Learn how UpToDate can help you.
Select the option that best describes you
- Medical Professional
- Resident, Fellow, or Student
- Hospital or Institution
- Group Practice
- Patient or Caregiver
- Find in topic

RELATED TOPICS
Contributor Disclosures
Please read the Disclaimer at the end of this page.
The following represent additions to UpToDate from the past six months that were considered by the editors and authors to be of particular interest. The most recent What's New entries are at the top of each subsection.
ADULT GENERAL INTERNAL MEDICINE
Smoking cessation strategies after failing initial pharmacotherapy (May 2024)
Several medications are effective for smoking cessation; however, optimal management of individuals who do not abstain with initial pharmacotherapy has been unclear. In a recent trial, participants who smoked at least five cigarettes daily and had previously been randomized to receive six weeks of varenicline (2 mg daily) or combination nicotine replacement therapy (NRT; 21 mg/day patch plus lozenges) but did not quit smoking were re-randomized to continue the same medication dose, increase the dose, or switch medications [ 1 ]. Among those who initially received varenicline, 12-week quit rates were highest with increasing the dose to 3 mg daily, compared with continuing the 2 mg dose or switching to NRT (20, 3, and 0 percent, respectively). Among those who initially received NRT, quit rates with increased dosing (two 21 mg/day patches) or switching to varenicline were higher than continuing standard dosing (14, 14, and 8 percent, respectively). These results suggest that for patients unable to quit with standard-dose varenicline or NRT, using higher doses is an effective option. (See "Pharmacotherapy for smoking cessation in adults", section on 'No response to treatment' .)
ACEP consensus guidelines on topical anesthetics for simple corneal abrasions (April 2024)
Dispensing or prescribing a topical anesthetic for management of corneal abrasions in emergency department (ED) patients is generally discouraged because of concern of causing permanent corneal damage. The American College of Emergency Physicians (ACEP) published consensus guidelines recommending that in adult ED patients with simple corneal abrasions, prescribing or providing a commercial topical anesthetic for 24 hours (no more than 1.5 to 2 mL total) after presentation was safe and improved analgesia and patient satisfaction [ 2 ]. Even though we agree that brief use of a topical anesthetic for a small, simple corneal abrasion is safe and provides superior analgesia, we disagree with these broader recommendations since errors in diagnosis of corneal abrasions are common and overuse is difficult to prevent because topical anesthetic is typically supplied in 4 to 15 mL bottles. (See "Corneal abrasions and corneal foreign bodies: Management", section on 'Pain control' .)
Electronic cigarettes for smoking cessation (March 2024)
Electronic cigarettes have played an uncertain role in smoking cessation because of a paucity of data regarding their efficacy and safety. However, recent randomized trials suggest that e-cigarettes are efficacious in helping adults stop smoking [ 3,4 ]. In a meta-analysis of seven randomized trials, nicotine e-cigarettes resulted in higher quit rates than nicotine replacement therapy (17.5 versus 10.2 percent) [ 5 ]. Rates of adverse events were similar between groups. Nicotine e-cigarettes also appear more effective than usual care, behavioral counseling, and nonnicotine e-cigarettes [ 5 ]. Although questions regarding their long-term safety remain, these data suggest a role for e-cigarettes as a smoking cessation aid, particularly for patients who have not had success with standard pharmacotherapies. (See "Vaping and e-cigarettes", section on 'Efficacy' .)
High-dose glucocorticoid therapy not preferred in patients with sudden sensorineural hearing loss (January 2024)
Glucocorticoid therapy is the initial treatment for patients with sudden sensorineural hearing loss (SSNHL), but optimal dosing is uncertain. In a trial among 325 patients with SSNHL, five days of either high-dose intravenous prednisolone (250 mg/d) or high-dose oral dexamethasone (40 mg/d) did not improve hearing more than low-dose oral prednisone (five days at 60 mg/d followed by five days of tapering doses), but increased adverse events [ 6 ]. In patients with SSNHL, we use a low-dose regimen of oral glucocorticoids. (See "Sudden sensorineural hearing loss in adults: Evaluation and management", section on 'Initial therapy' .)
Macular changes related to pentosan polysulfate sodium (November 2023)
Macular eye disease has been reported in patients who have taken pentosan polysulfate sodium (PPS), which is used for the treatment of interstitial cystitis. In a prospective cohort study of 26 eyes with PPS maculopathy and >3000 g cumulative PPS exposure, progression of macular changes continued 13 to 30 months after drug cessation [ 7 ]. Median visual acuity decreased slightly; most patients reported progression of symptoms, including difficulty in low-light environments and blurry vision. These results indicate that PPS maculopathy progresses despite drug discontinuation, underscoring the importance of regular screening for maculopathy in patients with current or prior PPS exposure. (See "Interstitial cystitis/bladder pain syndrome: Management", section on 'Pentosan polysulfate sodium as alternative' .)
Point-of-care decision support tool for older adult care (February 2024)
Overtesting and overtreatment can lead to adverse health outcomes in older adults. In a trial conducted among 60 outpatient practices, a point-of-care, clinical decision support tool utilizing behavioral principles plus brief case-based education resulted in lower annual rates of three outcomes (prostate-specific antigen testing in men aged 76 years and older without previous prostate cancer, urine testing for nonspecific reasons in women aged 65 years and older, and overtreatment of diabetes in patients aged 75 years and older) when compared with brief case-based education alone [ 8 ]. Clinical decision support tools may aid in preventing unnecessary testing and treatments. (See "Geriatric health maintenance", section on 'Appropriate goals of care for older adults' .)
Risk of fractures with benzodiazepine receptor agonists (January 2024)
Benzodiazepine receptor agonists (BZRAs), including benzodiazepines and nonbenzodiazepine BZRAs such as zolpidem , can cause excess drowsiness and imbalance leading to falls and fractures. In a recent meta-analysis of 20 observational studies in over six million individuals, BZRAs were associated with increased risk of osteoporotic fractures across a range of drug classes and fracture types, with odds ratios ranging from 1.2 to 1.4 [ 9 ]. Most but not all studies included adults 50 years of age or older. These data reinforce the need for caution in prescribing BZRAs for insomnia and other indications, particularly in older adults. (See "Pharmacotherapy for insomnia in adults", section on 'Special populations' .)
IMMUNIZATIONS
Second dose of a 2023-2024 COVID-19 vaccine for individuals 65 years and older (April 2024)
In the United States, a single dose of an updated 2023-2024 formula COVID-19 vaccine is recommended for all immunocompetent adults and adolescents, regardless of prior vaccination history. In February 2024, the Centers for Disease Control and Prevention (CDC) updated its guidance to recommend a second dose (at least four months after the prior dose) for individuals 65 years and older [ 10 ]. Rates of COVID-19-associated hospitalization and death are higher in this age group than in any other, and the repeat dose is intended to improve protection by restoring the waning immune response; the 2023-2024 vaccine elicits response against currently circulating variants. Our recommendations are consistent with those of the CDC. (See "COVID-19: Vaccines", section on 'Adults 65 years and older' .)
2024 immunization schedule for adults (January 2024)
The United States Centers for Disease Control and Prevention has published the 2024 immunization schedule for adults ( figure 1 and figure 2 ) [ 11 ]. Respiratory syncytial virus (RSV) vaccine is a new addition to the schedule; it is recommended for pregnant people 32 to 36 weeks' gestation during RSV season and is an option for adults ≥60 years of age. Mpox vaccine has also been added and is recommended for adults of all ages who are at risk for infection. Other changes include updates to COVID-19, polio, and meningococcal vaccine recommendations. Our approach to immunization is largely consistent with these updated recommendations. (See "Standard immunizations for nonpregnant adults", section on 'Immunization schedule for nonpregnant adults' .)
Nirsevimab to prevent severe respiratory syncytial virus in infants (January 2024)
Nirsevimab is a new antibody that prevents severe respiratory syncytial virus (RSV) infection in infants. In a trial conducted in France, Germany, and the United Kingdom, more than 8000 otherwise healthy infants ≤12 months, born at ≥29 weeks' gestation, and entering their first RSV season were assigned to receive one dose of nirsevimab or no intervention [ 12 ]. The group who received nirsevimab had fewer hospitalizations for RSV-associated lower respiratory tract infection (0.3 versus 1.5 percent, efficacy 83.2 percent, 95% CI 67.8-92.0) and fewer infants with an oxygen saturation <90 percent (0.1 versus 0.5 percent, efficacy 75.7 percent, 95% CI 32.8-92.9). These findings further support the use of nirsevimab for RSV immunoprophylaxis in infants. (See "Respiratory syncytial virus infection: Prevention in infants and children", section on 'Immunoprophylaxis' .)
ADULT CARDIOVASCULAR MEDICINE
Intravenous iron in heart failure (April 2024)
Individuals with heart failure (HF) and iron deficiency should be treated, but expert groups differ on the perceived benefits. In a new meta-analysis that included over 4500 patients participating in randomized trials, intravenous iron reduced the rate of cardiovascular hospitalizations compared with placebo; all-cause mortality was not reduced [ 13 ]. This supports our suggested approach of using intravenous iron, although oral iron may be reasonable. Iron supplementation should be stopped once stores are repleted, as excess iron deposition is cardiotoxic. (See "Evaluation and management of anemia and iron deficiency in adults with heart failure", section on 'Iron supplementation' .)
Phosphodiesterase-5 inhibitors and cardiovascular disease (March 2024)
Erectile dysfunction is common among individuals with established cardiovascular disease and is independently associated with future cardiovascular events in those without cardiovascular disease. Updated recommendations from the Princeton IV conference on phosphodiesterase-5 (PDE-5) inhibitors and cardiac health provide guidance on cardiovascular risk stratification of individuals with erectile dysfunction and the management of erectile dysfunction in men with cardiovascular disease [ 14 ]. The guidelines emphasize that in men with cardiovascular disease and erectile dysfunction who are prescribed nitrates, clinicians should assess the patient's current need for nitrate therapy, consider nitrate deprescription, and determine whether PDE-5 inhibitors can safely be prescribed. These guidelines help clinicians evaluate and manage men with erectile dysfunction and cardiovascular disease. (See "Sexual activity in patients with cardiovascular disease", section on 'Coadministration with nitrates contraindicated' .)
The Preventing Risk of Cardiovascular Disease EVENTS (PREVENT) calculator (February 2024)
Guidelines for primary prevention of cardiovascular disease (CVD) recommend using a risk calculator to estimate atherosclerotic CVD (ASCVD) risk. However, risk calculators derived from older databases may not reflect current risk in diverse populations. To provide contemporary estimates of ASCVD risk, the PREVENT calculator was derived and validated in over 6.6 million adults to estimate 10- and 30-year risks of CVD and its subtypes, heart failure and ASCVD [ 15,16 ]. The PREVENT calculator inputs include standard CVD risk measures (eg, age, sex, body mass index, diabetes, lipid levels, smoking history, blood pressure, and kidney function); the full model also includes albuminuria, hemoglobin A1C, and zip code (which estimates social deprivation). The PREVENT calculator is a valuable tool for individualizing risk assessment and discussing the primary prevention of ASCVD with patients. (See "Atherosclerotic cardiovascular disease risk assessment for primary prevention in adults: Our approach", section on 'Choosing a risk calculator' .)
ADULT ENDOCRINOLOGY AND DIABETES
Glucagon-like peptide 1 receptor agonist use and thyroid cancer risk (April 2024)
Preclinical studies suggest that glucagon-like peptide 1 (GLP-1) receptor agonists may increase risk of thyroid neoplasia, but whether clinical use of these agents increases thyroid cancer risk is uncertain. A recent cohort study evaluated thyroid cancer incidence in individuals initiating treatment with a GLP-1 receptor agonist (predominantly liraglutide and semaglutide ) compared with a dipeptidyl peptidase 4 (DDP-4) inhibitor. After a mean follow-up of 3.9 years, GLP-1 receptor agonist use was not associated with an increased risk of any thyroid cancer or medullary thyroid cancer [ 17 ]. DPP-4 inhibitors raise endogenous GLP-1 levels and therefore may not be an optimal comparator. Until more data are available, this study does not change our practice of avoiding GLP-1-based therapies in individuals with a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia type 2A or 2B. (See "Glucagon-like peptide 1-based therapies for the treatment of type 2 diabetes mellitus", section on 'Other' .)
Continuous glucose monitoring in individuals with type 2 diabetes (April 2024)
In individuals with type 2 diabetes, the utility of continuous glucose monitoring (CGM) is uncertain. In a meta-analysis of 14 trials in 1647 people with type 2 diabetes not meeting glycemic goals (variably defined, usually A1C ≥7, 7.5, or 8 percent), use of either flash or real-time CGM modestly reduced A1C compared with fingerstick blood glucose monitoring (BGM; mean difference -0.32 percentage points) [ 18 ]. Most participants were taking oral glucose-lowering medications with or without insulin, and trial duration varied from 10 to 52 weeks. In a separate meta-analysis with similar trial durations, CGM similarly reduced A1C [ 19 ]. In individuals with type 2 diabetes and A1C above target, CGM provides modest glycemic benefit. In this population, CGM may be helpful in identifying glycemic patterns that direct changes in behaviors and/or pharmacologic therapy. (See "Glucose monitoring in the ambulatory management of nonpregnant adults with diabetes mellitus", section on 'Insulin treated' .)
Tirzepatide for weight loss in adults (March 2024)
The US Food and Drug Administration recently approved subcutaneous tirzepatide , a dual glucagon-like peptide 1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist, for chronic weight management [ 20 ]. Two randomized trials in adults with obesity demonstrated mean losses of 15 to 21 percent body weight with the highest dose of tirzepatide (15 mg weekly) [ 21,22 ]. In the larger of the two trials, over 80 percent of participants in all tirzepatide treatment groups (5 to 15 mg weekly) lost ≥5 percent of body weight, compared with 35 percent of those assigned to placebo [ 21 ]. Dose-related gastrointestinal side effects (nausea, diarrhea, constipation) were common but generally mild. Although direct comparisons are limited, the magnitude of weight loss with tirzepatide appears greater than that with other agents; thus, we consider tirzepatide a preferred medication for chronic weight management. (See "Obesity in adults: Drug therapy", section on 'Efficacy for weight loss' .)
Monitoring after negative confirmatory testing for primary aldosteronism (February 2024)
After a positive screening test for primary aldosteronism, confirmatory testing is required for diagnosis. In individuals with a positive screening test but negative confirmatory testing, the optimal monitoring strategy is uncertain. In a study that prospectively followed 184 individuals with a positive screening test for primary aldosteronism but negative confirmatory testing, a screening test was repeated after at least two years of follow-up [ 23 ]. If positive, confirmatory testing was performed again. Over a mean follow-up of five years, 20 percent of participants were diagnosed with primary aldosteronism. Those who developed primary aldosteronism exhibited higher blood pressure between initial and repeat testing despite similarly aggressive antihypertensive therapy. These findings support repeat testing for primary aldosteronism in individuals with initially negative confirmatory testing, particularly in those with progressively treatment-refractory blood pressure. (See "Diagnosis of primary aldosteronism", section on 'Negative confirmatory testing' .)
Effects of tirzepatide discontinuation on weight (February 2024)
Glucagon-like peptide 1-based therapies for the treatment of obesity result in substantial weight loss. Although earlier data suggested that stopping treatment with semaglutide results in weight regain, it was unclear whether the same occurs with tirzepatide . Among adults with obesity who had previously lost weight (21 percent mean weight reduction) during a 36-week, open-label trial of tirzepatide, those randomly assigned to continue tirzepatide for 52 weeks experienced additional weight loss, whereas those assigned to placebo partially regained (-5.5 versus +14 percent mean weight change, respectively) [ 24 ]. These results, in line with those of previous studies, suggest that most individuals with obesity who opt for pharmacotherapy will require long-term treatment for weight loss maintenance. (See "Obesity in adults: Drug therapy", section on 'Duration of therapy' .)
Semaglutide and cardiovascular outcomes (January 2024)
Semaglutide and other glucagon-like peptide 1 receptor agonists can reduce rates of adverse cardiovascular events in individuals with type 2 diabetes who have established cardiovascular disease or are at high risk of cardiovascular disease. In a newly published trial of 17,604 individuals with overweight or obesity and cardiovascular disease but not diabetes, once-weekly subcutaneous semaglutide 2.4 mg reduced rates of adverse cardiovascular outcomes compared with placebo (6.5 versus 8.0 percent) [ 25 ]. Discontinuation of the study drug due to side effects occurred more often with semaglutide (17 versus 8 percent). For individuals with overweight or obesity and established cardiovascular disease, semaglutide is a particularly attractive option for chronic weight management. (See "Obesity in adults: Drug therapy", section on 'Cardiovascular benefits' .)
ADULT GASTROENTEROLOGY
Dupilumab for refractory eosinophilic esophagitis (February 2024)
Few data are available on the use of dupilumab (a monoclonal antibody) for treating refractory eosinophilic esophagitis. In a cohort study of 46 patients with refractory eosinophilic esophagitis, dupilumab therapy was associated with histologic remission (defined as <15 eosinophils/high-power field) in 37 patients (80 percent) and with symptomatic improvement in 42 patients (91 percent) after a median of six months [ 26 ]. These data support our approach of using dupilumab for patients with eosinophilic esophagitis who have not responded to other therapies (eg, topical glucocorticoids). (See "Treatment of eosinophilic esophagitis (EoE)", section on 'Dupilumab' .)
Mortality risk in alcohol-associated liver disease (January 2024)
Few studies have reported the long-term outcomes of patients with alcohol-associated liver disease (ALD). In a national registry study including over 23,000 patients with ALD diagnosed at median age 58 years, 67 percent died during >100,000 person-years of follow-up and liver disease was the primary cause of death in 45 percent [ 27 ]. The 5- and 10-year mortality rates due to liver disease were 26 and 31 percent, respectively. These data emphasize the importance of treating patients with alcohol use disorder and may inform strategies to prevent liver-related mortality in those with ALD. (See "Management of alcohol-associated steatosis and alcohol-associated cirrhosis", section on 'Mortality' .)
Clinical practice update on risk stratification for colorectal cancer screening and postpolypectomy surveillance (December 2023)
The American Gastroenterological Association (AGA) recently published nine statements of best practice advice on risk stratification for colorectal cancer (CRC) screening and postpolypectomy surveillance [ 28 ]. They advise basing risk stratification on an individual's age, a known or suspected predisposing hereditary CRC syndrome, other CRC predisposing conditions (eg, inflammatory bowel disease), and/or a family history of CRC. They also suggest that the decision to continue postpolypectomy surveillance for individuals older than 75 years should be individualized. Shared decision-making discussions should include an assessment of the risks of incident CRC, procedure-related risks, comorbidities, and life expectancy (>5 years). Our approach is consistent with this guidance. (See "Overview of colon polyps", section on 'Risk assessment for subsequent colorectal cancer' .)
ADULT HEMATOLOGY AND ONCOLOGY
Mirtazapine in patients with cancer-related anorexia (April 2024)
Patients with advanced cancer are at risk for cancer-related anorexia and weight loss; studies are evaluating strategies to manage these issues. In a randomized trial in 86 patients with advanced non-small cell lung cancer, mirtazapine improved mean daily energy intake by 379 kcal versus placebo and reduced the proportion of patients with sarcopenia (57 versus 83 percent), although appetite scores were not higher [ 29 ]. Despite these results, previous data are inconsistent. As such, we prefer other strategies including dietary counseling and olanzapine for cancer-related anorexia. (See "Management of cancer anorexia/cachexia", section on 'Mirtazapine' .)
Improvement in breast cancer mortality from 1975 to 2019 (January 2024)
Improvements in breast cancer screening and treatments are decreasing breast cancer mortality. In a study using four simulation models of breast cancer mortality rates in the United States (US), breast cancer screening and treatment in 2019 were associated with a 58 percent reduction in US breast cancer mortality compared with 1975 [ 30 ]. Approximately half of this reduction was due to treatment of early breast cancer, while the rest was divided roughly equally between treatment of metastatic breast cancer and breast cancer screening. We support breast cancer screening for appropriate candidates and incorporate novel, data-driven strategies into our treatment recommendations for breast cancer. (See "Overview of the treatment of newly diagnosed, invasive, non-metastatic breast cancer", section on 'Introduction' and "Screening for breast cancer: Strategies and recommendations" .)
ADULT INFECTIOUS DISEASES
Hepatitis C virus antiviral treatment for patients with opioid use disorder (May 2024)
Despite concerns about adherence to antiviral therapy among individuals with opioid use disorder, hepatitis C virus (HCV) treatment can be highly successful in this population, particularly in nontraditional care settings. In a cluster-randomized trial that included 600 individuals with chronic HCV infection who were engaged in an opioid treatment program, provision of antiviral therapy through the program, directed by an HCV specialist over telemedicine, increased rates of antiviral initiation (92 versus 40 percent) and sustained virologic response (85 versus 30 percent) compared with traditional referral to a specialist clinic for treatment [ 31 ]. These data highlight the impact of reducing barriers to care for individuals with opioid use disorder and support our recommendation to treat all patients for chronic HCV, regardless of active drug use. (See "Patient evaluation and selection for antiviral therapy for chronic hepatitis C virus infection", section on 'Active drug use' .)
Pemivibart for prevention of COVID-19 in selected immunocompromised patients (April 2024)
Monoclonal antibodies have been used as adjunctive pre-exposure prophylaxis to reduce the risk of COVID-19 in individuals expected to have suboptimal response to vaccination, although emergence of variants that escape neutralization limit their utility. In March 2024 in the United States, the novel monoclonal antibody pemivibart received emergency use authorization (EUA) to prevent COVID-19 in individuals age 12 years or older (weighing at least 40 kg) who have moderate-to-severe immunocompromising conditions ( table 1 ) [ 32 ]. Pemivibart is active against JN.1, the dominant SARS-CoV-2 variant. We suggest pemivibart in individuals at the highest risk for vaccine nonresponse (eg, those with hematologic malignancy or recent history of transplantation) as long as it remains active against the main circulating variants. (See "COVID-19: Epidemiology, virology, and prevention", section on 'Limited role for monoclonal antibodies in selected patients' .)
Demographic disparities in tuberculosis incidence among US-born individuals (April 2024)
In the United States (US), the incidence of tuberculosis (TB) is increased among certain populations. A study including national TB registry data for 2011 to 2021 among US-born individuals found that, compared with individuals who identify as White, TB incidence rate ratios were 4.4 to 14.2 times higher among individuals who self-identified as American Indian/Alaska Native, Asian, Black, or Hispanic [ 33 ]. Genotyping data suggested an important role of recent transmission in the observed disparities, supporting the need for timely identification and prevention of ongoing chains of transmission. These findings warrant targeted efforts by TB prevention and control programs. (See "Epidemiology of tuberculosis", section on 'In the United States' .)
Precautions for individuals with COVID-19 in the community (April 2024)
In March 2024, the United States Centers for Disease Control and Prevention updated guidance for precautions for people with COVID-19 in the community [ 34 ]. Such individuals should stay at home until their symptoms are improving and they have been afebrile for 24 hours without the use of antipyretics. They can subsequently resume normal activities but are encouraged to use other precautions (eg, masking, social distancing, good ventilation) for an additional five days to further reduce the risk of transmission to others. These measures are particularly important when around persons who are at increased risk for severe disease (eg, advanced age, immunocompromise, cardiopulmonary disease). (See "COVID-19: Infection prevention for persons with SARS-CoV-2 infection" .)
Simnotrelvir-ritonavir for mild to moderate COVID-19 (January 2024)
Although nirmatrelvir-ritonavir reduces hospitalization and death from COVID-19, the many drug interactions make it difficult to use in some patients. Simnotrelvir-ritonavir is a similar protease inhibitor combination that inhibits viral replication but does not have as many drug interactions. In a randomized, double-blinded study of over 1000 patients with mild to moderate COVID-19 (majority fully vaccinated), 5 days of simnotrelvir-ritonavir reduced time to symptom resolution by 1.5 days [ 35 ]. Since no participant progressed to severe disease or died by day 29, it is unknown whether the drug prevents hospitalizations or death from COVID-19. Simnotrelvir-ritonavir has emergency use approval in China but is not yet approved for use in other countries. (See "COVID-19: Management of adults with acute illness in the outpatient setting", section on 'Therapies of limited or uncertain benefit' .)
Statins for primary prevention of cardiovascular disease in persons with HIV (September 2023)
HIV infection is associated with an excess risk of cardiovascular disease. A randomized trial evaluated the efficacy of lipid-lowering therapy with pitavastatin for primary prevention in over 7700 persons with HIV ≥40 years of age receiving antiretroviral therapy who had a 10-year atherosclerotic cardiovascular disease (ASCVD) risk score <15 percent [ 36 ]. Pitavastatin reduced the relative risk of major cardiovascular events (eg, myocardial infarction, stroke) by 35 percent compared with placebo; the trial was stopped early for this apparent benefit. Based on these data, we now advise statins in all persons ≥40 years of age with an ASCVD score ≥5 percent; for those with lower baseline risk, we also discuss statin use, although the absolute benefit is smaller. For persons younger than 40 and older than 75 years of age, our approach is the same as in persons without HIV. (See "Management of cardiovascular risk (including dyslipidemia) in patients with HIV", section on 'Indications for statins' .)
ADULT NEPHROLOGY AND HYPERTENSION
Drug therapy to prevent recurrent urinary stone disease (May 2024)
In patients with kidney stones, drug therapy to reduce stone recurrence is indicated if the stone disease remains active or there is insufficient improvement in urine chemistries despite dietary modification; however, evidence for its effectiveness is limited. In a study of over 5600 adults with urinary stone disease and at least one urinary abnormality (hypercalciuria, hypocitraturia, or hyperuricosuria), drug therapy (thiazide diuretics, alkali therapy, or uric acid-lowering medications) was associated with a 19 percent lower risk of clinically significant recurrent stone disease over 12 to 36 months compared with no treatment [ 37 ]. This benefit did not reach statistical significance over longer follow-up periods; however, important factors that could potentially affect treatment efficacy (eg, use of appropriate drug doses, treatment adherence) were not reported. For patients with recurrent calcium oxalate stones, we tailor drug therapy based upon the presence of specific metabolic abnormalities. (See "Kidney stones in adults: Prevention of recurrent kidney stones", section on 'Drug therapy for specific metabolic abnormalities' .)
Association between obesity in adolescence and development of chronic kidney disease (April 2024)
Observational studies have suggested that adolescents with obesity are at increased risk for impaired kidney function. In a new study of 630,000 adolescents in Israel, high body mass index (BMI) in late adolescence was associated with development of chronic kidney disease in early adulthood, as measured by albuminuria [ 38 ]. For severe obesity, the adjusted hazard ratio for early chronic kidney disease was 9.4 for males and 4.3 for females. These findings support our suggestion to screen for impaired kidney function in patients with risk factors for chronic kidney disease, including severe obesity, hypertension, or type 2 diabetes. Screening consists of measuring urine albumin-to-creatinine ratio. (See "Overview of the health consequences of obesity in children and adolescents", section on 'Kidney' .)
Tenapanor for refractory hyperphosphatemia in patients on dialysis (November 2023)
Despite adequate dialysis, dietary restriction, treatment of hyperparathyroidism, and phosphate binders (PBs), hyperphosphatemia is common among patients on dialysis and associated with adverse outcomes. In a trial in which nearly 170 patients on hemodialysis with hyperphosphatemia despite PB therapy were randomly assigned to PBs plus either tenapanor (an inhibitor of intestinal sodium/hydrogen exchanger 3) or placebo for eight weeks, serum phosphorus levels were 1.76 mg/dL lower in the tenapanor group [ 39 ]. Diarrhea was more frequent among patients receiving tenapanor but was mild or moderate in all cases. These data, in conjunction with prior trial data, support our approach of using tenapanor as add-on therapy in patients on dialysis who have an inadequate response to PBs. (See "Management of hyperphosphatemia in adults with chronic kidney disease", section on 'Refractory hyperphosphatemia' .)
ADULT NEUROLOGY AND PSYCHIATRY
Risk of epilepsy after aneurysmal subarachnoid hemorrhage (May 2024)
Epilepsy is a known sequelae of aneurysmal subarachnoid hemorrhage (SAH), but risk factors are poorly understood. In a retrospective analysis of 419 patients with SAH who were followed for a median of 4.2 years, epilepsy was diagnosed in 12 percent at a median of seven months after SAH [ 40 ]. Incidence was modified by several variables: premorbid functional impairment, SAH-associated cerebral ischemia, surgical treatment of the aneurysm, and early-onset seizures. A predictive model for the risk of epilepsy was developed using these data, with predicted risk ranging from 3 to 76 percent depending on the score. These results may provide insight into the individual risk of epilepsy after SAH. (See "Aneurysmal subarachnoid hemorrhage: Treatment and prognosis", section on 'Epilepsy' .)
Calcitonin gene-related peptide antagonists as a first-line preventive therapy for migraine (April 2024)
Several calcitonin gene-related peptide (CGRP) antagonists available for migraine prevention have frequently been reserved for patients with an inadequate response to initial therapy. However, in a position statement by the American Headache Society, CGRP antagonists are now considered among first-line therapies for migraine prevention, based on cumulative evidence of efficacy, safety, and tolerability from several clinical trials, meta-analyses, and postapproval open-label cohort studies [ 41 ]. They may be effective for patients with severe symptoms or frequent migraines and may provide earlier benefit than other preventive agents, and the formulations given by injection may also be helpful for those who have difficulty with daily dosing. However, cost or insurance approval may limit access to these agents as first-line therapy for some patients. (See "Preventive treatment of episodic migraine in adults", section on 'Choosing pharmacologic therapy' .)
Exercise for treating depression (March 2024)
Evidence supports moderate to vigorous aerobic exercise for treating depression; however, the efficacy of other types of physical activity is less clear. A recent network meta-analysis of 218 randomized trials suggests that even light to moderate physical activity can improve depression [ 42 ]. Walking or jogging, dance, yoga, strength training, and tai chi significantly reduced depressive symptoms compared with active controls, and the magnitude of the effects was similar to those with standard treatments (ie, cognitive behavioral therapy or antidepressant treatment). Although the quality of evidence from most trials was low, these results support specific activity options for patients with depression who cannot engage in aerobic exercise. (See "Major depressive disorder in adults: Treatment with supplemental interventions", section on 'Type, intensity, and frequency' .)
Cerebral amyloid angiopathy as a risk for isolated subdural hematoma (February 2024)
Cerebral amyloid angiopathy (CAA) commonly presents with acute intracerebral hemorrhage that may extend into the subarachnoid or subdural spaces in some instances, but the risk of isolated spontaneous subdural hematoma (SDH) from CAA is uncertain. In a retrospective study of data from two large population-based cohorts, CAA was associated with an elevated risk of SDH after adjustment for patient demographics, cardiovascular risks, and antithrombotic medication use [ 43 ]. Leptomeningeal amyloid deposition may predispose such patients to spontaneous SDH. These results expand our understanding of the varied hemorrhagic presentations associated with CAA. (See "Cerebral amyloid angiopathy", section on 'Imaging features' .)
Time window to start dual antiplatelet therapy for high-risk TIA or minor ischemic stroke (January 2024)
There is evidence from several randomized trials that early initiation of short-term dual antiplatelet therapy (DAPT) for select patients with high-risk transient ischemic attack (TIA) or minor ischemic stroke reduces the risk of recurrent ischemic stroke. The evidence comes from trials that started DAPT within 12 to 24 hours of symptom onset. Results from the recent INSPIRES trial suggest that DAPT is still beneficial when started up to 72 hours after symptom onset [ 44 ]. Although the time window is extended by the results from INSPIRES, we start DAPT as soon as possible for patients with high-risk TIA or minor ischemic stroke. (See "Early antithrombotic treatment of acute ischemic stroke and transient ischemic attack", section on 'High-risk TIA and minor ischemic stroke' .)
Botulinum toxin injections for essential head tremor (November 2023)
Botulinum toxin (BoNT) injections have been used for refractory head tremor in patients with essential tremor (ET) based on limited data. In a randomized trial of 117 patients with essential or isolated head tremor, BoNT type A injections into each splenius capitis muscle improved subjective and objective head tremor severity measurements compared with placebo injections, with expected waning of response by 12 weeks after each injection [ 45 ]. Adverse effects were more frequent with BoNT (47 versus 16 percent), most commonly headache or neck pain, dysphagia, and posterior neck weakness. BoNT type A injections are an option for patients with bothersome head tremor due to ET who do not tolerate oral medications or whose tremor does not respond, but side effects are common and may outweigh potential benefits in some patients. (See "Essential tremor: Treatment and prognosis", section on 'Administration and efficacy' .)
Early use of ubrogepant to abort migraine headache (November 2023)
Acute migraine treatments, including calcitonin gene-related peptide (CGRP) antagonists, are typically given at headache onset, but the benefit of earlier dosing is uncertain. In a trial of 477 patients with migraine who were treated at the onset of prodromal symptoms (prior to headache), ubrongepant improved the proportion of patients who remained free of moderate to severe headache at 24 hours compared with placebo (46 versus 29 percent) [ 46 ]. Enrolled patients had migraines that consisted of prodromal symptoms (eg, photophobia, fatigue, neck pain) occurring one to six hours before headache onset in at least 75 percent of attacks. These results support our practice to administer acute migraine treatments, such as ubrogepant , early in the course of migraine symptoms. (See "Acute treatment of migraine in adults", section on 'CGRP antagonists' .)
ADULT RHEUMATOLOGY
Risk of autoimmune inflammatory rheumatic disease following COVID-19 (May 2024)
The risk of developing autoimmune inflammatory rheumatic diseases (AIRDs) following COVID-19 has recently been studied (eg, rheumatoid, psoriatic, and spondyloarthritides and connective tissue disorders) [ 47 ]. A Korean and Japanese cohort analysis of 22 million patients reported an increased risk of AIRDs in patients who had COVID-19 compared with uninfected patients (hazard ratio [HR], 1.25 [Korea], 1.79 [Japan]) and with patients who had influenza (HR, 1.30 [Korea], 1.14 [Japan]). The risk appeared to diminish over time and was likely reduced by vaccination. Clinicians should be aware of the risk of AIRD following COVID-19 and investigate appropriately when suspected. (See "COVID-19: Clinical presentation and diagnosis of adults with persistent symptoms following acute illness ("long COVID")", section on 'Physical symptoms' .)
Adverse effects of low-dose glucocorticoids in patients with systemic lupus erythematosus (April 2024)
Glucocorticoids (GCs) are frequently required for disease control in patients with systemic lupus erythematosus (SLE) but can cause multiple adverse effects; whether low doses of GCs offer a more acceptable balance of risks and benefits is uncertain. In a national cohort study in Sweden that followed over 5300 adults with SLE for up to 15 years, compared with patients not taking oral GCs, those taking GCs had higher rates of multiple adverse outcomes, including overall mortality, various bacterial and viral infections, gastroduodenal ulcers, hypertension, osteoporosis, osteonecrosis, and cataracts [ 48 ]. Patients taking low-dose GCs (<5 mg/day) had relatively lower risks for adverse effects compared with those taking higher doses, but still had higher risks compared with patients who were not taking GCs. These results underscore the importance of using the lowest GC dose possible to control SLE activity and monitoring for adverse effects, even in patients taking low doses. (See "Systemic lupus erythematosus in adults: Overview of the management and prognosis", section on 'Prognosis' .)
Investigational use of denosumab for erosive hand osteoarthritis (April 2024)
There are limited treatment options for erosive osteoarthritis (OA) of the hand. Denosumab , a RANK ligand inhibitor used for the treatment of osteoporosis, appears promising. In a randomized trial of 100 patients with erosive hand OA, denosumab reduced radiographic progression and new erosive joint development at 48 weeks compared with placebo [ 49 ]. Pain and disability scores improved from baseline with denosumab during the open-label extension at 96 weeks, but not at earlier time points. This is the first study to demonstrate that targeted therapy can reduce structural damage in erosive hand OA, but further data on patient-important outcomes are necessary to clarify its potential role. (See "Management of hand osteoarthritis", section on 'Therapies with limited efficacy or of uncertain benefit' .)
Ultrasound for the diagnosis of giant cell arteritis (April 2024)
Vascular ultrasound is being investigated as a substitute for biopsy for the diagnosis of giant cell arteritis (GCA). In a prospective cohort study including 229 patients with suspected GCA, a prediction model using both a clinical prediction algorithm and a quantitative ultrasound was able to classify 74 percent of patients as having either a low or high probability for GCA [ 50 ]. The prediction model misclassified 2 percent of patients as low probability who eventually were diagnosed as having GCA; an additional 3 percent of patients classified as high probability for GCA were eventually reclassified as having other diagnoses. Although this study suggests that temporal artery biopsy may not be necessary to evaluate all patients with suspected GCA, it was conducted by rheumatologists who were specifically trained to use ultrasound for GCA. Until such expertise is more broadly available, we continue to evaluate patients with suspected GCA with temporal artery biopsies. (See "Diagnosis of giant cell arteritis", section on 'Patients with a positive biopsy or imaging' .)
Extra-articular rheumatoid arthritis and mortality (March 2024)
Rheumatoid arthritis (RA) is a systemic inflammatory disease that can have extra-articular manifestations, which may be severe (eg, rheumatoid vasculitis) or nonsevere (eg, rheumatoid nodules). In a study that examined outcomes of 296 patients diagnosed with RA from 1985 to 1999 and 611 patients diagnosed from 2000 to 2014, extra-articular manifestations were associated with an increased risk of mortality among all patients (hazard ratio 3.0 for severe and 1.8 for nonsevere manifestations) [ 51 ]. However, the 10-year cumulative incidence of extra-articular RA declined between the two cohorts (45 versus 32 percent). Despite the declining incidence of extra-articular RA, the presence of any extra-articular features continues to be associated with a poor prognosis. (See "Disease outcome and functional capacity in rheumatoid arthritis", section on 'Risk factors for premature mortality' .)
Diagnosis of axial spondyloarthritis using nonsteroidal anti-inflammatory agents (March 2024)
There is a long-standing belief that a dramatic response to nonsteroidal anti-inflammatory agents (NSAIDs) differentiates axial spondyloarthritis (axSpA) from other causes of lower back pain. However, in a recent prospective study of 68 consecutive patients with axSpA and 165 patients with chronic back pain from other causes who were treated with NSAIDs for four weeks, patients with axSpA were only modestly more likely to report at least 50 percent improvement in back pain (23 versus 16 percent), and the difference was not statistically significant [ 52 ]. Although this result casts some doubt on the diagnostic utility of an NSAID trial, the study was small and nonrandomized, and it does not exclude the possibility that some NSAIDs may be better than others at distinguishing axSpA from other diagnoses. (See "Diagnosis and differential diagnosis of axial spondyloarthritis (ankylosing spondylitis and nonradiographic axial spondyloarthritis) in adults", section on 'History' .)
Plain radiographs in the initial evaluation of rheumatoid arthritis (March 2024)
Patients suspected of having rheumatoid arthritis (RA) are routinely evaluated with plain radiographs of the hands and feet. However, whether this is an effective strategy has not been well established. In a study of 724 patients suspected of having RA, erosions were found in only 32 patients (4.4 percent), and radiographs led to a change in disease classification for only 2 patients (0.3 percent) [ 53 ]. Patients who lacked RA-associated autoantibodies and/or acute phase reactant elevation were less likely to demonstrate RA-associated erosions. Although the yield for these outcomes was low, plain radiographs may be useful for establishing alternate diagnoses that can mimic RA (eg, pseudogout) and can identify other findings associated with RA that guide management (eg, periarticular osteopenia). (See "Diagnosis and differential diagnosis of rheumatoid arthritis", section on 'Radiologic studies' .)
Phosphodiesterase type 5 inhibition for Raynaud phenomenon (January 2024)
Phosphodiesterase type 5 (PDE5) inhibitors such as sildenafil and tadalafil are widely used to treat digital ischemia from Raynaud phenomenon. In an updated meta-analysis of nine randomized trials comprising 411 patients with Raynaud phenomenon (most of whom had scleroderma), treatment with PDE5 inhibition resulted in three fewer attacks weekly and a reduction in the average duration of the attacks by five minutes [ 54 ]. However, PDE5 inhibition led to minimal to no reduction in the pain associated with Raynaud phenomenon. This study implies that while PDE5 inhibition has a modest impact on the duration and frequency of Raynaud attacks, it might not be adequate to address all symptoms experienced by patients with severe disease. (See "Treatment of Raynaud phenomenon: Initial management", section on 'Phosphodiesterase type 5 inhibitor' .)
Same-day contraceptive start and pregnancy risk (May 2024)
Individuals who desire contraception often want to start the method on the same day as their office visit, but the risk of pregnancy for those >7 days from the onset of their last menstrual period has been a concern. However, in a prospective study of over 3500 individuals seeking contraception, first-cycle unintended pregnancy rates were low for both those with same-day starts >7 days from the onset of menses and those who waited to start the method within 7 days of onset of menses (0.4 and 0.1 percent, respectively), even though approximately 20 percent of same-day start participants had at least one episode of unprotected intercourse within the prior 14 days [ 55 ]. For individuals who prefer a same-day start and understand the potential need for follow-up pregnancy testing, contraceptives (any method) may be started on the same day as the visit with low overall pregnancy risk. (See "Contraception: Counseling and selection", section on 'Starting a method' .)
Risk of subsequent hysterectomy after endometrial ablation (January 2024)
Endometrial ablation is an alternative to hysterectomy in selected premenopausal patients with heavy menstrual bleeding. Most ablations are performed using a non-resectoscopic technique; however, the long-term efficacy of this approach is unclear. In a meta-analysis of 53 studies including over 48,000 patients managed with non-resectoscopic endometrial ablation (NREA), the rates of subsequent hysterectomy were 4 percent at 12 months, 8 to 12 percent at 18 to 60 months, and 21 percent at 120 months [ 56 ]. Hysterectomy rates were similar for the different NREA devices (eg, thermal balloon, microwave, radiofrequency). These findings are useful for counseling patients about the long-term risk for hysterectomy after NREA. (See "Endometrial ablation: Non-resectoscopic techniques", section on 'Efficacy' .)
Pregnancy outcome among individuals with obesity and low gestational weight gain (May 2024)
For individuals with obesity, increasing evidence suggests that gestational weight gain (GWG) below standard recommendations (5 kg) is safe and may result in a more favorable pregnancy outcome. In an observational study including over 11,000 pregnancies with class I obesity, 3000 with class II obesity, and 900 with class III obesity, GWG below 5 kg was not associated with an increased risk of the composite adverse outcome in those with class I or II obesity and was associated with a 20 percent risk reduction in those with class III obesity [ 57 ]. These findings suggest that GWG recommendations should be revised downward for individuals with obesity, particularly those with class III obesity. We do not advise pregnant people with obesity and GWG below 5 kg to increase weight gain if the fetus is growing appropriately on ultrasound examination. (See "Gestational weight gain", section on 'Approach to weight gain below IOM recommendations' .)
Reducing alcohol use during pregnancy (May 2024)
Clinicians caring for pregnant persons are advised to routinely educate and counsel about the harms of alcohol use during pregnancy. A meta-analysis of three trials reported more pregnant patients continuously abstained from alcohol consumption after receiving psychosocial interventions compared with usual care (69 versus 51 percent) [ 58 ]. We encourage clinicians caring for pregnant individuals to offer access to psychosocial interventions (eg, information sessions, self-help groups, cognitive behavioral therapy) in addition to routinely educating them about the dangers of alcohol use during pregnancy. (See "Alcohol intake and pregnancy", section on 'Management of screen-positive pregnant persons' .)
Acetaminophen use in pregnancy not associated with adverse neurodevelopment in offspring (April 2024)
Although older studies raised concerns about a possible adverse association between in utero exposure to acetaminophen and neurodevelopment, more recent studies with a lower risk of bias have not reported an association. In a population-based study in which acetaminophen use was prospectively recorded, siblings with any in utero exposure had no increased risk for attention deficit hyperactivity disorder, autism spectrum disorder, or intellectual disability at age 10 years compared with their unexposed siblings [ 59 ]. Although an association cannot be definitively excluded, these data are reassuring when a short course of acetaminophen is desirable to manage pain or fever during pregnancy. (See "Prenatal care: Patient education, health promotion, and safety of commonly used drugs", section on 'Acetaminophen' .)
Congenital anomaly risk with methadone or buprenorphine exposure (April 2024)
Data regarding the teratogenic risk of medications for opioid use disorder (MOUD) are limited. In a population-based study comparing over 9500 pregnancies exposed to buprenorphine in the first trimester with nearly 3900 methadone-exposed pregnancies, buprenorphine use was associated with a lower overall risk of congenital anomalies (5 versus 6 percent) [ 60 ]. Although the analysis adjusted for multiple potential confounding factors, unmeasured confounders may explain some of the observed associations. We base the choice of buprenorphine versus methadone for MOUD on other factors ( table 2 ). (See "Opioid use disorder: Pharmacotherapy with methadone and buprenorphine during pregnancy", section on 'Risk of structural anomalies' .)
Dexmedetomidine and postpartum depression (April 2024)
Dexmedetomidine is an anesthetic that is also used to treat acute psychotic or manic agitation. In a randomized trial of 338 individuals who were undergoing elective cesarean delivery and screened positive for antenatal depression, adding dexmedetomidine to standard patient-controlled intravenous analgesia reduced subsequent rates of depression at 42 days postpartum (11 versus 30 percent with standard analgesia plus saline placebo) [ 61 ]. However, the study sample represents a relatively small portion of the population at risk for postpartum depression, and the drug remains an investigational approach until additional data confirm its benefit. (See "Postpartum unipolar depression: Prevention", section on 'Investigational interventions' .)
Maternal sepsis risk with membrane rupture before 23 weeks of gestation (April 2024)
Chorioamnionitis can be a cause or a consequence of preterm prelabor rupture of membranes (PPROM), especially before 24 weeks of gestation. Development of maternal sepsis is a major concern in these pregnancies. In a prospective study of 364 patients with PPROM between 16 weeks 0 days and 22 weeks 6 days, maternal sepsis developed in 10 percent of patients with singleton pregnancies who chose to undergo pregnancy termination soon after diagnosis of PPROM and in 13 percent of those who initially chose to continue the pregnancy [ 62 ]. Two patients died. These findings underscore the importance of close maternal monitoring, early diagnosis of chorioamnionitis, timely fetal extraction, and appropriate antibiotic treatment in patients with PPROM. (See "Prelabor rupture of membranes before and at the limit of viability", section on 'Maternal sepsis and death' .)
Noninsulin antidiabetic medications and pregnancy (February 2024)
Noninsulin antidiabetic medications such as glucagon-like peptide 1 (GLP-1) agonists, sodium-glucose cotransporter 2 (SGLT-2) inhibitors, and dipeptidyl peptidase 4 (DPP-4) inhibitors are commonly used in nonpregnant individuals but avoided in pregnancy because of lack of safety data in humans and harms observed in animal studies. However, in a multinational population-based cohort study including nearly 2000 individuals with preconception/first trimester exposure to these medications, the frequency of congenital anomalies was not increased compared with insulin [ 63 ]. A limitation of the study is that it did not adjust for potential differences in A1C, diabetes severity, or diabetes duration, which could obscure true effects on risk for congenital anomalies. We continue to avoid use of GLP-1 agonists, SGLT-2 inhibitors, and DPP-4 inhibitors in females planning to conceive and in pregnancy. (See "Pregestational (preexisting) diabetes: Preconception counseling, evaluation, and management", section on 'Patients on preconception noninsulin antihyperglycemic agents' .)
Combined use of metformin and insulin for treating diabetes in pregnancy (February 2024)
In patients with type 2 diabetes, insulin is the mainstay for managing hyperglycemia in pregnancy. The addition of metformin improves maternal glucose control and reduces the chances of a large for gestational age newborn, but a prior randomized trial reported an increased risk for birth of a small for gestational age (SGA) infant. A recent randomized trial comparing use of insulin alone with insulin plus metformin in nearly 800 adult pregnant patients with either preexisting type 2 diabetes or diabetes diagnosed in early pregnancy confirmed the previously reported benefits but found that both treatment groups had low and similar rates of SGA [ 64 ]. The discordancy in SGA risk needs to be explored further, as metformin cotreatment would be undesirable if this risk is real. (See "Pregestational (preexisting) diabetes mellitus: Antenatal glycemic control", section on 'Metformin' .)
Fetoplacental GDF15 linked to nausea and vomiting of pregnancy (February 2024)
Almost all pregnant people experience nausea with or without vomiting in early pregnancy; however, the pathogenesis of the disorder has been unclear. Previous studies have shown that GDF15 is expressed in a wide variety of cells, with the highest expression in placental trophoblast, and that its protein (GDF15) appears to regulate appetite. A recent study confirmed the fetoplacental unit as a major source of GDF15 and also found that higher GDF15 levels correlated with more severe nausea and vomiting of pregnancy [ 65 ]. In the future, drugs targeting the production or action of GDF15 are a potential novel pathway for treating nausea and vomiting of pregnancy, if safety and efficacy are established. (See "Nausea and vomiting of pregnancy: Clinical findings and evaluation", section on 'Pathogenesis' .)
Use of cerebroplacental ratio at term does not reduce perinatal mortality (February 2024)
Cerebral blood flow may increase in chronically hypoxemic fetuses to compensate for the decrease in available oxygen and can be assessed by the cerebroplacental ratio (CPR; middle cerebral artery pulsatility index divided by the umbilical artery pulsatility index). However, increasing evidence indicates that use of the CPR does not reduce perinatal mortality in low-risk pregnancies. In a randomized trial comparing fetal growth assessment plus revealed versus concealed CPR in over 11,000 low-risk pregnancies at term, knowledge of CPR combined with a recommendation for delivery if the CPR was <5th percentile did not reduce perinatal mortality compared with usual care (concealed group) [ 66 ]. We do not perform umbilical artery Doppler surveillance, including the CPR, in low-risk pregnancies. (See "Doppler ultrasound of the umbilical artery for fetal surveillance in singleton pregnancies", section on 'Low-risk and unselected pregnancies' .)
Intrauterine postpartum hemorrhage control devices for managing postpartum hemorrhage (February 2024)
Intrauterine balloon tamponade and vacuum-induced uterine compression are the most common devices used for intrauterine postpartum hemorrhage (PPH) control in patients with atony, but it is unclear which device is superior as few comparative studies have been performed. In a retrospective study including nearly 380 patients with PPH, quantitative blood loss after placement, rate of blood transfusion, and discharge hematocrit were similar for both devices [ 67 ]. Based on these and other data, in the setting of ongoing uterine bleeding, rapid use of one of these devices is likely to be more important than the choice of device when both devices are available. (See "Postpartum hemorrhage: Use of an intrauterine hemorrhage-control device", section on 'Choice of method' .)
Low- versus high-dose calcium supplements and risk of preeclampsia (January 2024)
In populations with low baseline dietary calcium intake, the World Health Organization recommends 1500 to 2000 mg/day calcium supplementation for pregnant individuals to reduce their risk of developing preeclampsia. However, a recent randomized trial that evaluated low (500 mg) versus high (1500 mg) calcium supplementation in over 20,000 nulliparous pregnant people residing in two countries with low dietary calcium intake found low and similar rates of preeclampsia in both groups [ 68 ]. These findings suggest that a 500 mg supplement is sufficient for preeclampsia prophylaxis in these populations. For pregnant adults in the United States, we prescribe 1000 mg/day calcium supplementation, which is the recommended daily allowance to support maternal calcium demands without bone resorption. (See "Preeclampsia: Prevention", section on 'Calcium supplementation when baseline dietary calcium intake is low' .)
Respectful maternity care (January 2024)
Respectful maternity care is variably defined but broadly involves both absence of disrespectful conduct and promotion of respectful conduct toward pregnant individuals. A systematic review found that validated tools to measure respectful maternity care were available, but the optimal tool was unclear and high quality studies were lacking on the effectiveness of respectful maternity care for improving any maternal or infant health outcome [ 69 ]. Respectful maternal care is a basic human right, but how to best implement and monitor it and assess outcomes requires further study. (See "Prenatal care: Initial assessment", section on 'Effectiveness' .)
Outcome of a multifaceted intervention in patients with a prior cesarean birth (January 2024)
Patients with a pregnancy after a previous cesarean birth must choose between a trial of labor (TOLAC) and a planned repeat cesarean. The optimal care of such patients is unclear. In a multicenter, cluster-randomized trial including over 20,000 patients with one prior cesarean birth, a multifaceted intervention (patient decision support, use of a calculator to assess chances of a vaginal birth after cesarean [VBAC], sonographic measurement of myometrial thickness, clinician training in best intrapartum practices during TOLAC) reduced perinatal and major maternal morbidity composite outcomes compared with usual care [ 70 ]. VBAC and uterine rupture rates were similar for both groups. Further study is needed to identify the most useful component(s) of the intervention for reducing morbidity. (See "Choosing the route of delivery after cesarean birth", section on 'Person-centered decision-making model' .)
Labor epidural analgesia and risk of emergency delivery (December 2023)
It is well established that contemporary neuraxial labor analgesia does not increase the overall risk of cesarean or instrument-assisted vaginal delivery. However, a new retrospective database study of over 600,000 deliveries in the Netherlands reported that epidural labor analgesia was associated with an increased risk of emergency delivery (cesarean or instrument-assisted vaginal) compared with alternative analgesia (13 versus 7 percent) [ 71 ]. Because of potential confounders and lack of detail on epidural and obstetric management, we consider these data insufficient to avoid neuraxial analgesia or change the practice of early labor epidural placement to reduce the potential need for general anesthesia in patients at high risk for cesarean delivery. (See "Adverse effects of neuraxial analgesia and anesthesia for obstetrics", section on 'Effects on the progress and outcome of labor' .)
Delayed cord clamping in preterm births (December 2023)
Increasing evidence supports delaying cord clamping in preterm births. In an individual participant data meta-analysis of randomized trials of delayed versus immediate cord clamping at births <37 weeks (over 3200 infants), delaying cord clamping for >30 seconds reduced infant death before discharge (6 versus 8 percent) [ 72 ]. In a companion network meta-analysis evaluating the optimal duration of delay, a long delay (≥120 seconds) significantly reduced death before discharge compared with immediate clamping; reductions also occurred with delays of 15 to <120 seconds but were not statistically significant [ 73 ]. For preterm births that do not require resuscitation, we recommend delayed rather than immediate cord clamping. We delay cord clamping for at least 30 to 60 seconds as approximately 75 percent of blood available for placenta-to-fetus transfusion is transfused in the first minute after birth. (See "Labor and delivery: Management of the normal third stage after vaginal birth", section on 'Preterm infants' .)
PEDIATRICS: GENERAL PEDIATRICS
High-flow nasal cannula oxygen therapy in children with bronchiolitis (April 2024)
High-flow nasal cannula (HFNC) oxygen therapy is increasingly used for children with bronchiolitis and significant respiratory distress, but the clinical benefit has been questioned. In a meta-analysis of eight trials (over 2100 patients <2 years old with bronchiolitis) that compared oxygen therapy using HFNC with standard (low-flow) oxygen, the risk of escalation of therapy was lower with HFNC oxygen therapy; rates of adverse events were similar in the two groups (four studies, nearly 1800 patients, approximately 1 percent) [ 74 ]. Interpretation of these results is limited by significant heterogeneity and risk of bias. These findings suggest that HFNC oxygen therapy provides modest benefit for children with bronchiolitis without increasing adverse events. For children with bronchiolitis, we suggest HFNC in patients with severe respiratory distress; we advise against routine use of HFNC for children with hypoxemia and mild-to-moderate increased work of breathing. (See "Bronchiolitis in infants and children: Treatment, outcome, and prevention", section on 'High-flow nasal cannula' .)
Pharmacotherapy for ADHD and mortality risk (April 2024)
Attention deficit hyperactivity disorder (ADHD) is associated with higher mortality than in the general population; whether treatment modifies that risk is unclear. In an observational study of nearly 149,000 individuals with ADHD in Sweden (mean age 17 years), initiation of medication within three months of diagnosis was associated with lower all-cause mortality (hazard ratio [HR] 0.79) as well as lower mortality from unnatural causes (eg, suicide, unintentional injury, and accidental poisoning; HR 0.75) over the ensuing two years [ 75 ]. While the study could not control for unmeasured confounders that may have impacted mortality risk (eg, lifestyle factors, social support), these data generally lend further support for pharmacotherapy of ADHD. (See "Attention deficit hyperactivity disorder in adults: Treatment overview", section on 'Benefits of stimulant treatment' .)
Multisystem inflammatory syndrome in children incidence and severity (March 2024)
Although multisystem inflammatory syndrome in children (MIS-C) is increasingly rare as the overall COVID-19 burden declines, it continues to be associated with substantial morbidity. In 2023, 117 patients with MIS-C were reported to the Centers for Disease Control and Prevention, resulting in an estimated incidence of 0.11 cases per million person-months [ 76 ]. Of these patients, 50 percent required care in an intensive care unit, 34 percent experienced shock, and 27 percent experienced cardiac dysfunction; mortality was 2.6 percent (3 patients). More than 80 percent of patients were SARS-CoV2 vaccine eligible but had not been vaccinated; among 20 patients who had been vaccinated, 60 percent likely had waning immunity at the time of diagnosis. This study suggests that MIS-C severity remains high, but that SARS-CoV2 vaccination may provide some degree of protection. (See "COVID-19: Multisystem inflammatory syndrome in children (MIS-C) clinical features, evaluation, and diagnosis", section on 'Epidemiology' .)
Concussion and mental health disorders in children and adolescents (March 2024)
Ongoing research continues to examine the complex relationship between concussion and mental health disorders. In a recent case-control study of over 18,000 children (≤17 years old) with concussion and over 37,000 matched controls, concussion was associated with an increased risk for a new diagnosis of a behavior disorder at two and four years after injury [ 77 ]. For most diagnoses, the absolute numbers were low. Confidence in a causal relationship is limited by risk of confounding and reliance on an electronic medical record for establishing lack of baseline behavioral problems prior to injury. Whether pediatric concussion is an independent risk factor for new behavioral problems after recovery remains unclear. (See "Concussion in children and adolescents: Management", section on 'Mental health disorders' .)
Nirsevimab effectiveness in infants (March 2024)
During the 2023-24 respiratory syncytial virus (RSV) season, infants could receive the monoclonal antibody nirsevimab for the first time to protect against RSV-related hospitalization. In a case-control study of almost 700 infants <8 months old who were hospitalized in the United States for an acute respiratory illness during this RSV season, almost 60 percent tested positive for RSV; almost all of these patients had not received nirsevimab [ 78 ]. Among infants who tested negative for RSV, 18 percent had received nirsevimab. Estimated effectiveness against RSV-associated hospitalization among nirsevimab recipients was 90 percent. These data provide additional support for recommendations to administer nirsevimab to all infants <8 months old upon entering their first RSV season and to all newborns during the RSV season unless the birthing parent received RSV vaccination during pregnancy. (See "Respiratory syncytial virus infection: Prevention in infants and children", section on 'Immunoprophylaxis' .)
Budesonide oral suspension for eosinophilic esophagitis (March 2024)
In patients with eosinophilic esophagitis (EoE), use of topical glucocorticoids has been limited by lack of regulatory approval and potentially inconsistent drug delivery. Budesonide oral suspension is a formulation that was recently approved by the US Food and Drug Administration for treating EoE in adults and pediatric patients ages 11 years and older [ 79,80 ]. Approval was informed by clinical trials showing that topical budesonide resulted in higher rates of histologic remission and symptomatic improvement compared with placebo. We anticipate using budesonide oral suspension as the preferred topical glucocorticoid for treating EoE. (See "Treatment of eosinophilic esophagitis (EoE)", section on 'Topical glucocorticoids' .)
Benign acute childhood myositis (January 2024)
Benign acute childhood myositis (BACM) is a self-limited syndrome associated with calf pain and creatinine kinase elevation, often following infection with influenza. In a retrospective study of 65 patients with BACM, the median age was 6.6 years and 66 percent of patients were male [ 81 ]. The most common symptoms were bilateral calf pain, refusal to walk, and diffuse weakness. The median creatinine kinase was 1827 U/L, which normalized after an average of seven days. Early recognition of this syndrome allows the clinician to avoid an unnecessary evaluation for other muscle diseases. (See "Overview of viral myositis", section on 'Benign acute childhood myositis' .)
High blood lead levels in US children after eating cinnamon applesauce pouches (November 2023)
The Centers for Disease Control and Prevention have issued a health alert following reports of high blood lead levels from several states for a total of 22 children who were fed cinnamon-containing applesauce pouches that were subsequently found to contain extremely high concentrations of lead [ 82 ]. Children who have eaten a recalled product should undergo blood lead testing. Clinicians should advise parents, primary caregivers, and guardians to not buy specific cinnamon-containing apple puree or applesauce products named in the US Food and Drug Administration announcement and to discard any recalled products that they have purchased. (See "Childhood lead poisoning: Exposure and prevention", section on 'Food' and "Childhood lead poisoning: Clinical manifestations and diagnosis", section on 'Laboratory evaluation' and "Childhood lead poisoning: Management" .)
Testing for hepatitis C virus infection in infants with perinatal exposure (November 2023)
Perinatally acquired hepatitis C virus (HCV) infection in the United States has increased sharply since 2010. New guidance from the Centers for Disease Control and Prevention recommends early testing for infants with perinatal exposure to HCV ( algorithm 1 ) [ 83 ]:
● Test for HCV RNA during early infancy after two months of age, and ideally before six months of age.
● After 18 months of age, test any infant who has not previously been tested by measuring anti-HCV antibodies, with reflexive testing for HCV RNA.
A negative HCV RNA result at any time point after two months of age virtually excludes HCV infection and further testing is not required. Children with a positive HCV RNA test before three years of age should have repeat testing for HCV RNA before initiating antiviral therapy to determine whether they have spontaneously cleared the infection. This new guidance is consistent with our previous recommendations for early testing for infants with perinatal exposure to HCV. (See "Hepatitis C virus infection in children", section on 'How to test' .)
PEDIATRICS: DEVELOPMENTAL AND BEHAVIORAL PEDIATRICS
Infertility and autism spectrum disorder (December 2023)
Patients with infertility often ask about the impact of the disorder and its treatment on risk of autism spectrum disorder (ASD) in offspring. In a large population-based cohort study comparing ASD risk among children whose parents had subfertility (an infertility consultation without treatment), infertility treatment, or neither (unassisted conception), children in the subfertility and infertility treatment groups had a small increased risk of ASD compared with unassisted conception but the absolute risk was low (2.5 to 2.7 per 1000 person-years versus 1.9 per 1000 person-years with unassisted conception) [ 84 ]. The increased risk was similar in the subfertile and infertility treatment groups, suggesting that infertility treatment was not a major risk factor. Obstetrical and neonatal factors (eg, preterm birth) appeared to mediate a sizeable proportion of the increased risk for ASD. (See "Assisted reproductive technology: Infant and child outcomes", section on 'Confounders' .)
Postoperative antibiotics in children with gangrenous appendicitis (April 2024)
For children with gangrenous appendicitis (microperforation with bacterial contamination outside of the appendix), the role of postoperative antibiotics (pABx) is being reevaluated. In a retrospective study of over 950 children with gangrenous appendicitis (573 who received pABx), unadjusted rates of postoperative surgical site infections were low in patients who did or did not receive pABx (3.3 and 2.1 percent, respectively). With propensity-matching in 404 patients to address treatment by intention, rates remained similar for surgical site infection, postoperative abdominal imaging, and hospital revisits [ 85 ]. These findings challenge the traditional practice of giving pABx to children with gangrenous appendicitis and provide a basis for future randomized trials. (See "Acute appendicitis in children: Management", section on 'Postoperative care' .)
Predicting venous thromboembolism risk in non-major orthopedic surgery (April 2024)
For patients with non-major extremity orthopedic injury or surgery, deciding who should undergo venous thromboembolism (VTE) prophylaxis is challenging due to the wide range of risk. The Thrombosis Risk Prediction for Patients with cast immobilization or TRiP(cast) score, which predicts VTE risk, was recently derived and validated in nearly 5000 patients with prolonged lower limb casting, mostly for ankle sprain [ 86 ]. Among those assessed as low VTE risk (score <7) and in whom anticoagulation was withheld, the rate of symptomatic VTE was 0.7 percent compared with 2.7 percent among those with a score ≥7 despite anticoagulation. The negative predictive value for this threshold was 99 percent. Use of the score reduced the prescription of anticoagulants by 26 percent compared with baseline prescription levels. While promising, further validation is needed. (See "Prevention of venous thromboembolism (VTE) in adults with non-major extremity orthopedic injury with or without surgical repair", section on 'Venous thromboembolism risk' .)
Antibiotics are required for nonoperative management of uncomplicated appendicitis (April 2024)
In uncomplicated appendicitis, antibiotic therapy alone is a widely accepted alternative to appendectomy. Whether antibiotic therapy can be omitted in some patients is unknown. In a trial that randomly assigned 100 patients with mild appendicitis (defined as white blood cell count <13,000/microliter, C-reactive protein <60 mg/dL) to piperacillin-tazobactam or observation for either disease regression or the need for surgical exploration, antibiotic therapy reduced the need for appendectomy both during the initial hospitalization (28 versus 53 percent) and at three-year follow-up (50 versus 63 percent) [ 87 ]. Thus, we continue to suggest routine antibiotic therapy for all patients managed nonoperatively for acute appendicitis. (See "Management of acute appendicitis in adults", section on 'Protocols' .)
Pregnancy and childbirth after urinary incontinence surgery (January 2024)
Patients with stress urinary incontinence (SUI) have historically been advised to delay midurethral sling (MUS) surgery until after childbearing because of concerns for worsening SUI symptoms following delivery. In a meta-analysis of patients with MUS surgery who were followed for a mean of nearly 10 years, similar low SUI recurrence and reoperation rates were reported for the 381 patients with and the 860 patients without subsequent childbirth [ 88 ]. Birth route did not affect the findings. Although the total number of recurrences and reoperations was small, this study adds to the body of evidence suggesting that subsequent childbirth does not worsen SUI outcomes for patients who have undergone MUS. (See "Surgical management of stress urinary incontinence in females: Retropubic midurethral slings", section on 'Subsequent pregnancy' .)
- Cinciripini PM, Green CE, Shete S, et al. Smoking Cessation After Initial Treatment Failure With Varenicline or Nicotine Replacement: A Randomized Clinical Trial. JAMA 2024.
- Green SM, Tomaszewski C, Valente JH, et al. Use of Topical Anesthetics in the Management of Patients With Simple Corneal Abrasions: Consensus Guidelines From the American College of Emergency Physicians. Ann Emerg Med 2024; 83:477.
- Auer R, Schoeni A, Humair JP, et al. Electronic Nicotine-Delivery Systems for Smoking Cessation. N Engl J Med 2024; 390:601.
- Lin HX, Liu Z, Hajek P, et al. Efficacy of Electronic Cigarettes vs Varenicline and Nicotine Chewing Gum as an Aid to Stop Smoking: A Randomized Clinical Trial. JAMA Intern Med 2024; 184:291.
- Lindson N, Butler AR, McRobbie H, et al. Electronic cigarettes for smoking cessation. Cochrane Database Syst Rev 2024; 1:CD010216.
- https://evidence.nejm.org/doi/full/10.1056/EVIDoa2300172?query=ev_TOC&cid=DM2312304_Non_Subscriber&bid=2005966377 (Accessed on January 08, 2024).
- Somisetty S, Santina A, Au A, et al. Progression of Pentosan Polysulfate Sodium Maculopathy in a Prospective Cohort. Am J Ophthalmol 2023; 255:57.
- Persell SD, Petito LC, Lee JY, et al. Reducing Care Overuse in Older Patients Using Professional Norms and Accountability : A Cluster Randomized Controlled Trial. Ann Intern Med 2024; 177:324.
- Xu C, Leung JCN, Shi J, et al. Sedative-hypnotics and osteoporotic fractures: A systematic review of observational studies with over six million individuals. Sleep Med Rev 2024; 73:101866.
- Interim Clinical Considerations for Use of COVID-19 Vaccines Currently Authorized in the United States. https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html (Accessed on March 06, 2024).
- Murthy N, Wodi AP, McNally V, et al. Advisory Committee on Immunization Practices Recommended Immunization Schedule for Adults Aged 19 Years or Older - United States, 2023. MMWR Morb Mortal Wkly Rep 2023; 72:141.
- Drysdale SB, Cathie K, Flamein F, et al. Nirsevimab for Prevention of Hospitalizations Due to RSV in Infants. N Engl J Med 2023; 389:2425.
- Ponikowski P, Mentz RJ, Hernandez AF, et al. Efficacy of ferric carboxymaltose in heart failure with iron deficiency: an individual patient data meta-analysis. Eur Heart J 2023; 44:5077.
- Kloner RA, Burnett AL, Miner M, et al. Princeton IV consensus guidelines: PDE5 inhibitors and cardiac health. J Sex Med 2024; 21:90.
- Khan SS, Coresh J, Pencina MJ, et al. Novel Prediction Equations for Absolute Risk Assessment of Total Cardiovascular Disease Incorporating Cardiovascular-Kidney-Metabolic Health: A Scientific Statement From the American Heart Association. Circulation 2023; 148:1982.
- Khan SS, Matsushita K, Sang Y, et al. Development and Validation of the American Heart Association's PREVENT Equations. Circulation 2024; 149:430.
- Pasternak B, Wintzell V, Hviid A, et al. Glucagon-like peptide 1 receptor agonist use and risk of thyroid cancer: Scandanavian cohort study. BMJ 2024; 385:e078225.
- Uhl S, Choure A, Rouse B, et al. Effectiveness of Continuous Glucose Monitoring on Metrics of Glycemic Control in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis of Randomized Controlled Trials. J Clin Endocrinol Metab 2024; 109:1119.
- Jancev M, Vissers TACM, Visseren FLJ, et al. Continuous glucose monitoring in adults with type 2 diabetes: a systematic review and meta-analysis. Diabetologia 2024; 67:798.
- ZEPBOUND (tirzepatide) injection. United States prescribing information. Revised November 2023. US Food and Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/217806s000lbl.pdf (Accessed on November 18, 2023).
- Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide Once Weekly for the Treatment of Obesity. N Engl J Med 2022; 387:205.
- Garvey WT, Frias JP, Jastreboff AM, et al. Tirzepatide once weekly for the treatment of obesity in people with type 2 diabetes (SURMOUNT-2): a double-blind, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet 2023; 402:613.
- Buffolo F, Pecori A, Reincke M, et al. Long-Term Follow-Up of Patients With Elevated Aldosterone-to-Renin Ratio but Negative Confirmatory Test: The Progression of Primary Aldosteronism Phenotypes. Hypertension 2024; 81:340.
- Aronne LJ, Sattar N, Horn DB, et al. Continued Treatment With Tirzepatide for Maintenance of Weight Reduction in Adults With Obesity: The SURMOUNT-4 Randomized Clinical Trial. JAMA 2024; 331:38.
- Lincoff AM, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and Cardiovascular Outcomes in Obesity without Diabetes. N Engl J Med 2023; 389:2221.
- Lee CJ, Dellon ES. Real-World Efficacy of Dupilumab in Severe, Treatment-Refractory, and Fibrostenotic Patients With Eosinophilic Esophagitis. Clin Gastroenterol Hepatol 2024; 22:252.
- Kann AE, Jepsen P, Madsen LG, et al. Cause-specific mortality in patients with alcohol-related liver disease in Denmark: a population-based study. Lancet Gastroenterol Hepatol 2023; 8:1028.
- Issaka RB, Chan AT, Gupta S. AGA Clinical Practice Update on Risk Stratification for Colorectal Cancer Screening and Post-Polypectomy Surveillance: Expert Review. Gastroenterology 2023; 165:1280.
- Arrieta O, Cárdenas-Fernández D, Rodriguez-Mayoral O, et al. Mirtazapine as Appetite Stimulant in Patients With Non-Small Cell Lung Cancer and Anorexia: A Randomized Clinical Trial. JAMA Oncol 2024; 10:305.
- Caswell-Jin JL, Sun LP, Munoz D, et al. Analysis of Breast Cancer Mortality in the US-1975 to 2019. JAMA 2024; 331:233.
- Talal AH, Markatou M, Liu A, et al. Integrated Hepatitis C-Opioid Use Disorder Care Through Facilitated Telemedicine: A Randomized Trial. JAMA 2024; 331:1369.
- US Food and Drug Administration. FDA Roundup: March 22, 2024. https://www.fda.gov/news-events/press-announcements/fda-roundup-march-22-2024 (Accessed on March 25, 2024).
- Li Y, Regan M, Swartwood NA, et al. Disparities in Tuberculosis Incidence by Race and Ethnicity Among the U.S.-Born Population in the United States, 2011 to 2021 : An Analysis of National Disease Registry Data. Ann Intern Med 2024; 177:418.
- United States Centers for Disease Control and Prevention. https://www.cdc.gov/respiratory-viruses/prevention/index.html (Accessed on March 25, 2024).
- Gordon WJ, Henderson D, DeSharone A, et al. Remote Patient Monitoring Program for Hospital Discharged COVID-19 Patients. Appl Clin Inform 2020; 11:792.
- Grinspoon SK, Fitch KV, Zanni MV, et al. Pitavastatin to Prevent Cardiovascular Disease in HIV Infection. N Engl J Med 2023; 389:687.
- Arivoli K, Valicevic AN, Oerline MK, et al. Preventive Pharmacological Therapy and Risk of Recurrent Urinary Stone Disease. Clin J Am Soc Nephrol 2024; 19:565.
- Tsur AM, Akavian I, Landau R, et al. Adolescent Body Mass Index and Early Chronic Kidney Disease in Young Adulthood. JAMA Pediatr 2024; 178:142.
- Nitta K, Itoyama S, Ikejiri K, et al. Randomized Study of Tenapanor Added to Phosphate Binders for Patients With Refractory Hyperphosphatemia. Kidney Int Rep 2023; 8:2243.
- Campos-Fernandez D, Rodrigo-Gisbert M, Abraira L, et al. Predictive Model for Estimating the Risk of Epilepsy After Aneurysmal Subarachnoid Hemorrhage: The RISE Score. Neurology 2024; 102:e209221.
- Charles AC, Digre KB, Goadsby PJ, et al. Calcitonin gene-related peptide-targeting therapies are a first-line option for the prevention of migraine: An American Headache Society position statement update. Headache 2024; 64:333.
- Noetel M, Sanders T, Gallardo-Gómez D, et al. Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials. BMJ 2024; 384:e075847.
- Rivier CA, Kamel H, Sheth KN, et al. Cerebral Amyloid Angiopathy and Risk of Isolated Nontraumatic Subdural Hemorrhage. JAMA Neurol 2024; 81:163.
- Gao Y, Chen W, Pan Y, et al. Dual Antiplatelet Treatment up to 72 Hours after Ischemic Stroke. N Engl J Med 2023; 389:2413.
- Marques A, Pereira B, Simonetta-Moreau M, et al. Trial of Botulinum Toxin for Isolated or Essential Head Tremor. N Engl J Med 2023; 389:1753.
- Dodick DW, Goadsby PJ, Schwedt TJ, et al. Ubrogepant for the treatment of migraine attacks during the prodrome: a phase 3, multicentre, randomised, double-blind, placebo-controlled, crossover trial in the USA. Lancet 2023; 402:2307.
- Kim MS, Lee H, Lee SW, et al. Long-Term Autoimmune Inflammatory Rheumatic Outcomes of COVID-19 : A Binational Cohort Study. Ann Intern Med 2024; 177:291.
- Frodlund M, Jönsen A, Remkus L, et al. Glucocorticoid treatment in SLE is associated with infections, comorbidities and mortality-a national cohort study. Rheumatology (Oxford) 2024; 63:1104.
- Wittoek R, Verbruggen G, Vanhaverbeke T, et al. RANKL blockade for erosive hand osteoarthritis: a randomized placebo-controlled phase 2a trial. Nat Med 2024; 30:829.
- Sebastian A, van der Geest KSM, Tomelleri A, et al. Development of a diagnostic prediction model for giant cell arteritis by sequential application of Southend Giant Cell Arteritis Probability Score and ultrasonography: a prospective multicentre study. Lancet Rheumatol 2024; 6:e291.
- Kimbrough BA, Crowson CS, Davis JM 3rd, et al. Decline in Incidence of Extra-Articular Manifestations of Rheumatoid Arthritis: A Population-Based Cohort Study. Arthritis Care Res (Hoboken) 2024; 76:454.
- Baraliakos X, Bergmann E, Tsiami S, et al. A Good Response to Nonsteroidal Antiinflammatory Drugs Does Not Discriminate Patients With Longstanding Axial Spondyloarthritis From Controls With Chronic Back Pain. J Rheumatol 2024; 51:250.
- Ulijn E, den Broeder N, Ten Cate D, et al. Limited Diagnostic and Prognostic Value of Routine Radiographs in Newly Presenting Arthritis Suspected of Rheumatoid Arthritis: A Retrospective Study. Arthritis Care Res (Hoboken) 2024; 76:497.
- Maltez N, Maxwell LJ, Rirash F, et al. Phosphodiesterase 5 inhibitors (PDE5i) for the treatment of Raynaud's phenomenon. Cochrane Database Syst Rev 2023; 11:CD014089.
- Torres E, Carter G, Gero A, et al. Frequency of same-day contraceptive initiation, recent unprotected intercourse, and pregnancy risk: a prospective cohort study of multiple contraceptive methods. Am J Obstet Gynecol 2024.
- Oderkerk TJ, Beelen P, Bukkems ALA, et al. Risk of Hysterectomy After Endometrial Ablation: A Systematic Review and Meta-analysis. Obstet Gynecol 2023; 142:51.
- Johansson K, Bodnar LM, Abrams B, Hutcheon JA. Safety of low weight gain or weight loss in pregnancies with class 1, 2, and 3 obesity: a population-based cohort study. Lancet 2024.
- Minozzi S, Ambrosi L, Saulle R, et al. Psychosocial and medication interventions to stop or reduce alcohol consumption during pregnancy. Cochrane Database Syst Rev 2024; 4:CD015042.
- Ahlqvist VH, Sjöqvist H, Dalman C, et al. Acetaminophen Use During Pregnancy and Children's Risk of Autism, ADHD, and Intellectual Disability. JAMA 2024; 331:1205.
- Suarez EA, Bateman BT, Straub L, et al. First Trimester Use of Buprenorphine or Methadone and the Risk of Congenital Malformations. JAMA Intern Med 2024; 184:242.
- Zhou Y, Bai Z, Zhang W, et al. Effect of Dexmedetomidine on Postpartum Depression in Women With Prenatal Depression: A Randomized Clinical Trial. JAMA Netw Open 2024; 7:e2353252.
- Goodfellow L, Care A, Curran C, et al. Preterm prelabour rupture of membranes before 23 weeks' gestation: prospective observational study. BMJ Med 2024; 3:e000729.
- Cesta CE, Rotem R, Bateman BT, et al. Safety of GLP-1 Receptor Agonists and Other Second-Line Antidiabetics in Early Pregnancy. JAMA Intern Med 2024; 184:144.
- Boggess KA, Valint A, Refuerzo JS, et al. Metformin Plus Insulin for Preexisting Diabetes or Gestational Diabetes in Early Pregnancy: The MOMPOD Randomized Clinical Trial. JAMA 2023; 330:2182.
- Fejzo M, Rocha N, Cimino I, et al. GDF15 linked to maternal risk of nausea and vomiting during pregnancy. Nature 2024; 625:760.
- Rial-Crestelo M, Lubusky M, Parra-Cordero M, et al. Term planned delivery based on fetal growth assessment with or without the cerebroplacental ratio in low-risk pregnancies (RATIO37): an international, multicentre, open-label, randomised controlled trial. Lancet 2024; 403:545.
- Shields LE, Foster M, Klein C, et al. 68 Prospective multicenter trial comparing balloon versus suction hemorrhage control devices for postpartum hemorrhage. Am J Obstet Gynecol 2024; 230:S51.
- Dwarkanath P, Muhihi A, Sudfeld CR, et al. Two Randomized Trials of Low-Dose Calcium Supplementation in Pregnancy. N Engl J Med 2024; 390:143.
- Cantor AG, Jungbauer RM, Skelly AC, et al. Respectful Maternity Care : A Systematic Review. Ann Intern Med 2024; 177:50.
- Chaillet N, Mâsse B, Grobman WA, et al. Perinatal morbidity among women with a previous caesarean delivery (PRISMA trial): a cluster-randomised trial. Lancet 2024; 403:44.
- Damhuis SE, Groen H, Thilaganathan B, et al. Effect of intrapartum epidural analgesia on rate of emergency delivery for presumed fetal compromise: nationwide registry-based cohort study. Ultrasound Obstet Gynecol 2023; 62:668.
- Seidler AL, Aberoumand M, Hunter KE, et al. Deferred cord clamping, cord milking, and immediate cord clamping at preterm birth: a systematic review and individual participant data meta-analysis. Lancet 2023; 402:2209.
- Seidler AL, Libesman S, Hunter KE, et al. Short, medium, and long deferral of umbilical cord clamping compared with umbilical cord milking and immediate clamping at preterm birth: a systematic review and network meta-analysis with individual participant data. Lancet 2023; 402:2223.
- Armarego M, Forde H, Wills K, Beggs SA. High-flow nasal cannula therapy for infants with bronchiolitis. Cochrane Database Syst Rev 2024; 3:CD009609.
- Li L, Zhu N, Zhang L, et al. ADHD Pharmacotherapy and Mortality in Individuals With ADHD. JAMA 2024; 331:850.
- Yousaf AR, Lindsey KN, Wu MJ, et al. Notes from the Field: Surveillance for Multisystem Inflammatory Syndrome in Children - United States, 2023. MMWR Morb Mortal Wkly Rep 2024; 73:225.
- Delmonico RL, Tucker LY, Theodore BR, et al. Mild Traumatic Brain Injuries and Risk for Affective and Behavioral Disorders. Pediatrics 2024; 153.
- Moline HL, Tannis A, Toepfer AP, et al. Early Estimate of Nirsevimab Effectiveness for Prevention of Respiratory Syncytial Virus-Associated Hospitalization Among Infants Entering Their First Respiratory Syncytial Virus Season - New Vaccine Surveillance Network, October 2023-February 2024. MMWR Morb Mortal Wkly Rep 2024; 73:209.
- Budesonide oral suspension. US Food & Drug Administration, approval letter. February 2024. https://www.accessdata.fda.gov/drugsatfda_docs/appletter/2024/213976Orig1s000ltr.pdf (Accessed on February 12, 2024).
- Budesonide oral suspension. United States Prescribing Information, February 2024. US Food & Drug Administration. https://www.accessdata.fda.gov/drugsatfda_docs/label/2024/213976s000lbl.pdf (Accessed on February 13, 2024).
- Attaianese F, Costantino A, Benucci C, et al. Benign acute children myositis: 5 years experience in a tertiary care pediatric hospital. Eur J Pediatr 2023; 182:4341.
- Health Alert Network: High Blood Lead Levels in Children Consuming Recalled Cinnamon Applesauce Pouches. HAN00500. Centers for Disease Control and Prevention. . Atlanta, GA, November 13, 2023. https://emergency.cdc.gov/han/2023/han00500.asp?ACSTrackingID=USCDC_511-DM117142&ACSTrackingLabel=HAN%20500%20-%20General%20Public&deliveryName=USCDC_511-DM117142 (Accessed on November 14, 2023).
- Panagiotakopoulos L, Sandul AL, DHSc, et al. CDC Recommendations for Hepatitis C Testing Among Perinatally Exposed Infants and Children - United States, 2023. MMWR Recomm Rep 2023; 72:1.
- Velez MP, Dayan N, Shellenberger J, et al. Infertility and Risk of Autism Spectrum Disorder in Children. JAMA Netw Open 2023; 6:e2343954.
- Cramm SL, Graham DA, Blakely ML, et al. Postoperative Antibiotics, Outcomes, and Resource Use in Children With Gangrenous Appendicitis. JAMA Surg 2024; 159:511.
- Nemeth B, Douillet D, le Cessie S, et al. Clinical risk assessment model to predict venous thromboembolism risk after immobilization for lower-limb trauma. EClinicalMedicine 2020; 20:100270.
- Iresjö BM, Blomström S, Engström C, et al. Acute appendicitis: A block-randomized study on active observation with or without antibiotic treatment. Surgery 2024; 175:929.
- Nahshon C, Abramov Y, Kugelman N, et al. The effect of subsequent pregnancy and childbirth on stress urinary incontinence recurrence following midurethral sling procedure: a meta-analysis. Am J Obstet Gynecol 2024; 230:308.
Family Medicine and Community Health
is an open access journal focusing on the topics of family medicine, general practice and community health.
Impact Factor 6.1 Citescore 8.4 All metrics >>
FMCH strives to be a leading international journal that promotes 'Health Care for All' through disseminating novel knowledge and best practices in primary care, family medicine, and community health. FMCH publishes original research, review, methodology, commentary, reflection, and case-study from the lens of population health. FMCH 's Asian Focus section features reports of family medicine development in the Asia-pacific region.
FMCH aims to serve a diverse audience including researchers, educators, policymakers and leaders of family medicine and community health. We also aim to provide content relevant for researchers working on population health, epidemiology, public policy, disease control and management, preventative medicine and disease burden. FMCH does not impose any article processing charges (APC) or submission charges.
FMCH was founded by the Beijing Huawei General Practice Research Institute (BHGPRI) as an internationally focused open access journal devoted to subjects that are common and relevant to family medicine, general practice and community health. FMCH is owned by BHGPRI
JOURNAL NEWS: Family Medicine and Community Health is now indexed in PubMed Central and Medline.
Access further content on the journal blog . Follow the journal on X and Facebook. FMCH has a Citescore of 8.4 (2022) and an Impact Factor of 6.1 (2022).

Highlighted Articles

Family Medicine and Community Health accepts submissions of a wide range of article types, including Editorials, Original research, Focus on Asia Pacific, Review articles, Reflections, Case reports and Letters to the Editor.
The Author Information section provides specific article requirements to help you turn your research into an article suitable for FMCH.
Information is also provided on editorial and data policies .
Latest Articles
Original research :
18 May 2024
Perspective :
10 April 2024
4 April 2024
Most Read Articles
16 October 2023
13 October 2023
Systematic review :
6 July 2023
31 July 2023
10 May 2022
In the Journal
18 February 2022
Uncategorized
16 December 2021
26 November 2021
20 August 2021

Featured Video
Family medicine and community health - our full story.
Listen to Editor-in-Chief of Family Medicine and Community Health, Prof. Li Li, talk about the journal's aims and scope, the advice he has for authors thinking about submitting to the journal, what the journal has to offer to readers, highlights from the journal and what the journal has planned for 2024.
Related Journals

BMJ Open Diabetes Research & Care
Bmj sexual & reproductive health.

Journal of Epidemiology and Community Health (JECH)
Recruiter: Leeds Teaching Hospitals NHS Trust
Recruiter: Avon and Wiltshire Mental Health Partnership NHS Trust
Weston Super Mare
Dundee City
Recruiter: NHS Tayside
Helston, Cornwall
Recruiter: Helston Medical Centre
AAFP Family Medicine Publications
American family physician.
The AAFP’s peer-reviewed, evidence-based clinical journal offers concise, practical, easy-to-read clinical review articles for physicians and other health care professionals.
Annals of Family Medicine
The peer-reviewed research journal published by the AAFP and six other family medicine organizations advances knowledge essential to understanding health and primary care.

The AAFP’s peer-reviewed, practice-improvement journal offers practical ideas to improve practice, enhance the patient experience, and develop a rewarding career.
FP Essentials
The AAFP's peer-reviewed, monthly monograph series, available by subscription only, offers in-depth learning on a carefully chosen clinical topic in each print and digital edition.
Get the AAFP app . Access digital replicas of American Family Physician, FPM, and FP Essentials from the AAFP app. Free to AAFP members and subscribers.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Family Medicine
Clinical research.
Physician-scientists in the Department of Family Medicine-Research at Mayo Clinic engage in clinical research efforts to understand the causes of disease and to identify effective methods of prevention and treatment.
Research in the Department of Family Medicine-Research covers a broad range of medical issues focused on family and community medicine, including headache, depression, calcium and vitamin D nutrition, obesity, women's health, and global health.
Through networking and access to resources across Mayo Clinic, the Department of Family Medicine-Research conducts research projects that ultimately enhance patient well-being. Researchers study patterns of patient care and specific common or important patient conditions, with specialists pursuing focused areas of research interest.
Much of the department's research is epidemiological, which involves reviewing medical records with patient consent and adherence to privacy policies and procedures of Mayo Clinic. All research studies in the department are reviewed for safety and ethical issues by the Mayo Clinic Institutional Review Board , which meets the highest national standards for research review and oversight.
More about research at Mayo Clinic
- Research Faculty
- Laboratories
- Core Facilities
- Centers & Programs
- Departments & Divisions
- Clinical Trials
- Institutional Review Board
- Postdoctoral Fellowships
- Training Grant Programs
- Publications
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
The Department of Family Medicine is committed to producing high-quality scholarship that improves patient care, medical education, and health policy. Benefiting from the renowned academic environment of the University of Chicago , our Family Medicine researchers apply rigorous qualitative and quantitative methods to practical problems.
Quick Links
- Reproductive Health Outcomes and Disparities (RHOADs) Research
- Research Consortium on Religious Healthcare Institutions
- ExPAND Mifepristone
Research Topics
Our current research projects have diverse funding sources, including National Institutes of Health, private foundations, and the University of Chicago's Urban Health Initiative .
We study topics relevant to Family Medicine practitioners, patients and students, including:
- Community-based medical education
Reproductive health outcomes and disparities
- Screening for diabetic retinopathy
- Clinical ethics and narrative medicine
Community Involvement
In addition to producing primary research, members of the Department of Family Medicine participate in systematic dissemination of new research from the medical literature into medical practice. We nominate and review papers as part of the PURLs surveillance system and write Help Desk Answers for Evidence-Based Practice , a publication of the Family Physician Inquiry Network.
Faculty, fellows and residents all participate in research activities, and we welcome students to get involved. Research takes place on both our south side Chicago campus, through Pritzker School of Medicine and the University of Chicago Medical Center , and at our north suburban sites through the NorthShore University HealthSystem.
Areas of Research
Religious hospitals and the doctor-patient relationship.
Debra Stulberg, MD, MAPP
In collaboration with the University of Chicago's Program on Medicine & Religion , these studies survey and interview family physicians, general internists, and obstetrician-gynecologists to explore their experiences working at religiously-affiliated hospitals or practices. These are among the first empiric studies of physician ethical and professional conflicts around religious patient-care policies. Funding: Greenwall Foundation.
Using hospital discharge and insurance data, this group of studies evaluates the association between race, socioeconomic status and health system factors on the incidence and outcomes of pregnancy complications. Special focus is on the effect of insurance status on processes and outcomes of care in ectopic pregnancy. Funding: National Institute of Child Health and Human Development; Chicago Center of Excellence for Health Promotions Economics.
Gorukanti AL, Kimminau KS, Tindle HA, Klein JD, Gorzkowski J, Kaseeska K, Ali R, Singh L, David SP, Halpern-Felsher B. Cross-sectional online survey of clinicians' knowledge, attitudes and challenges to screening and counselling adolescents and young adults for substance use. BMJ Open. 2022 Nov 22;12(11):e059019.
Jang SK, Evans L, Fialkowski A, Arnett DK, Ashley-Koch AE, Barnes KC, Becker DM, Bis JC, Blangero J, Bleecker ER, Boorgula MP, Bowden DW, Brody JA, Cade BE, Jenkins BWC, Carson AP, Chavan S, Cupples LA, Custer B, Damrauer SM, David SP, de Andrade M, Dinardo CL, Fingerlin TE, Fornage M, Freedman BI, Garrett ME, Gharib SA, Glahn DC, Haessler J, Heckbert SR, Hokanson JE, Hou L, Hwang SJ, Hyman MC, Judy R, Justice AE, Kaplan RC, Kardia SLR, Kelly S, Kim W, Kooperberg C, Levy D, Lloyd-Jones DM, Loos RJF, Manichaikul AW, Gladwin MT, Martin LW, Nouraie M, Melander O, Meyers DA, Montgomery CG, North KE, Oelsner EC, Palmer ND, Payton M, Peljto AL, Peyser PA, Preuss M, Psaty BM, Qiao D, Rader DJ, Rafaels N, Redline S, Reed RM, Reiner AP, Rich SS, Rotter JI, Schwartz DA, Shadyab AH, Silverman EK, Smith NL, Smith JG, Smith AV, Smith JA, Tang W, Taylor KD, Telen MJ, Vasan RS, Gordeuk VR, Wang Z, Wiggins KL, Yanek LR, Yang IV, Young KA, Young KL, Zhang Y, Liu DJ, Keller MC, Vrieze S. Rare genetic variants explain missing heritability in smoking. Nat Hum Behav. 2022 Nov;6(11):1577-1586.
Nguyen LH, Anyane-Yeboa A, Klaser K, Merino J, Drew DA, Ma W, Mehta RS, Kim DY, Warner ET, Joshi AD, Graham MS, Sudre CH, Thompson EJ, May A, Hu C, Jørgensen S, Selvachandran S, Berry SE, David SP, Martinez ME, Figueiredo JC, Murray AM, Sanders AR, Koenen KC, Wolf J, Ourselin S, Spector TD, Steves CJ, Chan AT. The mental health burden of racial and ethnic minorities during the COVID-19 pandemic. PLoS One. 2022;17(8):e0271661.
Saulsberry L, Singh L, Pruitt J, Ward C, Wake DT, Gibbons RD, Meltzer DO, O'Donnell PH, Cruz-Knight W, Hulick PJ, Dunnenberger HM, David SP. Effect Modification by Social Determinants of Pharmacogenetic Medication Interactions on 90-Day Hospital Readmissions within an Integrated U.S. Healthcare System. J Pers Med. 2022 Jul 15;12(7).
Menni C, Valdes AM, Polidori L, Antonelli M, Penamakuri S, Nogal A, Louca P, May A, Figueiredo JC, Hu C, Molteni E, Canas L, Österdahl MF, Modat M, Sudre CH, Fox B, Hammers A, Wolf J, Capdevila J, Chan AT, David SP, Steves CJ, Ourselin S, Spector TD. Symptom prevalence, duration, and risk of hospital admission in individuals infected with SARS-CoV-2 during periods of omicron and delta variant dominance: a prospective observational study from the ZOE COVID Study. Lancet. 2022 Apr 23;399(10335):1618-1624.
Reiner AP, Raffield LM, Franceschini N, Auer PL,Lange EM, Nickerson DA, Zakai NA, Correa A, Olson N, David SP with the NHLBITrans-Omics for Precision Medicine Consortium. Effect of Sickle CellTrait and APOL1 Genotype on the Association of Soluble uPARwith Kidney Function Measures in Black Americans. Clin J Am Soc Nephrol. 2021 Feb 8;16(2):287-289. 16(2021):287-289.
Taliun D, Harris DN, Kessler MD, Carlson J,Szpiech ZA, Torres R, Taliun SAG, Corvelo A, Gogarten SM, Kang HM, Pitsillides AN, LeFaive J, Lee SB, Tian X, Browning BL, Das S, Emde AK, Clarke WE, LoeschDP, Shetty AC, Blackwell TW, Smith AV, Wong Q, Liu X, Conomos MP, Bobo DM, Aguet F, Albert C, Alonso A, Ardlie KG, Arking DE, Aslibekyan S, Auer PL, Barnard J, Barr RG, Barwick L, Becker LC, Beer RL, Benjamin EJ, Bielak LF, Blangero J, Boehnke M, Bowden DW, Brody JA, Burchard EG, Cade BE, Casella JF, Chalazan B, Chasman DI, Chen YI, Cho MH, Choi SH, Chung MK, Clish CB, Correa A, Curran JE,Custer B, Darbar D, Daya M, de Andrade M, DeMeo DL, Dutcher SK, Ellinor PT, EmeryLS, Eng C, Fatkin D, Fingerlin T, Forer L, Fornage M, Franceschini N, Fuchsberger C, Fullerton SM, Germer S, Gladwin MT, Gottlieb DJ, Guo X, Hall ME,He J, Heard-Costa NL, Heckbert SR, Irvin MR, Johnsen JM, Johnson AD, Kaplan R, Kardia SLR, Kelly T, Kelly S, Kenny EE, Kiel DP, Klemmer R, Konkle BA, Kooperberg C, Köttgen A, Lange LA, Lasky-Su J, Levy D, Lin X, Lin KH, Liu C, Loos RJF,Garman L, Gerszten R, Lubitz SA, Lunetta KL, Mak ACY, Manichaikul A, Manning AK, Mathias RA, McManus DD, McGarvey ST, Meigs JB, Meyers DA, Mikulla JL,Minear MA, Mitchell BD, Mohanty S, Montasser ME, Montgomery C, Morrison AC, Murabito JM, Natale A, Natarajan P, Nelson SC, North KE, O'Connell JR, Palmer ND, Pankratz N, Peloso GM, Peyser PA, Pleiness J, Post WS, Psaty BM, Rao DC,Redline S, Reiner AP, Roden D, Rotter JI, Ruczinski I, Sarnowski C, Schoenherr S, Schwartz DA, Seo JS, Seshadri S, Sheehan VA, Sheu WH, Shoemaker MB, SmithNL, Smith JA, Sotoodehnia N, Stilp AM, Tang W, Taylor KD, Telen M, Thornton TA,Tracy RP, Van Den Berg DJ, Vasan RS, Viaud-Martinez KA, Vrieze S, Weeks DE,Weir BS, Weiss ST, Weng LC, Willer CJ, Zhang Y, Zhao X, Arnett DK, Ashley-KochAE, Barnes KC, Boerwinkle E, Gabriel S, Gibbs R, Rice KM, Rich SS, SilvermanEK, Qasba P, Gan W, David SP with the NHLBI Trans-Omics for PrecisionMedicine (TOPMed) Consortium, Papanicolaou GJ, Nickerson DA, Browning SR, Zody MC, Zöllner S, Wilson JG, Cupples LA, Laurie CC, Jaquish CE, Hernandez RD,O'Connor TD, Abecasis GR. Sequencing of 53,831 diverse genomes from the NHLBITOPMed Program. Nature. 2021 Feb;590(7845):290-299.
Ikagami S, BenirschkeR, Fakhrai-Rad H, Motamedi MH, Hockett R, David S, Lee HK, Kang J,Gniadek TJ. Target specific serology analysis of COVID-19 convalescent plasma. PLoS One. 2021 Apr 28;16(4):e0249938.
McGuire D, JiangY, Liu M, Weissenkampen JD, Eckert S, Yang L, Chen F, Berg A, Vrieze S, JiangB, Li Q, Liu DJ, David SP as part of the GSCAN Consortium. Model-based assessment ofreplicability for genome-wide association meta-analysis. Nat Commun. 2021 Mar 30;12(1):1964. 12(2021):1964.
Natarajan P, Pampana A, Graham SE, RuotsalainenSE, Perry JA, de Vries PS, Broome JG, Pirruccello JP, Honigberg MC, Aragam K,Wolford B, Brody JA, Antonacci-Fulton L, Arden M, Aslibekyan S, Assimes TL,Ballantyne CM, Bielak LF, Bis JC, Cade BE, Do R, Doddapaneni H, Emery LS, HungYJ, Irvin MR, Khan AT, Lange L, Lee J, Lemaitre RN, Martin LW, Metcalf G,Montasser ME, Moon JY, Muzny D, O'Connell JR, Palmer ND, Peralta JM, Peyser PA,Stilp AM, Tsai M, Wang FF, Weeks DE, Yanek LR, Wilson JG, Abecasis G, Arnett DK,Becker LC, Blangero J, Boerwinkle E, Bowden DW, Chang YC, Chen YI, Choi WJ,Correa A, Curran JE, Daly MJ, Dutcher SK, Ellinor PT, Fornage M, Freedman BI, Gabriel S, Germer S, Gibbs RA, He J, Hveem K, Jarvik GP, Kaplan RC, Kardia SLR,Kenny E, Kim RW, Kooperberg C, Laurie CC, Lee S, Lloyd-Jones DM, Loos RJF,Lubitz SA, Mathias RA, Martinez KAV, McGarvey ST, Mitchell BD, Nickerson DA,North KE, Palotie A, Park CJ, Psaty BM, Rao DC, Redline S, Reiner AP, Seo D,Seo JS, Smith AV, Tracy RP, Vasan RS, Kathiresan S, Cupples LA, Rotter JI,Morrison AC, Rich SS, Ripatti S, Willer C, Peloso GM, David SP with the NHLBITrans-Omics for Precision Medicine (TOPMed) Consortium. Chromosome Xq23 isassociated with lower atherogenic lipid concentrations and favorable cardiometabolicindices. Nat Commun. 2021 Apr 12;12(1):2182.
Kasela S, OrtegaVE, Martorella M, Garudadri S, Nguyen J, Ampleford E, Pasanen A, Nerella S,Buschur KL, Barjaktarevic IZ, Barr RG, Bleecker ER, Bowler RP, Comellas AP,Cooper CB, Couper DJ, Criner GJ, Curtis JL, Han MK, Hansel NN, Hoffman EA,Kaner RJ, Krishnan JA, Martinez FJ, McDonald MN, Meyers DA, Paine R 3rd, PetersSP, Castro M, Denlinger LC, Erzurum SC, Fahy JV, Israel E, Jarjour NN, Levy BD,Li X, Moore WC, Wenzel SE, Zein J, Langelier C, Woodruff PG, Lappalainen T, Christenson SA, David SP with the NHLBI Trans-Omicsfor Precision Medicine (TOPMed) Consortium. Genetic and non-genetic factors affecting the expression ofCOVID-19-relevant genes in the large airway. Genome Med. 2021 Apr 21;13(1):66. 13(2021):66.
Sofer T, Zheng X, Laurie CA, Gogarten SM, BrodyJA, Conomos MP, Bis JC, Thornton TA, Szpiro A, O'Connell JR, Lange EM, Gao Y, Cupples LA, Psaty BM, Rice KM, David SP with the NHLBI Trans-Omics for Precision Medicine (TOPMed) Consortium. Variant-specific inflation factors forassessing population stratification at the phenotypic variance level. NatCommun. 2021 Jun 9;12(1)3506.
Keramati AR, Chen MH, Rodriguez BAT, Yanek LR,Bhan A, Gaynor BJ, Ryan K, Brody JA, Zhong X, Wei Q, Kammers K, Kanchan K, IyerK, Kowalski MH, Pitsillides AN, Cupples LA, Li B, Schlaeger TM, Shuldiner AR,O'Connell JR, Ruczinski I, Mitchell BD, Faraday N, Taub MA, Becker LC, LewisJP, Mathias RA, Johnson AD, David SP with the NHLBI Trans-Omics for PrecisionMedicine (TOPMed) Consortium. Genome sequencing unveils a regulatorylandscape of platelet reactivity. NatCommun. 2021 Jun 15;12(1):3626. 12(2021):3626.
David SP, Dunnenberger HM, Ali R,Matsil A, Lemke, AA, Singh L, Zimmer A, Hulick PJ. Implementing Primary CareMediated Population Genetic Screening within an Integrated Health System. JAm Board Fam Med. Jul-Aug 2021;34(4):861-865.
Cade BE, Lee J, Sofer T, Wang H, Zhang M, Chen H, Gharib SA,Gottlieb DJ, Guo X, Lane JM, Liang J, Lin X, Mei H, Patel SR, Purcell SM,Saxena R, Shah NA, Evans DS, Hanis CL, Hillman DR, Mukherjee S, Palmer LJ,Stone KL, Tranah GJ, Abecasis GR, Boerwinkle EA, Correa A, Cupples LA, KaplanRC, Nickerson DA, North KE, Psaty BM, Rotter JI, Rich SS, Tracy RP, Vasan RS,Wilson JG, Zhu X, Redline S, David SP with the NHLBI Trans-Omics for PrecisionMedicine (TOPMed) Consortium. Whole genome association analysesof sleep-disordered breathing phenotypes in the NHLBI TOPMed program. Genome Med. 2021 Aug 26;13(1):136.
Bello, J.K. , Chavez, J., Liederbauer, V. et al. Perceptions of a Spanish language Reproductive Health Self-assessment Tool Among Spanish-Speaking Women at a Federally Qualified Health Center. J Immigrant Minority Health (2020). https://doi.org/10.1007/s10903-020-00988-6
Hasselbacher, L.A., Hebert, L.E., Liu, Y. and Stulberg, D.B . (2020), “My Hands Are Tied”: Abortion Restrictions and Providers’ Experiences in Religious and Nonreligious Health Care Systems. Perspect Sex Repro H. doi:10.1363/psrh.12148
Jocelyn M. Wascher, Debra B. Stulberg & Lori R. Freedman (2020): Restrictions on Reproductive Care at Catholic Hospitals: A Qualitative Study of Patient Experiences and Perspectives, AJOB Empirical Bioethics, DOI: 10.1080/23294515.2020.1817173
B. Song , E. White VanGompel, C. Wang, S. Guzman, F. Carlock, K. Schueler, D.Stulberg , Effects of Clinic-level Implementation of One Key Question® on Reproductive Health Counseling andPatient Satisfaction, Contraception (2020), doi: https://doi.org/10.1016/j.contraception.2020.10.018 .
Wingo, E.E., Wascher, J.M., Stulberg, D.B . and Freedman, L.R. (2020), Anticipatory Counseling About Miscarriage Management in Catholic Hospitals: A Qualitative Exploration of Women's Preferences. Perspect Sex Repro H, 52: 171-179. https://doi.org/10.1363/psrh.12157
Oshman L, Caplan A, Ali R, Singh L, Khalid R, Jameel M, David SP . Whom Should We Test for COVID-19? Performance of a Symptom and Risk Factor Questionnaire on COVID-19 Test Results and Patient Outcomes in an Immediate Care Setting. J Prim Care Community Health. 2020 Jan-Dec;11:2150132720981297. PMID: 33300408
Luvsantseren S, Whirl-Carrillo M, Sangkuhl K, Shin N, Wen A, Empey P, Alam B, David S , Dunnenberger HM, Orlando L, Altman R, Palaniappan L. Variant Interpretation in Current Pharmacogenetic Testing. J Pers Med. 2020 Oct 31;10(4):204. doi: 10.3390/jpm10040204. PMID: 33142667 Free PMC article.
Rosas LG, Nasrallah C, Park VT, Vasquez JJ, Duron Y, Garrick O, Hattin R, Cho M, David SP , Evans J, McClinton-Brown R, Martin C. Perspectives on Precision Health Among Racial/Ethnic Minority Communities and the Physicians That Serve Them. Ethn Dis. 2020 Apr 2;30(Suppl 1):137-148. PMID: 32269455 Free PMC article.
Eng VA, David SP , Li S, Ally MS, Stefanick M, Tang JY. The association between cigarette smoking, cancer screening, and cancer stage: a prospective study of the women's health initiative observational cohort. BMJ Open. 2020 Aug 13;10(8):e037945. doi: 10.1136/bmjopen-2020-037945. PMID: 32796021
David SP , Dunnenberger HM, Ali R, Matsil, Lemke, AA, Singh L, Zimmer A, Hulick PJ. Implementing Primary Care Mediated Population Genetic Screening within an Integrated Health System. medRxiv. Prepublication. https://urldefense.com/v3/__https://www.medrxiv.org/content/10.1101/2020.07.16.20140228v1__;!!OaZRxjSJGsACmqMyc8s!ZEqvLH-ckcFgBfuNGMXK7BMng6kBUkxqRIr_tKZmNFdPKOF_p_Fomn_QEYqSO5vYwoO-XOE$
Bick AG, Weinstock JS, Nandakumar SK, Fulco CP, Bao EL, Zekavat SM, Szeto MD, Liao X, Leventhal MJ, Nasser J, Chang K, Laurie C, Burugula BB, Gibson CJ, Lin AE, Taub MA, Aguet F, Ardlie K, Mitchell BD, Barnes KC, Moscati A, Fornage M, Redline S, Psaty BM, Silverman EK, Weiss ST, Palmer ND, Vasan RS, Burchard EG, Kardia SLR, He J, Kaplan RC, Smith NL, Arnett DK, Schwartz DA, Correa A, de Andrade M, Guo X, Konkle BA, Custer B, Peralta JM, Gui H, Meyers DA, McGarvey ST, Chen IY, Shoemaker MB, Peyser PA, Broome JG, Gogarten SM, Wang FF, Wong Q, Montasser ME, Daya M, Kenny EE, North KE, Launer LJ, Cade BE, Bis JC, Cho MH, Lasky-Su J, Bowden DW, Cupples LA, Mak ACY, Becker LC, Smith JA, Kelly TN, Aslibekyan S, Heckbert SR, Tiwari HK, Yang IV, Heit JA, Lubitz SA, Johnsen JM, Curran JE, Wenzel SE, Weeks DE, Rao DC, Darbar D, Moon JY, Tracy RP, Buth EJ, Rafaels N, Loos RJF, Durda P, Liu Y, Hou L, Lee J, Kachroo P, Freedman BI, Levy D, Bielak LF, Hixson JE, Floyd JS, Whitsel EA, Ellinor PT, Irvin MR, Fingerlin TE, Raffield LM, Armasu SM, Wheeler MM, Sabino EC, Blangero J, Williams LK, Levy BD, Sheu WH, Roden DM, Boerwinkle E, Manson JE, Mathias RA, Desai P, Taylor KD, Johnson AD; NHLBI Trans-Omics for Precision Medicine Consortium ( TOPMed co-author David SP ), Auer PL, Kooperberg C, Laurie CC, Blackwell TW, Smith AV, Zhao H, Lange E, Lange L, Rich SS, Rotter JI, Wilson JG, Scheet P, Kitzman JO, Lander ES, Engreitz JM, Ebert BL, Reiner AP, Jaiswal S, Abecasis G, Sankaran VG, Kathiresan S, Natarajan P. Inherited causes of clonal haematopoiesis in 97,691 whole genomes. Nature. 2020 Oct;586(7831):763-768. doi: 10.1038/s41586-020-2819-2. PMID: 33057201
Li X, Li Z, Zhou H, Gaynor SM, Liu Y, Chen H, Sun R, Dey R, Arnett DK, Aslibekyan S, Ballantyne CM, Bielak LF, Blangero J, Boerwinkle E, Bowden DW, Broome JG, Conomos MP, Correa A, Cupples LA, Curran JE, Freedman BI, Guo X, Hindy G, Irvin MR, Kardia SLR, Kathiresan S, Khan AT, Kooperberg CL, Laurie CC, Liu XS, Mahaney MC, Manichaikul AW, Martin LW, Mathias RA, McGarvey ST, Mitchell BD, Montasser ME, Moore JE, Morrison AC, O'Connell JR, Palmer ND, Pampana A, Peralta JM, Peyser PA, Psaty BM, Redline S, Rice KM, Rich SS, Smith JA, Tiwari HK, Tsai MY, Vasan RS, Wang FF, Weeks DE, Weng Z, Wilson JG, Yanek LR; NHLBI Trans-Omics for Precision Medicine (TOPMed) Consortium ( TOPMed co-author David SP ); TOPMed Lipids Working Group, Neale BM, Sunyaev SR, Abecasis GR, Rotter JI, Willer CJ, Peloso GM, Natarajan P, Lin X. Dynamic incorporation of multiple in silico functional annotations empowers rare variant association analysis of large whole-genome sequencing studies at scale. Nat Genet. 2020 Sep;52(9):969-983. doi: 10.1038/s41588-020-0676-4. PMID: 32839606
De novo mutations across 1,465 diverse genomes reveal mutational insights and reductions in the Amish founder population. Kessler MD, Loesch DP, Perry JA, Heard-Costa NL, Taliun D, Cade BE, Wang H, Daya M, Ziniti J, Datta S, Celedón JC, Soto-Quiros ME, Avila L, Weiss ST, Barnes K, Redline SS, Vasan RS, Johnson AD, Mathias RA, Hernandez R, Wilson JG, Nickerson DA, Abecasis G, Browning SR, Zöllner S, O'Connell JR, Mitchell BD; National Heart, Lung, and Blood Institute Trans-Omics for Precision Medicine (TOPMed) Consortium ( TOPMed co-author David SP ); TOPMed Population Genetics Working Group, O'Connor TD. Proc Natl Acad Sci U S A. 2020 Feb 4;117(5):2560-2569. PMID: 31964835
D. Stulberg , A. Datta, E. White VanGompel , K. Schueler, C.H. Rocca, One Key Question® and the Desire to Avoid Pregnancy Scale: A Comparison of Two Approaches to Asking About Pregnancy Preferences, Contraception (2019), doi: https://doi.org/10.1016/j.contraception.2019.12.010
Saigal, Pooja . Diving for PURLs: Alkaline water and plant-based Mediterranean diet for laryngopharyngeal reflux. Evidence-Based Practice. 2019; 22(11).
Oyola, Sonia . Diving for PURLs: Increasing colorectal cancer screening rates. Evidence-Based Practice. 2019; 22(8).
Wake DT, Ilbawi N, Dunnenberger HM, Hulick PJ. Pharmacogenomics: Prescribing Precisely. Med Clin North Am. 2019 Nov;103(6):977-990. doi: 10.1016/j.mcna.2019.07.002. Epub 2019 Aug 24. Review. PMID: 31582008
Panagiotou OA, Schuit E, Munafò MR, Bennett DA, Bergen AW, David SP . Smoking Cessation Pharmacotherapy Based on Genetically-Informed Biomarkers: What is the Evidence? Nicotine Tob Res. 2019 Aug 19;21(9):1289-1293. doi: 10.1093/ntr/ntz009. PMID: 30690475
Nussbaum SE, Oyola S, Egan M, Baron A, Wackman S, Williams S, Benson J, Limaye S, Levine S. Incorporating Older Adults as "Trained Patients" to Teach Advance Care Planning to Third-Year Medical Students. Am J Hosp Palliat Care. 2019 Jul;36(7):608-615. doi: 10.1177/1049909119836394. Epub 2019 Mar 25. PMID: 30909719
Weidner A, Ewigman B , Peterson LE, Mainous AG 3rd. Response to "The Importance of Support Staff to Research Capacity". Fam Med. 2019 Jul;51(7):619. doi: 10.22454/FamMed.2019.332787. No abstract available. PMID: 31287911
Fazio, Lindsay . Diving for PURLs: Which is best for chronic low back pain: Yoga, physical therapy, or education? Evidence-Based Practice. 2019; 22(7).
Bergen AW, Do EK, Chen LS, David SP . Tobacco Genomics: Complexity and Translational Challenges. Nicotine Tob Res. 2019 May 21;21(6):705-706. doi: 10.1093/ntr/ntz033. No abstract available. PMID: 31111930
White VanGompel E , Perez S, Datta A, Wang C, Cape V, Main E. Cesarean overuse and the culture of care. Health Serv Res. 2019 Apr;54(2):417-424. doi: 10.1111/1475-6773.13123. Epub 2019 Feb 20. PMID: 30790273
Fudala, Monica . Diving for PURLs: Gastric acid suppression and recurrent Clostridium difficile infection. Evidence-Based Practice. 2019; 22(3).
Zhuri, Henri and Miller, Deborah . HelpDesk Answers: In adults who are overweight or obese, does treatment of depression improve weight loss? Evidence-Based Practice. 2019; 22(3).
Ward, William and Miller, Debra . HelpDesk Answers: In athletes, does cold therapy promote better exercise performance recovery? Evidence-Based Practice. 2019; 22(2).
Weidner A, Peterson LE, Mainous AG 3rd, Datta A, Ewigman B . The Current State of Research Capacity in US Family Medicine Departments. Fam Med. 2019 Feb;51(2):112-119. doi: 10.22454/FamMed.2019.180310. PMID: 30736036
Liaw W, Petterson S, Jiang V, Bazemore A, Pecsok J, McCorry D, Ewigman B . The Scholarly Output of Faculty in Family Medicine Departments. Fam Med. 2019 Feb;51(2):103-111. doi: 10.22454/FamMed.2019.536135. PMID: 30736035
Liu M, Jiang Y, Wedow R, Li Y, Brazel DM, Chen F, Datta G, Davila-Velderrain J, McGuire D, Tian C, Zhan X; 23andMe Research Team; HUNT All-In Psychiatry, Choquet H, Docherty AR, Faul JD, Foerster JR, Fritsche LG, Gabrielsen ME, Gordon SD, Haessler J, Hottenga JJ, Huang H, Jang SK, Jansen PR, Ling Y, Mägi R, Matoba N, McMahon G, Mulas A, Orrù V, Palviainen T, Pandit A, Reginsson GW, Skogholt AH, Smith JA, Taylor AE, Turman C, Willemsen G, Young H, Young KA, Zajac GJM, Zhao W, Zhou W, Bjornsdottir G, Boardman JD, Boehnke M, Boomsma DI, Chen C, Cucca F, Davies GE, Eaton CB, Ehringer MA, Esko T, Fiorillo E, Gillespie NA, Gudbjartsson DF, Haller T, Harris KM, Heath AC, Hewitt JK, Hickie IB, Hokanson JE, Hopfer CJ, Hunter DJ, Iacono WG, Johnson EO, Kamatani Y, Kardia SLR, Keller MC, Kellis M, Kooperberg C, Kraft P, Krauter KS, Laakso M, Lind PA, Loukola A, Lutz SM, Madden PAF, Martin NG, McGue M, McQueen MB, Medland SE, Metspalu A, Mohlke KL, Nielsen JB, Okada Y, Peters U, Polderman TJC, Posthuma D, Reiner AP, Rice JP, Rimm E, Rose RJ, Runarsdottir V, Stallings MC, Stančáková A, Stefansson H, Thai KK, Tindle HA, Tyrfingsson T, Wall TL, Weir DR, Weisner C, Whitfield JB, Winsvold BS, Yin J, Zuccolo L, Bierut LJ, Hveem K, Lee JJ, Munafò MR, Saccone NL, Willer CJ, Cornelis MC, David SP , Hinds DA, Jorgenson E, Kaprio J, Stitzel JA, Stefansson K, Thorgeirsson TE, Abecasis G, Liu DJ, Vrieze S. Association studies of up to 1.2 million individuals yield new insights into the genetic etiology of tobacco and alcohol use. Nat Genet. 2019 Feb;51(2):237-244. doi: 10.1038/s41588-018-0307-5. Epub 2019 Jan 14. PMID: 30643251
Erzurumluoglu AM, Liu M, Jackson VE, Barnes DR, Datta G, Melbourne CA, Young R, Batini C, Surendran P, Jiang T, Adnan SD, Afaq S, Agrawal A, Altmaier E, Antoniou AC, Asselbergs FW, Baumbach C, Bierut L, Bertelsen S, Boehnke M, Bots ML, Brazel DM, Chambers JC, Chang-Claude J, Chen C, Corley J, Chou YL, David SP , de Boer RA, de Leeuw CA, Dennis JG, Dominiczak AF, Dunning AM, Easton DF, Eaton C, Elliott P, Evangelou E, Faul JD, Foroud T, Goate A, Gong J, Grabe HJ, Haessler J, Haiman C, Hallmans G, Hammerschlag AR, Harris SE, Hattersley A, Heath A, Hsu C, Iacono WG, Kanoni S, Kapoor M, Kaprio J, Kardia SL, Karpe F, Kontto J, Kooner JS, Kooperberg C, Kuulasmaa K, Laakso M, Lai D, Langenberg C, Le N, Lettre G, Loukola A, Luan J, Madden PAF, Mangino M, Marioni RE, Marouli E, Marten J, Martin NG, McGue M, Michailidou K, Mihailov E, Moayyeri A, Moitry M, Müller-Nurasyid M, Naheed A, Nauck M, Neville MJ, Nielsen SF, North K, Perola M, Pharoah PDP, Pistis G, Polderman TJ, Posthuma D, Poulter N, Qaiser B, Rasheed A, Reiner A, Renström F, Rice J, Rohde R, Rolandsson O, Samani NJ, Samuel M, Schlessinger D, Scholte SH, Scott RA, Sever P, Shao Y, Shrine N, Smith JA, Starr JM, Stirrups K, Stram D, Stringham HM, Tachmazidou I, Tardif JC, Thompson DJ, Tindle HA, Tragante V, Trompet S, Turcot V, Tyrrell J, Vaartjes I, van der Leij AR, van der Meer P, Varga TV, Verweij N, Völzke H, Wareham NJ, Warren HR, Weir DR, Weiss S, Wetherill L, Yaghootkar H, Yavas E, Jiang Y, Chen F, Zhan X, Zhang W, Zhao W, Zhao W, Zhou K, Amouyel P, Blankenberg S, Caulfield MJ, Chowdhury R, Cucca F, Deary IJ, Deloukas P, Di Angelantonio E, Ferrario M, Ferrières J, Franks PW, Frayling TM, Frossard P, Hall IP, Hayward C, Jansson JH, Jukema JW, Kee F, Männistö S, Metspalu A, Munroe PB, Nordestgaard BG, Palmer CNA, Salomaa V, Sattar N, Spector T, Strachan DP; Understanding Society Scientific Group, EPIC-CVD, GSCAN, Consortium for Genetics of Smoking Behaviour, CHD Exome+ consortium, van der Harst P, Zeggini E, Saleheen D, Butterworth AS, Wain LV, Abecasis GR, Danesh J, Tobin MD, Vrieze S, Liu DJ, Howson JMM. Mol Psychiatry. 2019 Jan 7. doi: 10.1038/s41380-018-0313-0. [Epub ahead of print] Meta-analysis of up to 622,409 individuals identifies 40 novel smoking behaviour associated genetic loci. PMID: 30617275
Saigal, Pooja and Sharman, Meera, Debra . HelpDesk Answers: Which treatment is most effective for individuals with anorexia nervosa? Evidence-Based Practice. 2019; 22(1).
Stulberg, Debra . Diving for PURLs: Acupuncture for pain; Give it a try. Evidence-Based Practice. 2019; 22(1).
Brazel DM, Jiang Y, Hughey JM, Turcot V, Zhan X, Gong J, Batini C, Weissenkampen JD, Liu M; CHD Exome+ Consortium; Consortium for Genetics of Smoking Behaviour, Barnes DR, Bertelsen S, Chou YL, Erzurumluoglu AM, Faul JD, Haessler J, Hammerschlag AR, Hsu C, Kapoor M, Lai D, Le N, de Leeuw CA, Loukola A, Mangino M, Melbourne CA, Pistis G, Qaiser B, Rohde R, Shao Y, Stringham H, Wetherill L, Zhao W, Agrawal A, Bierut L, Chen C, Eaton CB, Goate A, Haiman C, Heath A, Iacono WG, Martin NG, Polderman TJ, Reiner A, Rice J, Schlessinger D, Scholte HS, Smith JA, Tardif JC, Tindle HA, van der Leij AR, Boehnke M, Chang-Claude J, Cucca F, David SP, Foroud T, Howson JMM, Kardia SLR, Kooperberg C, Laakso M, Lettre G, Madden P, McGue M, North K, Posthuma D, Spector T, Stram D, Tobin MD, Weir DR, Kaprio J, Abecasis GR, Liu DJ, Vrieze S. Exome Chip Meta-analysis Fine Maps Causal Variants and Elucidates the Genetic Architecture of Rare Coding Variants in Smoking and Alcohol Use. Biol Psychiatry. 2019 Jun 1;85(11):946-955. doi: 10.1016/j.biopsych.2018.11.024. Epub 2018 Dec 6. PMID: 30679032
White VanGompel E, Perez S, Wang C, Datta A, Cape V, Main E. Measuring labor and delivery unit culture and clinicians' attitudes toward birth: Revision and validation of the Labor Culture Survey. Birth. 2019 Jun;46(2):300-310. doi: 10.1111/birt.12406. Epub 2018 Nov 8. PMID: 30407646
Oshman, Lauren . Diving for PURLs: How many mammograms? Let breast density and risk factors guide screening intervals. Evidence-Based Practice. 2018; 21(9).
Benson, Janice and VanGompel, Emily White . Diving for PURLs: A risk score to guide anticoagulant choice in patients with Afib. Evidence-Based Practice. 2018; 21(9).
Roberson, Kortnee . Diving for PURLs: Bariatric surgery for treatment of diabetes. Evidence-Based Practice. 2018; 21(9).
Temple LM, Lampert SL, Ewigman B . Barriers to Achieving Optimal Success with Medical Cannabis: Opportunities for Quality Improvement. J Altern Complement Med. 2019 Jan;25(1):5-7. doi: 10.1089/acm.2018.0250. Epub 2018 Sep 6. PMID: 30188174
Gibes, Joseph P . Diving for PURLs: Diving for Chocolate PURLs. Evidence-Based Practice. 2018; 21(8).
Viollt, Anne and Oshman, Lauren . HelpDesk Answers: For adults with chronic low back pain, is a prescribed walking program as effective as formal physical therapy? Evidence-Based Practice. 2018; 21(8).
Moore, Lisa Marie and Whiteley, Miriam . HelpDesk Answers: In pregnant women with a positive BUN screen or quad screen, does secondary screening with cell-free DNA reduce the incidence of invasive testing for fetal aneuploidy? Evidence-Based Practice. 2018; 21(7).
Whiteley, Miriam . Diving for PURLs: Metformin versus insulin for GDM. Evidence-Based Practice. 2018; 21(7).
Tetreault, Stephanie and Oshman, Lauren . HelpDesk Answers: In women desiring postpartum contraception with an IUD, does immediate IUD insertion after delivery increased continued IUD use at 6 months compared with delayed IUD insertion? Evidence-Based Practice. 2018; 21(6).
Longo, Katie and Gibes, Joseph . HelpDesk Answers: In women with dense breast tissue,does the addition of automated whole-breast ultrasound to mammography lead to increased invasive testing? Evidence-Based Practice. 2018; 21(5).
Roberson, Kortnee and White VanGompel, Emily . Diving for PURLs: Dietary changes to improve depression. Evidence-Based Practice. 2018; 21(4).
Stombaugh, Sarah and Whiteley, Miriam . HelpDesk Answers: In adolescent girls using contraceptives, do long-acting reversible contraceptives (LARC) have a higher rate of continuation than other forms of contraception? Evidence-Based Practice. 2018; 21(4).
Oyola, Sonia . Diving for PURLs: Consider acupuncture for chronic constipation. Evidence-Based Practice. 2018; 21(1).
The University of Chicago has long been known for research that crosses traditional boundaries of disciplines. In studying health and health care, Family Medicine researchers collaborate with physicians and scholars from a wide array of departments, schools and programs.
Opportunities for interdisciplinary work are facilitated at the University of Chicago by centers that bring scholars together to share ideas and generate new knowledge.
The Center for Health and the Social Sciences
The mission of The Center for Health and the Social Sciences (CHeSS) is to support and encourage interdisciplinary health and social science research at The University of Chicago. The Center provides infrastructure including: administrative assistance for collaborations; pre- and post-award grants management; computer, data, and methodological support; and shared space.
Program on Medicine and Religion
The Program on Medicine and Religion at the University of Chicago seeks to promote rigorous study of and robust dialogue about the moral and spiritual dimensions of the practice of medicine. The Program reflects a collaboration between the Department of Medicine--and its MacLean Center for Clinical Medical Ethics, and the Divinity School--and its Marty Center for the Advanced Study of Religion.
The MacLean Center for Clinical Medical Ethics
Clinical medical ethics examines ethical issues that arise in encounters between patients, families, and physicians, and aims to improve the process and outcome of patient care. After twenty years, the MacLean Center is the leading program in the country devoted to the study and teaching of clinical ethics. The program has gained national and international prominence for its groundbreaking research and training in medical ethics.
Medical Education Research, Innovation, Teaching and Scholarship
MERITS is a University of Chicago-sponsored initiative to support and promote research, innovation, teaching, and scholarship in medical education with the goal of advancing patient care and the health of the public by improving the education of physicians.
Every month, thousands of primary research articles are published that may be relevant to the practicing family physician. PURLs (Priority Updates from the Research Literature) are those that should change practice and can be implemented immediately by family physicians. The PURLs surveillance system, to identify and disseminate these practicing-changing research studies, was developed as an objective of the University of Chicago Institute for Translational Medicine , in partnership with the Family Physician Inquiry Network and the Journal of Family Practice .
In order to be a PURL, a research article must first be nominated by a group of family physicians who actively survey the primary clinical research literature; the article must then be reviewed and determined to be relevant to family medicine, scientifically valid, applicable in a medical care setting, immediately implementable, and to lead to a change in current practice.
Department of Family Medicine physicians are active participants as PURL nominators, reviewers, authors, and editors.
Link: PURLs website at the Journal of Family Practice
NorthShore University HealthSystem is recognized as one of the nation's top Comprehensive Independent Research Hospitals. With extensive funding from the National Institutes of Health, the NorthShore Research Institute houses approximately 1,000 clinical trials, and provides training and infrastructure support for diverse clinical and translational research projects.
Research and scholarship are core elements of the academic affiliation between the University of Chicago and NorthShore University HealthSystem. The Family Medicine residency takes full advantage of this affiliation by offering residents mentorship and learning opportunities on both campuses. Residents each complete a core rotation in evidence-based medicine as part of a curriculum that emphasizes skills in synthesizing and applying the research literature.
Primary Care and Population Health Investigators Group
The Primary Care and Population Health (PCPH) Investigators Group (formerly called the "Ambulatory Primary Care Innovation Group" (APCIG)) is a team of investigators associated with the Northshore Outcomes Research Network and the Univeristy of Chicago Institute for Translational Medicine who are committed to research in areas of germane to primary care and population health (e.g., family planning, reproductive health, quality and care transformation, "personalized" or "precision medicine" in primary care, population-based surveys, etc.). PCPH has a monthly meeting and represents numerous active studies, grand-funded projects, development of new research opportunities, promotion of team science, and mentoring of junior scientists.
Outcomes Research Network
The NorthShore University HealthSystem Outcomes Research Network (ORN) was launched in December 2018 as the result of a system-wide planning process which identified research with immediate benefit to patients as a strategic goal. ORN is a networked structure with key academic leadership, providing support to propel research productivity across NorthShore (e.g., literature reviews, project management assistance, grant review). ORN houses two core research groups - PCPH, led by Dr. Sean P. David, and Child and Family Health Studies, led by Dr. Madeleine Shalowitz. ORN core faculty include Dr. Bernard Ewigman (Director), Drs. Sean P. David (Program Director for Translationsal Science), Madeleine Shalowitz (Program Director for Pediatrics), and Anthony Solomonides (Program Director for Bioformatics), and numerous affiliated ORN Program Directors (e.g., Drs. Amy Lemke, Personalized Medicine and Dr. Nirav Shah, Care Transformation).
Outcomes research at NorthShore is a collaborative, transdisciplinary science that uses a range of techniques and tools: quality improvement, health services research, cost effectiveness, comparative effectiveness, implementation science, actuarial science, practice-based research and community-based participatory research. At the community level, outcomes research emphasized actionable information leading to uniform access to care that is effective, efficient and equitable. For providers, it can provide insight that will enrich the experience of practicing medicine. Outcomes research yields valid, reliable, and impactful knowledge that can be used to support key strategic clinical, quality, and operational decision-making.
Contacts for Research programs at NorthShore University HealthSystem:
Research Resources
Office of clinical research, center for research informatics, institute for translational medicine, north american primary care research group (napcrg).
- STFM Journals
- Family Medicine
- Annals of Family Medicine

Recently Published
- Collections
CURRENT ISSUE
Family Medicine , an official journal of the Society of Teachers of Family Medicine, aims to publish high-quality, original scholarship about education in family medicine and primary care. The journal publishes original research, systematic reviews, narrative essays, and policy analyses relevant to the discipline of family medicine, particularly focusing on primary care medical education, health workforce policy, and health services research. The journal does not publish clinical review articles.
Family Medicine is committed to advancing efforts toward inclusion and antiracism in all journal-related activities. We endeavor to eliminate bias and racism in our editorial process and published content. Read the full diversity statement .
Submit Issue Cover Art for Family Medicine Interested in submitting a photograph, painting, or artwork for consideration for a future Family Medicine issue cover? Send the high-quality digital image to [email protected].
E-ISSN: 1938-3800
Loading Articles...
Call for papers— recruit, mentor, and promote a diverse family medicine workforce..
Submission deadline: August 15
Family Medicine seeks submissions for a theme issue on recruiting, mentoring, and promoting a diverse family medicine workforce. Family medicine is one of the most gender and racially diverse specialties, yet the discipline lags behind the general population in diversity, particularly in academic settings. Yet a diverse workforce is paramount to the health of patients and communities and success within organizations. Therefore our goal is to collect high-quality articles on pathway programs, recruitment initiatives, and meaningful retention and promotion strategies aimed to diversify the family medicine workforce. Original research and brief reports are welcome. FM Focus submissions must have high yield, concise information that will be published as an infographic. Narrative essay submissions should share original stories from the perspective of students, residents, faculty members, or practicing physicians.
The STFM Medical Editing Fellowship: A Gateway to Scholarly Growth for Community Physicians
by Priyanka Tulshian, MD, MPH, current fellow
Most Read (2022)
The Diabetes Code . Scherger JE. Fam Med. 2019;51(3):286-287.
Racism as Experienced by Physicians of Color in the Health Care Setting . Serafini K, Coyer C, Brown Speights J, et al. Fam Med. 2020: 52(4):282-287.
PedHITSS: A Screening Tool to Detect Childhood Abuse in Clinical Settings . Shakil A, Day PG, Chu J, Woods SB, Bridges K. Fam Med. 2018;50(10):763-769.
The Shared Principles of Primary Care: A Multistakeholder Initiative to Find a Common Voice . Epperly T, Bechtel C, Sweeney R, et al. Fam Med. 2019;51(2):179-184.
Joint Guidelines for Protected Nonclinical Time for Faculty in Family Medicine Residency Programs. Griesbach S, Theobald M, Kolman K, et al. Fam Med. 2021;53(6):443-452.
The Political Determinants of Health . Lin KW. Fam Med. 2022;54(1):65-66.
A Time-Motion Study of Primary Care Physicians’ Work in the Electronic Health Record Era . Young RA, Burge SK, Kumar KA, Wilson JM, Ortiz DF. Fam Med. 2018;50(2):91-99.
The Virginal Speculum and Its Myths. Walser SA. Fam Med. 2020;52(9):672-673.
Addressing Racism in Medical Education: An Interactive Training Module . White-Davis T, Edgoose J, Brown Speights JS, et al. Fam Med. 2018;50(5):364-368.
Family Physicians Delivering Babies? It’s Time to Decide . Winnie K, Saultz J. Fam Med. 2021;53(5):325-327.

Contact STFM
2024 © Society of Teachers of Family Medicine. All Rights Reserved.

- Patient Care
- School of Medicine
- Medical Student Education
- Residency Network
- Sports Medicine
- Palliative Care
- Osher Center
- MAKE A GIFT
Department of family medicine
An internationally-recognized research organization focused on increasing the quality, effectiveness, accessibility and sustainability of primary care. We conduct research and develop methods to answer vital healthcare questions in collaboration with colleagues in diverse disciplines and settings. We disseminate results to health practitioners and policymakers locally, nationally and internationally, aiming to inform practice and policy.
research areas

Health Workforce Studies
The health workforce is the backbone of any health care delivery system. Our research group houses three federally funded centers conducting quality research necessary to develop a strong and quality health workforce in the US.

Rural Health Research
Rural U.S. residents overall are poorer, have a higher burden of disease, are more likely to live in Health Professional Shortage Areas, and travel farther to access health care than their urban counterparts. Our research aims to inform local, regional, and national policy and practice to improve the health of vulnerable and minority rural populations.

WWAMI region Practice and Research Network (WPRN)
The WPRN is a network of more than 97 primary care practices across the five-state WWAMI (Washington, Wyoming, Alaska, Montana and Idaho) region that collaborate on research. The mission of the WPRN is to improve the health and well-being of patients in their communities, through the conduct of collaborative research that informs and enhances primary care clinical practice.

Cancer Prevention and Detection
Our research aims to improve cancer health outcomes through implementation of evidence-based cancer intervention in primary care practices.

Integrated Behavioral Health
Our research aims to address discovery and dissemination of evidence informed mental and behavioral health treatment s in primary care to address mental and physical health conditions.

Primary Care Innovation Lab
The PCI Lab researches the design, development, testing and implementation of new technologies and innovations in primary care.

Treatment and Prevention of Substance Use Disorders
Primary care practice is a critical setting for substance use disorder (SUD) prevention, diagnosis, and treatment, yet significant numbers of patients with SUDs go unrecognized. Opioid use and opioid use disorder are of particular relevance to primary care, as primary care providers, who are on the front lines of pain management, write half of all opioid prescriptions each year, and some of the individuals for whom they write prescriptions develop opioid use disorder. Our research tackles these important problems by addressing optimal management of chronic pain, opioid prescribing, and opioid use disorder in primary care practice.

Clinical Research Informatics
Clinical Research Informatics is a subdiscipline within biomedical informatics (an interdisciplinary field that studies use of biomedical data, information and knowledge to improve human health) focused on development of informatic theories, tools and solutions to accelerate translational science. Our research aims to target improvements in primary care to improve patient health through the use of informatics tools and solutions.

Reproductive and Women’s Health
Family Medicine researchers work within the Division of Family Planning in the Department of Obstetrics and Gynecology. Our mission is to investigate critical clinical questions and conduct innovative research to advance the field of family planning…

The COVID pandemic has profoundly impacted our healthcare system and patients worldwide. Our team participates in a broad range of COVID-related research. Examples include examining diagnostic testing modalities and access, predictors of long-term health impacts of COVID-19, impact of COVID on mental health and healthcare utilization, health disparities related to COVID, as well as disease severity, associated symptoms and comorbidities in acute and post-acute sequelae of COVID-19 (PASC). We have developed a robust research program centered on investigating long COVID-related pain and potential treatments in partnership with the Post-COVID Rehabilitation and Recovery Clinic, Rehabilitation Medicine, the CLEAR Center, and Osher Center for Integrative Medicine.
**Under Construction**
other department section research
Sports medicine research, medical student education research & scholarship, palliative care research.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 30, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Researchers develop easy-to-use screening tool to help improve family access to federal nutrition programs
by Children's Hospital of Philadelphia

Researchers from The Possibilities Project and Clinical Futures at Children's Hospital of Philadelphia (CHOP) have developed, implemented and successfully tested a nutrition screener to improve access to healthy resources for families eligible for federally-funded food benefits. The findings were published this week in the journal Annals of Family Medicine .
Many low-income families rely on the federally-funded Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and the Supplemental Nutrition Assistance Program (SNAP) for nutritional support, and both programs have been linked to improved health outcomes and decreased health care costs . However, many eligible families do not receive these program benefits because of the complex application and enrollment process.
"Prior studies at CHOP show that 50% of people who are eligible for services like WIC might not actually be taking advantage of them," said study co-author George Dalembert, MD, Associate Director of the Center for Health Equity at CHOP.
The Possibilities Project at CHOP aims to design innovative strategies and implement new ideas to better serve patients. In this study, to help eligible families navigate this system, researchers designed and tested a standardized process for linking families to WIC and SNAP during pediatric primary care visits. This nutrition screener was a tablet-based questionnaire that asked eligible families whether they were interested in help applying for WIC or SNAP or wanted information about local food banks.
Caregivers who requested help applying for WIC or SNAP received a phone call within a week offering targeted assistance with benefits enrollment. Information was also printed out during the office visit and linked to their child's patient portal.
In the first month of the pilot in November 2022, 433 families completed the screener (74% in person, 26% via patient portal), and 73 (17%) requested nutrition resources, including 17 who requested information about local food banks, and 56 families who requested benefits application support. Of these 56 families, 25 (45%) were reached by telephone and 21 (38%) were successfully connected to WIC and/or SNAP or given the information they requested. However, many families (55%) could not be reached as they either had incorrect contact information listed in the electronic health record (12%) or did not respond to telephone calls from our resource navigator (43%).
"The approach we developed may be one important way to normalize social needs assessment and provide families with additional nutrition support," said lead study author Aditi Vasan, MD, an attending physician with the Division of General Pediatrics at CHOP.
"To ensure all families in need are able to receive appropriate support, clinics should consider priming caregivers to expect follow-up from a resource navigator, as well as asking about preferred contact method and incorporating additional outreach approaches like text messaging."
Explore further
Feedback to editors

Cancer patients often do better with less intensive treatment, new research finds
7 hours ago

Study sheds new light on the contribution of dopamine to reinforcement learning
14 hours ago

Almost 1 in 3 Americans know someone who's died from a drug overdose
Jun 1, 2024

Antibody discovery promises new hope in influenza B battle, paves way for universal vaccine

Eye-tracking techniques could help primary care providers diagnose autism sooner, more accurately
May 31, 2024

This self-powered sensor could make MRIs more efficient

Not eating can hinder weight loss, study in fruit flies suggests

Neuroscience research suggests ketones can enhance cognitive function and protect brain networks

New research finds antidepressants may help deliver other drugs into the brain

Mediterranean diet tied to one-fifth lower risk of death in women
Related stories, effects of the proposed snap eligibility changes.
Mar 9, 2020

US families of children with leukemia may experience food insecurity despite a federal assistance program
Sep 16, 2022


Study finds cost-driven housing moves lead to disruptions in federal assistance programs
Feb 6, 2024

Confusing assistance requirements contribute to food insecurity among college students
Mar 25, 2024

Unhealthy drink consumption highest among economically-vulnerable households on multiple food assistance programs: Study
Jul 10, 2023

Extra food assistance cushioned the early pandemic's blow on kids' mental health
Mar 27, 2023
Recommended for you

Study shows most doctors endorsing drugs on X are paid to do so

Study finds use of in-hospital mortality as a sepsis quality metric may unfairly penalize safety-net hospitals

Scientists develop visual tool to help people group foods based on their levels of processing

Study finds even low lead levels in US water are linked to lead poisoning among susceptible people

Tobacco firms invest billions in medical products: Call for journals to ban research by the firms, their subsidiaries
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
30 Best universities for Family medicine in Russia
Updated: February 29, 2024
- Art & Design
- Computer Science
- Engineering
- Environmental Science
- Liberal Arts & Social Sciences
- Mathematics
Below is a list of best universities in Russia ranked based on their research performance in Family medicine. A graph of 47.2K citations received by 7.64K academic papers made by 30 universities in Russia was used to calculate publications' ratings, which then were adjusted for release dates and added to final scores.
We don't distinguish between undergraduate and graduate programs nor do we adjust for current majors offered. You can find information about granted degrees on a university page but always double-check with the university website.
1. Moscow Medical Academy
For Family medicine

2. Russian National Research Medical University

3. Moscow State University

4. Pavlov First Saint Petersburg State Medical University
5. Volgograd State Medical Academy

6. St. Petersburg State University

7. RUDN University

8. Kazan State Medical University

9. Siberian State Medical University

10. Saint Petersburg State Pediatric Medical Academy
11. National Research University Higher School of Economics
12. Rostov State Medical University
13. Kazan Federal University

14. Omsk State Medical Academy

15. Kuban State Medical University
16. perm state university.

17. Voronezh State Medical Academy

18. Privolzhsky Research Medical University
19. Novosibirsk State University
20. Novosibirsk State Medical University
21. mendeleev university of chemical technology of russia.
22. Saratov State University

23. Moscow Institute of Physics and Technology

24. ITMO University

25. Tomsk State University

26. Pacific State Medical University

27. Belgorod State University

28. Chelyabinsk State Medical Academy
29. kursk state medical university.

30. Russian Presidential Academy of National Economy and Public Administration

The best cities to study Family medicine in Russia based on the number of universities and their ranks are Moscow , Saint Petersburg , Volgograd , and Kazan .
Medicine subfields in Russia

“The Doctor as a Humanist”: The Viewpoint of the Students
Conference Report and Reflection by Poposki Ognen (University Pompeu Fabra); Castillo Gualda Paula (University of Balearic Islands); Barbero Pablos Enrique (University Autonoma de Madrid); Pogosyan Mariam (Sechenov University); Yusupova Diana (Sechenov University); and Ahire Akash (Sechenov University)

The practice of Medicine as a profession has become very technical; doctors rely on fancy investigations, treatment algorithms and standardized guidelines in treating patients. In a lot of universities, medical students and residents are trained without appreciating the importance of art and the humanities in delivering good care to patients and their families. Factual knowledge is imposed on us, as students, from scientific evidence delivered by highly specialized professionals: those who know more and more about niche subjects.
As a result, when someone decides to become a doctor , it seems that scientific training is the sole priority, with most attention being given to the disease-treatment model. As medical students, we are taught very specific subjects, leaving little or no space or time for any cultural enrichment programs. And yet, Personal growth as a doctor and a human being cannot be achieved unless one is exposed to the whole range of human experience. Learning from art and artists can be one such means of gaining these enriching experiences. We can learn from historians, and from eminent painters, sculptors, and writers, as well as from great scientists. How do we achieve these ends? The following essay summarizes and reviews one attempt at providing answers. The 2nd “Doctor as a Humanist” Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment.
To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference. Culture is a complex phenomenon that includes knowledge, beliefs, artistic production, morals, customs and skills acquired by being part of a society, which can be transmitted consciously or unconsciously, by individuals to others and through different generations.
The humanities are academic disciplines that study the cultural aspects and frailties of being human, and use methods that are primarily analytical, critical, or speculative, which distinguish them from the approaches of the natural sciences. Humanism is the practice of making the human story central. Consequently, the studies of humanities, so invested in human stories, is one aspect of practicing humanism.
Technological and practical progress in medicine has been impressive in the past fifty years. Nevertheless, patients still suffer from chronic conditions such as heart failure, chronic lung disease, depression, and many others. These are conditions where technology cannot significantly change the outcomes or reverse the underlying condition. One of the ways to alleviate suffering is through compassion and empathy where the doctor is a professional who listens to, understands and comforts the patient, as well as engaging the patient as a fellow human being. We need arts and humanities as doctors’ tools to comfort and, perhaps, even to heal. We also need them to remind us that we are ‘merely human’ ourselves, and that we share our humanity with our patients, as equals.
Unquestionably, there are fundamental requirements that every physician must internalize; the conference goal was to explain that one such requirement is the humanistic view. Opera, poetry, philosophy, history, the study of dialectics, biographical readings, and even volunteering abroad can be means of engaging the world for positive change. Sometimes called “soft” skills, these are in fact necessary and valuable qualities to empower ourselves as persons, as well as doctors. The 2nd The Doctor as a Humanist Symposium placed the corner stone in a global project that aims to understand medicine as a multidisciplinary subject, and to establish the concept of humanistic medicine both as a science and an art where the patient and the doctor are human beings working together.

STUDENT PARTICIPATION
The event united experts in Medicine and the Humanities from all over the world. The speakers (doctors, nurses and students) were from Russia, the USA, the UK, Spain, Italy, Germany, Mexico and more. Each day’s program was both intense and diverse, and included plenary lectures and panel sessions. Medical students were highly involved in all parts of the conference, offering us a great chance to introduce our projects, share our opinions on various topics, and discuss our questions connected with the role of the humanities in medicine.We participated in roundtable discussions, which were chaired by experts from different countries. Even though this made us nervous, at the same time it was very important for us, as students, to be a part of it. We discussed the future of medical humanities from various perspectives, and above all our thoughts and ideas were listened to and commented on, on an equal basis with the world’s experts. For once, we could see that our views were being taken into consideration, and we hope that in the future this will be the norm and NOT the exception. We are the future of medicine, and our voices should be heard, too.
At the end of the first day there was a students’ session, where we gave our opinions on the relative importance of the medical humanities from a multicultural viewpoint, and on this particular roundtable there were students from Russia, Spain, Iran, Mexico, Italy, as well as a Nursing resident. One of the students during the session shared her view that “I would like to see medicine through the lens of humanism and empathy, and also implement all its principles in my professional life on a daily basis”. All participants agreed, and although we were representing different countries and cultures there was no disagreement about this. Even though we have not yet faced many of the obstacles of the world of medicine, we can see the role of compassion in clinical practice better perhaps than our seniors. We shared our points of view about this question and its relevance in the different countries. It was an incredible moment, as experts and professors demonstrated a great interest in our ideas.
The program was extremely diverse; however, the main idea that most speakers expressed was how to find, sustain and not lose humanist goals. Brandy Schillace gave an impressive presentation entitled “Medical Humanities today: a publisher’s perspective”, which studied the importance of writing and publishing not only clinical trials, but also papers from historians, literary scholars, sociologists, and patients with personal experiences. The nurses Pilar d’Agosto and Maria Arias made a presentation on the topic of the Nursing Perspective that is one of the main pillars of medical practice. Professor Jacek Mostwin (Johns Hopkins University) shared his thoughts on patients’ memoirs. An Italian student, Benedetta Ronchi presented the results of an interview on medical humanities posed to the participants and speakers during the symposium. The plurality of perspectives made this conference an enriching event and showed us how diverse ideas can help us become better doctors. More importantly, it reminded us of our common humanity.
A significant part of the symposium was dedicated to Medicine and Art. Prof Josep Baños and Irene Canbra Badii spoke about the portrayal of physicians in TV medical dramas during the last fifty years. The book “The role of the humanities in the teaching of medical students” was presented by these authors and then given to participants as gifts. Dr Ourania Varsou showed how Poetry can influence human senses through her own experience in communicating with patients. She believed that many of the opinions and knowledge that we have internalized should be unlearned in order to have a better understanding of the human mind. The stimulus of poetry makes this possible. Poetry allows us to find new ways to express ourselves, and thus increase our emotional intelligence and understanding of other people’s feelings.
One of the most impressive lectures was by Dr Joan.B Soriano, who spoke about “Doctors and Patients in Opera” and showed how the leading roles of physicians in opera have changed over the centuries. People used to consider the doctor as the antihero, but with time this view has transformed into a positive one that plays a huge role in history.
It is important to be professional in your medical career, but also to be passionate about the life surrounding you; for instance, Dr Soriano is also a professional baritone singer. For students, this Symposium was full of obvious and hidden messages, which gave us much lot of food for thought. As Edmund Pellegrino, the founding editor of the Journal of Medicine and Philosophy , said: “Medicine is the most humane of sciences, the most empiric of arts, and the most scientific of humanities.”

CHOOSING ONE WORD
To conclude our summary of the students’ viewpoint each of us chose One word to encapsulate our thoughts about the symposium.
The Doctor as a Humanist is a multicultural event where everyone can learn and contribute to this global necessity to put the heart and soul back into medicine. Of course, we are aware and delighted that other organizations are championing the cause of the Humanities in Medicine, and in some cases, such as https://www.dur.ac.uk/imh/ , they have been doing so for many years.
As medical students, we appreciate how we have been placed at the centre of the symposium, which we believe has made this new initiative rather special. We hope that students of Medicine and from other disciplines come and participate in future symposia.
If you want to learn more, and see how you can participate, please contact the International student representatives, Mariam ( [email protected] ) and David ( [email protected] ).
Acknowledgements
Assistance provided by Jonathan McFarland (c) and Joan B. Soriano (University Autonoma de Madrid) was greatly appreciated during the planning and the development of the article.
Analysis and discussion of research | Updates on the latest issues | Open debate
All BMJ blog posts are published under a CC-BY-NC licence
BMJ Journals
- What is DPC?
- Our Providers
- Vaccines at SFM
- Vaccination Guidance
- Vaccination & Stem Cells
- Patient Handbook
- Dr. Story's Podcast
- Ear Piercing
- Forms and Agreements
.png/:/rs=h:320,cg:true,m/qt=q:95)
Andrew Becker PA-C
Andrew Becker, PA-C, was born in Pullman, WA, and graduated from WSU with a degree in Sports Medicine in 2005. In 2010 he received his EMT certification and in 2011 he graduated from the University of Washington’s MEDEX program with a Master of Clinical Health Services degree. He has spent nearly 10 years back on the Palouse practicing internal medicine, urgent care, and wound care as a Physician Assistant. He also serves as a volunteer EMT in Moscow and as Athletic Trainer for Logos School. Andrew loves building lasting relationships with his patients and is looking forward to continuing to build relationships with patients on the Palouse at Story Family Medicine.

Dr. Matthew Rice
Dr. Matthew Rice graduated from Oklahoma State University College of Osteopathic Medicine in Tulsa, OK in 1993. He also completed his Family Medicine Residency in Tulsa. DOs receive the full MD medical school education which additionally includes two years training in musculoskeletal treatment. DOs are also encouraged to view patients holistically (treating both body and soul/spirit). Dr. Rice is double board certified in Family Medicine and has a wide range of experience, having worked in private practice, various rural clinics, Indian Health Services, the Veteran’s Administration and as an ER physician. His practice philosophy is to treat his patients as he would his own beloved family. Speaking of which, he is married to his wonderful wife Doris, has two grown daughters and six delightful and unique grandchildren, whom he delights in!
Dr. Matthew McCabe
Dr. Matthew McCabe graduated with his Bachelor's degree from New Saint Andrews College, right here in Moscow. After a career as a teacher, he completed his MD degree at the University of Calgary and his residency training in Family Medicine at the University of Alberta. He has practiced family medicine in a variety of settings including with the Canadian Armed Forces and has provided hospital and ER coverage in rural Alberta. Dr. McCabe is looking forward to growing his practice through care and skill.
Dr. McCabe cares for patients of all ages.
Lisa Halpert, NP
Meet our Nurse Practitioner, Lisa Halpert. Lisa has worked primarily in internal medicine and urgent care.
Lisa is upbeat, loves a good cup of coffee, and is ready to lend a patient and attentive listening ear. While she primarily works alongside Dr. Story to support his panel, she is available on a case-by-case basis for well-woman exams of all our providers' patients.
Dr. Rod Story
Dr. Rod Story is a highly trained, Board-Certified family physician. He has provided medical care for 18 years in many settings, including the ER, hospital, hospice, and nursing homes. His broad experience and skills can provide for most of your medical needs, including office procedures and advanced testing.
In 2017 Dr. Story received the Physician Excellence Award from Pullman Regional Hospital.
Panel is full.
Story Family Medicine. All rights reserved.
Powered by GoDaddy Website Builder
- Patient Care & Health Information
- Diseases & Conditions
- Neurofibromatosis type 1
Neurofibromatosis type 1 (NF1) is a genetic condition that causes changes in skin pigment and tumors on nerve tissue. Skin changes include flat, light brown spots and freckles in the armpits and groin. Tumors can grow anywhere in the nervous system, including the brain, spinal cord and nerves. NF1 is rare. About 1 in 2,500 is affected by NF1.
The tumors often are not cancerous, known as benign tumors. But sometimes they can become cancerous. Symptoms often are mild. But complications can occur and may include trouble with learning, heart and blood vessel conditions, vision loss, and pain.
Treatment focuses on supporting healthy growth and development in children and early management of complications. If NF1 causes large tumors or tumors that press on a nerve, surgery can reduce symptoms. A newer medicine is available to treat tumors in children, and other new treatments are being developed.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Neurofibroma
Neurofibromatosis type 1 (NF1) usually is diagnosed during childhood. Symptoms are seen at birth or shortly afterward and almost always by age 10. Symptoms tend to be mild to moderate, but they can vary from person to person.
Symptoms include:
- Flat, light brown spots on the skin, known as cafe au lait spots. These harmless spots are common in many people. But having more than six cafe au lait spots suggests NF1. They often are present at birth or appear during the first years of life. After childhood, new spots stop appearing.
- Freckling in the armpits or groin area. Freckling often appears by ages 3 to 5. Freckles are smaller than cafe au lait spots and tend to occur in clusters in skin folds.
- Tiny bumps on the iris of the eye, known as Lisch nodules. These nodules can't easily be seen and don't affect vision.
- Soft, pea-sized bumps on or under the skin called neurofibromas. These benign tumors usually grow in or under the skin but can also grow inside the body. A growth that involves many nerves is called a plexiform neurofibroma. Plexiform neurofibromas, when located on the face, can cause disfigurement. Neurofibromas may increase in number with age.
- Bone changes. Changes in bone development and low bone mineral density can cause bones to form in an irregular way. People with NF1 may have a curved spine, known as scoliosis, or a bowed lower leg.
- Tumor on the nerve that connects the eye to the brain, called an optic pathway glioma. This tumor usually appears by age 3. The tumor rarely appears in late childhood and among teenagers, and almost never in adults.
- Learning disabilities. It's common for children with NF1 to have some trouble with learning. Often there is a specific learning disability, such as trouble with reading or math. Attention-deficit/hyperactivity disorder (ADHD) and speech delay also are common.
- Larger than average head size. Children with NF1 tend to have a larger than average head size due to increased brain volume.
- Short stature. Children who have NF1 often are below average in height.
When to see a doctor
See a healthcare professional if your child has symptoms of neurofibromatosis type 1. The tumors are often not cancerous and are slow growing, but complications can be managed. If your child has a plexiform neurofibroma, a medicine is available to treat it.
Neurofibromatosis type 1 is caused by an altered gene that either is passed down by a parent or occurs at conception.
The NF1 gene is located on chromosome 17. This gene produces a protein called neurofibromin that helps regulate cell growth. When the gene is altered, it causes a loss of neurofibromin. This allows cells to grow without control.
Risk factors
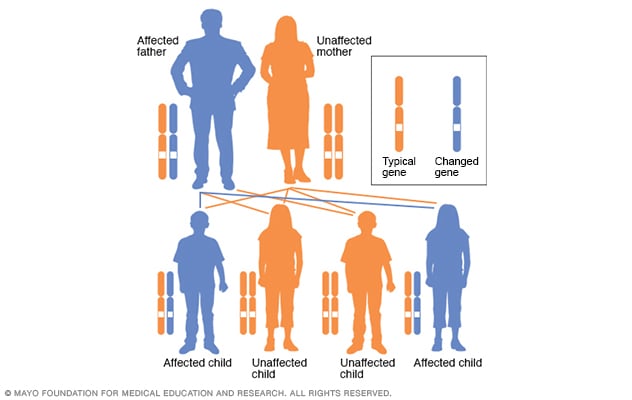
Autosomal dominant inheritance pattern
In an autosomal dominant disorder, the changed gene is a dominant gene. It's located on one of the nonsex chromosomes, called autosomes. Only one changed gene is needed for someone to be affected by this type of condition. A person with an autosomal dominant condition — in this example, the father — has a 50% chance of having an affected child with one changed gene and a 50% chance of having an unaffected child.
The biggest risk factor for neurofibromatosis type 1 (NF1) is a family history. For about half of people who have NF1, the disease was passed down from a parent. People who have NF1 and whose relatives aren't affected are likely to have a new change to a gene.
NF1 has an autosomal dominant inheritance pattern. This means that any child of a parent who is affected by the disease has a 50% chance of having the altered gene.
Complications
Complications of neurofibromatosis type 1 (NF1) vary, even within the same family. Generally, complications occur when tumors affect nerve tissue or press on internal organs.
Complications of NF1 include:
- Neurological symptoms. Trouble with learning and thinking are the most common neurological symptoms associated with NF1. Less common complications include epilepsy and the buildup of excess fluid in the brain.
- Concerns with appearance. Visible signs of NF1 can include widespread cafe au lait spots, many neurofibromas in the facial area or large neurofibromas. In some people this can cause anxiety and emotional distress, even if they're not medically serious.
- Skeletal symptoms. Some children have bones that didn't form as usual. This can cause bowing of the legs and fractures that sometimes don't heal. NF1 can cause curvature of the spine, known as scoliosis, that may need bracing or surgery. NF1 also is associated with lower bone mineral density, which increases the risk of weak bones, known as osteoporosis.
- Changes in vision. Sometimes a tumor called an optic pathway glioma develops on the optic nerve. When this happens, it can affect vision.
- Increase in symptoms during times of hormonal change. Hormonal changes associated with puberty or pregnancy might cause an increase in neurofibromas. Most people who have NF1 have healthy pregnancies but will likely need monitoring by an obstetrician who is familiar with NF1.
- Cardiovascular symptoms. People who have NF1 have an increased risk of high blood pressure and may develop blood vessel conditions.
- Trouble breathing. Rarely, plexiform neurofibromas can put pressure on the airway.
- Cancer. Some people who have NF1 develop cancerous tumors. These usually arise from neurofibromas under the skin or from plexiform neurofibromas. People who have NF1 also have a higher risk of other forms of cancer. They include breast cancer, leukemia, colorectal cancer, brain tumors and some types of soft tissue cancer. Screening for breast cancer should begin earlier, at age 30, for women with NF1 compared to the general population.
- Benign adrenal gland tumor, known as a pheochromocytoma. This noncancerous tumor produces hormones that raise your blood pressure. Surgery often is needed to remove it.
Neurofibromatosis type 1 care at Mayo Clinic
- Ferri FF. Neurofibromatosis. In: Ferri's Clinical Advisor 2024. Elsevier; 2024. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Neurofibromatosis. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Neurofibromatosis-Fact-Sheet. Accessed Feb. 21, 2024.
- Korf BR, et al. Neurofibromatosis type 1 (NF1): Pathogenesis, clinical features, and diagnosis. https://www.uptodate.com/contents/search. Accessed Feb. 21, 2024.
- Saleh M, et al. Neurofibromatosis type 1 system-based manifestations and treatments: A review. Neurological Sciences. 2023; doi:10.1007/s10072-023-06680-5.
- Neurofibromatosis. American Association of Neurological Surgeons. https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Neurofibromatosis. Accessed Feb. 21, 2024.
- Neurofibromatosis. Merck Manual Professional Version. https://www.merckmanuals.com/professional/pediatrics/neurocutaneous-syndromes/neurofibromatosis. Accessed Feb. 21, 2024.
- Jankovic J, et al., eds. Neurocutaneous syndromes. In: Bradley and Daroff's Neurology in Clinical Practice. 8th ed. Elsevier; 2022. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Armstrong AE, et al. Treatment decisions and the use of the MEK inhibitors for children with neurofibromatosis type 1-related plexiform neurofibromas. BMC Cancer. 2023; doi:10.1186/s12885-023-10996-y.
- Zitelli BJ, et al., eds. Neurology. In: Zitelli and Davis' Atlas of Pediatric Physical Diagnoses. 8th ed. Elsevier; 2023. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Kellerman RD, et al. Neurofibromatosis (type 1). In: Conn's Current Therapy 2024. Elsevier; 2024. https://www.clinicalkey.com. Accessed Feb. 21, 2024.
- Babovic-Vuksanovic D (expert opinion). Mayo Clinic. March 26, 2024.
- Tamura R. Current understanding of neurofibromatosis type 1, 2 and schwannomatosis. International Journal of Molecular Sciences. 2021; doi:10.3390/ijms22115850.
- Legius E, et al. Revised diagnostic criteria for neurofibromatosis type 1 and Legius syndrome: An international consensus recommendation. Genetics in Medicine. 2021; doi:10.1038/s41436-021-01170-5.
- Find a doctor. Children's Tumor Foundation. https://www.ctf.org/understanding-nf/find-a-doctor/. Accessed Feb. 26, 2024.
- Ami TR. Allscripts EPSi. Mayo Clinic. April 18, 2024.
- Collecting Pennies Through the Pain
Associated Procedures
- Chemotherapy
- Cochlear implants
- Genetic testing
- Radiation therapy
- Stereotactic radiosurgery
Mayo Clinic in Rochester, Minnesota, Mayo Clinic in Phoenix/Scottsdale, Arizona, and Mayo Clinic in Jacksonville, Florida, have been ranked among the best Neurology & Neurosurgery hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.

IMAGES
VIDEO
COMMENTS
In 2019, regular surveillance of 110 English-language research journals identified 254 studies that met the criteria to become POEMs (patient-oriented evidence that matters). Physician members of ...
Family Medicine Topics. Adolescent Medicine. Adverse Drug Events Reporting. Antibiotic Resistance. Asthma. Cardiovascular Risk Reduction. Chronic Kidney Disease. Coronavirus (COVID-19)
Intrauterine tamponade (with a balloon, packing, or vacuum) may be used to manage patients with postpartum hemorrhage (PPH) resulting from uterine atony that is not controlled by uterotonic medications and uterine massage. However, outcome data regarding vacuum-induced tamponade are limited.
India's need to integrate its socio-cultural and scientific epistemology to position itself as a global leader. Raina, Sunil K.; Kumar, Raman. Journal of Family Medicine and Primary Care. 13 (3):811-813, March 2024. Abstract. Abstract. Favorite. PDF. Permissions. Open.
Priority Updates to the Research Literature (PURLs) Series Now Featured in the JABFM. Gregory Castelli. The Journal of the American Board of Family Medicine March 2024, 37 (2) 165; ... The Journal of the American Board of Family Medicine March 2024, 37 (2) 303-308; DOI: ...
Get daily research topics, journal summaries & news from MDLinx. Create a free account to access exclusive CME content, conference listings & more.
Of more than 20,000 research studies published in 2022 in the journals reviewed by the POEMs team, 253 met criteria for validity, relevance, and practice change. These POEMs are emailed daily to ...
A family medicine, public and community health journal publishing original research, reviews, methodology and case-studies from the lens of population health. ... Family Medicine and Community Health. is an open access journal focusing on the topics of family medicine, general practice and community health. Impact Factor 6.1
Research in the Department of Family Medicine-Research focuses on two areas: Clinical research. Our clinical research efforts help pinpoint the causes of disease and identify effective methods of prevention and treatment. Read more about clinical research. Quality and practice improvement research. Research efforts related to quality and ...
We are now entering the third decade of the 21st Century, and, especially in the last years, the achievements made by scientists have been exceptional, leading to major advancements in the fast-growing field of Family Medicine and Primary Care. Frontiers has organized a series of Research Topics to highlight the latest advancements in science in order to be at the forefront of science in ...
Palliative and End of Life Care in the Post-Pandemic Era: Old Problems and New Perspectives. Barbara Sena. Enrico De Luca. Guido Giarelli. 836 views. 1 article. This section focuses on real life primary health care topics, such as prevention, diagnosis, treatment, and management of important health problems.
Family Medicine and Primary Care redhwan ahmed al-naggar. Faculty of Medicine, National University of Malaysia. Cheras, Malaysia. ... Research Topics See all (110) Learn more about Research Topics. Footer. Guidelines. Author guidelines; Editor guidelines; Policies and publication ethics ...
American Family Physician. The AAFP's peer-reviewed, evidence-based clinical journal offers concise, practical, easy-to-read clinical review articles for physicians and other health care ...
Research in the Department of Family Medicine-Research covers a broad range of medical issues focused on family and community medicine, including headache, depression, calcium and vitamin D nutrition, obesity, women's health, and global health. Through networking and access to resources across Mayo Clinic, the Department of Family Medicine ...
Research. Mayo Clinic family medicine researchers study many aspects of care for families and communities, including cancer screenings, depression, obesity, virtual care and prenatal care. Their goal is to improve how care is delivered and to build on a foundation of scientific evidence that supports the team-based model of care. Learn about ...
0.50 CME / ABIM MOC / CE. Medscape Now! Hot Topics in Family Medicine August 2023 Part 1. Learn about recent findings in acetaminophen poisoning treatment guidelines, diet-related gut inflammation, and autism-linked self-harm. Authors: News Authors: Pauline Anderson and Sarah Amandolare; CME Author: Kayla Naas, MA.
We study topics relevant to Family Medicine practitioners, patients and students, including: Community-based medical education; ... The Current State of Research Capacity in US Family Medicine Departments. Fam Med. 2019 Feb;51(2):112-119. doi: 10.22454/FamMed.2019.180310. PMID: 30736036.
Family Medicine, an official journal of the Society of Teachers of Family Medicine, aims to publish high-quality, original scholarship about education in family medicine and primary care.The journal publishes original research, systematic reviews, narrative essays, and policy analyses relevant to the discipline of family medicine, particularly focusing on primary care medical education, health ...
The WPRN is a network of more than 97 primary care practices across the five-state WWAMI (Washington, Wyoming, Alaska, Montana and Idaho) region that collaborate on research. The mission of the WPRN is to improve the health and well-being of patients in their communities, through the conduct of collaborative research that informs and enhances ...
Discover the components of a rewarding family medicine residency. Find out how to select a program that helps you develop the expertise you need for a successful clinical or academic career. ... Potential Research Project Topics; Site Index. Department of Family Medicine . 11/1/21 About Us; 2/7/19 Education and Training; 9/8/22 Family Medicine ...
The goal of this activity is for learners to be better able to evaluate and implement emerging data and guidelines into patient care. Upon completion of this activity, participants will: Have increased knowledge regarding the. Recent advances in family medicine that are improving patient care. Implications for the healthcare team.
More information: Aditi Vasan et al, Connecting Families to Benefit Programs Through a Standardized Nutrition Screener, The Annals of Family Medicine (2024). DOI: 10.1370/afm.3095 Journal ...
Toxicology 5. Urology 17. Veterinary 14. Virology 40. Below is the list of 30 best universities for Family medicine in Russia ranked based on their research performance: a graph of 47.2K citations received by 7.64K academic papers made by these universities was used to calculate ratings and create the top.
The 2nd "Doctor as a Humanist" Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment. To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference.
The clinic is across the street from a large church for West Sacramento's growing Russian population. Leaders of Vida Family Health Center hope the new family medicine residency training site will result in more physician hires from UC Davis Health. CommuniCare, as the Yolo County health care organization was known before recently merging ...
Highlighted Topics. Alzheimer's and Dementia. Brain Health. Caregiving. Clinical Trials and Studies. Exercise and Physical Activity. Healthy Eating. Menopause. NIA provides health information informed by research and reviewed by experts to help you learn about healthy aging and common health conditions in older adults.
NEJM Evidence NEW! A digital journal for innovative original research and fresh, bold ideas in clinical trial design and clinical decision-making.
Dr. Rod Story. Dr. Rod Story is a highly trained, Board-Certified family physician. He has provided medical care for 18 years in many settings, including the ER, hospital, hospice, and nursing homes. His broad experience and skills can provide for most of your medical needs, including office procedures and advanced testing.
Neurofibromatosis type 1 (NF1) is a genetic condition that causes changes in skin pigment and tumors on nerve tissue. Skin changes include flat, light brown spots and freckles in the armpits and groin. Tumors can grow anywhere in the nervous system, including the brain, spinal cord and nerves. NF1 is rare. About 1 in 2,500 is affected by NF1.