory and Critical Care Medicine. 1996; 154 (5):1290–5. [ PubMed : 8912738 ]
- Green GM, Carolin D. The depressant effect of cigarette smoke on the in vitro antibacterial activity of alveolar macrophages. New England Journal of Medicine. 1967; 276 (8):421–7. [ PubMed : 6019163 ]
- Greenland S. Relation of probability of causation to relative disease risk and doubling dose: a methodologic error that has become a social problem. American Journal of Public Health. 1999; 89 (8):1166–9. [ PMC free article : PMC1508676 ] [ PubMed : 10432900 ]
- Greenland S, Robins JM. Conceptual problems in the definition and interpretation of attributable fractions. American Journal of Epidemiology. 1988; 128 (6):1185–97. [ PubMed : 3057878 ]
- Gulsvik A, Fagerhol MK. Smoking and immunoglobulin levels [letter] Lancet. 1979; 1 (8113):449. [ PubMed : 84306 ]
- Gwaltney JM Jr. Acute bronchitis. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 4th ed. New York: Churchill Livingston; 1995a. pp. 606–8.
- Gwaltney JM Jr. Pharyngitis. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 4th ed. New York: Churchill Livingston; 1995b. pp. 566–72.
- Gwaltney JM Jr. The common cold. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 4th ed. New York: Churchill Livingston; 1995c. pp. 561–6.
- Hall CB, Hall WJ. Bronchiolitis. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 4th ed. New York: Churchill Livingston; 1995. pp. 612–9.
- Hanrahan JP, Tager IB, Segal MR, Tosteson TD, Castile RG, Van Vunakis H, Weiss ST, Speizer FE. The effect of maternal smoking during pregnancy on early infant lung function. American Review of Respiratory Disease. 1992; 145 (5):1129–35. [ PubMed : 1586058 ]
- Hansen EF, Rappeport Y, Vestbo J, Lange P. Increase in prevalence and severity of asthma in young adults in Copenhagen. Thorax. 2000; 55 (10):833–6. [ PMC free article : PMC1745615 ] [ PubMed : 10992534 ]
- Hawthorne VM, Fry JS. Smoking and health: the association between smoking behaviour, total mortality, and cardiorespiratory disease in west central Scotland. Journal of Epidemiology and Community Health. 1978; 32 (4):260–6. [ PMC free article : PMC1060966 ] [ PubMed : 744817 ]
- Haynes WF Jr, Krstulovic VJ, Bell ALL Jr. Smoking habit and incidence of respiratory tract infections in a group of adolescent males. American Review of Respiratory Disease. 1966; 93 (5):730–5. [ PubMed : 5936934 ]
- Helms PJ. Lung growth: implications for the development of disease [editorial] Thorax. 1994; 49 (5):440–1. [ PMC free article : PMC474862 ] [ PubMed : 8016762 ]
- Higenbottam T, Clark TJ, Shipley MJ, Rose G. Lung function and symptoms of cigarette smokers related to tar yield and number of cigarettes smoked. Lancet. 1980; 1 (8165):409–11. [ PubMed : 6101856 ]
- Higham MA, Pride NB, Alikhan A, Morrell NW. Tumour necrosis factor-α gene promoter polymorphism in chronic obstructive pulmonary disease. European Respiratory Journal. 2000; 15 (2):281–4. [ PubMed : 10706492 ]
- Hirschtick RE, Glassroth J, Jordan MC, Wilcosky TC, Wallace JM, Kvale PA, Markowitz N, Rosen MJ, Mangura BT, Hopewell PC. Bacterial pneumonia in persons infected with the human immunodeficiency virus. New England Journal of Medicine. 1995; 333 (13):845–51. [ PubMed : 7651475 ]
- Holt PG. Immune and inflammatory function in cigarette smokers. Thorax. 1987; 42 (4):241–9. [ PMC free article : PMC460693 ] [ PubMed : 3303428 ]
- Hoo A-F, Henschen M, Dezateux C, Costeloe K, Stocks J. Respiratory function among preterm infants whose mothers smoked during pregnancy. American Journal of Respiratory and Critical Care Medicine. 1998; 158 (3):700–5. [ PubMed : 9730993 ]
- Howie JGR, Clark GA. Double-blind trial of early demethylchlortetracycline in minor respiratory illness in general practice. Lancet. 1970; 2 (7683):1099–102. [ PubMed : 4097904 ]
- Hubbard R, Lewis S, Richards K, Johnston I, Britton J. Occupational exposure to metal or wood dust and aetiology of cryptogenic fibrosing alveolitis. Lancet. 1996; 347 (8997):284–9. [ PubMed : 8569361 ]
- Hueston WJ. Albuterol delivered by metered-dose inhaler to treat acute bronchitis. Journal of Family Practice. 1994; 39 (5):437–40. [See also comments in Journal of Family Practice 1994;39(5):43–5; Journal of Family Practice 1995;40(1):92; Journal of Family Practice 1995;40(4):328.] [ PubMed : 7864949 ]
- Iwai K, Mori T, Yamada N, Yamaguchi M, Hosoda Y. Idiopathic pulmonary fibrosis: epidemiologic approaches to occupational exposure. American Journal of Respiratory and Critical Care Medicine. 1994; 150 (3):670–5. [ PubMed : 8087336 ]
- Jaakkola JJK, Heinonen OP. Shared office space and the risk of the common cold. European Journal of Epidemiology. 1995; 11 (2):213–6. [ PubMed : 7672078 ]
- Jaakkola MS, Ernst P, Jaakkola JJK, N’gan’ga LW, Becklake MR. Effect of cigarette smoking on evolution of ventilatory lung function in young adults: an eight year longitudinal study. Thorax. 1991a; 46 (12):907–13. [ PMC free article : PMC463497 ] [ PubMed : 1792639 ]
- Jaakkola MS, Jaakkola JJK, Ernst P, Becklake MR. Ventilatory lung function in young cigarette smokers: a study of susceptibility. European Respiratory Journal. 1991b; 4 (6):643–50. [ PubMed : 1889490 ]
- Janoff A, Pryor WA, Bengali ZH. NHLBI workshop summary: effects of tobacco smoke components on cellular and biochemical processes in the lung. American Review of Respiratory Disease. 1987; 136 (4):1058–64. [ PubMed : 3310769 ]
- Jansen DF, Schouten JP, Vonk JM, Rijcken B, Timens W, Kraan J, Weiss ST, Postma DS. Smoking and airway hyperresponsiveness especially in the presence of blood eosinophilia increase the risk to develop respiratory symptoms: a 25-year follow-up study in the general adult population. American Journal of Respiratory and Critical Care Medicine. 1999; 160 (1):259–64. [ PubMed : 10390409 ]
- Johnson JD, Houchens DP, Kluwe WM, Craig DK, Fisher GL. Effects of mainstream and environmental tobacco smoke on the immune system in animals and humans: a review. Critical Reviews in Toxicology. 1990; 20 (5):369–95. [ PubMed : 2202327 ]
- Johnston RN, Lockhart W, Smith DH, Cadman NK. A trial of phenethicillin in chronic bronchitis. British Medical Journal. 1961; 4 (5258):985–6. [ PMC free article : PMC1970174 ] [ PubMed : 14452159 ]
- Johnston RN, McNeill RS, Smith DH, Dempster MB, Nairn JR, Purvis MS, Watson JM, Ward FG. Five-year winter chemoprophylaxis for chronic bronchitis. British Medical Journal. 1969; 4 (678):265–9. [ PMC free article : PMC1629696 ] [ PubMed : 4899454 ]
- Jørgensen AF, Coolidge J, Pedersen PA, Petersen KP, Waldorff S, Widding E. Amoxicillin in treatment of acute uncomplicated exacerbations of chronic bronchitis: a double-blind, placebo-controlled multicentre study in general practice. Scandinavian Journal of Primary Health Care. 1992; 10 (1):7–11. [ PubMed : 1589668 ]
- Kanner RE, Anthonisen NR, Connett JE. Lower respiratory illnesses promote FEV 1 decline in current smokers but not ex-smokers with mild chronic obstructive pulmonary disease: results from the Lung Health Study. American Journal of Respiratory and Critical Care Medicine. 2001; 164 (3):358–64. [ PubMed : 11500333 ]
- Kanner RE, Connett JE, Williams DE, Buist AS. Effects of randomized assignment to a smoking cessation intervention and changes in smoking habits on respiratory symptoms in smokers with early chronic obstructive pulmonary disease: the Lung Health Study. American Journal of Medicine. 1999; 106 (4):410–6. [ PubMed : 10225243 ]
- Kaplan BA, Mascie-Taylor CGN. Smoking and asthma among 23-year-olds. Journal of Asthma. 1997; 34 (3):219–26. [ PubMed : 9168849 ]
- Kark JD, Lebiush M. Smoking and epidemic influenza-like illness in female military recruits: a brief survey. American Journal of Public Health. 1981; 71 (5):530–2. [ PMC free article : PMC1619723 ] [ PubMed : 7212144 ]
- Kark JD, Lebiush M, Rannon L. Cigarette smoking as a risk factor for epidemic A(H 1 N 1 ) influenza in young men. New England Journal of Medicine. 1982; 307 (17):1042–6. [ PubMed : 7121513 ]
- Kennedy SM, Burrows B, Vedal S, Enarson DA, Chan-Yeung M. Methacholine responsiveness among working populations: relationship to smoking and airway caliber. American Review of Respiratory Disease. 1990; 142 (6 Pt 1):1377–83. [ PubMed : 2252256 ]
- Kilpelainen M, Terho EO, Helenius H, Koskenvuo M. Validation of a new questionnaire on asthma, allergic rhinitis, and conjunctivitis in young adults. Allergy. 2001; 56 (5):377–84. [ PubMed : 11350300 ]
- King DE, Williams WC, Bishop L, Shechter A. Effectiveness of erythromycin in the treatment of acute bronchitis. Journal of Family Practice. 1996; 42 (6):601–5. [See also comments in Journal of Family Practice 1996;43(3):230–1; Journal of Family Practice 1996;43(6):527–9] [ PubMed : 8656171 ]
- Kotaniemi JT, Lundback B, Nieminen MM, Sovijarvi AR, Laitinen LA. Increase of asthma in adults in northern Finland?--a report from the FinEsS study. Allergy. 2001; 56 (2):169–74. [ PubMed : 11167379 ]
- Krzyzanowski M, Lebowitz MD. Changes in chronic respiratory symptoms in two populations of adults studied longitudinally over 13 years. European Respiratory Journal. 1992; 5 (1):12–20. [ PubMed : 1577133 ]
- Krzyzanowski M, Sherrill DL, Paoletti P, Lebowitz MD. Relationship of respiratory symptoms and pulmonary function to tar, nicotine, and carbon monoxide yield of cigarettes. American Review of Respiratory Disease. 1991; 143 (2):306–11. [ PubMed : 1990944 ]
- Kurtti P, Isoaho R, von Hertzen L, Keistinen T, Kivelä S-L, Leinonen M. Influence of age, gender and smoking on Streptococcus pneumoniae, Haemophilus influenzae and Moraxella (Branhamella) catarrhalis antibody titres in an elderly population. Scandinavian Journal of Infectious Diseases. 1997; 29 (5):485–9. [See also erratum in Scandinavian Journal of Infectious Diseases 1998;30(1):95.] [ PubMed : 9435037 ]
- Laan M, Qvarfordt I, Riise GC, Andersson BA, Larsson S, Lindén A. Increased levels of interleukin-16 in the airways of tobacco smokers: relationship with peripheral blood T lymphocytes. Thorax. 1999; 54 (10):911–6. [ PMC free article : PMC1745375 ] [ PubMed : 10491454 ]
- Lam TH, Chung SF, Betson CL, Wong CM, Hedley AJ. Respiratory symptoms due to active and passive smoking in junior secondary school students in Hong Kong. International Journal of Epidemiology. 1998; 27 (1):41–8. [ PubMed : 9563692 ]
- Lange P, Groth S, Nyboe J, Mortensen J, Appleyard M, Jensen G, Schnohr P. Decline of the lung function related to the type of tobacco smoked and inhalation. Thorax. 1990; 45 (1):22–6. [ PMC free article : PMC475634 ] [ PubMed : 2321172 ]
- Lange P, Nyboe J, Appleyard M, Jensen G, Schnohr P. Relationship of the type of tobacco and inhalation pattern to pulmonary and total mortality. European Respiratory Journal. 1992; 5 (9):1111–7. [ PubMed : 1426222 ]
- Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. New England Journal of Medicine. 1998; 339 (17):1194–200. [ PubMed : 9780339 ]
- Larsson L. Incidence of asthma in Swedish teenagers: relation to sex and smoking habits. Thorax. 1995; 50 (3):260–4. [ PMC free article : PMC1021189 ] [ PubMed : 7660339 ]
- Lee PN, Garfinkel L. Mortality and type of cigarette smoked. Journal of Epidemiology and Community Health. 1981; 35 (1):16–22. [ PMC free article : PMC1052113 ] [ PubMed : 7264528 ]
- Lehmann D, Coakley KJ, Coakley CA, Spooner V, Montgomery JM, Michael A, Riley ID, Smith T, Clancy RL, Cripps AW, Alpers MP. Reduction in the incidence of acute bronchitis by an oral Haemophilus influenzae vaccine in patients with chronic bronchitis in the highlands of Papua New Guinea. American Review of Respiratory Disease. 1991; 144 (2):324–30. [ PubMed : 1859055 ]
- Leynaert B, Bousquet J, Henry C, Liard R, Neukirch F. Is bronchial hyperresponsiveness more frequent in women than in men: a population-based study. American Journal of Respiratory and Critical Care Medicine. 1997; 156 (5):1413–20. [ PubMed : 9372654 ]
- Liippo K, Pelliniemi T-T, Lehto H. Trimethoprim prophylaxis of acute exacerbations in chronic obstructive pulmonary diseases. Acta Medica Scandinavica. 1987; 221 (5):455–9. [ PubMed : 3300178 ]
- Liu B-Q, Peto R, Chen Z-M, Boreham J, Wu Y-P, Li J-Y, Campbell TC, Chen J-S. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. British Medical Journal. 1998; 317 (7170):1411–22. [ PMC free article : PMC28719 ] [ PubMed : 9822393 ]
- Locksley RM, Fowell DJ, Shinkai K, Wakil AE, Lacy D, Bix M. Development of CD4+ effector T cells and susceptibility to infectious diseases. Advances in Experimental Medicine and Biology. 1998; 452 :45–52. [ PubMed : 9889958 ]
- Lødrup Carlsen KC, Jaakkoka JJ, Nafstad P, Carlsen KH. In utero exposure to cigarette smoking influences lung function at birth. European Respiratory Journal. 1997; 10 (8):1774–9. [ PubMed : 9272918 ]
- MacNee W, Rahman I. Oxidants and antioxidants as therapeutic targets in chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1999; 160 (5 Pt 2):S58–S65. [ PubMed : 10556172 ]
- Mancini DAP, Mendonca RMZ, Mendonca RZ, do Prado JA, Andrade CdM. Immune response to vaccine against influenza in smokers, non-smokers and, in individuals holding respiratory complications. Bollettino Chimico Farmaceutico. 1998; 137 (1):21–5. [ PubMed : 9595830 ]
- Mandell GL, Bennett JE. Mandell, Douglas and Bennett’s Principles and Practice of Infectious Diseases. 4th ed. Dolin R, editor. New York: Churchill Livingston; 1995.
- Mannino DM, Brown C, Giovino GA. Obstructive lung disease deaths in the United States from 1979 through 1993: an analysis using multiple-cause mortality data. American Journal of Respiratory and Critical Care Medicine. 1997; 156 (3 Pt 1):814–8. [ PubMed : 9309998 ]
- Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988– 1994. Archives of Internal Medicine. 2000; 160 (11):1683–9. [ PubMed : 10847262 ]
- Mapel DW, Hurley JS, Frost FJ, Petersen HV, Picchi MA, Coultas DB. Health care utilization in chronic obstructive pulmonary disease: a case-control study in a health maintenance organization. Archives of Internal Medicine. 2000; 160 (17):2653–8. [ PubMed : 10999980 ]
- Marrie TJ, Durant H, Yates L. Community-acquired pneumonia requiring hospitalization: 5-year prospective study. Reviews of Infectious Diseases. 1989; 11 (4):586–99. [ PubMed : 2772465 ]
- Martinez FD, Antognoni G, Macri F, Bonci E, Midulla F, DeCastro G, Ronchetti R. Parental smoking enhances bronchial responsiveness in nine-year-old children. American Review of Respiratory Disease. 1988; 138 (3):518–23. [ PubMed : 3202406 ]
- McAllister-Sistilli CG, Caggiula AR, Knopf S, Rose CA, Miller AL, Donny EC. The effects of nicotine on the immune system. Psychoneuroendocrinology. 1998; 23 (2):175–87. [ PubMed : 9621397 ]
- McMillan SA, Douglas JP, Archbold GPR, McCrum EE, Evans AE. Effect of low to moderate levels of smoking and alcohol consumption on serum immunoglobulin concentrations. Journal of Clinical Pathology. 1997; 50 (10):819–22. [ PMC free article : PMC500261 ] [ PubMed : 9462262 ]
- McVay LV Jr, Sprunt DH. Antibiotic prophylaxis in chronic respiratory diseases. Archives of Internal Medicine. 1953; 92 :833–46. [ PubMed : 13103837 ]
- McWhorter WP, Polis MA, Kaslow RA. Occurrence, predictors, and consequences of adult asthma in NHANESI and follow-up survey. American Review of Respiratory Disease. 1989; 139 (3):721–4. [ PubMed : 2923372 ]
- Medical Research Council. Value of chemoprophylaxis and chemotherapy in early chronic bronchitis: a report to the Medical Research Council by their working party on trials of chemotherapy in early chronic bronchitis. British Medical Journal. 1966; 1 (5499):1317–22. [ PMC free article : PMC1844936 ] [ PubMed : 5327220 ]
- Melbostad E, Eduard W, Magnus P. Determinants of asthma in a farming population. Scandinavian Journal of Work, Environment and Health. 1998; 24 (4):262–9. [ PubMed : 9754857 ]
- Meliska CJ, Stunkard ME, Gilbert DG, Jensen RA, Martinko JM. Immune function in cigarette smokers who quit smoking for 31 days. Journal of Allergy and Clinical Immunology. 1995; 95 (4):901–10. [ PubMed : 7722172 ]
- Mikuniya T, Nagai S, Tsutsumi T, Morita K, Mio T, Satake N, Izumi T. Proinflammatory or regulatory cytokines released from BALF macrophages of healthy smokers. Respiration. 1999; 66 (5):419–26. [ PubMed : 10516538 ]
- Mili F, Flanders WD, Boring FR, Annest JL, Destefano F. The associations of race, cigarette smoking, and smoking cessation to measures of the immune system in middle-aged men. Clinical Immunology and Immunopathology. 1991; 59 (2):187–200. [ PubMed : 2009639 ]
- Miller LG, Goldstein G, Murphy M, Ginns LC. Reversible alterations in immunoregulatory T cells in smoking: analysis by monoclonal antibodies and flow cytometry. Chest. 1982; 82 (5):526–9. [ PubMed : 6982152 ]
- Mills PR, Davies RJ, Devalia JL. Airway epithelial cells, cytokines, and pollutants. American Journal of Respiratory and Critical Care Medicine. 1999; 160 (5 Pt 2):S38–S43. [ PubMed : 10556168 ]
- Milner AD, Marsh MJ, Ingram DM, Fox GF, Susiva C. Effects of smoking in pregnancy on neonatal lung function. Archives of Disease in Childhood. Fetal and Neonatal Edition. 1999; 80 (1):8F–14F. [ PMC free article : PMC1720884 ] [ PubMed : 10325804 ]
- Miravitlles M, Espinosa C, Fernández-Laso E, Martos JA, Maldonado JA, Gallego M. Relationship between bacterial flora in sputum and functional impairment in patients with acute exacerbations of COPD. Chest. 1999; 116 (1):40–6. [ PubMed : 10424501 ]
- Monsó E, Ruiz J, Rosell A, Manterola J, Fiz J, Morera J, Ausina V. Bacterial infection in chronic obstructive pulmonary disease: a study of stable and exacerbated outpatients using the protected specimen brush. American Journal of Respiratory and Critical Care Medicine. 1995; 152 (4 Pt 1):1316–20. [ PubMed : 7551388 ]
- Monto AS, Higgins MW, Ross HW. The Tecumseh study of respiratory illness. VIII: acute infection in chronic respiratory disease and comparison groups. American Review of Respiratory Disease. 1975; 111 (1):27–36. [ PubMed : 163065 ]
- Monto AS, Ross H. Acute respiratory illness in the community: effect of family composition, smoking, and chronic symptoms. British Journal of Preventive and Social Medicine. 1977; 31 (2):101–8. [ PMC free article : PMC479004 ] [ PubMed : 884394 ]
- Monto AS, Ross HW. The Tecumseh study of respiratory illness. X: relation of acute infections to smoking, lung function and chronic symptoms. American Journal of Epidemiology. 1978; 107 (1):57–64. [ PubMed : 623090 ]
- Morgan WJ, Martinez FD. Maternal smoking and infant lung function: further evidence for an in utero effect. American Journal of Respiratory and Critical Care Medicine. 1998; 158 (3):689–90. [ PubMed : 9730991 ]
- Mullen J, Hodgson MJ, DeGraff CA, Godar T. Case-control study of idiopathic pulmonary fibrosis and environmental exposures. Journal of Occupational and Environmental Medicine. 1998; 40 (4):363–7. [ PubMed : 9571528 ]
- Murphy TF, Sethi S. Bacterial infection in chronic obstructive pulmonary disease. American Review of Respiratory Disease. 1992; 146 (4):1067–83. [ PubMed : 1416398 ]
- Murphy TF, Sethi S, Niederman MS. The role of bacteria in exacerbations of COPD: a constructive view [comment] Chest. 2000; 118 (1):204–9. [ PubMed : 10893380 ]
- Murray RP, Anthonisen NR, Connett JE, Wise RA, Lindgren PG, Greene PG, Nides MA. Effects of multiple attempts to quit smoking and relapses to smoking on pulmonary function. Journal of Clinical Epidemiology. 1998; 51 (12):1317–26. [ PubMed : 10086826 ]
- Nair MPN, Kronfol ZA, Schwartz SA. Effects of alcohol and nicotine on cytotoxic functions of human lymphocytes. Clinical Immunology and Immunopathology. 1990; 54 (3):395–409. [ PubMed : 1689229 ]
- National Cancer Institute. Risks Associated with Smoking Cigarettes with Low Machine-Measured Yields of Tar and Nicotine. Smoking and Tobacco Control Monograph No 13. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 2001. NIH Publication No. 02–5074.
- National Heart, Lung, and Blood Institute. Guidelines for the Diagnosis and Management of Asthma: Expert Panel Report 2. Bethesda (MD): National Institutes of Health, National Heart, Lung, and Blood Institute; 1997. NIH Publication No. (NIH) 97–4051.
- National Research Council. Environmental Tobacco Smoke: Measuring Exposures and Assessing Health Effects. Washington: National Academy Press; 1986. [ PubMed : 25032469 ]
- Nicholson KG, Kent J, Hammersley V, Cancio E. Risk factors for lower respiratory complications of rhinovirus infections in elderly people living in the community: prospective cohort study. British Medical Journal. 1996; 313 (7065):1119–23. [ PMC free article : PMC2352467 ] [ PubMed : 8916700 ]
- Nicotra MB, Rivera M, Awe RJ. Antibiotic therapy of acute exacerbations of chronic bronchitis: a controlled study using tetracycline. Annals of Internal Medicine. 1982; 97 (1):18–21. [ PubMed : 7092002 ]
- Nieman RB, Fleming J, Coker RJ, Harris JRW, Mitchell DM. The effect of cigarette smoking on the development of AIDS in HIV-1-seropositive individuals. AIDS. 1993; 7 (5):705–10. [ PubMed : 8318178 ]
- Norrman E, Nystrom L, Jonsson E, Stjernberg N. Prevalence and incidence of asthma and rhinoconjunctivitis in Swedish teenagers. Allergy. 1998; 53 (1):28–35. [ PubMed : 9491226 ]
- Nuorti JP, Butler JC, Farley MM, Harrison LH, McGeer A, Kolczak MS, Breiman RF. Cigarette smoking and invasive pneumococcal disease. New England Journal of Medicine. 2000; 342 (10):681–9. [ PubMed : 10706897 ]
- Omenaas E, Bakke P, Eide GE, Haukenes G, Gulsvik A. Serum respiratory virus antibodies: predictor of reduced one-second forced expiratory volume (FEV 1 ) in Norwegian adults. International Journal of Epidemiology. 1996; 25 (1):134–41. [ PubMed : 8666481 ]
- Orcel B, Delclaux B, Baud M, Derenne JP. Oral immunization with bacterial extracts for protection against acute bronchitis in elderly institutionalized patients with chronic bronchitis. European Respiratory Journal. 1994; 7 (3):446–52. [ PubMed : 8013600 ]
- O’Shaughnessy TC, Ansari TW, Barnes NC, Jeffery PK. Inflammation in bronchial biopsies of subjects with chronic bronchitis: inverse relationship of CD8 + T lymphocytes with FEV 1 . American Journal of Respiratory and Critical Care Medicine. 1997; 155 (3):852–7. [ PubMed : 9117016 ]
- Parnell JL, Anderson DO, Kinnis C. Cigarette smoking and respiratory infections in a class of student nurses. New England Journal of Medicine. 1966; 274 (18):979–84. [ PubMed : 5909741 ]
- Petersen BH, Steimel LF, Callaghan JT. Suppression of mitogen-induced lymphocyte transformation in cigarette smokers. Clinical Immunology and Immunopathology. 1983; 27 (1):135–40. [ PubMed : 6872351 ]
- Petersen ES, Esmann V, Honcke P, Munkner C. A controlled study of the effect of treatment on chronic bronchitis: an evaluation using pulmonary function tests. Acta Medica Scandinavica. 1967; 182 (3):293–305. [ PubMed : 6069924 ]
- Petitti DB, Friedman GD. Cardiovascular and other diseases in smokers of low yield cigarettes. Journal of Chronic Diseases. 1985a; 38 (7):581–8. [ PubMed : 4008601 ]
- Petitti DB, Friedman GD. Respiratory morbidity in smokers of low- and high-yield cigarettes. Preventive Medicine. 1985b; 14 (2):217–25. [ PubMed : 4048084 ]
- Petitti DB, Kipp H. The leukocyte count: associations with intensity of smoking and persistence of effect after quitting. American Journal of Epidemiology. 1986; 123 (1):89–95. [ PubMed : 3940445 ]
- Piatti G, Gazzola T, Allegra L. Bacterial adherence in smokers and non-smokers. Pharmacological Research. 1997; 36 (6):481–4. [ PubMed : 9446715 ]
- Pines A. Controlled trials of a sulphonamide given weekly to prevent exacerbations of chronic bronchitis. British Medical Journal. 1967; 3 (559):202–4. [ PMC free article : PMC1842518 ] [ PubMed : 5339171 ]
- Pines A, Raafat H, Greenfield JSB, Linsell WD, Solari ME. Antibiotic regimens in moderately ill patients with purulent exacerbations of chronic bronchitis. British Journal of Diseases of the Chest. 1972; 66 (2):107–15. [ PubMed : 4556292 ]
- Pines A, Raafat H, Plucinski K, Greenfield JSB, Solari M. Antibiotic regimens in severe and acute purulent exacerbations of chronic bronchitis. British Medical Journal. 1968; 2 (607):735–8. [ PMC free article : PMC1991661 ] [ PubMed : 4872151 ]
- Pirdie RB, Datta N, Massey DG, Poole GW, Schneeweiss J, Stradling P. A trial of continuous winter chemotherapy in chronic bronchitis. Lancet. 1960; 2 :723–7. [ PubMed : 13737993 ]
- Plaschke PP, Janson C, Norrman E, Bjornsson E, Ellbjar S, Jarvholm B. Onset and remission of allergic rhinitis and asthma and the relationship with atopic sensitization and smoking. American Journal of Respiratory and Critical Care Medicine. 2000; 162 ( 3 Pt 1):920–4. [ PubMed : 10988106 ]
- Pollard RB, Melton LJ III, Hoeffler DF, Springer GL, Scheiner EF. Smoking and respiratory illness in military recruits. Archives of Environmental Health. 1975; 30 (11):533–7. [ PubMed : 1217913 ]
- Prescott E, Lange P, Vestbo J. Chronic mucus hypersecretion in COPD and death from pulmonary infection. European Respiratory Journal. 1995; 8 (8):1333–8. [ PubMed : 7489800 ]
- Prescott E, Lange P, Vestbo J. Effect of gender on hospital admissions for asthma and prevalence of self-reported asthma: a prospective study based on a sample of the general population. Copenhagen City Heart Study Group. Thorax. 1997; 52 (3):287–9. [ PMC free article : PMC1758523 ] [ PubMed : 9093349 ]
- Rahman I, MacNee W. Lung glutathione and oxidative stress: implications in cigarette smoke-induced airway disease. American Journal of Physiology. 1999; 277 (6 Pt 1):L1067–L1088. [ PubMed : 10600876 ]
- Razma AG, Lynch JP III, Wilson BS, Ward PA, Kunkel SL. Human alveolar macrophage activation and DR antigen expression in cigarette smokers. Chest. 1984; 85 (6):41S–43S.
- Repine JE, Bast A, Lankhorst I. Oxidative stress in chronic obstructive pulmonary disease: the Oxidative Stress Study Group. American Journal of Respiratory and Critical Care Medicine. 1997; 156 (2 Pt 1):341–57. [ PubMed : 9279209 ]
- Rijcken B, Schouten JP, Mensinga TT, Weiss ST, De Vries K, Van Der Lender R. Factors associated with bronchial responsiveness to histamine in a population sample of adults. American Review of Respiratory Disease. 1993; 147 (6 Pt 1):1447–53. [ PubMed : 8503555 ]
- Rijcken B, Schouten JP, Xu X, Rosner B, Weiss ST. Airway hyperresponsiveness to histamine associated with accelerated decline in FEV 1 . American Journal of Respiratory and Critical Care Medicine. 1995; 151 (5):1377–82. [ PubMed : 7735588 ]
- Rimpela A, Teperi J. Respiratory symptoms and low tar cigarette smoking—a longitudinal study on young people. Scandinavian Journal of Social Medicine. 1989; 17 (2):151–6. [ PubMed : 2749202 ]
- Riordan T, Cartwright K, Andrews N, Stuart J, Burris A, Fox A, Borrow R, Douglas-Riley T, Gabb J, Miller A. Acquisition and carriage of meningococci in marine commando recruits. Epidemiology and Infection. 1998; 121 (3):495–505. [ PMC free article : PMC2809555 ] [ PubMed : 10030697 ]
- Robbins RA, Gossman GL, Nelson KJ, Koyama S, Thompson AB, Rennard SI. Inactivation of chemotactic factor inactivator by cigarette smoke: a potential mechanism of modulating neutrophil recruitment to the lung. American Review of Respiratory Disease. 1990; 142 (4):763–8. [ PubMed : 2221580 ]
- Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. American Journal of Public Health. 1998; 88 (1):15–9. [ PMC free article : PMC1508384 ] [ PubMed : 9584027 ]
- Rona RJ, Gulliford MC, Chinn S. Effects of prematurity and intrauterine growth on respiratory health and lung function in childhood. British Medical Journal. 1993; 306 (6881):817–20. [ PMC free article : PMC1677317 ] [ PubMed : 8490372 ]
- Roszman TL, Elliott LH, Rogers AS. Suppression of lymphocyte function by products derived from cigarette smoke. American Review of Respiratory Disease. 1975; 111 (4):453–7. [ PubMed : 1124887 ]
- Roszman TL, Rogers AS. The immunosuppressive potential of products derived from cigarette smoke. American Review of Respiratory Disease. 1973; 108 (5):1158–63. [ PubMed : 4746572 ]
- Sachs APE, Koëter GH, Groenier KH, van der Waaij D, Schiphuis J, Meyboom-de Jong B. Changes in symptoms, peak expiratory flow, and sputum flora during treatment with antibiotics of exacerbations in patients with chronic obstructive pulmonary disease in general practice. Thorax. 1995; 50 (7):758–63. [ PMC free article : PMC474649 ] [ PubMed : 7570411 ]
- Saetta M. Airway inflammation in chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1999; 160 (5 Pt 2):S17–S20. [ PubMed : 10556163 ]
- Saetta M, Di Stefano A, Turato G, Facchini FM, Corbino L, Mapp CE, Maestrelli P, Ciaccia A, Fabbri LM. CD8+ T-lymphocytes in peripheral airways of smokers with chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1998; 157 (3 Pt 1):822–6. [ PubMed : 9517597 ]
- Saetta M, Turato G, Maestrelli P, Mapp CE, Fabbri LM. Cellular and structural bases of chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 2001; 163 (6):1304–9. [ PubMed : 11371392 ]
- Saint S, Bent S, Vittinghoff E, Grady D. Antibiotics in chronic obstructive pulmonary disease exacerbations: a meta-analysis. Journal of the American Medical Association. 1995; 273 (12):957–60. [See also comments in Journal of the American Medical Association 1995;274(14):1131–2] [ PubMed : 7884956 ]
- Sakao S, Tatsumi K, Igari H, Shino Y, Shirasawa H, Kuriyama T. Association of tumor necrosis factor α gene promoter polymorphism with the presence of chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 2001; 163 (2):420–2. [ PubMed : 11179116 ]
- Samet JM. Definitions and methodology in COPD research. In: Hensley MJ, Saunders NA, editors. Clinical Epidemiology of Chronic Obstructive Pulmonary Disease. New York: Marcel Dekker; 1989. pp. 1–22.
- Samet JM. National Cancer Institute. The FTC Cigarette Test Method for Determining Tar, Nicotine, and Carbon Monoxide Yields of US Cigarettes. Report of the NCI Expert Committee Smoking and Tobacco Control Monograph No 7. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 1996. The changing cigarette and disease risk: current status of the evidence; pp. 77–92. NIH Publication No. 96–4028.
- Samet JM, Lange P. Longitudinal studies of active and passive smoking. American Journal of Respiratory and Critical Care Medicine. 1996; 154 (6 Pt 2):S257–S265. [ PubMed : 8970398 ]
- Samet JM, Tager IB, Speizer FE. The relationship between respiratory illness in childhood and chronic air-flow obstruction in adulthood. American Review of Respiratory Disease. 1983; 127 (4):508–23. [ PubMed : 6340572 ]
- Sandford AJ, Chagani T, Weir TD, Connett JE, Anthonisen NR, Paré PD. Susceptibility genes for rapid decline of lung function in the Lung Health Study. American Journal of Respiratory and Critical Care Medicine. 2001; 163 (2):469–73. [ PubMed : 11179124 ]
- Sandford AJ, Weir TD, Paré PD. Genetic risk factors for chronic obstructive pulmonary disease. European Respiratory Journal. 1997; 10 (6):1380–91. [ PubMed : 9192947 ]
- Sandvik L, Erikssen G, Thaulow E. Long term effects of smoking on physical fitness and lung function: a longitudinal study of 1393 middle aged Norwegian men for seven years. British Medical Journal. 1995; 311 (7007):715–8. [ PMC free article : PMC2550717 ] [ PubMed : 7549684 ]
- Sankilampi U, Isoaho R, Bloigu A, Kivelä S-L, Leinonen M. Effect of age, sex and smoking habits on pneumococcal antibodies in an elderly population. International Journal of Epidemiology. 1997; 26 (2):420–7. [ PubMed : 9169180 ]
- Scanlon PD, Connett JE, Waller LA, Altose MD, Bailey WC, Buist AS, Tashkin DP. Smoking cessation and lung function in mild-to-moderate chronic obstructive pulmonary disease: the Lung Health Study. American Journal of Respiratory and Critical Care Medicine. 2000; 161 (2 Pt 1):381–90. [ PubMed : 10673175 ]
- Schenker MB, Samet JM, Speizer FE. Effect of cigarette tar content and smoking habits on respiratory symptoms in women. American Review of Respiratory Disease. 1982; 125 (6):684–90. [ PubMed : 7091875 ]
- Scherl ER, Riegler SL, Cooper JK. Doxycycline in acute bronchitis: a randomized double-blind trial. Journal of the Kentucky Medical Association. 1987; 85 (9):539–41. [ PubMed : 3668366 ]
- Scott J, Johnston I, Britton J. What causes cryptogenic fibrosing alveolitis? A case-control study of environmental exposure to dust. British Medical Journal. 1990; 301 (6759):1015–7. [ PMC free article : PMC1664043 ] [ PubMed : 2249047 ]
- Sherman CB. The health consequences of cigarette smoking: pulmonary diseases. Medical Clinics of North America. 1992; 76 (2):355–75. [ PubMed : 1548966 ]
- Sherman CB, Xu X, Speizer FE, Ferris BG Jr, Weiss ST, Dockery DW. Longitudinal lung function decline in subjects with respiratory symptoms. American Review of Respiratory Disease. 1992; 146 (4):855–9. [ PubMed : 1416410 ]
- Sherrill DL, Holberg CJ, Enright PL, Lebowitz MD, Burrows B. Longitudinal analysis of the effects of smoking onset and cessation on pulmonary function. American Journal of Respiratory and Critical Care Medicine. 1994; 149 (3 Pt 1):591–7. [ PubMed : 8118623 ]
- Sherrill DL, Lebowitz MD, Knudson RJ, Burrows B. Smoking and symptom effects on the curves of lung function growth and decline. American Review of Respiratory Disease. 1991; 144 (l):17–22. [ PubMed : 2064125 ]
- Silverman NA, Potvin C, Alexander JC Jr, Chretien PB. In vitro lymphocyte reactivity and T-cell levels in chronic cigarette smokers. Clinical and Experimental Immunology. 1975; 22 (2):285–92. [ PMC free article : PMC1538287 ] [ PubMed : 1082401 ]
- Simberkoff MS, Cross AP, Al-Ibrahim M, Baltch AL, Geiseler PJ, Nadler J, Richmond AS, Smith RP, Schiffman G, Shepard DS, Van Eeckhout JP. Efficacy of pneumococcal vaccine in high-risk patients: results of a Veterans Administration Cooperative Study. New England Journal of Medicine. 1986; 315 (21):1318–27. [ PubMed : 3534568 ]
- Sippel JM, Pedula KL, Vollmer WM, Buist AS, Osborne ML. Associations of smoking with hospital-based care and quality of life in patients with obstructive airway disease. Chest. 1999; 115 (3):691–6. [ PubMed : 10084477 ]
- Siroux V, Pin I, Oryszczyn MP, Le Moual N, Kauffman F. Relationships of active smoking to asthma and asthma severity in the EGEA study. European Respiratory Journal. 2000; 15 (3):470–7. [ PubMed : 10759439 ]
- Soler N, Torres A, Ewig S, Gonzalez J, Celis R, El-Ebiary M, Hernandez C, Rodriguez-Roisin R. Bronchial microbial patterns in severe exacerbations of chronic obstructive pulmonary disease (COPD) requiring mechanical ventilation. American Journal of Respiratory and Critical Care Medicine. 1998; 157 (5 Pt 1):1498–505. [ PubMed : 9603129 ]
- Soliman DM, Twigg HL III. Cigarette smoking decreases bioactive interleukin-6 secretion by alveolar macrophages. American Journal of Physiology. 1992; 263 (4 Pt 1):L471–L478. [ PubMed : 1415725 ]
- Sopori ML, Kozak W. Immunomodulatory effects of cigarette smoke. Journal of Neuroimmunology. 1998; 83 (1–2):148–56. [ PubMed : 9610683 ]
- Sopori ML, Kozak W, Savage SM, Geng Y, Kluger MJ. Nicotine-induced modulation of T Cell function: implications for inflammation and infection. Advances in Experimental Medicine and Biology. 1998; 437 :279–89. [ PubMed : 9666281 ]
- Sparrow D, Stefos T, Bosse R, Weiss ST. The relationship of tar content to decline in pulmonary function in cigarette smokers. American Review of Respiratory Disease. 1983; 127 (1):56–8. [ PubMed : 6849551 ]
- Speizer FE, Tager IB. Epidemiology of chronic mucus hypersecretion and obstructive airways disease. Epidemiologic Reviews. 1979; 1 :124–42. [ PubMed : 398264 ]
- Stanley PJ, Wilson R, Greenstone MA, MacWilliam L, Cole PJ. Effect of cigarette smoking on nasal mucociliary clearance and ciliary beat frequency. Thorax. 1986; 41 (7):519–23. [ PMC free article : PMC460384 ] [ PubMed : 3787531 ]
- Stick SM, Arnott J, Turner DJ, Young S, Landau LI, Lesouëf PN. Bronchial responsiveness and lung function in recurrently wheezy infants. American Review of Respiratory Disease. 1991; 144 (5):1012–5. [ PubMed : 1952425 ]
- Stick SM, Burton PR, Gurrin L, Sly PD, LeSouëf PN. Effects of maternal smoking during pregnancy and a family history of asthma on respiratory function in newborn infants. Lancet. 1996; 348 (9034):1060–4. [ PubMed : 8874457 ]
- Stott NCH, West RR. Randomised controlled trial of antibiotics in patients with cough and purulent sputum. British Medical Journal. 1976; 2 (6035):556–9. [ PMC free article : PMC1688091 ] [ PubMed : 786428 ]
- Strachan DP, Butland BK, Anderson HR. Incidence and prognosis of asthma and wheezing illness from early childhood to age 33 in a national British cohort. British Medical Journal. 1996; 312 (7040):1195–9. [ PMC free article : PMC2350975 ] [ PubMed : 8634562 ]
- Straus WL, Plouffe JF, File TM Jr, Lipman HB, Hackman BH, Salstrom S-J, Benson RF, Breiman RF. Ohio Legionnaires Disease Group. Risk factors for domestic acquisition of legionnaires disease. Archives of Internal Medicine. 1996; 156 (15):1685–92. [ PubMed : 8694667 ]
- Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest. 2000; 117 (2):5S–9S. [ PubMed : 10673466 ]
- Sunyer J, Antó JM, Kogevinas M, Soriano JB, Tobías A, Muñoz A. Smoking and bronchial responsiveness in nonatopic and atopic young adults: Spanish Group of the European Study of Asthma. Thorax. 1997; 52 (3):235–8. [ PMC free article : PMC1758517 ] [ PubMed : 9093338 ]
- Tager I, Speizer FE. Role of infection in chronic bronchitis. New England Journal of Medicine. 1975; 292 (11):563–71. [ PubMed : 802896 ]
- Tager IB, Hanrahan JP, Tosteson TD, Castile RG, Brown RW, Weiss ST, Speizer FE. Lung function, pre- and post-natal smoke exposure, and wheezing in the first year of life. American Review of Respiratory Disease. 1993; 147 (4):811–7. [ PubMed : 8466114 ]
- Tager IB, Muñoz A, Rosner B, Weiss ST, Carey V, Speizer FE. Effect of cigarette smoking on the pulmonary function of children and adolescents. American Review of Respiratory Disease. 1985; 131 (5):752–9. [ PubMed : 4003920 ]
- Tager IB, Ngo L, Hanrahan JP. Maternal smoking during pregnancy: effects on lung function during the first 18 months of life. American Journal of Respiratory and Critical Care Medicine. 1995; 152 (3):977–83. [ PubMed : 7663813 ]
- Tager IB, Segal MR, Speizer FE, Weiss ST. The natural history of forced expiratory volumes: effect of cigarette smoking and respiratory symptoms. American Review of Respiratory Disease. 1988; 138 (4):837–49. [ PubMed : 3202458 ]
- Takizawa H, Tanaka M, Takami K, Ohtoshi T, Ito K, Satoh M, Okada Y, Yamasawa F, Nakahara K, Umeda A. Increased expression of transforming growth factor-β1 in small airway epithelium from tobacco smokers and patients with chronic obstructive pulmonary disease (COPD). American Journal of Respiratory and Critical Care Medicine. 2001; 163 (6):1476–83. [ PubMed : 11371421 ]
- Tandon MK, Gebski V. A controlled trial of a killed Haemophilus influenzae vaccine for prevention of acute exacerbations of chronic bronchitis. Australian and New Zealand Journal of Medicine. 1991; 21 (4):427–32. [ PubMed : 1953532 ]
- Tang J-L, Morris JK, Wald NJ, Hole D, Shipley M, Tunstall-Pedoe H. Mortality in relation to tar yield of cigarettes: a prospective study of four cohorts. British Medical Journal. 1995; 311 (7019):1530–3. [ PMC free article : PMC2548184 ] [ PubMed : 8520394 ]
- Tanigawa T, Araki S, Nakata A, Kitamura F, Yasumoto M, Sakurai S, Kiuchi T. Increase in memory (CD4+CD29+ and CD4+CD45RO+) T and naive (CD4+CD45RA+) T-cell subpopulations in smokers. Archives of Environmental Health. 1998; 53 (6):378–83. [ PubMed : 9886155 ]
- Tashkin DP, Altose MD, Connett JE, Kanner RE, Lee WW, Wise RA. Methacholine reactivity predicts changes in lung function over time in smokers with early chronic obstructive pulmonary disease. American Journal of Respiratory and Critical Care Medicine. 1996; 153 (6 Pt 1):1802–11. [ PubMed : 8665038 ]
- Thun MJ, Day-Lally CA, Calle EE, Flanders WD, Heath CW Jr. Excess mortality among cigarette smokers: changes in a 20-year interval. American Journal of Public Health. 1995; 85 (9):1223–30. [ PMC free article : PMC1615570 ] [ PubMed : 7661229 ]
- Thun MJ, Day-Lally C, Myers DG, Calle EE, Flanders WD, Zhu B-P, Namboodiri MM, Heath CW Jr. Trends in tobacco smoking and mortality from cigarette use in Cancer Prevention Studies I (1959 through 1965) and II (1982 through 1988). In: Shopland DR, Burns DM, Garfinkel L, Samet JM, editors. Changes in Cigarette-Related Disease Risks and Their Implication for Prevention and Control. Smoking and Tobacco Control Monograph No 8. Bethesda (MD): Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 1997a. pp. 305–82. NIH Publication No. 97–4213.
- Thun MJ, Myers DG, Day-Lally C, Namboodiri MM, Calle EE, Flanders WD, Adams SL, Heath CW Jr. Age and the exposure-response relationships between cigarette smoking and premature death in Cancer Prevention Study II. In: Shopland DR, Burns DM, Garfinkel L, Samet JM, editors. Changes in Cigarette-Related Disease Risks and Their Implication for Prevention and Control. Smoking and Tobacco Control Monograph No 8. Bethesda (MD): Department of Health and Human Services, Public Health Service, National Institutes of Health, National Cancer Institute; 1997b. pp. 383–475. NIH Publication No. 97–4213.
- Thurlbeck WM. Emphysema then and now. Canadian Respiratory Journal. 1994; 1 (1):21–39.
- Tollerud DJ, Brown LM, Blattner WA, Mann DL, Pankiw-Trost LK, Hoover RN. T cell subsets in healthy black smokers and nonsmokers: evidence for ethnic group as an important response modifier. American Review of Respiratory Disease. 1991; 144 ( 3 Pt 1):612–6. [ PubMed : 1892301 ]
- Tollerud DJ, Clark JW, Brown LM, Neuland CY, Mann DL, Pankiw-Trost LK, Blattner WA, Hoover RN. Association of cigarette smoking with decreased numbers of circulating natural killer cells. American Review of Respiratory Disease. 1989a; 139 (1):194–8. [ PubMed : 2912340 ]
- Tollerud DJ, Clark JW, Brown LM, Neuland CY, Mann DL, Pankiw-Trost LK, Blattner WA, Hoover RN. The effects of cigarette smoking on T-cell subsets: a population-based survey of healthy Caucasians. American Review of Respiratory Disease. 1989b; 139 (6):1446–51. [ PubMed : 2786361 ]
- Torén K, Brisman J, Järvholm B. Asthma and asthma-like symptoms in adults assessed by questionnaires: a literature review. Chest. 1993; 104 (2):600–8. [ PubMed : 7802735 ]
- Torén K, Hermansson BA. Incidence rate of adult-onset asthma in relation to age, sex, atopy and smoking: a Swedish population-based study of 15813 adults. International Journal of Tuberculosis and Lung Disease. 1999; 3 (3):192–7. [ PubMed : 10094318 ]
- Torres A, Dorca J, Zalacaín R, Bello S, El-Ebiary M, Molinos L, Arévalo M, Blanquer J, Celis R, Iriberri M, Prats E, Fernández R, Irigaray R, Serra J. Community-acquired pneumonia in chronic obstructive pulmonary disease: a Spanish multicenter study. American Journal of Respiratory and Critical Care Medicine. 1996; 154 (5):456–61. [ PubMed : 8912764 ]
- Townsend MC, DuChene AG, Morgan J, Browner WS. Pulmonary function in relation to cigarette smoking and smoking cessation. Preventive Medicine. 1991; 20 (5):621–37. [ PubMed : 1758842 ]
- Troisi RJ, Speizer FE, Rosner B, Trichopoulos D, Willet WC. Cigarette smoking and incidence of chronic bronchitis and asthma in women. Chest. 1995; 108 (6):1557–61. [ PubMed : 7497760 ]
- US Department of Health and Human Services. The Health Consequences of Smoking: Chronic Obstructive Lung Disease A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office on Smoking and Health; 1984. DHHS Publication No. (PHS) 84–50205.
- US Department of Health and Human Services. The Health Consequences of Smoking: Cancer and Chronic Lung Disease in the Workplace A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service; 1985. DHHS Publication No. (PHS) 85–50207.
- US Department of Health and Human Services. The Health Consequences of Involuntary Smoking: A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Health Promotion and Education, Office on Smoking and Health; 1986. DHHS Publication No. (CDC) 87–8398.
- U.S. Department of Health and Human Services. Reducing the Health Consequences of Smoking: 25 Years of Progress. A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1989a. DHHS Publication No. (CDC) 89–8411.
- US Department of Health and Human Services. The International Classification of Diseases, 9th Revision, Clinical Modification Vol 1 Diseases: Tabular List. 3rd ed. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Health Care Financing Administration; 1989b. DHHS Publication No. 89–1260.
- US Department of Health and Human Services. The Health Benefits of Smoking Cessation A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control, Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1990. DHHS Publication No. (CDC) 90–8416.
- US Department of Health and Human Services. Preventing Tobacco Use Among Young People A Report of the Surgeon General. Atlanta: US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994.
- US Department of Health and Human Services. Women and Smoking A Report of the Surgeon General. Rockville (MD): U.S. Department of Health and Human Services, Public Health Service, Office of the Surgeon General; 2001.
- US Department of Health, Education, and Welfare. Smoking and Health Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Communicable Disease Center; 1964. DHEW Publication No. 1103.
- US Department of Health, Education, and Welfare. Smoking and Health A Report of the Surgeon General. Washington: U.S. Department of Health, Education, and Welfare, Public Health Service, Office of the Assistant Secretary for Health, Office on Smoking and Health; 1979. DHEW Publication No. (PHS) 79–50066.
- U.S. Environmental Protection Agency. Respiratory Health Effects of Passive Smoking: Lung Cancer and Other Disorders. Washington: Environmental Protection Agency, Office of Research and Development, Office of Air and Radiation; 1992. Publication No. EPA/600/6-90/006F.
- Verbrugge LM, Patrick DL. Seven chronic conditions: their impact on US adults’ activity levels and use of medical services. American Journal of Public Health. 1995; 85 (2):173–82. [ PMC free article : PMC1615320 ] [ PubMed : 7856776 ]
- Verheij TJM, Hermans J, Mulder JD. Effects of doxycycline in patients with acute cough and purulent sputum: a double blind placebo controlled trial. British Journal of General Practice. 1994; 44 (386):400–4. [ PMC free article : PMC1238988 ] [ PubMed : 8790652 ]
- Vestbo J, Prescott E, Lange P. Association of chronic mucus hypersecretion with FEV 1 decline and chronic obstructive pulmonary disease morbidity: Copenhagen City Heart Study Group. American Journal of Respiratory and Critical Care Medicine. 1996; 153 (5):1530–5. [ PubMed : 8630597 ]
- Vesterinen E, Kaprio J, Koskenvuo M. Prospective study of asthma in relation to smoking habits among 14,729 adults. Thorax. 1988; 43 (7):534–9. [ PMC free article : PMC461360 ] [ PubMed : 3269222 ]
- Villar MTA, Dow L, Coggon D, Lampe FC, Holgate ST. The influence of increased bronchial responsiveness, atopy, and serum IgE on decline in FEV 1 : a longitudinal study in the elderly. American Journal of Respiratory and Critical Care Medicine. 1995; 151 ( 3 Pt 1):656–62. [ PubMed : 7881652 ]
- Voelkel NF, Tuder R. COPD: exacerbation. Chest. 2000; 117 (5 Suppl 2):376S–379S. [ PubMed : 10843980 ]
- Vollmer WM, Enright PL, Pedula KL, Speizer F, Kuller LH, Kiley J, Weinmann GG. Race and gender differences in the effects of smoking on lung function. Chest. 2000; 117 (3):764–72. [ PubMed : 10713004 ]
- von Hertzen L, Kaprio J, Koskenvuo M, Isoaho R, Saikku P. Humoral immune response to Chlamydia pneumoniae in twins discordant for smoking. Journal of Internal Medicine. 1998a; 244 (3):227–34. [ PubMed : 9747745 ]
- von Hertzen L, Surcel H-M, Kaprio J, Koskenvuo M, Bloigu A, Leinonen M, Saikku P. Immune responses to Chlamydia pneumoniae in twins in relation to gender and smoking. Journal of Medical Microbiology. 1998b; 47 (5):441–6. [ PubMed : 9879945 ]
- Wakefield M, Ruffin R, Campbell D, Roberts L, Wilson D. Smoking-related beliefs and behaviour among adults with asthma in a representative population sample. Australian and New Zealand Journal of Medicine. 1995; 25 (1):12–7. [ PubMed : 7786238 ]
- Wang Z, Chen C, Niu T, Wu D, Yang J, Wang B, Fang Z, Yandava CN, Drazen JM, Weiss ST, Xu X. Association of asthma with beta (2)-adrenergic receptor gene polymorphism and cigarette smoking. American Journal of Respiratory and Critical Care Medicine. 2001; 1653 (6):1404–9. [ PubMed : 11371409 ]
- Warner JO. Worldwide variations in the prevalence of atopic symptoms: what does it all mean? Thorax. 1999; 54 (Suppl 2):S46–S51. [ PMC free article : PMC1765934 ] [ PubMed : 10451693 ]
- Weiss ST, O’Connor GT, Sparrow D. The role of allergy and airway responsiveness in the natural history of chronic airflow obstruction (CAO). In: Weiss ST, Sparrow D, editors. Airway Responsiveness and Atopy in the Development of Chronic Lung Disease. New York: Raven Press; 1989. pp. 181–240.
- Williamson HA Jr. A randomized, controlled trial of doxycycline in the treatment of acute bronchitis. Journal of Family Practice. 1984; 19 (4):481–6. [ PubMed : 6384419 ]
- Wise RA. Changing smoking patterns and mortality from chronic obstructive pulmonary disease. Preventive Medicine. 1997; 26 (4):418–21. [ PubMed : 9245659 ]
- Wise RA, Enright PL, Connett JE, Anthonisen NR, Kanner RE, Lindgren P, O’Hara P, Owens GR, Rand CS, Tashkin DP. Effect of weight gain on pulmonary function after smoking cessation in the Lung Health Study. American Journal of Respiratory and Critical Care Medicine. 1998; 157 (3 Pt 1):866–72. [ PubMed : 9517604 ]
- Withers NJ, Low L, Holgate ST, Clough JB. The natural history of respiratory symptoms in a cohort of adolescents. American Journal of Respiratory and Critical Care Medicine. 1998; 158 (2):352–7. [ PubMed : 9700106 ]
- Withey CH, Papacosta AO, Swan AV, Fitzsimons BA, Burney PGJ, Colley JRT, Holland WW. Respiratory effects of lowering tar and nicotine levels of cigarettes smoked by young male middle tar smokers. I: design of a randomised controlled trial. Journal of Epidemiology and Community Health. 1992a; 46 (3):274–80. [ PMC free article : PMC1059567 ] [ PubMed : 1645086 ]
- Withey CH, Papacosta AO, Swan AV, Fitzsimons BA, Ellard GA, Burney PG, Colley JR, Holland WW. Respiratory effects of lowering tar and nicotine levels of cigarettes smoked by young male middle tar smokers. II: results of a randomised controlled trial. Journal of Epidemiology and Community Health. 1992b; 46 (3):281–5. [ PMC free article : PMC1059568 ] [ PubMed : 1645087 ]
- Woo J, Chan HS, Hazlett CB, Ho SC, Chan R, Sham A, Davies PDO. Tuberculosis among elderly Chinese in residential homes: tuberculin reactivity and estimated prevalence. Gerontology. 1996; 42 (3):155–62. [ PubMed : 8796374 ]
- Wright JL. Small airways disease: its role in chronic airflow obstruction. Seminars in Respiratory Medicine. 1992; 13 (2):72–84.
- Xu X, Dockery DW, Ware JH, Speizer FE, Ferris BG Jr. Effects of cigarette smoking on rate of loss of pulmonary function in adults: a longitudinal assessment. American Review of Respiratory Disease. 1992; 146 (5 Pt 1):1345–8. [ PubMed : 1443894 ]
- Xu X, Laird N, Dockery DW, Schouten JP, Rijcken B, Weiss ST. Age, period, and cohort effects on pulmonary function in a 24-year longitudinal study. American Journal of Epidemiology. 1995; 141 (6):554–66. [ PubMed : 7900723 ]
- Xu X, Wang L. Synergistic effects of air pollution and personal smoking on adult pulmonary function. Archives of Environmental Health. 1998; 53 (1):44–53. [ PubMed : 9570308 ]
- Xu X, Weiss ST, Rijcken B, Schouten JP. Smoking, changes in smoking habits, and rate of decline in FEV 1 : new insight into gender differences. European Respiratory Journal. 1994; 7 (6):1056–61. [ PubMed : 7925873 ]
- Yamaguchi E, Okazaki N, Itoh A, Abe S, Kawakami Y, Okuyama H. Interleukin 1 production by alveolar macrophages is decreased in smokers. American Review of Respiratory Disease. 1989; 140 (2):397–402. [ PubMed : 2788378 ]
- Young S, Le Souëf PN, Geelhoed GC, Stick SM, Turner KJ, Landau LI. The influence of a family history of asthma and parental smoking on airway responsiveness in early infancy. New England Journal of Medicine. 1991; 324 (17):1168–73. [ PubMed : 2011160 ]
- Zhang J, Qian Z, Kong L, Zhou L, Yan L, Chapman RS. Effects of air pollution on respiratory health of adults in three Chinese cities. Archives of Environmental Health. 1999; 54 (6):373–81. [ PubMed : 10634226 ]
Pack-years = The number of years of smoking multiplied by the number of packs of cigarettes smoked per day.
- Cite this Page Office of the Surgeon General (US); Office on Smoking and Health (US). The Health Consequences of Smoking: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2004. 4, Respiratory Diseases.
- PDF version of this title (8.3M)
- Disable Glossary Links
In this Page
Other titles in these collections.
- Reports of the Surgeon General
- Health Services/Technology Assessment Text (HSTAT)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Respiratory Diseases - The Health Consequences of Smoking Respiratory Diseases - The Health Consequences of Smoking
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Health impact of smoking. Table Table1 1 lists the main causes of death from smoking. Tobacco smoking is estimated to lead to the premature death of approximately 6 million people worldwide and 96,000 in the UK each year (Action on Smoking and Health, 2016b; World Health Organization, 2013).A 'premature death from smoking' is defined as a death from a smoking-related disease in an ...
Foremost among the cancers caused by tobacco use is lung cancer. Cigarette smoking has been linked to about 80 to 90 percent of all cases of lung cancer, the leading cause of cancer death for both men and women, and it is responsible for roughly 80 percent of deaths from this disease. 22,47 Smoking increases lung cancer risk five to tenfold ...
For the essay, the article explains one of the few pro-tobacco arguments (that smoking has a calming effect) and proves that it is false and harmful. As a result, the article is an important contribution that provides some information on the opposite point of view, according to which there are benefits to smoking, and proves it wrong.
Smoking can affect a person's health in many other ways as well, harming nearly every organ in the body. Here are a few examples of other ways smoking tobacco can affect your health: Increased risk of gum disease and tooth loss. Lowered immune system function. Increased risk of type 2 diabetes.
Key facts. Tobacco kills up to half of its users who don't quit (1-3).; Tobacco kills more than 8 million people each year, including an estimated 1.3 million non-smokers who are exposed to second-hand smoke (4).; Around 80% of the world's 1.3 billion tobacco users live in low- and middle-income countries.
Tobacco smoking is the leading cause of preventable disease, disability, and death in the United States (U.S. Department of Health and Human Services [USDHHS] 2014). Smoking harms nearly every organ in the body and costs the United States billions of dollars in direct medical costs each year (USDHHS 2014). Although considerable progress has been made in reducing cigarette smoking since the ...
History Pre-cigarette. Texts on the harmful effects of smoking tobacco were recorded in the Timbuktu manuscripts.. James I wrote a book that denounced tobacco smoking as: "...loathsome to the eye, hateful to the nose, harmful to the brain, dangerous to the lungs...". Pipe smoking gradually became generally accepted as a cause of mouth cancers following work done in the 1700s.
We identified three outcomes with a 4-star association with smoking: COPD (72% increase in risk based on the BPRF, 0.54 ROS), lower respiratory tract infection (54%, 0.43) and pancreatic cancer ...
Smoking can result in stroke and heart attacks since it hinders blood flow, interrupting oxygen to various parts of the body, such as feet and hands. Introduction of cigarettes with low tar does not reduce these effects since smokers often prefer deeper puffs and hold the smoke in lungs for a long period. This smoking practice draws the tar ...
Abstract. Tobacco smoking is a major determinant of preventable morbidity and mortality worldwide. More than a billion people smoke, and without major increases in cessation, at least half will ...
Smoking is the practice of inhaling smoke from burning plant material. Nicotine works on your brain to create a relaxing, pleasurable feeling that makes it tough to quit. But smoking tobacco puts you at risk for cancer, stroke, heart attack, lung disease and other health issues. Nicotine replacements and lifestyle changes may help you quit.
Risk of other cancers. Digestive system. Central nervous system. Secondhand smoke. Quitting. Summary. Smoking cigarettes can have many adverse effects on the body. It increases a person's risk ...
Smoking causes about 90% (or 9 out of 10) of all lung cancer deaths. 1,2 More women die from lung cancer each year than from breast cancer. 5. Smoking causes about 80% (or 8 out of 10) of all deaths from chronic obstructive pulmonary disease (COPD). 1. Cigarette smoking increases risk for death from all causes in men and women. 1.
The scope of the burden of disease and death that cigarette smoking imposes on the public's health is extensive. Cigarette smoking is the major focus of this chapter because it is the central public health problem, but the topics of secondhand smoke exposure, smoking of other combustible tobacco products, smokeless tobacco, and electronic nicotine delivery systems (ENDS) are also considered.
It has many ill-effects on the human body which we will go through in the essay on smoking. Ill-Effects of Smoking. Tobacco can have a disastrous impact on our health. Nonetheless, people consume it daily for a long period of time till it's too late. Nearly one billion people in the whole world smoke.
Smoking affects the lungs and respiratory organs causing such terrible diseases as cancer. Among the most wider spread diseases are peptic ulcers, cancer of the larynx, kidney, pancreas, and other major organs. The resins from the smoke enter the blood and ruin cells. This process is inevitable if a person smokes for years.
500 Words Essay on Harmful Effects Of Tobacco Introduction. Tobacco is a plant that is grown for its leaves. These leaves are dried and then used in many ways, including cigarettes, cigars, and chewing tobacco. While many people use tobacco, it can cause serious health problems. This essay will discuss the harmful effects of tobacco on the ...
500 Words Essay on Harmful Effects of Smoking Introduction. Smoking is a prevalent habit, often started out of curiosity, peer pressure, or stress management. However, its harmful effects are well-documented, impacting nearly every organ in the human body. Despite the widespread knowledge of its adverse effects, smoking continues to be a ...
These means the cells cannot sweep clean the lining of your airways and protect you against infections. Tiny particles in tobacco smoke irritate your throat and lungs and cause 'smoker's cough'. This makes you produce more mucus and damages lung tissue. Ammonia and formaldehyde irritate your eyes, nose and throat.
Objective: Smoking electronic cigarettes (E-cig) has been promoted as a safer alternative to conventional tobacco cigarettes (CIG) and thus become popular, especially among younger generations. However, one mode of smoking nicotine containing products vs. another on the effects on health and gender are largely unknown. Hypothesis: Both E-cig and CIG have adverse effects on body weight as well ...
The topic of passive or involuntary smoking was first addressed in the 1972 U.S. Surgeon General's report (The Health Consequences of Smoking, U.S. Department of Health, Education, and Welfare [USDHEW] 1972), only eight years after the first Surgeon General's report on the health consequences of active smoking (USDHEW 1964). Surgeon General Dr. Jesse Steinfeld had raised concerns about ...
Smokeless tobacco causes cancer of the mouth, esophagus, and pancreas. 1. Many smokeless tobacco products contain cancer-causing chemicals. 1 6. The most harmful chemicals are tobacco-specific nitrosamines. 1 These are organic compounds that may increase the risk of cancer. They form during the growing, curing, fermenting, and aging of tobacco.
Overview. In the United States, youth use e-cigarettes, or vapes, more than any other tobacco product. 1. No tobacco products, including e-cigarettes, are safe, especially for children, teens, and young adults. 2. Most e-cigarettes contain nicotine, which is highly addictive. Nicotine can harm the parts of an adolescent's brain that control ...
Almost 35 years ago, the Office of the Surgeon General of the United States Health Service reviewed over 7000 research papers on the topic of smoking and health, and publicly recognized the role of smoking in various diseases, including lung cancer. ... Because of the antiestrogenic protective effects of smoking, the role of smoking in breast ...
Chantix and Zyban are two popular prescription medications for smoking cessation that you can discuss with your doctor. Pfizer shared research on the. effectiveness of Chantix. , with various ...
Cannabis use may have a wide range of health effects on the body and brain. ... Impact of changes in regular use of marijuana and/or tobacco on chronic bronchitis. COPD. 2012;9(4):367-374. doi: 10.3109/15412555.2012.671868. Wang X, Derakhshandeh R, Liu J, et al. One minute of marijuana secondhand smoke exposure substantially impairs vascular ...
Smoking has adverse health effects on the entire lung—affecting every aspect of lung structure and function—including impairing lung defenses against infection and causing the sustained lung injury that leads to chronic obstructive pulmonary disease (COPD). In fact, among the postulated causes of COPD are acute respiratory infections, for which smokers are at an increased risk. This ...