
Quick Links
- UW HR Resources
Impressing: Personal Statement
Personal statement, personal statements usually fall into 3 categories:.
- The top 5% are works of writing wonder which is appreciated by all who read them but add only a little to your interview chances.
- The middle 85% are not necessarily memorable but they are well written and get a sense of you across; these may not add a whole lot to your interview chances but they don’t detract and they will hopefully create a memorable image that will be yours for the season.
- The bottom 10% are poorly written with grammatical mistakes, spelling errors, a lack of organization, or some combination of the three; these will truly hurt your chances for an interview – some committees have a zero-tolerance policy for spelling or grammar errors.
Those who write papers in the bottom 10% are often the ones who are shooting for the top 5%; we, therefore, recommend that your goal should be the middle 85%. The goal of your statement should be to explain why you want to go into emergency medicine and why you think emergency medicine is the right specialty for you.
Overarching theme
Look over your CV and think about the experiences before and during medical school that might inform what kind of emergency physician you will become. Often there is a common thread that holds together even the most disparate of experiences – this common thread is usually one of your core values as a person. This may be a good theme to weave throughout and hold together your personal statement.
Experiences to highlight
Use your experiences to give programs an idea of who you are. Be specific – talking about the aspects of care that you like in emergency medicine is good but it’s even better when programs can see how your personal experiences reinforce aspects of emergency medicine that resonate with you as a person. It’s OK to include patient vignettes and talk about your accomplishments, but be sure to relate them back to yourself. How did the experience impact you? What did you learn about yourself? How will the experience make you a better family physician? What about the experience demonstrates your commitment to the discipline of emergency medicine, your ability to work with others, and your ability to work with patients? Often choosing one experience and telling the story is a good way to open your statement, develop your theme, and make it memorable.
Commitment to specialty
Talk about why you are choosing emergency medicine. What experiences convince you that this is the right field for you?
Strengths that you bring
What do you bring to a program? What are you naturally good at? What specific skills do you have that will serve you well in residency? Give examples.
Future plans/what you are looking for in a residency program
At the end of this long road of school and training, what kind of work do you see yourself doing? This is not necessary but if you do have a sense then you should bring it up – it will help paint a better picture of you and give you something to discuss during the interviews.
Organizing your statement
There are many ways to organize your statement to get these points across. One common way of organizing the personal statement is a three to five-paragraph form reminiscent of those essays you had to write in high school. To use this approach the first paragraph tells a story to open the theme, the middle paragraph(s) fleshes out other experiences that highlight the theme and discuss your commitment to emergency medicine and what you have to bring to it, and the third paragraph reviews your strengths and future plans/training desires. However, this is a personal statement and you are free to write and organize it as you desire.
- Write in complete sentences.
- Have transitions between paragraphs
- Use the active voice.
- Make your writing interesting – use a thesaurus and vary sentence length.
- Have at least two other people (one who knows you well and one who knows the process of applying to EM residency well) read your personal statement and give feedback.
- Give yourself plenty of time to work on your statement and revise it based on feedback.
- Rehash your CV or write an autobiography.
- Discuss research or experiences that you can’t expand significantly on in an interview.
- Be overly creative ‐‐ no poems or dioramas.
- Use abbreviations – spell things out.
- Say “emergency room” or “emergency room doctor” – use the emergency department and emergency physician
- Start every sentence with “I”.
- Make it longer than one page, in single‐spaced, 12-point font.
- Have ANY spelling or grammatical errors.
- Write a statement that could be used for several different specialties (i.e. one that talks about wanting a primary care career but not specifically emergency medicine). If you are still deciding on a specialty and applying to different fields, write two different statements.
- End your essay speaking to the reader (e.g., thanking them for their time).
- Be arrogant or overly self‐deprecating.
- Focus on lifestyle issues or what you will do with all your free time as an EP.
- Focus on your being an adrenalin junkie.
- Use hackneyed stories of growth, travel, or adventure unless it really is personal and you can express that.
Adapted with permission from the copyrighted career advising resources developed by Amanda Kost, MD, and the University of Washington Department of Family Medicine
5 Emergency Medicine Personal Statement Samples
Looking at emergency medicine personal statement samples can be very useful when preparing your residency applications. Your personal statement is one of the most challenging components of the ERAS or CaRMS residency applications, but it is also one of the most important ones. Especially when you consider the fact that emergency medicine is one of the most competitive residencies . Your residency personal statement is a one-page essay that is supposed to tell the residency directors who you are, why you've chosen to pursue your chosen medical specialty - which in this case is emergency medicine - and why you are a good fit it. This blog will give you some tips for writing a strong personal statement and share five different winning emergency medicine personal statement samples that you can use as a frame of reference as you prepare for residency applications .
>> Want us to help you get accepted? Schedule a free initial consultation here <<
Article Contents 19 min read
What is the purpose of a personal statement .
If you want to write a compelling residency personal statement , you need to understand what this document is supposed to achieve. Your personal statement should highlight the "why" behind your decision to apply to a particular residency program. Essentially, you want your statement to answer the following three questions:
Imagine that you've been called for your residency interview, and the interviewer has asked \" How Will You Contribute to Our Program? \" or \u201cwhat kind of doctor will you be?\u201d. When they ask these questions, they are trying to find out what you have to offer as a candidate, and that's one of the things that your personal statement should tell them. Talk about your reasons for choosing the specialty, how your values align with theirs, your strengths and abilities, and what makes you unique as a candidate. ","label":"What will you bring to the program?","title":"What will you bring to the program?"}]" code="tab2" template="BlogArticle">
We know that it sounds like a lot of information to fit in a one-page essay. It can be challenging to get right, but it is doable. Take a look at the emergency medicine personal statement samples below and pay attention to the way that the candidates answer these questions in their essays.
On the second day of my medical school rotations, one of the attendings pointed at me and said, "Now he looks like an ER doc." I laughed because I was not surprised at all. I have always gravitated toward Emergency Medicine because it fits my personality. I am naturally energetic and drawn to a high-paced environment.
I have been convinced that Emergency Medicine is the right fit for me since my first year of medical school, and I got to put my theory to the test during my Emergency Medicine rotation. In the space of a week, we saw gunshot wounds, infections, overdoses, broken bones, common colds, and motor vehicle accidents. At first, I wasn't sure I would be able to keep up with the pace of the trauma bay, but I thrived on it.
A few weeks ago, I celebrated my upcoming medical school graduation by purchasing a 7500-piece jigsaw puzzle. It is the biggest puzzle I have ever attempted to solve, and I can't wait to get started. See, the thing is that solving puzzles of any sort makes me happy. It is one of the many reasons I hope to have a long and rewarding career as an emergency physician.
As a third-year medical student, several factors motivated me to choose a residency in emergency medicine. During my clerkship, I got to experience the fast-paced, unpredictable nature of the emergency room. I quickly found a mentor in one of the attendings that I worked with. His breadth of knowledge, enthusiasm, and calm efficiency - even when all hell seemed to be breaking loose around us - showed me how challenging emergency medicine could be. My interest was certainly piqued, and the more I learned, the more I wanted to know.
I especially enjoyed the challenges of the undifferentiated patient. Often in the emergency room, you are the first to assess and treat a patient who's come in with little more than a chief complaint. You, therefore, have to start the process of diagnosing them from the very beginning. I loved the challenge of being faced with a set of symptoms and having to identify their common etiology.
That said, the most gratifying part for me was the interactions that I had with my patients. Behind all the symptoms that I was presented with were real people from all walks of life. I specifically remember a 62-year-old man who had been brought in after losing consciousness, falling in his kitchen, and getting a deep laceration on his forehead. He was presenting with vertigo and showing symptoms of malnutrition. While I attended to his bleeding forehead, we got to talking, and he explained to me how he had recently lost his wife and had been on a juice fast so that he could try to live longer. I was able to have a conversation with him and advise him on the kind of diet that was better suited for him.
I pride myself on my ability to quickly build rapport with people, especially patients. It is a skill that has always served me well, but it had never felt so useful as it did in the emergency room. Every patient has a story, and sometimes part of treating them is taking a few minutes to ask the right questions and make them feel heard. I was honestly surprised to learn that immersing myself in the unpredictable nature of the emergency room did not mean that I had to interact less with patients. On the contrary, I feel like I got a chance to connect with more people during my emergency medicine rotation than on any other service.
It taught me that emergency physicians wear many different hats throughout the day, and depending on the situation, they can call on various aspects of their medical training. Some cases require the kind of patience and bedside manner that people typically associate with internal and family medicine, while others need a physician who is as quick, decisive, and creative as a trauma surgeon. You never know which hat you will need to wear until your patient is in front of you, and then you simply have to adapt so that you can provide them with the best care possible.
For these reasons, a career in emergency medicine would satisfy my curiosity, constant need to be challenged, and need to connect with patients. I know that I have the skills and the drive required to pursue my training and become a competent emergency physician. Leading a musical band has taught me the importance of communication and shown me that while I am capable of working on my own, I enjoy being a part of a team, and I know how to reach out for assistance when need be.
I look forward to joining a residency program that will help me develop my medical skills and that values patient care and will help me achieve my goal of becoming a caring, competent emergency physician.
When I was a child, my mother often asked me what I wanted to become when I grew up, and up until high school, the answer was never a doctor. My parents are both family physicians, as are my grandmother and my oldest sister. No one ever said anything to me, but I always assumed they wanted me to follow in their footsteps. And I felt like although I didn't want to be, I was different from them because I had no desire to pursue a career in medicine at all.
That said, when you grow up in a house full of physicians, you learn a few things without knowing it. I found that out during a camping trip with my 7th-grade class when one of my friends had an allergic reaction, and we couldn't find an adult to help. Ms. XY was in the bathroom for a maximum of five minutes, but it felt like hours for us as we watched our friend break out in hives and struggle to breathe. I decided to call my mum instead of waiting for our teacher. Whenever she tells this story, she insists that I sounded like an intern on her first day when she picked up, and I said: "X seems to be reacting to something, we are not sure what it is, but she has raised patches of skin all-over her neck and her pulse feels slower than it should be. She needs Epi, right?"
This was not a ground-breaking diagnosis, by any means but it was my first time dealing with someone who was having an allergic reaction. I remember feeling a sense of pride at the fact that I had been level-headed enough to take note of the symptoms that my friend was having and seek help and communicate effectively. After confirming that my classmate did indeed need a shot from an epi-pen, so I went to get one from Ms. X, and she administered the shot.
Even though I had a few experiences of this nature, I was still going back and forth between four different professions, and I could not decide on one. First, I wanted to be a chemist, then a teacher, then a therapist, and then a police officer, and back and forth. It was my guidance counselor in high school that helped me figure out that the right medical career could combine all the things that I love about the professions I grappled with.
I didn't believe her at first, but she was right. After a few conversations with her on the topic, I finally started looking into the different fields that medical doctors can work in. I read an article describing emergency physicians as decisive jacks of all trades, who thrive in high-energy, fast-paced environments, and it felt like they were describing me. That was when my interest in emergency medicine was piqued.
It turned into a mission during my first week of clinical rotations when I worked in the emergency room and loved every minute of it. Every single day in the x general hospital emergency department, I saw at least one gunshot wound, a person with one or multiple broken bones, a motor vehicle accident, and a person whose medical condition is nonurgent. On many days, we had to treat several of those cases simultaneously.
My time at X general hospital confirmed that emergency medicine could give me a platform to do everything I love about the other professions I had considered. As an emergency physician, I get to be on the front lines and occasionally provide preventive care. I also have to listen to my patients and make sure they feel heard and understood, all while teaching them how to take care of their bodies in order to heal correctly.
Now, I can think of no better place to spend my professional career than the emergency department, and I know that with the right training, I will be able to provide my patients with the best care possible because that is exactly what every single patient deserves.
Want an overview of the tips that we cover later in this blog? Check out this infographic:
I didn't always want to be an emergency medicine physician. Actually, when I was in elementary school, I remember telling my dad that I wanted to be an engineer because someone had said to me that they fixed broken things, and I thought that was the coolest thing in the world. I wanted to fix broken things and make people happy. It wasn't until much later that I realized that medicine allows you to do something far cooler, in my opinion: fix people's bodies.
While in college, I got the opportunity to explore the intense, fast-paced world of critical care through an internship. Within a few months of working as a scribe at the X medical center emergency department, I fell in love with emergency medicine. I worked the same hours as some doctors and saw the same number of patients they saw. As I transcribed their medical decision-making, I would imagine myself in their shoes and wonder how I would react to similar situations. The time that I spent in that emergency department gave me an in-depth look at what being an emergency room physician means daily. I got to see them be radiologists, intensivists, orthopedists, and so much more. I admired the physicians who worked in the Emergency Department and loved that they got to wear so many different hats on a given day.
Some days were busy from the moment I came in for my shift to when I would leave to go home. Other days were so quiet that I could actually study for my MCAT right in the middle of the emergency room. The calm rarely lasted long, though, and I always looked forward to the next patient because you never knew what to expect. Sometimes it was a child with a broken bone or a pregnant woman with vaginal bleeding and abdominal pain. Other times it was a drunken man who wanted to tackle everybody in his way or a police officer with a gunshot wound. I found myself excited to get to work, and I just knew that emergency medicine was the perfect specialty for me. It promised to give me a platform to make medical decisions, use the full breadth of the skills I would have as a doctor, be hands-on with my patients, and experience something different every day.
There was no doubt in my mind that emergency medicine was right for me, but I was yet to figure out whether I was a good fit for emergency medicine. When I finally got into medical school, I spent a lot of time reflecting on the qualities that I was told a good emergency physician should have. I knew that I was a good team player because I have been part of a team my whole life. As one of the founding members of a small African dance group in my city, I have always taken the opportunity to be both a leader and a team member in great stride, and we have danced together for thirteen years now. My time as president of the Pre-med Student Union at X university taught me that sometimes you have to take control, and other times, you have to ask for help and work with others. I now know how o recognize those times, and I feel comfortable in both situations.
By my third year of medical school, I was more confident in my skills, and I started to believe that I am well suited to be an emergency physician. On one particular day, I was in the residence cafeteria when a small fire broke out, and chaos erupted around me. I didn't have to think about my actions; I just knew that I needed to remain calm, look for the nearest exit, and help as many people as possible get there. One of my classmates thanked me when we got outside and told me that I was very calm under pressure, a quality that I did not realize I possessed but looking back, I could see right away that she was right. I have always thrived under pressure. I can keep a level head in busy, fast-paced environments and focus on the task I have in front of me.
This theory was tested when I saw my first patient on the first shift of my first emergency medicine rotation. I had arrived five minutes before my shift to get acclimated to the department that I would be working in that day. Right behind me were paramedics, bringing in a two-month-old male who was hypothermic, hypotensive, and barely breathing. I watched in awe as the entire medical team coordinated to intubate, place a peripheral line, administer medications, and work to save this infant's life. Everyone worked together like it was a choreographed dance, and I was able to step back, look for the place where I'd be most helpful, and jump in. I helped one of the residents run the labs, and within an hour, the little boy was stabilized and on his way to the intensive care unit.
I went home many hours and patients later, still thinking about that little boy and how the emergency team's quick and coordinated efforts potentially saved his life. Each day after that, I continued to learn. I learned during my rotations on other services and in medical school. Now, I hope to get the chance to learn from one of the best residency programs in the country so that one day, I, too, can be a part of a coordinated effort to save lives as a skilled emergency medicine physician.
Use a Residency Match Calculator will to assess your match chances this year. It's a quick and easy way to find out how competitive you are for your chosen medical specialty! ","label":"Bonus tip:","title":"Bonus tip:"}]" code="tab3" template="BlogArticle">
I am the youngest of nine children and my parent’s only daughter, so I am used to commotion, and I have learned to thrive within it. When I was growing up, our house was only quiet in the dead of night, and even then, my older brothers would sometimes be playing around in the basement. By the time I was in high school, I'd gotten so used to the chaos around me that very little could break my concentration. I am very aware of my surroundings, but I've learned to decipher what requires my attention and what doesn't. My partner often refers to it as my superpower, and I guess it is in some ways.
This superpower served me well when I first moved to the United States at the age of sixteen and had to spend most of my free time studying. I was able to study in the busy cafeteria during lunch period and in loud classrooms during free periods. I even managed to do my homework in the stands at football games while my brother was playing on a few occasions. I grew up in France, so moving to America meant learning a new curriculum in a language that I did not speak very well at the time. The first few weeks were challenging, but once I figured out how to use my superpower to put in more study hours, I started making progress. Eventually, I graduated in the top 25% of my class.
I approach everything that I do with this same dedication and work ethic. I did it throughout my undergrad years, when I worked as a teacher's assistant, ran track for the school team, and completed my degree in biotechnology. I also did it in medical school, where I discovered that I genuinely enjoy teaching by offering tutoring lessons. I plan to continue in this way during my residency and during what I will work to ensure is a long and fulfilling career.
I believe that my perseverance and passion will help me along the way as I train to become a doctor, but it is because of my curiosity, compassion, and love for the field that I know that with the proper training, I can be a great emergency physician. When I was in primary school, we had a career day, and one of my classmates' friends came in and told us all about his work as an ER doctor. He talked about how he got to heal kids and adults who were hurting, and then he gave us lollipops and told us that if we worked hard, we could do it too. I was sold! At the dinner table that evening, I explained to my family that I was going to become a doctor. They all assumed it was because of the lollipop, but my interest had just been piqued, and the more I've learned about medicine since then, the more I've wanted to know.
I had always been drawn to emergency medicine because of the fast-paced and unpredictable nature of the emergency room. During my clerkship, I got to learn more about the core specialties in medicine, and I confirmed that emergency medicine was perfect for me. One of the attendings that I worked with in the ER told me that "emergency doctors are people who just like doing things, all the time." She told me that she knew it was right for her when she realized that she was just as comfortable around big scary things like traumas and codes as when dealing with children with appendicitis.
Her words stayed with me because they described precisely how I felt during my time in the emergency room. I loved the diversity in patients' presentations—surgical, medical, social, psychiatric, etc. I loved being required to think on my feet and act quickly to provide lifesaving or limb-saving care at a moment's notice.
Emergency medicine is the perfect platform for me to utilize my superpower, work ethic, and passion for medicine to provide patient care in an environment that is almost reminiscent of the home I grew up in. I cannot imagine a more fulfilling career path for myself.
Five Tips for a strong personal statement
1. start early.
Writing a residency personal statement, especially for a competitive field like emergency medicine, is not something that you can rush through. We recommend that you give yourself at least six to eight weeks to brainstorm, write, edit and polish your personal statement. The earlier you start, the more time you will have to review your statement and get a second pair of eyes to look at it to ensure it is as compelling as possible. You do not want to be scrambling at the last minute and end up with a subpar essay because you waited until the last minute to get the job done.
The key to an excellent personal statement is preparation. You should take the time to brainstorm and plan the structure of your essay for two reasons: First, because having a structure will guide you and keep you on track as you write. Secondly, because we tend to get attached to our work, and if we get to a point where we realize that the flow of the personal statement is off, it is harder to delete a whole paragraph than it is to just rewrite a few sentences. We suggest that you brainstorm first. Think about the questions that we mentioned earlier and write down your answers to those questions, as well as any memorable experiences that have contributed to your decision to become a physician.
4. Stay true to yourself
Students often make the mistake of writing what they think the program directors want to hear instead of the truth. This usually backfires because it can end up sounding cliché and generic, but also because it will likely not be consistent with the rest of your application. Your personal statement should be about you and your suitability for the residency program. So, be honest and don't try to fabricate your statement or exaggerate your experiences. Instead, tell the residency program directors about your exposure to medicine, what you've learned, and how your experiences led to you wanting to pursue this vocation.
Have you started preparing for your residency interviews? This video is for you:
5. Seek feedback
It's not enough to make statements about yourself. If you want to write a compelling statement, you need to back your claims up with specific examples or short anecdotes. Not only do people tend to remember such things more, but it is just a more impactful way to write. For example, instead of saying, "I am good at handling stress," you could say, "My role as the oldest sister of five children has often tested my ability to handle stressful situations." The second sentence is more memorable, and if you followed it up with an anecdote about one of those stressful situations, it would be even more impactful. It shows the directors that you have experience dealing with stressful situations, and it also gives them some new information about your background.
Your residency personal statement shouldn't be longer than one page unless otherwise specified. You should aim for an essay that is between 650 and 800 words.
Your personal statement should tell the program directors why you've chosen to pursue your specialty, why you're suited for it, and their program.
They are an essential part of your residency application as they give you a chance to tell the program directors why you are a good fit for your chosen field and their program in your own words. You should definitely not underestimate their importance.
While you can certainly send different versions of your personal statement to different programs, we do not recommend that you address them to any program in particular because this would mean writing several different personal statements. Instead, focus on writing personal statements that are tailored to specific specialties.
That depends on the concern in question. You should only discuss issues that you haven't addressed in other application components and that are relevant to the rest of your statement. If you address any red flags, make sure you demonstrate maturity and honesty by taking ownership of the problem and explaining how you've learned and grown from your mistakes.
Yes. Emergency medicine is one of the most competitive residencies, so you need to ensure your residency application is compelling if you want to secure a spot in a top program.
No, you do not. Most students apply to 15 - 30 residency programs in one application cycle, so writing a letter for each one is simply not feasible. Instead, you should write a letter for each specialty that you are considering.
You can write a strong personal statement if you take the time to brainstorm and plan for your essay early, use specific examples in your writing, and seek feedback from experts.
Want more free tips? Subscribe to our channels for more free and useful content!
Apple Podcasts
Like our blog? Write for us ! >>
Have a question ask our admissions experts below and we'll answer your questions, get started now.
Talk to one of our admissions experts
Our site uses cookies. By using our website, you agree with our cookie policy .
FREE Training Webinar:
How to make your residency application stand out, (and avoid the top 5 reasons most applicants don't match their top choice program).

Tips for Writing Your Personal Statement
Writing an amazing residency personal statement on your ERAS application is about telling your story in your own voice. It’s about telling the reader something about you that cannot be gathered from other parts of the application.
The personal statement is a longer discussion of yourself, motivation, and experiences. It is also an important element of your application as 67% of residency programs cite personal statements as a factor in selecting students to interview. We’ve put together some tips to help you below.
“Do’s” of writing personal statements :
🗸 DO tell a story about yourself or share a unique situation. You are showing the reader your narrative about why you are a great candidate for residency.
🗸 DO make it human. Approach the statement as an opportunity to process life experiences and articulate the arc of your journey.
🗸 DO be specific. Clearly outline your interest in the specialty, and use concrete examples where able.
🗸 DO be candid and honest.
🗸 DO pay attention to grammar and writing style.
🗸 DO keep the statement to one page.
🗸 DO get an early start. We recommend to begin writing your personal statement during the summer between your third and fourth years of medical school to allow ample time for revisions and reviews. Be prepared to do many drafts.
🗸 DO include personal challenges you have overcome in your medical education journey so far.
🗸 DO get feedback. Have multiple people read your statement including faculty in your field.
What to avoid :
✖ DON’T tell the reader what an emergency physician does; he or she already knows this.
✖ DON’T belittle another person or specialty.
✖ DON’T overestimate your personal statement. The benefit gained from even an outstanding personal statement is still marginal compared with other aspects of your application which carry more weight.
✖ DON’T underestimate your personal statement. A poorly written or error-filled personal statement can drag down your candidacy.
✖ DON’T just focus on activities that the admissions committee can learn about from your application. Use this opportunity to give NEW information that is not available anywhere else.
Questions to Consider When Writing
Crafting a strong personal statement begins with self-reflection. Before you even begin writing, lay the groundwork for your statement by asking yourself the following questions:

Why are you choosing emergency medicine? If you want to help people, why don’t you want to be a social worker or a teacher (for example)? What interests, concerns, or values drive you in your studies, work, and career choice?
Think back to volunteer, shadowing, global health, research, work, and coursework experiences. What has been defining? Are there any moments that stick out? What did you learn about yourself or your future profession? How did you change after that experience?
What do you want the residency program to know about you as a person, a student, and a future colleague? What makes you a good fit for the profession and the profession a good fit for you?
What makes you unique from other applicants?
Additional Resources

Most universities and colleges also have writing centers that may be able to help you focus your ideas into a theme or read and give feedback on your personal statement.
*This resource is intended to serve as inspiration and a compass to guide your own writing. All personal statements or parts thereof may not be reproduced in any form without written permission of the author.
- AI Content Shield
- AI KW Research
- AI Assistant
- SEO Optimizer
- AI KW Clustering
- Customer reviews
- The NLO Revolution
- Press Center
- Help Center
- Content Resources
- Facebook Group
Emergency Medicine Personal Statements: a Free Guide
Table of Contents
With the examples and tips shared in this article, crafting an effective personal statement for emergency health workers should no longer be a problem.
Admittedly, this can be daunting, especially with limited guidance and resources available. But fear not. This free guide provides you with everything needed to compose a unique and compelling essay that will stand out from the rest.
To make things easier, you’ll also find an emergency medicine personal statement sample to help you get started.
Tips for Writing Emergency Medicine Personal Statements
Convey a clear purpose.
When writing an emergency medicine personal statement , it is important to capture the essence of why you want to pursue the career.
In addition, show how your current experiences have shaped your passion for the profession. Ensure that your introduction conveys a clear purpose and concisely explains your motivation and inspiration.
Structure It Logically
A major key when crafting a compelling essay is effectively structuring the content. Begin with a succinct paragraph outlining your objectives before delving into details about your academic background.
Go on to discuss any relevant skills or experience, as well as other attributes which would make you an ideal candidate for emergency medicine. Be creative in showcasing your strengths but be mindful not to stray from the primary topic of the essay.
Maintaining focus throughout the personal statement is essential. Ensure that each sentence adds value toward reinforcing your overall message and goal. Vague descriptions and rambling should be avoided.
Try to get to the point quickly and stick to facts rather than opinions. Additionally, consider using active voice sentences, as they usually create more engaging content.
Stay Honest
Remember to stay grounded. Although it is good practice to showcase yourself in a positive light, do not go overboard by listing unsubstantiated claims or unrealistic accomplishments. Stay honest, humble and realistic throughout the entire statement. Provide evidence for every assertion you make within the essay instead of relying on mere words alone.
Adhere to Proper Grammar Rules
Adherence to proper grammar rules is vital for creating an effective piece of writing. No matter how interesting or complex your ideas may be, it won’t count for much if your essay is riddled with errors.
Emergency Medicine Personal Statement Sample

This section contains good examples that can inspire you as you write yours. Read through and select the emergency medicine personal statement sample that best reflects your aspirations.
I am a passionate medical professional with an unwavering commitment to providing the highest quality of emergency care. Throughout my career, I have continually sought out opportunities to develop and hone my expertise in this field. I shadowed experienced physicians during medical school, and I completed several residencies in emergency medicine. My ultimate goal is to combine my dedication to patient-centered care with my enthusiasm to provide the best outcomes possible for patients.
A major source of motivation throughout my studies has been the opportunity to gain insight into different facets of emergency medicine. To supplement these experiences, I have also pursued additional coursework on topics such as environmental health and injury prevention. My studies have not only sharpened my clinical judgment but have allowed me to appreciate the complexities of healthcare provision in today’s world.
I strive to be an advocate for those in need of emergency medical attention, regardless of their background or identity. In everything that I do, I aim to provide personalized and compassionate care while always putting safety first. Moreover, I prioritize a continual exchange of information between myself and the patient so that we can collaborate together toward achieving better health outcomes. This holistic approach is something I take great pride in, especially when it comes to ensuring that each patient leaves the ER feeling safe.
As someone eager to challenge themselves in this exciting field, I’m confident that I will bring energy and enthusiasm to any emergency medicine role. By continuing to pursue opportunities to expand my knowledge base and training, I believe I could make a positive contribution to any organization.
I have had a lifelong passion for emergency medicine, and I am determined to pursue a career in it. With over seven years of experience working as an Emergency Medical Technician, I bring an extensive set of skills and abilities to the field. My experience has enabled me to develop a holistic approach to patient care. At the same time, I try to be aware of every detail needed to provide fast and effective treatment. From traumas to cardiac emergencies, I always display poise, confidence and decisiveness, even when faced with chaos and pressure.
Furthermore, my involvement in several research projects, including one related to improving stroke care outcomes, has helped me understand the importance of evidence-based practice. Additionally, through medical residencies and volunteering at free clinics, I was able to hone my communication and collaboration skills. These skills enable me to work well within teams, discuss complex topics with patients and form meaningful relationships. This knowledge and my unwavering commitment to contribute to the betterment of healthcare have enhanced my enthusiasm for pursuing residency training in emergency medicine.
I firmly believe that these qualities make me highly qualified for a residency position. With ambition and determination, I’m sure that I can help foster team spirit and promote safe clinical environments that provide quality patient care.
Personal statements are like formal advertisements . They allow you to sell yourself and your ability to people in authority . This article focuses on writing personal statements for emergency medicine. The tips and examples therein can help you create a convincing personal statement.

Abir Ghenaiet
Abir is a data analyst and researcher. Among her interests are artificial intelligence, machine learning, and natural language processing. As a humanitarian and educator, she actively supports women in tech and promotes diversity.
Explore All Write Personal Statement Articles
How to draft meaningful length of law school personal statement.
Are you confused on how to write a law school personal statement? One of the essential elements of your application…
- Write Personal Statement
Effective History and International Relations Personal Statement to Try
Are you considering studying history and international relations? Or you may be curious about what a degree in this field…
Guide to Quality Global Management Personal Statement
Are you applying for a global management program and want to stand out from the crowd? A well-written personal statement…
How to Draft Better Examples of Personal Statements for Residency
Achieving a residency can be a massive accomplishment for any aspiring medical professional. To secure your spot in one of…
Tips for Drafting a Free Example of Personal History Statement
A personal history statement can be crucial to many applications, from university admissions to job search processes. This blog will…
Writing Compelling Dietetic Internship Personal Statement
Applying for a dietetic internship is a rigorous process and requires submitting a personal statement, which is an essential part…
- EM Resident
- Publications
- Join/Renew EMRA
Popular Recommendations
- Board of Directors
- EMRA Committees

PEM Personal Statement Example
Provided by michele mcdaniel.
From the moment I took my first, tremulous step through the doors of the hospital with my freshly ironed white coat and my newly minted title of MD, I knew I wanted to have a career in the field of pediatric emergency medicine. To anyone who loves kids, the reasons are obvious, plentiful, and easy to understand. Children are fun! They are vibrant and happy, and, for the most part, when they present to your ED, some combination of a silly face, a sticker, a popsicle, and your flavored antipyretic of choice cures what ails them and they go home to continue being cute little monsters. However, to people like you and me, who are passionate about the field of pediatric emergency medicine, the reasons for choosing this career resonate much deeper.
I can remember one specific case which will stick in my mind forever. As an intern, I picked up a chart with the chief complaint "fever". When I opened the door to walk into the room I found a mother, sobbing, clutching her toddler son to her chest. It didn't take me long to realize that the fever wasn't the only reason she had come. On speaking with her, I discovered that her son had suffered a febrile seizure. She was terrified, and visibly much more upset than her peacefully sleeping child. After listening to her story, we proceeded to discuss what had happened. She had no idea that a simple febrile illness could cause a seizure, and was relieved to know that her child most likely would never have another event. Over the course of our conversation, I could see her relax, and she left at peace and thanked me for doing something which required no medical skill at all, simply being available to talk - one human to another.
This case illustrates well those things that attract me to pediatric emergency medicine. I challenge anyone to find another specialty in which you see a comparable breadth of disease. Take for example the case of a febrile seizure. Do you know any adult who has seized during the course of his or her febrile URI? It never ceases to amaze me just how much medicine you need to know in order to complete even one shift in the peds ED. There are an endless number of diseases that present more commonly in a certain age group, have a symptom complex congruent with a variety of disease processes dependent upon the patient's age, or have a completely different presentation based on whether your patient is 6 months or 6 years old.
But it's not only the diagnostic challenge that excites me. I also enjoy the non-medical aspects of working with children as patients. The pediatric emergency department is a venue where communication skills go a long way. Whether you're demonstrating the superpowers of your "magic flashlight" in order to look in a three year old's ears, easing a mom's worries about a high fever, or making a consult, effective communication is extremely important. It is also helpful in identifying ways to make a difference for your patients beyond the prescription pad. The pediatric ED is perfect place to discuss prevention - bike helmets, proper car seat placement and seat belts, avoiding tobacco/alcohol/drug use, safe sex practices - the list is endless. The pediatric emergency department is also a fertile ground where advocacy takes root and flourishes. There are so many opportunities to reach out to young, malleable minds that you only have to dream up an initiative and you can make a difference that can span generations.
I have been fortunate to be a part of several different advocacy projects during my time at Indiana University. Whether it was fitting bike helmets and guiding young bike riders through an obstacle course, teaching mentally and physically handicapped children how to tell their life stories through photography, or coaching elementary students who'd never swum an entire length of the pool through a triathlon, I've enjoyed every opportunity to reach out into my community. This is something I intend to carry on through my time in fellowship. I have a particular interest in the area of non-accidental trauma, and I hope that, between the skills I've learned in my past advocacy work, my upcoming elective with the child protection team, and the knowledge I'll gain during my fellowship training, I'll be able to translate community-based research into community-based initiatives that will aid in prevention of child abuse in the future.
Beyond being a venue for furthering my interest in advocacy and research, I also know that a fellowship in pediatric emergency medicine will allow me to develop the skill set I need to achieve my career goals. I hope to one day work in both the adult and pediatric emergency departments at a large academic center and pass on the fruits of my education and experience to the next generation of emergency physicians. Having past experience in coaching and teaching, and having recently begun to have "staffing shifts", I know my passion lies in sharing my knowledge with others, and I look forward to each opportunity I'll have to gain more experience in the field of teaching and mentoring. I hope to one day be a successful clinician educator and I know that, by combining the knowledge and skill I'll gain from fellowship and my existing passion for emergency medicine (especially pediatric emergency medicine), I'll have a fulfilling and exciting career for many years to come.
I love what I do, and I'm looking forward to the next few years in which I'll be able to build a strong foundation for my future career. I know that I'll be able to provide as much enthusiasm and dedication to my program as I will gain knowledge and skill that I'll carry forward. I can't wait to be a part of the pediatric emergency medicine family, and I'll be proud to call myself your colleague one day.
Related Content

Aug 25, 2017
The Emergency Medicine Residents' Association EMRA is the voice of emergency medicine physicians-in-training and the future of our specialty and the largest and oldest independent resident organization in the world. EMRA was founded in 1974 and today has a membership over 18,000 residents, medical students, and alumni.
Jan 19, 2018
Emergency Medicine Wellness Week

When Lightning Strikes
- EM RESIDENT
- ADVERTISE & EXHIBIT
- Connect with us

EM can lead the way in addressing healthcare inequities. But first we must face the deficiencies of diversity, equity, and inclusion in our field. It starts with training.
Make sense of the chaos of the trauma bay with the emra trauma guide., mobilem put every emra guide in your pocket..
© 2021 Emergency Medicine Residents' Association | Privacy Policy | Website Links Policy | Social Media Policy
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Thematic Analysis of Emergency Medicine Applicants’ Personal Statements
Xiao chi zhang , md, ms, jeremy lipman , md, randy jensen , md, phd, kendra parekh , md.
- Author information
- Article notes
- Copyright and License information
Corresponding author.
Collection date 2019 Sep.
The personal statement is an important part of the residency application. Although guidance exists, the composition of personal statements is not standardized; each statement reflects an applicant’s unique personality. In emergency medicine (EM), the personal statement could thus provide insight into why applicants are choosing EM and what they hope to accomplish in the field that could guide advisors and applicants.
To perform a thematic analysis of personal statements from applicants accepted into an academic EM residency program to gain insight into what successful applicants include in their personal statements, why applicants are pursuing careers in emergency medicine, and anticipated career goals.
Thematic analysis was performed on ten randomly selected personal statements from matched allopathic, U.S. applicants at a single, large, urban 3-year EM residency program between 2008 and 2015. Themes and sub-themes were identified and analyzed for frequency.
Ten personal statements were analyzed. Thirty-one (31) unique themes were identified and grouped into five main themes: personal characteristics related to a career in EM (38.3%, 116/303), why I love EM (36%, 109/303), my story (13.5%, 41/303), my career in EM (8.9%, 27/303), and ideal characteristics of a residency program (3.3%, 10/303). The most common personal characteristics described were altruism and the ability to work well under pressure. Applicants love EM due to the diversity of patients and disease presentations and the ability to perform procedures.
Conclusions
Thematic analysis of EM applicants’ personal statements highlights the uniqueness of EM as a specialty and what draws applicants to EM.
Keywords: Emergency medicine, Medical student, Personal statement, Residency application, Texual analysis
Emergency medicine (EM) is becoming a highly competitive specialty with 1.2 to 1.3 applicants for each available spot [ 1 ]. In 2017, there were 3575 medical students who entered the National Resident Matching Program (NRMP), hoping to pursue a career in EM, and each EM residency program received an average of 941.8 applications [ 1 ]. As the number of applications per program increases, it becomes more challenging for the selection committee, usually comprised of program directors and associate program directors, to screen and select applicants for interviews. While a universal medical application includes academic achievements, transcripts, United States Medical Licensing Examination (USMLE) scores, and standardized letters of evaluation (SLOEs), one of the most uniquely personal aspects of the Electronic Residency Application Service (ERAS) application is the personal statement.
A compelling personal statement plays a significant role in the overall application process by providing the opportunity for applicants to embed their personality, interests, and passion for EM into their application beyond the constraints of a curriculum vitae [ 2 , 3 ]. Personal statements also provide program directors insights into applicants’ understanding and expectations of a career in EM. In the NRMP’s 2016 Program Directors survey, 66% of program directors cited personal statements as a crucial determinant in selecting applicants for interviews with an importance rating of 3.3 out of 5 [ 4 ]. Program directors also cited professionalism and personality with respective importance ratings of 4.9 and 4.5 out of 5, factors which are often reflected in the personal statement [ 4 ]. Some have even viewed the personal statement as an applicant’s perceived professional identity [ 5 ].
While formal and informal guidelines for writing personal statements are available from the American Medical Association (AMA), the Council of Emergency Medicine Residency Directors (CORD), medical school writing workshops, and student-centered websites, the impact of these efforts is unknown [ 6 ].
To our knowledge, the content of EM applicants’ personal statements has neither been explored nor previously published. Thus, the purpose of this study is to perform a thematic analysis of personal statements from applicants accepted into an EM residency program to better determine what successful applicants include in their personal statements and their perceptions of the specialty.
Personal statements of matched allopathic, U.S. applicants at a single, large, urban 3-year EM residency program between 2008 and 2015 were considered for inclusion in the study to ensure that no current residents at the time of the study would be included in the sample. Osteopathic and international medical graduates were excluded from this analysis as they make up a small portion of the EM applicant pool. During the study selection period, the EM residency admission committee was comprised of one program director and two associate program directors, all with various levels of education and leadership experience.
All eligible personal statements were screened for completeness and fully de-identified prior to analysis. Purposive sampling was used to create a sample representing the majority of applicants to EM residencies. Thematic analysis was used to explore the contents of EM applicants’ personal statements using an inductive coding approach to ground the study [ 7 ]. Manifest and latent coding were used to optimize the reliability of the thematic analysis. From the 100 available personal statements, two were randomly selected for generation of themes. All four authors, each with extensive experiences in residency selection (two authors were non-EM program directors, one author was the Director of Undergraduate Medical Education and EM Clerkship Director, and one author was Core Faculty and Assistant Director of an EM Clerkship), independently generated themes from these two personal statements. The authors then met to review and edit the themes through a collaborative, iterative process until the final themes were generated in consensus. Common themes identified by the authors were similar to those identified in prior studies in surgical specialties [ 8 ]. After thematic generation, ten (10) statements were randomly selected for analysis with plans to supplement these statements with additional personal statements as necessary to achieve theme saturation.
To identify themes, the authors divided themselves into teams of two; each team was responsible for independently identifying themes in half (5) of the personal statements. To minimize researcher bias, each team included a non-EM trained physician and an EM-trained physician. The authors utilized Dedoose [ 9 ], a qualitative data management software program, to code the statements and analyze the data for frequency of themes and sub-themes. Once each team concluded its independent review, both teams would review the personal statements coded by the other team before reaching consensus on the identification of the themes for all ten personal statements. This study was deemed exempt by the Thomas Jefferson University Institutional Review Board.
Ten (10) personal statements were analyzed. Thirty-one (31) unique themes were identified and grouped into the following five main themes (Table 1 ):
Personal characteristics related to a career in EM (38.3% of themes): This theme includes personal characteristics that make the applicant suitable for a career in EM such as being altruistic or working well under pressure.
Why I love EM (36% of themes): This theme includes the reasons why an applicant specifically chose emergency medicine for a career, such as the diversity of patients and the ability to perform procedures.
My story (13.5% of themes): This theme includes a personal story of growth and overcoming challenges and personal experiences with the medical system that inspired the applicant to pursue medicine as a career.
My career in EM (8.9% of themes): This theme includes what applicants aspire to in their future careers as emergency medicine physicians and includes goals such as pursuing specific research interests or fellowships.
Ideal characteristics of a residency program (3.3% of themes): This theme focuses on the characteristics of the applicant’s ideal residency program such as a challenging environment that offers autonomy or caring for an underserved population.
Frequency of themes and sub-themes determined by a random selection of personal statements for emergency medicine (EM) residency from a tertiary academic center from 2008 to 2015
| Codes grouped by theme | Frequency ( ) | Percent of total codes |
|---|---|---|
| My story | 41 | 13.5 |
| Clinical vignette | 9 | 3.0 |
| Volunteer experience in medical setting | 11 | 3.6 |
| Personal experience with medical system | 5 | 1.7 |
| Story of personal growth | 16 | 5.3 |
| My career in EM | 27 | 8.9 |
| Leadership | 8 | 2.6 |
| Academic and research | 11 | 3.6 |
| Clinical medicine | 8 | 2.6 |
| Personal characteristics | 116 | 38.3 |
| Identifying problems | 11 | 3.6 |
| Part of a team | 8 | 2.6 |
| Thrive in chaos | 5 | 1.7 |
| Work ethic | 6 | 2.0 |
| Work unusual schedule | 3 | 1.0 |
| Work well under pressure | 15 | 5.0 |
| Altruistic | 24 | 7.9 |
| Decision making | 7 | 2.3 |
| Demonstrate EM knowledge | 5 | 1.7 |
| Determination | 11 | 3.6 |
| Manage complex situations | 5 | 1.7 |
| Personal accomplishments | 16 | 5.3 |
| Residency program characteristics | 10 | 3.3 |
| Better doctor | 6 | 2.0 |
| Independence | 1 | 0.3 |
| Challenging | 3 | 1.0 |
| Why I love EM | 109 | 36.0 |
| Alleviate suffering | 6 | 2.0 |
| Differential diagnosis | 14 | 4.6 |
| Diversity of patients | 31 | 10.2 |
| First point of contact | 6 | 2.0 |
| Impact long term health | 10 | 3.3 |
| Motivating patients | 3 | 1.0 |
| Procedures | 15 | 5.0 |
| Acuity of patients | 14 | 4.6 |
| Preventive care | 10 | 3.3 |
A total of 303 theme statements were applied across the 10 personal statements, with an average of 30.3 themes per personal statement (SD = 8.01, range = 21–46). Table 1 displays the frequency of themes. Table 2 displays selected quotes from the common themes and sub-themes.
Selected quotes or emergency medicine personal statements as characterized by the five main themes
| Themes | Selected quotes |
|---|---|
| Personal characteristics related to a career in EM | Altruism: “Contributing to the community has been a standard that I have upheld throughout my adulthood.” “I am driven to provide for the needs of my patients and provide them with the best possible service.” Personal accomplishments: “I founded the international health interest group, Global Health Forum, which introduces medical students to current issues in international health and helps them gain medical experience abroad during their education.” Work well under pressure: “My even-tempered, quick, logical thinking during stressful situations will complement nicely my other attributes.” “I am well suited for emergency medicine because of my ability to work under pressure, and to stay calm and think logically in stressful situations.” |
| Why I love EM | Broad patient and disease presentations: “I can deal with the drunk who is uncooperative, the rambling schizophrenic or the demented elderly person.” “What fascinated me the most was the variety of the field, as no two shifts in the emergency room are ever the same. The profession has elements of nearly every field of medicine - from procedures, to primary care, to obstetrics/gynecology, to psychology, and everything in between.” Patient acuity: “Although Emergency Medicine can be considered the ‘jack of all trades’ specialty in certain regards, it is commonly misunderstood that they are, in fact, masters of acute intervention and prioritization.” “…stabilizing the unstable patient…” Forming differential diagnoses: “What I enjoy about emergency medicine is the constant need to think about atypical presentations for common diagnoses.” “I enjoy the responsibility of formulating a differential based on the history and interrogating those suspects with a complete, but directed physical exam and laboratory studies.” |
| My story | Personal growth: “…these changes have been immeasurable treasures that allowed me to grow into the person I have become.” “During this time, I learned the valuable lesson of how to deal with adversity while fulfilling my professional commitments.” Volunteer/personal experiences: “I learned that my mother had been living with the secret of advancing breast cancer which she had kept from her family, her friends, and even her doctor.” “In my undergraduate years I volunteered for 4 years at a community emergency department, as well as with Habitat for Humanity.” Clinical vignette: “I remember one patient with an asthma exacerbation due to crack cocaine use. The medical team gave him some nebulizer treatments. It soon became obvious he was not responding to the treatment and the attending physician performed a rapid sequence intubation. The experience inspired me.” |
| My career in EM | Future goals in emergency medicine: “Beyond residency, I hope to complete a fellowship in International Emergency Medicine.” “I plan on continuing to make research a part of my career and hope to bring more evidence-based practice to the field of Emergency Medicine.” |
| Ideal characteristics of a residency program | “I seek a residency program that is as excited at producing excellent physicians as caring for anyone, with anything, at any time.” |
All personal statements included a discussion of such personal characteristics. Some applicants provided specific examples of characteristics, while other applicants simply stated that they possessed the characteristic. The most commonly cited personal characteristic was being altruistic, followed by personal accomplishments and specific examples of how they work well under pressure.
The next most commonly identified theme was why I love EM, and all ten personal statements included comments reflecting this theme. Applicants discussed a myriad of reasons why they love the field of emergency medicine. The most commonly cited reason was the diversity of patients and disease presentations, being able to perform procedures, the acuity of patients, and building a differential diagnosis. Patient acuity was described in specific terms by listing acute conditions such as acute stroke and acute coronary syndrome as well as in general terms about managing acute needs..
This theme was identified in nine out of ten personal statements. There was diversity in how applicants discussed their story, from accounts of personal growth to experiences within the medical system, and specific clinical vignettes that inspired them to choose EM. Finally, all personal statements included comments about the applicant’s expected future career, which included post-residency goals as well as ideal residency program characteristics..
Occurrence of themes was also identified among the personal statements. The most commonly co-occurring themes were personal accomplishment and leadership, preventive care, and impacting long-term health. The next most common co-occurring themes were identifying problems and working under pressure, altruism and determination, and differential diagnosis and diversity of patients.
This study marks the first published report on personal statement contents from successful applicants to emergency medicine residency programs. The most commonly expressed themes in applicants’ personal statements were the description of personal characteristics that made the applicant well suited for the specialty. Applicants often provided specific characteristic examples that made them particularly prepared for a career in EM (Table 1 ). Previous work focusing on applicants’ personal statements to other residencies (internal medicine, general surgery, ophthalmology, and pediatrics) also identified similar themes to those characterized in our study [ 5 , 8 , 10 , 11 ]. Our analysis identified that EM applicants frequently discussed their ability to work well under pressure and altruism, which appears to be a theme unique to EM personal statements when compared with the work done in other specialties. Describing personal characteristics is in keeping with the American Association of Medical Colleges (AAMC)’s advice to portray marketable abilities [ 12 ]. Additionally, the characteristics mentioned by applicants—altruism and ability to work well under pressure—represent distinct personality characteristics of EM residents when compared to the general physician population [ 13 ].
It is noteworthy that discussion of why I love EM is included in all the personal statements examined in this study. The most commonly cited reason was the diversity of patients and disease presentations. This element has been identified in personal statements from internal medicine applicants, and we posit the frequency of this theme within EM applicants may be attributable to publications that recommend including this element [ 5 , 10 , 14 ]. Interestingly, this theme was not found in personal statements of those pursuing anesthesia or radiology residencies [ 3 , 15 ]. This discrepancy may relate to different resources and advising strategies for students applying to these fields or specialty-specific differences in expectations. The next most commonly mentioned reason for pursuing a career in EM was the opportunity to perform procedures; this reason was also identified as a common theme in applicants to surgical residences but not by applicants to internal medicine and pediatrics [ 8 , 10 , 11 ].
EM applicants also expressed an attraction to the acuity of care and taking care of patients in the acute phase of illness. This provides a unique perspective compared to themes identified in the literature concerning other specialties [ 3 , 5 , 8 , 10 , 15 – 17 ]. This finding along with the identification of specialty-specific personal characteristics again highlights the specialty-specific information that can be gleaned from personal statements. This may inform program directors of the alignment between applicant and program goals for training.
Almost all applicants discussed my story, which was their personal narrative for why they chose EM. This theme was presented in a wide variety of ways, but universally, the applicants explained their journey from an influential tipping point (e.g., personal experience or volunteer experience) to the present state of applying for an EM residency. This theme was also identified in dermatology, general surgery, internal medicine, ophthalmology, and pediatrics residency applicants [ 5 , 8 , 10 , 11 , 18 ]. This is also in keeping with the AAMC’s Careers in Medicine advice that the personal statement “be personal” [ 12 ]. The presence of this theme across multiple specialties may indicate good penetrance of the AAMC’s Careers in Medicine advice or natural concordance and agreement among program directors about what is important in a personal statement.
Due to a high prevalence of common features within personal statements across specialties, there is an overall perception that these documents are becoming more impersonal over time [ 3 ]. We have identified common themes found in personal statements written by applicants who ultimately matriculated to academic EM residency programs. Thus, an argument can be made in favor of standardizing the personal statement. This could potentially be advantageous to both programs and applicants if executed appropriately. If there was consensus among program directors for a given specialty on which theme(s) they find most useful in selecting applicants for interview, applicants could be encouraged to focus their statements on those theme(s). Program directors would have additional information perceived as valuable and applicants could more clearly focus on their narratives.
However, the goal of the residency application process is to identify which applicants best fit at a training program, and although the residency application incorporates information from a variety of sources, the personal statement remains the only portion of the application that provides a direct dialogue from the applicant to the program. As such, it allows for creativity and provides a tremendous opportunity for the applicant to identify and accentuate the elements of their application and background they believe would be most helpful to a selection committee. Our study identified unique characteristics discussed in personal statements that reflect the unique characteristics of emergency physicians demonstrating that it is possible to have distinction among personal statements. This could be lost with standardization of personal statements.
Limitations
This study was conducted at a single institution, with randomly selected statements, over an 8-year time frame, and only included applicants who matched into EM. Common themes may be different for applicants who go unmatched. Similarly, the statements were from applicants who matched at an academic residency program. Themes from applicants applying to a primary community program may be different. Osteopathic and international applicants were excluded, and these personal statements may express different themes than those captured in this study. Additionally, we acknowledge our sample size was small, and we did not consider other factors that might influence personal statements, nor did we attempt to analyze whether these personal statements improved or hindered the applicant’s likelihood of matching.
This study marked the first attempt at thematic analysis of personal statements of accepted applicants at an allopathic 3-year EM residency program. All statements included discussion of personal characteristics that make the applicant suitable for EM, why the applicant loved EM, and the applicants’ future goals. The most commonly cited personal characteristics were altruism and an ability to work under pressure. The most commonly discussed reasons for loving EM included the diversity of patients and being able to perform procedures. While this study was limited to a small sample of personal statements at a single institution, the themes identified in personal statements can be helpful in informing program directors how applicants view the practice of emergency medicine and can help guide prospective applicants on how to structure their personal statements. Future studies will be conducted to expand this pilot study by analyzing personal statements from multiple EM residencies and including osteopathic, international, and unmatched applicants. Further exploration could also include the impact of gender and underrepresented minority status on personal statements.
Compliance with Ethical Standards
This study received an ethical approval (IRB-Exempt no. 18E.436).
Conflict of Interest
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Xiao Chi Zhang, Email: [email protected].
Jeremy Lipman, Email: [email protected].
Randy Jensen, Email: [email protected].
Kendra Parekh, Email: [email protected].
- 1. AAMC. Electronic Residency Application Service Statistics 2017. https://www.aamc.org/services/eras/stats/359278/stats.html .
- 2. Association of American Medical Colleges. (2018). Historical Specialty Specific Data: Emergency Medicine. Retrieved from https://www.aamc.org/download/359222/data/emergencymed.pdf . Accessed 10 May 2018.
- 20. Association of American Medical Colleges. (2019). About ERAS. Retrieved from https://students-residents.aamc.org/applying-residency/article/abouteras/
- 3. Max BA, Gelfand B, Brooks MR, Beckerly R, Segal S. Have personal statements become impersonal? An evaluation of personal statements in anesthesiology residency applications. J Clin Anesth. 2010;22(5):346–351. doi: 10.1016/j.jclinane.2009.10.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. National Resident Matching Program. Results of the 2016 NRMP Program Director Survey. 2016 (June):79–80. http://www.nrmp.org/wp-content/uploads/2016/09/NRMP-2016-Program-Director-Survey.pdf . 8 June 2018
- 5. Osman NY, Schonhardt-Bailey C, Walling JL, Katz JT, Alexander EK. Textual analysis of internal medicine residency personal statements: themes and gender differences. Med Educ. 2015;49(1):93–102. doi: 10.1111/medu.12487. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. Campbell BH, Havas N, Derse AR, Holloway RL. Creating a residency application personal statement writers workshop: fostering narrative, teamwork, and insight at a time of stress. Acad Med. 2016;91(3):371–375. doi: 10.1097/ACM.0000000000000863. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Glaser BGSAL. The discovery of grounded theory: strategies for qualitative research. Chicago; 1967.
- 8. Ostapenko L, Schonhardt-Bailey C, Sublette JW, Smink DS, Osman NY. Textual analysis of general surgery residency personal statements: topics and gender differences. J Surg Educ. 2018;75(3):573–581. doi: 10.1016/j.jsurg.2017.09.021. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. Dedoose. https://www.dedoose.com/ . Published 2018. Accessed June 12, 2018
- 10. Lee AG, Golnik KC, Oetting TA, Beaver HA, Boldt HC, Olson R, Greenlee E, Abramoff MD, Johnson AT, Carter K. Re-engineering the resident applicant selection process in ophthalmology: a literature review and recommendations for improvement. Surv Ophthalmol. 2008;53(2):164–176. doi: 10.1016/j.survophthal.2007.12.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Nield LS, Nease EK, Mitra S, Van Den Langenberg E, Saggio RB. Major themes in the personal statements of pediatric resident applicants. Clin Pediatr. 2016;55(7):671–672. doi: 10.1177/0009922815600440. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. AAMC. 2019 AMCAS applicant guide. American Medical College Application Service. https://aamc-orange.global.ssl.fastly.net/production/media/filer_public/2d/5d/2d5d7c94-6b23-4edf-ab1b-d574221bf6e3/2019-amcas-applicant-guide.pdf . Accessed May 10, 2019
- 13. Jordan J, Linden JA, Maculatis MC, Hern HG, Jr, Schneider JI, Wills CP, Marshall JP, Friedman A, Yarris LM. Identifying the emergency medicine personality: a multisite exploratory pilot study. AEM Educ Train. 2018;2(2):91–99. doi: 10.1002/aet2.10078. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Olson DP, Oatts JT, fields BG, Huot SJ. The residency application Abyss: insights and advice. Yale J Biol Med. 2011;84(3):195–202. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Smith EA, Weyhing B, Mody Y, Smith WL. A critical analysis of personal statements submitted by radiology residency applicants. Acad Radiol. 2005;12(8):1024–1028. doi: 10.1016/j.acra.2005.04.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 16. Mathur A, Kamat D. The personal statement. J Pediatr. 2014;164(4):682–682.e1. doi: 10.1016/j.jpeds.2014.01.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. White BAA, Sadoski M, Thomas S, Shabahang M. Is the evaluation of the personal statement a reliable component of the general surgery residency application? J Surg Educ. 2012;69(3):340–343. doi: 10.1016/j.jsurg.2011.12.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 18. Olazagasti J, Gorouhi F, Fazel N. A critical review of personal statements submitted by dermatology residency applicants. Dermatol Res Pract. 2014;2014:934874. doi: 10.1155/2014/934874. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Badal JJ, Jacobsen WK, Holt BW. Behavioral evaluations of anesthesiology residents and overuse of the first-person pronoun in personal statements. J Grad Med Educ. 2011;3(2):151–154. doi: 10.4300/JGME-D-10-00117.1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (233.3 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Where to start
- Ultimate Guides
- Virtual Work Experiences
- Chat to students
- UCAS events
- Apprenticeships
Subject guides
- Subject tasters
Industry guides
Where to go.
- Universities and colleges
City guides
- Types of employment
- Write a cover letter
- Starting work
- Career quiz
Before you apply
- Campus open days
- What and where to study
- Distance learning
- Higher Technical Qualifications (HTQs)
- Studying at a college
- Pros and cons of university
Applying to university
- Dates and deadlines
Personal statement
- UCAS Tariff points
- Individual needs
After applying
- Track your application
- Decisions and offers
Results day
Clearing and results day, conservatoires.
- Fees and finance
- How to apply
Replying to offers
- Tracking your application
Postgraduate
- Choosing a course
- Fees, loans, and funding
- Teacher training
- International students
- Student finance
- Scholarships, grants, and bursaries
Additional funding
- Managing money
Student life
- Starting uni or college
- Mental health and wellbeing
Accommodation
- Accommodation for apprentices
- Accommodation for disabled students
- Apply for student accommodation
- Find the right accommodation
- The ultimate packing list
- Visas and immigration
- English Language Tests (ELTs)
- Choosing the right course
- Entry requirements
- International clearing guide
Financial information
- Available finance options
- Saving money
- UK bank accounts
- Support for refugees and asylum seekers
Extra support
- Adjusting to the UK
- Application tips
- Available support
- Checklist for moving to the UK
- International FAQs
- Support organisations
Student recruitment and marketing
- Drive applications through Clearing
- Drive applications through Extra
- Exhibiting as a university or college
- Improve conversions
- Improve your competitive strategy
- Increase brand awareness
- International
- Provider pages
Data products and solutions
- Application and decision tracker
- Competitor insight dashboard
- Course feasibility
- Leaky Hosepipe solution
- Outreach Elevator
- Student decision report
- Untapped Geographies
Managing applications
- Availability of UCAS data
- Fraud and similarity
- HESA return
- Link services
- Record of Prior Acceptance (RPA)
- Results Processing Service (ABL)
- Systems and services guides
Qualification Information Services
- Qualification Information Profiles (QIPs)
- Qualification guides and resources
- UCAS Tariff
Products as part of your membership
- Recruitment, marketing and admissions services
Provider news and updates
- UCAS correspondents bulletin
Provider developments
- Upcoming developments
- Previous updates
- UCAS maintenance schedule
- Service status
Test and training environments
- HEP1 and HEP2
Link product development
- Availability of new features
- UCAS Link API strategy
- Groups and forums
Admissions guides and resources
- Conservatoire admissions guide and resources
- Provider contact types
- Undergraduate admissions guide and resources
Good practice
- Admissions policies
- Admissions processes
- Applicant experience
- Collection tool help
- Contextualised admissions
- Equality and diversity
- Supporting disadvantages and under-represented groups
- Unconditional offers
- Widening access and participation
Online learning
Provider engagement.
- Annual provider update
Adviser news
- Adviser portal
- Key dates timeline
- Newsletters
- Adviser lives
- Qualification reform
Discovery events
- Getting ready for UCAS Discovery
- Events training
Create your future events
Conferences.
- Teacher and adviser conference 2024
- International Teachers and Advisers Conference
Events calendar 2024
Cycle toolkits.
- Adviser 2025 toolkit
- Conservatoire application toolkit
- Supporting students with individual needs
Lesson activities
- Classroom resources
- Lesson plans

Develop your adviser skills
- Practical ways to guide students
- Help finding work experience
- Events and summer school
- Positive career discussions
- Advice about GCSE choices
Online training
- Personal development platform
- Adviser tips
Tools and resources
- UCAS hub guide
- Digital training
- Progression pathways
Pre application support
- Bursaries, scholarships, and financial support
- Help writing personal statements
- Student budget planner
- Alternatives to A Levels
- Higher education options
Application overview
- Application deadlines
- Application process
- Exam results process
- Monitor student progression
- Predicted grades
- Undergraduate references 2024
- Reference processes and terminology
- Conservatoire references
UCAS registered centres
- Becoming a UCAS registered centre
- Getting started
- Teachers and advisers
International advisers
- Clearing guide for international students
- Qualifications advice
- Supporting international students
Confirmation and Clearing
- ACSL guidance
- Clearing essentials
- Conservatoires confirmation
- International students guide
- Reach talent and acquisition
Apprentices with UCAS
Career finder, employer profiles, multichannel campaigns, apprentices, international guides, make the most of clearing, smart financial decisions.
- Filling in your application
Making changes to your application
- How to get a reference
Results process
Application cancellation request form.
- Requests for personal data
- Notifications
- Preferences
- Provider Homepage
- Provider Dashboard
- Student Hub
- Adviser Homepage
- Adviser Portal
Writing your personal statement
- Admissions tests
- Deferred entry
- Staying safe online
- How to write a personal statement that works for multiple courses
- The new personal statement for 2026 entry
- How To Write Your Undergraduate Personal Statement
- How to start a personal statement: The attention grabber
How to end your personal statement
- Introducing the personal statement tool
Personal statement dos and don'ts
- What to include in a personal statement
- Using AI and ChatGPT to help you with your personal statement
Using your personal statement beyond a university application
- Carers, estranged students, refugees, asylum seekers, and those with limited leave to remain
- Personal statement advice: animal science
- Personal statement advice: biology
- Personal statement advice: business and management
- Personal statement advice: chemistry
- Personal statement advice and example: computer science
- Personal statement advice: dance
- Personal statement advice: dentistry
- Personal statement advice: drama
- Personal statement advice: economics
- Personal statement advice: engineering
- Personal statement advice: english
- Personal statement advice: geography
- Personal statement advice: history
- Personal statement advice: law
- Personal statement advice: maths
- Personal statement advice: media studies and journalism
- Personal statement advice: medicine
- Personal statement advice: midwifery
- Personal statement advice: modern languages
- Personal statement advice: music
- Personal statement advice: nursing
- Personal statement advice: pharmacy
- Personal statement advice: physiotherapy
- Personal statement advice: politics
- Personal statement advice: psychology
- Personal statement advice: social work
- Personal statement advice: sociology
- Personal statement advice: sports science
- Personal statement advice: statistics
- Personal statement advice: teacher training and education
- Personal statement advice: veterinary medicine
- Personal statement: finance and accounting
- Personal statement advice: architecture, building and planning
- Personal statement advice: art and design
- Personal statement advice: environmental science
- Personal statement advice: marketing
- Personal statement advice: philosophy
- Personal statement advice: photography
- Personal statement advice: physics
- Financial challenges as a mature student
- References for mature students
- Mature students – getting ready to start your course
- Mature student case studies
- The application process for mature students
- Mature students: five things to include in your personal statement
- Student finance for mature students
- Preparing for study as a mature student – student support
- Preparing for study as a mature student – your qualifications
- Preparing for study as a mature student – choosing where to study
- UCAS Undergraduate for mature students
- Contextual admissions
- How to apply in Welsh
- First-generation students
- Disabled students: Researching your choices
- Sharing a disability or mental health condition in the UCAS application
- Speaking to the disability adviser, mental health adviser or student support team
- Disabled students: Financial support
- Disabled students: Support with transition to university
- Disabled international students
- Disabled students: Further information and support
- UCAS Undergraduate: support for care leavers
- Student carers
- Student-parent’s guide to open days
- Chloe's story
- Funding for estranged student in Scotland
- Students from a UK Armed Forces background
- Patricka, UK Armed Forces Service leaver
- Support for students who have been bereaved as a child
- Criminal convictions – what you need to know
- Students with imprisoned parents
How to write your undergraduate personal statement
Stand out from the crowd by showcasing who you are and what you can bring to a university as you begin your undergraduate journey.
How to start a personal statement: the attention grabber
The personal statement is your opportunity to talk about you, and why you want to enrol on a particular course. But how do you start it strongly? Read our advice below on what to include, what not to do, and how to approach it.
The personal statement is your opportunity to talk about you, and why you want to enrol on a particular course. You’ve got this far – showing your passion for the subject. But how do you end your personal statement in a way that truly does it justice?
Introducing the personal statement builder
The personal statement is your opportunity to talk about you, and why you want to enrol on a particular course. But it can be hard to know how to structure the information, which is where the personal statement builder can really help.
The personal statement is your opportunity to talk about you, and why you want to enrol on a particular course. Use these easy-to-digest bullet points to help you decide what you should and shouldn’t include in your personal statement.
What to include in your personal statement
The five things every student should include on their personal statement.
start_your_application_400x400.png
You’ve done all the hard work creating your personal statement, but have you thought about how you can use what you’ve written for different purposes? Whether you’re thinking about applying for an apprenticeship, or there’s a job you’d love, and you need a covering letter, your personal statement can be a great place to start.
Find out more
Postgraduate personal statements
How to write your postgraduate personal statement.
Stand out from the crowd by showcasing your expertise and passion for your subject.
What are the differences between an undergraduate and postgraduate personal statement?
We’ve asked experts in the field and created a simple list to tell you about the important differences between undergraduate and postgraduate personal statements.
Dr Phil Porter – Associate Dean Education (Student Experience)
Michael, ba (hons) film and television studies, personal statement advice for other applicants, how to write a personal statement for a conservatoire.
The personal statement is your opportunity to talk about you, and why you want to enrol on a particular course. You should describe the ambitions, skills, and experience that’ll make you suitable for the course.
Mature students: Five things to include in your personal statement
The personal statement is your opportunity to talk about you, and why you want to enrol on a particular course. Applying to university if you’re 21 or over isn’t unusual, but how can you best make that life experience shine through?
Writing your personal statement: carers, estranged students, refugees or asylum seekers
Sponsored articles ucas media service, discover smu in london, do you need to take an english test to study at university in the uk, top 5 things to do at an open day.

Know Your Zone
- Find out your coastal Evacuation zone and how to prepare for hurricanes and coastal storms.

Strengthening Communities Program
The program offers grants to community networks to build their emergency preparedness plan and support local community resources. Apply now!
2022-2026 Strategic Plan
- NYC Emergency Management has released its 2022-2026 strategic plan, which highlights the agency's vision and key priorities through 2026.

Tune in to NYC Emergency Management's Podcasts
NYC Emergency Management's podcast, "Prep Talk," discusses all things emergency management. Listen to the latest episode by selecting one of the links below.
- Follow NYC Emergency Management - "Prep Talk" on SoundCloud
- Follow NYC Emergency Management - "Prep Talk" on Apple Podcasts
- Follow NYC Emergency Management - "Prep Talk" on Spreaker
- Get the RSS feed
¡Prepárate! , el primer podcast en español de la agencia, dedicado a educar a los Neoyorquinos como prepararse para las emergencias.
- NYC Emergency Management - ¡Prepárate! en SoundCloud
- ¡Prepárate! en Spreaker
Disasters Don't Plan Ahead. You Can.
You can't be prepared for every little disaster, but you can prepare for a big one. Make an emergency plan today .
Website Accessibility Statement
Are you having trouble accessing any part of our website because of a disability? Report website accessibility issues using our Website Accessibility Statement .
NYC Weather Updates
- Hurricane Evacuation Zone Finder
- Beat the Heat
- MOUs & Settlements
Programs & Initiatives

Learn more information about how severe weather emergencies are affecting New York City.

Sign up to receive alerts from the City's official source for information about emergencies.

COVID-19 Citywide Information & Updates
Get the latest health guidance, resources for individuals, businesses, nonprofits, and ways to help.

Know Your Zone is your destination for everything you need to know about hurricanes in NYC.

Ready New York
Learn how you can be best prepared for all types of emergencies.

Help prepare & respond to emergencies by joining NYC Community Emergency Response Teams.

Partners in Preparedness
Organizations can learn how to better prepare its employees, services, and facilities for disasters.

John D. Solomon Fellowship
First student fellowship with the City devoted specifically to emergency management.
Stay Connected

| See more in , , , , , | |
| --> |
| | | | |
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Consensus Statement
- Published: 22 October 2024
International expert consensus statement on the diagnosis and management of congenital nephrogenic diabetes insipidus (arginine vasopressin resistance)
- Elena Levtchenko ORCID: orcid.org/0000-0002-8352-7312 1 ,
- Gema Ariceta 2 ,
- Olga Arguedas Flores 3 ,
- Daniel G. Bichet ORCID: orcid.org/0000-0003-2856-6850 4 ,
- Detlef Bockenhauer ORCID: orcid.org/0000-0001-5878-941X 5 , 6 ,
- Francesco Emma ORCID: orcid.org/0000-0002-0383-3468 7 ,
- Ewout J. Hoorn ORCID: orcid.org/0000-0002-8738-3571 8 ,
- Linda Koster-Kamphuis ORCID: orcid.org/0000-0002-9971-995X 9 ,
- Tom Nijenhuis ORCID: orcid.org/0000-0002-4375-7236 10 ,
- Francesco Trepiccione ORCID: orcid.org/0000-0002-0622-6612 11 , 12 ,
- Rosa Vargas-Poussou 13 ,
- Stephen B. Walsh 14 &
- Nine V.A.M. Knoers ORCID: orcid.org/0009-0001-2916-1524 15
Nature Reviews Nephrology ( 2024 ) Cite this article
Metrics details
- Acid, base, fluid, electrolyte disorders
- Genetic testing
- Paediatric kidney disease
Congenital nephrogenic diabetes insipidus (NDI; also known as arginine vasopressin resistance) is a rare inherited disorder of water homeostasis, caused by insensitivity of the distal nephron to arginine vasopressin. Consequently, the kidney loses its ability to concentrate urine, which leads to polyuria, polydipsia and the risk of hypertonic dehydration. The diagnosis and management of NDI are very challenging and require an integrated, multidisciplinary approach. Here, we present 36 recommendations for diagnosis, treatment and follow-up in both children and adults, as well as emergency management, genetic counselling and family planning, for patients with NDI. These recommendations were formulated and graded by an international group of experts in NDI from paediatric and adult nephrology, urology and clinical genetics from the European Rare Kidney Disease Reference Network and the European Society of Paediatric Nephrology, as well as patient advocates, and were validated by a voting panel in a Delphi process. The goal of these recommendations is to provide guidance to health care professionals who care for patients with NDI and to patients and their families. In addition, we emphasize the need for further research on different aspects of this potentially life-threatening disorder to support the development of evidence-based guidelines in the future.
Introduction
Congenital nephrogenic diabetes insipidus (NDI) is a rare inherited disorder of water homeostasis, characterized by insensitivity of the distal nephron to antidiuretic hormone (ADH; also known as arginine vasopressin (AVP)) (Fig. 1 ). Consequently, the kidney loses its ability to concentrate urine, which leads to polyuria, polydipsia and the risk of hypertonic dehydration 1 .

Arginine vasopressin (AVP) binds to the vasopressin V 2 receptor (V2R) expressed on the basolateral membrane of collecting duct cells and initiates a cascade of events that involves receptor-linked activation of G protein, activation of adenylyl cyclase, production of cyclic adenosine monophosphate (cAMP) and stimulation of protein kinase A (PKA). These processes lead to the final step of the antidiuretic action of AVP — the exocytic insertion of aquaporin water channels into the luminal membrane — thereby increasing the water permeability of that membrane and allowing water to flow from the tubule lumen to the hypertonic medullary interstitium. This water transport occurs via AQP2 in the apical membrane and via AQP3 and AQP4 (constitutive water channels) in the basolateral membrane, and enables the formation of concentrated urine.
In 2022, the Working Group for Renaming Diabetes Insipidus, representing the global endocrinology community, proposed changing NDI to arginine vasopressin resistance, which distinguishes it from arginine vasopressin deficiency for central aetiologies 2 . However, this new terminology has not been officially adopted and is not yet included in the International Statistical Classification of Diseases and Related Health Problems (ICD-11) 3 . Therefore, here we will use the term NDI to describe the disease caused by insensitivity of the kidney to AVP.
Patients with NDI are usually born at term; polyuria in utero is absent or mild and polyhydramnios is not observed 1 . The urinary concentration defect is present at birth but rarely causes overt symptoms in breastfed infants because human milk is relatively poor in salt and protein, thereby limiting polyuria and preventing hypernatraemia. Conversely, formulas and solid foods increase the kidney solute load and cause polyuria.
The mean age at diagnosis is ~4 months 4 , with polyuria, failure to thrive and signs of dehydration as typical presenting symptoms (Box 1 ). Serum osmolality is usually >300 mOsm/kg H 2 O owing to hypernatraemia 4 , whereas urine is inappropriately diluted, with osmolality usually <200 mOsm/kg H 2 O (urine osmolality < plasma osmolality). However, urine osmolality can be higher than 200 mOsm/kg H 2 O in milder cases 5 , 6 . Infants are particularly at risk of dehydration as they have no free access to fluid. In addition, the intake of large fluid volumes can cause gastro-oesophageal reflux and vomiting 7 . In older children and adults, polydipsia is the predominant symptom at diagnosis.
The exact incidence and prevalence of congenital NDI are unknown, but the disease is considered to be rare. Secondary forms of NDI are more frequent and can be caused by other (inherited) kidney diseases that affect the ability to concentrate urine or medications 1 , 7 . Owing to the rarity of the condition, many practitioners are unfamiliar with this diagnosis, let alone its pathophysiology and management. Consequently, the diagnosis of NDI is frequently delayed and no evidence-based treatment recommendations have been formulated to date. Therefore, the European Reference Network on Rare Kidney Diseases (ERKNet), the European Society for Paediatric Nephrology and patient advocates took the initiative to develop Clinical Practice Recommendations (CPR).
In this Consensus Statement, we provide CPR for clinicians who are confronted in their practice with the diagnosis, treatment and genetic counselling of NDI, which is a challenging and potentially life-threatening condition. In addition, we have aimed to set up a research agenda that can aid the development of novel therapies and evidence-based guidelines in the future. Of note, our recommendations do not address secondary genetic or acquired forms of NDI.
Box 1 Clinical signs and symptoms at presentation of nephrogenic diabetes insipidus
Weight and height gain
Failure-to-thrive
Poor growth
Low skin turgor
Sunken fontanel
Increased periorbital folding
Sunken eyeballs
Tachycardia
Sunken abdomen
Neurological symptoms
Irritability
Gastrointestinal symptoms
Excessive thirst, preference for water
Poor appetite
Expert groups
For this CPR consensus paper, we followed the Reporting Items for Practical Guidelines in Healthcare statement 8 . The core group of experts comprised specialists from paediatric (G.A., D.Bo., F.E., L.K.K., E.L., R.V-P.) and adult (D.Bi., E.H., T.N., F.T., S.W.) nephrology, urology (O.A.F.), a clinical geneticist (N.K.) and patient advocates. The voting panel comprised 30 members with expertise in paediatric and adult inherited kidney diseases, and included members of the supporting societies and networks (voting members are listed in the Supplementary Information). Members of the voting panel provided their expert opinion on the recommendations based on a five-point scale (strongly disagree, disagree, neither agree nor disagree, agree, or strongly agree) according to the Delphi method using an electronic questionnaire. When a 70% level of consensus was not reached among the voting panel members, recommendations were adjusted after discussion in the core group and reviewed again by the voting panel until a consensus level of at least 70% was achieved.
Development of PICO questions
To ensure that the statements derived from this work could be translated into actionable recommendations, the core group developed patient population, intervention, comparator and outcomes (PICO) questions 9 (Supplementary Table 1 ) to be addressed in the literature searches. Each PICO question formed the basis for one recommendation and the population included children and adults with congenital NDI. Recommendations were developed based on available studies investigating the clinical phenotype, genetics and management of NDI. Regarding outcomes, we provide recommendations for diagnosis, genetic counselling, family planning, follow-up and treatment with respect to kidney and urinary tract diseases, children’s growth and emergency situations, as well as treatment-associated or disease-associated complications and comorbidities.
Literature search
A literature search was conducted for each PICO question. The PubMed database was searched for papers published between 1950 and December 2023. All papers regarding human studies in English were considered, including prospective randomized controlled trials, uncontrolled or observational studies, registries, summaries and case series. In vitro and animal studies were selected to inform the future research agenda for the development of new targeted therapies. The following key medical subject headings terms were identified: nephrogenic diabetes insipidus, NDI, arginine vasopressin type 2 receptor (AVPR2; also known as vasopressin V 2 receptor (V2R)) and aquaporin 2 (AQP2). The search retrieved 231 results and 102 articles (85 in the main text and 17 additional non-overlapping articles listed in the Supplementary Information).
Grading of recommendations
We followed the grading system from the American Academy of Paediatrics to evaluate and grade the recommendations 10 , 11 . The quality of evidence is graded high (A), moderate (B), low (C), very low (D) or not applicable (X). Grade X was used for exceptional situations in which validating studies cannot be performed, and benefit or harm clearly predominate. The strength of a recommendation is graded strong, moderate, weak or discretionary (when no recommendation can be made).
Diagnostic approach
Rationale for diagnostic approach.
We recommend suspecting NDI in infants and children who present with polyuria, polydipsia, failure to thrive and hypernatraemic dehydration, and in adults with unexplained polyuria and polydipsia. A comprehensive family history and pedigree construction is essential to identify family cases. The initial work-up consists of measuring serum sodium, serum osmolality and urine osmolality. The detection of inappropriately diluted urine (that is, urinary osmolality <200 mOsm/kg H 2 O), in combination with high–normal or elevated serum sodium is pathognomonic for the diagnosis of diabetes insipidus (nephrogenic or central) and warrants early genetic testing if NDI is suspected (Fig. 2 ).
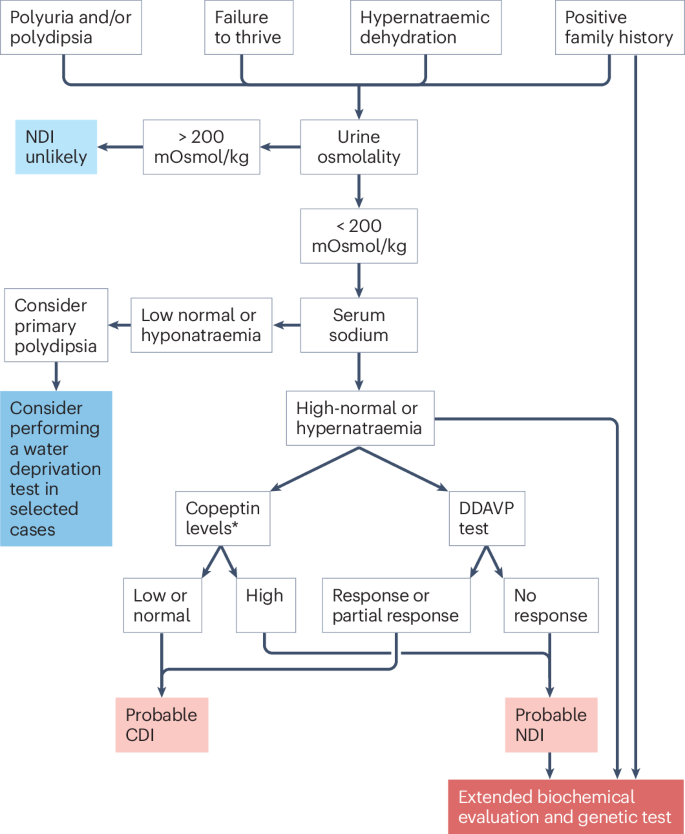
Nephrogenic diabetes insipidus (NDI) should be suspected in patients with unexplained polyuria, polydipsia, failure to thrive and/or hypernatraemic dehydration. The initial biochemical work-up consists of measuring urine and serum osmolality, and serum sodium. In patients with urine osmolality <200 mOsm/kg H 2 O and normal or high serum sodium, the diagnosis of DI is probable and early genetic testing is recommended. Early genetic testing should also be performed in patients at risk of NDI (for example, male offspring of a mother carrying an AVPR2 mutation). When early genetic testing is not available, other diagnostic tests can be recommended. Extended biochemical evaluation is performed to exclude polyuric disorders other than NDI. Plasma copeptin measurements are validated in adults, but not in children. The desmopressin (DDAVP) test can distinguish patients with central DI (CDI) (normal urine concentration capacity after the administration of DDAVP) and NDI (no response to DDAVP). Partial response to DDAVP is defined as an ability to increase urine osmolality above the baseline, but not reaching the reference values (600 mOsm/kg H 2 O in children <1 year; 600–800 mOsm/kg H 2 O in children aged 1–2 years; 800 mOsm/kg H 2 O in children aged >2 years). In patients with suspected primary polydipsia, a water deprivation test can be considered, although its diagnostic accuracy is limited. Of note, a water deprivation test is contraindicated in patients with a history of hypernatraemic dehydration and inappropriately diluted urine. In adults, copeptin levels after stimulation with hypertonic saline or arginine can help to distinguish primary polyuria and DI. *An assessment of copeptin levels is only useful to exclude CDI (arginine vasopressin (AVP) deficiency) if they are ≥21.4 pmol/l (indicative of NDI) and sodium levels are above 147 mmol/l because there is a large overlap between unstimulated copeptin levels in patients with AVP deficiency and primary polydipsia.
We recommend, when possible, starting the diagnostic process with genetic testing in all patients with clinical and biochemical symptoms of NDI. For practical reasons, in patients who present with polyuria and polydipsia, an extended biochemical work-up is usually performed simultaneously with the initial work-up to exclude other polyuric disorders, including diabetes mellitus, renal Fanconi syndrome or Bartter syndrome (Table 1 ).
Rationale for early genetic testing
Approximately 90% of all affected patients have the X-linked form of NDI (OMIM #304800) caused by pathogenic variants in AVPR2 (chromosome Xq28), and most patients are male 6 . A minority of patients (<10%) have autosomal forms of NDI caused by pathogenic variants in AQP2 (chromosome 12q13.12), which encodes the AQP2 water channel. These autosomal forms are inherited as autosomal-recessive (OMIM #222000) or autosomal-dominant (OMIM #125800) traits, affecting males and females equally 7 , 12 , 13 , 14 , 15 . Autosomal-dominant NDI caused by pathogenic AQP2 variants might be underdiagnosed, as these patients might be able to compensate for the AQP2 loss and therefore not show all symptoms.
Genetic testing can provide an early and definite diagnosis, with important implications for clinical management and outcome, and can avoid unpleasant, challenging, and potentially harmful diagnostic procedures, including the desmopressin (DDAVP) test or the water deprivation test. An early diagnosis also prevents prolonged, unrecognized periods of severe hypertonic dehydration, which can result in seizures, developmental delay and cognitive impairment 16 , 17 , 18 .
A minority of individuals with X-linked NDI have AVPR2 pathogenic variants associated with partial insensitivity to AVP 15 , 19 , 20 . A genetic diagnosis can help to identify these patients with partial NDI, in whom laboratory test results can be difficult to interpret and distinction from (partial) central diabetes insipidus (AVP deficiency) is challenging.
An early genetic diagnosis is also crucial for precise genetic counselling. It informs recurrence risks and can support patient decision-making regarding family planning, including reproductive options such as prenatal and preimplantation genetic testing. In addition, a genetic diagnosis offers presymptomatic testing opportunities for family members at risk. Especially in cases of X-linked NDI, awareness of carrier status of a familial AVPR2 pathogenic variant in female family members can support them and their partners in making an informed decision regarding their reproductive options. Finally, the identification of a genetic cause of NDI can have implications for determining the eligibility of patients for future genetically stratified clinical trials.
In families without a history of NDI, molecular genetic testing might identify de novo pathogenic variants, which is important to determine the genetic risk status of the extended family. A study of a large global cohort of patients with NDI revealed that a de novo pathogenic variant arose during oogenesis in the mother in 20% of isolated cases 21 .
In male offspring of heterozygote AVPR2 mutation carriers, we strongly recommend genetic testing in umbilical cord blood directly after birth (when this has not been performed at the prenatal stage), as it might prevent primary manifestations of the disorder by facilitating early treatment and monitoring 18 .
We strongly recommend performing genetic testing in a laboratory accredited for diagnostic genetic testing. We recommend the use of a massively parallel sequencing-based multigene panel that includes at least AQP2, AVPR2 and AVP (for differential diagnosis of central diabetes insipidus) to identify the genetic cause of NDI at the most reasonable cost while limiting incidental findings. The use of a multigene panel that additionally includes copy number variant analysis is highly recommended. Of note, genetic testing with such a multigene panel is recommended even for females with overt NDI. Overt NDI in females can be caused by biallelic pathogenic variants in AQP2 , but some females with AVPR2 pathogenic variants (10%) also develop the complete NDI phenotype 22 , 23 . The latter phenomenon is most likely due to X-inactivation of the chromosome that does not carry the AVPR2 pathogenic variant 24 , 25 .
Other diagnostic tests
If genetic testing is not available or inconclusive (5–10% of cases, personal communication of Daniel G. Bichet, Rosa Vargas-Poussou), we recommend performing the following diagnostic tests (Box 2 and Fig. 2 ).
Box 2 Recommendations for NDI diagnostic approach
Recommendation 1
We recommend suspecting diabetes insipidus (DI) in children with polyuria, polydipsia, failure to thrive and hypernatraemic dehydration with inappropriate low urine osmolality (mostly <200 mOsm/kg H 2 O) (level B, strong).
Recommendation 2
We recommend suspecting DI in adults with unexplained polydipsia and polyuria (level B, moderate).
Recommendation 3
We recommend measuring serum sodium, serum osmolality and urine osmolality as an initial biochemical work-up in patients with suspected nephrogenic DI (NDI) (level B, strong).
Recommendation 4
We recommend extended evaluation to exclude other disorders causing polyuria (level B, strong):
serum K, Cl, HCO 3 , Ca, Pi, Mg
serum creatinine, urea
serum glucose, HbA1C
urine glucose, amino acids, low-molecular-weight proteins
Recommendation 5
We recommend early genetic testing in a patient with clinical symptoms of suspected NDI (level X, strong).
Recommendation 6
We recommend genetic testing using umbilical cord blood in male offspring of a known heterozygote female carrier of an AVPR2 mutation (level X, strong).
Recommendation 7
We recommend genetic testing of AVPR2 and AQP2 in all symptomatic females (level B, strong).
Recommendation 8
We recommend performing genetic testing in laboratories accredited for diagnostic genetic testing (level X, strong).
Plasma copeptin
Measurement of blood AVP is challenging as the hormone is unstable and the measurement is cumbersome. In adults, we recommend measuring plasma copeptin as a suitable alternative, as copeptin (CT-proAVP) is released in an equimolar 1:1 ratio with AVP 26 . Baseline plasma copeptin levels above 21.4 pmol/l have been reported as diagnostic for NDI in adult patients 26 . Because these copeptin values are significantly higher than those observed in patients with other polyuric disorders 27 , 28 , 29 , for most adult patients with NDI no additional testing is necessary. Adults with plasma copeptin <21.4 pmol/l should be tested for AVP deficiency (central DI) and primary polydipsia using infusion tests with hypertonic saline or arginine 28 , 30 , 31 . Only a few reports have evaluated the diagnostic values of plasma copeptin in paediatric polyuric disorders 32 , 33 , 34 , 35 , 36 .
The urine concentration test uses DDAVP, a synthetic AVP analogue with specific affinity for AVPR2, to assess the responsiveness of the kidney to AVP 1 , 37 . The test should be performed with caution, especially in patients who cannot adapt their fluid intake according to thirst (for example, infants or patients who receive water through intravenous lines or nasogastric tubes). Patients with NDI usually show complete unresponsiveness to DDAVP. Patients need to be carefully monitored for their fluid intake, as ongoing fluid intake in patients with intact urinary concentration (for example, those with habitual polydipsia, can cause severe hyponatraemia). Protocols for intranasal and intravenous DDAVP tests are provided (Supplementary Boxes 1 and 2 ).
Water deprivation test
A water deprivation test (Supplementary Boxes 3 and 4 ) can be of value to assess a urinary concentration defect in selected patients (children and adults) with polyuria of unclear aetiology. However, in patients who present with high-normal or elevated serum sodium, and inappropriately diluted urine, the diagnosis of diabetes insipidus is already established. In such situations, performing a water deprivation test is not only unnecessary but poses a risk of severe dehydration 38 . Of note, the interpretation of urinary concentration ability after water deprivation can be difficult, as individuals with long-standing polydipsia do not concentrate urine up to the normal limits 39 , presumably owing to decreased AQP2 expression in the renal collecting duct, limiting the response to exogenous ADH 40 .
Treatment and follow-up in children
Rationale for treatment in children.
Treating children with NDI is particularly challenging, especially in infants and toddlers who cannot clearly express their thirst. Feeding difficulties and frequent vomiting place a significant burden on families. Managing these patients requires specialized expertise, not only from the responsible physician but also from the entire paramedic team, including specialized nurses, dietitians, psychologists and social workers 1 .
Fluid intake
We recommend ad libitum access to fluid in all patients with NDI to prevent dehydration, hypernatraemia, growth failure and constipation (Box 3 ). In patients who are old enough and capable of self-regulating their fluid intake, the determination of the optimal amount of fluid is best left to their own thirst sensation; the patient’s osmosensors and the subsequent development (or suppression) of thirst 1 tend to be more sensitive and accurate than any medical calculation. Consequently, most patients exhibit normal serum sodium levels at steady state and with free access to water. For patients who cannot self-regulate their fluid intake (for example, infants or individuals with a cognitive impairment), water should be offered frequently on top of their regular fluid intake. If patients need to fast for prolonged periods (>4 h), for example, prior to anaesthesia, intravenous water administration should be provided. A reasonable initial approach is 5% dextrose (glucose) in water at the usual maintenance rate 41 . In these patients, close monitoring of weight, fluid balance and biochemistry is crucial to inform adjustments to the rate of administration and fluid composition. Of note, given that this intravenous fluid provides no renal osmotic load, urine volume typically decreases considerably. Moreover, the infusion of glucose can lead to hyperglycaemia with subsequent osmotic diuresis 42 and regular control of blood glucose is therefore recommended.
Box 3 Recommendations for treatment and follow-up in children
We recommend free access to fluid in all children with nephrogenic diabetes insipidus (NDI) (level X, strong).
We recommend normal-for-age milk intake (instead of water) in infants with NDI to guarantee adequate caloric intake (level B, moderate).
We recommend considering tube feeding in infants and children with repeated episodes of vomiting and dehydration and/or failure to thrive (level B, moderate).
We recommend that every patient with NDI receives dietetic counselling from a dietitian who has experience with the disease (level D, strong).
We recommend monitoring dietary salt and protein intake to reduce renal osmotic load and thereby minimize urine volume. Excessive restriction of salt and protein intake can compromise growth (level B, moderate).
In symptomatic infants and children, we recommend starting treatment with a thiazide and prostaglandin synthesis inhibitors (level B, moderate).
We recommend adding amiloride to thiazide in patients with hypokalaemia induced by thiazides (level B, moderate).
Treatment efficacy can be evaluated via urine osmolality, urine output, weight gain and growth (level D, strong).
Recommendation 9
Ongoing drug treatment should be based on the balance of apparent efficacy and concern over development of side effects (level B, strong).
Recommendation 10
We recommend toilet training in children with NDI as in any other child, although full continence is usually only reached in the second decade of life (level D, moderate).
Recommendation 11
We recommend performing a kidney ultrasound at least once every 2 years to monitor for dilatation of the urinary tract and/or bladder dysfunction caused by polyuria (level D, moderate).
Recommendation 12
We recommend that patients with NDI are followed by a multidisciplinary team that includes a (paediatric) nephrologist, dietitian, psychologist, social worker and urologist (level X, strong).
Adequate caloric intake and tube feeding
We recommend normal-for-age milk intake (instead of water) in infants with NDI to guarantee adequate caloric intake. ‘Greedy’ drinking followed by vomiting is commonly reported, especially in infants, and is thought to reflect gastro-oesophageal reflux exacerbated by the large fluid volume 43 . Careful spacing of oral feeds and fluid might ease this problem and reduce the vomiting.
The commencement of tube feeding (either by nasogastric tube or gastrostomy) is a case-by-case decision that should be carefully discussed and considered with the family. In NDI, as in other kidney diseases, we recommend tube feeding if patients have repeated episodes of vomiting and dehydration and/or growth failure 44 . This can be helpful to ensure adequate fluid, energy and nutritional intake. Especially for parents of young infants, the use of tube feeding can reduce the stress associated with trying to achieve adequate nutrition. Many infants and young children with NDI will show a preference for water over more nutritional fluids and the transition to solid foods can be delayed. However, many infants and children manage to grow well and avoid serious dehydration with oral intake alone 45 , 46 . In three retrospective studies, 20–30% of children with NDI had received tube feeding at some point, with ~25% of them having had a gastrostomy 4 , 46 , 47 . Tube feeding is rarely continued beyond 4 years of age.
Slow tube feeding by use of a feeding pump will allow a steady administration of the fluid or feed volume, which can reduce vomiting and improve growth. For infants and children who receive tube feeding for more than 3 months, insertion of a gastrostomy should be considered. A gastrostomy allows continuous tube feeds to be administered safely overnight without the risks associated with dislodgement of a nasogastric tube (that is, inadvertent fluid aspiration and associated respiratory infections). For many parents, provision of a continuous overnight nutritious feed (especially in infancy) relieves anxiety. This approach enables families to encourage oral intake of liquid or solid food during the day without the added pressure of nutritional concerns. The volume of administered fluid and food should be gradually tailed off once consistent growth and weight gain have been achieved. This will allow reassessment of the benefit of tube feeding and ensure the development and maintenance of oral feeding skills.
We recommend support from a dietitian who has experience with NDI to ensure nutritional adequacy and provide practical advice on energy supplementation of oral fluids, salt and protein intake, or tube feeds if required.
Dietary salt and protein intake
We recommend monitoring dietary salt and protein intake to reduce renal osmotic load and hence minimize urine volume. As maximal urine osmolality is reduced in NDI, patient urinary output is mainly dependent on their renal osmotic load, which, in turn, is mainly determined by salt and protein intake. In infancy, a feed with a low renal osmotic load (15 mOsm/kg body weight/day) is recommended to reduce polyuria and polydipsia, and to achieve feed tolerance, weight gain and growth. In clinical practice, a simplified formula is used to quantify the renal osmotic load: mOsm = total protein content (g) × 4 + 2 × (sodium mmol + potassium mmol) 48 (Supplementary Box 5 ).
Beyond infancy, this calculation is usually not necessary, although for patients on tube feeding, it can be helpful to minimize the renal osmotic load of the feed to allow a more liberal oral diet. Salt control can be gradually eased, transitioning to a reduced-salt diet (or ‘no added salt diet’) by the age of 2 years. Strict avoidance of salt is not necessary and can contribute to growth failure 49 as salt has a crucial role in growth by stimulating cell proliferation, enhancing protein synthesis and increasing cell mass 50 . Salt tolerance will vary between children, and this will usually be self-regulated to minimize problems related to polyuria and bedwetting. In clinical practice, the reduction in dietary salt intake advised is broadly in line with population goals for salt or sodium consumption 51 (Table 2 ).
Protein and electrolytes other than sodium also contribute to renal solute load but restriction of these solutes is usually not necessary beyond infancy as it can compromise nutrition and contribute to poor growth 1 , 15 , unless intake is excessive (for example, protein supplements for bodybuilding). Protein intake should match the recommended dietary intake to support growth 52 . However, for children with problematic polyuria, adjusting protein intake closer to the theoretical minimum requirements for age (or height-age) might be helpful.
Drug treatment for reducing polyuria
In addition to dietary modifications, which decrease the renal osmotic load, medications to reduce urine output are available, most notably diuretics and prostaglandin synthesis (cyclooxygenase (COX)) inhibitors 4 , 43 , 46 , 53 , 54 (Table 3 and Supplementary Box 6 ).
In symptomatic infants and children with NDI, we recommend starting treatment with a thiazide and prostaglandin synthesis inhibitors. Thiazide diuretics act by inducing mild volume depletion and can reduce diuresis by up to 50% in the short term, when combined with a low-salt diet. This effect is presumably mediated by hypovolaemia-induced increase in proximal sodium and water reabsorption, thereby diminishing water delivery to the anti-diuretic hormone-sensitive sites in the collecting tubules and reducing the urine output 55 . Of note, in the long term, a much more moderate reduction in urine volume is usually observed.
Drug treatment can be very effective in infancy, with reported instances of marked hyponatraemia in patients who maintained an unchanged high fluid intake after commencement of drug treatment 56 , 57 . Thus, close monitoring of fluid balance, weight and biochemistry is recommended at the start of treatment and patients should be given as much control as possible to self-determine their fluid intake. In patients with hypokalaemia induced by thiazides, we recommend the addition of amiloride 58 .
Drug treatment is often discontinued with increasing age — in a multi-centre study, treatment with at least one medication decreased from 85% in childhood to 56% in adulthood, likely reflecting a perceived lack of efficacy and/or concern about side effects 47 . Whether lack of efficacy reflects inadequate dose adjustment, non-adherence to the prescribed medications or a true change in the physiological response to the treatment is currently unclear.
Similarly, the extent to which chronic use of prostaglandin synthesis inhibitors contributes to the progression of chronic kidney disease (CKD) — ~50% of adult patients with NDI also have CKD stage ≥2 — remains unclear 47 . Arguably, effective reduction in urine volume not only improves quality of life but can help to preserve kidney function by ameliorating urinary tract dilatation, bladder dysfunction and/or bladder-emptying problems. Thus, we recommend regular assessment of ongoing drug treatment based on a careful balance of risks and benefits.
Rationale for follow-up in children
A key symptom of NDI, especially in infancy, is growth failure. Consequently, height and weight are key parameters at each follow-up (Table 4 ). Basic plasma (Na, K, Cl, HCO 3 , creatinine, osmolality) and urine (osmolality) biochemistry also helps to monitor treatment, including the potential side effects of diuretics (if used).
Toilet training
No studies have investigated toilet training in patients with NDI. No data suggest that control of bladder function by the nervous system is different in children with NDI from that in others. Hence, we recommend performing toilet training in children with NDI as in any other child 59 . However, given the large urine volumes in NDI, accidents can be more frequent and noticeable than in children with intact urinary concentrating ability, and full continence is usually reached only in the second decade of life.
Some studies report a high incidence of night incontinence (referred to as ‘bed flooding’ by some parents because of the large urine volumes) in children with NDI, with urine continence at night achieved at a median age of 8–11 years 46 , 47 . Some parents use ‘double nappies’ to contain the urine volumes at night (that is, the use of a larger (for example, adult) nappy around the child’s usual nappy, so that overflow from the inner nappy is absorbed by the outer one). As indicated by our patient representatives, some parents use one or two mattress covers and change diapers several times during the night.
Urinary tract pathology
Based on our clinical experience, we recommend kidney ultrasound at least once every 2 years to monitor for urinary tract pathology, referred by some clinicians as ‘flow uropathy’, to describe the dilatation of the upper urinary tract, and/or bladder dysfunction caused by polyuria 46 , 47 .
In a single-centre retrospective study, urological complications were noted in 46% of patients with NDI. Nocturnal enuresis and incomplete voiding were most frequently observed, but large bladder capacity and unilateral or bilateral hydronephrosis were also reported 46 . In a retrospective study involving 315 patients with NDI, hydronephrosis was reported in 34% of cases 47 . However, in some patients, this alteration can be physiological and radiologists therefore commonly advise performing an ultrasound of the urinary tract with a filled bladder, which can lead to a transient upper tract dilatation that resolves after voiding. However, repeated or ongoing dilatation can lead to permanent damage to the urinary tract and/or the kidneys.
Anecdotal reports show evidence of obstruction in patients with a thick-walled bladder and post-micturition residual volume, which can be managed by cystostomy button drainage 60 . In another small retrospective study of 26 patients with diabetes insipidus (CDI and NDI) and hydroureteronephrosis, diagnostic tests revealed detrusor underactivity (42.3%), a contractile detrusor (15.4%) and reduced bladder sensations (53.9%) 61 .
For diagnostic evaluation, uroflowmetry is advised to exclude dysfunctional voiding. In addition, (video)urodynamic studies can be performed to assess bladder dysfunction in more detail. In patients with signs of urinary tract pathology, we recommend involvement of urologists, especially when invasive diagnostic tests or treatments such as clean intermittent catheterization are considered. Obviously, the importance of regular and frequent bladder emptying should be discussed with the patient to minimize further damage from ongoing dilatation. In addition, maximizing medical treatment to reduce urine volume can be considered.
Treatment and follow-up in adults
Rationale for dietary recommendations.
As NDI is characterized by water diuresis, patients should be advised to primarily drink water or other non-caloric beverages. The consumption of high-calorie drinks can contribute to the high incidence of obesity (41% versus 16% European average; P < 0.001) that is observed in adult patients with NDI 47 . To reduce the renal osmotic load, the recommended dietary targets are reduction of salt intake to ≤6 g/day and protein intake to ≤1 g/kg/day (Box 4 ). In practice, adherence to these recommendations is often challenging and malnutrition should be avoided. We recommend dietetic counselling to assess salt and protein intake, and provide individualized advice based on these recommendations.
Box 4 Recommendations for treatment and follow-up in adults
We recommend a low salt (≤6 g/day) and protein diet (<1 g/kg/day), supported by dietetic counselling (level B, moderate).
We recommend that the initiation, continuation or discontinuation of diuretics (thiazides, potassium-sparing diuretics) should be guided by the patient’s preference (level D, moderate).
We recommend discontinuing prostaglandin synthesis inhibitors once patients reach adulthood, or even earlier when complete continence is achieved (level D, moderate).
Prostaglandin-synthesis inhibitors are contraindicated in pregnancy (level X, strong).
We recommend that patients are assessed in a specialized centre at least once and that contact with this centre is made in situations of emergency medical care (level X, strong).
We recommend revising dietary and pharmacological prescriptions in older patients with NDI as their urinary output tends to decrease, independently of the natural decrease in glomerular filtration rate (level D, moderate).
Rationale for drug treatment in adults
Adults typically have an intact thirst drive and can maintain appropriate fluid intake to match their large urinary output. No studies have systematically investigated the impact of tapering or withdrawing COX inhibitors and/or thiazides in adult patients with NDI. Therefore, we recommend continuing or withdrawing thiazide diuretics depending on patient preference and on medical reasons (for example, development of thiazide-induced chronic hypokalaemia, gout, hypercholesterolaemia or non-melanoma skin cancer 62 ). Owing to concerns of nephrotoxicity, we recommend discontinuing COX inhibitors once patients reach adulthood (≥18 years of age), or even earlier if full continence is achieved. Our personal observation (Stephen B. Walsh) suggests that most patients do not experience or mind a change in urine volume after discontinuing COX inhibitors or thiazide diuretics. However, our patient representatives mentioned that some patients drink more after discontinuation of these medications and feel more tired than before. In patients who prefer to continue treatment with thiazide diuretics, hydrochlorothiazide 25 mg once or twice daily is typically recommended. Moreover, we recommend reducing salt intake as salt restriction potentiates the efficacy of diuretics.
In the case of thiazide-induced hypokalaemia, thiazide diuretics can be combined with amiloride, potentially leading to a further reduction in urine output 63 , 64 . The effects of chronic thiazide use on long-term kidney outcomes are unknown.
Rationale for follow-up in adults
For adults with stable disease and stable estimated glomerular filtration rate, annual follow-up can be sufficient (Table 4 ). For those with unresolved bladder dysfunction, more frequent follow-up by nephrologists and urologists might be desirable (for example, every 3–4 months). A more frequent follow-up schedule is warranted when withdrawing diuretics and COX inhibitors. As mentioned earlier, NDI is associated with an increased prevalence of CKD compared with a population-based cohort 47 . which is probably related to voluntary retention of urine leading to ‘flow uropathy’. Patients with progressive CKD or CKD stage ≥G4 benefit from more frequent follow-up as per KDIGO 65 or local guidelines. Unless an acute indication for imaging is present, we recommend conducting surveillance imaging once every 2 years (extended to 5 years, if the patient is stable). Kidney ultrasound for evaluating dilatation of ureters and the kidney pelvis should ideally be performed before and after emptying the bladder because in approximately one third of patients, dilatation will improve with double voiding rather than urological interventions (personal experience of Daniel G. Bichet).
As NDI is a rare disease and inadequate treatment, particularly of functional bladder outflow obstruction, is associated with poorer long-term outcome, we recommend that patients should have access to tertiary care centres with experience in NDI management. This approach facilitates clinical and genetic diagnosis, as well as access to specialist bladder outflow urology, if needed, and optimizes treatment and patient education. For patients who reside far from a specialist centre, follow-up can be shared with a local nephrologist and urologist.
Polyuria and polydipsia seem to ameliorate with age, independent of estimated glomerular filtration rate (personal experience of Daniel G. Bichet). Therefore, we suggest revising dietary and pharmacological prescriptions in patients from the age of 60. Finally, we emphasize that patient education and attention to psychosocial aspects of the disease are important, including sleep problems and limitations during work and daily life.
Emergency management
When patients with NDI have incidental disease, especially when they are admitted to hospital, their specific fluid requirements are often not appreciated by medical and nursing staff. This oversight is especially problematic if patients cannot maintain adequate oral intake and/or receive parenteral fluids. Close liaison with a specialist from the tertiary specialized centre should be sought in these circumstances (Box 5 ); patients should have contact details of their specialist physicians and wear medic alert bracelets or cards (Supplementary Box 7 ).
The typical emergency in NDI is hypernatraemic dehydration because of excessive water loss (for example, due to diarrhoea) and/or the inability to maintain adequate fluid intake (for example, vomiting). Hypernatraemic dehydration indicates a deficiency in water and consequently patients should be treated with water. By the time a patient with NDI presents with hypernatraemic dehydration, oral rehydration has usually failed and consequently, there should be a low threshold for intravenous rehydration.
Salt-containing solutions, especially NaCl 0.9% solutions, should be avoided because of their large renal osmotic load. The tonicity of such fluids (~300 mOsm/kg H 2 O) exceeds the typical urine osmolality in NDI (~100 mOsm/kg H 2 O) by about 3-fold. Consequently, around 3 l of urine are needed to excrete the renal osmotic load provided by 1 l of isotonic fluid, risking serious hypernatraemia 43 , 66 . Therefore, we recommend using water with dextrose (for example, 5% dextrose) and to calculate the initial rate of fluid administration based on a physiological demand. Routine maintenance rate (in children — first 10 kg: 100 ml/kg/24 h; 10–20 kg: 50 ml/kg/24 h; remaining 50 kg: 20 ml/kg/24 h; in adults — 25–30 ml/kg/24 h) is usually a good starting volume 67 , 68 . As 5% dextrose delivers no renal osmotic load, application at this rate will result in a slow decrease in plasma osmolality, unless there are excessive ongoing fluid losses (for example, diarrhoea). A common concern associated with the use of dextrose 5% solutions is a rapid decrease in plasma sodium concentration, which poses the risk of brain oedema. This concern does not usually apply to patients with NDI, as their urine is diluted with a very low sodium concentration and consequently, the hypotonic intravenous fluid matches the urinary losses. Importantly, dextrose 5% solution should not be administered as a bolus because of the risk of a rapid decrease in serum sodium. Isotonic fluids are appropriate for acute fluid resuscitation in patients in hypovolaemic shock. However, as intravascular volume is relatively well preserved in hypernatraemic dehydration, this is an exceedingly rare scenario in patients with NDI. Following the administration of isotonic fluid, sufficient free water should be provided to allow excretion of the renal osmotic load. If possible, the patient should be allowed to drink to thirst. Oral feeding should be provided as soon as tolerated and oral fluids should be included in the fluid balance.
In hospitalized patients, we recommend a close observation of clinical status, including neurological condition, fluid balance, weight and electrolytes. Placement of a urinary catheter should be considered to ensure proper monitoring of diuresis. Fluid composition and administration rate might need to be adjusted based on the rate and composition of ongoing losses — if the losses contain substantial concentrations of sodium, replacement of those losses with a fluid that contains a similar sodium concentration is appropriate. The aim for the overall administration rate is to balance losses, plus replacement of the fluid deficit over 48 h, and to avoid a decrease in serum sodium above 8 mmol/l/day in case of hypertonic dehydration.
We recommend treatment of patients with NDI and hypernatraemic dehydration in specialized centres to avoid potential life-threatening complications of inadequate fluid administration. Expert consultations are recommended for patients undergoing anaesthesia or surgery.
Box 5 Recommendations for emergency management
We recommend that each patient with nephrogenic diabetes insipidus (NDI) has an emergency plan, including a letter explaining their diagnosis and containing advice regarding intravenous fluid management and a contact number. Wearing a medical alert bracelet or card is also recommended (level X, strong).
We recommend using water with dextrose or glucose (for example, 5% dextrose) for intravenous rehydration (level X, strong).
We recommend calculating the initial rate of fluid administration to avoid a decrease in serum sodium above 8 mmol/l/day (level B, strong).
We recommend close observation of clinical status, including neurological condition, fluid balance, body weight and serum electrolytes (level X, strong).
We recommend that patients with NDI and hypernatraemic dehydration are treated in specialized centres with experience of the disease or under consultation with an expert centre (level X, strong).
We recommend that patients with NDI undergoing anaesthesia or surgery, or with an acute illness that carries the risk of acute hypernatraemia and dehydration, are closely monitored for fluid balance and electrolytes, and expert consultation is sought (level X, strong).
Genetic counselling and family planning
The detection of pathogenic variant(s) in either AVPR2 or AQP2 is crucial for genetic counselling. We strongly recommend counselling for young adults who are affected (hemizygous for AVPR2 pathogenic variant), who are heterozygotes for an AVPR2 or AQP2 pathogenic variant, or who are at risk of being heterozygous (Box 6 ). They should be informed about the inheritance of NDI, the related recurrence risks, and the implications of the results of the genetic test for family planning, including reproductive options. This discussion should take place soon after the genetic diagnosis has been confirmed and certainly before pregnancy 15 . Prenatal testing for a pregnancy at increased risk and preimplantation genetic testing (PGT) are, however, only possible if the disease-causing pathogenic variant(s) has/have been identified. The use of these tests should be discussed by a multidisciplinary team, according to the legislation of each country.
In the case of X-linked NDI or dominant NDI, counselling should also include information about the potential implications of the pathogenic variant(s) for family members. Patients should be encouraged to share that information with their family members at risk. These family members can then be counselled and, when applicable, undergo genetic testing.
Box 6 Recommendations for genetic counselling and family planning
We strongly recommend offering genetic counselling, including reproductive options, to parents of affected children and to young adults who are known to be heterozygotes or are at risk of being heterozygous (level B, moderate).
Prenatal and preimplantation genetic testing can be offered as reproductive options, depending on the legislation of the country (level D, moderate).
Unanswered questions and research agenda
The expert group identified several knowledge gaps and unmet needs regarding NDI that demand further research (Box 7 ). One important unanswered question concerns the long-term psychosocial outcomes of patients with NDI. Although a few studies have indicated that mental health conditions are more prevalent in patients with NDI than in the general population 4 , 17 , 46 , 47 , the degree of these problems remains to be determined, as well as their aetiology (for example, these conditions might reflect a primary manifestation of the disease or a secondary manifestation owing to complications such as dehydration-induced brain alterations).
Another pressing need is the development of targeted therapies for NDI based on the current knowledge of the underlying molecular defects. Here, we discuss some potential targeted therapies studied in vitro and/or in animal models in vivo. Only very few clinical trials in NDI have been performed, and these ended prematurely, owing to safety issues or lack of efficacy.
In vitro expression studies have demonstrated that most AVPR2 pathogenic variants associated with X-linked NDI, as well as all AQP2 pathogenic variants related to autosomal-recessive NDI, lead to the production of fully translated proteins. However, these proteins are misfolded and are consequently retained within the endoplasmic reticulum (ER). Agents that restore routing from the ER to the plasma membrane are under investigation as potential treatments. Promising agents for X-linked NDI include cell-permeable AVPR2 antagonists and agonists that rescue the intracellular retention of several AVPR2 mutants 69 , 70 , 71 , 72 . Remarkably, certain cell-permeable AVPR2 agonists have been shown to activate NDI-causing V2R mutant proteins at their intracellular location without changing their maturation and at a sufficient level to induce the translocation of AQP2 to the apical membrane. This finding indicates that non-peptide AVPR2 agonists constitute another promising treatment for NDI resulting from intracellularly retained AVPR2 mutants 73 . A clinical study in which patients with NDI and AVPR2 missense mutations were treated with a vasopressin 1a receptor (AVPR1A) antagonist had to be terminated early owing to possible interference with the cytochrome P450 metabolic pathway 74 , despite having beneficial effects on urine volume and osmolality.
Other therapeutic approaches relying on AVP-independent trafficking of AQP2 to the apical membrane have been proposed and tested in vitro and/or in animal models. One example of these AVP-independent approaches relies on activation of the cyclic adenosine monophosphate (cAMP) pathway by stimulating other G protein coupled receptors (GPCRs) such as the E-prostanoid receptors. Stimulation of the E-prostanoid receptor EP4 greatly reduced urine volumes in a conditional Avpr2 -deletion mouse model by raising AQP2 levels 75 . The rise in AQP2 levels most probably resulted from enhanced cAMP production induced by EP4 stimulation. A similar effect was observed after stimulation of the EP2 receptor with the agonist butaprost 76 . The EP2 receptor is a more interesting candidate for treatment of NDI than the EP4 receptor because EP2 agonists have already been tested in clinical studies for other diseases with promising results and an acceptable safety profile 77 , 78 , 79 . Another potential AVP-independent therapeutic strategy involves the activation of the cyclic guanosine monophosphate (cGMP) signalling pathway. Several research groups have shown that nitric oxide donors and atrial natriuretic factor stimulate the insertion of AQP2 in kidney epithelial cells in vitro and in vivo via a cGMP-dependent pathway 80 , 81 . The selective cGMP phosphodiesterase inhibitor sildenafil citrate (also known as Viagra), prevents degradation of cGMP, resulting in increased membrane expression in AQP2 in vitro and in vivo 82 . However, in a small clinical trial in patients with NDI, treatment with sildenafil citrate or riociguat (soluble guanylate cyclase stimulator) neither decreased urine volume nor increased urine osmolality 83 . Given that the oral antidiabetic drug metformin increases AQP2 phosphorylation and accumulation in the apical membrane in animal models, a trial in a small number of individuals with hereditary NDI was started in 2015 but was quickly terminated because of lack of efficacy 84 . Interestingly, a 2021 report demonstrated that a direct activator of AMP-activated protein kinase (AMPK), which also phosphorylates AQP2, increased urine concentration in NDI rats treated with the V2R blocker tolvaptan and in V2R-deficient mice 85 .
In knock-in-dominant NDI mice, the phosphodiesterase-4 inhibitor rolipram increased cAMP levels, leading to increased AQP2 phosphorylation and translocation to the apical membrane 86 . However, phosphodiesterase-4 is an abundantly expressed protein involved in immunosuppressive and anti-inflammatory pathways, and its inhibition can therefore have severe side effects. Rolipram was tested decades ago in two male patients with X-linked NDI and did not cause any relief of symptoms 87 , but the potential for other PDE inhibitors in the treatment of NDI should be examined further. Another drug that has recently received attention is the antifungal fluconazole, which increased plasma membrane AQP2 expression in collecting duct principal cells, independently from AVP, and reduced urinary output in mice treated with tolvaptan 88 . An ongoing clinical trial will test the efficacy of fluconazole in patients with NDI 89 . Gene therapy might represent a future treatment option for NDI but many challenges remain for gene-therapeutic approaches, especially in terms of efficiency 90 .
Box 7 Unanswered questions and future research agenda
Clinical research questions :
Can copeptin measurements replace desmopressin (DDAVP) or water deprivation tests in children?
What are pregnancy complications in females with nephrogenic diabetes insipidus (NDI)?
What is the natural history of NDI in ageing patients?
What are long-term psychosocial outcomes of patients with NDI?
Should NDI be included in neonatal screening?
How can testing of pharmacological agents in clinical trials be accelerated?
Fundamental research questions :
Can mutant AVPR2 stimulate alternative pathways leading to aquaporin 2 phosphorylation?
Can altered trafficking of arginine vasopressin type 2 receptor be improved by pharmacological chaperones?
Is gene therapy feasible in NDI?
Conclusions
Despite enormous advances in the understanding of the genetic causes and pathophysiology of congenital NDI in recent decades, the clinical care for patients remains challenging. Here, we formulate clinical practice recommendations for diagnostics, treatment, follow-up, emergency management, genetic counselling and family planning in patients with NDI (Boxes 2 – 6 ). These recommendations are largely expert-based consensus opinions of the core group, validated by a voting panel in a Delphi process. For most of these recommendations, full supportive evidence is not yet available; one-third of these recommendations are graded at level X, indicating exceptional situations where validating studies cannot be performed. To generate additional evidence for the other recommendations, longitudinal studies in large patient groups (both children and adults), and clinical trials are necessary. For now, we hope that the recommendations presented here can serve as a foundational framework to guide clinicians in their care for patients with NDI.
Knoers, N. V. A. M., Levtchenko, E. & Bichet, D. G. In Pediatric Nephrology (eds Francesco, E. et al.) 1063–1085 (Springer International, 2022).
Arima, H. et al. Changing the name of diabetes insipidus: a position statement of the working group for renaming diabetes insipidus. J. Clin. Endocrinol. Metab. 108 , 1–3 (2022).
Article PubMed PubMed Central Google Scholar
Bockenhauer, D., Knoers, N. & Bichet, D. G. What’s in a name? That which we call diabetes does not taste sweet! Pediatr. Nephrol. 38 , 937–939 (2023).
Article PubMed Google Scholar
D’Alessandri-Silva, C. et al. Diagnosis, treatment, and outcomes in children with congenital nephrogenic diabetes insipidus: a pediatric nephrology research consortium study. Front. Pediatr. 7 , 550 (2019).
Prosperi, F. et al. Characterization of five novel vasopressin V2 receptor mutants causing nephrogenic diabetes insipidus reveals a role of tolvaptan for M272R-V2R mutation. Sci. Rep. 10 , 16383 (2020).
Bichet, D. G. & Bockenhauer, D. Genetic forms of nephrogenic diabetes insipidus (NDI): vasopressin receptor defect (X-linked) and aquaporin defect (autosomal recessive and dominant). Best. Pract. Res. Clin. Endocrinol. Metab. 30 , 263–276 (2016).
Article CAS PubMed Google Scholar
Bockenhauer, D. & Bichet, D. G. Pathophysiology, diagnosis and management of nephrogenic diabetes insipidus. Nat. Rev. Nephrol. 11 , 576–588 (2015).
Chen, Y. et al. A reporting tool for practice guidelines in health care: the RIGHT Statement. Ann. Intern. Med. 166 , 128–132 (2017).
Guyatt, G. H. et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J. Clin. Epidemiol. 64 , 395–400 (2011).
Management, A. A. O. P. S. C. O. Q. I. a. Classifying recommendations for clinical practice guidelines. Pediatrics 114 , 874–877 (2004).
Article Google Scholar
Flynn, J. T. et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140 , e20171904 (2017).
Wesche, D., Deen, P. M. & Knoers, N. V. Congenital nephrogenic diabetes insipidus: the current state of affairs. Pediatr. Nephrol. 27 , 2183–2204 (2012).
Moeller, H. B., Rittig, S. & Fenton, R. A. Nephrogenic diabetes insipidus: essential insights into the molecular background and potential therapies for treatment. Endocr. Rev. 34 , 278–301 (2013).
Article CAS PubMed PubMed Central Google Scholar
Joshi, S. et al. Novel and recurrent variants in AVPR2 in 19 families with X-linked congenital nephrogenic diabetes insipidus. Eur. J. Pediatr. 177 , 1399–1405 (2018).
Knoers, N. & Lemmink, H. Hereditary nephrogenic diabetes insipidus. in: M. P. Adam et al. (eds) GeneReviews(®) (University of Washington, Seattle Copyright © 1993–2023, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved., 1993) (2000, updated 2020).
Forssman, H. Is hereditary diabetes insipidus of nephrogenic type associated with mental deficiency? Acta Psychiatr. Neurol. Scand. 30 , 577–587 (1955).
Hoekstra, J. A., van Lieburg, A. F., Monnens, L. A., Hulstijn-Dirkmaat, G. M. & Knoers, V. V. Cognitive and psychosocial functioning of patients with congenital nephrogenic diabetes insipidus. Am. J. Med. Genet. 61 , 81–88 (1996).
Bichet, D. G. Genetics in endocrinology pathophysiology, diagnosis and treatment of familial nephrogenic diabetes insipidus. Eur. J. Endocrinol. 183 , R29–r40 (2020).
Hureaux, M. & Vargas-Poussou, R. Genetic basis of nephrogenic diabetes insipidus. Mol. Cell Endocrinol. 560 , 111825 (2023).
Ishida, A. et al. Partial nephrogenic diabetes insipidus with a novel arginine vasopressin receptor 2 gene variant. Clin. Pediatr. Endocrinol. 31 , 44–49 (2022).
Arthus, M. F. et al. Report of 33 novel AVPR2 mutations and analysis of 117 families with X-linked nephrogenic diabetes insipidus. J. Am. Soc. Nephrol. 11 , 1044–1054 (2000).
Moses, A. M., Sangani, G. & Miller, J. L. Proposed cause of marked vasopressin resistance in a female with an X-linked recessive V2 receptor abnormality. J. Clin. Endocrinol. Metab. 80 , 1184–1186 (1995).
CAS PubMed Google Scholar
van Lieburg, A. F. et al. Clinical phenotype of nephrogenic diabetes insipidus in females heterozygous for a vasopressin type 2 receptor mutation. Hum. Genet. 96 , 70–78 (1995).
Migeon, B. R. X inactivation, female mosaicism, and sex differences in renal diseases. J. Am. Soc. Nephrol. 19 , 2052–2059 (2008).
Satoh, M., Ogikubo, S. & Yoshizawa-Ogasawara, A. Correlation between clinical phenotypes and X-inactivation patterns in six female carriers with heterozygote vasopressin type 2 receptor gene mutations. Endocr. J. 55 , 277–284 (2008).
Morgenthaler, N. G., Struck, J., Alonso, C. & Bergmann, A. Assay for the measurement of copeptin, a stable peptide derived from the precursor of vasopressin. Clin. Chem. 52 , 112–119 (2006).
Timper, K. et al. Diagnostic accuracy of copeptin in the differential diagnosis of the polyuria-polydipsia syndrome: a prospective multicenter study. J. Clin. Endocrinol. Metab. 100 , 2268–2274 (2015).
Fenske, W. et al. A copeptin-based approach in the diagnosis of diabetes insipidus. N. Engl. J. Med. 379 , 428–439 (2018).
Christ-Crain, M. & Gaisl, O. Diabetes insipidus. Presse Med. 50 , 104093 (2021).
Winzeler, B. et al. Arginine-stimulated copeptin measurements in the differential diagnosis of diabetes insipidus: a prospective diagnostic study. Lancet 394 , 587–595 (2019).
Refardt, J. et al. Arginine or hypertonic saline-stimulated copeptin to diagnose AVP deficiency. N. Engl. J. Med. 389 , 1877–1887 (2023).
Vergier, J. et al. Rapid differential diagnosis of diabetes insipidus in a 7-month-old infant: the copeptin approach. Arch. Pediatr. 25 , 45–47 (2018).
Tuli, G., Tessaris, D., Einaudi, S., Matarazzo, P. & De Sanctis, L. Copeptin role in polyuria-polydipsia syndrome differential diagnosis and reference range in paediatric age. Clin. Endocrinol. 88 , 873–879 (2018).
Article CAS Google Scholar
Bitencourt, L. et al. The usefulness of copeptin for the diagnosis of nephrogenic diabetes insipidus in infancy: a case report. J. Pediatr. Endocrinol. Metab. 34 , 1475–1479 (2021).
Bonnet, L. et al. Copeptin assays in children for the differential diagnosis of polyuria-polydipsia syndrome and reference levels in hospitalized children. Clin. Endocrinol. 96 , 47–53 (2022).
Binder, G., Weber, K., Peter, A. & Schweizer, R. Arginine-stimulated copeptin in children and adolescents. Clin. Endocrinol. 98 , 548–553 (2023).
Monnens, L., Smulders, Y., van Lier, H. & de Boo, T. DDAVP test for assessment of renal concentrating capacity in infants and children. Nephron 29 , 151–154 (1981).
Bichet, D. G. Evaluation of Patients with Polyuria . http://www.uptodate.com (2023).
De Wardener, H. E. & Herxheimer, A. The effect of a high water intake on the kidney’s ability to concentrate the urine in man. J. Physiol. 139 , 42–52 (1957).
Verbalis, J. G. Whole-body volume regulation and escape from antidiuresis. Am. J. Med. 119 , S21–S29 (2006).
Moritz, M. L. & Ayus, J. C. Maintenance intravenous fluids in acutely Ill patients. N. Engl. J. Med. 373 , 1350–1360 (2015).
Gennari, F. J. & Kassirer, J. P. Osmotic diuresis. N. Engl. J. Med. 291 , 714–720 (1974).
Bockenhauer, D. & Bichet, D. G. Nephrogenic diabetes insipidus. Curr. Opin. Pediatr. 29 , 199–205 (2017).
Rees, L. et al. Delivery of a nutritional prescription by enteral tube feeding in children with chronic kidney disease stages 2–5 and on dialysis — clinical practice recommendations from the Pediatric Renal Nutrition Taskforce. Pediatr. Nephrol. 36 , 187–204 (2021).
Lejarraga, H., Caletti, M. G., Caino, S. & Jiménez, A. Long-term growth of children with nephrogenic diabetes insipidus. Pediatr. Nephrol. 23 , 2007–2012 (2008).
Sharma, S. et al. Long-term outcome in inherited nephrogenic diabetes insipidus. Clin. Kidney J. 12 , 180–187 (2019).
Lopez-Garcia, S. C. et al. Treatment and long-term outcome in primary nephrogenic diabetes insipidus. Nephrol. Dial. Transpl. https://doi.org/10.1093/ndt/gfaa243 (2020).
Qizalbash, L., Cleghorn, S., McAlister, L. in: V. Shaw (ed.) Clinical Paediatric Dietetics. 238 (Wiley-Blackwell 2020).
Sasaki, G. et al. Growth failure in an infant with congenital nephrogenic diabetes insipidus during sodium restriction. Clin. Pediatr. Endocrinol. 16 , 95–98 (2007).
Haycock, G. B. The influence of sodium on growth in infancy. Pediatr. Nephrol. 7 , 871–875 (1993).
Scientific advisory committee on nutrition. Salt and Health . (The Stationery Office, 2003).
Coleman, J. in: V. Shaw, Lawson, M. (eds) Clinical Paediatric Dietetics . 1324, (Blackwell Science Ltd, 2001).
Bockenhauer, D. & Bichet, D. G. Urinary concentration: different ways to open and close the tap. Pediatr. Nephrol. 29 , 1297–1303 (2014).
Mortensen, L. A., Bistrup, C., Jensen, B. L. & Hinrichs, G. R. A mini-review of pharmacological strategies used to ameliorate polyuria associated with X-linked nephrogenic diabetes insipidus. Am. J. Physiol. Renal Physiol. 319 , F746–F753 (2020).
Earley, L. E. & Orloff, J. The mechanism of antidiuresis associated with the administration of hydrochlorothiazide to patients with vasopressin-resistant diabetes insipidus. J. Clin. Invest. 41 , 1988–1997 (1962).
Anton-Gamero, M., Garcia-Martinez, E., Fernandez-Ramos, J., Rodríguez-Salas, M. & Gil-Campos, M. Nephrogenic diabetes insipidus: the key element of paradoxical hyponatremia. Pediatr. Nephrol. 24 , 2277–2278 (2009).
Boussemart, T., Nsota, J., Martin-Coignard, D. & Champion, G. Nephrogenic diabetes insipidus: treat with caution. Pediatr. Nephrol. 24 , 1761–1763 (2009).
Kirchlechner, V., Koller, D. Y., Seidl, R. & Waldhauser, F. Treatment of nephrogenic diabetes insipidus with hydrochlorothiazide and amiloride. Arch. Dis. Child. 80 , 548–552 (1999).
Wu, H. Y. Achieving urinary continence in children. Nat. Rev. Urol. 7 , 371–377 (2010).
Colliver, D., Storey, R., Dickens, H. & Subramaniam, R. Nonobstructive urinary tract dilatation in children with diabetes insipidus. J. Pediatr. Surg. 47 , 752–755 (2012).
Wang, X. et al. Upper urinary dilatation and treatment of 26 patients with diabetes insipidus: a single-center retrospective study. Front. Endocrinol. 13 , 941453 (2022).
Pedersen, S. A. et al. Hydrochlorothiazide use and risk of nonmelanoma skin cancer: a nationwide case-control study from Denmark. J. Am. Acad. Dermatol. 78 , 673–681.e679 (2018).
Alon, U. & Chan, J. C. Hydrochlorothiazide-amiloride in the treatment of congenital nephrogenic diabetes insipidus. Am. J. Nephrol. 5 , 9–13 (1985).
Konoshita, T. et al. Treatment of congenital nephrogenic diabetes insipidus with hydrochlorothiazide and amiloride in an adult patient. Horm. Res. 61 , 63–67 (2004).
Levin, A. et al. Kidney disease: improving global outcomes (KDIGO) CKD work group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3 , 1–150 (2013).
Google Scholar
Guarino, S. et al. Nephrogenic diabetes insipidus in childhood: assessment of volume status and appropriate fluid replenishment. Pediatr. Emerg. Care 36 , e402–e404 (2020).
Holliday, M. A. & Segar, W. E. The maintenance need for water in parenteral fluid therapy. Pediatrics 19 , 823–832 (1957).
National Institute for Health and Care Excellence. Intravenous fluid therapy in adults in hospital. Clinical guideline [CG174], http://www.nice.org.uk/Guidance/CG174 (2013, updated 2017).
Erdem Tuncdemir, B., Mergen, H. & Saglar Ozer, E. Evaluation of pharmacochaperone-mediated rescue of mutant V2 receptor proteins. Eur. J. Pharmacol. 865 , 172803 (2019).
Morello, J. P. et al. Pharmacological chaperones rescue cell-surface expression and function of misfolded V2 vasopressin receptor mutants. J. Clin. Invest. 105 , 887–895 (2000).
Ranadive, S. A. et al. Identification, characterization and rescue of a novel vasopressin-2 receptor mutation causing nephrogenic diabetes insipidus. Clin. Endocrinol. 71 , 388–393 (2009).
Robben, J. H., Sze, M., Knoers, N. V. & Deen, P. M. Functional rescue of vasopressin V2 receptor mutants in MDCK cells by pharmacochaperones: relevance to therapy of nephrogenic diabetes insipidus. Am. J. Physiol. Renal Physiol. 292 , F253–F260 (2007).
Robben, J. H. et al. Intracellular activation of vasopressin V2 receptor mutants in nephrogenic diabetes insipidus by nonpeptide agonists. Proc. Natl Acad. Sci. USA 106 , 12195–12200 (2009).
Bernier, V. et al. Pharmacologic chaperones as a potential treatment for X-linked nephrogenic diabetes insipidus. J. Am. Soc. Nephrol. 17 , 232–243 (2006).
Li, J. H. et al. A selective EP4 PGE2 receptor agonist alleviates disease in a new mouse model of X-linked nephrogenic diabetes insipidus. J. Clin. Invest. 119 , 3115–3126 (2009).
Olesen, E. T., Rützler, M. R., Moeller, H. B., Praetorius, H. A. & Fenton, R. A. Vasopressin-independent targeting of aquaporin-2 by selective E-prostanoid receptor agonists alleviates nephrogenic diabetes insipidus. Proc. Natl Acad. Sci. USA 108 , 12949–12954 (2011).
Aihara, M. et al. Pharmacokinetics, safety, and intraocular pressure-lowering profile of omidenepag isopropyl, a selective, nonprostaglandin, prostanoid EP2 receptor agonist, in healthy Japanese and Caucasian volunteers (phase I study). J. Ocul. Pharmacol. Ther. 35 , 542–550 (2019).
Steinwall, M., Akerlund, M., Bossmar, T., Nishii, M. & Wright, M. ONO-8815Ly, an EP2 agonist that markedly inhibits uterine contractions in women. BJOG 111 , 120–124 (2004).
Aihara, M. et al. Phase 2, randomized, dose-finding studies of omidenepag isopropyl, a selective EP2 agonist, in patients with primary open-angle glaucoma or ocular hypertension. J. Glaucoma 28 , 375–385 (2019).
Boone, M., Kortenoeven, M., Robben, J. H. & Deen, P. M. Effect of the cGMP pathway on AQP2 expression and translocation: potential implications for nephrogenic diabetes insipidus. Nephrol. Dial. Transpl. 25 , 48–54 (2010).
Bouley, R. et al. Nitric oxide and atrial natriuretic factor stimulate cGMP-dependent membrane insertion of aquaporin 2 in renal epithelial cells. J. Clin. Invest. 106 , 1115–1126 (2000).
Bouley, R. et al. Stimulation of AQP2 membrane insertion in renal epithelial cells in vitro and in vivo by the cGMP phosphodiesterase inhibitor sildenafil citrate (Viagra). Am. J. Physiol. Renal Physiol. 288 , F1103–F1112 (2005).
Hinrichs, G. R. et al. Treatment of nephrogenic diabetes insipidus patients with cGMP-stimulating drugs does not mitigate polyuria or increase urinary concentrating ability. Kidney Int. Rep. 5 , 1319–1325 (2020).
ClinicalTrials.gov. US National Library of Medicine . https://clinicaltrials.gov/study/NCT02460354 (2018).
Klein, J. D. et al. An AMPK activator as a therapeutic option for congenital nephrogenic diabetes insipidus. JCI Insight 6 , e146419 (2021).
Sohara, E. et al. Pathogenesis and treatment of autosomal-dominant nephrogenic diabetes insipidus caused by an aquaporin 2 mutation. Proc. Natl Acad. Sci. USA 103 , 14217–14222 (2006).
Bichet, D. G., Ruel, N., Arthus, M. F. & Lonergan, M. Rolipram, a phosphodiesterase inhibitor, in the treatment of two male patients with congenital nephrogenic diabetes insipidus. Nephron 56 , 449–450 (1990).
Vukićević, T. et al. Fluconazole increases osmotic water transport in renal collecting duct through effects on aquaporin-2 trafficking. J. Am. Soc. Nephrol. 30 , 795–810 (2019).
Treatment of congenital nephrogenic diabetes insipidus with fluconazole, an antifungal medication. https://www.clinicaltrialsregister.eu/ctr-search/trial/2020-002204-38/DK .
Davis, L. & Park, F. Gene therapy research for kidney diseases. Physiol. Genomics 51 , 449–461 (2019).
Bockenhauer, D. & Bichet, D. G. Inherited secondary nephrogenic diabetes insipidus: concentrating on humans. Am. J. Physiol. Renal Physiol. 304 , F1037–F1042 (2013).
Hudson, J. L., Baum, J. I., Diaz, E. C. & Børsheim, E. Dietary protein requirements in children: methods for consideration. Nutrients 13 , 1554 (2021).
Richter, M. et al. Revised reference values for the intake of protein. Ann. Nutr. Metab. 74 , 242–250 (2019).
Crawford, J. D. & Kennedy, G. C. Chlorothiazid in diabetes insipidus. Nature 183 , 891–892 (1959).
Kennedy, G. C. & Crawford, J. D. Treatment of diabetes insipidus with hydrochlorothiazide. Lancet 1 , 866–867 (1959).
Knoers, N. & Monnens, L. A. Amiloride-hydrochlorothiazide versus indomethacin-hydrochlorothiazide in the treatment of nephrogenic diabetes insipidus. J. Pediatr. 117 , 499–502 (1990).
Gambaro, G. & Perazella, M. A. Adverse renal effects of anti-inflammatory agents: evaluation of selective and nonselective cyclooxygenase inhibitors. J. Intern. Med. 253 , 643–652 (2003).
Jakobsson, B. & Berg, U. Effect of hydrochlorothiazide and indomethacin treatment on renal function in nephrogenic diabetes insipidus. Acta Paediatr. 83 , 522–525 (1994).
Monnens, L., Jonkman, A. & Thomas, C. Response to indomethacin and hydrochlorothiazide in nephrogenic diabetes insipidus. Clin. Sci. 66 , 709–715 (1984).
Rascher, W., Rosendahl, W., Henrichs, I. A., Maier, R. & Seyberth, H. W. Congenital nephrogenic diabetes insipidus-vasopressin and prostaglandins in response to treatment with hydrochlorothiazide and indomethacin. Pediatr. Nephrol. 1 , 485–490 (1987).
Harris, R. C. Jr Cyclooxygenase-2 inhibition and renal physiology. Am. J. Cardiol. 89 , 10d–17d (2002).
Libber, S., Harrison, H. & Spector, D. Treatment of nephrogenic diabetes insipidus with prostaglandin synthesis inhibitors. J. Pediatr. 108 , 305–311 (1986).
Pattaragarn, A. & Alon, U. S. Treatment of congenital nephrogenic diabetes insipidus by hydrochlorothiazide and cyclooxygenase-2 inhibitor. Pediatr. Nephrol. 18 , 1073–1076 (2003).
Download references
Acknowledgements
This project was initiated by the Working Group for Tubulopathies of ERKNet. ERKNet is funded by the European Union within the framework of the EU4Health Programme (101085068). We thank patient advocates, Elodie Martin and Lucas van Baelen, for their important participation in our discussions, bringing in their personal experiences and those of other patients, Louise McAlister (Great Ormond Street Hospital for Children NHS Foundation Trust, UK) for dietary advice, Tanja Wlodkowski and Stefanie Häberle (ERKNet project managers) for project support, and members of the voting panel for their careful evaluation of the recommendations.
Author information
Authors and affiliations.
Department of Paediatric Nephrology, Emma Children’s Hospital, Amsterdam University Medical Centre, Amsterdam, The Netherlands
Elena Levtchenko
Department of Paediatric Nephrology, Hospital Vall d’ Hebron, Autonomous University of Barcelona, Barcelona, Spain
Gema Ariceta
Department of Paediatric Urology, Emma Children’s Hospital, Amsterdam University Medical Centre, Amsterdam, The Netherlands
Olga Arguedas Flores
Nephrology Service, Hôpital du Sacré-Coeur de Montréal, Departments of Medicine, Pharmacology and Physiology, University of Montreal, Québec, Canada
Daniel G. Bichet
Paediatric Nephrology, University Hospital and Catholic University Leuven, Leuven, Belgium
Detlef Bockenhauer
Great Ormond Street Hospital for Children NHS Foundation Trust and Department of Renal Medicine, University College London, London, UK
Division of Nephrology, Bambino Gesù Children’s Hospital, IRCCS, Rome, Italy
Francesco Emma
Division of Nephrology and Transplantation, Department of Internal Medicine, Erasmus Medical Center, University Medical Center Rotterdam, Rotterdam, The Netherlands
Ewout J. Hoorn
Department of Paediatric Nephrology, Amalia Children’s Hospital, Radboud University Medical Center, Nijmegen, The Netherlands
Linda Koster-Kamphuis
Department of Nephrology, Radboud University Medical Center, Nijmegen, The Netherlands
Tom Nijenhuis
Department of Medical Translational Sciences, University of Campania “Luigi Vanvitelli”, Naples, Italy
Francesco Trepiccione
Biogem Institute of Molecular Biology and Genetics, Ariano Irpino, Italy
Department of Genomic Medicine for Rare Diseases, Reference Centre for Hereditary Kidney Diseases of Children and Adults MARHEA, Assistance Publique Hôpitaux de Paris — Hôpital Européen Georges Pompidou, Paris, France
Rosa Vargas-Poussou
London Tubular Centre, Department of Renal Medicine, Department of Renal Medicine, University College London, London, UK
Stephen B. Walsh
Department of Genetics, University Medical Center Groningen, Groningen, The Netherlands
Nine V.A.M. Knoers
You can also search for this author in PubMed Google Scholar
Contributions
All authors researched data for the article, made substantial contributions to discussions of the content, and wrote, reviewed or edited the manuscript before submission.
Corresponding authors
Correspondence to Elena Levtchenko or Nine V.A.M. Knoers .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Reviews Nephrology thanks Gitte Hinrichs, Julie Refardt and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Levtchenko, E., Ariceta, G., Arguedas Flores, O. et al. International expert consensus statement on the diagnosis and management of congenital nephrogenic diabetes insipidus (arginine vasopressin resistance). Nat Rev Nephrol (2024). https://doi.org/10.1038/s41581-024-00897-z
Download citation
Accepted : 13 September 2024
Published : 22 October 2024
DOI : https://doi.org/10.1038/s41581-024-00897-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

IMAGES
VIDEO
COMMENTS
Personal Statement Personal statements usually fall into 3 categories: ... Say "emergency room" or "emergency room doctor" - use the emergency department and emergency physician; Start every sentence with "I". Make it longer than one page, in single‐spaced, 12-point font.
Looking at emergency medicine personal statement samples can be very useful when preparing your residency applications. Your personal statement is one of the most challenging components of the ERAS or CaRMS residency applications, but it is also one of the most important ones. Especially when you consider the fact that emergency medicine is one of the most competitive residencies.
"Do's" of writing personal statements: 🗸 DO tell a story about yourself or share a unique situation. You are showing the reader your narrative about why you are a great candidate for residency. 🗸 DO make it human. Approach the statement as an opportunity to process life experiences and articulate the arc of your journey.
Emergency Management Personal Statement. Decent Essays. 188 Words; 1 Page; Open Document. First and foremost, I have earned a master's degree in Emergency Management and Homeland Security from Arizona State University. This degree required hundreds of hours of training and education in every aspect of emergency management and continuity.
To make things easier, you'll also find an emergency medicine personal statement sample to help you get started. Tips for Writing Emergency Medicine Personal Statements Convey a Clear Purpose. When writing an emergency medicine personal statement, it is important to capture the essence of why you want to pursue the career.
The Medfools Emergency Medicine Sample Residency Personal Statement Library is now open! These sample ER - Emergency Medicine personal statements are here for your viewing pleasure (fully anonymous). We're hoping to add more in the future, including Pre-Med personal statements. If you've got one to add to the free library, don't forget to contribute yours. Emergency Medicine became […]
Emergency Medicine Personal Statement Example: Résumés and Personal Statements for Health Professionals James W. Tysinger,1999 Helps the user prepare a resume and personal statement The Premed Playbook Ryan Gray,2018-06-19 How to craft a personal statement that secures interviews and admissions Reliable advice a gift to premeds Sujay Kansagra ...
Personal Statement Emergency Medicine First Choice, a 47-foot sailboat that completed an 11-year voyage around the world caught my eye. Although the 25-year-old sturdy vessel showed signs of the journey, it was in no way antiquated. ... and management are areas that I want my training to emphasize. In addition, I would like to be in a
The Medfools Emergency Medicine Sample Residency Personal Statement Library is now open! These sample ER - Emergency Medicine personal statements are here for your viewing pleasure (fully anonymous). We're hoping to add more in the future, including Pre-Med personal statements. If you've got one to add to the free library, don't forget to contribute yours. It was a […]
The Medfools Emergency Medicine Sample Residency Personal Statement Library is now open! These sample ER - Emergency Medicine personal statements are here for your viewing pleasure (fully anonymous). We're hoping to add more in the future, including Pre-Med personal statements. If you've got one to add to the free library, don't forget to contribute yours. The wind whipped […]
PEM Personal Statement Example Provided by Michele McDaniel From the moment I took my first, tremulous step through the doors of the hospital with my freshly ironed white coat and my newly minted title of MD, I knew I wanted to have a career in the field of pediatric emergency medicine.
Personal preparedness is basic components of any group or association 's emergency planning. Regardless of different helpers, for example, real occasions and open data, people and families remain to a great extent ill-equipped to react to crisis and debacle circumstances (Rumbach and Foley, 2014).
Personal Statement: A Career In Emergency Management. Decent Essays. 580 Words; 3 Pages; Open Document. ... Thus, in emergency management, to enhance the agency's vision, changes may arise from policies and procedures, technology advancement, and equipment, shift in priorities, increase on mitigation and prevention measures, and methodologies ...
The personal statement is an important part of the residency application. Although guidance exists, the composition of personal statements is not standardized; each statement reflects an applicant's unique personality. ... The authors utilized Dedoose , a qualitative data management software program, to code the statements and analyze the ...
Or can you generally just use one personal statement (just addressing why you want to go into EM as a specialty) to apply to all EM residencies? Thanks in advance. ... /r/emergencymedicine is a subreddit for healthcare providers in the emergency setting to discuss their encounters and find ways to improve their knowledge of various parts of EM.
EMERGENCY MEDICINE PERSONAL STATEMENT The wind whipped through the airplane cabin as the door opened at 13,800 feet. As I sat waiting for my turn to jump, I felt more anxious and uncertain than I'd ever been in my life. "Ready?" the jumpmaster yelled. I didn't have time to respond.
Emergency Management protects communities by coordinating and integrating all activi-ties necessary to build, sustain, and improve the capability to mitigate against, prepare for, respond to, and recover from threatened or actual natural disasters, acts of terrorism, or other man-made disasters. Principles Emergency Management must be: 1.
Using your personal statement beyond a university application; Carers, estranged students, refugees, asylum seekers, and those with limited leave to remain; Personal statement guides. Personal statement advice: animal science; Personal statement advice: biology; Personal statement advice: business and management; Personal statement advice ...
The Medfools Emergency Medicine Sample Residency Personal Statement Library is now open! These sample ER - Emergency Medicine personal statements are here for your viewing pleasure (fully anonymous). We're hoping to add more in the future, including Pre-Med personal statements. If you've got one to add to the free library, don't forget to contribute yours. Born and raised […]
Follow NYC Emergency Management - "Prep Talk" on SoundCloud; Follow NYC Emergency Management - "Prep Talk" on Apple Podcasts; Follow NYC Emergency Management - "Prep Talk" on Spreaker; Get the RSS feed ¡Prepárate!, el primer podcast en español de la agencia, dedicado a educar a los Neoyorquinos como prepararse para las emergencias. NYC ...
emergency medicine residency personal statement
Here, we present 36 recommendations for diagnosis, treatment and follow-up in both children and adults, as well as emergency management, genetic counselling and family planning, for patients with NDI.