- CPSolvers Academy
- Morning Report
- Diagnostic frameworks
- Illness scripts
- Residency Match
- Spaced Learning

Problem Representation
- by Ankit Bansal
- June 12, 2022 June 12, 2022
Clinical Reasoning Corner: Problem Representation
By: Marcela A. de Oliveira Santana and Franco Murillo
Reviewed by: Jack Penner
Welcome back, Clinical Problem Solvers!
Today we are going to talk about the Problem Representation. Let’s go!
Objectives:
Define Problem Representation
Describe the core components of a Problem Representation
Summarize the value of the Problem Representation during the clinical reasoning process
Create a Problem Representation based on data from a clinical case
So, what exactly is a Problem Representation?
A problem representation (PR, or Summary Statement) is an evolving, concise summary that highlights the defining features of a case , helping clinicians generate a focused differential diagnosis and identify the next steps in diagnosis and treatment.
For those who like to use Twitter, you can ask yourself: What if I had to summarize this case and only had one tweet to do it?
The problem representation during the clinical reasoning process
The PR is linked to hypothesis-generation and can act as a guide during the diagnostic journey. It allows clinicians to distill the case into its most relevant features, which facilitates efficient diagnostic schema and illness script selection. As a teaching tool, it helps learners practice identifying key and differentiating case details as they practice and narrate their clinical reasoning.
To create a problem representation you need to be able to abstract critical information from a clinical scenario using semantic qualifiers; for example, young/old, constant/recurrent, diffuse/localized, mild/moderate/severe, and acute/subacute/chronic. By extracting key case details and translating them into generalizable terms, you can more effectively link the case in front of you to your own bank of diagnostic schemas and illness scripts. This will help you identify what new data you need to collect to support or falsify your diagnostic hypotheses.
One more important point: the problem representation is dynamic. It can and should evolve as you gather new information.
Let’s look at a few strategies for constructing a Problem Representation:
Try to answer 3 main questions in your PR: Who? When? What?
Who is the patient?
Relevant demographics, epidemiology, and risk factors
When did this happen?
The temporal pattern of the illness – the duration (hyperacute, acute, subacute, or chronic) and tempo (stable, progressive, fluctuating)
What is the clinical syndrome?
Key signs, symptoms, and differentiating features of the clinical syndrome.
Exclude extraneous information – Example: In a patient presenting with fever, cough, and shortness of breath, their history of chronic knee osteoarthritis does not belong in the PR.
Consider what information we need to keep in the background of our mind, not in the initial PR – Example: In a patient presenting with fevers and joint pain, you may not initially include that they have cats/dogs in your PR. However, this may become relevant if you discover in the workup that they have an aortic valve vegetation and negative blood cultures (i.e., culture negative endocarditis). At that point in the case, their exposure to cats can help frame the probability of different organisms that cause culture-negative endocarditis, making it a useful part of your PR.
We often have to pick and choose what to include to avoid overloading the one-liner. The information we include should help us frame someone’s clinical syndrome (e.g., including risk factors for cardiovascular disease in the PR for someone with chest pain).
It is important to understand that each clinician will have their own approach to PR. We should learn that PRs are not “right or wrong”. They can be “better” when all relevant attributes are addressed using the appropriate semantic qualifiers for the specific clinical problem.
Let’s see an example to illustrate what we learned:
You are at the emergency department evaluating a middle-aged male. He reports 3 days of headache, myalgia, and fever. When you hear these initial symptoms, you may not be able to select an illness script because many diseases present with “headache, myalgia, and fever.” However, you can choose between those symptoms and activate the most useful schema to start your diagnostic process. For example, you may start with a fever schema, such as “Fever – Overview” or “Fever – Path to inflammation ,” and then examine what diseases on those lists can also present with myalgias and headache,
At this time, your initial PR could be: “A middle-aged male presenting with acute fever associated with headache and myalgia.”
One day later the patient also develops a rash. At this time, you might want to activate another schema, for example, “Fever + Rash” . His past medical history is significant for hypertension and diabetes mellitus. He lives with his wife and 2 cats. He was traveling to Brazil last week to visit some friends, giving you an important clue about the patient’s epidemiological risk and prompting you to think about a new schema: “Fever in a Returning Traveler”.
His labs show leukopenia, lymphopenia, and thrombocytopenia.
At this moment, you can go back to your PR:
“A middle-age male with HTN, diabetes, and recent travel to Brazil presenting with acute headache, myalgia, fever, and rash and found to have leukopenia, lymphopenia, and thrombocytopenia”
Our PR helped us select two schemas (Fever in a Returning Traveler and Fever + Rash). We can look for diseases that may be present in one or both schemas to help identify which illness scripts to compare against the patient’s script. In this case, we see that Dengue is a differential diagnosis present in both the schemas. You compare the PR with the illness script for Dengue and notice that they match, guiding you to order the confirmatory exams for the final diagnosis.
“A middle-age male with HTN, diabetes, and recent travel to Brazil presenting with acute headache, myalgia, fever, and rash and found to have leukopenia, lymphopenia, and thrombocytopenia. A positive NS1 test result confirmed the final diagnosis of Dengue.”
That covers it, Clinical Problem Solvers! Don’t forget to check the Clinical Reasoning BootCamp VMR episode about the problem representation and see a great example of how the problem representation evolves during the case presentation!
A problem representation is a summary that highlights the defining features of a case and will guide you through the clinical reasoning process
It allows clinicians to use pattern recognition to quickly develop a differential diagnosis and allows learners to develop their reasoning skills.
The problem representation is dynamic. It would evolve as soon as you get clinically relevant information.
When you are making a problem representation try to answer 3 main questions: Who? When? What?
References:
Problem Representation Overview. CLINICAL REASONING EXERCISES. JGIM. https://www.sgim.org/web-only/clinical-reasoning-exercises/problem-representation-overview#
Diagnostic Schema. CLINICAL REASONING EXERCISES. JGIM. https://www.sgim.org/web-only/clinical-reasoning-exercises/diagnostic-schema#
- Principles and Practice of Case-based Clinical Reasoning Education A Method for Preclinical Students by Olle ten Cate, Eugène J.F.M. Custers, Steven J. Durning (eds.)
- Denise M. Connor. Key Clinical Reasoning Concepts. Developing Medical Educators of the 21st Century, San Francisco, CA . Feb 25-27,2019. https://meded21.ucsf.edu/sites/g/files/tkssra796/f/wysiwyg/W04%20Handout.pdf
- Martin M, Sedighi Manesh R, Henderson MC, Critchfield JM. Diagnostic Scheming. J Gen Intern Med. 2015;30(12):1874-1878. doi:10.1007/s11606-015-3478-0
- Minter DJ, Manesh R, Cornett P, Geha RM. Putting Schemas to the Test: An Exercise in Clinical Reasoning. J Gen Intern Med. 2018;33(11):2010-2014. doi:10.1007/s11606-018-4599-z
Discover more from The Clinical Problem Solvers
Subscribe now to keep reading and get access to the full archive.
Type your email…
Continue reading
Diagnosis of hypokalemia: a problem-solving approach to clinical cases
Affiliation.
- 1 Section of Pediatric Nephrology, Rush University Medical Center, Chicago, Illinois 60612, USA. [email protected]
- PMID: 19377223
In situations where the cause of hypokalemia is not obvious, measurement of urinary potassium excretion and blood pressure and assessment of acid-base balance are often helpful. A random urine potassium-creatinine ratio (K/C) less than 1.5 suggests poor intake, gastrointestinal losses, or a shift of potassium into cells. If hypokalemia is associated with paralysis, we should consider hyperthyroidism, familial or sporadic periodic paralysis. Metabolic acidosis with a urine K/C ratio less than 1.5 suggests lower gastrointestinal losses due to diarrhea or laxative abuse. Metabolic acidosis with K/C ratio of 1.5 higher is often due to diabetic ketoacidosis or type 1 or type 2 distal renal tubular acidosis. Metabolic alkalosis with a K/C ratio less than 1.5 and a normal blood pressure is often due to surreptitious vomiting. Metabolic alkalosis with a higher K/C ratio and a normal blood pressure suggests diuretic use, Bartter syndrome, or Gitelman syndrome. Metabolic alkalosis with a high urine K/C ratio and hypertension suggests primary hyperaldosteronism, Cushing syndrome, congenital adrenal hyperplasia, renal artery stenosis, apparent mineralocorticoid excess, or Liddle syndrome. Hypomagnesemia can lead to increased urinary potassium losses and hypokalemia. The differential rests upon measurement of blood magnesium, aldosterone and renin levels, diuretic screen in urine, response to spironolactone and amiloride, measurement of plasma cortisol level and the urinary cortisol-cortisone ratio, and genetic testing.
Publication types
- Practice Guideline
- Acid-Base Imbalance / complications
- Acid-Base Imbalance / diagnosis*
- Acid-Base Imbalance / genetics
- Creatinine / blood
- Creatinine / urine
- Hypertension / complications*
- Hypertension / etiology
- Hypertension / genetics
- Hypokalemia / complications*
- Hypokalemia / diagnosis*
- Hypokalemia / genetics
- Potassium / blood
- Potassium / urine
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Clinical problem solving and diagnostic decision making: selective review of the cognitive literature
Arthur s elstein, alan schwarz.
- Author information
- Article notes
- Copyright and License information
Correspondence to: A S Elstein [email protected]
Series information
Evidence base of clinical diagnosis
This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential approaches: problem solving 1 – 3 and decision making. 4 – 8 Problem solving research was initially aimed at describing reasoning by expert physicians, to improve instruction of medical students and house officers. Psychological decision research has been influenced from the start by statistical models of reasoning under uncertainty, and has concentrated on identifying departures from these standards.
Summary points
Problem solving and decision making are two paradigms for psychological research on clinical reasoning, each with its own assumptions and methods
The choice of strategy for diagnostic problem solving depends on the perceived difficulty of the case and on knowledge of content as well as strategy
Final conclusions should depend both on prior belief and strength of the evidence
Conclusions reached by Bayes's theorem and clinical intuition may conflict
Because of cognitive limitations, systematic biases and errors result from employing simpler rather than more complex cognitive strategies
Evidence based medicine applies decision theory to clinical diagnosis
Problem solving
Diagnosis as selecting a hypothesis.
The earliest psychological formulation viewed diagnostic reasoning as a process of testing hypotheses. Solutions to difficult diagnostic problems were found by generating a limited number of hypotheses early in the diagnostic process and using them to guide subsequent collection of data. 1 Each hypothesis can be used to predict what additional findings ought to be present if it were true, and the diagnostic process is a guided search for these findings. Experienced physicians form hypotheses and their diagnostic plan rapidly, and the quality of their hypotheses is higher than that of novices. Novices struggle to develop a plan and some have difficulty moving beyond collection of data to considering possibilities.
It is possible to collect data thoroughly but nevertheless to ignore, to misunderstand, or to misinterpret some findings, but also possible for a clinician to be too economical in collecting data and yet to interpret accurately what is available. Accuracy and thoroughness are analytically separable.
Pattern recognition or categorisation
Expertise in problem solving varies greatly between individual clinicians and is highly dependent on the clinician's mastery of the particular domain. 9 This finding challenges the hypothetico-deductive model of clinical reasoning, since both successful and unsuccessful diagnosticians use hypothesis testing. It appears that diagnostic accuracy does not depend as much on strategy as on mastery of content. Further, the clinical reasoning of experts in familiar situations frequently does not involve explicit testing of hypotheses. 3 , 10 – 12 Their speed, efficiency, and accuracy suggest that they may not even use the same reasoning processes as novices. 11 It is likely that experienced physicians use a hypothetico-deductive strategy only with difficult cases and that clinical reasoning is more a matter of pattern recognition or direct automatic retrieval. What are the patterns? What is retrieved? These questions signal a shift from the study of judgment to the study of the organisation and retrieval of memories.
Problem solving strategies
Hypothesis testing
Pattern recognition (categorisation)
By specific instances
By general prototypes
Viewing the process of diagnosis assigning a case to a category brings some other issues into clearer view. How is a new case categorised? Two competing answers to this question have been put forward and research evidence supports both. Category assignment can be based on matching the case to a specific instance (“instance based” or “exemplar based” recognition) or to a more abstract prototype. In the former, a new case is categorised by its resemblance to memories of instances previously seen. 3 , 11 This model is supported by the fact that clinical diagnosis is strongly affected by context—for example, the location of a skin rash on the body—even when the context ought to be irrelevant. 12
The prototype model holds that clinical experience facilitates the construction of mental models, abstractions, or prototypes. 2 , 13 Several characteristics of experts support this view—for instance, they can better identify the additional findings needed to complete a clinical picture and relate the findings to an overall concept of the case. These features suggest that better diagnosticians have constructed more diversified and abstract sets of semantic relations, a network of links between clinical features and diagnostic categories. 14
The controversy about the methods used in diagnostic reasoning can be resolved by recognising that clinicians approach problems flexibly; the method they select depends upon the perceived characteristics of the problem. Easy cases can be solved by pattern recognition: difficult cases need systematic generation and testing of hypotheses. Whether a diagnostic problem is easy or difficult is a function of the knowledge and experience of the clinician.
The strategies reviewed are neither proof against error nor always consistent with statistical rules of inference. Errors that can occur in difficult cases in internal medicine include failure to generate the correct hypothesis; misperception or misreading the evidence, especially visual cues; and misinterpretations of the evidence. 15 , 16 Many diagnostic problems are so complex that the correct solution is not contained in the initial set of hypotheses. Restructuring and reformulating should occur as data are obtained and the clinical picture evolves. However, a clinician may quickly become psychologically committed to a particular hypothesis, making it more difficult to restructure the problem.
Decision making
Diagnosis as opinion revision.
From the point of view of decision theory, reaching a diagnosis means updating opinion with imperfect information (the clinical evidence). 8 , 17 The standard rule for this task is Bayes's theorem. The pretest probability is either the known prevalence of the disease or the clinician's subjective impression of the probability of disease before new information is acquired. The post-test probability, the probability of disease given new information, is a function of two variables, pretest probability and the strength of the evidence, measured by a “likelihood ratio.”
Bayes's theorem tells us how we should reason, but it does not claim to describe how opinions are revised. In our experience, clinicians trained in methods of evidence based medicine are more likely than untrained clinicians to use a Bayesian approach to interpreting findings. 18 Nevertheless, probably only a minority of clinicians use it in daily practice and informal methods of opinion revision still predominate. Bayes's theorem directs attention to two major classes of errors in clinical reasoning: in the assessment of either pretest probability or the strength of the evidence. The psychological study of diagnostic reasoning from this viewpoint has focused on errors in both components, and on the simplifying rules or heuristics that replace more complex procedures. Consequently, this approach has become widely known as “heuristics and biases.” 4 , 19
Errors in estimation of probability
Availability —People are apt to overestimate the frequency of vivid or easily recalled events and to underestimate the frequency of events that are either very ordinary or difficult to recall. Diseases or injuries that receive considerable media attention are often thought of as occurring more commonly than they actually do. This psychological principle is exemplified clinically in the overemphasis of rare conditions, because unusual cases are more memorable than routine problems.
Representativeness —Representativeness refers to estimating the probability of disease by judging how similar a case is to a diagnostic category or prototype. It can lead to overestimation of probability either by causing confusion of post-test probability with test sensitivity or by leading to neglect of base rates and implicitly considering all hypotheses equally likely. This is an error, because if a case resembles disease A and disease B equally, and A is much more common than B, then the case is more likely to be an instance of A. Representativeness is associated with the “conjunction fallacy”—incorrectly concluding that the probability of a joint event (such as the combination of findings to form a typical clinical picture) is greater than the probability of any one of these events alone.
Heuristics and biases
Availability
Representativeness
Probability transformations
Effect of description detail
Conservatism
Anchoring and adjustment
Order effects
Decision theory assumes that in psychological processing of probabilities, they are not transformed from the ordinary probability scale. Prospect theory was formulated as a descriptive account of choices involving gambling on two outcomes, 20 and cumulative prospect theory extends the theory to cases with multiple outcomes. 21 Both prospect theory and cumulative prospect theory propose that, in decision making, small probabilities are overweighted and large probabilities underweighted, contrary to the assumption of standard decision theory. This “compression” of the probability scale explains why the difference between 99% and 100% is psychologically much greater than the difference between, say, 60% and 61%. 22
Support theory
Support theory proposes that the subjective probability of an event is inappropriately influenced by how detailed the description is. More explicit descriptions yield higher probability estimates than compact, condensed descriptions, even when the two refer to exactly the same events. Clinically, support theory predicts that a longer, more detailed case description will be assigned a higher subjective probability of the index disease than a brief abstract of the same case, even if they contain the same information about that disease. Thus, subjective assessments of events, while often necessary in clinical practice, can be affected by factors unrelated to true prevalence. 23
Errors in revision of probability
In clinical case discussions, data are presented sequentially, and diagnostic probabilities are not revised as much as is implied by Bayes's theorem 8 ; this phenomenon is called conservatism. One explanation is that diagnostic opinions are revised up or down from an initial anchor, which is either given in the problem or subjectively formed. Final opinions are sensitive to the starting point (the “anchor”), and the shift (“adjustment”) from it is typically insufficient. 4 Both biases will lead to collecting more information than is necessary to reach a desired level of diagnostic certainty.
It is difficult for everyday judgment to keep separate accounts of the probability of a disease and the benefits that accrue from detecting it. Probability revision errors that are systematically linked to the perceived cost of mistakes show the difficulties experienced in separating assessments of probability from values, as required by standard decision theory. There is a tendency to overestimate the probability of more serious but treatable diseases, because a clinician would hate to miss one. 24
Bayes's theorem implies that clinicians given identical information should reach the same diagnostic opinion, regardless of the order in which information is presented. However, final opinions are also affected by the order of presentation of information. Information presented later in a case is given more weight than information presented earlier. 25
Other errors identified in data interpretation include simplifying a diagnostic problem by interpreting findings as consistent with a single hypothesis, forgetting facts inconsistent with a favoured hypothesis, overemphasising positive findings, and discounting negative findings. From a Bayesian standpoint, these are all errors in assessing the diagnostic value of clinical evidence—that is, errors in implicit likelihood ratios.

Educational implications
Two recent innovations in medical education, problem based learning and evidence based medicine, are consistent with the educational implications of this research. Problem based learning can be understood as an effort to introduce the formulation and testing of clinical hypotheses into the preclinical curriculum. 26 The theory of cognition and instruction underlying this reform is that since experienced physicians use this strategy with difficult problems, and since practically any clinical situation selected for instructional purposes will be difficult for students, it makes sense to provide opportunities for students to practise problem solving with cases graded in difficulty. The finding of case specificity showed the limits of teaching a general problem solving strategy. Expertise in problem solving can be separated from content analytically, but not in practice. This realisation shifted the emphasis towards helping students acquire a functional organisation of content with clinically usable schemas. This goal became the new rationale for problem based learning. 27
Evidence based medicine is the most recent, and by most standards the most successful, effort to date to apply statistical decision theory in clinical medicine. 18 It teaches Bayes's theorem, and residents and medical students quickly learn how to interpret diagnostic studies and how to use a computer based nomogram to compute post-test probabilities and to understand the output. 28
We have selectively reviewed 30 years of psychological research on clinical diagnostic reasoning. The problem solving approach has focused on diagnosis as hypothesis testing, pattern matching, or categorisation. The errors in reasoning identified from this perspective include failure to generate the correct hypothesis; misperceiving or misreading the evidence, especially visual cues; and misinterpreting the evidence. The decision making approach views diagnosis as opinion revision with imperfect information. Heuristics and biases in estimation and revision of probability have been the subject of intense scrutiny within this research tradition. Both research paradigms understand judgment errors as a natural consequence of limitations in our cognitive capacities and of the human tendency to adopt short cuts in reasoning.
Both approaches have focused more on the mistakes made by both experts and novices than on what they get right, possibly leading to overestimation of the frequency of the mistakes catalogued in this article. The reason for this focus seems clear enough: from the standpoint of basic research, errors tell us a great deal about fundamental cognitive processes, just as optical illusions teach us about the functioning of the visual system. From the educational standpoint, clinical instruction and training should focus more on what needs improvement than on what learners do correctly; to improve performance requires identifying errors. But, in conclusion, we emphasise, firstly, that the prevalence of these errors has not been established; secondly, we believe that expert clinical reasoning is very likely to be right in the majority of cases; and, thirdly, despite the expansion of statistically grounded decision supports, expert judgment will still be needed to apply general principles to specific cases.
This is the fourth in a series of five articles
Series editor: J A Knottnerus
Preparation of this review was supported in part by grant RO1 LM5630 from the National Library of Medicine.
Competing interests: None declared.
- 1. Elstein AS, Shulman LS, Sprafka SA. Medical problem solving: an analysis of clinical reasoning. Cambridge, MA: Harvard University Press; 1978. [ Google Scholar ]
- 2. Bordage G, Zacks R. The structure of medical knowledge in the memories of medical students and general practitioners: categories and prototypes. Med Educ. 1984;18:406–416. doi: 10.1111/j.1365-2923.1984.tb01295.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 3. Schmidt HG, Norman GR, Boshuizen HPA. A cognitive perspective on medical expertise: theory and implications. Acad Med. 1990;65:611–621. doi: 10.1097/00001888-199010000-00001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Kahneman D, Slovic P, Tversky A, editors. Judgment under uncertainty: heuristics and biases. New York: Cambridge University Press; 1982. [ DOI ] [ PubMed ] [ Google Scholar ]
- 5. Sox HC, Jr, Blatt MA, Higgins MC, Marton KI. Medical decision making. Stoneham, MA: Butterworths; 1988. [ Google Scholar ]
- 6. Mellers BA, Schwartz A, Cooke ADJ. Judgment and decision making. Ann Rev Psychol. 1998;49:447–477. doi: 10.1146/annurev.psych.49.1.447. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Chapman GB, Sonnenberg F, editors. Decision making in health care: theory, psychology, and applications. New York: Cambridge University Press; 2000. [ Google Scholar ]
- 8. Hunink M, Glasziou P, Siegel J, Weeks J, Pliskin J, Elstein AS, et al. Decision making in health and medicine: integrating evidence and values. New York: Cambridge University Press; 2001. [ Google Scholar ]
- 9. Patel VL, Groen G. Knowledge-based solution strategies in medical reasoning. Cogn Sci. 1986;10:91–116. [ Google Scholar ]
- 10. Groen GJ, Patel VL. Medical problem-solving: some questionable assumptions. Med Educ. 1985;19:95–100. doi: 10.1111/j.1365-2923.1985.tb01148.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Brooks LR, Norman GR, Allen SW. Role of specific similarity in a medical diagnostic task. J Exp Psychol Gen. 1991;120:278–287. doi: 10.1037//0096-3445.120.3.278. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Norman GR, Coblentz CL, Brooks LR, Babcock CJ. Expertise in visual diagnosis: a review of the literature. Acad Med. 1992;66(suppl):S78–S83. doi: 10.1097/00001888-199210000-00045. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Rosch E, Mervis CB. Family resemblances: studies in the internal structure of categories. Cogn Psychol. 1975;7:573–605. [ Google Scholar ]
- 14. Lemieux M, Bordage G. Propositional versus structural semantic analyses of medical diagnostic thinking. Cogn Science. 1992;16:185–204. [ Google Scholar ]
- 15. Kassirer JP, Kopelman RI. Learning clinical reasoning. Baltimore: Williams and Wilkins; 1991. [ Google Scholar ]
- 16. Bordage G. Why did I miss the diagnosis? Some cognitive explanations and educational implications. Acad Med. 1999;74(suppl):S138–S142. doi: 10.1097/00001888-199910000-00065. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Sackett DL, Haynes RB, Guyatt GH, Tugwell P. Clinical epidemiology: a basic science for clinical medicine. 2nd ed. Boston: Little, Brown; 1991. [ Google Scholar ]
- 18. Sackett DL, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine: how to practice and teach EBM. New York: Churchill Livingstone; 1997. [ Google Scholar ]
- 19. Elstein AS. Heuristics and biases: selected errors in clinical reasoning. Acad Med. 1999;74:791–794. doi: 10.1097/00001888-199907000-00012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1982;211:453–458. doi: 10.1126/science.7455683. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Tversky A, Kahneman D. Advances in prospect theory: cumulative representation of uncertainty. J Risk Uncertain. 1992;5:297–323. [ Google Scholar ]
- 22. Fischhoff B, Bostrom A, Quadrell M J. Risk perception and communication. Annu Rev Pub Health, 1993;4:183–203. doi: 10.1146/annurev.pu.14.050193.001151. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Redelmeier DA, Koehler DJ, Liberman V, Tversky A. Probability judgment in medicine: discounting unspecified probabilities. Med Decis Making. 1995;15:227–230. doi: 10.1177/0272989X9501500305. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Wallsten TS. Physician and medical student bias in evaluating information. Med Decis Making. 1981;1:145–164. doi: 10.1177/0272989X8100100205. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Bergus GR, Chapman GB, Gjerde C, Elstein AS. Clinical reasoning about new symptoms in the face of pre-existing disease: sources of error and order effects. Fam Med. 1995;27:314–320. [ PubMed ] [ Google Scholar ]
- 26. Barrows HS. Problem-based, self-directed learning. JAMA. 1983;250:3077–3080. [ PubMed ] [ Google Scholar ]
- 27. Gruppen LD. Implications of cognitive research for ambulatory care education. Acad Med. 1997;72:117–120. doi: 10.1097/00001888-199702000-00012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Schwartz A. Nomogram for Bayes's theorem. http://araw.mede.uic.edu/cgi-bin/testcalc.pl (accessed 28 December 2001).
- View on publisher site
- PDF (219.1 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List

Comparing the Efficacy of Individual Approaches and Team-Based Approaches in Solving Clinical Case Vignettes
Amita singh, amita kumari, anita kumari, ayesha juhi, anup kumar d dhanvijay, mohammed j pinjar, himel mondal, pratima gupta.
- Author information
- Article notes
- Copyright and License information
Himel Mondal [email protected]
Corresponding author.
Accepted 2023 Oct 26; Collection date 2023 Oct.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Clinical case vignettes are a widely adopted pedagogical approach in medical education. The cases may be presented to students with a closed response option for objectivity. While solving clinical cases has demonstrated its effectiveness in enhancing medical students' clinical reasoning, there is an ongoing debate regarding the most effective approach: individual problem-solving or team-based problem-solving.
To observe and compare the score obtained from individual clinical problem-solving approaches versus team-based clinical problem-solving approaches.
After obtaining consent, a total of 100 students were randomly selected for the study. The participants were divided into two groups: an individual approach group (IAG) (n=25) and a team-based approach group (TAG) comprising 25 groups of three students each. Both groups were presented with a set of 10 clinical problems, each requiring a closed-answer response of "yes", "no", or "don't know". The participants' responses were recorded and analyzed to evaluate their problem-solving efficacy.
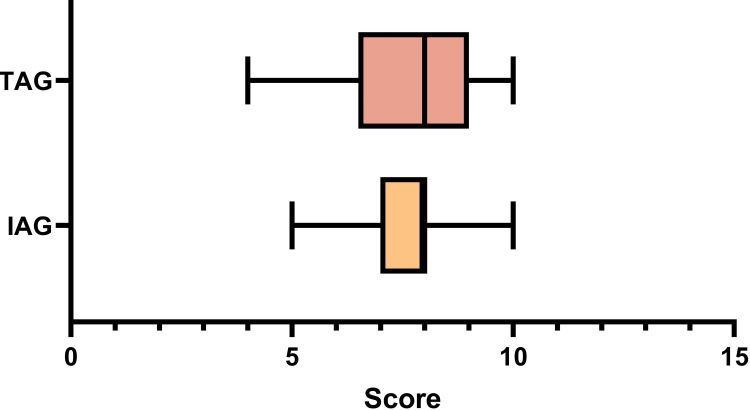
A total of 25 responses were obtained from 25 students from the IAG group and 25 responses from 25 groups from the TAG group. There was no difference between the score in IAG (7.44±1.12) and TAG (7.52 1.66) p-value=0.58. There was no difference between individual scores in 10 questions between IAG and TAG groups.
The study found no significant score differences between individual and team-based clinical case-solving groups. Hence, for the objective type of case-solving pattern used in this study, a team-based approach may not be necessary. Further research is needed to explore factors for such findings in future studies.
Keywords: objective question, physiology, clinical problem-solving, decision-making, group size, collaborative learning, medical education, team-based approaches, individual approaches, problem-based learning
Introduction
Clinical case vignette-based learning is a widely adopted pedagogical approach in medical education that emphasizes active learning, critical thinking, and collaborative problem-solving. In case-based learning, students are presented with real-world clinical scenarios or problems and are tasked with finding solutions based on their existing knowledge and resources [ 1 , 2 ]. While case-based learning has demonstrated its effectiveness in enhancing medical students' clinical reasoning and problem-solving skills, there is an ongoing debate regarding the most effective approach: individual problem-solving or team-based learning (TBL) [ 3 ].
Individual problem-solving in case-based learning allows students to work independently, relying solely on their own knowledge and problem-solving abilities. In contrast, team-based case-based learning encourages students to work collaboratively in groups, pooling their collective knowledge and skills to arrive at solutions. The combination of team-based learning principles within the framework of case-based learning offers a synergistic approach to medical education [ 4 ]. In this integrated approach, students can engage in collaborative problem-solving within their teams but also bring their collective insights to the larger case-based learning group.
However, clinical problem-solving may not always benefit from a team-based approach due to potential challenges such as differing opinions leading to debates, the risk of groupthink, uneven participation, communication issues, decision-making delays, accountability concerns, and compatibility issues within the team. In certain situations, especially those requiring quick and decisive actions or clear individual responsibility, individual problem-solving approaches may be more efficient and effective in ensuring optimal patient care [ 5 , 6 ]. The choice between individual and team-based approaches should be context-specific and consider the unique demands of each clinical scenario.
The gradual introduction of case-based questions in preclinical subjects for both objective and written examinations represents a forward-thinking pedagogical approach. This shift benefits students by encouraging the practical application of theoretical knowledge, fostering critical thinking, and demonstrating the real-world relevance of their studies. With careful implementation, case-based questions can enhance the overall educational experience and better equip students for their future roles in healthcare or related fields [ 7 , 8 ]. However, as these examinations are written by individual students, their individual competency is of great importance for academic progression.
Given these considerations, this study aimed to observe and compare the efficacy of individual and team-based problem-solving capability for objective types of questions related to a clinical scenario in physiology among first-year medical students.
Materials and methods
Type and settings
This cross-sectional study was conducted in a medical school of national importance in the eastern part of India. The study was conducted with first-year medical students studying pre-clinical subjects. The study was conducted on the subject of physiology. This study was approved by the Institutional Ethics Subcommittee of All India Institute of Medical Sciences, Deoghar, Jharkhand, India as an individual project (2023-210-IND-03).
Sample and recruitment
Total number of students in the medical school is 125. All the students were approached for the study, and 121 students consented to participate in the study. Among the willing students, a randomly selected 100 students were recruited for the study. They were randomly assigned to two groups: the individual approach group (IAG) (n=25) and the team-based approach group (TAG) (n=25; each team contains three students). The process is shown in Figure 1 .
Figure 1. Number of participants and brief study method.
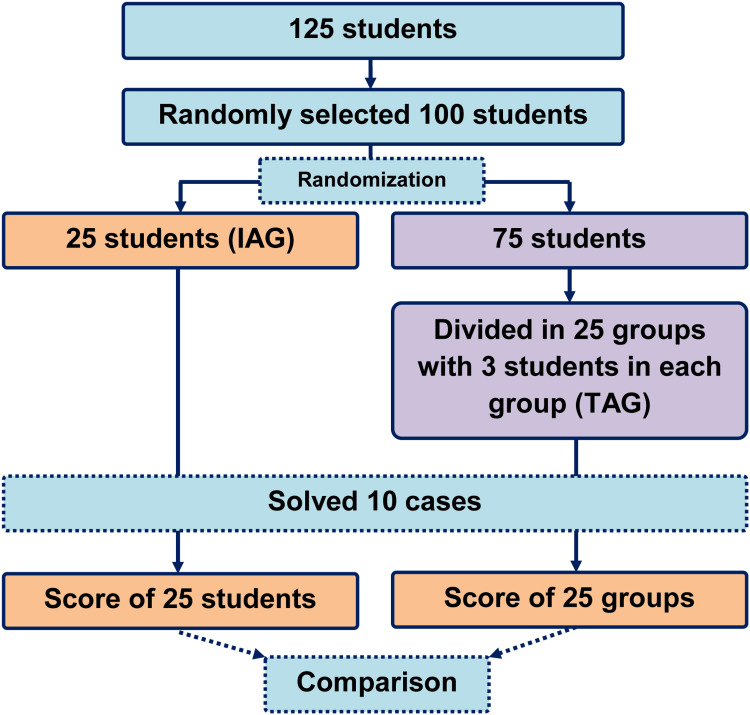
IAG - individual approach group; TAG - team-based approach group
Case-based learning questions preparation and validation
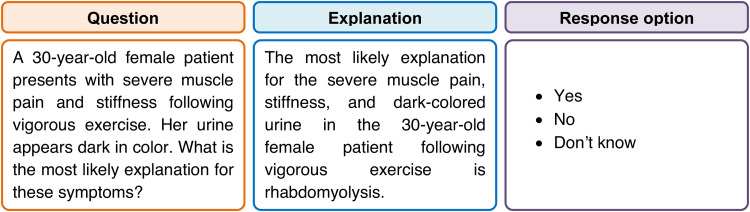
To ensure the validity and reliability of the case-based learning questions, a panel of subject matter experts (n=3) who are experienced in medical education (more than 10 years) in physiology developed the questions and answers. These scenarios and questions are reviewed for face and content validity and clarity by another two experts. Additionally, a pilot test was conducted with a small group (n=10) of second-year undergraduate medical students to find the suitability and comprehension of the questions. Based on feedback and pilot results, necessary adjustments were made to the questions, and finally, 10 questions were prepared and printed on white paper for application. One such question is shown in Figure 2 . In this example, the score for the answer yes = 1, don't know = 0, and no = -1.
Figure 2. An example of a case, its explanation, and response options.
Data collection
Participants from both the IAG and TAG engage in case-based learning sessions where they work on the provided scenarios and answer associated questions. Their responses were analyzed with pre-defined answer keys. The correct answer was scored 1, the wrong answer was -1, and don't know was 0. The grading system incentivizes correct responses, penalizes incorrect ones, and recognizes instances where students openly admit their lack of knowledge, contributing to a more nuanced understanding of their problem-solving skills.
Statistical analysis
Descriptive statistics were used to summarize the data. The scores obtained by the IAG and TAG groups were compared by the Mann-Whitney U test. We used GraphPad Prism 9.5.0 for statistical analysis, and a p-value <0.05 was considered statistically significant.
A total of 100 undergraduate medical students in their first year of study participated in this study. Among these 100 students, 25 students comprised the individual group, and 75 students were in the team-based group (each group was composed of three students). The score between the IAG (7.44±1.12) and TAG (7.52 1.66) was similar (p-value = 0.58). This indicates that a student alone and in a group have similar performance in solving objective-type clinical case solving. The score in the box plot is shown in Figure 3 .
Figure 3. Score of individual approach group (IAG) and team approach group (TAG).
The case-wise average score is shown in Table 1 . There was no difference between the scores in IAG and TAG. This indicates that not only in overall performance, question-wise performance of students in individual or in a group perform equally.
Table 1. Problem-wise score in individual approach group (IAG) and team-based approach group (TAG).
Q - question
TBL is a valuable pedagogical approach with several advantages in case-based learning contexts. TBL fosters collaboration and teamwork skills, which are crucial in healthcare settings where professionals often work in interdisciplinary teams [ 9 ]. TBL encourages students to collectively solve complex problems and share diverse perspectives. TBL promotes active engagement by dividing students into teams, requiring them to actively participate in discussions, and holding them accountable for their contributions. This dynamic interaction enhances critical thinking [ 10 ].
However, TBL may not be an ideal method for all aspects of case-based learning. The effectiveness of TBL relies on cohesive team dynamics, and if teams experience conflicts or imbalances in participation, it can hinder the learning process. Case-based learning's individual approach may provide students with a more self-directed learning experience, enabling them to tailor their problem-solving strategies to their unique needs [ 11 ]. It may build self-confidence and help in memory retention [ 12 ]. Therefore, the choice between TBL and individual learning should be made judiciously, considering the specific learning objectives, context, and desired outcomes in medical education [ 13 ].
In our study, the lack of a significant difference in scores between the IAG and the TAG could be attributed to several underlying factors. The composition of both groups was relatively homogeneous in terms of academic backgrounds, prior knowledge, and problem-solving skills. Such homogeneity could have led to similar performance outcomes for both groups and individuals. Additionally, the level of complexity of the cases could have played a role. As for objectivity, we used choice-based closed answers. Hence, actual collaborative problem-solving might not take place. The dynamics within each TAG team may have also influenced outcomes, as issues with communication, cooperation, or leadership could have hindered their collective performance. Moreover, some students in the IAG may have taken a highly self-directed approach to problem-solving, compensating for the absence of teamwork [ 14 , 15 ].
The study's limitations include a relatively small sample size, potential variations in the complexity of case scenarios, and the focus solely on academic performance as an outcome measure. Additionally, the study's cross-sectional design may not capture the long-term impact of case-based learning approaches on students' clinical reasoning and problem-solving abilities.
Conclusions
In conclusion, this study examined the effectiveness of individual and team-based case-based learning approaches in a medical education context. The results indicate that, within the parameters of this study, there were no significant differences in academic performance scores between the two approaches for objective case-solving in physiology. These findings suggest that the choice between individual and team-based case-based learning methods may not significantly impact immediate academic performance. Further research on other subjects with larger sample sizes may provide deeper insights into the topic.
Acknowledgments
We thank all the students who participated in the study. Some portion of the text in the introduction and discussion was edited for language and grammar by ChatGPT-3.5 free research version (September 25, 2023)
The authors have declared that no competing interests exist.
Author Contributions
Concept and design: Himel Mondal, Amita Singh, Amita Kumari, Ayesha Juhi, Anup Kumar D. Dhanvijay, Anita Kumari, Mohammed J. Pinjar, Pratima Gupta
Acquisition, analysis, or interpretation of data: Himel Mondal, Amita Singh, Amita Kumari, Ayesha Juhi, Anup Kumar D. Dhanvijay, Anita Kumari, Mohammed J. Pinjar, Pratima Gupta
Drafting of the manuscript: Himel Mondal, Amita Singh, Amita Kumari, Ayesha Juhi, Anup Kumar D. Dhanvijay, Anita Kumari, Mohammed J. Pinjar, Pratima Gupta
Critical review of the manuscript for important intellectual content: Himel Mondal, Amita Singh, Amita Kumari, Ayesha Juhi, Anup Kumar D. Dhanvijay, Anita Kumari, Mohammed J. Pinjar, Pratima Gupta
Supervision: Himel Mondal
Human Ethics
Consent was obtained or waived by all participants in this study. Institutional Ethics Subcommittee of All India Institute of Medical Sciences, Deoghar issued approval 2023-210-IND-03. This study was approved by the Institutional Ethics Subcommittee of All India Institute of Medical Sciences, Deoghar, Jharkhand, India, as an individual project.
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
- 1. Case-based learning and its application in medical and health-care fields: a review of worldwide literature. McLean SF. J Med Educ Curric Dev. 2016;3:20377. doi: 10.4137/JMECD.S20377. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Collaborative case-based learning with programmatic team-based assessment: a novel methodology for developing advanced skills in early-years medical students. James M, Baptista AM, Barnabas D, Sadza A, Smith S, Usmani O, John C. BMC Med Educ. 2022;22:81. doi: 10.1186/s12909-022-03111-5. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 3. A systematic review examining the effectiveness of blending technology with team-based learning. River J, Currie J, Crawford T, Betihavas V, Randall S. Nurse Educ Today. 2016;45:185–192. doi: 10.1016/j.nedt.2016.08.012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 4. Conceptualizing problem-based learning: an overview. Virk A, Mahajan R, Singh T. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8848565/ Int J Appl Basic Med Res. 2022;12:1–3. doi: 10.4103/ijabmr.ijabmr_827_21. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Use of individualized learning plans to facilitate feedback among medical students. Kiger ME, Riley C, Stolfi A, Morrison S, Burke A, Lockspeiser T. Teach Learn Med. 2020;32:399–409. doi: 10.1080/10401334.2020.1713790. [ DOI ] [ PubMed ] [ Google Scholar ]
- 6. The effectiveness of self-directed learning in health professions education: a systematic review. Murad MH, Coto-Yglesias F, Varkey P, Prokop LJ, Murad AL. Med Educ. 2010;44:1057–1068. doi: 10.1111/j.1365-2923.2010.03750.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Case-based learning in endocrine physiology: an approach toward self-directed learning and the development of soft skills in medical students. Gade S, Chari S. Adv Physiol Educ. 2013;37:356–360. doi: 10.1152/advan.00076.2012. [ DOI ] [ PubMed ] [ Google Scholar ]
- 8. Students' perception and learning on case based teaching in anatomy and physiology: an e-learning approach. Vedi N, Dulloo P. J Adv Med Educ Prof. 2021;9:8–17. doi: 10.30476/jamp.2020.87332.1304. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Maximizing the benefits of team-based learning. Chong JW, Lee JC. Adv Physiol Educ. 2022;46:365. doi: 10.1152/advan.00071.2022. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Team-based learning (TBL) in the medical curriculum: better than PBL? Burgess A, Bleasel J, Haq I, Roberts C, Garsia R, Robertson T, Mellis C. BMC Med Educ. 2017;17:243. doi: 10.1186/s12909-017-1068-z. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 11. Case-oriented self-learning and review in pharmacology teaching. Li S, Yu B, Yue J. Am J Med Sci. 2014;348:52–56. doi: 10.1097/MAJ.0000000000000197. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Comparison of lecture and team-based learning in medical ethics education. Ozgonul L, Alimoglu MK. Nurs Ethics. 2019;26:903–913. doi: 10.1177/0969733017731916. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. A comparison of conventional lecture and team-based learning methods in terms of student learning and teaching satisfaction. Jafari Z. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4154282 . Med J Islam Repub Iran. 2014;28:5. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 14. Group problems in problem-based learning. Hendry GD, Ryan G, Harris J. Med Teach. 2003;25:609–616. doi: 10.1080/0142159031000137427. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. Contemporary issues in group learning in undergraduate science classrooms: a perspective from student engagement. Hodges LC. CBE Life Sci Educ. 2018;17:3. doi: 10.1187/cbe.17-11-0239. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (399.7 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections

IMAGES
COMMENTS
In this review article, the author introduces a problem-solving approach to dissect the different clinical cases with hyponatremia and presents simple algorithms for the evaluation and management of hyponatremia that are useful at the bedside to improve quality, safety and cost-effectiveness of the patient's care.
Create a Problem Representation based on data from a clinical case So, what exactly is a Problem Representation? A problem representation (PR, or Summary Statement) is an evolving, concise summary that highlights the defining features of a case , helping clinicians generate a focused differential diagnosis and identify the next steps in ...
In situations where the cause of hypokalemia is not obvious, measurement of urinary potassium excretion and blood pressure and assessment of acid-base balance are often helpful. A random urine potassium-creatinine ratio (K/C) less than 1.5 suggests poor intake, gastrointestinal losses, or a shift of …
This chapter introduces the concept of clinical reasoning. It attempts to define what clinical reasoning is and what its features are. Solving clinical problems involves the ability to reason about causality of pathological processes, requiring knowledge of anatomy and the working and pathology of organ systems, and it requires the ability to compare patient problems as patterns with instances ...
This article reviews our current understanding of the cognitive processes involved in diagnostic reasoning in clinical medicine. It describes and analyses the psychological processes employed in identifying and solving diagnostic problems and reviews errors and pitfalls in diagnostic reasoning in the light of two particularly influential approaches: problem solving 1 - 3 and decision making ...
In this article, we present a comprehensive approach to solving complex clinical problems based on the work by Weed, 12,13,14 Eddy and Clanton, 15 and Evans and Gadd 16 and elaborated at the Medical Faculty at the University of Nijmegen, Nijmegen, The Netherlands. This approach, called clinical problem analysis (CPA), has three major goals:
You've read your textbook and your course notes. Now you need to apply your knowledge to real-life clinical situations.The problem-solving approach of Core Clinical Cases guides you to think of the patient as a whole, rather than as a sequence of unconnected symptoms. With its emphasis on everyday practice strongly linked to underlying theory, the
Hyponatremia: a problem-solving approach to clinical cases REVIEW DOI: 10.5301/jn.5000060 Key words: Cerebral salt-wasting, Hyponatremia, Hy-ponatremic encephalopathy, Neurogenic syndrome of
The cases may be presented to students with a closed response option for objectivity. While solving clinical cases has demonstrated its effectiveness in enhancing medical students' clinical reasoning, there is an ongoing debate regarding the most effective approach: individual problem-solving or team-based problem-solving. Objective
Clinical Problem-Solving. William C. Mundell, MD. Division of General Internal Medicine, College of Medicine, Mayo Clinic, Rochester, Minn ... A multiauthored case-based book structured to improve the clinician's approach to clinical decision making.