Understanding Communication in Nursing (With Examples, Importance, & How to Improve)

Communication is one of the most powerful tools nurses use when providing patient care. Because communication can impact every aspect of work and nurse-patient relationships, nurses must learn how to improve communication in nursing and implement measures for effective communication. In this article, you will learn the importance of therapeutic communication and find 18 useful tips to improve communication in nursing.

Who Do Nurses Communicate With?
7 reasons why communication is so important in nursing, 1. effective communication in nursing is essential in assessing a patient’s response to treatment., 2. communication with patients and their loved ones helps relieve stress and improves patient outcomes., 3. effective communication among the healthcare team can help reduce the risk of errors in patient care., 4. effective communication in nursing care is necessary to advocate for patients., 5. communicating with patients and their families will help identify special needs., 6. communication with your patients will help you identify and understand the social determinants impacting their health., 7. effective communication in nursing is vital for understanding the status of your patient's emotional and physical well-being., what are the 8 essential components of good communication in nursing, 1. eye contact:, 2. an attentive listener:, 3. a clear message:, 4. patience:, 5. being receptive:, 6. body language:, 7. understanding:, 8. feedback:, examples of bad communication vs. good communication in nursing, 1. scenario:, bad communication:, good communication:, 2. scenario:, 3. scenario:, 4. scenario:, how to improve communication in nursing, 1. use the right tone when speaking to others., 2. be aware of others’ body language., 3. be mindful of your own body language., 4. show interest in what others say., 5. be patient., 6. demonstrate a positive attitude., 7. create an atmosphere conducive to effective communication., 8. practice active listening., 9. exercise emotional intelligence., 10. ask open-ended questions., 11. be attentive to your patient’s efforts at communicating with you., 12. practice cultural awareness., 13. ask for input from colleagues., 14. be mindful of your patient’s situation., 15. exercise diverse types of communication., 16. incorporate role-play when appropriate., 17. involve your patient’s friends and/or family., 18. show compassion., 7 consequences of bad communication in nursing, 1. miscommunication of vital patient information:, 2. poor communication skills in nursing can cause increased workload pressure., 3. patients may not understand important information such as when to take a medication or possible side effects to report., 4. when there is bad communication in nursing, there is an increased risk to the patient's safety., 5. when nurses communicate poorly with one another, there is an increased risk of malpractice suits., 6. poor patient satisfaction scores:, 7. increased chance of medication errors., useful resources to improve communication in nursing, • the importance of listening in healthcare, • empowering communication, • therapeutic communication, calming people down and dealing with patient complaints, • how can i improve my communication skills with my patients, • communication mishaps between patients and nurses, youtube videos, • nursing fundamentals: therapeutic communication & coping, • nurse to nurse communication skills, • therapeutic communication for nurses: avoid these 5 traps, • nursing standard: inclusive communication and how to avoid making assumptions, • stitcher: healthcare communication- effective techniques for clinicians, • audible: healthcare communication solutions, • therapeutic communication: knowing what to say when, • communication for nurses: how to prevent harmful events and promote patient safety, • 4 essential keys to effective communication, my final thoughts, frequently asked questions answered by our expert, 1. as a nurse, how do i know if i am a good communicator, 2. will lack of communication impact my nursing career, 3. usually, how long does it take for a nurse to improve the skill of therapeutic communication, 4. do all types of nurses require very good communication skills, 5. as a nurse, do i need to be good at all types of communication.

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021.

Nursing Fundamentals [Internet].
- About Open RN
Chapter 2 Communication
2.1. communication introduction, learning objectives.
- Assess one’s own communication skills and effectiveness [ 1 ]
- Demonstrate cultural humility, professionalism, and respect when communicating [ 2 ]
- Use communication styles and methods that demonstrate caring, respect, active listening, authenticity, and trust [ 3 ]
- Maintain communication with interprofessional team members and others to facilitate safe transitions and continuity in care delivery [ 4 ]
- Use therapeutic communication techniques
- Confirm the recipient of the communication heard and understands the message [ 5 ]
- Apply principles of distance and space
- Discuss strategies for maintaining confidentiality
- Use technology to access current and reliable information
- Use correct medical terminology and abbreviations
- Report significant patient information verbally and in writing
- Document according to legal guidelines
Strong communication skills are essential to provide safe, quality, patient-centered care. Nurses develop therapeutic relationships with patients and family members each day to ensure that health care concerns and needs are addressed. If communication breaks down, information exchange stops and needs go unidentified. Nurses optimize communication channels with patients and families by establishing trust and actively listening to health care concerns. Additionally, the nurse is vital for ensuring that information transfer occurs within the multidisciplinary team. Communication with other health care team members is professional, organized, accurate, complete, and concise. This chapter will review methods for establishing good communication.
Before getting started, view the following video and reflect on the often invisible needs of those around us and the difference we can make by creating caring human connections.
View the video: Empathy: The Human Connection to Patient Care . [ 6 ]
2.2. basic communication concepts.
Effective communication is one of the Standards of Professional Performance established by the American Nurses Association. The standard states, “The registered nurse communicates effectively in all areas of practice.” [ 1 ] There are several concepts related to effective communication such as demonstrating appropriate verbal and nonverbal communication, using assertive communication, being aware of personal space, and overcoming common barriers to effective communication.
Types of Communication
Verbal communication.
Effective communication requires each interaction to include a sender of the message, a clear and concise message, and a receiver who can decode and interpret that message. The receiver also provides a feedback message back to the sender in response to the received message. See Figure 2.1 [ 2 ] for an image of effective communication between a sender and receiver.
Effective Communication
Nurses assist patients and their family members to understand health care needs and treatments by using verbal, nonverbal, and written communication. Verbal communication is more than just talking. Effective verbal communication is defined as an exchange of information using words understood by the receiver in a way that conveys professional caring and respect. [ 3 ] Nurses who speak using extensive medical jargon or slang may create an unintended barrier to their own verbal communication processes. When communicating with others, it is important for the nurse to assess the receiver’s preferred method of communication and individual receiver characteristics that might influence communication, and subsequently adapt communication to meet the receiver’s needs. For example, the nurse may adapt postsurgical verbal instruction for a pediatric versus an adult patient. Although the information requirements regarding signs of infection, pain management, etc., might be similar, the way in which information is provided may be quite different based on developmental level. Regardless of the individual adaptations that are made, the nurse must be sure to always verify patient understanding.
Nonverbal Communication
In addition to communicating verbally, the nurse must also be aware of messages sent by nonverbal communication . Nonverbal communication can have a tremendous impact on the communication experience and may be much more powerful than the verbal message itself. You may have previously learned that 80% of communication is nonverbal communication (see Figure 2.2 [ 4 ] ). The importance of nonverbal communication during communication has also been described in percentages of 55, 38, and 7, meaning 55% of communication is body language, 38% is tone of voice, and 7% is the actual words spoken. [ 5 ]
Nonverbal communication includes body language and facial expressions, tone of voice, and pace of the conversation. For example, compare the nonverbal communication messages in Figures 2.3 [ 6 ] and 2.4 . [ 7 ] What nonverbal cues do you notice about both toddlers?
Toddler’s Nonverbal Communication
Nurses should be attentive to their nonverbal communication cues and the messages they provide to patients and their families. Nurses should be purposeful in their use of nonverbal communication that conveys a feeling of caring. [ 8 ] What nonverbal cues do you notice about the nurse in Figure 2.5 [ 9 ] that provide a perception of professional caring?
Nurse’s Nonverbal Communication
Nurses use nonverbal communication such as directly facing patients at eye level, leaning slightly forward, and making eye contact to communicate they care about what the person is telling them and they have their full attention. [ 10 ]
It is common for health care team members in an acute care setting to enter a patient’s room and begin interacting with a patient who is seated or lying in bed. However, it is important to remember that initial or sensitive communication exchanges are best received by the patient if the nurse and patient are at eye level. Bringing a chair to the patient’s bedside can help to facilitate engagement in the communication exchange. SOLER is common mnemonic used to facilitate nonverbal communication (sit with open posture and lean in with good eye contact in a relaxed manner).
Communication styles.
In addition to verbal and nonverbal communication, people communicate with others using three styles. A passive communicator puts the rights of others before their own. Passive communicators tend to be apologetic or sound tentative when they speak and often do not speak up if they feel as if they are being wronged. Aggressive communicators, on the other hand, come across as advocating for their own rights despite possibly violating the rights of others. They tend to communicate in a way that tells others their feelings don’t matter. However, assertive communicators respect the rights of others while also standing up for their own ideas and rights when communicating. An assertive person is direct, but not insulting or offensive. [ 11 ] Assertive communication refers to a way of conveying information that describes the facts and the sender’s feelings without disrespecting the receiver’s feelings. Using “I” messages such as, “I feel…,” “I understand…,” or “Help me to understand…” are strategies for assertive communication. This method of communicating is different from aggressive communication that uses “you” messages and can feel as if the sender is verbally attacking the receiver rather than dealing with the issue at hand. For example, instead of saying to a coworker, “Why is it always so messy in your patients’ rooms? I dread following you on the next shift!,” an assertive communicator would use “I” messages to say, “I feel frustrated spending the first part of my shift decluttering our patients’ rooms. Help me understand why it is a challenge to keep things organized during your shift?”
Using assertive communication is an effective way to solve problems with patients, coworkers, and health care team members.
View this humorous video demonstrating assertive communication techniques being used by the actors on a TV show: Everybody Loves Raymond Uses Active Listening – from Parent Effectiveness Training.
Personal space.
While being aware of verbal and nonverbal messages and communicating assertively, it is also important to be aware of others’ personal space. Proxemics is the study of personal space and provides guidelines for professional communication. The public zone is over 10 feet of distance between people and generally avoids physical contact. The social zone is four to 10 feet of distance between people. It is used during social interactions and business settings. The personal zone is 18 inches to four feet of space and is generally reserved for friends and family. Less than 18 inches is reserved for close relationships but may be invaded when in crowds or playing sports. [ 12 ] Nurses usually communicate within the social zone to maintain professional boundaries. However, when assessing patients and performing procedures, nurses often move into a patient’s personal zone. Nurses must be aware of patients’ feelings of psychological discomfort that can occur when invading this zone. Additionally, cultural considerations may impact the appropriateness of personal space when providing patient care. See Figure 2.6 for example of personal space zones. [ 13 ]
Personal Space Zones
Overcoming Common Barriers to Communication
It is important for you to reflect on personal factors that influence your ability to communicate effectively. There are many factors that can cause the message you are trying to communicate to become distorted and not perceived by the receiver in the way you intended. It is important to seek feedback that your message is clearly understood. Nurses must be aware of these potential barriers and try to reduce their impact by continually seeking feedback and checking understanding. [ 14 ]
Common barriers to communication in health care and strategies to overcome them are described in the following box. [ 15 ]
Common Barriers to Communication in Health Care
- Jargon: Avoid using medical terminology, complicated, or unfamiliar words. When communicating with patients, explain information in plain language that is easy to understand by those without a medical or nursing background.
- Lack of attention: Nurses are typically very busy with several tasks to complete for multiple patients. It is easy to become focused on the tasks instead of the patient. When entering a patient’s room, it is helpful to pause, take a deep breath, and mindfully focus on the patient in front of you to give them your full attention. Patients should feel as if they are the center of your attention when you are with them, no matter how many other things you have going on.
- Noise and other distractions: Health care environments can be very noisy with people talking in the room or hallway, the TV blaring, alarms beeping, and pages occurring overhead. Create a calm, quiet environment when communicating with patients by closing doors to the hallway, reducing the volume of the TV, or moving to a quieter area, if possible.
- Light: A room that is too dark or too light can create communication barriers. Ensure the lighting is appropriate according to the patient’s preference.
- Hearing and speech problems: If your patient has hearing or speech problems, implement strategies to enhance communication. See the “Adapting Your Communication” section below for strategies to address hearing and speech problems.
- Language differences: If English is not your patient’s primary language, it is important to seek a medical interpreter and to also provide written handouts in the patient’s preferred language when possible. Most agencies have access to an interpreter service available by phone if they are not available on-site.
- Differences in cultural beliefs: The norms of social interaction vary greatly in different cultures, as well as the ways that emotions are expressed. For example, the concept of personal space varies among cultures, and some patients are stoic about pain whereas others are more verbally expressive. Read more about caring for diverse patients in the “ Diversity ” chapter.
- Psychological barriers: Psychological states of the sender and the receiver affect how the message is sent, received, and perceived. For example, if nurses are feeling stressed and overwhelmed with required tasks, the nonverbal communication associated with their messages such as lack of eye contact, a hurried pace, or a short tone can affect how the patient perceives the message. If a patient is feeling stressed, they may not be able to “hear” the message or they may perceive it differently than it was intended. It is important to be aware of signs of the stress response in ourselves and our patients and implement appropriate strategies to manage the stress response. See the box below for more information about strategies to manage the stress response.
- Physiological barriers: It is important to be aware of patients’ potential physiological barriers when communicating. For example, if a patient is in pain, they are less likely to hear and remember what was said, so pain relief should be provided as needed before providing patient education. However, it is also important to remember that sedatives and certain types of pain medications often impair the patient’s ability to receive and perceive messages so health care documents cannot be signed by a patient after receiving these types of medications.
- Physical barriers for nonverbal communication: Providing information via e-mail or text is often less effective than face-to-face communication. The inability to view the nonverbal communication associated with a message such as tone of voice, facial expressions, and general body language often causes misinterpretation of the message by the receiver. When possible, it is best to deliver important information to others using face-to-face communication so that nonverbal communication is included with the message.
- Differences in perception and viewpoints: Everyone has their own beliefs and perspectives and wants to feel “heard.” When patients feel their beliefs or perspectives are not valued, they often become disengaged from the conversation or the plan of care. Nurses should provide health care information in a nonjudgmental manner, even if the patient’s perspectives, viewpoints, and beliefs are different from their own.
Read more about Barriers to Effective Communication.
Managing the Stress Response [ 16 ]
The stress response is a common psychological barrier to effective communication. It can affect the message sent by the sender or how it is received by the receiver. The stress response is a common reaction to life events, such as a nurse feeling stressed by being overwhelmed with tasks to complete for multiple patients, or a patient feeling stressed when admitted to a hospital or receiving a new diagnosis. Symptoms of the stress response include irritability, sweaty palms, a racing heart, difficulty concentrating, and impaired sleep. It is important to recognize symptoms of the stress response in ourselves and our patients and use strategies to manage the stress response when communicating. Strategies to manage the stress response are as follows:
Use relaxation breathing . Become aware of your breathing. Take a deep breath in your nose and blow it out through your mouth. Repeat this process at least three times in succession and then as often as needed throughout the day.
Make healthy diet choices. Avoid caffeine, nicotine, and junk food because these items can increase feelings of anxiety or being on edge.
Make time for exercise. Exercise stimulates the release of natural endorphins that reduce the body’s stress response and also helps to improve sleep.
Get enough sleep. Set aside at least 30 minutes before going to bed to wind down from the busyness of the day. Avoid using electronic devices like cell phones before bedtime because the backlight can affect sleep.
Use progressive relaxation . There are several types of relaxation techniques that focus on reducing muscle tension and using mental imagery to induce calmness. Progressive relaxation generally includes the following steps:
- Start by lying down somewhere comfortable and firm, like a rug or mat on the floor. Get yourself comfortable.
- Relax and try to let your mind go blank. Breathe slowly, deeply, and comfortably, while gradually and consciously relaxing all your muscles, one by one.
- Work around the body one main muscle area at a time, breathing deeply, calmly, and evenly. For each muscle group, clench the muscles tightly and hold for a few seconds, and then relax them completely. Repeat the process, noticing how it feels. Do this for each of your feet, calves, thighs, buttocks, stomach, arms, hands, shoulders, and face.
2.3. COMMUNICATING WITH PATIENTS
Therapeutic communication is a type of professional communication used by nurses with patients and defined as, “The purposeful, interpersonal information-transmitting process through words and behaviors based on both parties’ knowledge, attitudes, and skills, which leads to patient understanding and participation.” [ 1 ] Therapeutic communication techniques used by nurses have roots going back to Florence Nightingale, who insisted on the importance of building trusting relationships with patients and believed in the therapeutic healing that resulted from nurses’ presence with patients. [ 2 ] Since then, several professional nursing associations have highlighted therapeutic communication as one of the most vital elements in nursing.
Read an example of a nursing student effectively using therapeutic communication with patients in the following box.
An Example of Nursing Student Using Therapeutic Communication

Ms. Z. is a nursing student who enjoys interacting with patients. When she goes to patients’ rooms, she greets them and introduces herself and her role in a calm tone. She kindly asks patients about their problems and notices their reactions. She does her best to solve their problems and answer their questions. Patients perceive that she wants to help them. She treats patients professionally by respecting boundaries and listening to them in a nonjudgmental manner. She addresses communication barriers and respects patients’ cultural beliefs. She notices patients’ health literacy and ensures they understand her messages and patient education. As a result, patients trust her and feel as if she cares about them, so they feel comfortable sharing their health care needs with her. [ 3 ] , [ 4 ]
Active Listening and Attending Behaviors
Listening is obviously an important part of communication. There are three main types of listening: competitive, passive, and active. Competitive listening happens when we are focused on sharing our own point of view instead of listening to someone else. Passive listening occurs when we are not interested in listening to the other person and we assume we understand what the person is communicating correctly without verifying. During active listening , we are communicating verbally and nonverbally that we are interested in what the other person is saying while also actively verifying our understanding with the speaker. For example, an active listening technique is to restate what the person said and then verify our understanding is correct. This feedback process is the main difference between passive listening and active listening. [ 5 ]
Touch is a powerful way to professionally communicate caring and empathy if done respectfully while being aware of the patient’s cultural beliefs. Nurses commonly use professional touch when assessing, expressing concern, or comforting patients. For example, simply holding a patient’s hand during a painful procedure can be very effective in providing comfort. See Figure 2.7 [ 6 ] for an image of a nurse using touch as a therapeutic technique when caring for a patient.
Using Touch as Therapeutic Communication
Therapeutic Techniques
Therapeutic communication techniques are specific methods used to provide patients with support and information while focusing on their concerns. Nurses assist patients to set goals and select strategies for their plan of care based on their needs, values, skills, and abilities. It is important to recognize the autonomy of the patient to make their own decisions, maintain a nonjudgmental attitude, and avoid interrupting. Depending on the developmental stage and educational needs of the patient, appropriate terminology should be used to promote patient understanding and rapport. When using therapeutic communication , nurses often ask open-ended statements and questions, repeat information, or use silence to prompt patients to work through problems on their own. [ 7 ] Table 2.3a describes a variety of therapeutic communication techniques. [ 8 ]
Therapeutic Communication Techniques
In addition to the therapeutic techniques listed in Table 2.3a , nurses and nursing students should genuinely communicate with empathy. Communicating honestly, genuinely, and authentically is powerful. It opens the door to creating true connections with others. [ 9 ] Communicating with empathy has also been described as providing “unconditional positive regard.” Research has demonstrated that when health care teams communicate with empathy, there is improved patient healing, reduced symptoms of depression, and decreased medical errors. [ 10 ]
Nurses and nursing students must be aware of potential barriers to communication. In addition to considering common communication barriers discussed in the previous section, there are several nontherapeutic responses to avoid. These responses often block the patient’s communication of their feelings or ideas. See Table 2.3b for a description of nontherapeutic responses. [ 11 ]
Nontherapeutic Responses
Strategies for Effective Communication
In addition to using therapeutic communication techniques, avoiding nontherapeutic responses, and overcoming common barriers to communication, there are additional strategies for promoting effective communication when providing patient-centered care. Specific questions to ask patients are as follows:
- What concerns do you have about your plan of care?
- What questions do you have about your medications?
- Did I answer your question(s) clearly or is there additional information you would like? [ 12 ]
Listen closely for feedback from patients. Feedback provides an opportunity to improve patient understanding, improve the patient-care experience, and provide high-quality care. Other suggestions for effective communication with hospitalized patients include the following:
- Round with the providers and read progress notes from other health care team members to ensure you have the most up-to-date information about the patient’s treatment plan and progress. This information helps you to provide safe patient care as changes occur and also to accurately answer the patient’s questions.
- Review information periodically with the patient to improve understanding.
- Use patient communication boards in their room to set goals and communicate important reminders with the patient, family members, and other health care team members. This strategy can reduce call light usage for questions related to diet and activity orders and also gives patients and families the feeling that they always know the current plan of care. However, keep patient confidentiality in mind regarding information to publicly share on the board that visitors may see.
- Provide printed information on medical procedures, conditions, and medications. It helps patients and family members to have multiple ways to provide information. [ 13 ]
Adapting Your Communication
When communicating with patients and family members, take note of your audience and adapt your message based on their characteristics such as age, developmental level, cognitive abilities, and any communication disorders. For patients with language differences, it is vital to provide trained medical interpreters when important information is communicated.
Adapting communication according to the patient’s age and developmental level includes the following strategies:
- When communicating with children, speak calmly and gently. It is often helpful to demonstrate what will be done during a procedure on a doll or stuffed animal. To establish trust, try using play or drawing pictures.
- When communicating with adolescents, give freedom to make choices within established limits.
- When communicating with older adults, be aware of potential vision and hearing impairments that commonly occur and address these barriers accordingly. For example, if a patient has glasses and/or hearing aids, be sure these devices are in place before communicating. See the following box for evidence-based strategies for communication with patients who have impaired hearing and vision. [ 14 ]
Strategies for Communicating with Patients with Impaired Hearing and Vision
Impaired Hearing
- Gain the patient’s attention before speaking (e.g., through touch)
- Minimize background noise
- Position yourself 2-3 feet away from the patient
- Facilitate lip-reading by facing the patient directly in a well-lit environment
- Use gestures, when necessary
- Listen attentively, allowing the patient adequate time to process communication and respond
- Refrain from shouting at the patient
- Ask the patient to suggest strategies for improved communication (e.g., speaking toward better ear and moving to well-lit area)
- Face the patient directly, establish eye contact, and avoid turning away mid sentence
- Simplify language (i.e., do not use slang but do use short, simple sentences), as appropriate
- Note and document the patient’s preferred method of communication (e.g., verbal, written, lip-reading, or American Sign Language) in plan of care
- Assist the patient in acquiring a hearing aid or assistive listening device
- Refer to the primary care provider or specialist for evaluation, treatment, and hearing rehabilitation [ 15 ]
Impaired Vision
- Identify yourself when entering the patient’s space
- Ensure the patient’s eyeglasses or contact lenses have current prescription, are cleaned, and stored properly when not in use
- Provide adequate room lighting
- Minimize glare (i.e., offer sunglasses or draw window covering)
- Provide educational materials in large print
- Apply labels to frequently used items (i.e., mark medication bottles using high-contrasting colors)
- Read pertinent information to the patient
- Provide magnifying devices
- Provide referral for supportive services (e.g., social, occupational, and psychological) [ 16 ]
Patients with communication disorders require additional strategies to ensure effective communication. For example, aphasia is a communication disorder that results from damage to portions of the brain that are responsible for language. Aphasia usually occurs suddenly, often following a stroke or head injury, and impairs the patient’s expression and understanding of language. Global aphasia is caused by injuries to multiple language-processing areas of the brain, including those known as Wernicke’s and Broca’s areas. These brain areas are particularly important for understanding spoken language, accessing vocabulary, using grammar, and producing words and sentences. Individuals with global aphasia may be unable to say even a few words or may repeat the same words or phrases over and over again. They may have trouble understanding even simple words and sentences. [ 17 ]
The most common type of aphasia is Broca's aphasia . People with Broca’s aphasia often understand speech and know what they want to say, but frequently speak in short phrases that are produced with great effort. For example, they may intend to say, “I would like to go to the bathroom,” but instead the words, “Bathroom, Go,” are expressed. They are often aware of their difficulties and can become easily frustrated. See the hyperlink in the box below for evidence-based strategies to enhance communication with a person with impaired speech. [ 18 ]
Read more about aphasia .
Strategies to improve communication with patients with impaired speech.
- Modify the environment to minimize excess noise and decrease emotional distress
- Phrase questions so the patient can answer using a simple “Yes” or “No,” being aware that patients with expressive aphasia may provide automatic responses that are incorrect
- Monitor the patient for frustration, anger, depression, or other responses to impaired speech capabilities
- Provide alternative methods of speech communication (e.g., writing tablet, flash cards, eye blinking, communication board with pictures and letters, hand signals or gestures, and computer)
- Adjust your communication style to meet the needs of the patient (e.g., stand in front of the patient while speaking, listen attentively, present one idea or thought at a time, speak slowly but avoid shouting, use written communication, or solicit family’s assistance in understanding the patient’s speech)
- Ensure the call light is within reach and central call light system is marked to indicate the patient has difficulty with speech
- Repeat what the patient said to ensure accuracy
- Instruct the patient to speak slowly
- Collaborate with the family and a speech therapist to develop a plan for effective communication [ 19 ]
Maintaining Patient Confidentiality
When communicating with patients, their friends, their family members, and other members of the health care team, it is vital for the nurse to maintain patient confidentiality. The Health Insurance Portability and Accountability Act (HIPAA) provides standards for ensuring privacy of patient information that are enforceable by law. Nurses must always be aware of where and with whom they share patient information. For example, information related to patient care should not be discussed in public areas, paper charts must be kept in secure areas, computers must be logged off when walked away from, and patient information should only be shared with those directly involved in patient care. For more information about patient confidentiality, see the “ Legal Considerations & Ethics ” section in the “Scope of Practice” chapter.
Read more information about the Health Insurance Portability and Accountability Act of 1996 (HIPAA) .
2.4. communicating with health care team members.
Professional communication with other members of the health care team is an important component of every nurse’s job. See Figure 2.8 [ 1 ] for an image illustrating communication between health care team members. Common types of professional interactions include reports to health care team members, handoff reports, and transfer reports.
Interprofessional Communication
Reports to Health Care Team Members
Nurses routinely report information to other health care team members, as well as urgently contact health care providers to report changes in patient status.
Standardized methods of communication have been developed to ensure that information is exchanged between health care team members in a structured, concise, and accurate manner to ensure safe patient care. One common format used by health care team members to exchange patient information is ISBARR , a mnemonic for the components of I ntroduction, S ituation, B ackground, A ssessment, R equest/Recommendations, and R epeat back.
- Introduction: Introduce your name, role, and the agency from which you are calling.
- Situation: Provide the patient’s name and location, why you are calling, recent vital signs, and the status of the patient.
- Background: Provide pertinent background information about the patient such as admitting medical diagnoses, code status, recent relevant lab or diagnostic results, and allergies.
- Assessment: Share abnormal assessment findings and your evaluation of the current patient situation.
- Request/Recommendations: State what you would like the provider to do, such as reassess the patient, order a lab/diagnostic test, prescribe/change medication, etc.
- Repeat back: If you are receiving new orders from a provider, repeat them to confirm accuracy. Be sure to document communication with the provider in the patient’s chart.
Read an example of an ISBARR report in the following box. A hyperlink is provided to a printable ISBARR reference card.
Sample ISBARR Report From a Nurse to a Health Care Provider
I: “Hello Dr. Smith, this is Jane White, RN from the Med Surg unit.”
S: “I am calling to tell you about Ms. White in Room 210, who is experiencing an increase in pain, as well as redness at her incision site. Her recent vital signs were BP 160/95, heart rate 90, respiratory rate 22, O2 sat 96%, and temperature 38 degrees Celsius. She is stable but her pain is worsening.”
B: “Ms. White is a 65-year-old female, admitted yesterday post hip surgical replacement. She has been rating her pain at 3 or 4 out of 10 since surgery with her scheduled medication, but now she is rating the pain as a 7, with no relief from her scheduled medication of Vicodin 5/325 mg administered an hour ago. She is scheduled for physical therapy later this morning and is stating she won’t be able to participate because of the pain this morning.”
A: “I just assessed the surgical site and her dressing was clean, dry, and intact, but there is 4 cm redness surrounding the incision, and it is warm and tender to the touch. There is moderate serosanguinous drainage. Otherwise, her lungs are clear and her heart rate is regular.”
R: “I am calling to request an order for a CBC and increased dose of pain medication.”
R: “I am repeating back the order to confirm that you are ordering a STAT CBC and an increase of her Vicodin to 10/325 mg.”
View or print an ISBARR reference card
Handoff Reports
Handoff reports are defined by The Joint Commission as “a transfer and acceptance of patient care responsibility achieved through effective communication. It is a real-time process of passing patient specific information from one caregiver to another, or from one team of caregivers to another, for the purpose of ensuring the continuity and safety of the patient’s care.” [ 2 ] In 2017, The Joint Commission issued a sentinel alert about inadequate handoff communication that has resulted in patient harm such as wrong-site surgeries, delays in treatment, falls, and medication errors. Strategies for improving handoff communication have been implemented at agencies across the country.
Although many types of nursing shift-to-shift handoff reports have been used over the years, evidence strongly supports that bedside handoff reports increase patient safety, as well as patient and nurse satisfaction, by effectively communicating current, accurate patient information in real time. [ 3 ] See Figure 2.9 [ 4 ] for an image illustrating two nurses participating in a handoff report. Bedside reports typically occur in hospitals and include the patient, along with the off-going and the oncoming nurses in a face-to-face handoff report conducted at the patient’s bedside. HIPAA rules must be kept in mind if visitors are present or the room is not a private room. Family members may be included with the patient’s permission. See a sample checklist for a bedside handoff report from the Agency for Healthcare Research and Quality in Figure 2.10 . [ 5 ] Although a bedside handoff report is similar to an ISBARR report, it contains additional information to ensure continuity of care across nursing shifts. For example, the “assessment” portion of the bedside handoff report includes detailed pertinent data the oncoming nurse needs to know, such as current head-to-toe assessment findings to establish a baseline; information about equipment such as IVs, catheters, and drainage tubes; and recent changes in medications, lab results, diagnostic tests, and treatments.
Bedside Handoff Report
Figure 2.10
Bedside Handoff Report Checklist
Print a copy of the AHRQ Bedside Shift Report Checklist. View Sample Information to Include in a Shift Report.
View a video on creating shift reports. [ 6 ].
Transfer Reports
Transfer reports are provided by nurses when transferring a patient to another unit or to another agency. Transfer reports contain similar information as bedside handoff reports, but are even more detailed when the patient is being transferred to another agency. Checklists are often provided by agencies to ensure accurate, complete information is shared.
2.5. DOCUMENTATION
Using technology to access information.
Most patient information in acute care, long-term care, and other clinical settings is now electronic and uses intranet technology for secure access by providers, nurses, and other health care team members to maintain patient confidentiality. Intranet refers to a private computer network within an institution. An electronic health record (EHR) is a real-time, patient-centered record that makes information available instantly and securely to authorized users. [ 1 ] Computers used to access an EHR can be found in patient rooms, on wheeled carts, in workstations, or even on handheld devices. See Figure 2.11 [ 2 ] for an image of a nurse documenting in an EHR.
Figure 2.11
Nurse Documenting in EHR
The EHR for each patient contains a great deal of information. The most frequent pieces of information that nurses access include the following:
- History and Physical (H&P): A history and physical (H&P) is a specific type of documentation created by the health care provider when the patient is admitted to the facility. An H&P includes important information about the patient’s current status, medical history, and the treatment plan in a concise format that is helpful for the nurse to review. Information typically includes the reason for admission, health history, surgical history, allergies, current medications, physical examination findings, medical diagnoses, and the treatment plan.
- Provider orders: This section includes the prescriptions, or medical orders, that the nurse must legally implement or appropriately communicate according to agency policy if not implemented.
- Medication Administration Records (MARs): Medications are charted through electronic medication administration records (MARs). These records interface the medication orders from providers with pharmacists and are also the location where nurses document medications administered.
- Treatment Administration Records (TARs): In many facilities, treatments are documented on a treatment administration record.
- Laboratory results: This section includes results from blood work and other tests performed in the lab.
- Diagnostic test results: This section includes results from diagnostic tests ordered by the provider such as X-rays, ultrasounds, etc.
- Progress notes: This section contains notes created by nurses and other health care providers regarding patient care. It is helpful for the nurse to review daily progress notes by all team members to ensure continuity of care.
View a video of how to read a patient’s chart. [ 3 ]
Legal Documentation
Nurses and health care team members are legally required to document care provided to patients. In a court of law, the rule of thumb used is, “If it wasn’t documented, it wasn’t done.” Documentation should be objective, factual, professional, and use proper medical terminology, grammar, and spelling. All types of documentation must include the date, time, and signature of the person documenting. Any type of documentation in the EHR is considered a legal document and must be completed in an accurate and timely manner. Abbreviations should be avoided in legal documentation.
Documentation is used for many purposes. It is used to ensure continuity of care across health care team members and across shifts; monitor standards of care for quality assurance activities; and provide information for reimbursement purposes by insurance companies, Medicare, and Medicaid. Documentation may also be used for research purposes or, in some instances, for legal concerns in a court of law.
Documentation by nurses includes recording patient assessments, writing progress notes, and creating or addressing information included in nursing care plans. Nursing care plans are further discussed in the “Planning” section of the “ Nursing Process ” chapter.
Common Types of Documentation
Common formats used to document patient care include charting by exception, focused DAR notes, narrative notes, SOAPIE progress notes, patient discharge summaries, and Minimum Data Set (MDS) charting.
Charting by Exception
Charting by exception (CBE) documentation was designed to decrease the amount of time required to document care. CBE contains a list of normal findings. After performing an assessment, nurses confirm normal findings on the list found on assessment and write only brief progress notes for abnormal findings or to document communication with other team members.
Focused DAR Notes
Focused DAR notes are a type of progress note that are commonly used in combination with charting by exception documentation. DAR stands for D ata, A ction, and R esponse. Focused DAR notes are brief. Each note is focused on one patient problem for efficiency in documenting and reading.
- Data: This section contains information collected during the patient assessment, including vital signs and physical examination findings found during the “Assessment” phase of the nursing process. The Assessment phase is further discussed in the “ Nursing Process ” chapter.
- Action: This section contains the nursing actions that are planned and implemented for the patient’s focused problem. This section correlates to the “Planning” and “Implementation” phases of the nursing process and are further discussed in the “ Nursing Process ” chapter.
- Response: This section contains information about the patient’s response to the nursing actions and evaluates if the planned care was effective. This section correlates to the “Evaluation” phase of the nursing process that is further discussed in the “ Nursing Process ” chapter.
View sample charting by exception paper documentation with associated DAR notes for abnormal findings.
For more information about writing dar notes, visit what is f-dar charting, view a video explaining f-dar charting. [ 4 ].
Narrative Notes
Narrative notes are a type of progress note that chronicles assessment findings and nursing activities for the patient that occurred throughout the entire shift or visit. View sample narrative note documentation according to body system in each assessment chapter of the Open RN Nursing Skills textbook.
SOAPIE Notes
SOAPIE is a mnemonic for a type of progress note that is organized by six categories: S ubjective, O bjective, A ssessment, P lan, I nterventions, and E valuation. SOAPIE progress notes are written by nurses, as well as other members of the health care team.
- Subjective: This section includes what the patient said, such as, “I have a headache.” It can also contain information related to pertinent medical history and why the patient is in need of care.
- Objective: This section contains the observable and measurable data collected during a patient assessment, such as the vital signs, physical examination findings, and lab/diagnostic test results.
- Assessment: This section contains the interpretation of what was noted in the Subjective and Objective sections, such as a nursing diagnosis in a nursing progress note or the medical diagnosis in a progress note written by a health care provider.
- Plan: This section outlines the plan of care based on the Assessment section, including goals and planned interventions.
- Interventions: This section describes the actions implemented.
- Evaluation: This section describes the patient response to interventions and if the planned outcomes were met.
Patient Discharge Summary
When a patient is discharged from an agency, a discharge summary is documented in the patient record, along with clear verbal and written patient education and instructions provided to the patient. Discharge summary information is frequently provided in a checklist format to ensure accuracy and includes the following:
- Time of departure and method of transportation out of the hospital (e.g., wheelchair)
- Name and relationship of person accompanying the patient at discharge
- Condition of the patient at discharge
- Patient education completed and associated educational materials or other information provided to the patient
- Discharge instructions on medications, treatments, diet, and activity
- Follow-up appointments or referrals given
See Figure 2.12 [ 5 ] for an image of a nurse providing discharge instructions to a patient. Discharge teaching typically starts at admission and continues throughout the patient’s stay.
Figure 2.12
Discharge Teaching
Minimum Data Set (MDS) Charting
In long-term care settings, additional documentation is used to provide information for reimbursement by private insurance, Medicare, and Medicaid. The Resident Assessment Instrument Minimum Data Set (MDS) is a federally mandated assessment tool created by registered nurses in skilled nursing facilities to track a patient’s goal achievement, as well as to coordinate the efforts of the health care team to optimize the resident’s quality of care and quality of life. [ 6 ] This tool also guides nursing care plan development.
Read more details about MDS charting in the Long-Term Care Facility Resident Assessment User Manual established by the Centers for Medicare and Medicaid Services (CMS).
2.6. putting it all together.
Patient Scenario
Mr. Hernandez is a 47-year-old patient admitted to the neurological trauma floor as the result of a motor vehicle accident two days ago. The patient sustained significant facial trauma in the accident and his jaw is wired shut. His left eye is currently swollen, and he had significant bruising to the left side of his face. The nurse completes a visual assessment and notes that the patient has normal extraocular movement, peripheral vision, and pupillary constriction bilaterally. Additional assessment reveals that Mr. Hernandez also sustained a fracture of the left arm and wrist during the accident. His left arm is currently in a cast and sling. He has normal movement and sensation with his right hand. Mrs. Hernandez is present at the patient’s bedside and has provided additional information about the patient. She reports that Mr. Hernandez’s primary language is Spanish but that he understands English well. He has a bachelor’s degree in accounting and owns his own accounting firm. He has a history of elevated blood pressure, but is otherwise healthy.
The nurse notes that the patient’s jaw is wired and he is unable to offer a verbal response. He does understand English well, has appropriate visual acuity, and is able to move his right hand and arm.
Based on the assessment information that has been gathered, the nurse plans several actions to enhance communication. Adaptive communication devices such as communication boards, symbol cards, or electronic messaging systems will be provided. The nurse will eliminate distractions such as television and hallway noise to decrease sources of additional stimuli in the communication experience.
Sample Documentation
Mr. Hernandez has impaired verbal communication due to facial fracture and inability to enunciate words around his wired jaw. He understands both verbal and written communication. Mr. Hernandez has left sided facial swelling, but no visual impairment. He has a left arm fracture but is able to move and write with his right hand. The patient is supplied with communication cards and marker board. He responds appropriately with written communication and is able to signal his needs.
2.7. LEARNING ACTIVITIES
Learning activities.
(Answers to “Learning Activities” can be found in the “Answer Key” at the end of the book. Answers to interactive activity elements will be provided within the element as immediate feedback.)
Practice what you have learned in this chapter by completing these learning activities. When accessing the online activities that contain videos, it is best to use Google Chrome or Firefox browsers.
To test understanding of these terms, try an online quiz: Therapeutic Communication Techniques vs. Non-therapeutic Communication Techniques Quizlet
Consider the following scenario and describe actions that you might take to facilitate the patient communication experience.
You are caring for Mr. Curtis, an 87-year-old patient newly admitted to the medical surgical floor with a hip fracture. You are preparing to complete his admission history and need to collect relevant health information and complete a physical exam. You approach the room, knock at the door, complete hand hygiene, and enter. Upon entry, you see Mr. Curtis is in bed surrounded by multiple family members. The television is on in the background and you also note the sound of meal trays being delivered in the hallway.
Based on the described scenario, what actions might be implemented to aid in your communication with Mr. Curtis?
- II GLOSSARY
A communication disorder that results from damage to portions of the brain that are responsible for language.
A way to convey information that describes the facts, the sender’s feelings, and explanations without disrespecting the receiver’s feelings. This communication is often described as using “I” messages: “I feel…,” “I understand…,” or “Help me to understand…”
A handoff report in hospitals that involves patients, their family members, and both the off-going and the incoming nurses. The report is performed face to face and conducted at the patient’s bedside.
A type of aphasia where patients understand speech and know what they want to say, but frequently speak in short phrases that are produced with great effort. People with Broca’s aphasia typically understand the speech of others fairly well. Because of this, they are often aware of their difficulties and can become easily frustrated.
A type of documentation where a list of “normal findings” is provided and nurses document assessment findings by confirming normal findings and writing brief documentation notes for any abnormal findings.
A type of documentation often used in combination with charting by exception. DAR stands for Data, Action, and Response. Focused DAR notes are brief, and each note is focused on one patient problem for efficiency in documenting, as well as for reading.
A digital version of a patient’s paper chart. EHRs are real-time, patient-centered records that make information available instantly and securely to authorized users.
A type of aphasia that results from damage to extensive portions of the language areas of the brain. Individuals with global aphasia have severe communication difficulties and may be extremely limited in their ability to speak or comprehend language. They may be unable to say even a few words or may repeat the same words or phrases over and over again. They may have trouble understanding even simple words and sentences.
A process of exchanging vital patient information, responsibility, and accountability between the off-going and incoming nurses in an effort to ensure safe continuity of care and the delivery of best clinical practices.
A mnemonic for the format of professional communication among health care team members that includes Introduction, Situation, Background, Assessment, Request/Recommendations, and Repeat back.
A federally mandated assessment tool used in skilled nursing facilities to track a patient’s goal achievement, as well as to coordinate the efforts of the health care team to optimize the resident’s quality of care and quality of life.
A type of documentation that chronicles all of the patient’s assessment findings and nursing activities that occurred throughout the shift.
Responses to patients that block communication, expression of emotion, or problem-solving.
Types of relaxation techniques that focus on reducing muscle tension and using mental imagery to induce calmness.
A breathing technique used to reduce anxiety and control the stress response.
A mnemonic for a type of documentation that is organized by six categories: Subjective, Objective, Assessment, Plan, Interventions, and Evaluation.
The purposeful, interpersonal information transmitting process through words and behaviors based on both parties’ knowledge, attitudes, and skills, which leads to patient understanding and participation.
Techniques that encourage patients to explore feelings, problem solve, and cope with responses to medical conditions and life events.
Exchange of information using words understood by the receiver.
Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/ .
- Cite this Page Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Fundamentals [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021. Chapter 2 Communication.
- PDF version of this title (216M)
In this Page
- COMMUNICATION INTRODUCTION
- BASIC COMMUNICATION CONCEPTS
- COMMUNICATING WITH PATIENTS
- COMMUNICATING WITH HEALTH CARE TEAM MEMBERS
- DOCUMENTATION
- PUTTING IT ALL TOGETHER
- LEARNING ACTIVITIES
Other titles in this collection
- Open RN OER Textbooks
Related Items in Bookshelf
- All Textbooks
Bulk Download
- Bulk download content from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Chapter 2 Communication - Nursing Fundamentals Chapter 2 Communication - Nursing Fundamentals
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Open access
- Published: 03 September 2021
A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward
- Abukari Kwame 1 &
- Pammla M. Petrucka 2
BMC Nursing volume 20 , Article number: 158 ( 2021 ) Cite this article
358k Accesses
158 Citations
97 Altmetric
Metrics details
Providing healthcare services that respect and meet patients’ and caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thereby fulfilling a significant aspect of patient-centered care requirement. Effective communication between patients and healthcare providers is crucial for the provision of patient care and recovery. Hence, patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns, beliefs, and contextual variables. Achieving patient-centered care and communication in nurse-patient clinical interactions is complex as there are always institutional, communication, environmental, and personal/behavioural related barriers. To promote patient-centered care, healthcare professionals must identify these barriers and facitators of both patient-centered care and communication, given their interconnections in clinical interactions. A person-centered care and communication continuum (PC4 Model) is thus proposed to orient healthcare professionals to care practices, discourse contexts, and communication contents and forms that can enhance or impede the acheivement of patient-centered care in clinical practice.
Peer Review reports
Providing healthcare services that respect and meet patients’ and their caregivers’ needs are essential in promoting positive care outcomes and perceptions of quality of care, thus constituting patient-centered care. Care is “a feeling of concern for, or an interest in, a person or object which necessitates looking after them/it” [ 1 ]. The Institute of Medicine (IOM) noted that to provide patient-centered care means respecting and responding to individual patient’s care needs, preferences, and values in all clinical decisions [ 2 ]. In nursing care, patient-centered care or person-centered care must acknowledge patients’ experiences, stories, and knowledge and provide care that focuses on and respects patients’ values, preferences, and needs by engaging the patient more in the care process [ 3 ]. Healthcare providers and professionals are thus required to fully engage patients and their families in the care process in meaningful ways. The IOM, in its 2003 report on Health Professions Education , recognized the values of patient-centered care and emphasized that providing patient-centered care is the first core competency that health professionals’ education must focus on [ 4 ]. This emphasis underscored the value of delivering healthcare services according to patients’ needs and preferences.
Research has shown that effective communication between patients and healthcare providers is essential for the provision of patient care and recovery [ 5 , 6 , 7 , 8 ]. Madula et al. [ 6 ], in a study on maternal care in Malawi, noted that patients reported being happy when the nurses and midwives communicated well and treated them with warmth, empathy, and respect. However, other patients said poor communication by nurses and midwives, including verbal abuse, disrespect, or denial from asking questions, affected their perceptions of the services offered [ 6 ]. Similarly, Joolaee et al. [ 9 ] explored patients’ experiences of caring relationships in an Iranian hospital where they found that good communication between nurses and patients was regarded as “more significant than physical care” among patients.
According to Boykins [ 10 ], effective communication is a two-way dialogue between patients and care providers. In that dialogue, both parties speak and are listened to without interrupting; they ask questions for clarity, express their opinions, exchange information, and grasp entirely and understand what the others mean. Also, Henly [ 11 ] argued that effective communication is imperative in clinical interactions. He observed that health and illness affect the quality of life, thereby making health communication critical and that the “intimate and sometimes overwhelming nature of health concerns can make communicating with nurses and other healthcare providers very challenging” [ 11 ]. Furthermore, Henly [ 11 ] added that patient-centered communication is fundamental to ensuring optimal health outcomes, reflecting long-held nursing values that care must be individualized and responsive to patient health concerns. Given the prevalence of face-to-face and device-mediated communications and interactions in healthcare settings, we must explore and clarify who, what, where, when, why, and how interactions with individuals, families, and communities are receiving care and health services [ 11 ].
The value of effective communication in nurse-patient clinical interactions cannot be overemphasized, as “research has shown that communication processes are essential to more accurate patient reporting and disclosure” [ 12 ]. Respectful communication between nurses and patients can reduce uncertainty, enhance greater patient engagement in decision making, improve patient adherence to medication and treatment plans, increase social support, safety, and patient satisfaction in care [ 12 , 13 ]. Thus, effective nurse-patient clinical communication is essential to enhancing patient-centered care and positive care outcomes.
Patient-centered communication, also known as person-centered communication or client-centered communication, is defined as a process that invites and encourages patients and their families to actively participate and negotiate in decision-making about their care needs, as cited in [ 7 ]. Patient-centered communication is crucial in promoting patient-centered care and requires that patients and their caregivers engage in the care process. As McLean [ 14 ] observed, patient-centered care can be enhanced through patient-centered communication by valuing patients’ dignity and rights. Through open communication and collaboration, where information and care plans are shared among care providers, patients, and their families, care provision becomes patient-centered [ 14 ].
Given the interconnected nature of patient-centered care and communication, we must identify the barriers and enablers of patient-centered care and communication and proposed efficient ways to enhance that because patient-centered communication is essential in achieving patient-centered care. Our aim in this paper is to identify the barriers and facilitators of patient-centered care and communication and propose and present a patient-centered care and communication continuum (PC4) Model to explain how patient-centered care can be enhanced in nurse-patient clinical interactions. As Grant and Booth argued, critical reviews are often used to present, analyse, and synthesized research evidence from diverse sources, the outcome of which is a hypothesis or a model as an interpretation of existing data to enhance evidence-based practice [ 15 ]. Thus, this critical literature review study explores the questions: what are the barriers and facilitators of patient-centered care and how can patient-centered care be enhanced through effective clinical communication?
An earlier version of this study was submitted as part of author AK’s doctoral comprehensive exams in February 2021. An interdisciplinary doctoral committee recommended many of the included literature and the questions explored in this study based on the current discourse of patient-centered care advocated for in many healthcare facilities and in recognition of the universal healthcare access objective of the health sustainable development goal. Additional searches for literature were conducted between September and November 2020 using keywords such as barriers and facilitators of nurse-patient interaction, patient-centered care, patient-centered communication , and nurse-patient communication . Databases searched included CINAHL, PubMed, Medline, and Google Scholar. Included studies in this critical review were empirical research on nurse-patient interactions in different care settings published in English and open access. All relevant articles were read, and their main findings relevant to our review questions were identified and organized into themes and subthemes discussed in this paper. Other published studies were read, and together with those that addressed the review question, a model was developed regarding how to enhance patient-centered care through effective communication.
Barriers to Patient-Centered Care and Communication
Nurses constitute a significant workforce of care providers whose practices can severely impact care outcomes (both positive and negative). Nurses spend much time with patients and their caregivers. As a result, positive nurse-patient and caregiver relationships are therapeutic and constitute a core component of care [ 9 , 13 ]. In many instances, nurses serve as translators or patients’ advocates, in addition to performing their primary care duties. Although good nurse-patient relationships positively impact nurse-patient communication and interaction, studies have shown that several factors impede these relationships with significant consequences on care outcomes and quality [ 6 , 16 , 17 ]. Thus, these barriers limit nurses’ and other care providers’ efforts to provide healthcare that meets patients’ and caregivers’ needs. We categorize the barriers to patient-centered care and communication into four kinds: institutional and healthcare system-related, communication-related, environment-related, and personal and behaviour-related barriers. Although these barriers are discussed in separate subheadings, they are interlinked in complex ways during clinical practice.
Institutional and Healthcare System Related Barriers
Many barriers to providing patient-centered care and communication during nurse-patient interactions emanate from healthcare institutional practices or the healthcare system itself. Some of these factors are implicated in healthcare policy or through management styles and strategies.
Shortage of nursing staff, high workload, burnout, and limited-time constituted one complex institutional and healthcare system-level barrier to effective care delivery [ 18 , 19 ]. For instance, Loghmani et al. [ 20 ] found that staffing shortages prevented nurses from having adequate time with patients and their caregivers in an Iranian intensive care unit. Limitations in nursing staff, coupled with a high workload, led to fewer interactions between nurses, patients, and caregivers. Similarly, Anoosheh et al. [ 16 ] found that heavy nursing workload was ranked highest as a limiting factor to therapeutic communication in nurse-patient interactions in Iran.
In a study on communication barriers in two hospitals affiliated with Alborz University of Medical Sciences, Norouzinia et al. [ 21 ] found that shortage of nurses, work overload, and insufficient time to interact with patients were significant barriers to effective nurse-patient interactions. Similar factors are identified as barriers to nurse-patient communication and interactions in other studies [ 13 , 16 , 18 ]. For instance, Amoah et al. [ 16 ] reported that nursing staff shortage and high workload were barriers to patient-centered care and therapeutic communication among Ghanaian nurses and patients. Amoah and colleagues reported a patient’s statement that:
[B]ecause there are few nurses at the ward, sometimes you would want a nurse to attend to you, but he or she might be working on another patient, so in such case, the nurse cannot divide him or herself into two to attend to you both [ 16 ].
Nurses and patients and their caregivers have noted that limited time affects nurse-patient interactions, communication, and care quality. Besides, Yoo et al. [ 22 ] reported that limited visiting hours affected communications between caregivers and nurses in a tertiary hospital in Seoul, Korea. Since the caregivers had limited time to spend with patients, they had little knowledge about the intensive care unit and distrusted the nurses.
Although nursing staff shortage is a significant barrier to patient-centered care and communication that healthcare institutions and managers must know, some healthcare scholars have critique nurses’ complaints of time limitation. For instance, McCabe [ 7 ] argued that the quality of nurse-patient interactions is what matters and not the quantity of time spent with patients and their caregivers. McCabe maintained that “spending long periods with patients does not always result in positive nurse-patient relationships” [ 7 ]. He argued that implementing patient-centered care does not require additional time; hence, nurses’ perceptions of being too busy cannot excuse poor therapeutic communication during clinical interactions. Instead, nurses are encouraged to develop self-awareness, self-reflection, and a commitment to ensuring that patients receive the needed care.
Another institution-related barrier to patient-centered care and communication is the healthcare system’s emphasis on task-centered care. Care providers are more focused on completing care procedures than satisfying patients’ and caregivers’ needs and preferences. This barrier to patient-centered care and communication is acknowledged in several studies [ 7 , 14 , 20 , 22 , 23 ]. For example, McLean [ 14 ] studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients’ care needs. However, in the other care home (Snow II), patient-centered care was enhanced as nurses, physicians, and the care home managers focused on addressing patients’ needs and values rather than completing care routines and tasks.
Similarly, Yoo and colleagues [ 22 ] observed that nurse-patient communication was affected when the ICU nurses placed urgency on completing tasks linked directly to patients’ health (e.g., stabilizing vital signs) than communicating to addressed patients’ specific needs. This evidence shows that when nurses are more task-focused, patients and caregivers are treated as bodies and objects, on which medical and care practices must be performed to restore health. Research has shown that when nurses focus on task-oriented care, it becomes hard to provide holistic care to patients or teach and communicate with patients even when nurses are less busy [ 20 ].
Nursing managers and their management styles can affect patient-centered care and communication. Studies have revealed that the management styles that nursing managers implement can either facilitate or impede patient-centered care [ 14 , 22 ]. When nurse managers orient their nursing staff towards task-centered care practices, it affects nurse-patient interaction and communication. Moreover, when nurse managers fail to address their staff’s mental health needs and personal challenges, it influences how nurses attend to patients’ care needs. For example, nurses have indicated that nurse-patient communication is affected when nurse managers are unsupportive or unresponsive to their needs [ 20 ].
In a study exploring nursing and midwifery managers’ perspectives on obstacles to compassion giving and therapeutic care across 17 countries, Papadopoulos et al. [ 24 ] discovered that nurses and midwifery managers’ characteristics and experiences could facilitate or impede compassion and therapeutic interactions in nursing care. Negative personal attitudes, including selfishness, arrogance, self-centeredness, rudeness, lack of leadership skills, the desire for power, and feelings of superiority among nurses and midwifery managers, were obstacles to compassion building. The study further showed that managers who emphasize rules, tasks, and results do not prioritize relationship-building and see their staff as workers rather than team members [ 24 ]. Therefore, nurse managers and care administrators must monitor nurse-patient interaction and communication to address nurses’ concerns and support them, especially in resource-constrained and high patient turnover contexts [ 25 , 26 ].
Communication-Related Barriers
Effective communication is essential to providing patient-centered care. Studies have shown that poor communication between care providers and patients and their caregivers affects care outcomes and perceptions of care quality [ 7 , 16 , 27 , 28 ]. A consistent communication-related barrier in nurse-patient interaction is miscommunication, which often leads to misunderstandings between nurses, patients, and their families [ 20 ]. Other communication-related barriers include language differences between patients and healthcare providers [ 6 , 16 , 27 ], poor communication skills, and patients’ inability to communicate due to their health state, especially in ICU, dementia, or end-of-life care contexts [ 13 , 22 ]. For instance, in their maternity care study, Madula et al. [ 6 ] noted that language barriers significantly affected effective communication between nurses/midwives and expectant mothers. A patient in their study indicated that although many nurses were polite and communicated well, some nurses had challenges communicating with patients in the Chitumbuka language, which affected those nurses’ ability to interact effectively with patients [ 6 ].
Furthermore, Norouzinia et al. [ 21 ] asserted that effective communication could not be established when nurses and patients have a language difference. Moreover, the meanings of certain non-verbal communication acts (e.g., head nodding, eye gaze, touch) can invoke different interpretations across different cultures, which could impede the interactions between patients and nurses. Even in healthcare contexts where nurses and patients speak the same language, “differences in vocabulary, rate of speaking, age, background, familiarity with medical technology, education, physical capability, and experience can create a huge cultural and communication chasm” between nurses and patients [ 12 ]. In ICU and other similar care settings, nurses find it difficult to effectively communicate with patients because the mechanical ventilators made it hard for patients to talk [ 22 ].
To overcome the communication-related barriers, healthcare institutions must make it a responsibility to engage translators and interpreters to facilitate nurse-patient interactions where a language barrier exists. Moreover, nurses working in ICU and other similar settings should learn and employ alternative forms of communication to interact with patients.
Environment-Related Barriers
The environment of the care setting can impact nurse-patient communication and the resulting care. Thus, “good health care experiences start with a welcoming environment” [ 29 ]. Mastors believed that even though good medicine and the hands working to provide care and healing to the sick and wounded are essential, we must not “forget the small things: a warm smile, an ice chip, a warm blanket, a cool washcloth. A pillow flipped to the other side and a boost in bed” [ 29 ]. The environment-related barriers are obstacles within the care setting that inhibit nurse-patient interaction and communication and may include a noisy surrounding, unkept wards, and beds, difficulties in locating places, and navigating care services. Noisy surroundings, lack of privacy, improper ventilation, heating, cooling, and lighting in specific healthcare units can affect nurse-patient communication. These can prevent patients from genuinely expressing their healthcare needs to nurses, which can subsequently affect patient disclosure or make nursing diagnoses less accurate [ 13 , 18 , 21 ]. For instance, Amoah et al. [ 16 ] revealed that an unconducive care environment, including noisy surroundings and poor ward conditions, affected patients’ psychological states, impeding nurse-patient relationships and communication. Moreover, when care services are not well-coordinated, new patients and their caregivers find it hard to navigate the care system (e.g., locating offices for medical tests and consultations), which can constrain patient-centered care and communication.
Reducing the environment-related barriers will require making the care setting tidy/clean, less noisy, and coordinating care services in ways that make it easy for patients and caregivers to access. Coordinating and integrating care services, making care services accessible, and promoting physical comfort are crucial in promoting patient-centered care, according to Picker’s Eight Principles of Patient-Centered Care [ 30 ].
Personal and Behaviour Related Barriers
The kind of nurse-patient relationships established between nurses and patients and their caregivers will affect how they communicate. Since nurses and patients may have different demographic characteristics, cultural and linguistic backgrounds, beliefs, and worldviews about health and illnesses, nurses’, patients’, and caregivers’ attitudes can affect nurse-patient communication and care outcomes. For instance, differences in nurses’ and patients’ cultural backgrounds and belief systems have been identified as barriers to therapeutic communication and care [ 12 , 13 , 21 ]. Research shows that patients’ beliefs and cultural backgrounds affected their communication with nurses in Ghana [ 16 ]. These scholars found that some patients refused a blood transfusion, and Muslim patients refused female nurses to attend to them because of their religious beliefs [ 16 ]. Further, when nurses, patients, or their caregivers have misconceptions about one another due to past experiences, dissatisfaction about the care provided, or patients’ relatives and caregivers unduly interfere in the care process, nurse-patient communication and patient-centered care were affected [ 16 , 21 ].
Similarly, nurse-patient communication was affected when patients or caregivers failed to observe nurses’ recommendations or abuse nurses due to misunderstanding [ 20 ], while patients’ bad attitudes or disrespectful behaviours towards nurses can inhibit nurses’ ability to provide person-centered care [ 31 ]. The above-reviewed studies provided evidence on how patients’ and caregivers’ behaviours can affect nurses’ ability to communicate and deliver patient-centered care.
On the other hand, nurses’ behaviours can also profoundly affect communication and care outcomes in the nurse-patient dyad. When nurses disrespect, verbally abuse (e.g., shouting at or scolding), and discriminate against patients based on their social status, it affects nurse-patient communication, care outcomes, and patient disclosure [ 6 , 32 ]. For instance, Al-Kalaldeh et al. [ 18 ] believe that nurse-patient communication is challenged when nurses become reluctant to hear patients’ feelings and expressions of anxiety. When nurses ignore patients’ rights to share ideas and participate in their care planning, such denials may induce stress, discomfort, lack of trust in nurses, thereby leading to less satisfaction of care [ 18 ].
Furthermore, when nurses fail to listen to patients’ and caregivers’ concerns, coerce patients to obey their rules and instructions [ 16 , 17 , 20 ], or fail to provide patients with the needed information, nurse-patient communication and patient-centered care practices suffer. To illustrate, in Ddumba-Nyanzia et al.‘s study on communication between HIV care providers and patients, a patient remarked that: “I realized no matter how much I talked to the counselor, she was not listening. She was only hearing her point of view and nothing else, [and] I was very upset” [ 17 ]. This quote indicates how care provider attitudes can constrain care outcomes. Due to high workload, limited time, poor remunerations, and shortage of personnel, some nurses can develop feelings of despair, emotional detachment, and apathy towards their job, which can lead to low self-esteem or poor self-image, with negative consequences on nurse-patient interactions [ 13 , 18 ].
Given the significance of effective communication on care, overcoming the above personal and behaviour related barriers to patient-centered care and communication is crucial. Nurses, patients, and caregivers need to reflect on the consequences of their behaviours on the care process. Thus, overcoming these barriers begins with embracing the facilitators of patient-centered care and communication, which we turn to in the next section.
Facilitators of patient-centered care and communication
Patient-centered care and communication can be facilitated in several ways, including building solid nurse-patient relationships.
First, an essential facilitator of patient-centered care and communication is overcoming practical communication barriers in the nurse-patient dyad. Given the importance of communication in healthcare delivery, nurses, patients, caregivers, nursing managers, and healthcare administrators need to ensure that effective therapeutic communication is realized in the care process and becomes part of the care itself. Studies have shown that active listening among care providers is essential to addressing many barriers to patient-centered care and communication [ 7 , 13 ]. Although handling medical tasks promptly in the care process is crucial, the power of active listening is critical, meaningful, and therapeutic [ 22 ]. By listening to patients’ concerns, nurses can identify patients’ care needs and preferences and address their fears and frustrations.
Another facilitator of patient-centered care is by understanding patients and their unique needs [ 25 ], showing empathy and attending attitudes [ 7 , 13 ], expressing warmth and respect [ 22 ], and treating patients and caregivers with dignity and compassion as humans. For instance, McCabe [ 7 ] noted that attending, which obligates nurses to demonstrate that they are accessible and ready to listen to patients, is a patient-centered care process; a fundamental requirement for nurses to show genuineness and empathy, despite the high workload. Showing empathy, active listening, respect, and treating patients with dignity are core to nursing and care, and recognized in the Code of Ethics for Nurses [ 33 ], and further emphasized in the ongoing revision of the Code of Ethics for nurses [ 34 ].
Besides, engaging patients and caregivers in the care process through sharing information, inviting their opinion, and collaborating with them constitutes another facilitator of patient-centered care and communication. When patients and caregivers are engaged in the care process, misunderstandings and misconceptions are minimized. When information is shared, patients and caregivers learn more about their health conditions and the care needed. As McLean [ 14 ] argued, ensuring open communication between care providers and patients and their families is essential to enhancing patient-centered care. Conflicts ensue when patients or their families are denied information or involvement in the care process. As a result, the Harvard Medical School [ 30 ] identified patient engagement, information sharing, and nurse-patient collaboration during care as essential patient-centered care principles.
Finally, health policy must be oriented towards healthcare practices and management to facilitate patient-centered care and communication. These policies, at a minimum, can involve changes in management styles within healthcare institutions, where nurse managers and healthcare administrators reflect on nursing and care practices to ensure that the Code of Ethics of Nurses and patients’ rights are fully implemented. Resource constraints, staff shortages, and ethical dilemmas mainly affect care practices and decision-making. Nonetheless, if patients are placed at the center of care and treated with dignity and respect, most of the challenges and barriers of patient-centered care will diminish. Empowering practicing nurses, equipping them with interpersonal communication skills through regular in-service training, supporting them to overcome their emotional challenges, and setting boundaries during nurse-patient interactions will enhance patient-centered care practices.
In line with the above discussion, Camara et al. [ 25 ] identify three core dimensions that nurses, patients, and caregivers must observe to enhance patient-centered care: treating the patient as a person and seeing the care provider as a person and a confidant. Regarding the first dimension, care providers must welcome patients, listen to them, share information with them, seek their consent, and show them respect when providing care. The second dimension requires that the healthcare provider be seen and respected as a person, and negative perceptions about care providers must be demystified. According to Camara et al. [ 25 ], care providers must not overemphasize their identities as experts but rather establish good relationships with patients to understand patients’ personal needs and problems. Lastly, patients and caregivers must regard care providers as confidants who build and maintain patients’ trust and encourage patients’ participation in care conversations. With this dimension, patients and caregivers must know that nurses and other care providers have the patient at heart and work to meet their care needs and recovery process.
Camara et al.‘s [ 25 ] three dimensions are essential and position patients, their caregivers, and nurses as partners who must engage in dialogic communication to promote patient-centered care. As a result, effective communication, education, and increased health literacy among patients and caregivers will be crucial in that direction.
Enhancing Patient-Centered Care and Communication: A Proposed Model
Nursing care practices that promote patient-centered communication will directly enhance patient-centered care, as patients and their caregivers will actively engage in the care process. To enhance patient-centered communication, we propose person-centered care and communication continuum (PC4) as a guiding model to understand patient-centered communication, its pathways, and what communication and care practices healthcare professionals must implement to achieve person-centered care. In this PC4 Model, we emphasize the person instead of the patient because they are a person before becoming a patient. Moreover, the PC4 Model is supposed to apply to all persons associated with patient care; thus, respect for the dignity of their personhood is crucial.
Although much is written about patient-centered communication in the healthcare literature, there is a gap regarding its trajectory and what communication content enhances patient-centered communication. Also, little is known about how different clinical discourse spaces influence communication and its content during nurse-patient clinical interactions. Using evidence from Johnsson et al. [ 3 ], Murira et al. [ 23 ], and Liu et al. [ 35 ], among other studies, we outline the components of the PC4 Model and how different discourse spaces in the clinical setting and the content of communication impact patient-centered care and communication.
The proposed PC4 Model in this paper has three unbounded components based on the purpose of and how communication is performed among care providers, patients, and their caregivers. Figure 1 illustrates the PC4 Model, its features, and trajectory.
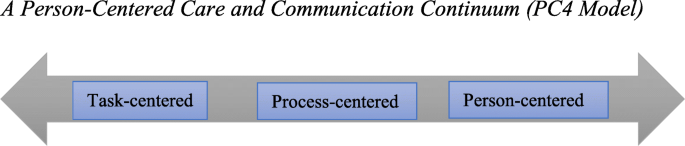
A Person-Centered Care and Communication Continuum (PC4 Model)
Task-Centered Communication
At the lowest end of the PC4 Model is task-centered communication. Here, the care provider’s role is to complete medical tasks as fast as possible with little or no communication with the patient and their caregivers. Patients and caregivers are treated as bodies or objects whose disease symptoms need to be studied, identified, recorded, treated, or cured. As Johnsson et al. [ 3 ] observed, communication content at this stage is mainly biomedically oriented, where nurses and other healthcare professionals focus on the precise medical information (e.g., history taking, medical examination, test results, medication, etc.) about the patient. With a task-centered orientation, nurses make journal entries about their patients’ disease state and ensure that treatment plans, diagnostic tests, and medical prescriptions are completed. Communication at this stage is often impersonal or rigid (see [ 23 ] for details). Care providers may address patients and their caregivers by using informal attributes (e.g., bed 12, the woman in the red shirt, card 8, etc.), thereby ignoring patients’ and caregivers’ personal and unique identities. Patients’ and caregivers’ nonverbal communication signs are mostly overlooked.
Motivations for task-centered communication can be attributed to time limitation, high workload, and staff shortage, thereby pushing nurses and other care providers to reach as many patients as possible. Moreover, the healthcare system’s orientation towards and preference for biomedically-focused care seems to favour task-centered communication [ 7 , 14 ].
Depending on the clinical discourse space under which patient-provider interactions occur, different forms of communication are employed. Clinical discourse spaces can be public (e.g., in the ward, patient bedside), private (e.g., consulting rooms, medical test labs, nurse staff station, etc.), or semi-private (e.g., along the corridor) [ 35 ]. In these clinical discourse spaces, nurse-patient communication can be uninformed (patients or caregivers are not informed about patients’ care conditions or why specific data and routines are performed). It can be non-private (others can hear what the nurse and patient are talking about) or authoritative (care providers demonstrate power and control and position themselves as experts) [ 23 ]. Finally, in task-centered communication, healthcare providers often use medical jargon or terminologies [ 3 ] since the goal of communication is not to engage the patient in the process. Usually, patients or their caregivers are not allowed to ask questions, or their questions get ignored or receive superficial, incomprehensible responses.
Process-Centered Communication
Process-centered communication is an intermediate stage on the continuum, which could slip back into the task-centered or leap forward into person-centered communication. Through process-centered communication, care providers make an effort to know patients and their caregivers as they perform care routines. Care providers ask patients or their caregivers questions to understand the care conditions but may not encourage patients or caregivers to express their thoughts about their care needs. Patients and caregivers are recognized as persons with uniques care needs but may not have the agency to influence the care process. Care providers may chit-chat with patients or their caregivers to pass the time as they record patients’ medical records or provide care. Unlike task-centered communication, there is informative and less authoritative communication between nurses and patients and their caregivers. The goal of process-centered communication could be a mixture of instrumental and relational, with less display of power and control by nurses.
Person-Centered Communication
This is the highest point of the PC4 Model, where patient-centered care is actualized. At this stage of the communication continuum, patients and caregivers are treated as unique persons with specific care needs and are seen as collaborators in the care process. As McLean [ 14 ] observed, caregiving becomes a transactional relationship between the care provider and receiver at the person-centered stage of the continuum. The care itself becomes intersubjective, a mutual relational practice, and an ongoing negotiation for care providers and receivers [ 14 ].
The content of communication at this stage of the continuum is both “personal” and “explanatory” [ 3 ]. Nurses and other healthcare providers create meaningful relationships with patients and their caregivers, understand patients’ concerns, needs, and problems, use open-ended questions to encourage patients or caregivers to express their thoughts and feelings about the care situation. Nurses and other healthcare professionals explain care routines, patients’ health conditions, and management plans in lay language to patients and caregivers through person-centered communication. Accomplishing this level includes employing alternative forms of communication to meet the needs of intensive care unit patients, deaf patients, and ventilated and intubated patients. For instance, it has been shown that “deaf people […] frequently do not have access to clear and efficient communication in the healthcare system, which deprives them of critical health information and qualified health care” [ 36 ]. Empathetic communication practices, including active listening, showing genuine interest in patients’ care, and respect and warmth, become a significant part of nursing care [ 3 , 7 , 14 , 22 ].
Different communication strategies are employed based on the care situation and context. Chit-chatting, as a form of personal communication [ 3 ], use of humor as a communication strategy [ 7 , 8 ], and even maintaining silence [ 28 ] are essential in enhancing person-centered care and communication. Both care providers and patients or their caregivers use relationship-building and -protecting humor (see [ 28 ] for details) to address difficult situations in the care process.
Implications of the PC4 Model for Nursing Practice
Given the values of effective communication in nurse-patient interactions and care outcomes, nurses and other healthcare providers must ensure that they develop therapeutic relationships with patients, their families, and caregivers to promote person-centered care and communication. Achieving that begins with knowing and reflecting on the barriers of therapeutic communication and ways to minimize them. The PC4 Model draws nurses and all healthcare providers’ attention to patient-centered care pathways and how effective communication is necessary. Healthcare professionals, including nurses, must be aware of how their communication orientation–––either oriented toward completing tasks, following care processes or toward addressing patients’ and their caregivers’ needs––can impact patient-centered care. Healthcare providers must observe the care context, patients’ unique situations, their non-verbal language and action, and whether they belong to historically marginalized groups or cultures.
Mastors [ 29 ] has offered healthcare providers some guidance to reflect on as they communicate and interact with patients and caregivers. Thus, (a) instead of asking patients, “What’s the matter?“ care providers must consider asking them, “What’s important to you?“ With this question, the patient is given a voice and empowered to contribute to their own care needs. Care providers should (b) check with patients in the waiting room to update patients whose waiting time has been longer than usual, based on the care context. They should also (c) try to remember their conversations with patients to build on them during subsequent interactions. This continuity can be enhanced by nurse managers reexamining how they deploy care providers to patients. The same nurse can be assigned to the same patients for the duration of the patient’s stay to help patients feel valued and visible [ 29 ].
Knowledge of cultural competence, sensitivity, humility, and interpersonal communication skills will help achieve and implement the PC4 Model. As Cuellar [ 37 ] argues, “[h]umility is about understanding and caring for all people [and] being empathetic.“ Cultural competence is a “dynamic process of acquiring the ability to provide effective, safe, and quality care to the patients through considering their different cultural aspects” [ 38 ]. The concept of cultural competence entails “cultural openness, awareness, desire, knowledge and sensitivity” during care [ 39 ]. It demands that care providers respect and tailor care to align with patients’ and caregivers’ values, needs, practices, and expectations, based on care and moral ethics and understanding [ 39 ]. Active listening and showing compassion as therapeutic relationship-building skills are essential, and continuous education and mentorship will be crucial to developing these skills among healthcare providers.
We invite qualitative and quantitative studies, especially on language use and communication strategies, to explore and evaluate the PC4 Model. Providing in-depth and experiential data on ways to increase its effectiveness as a tool to guide healthcare providers is highly desired. More knowledge can support healthcare providers in offering evidence-based patient-centered care in different healthcare settings and units.
Conclusions
Effective communication is an essential factor in nurse-patient interactions and a core component of nursing care. When communication in the nurse-patient dyad is patient-centered, it becomes therapeutic. It allows for trust and mutual respect in the care process, thereby promoting care practices that address patients’ and caregivers’ needs, concerns, and preferences. We have identified the barriers and facilitators of patient-centered care and communication and proposed a person-centered care and communication continuum (PC4 Model) to demonstrate how patient-centered communication intersects with patient-centered care.
Availability of data and materials
Not applicable.
Abbreviations
Intensive Care Unit
Institution of Medicine
Person-Centered Care and Communication Continuum
Etheredge HR. “Hey sister! Where’s my kidney?“ Exploring ethics and communication in organ transplantation in Gauteng, South Africa, Ph.D. dissertation, Johannesburg. University of the Witwatersrand; 2015.
Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. National Academy Press; 2001.
Johnsson A, Wagman P, Boman A, Pennbrant S. What are they talking about? Content of the communication exchanges between nurses, patients and relatives in a department of medicine for older people: An ethnographic study. J Clin Nurs. 2018 Apr;27(7–9):e1651-9. doi: https://doi.org/10.1111/jocn.14315 .
Long KA. The Institute of Medicine report on health professions education: A bridge to quality. Policy Polit Nurs Pract. 2003 Nov;4(4):259–62. doi: https://doi.org/10.1177/1527154403258304 .
Crawford T, Candlin S, Roger P. (2017). New perspectives on understanding cultural diversity in nurse-patient communication. Collegian, 2017 Feb 1;24(1):63 – 9. https://doi.org/10.1016/j.colegn.2015.09.001 .
Madula P, Kalembo WF, Yu H, Kaminga CA. Healthcare provider-patient communication: A qualitative study of women’s perceptions during childbirth. Reprod Health. 2018 Dec;15(135):1–10. https://doi.org/10.1186/s12978-018-0580-x .
McCabe C. Nurse-patient communication: An exploration of patients’ experiences. J Clin Nurs. 2004 Jan;13(1):41–9.
Schöpf AC, Martin GS, Keating MA. Humor as a communication strategy in provider-patient communication in a chronic care setting. Qual Health Res. 2017 Feb;27(3):374–90. doi: https://doi.org/10.1177/1049732315620773 .
Joolaee S, Joolaei A, Tschudin V, Bahrani N, Nikbakht NA. Caring relationship: the core component of patients’ rights practice as experienced by patients and their companions. J Med Ethics Hist Med. 2010;3(4):1–7.
Google Scholar
Boykins AD. Core communication competences in patient-centered care. The ABNF J. 2014 Apr 1;25(2):40 – 5.
Henly SJ. Health communication research for nursing science and practice. Nurs Res [Editorial] 2016:257–8. doi: https://doi.org/10.1097/NNR.0000000000000171 .
Ruben BD. Communication theory and health communication practice: The more things change, the more they stay the same. Health Commun. 2016 Jan 2;31(1):1–11. doi: https://doi.org/10.1080/10410236.2014.923086 .
Bello P. Effective communication in nursing practice: A literature review. BSc Nursing Thesis. Arcada; 2017. Available at https://core.ac.uk/download/pdf/84798372.pdf Accessed 20 Jan 2021.
McLean A. The person in dementia: A study of nursing home care in the US. Toronto, University of Toronto Press; 2007.
Grant MJ, Booth A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Info Libraries J. 2009;26:91–108. Doi: https://doi.org/10.1111/j.1471-1842.2009.00848.x .
Article Google Scholar
Amoah KMV, Anokye R, Boakye SD, Acheampong E, Budu-Ainooson A, Okyere E, Kumi-Boateng G, Yeboah C, Afriyie OJ. A qualitative assessment of perceived barriers to effective therapeutic communication among nurses and patients. BMC Nurs. 2019 Dec;18(4)1–8. https://doi.org/10.1186/s12912-019-0328-0 .
Ddumba-Nyanzia I, Kaawa-Mafigiria D, Johannessen H. Barriers to communication between HIV care providers (HCPs) and women living with HIV about childbearing: A qualitative study. Patient Educ Couns. 2016 May 1:99(5):754–9. https://doi.org/10.1016/j.pec.2015.11.023 .
Al-Kalaldeh M, Amro N, Qtait M. Barriers to effective nurse-patient communication in the emergency department. Emerg Nurse. 2021 Mar 2;29(2). doi: https://doi.org/10.7748/en.2020.e1969 .
Sethi D, Rani MK. Communication barrier in health care setting as perceived by nurses and patient. Int J Nurs Educ 2017 Oct. 2016;9(4):30. doi: https://doi.org/10.5958/j.2320-8651.2.1.001 .
Loghmani L, Borhani F, Abbaszadeh A. Factors affecting the nurse-patients’ family communication in intensive care unit of Kerman: A qualitative study. J Caring Sci. 2014 Mar;3(1):67–2. doi: https://doi.org/10.5681/jcs.2014.008 .
Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication barriers perceived by nurses and patients. Glob J Health Sci. 2016 Jun;8(6):65–4. https://doi.org/10.5539/gjhs.v8n6p65 .
Yoo HJ, Lim OB, Shim JL. Critical care nurses’ communication experiences with patients and families in an intensive care unit: A qualitative study. PLoS One. 2020 Jul 9;15(7):e0235694. https://doi.org/10.1371/journal.pone.0235694 .
Murira N, Lützen K, Lindmark G, Christensson K. Communication patterns between healthcare providers and their clients at an antenatal clinic in Zimbabwe. Health Care Women Int. 2003 Feb 1;24(2):83 – 2. https://doi.org/10.1080/07399330390170060 .
Papadopoulos I, Lazzarino R, Koulouglioti C, Aagard M, Akman O, Alpers L-M, Apostolara P, Araneda Bernal J, Biglete-Pangilinan S, Eldar-Regev O, Gonzalez-Gil MT, Kouta C, Zorba A. Obstacles to compassion-giving among nursing and midwifery managers: An international study. Int Nurs Rev. 2020 Aug;11:1–13.
Camara BS, Belaid L, Manet H, Kolie D, Guilard E, Bigirimana T, Delamou A. What do we know about patient-provider interactions in sub-Saharan Africa? A scoping review. Pan Afr Med J. 2020;88(88):1–13. doi: https://doi.org/10.11604/pamj.2020.37.88.24009 .
Kwame A, Petrucka PM. Communication in nurse-patient interaction in healthcare settings in sub-Saharan Africa: A scoping review. Int J Afr Nurs Sci. 2020 Jan 1;12:100198. https://doi.org/10.1016/j.ijans.2020.100198 .
Anoosheh M, Zarkhah S, Faghihzadeh S, Vaismoradi M. Nurse-patient communication barriers in Iranian nursing. Int Nurs Rev. 2009 Jun;56(2):243–9.
Vuković M, Gvozdenović BS, Stamatović-Gajić B, Ilić M, Gajić T. Development and evaluation of the nurse quality of communication with patient questionnaire. Srp Arh Celok Lek. 2010;138(1–2):79–4. doi: https://doi.org/10.2298/SARH1002079V .
Article PubMed Google Scholar
Mastors P. (2018). What do patients want, need, and have the right to expect? Nurs Adm Q. 2018 Jul 1;42(3):192-8. doi: https://doi.org/10.1097/NAQ.0000000000000297 .
Harvard Medical School. The Eight Principles of Patient Centered Care; 2015 Nov 18. Available from OneView: https://www.oneviewhealthcare.com/the-eight-principles-of-patient-centered-care/ Accessed 28 Dec 2020.
White J, Phakoe M, Rispel LC. ‘Practice what you preach’: Nurses’ perspectives on the Code of Ethics and Service Pledge in five South African hospitals. Glob Health Action. 2015 Dec 1;8(1):26341. https://doi.org/10.3402/gha.v8.26341 .
Kruger L-M, Schoombee C. The other side of caring: abuse in a South African maternity ward. J Reprod Infant Psychol. 2010 Feb 1;28(1):84–101. doi: https://doi.org/10.1080/02646830903294979 .
International Council of Nurses. ICN Code of Ethics for Nurses; 2012. Available from www.icn.ch/images/stories/documents/about/icncode_english.pdf . Accessed 20 Dec 2020.
Stievano A, Tschudin V. The ICN code of ethics for nurses: A time for revision. Nurs Health Policy Perspect. 2019 Jun;66(2):154–6.
Liu W, Manias E, Gerdtz M. Medication communication during ward rounds on medical wards: Power relations and spatial practices. Health 2012 Mar. 2012;17(2):113–34. doi: https://doi.org/10.1177/1363459312447257 .
Hoglind TA. Healthcare language barriers affect deaf people, too. 2018 Oct 11. Retrieved from Boston University [BU] School of Public Health: Available from https://www.bu.edu/sph/news/articles/2018/healthcare-language-barriers-affect-deaf-people-too/ Accessed 15 Jan 2021.
Cuellar NG. Humility. A concept in cultural sensitivity. JTranscult Nurs [Editorial]. 2018 Apr 26; 29(4):317. https://doi.org/10.1177/1043659618772384 .
Sharifi N, Adib-Hajbaghery M, Najafi M. Cultural competence in nursing: A concept analysis. Int J Nurs Stud. 2019 Nov 1;99(103386):1–8. https://doi.org/10.1016/j.ijnurstu.2019.103386 .
Henderson S, Horne M, Hills R, Kendall E. Cultural competence in healthcare in the community: A concept analysis. Health Soc Care Community. 2018 Jul;26(4):590–603. doi: https://doi.org/10.1111/hsc.12556 .
Download references
Acknowledgments
We express our gratitude to the first author’s doctoral committee members for their valuable comments, suggestions, and critique of an earlier version of this paper. We are also grateful to the anonymous reviewers for the insightful comments and suggestions that have helped us improve the study’s quality.
Authors' information
Abukari Kwame is a Ph.D. candidate in Interdisciplinary Studies in the College of Graduate and Postdoctoral Studies, University of Saskatchewan, interested in patients' rights in nurse-patient clinical communications and interactions in the hospital setting. He holds two Master of Philosophy degrees in Indigenous Studies and English Linguistics. Abukari's research interests include language use in social interaction, health communication, First/Second language acquisition, African traditional medical knowledge, and Indigenous and qualitative research methodologies.
Pammla M. Petrucka is a professor in Nursing and has international research experience with many of her graduate students from Africa, Asia, and the Caribbean. Pammla has published extensively in the field of nursing. Her research interests are vast, including child and maternal health, Indigenous peoples' health, global health, and vulnerable populations, with extensive experiences in qualitative research and indigenous research methodologies. Pammla is co-editor of the BMC Nursing journal and a reviewer for many other academic journals.
The authors have not received any funding for the conduct, preparation, and publication of this paper.
Author information
Authors and affiliations.
College of Graduate and Postdoctoral Studies, University of Saskatchewan, Saskatoon, Canada
Abukari Kwame
College of Nursing, University of Saskatchewan, Regina Campus, Regina, Canada
Pammla M. Petrucka
You can also search for this author in PubMed Google Scholar
Contributions
Both authors conceived the topic. PMP recommended the literature, AK searched and added more sources, and drafted the paper. PMP reviewed the paper for intellectual content. Both AK and PMP read and approved the final version.
Corresponding author
Correspondence to Abukari Kwame .
Ethics declarations
Ethics approval and consent to participate.
Not Applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions

About this article
Cite this article.
Kwame, A., Petrucka, P.M. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, facilitators, and the way forward. BMC Nurs 20 , 158 (2021). https://doi.org/10.1186/s12912-021-00684-2
Download citation
Received : 05 May 2021
Accepted : 18 August 2021
Published : 03 September 2021
DOI : https://doi.org/10.1186/s12912-021-00684-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Patient-centered care
- Therapeutic communication
- Nurse-patient interactions
- Clinical discourse space
- Patient-centered care and communication continuum
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Open Access is an initiative that aims to make scientific research freely available to all. To date our community has made over 100 million downloads. It’s based on principles of collaboration, unobstructed discovery, and, most importantly, scientific progression. As PhD students, we found it difficult to access the research we needed, so we decided to create a new Open Access publisher that levels the playing field for scientists across the world. How? By making research easy to access, and puts the academic needs of the researchers before the business interests of publishers.
We are a community of more than 103,000 authors and editors from 3,291 institutions spanning 160 countries, including Nobel Prize winners and some of the world’s most-cited researchers. Publishing on IntechOpen allows authors to earn citations and find new collaborators, meaning more people see your work not only from your own field of study, but from other related fields too.
Brief introduction to this section that descibes Open Access especially from an IntechOpen perspective
Want to get in touch? Contact our London head office or media team here
Our team is growing all the time, so we’re always on the lookout for smart people who want to help us reshape the world of scientific publishing.
Home > Books > Nursing
Effective Communication in Nursing
Submitted: 27 October 2017 Reviewed: 06 February 2018 Published: 21 March 2018
DOI: 10.5772/intechopen.74995
Cite this chapter
There are two ways to cite this chapter:
From the Edited Volume
Edited by Nilgun Ulutasdemir
To purchase hard copies of this book, please contact the representative in India: CBS Publishers & Distributors Pvt. Ltd. www.cbspd.com | [email protected]
Chapter metrics overview
12,476 Chapter Downloads
Impact of this chapter
Total Chapter Downloads on intechopen.com
Total Chapter Views on intechopen.com
Nurses are critical in the delivery of essential health services and are core in strengthening the health system. They bring people-centred care closer to the communities where they are needed most, thereby helping improve health outcomes and the overall cost-effectiveness of services. Nurses usually act as first responders to complex humanitarian crises and disasters; protectors and advocates for the community and communicators and co-ordinators within teams. Communication is a core component of sound relationships, collaboration and co-operation, which in turn are essential aspects of professional practice. The quality of communication in interactions between nurses and patients has a major influence on patient outcomes. Increases in nursing communication can lessen medical errors and make a difference in positive patient outcomes. This chapter explores how effective communication and interpersonal skills can enhance professional nursing practice and nursing relationships with various stakeholders. It explains principles of communication, communication process, purpose of communication, types of communication, barriers to effective communication, models of communication and strategies of improving communication and guidelines for successful therapeutic interactions.
- communication
- communication skills
- non-verbal communication
- nurse–patient relationship
- nursing verbal communication
Author Information
Maureen nokuthula sibiya *.
- Durban University of Technology, Durban, South Africa
*Address all correspondence to: [email protected]
1. Introduction
Nurses are critical in the delivery of essential health services and are core in strengthening the health system [ 1 , 2 ]. They bring people-centred care closer to the communities where they are needed most, thereby helping improve health outcomes and the overall cost-effectiveness of services [ 3 ]. Nurses usually act as first responders to complex humanitarian crises and disasters; protectors and advocates for the community and communicators and co-ordinators within teams. Communication skills for nurses are essential but may be difficult to master. Communication is the exchange of information between people by sending and receiving it through speaking, writing or by using any other medium. Clear communication means that information is conveyed effectively between people. To be a successful nurse, excellent communication skills are required [ 4 ]. Nurses speak to people of varying educational, cultural and social backgrounds and must do so in an effective, caring and professional manner, especially when communicating with patients and their families [ 5 ]. The quality of communication in interactions between nurses and patients has a major influence on patient outcomes. This influence can play a very important role in areas such as patient health, education and adherence [ 6 ]. Good communication plays an important role in the organization’s effective functioning [ 7 , 8 , 9 ]. A nurse must therefore, continuously try to improve his/her communication skills as poor communication can be dangerous and lead to confusion.
2. Principles of communication
Communication is a process;
Communication is not linear, but circular;
Communication is complex;
Communication is irreversible; and
Communication involves the total personality [ 5 ].
3. Communication process
A clear message; and
A receiver [ 12 ].
4. Purpose of communication
To convey information/opinion, for example, “I have headache” or “I am here to give you medication”.
To request information/opinion/behavior, for example, “Are you allergic to penicillin?” or “Tell me more about the injury”.
To give social acknowledgement, for example, “Hello” or “Good morning”.
These three primary types of messages can be combined in many ways so that they form an interaction (conversation). The goals of the interaction can be comprehensive. Nurses strive to make all their communication with patients therapeutic, that is, their communication is purposefully and consciously planned to promote the patient’s health and wellbeing.
5. Types of communication
Verbal and non-verbal communications are the two main types of communication used by human beings.
5.1. Verbal communication
Verbal communication is associated with spoken words and is vitally important in the healthcare context. Members of the multi-disciplinary healthcare team communicate verbally with one another and with patients as well as family members.
5.2. Verbal communication
Bodily contact
Direction of gaze
Emotive tone in speech
Facial and gestural movements
Physical appearance
Speech errors
Timing of speech [ 5 , 8 , 9 , 10 ].
6. Communication process
The communication process may be explained by means of a linear model of communication, interactive model of communication or transactional model of communication [ 11 ].
6.1. Linear model of communication
Linear model of communication entails a sender, a message, a receiver and noise ( Figure 1 ).

Linear model of communication.
6.2. Interactive model of communication
Interactive model of communication gives a slightly more complex explanation of the communication process. Communication is seen as a process in which the listener gives feedback or responds to a message after a process of interpretation. A communicator creates and interprets a message with a personal field of expertise and/or a frame of reference Figure 2 ).

Interactive model of communication.
6.3. Transactional model of communication
Transactional model of communication acknowledges and gives emphasis to the dynamic nature of interpersonal communication and the multiple roles of the communicators. Features such as time, messages, noise, fields of experience, frames of reference, meanings, shared systems of communicators and personal systems all pay a role in the process of communication. Communicators often participate simultaneously (sending, receiving and interpreting). The unique interpretive and perceptual processes of individuals thus play an essential role in the communication process.
7. Barriers to effective communication
Effective communication skills and strategies are important for nurses. Clear communication means that information is conveyed effectively between the nurse, patients, family members and colleagues. However, it is recognized that such skills are not always evident and nurses do not always communicate well with patients, family members and colleagues. The message sent may not be the message received. The meaning of a message depends on its literal meaning, the non-verbal indicators accompanying it and the context in which it is delivered. It is therefore, easy to misinterpret the message, or to interpret it correctly, but to decide not to pursue its hidden meaning this leads to obstruction to communication. Continuous barriers to effective communication brings about a gradual breakdown in relationships. The barriers to effective communication outlined below will help nurses to understand the challenges [ 8 ].
7.1. Language barrier
Language differences between the patient and the nurse are another preventive factor in effective communication. When the nurse and the patient do not share a common language, interaction between them is strained and very limited [ 9 , 10 , 11 ]. Consequently, a patient may fail to understand the instructions from a nurse regarding the frequency of taking medication at home.
7.2. Cultural differences
Culture is another hindrance. The patient’s culture may block effective nurse–patient interactions because perceptions on health and death are different between patients [ 12 , 13 , 14 ]. The nurse needs to be sensitive when dealing with a patient from a different culture [ 9 , 15 , 16 ]. What is acceptable for one patient may not be acceptable for another. Given the complexity of culture, no one can possibly know the health beliefs and practices of every culture. The nurse needs check with the patient whether he/she prefers to be addressed by first name or surname. The use of eye contact, touching and personal space is different in various cultures and rules about eye contact are usually complex, varying according to race, social status and gender. Physical contact between sexes is strictly forbidden in some cultures and can include handshakes, hugging or placing a hand on the arm or shoulder. A ‘yes’ does not always mean ‘yes’. A smile does not indicate happiness, recognition or agreement. Whenever people communicate, there is a tendency to make value judgements regarding those perceived as being different. Past experiences can change the meaning of the message. Culture, background and bias can be good if they allow one to use past experiences to understand something new; it is when they change meaning of the message that they interfere with the communication process [ 12 ]. It is important for nurses to think about their own experiences when considering cultural differences in communication and how these can challenge health professionals and service users.
7.3. Conflict
Conflict is a common effect of two or more parties not sharing common ground. Conflict can be healthy in that it offers alternative views and values. However, it becomes a barrier to communication when the emotional ‘noise’ detracts from the task or purpose. Nurses aim for collaborative relationships with patients, families and colleagues.
7.4. Setting in which care is provided
The factors in care setting may lead to reduction in quality of nurse–patient communication. Increased workload and time constraints restrict nurses from discussing their patients concerns effectively [ 16 ]. Nurses work in busy environments where they are expected to complete a specific amount of work in a day and work with a variety of other professionals, patients and their families. The roles are hard, challenging and tiring. There is a culture to get the work done. Some nurses may consider colleagues who spend time talking with patients to be avowing the ‘real’ work and lazy. Nurses who might have been confident in spending time with patients in an area where this was valued, when faced with a task-orientated culture have the dilemma of fitting into the group or being outside the group and spending time engaging with patients. Lack of collaboration between the nurses and the doctors in information sharing also hinder effective communication. This leads to inconsistencies in the information given to patients making comprehension difficult for the patient and their families.
7.5. Internal noise, mental/emotional distress
Internal noise has an impact on the communication process. Fear and anxiety can affect the person’s ability to listen to what the nurse is saying. People with feelings of fear and anger can find it difficult to hear. Illness and distress can alter a person’s thought processes. Reducing the cause of anxiety, distress, and anger would be the first step to improving communication.
7.6. Perception
If a healthcare professional feels that the person is talking too fast, not fluently, or does not articulate clearly etc., he/she may dismiss the person. Our preconceived attitudes affect our ability to listen. People tend to listen uncritically to people of high status and dismiss those of low status.
7.7. Difficulty with speech and hearing
People can experience difficulty in speech and hearing following conditions like stroke or brain injury. Stroke or trauma may affect brain areas that normally enable the individual to comprehend and produce speech, or the physiology that produces sound. These will present barriers to effective communication.
7.8. Medication
Medication can have a significant effect on communication for example it may cause dry mouth or excess salivation, nausea and indigestion, all of which influence the person’s ability and motivation to engage in conversation. If patients are embarrassed or concerned that they will not be able to speak properly or control their mouth, they could be reluctant to speak.
Equipment or environmental noise impedes clear communication. The sender and the receiver must both be able to concentrate on the messages they send to each other without any distraction.
8. Improving communication
Listen without interrupting the sender.
Show empathy at all times and try to understand.
Try to stay focused on the conversation. Do not however, force the patient to continue if he/she becomes anxious or seems to wish to change the subject.
Use the body language that indicates your interest and concern. Touch the patient if it seems appropriate. Lean forward, listen intently and maintain eye contact if it culturally acceptable.
Offer factual information. This relieves anxiety. Do not offer your personal opinion. Assure the patient that you have professional discretion.
Try to reflect the feelings and thoughts the patient is expressing by rephrasing questions and comments using their own words.
Avoid unclear or misleading messages.
Avoid giving long explanations.
Give your co-workers your full attention when communicating with them.
Ask questions to clarify unclear messages.
Do not interrupt until the sender has completed the message.
Provide a quiet environment without distractions.
Be convincing wen communicating [ 17 ].
9. Communicating with patients
Be open, respectful and gracious in all your interactions with the patient and keep his/her cultural preferences in mind.
Answer nurses’ bells promptly.
Make sure you have the patients’ attention when communicating.
Use words that are non-threatening – explain what you would like to do and do not give orders to the patient.
Use simple, understandable phrases, not medical terms as most patients do not understand these terms.
Speak clearly and courteously.
Use a pleasant and normal tone of voice to the hard of hearing.
Always stand so that the patient can see the nurse’s face when communicating, as lip reading is part of all normal hearing.
Use body language that is appropriate.
Explain facts and procedures before donning a mask that covers the wearer’s mouth and lower face.
Be alert to the patient’s needs. Allow time for answers to your requests and to answer patient’s questions [ 17 ].
10. Communicating by phone
Always speak clearly into the mouthpiece of the phone.
Offer a greeting for example, good morning or good afternoon.
Identify the unit or place of work.
Identify yourself by indicating who you are and where you are phoning from.
Identify the person to whom you are speaking.
Politely listen to the message and make notes if you think you may not remember all the information.
If you are asked to call another person, note the date, time, caller’s name and telephone number together with the message.
Date and sign the message [ 17 ].
11. Assertive communication
Content – where the rights of the people involved are embedded gently in the statement. This could be done by using an explanation, empathy for the listener, and praise for the listener, an apology for the consequence for the listener or a compromise that is favorable to both people.
Covert elements – where the speaker is able to recognize their rights and the rights of the listener in the communication process. These include respect, expressing feelings, having your own priorities, being able to say ‘no’, being able to make mistakes and choosing to say nothing.
Process – concerned with how people express themselves assertively. Is their body language, intonation and choice of language reflective of a confident assertive person? Are the processes that make up communication congruent, in keeping with what is being said? The process also involves managing the setting so that people are not embarrassed, or the noise levels are kept to a minimum. Increasing the likelihood of assertive communication happening again involves feedback to the listener to show that their accomplishment is appreciated.
Non-verbal cues – gesture, touch, proxemics and posture – also need to reflect confidence, regard and respect for self and others.
12. Therapeutic interactions
Assess a patient : The nurse wants to know more about a patient to identify his/her problems. This type of conversation can be a structured interview using an interview schedule. The purpose of this conversation is always a better understanding of the patient.
Instruct a patient : Patient instruction may vary from an informal conversation during which few facts are conveyed to an elaborate instruction session.
Problem solving : If a patient discuss his/her problems with a nurse, the nurse helps the patient to analyze the problem, consider possible alternative ways of handling it and how to decide which way is the best. Problem solving is done with the patients and not for them.
Give emotional support : The presence of an empathetic nurse, that is, one who can enter into the patient’s shoes and understand the patient’s experience, is immensely supportive of the patient. Emotional support alleviates the loneliness of the patient’s experience of illness and increases his/her dignity [ 17 ].
13. Guidelines for successful therapeutic interactions
After the purpose of the therapeutic interaction has been established, the following guidelines assist in conducting a successful interaction:
13.1. Maintaining a low-authority profile
The nurse must strive to maintain a low-authority profile at the beginning of the conversation. As the conversation progresses, the nurse can use more directive techniques to find out specific information. There are usually differences in age, sex, occupation, cultural background, moral and religious convictions between the nurse and the patient. These differences make it impossible for the nurse to fully understand the patient’s behavior and reactions. It is therefore, important for the nurse to understand and accept differences in patients’ cultures and beliefs. When in doubt, check with the patient. If trust is established, patient will be willing to teach the nurse.
13.2. Use of understandable language
The nurse should determine the patient’s level of understanding and if necessary change the use of language, comments and questions. Using the terminology which the patient does not understand can also frighten the patient and make him/her think that he/she has a more serious problem than he/she originally wanted help for. At the same time, the patient could give incorrect information because due to confusion, he/she may give affirmative answers to questions about symptoms that he/she has not actually experienced [ 18 ]. Nurses should share their aims with patients before expecting them to participate in the interaction. They should understand that there is a mutual understanding of each other’s point of departure. In an assessment interview, the nurse can, for instance, say: “Mr Jones, I would like to give you information on how to lose weight so as to bring down you high blood pressure, but I first need to find out what you already know about the condition”. It is not only important that the patients understand what nurses expect from the conversation; it is also essential that nurses understand the patients and convey this understanding before they participate in the conversation. When providing emotional support, this understanding is often all that is necessary. For nurses to understand patients, they must encourage them to talk – not just about facts, but also about their feelings. The nurse must listen more than speak, both to what the patient is saying verbally and what is being said non-verbally. Having listened carefully, the nurse then concentrates and responds empathetically to the patients’ feelings. Only when the nurse has a reasonably complete understanding of the patient’s situation and has communicated this understanding, can she proceed to interventions, such as giving information or solving a problem.
13.3. Tailor the message to the totality of the person
Saying something does not necessary mean that the message has been received and understood. It is the responsibility of the nurse to ensure that the person with whom he/she is conversing understands the message. To ensure this, the message has to be adapted to the language, culture and socio-economic status of the patient. The emotional or physical condition of patients may also make it difficult for them to receive long of complicated messages or even any message. There may also be other disturbances in the immediate environment for example, noise that can make the patient not to hear or understand the message. The message must also be adapted to the age of the patient [ 10 ].
13.4. Validate the interpretation with the patient
Validation means that you ask the patient whether your interpretation is correct or not. You therefore, ask him/her to confirm your understanding of what he/she said. Many misunderstandings arise because people interpret other people’s words without checking their interpretation. The nurse should try to eliminate misunderstandings in the conversations by checking meaning with the patient.
13.5. Active listening
Is the eye contact maintained with the person who is speaking?
Are the body and face turned towards the speaker?
Are there regular verbal responses, even if these consist only of encouraging sounds?
Does the response indicate understanding, not only of the facts, but also of the feelings and the implications of the facts?
It is much easier to speak than to listen. Nurses are, in general, very active people, who want help b acting quickly. To ‘just listen’ without expressing opinions or offering advice is therefore, often not in their nature. Active listening is a valuable skill to acquire [ 10 , 17 , 18 ].
13.6. Evaluate own communication
Simplicity : Say what you want to say concisely and without using difficult or unfamiliar terms.
Clarity : Say precisely what you want to say without digressing, and support your verbal message with non-verbal indicators.
Relevance : Make sure that your message suits the situation, the time and the person you are speaking to.
Adaptability : Adapt your response to the clues the patient that the patient gives you.
Respect : Always show respect for the individuality and dignity of the person you are speaking to [ 17 ].
14. Therapeutic communication techniques
Table 1 gives an overview of therapeutic communication techniques and provides examples of each technique [ 10 , 13 ].
Therapeutic communication techniques.
15. Counter-productive communication techniques
There are certain counter-productive communication techniques that the nurse should avoid as they do not assist in the recovery of the patient and do not have any therapeutic value. Table 2 shows counter-productive communication techniques, explains why these should be avoided and gives examples [ 10 , 18 ].
Non-therapeutic communication techniques that should be avoided.
16. Conclusion
Promoting effective communication in health care is demanding and challenging because of the nature of the work environment. Nurses who have received training in communication skills communicate effectively and show increased confidence in communicating with patients. Many nurses choose to work in other countries, providing an opportunity to broaden their experience and knowledge. However, it is important that nurses who have the opportunity to work in other countries develop communication skills, cultural awareness and sensitivity before arriving. For example, in China talking about death is taboo [ 19 ]. In South Africa, maintaining eye during communication may be regarded as being disrespectful by Black people [ 11 ]. This article provides a reflective account of the experiences of one of the authors of working overseas. This chapter provides the effective communication and interpersonal skills that enhance professional nursing practice and nursing relationships by explaining principles of communication, communication process, purpose of communication, types of communication, barriers to effective communication, models of communication and strategies of improving communication and guidelines for successful therapeutic interactions.
Acknowledgments
The author wishes to acknowledge the Durban University of Technology for funding this book chapter.
Conflict of interest
The author declares that there is no conflict of interest in this chapter.
- 1. World Health Organization (WHO). Global strategic directions for strengthening nursing and midwifery 2016-2020. 2016. Geneva: WHO
- 2. Mokoka KE, Ehlers VJ, Oosthuizen MJ. Factors influencing the retention of registered nurses in the Gauteng Province of South Africa. Curationis. 2011; 34 (1):1-9
- 3. Mokoka E, Oosthuizen MJ, Ehlers VJ. Retaining professional nurses in South Africa: Nurse managers’ perspectives. Health SA Gesondheid. 2010; 15 (1):1-9
- 4. Neese B. Effective Communication in Nursing: Theory and Best Practices. [Internet]. 2015. Available from: http://online.seu.edu/effective-communication-in-nursing/ [Accessed: December 28, 2017]
- 5. Bush H. Communication Skills for Nurses. [Internet]. 2016. Available from: https://www.ausmed.com/articles/communication-skills-for-nurses/ [Accessed: December 28, 2017]
- 6. O’Hagan S, Manias E, Elder C, Pill J, Woodward-Kron R, McNamara T, Webb G, McColl G. What counts as effective communication in nursing? Evidence from nurse educators’ and clinicians’ feedback on nurse interactions with simulated patients. Journal of Advanced Nursing. 2013:1344-1355
- 7. Sibiya MN. People management. In: Booyens S, Jooste K, Sibiya N, editors. Introduction to Health Services Management for the Unit Manager. 4th ed. Claremont: Juta and Company (Pty) Ltd; 2015. pp. 194-205. ISBN: 978-0-70218-866-4
- 8. van Niekerk V. Relationship, helping and communication skills. In: van Rooyen, D, Jordan PJ, editors. Foundations of Nursing Practice: Fundamentals of Holistic Care. African Edition. 2nd ed. Edinburgh: Mosby Elsevier; 2016. pp. 181-207. ISBN: 978-0-7020-6628-3
- 9. Jooste K. Effective leadership communication. In: Jooste K, editor. Leadership in Health Services Management. 2nd ed. Claremont: Juta and Company (Pty) Ltd; 2011. pp. 205-220. ISBN: 9-780702-180347
- 10. Uys L. Interpersonal needs. In: Uys L, editor. Integrated Fundamental Nursing. 2nd ed. Cape Town: Pearson; 2017. pp. 453-571. ISBN: 978-1-775-95450-7
- 11. du Plessis E, Jordaan EJ, Jali MN. Communication in a health care unit. In: Jooste K, editor. The Principles and Practice of Nursing and Health Care. Pretoria: Van Schaik Publishers; 2010. pp. 205-220. ISBN: 9-780627-027857
- 12. Kai J, Beavan J, Faull C. Challenges of mediated communication, disclosure and patient autonomy in cross-cultural cancer care. British Journal of Cancer. 2011; 105 (7):918-924
- 13. McCarthy J, Cassidy I, Margaret MG, Tuohy D. Conversations through barriers of language and interpretation. Bristish Journal of Nursing. 2013; 22 (6):335-340
- 14. Tay LH, Ang E, Hegney D. Nurses’ perceptions of the barriers in effective communication with inpatient cancer adults in Singapore. Journal of Clinical Nursing. 2012; 21 (17-18):2647-2658
- 15. Aslakson RA, Wyskiel R, Thornton I, Copley C, Shaffer D, Zyra M, Pronovost PJ. Nurse-perceived barriers to effective communication regarding prognosis and optimal end-of-life care for surgical ICU patients: A qualitative exploration. Journal of Palliative Medicine. 2012; 15 (8):910-915
- 16. Helft PR, Chamness A, Terry C, Uhrich M. Oncology nurses’ attitudes toward prognosis-related communication: A pilot mailed survey of oncology nursing society members. Oncology Nursing Forum. 2011; 38 (4):468-474
- 17. Booyens L, Erasmus I, van Zyl M. The Auxiliary Nurse. 3rd ed. Cape Town: Juta and Company Ltd; 2013. 504 p. ISBN: 978-0-702 19-794-9
- 18. Viljoen MJ, Sibiya N. History Taking and Physical Examination. 2nd ed. Cape Town: Pearson Education South Africa (Pty) Ltd; 2009. ISBN: 978-1-86891-976-5
- 19. Zheng RS, Guo QH, Dong FQ, Owens RG. Chinese oncology nurses’ experience on caring for dying patients who are in their final days: A qualitative study. International Journal of Nursing Studies. 2015; 52 (1):288-296
© 2018 The Author(s). Licensee IntechOpen. This chapter is distributed under the terms of the Creative Commons Attribution 3.0 License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Continue reading from the same book
Published: 19 September 2018
By Vasfiye Bayram Değer
3658 downloads
By Mayumi Uno
1132 downloads
By Nilgun Ulutasdemır
1469 downloads
Principles of Communication in Nursing Essay
Introduction, principles of communication, verbal vs. non-verbal communication, sbar communication.
Effective communication is crucial in nursing because it allows healthcare professionals to choose the optimal strategy for helping their patients and interacting with their co-workers. Verbal and non-verbal communication is equally essential for nurses, and it is possible to evaluate communication effectiveness using the SBAR tool. Registered nurses should know the principles that make professional interaction prolific and ethical (Wagner, 2018). The purpose of the paper is to understand that the principles of communication are essential while delegating the duties of the registered nurse to other healthcare providers without endangering the patient’s safety. Effective communication is a vital competency in nursing that allows the healthcare professional to promote the patient’s interests and delegate tasks between the team members.
Even though the communication principles between nurses and other healthcare specialists, and nurses and patients are slightly different, they are based on the same code of professional ethics. According to this, pursuing the patient’s safety and well-being is the main communication issue (Wagner, 2018). This aim determines the communicative process or the way registered nurses interact with co-workers and patients. Nurses often deal with emotionally complicated tasks when interacting with patients and adapt to the interlocutor using various communication modes (Wagner, 2018). For instance, the nurse should develop listening skills to understand the needs of the patient or the co-worker and to find the appropriate communication mode based on internal and external factors. In this case, the registered nurse must balance professional objectivity and providing the patient with the required support.
Professional interaction of the nurse is consistent with the s of modes of communication. There is a difference between interpersonal, presentational, and interpretive communication modes that reflect the motivation of the speaker (Wittenberg et al., 2018). Internal communication is the process of interaction with co-workers, while external communication is the interaction with patients in the clinical setting (Wittenberg et al., 2018). Paying equal attention to internal and external factors that affect communication allows nurses to preserve professionalism and empathy in approaching people.
At the same time, when the nurse prepares the summary of the information about the patient, they should also describe their subjective perception of the case. For example, suppose the patient needs to speak English at an adequate level, and it is challenging to communicate the clinical recommendations to them (Wittenberg et al., 2018). In that case, the nurse should emphasize this in interacting with co-workers (Wittenberg et al., 2018). It allows the assumption that pursuing the patient’s interests is the main principle in the communication of the registered nurse, and they should combine objectivity and empathy in their reports to their co-workers.
Verbal communication can be oral and written; in both cases, the person articulates their thoughts using the language. Precision and accuracy are the key characteristics that the registered nurse should remember in professional verbal communication (Fuoto & Turner, 2019). There should not be controversial personal opinions about the discussed issues in professional verbal communication. The way nurse communicates using verbal channels should reflect their competencies (Fuoto & Turner, 2019). In this case, the data obtained by the nurse about the clinical issue can be used as the basis for the work of another healthcare professional, which facilitates interaction within the team.
Professionalism is also a significant component of the non-verbal communication of the registered nurse. At the same time, it is challenging to measure and evaluate it, making demonstrating professionalism difficult. Such elements of non-verbal communication as the nurse’s gestures, eye contact, posture, movement, and voice tone are vital in creating the appropriate professional image (Barrow & Sharma, 2022). Even though the perception of these characteristics is subjective in some cases, most people share a similar opinion about their importance (Barrow & Sharma, 2022). It foregrounds the need to consciously apply non-verbal communicative tools to achieve the required results in interacting with patients and co-workers.
It is possible to find numerous examples from clinical practice that illustrate the importance of using non-verbal communicative signs in the evaluation of the nurse’s professionalism and judgment. For example, when the nurse speaks to the patient in a confident voice, her appearance is tidy and clean, and her gestures are calm, the patient sees that the professional cares for them (Barrow & Sharma, 2022). Suppose the nurse displays such non-verbal signs as a hysterical voice, dirty clothes, and panic in gestures. In that case, the patient will not think about them as a professional whose opinion is credible. A similar example can be applied to the communication between co-workers. In case the nurse avoids eye contact with another healthcare professional while talking about the patient’s case, there is the chance that they are not assured in their descriptions (Barrow & Sharma, 2022). These examples illustrate the notion of congruence of verbal and non-verbal communication that supposes that verbal and non-verbal signs should convey a similar message (Barrow & Sharma, 2022). In other words, these two channels of communication should provide coherent data to the audience and create the appropriate image in the professional interaction of the registered nurse.
The SBAR approach to communication supposes equal attention to the situation in the clinical practice, its background, the assessment, and the recommendations on the issue. This framework is convenient to use in critical situations requiring the healthcare professional’s attention within a limited period (Abbaszade et al., 2021). The SBAR method allows the registered nurse to articulate the information on the case concisely, which is essential in communication between the team members (Abbaszade et al., 2021). It is vital to mention that this approach promotes patient safety, which is the fundamental component of the ethical behavior of the professional nurse (Abbaszade et al., 2021). Therefore, the SBAR framework can be used in various clinical settings to communicate the message to colleagues precisely and to ensure the patient receives adequate help.
The SBAR communicative tool supposes high accuracy in conveying the message to another healthcare professional who might not be acquainted with the case. For this reason, delegating tasks between the team members is crucial because it supposes that all professionals understand the clinical background and the peculiarities of the case (Barrow & Sharma, 2022). The active use of the SBAR technique allows healthcare specialists to increase the quality of their services and improve the team’s interaction (Lo et al., 2021). In other words, situations when the nurse has to delegate a task to another co-worker, are common in clinical practice. It requires the ability to articulate the information about the patient, their state, and the previous clinical intervention precisely and to convey this message to another nurse (Lo et al., 2021). The SBAR technique is the optimal solution for this task that supposes a clear written summary for the subsequent multifaceted clinical interventions.
Verbal, non-verbal, and SBAR communicative tools are critical in effective communication between team members. Interaction between healthcare professionals in the clinical setting should be based on the central principles of ethical behavior. The focus on the patient’s safety is the most vital concern for nurses and doctors, which determines the communicative tools they choose. For this reason, communication between healthcare specialists should be accurate, precise, and detailed. It allows them to delegate tasks within the team without endangering the patient’s health, which is essential in their work. Nurses often focus on verbal communication and disregard non-verbal interaction, which is a potential problem. Moreover, they focus on written interaction because conveying the message is usually associated with professionalism. At the same time, verbal and non-verbal communication types are equally important in the practical work of the registered nurse.
Abbaszade, A., Assarroudi, A., Armat, M. R., Stewart, J. J., Rakhshani, M. H., Sefidi, N., & Sahebkar, M. (2021). Evaluation of the impact of handoff based on the SBAR technique on quality of nursing care . Journal of Nursing Care Quality, 36 (3), E38–E43. Web.
Barrow, J. M., & Sharma, S. (2022) . Five rights of nursing delegation. StatPearls Publishing.
Fuoto, A., & Turner, K. M. (2019). Palliative care nursing communication: An evaluation of the COMFORT model . Journal of Hospice and Palliative Nursing: JHPN: The Official Journal of the Hospice and Palliative Nurses Association, 21 (2), 124–130. Web.
Lo, L., Rotteau, L., & Shojania, K. (2021). Can SBAR be implemented with high fidelity and does it improve communication between healthcare workers? A systematic review . BMJ Open, 11 (12), e055247. Web.
Wagner E. A. (2018). Improving patient care outcomes through better delegation-communication between nurses and assistive personnel . Journal of Nursing Care Quality, 33 (2), 187–193. Web.
Wittenberg, E., Ferrell, B., Kanter, E., & Buller, H. (2018). Health literacy: Exploring nursing challenges to providing support and understanding . Clinical Journal of Oncology Nursing, 22 (1), 53–61. Web.
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, January 29). Principles of Communication in Nursing. https://ivypanda.com/essays/principles-of-communication-in-nursing/
"Principles of Communication in Nursing." IvyPanda , 29 Jan. 2024, ivypanda.com/essays/principles-of-communication-in-nursing/.
IvyPanda . (2024) 'Principles of Communication in Nursing'. 29 January.
IvyPanda . 2024. "Principles of Communication in Nursing." January 29, 2024. https://ivypanda.com/essays/principles-of-communication-in-nursing/.
1. IvyPanda . "Principles of Communication in Nursing." January 29, 2024. https://ivypanda.com/essays/principles-of-communication-in-nursing/.
Bibliography
IvyPanda . "Principles of Communication in Nursing." January 29, 2024. https://ivypanda.com/essays/principles-of-communication-in-nursing/.
- SBAR in Healthcare Contexts: Interpersonal Communication
- Handoff Communication in the Clinical Setting
- Nurse Leader-Directed Nurse-To-Nurse Handoff
- Leadership SMART Goal: Effective Communication
- Bedside Shift Report in the Nursing
- Medical Errors Caused by Miscommunication
- Role of Communication and Teamwork in Improving Patient Safety
- Guidance and Coaching in Advanced Nursing Practice
- Trustee vs. Delegate Models of Representation
- Nonverbal Cues and Advance Nonverbal Communication Skills
- Aspects of the Comfort and Pain Management
- Applying New Methods in Nursing Practice
- Managing Joint Pain and Gait Abnormalities
- Quantifying Nursing Care and Services
- Choosing an Evidence-Based Practice Framework
Effective communication between nurses and patients: an evolutionary concept analysis
Affiliation.
- 1 Student Nurse, University of West London, Brentford.
- PMID: 32881615
- DOI: 10.12968/bjcn.2020.25.9.438
Communication can be considered as the basis of the nurse-patient relationship and is an essential element in building trust and comfort in nursing care. Effective communication is a fundamental but complex concept in nursing practice. This concept analysis aims to clarify effective communication and its impact on patient care using Rodgers's (1989) evolutionary framework of concept analysis. Effective communication between nurses and patients is presented along with surrogate terms, attributes, antecedents, consequences, related concepts and a model case. Effective communication was identified to be a multifactorial concept and defines as a mutual agreement between nurses and patients. This influences the nursing process, clinical reasoning and decision-making. Consequently, promotes high-quality nursing care, positive patient outcome and patient's and nurse's satisfaction of care.
Keywords: Communication; Concept analysis; Nurse-patient relationship; Nursing traits; Trust.
- Communication*
- Models, Nursing
- Nurse's Role
- Nurse-Patient Relations*
- Nursing Process
Home — Essay Samples — Nursing & Health — Nursing — Nursing and Effective Communication
Nursing and Effective Communication
- Categories: Effective Communication Nursing
About this sample

Words: 514 |
Published: Jan 25, 2024
Words: 514 | Page: 1 | 3 min read
Benefits of Effective Communication in Nursing
Works cited.
- Barton, G., Bruce, A., & Schreiber, R. (2018). Teaching nurses teamwork: Integrative review of competency-based team training in nursing education. Nurse education in practice, 32, 129-137.
- Kourkouta, L., & Papathanasiou, I. V. (2014). Communication in nursing practice. Material socio-medica, 26(1), 65.
- The Importance of Effective Communication in Nursing (2022). The University Of St. Augustine for Health Sciences. Retrieved from, www.usa.edu/blog/communication-in-nursing/

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Dr. Karlyna PhD
Verified writer
- Expert in: Sociology Nursing & Health

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
2 pages / 777 words
1 pages / 599 words
4 pages / 1784 words
4 pages / 2141 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Nursing
When driving around Miami, FL there are a copious number of billboards that I see advertising for people to become nurses throughout the city. When doing research, I’ve only come across a couple of news articles, advertising on [...]
Gagnon, K., & Sabus, C. (2015). Professionalism in a Digital Age: Opportunities and Considerations for Using Social Media in Health Care. Physical Therapy, 95(3), 406–414.Nayak, S. G. (2018). Time Management in Nursing -- Hour [...]
A Better NHS. (2011). Patient autonomy and choice. Retrieved from 71-77.
Smith, J. (2021). The Essence of Nursing: Compassionate Care and Patient Well-being. Journal of Nursing Education and Practice, 11(5), 26-31.Johnson, M., & Higgins, I. (2018). Nursing Care: A Compassionate Approach. Elsevier [...]
Postpartum hemorrhage is a significant risk in the postpartum period, requiring prompt recognition, assessment, prevention, and management. Nursing care plays a pivotal role in ensuring the well-being of women experiencing [...]
In the world of healthcare, professionalism is the cornerstone of nursing practice. It encompasses a set of qualities and behaviors that not only uphold the standards of the profession but also ensure the delivery of safe and [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
Importance of Therapeutic Communication in Nursing
This essay about therapeutic communication in nursing highlights its pivotal role in fostering trust, understanding, and healing between nurses and patients. It explores the significance of human connection through communication in healthcare settings, emphasizing active listening, empathy, and respect. The essay discusses how therapeutic communication builds trust, gathers crucial patient information, enhances satisfaction, and benefits both patients and nursing professionals. It underscores the importance of honing communication skills for delivering high-quality, patient-centered care in the evolving healthcare landscape.
How it works
Therapeutic communication stands as the secret sauce in the rich recipe of nursing care, infusing the clinical setting with warmth, understanding, and healing. In the hustle and bustle of healthcare, where technology often takes the spotlight, the human touch through communication emerges as the unsung hero, weaving bonds of trust and empathy between nurses and their patients. It’s a symphony of verbal and nonverbal gestures aimed not just at conveying information, but at creating a safe space where patients feel truly seen, heard, and valued.
At its essence, therapeutic communication embodies the art of active listening, empathy, and honoring the patient’s autonomy. It’s about more than just exchanging words—it’s about building bridges of understanding that traverse the chasm between illness and wellness. Nurses who excel in this dance of dialogue understand that each interaction is an opportunity to forge a connection, to reach beyond the clinical veneer and touch the human heart beneath.
One of the magical outcomes of therapeutic communication is its ability to sow the seeds of trust and camaraderie between nurse and patient. Trust is the cornerstone of healing, the bedrock upon which patients feel empowered to share their deepest fears, concerns, and hopes. By lending an empathetic ear and a caring presence, nurses cultivate a fertile ground where patients feel safe to be vulnerable, to express themselves without fear of judgment.
Moreover, therapeutic communication serves as a treasure trove of insights, a window into the inner world of the patient. Through attentive listening and skillful questioning, nurses unlock the mysteries that lie beyond the surface—a twinge of pain hidden behind a smile, a flicker of anxiety concealed beneath a brave facade. This holistic approach to communication enables nurses to tailor their care plans to fit the unique contours of each patient’s journey, ensuring that no voice goes unheard, no need goes unmet.
Beyond the tangible benefits for patients, therapeutic communication casts a radiant glow upon the nursing profession itself. Engaging in genuine, meaningful interactions with patients becomes a source of nourishment for the soul, a reminder of why nurses embarked on this noble calling in the first place. In the shared moments of laughter, tears, and everything in between, nurses find fulfillment, purpose, and a deep sense of belonging to a profession built on the pillars of compassion and humanity.
In the grand tapestry of healthcare, therapeutic communication emerges as a golden thread, weaving its way through the fabric of healing and transforming sterile clinical environments into havens of compassion and empathy. As the healthcare landscape continues to evolve, one thing remains constant—the profound impact of human connection, forged through the simple yet profound act of communication. In the words left unspoken, in the gestures of kindness, lies the transformative power to heal, to uplift, and to remind us all of our shared humanity
Cite this page
Importance Of Therapeutic Communication In Nursing. (2024, Apr 29). Retrieved from https://papersowl.com/examples/importance-of-therapeutic-communication-in-nursing/
"Importance Of Therapeutic Communication In Nursing." PapersOwl.com , 29 Apr 2024, https://papersowl.com/examples/importance-of-therapeutic-communication-in-nursing/
PapersOwl.com. (2024). Importance Of Therapeutic Communication In Nursing . [Online]. Available at: https://papersowl.com/examples/importance-of-therapeutic-communication-in-nursing/ [Accessed: 7 May. 2024]
"Importance Of Therapeutic Communication In Nursing." PapersOwl.com, Apr 29, 2024. Accessed May 7, 2024. https://papersowl.com/examples/importance-of-therapeutic-communication-in-nursing/
"Importance Of Therapeutic Communication In Nursing," PapersOwl.com , 29-Apr-2024. [Online]. Available: https://papersowl.com/examples/importance-of-therapeutic-communication-in-nursing/. [Accessed: 7-May-2024]
PapersOwl.com. (2024). Importance Of Therapeutic Communication In Nursing . [Online]. Available at: https://papersowl.com/examples/importance-of-therapeutic-communication-in-nursing/ [Accessed: 7-May-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
Nursing Essay Examples

Nursing Essay Examples That Will Help You Write a Stellar Paper
Published on: May 6, 2023
Last updated on: Jan 29, 2024

Share this article
Many nursing students struggle with writing effective nursing essays, which are an essential part of their education and professional development.
Poor essay writing skills can lead to low grades and an inability to effectively communicate important information.
This blog provides a comprehensive guide to writing nursing essays with examples and tips for effective writing. Whether you are a nursing student or a professional looking to improve your writing skills, this blog has something for you.
By following the tips and examples provided, you can write compelling nursing essays that showcase your dedication to the field.
Let’s get started.
On This Page On This Page -->
What is a Nursing Essay?
A nursing essay is a type of academic writing that aims to explore a particular topic related to nursing. It also presents a clear and concise argument or viewpoint supported by evidence.
Nursing essays can take many forms, including:
- Descriptive essays
- Reflective essays
- Analytical essays
- Persuasive essays
What is the Importance of the Nursing Essay?
Nursing essays are important for several reasons. First, they help nursing students develop critical thinking skills by requiring them to analyze and evaluate information.
Second, they help students develop research skills by requiring them to locate and use credible sources to support their arguments.
Third, nursing essays help students develop communication skills by requiring them to present their ideas clearly and concisely in writing. Finally, nursing essays are important for nursing education because they prepare students for the types of writing.
Paper Due? Why Suffer? That's our Job!
To help students better understand how to write nursing essays, it can be helpful to review examples.
Below are some examples of nursing essays.
Nursing School Essay Examples
College Nursing Essay Examples
Graduate Nursing Essay Examples
Nursing Scholarship Essay Examples
Nursing Essay Conclusion Examples
Nursing Essay Examples of Different Fields
Nursing is a diverse field with many different specialties and areas of focus. As a result, nursing essays can take many different forms and cover a wide range of topics.
Given below are some examples of different types of nursing essays:
Personal Philosophy Of Nursing - Essay Examples
Cal State Fullerton Nursing Essay Examples
Evidence Based Practice Nursing In Medical Field - Essay Examples
Leadership In Nursing And Healthcare Professionals - Essay Examples
Principles Of Professional Practice Of Nursing Professionals And Pharmacists
If you're seeking additional examples of nursing essays, you're in luck!
Below are some more examples that can help you gain a better understanding of nursing essays:
Health Care And Reflective Models For Nursing - Essay Examples
History Of Nursing Essay Examples
Ethical Dilemma In Nurses Work - Essay Examples
Mental Health Nursing Essay Examples
Why I Want To Be A Nurse Essay
Working In A Team And Collaboration In Nursing
How to Write a Nursing Essay
Writing a nursing essay can seem daunting, but with the right approach, it can be a rewarding experience.
Here are the key steps involved in writing a nursing essay:
Understanding the Topic and Question
The first step in writing a nursing essay is to carefully read and understand the topic and question.
This will help you determine what information you need to research and include in your essay. Make sure you understand any key terms or concepts related to the topic. Consider different perspectives or viewpoints that may be relevant.
Researching the Topic
Once you have a clear understanding of the topic and question, it's time to research.
Start by gathering information from credible sources such as academic journals, textbooks, and government websites.
Consider both primary and secondary sources, and make sure to take detailed notes as you read.
Organizing and Outlining the Essay
Once you have completed your research, it's time to organize your ideas and create an outline for your essay.
Start by identifying the main points or arguments you want to make, and then organize them into a logical order that flows well.
Your outline should include an introduction, body paragraphs, and a conclusion.
Writing the Essay
With your outline in place, it's time to start writing your essay. Make sure to follow your outline closely, and use clear and concise language that effectively communicates your ideas.
Use evidence from your research to support your arguments, and cite your sources appropriately.
Editing and Revising the Essay
Once you have completed a first draft of your essay, take some time to edit and revise it. Look for any errors in grammar, spelling, or punctuation, and make sure your essay is well-organized and flows well.
Consider asking a peer or instructor to review your essay and provide feedback.
What To Include In Your Nursing Essay
When writing a nursing essay, there are several key elements that you should include. Here are some important things to keep in mind:
- Introduction
Your introduction should provide a brief overview of the topic and purpose of your essay. It should also include a clear thesis statement that presents your main argument or point of view.
- Background Information
Provide some background information on the topic to help the reader better understand the context of your essay. This can include relevant statistics, historical information, or other contextual details.
- Evidence and Examples
Use evidence and examples from your research to support your arguments and demonstrate your knowledge of the topic. Make sure to cite your sources appropriately and use a variety of sources to strengthen your argument.
- Analysis and Evaluation
Provide analysis and evaluation of the evidence and examples you've presented. This can include discussing strengths and weaknesses, comparing and contrasting different viewpoints, or offering your own perspective on the topic.
Your conclusion should summarize the main points of your essay and restate your thesis statement. It should also offer some final thoughts or suggestions for further research or action.
Nursing Essay Topic Ideas
Choosing a topic for your nursing essay can be challenging, but there are many areas in the field that you can explore. Here are some nursing essay topic ideas to consider:
- The role of technology in nursing practice
- The impact of cultural diversity on healthcare delivery
- Nursing leadership and management in healthcare organizations
- Ethical issues in nursing practice
- The importance of patient-centered care in nursing practice
- The impact of evidence-based practice on nursing care
- The role of nursing in promoting public health
- Nursing education and the importance of lifelong learning
- The impact of nursing shortages on healthcare delivery
- The importance of communication in nursing practice
These are just a few ideas to get you started. You can also explore other topics related to nursing that interest you or align with your academic or professional goals.
Remember to choose a topic that is relevant, interesting, and feasible to research and write about.
Tips for Writing an Effective Nursing Essay
Writing a successful nursing essay requires careful planning, research, and attention to detail. Here are some tips to help you write an effective nursing essay:
- Writing Concisely and Clearly
Nursing essays should be written in clear and concise language, avoiding unnecessary jargon or technical terms. Use simple language and short sentences to help ensure that your ideas are communicated clearly and effectively.
- Stating a Clear Thesis Statement
Your thesis statement should clearly state your main argument and provide a roadmap for the rest of your essay. It should be clear, concise, and located at the end of your introduction.
- Using Proper Citation and Referencing
Citing and referencing your sources is crucial in any academic writing, including nursing essays. Make sure to use proper citation and referencing styles, such as APA or MLA. Include a reference list or bibliography at the end of your essay.
- Seeking Feedback and Revising
Before submitting your nursing essay, seek feedback from peers, professors, or writing tutors. Use their feedback to revise and improve your essay. Make sure that it is well-structured, coherent, and effectively communicates your point of view.
By following these tips, you can write a nursing essay that demonstrates your knowledge and skills in the field.
In conclusion, writing a successful nursing essay requires careful planning, research, and attention to detail.
To showcase your knowledge in the field of nursing, it is important to have a clear understanding of the topic at hand. When writing your nursing essay, be sure to include relevant examples, incorporate current research, and use proper citation and referencing.
And remember , seeking feedback and revising your essay is key to ensuring that it effectively communicates your ideas and arguments.
If you need help with your nursing essay or any other type of academic writing, consider using our AI essay writer .
Our nursing essay writing service can provide personalized support to help you succeed in your academic goals.
So, why wait? Contact us to get college essay writing help today!
Cathy A. (Literature)
For more than five years now, Cathy has been one of our most hardworking authors on the platform. With a Masters degree in mass communication, she knows the ins and outs of professional writing. Clients often leave her glowing reviews for being an amazing writer who takes her work very seriously.
Paper Due? Why Suffer? That’s our Job!
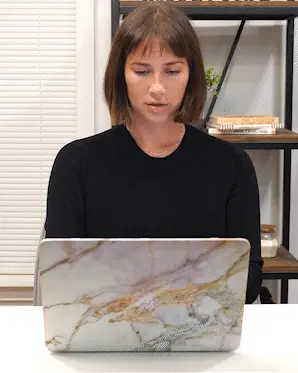
Legal & Policies
- Privacy Policy
- Cookies Policy
- Terms of Use
- Refunds & Cancellations
- Our Writers
- Success Stories
- Our Guarantees
- Affiliate Program
- Referral Program
- AI Essay Writer
Disclaimer: All client orders are completed by our team of highly qualified human writers. The essays and papers provided by us are not to be used for submission but rather as learning models only.

IMAGES
VIDEO
COMMENTS
1. Use the right tone when speaking to others. Effective communication skills in nursing include the way you relate to patients, their loved ones, and your peers. When speaking with patients or their caregivers, use concise language without talking to them in a demeaning way.
Communication is a fundamental element in nursing practice. This element can possibly determine patients' satisfaction and even the outcomes of their treatment (Lotfi et al., 2019). The situation described in the paper will exemplify the potential role of communication, which is why it will serve as a Gibbs Reflective Cycle nursing example.
Importance Of Communication Of Nurses Nursing Essay. Communication involves the exchange of messages and is a process which all individuals participate in. Whether it is through spoken word, written word, non-verbal means or even silence, messages are constantly being exchanged between individuals or groups of people (Bach & Grant 2009).
2. PRINCIPLES OF COMMUNICATION. Communication can be defined as a transaction and message creation. The entire process occurs in a context consisting of physical space, cultural and social values and psychological conditions ().Communication assists in the performance of accurate, consistent and easy nursing work, ensuring both the satisfaction of the patient and the protection of the health ...
Strong communication skills are essential to provide safe, quality, patient-centered care. Nurses develop therapeutic relationships with patients and family members each day to ensure that health care concerns and needs are addressed. If communication breaks down, information exchange stops and needs go unidentified. Nurses optimize communication channels with patients and families by ...
For example, McLean studied dementia care in nursing homes in the United States. She found that patient-centered care and communication in one nursing home (Snow I) were severely affected when nurses, physicians, and care managers focused on completing tasks or observing care and institutional routines to the detriment of satisfying patients ...
Introduction. In the nursing field, productive communication is an important aspect of successful activities and the key to effective patient care. In case the management of a particular medical institution promotes creating conditions for such interaction, performance increases due to the minimization of errors and the exchange of experience ...
Sample of a Nursing Reflective Essay . The following is a sample of a nursing Reflective essay using Gibb's Model of Reflection. Use this sample to guide you when writing your own. Introduction . Communication is an important element in healthcare practice as it determines patient satisfaction and treatment outcomes.
EXAMPLE ANALYTICAL ESSAY This example of an analytical essay is presented in association with Price, B and Harrington, A (2010) Critical Thinking and Writing for Nursing Students, Exeter, Learning Matters. Readers are introduced to the process of critical and reflective thinking and the translation of these into coursework that will help them ...
Nurses are critical in the delivery of essential health services and are core in strengthening the health system. They bring people-centred care closer to the communities where they are needed most, thereby helping improve health outcomes and the overall cost-effectiveness of services. Nurses usually act as first responders to complex humanitarian crises and disasters; protectors and advocates ...
For example: Nod your head, but never interrupt. Lean forward and maintain eye contact to let the person know you're engaged. Include minimal verbal encouragement, such as "I understand," and "go on.". 4. Written Communication. Written communication skills are also essential for effective nurse-to-nurse communication.
These examples illustrate the notion of congruence of verbal and non-verbal communication that supposes that verbal and non-verbal signs should convey a similar message (Barrow & Sharma, 2022). In other words, these two channels of communication should provide coherent data to the audience and create the appropriate image in the professional ...
Effective communication was identified to be a multifactorial concept and defines as a mutual agreement between nurses and patients. This influences the nursing process, clinical reasoning and decision-making. Consequently, promotes high-quality nursing care, positive patient outcome and patient's and nurse's satisfaction of care.
Published: Jan 25, 2024. In Nursing, communication is crucial in that it facilitates the improvement of outcomes, fosters relationships, and helps in facilitating effective teamwork. When carrying out nursing activities, information is needed from the patient for the nurses to offer care that will lead to achieving the best outcomes.
The Importance Of Communication Nursing Essay. This assignment will critically analyse the concept of communication within nursing. A concept is said to be 'a label given to an observed phenomenon' (Bell, 2009, P46-51). Cutcliffe and McKenna, (2005, P3) suggested that concepts are 'the building blocks of a theory', Mcewan and Willis ...
Cite this essay. Download. Communication is an exchange of information between people through either verbal or non-verbal forms. Dëger, Sibiya, Johnson & Uno (2018) stated that communication is an essential component in cooperation, collaboration, and relationships, which makes communicating in professional practice such as nursing vital.
Essay Example: Therapeutic communication stands as the secret sauce in the rich recipe of nursing care, infusing the clinical setting with warmth, understanding, and healing. In the hustle and bustle of healthcare, where technology often takes the spotlight, the human touch through communication
As a result, nursing essays can take many different forms and cover a wide range of topics. Given below are some examples of different types of nursing essays: Personal Philosophy Of Nursing - Essay Examples. Cal State Fullerton Nursing Essay Examples. Evidence Based Practice Nursing In Medical Field - Essay Examples.
Importance Of Communication Of Nurses Nursing Essay. Communication involves the exchange of messages and is a process which all individuals participate in. Whether it is through spoken word, written word, non-verbal means or even silence, messages are constantly being exchanged between individuals or groups of people (Bach & Grant 2009).
Effective communication is an essential factor in establishing a positive helping relationship. The ways in which care-workers communicate convey to the service user how they value that person. For communication to be effective, a person must use all the means at their disposal to make sure that they send a clear message.
A number of potential barriers exist to effective inter-professional collaboration which Nursing Associates need to be aware of, including poor communication and opportunities for group meetings particularly during the COVID-19 pandemic, different leadership styles and management structures (Seaton, et al., 2021), professional language and ...